


















The only way to stop it is to willingly not pay attention. The problem is, readers of this magazine find it very difficult to do this – we are compelled to attend the webinar, follow that email, open these pages.
We are continual learners. That’s part of the definition of ‘Professionals’ assigned by Dr. Pankey and others. Constantly seeking new answers for clinical puzzles gives us confidence to welcome the next health seeker to our offices. We want to be able to look our patients in the eye and transmit this confidence to them – everyone who puts themselves in a health care professional’s hand wants to believe they are safe.
How do we know what we are learning is the ‘right thing?’ If you have a foolproof answer for that question, please, share it with the world. No one else has figured it out. What we believe to be true and worthy of using for our patients’ benefit must be filtered through prior learning, personal experiences, our values, and our commitment to ethical behavior, however those things are defined by each of us.
Puts a lot of responsibility on each of us, doesn’t it? Yet, we willingly embrace that ‘burden’ because we enjoy the rewards of wellserved patients and the satisfaction of sorting out the riddles, piecing together the pictures, imagining the best outcome, and encouraging changes of behavior that produce the high perceived value sought by our patients.
Where does that start? How can we become confident we can be the change agent most likely to achieve such positive results? I believe we must become upstream advocates.
One of the many helpful books Dan Heath has written is Upstream, The Quest to Solve Problems Before They Happen. By telling stories of success looking at what is happening not as a current event but as part of a line of events, Heath points out that we can often change expectations by catching problems
far earlier than we have been taught to see them.
Medicine is a symptom-treatment system, despite decades of effort to promote prevention through diet, exercise, and mindfulness. Dentistry, with an emphasis on controlling triggers to inflammation and adding fluoride, has a long and proud history of preventive focus. But dentists still face high demand for restorative services – the equivalent of medicine’s prescription page. Both address downstream problems.
Steve Carstensen, DDS Diplomate, American Board of Dental Sleep Medicine
Back to continual learning. Exploring the root causes of the symptoms presented allows us to think upstream. Since most of our therapies do not cure, but manage, chronic disease, there may be a way for the patient to work themselves upstream, if given a vision of the benefit.
Imagine the next sleepy patient in your clinic. They need help now for their downstream problems. PAP or OAT gets their airway, and their ability to see other choices, open. If we stop at these management devices, we do not honor our learning. We don’t apply the best of what we can do. Let’s lead them upstream.
What have you learned lately about endotypes, precision medicine, more targeted and easier diagnostics? Is there a way for you to direct your sleepy patient to make changes in lifestyle, in breathing patterns, in structure and function of the airway? These are moving treatment upstream and away from symptom-focused advice.
Continually seeking new knowledge allows you to keep up. Being a great doctor requires you to bring your patients up with you.
Provider of the Year?
by Len Liptak, ProSomnus Co-founder and CEO, and Mark T. Murphy, DDS, D.ABDSM Merging design, materials, and research to focus on
outcome.
Medical Insight
Desaturation Patterns Versus Apnea Hypopnea Index: Which is More Reliable?
by Dr. Jagdeep BijwadiaA discussion of the limitations and strengths of various measures of oxygen saturation and exploring newer metrics.

Acquired from Sleep Related
Breathing Disorders is the Cause of Most Non-Communicable Diseases


 by Dr. Steve Lamberg
by Dr. Steve Lamberg
Tiny things are the foundation of health and disease.
2 CE CREDITS
Medical Insight
Looking at the new paradigm in physician acceptance of oral appliance therapy in the treatment of OSA.

35
AADSM Special Section
Visit with these innovative companies at the AADSM.
Each drug-free treatment plan is tailored to address the individual patient’s symptoms, and includes the use of several tested technologies, including ultrasound, photobiomodulation, microcurrent, and muscle manipulation.






Clinician Spotlight The Duck Wrangler
DSP interview with Rose Nierman
8
6 Publisher’s Perspective
Be the Lotus
by Lisa Moler, Founder/CEO, MedMark Media

23 Team Effort LIAISONS: Moving Collaborative Care from Idea to Reality
by Stacey Larkin, RDH, OMT
The more connections we can make, the better we can serve our community health.
26 Cardio-Sleep Corner Addressing Poor Sleep May Help Heart Health
by Lee A. Surkin, MD, FACC, FCCP, FASNC, FAASM
Poor sleep can negatively affect the heart; a recent study emphasizes this.

48 Bigger Picture Happy 57th Birthday to the Beast Known as Sleep Apnea!
by David E. McCarty, MD, FAASM
All these years, and we’re still figuring it out.
Getting paid has always been part of the service.
52 Adjunctive Therapy
Management of Temporomandibular Disorders with Orofacial Myofunctional Therapy
by Zareth Jana Hernández, DMD
Be alert for how other therapies can help clinical management.
55 Practice Growth Helping Your Community with WatchPAT® ONE
by Glennine Varga
The pandemic opened new ways of addressing patient concerns.
58 Practice Management Does Selling Have a Place in Dentistry?
by Dr. Chelsea Erickson
Achieving health goals means helping people decide with integrity.
60 Legal Ledger Legal Misalignment
by Daniel B. Brown, Esq.
How corporate practice doctrines bite against sleep doctors and sleep dentists.
64 Seek and Sleep DSP Waffle
Expert View Sleep and Pain: Can’t We Pick Just One?
16
by Steven D. Bender, DDS
The fascinating connection between two common conditions.
Summer 2023
Publisher | Lisa Moler lmoler@medmarkmedia.com
Chief Dental Editor
Steve Carstensen, DDS, D.ABDSM stevec@medmarkmedia.com
Chief Medical Editor
Lee A. Surkin, MD, FACC, FCCP, FASNC drsurkin@n3sleep.com
Associate Editor | Lou Shuman, DMD, CAGS lou@medmarkmedia.com
Editorial Advisors
Steven Bender, DDS
Jagdeep Bijwadia, MD (Pulmonary, Sleep)
Kevin Boyd, DDS
Karen Parker Davidson, DHA, MSA, M.Ed., MSN, RN
Kristie Gatto, MA, CCC-SLP, COM
Amalia Geller, MD (Neurology, Sleep)
William Hang, DDS, MSD
Steve Lamberg, DDS, D.ABDSM
Christopher Lettieri, MD (Pulmonary, Critical Care, Sleep)
Pat McBride, PhD, CCSH
Jyotsna Sahni, MD (Internal Medicine, Sleep)
Ed Sall, MD (ENT, Sleep)
Alan D. Steljes, MD (Cardiology, Sleep)
Laura Sheppard, CDT, TE
DeWitt Wilkerson, DMD
Scott Williams, MD (Psychiatry, Sleep)
Gy Yatros, DMD
National Account Manager

Adrienne Good | agood@medmarkmedia.com
Sales Assistant & Client Services
Melissa Minnick | melissa@medmarkmedia.com
Creative Director/Production Manager
Amanda Culver | amanda@medmarkmedia.com
Marketing & Digital Strategy
Amzi Koury | amzi@medmarkmedia.com
eMedia Coordinator
Michelle Britzius | emedia@medmarkmedia.com
Social Media & PR Manager
April Gutierrez | medmarkmedia@medmarkmedia.com
Webmaster
Eileen Kane | webmaster@medmarkmedia.com
MedMark, LLC
15720 N. Greenway-Hayden Loop #9 Scottsdale, AZ 85260
Tel: (480) 621-8955 | Toll-free: (866) 579-9496 www.DentalSleepPractice.com
Subscription Rate: 1 year (4 issues) $149
©MedMark, LLC 2023. All rights reserved. The publisher’s written consent must be obtained before any part of this publication may be reproduced in any form whatsoever, including photocopies and information retrieval systems. While every care has been taken in the preparation of this magazine, the publisher cannot be held responsible for the accuracy of the information printed herein, or in any consequence arising from it. The views expressed herein are those of the author(s) and not necessarily the opinion of either Dental Sleep Practice magazine or the publisher.
The MandiTrac will target the three main jaw muscles for better functionality , improved airway and decreased facial pain . The exercises are to be done once per day and takes about 1 minute to complete.

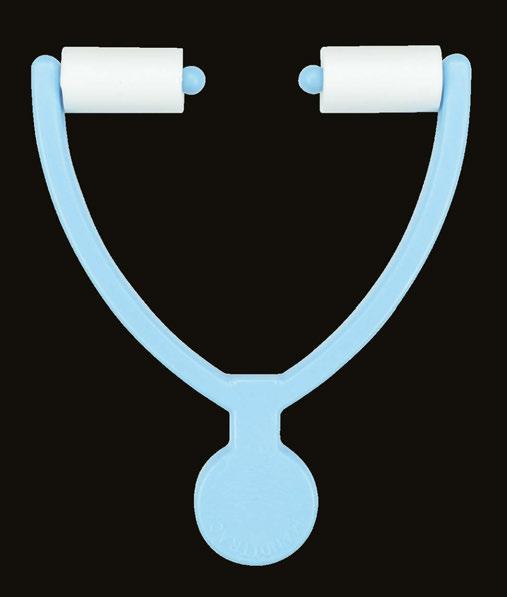
We put a lot of stress on our jaw with grinding, clenching, sleep apnea, dental sleep devices, but often times we do not exercise or stretch our jaw muscles back out.

“Working on orofacial muscular strength and awareness takes time and dedication. I am grateful for the MandiTrac, as it provides an easy way for my patients to take less than 3 minutes of their time to enhance the muscles that support their tongue posture and jaw function.”
In an array of colors, blue, white, purple, red, or pink, lotuses are touted as symbols of peace, beauty, and longevity. I love lotus flowers. Earth.com describes them as extremely strong with the first one estimated to have sprouted millions of years ago. For all of its breathtaking beauty, the lotus flower grows out of the mud, rising above the water. As a result, it also has gained a reputation as a symbol of persistence. What does this flower have to do with anything dental, anyway? Well, like the lotus flower, on our professional and personal journeys, we may have to find the strength to grow out of somewhat messy circumstances or humble beginnings. How do we do it? Persistence, innovation, and constantly reaching for a higher standard.
Lisa Moler Founder/CEO, MedMark Media
One way to get out of our rut when we are stuck in the mud is by purging – getting rid of old perceptions, equipment, or materials that hold us back from growing. After freeing up some space, invite future growth by researching and adding new things that can improve life around your office and for your patients. Imaging, 3D printing, AI software, instrumentation – you name it – dental visionaries and entrepreneurs are introducing amazing inventions every day. You just have to find the ones that fit your own space and needs, and maybe even help you grow outside your comfort zone. We hope to be able to help you on your journey.
We have lots of ideas in this issue to help you expand your mind and office. Dr. Steve Lamberg delves into how mitochondria can affect sleep-related breathing disorders and interfere with healthy cellular function. Our cover story, “Dental Sleep Medicine Provider of the Year?” discusses precision intraoral medical devices, a new category of OAT devices. This category now includes the EVO® by ProSomnus®, engineered to consis-
tently protrude and stabilize the mandible within one millimeter of the target mandibular position for each patient. This device utilizes AI-driven software and manufacturing robots to virtually eliminate protrusion inconsistencies. Our AADSM Special Section features companies that run the gamut of innovation from a custom TAP appliance to Dental Sleep Medicine Systems for software and billing to sleep-changing oral appliance therapies.
At MedMark, we don’t want your practices to be stuck in the mud of mediocrity. Ora Nadrich, life coach and mindfulness teacher said, “On the path of self-realization, there is no one big awakening, but many along the way of varying degrees: some small, some big; and each one of them is like the lotus flower, which grows out of muddy waters.” So my message this issue is: No matter how small or big your practice, be a lotus; keep growing, changing, and reaching for whatever it takes to make you blossom.
To your best success,
Lisa MolerDo you like what you are reading in DSP? Do you have ideas you want to share about what works in your practice? Our Chief Dental Editor Dr. Steve Carstensen is happy to consider essays from any reader! Contact him at stevec@medmarkmedia.com.

Rose Nierman has been the go-to source for dentists getting paid for new services since before the first mandibular advancement devices hit the market. She feels that managing patient success includes making financial barriers as low as possible. To help current dentists appreciate how medical billing has become the norm for TMD and airway support services, DSP engaged Rose in a lively conversation.

DSP: Rose, let’s start at the beginning. How did you get involved in medical billing?
Rose Nierman: I was a dental hygienist. Our dentist took us all to see Brendon Stack – he talked about success treating TMD in our practice. My dentist asked me to learn how to be the TMD assistant, so I started helping with appliances. We got started with American Academy of Craniofacial Pain and treated these patients for quite a while. When our admin staff attended a course on billing and came back to the practice and refused to take that on, I thought “I could do that.” Soon, I wasn’t doing hygiene any longer –TMD assisting and medical billing became my role. The more I got into it, the more I wanted to do. Our practice was mostly fee for service, so we’d give patients superbills and a narrative report of medical necessity, and they would get reimbursed. I became good at talking patients through this process, so I learned a lot about coding and documentation.
DSP: That’s the same today, isn’t it? Administrative staff still must take on medical billing, some offices are fee for service, and documentation is required, right?
RN: Yes, but it’s also different. The documentation requirements for sleep appliances have undergone changes. It got a lot easier when CMS (Medicare) started allowing for mandibular advancement devices and set down the rules for what information is necessary for a complete claim. By giving us a list of what is needed, it made it simpler for dentists to gather everything from the physicians. Many of our clients initially tried to stay fee for service, so they collect upfront, but they are finding out that the insurance companies are turning around and calling them to get documents when the patient submits the claim on their own. So, the dental practices are still having to put some effort in for claims to be paid, but they have the money upfront. By the way, we still hear from some physicians that they don’t think oral appliances are covered by medical insurance and say that’s one of the reasons they don’t prescribe them. One doctor I know told me he ‘just refers them to Inspire,’ because he thinks the “dental device” won’t be covered, but the implant will. I think this comes from being told about fee for service in dentistry, so they think all dentists do it this way. This highlights the importance of notifying physicians that you are billing medical insurance for these devices.
DSP: Have there been any changes that make this easier?
RN: The biggest has been the advent of telemedicine – by both physicians and dentists. Now, instead of having to tell your dental patient to wait for weeks or months to see a physician about sleep breathing, you can get this done very quickly. Several companies provide this service. There are also a lot of articles written about what documentation is needed; dentists can share these with referring physicians to make that process go smoother.

DSP: Do you think physicians know how billing works? Do they understand what their (and our) team have to do to get a claim paid?
RN: I don’t think they have a strong understanding of all the requirements. One helpful tip is for dental admin team members to connect with their counterpart in the physician’s office and tell them what we need is the same as what CPAP requires. I have noticed that some insurers request data about other treatments the patient has tried before paying. One company insists, for example, that patients must try diazepam and a soft diet before they will pay for any other TMD therapy. Can you imagine? Proof of delivery is another sticking point we are finding that’s relatively new. We are getting reports of denial of payment because the dentist didn’t have the patient sign a paper that says they received their custom device. We are advising all our clients to make sure they get those signatures!
DSP: What about Medicare – CMS. Do you think dentists should sign up?

RN: Yes, we believe this is a beneficial step. Most physicians expect dentists to be enrolled, and we still advise dentists to enroll as non-participating DME suppliers. That gives the dental practice the ability to balance bill – meaning they have the option of collecting their full fee. We also think Medicare has done the best job detailing the information needed for a claim, so we advise all our clients to ‘document like the claim is going to Medicare,’ even for commercial carriers. It makes it simpler to do it all the same way.
DSP: Medicare restricts us to using PDAC-listed devices. Now we see commercial carriers doing the same thing. What do you think about that?
RN: This is an area I wish the dental academies and organizations could help change. I think dentists should be in charge of choosing the right device for the patient.
DSP: Do you think dentists should be in network with medical carriers?

RN: In the early days, some dentists were quite successful in negotiating good fees on insurance contracts. Some still are, but I think many dentists are staying fee for service and assisting patients in obtaining reimbursement. I hear some consultants making big promises to dentists about getting them in-network with big fees, but those promises make me worry – it’s not always a slam dunk.
DSP: What about E&M codes and Medicare? – that’s another point of dispute.
RN: Medicare has come out pretty
 Rose Nierman and Dr. Steve Carstensen at a CE event.
Rose Nierman and Dr. Steve Carstensen at a CE event.
Rose always strives to provide the most relevant data and products. If she doesn’t have the answer today, she will find out what she can to provide information tomorrow. For over 20 years, she has provided me with guidance on understanding medical billing for dentists. She has worked her entire career to provide solutions intended to lighten the struggles of the dental to medical translation for insurance and letters. Personally, I’ve seen her solutions succeed for thousands of offices, and I look forward to watching her lasting impressions help dentists help patients. Thank you for everything Rose!

 – Glennine Varga
– Glennine Varga

Rose Nierman unequivocally made it possible for dental practices to significantly increase patient access to care for Dental Sleep Medicine (DSM) services by providing the education, software, and support required for successful and ethical medical documentation, coding, and billing. This profound impact on the DSM industry continues to tranform practices, improve lives, and cultivate dental-medical community collaboration.
– Courtney SnowSeveral decades ago, while building a unique medical referral only TMD and Dental Sleep practice, I was struggling to keep up with reports seeing 30-50 new patients a month. I believe I was among the first clients that embraced Rose Nierman’s Dentalwriter program. Frankly, the practice was beyond capabilities of software. Rose has an infectious can do attitude. Her team adapted to me. Writing new code to handle my practice. 10k patients in my system. Full practice including billing and scheduling....dialed!


Over 30 years when I pivot, she’s a step ahead of me. A jewel of a human and a treasure of the profession.
Yes, “There’s a code for that”!
– Tim Mickiewicz, DDSstrongly against dentists charging evaluation and management fees, including at a panel at the last AADSM meeting. On the other hand, their new rules consider the time spent seeing patients, reading sleep reports, physician notes, and writing up the dentist’s own notes as the basis for E&M coding. These conflicting directives keep us guessing. I know offices that submit E&M codes and others that don’t without facing any definite Medicare response so far. I would recommend that dentists error on the side of caution and seek guidance about protocols. Either way, dentists still can’t bill anything for 90 days after delivery – that much is clear.
DSP: What’s the future look like, Rose?
RN: It’s not that much different than the past! Just like I changed from dental hygienist to become the TMD, then Sleep, Champion in my office, each dental practice must identify one team member who takes ownership and becomes passionate about helping people. Yes, there are challenges in staffing – we’ve all felt them – but those seem to be resolving and dentists can get on with the health improvements they offer. We celebrate when we can help our clients either bill on their own or guide them in how to succeed with a billing company. There are several billing companies, so there is no need to bill in-house if you don’t want to, at least at first. But even with a billing service, there needs to be that team member eager to coordinate. Treating sleep and TMD problems is a great service to dental patients. I always say, “Get your ducks in a row! Don’t let billing problems keep you from rewarding your team, yourself, and your practice by creating happy healthy patients!”
Rose teaching medical billing.Hosting a CE course in Jupiter, FL.
The Academy of Clinical Sleep Disorders Disciplines is the only organization offering a fully online and on-demand certificate in Dental Sleep Medicine. Study the lectures and course materials at your own pace, then when you are ready, take the exam. The C.DSM certificate from ACSDD provides the necessary medical and dental knowledge to confidently approach physicians and seek insurance reimbursement.
The certificate is a prerequisite for ACSDD Fellow and Diplomate.
The Academy of Clinical Sleep Disorder Disciplines is the only organization offering a fully online and on-demand certificate in Dental Sleep Medicine. Study the lectures and course materials at your own pace, then when you are ready, take the exam. 12 modules present both the medical and dental science of sleep medicine providing a solid foundation for understanding clinical applications. Most dentists are able to complete the 13 CE program in 4-6 months.
The certificate is a prerequisite for ACSDD Fellow and Diplomate


Picture yourself on the cover of this journal, being praised by your peers for crossing the chasm with sleep physicians. It is likely you did not do it alone. You had the help of modern medical device manufacturing, artificial intelligent design with efficacy and adherence that was finally on par with CPAP. You used advanced medical grade class VI materials and had evidence-based logic that guided AADSM AASM treatment protocols.
Inconsistent efficacy is the cardinal reason physicians are reluctant to refer patients for Oral Appliance Therapy (“OAT”). Studies, surveys, and focus groups have been conducted on this topic, ad nauseum. The feedback is clear: convince physicians that DSM providers have resolved the problem of inconsistent efficacy and physicians will refer patients for OAT. In other words, if you can provide OAT that delivers consistent efficacy you will be the DSM provider of the year. You even might find yourself on the cover of DSP.
How does one resolve inconsistent efficacy? Where is that data going to come from? All oral appliances are the same, right?
In DSM, before the advent of precision medical device designs for OSA therapy, research studies indicated that all traditional oral appliances had similarly inconsistent efficacy. All oral appliances do share the same mechanism of action: 1. protrude and 2. stabilize the mandible at a target position where the airway is patent. This mechanism of action is well-established in medical guidelines. It is evidence based, constructed upon systemic literature reviews.
Yet, what DSM providers might not be aware of is that traditional oral appliances are inconsistent at performing this mechanism of action.
Traditional oral appliances do not consistently protrude the mandible at the target position. We measured this before founding ProSomnus. Protrusive positions deviated from target by an average of three millimeters. A more recent study reported an average protrusion variance of 3.7 +/- 1.4 millimeters relative to target. For those familiar with dental laboratory methods for fabricating oral appliances, this inconsistency is understandable. Building a complex, patient-specific, oral appliance by hand is very difficult, even if CAD/CAM assisted.
Nor do traditional oral appliances consistently stabilize the mandible at the target position. On average, traditional oral appliances allow the mandible to retrude approximately two millimeters for every five millimeters of mouth opening. Herbst arms and angled dorsal posts allow the mandible to retrude if a patient opens their mouth during sleep. Nylon and elastomeric strap titration mechanisms allow several millimeters of anterior-posterior play, in addition to stretching and deforming over time.

Might inconsistent efficacy be the consequence of traditional oral appliances’ inability to consistently protrude and stabilize the mandible at the target position? Do five or six millimeters of error affect efficacy? Consider that the mean minimum upper airway

“The
peer reviewed independent research on ProSomnus EVO demonstrates efficacy on par with CPAP. Because of superior objective adherence, ProSomnus EVO is likely to be more effective than CPAP. This is what physicians have been waiting for, better treatment options for OSA than CPAP or HNS. The results of the FLOSAT and Severe OSA trials, currently underway, will be transformative for sure. The new ProSomnus sensor technology will give physicians the final link to engage with us. Incredible stuff.” – John E. Remmers, MD
cross section for an OSA patient is 4.6 +/1.2mm (Ogawa, 2006). The magnitude of the inconsistency of traditional oral appliances exceeds the mean minimum upper airway cross section!
Not surprising, scientific investigations by Esaki in 1997, Kato in 2000, Walker in 2003, Gindre in 2008, and Aarab in 2010 report a “dose dependent” relationship between efficacy and mandibular protrusion. After standardizing definitions, these studies suggest a one-millimeter change in mandibular protru-
Len Liptak is the CEO of ProSomnus® Sleep Technologies. An award-winning executive with expertise growing and operating innovation-oriented businesses, Len is a founding member of ProSomnus, and co-inventor of the company’s flagship product. Len also serves on the company’s Board of Directors. Prior to starting ProSomnus, Len was President of MicroDental Laboratories, where he led the commercializationof multiple, award-winning new products, guided business unit operations, and directed the expansion of the company’s digital supply chain. During Len’s tenure, the company grew three times faster than the industry average, expanded gross margins, and set company records for profitability. Len was named to ExecRank’s list of top executives for privately held companies in 2012 and 2013. In 2016, Len led the sale of MicroDental Laboratories to the Modern Dental Group (HKG:3600). Len also spent 10 years at 3M Company and Stryker Corporation in strategic business development, business unit management, and product development capacities. Len earned an M.B.A. from the University of Minnesota’s Carlson School of Management and a B.A. from Brown University. A lifelong learner, Len has completed executive education programs at John’s Hopkins, and is a member of the Young President’s Organization (YPO).
Mark T. Murphy, DDS, D.ABDSM, is an American Board of Dental Sleep Medicine Diplomate and has practiced in the Rochester, MI area for 40 years. He is the Chief Growth Officer at ProSomnus Sleep Technologies, serves on the DSM faculty at University of Detroit Mercy School of Dentistry, and is a regular presenter on Dental Sleep Medicine at the Pankey Institute. He has served on the Board of Directors of the Pankey Institute, National Association of Dental Laboratories, the Identalloy Council, the Foundation for Dental Laboratory Technology, St. Vincent DePaul’s Dental Center, and the Dental Advisor. He lectures internationally on Leadership, Strategic Planning, and Dental Sleep Medicine.


recent
sion is associated with a 10% change in efficacy. It seems logical that a five- or six-millimeter variance in mandibular protrusion might affect efficacy.
To clarify, this is not to suggest more consistent protrusion and stabilization transforms non-responders into responders. Non-responders are non-responders. What this is suggesting is that there are responders who end up as non-responders because the oral appliance does not reposition and stabilize their mandible within an acceptable tolerance of the target position. When this happens, a patient who would respond, might not respond, despite the best efforts for the DSM provider to titrate and adjust the appliance. This inconsistency drags down the mean efficacy for the population treated with traditional oral appliances.
Why not adjust the traditional oral appliance to maximum protrusion? The same dose dependency research finds that the risk of side effects increases with protrusion. Each millimeter of incremental protrusion is, in general, associated with an incremental increase in side effect risk. It is important to find the target and select a device that can protrude and stabilize the mandible at that target position.
Yes, in the hands of select providers, or by following preferred protocols, or appliance titration, one could sometimes eke out a few more points of efficacy with traditional oral appliances. With inconsistent efficacy somewhat assumed, choosing an oral appliance was far more about patient preferences, dental considerations, comfort, management

of side effects, ease of delivery and use. The initial price of the device along with the full cost of repair, remake and chair time were also fair game in the provider decision matrix. Most of the above choices might help improve patient adherence, create practice efficiencies, and save the provider money to round out the business case in DSM. This is all good. But none of it adequately addresses the root cause issues of inconsistent efficacy.

What if a new type of precision intraoral medical device could more consistently protrude and stabilize the mandible relative to target? What if a new type of precision intraoral medical device could virtually eliminate the five or six millimeters of inconsistency relative to the target mandibular position? Might eliminating these inconsistencies in mandibular protrusion yield more consistent efficacy? Might this also reduce the risk of side effects, with the assumption that providers would be less likely to over-protrude while chasing efficacy?
Precision intraoral medical devices are a new category of OAT devices. Precision intraoral medical devices, such as the EVO® by ProSomnus®, are engineered to consistently protrude and stabilize the mandible within one millimeter of the target mandibular position for each patient. ProSomnus precision devices, for example, have a quality control specification of 0.5mm of global variance. The term global refers to six axis total variance, including anterior posterior, vertical, lateral, roll, pitch, and yaw variances. The actual mean global variance for ProSomnus devices is 0.32mm, about 12x less global protrusion variance than the typical traditional oral appliance.
Precision intraoral medical devices such as EVO by ProSomnus stabilize the mandible in the target position. The ProSomnus EVO, for example, features a 90-degree post. This 90-degree post allows the mandible to move side to side and even vertically while still stabilizing the mandible in the target protrusive position.
Utilizing AI-driven software and manufacturing robots to virtually eliminate protrusion inconsistencies, precision intraoral devices by ProSomnus that have demonstrated 94% success treating mild and moderate OSA patients to an AHI/ODI below 10 events per hour. This is approximately 26% points better than what has been previously reported

for traditional oral appliances. These types of efficacy results suggest the overall effectiveness (efficacy times adherence) of precision intraoral devices may be on par with CPAP for mild and moderate OSA patients.
Outcomes data consistently demonstrating greater than 90% efficacy with precision intraoral devices, although more data is warranted and those studies are in-process, may convince physicians to reconsider Oral Appliance Therapy as part of their overall prescription mix. It is estimated that there are over six million CPAP placements annually in North America. The prescription OAT market may represent as high as 5% or 300,000 devices. That estimated ratio has remained unchanged over the years and the CAGR for PAP and OAT have grown in parallel. A simple 10% shift in prescribing patterns will triple the demand for OAT. Traditional oral appliances will not drive this change; they haven’t for decades. Precision, intraoral devices that provide medical grade outcomes data, delivered by caring qualified therapy providers striving for improved efficacy, better adherence, and improved health outcomes likely will be what it takes.
The environment is ripe to educate physicians about the merits of precision Oral Appliance Therapy relative to traditional oral appliances. Physicians and their patients have very quickly learned that not all CPAPs are the same. Like oral appliances, for years physicians assumed that all CPAPs were the same. Like oral appliances, all CPAPs share the same mechanism of action. The mechanism of action for a CPAP is to overcome airway obstruction by applying an appropriate amount of pressure. Not enough pressure and the airway might still collapse. Too much pressure and the patient may be less likely to tolerate it.
Yet all CPAPs are irrefutably not the same. One specific brand of CPAP is under FDA recall. Why not recall all CPAPs, if they are all the same? The brand under recall uses different materials than the other brands. And those materials are associated with a higher risk to patient safety. Same mechanism of action as the other CPAP brands? Yes. Same performance profile as the other CPAP brands? No.
Moving forward, ProSomnus will continue to pursue efficacy. If we want to boost treatment effectiveness, there is no other
“I switched to ProSomnus precision devices based on patient experience and clinical outcomes. I published a retrospective analysis of 115 consecutively treated patients at the World Sleep Congress in Rome, March of 2022. The data showed that a precision oral appliance is capable of successfully treating patients with all levels of severity with most patients treated to an AHI < 5 and 29 severe patients with an average AHI of 51.5 were treated to a final AHI average of 9.9.”
– Edward T. Sall, MD, DDS, MBA
option. Multiple studies have reported objectively recorded adherence rates of over 90% with ProSomnus precision intraoral devices. There really isn’t much opportunity to get better in the realm of adherence.
ProSomnus will also continue to invest in research that evaluates the role of precision intraoral devices on efficacy criteria beyond AHI. For example, ProSomnus devices are associated with some of the only papers published in medical journals that use Oxygen Desaturation Index endpoints. ProSomnus devices are being utilized for investigations evaluating the impact of OAT on sleep apnea specific hypoxic burden and sleep apnea specific delta heart rate.
Wrapping up, consistent efficacy was the key barrier to OAT earning more prescriptions from physicians. Today, precision intraoral medical devices are engineered to optimize efficacy by virtually eliminating the mandibular protrusion and stabilization errors inherent with traditional oral appliances. Precision intraoral medical devices, specifically ProSomnus devices, have demonstrated excellent efficacy for patients with mild and moderate OSA, and severe OSA too. The levels of efficacy associated with precision intraoral devices, combined with objective reported adherence, place precision oral appliances at least on par with CPAP when it comes to treatment effectiveness (efficacy times adherence). DSM providers who have evolved their appliance selection criteria to precision intraoral medical devices are seeing significantly more prescriptions from sleep physicians, better efficacy and improved outcomes. Precision intraoral medical devices are the bridge that crossed the chasm.
The relationship between pain and sleep has been extensively studied but continues to remain ambiguous. It is widely accepted that poor sleep often precedes pain disorders, including temporomandibular disorders (TMDs)1 and that pain disorders can negatively impact sleep quality. It is therefore essential for dental teams involved in the clinical management of orofacial pains and dental sleep medicine to understand and recognize the frequent comorbidity of these two entities. Dental teams need also to understand the importance of working closely with physicians and when appropriate, comfortably refer patients to the appropriate provider in sleep medicine for further evaluation of any suspected sleep disorder. The aim of this article is to provide a brief overview of the current understanding of pain and sleep interactions in hopes that the dental team will be better prepared to confidently address these when encountered in practice.
Sleep and pain both serve vital functions necessary for human survival. Dysregulation of either has the capacity to affect the other and ultimately interfere with optimum health. Approximately 10-25% of adults will experience some form of chronic pain defined as persistent or recurrent pain lasting ≥ 3 months.2,3,4 Recent data suggests that 5090% of people with chronic pain also report poor sleep, specifically insomnia, prolonged sleep latency, poor sleep efficiency, and frequent awakenings after sleep onset.5-7
While various theories have been proposed as to the directionality of the relationship between sleep and pain, more recent longitudinal studies have shown that poor sleep tends to be more predictive of the on-

set of various pain disorders such as headaches,8,9 fibromyalgia,10 and musculoskeletal pains11 as opposed to pain conditions leading to poor sleep. The Orofacial Pain Prospective Evaluation and Risk Assessment (OPPERA) study found that patients often experience a period of poor sleep months before the onset of new TMD related pains, independent from other variables.1
Nonrestorative sleep is defined as an unrefreshed feeling on awakening and is experienced in approximately 10% of the general population, particularly in older individuals. Patients with chronic pain conditions such as TMDs commonly report poor or unrefreshing sleep as indicated by frequent awakenings throughout the night, daytime drowsiness, issues with restless leg syndrome, and sleep-related breathing disorders (SRBDs). For some individuals, the restoration of a restful sleep (sleep that makes them feel refreshed and energized) has been associated with the resolution of chronic widespread pain.12
36% of patients with TMDs meet the criteria for insomnia.13,14 Insomnia may be suspected when sleep onset is longer than 20 to 30 minutes, and occurs three to five times a week, or if spontaneous awakening is pres-
Steven D. Bender, DDS, is a Clinical Associate Professor at Texas A&M School of Dentistry in Dallas, Texas, and serves as the director of the Clinical Center for Facial Pain and Sleep Medicine, Texas A&M Health, Dallas, Texas. He is a Diplomate of the American Board of Orofacial Pain and has earned Fellowships in the American Academy of Orofacial Pain, the American Headache Society, the International Academy of Oral Oncology, and the American College of Dentists. He earned his Doctor of Dental Surgery degree from Baylor College of Dentistry in Dallas, Texas, in 1986 and practiced general and restorative dentistry in Plano, Texas, for 12 years. From 1998-2000, he studied orofacial pain and temporomandibular disorders at the Parker E. Mahan Facial Pain Center at the University of Florida College of Dentistry, Gainesville, Florida. From 2000-2015, Dr. Bender maintained a private practice limited to orofacial pain and sleep disorders before becoming a full-time faculty member at the School of Dentistry in 2016. He is a past president of the American Academy of Orofacial Pain as well as the Fourth District Dental Society of Texas and the Dallas Academy of General Dentistry. Dr. Bender has authored and coauthored numerous articles and book chapters and has lectured locally, nationally, and internationally on the topics of headache, TMD, facial pains, pharmacology, anatomy, and sleep topics. Dr. Bender regularly mentors post graduate students during their research projects and dissertation preparation at the School of Dentistry.
ent during the night without the ability to resume sleeping.15,16 It is estimated that approximately 10% of the general population suffers from chronic insomnia. However, the prevalence is reported to be approximately 30% in chronic pain patients.17
Factors such as lifestyle, beliefs, difficulties in coping with anxiety, poor physical fitness, and chronic fatigue can be considered risk factors for insomnia. Orofacial pain patients tend to report more problems in coping with fatigue, psychologic distress, headaches, abdominal pains, and sleep disturbances.14,18-20

As it is estimated that 5.9 million U.S. adults have obstructive sleep apnea (OSA) with up to 80% remaining undiagnosed, it is the responsibility of the dental team that participates in the care of orofacial pain patients to screen for any suspected sleep disorders that if present, could hinder treatment outcomes in the pain patient. Conversely, it is also critical for the dental sleep medicine practice to meticulously screen for the presence of TMDs or other orofacial pains that may interfere with the initiation of care of the patient with a sleep related breathing disorder. 21 Additionally, when indicated, the appropriate referral should be made for further evaluation, diagnosis, and any necessary therapies that may fall outside the scope of a dental practice. Management strategies for sleep disorders and orofacial pains will vary depending on the diagnosis and should be patient centered and individualized accordingly.
Oral appliances may be utilized for both TMDs and SRBDs. While positive airway pressure (PAP) therapy is currently considered the gold standard treatment for SRBDs, oral devices designed to hold the mandible in a protruded position in relation to the maxilla during sleep, known as mandibular advancement devices (MADs), may also be offered as a first line of treatment for a large number of patients, especially with mild to moderate severity.22 MADs have been shown to provide comparable benefit in terms of quality of life, cognitive and functional out-

Join DreamSleep – a nationwide network of dentists & physicians fighting sleep apnea. Our Whole Patient Program is a comprehensive plan that empowers dental practices with the knowledge, resources, and tools in order to provide patients with the highest standard of care for dental sleep medicine. The Whole Patient Program consists of four principles: Raise public awareness of Obstructive Sleep Apnea, DMSD, TMD, migraine and associated symptoms; train dentists to work with physicians and implement medical treatments; create screening and therapy programs for the industry; and connect patients with providers.
Through state of the art, individualized training and implementation processes, we help you seamlessly integrate these medical treatments into your dental practice to increase your patients’ quality of life and add a valuable revenue stream. Call 844.363.7533 today for details.
Comprehensive education you and your whole team: •Online, on-demand academic certification
•Individualized training programs
• In-office clinical training
•Team Coaching •Screening
comes as compared to PAP, and appear to have greater treatment compliance.23 Also, there is data to suggest that MADs may reduce the rhythmic masticatory muscle activity (RMMA) associated with some forms of sleep bruxism (SB).24-27 However, most of these studies are short term in duration (approximately 2 weeks). It should be noted that a recent scoping review found that in instrument-based studies utilizing electromyography and polysomnography, there was no significant correlation found between SB and TMDs.28 It should also be mentioned that while SRBDs may play a role in some SB manifestations, recent reviews have concluded that to date, there is insufficient evidence to support a conclusive cause and effect relationship between the two.29,30 Other types of oral appliances have long been utilized to help manage various TMD complaints. While many hypotheses have been reported, there is currently no significant data to support any specific mechanism of action for these devices in their role as therapy for TMDs. Importantly, some reports have suggested that devices fabricated for the maxillary arch may increase the severity of OSA in some patients.31-33 The mechanism for this adverse response is currently not known.
The goals of pharmacotherapy in orofacial pain and sleep disturbances will vary depending on the specific diagnosis and individual patient characteristics but will have the common objective of reducing pain and improving sleep. Mild analgesics are commonly used alone or in combination with muscle relaxants or other sedating agents to help manage some orofacial pain conditions. Benzodiazepines, which act on gamma amino butyric acid (GABA)-A receptors in the CNS, tend to shorten sleep latency and increase sleep duration in most individuals. They are anxiolytic and sedating and have demonstrated positive outcomes in chronic TMD pain34,35 and in patients with SB.36 However, benzodiazepines will tend to decrease REM stage sleep.37 Cyclobenzaprine, used commonly in the management of musculoskeletal pains, is frequently used in the management of muscle related TMDs. It has been
shown to be beneficial in reducing morning TMD related pain as well as improving subjective sleep quality.38 Duloxetine, a selective serotonin and norepinephrine reuptake inhibitor (SNRI), is approved by the US Food and Drug Administration (FDA) for the treatment of widespread pain/fibromyalgia. While there appears to be an increase in deeper stages of sleep with duloxetine, REM stage sleep is often suppressed.39 Other medications, such as tricyclic antidepressants (e.g., amitriptyline) have mild to moderate positive effects on both pain and sleep. The positive effects of amitriptyline have been documented for the management of some orofacial neuropathic pains40 as well as chronic tension-type headache.41 Gabapentin and pregabalin, which appear to work at the voltage sensitive calcium channels, also appear to improve pain and sleep quality and continuity.42 The use of opioids in the management of chronic pain is still common despite the potential for tolerance and substance use disorders, as well as the development of opioid induced hyperalgesia. In addition, the risk of respiratory depression associated with opioid use is of significant concern, particularly in patients with SRBDs.
While it has been traditionally believed that some psychotropic medications may induce or worsen both awake bruxism and SB, a recent review found that there is insufficient evidence to draw any such conclusions.43
Sleep is a vital physiologic activity that normally occupies approximately ⅓ of an individual’s life. There appears to be a bidirectional relationship between pain and sleep. Sleep disturbances and sleep disorders can lead to pain disorders and can negatively impact pain management therapy, and acute and chronic pain conditions can disturb sleep. Dental teams should be acutely aware that many patients presenting with orofacial pains frequently suffer with sleep disorders. When sleep disorders are suspected in the orofacial pain patient, the team should understand their role in screening and how to make the most appropriate referrals for accurate diagnosis and comprehensive care.
In addition, the dental sleep medicine team should be acutely aware of the impact of any existing orofacial pains, including TMDs
Treatment strategies depend on the diagnosis and should be patient centered.






1. Sanders AE, Akinkugbe AA, Bair E, et al. Subjective Sleep Quality Deteriorates Before Development of Painful Temporomandibular Disorder. J Pain 2016;17(6):669-77.
2. Scholz J, Finnerup NB, Attal N, et al. The IASP classification of chronic pain for ICD-11: chronic neuropathic pain. Pain 2019;160(1):53-59.
3. Goldberg DS, McGee SJ. Pain as a global public health priority BMC Public Health 2011;11:770.
4. Henderson JV, Harrison CM, Britt HC, Bayram CF, Miller GC. Prevalence, causes, severity, impact, and management of chronic pain in Australian general practice patients. Pain Med 2013;14(9):1346-61.
5. Cheatle MD, Foster S, Pinkett A, et al. Assessing and Managing Sleep Disturbance in Patients with Chronic Pain. Anesthesiol Clin 2016;34(2):379-93.
6. de Tommaso M, Delussi M, Vecchio E, et al. Sleep features and central sensitization symptoms in primary headache patients. J Headache Pain 2014;15:64.
7. Odegard SS, Sand T, Engstrom M, Zwart JA, Hagen K. The impact of headache and chronic musculoskeletal complaints on the risk of insomnia: longitudinal data from the Nord-Trondelag health study. J Headache Pain 2013;14:24.
8. Boardman HF, Thomas E, Millson DS, Croft PR. The natural history of headache: predictors of onset and recovery. Cephalalgia 2006;26(9):1080-8.
9. Odegard SS, Sand T, Engstrom M, et al. The long-term effect of insomnia on primary headaches: a prospective population-based cohort study (HUNT-2 and HUNT-3). Headache 2011;51(4):570-80.
10. Mork PJ, Nilsen TI. Sleep problems and risk of fibromyalgia: longitudinal data on an adult female population in Norway. Arthritis Rheum 2012;64(1):281-4.
11. Nitter AK, Pripp AH, Forseth KO. Are sleep problems and non-specific health complaints risk factors for chronic pain? A prospective population-based study with 17 year follow-up. Scand J Pain 2012;3(4):210-17.
12. Lavigne GJ, Nashed A, Manzini C, Carra MC. Does sleep differ among patients with common musculoskeletal pain disorders? Curr Rheumatol Rep 2011;13(6):535-42.
13. Davies KA, Macfarlane GJ, Nicholl BI, et al. Restorative sleep predicts the resolution of chronic widespread pain: results from the EPIFUND study. Rheumatology (Oxford) 2008;47(12): 1809-13.
14. Smith MT, Wickwire EM, Grace EG, et al. Sleep disorders and their association with laboratory pain sensitivity in temporomandibular joint disorder. Sleep 2009;32(6):779-90.
15. The International Classification of Sleep Disorders: (ICSD-3): American Academy of Sleep Medicine; 2014.
16. Lavigne GJ HR, Cistulli PA, Smith MT. Classification of sleep disorders. In: Lavigne GJ CP, Smith MT editor. Sleep Medicine for Dentists: A Practical Overview. Chicago: Quintessence; 2009. p. 21-31.
17. Lavigne GJ SM, Denis R, Zucconi M. Pain and Sleep. In: Kryger HM RT, Dement WC, editor. Principles and Practice of Sleep Medicine. Philadelphia: Elsevire Saunders; 2011. p. 1442-51.
18. de Leeuw R, Studts JL, Carlson CR. Fatigue and fatigue-related symptoms in an orofacial pain population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99(2):168-74.
19. Goncalves DA, Camparis CM, Speciali JG, et al. Temporomandibular disorders are differentially associated with headache diagnoses: a controlled study. Clin J Pain 2011;27(7):611-5.
20. Macfarlane TV, Blinkhorn AS, Davies RM, et al. Orofacial pain: just another chronic pain? Results from a population-based survey. Pain 2002;99(3):453-58.
21. Peppard PE, Young T, Barnet JH, et al. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 2013;177(9):1006-14.
22. Ramar K, Dort LC, Katz SG, et al. Clinical Practice Guideline for the Treatment of Obstructive Sleep Apnea and Snoring with Oral Appliance Therapy: An Update for 2015. J Clin Sleep Med 2015;11(7):773-827.
23. Schwartz M, Acosta L, Hung YL, Padilla M, Enciso R. Effects of CPAP and mandibular advancement device treatment in obstructive sleep apnea patients: a systematic review and meta-analysis. Sleep Breath 2018;22(3):555-68.
24. Landry-Schonbeck A, de Grandmont P, Rompre PH, Lavigne GJ. Effect of an adjustable mandibular advancement appliance on sleep bruxism: a crossover sleep laboratory study. Int J Prosthodont 2009;22(3):251-9.
25. Landry ML, Rompre PH, Manzini C, et al. Reduction of sleep bruxism using a mandibular advancement device: an experimental controlled study. Int J Prosthodont 2006;19(6):549-56.
26. Franco L, Rompre PH, de Grandmont P, Abe S, Lavigne GJ. A mandibular advancement appliance reduces pain and rhythmic masticatory muscle activity in patients with morning headache. J Orofac Pain 2011;25(3):240-9.
27. Saueressig AC, Mainieri VC, Grossi PK, et al. Analysis of the influence of a mandibular advancement device on sleep and sleep bruxism scores by means of the BiteStrip and the Sleep Assessment Questionnaire. Int J Prosthodont 2010;23(3):20413.
28. Manfredini D, Lobbezoo F. Sleep bruxism and temporomandibular disorders: A scoping review of the literature. J Dent 2021;111:103711.
29. da Costa Lopes AJ, Cunha TCA, Monteiro MCM, et al. Is there an association between sleep bruxism and obstructive sleep apnea syndrome? A systematic review. Sleep Breath 2020;24(3):913-21.
30. Pauletto P, Polmann H, Conti Reus J, et al. Sleep bruxism and obstructive sleep apnea: association, causality or spurious finding? A scoping review. Sleep 2022;45(7).
31. Nikolopoulou M, Ahlberg J, Visscher CM, et al. Effects of occlusal stabilization splints on obstructive sleep apnea: a randomized controlled trial. J Orofac Pain 2013;27(3):199-205.
32. Gagnon Y, Mayer P, Morisson F, Rompre PH, Lavigne GJ. Aggravation of respiratory disturbances by the use of an occlusal splint in apneic patients: a pilot study. Int J Prosthodont 2004;17(4):447-53.
33. Hans MG, Nelson S, Luks VG, Lorkovich P, Baek SJ. Comparison of two dental devices for treatment of obstructive sleep apnea syndrome (OSAS). Am J Orthod Dentofacial Orthop 1997;111(5):562-70.
34. Harkins S, Linford J, Cohen J, Kramer T, Cueva L. Administration of clonazepam in the treatment of TMD and associated myofascial pain: a double-blind pilot study. J Craniomandib Disord 1991;5(3):179-86.
35. Singer E, Dionne R. A controlled evaluation of ibuprofen and diazepam for chronic orofacial muscle pain. J Orofac Pain 1997;11(2):139-46.
36. Saletu A, Parapatics S, Saletu B, et al. On the pharmacotherapy of sleep bruxism: placebo-controlled polysomnographic and psychometric studies with clonazepam. Neuropsychobiology 2005;51(4):214-25.
37. de Mendonca FMR, de Mendonca G, Souza LC, et al. Benzodiazepines and Sleep Architecture: A Systematic Review. CNS Neurol Disord Drug Targets 2023;22(2):172-79.
38. Herman CR, Schiffman EL, Look JO, Rindal DB. The effectiveness of adding pharmacologic treatment with clonazepam or cyclobenzaprine to patient education and self-care for the treatment of jaw pain upon awakening: a randomized clinical trial. J Orofac Pain 2002;16(1):64-70.
39. Kluge M, Schussler P, Steiger A. Duloxetine increases stage 3 sleep and suppresses rapid eye movement (REM) sleep in patients with major depression. Eur Neuropsychopharmacol 2007;17(8):527-31.
40. Sharav Y, Singer E, Schmidt E, Dionne RA, Dubner R. The analgesic effect of amitriptyline on chronic facial pain. Pain 1987;31(2):199-209.
41. Ashina S, Bendtsen L, Jensen R. Analgesic effect of amitriptyline in chronic tension-type headache is not directly related to serotonin reuptake inhibition. Pain 2004;108(1-2):108-14.
42. Hindmarch I, Dawson J, Stanley N. A double-blind study in healthy volunteers to assess the effects on sleep of pregabalin compared with alprazolam and placebo. Sleep 2005;28(2): 187-93.
43. de Baat C, Verhoeff M, Ahlberg J, et al. Medications and addictive substances potentially inducing or attenuating sleep bruxism and/or awake bruxism. J Oral Rehabil 2021;48(3): 343-54.
may have on their ability to successfully manage SRBDs.
Public and practitioner interest in airway, sleep and breathing issues (ASB) is growing like wildfire. ASB issues affect health, performance, learning, and behavior of men, women, and children of all ages across all social and economic strata. The increasing awareness has attracted practitioners of different disciplines to offer treatment ranging from medication, CPAP, oral appliances, orthodontics, myofunctional and physical therapy, nutrition, and surgery. In many cases treatment is limited in focus, determined by what the treating practitioner offers. As a result, patients may receive incomplete diagnosis and treatment. Best treatment outcomes for ASB are often achieved through a collaborative interdisciplinary diagnostic and treatment approach. Practitioners who have committed to this approach of being part of a networking community have been gratified by patient results and have seen their practices flourish.
But developing an ASB collaborative practice is challenging. Practitioners ask, “What additional diagnostic and consultations does my patient require? Who is available in my community? How do I find them and learn to communicate? Who will be the quarterback?” The demographics of one community may differ from another. Specialists may not be available. Social and economic factors also come into play.
The American Academy of Physiologic Medicine and Dentistry, AAPMD, realized these obstacles to collaboration and with the guidance and support of Leyli Norouz-Knutsen, created the LIAISONS.

The LIAISONS are AAPMD members who have committed to raise awareness and to connect and collaborate with other like-minded
practitioners to provide better ASB care for their community. LIAISONS represent a variety of specialties including:
• Physicians, Osteopaths – Pediatricians, ENTs, Pulmonologists, Sleep Medicine Specialists, Cardiologists, Gynecologists, Functional Medicine Doctors
• Dentists, Dental Hygienists – Orthodontists, Prosthodontists, Sleep Medicine Specialists, TMJ Specialists


• Physical Therapists, Orofacial Myofunctional Therapists, Speech Language Pathologists, Chiropractors
• Breathing Practitioners, Clinical Massage Therapists, Acupuncturists, Psychotherapists, IBCLCs
• Additionally, Non-Practitioner Supporters (i.e. teachers, parents, etc.) are welcome to participate!
• Working together with other practitioners to better serve patients
• Advocate to enlighten the public about airway issues and treatment options
• Collaborate to develop screening tools
• Educate and share information between practitioners with monthly meetings
• Organize AAPMD satellite study clubs that meet virtually or in-person to collaborate on patient case studies, discuss challenges and successes, invite guest speakers
• Liaisons are able to join other virtual study club meetings to continue collaboration
• Quarterly CoLAB webinar meetings are held for the Liaisons to discuss what the Liaisons’ needs are for their local communities in outreach, supporting each other by networking along with brainstorming on how to improve public awareness
• Through the LIAISON Section page on the AAPMD website, LIAISONS can share information, successes and obstacles, protocols, and view recorded local meetings
In 2023 the LIAISONS, along with the Foundation for Airway Health, will raise more awareness and provide more extensive knowledge to the public – reaching out to schools, houses of worship, social media groups, childcare facilities, community public health events, and others.
Want to be a leader in your community? Network, cross-refer, and collaborate? Become part of our growing community by signing up directly on the AAPMD website. If you are already an AAPMD member and want to learn more about the Liaison group, feel free to reach out to stacey@aapmd.org. The AAPMD, leader in interdisciplinary collaboration and education for optimal airway growth and function, has grown to a world-wide network approaching 1,000 members across 6 continents.
Stacey Larkin is a Registered Dental Hygienist and Orofacial Myofunctional Therapist located in east Texas. With more than 20 years of dental experience with adults and children, and also being a MyoMasterminds graduate with The Breathe Institute, she is passionate about helping people improve their quality of life. She is the AAPMD Liaison Coordinator, helping Liaisons network, increase outreach in their local community, and nurture AAPMD satellite study clubs across the globe.
Best treatment outcomes for airway, sleep and breathing issues are often achieved through a collaborative interdisciplinary diagnostic and treatment approach.

The heart is the key element of the circulatory system which makes sure that all the organs and tissues get the oxygen needed. So, being responsible for pumping blood throughout the body, we should never underestimate the importance of heart health.
We are already aware that factors like smoking, poor diet, and lack of physical exercise may lead to heart problems. But, did you know that sleep and heart health are also closely connected? Namely, poor sleep can also negatively affect the heart as sleep allows the body to restore and recharge.

Sleep deprivation can indeed contribute to many heart problems including high blood pressure or an increased risk of heart failure, heart attack, arrhythmias, diabetes, and stroke. Logically, we can conclude that addressing poor sleep may help heart health and help prevent damage to the entire cardiovascular system.
So, given the strong link between sleep and heart health and the importance of both for optimal physical health, researchers have done an extensive study on the topic. To find out more, continue reading below.
A recent study found that the risk of heart disease may nearly triple for those who have a mix of sleep issues like trouble falling asleep,
waking up way too early, or not getting the recommended amount of sleep each night.1 So, the evidence once again highlights the connection between sleep and heart health. To be more precise, the study was conducted on 7,483 American adults in midlife who provided detailed information about their sleep and heart health, everything from their sleep habits to their heart disease history. In addition, 663 participants were given a wrist-worn device to record their sleep activity.
Furthermore, a little bit more than half of the participants were women, three-quarters were white and 16% were black. Their average age was 53. And, if you were asking yourself why the study included only middle-aged people, the reason is that adults, in that period, typically go through diverse and stressful experiences, age-related sleep problems and early signs of heart disease appear.
To find out how sleep affects heart health, researchers conducting the study focused on several aspects of sleep, including:
A recent study found that the risk of heart disease may nearly triple for those who have a mix of sleep issues...1
• Sleep regularity – whether participants followed a consistent sleep schedule, i.e. went to bed and woke up at the same time during workdays and at weekends.
• Sleep satisfaction – whether participants faced issues falling asleep and staying asleep throughout the entire night, and if they woke up, were they able to go back to sleep easily.
• Alertness – whether they felt sleepy and tired during the day, and how often they had naps longer than five minutes.
• Sleep latency – how long it took participants to fall asleep after getting in bed.
• Sleep duration – how long they slept each night.
What’s more, to be able to identify the connection between sleep and heart health, participants were also asked questions about their heart disease history, whether they had suspected they had heart problems at any time in their life, and whether they sometimes experienced chest pain longer than 30 minutes.
The study found that each increase in self-reported poor sleep was linked to a 54% increased risk of heart problems compared to those with normal sleep schedules. Still, this increase in risk goes up to 141% in those
Increased risk of heart problems goes up to 141%

in those who not only self-reported sleep issues but also had the wristworn device...
who not only self-reported sleep issues but also had the wrist-worn device which is considered to be more accurate.

Therefore, if you are experiencing poor sleep, ensure you consult your doctor about how you can improve your sleep so as not to affect your heart health because sleep and heart health are closely connected.
Lee A. Surkin, MD, is the Chief Medical Officer of Nexus Dental Systems. A private practitioner in cardiology, sleep medicine, and obesity medicine, he is one of a small group of physicians to be triple board certified in cardiology, sleep medicine, and nuclear cardiology. In 2009, he created Carolina Sleep – the only dedicated sleep medicine practice in eastern NC. Dr. Surkin has created a cardiovascular and sleep healthcare model that includes a multi-faceted diagnostic and treatment approach that is enhanced by a network of relationships with physicians, dentists, respiratory therapists, sleep technologists, and public officials who recognize the important role that sleep medicine has in our daily life. In 2012, Dr. Surkin founded the American Academy of Cardiovascular Sleep Medicine which is a not-for-profit academic organization dedicated to educating healthcare providers, supporting research, and increasing public awareness of the convergence between cardiovascular disease and sleep disorders. In 2014, Dr. Surkin created a new multi-specialty practice called Carolina Clinic for Health and Wellness which combines his specialties with primary care, gynecology, behavioral health and a medical spa. Dr. Surkin is married with three daughters and a golden retriever and resides in Greenville, NC.
Obstructive sleep apnea is a significant and common medical disorder characterized by recurrent total or partial pharyngeal collapse causing temporary upper airway obstruction and drops in oxygen saturation during sleep.
Obstructive sleep apnea is recognized as an independent risk factor for hypertension, arrhythmias (such as atrial fibrillation), coronary artery disease, and stroke. Metabolic disorders such as diabetes and disorders of lipid metabolism are also associated with obstructive sleep apnea. Hypoxemia, oxidative stress, systemic inflammatory responses, sympathetic activation, and sleep fragmentation have all been studied as markers for these subsequent cardio-metabolic disorders.
Obstructive sleep apnea impacts over a billion people worldwide. The overall incidence of obstructive sleep apnea in the US is estimated at 30% with men having a higher incidence than premenopausal women.1 Defining the disease using a reliable metric is critical. The ideal metric should be able to differentiate a disease state from normal,
categorize the severity of the disease, predict outcomes, and allow us to measure and reduce the impact of the disease with treatment.
A recent special article published in the journal Sleep2 emphasized the need for alternative metrics to AHI for sleep apnea severity. This article will compare the apnea hypopnea index to various measures of oxygen saturation discussing the limitations and strength of each measure as well as exploring some of the newer metrics such as hypoxic burden that have been recently described.
Historically the apnea-hypopnea index (AHI) has been the central metric for obstructive sleep apnea assessment. Although traditionally measured in polysomnographic studies, more recently home sleep testing has been demonstrated to be more cost effective and has been accepted as having equivalent accuracy in determining AHI for patients with a high suspicion of obstructive sleep apnea.

Using the AHI as the metric for obstructive sleep apnea however has several signif-

icant limitations. Inconsistency in the definition of sleep-disordered breathing events especially when measuring hypopneas is a significant concern. While first described by Block et al. as a respiratory event causing a 4% oxygen desaturation, subsequent task forces have variously defined hypopneas as a 50% reduction in airflow or a “clear amplitude” reduction or most recently a 30% airflow reduction. Associated drops in oxygen level during hypopneas has been defined as 3% or 4% or more recently 3% with an “option to report” a 4% desaturation. Hypopneas can also be considered present when there is limited airflow in the presence of an EEG based arousal. Note that some home sleep test devices use surrogates for EEG arousals such as changing snoring, pulse rate change or movement to identify hypopneas.2
Curiously the length of an apnea or hypopnea is not considered in the definition. One would imagine that a patient with prolonged apneas or hypopneas has significantly worse disease burden, but paradoxically, these patients with prolonged events may have a lower AHI as calculated by current standard definitions. Night-to-night variability in the AHI due to differing sleep stages, body position, or sleep fragmentation also represents a challenge.
One of the main strengths of the AHI is a large body of literature using AHI linking untreated obstructive sleep apnea and to a variety of comorbid conditions.
Some of the largest epidemiologic studies conducted in the past including the Sleep Heart Health Study,3 and the Wisconsin Cohort Study4 as well as many others have used the AHI as the metric linking increasing severity of obstructive sleep apnea to various adverse health outcomes including all-cause mortality, cardiovascular disease, stroke, motor vehicle accidents, quality of life, and daytime sleepiness.

When compared to the AHI, oxygen desaturation metrics may have some significant advantages. Two patterns of hypoxemia can be observed during sleep. Short intermittent and high frequency hypoxemia is seen in patients with obstructive sleep apnea due to recurrent airway collapse. Prolonged low frequency hypoxemia is seen in chronic obstructive lung disease and other pulmonary
Estimated prevalence of obstructive sleep apnea based on different scoring rules. Image inspired by Benjafield AV, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019 Aug;7(8):687-698.
diseases as well as at high altitude. The major difference between these two is cycles of reoxygenation. The cyclic changes and hypoxemia and reoxygenation are similar to those observed with ischemia reperfusion injury and contribute to an increased production of reactive oxygen species which may be directly causative to adverse cardio-metabolic consequences.5
A commonly used oxygen desaturation metric is the ODI that represents the number of occurrences of desaturation 3% or 4% per hour of sleep. Note that it does not necessarily mean that the oxygen saturation falls below 90% since drops from 96-92% may be observed for example. Data from the European Sleep Apnea Database (ESADA) have shown that when both AHI and ODI are used in the same statistical model only ODI is independently associated with the prevalence of hypertension in patients with obstructive sleep apnea.
Dr. Jagdeep Bijwadia is board certified in internal medicine, pulmonary, and sleep medicine. He is founder and CEO of a national sleep telemedicine practice (Sleepmedrx) serving all 50 US states. He also serves as Chief Medical Officer for Whole You and is a clinical consultant for Ectosense. He currently holds a faculty position as Assistant Professor in the Department of Pulmonary Critical Care and Sleep Medicine at the University of Minnesota and has a private practice in Saint Paul, Minnesota. Dr. Bijwadia has been named top doc by the Minneapolis magazine as well as US News and World Report. He served as president for the Minnesota Sleep Society from 2016 to 2018 and is active in promoting sleep health in Minnesota. He also has an MBA from the University of St. Thomas in Minneapolis.

The ODI, however, does not assess the length of oxygen desaturation consecutive to an obstructive apnea or hypopnea thus limiting its ability to assess obstructive sleep apnea effects accurately. To address this, two additional parameters have been recently suggested: the T90 and hypoxic burden.
T90 represents the amount of time the patient spent with saturations below 90% during their sleep.
A major limitation of the ODI is that it measures both hypoxemia due to obstructive sleep apnea as well as any underlying pulmonary causes. To overcome this limitation, a numeric was proposed by Azerbaijan et al.6 to measure hypoxic burden. Hypoxic burden was defined as a value reflecting the area under the curve on the oxygen saturation curve during desaturation episodes. This value considers the frequency, length, and depth of respiratory related oxygen desaturation.
This measure of hypoxic burden related to obstructive sleep apnea in the occurrence of cardiovascular complications was studied in two different large cohorts: The osteoporotic fractures in men study (MrOS)6 and the Sleep Heart Health Study. Researchers were able to demonstrate that the respiratory events related to hypoxic burden were independently associated with cardiovascular mortality. This association persisted after adjusting for a large number of potential confounders including prevalent cardiovascular disease as well as a AHI, T90, and sleep duration
In summary, hypoxia based metrics may be less prone to error, can be reliably mea-

ANNOUNCING
a new YouTube series: Nexus Connexus. This series will embody our Nexus Dental Systems’ vision and mission to inspire others to take action and be informed. We are all extensions of this great cause and your efforts can benefit so many!



sured by both polysomnography and home sleep tests, and be more reflective of disease burden and ability predict outcomes. It is likely that hypoxic burden and several other newer metrics will be used in conjunction to provide a much more accurate picture of OSA disease burden as research continues to uncover other markers.
1. Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MSM, Morrell MJ, Nunez CM, Patel SR, Penzel T, Pépin JL, Peppard PE, Sinha S, Tufik S, Valentine K, Malhotra A. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019 Aug;7(8):687-698. doi: 10.1016/S2213-2600(19)30198-5. Epub 2019 Jul 9. PMID: 31300334; PMCID: PMC7007763.
2. Malhotra A, Ayappa I, Ayas N, Collop N, Kirsch D, Mcardle N, Mehra R, Pack AI, Punjabi N, White DP, Gottlieb DJ. Metrics of sleep apnea severity: beyond the apnea-hypopnea index. Sleep. 2021 Jul 9;44(7):zsab030. doi: 10.1093/sleep/zsab030. PMID: 33693939; PMCID: PMC8271129.
3. Gottlieb, Daniel J. ; Yenokyan, Gayane ; Newman, Anne B. ; O’Connor, George T. ; Punjabi, Naresh M. ; Quan, Stuart F. ; Redline, Susan ; Resnick, Helaine E. ; Tong, Elisa K. ; Diener-West, Marie ; Shahar, Eyal Prospective study of obstructive sleep apnea and incident heart disease and heart failure: a prospective study. Circulation (New York, N.Y.), 2010, Vol.122 (4), p.352-360
4. Hla KM, Young T, Hagen EW, Stein JH, Finn LA, Nieto FJ, Peppard PE. Coronary heart disease incidence in sleep disordered breathing: the Wisconsin Sleep Cohort Study. Sleep. 2015 May 1;38(5):677-84. doi: 10.5665/sleep.4654. PMID: 25515104; PMCID: PMC4402672.
5. Blekic N, Bold I, Mettay T, Bruyneel M. Impact of Desaturation Patterns versus Apnea-Hypopnea Index in the Development of Cardiovascular Comorbidities in Obstructive Sleep Apnea Patients. Nat Sci Sleep. 2022 Aug 25;14:1457-1468. doi: 10.2147/NSS.S374572. PMID: 36045914; PMCID: PMC9423119.
6. Azarbarzin A, Sands SA, Stone KL, Taranto-Montemurro L, Messineo L, Terrill PI, Ancoli-Israel S, Ensrud K, Purcell S, White DP, Redline S, Wellman A. The hypoxic burden of sleep apnoea predicts cardiovascular disease-related mortality: the Osteoporotic Fractures in Men Study and the Sleep Heart Health Study. Eur Heart J. 2019 Apr 7;40(14):1149-1157. doi: 10.1093/eurheartj/ehy624. Erratum in: Eur Heart J. 2019 Apr 7;40(14):1157. PMID: 30376054; PMCID: PMC6451769.








 by Edward T. Sall, MD, DDS, MBA
by Edward T. Sall, MD, DDS, MBA
In 1981, a landmark paper by Sullivan et al. reported on 5 patients treated with a nasal mask that eliminated their obstructive sleep apnea. Since that time, multiple mask interfaces have been introduced in an attempt to allow physicians to customize the mask interface to the patient’s anatomy and improve patient compliance or adherence. CPAP, stamped and branded as the “gold standard” in the treatment of Obstructive Sleep Apnea, remains the bar by which all of the other treatments are compared.
Although the standard of care for the treatment of OSA is the highly efficacious CPAP, the real-world long-term health effects of CPAP are compromised by low compliance and suboptimal hours of treatment. Compliance has been defined as greater than

4 hours of use of CPAP over 7-10 days. This arbitrary definition is not evidence based and fails to take into account the sleep time off treatment. In fact, according to this definition, a patient only has to use CPAP 86/hrs. per month or 35% of the total sleep time to be considered adherent. Weaver et al. (2007) showed that normalization of subjective sleepiness (ESS), objective sleepiness (as tested by the MSLT), and disease specific functional status (as measured by the functional outcomes of sleep questionnaire [FOSQ]) requires 4, 6, and 7.5 hours, respectively, of nightly CPAP usage.
Sleep physicians often continue to recommend CPAP over Oral Appliance Therapy for all levels of severity of OSA because of the highly efficacious nature of CPAP without critically accounting for the poor com-
pliance. Sutherland K. et al. (2015) have stressed that “Efficacy” must be differentiated from ”Effectiveness” and introduced the term Sleep Adjusted Residual AHI (SARAH Index) to critically assess the “effectiveness” of treatment as it properly accounts for compliance. That being said, Oral Appliance Therapy may be as equally effective as CPAP when compliance is factored into the equation. Boyd et al. (2016) introduced the term Effective AHI as a new measure of the effectiveness of PAP therapy as it accounts for sleep disorderedbreathing events during the time PAP is (PAP on) and is not (PAP off) being used.
Rotenberg et al. (2016) reported that there was no clinical improvement in CPAP adherence in recent years despite efforts toward behavioral intervention and patient coaching. He concluded that these findings (20 years of data collection) calls into question the concept of CPAP as the “gold standard” of therapy for OSA. Despite these findings, sleep physicians still have reservations about referring patients for Oral Appliance Therapy. An online survey of sleep physicians was reported in Sleep Review in 2016 to poll the participants as to the top reasons for not referring patients to a dentist for OAT. They were as follows:
1. “I want to try other strategies to get the patient CPAP adherent.”

2. “The patient won’t be able to afford an appliance.”
3. “The oral appliance may not be efficacious.”
4. “The oral appliance won’t record the patient’s adherence with the therapy.”
5. “The patient may develop side effects from using the oral appliance.”
6. “I worry dentists are acting outside the scope of practice in all or part when treating OSA.”
7. “Patients disappear when I refer them to a dentist.”
8. “I don’t know a local dentist who I trust with my patients.”
The fundamental issue that all dentists delivering Oral Appliance Therapy for the treatment of patients with OSA is how to move the needle for more physician acceptance of that paradigm. Clearly, physicians have reservations about the efficacy, predictability, adherence monitoring, and side effects of OAT which prevents them from embracing this form of treatment. By addressing the primary
concerns of physicians, we should be able to dramatically increase acceptance of Oral Appliance Therapy.
In the field of Dental Sleep Medicine, before the advent of precision medical devices for the treatment of OSA, most of the available custom oral appliances had similar efficacy. It was often reported, in general terms, that over a third of patients will show a complete response to oral appliance therapy with a reduction in AHI to <5/hr (or no OSA). Another third will have a clinically important response showing >50% reduction in AHI, although AHI remains >5/hr, and a third will not achieve >50% reduction in AHI. These traditional results have made physicians reluctant to refer patients for OAT because they feel it is too difficult to predict how one will respond to this treatment. The irony of this resistance is that sleep physicians often neglect concepts of the SARAH Index and Effective AHI in prescribing the “gold standard” of CPAP. Additionally, the FDA approved implantation of the neurostimulation devices (Inspire) with “the surgical success” criteria of <50% reduction of the AHI and an AHI <20/hr. When viewed in this context, OAT may be more effective than the Inspire at a fraction of the cost.
For many years, oral appliance design and performance have remained stagnant. At that time, choosing a device was far more about patient preference, comfort, ease of delivery and use. The initial price of the device along with the full cost of repair, remakes, and chair time influenced the selection of the appliance by the sleep dentist. While these
Edward T. Sall, MD, DDS, MBA, is a licensed dentist and physician. He is board-certified in both Otolaryngology/ Head & Neck Surgery, and Sleep Medicine. Currently, he is in full-time private practice in Syracuse, New York as an Otolaryngologist and Sleep Physician. In 2019, Dr. Sall accepted the position as medical director of ProSomnus Sleep Technologies with the role of increasing physician acceptance of OAT in the treatment of OSA. In 2020, Dr. Sall became the President and CEO of BetterNight Medical group as well as SD Diagnostics, Inc, a home sleep testing company. Currently, Dr. Sall has medical licenses in 40 states which allows him to do telemedicine consultations in sleep medicine for BetterNight. In 2021, Dr. Sall accepted a position as a consultant to Aerin Medical. His role at Aerin Medical is to increase collaboration between sleep dentists and otolaryngologists in order to improve outcomes in patients with OSA treated with both OAT and CPAP.

factors may have been important in the economics of a sleep dentistry practice, they are not the concerns of the sleep physicians. The sleep physicians remain concerned about efficacy, predictability, adherence, and absence of side effects.
The root cause issue is that traditional oral appliances are not particularly consistent at satisfying their stated mechanisms of action. Medical guidelines (AASM and AADSM) have established that the mechanisms of action of oral appliances are to reposition and stabilize the mandible to achieve and maintain airway patency. Laboratory testing has demonstrated that traditional oral appliances can express up to 6mm of variance to the prescribed mandibular position. Furthermore, engineering testing has demonstrated that traditional or ”legacy” oral appliance designs feature titration mechanisms like straps, hinges, herbst attachment arms, and angled posts that can express up to 5mm of additional variance when attempting to stabilize the mandible. Clearly, inconsistent efficacy is the consequence of these variances, among other factors including compliance, side effects, and durability.
AI design and robotic manufacturing have created a new class of Oral Appliances. They have resulted in Precision Oral Appliances (ProSomnus Sleep Technologies, Inc.) that offer 26% better efficacy than the older “legacy oral appliances” and have been found to have an objectively measured adherence (via compliance monitoring) of 90%. The accuracy of bite transfer, smaller profile (allowing for more space for the tongue), the minimization of side effects, the ability to maintain the prescribed bite position, and lack of biogunk have all contributed to this increased efficacy and objectively measured adherence. Taking all this into account, Precision Oral Appliance Therapy may be comparable or better than CPAP or Hypoglossal Nerve Stimulation in effectiveness for patients with mild, moderate, and even severe OSA.
Obstructive Sleep Apnea is a global epidemic, and in 2019 in the Lancent article, the WHO and ATS estimated the global prevalence of OSA at 1 billion people. As we know, 80-85% of the people remain undiagnosed of their disease. While OSA has multiple phenotypes, it should be clear that there is poor support of the notion that CPAP is the “gold standard” for therapy. Moving the
needle for physician acceptance of Oral Appliances for the treatment of OSA requires an individualized approach to therapy. Utilizing Precision Oral Appliance Therapy (ultimately with compliance monitoring) will become the new paradigm for physician acceptance. It is in the best interest of their patients that dental sleep specialists choose the most precise and most researched appliance available. Increasing the predictability of the results, minimizing the incidence of side effects, and monitoring adherence will increase the acceptance by your referring physicians.
Inspire spent over 100 million dollars in marketing for HNS in 2022 and plans to increase that to 200 million in 2023. That amount of marketing dollars has created unprecedented awareness of an alternative treatment to CPAP. That being said, roughly only 10% of those patients that seek a consultation for HNS actually have the surgery. The message is very clear; patients want alternatives to CPAP because it isn’t the “gold standard”. Oral Appliance Therapy suffers from an awareness issue as many patients simply don’t know the option exists. The introduction of this new class of Oral Appliances has the potential to change the perception and acceptance of Oral Appliances as the preferred form of therapy for the majority of patients with OSA.
1. Sullivan C Berthon-Jones M, Issa L. Reversal of obstructive sleep apnoea by continuous positive pressure applied through the nares. Lancet 1981; 317: 862-865.
2. Lettieri, CJ, Williams, SG, Collen, JF, Wickwire, EM, “Treatment of Obstructive Sleep Apnea: Achieving Adherence to Positive Airway Pressure Treatment and Dealing with Complications”, Sleep Med Clin 12 (2017): 551-564.

3. Weaver, TE, Maislin, et al. Relationship Between Hours of CPAP Use and Achieving Normal Levels of Sleepiness and Daily Functioning. Sleep. 2007 Jun 1; 30(6): 711-719.
4. Sutherland, K, Phillips CL, Cistulli, PA. Efficacy versus Effectiveness in the Treatment of Obstructive Sleep Apnea: CPAP and Oral Appliances. Journal of Dental Sleep Medicine 2015; Vol. 2, No 4:175-181.
5. Boyd, SB, Upender, R, et al. Effective Aphea-Hypopnea Index (”Effective AHI”): A New Measure of Effectiveness for Positive Airway Pressure Therapy. Sleep. 2016 Nov 1; 39 (11): 1961-1972.
6. Rotenberg, BW, Murariu, D, Pang KP. Trends in CPAP adherence over twenty years of data collection: a flattened curve. Journal of Otolaryngology-Head and Neck Surgery. 2016 45:43.
7. Schoch OD, Baty, F et al. Baseline Predictors of Adherence to Positive Airway Pressure Therapy for Sleep Apnea: A 10-Year Single-Center Observational Cohort Study. Respiration. 2014; 87: 121-128.
8. Sutherland, K, Cistulli PA. Oral Appliance Therapy for Obstructive Sleep Apnoea: State of the Art. J Clin Med. 2019 Dec; 8(12): 2121.
9. Marklund, M. Update on Oral Appliance Therapy for OSA. Curr Sleep Med Rep. 2017: 3(3): 143-151.
10. Benjafield, AV, Ayas, NT et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019 Aug: 7(8): 687-698.



Looking for an easy and effective solution to your patients’ snoring and OSA? As the first customTAP with no metal parts, flexTAP is an oral appliance that is customized for personal comfort and equipped with a self-adjustor for at-home ease. Its new ThermAcryl® liner allows for easier chairside adjustments using warm water.
flexTAP is the first of its kind to utilize our proprietary Vertex Technology® paired with the flexTAP Mouth Shield comfort accessory to promote nasal breathing, prevent dry mouth, and minimize excess saliva for extra comfort. Uniquely designed with a wide range of advancement (14mm) without

the need for bite registration or exchanging hooks, Vertex Technology allows the mouth to open vertically and horizontally simultaneously during advancement of the jaw.
“Vertex Technology allows for more tongue space and minimizes jaw advancement,” says Dr. Keith Thornton, inventor of the Thornton Adjustable Positioner (TAP®). “Not only will this help patients achieve better treatment outcomes, but it will ease joint impact.”
flexTAP is our lowest priced custom TAP, PDAC coded (E0486) and includes a standard 3-year warranty. It is available to order through Airway Labs and participating partner labs.
DynaFlex would like to introduce you the newest member of the TAP family; The flexTAP, now with Vertex Technology. This is a premium lab-made custom oral appliance for the treatment of snoring and obstructive sleep apnea.
As the first custom TAP® with no metal parts, flexTAP is an oral appliance that is customized for personal comfort and equipped with a self-adjuster for at-home ease. flexTAP’s new blue ThermAcryl liner is thinner, more durable, and easy to adjust chair side using warm water. The key to flexTAP’s success is the new patented Vertex Technology. Vertex Technology is the design of the post angulation in the flexTAP hardware. The post is angled at a 45-degree angle, allowing the patient to advance their lower jaw both vertically and horizontally at the same time.

The flexTAP is also the first custom oral appliance to include a standard nasal breathing component, the flexTAP Mouth Shield, to improve comfort and treatment outcomes. Recent literature shows nasal breathing as the proper way to breathe. The flexTAP Mouth Shield slips onto the post to increase comfort and provide better treatment outcomes. It also helps prevent dry mouth or excess saliva.

Scan the QR code to order a custom Flextap for your next patient.



One of my favorite sayings is “Dental Sleep Medicine isn’t difficult, it’s just different.” Most dental practices have great processes, but dental systems don’t account for the unique elements involved in dental sleep cases, mainly:
• Collaboration with physicians for diagnosis and referrals.
• Documentation of medical necessity.
• Medical billing reimbursement.
So, you need a system that solves these workflow, referral, and reimbursement challenges. Simple right? Yet, many dental practices acquire a solution and struggle to adopt it and implement DSM successfully. Does it have to be this way? The answer is no. User
experience (UX) design is a scientific field to make products efficient, rewarding, and easy to use. UX is not just about software, it is made of all the interactions a client has with a product or service.
Intuitive systems that have reliable support reduce friction and stress, enabling dental teams to succeed with dental sleep medicine and medical billing.
At Nierman Practice Management, we have re-imagined the user experience of dental sleep medicine systems with our innovative platform, DentalWriter Plus+ and Nierman Medical Billing Service. Our user-friendly cloud software and dedicated billing and client success team work together seamlessly to make it easy for your dental sleep practice.

ProSomnus will be featured again in this year’s scientific abstracts and case submission for the AADSM Annual Meeting, May 19-20, 2023 in Philadelphia, PA. These publications continue to demonstrate the efficacy and compliance of precision Oral Appliance Therapy. Abstracts include:
Precision vs. Traditional Oral Appliance Therapy: A Comparison of Therapeutic Efficacy



• Literature review comparing efficacy between precision and traditional oral appliances (OAs)
• Median efficacy: 92% for precision and 75% for traditional OAs (mild/moderate OSA)
Comparison of Clinical Effectiveness and Patients’ Preference for Two Non-Invasive Treatment Options for Patients
Diagnosed with Moderate to Severe Obstructive Sleep
Apnea: The FLOSAT Study
• Crossover study comparing mean disease alleviation in patients using CPAP and ProSomnus EVO®
• Preliminary results indicate that ProSomnus EVO is non-inferior to CPAP
Adverse Event Reports for CPAP, Hypoglossal Nerve Stimulation and OAT Devices

• Winner of an AADSM Clinical Research Award
• FDA MAUDE database review of adverse events (AEs) by device type
• In 2022, only 30 AEs were reported for OAT OAT Device Designs Are Not the Same When it Comes to FDA Adverse Event Reports
• FDA MAUDE database review of AEs by device material/ design
• Linerless OAs with 90° twin post mechanisms were associated with fewer AEs than other designs

SleepImage is the home sleep test of choice for dentists. It provides the ability to test multiple consecutive nights for efficacy studies and titrations while remaining the lowest cost home sleep test in the market. SleepImage uses a proprietary method called cardiopulmonary coupling and has been featured in over 100 peer reviewed articles. SleepImage utilizes a ring that features a single sensor and connects to a mobile application to send data to a unique cloud-based portal. SleepImage is an FDA cleared (K182618) product to diagnose sleep apnea, measure health during sleep through the sleep quality index and to manage sleep disorders such as insomnia and sleep apnea (obstructive and central) for adults and children as young as 2 years old.
The SleepImage system has been validated against manually scored in lab PSG. The ring is comfortable for patients to wear overnight, the system works without any consumables,

and can lower the costs of diagnosing sleep apnea and other sleep disorders.
ADA recommends every dental practice screen for sleep-related breathing disorders as a part of the comprehensive examination, including ongoing monitoring when supplying oral appliance therapy.

For additional information on the SleepImage device and usage, please visit www.sleepimage.com


VirtuOx has developed the only end-to-end solution for sleep dentistry that simplifies the testing and treatment pathway from OSA diagnosis through titration of your patient’s new oral appliance.
Dentists utilize our telemedicine platform to easily refer their patients to board certified sleep physicians who will order home sleep apnea tests and prescribe oral appliances.



Dentists are provided with NightOwl® Home Sleep Apnea Testing (HSAT) devices on consignment (no cost to the dentist) to send home with their patients. These disposable sensors allow the patient to test both with and without a dental device for up to 10 nights. The first 1-2 nights of testing will be used by VirtuOx to diagnose sleep apnea.¹ Once the patient is fitted with their custom oral appliance, the dentist

may reuse the NightOwl for repeat tests to titrate the device to an optimal setting. A final efficacy test, as recommended by the AADSM, will then be completed by VirtuOx.¹
Dentists have full visibility into this entire patient journey through our HIPAA secure platform.
ZOLL® Itamar®, a division of ZOLL® Medical, is a leading company in sleep apnea diagnosis and pioneering innovative sleep apnea management programs for patients and healthcare professionals.

Our mission is to improve access to the millions of undiagnosed sleep apnea patients with diagnostic testing and cardio sleep solutions through our breakthrough WatchPAT® products and services.
Itamar® Medical was founded in 1995 and acquired by ZOLL® in 2021.

This self-instructional course for dentists aims to show that mitochondria are more than just ATP factories. They are now considered central hubs in regulating calcium homeostasis, orchestrating apoptosis, creating chronic inflammation, and regulating innate immunity. Hypoxia and fragmented sleep associated with sleep related breathing disorders promote dysfunctional mitochondria alterations that increase reactive oxygen species which lead to inflammatory processes which contribute to aging and cellular health. This article connects the dots between SRBD and non-communicable diseases, and mitochondrial dysfunction is exposed as the smoking gun. As mitochondria represent the future of medicine, there will always be a seat at that table for SRBD management.
Wouldn’t you love a deeper understanding of the underlying pathophysiology of sleep related breathing disorders “SRBD” and how they cause so many medical conditions? I certainly would. After “peeling this onion” to connect the dots, it’s clear that one’s level of health and wellness is a result of mitochondrial function. A growing body of research reveals that mitochondrial dysfunction is very common and is associated with most chronic disease and early aging. Several recent studies show the intermittent breathing disruptions that characterize obstructive sleep apnea stress mitochondria. The research supports that the free radical production from hypoxic events along with sleep fragmentation are both underlying contributors to mitochondrial dysfunction. The significance of this mitochondrial-SRBD relationship cannot be overstated and should earn it a place in any sleep and airway educational curriculum.
Dental Sleep Practice subscribers can answer the CE questions online at https://dentalsleeppractice.com/continuing-education/ to earn 2 hours of CE from reading the article. Correctly answering the questions will demonstrate the reader can:
1. Review the components of the eukaryote cell.
2. Review the structure and function of mitochondria.
3. Learn where and how ROS are formed.
4. Understand why triglycerides are increased in SRBD.
5. Examine how sleep loss really affects brain function.
6. Learn the components of the microbiota-gut-brain-axis.
7. Discover how SRBD leads to mitochondrial dysfunction.
8. Learn how mitochondrial dysfunction leads to disease.
Despite advances in health care, the CDC reports over 60% of US population has at least one chronic disease, and this statistic is trending upward. While scientific literature supports the role of poor breathing and sleeping habits as a causal factor in almost all chronic illnesses, we are just beginning to appreciate that maintaining healthy cellular function is at the core of healthy tissues and organ systems. So how does one go about attaining good cellular function? Current research shows the underlying mechanism by which SRBD cause problems with every one of our body’s systems is by disrupting the normal function of our mitochondria. The necessary balancing act between pro-oxidative productions and a concomitant antioxidant defense systems is referred to as redox homeostasis and is a
crucial determinant of physiologic processes to maintain optimal health.1 Although mitochondrial dysfunction can be acquired from aging, trauma, poor diet, and drugs, hypoxia and sleep fragmentation associated with SRBD has recently stolen the limelight. As SRBD is associated with cyclic alterations of arterial oxygen saturation and desaturation as well as sleep fragmentation, these hypoxic and fragmenting events trigger pro-inflammatory processes and interfere with healthy mitochondrial function2 which interferes with healthy cellular function.
A quick review of the composition of a cell (Figure 1), the structure of the mitochondria (Figure 2), the general energy producing operations (Figure 3), and a more detailed view of the metabolic pathways of energy production (Figure 4) is necessary to appreciate the mitochondrial-SRBD connection.
Mitochondria are double membrane cell organelles (Figure 2) which have their own DNA “mDNA” and are primarily tasked with cellular respiration and regulating the metabolic activity of the cell. Evidence shows they evolved from primitive bacteria and each cell has thousands of them. They produce the majority of ATP through the process of oxidative phosphorylation (2 ATP from the Krebs Cycle (also known as the Citric Acid Cycle or the TCA cycle) and 34 ATP from the electron transport chain “ETC”). They can promote cell growth as well as programmed
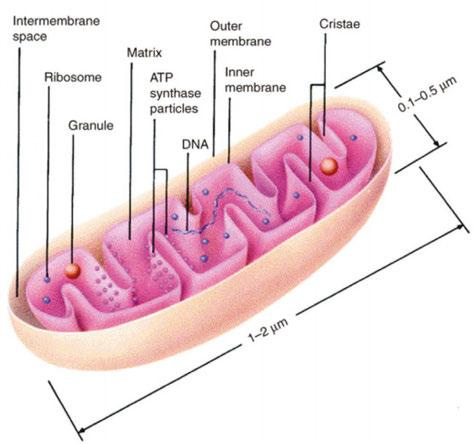

cell death (apoptosis). Additionally mitochondria regulate calcium homeostasis and detoxify ammonia in the liver cells. Reactive oxygen species “ROS” are produced in all cell types as byproducts of the mitochondrial election transport chain (ETC) during ATP synthesis (the sequential passage of electrons from high (NADH or FADH2) to low (molecular oxygen), or formed by NADPH oxidase (NOS) in a controlled manner for targeted purposes such as the respiratory burst in macrophages and neutrophils to defend against microbial invasion.4 Sleep fragmentation is inflammatory as well and increases ROS (oxidative stress).
Dr. Steve Lamberg has been practicing comprehensive restorative dentistry in Northport, NY for 40 years. Always passionate about sleep and wellness, he became a Diplomate of the American Board of Dental Sleep Medicine in 2011 and has served on their board review faculty. He holds several patents, and is the inventor of the Lamberg SleepWell Appliance, which is FDA-cleared for the treatment of OSA. Dr. Lamberg also launched and serves as the director of the Pediatric and Adult Airway Network of New York (PAANNY), to provide a local platform where dentists, physicians, orofacial myologists, and other related professionals learn and collaborate on treatment patients of all ages. Additionally, Dr. Lamberg serves as a Scientific Advisor at the Kois Center in Seattle. His recently published book for the general public, “Treat the Cause…Treat the Airway” correlates many common medical conditions to airway and sleep and is available on Amazon.

As oxidative stress from the ROS injures the mitochondria, it affects changes in mitochondrial metabolism which trigger systemic
inflammation, accelerated aging and apoptosis. Blocking the electron transport chain and fumbling of electrons in the mitochondria result in more oxidation which leads to: accumulation of free radicals, DNA damage accumulation (deletions and mutations) leading to chronic inflammation, damage to lipids, damage to proteins, and increase in mitochondrial membrane permeability. Mitochondria DNA “mDNA” deletions cause major disruption of metabolism and can result in severe cellular impairment or death.5
ROS has another important job as it is linked to the hypoxia-inducible factor 1 “HIF-1” system and it allows anticipating multiple layers of reciprocal interaction to help the mitochondria adapt to hypoxia. The HIF-1 system regulates mitophagy - the reduction of mitochondrial mass by removal of damaged mitochondria.6
In SRBD, mitochondrial dysfunction as a result of redox imbalance can prevent pyruvate, a byproduct of glycolysis, from even en-
Figure 4: A more detailed view of the energy producing metabolic pathways and where they take place in the cell. Note that glycolysis produces pyruvate. Under aerobic conditions, pyruvate can diffuse into mitochondria where it enters the citric acid cycle and generates reducing equivalents in the form of NADH and FADH2. During the ischemia from intermittent hypoxia “IH” the inefficient electron transfer in the ETC (Shown above titled OSPHOS) which is due to the insufficient amount of the recipient O2, causes an accumulation in Reactive Oxygen Species “ROS” (free radicals) which include: superoxide anion, hydrogen peroxide, and hydroxyl radical. These free radicals inflict damage to adjacent structures. The increase of ROS is also referred to as oxidative stress.3
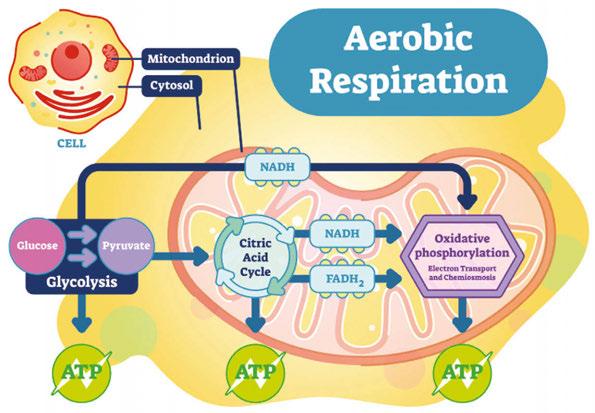

tering the mitochondria and leads instead to the pyruvate being converted into the fatty acid palmitic acid (“de novo lipogenesis”), which in turn is exported from the liver and increases triglyceride levels.7 This has a tendency to hinder glucose uptake into the cells which can lead to insulin resistance and T2DM.
Sleep and wakefulness can affect changes in mitochondrial gene expression, oxidative phosphorylation activity, and morphology in the brain.8 Sleep loss affects brain function in numerous ways including disrupting both short and long-term memory, attention, decision making, and has even been proposed as a trigger for manic episodes in bipolar disorder in humans. Morphological changes to neuronal mitochondria have been reported after prolonged sleep deprivation “SD”. Morphological changes relate to SD-driven changes in mitochondrial cristae functions such as cytochrome c storage or ETC activity. Taken together the reported effects of SD on mitochondrial morphology suggest a major impact on neuronal energy production, and potentially also on neuronal viability. In fact, available data suggest that sleep loss disrupts such fundamental cellular processes as transcription, translation, intracellular transport, and metabolism.9
The regulation of hypoxia has recently emerged as having a central role in mitochondrial function and dysfunction in various diseases, including the major disorders worldwide: CVD and cancer. Accumulating evidence demonstrates that mitochondria are the major target of hypoxic injury, the most common source of ROS during hypoxia, and are the key elements for inflammation regulation during the development of both CVDs and cancer. Taken together, observations propose that hypoxia, mitochondrial abnormality, oxidative stress, inflammation in CVDs, and cancer are closely linked.10
Oxidative stress and mitochondrial damage have also been implicated in pathogenesis of several neurodegenerative diseases, including Alzheimer’s disease, Parkinson’s disease, and amyotrophic lateral sclerosis.11
Abnormalities in mitochondrial metabolism have also been shown to contribute to hypoxia-induced placental oxidative stress. Intermittent hypoxia resulted in reductions in mitochondrial content, decreased abundance of key molecules involved in the electron transport chain and increased expression
and activity of glycolytic enzymes. Expression levels of key regulators of mitochondrial biogenesis were decreased while the abundance of constituents of mitophagy, autophagy and mitochondrial fission machinery was increased in response to hypoxia. Placental hypoxia was associated with mitochondrial-generated ROS, increased oxidative stress, alterations in molecular pathways controlling mitochondrial content and function, inflammation, and apoptosis.12
The microbiota-gut-brain axis is a complex multidirectional crosstalk system between the gut microbiota, the enteric nervous system, and the brain. It acts as an adaptive interface with the environment. A strong interplay also exists with the neuroendocrine-immune network and therefore, the functional integrity of this axis is required for the homeostasis of several systems.13 Mitochondria emerged from bacterial ancestors during endosymbiosis. Mitochondria and bacteria had analogous genomic characteristics, similar bioactive compounds, and comparable energy metabolism pathways. The interactions of intestinal microbiota with neural mitochondria have become an area of investigation. Recent studies have identified neural mitochondrial dysfunction as a critical pathogenic factor for the onset and progress of multiple neurological disorders, in which the role of altered gut flora composition was increasingly noticed. It has been proposed that the communicating channel from gut to brain involves the interaction between intestinal microbiota and neural mitochondria.14 As mitochondria supply the necessary energy and messaging capacity to maintain this complex neuronal network, any mitochondrial dysfunction that results from oxidative stress in SRBD will have a negative impact on the overall health of this system. Emerging evidence suggests that gut microbiota also communicate with the mitochondria of mucosal cells, including epithelial cells and immune cells. Gut microbiota signaling to mitochondria has been shown to alter mitochondrial metabolism, activate immune cells, induce inflammasome signaling, and even alter epithelial barrier function. Both dysbiosis of the gut microbiota and mitochondrial dysfunction are associated with inflammatory bowel disease “IBD” and colorectal cancer.15
60%
Another area of interest is the role of mitochondria in skeletal muscle tissue in obesity. Recent studies reveal that disorder in the balance between mitochondrial fission and fusion is implicated in mitochondrial damage and dysfunction in skeletal muscle in obesity. Genioglossus injury in obese mice that were fed a high fat diet was mediated by mitochondrial disturbance.16
A short list of pro-mitochondrial health suggestions include:
1. Eat a balanced diet which includes healthy fats such as omega-3s and avoid processed foods and refined carbohydrates which interfere with mitochondrial molecular pathways. Restrict calories and try to eat within a 10-hour window.
2. Maintain a daily exercise routine that includes high intensity interval training that includes aerobic activities like swimming biking and hiking.
3. Prioritize getting 7 hours of quality sleep. Sleep related breathing disorders cause hypoxia and sleep fragmentation, both of which compromise mitochondrial health by increasing ROS which leads to chronic inflammation.
4. Supplementation can reduce oxidative stress and stimulate mitochondrial health. Melatonin and αlpha-lipoic acid are strong mitochondrial antioxidants. Resveratrol is another antioxidant which is found in red wine and dark chocolate, however you would
get rather drunk and fat getting your therapeutic dosing this way. Stick to the inexpensive pill. Caffeine increases mitochondrial function.
5. Heat therapy from a sauna or steam bath has been shown to increase the efficiency of mitochondria. Be vigilant about electromagnetic fields “EMFs” which are prevalent in some far infrared saunas. EMFs have been shown to cause mitochondrial stress and dysfunction which will easily outweigh any benefits.
6. Practice relaxation techniques like meditation and massage to reduce stress hormones such as cortisol which negatively effects immune, nervous, and endocrine systems. Simply hiking in nature has been shown to decrease amygdala activity.
This “mitochondriac journey” is not just for your patients, it’s for you too! Look at your own concept of wellness and illness. Reboot your own mitochondria to prevent chronic degenerative disease before it becomes irreversible! Where there are healthy mitochondria there is absence of disease. Understanding the mechanisms by which SRBD cause mitochondrial dysfunction, and eventually disease, will hopefully provide health care providers with therapeutic targets as solutions to optimize mitochondrial health and therefore total body health. “Great things are done by a series of small things brought together.” – Vincent Van Gogh
Inflammatory Diseases, Hindawi, BioMed Research International Volume April 2022, Article ID 9813486
2. Lacedonia et al. Mitochondrial DNA alteration in obstructive sleep apnea. Respiratory Research (2015) 16:47
3. K. Schroder, “NADPH oxidases in bone homeostasis and osteoporosis,” Free Radical Biology & Medicine, vol. 132, pp. 67– 72, 2019.
4. Levy P, Tamisier R, Arnaud C, Monneret D, Baguet JP, Stanke-Labesque F, et al. Sleep deprivation, sleep apnea and cardiovascular diseases. Front Biosci. 2012;1(4):2007–21.
5. Elizabeth Murphy, Hossein Ardehali, Robert S. Balaban, Fabio DiLisa, Gerald W. DornII, Richard N. Kitsis, Kinya Otsu, Peipei Ping, Rosario Rizzuto, Michael N. Sack, Douglas Wallace and Richard J. Youle, Mitochondrial Function, Biology, and Role in Disease - A Scientific Statement From the American Heart Association, Circulation Research. 2016;118:1960–1991
6. Fuhrmann, Brune, Mitochondrial composition and function under the control of hypoxia, Redox Biology, 12 (2017) 208-215
7. Kollar et al. The impact of sleep apnea syndrome on the altered lipid metabolism and the redox balance, Lipids in Health and Disease (2021) 20:175
8. Kim et al: Increased mtDNA Copy Number in the Rat Hippocampus After REM-Sleep Deprivation in vivo 36: 1726-1733 (2022)
9. Lijing Wang and Sara J. Aton, Perspective – ultrastructural analyses reflect the effects of sleep and sleep loss on neuronal cell biology, SLEEPJ, 2022, Vol. 45, No. 5
10. Bouhamida E, Morciano G, Perrone M, Kahsay AE, Della Sala M, Wieckowski MR, Fiorica F, Pinton P, Giorgi C, Patergnani S. The Interplay of Hypoxia Signaling on Mitochondrial Dysfunction and Inflammation in Cardiovascular Diseases and Cancer: From Molecular Mechanisms to Therapeutic Approaches. Biology (Basel). 2022 Feb 12;11(2):300.
11. Giovanna Cenini, Ana Lloret , and Roberta Cascella, Review Article: Oxidative Stress in Neurodegenerative Diseases: From a Mitochondrial Point of View, Hindawi, Oxidative Medicine and Cellular Longevity Volume 2019, Article ID 2105607
12. Vangrieken P, Al-Nasiry S, Bast A, Leermakers PA, Tulen CBM, Janssen GMJ, Kaminski I, Geomini I, Lemmens T, Schiffers PMH, van Schooten FJ, Remels AHV. Hypoxia-induced mitochondrial abnormalities in cells of the placenta. PLoS One. 2021 Jan 12;16(1)
13. Laura Dumitrescu, Iulia Popescu-Olaru, Liviu Cozma, Delia Tulbă, Mihail Eugen Hinescu , Laura Cristina Ceafalan ,Mihaela Gherghiceanu and Bogdan Ovidiu Popescu, Oxidative Medicine and Cellular Longevity, Hindawi, Volume 2018, Article ID 2406594
14. Zhu Y, Li Y, Zhang Q, Song Y, Wang L and Zhu Z, Interactions Between Intestinal Microbiota and Neural Mitochondria: A New Perspective on Communicating Pathway From Gut to Brain. Front. Microbiol. (2022) 13:798917
15. Dakota N Jackson , Arianne L, Theiss Gut bacteria signaling to mitochondria in intestinal inflammation and cancer, 2020 May 3;11(3):285-304.
16. Chen, Han, Chen, Zhao, Sun, Sun ,Zhang, Yu, Lui, High-Fat Diet-Induced Mitochondrial Dysfunction Promotes Genioglossus Injury - A Potential Mechanism for Obstructive Sleep Apnea With Obesity, Nature and Science of Sleep 2021:13 2203-2219
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 8 CE credits for only $149 by visiting https://dentalsleeppractice.com/subscribe/.
AGD Code: 010
Date Published: April 20, 2023 Course Expires: April 20, 2026
Legal disclaimer: Course expires 3 years after publication date. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
n To receive credit: Go online to dentalsleeppractice.com/continuing-education/, click on the article, then click on the take quiz button, and enter your test answers
To provide feedback on this article and CE, email us at education@medmarkmedia.com.
1. The CDC reports _________ of US population has at least one chronic disease.
a. 10%
b. 30%
c. 60%
d. 80%
2. Oxidative Phosphorylation takes place in the ___________ of the cell.
a. Cytoplasm
b. Mitochondrion
c. Nucleus
d. Endoplasmic Reticulum
3. The majority of ATP production is accomplished by ________.
a. Glycolysis
b. Krebs cycle
c. Electron Transport Chain
d. Facilitated diffusion
4. Oxidative stress injures the mitochondria and changes mitochondrial metabolism which leads to ______________.
a. systemic hypocarbia
b. accelerated glycolysis
c. apoptosis
d. increased cell wall thickness
5. Sleep deprivation can cause morphological changes in neuronal mitochondria.
a. True
b. False
6. Placental hypoxia is associated with _____________.
a. mitochondrial generated ROS
b. increased oxidative stress
by Dr.
Steve Lambergc. alterations in molecular pathways controlling mitochondrial function
d. inflammation
e. apoptosis
f. all of the above
7. The communicating channel from gut to brain (microbiotagut-brain axis) involves the interaction between intestinal microbiota and neural mitochondria. Gut microbiota signaling to mitochondria has been shown to ______________.
a. alter synaptic fluid metabolism
b. activate immune cells
c. induce diuretic protein signaling
d. alter epithelial cell bonding
8. Pro-mitochondrial health suggestions include all of the following except which one?
a. Maintaining a balanced diet
b. Regular exercise including high intensity
c. Heat therapy (like saunas)
d. Consuming gluten, sugar, and dairy products frequently
9. Sleep and wakefulness can affect changes in mitochondrial gene expression, oxidative phosphorylation activity, and morphology in the brain.
a. False
b. True
10. Cancer, Inflammatory Bowel Disease, Neurodegenerative Diseases, and CVD have recently emerged as having links to mitochondrial function and dysfunction through _________.
a. statin hypersensitivity
b. having homozygous gene PANY33
c. intermittent hypoxia
d. insulin resistance
If Sleep Apnea – as a construct – can be said to have a birthday, you could say it happened in February 1966. That would make this year Sleep Apnea’s 57th birthday.
It was during that cold winter that French epileptologist Henri Gastaut and colleagues strapped electrodes to a patient with Pickwickian syndrome, with a specific intent to study his sleep, finding a certain breathing pattern that would later spawn a new specialty of medicine, a multi-billion-dollar industry, and ongoing feuds between providers with differing opinions for how the problem should be managed.
But I’m getting ahead of myself.
By 1966, the concept of Pickwickian Syndrome had been puzzled over by scientists for various reasons for over half a century. It was well-understood that patients with a combination of snoring, obesity, and daytime somnolence tended to die younger. Their mode of exit was typically cardiovascular: right heart failure, pulmonary hypertension, strokes, cardiac arrhythmias.
The pattern was called “Pickwickian Syndrome” because the great Dr. William Osler noticed a similarity his patients shared with a character created by Charles Dickens for his first novel The Posthumous Papers of the Pickwick Club, first published in serial form in 1836-1837. In the story, an obese young lad (often called “Fat Joe”) makes his appearance to the other characters by literally falling asleep on his feet while knocking at the door.
Back in 1966, Sleep Apnea didn’t have a name, because nobody even knew it existed. Nobody ever thought to study Pickwickian sleep before. Back then, there was only the knowledge that obesity and sleepiness often went together.

To hear Dr. Osler describe it in 1918: “A remarkable phenomenon associated with excessive fat in young persons is an uncontrollable tendency to sleep – like the fat boy in Pickwick.”1
In 1956, Burwell reported a case involving an obese patient with excessive sleepiness, who was found to be in heart failure with chemical evidence of respiratory acidosis.2 From this case, a new mindset emerged. Burwell’s case definitively demonstrated a link between sleepiness and inadequate clearance of CO2.
After Burwell’s report, the prevailing presumption in the medical community was that, in Pickwickian patients, excess abdominal fat acted as a barrier to pulmonary excursion, thus limiting proper ventilation. The follow up logic was that the hypoventilation (i.e.: lack of clearance of CO2) was the mechanism for the daytime hypersomnia. In other words, patients like Fat Joe were sleepy, they reasoned, because the arterial CO2 level was constantly too high.
Obesity-hypoventilation syndrome, nice to make your acquaintance!
In 1966, Henri Gastaut was known to his peers as a diligent and highly intelligent man, possessing a voracious appetite for learning and exploring, and a supernatural talent for seeing patterns within patterns. Gastaut’s observations of squiggles obtained by the relatively new technique known as electroencephalography (EEG) – the science of interpreting brain waves – established the new field of epileptology as a legitimate science, putting him on the international map as a medical pioneer and a force to be reckoned with.
Gastaut’s work to understand seizure semiology must have prepared him to think about medical challenges with a different
frame of mind than his peers. Perhaps the experience of having seen seizures that transition to a state indistinguishable from sleep positioned him to challenge the dominant paradigm, the one that said that sleepiness in Pickwickian patients was chemical in nature, the result of persistent hypercapnia.
In the winter of 1965, Gastaut seized the idea to apply his genius for pattern recognition and his familiarity with EEG patterns, to scientifically deconstruct the sleep of a person suffering from Pickwickian Syndrome.
The beast known as Sleep Apnea opened its eyes and choked its first breaths in February 1966, when Gastaut, Tassarini, and Duron published a case report in the second issue of the journal Brain Research, entitled “Polygraphic study of the episodic diurnal and nocturnal (hypnic and respiratory) manifestations of the pickwick syndrome”.3
It says a lot for Gastaut’s prominence that he was afforded an astonishing 19 pages to tell the story of a single patient with “authentic Pickwickian syndrome, the symptomotology may be confined to obesity and diurnal drowsing epsiodes of the type described by Dickens in his novel.”
You can almost feel the glee of discovery as Gastaut describes the pattern he found. He was smart enough to know he was seeing something no one had ever described before:
“Nocturnal polygraphic registrations disclosed respiratory pauses which occurred in the initial phase of sleep… so rapid and pronounced that the tongue moves back and causes the obstructive apnoea responsible for a hypoxia, which arouses the subject, who returns to sleep after a short while.
The cyclic repetition of arousal and slumber reduces the nocturnal sleep to 2-3 hours a night. This loss of nocturnal sleep is held responsible for the diurnal somnolence.”
Cue crash of thunder, as lightning flashes reveal a silhouette of a brash young neurologist crying out into the night, as the creature opens its eyes: “C’est vivant!....VIVANT!!”. Meanwhile a nearby transistor radio plays the number one pop song on the planet, over and over: Lou Christie’s falsetto-infused teen anthem Lightnin’ Strikes Again.
The concept of “Sleep Apnea” as a cause of daytime sleepiness wouldn’t enter the public consciousness until over two decades later, because, quite frankly, there wasn’t much one could do about it, back then. The prevailing wisdom at the time was for doctors to tell Pick-
wickian patients to lose weight, because… what else was there? For those who had problems deemed too severe to live with, a tracheostomy was a last-ditch option that almost no one wanted to talk about.
For nearly three decades following his birth, Sleep Apnea lived primarily behind closed doors, the diagnosis mostly being made in academic institutions, populated by nerdy eggheads who idolized people like Henri Gastaut enough to spend two years of their life learning how to decode the erratic squiggles of a polysomnogram.


It would take a treatment strategy more appealing than tracheostomy and more immediate than diet advice to propel Sleep Apnea into the public consciousness. That strategy wouldn’t arrive until Sleep Apnea’s 25th birthday.
In April 1981, while fellow Aussies The Bee Gees established their own falsetto chart supremacy, Dr. Colin Sullivan quietly published a case series of five patients with “severe obstructive sleep apnea,” who experienced complete remediation of the breathing pauses and restoration of “an entire night of uninterrupted
David E McCarty, MD, FAASM is a Sleep Medicine clinician, author, cartoonist, and podcast creator/host. He is the coauthor of Empowered Sleep Apnea: A Handbook for Patients and the People Who Care About Them, and the creator and co-host of Empowered Sleep Apnea: THE PODCAST.
sleep” as a result of using a device he cobbled together from ventilator parts and an emancipated vacuum cleaner pump, a treatment he called Continuous Positive Airway Pressure.3
Almost overnight, a new paradigm of medical treatment was born, and not surprisingly, much debate would ensue in the coming years about what does and does not constitute Sleep Apnea, much of it initiated by insurance payors, having done the math to find out how expensive it could get, if every sleepy person on their “covered life” list decided they needed a sleep study and wanted treatment.
I felt compelled to tell the story of Sleep Apnea’s birthday, because his origin story – the very notion of the construct known as Sleep Apnea – creates strange new ways for individuals to suffer. The concept itself creates siloed thinking that can ironically block patients suffering with airway problems from obtaining care, whilst simultaneously placing vulnerable people in a situation of being offered treatments that they don’t necessarily need.
To understand how the construct of Sleep Apnea can ironically become a barrier to care, I spoke with Katy, an outspoken physical therapist and mother of four who has Sleep Apnea with a respiratory effort related arousal (RERA) predominance. In other words, she has obstructive events which ONLY cause arousals from sleep, not oxygen desaturations. Katy says she literally had to lie to her doctor to obtain access to polysomnographic testing.
“The problem was: I’m young, and my breathing events don’t cause desaturations. On the oximetry test, my oxygen levels were normal, and didn’t drop. My doctor told me that I couldn’t possibly have Sleep Apnea because I was slender, and my oxygen level was normal. Meanwhile I was snoring and feeling terrible, and I couldn’t breathe through my nose. I knew something was wrong, and the doctor just made me feel like it was all in my head.”
Dr. Barry Raphael, an Airway Centered Orthodontist in New Jersey, agrees that the construct known as Sleep Apnea can sometimes represent a barrier to care. “I think we are seeing a different phenotype of the larger problem. The disease we call “obstructive sleep apnea” is an end stage of a long process that involves chronic airflow limitation. Patients we see have difficulty with their breathing not just during sleep, but during the daytime, too. We are just more susceptible to the consequences of suboptimal breathing during sleep.”
Raphael says that patients seen by Airway Centered Dentists are fundamentally different than the Pickwickian patient studied by Gastaut that fateful winter, so long ago: “Patients we see are not just overweight old men, but may be thin, fit women, with evidence of upper airway resistance and sympathetic overdrive…they have fragmented sleep, headaches, TMJ dysfunction, dental breakdown, and comorbidities that aren’t mentioned in the ICSD-3, like migraine headaches, and we are seeing these signs and symptoms improve when we work on the airway.”
These obvious differences aside, these patients are still labeled with Sleep Apnea, if they happen to undergo testing in the sleep lab. The label, it seems, now represents problems that are decidedly not Pickwickian.
I think it’s fair to say that even the great Dr. Osler wouldn’t recognize the connection between Raphael’s patients and Dickens’ character.
If a Pickwickian lens applied to the diagnostic process is capable of blocking slender, RERA-predominant cases from being recognized, a culture of relying on the apnea-hypopnea index (AHI) as the gold-standard indicator of “disease” creates another potential problem: needless overtreatment of vulnerable patients, at the expense of an algorithmic payor.
In 2008, Milena Pavlova and colleagues published a paper that blew my mind, revealing that, in a group of seniors (over age 65) who specifically denied any sleep-wake complaints and had ZERO evidence of medical disease, more than half had an AHI greater than 15 per hour – a metric which, according to the ICSD3, allows the diagnosis of “obstructive sleep apnea” to be awarded with no other supportive information.
Let that sink in.
When Sleep Apnea was confined to his nerdy academic home (that is to say, when the world was young, and the diagnosis was still rare) the discussion of the WHY? of therapy could be a lot more nuanced. Scientific investigators are often the first to tell you what they don’t know.
The truth of the matter is: nobody knows what to do with the inconvenient truth that more than half of “perfectly well” seniors would test positive for Sleep Apnea, if somebody just bothered to screen them. Nobody knows whether treating a person like this with CPAP (or anything else) will prolong life, prevent disease, or enhance cognition. It’s quite
The disease we call “obstructive sleep apnea” is an end stage of a long process.
possible that “treatment” in this setting could make a person’s life worse. Those are the facts.
It really should be presented that way.
But.
That’s not how it goes, in the “real world,” where patients are seen on a rotating 15-minute schedule, where providers are overworked and stressed, and defensive medicine is on display. A 65-year-old who raises objections to being treated is quite likely to be subjected to an “educational” session about the “risks of non-treatment,” which inevitably includes a crisp discussion on how untreated Sleep Apnea raises the risk for stroke, a process which feels a lot like a browbeating.
In my experience, this sort of algorithmic approach pushes many patients to reject the system altogether, after only a short introduction, and never…ever, come back.
If that’s not harm, what is?
Sleep Apnea is no longer confined to an academic dungeon, but indeed has “escaped” to the consideration of the individual patient, who is presented with an increasing array of options for how to proceed. Sleep Apnea diagnostic testing has likewise escaped from the nerdy laboratory to the realm of wearable technology, making the diagnostic test more efficient and available than ever before, and making access to Sleep Apnea treatment almost as easy as stepping up to a vending machine.
So, what’s missing? While we providers who have watched the beast grow and mature understand the nuance and complexity that exist under the black and white rules of diagnostic classifications and event scoring criteria, new trainees have internalized these rules as core beliefs, as ground truth.
The construct has become the reality. The monster is fully awake.
To Katy’s provider, her absence of daytime sleepiness constituted an “evidence-based reason” to deny her access to a sleep study. “I practice evidence-based medicine,” he said, the evidence apparently being the rules he had memorized.
To a senior citizen who feels perfectly well and has no evidence of medical disease, on the other hand, a well-intentioned “screening test” has more than a coin-flip’s chance of disclosing a “disease” that will require a hefty amount of counseling to understand (and may only represent a natural consequence of ag-
ing). The growing trend towards more algorithmic delivery of treatments for Sleep Apnea will doubtless see many more individuals talked into starting therapy for dubious reasons, by inexperienced providers reading from an algorithm provided by the company they work for.
So, if the current definition of Sleep Apnea can’t be trusted not to exclude atypical patients with non-Pickwickian phenotypes, nor can it be trusted to prevent well persons from being exposed to unnecessary treatments, where does that leave us?
In other words: What Do We Do?
My answer: Empower the patient.
Educate the patient early in the process about the Five Reasons to Treat Sleep Apnea: (1) risk, (2) snoring, (3) sleep, (4) wake, (5) comorbidities.5 Help the patient understand that if there are no reasons to treat, there is no reason to treat.
Help the patient understand that the discussion about the first reason – risk – is a nuanced one, requiring attentive deliberation to the types of breathing events that the patient experienced, a review of the patient’s comorbid conditions, as well as the patient’s perceived medical vulnerability. Help the patient understand that there is no “one size fits all” solution. Give the patient guidance in the creation of goals of therapy, based upon the reasons to treat that matter to them. Help the patient along on their journey towards achieving those goals.
Above all: Create the expectation that you will care for the person, not for the label. That’s what you do.
So raise a glass with me, as I toast a happy 57th birthday to the beast known as Sleep Apnea, as he emerges to walk amongst us, with a life of his own.
May we someday truly understand him, in all his glory, beyond the lens of his Pickwickian origins, for the better health of our patients! In the meantime… Brace yourself.
1. Osler W. The Principle and Practice of Medicine. Eighth Edition. 1918.
2. Burwell CS, Robin ED, Whaley RD, Bickelman AG. Extreme obesity associated with alveolar hypoventilation—A Pickwickian Syndrome. Am J Med. 21:811, 1956
3.
4. Pavlova MK, Duffy JF, Shea SA. Polysomnographic Respiratory Abnormalities in Asymptomatic Individuals. SLEEP 2008;31(2):241-248
5.
Help the patient understand that if there are no reasons to treat, there is no reason to treat.
Temporomandibular disorders (TMDs) are debilitating conditions that may cause pain, dysfunction, and impaired quality of life.1 TMD patients may present with dysfunctional breathing, chewing, and speech patterns. They may compensate by recruiting orofacial muscles that should not be activated to perform these essential stomatognathic functions, which turns this into a vicious cycle that potentiates pain and dysfunction.2-4 Non-invasive therapies reported in the literature to alleviate pain are self-care guidelines, orthotics, and laser therapy.5-7 In addition to reducing pain, healthcare providers should aim to improve dysfunction.

Myofunctional therapy (OMT) involves neurologic reeducation through daily exercises that assist in breathing, chewing, speech,8 and even facial expressions in a social context.9 Modifying dysfunctional muscle patterns associated with TMDs may be achieved due to the principle of neuroplasticity.
Myofunctional therapy has three main goals:
1. The tongue should rest on the palate
2. Lips together, teeth apart
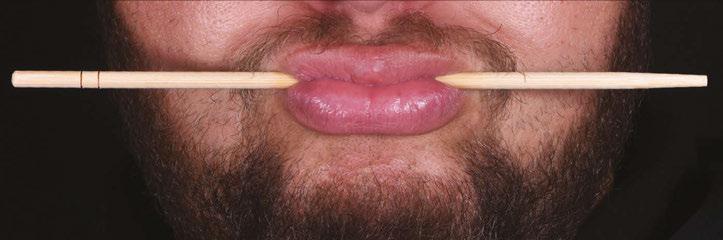
3. Primarily nasal breathe10 Collaboration with dentists, ENTs, and osteopaths, among other specialties, is often

required for comprehensive diagnosis and treatment planning.
Figures 1-3 show examples of myofunctional exercises. During the first phase, myofunctional therapists may provide these and other exercises in weekly treatment sheets after thoroughly assessing orofacial functions.10
The role of OMT in improving health and quality of life cannot be emphasized enough. A recent international consensus statement reported that OMT should be considered an integral part of the interdisciplinary management of obstructive sleep apnea.11 Studies have found that OMT reduces the AHI by 50% in adults and 62% in children.12 Interestingly, the clinical and radiographic findings of TMD patients are often indistinguishable from those of airway patients.13
A systematic review that evaluated the evidence of OMT to manage TMD found a reduction in pain and dysfunction from baseline in symptomatic subjects that performed OMT. Results should be interpreted cautiously since the overall risk of bias was “High” and the certainty of the evidence for both outcomes was “Very low.”14 In this review, the primary outcome was pain which was measured subjectively via validated instruments,15 and the secondary outcome was dysfunction, measured with the validated Orofacial Myofunctional Evaluation with Scores (OMES) protocol.16
Most subjects were female (F= 92, M= 7) in all studies17-20 included in the review.14 The TMD diagnoses were made using the Research Diagnostic Criteria.21-22 Three-di-
Total Appearance and Posture Result (Sum)
(Dysfunctions or alterations were considered to be present when lack of precision in the movement, tremor, associated movements of other components (e.g., lips accompanying the movements of the tongue) and inability to perform the movement were observed)

Felício CM, Ferreira CLP. Protocol of orofacial myofunctional evaluation with scores. International Journal Pediatric Otorhinolaryngology 2008;7(3)367-375.
mensional imaging was not reported in any of the studies for TMD diagnosis, which can be considered a limitation.23
Claudia María de Felício, a speech pathologist and myofunctional therapist from
Zareth Jana Hernández, DMD, is a graduate of the University of Puerto Rico School of Dental Medicine and completed a 12-month Advanced Education in General Dentistry Postdoctoral Program with NYU Langone Hospitals’ affiliated institution in Puerto Rico. Dr. Jana trained in Orofacial Myofunctional Therapy with the Academy of Orofacial Myofunctional Therapy in 2020. She is in her senior year of Prosthodontics Residency at Puerto Rico’s Medical Sciences Campus. After residency, Dr. Jana will pursue further education in craniofacial development, airway, sleep, and TMD. She enjoys research, running, and spending time with her partner, Armando.

Brazil, developed an OMT protocol for TMD patients. The clinical trials included in the Jana et al. systematic review14 applied de Felício’s original or adapted protocol. Although this protocol is available, having the appropriate training is critical to individualizing the treatment exercises depending on the needs of each patient.8,17-20 de Felício’s protocol is completed in 120 days. Patients receive a treatment sheet with exercises that change weekly during the first month and every two weeks afterward. Patients should be sitting with their backs straight while completing the exercises. They should also use a mirror for immediate feedback. The myofunctional therapist assesses compliance and reviews the exercises at each appointment.
In the first stage of de Felício’s protocol, mobility exercises are done in which oral structures are trained individually. Patients should slowly move the tongue and oral structures to maintain the target position for at least three seconds. The therapist decides on the number of repetitions based on the tonicity and fatigue limit of the orofacial muscles. After the mobility stage, strength and resistance exercises are implemented. Finally, coordination exercises are prescribed; in this phase, multiple orofacial muscles synchronize to assist stomatognathic functions.8
Take-home Message:
1. OMT is a tool for healthcare providers to improve TMD patients’ pain and dysfunction.
2. An OMT practitioner familiar with de Felício’s protocol would be a valuable member of the treatment team.
1. Hoffmann RG, Kotchen JM, Kotchen TA, Cowley T, Dasgupta M, Cowley Jr AW. Temporomandibular disorders and associated clinical comorbidities. The Clinical journal of pain. 2011 Mar 1;27(3):268-74.
2. Rosa RR, Bueno MD, Migliorucci RR, Brasolotto AG, Genaro KF, Berretin-Felix G. Tongue function and swallowing in individuals with temporomandibular disorders. Journal of Applied Oral Science. 2020 Apr 3;28.
3. Ferreira CL, Machado BC, Borges CG, Da Silva MA, Sforza C, De Felício CM. Impaired orofacial motor functions on chronic temporomandibular disorders. Journal of Electromyography and Kinesiology. 2014 Aug 1;24(4):565-71.
4. Marim GC, Machado BC, Trawitzki LV, de Felício CM. Tongue strength, masticatory and swallowing dysfunction in patients with chronic temporomandibular disorder. Physiology & behavior. 2019 Oct 15;210:112616.
5. de Freitas RF, Ferreira MA, Barbosa GA, Calderon PS. Counselling and self-management therapies for temporomandibular disorders: a systematic review. Journal of oral rehabilitation. 2013
Nov;40(11):864-74.
6. Ebrahim S, Montoya L, Busse JW, Carrasco-Labra A, Guyatt GH, Medically Unexplained Syndromes Research Group. The effectiveness of splint therapy in patients with temporomandibular disorders: a systematic review and meta-analysis. The Journal of the American Dental Association. 2012 Aug 1;143(8):847-57.
7. Maia ML, Bonjardim LR, Quintans JD, Ribeiro MA, Maia LG, Conti PC. Effect of low-level laser therapy on pain levels in patients with temporomandibular disorders: a systematic review. Journal of Applied Oral Science. 2012;20:594-602.
8. Connelly S, Tartaglia G, Silva R., Oral Motor Treatment of TMD. In: de Felício CM, editor. Contemporary management of temporomandibular disorders. Springer International Publishing; 2019. p. 149-162.
9. Kuć J, Szarejko KD, Gołȩbiewska M. Smiling, Yawning, Jaw Functional Limitations and Oral Behaviors With Respect to General Health Status in Patients With Temporomandibular Disorder—Myofascial Pain With Referral. Frontiers in Neurology. 2021:754.
10. Academy of Orofacial Myofunctional Therapy. https://aomtinfo. org
11. Mediano O, Mangado NG, Montserrat JM, Alonso-Álvarez ML, Almendros I, Alonso-Fernández A, Barbé F, Borsini E, Caballero-Eraso C, Cano-Pumarega I, de Carlos Villafranca F. Documento internacional de consenso sobre apnea obstructiva del sueño. Archivos de Bronconeumología. 2022 Jan 1;58(1):52-68.
12. Camacho M, Certal V, Abdullatif J, Zaghi S, Ruoff CM, Capasso R, Kushida CA. Myofunctional therapy to treat obstructive sleep apnea: a systematic review and meta-analysis. Sleep. 2015 May 1;38(5):669-75.
13. Rouse, J, McKee, J. Are we treating the same patient? The Blend of Airway and TMJ. SpearEducation. 04/17/2020. https://online.speareducation.com/course/are-we-treating-the-same-patient/lesson/are-we-treating-the-samepatient#_ga=2.130040207.1843449027.16777752721718351918.1677775272 Accessed: 01/02/2023.
14. Jana Z, Blanco A, Elías A, López L. Efficacy of orofacial myofunctional therapy to manage pain and dysfunction in patients with temporomandibular disorders: a systematic review. (unpublished). 2023
15. de Felício CM, de Oliveira Melchior M, Rodrigues Da Silva MA. Clinical validity of the protocol for multi-professional centers for the determination of signs and symptoms of temporomandibular disorders. Part II. CRANIO®. 2009 Jan 1;27(1):62-7.
16. de Felício CM, Medeiros AP, de Oliveira Melchior M. Validity of the ‘protocol of orofacial myofunctional evaluation with scores’ for young and adult subjects. Journal of oral rehabilitation. 2012 Oct;39(10):744-53.
17. Felício CM, Ferreira CLP. Protocol of orofacial myofunctional evaluation with scores. International Journal Pediatric Otorhinolaryngology 2008;7(3)367-375.
18. de Felício CM, Melchior MD, da Silva MA. Effects of orofacial myofunctional therapy on temporomandibular disorders. CRANIO®. 2010 Oct 1;28(4):249-59.
19. Machado BC, Mazzetto MO, Da Silva MA, de Felício CM. Effects of oral motor exercises and laser therapy on chronic temporomandibular disorders: a randomized study with follow-up. Lasers in medical science. 2016 Jul;31:945-54.
20. de Felício CM, de Oliveira Melchior M, Lúcia Pimenta Ferreira C, Rodrigues Da Silva MA. Otologic symptoms of temporomandibular disorder and effect of orofacial myofunctional therapy. CRANIO®. 2008 Apr 1;26(2):118-25.
21. Brandão RD, Mendes CM, Brandão Filho RA, De Sena EP. Isotonic exercises and relaxing techniques in individuals with temporomandibular dysfunction. CRANIO®. 2022 May 4;40(3):199-206.
22. LeResche L, Von Korff M. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J craniomandib Disord. 1992;6(4):30155.
23. Schiffman E, Ohrbach R, Truelove E, Truelove E, Look J, Anderson G, Ceusters W, Smith B. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications.
24. Schnabl D, Rottler AK, Schupp W, Boisserée W, Grunert I. CBCT and MRT imaging in patients clinically diagnosed with temporomandibular joint arthralgia. Heliyon. 2018 Jun 1;4(6):e00641.
The role of OMT in improving health and quality of life cannot be emphasized enough.
It was my fourth day on the job and my last day of training
– Thursday, February 27, 2020, Atlanta. Most of my conversations during breaks with new work colleagues at the ItamarMedical headquarters were about how excited I was to be headed to Europe for the first time in April 2020 with my family. However, news started to hit regarding COVID and how things may be different at the airport on the way home. Would this impact our Europe trip? Little did I know cancelling the Europe trip would be the least of our problems. On March 17, huge headlines hit Las Vegas, where I live – The Strip is Closed! I just started my new job and within 30 days, my clients (dental offices) are also closing. My wonderful work team encouraged me to keep learning about the product and helping clients as much as I could. To be honest, there really wasn’t time for me to speculate how this was going to turn out. It was panic mode time. A lot of dental teams fell apart and dental sleep medicine seemed to be at a standstill.
Then the phone started ringing – dentists called asking about WatchPAT® ONE (WP1) the fully disposable home sleep apnea test
device. They asked: Can WP1 be shipped to patients? Is it possible to instruct patients remotely? Are results easily accessible? Do we work directly with physicians? Are we able to use local physicians? The answers are all YES, and I noticed an immediate shift. Dentists were pivoting!
I can’t remember the exact date on this one because I was busy with WP1 calls, but there was a day when the American Academy of Sleep Medicine (AASM) announced sleep testing should only be done with a fully disposable sleep test. That was it! We were off to the races!
In my 27 years in dentistry, I’ve been using the WatchPAT® for 18 years. I’ve seen success because it’s simple, accurate and reliable… and now disposable. To say this is a game changer is an understatement! Many centers of excellence using WP1 have found it to be much more profitable than non-disposable devices for many reasons – there is no need to track the device or clean it and prepare it for the next patient. Why limit your test device to one patient per night, and factor in travel days and ‘slow return’ patients? Now, a medical facility can hand out hundreds of

tests a day and retrieve reports in the secure HIPAA compliant portal, CloudPAT®. Time is what counts the most here.
Here are three examples I’ve come across recently where a dental office uses WP1 to be a game changer for the community. I talk with many dentists working with local physicians utilizing WP1 during the screening, diagnosis, and treatment recommendation processes.

Desert Dental Group – Brett Barney, DDS, also owns what his team calls the “REO Sleep Wagon.” Dr. Barney has been providing dental sleep medicine to his patients for several years and recently has added the WP1. He feels he can provide patients an affordable way to obtain a diagnosis. He spends time in his RV mobile office visiting patients unable to visit him – recently he has been able to branch out of state. His office manager Pete says, “We received 10 referrals the first week we started using WP1, patients are willing to pay cash to know if there is an issue and how to go about managing it.” Pete says now that they have the disposable, they will be able to help even more patients. Not lending out a $5k home sleep test will allow more confidence, fewer logistical problems, and increase the volume.

Glennine Varga is a Clinical Sales Specialist Zoll® Itamar® Medical. She has been employed in dental education for 20 years. She is a member of the Academy of Dental Management Consultants (ADMC) and a professional member of the National Speakers Association (NSA). She is also a visiting faculty member of The Pankey Institute and Spear Education’s Dental Sleep Medicine courses. Glennine is an expanded duties dental assistant certified in TMD with the American Academy of Craniofacial Pain (AACP).

Christensen Orthodontics – Bret Christensen, DDS, is one of the few orthodontists to whom I have the pleasure of providing our products. He has been using WP300 and once he added WP1 his team member Kris noticed an uptick in patient acceptance. She explained to me it was time. What once took 7 days now takes 3 days. WP1 dispensed, the next day a study is in the portal, an interpretation is made by a board-certified sleep physician, a phone call is made and soon the patient is in therapy. Kris explains with multiple office locations, WP1 really multiplies the speed of this process. There is not much time between steps which really helps the patients to choose their best therapy option.
Eugene Dental Sleep Center (EDSC) –Donald Dexter, DMD, also owner of Don Dexter Gallery. Last month, I was able to visit Dr. Dexter’s center for the first time. As I arrived, I noticed both of his businesses are listed on the building map. He explained his practice is based on ABC…Always Building Community. Including art builds community. He brings his community together through art sections, wellness presentations, and collaboration in a pleasant meeting space. The wellness presentation series is intended to bring awareness to sleep quality. Dr. Dexter says “Sleep and wellness is a two-way street, we live as we sleep and we sleep as we live, so everything that we do to improve our health and wellness will impact our sleep. Sleep isn’t simply the event at the end of the day, it’s the consequences of the day that we lived…so live well, sleep well.” Dr. Dexter feels everything he and his team do is based on building healthy patient relationships, connecting providers, and contributing to a thriving community. I will be representing WP1 at the EDSC to see Ariel Yabek, a local licensed marriage and family therapist present “Mindfulness from a Relational Model of Care: Education & Practices to Promote Connection and Wellness.” Excited to participate and happy WatchPAT® is along for the ride. Pivot, collaborate and survive, increase your production, and focus on community through education and art. Powerful results for a home sleep apnea test – I suppose I should give some credit to the dentists and teams making this happen. Take a few minutes with your team and brainstorm how you can be creative and help your community more. We all win when we all win.




Do you ever read something that just makes you think about why you do what you do? I recently read an article written by Ben Waldman for DSP that was titled “Schrödinger’s Dentist”. In the article, he talks about dentists being poor at understanding selling and why that is a detriment to our patients.

The idea of selling dentistry is one that evokes strong feelings in dentists and patients alike. When researching the definition of “sell” there were two that struck me because of how at odds they were with each other. The first was the verb definition meaning to persuade someone the merits of. The second was the noun definition meaning a disappointment arising from being deceived. So when I asked dentists how they felt about “selling dentistry,” all that I interviewed stated some version of the first verb definition where selling is necessary for a patient to make the best choices for their health. However, when I asked non-dentists, potential patients, they tended to have a more negative outlook more closely aligned with the second definition. As many of us have likely
experienced, when a patient is feeling “sold” they may make comments like, “You’re just trying to pay for that new car in the parking lot.” They said they didn’t want to be “sold.” They wanted to be cared for.
These conversations with the two groups revealed a glaring disparity in how dentists care for their patients and how patients perceive this care. Why does this discrepancy exist? How do we influence or persuade with integrity in a way that our patients can feel? Why is doing so important?
The last question is the easiest to answer, especially in the context of dental sleep medicine. If patients with sleep disordered breathing go undiagnosed or untreated, they are likely to suffer from one or more comorbidities such as heart attack, stroke, depression, and motor vehicle accidents. Clearly controlling these sleep issues can be very impactful not only to the patient being treated but also for their family and community. But, how then, do we get our patients to say yes to the treatment that they need, but don’t necessarily want?
LD Pankey’s cross of dentistry is a useful tool to help dentists influence with integrity. The four sides are “Know your Work,” “Know Your Patient,” “Know Yourself,” and “Apply Your Knowledge.” He taught us that suc-
cessful application of these four principles rewards both the clinician and the patient.
“Know Your Work” is the first key to exceptional patient care. You can’t sell what you don’t have on the shelf and you can’t diagnose what you don’t know how to see. From a comprehensive care standpoint, a dentist having an understanding of sleep and its impact on a patient and their oral health is a necessity. We are required to screen for sleep related issues. “Knowing your work” is also critical for getting patients to trust you. When a dentist is deeply knowledgeable in their recommendations, they are perceived as being confident and trustworthy. This creates a feeling of safety and reassurance for the patient.
The second side of the cross , “Know Your Patient”, is the most crucial in crossing the divide between a patient feeling like they’re being “sold” or the patient feeling like they are being persuaded with integrity. Taking the time to get to know who your patient is on a deeper level goes a long way towards building trust. Understanding what motivates an individual patient, what their values are, how they make decisions and what barriers they have towards moving forward with care is essential. Knowing a patient at a personal level helps a dentist cater the care they are providing to the individual and helps them move towards health.
The third side of the cross of “Know Yourself” as it applies to “selling” patients optimal care, I interpret as obstacles and assumptions dentists might put in their own way unknowingly. Obstacles like thinking they don’t have enough time to connect with a patient. Or assuming a patient is going to say no because of cost. Assuming we have effectively communicated when we have not. When we become aware of our tendencies to add these obstacles and assumptions, we can be more proactive about identifying and removing them.

The last side of “Apply your Knowledge” is done most successfully after the knowledge of the work can be connected skillfully to knowledge about each individual patient. When applied properly, “selling” the same treatment may look different depending on the motivations of each patient. Take, for example, treatments involving a Mandibular Advancement Device. For one patient, you may have discovered that they love running
and are always aiming for a personal record time. You can connect with their goals by having a conversation about how addressing their sleep will not only help them be healthier, it may even help them improve their running times. For another patient, you might have discovered that they are becoming more self conscious about the chipping and wear of their teeth. For them, explaining how the proper device will also prevent more chipping and wear from occurring might motivate them towards health.
We can become highly educated by seeking out quality courses. We can also learn how to proficiently connect with our patients through the lens of their wants, needs and values. We can learn about ourselves and how our own biases get in our way. When we master these and apply them effectively we move more towards the persuading of the merits of and away from disappointment by deception. And so we are “selling” in ways that benefit our patients by helping them move towards health and in turn the health of our practice.
Dr. Chelsea Erickson is a North Dakota native who grew up near the Turtle Mountains in Bottineau, North Dakota. She graduated in 2006 from the University of North Dakota with a Bachelor of Science in Chemistry. She then attended Creighton University where she graduated with her Doctor of Dental Surgery degree in 2010. She comes from a medical background and knew from an early age she wanted to become a medical professional. Dr. Erickson felt that dentistry was right for her for several reasons. Of the many medical fields she observed, she felt the dental profession had the privilege of getting to know their patients very well. It also grants practitioners the benefit of autonomy where decisions about treatment are made based on the patients’ needs and not dictated by a governing hospital or insurance company. Dentistry also provides regular hours allowing her to enjoy more time being a mother and wife. Dr. Erickson is in private practice at DeMers Dental and is a visiting faculty member at the Pankey Institute.

LD Pankey’s cross of dentistry is a useful tool to help dentists influence with integrity. The four sides are “Know your Work,” “Know Your Patient,” “Know Yourself,” and “Apply Your Knowledge.”
Nobody goes to dental school to become a durable medical equipment supplier. And few dentists seek employment at a medical practice to ply their trade.
But dentists who practice dental sleep medicine find themselves in just this position. Payors characterize the oral appliance service as an item of durable medical equipment (DME). So a dentist needs to call himself a DME supplier to get paid. But getting a commercial insurance company to cover a dentist’s work for providing DME can be a difficult maze.
Reimbursement for the DME service could be easier if a physician billed the service under his or her provider contract with the payor. So, it seems like a sound business proposition for the dentist to be part of the sleep doctor’s practice.
Assume a dentist seeks employment or an independent contractor arrangement with a sleep physician practice. The physician might ask the staff dentist to fabricate and fit an oral appliance to treat the practice’s obstructive sleep apnea (OSA) patient. The practice could bill the patient’s insurance for the DME service, and the practice could share a portion of the collected fee to compensate the dentist for his work.
Though it’s a solid economic and clinical proposition, it is also illegal in states that follow the corporate practice of medicine (COPM) doctrine.
The corporate practice of medicine doctrine walls off persons licensed to practice one profession (law, medicine, dentistry, etc.) from any person who does not also hold a license to practice the same profession. The doctrine generally allows individual doctors or dentists to practice in the corporate or limited liability company form, but only if all of the shareholders or owners of the legal entity are members of the same profession.
Subject to certain exceptions, the COPM prohibits lay entities (ie, those owned in any part by non-doctors or non-dentists) from employing or contracting with licensed practitioners to provide professional services for or on behalf of the lay business. In addition, most COPM laws permit entities to perform only one profession. This means that doctors and dentists in COPM states cannot own a single practice from which each can perform his or her own profession.
The rationale is to keep lay persons from interfering with the professional’s exercise of independent medical or dental judgment. The concern is that the professional will be induced to chase profits to benefit the unlicensed business owner instead of choosing efficient cures for the patient.




Air quality is CRITICAL to your practice. Contaminants are everywhere: Pathogens, Pollutants, Viruses, Bacteria & Fungi all threaten our air quality and quality of care.
Benefits of Air Quality Guard:
• Arm and ceiling intakes capture aerosols at the source and move them away from occupants
• Contaminated air is filtered through a 3 layer system, removing greater than 99.99% of all contaminants
• Reduces the spread of COVID-19 and reduces sick leave
• Negative pressure airflow cycle ensures that contaminants are captured before they can circulate
• Quietly and efficiently filters & replaces up to 100% of air with pure, clean air
• Power ful enough to replace all the air in the room every 7 minutes*
Though several states have abandoned the doctrine in light of changing technologies, a majority of states still recognize the doctrine. Some of the more strict followers of COPM include California, New Jersey, New York, North Carolina, Ohio, Colorado, Illinois, Maryland, Tennessee, and Texas.
The Texas’ Professional Entity law, Tex. Bus. Org. Code 300.001, et seq. is representative. The law says that physicians, dentists and certain other professionals may practice their profession under a limited liability vehicle (i.e., a corporation, limited liability company or other association) only if all of the owners of the entity are practitioners of the same profession. The professional entity is limited to practice only one profession.
Other than hospitals and certain other specified health care entities, businesses not owned 100% by physicians or 100% by dentists may not employ or contract a physician or a dentist, respectively, to perform their professional services for or on behalf of the lay company.
Dentists have even more stringent Corporate Practice of Dentistry (COPD) restrictions. Dental Boards across the country protect their licensees by making sure that their dentists aren’t answering to non-dentists or sharing dental fees with non-dentists.
Colorado is particularly strict in this regard. Not only are Colorado dentists prohib-
Daniel B. Brown is the principal health care partner at Taylor English Duma LLP, a full-service law firm of over 150 attorneys headquartered in Atlanta, Georgia. Dan is an accomplished corporate and health care attorney who regularly advises clients on transactions and the legal and regulatory aspects associated with the operation and sale of health care businesses. Dan regularly advises physician practices, diagnostic facilities, sleep centers, dentists, DME suppliers and other health care providers in mergers, asset acquisitions, and joint ventures. He regularly assists clients on structuring health care business operations and maintaining regulatory compliance. He is a frequent speaker and author on the legal aspects of sleep medicine, home medical equipment, oral appliance therapy for obstructive sleep apnea, and other health law matters.
In 2004, Mr. Brown published “Sleep Lab Compliance and the Law,” a multi-volume publication addressing the licensing, staffing, and joint venturing of sleep labs and the dispensing of treatment therapies for obstructive sleep apnea. He served as Treasurer and a member of the Executive Committee of the National Sleep Foundation during 2010’s.

ited from practicing dentistry in any entity not owned 100% by dentists, Colorado dentists are allowed to share dental fees only with another licensed dentist or a dental hygienist with whom the dentist is lawfully associated in the practice of dentistry. See, Mason v. Orthodontic Ctrs. of Colorado, Inc., 516 F. Supp. 2d 1205 (D. Colo. 2007). See also, Weinbach v. Orthodontic Ctrs. of Colorado, Inc., 2007 WL 2786426, at *3 (D. Colo. 2007)
One business model bandied about is for a well-established DME supplier to hire a local dentist to fit and fabricate OAT for OSA patients referred to the supplier. The supplier would bill the OAT service under the supplier’s long-standing DME payor provider agreements. The supplier would share a portion of the insurance reimbursement with the dentist.
COPD forecloses this arrangement as well. As a lay entity, the DME supplier cannot hire the dentist to perform dentistry (OAT fitting and fabrication) for the supplier.
Penalties for violating corporate practice doctrines vary by state. However, doctors and dentists who violate a state’s corporate practice rules may be subject to disciplinary action. Some state dental boards penalize persons who promote the unlawful practice of dentistry. So a physician who seeks to hire a dentist in a COPD state could face trouble from a state dental board. A key financial risk is that, upon audit, the insurance company payor of the oral appliance could claim that all payments made to a physician or DME supplier for OAT in violation of state law are subject to recoupment and must be repaid.
Recall that most states authorize licensed professionals to practice only one profession in the professional entity. Even strict states permit some professionals to practice under one roof, such as doctors and nurses. Georgia recognizes the practices of architecture, professional engineering, and land surveying as the practice of only one profession for this purpose.
In light of these corporate practice restrictions, is it ever possible for a doctor and dentist to practice in the same professional entity, where the physician can determine sleep apnea and the doctor can hire a dentist to fabricate and fit the oral appliance therapy? In rare cases the answer is yes.
One instance could be Utah, where there is no COPM or COPD. Another outlier is California. The first part of California Corp Code § 13401.5 generally says that only licensed physicians can become employees of a medical professional corporation. But a later section more recently adopted takes it back by saying that the section does not limit employment by a professional corporation of persons who hold certain types of other health care licenses. Dentists appear on the list of approved professionals. This means that a California professional medical corporation can employ a dentist to render professional dental services at and for the medical professional corporation.
But that is not the end of the story. Doctors and dentists must comply with applicable fee splitting and anti-kickback laws. These laws limit how and how much, if any, a person can pay the other for referring patients. Exceptions exist for employed persons in certain instances, so a review by knowledgeable health care counsel is critical. However, there is likely no exception under the Stark law for a physician who owns a sleep or other practice to refer oral appliance therapy to a dentist employed at the practice if the appliance and service is reimbursable by Medicare.
The Stark law prohibits a physician from referring a designated health service (DHS) reimbursable by Medicate to an entity in which the referring physician (or an immediate family member) has a financial interest. Here the physician refers the oral appliance to the staff dentist to furnish. Stark law exceptions do exits to permit physician referrals of certain DHS furnished within a single group practice. The exception does not apply with respect to almost all items of DME. Because oral appliance therapy, like CPAP, is an item of DME, the joint-practice entity cannot bill Medicare for oral appliance therapy if the physician-owner of the practice referred the services to the practice’s staff dentist. Some states have “little Stark” acts that could apply to these referrals even in the absence of Medicare reimbursement. Have your attorney check these laws as well.
Like any new venture in health care, the regulatory traps area everywhere. Know the scope of COPM and COPD rules in your state before getting too far along in your business planning. Next time, we will visit some of the legal issues surrounding being a part of dental service organization for a sleep dental practice.
Note: This article is for informational purposes only and does not constitute legal advice.

Like any new venture in health care, the regulatory traps are everywhere.
Rearrange the letters in the grid to create 6 words that make sense both horizontally and vertically. Letters in green blocks are already in the correct location. Letters in white blocks need to be moved to a different word. Letters in gold blocks indicate the letter belongs somewhere within the word but not in its current location.
H I A E T
O
P T A E S E T
A Y
N R
R E

B S
For the solution, visit www.dentalsleeppractice.com.
Sapphire is uniquely positioned “Expand North American sales and

Sapphire is uniquely positioned to impact the dental strategic “Expand North American sales and leverage the marketing organization

pillars. organization to drive adoption of a national turnkey brand”


OSA public awareness activities: website, social media, brochures, posters, videos, events and most importantly the B to C products
Complete turn on approach to Sleep implementation, ongoing coaching & support and new sales of equipment, software and services
Unique therapeutic framework for Chronic Headache, Migraine, TMD, Tinnitus, Vertigo, Pain Head, Neck, and Face
OSA public awareness media, brochures, importantly the Complete turn-key, implementation, new sales of equipment, Unique therapeutic Headache, Migraine, Head, Neck, and
501C3 Non-Profit Fully accredited, online, ondemand Dental Sleep Medicine credentialing. The only one of its kind in the world.



Medmark LLC is proud to be the leading interactive marketing and multi-platform advertising company focused on the niche specialties of dentistry. We are creating a healthier America through knowledge, due diligence, and experience, by empowering dental professionals with high quality clinical information in clear and concise language and showcasing innovative technologies.


www.nexusdentalsystems.com
 Nexus Bill
Nexus Airway
Nexus Bill
Nexus Airway


