Learn more at high5health.com PROMOTING EXCELLENCE IN ENDODONTICS Communicating periodontal issues across dental implant platforms Drs. Stuart Segelnick and Mea A. Weinberg Dental infections, part 2 — prophylaxis: help avoid antimicrobial resistance Wiyanna K. Bruck, PharmD, and Jessica Price
Dr. Jason Putnam: owning his future Winter 2022 Vol 15 No 4 endopracticeus.com Implant & Endo Connection n 4 CE Credits Available in This Issue* Judy McIntyre, DMD, MS
You’re passionate about teeth. We’re passionate about payroll, recruiting, and human resources. HighFive is your expert team at wrangling all those business necessities before they consume your practice.
Practice spotlight

Winter 2022 n Volume 15 Number 4
Editorial Advisors
Dennis G. Brave, DDS
David C. Brown, BDS, MDS, MSD
L. Stephen Buchanan, DDS, FICD, FACD
Gary B. Carr, DDS
Arnaldo Castellucci, MD, DDS
Gordon J. Christensen, DDS, MSD, PhD
Stephen Cohen, MS, DDS, FACD, FICD
Samuel O. Dorn, DDS
Josef Dovgan, DDS, MS
Luiz R. Fava, DDS
Robert Fleisher, DMD
Marcela Fridland, DDS

Gerald N. Glickman, DDS, MS
Jeffrey W Hutter, DMD, MEd
Syngcuk Kim, DDS, PhD
Kenneth A. Koch, DMD
Gregori M. Kurtzman, DDS, MAGD, FPFA, FACD, DICOI
Joshua Moshonov, DMD
Richard Mounce, DDS
Yosef Nahmias, DDS, MS
David L. Pitts, DDS, MDSD
Louis E. Rossman, DMD
Stephen F. Schwartz, DDS, MS
Ken Serota, DDS, MMSc
E Steve Senia, DDS, MS, BS
Michael Tagger, DMD, MS
Martin Trope, BDS, DMD
Peter Velvart, DMD
Rick Walton, DMD, MS
John West, DDS, MSD
CE Quality Assurance Board
Bradford N. Edgren, DDS, MS, FACD

Fred Stewart Feld, DMD
Gregori M. Kurtzman, DDS, MAGD, FPFA, FACD, FADI, DICOI, DADIA
Justin D. Moody, DDS, DABOI, DICOI
Lisa Moler (Publisher)
Mali Schantz-Feld, MA, CDE (Managing Editor)
Lou Shuman, DMD, CAGS
© MedMark, LLC 2022. All rights reserved. The publisher’s written consent must be obtained before any part of this publication may be reproduced in any form whatsoever, including photocopies and information retrieval systems. While every care has been taken in the preparation of this magazine, the publisher cannot be held responsible for the accuracy of the information printed herein, or in any consequence arising from it. The views expressed herein are those of the author(s) and not necessarily the opinion of either Endodontic Practice US or the publisher.
number 2372-6245
INTRODUCTION
Asking for insights leads to good decisions
As endodontists, keeping up with the latest advancements in technology is simply part of the job. As we endeavor to provide our patients with the best possible care, it’s our responsibility to ensure we’re up-to-date on the best possible tools and technologies to help us provide that care. It’s what our patients deserve and what our profession promises. But amidst our long hours and packed waiting rooms, how can we use our limited capacity to separate the gimmicks from the legitimately important advancements in our profession? In a world of finite resources, how do we ensure we’re investing our time, effort, and money on things that will actually improve our patients’ lives as well as our own?
I remember when I finally decided to take the leap and invest in cone beam computed tomography. It wasn’t an easy decision. Navigating how to incorporate this new technology, as well as the financial investment of the CBCT equipment and the financial impact on patients, was a challenge. And then there’s simply the resistance to change. So many aspects of endodontics are tried and true. We all become proficient in a certain way of doing things and become hesitant to anything new that deviates from that trusted path. But next to the microscope, the use of CBCT imaging has become the most important development in endodontics. It has increased our ability to diagnose and treat pathology efficiently and correctly. The switch wasn’t easy, but the long-term positive impact for my patients and my practice has been worth the effort.
But how did I come to that decision? Of course, I stayed current on the latest literature and attended continuing education courses. But more than anything, I relied on what I consider to be the most important tool in any endodontist’s arsenal — my colleagues.
No advancement, no new piece of technology, no exciting new technique will ever be more valuable than the minds, experience, insight, and fellowship of our fellow endodontists. Being a partner with HighFive Healthcare, I have access to a network of brilliant, hardworking, and generous people who all bring their own unique perspectives, knowledge, and history to the table and whose advice and guidance I can rely on when faced with challenging decisions. I didn’t just read articles about the CBCT; I asked my colleagues. I got their first-hand experiences. I learned the ups and the downs, the pros and the cons. I had people I trusted to help me make that important decision and help make it the right one.
Technology is always changing. There’s always some new thing on the horizon that claims to change the way we practice for the better. And some of them actually will. But nothing will ever be more important than the relationships we build with each other. And anything that allows us, as endodontists, to increase those connections, to improve our communications, to bring us closer together in order to share our expertise with one another, that is the most important innovation possible.
Kristy Goff Jones, DMD, graduated Millsaps College in 2003 with a BS in Biology and then attended the University of Mississippi School of Dentistry. After receiving her DMD in 2007, she started the postgraduate program in endodontics at Tufts University School of Dental Medicine in Boston, Massachusetts. In 2009, she began practicing with Endodontic Associates where she currently works alongside Dr. Jeffery Pride in three locations in Ridgeland, Brandon, and Vicksburg, Mississippi. You can reach out to Dr. Jones at https://endoofms.com/.
1 endopracticeus.com Volume 15 Number 4
ISSN
Kristy Goff Jones, DMD



2 Endodontic Practice US Volume 15 Number 4 TABLE OF CONTENTS TECHNIQUE Negative and positive pressure irrigation: all-in-one! Dr. Allen Ali Nasseh explores whether the positive and negative pressure needs of clinicians can be met with a simple and inexpensive device
PERSPECTIVE Telling the world about you
Founder/CEO, MedMark Media............................... 6 CLINICAL Internal root resorption: morphological aspects and clinical management
Fernando Goldberg, Denise Alfie, Juan Pablo Miraglia, Carlos Cantarini,
Gonzalo
discuss treatment for
inflammatory condition ..............18 TECHNIQUE Rotary negotiation as first file to length Drs. L. Stephen Buchanan and Christophe L.M. Verbanck discuss a modern answer to
age-old issue .............................. 24 SERVICE PROFILE US Endo Partners Building culture delivers financial returns .............................................. 28 CONTINUING EDUCATION Communicating periodontal issues across dental implant platforms Drs. Stuart Segelnick and Mea A. Weinberg review typical challenges and management at the dental implant-abutment connection ...................................... 30 8 12
STORY
McIntyre, DMD, MS
image of Dr. McIntyre courtesy of DEXIS.
PUBLISHER’S
Lisa Moler,
Drs.
and
Garcia
an
an
COVER
Judy
Cover



2023 YOUR MAKE
your practice growing strongly and more profitable than ever. Enjoy productive stress-free scheduling driven by incredible teamwork and efficiency. Improve referrals and patient flow with powerful strategies for engaging GP relationships.
one year, the Endo Mastery team can help you transform your practice and transform your life. Pay off debt fast, eradicate financial stress, empower personal and family goals, and love your practice like never before. Learn more about Endo Mastery’s coaching programs and why our clients love us. BEST YEAR! 1-800-482-7563 info@endomastery.com
Imagine
In
CONTINUING EDUCATION
Dental infections, part 2 — prophylaxis: help avoid antimicrobial resistance


Wiyanna K. Bruck, PharmD, and Jessica Price continue their discussion of concepts surrounding antibiotic prophylaxis in dentistry ............. 35

TECHNOLOGY
Healing and longterm results with the GentleWave® Procedure
Dr. Scott K. Hetz illustrates minimally invasive endodontic treatment with predictable results 40
PRODUCT PROFILE
Sealing the deal with a bioceramic root canal sealer
CeraSeal from Meta Biomed provides antimicrobial properties, high biocompatibility, and a hermetic seal 44
PRODUCT SPOTLIGHT

Optimizing surgical visualization with the ZEISS EXTARO® 300
Dr. Jon Irelan discusses innovations in endodontic microsurgery 46
LEGAL MATTERS
Implications of the False Claims Act
Kerry Cahill, Esq., discusses how practitioners need to protect themselves even in altruistic circumstances
PRACTICE MANAGEMENT
Life sentence practice or lifestyle practice?
Dr. Albert (Ace) Goerig describes the foundation to his philosophy and vision...................................... 54
SMALL TALK
PRODUCT PROFILE ES Vac ES Vac is changing irrigation! ... 48
LEGAL MATTERS Navigating dental malpractice lawsuits


Kristin Tauras, JD, guides dental specialists through the legal elements
50
Thoughts on why we lose staff
Drs. Joel C. Small and Edwin McDonald discuss the rewards of appreciating your team 55
PRACTICE PROFILE Dr. Jason Putnam: owning his future
4 Endodontic Practice US Volume 15 Number 4 TABLE OF CONTENTS
......................................
............................ 52
.........................................................
Connect. Be Seen. Grow. Succeed. | www.medmarkmedia.com READ the latest industry news and business WATCH DocTalk Dental video interviews with KOLs LEARN through live and archived webinars RECEIVE news and event updates in your inbox by registering for our eNewsletter CONNECT with us on social media www.endopracticeus.com *Paid subscribers can earn 4 continuing education credits per issue by passing the 2 CE article quizzes online at https://endopracticeus.com/category/continuing-education/
56
You handle the teeth.
At HighFive Healthcare, we’re passionate about the business of endodontics. That’s why we partner with Endodontists who are equally passionate about helping their patients. Our family of experts handle just about everything outside of root canals, so you can focus on what you love and create your own tomorrow.
Learn more at high5health.com
Telling the world about you
Published by
Our worlds are so busy with our time consumed with improving clinically, professionally, and personally. We work hard and hopefully find the time to play hard. From my view as a publisher of four and soonto-be five dental publications, I see and hear about so much innovation going on in the dental community. Dentists are showing patients that dental health means better overall health, and there are so many ways to add technology, expand clinical options, and create your own new protocols and inventions that can change the face of your specialties. My team at MedMark is always searching for your stories — for your journeys, your successes, and even your speed bumps along the way. Entrepreneur Gary Vaynerchuk said, “Regardless of what you are trying to accomplish, you’ve got to tell the world about it.” I wholeheartedly agree. And that’s what we at MedMark Media have been doing over the past 17 years. We’ve been telling the world about you.
Publisher
Lisa Moler lmoler@medmarkmedia.com
Managing Editor
Mali Schantz-Feld, MA, CDE mali@medmarkmedia.com Tel: (727) 515-5118
Moler Founder/Publisher, MedMark Media
All of the new advancements in dental specialty fields are amazing — artificial intelligence (AI), virtual reality, 3D printing, robotics, the field of dental sleep medicine, braces and aligners that move teeth faster and more efficiently, and imaging in 2D and 3D that makes diagnostics more precise. Advances in endodontic materials such as bioceramics contribute significantly to that specialty’s incredible growth. Let’s not forget implants — according to iData Research, over 3 million dental implants are placed each year in the United States, and the U.S. market is expected to exceed $1.5 billion in 2027.
Here’s more good news! Our Cover Story is a conversation with Dr. Judy McIntyre, who talks about how DEXIS™ CBCT imaging helps her to confidently offer a realistic prognosis and gives her essential information for treatment planning. Our CE article by Drs. Stuart Segelnick and Mea Weinberg, titled “Communicating periodontal issues across dental implant platforms,” explores common problems and management at the dental implant-abutment connection. For our Technique column, Dr. Allen Ali Nasseh tells how the TotalVac Irrigation System allows for both positive and negative pressure application of the multiple liquids necessary for the root canal process. Drs. L. Stephen Buchanan and Christophe L.M. Verbanck discuss rotary negotiation as the first files to length and the progress that has been made by different files over the years.
Back to you — how can we help you tell the world about your innovations, techniques, and life-changing treatments? Our articles and advertisers show you what is possible and practice changing, and promises to help differentiate you from the rest. To change Gary Vaynerchuk’s quote just a bit: Regardless of what you are trying to accomplish, MedMark is here to help you tell the world about it.
To your best success,
Assistant Editor Elizabeth Romanek betty@medmarkmedia.com
National Account Manager Adrienne Good agood@medmarkmedia.com Tel: (623) 340-4373
Sales Assistant & Client Services Melissa Minnick melissa@medmarkmedia.com

Creative Director/Production Manager Amanda Culver amanda@medmarkmedia.com
Marketing & Digital Strategy Amzi Koury amzi@medmarkmedia.com
eMedia Coordinator Michelle Britzius emedia@medmarkmedia.com
Social Media Manager April Gutierrez socialmedia@medmarkmedia.com
Digital Marketing Assistant Hana Kahn support@medmarkmedia.com
Website Support Eileen Kane webmaster@medmarkmedia.com
MedMark, LLC 15720 N. Greenway-Hayden Loop #9 Scottsdale, AZ 85260
Lisa
Moler Founder/Publisher MedMark Media

Tel: (480) 621-8955 Toll-free: (866) 579-9496 www.medmarkmedia.com
www.endopracticeus.com
Subscription Rate
1 year (4 issues) $149 https://endopracticeus.com/subscribe/
6 Endodontic Practice US Volume 15 Number 4 PUBLISHER’S PERSPECTIVE
Lisa


two
help patients
You proactively recommend the CareCredit credit card to patients. Have patients scan your custom link QR code where they can privately see if they prequalify, apply and pay with CareCredit. #1: #2: It’s financing simplified. Get everything you need with the Contactless Financing Kit — Scan this QR code, or visit carecredit.com/contactless-kit. MM2SQ4DA Data fees may apply. Not yet enrolled with CareCredit? Call 800.300.3046 (option 5).
It takes
steps to
get care
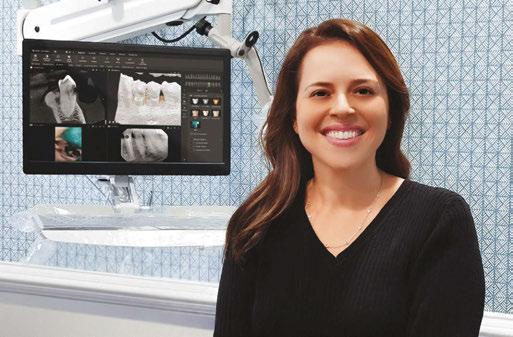
Judy McIntyre, DMD, MS
Why did you become an endodontist?
I always knew I wanted to be a dentist. As a child, I had a traumatic dental injury, and I had positive experiences with my dentist; I wanted to be able to provide the same kind of care to others. I’ve always enjoyed working with my hands, and endodontics suited my skill set and personality.
During my residency at the Adams School of Dentistry (UNC-Chapel Hill), I was fortunate to have great mentors and was exposed to many dental trauma cases. In my practice, Hopkinton Endodontics, I treat pediatric and adult patients with dental trauma as well as my traditional endodontic patients, so I can combine both passions. It’s the perfect fit.
What is the most rewarding aspect of your practice?
I find it incredibly rewarding to save teeth and relieve patients’ pain. Being able to put patients at ease and give them their smiles and confidence back is very gratifying. Our pediatric patients are surprisingly good; typically they have fewer past dental experiences, and with the right approach, they turn out to be very cooperative with local anesthesia alone! The parents are so appreciative, especially when they’ve previously been told that nothing can be done for their children/tooth. My young patients with dental trauma have a lot on the line — trying to save a tooth in a growing patient. Treating kids is extremely rewarding.
I also find current technology such as CBCT imaging helps to identify the cause of patients’ pain and to treat issues that have been missed or misdiagnosed. Often, patients have seen other practitioners and have been told that everything appears normal. It makes my day when I’m able to reveal the cause of their pain and problems, to show them on their 3D scan that they were correct in thinking something was not quite right, and then correct and treat the issue. The patients are extremely grateful and relieved. My CBCT unit plays a key role in that.
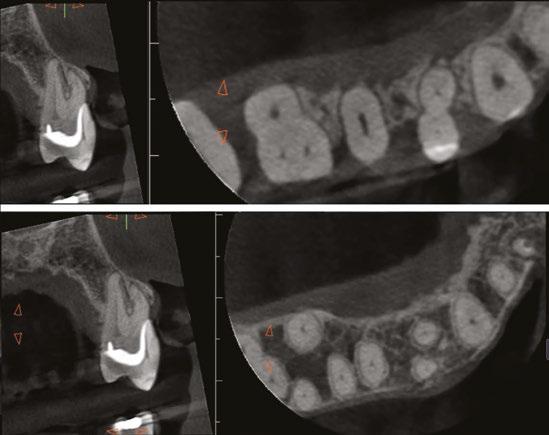
As endodontists, our priority is to save teeth whenever possible. Sometimes we forget that; we’re doing more than just a root canal procedure — we’re preventing or treating apical periodontitis — we are saving teeth! CBCT enables me to save more teeth and do it more predictably; patients appreciate when they can avoid losing the tooth.

When did you start using CBCT in your practice?

I was first introduced to cone beam technology during my endodontics residency. UNC had a CBCT unit and was one of only a few institutions in the country that did almost 20 years ago. At the time, the technology was new, and we didn’t use it often. Reflecting back, I wish we had used it
8 Endodontic Practice US Volume 15 Number 4 COVER STORY
Judy McIntyre, DMD, MS
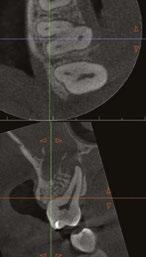
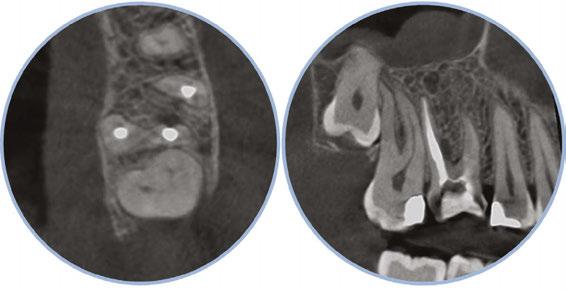
Figure 1: Acutely curved and calcified buccal canal right under upper left premolar crown margin; valuable information for access and management. No. 9 also has a PARL, which was only incidentally captured
Figure 2: Large PARL with destruction of the maxillary sinus floor and sinusitis as a result
more. In residency, I planned an autotransplantation on a patient in her early 20s whose lower left first molar had to be extracted. My plan was to move her upper right third molar to the extracted tooth’s position. I measured for this using a panoramic x-ray unit and ended up being far off — even after calculating for the known magnification of the pan. I published a paper about this case. Although it was successful, I could’ve done it better had I used the CBCT with more accurate information while I was planning. That was my first of many aha moments that has helped to shape my current imaging protocols.
About 10 years after completing residency, I opened my own practice and invested in a DEXIS CBCT. Initially, I only used it for apicoectomies and retreatments. In time, I began to realize how helpful it was for all my cases. With the 3D-scan information (Figure 1), I could have saved myself some humbling experiences and surprises. Endodontists hate surprises, and we really hate failures! Once I started using my CBCT more frequently, I was able to appreciate things that would have otherwise been intra-op surprises and plan for them prior to starting the procedure. The 3D data allows me to properly assess prognosis, determine the best course of treatment, and plan that treatment with a level of precision that is impossible otherwise.
CBCT also allows me to capture issues I might have previously missed, whether related or solely incidental findings. Practitioners can visualize pathology/issues even when a patient is completely asymptomatic. I had a patient referred to me with an issue on one tooth. Cone beam revealed the patient had four teeth that unfortunately needed extractions, and all previous imaging gave no indication of this. Another patient presented for one tooth, but the CBCT showed several cracked molars and a perforated post. I was able to properly diagnose those problems as well. Sadly, those couldn’t be saved with endodontics, but knowing that up front saved time, unnecessary treatment, and resources for the patient.
On a recent second molar case where I did not take a 3D scan prior to root canal treatment, the patient returned several days later still in pain! I took a scan and appreciated their deep split, forked in the last 5 mms of the distal canal (Figure 8). Without a CBCT scan, it’s easy to miss — I did! CBCT helps prevent this from happening by catching those variants and hard-to-find issues, which are not as rare as we think. This was another case that helped shape my current imaging protocol, so that now I scan nearly all of my patients. I honestly can’t imagine practicing without my CBCT unit — similar to when the microscope was introduced to endodontics.

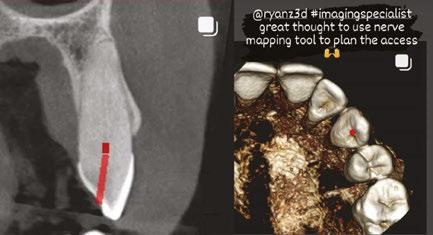
As I did not train with CBCT in residency, I really did have to “invest” the time into improving my interpretation with it. I purchased a CBCT/endodontics book, attended every webinar and lecture I could, began working more closely with oral radiologists, and did more training with my DEXIS Imaging Specialist, Ryan Zager. All of these were really worthwhile, and I’m still learning, but now I can better distinguish a true crack from beam hardening, etc. I feel way more confident in my interpretation. I have
to thank DEXIS mainly for that. Their technology and support is unparalleled.
How has CBCT affected your patient experience and outcomes?
CBCT has greatly improved the patient experience. As an endodontist, a good portion of the teeth I’m treating have already had endodontic treatment. CBCT allows me to figure out why the root canal didn’t work the first time: Sometimes there is a missed canal or a fracture. If something is failing, I need to know why it is failing in order to plan my treatment appropriately and to give the patient the best chance of saving the tooth, as well as

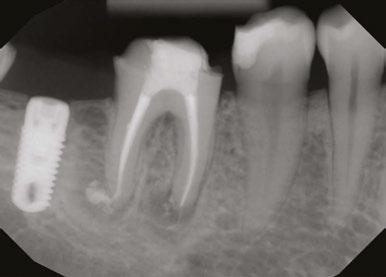
9 endopracticeus.com Volume 15 Number 4 COVER
STORY
Figure 3: Second maxillary molar with external root resorption (ERR) with incidentally captured ERR on the lower mandibular first molar as well. When there is one tooth with resorption, be suspicious of other teeth with resorption, especially on younger patients
Figure 6: No PARL on PA film. Clear PARL on scan taken with medicament
Figures 4 and 5: 4. Mandibular molar with a J-shaped lesion due to endo — not a vertical root fracture. Path of least resistance happens to be through a distal perio pocket, but this is an endo-perio lesion and not a VRF. Incidentally, a mucous retention cyst was captured in the sinus. 5. Healing after bridge removal and retreatment
a realistic prognosis. Unfortunately, not all teeth can be saved. Some are not candidates for retreatment (Figure 11). Without a CBCT scan, it would be easy to attempt these retreatments only to discover the true problem mid-treatment, or worse — to think I had caused one (Figures 10 and 11). This added information not only helps the practitioner, but also provides patients a higher level of confidence and trust in you.
With retreatments, maybe the root canal looks completely fine on a PA or panoramic x-ray, but the patient says that it just doesn’t feel right. A cone beam can often reveal the cause of the patient’s discomfort. This could be that the tooth was perforated, cracked or has an unfilled canal, and the patient is totally justified in feeling like something’s wrong. Or sometimes the scan will show that there is another issue on an adjacent tooth or in the patient’s sinuses (causing their discomfort). When patients sense a problem but are told that there is not one (usually based on 2D radiographs), that’s not a great feeling. Being able to show the patient the CBCT scan and say, “You were right, and here’s the issue,” improves the patient experience.


I also find with 2D radiographs, patients don’t always understand what we’re trying to share with them in the image, even when they say they do. However, I’ve noticed when I review a 3D scan with patients, their eyes widen and they start nodding, especially when reviewing their volume rendering; it’s definitely helped with patient education and case acceptance. They see their teeth, their jaw, the infection in their bone (as a hole), and they understand this since they recognize themselves in 3D. This better understanding makes them more likely to accept the recommended treatment plan, leading to better outcomes. Ultimately, the patient is glad we took the CBCT scan. They’re thankful to have that information.
I also see a good amount of resorption cases. Without the scan, I can’t determine how large or destructive the lesion is. I cannot accurately determine the best course for these resorptive cases without knowing what they look like in 3D (Figure 3). I might approach it surgically without endo, or I might plan only for the endo and monitor it after. And, some cases need both at
the same time, or closely planned together, or a resorptive defect could be taken care of internally with the endo — all of that thought and planning comes from the scan; usually not possible with 2D imaging alone.
How has CBCT changed your treatment approach?
CBCT has transformed the way I treat patients in many ways. First, with cone beam, I can confidently offer a realistic prognosis on a tooth. Sometimes this means no treatment, saving me — and the patient — the time of pursuing a treatment that may not work, or has a poor prognosis.
The 3D scan also provides essential information to better treatment planning. Sometimes, this means knowing exactly the number of canals in a tooth, instead of hunting and based on
10 Endodontic Practice US Volume 15 Number 4 COVER STORY
Figure 7: Planned-for access with the scan info on this extremely calcified canine
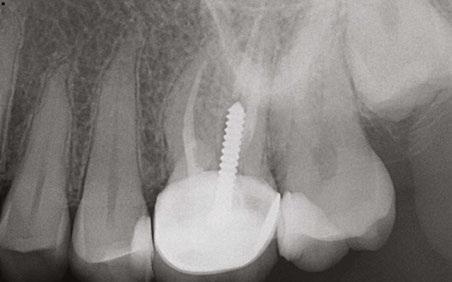
Figures 8 and 9: 8. Deep distal split with PARL. 9. Missed buccal canal; history of previous RCT, post, crown and apico
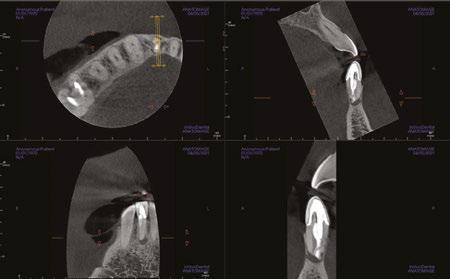
Figure 10: Retreatment consultation. PA from GD
Figure 11: Scan images show a previously existing strip perforation
what the literature suggests. And, when I know how many and where the canals are (Figure 13), I can take measurements on the scan and work more efficiently — measuring my working lengths of each canal, appreciating severe curves or calcifications, and knowing where canals can be expected to be located, again, rather than removing unnecessary tooth structure to find if it is there, or not!
As an endodontist, I often treat heavily restored teeth. I am often planning my accesses based on the scan’s information. This saves time and conserves more tooth structure. I’m not looking for canals that may or may not be there, and I’m looking for canals under the targeted/planned access — with the scan, I have an actual map (Figure 7)! CBCT directs me where to go and where to end. It reveals anomalies, which are more common than we think, so I can avoid iatrogenic incidents and provide less invasive treatments. Lower second molars with only two canals occur — often!
I’m also changing my treatment plans based on the data from my CBCT. Sometimes I look at a root canal treated PA and presume I know what I will do: a retreatment or an apico. Another recent, poignant case: a lower incisor with a previous RCT and a previous apico (Figure 9). Usually, once a tooth has had an apico, there may not be much left to offer and most of the time, the default is another apico, especially as there was very little room for an implant on the lower anteriors. I scanned the tooth and saw that a whole canal had been missed — twice! The RCT and the apico had left the buccal canal completely untouched. I changed my treatment plan based on this information!
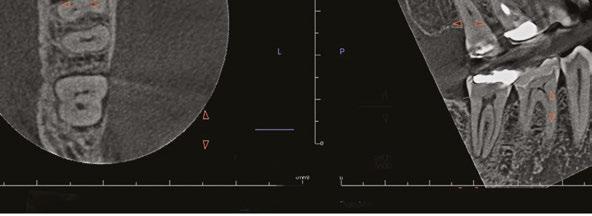
Cracked teeth are also quite prevalent (Figure 12). Of course, I can suspect them clinically and with transillumination and other tests, I’m fairly confident in my diagnosis. Thankfully, the 3D scan proves it and shows the depth of these cracks and the angular defect. Without a CBCT, sometimes these cases are started unnecessarily.
Lastly, using CBCT also allows me to find issues that should be evaluated by another specialist. For example, when I capture incidental sinusitis, I can inform my patient to see an MD or ENT and can provide the 3D images to share with their physicians; or, to involve another dental specialist. (Figures 2, 4, 6, and 11 show incidental sinus findings.)
What advice would you give to your younger self?
I would tell my younger self that CBCT is as important of a tool for endodontics as a microscope and that I should get proficient with it early. I wish I had started using cone beam technology a lot earlier, on a lot more cases. Thankfully, I had tremendous support from DEXIS to help with my 3D-learning curve, but I wish I had become better with it earlier so that I could have used it to its potential even earlier.

What does the future of endodontics look like?
I would say that the impact of COVID will shape the future of endodontics. Many people delayed dental care during the pandemic, and now that they’re coming back into our practice, we’re seeing more complex cases and bigger problems. We’re seeing a phenomenal number of cases with cracked teeth, for example. Patients are stressed and anxious. All of this can be harder to manage and more challenging to treat.
We need to adapt to this new reality by staying calm, reassuring patients, and having empathy. We should also be taking advantage of all the technological advancements available to us — such as the OP 3D CBCT system from DEXIS — to support better diagnosis, treatment, and patient outcomes for these complex cases. When we have more confidence in our work, patients have more confidence in us. EP

11 endopracticeus.com Volume 15 Number 4
COVER STORY
Figure 12: Cracked tooth
Figure 13: Five canaled maxillary molar with five portals of exit
Negative and positive pressure irrigation: all-in-one!
Dr. Allen Ali Nasseh explores whether the positive and negative pressure needs of clinicians can be met with a simple and inexpensive device
During a conventional root canal procedure, the operator must manage the multiple liquids used to facilitate the access, chemomechanical instrumentation, and final obturation steps of the procedure. These liquids are used at each phase of the procedure and have specific functions.1 The access preparation phase requires water coolant spray from high- speed handpieces. Chemomechanical instrumentation requires positive pressure irrigation of disinfectants and chelators in the coronal and apical segments of the root canal, and finally, a bout of negative pressure irrigation is used by some clinicians to safely run a high-volume of disinfectant and chelating agents at the end of the procedure for enhanced apical cleaning prior to obturation.1-3 During each phase, multiple solutions including water, sodium hypochlorite, chelators, and lubricants help facilitate the process of root canal therapy and allow us to get rid of the infected pulp and biofilm, clear dentinal debris, and prepare a clean root canal surface ready for obturation.2

To manage these fluids, suction (negative pressure) is required to clear excess fluids and macro debris from the area. The operator, generally aided by a dental assistant, starts the procedure by a sequence of high-speed evacuation to remove the water coolant from the area after it is expressed from the handpiece, then switch to surgical suction to manage the debris and added irrigants during root canal instrumentation, and finally switch to another device for negative pressure suction at the end of
Allen Ali Nasseh, DDS, MMSc, received his dental degree from Northwestern University Dental School in Chicago, Illinois, in 1994 and completed his postdoctoral endodontic training at Harvard School of Dental Medicine in 1997, where he also received a Master of Medical Sciences (MMSc) degree in the area of bone physiology. He has been a clinical instructor and lecturer in the postdoctoral endodontic program at Harvard School of Dental Medicine since 1997 and the Alumni Editor of Harvard Dental Bulletin. Dr. Nasseh is the endodontic advisor to several educational groups and study clubs and is endodontic editor to several peer-reviewed journals and periodicals. He has published numerous articles and lectures extensively both nationally and internationally in surgical and nonsurgical endodontic topics. Dr. Nasseh is in solo private practice (MSEndo.com) in downtown Boston, Massachusetts. Dr. Nasseh is the President and Chief Executive Officer for the endodontic education company Real World Endo® (RealWorldEndo.com).
Disclosure: Dr. Nasseh is a speaker and key opinion leader for Brasseler USA® and has received compensation for lecture presentations showcasing the company’s bioceramics.

Figure 1: The TotalVac Irrigation System showing its three main components: 1) The High-Speed Evacuation tip. 2) The Surgical Suction Adaptor. 3) The Negative Pressure Tubing
Figure 2: The high-volume evacuation tip is used during access and high-volume needs of cleaning and shaping procedure
instrumentation.3 These three phases often require three separate HVE suction outlets from the operatory unit with three separate components and a complicated workflow.
Recently, a novel modular device has been developed by the author that may help address the clinical needs for positive and negative pressure irrigation during these three phases of treatment through the application of a single system. The TotalVac Irrigation System (Brasseler USA®, Savannah, Georgia) is a disposable kit that allows the operator to use the aforementioned positive and negative pressure application of fluids during the root canal procedure through modular use of its components (Figure 1). The kit consists of three main parts:
1. High-Speed Evacuation Tip
2. The Surgical Suction Adaptor
3. The Negative Pressure Tubing
High-Volume Evacuation
This is the most intuitive component of the system. It duplicates the conventional high-volume evacuation; however, the nozzle size is in-between a large high-volume evacuation tip and a surgical suction tip. Therefore, this tip can generally be used for both applications during access preparation and normal evacuation of fluids during instrumentation. This item requires a single suction inlet from the operatory unit (Figure 2).

12 Endodontic Practice US Volume 15 Number 4 TECHNIQUE





Order online at Shop.BrasselerUSA.com
our
at
order
diameters to suit your specific needs Retail: $200.00 Special: $163.00 Kit includes: 25 high volume evacuation and surgical suction adaptors, 25 TotalVac tubings, 25 plastic suction tips, 25 25ga short delivery tips, and 25 30ga side vented long delivery tips *While supplies last. Offer subject to change. Promotion expires January 31, 2023. Invoice or statement prices may reflect or be subjected to a bundled discount or rebate pursuant to purchase offer, promotion, or discount program. You must fully and accurately report to Medicare, Medicaid, Tricare and/or any other
program,
such program, the discounted price(s) or net price(s) for each invoiced item, after giving effect to any applicable discounts or rebates, which price(s) may differ from the extended prices
and
information for your records.
your responsibility to review any agreements or other documents, including offers or promotions,
discount or rebate.
discounts must
calculated pursuant to the terms of the
purchase offer, promotion, or discount
B-5699-EP-12.22 ©2022 Brasseler USA. All rights reserved. Visit
website
BrasselerUSADental.com To
call 800.841.4522 or fax 888.610.1937.
federal or State
upon request by
set forth on your invoice. Accordingly, you should retain your invoice
all relevant
It is
applicable to the invoiced products/prices to determine if your purchase(s) are subject to a bundled
Any such
be
applicable
program. Participation in a promotional discount program is only permissible in accordance with discount program rules. By participation in such program, you agree that, to your knowledge, your practice complies with the discount program requirements.
TECHNIQUE
Surgical Suction Adaptor

If more precise suction application is needed than that provided by the High-Volume Evacuator, a Surgical Suction Adaptor can be fitted to the High-Volume Evacuator Tip, transforming it into a surgical suction (Figure 3). This allows an efficient conversion of high-speed evacuation to surgical suction, and vice versa. The dental assistant can merely take on-and-off this adaptor to switch between two types of suction instead of replacing the entire suction tip or requiring two separate HVE inlets with two separate suction tips on the operatory unit.



Negative Pressure Tubing
While high-volume evacuator and surgical suction are used by all clinicians doing endodontic therapy, applying suction capability closer to the treatment site without the aid of an assistant may be necessary in some clinical settings where a dental assistant may not be available during this phase of the procedure. This is common in dental school/residency and some private practice settings. Furthermore, some astute clinicians prefer using a large volume of irrigation inside the root canal with the safety of negative pressure techniques instead of mere positive pressure irrigation at the end of instrumentation.3 The purpose of the TotalVac Tubing is to address both of these needs through its modular design (Figure 4). The HVE fitting end of the tubing can be connected directly to an available HVE inlet in the operatory, or if an extra inlet is not available, the HVE fitting can be attached directly to the Surgical Suction Adaptor and connected to the High-Speed Evacuation Tip. This gives the operator the option of using only a single HVE inlet for all the various phases and applications of this device from access to obturation by using different configurations of tips in a modular manner. However, direct connection of the HVE connection into an available HVE inlet in the operatory is generally the most convenient configuration of this tubing according to the author.
The TotalVac Tubing bifurcates in two separate suction tubes. One end of tubing is connected to the manifold, a sleeve that houses a short Luer Lock needle that connects to the irrigation syringe for delivery of irrigation solution with simultaneous suction of excess fluid (Figure 5). The other end accommodates a handpiece that can be fitted with conventional Luer Lock delivery tips or needles to allow suction inside the root canal (Figure 6). The kit is supplied with a flexible plastic suction tip for average-size canals and a 30 gauge close-ended, side-vented needle that can be used for thinner canals. The same 30 gauge needle can also be used for positive pressure irrigation in combination with the plastic manifold at the other end of the TotalVac Tubing (Figure 7).
However, in negative pressure applications, it’s important to recognize that the use of this macro and micro level of suction deep in the root canal should really be limited to the end of instrumentation and after all the large pulp and dentinal debris have been removed from the canal to avoid clogging of the applicators tips.
The TotalVac Tubing assembly can operate under four distinct modes of operation. These modes are used based on the
Figure 3: The Surgical Suction Adaptor is connected to the High-Volume Evacuation Tip converting it into a surgical suction in a reversible manner
Figure 4: The bifurcated TotalVac Suction Tubing has an HVE connection end and two separate ends with a handpiece and a manifold for irrigation and suction
Figure 5: The TotalVac Manifold can accommodate various Luer Lock needles. In the kit, this is pre-fitted with a removable short needle that connects to an irrigation syringe
Figure 6: The Handpiece end of the suction tubing can accommodate the Plastic Suction Tip for macro suction or the 30 gauge needle for micro suction deep in the canal

Figure 7: The 30 gauge needle can also be used through the manifold to achieve deep positive pressure irrigation
stage of chemomechanical instrumentation (early or late) or the need for negative or positive pressure during irrigation (operator preference). Not all four modes are required during a single procedure, and the modularity of this device makes it possible for each operator to choose the modes he/she prefers for positive or negative pressure irrigation throughout the procedure.
14 Endodontic Practice US Volume 15 Number 4
TECHNIQUE
The four possible modes of application consist of two positive pressure (irrigation) modes and two negative pressure (suction) modes.
Coronal Irrigation (Mode 1)
The short needle in the manifold is connected to your irrigation solution of choice, and irrigation is deposited into the chamber while excess is suctioned up through the manifold (Figure 8). This allows single-handed operation of the syringe combining irrigation with suction. The manifold suction assembly should be kept very close to the cavosurface area of the access to allow suctioning of the excess fluid. (Note: The use of a caulking material to achieve secondary isolation of a fluid tight seal around the rubber dam is generally recommended prior to all root canal therapy.) Since the manifold needle is short and does not reach in the depths of the canal, this form of irrigation allows effective irrigation in only the coronal half of the root canal. This mode can be combined with the handpiece applicator to achieve high-volume negative pressure toward the end of the procedure (Modes 3 and 4).
Apical Irrigation (Mode 2)
To achieve deeper irrigation using this one-handed technique, the short needle can be removed from the manifold and replaced with the 30 gauge needle. After threading the needle through the manifold, the tip can be bent 90 degrees for better access to the canal orifice (Figure 9). The needle can protrude up to 17 mm from the manifold reaching deep in the root canal. Longer needles are available for longer roots if deeper insertion is desired. Since the manifold has to be close to the cavosurface area of the access to achieve effective suction of excess fluids in the canal, it’s recommended to continue to use the Coronal Irrigation needle (Mode 1) until working length has been established and confirmed, and the canal has been enlarged adequately to accommodate the 30 gauge needle to a depth of 17 mm. Otherwise, inadequate insertion depth will not allow the simultaneous suction through the manifold as the suction nozzle won’t be close enough to the cavosurface area to capture the fluids. Establishing working length and some initial enlargement first also allows the operator to avoid accidental insertion of the tip beyond the apex.



Macro Suction (Mode 3)
After instrumentation is complete using positive pressure irrigation and all macro debris is removed, the canal is ready for obturation. At this point, many operators may elect to run a high-volume of disinfectant safely in the canal to remove any remnant tissue at the apical third of the canal.3 Here, the goal is to place a suction tube deep in the canal while irrigation solution is added coronally (Figure 10). The negative pressure created apically by suction will pull the coronally deposited fluids apically toward the suction tip and clear up the suction. This allows a large volume to flow through the canal without the risk of extru-
Figure 8: During Coronal Irrigation (Mode 1), the short needle deposits the solution inside the access preparation, and the suction through the manifold will capture the excess overflow. It’s important to keep the manifold as close to the cavosurface margin of the access for effective suction
Figure 9: During Apical Irrigation (Mode 2), the short needle in the manifold is replaced with the long 30 gauge needle allowing positive pressure irrigation up to 17 mm deep with simultaneous suction. This is used later in instrumentation after 17 mm depth can be achieved with the 30 gauge needle

Figure 10: Macro Suction (Mode 3) is the simultaneous use of coronal irrigation (Mode 1) with plastic suction tip inserted deep in the canal
Figure 11: Micro Suction (Mode 4) is the simultaneous use of coronal irrigation (Mode 1) with the 30 gauge needle on the suction handpiece inserted deep in the canal
sion. In this mode, the operator may insert the plastic dispensing tip on the handpiece to achieve suction deep in the canal while the assistant is depositing the irrigant on top with the aid of the coronal suction assembly (Mode 1). Therefore, Mode 3 can be summarized with the simultaneous use of the plastic suction tip on the handpiece with Mode 1. It’s important to use this mode toward the end of instrumentation to avoid clogging of the tip of the plastic suction tip with large tissue and debris remaining in the canal.
Micro Suction (Mode 4)
This mode of operation is identical to the Macro Suction (Mode 3), except that instead of using the plastic suction tip on the handpiece, the thinner 30 gauge needle is used on the handpiece in order to achieve an even deeper depth of insertion in thinner canals (Figure 11). The insertion depth is limited to inside the root canal and should only be used at the very end of the procedure after all large pulp debris and dentinal chips have already been removed to avoid clogging of the small needle port with large debris in this negative pressure mode.
15 endopracticeus.com Volume 15 Number 4
Clinical Adaptation
TECHNIQUE
TotalVac is a modular irrigation device that has been designed to address the positive pressure and negative pressure irrigation needs of clinicians during root canal therapy.
Most clinicians will find their own preference for the combined use of positive or negative pressure irrigation when using this device. Most people will use the high-speed evacuation and adaptor for most suction needs and use the 30 gauge needle for conventional positive pressure irrigation on a syringe while using the plastic suction tip and the short needle on the manifold (as preassembled in the kit) for negative pressure irrigation toward the end of the procedure prior to obturation. Furthermore, having the plastic tip available during the procedure helps manage the fluid levels in the chamber and dry the canal from fluid during apex location stage for a more accurate measurement or drying the canals just prior to obturation.
The most practical clinical tip for using this system involves connecting the negative pressure tubing to a separate HVE inlet and resting the coronal suction manifold and short dispensing needle along with the handpiece and the plastic dispensing tip on a waterproof apron or tray on or near the patient’s chest for quick access. Then use the system for positive pressure irrigation at the beginning of the procedure and negative pressure at the end of the procedure. The plastic suction tubing can be used throughout the procedure to control the fluids in the chamber and canal with precision.
Limitations
Like every clinical device, this device has its limitations too. The depth of insertion of needle in Mode 1 is limited to the coronal area of the root and chamber or to 17 mm at the longest end in combination with the 30 gauge needle (Mode 2). Even though most clinicians limit their needle insertion in the canal to these same average depths, some operators may prefer needle insertion down to 1 mm short of the apex. In longer roots, a different length needle should then be used than that which is provided in the kit. Alternatively, normal positive irrigation with the 30 gauge needle and conventional syringe can be used, and this device’s use could be limited to its negative pressure and micro suction applications throughout the procedure. Another challenge is the use of multiple syringes with different solutions during Modes 1 and 2, which would require removing and reconnecting different solution syringes to the manifold using the same syringe tip, which may feel cumbersome if repeated multiple times.4 The most practical solution is combining TotalVac with and all-in-one irrigation solution such as Triton™ (Brasseler USA®, Savannah, Georgia) that can bypass the need for multiple syringes by combining all required solutions in one syringe. Triton contains sodium hypochlorite, chelating agents as well as surfactants and lubricants, all in a single syringe and can provide additional efficiency of using a
single syringe of solution from the beginning to the end of the procedure in conjunction with this device.5
Advantages
The most important advantage of this system is that it’s more versatile than other similar negative pressure devices in the past and can achieve the same negative pressure principles plus additional modes — all at a much lower cost than alternative options on the market. The system allows each operator to use it based on his/her own needs and priorities. Some operators may use all four modes, some may only use it for modes 1 and 2, and others may just apply deep negative pressure disinfection prior to obturation. Lastly, some may only want to use the plastic dispensing tip to manage the level of fluids in the canal with precision during chemomechanical instrumentation, apex location, and obturation while using conventional syringe irrigation.
Conclusion
TotalVac is a modular irrigation device that has been designed to address the positive pressure and negative pressure irrigation needs of clinicians during root canal therapy. This system can be customized based on each operator’s preference for positive or negative pressure irrigation at different phases of treatment through four modes of operation. Each clinician will find the optimum workflow that works best for him/her after understanding the various applications of this device.
While the system has some limitations, its relatively low cost and versatility can make it a practical solution for most irrigation needs chairside.
REFERENCES
1. Konstantinidi E, Psimma Z, Chávez de Paz LE, Boutsioukis C. Apical negative pressure irrigation versus syringe irrigation: a systematic review of cleaning and disinfection of the root canal system. Int Endod J. 2017;50(11):1034-1054.
2. Basrani, B. And Haapasalo, M. Update on Endodontic Irrigating Solutions. Endod Topics. 2012,27(1):74-102.
3. Kungwani ML, Prasad KP, Khiyani TS. Comparison of the cleaning efficacy of EndoVac with conventional irrigation needles in debris removal from root canal. An in-vivo study. J Conserve Dent. 2014;17(4):374-378.
4. Grawehr M, Sener B, Waltimo T, Zehnder M. Interactions of Ethylenediamine Tetraacetic Acid with Sodium Hypochlorite in aqueous solution. Int Endod J. 2003; 36(6):411-415.
5. Nasseh AA. Streamlining Effective Irrigation. Endodontic Practice US. 2022;15:(3) 10-12.
16 Endodontic Practice US Volume 15 Number 4
EP

 Lorem ipsum
Lorem ipsum
Internal root resorption: morphological aspects and clinical management
Drs. Fernando Goldberg, Denise Alfie, Juan Pablo Miraglia, Carlos Cantarini, and Gonzalo Garcia discuss treatment for
an inflammatory condition
Introduction
According to the American Association of Endodontists,1 internal root resorption (IRR) is a unique entity, unlike external root resorption, which can take different shapes. For IRR to occur, a damage or loss of the predentin and odontoblast layer must precede it, leaving the mineralized dentin wall exposed.2,3 A chronic pulpal inflammation is an additional factor needed to activate the action of the clastic cells on the dentin wall triggering its resorption. For the IRR to start, part of the pulp tissue must be vital to provide the clastic cells responsible for the resorption (active resorption).
This chronic inflammatory condition progresses until the pulp is removed or becomes totally necrotic, and at that point, the resorption ceases (inactive resorption). Haapasalo and Endal3 reported that the progress of internal root resorption is dependent on two things: 1) the pulp tissue at the resorption area must be vital, and 2) the pulp coronal to the resorption must be partially or completely necrotic, allowing bacterial infection and microbial antigens to enter the root canal. If the progression of the infection is slow and the necrosis of the whole pulp takes time, the IRR can continue and create a communication between the root canal and the surrounding periodontium, complicating the treatment with a poor prognosis. The IRR can be very small and radiographically not visible or produce a noticeable cavity of different shapes and sizes, generally with symmetrical walls, which appears as a radiolucent area that deforms the dentin wall.
In the radiographic image, the internal resorption cavity continues with the walls of the root canal. In contrast, in the case of an external resorption, the original shape of the canal remains radiographically intact because the resorption only projects over the root canal. The prevalence of IRR is very low. Haapasalo
Dr. Fernando Goldberg is from the Department of Endodontics, School of Dentistry, University del Salvador-AOA, Argentina.
Dr. Denise Alfie is in private practice.
Dr. Gonzalo Garcia is from the Department of Endodontics, School of Dentistry, University of Buenos Aires, Argentina.
Dr. Carlos Cantarini is from the Department of Endodontics, School of Dentistry, University del Salvador-AOA, Argentina.
Dr. Juan Pablo Miragila is a professor of Master of Endodontics at the Rey Juan Carlos University, Madrid, Spain.
Disclosure: The authors have stated explicitly that there are no conflicts of interest in connection with this article.
and Endal3 suggest that this prevalence is between 0.01% and 1%, and it can be in any third of the root canal. Patel, et al.,4 detail several etiological factors proposed as antecedents of IRR: trauma, caries, periodontal infections, excessive heat generated during restorative procedures on vital teeth, orthodontic treatment, etc.
There is always a determining factor that is the reason for its initiation. However, the advancement of internal root resorption depends on bacterial stimulation. Patel, et al.,4 emphasize that without this stimulation, the resorption will be self-limiting.
Wedenberg and Lindskog5 divide IRR into two types: transient and progressive. The authors mention that the transient type develops in the absence of pulpal infection, while the progressive type requires continuous stimulation by bacterial inflammation.
Many lesions are found accidentally during routine checkup radiographs, as teeth with internal resorption are typically symptom- free, and in cases of doubt, the CBCT can be of great help to clarify the diagnosis.6,7
Purpose
The purpose of this article is to analyze morphological and therapeutic aspects of IRR in different clinical situations.
Materials and methods
This study was performed with the approval of the Ethics Committee of the Department of Coordination of General Research of the Argentinian Dental Association (resolution number 0422). The STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) checklist and statement were followed.
18 Endodontic Practice US Volume 15 Number 4 CLINICAL
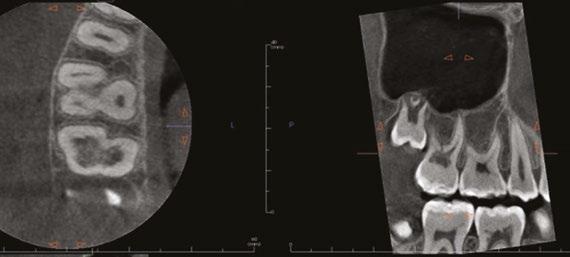
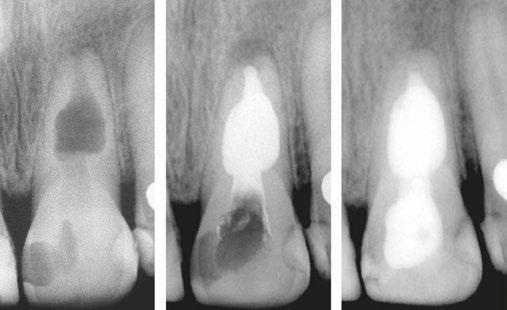
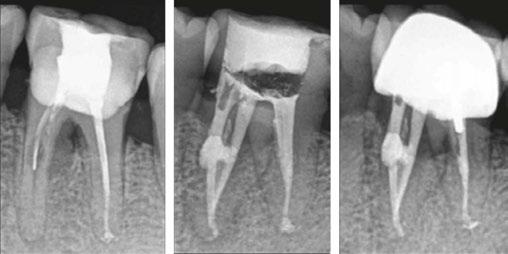
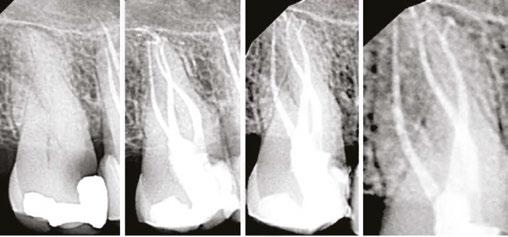
Figures 1A-1C: 1A. Preoperative X-ray. 1B. Immediate postoperative X-ray. 1C. Follow-up after 9 years and 10 months





Periapical radiographs and medical records corresponding to 48 teeth with IRR were collected from five different dental offices. The following aspects of the IRR were then analyzed: number of tooth in which it was found, location, presence or absence of periapical radiolucency, shape of the affected dentin walls, type of treatment performed, filling technique used, degree of adaptation of the filling to the resorption, presence of perforation communicating with the periodontium. Of the 48 cases diagnosed with IRR, all have been endodontically treated, and 29 of them have received initial treatments and 19 retreatments. Of the total number of cases, 29 had long-term follow-ups, while 19 do not have them.
The observations of the different aspects analyzed were carried out by five specialists in endodontics, and data were tabulated.
Results
The results of the items proposed in materials and methods are described in Tables 1 and 2.
Of the total, 29 had long-term radiographic follow-ups that ranged from a minimum of 6 months to a maximum of 25 years, with an average of 5 years, 4 months. Of the cases with radiographic follow-ups, 28 were considered successful and one failure (Table 2). Of the successful cases, 17 corresponded to treatments and 11 to retreatments (Figures 1A, 1B, 1C, and 2A, 2B, 2C). The tooth considered failed was a retreatment.
Discussion
IRR is a disease of the dental pulp that affects the dentin wall, which is reabsorbed by clastic action. It can occur in any tooth, although its presence is more frequent in those more susceptible to different kind of trauma. According to what was observed in this study, the upper incisors and the lower first molars are the most likely to present IRR, and this could be since the former are the ones that often suffer traumatic injuries, while the lower molars suffer more the action of orthodontic forces (Figures 3A, 3B, 3C).
The results of the present retrospective study are consistent with previous findings.8 Çaliişkan and Türkün8 reported that the most affected teeth with IRR were the upper incisors and agreed that the middle-third of the root was the area where it was located most frequently after an evaluation of 28 cases.
The radiographic appearances that generates the IRR are varied. The most common one observed in the present study was a circular shape with regular and symmetrical walls specially in single-rooted teeth (Figure 4A), although there were also some
Figures 2A-2C: 2A. Preoperative X-ray. 2B. Immediate postoperative X-ray. 2C. Follow-up after 18 years and 6 months
Figures 3A-3C: 3A. Preoperative X-ray. 3B. Immediate postoperative X-ray. 3C. Follow-up after 4 years
irregular ones with asymmetrical walls (Figure 4B). In molars, when resorption affects the pulp chamber, it was commonly seen as an irregularly shaped radiolucent cavity2 (Figure 4C).
Most of the IRR develop without clinical symptoms, although as they progress, necrosis of the pulpal tissue may progress, and pulpal symptoms become noticeable.3
When the IRR is diagnosed, root canal treatment is the treatment of choice. The prognosis is, in general, very good except when the resorption has perforated the dentin wall connecting the root canal with the periodontium.3,4,8 In many cases, this communication can’t be observed radiographically. Before performing endodontic therapy, it is always important to evaluate if the tooth is deemed restorable and what kind of reconstruction is needed. Properly cleaning and shaping the area of resorption may be very challenging because in many cases, it presents a complex access.

20 Endodontic Practice US Volume 15 Number 4
CLINICAL
2: Treatments and results
29From 6 months to 25 years Successes 28Treatments 17 Retreatments 11 Failures 1 Retreatment
Characteristics
the IRR
Max. Cl (17) Max. LI (9) and 1st MM (9) Others (13)
middle third (19), apical (16), coronal (13)
regular 31, irregular 17
radiolucencyYes 36, No 12
29, Retreatment 19
technique Thermoplasticized gutta-percha 45, Others 3
Very
43, Poor 5
Table
Follow-ups
Table 1:
of
Teeth
Location
Shapes
Periapical
Treatment performedTreatment
Obturation
Filling adaptation
good
42
Periodontal communicationYes 6, No


Different strategies have been proposed for instrumentation, such as use of sonic and ultrasonic activation of sodium hypochlorite,9,10 activation with the XP-Endo® Finisher file10 (FKG, Dentaire SA, La Chaux de Fonds, Switzerland), the use of precurved files in the RDI area,11 multiple visits using calcium hydroxide as intracanal medication, and sodium hypochlorite as irrigant in order to improve the disinfection of areas that are difficult to access.3,4
In the present study, calcium hydroxide was used as intracanal medication in only three of the 48 cases, while in 45 cases, the treatment was carried out in one single visit. However, complete removal of the calcium hydroxide used as temporary medication can be difficult in canals with normal morphology,12-14 so the situation would be aggravated in teeth with IRR given the difficulty of removing it from the retentive cavity of the resorption. Topçuoğlu, et al.15 and Marques-da-Silva, et al.16 used different irrigation techniques in simulated IRR, observing that none of them completely removed the calcium hydroxide from the resorptive cavities.
Regarding the obturation, the best results were observed with the use of thermoplasticized gutta-percha injection techniques.3,4,8,17-20 In this study, a thermofluid gutta-percha technique was used in 45 teeth, presenting adequate filling adaptation to the dentin walls in 43 of those cases. It is important to high-
light the studies by Ulusoy, et al.,21 who mention that the ex vivo use of System B™ and Obtura II in IRR fillings produced a temperature increase above the critical limit. In any case, these authors consider that the few seconds of thermal increase and the cooling action of the periodontium ligament in vivo would be a barrier to avoid thermal damage.
When the IRR communicates with the periodontium area, MTA, Biodentine® (Septodont USA) or similar product is the filling of choice,3,4 (Figures 5A, 5B, 5C).
Conclusions
The prevalence of IRR was higher in the upper incisors and lower molars, being located predominantly in the middle and apical thirds of the root canal. Its walls are generally regular and continuous. The use of thermoplasticized gutta-percha techniques allowed the adequate filling of the IRR cavities. Root canal treatment and retreatment provided adequate conditions to achieve a successful outcome.
REFERENCES
1. American Association of Endodontists, Communique, By Blicher B. Differentiating resorption January 2021;5:1-5.
2. Tronstad L. Root resorption-etiology, terminology, and clinical manifestations. Endod Dent Traumatol. 1988;4:241-252
3. Haapasalo M, Endal U. Internal inflammatory root resorption: the unknown resorption of the teeth. Endod Topics. 2006;14:60-79.
4. Patel S, Ricucci D, Durak C, Tay F. Internal root resorption: a review. J Endod. 2010;(36)7:1107-1121.
5. Wedenberg C, Lindskog S. Experimental internal resorption in monkey teeth. Endod Dent Traumatol. 1985;1:221-227.

6. Patel S, Dawood A, Wilson R, Horner K, Mannocci F. The detection and management of root resorption lesions using intraoral radiography and cone beam computed tomography: an in vivo investigation. Int Endod J. 2009;42(9):831-838
7. Kamburoğlu K, Kurşun Ş, Yüksel S, Öztaş B. Observer ability to detect ex vivo simulated internal or external cervical root resorption. J Endod. 2011;37(2):168-175.
8. Çaliişkan MK, Türkün M. Prognosis of permanent teeth with internal resorption: a clinical review. Endod Dent Traumatol. 1997;13(2):75-81.
9. Stamos DE, Stamos DG. A new treatment modality for internal resorption. J Endod. 1986;12(7):315-319.
10. Hernandez Restrepo C, García G, Alfie D, Oyhanart SR, Goldberg F. Efficacy of different procedures in removing radiopaque organic material from simulated internal root resorption cavities: an ex vivo study. Endod Practice US. 2020;13:24-27.
11. Manzur E. Evaluación in vitro de diferentes técnicas para la instrumentación de reabsorciones dentinarias internas simuladas. Rev Asoc Odontol Argent. 2003;63(5-6):107-111.
Figure 4A-4C: 4A. Maxillary lateral incisor with an internal resorption at the coronal third. 4B. Mandibular canine with an internal resorption in the middle-apical area. 4C. Mandibular molar with an irregular internal resorption in the coronal portion Figures 5A-5C:
12. Wiseman A, Cox TC, Paranjpe A, et al. Efficacy of Sonic and Ultrasonic Activation for Removal of Calcium Hydroxide from Mesial Canals of Mandibular Molars: A Microtomographic Study. J Endod. 2011;37(2):235-28.
13. Alturaiki S, Lamphon H, Edrees H, Ahlquist M. Efficacy of 3 different irrigation systems on removal of calcium hydroxide from the root canal: a scanning electron microscopic study. J Endod. 2015;41:97-101.
14. Zorzin J, WieBner J, WieBner T, et al. Removal of radioactively marked calcium hydroxide from the root canal: influence of volume of irrigation and activation. J Endod. 2016;42(4):637-40.
15. Topçuoğlu HS, Düzgün S, Ceyhanlı KT, et al. Efficacy of different irrigation techniques in the removal of calcium hydroxide from simulated internal root resorption cavity. Int Endod J. 2015;48:309-16.
16. Marques-da-Silva B, Alberton CS, Tomazinho FSF, et al. Effectiveness of five instruments when removing calcium hydroxide paste from simulated internal root resorption cavities in extracted maxillary central incisors. Int Endod J. 2020;53(3):366-375.
17. Goldberg F, Massone EJ, Esmoris M, Alfie D. Comparison of different techniques for obturating experimental internal resorptive cavities. Endod Dent Traumatol. 2000;16(1):116-1121.
18. Goldberg F, Manzur E, Mignanelli ME. Estudio comparativo entre diferentes técnicas para la obturación de reabsorciones internas creadas artificialmente. Rev Asoc Odontol Argent. 2001;89:125-1259.
19. Gencoglu N, Yildirim T, Garip Y, Karagenc B, Yilmaz H. Effectiveness of different gutta-percha techniques when filling experimental internal resorptive cavities. Int Endod J. 2008;41(10):836-842.
20. Keles A, Ahmetoglu F, Uzun I. Quality of different gutta-percha techniques when filling experimental internal resorptive cavities: A micro-computed tomography study. Aust Endod J. 2013;40:131-135.
21. Ulusoy ÖI, Yilmazoglu Z, Görgül. Effect of several thermoplastic canal filling techniques on surface temperature rise on roots with simulated internal resorption cavities: an infrared thermographic analysis. Int Endod J. 2015,48(2):171-176.
22 Endodontic Practice US Volume 15 Number 4
CLINICAL
5A. Preoperative X-ray. 5B. Immediate postoperative X-ray. 5C. Follow-up after 1 year and 9 months EP





YOU’LL BE SMILING... KNOWING WE ARE THE ONLY
solely focusing on the “practice” part of your endodontic practice. We partner with endodontists
to empower them
that, while
you to
your
Partners
partners
administrative
Endodontic Partnership led by Endodontists. Our family of brands 305-206-7388 I Endo1partners.com
Imagine
nationwide
to do just
helping
achieve
goals. Endo1
supports our endodontic
by implementing business best practices to reduce
burden, increase efficiency, and prioritize growth.
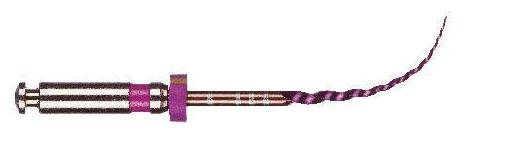
Rotary negotiation as first file to length
Drs. L. Stephen Buchanan and Christophe L.M. Verbanck discuss a modern
answer to an age-old issue
Functional characteristics of file geometry and metallurgy
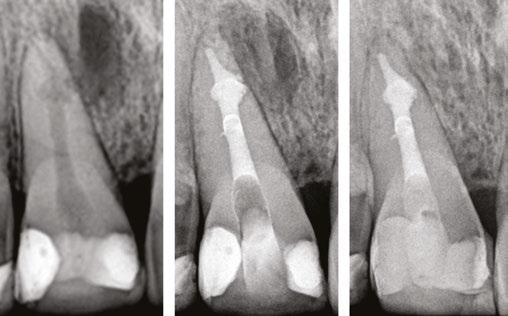
The rotary file rule
Since the beginning of the nickel-titanium (NiTi) rotary file revolution, we have been nearsighted in our expectations of what is possible. For the 30-plus years we have had them in our arsenal (Haapasalo and Shen, 2013), our wonder over what mechanized instrumentation could do for us was limited by the instruments we had at the time, by our conceptual misunderstanding of what is really going on when we use hand files to negotiate small complex canal forms, and by our fear of damaging patient’s teeth. This is completely understandable considering the hidden and tortuous canal paths we encounter when we thread the first file to length (Figure 1). For these reasons, endodontic educators and clinicians came to believe that rotary files should only be used for shaping after a glide path to the terminus has been secured with hand-operated K-files. The realistic concerns were that rotary files would break if used as first file to length; that rotary files used this way would block, ledge, or lacerate apical anatomy; and that rotary files would resist advancing through apical curvatures or beyond apical impediments.
Figure 1: This CT reconstruction of the apical third of a premolar root shows the challenge we often encounter when negotiating root canals to their terminal lengths. In just these two canals, there are five potential impediments to passage of the first negotiating file to length

At the advent of the rotary file revolution, before heat treatment was used to reduce the shape memory of NiTi alloy, file breakage was a serious problem that was mostly resolved by procedural workarounds such as crown-down shaping (using a big-to-small file order) to reduce torsional stresses delivered to the smallest files (Peters, 2004). This has changed radically as today’s heat-treated rotary files have the ability to unravel and wind up backwards before coming apart under stress (Peters, et al., 2012; Santos, et al., 2013); so for the first time, they can be used as first file to length (FFL) before any coronal shape has been cut (Buchanan, 2019). Conversely, without heat-treated NiTi files, rotary negotiation as FFL is untenable.
L. Stephen Buchanan, DDS, FICD, FACD, Dipl. ABE, has been lecturing and teaching hands-on endodontic continuing education courses for over 30 years, both in his state-of-the-art training facility in Santa Barbara, California, as well as in dental schools and at meetings around the world. He currently serves as a part-time faculty member in the endodontic departments at the University of the Pacific’s Arthur Dugoni School of Dentistry and the University of California at Los Angeles as well as being the Endodontic Advisory Board Member to the Academy of General Dentistry. Dr. Buchanan is nationally and internationally known for his 50-plus endodontic procedural articles as well as his expertise in the research and development of new endodontic technology, instruments, and techniques. He is a Diplomate of the American Board of Endodontists, a Fellow of the International and American College of Dentists. Dr. Buchanan also maintains a private practice limited to Endodontics in Santa Barbara, California.
Christophe L.M. Verbanck, DDS, MSc, obtained his Master of Dentistry at Gent University in 2009. He specialized in endodontics, graduating after a 3-year postgraduate training program from the same university. Since 2010 he has worked in several multi-disciplinary and endodontic referral practices all over Flanders. In January 2016, together with his wife, he started his own referral practice for Endodontics, Lovendo, in Lovendegem (Belgium). He regularly teaches endodontics to general dentists and holds workshops on the application of endodontic techniques.
Disclosures: Dr. L. Stephen Buchanan is a co-founder of PlanB Dental.
The other technological advances in rotary file manufacturing have been achieved through improved flute angles, file tip geometry, and cross-sectional core strength (Figure 2). Typical tapered-file flute geometry has flute angles that are tighter at the shank end and more open near the file tip, which contributes to files threading into canals when their shank end flutes approach the orifice level. When that happens, file tips are propelled into the canal; and if they have lesser flute angles, they are more likely to hang an edge, a major cause of file separation. Files with consistent flute angles have greater tip flexibility and strength, while their shank end flutes resist threading and cut more effectively. This flute-angle geometry is imperative when using rotary instruments as FFL (Buchanan, 2019). Without it, breakage too easily occurs, even when using a light touch and a low-torque limit. Adequate core strength is also critical in these narrowest of files; miniKUT Rotary Files have different cross-sectional geometries, depending on their purpose — just two flutes for the larger shaping files to aid cutting function, and four flutes for the smaller EZP rotary negotiating files to add torsional strength (Oh, et al., 2010).
With these engineered solutions that minimize breakage, the only remaining concern about using rotary negotiation as FFL is the possibility of rotary file tips blocking, ledging, or perforating the often tortuous apical regions of canals. This is why file tips on these rotary negotiators are fully radiused. This extremely passive tip geometry not only prevents ledging and perforation, but also actually causes these rotary files to kind of “bump” around impediments that would absolutely be engaged by an unbent hand file. While blockage is always a concern when advancing a file into apical regions of vital canals during negotiation procedures, it turns out that the way hand files function when used in a watch-wind, push-pull manner is actually the cause of most apical blockage.
24 Endodontic Practice US Volume 15 Number 4 TECHNIQUE
“If you obey all the rules, you miss all the fun” — Katharine Hepburn
TECHNIQUE
Deconstructing hand file negotiation, learning to love motor-driven negotiating files
Before we move on, it’s important to thoroughly understand what happens in apical regions when hand K-files are used as first file to length during negotiation. It’s not quite what you think. Hand K-files are used in many ways, including watchwind, push-pull, 1/4 turn-pull, and the Balanced Force method.
Forty-seven years ago, 1/4 turn-pull was shown to ledge curved canals, so that’s out (Weine, et al., 1975). The Balanced Force (Roane, et al., 1985) manner of cutting with K-files, while the most effective way to move a hand-operated K-file through dentin, is not a good technique when using files smaller than a No. 15 K-file. That leaves us with watch-wind, push-pull.
Watch-wind, Push-Pull (WWPP) filing action is accomplished by inserting the file into the canal (with a lubricant filling the access cavity) until it binds. Apical pressure is applied to the file and it is then rotated back and forth (watch-winding), limiting the movements to a 1/4 turn in either direction, wherein the file usually moves apically and tightens in the canal. The file is then used in three to four push-pull filing motions to loosen it at that position in the canal. After that, apical pressure is reapplied to the file; it is again watch-wound to advance it further in the canal, followed by push-pull filing to advance again. Rinse and repeat until the file does not advance during watch-winding with moderate apical pressure.
What actually happens near the canal terminus during apical advancement with this method? As the first file progresses to length in these small canals, it pierces and macerates pulp tissue, then leaves it in the apical third, risking compaction by the next larger file used. That is why we need to use lubricants and patency files during this procedure to avoid apical blockage by pulp remnants or, when it occurs, to pick a hole through the apically compacted debris, break it loose, irrigate it out of the canal, and then run another cutting cycle. Reciprocating motor-driven files cut and move even more debris in an apical direction in less time than a hand file when used with the WWPP technique, so it is too dangerous to use for rotary negotiation. In the authors’ opinion, reciprocating handpieces are a step backward in apical function.
The only motion that won’t work at all with hand K-files is continuous rotational cutting by hand. When small K-files are in use, continuous rotation in the same clockwise direction threads the file into the canal until its tip binds canal walls; whereafter, if CW rotation is continued, the file shank is literally twisted off the bound-up file tip. Constant rotary file rotation works because of a) the torsional strength of NiTi, and b) the centripetal force provided by the file spinning at 500 rpm (8 times a second), which bangs the flutes against the dentin, cutting it with a fraction of the torsional stresses delivered by hand files continuously rotating in a CW direction.
In fact, one of the greatest, but least appreciated, advantages of even the earliest rotary files was that for the first time, these rotary files removed the debris cut from the canal — carried in its flute spaces — instead of leaving cut debris in place to cause trouble. This functional characteristic of rotary files once again comes to play a major role when they are used as FFL.
During the development of rotary negotiation files, the overriding concern was preventing file breakage and avoiding apical blockage, ledging, and perforation (Plotino, et al., 2020). Surprisingly, the outcome was not a technique just as safe as hand-driven K-files. The outcome was a technique that is faster, easier, better, and safer than hand file manipulation.
Figure 2: PlanB’s 15-.03 miniKUT EZP Rotary Negotiation File. Note the square cross section and the aggressive rake angles of the four flutes, providing torsional strength with cutting efficiency (middle). The completely passive “duckbill” file tip geometry eliminates the chance of ledging curved canals during rotary negotiation as FFL (right). The side view shows flute angles that are consistent from tip to shank, preventing file threading and tip breakage (left)

No.
EZP
With rotary negotiation, patency is not an issue because pulp tissue is broached out of the canal and augured into the pulp chamber by the constantly spinning file (Ha, et al., 2016). Conversely, hand K-files used with WWPP motions encourage apical blockage and tend to engage the smallest canalar impediments rather than glance by them as rotary negotiation files do.
The simple fact is that rotary negotiation as FFL is superior to hand file negotiation (Figures 3,4 and 6).
Handpiece + EAL = Smart Handpiece + EAL + Rotary Negotiation = Genius
While having a heads-up display of handpiece and apex locator functions will likely be available in the future, we already have remarkably sophisticated functionality in the latest endo handpieces with electronic apex locators (EAL) inside (Figure 5). Motors with a resident EAL have a file lead conductor that runs through the handpiece attachment to its chuck where it contacts the latch-grip handle of the file, eliminating the need for a separate apex locator and file lead.
While these handpieces still require a ground lead be connected to the patient, eliminating the file lead and automating important handpiece functions is a game changer. Above all, the Apical Stop function of these handpieces improves clinicians’ accuracy during instrumentation. This is chosen during initial programming as opposed to Apical Slow, or the worst, Apical
25 endopracticeus.com Volume 15 Number 4
Figure 3: The canals in this case were negotiated with a 15-.05 miniKUT
Rotary Negotiation File (PlanB Dental) after multiple unsuccessful attempts to get through the DB canal beyond mid-root with prebent No. 06,
08, and No. 10 SS K-files. Case by Dr. L. Stephen Buchanan
TECHNIQUE
Reverse. Apical Slow isn’t helpful as some files break more easily when used at speeds lower than the manufacturer’s recommendation. Apical Reverse causes the file to back up when the preset apex locator position is reached, which dumps all the cut debris in tip flute spaces into the apical constriction, a perfect setup for apical blockage. Apical Stop is ideal: When the file stops spinning in the canal, it lightly binds at length, providing stability of the file as the stop is moved to position at the chosen reference point.
When positioning a hand file with a traditional EAL, besides the awkwardness of holding a hand file with an EAL clip hanging off of it, it requires rotating the file back and forth, so the helical flutes move the file in and out with vernier movements until the apex locator shows a steady bar at the position set on the EAL. Then the stop on the file shank is set to a reference point on the tooth, the file is removed, measured, and the next file to be used has its stop set at the referenced length. Rotary positioning of the file based on electronic signals is dead-on, immediate, and it cuts out at least four to five opportunities for error during length determinations with traditional methods.
First off, having the EAL inside provides Auto Start and Auto Stop functions. The Auto Start and Auto Stop functions not only significantly boost productivity during instrumentation, but also eliminate one of the most irritating aspects of using a cordless endo handpiece — having to hit the on/off button instead of actuating it by foot control. We use foot controls in a car (gas, brake, clutch) because we need to use our hands to steer, and humans are quite good at moving all of their limbs to control simultaneous but different functions. When we have to turn a cordless handpiece on and off, we momentarily lose our dexterity in directing the handpiece physically through space. With Auto Start, the moment the file tip touches irrigants or lubricants in the access cavity, the motor spools up. Auto Stop then happens as soon as the file clears the pulp chamber, allowing immediately cleaning and inspection of the file, thus shortening the time it takes to get the file back in the canal to do more work.
So what do we do when a rotary file doesn’t want to progress to length, and we need to use a hand K-file? These handpieces all have a secondary file lead (plus the file lead running through the handpiece) if a hand file needs to be brought into service.
Single-file canal treatment
Great progress has been made over the past years in endodontic procedural concepts, tools, and techniques. For those who resist the idea of using rotary negotiating files as first file to length because they believe hand files provide the chance to shape complex apical anatomy, this is both wishful thinking and sophistry. Fortunately, there are increasing numbers of clinicians who understand that instrumentation is solely meant to cut enough space in canals (if it doesn’t already exist) to allow adequate irrigation and obturation of the space in all of its natural complexity.
The benefit of this conceptual leap? Fewer files, less breakage, less time spent instrumenting before irrigation, and less loss of structural integrity. When you use three to five hand files before you meet the apex, that is not a Single-File Case. A Single-File Case is when a 15-.05 miniKUT EZP rotary negotiation file cuts to length without pause and the canal then gauges at a No. 15 K-file, indicating that shaping is complete. That is a true Single-File Case. Welcome to the 21st century.
Look for our next article on the broader topic of instrumentation in the spring edition of Endodontic Practice US.
EP
Figure 4: First full-rotary negotiation case. Rotary negotiation with a Hyflex EDM 10-.05 Glidepath File (Coltene) was the easy way to go because of the limited inter-occlusal distance. Case by Dr. Christophe Verbanck
Figure 5: PlanB cordless endodontic handpiece with an electronic apex locator inside, providing automatic on/off function as well as highly accurate apex location

Figure 6: Rotary negotiation case done with miniKUT 15- .03 EZP Rotary Negotiating File (PlanB Dental), used with a cordless endo handpiece with built-in apex locator. Case by Dr. Christophe Verbanck
REFERENCES
1. Buchanan LS. Rotary Negotiation Procedures. April 2019. www.dentistrytoday.com. Accessed November 8, 2022.
2. Ha JH, Kim SK, Kwak SW, stal. Debris extrusion by glide-path establishing endodontic instruments with different geometries. J Dent Sci. 2016;11(20):136-140.
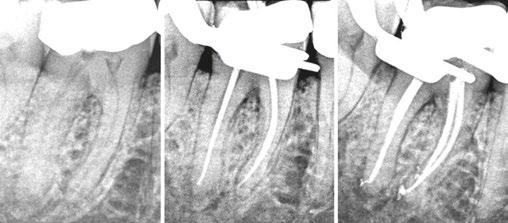
3. Haapasalo M, Shen Y. Evolution of nickel-titanium instruments: from past to future. Endod Topics. 2013;29, 3-17.
4. Oh S-R, Chang S-W, Lee Y, et al. A comparison of nickel-titanium rotary instruments manufactured using different methods and cross-sectional areas: ability to resist cyclic fatigue. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(4):622-628.
5. Peters OA. Current challenges and concepts in the preparation of root canal systems: a review. J Endod. 2004;30(8)559-567.

6. Peters OA, Gluskin AK, Weiss RA, Han JT. An in vitro assessment of the physical properties of novel Hyflex nickel-Titanium instruments. Int Endod J. 2012;45(11):1027-1034.
7. Plotino G, Nagenddrababu V, Bukiet F, et al. Influence of Negotiation, Glide Path, and Preflaring Procedures on root canal shaping-terminology, basic concepts, and a systematic review. J Endod. 2020;46(6):707-729.
8. Roane JB, Sabala CL, Duncanson MG Jr. The “balanced force” concept for instrumentation of curved canals. J Endod. 1985;11(5):203-211.
9. Santos LA, Bahia MG, de Las Casas EB, Buono, VT. Comparison of the mechanical behaviour between controlled memory and superelastic nickel-titanium files via finite element analysis. J Endod. 2013;39(11):1444-1447.
10. Weine FS, Kelly RF, Lio PJ The effect of preparation procedures on original canal shape and on apical foramen shape. J Endod. 1975;1(8):255-262.
26 Endodontic Practice US Volume 15 Number 4

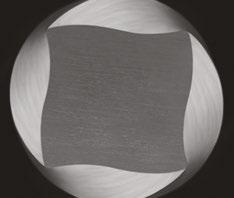




Fearless Rotary Negotiation
cross section ensures strength Fully radiused tip protects against ledging Trust to be First File to Length SAVE Time Money Apical Integrity
Four-bladed
US Endo Partners
Building culture delivers financial returns
As today’s endodontists look to the future of their practices and careers, more are exploring the trend of practice partnerships and weighing the notion of an ideal culture and community against a lucrative financial opportunity. At US Endo Partners, we know the two go hand-in-hand.

US Endo Partners — a unique Specialty Dental Service Organization (SDSO) founded in 2018 — is built on an exciting mission to drive meaningful opportunity and growth for our team members as we pursue excellence together. We also share a compelling vision to spread the life-changing power of saving teeth while proactively shaping our specialty and the next generation of endodontic leaders. We were the nation’s first SDSO exclusively for endodontists, and now we are proud to announce that we were the nation’s first endodontic SDSO to enjoy a successful equity event.
“Clarity, alignment, and unity of purpose define our culture and create value,” said Ronny Rowell, US Endo Partners Chief Operating Officer. “Our successful equity event shows that our intentional focus on outstanding patient care, united with our commitment to fostering the growth of the whole person, pays big dividends.”
The US Endo Partners model is attractive on multiple levels. First, we believe that the success we generate from our aligned pursuit of excellence should be rewarded. Our Partners have a stake in the company’s proven financial success. Our Partners are Class A shareholders in our company, which means you invest in your Partners, and they invest in you. Moreover, as a practicing endodontist, your work continues to produce for you at the same time as your investment does. This allows our Partners to realize the benefits of retirement while they’re still building — and benefiting from — their careers.

The additional allure of US Endo Partners for endodontists in all career stages is multifaceted, starting with our partnership model, which allows you to stay uniquely you. With US Endo, you retain your clinical autonomy, practice culture, valued team members, and local brand identity. Dedicated to you, your team, and your work-life balance, our Support Team works with the business side of your practice in areas from marketing and human resources to revenue-cycle management and compliance. This supportive-community dimension of US Endo Partners develops and insulates our endodontists. In short, we do what we do best, so you and your team can do what you do best.
Partners and their practice teams feel the empowering connection and support of belonging to a special community invested in each other’s success.
Our annual Vision Summit brings us all together to focus on personal and professional growth while building strong friendships, and our innovation of a track of comprehensive development programs drives fulfillment among our clinicians. In 2022, nearly 200 Partners assembled in Dallas for the Summit, and to take advantage of the opportunity to connect with their peers from across the country and plan for the future — and the excitement was palpable!
We also feel the power of giving back to our local communities. US Endo was proud to join forces with the Foundation for Endodontics to launch the Domestic Access to Care Program in a quest to provide exceptional treatment to underserved patients across the country.
“Partnering with US Endo is so much more than a great business opportunity. Our culture is about growth in every aspect of our lives — from improving our communication skills to leadership training, to advanced clinical training courses and beyond,” said Dr. Jeremy M. Young, US Endo Partners Operational Excellence Leader. “I truly believe that being part of US Endo offers the chance to become not only a better endodontist, but also a better boss, a better spouse, and a better friend. What we are building is unique; I’m truly thrilled to get to be a part of it.”
When it’s time to talk, talk to the first and only SDSO with proven financial results and a supportive, growth-minded culture — US Endo Partners. We’re in active discussions with top-tier endodontists, and we have openings for associates and recent graduates who are looking to start their careers at a flourishing practice. Learn more about US Endo Partners by visiting www. usendopartners.com or scanning the QR code above.
This information was provided by US Endo Partners.
28 Endodontic Practice US Volume 15 Number 4 SERVICE PROFILE
EP
At US Endo’s annual Vision Summit in Dallas, Partners came together to talk about the future, strengthen connections, and have a little fun
Learn more about US Endo Partners
How to submit an article to Endodontic Practice US
Endodontic Practice US is a peer-reviewed, quarterly publication containing articles by leading authors from around the world. Endodontic Practice US is designed to be read by specialists in Endodontics, Periodontics, Oral Surgery, and Prosthodontics.
Submitting articles
Endodontic Practice US requires original, unpublished article submissions on endodontic topics, multidisciplinary dentistry, clinical cases, practice management, technology, clinical updates, literature reviews, and continuing education.
Typically, clinical articles and case studies range between 1,500 and 2,400 words. Authors can include up to 15 illustrations. Manuscripts should be double-spaced, and all pages should be numbered. Endodontic Practice US reserves the right to edit articles for clarity and style as well as for the limitations of space available.
Articles are classified as either clinical, continuing education, technology, or research reports. Clinical articles and continuing education articles typically include case presentations, technique reports, or literature reviews on a clinical topic. Research reports state the problem and the objective, describe the materials and methods (so they can be duplicated and their validity judged), report the results accurately and concisely, provide discussion of the findings, and offer conclusions that can be drawn from the research. Under a separate heading, research reports provide a statement of the research’s clinical implications and relevance to endodontics. Clinical and continuing education articles include an abstract of up to 250 words. Continuing education articles also include three to four educational aims and objectives, a short “expected outcomes” paragraph, and a 10-question, multiple-choice quiz with the correct answers indicated. Questions and answers should be in the order of appearance in the text, and verbatim. Product trade names cited in the text must be accompanied by a generic term and include the manufacturer, city, and country in parentheses.
Additional items to include:
• Include full name, academic degrees, and institutional affiliations and locations
• If presented as part of a meeting, please state the name, date, and location of the meeting
• Sources of support in the form of grants, equipment, products, or drugs must be disclosed
• Full contact details for the corresponding author must be included
• Short author bio
• Author headshot
Pictures/images
Illustrations should be clearly identified, numbered in sequential order, and accompanied by a caption. Digital images must be high resolution, 300 dpi minimum, and at least 90 mm wide. We can accept digital images in all image formats (preferring .tif or jpeg).
Tables
Ensure that each table is cited in the text. Number tables consecutively, and provide a brief title and caption (if appropriate) for each.
References
References must appear in the text as numbered superscripts (not footnotes) and should be listed at the end of the article in their order of appear-
ance in the text. The majority of references should be less than 10 years old. Provide inclusive page numbers, volume and issue numbers, date of publication, and all authors’ names. References should be submitted in American Medical Association style. For example:
Journals: (Print)
White LW. Pearls from Dr. Larry White. Int J Orthod Milwaukee. 2016;27(1):7-8. (Online)
Author(s). Article title. Journal Name. Year; vol(issue#):inclusive pages. URL. Accessed [date].
Or in the case of a book: Pedetta F. New Straight Wire. Quintessence Publishing; 2017.
Website: Author or name of organization if no author is listed. Title or name of the organization if no title is provided. Name of website. URL. Accessed Month Day, Year. Example of Date: Accessed June 12, 2011.
Author’s name: (Single) (Multiple) Doe JF Doe JF, Roe JP
Permissions
Written permission must be obtained by the author for material that has been published in copyrighted material; this includes tables, figures, pictures, and quoted text that exceeds 150 words. Signed release forms are required for photographs of identifiable persons.
Disclosure of financial interest
Authors must disclose any financial interest they (or family members) have in products mentioned in their articles. They must also disclose any developmental or research relationships with companies that manufacture products by signing a “Conflict of Interest Declaration” form after their article is accepted. Any commercial or financial interest will be acknowledged in the article.
Manuscript review
All clinical and continuing education manuscripts are peer-reviewed and accepted, accepted with modification, or rejected at the discretion of the editorial review board. Authors are responsible for meeting review board requirements for final approval and publication of manuscripts.
Proofing
Page proofs will be supplied to authors for corrections and/or final sign off. Changes should be limited to those that are essential for correctness and clarity.
Articles should be submitted to:
Mali Schantz-Feld, managing editor, at mali@medmarkmedia.com
Reprints/Extra issues
If reprints or additional issues are desired, they must be ordered from the publisher when the page proofs are reviewed by the authors. The publisher does not stock reprints; however, back issues can be purchased.
29 endopracticeus.com Volume 15 Number 4 AUTHOR GUIDELINES
Communicating periodontal issues across dental implant platforms
Drs. Stuart Segelnick and Mea A. Weinberg review typical challenges and management at the dental implant-abutment connection

Introduction
Dental implants have a record of long-term success with a cumulative survival rate of about 96% up to 10 years post-loading.1,2 It is important to realize the various factors that can influence implant survival or failure. A higher rate of implant failure occurs in patients with a smoking history, hypertension without medication, and uncontrolled diabetes.3-5 In addition to systemic reasons, there are other properties of dental implants that could influence their long-term success, including crestal bone loss, placement of the platform at or below gingival margin, presence of excess cement from restoration cementation, presence of a microgap between the implant connector and the abutment, and non-submerged versus submerged implants. This article will review common problems and management at the dental implant-abutment connection.
Periodontal issues in implant failure

The first issue to consider is the location of the implant-abutment connection (IAC) in regard to the bone level. This is important when considering that excessive marginal bone loss can result in implant failure.6,7 The question is whether there is a difference in success rates between having the platform placed below crestal bone (termed subcrestal implants), or at the level of bone (termed bone-level implants).6,8 There are mixed results regarding bone level placements that reduce marginal bone loss. Some articles found no difference if implants were placed at the level of bone or subcrestally.9,10,6 However, most articles, including a systematic review and meta-analysis article, found
Educational aims and objectives
This self-instructional course for dentists aims to review common problems and management at the dental implant-abutment connection.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions by taking the quiz online at endopracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
• Understand how platform switching is important in preserving crestal bone.
• Describe the microgap and its importance in implant failure.
• Describe how excessive cement around an implant crown can result in implant failure.
• Explain the role of keratinized tissue around the implant. Understand how non-keratinized mucosa around an implant can cause inflammation. Explain the oral hygiene process for implant care.
that subcrestal placement of implants is ideal because there is less chance for the implant to become exposed, thereby increasing stability and reducing the risk of peri-implantitis.7,11 In the review article, it was concluded that recommendations are to place tissue level implants at the level of the crest and bone level implants subcrestally (Figure 1).12,13
Additionally, non-submerged implants stabilize the soft tissue seal around the implant, preventing abutment movement that affects the soft tissue seal and thus preserving marginal bone.13 On the other hand, non-submerged implants cannot transfer stress or masticatory load as well as submerged implants (implants placed below the gingival margin), which can lead to marginal bone resorption.14 Non-submerged implants are ideal for immediate and early loading.
Standard platform implants that range in size from 3.5 mm to 4.2 mm in diameter are available in shorter lengths and narrower diameters, which is ideal for the anterior area. Wide platform implants are ideal for the posterior area; the sizes available are 4.5 mm to 6 mm. To prevent crestal bone loss, the question arises whether the abutment should be platform-matched, whereby the
30 Endodontic Practice US Volume 15 Number 4 CONTINUING EDUCATION
Stuart Segelnick, DDS, MS, is immediate past president of the American Association of Dental Editors and Journalists. He is editor of the Northeastern Society of Periodontists NESP Bulletin and the Second District Dental Society of New York SDDS Bulletin. Dr. Segelnick has co-edited five books on dentistry. He is a Diplomate of the American Board of Periodontology and the International Congress of Oral Implantologists. Dr. Segelnick is an Adjunct Clinical Professor at NYU Dentistry in the Department of Periodontology and Implant Dentistry.
Mea A. Weinberg, DMD, MSD, RPh, is a clinical professor in the Department of Periodontology and Implant Dentistry at New York University College of Dentistry. A Diplomate of the American Board of Periodontology, she has published many articles, chapters, and books on periodontics and pharmacology.
2 CE CREDITS
abutment has the same diameter as the platform of the implant (Figure 2), or if the abutment should be platformed-switched (PLS), using a smaller diameter abutment on a larger diameter implant collar, making the implant-abutment connection (IAC) more distinct (Figure 3).15 This type of connection shifts the perimeter of the IAC inward toward the central axis of the implant, allowing a thicker soft tissue cuff around the implant prosthesis, which is easier to maintain. Lazzara and Porter have hypothesized that shifting the IAC inward also shifts the inflammatory cell infiltrate inward and away from the crestal bone.16
Platform switching, which was initially proposed by Gardner in 2005 and further described by Lazzara in 2006, is an IAC modification to control marginal bone loss (MBL) around an implant.16-18 Additionally, PLS is a process to improve long-term bone maintenance around implants as well as improved tissue response. A 2015 systematic review as well as the majority of more current articles conclude that the majority of clinical studies showed that there was significantly less mean MBL at implants with PLS versus platform-matching implant-abutment configuration.19,20 Mean crestal bone loss that was reported was 0.22 mm in platform-switched implants and 2.02 mm in nonplatform-switched implants. Also, the reduction of the abutment width by the platform circumferentially of 0.45 mm is sufficient to avoid peri-implant bone loss.15 Before placing implants, the surgeon should consider using platform-switching, which not only increases the distance between IAC and the crestal bone, but also increases the microgap to crestal bone distance and thus potentially preserving crestal bone.21
The microgap, the space between the implant and the abutment, presents a reservoir of bacteria, and if in close proximity

to the bone, can result in peri-implantitis and bone loss.22 The bacteria adhere and proliferate in this gap causing an increase in inflammation around the IAC during soft tissue manipulation for the crown insertion and during function.22 Since there is no complete seal at the IAC with any implant systems, it is ideal to have the smallest microgap between the implant and abutment and position it a distance from the outer perimeter of the implant. A pumping effect occurs when there is a larger microgap, allowing for bacterial movement inside and outside the connection during pressure changes as the restoration is loaded.6 A clinical review concluded that conical and mixed connections were better than implants with an external connector.22 An advantage of a onepiece implant is that there is no microgap; however, it must be cemented, and then there are possible problems with excess subgingival cement that is not removed. Ideally, the smallest amount of bone loss that occurs around implants is when the microgap between the abutment and implant is placed 1–2 mm above the bone (supracrestally).6,23 Other studies have shown tissue level implants can be restored with a screw-retained crown.24 Different studies found varied results relating the association of abutment height and marginal bone loss. Long abutments showed less interproximal marginal bone resorption than shorter abutments in screw-retained crowns and cement-retained crowns. It is speculated the decreased vertical height of the abutments
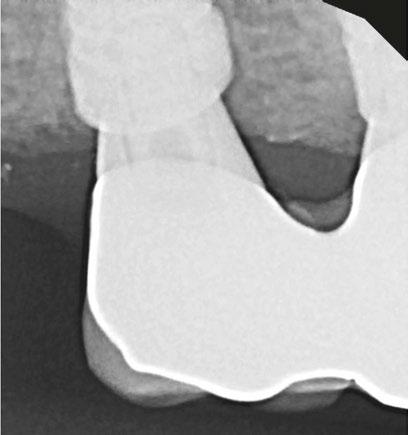
31 endopracticeus.com Volume 15 Number 4 CONTINUING EDUCATION
Figure 1: Subcrestal placement of implant platform
Figure 2: Platform is the same size as the abutment/crown screw down
The microgap, the space between the implant and the abutment, presents a reservoir of bacteria, and if in close proximity to the bone, can result in periimplantitis and bone loss.
would cause an encroachment on the supracrestal tissue attachment formation leading to an increase in bone loss around the implant.25,26
There are different implantabutment connection systems used to support a single or multiunit restoration with the purpose of reducing stress on the prosthetic component and on the bone-implant interface and to provide good prosthetic stability.18 The platform may have an internal (internal hexagon, tri-lobe, and octagon) (Figure 4), conical (Morse taper), external (external hex), or tubein-tube connection.27 The internal connection is best to reduce bone loss and increase implant stability.6 The majority of articles concluded that dental implants with internal connections showed less MBL than implants with external connections, which was the result of platform switching.28,29 Moreover, abutment disconnection and reconnection multiple times were found to significantly cause marginal bone loss compared to implants with final abutment placement at the time of implant placement.30 Thus, it is recommended to limit the removal of the abutment once it is placed.
Levine, Present, and Wilson described complications with excess cement around dental implants, precisely at the restoration-abutment connection. There are advantages and disadvantages of cement retention versus screw-retention crowns.31 Excessive remaining cement results in peri-implantitis which can lead to implant failure.32,33 Proper cementing technique is helpful to prevent excessive cement.34 Screw-retained restorations had 16.9% less inflammation than cemented restorations.35 One of the disadvantages of cement retention that can affect the IAC is the presence of excessive subgingival cement, and if the margins of the restorations were subgingival, particularly 2 mm or deeper, it made removal of excess cement difficult.36 Additionally, the time after cementation to finding signs of peri-implant disease was from 6 weeks to 4 months but can be up to many years.36 It is recommended that the margin of a restoration be either supragingival or no more than 1.5 mm subgingival.31 Ideally, it is recommended to have the restoration-abutment connection far from the IAC to reduce marginal bone loss and not impede on the implants supracrestal tissue attachment (once known as biologic width).37

Most evidence supports that implants with non-keratinized tissue allow for more oral biofilm (plaque) accumulation, marginal tissue recession, marginal inflammation and patient discomfort.38-41 One article found having < 2 mm of keratinized mucosa around an implant was a good indicator for future peri-implant disease.41
There are benefits in good oral biofilm control as well as regular professional maintenance visits in preventing periimplant disease.42 It is important to have the proper instruments such as plastic instruments or plastic sleeves on ultrasonic power scalers to prevent damage to the peri-implant tissues as well as the implant.44 Titanium or plastic brushes, curettes, scalers, and lasers have all been used effectively in oral biofilm removal. More recent professional oral hygiene recommendations to reduce peri-implant inflammation include use of glycine powder air polishing and erythritol powder air polishing.45 Time must be taken to scale around implants due to the configuration of the restoration. When the emergence profile on a crown is ≥ 30 degrees and convex, it is more difficult to scale, thus increases the prevalence of peri-implantitis.46
Conclusion
There are many factors of the dental implant-abutment connection that can influence periodontal issues. Management of these potential problems should be addressed when possible by placing the platform subcrestally, platform switching, using longer abutments to place the restorative margin closer to the gingival soft tissue margin, decreasing abutment disconnection and reconnection times, using screw-retained abutments, having adequate keratinized gingiva, and limiting bulbous prostheses. Including these factors in treatment planning can help reduce inflammation, marginal bone loss, and implant failure. Ultimately, patients must be compliant with oral hygiene and maintenance care to have better outcomes of implant success.
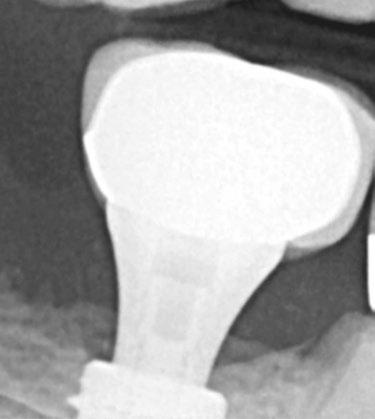
REFERENCES
1. Moraschini V, Poubel LADC, Ferreira VF, Barboza EDSP. Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: A systematic review. Int J Oral Maxillofac Surg. 2015; 44(3):377-388.
32 Endodontic Practice US Volume 15 Number 4 CONTINUING EDUCATION
Figure 3: Platform is larger than the abutment circumference
EP
Figure 4: Internal hex implant. Photo by Ye Shi, BDS, MS
CONTINUING EDUCATION
2. Howe MS, Keys W, Richards D. Long term (10-year) dental implant survival: A systematic review and sensitivity meta-analysis. J Dent. 2019:84:9-21.
3. Kasat V, Ladda R. Smoking and dental implants. J Int Soc Prev Community Dent. 2012;2(2):38-41.
4. Wu X, Al-Abedalla K, Eimar H, et al. Antihypertensive medications and the survival rate of osseointegrated dental implants: A cohort study. Clin Implant Dent Relat Res. 2016;18(6):1171-1182.
5. Wagner J, Spille JH, Wiltfang J, Naujokat H. Systematic review on diabetes mellitus and dental implants: an update. Int J Impl Dent. 2022;8(1).
6. Kowalski J, Lappinska B, Nissan J, Lukomaska Szymanska M. Factors influencing marginal bone loss around dental implants: a narrative review. Coatings. 2021;11(7):865.
7. Galindo-Moreno P, Catena A, Pérez-Sayáns, et al. Early marginal bone loss around dental implants to define success in implant dentistry: A retrospective study. Clin Implant Dent Relat Res. 2022; 24(5):630-642.
8. Esposito M. Impact of 0.5mm vs 1.5 mm subcrestal implant placement on marginal bone and aesthetics - 3-year results of a multicenter RCT. Clin Oral Implants Res. 2019;30(S19):31.
9. Nagarajan B, Murthay V, Lingstone D, Surendra MP, Jayaraman S. Evaluation of crestal bone loss around implants placed at equicrestal and subcrestal levels before loading: a prospective clinical study. J Clin Diagn Res. 2015;9(12): ZC47-ZC50.
10. Sargolzaie N, Zarch HH, Arab H, Koohestani T, Ramandi MF. Marginal bone loss around crestal or subcrestal dental implants: prospective clinical study. J Korean Assoc Oral Maxillofac Surg. 2022;30;48(3):159-166.
11. Chatterjee P, Shashikala R, Navneetham A. Comparative study of the crestal vs subcrestal placement of dental implants via radiographic and clinical evaluation. J Contemp Dent Pract. 2022;23(6):623-627.
12. Palacios-Garzón N, Velasco-Ortega E, López-López J. Bone Loss in Implants Placed at subcrestal and crestal level: A systematic review and seta-analysis. Materials (Basel). 2019; 12(1):154-173.
13. Saleh MHA, Ravidà A, Suárez-López del Amo, F, L GH, Asa´ad F, Wang HL. The effect of implant-abutment junction position on crestal bone loss: A systematic review and meta-analysis. Clin Implant Dent Relat Res. 2018;20(4):617-633.
14. Kim JC, Lee M, Yeo IL. Three interfaces of the dental implant system and their clinical effects on hard and soft tissues. Mater Horiz. 2022;9(5):1387-1411.
15. Gupta S, Sabharwal R, Nazeer J, et al. Platform switching technique and crestal bone loss around the dental implants: A systematic review. Ann Afr Med. 2019;18(1):1-6.
16. Lazzara RJ, Porter SS. Platform switching: A new concept in implant dentistry for controlling postrestorative crestal bone levels. Int J Periodontics Restorative Dent. 2006;26(1):9-17.
17. Gardner DM. Platform switching as a means to achieving implant esthetics. N Y State Dent J. 2005;71(3):34-37.
18. Singla S, Kumar L, Rathee M. Know your implant connections. African Journal of Oral Health. 2018;6(2).
19. Strietzel FP, Neumann K, Hertel M. Impact of platform switching on marginal peri-implant bone-level changes. A systematic review and meta-analysis. Clin Oral Implantsl Res. 2015;26:342-358.
20. Tokgöz SE, Bilhan H. The influence of the implant abutment complex on marginal bone and peri-implant conditions: A retrospective study. J Adv Prosthodont. 2021;13(1):46-54.
21. Nayak R, Devanna R, Dharamsi AM, et al. Crestal bone loss around dental implants: platform switching vs platform matching – A retrospective study. J Contemp Dent Pract. 2018;19(5):574-578.
22. Lauritano D, Moreo G, Lucchese A, et al., The impact of implant-abutment connection on clinical outcomes and microbial colonization: a narrative review. Materials. 2020;13(5):1131.
23. Piattelli A, Vrespa G, Petrone G, et al. Role of the microgap between implant and abutment: A retrospective histologic evaluation in monkeys. J Periodontol. 2003;74(3):346-352.
24. Agustín-Panadero R, Bermúdez-Mulet I, Fernández-Estevan L, et al. Peri-Implant Behavior of Tissue Level Dental Implants with a Convergent Neck. Int J Environ Res Public Health. 2021; 18(10):5232.
25. Blanco J, Pico A, Caneiro L, Nóvoa L, et al., Effect of abutment height on interprox-
imal implant bone level in the early healing: A randomized clinical trial. Clin Oral Implants Res. 2018;29(1):108-117.
26. Spinato S, Galindo-Moreno P, Bernardello F, Zaffe D. Minimum abutment height to eliminate bone loss: influence of implant neck design and platform switching. Int J Oral Maxillofac Implants. 2018;33(2):405-411.
27. Bittencourt ABBC, Neto CLMM, Penitente PA, et al. Comparison of the Morse Cone Connection with the Internal Hexagon and External Hexagon Connections Based on Microleakage - Review. Prague Med Rep. 2021;122(3):181-190.
28. de Medeiros RA, Pellizzer EP, Filho AJV, dos Santos DM, da Silva EVF et al. Evaluation of marginal bone loss of dental implants with internal or external connections and its association with other variables: A systematic review. J Prosthet Dent. 2016;116(4):501-506.
29. Kim DH, Kim HJ, Kin S, et al. Comparison of marginal bone loss between internaland external-connection dental implants in posterior areas without periodontal or peri-implant disease. J Periodontal Implant Sci. 2018;48(2):103-113.
30. Koutouzis T, Gholami F, Reynolds J, Lundgren T, Kotsakis GA. Abutment disconnection/reconnection affects peri-implant marginal bone levels: A meta-analysis. Int J Oral Maxillofac Implants. 2017;32(3):575-581.
31. Levine RA, Present S, Wilson Jr. TG. Complications with excess cement and dental implants: Diagnosis, recommendations and treatment of 7 clinical cases. Implant Realities. 2014;1:51-159.
32. Pesce P, Canullo L, Grusovin MG, et al. Systematic review of some prosthetic risk factors for periimplantitis. J Prosthet Dent. 2015;114(3):346-350.
33. Staubli N, Walter C, Schmidt JC, Weiger R, Zitzmann NU. Excess cement and the risk of periimplant disease – a systematic review. Clin Oral Implants Res. 2017; 28(10):1278-1290.
34. Reda R, Zanza A, Cicconetti A, et al. A systematic review of cementation techniques to minimize cement excess in cement—retained implant restorations. Methods Protoc. 2022;5(1):9.
35. Agustín-Panadero R, Bustamante-Hernández N, Labaig-Rueda C, et al. Influence of biologically oriented preparation technique on peri-implant tissues; prospective randomized clinical trial with three-year follow-up. Part II: Soft tissues. J Clin Med. 2019;8:2223.
36. Linkevicius T, Vindasiute E, Puisys A, Peciuliene V. The influence of margin location on the amount of undetected cement excess after delivery of cement-retained implant restorations. Clin Oral Implants Res. 2011;22(12):1379-1384.
37. Tokgöz SE, Bilhan H. The influence of the implant-abutment complex on marginal bone and peri-implant conditions: A retrospective study. J Adv Prosthodont. 2021;13(1):46-54.
38. Kungsadalpipob K, Supanimitkul K, Manopattanasoontorn S, et al. The lack of keratinized mucosa is associated with poor peri-implant tissue health: a cross-sectional study. Int J Implant Dent. 2020;6(1):28.
39. Kamal, RK. Necessity of Keratinized Tissue Around Dental Implants to Maintain Peri-Implant Tissue Health: A Systematic Review. Dental Theses. 2018;33.
40. Saltz AE. Impact of keratinized mucosa in dental implant treatment. Decisions in Dentistry. 2020;6(8):40-44.
41. Grischke J, Karch A, Wenzlaff A, et al. Keratinized mucosa width is associated with severity of peri-implant mucositis. A cross-sectional study. Clin Oral Implants Res. 2019;30(5):457-465.
42. Cortellini S, Favril C, De Nutte M, Teughels, Quirynen M. Patient compliance as a risk factor for the outcome of implant treatment. Periodontology 2000. 2019; 81(1):209-225.
43. Gulati M, Govila V, Anand V, Anand B. Implant Maintenance: A Clinical Update. Int Sch Res Notices. 2014; 9:908534.
44. Baldi D, De Giorgis L, Menini M, Motta F, Colombo J. Efficacy of Instruments for Professional Oral Hygiene on Dental Implants: A Systematic Review. Appl Sci. 2022;12(1):26-44.
45. Tan SL, Grewal GK, Mohamed Nazari NS, Mohd-Dom TN, Baharuddin NA. Efficacy of air polishing in comparison with hand instruments and/or power-driven instruments in supportive periodontal therapy and implant maintenance: a systematic review and meta-analysis. BMC Oral Health. 2022;22(1):85-102.
46. Yi Y, Koo KT, Schwarz F, Amara HB, Heo-SJ. Association of prosthetic features and periimplantitis: A cross-sectional study. J Clin Periodontol. 2020; 47(3):392-403.
33
Volume 15 Number 4
endopracticeus.com
Continuing Education Quiz
Communicating periodontal issues across dental implant platforms SEGELNICK/WEINBERG
1. Dental implants have a record of long-term success with a cumulative survival rate of about ______ up to 10 years post-loading.
a. 82% b. 89% c. 96% d. 99%
2. A higher rate of implant failure occurs in patients with __________.
a. a smoking history b. hypertension without medication c. uncontrolled diabetes d. all of the above
3. In addition to systemic reasons, dental implants’ long-term success could be influenced by crestal bone loss and placement of the platform at or below gingival margin as well as __________.
a. presence of excess cement from restoration cementation b. presence of a microgap between the implant connector and the abutment c. nonsubmerged versus submerged implant d. all of the above
4. The ________, the space between the implant and the abutment, presents a reservoir of bacteria, and if in close proximity to the bone, can result in peri-implantitis and bone loss. a. microgap b. platform c. platform match d. none of the above
5. A _________ occurs when there is a larger microgap, allowing for bacterial movement inside and outside the connection during pressure changes as the restoration is loaded. a. pressure gap b. pumping effect c. platform switch d. thicker soft tissue
6. Ideally, the smallest amount of bone loss that occurs around implants is when the microgap between the abutment and implant is placed _______ above the bone (supracrestally).
a. 1–2 mm
b. 3-4 mm
c. 5-6 mm d. 7-8 mm
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 16 CE credits for only $149; call 866-579-9496, or visit https://endopracticeus.com/ subscribe/ to subscribe today.
n To receive credit: Go online to https://endopracticeus.com/continuingeducation/, click on the article, then click on the take quiz button, and enter your test answers.
AGD Code: 490
Date Published: December 18, 2022 Expiration Date: December 18, 2025
2 CE CREDITS
7. Abutment disconnection and reconnection multiple times were found to significantly cause marginal bone loss compared to implants with final abutment placement at the time of implant placement. a. True b. False
8. Screw-retained restorations had _________ less inflammation than cemented restorations. a. 5.7% b. 16.9% c. 24% d. 45%
9. Additionally, the time after cementation to finding signs of periimplant disease was from __________. a. the day of placement up to 4 days after b. 1 week to a month after placement c. 6 weeks to 4 months but can be up to many years d. none of the above
10. When the emergence profile on a crown is _________ and convex, it is more difficult to scale, thus increases the prevalence of peri-implantitis.
a. ≥ 10 degrees b. ≥ 30 degrees c. ≥ 40 degrees d. ≥ 50 degrees
To provide feedback on CE, please email us at education@medmarkmedia.com
Legal disclaimer: Course expires 3 years from date of publication. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
34 Endodontic Practice US Volume 15 Number 4 CONTINUING EDUCATION
Dental infections, part 2 — prophylaxis: help avoid antimicrobial resistance

Wiyanna
K. Bruck, PharmD,

and Jessica Price continue their discussion of concepts surrounding antibiotic prophylaxis in dentistry
Introduction
Use of antimicrobials in the field of dentistry is not limited to treating active dental infections. Many dentists prescribe antibiotics as a onetime dose prior to performing procedures. In fact, in the United States, general and specialty dentists are the third-highest prescribers of antibiotics in all outpatient settings.1 Moreover, looking at data from 2017 to 2019, it is estimated that somewhere between 30% to 85% of dental antibiotic prescriptions are “suboptimal or not indicated.”2-4 Appropriate use of antibiotics for prevention of infections surrounding dental procedures has received a lot of attention recently, which was illustrated by the American Dental Association (ADA) updating its antibiotic stewardship recommendations in the fall of 2020.5 It is well-known that antibiotics are one of the greatest medical advances that laid a foundation for an area of medicine, which has allowed once deadly infections to be readily treatable.6 However, excessive antibiotic use, even if it is just one dose, comes with consequences of side effects, antibiotic resistance, and superinfections like Clostridioides difficile.
Being attentive to appropriate antimicrobial prescribing is vital in all fields of healthcare, including dentistry, which is not limited to treatment, but also applies to antimicrobial prophylaxis.7,8 To aid in considering the threats of overusing antibiotics, but also being able to recognize when antibiotics are warranted, the Centers for Disease Control and Prevention (CDC) has constructed a Checklist for Antibiotic Prescribing in Dentistry (see
Wiyanna K. Bruck, PharmD, BCPS, BCIDP, BCPPS, is an assistant professor of Pharmacy Practice at South College School of Pharmacy as well as an Antimicrobial Stewardship and Emergency Medicine Clinical Pharmacist practicing at a community hospital. She teaches infectious diseases as well a pediatric pharmacotherapy to both pharmacy and physician assistant students. Dr. Bruck received her bachelor of science in biology, followed by a Doctorate of Pharmacy degree, and then completed a postgraduate pharmacy residency program at William Beaumont Hospital in Troy, Michigan. Her research interests include antimicrobial stewardship, infectious diseases, as well as food allergy awareness. Dr. Bruck is Boardcertified in pharmacotherapy, infectious diseases, and pediatrics.
Jessica Price is a Doctor of Pharmacy candidate at South College School of Pharmacy in Knoxville, Tennessee. She has a Bachelor of Arts degree in Advertising and Public Relations, with minors in Business and English Writing from the University of Central Florida. Price completed her post-baccalaureate track in Biology at Florida International University and at the University of Tennessee, Knoxville.
Educational aims and objectives
This self-instructional course for dentists aims to provide an overview of judicious use of antibiotics in the dental practice to avoid antimicrobial resistance.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions by taking the quiz online at endopracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
• Observe some data regarding indications for appropriate use of antibiotics.
• Identify some ways to prevent transient bacteremia from dental procedures. Realize some published guidelines related to the prevention of infective endocarditis.
• Recognize antibiotic prophylaxis in regard to prosthetic joint Infections.
• Identify some pediatric considerations in antimicrobial prophylaxis.
Table 1). This checklist serves as an excellent supplement to concepts surrounding antibiotic prophylaxis in dentistry that will be discussed in further detail.9
Prevention of transient bacteremia from dental procedures
There are antibiotic prophylaxis recommendations for two types of patients undergoing invasive dental procedures, which include those with heart conditions who may be at an increased risk of infective endocarditis and those with prosthetic joint(s) who may be predisposed to the development of a hematogenous infection at the site of the prosthetic(s). The oral cavity is colonized with numerous microorganisms that comprise between 300 to 600 species of bacteria, fungi, and protozoa. The rationale for antibiotic prophylaxis is to reduce or eliminate transient or intermittent bacteremia (bacteria in the bloodstream) caused by invasive dental procedures that might result in more severe infections for these high-risk patients.10 Theoretically, patients with certain conditions and/or a compromised immune system might not be able to mount an immune response adequate to clear intermittent bacteremia originating from their oral flora. However, the exact risk is unknown as transient bacteremia from everyday activities (e.g., brushing teeth, chewing) might pose
35 endopracticeus.com Volume 15 Number 4 CONTINUING EDUCATION
2 CE CREDITS
Table 1: Checklist for antibiotic prescribing in dentistry
Pretreatment
• Correctly diagnose an oral bacterial infection.
• Consider therapeutic management interventions, which may be sufficient to control a localized oral bacterial infection.
• Weigh potential benefits and risk (i.e., toxicity, allergy, adverse effects, risk for Clostridioides difficile infection) of antibiotics before prescribing.
• Prescribe antibiotics only for patients of record and only for bacterial infections you have been trained to treat. DO NOT prescribe antibiotics for oral viral infections, fungal infections, or ulcerations related to trauma or aphthae.
• Implement national antibiotic prophylaxis recommendations for medical concerns for which guidelines exist (e.g., cardiac defects).
• Assess patients’ medical history and conditions, pregnancy status, drug allergies, and potential for drug-drug interactions and adverse events, any of which may impact antibiotic selection.
Prescribing
• Ensure evidence-based antibiotic references are readily available during patient visits. AVOID prescribing based on non-evidence-based historical practices, patient demand, convenience, or pressure from colleagues.
• Make and document the diagnosis, treatment steps, and rationale for antibiotics (if prescribed) in the patient chart.
• Prescribe only when clinical signs and symptoms of a bacterial infection suggest systemic immune response such as fever or malaise along with local oral swelling.
• Revise empiric antibiotic regimens on the basis of patient progress and, if needed, culture results.
• Use the most targeted (narrow-spectrum) antibiotic for the shortest duration possible (2 to 3 days after clinical signs and symptoms subside) for otherwise healthy patients.
• Discuss antibiotic use and prescribing protocols with referring specialists.
Patient Education
• Educate your patients to take antibiotics exactly as prescribed, take antibiotics only prescribed for them, and not save antibiotics for future illness.
Staff Education
• Ensure staff members are trained in order to improve probability of patient adherence to antibiotic prescriptions .
Reference: Printable checklist for antibiotic prescribing in dentistry available at: https://www.cdc.gov/oralhealth/infectioncontrol/faqs/antibiotic-stewardship.html
a higher risk for closed-spaced infections in these populations than transient bacteremia after a dental procedure in a patient without an active dental infection.11,13
Antibiotic prophylaxis: infective endocarditis
In 2008, the American Heart Association (AHA) published guidelines related to the prevention of infective endocarditis, which included guidance from the American Dental Association (ADA).13 The first iteration of the guidelines were supplemented with an updated scientific statement by the AHA in 2021.14,15 The scientific statement reaffirmed previous recommendations that prophylaxis is warranted in only a small subset of patients at highest risk of adverse outcomes. The recommendations consider the available evidence, weighing the benefits of preventing infective endocarditis with the risks, which include undue adverse effects as well as contribution to antimicrobial resistance. Moreover, these recommendations only apply to invasive dental procedures in which there is manipulation of the gingival tissue or periapical region of teeth, or perforation of the oral mucosa.16-18 The four broad categories of underlying conditions for which antimicrobial prophylaxis is advised are summarized in Table 2. The antibiotics suggested for use in those who are deemed to be at highest risk have empiric activity against the most common oral bacterial pathogens, most notably viridans group streptococci. The antibiotic regimen is chosen based on patients’ age, history of antibiotic allergy, and whether they can take oral medications (see Table
3). The antibiotic is given as a one time by mouth dose 30 to 60 minutes prior to the invasive dental procedure; hence, prior to the dental appointment, patients would need to have a prescription written with enough time to have it filled and administered. If the prescription is inadvertently not taken by patients before the procedure, then it can be given up to 2 hours after the procedure.19
One notable change in the 2021 AHA recommendations is that clindamycin has been removed from the options for prophylaxis because it may cause more frequent and severe reactions than other antibiotics used for prophylaxis.19 Clindamycin used to be the recommended prophylactic agent for patients with severe penicillin allergies. However, clindamycin has a listed a black box warning for Clostridioides difficile infection (CDI), which can be seen with onetime doses. The Minnesota Health Department found that patients were significantly more likely to have received a prescription for clindamycin in comparison to patients who received prescriptions from other non-dental providers. In this same study between the years of 2009 to 2015, it was found that 15% of patients with community-acquired CDI were treated by their dentist showing that a onetime prescription can produce undue downstream effects.20 The suggested alternatives for individuals unable to tolerate penicillin and β-lactam agents are azithromycin, clarithromycin, or doxycycline. If a patient has a non-IgE mediated allergy to penicillin or ampicillin, first- or second-generation cephalosporins can be chosen.19
36 Endodontic Practice US Volume 15 Number 4 CONTINUING EDUCATION
Table 2: Underlying conditions for which antimicrobial prophylaxis is suggested (before certain dental procedures)19
Prosthetic cardiac valve or material
• Transcatheter implanted prosthetic valves
• Annuloplasty, rings, or clips
• Left ventricular assist devices or implantable heart
Previous, relapse, or recurrent infective endocarditis
Congenital heart disease [CHD]
• Unrepaired cyanotic congenital CHD (including palliative shunts, conduits)
• Completely repaired defect with prosthetic material/device within 6 months after procedure
• Repaired CHD with residual defects at/or adjacent to the site of prosthetic material
• Surgical or transcatheter pulmonary artery valve or conduit placement
Cardiac transplant recipients who develop cardiac valvulopathy
Antibiotic prophylaxis: prosthetic joint Infections
In contrast with antibiotic prophylaxis to prevent infective endocarditis, the ADA Council on Scientific Affairs concluded that “Evidence fails to demonstrate an association between dental procedures and prosthetic joint infections or any effectiveness for antibiotic prophylaxis.” Given this information in conjunction with the potential harm from antibiotic use, using antibiotics before dental procedures is not recommended to prevent prosthetic joint infections. Additional case control studies are needed to increase the level of certainty in the evidence to a level higher than moderate.21 Due to the paucity of available literature in this area, there may be individual scenarios when it is not apparent if antibiotic prophylaxis is indicated. In these cases, all patients, their risk of invasive infection due to oral pathogens after a dental procedure, as well as the risks and the benefits of antibiotic prophylaxis should be carefully weighed.21-26 However, the ADA guidelines cite that in cases where antibiotics are deemed necessary, it is most appropriate that the orthopedic surgeon recommend the appropriate antibiotic regimen and, when reasonable, write the prescription.
Pediatric considerations in antimicrobial prophylaxis
Pediatric dosing considerations for antimicrobial prophylaxis are also found in the AHA guidelines as seen in Table 3. Recommendations for pediatric patients are similar to adults with respect to empiric pathogen coverage, type of dental procedure warranting prophylaxis, and the use of a single oral prophylactic antibiotic dose. Clinicians should ensure the pediatric weightbased dose does not exceed a single adult dose.26 Pediatric patients are approached with less concrete guidance than adult patients, which has been described in separate documents. More discussion regarding pediatric patients with a compromised immune system who may be at an increased risk of complications of bacteremia are discussed in the Reference Manual of Pediatric Dentistry.16,27 In the Best Practice Report provided by the ADA Council on Scientific Affairs, it is mentioned that there is a lack of data to fully support antimicrobial prophylaxis as well
which high-risk patients should be considered for antimicrobial prophylaxis. Several additional conditions could also warrant prophylaxis for pediatric patients, including the following:
• immunosuppression secondary to human immunodeficiency virus (HIV)
• severe combined immunodeficiency (SCIDS)
• neutropenia
• cancer chemotherapy
• stem cell or solid organ transplantation
• history of head and neck radiotherapy
• autoimmune disease
• sickle cell anemia or other asplenia
• chronic high dose steroid use
• uncontrolled diabetes
• bisphosphonate therapy
• hemodialysis27
Additionally, if a patient undergoing an invasive dental procedure has a vascular shunt, a consultation with the child’s physician is warranted to guide the need for and selection of antibiotic prophylaxis.
Summary
It is not only imperative to be cautious with antibiotic overprescribing for the intended treatment of dental infections, but also equally important that careful consideration is taken prior to prescribing antibiotics for dental infection prophylaxis. Although prophylaxis is generally a onetime dose of antibiotics, there is still the potential for negative downstream effects of antimicrobial resistance and/or undue side effects. Table 1 provides a summary of tools that can be utilized to assist dental practitioners in curbing antimicrobial threats surrounding dental prophylaxis as well as dental infection treatment.
EP
REFERENCES
1. Durkin MJ, Hsueh K, Haddy Y, et al. An evaluation of dental antibiotic prescribing practices in the United States. J Am Dent Assoc. 2017;148(12):878-886.
2. Gross AE, Hanna D, Rowan SA, et al. Successful implementation of an antibiotic stewardship program in an academic medical practice. Open Forum Infect Dis. 2019;6(3): 1-6.
37 endopracticeus.com Volume 15 Number 4 CONTINUING EDUCATION
Table 3: Single-dose antibiotics for prophylaxis prior to certain dental procedures: given 30 to 60 minutes prior to procedure19
Situation Antibiotic Single Dose for Adults
Able to take PO
Single Dose for Children¥
amoxicillin 2000 mg 50 mg/kg
Able to take PO, but allergic to penicillin or ampicillin cephalexin* 2000 mg 50 mg/kg
azithromycin 500 mg 15 mg/kg clarithromycin doxycycline 100 mg < 45 kg = 2.2 mg/kg > 45 kg = 100 mg
Unable to take PO (give agents IV or IM)ampicillin 2000 mg 50 mg/kg cefazolin∆» 1000 mg 50 mg/kg ceftriaxone∆» 1000 mg 50 mg/kg
IM = intramuscular; IV = intravenous; PO = oral
* Or other 1st or 2nd generation cephalosporin in equivalent adult or pediatric dosing
∆ Cephalosporins should not be used in patients with a history of anaphylaxis, angioedema, or urticaria with penicillin or ampicillin
» Allergic to penicillin or ampicillin and unable to take PO medications
¥ Pediatric weight-based dosing should NOT exceed adult single dose recommendations
3. Suda KJ, Henschel H, Patel MA, et al. Use of antibiotic prophylaxis for tooth extractions, dental implants, and periodontal surgical procedures. Open Forum Infect Dis. 2018;5(1): 1-5.
4. Loffler C, Bohmer F. The effect of interventions aiming to optimise the prescription of antibiotics in dental care: a systematic review. PLoS One. 2017:12(11):1-23.
5. American Dental Association. Oral health topics: Antibiotic prophylaxis prior to dental procedures. American Dental Association website. Last updated January 5, 2022. Available at: https://www.ada.org/resources/research/science-and-research-institute/ oral-health-topics/antibiotic-prophylaxis Accessed October 27, 2022.
6. Macfarlane G. Alexander Fleming: The Man and the Myth. Harvard University Press; 1984.
7. Fluent MT, Jacobsen PL, Hicks LA. Considerations for responsible antibiotic use in dentistry. J Am Dent Assoc. 2016;147(8):683-686.
8. Dana R, Azarpazhooh A, Laghapour N, Suda KJ, Okunseri C. Role of dentists in prescribing opioid analgesics and antibiotics: an overview. Dent Clin North Am. 2018;62(2):279-294.
9. Centers for Disease Control and Prevention. Printable Checklist for Antibiotic Prescribing in Dentistry: https://www.cdc.gov/oralhealth/infectioncontrol/faqs/antibiotic-stewardship.html. Accessed October 27, 2022.
10. American Dental Association. Oral health topics: Antibiotic prophylaxis prior to dental procedures. American Dental Association website. Last updated January 5, 2022. Available at: https://www.ada.org/resources/research/science-and-research-institute/ oral-health-topics/antibiotic-prophylaxis Accessed October 27, 2022.
11. Duval X, Leport C. Prophylaxis of infective endocarditis; current tendencies, continuing controversies. Lancet Infect Dis. 2008; 8:225-232.
12. Goff DA, Mangino JE, Glassman AH, et al. Review of guidelines for dental antibiotic prophylaxis for prevention of endocarditis and prosthetic joint infections and need for dental stewardship. Clin Infect Dis. 2020;71(2):455-462.
13. Wilson W, Taubert KA, Gewitz M, et al. Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. J Am Dent Assoc. 2008;139(suppl):3S-24S.
14. Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients with Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135(25): e1159-e1195.
15. Wilson WR, Gewitz M, Lockhart PB, et al. Prevention of Viridans Group Streptococcal
Infective Endocarditis: A Scientific Statement from the American Heart Association. Circulation. 2021;143:e963-e978.
16. Loyola-Rodriguez JP, Franco-Mrianda AF, Loyola-Leyva A, et al. Prevention of infective endocarditis and bacterial resistance to antibiotics: A brief review. Spec Care Dentist. 2019;39:603-609.
17. Goff DA, Mangino JE, Glassman AH, et al. Review of guidelines for dental antibiotic prophylaxis for prevention of endocarditis and prosthetic joint infections and need for dental stewardship. Clin Infect Dis. 2020;71(2):455-462.
18. Chen TT, Yeh YC, Chien KL, et al. Risk of infective endocarditis after dental treatments. Circulation. 2018; 138(4):356-363.
19. Thornhill MH, Dayer M, Lockhart PB, Prendergast B. Antibiotic prophylaxis of infective endocarditis. Curr Infect Dis Rep. 2017;19(2):9.
20. Bye M, Whitten T, Holzbauer S. Antibiotic Prescribing for Dental Procedures in Community-Associated Clostridium difficile cases, Minnesota, 2009-2015. Open Forum Infect Dis. 2017;4(Suppl 1):S1.
21. Sollecito TP, Abt E, Lockhart PB, et al. The use of prophylactic antibiotics prior to dental procedures in patients with prosthetic joints: Evidence-based clinical practice guideline for dental practitioners — a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2015;146(1):11-16 e8.
22. Watters W 3rd, Rethman MP, Hanson NB. Prevention of Orthopaedic Implant Infection in Patients Undergoing Dental Procedures: J Am Acad Orthop Surg. 2013;21(3): 180-189.
23. Rethman MP, Watters W,3rd, Abt E, et al. The American Academy of Orthopaedic Surgeons and the American Dental Association clinical practice guideline on the prevention of orthopaedic implant infection in patients undergoing dental procedures. J Bone Joint Surg Am. 2013;95(8):745-747.
24. Meyer DM. Providing clarity on evidence-based prophylactic guidelines for prosthetic joint infections. J Am Dent Assoc. 2015;146(1):3-5.
25. American Dental Association-Appointed Members of the Expert Writing and Voting Panels Contributing to the Development of American Academy of Orthopedic Surgeons Appropriate Use Criteria. American Dental Association guidance for utilizing appropriate use criteria in the management of the care of patients with orthopedic implants undergoing dental procedures. J Am Dent Assoc. 2017;148(2):57-59.
26. Quinn RH, Murray JN, Pezold R, Sevarino KS. The American Academy of Orthopaedic Surgeons Appropriate Use Criteria for the Management of Patients with Orthopaedic Implants Undergoing Dental Procedures. J Bone Joint Surg Am. 2017;99(2):161-163.
27. American Academy of Pediatric Dentistry. Antibiotic prophylaxis for dental patients at risk of infection. The Reference Manual of Pediatric Dentistry. American Academy of Pediatric Dentistry. 2019:416-421.
38 Endodontic Practice US Volume 15 Number 4 CONTINUING EDUCATION
Continuing Education Quiz
Dental infections,
part 2
— prophylaxis: help avoid antimicrobial resistance BRUCK/PRICE
1. In the United States, general and specialty dentists are the _______ prescribers of antibiotics in all outpatient settings.
a. highest b. second highest c. third highest d. fourth highest
2. Looking at data from 2017 to 2019, it is estimated that somewhere between 30% to _________ of dental antibiotic prescriptions are “suboptimal or not indicated.”
a. 40% b. 60% c. 85% d. 92%
3. The oral cavity is colonized with numerous microorganisms that comprise between 300 to 600 species of _______. a. bacteria b. fungi c. protozoa d. all of the above
4. Regarding guidelines related to the prevention of infective endocarditis from the American Heart Association and American Dental Association, antibiotic prophylaxis is warranted ________. a. for every patient undergoing a dental procedure b. in only a small subset of patients at highest risk of adverse outcomes c. only for patients prone to joint infections d. only for patients who ask for it
5. One notable change in the 2021 AHA recommendations is that ______ has been removed from the options for prophylaxis because it may cause more frequent and severe reactions than other antibiotics used for prophylaxis.
a. clindamycin b. penicillin c. azithromycin d. doxycycline
6. ____________ used to be the recommended prophylactic agent for patients with severe penicillin allergies.
a. Doxycycline b. Azithromycin c. Clindamycin d. Penicillin
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 16 CE credits for only $149; call 866-579-9496, or visit https://endopracticeus.com/ subscribe/ to subscribe today.
n To receive credit: Go online to https://endopracticeus.com/continuingeducation/, click on the article, then click on the take quiz button, and enter your test answers.
AGD Code: 010
Date Published: December 18, 2022 Expiration Date: December 18, 2025
2 CE CREDITS
7. If a patient has a non-IgE mediated allergy to penicillin or ampicillin, ________ can be chosen. a. first- or second-generation cephalosporins b. clarithromycin c. doxycycline d. levaquin
8. (Regarding prosthetic joint infections) The ADA guidelines cite that in cases where antibiotics are deemed necessary, it is most appropriate that the ________ recommend the appropriate antibiotic regimen and, when reasonable, write the prescription. a. oral surgeon b. orthopedic surgeon c. orthodontist d. internist
9. When prescribing antibiotics for pediatric patients, clinicians should ensure the pediatric weight-based dose does not exceed a single adult dose. a. True b. False
10. As shown in Table 3, single-dose antibiotics for prophylaxis prior to certain dental procedures should be given _____ prior to procedure. a. 30 to 60 minutes b. 2 to 3 hours c. the night before d. the day before
To provide feedback
on CE, please email us at education@medmarkmedia.com
Legal disclaimer: Course expires 3 years from date of publication. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
39 endopracticeus.com Volume 15 Number 4 CONTINUING EDUCATION
Healing and long-term results with the GentleWave ® Procedure
Dr. Scott K. Hetz illustrates minimally invasive endodontic treatment with predictable
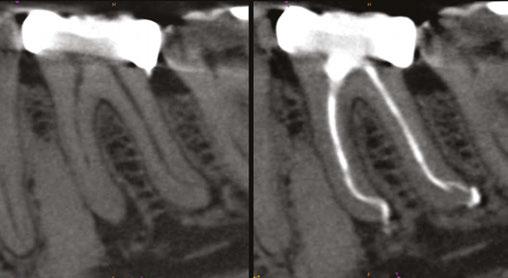

results
Our patients are primarily concerned with two things: getting a painless procedure and knowing how long this will take. It is not often that we receive an initial inquiry about outcomes before the game even begins. Outcomes matter; in fact, that is where my mind goes every time I begin gathering diagnostic data and discovering the details about my patient’s chief complaint. Endodontics is not a game or a sport, yet we aspire to gain any advantage and win nonetheless.
Whether we like it or not, change is inevitable. New technology options will continue to evolve, allowing each of us the opportunity to be an active participant in the direction of our own practice. I was initially fascinated by the science supporting the GentleWave® Procedure (Sonendo®, Laguna Hills, California). This technology’s mechanism of action offers a different option for actively dissolving pulp tissue and removing biofilm, which are just a couple of the many advantages that I have come to rely on over the past 4 years.
In the AAE 2010 Colleagues for Excellence article, titled “Access Opening and Canal Location,” the authors wrote, “The ultimate goal of endodontic treatment is to create an environment in which the body can heal itself.”1 In other words, our job as endodontists is to clean and disinfect the root canal system as thoroughly as possible, to then allow the body’s natural healing process to take over, and to repair the damage created by either infection or inflammation, or both. Our objective then should be to minimize our “touch” to the tooth, thereby promoting lasting sustainability of the remaining structure and, ultimately, full healing.
Case 1: The thrill of the clean
For many of us specialists, it is rewarding to see some of the amazing canal anatomy displayed on the final radiograph after
Scott K. Hetz, DMD, is a Board-certified specialist in Endodontics. He is a 1997 graduate of the University of Pittsburgh School of Dental Medicine. Dr. Hetz served in the United States Air Force for 9 years, including an Advanced Education in General Dentistry program. Also, while on active duty, he received his specialty certificate in Endodontics from the University of Southern California in 2004.
Dr. Hetz volunteers as affiliate faculty in the Department of Endodontics Naval Postgraduate Dental School at Walter Reed National Military Medical Center. He maintains a full-time practice as a partner with Advanced Endodontic Associates in Washington, DC. Dr. Hetz can be reached at scotthetz@mac.com.
Disclosure: Dr. Scott Hetz is a key opinion leader for Sonendo®

putting all that effort into your root canal treatment — it is the “Thrill of the Fill,” as quoted by one of the masters of endodontics. However, the real game changer is the “Thrill of the Clean.” We know from the Pauli’s exclusion principle that two objects cannot occupy the same space at the same time, so you cannot fill if there is debris remaining. The GentleWave Procedure offers an option to dissolve both vital and necrotic tissues in previously inaccessible isthmus anatomy, fins, and lateral canals.
Case 1 poses a number of shaping challenges, but let us approach it from a place of opportunity. Cutting a more traditional shape for this specific anatomy would block out most of this distal apical delta and risk file separation. Shortly after adopting GentleWave, my mindset had shifted. I now ask, “How will I accommodate my approach to any case to best utilize this technology?”
Instead of shaping, the new goal is to secure a minimally invasive fluid pathway to deliver the GentleWave System’s efficient and powerful mechanism of action into this complex anatomy.
40 Endodontic Practice US Volume 15 Number 4 TECHNOLOGY
Figure 1: Case 1. Immediate post-op with GentleWave® Procedure Figure 2: Case 1. 3 months post-GentleWave® Procedure
Once cleaned and thoroughly dried, the root canal system can be predictably obturated with a single-cone, sealer-based technique using bioceramic sealer.
The early healing observed by most clinicians using these techniques is validated with comparative CBCT images at 3 months.
Case 2: Endo-perio: Single-appointment resolution with longer-term results
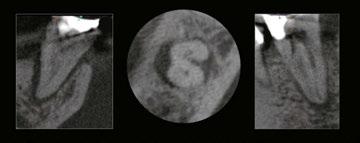
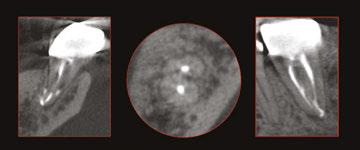
In this case, the endo-perio lesion was the result of periodontal and pulpal disease occurring within the same dental element. Diagnosis, prognosis, and treatment planning were complicated by the inter-relationships and simultaneous existence of both processes. Many of us were trained to treat a case like this just one way — multiple visits. Only shape and clean initially, and we should definitely be medicating.
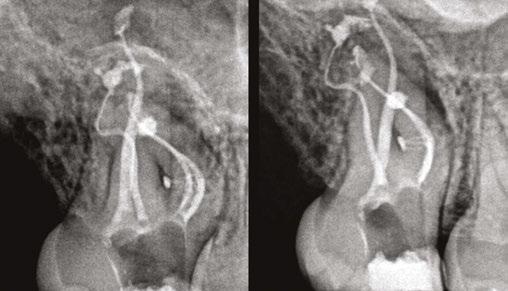
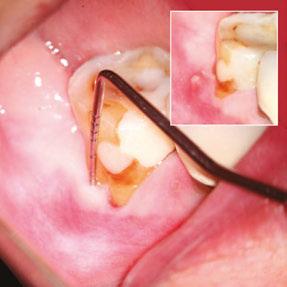
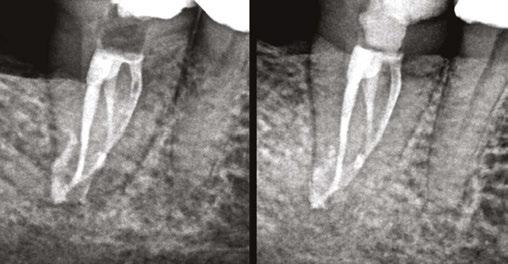

Legacy workflow involved bringing the patient back to assess the periodontal status, followed by another treatment session with more anesthesia and a rubber dam.
An additional level of difficulty to consider was the “C-shaped” root form. It must be explained that the prognosis remains questionable, and only the desired periodontal healing can confirm a diagnosis of primary endo etiology. So successful resolution of periodontal symptoms after endodontic therapy is diagnostic in itself. Now we can offer same-day, unscheduled, single-appointment, and predictable endodontics for this patient using the GentleWave Procedure.
A differential diagnosis to include root fracture and treatment options was discussed, and this patient consented to my primary recommendation for nonsurgical RCT.
Resolution of the current symptoms was certainly important, but confirming longerrange healing and tooth retention carried equal value. The probing depths and sinus tract resolved in 1 month, providing an immediate upgrade to the periodontal prognosis. The 3.5-year recall demonstrated continued and lasting healing of the endodontic component. This patient had completely regenerated hard tissues.
Case 3: A minimalistic approach with small shapes
With the GentleWave System, the emphasis on the decadesold endodontic triad of shape, clean, and obturate has shifted to cleaning, with shaping taking on a much lesser role. In my practice, a 6% taper now only has historical value. I no longer use files to shape in the traditional sense, but instead to provide a fluid pathway to dissolve vital pulp tissues, necrotic remnants, and remove biofilm from intricate canal anatomies previously inaccessible by traditional means of irrigation.
This case highlights a minimalistic approach with no shape exceeding .17 tip size or .04 taper. The DB and MB2 remained at .16 tip size with a .02 taper! The obturation optics would not have projected “a sense of clean” in years past, but now the GentleWave Procedure’s mechanism of action leaves areas of
41 endopracticeus.com Volume 15 Number 4
TECHNOLOGY
Figure 3: Case 2. Pre-GentleWave® Procedure
Figure 4: Case 2: Post-GentleWave® Procedure and 3.5-year recall postGentleWave® Procedure
Figures 5, 6A, and 6B: Case 2. 5. Resolution of probing depths and sinus tract. 6A. Pretreatment images. 6B. 3.5-year recall post-GentleWave® Procedure
Figure 7: Case 3. Post-GentleWave® Procedure
confluent isthmus and lateral canals free of debris. This style of endodontics is now possible due to the perfect storm of conservative shapes, bioceramic sealer, and an enhanced irrigation delivery system.
Evidence of accelerated healing was observed at the 3-month recall, and complete healing was verified at the 16-month recall.
Case 4: Non-instrumentation endodontics
This next case represents a huge paradigm shift in how I treatment-plan emergency endodontic care and is a great opportunity to share how we can let go of deep-rooted protocols and embrace new technologies.
This young adult presented with buccal edema and significant pain. Upon access, purulent drainage was allowed to passively flow, but not for long. After a few brief moments to build a custom platform, the 9-minute GentleWave Procedure applied negative pressure to this closed-loop system, which enhanced the evacuation of drainage. It simultaneously provided a clean canal space, free of debris, and ready for same-day obturation with a combination of bioceramic putty/bioceramic sealer to address the open apex.

The canal walls of this 28 mm lateral incisor remained untouched. No files were used, not one! A fluid pathway to the portal of exit allowed for continuous exchange of irrigation fluids throughout the procedure. Once the procedure was completed, my patient reported, “Hey, Doc, the swelling in my face is nearly gone!” Continued follow-up care demonstrated complete regeneration of the buccal cortical plate.
Implementing the GentleWave® System
My goal always is to make the canal anatomy as clean as possible, and GentleWave more than satisfies this criterion in a single-appointment model. Often, I am asked about the level of difficulty to expect while implementing the GentleWave System. It is not difficult, but it does require a commitment from the whole office. There is a lot of preparation to get your staff and practice ready, but once you integrate the system, you will discover it is worth it.
REFERENCES
1. Paul Krasner, Rankow HJ, Abrams ES. Access Opening and Canal Location. ENDONDONTICS: Colleagues for Excellence newsletter. Spring 2010:2. https://www.aae.org/ specialty/newsletter/access-opening-canal-location/. Accessed November 10, 2022.
Figure 9: Case 4. Pre-op scan and interop photos
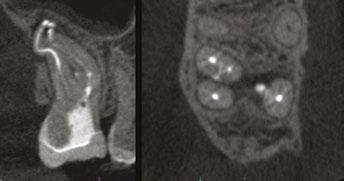

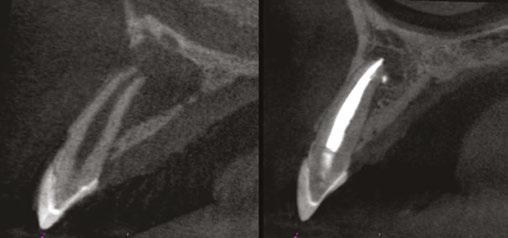
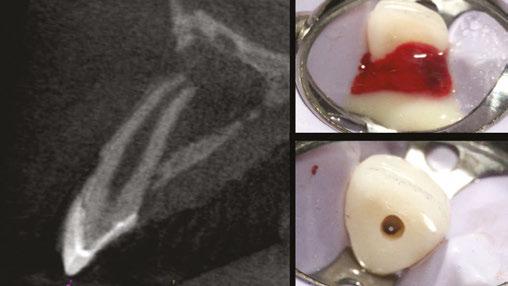
Figure 10: Case 4. 3-month recall post-GentleWave® Procedure

Figure 11: Case 4. Side-by-side comparison — Pre-op and 2-year recall post-GentleWave® Procedure
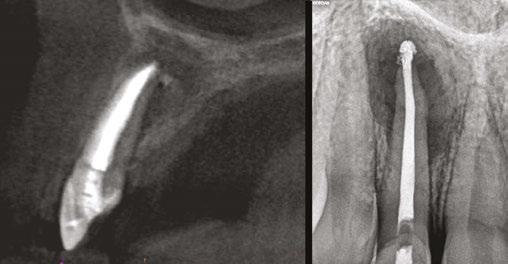
42 Endodontic Practice US Volume 15 Number 4 TECHNOLOGY
EP
Figures 8A–8C: Case 3. A. Pre-op scan. B. 3-month recall post-GentleWave® Procedure. C. 16-month recall post-GentleWave® Procedure A. B. C.
Now we can offer same-day,
unscheduled,
singleappointment, and predictable endodontics for this patient using the
GentleWave® Procedure.”

Sealing the deal with a bioceramic root canal sealer
CeraSeal from Meta Biomed provides antimicrobial properties, high biocompatibility, and a hermetic seal
Successful root canal treatment means the complete elimination of microbial entity and prevention of future predilection of reinfection. Achieving that objective requires a proper seal, thereby diminishing the chance of bacteria proliferation and future occurrence of pathology. However, with so many different categories and brands of sealer available, it can be difficult to determine the best choice for effective treatment.

Let’s consider the key properties of root canal sealer. The material must close the space around the gutta percha and extend to the dentinal wall, forming a bond between the core of the filling material and the root canal wall. The root canal sealer must fill in potential gaps and voids, and flow into and seal off lateral and accessory canals.
While Grossman described 11 properties of root canal sealer — including providing good adhesion, a hermetic seal, radiopacity, and nonshrinkage — it’s been widely accepted that there may be no perfect sealer that accomplishes all criteria. Clinicians have had to choose among types of sealer categorized according to their main chemical constituents: zinc oxide eugenol, calcium hydroxide, glass ionomer, silicone, resin, and bioceramic-based sealers.
Introduced to endodontics in the 1990s and advancing to newer generations, bioceramic sealers have several major advantages. Importantly, their biocompatibility prevents rejection by the surrounding tissues, and they contain calcium phosphate, which enhances the setting properties of bioceramics and results in a chemical composition and crystalline structure similar to tooth and bone apatite materials, thereby improving sealer-toroot dentin bonding.
Optimal biocompatibility
CeraSeal, a calcium silicate-based bioceramic root canal sealer from Meta Biomed, represents the next generation, providing high flowability and excellent sealing ability while creating an optimal biocompatible environment to tissues in the root canal.

The calcium silicate produces calcium aluminate hydrate (CAH) gel and calcium silicate hydrate (CSH) gel by absorbing the moisture from surrounding tissues in the root canal and some
crystallization of calcium hydroxide. Thanks to the high pH of calcium hydroxide, the material has an antimicrobial action that suppresses the bacteria in the root canal.
Stronger seal and faster set
Moisture in the dentinal tubules and calcium silicate’s chemical reaction produce crystallization of calcium hydroxide. As a result of this reaction, CeraSeal is fully hermetic in the root canal and prevents the propagation of bacteria. And while sealers such as those that are resin-based will shrink upon setting, CeraSeal neither shrinks in the root canal nor expands. Therefore, CeraSeal not only prevents bacteria, but also protects against odontoclasis because of the high-volumetric stability. The hermetic sealing also allows for single-cone technique obturation.
Radiopacity is a key property of root canal sealers, so they can be distinguishable from adjacent anatomical structures. CeraSeal’s high radiopacity of 8 mm allows the quality of the root filling to be sufficiently evaluated through radiographic examination.
Another benefit of CeraSeal is its short setting time (3.5 hours). This prevents the washout phenomenon. And while the science behind CeraSeal makes it a viable option for permanent root canal sealing and permanent root canal filling, there is one more benefit for the clinicians — it’s easy to use. CeraSeal comes in a premixed syringe with no mixing required. This information was provided by Meta Biomed.
EP
44 Endodontic Practice US Volume 15 Number 4 PRODUCT PROFILE
Clinical cases

| Half the leakage, Half the Cost Anti-microbial Optimal biocompatibility Excellent sealing ability Unique stability Calcium silicate-based CeraSeal provides an optimal biocompatible environment to periapical and root canal tissues. No shrinkage or expansion, with next generation sealing abilities. SCAN TO SHOP CeraSeal Clinical Review Article Address: 3015 Advance Lane, Colmar, PA 18915 Website: metabiomedamericas.com | metabiomedshop.com Email: america@metabiomed-inc.com Phone: 267.282.5893
Optimizing surgical visualization with the ZEISS EXTARO ® 300
Dr. Jon Irelan discusses innovations in endodontic microsurgery

With advances in 3D-imaging techniques and the advent of microtomography, our understanding of root canal anatomy has evolved markedly over recent decades. Through this understanding comes the realization that root-end anatomy presents with profound complexity and variability. Further complicated by the intricate mechanism of periapical disease and biofilms, the challenge we face as clinicians is the necessity for diligent and accurate detection of etiologies associated with the pathoses we seek to resolve.
Figures 1A-1C: A. Tooth No. 13 root-end inspection Fluorescence Mode. B. Tooth No. 2 root-end inspection methylene blue. C. Tooth No. 2 root-end inspection Fluorescence Mode
Historically, my practice has been largely centered on endodontic retreatment and microsurgery. With many microsurgeries involving the treatment of molar teeth, ideal visualization of the surgical site is a main concern. In addition to properly accessing the surgical site, great effort must be made to achieve proper positioning of the patient in order to remain comfortable throughout the procedure. Furthermore, this must be done while also allowing the clinician to maintain ideal posture throughout the surgery. Thanks to features offered by the EXTARO® 300 from ZEISS, these goals can be readily accomplished.
With the MORA Interface, eyepieces are kept level while the lens can be angled sharply to accommodate the patient’s position. While the Foldable Tubes are a lesser-known feature of the EXTARO 300, they allow the clinician to remain a greater distance
Jon P. Irelan DDS, MS, MS, earned a Bachelor of Science from Marquette University. He went on to graduate Magna Cum Laude from Marquette University School of Dentistry, earning his DDS in 2013. During dental school, he served as an instructor in anatomy and occlusion courses and worked as a lab technician for a prosthodontic practice. Dr. Irelan was the recipient of the American College of Prosthodontists Outstanding Undergraduate Achievement Award, as well as Hanau’s Best of the Best Excellence in Prosthodontics Award and the Quintessence Award in Research. He later completed a 3-year prosthodontic residency in 2016 at Marquette University School of Dentistry, earning a Master of Science degree, and continued as the sole prosthodontist for a 60-practice dental group. Dr. Irelan completed his endodontic residency in 2018 at Marquette University School of Dentistry earning an additional Master of Science degree, and is continuing as an Adjunct Assistant Professor for dental students and endodontic residents. He lectured at the 2018 American Association of Endodontics Annual Session in Denver, Colorado, and again in 2019 in Montreal, Quebec. Dr. Irelan is an endodontist in Franklin, Tennessee.
Disclosure: Dr Irelan is a Key Opinion Leader. This article is sponsored by ZEISS.
from the scope and can even allow the lens to be angled back toward the clinician. The Varioskop® 230 from ZEISS allows for even greater flexibility with a focal length of 200 mm to 430 mm, which accommodates a wider in-focus range of distance between the scope and the patient than other endodontic microscopes.
While I regularly employ methylene blue dye for evaluation of root structure and apical anatomy, I have found Fluorescence Mode on the EXTARO 300 invaluable. Fluorescence Mode allows for the detection of cariogenic bacteria by exciting fluorophores, which give off an orange-red light, a technology that does not require the application of any additional substances. While its intended use allows for caries detection with high sensitivity and specificity, I have personally found it to act as an excellent contrasting tool during microsurgery. Using this augmented visualization mode, dentin and cementum fluoresce brilliantly relative to osseous and soft tissue. This distinction between tissues allows for ready identification and evaluation of the root structure, providing another important tool for locating critical root canal anatomy during microsurgical procedures. EP

46 Endodontic Practice US Volume 15 Number 4 PRODUCT SPOTLIGHT
300 MORA Interface
ZEISS EXTARO®

We’ve got your back while you take care of your patients. ZEISS EXTARO 300 Benefits of an ergonomically designed microscope help to • Reduce neck and back pain • Sit in a comfortable, neutral posture • Reduce musculoskeletal injuries • Fully focus on your patient and increase your productivity en-US_30_030_0150I ©2021 Carl Zeiss Meditec, Inc. All rights reserved.
ES Vac
ES Vac is changing irrigation!
ES Vac is the ONLY single-handed apical negative pressure irrigation system on the market! ES Vac uses suction to pull irrigants down the canal of the tooth and out of the canal via the suction dual port cannula. Many companies have tried to make negative pressure irrigation simple and easy, but nothing comes close to the ease and clinical effectiveness of ES Vac.
Research shows that patients have less post-op pain when negative pressure irrigation is performed during their root canal therapy.1,2,3
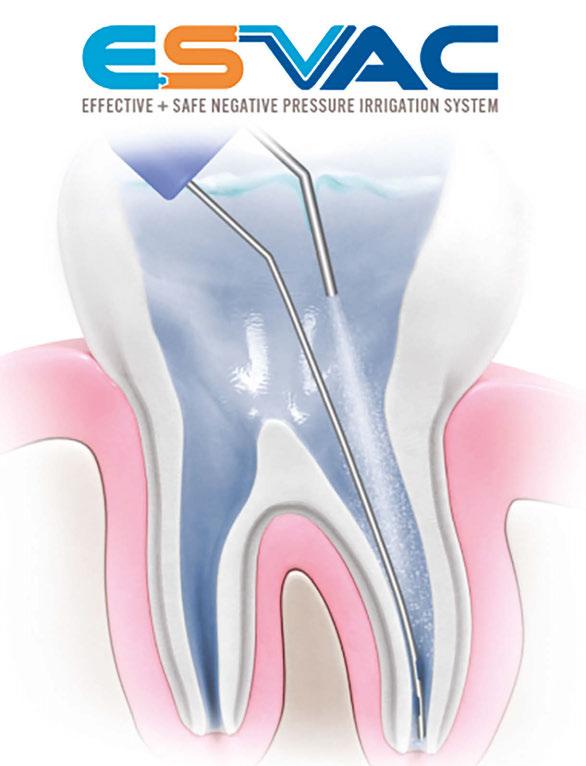
Single-handed operation is like no other device on the market. Why? ES Vac’s ease-of-design the clinician can use ES Vac with ONE HAND!
ES Vac comes fully assembled!
ES Vac is the ONLY device on the market that comes preassembled. Gone are the days of having to “build” your irrigation device. ES Vac is ready to go right out of the pouch.
Simply plug in the suction connector to your Hi-Lo suction, fill the provided syringe with your irrigant, and lock your syringe onto irrigation/suction manifold, and you’re ready to clean!
All ES Vac devices have dual-port suction cannulas to ensure constant suction of debris. ES Vac comes in 23, 27, and 30 gauge suction cannulas for gross- to micro-debris removal.
No timely waiting — ES Vac is so effective you only need seconds per canal! Gone are the days of leaving your patients waiting for minutes with devices stuck in their mouths.
Proven technique with over a decade of research — negative pressure has been proven to work and has been a tried-and-true method for irrigation with over a decade of clinical research to support it.
EP
REFERENCES
1. Topçuoğlu HS, Topçuoğlu G, Arslan H. The Effect of Apical Positive and Negative Pressure Irrigation Methods on Postoperative Pain in Mandibular Molar Teeth with Symptomatic Irreversible Pulpitis: A Randomized Clinical Trial. J Endod. 2018;44(8):1210-1215.
2. Gondim E Jr, Setzer FC, Dos Carmo CB, Kim S. Postoperative pain after the application of two different randomized clinical trial irrigation devices in a prospective. J Endod. 2010;36(8):1295-1301.
3. Heilborn C, Reynolds K, Johnson JD, Cohenca N. Cleaning efficacy of an apical negative-pressure irrigation system at different exposure times. Quintessence Int. 2010;41(9):759-767.
48 Endodontic Practice US Volume 15 Number 4 PRODUCT PROFILE
ES Vac makes total debris evacuation and irrigation easy!”
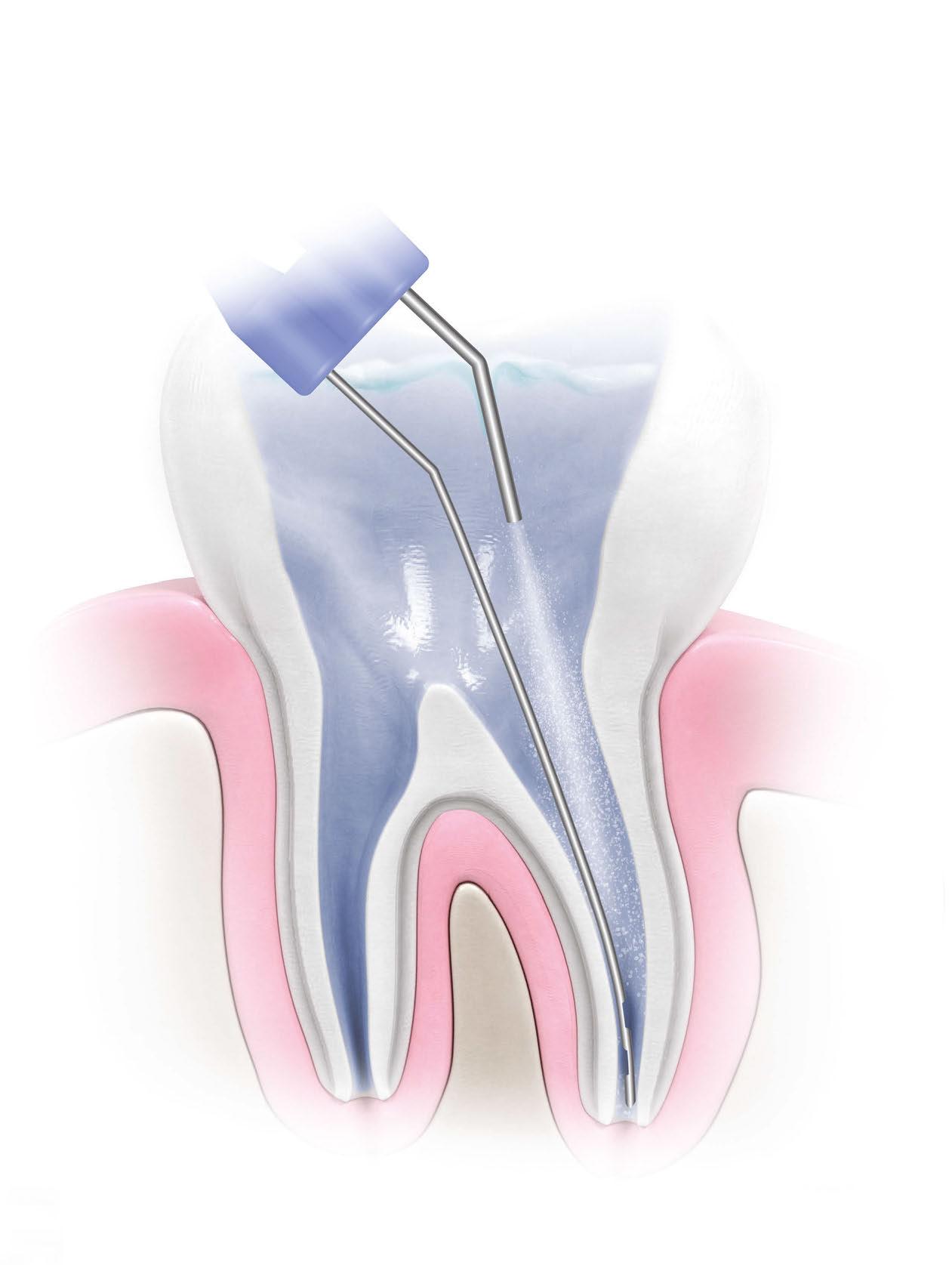

Navigating dental malpractice lawsuits — part 1
 Kristin Tauras, JD, guides dental specialists through the legal elements
Kristin Tauras, JD, guides dental specialists through the legal elements
Dental specialists are increasingly being sued for professional malpractice. As one plaintiff’s counsel explained, it is easier to get a dental specialist to settle than any other medical professionals these days. While most other medical professionals are aware that they are the target of lawsuits and have themselves been sued or see their colleagues getting sued, the same cannot be said for the dental profession. While not new, dental malpractice lawsuits are still a novelty to most in the profession. Dental specialists are unprepared for the havoc a lawsuit can cause in their practice, are embarrassed when they are sued, are less likely to tell colleagues that they have been sued or seek advice, and are more apt to settle quickly and quietly than fight what is oftentimes a defensible case.
The term dental specialist used throughout this article encompasses all dental and medical providers who treat diseases and problems of the teeth, gums, and jaw — including dentists, cosmetic dentists, pediatric dentists, prosthodontists, periodontists, endodontists, oral and maxillofacial surgeons, and orthodontists. This also encompasses the liability of the dental specialist’s staff — including dental hygienists, dental assistants, nurses, anesthesiologists, and other medical providers who assist with the dental treatment and potentially can be named in a dental malpractice lawsuit.
Proving professional malpractice
In every state, a patient may pursue a malpractice claim against a dental healthcare provider if the healthcare provider causes injury or death to the patient through a negligent act or omission. In dental treatment, professional malpractice is defined as any act or omission by a dental specialist, or someone under their direction, during the treatment of a patient that deviates from the accepted standard of care and causes harm to the patient.
To recover for alleged dental malpractice, the plaintiff must allege and prove that the dental specialist (or someone under his/her supervision) was negligent in the treatment of a patient,
Kristin Tauras, JD, is a partner in the law firm of McKenna Storer in Chicago, Illinois. She has a litigation practice in the areas of employment law, insurance coverage, and professional malpractice. McKenna Storer is a fullservice law firm providing legal services to individuals and small to midsize companies, including defending professional malpractice negligence lawsuits and Illinois Department of Professional Regulation investigation, as well as advising dental and medical professionals regarding business and employment matters.
and that the negligence caused harm to the patient. The elements may be broken down further:
• Duty of care owed by the dental specialist to the patient
• Breach of duty of care by the dental specialist
• Injury caused to the patient by the breach of duty of care by the dental specialist
• Damages to the patient
Duty of care
First, the plaintiff must establish that the dental specialist owed the patient a duty of care. This first element requires that there is a relationship between the dental specialist and the patient. Usually this element is easily proven through the use of medical records showing that the dental specialist treated the patient.
Other times though, the patient relationship falls within a gray area — for example, where the patient does not return for the treatment, the dental specialist declines or refuses to treat the patient for a dental issue, or the dental specialist refers the patient to someone else before the malpractice occurs.
It is also important to note that dental specialists are also liable in most states for those who work under their supervision with them and, in some cases, those to whom they refer cases. Just because the dental professional did not cause the injury, he/ she may still be liable for the acts of others. This includes their dental hygienist, nurse, or anesthesiologist.
50 Endodontic Practice US Volume 15 Number 4 LEGAL MATTERS
LEGAL MATTERS
Breach of duty of care
Second, the plaintiff must establish a breach of duty of care. To do so, the plaintiff must establish the standard of care. The standard of care is a “reasonable person standard,” which is a legal fiction, created by laws, referencing a standard of care that all dental professionals in a similar situation and similar locale should follow. A breach of the standard of care occurs when the provider fails to act as a reasonably prudent and trained dental professional would under the same or similar circumstances when treating a patient. Both the standard of care and the breach of the standard of care must almost always be established through expert witnesses. The exception is where the breach is of such an obvious nature that the breach speaks for itself.
Breach of standard of care
Third, the breach of the standard of care must cause an injury. A plaintiff must prove that the healthcare provider caused the injury or made an existing condition worse by his/her action (or inaction). The patient must show a direct relationship between the alleged breach and the subsequent injury. This is known as “proximate cause.” The malpractice must proximately cause the injury suffered by the patient.
Damages
Fourth, there must be damages. Damages can be in the form of medical bills (the cost of medical treatment and corrective treatment), disfigurement, pain and suffering, loss of normal life, and economic losses (lost wages).
When dental errors result in permanent disability or death, family members may also, in most states, recover for the “loss of society” and/or wrongful death of the patient.
In rare cases, punitive damages may also be awarded. For this to occur, there must usually be malfeasance or malintent alleged.
Types of dental malpractice
Any deviation from the standard of care can constitute malpractice if it proximately causes a patient injury. There are an infinite number of ways dental practitioners can deviate from the standard of care. Examples of deviations from the standard of care that may result in a malpractice claim follow.
• Ignoring the current standards when recommending or pursuing a course of treatment.
• Improperly treating or failing to treat the dental condition.
• Failing to accurately diagnose an infection, lesion, cancer, periodontal disease, or other oral diseases.
• Causing an infection.
• Failing to adequately supervise employees under their direction or control.
• Improperly administering anesthesia that leads to complications such as brain damage or death.
• Causing nerve injuries that lead to complications such as neuropathy or paralysis.
• Causing damage to bone or soft tissue.
• Drilling too deeply, resulting in permanent injury to the tooth.
• Performing an improper extraction.
• Misaligning the teeth by improperly fitting fillings, crowns, or implants, resulting in issues with bite and speech.
• Using excessive force on patients.
• Recommending unnecessary dentures or failing to correctly fit dentures.
• Using improper instrumentation, improperly maintained instrumentation, or using outdated tools.
• Failing to consider a patient’s existing medical conditions, allergies, and physiology before treating the patient.
• Recommending and performing treatments that are not medically necessary.
• Failing to refer the patient to the proper dental specialist such as an oral surgeon or an endodontist.
• Failing to obtain informed consent and failing to explain the risks of the procedure to the patient in a manner and language in which the patient can understand.
Art of dentistry
Dental specialists are familiar with the term art of dentistry. Despite enormous advances in the practice of dentistry, the personal encounter between patient and physician remains the cornerstone of dental care. The dental professional becomes the diagnostic and therapeutic expert who applies the knowledge and skills of dentistry. It includes not only what is required for a diagnosis and healing, but also the ability to apply the generalized knowledge of dentistry to individual patients. Dental specialists should not allow the fear of a malpractice suit to hamper their judgment and their application of the art of dentistry, but they should be aware of the types of claims so they may make sure to protect themselves against a claim that they committed dental malpractice.
Best practice
Dental specialists should make sure they chart their thought processes, conversations with patients, and treatments thoroughly so that they may defend themselves against claims of malpractice.
The lack of charting is not listed as a basis of the typical allegation of negligence against a dental specialist, but lack of adequate charting may be a factor in a lawsuit against the dental specialist. A plaintiff’s counsel may argue that if it wasn’t charted, it didn’t happen; or if it wasn’t charted, it wasn’t considered. The failure to chart essential aspects of the patient’s care may lead to difficulties in defending the dental specialists’ reasons for their decisions and treatment.
While all dental specialists know that a substantial part of their treatment of a patient is the “art of dentistry,” taking into account the patients they see, their knowledge, training, and expertise, it makes it easier to defend their actions when these considerations are included in the chart.
EP
51 endopracticeus.com Volume 15 Number 4
Dental specialists are unprepared for the havoc a lawsuit can cause in their practice. ...
Implications of the False Claims Act

Kerry Cahill, Esq., discusses how practitioners need to protect themselves even in altruistic circumstances

Altruism and the ability and competency to help others are replete in the dental profession. In most providers’ experience, patients who may not be able to afford their services have approached them. With inflation continuing to rise, many patients may not have the financial means to afford reconstructive or cosmetic dentistry, orthodontics, or endodontics. However, if a practice accepts federal funds such as Medicaid, FEDVIP, or the Enhanced Provider Relief Fund Payments, and the practitioner is considering offering discounted rates, be forewarned — these discounts have the potential to run afoul of the federal False Claims Act (FCA), 31 U.S.C. § 3729 et seq., and its equivalent statutory state counterparts.
The False Claims Act
Under the FCA, there are four primary provisions that practitioners should understand.
• First, it is unlawful to knowingly submit a false or fraudulent claim to the federal government for payment or approval, 31 U.S.C. § 3729(a).
• Second, it is unlawful to directly or indirectly make or use a false record or statement in support of a false or fraudulent claim, 31 U.S.C. § 3729(b).
• Third, it is unlawful to possess, have custody, or control of property or money used by the government, while delivering less than its full value, 31 U.S.C. § 3729(d).
• Fourth, conspiring to participate in any of the foregoing activities is also prohibited, 31 U.S.C. § 3729(c).
Although there is no statutory definition as to what constitutes a “false” claim, relevant case law provides that a claim is factually false “when the claimant misrepresents what goods or services that it provided to the Government,” (United States ex rel. Wilkins v. United Health, 659 F.3d 295, 305 [3d Cir. 2011]).
Indisputably, billing for services not provided, upcoding, and illegal kickbacks are unlawful and would warrant FCA claims. Conversely, providers may have the most altruistic intentions with respect to rendering clinical services and unknowingly subject themselves to a potential FCA claim. A provider who offers discounted rates or prepayment incentives to patients who he/she knows are uninsured or underinsured, or who are asset limited, income constrained, and employed (ALICE) may be problematic.
Kerry Cahill, Esq., is an attorney with Lindabury, McCormick, Estabrook & Cooper, P.C. (www.lindabury.com) based in Westfield, New Jersey. Her practice focuses on advising clients in the healthcare industry — including dentists, orthodontists, and endodontists. She can be reached at kcahill@lindabury.com.
As a matter of practicality, when a provider offers or accepts discounted rates or fails to universally balance bill and collect from his/her patients, the provider may have exposure under the FCA. For example, if a provider receives $250.00 per hour from Medicaid, is reimbursed on average $200.00 per hour after balance billing privately insured individuals, and charges his/her uninsured patients $150.00 per hour, there is an inherent question as to the true value of the provider’s services. Is the true value of the services $150.00 or $250.00? With niche orthodontic, endodontic, or implant practices, these payment discrepancies may be very large. As a result, this discrepancy in valuation often leads to costly protracted litigation, which can include a lengthy trial. At present, if found liable for an FCA violation, a civil penalty of between $5,500 and $11,000 is assessed per claim, plus 3 times the amount of damages which the government sustains because of the act, 31 U.S.C. § 3729(a)(1).
“Qui tam” cases are on the rise
Additionally, providers should note that it is not just the government that may institute suit. In addition to allowing the United States to pursue FCA violators, the FCA allows private citizens (called relators) to file suits on behalf of the U.S. government (called “qui tam” suits) against those who have defrauded the government. Private citizens who successfully bring qui tam actions may receive a portion of the government’s recovery, 31 U.S.C. §3730(d). If the government declines to pursue the claim, and the relator prevails, it is statutorily entitled to recover 25% to 30% of the damages, in addition to being reimbursed reasonable counsel fees. The significant reward in assertion of these claims is evidenced by the U.S. Department of Justice’s collection of more than $5.6 billion settlements and judgments for the fiscal year ending on September 30, 2021.*
52 Endodontic Practice US Volume 15 Number 4 LEGAL MATTERS
LEGAL MATTERS
Insurance coverage is questionable
Generally, practitioners can obtain Commercial General Liability (CGL), Employment Practices Liability (ELI/EPLI), malpractice, and umbrella policies to offset a large amount of risk associated with maintaining their practices. Also, practitioners may maintain a Directors and Officers (“D&O”) policy, in order to protect the personal assets or corporate directors and officers from liability resulting from their management decisions. However, be forewarned that FCA claims may be excluded from coverage under any potentially applicable insurance policies that the practitioner and practice may have. As a result, a practitioner without insurance coverage may have to pay any damages awarded against it.
Practice mitigation of liability

In spite of risk of potential FCA claims, there are a number of preemptive measures a practitioner can take to mitigate its risk. Ensuring that a practice is adequately structured is imperative. When forming a practice, practitioners should take into consideration the roles and responsibilities that they will directly and indirectly undertake — for example, whether they will be handling their own billing, contracting with a third-party billing service, or partnering with a Management Services Organization (MSO).
Additionally, having a well-defined Operating Agreement and up-to-date policies and procedures is integral. Together, these should delineate the responsibilities of the practitioners, their staff, and the patients with respect to handling billing
matters. For practitioners in a group practice, the Operating Agreement should address insurance and the apportionment of liability for potential FCA claims among the practitioners. Even if a practice relies upon a separate business entity such as an MSO, this may not insulate the practitioner’s liability. Under the FCA, if a provider has actual knowledge or is deliberately ignorant or recklessly disregards the truth or falsity of the information, it may face liability, 31 U.S.C. § 3729(b)(1). As a result, it is imperative to have contractual provisions with third-party billing agencies regarding the communication and status of billing practices, adequate levels of insurance, and indemnification provisions.
Next, diligent record keeping and records retention are of the utmost importance. This obligation extends to all records relating to the treatment of a patient. For some FCA claims, the issue in question is whether the services for which payment was requested or received from the federal government were actually rendered. By following best practices, practitioners can provide an affirmative defense that they relied upon universally accepted industry practices, which can help to mitigate damages.
Finally, conducting periodic audits and reviews of patient reimbursement rates is wise. Similar to the preceding, these audits and reviews help the practice to implement practical policies and procedures, which can be timely modified — if necessary.
EP 3 REASONS TO SUBSCRIBE • 16 CE credits available per year • 1 subscription, 2 formats – print and digital • 4 high-quality, clinically focused issues per year 3 SIMPLE WAYS TO SUBSCRIBE • Visit www.endopracticeus.com • Email subscriptions@medmarkmedia.com • Call 1-866-579-9496
Endodontic Practice US 1 year $149 / 1 year digital only $79

Summer2022 Vol15 No2
Fall2022 Vol15 No3
endopracticeus.com FAQSpecialSection n 4CECreditsAvailableinThisIssue effectiveStreamlining irrigation Dr.AllenAliNasseh
Buildingconfidenceand improvingrepeatabilityin yourendodonticpractice Dr.MarkAnthonyLimosani Corporateprofile EndoPracticePartners Practiceprofile MicroSurgicalEndodontics Companyspotlight CareCredit—FinancingSimplified
endopracticeus.com Implants n 4CECreditsAvailableinThisIssue Blueprintforthefuture NorthernColoradoEndodontics PROMOTING EXCELLENCE IN ENDODONTICS

53 endopracticeus.com Volume 15 Number 4
* Department of Justice. Office of Public Affairs. Justice News. Justice Department’s False Claims Act Settlements and Judgments Exceed $5.6 Billion in Fiscal Year 2021. https:// www.justice.gov/opa/pr/justice-department-s-false-claims-act-settlements-and-judgmentsexceed-56-billion-fiscal-year. Accessed June 24, 2022. Connect. Be Seen. Grow. Succeed. | www.medmarkmedia.com
Life sentence practice or lifestyle practice?
 Dr. Albert (Ace) Goerig describes the foundation to his
Dr. Albert (Ace) Goerig describes the foundation to his
Ispent my first 20 years practicing endodontics in the army, so I was a newbie to private practice endodontics in my mid-40s. I was 20 years behind my residency peers! However, within 10 years, I was far ahead of them. After talking with my contemporaries, I knew there had to be a better way than what they were describing:
• Meaningful growth had stalled, and my peers were frustrated.
• On average, they were completing only 3 or 4 cases a day.
• Most still had debt and financial stress, even after 20 years.
• Most felt seriously behind in preparing financially for retirement.
• Many felt worn-out or tired but avoided time off to be available for referrers.
• Many experienced daily stresses with team and practice management issues.
• They weren’t having fun and felt locked in by the profession.
In short, the overall impression I got was that most of my peers were feeling that their practice life should be easier and better by that point, and their personal life was stuck as a result. The practice was taking up too much time, and they didn’t have the flexibility in their economics to do anything about it.
Defining the lifestyle practice
The list above became my focused checklist of things to avoid when setting up and leading my practice. Therefore, the lifestyle practice is defined as having:
• Powerful, effective marketing systems to drive referral relationships and growth.
• The doctor only does what is medically necessary for the doctor to do.
Albert Goerig, DDS, MS, is a Diplomate of the American Board of Endodontics and a sought-after speaker who has lectured extensively on the field of endodontics and practice success throughout the United States, Canada, and abroad. He is the author of more than 100 published articles and contributing author to numerous endodontic textbooks. Dr. Goerig has a private endodontic practice in Olympia, Washington, in the top 1% nationwide for practice profitability. He has almost 40 years of experience as an endodontic educator and practice coach to over 1,000 endodontists. www.endomastery.com | 1-800-482-7563 | info@endomastery.com

philosophy and vision
• Complete at least two more cases per day than average with effortless team efficiency.
• Empowered and accountable office manager to deal with daily issues.
• 4 days/week at first, 3 days/week as productivity grows, plus 10 weeks off annually. (Time flexibility grows when you add another endodontist to your practice.)
• Practice profitability at least 2 times higher than average.
• Quick debt elimination and freedom from financial stress forever.
• Time and income to enjoy your family and your life together.
Achieving your lifestyle vision
The lifestyle model for endodontic practices is the foundation of our philosophy and vision at Endo Mastery. We want every endodontist to have the most amazing life, supported by the most amazing practice. It is what our coaching program is designed to do. In a year or two, you can close all the gaps that tell you things should be easier or better. In fact, we have clients in their early 30s who have done this already. They are living such an abundant life that every day inside and outside the practice is a dream.
It’s not about how old you are, or how many years in practice. It’s just about making the decision to optimize and grow the practice so that you get enjoyment back and get your life back. Stop feeling like your practice is a life sentence!
For more information, visit www.endomastery.com, or call 1-800-482-7563.
54 Endodontic Practice US Volume 15 Number 4 PRACTICE MANAGEMENT
EP
Thoughts on why we lose staff
Drs. Joel C. Small and Edwin McDonald discuss the rewards of appreciating your team


We are currently experiencing an unprecedented shortage of clinical and administrative staff for healthcare practices. Without question, the loss of qualified staff has had a financial impact on doctors and their teams. Many studies have validated the negative financial impact of staff turnover for dental practices. We have personally seen studies indicating that the loss of a valuable staff person can create actual losses of production in the tens of thousands of dollars.
Many of our client doctors have expressed dismay and negative emotions over losing valuable staff. These are the recurring refrains that we are hearing from many clients.

• “Why did my staff leave for an opportunity that paid a few dollars more?”
• “What could I have done differently to maintain my staff?”
• “I thought I treated my staff well, and they left anyway.”
The loss of staff is becoming a personal and highly emotional issue for doctors as they search for answers.
Little has been written regarding the negative emotional impact that staff shortages have created for doctors and their teams; and although this topic has received little attention, it has serious implications. Many clinicians and their teams are currently having to compensate for staff shortages by working longer hours and enduring more stress as they struggle to maintain production with fewer staff. Consequently, we are hearing increased reports of staff and doctor burnout as the hours and workload increase with no end in sight.
The easiest and most psychologically safe justification for staff loss is to assume that staff leaves for higher pay. We can rationalize a staff exodus by claiming that employees today have no loyalty and are financially driven. They will simply offer their services to the highest bidder. Our experience, however, would indicate that this is a false narrative.
What we are observing is that staff who feel listened to and are encouraged by their doctor to offer unfiltered feedback regarding their working environment with no fear of repercus-
Drs. Joel C. Small and Edwin (Mac) McDonald have a total of over 75 years of dental practice experience. Both doctors are trained and certified Executive Leadership Coaches. They have joined forces to create Line of Sight Coaching, a business dedicated to helping their fellow dentists discover a better and more enjoyable way to create and lead a highly productive clinical dental practice. Through their work, clients experience a better work/life balance, find more joy in their work, and develop a strong practice culture and brand that positively impact their bottom line. To receive their free ebook, 7 Surprising Steps to Grow Your Practice Through Leadership, go to www.lineofsightcoaching.com.
sions are less likely to leave their current job for one that offers a few dollars more in compensation. Simply put, if a person feels powerless and unable to offer input regarding negative aspects of their work environment, he/she will be more likely to leave regardless of their level of compensation.
The loss of highly motivated and skilled staff can have a devastating effect on a practice’s culture, especially if those departing are seen as team leaders, and those who remain are there just to collect their paycheck and have no interest in a transformational culture or being part of a peak-performing team.
Working in our offices is our staff’s choice. How we communicate with our staff during times of increased workload and stress is our choice and will likely determine whether our staff chooses to stay or seek employment elsewhere.
During periods of staff shortage, we must be sensitive to the increased demand and stress our staff is experiencing. In order to avoid any further crippling loss of staff, we at Line of Sight Coaching are suggesting that doctors spend more time checking in with their teams by listening more and providing much needed support during these stressful times. Just the simple fact that we show appreciation and concern for their well-being sends a powerful and positive message to our staff.
Another worthwhile suggestion is to schedule more frequent staff meetings during periods of stress to allow the staff to collaborate about ways to reduce stress and lighten the workload in the office. We are often surprised at how resourceful and creative our teams can be when given the opportunity to solve problems, and as a general rule, staff is more motivated to implement solution-oriented plans when they have had input into the solution.
55 endopracticeus.com Volume 15 Number 4 SMALL TALK
EP
Dr. Jason Putnam: owning his future
After more than 15 years of running a successful solo practice in idyllic Bluffton, South Carolina, Dr. Jason Putnam began to feel isolated and burned-out. He knew he needed more — a new goal, mission, or direction in his professional career.
“I was finding myself not enjoying practicing as much as I had in the past, and it was really weighing on me,” Dr. Putnam said.
His practice, Coastal Carolina Endodontics, is situated just 15 minutes from iconic Hilton Head Island. Known primarily as a vacation and retirement spot, Bluffton proved the perfect place for Dr. Putnam and his wife, Casey, who serves as Practice Manager, to put down roots and raise their two sons.

“My family is number one and always has been, but what we do for patients in this community is a close number two for me,” he said. Dr. Putnam wanted to continue to serve his neighbors but was struggling with the idea of continuing his career as a clinician for much longer.
“Burnout is a real thing in endo,” Dr. Putnam said. “It happens to all of us because it is a difficult and technical procedure.”
He and Casey were advised by a colleague from his residency at the University of Iowa to look at US Endo Partners, a specialty dental service organization, as a potential catalyst for change.
“I hadn’t heard of US Endo, but it sounded like something that would give us options and possibly rejuvenate us a little bit,” he said. “I was really interested in experiencing camaraderie with other doctors, exchanging ideas, and finding new motivations for myself and my team.”
Dr. Putnam partnered with US Endo in August 2021 and then attended his first Vision Summit, the annual Partners’ meeting, that October in Dallas, Texas. He expected to establish positive relationships with his new business partners but didn’t expect to be inspired by the gathering.

“It was the most profound experience of my career. I left the Summit bursting with motivation and new ideas that I could not
wait to share with my team,” Dr. Putnam said. “I knew something big was about to happen. I didn’t really have a specific goal. I just knew we were going to take a huge step toward our true potential.”
Dr. Putnam called a team meeting upon arrival back in South Carolina and was blown away by his team’s interest in improving efficiencies to increase access to care and to get more patients out of pain each day. It didn’t take long to see a significant impact.
Within a two-month time span — and without working more hours — Dr. Putnam and his team were able to increase the number of patients they could help each day by 50% over the previous year. In the third month after the Summit, Dr. Putnam and his team had dialed in their new motivations and efficiencies resulting in a staggering 103% improvement — more than doubling the number of patients they were able to help. And those numbers continue to soar 1 year later.
“US Endo completely and utterly changed my life. It was an awakening — a resurrection of my career and passion for this specialty,” Dr. Putnam said. “My team and I are absolutely jamming! We are helping twice as many patients each day, and we’ve never been so motivated and happy. We’re having fun again.”
This information was provided by US Endo Partners.

56 Endodontic Practice US Volume 15 Number 4 PRACTICE SPOTLIGHT
EP
US Endo Partners has completely and utterly changed my life. It has been an awakening — a resurrection of my career and passion for this specialty.”
— Jason Putnam, DMD, Coastal Carolina Endodontics
Dr. Jason Putnam serving his neighbors in Bluffton, South Carolina
Dr. Jason Putnam telling his inspiring story at the US Endo Partners 2022 Vision Summit
Scan to watch Jason and Casey tell their story
Reclaim
Spark.
Successful solo practitioner Dr. Jason Putnam was struggling with burnout and isolation when he joined US Endo. He found the camaraderie he was craving, and the spark he needed to dig deeper and to rekindle his passion for the specialty. When you share ideas and foster a positive mindset, growth quickly follows.



possible
life-changing” The Endo Files™ Podcast Deep dives and unexpected conversations with the top names in Endo. Scan to listen!
Partner and believer since 2021
“Recognizing within ourselves what is
is
– Jason Putnam, DMD, Coastal Carolina Endodontics, Bluffton, SC
your The Spirit of US



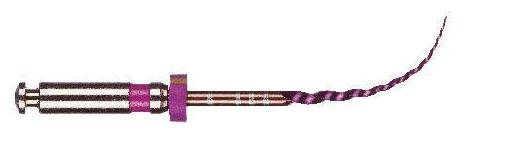


avalonbiomed.com ENDO YOUR WAY S This distinctive multi-alloy system provides superior durability, efficiency and flexibility. RYAN WALSH, DDS, MS Co-Owner Advanced Endodontics of Texas Keller, TX ™ SCAN FOR A FREE SAMPLE















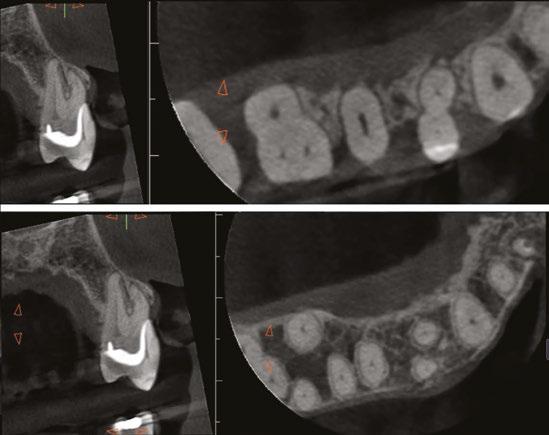

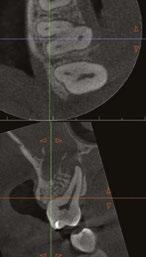

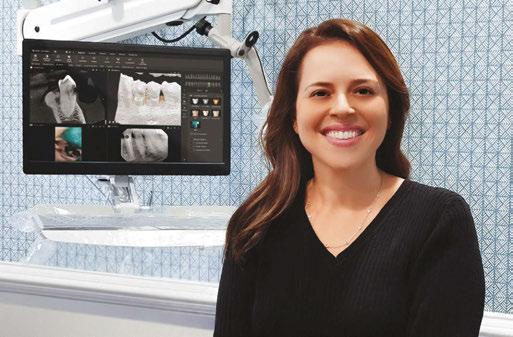
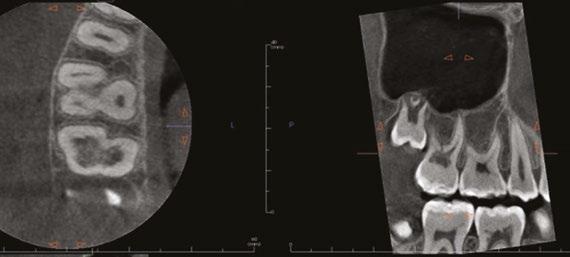


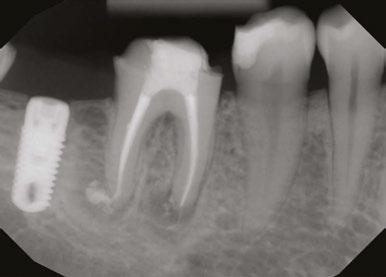

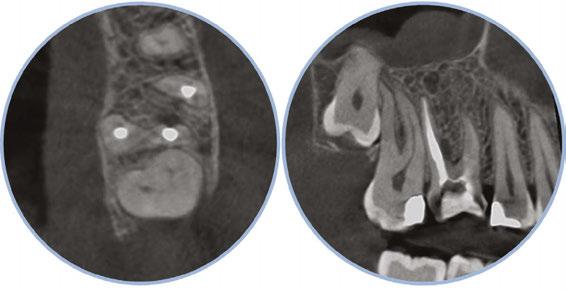
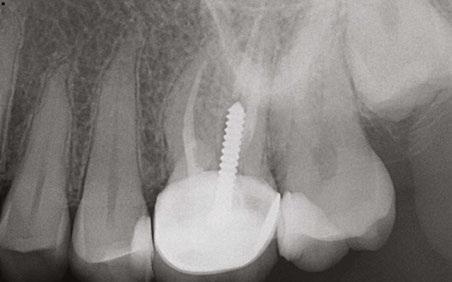

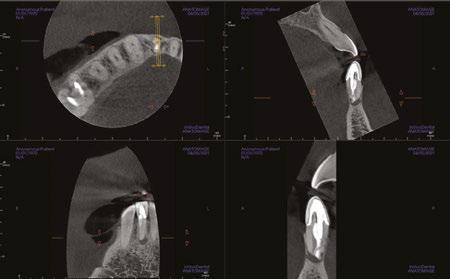
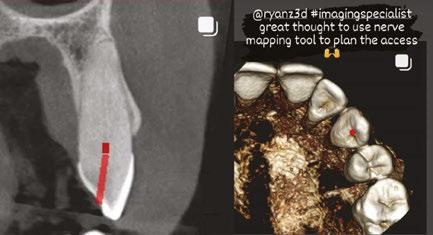
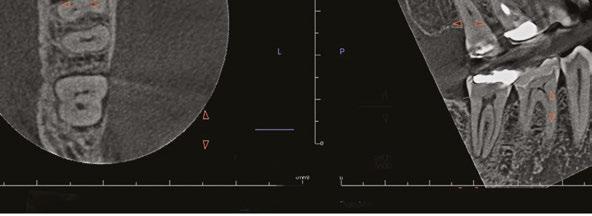



















 Lorem ipsum
Lorem ipsum
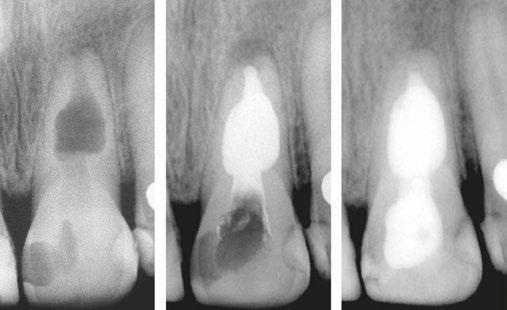





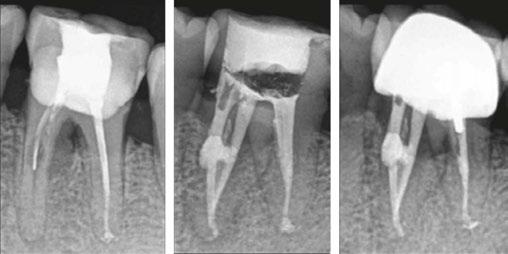



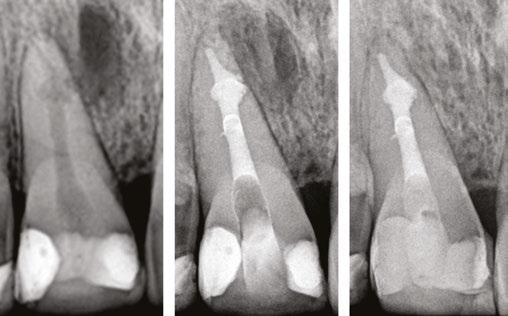





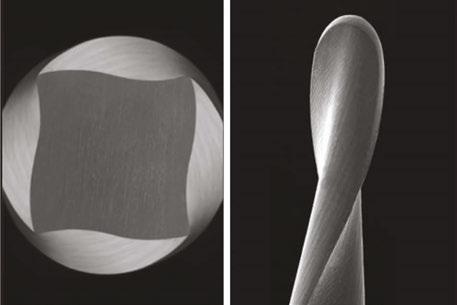
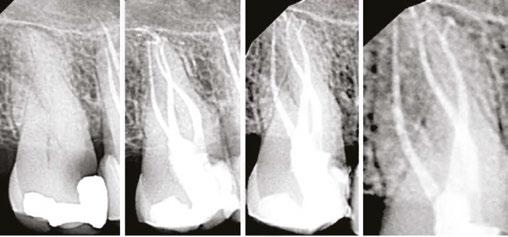

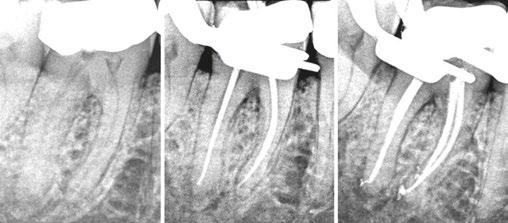


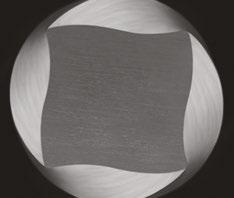

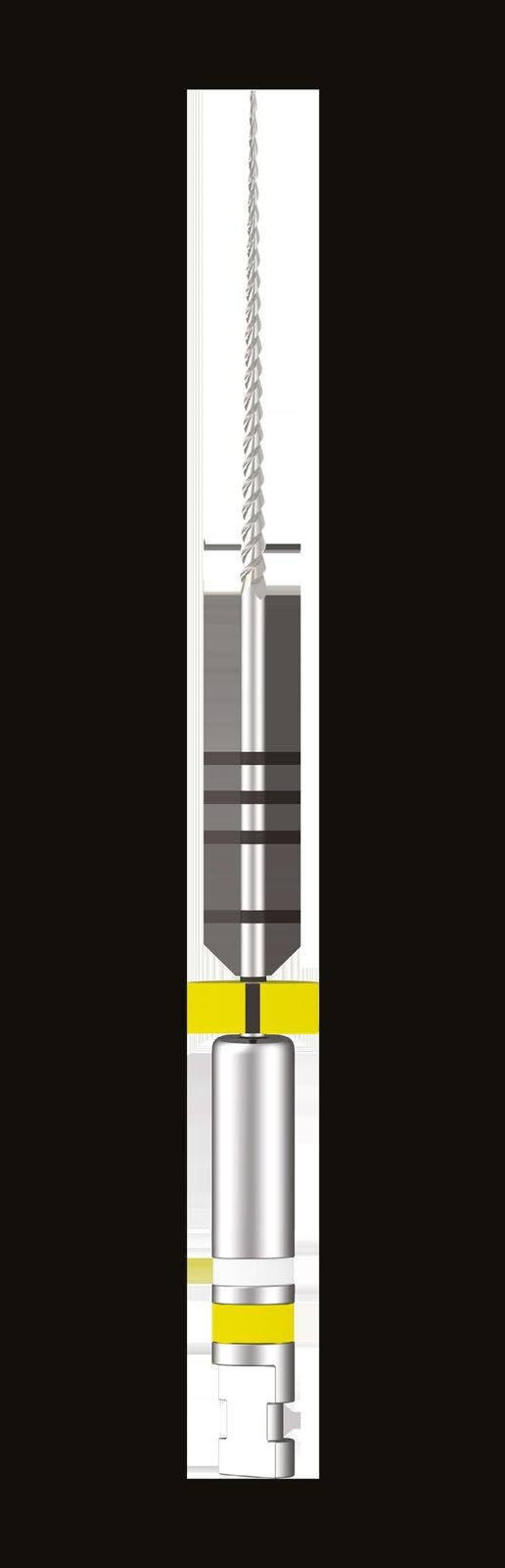








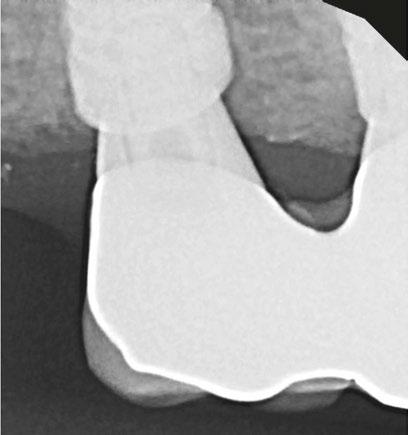

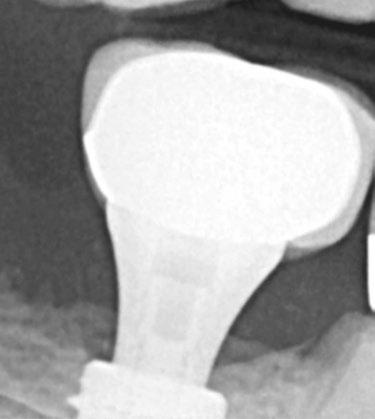


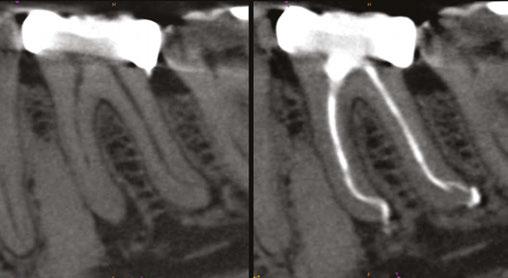


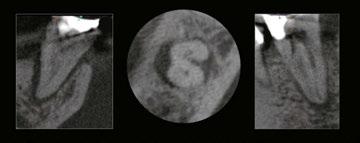
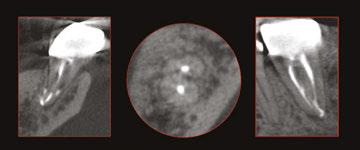
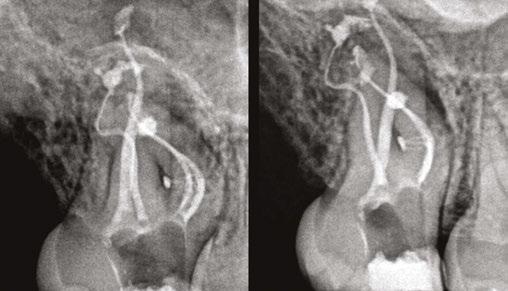
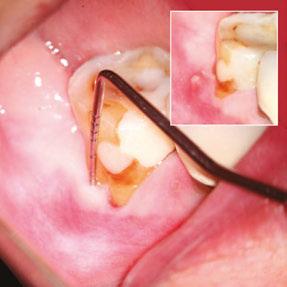
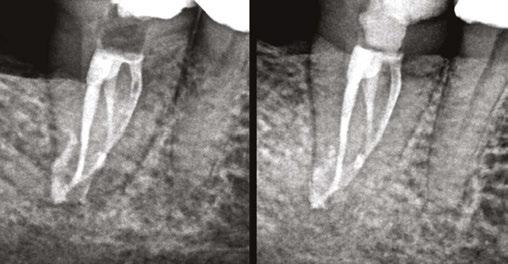


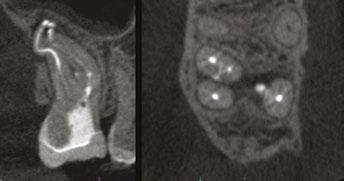

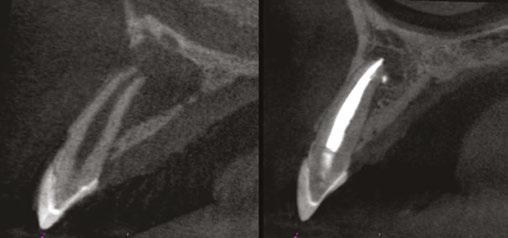
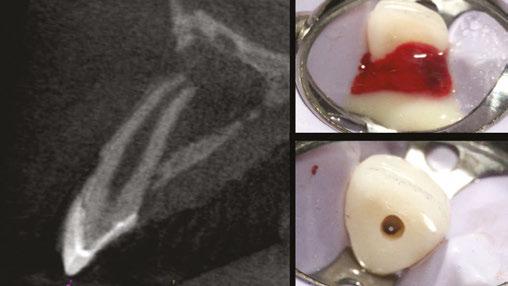

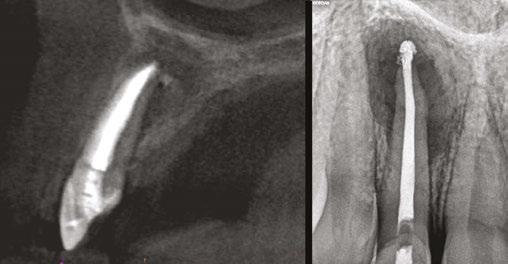







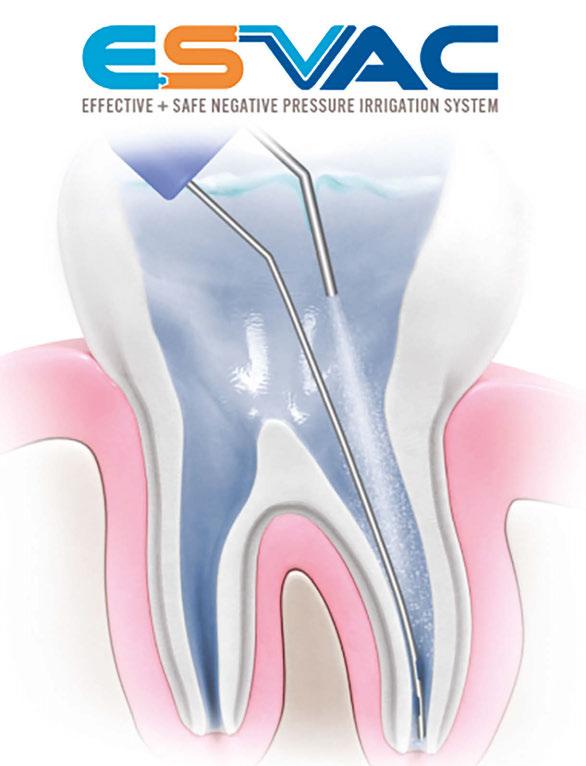
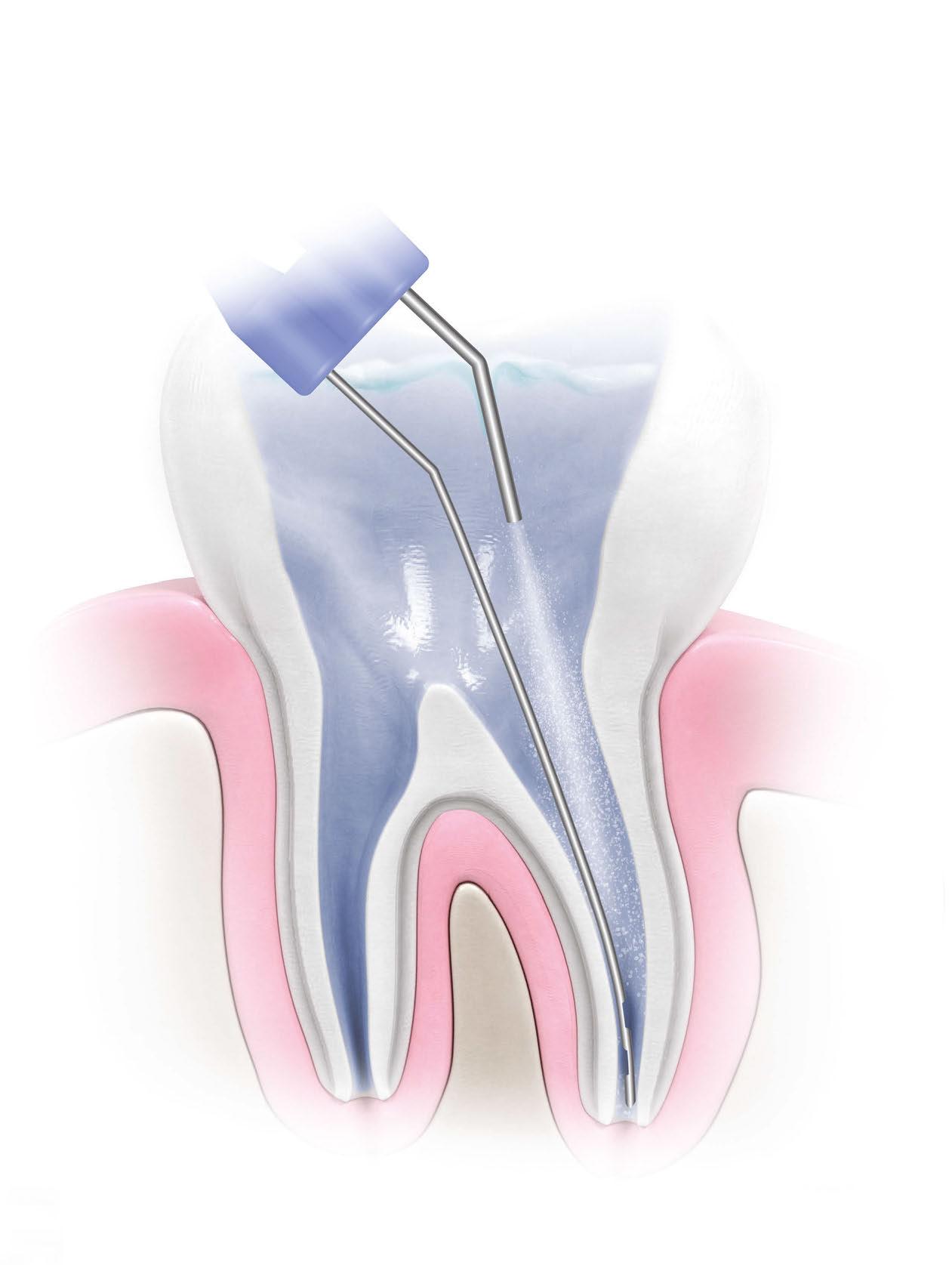

 Kristin Tauras, JD, guides dental specialists through the legal elements
Kristin Tauras, JD, guides dental specialists through the legal elements





 Dr. Albert (Ace) Goerig describes the foundation to his
Dr. Albert (Ace) Goerig describes the foundation to his