


















New Orleans is an inspiring city. Walking around the Garden District with its flowers and big houses, or when seeking out live music, one takes in history mixed with day-to-day joy of living. It’s a city of contrasts with very old buildings in disrepair side-by-side with new, vibrant businesses and homes.
While it’s easy to convince me to visit New Orleans, an invite to speak at a remarkable conference, Airway Palooza, was enticing – it’s one of the best times to gather with peers and learn from each other. After these happy events, it’s interesting to take stock of how it went – what did I learn, what connections were made or enhanced, what new opportunities are available.
The organizer asked me for an ‘update on dental sleep medicine.’ With that open direction, I gave a talk about when we make a difference in patients’ lives. I said there are three chances: First, Best, and Last chances, depending on how long the person has had to deal with the consequences of poor breathing, daytime and during sleep. It felt good to hear kudos after the talk.
There are many ideas that came to me afterwards I wish I had time and thought to say. ‘Great’ points I could have made. ‘Important’ details that would have enhanced the message. Things I wish I would have said.
The only one who knows what I ‘left out’ is me. My audience has no idea. They have access to what they heard, and control over how it applies, or doesn’t, to their lives. As an educator, I’ve come to realize a presentation is like a gift – the content becomes the receiver’s, to use as they wish. The (amazing!) pearls I left out might have been super well-received, or completely passed over.
Isn’t clinic like that? You take in all the details you can gather, consider your medical choices, and recommend therapy accompanied by explanation. How is that different from my talk? We give our patients a gift of our clinical wisdom – that’s why they sought us out – but we cannot control what they do with that gift. We can communicate details, a sense of urgency, a list of possible consequences of treatment and no treatment. What they do with everything we give them is completely out of our control.
And they know only the things we tell them. They don’t know what we don’t say any more than we know what they learned online, from other health care professionals, or from friends.
Communication is a mess. From the front of the room, I hope my gift to the learners will be found valuable and create action. What I leave out bothers me, not them. In my clinic, I hope to support value for the choices my patients own. I think of what else I could have said every day. Especially when outcomes don’t meet expectations.
Next time you find yourself ruminating about what you wish you’d said, give yourself credit for the gifts you provided, and look for the next chance to help. Like an old building that is still standing despite neglect, your relationship with your patient will survive. Remember, they don’t know what you didn’t say.
Do you like what you are reading in DSP? Do you have ideas you want to share about what works in your practice? As Chief Dental Editor, I am happy to consider essays from any reader! Contact me at stevec@medmarkmedia.com.
 Steve Carstensen, DDS Diplomate, American Board of Dental Sleep Medicine
Steve Carstensen, DDS Diplomate, American Board of Dental Sleep Medicine
Cover Story
SomnoMed Elevates Oral Appliance Therapy Through Its Medical Initiative™ with Research-Backed Efficacy, Quality, Comfort, and Durability
Increasing the bonds between health care professionals.


Continuing Education
Pediatric Sleep-Disordered Breathing and Obstructive Sleep Apnea: The Role of the Speech-Language Pathologist by Ann Blau, MS, CCC-SLP, CMT® and Kaitlyn Shrum, MA, CCC-SLP, QOM, CMT®
FAIREST-6 – Find children at risk in your practice.


Medical Insight Sleep & Cannabis: Exploring the Potential by Jamila Battle, MD
A look at the use of cannabis products for sleep disorders.

2 CE CREDITS
Medical Insight Sleep Through Her Eyes: Unpacking Gender Differences in Sleep and OSA by Alison S. Kole, MD, MPH, FCCP
Exploring the unique characteristics and challenges of sleep in women.

• Offer FDA-cleared therapeutic procedures that provide pain relief and rehabilitate force imbalances for new and existing patients
• Provide medically necessary dentistry using tested technologies including ultrasound, photobiomodulation, microcurrent, and muscle manipulation.
• Precisely diagnose and deliver state-of-the-art treatment for chronic migraines and headaches, tinnitus, and other neck/jaw/face pain
• Address an individual patient’s symptoms with a drug-free, needle-free treatment plan that has a 95%-100% clinical success rate
• Receive clinical training along with ongoing implementation assistance
• Add a revenue stream to your practice, increasing your non-doctor revenue
• See nearly 389% ROI and only 30 minutes of doctor chair time per case.



44 Practice Management What’s All the Buzz about the ‘K’ Code in Dental Sleep Medicine? by Rose Nierman, CEO, Nierman Practice Management
New codes can be confusing. Here’s what we know today.
6 Publisher’s Perspective My Rx for Summer by Lisa Moler, Founder/CEO, MedMark Media
12 The Bigger Picture Optimizing Healthspan: A Resounding Victory, A Probable Failure, And A Call To Action by Bill Hang, DDS, MSD When we consider all the benefits early treatment can provide...
16 The Bigger Picture Dentistry 3.0 by Steven Lamberg, DDS Evidence plus clinical wisdom is better medicine.
18 Cardio-Sleep Corner The Biggest Sleep Myths by Lee A. Surkin, MD, FACC, FCCP, FASNC, FAASM
Let’s dispel some common misconceptions about sleep.
25 Communication Corner “The First Thing I Got Wrong” by Kalli Hale, DDS, MPH, D.ABDSM, D.ABSB
Second in a series of real-world experience.
42 Education Spotlight Dental Sleep Medicine and Craniofacial Pain Education Makes Global Impact by Drs. Terry Bennett and Mayoor Patel Are you curious what your colleagues in other countries are learning?
48 Clinical Focus Titration Before Fabrication or “Try It Before You Buy It” by Allen J. Moses, DDS, DABCP, D.ABDSM
Rethink your workflow to get to predictable solutions faster.
54 Sleep Humor The Lighter Side of Sleep Apnea
Summer 2024
Publisher | Lisa Moler lmoler@medmarkmedia.com
Chief Dental Editor
Steve Carstensen, DDS, D.ABDSM stevec@medmarkmedia.com
Chief Medical Editor
Lee A. Surkin, MD, FACC, FCCP, FASNC drsurkin@n3sleep.com
Associate Editor | Lou Shuman, DMD, CAGS lou@medmarkmedia.com
Editorial Advisors
Jamila Battle, MD (Family/Sleep/Addiction)
Steven Bender, DDS
Jagdeep Bijwadia, MD (Pulmonary, Sleep)
Kevin Boyd, DDS
Alison Kole, MD, MPH, FCCP, FAASM (Sleep, Pulmonary, Critical Care)
Karen Parker Davidson, DHA, MSA, M.Ed., MSN, RN
Bertrand de Silva, MD, FCCP, D.ABSM
Kristie Gatto, MA, CCC-SLP, COM
Amalia Geller, MD (Neurology, Sleep)
William Hang, DDS, MSD
Steve Lamberg, DDS, D.ABDSM
Christopher Lettieri, MD (Pulmonary, Critical Care, Sleep)
Pat McBride, PhD, CCSH
Jyotsna Sahni, MD (Internal Medicine, Sleep)
Ed Sall, MD (ENT, Sleep)
Alan D. Steljes, MD (Cardiology, Sleep)
Laura Sheppard, CDT, TE
DeWitt Wilkerson, DMD
Scott Williams, MD (Psychiatry, Sleep)
Gy Yatros, DMD

National Account Manager
Adrienne Good | agood@medmarkmedia.com
Sales Assistant & Client Services
Melissa Minnick | melissa@medmarkmedia.com
Creative Director/Production Manager
Amanda Culver | amanda@medmarkmedia.com
Marketing & Digital Strategy
Amzi Koury | amzi@medmarkmedia.com
eMedia Coordinator
Michelle Britzius | emedia@medmarkmedia.com
Social Media
Felicia Vaughn | felicia@medmarkmedia.com
Website Support
Eileen Kane | webmaster@medmarkmedia.com
MedMark, LLC 15720 N. Greenway-Hayden Loop #9 Scottsdale, AZ 85260
Tel: (480) 621-8955 | Toll-free: (866) 579-9496
www.DentalSleepPractice.com
Subscription Rate: 1 year (4 issues) $149










 Lisa Moler Founder/CEO, MedMark Media
Lisa Moler Founder/CEO, MedMark Media
How many times have you written prescriptions for your patients? Even after they leave your office, you strive to ease their pain, head off their infections, and get them back to healthy lives. I’m not a dentist, but I have played one for almost 20 years now! So, for this summer issue, it’s my turn to write a prescription – to encourage ongoing mental and physical health for our dedicated readers.
My Rx for a Productive and Rejuvenating Summer
Vitamin D: Take some time to get out in the sun and soak up the relaxing rays! Change out of your scrubs and breathe some fresh air – and don’t forget your hat and sunscreen. You will return to work revitalized and ready to tackle any patient.
Get moving: Even if you don’t have time to get to the beach or take a longer vacation, exercise is one of the best ways to relieve tension and clear your mind. The CDC recommends 150 minutes of moderate-intensity physical activity per week. You don’t even need to join a gym – a daily walk will keep that blood flowing. Breaking the time up into 30 minutes a day for 5 days is very doable and can become a healthy habit.
Give your mind some thought: Every day, take some time for mindful thought or meditation. It doesn’t have to be the same time every day, or even done in the same way. Just pick a comfortable spot, close your eyes, breathe deeply, and focus on your breathing. Picture the beach, a mountain trail, or any spot that brings you peace. Taking a few minutes can reduce stress, ease frustration, and open the door to serenity.
Read, watch television, or listen to music: Having a way to unwind first thing in the morning or before bed can calm your mind and body.
Eat healthy, but give yourself a treat: We all know the drill – eat healthy fruits, vegetables and grains, go big on the protein and low on fats and sugars. But, as with all things under heaven, there is a time for ice cream and cake too (in moderation).
Build a trusted team, in and out of the office: Having support people to boost you when you are sad, and laugh with you when
you are happy can make life a warmer, more welcoming place.
Forgive yourself! One of my main mantras throughout this journey of life is to give yourself a break. Everyone makes mistakes, and no matter what some people think, no one is perfect. Every mistake is an opportunity to learn from and grow.
Keep learning: Whether you are in the office or on vacation, take MedMark specialty publications with you! Keep learning new concepts so when you return to work, you can expand your patients’ options for care.
In this summer issue, our Cover Story talks about the mission of SomnoMed’s Medical Collaborative™ that is providing the most effective and accessible treatment options for obstructive sleep apnea (OSA) patients, including oral appliance therapy as a primary treatment option alongside CPAP or surgery. The CE by Ann Blau and Kaitlyn Shrum,“Pediatric Sleep-Disordered Breathing and Obstructive Sleep Apnea: The Role of the Speech-Language Pathologist,” explains the use of the Fairest-6 pediatric clinical airway screening tool for objective screening alongside speech-language pathology. In the Medical Insight column, Dr. Allison Kole looks at gender differences in sleep and OSA for more precisely tailored diagnostic and therapeutic approaches. Check out the AADSM Special Section to discover products and treatment options that bring your DSM practices to a higher level, and increase your clinical and financial success.
Even if your summer is busy with patients, there are plenty of ways to keep a healthy outlook on life. Journalist Charles Bowden once said, “Summertime is always the best of what might be.” Try a few of my Rx recommendations, and you will feel that endless summer in your hearts and minds for all future seasons.

• Whole-Team Training
• Ongoing Coaching
• Streamlined Protocols
• Precision Bite Technology
• Patient Education
• In-Network Medical Billing
SomnoMed’s Medical Initiative™
In sleep medicine, advancements pave the way for enhanced treatment modalities and improved patient outcomes. SomnoMed, the global leader in oral appliance therapy, with a presence in 28 countries and treatment of more than 860,000 patients to date, continues to spearhead innovation.

SomnoMed’s Medical Initiative™ fosters collaboration, promotes awareness, and helps drive research to facilitate adoption, acceptance, and treatment of oral appliance therapy as a primary therapy option among physicians, patients, and insurers. At the heart of this mission lies a dedication to providing the most effective and accessible treatment options for obstructive sleep apnea (OSA) patients. Keith E. Matheny, MD, FARS, is a staunch advocate for the Medical Initiative, emphasizing its critical nature: “SomnoMed’s Medical Initiative is brilliant and fundamental in so many ways. We, as healthcare professionals collectively, are doing a poor job caring for obstructive sleep apnea. This endeavor, spearheaded by SomnoMed, changes that, by aligning sleep physicians and sleep dentists cohesively to offer oral appliance therapy as a primary treatment option alongside CPAP or surgery. It does so in a way that benefits a wider spectrum of both patients and providers from both an economic and accessibility standpoint.”
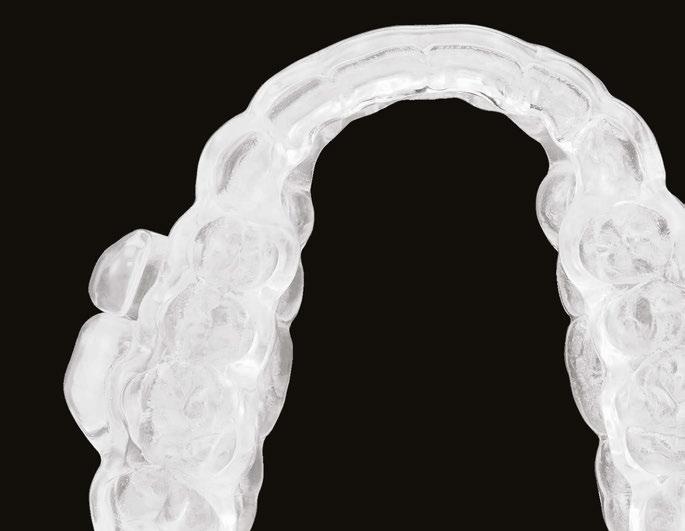
An important pillar of SomnoMed’s Medical Initiative is the quality of SomnoMed oral appliances, a primary factor that contributes to patient compliance and thereby efficacy of treatment. A recent study published in Sleep Medicine underscores how the selection of MAD design may influence treatment therapeutic effectiveness and emerge as a crucial factor in choosing the most suitable MAD for personalized treatment of individuals with moderate to severe OSA.1 The study follows 209 patients over a three-month period, comparing traditional wing-based devices with SomnoMed’s innovative SomnoDent® Avant™ – and the results were nothing short of groundbreaking.
Advancing Oral Appliance Therapy: The Cornerstone of SomnoMed’s Mission
Supporting SomnoMed’s commitment to quality, comfort, and efficacy, the recent aforementioned study featured in Sleep Medicine sheds light on the efficacy of oral appliances as a promising first-line treatment in OSA patients.1 Analyzing 91 patients using a wingbased device and 118 using the SomnoDent Avant, the study compared efficacy of both types of devices. While the wing-based device was clinically effective, with an average reduction in Apnea-Hypopnea Index (AHI) from 23.6 to 11 or 63% reduction in treatment (equal to the results reported by other OAT devices), the SomnoDent Avant demonstrated a remarkable statistically significant reduction in AHI from 21.6 to 6, or 70% reduction in treatment, approaching the efficacy of Continuous Positive Airway Pressure (CPAP) therapy.1
The unique design of the SomnoDent Avant, with its passive mouth closing feature, plays a pivotal role in its superior effectiveness. As the recent study states: “While the results of the traditional wing-based MAD design were comparable to the therapeutic outcome with other titratable, custom-made MADs, the MAD with the passive mouth closing feature (SomnoDent Avant) showed significantly greater reduction in total AHI potentially due to encouraged nasal breathing, reduced mouth breathing, and lesser vertical opening”.1 This study is the first to differentiate efficacy among custom appliance designs and puts the unique design of SomnoDent Avant in a class entirely on its own. “Design does matter,” notes Olivier M. Vanderveken, MD, PhD. “A well thought out design in terms of the whole pathophysiology and working mechanism, high quality material that can be reproducible, supports the notion that there is a high probability that OSA patients will get better therapy outcomes.”
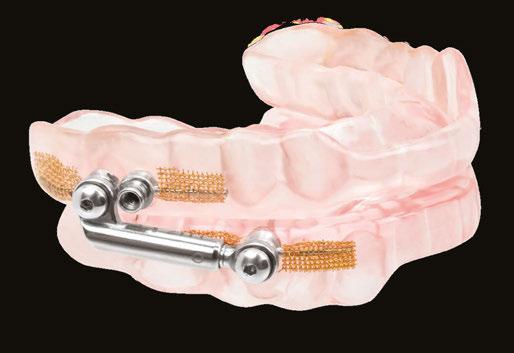
SomnoMed’s commitment to quality underscores the Medical Initiative’s goal to help “Treat More OSA Patients, More Effectively.” Devices milled from a single piece of dental material, like the SomnoDent Avant and the SomnoDent® Herbst Advance Elite™, feature SomnoMed’s proprietary b-flex Comfort Liner™ and a First Time Fit™, every time promise, cradling and supporting each tooth and thereby enhancing long-term patient compliance. In addition to b-flex, the PDAC-approved for Medicare E04486 Herbst Advance Elite offers the first and only full 5 Year War-
ranty in the industry due to utmost confidence in the device’s strength, durability, and comfort, and requires no Medicare insurance verification.
Expanding upon its innovative approach, SomnoMed’s first ever inbuilt technology-enabled oral appliance, soon to be featured in both SomnoMed’s SomnoDent Avant and SomnoDent Herbst Advance Elite, further addresses a major barrier to prescription and reimbursement rates to date: the lack of overnight monitoring in continuous open airway therapy (COAT™). With sensors that measure treatment efficacy and adherence, both physicians and dentists can view personalized patient data on a web-based portal, alongside a phone app for patients that allows them to view their own sleep data. This analysis supports SomnoMed’s Effectiveness Equation (Effectiveness = Efficacy x Compliance) and drives acknowledgement of equivalent clinical effectiveness for COAT and CPAP when considering both efficacy and compliance together.
SomnoMed’s Medical Initiative extends beyond research and development; it’s also about granting providers the tools and relationships they need for effective patient treatment while empowering patients to take control of their sleep health. Suzanne Thai, DDS, highlights the transformative impact of the medical collaboration SomnoMed helps facilitate, stating: “I’m incredibly thankful for SomnoMed’s Medical Initiative! It has been a game-changer in treating sleep apnea patients. By teaming up with physicians and raising awareness, we are not just addressing sleep issues but changing lives!”


The role of SomnoMed’s Business Development Managers (BDMs) is pivotal in bridging the gap between dental professionals and medical prescribers. Located throughout the US and Canada, SomnoMed’s BDMs dedicate their time educating the medical community of MDs, DOs, PAs, NPs, and their professional staff members on oral appliance therapy as an effective, first-line treatment option for mild to moderate OSA patients. They are experts at bringing medical prescribers and SomnoMed’s robust network of sleep dentists together, with
An OSA patient is shown SomnoMed oral appliances.
the shared goal of getting all OSA patients into the right OSA therapy at the right time. BDMs introduce sleep physicians – often personally – to highly qualified and experienced SomnoMed sleep dentist(s).
With our industry partners aligned, we can continue the journey to building the most effective and efficient treatment pathways for the patient, sleep dentist, and physician. As Brad Mechor, MD, FRCSC, notes: “There was a time when Otolaryngology encompassed EENT – eyes, ears, nose and throat. Now, I believe it should be ENTT –Ear, nose, throat and teeth! Being able to assess the nasal-oropharyngeal airway is an important part of the treatment pathway for all patients with sleep disordered breathing/OSA and being able to provide early, minimally invasive intervention will help to improve patient treatment outcomes. A strong working relationship between ENT and sleep dentists is essential.”

SomnoDent® Herbst Advance Elite™ and SomnoDent® Avant™, respectively.
Through strategic partnerships, SomnoMed streamlines the diagnosis and treatment process for OSA, making it more accessible and efficient for patients and providers alike.
One such valuable collaboration is exemplified in SomnoMed’s partnership with Nexus Dental Systems, allowing for increased access to dental sleep medicine. Acting as a training and billing company, Nexus protocols increase office efficiency and result in more patients getting tested for OSA. National billing contracts allow Nexus dentists to bill In-Network with major insurance plans. Our partnership will raise public awareness of sleep apnea, train dentists to implement dental sleep medicine, create sleep apnea programs for the industry, and connect patients with providers by creating sustainable and resilient systems for both providers and patients.
Another of SomnoMed’s partnerships allows for an automated process in which patient symptoms are assessed, diagnosed, and matched with treatment for obstructive sleep apnea. Board-certified sleep physicians guide patients through an automated program for less time and money than a traditional office visit and sleep study. Speaking to the impact
of SomnoMed’s Medical Initiative, Jean-Maria Langley, DO, FAOCO-HNS, remarks: “As an ENT surgeon, we hope to reduce if not eliminate obstruction leading to hypopnea and apnea. With SomnoMed’s help, we’ve built a strong collaboration with our sleep dentistry team to integrate oral appliance therapy to treat our patients’ upper airway obstruction, increase compliance to treatment, and reduce comorbidities associated with obstructive sleep apnea.”
SomnoMed’s Medical Initiative is not just about advancing oral appliance therapy as a treatment option; it’s also about fostering a collaborative, interdisciplinary approach to healthcare with the objective of changing patient lives. Dental sleep provider Carrie Sessom, DDS, D-ASBA, highlights: “The impact of SomnoMed’s Medical Initiative has been multifold. It has brought to light the importance of medical/dental collaboration and the value of personal relationships between physicians and dental sleep providers, putting oral appliance therapy front and center as an effective, preferred patient therapy for more and more medical prescribers. It’s certainly helping to ease the CPAP supply pinch.”
With the right referral pathways, it can be just as easy and seamless to refer patients for OAT as it is to send an order for CPAP to a durable medical equipment company (DME).
“We’re optimizing OAT treatment accessibility for the millions of patients suffering from mild to moderate OSA,” says Matt Conlon, Executive Vice President, SomnoMed North America. “And in light of certain PAP supply challenges for years to come, we’re committed to helping more physicians consider oral appliance therapy as a patient preferred, effective treatment solution for their patients.”
Here at SomnoMed, we’re paving the way for a future where the treatment of sleep apnea is more integrated, accessible, and effective for all involved. Join us. Connect with our team at insidesales@somnomed.com.
1. Olivier M. Vanderveken, Margot Van Daele, Johan Verraecken, Marc J. Braem, Marijke Dieltjens, Comparative analysis of two custom-made mandibular advancement devices with varied designs for treating moderate to severe obstructive sleep apnea; Sleep Medicine, 2024. https://www.sciencedirect.com/science/ article/abs/pii/S1389945724000777
Jeremy Powers, Global Clinical Affairs Director, SomnoMed (left), pictured with David M. Rapoport, MD, SomnoMed Clinical Advisory Board member.
I recently finished reading one of the dozens of books on health/longevity that I’ve read in the last few decades. Outlive by Peter Attia, MD, is one of the better written, comprehensive, well documented, and practical books on the subject of longevity. It is the first one I’ve seen making liberal use of the word “healthspan” vs. “lifespan”. This is an important distinction which makes sense to most people. Attia encourages the reader to think rather than blindly follow the supposed one and only path to longevity which typically is the goal of so many books selling a specific diet, supplement, exercise plan, etc. He emphasizes lifestyle, personal choice, and personal responsibility decisions as being the path to achieve a long “healthspan”. He encourages each reader to develop his/her own “evidence-informed” plan which, to me, is the only way forward.


success I had hinged on the patient accepting a significant role in their own treatment. How refreshing it is to see a book like Outlive recognize and address these issues from a medical perspective!
I’ve spent the last 30 years of my professional life trying to help patients reverse or prevent problems which occur due to lifestyle choices endemic in all industrialized societies. Specifically, we sought to help growing children have better “healthspans” by becoming 100% nasal breathers with proper rest oral posture which develops the face forward to optimize their airways. I’ve also treated hundreds of teens and adults whose airways were reduced by poor rest oral posture causing unfavorable vertical facial growth. Others we treated had their forward facial growth stunted with retractive orthodontic treatments. Like everyone, I had my successes and my failures. Much of the
The significance of this all came together in the space of less than 15 minutes this past week when my wife and I went to breakfast at a popular local restaurant in a town where we practiced orthodontics for many years. Sitting at the table next to us was a now 103 year old man we first met soon after we moved there. In 1975, he was to me “an older man” I played tennis with and looked up to. He physically resembled my mother’s father in every way down to the exact same balding pattern! He and my grandfather also shared the same gentle personality type, were both funeral directors in small towns, never spoke negatively about others, and were universally loved by all. My grandfather smoked and died at 76. This man never smoked, continued an active lifestyle, and apparently to this day has a good “healthspan”. I suspect that he has done many things right as described

12 modules cover both the medical and dental science of sleep medicine. Dentists who complete the coursework and pass the exam are qualified to submit cases for board review to achieve Diplomate status. The certificate is a prerequisite for ACSDD Fellow and Diplomate



I have responsibility to share the valuable
lessons
my patients taught me.

Top: Enjoying “tractor therapy” in Vermont
Bottom: Enjoying semi-retirement in the National Parks of Utah
in Outlive. He is a victorious poster child for that book and role model for all.
At the very same breakfast, we talked with a woman who was lamenting about her 14.5 year old grandson. The boy and his mother (the woman’s daughter) live with her and her husband. Grandma is very involved in raising this boy. She described him as being very fidgety, diagnosed with ADHD, impossible to get out of bed in the morning, late to school most mornings, etc. She noted that he has been told by teachers that “you will never amount to anything unless you learn to sit still” and has indicated he plans on quitting school as soon as he is old enough to legally do so. My heart sank as I remembered similar children with very unfortunate lives. I asked her all the usual questions that anyone involved with sleep/breathing disorders knows to ask. Her responses were 100% predictable and confirmed my concerns.
Dr. Steven Sheldon, now retired as head of Lurie Children’s Hospital Pediatric Sleep Clinic, often said, “I do not believe there is such a thing as ADHD. I believe it is ALWAYS a sleep/breathing disorder.” He would always footnote that statement with the fact that he cannot prove it, but those are pretty strong words for a published researcher like Dr. Sheldon. I related his statement to this grandmother, and she listened intently. I could see some hope in her eyes.
In 14.5 years, no one in medicine, dentistry, or the educational establishment recognized the obvious sleep/breathing disorder. Sadly, there are only a few communities in the U.S. where his problems would have been recognized very early – if they were recognized at all. I gave the woman some ideas for her to explore and the name of a person I have trained in my E.C.H.O. Men-

Bill Hang, DDS, MSD, practiced orthodontics in Vermont from 1975 to 1996 and in California from 1997 until his retirement in November 2022. He currently lives in Flat Rock, NC. Having been traditionally trained, he extracted teeth for crowding and often retracted the teeth. For the last 40 years, however, he has been a pioneer in non-retractive treatments to improve the airway in patients of all ages and founded OrthO2Health.
torship who lives about 2 hours away in a neighboring state. I know there are treatments that may help him, but also know there are no guarantees with any treatment. I also know the incredibly bad consequences which may occur by doing nothing. Were he my grandson, I would be moving mountains to find and try solutions which have proven to help so many others in hopes that he might be helped also
In my practice, I had many kids who’ve confronted similar failure in unfortunate ways. I had more than one become involved in drugs and die of drug overdoses. Others got on the wrong side of the law. A poster child for this is the story of a close friend from my grade school years. Ron was in my class but a year older, because he had “flunked” a grade. He was a chronic mouth breather with a nasal voice, narrow maxilla with a V-shaped incisor segment, long face, and a sugar addiction. When he was doing poorly in elementary school, his dad told him he would “never amount to anything”. His older sister did well in school which didn’t help his feeling of failure. As the object of much teasing, his main coping mechanism was to be the “class clown”. At lunch time, he gave away bagfuls of candy to buy friendship from classmates. He couldn’t sit still and would have received the ADHD label had that diagnosis existed when we were kids.
He graduated high school unable to write a complete sentence. I strongly suspect he suffered brain damage from what we now call OSA. Today, researchers like Ron Harper, PhD, at UCLA or David Gozal, MD, might use MRI’s to document which specific areas of the brain were affected. His sugar addiction resulted in him ballooning from a string bean as an adolescent to obese by his early adulthood. He lost all his teeth by his late 30s as a consequence of his massive sugar intake, chronic mouth breathing, etc. Although, as adults, we lived a thousand miles apart in different states we stayed connected via phone and occasional personal visits when I returned home to visit my parents. Sadly, he died of liver cancer in his early 60s. The memory of his appearance 2 weeks before he died still haunts me. Everyone working in the airway arena probably knows similar stories with similar tragic outcomes.
I hope that my words and suggestions to this grandmother gave her hope and guidance to find help for her grandson to have a more favorable outcome.
In less than 15 minutes, I had concrete examples of victory and tragedy in the battle to optimize “healthspan” as described by Peter Attia in Outlive. Reflecting on one year of retirement after 50+ years of orthodontic practice, I’m indebted to the patients who trusted me to treat them. I now have responsibility to share with other professionals the valuable lessons my patients taught me. Books and days like I just experienced motivate me to help others develop skills which can bring change for the better. We can’t rest until every town of any significant size in North America has teams of people who can collaborate, recognize airway problems early, and provide effective treatments to
produce better healthspans for all. And why stop with North America? The World needs our help.
Every dental practice has patients with similar issues (or worse) than my friend Ron. We cannot turn our backs on these kids by pretending there is no problem just because there is no guaranteed solution. Not having bulletproof RCT’s at the top of the “evidence pyramid” supporting our every action is no excuse for inaction. We must act forcefully with the best “evidence-informed” treatment approaches as Peter Attia suggests. We are in our infancy understanding the airway pandemic. We do not have all the answers, and must find better solutions than the current ones. It is my hope that this story helps motivate others to work together, to act, to do the research, and improve our batting average of success for the people we seek to help. Future generations are depending on new leaders – perhaps like YOU – to carry the torch for others to see.

 by Steven Lamberg, DDS
by Steven Lamberg, DDS
T3.0
he context of this new term, Dentistry 3.0, is derived from Dr. Peter Attia’s recent book Outlive in which he introduces the emerging philosophy of Medicine 3.0. Our drive to be great fixers of what’s broken has supplanted the practicality of prevention. Although Attia’s major theme is about longevity, the concept of approaching one’s health status more proactively is essential. Interwoven into this thinking is the reality that medicine and dentistry have evolved into a somewhat unnatural professional separation that is helpful to no one. It seems however that, driven by our greater understanding of the links between medical and dental outcomes, we find ourselves in a unique period of what we could call “healthcare self-awareness”. A recent push to integrate the two fields will undoubtedly prove beneficial for fulfilling our patient’s needs.
Attia’s thesis rests on the distinction between the current approach of Western medicine, “Medicine 2.0”, and an updated framework, “Medicine 3.0”. The former focusing on treating what’s broken while the later has optimal health as its target. Optimal health is dependent on prevention and the appreciation of treating the root cause(s)
of existing conditions. As an example, Attia lists the most common medical conditions causing death which include the following: Cardiovascular disease, Cancer, Neurodegenerative disease, and Metabolic disease. Medicine 2.0 provides treatments to mitigate their impact. Medicine 3.0 tries to prevent them by working upstream.
Why the need for this new term, Dentistry 3.0? In the current world of dentistry, Dentistry 2.0 is focused on treatment of problems which can be nicely separated into categories such as; periodontal conditions, biomechanical conditions, functional occlusal conditions and esthetic concerns. The progress Dentistry 2.0 has made within the last 40 years has been nothing short of meteoric. Technology and our understanding of biologic systems have led to a new age of proficiency in restoring patients to a place superior to their natural dentitions. Although we know how to diagnose and elegantly plan treatment, the missing piece is the why. Why did this particular patient have the problem becomes the question which should lead us to exposing the root cause. The importance of this step cannot be overstated. This is the essence of
Dentistry 3.0, and is parallel to Attia’s Medicine 3.0. Intervening as early as possible always leads to a less invasive solution. As the earliest intervention and prevention are essentially first cousins, we need to up the ante on screening for medical conditions based on evidence uncovered in the mouth.
My book Treat the Cause…Treat the Airway examines every system of the body and connects the dots between the medical conditions and sleep related breathing disorders “SRBD”. There are many ways dentistry can help patients achieve optimal health by improving the airway and sleep. Dentistry 3.0 recognizes airway problems as a root cause of most dental problems. Clinicians who focus on treating a specific symptom without considering what caused it may allow that root cause to take down other systems in the body. Treatment becomes less predictable. Noticing whole-body disruptions, such as chronic inflammation, and looking for what’s causing them, is what is bringing medicine and dentistry closer together.
As Dentistry 3.0 focuses more on prevention and early intervention, there is a need for more robust data collection and screening tools. Because most medical conditions correlate with airway problems, the Lamberg Questionnaire v 16 is an excellent way to use the patient’s medical history to screen for airway problems. Although data collection is related to screening, it goes well beyond that. In Dentistry 3.0 data collection is used for the purpose of revealing the root cause of the problem. Dentistry 3.0 realizes we cannot treat an AHI and focuses instead on what is causing an increase in the number of apneas, hypopneas, and respiratory effort related arousals. The concept of treating what’s actually causing the airway problem elevates the discussion to Airway 3.0 which will be explored in a follow-up article. Both the Lamberg Questionnaire v16 and Data Collection Form v4 are available on my website for free.
When we have young patients under the curve of orthopedic growth and development for their age, Dentistry 3.0 asks why.
When we have attrition and abrasion of the teeth, Dentistry 3.0 asks why. When the dentition is crowded or the jaws don’t align in crossbite relationships, Dentistry 3.0 asks why. When our dental patients are on cholesterol medications or have prediabetes, atrial
Intervening as early as possible always leads to a less invasive solution.
fibrillation, hypertension or reflux, Dentistry 3.0 asks why. When young children have problems sleeping which translates into behavioral or learning problems, Dentistry 3.0 asks why.
Are you ready to look at a complex medical history of a patient and then look for signs or symptoms of an airway problem? Do you think yourself a sentinel for airway disease as a dentist?
Do you appreciate the impact of mouth breathing on not just the mouth but the entire body? Is the opportunity to help people maintain a high level of health, free of disease, as significant to you as doing Dentistry 2.0?
As medicine 3.0 and dentistry 3.0 find their paths merging more and more, perhaps the unnatural separation of medicine and dentistry is self-correcting. Hopefully the 3.0s will lead us to a new era where our lifespan and our health span will be much closer than they are today. It is only through prevention and early intervention that medicine and dentistry can join for the benefits of all of our patients. This new mindset will forever change how you feel going to your office each morning. Optimal health is a worthy goal and I believe the juice is worth the squeeze.

Dr. Steve Lamberg has been practicing comprehensive restorative dentistry in Northport, NY for 40 years. Always passionate about sleep and wellness, he became a Diplomate of the American Board of Dental Sleep Medicine in 2011 and has served on their board review faculty. He holds several patents, and is the inventor of the Lamberg SleepWell Appliance, which is FDA-cleared for the treatment of OSA. Dr. Lamberg also launched and serves as the director of the Pediatric and Adult Airway Network of New York (PAANNY), to provide a local platform where dentists, physicians, orofacial myologists, and other related professionals learn and collaborate on treatment patients of all ages. Additionally, Dr. Lamberg serves as a Scientific Advisor at the Kois Center in Seattle and teaches a course there titled Restorative Dentistry for the Airway Compromised Patient. His recently published book for the general public, “Treat the Cause…Treat the Airway” correlates many common medical conditions to airway and sleep and is available on Amazon.
During the last couple of decades, sleep science has developed remarkably, providing significant findings about the importance of sleep, how it is disrupted, and the biological mechanisms controlling sleep. However, although scientific knowledge and evidence have increased, many people still have some misconceptions about sleep mainly read online or heard by word-of-mouth.
Unfortunately, many of these sleep myths get so widely spread that people consider them as sleep facts. Usually, the belief in such sleep myths leads to poor sleep habits and lack of sleep. For that reason, experts have identified the most common sleep myths and provided the true sleep facts to help people get informed. So now, let’s get these sleep myths debunked!
Myth #1: The hours of sleep needed decrease with age
One of the major sleep myths people believe is that the older you get, the less sleep

you need. However, sleep experts recommend seven to eight hours of sleep each night for an average adult. This also applies to older people. Although they experience a change in their sleep patterns with less slow wave or deep sleep and less REM sleep with increased sleep fragmentation, they still need the same amount of sleep as younger adults. That’s why they typically nap during the day to compensate for the lack of sleep during the night.
Another popular sleep myth is that the brain rests during sleep. But, one of the mind-blowing facts about sleep is that the brain remains pretty active while the body rests during sleep. The brain indeed recharges during sleep but it still keeps control of many vital body functions, like breathing for example. Indeed, the brain remains active and is able to process information even in the deepest non-REM sleep stages when awakenings are difficult and the most restorative sleep occurs.

Next on the list of our sleep myths debunked is the one that says that daytime sleepiness always, with no exceptions, means that a person lacks sleep. In reality, excessive daytime sleepiness may be a medical condition or point to a sleep disorder like Narcolepsy, Sleep Apnea, Restless Legs Syndrome and associated Periodic Limb Movements of Sleep. Yes, these might be one of the

mind-blowing facts about sleep, but the truth is that daytime sleepiness is one of the major symptoms of these sleep disorders.
Myth #4: In case of nighttime awakenings, just lie in bed
Here’s yet another of the sleep myths debunked – if you wake up in the middle of the night, you should lie in bed, toss and turn, and try to fall back asleep forcefully. Yet, this isn’t really a solution and may result in a lack of sleep and negative associations to their actual bed. Instead, you should try some relaxation or breathing techniques to induce sleep. If you are still unable to fall back asleep within 20 minutes, get out of bed and engage in another relaxing activity, like reading in dim light (do not use an electronic device or watch TV), in another room. Return to bed only when you feel sleepy.
Myth #5: Sleep apnea is just snoring
Last but not least, one of the clear facts is that sleep apnea isn’t just snoring. Mistakenly, people think of them as interchangeable. Snoring is a sign of airway resistance and is not always associated with sleep apnea. Statistics show that nearly half of the population snores from time to time, whereas one in four adults snores chronically 1 Plus, about 20-40 million Americans suffer from OSA. So yes, they are connected, but not interchangeable.
1. J Davey MSc, M. (n.d.). Epidemiological study of snoring from a random survey of 1075 participants. https://britishsnoring. co.uk/pdf/epidem.pdf
Statistics show that nearly half of the population snores from time to time, whereas one in four adults snores chronically.
Lee A. Surkin, MD, is the Chief Medical Officer of Nexus Dental Systems. A private practitioner in cardiology, sleep medicine, and obesity medicine, he is one of a small group of physicians to be triple board certified in cardiology, sleep medicine, and nuclear cardiology. In 2009, he created Carolina Sleep – the only dedicated sleep medicine practice in eastern NC. Dr. Surkin has created a cardiovascular and sleep healthcare model that includes a multi-faceted diagnostic and treatment approach that is enhanced by a network of relationships with physicians, dentists, respiratory therapists, sleep technologists, and public officials who recognize the important role that sleep medicine has in our daily life. In 2012, Dr. Surkin founded the American Academy of Cardiovascular Sleep Medicine which is a not-for-profit academic organization dedicated to educating healthcare providers, supporting research, and increasing public awareness of the convergence between cardiovascular disease and sleep disorders. In 2014, Dr. Surkin created a new multi-specialty practice called Carolina Clinic for Health and Wellness which combines his specialties with primary care, gynecology, behavioral health and a medical spa. Dr. Surkin is married with three daughters and a golden retriever and resides in Greenville, NC.
Looking for an easy and effective solution to your patients’ snoring and OSA? As the first customTAP with no metal parts, flexTAP is an oral appliance that is customized for personal comfort and equipped with a self-adjustor for at-home ease. Its new ThermAcryl® liner allows for easier chairside adjustments using warm water.
flexTAP is the first of its kind to utilize our proprietary Vertex Technology® paired with the flexTAP Mouth Shield comfort accessory to promote nasal breathing, prevent dry mouth, and minimize excess saliva for extra comfort. Uniquely designed with a wide range of advancement (17mm) without the need for bite registration or exchanging hooks, Vertex Technology allows the mouth to open vertically and horizon-

tally simultaneously during advancement of the jaw.
“Treatment success relies on how far the jaw can open,” says Dr. Keith Thornton, inventor of the Thornton Adjustable Positioner (TAP). “Since people breathe in various positions, healthcare providers need the flexibility to adjust the device according to individual patient night-tonight needs.”
flexTAP is our lowest priced customTAP, PDAC coded (E0486) and includes a standard 3-year warranty. It is available to order through Airway Labs and participating partner labs.
•Promotes nasal breathing
•Included with every flexTAP and myTAP device
•Enhances treatment outcomes
•Slides over post and seals inside the lips

Non-custom oral appliance

Appliance selection remains our most powerful resource to ensure desired outcomes. The Respire Pink AT (Advanced Titration) Herbst by DynaFlex has become one of the most effective appliances applicable for many patients due to several key innovations. The adjustment tool (Figure 1) has a userfriendly handle. Patented technology ensures the screw does not turn back on itself during wear. The measuring scale on the arm allows both patient and dentist to closely monitor acute advancements.
When looking to innovate further on the Respire Pink AT, DynaFlex focused on patient comfort. We have been able to maintain all the current AT features, while creating one of the smallest PDAC approved hinges on
the market. Reducing the length of the hinge by 24% prevents irritation of the commissures of the lip while the mandible is being advanced. We were able to achieve a much smaller and more comfortable arm without sacrificing advancement range. Thanks to one of the key features in the new Micro design you can titrate up to 8mm, if needed.
Knowing your options for appliance selection gives you the opportunity to provide precision therapy for your sleep apnea patients. Using an experienced oral appliance manufacturer like DynaFlex, who has a large variety of appliance choices, allows you to treat each patient according to their needs and helps achieve the goal of personalized medicine.
Allowing up to 8mm of advancement over the course of treatment.
1mm advancement with only 4 turns and a measuring scale for precise adjustments.


Anew, uniquely sophisticated mandibular advancement device clinically proven to treat obstructive sleep apnea and snoring.
The appliance features an extremely smooth and comfortable finish. There are no metal components to irritate mucosa. The sintered nylon allows for a small buccal profile for patients with a small buccal corridor.
The clinician can choose various mandibular positions. The appliance is ideal for bruxers because of the occlusal support and the strength of the material. A rigid, precise fit reduces the possibility of tooth movement. The unique cam design provides for freedom of movement allowing TM joints to move without restriction.
Mandibular advancement devices are suitable for patients who suffer from mild to moderate obstructive sleep apnea. The device can be recommended for patients who are intolerant to other treatments and patients who snore during sleep.

Great Lakes Dental Technologies is an employee-owned company, with 200 employee-owners who design, develop, manufacture, and market appliances and products for use in the orthodontic, dental, and sleep and airway markets.
Great Lakes is one of North America’s largest orthodontic laboratories and offers more than 4,000 products and services. Training and education are offered at the onsite training center in the company’s headquarters, located in Tonawanda, NY.

The custom OrthoApnea NOA features two individual low-profile splints that hold the jaw in a controlled forward position to facilitate breathing and provide a more comfortable experience for the patient.
The flexible, controlled advancement allows for lateral jaw movement while preventing joint discomfort.



Mandibular advancement is defined by the doctor and performed in a progressive and controlled sequence through a series of lower splints.
greatlakesdentaltech.com 800.828.7626
“The right tools for the right job.” The convergence of dentistry and sleep medicine has brought forth a critical need for a specialized system in addressing medical model workflows for obstructive sleep apnea (OSA) treatment. Sleep testing, physician collaboration, medical billing, documentation, progress reports... while conventional dental software or medical EMR's serves some needs, it lacks the nuanced features designed specifically for effective dental sleep medicine management.

DentalWriter Plus revolutionizes dental sleep medicine with its comprehensive suite of features tailored to streamline workflows. Interactive checklists guide practitioners through each step of the sleep patient process, ensuring efficiency and
accuracy. Dedicated questionnaire and exam forms for every visit facilitate detailed clinical notes while generating SOAP reports. Optimized referral reports foster seamless collaboration between dentists and physicians, igniting referral networks.
This user-friendly platform boasts robust features, allowing for customization and detailed production, referral, and analytics reporting to meet the needs of dental practices treating obstructive sleep apnea. Integrated with medical billing services, DentalWriter Plus ensures accurate and seamless reimbursement, supported by an expert team dedicated to transparency and efficiency.
As you embark on your dental sleep medicine journey, ask yourself “Do I have my ducks in a row?”

ZOLL® Itamar®, a division of ZOLL® Medical, is a leading company in sleep apnea diagnosis and pioneering innovative sleep apnea management programs for patients and healthcare professionals. Our mission is to improve access to the millions of undiagnosed sleep apnea patients through our breakthrough WatchPAT® products and services.
WatchPAT® is an innovative Home Sleep Apnea Device (HSAT) that utilizes the peripheral arterial tonometry signal for sleep apnea diagnosis. It measures up to 7 channels (Peripheral arterial tonometry, heart rate, oximetry, actigraphy, body position, snoring, and chest motion) via three points of contact. Within one-minute post-study, the raw data is downloaded and auto-scored identifying all types of sleep apnea events. WatchPAT® home sleep apnea test provides AHI, AHIc, RDI, and ODI based upon True Sleep Time and
Visit ZOLL Itamar at AADSM Booth No. 204

Sleep Staging. The WatchPAT® Home Sleep Test (HST) is clinically validated with an 89% correlation to PSG.1
1.

can help you optimize the potential of your dental practice.
learn more, scan here to visit our website or call

During a break session at a collaborative conference for sleep, a physician colleague caught me checking a sleep test from my computer. Recognizing I was disappointed in the numbers, he patted me on the back and said “...don’t be upset, those are good results. You can’t cure them all.”
As I mentioned in my first article, my journey as a dental sleep medicine dentist turned my world upside down. Transitioning from full time general dentistry to a focused practice of airway dentistry, while simultaneously being blessed to bring my passion into many lecture circuits has been a wild ride! But even with all of my wins in my private practice cases, behind the scenes, I was struggling. I had never felt more fulfilled, or experienced more growth in my practice, but at the same time, I was somewhat discouraged. I realized I wanted to cure them all!
Ingrained in our profession is a level of self criticism and extreme precision (where “a millimeter is a mile”) that is rarely seen in other parts of healthcare. The contacts must be tight, the crown margins must be sealed, and the shade match must be perfect. While I have come to realize we hold ourselves to unrealistic expectations of perfection in general dentistry, this is where dental sleep medicine stands in stark contrast…
When you first start out, by screening your patients, you get a slew of objective data: O2 scores, AHI stats, heart rates, etc.. I stumbled into the impossible universe where I believed I would have a positive impact on all these metrics every time. Impossible goals lead to a sense of personal failure and inadequacy that has no place in our minds. We fail to remember that the airway is dynamic; the level and severity of the soft tissue collapse is just one of many factors determining

the success of oral appliance therapy (OAT). For example, one person may titrate perfectly with your go-to mandibular advancemen device (MAD), but not the other. While I was successful hundreds of times more than I was not, there were times that the burden of managing this disease was heavy. When questioning dentists who “dabbled in sleep” why they stopped offering the services, the common response was “it was too hard and didn’t always work.” What I can assure you is, with time and more experience, the conversations with your patients will drastically improve, as did mine! You can help your patients with their sleep, their quality (and longevity) of life, and improve their healthspan better than any other provider in this space!
Communication and setting expectations are the hardest part of dental sleep medicine. Understanding that this is “healthcare in the mouth” (not general dentistry) is important! Dentistry is just as integral to overall patient health as any other medical discipline. Did you know, in medicine, a 10-20% success rate with a new therapy is considered a “success”?1 This blew my mind! Can you imagine if 80-90% of our fillings failed? I hope that helps give context to the difference in treating a simple disease (e.g., cavities) versus a complex disease (e.g., OSA).
As you progress into airway dentistry, the patient cycle will remain the same: screen, sleep test, diagnosis, appliance selection, and titration sleep test. The rubber meets the road when you are forced to go backwards in that cycle. This is the hard part. “Why isn’t the appliance working?”, or “I should have
You can help improve healthspan better than any other provider.

Kalli Hale, DDS, MPH, D.ABDSM, D.ABSB, is passionate about how our teeth affect our systemic health – the link between chronic jaw infections, periodontal disease, and subsequent heart problems. Her training in obstructive sleep apnea has transformed both her personal and professional career. Dr. Hale is a Clinical Advocate for VIVOS Therapeutics and works with dentists around the country to develop clinical protocols for the treatment of mild to moderate obstructive sleep apnea and sleep-disordered breathing. Her work in pediatric expansion and sleep-disordered breathing catapulted her speaking career and she lives by the slogan “we have to stop getting it wrong, for our kids.” She is faculty for the Dental Success Network, a key-opinion leader for Candid, and the Chief Dental Officer for Toothpillow. She travels monthly across the U.S. and abroad to teach dentists about Obstructive Sleep Apnea. Learn more about her sleep mentorship program at https://sleepwelljourney.com/.






Sleep is one of the greatest public health challenges of the 21st century. The American Academy of Pediatrics estimates that sleep problems affect 25-50% of children and 40% percent of adolescents. At least 12-14% of children have some form of sleep-disordered breathing (SDB) and roughly one to five percent have a formal diagnosis of obstructive sleep apnea (OSA). SDB and OSA can adversely impact children’s speech, language, and cognitive development as well as their craniofacial and upper airway growth.
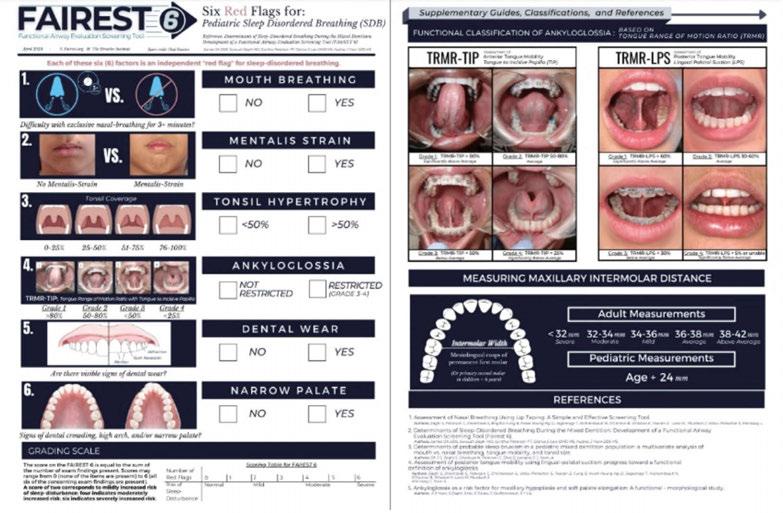
This self-instructional course for dentists aims to present the FAIREST-6 tool. All professionals assessing children for possible sleep-related breathing disorders, poor growth of the craniofacial respiratory complex (CFRC), and potential speech and swallowing dysfunctions need a tool to make screening more objective. This article presents the most well-developed tool for this process, the FAIREST-6. It also highlights the role of the Speech-Language Pathologist as a key player in identifying these at-risk children.
Dental Sleep Practice subscribers can answer the CE questions online at https://dentalsleeppractice.com/continuing-education/ to earn 2 hours of CE from reading the article. Correctly answering the questions will demonstrate the reader can:
1. Easily document several objective measurements of the CFRC.
2. Be able to communicate the importance of these measures with families.
3. Feel confident in collaborative care with other health care providers in this field.
Since speech-language pathologists (SLPs) are often involved early in the assessment and treatment of communication and swallowing difficulties in the pediatric population, they are uniquely positioned to screen for sleep problems in these children. SLPs can incorporate The Functional Airway Evaluation Screening Tool (FAIREST-6) as part of their comprehensive speech and swallowing assessments to identify at-risk children and make appropriate and timely referrals when needed.
The Functional Airway Evaluation Screening Tool (FAIREST-6) is a concise and validated clinical airway screening tool that was developed to identify pediatric dental patients at risk for sleep-disordered breathing (SDB). It is comprised of six clinical determinants, each of which have been found to be independent red flags for SDB in children during the mixed dentition (the stage where both primary and permanent teeth are present). These include mouth breathing, mentalis strain, tonsil hypertrophy, ankyloglossia, dental wear, and a narrow palate.
The FAIREST-6 can be used by dentists, physicians, and allied health professionals to screen for pediatric SDB, aiding in early diagnosis and intervention in pediatric SDB. As SLPs, this is an easy-to-administer screening tool that can be used in a variety of settings to identify at-risk pediatric patients on our caseloads. Although the FAIREST-6 was initially validated on children between the ages of 6 and 12, there exists a potential for extended application to children above the age of 2.5- to 3-years-old, since the signs of pediatric SDB can be present from a young

Ann Blau, MS, CCC-SLP, CMT® is a licensed Speech-Language Pathologist and Certified Myofunctional Therapist. She graduated with a Master’s Degree in Communication Sciences and holds a Certificate of Clinical Competence from The American Speech-Language-Hearing Association. Ann is the founder and owner of All Access Speech Therapy, a private telepractice providing speech therapy services in the states of NY and FL. Based in New York, her practice specialty is in the assessment and treatment of Orofacial Myofunctional Disorders. She provides Orofacial Myofunctional Therapy as part of a collaborative, multidisciplinary approach to patient care. Ann has trained with the Academy of Orofacial Myofunctional Therapy and is certified in The Myo Method® and Simon Says Myofunctional Therapy programs. She mentors post-graduate clinicians privately and through The Myo Membership®. Ann is also the voluntary editor-in-chief of Airway Circle. She has developed and presented CE webinars on the topic of OMDs and OMT. Ann has over 15 years of professional experience in the evaluation and treatment of adults with neurogenic speech, swallowing, cognitive, and voice disorders in acutecare, inpatient and outpatient rehabilitation settings.
Kaitlyn Shrum MA, CCC-SLP, QOM, CMT, certBBM, is the owner and founder of Southern Speech & Myo. She graduated from the University of Central Florida with a Master’s degree in communication sciences and disorders. Kaitlyn holds a Certificate of Clinical Competence from the American Speech-Language and Hearing Association, is a Certified Myofunctional Therapist (CMT) and is a Qualified Orofacial Myologist (QOM). Kaitlyn is also a certified Buteyko Breathing Method (certBBM) instructor. She has completed continuing education focusing on dysphagia, orofacial myofunctional disorders, Buteyko Breathing, TOTS Training, sensory-motor based feeding, the SOFFI method, Beckman Oral Motor Protocol, and the Kaufman approach to treat childhood apraxia of speech. She has been published in several professional journals for her research on phonemic awareness in children with disabilities and the benefits of dialogic book reading for vocabulary development. Kaitlyn also works as a mentor and continuing education provider.
age and early identification is critical. While the FAIREST-6 does have some validity in older cohorts as well, there are other assessment tools that can be used that are more specific to those populations.
Visit https://www.fairest.org/ or scan the QR code above to download a copy of the FAIREST-6.
Each of the six red flags on the FAIREST-6 are discussed in detail below:
1. Mouth Breathing refers to difficulty breathing through the nose with the lips sealed for >3 minutes.
Potential methods of assessment include:
a. having the patient hold water in the mouth with the lips sealed for 3 minutes
b. placing a tongue depressor between gently closed lips while the patient breathes through the nose for 3 minutes
c. having the patient keep their lips closed while breathing through the nose for 3 minutes
If (c) is not possible, the lips may be gently sealed with MicroPore paper tape* while the patient breathes through the nose for three minutes. This protocol was implemented in the Zaghi et al. (2020) cross-sectional, multi-center cohort study. Among the 663 study participants between the ages of 3 and 83, those who were unable to breathe exclusively through the nose for 3 minutes while the lips were taped were found
to have a significantly increased likelihood of mouth breathing while awake and asleep.
*Disclaimer: MicroPore paper tape in the pediatric population specifically should be utilized with extreme caution under the direct supervision of a knowledgeable healthcare provider and should be removed immediately at the first sign of respiratory distress.
If the patient cannot comply for the full three minutes, referral to an otolaryngologist for further assessment of upper airway patency is advised.
According to Warnier et al. (2023), the most efficient way for SLPs to assess mouth breathing in preschool children is via observation of the child at rest (i.e., time spent with an open/closed mouth and position of the tongue/ lips). The child’s breathing pattern while chewing (open/closed mouth) and after swallowing (open/closed mouth just after swallowing) can provide additional clinically relevant data.
Characteristic features of mouth breathers include: lips open or parted at rest (instead of resting gently together), a shortened upper lip (showing the upper front teeth), a protruding or flaccid lower lip, an elongated face, venous pooling or dark circles under the eyes, narrow nostrils, weak cheek muscles, a high palate, narrowing of the upper jaw and malocclusion (misalignment of the teeth), altered head posture, dry lips and mouth, swollen and red gums that bleed easily. Additionally, mouth breathing patients may report symptoms such as snoring and open mouth while sleeping, chronic sinus and ear infections and colds, and chronic halitosis. During sleep, mouth breathing decreases intra oral pH which can lead to greater risk of tooth erosion, tooth decay, and increased tooth sensitivity. Chronic mouth breathing in growing children is associated with palatal growth restriction, alterations in craniofacial development, low tongue tone, reduced tongue strength, chewing inefficiency, sleep-disordered breathing, and increased risk for obstructive-sleep apnea later in life. The most important factors in ensuring adequate craniofacial and airway development in children are exclusive nasal breathing and proper oral rest posture.
2. Mentalis Strain refers to lip incompetence characterized as moderate-severe straining of the chin muscle upon mouth closure.
At rest, the lips should remain closed with a relaxed mentalis. When there is a struggle to bring or keep the lips together, a strain or dim-
pling in the chin is seen. Mentalis strain is an extra-oral indicator of altered facial growth. It can be accompanied by a gummy smile due to a long, vertical face, a retrognathic (recessed) mandible, or underdevelopment of both the maxilla and the mandible. Mentalis strain can be indicative of oral incompetence, lip ties, weakness in the lips and skeletal discrepancies or changes.
3. Tonsil Hypertrophy refers to enlarged tonsils that occupy >50% of the oropharyngeal width.
Enlarged tonsils can make the upper airway smaller, increase resistance to nasal breathing and (potentially) worsen SDB. The tonsils can be seen by asking the patient to open their mouth widely and depressing the tongue with a tongue depressor to better visualize the tonsils at the back of the throat. Tonsillar tissue is hypertrophic if it occupies more than 50% of the oropharynx upon opening. Tonsil size can be assessed using the Brodsky tonsillar grading scale. Brodsky Grade 3 (tonsils occupying 51-75% of the oropharynx) and Grade 4 (tonsils occupying greater than 75% of the oropharynx) are predictive of SDB. Since the peak period of tonsillar growth is between the ages of two and eight, that is the time when the lymphoid tissue is disproportionately large in relation to the craniofacial profile, which can be a risk factor for SDB. Tonsillar hypertrophy is associated with mouth breathing and a retrognathic mandible, which diminishes retroglossal airway space. Together with adenoid hypertrophy, it is the most common risk factor for obstructive sleep apnea (OSA) in children, as the resulting upper airway stenosis can obstruct airflow, thereby contributing to OSA development.
4. Ankyloglossia, also known as tongue tie, refers to a congenital condition that impairs tongue movement due to a restrictive lingual frenulum.
A tongue tie restricts tongue mobility when the lingual frenulum, the midline fold of fascia and overlying mucosa that lies between the ventral surface of the tongue and the floor of the mouth, is unusually short, thick, or tight. Ankyloglossia interferes with normal tongue function by preventing the tongue from resting along the palate in its entirety, thereby affecting proper development of the craniofacial structures. Alterations of the lingual frenulum may contribute to orofacial myofunctional disorders, speech (e.g., lisps) and swallowing
Each of the six determinants on the FAIREST-6 screening tool is an independent red flag for SDB, and a sign of orofacial myofunctional impairment.
impairments (a tongue thrust or poor swallowing pattern) and even SDB. Ankyloglossia has also been associated with underdevelopment of the maxilla (or narrowing of the maxillary arch) and elongation of the soft palate, resulting in an anatomically smaller upper airway with increased risk of collapsibility.
A functional classification of restricted tongue mobility is the tongue range of motion ratio (TRMR), an independent measure of tongue mobility. Objective measurements of tongue mobility using the TRMR are taken with the tongue tip extended towards the incisive papilla (TIP) and with the tongue body held against the palate in lingual-palatal suction (LPS). The incisive papilla is a cartilaginous landmark on the hard palate that is posterior to the upper front teeth and anterior to the first palatal ridge. The TIP functional measurement is obtained by instructing the patient to lift the tip of the tongue behind the upper front teeth and opening the mouth as widely as comfortably possible without discomfort or pain. The TRMR-TIP serves as a measure of the variation in functional mobility of the anterior one-third (tongue tip and apex) of the tongue. It is calculated as the ratio between maximum mouth opening with vertical tongue extension to the incisive papilla (TIP) and maximum comfortable mouth opening capacity. Measurements are rated according to the following grading scale: Grade 1 = >80% (significantly above average), Grade 2 = 50-80% (average), Grade 3 = < 50% (below average), and Grade 4 = < 25% (significantly below average). TRMRTIP Grades 3 and 4 are considered independent red flags for SDB.
The LPS functional measurement is obtained by instructing the patient to lift and suction the entire tongue to the palate (as if about to make a click sound) and opening the mouth as widely as possible without discomfort or pain. The TRMR-LPS serves as a measure of the variation in functional mobility of the posterior one-third (body) of the tongue. It is calculated as the ratio between maximum mouth opening with the tongue in lingual-palatal suction (LPS) and maximum comfortable mouth opening capacity. Measurements are rated according to the following grading scale: Grade 1 = > 60% (significantly above average), Grade 2 = 30-60% (average), Grade 3 = < 30% (below average), and Grade 4 = < 5% or unable (significantly below average). TRMR-LPS Grades 3
and 4 are considered independent red flags for SDB.
Overall, TRMR-TIP of less than 50% and TRMR-LPS of less than 30% are considered representative of moderately restricted anterior and posterior tongue mobility, respectively. It is also important to consider the influence of other clinical factors such as tension and compensation patterns when calculating these measurements.
An alternative functional classification system to the TRMR is the Kotlow free tongue measurement, an independent measure of tongue length and mobility. It is measured in millimeters as the distance from the tip of the tongue to the superior attachment of the lingual frenulum along the ventral tongue surface. Less than 16 mm is considered a clinically unacceptable value of free tongue movement and is classified as ankyloglossia.
5. Dental Wear refers to irreversible moderate-severe deterioration of dental hard tissue resulting in dentin exposure by a mechanical or chemical process rather than tooth decay.
Two etiological factors implicated individually or synergistically (Nota et al., 2022) in dental wear are bruxism, a mechanical process, and gastroesophageal reflux disease (GERD), a chemical process.
Bruxism is defined as a repetitive masticatory muscle activity characterized by clenching or grinding of the teeth and/or by bracing or thrusting of the mandible. Sleep bruxism (or bruxism that occurs during sleep) is considered a major contributor to observable dental wear. It is thought that frequent arousals during sleep may signal activation of the jaw muscles to compensate for a restricted airway. In doing so, the lower jaw slides forward, opening the collapsed airway. A consequence of the protrusive sliding movement of the lower jaw against the upper jaw is friction on the teeth, which can lead to loss of tooth structure, cracked teeth and even tooth loss. Dental wear is considered a significant risk factor for SDB if dentin, the middle layer underneath the enamel of the tooth, can be seen.
GERD is a condition resulting in troublesome symptoms and/or complications due to retrograde flow of acidic stomach contents (digestive juices or food and fluid) into the esophagus. Sleep-related GERD in children is considered a risk factor for dental wear because gastric acid can displace saliva from tooth surfaces, resulting in dental erosion and demineralization.
GERD is common in pediatric patients with digestive problems and obstructive sleep apnea.
6. Narrow Palate refers to maxillary constriction which cannot accommodate the tongue at rest due to inadequate space.
To achieve proper growth and development of the maxilla, the tongue must reside in the palate, its physiological resting position. The constant pressure generated by the tongue resting in the roof of the mouth stimulates forward and lateral jaw growth as well as the development of the nasomaxillary complex and upper airway. When the tongue posture is low (such as in mouth breathing), the maxillary arch is often restricted with a V-shaped arch, high palatal vault and increased nasal airway resistance (since the same structure that forms the roof of the oral cavity serves as the floor of the nasal cavity). Dental crowding (a discrepancy between tooth size and jaw size), other malocclusions (misalignments of the teeth) such as an open bite (when the upper and lower teeth do not come in contact when biting down) or crossbite (when the upper teeth fit inside the lower teeth while biting down), a history of dental extractions due to limited space and increased facial height (an abnormally long inferior third of the face) can all be the result of an underdeveloped airway. A narrow maxilla leads to increased nasal resistance which promotes mouth breathing and subsequently SDB.
There are several different ways to measure palatal restriction. The Supplementary Guide of the FAIREST-6 provides an up-to-date and reliable method of assessing for maxillary transverse deficiency. In children, what constitutes ‘narrow’ can be referenced to the Bogue Index, which uses the algorithm of “chronological age + 24” to indicate sufficient development of the palatal arch. This indexed algorithm is based upon Dr. E.A. Bogue’s analysis of intermolar arch width in a large population of children under six years of age from the late 19th century through the early 20th century. Dr. Bogue postulated that in the absence of an intermolar distance of 28 mm between the mesiolingual cusps (the anterior cusps situated on the lingual side of the mandibular molar teeth) of the primary second molars in children under 6 years of age, and the permanent first molars in children above the age of 6, maxillary transverse deficiency was present.
In adults, an intermolar distance of less than 32 mm between the mesiolingual cusps
of the first permanent molars is transverse deficient, which is comorbid with an SDB.
[Maxillary arch width can be estimated by assessing whether a cotton roll fits between the first permanent molars. A standard cotton roll is generally 37 mm long. A tool that can be used to measure arch length more accurately (in children or adults) is a dental caliper.]
The score on the FAIREST-6 is equal to the sum of the number of red-flag items present. Scores may range from 0 (none of the items are present) to 6 (all six of the concerning items are present). A score of 2 is associated with mildly increased risk of sleep-disturbance, a score of 4 is associated with moderately increased risk, and a score of 6 is associated with severely increased risk. Those with scores indicative of greater risk of SDB should be referred for a more comprehensive evaluation.
Each of the six determinants on the FAIREST-6 screening tool is an independent red flag for SDB, and a sign of orofacial myofunctional impairment.
A recent publication in the ASHA Leader outlines a guide for the role of the SLP in children’s airway health. The article states, “SLPs can play a critical role in the prevention of, screening for, and interdisciplinary collaboration to diagnose SDB and related airway problems. We are able to intervene before significant problems take hold and become bigger issues for children, families, schools and society. By getting to the cause of the symptoms we see, we can help improve treatment outcomes, while ensuring that all our young clients live, learn and sleep with optimal airway function, 24/7” (Archambault 2018).
SLPs can identify signs and symptoms of SDB during their comprehensive speech, language, and swallowing evaluations via oral mechanism examination (including an assessment of structure and function), questionnaires, and a thorough parent/caregiver interview. They can screen for tongue space, tongue ties and mouth breathing habits, and refer to other medical professionals for further assessment of the upper airway. They can also observe behavioral signs of a possible SDB, such as excessive fidgeting, difficulty attending to tasks and emotional outbursts. SLPs may utilize informa-
tion from standardized questionnaires and an in-depth intake to construct a comprehensive profile of the child’s sleep patterns, nighttime symptoms, and daytime functioning.
In addition to identification, SLPs can provide education to families regarding the possible impact of SDB on speech, language and swallowing. The SLP works closely with other health care professionals, including otolaryngologists, pediatricians, sleep specialists, allergists, etc. and can help develop a collaborative team to ensure the most comprehensive plan of care.
SLPs can therefore play a critical role in disease prevention in the children they serve by identifying those at highest risk for sleep disorders and other airway-related conditions via routine screening. Furthermore, since orofacial myofunctional disorders are prevalent in children displaying symptoms of SDB, we can also diagnose and treat concomitant orofacial myofunctional disorders to normalize orofacial resting posture and muscle function, which will in turn promote the development of a healthy airway.
1. Alexander, N., Boota, A., Hooks, K., & White, J. R. (2019). Rapid maxillary expansion and adenotonsillectomy in 9-year-old twins with pediatric obstructive sleep apnea syndrome: An interdisciplinary effort. Journal of Osteopathic Medicine, 119(2), 126–134. https://doi.org/10.7556/ jaoa.2019.019
2. Alhazmi, W. (2022). Mouth breathing and speech disorders: A multidisciplinary evaluation based on the etiology. Journal of Pharmacy And Bioallied Sciences, 14(5), 911. https://doi.org/10.4103/jpbs. jpbs_235_22
3. Archambault, N. (2018). Healthy Breathing, ’Round the Clock: Problems with airway functioning during sleep can hurt children’s health. And SLPs, alongside other professionals, are on the front lines of identification and intervention. The ASHA Leader, 23(2), 48–54. https://doi. org/10.1044/leader.FTR1.23022018.48
4. Becker, S., Brizuela, M., & Mendez, M. D. (2023). Ankyloglossia(Tongue-tie). In StatPearls. StatPearls Publishing. http://www.ncbi. nlm.nih.gov/books/NBK482295/
5. Bhargava, S. (2011). Diagnosis and management of common sleep problems in children. Pediatrics In Review, 32(3), 91–99. https://doi. org/10.1542/pir.32.3.91
6. Bogue, E. A. (1915). Judgment in orthodontics. International Journal of Orthodontia, 1(7), 354–356. https://doi.org/10.1016/S10723471(15)80060-1
7. Bonuck, K., Battino, R., Barresi, I., & McGrath, K. (2021). Sleep problem screening of young children by speech-language pathologists: A mixed-methods feasibility study. Autism & Developmental Language Impairments, 6, 23969415211035066. https://doi. org/10.1177/23969415211035066
8. Bonuck, K., Freeman, K., Chervin, R. D., & Xu, L. (2012). Sleep-disordered breathing in a population-based cohort: Behavioral outcomes at 4 and 7 years. Pediatrics, 129(4), e857–e865. https://doi.org/10.1542/ peds.2011-1402
9. Blunden, S., Lushington, K., Kennedy, D., Martin, J., & Dawson, D. (2000). Behavior and neurocognitive performance in children aged 5-10 years who snore compared to controls. Journal of clinical and experimental neuropsychology, 22(5), 554–568. https://doi. org/10.1076/1380-3395(200010)22:5;1-9;FT554
10. Bozzini, M. F., & Di Francesco, R. C. (2016). Managing obstructive sleep apnoea in children: the role of craniofacial morphology. Clinics (Sao Paulo, Brazil), 71(11), 664–666. https://doi.org/10.6061/clinics/2016(11)08
11. Brennan, L. C., Kirkham, F. J., & Gavlak, J. C. (2020). Sleep-disordered breathing and comorbidities: role of the upper airway and craniofacial skeleton. Nature and science of sleep, 12, 907–936. https://doi.
org/10.2147/NSS.S146608
12. Brzęcka, D., Garbacz, M., Micał, M., Zych, B., & Lewandowski, B. (2019). Diagnosis, classification and management of ankyloglossia including its influence on breastfeeding. Developmental period medicine, 23(1), 79–87. https://doi.org/10.34763/devperiodmed.20192301.7985
13. Bulanda, S., Ilczuk-Rypuła, D., Nitecka-Buchta, A., Nowak, Z., Baron, S., & Postek-Stefańska, L. (2021). Sleep Bruxism in Children: Etiology, Diagnosis, and Treatment-A Literature Review. International journal of environmental research and public health, 18(18), 9544. https://doi. org/10.3390/ijerph18189544
14. Byrd, R. S., Weitzman, M., Lanphear, N. E., & Auinger, P. (1996). Bed-wetting in US children: epidemiology and related behavior problems. Pediatrics, 98(3 Pt 1), 414–419.
15. Carter, K. A., Hathaway, N. E., & Lettieri, C. F. (2014). Common sleep disorders in children. American Family Physician, 89(5), 368–377.
16. Chervin, R. D., Archbold, K. H., Dillon, J. E., Panahi, P., Pituch, K. J., Dahl, R. E., & Guilleminault, C. (2002). Inattention, hyperactivity, and symptoms of sleep-disordered breathing. PEDIATRICS, 109(3), 449–456. https://doi.org/10.1542/peds.109.3.449
17. Corrêa, C. D. C., Cavalheiro, M. G., Maximino, L. P., & Weber, S. A. T. (2017). Obstructive sleep apnea and oral language disorders. Brazilian Journal of Otorhinolaryngology, 83(1), 98–104. https://doi. org/10.1016/j.bjorl.2016.01.017
18. Crabtree, V. M., Varni, J. W., & Gozal, D. (2004). Health-related quality of life and depressive symptoms in children with suspected sleep-disordered breathing. Sleep, 27(6), 1131–1138. https://doi.org/10.1093/ sleep/27.6.1131
19. Ebert, C. S., & Drake, A. F. (2004). The impact of sleep-disordered breathing on cognition and behavior in children: A review and meta-synthesis of the literature. Otolaryngology–Head and Neck Surgery, 131(6), 814–826. https://doi.org/10.1016/j.otohns.2004.09.017
20. Gottlieb, D. J., Chase, C., Vezina, R. M., Heeren, T. C., Corwin, M. J., Auerbach, S. H., Weese-Mayer, D. E., & Lesko, S. M. (2004). Sleep-disordered breathing symptoms are associated with poorer cognitive function in 5-year-old children. The Journal of pediatrics, 145(4), 458–464. https://doi.org/10.1016/j.jpeds.2004.05.039
21. Gozal, D., & Pope, D. W. (2001). Snoring during early childhood and academic performance at ages thirteen to fourteen years. Pediatrics, 107(6), 1394–1399. https://doi.org/10.1542/peds.107.6.1394
22. Guilleminault, C., Huang, Y. S., Monteyrol, P. J., Sato, R., Quo, S., & Lin, C. H. (2013). Critical role of myofascial reeducation in pediatric sleep-disordered breathing. Sleep Medicine, 14(6), 518–525. https:// doi.org/10.1016/j.sleep.2013.01.013
23. Harding, R., Haszard, J. J., Schaughency, E., Drummond, B., & Galland, B. (2020). Parent report of children’s sleep disordered breathing symptoms and limited academic progress in reading, writing, and math. Sleep medicine, 65, 105–112. https://doi.org/10.1016/j.sleep.2019.07.018
24. Harding, R., Schaughency, E., Haszard, J. J., Gill, A. I., Luo, R., Lobb, C., Dawes, P., & Galland, B. (2021). Sleep-related breathing problem trajectories across early childhood and academic achievement-related performance at age eight. Frontiers in Psychology, 12, 661156. https:// doi.org/10.3389/fpsyg.2021.661156
25. Heit, T., Tablizo, B. J., Salud, M., Mo, F., Kang, M., Tablizo, M. A., & Witmans, M. (2022). Craniofacial Sleep Medicine: The Important Role of Dental Providers in Detecting and Treating Sleep Disordered Breathing in Children. Children (Basel, Switzerland), 9(7), 1057. https://doi. org/10.3390/children9071057
26. Helwany, M., & Rathee, M. (2023). Anatomy, head and neck, palate. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/ NBK557817/
27. Hoang, D. A., Le, V. N. T., Nguyen, T. M., & Jagomägi, T. (2023). Orofacial dysfunction screening examinations in children with sleep-disordered breathing symptoms. The Journal of clinical pediatric dentistry, 47(4), 25–34. https://doi.org/10.22514/jocpd.2023.032
28. Honaker, S. M., Gozal, D., Bennett, J., Capdevila, O. S., & Spruyt, K. (2009a). Sleep-disordered breathing and verbal skills in school-aged community children. Developmental Neuropsychology, 34(5), 588–600. https://doi.org/10.1080/87565640903133582
29. Honaker, S. M., Gozal, D., Bennett, J., Capdevila, O. S., & Spruyt, K. (2009b). Sleep-disordered breathing and verbal skills in school-aged community children. Developmental Neuropsychology, 34(5), 588–600. https://doi.org/10.1080/87565640903133582
30. Huynh, N. T., Morton, P. D., Rompré, P. H., Papadakis, A., & Remise, C. (2011). Associations between sleep-disordered breathing symptoms and facial and dental morphometry, assessed with screening examinations. American journal of orthodontics and dentofacial orthopedics : official publication of the American Association of Orthodontists, its constituent societies, and the American Board of Orthodontics, 140(6), 762–770. https://doi.org/10.1016/j.ajodo.2011.03.023
31. Isaiah, A., Ernst, T., Cloak, C. C., Clark, D. B., & Chang, L. (2021). Associations between frontal lobe structure, parent-reported obstructive sleep disordered breathing and childhood behavior in the ABCD dataset. Nature Communications, 12(1), 2205. https://doi.org/10.1038/ s41467-021-22534-0
32. Isono, S., Shimada, A., Utsugi, M., Konno, A., & Nishino, T. (1998). Comparison of static mechanical properties of the passive pharynx between normal children and children with sleep-disordered breathing. American journal of respiratory and critical care medicine, 157(4 Pt 1), 1204–1212.
33. Kaditis, A. G., Alonso Alvarez, M. L., Boudewyns, A., Alexopoulos, E. I., Ersu, R., Joosten, K., Larramona, H., Miano, S., Narang, I., Trang, H., Tsaoussoglou, M., Vandenbussche, N., Villa, M. P., Van Waardenburg, D., Weber, S., & Verhulst, S. (2016). Obstructive sleep disordered breathing in 2- to 18-year-old children: Diagnosis and management. European Respiratory Journal, 47(1), 69–94. https://doi. org/10.1183/13993003.00385-2015
34. Kazakova, T., Danoff, R., Esteva, I., & Shchurin, A. (2023). Gastro-esophageal reflux disease in primary care practice: A narrative review. Annals of Esophagus, 6, 25–25. https://doi.org/10.21037/aoe-21-62
35. Kumar, D. S., Valenzuela, D., Kozak, F. K., Ludemann, J. P., Moxham, J. P., Lea, J., & Chadha, N. K. (2014). The reliability of clinical tonsil size grading in children. JAMA otolaryngology-- head & neck surgery, 140(11), 1034–1037. https://doi.org/10.1001/jamaoto.2014.2338
36. Lam, D. J., Jensen, C. C., Mueller, B. A., Starr, J. R., Cunningham, M. L., & Weaver, E. M. (2010). Pediatric sleep apnea and craniofacial anomalies: a population-based case-control study. The Laryngoscope, 120(10), 2098–2105. https://doi.org/10.1002/lary.21093
37. Lau, E. Y., Choi, E. W., Lai, E. S., Lau, K. N., Au, C. T., Yung, W. H., & Li, A. M. (2015). Working memory impairment and its associated sleep-related respiratory parameters in children with obstructive sleep apnea. Sleep medicine, 16(9), 1109–1115. https://doi.org/10.1016/j. sleep.2015.04.025
38. Lin, L., Zhao, T., Qin, D., Hua, F., & He, H. (2022). The impact of mouth breathing on dentofacial development: A concise review. Frontiers in Public Health, 10, 929165. https://doi.org/10.3389/fpubh.2022.929165
39. Lobbezoo, F., Ahlberg, J., Raphael, K. G., Wetselaar, P., Glaros, A. G., Kato, T., Santiago, V., Winocur, E., De Laat, A., De Leeuw, R., Koyano, K., Lavigne, G. J., Svensson, P., & Manfredini, D. (2018). International consensus on the assessment of bruxism: Report of a work in progress. Journal of oral rehabilitation, 45(11), 837–844. https://doi.org/10.1111/ joor.12663
40. Luo, R., Galland, B. C., Gill, A. I., Dawes, P., & Schaughency, E. (2018). Habitual snoring at age 3 years: Links with parent-rated remembering in daily life and academic achievement at age 7 years. Journal of Developmental & Behavioral Pediatrics, 39(2), 144–153. https://doi. org/10.1097/DBP.0000000000000524
41. Luo, R., Harding, R., Galland, B., Sellbom, M., Gill, A., & Schaughency, E. (2019). Relations between risk for sleep-disordered breathing, cognitive and executive functioning, and academic performance in six-yearolds. Early Education and Development, 30(7), 947–970. https://doi.org /10.1080/10409289.2019.1593075
42. Marino, A., Malagnino, I., Ranieri, R., Villa, M. P., & Malagola, C. (2009). Craniofacial morphology in preschool children with obstructive sleep apnoea syndrome. European journal of paediatric dentistry, 10(4), 181–184.
43. Menzies, B., Teng, A., Burns, M., & Lah, S. (2022). Neurocognitive outcomes of children with sleep disordered breathing: A systematic review with meta-analysis. Sleep Medicine Reviews, 63, 101629. https://doi. org/10.1016/j.smrv.2022.101629
44. Mills, N., Geddes, D. T., Amirapu, S., & Mirjalili, S. A. (2020). Understanding the lingual frenulum: Histological structure, tissue composition, and implications for tongue tie surgery. International Journal of Otolaryngology, 2020, 1820978. https://doi.org/10.1155/2020/1820978
45. Moeller, J. L., Paskay, L. C., & Gelb, M. L. (2014). Myofunctional therapy. Sleep Medicine Clinics, 9(2), 235–243. https://doi.org/10.1016/j. jsmc.2014.03.002
46. Mohammed, D., Park, V., Bogaardt, H., & Docking, K. (2021). The impact of childhood obstructive sleep apnea on speech and oral language development: A systematic review. Sleep Medicine, 81, 144–153. https://doi.org/10.1016/j.sleep.2021.02.015
47. Nota, A., Pittari, L., Paggi, M., Abati, S., & Tecco, S. (2022). Correlation between Bruxism and Gastroesophageal Reflux Disorder and Their Effects on Tooth Wear. A Systematic Review. Journal of Clinical Medicine, 11(4), 1107. https://doi.org/10.3390/jcm11041107
48. O’Brien, L. M., Mervis, C. B., Holbrook, C. R., Bruner, J. L., Klaus, C. J., Rutherford, J., Raffield, T. J., & Gozal, D. (2004). Neurobehavioral implications of habitual snoring in children. Pediatrics, 114(1), 44–49. https://doi.org/10.1542/peds.114.1.44
49. Oh, J. S., Zaghi, S., Peterson, C., Law, C. S., Silva, D., & Yoon, A. J. (2021). Determinants of sleep-disordered breathing during the mixed dentition: Development of a functional airway evaluation screening tool(FAIREST-6). Pediatric Dentistry, 43(4), 262–272.
50. Owens, J. A., Spirito, A., McGUINN, M., & Nobile, C. (2000). Sleep habits and sleep disturbance in elementary school-aged children: Journal of Developmental & Behavioral Pediatrics, 21(1), 27–36. https://doi. org/10.1097/00004703-200002000-00005
51. Pacheco, M. C., Fiorott, B. S., Finck, N. S., & Araújo, M. T. (2015).
Craniofacial changes and symptoms of sleep-disordered breathing in healthy children. Dental press journal of orthodontics, 20(3), 80–87. https://doi.org/10.1590/2176-9451.20.3.080-087.oar
52. Ranjitkar, S., Kaidonis, J. A., & Smales, R. J. (2012). Gastroesophageal reflux disease and tooth erosion. International Journal of Dentistry, 2012, 1–10. https://doi.org/10.1155/2012/479850
53. Shirke, S. R., & Katre, A. N. (2023). Association of Sleep-Disordered Breathing and Developing Malocclusion in Children: A Cross-Sectional Study. Cureus, 15(6), e39813. https://doi.org/10.7759/cureus.39813
54. Singh, H., Chandwani, B., & Finkelman, M. (2011). Sleep Bruxism Related Tooth Wear as a Clinical Marker for Obstructive Sleep Apnea/Hypopnea Syndrome in Children [Master’s thesis, Tufts University School of Dental Medicine]. https://dl.tufts.edu/concern/pdfs/rn301c544
55. Svingos, A., Greif, S., Bailey, B., & Heaton, S. (2018). The Relationship Between Sleep and Cognition in Children Referred for Neuropsychological Evaluation: A Latent Modeling Approach. Children (Basel, Switzerland), 5(3), 33. https://doi.org/10.3390/children5030033
56. Tamkin J. (2020). Impact of airway dysfunction on dental health. Bioinformation, 16(1), 26–29. https://doi.org/10.6026/97320630016026
57. Thomas, W. (1966). A statistical assessment of tooth sizes, arrangement and arch form obtained from dental casts preparatory to the development of computer programming of malocclusions. Master’s Theses. https://ecommons.luc.edu/luc_theses/2068
58. Urschitz, M. S., Eitner, S., Guenther, A., Eggebrecht, E., Wolff, J., Urschitz-Duprat, P. M., Schlaud, M., & Poets, C. F. (2004). Habitual snoring, intermittent hypoxia, and impaired behavior in primary school children. Pediatrics, 114(4), 1041–1048. https://doi.org/10.1542/ peds.2003-1145-L
59. Wang, R., Zhu, Y., Chen, C., Han, Y., & Zhou, H. (2022). Tooth Wear and Tribological Investigations in Dentistry. Applied bionics and biomechanics, 2022, 2861197. https://doi.org/10.1155/2022/2861197
60. Warnier, M., Piron, L., Morsomme, D., & Maillart, C. (2023). Assessment of mouth breathing by Speech-Language Pathologists: an international Delphi consensus. CoDAS, 35(3), e20220065. https://doi. org/10.1590/2317-1782/20232022065
61. Yoon, A., Zaghi, S., Weitzman, R., Ha, S., Law, C. S., Guilleminault, C., & Liu, S. Y. C. (2017). Toward a functional definition of ankyloglossia: validating current grading scales for lingual frenulum length and tongue mobility in 1052 subjects. Sleep & breathing = Schlaf & Atmung, 21(3), 767–775. https://doi.org/10.1007/s11325-016-1452-7
62. Zaghi, S., Peterson, C., Shamtoob, S., Fung, B., Kwok-keung Ng, D., Jagomagi, T., Archambault, N., O’Connor, B., Winslow, K., Peeran, Z., Lano, M., Murdock, J., Valcu-Pinkerton, S., & Morrissey, L. (2020). Assessment of nasal breathing using lip taping: A simple and effective screening tool. International Journal of Otorhinolaryngology, 6(1), 10. https://doi.org/10.11648/j.ijo.20200601.13
63. Zaghi, S., Shamtoob, S., Peterson, C., Christianson, L., Valcu-Pinkerton, S., Peeran, Z., Fung, B., Kwok-Keung Ng, D., Jagomagi, T., Archambault, N., O’Connor, B., Winslow, K., Lano, M., Murdock, J., Morrissey, L., & Yoon, A. (2021). Assessment of posterior tongue mobility using lingual-palatal suction: Progress towards a functional definition of ankyloglossia. Journal of oral rehabilitation, 48(6), 692–700. https://doi. org/10.1111/joor.13144
64. Xiao, L., Su, S., Liang, J., Jiang, Y., Shu, Y., & Ding, L. (2022). Analysis of the Risk Factors Associated With Obstructive Sleep Apnea Syndrome in Chinese Children. Frontiers in pediatrics, 10, 900216. https://doi. org/10.3389/fped.2022.900216
65. Zhang, W., & Si, L. Y. (2012). Obstructive sleep apnea syndrome (OSAS) and hypertension: pathogenic mechanisms and possible therapeutic approaches. Upsala journal of medical sciences, 117(4), 370–382. https:// doi.org/10.3109/03009734.2012.707253
66. Zettergren-Wijk, L., Forsberg, C. M., & Linder-Aronson, S. (2006). Changes in dentofacial morphology after adeno-/tonsillectomy in young children with obstructive sleep apnoea--a 5-year follow-up study. European journal of orthodontics, 28(4), 319–326. https://doi.org/10.1093/ ejo/cji119
67. Ziliotto, K. N., dos Santos, M. F., Monteiro, V. G., Pradella-Hallinan, M., Moreira, G. A., Pereira, L. D., Weckx, L. L., Fujita, R. R., & Pizarro, G. U. (2006). Auditory processing assessment in children with obstructive sleep apnea syndrome. Brazilian journal of otorhinolaryngology, 72(3), 321–327. https://doi.org/10.1016/s1808-8694(15)30963-0
Similar content was also presented as an iPoster at the American Speech-Language-Hearing Association Annual Convention, November 16-18, 2023, Boston, MA.
Acknowledgment: We would like to express our gratitude to Dr. Soroush Zaghi and his colleagues for granting us permission to share the latest version of the FAIREST-6 airway screening tool.
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 8 CE credits for only $149 by visiting https://dentalsleeppractice.com/subscribe/.
AGD Code: 730
Date Published: May 1, 2024 Course Expires: May 1, 2027
Legal disclaimer: Course expires 3 years after publication date. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
n To receive credit: Go online to dentalsleeppractice.com/continuing-education/, click on the article, then click on the take quiz button, and enter your test answers
To provide feedback on this article and CE, email us at education@medmarkmedia.com.
1. FAIREST stands for _____________.
a. Free Airway Impairment Resource Estimating Size of the Throat
b. Functional Airway Evaluation Screening Tool
c. First Assessment Intending to Recruit Every Snorer for Testing
d. Fun And Interesting Result of Every Speechie’s Training
2. Speech-Language Pathologists are involved ______________.
a. When other therapies are not successful
b. Only when covered by medical insurance
c. Early in the assessment and treatment of communication and swallowing difficulties in the pediatric population
d. Side by side with surgeons to ensure proper tethered tissue removal
3. Mouth Breathing can be best objectively assessed by ____________.
a. Asking the patient if they ever breathe through their mouth
b. Looking for signs such as chapped lips or red gums
c. Asking the parent to bring in video evidence
d. Having the patient keep their lips closed while breathing through their nose for three minutes
4. Mentalis Strain is ______________.
a. Difficulty remembering clinical instructions
b. Associated with Class 2, Div2 occlusion
c. Lip incompetence with strain of chin muscles upon mouth closure
d. Corrected by jaw repositioning
5. Tonsil Hypertrophy refers to ______________.
a. Tissue that can be easily seen with mouth opening
b. Troubles that patients report
c. A condition otherwise known as “Waldeyer’s Ringing”
d. Enlargements of tissue occupying >50% of the oropharyngeal width
6. Ankyloglossia, also known as tongue-tie, ______________.
a. Restricts tongue mobility so the patient cannot lick their lips
b. Should always be corrected by age 10
c. Is graded by comparing the amount of vertical jaw opening to tongue mobility and also by functional measurements of tongue positioning
d. Is a subject of wide consensus agreement in dentistry and medicine
7. Dental Wear is important to assess because ______________.
a. It is a cardinal sign of weakening of the enamel surface from caries
b. May be a combination of parafunction and gastroesophageal reflux disease
c. Baby teeth are smaller and may wear out faster
d. Only happens during deep sleep so lack of wear means poor sleep quality
8. Narrow Palate is a maxillary constriction that can be measured _______.
a. By the Bogue Index
b. By a cotton roll in adults
c. By a dental caliper
d. Any or all of these answers, as long as it is objective and recorded
9. Advantages of working with Speech-Language Pathologists include ______________.
a. They often help address many of the root cause(s) identified on the Fairest-6
b. They do not use up insurance benefit resources
c. They are adept at observing behavioral signs of possible sleep disordered breathing
d. A and C; B should not be a limiting factor when the lifetime health of a child is at stake
10. The single most important factors in ensuring adequate craniofacial and airway development in children are ______________.
a. Non extraction orthodontics and whole-food diets
b. Breast feeding and baby-led weaning
c. Exclusive nasal breathing and proper oral rest posture
d. Avoidance of allergens and thumb sucking habit







The use of cannabis products for sleep disorders has gained popularity, but there is limited scientific evidence to support their efficacy. Discontinuation of cannabis use has also been linked to significant sleep-related symptoms that can increase the likelihood of relapse.
Medical cannabis raises several questions:
1. Does it work, and for which sleep related conditions?
2. Is it safe?
3. Can it be prescribed?
4. What lies ahead?
Understanding the distinctions between Cannabis, Marijuana, and Cannabinoids is important. Cannabis refers to the plant itself, which can be classified into different strains such as Indica and Sativa. Marijuana refers to the dried leaves or flowers of the cannabis plant. Compounds within the plant can be classified as Phyto cannabinoids (such as THC, CBD, CBN…etc) and non-cannabinoids (including terpenes, phenolic compounds, and alkaloids). Cannabinoid varieties include endocannabinoids (Anandamide, 2-AG…etc), Phyto cannabinoids and Synthetic cannabinoids (Dronabinol, Nabilone).
In the United States, ∆9-THC (the psychoactive cannabinoid in cannabis) is classified as a schedule I drug. However, recreational cannabis use has been legalized in 24 states and the District of Columbia, while medical
cannabis use is permitted and/or decriminalized in 37 states.
The Hemp Farming Act of 2018 legalized industrial hemp with a ∆9-THC concentration of less than 0.3%. However, the legal landscape surrounding CBD is complex. CBD derived from cannabis plants with more than 0.3% THC is considered illegal by the DEA. The FDA has not approved CBD derived from hemp plants for medicinal or food and drink products. Epidiolex™, an FDA-approved prescription CBD, is the only drug classified as a schedule V substance, containing less than 0.1% THC.
Cannabis products for sleep disorders are on the rise but scientific evidence supporting their effectiveness is limited. The legal status of cannabis and CBD adds further complexity. Caution is necessary as research continues and regulations evolve. The FDA warns consumers that these products are not approved for diagnosing, preventing, or treating diseases, although CBD and THC remain widely available.
A survey of medical cannabis users found the top conditions for using medical cannabis were anxiety, pain, stress, and insomnia.1
Three systematic reviews have examined the effectiveness of cannabis in aiding sleep. The first review concluded that there is insufficient evidence to support the routine clinical use of cannabinoid therapies for any sleep disorder.2
A meta-analysis published in JAMA found potential benefits of cannabinoids for chemotherapy-induced nausea, weight loss in HIV or cancer patients, and spasticity in certain conditions. Positive results were observed for sleep improvement in patients with fibromyalgia using synthetic cannabinoids. However, sleep was not the primary focus of these studies.3
A recent scoping review analyzed studies from the past five decades and found that cannabis improved sleep in approximately 21% of the studies, worsened sleep in 48%, had mixed results in 14%, and had no impact in 17%. These studies collectively provide limited evidence supporting the use of cannabis for sleep.4
Cannabis has been shown to increase stage 3 non-rapid eye movement sleep in some studies, but not consistently. The effects on rapid eye movement sleep vary as well. Studies have reported a faster onset of sleep, subjective decrease in insomnia and nightmares, and improved sleep quality, but these benefits tend to decline with chronic cannabis use.5,6,7
Regular medical cannabis use may be associated with a slight increase in middleof-the-night awakenings. Regular cannabis use is more likely to be linked to short sleep or long sleep, and heavy cannabis users are even more likely to experience extreme sleep durations.8,9
One randomized controlled trial found no improvement in sleep with various combinations of CBD/CBN, two compounds found in cannabis.10
Insomnia has been studied extensively. Two recent trials showed that THC improved sleep in patients with insomnia but had flaws in study design and lacked objective measures of improvement.11,12
Overall, the evidence for cannabis helping with insomnia is weak. Negative studies and inconsistent positive findings suggest caution when considering cannabis as a treatment for this sleep disorder.
Cannabis has been explored for excessive daytime sleepiness. While some studies have shown that cannabinoids promote wakefulness, cannabis products are also associated with significant daytime sedation.13
Research on cannabis-based treatments for sleep apnea has yielded mixed results. Synthetic THC has shown a slight decrease in sleep apnea severity, but the clinical significance is questionable.14,15 AASM issued a statement opposing the use of cannabis for treatment of OSA.
Some case series have shown promise in CBD treatment for rapid eye movement sleep behavior disorder16 but an RCT showed no difference.17 Military veterans are increasingly using cannabinoids to treat symptoms of PTSD including nightmares. A study found that treatment with Nabilone produced a reduction in nightmare presence and intensity and increased hours of sleep per night.18 A case series of 6 patients showed 100% improvement restless legs syndrome with cannabis but there have been no RCTs.19
From an addiction standpoint, medical cannabis use can be more problematic than recreational cannabis uses because one of the main risk factors to going on to developing cannabis use disorder or cannabis addiction is regular use. People who use it for medical purposes use it much more regularly and in larger quantities than those who are recreational users alone.20 Other risks include tolerance and withdrawal which increases in sleep disturbances.13,23 Then these sleep disturbances led to relapse back to cannabis.13 Cannabis use, whether for medical or recreational purposes, has been associated with various adverse health effects, including addiction to marijuana and other substances,

While there is ongoing interest in the potential benefits of cannabis for sleep-related issues, the scientific evidence remains inconclusive.
Dr. Jamila Battle, triple board certified in family medicine, sleep, and addiction, is the creator of Reboot Repair Rebirth®. This innovative model helps victims who have suffered trauma truly forgive themselves. The ability of the body, mind and spirit to repair is underutilized. Furthermore, uninterrupted sleep is at the foundation of repair and restoration. She focuses on the relationship between adverse childhood experiences, toxic stress and the leading causes of morbidity, mortality, and disability to include chronic physical health problems, sleep disorders, depression, obesity, and drug abuse. Her passion is to not only serve the emotional, physical, and spiritual needs of her clients but also motivate others to identify unique talents they possess and succeed despite adversity and struggle. She volunteers with at risk families and enjoys not only health and fitness but also spending time with her husband and three children. She is a consultant physician for Dr. Jamila Battle & Associates, PA.

motor vehicle accidents, cardiovascular complications, chronic bronchitis, and decreased lifetime achievement. Cannabis use has also been linked to the development of mental health conditions such as schizophrenia, depression, and anxiety. Long-term or heavy cannabis use has been associated with a low risk of lung cancer and other cancers.13
Cannabis products can lead to increased daytime sleepiness, especially with higher THC doses.21 A meta-analysis revealed an increased risk of fatal motor vehicle collisions with THC use. Sleep difficulties during cannabis abstinence can contribute to relapse in some individuals.22
Cannabis can also interact with certain medications, affecting their serum concentrations. Delta-9 THC decreases the serum concentrations of medications such as clozapine, duloxetine, naproxen, cyclobenzaprine, olanzapine, haloperidol, and chlorpromazine. CBD is a competitive inhibitor of CYP2C9 and CYP3A4.13
Consultation with healthcare professionals and consideration of alternative sleep management strategies is important before using cannabis products for sleep.
In recent years, there has been a surge in the availability and promotion of cannabis products as sleep aids. However, it is crucial to examine their efficacy and potential risks. While the legal debate surrounding cannabis may not directly impact its addictive properties, healthcare professionals should counsel patients about the potential risks involved.
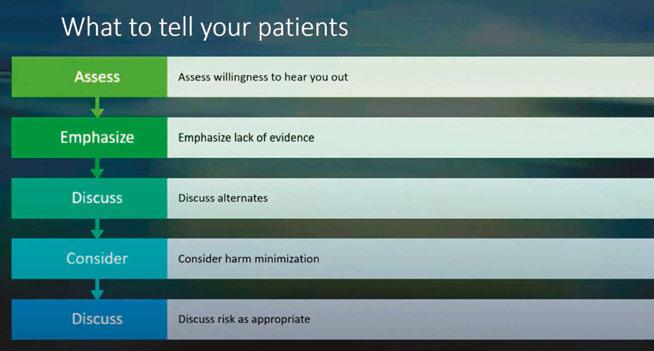
When considering the use of cannabis products for sleep, clinicians should have open discussions with patients. It is important to emphasize the lack of scientific evidence supporting the efficacy of these products for sleep-related conditions. Alternative treatments and potential risks should be thoroughly discussed. Harm minimization strategies may be considered in certain cases.13
Although some studies have reported modest improvements in subjective sleep when cannabis products were used to manage chronic pain, evidence for significant improvements in sleep disorders like insomnia and restless leg syndrome is unconvincing. Cannabis may show promise for nightmares in a military population but there is limited evidence for RBD. Dronabinol, a synthetic form of THC, has shown a slight decrease in the severity of sleep apnea, but the clinical significance is questionable. Withdrawal from cannabis use can lead to significant sleep disruption and a higher risk of relapse.
The effects of THC and CDB depend on many factors including plant species, method of preparation, and how it is consumed. Significant variations in cannabinoids available on the market present challenges in studying their effects on sleep. The consensus indicates a lack of evidence supporting the use of over-the-counter CBD products for sleep improvement. Drug interactions and contamination with psychoactive THC are concerns that should not be overlooked. Dependence and other side effects should be carefully considered.
Further research is needed to explore the potential benefits and risks of cannabis products for sleep. An evidence-based approach and prioritizing patient safety are crucial in navigating this emerging field.
Critically evaluating the role of cannabis products in managing sleep-related conditions is essential. By considering the limited evidence and potential risks, healthcare professionals can guide informed decision-making processes for their patients’ sleep needs. References available online.



Sleep, a fundamental aspect of health and well-being,1 exhibits unique characteristics and challenges in women, influenced by biological, hormonal, and life cycle factors. These distinctions not only shape sleep patterns but also affect the presentation and diagnosis of sleep disorders, including Obstructive Sleep Apnea (OSA). This article delves into the unique sleep characteristics in women and how OSA presents differently in females compared to males, shedding light on the necessity for tailored diagnostic and therapeutic approaches.
Gender differences in sleep quality correlate with the onset of puberty.2 The female reproductive hormones, estrogen and progesterone, play crucial roles in regulating sleep. Their levels fluctuate throughout the menstrual cycle, pregnancy, and menopause, impacting sleep quality and patterns. For instance, during the luteal phase of the menstrual cycle, progesterone levels peak, increasing core body temperature at night, which contributes to more daytime sleepiness and more awakenings during the night.3 Similarly, during pregnancy, especially in the third trimester, sleep can be significantly disrupted due to hormonal changes, physical discomfort, restless legs (RLS), and anxiety.4
Menopause is a pivotal period in a woman’s life, marked by significant hormonal changes that can profoundly impact sleep. The decline in estrogen and progesterone
levels lead to vasomotor symptoms (hot flashes) which can contribute to sleep disturbances, insomnia, increased sleep latency, and decreased sleep efficiency. Women may find an uptick in RLS symptoms, particularly if their transition leaves them with heavier periods and resultant loss of iron.5 The protective effect of these hormones on the upper airway muscle tone diminishes, leading to an increased likelihood of airway obstruction during sleep (OSA).6
OSA in women often presents with symptoms that differ from the classic signs observed in men, across the lifespan. While loud snoring and prolonged apneas are hallmark symptoms in men, women may exhibit more subtle signs such as fatigue, insomnia, morning headaches, mood disturbances, and unrefreshing sleep. This difference in symptomatology can lead to underdiagnosis or misdiagnosis of OSA in women, as their symptoms might be attributed to stress, anxiety, or depression instead.7
Women diagnosed with OSA often present with what appears to be a less severe variant of the condition when evaluated using the Apnea-Hypopnea Index (AHI), a tool for assessing sleep apnea severity. Nonetheless, this perceived mildness does not imply a minimal effect on their overall health and well-being. In fact, women experience brief apneic incidents but face more intense drops in oxygen levels during these moments. They
also show a reduced frequency of OSA when lying on their back and a concentration of apneic events during REM sleep phases.8–10 Women, especially those in the premenopausal or perimenopausal stages, often exhibit a pattern of frequent increases in respiratory effort that end with brief awakenings. Unlike typical OSA, these do not involve as significant collapse of the airway, hypoventilation, or oxygen desaturations, a condition known as “upper airway resistance syndrome” (UARS).11 These less obvious disturbances might not affect the Apnea-Hypopnea Index (AHI) scores, suggesting normal sleep. However, evaluating the Respiratory Disturbance Index (RDI) may offer a more comprehensive assessment of sleep disruption in women.
The unique characteristics of sleep and OSA in women pose diagnostic challenges. For example, the Centers for Medicare and Medicaid Services (CMS) policy for local coverage determination (LCD) of both oral appliances as well as Positive Airway Pressure (PAP) devices for treatment of OSA states: “The respiratory disturbance index (RDI) is defined as the average number of apneas plus hypopneas per hour of recording without the use of a positive airway pressure device. For purposes of this policy, respiratory effort related arousals (RERAs) are not included in the calculation of the RDI.”12,13 There is an enormous potential to miss the diagnosis of OSA in women who tend to have more RERAs and a lower AHI. Since home sleep apnea testing (HSATs) are both more economical and more convenient, home testing has become the new norm for evaluating OSA. However, particularly with more mild disease, there is the potential to underestimate OSA severity.14 This is why the clinical presentation is so key in women. Do not stop at HSAT when there is a clinical suspicion. Crossfunctional collaboration between medical sleep specialist and dental sleep specialist is paramount to protecting the sleep health of women.
Recognizing and addressing the unique aspects of sleep in women are crucial steps towards personalized medicine. Healthcare providers should be aware of the gender differences in sleep disorders and consider
these factors when diagnosing and treating female patients. Moreover, women should be encouraged to report sleep-related issues and seek professional help, emphasizing that sleep disturbances are not merely stress-related but could be indicative of a sleep disorder. Ladies, we do not need to be stoic about our sleep!
Sleep in women is influenced by a myriad of factors, including hormonal changes that can lead to unique sleep characteristics and distinct presentations of disorders such as OSA. Understanding these differences is essential for providing appropriate care and improving the overall health and well-being of women. As research continues to evolve, it is hoped that more gender-specific approaches in sleep medicine will emerge, offering more effective diagnosis and treatment options for sleep disorders in women.
1. Chow CM. Sleep and Wellbeing, Now and in the Future. Int J Environ Res Public Health. 2020 Apr 22;17(8):2883.
2. Sadeh A, Dahl RE, Shahar G, et al. Sleep and the transition to adolescence: a longitudinal study. Sleep. 2009 Dec;32(12):1602-9.
3. Jehan S, Auguste E, Hussain M, et al. Sleep and Premenstrual Syndrome. J Sleep Med Disord. 2016;3(5):1061.
4. Po Fung Wong, Rebecca D’Cruz, Alanna Hare. Sleep disorders in pregnancy. Breathe. 2022;18(2):220004. doi:10.1183/20734735.0004-2022
5. Hensley J. Menopause and RLS. Restless Legs Syndrome Foundation Blog. (2020) https://rlsfoundation.blogspot. com/2020/09/menopause-and-rls.html Accessed 09 March 2024.
6. Tandon VR, Sharma S, Mahajan A, et al. Menopause and Sleep Disorders. J Midlife Health. 2022 JanMar;13(1):26-33.
7. Pataka A, Kotoulas S, Kalamaras G, et al. Gender Differences in Obstructive Sleep Apnea: The Value of Sleep Questionnaires with a Separate Analysis of Cardiovascular Patients. J Clin Med. 2020 Jan 3;9(1):130.
8. Kapsimalis F, Kryger MH. Gender and obstructive sleep apnea syndrome, part 1: clinical features. Sleep 2002; 25: 412–419.
9. Kulkas A, Duce B, Leppänen T, et al. Gender differences in severity of desaturation events following hypopnea and obstructive apnea events in adults during sleep. Physiol Meas 2017; 38: 1490–1502.
10. Maria R. Bonsignore, Tarja Saaresranta, Renata L. Riha. Sex differences in obstructive sleep apnoea. Eur Respir Rev. 2019;28(154):190030. doi:10.1183/16000617.0030-2019
11. Guilleminault, C., & Chowdhuri, S. (2000). Upper airway resistance syndrome is a distinct syndrome. American journal of respiratory and critical care medicine, 161(5), 1412-1413.
12. Local Coverage Determination (LCD). Positive Airway Pressure (PAP) Devices for the Treatment of Obstructive Sleep Apnea. https://www.cms.gov/medicare-coverage-database/view/lcd.aspx?LCDId=33718 Accessed 09 March 2024.
13. Local Coverage Determination (LCD). Oral Appliances for Obstructive Sleep Apnea. https://www.cms.gov/ medicare-coverage-database/view/lcd.aspx?LCDId=33611. Accessed 09 march 2024.
14. Bianchi MT, Goparaju B. Potential Underestimation of Sleep Apnea Severity by At-Home Kits: Rescoring In-Laboratory Polysomnography Without Sleep Staging. J Clin Sleep Med. 2017 Apr 15;13(4):551-555.

Alison S. Kole, MD, MPH, FCCP, FAASM, is Board Certified in Sleep, Pulmonary, and Critical Care Medicine. She is currently host of the Sleep Is My Waking Passion podcast, Medical Director of the Oak Health Center Sleep Telemedicine program, and Director of Medical Affairs and Strategy for TotalCME. Dr. Kole believes that empowerment and advocacy through patient and provider education and interdisciplinary collaboration are key components to improving Sleep health globally.

Tufts University School of Dental Medicine (TUSDM) has long stood at the forefront of dental education, pioneering research, and community service. With a mission deeply rooted in the belief that access to quality dental care is a cornerstone of global health, TUSDM is now taking significant strides to spread dental education globally, particularly in the specialized areas of obstructive sleep apnea, craniofacial pain, and temporomandibular joint disorders (TMD).
This ambitious endeavor aims to train the world’s dentists here in Boston and around the globe to transform the landscape of dental medicine. It’s an opportunity for dentists worldwide to expand their practices to reach more patients.
Obstructive sleep apnea (OSA), craniofacial pain, and TMD represent a trio of conditions that not only affect oral health but also have far-reaching implications on overall well-being. OSA, a condition marked by repeated breathing interruptions during sleep, has been linked to cardiovascular disease, type 2 diabetes, and stroke.
Globally, OSA affects a significant portion of the adult population with some research signaling nearly 1 billion adults between the ages of 30 and 69 suffering from mild to severe OSA. In that same age range, about 425 million may have moderate to severe OSA. These estimations highlight the widespread nature of the condition and underscore the need for effective diagnostic and treatment strategies worldwide.
Mayoor Patel, DDS, MS, D.ABDSM, DABOP, DABCP, DABCDSM, DAIPM, RPSGT, FAAOP, FICCMO, FAACP, FAGD, FPFA, received his dental degree from the University of Tennessee in 1994 and then went on to complete a one-year residency in Advanced Education in General Dentistry. He also earned a Masters in Science from Tufts University in 2011. Dr. Patel served as an Adjunct Clinical Instructor at the Craniofacial Pain Center at Tufts Dental School from 2011-2014 and presently again. Since 2003, he has limited his practice, Craniofacial Pain & Dental Sleep Medicine Center of Georgia, to the treatment of TMJ Disorders, Headaches, Facial Pain, Sleep Apnea, and Snoring.
Terry Bennett, DMD, DABCP, D.ABDSM, has had more than 40 years of experience in private dental practice. Dr. Bennett graduated from the University of Louisville School of Dentistry with his dental degree in 1977. For the past three decades, Dr. Bennett has limited his practice, The Tulsa Orofacial Pain & Sleep Disorders Clinic, to the conservative treatment of temporomandibular joint dysfunction (TMD) and sleep apnea.
Similarly, craniofacial pain and TMD can lead to chronic discomfort, impairing quality of life and overall health. The numbers affected speaks to the urgency of increasing education and treatment options in dental offices everywhere. Research estimates the prevalence of TMD to be between 5% and 12% around the world, a global burden that varies by age, gender, and other demographic factors. It presents a considerable public health issue due to its impact on quality of life and association with other craniofacial pain conditions.
Beyond the global impact of TMD, craniofacial pain and sleep apnea on their own, there is also a connection that needs to be addressed. In a study published in the International Journal of General Medicine, researchers found individuals with sleep disorders had a higher risk for TMD than those who did not have a sleep disorder. This places even more emphasis on the need for dentists to offer treatments for both TMD and sleep apnea. And it starts with education.
Recognizing the critical need for specialized training in these areas, TUSDM has developed comprehensive programs aimed at equipping dental professionals with the knowledge and skills necessary to diagnose, treat, and manage these complex conditions. By integrating cutting-edge research, clinical expertise, and a multidisciplinary approach, TUSDM’s curriculum is uniquely designed to address this global challenge. Through partnerships with dental schools and health organizations around the world, TUSDM is extending its reach, offering hands-on training sessions that are accessible to dental professionals regardless of location. This will create a worldwide network of trained dental professionals who can make a difference in their communities.
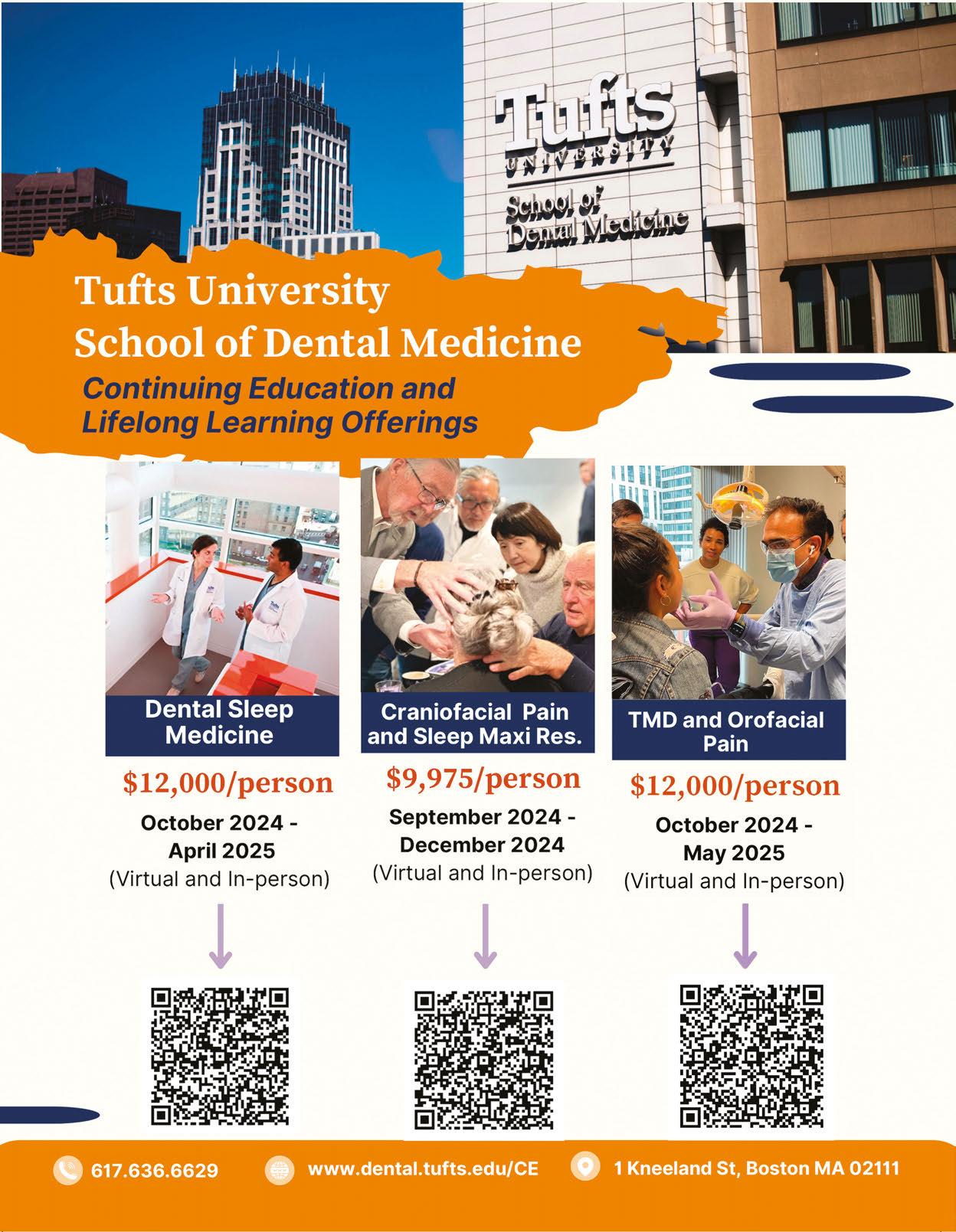
The landscape of billing for oral appliances in dental sleep medicine is constantly shifting. As a dental office delving into the intricacies of dental sleep medicine billing, you've likely encountered the buzz surrounding the new
“K” code, K1027. In this article, we'll embark on a journey through oral appliance billing, and discuss some of the updates Nierman Practice Management has found.
For years, we’ve relied on E0486, the established code for custom oral appliances. But now, enter stage left: K1027, the new code on the block. What sets this code apart? Well, it's essentially E0486's cousin, minus the mechanical hinge.
• E0486: Oral device/appliance used to reduce upper airway collapsibility, adjustable or non-adjustable, custom fabricated, includes fitting and adjustment
• K1027: Oral device/appliance used to reduce upper airway collapsibility, without fixed mechanical hinge, custom fabricated, includes fitting and adjustment
In 2012, Medicare added written criteria for a hinge relating to E0486 which has sparked considerable discussion about reimbursement. This stipulation was puzzling to many dental professionals as there was no evidence suggesting that a device with a mechanical hinge outperformed one without. The emergence of two codes for oral appliance therapy stemmed from the inability to amend the hinge criteria associated with E0486. As a result, the creation of a new code, K1027, tailored specifically for nonhinged appliances, was pursued as an alternative solution with the hope that it will pave the way for a broader range of choices for reimbursable appliances. Now, you may find yourself wondering, “Why didn't they just amend the criteria?” It’s a valid question, and the answer lies in the intricacies of bureaucratic processes
and the sometimes-perplexing decisions made by regulatory bodies.
The connection between a hinge and reimbursement for the E0486 started with PDAC. PDAC stands for Pricing, Data Analysis, and Coding. It's an organization contracted by the Centers for Medicare & Medicaid Services (CMS) to provide coding and pricing determinations for durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS). PDAC is crucial in establishing coding guidelines for medical equipment and supplies covered by Medicare. The PDAC criteria are embedded in Medicare's Local Coverage Decision (LCD) for Oral Appliances for Obstructive Sleep Apnea, established in 2015. Here are the PDAC criteria:
To be coded as E0486, custom fabricated mandibular advancement devices must meet all the criteria below:
• Have a fixed mechanical hinge at the sides, front or palate; and,
• Be able to protrude the individual beneficiary's mandible beyond the front teeth when adjusted to maximum protrusion; and,
• Incorporate a mechanism that allows the mandible to be easily advanced by the beneficiary in increments of one millimeter or less; and,
• Retain the adjustment setting when removed from the mouth; and,
• Maintain the adjusted mouth position during sleep; and,
• Remain fixed in place during sleep to prevent dislodging the device; and,
• Require no return dental visits beyond the initial 90-day fitting and adjustment period to perform ongoing modification and adjustments to maintain effectiveness.
A fixed hinge is defined as a mechanical joint, containing an inseparable pivot point. Interlocking flanges, tongue and groove mechanisms, hook and loop or hook and eye clasps, elastic straps or bands, mono-block articulation, traction-based articulation, compression-based articulation, etc. (not all-inclusive) do not meet this requirement.
PDAC has verified 98 appliances for E0486 and 23 for K1027, and they are continually adding additional manufacturers and laboratories to the PDAC list. To check for PDAC ver-
ified devices, visit DMEPDAC.com and enter the codes in the product classification area.
With the introduction of these policy additions, numerous DSM providers are requesting coverage guidelines for both codes when making insurance verification calls. Nierman Practice Management recently tracked 200 verification calls to payers and received EOB data from several providers for K1027. This is what our sampling revealed:
• Many insurance plans indicated both codes as covered, although a few plans only have coverage for E0486.
• A major finding was that K1027 did not require preauthorization as often as E0486 with some of the insurers.
• In our billing sample, we saw a relatively consistent reimbursement range for E0486 whereas the reimbursement for K1027 varied with carriers. We saw lower payments here and there, but with some payers, we had higher reimbursements than with E0486.
It's worth noting that many of these policy additions have taken place in recent months and are still evolving. January 2024 marked a significant milestone, with many payers incorporating K1027 into their policies.
1. Optimize Verification Processes: It’s what you do upfront that counts. Verify insurance benefits for both K1027 and E0486. During a verification call, the biller should ask if preauthorization is required for each individual code.
2. Optimize Billing Processes: Avoid billing oral device codes as morning repositioner appliances, which can inadvertently lower the allowed fees.
3. Analyze Your Reimbursement Trends: Monitor and track billing your pay-

“You can navigate K1027 effectively and optimize reimbursement.”
A pioneer of medical billing in dentistry, Rose Nierman is the CEO of Nierman Practice Management (NPM) and creator of DentalWriter Plus Software. For more than 30 years, Rose has taught dental practices successful and ethical medical billing through the iconic Successful Medical Insurance in Dentistry seminars. Contact NPM at 1-800-879-6468 or at Coding@dentalwriter.com.
ments for E0486. If you bill any with K1027, track those EOB’s as well.
4. Get your Ducks in a Row with Documentation: When billing new codes, create detailed SOAP narrative reports including appliance type and design.
5. Educate Team and Providers: Keep upto-date with the continually shifting terrain of dental sleep medicine with educational courses and billing updates.
6. Engage with Professional Networks: Stay in touch with other providers and billers. Attend meetings to exchange insights and best practices regarding the implementation of K1027.
7. Evaluate Patient Impact: Assess how the availability of K1027 impacts patient appliance choices and satisfaction. Consider any adjustments to typical treatment approaches accordingly.
By taking these steps, you can navigate the evolving landscape surrounding K1027 effectively and optimize reimbursement outcomes for your practice. For Medicare claims, a definitive shift may hinge upon Medicare's establishment of an LCD for K1027.
The introduction of K1027 has ushered in a new era in dental sleep medicine, sparking discussions, challenges, and opportunities. As we adapt to new reimbursement policies and continue to advocate for patient-centered care, it’s crucial to stay informed, embrace change, and advocate for policies that prioritize patient choice and quality of care. With dedication, collaboration, and a commitment
E0486
Effective Jan. 1, 2006
Oral device/appliance used to reduce upper airway collapsibility, adjustable or non-adjustable, custom fabricated, includes fitting and adjustment
No Hinge Reference
See PDAC criteria
K1027
Effective Oct. 1, 2021
Oral device/appliance used to reduce upper airway collapsibility, without fixed mechanical hinge, custom fabricated, includes fitting and adjustment
Without Fixed Mechanical Hinge
to excellence, we can ensure that dental sleep medicine remains at the forefront of improving patients’ lives.
New codes for Neuromuscular Electric
Stimulation of the Tongue, (NMES) represent an innovative approach to managing mild OSA and snoring. Here's a breakdown of the relevant codes and their descriptions:
• E0492: Power source and control electronics unit for the oral device or appliance used for NMES of the tongue muscles. You will utilize this code to bill the eXciteOSA® starter kit, which includes not only the mouthpiece but also the control unit, eXciteOSA app download instructions, USB-C charging cable, and cleaning cap.
• E0493: An oral device or appliance specifically designed for neuromuscular electrical stimulation of the tongue muscles. It includes the device, the power source and control electronics units controlled by a phone application. This code covers a 90-day supply of the device. This code is specifically for billing the replacement mouthpiece. NMES has been used for increasing and maintaining muscle strength and preventing atrophy in other areas of the body, particularly helping spinal cord injury patients walk. For breathing disorders, therapy involves sending electrical impulses to the tongue muscles, causing them to contract and strengthen. eXciteOSA indicates this daytime therapy is designed to reduce airway blockage and alleviate symptoms of OSA and snoring. Patients typically undergo 20-minute sessions daily for six weeks, then maintain muscle tone by using the device one to four times a week afterward. Clinically proven results of symptom reduction are usually found within the six weeks onboarding process. Given the novelty of NMES technology for OSA treatment, national insurance guidelines have yet to be established. Insurers are gradually becoming aware of these devices and may require additional information for coverage determinations on a case-by-case basis. These new E-codes, alongside the K-codes, contribute to the evolving landscape of dental sleep medicine, offering practitioners comprehensive tools for managing sleeprelated breathing disorders and improving patient outcomes.
Introduction
The recent confluence of scientific advances in dental sleep medicine is resulting in a paradigm change that will revolutionize effective treatment.
• Digital registration of jaw position and computer-generated oral sleep appliances
• A Molar Stabilization device for multidimensional bite registration of oral appliances
• Recognition of the obsolescence and demise of mechanical adjustment mechanisms on oral sleep appliances
• Elucidation of the complex relationship of the anatomic components involved in oral airway maintenance during sleep
• Ergonomic design of oral sleep appliances
• Advent of noninvasive, accurate, safe, easy to use and low-cost home sleep testing
The culmination of these advances presents to dental clinicians an ergonomic, extremely low-cost, multidimensional monoblock trial sleep appliance. It is fabricated using the following simple instructions:
1. Using the X-Slant™ Molar Stabilization System, multidimensionally establish, then digitally scan and transmit the parallel, physiologic interarch jaw relationship (with minimum 3.0mm. interarch clearance) to the dental lab.
2. Digitally scan and transmit upper and lower impressions of the patient’s dental arches to your dental laboratory.
3. Request a monoblock trial sleep appliance consisting of 0.40mm. acrylic upper and lower retainers fused into the trial interarch position by selfcured methyl-methacrylate (Figure 1).
This article deals with how a simple ergonomic, extremely low-cost, generic multidimensional monoblock trial sleep appliance

Figure 1*: The generic monoblock custom sleep appliance shown is specifically the trial appliance being discussed in this article. It is not intended for a single night trial right after insertion, but rather used until the patient has accommodated to sleeping with an oral device, is comfortable, and responds favorably. Then it is tested.
can enhance the quality and economics of future dental practice.
The interarch relationship for an intraoral sleep appliance is not a normally sustained biofunctional position for the mouth. The ideal interarch jaw position for an oral sleep appliance is optimal airway dilation and stenting with the lips comfortably closed. Dilation refers to getting the airway enlarged and stenting is keeping it open. Five specific dimensions need to be considered to determine treatment position for an oral sleep appliance: protrusive, lateral, vertical, cant and slant; and the device must be capable of registering asymmetric movement.1 X-Slant Molar Stabilization System is the only registration device commercially available that can properly establish all the necessary dimensional parameters.
In an incisor stabilized interarch jaw registration, an acute angle seen between the
plane of the mandibular teeth relative to the plane of the maxillary teeth and narrower at the posterior than anterior is referred to as “slant” (Figure 2). When the brain acts on the neural signal, “Close teeth on stabilizer”, to establish the interarch jaw relationship using an (anterior) incisor stabilization device, the focus of action is dictated by the elevator muscles in the molar area. With incisal stabilization there is a firm stop in the incisal area and no resistance in the molar area. The result is “slant”, an iatrogenic artifact.2 The negative physiologic consequence of slant, also referred to as “Elevator Muscle Squeeze”, is a reduced posterior oral airway diameter at the pharyngeal opening. There are no scientific bases to substantiate slant as a beneficial characteristic in an oral sleep appliance. To adequately achieve proper airway dilation at the oropharynx, slant may over-stent the mouth vertically at the anterior, making lip closure difficult, and consequently facilitate mouth breathing, another negative consequence. The good news is that slant is an avoidable phenomenon.
Molar stabilization devices, of which X-Slant is the prime example, focus the resistance at the molar area, and with no appreciable contractile force in the anterior, the result is parallel interarch planes, no slant and no diminution of mouth volume at the pharyngeal opening. The substantiating science is applied human anatomy.
The unique and inherent feature of molar stabilization devices such as X-Slant is that mandibular molar teeth are able to freely slide anteriorly, posteriorly and laterally. X-Slant takes up no tongue space, does not interfere with tongue movement, offers no arbitrary mechanical interference to jaw movement and accurately accommodates natural asymmetric and multidimensional jaw movement. Facilitating the full range of multi-dimensional movement to establish the optimal position for appliance fabrication is essential for biologic compatibility, comfort and optimal oropharyngeal positioning of a sleep appliance.
Unidirectional movement does not describe how airway dilation occurs with use of an oral sleep appliance. Optimal airway volume is based on multidimensional posi-
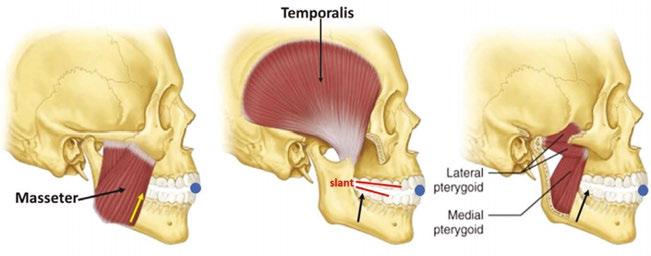
Figure 2: Medical illustration of three skulls, identifying the elevator muscles, showing their direction of closure with arrows. The blue balls represent anterior/incisal stabiizers. With no posterior resistance to the overpowering force of the elevators, the result is registration of slant.
tioning. Unidirectional however, describes the adjustment mechanisms in virtually all mechanically advanceable oral sleep appliances. Any proposition that the neurologically coordinated movement of over 20 muscles moving in multiple directions with unpredictable firing sequences, anchored and guided by the irregular, asymmetric shapes of the hyoid bone, condyles and glenoid fossae could move in tandem and in a straight unidirectional dimension that can be set arbitrarily in
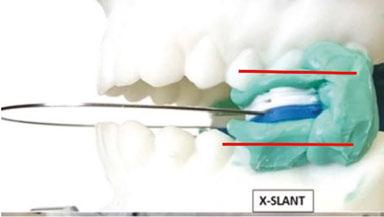
Figure 3: A set of patient models mounted on an articulator to demonstrate how a posterior/molar stabilization device registers parallel dental arches and accurately sets the vertical height for the case with stackable shims

Allen J. Moses, DDS, DABCP, D.ABDSM, was in private dental practice for 48 years in Chicago Illinois and assistant professor at Rush University Medical School in the Department of Sleep Disorders and Research for 13 years. He holds three US Patents for intraoral sleep devices and a Patent Pending for a shim system for registering the posterior interarch jaw relationship for intraoral sleep appliances. He was a member of the United States Food and Drug Administration Dental Products Panel for 10 years, has authored a book on temporomandibular disorders and over 30 scientific papers on TMDs and sleep dentistry. He was book review editor of Cranio for 10 years.
a dental lab or by a clinician is contrary to any known anatomic principles3 and has no more credibility than guesswork.
Current mechanical adjustment mechanisms consisting of tubes, straps, set-screws, rubber bands, hinges, hooks and springs are unidirectional and do not replicate human condylar movement. Built-in adjustment mechanisms in oral sleep appliances are not specifically pre-calibrated for the direction necessary to achieve optimal airway dilation/stenting. Built-in mechanical expansion mechanisms are unidirectional, never having concurrent multi-dimensionality, almost universally horizontal in direction, very rarely vertical or programmed to register asymmetric movement. The presence of a unidirectional mechanical adjustment mechanism in an oral sleep appliance limits its characterization to temporary or trial device, and it will remain as such until it is objectively validated by HSAT.
The old idea that oral appliances are merely mandibular advancement devices (MADS), moving the tongue forward to prevent its collapse on the airway is an oversimplification. It does not account for the dilation of the sides and back of the pharynx. The pharyngeal constrictors are not attached to either the tongue or the mandible. The multidimensional airway dilation shown cannot be accounted for solely by active anterior movement of the mandible and the attendant passive pull-forward of the tongue base.

Finding a mouth position that dilates the throat has a complex effect on the musculature of the entire airway.4
Maintaining a dilated airway during sleep has also been shown to be problematic. Mandibular movement during sleep changes the shape of the oropharynx. Intraoral sleep appliances that allow mandibular movement do not maintain a stable, stented airway position during sleep. Airway size changes multidimensionally with repositioning of the anatomic parts of the oral apparatus, i.e. lips tongue, soft palate, pharynx and hyoid bone.
Note: The Monoblock Generic Custom Sleep Appliance shown in Figure 1. maintains a stable oral airway during sleep.
The combined interaction of the collapsible pharynx, tongue, temporomandibular joints, soft palate, hyoid bone, musculature, head posture, and nervous system to optimally dilate and stent the airway during sleep has been discussed in a previous paper.5 It is a movement so complex that any concept of definitively effecting a multidimensional airway dilation by advancing a single, unidirectional mechanism is an oversimplification.
Ergonomics is the process of designing products so they optimally perform and fit, enhancing their efficiency. The field of ergonomics considers anthropometry, physiology, biomechanics, design, kinesiology, comfort, ease of use, esthetics and satisfaction. Ergonomically designed oral sleep appliances integrate these principles into overall performance. Examples of non-ergonomic oral appliances are those that compromise tongue and mouth space, such as those with wires or hardware that prevent the tongue from resting on the palate, those with restrictive anterior devices that prevent the tongue from reaching the lips or those whose vertical anterior height prohibits comfortable lip closure.
Custom-made oral appliances are those in which all components are fabricated to the unique personal proportions of the individual’s anatomy. Store-bought mechanical parts
built into an oral appliance do not make it custom or ergonomic. A unidirectional adjustment mechanism on an oral appliance determines definitively that the device is not custom and not ergonomic.
The clinical practice guideline for diagnostic testing for adult sleep apnea by the American Academy of Sleep Medicine (AASM) formulated a strong recommendation that home sleep apnea testing (HSAT) is an appropriate diagnostic testing option for uncomplicated adult patients who are at increased risk of moderate to severe sleep apnea.6 HSAT devices that analyze changes in peripheral arterial tone (PAT) in combination with actigraphy and blood oxygen saturation (SpO2) have been determined to be adequate to diagnose OSA in patient populations with a high pretest probability.7
Typical systems consist of a small optical sensor device which is placed on the finger, fingertip or chin. The sensors are designed to be easily self-applied by the patient. The sensor acquires accelerometer data and reflectance-based photoplethysmography (PPG) signals. The software derives SpO2, PAT, pulse rate and other biophysical parameters recommended by The AASM Manual for the Scoring of Sleep and Associated Events for home sleep apnea testing. Collected data from the sensor is continuously streamed to a user’s smartphone via Bluetooth then pro-
cessed by a state-of-the-art sensor’s data algorithm and results are displayed via an online dashboard for doctors to login to on their smartphone.
The main limitation of PSG has been its prohibitive expense which determined that it be a single-night in-laboratory, clinician attended sleep study. Repeated unattended sleep testing in the home environment is now recognized as a more thorough approach. With the costs for some HSATs now being below $100 US dollars,9 good clinical practice would seem to mandate home testing the efficacy of oral asleep apnea devices as many times as the clinical guidelines determine is reasonable, to achieve successful treatment. Dentists trained to treat sleep apnea should be knowledgeable to read an HSAT and titrate an appliance when necessary.
1. Reorientation of the clinical protocol to “Validate Before Delivery” or “Try Before You Buy”, really does not introduce new science but is an example of a major paradigm change that calls for rearranged integration of the several existing parts.
2. Present technology as well as ergonomics, cost efficiency and science create the possibility to objectively evaluate the efficacy of a trial sleep appliance before incurring the expense of laboratory fabrication of the permanent appliance.

5**: A monoblock, non-adjustable, ergonomic, custom, definitively effective, simple, low-cost oral sleep appliance fabricated after satisfactory home sleep testing of the generic trial sleep appliance shown in Figure
It was made from the original digitally transmitted models and the successful X-Slant™ bite registration from the successfully (HSAT) tested trial device.

3. Use of a simple, new, low-cost, molar bite registration system (such as X-Slant™) with no mechanical restriction of natural asymmetric movement, and no tongue interference, establishes the multidimensional parameters of vertical, lateral, protrusive cant and eliminates slant completely, with a high degree of accuracy.
4. The trial sleep appliance presented in Figure 1 can be handcrafted, or inexpensively fabricated, yet virtually replicates or clones the function of the permanent oral sleep appliance shown in Figure 5.
5. It may be necessary to test more than one trial device, but the low cost of the monoblock device shown in Figure 1 is so nominal several can be tried.
6. Built-in mechanical adjustment mechanisms in oral sleep appliances such as tubes, hinges, springs, screws and straps are presented as being impractical, obsolete and not ergonomic because their movement is unidirectional and does not replicate multidimensional TMJ movement.
7. The low-cost trial device can be tested, objectively validated and manufactured before delivery of a “final version”.
8. Additional recognized ergonomic factors for validation before delivery are
comfort, simplicity, very low cost and durability.
9. The recent innovation of accurate, efficient, low cost and simple home sleep apnea testing technology based on easy, self-applied disposable sensors and smartphone software is the culminating event for the reality of a “Try it before you buy it” sleep dentistry protocol,
The demise and obsolescence of the traditional concept of non-custom, non-ergonomic, expensive, unidimensional, appliances having built-in adjustment mechanisms and being represented at delivery as more than a trial device was thoroughly explained. The new paradigm, that an inexpensive “Trial” oral sleep appliance, based on an improved bite registration system and incorporating the confluence of scientific advances discussed, can simultaneously capture all multidimensional parameters, be made from scratch, tested, and validated before fabrication of the permanent nonadjustable appliance just makes more sense.
Addendum: Dentists are offered a complimentary sample of X-Slant, the molar bite stabilization system discussed in this article by sending their complete mailing address to info@themoses.com and simply writing “Yes, send me one” in the subject line.
1. Moses AJ, Interarch Jaw Registration Devices for Oral Sleep Appliances: Consequences of Anterior vs Posterior Stabilization. Dental Sleep Practice, Winter 2022, p.30-35
2. Moses AJ, Interarch Jaw Registration Devices for Oral Sleep Appliance: Part 2, Shift Happens. Dental Sleep Practice, Spring 2022, p.16-19
3. DuBrul EL, Sicher’s Oral Anatomy by DuBrul. CV Mosby, Philadelphia 7ed, 1980
4. Schwab RJ, Kuna SJ, Remmers JE, Anatomy and Physiology of Upper Airway Obstruction 82: 983-1000; In Princ and Pract Sleep Med; 4ed. Kryger, Roth, Dement, 2005 Elsevier Saunders, Philadelphia
5. Moses AJ, Relating Oral Physiology to Sleep Apnea Positioning. Dental Sleep Practice, Winter 2023, p.44 - 48
6. Kapur VK, Auckley DH, Chowdhuri Set al.Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med; 2017;133:479-504
7. Collop NA, Anderson WM, Boehlecke B, et al. Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. Portable Monitoring Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med; 2007;37:737-747
8. Berry RB, Brooks R, Gamaldo CE,et al. for the American Academy of Sleep Medicine The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications Darien, IL: American Academy of Sleep Medicine Version 2.4; 2017.
9. https://www.sleepon.us/go2sleep/?utm_source=google&utm_medium=cpc&utm_campaign=19668111319&gclid=Cj0KCQjw1aOpBhCOARIsACXYv-fN0esw-xnX6wTMleBa3Gv5A4wiSjtvOTChmX4aQO153dQBUZ_jy4caAlL5EALw_wcB
*The device shown in Figure 1 is a generic device, not trademarked, not patent protected, not patentable by its common use and does not require FDA 510K clearance. The dental lab has no license fee or royalty or use a proprietary part so the expected charge for fabricating this device might be $80 – $110. A dentist’s work order to the lab should accurately describe the structure of the device and specify that materials used be FDA approved for safety.
FDA 510K Clearance is required for U.S. manufacture and/or sale of oral sleep appliances using proprietary, trademarked, prefabricated or non-custom parts. Approval is based on demonstrating safety by use of specified FDA approved materials and confirmation of “substantial equivalence” in structure to two previously 510K cleared oral sleep devices.
**Figure 5 shows a Moses Alpha™, a definitively effective, proprietary patented, trademarked, licensed and FDA 510K cleared oral sleep device. Its cost from Modern Dental Lab USA and Micro Dental Labs is $250 U.S. If the device needs to be remade, the upper component is re-used and the lower component is replaced for a charge of $175.
Dental Sleep Practice magazine is the sleep apnea publication for dentists –encompassing everything they need to know to properly treat this condition.
SUBSCRIBERS BENEFIT FROM:
s 4 fantastic issues per year
s 8 continuing education credits each year
s Clinical articles enhanced by high quality photography
s Practice management advice on how to make dental sleep more profitable
s Analysis of the latest groundbreaking developments in dental sleep
s Real-life profiles of successful dental sleep practices
s Technology reviews of the latest products





Billing Information
• Accurate – bite notches on the horizontal keys are deep and oval shaped, making for a more secure fit on the tooth
• Fast Streamlined Workflow – keys are tested in order from left to right, with no flipping and only one set of numbers visible on all sides
• Easy – no calculations, the number you see is the measurement
• Built for 3D Scanning – keys are compact and have a non-reflective surface, so they do not block any teeth nor cause errors due to reflections


