Simple endodontic irrigation

Dr. Allen Ali Nasseh
Closed-system negative pressure irrigation
Drs. L. Stephen Buchanan and Christophe Verbanck
Allowing technology to help you navigate inevitable challenges
Dr. James A. Smith, Jr.
Minimally invasive

Dr. Chafic Safi discusses preserving as much healthy tooth structure as possible

PROMOTING EXCELLENCE IN ENDODONTICS Fall 2023 Vol 16 No 3 endopracticeus.com Irrigation & Obturation n 4 CE Credits Available in This Issue*
endodontics





Fall 2023 n Volume 16 Number 3
Editorial Advisors
Dennis G. Brave, DDS
David C. Brown, BDS, MDS, MSD
L. Stephen Buchanan, DDS, FICD, FACD
Gary B. Carr, DDS
Arnaldo Castellucci, MD, DDS
Gordon J. Christensen, DDS, MSD, PhD
Stephen Cohen, MS, DDS, FACD, FICD
Samuel O. Dorn, DDS
Josef Dovgan, DDS, MS
Luiz R. Fava, DDS
Robert Fleisher, DMD
Marcela Fridland, DDS
Gerald N. Glickman, DDS, MS
Jeffrey W Hutter, DMD, MEd
Syngcuk Kim, DDS, PhD
Kenneth A. Koch, DMD
Gregori M. Kurtzman, DDS, MAGD, FPFA, FACD, DICOI
Joshua Moshonov, DMD
Richard Mounce, DDS
Yosef Nahmias, DDS, MS
David L. Pitts, DDS, MDSD
Louis E. Rossman, DMD
Stephen F. Schwartz, DDS, MS
Ken Serota, DDS, MMSc
E Steve Senia, DDS, MS, BS
Michael Tagger, DMD, MS
Martin Trope, BDS, DMD
Peter Velvart, DMD
Rick Walton, DMD, MS
John West, DDS, MSD
CE Quality Assurance Board
Bradford N. Edgren, DDS, MS, FACD

Fred Stewart Feld, DMD
Gregori M. Kurtzman, DDS, MAGD, FPFA, FACD, FADI, DICOI, DADIA
Justin D. Moody, DDS, DABOI, DICOI
Lisa Moler (Publisher)
Mali Schantz-Feld, MA, CDE (Managing Editor)
Lou Shuman, DMD, CAGS
Keeping up
It was exactly 3 years ago, in the midst of the COVID-19 pandemic, when I wrote the introduction letter in the Summer 2020 issue. Back then, I used “From Evolution to Revolution (while remaining a clinician)” as the title. Today, this title is still applicable, particularly for anyone who is setting up a new practice or even for a newly graduated endodontist. However, there is a lot of “keeping up” to do in order to stay afloat in a sea of technological advancements and new concepts and not lose track of our mission — saving natural teeth!
Here are three tips to follow to keep up with the profession:
1. Think like a clinician: The success rate of endodontic therapy has always been reported to be in the top 90%, and we want it to remain this way. This raises the following question: When was the last time a new concept or a new trend was proven to yield a higher success rate? “Keeping up” means knowing which changes to embrace while staying mindful of their shortterm and long-term clinical significance. In today’s world, only “valuable” changes should be embraced such as minimally invasive endodontics, vital pulp therapy, artificial intelligence, etc. These are the advancements that will ultimately have a positive impact on our field and on our patients.
2. Sharpen your scientific data — the non-endodontic one as well: It is easy to be distracted by our area of expertise and miss out on other information that could potentially affect our diagnosis and treatment plan. Surely, it is important to stay up-to-date with our endodontic education and our skills; however, we cannot ignore an important phenomenon happening: higher life expectancy amongst our patients. This comes hand-in-hand with complex medical histories and a high rate of natural teeth retention — and a bigger percentage of our patient population will be considered medically compromised. Medical conditions such as diabetes, infective endocarditis, cancer, medication-related osteonecrosis of the jaw, coagulative therapy — just to name a few — all have an impact on the patient’s capacity to withstand dental treatment and could lead to compromised healing. Keeping up with this information is crucial to the success of our treatment.
Moreover, when odontogenic pain is ruled out, one has to be able to evaluate the patient for other pain etiologies, such as neuropathic pain, myogenous pain, arthralgia, etc. Hence, the importance of keeping up by having a diverse continuing dental education portfolio.
3. Adopt a patient-centered philosophy: Patient-centeredness is essential to any healthcare professional; therefore, presenting the best outcomes and patient experience remains one of our core responsibilities. “Keeping up” implies employing our best clinical skills, knowledge, and qualifications in order to render the best service in a simple, cost-effective, and affordable manner. Finally when we look at the trends, one can say that 3 years from now, the field of Endodontics will be looked upon by other fields with one thing in mind: keeping up with us.
© MedMark, LLC 2023. All rights reserved. The publisher’s written consent must be obtained before any part of this publication may be reproduced in any form whatsoever, including photocopies and information retrieval systems. While every care has been taken in the preparation of this magazine, the publisher cannot be held responsible for the accuracy of the information printed herein, or in any consequence arising from it. The views expressed herein are those of the author(s) and not necessarily the opinion of either Endodontic Practice US or the publisher.
ISSN number 2372-6245
Chafic Safi, DMD, MS, completed his postgraduate residency in Endodontics at the University of Pennsylvania in 2015 where he also completed a Master of Science in Oral Biology researching the outcome of endodontic microsurgery and factors affecting prognosis. Dr. Safi is a published researcher and lectures on various endodontic topics. He is certified by the American Board of Endodontics. Dr. Safi remains on the faculty at the University of Pennsylvania’s Department of Endodontics as well as University of Montreal, as an adjunct professor. He is also a faculty lecturer for Next Level Endodontics. He founded Centre Endodontique Saint-Laurent in Montreal, Canada where he lives and practices since 2016.

1 endopracticeus.com Volume 16 Number 3 INTRODUCTION




2 Endodontic Practice US Volume 16 Number 3 TABLE OF CONTENTS PUBLISHER’S PERSPECTIVE Staying informed and safe Lisa Moler, Founder/CEO, MedMark Media............................... 6 TECHNOLOGY Allowing technology to help you navigate inevitable challenges Dr. James A. Smith, Jr. discusses simplifying the root canal process with the GentleWave® Procedure 16 CONTINUING EDUCATION Simple endodontic irrigation Allen Ali Nasseh, DDS, MMSc, outlines innovations and concepts for effective cleaning and disinfection .............................18 8 COVER STORY Minimally invasive endodontics Dr. Chafic Safi discusses preserving as much healthy tooth structure as possible Cover
WELLNESS WATCH Endodontist self-care: Dealing with dental mental and physical trauma in your practice Dr. Reid Pullen offers guidance on staying healthy as a practitioner 12
image of Dr. Chafic Safi courtesy of Brasseler USA.





2-DAY LIVE SEMINAR: LAS VEGAS, NEVADA JAN 19TH & 20TH, 2024 Endo Mastery (Inner Peace Seminars) Nationally Approved PACE Program Provider for FAGD/MAGD credit. Approval does not mean acceptance by any regulatory authority or AGD endorsement 5/1/2022 to 4/30/2025 Provider ID# 358761 1-800-482-7563 info@endomastery.com YOU’RE INVITED TO THE NEXT LEVEL OF ENDO SUCCESS! MASTERING THE EFFORTLESS ENDODONTIC PRACTICE “Endo Mastery increased my take home pay by 60% in 1 year! Not only that, they made my team more cohesive and efficient. Having a coach helped me to feel supported and confident.” DR. GEOFFREY CLIVE Join endo’s top practice and financial coach, Dr. Ace Goerig, for insights and practical advice to create the ultimate lifestyle practice. DDS, MS, ABE DIPLOMAT ENDOMASTERY OWNER endomastery.com/LV24/





4 Endodontic Practice US Volume 16 Number 3 TABLE OF CONTENTS CONTINUING EDUCATION Closed-system negative pressure irrigation Drs. L. Stephen Buchanan and Christophe Verbanck explore irrigation of root canal systems 23 GOING VIRAL Is social media placing your personal privacy or your small business at risk? Mark Pribish offers guidance on minimizing risks of social media ........................................................ 30 LEGAL MATTERS Anatomy of a dental malpractice action Kristin Tauras, JD, defines the various complex parts of a malpractice claim 34 MARKETING MOMENTUM A good “NAP” is 1 of 3 ways to improve practice success Chad Erickson discusses how to generate more revenue from your local listings 38 INDUSTRY NEWS ........................ 39 PRODUCT SPOTLIGHT MANI JIZAI NiTi File System Story of JIZAI .................................. 40 SMALL TALK The curse of perfectionism Drs. Joel C. Small and Edwin McDonald discuss perfectionism versus consistent improvement ......................................................... 43 PRODUCT PROFILE For the life of your practice: the vision of Endodontic SuperSystems (ESS) ............................................................. 44 PRODUCT PROFILE New RoTAC Rotary File Grips RoTAC Rotary File Grips change rotary files into hand files to prepare difficult tight-curved canals safely and efficiently .............................................................. 46 SOUND ADVICE The Endo Files: the endodontic experts podcast Specialized Dental Partners amplifying the voices of clinicians and industry insiders ................. 48 Connect. Be Seen. Grow. Succeed. | www.medmarkmedia.com READ the latest industry news and business WATCH DocTalk Dental video interviews with KOLs LEARN through live and archived webinars RECEIVE news and event updates in your inbox by registering for our eNewsletter CONNECT with us on social media www.endopracticeus.com *Paid subscribers can earn 4 continuing education credits per issue by passing the 2 CE article quizzes online at https://endopracticeus.com/category/continuing-education/
Most endodontists have to master multitasking. Ours just have to master root canals.

Do what you do best and we’ll handle the rest. We aren’t your typical DSO. When you partner with HighFive Healthcare, you join an exclusive network of top endodontists dedicated to exceptional patient care. Our doctor-owned practices and seasoned team of experts nurture a fun and collaborative culture like no other. While we optimize and scale the business side of endodontics, clinical autonomy is left in your skilled hands. Together, we’ll help you take ownership of something bigger than a single practice and support you as you create your own tomorrow.
Learn more at high5health.com
RECRUITING | SCHEDULING OPTIMIZATION | SCALABILITY | BRANDING & MARKETING | PAYROLL | IT SERVICES | AND MORE
Staying informed and safe
Recently, I saw a movie called “The Sound of Freedom,” the story of Tim Ballard, a federal agent who quits his job with the Department of Homeland Security to start his own independent team to rescue child trafficking victims. One of the movie’s executive producers is Tony Robbins. Tony has been a mentor and inspiration to me. The movie was emotional and moving for me, watching (as Tony describes on his website), “the harrowing experiences faced by victims of human trafficking and the relentless dedication of those fighting to dismantle these dark criminal networks, which continue to enslave millions of children globally each year.”
Human trafficking is not just a movie. The U.S. Department of Homeland Security (DHS) notes, “Every year, millions of men, women, and children are trafficked worldwide — including right here in the United States. It can happen in any community, and victims can be any age, race, gender, or nationality.” Violence, manipulation, false promises of well-paying jobs, and even the promise of romantic relationships can lead to imprisonment of these innocent, frightened victims. DHS adds, “Language barriers, fear of their traffickers, and/or fear of law enforcement frequently keep victims from seeking help, making human trafficking a hidden crime.”
At-risk victims may be hiding in plain sight. Dental professionals may not realize that patients who visit their offices may impacted by this terrible crime. Because of signs and symptoms of human trafficking, dentists may be able to help a victim of human trafficking during the course of the dental visit. Several states mandate that dentists need a human trafficking continuing education course to renew their licenses. In these courses, dentists learn details such as:
• Work-settings that may employ trafficking victims.
• Physical and psychological clues that the patient may be being trafficked.
• Some key words that the victim or perpetrator may say to the dentist to avoid being identified as a trafficking situation.
• Reasons why a victim may try to avoid being identified.
• Oral injuries that may indicate a trafficking victim.
• Resources for intervention specialists in human trafficking.
• What steps the clinician can take if the patient is identified as a trafficking victim.
The DHS says that in helping these victims, the healthcare professional also needs to pay careful attention to the safety of themselves and their teams. They warn, “Do not attempt to confront a suspected trafficker directly or alert a victim to any suspicions. It is up to law enforcement to investigate suspected cases of human trafficking.”
Back to our fall issue, our CE on closed-system negative pressure irrigation by Drs. L. Stephen Buchanan and Christophe Verbanck focuses on some challenges of irrigation and discusses various traditional and new irrigation techniques and technologies. Dr. Allen Ali Nasseh also discusses strategies and efficient combined solutions for the disinfection phase of irrigation. In our Cover Story, read about how Dr. Chafic Safi preserves tooth structure and practices minimally invasive endodontics with products from Brasseler USA.
In my Publisher’s Perspective column, I always share topics that are important to my growth not just as a publisher and entrepreneur, but also as a human being. Human trafficking is an outrageous and evil crime. Take a CE class on this topic to know warning signs and also to stay safe. Human trafficking “exists nationwide — in cities, suburbs, and rural towns — and possibly in your own community,” says DHS. Be aware, smart, and cautious — as you help patients to survive and thrive.
To your best success,
Lisa Moler Founder/Publisher, MedMark Media
Published by
Publisher Lisa Moler lmoler@medmarkmedia.com
Managing Editor Mali Schantz-Feld, MA, CDE mali@medmarkmedia.com
Tel: (727) 515-5118
National Account Manager Adrienne Good agood@medmarkmedia.com
Tel: (623) 340-4373
Sales Assistant & Client Services Melissa Minnick melissa@medmarkmedia.com

Creative Director/Production Manager Amanda Culver amanda@medmarkmedia.com
Marketing & Digital Strategy Amzi Koury amzi@medmarkmedia.com
eMedia Coordinator Michelle Britzius emedia@medmarkmedia.com
Social Media Manager April Gutierrez socialmedia@medmarkmedia.com
Digital Marketing Assistant Hana Kahn support@medmarkmedia.com
Website Support Eileen Kane webmaster@medmarkmedia.com
MedMark, LLC

15720 N. Greenway-Hayden Loop #9 Scottsdale, AZ 85260
Tel: (480) 621-8955
Toll-free: (866) 579-9496 www.medmarkmedia.com
www.endopracticeus.com
Subscription Rate
1 year (4 issues) $149
https://endopracticeus.com/subscribe/
6 Endodontic Practice US Volume 16 Number 3 PUBLISHER’S PERSPECTIVE
Lisa Moler Founder/Publisher, MedMark Media


S3100LC ENDODONTICS TREATMENT CHAIR GET YOUR CUSTOMIZED QUOTE TODAY! Durable and customizable Endodontics equipment addresses the functional and ergonomic requirements of dental professionals. Personalize the S3100LC to suite your needs. Elevate your practice with Boyd and experience innovation that is: Built to Last, Built for You, Built by Boyd! 800-255-2693 • www.BoydIndustries.com
Minimally invasive endodontics

Dr.
It has been almost 100 years since 1925, when Walter Hess discovered the extensive and intricate nature of root canal anatomy. From that moment, the focus has always been on how to effectively clean, disinfect, and seal the root canal system. This has fueled multiple developments and technological advancements, making way for fascinating concepts and treatment philosophies, especially in the recent decade. Perhaps, the most spoken about recent development is minimally invasive endodontics (MIE).
What does “minimally invasive endodontics” mean?
To understand MIE, one has to understand minimally invasive dentistry. Minimally invasive dentistry can be defined as the preservation of healthy dental structure by preventing disease from occurring, intercepting its progress, but also removing and replacing with as little tissue loss as possible. In other words, the objective is minimal intervention.1
MIE is a technique that aims first and foremost at maintaining the vitality of the pulp. Should this vitality not be maintainable and root canal treatment indicated, healthy coronal, cervical, and radicular tooth structure should be preserved as much as possible.2 From treatment selection — root canal treatment versus vital pulp therapy to access opening, root canal cleaning and shaping, and obturation — the preservation of maximal dentin mass is of utmost importance.
With this objective in mind and in the context of biomechanical instrumentation, cleaning the canals while respecting their natural morphology is one of the minimally invasive approaches that can preserve radicular tissue. Recently, newly developed technologies and materials have emerged that allow minimally invasive endodontic procedures during instrumentation.
Root canal instrumentation, the traditional way
The primary goal of endodontic treatment is to access, shape, clean, and fill the complicated anatomy while leaving the tooth strong enough in order to maintain function. Today, many file systems with different taper and cutting efficiencies are avail-
able. These instruments cause varying levels of removed dentin volume and surface area in the root canals. During mechanical preparation, removing excessive amounts of dentin tissue or

8 Endodontic Practice US Volume 16 Number 3 COVER STORY
Chafic Safi discusses preserving as much healthy tooth structure as possible
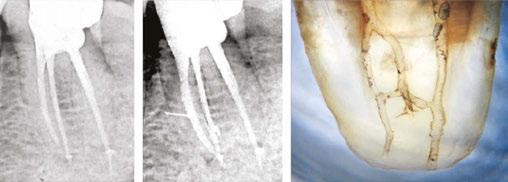
Figure 1: A PA X-ray showing a failed root canal treatment on a lower incisor (left) and the corresponding endodontic microsurgery (right) showing the original oval and missed anatomy of the canal. Courtesy Dr. Bertrand Khayat, Paris, France
Dr. Chafic Safi treating a patient at his practice, Centre Endodontique Saint-Laurent, in Montreal, Canada
leaving behind uninstrumented areas cause failure. Thus, the target is to allow effective disinfection by being faithful to the original root canal anatomy and reaching an apical enlargement sufficient enough to achieve strong antimicrobial efficacy.
Traditional endodontic files cannot enlarge the natural cross section of the root in all directions; rather they induce a round shape, leaving large areas untouched and packing debris in the oval extremities.3 This prevents adequate cleaning and disinfection (Figure 1). Moreover, the more a canal is tapered with traditional instruments, the thinner and the weaker the tooth becomes. Traditional rotary instruments have consistently been shown to create dentinal defects and cracks that are suspected to lead to root fractures.4 Even reciprocating techniques create dentinal cracks, without mentioning their debris extrusion into the periapical tissues.5,6
Root canal instrumentation, the minimally invasive way
There are three important facts to remember:
1. Traditional NiTi instrumentation techniques are deficient.
2. Bacteria organize themselves as biofilm that is more difficult to remove than planktonic bacteria.
3. Teeth are weakened by conventional instrumentation. In order to address these shortcomings, a paradigm shift was needed whereby we move from the school of thought of the file shaping the canal to the canal shaping the file. In 2016, two unique instruments were launched with the promise of anatomical shaping and deep disinfection: the XP-3D™ Shaper and the XP-3D™ Finisher. These instruments were made using a newly patented NiTi alloy called MaxWire (Brasseler USA, Savannah, Georgia) with the special ability to change molecular structure, from the martensitic phase at room temperature to the austenitic phase at body temperature, allowing them to expand and adapt

to the root canal wall in all directions and enhance irrigation. Both instruments when rotated at speeds of 800-1000 rpm would engage in a wider envelope of motion, creating a cleaner canal while conserving its original shape — minimally invasive anatomical instrumentation.
This year, the XP-3D Shaper got a new upgrade. It now comes in the austenitic phase regardless of temperature, making it more effective at cutting dentin while still offering the biological properties of anatomical shaping. This new XP-3D Shaper+ with the combination of the XP-3D Finisher, offer the clinician an easy, safe, and minimally invasive approach at performing root canal treatments as well as non-surgical retreatments.
So, what is this XP-3D Shaper+, and how does it work?
Just like its predecessor, The XP-3D Shaper+ features a small flexible core (#30/.01) that is extremely resistant to cyclic fatigue. The unique serpentine design allows the instrument to gently abrade the inner walls of the root canal, keeping the debris in suspension while the MaxWire® alloy allows its adaptation to the canal morphology without the stress associated with conventional NiTi file. With an initial taper of 1%, the XP-3D Shaper+ expands inside the canal to achieve a taper of 4%.

9 endopracticeus.com Volume 16 Number 3 COVER STORY
Figure 2: The newly redesigned Booster Tip with 6 cutting edges and 6 facets
Figure 3: The new XP-3D Shaper+ sequence. Both files can be used at 1000 rpm and 1Ncm torque. Once a glide path of 15.04 is reached, the shaper is taken to working length using 2-5 strokes, followed by 8 additional long strokes to get 30.04
This new XP-3D Shaper+ with the combination of the XP-3D Finisher, offer the clinician an easy, safe, and minimally invasive approach at performing root canal treatments as well as non-surgical retreatments.
Another cutting-edge technology included in the XP-3D Shaper+ is the tip which has a unique geometry. It comes with the Booster Tip made of six cutting edges aligned with six facets — versus three for the conventional XP-3D Shaper. This tip enables the instruments to start cleaning and cutting dentin at 0.6 mm from the tip with an initial cutting diameter of 0.12 mm, ensuring 0.30 mm diameter is reached at 0.6 mm from the tip (Figure 2). A glide path of at least 15.04 is required, which will be gradually increased to achieve 30.04. This design makes treatment shorter and easier to perform, reducing the risk of errors and incidents while preserving the natural shape of the canal. The XP-3D Shaper+ is employed at a speed of 1000 rpm and 1Ncm torque and can be used up to eight canals according to the following protocol: once working length is confirmed, a glide path up to size 15.04 is recommended. This is easily achievable with the XP-3D Scout (Brasseler USA, Savannah, Georgia) 15.04 file. Following that, the XP-3D Shaper+ can be used giving 2-5 strokes until working length is reached. The canal is then flushed with NaOCl or another irrigation solution like Triton® (Brasseler USA, Savannah, Georgia) and the XP-3D Shaper+ reintroduced with eight full strokes to working length, at which point the canal would have been anatomically cleaned and instrumented to a size 30.04.7 The advantage of using the aforementioned 15.04 file is that it functions at the same speed and torque as the XP-3D
Shaper+, hence streamlining the procedure (Figure 3). This new instrument offers clinicians the possibility of letting the canal shape the file and solves two of the previously mentioned challenges: the deficiency of traditional NiTi instruments and their weakening of the dental structure.

Additionally, the XP-3D Shaper+ can also be used in retreatments. Thanks to its shape, it acts like a corkscrew engaging itself around gutta percha and pulling it out in large pieces (Figure 4). This way, there is no burnishing of the material against the root canal. A speed of 2500 rpm is required in order for the XP-3D Shaper+ to pull out the gutta percha. The XP-3D Shaper+ has been shown to remove gutta percha twice as fast as conventional files.8

What about the XP-3D Finisher?
The XP-3D Finisher file (Brasseler USA, Savannah, Georgia) has been designed with the aim of contacting areas in the longer aspect of the canal, where any conventional round file cannot reach. It is made using the MaxWire alloy which allows shifts in conformation from the martensite soft phase to the austenite robust phase, yielding a sickle/spoon shape at its tip. Additionally the XP-3D Finisher has no taper, making it extremely flexible and resistant to cyclic fatigue, so it does not enlarge the canal. When the tip is squeezed, the bulb can be expanded to
Figures 4A-4C: 4A. Non-surgical retreatment protocol using the XP-file family. After creating a well in the gutta percha, solvent is placed and left to react for 2 minutes with gutta percha. The XP-3D Shaper+ is then inserted into the prepared space and rotated at 2500 rpm with gentle strokes at an estimated working length in order to remove the bulk of gutta percha. Once the bulk gutta percha is removed, the working length is established and the Shaper+ reinserted and given 15 strokes to working length at 1000-2500 rpm, followed by 60 seconds with the XP-3D Finisher, ensuring removal of biofilm and gutta-percha tags. The Shaper acts like a corkscrew pulling out the gutta percha. The Finished acts like a scrapper, detaching stubborn gutta-percha tags. 4B. Shaper in retreatment action. Courtesy Dr. Klaus Lauterback, Germany. 4C. Finisher in retreatment action. Courtesy Dr. Rina Campbell, Union City, California

10 Endodontic Practice US Volume 16 Number 3 COVER STORY
A.
B.
C.
6 mm; and when the bulb is compressed, the tip will expand to 6 mm. The expansion of the bulb and tip act like a periodontal scaler but within the root canal, hence scraping and dislodging all the debris attached to the root canal walls, namely biofilm and stubborn gutta-percha tags in cases of retreatment. It is more effective than passive ultrasonic irrigation in reducing biofilm and the remaining root canal filling.9,10 This instrument comes in two tip sizes, a No. 25 and a No. 30. The No. 30 is also known as the Finisher-R, indicating its usefulness in retreatments. The No. 30 is slightly stiffer than the No. 25, making it an ideal wire to whip and detach stubborn gutta percha.
Finally, the XP-3D Finisher causes turbulence of the irrigant, maximizing the anti-microbial effect and therefore achieving deep disinfection in a safe and anatomical fashion.
Once inside the canal, the XP-3D Finisher is rotated for 60 seconds at 1000 rpm, moving it up and down at an amplitude of 7 mm to 8 mm in order to adequately spread the action of the tip and the bulb. The canal has to be filled with NaOCl or Triton and should be minimally prepared to a size ISO25 for the No. 25 Finisher and to a size ISO30 for the No. 30 Finisher.
The XP-3D Finisher is indicated to be used (Figure 5):
1. After conventional NiTi instrumentation
2. After XP-3D Shaper+ especially in oval canals
3. In retreatment cases
4. In special anatomical cases such as internal resorptions, dens in dente, and immature roots
With the XP-3D Finisher in a clinician’s armamentarium, eliminating biofilm and maximizing disinfection is now possible in a minimally invasive fashion.
Where do we go from here?
Minimally invasive instrumentation during root canal treatment aims at exerting microbial control while preserving tooth structure and supporting tissues, especially coronal and radicular dentin. Many instruments varying in flexibility and metallurgical
properties have been produced in the past, however none have been able to clean the root canal system anatomically. Today, the combination of two instruments, the XP-3D Shaper+ and the XP-3D Finisher, offer the possibility to debride, clean, and disinfect, while adapting to the canal’s natural anatomy in a simple, safe, efficient, and conservative fashion. All of these factors make minimally invasive endodontic treatment more possible and successful.
REFERENCES
1. Ericson D. What is minimally invasive dentistry? Oral Health Prev Dent. 2004;2 Suppl 1:287-292.
2. Gluskin AH, Peters CI, Peters OA. Minimally invasive endodontics: challenging prevailing paradigms. Br Dent J. 2014 Mar;216(6):347-353.
3. Paqué F, Balmer M, Attin T, Peters OA. Preparation of oval-shaped root canals in mandibular molars using nickel-titanium rotary instruments: a micro-computed tomography study. J Endod. 2010 Apr;36(4):703-707.
4. Shemesh H, Bier CA, Wu MK, Tanomaru-Filho M, Wesselink PR. The effects of canal preparation and filling on the incidence of dentinal defects. Int Endod J. 2009 Mar;42(3):208-213.
5. Elayouti A, Chu AL, Kimionis I, Klein C, Weiger R, Löst C. Efficacy of rotary instruments with greater taper in preparing oval root canals. Int Endod J. 2008 Dec;41(12): 1088-1092.
6. Caviedes-Bucheli J, Castellanos F, Vasquez N, Ulate E, Munoz HR. The influence of two reciprocating single-file and two rotary-file systems on the apical extrusion of debris and its biological relationship with symptomatic apical periodontitis. A systematic review and meta-analysis. Int Endod J. 2016 Mar;49(3):255-270. Epub 2015 Apr 22.
7. Azim AA, Piasecki L, da Silva Neto UX, Cruz ATG, Azim KA. XP Shaper, A Novel Adaptive Core Rotary Instrument: Micro-computed Tomographic Analysis of Its Shaping Abilities. J Endod. 2017 Sep;43(9):1532-1538.
8. Azim AA, Wang HH, Tarrosh M, Azim KA, Piasecki L. Comparison between Single-file Rotary Systems: Part 1-Efficiency, Effectiveness, and Adverse Effects in Endodontic Retreatment. J Endod. 2018 Nov;44(11):1720-1724.
9. Bao P, Shen Y, Lin J, Haapasalo M. In Vitro Efficacy of XP-endo Finisher with 2 Different Protocols on Biofilm Removal from Apical Root Canals. J Endod. 2017 Feb;43(2):321-325.
10. Alves FR, Marceliano-Alves MF, Sousa JC, Silveira SB, Provenzano JC, Siqueira JF Jr. Removal of Root Canal Fillings in Curved Canals Using Either Reciprocating Single- or Rotary Multi-instrument Systems and a Supplementary Step with the XP-Endo Finisher. J Endod. 2016 Jul;42(7):1114-1119.

11 endopracticeus.com Volume 16 Number 3 COVER STORY EP
Figure 5: The XP-3D Finisher can be used in many situations. Its ability to expand and scrape the root canal walls make it an ideal instrument to remove biofilm and previous root canal filling as well to adapt and clean special anatomical cases such as a dens in dente
Endodontist self-care: Dealing with dental mental and physical trauma in your practice
Dr. Reid Pullen offers guidance on staying healthy as a practitioner


Repetitive work trauma is a phrase that recently came to my attention. I did not have to hear the definition to understand the meaning because I live it each week. I feel its effects in my body every day. My lower back and hips feel eternally tight with a ball of pain that usually centers in my left buttock and lower back area. Many days, I struggle to walk upright for the first 5 minutes after the last patient. Twenty-four years as a practicing dentist (general for 5 years and endodontics for 19 years) has made the meaning of repetitive work trauma crystal clear.
According to Bluestein Attorneys, repetitive work trauma “occurs gradually over time, as a result of repetitive motion, strain, or pressure on a particular body part.”1 I would like to add two more phrases that serve as a subset to repetitive work trauma: Dental Mental Trauma (DMT) and Dental Physical Trauma (DPT). These two phrases sum up as a whole the body and mind trauma that can occur daily in a dental or specialty practice.
Why am I interested in talking about mind and body trauma? I turned 50 a few months ago, and I am not sure how long I will be able to practice endodontics and stay physically healthy. My goal is not to let my body dictate my retirement date. After 17 years of clinical endodontic practice, I enjoy what I do (most of the time), and I’m good at it (most of the time). But enter the two dragons: DMT and DPT. Year after year, case after case, we dutifully go to work. We are dentists and have a professional skill that can take people out of pain and save teeth.
Duty and obligation are good things. We do our duty because we must, but over time this “duty” chips away at us both mentally and physically. Sitting every day in a frozen position, focused intently inside a tooth slowly scrapes away at our physical health. Crying, anxious, mean, and uncooperative patients slowly chip away at our mental health. Some weeks, the experience of truly difficult patients has eroded my mental strength more than months of normal everyday life.
Add DMT and DPT to an aging body; we aren’t getting any looser, trimmer, or stronger because of the second law of thermodynamics (law of entropy). We are slowly edging from order to disorder; order to chaos. The natural order of aging is difficult but much more difficult if you are in constant pain.
In this article, I will discuss self-care tactics that can combat Dental Mental Trauma (DMT) and Dental Physical Trauma (DPT). The goal of self-care is to practice and live a healthier, happier life. I do not just want us to survive; I want us all to thrive.
Physical self-care
I have purchased and used nearly every body “self-care” gadget or device on the market. I have gone to cryotherapy for years (sometimes 2 times a day. I’m lucky to have a million dollar cryotherapy chamber located 200 yards from my door.). I have sat in saunas and 104° hot tubs. I have spent hours in hyperbaric chambers, used infrared and near infrared full-body red light therapy (Joovv), hip and leg compression therapy (Normatec from Hyperice), and Pulse Electromagnetic Field (PEMF) therapy devices like the Haelo. I have two massage chairs, a vibrating standing plate (HyperVibe™), and three different Hypervolt compression guns from HyperIce. I have two different full body rollers and nine different types of ball rollers including a lacrosse ball and a softball.
I have found that some of these therapies and devices are excellent in decreasing inflammation and promoting muscle and connective tissue recovery. But the No. 1 way I have found to take care of my body and mind, is to have a morning workout routine. In real estate, the famous catch phrase is, “location, location, location.” In self-care, the catch phrase should be, “routine, routine, routine.” Do not let life and all its distractions rob you of your consistent daily workout routine.
12 Endodontic Practice US Volume 16 Number 3 WELLNESS WATCH
Reid V. Pullen, DDS, graduated from USC Dental School in 1999. He completed an advanced education in general dentistry in 2000 while serving in the Army Dental Corps in Landstuhl, Germany. He graduated from the Long Beach VA Endodontic Residency in 2006 and opened a private practice in Brea, California, in 2007. Dr. Pullen founded and runs Rootcanalacademy. com and The 2 Day Root Camp Boot Camp. Dr. Pullen became a Diplomate of the American Board of Endodontics in 2013.
ANATOMICAL CLEANING JUST GOT BETTER
Everything you love about Brasseler USA’s minimally invasive XP-3D Shaper—now with an improved tip for optimal guidance and scouting.


✓ Transitions from an ISO# 15 to ISO# 30 within 1mm from the tip, functioning as a scouting and finishing file.
✓ Featuring our exclusive MaxWire® Technology, XP-3D Shaper+ adapts to the canal’s natural anatomy by expanding once exposed to body temperature.
✓ Adaptive Core™ Technology allows XP-3D’s smaller central core to move freely and adapt to the canal’s natural morphology.


Watch the Video to Learn More & Request an In-office Demo at XP-3D.com B-5788-EP-10.23 ©2023 Brasseler USA. All rights reserved. Visit our website at BrasselerUSADental.com To order call 800.841.4522 or fax 888.610.1937.
NEW!
My daily routine goal is 30-30-30. Thirty minutes of resistance training (lifting), 30 minutes of cardio (my body feels the best with the elliptical, bike, or swimming because it is low impact), and 30 minutes of stretching (often I mix resistance training and stretching and stretch between sets). I also transitioned to using machines for resistance training to lessen the stress on the joints. On workdays, I perform a 20-20-20 workout and then 30-30-30 on non-workdays since there is more time. I enjoy resistance training more than cardio and cardio more than stretching. In my routine, if I lift for 40 minutes and perform cardio (elliptical) for 20 minutes, I realize I do not have enough time to stretch or perform yoga.
After doing this for years and then finally making the commitment to stretching, I have realized that stretching and yoga is one of the most important things we can do for self-care. I have noticed that just after 10 minutes of stretching, my body feels 60%-70% better, and my back and hip pain is greatly reduced. If I add another 10 minutes or perform a 15 minute yoga routine in conjunction with cardio, rolling on a foam roller, and using a lacrosse ball to pinpoint the knotted areas, I can often decrease my body pain to 80%-90% and actually feel free and loose again. A 30 minute stretch is a gift that keeps on giving sometimes even days later. But, this takes work and discipline and sometimes it’s just easier to sit in the easy chair and watch television. The best part about a routine that involves the movement triad of resistance-cardio-stretching is that it is self-care for both the physical and mental components of life helping combat daily DMT and DPT.
There are three books that I use to help with stretching and yoga that I recommend: Foundations: Redefine your Core, Conquer Back Pain, and Move with Confidence by Dr. Eric Goodman and Peter Park, Knee Ability Zero by Ben Patrick (knees over toes guy), and Yoga Fitness for Men by Dean Pohlman (or any good yoga book or video that has different routines that target different areas of the body).
My daily routine usually consists of a 15 to 30 minute hot tub soak at 102°-104° at 5 a.m. while I read, pray, or meditate, and drink my coffee. I then drive to the gym and perform resistance training, cardio, and stretching for 45 minutes to 1-1/2 hours depending on the day. I then eat a nutritious breakfast with low sugar and higher protein. After work, I usually go in the cryotherapy chamber for 3-1/2 minutes at -175°F. I then go home and attempt to stretch and roll for 15 minutes. Sometimes after dinner, my wife and I will go on a walk, and if we do watch television, I use the Normatec compression therapy and a PEMF device (Haelo) concurrently to help reduce inflammation and promote healing.
Mental self-care
The second component to self-care is taking care of your mental health. Every day as dentists, we absorb little trauma packets from our patients. These trauma packets can build up in our body and mind and affect our peace and happiness. This Mental Dental Trauma that we receive from our patients can impact our family relationships and lead to depression, anxiety, and anger. I did not realize how much DMT I have absorbed
from my patients crying and acting out in my dental chair for the past 24 years. Along with DMT, a few years ago, my family and I went through significant trauma. This trauma brought incredible grief and led me to start therapy with a licensed marriage and family therapist. I did not think I needed it and was resistant to going. I started 3 years ago, am still going, and I can wholeheartedly say it is one of the best things that I have ever done for mental self-care.
Therapy has helped me work through and reframe poor thinking and negative self-talk. I have dealt with insecurities, fear, and childhood traumas and have learned to be kind to myself, allowing much more grace in my life. I have become a much better listener, and this has helped me in my interactions with family and patients. I understand true grief and can empathize with patients when they discuss their fear or anxiety. Therapy has allowed me to truly feel and work through sadness, which believe it or not, has greatly increased my true joy for life. I am much happier because I do not take things for granted, and my new life motto is, “Live simply, live with joy, and live in the present.”
I just live today and try to wring as much joy as possible out of today. I feel grateful and blessed for today. I am not sure about tomorrow, but I know we have today, and I want to live today because we are not promised tomorrow. I am 50 now, and if I die at 80 that means I only have 10,950 days left. I want to really live each day, if possible, with joy and happiness, full of love to my family, friends, and patients. I recommend therapy to many of my friends and family, and to be honest, most say they do not need it. I believe they are missing out on a better, more fulfilled life. I encourage you to be vulnerable and seek a professional therapist (even if it’s the hardest thing you’ve had to do). It can change your life and make you a better dentist and, most importantly, person.
Conclusion
The bottom line to taking care of our body and mind starts with a daily movement routine to help combat Physical Dental Trauma. Then add chiropractic care, massages, and consistent daily stretching and yoga. Devices like the Normatec (HyperIce) and a PEMF (Haelo) device used concurrently have increased my recovery by decreasing inflammation and promoting mitochondrial health. Next, incorporate talk therapy to work through life’s emotional stress and lessen the impact of Dental Mental Trauma. In conclusion, routine, routine, routine can change your life, make you a better spouse, parent, and clinician. When you feel better both mentally and physically, life is so much more enjoyable. So, let’s take care of ourselves for our family and for our grandkids and be kind to both our body and mind.
14 Endodontic Practice US Volume 16 Number 3 WELLNESS WATCH
REFERENCE
1. Bluestein Attorneys. Repetitive Trauma. https://bluesteinattorneys.com/areas-of-practice/workers-compensation/types-of-injuries/repetitive-trauma/. Accessed May 2, 2023.
EP
When you feel better both mentally and physically, life is so much more enjoyable.”

800 - 605 - 3437 | Specialty1partners.com YOUR SPECIALTY IS OUR SPECIALTY . The Only Doctor-Founded, Doctor-Led Specialty Partnership Organization. #1 in Dental Services “It’s a partnership of specialists and we are all specialty strong.”
Dr. Joanne Jensen Endodontic Artistry
Allowing technology to help you navigate inevitable challenges
Dr. James A. Smith, Jr. discusses simplifying the root canal process with the GentleWave® Procedure

We all know that endodontics is not simple.
One of the most significant challenges that endodontists face is canals that cannot be located within the root canal system or are inaccessible through traditional instruments. In fact, I’d be confident in saying that this is the top challenge within the specialty.


Another difficulty is knowing for certain when a root canal system is fully cleaned and disinfected.
And on top of these clinical challenges, many of our patients are afraid of undergoing root canal treatment. This is understandable, as many people fear the unknown, but it’s our job as endodontists to help our patients overcome any fears or anxiety.
Knowledge is power
According to a consumer survey from the dental technology company Sonendo®, 77% of Americans would rather be forced to sleep at the airport after a cancelled flight than undergo a root canal procedure. This underscores the widespread fear and anxiety surrounding traditional treatment.
I chalk this up to patients not fully understanding what a root canal procedure is or having prior misconceptions about intense pain and a slow healing process.
As endodontists, the more we can explain to our patients about what’s really going on, the better. This includes before the procedure with a thorough consultation and on the day of treatment. I suggest verbally walking patients through what you’re going to do throughout the process. This way, the patient is armed with information and knows what to expect.
Technology is your friend
While I am confident in my professional ability and skill, I am not hesitant to use technology to help me successfully navigate challenges that arise.
In my practice, my partner and I use the GentleWave® System with CleanFlow™ Technology to simplify and modernize the root canal procedure process. I adopted the GentleWave System nearly 7 years ago, and since then, it has proven its worth time and time again.
It’s important to note that Sonendo, the developer of the GentleWave System, is continuously gathering feedback from clinicians and optimizing its technology. This is evident in its enhanced CleanFlow Procedure Instrument, which is now indicated for use on anterior teeth and comes with a new matrix design.
I’ve been using the enhanced CleanFlow Procedure Instrument exclusively for all case types for several months. Some of the benefits are listed below:
• It provides a streamlined workflow.
• It offers superior tissue dissolution.
• The anterior indication allows me to use one procedure instrument for every case type, simplifying my inventory needs.
• The new matrix cradles the instrument which provides procedural consistency.
16 Endodontic Practice US Volume 16 Number 3 TECHNOLOGY
James A. Smith, Jr., DMD, received his dental degree in 1980 from The University of Alabama School of Dentistry and completed his endodontic residency there in 1982. He has been practicing for over 41 years and is an Adjunct Professor with the Department of Endodontics at the University of Alabama in the Birmingham School of Dentistry. Dr. Smith has co-authored an article that was published in the November 2014 Journal of Endodontics. His practice is located in Birmingham, Alabama.
In my practice, my partner and I use the GentleWave® System with CleanFlow™ Technology to simplify and modernize the root canal procedure process.”
Necrotic case — Pretreatment (left) and post GentleWave treatment (right)
With the enhanced CleanFlow Procedure Instrument, I am able to shave about 5 to 7 minutes off each root canal procedure I perform, as compared to the prior procedure instrument.


Overcoming skepticism


CleanFlow Technology enables the inside of the tooth to be cleaned from the outside. When I first tried it, I was a bit skeptical that a cleaning action generated outside the tooth could be as effective as when the cleaning action is produced in the pulp chamber. Now, I am highly confident in it.
Improved patient experience


As endodontists, we know that patients don’t want to have to come to our offices for treatment more than once. With the GentleWave System, single-visit procedures are more likely than ever before. Additionally, most of my patients have little to no postoperative issues with the Gen tleWave System with CleanFlow Technology. Not only is this incredible for my patients, but it also frees up time and resources for my staff.
And believe it or not, the white noise generated by the GentleWave System with CleanFlow Technology has even led a few of my patients to fall asleep during the procedure.
Locally, word has spread about how I use this technology in my office. Some patients specifically ask for it, and refer ring general dentists know about it too, touting that it can offer a modernized patient experience.
Advice for colleagues
If you’re a GentleWave System user, the enhanced Clean Flow Procedure Instrument is a win for practitioners and our patients.
For those who are not currently using the GentleWave System, I encourage you to schedule a test drive here: https:// gentlewave.com/doctor/contact?form_type=test_drive. If you are open to it, the GentleWave System can replace much of the traditional root canal procedure process. It doesn’t add to the process; rather, it simplifies it.



I want to help empower my fellow endodontists to stop “knocking their heads against a wall” when faced with inev itable challenges. Instead, leverage innovative technology to help you navigate them smoothly.

TECHNOLOGY
This article was provided by Sonendo®
EP
Simple endodontic irrigation
Allen Ali Nasseh, DDS, MMSc, outlines innovations and concepts for effective cleaning and disinfection

Endodontic irrigation plays a pivotal role in the success of clinical endodontics.1,2 Traditionally, the term “irrigation” has been used broadly to explain disinfection of root canal spaces. However, recent advancements in powered devices and chemical solutions have led the author to conclude that the term irrigation is better understood if broken down into its two distinct subcategories: cleaning and disinfection.3 This conceptual breakdown helps the clinician focus on the specific needs of each component of irrigation, focusing on optimizing its requirements for better efficiency. The overall goals of irrigation can be described as the chemical and physical removal of organic and inorganic debris followed by disinfection and removal of microbes and microbial components from the root canal space.1,4
During the cleaning component of irrigation, techniques, and processes aim at the physical removal of the macro debris generated during the act of instrumentation, referred to by the author as Macro Debris Removal (MDR), while disinfection primarily focuses on chemical and physical means to eliminate microorganisms in the root canal space3 (Figure 1).
The Macro Debris Removal (MDR) steps are those cleaning steps that remove the vital or diseased pulpal tissue, dentinal chips, and other debris produced by shaping instruments, as well as the naturally existing loose organic and inorganic debris in the root canal system. These types of macro debris have traditionally been removed by positive pressure syringe irrigation using various irrigation solutions.1
Disinfection, on the other hand, attempts to chemically destroy the biofilm and microorganisms in the root canal system during or after MDR has been accomplished. This article aims to explore concepts and innovations in endodontic irrigation, with specific focus on the use of uncomplicated and affordable sonic/ultrasonic devices to activate or agitate solutions during the cleaning phase, while using more efficient combined disinfecting solutions during the disinfection phase of irrigation.
Educational aims and objectives
This self-instructional course for dentists aims to explore concepts and innovations in endodontic irrigation, with specific focus on the use of uncomplicated and affordable sonic/ultrasonic devices to activate or agitate solutions during the cleaning phase, while using more efficient combined disinfecting solutions during the disinfection phase of irrigation.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions by taking the quiz online at endopracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
• Define the overall goals of irrigation.

• Define Macro Debris Removal (MDR) and its role in the process.
• Identify the importance of agitation and activation techniques in the cleaning process. Recognize the main requirements for adequate disinfection.
• List the three steps to highly expedite the cleaning and disinfection components of irrigation.
• Identify the three main chemical needs of all endodontic irrigation.
2 CE CREDITS
Allen Ali Nasseh, DDS, MMSc, is an endodontist practicing in Boston Massachusetts and the CEO and President of Real World Endo® an education, innovation, and medical device company.
Dr. Nasseh is a clinical advisor to NIH/NIDCR Consortium for Regenerative Sciences and the ADA Instruments and Materials Committee. He is an international speaker and a senior clinical instructor and lecturer at Harvard School of Dental Medicine and is on the editorial staff of several peer-reviewed journals and periodicals.
Disclosure: Dr. Nasseh has helped develop many of the products and techniques discussed in this article and receives royalties from his developments and innovations.
Cleaning: the importance of agitation and activation techniques
Cleaning the root canal space prior to engaging in disinfection is crucial because clumped macro debris and smear layer
18 Endodontic Practice US Volume 16 Number 3 CONTINUING EDUCATION
Figure 1: The broad term “endodontic irrigation” should be subdivided into its main components: cleaning, responsible removal of macro debris from the canal, and disinfection, which removes microbes and microbial byproducts from the canal
in the canal can prevent disinfectant solutions from reaching or contacting the biofilm and microorganism in fins and fissures of the root canal space and can act as a protective barrier for the microorganisms in the canal.5 This smear layer can clog dentinal tubules and physically prevent disinfectants from penetrating into them. Furthermore, we know that our gold standard disinfectant, sodium hypochlorite, is chemically deactivated and buffered rapidly by loose dentinal chips and dentinal walls and loses its efficacy6; therefore, removal of the loose macro debris and dentinal chips will not only expedite shaping, but more importantly, it will help improve the efficacy of the disinfection phase.
Root canal instrumentation produces loose chunks of dentin during the enlargement and advancement of rotary or reciprocating files in the root canal. Although some instrumentation motions generate more debris than others, all instrumentation motions, including reciprocation, rotation, and filing create debris that must be managed promptly to improve disinfection.
Persistent debris in the root canal during instrumentation will cause packing of debris laterally and apically, causing a variety of undesirable mid-operative and postoperative problems including canal blockage, ledging, and post-op pain. Furthermore, packed debris into a file’s dentinal chips will prevent file advancement and can cause file fractures by over-torqueing the instrument. This is why debris management is crucial during all phases of instrumentation.
Historically, most clinicians have used alternating use of sodium hypochlorite, a disinfectant capable of organic tissue dissolution, with a chelating agent like EDTA that removes inorganic components of the dentinal smear layer. This combination has constituted the positive pressure syringe irrigation that has been the standard irrigation for the past century. However, the use of a caustic irrigant such as NaClO in positive pressure to flush out debris bears its own risks. NaClO solution extrusion from the apex can lead to acute postoperative pain, or worse, a hypochlorite accident. This fear has prevented users from imposing a strong flushing action on the syringe solution to avoid these potential procedural accidents, thus resorting to passive needle irrigation to reduce risk. This physically gentler form of irrigation is not as efficient in flushing out loose debris from the canal. This is why the author believes continuous irrigation and activation of gentler solutions, such as distilled or iodinated water, from an ultrasonic or sonic device connected to the fluid source throughout instrumentation, is not only a more efficient method of MDR; but also, it’s a safer method of positive pressure flushing since the activated solution is water and not a toxic chemical.
This process of continuous water flushing using a powered device during instrumentation is often referred to as continuous ultrasonic irrigation.7 The technique involves short interval ultrasonic/sonic use with a wet tip (an ultrasonic or sonic tip with a water port) at a low power setting in each canal in between instrumentation. This can be a 10-15 second burst of water flushing by
activating the ultrasonic tip inside the canal and moving up and down. The expressed water from the powered device’s tip will quickly flush the canal from loose macro debris. Since this powered action of water can be used either through ultrasonic or sonic power, the author refers to this technique as “powered flushing” — the act of flushing out the loose content of the canal with a powered ultrasonic or sonically energized continuous flow of water used in a short burst.
However, since water is chemically inert in the canal, once the flushing action is complete, it should be replaced with a chemically active disinfectant. This can be accomplished efficiently with the insertion of a thin negative-pressure suction tip in the canal (Figure 2), creating negative pressure to suction out the water.3 A side benefit of using negative pressure (suction) at this stage to remove the water is the simultaneous removal of any remaining loose debris in the canal suspended in the water or loose that was not removed by powered flushing.
Why are activation and agitation methods important during root canal cleaning procedures? These physical processes are essential because they increase the kinetic energy of the solutions used, which catalyzes the chemical effect of irrigants and enhances the physical removal of debris from the walls of the root canal.7,8 The use of activation or agitation methods, such as ultrasonics or sonic devices, creates an energy wave that propagates throughout the solution, aiding in the removal of loose debris. In case of ultrasonics, this can include cavitation, agitation, and acoustic streaming, all of which increase the kinetic energy of water molecules and their Brownian motion. This

19 endopracticeus.com Volume 16 Number 3 CONTINUING EDUCATION
Figure 2: A small suction tip attached to a negative pressure system such as TotalVac™ (Brasseler USA, Savannah Georgia) or equivalent, can be used to quickly remove the water after powered flushing and replace it with a chemically active disinfectant
continuous flushing of water also facilitates cleaning by creating a streaming effect that washes out the loosened debris from the root canal. To achieve this, connecting an ultrasonic or sonic handpiece to the dental unit with a wet tip that can support continuous water flow during use is recommended.
The only limitation with the use of ultrasonic tips in this step is the stiffness of ultrasonic tips and the curve of some root canals. Stiff tips cannot negotiate around curves, and this limits their penetration to the straight portion of the root canal. However, even though true ultrasonic activation through cavitation may not occur far beyond the tip of the instrument, agitation and acoustic streaming can still occur several millimeters beyond the instrument tip, thus still improving the kinetic energy of the solution beyond the tip of the instrument and still providing an environment that is superior to mere passive action of the fluids at the apex to flush loose debris.
Therefore, during the cleaning phase of irrigation, which is generally during instrumentation and between files, MDR is safely and efficiently implemented when an ultrasonic or sonically powered wet tip produces continuous flow of energized water to flush out the cut debris from the root canal with positive pressure agitation. This is referred to by the author as “powered flushing.” The remaining water in the root canal is then quickly removed using a negative pressure tip (suctioned out) and is immediately replaced with a disinfectant.
Disinfection: the main requirements for adequate disinfection
After effective MDR has been achieved using powered flushing, the remaining water in the canal is removed with negative pressure suction and replaced with a chemically active solution to achieve deep disinfection.
The requirement for adequate disinfection of the root canal can be summarized as the physical and chemical removal of loose and attached biofilms, as well as their antigenic organic byproducts (e.g., LPS, EPS, etc.). MDR is responsible for the physical removal of the macro debris and physical flushing of some of the biofilm and its associated bacteria, but disinfection is the next level of chemical warfare needed to eradicate the remaining microorganisms and biofilms; and therefore, requires solutions that are optimized for that purpose.
To achieve such chemistry, we need to pay attention to the three main chemical needs of all endodontic irrigation: the removal of the organic debris, the inorganic debris, and the remaining microorganisms and their byproducts.
Over the past 3 decades, we’ve come to consensus that sodium hypochlorite (NaClO) is the gold standard for endodonic disinfection.9 This is due to the fact that higher concentrations (above 2.5%) of NaClO can kill microorganisms as well as dissolve collagen found in tissues. This organic tissue dissolution and simultaneous disinfection has made NaClO an excellent
double action irrigant.9 However, since it’s unable to do any inorganic debris removal, the third requirement of irrigation has been assigned to a separate irrigant that is an acid chelator. Recently, the use of EDTA 17% has become popular; however, EDTA and NaClO have a chemically antagonistic relationship and neutralize and buffer each other readily when combined. Furthermore, NaClO is also buffered by dentinal chips. This means that the use of a chelator to remove dentinal chips is necessary in order to improve the disinfecting function of NaClO. This antagonistic relationship between these two solutions has led clinicians to develop complicated protocol-and-use-separate NaClO and EDTA syringes alternating their use during instrumentation to achieve chelation of dentinal chips followed by disinfection and tissue dissolution.
Since this is a redundant and cumbersome protocol, combining solutions that can achieve these three main objectives of irrigation chemicals has been a long goal in the field. Recently, a new combined irrigation solution has been developed that is a combined 4% NaClO and 11 gentle chelators that substitute EDTA, chemical surfactants, and saponification agents. The replacement of EDTA with other chelators instead of replacing NaClO as a disinfectant allowed the use of the gold standard disinfectant in our field and simultaneous chelation using other chelating agents that are more resistant to the corrosive effect of NaClO. A mix-to-use delivery method was designed to mix the chelators and NaClO before use, allowing ample time for any given procedure using a single irrigation syringe that contains all the necessary components of disinfection and smear layer removal with added surfactants.10
The antimicrobial properties of the new solution, Triton® (Brasseler USA, Savannah, Georgia) have shown it to be 210 times more effective at killing C. albicans compared to NaClO with EDTA.11 Additionally, another study at University of British Columbia has shown that Triton can cut irrigation time by up to 50% thus allowing for a more efficient disinfection routine.12
This combined irrigant has made it possible to achieve simultaneous chelation during disinfection, which was long promised to expedite disinfection and be more efficacious in its action.11,12 Furthermore, adding surfactants to this solution can help deeper penetration into dentinal tubules.11 Recent studies on this combined disinfectant are very promising.13 Given its chemical and ergonomic advantages, this makes this mixture an ideal replacement solution for water immediately after powered
20 Endodontic Practice US Volume 16 Number 3 CONTINUING EDUCATION
The overall goals of irrigation can be described as the chemical and physical removal of organic and inorganic debris followed by disinfection and removal of microbes and microbial components from the root canal space.”
flushing of the root canal space during the cleaning phase of irrigation.
Therefore, removing the macro debris using powered flushing followed by replacing the water in the canal with a combined irrigation solution can help create a more efficient and thorough cleaning and disinfection process. The following three steps highly expedite the cleaning and disinfection components of irrigation:
1. Powered flushing
2. Negative pressure to remove water
3. Replacement with a multi-action irrigant (Figure 4).
Since we know that utilizing passive, positive pressure irrigation, 40 minutes of exposure to NaClO is necessary to kill e. faecalis, it’s possible that a protocol that allows powered flushing with a more efficient irrigation solution can help us overcome this rate-limiting step of disinfection during our root canal proce-
dures by catalyzing the rate of reactions inside the root canal.14 Further research in this area is necessary to validate this claim.
The additional use of Passive Ultrasonic Irrigation (PUI) at the end of the cleaning and shaping procedure, by applying sonic or ultrasonic energy without water in a canal flooded with this combined solution and agitating for an additional 30-60 seconds may achieve an even deeper smear layer removal and disinfection prior to drying and filling the root canal.

Conclusion
In conclusion, it is vital to break down the term irrigation into its two primary components: cleaning and disinfection. The first step, cleaning, involves the removal of macro debris through the use of agitation or activation by a powered device using a safe irrigant like water. The second step entails using negative pressure, specifically micro-suction, to evacuate the water and any loose debris from the root canal. Finally, in the third step, a combined chelator and disinfectant is introduced to fill the canal and allow for continuous chelation during instrumentation. With the availability of simple and cost-effective technology, these three steps can be seamlessly executed, ensuring safe and efficient irrigation during chemomechanical instrumentation.
REFERENCES
1. Zehnder M. Root canal irrigants. J Endod. 2006 May;32(5):389-398.
2. Bergenholtz G. Assessment of treatment failure in endodontic therapy. J Oral Rehabil. 2016 Oct;43(10):753-758.
3. Nasseh AA. Streamlining effective irrigation. Endodontic Practice US. 2022;15(3): 10-12.
4. Haapasalo M, Shen Y, Wang Z, Gao Y. Irrigation in endodontics. Br Dent J. 2014 Mar;216(6):299-303.
5. Wang Z, Shen Y, Haapasalo M. Effect of smear layer against disinfection protocols on Enterococcus faecalis-infected dentin. J Endod. 2013 Nov;39(11):1395-1400.
6. Macedo RG, Herrero NP, Wesselink P, Versluis M, van der Sluis L. Influence of the dentinal wall on the pH of sodium hypochlorite during root canal irrigation. J Endod. 2014 Jul;40(7):1005-1008.
7. Machado R, Rother A, Comparin D, Pawar AM, Matos FDS, Cunha TC, Alberton LR, Paranhos LR. Removal of the smear layer by passive and continuous ultrasonic irrigation: a scanning electron microscopy study. J Oral Res. 2021;10(6): 1-8.
8. Al-Zuhair H, Su Z, Liu H, Wang Z, Haapasalo M, Hieawy A, Gao Y, Shen Y. Antimicrobial effects of agitational irrigation on single- and multispecies biofilms in dentin canals. Odontology. 2023 Jan;111(1):49-56.
can help achieve simultaneous flow of water during activation creating some level of cavitation, agitation, and acoustic streaming of the water expressed through the tip. This will act as powered flushing of the root canal debris out of the canal efficiently
Irrigation Sequence
1. Powered Flushing (Flush out lose debris)
2. Negative Pressure (Remove water)
3. Add Multi Action Solution
Figure 4: The procedural steps recommended between files during instrumentation are: a 10-15 second burst of ultrasonic/sonic powered flushing with water, removal of the water and loose debris from the canal with negative pressure, and replenishing the canal with a multifunctional chelator/disinfectant for continued chemical action during instrumentation
9. Stojicic S, Zivkovic S, Qian W, Zhang H, Haapasalo M. Tissue dissolution by sodium hypochlorite: effect of concentration, temperature, agitation, and surfactant. J Endod. 2010 Sep;36(9):1558-1562.
10. Clarkson RM, Kidd B, Evans GE, Moule AJ. The effect of surfactant on the dissolution of porcine pulpal tissue by sodium hypochlorite solutions. J Endod. 2012 Sep;38(9): 1257-1260.
11. La Rosa GRM, Plotino G, Nagendrababu V, Pedullà E. Effectiveness of continuous chelation irrigation protocol in endodontics: a scoping review of laboratory studies. Odontology. 2023 Jul.
12. Andrabi SM, Kumar A, Mishra SK, Tewari RK, Alam S, Siddiqui S. Effect of manual dynamic activation on smear layer removal efficacy of ethylenediaminetetraacetic acid and SmearClear: an in vitro scanning electron microscopic study. Aust Endod J. 2013 Dec;39(3):131-136.
13. Sheng X, Yu J, Liu H, Wang Z, Deng S, Shen Y. Dual effectiveness of a novel all-in-one endodontic irrigating solution in antibiofilm activity and smear layer removal. Front Bioeng Biotechnol. 2023 Aug 1;11:1254927.
14. Retamozo B, Shabahang S, Johnson N, Aprecio RM, Torabinejad M. Minimum contact time and concentration of sodium hypochlorite required to eliminate Enterococcus faecalis. J Endod. 2010 Mar;36(3):520-523.
21 endopracticeus.com Volume 16 Number 3 CONTINUING EDUCATION
Figure 3: Using a wet tip (a powered tip with a water port) on an ultrasonic
EP
Continuing Education Quiz
Simple endodontic irrigation
NASSEH
1. Endodontic irrigation _________.
a. plays a pivotal role in the success of clinical endodontics
b. is only important if the pulp is non-vital
c. is more important if there is external root resorption
d. is not as important as shaping procedures
2. Recent advancements in powered devices and chemical solutions have led the author to conclude that the term irrigation is better understood if broken down into its two distinct subcategories: ____________.
a. cleaning and disinfection
b. powered and non-powered
c. sonic and ultrasonic irrigation
d. active and passive irrigation
3. The cleaning component of irrigation, techniques, and processes that aim at the physical removal of the macro debris generated during the act of instrumentation are referred to by the author as _________.
a. Macro Debris Removal (MDR)
b. ultrasonic use
c. NaClO irrigation
d. syringe irrigation
4. Disinfection attempts to _____________ during or after MDR has been accomplished.
a. chemically destroy the biofilm and microorganisms in the root canal system
b. apply chelating agents
c. apply powered devices
d. use copious use of water
5. Cleaning the root canal space prior to engaging in disinfection is crucial because clumped macro debris and smear layer in the canal _________.
a. can prevent disinfectant solutions from reaching and contacting the biofilm and microorganisms in fins and fissures of the root canal space
b. can cause decay
c. can stick to paper points during drying
d. can make the sealer set quickly
6. Although some instrumentation motions generate more debris than others, ___________ create(s) debris that must be managed promptly to improve disinfection.
a. reciprocation
b. rotation
c. filing
d. all of the above
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 16 CE credits for only $149; call 866-579-9496, or visit https://endopracticeus.com/ subscribe/ to subscribe today.
n To receive credit: Go online to https://endopracticeus.com/continuingeducation/, click on the article, then click on the take quiz button, and enter your test answers.
AGD Code: 070
Date Published: September 1, 2023
Expiration Date: September 1, 2026
2 CE CREDITS
7. Persistent debris in the root canal during instrumentation will cause packing of debris laterally and apically, causing a variety of undesirable mid-operative and postoperative problems including canal blockage, ledging, and post-op pain.
a. True
b. False
8. The requirement for adequate disinfection of the root canal can be summarized as ________.
a. the physical and chemical removal of loose and attached biofilms, as well as their antigenic organic byproducts
b. removal of organic tissue in the canal
c. placement of chelators in the canal
d. placement of chemicals to remove e fecalis
9. The main chemical need(s) of all endodontic irrigation is/are: _______.
a. Removal of organic debris
b. Removal of inorganic debris
c. Removal of remaining microorganisms and their byproducts
d. All of the above
10. The author notes, “Since we know that utilizing passive, positive pressure irrigation, 40 minutes of exposure to NaClO is necessary to kill e. faecalis, it’s possible that a protocol that allows powered flushing with a more efficient irrigation solution can help us overcome this rate-limiting step of disinfection during our root canal procedures by catalyzing the rate of reactions inside the root canal.”
a. True
b. False
To provide feedback on CE, please email us at education@medmarkmedia.com
Legal disclaimer: Course expires 3 years from date of publication. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
22 Endodontic Practice US Volume 16 Number 3 CONTINUING EDUCATION
Closed-system negative pressure irrigation
Drs. L. Stephen Buchanan and Christophe Verbanck explore irrigation of root canal systems
Irrigation of root canal systems is the most important aspect of RCT,1,2,3 yet it may also be the least understood action we do inside these complex spaces.4 Evidence for that statement is the fact that, to this day, very few endodontists understand how the introduction of rotary shaping files caused an increase in our irrigation failures,5 including the fact that a large proportion of endodontists instrument with NaOCl6,7 and still think we clean canals with files.5,8
Does this lack of understanding about irrigation fundamentals translate into RCT failures? The answer is yes, although these cases are seldom correctly diagnosed after the fact.
A randomized multi-center study done by Nixdorf, et al.,9 showed that 11% of patients in pain and seen by endodontists were not pain-free 6 months later! Half of these patients were misdiagnosed myofascial pain cases — they didn’t need RCT. The other half did need RCT, but 40% of this group received RCT on an adjacent tooth — so much for pulp testing — leaving the remaining cases that did need RCT, had the correct tooth treated, but remained symptomatic.
Virtually all of these cases had a history of severe pulpitis or partial necrosis before RCT, indicating to the authors that the most likely etiology for those teeth to continue to be symptomatic was due to pulp remnants left by the irrigation procedure; said irrigation failure rate being 3.3% of the patients presenting in pain.
Of the eleven percent of those still in pain 6 months later, half of those — 5.5% didn’t need RCT, and 40% of the other half had
L. Stephen Buchanan, DDS, FICD, FACD, Dipl. ABE, has been lecturing and teaching hands-on endodontic continuing education courses for over 30 years, both in his state-of-the-art training facility in Santa Barbara, California, as well as in dental schools and at meetings around the world. He currently serves as a part-time faculty member in the endodontic departments at the University of the Pacific’s Arthur Dugoni School of Dentistry and the University of California at Los Angeles as well as being the Endodontic Advisory Board Member to the Academy of General Dentistry. Dr. Buchanan is nationally and internationally known for his 50-plus endodontic procedural articles as well as his expertise in the research and development of new endodontic technology, instruments, and techniques. He is a Diplomate of the American Board of Endodontists and a Fellow of the International and American College of Dentists. Dr. Buchanan also maintains a private practice limited to Endodontics in Santa Barbara, California.
Christophe L.M. Verbanck, DDS, MSc, obtained his Master of Dentistry at Gent University in 2009. He specialized in endodontics, graduating after a 3-year postgraduate training program from the same university. Since 2010 he has worked in several multi-disciplinary and endodontic referral practices all over Flanders. In January 2016, together with his wife, he started his own referral practice for Endodontics, Lovendo, in Lovendegem (Belgium). He regularly teaches endodontics to general dentists and holds workshops on the application of endodontic techniques.
Disclosures: Dr. L. Stephen Buchanan is a co-founder of PlanB Dental.
Educational aims and objectives
This self-instructional course for dentists aims to focus on some challenges of irrigating anatomic complexities.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions by taking the quiz online at endopracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
• Distinguish between the mechanism of action, benefits, drawbacks and safety issues of Positive Pressure Irrigation (PPI), Negative Pressure Irrigation (NPI), Closed System Negative Pressure Irrigation (CSNPI), and Multisonic Ultracleaning Systems (MUS).
• Realize some statistics about the causes of root canal failures.
• Identify some more recent root canal technologies.
• Identify what could happen if the direction of vacuum is reversed.
• Realize the concept and advantages of “The Forward Effect” caused by the vacuum on multi-cannular drawn NaOClirrigation in MIE preparations.
2 CE CREDITS
Figures 1A-1C: 1A. This tooth continued to refer pain (in the endodontic zone) for 18 months after RCT. Two different endodontists recommended apicoectomy to remove the overextended filling material beyond the MB and D roots. Instead, the patient was told the case could be cut at any time in the future, but that surgery might be avoided by simply retreating the underfilled ML canal. 1B. Post-op radiography revealed a mid-mesial canal with its own blood supply. 1C. Cleared mesial root of an extracted lower molar illustrates the impossibility of cleaning this root canal system with instruments and the necessity of irrigating effectively
the wrong tooth treated, leaving 60% of 5.5% which calculates at 3.3 of our cases. That’s not a small issue if you consider the fact that 25 million RCTs10 are done in the U.S. alone every year, revealing approximately 825,000 RCT irrigation failures per year — a number that closely relates to the findings in a previous study by Nixdorf, et al., on persistent tooth pain after RCT.11
23 endopracticeus.com Volume 16 Number 3 CONTINUING EDUCATION
The challenge of irrigating anatomic complexities
Complete removal of pulp tissue during RCT is not a simple job due to the anatomic complexity of root canal systems and the fact that NaOCl dissolves pulp tissue in a linear fashion, not as a catalytic reaction (Figure 2).7,8 While a broached pulp can be completely dissolved in a minute or two when dropped into a dappen dish of bleach, it can take 40 minutes of passive positive pressure irrigation to digest the same volume of pulp tissue out of an MB canal system contained inside an upper molar. Fortunately, irrigation technology is rapidly improving our ability to eliminate lateral pulp remnants in spite of the current trend toward minimally invasive instrumentation.


Stojicic, et al., in 2010, looked at the effects of concentration, temperature, and agitation on NaOCl efficacy and found that dissolution efficacy increased almost linearly with the concentration of NaOCl. Higher temperatures and agitation considerably enhanced the efficacy of NaOCl, although agitation had a greater effect than temperature, and continuous agitation resulted in the fastest tissue dissolution. Their comment that “Optimiz-
ing the concentration, temperature, flow, and surface tension can improve the tissue dissolving effectiveness of NaOCl even 50-fold” seemed a bit far-fetched when first read;12 however, our own research (unpublished data) on the rates of pulp dissolution from isthmus spaces have confirmed that this is possible.
New irrigation technologies
There are many ways to intermittently agitate (cavitate) NaOCl in root canal systems — sonic, ultrasonic, and laser activation, but GentleWave® irrigation (GW), developed by Sonendo® (Sonendo Inc., Laguna Hills, California), is one of the few irrigation methods that delivers continuous agitation to all canals simultaneously. They pump the irrigating fluids up to 9000 psi, and blast them into and out of the access cavity, creating a negative pressure Bernoulli effect in the RCS to prevent NaOCl from escaping into peri-radicular tissues. Much is made of the sonic energy GW imparts to the solutions, but the greatest mechanism of action is more likely the 250 ml of NaOCl shot through the tooth during the 5-minute NaOCl cycle, allowing accelerated dissolution of pulp tissue in canals (Figure 4).13
After 40 to 50 RCT procedures successfully done with GW, the senior author had his first case failure in a red-hot C-shaped lower molar that remained symptomatic after RCT was completed (Figure 5). The case looked pretty nice when finished — several filled lateral aberrations were seen postoperatively, but the patient complained about pain that continued to be referred

Figures 2A-2C: 2A. MicroCT reconstruction of an upper first molar, highlighting the complexity of the MB canal system. 2B. By segmenting the root canal space from the root, the lateral morphology is more apparent. 2C. Superimposition of typical MIE canal shaping reveals the very narrow interface of lateral pulp remnants exposed to irrigating solutions, requiring linear dissolution rather than circumferential dissolution
Figures 3A-3C: 3A. This MIE RCT was cleaned with conventional positive pressure irrigation with 6% NaOCl, delivered with a 12cc syringe and a 30 Ga. closed-end side-vented cannula. This is simple, inexpensive, but uni-canular and very time dependent (20-40 mins). 3B. The lower molar RCT was treated by Dr. Filippo Santarcangelo using EndoVac™ by Kerr Endodontics. This tooth was irrigated continuously for 45 minutes because he could not negotiate the last 3 mm of the distal canal. Post-op radiography reveals the distal primary canal cleaned and filled 3 mm beyond the apical extent of instrumentation with multiple microscopic lateral canals filled in both roots. 3C. The complete healing seen at the 4-month recall is testament to the thoroughness of the irrigation. Like conventional irrigation, EndoVac is uni-canular, but completely safe due to the cannula being used for suction instead of irrigant delivery

24 Endodontic Practice US Volume 16 Number 3 CONTINUING EDUCATION
Figure 4: Lower cuspid with extensive internal resorption treated with GentleWave® irrigation. Note the myriad of resorptive lacuna trails filled postoperatively after the vital tissue that caused them was dissolved during two complete cycles of GW (Case by Buchanan)
Figure 5A-5D: 5A. This lower C-shaped molar presented with a severely inflamed pulp. 5B-5C. Post-op radiographs show abrupt mesial and distal apical canal curvatures as well as significant isthmus morphology. 5C. Extending toward the centerline from the MB and D canals. 5D. This CBCT view shows the MB canal possibly treated short of terminal length
to his right endo zone (below the malar eminence, above the lower border of the mandible). This being a C-shaped molar, the best hypothesis for the etiology of this failure was incomplete debridement of pulp tissue in the large isthmus spaces (Figure 6).
A novel isthmus replica
To test this hypothesis, a research device was designed to replicate the isthmus morphology seen in these molars. This was 3D-printed in two halves so a pulp replica (porcine muscle tissue) could be inserted into the isthmus form before they were assembled with light-cure adhesive (Figure 7). This novel in vitro device was capable of displaying how pulp dissolution occurs in isthmus spaces when a number of variables are compared, said variables being NaOCl concentration, temperature, fluid flow, and agitation.
The first irrigation method tested in the isthmus block was of course GW, and it confirmed my hypothesis about the cause of my C-shaped molar failure — at the end of the 5-minute NaOCl cycle, significant amounts of pulp replica remained. Also confirmed by this test was the fact that EDTA — even when activated by multi-sonic energy — has zero ability to digest organic tissue, so it could be said that GW’s primary mechanism of action
(MOA) for pulp dissolution is hosing root canal systems with enormous volumes of NaOCl (Figure 8).


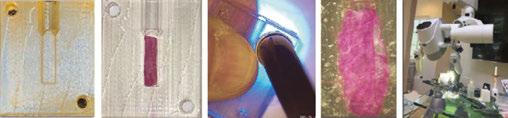
Negative pressure irrigation (NPI) versus positive pressure irrigation (PPI)
The isthmus research blocks were then used to investigate NPI because the literature shows excellent cleaning of isthmus spaces with EndoVac™ (EV) by Kerr Endodontics.14,15,16 Is it the direction the solutions are moving through the canal? Is it because EV eliminates “vapor lock” — the gas bubbles liberated during pulp saponification?17 Isthmus block studies showed the only difference between PPI and NPI was that the latter requires constant replenishing of solutions, whereas dentists using PPI tend to irrigate and let the solutions soak in the patient’s tooth — radically decreasing the volume of solutions run through root canals. When constant irrigation was used for both NPI and PPI, the results were identical (Figure 9).
Therefore, while EV is 100% safe from irrigation accidents,18,19 it was poorly designed and was pedantic to use because of the constant attention needed and because of its propensity to clog up every 5 minutes of use. Worse than that, EV is uni-canular, meaning it only irrigates a single canal at a time so a four-canal molar requires 20 minutes of intensive hands-on work.
Investigating closed-system negative pressure irrigation (CSNPI)
Eliminating intensive hands-on requirements was simple in a closed system as the solutions could then be pulled into the pulp
6:
CBCT
(left, originally published in: Fan B, Cheung GSP, Fan M, Gutmann JL, Bian Z. C-shaped canal systems In mandibular second molars: part 1- Anatomical features. J Endod. 2004 Dec; 30(12): 899-903) and computer reconstructions (right, originally published in: Solomon M, Piqué F, Fan B, Eilat Y, Berman LH. The challenge of C-shaped canal systems: A comparative study of the Self-Adjusting File and ProTaper. J Endod. 2012 Feb; 38(2): 209-214) of C-shaped molars, showing isthmus spaces extending from MB to D canals. Generally impossible to instrument, some of these isthmus spaces are wider than 5 mm presenting the ultimate challenge to any irrigation procedure

Figures 7A-7E. 7A. Isthmus research block half after printing with UV-cured clear polymer. 7B. A cut and dyed pulp replica (prosciutto) after placement in the isthmus space. 7C. A second block half is bonded over this, trapping the isthmus replica inside. D. Isthmus block assembled, prior to cutting pulp replica out of the two canal paths. 7E. Isthmus block mounted in a PanaVise in front of an operating microscope connected to a digital video recorder
block after the 30-second distilled water cycle — no pulp replica dissolved. 8B. The block after 2.5 minutes of the NaOCl cycle. 8C The block after the end of the 5-minute NaOCl cycle. 8D. The block after the 2 minute EDTA cycle. 8E. Another GW procedure instrument was installed in the console, and after an additional 2.5 minutes of the NaOCl, cycle all remaining tissue was gone, revealing that although GW greatly accelerates NaoCl tissue dissolution, it is still a linear process needing adequate time to do its job
25 endopracticeus.com Volume 16 Number 3 CONTINUING EDUCATION
Figure
Axial
views
Figure 8A-8E. 8A. Isthmus research
A. B. C. D. E.
Figure 9: Isthmus research blocks showing no difference between PPI and NPI when constant irrigation was done (Buchanan)
A. B. C. D. E.
chamber by the vacuum coming through the micro-cannulas from the chairside evac system (Figure 10). The results from the extracted tooth experiment (Figure 11) as seen in SEM imaging were exceptional, but it took 30 minutes due to the repeated clogging of the microcannula.
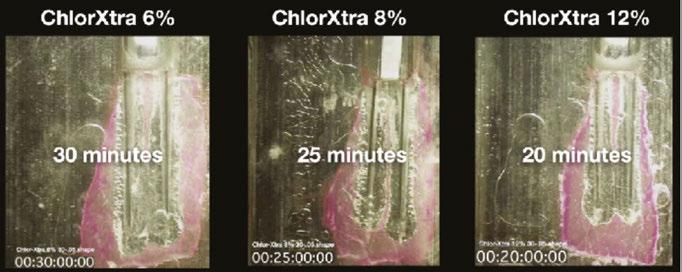

The reversal
The senior author then had the epiphany that clogging would never be an issue if the direction of vacuum were reversed, so that change was made, and another isthmus block study was
kicked off. Shortly after beginning, it became apparent that not only was the cannula blockage issue solved, but that the vacuum-drawn outflow of NaOCl through the end of the blunt-cut cannula was dissolving pulp replica at a remarkable rate (Figure 12), most likely due to the constant, rapid fluid flow of sodium hypochlorite exiting the cannula ends.
There was initial concern about the inherent safety of NaOCl flowing out of an open-ended cannula, until it was realized that vacuum-drawn irrigation immediately ceased the moment an

Figures 10A-10B. 10A. Illustration of experimental closed system EV. The irrigating canula is the vacuum source pulling the NaOCl from an IV bag through an inlet sealed into the access cavity. 10B. This was run for 30 minutes, unclogging the cannula every 5 minutes. 10C. The ultimate objective for this irrigating system was to have manifolds and cannulae for each canal so multicanalar irrigation can happen. Originally the vacuum was connected to the cannula, and the irrigants inlet was placed just inside the access cavity
Figure 12: The isthmus block result after just 13 minutes when the vacuum was reversed to prevent cannula blockage and found that the constant vacuum-drawn outflow through the end of the cannula radically increased dissolution speed


Figure 13: Illustration showing the safety difference between NaOCl being pushed out the end of an irrigating cannula by a syringe (the reason to only use closed-end side-vented irrigating cannulas for PPI) and NaOCl being drawn out by resident vacuum pressures. Vacuum-drawn irrigant flow ceases the moment a cannula binds circumferential canal walls

26 Endodontic Practice US Volume 16 Number 3 CONTINUING EDUCATION
Figures 11A-11C: SEM imaging of root canal walls in the coronal, middle, and apical thirds (from the experimental tooth in Figure 10) showing exceptional cleaning results (Buchanan)
Figures 14A-14D: 14A. This isthmus block shows the Forward Effect that occurs because NaOCl is being drawn straight out the end of the blunt-cut cannula. EV only irrigates to the depth the micro-cannula fits in the canal, requiring a larger apical shape. 14B-14D: Isthmus research blocks displaying increases in dissolution time with increases in NaOCl concentration
A.
B. C.
A.
B.
C.
A.
B.
C.
D.
Figures 16A-16C: 16A-16B. Isthmus research blocks showed a dramatic 100% increase in effect when NaOCL was aerated versus non-aerated. 16C. The replica canal on the left was irrigated with aerated NaOCl, the canal on the right with non-aerated NaOCl.
open-ended needle was locked in a canal, rendering it impossible to cause a hypochlorite accident with this MOA (Figure 13).


The Forward Effect
Then, as the studies continued, it became apparent that drawing the NaOCl out the end of the cannula with vacuum pressure was having its effect at least 5 mm forward of the cannula end. This was very providential as it meant that irrigating cannulae had only to be placed to mid-root in most canals, a definite advantage when dealing with severely curved canals, especially when cutting minimally-invasive canal preparations.20 EV, by comparison, requires a .35 mm 4 % apical preparation diameter,21 a shaping objective that invites apical damage in curved canals.5
Over the following months, the isthmus research block was used to compare the effects of different irrigation variables. Simply choosing a higher NaOCl concentration has significant effect on the speed of dissolution (Figure 14). Raising the irrigant’s temperature from 70ºF (21.1C) to 100ºF (37.7C) increasinged the speed of dissolution by 33% (Figure 15), and the shear forces of agitation — provided in this case by aerating the solution to cause gas bubble cavitation — doubled the speed of dissolution (Figure 16), confirming Stojicic, et al.’s findings12 that agitation brought more effect than temperature. All irrigation tests were done with a constant flow of solutions — another variable critical to GW’s MOA.
Figures 17A-17C: Isthmus research blocks showing the isthmus replica dissolved in 7 minutes with higher NaOCl concentrations, temperatures, and continuous agitation from aeration bubbles
Finally, a study was done with 12% NaOCl irrigant that was aerated and heated to 120° F (48,9°C), and the isthmus pulp replica was gone in just over 7 minutes (Figure 17).

Case outcomes
Closed-System Negative Pressure Irrigation device staged on a lower molar (PulpSucker® by PlanB® Dental). 18B. Post-op radiograph showing a 7 mm long mid-mesial canal that was never touched with a file but was cleaned of vital tissue. 18C. Close-up shows an apical delta system of lateral canals in the apical third of the distal canal

Figures 19A-19E: 19A. Recent clinical case that presented with severe irreversible pulpitis. 19B. Cone fit radiograph, after PulpSucker irrigation in a single-visit procedure, showing perfect cone fit in the mesial canals, but inadequate cone fitting in the very complex distal canal. 19C. Multiple impediments at the end of the virtually non-instrumented distal canal were the ideal indication for carrier-based obturation. 19D. Post-obturation image shows a loop off the distal canal that is hidden in all the other radiographs. 19E. A postoperative radiograph showing the independent MIE access entries for mesial and distal canals and the multiplicity of lateral canals in both roots
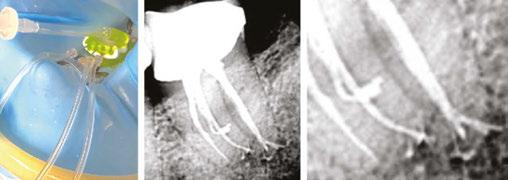
27 endopracticeus.com Volume 16 Number 3 CONTINUING EDUCATION
Figure 15A-15B: Isthmus research blocks showing a 33% increase in speed of dissolution when the temperature of the solution was raised from room temperature to body temperature
Figures 18A-18C.
A. B.
A. B.
C.
A. B. C.
A.
B. C.
A.
B.
C.
D.
E.
In conclusion: features, advantages, and benefits of CSNPI
Closed-system negative pressure irrigation (CSNPI) has several advantages over conventional open-system irrigation (PPI or NPI):
1. CSNPI can be multi-cannular. Multi-cannular means that it can clean all of the canals in a given tooth at the same time. Only laser-driven PIPS (photo-induced photo-acoustic streaming), GentleWave, and PulpSucker irrigation can do this. Why is this important? Because endodontists treat mostly multi-cannular molars, so any irrigation method that is uni-cannular is non-optimal and time consuming.
2. CSNPI is more effective than open-system irrigation. Open-system NPI can have constant irrigation flow but only in a single canal at a time, so even though EV ads say they can reduce a 40 minute irrigation time to 5 minutes, clinicians have to hang onto an EV syringe for 20 minutes in a 4-canal molar. That is just untenable for specialists doing 4 to 8 cases a day.
3. CSNPI can be hands-free. CSNPI can do its work without dentist or assistant in the operatory. GentleWave irrigation is fast, but operators must hold onto the GW procedure instrument in a very focused manner for 8 minutes after the preparatory 3-5 minutes of hands-on work. PulpSucker irrigation can be staged in less than 5 minutes, after which it is entirely hands-off.
4. CSNPI decreases immediate post-op symptoms. All pain of endodontic origin is a pressure phenomena. “Hot teeth” are exquisitely tender to touch because of the peri-radicular tissue pressure induced by severe inflammation. Closed-system irrigation applies vacuum pressures to the RCS but also to PA tissues beyond the root, and although evidenced-based clinical trials have not been completed yet, clinical experiences indicate that patients who had RCT with CSNPI experience much less post-op pain when the anesthesia wears off than patients who had RCT in teeth irrigated conventionally.
REFERENCES
JR, Ling J, Choi KK, Pashley DH, Tay FR. Review of contemporary irrigant agitation techniques and devices. J Endod. 2009 Jun;35(6):791-804.
2. Liu H, Shen Y, Haapasalo M. Effectiveness of Six Irrigation Techniques With Sodium Hypochlorite in Tissue Dissolution. Cureus. 2023 May 18;15(5):e39208.
Some RCT considerations
1. To avoid complications or failures of treated endodontic cases, it is important to understand that mechanical/rotary instruments do not clean canals. They are merely an aid for better irrigation of the complex root canal system.
2. NaOCl is still the irrigant of choice.
3. Irrigation can only come from coronal directions. Although NaOCl is capable of dissolving organic tissue in under 2 minutes in a dappen dish, the complexity of the root canal system prevents this rapid break down. Further developments in irrigation technology are trying to improve this obstacle.
4. The efficacy of tissue dissolution can be enhanced by concentration, temperature, and agitation of NaOCl. A higher or constant volume/time will give the best results.
3. Gulabivala K, Ng YL, Gilbertson M, Eames I. The fluid mechanics of root canal irrigation. Physiol Meas. 2010 Dec;31(12):R49-84.
4. Boutsioukis C, Arias-Moliz MT. Present status and future directions - irrigants and irrigation methods. Int Endod J. 2022 May;55 Suppl 3(Suppl 3):588-612.
5. Buchanan LS, Verbanck CLM. Root canal shaping in the age of minimally invasive endodontics (MIE). Endod Practice US. 2023; 16(1): 20-24.
6. McComb D, Smith DC. A preliminary scanning electron microscopic study of root canals after endodontic procedures. J Endod. 1975 Jul;1(7):238-242.
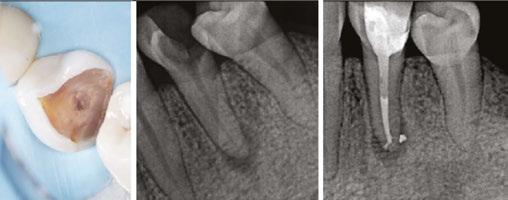
7. Zehnder M. Root canal irrigants. J Endod. 2006 May;32(5):389-398.
8. Peters OA. Current challenges and concepts in the preparation of root canal systems: a review. J Endod. 2004 Aug;30(8):559-567.
9. Nixdorf DR, Law AS, John MT, Sobieh RM, Kohli R, Nguyen RH; National Dental PBRN Collaborative Group. Differential diagnoses for persistent pain after root canal treatment: a study in the National Dental Practice-based Research Network. J Endod. 2015 Apr;41(4):457-463.
10. American Association of Endodontists. AAE Root canal safety talking points. https:// www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/rootcanalsafetytalkingpoints.pdf. Accessed August 10, 2023.
11. Nixdorf DR, Moana-Filho EJ, Law AS, McGuire LA, Hodges JS, John MT. Frequency of persistent tooth pain after root canal therapy: a systematic review and meta-analysis. J Endod. 2010 Feb;36(2):224-230.
12. Stojicic S, Zivkovic S, Qian W, Zhang H, Haapasalo M. Tissue dissolution by sodium hypochlorite: effect of concentration, temperature, agitation, and surfactant. J Endod. 2010 Sep;36(9):1558-1562.
13. Haapasalo M, Wang Z, Shen Y, Curtis A, Patel P, Khakpour M. Tissue dissolution by a novel multisonic ultracleaning system and sodium hypochlorite. J Endod. 2014 Aug;40(8):1178-1181.
14. Versiani MA, Alves FR, Andrade-Junior CV, Marceliano-Alves MF, Provenzano JC, Rôças IN, Sousa-Neto MD, Siqueira JF Jr. Micro-CT evaluation of the efficacy of hard-tissue removal from the root canal and isthmus area by positive and negative pressure irrigation systems. Int Endod J. 2016 Nov;49(11):1079-1087.
15. Yoo YJ, Lee W, Kim HC, Shon WJ, Baek SH. Multivariate analysis of the cleaning efficacy of different final irrigation techniques in the canal and isthmus of mandibular posterior teeth. Restor Dent Endod. 2013 Aug;38(3):154-159.
16. Siu C, Baumgartner JC. Comparison of the debridement efficacy of the EndoVac irrigation system and conventional needle root canal irrigation in vivo. J Endod. 2010 Nov;36(11):1782-1785.
17. Estrela C, Estrela CR, Barbin EL, Spanó JC, Marchesan MA, Pécora JD. Mechanism of action of sodium hypochlorite. Braz Dent J. 2002;13(2):113-117.
18. Desai P, Himel V. Comparative safety of various intracanal irrigation systems. J Endod. 2009 Apr;35(4):545-549.
19. Azim AA, Aksel H, Margaret Jefferson M, Huang GT. Comparison of sodium hypochlorite extrusion by five irrigation systems using an artificial root socket model and a quantitative chemical method. Clin Oral Investig. 2018 Mar;22(2):1055-1061.
20. Buchanan LS. Closed-system negative pressure irrigation: A serious inflection point in root canal cleaning. Dentistry Today. April 2020 [Online]. https://www.dentistrytoday. com/closed-system-negative-pressure-irrigation-a-serious-inflection-point-in-root-canal-cleaning/. Accessed August 10, 2023.
21. Kerr Endodontics. EndoVac Apical Negative Pressure Irrigation System Instructions for use. Download for instructions can be found at: https://www.kerrdental.com/download-centre?f%5B0%5D=field_resource_document_type%3A633. Accessed August 10, 2023.
28 Endodontic Practice US Volume 16 Number 3 CONTINUING EDUCATION EP
Figures 20A-20C: 20A-20B. Pre-op situation showing severely broken down lower left premolar with a partial necrosis of the pulp. 20C. Post-op image showing complete obturation of the apical pulp space and delta after PulpSucker irrigation in a single-visit treatment. Immediate placement of a fiberpost was done for future indirect restoration
1. Gu LS, Kim
A. B.
C.
Continuing Education Quiz
Closed-system negative pressure irrigation
BUCHANAN
1. A randomized multi-center study done by Nixdorf, et al., showed that 11% of patients in pain and seen by endodontists were not pain-free ________ later.
a. 2 weeks
b. 4 weeks
c. 6 weeks
d. 8 weeks
2. __________ RCTs are done in the U.S. alone every year.
a. 1 million
b. 10 million
c. 25 million
d. 50 million
3. Complete removal of pulp tissue during RCT is not a simple job due to ________.
a. the anatomic complexity of root canal systems
b. the fact that NaOCl dissolves pulp tissue in a linear fashion, not as a catalytic reaction
c. those patients with undetected pulpitis
d. both a and b
4. While a broached pulp can be completely dissolved in a minute or two when dropped into a dappen dish of bleach, it can take 40 minutes of passive positive pressure irrigation to digest the same volume of pulp tissue out of an MB canal system contained inside an upper molar.
a. True
b. False
5. Stojicic, et al., in 2010, looked at the effects of concentration, temperature, and agitation on NaOCl efficacy and found that dissolution efficacy _________ the concentration of NaOCl.
a. decreased almost linearly with
b. increased almost linearly with
c. stayed the same despite
d. was completely eliminated by
6. Higher temperatures and agitation considerably enhanced the efficacy of NaOCl, _______, and continuous agitation resulted in the fastest tissue dissolution.
a. although agitation had a greater effect than temperature
b. although temperature had a greater effect than agitation
c. while agitation and temperature had the same effect
d. none of the above
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 16 CE credits for only $149; call 866-579-9496, or visit https://endopracticeus.com/ subscribe/ to subscribe today.
n To receive credit: Go online to https://endopracticeus.com/continuingeducation/, click on the article, then click on the take quiz button, and enter your test answers.
AGD Code: 070
Date Published: September 1, 2023
Expiration Date: September 1, 2026
2 CE CREDITS
7. There are many ways to intermittently agitate (cavitate) NaOCl in root canal systems — sonic, ultrasonic, and laser activation.
a. True
b. False
8. Then, as the studies continued, it became apparent that drawing the NaOCl out the end of the cannula with vacuum pressure was having its effect at least ________ forward of the cannula end.
a. 5 mm
b. 7 mm
c. 8 mm
d. 10 mm
9. CSNPI can be _________.
a. laser-driven
b. multi-cannular
c. only unicannular
d. untenable for specialists doing 4 to 8 cases a day
10. Open-system NPI can have constant irrigation flow but only in a single canal at a time, so even though EV ads say they can reduce a 40 minute irrigation time to 5 minutes, clinicians have to hang onto an EV syringe for _________ in a 4-canal molar.
a. 7 minutes
b. 12 minutes
c. 20 minutes
d. 35 minutes
To provide feedback on CE, please email us at education@medmarkmedia.com
Legal disclaimer: Course expires 3 years from date of publication. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
29 endopracticeus.com Volume 16 Number 3 CONTINUING EDUCATION
Is social media placing your personal privacy or your small business at risk?
Mark Pribish offers guidance on minimizing risks of social media

Some critics of social media say our addiction to apps in general and social media (in particular) open ourselves up to privacy risks. My question to app and social media users is, “When was the last time you read the terms and conditions or adjusted the privacy settings of your app or social media accounts?”
While apps and social media offer convenience, entertainment, and networking opportunities — cyber thieves and ID theft criminals are leveraging social networks and apps to do their dirty work.

According to the second quarter 2022 Brand Phishing Report from Check Point Research, which “highlights the brands that were most frequently imitated by cybercriminals in their attempts to steal individuals’ personally identifiable information (PII) or payment credentials over the quarter,” LinkedIn remains the most impersonated brand by phishing campaigns.1
As most know, LinkedIn is not only a social media site but also the world’s leading professional networking site. Hackers have imitated brands in business sectors such as social media (LinkedIn), technology (Microsoft), shipping/courier services (DHL), and online shopping (Amazon) and highlights the ongoing risks facing users of trusted business platforms.
I have listed below from the Check Point Research Brand Phishing Report the top-ranked brands by their overall appearance in brand phishing attempts.2
1. LinkedIn (45%)
These imitation phishing scams of leading brands are effective and lucrative for cyber thieves and ID theft criminals because both consumers and business executives are more likely to click on a well-known name/brand.
But sometimes it’s more than just the hacker you must worry about. Consumers and business executives need to know that apps and social media can track your search engine history, purchasing habits, geographical location, and even investigate your files and contact list — all without your knowledge and sometimes without your permission.
For example, when you install an app, most apps will require you to “accept” their terms and conditions — but did you read and really understand the type of information that is being collected and the kind of privacy threats you now are exposed to?
How bad can these “privacy threats” be? Just imagine an app vendor or third-party marketer collecting and selling your smartphone’s unique device ID, phone’s location, phone number, your age, gender, likes, dislikes, search engine habits, emails, usernames, and more to data brokers. And then imagine how these data brokers collect, analyze, and package your most sensitive personal information in a unique profile and sell it over and over again — without your knowledge.
But it gets worse as The Federal Bureau of Investigation (FBI) released its Internet Crime Complaint Center (IC3) 2021 Internet Crime Report and accompanying 2021 State Reports last March.3 The FBI reported 847,376 complaints of suspected Internet crime in 2021, a 7% increase from 2020 that resulted in losses exceeding $6.9 billion. This is happening even though small and big businesses along with state and Federal governments spend billions of dollars to fight daily cybersecurity attacks.
30 Endodontic Practice US Volume 16 Number 3 GOING VIRAL
2. Microsoft (13%)
3. DHL (12%)
4. Amazon (9%)
5. Apple (3%)
6. Adidas (2%)
7. Google (1%)
8. Netflix (1%)
9. Adobe (1%)
10. HSBC (1%)
Mark Pribish is the Practice Leader, Identity Theft and Data Breach Solutions at Scottsdale, Arizona-based Vero, LLC. He has authored hundreds of articles and is frequently interviewed by local and national media as an identity theft and data breach risk management expert. He is a member of the Identity Theft Resource Center Board of Directors and is a graduate of the University of Dayton.

















Microsoft is an example of a large and sophisticated technology company with annual revenue of $168 billion that spends about $2 billion annually to respond to current and future cybersecurity challenges and threats. At the same time, hackers focusing on Microsoft vulnerabilities have successfully beached Microsoft 4 times, creating four significant data breach incidents that have exposed customer data and placed clients at risk during the last 12 months.4
In addition, the FBI Internet Crime Report stated that of the more than 30 crime types reported, the top three cybercrimes were phishing scams, non-payment/non-delivery scams and personal data breach, closely followed by identity theft and extortion.
The reality is that small- and mid-sized businesses such as dental and medical practices are viewed as easy targets because of limited resources and poor information security best practices.
The fact is that cyber thieves and ID theft criminals love the trail we leave on social media. Specific to individual consumers and small business employees, here are my five tips to help you minimize your social media privacy risks:
1. Limit and/or eliminate sharing your personal information online.
2. Increase your privacy awareness by reviewing and adjusting your privacy settings.
3. Be aware that some apps reset your privacy settings during major upgrades.
4. Learn more on how your personal information is used and for what purposes.
5. Consider using “privacy assistant or automation software” to help keep your privacy preferences current.
Specific to small (and big) businesses, no one company can ever prevent itself from ever experiencing a data breach event — especially with how apps and social media can place a small business at risk. Some of the most notable data breaches in 2021 and 2022 include CNA, Experian, Facebook, GEICO, Instagram, LinkedIn, Marriott, Microsoft, Tesla, and Twitter.
The irony to these data breaches is that these businesses pride themselves on safeguarding PII, and these businesses have more financial and information technology resources than most other business. Yet they still cannot prevent a data breach event from happening.
The reality of data breaches is that they occur almost every day — whether it is an accidental release (which is a polite phrase for carelessness or incompetence) or malicious intent (with the insider threat a common focal point, although the media heavily focuses on IT and hacking events).
The 2021 Verizon Data Breach Investigations Report can help both consumers and small businesses be proactive in mitigating their exposure to identity theft and data breaches. Last year’s Data Breach Investigations Report (DBIR) highlights the reality of data breaches that can support a cyber-risk management strategy for all businesses in general but small business in particular, including these findings.5
• Social engineering is the most successful attack.
• 85% of breaches involved a human element.
• Older vulnerabilities that haven’t been patched are being exploited by attackers.
• Credentials remain one of the most sought-after data types, followed by personal information.
• Employees continue to make mistakes that cause incidents and breaches.
• Business email compromises were the second most common form of social engineering.
• Most social engineering incidents were discovered externally.
This year’s 2022 Verizon Data Breach Investigations Report highlights “the importance of building a culture of cybersecurity vigilance,” including these findings.6
• There are four key paths leading to your estate: credentials, phishing, exploiting vulnerabilities, and botnets.
• All four are pervasive in all areas of the DBIR, and no organization is safe without a plan to handle each of them.
• This year ransomware has continued its upward trend with an almost 13% rise — an increase as big as the past 5 years combined.
• The human element continues to drive breaches. Whether it is the use of stolen credentials, phishing, or simply an error, people continue to play a large part in incidents and breaches alike.
• Error continues to be a dominant trend, and the fallibility of employees should not be discounted.
Whether you are an individual consumer, employee, or a small business owner, you need to be aware that social media can place your personal privacy and/or small business at risk. Be aware of the latest social engineering trends including apps and social media where hackers imitate leading business brands.
As for receiving links of well-known brands on social media, my recommendation on receiving notifications from LinkedIn, Facebook, or any other social media is to ignore the links or attachments. If a social media notification is legitimate, you will receive it again, and then you can go to the social media network login page to retrieve it directly.
REFERENCES
1. 2022 Brand Phishing Report from Check Point Research. LinkedIn remains the most impersonated brand by phishing campaigns. Accessed August 16, 2022.
2. 2022 Brand Phishing Report from Check Point Research. https://www.securitymagazine.com/articles/98046-linkedin-remains-most-impersonated-brand-by-phishing-campaigns#:~:text=Below%20are%20the%20top%20brands,DHL%20(12%25). Accessed August 16, 2022.
3. FBI Internet Crimes Report. https://www.ic3.gov/Media/PDF/AnnualReport/2021_ IC3Report.pdf. Accessed August 16, 2022.
4. Microsoft Data Breaches: Full Timeline Through 2022. https://firewalltimes.com/microsoft-data-breach-timeline/. Accessed August 16, 2022.
5. 2021 Verizon Data Breach Investigations Report. https://www.verizon.com/about/ news/verizon-2021-data-breach-investigations-report. Accessed August 16, 2022.
6. 2022 Verizon Data Breach Investigations Report. https://www.verizon.com/business/resources/reports/2022/dbir/2022-data-breach-investigations-report-dbir.pdf. Accessed August 16, 2022.
32 Endodontic Practice US Volume 16 Number 3 GOING VIRAL
EP
How to submit an article to Endodontic Practice US
Endodontic Practice US is a peer-reviewed, quarterly publication containing articles by leading authors from around the world. Endodontic Practice US is designed to be read by specialists in Endodontics, Periodontics, Oral Surgery, and Prosthodontics.
Submitting articles
Endodontic Practice US requires original, unpublished article submissions on endodontic topics, multidisciplinary dentistry, clinical cases, practice management, technology, clinical updates, literature reviews, and continuing education.
Typically, clinical articles and case studies range between 1,500 and 2,400 words. Authors can include up to 15 illustrations. Manuscripts should be double-spaced, and all pages should be numbered. Endodontic Practice US reserves the right to edit articles for clarity and style as well as for the limitations of space available.
Articles are classified as either clinical, continuing education, technology, or research reports. Clinical articles and continuing education articles typically include case presentations, technique reports, or literature reviews on a clinical topic. Research reports state the problem and the objective, describe the materials and methods (so they can be duplicated and their validity judged), report the results accurately and concisely, provide discussion of the findings, and offer conclusions that can be drawn from the research. Under a separate heading, research reports provide a statement of the research’s clinical implications and relevance to endodontics. Clinical and continuing education articles include an abstract of up to 250 words. Continuing education articles also include three to four educational aims and objectives, a short “expected outcomes” paragraph, and a 10-question, multiple-choice quiz with the correct answers indicated. Questions and answers should be in the order of appearance in the text, and verbatim. Product trade names cited in the text must be accompanied by a generic term and include the manufacturer, city, and country in parentheses.
Additional items to include:
• Include full name, academic degrees, and institutional affiliations and locations
• If presented as part of a meeting, please state the name, date, and location of the meeting
• Sources of support in the form of grants, equipment, products, or drugs must be disclosed
• Full contact details for the corresponding author must be included
• Short author bio
• Author headshot
Pictures/images
Illustrations should be clearly identified, numbered in sequential order, and accompanied by a caption. Digital images must be high resolution, 300 dpi minimum, and at least 90 mm wide. We can accept digital images in all image formats (preferring .tif or jpeg).
Tables
Ensure that each table is cited in the text. Number tables consecutively, and provide a brief title and caption (if appropriate) for each.
References
References must appear in the text as numbered superscripts (not footnotes) and should be listed at the end of the article in their order of appear-
ance in the text. The majority of references should be less than 10 years old. Provide inclusive page numbers, volume and issue numbers, date of publication, and all authors’ names. References should be submitted in American Medical Association style. For example:
Journals:
(Print)
White LW. Pearls from Dr. Larry White. Int J Orthod Milwaukee. 2016;27(1):7-8.
(Online)
Author(s). Article title. Journal Name. Year; vol(issue#):inclusive pages. URL. Accessed [date].
Or in the case of a book: Pedetta F. New Straight Wire. Quintessence Publishing; 2017.
Website:
Author or name of organization if no author is listed. Title or name of the organization if no title is provided. Name of website. URL. Accessed Month Day, Year. Example of Date: Accessed June 12, 2011.
Author’s name: (Single) (Multiple)
Doe JF Doe JF, Roe JP
Permissions
Written permission must be obtained by the author for material that has been published in copyrighted material; this includes tables, figures, pictures, and quoted text that exceeds 150 words. Signed release forms are required for photographs of identifiable persons.
Disclosure of financial interest
Authors must disclose any financial interest they (or family members) have in products mentioned in their articles. They must also disclose any developmental or research relationships with companies that manufacture products by signing a “Conflict of Interest Declaration” form after their article is accepted. Any commercial or financial interest will be acknowledged in the article.
Manuscript review
All clinical and continuing education manuscripts are peer-reviewed and accepted, accepted with modification, or rejected at the discretion of the editorial review board. Authors are responsible for meeting review board requirements for final approval and publication of manuscripts.
Proofing
Page proofs will be supplied to authors for corrections and/or final sign off. Changes should be limited to those that are essential for correctness and clarity.
Articles should be submitted to:
Mali Schantz-Feld, managing editor, at mali@medmarkmedia.com
Reprints/Extra issues
If reprints or additional issues are desired, they must be ordered from the publisher when the page proofs are reviewed by the authors. The publisher does not stock reprints; however, back issues can be purchased.
33 endopracticeus.com Volume 16 Number 3 AUTHOR GUIDELINES
Anatomy of a dental malpractice action
Kristin Tauras, JD, defines the various complex parts of a malpractice claim
Today’s reality is that most dental and medical providers have a high probability of being sued. Below is a primer on the “anatomy” of a dental malpractice case. Lawsuits are controlled by state and federal law, but the basic anatomy of the lawsuit is the same in each state and follows the same general timeline.
The term used in the lawsuit may be “professional malpractice” or “dental malpractice,” but this article encompasses all professional negligence claims against dental specialists, including dentists, cosmetic dentists, pediatric dentists, prosthodontists, periodontists, endodontists, oral and maxillofacial surgeons, and orthodontists. It also encompasses the liability of the dental specialist(s) staff who assist with the dental treatment and may be named in the dental malpractice lawsuit, including dental hygienists, dental assistants, nurses, anesthesiologists, and other dental care providers.
Parties
There are at least two parties to a lawsuit: the plaintiff and the defendant.

The plaintiff is usually the patient or the parent/guardian of a minor patient. The lawsuit may be brought by the estate of a deceased or incapacitated plaintiff.
The primary defendant is the treating dental specialist, but there may be multiple defendants. Defendants may include any individual involved in the patient’s care and treatment leading up to and through the alleged malpractice event, including consulting dental specialists, nurses, radiologists, surgeons, dental hygienists, and even the medical malpractice insurance companies in some states. The lawsuit may also name the practice group, corporation, or limited liability company that employs the dental specialist(s).
Pleading stage
A dental malpractice lawsuit begins with a pleading or complaint that is filed with the court. It is the story the patient wants to tell the jury of what the dental specialist(s) did wrong and why the jury should award the patient money. The complaint must set forth that there was a patient and dental specialist(s) relationship, the dental specialist owed a duty of care to the patient, the den-
tal specialist(s) violated the duty of care, and that the violation of the dental specialist(s) duty to the patient proximately caused the patient’s injuries, and the patient (or patient’s estate) suffered damages.
Twenty-eight states have the additional requirement to file a certificate of merit for a dental malpractice claim to move forward.
The complaint must be served on each defendant. The date of service of the complaint on the defendant governs the timing of when the defendant must respond to the complaint. The defendant typically has 21 to 28 days to respond to the complaint. The response may either be an answer to the complaint (admitting, denying, or claiming insufficient information with respect to the allegations), or a motion to dismiss the complaint for technical errors or substantive reasons why the dental professional is not liable.
The pleading stage is also where the defendant may want to file a third-party action against another entity to bring them into the suit. While most attorneys will advise against filing a thirdparty action against another dental treater so that they can bring a unified defense, there may be an occasion to file a third-party suit against the manufacturer of a faulty instrument that caused or contributed to the problem. Most dental malpractice claims do not have third-party actions.
Respondents in discovery
Some states allow for complaints to be filed against an individual, but not name the individual as a defendant. Called a Respondent in Discovery, these individuals are named for discovery purposes only. A Respondent in Discovery may be converted to a direct defendant so long as the plaintiff follows the rules of the state for converting the Respondent in Discovery to a proper party defendant.
Notifying the insurer
The dental specialist(s) must notify their insurance company at the time they know of a claim or are served with a lawsuit. Every insurance policy contains a duty to notify the insurance
34 Endodontic Practice US Volume 16 Number 3 LEGAL MATTERS
Kristin Tauras, JD, is a partner in the law firm of McKenna Storer in Chicago, Illinois. She has a litigation practice in the areas of employment law, insurance coverage, and professional malpractice. McKenna Storer is a fullservice law firm providing legal services to individuals and small-to-midsize companies, including defending professional malpractice negligence lawsuits and Illinois Department of Professional Regulation investigations, as well as advising dental and medical professionals regarding business and employment matters.
With
High Cutting Efficiency
Proprietary heat treatment and triangular cross-section design preserve the sharp cutting edges of the flute that lets you reach full working length with less resistance and more control during the procedure.
Minimally Invasive
A maximum flute diameter of 1mm and a non-cutting tip work together to minimize transportation and preserve the tooth’s structural integrity.
Exceptional Strength
Superior resistance to failure, minimizing file breakage.

Corresponding Gutta Percha and Paper Points
Gutta
and paper points match canals shaped by ZenFlex ONE
Reciprocating
percha
files.
ZenFlex ONE gives you more
and
you can trust.
the perfect balance of durability and high cutting efficiency.
confidence
a smooth finish
“I liked the ZenFlex
ONE
system because of its better cutting ability and flexibility. I felt more confident instrumenting with this system.”
| kerrdental.com
Kerr Corporation. All trademarks are property of Kerr Corporation. All Rights Reserved. MKT-23-0954 Rev 0
10 Packs of ZenFlex ONE Files, GET 5 Packs of ZenFlex ONE Files FREE!*
August 1, 2023 - December 30, 2023
goods must be of equal or lesser value and may not be combined with any other offers. Purchase must be made on one invoice between 8/1 and 12/31 unless otherwise noted. Redemptions after 1/31/24 will not be honored. To receive your promotional goods, email or fax a copy of your authorized Kerr dealer invoice noting promo code ZFOMM23 and product(s) desired to: kerrpromo@kerrdental.com or FAX: 888.727.2614. Limit to 3 redemptions per location. Incomplete submissions will not be processed. Allow 8 weeks for delivery. Offers valid in the 50 United States only. Promotions are subject to change or cancellation without notice. Offer void if purchased product is returned and you will automatically be billed the full MSRP for any promotional product that you retain. Note that you may have an obligation under federal, state, or local law to reflect discounts on products given pursuant to this promotion on any cost report forms submitted to a federal or state government or private payer who provides reimbursement for that product. See it in Action
your Order Today!
- Dr. Alma Cecilia Perez Pulido
1-800-KERR-123
©2023
BUY
Valid:
Promotional
Place
company upon learning of the potential claim when served with a lawsuit. If the dental specialist(s) fails to notify the insurance company, the insurer may refuse to defend and indemnify the claim.
Notice of the claim allows the insurance company to assign the dental specialist(s) an attorney, direct them on what records to keep, and how they should proceed. Some policies allow the dental specialist(s) to choose their own counsel.
Immediately retain documents and preserve evidence
Upon knowing of a claim and/or being served with a lawsuit, it is imperative that the dental specialist(s) retain all medical and dental records, notes, bills, x-rays or other imaging, correspondence with the patient, and machines used in the treatment of the patient, essentially “preserving” all evidence of the alleged malpractice. Your attorney and/or the insurance company will advise you what they need you to retain and send to them to defend the case as well. If you do not, or if you destroy relevant evidence, some states will allow a “spoliation of evidence” claim to be filed against you, which may include a putative finding of liability with just damages to be assessed.
Discovery stage
After the answer is filed or the motion to dismiss is resolved, the case will enter the discovery phase.
Discovery is broken down into three types: fact written discovery, fact oral discovery, and expert discovery.
Written discovery
All parties may issue written discovery against the other parties. Where there are multiple defendants, each plaintiff may issue discovery against each defendant, and each defendant may issue discovery against the plaintiff, as well as against each of the other defendants.
Written discovery is divided into four types: Interrogatories, Requests to Produce, Third-Party Subpoenas, and Requests to Admit.
Interrogatories are questions submitted to the other parties. The plaintiff’s Interrogatories to the defendant(s) will include requests for information such as the identity of all treaters (both dental and non-dental), dates of treatment, types of treatment, types of tests done prior to the treatment, cost of the treatment, and information regarding the insurance. The defendant(s) Interrogatories will include the basis for the negligence allegations, identify the claimed negligent treatment, damages (including alleged injury, days off work, cost of alleged repair or further treatment, as well as pain and suffering and disfigurement), and identity of witnesses.
The Requests to Produce are written requests for documents. The plaintiff’s Requests to Produce will usually include the patient’s dental records, bills, x-rays or other imaging, correspondence, as well as the office policies and procedures. The defendant’s Request to Produce will usually include the plaintiff’s dental and medical records, bills from additional treatment, and proof of damages such as time off work.
The parties may also issue Subpoenas to other entities not involved in the lawsuit, including other medical and dental treaters who have treated the patient both in the past and with respect to the claimed malpractice.
The parties may also issue Requests to Admit. These are statements that the parties must either admit or deny or set forth a reason they can neither admit nor deny the statements. Depending on the state law, these Requests to Admit may become binding on the parties at the time of trial.
Oral fact discovery
Discovery also includes non-expert testimony from the plaintiff, defendant(s), and any other fact witness.
The patient’s deposition is usually the first deposition taken in a case. If the patient is unable to testify, such as when the patient is a minor or the patient is disabled or deceased, the family members or next of kin who brought the lawsuit may testify about the patient’s treatment and injuries.
The defendant(s) depositions then take place. The defendant(s) include the dental specialist(s) sued in the case, as well as the other individuals in the office that took part in the care. The depositions of the defendant(s) usually center around the issues of informed consent, care provided to the patient, policies and procedures of the office, and the dental specialist(s) training and experience to perform the procedures that form the basis of the lawsuit.
After the defendant(s) depositions are taken, the parties will take the depositions of the other dental and medical treaters who have seen the patient.
Additional fact witness(es) depositions may also be taken. These fact witness(es) may include the office manager(s) to testify regarding bills and the office policies and procedures, and family members that can testify to the condition of the patient before and after the procedure.
Expert discovery
In all states, almost without exception, the plaintiff must have dental specialist(s) testify to the standard of care and whether the care deviated from that standard. While technically the defendant(s) may be qualified to testify to the standard of care and alleged deviation, standard of care experts are usually paid experts who evaluate the patient’s records and testify regarding their expertise. Expert testimony may be excused when it is readily apparent that malpractice occurred (such as inexcusably removing the wrong tooth) and that an expert’s testimony might be redundant. Many trials rise and fall on the strength of the dental specialist(s) expertise.
Other experts may also testify regarding damages, including financial experts who testify about the financial harm the plaintiff suffered because of the sub-standard care.
36 Endodontic Practice US Volume 16 Number 3 LEGAL MATTERS
Under most insurance policies, the dental specialist has the ultimate right to make all decisions regarding settlement.
Dispositive motions
Most states have a mechanism for filing a dispositive motion, such as a motion for summary judgment or summary decision, after the close of discovery. The dispositive motion requests that the judge review the law and the facts to see if there is an issue of fact that requires that the matter be tried. Usually, this motion is filed by the defendant(s), alleging that the plaintiff cannot prove a required element of their case.
Settlement
While settlement discussions can happen at any time during the case, most parties will engage in settlement discussions after the close of discovery or before the trial begins. In dental cases, there is the notion that the case is either in a “settlement posture” or a “trial posture.” Nevertheless, many cases do settle on the eve of trial. Under most insurance policies, the dental specialist(s) has the ultimate right to make all decisions regarding settlement.
Trial
Many dental malpractice cases go to trial. A trial date is usually set between 18 months to 36 months after the date the lawsuit was filed. The dental specialist(s) should sit at counsel’s table through the duration of the trial.
Professional malpractice trials are long, lasting a week or longer. The first day is usually a “pretrial conference.” The judge will attempt to settle the case and then rule to either admit or exclude evidence from trial (called the motions in limine), and review jury instructions.
Day 2 and Day 3 are spent with jury selection. Jury selection is heavily individualized by the judge who presides over the case. The judge may ask the jury questions or let the attorney ask the questions.
Once the jury is empaneled, the trial begins. The attorneys will give their opening statements, explaining to the jury what they believe the evidence will show. After that, the plaintiff will present their case in chief, and the defendant(s) will then present their case in chief.
At the end of the evidence phase, the judge will instruct the jury on the law, and the deliberation process begins. The jury will deliberate until either they reach a decision, or they inform the court that they are unable to reach a decision.
Motion to overturn the verdict or appeal
After the jury reaches its verdict, the jury foreman will read the verdict. This does not end the proceedings. The parties in all states have the right to file a motion to contest the jury verdict and/or file an appeal from the jury’s verdict.
If the jury verdict is affirmed by the appellate court, and the appellate process is exhausted, the matter ends. If the jury verdict is overturned by the judge and/or the appellate courts, then it is possible the matter will be retried.
Reporting
Some states require that any settlement or an adverse judgment be reported to the state licensing board. In that case, the dental specialist(s) should retain defense counsel to assist with the defense of the dental license. EP


37 endopracticeus.com Volume 16 Number 3 LEGAL MATTERS
Connect. Be Seen. Grow. Succeed. | www.medmarkmedia.com 3 REASONS TO SUBSCRIBE • 16 CE credits available per year • 1 subscription, 2 formats – print and digital • 4 high-quality, clinically focused issues per year 3 SIMPLE WAYS TO SUBSCRIBE • Visit www.endopracticeus.com • Email subscriptions@medmarkmedia.com • Call 1-866-579-9496 Endodontic Practice US 1 year $149 / 1 year digital only $79 Fall2023 Vol16 No3 endopracticeus.com Irrigation&Obturation n 4CECreditsAvailableinThisIssue * Minimallyinvasive endodontics preservingDr.ChaficSafidiscusses asmuchhealthy toothstructureaspossible Simpleendodontic irrigation Dr.AllenAliNassehClosed-systemnegative PROMOTING EXCELLENCE IN ENDODONTICS Summer2023 Vol16 No2 endopracticeus.com Irrigation&Obturation n 4CECreditsAvailableinThisIssue * CaliforniaDreamin' Dr.ReidPullenhelpsnewassociate Dr.AllenAbrishamitoaccomplishlife goalsthroughmentorship Theimportanceofsuturing indentalimplantsurgery Dr.StevenVorholtDentalsedation: anoverview Dr.BrianMcGueExpandingendodontic treatmentsand procedureswith dentallasers Dr.FernandoMeza
A good “NAP” is 1 of 3 ways to improve practice success
Chad Erickson discusses how to generate more revenue from your local listings
With an estimated 46% of all searches containing local terms such as “near me,” it’s clear that local search that contains more than just your name, address, and phone data (NAP) is more important than ever. If you aren’t optimizing your local search profiles to generate the newest business possible — and, therefore, the most revenue possible, you’re missing out on connecting with the people who conduct these searches. You also risk frustrating the people who are searching directly for your practice, as improperly maintained local search profiles often contain inaccurate information, which means more lost revenue from patients who choose not to work with you in favor of practices that are easier to get ahold of. Here are three easy ways to make your local search listings start (and continue) to generate more revenue.

1. Make inaccuracies your No. 1 enemy.
Inaccurate information on a local listing profile is incredibly frustrating. If you’ve encountered it, you know exactly how it feels. Driving to a business only to find out its hours are incorrect or their address is wrong is more than enough to cause potential patients to not want to do business with you. You might not have any inaccuracies in your online listings, but the thing that makes these such a problem is that they pop up so frequently. Whether through Google indexing new information about your practice, a suggestion from a user, or through data collected from thirdparty companies, the truth is that your online listings are subject to change at any time. The best way to avoid losing revenue through inaccurate listings is to audit your listings as frequently as possible. At the bare minimum, checking all of your directory listings at least once per month will help cut down on these incidents.
2. Work on optimizing your listings.
Once your listings are straightened out, it’s time to start optimizing them. That means adding information beyond the basics, like your name, address, and phone number (NAP). Google and other search engines utilize “relevance” as one of the search metrics to rank local search profiles, which measures how likely
Chad Erickson, VP Strategy and co-owner of MyAdvice, has been consulting clients on the best marketing strategies for their businesses since 1999. With a focus on both the internal and external aspects of effective marketing, he understands the complex aspects of owning and running a business. He has a proven record of raising capital, acquiring companies, and developing strategic alliances within the industry. He is also a faculty member for many top medical and dental conferences. For more information on local listings management, reviews, and digital marketing campaigns, visit myadvice.com.
your practice is to provide the service or product the searcher is looking for. Without complete profile information, it’s hard for search engines to tell precisely what your practice does. So adding this information can make a huge difference:
• Filling out the primary and secondary categories your business falls under
• Adding photos of your business
• Including all of the services you provide
• Including your business attributes and hours
• Any additional contact information like your social media and website links
• Regularly posting new photos and updates on your profile to show that your profile has active updates
3. Generate new reviews.
Reviews are massively important to local search. In fact, in a survey we conducted earlier this year, 57% of the practices we polled told us that generating new reviews had the most positive impact on their local search performance. They’re incredibly important to potential patients interested in your practice as well as search engines. That’s right, search engines are indexing your reviews! Another metric used by search engines to rank local search profiles is called “prominence,” and it consists of every mention of your business online. That includes your online reviews. Setting up an automated system to request reviews from your patients and making sure to respond to the reviews you do get goes a long way towards helping your local search profile generate more revenue. Make auditing your reviews a part of your local search audit system to avoid missing a review that needs a response.
38 Endodontic Practice US Volume 16 Number 3 MARKETING MOMENTUM
EP
Envista Smile Project completes second oral care mission trip to the Dominican Republic

The Envista Smile Project completed its second mission trip to the Dominican Republic, where volunteers treated a combination of 782 juvenile and adult patients who otherwise would not have access to dental services. For many of these patients in the rural village of San Francisco de Macoris, this was their first time ever receiving professional dental care. The team of 25 volunteers performed oral examinations, scaling, oral prophylaxis, fillings, root canals, and routine and surgical extractions, providing the equivalent of $315,000 in free dental work. Envista Smile Project is a philanthropic foundation designed to improve the smiles and oral health of disadvantaged communities by supporting increased access to oral care and oral health education and collaborating with dental professionals and Envista employee volunteers to donate products, treatment, and oral health education to communities in need around the world. For more information about the Envista Smile Project, visit envistasmileproject.com.
Bright Referral brings referral tracking to the 21st Century
Imagine exchanging patient referral information with just a tap of a card. Thanks to Bright Referral, that’s now a reality. Up until now, referring doctors used a notepad and “hoped” that the patient would follow up. But just like the typewriter and fax machine, notepads are soon becoming a thing of the past. Using new technology, patients simply tap their phone to the Bright Card provided by the referring doctor. The patient then receives all of the referral information on their phone. Doctors get a wealth of new information — patient contact information to follow-up right away, and the ability to track referrals by source, time period, volume, and starts. It’s a total game-changer.
Bright Referral is now offering one month free to the first 10 endodontists to sign up with this discount code: ENDO10. For more information, visit brightreferral.co.
Weave launches AI-driven email marketing and product suite for payments

Weave has launched Email Assistant that provides an innovative way for healthcare providers to communicate and connect with their patients and clients. By inputting the themes that need to be covered in the email, Weave Email Assistant will generate the email text in a matter of seconds, which can then be edited before sending. This tool allows healthcare providers to quickly create, personalize, and automate email marketing campaigns, resulting in improved patient engagement and retention, a higher patient growth rate, and increased awareness of services offered by a practice.
The company also expanded its payments platform with the addition of Mobile Tap to Pay feature that allows patients and clients to make contactless payments by simply tapping their credit or debit card on the provider’s mobile device. This feature enables Weave customers to seamlessly collect payments from anywhere and aims to cater to the evolving needs of on-the-go patients, clients, and mobile-first businesses. Mobile Tap to Pay is seamlessly integrated into Weave’s existing payments platform.
For more information, visit https://www.getweave.com/.
Introducing Ultracare™ Topical Anesthetic Gel

Ultradent has announced the return of Ultracare™ topical anesthetic gel — a delightfully flavored 20% benzocaine oral gel formulated for rapid, profound topical anesthesia. Dental professionals can administer Ultracare gel directly on a cotton swab for increased patient comfort. The gel’s trio of benefits include 20% benzocaine for effective numbing, as well as rapid onset — numbing tissues in 15–20 seconds.
For information, call 800-552-5512 or visit ultradent.com.
39 endopracticeus.com Volume 16 Number 3 INDUSTRY NEWS
MANI JIZAI NiTi File System
Story of JIZAI

“JIZAI” in Japanese means “being at will.” This phrase represents its features. Tochigi Prefecture, Japan, where MANI is located, is renowned for the 400-year old craftsmen of the woodworking art of Kanuma Kumiko. MANI celebrates and respects this tradition and is still brushing up their techniques and products to meet the needs of contemporary life. We have incorporated the exquisite and beautiful structure of Kanuma Kumiko into the JIZAI brand image.
This system is the newest addition to our endodontic product line. The three foundational concepts that form the basis of JIZAI are the following:
1. Smooth – The unpredictable screw-in effect is one of the biggest problems during root canal shaping. JIZAI enables smooth cutting with less screw-in effect as a result of its original crosssection and flute pitch. Radial lands help to prevent overinstrumentation and excessive engagement on the root canal walls. The off-center file axis is uniquely designed to provide a larger “pocket” space for debris removal during instrumentation.
2. Flexible – Respects the original anatomy. As a result of the heat treatment that each JIZAI file undergoes, there is a significantly lower risk of ledge, transportation, and perforation. Centering ability test shows high centering ability as shown in the chart below.

3. Simple – JIZAI is designed to be used in a single length technique along with sequence numbers. Tip size, taper, and sequence number are etched on the shank for easy recognition.
Each file is fully heat-treated, highly flexible, and designed to cut smoothly and efficiently. The cross-sectional shape and flute pitch help to prevent overinstrumentation and file binding.
Each file can be pre-bent and will hold its shape. Available in individual ISO-sized packs of three files or as part of a Standard Kit which includes a sequence of 25.04, 25.06, and 35.04 files that are designed to instrument straight and slightly curved canals. Manufactured in Japan.
Our recommended sequence is in the following charts:

• 01 Straight-line Access
° JIZAI Orifice Opener (025 .14)
° Use JIZAI Orifice Opener (025.14), and prepare the coronal part of the root canal. Coronal flaring secures unimpeded entry and reduces the stress loading on subsequent files.
° Allowable engine speed: 500min-1 or less
°Allowable torque setting: 3.0N·cm or less
• 02 Patency
° D Finders (010 .02)
° Glide Finders (010 Multi taper .03-.02)

40 Endodontic Practice US Volume 16 Number 3 PRODUCT SPOTLIGHT
JIZAI standard kit
JIZAI quality control, above. JIZAI cross section, left


° Use D Finders to achieve patency. D Finders work efficiently even in calcified and severely curved canals. Glide Finders are recommended for canals requiring more cutting force.
• 03 Glide Path
° JIZAI Glider (013 .04)
° Use the JIZAI Glider to create a glide path. Featuring a 013 tip size and .04 taper, JIZAI Glider provides a smooth transition to shaping with JIZAI I (025 .04).
° Allowable engine speed: 300min-1 or less
° Allowable torque setting: 1.0N·cm or less
° Use with a gentle pecking motion. Irrigate and recapitulate after instrumentation. Always use files with recommended speed and torque, and do not force files apically.
• 04 Shaping
° JIZAII(025 .04)
° JIZAIII(025 .06)
° JIZAIIII(035 .04)
° JIZAI is designed to be used in a single length technique along with the sequence numbers.
° Use JIZAI I, II, and III for shaping straight or slightly curved root canals.

° For severely curved canals, use only JIZAI I and II.


° Allowable engine speed: 500 min-1 or less
° Allowable torque setting: 3.0N·cm or less
Related products for patency
• D Finders
° The D-shaped cross section increases blade strength and prevents excessive filing and binding in calcified or curved root canals.
° Size: 08, 10, 12, 15
° Length: 21 mm, 25 mm
° Product name: MANI® D Finders
• Glide Finders
° The Glide Finders are multi-tapered files with a varying cross section from tip to handle. This design provides optimal tip resilience and shank flexibility near the handle.
° Size: 08, 10, 12, 15
° Length: 21mm, 25mm
° Product name: MANI K-Files
MANI is a manufacturer of medical devices and dental instruments. Ever since we began manufacturing suture needles in 1956, we have contributed to society as a medical device manufacturer supplying medical and dental instruments. We made this possible by establishing microfabrication technologies using wire as a base material.
Our products are safe, high-quality medical devices that satisfy the needs of doctors and patients, which have also passed the strict standards of various countries around the world.
42 Endodontic Practice US Volume 16 Number 3 PRODUCT SPOTLIGHT
This information was provided by MANI.
EP
The curse of perfectionism
Drs. Joel C. Small and Edwin McDonald discuss perfectionism versus consistent improvement


Professional athletes train to perfect their skills throughout their lifetime, and yet few of them can attain perfection.
Olympic gymnasts, for example, spend hours upon hours in training to perfect their skills yet rarely achieve a perfect 10 score. Ty Cobb, a renowned baseball player, had a .366 batting average over 24 seasons as a professional player. This is the highest career batting average ever recorded in major league baseball. Even Babe Ruth, one of the most revered baseball sluggers of all time, had a career batting average of .342. To put this in a more understandable perspective, two of the very best batters in the history of professional baseball had successful at-bats a little more than one out of every three attempts, and yet they are, to this day, considered to be among the best to ever have played the game.
What is it that allows professional athletes to continue their rigorous training and all that it entails when they find themselves incapable of achieving consistent perfection? Perhaps they have a healthier understanding of their aspirations and goals. Perhaps they have accepted the reality that batting a thousand or consistently receiving a perfect 10 is unattainable and unrealistic. Recognizing and accepting this reality allows them to adopt more reasonable and achievable goals.
Sure, they would love to be perfect in every aspect of their sport, but holding this unattainable goal of perfection as their standard has negative psychological consequences. Setting a standard of perfection and never being able to achieve it creates a state of cognitive dissonance and brings with it all the accompanying stress, frustration, and loss of self-esteem. Rather than setting perfection as their standard, most successful athletes set a more realistic goal of constant improvement. Quite simply, their goal is to be better tomorrow than they were today.
Dentists and other health care professionals would be much better off adopting a similar mindset.
We have seen too many of our colleagues suffer the ravages of perfectionism, as they seek validation and self-esteem
through perfection. Ultimately, they suffer the severe and predictable psychological consequences when they fail to achieve the unachievable. This is a no-win scenario with a significant downside.
Dentistry is a highly skillful and precise profession in which perfection is often the difference of a millimeter or two. Furthermore, factors beyond our control often limit our ability to achieve clinical perfection. How we view this reality is critical. Do we accept our imperfection knowing that we gave our very best effort to achieve an optimal result, or do we demean ourselves and find ourselves unworthy or not enough?
The truth is that we were trained to be perfectionists, and yet we live in an imperfect world where perfection is seldom attained. Being a perfectionist in an imperfect world creates an incongruous reality in which a gap exists between where we are currently and where we ideally want to be. Closing the gap is only possible if the preferred reality is attainable. Otherwise, our inability to close the gap creates ongoing mental anguish.
Holding ourselves to an unachievable standard will often result in depression, severe burnout, drug and alcohol abuse, stressed relationships, and loss of self-esteem. It is not uncommon for colleagues to suffer from “imposter syndrome” when they consistently fail to meet an impossible standard, and therefore feel unworthy and diminished. Sadly, some of our colleagues have left our profession because the psychological consequences of perfectionism were more than they could bear.
Rejecting perfection as our standard does not mean that we submit to imperfection or accept mediocrity as a new standard. In fact, striving for constant improvement is a much healthier and more realistic goal that recognizes our professional development as an ongoing journey. This mindset, often referred to as a “growth mindset,” acknowledges that we are constantly in a state of imperfection as we continually seek more knowledge and skill. Scaling our capabilities and capacity to meet the changing technical demands of our profession is a life-long endeavor that requires continual learning and adjustment. In today’s world, it is an organizational imperative if we are to remain relevant. Believing that perfection is an end point or achievable destination, however, shuts down future growth because there is no motivation to grow beyond perfection.
It has been our experience as professional healthcare coaches that the happiest and most successful doctors acknowledge their shortcomings but refuse to be psychologically victimized by them. Instead, they are constantly seeking self-improvement through continuing education and other means of self-enrichment. Like professional athletes, they too would like to be perfect in every aspect of their profession, but they refuse to let imperfection serve as an excuse to quit trying to be better tomorrow than they were today.
43 endopracticeus.com Volume 16 Number 3 SMALL TALK
EP
Drs. Joel C. Small and Edwin (Mac) McDonald have a total of over 75 years of dental practice experience. Both doctors are trained and certified Executive Leadership Coaches. They have joined forces to create Line of Sight Coaching, a business dedicated to helping their fellow dentists discover a better and more enjoyable way to create and lead a highly productive clinical dental practice. Through their work, clients experience a better work/life balance, find more joy in their work, and develop a strong practice culture and brand that positively impact their bottom line. To receive their free ebook, 7 Surprising Steps to Grow Your Practice Through Leadership, go to www.lineofsightcoaching.com.
For the life of your practice: the vision of Endodontic SuperSystems (ESS)
Efficiency and collaboration are vital in the dynamic world of endodontic practice! Endodontic SuperSystems (ESS) has emerged as transformative executive technology empowering the entire team in the office. Driven by the vision of effortless coordination, the revolutionary SaaS platform Seneca™ has set a new standard in endodontic practice management. ESS raises the tide for all ships by offering the game-changing solution designed to keep the office running consistently smooth.
Converting busy to productive!
ESS offers a future where your endodontic practice is seamlessly optimized, giving practitioners and their teams the most time to focus on providing their best patient care. ESS transparently connects the front and back office teams allowing all team members to take action for the practice’s growth and success. This new level of flow, typical in modern times, elevates the entire experience for patients.

On-board a new hire at lightning speed!
At the core of ESS lies a profound financial return by providing the standardized training and crystal-clear digital guidance throughout the workday. ESS understands that every member of the endodontic office plays a critical role in delivering exceptional patient care — includ-
ing marketing and management. Reducing the time it takes to convert a new hire to a fully functioning member creates huge financial returns far greater than the cost of the subscription.
See the unseen!
ESS’s groundbreaking platform equips the owner or manager with objective real-time insights. Much like a digital map guides a driver, the Seneca™ platform guides each role. During the workday, the Seneca™ data identifies potential bottlenecks in advance so the team can respond and overcome challenges proactively while maximizing productivity. Also, standardized objective data allows management to monitor, compare, and improve employees’ flow and relative work amount.
Always improving!
ESS remains committed to staying at the forefront of advancements in the industry. With built-in improvement suggestions, ESS ensures that the platform is constantly evolving to meet the changing business needs of our endo community. This is the future!

Book a demo or webinar today to learn more and start your free trial!
This information was provided by Endodontic SuperSystems.
44 Endodontic Practice US Volume 16 Number 3 PRODUCT PROFILE
EP






Have you ever felt the chaos of losing an employee? Minimize your pain with ESS's Executive Technology *Case Study: One CA Endo office's savings. ESS more than pays for itself! For The Life of Your Endodontic Practice Download White Paper ROLE NUMBER OF EE TURNOVER IN A YEAR COST OF TRAINING PERIOD NUMBER OF EE TURNOVER IN A YEAR COST OF TRAINING PERIOD SAVINGS WITH ESS DA 4 $36,288.00 4 $8,640.00$27,648.00 RDA 3 $60,480.00 3 $14,400.00$46,080.00 RDAEF 3 $161,280.00 3 $38,400.00$122,880.00 RDH 3 $60,480,00 3 $9,600.00$50,880.00 Front Office 5 $85,680.00 5 $10,200.00$75,480.00 Marketer 2 $104,832.00 2 $4,160.00$100,672.00 Manager 1 $68,544.00 1 $8,160.00$60,384.00 Side by Side OnboardingESS Executive Tech
New RoTAC Rotary File Grips
RoTAC Rotary File Grips change rotary files into hand files to prepare difficult tight-curved canals safely and efficiently
Why develop RoTAC File Grips
Motor file separation is a major, but preventable, problem. The common thread running through this difficulty is the device controlling the file. Most of the journal articles written on ways to prevent motor file separation give us good ideas, but don’t tell us to stop using the motor in difficult cases! It’s agreed there is a high risk of motor file separation in tight curved canals, especially in molar teeth. Early assessment of this risk is critical.
The idea behind the development of RoTAC File Grips is to eliminate motor file separation. Having the option to switch to manual rotary file control in difficult cases can avoid the embarrassment of motor file separation and its complications.
How to reduce motor file separation
In high-risk cases, “motor power control” can become “out of control.”

Imagine taking back control of the file. First let’s find the most successful manual file instrumentation of the past then build on that foundation as we use all the good qualities and benefits of today’s tapered files.
The classic article by Dr. James Roane in the Journal of Endodontics in 1985 significantly improved our way of using hand files in curved canals.1 This technique was accepted worldwide and became a big part of dental school endodontic training. It was known for cutting the most dentin with the most control.
Dr. Steven S. Larsen notes that applying Dr. Roane’s manual “Balance Force Concept” with tapered files is the key to eliminating motor file separation.
What elements of Dr. Roane’s technique help prevent separation?
1. Select the right file design
• A file that cuts dentin in both clockwise and counterclockwise directions
• Sharp triangular cross-section tapered files (examples: Brasseler EndoSequence® CM, Dentsply Vortex Blue® , or other similar files).
2. Move the file with efficiency
• Simple watch-winding or back-and-forth Balance Force motion of a triangular-designed file cuts the full 360-degree circumference of the canal with a reciprocating arch of only 60º. (Quarter turn 90º works even better.) This advances the file toward working length.
• Remove the cut dentin debris with a few gentle clockwise turns.
3. New way to control the rotary file with tactile sensitivity
• RoTAC rotary file grips were developed by Dr. Steven S. Larsen and a team of endodontists and engineers


• Slip-on, color-coded easy identification
• Big, soft, comfortable hand control grip
• Autoclavable for multiple uses
Results: Do they really work?
This technique was introduced to dental students prior to their clinical experience. Comments from students and instructors include: “Manual rotary tapered file instrumentation with Rotary File Grips is easy to teach, easy to learn, and easy to apply.” The department recorded over 750 clinical cases with less of the usual treatment mishaps and not one file separation. Endodontists, general dentists, and students find this simple technique a welcome option to safeguard file separation in difficult cases. REFERENCE
46 Endodontic Practice US Volume 16 Number 3 PRODUCT PROFILE
1. Roane JB, Sabala CL, Duncanson MG Jr. The “balanced force” concept for instrumentation of curved canals. J Endod. 1985 May; 11(5):203-211.
EP
This information was provided by Venta Endo.
Slip-on colored grips identify file sizes
60º arch of triangular file cuts 360º circumference



 le grips
le grips
The Endo Files: the endodontic experts podcast

Specialized Dental Partners amplifying the voices of clinicians and industry insiders
The Endo Files Podcast is a show for endodontists and other dental specialists looking to gain insights, education, and inspiration from their peers. Brought to you by Specialized Dental Partners (formerly US Endo Partners), each episode features a rich conversation between industry experts, highlighting personal perspectives on the specialty, including clinical best practices, hot topics, work-life balance, innovative technologies, and so much more!
From harnessing mental toughness to thriving in the demanding field of endodontics and other specialties, to the importance of giving back and investing your time to help develop the next generation of leaders, Season One covered myriad topics appealing to clinicians in every stage of career. Season Two is digging even deeper!
Season two: new co-hosts and deeper dives
The Endo Files is hosted by a rotating line-up of experts, each bringing a different perspective to the table! You’ll hear dynamic conversations led by Dr. Diwakar Kinra and Dr. Brett Gilbert, among other clinicians, along with longtime industry insider and seasoned podcast host, Kim Livesay Brownell of Specialized Dental.
New and notable from season two Securing Your Spot: Insider Tips for Standout Residency Applications — Dr. Adham Azim and Dr. Diwakar Kinra
Dr. Adham Azim is an Associate Professor and the Chair of the Endodontic Department at the University of the Pacific’s School of Dentistry and CEO of Endolit.
Dr. Kinra leads an in-depth discussion on the requirements and considerations for dental students interested in pursuing specialty programs like Endodontics, highlighting strategies and tips that students can use to help their applications stand out from the rest.
In
Conversation
with the Dean of Harvard’s School of
Medicine — Dr. William Giannobile
ICYMI: highlights from season one
• Endo Never Sleeps: Setting Boundaries and Thriving Through Grind — Dr. David Landwehr, Capital Endodontics
• Why Mental Toughness is the Endodontist’s Superpower
— Dr. Reid Pullen, Brea Endodontics
• Why Chasing Excellence is More Sustainable than Chasing Perfection — Dr. Brett Gilbert, King Endodontics
• The Symbiotic Relationship Between Radiology and Endodontics, and Going Back to School — Dr. Bruno Azevedo aka “The Cone Beam Guy”
• Resident Lessons, Side Hustles, and the Importance of Work-Life Balance — Dr. Diwakar Kinra, Contemporary Endodontics
• Paying it Forward: Investing in the Specialty to Shape the Future — Dr. Scott Doyle, Metropolitan Endodontics
• Advice for Current Residents and New Endodontic Associates — Dr. Allen Abrishami, Brea Endodontics
• In Conversation with The Pulpinato — Dr. Daniel Tran, Belle Meade Endodontics
• The Case for Faster Procedures: Leaning Down to Maximize Efficiency — Dr. Tim Adams, Summit Boulevard Endodontics
• And MORE!
Dental
An alumnus of Harvard himself, possessing advanced degrees in periodontology and oral biology, Dr. Giannobile shares his career journey while reflecting on the evolving process of applying to specialty programs and offers his perspective on the integrated healthcare model and its pivotal role in the future of dentistry.
If you’re looking to differentiate yourself and your practice, to stay up-to-date on the latest happenings in the field, and to connect with other specialists on a personal level, The Endo Files is an excellent resource to add to your toolkit.
The podcast is available for free on all major podcast platforms, including Apple Podcasts, Spotify, and Google Podcasts. Subscribe today so you never miss an episode!
EP
This information was provided by Specialized Dental Partners.
48 Endodontic Practice US Volume 16 Number 3 SOUND ADVICE
Specialized is energized.
We were the first specialty DSO to champion endodontists and remain committed to the specialty—now, we’re expanding our impact and welcoming periodontists and oral surgeons to our community to revolutionize oral health care. Together, we’re delivering worldclass patient experiences and creating brighter tomorrows for all.


Welcome to the future of oral health care.
Energized care.
Elevate patient experiences with unparalleled support.

Energized excellence.
Advance oral health care with innovative technologies.
Energized connection.
Thrive in a community of growth-minded peers.

Energized future.
Secure your legacy while doing what you love.
specializeddental.com
Dr. Tyler Peterson, Metropolitan Endodontics Partner and believer since 2021
























































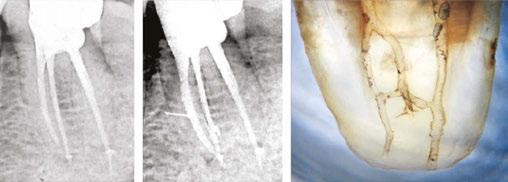






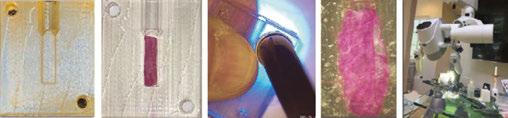

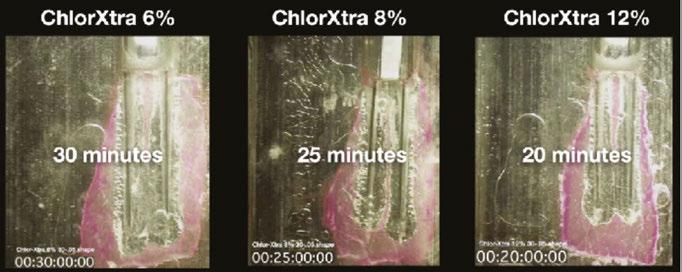









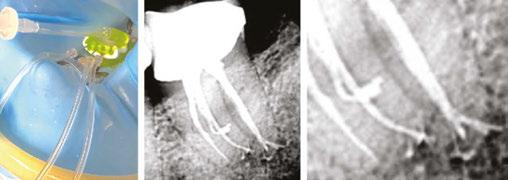
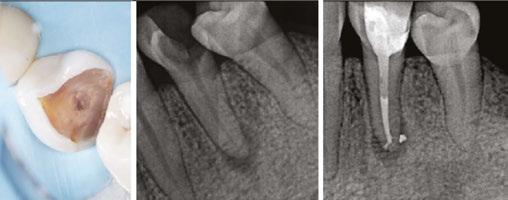

















































 le grips
le grips






