Restoratively driven endodontic access and instrumentation
Dr. Gregori M. Kurtzman
Building a team of rock stars
Dr. Garth Hatch
Root canal shaping in the age of minimally invasive endodontics

Drs. L. Stephen Buchanan and Christophe Verbanck
A technological innovation that has made
Dr. Josh Todd

PROMOTING EXCELLENCE IN ENDODONTICS
Spring 2023 Vol 16 No 1 endopracticeus.com AAE Special Section n 4 CE Credits Available in This Issue*
the difference



Spring 2023 n Volume 16 Number 1
Editorial Advisors
Dennis G. Brave, DDS
David C. Brown, BDS, MDS, MSD
L. Stephen Buchanan, DDS, FICD, FACD
Gary B. Carr, DDS
Arnaldo Castellucci, MD, DDS
Gordon J. Christensen, DDS, MSD, PhD
Stephen Cohen, MS, DDS, FACD, FICD
Samuel O. Dorn, DDS
Josef Dovgan, DDS, MS
Luiz R. Fava, DDS
Robert Fleisher, DMD
Marcela Fridland, DDS
Gerald N. Glickman, DDS, MS
Jeffrey W Hutter, DMD, MEd
Syngcuk Kim, DDS, PhD
Kenneth A. Koch, DMD
Gregori M. Kurtzman, DDS, MAGD, FPFA, FACD, DICOI
Joshua Moshonov, DMD
Richard Mounce, DDS
Yosef Nahmias, DDS, MS
David L. Pitts, DDS, MDSD
Louis E. Rossman, DMD
Stephen F. Schwartz, DDS, MS
Ken Serota, DDS, MMSc
E Steve Senia, DDS, MS, BS
Michael Tagger, DMD, MS
Martin Trope, BDS, DMD
Peter Velvart, DMD
Rick Walton, DMD, MS
John West, DDS, MSD
CE Quality Assurance Board
Bradford N. Edgren, DDS, MS, FACD Fred Stewart Feld, DMD

Gregori M. Kurtzman, DDS, MAGD, FPFA, FACD, FADI, DICOI, DADIA
Justin D. Moody, DDS, DABOI, DICOI

Lisa Moler (Publisher)
Mali Schantz-Feld, MA, CDE (Managing Editor)
Lou Shuman, DMD, CAGS
Navigating innovation
When it comes to innovation, consider the following statement associated with Henry Ford’s development of the Ford Model T: “If I had asked people what they wanted, they would have said faster horses.” At the time, people didn’t realize that a motor vehicle was even in the realm of possibility. This concept can be applied to almost every industry, including endodontics. Thinking creatively and maintaining a forward-looking mindset is critical to progress.
There’s more to innovation than launching a new product. Without adoption and utilization, a new technological offering is futile. Awareness and understanding are two key components. In endodontics, it’s common for clinicians to be unaware of a brand new technology. Also, a clinician may be aware of a new product, but lack a proper understanding of how it works and its potential impact on procedural and clinical outcomes.
Here are four products that have had positive impact:
• Cone-beam computed tomography (CBCT): CBCT allows clinicians to gain a deeper understanding of their patient’s tooth and the surrounding structures. This allows for doctors to unveil the possibility of cracks, fractures, and resorption, which eliminates guesswork significantly and limits the need to surgically explore a tooth.
• Microscope: The microscope truly revolutionized the way clinicians operate. Endodontics has transitioned from a largely tactile specialty to heavily relying on the enhanced visual cues that provide unparalleled precision. The microscope increases predictability and allows clinicians to visually map out the floor of the chamber while minimizing the sacrifice of healthy tooth structure. With it, we can better prepare for and address any areas that could cause heightened discomfort for patients, while also improving procedural predictability by more thoroughly addressing the internal anatomy.
• Heat-treated rotary instruments: Prior to rotary instruments being heattreated, clinicians were forced to create an access into the chamber and the mid/apical third of the canals to accommodate these more rigid instruments and mitigate the liability of their separation. Now, flexible and pre-bent instruments allow us to cut smaller and manage cases with more limited access.
• GentleWave® System: The GentleWave System is an innovative technology platform designed to treat the infected or inflamed dental pulp by cleaning and disinfecting the microscopic spaces within teeth for greater dentin preservation. It enables thorough treatment with less collateral damage.
With all new technology comes unfamiliarity. While it can be intimidating to change a long-standing way of thinking or process, discomfort can represent great opportunity. When researching a new technology, I always consider how it could positively impact my practice and my patients, rather than focusing on the learning curve.
I encourage endodontists to think about our profession through the lens of possibility. Make time to learn about disruptive product offerings that are available today, and then push yourself to move past the discomfort to obtain better outcomes for yourself and your patients.
© MedMark, LLC 2023. All rights reserved. The publisher’s written consent must be obtained before any part of this publication may be reproduced in any form whatsoever, including photocopies and information retrieval systems. While every care has been taken in the preparation of this magazine, the publisher cannot be held responsible for the accuracy of the information printed herein, or in any consequence arising from it. The views expressed herein are those of the author(s) and not necessarily the opinion of either Endodontic Practice US or the publisher.
ISSN number 2372-6245
Mark Anthony Limosani, DMD, received his dental degree from the University of Montreal in 2007. Since then, he completed a 1-year multi-disciplinary residency at the Queen Elizabeth Oral Health Center, a McGill University affiliated program. Following 1 year of private practice and many hours of continuing education, he then followed his dream and attended the specialty program in endodontics at Nova Southeastern University where he also received his Master’s degree in Dental Science. He is an international speaker and the recipient of the “Robert A. Uchin Endodontic Award” for his presentation during Nova’s endodontic alumni day. He is a past president of the South Broward Dental Society as well as the South Florida District Dental Association and currently serves as a Trustee to the Florida Dental Association.
1 endopracticeus.com Volume 16 Number 1 INTRODUCTION

2 Endodontic Practice US Volume 16 Number 1 TABLE OF CONTENTS ENDOSPECTIVE The ultimate look Dr. John D. West looks at the new ProTaper Ultimate and says, “It’s not one thing, it’s everything” PUBLISHER’S PERSPECTIVE Reflections from a grateful GOAL-getter Lisa Moler, Founder/CEO, MedMark Media............................... 6 TECHNOLOGY Root canal shaping in the age of minimally invasive endodontics Drs. L. Stephen Buchanan and Christophe Verbanck discuss the benefits of files with conservative tapers ............................................... 20 AAE SPECIAL SECTION Endo Mastery ................... 26 Endodontic Practice Partners ..................................... 27 Endodontic SuperSystems .................... 28 Endo1 Partners/ Specialty1 Partners ..... 29 HighFive Healthcare... 30 Produits Dentaires SA IrriFlex .......................................... 31 Quintessence Publishing 32 Seiler ............................................. 33 Sonendo GentleWave 34 US Endo Partners 35 ZEISS ............................................. 36 8 12
STORY A technological innovation that has made the difference
Josh Todd has a conversation about his commitment to changing perceptions about root canal treatment and how the GentleWave® System helps him achieve that goal
COVER
Dr.
Cover image of Dr. Josh Todd courtesy of Sonendo®.



Imagine your practice growing strongly and more profitable than ever. Enjoy productive stress-free scheduling driven by incredible teamwork and efficiency. Improve referrals and patient flow with powerful strategies for engaging GP relationships. In one year, the Endo Mastery team can help you transform your practice and transform your life. Pay off debt fast, eradicate financial stress, empower personal and family goals, and love your practice like never before. Learn more about Endo Mastery’s coaching programs and why our clients love us. 1-800-482-7563 info@endomastery.com VISIT US AT AAE23-CHICAGO BOOTH #239! VIEW OUR SHOW SPECIALS AND DR. ACE GOERIG’S SPEAKING SCHEDULE THISYour MAKE BEST YEAR! endomastery.com/offers






4 Endodontic Practice US Volume 16 Number 1 TABLE OF CONTENTS CONTINUING EDUCATION The importance of maintaining indoor air quality in dentistry Drs. Tyler Orehek and Troy Roeder discuss the reasons for maintaining diligent air quality standards in the office ............... 43 PRACTICE MANAGEMENT Sailing into practice ownership Dr. Albert (Ace) Goerig discusses several ways to navigate practice ownership .................................... 48 PRACTICE DEVELOPMENT Building a team of Rock Stars Dr. Garth Hatch covers essential elements for a practice that runs in perfect harmony ...................... 50 PRODUCT SPOTLIGHT Boyd Industries 52 SMALL TALK People growth precedes practice growth Drs. Joel C. Small and Edwin McDonald discuss the beliefs behind a growth mindset ........ 54 MILITARY MATTERS A commemoration of oral health services to soldiers Dr. Francis Nasser, Jr. discusses the important role of military dentists and a special way to recognize their contribution .... 55 SERVICE PROFILE A strategy for growth A conversation with Dr. Scott Doyle, Metropolitan Endodontics ......................................................... 56 Connect. Be Seen. Grow. Succeed. | www.medmarkmedia.com READ the latest industry news and business WATCH DocTalk Dental video interviews with KOLs LEARN through live and archived webinars RECEIVE news and event updates in your inbox by registering for our eNewsletter CONNECT with us on social media www.endopracticeus.com *Paid subscribers can earn 4 continuing education credits per issue by passing the 2 CE article quizzes online at https://endopracticeus.com/category/continuing-education/ 37 CONTINUING EDUCATION Restoratively driven endodontic access and instrumentation Dr. Gregori M. Kurtzman discusses preserving sound tooth structure and gaining endodontic access





To learn more about TotalVac, visit BrasselerUSADental.com/Discover-TotalVac B-5699-EP-04.23 ©2023 Brasseler USA. All rights reserved. Visit our website at BrasselerUSADental.com To order call 800.841.4522 or fax 888.610.1937. diameters to suit your specific needs Retail: $200.00 Special: $163.00 Kit includes: 25 high volume evacuation and surgical suction adaptors, 25 TotalVac tubings, 25 plastic suction tips, 25 25ga short delivery tips, and 25 30ga side vented long delivery tips *While supplies last. Offer subject to change. Promotion expires June 30, 2023. Invoice or statement prices may reflect or be subjected to a bundled discount or rebate pursuant to purchase offer, promotion, or discount program. You must fully and accurately report to Medicare, Medicaid, Tricare and/or any other federal or State program, upon request by such program, the discounted price(s) or net price(s) for each invoiced item, after giving effect to any applicable discounts or rebates, which price(s) may differ from the extended prices set forth on your invoice. Accordingly, you should retain your invoice and all relevant information for your records. It is your responsibility to review any agreements or other documents, including offers or promotions, applicable to the invoiced products/prices to determine if your purchase(s) are subject to a bundled discount or rebate. Any such discounts must be calculated pursuant to the terms of the applicable purchase offer, promotion, or discount program. Participation in a promotional discount program is only permissible in accordance with discount program rules. By participation in such program, you agree that, to your knowledge, your practice complies with the discount program requirements.
Reflections from a grateful GOAL-getter
In my columns, I have always shared my thoughts on professional and personal success. I’ve shared MedMark Media’s triumphs, and in recent years searched with you for solutions to some very tough challenges. As always, I am so proud of MedMark Media’s publications and the team that has been the center of my life for so many years. With this column, I am thrilled to announce some amazing news. I just got back from Dallas where I won a 2023 Denobi Award! This prestigious honor is incredibly humbling and inspiring. The Denobi Awards recognize leaders in the dental industry worldwide — including, as the Denobi website notes, “clinicians, educators, brand leaders, students, administrative personnel, sales, advocates, speakers, and leading experts.” From the nominations, finalists include 10 individual winners, one dental team, and one individual that receives the esteemed Dr. Lou Shuman Denobi Pinnacle Achievement Award. Right now, I think back to the years when I ran MedMark out of my tiny condo. Step by step the company has grown into publishing of five magazines, many digital platforms, podcasts, webinars, and opportunities. Some have described me as a “go-getter,” but I like to define myself as a “goal-getter.”
Speaking of setting and reaching new goals, you all know that specialty dentistry is our focus and our passion. So some more good news is the debut this spring of our newest national publication, Pediatric Dental Practice US. Articles will focus on oral health from infancy through teens and offer pediatric dentists new insights on helping young patients. As we strive to inform and improve the practices of endodontists, implant specialists, orthodontists, and dental sleep medicine professionals, reaching clinicians who care for the youngest patients seems like a perfect fit into our coverage of dental care that spans a lifetime.
In the cover story of this issue of Endodontic Practice US, Dr. Josh Todd relates some common challenges to the endodontic practice when treating individual patients’ unique anatomies. He has found that his patients experience less pain, and he achieves more thorough cleaning when using the GentleWave system. In his CE, “Restoratively driven endodontic access and instrumentation,” Dr. Gregori Kurtzman reviews tooth anatomy and canal orifices so that readers can better preserve tooth structure when locating and accessing canals. Pass the quiz and receive 2 CE credits! Our AAE Special Section shines a spotlight on innovations to help the endodontic practice become more efficient and effective in terms of fulfilling partnerships, irrigation, instrumentation, and coaching for endodontic success.
I struggled over whether to announce winning the Denobi Award in my column. That humble voice in my head didn’t want to seem boastful. But, I know that my team, friends, readers, and advertisers would want to share in my excitement of this recognition. This is not just about me. I always try to encourage you all to take some chances, believe in yourself, and as inspirational author Norman Vincent Peale advises have a “humble but reasonable confidence in your own powers.” I also try to emphasize my philosophy of “know your worth.” It sure is a fantastic feeling when others realize your worth too.
To your best success,
Lisa Moler Founder/Publisher MedMark Media
Published by
Publisher
Lisa Moler lmoler@medmarkmedia.com
Managing Editor Mali Schantz-Feld, MA, CDE mali@medmarkmedia.com
Tel: (727) 515-5118
Assistant Editor Elizabeth Romanek betty@medmarkmedia.com
National Account Manager Adrienne Good agood@medmarkmedia.com
Tel: (623) 340-4373
Sales Assistant & Client Services
Melissa Minnick melissa@medmarkmedia.com
Creative Director/Production Manager

Amanda Culver amanda@medmarkmedia.com
Marketing & Digital Strategy
Amzi Koury amzi@medmarkmedia.com
eMedia Coordinator
Michelle Britzius emedia@medmarkmedia.com
Social Media Manager
April Gutierrez socialmedia@medmarkmedia.com

Digital Marketing Assistant Hana Kahn support@medmarkmedia.com
Website Support
Eileen Kane webmaster@medmarkmedia.com
MedMark, LLC
15720 N. Greenway-Hayden Loop #9 Scottsdale, AZ 85260
Tel: (480) 621-8955
Toll-free: (866) 579-9496
www.medmarkmedia.com
www.endopracticeus.com
Subscription Rate 1 year (4 issues) $149
https://endopracticeus.com/subscribe/
6 Endodontic Practice US Volume 16 Number 1 PUBLISHER’S PERSPECTIVE
Lisa Moler Founder/Publisher, MedMark Media
Most endodontists have to master multitasking. Ours just have to master root canals.

Do what you do best and we’ll handle the rest. We aren’t your typical DSO. When you partner with HighFive Healthcare, you join an exclusive network of top endodontists dedicated to exceptional patient care. Our doctor-owned practices and seasoned team of experts nurture a fun and collaborative culture like no other. While we optimize and scale the business side of endodontics, clinical autonomy is left in your skilled hands. Together, we’ll help you take ownership of something bigger than a single practice and support you as you create your own tomorrow.
Learn more at high5health.com
RECRUITING | SCHEDULING OPTIMIZATION | SCALABILITY | BRANDING & MARKETING | PAYROLL | IT SERVICES | AND MORE
A technological innovation that has made the difference
Dr. Josh Todd has a conversation about his commitment to changing perceptions about root canal treatment and how the GentleWave® System helps him achieve that goal


Why did you choose to enter the field of endodontics?
I received a scholarship through the Army to attend dental school at the University of Louisville in Kentucky, where I
Josh Todd, DMD, is a dual board-certified general dentist and endodontist. He received his undergraduate degree from Auburn University and went on to earn his DMD at the University of Louisville School of Dentistry. From there he took his commission as an officer in the Army, where he completed two advanced residency programs in general dentistry and endodontics. He practiced general dentistry for 7 years before returning to pursue his endodontic training. He served as the Chief Dental Officer from 2010 to 2013 in Hohenfels, Germany and was the lead endodontic mentor at the Advanced Dental Education program at Fort Campbell, Kentucky from 2017 to 2020. He opened Elite Endodontics in Pensacola, Florida in August 2020.
Disclosure: The author declares that there are no conflicts of interest in connection with this article.
received a great education with valuable access and exposure to highly trained specialists. After dental school, I attended an advanced dental education residency at Fort Bragg, North Carolina, where I worked with professionals in endodontics, oral surgery, periodontics, and pediatric dentistry. My endodontic mentor, COL Lindsay, encouraged me to seriously consider the specialty. At the time, I was against this idea because I really enjoyed general dentistry. But, after several years of practicing, and as her words continued to echo in my ear, I spoke with my wife — who is also a general dentist — and decided to apply for an endodontic residency program through the Army. I was accepted into the program at Fort Gordon, Georgia, and my endodontic mentor was the director of residency. It all came full circle.
What inspired you to open your own practice?
I was in the Army for 12 years, and we were moving every 2-to-3 years to a different base. My wife and I wanted our chil-
8 Endodontic Practice US Volume 16 Number 1 COVER STORY
Case 1: This case was a 54-year-old male that the general dentist had initiated root canal therapy on tooth No. 31. During the procedure, a large file was separated in the mesial buccal canal. The patient was still in pain and was seen in one of our emergency appointments. The CBCT reveals that not only was the file separated around the curvature in the root, but the IAN was in direct contact with the apex of tooth No. 31. From the CBCT, the ML/MB joined so the plan was to negotiate the ML canal to length, and then, run GentleWave to allow for cleaning of the very complex anatomy that was present. I did minimal instrumentation in this case due to the other canals already having been prepared by the general dentist. I ran the GentleWave through the entire cycle without any issues; the patient was comfortable the entire time. Upon injection of sealer in the ML canal, I could see it start to come up in the MB canal revealing that it had cleaned around the file. The final obturation reveals that nothing was extruded into the IAN canal. The patient was pain free the next day when we called him


dren to grow up around family members living in Pensacola, Florida. As I was conducting research and sending out feelers to inquire about who was hiring in the area, I was surprised to learn that no one was. It became clear that this location was underserved by endodontists. My wife was the one who really encouraged me to open our own practice.
So, we started an endodontic practice in a town where we knew almost nobody in August 2020, shortly after the COVID-19 shutdown. Due to the restrictions placed on me by the Army during the pandemic, I was not allowed to travel outside of Tennessee. So, ahead of opening day, my wife and our office manager were able to visit the local general dentists’ offices, make connections, and market the practice. We’re so grateful to have had referrals from day one. It’s been a wild ride — but it’s been a great success.
What are some common challenges that clinicians face when performing traditional root canal treatment?


There is rarely a straightforward root canal, with every tooth having unique curves and delicate nuances within the anatomy. Working in Florida, I have grown accustomed to treating an older patient population. These cases are not often easy, with hidden canals, highly complex anatomies, and more.
Treating calcified root canals is one of the most common challenges I face. As a clinician, when I’m fighting a calcified canal, I sometimes feel like I am spending too much time, effort, and energy trying to get down to hard-to-reach places. When this happens, my biggest concern is my patients, who are sitting in the chair and feeling the amount of time I’m spending on them. This can be very stressful.
While files have significantly improved over the years, they still have physical limitations that prevent them from negotiating certain aspects of the root canal anatomy (lateral canals, accessory canals, isthmuses, etc.). It can also be challenging to get the appropriate amount of disinfecting solutions into those areas.
Long-time challenges like this are why it’s important for endodontists to consider new technology. At my practice, I use the GentleWave® System, which is redefining the standard of root

9 endopracticeus.com Volume 16 Number 1 COVER STORY
Dr. Todd discussing the patient’s treatment plan in his office, Elite Endodontics
canal treatment with a minimally invasive process that preserves tooth structure and promotes early healing. With it, I’m able to better disinfect those hard-to-reach places. And I have the confidence of knowing the additional anatomy that files can’t reach is cleaned and disinfected by the fluids in the GentleWave System.
Can you describe patient sentiment surrounding traditional root canal treatment?
Root canal treatment is what everyone compares to the most horrible things they can think of — “At least it’s not a root canal!” It’s no surprise that the overwhelming connotation behind root canals is negative. In my opinion, much of this stems from the history of root canal therapy, which was not always as effective or seamless as it is today.
My patients have told me time and time again that the GentleWave® Procedure is less painful and easier than traditional therapy. Patients who have received traditional treatment in the past can, hopefully, relax a bit more when undergoing a GentleWave Procedure and allow me to treat them without being overburdened with fear and anxiety. Some patients even like the noise that the machine makes, and several have compared it to a calming sound machine!
When and how did you learn about the GentleWave® Procedure?

In 2019, a friend of mine invited me to the TDO Software meeting (now known as EndoCon). I attended a continuing education (CE) event about the GentleWave Procedure while I was there. During the presentation I thought to myself, “I have never had a root canal look like that, ever.” In my head, I knew that was what I wanted to be able to offer my patients when I started my own practice because I recognized it was a higher level of cleaning and disinfection, and therefore, the best treatment available. I have used the GentleWave System since opening day.
When adopting new technology, clinicians will always have to unlearn some of their traditional instrumentation techniques.
This was challenging — especially as I was opening a new practice and training staff all at the same time. To make this learning curve easier, I followed the advice of my GentleWave trainer and trusted the technology to do what it says it does. I adhered to necessary protocols and encouraged myself to forge ahead. With this, it didn’t take more than a few short weeks to get fully up to speed on the GentleWave System. I was committed to it — and it more than paid off. I have also spent a lot of time discussing clinical protocols with other GentleWave providers who have been using the technology longer than I have and have gained wisdom from their techniques.
How did the GentleWave® System help overcome some of the challenges you described earlier and others?
In addition to helping me navigate complex anatomies and calcified root canals, the GentleWave Procedure has limited the number of re-treat and multi-visit cases that I see. It does such a thorough job of cleaning, all without having to remove nearly as much tooth structure as with traditional therapy. By having the unique ability to find additional canals and reach complex areas, about 98 to 99% of my patients come in for one visit only. I love this, and so do my patients — their time is valuable. Additionally, several of my referring dentists have noticed, the GentleWave System allows me to be as minimally invasive as possible — all while keeping tooth structure intact. The GentleWave Procedure gives restorative dentists more tooth structure to work with after treatment, which benefits the patient and offers a better long-term prognosis for that tooth. Using the GentleWave System not only helps endodontists and patients, but it also helps other industry professionals.
How has integrating the GentleWave System helped you as a business owner?
Nearly everyone is relatively tech-savvy today, and patients notice that we have updated equipment and the latest technology

10 Endodontic Practice US Volume 16 Number 1 COVER STORY
At left, Dr. Todd explaining how the GentleWave G4 system is a modern way to treat root canal infections and promotes pain-free fast healing. Dr. Todd leverages the latest technology, including the GentleWave G4 system, to differentiate his practice
Case 2: This is a 23-year-old male that presented with a constant dull ache in his tooth. Tooth No. 30 tested necrotic with SAP. The CBCT did not reveal any odd anatomy and appeared to be fairly straight forward. After running GentleWave and drying the canals, I injected Endosequence BC Sealer into the ML canal. I could immediately see sealer filling in the MB and then in a mid-mesial canal. The mesial canals were obturated with single cones and the distal using thermomechanical compaction. This case was instrumented using Brasseler Endosequence CM files in the following sequence: 15/.04, 20/.04. The final shift shot radiograph captures the midmesial canal and the split into both the MB/ML


in our office. We differentiate our practice by using the GentleWave System, and we see patients coming in specifically because they know it’s what they want. More people are making informed choices about their healthcare and doing their own research about various procedures and techniques. When patients are looking for an endodontic practice in our area, they quickly realize that we’re the only one offering the GentleWave Procedure.
Sonendo, the developer of the GentleWave System, has made our marketing efforts as seamless and straightforward as possible. We have implemented Sonendo’s library of marketing materials, joined a community of GentleWave users, and more. The GentleWave Portal consists of various digital resources, including brochures, that are easy to customize with our practice name and logo, which makes marketing very easy.
Additionally, as practice owners, we have many pieces of equipment that must be maintained, serviced, or repaired on a regular basis, and the staff is tasked with keeping track of it all. The GentleWave System removes the administrative work, telling us when it’s ready for maintenance and outlining the necessary steps. It then sends this data to Sonendo, so our team doesn’t have to keep any records on hand. While having one less thing to worry about from a maintenance standpoint may seem small, it makes our lives as business owners much easier.
There is clear evidence showing that the GentleWave Procedure provides excellent clinical results. But, what’s exceptional about Sonendo is the amount of support it shows its customers.
They have fostered a community of like-minded professionals who support one another. They are also always offering a wide variety of educational content to help us become better clinicians and business owners. The company is unparalleled in this way.
In your opinion, why do some clinicians remain hesitant to adopt innovative technology like the GentleWave System? What is your advice?
It’s almost always uncomfortable to learn something new. We’re creatures of habit, and clinicians tend to develop their own treatment protocols. However, to fully embrace the future of endodontics, we must be willing to unlearn years’ worth of habits. I would advise endodontists to take a step back and give themselves room to change and grow. I recognize that adopting new technology can be a leap of faith, but it can be worth it.
When it comes to the GentleWave System, it will benefit you and your practice long-term. In fact, I have recommended this technology to many of my colleagues, who have adopted it for their own practices and are very glad that they did.
From my experience, it will improve your life as a clinician and business owner. It will differentiate you and your practice in the market, helping to ensure that you are providing the best possible care for your patients. It will offer access to a community of like-minded and supportive endodontists, who can serve as mentors and friends. Together, these factors add up to make the GentleWave System completely worth the investment.
11 endopracticeus.com Volume 16 Number 1 COVER STORY EP
The ultimate look
Introduction
Can you feel it? We all feel the stress of doing our next endodontic treatment to one extent or another. Why is that?

Stress is present because endodontics is the only dental discipline where we “do it in the dark,” and doing dentistry blind is stressful for any dentist. After entering an endodontic root canal system, we cannot “see” and “do” simultaneously. We lose our precious control. This loss is felt deep in our gut, and our mind agrees. Or maybe it is the other way around. Either way, we have all been there, looking at a pretreatment endodontic image, feeling anxiety, and sometimes even threatened. You feel it, your staff feels it, and your patient feels it. It is not fun.
In preparation to receive this article’s full clinical value, I invite you to imagine for a moment that it’s Monday morning, and you have found the canal entrance of your first scheduled endodontic patient. At this crucial treatment point, you find yourself experiencing the fear of one or more of the most common endodontic “stress points.” Stress is produced for these reasons:
1. because you cannot prepare or preserve the glidepath for mechanical preparation
2. because the canal is too calcified, coronally restrictive dentin prevents your “following” the canal to length, or you simply “can’t get down”
3. because your mechanical NiTi file could break, stretch, or result in a preparation that you cannot conefit, 3D clean, and 3D fill
4. from failing to prepare the proper shape for safe and predictable obturation in large or open apex canals
5. from fear of canal blocking, ledging, transportation, or breaking a file in a sharp apical canal hook
6. because the master gutta-percha cone does not fit after all your effort
Yes, all these things are stressful. They don’t have to be. These endodontic treatment stress points and concerns are real. What if these stresses could instead be turned into fun, confidence, and successful production? What if a Shaping System allowed you to master your endodontic endgame? What if the stress that you experience while waiting for the final obturation
John West, DDS, MSD, received his DDS degree from the University of Washington, where he is an affiliate professor and his MSD degree in endodontics from Boston University, where he was honored with the Distinguished Alumni Award. Dr. West is founder and director of the Center for Endodontics in Tacoma, Washington, where he is also in private endodontic practice. He can be reached at (253) 377-2007 or via email at johnwest@centerforendodontics.com.
Disclosure: Dr. West is co-inventor of ProTaper, ProGlider, WaveOne, Gold Glider, and
image to appear was replaced with the excitement of anticipating a solid, well-designed obturation with multiple portals of exit visibly sealed? What if in seeing the final obturation image, your inner child exploded with joy and satisfaction? Allow me to introduce ProTaper Ultimate (Dentsply Sirona). The motivation for creating ProTaper Ultimate was to transform these endodontic stresses into stressless endodontics. Here is how it was done.
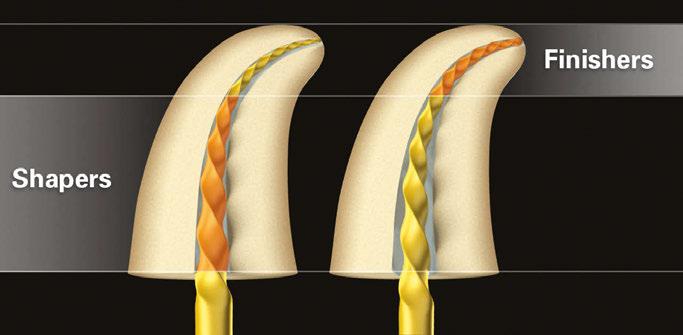
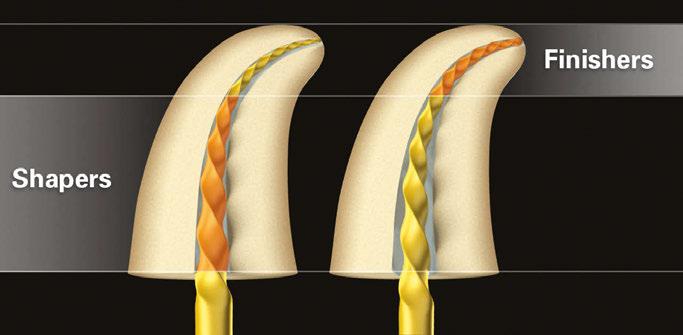
In May 2001, I wrote an article for another publication titled “Introducing a New Rotary System: Progressively Tapering Files.”1 The revolutionary distinction of Shapers (progressive geometries) and Finishers (regressive geometries) was a first and lasting clinical value (Figure 1).2 Today almost 20 years to the day of that first article, I wrote the introductory article for ProTaper Ultimate — an exploration and assembly of the essentials of endodontic preparation requirements for “appropriate” shaping, 3D cleaning, and 3D filling.3,4 Since 2001, ProTaper has saved more than 200 million teeth; 1,200 scientific articles have been written about ProTaper; and ProTaper has become the world’s most popular and recognizable endodontic file system brand. And yet 2 years ago, it became clear that the endodontic landscape was changing due to further improved metallurgy, cleaning, and filling counterparts.
ProTaper Ultimate’s goals are to perform the following:
1. Advance minimally invasive endodontics (MIE)
2. Simplify the technique
3. Facilitate a safer procedure
4. Treat a wider range of anatomy
5. Start with rotary file first to secure canal
6. Discover the carefully balanced and essential engineering transition elements from Glidepath through Finisher. The intended result was to design a fresh and almost
12 Endodontic Practice US Volume 16 Number 1 ENDOSPECTIVE
Dr. John D. West looks at the new ProTaper Ultimate and says, “It’s not one thing, it’s everything”
Calamus products.
Figure 1: ProTaper Ultimate’s (Dentsply Sirona) two critical distinctions are Shapers designed to remove restrictive dentin where present and Finishers to “connect the dots” from the terminal portal of exit and through the chamber orifice in order to prepare an appropriate continuously tapering preparation funnel while mechanically maintaining the portal of exit position, i.e., Deep Shape
peaceful clinical experience that fosters fun, predictability, and improved productivity. The most important task of all was to create a desirable Shaping System that dentists would want to use.
ProTaper Ultimate is not just a Shaping System but the first of a three-part launch from Dentsply Sirona. The first part of this trifecta is ProTaper Ultimate. Part 2, the 3D cleaning system (SmartLite Pro, Dentsply Sirona), and part 3, the revolutionary 3D filling system (carrier-based obturation with AH Plus® Bioceramic Sealer (Dentsply Sirona) will be coming soon.
The ultimate answer to endodontic stress: the making of a “wow”
When given the opportunity 2 years ago to reinvent a revelatory endodontic Shaping System that would produce a gap between “what is” and “what could be,” we knew the assignment would be an overwhelming invitation since most metallurgies, rake angles, tip designs, sizes, and shapes had been tried in endodontics. Given the enormous success of ProTaper, which is identified as the most recognizable Shaping System in the world, we knew we had a challenge on our hands. ProTaper Gold™ is also the overwhelming choice of North American endodontists, but could it be made even better?5 Dentsply Sirona designers
Dr. Cliff Ruddle, Professor Pierre Machtou, and I all agreed that if we could not produce a “WOW” (our adopted working title), the project should end. The endodontic world did not need just another file. In fact, since ProTaper’s first-generation launch 20 years ago, there have been an estimated 300 file systems that have come and gone. Their clinical value was not sustainable. In fact, as I am writing this article, there are three new file system advertisements on my desk promising, at one point or another, everything from total enlightenment to financial freedom. No wonder they come and go. Dentists want to trust that a product does what it promises to do.
Standing still was never a ProTaper option, but the first months attempting to pioneer a WOW felt like standing still. Special things don’t just happen; it is always about intention. Making a WOW took Dentsply Sirona backing; Swiss master engineers Nicolas Crevoisier and Gilbert Rota (the original ProTaper engineer in 1995); an acclaimed machine factory in Ballaigues, Switzerland; craft, passion, patience, vision, and decades of experience. Finally, we needed an additional “creative” ingredient: imagination. Imagination allowed an opening into a future that could forge the fusion of technical precision, uncompromised functionality, and exclusive design augmentation.
In the beginning, the development team was searching for our WOW, but our efforts were all in the wrong places. We were looking for this big WOW, and yet our breakthrough was instead found in many little places. Some believe the relationship between effort and results is not linear and follows what scientists call a “Power Law.”6 According to the Power Law Theory, certain small changes in a complex system can produce exponentially more and often sudden results than others. These small changes can cause a cascade among the connected parts such as knocking over the first domino in a long row. We just had to find the right changes. In short, by paying attention to the essential few elements of an endodontic Shaping System, a “less but better” complex was discovered — at last, the WOW we
had been looking for. The answer that had been so hard to find suddenly became clear and simple. Certain critical little changes throughout the ProTaper Ultimate system produced exceptional and expanding performance values.
ProTaper Ultimate has made incredible advancements in the foundational technology for designing, developing, and building an endodontic Shaping System that makes radicular preparations more accessible, more predictable, and more affordable for all dentists. The endodontic transformational power of ProTaper Ultimate was discovered. Time is our biggest cost, and Ultimate’s efficiency and file-robustness result in an endodontic treatment that is energizing and time-saving, and frees you to do more. This feeling is deeply rewarding, fulfilling, and gratifying all at once.
New file features and clinical value
The mantra, the sequence, and the ProTaper confidence have always come from a plan for predictability. Look how simple Ultimate makes it: purple, white, and yellow — sculpted endodontic preparations as easy as 1, 2, 3. I will now introduce the entire ProTaper Ultimate family: a simple, wide range of endodontic shaping solutions (Figure 2A).
1. Slider (purple) (Figure 2B)
Goal: As always, determine working length. The Slider then prepares a safe, mechanical “Glidepath” for the Shaper. The use of “rotary first” invites you to think profoundly different (both with confidence and caution).
Distinguishing features and clinical value:
• We have thought about the Glidepath differently for some time now.7-10 Nature’s untouched root canal walls often provide a sufficiently smooth tunnel or slide from orifice to physiologic terminus that can be safely followed by this newly designed mechanical file. Simply changing the word Glidepath to “Slidepath” immediately changes a clinician’s mindset and makes the preparation for rotary a much easier game. Nature presents what we now prefer to call “nature’s Slidepath.” Studies show that the Slider can successfully follow nature’s untouched canals ~63% to 80% of the time if we use masterful restraint with professional patience and supreme delicacy (as discovered by the designers and Dentsply Sirona user evaluations). The Slider will find its way by following nature’s natural tunnel, usually in 1 to 3 passive passes, while cradling the handpiece in the palm of your hand. Do not push or peck with your index finger; resist this temptation that will always be present. The index finger is the most dangerous finger in all rotary or reciprocation shaping because it wants to do something, and that something is to push, which leads to breakage, blocks, ledges, transportations, and perforations. If the Slider does not slide after a few self-restrained “follow” passes, return to K-files 6, 8, or 10, and manually prepare a Slidepath.11
• The Slider is a purpose-specific M-wire mix of variable parallelogram cross sections producing enhanced performance versus ProGlider square cross sections.
• Using the Slider at 400 rpm and 5 Ncm versus ProGlider at 300 rpm contributes to enhanced cutting efficiency.
• The Slider’s alternating, offset machining produces reduced friction and greater space for debris removal.
13 endopracticeus.com Volume 16 Number 1 ENDOSPECTIVE
preparing the “Slidepath”
the Shaper
Finisher. 2C.
(white) is for preparing a minimally invasive endodontic (MIE) body. 2D. Two Shapers become one Ultimate super Shaper. The Slider and Shaper maximum flute diameter (MFD) has been reduced from 1.2 mm to 1.00 mm, producing a profound increase in flexibility while also preserving pericervical dentin. 2E. The exclusive design of the Finisher (yellow), is characterized by apical progressive tapers (for preparing Deep Shapes) and coronal regressive tapers (for preparing MIE bodies) — as simple as 1, 2, 3 or purple, white, yellow. 2F. The ProTaper Ultimate Manual Shapers and Finishers are used for preparing delicate root canal system anatomy and abrupt canal termini or if motors were either not available or simply not preferred

2. Shaper (white) (Figures 2C and 2D)
Goal: Simplify the system by combining two Shapers into one. Integrate ProTaper Gold S1 and S2 in order to design a unique and harmonious transition from the Slider through the Finishers.


Distinguishing features and clinical value:
• The Shaper is a single Shaper.
• The Shaper uses purpose-specific gold heat treatment.
• The Shaper is produced from a 1.0-mm maximum flute diameter (MFD) versus 1.2 mm MFD of ProTaper Shaper S1 and S2, increasing flexibility and preparing an MIE narrower body.
• The Shaper has alternating offset machining and a variable parallelogram cross section generating flexibility without compromising cutting efficiency and resulting in greater resistance to cyclic fatigue.
3. Finisher 1 (F1) (yellow)
Goal: Achieve an MIE body while maintaining the iconic ProTaper Deep Shape.
Distinguishing features and clinical value:
• Made from purpose-specific gold heat treatment (Figure 2E).
• 1.0 mm MFD metal versus 1.2-mm MFD metal, enhancing flexibility and apical preparation control and fashioning a slimmer body shape.
• Alternating, offset machining.
• Carefully balancing better flexibility without compromising cutting efficiency.
• Bernoulli’s principle funnel shapes facilitate 3D filling. (Bernoulli’s principle of fluid dynamics is named after Daniel Bernoulli, who published it in his book Hydrodynamica in 1738.)
4. Finisher 2 (F2) and Finisher 3 (F3) (red and blue, respectively, when needed)
The goal, features, and clinical value are the same as with F1. Note that the Slider through the F3 represents the ProTaper Ultimate core.
5. Auxiliary Finishers FX and FXL (when needed)
Goal: Expand ProTaper Deep Shape preparations with Finishers for larger canals.


Distinguishing features and clinical value:
• Same as F1 to F3, except for 1.2 mm MFD for FX and 1.0 mm MFD for FXL, with purpose-specific blue heat treatment.
6. SX Auxiliary Shaping File (when needed)
Goal: To improve flexibility and preserve superb cutting efficiency.

Distinguishing features and clinical value:
• The new Ultimate SX file, thanks to a variable parallelogram cross section and alternating offset machining, is an auxiliary instrument that combines flexibility without compromising cutting efficiency. This advantage was not the case with the current ProTaper Gold SX version. The new Ultimate SX file has the flexibility advantage of the current ProTaper Gold SX and the cutting efficiency behavior of the traditional, non-heat-treated ProTaper Universal SX file.
7. Manual files (when needed)
Goal: Shape anatomy that has an abrupt and sharp apical turn or all anatomy where rotary is not available or not preferred. Distinguishing Features and Clinical Value:
• Same as rotary counterparts (Figure 2F).
14 Endodontic Practice US Volume 16 Number 1 ENDOSPECTIVE
A.
Figures 2A-2F: The ProTaper Ultimate family and the Ultimate “Look.” 2A. The complete Ultimate family from SX to FXL. 2B. The Slider Rotary (purple) is the first instrument in
for
and the subsequent
The Shaper
B.
D.
C.
E.
F.


Figures 3A-3I. ProTaper Ultimate’s iconic Deep Shape and Minimally Invasive Body. 3A. Allow all ProTaper Ultimate Shapers and Finishers to follow canals without an intended direction or rate. Cradle the handpiece in the webbing of your hand, and simply let the weight of the handpiece enable the file to advance while repeating to yourself, “Let it run.” Do not ever push. Never break this rule. It works. Instead, use the watchwords: restraint, restraint, restraint. Take your time; the canal is not going anywhere unless you make it do so by blocking, ledging, or transporting. 3B. Pretreatment of a maxillary right molar. 3C. Radiograph of the Slider having slid to length. 3D. Radiograph of the Shaper having patiently carved its way to length. Notice the maintaining of the apical portal of exit position! 3E. The downpack reveals apical Deep Shapes in all four canals of varying curvatures. 3F. Distal oblique radiograph of the finished obturation, displaying maintenance of the original anatomy of the severely curved MB1 and MB2 system while the DB has an abrupt apical curvature into or out of the plane of the image. (Courtesy of Dr. Jason West, Tacoma, Washington) 3G. Pretreatment of a mandibular first molar with a gutta-percha clinical cone tracing the sinus tract. 3H. Perpendicular posttreatment radiograph illustrating foraminal hydraulics sufficient to press surplus sealer through the entire length of the sinus tract. 3I. Oblique posttreatment view
• The ability to produce a deep shape and an MIE body with just a few manual and safe rotations.
When comparing ProTaper Ultimate to ProTaper Gold F1 and F2:

• Ultimate F1 is 13% more flexible than ProTaper Gold F1.
• Ultimate F1 is 75% more resistant to cyclic fatigue than ProTaper Gold F1.
• Ultimate F2 is 30% more flexible than ProTaper Gold F2.
• Ultimate F2 is 30% more resistant to cyclic fatigue than ProTaper Gold F2.
How does this new system overcome the six most common endodontic stresses?








Common Stress Point No. 1: Glidepath failure.
Ultimate solution: The Slider is intended to be the first instru-
ment to slip and slide down the virgin canal. Fill the chamber with viscous chelator. Cradling the handpiece in the web of your hand (no pushing or “trying” to reach length) allows the file to follow nature’s canal walls to length (Figure 3A). If the file slows, remove it, clean the flutes, irrigate with NaOCl or an additional viscous chelator, and repeat until length is reached. If the Slider does not easily progress to length, manually prepare the Slidepath in those last few millimeters. Remember that the Slider reaches length ~63% to 80% of the time, as discovered by the designers and Dentsply Sirona user evaluations. For the other 20% to 37% of the time, return to a manual Glidepath. Please note the newly engineered SX Auxiliary file consistently removes canal access dentin triangles that may prevent easy entrance and apical progression of the Slider. The watchword for the Slider is restraint.
16 Endodontic Practice US Volume 16 Number 1 ENDOSPECTIVE
A.
B.
C.
G.
H.
I.
D.
E.
F.
YOU’LL BE SMILING...
KNOWING WE ARE THE ONLY
Dental Surgical Specialty Partnership
Led by Doctors.
You deserve to control your business while also having the peace of mind from a support system designed by doctors for doctors.
As an Endodontist, Specialty1 Partners enables you to focus on patient care because we focus on ensuring your ability to do so.
YOUR SPECIALTY IS OUR SPECIALTY.

305 - 206 - 7388 | Specialty1partners.com
Common Stress Point No. 2: Calcification
Ultimate Solution: The Shaper is a single Shaper replacing ProTaper’s S1 and S2 Shapers. The Shaper’s reduced MFD and improved cutting efficiency make it easy to remove restrictive dentin along the Slider-prepared walls. It may take several passes while cleaning flutes between passes and irrigating with NaOCl. Finishers will gracefully follow the Shaper’s path. The watchword for the Shaper is patience (Figures 3B to 3D).

Common Stress Point No. 3: The finishing file breaks or stretches, or the prep does not produce 3D cleaning or 3D filling
Ultimate Solution: As already noted, core Finishers F1, F2, and F3 have more flexibility and greater resistance to cyclic fatigue than ProTaper Gold Finishers. The new design makes them more robust yet highly efficient and produces repeated shapes within the same tooth without metal distortion. This feature produces consistent and accurate Deep Shapes for confidence in 3D cleaning and 3D filling. The watchword for Finishers F1 to F3 and the “Ultimate Look” is effortless (Figures 3E to 3K).

Common Stress Point No. 4: Treating larger canals

Ultimate Solution: The FX and FXL enable clinicians to predictably prepare larger canals where there is sufficient tooth structure. If severe apical reverse architecture is present, an apical plug may be required. The watchword for the FX and FXL is easy (Figures 3L to 3N).




Common Stress Point No. 5: Fear of breaking a rotary file or blocking, ledging, or transporting sharp apical curvatures
Ultimate Solution: Manual files have all the same geometries as Ultimate Rotary files and enable the clinician to prepare sharp apical canal curvatures in 1 to 3 turns of the handle. The watchword for Manual files is safety.
Common Stress Point No. 6: Conefit12
Ultimate Solution: Precision-machined Ultimate gutta-percha master cones exactly replicate and fit the last 3 mm of the Ultimate apical preparations and also are designed to have an intimate fit throughout the canal preparation, making single-cone, vertical-compaction-of-warm-gutta-percha, and carrier-based obturation easy and predictable. The watch phrase for conefit is conefit is a fit (Figures 30 and 3P).
Six cardinal rules
Never deviate from these six rules; they will always work.
1. Always start with the Slider. This allows you to slide down nature’s very own, already existing Slidepath without using a manual file anywhere from ~63% to 80% of the time. Otherwise, return to a manual Slidepath. Never force it. Once you have the Slidepath, the rest is easy!
2. Always shape the coronal two-thirds of restrictive dentin with the Shaper. This allows you freedom and effortlessness in preparing a Deep Shape apically while preserving pericervical coronal dentin.
3. Always finish radicular preparation with the Finisher that
18 Endodontic Practice US Volume 16 Number 1 ENDOSPECTIVE
J.
O.
K. L. M.
Figures 3J-3P. ProTaper Ultimate’s iconic Deep Shape and Minimally Invasive Body. 3J. Pretreatment radiograph of a maxillary second molar FPD abutment. 3K. Posttreatment radiograph divulging a deep curvature shape plus a simultaneous MIE body shape. (Courtesy of Dr. Jason West) 3L. Pretreatment radiograph of a previous nonsurgical and surgical attempt with a continued lesion of endodontic origin. 3M. Nonsurgical retreatment downpack after removing the post and the FXL standalone rotary shaping file. 3N. Posttreatment periapical radiograph. 3O. ProTaper Ultimate 100% conefit. An example of Ultimate F2 precision Deep Shape and MIE body conform fit combined into a single intimate preparation fitting the gutta-percha cone. 3P. Six clinically beneficial innovations of ProTaper Ultimate master gutta-percha cones
N.
P.
cuts apically. If F1 does not visually cut dentin seen in its apical flutes, advance to F2; and if F2 does not visually cut dentin in its few apical millimeters, then advance to F3. If F3 is devoid of apical dentin shavings, then consider FX; and if FX is not cutting dentin on visual inspection, advance to FXL. If the FXL fails to prep the few apical millimeters, then consider an apical barrier due to reverse apical architecture (Figure 4A). This allows you to prove that you are finished shaping and are ready to confidently fit cone.
4. Always conefit after Ultimate flutes are filled with apically carved dentin while the canals are still wet. This allows you to confirm that the Deep Shape and Body Shape are present in your preparation and correspond perfectly with the last finisher used.
5. Always use EDTA, then NaOCl 3D cleaning protocol with EndoActivator (Dentsply Sirona) or SmartLite Pro after conefit. This allows you to remove the smear layer, eliminate tenacious bacteria still present after shaping, and digest remaining pulp.
6. Always obturate at the time of shaping unless the patient is symptomatic, or if you first want evidence of healing such as sinus tract closure or endo-perio improvement. This allows you to obturate when you are most knowledgeable and familiar with the root canal system anatomy.
The ultimate challenge: an invitation to discover for yourself
It’s now time for the “Ultimate challenge”: Test ProTaper

Ultimate’s performance against your current preferred rotary Shaping System (Figure 4B) by keeping a diary of preparation comparisons — simplicity, efficiency, safety, durability, consistency, predictability, control, and conefit accuracy, and ease the first time.
Closing comments
As dentists, we have the same goals. We are self-selected. We want to help people, we do not want to cause any harm, and we are artists in our own way. We are Michelangelos in a different medium. Even though our desired outcomes are different, our intentions are the same as a Michelangelo sculpture: “Trifles make perfection, and perfection is no trifle.” My purpose in writing this article is to have you experience your own endodontic artistry in your practice through ProTaper Ultimate’s transformational potential.
Twenty-five years ago, the groundbreaking ProTaper concepts were conceived, and in 2001, they were first embraced by ProTaper advocates in difficult cases, then in easy cases, and eventually in all cases. ProTaper Ultimate is a fresh story in the ProTaper legacy, and, as we venture into the future, I predict Ultimate will be the world’s go-to endodontic-preparation rotary system.

Today is a historical milestone for dentistry as thoughtful endodontic technologies have been brought together to build a generation of dentists free from endodontic stress and serving a greater patient condition. We stand on the precipice of a new era of endodontic performance and experience.
Until the present, “root canal words” such as “tranquil,” “bliss,” and “fun” would never have found their way into mainstream endodontic language. But now, it’s too good, and it’s true. Finally, we’re back to my beginning question: Can you feel it?
What are you waiting for?
Acknowledgment
Graphics in this article were produced in collaboration with Advanced Endodontics, Santa Barbara, California.
REFERENCES
1. West JD. Introduction of a new rotary endodontic system: progressively tapering files. Dent Today. 2001;20(5):50-52,54-57.
2. West JD. The Evolving Look of “The Look.” Dent Today. 2019;38(6):62-66.
3. West JD. The pendulum swings: “minimally invasive” vs “maximally appropriate.” Dent Today. 2019;38:8-10.
4. West JD. The Endodontic Triad: ‘Dead or Alive?’ Dent Today. 2021;28-35.
5. West JD. Survey from American Academy of Endodontists. Scientific Zoom Session; April 2021.
6. McKeown G. Essentialism: The disciplined pursuit of less. Crown Publishing Group; 2020.
7. West JD. The endodontic glidepath: “secret to rotary safety.” Dent Today. 2010;29:86-93.
8. West JD. Manual vs. mechanical endodontic glidepath. Dent Today. 2011;30:136-140.
9. West JD. Glidepath implementation: “return to the beginning.” Dent Today. 2011; 30:90-97.
10. West JD. Restraint: The lost art of endodontics. Dent Today. 2018:100-103.
Figures 4A-4B: The ProTaper Ultimate shaping protocol and the “Ultimate challenge.” 4A. The ProTaper Ultimate decision-making process. 4B. The best education in the world is your own via pitting ProTaper Ultimate versus your current Shaping System. This is an invitation to find out for yourself if ProTaper Ultimate can transform your endodontic performance
11. West JD. Perforations, blocks, ledges, and transportations. Overcoming barriers to endodontic finishing. Dent Today. 2005;24(1):68-73.
12. West JD. The cone fit: An essential step to creating exceptional endodontic obturation. Dent Today. 2005;24(5):102-105.
This article has been reprinted with permission from Dentistry Today.
19 endopracticeus.com Volume 16 Number 1 ENDOSPECTIVE
EP
A.
B.
Root canal shaping in the age of minimally invasive endodontics (MIE)

Drs. L. Stephen Buchanan and Christophe Verbanck discuss the benefits of files with conservative tapers
Introduction
We are entering a new golden age of endodontics where instrumentation with root canal files is safer, easier, and more efficient. In 1980, when the senior author matriculated from his endo residency at Temple University, the most difficult art form in clinical endodontics was serial step-back (SSB) root canal shaping. Today, endodontic instrumentation can be as simple as cutting a single rotary file to length, and it’s time to irrigate and fill the RC system. This is the story about how we got here.
The Apical Stop Preparation

The Apical Stop Preparation (ASP) described by Kuttler,1 based on the standardized technique,2,3 gained widespread popularity at the end of the 1950s. The technique was to work small files to length, subtract 0.5 mm-1.0 mm from the full length of the canal as determined by radiograph, then progressively enlarge the preparation diameter at that working length to a minimum of 0.35 mm (a #35 KF) in small roots and to at least 0.45 mm (a #45 KF) in larger roots. The intention was to cut — using 1/4-turn,
L. Stephen Buchanan, DDS, FICD, FACD, Dipl. ABE, has been lecturing and teaching hands-on endodontic continuing education courses for over 30 years, both in his state-of-the-art training facility in Santa Barbara, California, as well as in dental schools and at meetings around the world. He currently serves as a part-time faculty member in the endodontic departments at the University of the Pacific’s Arthur Dugoni School of Dentistry and the University of California at Los Angeles as well as being the Endodontic Advisory Board Member to the Academy of General Dentistry. Dr. Buchanan is nationally and internationally known for his 50-plus endodontic procedural articles as well as his expertise in the research and development of new endodontic technology, instruments, and techniques. He is a Diplomate of the American Board of Endodontists and a Fellow of the International and American College of Dentists. Dr. Buchanan also maintains a private practice limited to Endodontics in Santa Barbara, California.
Christophe L.M. Verbanck, DDS, MSc, obtained his Master of Dentistry at Gent University in 2009. He specialized in endodontics, graduating after a 3-year postgraduate training program from the same university. Since 2010 he has worked in several multi-disciplinary and endodontic referral practices all over Flanders. In January 2016, together with his wife, he started his own referral practice for Endodontics, Lovendo, in Lovendegem (Belgium). He regularly teaches endodontics to general dentists and holds workshops on the application of endodontic techniques.
Disclosures: Dr. L. Stephen Buchanan is a co-founder of PlanB Dental.
pull motions — an intentional ledge near the end of the canal as resistance-form to contain obturation materials within the canal and prevent overfills.4
The ASP’s unforgiveness of length determination errors, combined with the inaccuracy of radiographic length determination (before apex locator use was widespread), meant that clinicians preferred treating root canals short of their entire length, despite the fact that undertreatment of root canal systems was the most common cause of RCT failure (Figure 1).5,6 The predominant, yet illogical, expert opinion at the time was to stay short of the ends of root canals because we don’t want to damage any apical tissues, however, if the RCT fails, those same experts recommended apicoectomy (cutting off the apical third of the root) because that is where all the lateral canals are found. That is, in essence, saying, “a #10 KF passed through the root canal terminus is bad, but hacking the root end off and cutting all the bone around it is OK.”
In fact, all of our clinical experience and all of our evidence-based research has proven the importance of treating the entire root canal system.7
20 Endodontic Practice US Volume 16 Number 1 TECHNOLOGY
“Y ou cannot clean a root canal with a larger file.” — LSB
Figure 1: These illustrations show how treating a root canal 2 mms short of the root apex — as recommended by Kuttler1 — can result in 6 mm-8 mms of untreated canal form. Endodontists will argue all day about treating RCs 0 mm-2mm short, but none of them say, “I treat root canals 6 mm short, and it works like a champ.”
Figure 2: Weine’s classic “hour-glass” preparation in the mesial root of a lower molar. This is the result when 1/4-turn, pull filing motions are used to cut increasingly larger SS K-files to working length — without the use of patency files to clear apical debris — in curved canals with apical blockage
Worse than undertreatment, the ASP encouraged damage of delicate apical anatomy when increasingly larger, more rigid stainless steel files were forced to cut to working length. In 1975, Weine showed how 1/4-turn, pull motions with SS K-files transport apical canal paths, creating ledges in curved canals (Figure 2).8


The ASP technique was the most common cause of overfills between 1950 and 1980 when most of the research correlating overfills with RCT failures was done (Figure 3). Sadly, only a few of the over 70 authors who published on this topic were able to understand that overextended filling material was coincidental to the failure, not the etiology for the failure. For the authors, this begs the question, “If the filling materials we use in endodontics must all pass regulatory biocompatibility tests, how does surplus filling material inhibit healing of periapical disease?” In fact, the belief that surplus filling material causes failure is a case of mass hysteria following mistaken etiology.9,10 Overfills are nearly always caused by derangement of the canal path during instrumentation (Figure 4).
The Schilder Serial Step-Back tapered preparation technique

In the 1970s, Dr. Herbert Schilder11 from Boston University popularized the “Serial Step-Back” (SSB) preparation technique, known for its large coronal shapes, its small apical preparations, and its incessant irrigation with sodium hypochlorite. For decades it was the most successful method of treating root canal systems to their full apical extents because he unapologetically espoused the use of patency files passed to and through the ends of primary canals to clear their apical thirds of pulp and dentin debris. Uniquely, his advice to keep the apical foramen as small as is practical empowered instrumentation and obturation of even the most dilacerated canals to their very ends, when clinicians cutting larger apical preps in small molar roots could never complete treatment at length — always ending up blocked out 1, 2, and even 3 mm short of the primary canal terminus.12
Schilder’s technique became best known for its post-op display of filled lateral canals because NaOCl was used to lavage canals after every other file was used, and nobody else in the specialty irrigated with that efficacy, so they seldom saw lateral canals filled. Because they seldom saw lateral canals filled, it was difficult for most of them to understand the importance of treating the commonly occurring lateral anatomy in RC systems. Meanwhile, Schilder and his acolytes cleaned and filled lateral anatomy routinely by using both his cleaning and shaping method as well as his “Vertical Condensation of Warm Gutta Percha” obturation technique.13
Schilder’s recommendation that clinicians cut bigger access cavities and bigger coronal canal shapes was logical considering the limitations of the instruments of his time, and at that time, dentist’s RCT results were improved by it. However, his enlargement concept has been obviated by the improvement of our material science, by the quality of our tool designs, and because the most progressive endodontists are currently pursuing minimally invasive access and shaping objectives. Sadly, some endodontists still equate overcut endo preparations with quality RCT.
Schilder was best known for his warm gutta percha obturation technique, however, in the author’s minds, his enduring
legacy in the specialty pivots around his advocacy for tapered apical resistance form, maintaining the apical foramen’s original diameter, and for the irrigation technique embedded in his shaping routine. Until recently, Schilder’s critics didn’t understand how his cases succeeded despite what looked to them like under-enlarged apical preparations because few of them knew how to use NaOCl to its potential in their own cases. Fortunately endodontists are coming to realize that if you optimize irrigation protocols, you can achieve predictable clinical success without cutting any dentin.14 Schilder knew this 50 years ago.
Ultimately, Schilder’s greatest genius was in defining a better objective for clinical RCT, namely, treatment to the full apical and lateral extents of root canal systems.
The variably-tapered rotary file revolution
Until 1989, there were no files with tapers greater than the ISO .02 mm/mm standard K-file, so SSB was the only way to cut a tapered prep with the relatively untapered files that were available. However, as the advantages of tapered preparations became apparent, the difficulties of learning, applying, and even
21 endopracticeus.com Volume 16 Number 1 TECHNOLOGY
Figure 3: These illustrations show how ripping open curved apical canal regions eliminates all resistance form, encouraging master GP cones to over-extend yet leave the end of the canal underfilled
Figure 4: CT reconstruction of a mesial root of a lower molar comparing the original canal path (red) and the deranged canal path (green) caused by misuse of a stiff, aggressive rotary file. This is the setup for overfilling
Figure 5: 20-.06 GT Hand File (Tulsa Dentsply) circa 1996 — the first single-file shaping instrument as well as the first variably tapered file designed with a maximum flute diameter limitation. (File design by Buchanan)
teaching SSB shaping routines also became evident, eventually becoming the inspiration for files with greater tapers.15 By posing the question, “Instead of using 12-18 instruments in multiple recapitulations, why not just use a single file with a shape matching the tapered shaping objective?” The answer learned through the development process that followed was that stainless steel is too stiff and too weak for files of greater taper to work. Serendipitously, after prototying in stainless steel failed, nickel titanium came to endo from orthodontics,16 and suddenly variably-tapered shaping files became a reality (Figure 5).
Originally, the objective was to make files with the same shapes we cut during SSB shaping with stainless steel files, namely, .04, .06, .08, .10, and even .12 tapers. During this design process, it became obvious that files with these tapers would be too large at their shank ends if they all had 16 mm flute lengths, so the original GT Hand and Rotary Files were designed with 1.0 mm maximum flute diameter limitations. The first MIE file feature, 20 years ahead of its time, one could also argue the GT Hand File was the industry’s first single-file shaping instrument. What we found out after giving files of greater taper to dental students (Figure 6)17 was that we did not need the same degree of taper with rotary shaping files that were required with SSB shaping because the quality of the shapes cut with variably-tapered files was so much more precise. Today most endodontists cut .06 tapers at the most, with many limiting their shaping files to .04 tapers and, with the advent of the miniKUT file system, even .03 tapers.
Current instrumentation concepts, tools, and procedures
In the 30 years since, conceptually, we’re finally beginning to accept the fact that to cut is not to cure when instrumenting canals. This offers so many advantages — less file breakage, less laceration of apical architecture, less post-op pain, fewer files to buy, and much less time spent using cutting instruments in canals. Successful MIE instrumentation does not revolve around using files; it hinges on upping our irrigation game. Files are the means, not the end. As proven to the authors by all the successfully treated canals done the past 5 years without cutting any dentin off a canal wall, just better irrigation.

The greatest improvement in our tools has been heat treatment of nickel-titanium files to remove the shape memory that is responsible for so many file separations due to cyclic fatigue.18,19 Before heat treatment, NiTi rotary files would exhibit what appeared to be spontaneous breakage. Now heat-treated files unwind and windup 9 or 10 turns backwards before they come apart. Heat-treated files cost less now than standard files did 10 years ago, so there is no reason for taking the greater risk of file separation associated with non-heat-treated NiTi files.

Another improvement in our tool design has been the realization that different file sizes in the same file set can never be optimized if they all have the same geometry. PlanB Dental’s miniKUT® MIE rotary files have variable geometry between their files; a square cross-section for their small EZPass rotary negotiating files, an aggressive two-bladed cross section in their shaping files, and three blades for their retreatment files (Figure 7). The advancements of variable geometry makes using rotaries as the “first files to length” a reality.20

Procedurally, the biggest sea change has been our realization that the mission of endodontic instrumentation is really only about confirming that canals have positive apical architecture before they are irrigated and filled. Once the apical diameter of the foramen has been determined — with gauging instruments, by observing whether there is debris in the last flutes of the first file of a larger diameter cut to length, and even with analysis of pre-op CBCT volumes as they display anatomic dimensions in an isotropic 1:1 scale21 — the only shaping requirement is that the narrowest canal diameter be at the terminus of the canal.
If the natural canal has an ideal shape preoperatively (most common in young adult teeth), the instrumentation plan is to broach the pulp, irrigate the canal, and stuff it.
we
22 Endodontic Practice US Volume 16 Number 1 TECHNOLOGY
When
Figures 7A-7C: PlanB Dental’s miniKUT files with specific cross sections for specific functions. 7A. Square for 15-.03 and 15-.05 rotary negotiating files. 7B. Two-bladed “S” flutes with big chip space for shapers. 7C. A three-bladed cross section for the greater torsional loads associated with retreatment
A. B. C.
Figure 6: CT reconstruction of a mesial root of a lower molar before (red) and after (green) instrumentation by novice dental students. The MB canal (bottom) was instrumented with five stainless steel .02 tapered K-files and three Gates-Glidden burs; the ML canal was instrumented with just a single nickel-titanium 20-.06 Hand GT File17
Figure 8: The upper molar RCT, done in 1989, represents Schilder’s larger coronal shaping style. The lower molar RCT, treated in 2018, shows the minimalistic MIE instrumentation style currently and virtuously in vogue (cases by Buchanan)




Scan our Case Gallery of world-class clinicians showing their work
Case by Dr. C. Verbanck
encounter canals with reverse apical architecture, meaning the narrowest diameter is coronal to the terminus, then our only instrumentation objective is to cut a shape that repositions the narrowest diameter in the canal to the end of the canal. So, the evolution of Endodontics has approached nearly prepless RCT where chemical cleaning will always play the most significant role (Figure 8).
Recently, reciprocation was touted as the key to single-file shaping, which is patently not true. The two authors, between them, have done thousands of single-file shaping cases with a myriad of rotary files years before reciprocation even existed. This shined a spotlight on the big advantage of rotary cutting tools — to effectively remove pulp tissue and dentin chips from apical regions instead of pushing them laterally and apically — it also revealed that reciprocation was a step backwards.22
State of the art of instrumentation
The current trend among progressive endodontists is toward the application of minimally invasive endodontic principles (Figures 9 and 10). An excellent example is the miniKUT file system of instruments, with conservative tapers of .03 and .05. The unconventional .03 taper is at the low end of the natural taper of small root canals and will work even if the canal has an even smaller or non-tapered canal outline, an extreme curvature, or apical impediment. The .05 taper is closer to an SSB tapered preparation with 1 mm step-back increments and creates the right amount of space for all contemporary methods of irrigation. Used at speeds ranging between 600 and 900 RPMs, their cutting efficiency feels effortless even in long canals. These rotational speeds create centripetal forces that center the file and
keep the flutes from stalling against the root canal wall during preparation. They can be used for rotary negotiation (the 15-.03 and 15-.05 EZP) as well as “single-file shaping” with minimal coronal enlargement.
One of the author’s referring prosthodontists once told him that if endodontists could just “suck the pulp out and not cut any dentin” he would be happier. Specialty Endodontics has spent the past 30 years delivering on that virtuous aspiration. The irony of these sea changes in the art and science of instrumentation is that as our conceptual understanding of our mission became more sophisticated, procedural instrumentation became inordinately simple.
Look for our next article, “Irrigation: The Final Frontier,” in the fall edition of Endodontic Practice US.
REFERENCES
1. Kuttler Y. Microscopic investigation of root apexes. J Am Dent Assoc. 1955 May;50(5):544-552.
2. Seidler B. Root canal filling: an evaluation and method. J Am Dent Assoc. 1956 Nov; 53(5):567-576.
3. Ingle JI. A standardized endodontic technique utilizing newly designed instruments and filling materials. Oral Surg Oral Med Oral Pathol. 1961 Jan;14:83-91.
4. Kerekes K, Tronstad L. Long-term results of endodontic treatment performed with a standardized technique. J Endod. 1979 Mar;5(3):83-90.
5. Hess W, Zürcher E, Dolamore W. The anatomy of the root-canals of the teeth of the permanent dentition. New York NY: William Wood and Co.; 1925.
6. Coolidge ED. Anatomy of the root apex in relation to treatment problems. J Am Dent Assoc. 1929; 16:1456-1465.
7. Arias A, Azabal M, Hidalgo JJ, de la Macorra JC. Relationship between postendodontic pain, tooth diagnostic factors, and apical patency. J Endod. 2009 Feb;35(2):189-192.
8. Weine FS, Kelly RF, Lio PJ. The effect of preparation procedures on original canal shape and on apical foramen shape. J Endod. 1975 Aug;1(8):255-62.
9. Ricucci D, Langeland K. Apical limit of root canal instrumentation and obturation, part 2. A histological study. Int Endod J. 1998 Nov;31(6):394-409.
10. Siqueira JF Jr. Aetiology of root canal treatment failure: why well-treated teeth can fail. Int Endod J. 2001 Jan;34(1):1-10.
11. Schilder H. Cleaning and shaping the root canal. Dent Clin North Am. 1974 Apr;18(2): 269-296.

12. Senia ES. Canal diameter: the forgotten dimension. Dent Today. 2001 May;20(5):58-62.
13. Schilder H. Filling root canals in three dimensions. Dent Clin North Am. 1967 Nov: 723-744.

Figure 9: MIE RCT of maxillary premolar. The access was 1 by 1.5 mm, and the canal shapes were limited to a 30-.03 size. Despite this minimalistic treatment, three separate lateral canals were cleaned and filled in this vital case (case by Verbanck)
14. Buchanan LS. Chapter 7: Cleaning and Shaping Root Canal Systems. Pathways of the Pulp 5th ed. Mosby-Yearbook 1989.
15. Buchanan LS. The art of endodontics: files of greater taper. Dent Today. 1996 Feb;15(2):42, 44-6, 48-9 passim.
16. Walia HM, Brantley WA, Gerstein H. An initial investigation of the bending and torsional properties of Nitinol root canal files. J Endod. 1988 Jul;14(7):346-351.
17. Gluskin AH, Brown DC, Buchanan LS. A reconstructed computerized tomographic comparison of Ni-Ti rotary GT files versus traditional instruments in canals shaped by novice operators. Int Endod J. 2001 Sep;34(6):476-484.
18. Kwak SW, Shen Y, Liu H, Wang Z, Kim HC, Haapasalo M. Heat treatment and surface treatment of Nickel-Titanium Endodontic instruments. Front. Dent. Med. 2021, 2: 769977. https://www.frontiersin.org/articles/10.3389/fdmed.2021.769977/full. Accessed February 14, 2023.
19. Pruett JP, Clement DJ, Carnes DL Jr. Cyclic fatigue testing of nickel-titanium endodontic instruments. J Endod. 1997 Feb;23(2):77-85.
20. Buchanan LS., Verbanck CLM. Rotary negotiation as first file to length. Endodontic Practice US. 2022; 15(4): 24-26.
Figure 10: RCT of a mandibular molar. The final canal shapes were a 30-.03 size for the distal canal and .25-.03 for the mesial canals. Blockage in the ML canal from the previous RCT attempt was bypassed with a 15-.03 miniKUT EZPass Rotary File (case by Verbanck)
21. Scarfe WC, Farman AG, Sukovic P. Clinical applications of cone-beam computed tomography in dental practice. J Can Dent Assoc. 2006 Feb;72(1):75-80.
22. Bürklein S, Benten S, Schäfer E. Quantitative evaluation of apically extruded debris with different single-file systems: Reciproc, F360 and OneShape versus Mtwo. Int Endod J. 2014 May;47(5):405-409.
24 Endodontic Practice US Volume 16 Number 1 TECHNOLOGY
EP


TO GET BUY1 GET1 FREE
SCAN
Endo Mastery
Seminars and practice coaching for incredible endodontic success!


Visit our booth No. 239 to meet our team and practice owners who have achieved incredible growth and success with Endo Mastery practice coaching.
Endo Mastery transforms your practice into a highly productive and profitable environment that is stress-free, effortless, and fun. Our coaching programs are tailored to your vision and goals, and we support you at every stage of practice ownership from startup to mid-career growth to maximizing practice value.

At this year’s meeting, we’re pleased to sponsor the entire Practice Management Educational Track. Teamwork, schedul-
ing, marketing, growth, finances — these are topics we love!
Come to our booth to get our AAE show special of the lowest seminar tuition we offer. Save 50% on seminars, including our popular 2-day doctor and team seminar, “Mastering the Effortless Endodontic Practice” in Orlando this September!
We are also excited to sponsor the AAE Career Fair to help residents and new endodontists get started. Visit our Career Fair table to get access to free career start resources, or to find out about our coaching program for your startup or buy-in.
26 Endodontic Practice US Volume 16 Number 1 SPECIAL SECTION AAE SPECIAL SECTION
Visit Endo Mastery at AAE Booth No. 239 THISYour MAKE BEST YEAR! CHECK OUT OUR SHOW SPECIALS AND DR. ACE GOERIG’S SPEAKING SCHEDULE: endomastery.com/offers LEARN MORE ABOUT WHY OUR CLIENTS LOVE US.
Dr. Ace Goerig: Endo’s top practice growth and financial coach
Endodontic Practice Partners
As the sole specialty partnership organization (SPO) in the industry, co-founded and led by a female endodontist, Endodontic Practice Partners (EPP) understands the changing market and the advantage an affiliation brings to a traditional practice.

EPP was founded on sound business principles: operate with purpose, maintain ethical practices, operate with integrity and compassion, and maintain our affiliates’ autonomy and brand. As a nationwide partnership of endodontic practices focused on patient care, clinical quality, and growth, EPP seeks those practices that want to be best in class, progressive, and realize the strength that comes from being part of a larger group.
Many practices don’t have the time, bandwidth, or resources to support their vision. EPP provides help with hiring and managing staff, supply ordering, IT support, insurance negotiation, and more to position our equity partners to grow their success.
We provide value to our affiliates by personalizing a stra-







tegic growth plan, by fully integrating all our affiliates, and by delivering on what we promise. EPP is not in competition to be the largest or fastest growing. Success speaks for itself.
Endodontic Practice Partners is a proud supporter of the AAE Annual Conference. Visit us at Booth No. 365 to converse about what a partnership could look like for you. And get an updated professional picture by MK Photography at the Headshot Booth. May 3: 11 a.m. – 4:30 p.m. | May 4: 11:30 a.m. – 6:30 p.m. | May 5: 11:30 a.m. – 5:30 p.m.
27 endopracticeus.com Volume 16 Number 1 SPECIAL SECTION AAE SPECIAL SECTION
Visit Endodontic Practice Partners at AAE Booth No. 365 IGNITE YOUR SUCCESS Your ultimate business partner. Our services support you and your growth. Learn more at endopracticepartners.com. Business Operations Hiring & Payroll Insurance Negotiation Marketing Accounting & Finance IT & Equipment Support Associate Recruiting
Transform your endodontic practice with ESS
Are you losing precious time to menial tasks and searching for a comprehensive solution for your endodontic practice? Endodontic SuperSystems (ESS) is the answer. Our platform is designed for service businesses such as the dental and endodontic sectors. The platform gives the team driving instructions on your smartphone from 8 a.m. to 5 p.m. to convert busy people into productive people.

ESS offers an adaptable plan for each stage of your practice’s growth, comprehensive training and workflows, and process technology to empower your team and improve productivity. Our learning management system and training tools streamline the onboarding process, allowing new team members to be productive sooner and increasing office income.

Our mission is to help small businesses thrive and enhance the quality of life for everyone. With a bottom-up approach,
transparency, and a focus on continuous improvement and collaboration, ESS provides you with the tools to create a successful and efficient endodontic practice. Say goodbye to stress and anxiety and hello to success and freedom with ESS. Request a demo today and see our revolutionary approach in action.
28 Endodontic Practice US Volume 16 Number 1 SPECIAL SECTION AAE SPECIAL SECTION
a Free Trial, Request a Demo or Group Webinar at www.EndoSuperSystems.com
For
Continuing our focus on serving specialists
Endo1 Partners’ successful transition to Specialty1 Partners
Specialty1 Partners remains the market-leading solution to meet the specific practice management needs of dental surgical specialists. Since its launch in 2019 as Endo1 Partners, the first dental surgical specialty organization founded by endodontists for endodontists, the company has expanded to also serve oral surgeons and periodontists.

“As working endodontists juggling the complexities of treating patients and running successful practices, we saw first-hand the need for a truly doctor-focused partnership for dental specialists,” said Matthew Haddad, founder and co-CEO of Specialty1 Partners.” There are a lot of competitors that claim to be doctor-led and doctor-founded, but that simply isn’t the case, and it’s misleading to potential partners. Our vision, culture
and leadership all start with dental specialists. This has allowed us to significantly outperform others in the dental surgical specialty space.”
Specialty1 Partners now supports more than 225 locations in 27 states.
“Our focus every day is supporting our partners while continuing to build partnerships with industry-leading, innovative surgical specialists,” said Daryl Dudum, founder and co-CEO of Specialty1 Partners. “It’s not just about growing our network — it’s about helping partner practices grow organically and succeed on their terms.”
Reach out to discuss what Specialty1 Partners can do for your practice. Specialty1Partners.com.
29 endopracticeus.com Volume 16 Number 1 SPECIAL SECTION AAE SPECIAL SECTION
Visit Specialty1 Partners at AAE Booth Nos. 404 and 439
HighFive Healthcare A

t HighFive Healthcare, we’re passionate about the business of endodontics. That’s why we partner with endodontists who are equally passionate about helping their patients. With more than 60 years of healthcare experience, our diverse team of experts works hand in hand with our partners to streamline and optimize every aspect of practice operations — recruiting, payroll, human services, IT services, data security, customer relations, branding, marketing, and office expansion. We take care of the business of teeth so our partners have more time to focus on what they do best.
Our partnership contract is simple — take care of your patients, and we’ll handle the rest. After all, it’s your practice; we just help make it better, easier, and more fulfilling. Our unrivaled culture of fun and family puts you in the lead of a robust team of experts ready to support you and the goals you have, not just for your practice, but for your life. Whether you’re after increased revenue, a more efficient operation, a larger office footprint, more time to spend with your family
or the golf course, or all of the above, at HighFive Healthcare, we’re dedicated to helping our partners create their own tomorrow.

30 Endodontic Practice US Volume 16 Number 1 SPECIAL SECTION AAE SPECIAL SECTION
Visit HighFive Healthcare at AAE Booth No. 281
RECRUITING | HUMAN RESOURCES | PAYROLL | ACCOUNTING | BRANDING & MARKETING | IT SERVICES | AND MORE themonstertamers.com
While you’re trying to help patients,your business is trying to devour everything else.
IrriFlex ®

Flexible root canal irrigation needle


Successful root canal therapy relies on the combination of proper instrumentation and proper irrigation. Efficient cleaning and disinfection of complex root canal anatomy with a conventional metal needle is a challenge. In fact, the design of a metal needle faces the limits of required flexibility and effectiveness for modern endodontic procedures. Based on this, Produits Dentaires SA engineered and manufactured a unique irrigation needle with several new characteristics. IrriFlex® is the first 30G tapered-shape plastic needle with two back-to-back openings. Consequently, IrriFlex® is flexible and slides easily down to the bottom of the canal with no resistance despite variations in root canal anatomy. The two back-to-back side vents deliver balanced jets directly towards dentinal walls. The 4% conicity replicates the shape of instrumented canals and consequently maximizes shear forces during manual back-
and-forth irrigation. As a result, debris, smear layer, and bio-film are disorganized and removed. Thanks to the depth marks, the working length can be controlled. IrriFlex® is the new reference needle to deliver irrigation solutions successfully during root canal treatments. It is game changer.
For more information, visit www.pd-irriflex.com.

31 endopracticeus.com Volume 16 Number 1 SPECIAL SECTION AAE SPECIAL SECTION
Visit Produits Dentaires SA at AAE Booth No. 490 SMART PRODUCTS FOR ENDO LOVERS Depth marks Two side vents Flexibility *Offer valid from May 3 to 6, 2023, limited to the purchase of 4 boxes (REF 21401).
us at Booth N°490 during AAE and benefit from the offer
boxes of IrriFlex® GET 1 FREE ,
Flexible root
canal
irrigation needle IrriFlex® Visit
Buy 2
Quintessence Publishing




Evidence-based standards evolve as the literature changes, and practitioners must adapt their clinical practice accordingly. The second edition of this study guide, titled Endodontics Review, — known in some circles as “The Orange Book” — has been updated based on new peer-reviewed journal articles, position statements, and guidelines, and thus provides an up-to-date and comprehensive review of all the key topics in endodontics, from examination, diagnosis and prognosis, and treatment to follow-up care and complications. Radiographs of teeth before and after treatment illustrate common and uncommon situations, and dozens of helpful charts and diagrams distill the most essential information in a way that can be easily memorized. The extensive bibliographies in each chapter emphasize the most important literature for each topic and direct the reader to further sources. This is an indispensable study guide for all things endo!









32 Endodontic Practice US Volume 16 Number 1 SPECIAL SECTION AAE SPECIAL SECTION
Visit Quintessence Publishing at AAE Booth No. 238 www.quintpub.com Visit us at our booth and receive or order online with code BLICHER25 Discount offer valid May 3–5, 2023 THIS TITLE 25% OFF
3D Dental Surgical Microscope


Lightweight, fluid maneuverability, and heads-up 3D display make Seiler’s 3D dental surgical microscope a breeze to work with. Watch a seamless, magnified video image at 1080p and 60 frames per second with the fastest image processing available. With up to 28X magnification, unprecedented depth-of-field and German apochromatic lenses, it’s revolutionizing the way surgical microscopes are used worldwide. Optical instruments have been a Seiler family tradition since 1913. Seiler Instruments is a U.S. manufacturer based in America’s Heartland, St. Louis, Missouri. The Seiler Medical Division offers a wide variety of dental scopes for Enhanced General Dentistry and Endodontics and LED Surgical Loupes for applications needing low power magnification.
2X-24X MAGNIFICATION
SEAMLESS VIEWING AT 60 FPS
UNPRECEDENTED DEPTH OF FIELD
HEADS-UP 3D VIEW
NATURAL 3D IMAGE

NORMAL DEPTH PERCEPTION
NO EYEPIECES
HD VIDEO CAPTURE SYSTEM Come

33 endopracticeus.com Volume 16 Number 1 SPECIAL SECTION AAE SPECIAL SECTION
Visit Seiler at AAE Booth No. 611
visit us at AAE Booth 611 to see the 3D in action!
Dr.
Jenner Argueta DDS, M.Sc.
“When you’re looking for equipment that can sa�sfy the current requirements to prac�ce biologically safe Den�stry, it’s the perfect choice.”
(800) 489-2282 | www.seilermedical.com
Dr. Tuong Nguyen Nguyen BDS, MSD “It’s
going to project you way forward because of the ability to see and therefore to make very well informed decisions.”
The GentleWave ® G4 System
Beyond irrigation. Beyond clean.
TheGentleWave System takes you beyond canal complexity that can hinder thorough disinfection and debridement.

Inside the console, the irrigant is thoroughly degassed, precisely diluted, and continuously refreshed. Next, it enters the sealed, closed-loop delivery system, where the system’s physicsaccelerated chemistry becomes truly remarkable.
The GentleWave procedure is a more effective way of cleaning teeth, including hard-to-reach areas such as the apical thirds and complex anatomies of the root canal system:
• Predictably removes up to 99.9% of biofilm
• Effectively disinfects and debrides undetected and intri cate anatomies2,3
• 4X - 8.5X greater penetration into dentinal tubules v sus ultrasonic systems4
This can lead to better patient outcomes and deliver a more comfortable patient experience with reduced risk of complications:

• 96.6% of patients report mild to no pain within 48 hours5 of the procedure
• 97.7% 12-month healing rate6
• Preserves the structural integrity of the tooth
SPECIAL SECTION AAE SPECIAL SECTION
Test-drive a GentleWave G4
C M Y CM MY CY CMY K SSA-Half-Page-Ad-v4-Outlines.pdf 1 2/3/2023 1:10:37 PM
1. Zhang D, Shen Y, de la Fuente-Núñez C, Haapasalo M. In vitro evaluation by quantitative real-time PCR and culturing of the effectiveness of disinfection of multispecies biofilms in root canals by two irrigation systems.
system at AAE Booth No. 501
US Endo Partners
When you share ideas, foster a growth mindset, and pursue excellence as a team, success quickly follows. This is the spirit of US Endo – the Spirit of US.
“Partnering with US Endo is so much more than a great business opportunity. Our culture is about growth in every aspect of our lives – from improving our communication skills to leadership training, to advanced clinical training courses, and beyond. Being a part of US Endo offers the chance to become not only a better endodontist, but also a better boss, a better spouse, and a better friend. What we are building is unique; I’m truly thrilled to get to be a part of it,” says Dr. Jeremy Young, US Endo Partner and Specialized Dental Director of Partner Engagement.
When it’s time to talk, talk to the first-and-only Specialized DSO with proven financial results and a supportive, growthminded culture. Talk to US.

Visit US at booth No. 451 at AAE 23 in Chicago! You’ll find:


• Expanded lounge space to relax and connect with other top-tier endodontists;
• A barista-manned coffee bar featuring made-to-order drinks and other treats;
• Multiple charging stations to keep your tech gadgets performance-ready;
• Live recordings of season two of our successful podcast, “The Endo Files,” plus a chance to tell your story for a future special episode!
35 endopracticeus.com Volume 16 Number 1 SPECIAL SECTION AAE SPECIAL SECTION
Visit US Endo Partners at AAE Booth No. 451 US. US. Connect with usendopartners.com Reid Pullen, DDS, Brea Endodontics US Endo Partner and believer since 2020 Visit US @ Booth
US Endo EPUS_AAE 23.indd 1 2/3/2023 3:57:59 PM
#451
Visit ZEISS at AAE Booth 339 this year to get a sneak peek of the new ZEISS Surgical Cloud for EXTARO® 300.
Connect with our experts in person to learn how ZEISS microscopes can enhance your view and advance your practice.


We want to help find the best scope for you.

Experiencing the power of digital communication.
• Benefit from a digital workflow
• Easily educate your patients
• Demonstrate the value of your work
SPECIAL SECTION AAE SPECIAL SECTION
ZEISS EXTARO 300
® 300 from ZEISS
The integrated HD camera of the EXTARO records wirelessly to the ZEISS Connect App — empowering patient interaction and informed decisions with images and videos directly transferred to your local network
CAP-en-US_30_030_0190I © Carl Zeiss Meditec, Inc., 2023. All rights reserved.
ZEISS
Restoratively driven endodontic access and instrumentation
Dr. Gregori M. Kurtzman discusses preserving sound tooth structure and gaining endodontic access

The endodontic component of treatment
The accepted goal of dental treatment the elimination of all decay. When treating the tooth endodontically, an accepted goal is removal of all decay. Any decay that remains weakens the tooth, which can allow the remaining decay to progress over time, leading to structural failure of the tooth. But the goal of restoration of the tooth is to preserve as much sound tooth structure as is feasible.
Thus, endodontic treatment is restoratively driven. If insufficient tooth structure remains after endodontic treatment is completed, then the tooth is weak and structurally will not last in the long-term. Therefore, preservation of healthy tooth structure is important. So, conservative endodontic treatment begins with understanding the tooth’s anatomy and where the canal orifices lay within that anatomy allowing us to preserve tooth structure when locating and accessing the canals.1
Cervical tooth structure and its importance
Teeth when loaded under function have forces directed in the long-axis in posterior teeth in the maxilla and mandible. Maxillary incisors due to the angulation to the opposing teeth (tipped facially with contact on the lingual aspect of the tooth) have their loads off-axis to the tooth’s long-axis. With that in mind, whether posterior or anterior teeth, forces concentrate at the cervical of the tooth2 (Figure 1). Therefore, teeth with a weakened cervical region will have a higher failure rate and have decreased ability to manage those loads under function than teeth with intact cervical areas. Maintenance of this important region of the tooth structure is critical to long-term survival of those teeth.
Gregori M. Kurtzman, DDS, MAGD, FPFA, FACD, FIADFE, DICOI, DADIA, DIDIA, in private general dental practice in Silver Spring, Maryland, was a former Assistant Clinical Professor at University of Maryland in the department of Restorative Dentistry and Endodontics, and a former AAID Implant Maxi-Course assistant program director at Howard University College of Dentistry. He has lectured internationally on the topics of restorative dentistry, endodontics and implant surgery, removable and fixed prosthetics, and periodontics and has over 800 published articles globally, several ebooks, and textbook chapters. He has earned Fellowship in the AGD, American College of Dentists (ACD), International Congress of Oral Implantology (ICOI), Pierre Fauchard, ADI, Mastership in the AGD and ICOI, and Diplomat status in the ICOI, American Dental Implant Association (ADIA), and International Dental Implant Association (IDIA).
Disclosure: In the past, SS White has provided lecture support to Dr. Kurtzman.
Educational aims and objectives
This self-instructional course for dentists aims to review tooth anatomy and the location of canal orifices within that anatomy leading to the preservation of tooth structure when locating and accessing the canals.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions by taking the quiz online at endopracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
• Understand the importance of cervical tooth structure and realize the tooth’s ability to manage loads under function.

• Identify access to the pulp chamber to preserve tooth structure.
• Realize the benefit of a smaller orificedirected access. Recognize some approaches to gaining access to anterior teeth, premolars, and molars.
2 CE CREDITS
This is also important in instrumentation of the canals within the tooth and preserving as much cervical tooth structure as possible. Use of wider taper files (0.08-0.12 or greater) results in over-instrumentation of the canals by removing greater amounts of cervical tooth structure (Figure 2). So, selection of the ideal taper should be dependent on which tooth is being treated as well as the cervical size of the canal prior to treatment. Typically, in the majority of cases treated, finalization with a 0.06
37 endopracticeus.com Volume 16 Number 1 CONTINUING EDUCATION
Figure 1: Stresses are concentrated in the cervical area of the tooth, and key to preservation of the tooth following endodontic treatment is to preserve the cervical tooth structure. (Courtesy of Dr. Gene McCoy)
taper file is sufficient in palatal canals of maxillary molars, distal canals of mandibular molars, maxillary central incisors, and all canines. All other teeth and canals typically can be effectively instrumented with a final 0.04 taper file. There will be exceptions to this, but wider taper files should be reserved for those rare clinical circumstances where a very wide canal is noted during diagnosis radiographically.

Initializing access
When the tooth to be endodontically treated does not have a crown present, but direct restorative material (amalgam or composite) is present, that needs to be addressed to access the pulp chamber. The old restorative materials and decay are removed so that only the necessary tooth structure needed to unroof the pulp chamber and locate the canal orifices will require removal. This aids in visualization of the tooth structure overlying the pulp chamber especially when treating posterior teeth. Additionally, preserving the important native tooth structure will contribute to long-term survival of the tooth.

Teeth with an existing crown can be a challenge as the practitioner loses anatomical reference to where the pulp chamber is oriented in the tooth, which is especially true with posterior teeth. The tooth may have been rotated or tipped prior to placement of the crown. Therefore, the pulp chamber and canal orifices may not be positioned based on the anatomy of the crown. As the crown will often require replacement following endodontic treatment, removal of the majority of the occlusal aspects of the crown to expose the underlying tooth structure improves visibility to unroof the pulp chamber. This avoids “rooting” around in a limited access through the crown that may lead to perforation in an attempt to locate the canal orifices and pulp chamber. Should the existing crown not be planned for replacement, or if there will be a period of time before the patient can replace the crown following endodontic treatment, access through the crown will be needed with preservation of its structure, and an understanding of the tooth’s anatomy is important. Ceramic crowns, especially zirconia monolithic materials, have become the predominate crown material. Access through zirconia can be a frustration to many practitioners due to its hard structure.
Initial penetration through the zirconia is accomplished with a medium-grit round diamond (Great White® Zirconia (GWZ) diamonds, SS White, Lakewood, New Jersey) centered on the occlusal surface in posterior teeth or lingual surface on anterior teeth3 (Figure 3). The diamond is used with light pressure outlining the access shape appropriate to the tooth being treated, while irrigation from the handpiece is used. This can also be utilized on other ceramic materials. Should any core material be present under the crown, that should be carefully removed to improve visibility as this will avoid inadvertent straying when trying to unroof the pulp chamber.
Access shape
Traditional access in molars for example was taught for many decades due to a poor understanding of the importance of preservation of tooth structure especially in the cervical aspect of the tooth. This involved a flared access that essentially removed most of the coronal aspect of the tooth, leaving thin walls on the mesial, distal, buccal, and lingual (Figure 4 left). As the
understanding of the importance of preservation of coronal and cervical tooth structure improved, a more conservative access developed. This new access, termed “orifice directed” utilizes canal projection related to the coronal anatomy to preserve coronal tooth structure (Figure 4 right). Preservation of the lateral tooth structure is important as crown preparation will remove the lateral aspects of the tooth’s coronal and affect the ability to achieve restorative ferrule that can lead to restorative failure under loading.
Straight-line access into the canals in molars specifically in the past required the file to be vertical to enter the canal, which

38 Endodontic Practice US Volume 16 Number 1 CONTINUING EDUCATION
Figure 2: As instrument taper increases, greater degrees of tooth structure are removed cervically during endodontic instrumentation
Figure 3: When access is performed through an existing crown, a GWZ round diamond is used to make initial penetration through the crown, and then an access outline is created to allow the pulp chamber to be accessed
Figure 4: Traditional access in molars (left) required significant removal of cervical tooth structure weakening the tooth, where orifice-directed access (right) preserves tooth structure and allows straight line access into each canal
leads to removal of tooth structure. With a better understanding of canal projection, we see that as the canal approaches the pulp chamber, it actually leans to the opposite side of the tooth. This means that straight-line access into the distal canal in a mandibular molar for example, actually comes from the mesial side of the tooth and enters the mesial canals from the distal aspect of the tooth (Figure 5). With this in mind, a smaller orifice-directed access aids in coronal tooth structure preservation while allowing straight line access into the canals.

Anterior teeth

Access in anterior teeth has a potential problem when the anatomy is not well understood. Approach to the pulp chamber on the lingual at an angle can lead to perforation of the facial cervical in an attempt to locate the pulp chamber, which becomes more likely in older patients where some calcification of the pulp chamber has occurred (Figure 6). As the canal runs down the center of the root, access needs to be parallel to the long-axis of the tooth and is through the incisal edge to drop down into the chamber and canal (Figure 7).
Utilization of burs designed for orifice location are key to simplifying access, and how they are used prevents accidental perforation or transportation of the canal. EndoGuide® burs (SS White) are conical-shaped carbide tips on a long shaft available various shapes for either friction grip (FG) (highspeed) or latch pin (slowspeed) handpieces (Figure 8). While there are other similar burs, the unique shape of the cutting blade makes these burs unique in accomplishing tooth conservation, in the author’s opinion. The instrument allows precision guidance to and into the canal orifice while preserving tooth structure. With the anatomy in mind, the maxillary anterior access will be centered on the incisal edge (Figure 9 left) or slightly lingual to the incisal edge (Figure 9 right). Initial penetration into the tooth is made with standard carbide bur (330 or round) then continued with an appropriate EndoGuide bur or can be performed only with the




39 endopracticeus.com Volume 16 Number 1 CONTINUING EDUCATION
Figure 5: With an orifice-directed access due to the tooth’s anatomy, the distal canal is approached from the mesial, and the mesial canals are approached from the distal, minimizing how large the access needs to be
Figure 8: EndoGuide burs available in various size heads for latch pin (slowspeed) and friction grip (highspeed) usage
Figures 6 and 7: 6. When access is attempted in anterior teeth, approaching from the lingual perforation may occur through the tooth’s facial cervical while trying to locate the tooth’s canal. 7. In the maxillary incisors, access to the canal orifice is parallel to the tooth’s root through the tooth’s incisal edge to prevent accidental perforation and preserve cervical and coronal tooth structure
Figure 9: In the maxillary incisors, the canal orifice will lie either centered in the incisal edge (left) or just lingual to the incisal edge (right)
Figure 10: Access in the anterior teeth should be through the incisal edge in a straight line parallel to the tooth’s root to avoid possible perforation. Once access has allowed identification of the canal orifice, a hand file is used to establish glide path to WL
EndoGuide bur. An alternative to prevent bur run-off and ledging is to use the EndoGuide bur for the initial access preparation due to its self-centering micro tip. Once the canal orifice has been identified, a handfile is used to explore the canal to ensure a glide path to working length (WL) is present. Depending on the size of the canal, a No. 6, 8, 10, or 15 initial file may be required (Figure 10). Progressive handfiles are used until a size 20 hand file reaches working length (WL).

Mandibular incisors are similar anatomically to maxillary incisors with access made through the incisal edge as this overlies the canal orifice and permits straight-line access to the canal (Figure 11). Ethnic variances should be considered as it has been reported that a percentage of the Asian4 and Middle Eastern5 population present with two canals in the mandibular incisors (Figure 12). These may converge into a single canal in the apical portion of the root but will require instrumentation of both canals in the coronal portion of the root.
Premolars
Maxillary and mandibular premolars may present with one or two canals. When initiating endodontic access on a premolar, access is made at the center of the tooth into the pulp chamber. When a single canal is present, it will lie centered in the tooth (Figures 13 and 14 left). Should this not be identifiable; two canals may be present, and access needs to be expanded

towards the cusp tips as the canal orifice will lie under where the cusp tip would be present (Figure 14 right). If the orifice cannot be identified, use of transillumination of the tooth by placement of a dedicated transilluminator on the buccal or lingual tooth may be necessary (Figure 15). In the absence of a transilluminator, a fiber optic handpiece may be used. Without a bur in the handpiece, place the head where the fiberoptic lights are on the tooth, and press the rheostat (foot pedal). The orifice will appear as a dark spot when the tooth is transilluminated.
Another consideration is when radiographically the canal disappears in the apical half of the premolars root and is prominent in the coronal aspect. This indicates that the canal has divided into two canals (Figure 16). Exploration with small handfiles along the buccal or lingual portion of the identifiable canal will allow a glide path to the two narrow canals to WL.
Molars
Maxillary and mandibular molars differ in how many roots and canals they have but are approached in a similar manner. As molars predominantly have been previously restored, they may have restorative material or a crown present. Following access as previously described, the orifices are identified. Should the EndoGuide bur be used, it is important that it should not be advanced into the orifice further than its head length to avoid the potential for transportation of the canal or perforation of the root



40 Endodontic Practice US Volume 16 Number 1 CONTINUING EDUCATION
Figure 11: In the mandibular incisors, the canal orifice will lie under the incisal edge, and access should be straight line through the incisal edge
Figure 12: In the mandibular anterior teeth, a majority of the time a single canal is present which lies under the incisal edge or just lingual to it (left), but in some patients, a second canal is present that is under the cingulum (right) and needs to be considered possible in some patient populations
Figures 13 and 14: 13. With regard to premolars, when the canal orifice is centered buccal lingually, this indicates a single canal in the root, and if not, there are two canals present, and access needs to be expanded buccal lingually to identify the canal orifices that typically in these cases lie under the two cusp tips. 14. An example of a premolar with a single canal with the orifice centered buccal lingually (left), and when two canals are present, the orifice lies under the cusp tips (right)
Figure 15: Transillumination of the tooth to aid in identifying the canal orifice is performed by placement of a light source on the buccal or lingual tooth structure
Figures 16 and 17: 16. With regard to premolars, when the canal disappears at mid root radiographically, this typically indicates the canal has split into two separate canals. 17. When using the EndoGuide bur for canal access, it is important to not place the bur into the canal further than the head to avoid possible canal transportation or perforation
(Figure 17). The bur is also used to remove any overhang of the chamber’s walls that may hamper file insertion into the canal.
Anatomically, the pulp chamber in maxillary molars lies more over the buccal half of the tooth (Figure 18). Identification of the canal orifices in these teeth is aided as a darker line can be observed on the chamber floor connecting the mesial, distal, and palatal orifices. When a mesial buccal 2 (MB2) is present, this will lay along a line between the mesial and palatal orifices requiring additional removal of tooth structure to access it. The MB1 should lie under the MB cusp tip, and if it does not, the MB2 may have to be identified, and further extension to the MB cusp is needed to MB1.
Mandibular molars typically present with three canals, with a single canal on the distal with the orifice centered between the buccal and lingual (Figure 19 left). Should the distal orifice not be centered on the distal, a second distal canal should be suspected, and extension of the access needs to be widened buccal-lingually to find the other orifice (Figure 19 right). If two distal canal orifices are identified, these may be two separate canals, or they may converge as they progress apically.
Completing instrumentation
Figure 18: The canal orifices in a maxillary molar are typically under the mesial half of the coronal portion of the tooth, and this needs to be considered during access for endodontic treatment. When a MB2 is present, it will be located palatally to MB1 under the marginal ridge portion of the tooth


Following access to the pulp chamber and identification of the canal orifices in any tooth, the canal is explored to WL with hand files to establish a glide path. Once WL has been established, rotary files such as the DCTaperH™ or ExactTaperH DC™ (SS White) are utilized to instrument the canal (Figure 20). First a size 17 file in the appropriate taper (canal and tooth dependent) is taken to WL, which is followed by a size 20, and then 25 file. Completion of instrumentation will be dependent on the tooth being treated with preservation of cervical tooth structure as the treatment goal. Following these guidelines, critical cervical tooth structure has been preserved, and the tooth is ready for obturation.
Conclusion
Figure 19: Most mandibular molars have three canals with a single distal canal (left) but some may present with two distal canal orifices (right) that may be two separate canals or converge in the root to a single distal canal
The practitioner may be able to find, instrument, and obturate the canals in the tooth, but if tooth structure is not preserved especially in the cervical area where the majority of functional loading occurs, long-term survival of the tooth is questionable. A conservative approach to endodontics that is restoratively driven aids in preservation of tooth structure that cannot be replicated with restorative materials. Instruments utilized to access the canal orifice play an important factor, as well as the taper to which the canals are instrumented so that critical cervical tooth is preserved.

References
1. Tang W, Wu Y, Smales RJ. Identifying and reducing risks for potential fractures in endodontically treated teeth. J Endod. 2010 Apr;36(4):609-617.

2. McCoy G. Occlusion confusion. Gen Dent. 2013 Jan-Feb;61(1):69-75; quiz 76.
3. Kurtzman G. Solving Ceramic Crown Removal and Endo Access Challenges. Dentistry Today. December 1, 2020. https://www.dentistrytoday.com/solving-ceramic-crownremoval-and-endo-access-challenges/. Accessed February 10, 2023.
4. Usha G, Muddappa SC, Venkitachalam R, Singh V P P, Rajan RR, Ravi AB. Variations in root canal morphology of permanent incisors and canines among Asian population: A systematic review and meta-analysis. J Oral Biosci. 2021 Dec;63(4):337-350.
5. Rahimi S, Milani AS, Shahi S, Sergiz Y, Nezafati S, Lotfi M. Prevalence of two root canals in human mandibular anterior teeth in an Iranian population. Indian J Dent Res. 2013 Mar-Apr;24(2):234-236.

41 endopracticeus.com Volume 16 Number 1 CONTINUING EDUCATION
EP
Figure 20: Sequence of exploration and instrumentation of the canal following identification of the canal orifice
Continuing Education Quiz
Restoratively driven endodontic access and instrumentation KURTZMAN
1. Teeth with a weakened cervical region will have ________ under function than teeth with intact cervical areas.
a. a higher failure rate
b. decreased ability to manage those loads
c. a lower failure rate
d. both a and b
2. Typically, in the majority of cases treated, finalization with a taper file is sufficient in palatal canals of maxillary molars, distal canals of mandibular molars, maxillary central incisors, and all canines.
a. 0.06
b. 0.08
c. 0.10
d. 0.12
3. ___________ can be a challenge as the practitioner loses anatomical reference to where the pulp chamber is oriented in the tooth, which is especially true with posterior teeth.
a. Teeth with no crown present
b. Teeth with an existing crown
c. Teeth with fillings
d. Incisors
4. (In the case of a Zirconia crown) Initial penetration through the zirconia is accomplished with a medium-grit ________ centered on the occlusal surface in posterior teeth or lingual surface on anterior teeth.
a. football-shaped diamond
b. bulk carbide
c. round diamond
d. straight-flat carbide
5. Traditional access in molars for many decades involved a flared access that essentially removed most of the coronal aspect of the tooth, leaving thin walls on the _________ and lingual.
a. mesial
b. distal
c. buccal
d. all of the above
6. This new access, termed utilizes canal projection related to the coronal anatomy to preserve coronal tooth structure.
a. “orifice directed”
b. “conservative focused”
c. “preservation centric”
d. “straight-line access”
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 16 CE credits for only $149; call 866-579-9496, or visit https://endopracticeus.com/ subscribe/ to subscribe today.
n To receive credit: Go online to https://endopracticeus.com/continuingeducation/, click on the article, then click on the take quiz button, and enter your test answers.
AGD Code: 070
Date Published: March 22, 2023
Expiration Date: March 22, 2026
2 CE CREDITS
7. (In anterior teeth) Approach to the pulp chamber on the lingual at an angle can lead to perforation of the facial cervical in an attempt to locate the pulp chamber, which becomes more likely in older patients where some calcification of the pulp chamber has occurred.
a. True
b. False
8. Ethnic variances should be considered as it has been reported that a percentage of the Asian and Middle Eastern population present with ______ in the mandibular incisors.
a. one canal
b. two canals
c. three canals
d. four canals
9. When initiating endodontic access on a premolar, access is made _______ into the pulp chamber.
a. on the lingual side of the tooth
b. on the buccal side of the tooth
c. at the center of the tooth
d. on the incisal edge of the tooth
10. The practitioner may be able to find, instrument, and obturate the canals in the tooth, but if tooth structure is not preserved, especially _______, long-term survival of the tooth is questionable.
a. on the coronal portion of the tooth
b. in the cervical area where the majority of functional loading occurs
c. in teeth with four canals
d. in maxillary molars
To provide feedback on CE, please email us at education@medmarkmedia.com
Legal disclaimer: Course expires 3 years from date of publication. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
42 Endodontic Practice US Volume 16 Number 1 CONTINUING EDUCATION
The importance of maintaining indoor air quality in dentistry



Drs. Tyler Orehek and Troy Roeder discuss the reasons for maintaining diligent air quality standards in the office
Three years into the Covid-19 pandemic, most industries and professions have undergone significant long-term changes. As more Americans resume their lives, each with a different definition of normalcy, all industries must adapt. New safety protocols, guidance, and equipment are the bare necessities for those looking to thrive in a post-pandemic world.
The dental industry is no stranger to these changes. A report from the National Library of Medicine explored how the industry must adapt to the challenges presented by the pandemic, namely through masking, sanitizing, and most importantly, indoor air purification.1 The prevalence of SARS-CoV-2, a highly contagious airborne virus, means that indoor air purification is crucial in any dental space. This is critical not only for patients who are unable to mask during cleanings and procedures, but for the dentists, hygienists, assistants, and office staff who spend hours of their days in these environments.
For dental offices, simply masking is not enough. During dental treatments, aerosols that may contain blood, saliva, oronasal secretions, microorganisms, filling particles, and tooth particles, are produced. Aerosols are created and spread through the air as a result of various devices used such as turbine handpieces, ultrasonic scalers, air and water syringes, polishing procedures, and surgical lasers. Given that most dental treatments involve the use of many of these instruments, the potential for viruses and infections to spread throughout a dental space is incredibly high.
Tyler Orehek, DC, MSc, CIEC, began his professional career in 2003, and he owned and operated a multidisciplinary practice in midtown Manhattan, serving as the primarycare physician and portal-of-entry healthcare practitioner, with a special emphasis on the treatment of pulmonary and neuromusculoskeletal conditions. Dr. Orehek has been an indoor air quality specialist since 2007. He is also a Council-Certified Indoor Environmental Consultant (CIEC), board-awarded by the American Council for Accredited Certification (ACAC).
Troy Roeder, DDS, is a general dentistry practitioner with over 30 years of experience based in Moline, Illinois. Dr. Roeder attended The University of Iowa, with studies in Biology and Chemistry, before completing his dental training at The University of Iowa College of Dentistry. Dr. Roeder’s dental practice provides both general and cosmetic dental treatments as well as orthodontics for teens and adults.
Disclosure: Dr. Orehek is the President of Airgle Corp., and Dr. Roeder employs Airgle air purification units at his dental practice.
Educational aims and objectives
This self-instructional course for dentists aims to discuss the importance of maintaining indoor air quality in dentistry.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions by taking the quiz online at endopracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can: Identify the primary causes of airborne pathogens in dentistry.
• Recognize the role that dental tools play in spreading aerosols and airborne pathogens.
• View the most effective tools to combat aerosols and airborne pathogens.
• Identify various strategies that can be put in place to maintain air quality.
• Observe how air purification units work to eliminate aerosols and airborne pathogens.
2 CE CREDITS
A recent study demonstrated that saliva may have a significant role in the virus’ ability to spread through airborne transmission.2 A patient infected in the early stages of COVID-19, potentially before they’re even aware of the infection, could have high viral loads in their saliva, and cases with multiple symptoms often
43 endopracticeus.com Volume 16 Number 1 CONTINUING EDUCATION
correlate with higher viral loads. These viruses can spread very far, quickly, and remain suspended in the air for very long periods of time.
Asymptomatic patients are also at risk of spreading high viral loads, as many can be unaware of their asymptomatic infection. Respiratory droplets are produced quickly, and heavier droplets can spread within 6 feet of the source in seconds. However, coughing and sneezing can produce even smaller droplets, which can linger in the air up to 20 feet from the source, hours after initially being produced and creating a hazardous environment for patients and dentists.3 Additionally, HVAC systems with poor specifications and efficiency can further contribute to the spread of such droplets.
Furthermore, dentists work in small, tight rooms, making it easy for infections to spread. This has forced the industry to become leaders in infection control in the past, and a similar opportunity presented itself over the past few years during the COVID-19 pandemic.
The pandemic forced dental practices to close for months in March 2020, providing yet another opportunity for the industry to reassess how to improve indoor air quality. For example, while high-volume evacuation (HVE) equipment is effective in sucking up aerosols, the smallest viral particles will often be able to escape, necessitating a more comprehensive solution. Alternative methods are required to improve air quality in dental offices, while also reducing the spread of airborne particles. The following are a few examples of the ways that the dental industry can prioritize indoor air quality, creating a safer environment for patients and practitioners alike.
Negative pressure rooms
One option for practices is to convert operatories into “negative pressure rooms,” which are typically found in hospitals. Designed to combat airborne infections, negative pressure rooms ideally undergo between six to 12 air changes per hour (ACH) and must have air pressure that is lower than the external air pressure. However, while negative pressure rooms protect those outside of the room, they do not provide additional protection to those inside. Additionally, this is a costly conversion, and out of reach for many practices.
HVAC and filtration
Another option is to modify existing HVAC systems, such as through adding high efficiency particulate air (HEPA) filtration. Unfortunately, older HVAC systems often use rudimentary filter stages and are also incapable of sustaining adequate air exchange. These systems are not as robust nor efficient in exchanging air as compared to stand-alone, medical-grade air purifiers, and the difference can be critical. One way to modify these systems is by incorporating UV light into existing HVAC systems, which works if microorganisms are consistently exposed to the UV light. However, this is far from a guarantee, and the modifications can be costly.
Oftentimes, HVAC systems are set to “auto” mode, which adversely affects indoor air quality as it turns off from time to time. This allows contaminants to remain in the air for longer periods of time. By switching the setting to “on,” HVAC systems can work more effectively, relatively speaking, by promoting constant air flow.
Medical grade air purification units
Ultimately, air purifiers are one of the most effective ways to improve indoor air quality. However, the quality and specifications are critical to examine when determining the kind of professional-grade air purifier to implement. While consumer-grade air purifiers are more economical, allowing numerous units to be installed throughout a practice, they are typically less effective than medical-grade air purification systems for a host of reasons. Lesser systems are often underpowered and have smaller cubic feet per minute (CFM) ratings compared to medical-grade purifiers. CFM represents how much air can be drawn into a system per minute. Dental operatories necessitate high CFM to be truly impactful. Additionally, consumer-grade purifiers cannot provide high ACH as compared to medical-grade systems. Lastly, many do not remove ultra-fine particles as small as the SARSCoV-2 virus, which is incredibly small, with an average diameter of only 0.1 microns.
High efficiency, medical-grade air purification systems are one of the most effective ways to combat this issue. Standalone, medical-grade air purification systems are far more effective than HVAC systems in filtering out pollutants as well as airborne viruses, bacteria, and mold. Medical-grade purifiers have the highest rate of CFM, meaning they purify more of the air in the same amount of time as compared to other methods of purification. This helps mitigate the potential risk of transmission between doctors, patients, and other staff. Medical-grade purifiers effectively draw aerosolized particles away from operatories and trap them within its filter media. Studies have found that exposure to droplets and contaminants dropped 80% to 95% when air purifiers were used in dental offices.4
Air purification systems must be engineered to combat airborne pathogens (including CoV-2), ultra-fine particulates, and volatile organic compounds (VOCs). For example, Airgle air purification systems utilize a cleanroom-grade cHEPA filter with a capture threshold down to 0.003 microns, which is 100 times more discriminating than traditional HEPA, to capture the smallest of ultra-fine airborne particulates and microbial con-
44 Endodontic Practice US Volume 16 Number 1 CONTINUING EDUCATION
Air purification systems are the only solutions that have discriminating enough filtration, the necessary CFM of delivered air, and the vitally important air changes per hour, resulting in the cleanest possible air in the shortest amount of time.
taminants. Medical-grade purifiers also have more adept cubic feet per minute (CFM), a critical consideration for dental practices. As aerosols linger and remain suspended in operatories for longer periods of time, the risk for cross-contamination can increase exponentially.

An air purifier’s ability to contain airborne contaminants such as pathogens and mold, in addition to volatile organic compounds and ultra-fine particulates, is primarily determined by the type of filter used. An air purification system’s effectiveness is largely correlated to the quality, specifications, and integrity of the purification filter media used within a system.
Putting it into practice
When treating patients, it is critical to keep operating rooms as clean and safe as possible, with a focus on removing aerosols. Installing two medical-grade air purification systems, one at each side of the chair in the main operating room, can ensure a
healthy and safe space for patients. These units also incorporate germicidal UV lights and a high number of air changes per hour, ensuring that rooms are as clean and safe as possible for patients and staff.
While it was standard operating procedure to employ standard screening questions and take patient and staff temperatures when re-opening, patients were looking for more preventative measures. They wanted assurances that every action possible was being taken to make the air safe to breathe. Employing air purification units that filter out the smallest particles gave patients peace of mind when visiting the dental office. In fact, it would serve patients well to have high quality air purifiers in their own home and workplace.
Four main takeaways to highlight, both from personal experience and published studies on the matter:
1. The pandemic is here to stay. Americans are starting to return to their pre-pandemic lives, and many are looking for assurance that they’ll be safe from being exposed to CoV-2 when doing so.
2. Dental practices have a unique challenge. Operating rooms are small, tight areas, where potentially hazardous aerosols can linger for hours if not properly purified and ventilated. This is why dental practices are consistently leaders in public safety.
3. Not all methods of air purification are equal. HVAC systems are effective, but are often unable to combat the smallest of airborne particles like SARS-CoV-2. Consumer-grade air purification systems can be economical, but frequently do not possess the more discriminating filter media, nor the necessary CFM and ACH rates required to keep operatories as safe as possible. Negative pressure room conversions are also an option, but are often too costly for the average dental office to afford.
4. Medical-grade air purifiers are imperative. Air purification systems are the only solutions that have discriminating enough filtration, the necessary CFM of delivered air, and the vitally important air changes per hour, resulting in the cleanest possible air in the shortest amount of time. Purifiers are the most appropriate approach for targeting and capturing the SARS-CoV-2 virus.
The time is now for dental offices to make adjustments if they have not done so already, and medical-grade air purification is the best way to ensure safety for dentists and patients alike.
REFERENCES
45 endopracticeus.com Volume 16 Number 1 CONTINUING EDUCATION
1. Ancuta G, Sandu D, Tatarciuc M, Luchian I. The Impact of the COVID-19 Pandemic on Dentistry and Dental Education: A Narrative Review. Int J Environ Res Public Health. 2022 Mar; 19(5):2537.
2. Carrouel F, Gadea E, Esparcieux A, Dimet J, Langlois ME, Perrier H, Dussart C, Bourgeois D. Saliva Quantification of SARS-CoV-2 in Real-Time PCR From Asymptomatic or Mild COVID-19 Adults. Front Microbiol. 2021; 12:786042.
3. Xie X, Li Y, Sun H, Liu L. Exhaled droplets due to talking and coughing. J R Soc Interface. 2009 Dec 6;6 Suppl 6(Suppl 6):S703-714.
EP
4. Chen C, Zhao B, Cui W, Dong L, An N, Ouyang X. The effectiveness of an air cleaner in controlling droplet/aerosol particle dispersion emitted from a patient’s mouth in the indoor environment of dental clinics. J R Soc Interface. 2010 Jul 6;7(48):1105-1118.
Operating rooms are small, tight areas, where potentially hazardous aerosols can linger for hours if not properly purified and ventilated.
Continuing Education Quiz
The importance of maintaining indoor air quality in dentistry
OREHEK/ROEDER
1. A report from the National Library of Medicine explored how the industry must adapt to the challenges presented by the pandemic, through ________.
a. masking
b. sanitizing
c. indoor air purification
d. all of the above
2. During dental treatments, aerosols that may contain __________, microorganisms, filling particles, and tooth particles are produced.
a. blood
b. saliva
c. oronasal secretions
d. all of the above
3. Aerosols are created and spread through the air as a result of various devices used such as turbine handpieces, ultrasonic scalers, air and water syringes, polishing procedures, and surgical lasers.
a. True
b. False
4. Respiratory droplets are produced quickly, and heavier droplets can spread within ________ of the source in seconds.
a. 6 feet
b. 10 feet
c. 12 feet
d. 14 feet
5. However, coughing and sneezing can produce even smaller droplets, which can linger in the air up to _________ from the source, hours after initially being produced and creating a hazardous environment for patients and dentists.
a. 20 feet
b. 30 feet
c. 35 feet
d. 40 feet
6. Designed to combat airborne infections, _____________ ideally undergo between six to 12 air changes per hour (ACH) and must have air pressure that is lower than the external air pressure.
a. positive pressure rooms
b. negative pressure rooms
c. high particulate rooms
d. auto-mode HVAC rooms
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 16 CE credits for only $149; call 866-579-9496, or visit https://endopracticeus.com/ subscribe/ to subscribe today.
n To receive credit: Go online to https://endopracticeus.com/continuingeducation/, click on the article, then click on the take quiz button, and enter your test answers.
AGD Code: 130
Date Published: March 22, 2023
Expiration Date: March 22, 2026
2 CE CREDITS
7. By switching the setting to ______, HVAC systems can work more effectively, relatively speaking, by promoting constant air flow.
a. “on”
b. “off”
c. “auto”
d “professional”
8. ___________ represents how much air can be drawn into a system per minute.
a. Pressure per minute (PPM)
b. High-volume evacuation per minute (HVEM)
c. Cubic feet per minute (CFM)
d. none of the above
9. Standalone, medical-grade air purification systems are far more effective than HVAC systems in filtering out pollutants as well as _________.
a. airborne viruses
b. bacteria
c. mold
d. all of the above
10. Studies have found that exposure to droplets and contaminants dropped when air purifiers were used in dental offices.
a. 25%-34%
b. 46%-53%
c. 65%-76%
d. 80%-95%
To provide feedback on CE, please email us at education@medmarkmedia.com
Legal disclaimer: Course expires 3 years from date of publication. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
46 Endodontic Practice US Volume 16 Number 1 CONTINUING EDUCATION













Sailing into practice ownership

Dr. Albert (Ace) Goerig discusses several ways to navigate practice ownership

Few things in life are as satisfying as home ownership, and the same is true for owning your “practice home.” The professional independence, economic self-sufficiency, and ability to achieve your vision are tremendously gratifying. Doctors currently seeking practice ownership typically include:
• Recently graduated from endodontic residency
• Exiting from an associate or employment environment
• Starting private practice after military or public service
• Making a long-distance move to a new city
Your comfort level with the ownership process usually depends on any past experience in private practice. Endodontic graduates who completed their residency immediately after dental school have both limited clinical experience and business experience in the real world, so they often have the highest perception of risk. Other doctors have previous clinical experience and sometimes previous business experience too.
Either way, it is common for doctors to have concern about risk because becoming a practice owner is a big investment in your long-term future. Here are some guidelines that can ease the process and ensure you’re making good decisions now that will set you up for the best success as a practice owner.
Economic realities
Most doctors begin their practice ownership journey already burdened by a high level of debt, particularly lingering education debt, but possibly a mortgage too if they are a homeowner already. A lender is going to look at your current debt obligations and living expenses compared to your potential income as a practice owner. The gap between the two effectively defines your available funding for ownership (unless you have other sources, such as family contributions).
Your current debt is a given, so your cost of living and income potential as a practice owner are the variables that really matter. Keep your living costs modest, minimized, and avoid unneces-
Albert Goerig, DDS, MS, is a Diplomate of the American Board of Endodontics and a sought-after speaker who has lectured extensively on the field of endodontics and practice success throughout the United States, Canada, and abroad. He is the author of more than 100 published articles and contributing author to numerous endodontic textbooks. Dr. Goerig has a private endodontic practice in Olympia, Washington, in the top 1% nationwide for practice profitability. He has almost 40 years of experience as an endodontic educator and practice coach to over 1,000 endodontists. www.endomastery.com | 1-800-482-7563 | info@endomastery.com
sary consumer debt (including expensive cars). As far as income potential, lenders are going to look at endodontic industry averages at best, which are lower than you would expect.
Whatever funding you are able to get is going to highly influence your path to practice ownership. Average solo doctor endodontic practices often sell for $600,000 to $900,000, which is a significant investment. Alternatively, you can go for a startup approach, which is notably less expensive but lacks the built-in goodwill and referral network you get by buying out a practice. If neither of these options work for you, you will need to reduce your debt and save for your ownership path. For many doctors, that means working as an associate first.
Associate pathways
Because of high current debt and uncertainty about risk, many doctors work as an associate before venturing to practice ownership. How soon you can move from an associate environment to ownership depends a lot on the associate position that you accept. If you associate in a practice that is motivated by growth and enables you to be highly productive, you can significantly reduce your debt and save for practice ownership within a few years.
If, however, you end up associating in a practice which is not providing you enough productivity, you may be spinning your wheels. Yes, you might be earning enough to make your debt payments and cost of living each month, but that’s not enough to effectively prepare for ownership. If your goal is practice ownership, the reason you are associating is to make money. Staying in a practice that is limiting you economically is self-defeating.
As a general guideline, if you are completing less cases as an associate than the average endodontist (at least 3 to 4 cases per day), you should consider looking around for a better situation in a practice that is highly efficient and has a better referral network. A full-time associate should reasonably expect more than
48 Endodontic Practice US Volume 16 Number 1 PRACTICE MANAGEMENT
part-time productivity! The good news is that endo associates are in high demand, and it’s easy to find better opportunities in highly successful practices where you can excel as an associate and earn far more income. One more case a day on average can make the difference of as much as $100,000 income in a year.
Acquisition versus startup versus transition
There are basically only three paths into practice ownership. The first path is acquisition where you buy out a doctor who is exiting their practice. Buyouts are usually 70% or more of the exiting doctor’s annual revenues, and most of that value is in the referral network goodwill. The exiting doctor usually stays for a short time (usually 6 months to a year) to coordinate your introduction to the referral network so you earn the right to their continued referrals and transfer as much goodwill as possible.
• Advantage: existing referral network and potential initial cash flow
• Disadvantage: most expensive upfront investment cost
The second approach is a new practice startup. A startup is exactly that: opening a brand-new practice in a new location and building everything from the ground up, including a referral network. Associates in most states who open startups usually have to locate outside the referral draw area of the practice they are associating in due to restrictive covenants, which is a good reason to avoid associating in the community you want to end up in.
• Advantage: less expensive (save half or more compared to acquisition)
• Disadvantage: zero revenues on Day 1 of ownership
The third approach is through an associate transition, which is when you start as an associate in the practice and eventually (in about 5 years typically) buy in to become a partner or buy out an exiting doctor. The agreement in principle for the transition is usually determined upfront as part of associateship engagement, depending on a trial period to ensure there is a good match in the case of an eventual partnership. Sometimes those partnerships are time-limited, with the senior doctor retiring well before you, and you have the right to buy out their final equity.
• Advantage: earn income now and prove your potential in the practice you will own
• Disadvantages: delayed approach, and being the “junior” if in an eventual partnership
Location and facility
In terms of location, I strongly recommend that you carefully select the community that your practice is located in. Ownership puts down roots that are hard to change, and you want to practice as near as possible to where you want to live and enjoy life with your family on a long-term basis. Commuting is a huge time loss in life, so think about where you want to be in your 30s, 40s, and 50s, and how quickly and easily you can get to work. The ultimate goal is to have a great life with endodontics as your professional and financial foundation.
In terms of facility, this is one area where less is more at the beginning. We all graduate into dentistry with our “dream practice” in our minds, and that is a great vision to work toward. However, it’s probably not going to be your first step into prac-
tice ownership. You need to maximize income and minimize expenses, so don’t “over buy” what you need to get established. Prioritize for early profitability, which can mean equipping a startup practice with second-hand equipment to save on upfront costs. When you are buying an existing practice, of course, everything is already second-hand.
The key to remember is that even though your path to ownership is financially limited by what lenders believe you can safely earn, your actual income potential as an endodontist is far higher. Doctors in Endo Mastery-coached practices typically earn 2 to 3 times the average endodontist within a few years, and that includes new owners in recent startups and acquisitions. When you achieve that level of success, you’ll quickly pay off all your debt and then easily afford building or moving to your dream facility.
Productivity and profitability
The level of productivity and profitability that you will achieve in your practice is directly linked to the performance of the team and the effectiveness of practice systems. Acquisition doctors tend to assume that the practice’s current team and systems are adequate. Startup doctors tend to assume that they (or someone on their newly hired team) will train and set up their systems once the practice is open. Both of these assumptions are mindsets that should be challenged.
Notwithstanding the fact that we are all quite brilliant as doctors, we are not taught the nuts and bolts of business ownership in dental school or residency. We are not taught the most efficient and effective marketing techniques, scheduling strategies, or financial systems for our offices. Most doctors try to learn it by the seat of their pants, and that’s why most endodontic practices significantly underperform their potential and cause stress for the doctor.
At Endo Mastery, we strive for doctors to achieve “effortless endodontics” in their practices, which means an optimized and empowered approach to teamwork, practice systems, and doctor productivity. Endo Mastery-coached doctors can achieve multiples higher than the average endodontist because they’ve invested in creating a stress-free but growth-driven business, driven by a highly-trained and motivated team.
Coaching for business success is just like any other advisor that you rely on as a new practice owner, such as your lawyer or accountant. If you’re serious about success as a practice owner, it’s a vital component to your journey that you should be building into your strategic plan from the beginning. That’s especially true in the current employment environment where it is so difficult to hire experienced team members.
Risk and reward
I started this article talking about the perception of risk, and certainly there are vital decisions that you make on the way to practice ownership that affect your future. However, the rewards of ownership make it all worthwhile. None of the issues you face are unsolvable, and navigating the initial concerns of debt and finances is the most difficult part. With vision, ingenuity, and coaching, you can find the right path and establish a practice that will drive incredible future success. EP
49 endopracticeus.com Volume 16 Number 1 PRACTICE MANAGEMENT
Building a team of Rock Stars

Dr. Garth Hatch covers essential elements for a practice that runs in perfect harmony
Have you ever wondered what your average day would look like at the clinic if your entire team functioned like a well-trained, motivated team of Navy Seals (with smiles on their faces)? This image may not be what you would imagine for a team of endodontic dental professionals, but the idea of having a team where everyone is clear on the practice mission, understands their essential role in the success of the team, and can execute at a high-level sounds amazing. This quality of a team is achievable yet doesn’t happen by accident. It only happens with systems in place that begin with hiring the right team members that align with your practice vision, train them on their essential role and responsibilities so they understand what success looks like, continue to monitor their progress, make friendly course corrections as needed, and then hold them accountable for their performance.
For our office, we integrated the theme of training Rock Stars that are well trained at their job, see the vision of the practice which is emphasized during the hiring and training phase, and can turn on the shine when it’s show time in front of our patients. We also borrowed the Disney theme for our team members of being “On-Stage” meaning they are in front of the public versus “Off-Stage” when they are behind the scenes in the breakroom, etc. This has helped remind all of us that despite what may be going on in our lives outside of the clinic, when it’s show-time, and we are on-stage with our patients and referring offices, we need to perform like rock stars. To accomplish this level of team, three things are critical to achieve this: hiring right, training, and monitoring progress. Let’s briefly cover each of these and then review essentials for Rock Star team members.
Hiring right
Hiring team members that are a good fit for the practice is critical to achieving a Rock Star team. All the training in the world won’t fix a person that isn’t aligned with the practice vision, has a negative attitude, or doesn’t “play well with others.”
When we hire new team members, our top priority is assessing their people skills, customer service ability, and whether they are team players. Some of our best team members had little to no dental experience when we hired them, and we’ve learned that most other skills can be trained on the job. We have at least three separate interactions with a new hire that includes an interview with our office manager or lead assistant, an interview with the doctor, and a “working interview” where they come to work for 1-2 hours and just interact with the team in a more casual way. Lots of discussions come up with the other team members that can solidify our desire to hire them or also notice red flags that we may want to keep looking for someone else. As my mentor Ace Georig would say, “Hire slow and fire fast.”
Training
Garth Hatch, DDS, is an endodontist who founded a multidoctor private specialty practice with locations in Kennewick and Yakima Washington. He is passionate about building strong teams, loyal dual-benefiting referral relationships, and creating happy patient experiences. He received his DDS at Indiana University School of Dentistry, an AEGD-1 at Fort Jackson South Carolina and a Certificate in Endodontics from the U.S. Army Endodontics Residency Program, Fort Gordon. He loves his family, faith, fitness, fun, freedom and flying (travel). He can be reached at garth@ourcre.com.
How are businesses like Ritz Carlton, Nordstrom, and Zappos so legendary in the customer service realm? Primarily from hiring well and training, training, and more training. According to Joseph Michelli, PhD, Ritz Carlton provides at least 250 hours of training to new employees in the first year alone. As business owners, we often expect our employees to do or say things we would do or say, but unless we have trained them specifically in these areas, we can only blame ourselves for less-than-ideal performance. Training is a continuous process that never ends and should be reviewed at least monthly and annually. We’ve tried various training times and methods but currently we do several days of onboarding training upfront with new hires and team training twice a month and one annual retreat training session. There’s no perfect way for each office to train team members, but you must establish and maintain a training process, or you likely won’t be happy with the unsaid training that is taking place.

50 Endodontic Practice US Volume 16 Number 1 PRACTICE DEVELOPMENT
Monitor progress
After hiring well and training your team, the next step is to monitor progress. This should be a continual process both formally and informally. Formally, we have annual reviews with our team members and provide goals for improvement that are established with both the team member and the office manager and or doctor. We also discuss issues and make corrections during our team meetings to try and fix performance that isn’t in alignment with our team vision. Warren Buffet recommends praising specifically and criticizing generally with employees, and I think this is wise to follow. If team members have been trained, retrained, spot corrected, and continue to perform below the standard, they may not be a good fit and need to be let free to find fulfillment elsewhere.
Building your Rock Star team
Here are some tips to help our office team members become R.O.C.K.S.T.A.R.S.
Results — What’s the big picture for your practice, and why do you do what you do every day? Clarity on the desired results and outcome for your practice will add excitement, fulfillment, and practice growth.
Ownership — This is everyone’s practice (not just the doctors)! You all derive your income from the same practice and should feel a sense of pride and ownership in your office. If things aren’t ideal now, be a positive catalyst for improvement.
Customer service excellence — You want to be customer service Rock Stars! See everything you do from the eyes of the
patient and referring office. How can you improve their experience? Your practice rewards are directly tied to your level of customer service excellence. Wow your patients!

Kaizen — A Japanese word meaning constant and neverending improvement. Small, incremental improvements over time make major, long lasting changes. Commit to continually improve professionally and personally.
Systems — The system is the secret! Everything your practice does should be systematized — from scheduling patients and phone calls to dental care and post-op instructions. The team should create, understand, and follow the system.

Team player — Your office should be a well-trained, energized, kick-butt team! Everyone is needed, appreciated, and supported. Office culture is critical to success. Your team is your tribe. You should have each other’s backs! Team means “together everyone achieves more.”
Action — Nothing happens until someone moves. Be engaged at the practice, and look for ways you can help. Remember, “That’s not in my job description” should never be an excuse for not acting when it’s required.
Resolve — Make a definite and serious decision to do or change something. Many people live their life half committed to everything they do. Go all in, be fully committed, or find something else you can fully commit to. Resolve to be the best you can be, and to make the practice the best it can be!
Serve — Be service oriented. Continually think, “How can you make someone’s life better today?” You are rewarded in life to the degree you sincerely serve others! EP
51 endopracticeus.com Volume 16 Number 1 PRACTICE DEVELOPMENT
Connect. Be Seen. Grow. Succeed. | www.medmarkmedia.com 3 REASONS TO SUBSCRIBE
16 CE credits available per year
1 subscription, 2 formats – print and digital
4 high-quality, clinically focused issues per year 3 SIMPLE WAYS TO SUBSCRIBE
Visit www.endopracticeus.com
Email subscriptions@medmarkmedia.com
Call 1-866-579-9496 Endodontic Practice US 1 year $149 / 1 year digital only $79
•
•
•
•
•
•
Boyd Industries
“Built to Last. Built for You. Built by Boyd” is more than a tagline; it signifies the commitment that everyone at Boyd makes to each and every one of our customers. Best known for the durability and reliability of our award-winning products — including treatment chairs, mobile storage, and clinical cabinetry — we combine over 60 years of design and manufacturing expertise to perfectly fit your unique space and personal style. We take great pride in the craftsmanship and longevity of all products built at our U.S.-based facility, so you can take pride in your office for years to come.
Boyd Industries is an award-winning manufacturer of high-quality operatory equipment specifically designed for endodontics.
Dental chairs are the centerpieces and a serious investment to any treatment room. Boyd makes certain to include reliability, performance, and longevity when designing each and every chair.

Our S3100LC treatment chair incorporates proven characteristics into a product that provides ergonomic features for the doctor, assistant, and patient. A smooth, lockable swivel base allows for 90 degrees of rotation from center to accommodate patient positioning and entry/egress. A lift column allows the chair to be raised or lowered in a fixed field of view. In addition to facilitating closer assistant positioning, the tapered back design provides a low-profile, single articulating headrest that helps place the patient’s head properly. The chair back base and
back adjustments are controlled by easy-to-access membrane switches. Three programmable settings for one-touch control can articulate the chair to frequently used positions. A home button easily returns to a lowered and upright position for patient egress. Our Ultraleather Pro™ fabric and memory-foam support ensures maximum patient comfort and is ink and stain resistant, with antimicrobial disinfecting ingredients making sanitizing quick and easy.
An unreliable piece of equipment can result in costly service calls and loss of productivity, becoming expensive and time-consuming to fix. Boyd engineers its products to encompass fewer moving parts, making installation easy, lowering the risk of failure, simplifying maintenance, and resulting in fewer service calls.
The Boyd team has made every effort to create specialized products that are truly “Built for You.” To create a cohesive office space, Boyd’s custom clinical and office cabinetry can be combined with nearly unlimited color and print laminate combinations. To meet the unique needs of every doctor, the Boyd Team offers the widest range of customization options.
Attend AAE23 to see our S3100LC chair and customizable workspace, creating comfort for you and your patients.
For more information or to request a quote, visit Boyd Industries at www.boydindustries.com.
52 Endodontic Practice US Volume 16 Number 1 PRODUCT PROFILE
This information was provided by Boyd Industries. EP
S3100LC chair



CREATING COMFORT Boyd Industries offers the widest range of durable and customizable endodontic equipment. We focus on your functional and ergonomic comfort so you can focus on your patient’s need. Built to Last. Built for You. Built by Boyd! CONTACT US TO DESIGN YOUR COMFORT TODAY. 727-561-9292 I 800-255- 2693 www.boydindustries.com Boyd will be at AAE23 Booth #627 showcasing the latest in endodontic technology. Get an in-depth consultation and special pricing. FOR YOU AND YOUR PATIENTS
People growth precedes practice growth
Drs. Joel C. Small and Edwin McDonald discuss the beliefs behind a growth mindset

Theories of leadership and organizational culture have undergone significant change in the modern era. During the industrial revolution, leadership was more of the “command-and-control” variety and “laborers” (a popular term at the time) were mostly performing mindless and repetitive tasks. Due to the nature of the work and the leaders’ mindset, laborers had no expectation or opportunity for growth other than to increase their capacity to produce more products.
Entering the modern era, we evolved from the Industrial Revolution to the information technology era which emphasizes mental capabilities and capacity. A command-and-control style of leadership is no longer effective. In fact, this leadership style has become counterproductive. Today’s best leaders now embrace a style of leadership that supports team building, individual creativity, and inclusiveness. Fundamental to this new leadership style is a different way of thinking known as a “growth mindset” — the belief that everyone on the team has the capacity for growth. This contrasts with a “fixed mindset” that believes basic qualities, like intelligence and talent, are fixed and unchangeable. Based on these contrasting mindsets, the resulting practice culture, which the leader creates, will reflect these underlying beliefs. Practice cultures based on a prevailing fixed mindset tend to become stagnant and decline over time, whereas growth-oriented cultures are able to scale individual and team capabilities and capacity to meet changing demands and future complexity.
We have identified three basic beliefs that are essential to the development of a growth mindset.
1. Growth is an organizational imperative

This recognizes that both individual and team growth are fundamental to our practice survival. Imagine that you practiced dentistry with a fixed skill set; that your skills were fixed and never improved from your graduation from dental school. As
years passed, your ability to meet modern standards would continue to diminish until you and your practice eventually became irrelevant, marginalized, and failed. Unfortunately, this scenario plays out in many practices. The onset and progression of decline is often slow and imperceivable until a developmental (growth) gap becomes so broad that recovery is extremely difficult.
2. Failure leads to success
Remember how you learned to ride a bike? Initially you may have fallen and experienced some minor bumps and bruises until finally, one day, off you went. A similar experience holds true for personal and professional growth. Failure will often precede success, and leaders must learn to accept failure as a necessary steppingstone for ultimate success and mastery. It is our job to support our team through these developmental experiences and make each failure a learning opportunity. We do this by creating a psychologically safe environment that prioritizes growth despite the failures inherent in the growth learning process. We must recognize that scaling our organizational capability and capacity to meet future demands is essential to our survival.
3. Perfection is a myth
At the risk of being considered heretical, I have spoken the unspeakable. Perfection is a myth, and the belief in perfectionism can even be destructive. If perfection is attainable, growth comes to a screeching halt because there is no growth beyond perfection. The reason that perfection is a myth is that what may be considered perfect today will likely be viewed as imperfect in the future. For example, when I graduated my endodontic residency, the ideal root canal had a large access and canals that were enlarged through aggressive cleaning and shaping procedures. Today, the ideal root canal has a small access and preserves critical tooth structure utilizing modern cleaning technology and shaping techniques. What was perfect then is considered imperfect now. Furthermore, we create unnecessary stress and frustration for ourselves and our team by doggedly adhering to a perfectionist mindset. It would be far better for everyone if we could alter our mindset to one that promoted constant improvement rather than unattainable perfection. Seeking constant improvement is more aligned with a growth mindset and more easily accepted by our staff.
Past research indicates that our expectations of our team will likely be reflected in the results they achieve. Believing in our team’s capacity for growth and expecting continuing improvement in their performance and skills will pay dividends for our practices if we create a work environment that is conducive to growth.
54 Endodontic Practice US Volume 16 Number 1 SMALL TALK
EP
Drs. Joel C. Small and Edwin (Mac) McDonald have a total of over 75 years of dental practice experience. Both doctors are trained and certified Executive Leadership Coaches. They have joined forces to create Line of Sight Coaching, a business dedicated to helping their fellow dentists discover a better and more enjoyable way to create and lead a highly productive clinical dental practice. Through their work, clients experience a better work/life balance, find more joy in their work, and develop a strong practice culture and brand that positively impact their bottom line. To receive their free ebook, 7 Surprising Steps to Grow Your Practice Through Leadership, go to www.lineofsightcoaching.com.
A commemoration of oral health services to soldiers
Dr. Francis Nasser, Jr. discusses the important role of military dentists and a special way to recognize their contribution to the field
The Association of Army Dentistry (AAD) dedicated the Army Dentistry Monument on Friday, March 24, 2023, in a ceremony at the U.S. Army Medical Department (AMEDD) Museum in San Antonio, Texas. According to Dr Ronald Lambert (COL USA DC ret, Past President of the AAD), “The monument is a lasting tribute to all the soldiers, civilians, and spouses who have served and continue to serve in the Army Dental Care System in support of the U.S. Army and its military mission. The monument recognizes and honors the selfless contributions made by the diverse members of the Army Dental Care System and its key supporting components in the overall mission of Army Medicine.”
Founded in March 1911, the Army Dental Corps has a long and distinguished history of providing global dental services to soldiers and ensuring the readiness of the nation’s fighting forces. Even before 1911, the Army contracted dental surgeons to provide dental care to soldiers deployed to the new territories of a growing nation. The tradition of providing oral health services to soldiers wherever they are assigned continues to this day.
During World War II, more than 18,000 dentists served in uniform. It was during this time that the role of Army Dentistry expanded to include not only all levels of dental services, but also non-dental support and leadership. In the battle of Saipan in the Pacific, a Dental Corps Officer, Captain Ben Salomon, took command of the battalion aid station on the island. During an ensuing and desperate attack by enemy forces, CPT Salomon, also a skilled infantry soldier, heroically fought and defended the battalion aid station. He lost his life in the battle, but his gallantry and sacrifice did not go unrecorded. He was awarded the Medal of Honor posthumously, the only Army dentist to ever receive the nation’s highest military award. The image of Dr. Ben Salomon was used in the design of the dental officer sculptured in the monument.
Army Dentistry was firmly established as a permanent and essential element in preserving the readiness and fitness of the fighting force. During the conflicts in Korea and Vietnam, Army Dentistry continued to provide direct support to soldiers in the field of operations.
The Persian Gulf War brought the largest expansion of Reserve Dental Support in Army Dentistry. Over 220 reserve dental officers and 320 reserve enlisted soldiers were called up to support the mission. Overall, 121 dental officers served in the theater. The expanded use of reserve forces continued throughout the later conflicts in Iraq and Afghanistan.
Today the Army Dental Care System is a highly trained and integrated team of military officers, non-commissioned officers (NCO), enlisted soldiers, and government service (GS) civilians. The Army Dental Corps has 970 dentists in uniform and is augmented with 455 GS and contracted civilian dentists. There are 1,225 NCOs and enlisted soldiers and 2,300 civilians providing clinical and administrative support. All services and specialties of the dental profession are provided to the nation’s service members. In addition, Army Dentistry is a leader in the postgraduate education and specialty training of young dentists, and the advanced training of enlisted soldiers and civilians. The mission of the Army requires that Army Dentistry be prepared to support soldiers wherever they are deployed. Colonel Tom Goksel, DDS, MD, says, “The Army Dental Corps is the leader in expeditionary dentistry and sustainment of force readiness … the mission is to have a ready Dental Corps capable of delivering global dental services in order to sustain the readiness of the total military force.”
The Association of Army Dentistry is proud to keep the legacy of the Army Dental Corps alive and preserve its rich history, in order to inspire those who choose to serve and support the nation’s military men and women. The Army Dentistry Monument Dedication commemorates this unique contribution to the U.S. Army and the nation.


55 endopracticeus.com Volume 16 Number 1 MILITARY MATTERS
EP
Dr. Francis Nasser, Jr. is a retired Colonel in the U.S. Army Dental Corps and a current member of the Association of Army Dentistry Board of Directors.
A strategy for growth
A conversation with Dr. Scott Doyle, Metropolitan Endodontics

Two years ago, it occurred to Dr. Scott Doyle and his partners at Metropolitan Endodontics in Minneapolis, Minnesota that it might be time to do a little fact finding about options for collaboration and support for their thriving practice.
“We didn’t need to do anything — we already had a very successful practice,” Dr. Doyle said. “But we thought we should go through the discovery phase and explore the idea of a Specialty Dental Service Organization. The landscape of endodontics is changing; it seemed better to have an answer now, rather than thinking 3 or 5 years down the line, ‘Why didn’t we do anything?’”
Dr. Doyle and his eight partners practice in four flourishing locations that serve the beautiful southern suburbs of the Twin Cities of Minneapolis and St. Paul. Founded by Dr. Eric Grutzner 30 years ago, the organization had an excellent reputation and was on solid footing — and the doctors had no intention of making a misstep that might jeopardize the future.
“It wasn’t an easy task. We brought it to the group; it was 5 or 6 months of discovery and discussion — difficult, candid discussion — with the partners about what we wanted to do to move forward,” he said. “Where do we want to be in 10 to 20 years?”
The answer? They wanted to grow.
“We went in open-minded, not expecting to do anything,” Dr. Doyle said. “Once we decided to go down the path, the decision about with whom to partner was easy. It was unanimous to partner with US Endo.”
Metropolitan Endodontics is currently building out one location to accommodate more doctor days and organically grow
the practice, as well as actively looking for new associates. “Partnering with US Endo was not an exit strategy. It was a growth strategy,” Dr. Doyle said.
He envisions that Metro’s partnership with US Endo will be a huge asset in recruiting new endodontic talent, given the national network of clinicians now looking out for their practice’s best interests.
“Connection is everything in endodontics,” he said. “We have nine fantastic partners who work really well together; now we have hundreds of partners across the country to rely on for support.”

Dr. Doyle cited a variety of intangibles as other feathers in US Endo’s cap, including an exciting track of professional and personal development programs, a focus on encouraging board certification among its partners to continue shaping the specialty, and grass roots support of the AAE Foundation’s Domestic Access to Care program. “The fact that US Endo even thought about Access to Care made them attractive to me,” he said. US Endo made a seed contribution of $235,000 in 2021 to help the Foundation kickstart the Domestic Access to Care initiative, which provides a high level of endodontic care to people in need across the United States and spreads the life-changing power of saving teeth.
Dr. Doyle said the commitment to patient care is only one facet of the dynamic US Endo Partners community. He added, “The aligned mission and vision between Metropolitan Endodontics and US Endo Partners was extremely important.”
56 Endodontic Practice US Volume 16 Number 1 SERVICE PROFILE
EP
This information was provided by US Endo Partners.
Roger Burke, DDS, MS; Eric Grutzner, DDS, MS; and Scott Doyle, DDS, MS
Dr. Scott Doyle
When you join US, you gain access to a nationwide recruiting network—and a team committed to helping you meet your professional match.




“I never would have met Dr. Abrishami if not for US Endo’s recruiting network. In my opinion, they found me the best associate in the entire nation.”
Reid Pullen, DDS, Brea Endodontics | US Endo Partner and believer since 2020
Network A proven usendopartners.com
Scan to hear Dr. Allen Abrishami talk about his experience being mentored by Dr. Reid Pullen as he begins his endodontic career.