Tongue Tie is Not Your Only Problem and Frenectomy is Not Your Only Answer
by Linda D'Onofrio, MS, CCC-SLP
They are Not Their Disease: Clinician and Providers Need to Feel That
by Pat McBride, PhD, CCSH















Readers know, as individuals, they don’t hold all the answers for the patient in their clinic. Each person presents a myriad of signs, symp toms, personal goals, biosignals, and interpretations that form the clinical puzzle we are charged with arranging into a pathway to health.
September was a busy month. Collabo ration Cures, a gathering of more than 750 dentists, physicians, speech pathologists, physical therapists, dental hygienists, and others interested in a whole-person, focuson-healthspan, approach, happened in Phoenix. The American Dental Association produced the 5th Children’s Airway Initiative CE Event, virtually, just a week later. Both meetings featured speakers and learners from around the globe. Dan Klauer, a dentist in South Bend, Indiana, hosted his 5th Sleep Symposium focused on pediatric interven tions, with a lineup of luminary leaders in the field. No doubt there were dozens of other events, large and small, bringing health care practitioners together to learn, grow, and gain confidence to help people reach the optimum health they seek.
Why do we all invest our resources –money, time, intellectual effort, commitment to teach our team, and disrupt our practices with new ideas? Why do we take the risk? I think it is because dedicated professionals cannot sit with a person needing help and be satisfied with yesterday’s answers. Or the information shared years ago in professional training. Or CE available from the experts in their own town. They seek a new story.

Why would Sharon Moore and Shereen Lim take more than two weeks away from their practices in Australia, spend thousands of dollars to travel to the United States, and share their experience with Collaboration Cures and the ADA? Not for the honoraria, I can assure you. These professionals do not seek fame. They simply cannot sit back and hold their expertise to themselves. Every speaker at these events stands up because they can’t stop learning. They must settle a need to share to bring balance to their lives.
They have sat in the chairs each of you sit in, invited patients to put the puzzle pieces onto their tables, and, just like you, have
looked for the corner pieces, the edges, and have done their best to bring the picture to focus. When their colleagues wonder about how they were able to see that big picture, stories came out about confusion, about frustration, and about reaching out to others for help before learning how to sort it for themselves. Above all, the stories are about not being satisfied until the picture comes together.
What happens when you get the best news of the day? The urge to share is the same as our courageous colleagues on the podium – life is out of balance until the next person can see a new path to success. As one learns from another, stories form about the journey from unaware to aware to mastery. When telling the story, don’t leave out the parts where things went south for a bit – say ing them out loud builds trust and enhances learning. Every time the story is told, the learning expands for both the teller and the receiver.
Post-pandemic Zoom meeting may be tiring, but they open every one of us to global expertise. Your clinical puzzles may become clearer after hearing a story from an ENT in Malaysia, a Brazilian speech pathol ogist, or a Chilean physical therapist. Be a consumer of global stories. Know that when you ask to hear their story, you help them learn, too. When you share your stories, we all get better.
Steve Carstensen, DDS Diplomate, American Board of Dental Sleep MedicineWhen telling the story, don’t leave out the parts where things went south for a bit – saying them out loud builds trust and enhances learning. Every time the story is told, the learning expands for both the teller and the receiver.
Peter J. Catalano, MD, and John Walker, DMD





by Colonel Scott Williams, MD, FAASM A review of the more common psychiatric diagnoses and how they both impact and are impacted by sleep.






Publisher’s Perspective
Telling the World About You by Lisa Moler, Founder/CEO, MedMark Media 8 Clinician
An interview with Dr. Alan Lowe It’s never been about the effect on tooth position.
16 Communications Corner Finn’s Journey to Health Started in His Dentist’s Office by Kelley Richardson You have the power to unlock mysteries – with profound results.
21 Product Spotlight THEFUTUREISNOWHERE Precision takes its place in our therapy decisions.
38 Product Spotlight
Achieving Long-term OSA Stabilization Despite CPAP Intolerance with Oral Appliance Therapy by Sal Rodas, MBA Seeing possibilites led to a great outcome in this case.
42 Team Effort
They are Not Their Disease by Pat McBride, PhD, CCSH Know your patient and youself for better health care.
44 Clinical Focus
4 Tips for Reducing Your Headaches And Chairtime at Appliance Delivery by Frank Madrigal, CDT
Tips for successful oral appliance workflow.
48
Practice Management Demystifying Medicare Advantage Plans for Oral Appliance Therapy by Rose Nierman and Courtney Snow Pulling on another thread to unravel the Medicare mystery.
50
Event Recap Panthera Dental 10th Anniversary Celebration by Adrienne Good
Continuous innovation keeps this company vital.
52 Adjunctive Therapy Good Doctoring
See how three early adopters integrate new therapy to their DSM practices.
56
Practice Management Getting Paid for Sleep Therapy by Jamison Spencer, DMD, MS Don’t let yourself believe there are no choices for how to expect payment.
59
Product Spotlight Dentists Have an Affordable New Option for Treating Medicare-Enrolled Patients Keeping business in mind doesn’t mean compromizing quality.
60
Practice Motivation
A Dentist Held the Keys to My Freedom by Julia Worrall, The Sleep RN New eyes to see leads to profound insight for individual patient care.
62
Legal Ledger Legally Fit by Daniel B. Brown, Esq. A look ahead at topics to be covered in this column.
Winter 2022
Publisher | Lisa Moler
lmoler@medmarkmedia.com
Chief Dental Editor
Steve Carstensen, DDS, D.ABDSM stevec@medmarkmedia.com
Chief Medical Editor
Lee A. Surkin, MD, FACC, FCCP, FASNC drsurkin@n3sleep.com
Associate Editor | Lou Shuman, DMD, CAGS lou@medmarkmedia.com
Editorial Advisors
Steven Bender, DDS
Jagdeep Bijwadia, MD (Pulmonary, Sleep)
Kevin Boyd, DDS
Karen Parker Davidson, DHA, MSA, M.Ed., MSN, RN
Kristie Gatto, MA, CCC-SLP, COM
Amalia Geller, MD (Neurology, Sleep)
William Hang, DDS, MSD
Christopher Lettieri, MD (Pulmonary, Critical Care, Sleep)
Pat McBride, PhD, CCSH
Jyotsna Sahni, MD (Internal Medicine, Sleep)
Ed Sall, MD (ENT, Sleep)
Alan D. Steljes, MD (Cardiology, Sleep)
Laura Sheppard, CDT, TE
DeWitt Wilkerson, DMD
Scott Williams, MD (Psychiatry, Sleep)
Gy Yatros, DMD
National Account Manager

Adrienne Good | agood@medmarkmedia.com
Sales Assistant & Client Services
Melissa Minnick | melissa@medmarkmedia.com
Creative Director/Production Manager
Amanda Culver | amanda@medmarkmedia.com
Marketing & Digital Strategy
Amzi Koury | amzi@medmarkmedia.com
eMedia Coordinator
Michelle Britzius | emedia@medmarkmedia.com
Social Media & PR Manager
April Gutierrez | medmarkmedia@medmarkmedia.com Webmaster
Eileen Kane | webmaster@medmarkmedia.com
MedMark, LLC
15720 N. Greenway-Hayden Loop #9 Scottsdale, AZ 85260
Tel: (480) 621-8955 | Toll-free: (866) 579-9496
www.DentalSleepPractice.com
Subscription Rate: 1 year (4 issues) $149
©MedMark, LLC 2022. All rights reserved. The publisher’s written consent must be obtained before any part of this publication may be reproduced in any form whatsoever, including photocopies and information retrieval systems. While every care has been taken in the preparation of this magazine, the publisher cannot be held responsible for the accuracy of the information printed herein, or in any consequence arising from it. The views expressed herein are those of the author(s) and not necessarily the opinion of either Dental Sleep Practice magazine or the publisher.






Our worlds are so busy with our time consumed with improving clin ically, professionally, and personally. We work hard, and hopefully find the time to play hard. From my view as a publisher of four and soon to be five dental publications, I see and hear about so much innovation going on in the dental community. Dentists are showing patients that den tal health means better overall health, and there are so many ways to add technology, expand clinical options, and create your own new protocols and inventions that can change the face of your specialties. My team at MedMark is always searching for your stories – for your journeys, your successes, and even your speed bumps along the way. Entrepreneur Gary Vaynerchuk said, “Regardless of what you are trying to accomplish, you’ve got to tell the world about it.” I wholeheartedly agree. And that’s what we at MedMark Media have been doing over the past 17 years. We’ve been telling the world about you.
Lisa Moler Founder/CEO, MedMark Media
All of the new advancements in dental specialty fields are amazing – augmented reality (AI), virtual reality, 3D printing, robot ics, the field of dental sleep medicine, braces and aligners that move teeth faster and more efficiently, and imaging in 2D and 3D that makes diagnostics more precise. Advances in endodontic materials such as bioceram ics, contribute significantly to that specialty’s incredible growth. Let’s not forget implants – according to iData Research, over 3 mil lion dental implants are placed each year in the United States, and the U.S. market is expected to exceed $1.5 billion in 2027.
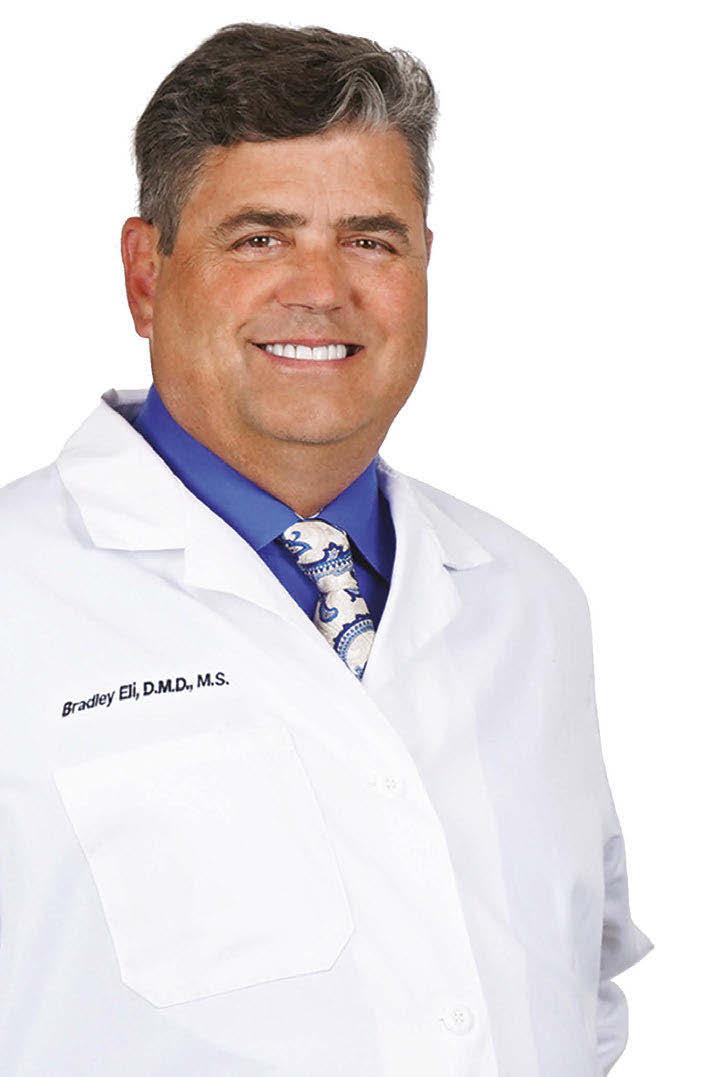
Here’s more good news. In this issue of Dental Sleep Practice, our Cover Story spotlights the latest in dental sleep medi cine solutions to treat OSA patients more effectively. SomnoMed’s second annual SomSummit focused on vetting the value of all sleep therapies and explored the fun damental research that supports them in improving, and even defining, OSA treat ment success. In our CE, “Interarch Jaw Registration Devices for Oral Sleep Appli ances,” Dr. Allen J. Moses explains bilat eral molar stabilization and creating a more open airway. In “Tongue Tie is Not Your Only
Problem, and Frenectomy is Not Your Only Answer,” Linda D’Onofrio discusses oromy ofunctional therapy (OMT) and the different myofunctional disorders that can be clinical markers of sleep-disordered breathing. In “They are Not Their Disease: Clinician and Providers Need to Feel That,” Pat McBride explains listening and communication can make you the one provider who captures the influence of illness on your patients. She says that great care providers understand science and help patients accept their diagnosis and process it. Patients who feel understood and cared for follow treatment recommenda tions and self-management protocols better, improving their quality of life and long-term health outcome.
Back to you – how can we help you tell the world about your innovations, tech niques, and life-changing treatments? Our articles and advertisers show you what is possible, practice-changing, and promises to help differentiate you from the rest. To change Gary Vaynerchuk’s quote just a bit –Regardless of what you are trying to accom plish, MedMark is here to help you tell the world about it.
To your best success!


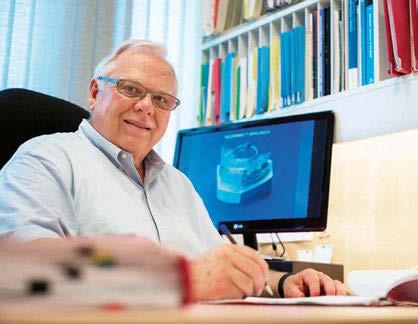
DSP continues to honor the founders of our profession in an ongoing series of interviews with those who were there at the beginning. This issue, we sat down with Dr. Alan Lowe, retired professor of orthodontics at University of British Columbia. Dr. Lowe was part of the group that started the Sleep Disorders Dental Society and has influenced count less dentists with his practical, yet scientifically sound, teaching.
You’ve been named as the developer of one of the first commercially avail able devices specific to treatment of obstructive sleep apnea, the Klearway. Can you tell us how you took the ‘snore appliance’ concept and developed a system to treat what was then a new disease?
The role of airway and tongue posture are important determinants in the development of the dentition which has been studied by ortho dontists for decades and several current clini cal therapies take these factors into account. The Canadian Federal government sponsored multicenter clinical trials of patented Canadi an inventions and Klearway was invented and patented specifically with the encouragement of the Industrial Liason Office at the University of British Columbia which created a signifi cant amount of interest in both the dental and medical professions. Klearway was licensed by the University to Space Maintainers Can ada and Great Lakes Orthodontics both clear national industry leaders in the field. These two companies assumed exemplary roles in manufacturing appliances to a high standard and actively supported educational programs for both dentists and physicians. The Universi ty of British Columbia was uniquely equipped to contribute to this field with an established medical sleep clinic that worked in close asso ciation with our dental sleep group especially as we tested and developed a number of oral appliances. One of our first priorities was to establish a clinical protocol for oral appliance use in sleep disordered breathing. Over time
and years of clinical testing, guidelines for ap pliance selection, titration protocols, quanti fication of side effects, post treatment studies and potential insurance options were devel oped to guide dentists and physicians in this newly developing field.
Dr. John Remmers credits you with recruiting him to support the dentist’s role. Collaboration with physicians has been a rocky road for our field –what are your thoughts about today’s state of affairs?

Dr. John Remmers and I shared common research interests in the late 1970s as he was especially interested in 3D reconstructions of tongue posture we had developed at UBC based on CT scans. Shortly thereafter, he served as external PhD examiner for one of my stu dents and we have collaborated on numerous projects and panel discussions ever since. He has been a strong advocate for the use of oral appliances in the treatment of sleep disordered breathing. Together we have encouraged den tists and sleep physicians to treat such patients and have fostered this educational role across North America and around the world. Unfor tunately both professions are primarily led by clinicians with an inherent suspicion of the others motives which has slowed down prog ress in this area. Initially, a lack of clinical trial data to support the efficacy of oral appliances slowed the field down but over time several comparative studies were eventually published and both therapies were found to be effective therapeutic options. Insurance companies were initially hesitant to fund oral appliances and the pros and cons of oral appliances vs. nCPAP took several decades to sort out.
It’s one thing to come up with a great idea, another entirely to promote this to an entire profession. What do
Sapphire is uniquely positioned “Expand North American sales and




Sapphire is uniquely positioned to impact the dental strategic “Expand North American sales and leverage the marketing organization
Nexus Bill
pillars. organization to drive adoption of a national turnkey brand”
OSA public awareness activities: website, social media, brochures, posters, videos, events and most importantly the B to C products
Complete turn on approach to Sleep implementation, ongoing coaching & support and new sales of equipment, software and services
Unique therapeutic framework for Chronic Headache, Migraine, TMD, Tinnitus, Vertigo, Pain Head, Neck, and Face

OSA public awareness media, brochures, importantly the Complete turn key, implementation, new sales of equipment, Unique therapeutic Headache, Migraine, Head, Neck, and


501C3 Non Profit Fully accredited, online, on demand Dental Sleep Medicine credentialing. The only one of its kind in the world.



Medmark LLC is proud to be the leading interactive marketing and multi platform advertising company focused on the niche specialties of dentistry. We are creating a healthier America through knowledge, due diligence, and experience, by empowering dental professionals with high quality clinical information in clear and concise language and showcasing innovative technologies.
www.nexusdentalsystems.com
you think of the ripple effects of your work, seen today in the number of dentists engaged in treating sleep re lated breathing disorders?
Over the next three decades revenue from royalties helped to sponsor research trainees from within and outside Canada many of whom continue to contribute to developments in this field today. Training dentists in the ba sics of sleep medicine and the required clinical and titration protocols took years to establish. The establishment of the American Association of Dental Sleep Medicine set a stan dard for training and certification of some 1,500 dentists which has been further defined over time. Problems with nCPAP adherence drove the oral appliance market in part and the general public actively sought out therapeutic options for both snoring and ob structive sleep apnea.
One of your signature lines is: “Teeth move, get over it.” Dentists are trained to make bites work – how do you reconcile your work as a professor of orthodontics with acceptance of changes to bites using oral devices?
Early on as we tested various oral appliance for sleep disordered breathing, we were sur prised to observe tooth movement in selected patients after prolonged oral appliance use. Initially this was a definite concern for many clinicians since so much time is spent creat ing straight and supposedly healthy dentitions. However we were also observing tooth move ment after prolonged nCPAP wear so both ther apies had an effect on tooth position although expressed in different ways. We quantified and published data from both therapies and trained dentists on how to recognize same and even reduce the progress of such movements in se lected patients. With time, tooth movement re lated to sleep therapies began to be recognized as common side effects and inappropriate cessation of either therapy was replaced with careful monitoring and appliance adjustments. Tooth movement in adults often in periodontal ly-compromised dentitions can occur rapidly due to reduced alveolar bone support but does not cause death of our patients and must be
accepted as a side effect. Training both profes sions to acknowledge and recognize this real ity has been an ongoing challenge especially when both professions can on occasion be oblivious to the long term effects of untreated obstructive sleep apnea.
What role do you see orthodontists playing in young children who are at risk of breathing disorders?
Orthodontists are trained to recognize ade noid faces in the waiting room and plan effective therapies to establish a functional occlusion. However, a number of tongue disorders con tribute to misaligned teeth and this in combina tion with compromised airways can be difficult to diagnose and effectively treat on the long term. Functional appliances which advance the mandible in growing children may have an important role in the control of disordered breathing but objective data of this common ly assumed concept has not been published to date other than in very small case studies. This represents an important field for growth in den tal sleep medicine and is beginning to get the attention it warrants.
Many dentists ask when dental schools will include airway growth/function/ management into their curriculum, and teach about sleep disturbances to undergraduate students. Obviously you can’t speak for all dental schools, but from your perspective as a professor, do you see this coming soon? Do you think a dentist-alumnus could have an influence on their local dental school?
As an academic orthodontist with some 53 years of experience in university and prac tice group settings, I have found this to be a frustrating and slow moving aspiration. Dental curriculum are full of new technologies and challenges as the science of dentistry advanc es very quickly and sleep disordered breath ing holds little weight in comparison to the demands of changing dental therapeutics. Traditional dentistry is hesitant to include oral appliance therapy in part because so few uni versities have adequately trained individuals to create such courses provide same. The need for more full time dental academics in the field is paramount to the inclusion of the field in a dental school curriculum.

Air quality is CRITICAL to your practice. Contaminants are everywhere: Pathogens, Pollutants, Viruses, Bacteria & Fungi all threaten our air quality and quality of care.

Benefits of Air Quality Guard:
• Arm and ceiling intakes capture aerosols at the source and move them away from occupants
• Contaminated air is filtered through a 3 layer system, removing greater than 99.99% of all contaminants
• Reduces the spread of COVID-19 and reduces sick leave

• Negative pressure airflow cycle ensures that contaminants are captured before they can circulate
• Quietly and efficiently filters & replaces up to 100% of air with pure, clean air
• Powerful enough to replace all the air in the room every 7 minutes*
*Based on recommended system design principles. Customization may increase or decrease this value.
 Effectively by Matthew Conlon, EVP of Sales & Marketing, SomnoMed North America
Effectively by Matthew Conlon, EVP of Sales & Marketing, SomnoMed North America
SomSummit ’22 co-chairs, Colleen Lance, MD, and David Rapport, MD, insightfully noted: “Never before has the specialty of sleep medicine been at such a turning point, poised with innovation in several key arenas. As a field, we are redefining what sleep apnea is and how to better measure and treat it.”

SomnoMed North America recently held our second annual SomSummit ’22, in Scottsdale, AZ. We showed, by example, the power of physician-dentist collaborations as our Medical Initiative is intended to facilitate. We also highlighted the enormous opportunity to success fully treat more OSA patients in light of the astonishing statistics we see of undiagnosed, untreated OSA suffer ers, and the growing recognition of PAP treatment shortcomings in effec tiveness – and now, access.
SomSummit ’22 presented an opportunity to go even further. The
focus wasn’t on Oral Appliance Therapy (OAT), and it wasn’t about SomnoMed prod ucts. Rather, it focused on vetting the value of all therapies, and the fundamental research that supports them in improving, and even defining, OSA treatment “success.” Topics included:
• The potentially waning value of AHI and myriad prospective future approaches to better define and mea sure successful treatment
• When and why to STOP likely-to-fail therapies based on “big data” statistics
• Patient endotyping and phenotyping as a means to predict the most successful treatments outcomes
• The potential to quickly triage patients from one failed or failing therapy to the next, and starting with patient choice as a likely factor in treatment success
• And of course, all too familiar remind ers of the stubborn and startling OSA prevalence and treatment statistics that unify sleep health professionals of wildly diverse interests and
expertise SomSummit ‘22 attendees in Sleep Medicine, Sleep Dentistry, Sleep Psychology, Otolaryngology, and Advanced Practice Modeling Danny Eckert, PhD, a Matthew Flinders Pro fessor at Flinders University and Director of the Adelaide Institute for Sleep Health in Adelaide, Australia, presents about Pheno typing OSA Patients and the Implications for Precision Sleep Medicine at SomSummit ‘22.around a “North Star” urgency to Treat More OSA Patients, More Effectively.
It’s truly humbling to gain a fuller perspective of the entire universe of solutions in sleep disordered breathing. It’s also daunting to contemplate the work needed to make an impact, to move the needle, to address the gaps, and to ease the frictions that stand in the way of broader and more effec tive treatment of the persistently underestimated condition of OSA. The goal – the mission –for SomnoMed, however, is sim ple: to bring OAT and the Dental Sleep Medicine (DSM) experts who provide it into the primary OSA treatment ecosystem as a prominent, clinically accepted, and accessible therapy for OSA sufferers…among other therapies.
Over the past year, SomnoMed assembled Clinical Advisory Boards, composed of both sleep dentists and physicians, in each of our global regions. This year, we were delighted to follow the lead of our Clinical Advisory Board members and SomSummit ’22 co-chairs, Colleen Lance, MD, and David Rapoport, MD. In con trast to last year’s Summit, while DSM was expertly and prom inently represented, DSM and OAT was but one specialty, one topic, interspersed and in relation to ALL current and future poten tial therapies and approaches to Treating More OSA Patients, More Effectively. The theme of SomSummit ’22 was “The Right Therapy for the Right Patient, at the Right Time.” As humbling –and daunting – as the challenge may be, the level and diversity of expertise, and the professional interest, courtesy, and admiration across all specialties, points toward an incredibly promising future for the field of DSM.
Sleep dentistry was superbly represented and fully engaged in the sleep ecosystem during SomSummit ’22, which was comprised of top key opinion leaders (KOLs) and practitioners in sleep medicine. A barometer of Som noMed’s Medical Initiative, this confirms for us, the DSM community, that OAT has earned a respected position within that primary ecosystem. Now, we must continue to translate this strong position with the goal of enabling OAT as a standard of care.
The growth of DSM and OAT to where it stands today as a clinically viable option for the treatment of OSA is a credit, almost exclusively, to the profession itself: both topdown, through formal organization of advocacy, education, and credentialing, and bottom-up, dentist-by-dentist treat ing patient-by-patient. One-by-one, expert DSM providers have cultivated rare, trusted rela tionships with local prescribers where only two or three strong local referral relationships has built many robust DSM practices. This, combined with lower-fric tion pathways for diagnosing via home sleep testing, the leverag ing of rapidly growing telemed icine opportunities, and greater adoption of direct-to-patient mar keting and treatment pathways, have contributed to the signif icant growth of SomnoMed’s –and our dental customers’ – treat ment impact. Yet, in relation to the enormous number of undiag nosed, untreated, or unsuccess fully treated OSA sufferers, it’s clear that the field of DSM has been lying outside of the primary sleep ecosystem where millions of patients are seen and treated, successfully or otherwise.
In the DSM arena, manufactur ers have historically sold features and benefits to dentists. They’ve swapped market share between themselves, adding little real value to the growth of the indus try or to their sleep dentistry cus tomers; “just another lab” selling feature, benefit, and price. Few dentists and fewer manufacturers were educating prescribers and investing in and leading clinical research and publication efforts to influence prescribing habits. The resulting frustration of DSM providers is expressed routinely. We’ve commonly heard: “They (sleep physicians) don’t get it. They won’t change.” It’s clear that regardless of enabling technologies, prescribers (treating physicians) must be educated and on board with the value of the therapy and the value of the therapist – the qual ified, expert, sleep dentist – before we, as an industry and a profession, “move the needle” to any significant degree.
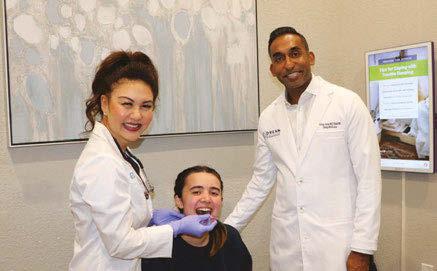

In context, the OAT journey to broad-scale prescriber
Asim Maqsood, MD, a sleep medicine physician with SSM Health Sleep Services, OKC, receives an intraoral scan from Beth Hamann, DDS, of Agave Sleep & Wellness.acceptance and adoption…to a standard of care, actually isn’t so different than that of many other medical therapy journeys in the past, including PAP therapies. In fact, it’s been widely reported that it takes an average of seventeen years for evidence-based practices to be incorporated into routine general health care practices.
From the inception of CPAP reimbursement in the mid 1980s, Respiratory DME companies have depended on prescriber referrals. The literature supported CPAP, and the guidelines and reimbursements were aligned with the clinical research, as we have today with OAT. However, this alone didn’t drive treating physicians to alter their treat ment routines. DMEs, together with the major manufacturers, needed to bring the literature, the “why?” (clinical proof sources), and the “how?” (the process) to them, office-by-office, physi cian-by-physician, and patientby-patient. The DMEs also had armies of sales reps. By the early 90’s, with PAP still in its infancy, there were no fewer than four local DME reps calling on each sleep physician to educate them and ask for patient referrals.
services (DME), and patient treatment pathways to support their practice and patient care needs.


The principles of operation of bi-level PAP devices, with flow algorithms and triggering mechanisms, that were being detailed to physicians in 1991 to enable clinical application of Non-Invasive Ventilation only “mattered” to prescribing physi cians after several more years of industry advocacy and education, supported by clinical research and publication. Thirty years later, non-invasive ventilation is a standard of care, and CPAP clings to the title of “gold standard” for OSA treatment. SomnoMed’s Medical Initiative is modeled around a similar proven approach to clinical adoption.
Session Moderator Colleen G. Lance, MD, opens SomSummit ‘22 with a slide addressing recovery from the pandemic. She addresses how, as a field, we are redefining what sleep apnea is and stresses the importance of coming together in a multidisci plinary fashion to approach patients with innovative therapies.
The respiratory DME com panies leaned on the leading manufacturers such as Res pironics and ResMed to help them win new referral sources with CE programs, explanation of technologies, features, and benefits. Manufacturers were likewise expected to know the literature of PAP to support an evidence-based decision tree. Prescribers needed to know the “why?” It was understood that prescribers don’t drink their morning coffee with jour nals in front of them; they don’t attend all of the relevant conferences. However, when they hear and see the same “drum beat” from various credible industry sources, and are brought together with their peers that may be a bit ahead of their curve, they gain a comfort level in moving toward newer recommendations and patient care routines. In short, they needed confidence that they were practicing evidence-based medicine. Then, and only then, did they move to the “how?” with the right product(s), patient care
As DSM participants of Som Summit ’22 will attest, leading Key Opinion Leaders in the field of Sleep Medicine view OAT as a valid, effective, and important “tool in the tool box,” and are eager to find more trusted and fric tionless treatment pathways,and better means of predicting suc cess. They are tremendously excited with the prospect of tech nologies to finally enable objec tive, reliable metrics of nightly oral appliance patient compliance and efficacy. DSM has the topdown support of these KOLs and formal guidelines. SomnoMed, with our Medical Initiative, and through strong collaboration with key industry stake holders who’s products and services are integral to frictionless patient and provider treatment journeys, is leading the charge to translate this resounding support into clinical adoption.
The parallels are clear: the sleep dentist replaces the DME in the CPAP model. What’s missing? AASM guidelines based their robust support of OAT use even as a first-line treatment option and the leading sleep KOLs are on board. So, what barriers remain?
While we can draw strong parallels of OAT to PAP relative to their DME status, there are significant departures, as well: • DMEs are mostly national and regional, with an addi tional churn of local providers. Their “armies” can be deployed at scale and with uniformity of patient care
and operational efficiencies across state lines. DME providers are also not “sleep medicine” professionals like DSM Providers (dentists), who are held to strict, state-by-state dental practice laws. While ensuring the integrity and quality of their services, these laws may also present barriers to scaled delivery of DSM care.
• DMEs compete ferociously on nuances of service, patient satisfaction, and treatment success. One of their most compelling offerings is providing the prescriber with assurance – through robust, routine communication – that the patients are being treated successfully. Data, by patient and in aggregate, of prescribers’ patient suc cess rates is critical. While DMEs provide objective data via CPAP compliance monitoring technologies, OAT has relied on widely varying, and mostly sub jective, reporting of ill-de fined OAT treatment suc cess. Future technologies will help to fill the void of objective metrics of nightly compliance and efficacy.
• Dentists are not DME providers. DSM providers walk a tightrope between their role as a commercial DME pro vider, eager for referrals, and that of a trusted colleague in the field of sleep medicine. Physicians can choose among many CPAP DMEs based on varying service and patient care metrics, but they need and want to know the dentist. Their historical perceptions are often based on poor experience or hearsay of sending the wrong patient to the wrong dentist with wildly exaggerated fees or billing methods, or simply no feedback or fol low-up from the dentist at all.
Under SomnoMed’s Medical Initiative structure and pro cess, our team of Business Development Managers, ded icated to calling on prescribing physicians, serve as facili tators of physician-to-dentist relationship building. They introduce only the most highly qualified DSM providers to prescribers, where Dentists are presented as the colleagues and patient care partners they are…not as another DME pro vider. Business Development Managers explore prescribers’ depth of awareness, understanding, and perceptions of OAT to address the barriers that prevent appropriate consideration of OAT as a means of achieving more successful OSA treat ment outcomes.
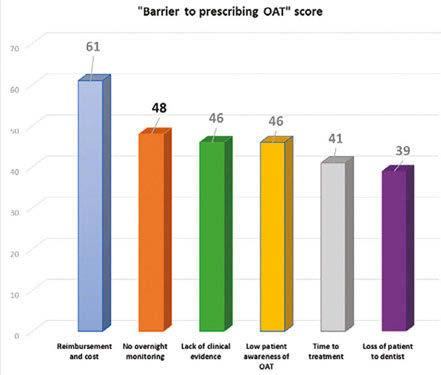
In 2019, SomnoMed surveyed 242 CPAP prescribers to
understand the barriers to greater adoption of OAT.
Do these survey results reflect these physicians’ under standing of OAT as a treatment option …or, rather, their per ceptions? After all, we know that over a five year span, CPAP patient costs are far greater than those of OAT. How could “lack of clinical evidence” rate so strongly when AASM guidelines are evidence-based? Does “time to treatment” still hold water when CPAP treatment times are now weeks and months in light of the CPAP supply issues stemming from the Philips recall?
While each of these are undoubtedly partial contributors to under-prescription of OAT, there are more significant, over arching barriers. Foremost is the physicians’ level of awareness… and their associated perceptions. Almost all PAP-prescribers are aware of OAT. If they had been merely aware of CPAP in the early 1990s, however, without having been reinforced of its clin ical value via a consistent drum beat of supporting clinical pub lications, podium presentations, and DME reps would PAP be the dominant therapy it is today? Can DSM address the per ceived barriers?
To be effective in representing and advocating for OAT and our expert DSM professionals who provide it, Som noMed is aware and fully educated in OAT’s potential and value that prescribers are obligated to assess, prioritize, and prescribe for their patients. CPAP is the right therapy for many patients, as are positional devices, surgeries, pharma ceuticals, and OAT. The goal must be one hundred percent treatment success.
DSM is not peripheral, but central to the broader discus sions surrounding sleep disordered breathing. SomSummit ’22 helped to further confirm that patients and their physi cians need us. Come SomSummit ’23, we’ll look back on progress made and move further ahead with new insight, experience, and perspective toward our common goal of one hundred percent effective OSA treatment.
The most important work to be done is at the local level; physician-by-physician, patient-by-patient. We’ll need a growing army of DSM and medical professionals, industry stakeholders, and key opinion leaders. As we show the suc cesses, identify the failures, and address the real and per ceived barriers to broader adoption of OAT as an effective choice, the right choice, for millions of OSA sufferers, the turning point becomes a tipping point.
Until our son, Finn, was 6 years old, he had not slept through the night… We thought we had tried every thing, and we were tired. It never occurred to us to look at how he was breathing.
Look closely… is your child breathing through their nose or mouth?
It turned out, Finn was a mouth breather. We had no idea his mouth breathing habit led to nasal congestion. We learned that an open mouth posture makes it harder to get restorative sleep. Sleep quantity is not always synonymous with deep, quality sleep.

He was a restless sleeper. Tossing and turning, he would repeatedly call out through the night for help. His breathing was labored, he was sweating profusely during naps and at night. He suffered from night mares and dark circles under his eyes. De spite waking up tired and yawning, he had an abundance of energy throughout the day. He developed eczema on his face and was congested to the point of trying to clear his nose and throat several times a minute. He was clearly in distress.
Was it Physiology? Allergies? Diet?
After years of doctor appointments and medications, we were still no closer to find ing the root cause. Until a conversation with a dentist. The dentist explained how the nose filters, warms, purifies and humidifies the air coming into our body. Mouth breath ing doesn’t do this but instead can lead to nasal congestion and enlargement of tonsils and adenoids, as well as other forms of in flammation. The first step to resolving his fragmented sleep and disordered breathing was to transform Finn’s breathing habit from mouth breathing to nose breathing.
This was the beginning of our journey to helping our son sleep and breathe better, but it was a very crucial first step. After breath ing retraining, Finn benefited from a lingual frenectomy (before frenuloplasty was taught), myofunctional therapy and expansion ortho dontics. Seeing first-hand the results of early treatment on Finn’s improved quality of sleep has made me an advocate of early interven tion. It’s not uncommon for me to discuss the phenotypes of sleep and breathing dis orders with teachers, coaches and parents. I am often handing out Breathe Right strips and demonstrating the Cottle maneuver on school trips, baseball fields, and playdates.
I feel fortunate to have learned this mes sage while my son was still young enough to benefit from early treatment. Having worked on the business side of dentistry for 25 years, I am encouraged and grateful for the growing number of dentists passionate about screen ing and treating Sleep Related Breathing Dis orders. When you are treating a child, you are helping the entire family breathe easier. As Ralph Waldo Emerson said, “To know even one life has breathed easier because you have lived. This is to have succeeded.”



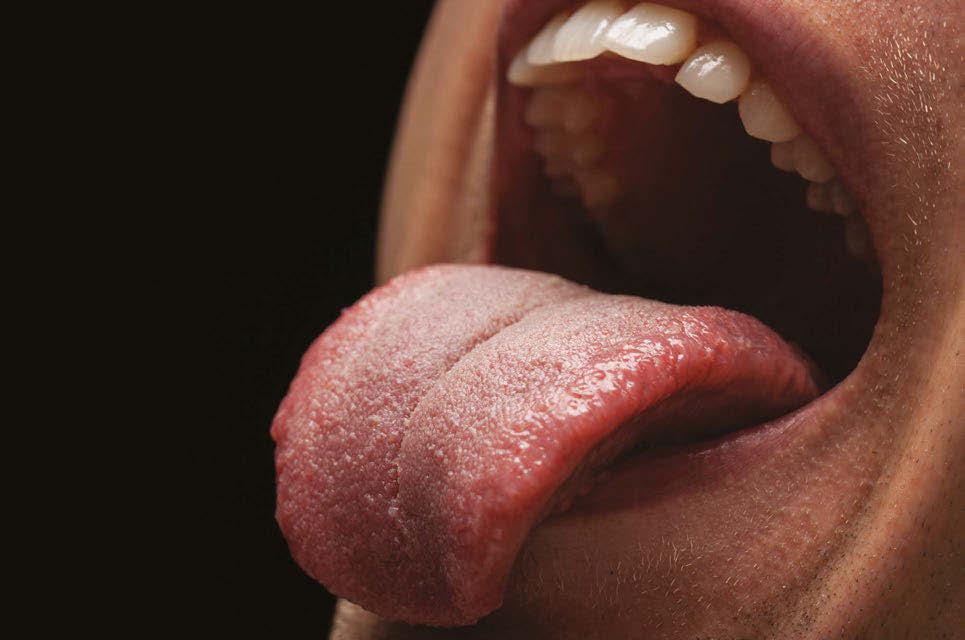 by Linda D’Onofrio, MS, CCC-SLP
by Linda D’Onofrio, MS, CCC-SLP
For many providers the correlation between sleep disorders and ankyloglossia feels like a fad. But for providers like myself who have been diagnosing and treating pediatric and adult oromyofunctional disorders for decades, it is an ev idence-based understanding of anatomy and physiology. This article will cover my approach to diagnosis and treatment in frenectomy patients three years and older.
I take calls regularly from potential adult patients asking to get on my caseload be cause they want a lingual frenectomy, and their doctor said they need to do some tongue stretches or something. They often balk when I tell them I need to conduct a full orofacial myofunctional evaluation be fore making recommendations for treatment, including frenectomy. Some of them tell me they found a bunch of exercises on YouTube, so they don’t understand why an evaluation is necessary. They’ve already been diagnosed with tongue tie. And I find myself saying the same thing again and again, because it’s true. Tongue tie is not your only problem and frenectomy is not your only answer.
Ankyloglossia is a very critical structural symptom of an orofacial myofunctional dis order (OMD) that has the potential to change other craniofacial structures, change muscu lar development, make some foods unsafe or unpleasant, change how we speak, and cause thousands of dollars of orthodontic

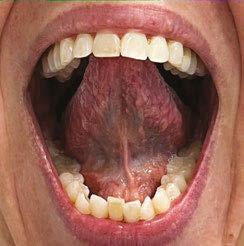
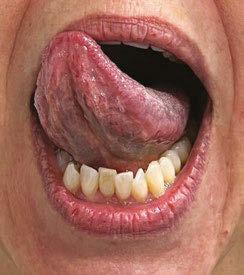
damage.3 As critical as this one symptom is, a restricted lingual frenulum is one of over a dozen structural and functional symptoms of an OMD. For those who treat sleep disor dered breathing (SDB), this is a critical but new understanding. “Orofacial myofunction al disorders can serve as clinical markers for SDB and include the following structural and functional symptoms: enlarged tonsils; elon gated uvula; narrow maxillary arch; tongue scalloping; restricted lingual frenum; orofa cial pain with or without headache; interden talized speech sounds (/s, z, t, d, n, l/); ab normal swallow patterns; impaired chewing; and picky eating.”1
Correcting the lingual structure, through frenectomy or frenuloplasty, does not nor malize lingual function. It won’t normalize the swallow or change breathing. It won’t end picky eating and it won’t resolve sleep apnea. It is generally accepted that surgeries impacting skeletal muscles require rehabili tation afterwards, and that includes the face and mouth. Rehabilitation ensures wound healing only, it does not teach normal func tion. That is the goal of oromyofunctional therapy (OMT).
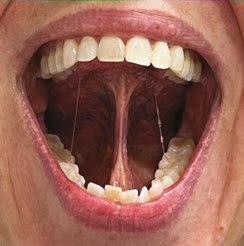
An OMD evaluation is an assessment of bony and soft tissue structure, including oral restrictions. It is an assessment of facial and oral function when at rest and sleeping, when swallowing, and when communicat ing. If performed by a speech-language pa thologist, it will include a feeding, voice,
and a speech sound assessment. Evaluation of lingual coordination and range of motion, especially the posterior tongue’s ability to el evate away from the mandible and fit com fortably in the posterior palate, is critical for sleep breathing.
Effective and efficient OMT, including pre and post lingual frenectomy care, is depen dent on a differential diagnosis and individ ualized treatment planning. Most patients want to get off CPAP – or better tolerate it, and reduce the triggers that interrupt good quality sleep.
My pre/post frenectomy routine is some thing that any three-year old can learn and every parent can understand. The patient must participate in their own post-procedural care. Developing that ability might take three sessions for one patient and ten for another. My experience preparing children and adults for this procedure for twenty years has been that what a patient does before the frenecto my is exactly what they will do afterwards. Surgery on a patient that is not ready increas es the likelihood of a less than optimal out come and the need for a secondary proce dure. Timing is everything.
Even in infants, the timing of lingual frenec tomy is critical to immediate and long-term success. Timing of lingual frenectomy, palatal expansion, and other oral interventions is its own topic).4 The timing of lingual frenectomy with maxillary-mandibular advancement sur geries is not generally agreed upon and does not have a robust research base.
The routine below is part of my diagnos tic process; it is what I teach patients that may not want frenectomy, it is what I teach before referral, and it’s what I teach to my many patients who had frenectomy in the past. Some of my patients are so restricted, they can barely manage this routine, so it is more important for them to intellectually un derstand normal function prior to referral. I break things down into five activities, exer cises, strategies, techniques, postures – what ever term fits your schema.
1. Unsupported stable extension. I call it a “diving board” since many of my re stricted patients have more of a “water slide” presentation. The mouth needs to be open, and the lips and teeth should
not support the tongue blade. This pos ture requires stability and balance of the extrinsic muscles of the tongue. This can be initially tricky if the tongue is flac cid or maintains a wide posture in the mandible.
2. Extended lateralization with an open stable mandible. I refer to this simply as “side to side” and with children I often teach this with a preferred flavor in the corners of the mouth. The goal is that the tongue moves independently from the mandible. This task, when slowed down, can support extension.
3. Elevation to the rugae/alveolar ridge with open jaw and (in my clinic) elevated posterior retraction with open jaw. In speech, these are essentially the sounds /el/ and /ar/ in the American English dia lect. The anterior elevation is both a di agnostic and therapeutic task for anterior restriction. The second posture I highly recommend, since a large segment those with posterior tongue tie languish for years in school speech therapy without proper diagnosis or treatment.
4. Circumlocution around lips, around teeth, and around the cheeks. Cleaning and clearing the oral space are the pri mary functions of the tongue after a safe swallow. In an exercise program, I would refer to circles around lips (always with an open jaw), circles around the outsides

Tongue elevation
Tongue lateralization

Linda D’Onofrio, MS, CCC-SLP, has a private practice in Portland, Oregon focusing in craniofacial disorders, oromy ofunctional disorders, feeding disorders and dysphagia, and sensory-motor speech disorders. She completed her Masters at the University of Oregon, her medical externship at the Or egon Health Sciences University Medical Center with a focus on inpatient neurological acute care and outpatient cognitive rehabilitation, and she completed her clinical fellowship at the Oregon VA Medical Center with a focus on dysphagia, aphasia, brain in jury, and oral cancer. In 2019, Linda published in the journal Orthodontics & Craniofacial Research, and she was awarded the most downloaded article for the journal that year. She participates on a local craniofacial team and on a lo cal sleep neurology team, and she has reviewed manuscripts for the Journal of Oral Rehabilitation and Folia Phoniatrica et Logopaedica. She is a member of the American Speech-Language Hearing Association, a past president of the Oregon Speech-Language Hearing Association, and she has lectured on oral physiology at several dental and orthodontic programs, including Stanford, Tufts, and the Vienna School for Interdisciplinary Dentistry.
of the teeth (with a big smile) and sweep ing the vestibules and sulci. Even when cleaning inside a molar, I encourage cir cular motions rather than sweeping ones to engage the intrinsic muscles of the tongue.
5. Full-blade lingual-palatal suction with wide open jaw. If you only perform one task, this should be it, as it engages many lingual and facial muscles and is the ex ercise that it critical to generalizing stable saliva swallows. Teaching this task can be tricky for some and depends on cra niofacial shape, jaw alignment, maxillary height, tori, degree of bruxing or lack of molar eruption. Function and structure depend on each other.
I’ve seen various recommendations on the time and length of treatment. My clini cal experience has been that a few minutes of engaging in these activities 3-5 times per day, for a minimum of a month post proce dure results in optimal healing and signifi cantly improved, if not normalized range of motion. I measure this several ways. Objec tively, I assess pre and post treatment mea surements for maximum mouth opening, open with elevated lingual tip, and open with full lingual-palatal suction. I am looking for as close to a 1:1:1 ratio as is appropriate for that patient. But I am re-assessing much more, including breathing, and swallowing at rest, during sleep, and during meals. I may have other feeding, chewing, articulation, or voice objectives. My work is often aligned with other medical and dental providers, so my success is measured by how efficiently and effectively my team members meet their goals. And most importantly, my outcomes are considered successful when my patient is satisfied, and their health has improved in a measurable way.
• To keep it simple for small children, I tell them their tongue can go out, it can go side to side, it can go up and down, it can go round and round, and it can suction to the roof of our mouth. (It can do so much more, but this is just for rehab.)
• To keep it functional for the many children with neurocognitive differences, much of this routine can be accomplished effectively with a peanut butter and jam
sandwich and a glass of chocolate milk. I always sit side by side in a mirror (or on zoom) with my patients so we can see ourselves and each other.
• To keep it relevant for adults, I show how these tasks are related to normal muscle function that reduces or eliminates ap nea triggers, helps with the mastication of foods, and improve speech clarity. I use language that they can relate to and connect strategies to their personal objec tives.
• My more mature patients get excited when I explain that these exercises tone the face and neck, make eating denser foods more enjoyable, and they are much cheaper and more effective than fillers for maintaining a youthful face.
All medical and dental providers need to screen and refer for ankyloglossia if they do not diagnose and treat it themselves. Validated protocols for diagnosing ankylo glossia include the Marchesan Lingual Fren ulum Protocol for children and adults from 2012,5 the Lingual Frenulum Protocol for Infants, updated in 2019,2 and the FAIREST 6 for children and adults.6 Multidisciplinary intervention of anatomical and physiological dysfunction should be the gold standard of care. Structural providers, including sleep dentistry and orthodontics, should collab orate with oromyofunctional providers like speech-language pathologists, occupational therapists, physical therapists, and specially trained dental hygienists to address the un derlying causes of dysfunction and maximize patient outcomes.
1. Archambault, N., Healthy Breathing ‘Round the Clock. ASHA Leader 2018 Feb 1. https://leader.pubs.asha.org/doi/10.1044/ leader.FTR1.23022018.48
2. Campanha SMA, Martinelli RLC, Palhares DB. Association between ankyloglossia and breastfeeding. Codas. 2019 Feb 25;31(1):e20170264. doi: 10.1590/2317-1782/20182018264. PMID: 30810632. https://www.scielo.br/j/codas/a/bxq8mdhZ wXvnxkxCCyyBHGf/?lang=en
3. D’Onofrio, L., Oral dysfunction as a cause of malocclusion. Orthod Craniofac Res. 2019;22(Suppl. 1):43-48. https://on linelibrary.wiley.com/doi/10.1111/ocr.12277
4. D’Onofrio, L., Coordinating orthodontics, oral surgery, OSA and oromyofunctional therapy. The Orofacial Myofunctional Lecture Series, 2020 July; Vimeo online. https://vimeo.com/ ondemand/orthooralsurgosaandomt
5. Marchesan IQ. Lingual frenulum protocol. Int J Orofacial My ology. 2012 Nov;38:89-103. PMID: 23367525. https://ijom. iaom.com/cgi/viewcontent.cgi?article=1063&context=journal
6. Oh, Zaghi, et al. Determinants of Sleep-Disordered Breathing During the Mixed Dentition: Development of a Functional Air way Evaluation Screening Tool (FAIREST-6). Pediatr Dent. 2021 Jul 15;43(4):262-272. https://www.fairest.org/tools/

The catenation above is most often read as THE FUTURE IS NOWHERE. But it can and should be read as THE FUTURE IS NOW HERE!
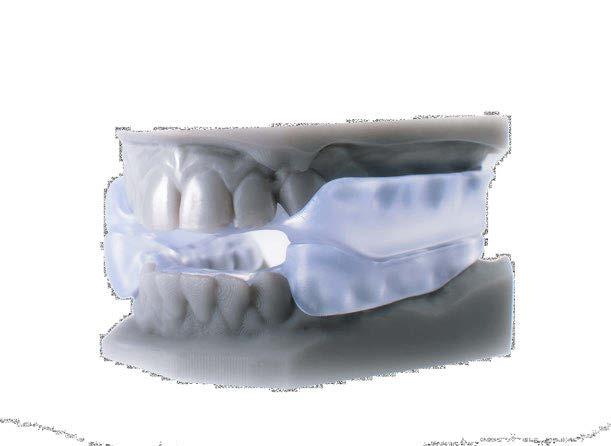
ProSomnus’ inaugural annual meeting, ‘ProSleep 2022 Users Conference’ was a shining example of just how NOW that future really is! The theme of ‘Making SHIFT Happen’ was on full display. Imagine a DSM in which preci sion OAT (like that engineered by ProSomnus) provides efficacy on par with CPAP for mild and moderate patients. Where adherence combines to offer a more effective treatment than positive pressure. Where design minimizes side effects, comfort is excellent, and repair and breakage are rare. Well, that FUTURE IS NOW HERE! P-OAT or precision Oral Appliance Therapy has become the new standard of care providing more patients with better outcomes than traditional custom devices. It gets better. The likelihood that ProSomnus® EVO™ could become the first P-OAT to be cleared for first line use for severe patients and robust sensor technology on the horizon will be transformational to Dental Sleep Medicine.
The fabulously elegant San Francisco Fairmont served as the backdrop for two days of intense evidence-based lectures, panels, and 25-minute TED-like talks. Dr. Olivier Vanderveken walked the room through the early results of the First Line OSA Therapy Study in Belgium. Designed to show that precision OAT can serve as an effective first line treatment for moderate and severe OSA and demonstrate patient preference. Hypoxic burden as the
next, perhaps more appropriate metric than AHI, was featured by Dr. Reza Radmand and his study at Harvard using precision OAT. Dr. John Remmers painted a picture of how precision OAT ‘WILL’ cross the chasm and become the new Gold Standard for effective OSA treatment. For a full list of topics and speakers, contact ProSomnus at Events@Pro Somnus.com. Visit ProSomnus.com for the ProSleep 2023 Save the Date, coming soon!
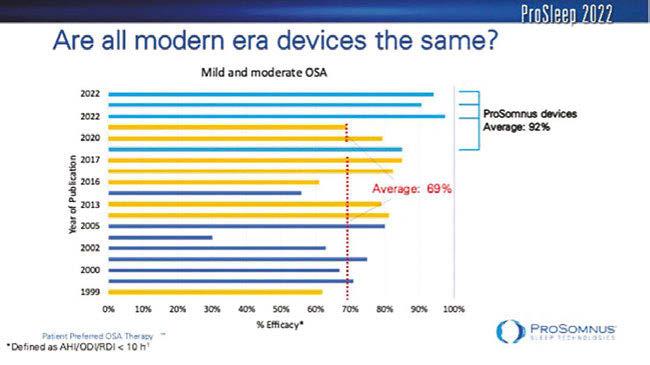
Dr. Erin Mosca, PhD’s presentation stim ulated lengthy discussions at breaks and at evening dinners. Her data analysis of pub lished studies framed first, how the AASM treatment guidelines came to be and have evolved, and second, how much better the efficacy and ergo effectiveness of precision OAT is. Her literature review of Efficacy, Adherence and Durability demonstrated that only recently have precision devices shifted the preponderance of evidence to support first line therapy use. Studies using custom non-precision devices, demonstrated 69% efficacy for mild and moderate compared to 92% for ProSomnus precision devices.
Similarly for severe cases, the custom non-precision devices demonstrated 50% efficacy compared to 63% for ProSomnus. This helps us position precision treatment to be comparable to CPAP and more effective. We now need randomized control trials to demonstrate the impact on outcomes and relevance of metrics. ProSomnus EVO may be uniquely positioned to become the first oral appliance to acquire a severe clearance indication for use.
If we want to cross the great divide with medicine, we must think, act, and be more like them. That includes making clin ical decisions based on what is best for the patient. Better efficacy and adherence along with durability and fewer side effects should be the goal. Today, the preponderance of evidence points us in the direction of preci sion OSA therapy. The resultant effectiveness is making it the preferred choice; not just of patients and providers, but ultimately physi cians and payers too…and that makes SHIFT HAPPEN!

 by Peter J. Catalano, MD, and John Walker, DMD
by Peter J. Catalano, MD, and John Walker, DMD
Abetter understanding of ADD and ADHD symptoms and a new way to reverse them has given new found hope to the parents of children who struggle with behavioral issues and learning disabilities in school and at home. The solution, according to recent medical research, is surprisingly simple and yet frustratingly elusive: healthy, unbroken sleep.
The key word in that phrase is “unbroken.” While parents do commonly strive to ensure that their children sleep for the recommend ed 8 to 10 hours each night, very few can at test to the real quality of that sleep. Increasing evidence is now coming to light that certain children with attention related or behavioral disorders can be treated without medication. The real culprits behind their behavior? Inter rupted sleep due to nasal obstruction.
The key to great sleep is healthy breath ing through the nose. Not all breath ing is equal. Many children with narrow or blocked nasal passag es are forced to breathe through their mouths all or part of the
time. For many, the nasal obstruction only oc curs at night. When the children lie down and fall asleep, their nasal tissues swell and their throat muscles relax making an already small airway even tighter. They don’t get the oxygen they need and effectively start to suffocate. The body goes into panic mode and partially reawakens not enough for the child to regain consciousness, but just enough for the throat muscles to reopen the airway.
The issue lies in the body’s need to arouse itself repeatedly throughout the night. When a sleeping child’s body reawakens, the child then gets the oxygen they need. The reawak ening occurs in response to adrenaline, the body’s natural stimulant that can be secret ed by our adrenal glands numerous times an hour in order to keep the child breathing. The child is forced into something called “sym pathetic dystrophy,” which basically means that they become over stimulated.
Hours of such chemical stim ulation during sleep leads to an anxious, hyperactive, unfocused child during the day. This is why we com
monly see young patients filled with nervous energy. Parents tell us that their son or daugh ter just can’t keep still. That’s the adrenaline at work; the repeated awakenings also cause the child to miss out on a complete sleep cycle. This happens over and over all night long. By morning, the child has failed to reach the deepest cycle of sleep and over the years this can have catastrophic consequenc es on behavior, physical health, and intellec tual development.

This chronic sleep problem, known in the medical community as “Sleep Disordered Breathing” (SDB), has begun to receive more and more attention in recent years as the number of ADD and ADHD diagnoses have skyrocketed. The symptoms of Sleep Disor dered Breathing in children are one cause of ADD and ADHD, and it is currently unclear how many children have sleep deprivation. For example, SDB symptoms can include problems such as hyperactivity, shorter atten tion spans, unexplained anger or depression, and poor school performance – all traditional hallmarks of ADD or ADHD. Children suffer ing from SDB may also exhibit other easily overlooked symptoms, including snoring, bed wetting, slouched posture, poor appe tite, messy eating habits, headaches, and fre quent open mouth breathing.
For many of the children their behavior-re lated struggles turn out to be a direct result of ongoing sleep deprivation. It is important to note that tiredness can also be a symptom of poor sleep, but it is mostly limited to older children and adults.
As years of improper sleep progress, a child’s symptoms can also begin to reveal more lasting damage. The deepest cycles of sleep are when a child’s body develops physically, emotionally, and intellectually. If enough time passes without healthy sleep, you can see issues like delayed cognitive de velopment, stunted physical growth, and ab normal upper and lower jaw development. The latter ultimately leads to orthodontic and dental problems.
New research coming out about sleep deprivation has emerged, surprisingly, from
the field of dentistry or more specifically, from a dental subfield called “Airway Ortho dontics.” Instead of simply correcting crook ed teeth with braces and sending patients on their way, more and more orthodontists have begun to ask a previously unconsidered question: Why are teeth getting crooked in the first place? The answer, it turns out, is the same root cause behind sleepless nights: mouth breathing brought on by a blocked nasal passage. In fact, studies show that over 90% of children with crooked teeth, teeth grinding issues, or poor jaw alignment also have compromised nasal breathing.
You really cannot overestimate the im pact that nasal breathing has on facial devel opment. Constant airflow through the mouth puts inward pressure on the jaw and teeth. This keeps the jaw from growing properly. Eventually, we end up with a child whose narrow jaw and face can’t hold all their adult teeth. From there, you can suffer from all types of orthodontic problems.
What does a narrow jaw have to do with sleep, though? Your jaw affects the size of your airway passage, thus if your jaw doesn’t develop to its proper width, then your airway is going to be too small for healthy breathing, especially when you lie down at night. Pa tients usually begin with a blocked nose and start mouth breathing at a young age (i.e.1 year to 4 years old). By the time they require braces, they’ve effectively been damaging their bodies and their airway for years.
The vast majority of children with Sleep-Disordered Breathing have nasal air
way obstruction that results in mouth breath ing that may be present day and night, or just when the child lies down. The latter occurs as fluid that had been drained out of the na sal tissues by gravity during the day, re-enters the nasal tissues when the child lies down and loses the benefit of gravity.
We are not supposed to breathe through our mouths at any time. Our noses have evolved to do a better job of breathing in almost every way from filtering impurities out of the air you breathe, to warming and humidifying the air for your body, to giv ing you a sense of smell. But when a child can’t breathe through their nose, they have no choice but to resort to mouth-breathing instead. From there, all sorts of problems arise.
The first step in helping a child, therefore, is to identify and correct any blockage in the nose. Possible reasons for nasal obstruction include anatom ical deformities, septal deviations, enlarged septal swell bodies and/or turbinates, enlarged adenoids, or en vironmental allergies. It’s not uncom mon for orthodontic patients to con sult with other specialists depending on what the dentist sees during their exam and sinus/airway CT scan. The latter is now commonplace in airway orthodontics. If the orthodontists see nasal and/or sinus prob lems, or large adenoids or tonsils, they will recommend an otolaryngology consult.
The correction of nasal obstruction in a child can be challenging due to the small size of the nasal passages and the severity of the intranasal deformities encountered. In addi tion, many ENT doctors simply focus on re moving the child’s adenoids and/or tonsils in an attempt to improve their breathing during sleep. However, studies have shown that only 1/3 of children with SDB are cured after T&A, with the rest requiring surgery on their nasal passages. We have pioneered many of the procedures to correct nasal obstruction using minimally invasive techniques that al low children and adults to return to school or work within 24 hours of surgery. There is no nasal packing or external evidence of surgery, and most children do not even re quire Tylenol after surgery. This newly devel oped ability to correct nasal obstruction in children, coupled with the breakthrough in understanding how ADD and ADHD devel
op from poor sleep, have revolutionized our treatment of this condition.
After healthy nasal breathing gets re stored, the orthodontist then begins the second important aspect of treatment: en suring proper jaw growth. The ideal time to help a child is before their jaw has finished growing. This allows the use of non-surgical and non-invasive methods to guide the jaw growth natural and wide enough to promote a healthy sized airway.
Typical orthodontists don’t see a child un til age 11 or 12, when their facial growth is already 90% complete. Airway Orthodontists argue that this is far too late. Even a 4-yearold has already completed 60% of their fa cial growth, thus the sooner a child can be seen, the easier it will be on them. However, this doesn’t mean hope is lost for a preteen, teenager, or even an adult with Sleep Disor dered Breathing. It’s never too late to address a breathing problem, it just may get more dif ficult to correct, but there are still treatment options.
While Sleep-Disordered Breathing has begun to receive more attention recently, only a small percentage of pediatric doctors are able to recognize the symptoms. We have amazing pediatric doctors out there taking care of children, but unfortunately they just haven’t been made aware of the opportunity to correct SDB through minimally invasive nasal surgery and proper orthodontic care. You combine that with the fact that SDB pro duces ADD or ADHD symptoms, and you end up with great doctors who are simply misdiagnosing some of their patients.
What can parents do in the meantime? “Keep an eye out for sleep deprivation symp toms in your child, and don’t be afraid to seek out a second or third opinion from an Airway Orthodontist or a pediatrician who keeps up with recent medical research on childhood sleep, especially if your child has been diagnosed with ADD or ADHD. There is a chance that your child’s issues are in fact reversible without needing medication or therapy. The improvements in these patients can be nothing short of life changing.
Republished with permission: Catalano PJ, Walker J. ADD & ADHD in Children: The Answer is Right in Their Nose. Am J Otolaryngol Head Neck Surg. 2018; 1(5): 1025.

The first step in helping a child is to identify and correct any blockage in the nose.



 by Colonel Scott Williams, MD, FAASM
by Colonel Scott Williams, MD, FAASM
Sleep and mental health are inextricably linked, and there is a large volume of evidence looking at the various rela tionships across disease states. While it is impractical to provide an exhaustive review of the literature here, this article will focus on a few of the more common psychiatric diagno ses and how they both impact and are impacted by sleep. As we know, there are three states of being. We are either awake, in Non-Rapid Eye Movement (NREM) sleep, or we are in REM sleep.1 There are a variety of neurotransmitters that affect both wake and sleep (Figures 1-3) and it is no coincidence that many of these neurotransmitters are the same ones affected by psychi atric disorders.2
Psychiatric conditions can change the rel ative percentage of time during a 24 hour pe riod that we are in these three states, and in so doing, markedly impact the subjective ex perience of the patient. In contrast, treatment of psychiatric conditions may also change the proportion of time spent in each state in a way that is different than those who are in remission.

Impaired sleep is a hallmark feature of depression and is a diagnostic criterion in the Diagnostic and Statistical Manual of Mental Disorders.3 It is estimated that 20-30% of pa tients suffering from Major Depressive Disor der (MDD) have difficulty falling or staying asleep.4,5 In addition, those with depression have been observed to have decreased REM latency.6 In contrast, serotonergic medica tions such as serotonin reuptake inhibitors (SSRIs) or dual serotonin and norepinephrine reuptake inhibitors (SNRIs) prolong REM la tency to a greater extent than is seen in those without depression.7 This can be understood when looking once again at the CNS neu rotransmitters and their impact on the var ious states of being (Figure 2: REM on and REM off neurons).
Figure 1: Neurotransmitters involved in REM sleep
Some antidepressants may also worsen sleep disorders such as insomnia. Bupropion, for example, is a dopamine and norepineph rine reuptake inhibitor (DNRI). There are different formulations of bupropion, and the shorter acting formulation, when taken too
close to bedtime, may increase overall sleep latency.8
While antidepressants have shown clear benefit in reducing many of the sequelae of depression, it is less clear whether the change in REM latency has a direct impact on overall subjective sleep quality and few studies have directly linked SSRI use with sleep improve ment.9 It is also unclear whether psychother apy, which in itself does not alter REM laten cy other than to return it to the premorbid state, has a differential impact on sleep when compared with medication management.

It can be difficult to determine the cause-effect relationship between sleep and depression because there is often a vicious cycle whereby one condition worsens the other. In some patients without a history of depression, there is data showing that the de velopment of a sleep disorder may increase the risk of subsequent depression. Just as many depressed individuals endorse insom nia, insomnia itself is a risk factor for the development of depression with an overall odds ratio of 2.1.10 One of the most common sleep disorders, Obstructive Sleep Apnea (OSA), causes profound sleep fragmentation and has been shown to increase the risk of subsequent MDD.11 There is scant data re garding the impact of OSA treatment on de pression, however. The few studies that have been conducted have shown a benefit with CPAP. El-Sherbini and colleagues found in a small population that the Hamilton Depres sion Rating Scale scores pre and post CPAP were significantly different.12
• GABA (VLPO)
Orexin (PLH)
Histamine (TMN)
Acetylcholine (LDT/PPT)
Serotonin (DR) Noradrenaline (LC) Dopamine (vlPAG)
Figure 2: Neurotransmitters involved in NREM sleep
There is even less data assessing the impact of mandibular advancement device (MAD) therapy in patients with OSA-induced depression, and there are no high-quality data discussing the relative impact of CPAP vs. MAD on depression.13 This is a critical gap in the literature and is deserving of sig nificant attention.
Bipolar disorder is a mental disorder characterized by shifts between depression and overly energetic, irritable or impulsive moods.2 The impact of bipolar depression on sleep quantity is largely the same as unipolar depression, but bipolar mania reduces sleep in a different way. Whereas in depression, patients often feel fatigued but have trou
Na tional Military Medical Center in 2012. Upon graduation from fellowship, Dr. Williams assumed duties as Chief of Sleep Medicine at Womack Army Medical Center. While there he served on the AASM Education Committee and obtained an academic appointment as assistant professor of medicine at USUHS, later rising to the rank of associate professor of Medicine (primary) and Psychiatry (secondary). He increased his involvement with the AASM after returning to WRNMMC to take charge of the Sleep Disorders Center. He is now the chair of the Sleep Technologist and Respiratory Therapist Education Committee and is part of the gold standard panel for the Inter-Scorer Reliability program.
 Colonel Scott Williams, MD, FAASM, is the director for Military Psychiatry and Neuroscience at the Walter Reed Army Institute of Research. LTC Williams was born in Bournemouth, England and was raised in Princeton, New Jersey. He graduated and was commissioned into the U.S. Army from The University of North Carolina at Chapel Hill in 2000. LTC Williams received his medical doctorate from the Uniformed Services University of the Health Sciences in 2004. He completed a dual residency in Internal Medicine and Psychiatry at the Walter Reed Army Medical Center in 2009. He completed fellowship training in Sleep Disorders Medicine at the Walter Reed
PLH BF VLPO TMN
DR LDT/PPT vlPAG LC
Colonel Scott Williams, MD, FAASM, is the director for Military Psychiatry and Neuroscience at the Walter Reed Army Institute of Research. LTC Williams was born in Bournemouth, England and was raised in Princeton, New Jersey. He graduated and was commissioned into the U.S. Army from The University of North Carolina at Chapel Hill in 2000. LTC Williams received his medical doctorate from the Uniformed Services University of the Health Sciences in 2004. He completed a dual residency in Internal Medicine and Psychiatry at the Walter Reed Army Medical Center in 2009. He completed fellowship training in Sleep Disorders Medicine at the Walter Reed
PLH BF VLPO TMN
DR LDT/PPT vlPAG LC
While neurophysiology and the interplay between psychiatry and sleep is complex, there are a few basic tenets that must be understood. First, each patient must be treated holistically. Second, it is important to treat these conditions in parallel, not in series.
must each be treated separately. Second, it is important to treat these conditions in par allel, not in series. Too often we see patients who are being treated for depression in the hopes that this will fix their chronic insom nia, or patients being treated for OSA in the hopes that this alone will allow their depres sion to remit. Each condition must be treat ed simultaneously, and once subjective and objective response is achieved, the treatment plan can be tapered.
ble transitioning to sleep, in hypomania or mania, patients lack the desire or need for sleep.1 During manic episodes, patients may not be aware that they are lacking the restorative properties of sleep. There are studies showing that toxic proteins can accumulate in patients with bipolar disorder, leading to neurodegeneration, and the cyclic lack of sleep may be a key part of this pathology.14 Treatment of bipolar disorder may slow this neurodegeneration, but currently there is lit tle evidence to show the absolute magnitude of the benefit.
While neurophysiology and the interplay between psychiatry and sleep is complex, there are a few basic tenets that must be un derstood. First, each patient must be treated holistically. Do not assume that treatment of one condition will completely treat another. Co-morbid sleep and psychiatric disorders
For dental sleep practitioners especially, it is important to recognize the association between emotional reactivity and sleep dis orders. One of the great advantages of den tistry over most medical clinics is the amount of time spent with a patient. If patients seem highly anxious, have a decreased tolerance for pain, or a heightened gag reflex, it is ab solutely appropriate to ask about other areas of hyper-reactivity in their lives.
1. Principles and Practices of Sleep Medicine, 6th Ed. Kryger MH, Roth T, Dement WC, eds. Elsevier, 2016.
2. Bassetti CL, et al. Neurology and psychiatry: waking up to op portunities of sleep. State of the art and clinical/research priori ties for the next decade. Eur J Neurol 2015;22:1337-54.
3. American Psychiatric Association (2013). Diagnostic and statis tical manual of mental disorders (5th ed.)

4. Buysse DJ, Angst J, et al. Prevalence, course and comor bidity of insomnia and depression in young adults. Sleep 2008;31(4):473-80.
5. Ohayon MM, Caulet M, Lemoine P. Comorbidity of mental and insomnia disorders in the general population. Compr Psychiatry 1998;39(4):185-97.
6. Kupfer D, Foster FG. Interval between onset of sleep and rap id-eye-movement sleep as an indicator of depression. Lan cet 1972;300:684-6.
7. Chen C-N. Sleep, depression and antidepressants. Br J Psychia try 1979;135:385-402.
8. Gandotra K, Jaskiw GE, Williams SG, et al. Development of insomnia associated with different formulations of bupropion. Prim Care Companion CNS Disord 2021;23(1):20br02621.
9. Everitt H, Baldwin DS, Stuart B, et al. Antidepressants for insom nia in adults. Cochrane Database Syst Rev 2018;5(5):CD010753.
10. Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epide miological studies. J Affect Disord 2011;135(1-3):10-9.
11. Harris M, Glozier N, Ratnavadivel R, Grunstein RR. Obstructive sleep apnea and depression. Sleep Med Rev. 2009;13:437–44.
12. El-Sherbini AM, Bediwy AS, El-Mitwalli A. Association between obstructive sleep apnea (OSA) and depression and the effect of continuous positive airway pressure (CPAP) treatment. Neuro psychiatric disease and treatment, 2011.
13. Povitz M, Bolo CE, Heitman SJ, et al. Effect of treatment of ob structive sleep apnea on depressive symptoms: systematic re view and meta-analysis. PLoS Med 2014,11(11):e1001762.
• Orexin (PLH)
• Histamine (TMN)
• Acetylcholine (LDT/PPT)
• Acetylcholine (BF)
• Serotonin (DR)
• Noradrenaline (LC) • Dopamine (vlPAG)
14. Naserkhaki R, Zamanzadeh S, Baharvand H, et al. cis pT231Tau drives neurodegeneration in bipolar disorder. ACS Chem Neurosci 2019;10(3):1214-21
Images inspired by Bassetti et al, European Journal of Neurology, 2015, 22:1337-1354

Q: What do you need from the office to start a case?
A: Many believe that laboratories need more informa tion than usual to design obstructive sleep apnea devices. The good news is this is not the case! As your custom sleep device manufacturer, DynaFlex® only needs a completed Rx form, your patient’s models or scans, and a bite record of where you would like our team to build the appliance. You or the patient can titrate the device to protrude the mandible forward from the start position. Keep in mind: most of these devices do not go backwards; it is always best to be con servative in the starting position. If the bite is too protrusive to start, and the patient cannot tolerate it, you will typically have to send the case back to the lab for a “Bite Reset”.
A: Most importantly, make sure your Rx is filled out com pletely and properly. While this may seem obvious, it’s one of the major causes of delay/case to be put on hold. Sec ondly, please make sure the scans/models are not distorted, and the bite has not shifted. We recommend verifying scans/ models while the patient is in office. Calling the patient back to the office for new records takes up valuable time and delays the case even further. These digital issues are easily avoidable with some simple checks in place. Most labs offer rush services to create devices faster for patients who need theirs quickly.
Keep in mind: most of these devices do not go backwards; it is always best to be conservative in the starting position.
rent position, then reset the hardware so that the patient can go further forward. This usually adds strength to the device, which is essential for heavy bruxers.


A: Many labs offer a “Bite Reset” service, which requires the device to be sent to the lab. They will mount it to its cur-
Have more questions on starting a case for oral appliance therapy? Worried about the details when it comes to a more complex case for edentulous patients? Give our laboratory a call at 1-800-489-4020 and speak to a dental sleep medicine expert – we are here to help!
Q: What if my patient needs to go further protru sive than their sleep device will allow?
Thank you to Dental Sleep Practice magazine for the opportunity to have ProSomnus answer the five most com mon questions about ProSomnus® EVO™. Counting down from number five.


EVO is PDAC verified. The issue is that it is PDAC verified for code K1027, not E0486. CMS is in the process of develop ing a coverage policy for K1027. A growing number of insur ance payors are beginning to cover K1027 as a benefit. We’ll know more later this year. Many of our customers are using a low cost PDAC approved appliance to fulfill the CMS rules and sign the POD for this. They then sell the patient a backup device like ProSomnus EVO, and then execute an ABN for that.
With a 70-degree post/strap/arm or similar mechanism that replicates mandibular rotation, you will lose 1.8mm of advancement if the patient opens 5.0mm. That means, with 70-degree posts you would need more dose/advancement and that could mean less comfort, more side effects and loss of some efficacy.
With Iterative Advancement like this, the numbers on the post indicate where you are at precisely. U0 + L0, is exactly where you took your bite. By trading out the other arches in any combination, the numbers add up to where you are in relation to that point. U0 + L1, would be forward 1.0mm, U2 + L0 would be forward 2.0mm, U2 + L1 would be 3.0mm, and so forth. You can even move backward if you accidentally started too far forward or if the patient develops muscle or lig ament discomfort. U-2 + L0 would be 2.0mm more retruded, then U-2 + L1 would be 1.0mm retruded. All very precisely.
2. ProSomnus EVO is comparable to other premium priced devices…but you say it can save me money?
EVO saves delivery time, has fewer side effects, less break age/repair, better compliance, and best-in-class outcomes.
Precision solutions like this have the potential to save your practice so much TIME, they can be considered the LEAST expensive device solution. ProSomnus takes great pride in being a Class II Medical Device Manufacturer. We accept the additional regulatory, testing and reporting requirements that accompany that responsibility. We invest in making devices with bite transfer precision (articulator mounting), accuracy in advancement, and with the smallest volume. We utilize best-in-class materials, including MG6™ Technology for our ProSomnus EVO products that are stronger, safer, and more biocompatible. All this serves our customers and patients with the best efficacy and adherence. Plus, we want to delight phy sicians and payers, so they appreciate the value of better, more efficacious, and adherent OAT with precision devices. Lower dose, fewer side effects and first-time fit saves our customers time and money. Other manufactures do not do the amount of research that we do. We are investing in the future of DSM in a way that results in better treatment experiences for the ben efit of patients and our dentist customers. We are proud of our fees, they represent the investment in precision, technology, and better outcomes that our customers have come to expect from us. Not to mention, that patients deserve; physicians will trust, and payers will reimburse better.
If we told you…we would have to, you know. The MG6 Technology is proprietary material resourced and designed using Artificial Intelligence and Robotic Manufacturing in such a way that it provides the most precise fit, bite trans fer, and biocompatibility of any material used today. The great success we continue to enjoy with the milled PMMA material is even better with the slightly flexible, more for giving, most biocompatible material. In the FDA MAUDE database (Manufacturer and User Facility Device Experience Complaint Database), 95% of the complaints were from 8 other manufacturers. 59% of those complaints are traceable to biocompatibility/hypersensitivity/allergic/inflammatory reactions. None of those were ProSomnus materials. In fact, 100% of them were cold cured/bench acrylics, Thermacryl, and soft liner materials.
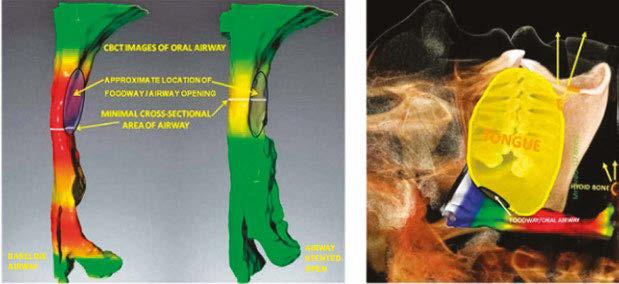
This self-instructional course for dentists aims to present the anatomic rationale for bilateral molar stabilization, an innovative alternative resulting in parallel arches that in fact establish a di lated posterior oral airway.
Two basic design principles for oral sleep apnea devices are: prevent collapse of the tongue on the pharynx and establish oral airway dilation (OAD). Commercially available devices for regis tering the interarch jaw relationship are based on anterior or in cisal stabilization, almost universally resulting in slant, an acute angle between the maxillary and mandibular teeth narrower at the posterior than the anterior, and a negative for OAD.
Dental Sleep Practice subscribers can answer the CE questions online at https://dentalsleeppractice.com/continuing-education/ to earn 2 hours of CE from reading the article. Correctly answering the questions will demonstrate the reader can:
1. Think three-dimensionally about the condylar position during bite registration 2. Reliably provide sufficient inter-arch space for device fabrication 3. Gain confidence in setting expectations for patient accommoda tion to oral appliance therapy
Human beings are the only mammals to have a shared foodway and airway. As a result, adult humans cannot breathe and swallow at the same time. Therein the human species is unique in its tendency to succumb to Obstructive Sleep Ap nea (OSA), a disorder having morbid health con sequences. OSA is a series of nocturnal periodic collapses of the tongue into the airway, causing obstructions.
It is known that the diameter and volume of the pharynx can be dilated and stented by appli ances that reposition parts of the oral apparatus. Dilation refers to getting the airway enlarged and stenting is keeping it open. Airway support during sleep is dependent on complex coordi nation of the interaction between the local bony architecture, neural, muscular, vascular, liga ments, cartilaginous disc and soft tissue.
Normal interarch jaw position varies de pending on the biological function being carried out, such as mastication, breathing, swallowing, incising, speaking, and screaming. Each distinct function utilizes different combinations of mus cle activity and different muscle pressures. Each person has a unique combination of facial fea tures and facial muscle alignment.
The interarch relationship for an intraoral sleep appliance is not a normally sustained biofunctional position for the mouth. The ide al interarch jaw position for an oral sleep ap pliance is optimal airway dilation and stenting with the lips comfortably closed. Four specific dimensions need to be considered to determine effective treatment position with an oral sleep appliance: protrusive, lateral, vertical and slant.
Figures 1A-1B: A: The oropharynx has no bony support walls, anatomy unique to humans. It is a soft tissue tube, not in the mouth but behind it. B: Directions the mandible can be manipulated and proximity of tongue to airway. CT renderings with superimposed illustrations.
In an anterior stabilized interarch jaw regis tration, the acute angle seen between the plane of the mandibular teeth and the plane of the maxillary teeth is referred to as slant. It will al
ways be narrower at the posterior than ante rior. Understanding slant can affect the reg istration of the interarch jaw position for an intraoral sleep appliance.
Slant can affect airway size and patency. Slant can often be changed, depending on how the mandible is stabilized relative to the maxilla in registering the interarch jaw posi tion for an intraoral sleep apnea appliance. Stabilization in the anterior incisor area will usually result in a different interarch jaw rela tionship, or slant, than from jaw stabilization in the molar area. Slant in a sleep appliance can compromise posterior airway diameter and volume, while simultaneously increas ing anterior opening, making lip closure dif ficult during sleep.
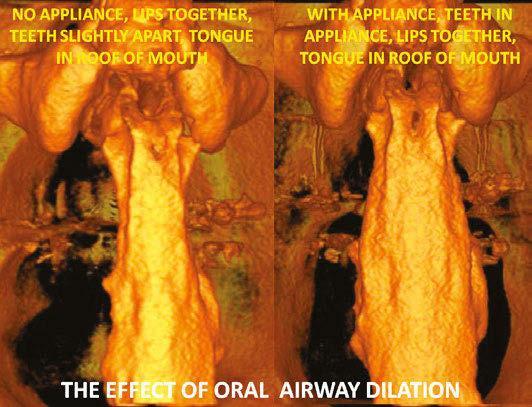

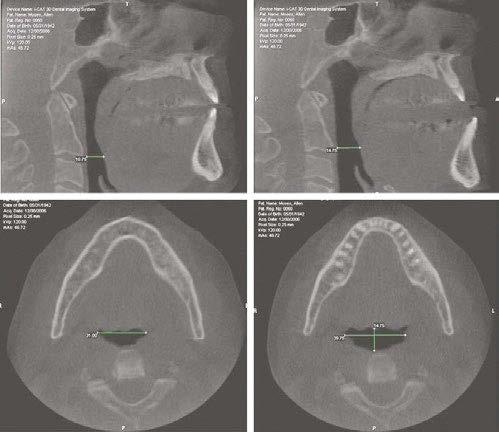
The interarch jaw position registered by an anterior stabilization device sets the man dibular condyles in an anterior and down
ward position outside the temporal fossae (See Figure 2). A hard anterior stabilization device resists jaw closure in the anterior seg ment of the mouth, but there is insufficient resistance to closure of the powerful eleva tor muscles in the posterior (see figure 6). In an anterior stabilized interarch position, the combined power of the masseters, pterygoids and temporalis pivots the condyles and discs back up toward the fossae and creates slant, reducing posterior airway space. Not only does anterior stabilization reduce posterior oral airway space, but the effect on the po sitions of the temporomandibular joints is not always desirable for patients having TMD problems.
Slant seen in an open mouth position with out any stabilization, such as when screaming or biting into a club sandwich is not relevant to design of a sleep appliance for airway dila tion. Such activity is within a normal range of movement and biological function of the oral
Figure 4: Sagittal sketches of three skulls. A. The arches are in centric occlusion. The upper arch is close to a flat plane to match the mandibular posterior teeth and create occlusal surfaces for mastication. B. The dental arches as they would be in the rest position, essentially parallel to each other with no teeth touching. C. Shows functional position as shouting or screaming. The condyles advance out of the tem poral fossae and an angle is created between the maxillary and mandibular arches identified as slant.
apparatus. Holding the jaws in a fixed protru sive position all night beyond the vertical of rest position, in a TMJ position of questionable merit, with excessive muscle stress from the elevators and less than optimal airway dila tion, is not within the normal function of the oral musculature. Slant in the interarch jaw registration for a sleep apnea patient appears to be a suboptimal treatment position.
The mandibular musculature is coor dinated and balanced by a central pattern generator and curbed by proprioceptive re flexes and hard tissue limitations. The neural feedback mechanism is subject to anomalies that lead to an imbalance of the delicate nor mally harmonized muscles. Displacement of the mandible by an anterior stabilized bite registration device disrupts the harmonious function and introduces a disproportionate vertical increase in the anterior segment. With anterior stabilization and its accompa nying slant, achieving the necessary posterior clearance may require introducing so much vertical in the anterior that the lips cannot stay comfortably closed at night and mouth breathing becomes an unwanted sequelae.
A posterior stabilization device posi tioned bilaterally in the molar areas to reg ister the interarch bite position of a sleep apnea patient prevents or completely elim inates slant. The maxillary and mandibular planes are very close to parallel. Vertical height is gained in the posterior, where it is needed to optimally dilate the oral airway. Most of the vertical height is not gained as a consequence of excessive anterior height where its effect may be deleterious. A pos terior stabilization device facilitates normal anatomic TMJ movement in registering the interarch jaw position for a sleep appliance.
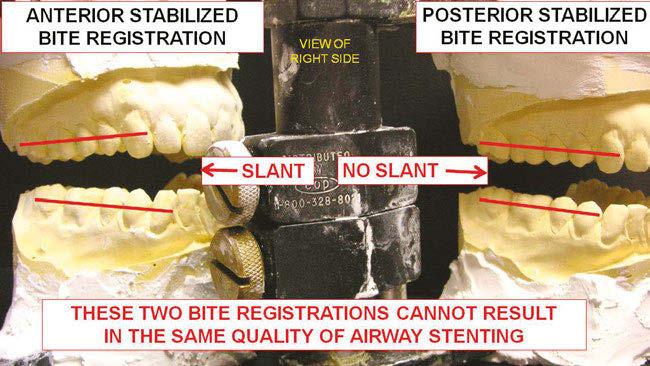
Figures 5A-5B: A. Illustrates that posterior stabilized bite shims result in less slant and probable larger circumference of posterior airway. B. illustrates the importance of adjustable shim placement in the posterior area to reduce or eliminate slant in the interarch jaw registration.
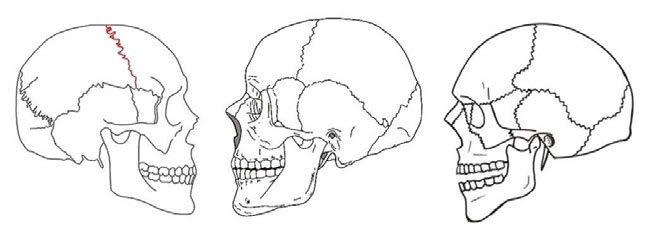
The objective of a dental sleep clinician is to establish a static position of the oro pharyngeal airway components at optimal dilation and stenting. It is a static position because any jaw movement will change the airway dimension. This position is arrived at by manipulating the complex interrelation ship between the temporomandibular joint, hyoid apparatus, elevator muscles and their antagonistic muscles, pharyngeal constrictor muscles, soft palate and tongue.

Oral sleep appliances are about a multi dimensional increase in airway volume; not pure protrusive mandibular advancement. The objective of a dental sleep clinician is to establish a static position of the oropharyn geal airway components of optimal dilation and stenting.

It is a static position because any jaw movement will change the airway dimen sion. This position is arrived at by manipu lating the complex interrelationship between the temporomandibular joint, hyoid appara tus, elevator muscles and their antagonistic muscles, pharyngeal constrictor muscles, soft palate and tongue.
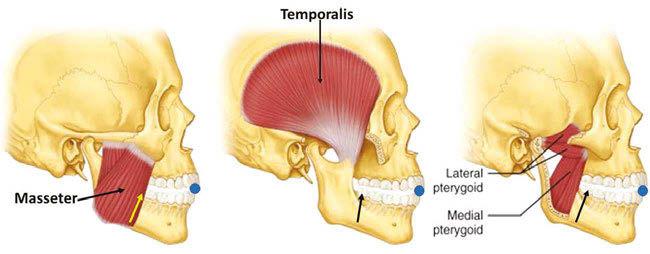
It is not a normal functional position gen erated by the central pattern generator. There is no hard tissue bony support to the pharynx. The sole support for this nonfunctional posi tion is in the interarch jaw registration and the fabricated oral sleep apnea appliance.
Registration of the optimal interarch jaw position presents a complex puzzle for sleep dentists. Finding the ideal position may be different for different face types and different case histories. Face types can change over the lifetime of a patient. Muscles have an abundance of contractile possibilities. Mus cles do not always function in the same way in similar circumstances. The same muscle does not always function the same way in all people.
In sleep apnea patients correct airway size is of paramount importance. In TMD cases correct jaw position is of paramount importance. Many patients may have both TMD and sleep apnea. Posterior vertical dimension may be increased without dis proportionately increasing anterior vertical dimension. There may not be one universal interarch jaw relationship that is correct for all patients.


Anterior stabilization interarch registra tion devices which appear to be the current mainstream method in dental sleep practices pose several difficult biological issues. Not only might anterior stabilization registration devices reduce posterior oral airway space, introducing an effect on the positions of the temporomandibular joints that is not desir able for patients having TMD problems, but they misdirect protrusive movement as much as 95% of the time. The directed movement of anterior stabilized bite registration devic es is unidirectional and not consistent with
Figure 7: The bilateral posterior bite registration device shown here consists of two elements, plastic stackable shims and a cross arch wire shim coupler. The shims can be stacked from 3.0 mm and up, in .5 mm increments. The wire fits in a groove on the top of one shim and is firmly fastened between shims when the shim above it is snapped into place.
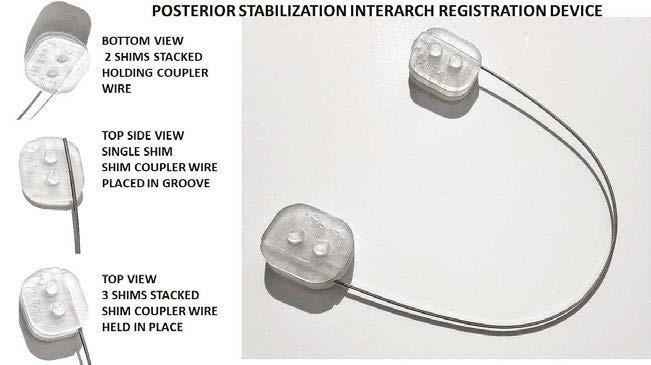
natural jaw movement. It would seem rea sonable to ask if there is another alternative.
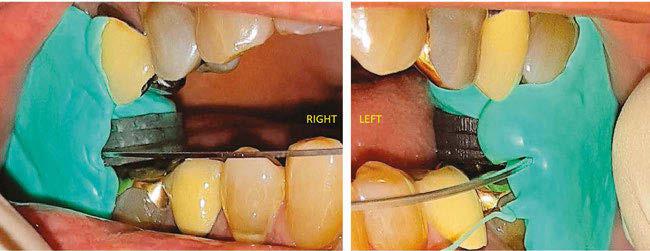
There is certainly logic and anatomical principles that validate using a posterior stabilization device to establish the optimal stented position for an oral sleep appliance. There is nothing that always works. Clini cians cannot always apply the same variables and factors to a universal patient model. Facts were presented here about differentiating an terior and posterior interarch jaw registration techniques. Clinicians now have a complex choice of whether to use anterior or posterior stabilization techniques to register the inter arch jaw position for sleep appliances.
Clinical objective studies are warranted to determine the merit and physiological signif icance of the suggested shortcomings of an terior stabilization devices for registering the interarch treatment position for an oral sleep appliance as well as comparative studies to evaluate whether there is one better registra tion technique for interarch jaw position.

AGD Code: 750
Date Published: November 10, 2022 Course Expires: November 10, 2025 Legal disclaimer: Course expires 3 years after publication date. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 8 CE credits for only $149 by visiting https://dentalsleeppractice.com/subscribe/.
n To receive credit: Go online to dentalsleeppractice.com/continuing-education/, click on the article, then click on the take quiz button, and enter your test answers
To provide feedback on this article and CE, email us at education@medmarkmedia.com.
1. The interarch jaw position registered by an anterior stabilization device sets the mandibular condyles ________.
a. Seated in the middle of the glenoid fossa b. In centric relation c. As far forward as possible d. In an anterior and downward position outside the temporal fossa
2. Holding the jaws in a fixed position of an interarch jaw registra tion is ___________.
a. Within the normally sustained function of the oral musculature b. Manageable for most people, with accommodation c. The same as biting into a club sandwich d. Contraindicated for people with arthritis
3. Slant refers to _______.
a. The change in position of the mandible between upright and supine posture b. The angle between the occlusal planes of the jaws c. The comparison between a line laid across the cuspids and the inter-ocular line d. The direction of the nasal septum when compared to the palate
4. Slant can compromise posterior airway diameter _________.
a. While increasing anterior opening b. While improving lip competency c. While providing more volume for the tongue d. While decreasing muscle forces on the oral device
5. The focus of contractile force of the elevator muscles is _______.
a. Able to position the condyle in any accessible position b. Evenly balanced across the body of the mandible c. Balanced by the positional muscles d. Concentrated at the posterior of the mouth
6. With posterior stabilization recording, the maxillary and mandib-
ular occlusal planes are _________. a. Recorded with three-point stabilization b. Allowed to assume a natural parallel orientation c. Distorted in patients with bicuspid extractions d. Kept at close to contact as possible for minimal vertical opening
7. The bony support of the lumen of the oropharynx comes from ______. a. The hyoid bone articulation with the cervical spine b. The posterior border of the mandibular ramus c. The palatine bone extension d. There is no bony support of the oropharynx lumen
8. The correct treatment position using an oral prosthesis for TMDs or OSA patients is _________. a. Always less protruded for TMDs than OSA b. More protruded for either disease in obese people c. Not universal – each person needs individual positioning d. Can only be determined by comparing pharyngeal dimensions
9. When using anterior interarch stabilization devices ________. a. The interincisal dimension can be minimized b. Clearance between posterior teeth is optimized c. Can result in too much pressure on front teeth d. May lead to insufficient airway space in the posterior segments
10. A posterior stabilization system positioned bilaterally in the molar areas to register the interarch jaw relationships ___________. a. Has the primary benefit of easy scanning for appliance fabri cation b. Provides a way to manage the complex anatomical interrelationships c. Takes less expensive bite registration material than other methods d. Is useful for OSA, but not TMD, patients.
 by Sal Rodas, MBA
by Sal Rodas, MBA
Like CPAP, oral devices are for managing and not curing OSA and will require patients to wear the devices long-term.
Therefore, consideration of effectiveness vs. efficacy of therapy should be analyzed when considering an ideal treatment for the patient.
However, there have been studies pub lished in the refereed literature suggesting that oral appliance therapy is an equivalent alternative for patients that suffer from mild to moderate OSA. Some of those studies highlight the benefits of using oral appliance therapy over CPAP because patients find oral appliances more convenient and comfortable, resulting in better compliance.

Compliance is an essential factor that patients should be made aware of when presented with therapy options. Studies have shown that CPAP intolerance can be as high as 60%. Despite studies showing how effec tive CPAP addresses OSA, it should be noted that this efficacy possibly comes at the cost of driving patients not to wear CPAP long-term.
The following case, courtesy of Dr. Joseph Yousefian in Bellevue, WA, showcases an effective and practical protocol to address CPAP-intolerant patients and demonstrates an effective option with oral appliance therapy.
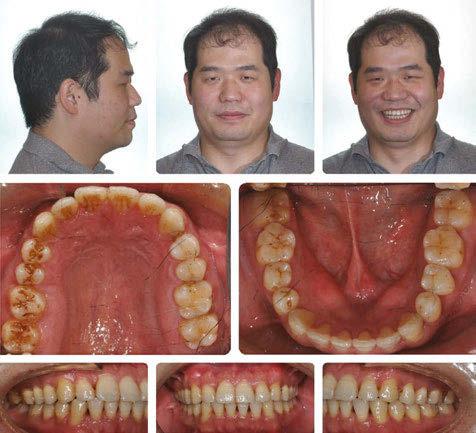
The patient presented to the practice with an ideal bite after orthodontic/equilibration treatment, as noted in the post-treatment pho tographs (Figure 1).
During the visit, the patient indicated he had been diagnosed with OSA and was pre scribed the use of CPAP to manage his con dition. However, the patient explained that he had not been using his CPAP. Therefore, a sleep disordered evaluation was performed on
Continuous Positive Airway Pressure (CPAP) therapy continues to be considered the gold-standard treatment option for patients that suffer from obstructive sleep apnea (OSA).Figure 1: Post orthodontic/equilibration treatment, extra and intraoral photographs. Courtesy: Joseph Yousefian, DMD

the patient that revealed symptoms of severe sleep bruxism, excessive daytime sleepiness, and snoring. The patient also complained of having chronic pain in the jaw and masseters, especially when waking up in the mornings. He reported gaining over 10 pounds in the last few years and the presence of hyperten sion which was not responsive to his daily medication.
The patient was referred to complete an in-lab polysomnogram (PSG) since it had been a long time since his previous sleep study.
The results of the PSG indicated the pres ence of severe OSA with an apnea/hypopnea index (AHI) of 43.1/Hr and respiratory dis turbance index (RDI) of 44.8/Hr. The PSG also indicated a REM dom inant OSA with an AHI of 58.6/Hr. The minimum SaO2 was 89.0% with a mean SaO2 of 98.8%. The sleep efficiency was cal culated at 93.4%.
Despite his severe OSA, the patient refused treatment with CPAP and was referred back to Dr. Yousefian’s office to be treated for his OSA and masticatory/temporoman dibular joint disorders (M/ TMJD). His treatment was initiated with bedtime use of the ApnoDent®, an FDA-approved oral appliance (Figure 2) designed to manage his bruxism, M/TMJD issues, snoring, and OSA.
An efficacy test was performed after four weeks of ApnoDent® use; the sleep test results indicated a reduction of AHI to 1.9/Hr with SpO2 nadir of 91%. The Mean SaO2 was 94.7%, and the sleep efficiency was 93.4%
The patient started his 2-year supervision phase and continued to use the ApnoDent

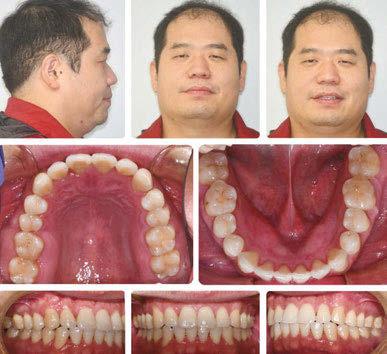
with a lower clear retainer at bedtime.
In the post-treatment phase, he was seen annually for clinical monitoring of his M/TMJD and OSA issues. His annual check in the fourth year revealed that his bite was still very stable with Shimstock still holding all the posterior teeth. He presented an absence of bruxism and M/TMJD symptoms as long as the patient wore the ApnoDent. The patient described waking up refreshed daily, that he has not gained any more weight, and his blood pressure is back to normal with no need for medication.
As noted in this case, oral appliance ther apy can be an effective alternative to CPAP, even in cases where the patient has been diag nosed with severe OSA.
The use of the novel ApnoDent device was ideal in this case because the device did not cause any of the known side effects that tradi tional dental sleep appliances cause: posterior open bites, joint discomfort, or unintended tooth movements, allowing the patient to suc cessfully wear the device long-term.
While CPAP remains the gold standard, educating patients on intolerance rates is essential to help patients make an informed decision about their treatment options. In this case, monotherapy was ideal for the patient. However, there are opportunities also to treat severe OSA patients with combination therapy, where CPAP and an oral appliance are worn together to help the patient be more successful and compliant with their treatment.
1. Almeida, F. R., & Bansback, N. (2013). Long-term effective ness of oral appliance versus CPAP therapy and the emerging importance of understanding patient preferences. Sleep, 36(9), 1271–1272. https://doi.org/10.5665/sleep.2938
2. Doff, M. H., Hoekema, A., Wijkstra, P. J., van der Hoeven, J. H., Huddleston Slater, J. J., de Bont, L. G., & Stegenga, B. (2013). Oral appliance versus continuous positive airway pressure in obstructive sleep apnea syndrome: A 2-year follow-up. Sleep, 36(9), 1289–1296. https://doi.org/10.5665/sleep.2948
3. Li, W., Xiao, L., & Hu, J. (2013). The comparison of CPAP and oral appliances in treatment of patients with OSA: A systematic review and meta-analysis. Respiratory Care, 58(7), 1184–1195. https://doi.org/10.4187/respcare.02245
4. Sutherland, K., Phillips, C. L., & Cistulli, P. A. (2015). Efficacy versus effectiveness in the treatment of obstructive sleep apnea: CPAP and Oral Appliances. Journal of Dental Sleep Medicine, 02(04), 175–181. https://doi.org/10.15331/jdsm.5120
5. Tong, B. K., Tran, C., Ricciardiello, A., Donegan, M., Chiang, A. K., Szollosi, I., Amatoury, J., Carberry, J. C., & Eckert, D. J. (2020). CPAP combined with oral appliance therapy reduces CPAP requirements and pharyngeal pressure swings in obstructive sleep apnea. Journal of Applied Physiology, 129(5), 1085–1091. https://doi.org/10.1152/japplphysiol.00393.2020
6. Virk, J. S., & Kotecha, B. (2016). When continuous positive airway pressure (CPAP) fails. Journal of Thoracic Disease, 8(10). https://doi.org/10.21037/jtd.2016.09.67






 by Pat McBride, PhD, CCSH
by Pat McBride, PhD, CCSH
In the United States, roughly half of the entire adult population suffers from at least one sort of chronic, incurable illness, in cluding diabetes, cancer, heart disease, arthritis, and sleep ap nea.1 Having any of these disorders can pose major challenges to an individual’s life, due to strict medication issues, access to appropriate care, ability to pay for or tolerate treatment offered, and lifestyle changes. While dealing with the medical nuts and bolts of a sudden life changing diagnosis, many patients may have trouble in dealing with the “idea” of the diagnosis and how they will psycho-socially incorporate it into their lives.
Much of the literature on how people deal with their disorders focuses on how people perceive and experience their illness. The focus here, being on the disease itself, not the person who is living with it. As pro viders, when looking at illness perceptions we immediately think of things like quality of life, adherence to therapy, treatment-seek ing-behavior and long-term management for the disorder. When treating obstructive sleep apnea, which by the way is one of the most the most highly contested diagnoses2 we must also be mindful of the concept of illness identity3 in the patient. Illness identi ty not only expresses how the patient views the disease process and treatments, but also how having the disease affects the way they think about themselves and their ability to integrate the disorder into their active identity. Simply put, patients who strong ly refute their diagnoses tend toward sub-optimal disease management and adherence to therapies which improve quality of life and clinical outcomes. Whereas those indi viduals who accept their disease process and integrate it into their lives aside from other self-defin ing identity assets tend to follow treatment recommendations and self-management protocols, im proving their quality of life and
long-term health outcome. How we as pro viders help navigate people from rejection to acceptance has, in my opinion, everything to do with our ability to show clinical empathy in a meaningful way to our patients.
When we think of empathy outside of the patient care setting most of us would agree that empathy is a mode of understanding that specifically involves emotional resonance. We react to and become attuned to other’s experiences. However, most clinical pro viders understand empathy as a form of de tached cognition, which in a post pandemic world is less than ideal. On the one hand, we must remain detached to care for patients reliably and objectively, while on the other, reconciling patients’ needs and desire for genuine empathy from their doctors. The op erative word here being genuine. Good care providers understand the science whereas great care providers understand science and how to apply it to people. Why? Because they can communicate effectively through clinical empathy and become emotionally attuned to the patient experience. Emotion al attunement is absolutely not the same as becoming emotionally “involved” in the pa tient’s disease process or emotional issues. Emotional attunement operates by shaping what we as providers can imagine about an other person’s experience.4 When clinicians can imagine what another person is going through, they can find themselves resonating authentically. It is not necessary that any of us have had the same or similar experience personally as the patients are. Emotional attunement provides a kind of involuntary backdrop to the situation at hand and is just part of ordinary communication between patient and provider in a clinical setting. By careful observation of and attuning to even small comments made by patients, we can get a nonverbal sense of where a person is emotionally in their disease process accep tance/denial or integration. Are they “sitting with it, or not?”
Emotional attunement to your patients will help you and your staff members ap preciate the personal meanings behind the patient’s gestures, body language and words. Using what is called associative reasoning helps. For example, when a female patient sits looking at the floor and states that she refuses to wear CPAP in front of her husband, and takes it off at night regardless of gained benefit from and tolerance to it, associative listening may allow her practitioner to “see through” the words to the underlying issue which may be that her husband is “turned off” by her wearing the CPAP. By holding on to the emotions of her words, establishing eye contact, and observing body language, the provider can delve deeper into what may be hindering her ability to positively inte grate her disorder to her identity.
The ability to use associative listening, repeating key words and phrases, noting change in vocal tone, body language and by imagining what the patient experiences can and will facilitate trust and further disclosure from patients which is essential in providing precision care. Gaining a high level of trust from patients in turn improves therapeutic ef ficacy overall.5 Establishment of patient trust in their provider has been directly correlated with better treatment adherence and accep tance of their disease process, regardless of what the disease process is. Better accep tance means positive identity integration. Furthermore, empathy in a clinical setting has the additional benefit of substantially de creasing depression and anxiety.6
Finally, treating patients in a post pandem ic world will never be what it once was, nor should it be. Most of us would likely agree, that it is imperative that we never lose our cu riosity about our patients and their lives, and frankly our place in their lives. Afterall, each and every patient brings something unique to our table that may improve our lives in ways they will never know. The old models of clini cal detachment in the world of medicine and dentistry no longer serve the patients or doc tors well, and post pandemic Zoom medical appointments are not always the appropriate answer to our current healthcare crises. We all need connection, and folks with chronic disease processes need far more “touches” than healthy people. Patients want their pro viders to be actively engaged and empathic to their needs, and if Roter et al. are to be
believed, those of you who engage patients with psychosocially oriented communica tion styles and empathy will experience burn out far less frequently than your colleagues.7 People may argue that clinical empathy is not practical but using objective reasoning alongside of empathy can enhance any diag nosis rather than detract from it.
Without thinking about it, a few small changes in your listening and communica tion style may make you the one provider who captures the influence of illness on your patient’s sense of self. If you do, it will be something they will never forget and always be grateful for. It’s powerful stuff at the end of the day. Whether or not you can help nav igate them from absolute rejection of their disorder towards a place of acceptance and even on to perceiving their lives as improved after diagnosis, the time you spend moving away from clinical detachment toward a place of true clinical empathy will serve you well.
1. Centers for Disease Control and Prevention. The Power of Prevention. (2009) Accessed at http://www.cdc.gov/ chronicdisease/pdf/2009-Power-of-Prevention.pdf
2. Zarhin D. Contesting medicalisation, doubting the diagnosis: patients’ ambivalence towards the diagnosis of Ob structive Sleep Apnoea. Sociol Health Illn. 2015 Jun;37(5):715-30. doi: 10.1111/1467-9566.12229. Epub 2015 Feb 13. PMID: 25683493.
3. Oris L, Rassart J, Prikken S, Verschueren M, Goubert L, Moons P, Berg CA, Weets I, Luyckx K. Illness identity in adolescents and emerging adults with type 1 diabetes: introducing the illness identity questionnaire. Diabetes Care. 2016; 39:757–763.
4. Charmaz, K. The body, identity, and self: Adapting impairment. Sociol Q 1995: 36: 657-680

5. Samantha Berridge, Nick Hutchinson, Staff experience of the implementation of intensive interaction within their places of work with people with learning disabilities and/or autism, Journal of Applied Research in Intellectual Disabilities, 10.1111/jar.12783, 34, 1, (1-15), (2020).
6. Hillel Gray, “We Need Something Different”, Journal of Religious Ethics, 10.1111/jore.12308, 48, 2, (247-277), (2020).
7. Julia Silver, Colleen Caleshu, Sylvie Casson Parkin, Kelly Ormond, Mindfulness Among Genetic Counselors Is Asso ciated with Increased Empathy and Work Engagement and Decreased Burnout and Compassion Fatigue, Journal of Genetic Counseling, 10.1007/s10897-018-0236-6, 27, 5, (1175-1186), (2018).
Pat Mc Bride, PhD, CCSH, has spent 38 years as a full time clinician, educator, and author in the fields of den tistry, respiratory medicine, and dental sleep medicine. Her extensive experience in clinical, laboratory, research, and educational arenas has led to the development of interdisciplinary care model delivery systems used in col laboration by physicians and dentists around the globe. Pat has a unique ability to intervene in the interstices of global systems, devel oping protocols which can be translated across demographics and cultures into improved clinical outcomes. In addition to teaching and writing, Pat continues to work hands on in the patient care arena. Serving the under served and marginalized patient remains a passion and priority for her. She sits on numerous Boards such as the AAPMD and is the Executive Director for The Foundation for Airway Health. She has one grown daughter who shares her passion for social justice and education, serving as a sixth grade teacher in the inner city Oakland.
Our ability to show empathy helps navigate people toward acceptance.
•
• Reduced chairtime
• Improved patient comfort which can lead to better com pliance
From the laboratory perspective, the cli nician should consider the following 4 items for improved success:
of True Function Lab devices produced have some form of digital process.
Did you know that at True Function, approximately 70% of cases received come from intraoral scans and that over 90% of our devices produced have some form of digital process? There are many advantages to using digital including:
• Efficiency – we receive the scans the day you send them
• Quality – you are able to QC your scans before the patient leaves the chair and make corrections
• Cost savings – because you can quali ty check your cases immediately, there is less of a possibility of the lab calling and requesting a new scan
• Repeatability – Dog ate the appli ance? No problem! If we have scans, no need to bring the patient back for impressions
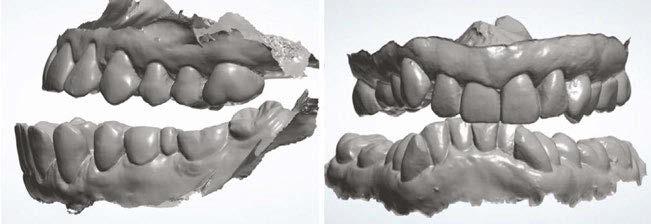
• We have begun offering some modelless appliances
• Do I need a PDAC Device?
If so, this will limit your device and design options. Devices like Panthera DSAD, True Herbst, OASYS Hinge, and TAPs are PDAC approved.
• The market is flooded with well over 100 devices. This can be overwhelm ing. If you are new to oral appliance therapy, try a few different appliance types for yourself and team members.
Consider using tried and true devices like: EMA, Dorsal, Herbst, TAP, Panthera, etc. These appliance designs have been around for over 20 years, providing confidence to any dentist.
Missing teeth, steep curve of Spee, open bites, tipped teeth, and other details affect the choices matching device to the patient. By sending an accurate scan and requesting a consult with the lab artist, you can work out the specifics. You may have to compro mise on your appliance and material choice, but staying open minded and collaborative will give you the best design for success.
I often get asked, “Frank, what type of bite do you prefer?”My response is “Well Doctor, as a technician, my favorite bite is perfectly symmetrical and provides sufficient vertical for the device and material choice.”
There are many variables that go into a great bite. Here are a couple to consider:
• Vertical
Depending on material choice, minimum vertical for devices is about
What if you could consistently get?
A great fit







3mm to 5mm inter-occlusally (in pos terior). The amount of opening need ed is typically material dependent. Check with your lab/manufacturer for minimum vertical requirements. When preparing to take a bite registra tion, place the instrument of choice; George Gauge, ProGauge, Airway Metrics, SomnGauge, etc. and look in the posterior. You should be able to see approximately 3-5mm of space between upper and lower most poste rior teeth. If vertical is not sufficient, change the size of bite fork or shim.
One of a laboratory’s most com mon reasons for reaching out to cli nicians is related to bite shifts. When taking a bite, document any bite shifts
and communicate on the prescrip tion. This will let us know that you are aware of the discrepancy and whether we should proceed with device as is.
Given the anatomical features of the im ages in Figure 1, think about appliance de sign, material choice and certain compro mises that might be necessary for successful Oral Appliance Therapy.
Communication is extremely important to us, and we will contact you if we see a challenge with your choice in appliance, material, retention,v ertical, biteshifts, etc.
At True Function, our goal is to deliver Peace of Mind to all stakeholders, including our customers, our team, and our partners. If you are ready for a more efficient device delivery experience, give us a call. We are ready to help.









 by Rose Nierman and Courtney Snow
by Rose Nierman and Courtney Snow
How important is Medicare billing to oral appliances for obstructive sleep apnea (OSA) treatment? Very import ant! To avoid a potentially disappointing outcome, den tists billing Medicare plans for oral appliances for OSA need to know the difference between original Medicare and Medicare Advantage plans. Our hope is that if we can save even one of fice from having a disappointing result, we have done our job as medical billing geeks in dentistry!
How do you know whether your patient has a Medicare Advantage plan or original Medicare? The first clue will be the patient’s medical insurance ID card. Original Medicare ID cards all look the same, colored red, white, and blue, and “Medicare Health Insurance” spans across the top of the card. On the other hand, Medicare Advantage plan ID cards look different depending on what insurance company administers the plan. Medicare Advantage ID cards will typically have the word “Medicare” somewhere on the front and another insurer’s name, for example, “Aetna Medicare”.
Identifying original Medicare vs. Medicare Advantage is critical to set prop er expectations for patients. Here are 5 essential differences between the two.
Medicare Advantage plans have varying deductible and coinsurance fig ures. Original Medicare plans all have the same deductible ($226 for 2023) and the same coinsurance (20%). Confirming the deductible and coinsur ance for Medicare Advantage plans will help estimate the patient’s out-ofpocket expenses.
Original Medicare plans have coverage for DME if “Medicare (Part B)” is listed on the front of the card. Medicare Advantage plans may or may not have DME coverage. Because custom oral sleep appliances fall under the DME benefit category, verifying DME coverage is critical.
Original Medicare plans do not offer pre-authorization for custom oral sleep ap pliances. On the other hand, Medicare Ad vantage plans may require pre-authoriza tion. This difference is especially crucial to understand, as we have seen practices move forward with delivering a custom oral sleep appliance under the assumption the patient has an original Medicare plan, only to find out when the claim is returned the patient has a Medicare Advantage plan that requires pre-authorization to be eligible for coverage.
Original Medicare will only reimburse for custom oral sleep appliances to dental prac tices enrolled as a Medicare DME supplier. While some Medicare Advantage plans do require the dental practice to be enrolled as a DME supplier with original Medicare to re imburse, not all do.
It is common for a patient with original Medicare to also have a supplement plan. On the other hand, Medicare Advantage plans are the patient’s sole policy.
tice Management: contactus@dentalwriter.com or 800879-6468.
Here at Nierman Practice Management, we advise our clients to treat Medicare Advan tage plans as you would a commercial policy, meaning always perform a thorough benefit verification and submit a pre-authorization when required. Knowing the differences be tween original Medicare and Medicare Advan tage plans will allow you to successfully treat your Medicare patients and avoid a potentially frustrating and expensive situation.
Rose Nierman is the CEO of Nierman Practice Manage ment (NPM) and creator of the DentalWriter Plus+ soft ware. For over 30 years, Rose has taught dental practices successful & ethical medical billing through the iconic Suc cessful Medical Insurance in Dentistry seminars.



 by Adrienne Good, National Account Manager, Dental Sleep Practice
by Adrienne Good, National Account Manager, Dental Sleep Practice
Panthera Dental asked me to attend their 10th Anniversary Party and Master Cup Award Ceremony at their headquar ters in Quebec City, in September this year. Over the years, I have been impressed with their versatility in the dental space, and I had to see this new facility in person. The owners, siblings Gabriel and Béatrice Robichaud, bring their own unique person alities to this more than 40,000 square foot building. From the bright distinct Panthera purple to the 1980s-themed game room, it seems like an awesome place to work. Esthet ics aside, they considered efficiency and workflow when designing every detail of their headquarters. We even got to meet the hardest worker of all, their robot courier, Alfred. Everything is strategically set up with the end goal of your patients receiving their order within a quick timeline and with an exceptional quality product.
After a lovely tour, the top three winners of their Master Cup were announced. Panthera,
in an effort to keep innovation with technol ogy in dental alive, has a contest every year where globally, technicians compete by craft ing a complete dental prosthesis. After mimo sas and media interviews, the real fun began. Guests arrived in the evening greeted by bartenders pouring drinks extending from aerial silk. The hors d’oeuvres were top notch, and the photo booth, along with their DJ playing throughout the night, were pure entertainment. The most memorable part of the night was when a school bus pulled up on the side of the building and took us to a small diner in downtown Quebec City. There, we got to try Quebec’s version of “diner food,” and network with colleagues from around the world.
I am not surprised Panthera’s party was a great success, because they put this kind of effort into everything they do. The quality in their work really shows, and I am fortunate to be able to witness the processes behind it all. Know that when you are purchasing a Pan thera Dental product, whether it be esthetic, sleep, or implant related, you are supporting a wonderful bunch of people, a facility with the best technology, and most importantly, top notch quality you can pass down to your patients.
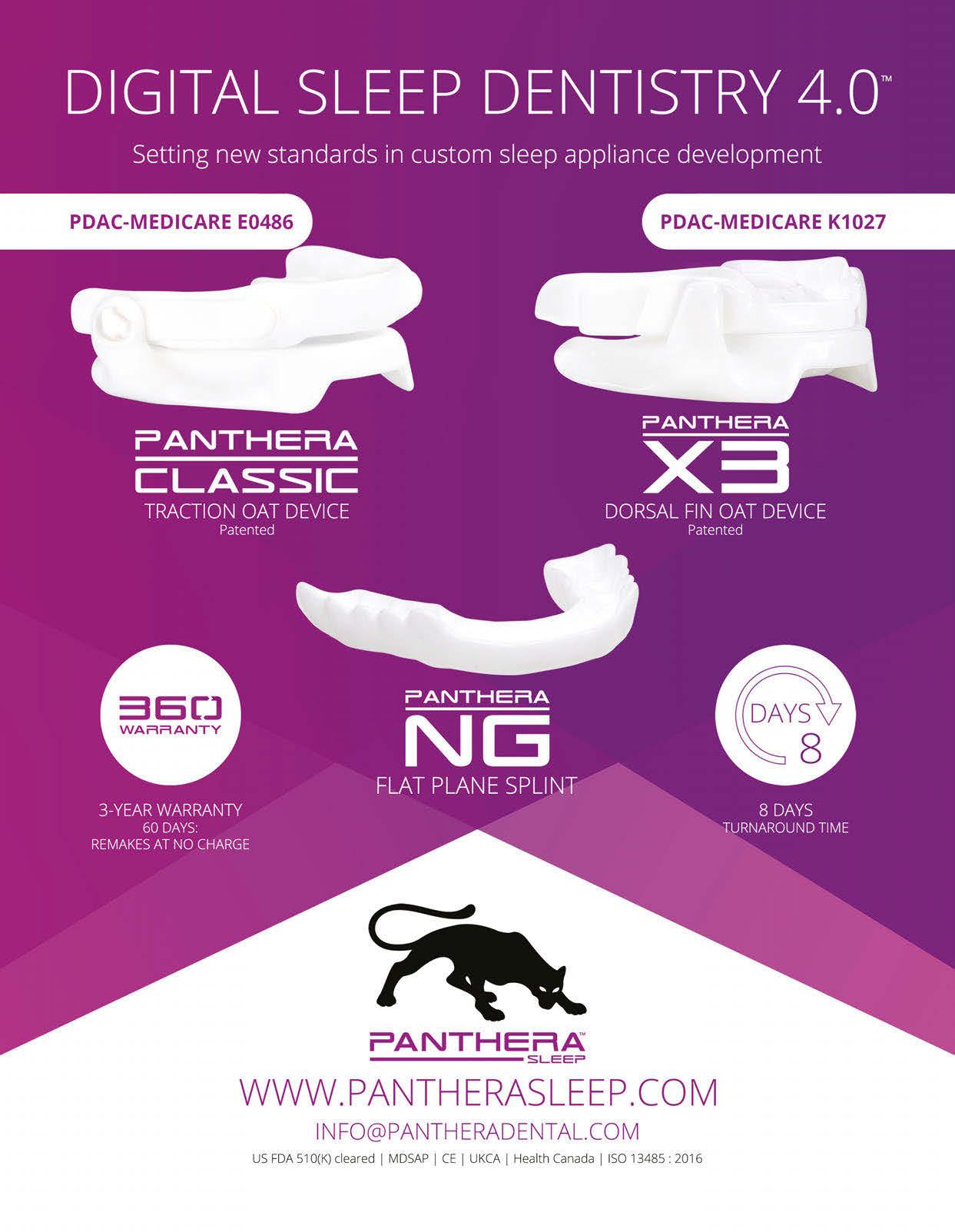
New to the United States is a novel device to affect tongue posture from the inside out. eXciteOSA uses electrical stimulation, which has been shown to convert skeletal muscle fast-twitch fibers into slow-twitch high-en durance fibers, to keep the tongue forward in the mouth and the airway open. To get some insight into how this is being used in dental practices, DSP talked with three experienced dentists who focus their practices on sleepy people, facial pain, and TMD therapy.
Aditi Desai, BDS, from London, UK; Max Kerr, DDS, from Austin; and Kent Smith, DDS, of Dallas have each been using eXcite OSA in their practices since the first days the device became available for dentists.
DSP: What interested you in this new device? What made you think it would be helpful for your patients?
Max Kerr (MK): Patients are always com ing in asking ‘what else can I do’ – I recall from your course, Kent, you showed us a di geridoo and talked about circular breathing. I understood about improving muscle tone from that. When I got an alert on my Google
desktop about Signifier’s FDA authorization, I wanted to see how it could fit into our prac tice. Like a jazz artist, I wanted to have more instruments to play – see what fits into that patient’s groove.
Aditi Desai (AD): I was excited about this product right from the start, getting involved as soon as I could. In the UK, the device went by the name ‘SnooZeal’ at first – that’s how long I’ve been using it. I’m the President of the British Society of Dental Sleep Medicine, so I get a lot of calls about new innovations. One of my ENT colleagues had been trialing this device in the UK, and he contacted me as the company was looking to introduce it to a dentist. I agreed to meet with the company representatives. Within a couple of hours, I met the CEO, Akhil Tripathi – and it was then that I realized how many medical and scien tific leaders in sleep medicine were involved. This all happened just a few days before we went into COVID lockdown.
Kent Smith (KS): At Sleep Dallas, we are always trying to find modalities to help peo ple sleep. Sometimes appliances don’t work, patients don’t have any teeth, sometimes AHI gets better but not enough better. I follow a sleep doctor I heard at AASM meeting – I don’t treat the polysomnogram. I embraced this pretty quickly because it is something that has some backbone to it, there was re search, I thought it was worth pursuing.

DSP: Kent, you mentioned edentulous patients. Together with people using clear aligners, those have been two populations that are very challenging and frustrating for therapy. CPAP, yes, but for intolerant patients, have you found eXciteOSA helpful?
KS: For edentulous patients, they can use it with or without their dentures – I just tell them to put it in. They want help, and noth ing else has worked so far.
MK: It’s not mentioned in the FDA regu lations, not a contraindication, so I say ‘just get it done.’
KS: I’ve never found an oral appliance I can use with clear aligners – there’s just noth ing that works well. I think excite is a good option for those who won’t use CPAP while they are getting their teeth straightened.
MK: I tried a few of the devices over clear aligners, but they are a mess. This is much better.

AD: I have been able to manage a few pa tients who are either completing orthodontic treatment or who are undergoing extensive dental rehabilitation prior to having oral ap pliance therapy while unable to tolerate CPAP.
DSP: How do you choose the patients for which you want to prescribe eXciteOSA?
KS: People come in looking for it because they’ve heard about it, or they might see it in our clinic. If they ask about it, my team knows what to say. I sometimes use it for mild OSA or simple snorers, but not as first line for moderate or severe patients.
MK: If a person seems not likely to be a responder in Oral Appliance Therapy, I’m already thinking about it. I try to let patients choose which therapy they think will work for them. I tell patients what I know about the literature, the scientific studies. I wish I had as much as we do for OAT. When a pa tient is leaning toward eXciteOSA, and they have a more severe diagnosis, I don’t dis courage it, but I let them know that it might not be sufficient and other therapy might be needed. This isn’t different than what I say for OAT for this life-threatening disease. I cite the literature, but I also keep in mind the reason many people aren’t getting their sleep apnea treated is how difficult the treat ment is.
AD: I’ve seen a lot of patients with a tongue base issue – high BMI, big floppy tongue. I can’t always manage them with a MAD only. If they’re not going to be CPAP compliant, I thought it would be an adjunct to MAD and CPAP. I actually don’t pay much attention to severity – AHI is on its way out. I now treat any patient who needs help no matter what the severity – some improve ment in their symptoms is better than none. If we limit ourselves to one particular therapy for severe apnoeacs for example, we are not serving our patients well.
DSP: After doing this for a while, what would you say to a dentist who is fairly new at this? How would eXciteOSA help them?
KS: if they’ve not done a lot of devices, they probably don’t have the verbal skills and office systems down yet to cover the cost fac tor. They can offer eXciteOSA as a cheaper option to keep the patient involved.
MK: A dentist who feels unprepared for side effects of dental appliances, such as
Aditi Desai, BDS, is a recognised dental sleep expert and dental surgeon located in London, UK. She is qualified from the University of Wales in 1977 and has 42 years of diverse experience. In 2004, she completed her MSc in Conservative Dentistry at University College London. She is currently Pres ident of the British Society of Dental Sleep Medicine. Dr. De sai is a founder of Global Sleep Solutions, an establishment whose principal intention is to raise awareness, provide education, and access to treatment for a wide range of sleep disorders.
Max Kerr, DDS, D.ABDSM, is a dental entrepreneur who owns a successful restorative dental practice, four dental sleep medicine offices, and is a coach\lecturer focused on building healthy, thriving practices. He devotes time and en ergy towards philanthropic dentistry and understanding effi cient business models.
Kent Smith, DDS, D.ABDSM, is the founding director of Sleep Dallas, a DSM practice serving the Dallas-Fort Worth metrop lex. Dr. Smith is president of the American Sleep and Breath ing Academy, a Diplomate of the American Board of Dental Sleep Medicine, and is on the advisory committee of the Aus tralasian Academy of Dental Sleep Medicine. In addition to running his practice, He is the founder and primary facilitator of 21st Century Sleep Seminars, a series of training events that prepares dental professionals to incorporate dental sleep medicine into their practices.


an open bite, may want to provide just this therapy and if it doesn’t work, they can find a more experienced dental sleep medicine doctor to refer for OAT.

AD: I have an interesting case – a fairly high-profile person was referred to me. He didn’t have OSA, so the ENT consultant sug gested he get a boil-in-a-bag device many years ago. It stopped working for him, and he had developed quite a significant bite change. I went ahead with a MAD and sug gested eXciteOSA. About three weeks later when I saw him to fit his MAD, he report ed that his snoring had reduced significant ly, and his wife was much happier. I went ahead with the MAD anyway, because I had confidence in it. About six months later at the follow up visit, he reported that he was not wearing the MAD, because his snoring had stopped, and all the bite changes were reversed. It’s only one case, but it made me and the patient very happy. So for MAD pa tients who have had bite changes, why not use eXciteOSA and see if it helps enough? That’s one case – it’s not something I count on, but it seems helpful. There are others who have reported snoring cessation or much re duced levels of snoring decibels.
DSP: Have you had any negative feedback from patients? Signifier offers a guarantee if it “doesn’t work.” What’s been your experience?
AD: I’ve prescribed 65 or 70 of the de vices, and recently we were able to do an audit of about 40 of them. A few complained
of mild pain from having to hold the device in the mouth, but they needed to be shown not to bite too hard on the mouthpiece. One woman couldn’t get over excessive saliva tion, another blamed it on making his tinni tus worse, but those two are the only ones who have returned their devices. So I don’t have much to say about negative side effects.
KS: Other than patients who say “It didn’t work,” just like we hear with mandibular ad vancement, the only other negative feedback came from a patient whose cardiologist told him to stop wearing it. More education is needed.
MK: At the highest levels, some patients have reported transient discomfort with eX citeOSA. Other than that, the only feedback that I have received has been regarding com pliance. Some patients have difficulty keep ing up with the treatment schedule.
DSP: How do you handle the cost factor?
AD: These are not within the NHS. We occasionally help with payment plans when the need arises, but I just let the patient choose. The guarantee helps, and not hav ing to charge VAT if the patient certifies they have OSA and not just snoring.
MK: It will be great if insurance would start paying for it, but until then, we have the patients pay cash. The price varies whether they are getting a MAD to go with it, we bun dle the replacement mouthpieces, and any other thing we can do to maximize patient outcomes. Retail is not any significant factor in Sleep Better Austin, anyway, so we don’t make it a barrier if the patient chooses this therapy.
KS: Same here. Sometimes we even give it away if seems to be the right thing for the pa tient. Maybe that’s not the best for business, but like Max, retail isn’t our thing – it’s creat ing the right therapy plan for that patient.
DSP: There are some codes for this therapy, K1028 and K1029, but reimbursement is mixed from private payors, so far. HSA accounts can be used. Thank you all, for a very interesting con versation! I know readers of DSP are always looking for ways to help – and having an other non-invasive, easy to use therapy might just be the right answer for the patient in your chair.








 by Jamison Spencer, DMD, MS
by Jamison Spencer, DMD, MS
Dentists treat sleep-related breathing disorders because of a strong desire to help patients prevent the negative health consequences associated with these conditions. The challenge, however, has been the complexity of obtaining reimbursement for these services. Dental insurance doesn’t cov er sleep appliances — and billing medical insurance is diffi cult and expensive. It’s difficult because it pays dentists only after patients have received a definitive diagnosis of sleep apnea from their physician, and it’s expensive because working with a billing company reduces your profit margin.
Fortunately, dentists don’t need to accept medical insurance to become involved in treating sleep-related breathing disorders. If you have a desire to treat snoring and sleep apnea, the win-win-win billing method is a strategy that can ensure victory.
Step 1: Develop a case fee
To determine your rate for providing oral appliance therapy, you must account for

multiple factors, such as how much capacity you have (available chair time and staff), your skill and expertise, and the skill and expertise of your staff. Evaluation, treatment planning, fitting and follow-up will all take longer in the beginning. The fee will depend on appli ance selection and the associated costs. Ap pliance choice will vary from patient to pa tient – there is no one-size-fits-all appliance. The fee will also depend on the ability for the office to use telemedicine appointments for follow-up, which reduces needed chair time and makes chair time more productive.
To determine your fee, do not use a for mula such as “three to five times the cost of the lab bill.” This may work fine for many procedures, but not for sleep therapy, which is follow-up intensive and therefore chairtime intensive. This chair time is not typi cally related to physical adjustments of the appliance, but is rather the time required to discuss with patients how they are respond ing to therapy and what, if any, side effects they are experiencing. Time is also needed for decision-making by the dentist and staff
Treating patients for sleep-related breathing disorders involves devel oping a case fee that’s both afford able for patients and profitable for the clinician.
regarding next steps. Handling follow-up via telemedicine can make these visits much more efficient.
For most dentists, an all-inclusive fee in the $1,800 to $3,200 range would be appro priate. Some dentists may decide to charge less as they are starting out because they rec ognize that they are “paying for their educa tion.” Dentists may use the profitability index formula to evaluate their profitability and create their case fee (See Table 1).
In most states, dentists can delegate the fitting and follow-up adjustments to welltrained staff members, resulting in very little chair time for the dentist. In addition, many follow-up visits can be conducted using tele medicine, further reducing required chair time.

Step 2: Discuss your case fee with patients, as well as options for immediate treatment and long-term care.
Ensure that your patients completely un derstand what you can and can’t do for them. Explain that the case fee is all-inclusive, just like it would be with orthodontics. Ortho dontics is a nice example because most peo ple know approximately how much braces cost in their area. As such, when your case fee is presented and it is less than orthodon tics, patients will feel it’s appropriate, and they may not be surprised.
Provisional mandibular advancement de vice (PMAD) therapy provides an option for the patient to get started immediately and use the outcomes of therapy as part of the decision-making process for moving forward with further diagnosis and treatment, work ing in conjunction with their primary care physician.
In the PMAD model, the provisional as pect of therapy may be presented as a por tion of the case fee. If long-term care is in dicated, then the rest of the case fee would be charged. The following is an example sit uation:
• Case example – The dentist’s case fee is $1,800 for PMAD therapy. The pa tient receives the physician’s definitive diagnosis of sleep apnea. The dentist uses what was learned from provision al therapy (i.e., mandibular position, including vertical) to prescribe a new
appliance. This treatment plan is an additional $1,000 and includes the necessary follow-up.
The EMA device and Silent Nite® Sleep Appliance, which are both available from Glidewell, are excellent choices for the PMAD model for the following reasons:
• Comfort – They are thin and comfort able for the patient to wear. Compli ance is the key to success with oral appliance therapy. Starting with a custom appliance that is small and easy to use helps set the patient up for success.

• Adjustment style – The straps or con nectors, and thus the mandibular po sition, are prescribed by the dentist. When only the straps appropriate to that stage of therapy are given to the patient, this eliminates the risk of the patient being lost to follow-up and adjusting their appliance farther and farther forward, which may lead to significant side effects.
• Long-term success – Both the Silent Nite and EMA appliances may also be used long term and are affordable enough that a patient could have sev eral appliances (e.g., one for home and one for their travel bag). Addition al cost savings are provided when two appliances are prescribed at the same time with the Glidewell Clinical Twin pak™.
For a simple way to treat snoring and sleep apnea, explore the PMAD protocol and download your free informed consent form at glidewell.com/pmad.
Let patients know that if they receive their physician’s diagnosis of sleep apnea, a por
With dental sleep therapy, fitting and follow-up appointments can often be delegated to well-trained staff members, resulting in very little chair time for the dentist.

The Silent Nite Sleep Appliance is an excellent choice for the PMAD model due to its comfort, connec tor adjustment style, and affordabil ity. The Glidewell Clinical Twinpak enables two appliances to be pre scribed at the same time at a spe cial discounted price.
He is an invited lecturer on the topics of dental sleep and TMD around the world. His “Spencer Study Club” is the premier, members only, education and mentoring forum for smart and ethical dentists looking to implement sleep and TMD in their practices effectively and profitably. For more practical and often irreverent information check out his podcast, “The Airway, Sleep & TMD Podcast.”
With the win-win-win billing meth od, dentists can provide sleep ther apy without having to deal with the extra hassles of medical insurance.
tion of the oral appliance therapy may be covered by their medical insurance — and if cost is most important, because you don’t work with medical insurance, you would be happy to refer them to a colleague who does.
Because of escalating deductibles, many patients would have to pay a significant amount out-of-pocket anyway, so they will be more likely to stay with their trusted fam ily dentist. However, when cost is the deter mining factor, patients will appreciate your referral, which builds more trust that you are looking out for their well-being and financial situation.
For most dentists, medical billing is the main obstacle as they try to start helping patients with snoring and sleep apnea prob lems. The win-win-win billing method allows you to start without having to deal with extra hassles, and you can refer patients to den tists who are in-network if that is the patient’s desire. This method is a practice builder, as it allows patients to start provisional therapy immediately, connects you to primary care doctors who may become referral sourc es, and strengthens the relationship of trust
between you and your patients. With this strategy, everyone wins, including patients. You and your team also win, as helping peo ple sleep better – which improves overall health and quality of life – is one of the most rewarding things healthcare professionals can do.

Learn more about the win-win-win billing method at glidewelldental.com/treating-sleepdisorders-simple-steps-to-get-started.
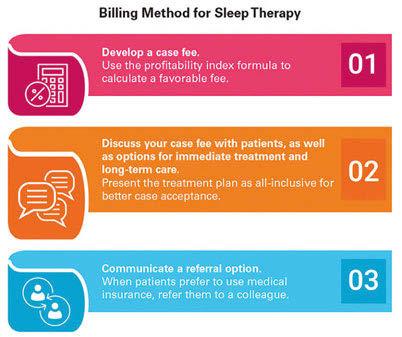
In the U.S., more than 60 million people are covered by Medi care,1 and it’s estimated that more than half of Americans aged 65 or older are at increased risk for obstructive sleep apnea (OSA).2 This condition is associated with cardiovascular disease, cognitive dysfunction, depression, metabolic syndrome, motor vehicle accidents and diminished quality of life.2 To help den tists serve their Medicare-enrolled patients, Glidewell has intro duced the Silent Nite® Sleep Appliance with Glidewell Hinge™. This device is an extension of the Silent Nite brand, which den tists have been using since 1996 to treat snoring and OSA.
Design Features: PDAC-Approved (E0486)
“Because of its low price point, the Silent Nite with Glidewell Hinge makes MAD therapy more accessible for Medicare-enrolled patients and more profitable in the dental office.”
– Randy Clare, subject matter expert in dental sleep therapy at Glidewell

For Medicare-enrolled patients, a mandibular advancement device (MAD) must meet strict design parameters for Pricing, Data Analysis and Coding (PDAC) approval using code E0486. The Glide well R&D department exam ined the Medicare requirements and designed the Glidewell Hinge to meet these standards. The Glidewell Hinge is made of surgical stainless steel and is micro-adjustable to provide dentists with the ability to set a therapeutic jaw position while the device is inside or outside of the mouth.
The appliance is flexible, thin and com fortable to wear throughout the night, help ing patients achieve a more restful sleep and enhanced quality of life. Each Silent Nite case includes an AM Aligner to aid patients in exercising and realigning the jaw after nighttime mandibular advancement.
The Silent Nite with Glidewell Hinge was developed to meet the needs of Medicare
patients and the needs of the den tist with a busy practice. The MAD is value priced at $227 and includes the comprehensive warranties for which Glidewell is known.
To learn more or to receive information about the Glidewell Clinical Twin pak™, which saves dentists $100 on a duplicate Silent Nite with Glidewell Hinge appliance to ensure uninterrupted treatment, call 877-210-3338 or visit glidewell.com/silent-nite-hinge.

1. Centers for Medicare & Medicaid Services [internet]. Balti more (MD): U.S. Centers for Medicare & Medicaid Services. CMS releases latest enrollment figures for Medicare, Medicaid, and Children’s Health Insurance Program (CHIP); 2021 Dec 21 [cited 2022 Aug 10]. Available from: https://www.cms. gov/newsroom/news-alert/cms-releases-latest-enrollment-fig ures-medicare-medicaid-and-childrens-health-insurance-pro gram-chip.

2. Braley TJ, Dunietz GL, Chervin RD, Lisabeth LD, Skolarus LE, Burke JF. Recognition and diagnosis of obstructive sleep apnea in older Americans. J Am Geriatr Soc. 2018 Jul;66(7):1296-1302.
AM Aligner is a product of Airway Management Inc.
Ihave this recurring nightmare where I am standing in a stuffy room full of dentists, psychologists, and physicians, all ex perts in their fields, milling about chatting enthusiastically.
Gratefully soaking up each of their pro found professional secrets, I suddenly realize to my utter shock and horror that each profession seems oblivious to what the other is saying!
It feels as if some kind of mental force field is blocking the very communication that could make all the difference for so many patients urgently needing their help.
Desperate for the groups to wake up and speak with one another, I start to scream...but no sound comes out.
Years ago, when attending my very first sleep conference, I was so excited to learn from Dentists discussing the value of struc tural and functional airway assessments. They shared science that demonstrated efficacy of successfully treating sleep apnea with Oral Appliances.
Then, when they packed up and left the convention center, Medical Providers moved in and discussed their research demonstrating the value of PAP Therapy, surgical interven tions, and medications to treat various sleep disorders.
It was all wonderfully illuminating. Yet my most prominent takeaway was the massive dis connect between the two entities.
I simply could not wrap my head around why these two groups – both passionately ded icated to successfully treating sleep disorders –are not working closely together to share their knowledge with the people who need it!
And I was one of them.
I thought that with all the specialists I had consulted for my sleep and killer migraines, all the tests I had done, all the medications I had tried, that I would have for sure found a suc cessful treatment plan.
After all, as a medical professional I had knowledge, and I had access.
But I never imagined that it would be a DENTIST who held the keys to my freedom from pain and fatigue.
MY MIND WAS TRULY BLOWN, so I set out on a journey of discovery, hungry to learn more.
How could it be that there is this whole world of knowledge out there that we (Med ical Model) know nothing about?
I started taking courses and attending con ferences in Sleep Medicine. The research, the studies, the data, the experts, the case studies, the assessment skills, the testing, the devices... copious amounts of knowledge were present ed that changed my whole mindset.
Everything I had thought I knew about Head-to-toe-Assessments, about Pathophysi ology and Treatment, about mind/body and stress response was blown to bits!
And this “aha!” moment changed my life forever.
I was so excited that I naively believed ev eryone would be yearning for this knowledge.
I went back to work in the Emergency De partment, but with the veil lifted, I started to see things in a whole new way.
The man who woke with palpitations and chest pain in the night showing a-fib on the monitor...look at his thick neck, bloated bel ly, skin colour, ground down teeth, high blood pressure, type 2 diabetes, high cholesterol….
Before, I would have assumed that this gen tleman was not careful with his health, mak ing poor choices in his diet, probably sitting around watching TV instead of exercising and not handling stress well.
My considerations all concerning his wake ful hours.
Now, I saw a man who probably tries his best to make good lifestyle choices, but is ex hausted from suffocating in his sleep, night af ter night, and probably has been for years!
He feels shame. He wishes he was healthi er, slimmer, more active.
He wishes he didn’t feel so down and is afraid to admit he may be depressed, because he can’t actually explain why he would be de pressed.
He has a supportive wife and a loving fam ily. He worked hard at a job he enjoyed and now has the means to travel and enjoy his re
tirement, except he has no motivation to go anywhere.
He knows his wife is disappointed and had looked forward to travelling but was so em barrassed during the one bus trip they went on because he kept falling asleep and snoring loudly, missing most of the tour so what was the point….
I proudly declared to the ER MD, “This man has sleep apnea!”
That explains all his symptoms.
Sighing in exasperation, the doctor looked at me and said, “He has congestive heart fail ure. It’s a chronic condition.”
I reply, “Yeah, but sleep apnea can cause congestive heart failure.” He looks at me like I’m an idiot.
He spends the next few hours pouring over lab results, ECGs, x-rays, vital signs, medica tions and possible interactions.
He will find a way to increase or add meds and then refer this patient to a cardiologist.
The cardiologist will do a stress test, an echo, and add more meds.
I suggest that he refer the patient for a sleep study. He replies that this is an emergency room and that the patient can take that up with his family doctor – except that he won’t.
I advise the patient that he really needs a sleep study and plead with him to ask his fam ily doctor to refer him for a sleep test. “I don’t have a sleep problem. I can fall asleep at the drop of a hat,” he proclaims, “I can sleep any where, anytime!”
I try to explain that these are all signs of a sleep breathing disorder, but I can tell he is not hearing me.
I implore him by showing him his vital signs while he was sleeping.
I SHOW him the apneic periods and the drops in his oxygen saturations.
I emphasized again that I had to provide oxygen while he was sleeping, and I even did a few sternal rubs to get him breathing again.
Of course, he doesn’t remember any of this.
He is distractedly looking for his shoes as I speak.
I turn to his wife, “Please, please make sure he gets a sleep test. I am worried about him.”
The wife replies, “All those sleep labs want to do is con us into buying that breathing ma chine. We’re not falling for that!”
I am flabbergasted.
Three weeks later the wife calls 911 to re vive her husband in the middle of the night.
They are unsuccessful. I feel sick to my stomach.
Working in the Emergency Department day after day, watching these poor folks inadver tently destroying their lives has become intol erable for me.
I resign. My 20+ year career in Critical Care is over.
My family cannot believe I have walked away from something I was so passionate about.
I LOVE my job. Correction, I LOVED my job.
The reason I loved my job was because I love people. I love helping people.
I am fascinated by the body and its intricacies...how intertwined our experi ences, beliefs and choices are in creating health and wellness and conversely illness and disease.
As challenging as this path has been, I still believe that we can truly help more people by uniting the medical, dental, and mental health communities in addressing what is happening during those elusive eight hours, or one-third of folks’ lives when THEY ARE UNCONSCIOUS.
THEY are not responsible for what happens during this time. WE ARE. As healthcare pro viders, we have knowledge readily available to us that the public lacks.
We will look back one day and be horri fied that we have treated sleep so lightly. It has been the LAST thing we considered, instead of the FIRST.
As a dedicated Airway Advocate and Ex pert Sleep Consultant, I look forward to shift ing the healthcare paradigm with you, one great night’s sleep at a time!
After spending 20+ years as a critical care nurse, Julia Worrall was introduced to an amazing, forward-thinking, dental provider that was able to successfully treat her in tractable migraines and sleep issues. This chance meeting opened up a whole new world! Applying herself to tak ing multiple sleep and craniofacial courses along with her insatiable appetite for research led to the discovery that sleep is so much more than simply ‘closing one’s eyes’. Realizing that this information is sorely lacking in all areas of healthcare as well as in the general population, Julia became a prolific researcher, pub lished author, and a member of multiple professional bodies. She lectures in ternationally and is an expert in applying sleep and craniofacial assessments in various healthcare environments.

I believe that we can truly help more people by uniting the medical, dental, and mental health communities in addressing what is happening during those elusive eight hours...
o,” my dentist client explains to me, “I’ve got it all set up. It’s a sleep medicine practice. It’s beautiful!”
“Great,” I tell him. “We haven’t talked about this new idea. Tell me about it.”
“Here’s how it works,” he says. “A retiring sleep doctor two states over said he’d join me. We formed a new practice – 50/50.
“I’ll send my patients who complain of snoring to our new practice. The doctor will do a telehealth visit and I’ll do the home sleep test. The doctor will review the test and order the appliance.
“Then I’ll fit the patient and the practice will bill the patient’s health plan. I can’t wait to get started! I signed a five-year lease this morning. What do you think?”
“Well,” I said, “I think we need to contact your landlord and try to get you out of this lease.”
In all honesty, this conversation never happened. But I’ve been advising clients in the dental sleep medicine space for about ten years and I won’t be surprised if I get on a phone call one day along these lines.
That’s because dental sleep medicine is complicated. It must coordinate two different health professions in the testing, diagnosis and treatment of a single condition – obstruc tive sleep apnea. The sleep doctor operates
in his or her own world of state and federal regulations. The dentist operates in a sepa rate universe of laws and regulations, many of which are more restrictive than those of the medical doctor.

And thorniest of all for the dentist is get ting paid for fabricating and fitting the oral appliance. The wizards who control reim bursement categorize oral appliance therapy as an item of Durable Medical Equipment (DME). That throws the dentist in the same pool as suppliers of oxygen, hospital beds, TENS units for chronic pain, and CPAP.
When a dentist files a claim for oral appliance therapy, insurance companies often reject the claim. Insurance plans could use a hall of mirrors approach to rejection – per haps the dentist isn’t a contracted provider in the insurance plan, or the claim might be viewed as a sleep apnea disease matter and shunted off to the carrier’s medical division, who might deflect payment by saying that the invoice is a claim for dental services to be processed by the dental service division, who rejects on the ground that the invoice is for DME to be processed by the carrier’s DME section, who might send it to the dental section and start the merry-go-round again.
Getting paid for oral appliance therapy by Medicare invites its own pain. First the den tist must enroll in the Medicare program as a DMEPOS supplier. As a DME supplier, the
dentist is subject to variety of restrictive sup plier standards. Worse, the dentist becomes subject to the federal Anti-Kickback and Stark laws. This means that the dentist must thoroughly vet the financial arrangements, if any, with the referring sleep doctor.
For example, in the joint practice de scribed by my hypothetical client above, the sleep doctor’s order of an oral appliance furnished by the dentist and billed by the practice to Medicare would likely violate the Stark law’s referral prohibition.
But that supposes that a dentist and phy sician are permitted by State law to practice together in the first place. Like I said, it gets complicated.
I’ve been asked by Dental Sleep Practice magazine to author a quarterly column ad dressing some of the legal issues facing den tal sleep practitioners. I plan to address one or two regulatory topics in this column each issue. I hope you find these helpful.
Here’s a quick run-down of some of the issues I’ll address in upcoming columns:
• Corporate Practice of Dentistry. Most states prohibit lay persons or medical doctors from owning any part of den tal practice or practicing medicine at a dental practice.
• Corporate Practice of Medicine. Most states prohibit lay persons or dentists from owning any part of a medical practice or practicing dentistry at a medical practice.
• Dental Service Organizations. This addresses when and how non-dentists participate in a dental sleep medicine business via a management services
arrangement. Some states make it hard. North Carolina, for example, requires that the proposed service agreements be submitted to the state for review and prior approval.
• Home Sleep Testing. Some states, like Georgia, absolutely forbid dentists from handling a home sleep test. Oth ers are more lenient and allow dentists to perform home sleep tests as long as sleep doctors interpret the results.
• Teledentistry. Can the dentist work up an oral appliance via telehealth?
• Leased or Mobile Dentist Office. Can a dentist lease space from a sleep doctor to provide oral appliance therapy? Or can the dentist drive a van to the sleep doctor’s parking lot to fit the appliance?
• HIPAA. Sleep dentistry requires sharing of patient information. How does HIPAA apply?
• Fraud and Abuse. When and how do patient self-referral and anti-kickback laws apply to financial arrangements among sleep physi cians and the dentist who furnishes the oral appliance.
• Dental Advertising Restrictions. Many state dental boards prohibit dentists from advertising a specialty, such as dental sleep, unless the dental board has taken action to recognize the specialty.
We will take a look at these items and more over the coming months. See you next time.
In 2004, Mr.

When a dentist files a claim for oral appliance therapy, insurance companies often reject the claim.

The Academy of Clinical Sleep Disorders Disciplines is the only organization offering a fully online and on-demand certificate in Dental Sleep Medicine. Study the lectures and course materials at your own pace, then when you are ready, take the exam. The C.DSM certificate from ACSDD provides the necessary medical and dental knowledge to confidently approach physicians and seek insurance reimbursement. The certificate is a prerequisite for ACSDD Fellow and Diplomate.
The Academy of Clinical Sleep Disorder Disciplines is the only organization offering a fully online and on-demand certificate in Dental Sleep Medicine. Study the lectures and course materials at your own pace, then when you are ready, take the exam. 12 modules present both the medical and dental science of sleep medicine providing a solid foundation for understanding clinical applications. Most dentists are able to complete the 13 CE program in 4-6 months.
The certificate is a prerequisite for ACSDD Fellow and Diplomate
The Academy of Clinical Sleep Disorders Disciplines (ACSDD) is an ADA CERP Recognized Provider.
ADA CERP is a service of the American Dental Association to assist dental professionals in identifying quality providers of continuing dental education. ADA CERP does not approve or endorse individual courses or instructors, nor does it imply acceptance of credit hours by boards of dentistry.
The Academy of Clinical Sleep Disorders Disciplines (ACSDD) is an ADA CERP Recognized Provider.

This program has been submitted for approval by the ACSDD for a maximum of 13 credits as meeting general dental requirements.
ADA CERP is a service of the American Dental Association to assist dental professionals in identifying quality providers of continuing dental education. ADA CERP does not approve or endorse individual courses or instructors, nor does it imply acceptance of credit hours by boards of dentistry. Concerns or complaints about a CE provider



