Dr. Josh Todd
Clinical implementation and future of AI in endodontic dentistry
Drs. Aaron Glick, David Jaramillo, Nisha Manila, and Jennifer Chang
Antibiotics in endodontics: a desktop reference
Dr. Joseph C. Stern
Odne — Swiss start-up transforming endo


PROMOTING EXCELLENCE IN ENDODONTICS AAE Special Section n 4 CE Credits Available in This Issue*
Spring 2024 Vol 17 No 1 endopracticeus.com A transformative innovation that continues to make a difference

Spring 2024 n Volume 17 Number 1
Editorial Advisors
Dennis G. Brave, DDS
David C. Brown, BDS, MDS, MSD
L. Stephen Buchanan, DDS, FICD, FACD
Gary B. Carr, DDS
Arnaldo Castellucci, MD, DDS
Gordon J. Christensen, DDS, MSD, PhD
Stephen Cohen, MS, DDS, FACD, FICD
Samuel O. Dorn, DDS
Josef Dovgan, DDS, MS
Luiz R. Fava, DDS
Robert Fleisher, DMD
Marcela Fridland, DDS
Gerald N. Glickman, DDS, MS
Jeffrey W Hutter, DMD, MEd
Syngcuk Kim, DDS, PhD
Kenneth A. Koch, DMD
Gregori M. Kurtzman, DDS, MAGD, FPFA, FACD, DICOI
Joshua Moshonov, DMD
Richard Mounce, DDS
Yosef Nahmias, DDS, MS
David L. Pitts, DDS, MDSD
Louis E. Rossman, DMD
Stephen F. Schwartz, DDS, MS
Ken Serota, DDS, MMSc
E Steve Senia, DDS, MS, BS
Michael Tagger, DMD, MS
Martin Trope, BDS, DMD
Peter Velvart, DMD
Rick Walton, DMD, MS
John West, DDS, MSD
CE Quality Assurance Board
Bradford N. Edgren, DDS, MS, FACD
Fred Stewart Feld, DMD
Gregori M. Kurtzman, DDS, MAGD, FPFA, FACD, FADI, DICOI, DADIA
Justin D. Moody, DDS, DABOI, DICOI
Lisa Moler (Publisher)
Mali Schantz-Feld, MA, CDE (Managing Editor)
Lou Shuman, DMD, CAGS

Advancing endodontics
As we embark on another promising year in the field of endodontics, it’s crucial to explore the transformative potential of cutting-edge technologies in reshaping our practice landscape. In this introduction, we’ll delve into four key areas poised to revolutionize the way we diagnose, communicate with patients, optimize operatory ergonomics, and enhance clinical outcomes: artificial intelligence (AI), large language models (LLMs), advanced irrigation technology, and augmented reality (AR).
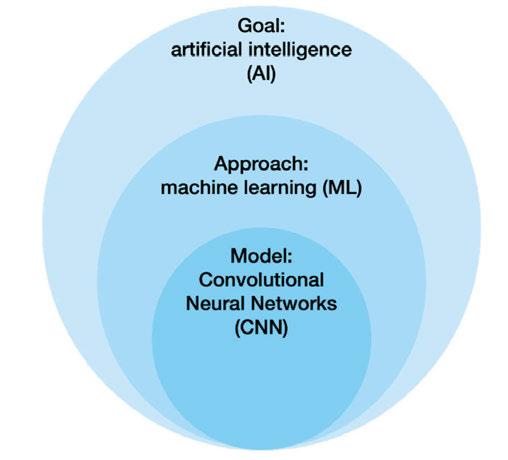
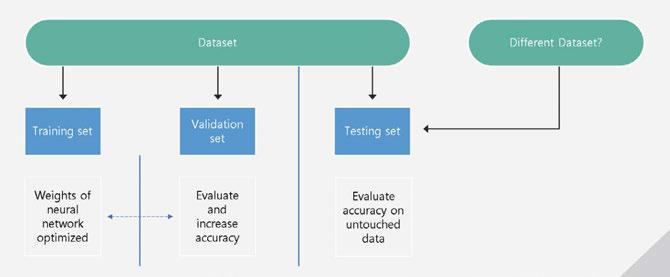
AI holds immense promise in revolutionizing the diagnostic process by augmenting our ability to detect and analyze abnormalities in cone beam computed tomography (CBCT) scans. By leveraging machine-learning algorithms, AI-driven systems can assist endodontists in identifying subtle nuances and potential areas of concern with unprecedented accuracy and efficiency. This not only enhances diagnostic capabilities but also enables early intervention and personalized treatment planning.
In addition to its diagnostic prowess, LLM technology serves as a powerful ally in enhancing patient communication and engagement. By harnessing the capabilities of LLMs, the endodontic administrative team can communicate with patients promptly, effectively, and empathetically, addressing their concerns and guiding them through every step of their treatment journey. Whether it’s collecting crucial information for appointment requests or addressing postoperative queries, LLM-powered communication platforms empower endodontists to seamlessly engage with their patients. These platforms have the unique ability to capture the nature of patients’ concerns in a compassionate manner. What’s more, this technology operates round-the-clock, virtually eliminating the limitations associated with staffing availability and regular business hours communications.
Moreover, the integration of advanced irrigation technology, exemplified by systems like the GentleWave, has redefined the standard of practice in endodontics. By harnessing the principles of multisonic technology and optimized fluid dynamics, advanced irrigation systems transcend conventional methods, delivering superior cleaning efficacy, enhanced debridement, and unparalleled disinfection. As a result, endodontists can achieve more predictable outcomes, reduce treatment times, and elevate the overall patient experience. Moreover, by minimizing postoperative discomfort and optimizing workflow efficiencies, advanced irrigation technologies empower endodontists to enhance practice productivity and patient satisfaction alike.
Furthermore, the integration of augmented reality (AR) holds immense potential in optimizing operatory ergonomics and communication systems within the endodontic office. By overlaying digital information onto the physical environment, AR technology enables endodontists to minimize the physical footprint of screens and equipment within the operatory, creating a more streamlined and ergonomic workspace. Moreover, AR-enhanced communication systems facilitate real-time collaboration between team members, enabling seamless information sharing and enhancing workflow efficiencies.
In conclusion, as we embrace the dawn of a new era in endodontics, these transformative technologies promise to redefine the standard of care, enhance patient experiences, optimize practice workflows, and elevate clinical outcomes. We can propel the field of endodontics forward, delivering unparalleled care and outcomes to our patients while advancing the profession as a whole.

Mark Anthony Limosani, DMD, received his dental degree from the University of Montreal in 2007. He attended the specialty program in Endodontics at Nova Southeastern University where he also received his Master’s Degree in Dental Science. Dr. Limosani is both a Fellow of the Royal College of Dentists of Canada and a diplomate of the American Board of Endodontics. He is a past president of the South Florida District Dental Association and serves on the Council of Communications at the ADA. He is currently in private practice in Weston and Aventura, Florida. Dr. Limosani has lectured locally and internationally on many topics in endodontics including: dental traumatology, the restoration of endontically treated teeth, restoratively minded endodontics, diagnosis and treatment planning and cone beam computed tomography (CBCT) use in endodontics. Dr. Limosani is a Key Opinion Leader for Sonendo and SS White.
ISSN number 2372-6245
1 endopracticeus.com Volume 17 Number 1 INTRODUCTION
© MedMark, LLC 2024. All rights reserved. The publisher’s written consent must be obtained before any part of this publication may be reproduced in any form whatsoever, including photocopies and information retrieval systems. While every care has been taken in the preparation of this magazine, the publisher cannot be held responsible for the accuracy of the information printed herein, or in any consequence arising from it. The views expressed herein are those of the author(s) and not necessarily the opinion of either Endodontic Practice US or the publisher.

Drs. Iris Slutzky-Goldberg, Rotem Ophek, Dar Slutzky, and David Keinan
2 Endodontic Practice US Volume 17 Number 1 TABLE OF CONTENTS CLINICAL Contemporary treatment of Dens Invaginatus type III
explore the use of CBCT, ultrasonics, strict biomechanical preparation, and bioceramics for a specific condition PUBLISHER’S PERSPECTIVE 2024 — appreci-8 your potential Lisa Moler, Founder/CEO, MedMark Media............................... 6 ENDODONTIC INSIGHT Endodontic retreatment that sets the stage for dental success Dr. Stephanie Tran discusses the tools she uses for minimally invasive endodontics .................. 16 ENDODONTIC CONCEPTS Sepsis is serious — recognize the signs Dr. Stuart L. Segelnick describes lifesaving warning signs ........... 20 AAE SPECIAL SECTION BIO-C® Sealer ION+ By Angelus ....................................... 22 Brasseler — a leader in Anatomically Centered Endodontics (ACE) 23 Unlock the future of your dental practice........................ 24 Endo Mastery .......................... 25 Endodontic Practice Partners — dynamic and focused ...... 26 Kerr Dental ............................... 27 Luman Dental: Specialists in CBCT Technology .................. 28 Odne — transforming endo ............................................. 29 Sonendo GentleWave .......... 30 Specialized Dental Partners 31 Continuing our focus on serving specialists ............... 32 SS White — landmark accomplishments .................. 33 8 12 COVER STORY A transformative innovation that continues to make a difference A conversation with Dr. Josh Todd about how the GentleWave® System is helping him create a win-win-win for patients, referring dentists, and his practice
Cover image of Dr. Josh Todd courtesy of Sonendo®.




Transform your practice, Transform your life! DOCTOR AND TEAM SEMINARS PRACTICE MANAGEMENT CONSULTING CLINICAL TEAM TRAINING LIFESTYLE AND FINANCIAL FREEDOM PREMIERE ENDODONTIC COACH FOR PRACTICE OWNERS AAE BOOTH #437 | www.endomastery.com | 1-800-482-7563
CONTINUING EDUCATION
Clinical implementation and future of AI in endodontic dentistry
Drs. Aaron Glick, David Jaramillo, Nisha Manila, and Jennifer Chang discuss the pros and cons of AI in endodontic and general dental practice 34 PRODUCT SPOTLIGHT Odne – Swiss start-up transforming

Dr. Joseph C. Stern discusses the benefits and drawbacks of prescribing antibiotics in endodontics
PRACTICE DEVELOPMENT
Elevating your practice’s referral marketing: a comprehensive approach
Stacy Hill discusses establishing credibility and building longterm, genuine relationships with your referral network 48
ZenSeal™ Bioceramic Root Canal Sealer features high flowability and excellent sealability with zero shrinkage, while also reducing material waste per application
50
MILITARY MATTERS
Freedom Day USA
Dr. Lou Shuman discusses how a lifetime of freedom can be repaid by giving a day for free ............... 52
FINANCIAL FOCUS 5 ways to help your practice reduce credit card processing fees
Matt Rej offers tips on how to mitigate the costs of accepting credit cards .................................. 54
ENDOSPECTIVE A collaborative shift Dr. Michael Winick’s endodontic odyssey with Specialized Dental Partners......................................... 56





4 Endodontic Practice US Volume 17 Number 1 TABLE OF CONTENTS
45
endo
PRODUCT PROFILE
deal
simpler root canals
Sealing the
on
.............................................................
Connect. Be Seen. Grow. Succeed. | www.medmarkmedia.com READ the latest industry news and business WATCH DocTalk Dental video interviews with KOLs LEARN through live and archived webinars RECEIVE news and event updates in your inbox by registering for our eNewsletter CONNECT with us on social media www.endopracticeus.com *Paid subscribers can earn 4 continuing education credits per issue by passing the 2 CE article quizzes online at https://endopracticeus.com/category/continuing-education/ 40 CONTINUING EDUCATION
in endodontics: a
Antibiotics
desktop reference


2024 — appreci-8 your potential
Numerology is the study of numbers that deal with their mystical meaning and effect on our lives. When you think of all of the numbers that surround us every day — our dates of birth, other special dates, births, anniversaries, and deaths of those near and dear to us, even your home address can have a deeper meaning. No better time to think about the power of numbers than this year. Add up the numbers in our new year, 2024, and the result is the number 8. Turn the number 8 on its side, and you get the infinity symbol — this year, you can harness the power of 8 — when opportunities to reach goals in our personal and private lives can be limitless.
 Lisa Moler Founder/Publisher, MedMark Media
Lisa Moler Founder/Publisher, MedMark Media
A little numerology research on the number 8 shows that it represents the achiever and goal-reacher. The number symbolizes good sense, a powerful presence, and strong success drive. Balance is also a hallmark of the number 8, as reflected in its symmetrical shape that promotes stability, potential, and productivity. The number 8 is ruled by the planet Saturn (as is the zodiac sign, Capricorn). Traits of this planet are perseverance and ambition, so during 2024, our “8” year, we should strive to find our places as strong leaders ready to transform our plans and words into actions.
For the Spring 2024 issue, we want to help turn your plans into prosperity with our clinical articles and marketing expertise. In our Cover Story, Dr. Josh Todd writes about overcoming endodontic challenges and providing a minimally invasive patient experience with the GentleWave System by Sonendo. Our CE by Dr. Joseph Stern explores the benefits and drawbacks of prescribing antibiotics in the endodontic practice. Another CE, by Dr. Aaron Glick and colleagues, looks into artificial intelligence (AI) and its possible endodontic applications. Check out the AAE Special Section to discover products and services that bring your practices to a higher level, lower stress, and increase your clinical and financial success.
What can you do to make the most of your “8” year? Keep achieving, be strategic, and fiercely tenacious. Be a leader, but listen to your team, and let them know that the most fulfilling achievements are the ones that you reach together. Give back when you can because the karma of the number 8 is connected to the infinite balance between success and gratitude. And remember like the balanced number 8, to make time for personal life, even while you pursue professional success. 2024 is the year to turn your potential into prosperity.
With appreci-8-tion for success in 2024,
Lisa Moler Founder/Publisher MedMark Media
Published by

Publisher Lisa Moler lmoler@medmarkmedia.com
Managing Editor
Mali Schantz-Feld, MA, CDE mali@medmarkmedia.com Tel: (727) 515-5118
National Account Manager Adrienne Good agood@medmarkmedia.com Tel: (623) 340-4373
Sales Assistant & Client Services
Melissa Minnick melissa@medmarkmedia.com
Creative Director/Production Manager Amanda Culver amanda@medmarkmedia.com
Marketing & Digital Strategy Amzi Koury amzi@medmarkmedia.com
eMedia Coordinator
Michelle Britzius emedia@medmarkmedia.com
Social Media Manager Felicia Vaughn felicia@medmarkmedia.com
Digital Marketing Assistant Hana Kahn support@medmarkmedia.com
Website Support Eileen Kane webmaster@medmarkmedia.com
MedMark, LLC 15720 N. Greenway-Hayden Loop #9 Scottsdale, AZ 85260
Tel: (480) 621-8955
Toll-free: (866) 579-9496 www.medmarkmedia.com www.endopracticeus.com
Subscription Rate 1 year (4 issues) $149 https://endopracticeus.com/subscribe/
6 Endodontic Practice US Volume 17 Number 1 PUBLISHER’S PERSPECTIVE

800 - 605 - 3437 | Specialty1partners.com YOUR SPECIALTY IS OUR SPECIALTY . The Only Doctor-Founded, Doctor-Led Specialty Partnership Organization. “It’s a partnership of specialists and we are all specialty strong.” Dr. Joanne Jensen Endodontic Artistry Visit Us at AAE Booth #819
A transformative innovation that continues to make a difference
A conversation with Dr. Josh Todd about how the GentleWave® System is helping him create a win-win-win for patients, referring dentists, and his practice
Why did you choose to enter the field of endodontics?
I gained a great education and valuable access to highly trained specialists during my years in dental school at the University of Louisville in Kentucky. I received a scholarship as well as a phenomenal dental school experience. After graduating, I worked with professionals in endodontics, oral surgery, periodontics, and pediatric dentistry while attending an advanced dental education residency at Fort Bragg, North Carolina. My endodontic mentor, COL Lindsay, encouraged me to seriously consider specializing. Because I really enjoyed general dentistry, at first, I was skeptical. But, after several years of practicing, my mentor’s words echoing in my ear, and conversations with my wife — who is also a general dentist — I decided to apply for an endodontic residency program at Fort Gordon, Georgia through the Army. I was accepted into the program, and in a full-circle and serendipitous moment, discovered that my endodontic mentor was the director of residency.

What
inspired you to open your own practice?
I was in the Army for 12 years, and we were moving every 2-to-3 years to a different base. My wife and I wanted our children to grow up around family members living in Pensacola, Florida. As I was conducting research and sending out feelers to inquire about who was hiring in the area, I was surprised to learn that no one was. It became clear that this location was underserved by endodontists. My wife was the one who really encouraged me to open our own practice.

Josh Todd, DMD, is a dual board-certified general dentist and endodontist. He received his undergraduate degree from Auburn University and went on to earn his DMD at the University of Louisville School of Dentistry. From there, he took his commission as an officer in the Army, where he completed two advanced residency programs in general dentistry and endodontics. He practiced general dentistry for 7 years before returning to pursue his endodontic training. He served as the Chief Dental Officer from 2010 to 2013 in Hohenfels, Germany and was the lead endodontic mentor at the Advanced Dental Education program at Fort Campbell, Kentucky from 2017 to 2020. He opened Elite Endodontics in Pensacola, Florida in August 2020.
Disclosure: The author declares that there are no conflicts of interest in connection with this article.
So, we started an endodontic practice in a town where we knew almost nobody in August 2020, shortly after the COVID-19 shutdown. Due to the restrictions placed on me by the Army during the pandemic, I was not allowed to travel outside of Tennessee. So, ahead of opening day, my wife and our office manager were able to visit the local general dentists’ offices, make connections, and market the practice. We’re so grateful to have had referrals from day one. It’s been a wild ride — but it’s been a great success.
What are some common challenges that clinicians face when performing traditional root canal treatment?
There is rarely a straightforward root canal, with every tooth having unique curves and delicate nuances within the anatomy.
8 Endodontic Practice US Volume 17 Number 1 COVER STORY
Working in Florida, I have grown accustomed to treating an older patient population. These cases are not often easy, with hidden canals, highly complex anatomies, and more.
Treating calcified root canals is one of the most common challenges I face. As a clinician, when I’m fighting a calcified canal, I sometimes feel like I am spending too much time, effort, and energy trying to get down to hard-to-reach places. When this happens, my biggest concern is my patients, who are sitting in the chair and feeling the amount of time I’m spending on them. This can be very stressful.
While files have significantly improved over the years, they still have physical limitations that prevent them from negotiating certain aspects of the root canal anatomy (lateral canals, accessory canals, isthmuses, etc.). It can also be challenging to get the appropriate amount of disinfecting solutions into those areas.
Long-time challenges like these are why it’s important for endodontists to consider new technology. At my practice, I use the GentleWave® System, which is redefining the standard of root canal treatment with a minimally invasive process that preserves tooth structure and promotes early healing. With it, I’m able to better disinfect those hard-to-reach places. And I have the confidence of knowing the additional anatomy that files can’t reach is cleaned and disinfected by the fluids in the GentleWave System.


Todd explaining how the GentleWave G4 system is a modern way to treat root canal infections and promote pain-free fast healing

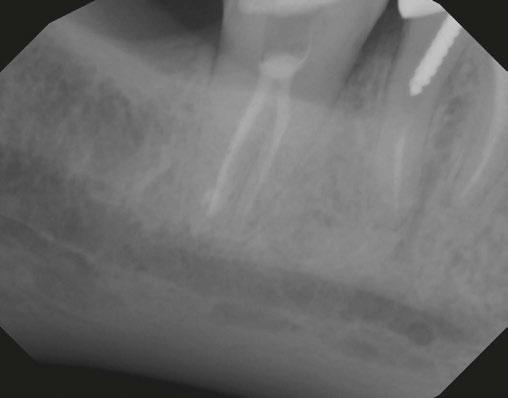
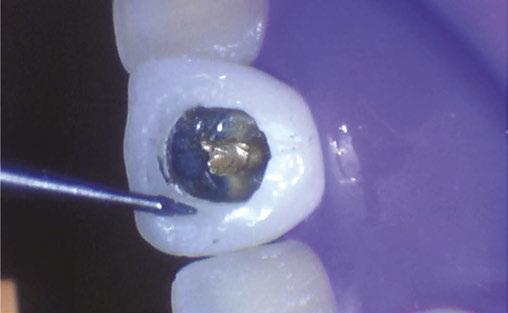
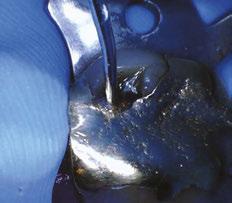
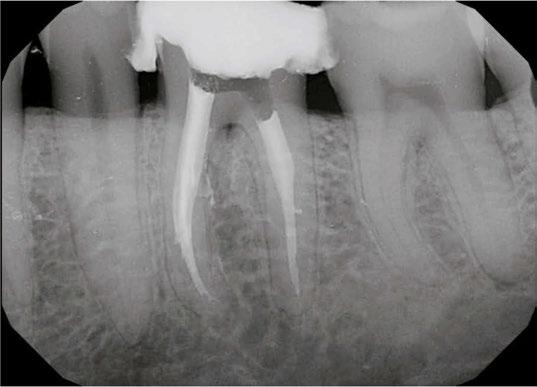
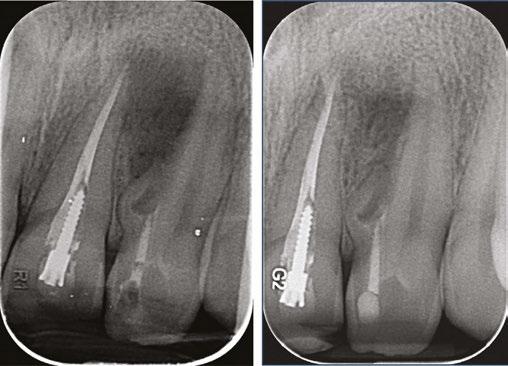
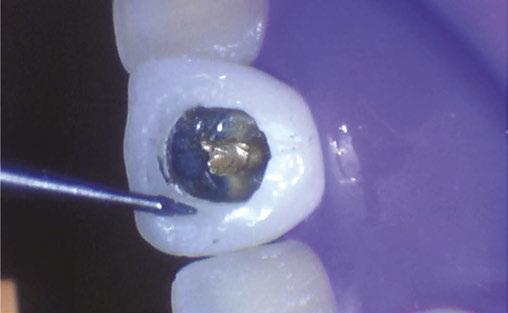
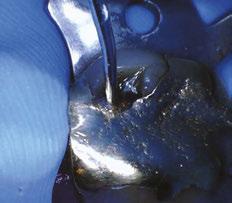
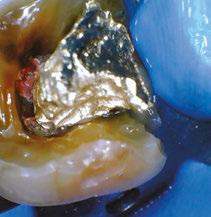
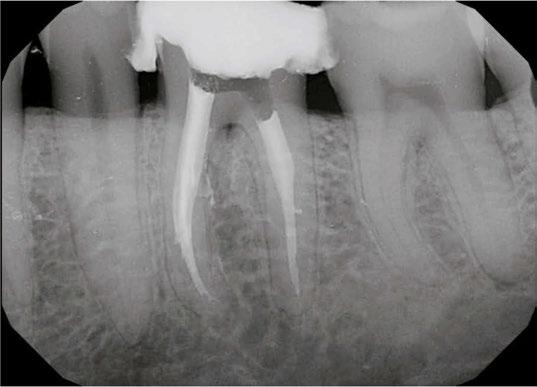
Case 1: Pre-op and diagnosis: A 68-year-old female presented with localized vestibular swelling buccal to tooth No. 30. No. 30 had been symptomatic for a few days, but the swelling started to alarm the patient and caused her to seek treatment. Upon evaluation, No. 30 was diagnosed as necrotic pulp with acute apical abscess. Two treatment options were discussed with the patient: 1) Tooth No. 30 non-surgical root canal therapy or 2) Tooth No. 30 extraction. The patient elected tooth No. 30 non-surgical root canal therapy (NSRCT). A pre-op Small FOV CBCT revealed a heavily calcified pulp chamber and calcified canals and a radix entomolaris. The CBCT revealed PARL’s at the apex of the mesial, distal, and radix entomolaris roots with the lesion extending coronally into the furcation. The patient was advised before treatment that this would be a very challenging case, and No. 30 NSRCT would be given a guarded prognosis, but she chose to proceed with No. 30 NSRCT. Treatment: No. 30 NSRCT, the patient was anesthetized with 68 mg Lidocaine with 0.034 mg EPI via IAN and 68 mg Septocaine with 0.017 mg EPI via buccal infiltration. Rubber dam isolation was utilized, and access was prepared through the PFM crown. 4 canals were located and then immediately after identification of the canal orifices, a platform was created with Soundseal, and the GentleWave Cleanflow handpiece was utilized to help break up the calcified tissue and negotiate each canal, alternating between a pathfile to slowly negotiate the coronal half of the canals and then running the GentleWave CleanFlow Procedure Instrument for 30-40 seconds to remove the accumulated debris. By alternating between files and the CleanFlow with GentleWave, all 4 canals were negotiated to length, and patency was achieved. The final working lengths were between 23 mm-24.5 mm for all 4 canals. All canals were instrumented to a Master Apical File of 20/.04 and obturated with high-flow BC Sealer. By utilizing the GentleWave and High-Flow BC Sealer, the apical delta of the distal root was cleaned, disinfected, and obturated in ways that would not have been possible with traditional endodontic therapy. Post-op: The patient was called 24 hours after treatment and reported she was pain-free, the swelling had reduced, and she was doing well.
9 endopracticeus.com Volume 17 Number 1 COVER STORY
Dr.
Can you describe patient sentiment surrounding traditional root canal treatment?
Root canal treatment is what everyone compares to the most horrible things they can think of — “At least it’s not a root canal!” It’s no surprise that the overwhelming connotation behind root canals is negative. In my opinion, much of this stems from the history of root canal therapy, which was not always as effective or seamless as it is today.
My patients have told me time and time again that the GentleWave® Procedure is less painful and easier than traditional therapy. Patients who have received traditional treatment in the past can, hopefully, relax a bit more when undergoing a GentleWave Procedure and allow me to treat them without being overburdened with fear and anxiety. Some patients even like the noise that the machine makes, and several have compared it to a calming sound machine!



When and how did you learn about the GentleWave® Procedure?
In 2019, a friend of mine invited me to the TDO Software meeting (now known as EndoCon). I attended a continuing education (CE) event about the GentleWave Procedure while I was there. During the presentation I thought to myself, “I have never had a root canal look like that, ever.” In my head, I knew that was what I wanted to be able to offer my patients when I started my own practice because I recognized it was a higher level of cleaning and disinfection, and therefore, the best treatment available. I have used the GentleWave System since opening day.
When adopting new technology, clinicians will always have to unlearn some of their traditional instrumentation techniques. This was challenging — especially as I was opening a new practice and training staff all at the same time. To make this learning curve easier, I followed the advice of my GentleWave trainer and trusted the technology to do what it says it does. I adhered to necessary protocols and encouraged myself to forge ahead.
With this, it didn’t take more than a few short weeks to get fully up to speed on the GentleWave System. I was committed to it — and it more than paid off. I have also spent a lot of time discussing clinical protocols with other GentleWave providers who have been using the technology longer than I have and have gained wisdom from their techniques.
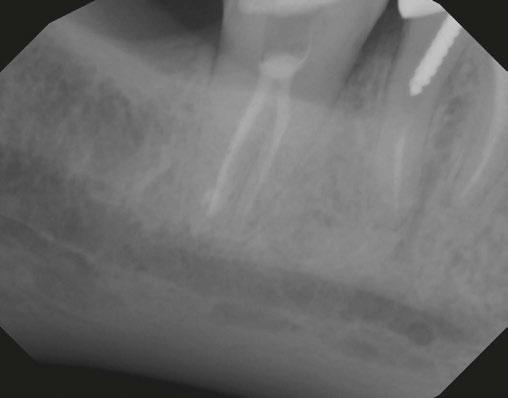
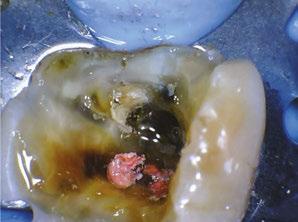
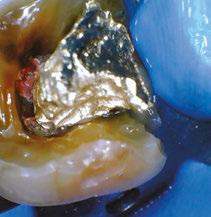
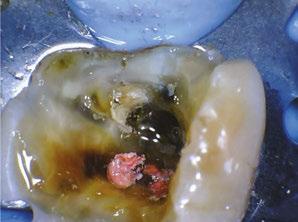
Case 2: Pre-op and diagnosis: A 52-year-old female presented with a chief complaint of pain to hot and cold. Pulpal sensitivity testing on tooth No. 31 revealed a lingering, aching response to thermal testing. A clinical exam revealed a small crack extending from the occlusal resin over the distal marginal ridge. Probing depths around No. 31 were all <3 mm. No. 31 was diagnosed symptomatic irreversible pulpitis with symptomatic apical periodontitis. A pre-op small FOV CBCT revealed No. 31 to have a C-shaped canal morphology. Two treatment options were discussed with the patient: 1) Tooth No. 31 non-surgical root canal therapy or 2) No. 31 extraction. The patient elected No. 31 non-surgical root canal therapy (NSRCT). Treatment: No. 31 NSRCT, the patient was anesthetized with 68 mg Lidocaine with 0.034 mg EPI via IAN and 68 mg Septocaine with 0.017 mg EPI via buccal Infiltration. Rubber dam isolation was utilized, and access was prepared. Due to the C-shaped canal morphology, only two canals could be identified. Prior to placement of the SoundSeal platform, a small amount of bonding agent was placed over the crack along the distal marginal ridge and distal portion of the pulp chamber. The SoundSeal platform was securely placed to create a vacuum seal. The two canals were negotiated to achieve patency by alternating rotary instrumentation and the GentleWave CleanFlow Procedure Instrument for 30-40 seconds to thoroughly debride the internal anatomy. The mesial canal was instrumented to a Master Apical File of 20/.04, while the distal canal to a 25/.04 Master Apical File. Due to the larger and more irregular canal morphology of the distal canal, various-sized gutta-percha cones were used to gauge the size to be used for obturation. The mesial canal was obturated with a Sealer-based obturation method with High Flow BC Sealer and a single 20/.04 master cone. The distal canal was obturated with High Flow BC Sealer and Warm Vertical Compaction. With the aid of the GentleWave and the CleanFlow Procedure Instrument, the C-Shaped canal anatomy was more deeply cleaned, pulp tissue more thoroughly removed, and this case was completed in a single visit which would have been much more difficult to accomplish with traditional endodontic therapy.
10 Endodontic Practice US Volume 17 Number 1 COVER STORY
Another example of constant and never-ending learning is my colleague, Dr. Terry Webb, a fellow of the International College of Dentists, and Diplomate of the American Board of Endodontics. After completing his 30-year naval career in 2023, he joined us at Elite Endodontics, has embraced the GentleWave System, and includes it in most of his cases.
How did the GentleWave® System help overcome some of the challenges you described earlier and others?
In addition to helping me navigate complex anatomies and calcified root canals, the GentleWave Procedure has limited the number of re-treat and multi-visit cases that I see. It does such a thorough job of cleaning, all without having to remove nearly as much tooth structure as with traditional therapy. By having the unique ability to find additional canals and reach complex areas, about 98% to 99% of my patients come in for one visit only. I love this, and so do my patients — their time is valuable.

Additionally, several of my referring dentists have noticed that the GentleWave System allows me to be as minimally invasive as possible — all while keeping tooth structure intact. The GentleWave Procedure gives restorative dentists more tooth structure to work with after treatment, which benefits the patient and offers a better long-term prognosis for that tooth. Using the GentleWave System not only helps endodontists and patients, but it also helps other industry professionals.
How has integrating the GentleWave System helped you as a business owner?
Nearly everyone is relatively tech-savvy today, and patients notice that we have updated equipment and the latest technology in our office. We differentiate our practice by using the GentleWave System, and we see patients coming in specifically because they know it’s what they want. More people are making informed choices about their healthcare and doing their own research about various procedures and techniques. When patients are looking for an endodontic practice in our area, they quickly realize that we’re the only one offering the GentleWave Procedure.
Sonendo, the developer of the GentleWave System, has made our marketing efforts as seamless and straightforward as possible. We have implemented Sonendo’s library of marketing materials, joined a community of GentleWave users, and more. The GentleWave Portal consists of various digital resources, including brochures, that are easy to customize with our practice name and logo, which makes marketing very easy. Additionally, as practice owners, we have many pieces of equipment that must be maintained, serviced, or repaired on a regular basis, and the staff is tasked with keeping track of it all. The GentleWave System removes the administrative work, telling us when it’s ready for maintenance and outlining the necessary steps. It then sends this data to Sonendo, so our team
doesn’t have to keep any records on hand. While having one less thing to worry about from a maintenance standpoint may seem small, it makes our lives as business owners much easier.
There is clear evidence showing that the GentleWave Procedure provides excellent clinical results. But, what’s exceptional about Sonendo is the amount of support it shows its customers. They have fostered a community of like-minded professionals who support one another. They are also always offering a wide variety of educational content to help us become better clinicians and business owners. The company is unparalleled in this way.
In your opinion, why do some clinicians remain hesitant to adopt innovative technology like the GentleWave System? What is your advice?
It’s almost always uncomfortable to learn something new. We’re creatures of habit, and clinicians tend to develop their own treatment protocols. However, to fully embrace the future of endodontics, we must be willing to unlearn years worth of habits. I would advise endodontists to take a step back and give themselves room to change and grow. I recognize that adopting new technology can be a leap of faith, but it can be worth it.
The GentleWave System will benefit you and your practice long-term. In fact, I have recommended this technology to many of my colleagues, who have adopted it for their own practices and are very glad that they did.
From my experience, it will improve your life as a clinician and business owner. It will differentiate you and your practice in the market, helping to ensure that you are providing the best possible care for your patients. It will offer access to a community of like-minded and supportive endodontists, who can serve as mentors and friends. Together, these factors add up to make the GentleWave System completely worth the investment.
11 endopracticeus.com Volume 17 Number 1 COVER STORY EP
Dr. Todd leverages the latest technology, including the GentleWave G4 system, to differentiate his practice
Contemporary treatment of Dens Invaginatus Type III
Drs.
Iris Slutzky-Goldberg, Rotem Ophek,
Dar
Slutzky,
and David Keinan explore the use of CBCT, ultrasonics, strict biomechanical preparation, and bioceramics for a specific condition
Abstract
In
Dens invaginatus is a rare developmental malformation of the tooth that mainly affects the permanent maxillary lateral incisors. Endodontic treatment might be challenging due to the complex canal anatomy of the tooth with the diagnosed invagination. This invagination is often not connected to the main canal, so if it becomes infected, the main canal is usually unaffected. CBCT imaging is necessary to evaluate the complex anatomy and accurately determine the source of the periapical lesion and, thereafter, the treatment plan. The purpose of this article is to describe the careful evaluation of the source of infection by combining data from clinical findings and the use of 3D imaging. The correct obturation material should be selected, and the biomechanical preparation should be adjusted to the complex anatomic irregularities to ensure success.
Introduction
order to visualize the complex anatomy, the use of a CBCT is an essential step. It is especially important to evaluate if there are any separate apical
foramina and communications between the main canal and the invagination.”
tal ligament and periradicular tissues. These types range from a minimal Invagination (Type I ) confined within the coronal to an invagination that extends to the root and communicates with the periradicular tissues, either laterally (Type IIIa) or at the apical foramen (Type IIIb).1
Dens invaginatus (DI), otherwise known as dens in dente, is a dental anomaly that occurs during tooth development and is characterized by an invagination of the enamel organ into the dental papilla before mineralization.1 The distortion of the enamel organ during tooth development can lead to a formation of an enamel-lined canal that ends at the cingulum and in some cases at the incisal edge, producing an irregular coronal shape.2
Dens invaginatus is observed mainly in maxillary lateral incisors, and its prevalence ranges from 0.3% to 10%.1,3 Oehlers (1957) classified dens invaginatus into three types based on the depth of invagination and communication with the periodon-
Dr. Iris Slutzky-Goldberg is from the Department of Endodontics, Galilee College of Dental Sciences, Nahriya and the Azrieli Faculty of Medicine, Bar Ilan University, Ramat Gan, Israel.
Dr. Rotem Ophek is in private practice in Rehovot, Israel.
Dr. Dar Slutzky is in the Faculty of Dental Medicine, Hebrew University of Jerusalem, Israel and Hadassah Medical Center, Jerusalem, Israel.
Dr. David Keinan is from the Department of Endodontology, Maurice and Gabriela Goldschleger School of Dental Medicine, Tel Aviv University, Tel Aviv, Israel.
Several treatment alternatives have been suggested for the treatment of teeth with Type III DI. These include nonsurgical endodontic treatment of the invagination alone,4 treatment of the main canal alone or along with the invagination, combined orthograde and surgical treatment,5,6 or extraction.
Conventional periapical radiographs, which are the gold standard for identification of DI7 provide only a two-dimensional illustration of the complex anatomy of the tooth7,8 and thus might not yield sufficient information to correctly evaluate the true anatomy of the invagination as well as the main canal.9
Cone beam computed tomography (CBCT) provides a three-dimensional (3D) representation of the tooth.8.9 It enables not only the understanding of the involvement of the main canal in the infection but also whether the invagination is completely separated from the main canal and may allow treatment of the DI without involvement of the main canal.8
The aim of this case report is to present two cases of dens invaginatus, treated by conservative endodontic treatment after a 3-dimensional illustration of the inner anatomy of the tooth using CBCT, ultrasonic, and additional means of improved irrigation.
Case No. 1
A 19-year-old male presented to the endodontic clinic with pain and swelling in the gingiva surrounding his upper left central and lateral incisors. The patient was generally healthy and received endodontic treatment for the maxillary left central incisor following a dental injury 6.5 years ago. A scar of a previous sinus tract was also observed in the oral mucosa. The left lateral incisor was sensitive to percussion and palpation, but positively
12 Endodontic Practice US Volume 17 Number 1 CLINICAL
responded to sensibility testing (Endo-Ice, Coltene). The central incisor did not present any irregular signs or symptoms.
A periapical radiograph demonstrated a DI with an apical radiolucency extending from the mesial aspect of the lateral incisor towards the apex and distal aspect of the central incisor. A slight inclination of the root of the maxillary left lateral incisor was observed in the periapical radiograph.
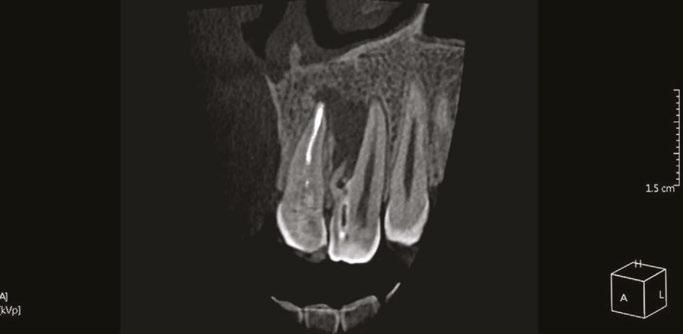
Considering the irregular anatomy of the tooth, the patient was referred for a CBCT scan.
The CBCT scan confirmed the presence of a Type IIIa invagination and a large radiolucent lesion that was associated with the invagination in the lateral incisor and extended mesially towards the apex of the central incisor. Since the apex of the main canal in the lateral incisor was not involved, it was decided to limit the treatment to the invagination. The diagnosis of the periapex of the previously treated central incisor was unclear; there was either periapical healing or asymptomatic apical periodontitis; therefore, no intervention was done, and the tooth was kept for follow-up.
During the first appointment, a palatal access cavity was prepared under a surgical operating microscope based on the external morphology of the tooth and the CBCT scan. After gaining access to the invagination, the enamel-lined canal was conservatively enlarged using an ultrasonic tip. Biomechanical preparation was based on copious irrigation with 2.5% Sodium hypochlorite (NaOCl) and 17% ethylene diamine tetra-acetic acid (EDTA) and the use of the XP Finisher (FKG Dentaire Sarl, La Chaux-de-Fonds, Switzerland). A calcium hydroxide dressing was placed using a spiral Lentulo, and the access cavity was temporized with Coltosol® (Coltene Whaledent) provisional filling material.
At the second appointment (2 weeks later), the patient was asymptomatic. The invagination was irrigated with 2.5% NaOCl and 17% EDTA, and the enamel-lined invagination was obturated with BC Putty (EndoSequence®, BC RRM™ Fast Set, Brasseler). The access cavity was then filled with a Coltosol F® (Coltene Whaledent) and Fuji Equia glass ionomer (GC America) as a temporary filling to seal the access. One week later, it was replaced by a permanent composite restoration.
One year later, the tooth was asymptomatic, with no tenderness to palpation or percussion, and normal mobility was observed. Radiographic examination demonstrated healing of the lesion. Complete healing was observed around the apex of the central incisor, which was symptom-free, and therefore no intervention was necessary for this tooth.
The patient has been scheduled for a follow-up appointment in 1 year.
Case No. 2
An 8.5-year-old girl was referred by her pediatric dentist due to extraoral swelling that extended into the infra-orbital space originating from the left lateral incisor. The immature tooth had only 2/3 of the root completed and therefore was staged as Nolla 8.10 The deciduous lateral incisor was extracted at the age of 2 years after a traumatic dental injury. She was administered Amoxycillin to manage the infection.
Considering the irregular anatomy of the tooth, which was seen in the periapical radiograph, the patient was referred


for a small-field CBCT scan. A Class III dens invaginatus was verified. A few days after undergoing emergency treatment, including incision and drainage at the oral surgery department, swelling in the buccal vestibule was still evident upon arrival at the follow-up appointment. Local anesthesia was administered before tooth isolation with a rubber dam. Access cavity was then achieved through the invagination alone, and a transpar-
13 endopracticeus.com Volume 17 Number 1 CLINICAL
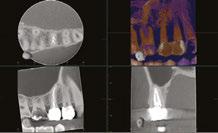
Figure 1: CBCT scan of the tooth demonstrating the radiolucent lesion surrounding the DI and extending to the apex of the central incisor
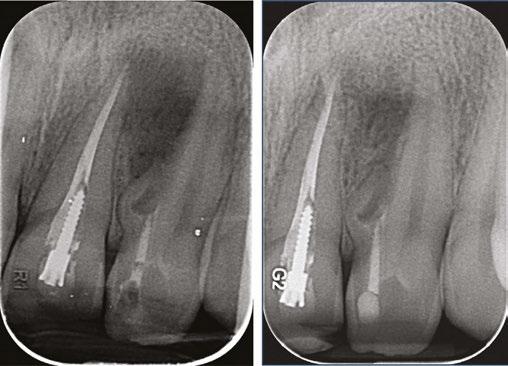
Figures 2A-2D: 2A. Periapical radiograph of the dens. 2B. Hedstrom file in the invagination. 2C. The obturated enamel lining of the invagination with BC putty. 2D. Healing of the periapical lesion in the 1-year follow-up
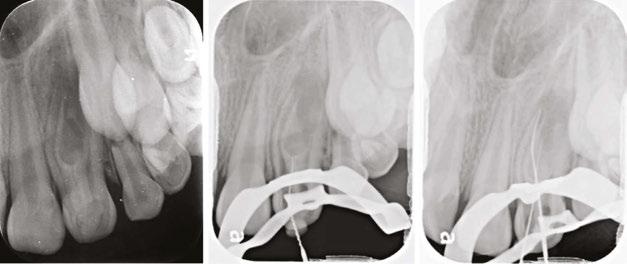

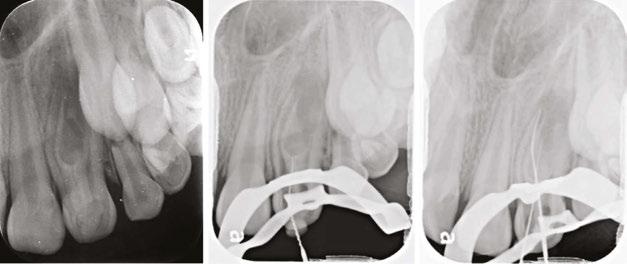
int the C-shaped main canal. 3D.The obturated enamel of lined canals with Biodentine. The radiopacity is similar to that of dentin. 3E. Healing of the periapical lesion in the 3-year follow-up and continued root formation
ent liquid leaked from the canal. The invagination was then irrigated with 3% NaOCl and 17% EDTA, dressed with CaOH2, and sealed with a temporary filling material (Coltosol), placed between appointments. Ten days later, at a follow-up appointment, there was still buccal swelling, so similar irrigation and dressing were repeated.
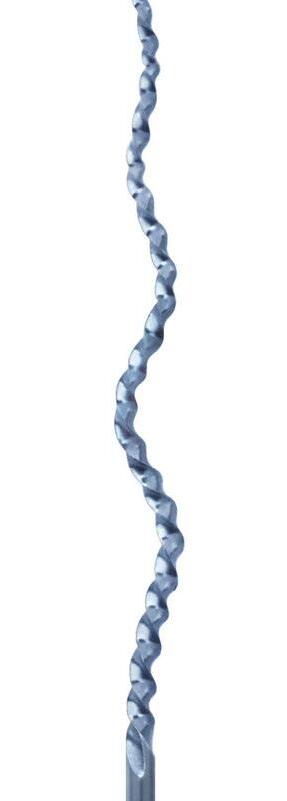
Two weeks later, since there was still swelling, it was decided to treat the main canal as well. The main canal was prepared and irrigated with copious irrigation with 3% NaOCl and 17% EDTA, combined with the use of SAF (Redent Nova, Raanana, Israel) owing to its ability to adapt three-dimensionally to the shape of the canal, and its continuous flow of irrigant through its hollow file, which facilitates better cleaning and debridement. Dressing of the invagination and the main canal were done with a slurry of calcium hydroxide (Ca(OH)2). This step led to the resolution of the swelling; therefore, at the next appointment, it was decided to obturate the canals with Biodentine® (Septodont), and the access cavity was filled with a composite resin.
Follow-up examinations were scheduled for 6 months and then yearly. At the 3-year follow-up, complete healing was observed; continuous PDL was observed around the root and resolution of the periapical lesion. The immature root canals continued to develop, and apical closure is evident in the periapical radiograph.
Discussion
Dens invaginatus is a relatively common anatomical aberration mainly found in the maxillary lateral incisors with a prevalence up to 10%.1,3 The invagination can be a simple enamel fold in the coronal or a complex anatomy with a separate communication to the periapical area.1 Diagnosing the source of infection and planning treatment for this complex anatomy can be challenging. A careful diagnosis is necessary to determine whether to treat the invagination alone, the main canal or both.4 Moreover, in certain cases, additional surgical intervention may be required after the orthograde endodontic treatment5 and even intentional replantation.6
In order to visualize the complex anatomy, the use of a CBCT is an essential step.8,9 It is especially important to evaluate if there are any separate apical foramina and communications between
the main canal and the invagination.8 This data should be evaluated in conjunction with clinical signs like swelling, sinus tract location and response to thermal tests.11 The use of high magnification and proper lighting is mandatory during access cavity preparation, negotiation of complex canal anatomy, and, if needed, during endodontic microsurgery.12 The use of a guided splint was also reported for the conservative pulp access during endodontic treatment of dens invaginatus.13
The two cases described were treated by a strict protocol for biomechanical preparation. The initial access cavity preparation includes penetration into the invagination using a small file, and then gradual enlargement with ultrasonic tips. Thereafter, copious irrigation with both 3% NaOCl and 17% EDTA, combined with the use of rotary file systems facilitates better availability of the solutions throughout the canal system.14,15 Irrigation with sodium hypochlorite and dressing with Ca(OH)2 are required to dissolve any necrotic tissue in the canals, or any isthmi and cul de sacs.16,17 In the first case, additional debridement and finishing were performed using the XP finisher files (FKG Dentaire Sarl, Switzerland),18 and in the second case, the self-adjusting file system (Redent Nova, Raanana, Israel) was used.19 Both file systems allow for more effective disinfection of the complex canal system with minimal tooth structure removal.20
During canal obturation, we used a bioceramic material to treat the invagination, similar to that of open apices,21 or for root perforation repair.22 The material is known for its excellent sealing ability and biocompatibility, which has made it widely used clinically.23 The high success rate of this material can be attributed to its antimicrobial properties, which result from its high pH during setting.24,25 The use of BC putty, with its higher radiopacity, allows for easy evaluation of radiographic sealing, whereas it may be more challenging with Biodentine due to its similar radiopacity to dentin.25
Conclusion
This article outlines the essential steps for the successful evaluation and treatment of a tooth diagnosed with type III dens invaginatus. These steps include the use of a 3D imaging, ultrasonic access cavity preparation, strict biomechanical protocol and dressing, and then obturation with a bioceramic material.
14 Endodontic Practice US Volume 17 Number 1 CLINICAL
Figures 3A-3E: 3A Periapical radiograph of the dens in dente. It is impossible to determine the accurate source of infection. 3B. Hedstrom file in the invagination. 3C. Files
Further study is recommended to evaluate the effect of a revascularization protocol as an alternative treatment option for those teeth.
REFERENCES
1. Alani A, Bishop K. Dens invaginatus. Part 1: Classification, prevalence and aetiology. Vol. 41, Int Endod J. 2008;41(12): 1123-1136.
2. Hülsmann M. Dens invaginatus: Aetiology, classification, prevalence, diagnosis, and treatment considerations. Int Endod J. 1997;30(2):79-90.
3. Siqueira JF Jr, Rôças IN, Hernández SR, Brisson-Suárez K, Baasch AC, Pérez AR, Alves FRF. Dens Invaginatus: Clinical Implications and Antimicrobial Endodontic Treatment Considerations. J Endod. 2022 Feb;48(2):161-170.
4. Tagger M. Nonsurgical endodontic therapy of tooth invagination. Report of a case. Oral Surg Oral Med Oral Pathol. 1977 Jan;43(1):124-129.
5. da Silva Neto UX, Hirai VH, Papalexiou V, Gonçalves SB, Westphalen VP, Bramante CM, Martins WD. Combined endodontic therapy and surgery in the treatment of dens invaginatus Type 3: case report. J Can Dent Assoc. 2005 Dec;71(11):855-858.
6. Li N, Xu H, Kan C, Zhang J, Li S. Retrospective Study of Intentional Replantation for Type IIIb Dens Invaginatus with Periapical Lesions. J Endod. 2022 Mar;48(3):329-336.
7. Kfir A, Flaisher Salem N, Natour L, Metzger Z, Sadan N, Elbahary S. Prevalence of dens invaginatus in young Israeli population and its association with clinical morphological features of maxillary incisors. Sci Rep. 2020 Oct 13;10(1):17131.
8. Patel S. The use of cone beam computed tomography in the conservative management of dens invaginatus: a case report. Int Endod J. 2010 Aug;43(8):707-713.
9. Kfir A, Telishevsky-Strauss Y, Leitner A, Metzger Z. The diagnosis and conservative treatment of a complex type 3 dens invaginatus using cone beam computed tomography (CBCT) and 3D plastic models. Int Endod J. 2013 Mar;46(3):275-288.
10. Nolla CM. The development of permanent teeth. J Dent Child. 1960;27:254-266.
11. Petersson K, Söderström C, Kiani-Anaraki M, Lévy G. Evaluation of the ability of thermal and electrical tests to register pulp vitality. Endod Dent Traumatol [Internet]. 1999 Jun [cited 2022 Jul 20];15(3):127–131. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10530156
12. Pecora G, Andreana S. Use of dental operating microscope in endodontic surgery. Oral Surg Oral Med Oral Pathol. 1993 Jun;75(6):751-758.
13. Mena-Álvarez J, Rico-Romano C, Lobo-Galindo AB, Zubizarreta-Macho Á. Endodontic treatment of dens evaginatus by performing a splint guided access cavity. J Esthet Restor Dent. 2017;29(6):396-402
14. Caron G, Nham K, Bronnec F, Machtou P. Effectiveness of different final irrigant activation protocols on smear layer removal in curved canals. J Endod. 2010 Aug;36(8):1361-1366
15. Haapasalo M, Shen Y, Wang Z, Gao Y. Irrigation in endodontics. Br Dent J. 2014 Mar;216(6):299-303.
16. Slutzky-Goldberg I, Hanut A, Matalon S, Baev V, Slutzky H. The effect of dentin on the pulp tissue dissolution capacity of sodium hypochlorite and calcium hydroxide. J Endod. 2013 Aug;39(8):980-983.
17. Hasselgren G, Olsson B, Cvek M. Effects of calcium hydroxide and sodium hypochlorite on the dissolution of necrotic porcine muscle tissue. J Endod. 1988 Mar;14(3):125-127.
18. Villalta-Briones N, Baca P, Bravo M, Solana C, Aguado-Pérez B, Ruiz-Linares M, Arias-Moliz MT. A laboratory study of root canal and isthmus disinfection in extracted teeth using various activation methods with a mixture of sodium hypochlorite and etidronic acid. Int Endod J. 2021 Feb;54(2):268-278.
19. Neves MA, Rôças IN, Siqueira JF Jr. Clinical antibacterial effectiveness of the self-adjusting file system. Int Endod J. 2014 Apr;47(4):356-365.
20. Sasanakul P, Ampornaramveth RS, Chivatxaranukul P. Influence of Adjuncts to Irrigation in the Disinfection of Large Root Canals. J Endod. 2019 Mar;45(3):332-337.
21. Torabinejad M, Smith PW, Kettering JD, Pitt Ford TR. Comparative investigation of marginal adaptation of mineral trioxide aggregate and other commonly used root-end filling materials. J Endod. 1995 Jun;21(6):295-299.
22. Main C, Mirzayan N, Shabahang S, Torabinejad M. Repair of root perforations using mineral trioxide aggregate: a long-term study. J Endod. 2004 Feb;30(2):80-83.
23. Fischer EJ, Arens DE, Miller CH. Bacterial leakage of mineral trioxide aggregate as compared with zinc-free amalgam, intermediate restorative material, and Super-EBA as a root-end filling material. J Endod. 1998 Mar;24(3):176-179.
24. Camilleri J. Staining Potential of Neo MTA Plus, MTA Plus, and Biodentine Used for Pulpotomy Procedures. J Endod. 2015 Jul;41(7):1139-1145.
25. Caron G, Azérad J, Faure MO, Machtou P, Boucher Y. Use of a new retrograde filling material (Biodentine) for endodontic surgery: two case reports. Int J Oral Sci. 2014 Dec;6(4):250-253.
Endodontic Practice US Webinars
LEARN about the lastest techniques and technology from industry leaders with our free live and archived educational webinars. Our online seminars are a convenient way to access great information and upskill. Check out our most recent webinars:
• The Science and Clinical Evidence Behind A ModernDay Disinfection and Debridement Technology with host Dr. Derek Peek
• Diagnosis & Cracked Teeth – How CBCT can change your practice with host Dr. Judy McIntyre
• Complete Endodontic Success: From Root Canals to Patient Reviews with host Dr. Ryan M. Walsh

15 endopracticeus.com Volume 17 Number 1 CLINICAL
EP
WATCH NOW at https://endopracticeus.com/webinars/ Connect. Be Seen. Grow. Succeed. | www.medmarkmedia.com
Endodontic retreatment that sets the stage for dental success
Dr. Stephanie Tran discusses the tools she uses for minimally invasive endodontics
“Begin with the end in mind.” That key principle from Stephen R. Covey’s book, The 7 Habits of Highly Effective People, can be used to describe the modern concept of restoratively driven endodontics. Root canal treatment has always been about maintaining the tooth so that it can be functional and free of disease, and in recent years we have seen a shift toward more minimally invasive treatment that also conserves more tooth structure and sets the stage for a successful long-term restoration.1,2 Endodontic retreatment aims to manage previously treated cases with persistent or recurrent apical periodontitis. Like modern restorative dentistry concepts trending toward more conservative prep designs and advancements in bonding, contemporary endodontic retreatment can also consequently enhance the survival rate and thus the options of direct and indirect restorative options for the restorative dentist.3


Minimally invasive techniques have emerged as a cornerstone in modern endodontic practice, focusing on preserving tooth structure while effectively managing endodontic cases. This idea of restoratively driven endodontics is a newer phenomenon that wasn’t always possible. With advancements in magnification

Stephanie Tran, DDS, is an endodontist who is passionate about endodontic education and helping patients relieve their dental pain while helping them maintain their teeth. Born in Connecticut and raised in California, Dr. Tran completed her undergraduate studies at the University of the Pacific in San Francisco, California. She completed a General Practice Residency program at SUNY Stony Brook University Medical Center, where she became experienced in managing advanced dental cases, trauma, and complex surgeries. After several years building her comprehensive dentistry background as a general dentist, Dr. Tran then decided to pursue her passion for endodontics. She completed her post-graduate endodontics specialty residency at the University of Tennessee Health Science Center, where she served as Chief Resident of the program. Dr. Tran is an experienced clinician who is trained in contemporary advanced endodontic techniques, microscopic surgical and nonsurgical endodontic treatment, and management of traumatic injuries. She provides endodontic treatment for both adults and pediatric patients in private practice, serving the New York City and Long Island, New York regions to help patients treat dental disease and save their teeth. She is also passionate about endodontic education and lectures both nationally and internationally to share her enthusiasm for endodontics with other clinicians along with posting on her social media @ her_holiness_the_pulp. In her free time, Dr. Tran enjoys traveling, snorkeling, exploring NYC’s many restaurants and museums, cooking, and going to the beach with her dog.
Disclosure: Dr. Tran uses and lectures on SS White products.
and visualization along with the contemporary armamentarium, we are able to conservatively remove the restorative material as well as remove less tooth structure. By removing less tooth structure and preserving the maximum amount of peri-cervical dentin, we’re helping to prevent future coronal and root fractures in the restored tooth.4,5
The chance of teeth with apical periodontitis to completely heal after initial treatment or retreatment is 74% to 86%, and their chance to be functional over time is 91% to 97%.6,7,8 Endodontic retreatment has a high success even with previous techniques, and with modern armamentarium and technology, we can improve the conservation of tooth structure and the efficacy of restorative material removal for retreatment. It has been shown that the endodontic access can affect the fracture load of crowns.9,10
SS White has a variety of burs that can reduce the microfractures and decrease the chance of crown fracture. For example, Great White®Z Diamonds are designed for Endo Access in all types of ceramic crowns such as Zirconia, Lithium Disilicate,
16 Endodontic Practice US Volume 17 Number 1 ENDODONTIC INSIGHT
Figures 1A and 1B: Retreatment with Tooth No. 3 (ExactTaperH DC)
Figure 2: Anterior post removal easily achieved using the EndoGuide (EG3) to delicately remove core build-up around the post.





That feeling when you know you’re providing great care and the best outcomes for your patients? It doesn’t get any better. Efficient crown removal and access creation with SS White® Great White® Z and Great White® Ultra burs expedites care to minimize chair time for your patients. By preserving more tooth structure with our DCTAPER™ files and EndoGuide® burs, you can expand restorative options for referring dentists and maintain the integrity of your patients’ teeth for improved long-term outcomes. Happy patients mean more referrals for your practice.
TFW you Preserve. Vital. Tooth. Structure. Conserve 40–70% More Tooth Structure with SS White® See show specials at AAE24 Booth #648 sswhitedental.com/aae
© 2024 SS White. All rights reserved. SS White, EndoGuide, DCTAPER and Great White are registered trademarks of SS White Dental. Market research and test studies available upon request.
e.max® and BruxZir®, reducing the chance of micro-fracture. The SS White SmartBursII® instruments are used with biomimetic principles to safely remove soft carious dentin and will not cut harder, healthier tissues (enamel, healthy dentin) or amalgam or composite, allowing for an increase of maintaining tooth structure.
Efficient, straight-line access to canals is achievable with EndoGuide, a unique set of eight carbide burs for nonsurgical root canal treatment. The funnel-shaped bur design improves canal visualization, removing less tooth structure while unveiling missed anatomy and untreated canals for root canal retreatment. The conical shaped micro-diameter tip acts as a self-centering guide for precision access to canals to remove root-filling materials and clean isthmuses while conserving healthy peri-cervical dentin. The minimally invasive high-speed carbides both from this kit as well as the SS White Great White carbides can be used in conjunction to conservatively remove restorative materials and loosen posts for retreatment of even some of the most daunting cases.
For removal of the root filling materials conservatively and efficiently, the Exact Retreatment File system uses heat treatment technology and a minimally invasive design to remove root canal obturating material such as gutta percha, carrier-based obturators, and fillers from coronal, middle, and apical thirds of root canal prior to canal reshaping. These heat-treated and controlled-memory NiTi rotary files are more flexible with increased resistance to cyclical and tortional fatigue. They also have a smaller maximum flute diameter which still allows for adequate instrumentation of the canal. These minimally invasive instruments allow for precise and controlled removal of gutta percha and sealer while minimizing stress on the root canal walls.
Through these contemporary techniques and technologies, restoratively driven endodontics results in more conservative yet effective management of the canal systems, and improved treatment options for the patient. Minimally invasive techniques have revolutionized the field of endodontic retreatment, offering a conservative yet effective approach to managing endodontic failures.14 By prioritizing tooth preservation and tissue conservation, these techniques ensure optimal treatment outcomes while minimizing patient discomfort and preserving long-term dental health. We are fortunate to work in a field that is constantly advancing, enabling us to work together to comprehensively take care of the patient by maintaining their teeth and giving it the greatest chance for long-term survival.
REFERENCES
1. Dietschi D, Duc O, Krejci I, Sadan A. Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature--Part 1. Composition and micro- and macrostructure alterations. Quintessence Int. 2007 Oct;38(9):733-743.
2. Dimitriu B, Vârlan C, Suciu I, Vârlan V, Bodnar D. Current considerations concerning endodontically treated teeth: alteration of hard dental tissues and biomechanical properties following endodontic therapy. J Med Life. 2009 Jan-Mar;2(1):60-65.
3. Nagasiri R, Chitmongkolsuk S. Long-term survival of endodontically treated molars without crown coverage: a retrospective cohort study. J Prosthet Dent. 2005 Feb;93(2):164-170.
4. Reeh ES, Messer HH, Douglas WH. Reduction in tooth stiffness as a result of endodontic and restorative procedures. J Endod. 1989 Nov;15(11):512-516.
5. Kishen, Anil. “Mechanisms and risk factors for fracture predilection in endodontically treated teeth.” Endodontic Topics. 2006;13(1):57-83.
6. Friedman S, Mor C. The success of endodontic therapy--healing and functionality. J Calif

Dent Assoc. 2004 Jun;32(6):493-503.
7. Farzaneh M, Abitbol S, Friedman S. Treatment outcome in endodontics: the Toronto study. Phases I and II: Orthograde retreatment. J Endod. 2004 Sep;30(9):627-633.
8. Stabholz A, Friedman S. Endodontic retreatment--case selection and technique. Part 2: Treatment planning for retreatment. J Endod. 1988 Dec;14(12):607-14.
9. Nejat AH, Dupree P, Kee E, Xu X, Zakkour W, Odom M, Bruggers K, Mascarenhas F. Effect of Endodontic Access Preparation on Fracture Load of Translucent versus Conventional Zirconia Crowns with Varying Occlusal Thicknesses. J Prosthodont. 2021 Oct;30(8):706-710.
10. Lucas TJ, Lawson NC, Englert B, Goldstein K, Goldstein R. Fracture strength of zirconia and lithium disilicate restorations following endodontic access. J Esthet Restor Dent. 2022 Apr;34(3):534-540.
11. Oguz Eİ, Kılıçarslan MA, Özcan M. Effect of endodontic access simulation on the fracture strength of lithium-disilicate and resin-matrix ceramic CAD-CAM crowns. J Esthet Restor Dent. 2020 Jul;32(5):472-479.
12. Qeblawi D, Hill T, Chlosta K. The effect of endodontic access preparation on the failure load of lithium disilicate glass-ceramic restorations. J Prosthet Dent. 2011 Nov;106(5):328-336.
13. Friedman S, Löst C, Zarrabian M, Trope M. Evaluation of success and failure after endodontic therapy using a glass ionomer cement sealer. J Endod. 1995 Jul;21(7):384-390.
14. Mandel E, Friedman S. Endodontic retreatment: a rational approach to root canal reinstrumentation. J Endod. 1992 Nov;18(11):565-569.
15. Friedman S, Stabholz A, Tamse A. Endodontic retreatment--case selection and technique. 3. Retreatment techniques. J Endod. 1990 Nov;16(11):543-549.
16. Plotino, G. Minimally Invasive Approaches in Endodontic Practice; Springer Nature: Cham, Switzerland, 2021
18 Endodontic Practice US Volume 17 Number 1 ENDODONTIC INSIGHT EP
Figures 3-7: Conservative removal of restoration and cast post using Great White Ultra
How to submit an article to Endodontic Practice US
Endodontic Practice US is a peer-reviewed, quarterly publication containing articles by leading authors from around the world. Endodontic Practice US is designed to be read by specialists in Endodontics, Periodontics, Oral Surgery, and Prosthodontics.
Submitting articles
Endodontic Practice US requires original, unpublished article submissions on endodontic topics, multidisciplinary dentistry, clinical cases, practice management, technology, clinical updates, literature reviews, and continuing education.
Typically, clinical articles and case studies range between 1,500 and 2,400 words. Authors can include up to 15 illustrations. Manuscripts should be double-spaced, and all pages should be numbered. Endodontic Practice US reserves the right to edit articles for clarity and style as well as for the limitations of space available.
Articles are classified as either clinical, continuing education, technology, or research reports. Clinical articles and continuing education articles typically include case presentations, technique reports, or literature reviews on a clinical topic. Research reports state the problem and the objective, describe the materials and methods (so they can be duplicated and their validity judged), report the results accurately and concisely, provide discussion of the findings, and offer conclusions that can be drawn from the research. Under a separate heading, research reports provide a statement of the research’s clinical implications and relevance to endodontics. Continuing education articles also include three to four educational aims and objectives, a short “expected outcomes” paragraph, and a 10-question, multiple-choice quiz with the correct answers indicated. Questions and answers should be in the order of appearance in the text, and verbatim. Product trade names cited in the text must be accompanied by a generic term and include the manufacturer, city, and country in parentheses.
Additional items to include:
• Include full name, academic degrees, and institutional affiliations and locations
• If presented as part of a meeting, please state the name, date, and location of the meeting
• Sources of support in the form of grants, equipment, products, or drugs must be disclosed
• Full contact details for the corresponding author must be included
• Short author bio and author headshot
Pictures/images/tables
Illustrations should be clearly identified, numbered in sequential order, and accompanied by a caption. Digital images must be high resolution, 300 dpi minimum, and at least 90 mm wide. We can accept digital images in all image formats (preferring .tif or jpeg).
Ensure that each table is cited in the text. Number tables consecutively, and provide a brief title and caption (if appropriate) for each.
Disclosure of AI use
Authors must disclose any AI used in researching, writing, or creating their articles. This includes a language model, machine learning, or similar technologies to create or assist with this submission. If AI was used, please provide a description of the AI-generated content and the name, model or tool used, and manufacturer. If AI was used, please confirm that you take responsibility for the integrity of the content that you are submitting.
References
References must appear in the text as numbered superscripts (not footnotes) and should be listed at the end of the article in their order of appearance in the text. The majority of references should be less than 10 years old. Provide inclusive page numbers, volume and issue numbers, date of publication, and all authors’ names. References should be submitted in American Medical Association style. For example:
Journals: (Print)
White LW. Pearls from Dr. Larry White. Int J Orthod Milwaukee. 2016;27(1):7-8. (Online)
Author(s). Article title. Journal Name. Year; vol(issue#):inclusive pages. URL. Accessed [date].
Or in the case of a book: Pedetta F. New Straight Wire. Quintessence Publishing; 2017.
Website:
Author or name of organization if no author is listed. Title or name of the organization if no title is provided. Name of website. URL. Accessed Month Day, Year. Example of Date: Accessed June 12, 2011.
Author’s name: (Single) (Multiple) Doe JF Doe JF, Roe JP
Permissions
Written permission must be obtained by the author for material that has been published in copyrighted material; this includes tables, figures, pictures, and quoted text that exceeds 150 words. Signed release forms are required for photographs of identifiable persons.
Disclosure of financial interest
Authors must disclose any financial interest they (or family members) have in products mentioned in their articles. They must also disclose any developmental or research relationships with companies that manufacture products by signing a “Conflict of Interest Declaration” form after their article is accepted. Any commercial or financial interest will be acknowledged in the article.
Manuscript review and extra issues
All clinical and continuing education manuscripts are peer-reviewed and accepted, accepted with modification, or rejected at the discretion of the editorial review board. Authors are responsible for meeting review board requirements for final approval and publication of manuscripts. If additional issues are desired, they must be ordered from the publisher when the page proofs are reviewed by the authors. The publisher does not stock back issues. Reprints can be purchased after the issue is published.
Proofing
Page proofs will be supplied to authors for corrections and/or final sign off. Changes should be limited to those that are essential for correctness and clarity.
Articles should be submitted to: Mali Schantz-Feld, managing editor, at mali@medmarkmedia.com
19 endopracticeus.com Volume 17 Number 1 AUTHOR GUIDELINES
Sepsis is serious — recognize the signs
Dr. Stuart
L.
Segelnick describes lifesaving warning signs
Acall comes in from an emergency patient soon after you remove a hopelessly infected tooth. Her major concern is having a fever, chills, and feeling downright terrible. She has no difficulty breathing or swallowing, though her mouth still feels swollen. Grace is a middle-aged woman who suffers from diabetes and recently finished chemotherapy for breast cancer. She doesn’t smoke or drink alcohol. Also, she relates getting home too late to pick up the antibiotics that were prescribed. What should she do?
Grace was fortunate to have gone directly to the hospital emergency room and had a CT scan, which didn’t show anything unusual. However, sepsis was suspected, and IV antibiotics were administered. Feeling much better after a night of observation, Grace went home the very next day with a prescription for oral antibiotics.
Untreated or poorly managed periodontal disease, caries, and endodontic and dental alveolar lesions can lead to sepsis. Case reports have been published in dental literature highlighting the morbidity and mortality of dental disease complications. Although rarely reported, post tooth extractions have also been linked to sepsis.1 According to the Centers for Disease Control and Prevention (CDC)2 and the Mayo Clinic,3 bacterial infections are the leading cause of sepsis (viral and fungal infections have also been implicated). When these microbes overwhelm your immune system, your body fights back, causing overt damage to your organs, which may progress to septic shock with the accompanying free fall in blood pressure, organ dysfunction, and ultimate death.
The World Health Organization (WHO) realizes the severity of sepsis and reported that in 2017, sepsis accounted for 20% of all deaths globally. In America, the CDC reports that almost 2 million adults develop sepsis, and 350,000 “die during their hospitalization or are discharged to hospice.” A third of the peo-

Stuart L. Segelnick, DDS, MS, currently serves as editor of the Second District Dental Society of New York Bulletin, the Northeastern Society of Periodontists Bulletin, and is Associate Editor of the New York State Dental Journal. He is a Diplomate of the American Board of Periodontology and International Congress of Oral Implantologists and President-Elect of the Northeastern Society of Periodontists. Dr. Segelnick is an adjunct clinical professor at NYU College of Dentistry Department of Periodontology and Implant Dentistry. He is a Certified Dental Editor (CDE), designated by the American Association of Dental Editors & Journalists, and serves as the association’s liaison to the American College of Dentists. Dr. Segelnick has been recognized multiple times by the International College of Dentists and the American Dental Education Association Gies Foundation for his newsletter production and editorials. He has co-edited five books on dentistry and authored/co-authored multiple scientific articles. He is a fellow of the Pierre Fauchard Academy, the International College of Dentists, and the American College of Dentists. Dr. Segelnick has a private periodontal practice in Brooklyn, New York.

ple who died at the hospital had sepsis during their stay. Even more frightening is that “among adult sepsis survivors, one in three died within a year, and one in six experienced significant, long-term morbidity.”4
Higher risks of acquiring sepsis are found in older people (over 65 years) and children who are under a year old, as well as those inflicted with chronic medical problems, immunocompromised individuals, sepsis survivors, and people recently hospitalized and with severe sickness. Some of the signs and symptoms of sepsis include fever, chills, shivering, sweating, severe pain, fast heart rate, fatigue, hypotension, confusion, and altered mental state.
Tests that your patient’s physician or the hospital will perform if they are suspected of having sepsis include a physical exam, blood cultures, full blood work-up, X-rays, CT scans, and ultrasounds to aid in making a sepsis diagnosis.5 High temperature, elevated heart and respiratory rate, and high white blood cell counts are red flags for sepsis.
Sepsis is considered a medical emergency, and the most important thing you can do is recognize and treat it quickly. Treatment usually includes broad spectrum IV antibiotics, IV fluids, and vasopressors. Monitoring serial lactate measurements is also important. Hospitals must report cases of sepsis to the federal and state government.
According to Mannan, et al., “Early antimicrobial intervention is associated with surviving severe sepsis, making it critical for dentists to understand local factors leading to the crisis and the signs and symptoms of the sepsis-septic shock continuum.”6 In a paper by Sato, et al., the authors stated that “When an oral infection is suspected in an elderly patient, antibiotics should be quickly administered, the patient’s local and systemic state should be confirmed. ... If no improvement is observed, medical attention should be quickly sought.”7
Organizations such as END SEPSIS, the Legacy of Rory Staunton (endsepsis.org) and the Sepsis Alliance (sepsis.org) have accomplished amazing work in bringing awareness to the seriousness of
20 Endodontic Practice US Volume 17 Number 1 ENDODONTIC CONCEPTS
sepsis. END SEPSIS has been very successful in advocating for guidelines, regulations, and increasing awareness of sepsis.8 A recent New York Times article by Emily Baumgaertner9 tells how the CDC has developed new guidelines in helping recognize and reduce sepsis in hospitals. The article also highlights that, “In 2013, New York became the first state to mandate that all hospitals adopt sepsis protocols, known as “Rory’s regulations.” Rory Staunton was only 12 years old when he died from undiagnosed sepsis, and his parents started a foundation and the END SEPSIS organization. With these wonderful organizations helping to eradicate sepsis, the future looks promising, so much so that even AIs are now being used to detect sepsis!10

1:
A month after my own gall bladder removal surgery, I had already returned to my office on a lighter schedule when I started feeling very fatigued and had pain in my right back flank. After 3 days of decline and pushing myself through the day, I noticed that my hands had started shaking at the end of a patient examination. At that point, I knew I couldn’t continue and had my receptionist cancel the rest of my appointments.
IV antibiotics
Almost falling asleep at the wheel, I barely managed to drive home. Once home, I made my way to bed and fell right to sleep. At 1 a.m., I awoke bathed in sweat, simultaneously yet uncontrollably shivering and feeling downright awful. I knew something was dangerously wrong. I woke up my wife, and we headed to the hospital ER, where they immediately took my vitals. My blood pressure was extremely low, my heart rate was racing out of control, and my temperature was burning up at 103.3 F. The diagnosis was sepsis! After a CT scan of the abdomen and blood work, I was placed on IV antibiotics. I won’t go into the horrible details of 8 miserable days in the hospital and 4 weeks of IV antibiotics, which were delivered through a picc line (Figure 1) inserted into my arm. I thank G-d every day that I’m alive and able to go back to caring for my family, friends, staff, colleagues,
and patients and cherishing every moment I’m still in this beautiful world.
It makes me wonder if I, as a healthcare professional, couldn’t make a timely diagnosis of my own sepsis setting in, how could the average person? Sepsis is a major life-threatening event that dentists must be aware of. Be prepared to advise your patients when sepsis is suspected to head to the hospital ER, because that timely response just might save their lives.
REFERENCES
1. Lee JJ, Hahn LJ, Kao TP, Liu CH, Cheng SJ, Cheng SL, Chang HH, Jeng JH, Kok SH. Post-tooth extraction sepsis without locoregional infection--a population-based study in Taiwan. Oral Dis. 2009 Nov;15(8):602-607.
2. Centers for Disease Control. What is Sepsis? https://www cdc.gov/sepsis/what-is-sepsis.html. Updated August 24, 2023, Accessed February 28, 2024.
3. Mayo Clinic. Sepsis. https://www.mayoclinic.org/diseasesconditions/sepsis/symptoms-causes/syc-20351214 Published February 20, 2023, Accessed February 28, 2024.
4. World Health Organization. Global Report on the Epidemiology and Burden of Sepsis. https://iris.who.int/bitstream/ handle/10665/334216/9789240010789-eng.pdf?sequence=1. Accessed February 28, 2024.
5. WebMD. Sepsis (Blood Infection): Symptoms and Treatment. https://www.webmd. com/a-to-z-guides/sepsis-septicemia-blood-infection. Reviewed February 1, 2024.
6. Mannan S, Tordik PA, Martinho FC, Chivian N, Hirschberg CS. Dental Abscess to Septic Shock: A Case Report and Literature Review. J Endod. 2021 Apr;47(4):663-670.
7. Sato H, Tamanoi T, Suzuki T, Moriyama H, Abe S, Yoshida K, Kawaai H, Yamazaki S. Risk Perception of Septic Shock with Multiple Organ Failure Due to Acute Exacerbation of an Infectious Dental Disease. Ther Clin Risk Manag. 2021 Apr 22;17:365-369.
8. End Sepsis. About End Sepsis. https://www. endsepsis.org/about/. Accessed February 28, 2024.
9. Baumgaertner E. C.D.C. Sets New Standards for Hospitals to Combat Sepsis. https:// www.nytimes. com/2023/08/24/health/sepsis-hospitals-cdc.html. Updated September 22, 2023.
10. Moor M, Bennett N, Plečko D, Horn M, Rieck B, Meinshausen N, Bühlmann P, Borgwardt K. Predicting sepsis using deep learning across international sites: a retrospective development and validation study. eClinicalMedicine Part of The Lancet. August 2023;62(102124) https://www.thelancet.com/journals/eclinm/article/ PIIS2589-5370(23)00301-2/fulltext. Accessed February 28, 2024.
This article was reprinted with permission from the Second District Dental Society of New York (SDDSNY) Bulletin.


21 endopracticeus.com Volume 17 Number 1 ENDODONTIC CONCEPTS
EP
3 REASONS TO SUBSCRIBE
16 CE credits available per year
1 subscription, 2 formats – print and digital
4 high-quality, clinically focused issues per year 3 SIMPLE WAYS TO SUBSCRIBE
Visit www.endopracticeus.com
Email subscriptions@medmarkmedia.com
Call 1-866-579-9496 Endodontic Practice US 1 year $149 / 1 year digital only $79 Winter2023 Vol16 No4 endopracticeus.com Implants&Endon 4CECreditsAvailableinThisIssue * Unleashingthe powerofteamdrivenendodontics Dr.SoniaChopra Thelateralpuffinendodontics Drs.MahmoodRezaKalantar Motamedi&BrettE.Gilbert Brokenfileretrievalin theageofminimally invasiveendodontics Drs.L.StephenBuchanan &ChristopheVerbanck Managementofpre-and postoperativedentaland surgicalpainduringthe opioidcrisis Drs.DianaBronstein&RitaSteiner
Figure
PICC line removed after 4 weeks, which went from the inner arm through the brachial vein towards the heart for delivery of
•
•
•
•
•
•
BIO-C ® Sealer ION+ By Angelus
BIO-C® Sealer ION+ comes in a syringe with intracanal tips for direct insertion into the root canal. In addition, it presents an innovative formula with modified calcium silicate with more ion release that will stimulate the production of hydroxyapatite, enhancing bone regeneration.
4 reasons to choose BIO-C® Sealer ION+
1. Resin-free and eugenol-free material
BIO-C® Sealer ION+ is resin-free and does not cause post-op symptoms. Being eugenol-free, it also does not interact negatively with cements and bonding agents.
2. Excellent flow

of a hermetic and three-dimensional filling.
3. Possible to use with cold or warm gutta percha
Root canal filling techniques that use the heated gutta percha reach a temperature of 392°F.

BIO-C® Sealer ION+ remains stable at this temperature unlike other sealers that degrade at temperatures close to 291°F.
4. Low solubility




SPECIAL SECTION AAE SPECIAL SECTION
Image courtesy of Warley Tavares, DDS, MSc, PhD
Brasseler — a leader in Anatomically Centered Endodontics (ACE)
For two decades, Brasseler has been spearheading advancements in root canal procedures with leading products in obturation, shaping, and disinfection. Now, Brasseler is simplifying the endodontic workflow for all clinicians by focusing on Anatomically Centered Endodontics. The “ACE” philosophy combines three leading, patented products: the XP-3D™ Shaper, Triton® Irrigation Solution, and BC Sealer™
BC Sealer simplified obturation, allowing doctors to embrace a single cone technique without the need for complicated heated condensation.
The XP Endo Shaper is the ultimate adaptive and minimally invasive shaping instrument. Adaptive core technology allows the instrument to move freely and adapt to the canal’s natural shape, reducing potential for damage to the tooth. Not only
is XP excellent at shaping, it also functions as an agitator for enhanced irrigation and debridement.
Triton All-in-One Irrigation Solution simultaneously disinfects while also debriding. No other irrigation solution can tackle tissue dissolution, smear layer removal, and disinfection in one step.
The ACE workflow combines the use of the XP-3D Shaper with Triton allowing for simultaneous shaping and disinfection. The canals are then obturated with BC Sealer and a matching single cone, making endodontics accessible to all clinicians by utilizing affordable, easy-to-use products in a simple, streamlined workflow.
To learn more about Brasseler’s leading patented products and the ACE philosophy, visit us at https://brasselerusadental. com/ace/.
EndoSequence BC Sealer
Simplified obturation allowing doctors to embrace a single cone technique without the need for complicated heated condensation.
XP-3D Shaper
Adaptive core technology allows the instrument to move freely and adapt to the canal’s natural shape, reducing potential for damage to the tooth.
Triton All-In-One Irrigation Solution
No other irrigation solution can tackle tissue dissolution, smear layer removal and disinfection in one step.




AAE SPECIAL SECTION
23 endopracticeus.com Volume 17 Number 1 SPECIAL SECTION
Visit Brasseler USA at AAE Booth No. 319
EP-04.24 ©2024 Brasseler USA. All rights reserved. Visit our website at BrasselerUSADental.com To order call 800.841.4522 or fax 888.610.1937 simplifying the endodontic workflow for all clinicians SCAN QR CODE TO LEARN MORE ABOUT THE ACE WORKFLOW or visit BrasselerUSADental.com/ACE
Unlock the future of your dental practice
Are you considering selling your practice in the next 12 months?
You could seamlessly transition your practice to a 100% endodontist-owned platform dedicated to preserving your legacy. We do not answer to any corporate interests. Our owner-centric model allows you to retain equity or choose a full cash transaction with no restrictive contracts or crawl-back clauses. With more than 20 years of experience, 50 clinicians, and over 1 million procedures completed by our network of endodontists, we are your perfect partner.
To explore possibilities and make your practice transition a triumph, connect with us at our booth No. 308.
For aspiring endodontists
Join us as an associate for the most competitive compensation, mentoring, and training to elevate your clinical skills. Shape a successful career with us, and secure the future you deserve. Connect with us at our booth No. 308.



“After looking at many options Cornerstone was the best. No regrets”
-DR. E. APAYDIN, DDS

“I was looking for a buyer who would respect my legacy, Cornerstone has exceeded my expectations”
-DR. P. GARRETT, DDS

“I love performing Endodontics, it is so nice now to only focus on my patients and not anything to do with operating the practice”
-DR. J. LIES, DDS

“After decades of running my practice, I needed a buyer I could trust to support my team. Cornerstone has been a wonderful partner, and my staff is so excited about the next chapter”
-DR. J. AIVAZ, DDS
24 Endodontic Practice US Volume 17 Number 1 SPECIAL SECTION AAE SPECIAL SECTION
Visit Cornerstone Dental Specialties at AAE Booth No. 308
Your Practice...Our Platform™ CDSDENTAL.COM
Endo Mastery
Seminars and practice coaching for incredible endodontic success!
Endo Mastery transforms your practice into a highly productive and profitable environment that is stress-free, effortless, and fun. Teamwork, scheduling, clinical efficiency, marketing, growth, profitability, and great lifestyle — these are topics we love and excel at with our clients!
Our coaching programs are tailored to your vision and goals, and we support you at every stage of practice ownership from startup to mid-career growth to maximizing practice value and owner equity.
our popular 2-day doctor and team seminar, “Mastering the Effortless Endodontic Practice” in Nashville this September!

Come to our booth to get our AAE show special of the lowest seminar tuition we offer. Save 50% on seminars, including
We are also excited to sponsor the AAE Career Fair to help residents and new endodontists get started. Visit our Career Fair table to access free careerstart resources, discover associate opportunities, or to find out about our coaching program for your startup or buy-in.
Visit our booth No. 437 to meet our team and network with other practice owners who have achieved incredible growth and success with Endo Mastery practice coaching.

Elevate teamwork, reduce stress, improve lifestyle, have fun and achieve incredible profitability.
Visit our AAE booth #437 1-800-482-7563 | www.endomastery.com
SPECIAL SECTION
25 endopracticeus.com Volume 17 Number 1 SPECIAL SECTION
AAE
Transform your practice, Transform your life! DR. ACE GOERIG DDS, MS, ABE
owners!
Visit Endo Mastery at AAE Booth No. 437
Endo’s top coach for practice
Discover our proven strategies for effortless practice management and endodontic success.
TEAM SEMINARS • PRACTICE COACHING • FINANCIAL FREEDOM
Endodontic Practice Partners (EPP) — dynamic and focused
Endodontic Practice Partners (EPP) is a dynamic business exclusively focused on affiliating with premiere endodontic practices. EPP provides expertise and resources to help practices focus on their clinical core responsibilities — delivering high-quality, patient-centered care. We assist in streamlining operations, enhancing growth opportunities, and optimizing efficiencies to reach personal and professional goals. The challenge for most busy practices is the lack of time, resources, and personnel to execute a business strategy. We strategically grow within a state to enhance negotiating power with reimbursement rates, supplies,

equipment, and more. Strength in numbers is the advantage of being a partner with EPP. We are seeking practices that want to be best in class, progressive, and have the advantage of being a part of a larger entity. Whether you are a solo or group practice, now is the time to consider an affiliation. Together, we lead the way.
Endodontic Practice Partners is a proud supporter of the AAE Annual Conference. Visit us at Booth No. 529 to learn what a partnership would look like for you. And be sure to stop by booth No. 829 to get an updated professional headshot at our sponsored headshot booth!
YOUR MOUNTAIN IS WAITING …SO
26 Endodontic Practice US Volume 17 Number 1 SPECIAL SECTION AAE SPECIAL SECTION
Visit Endodontic Practice Partners at AAE Booth No. 829
YOUR
GET ON
WAY. – Dr. Seuss
Kerr Dental
Kerr Dental, a renowned name in dental care, offers a range of Endodontic, Restorative, Rotary, and TotalCare products. Kerr has introduced several innovations in endodontics, including the minimally invasive ZenFlex™ NiTi Rotary Shaping File, elements™ IC obturation unit, and the new cordless motor elements™ Connect. Kerr also put the “K” in K-File, defining a new category of endo products found in most doctors’ practices.

We collaborate closely with our industry’s key opinion leaders to make sure we’re responding to the needs of doctors, practices, and their patients. “Kerr truly listens to the feedback from dentists and incorporates our input into their design. This results in products that are intuitive to use, drive workflow efficiencies, adapt to the doctor’s preferred techniques, and support improved patient outcomes with excep-
tional results,” says Dr. Matthew Miller, a member of Kerr’s Endodontic and Restorative Advisory Board.
Kerr Endodontics offers a comprehensive solution for endodontic procedures to address the needs of your practice. Stop by the Kerr Dental Booth No. 519, and see how we can help you save on your everyday products.

27 endopracticeus.com Volume 17 Number 1 SPECIAL SECTION
AAE SPECIAL SECTION
Visit Kerr Dental at AAE Booth No. 519
Luman Dental: Specialists in CBCT Technology
Family-owned and operated Luman Dental, LLC, has been assisting dental professionals in acquiring and utilizing CBCT imaging equipment since 2014. Founder Jeremy Luman has assisted endodontic practices with their implementation of CBCT imaging for the past decade. Thanks to his history of assisting in an endodontic practice, he has mastered all aspects of the practice, including chairside procedures, frontoffice billing and insurance, supply logistics, and marketing. Company COO Matt Sakaluk has 13 years of experience in dental imaging technologies. Together, they strive to meet the specific requirements of their specialty clients.

Around-the-clock customer service ensures that each practice gets the appropriate equipment and training to meet its
unique needs. The company also offers small equipment sales with service plans for both lasers and CBCT machines. And, for those who want a change, Luman has a CBCT trade-in/buyback program. The company is a prominent nationwide dealer of CBCT imaging equipment, including trusted brands, JMorita, Prexion, and HDX Will.
Because of its excellence in installation, training, and ongoing technical support, Luman Dental has become a trusted partner for dental practices who want to enhance their capabilities. Whether it's helping practitioners select the right CBCT equipment, ensuring seamless installation, or providing comprehensive training and support, Luman Dental is dedicated to helping dental professionals obtain technologies that lead to superior patient care.


Luman Dental is a leader in 3D imaging.
As one of the few full-service dealers in the country for Morita, PreXion, and HDX WILL, we will be with you for the life of your machine. We also have a CBCT trade-in/buyback program.
From choosing the right option to installation, training, and ongoing support, we have you and your dental practice covered. And if your practice is looking forward to a relocation, we can even move your imaging system for you. All of our solutions are 100% certified new and preowned from the manufacturer. And our clients love us! Check out our CBCT



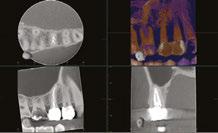


28 Endodontic Practice US Volume 17 Number 1 SPECIAL SECTION AAE SPECIAL SECTION
Visit Luman Dental at AAE booth No. 128 Your Go-To Specialists in CBCT Technology! Experience the Luman Dental Difference • lumandental.com • (480) 331-2284
trade-in/buyback program!
Odne — transforming endo
Visit our booth No. 747 to meet the Odne Team and get a first view and hands-on of our innovative Root Preservation Therapy (RPT) technology platform. Provide us with your feedback and discuss with us how Odne can become a practice builder for you.
Odne™Clean, saline cavitation — minimally invasive endodontic debridement
A cleaning tip as thin as 190µm creates a hydrodynamic cavitation cloud inside the root canal, using saline solution. The cavitation jet removes debris inside the canals and tubules. Depending on the clinical protocol, various cycles of Odne™Clean (30-60 sec.) are applied. Final disinfection is reached with a NaOCl rinse.
Odne™Fill, light-cured obturation — all-in-one endodontic filling material
This is the first FDA-cleared light-curing, injectable, singlecomponent endodontic material for root canal obturation.

Odne™Fill is a highly stable hydrogel. It forms a very tight interface with the hydrophilic dentin. Due to its water-like viscosity and the ultra-high hydrophilicity in its uncured state, it can reach the smallest endodontic structures.
Odne™Cure, high-precision laser curing — thinnest dental light-curing device
Odne™Cure is the micro-laser curing light to cure Odne™Fill directly in the root canal — equipped with the thinnest light conductor currently used in dental (220µm).
Odne’s Root Preservation Therapy (RPT) supports patientfriendly and economic treatment, minimizing postoperative pain, reducing chair time, and delivering long-standing restorations. Odne’s solutions offer excellent price value and affordability, enabling the endo leader to standardize the treatment workflow within its referral base. Referred retreatments will become easier, as the initial treatment preserves tooth structure. Removal of an obturation becomes less complex. Transforming the practice network to RPT with Odne enables successful practice building.

World Premiere. After 6 years of R&D we exhibit our innovations for debridement and obturation to the endo community, for the first time. We are welcoming you for an in-depth demo and look forward to your feed-back.
Participate in our Priority Access Program and become a Priority Access Program Associate (P.A.P.A.). Limited spaces available.

SPECIAL SECTION
29 endopracticeus.com Volume 17 Number 1 SPECIAL SECTION AAE
Visit Odne at AAE Booth No. 747
Become a P.A.P.A www.odne.co M-EA-0007-V1.0-ADV-EN-2403
The GentleWave ® G4 System
Beyond irrigation. Beyond clean.
The GentleWave System takes you beyond canal complexity that can hinder thorough disinfection and debridement.
Inside the console, the irrigant is thoroughly degassed, precisely diluted, and continuously refreshed. Next, it enters the sealed, closed-loop delivery system, where the system’s physicsaccelerated chemistry becomes truly remarkable.
The GentleWave procedure is a more effective way of cleaning teeth, including hard-to-reach areas such as the apical thirds and complex anatomies of the root canal system:
• Predictably removes up to 99.9% of biofilm
• Effectively disinfects and debrides undetected and intri cate anatomies2,3
• 4X - 8.5X greater penetration into dentinal tubules v sus ultrasonic systems4
This can lead to better patient outcomes and deliver a more comfortable patient experience with reduced risk of complications:
• 96.6% of patients report mild to no pain within 48 hours5 of the procedure
• 97.7% 12-month healing rate6

• Preserves the structural integrity of the tooth
Test-drive a GentleWave G4 system at AAE Booth No. 701
SSA-Half-Page-Ad-v4-Outlines.pdf 1 2/3/2023 1:10:37 PM

SPECIAL SECTION AAE SPECIAL SECTION
1. Zhang D, Shen Y, de la Fuente-Núñez C, Haapasalo M. In vitro evaluation by quantitative real-time PCR and culturing of the effectiveness of disinfection of multispecies biofilms in root canals by two irrigation systems.
C M Y CM MY CY CMY K
Specialized Dental Partners
Champion of Specialists
As today’s dental specialists look to the future of their practices and careers, more are exploring the trend of practice partnerships — weighing the notion of a vibrant culture and community against a lucrative financial opportunity. At Specialized Dental Partners, we know the two go hand-in-hand.
Since 2018, Specialized Dental Partners has championed endodontists — building a community of over 300 premiere specialists that share our core values and are moved by our mission. Our culture is about growth in every aspect of our lives — from improving our communication skills to leadership training, to advanced clinical training courses, and beyond.
“Specialized Dental Partners offers the chance to become not only a better endodontist, but also a better boss, a better spouse, and a better friend. What we are building is unique; I’m truly thrilled to get to be a part of it,” ~ Dr. Jeremy Young, Director of
Partner Engagement.
You deserve a champion to support you in designing a future that surpasses expectations. We would love to join you on that journey.
We are proud to again be a Diamond Sponsor at AAE24. Come meet us at Booth No. 901 and enjoy:
• An expansive lounge space to relax and chat with our doctors about life as a partner
• A barista-manned coffee bar featuring made-to-order drinks and other treats
• Multiple charging stations to keep your tech gadgets performance-ready
• Live recordings of season three of our successful podcast, Specialized, (previously The Endo Files), and get a chance to tell your story on a future episode!

AAE SPECIAL SECTION
31 endopracticeus.com Volume 17 Number 1 SPECIAL SECTION
Visit Specialized Dental Partners at AAE Booth No. 901
Continuing our focus on serving specialists
Better Care. Better Business. Better Oral Health.
Specialty1 Partners remains the market-leading solution to meet the specific practice management needs of dental surgical specialists. Specialty1 Partners, the first dental surgical specialty organization founded by endodontists, has consistently achieved impressive growth, now providing support to over 225 locations across 28 states. This remarkable achievement is a testament to our continuous commitment to excellence, innovation, and collaborative efforts.
“As working endodontists juggling the complexities of treating patients and running successful practices, we saw first-hand the need for a truly doctor-focused partnership for dental specialists,” said Matthew Haddad, founder and co-CEO of Specialty1 Partners. “There are a lot of competitors that claim to be
doctor-led and doctor-founded, but that simply isn’t the case, and it’s misleading to potential partners. Our vision, culture, and leadership all start with dental specialists. This has allowed us to significantly outperform others in the dental surgical specialty space.”
“Our focus every day is supporting our partners while continuing to build partnerships with industry-leading, innovative surgical specialists,” said Daryl Dudum, founder and co-CEO of Specialty1 Partners. “It’s not just about growing our network — it’s about helping partner practices grow organically and succeed on their terms.”
Reach out to discuss what Specialty1 Partners can do for you and your practice: www.Specialty1Partners.com.
32 Endodontic Practice US Volume 17 Number 1 SPECIAL SECTION AAE SPECIAL SECTION
Visit Specialty1 Partners at AAE Booth No. 819 BETTER CARE. BETTER BUSINESS. BETTER ORAL HEALTH. VISIT US AT AAE BOOTH 819 www.specialty1partners.com 800 - 605 - 3437
SS White — landmark accomplishments
Albert Einstein once said, “Only one who devotes himself to a cause with his whole strength and soul can be a true master.” A tireless inventor, Samuel Stockton White, the founder of SS White Dental, meets these qualifications perfectly. A young dentist who started a business out of an attic in downtown Philadelphia making porcelain teeth, Mr. White never could have imagined his little “tooth factory” would grow to become one of the largest dental instrument manufacturers in the world.
From inventing the carbide bur to introducing the first single-use, sterile diamonds, here we highlight some of SS White’s landmark accomplishments in endodontics that have revolutionized minimally invasive dentistry. From the first — ORIGINAL minimally invasive endodontic file on the market, DCTaper®, in 2012 (formerly V-Taper) to the next generation NiTi file for those wanting to transition to a strong, yet flexible, MI file system, EXACTTaperH DC™ file system was designed with multiple tapers that cut dentin in specific canal zones,
while utilizing a 0.8 mm maximum flute diameter for the highest level of pericervical dentin conservation to reduce the chance of over-preparation. MantaTM, a portable and compact precision handpiece motor, uses precision processing technology to minimize vibration and offers 8 hours of battery life on a fast, 2.5-hour charge. Its mini contra-angle head enhances visibility during root canals, while five programmable settings for speed and torque can be adjusted to meet clinicians’ needs and preferences.
Visit endo.sswhitedental.com.
$3,000 or more in SS White products and get that feeling when you receive your FREE Ray-Ban® Meta SM Smart Glasses.*
more and schedule a consultation with an SS White representative: sswhitedental.com/aae


33 endopracticeus.com Volume 17 Number 1 SPECIAL SECTION AAE SPECIAL SECTION
Visit SS White at AAE
648 TFW you get FREE tech at AAE Visit SS White®
Exclusive
Promotions Purchase
With livestream & AI technology!
*To qualify for in-booth promotions, orders must be taken at trade show booth with an SS White representative. All offers are limited to stock on hand and are not valid on prior purchases. Meta Ray-Ban Smart Glasses will be shipped to invoice address. Please allow 4-6 weeks for delivery. Offers may not be combined with any other sale, promotion, discount, code, coupon and/or offer. Sales promotion choice must be indicated on invoice sent to SS White on applicable order. © 2024 SS White. All rights reserved. SS WHITE is a registered trademark of SS White Dental. Ray-Ban is a registered trademark of Luxottica Group SPA. Meta is a registered service mark of Meta Platforms, Inc.
Booth No.
Booth #648 for
AAE24
Learn
Clinical implementation and future of AI in endodontic dentistry
Drs. Aaron Glick, David Jaramillo, Nisha Manila, and Jennifer Chang discuss the pros and cons of AI in endodontic and general dental practice
Introduction
Although artificial intelligence (AI) has been integrated in daily life, most are not aware that it has become an integral part of many aspects of modern life over the past decades given the increased computing power, digitization of data, advances in

Aaron Glick, DDS, works in healthcare innovation and is on faculty at the University of Texas Health Science Center at Houston School of Dentistry and Sam Houston State University College of Osteopathic Medicine. He is a Diplomate of the ABDSM, faculty member of the AADSM Mastery Program, and holds fellowship credentials with Academy of General Dentistry and International Congress of Oral Implantology. He enjoys all technologies and has a background in software programming for neuroscience research at Brandeis University and Harvard University using 3D modeling, AI, and fMRI technologies. Dr. Glick has been published in medical and dental journals and lectures nationally on dental sleep medicine and digital/software technologies.

David Jaramillo, DDS, is a tenured professor at the Department of Endodontics at UTHealth School of Dentistry. He has taught non-stop since 1990 at the University of Southern California and Loma Linda University in California as a clinic director of endodontics and course director of endodontics in the International Dentist Program. Dr. Jaramillo’s main research focus is in the irrigation of the root canal system. He has dictated more than 100 conferences worldwide, published over 22 peer-reviewed papers, written seven book chapters, and is a member of the International College of Dentists, AAE, and IFEA.

Nisha Manila BDS, PhD, is an Associate Professor and Director of Oral and Maxillofacial Radiology at California Northstate University College of Dental Medicine. With a dental degree from India, and a Ph.D. in Oral Radiation Oncology from Tokyo Medical and Dental University, Japan, she completed Oral and Maxillofacial Radiology training at Texas A&M University. Dr. Manila is a fellow of the American College of Dentists, and her research interests include applications of AI in dentistry, CBCT imaging, and advanced diagnostic imaging modalities. Dr. Manila is an active member of several professional organizations.

Jennifer Chang DDS, MSD, is an assistant professor and program director in the Department of Periodontics at The University of Texas School of Dentistry at Houston. She completed her Doctor of Dental Surgery degree and 2 years of general practice residency in Taiwan. She obtained her Master of Science in Dentistry degree in periodontics from Indiana University School of Dentistry. Dr. Chang is a board-certified Diplomate in Periodontology and Dental Implant Surgery. She maintains a part-time practice at the school’s faculty group practice and in the greater Houston area. Her clinical and research interests focus on improving treatment options for periodontal/peri-implant disease.
Educational aims and objectives
This self-instructional course for dentists aims to identify how artificial intelligence (AI) works, as well as its advantages and disadvantages in the endodontic and general dental practice.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions by taking the quiz online at endopracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
• Define AI and the evolving types of AI.
• Identify the basics of how the data is used in a clinical way by interacting with AI-enabled systems and machines.
• Recognize how AI systems are being used to improve aspects of the implant process.
• Realize some of the issues that need to be addressed to ensure patient safety, clinical success, and to safeguard the practice from legal complications. 2 CE CREDITS
algorithm, and improvements in accuracy. In fact, when a group of Americans were surveyed, over half were not able to identify that AI was powering wearable fitness trackers, automated chatbots, product recommendations, security cameras that identify unrecognized people, music playlist recommendations, and email services identifying spam messages.1 In dentistry, some of these same AI systems, such as chatbots, have been integrated for general office support and software automations. Other AI systems that are more dental-specific have also been used for approximately a decade. These include systems that automatically identify dental landmarks in CBCT,2 maxillary/mandibular segmentation from radiographic images,3 and digital reconstruction of tooth surfaces.4
Some examples of more current AI systems in dentistry are decision-support systems to aid clinicians in the diagnosis of caries and periodontal conditions, AI-enabled robotic surgeries, and creation of AI-generated dental restorations/appliances.5 Since AI is a tool, it can be used in multiple applications within the dental field; as the algorithms advance in accessibility and accuracy, the amount of products with embedded AI will likely increase (Table 1). Therefore, it is important as a dental practitioner to understand the tools used, particularly if they can have a direct or indirect effect on patients.
34 Endodontic Practice US Volume 17 Number 1 CONTINUING EDUCATION
How AI works
AI is a broad term that generally refers to the ability for computers to perform tasks that typically require human intelligence (Figure 1); for example, viewing a dental X-ray and identifying interproximal caries. Machine learning (ML) refers to the mathematical approach to accomplish this perceived human intelligence. These algorithms are programmed to take information and “learn” from these datasets. Since there are alternative methods for artificial intelligence, machine learning is considered a subset of the approaches to achieve artificial intelligence. Multiple types of algorithms can be programmed by the user. In one approach, a convolutional neural network (CNN) can feed a large dataset to identify the features that are most salient in a classification task. For instance, with multiple pictures of apples or cats, the neural network would be a mathematical model used to make the binary decision on if the currently presented image should be classified as an apple or cat. The CNN approach is typically selected for image operations since this algorithm is optimized to process images based on the extraction of spatial features.
Depending on the task to be performed, there are multiple types of models that are specific to optimizing for the type of data or output intended. For instance, chatbots require a text-based approach with grammatical rules built into sequences of words. Therefore, language-specific models would be used for textbased tasks, typically called natural language processing (NLP).
Further into the black box
While most dentists today don’t consider building custom AI products, there are products that will democratize the use of AI through no-coding technologies.6 Whether coding the algorithms or not, understanding the basics of how the data is used to derive a clinical decision/outcome is important since dentists are increasingly interacting with AI-enabled systems and machines. When software manufacturers train an AI model, they require a large amount of data to process. In general, the full dataset is split into 3 distinct groups: 1) training set, 2) validation set, and 3) testing set (Figure 1). In a supervised model, a team of clinicians will label the full dataset. For instance, if the classification task is to automatically identify caries in bitewing radiographs, the clinician would identify areas of the radiographs with caries. These labeled radiographs serve as the “ground truth” for the algorithm. The bulk of the data is used in the training set to optimize the weights of the neural network identifying salient features of the categorized dataset. The model is then further optimized by using a validation dataset, where additional processes can improve the accuracy. The final step is to understand how accurate the fully trained AI model can perform on the similar dataset. Therefore, the testing dataset is then categorized by the trained model to provide an accuracy typically reported as a percentage of accurately categorized responses and Receiver Operating Characteristics (ROC) curve/area under the curve (AUC). The ROC curve and AUC offers additional details similar to the true positive rate and false positive rate. Ultimately, the large dataset is trained, and the same isolated dataset is used to assess the accuracy in a non-clinical setting.
Table 1: Multifaceted uses of AI in dentistry
Dental specialtyUse case
Endodontics
Implant dentistry
Oral surgery
Orthodontics and pediatric dentistry
Pathology
Periodontics
Prosthodontics and restorative dentistry
Radiology
Non-clinical
• Identify root morphology, minor apical foramen
• Diagnosis of apical lesion, root fracture
• Risk of peri-implant diseases
• Surgical procedures
• Identification of anatomic features
• Screening and classification of oral cancer
• Cephalometric analysis
• Treatment needs and outcome evaluation
• Vertebral growth assessment
• Analyze histologic slides and cytologic specimens
• Clinical and radiographic assessment
• Immunologic and microbiologic analysis
• Caries detection
• Shade selection, tooth preparation, restoration design
• Radiographic mounting
• Caries detection, oral cancer diagnosis
• Patient education and engagement
• Dental research
• Practice management (i.e., HR and insurance automations, financial projections, scheduling chatbots)
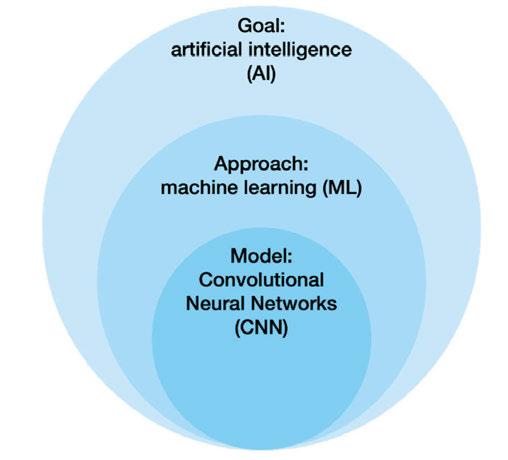
When building these algorithms, there are some additional key considerations as to how the algorithm uses data. In an oversimplification, an algorithm can be delineated as 1) supervised/
35 endopracticeus.com Volume 17 Number 1 CONTINUING EDUCATION
Figure 1: Visualization of the distinction between terminology for artificial intelligence (AI), machine learning (ML), and Convolutional Neural Networks (CNN)
unsupervised or 2) static/continuous learning. Supervised learning is based on a clinician providing the algorithm with a ground truth for labelled data, similar to the previous example. Unsupervised learning is where the model learns without explicitly provided information to classify and can be accomplished through patterns within the data. Static learning algorithms are the traditional type of AI; however, some current algorithms are designed to update and improve themselves based on additional data acquired during use.
AI in endodontics
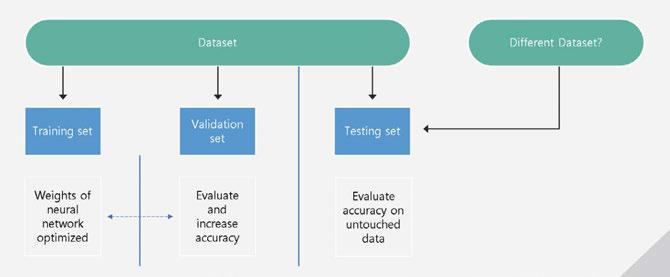
AI is changing our daily lives and approaches to dentistry in general. In endodontics, AI is being used for the following:
1. Radiographic detection of periapical lesions and root fractures
2. Treatment assistance for determining working length and root morphology
3. Treatment outcome predictions for retreatment and stem cell therapies
Innovations in radiographic identification of endodontic specific features focus mainly on periapical and root fractures.5 Multiple types of radiographs have been used as inputs for machine learning systems, such as periapical, panoramic, and cone-beam computed tomographic (CBCT). Accuracies of periapical lesion identification have been shown to have classification accuracies up to 97%, 84%, and 96% using periapical, panoramic, and CBCT radiographs respectively with generally higher average accuracy with CBCT in published literature.7,8 Similarly, vertical root fracture detection has higher diagnostic accuracy when using machine learning in CBCT versus periapical radiographs.9
AI has been applied in multiple facets for the treatment of endodontic practice such as determining working lengths, assistive tools to navigate root morphology, optimal selection of force/torque during canal preparation, implementing imageguided robotic surgery, and other integrations of AI within hardware used for treatment purposes.10 Another interesting future application to endodontics that has been used in other areas of healthcare is drug delivery and biofilm disruption using nanorobots controlled by machine learning.11
Leveraging one of the key values of AI is complex pattern recognition beyond the human ability. Applying machine learning to large-scale datasets of clinical endodontics information can facilitate predictions of treatment success. For instance, complex patient and clinical interactions hold patterns that can elucidate patient-specific chances for treatment success or failure. AI-powered tools have the potential to discriminate optimal first-line treatment approaches despite these complex interactions. Currently, machine learning techniques have been applied to the prognosis of endodontic microsurgeries, decision to retreat the root canal system, and regeneration technique of dental pulp.12,13 Additionally, clinical decisions such as selecting the patient-specific appropriate course of antibiotics or pain medications could
potentially be identified using AI tools. Currently, AI algorithms have been developed to identify the occurrence and severity of postoperative pain based on patient-specific factors.14
A light in the black box
AI presents an exciting tool to simulate human intelligence to help dentists achieve a higher quality of life, better decision-making capability, and fewer postoperative complications.15 However, despite these advances, AI in dentistry is in its infancy. On the horizon are more autonomous systems that do not require human input at the clinical stage within the AI algorithm. While a good understanding of the basics of AI is useful, the actual processes of most algorithms and datasets are not transparent to clinicians. Accuracy, trust, data stewardship, and equity/sustainability are concerns that clinicians and AI software manufacturers need to address to ensure patient safety, clinical success, and safeguarding from legal complications.
Accuracy
The accuracy of an AI system is based on a predefined gold standard. Most clinical decision support tools are supervised algorithms and labeled by clinical dentists without histologic confirmation. Since the amount of data that is required to train the models is so large, it is impractical to build highly accurate datasets that are verified with high-quality standards. In fact, the sensitivity for dentists to detect interproximal caries in bitewings in dentin is low (.36),16 and provider agreement also is low (.4 kappa).17 Similar findings have been seen in other fields such as in periodontal conditions yet are task specific.18 While the quality of the dataset will likely not be transparent, the process for labeling the data as an important factor in the accuracy of the system could be stated by the manufacturer. Another issue that can affect AI is the imbalance of certain conditions like rare pathology that limit the number of instances for the algorithm to learn.
What is the clinical accuracy of these AI models? Is the trained dataset similar to your patient population or data in your EHR? Most report accuracies on the original dataset that was used, yet the true accuracies with different datasets or after clinicians have interacted with the AI system remain limited, and independent testing remains even more limited. In fact, some studies have shown that when AI presents incorrect informa-
36 Endodontic Practice US Volume 17 Number 1 CONTINUING EDUCATION
Figure 2: Use of data with a supervised AI model
tion, clinicians are more likely to be misled by this recommendation which could result in poor patient outcomes.19,20 Should incorrect guidance be provided by the AI system and patient harm occurs, the current legal climate would hold the clinician liable.21 Additionally, when the AI system is accurate, there are concerns of other biases and trust.
Trust
A human-computer interaction exists between the dentist and AI system that can affect the perception of clinical information and ultimately treatment performance and decision. Trust is a well-studied concept that is affected by many factors with transparency, reliability, and tangibility as some of the commonly cited values that apply most to human-computer interaction.22
Transparency is inherent in trust, and AI systems can be built to be explainable. While most traditional forms of AI suffer from the “black box problem,” some offer detection strategies through computer vision,23 and others provide embeddings through natural language processing.24 Reliability offers a perception that the algorithm is making similar decisions in seemingly similar circumstances. For continuously learning algorithms, there is a potential risk that adaptive learning could introduce new errors and reduce reliable performance.25,26 Tangibility refers to the physical or virtual presence of the AI system and when it appears more real or anthropomorphic, which improves trust.27
Data stewardship
Machine learning sits at the intersection of big data and software algorithms. Given the need for large datasets to train models, the data stewardship in regulated industries, especially dentistry, is important. Dental offices handle private data on patients within their electronic health record system such as financial, demographic, disease state information, and other sensitive clinical information. With the digitization of records and equipment, the dental industry is a prime target for hackers and also lacks adequate knowledge about the prevention of these crimes.28 In fact, Henry Schein, a large distribution, and software company with more than 23,000 employees and 1-million customers globally, halted operations due to a cyber-security incident.29 Large, consolidated datasets with patient data are vulnerable to attacks. Additionally, generative AI that ingests data from multiple sources feeding back into the algorithm can pose a risk if patient data is used. For instance, divulging patient data on a generative AI platform to write patient notes more efficiently could put the dentist at risk of breaching HIPAA with patient data being used to continuously train the model. For example, Sarah Silverman is suing openAI and Meta over violations of her copyrighted book that surfaced when these platforms regurgitated substantial elements of her copyrighted materials.30
Equitability/sustainability
The equitable treatment of patients is an ethical value upheld by the American Dental Association where all treatment decisions should be determined on the same basis as all other
Currently, machine learning techniques have been applied to the prognosis of endodontic microsurgeries, decision to retreat the root canal system, and regeneration technique of dental pulp.
patients. As AI systems are built with human inputs, biases can be encoded into the model.32 In one example of this Optum, a health service company, created an AI program to spot high-risk patients that should receive medical follow-up care. However, the follow-up care disproportionately identified white patients with 82% white and 18% black patients identified compared to an independent analysis finding that 53% white and 46% black patients should have been identified based on medical need. Before this error could be detected, the program had already been applied to 100 million patients.33 Additionally, the hardware that powers AI requires high energy and a large local ecological footprint.34 In fact, GPT3 took 1.287 gigawatt hours of electricity and 700,000 liters of clean freshwater.
35
Implementation of AI systems
As manufacturers continue to release new and update current AI embedded technologies, dentists should be aware of how these tools operate and can potentially change patient care. Many dentists are likely to already implement embedded AI technologies without fully realizing it since AI is commonly used as a tool to accomplish a task or optimize tasks, and most backend systems are not transparent to the user.
In order to implement new technologies with AI into a dental office, technology acceptance and continual quality assurance should be a consideration. The primary factors for technology acceptance are perceived usefulness and perceived ease of use.36 Therefore, removing barriers to trust within the human-computer interaction can improve usage. Training with technology in a safe environment can build confidence and improve ease of use. Additionally, having a plan for continuous quality assurance with the use of AI can aid in patient safety given that the systems can change with updates or continuously learning models. AI behavior should be periodically monitored, and a set of well-defined metrics are needed to guide regularly scheduled testing.37
The US government also functions to protect patients and dental offices’ implementation of AI through the FDA clearance process of software as a medical device. FDA has become increasingly more stringent on this type of software that predicts and identifies medical/dental conditions.38 As dentists expand their appetite for additional functionality of these software systems, there needs to be a balance between the regulatory burden and the ability to innovate.
Exciting future of AI in dentistry
With the digitization of dental records and radiographs, dentistry is an ideal profession to harness AI. Current applications
37 endopracticeus.com Volume 17 Number 1 CONTINUING EDUCATION
of AI are already being implemented to change the workflow of dental offices and patient care. Despite risks of inaccuracies, human-computer mistrust, data security concerns, and inequities in applications, it is easy to imagine overcoming these obstacles as the perceived future benefits outweigh the risks.39 Healthcare in general is expected to see an increase in venture investments as the value of AI in health is expected to grow from $4.9B in 2020 to $45.2B in 2026. Dentistry, however, is lacking in the amount and accuracy of data.40 To accelerate the advancement of AI, manufacturers need access to large, structured datasets that contain valid and reliable data. In fact, each of our practices holds valuable data that has the potential to improve the field.
REFERENCES
1. Kennedy B, Tyson A, Saks E. Public awareness of artificial intelligence in everyday activities. Pew Research Center. (Published February 15, 2023.) https://www.pewresearch.org/science/2023/02/15/public-awareness-of-artificial-intelligence-in-everyday-activities/. (Accessed: November 24, 2023.)
2. Cheng E, Chen J, Yang J, Deng H, Wu Y, Megalooikonomou V, Gable B, Ling H. Automatic Dent-landmark detection in 3-D CBCT dental volumes. Annu Int Conf IEEE Eng Med Biol Soc. 2011;2011:6204-6207.
3. El-Bialy A. Towards a Complete Computer Dental Treatment System. 2008 Cairo International Biomedical Engineering Conference, Cairo, Egypt. 2008:1-8.
4. Sporring J., Hommelhoff Jensen K. Bayes Reconstruction of Missing Teeth. J Math Imaging Vis. 2008;31:245–254.
5. Chang J, Glick A. Clinical implementation of artificial intelligence systems. J Greater Houston Dent Soc. 2023; 94(2):18-19.
6. Sundberg L, Holmström J. Democratizing artificial intelligence: How no-code AI can leverage machine learning operations. Business Horizons. 2023;66(6):777-778.
7. Leonardi Dutra K, Haas L, Porporatti AL, Flores-Mir C, Nascimento Santos J, Mezzomo LA, Corrêa M, De Luca Canto G. Diagnostic Accuracy of Cone-beam Computed Tomography and Conventional Radiography on Apical Periodontitis: A Systematic Review and Meta-analysis. J Endod. 2016 Mar;42(3):356-364.
8. Sadr S, Mohammad-Rahimi H, Motamedian SR, Zahedrozegar S, Motie P, Vinayahalingam S, Dianat O, Nosrat A. Deep Learning for Detection of Periapical Radiolucent Lesions: A Systematic Review and Meta-analysis of Diagnostic Test Accuracy. J Endod. 2023 Mar;49(3):248-261.e3.
9. Salineiro FCS, Kobayashi-Velasco S, Braga MM, Cavalcanti MGP. Radiographic diagnosis of root fractures: a systematic review, meta-analyses and sources of heterogeneity. Dentomaxillofac Radiol. 2017 Dec;46(8):20170400.
10. Khanagar SB, Alfadley A, Alfouzan K, Awawdeh M, Alaqla A, Jamleh A. Developments and Performance of Artificial Intelligence Models Designed for Application in Endodontics: A Systematic Review. Diagnostics (Basel). 2023 Jan 23;13(3):414.
11. Singh AV, Chandrasekar V, Janapareddy P, Mathews DE, Laux P, Luch A, Yang Y, Garcia-Canibano B, Balakrishnan S, Abinahed J, Al Ansari A, Dakua SP. Emerging Application of Nanorobotics and Artificial Intelligence To Cross the BBB: Advances in Design, Controlled Maneuvering, and Targeting of the Barriers. ACS Chem Neurosci. 2021 Jun 2;12(11):1835-1853.
12. Qu Y, Lin Z, Yang Z, Lin H, Huang X, Gu L. Machine learning models for prognosis prediction in endodontic microsurgery. J Dent. 2022 Mar;118:103947.
13. Aminoshariae A, Kulild J, Nagendrababu V. Artificial Intelligence in Endodontics: Current Applications and Future Directions. J Endod. 2021 Sep;47(9):1352-1357.
14. Gao X, Xin X, Li Z, Zhang W. Predicting postoperative pain following root canal treatment by using artificial neural network evaluation. Sci Rep. 2021 Aug 26;11(1):17243.
15. Nguyen TT, Larrivée N, Lee A, Bilaniuk O, Durand R. Use of Artificial Intelligence in Dentistry: Current Clinical Trends and Research Advances. J Can Dent Assoc. 2021 May;87:l7.
16. Schwendicke F, Tzschoppe M, Paris S. Radiographic caries detection: A systematic review and meta-analysis. J Dent. 2015 Aug;43(8):924-933. Epub 2015 Feb 24. Erratum in: J Dent. 2021 Nov;114:103783.
17. Naitoh M, Yuasa H, Toyama M, Shiojima M, Nakamura M, Ushida M, Iida H, Hayashi M, Ariji E. Observer agreement in the detection of proximal caries with direct digi-
tal intraoral radiography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998 Jan;85(1):107-112.
18. Meusburger T, Wülk A, Kessler A, Heck K, Hickel R, Dujic H, Kühnisch J. The Detection of Dental Pathologies on Periapical Radiographs-Results from a Reliability Study. J Clin Med. 2023 Mar 13;12(6):2224.
19. Glick A, Clayton M, Angelov N, Chang J. Impact of explainable artificial intelligence assistance on clinical decision-making of novice dental clinicians. JAMIA Open. 2022 May 17;5(2):ooac031.
20. Gaube S, Suresh H, Raue M, Merritt A, Berkowitz SJ, Lermer E, Coughlin JF, Guttag JV, Colak E, Ghassemi M. Do as AI say: susceptibility in deployment of clinical decision-aids. NPJ Digit Med. 2021 Feb 19;4(1):31.
21. Maliha G, Gerke S, Cohen IG, Parikh RB. Artificial Intelligence and Liability in Medicine: Balancing Safety and Innovation. Milbank Q. 2021 Sep;99(3):629-647.
22. Glikson E, Williams Woolley A. Human trust in artificial intelligence: Review of empirical research. Academy of Management Annals. 2020;14.2: 627-660.
23. Meske C, Bunde E. “Transparency and trust in human-AI-interaction: The role of model-agnostic explanations in computer vision-based decision support.” Artificial Intelligence in HCI. First International Conference, AI-HCI 2020, Held as Part of the 22nd HCI International Conference, HCII 2020, Copenhagen, Denmark, July 19–24, 2020, Proceedings 22. Springer International Publishing, 2020.
24. Zini, JR, Awad M. On the explainability of natural language processing deep models. ACM Computing Surveys. 2022;55.5:1-31.
25. Vokinger KN, Feuerriegel S, Kesselheim AS. Continual learning in medical devices: FDA’s action plan and beyond. Lancet Digit Health. 2021 Jun;3(6):e337-e338.
26. Pianykh OS, Langs G, Dewey M, Enzmann DR, Herold CJ, Schoenberg SO, Brink JA. Continuous Learning AI in Radiology: Implementation Principles and Early Applications. Radiology. 2020 Oct;297(1):6-14.
27. Kim K, Bölling L, Haesler S, Bailenson, Bruder G, Welch G. Does a digital assistant need a body? The influence of visual embodiment and social behavior on the perception of intelligent virtual agents in AR. 2018 IEEE International Symposium on Mixed and Augmented Reality (ISMAR).
28. Melon E, Hernandez W. Cybersecurity in the dental healthcare sector: The need of knowledge for small practitioners. Issues in Information Systems. 2020;21(1):118-124.
29. Henry Schein. “Henry Schein provides information on cybersecurity incident.” [Press release]. Available at: https://investor.henryschein.com/news-releases/news-release-details/henry-schein-provides-information-cybersecurity-incident. (Accessed November 25, 2023).
30. Hayes, Carol Mullins, Generative Artificial Intelligence and Copyright: Both Sides of the Black Box (July 21, 2023). Available at SSRN: https://ssrn.com/abstract=4517799 or http://dx.doi.org/10.2139/ssrn.4517799. Accessed January 4, 2024.
31. American Dental Association. Principles of Ethics & Code of Professional Conduct. https://www.ada.org/-/media/project/ada-organization/ada/ada-org/files/about/ ada_code_of_ethics.pdf?rev=ba22edfdf1a646be9249fe2d870d7d31&hash=CCD76FCDC56D6F2CCBC46F1751F51B96. Accessed November 25, 2023.
32. Schönberger, Daniel. Artificial intelligence in healthcare: a critical analysis of the legal and ethical implications. International Journal of Law and Information Technology. 2019;27(2):171-203.
33. Obermeyer Z, Powers B, Vogeli C, Mullainathan S. Dissecting racial bias in an algorithm used to manage the health of populations. Science. 2019 Oct 25;366(6464):447-453.
34. Kopka A, Grashof N. Artificial intelligence: Catalyst or barrier on the path to sustainability? Technological Forecasting and Social Change. 2022;175:121318.
35. Baxter K, Schlesinger Y. Managing the risks of generative AI. Harvard Business Review. https://hbr.org/2023/06/managing-the-risks-of-generative-ai. (Accessed November 11, 2023).
36. Alhashmi SFS, Alshurideh M, Al Kurdi B, Salloum S. “A systematic review of the factors affecting the artificial intelligence implementation in the health care sector.” Proceedings of the International Conference on Artificial Intelligence and Computer Vision (AICV2020). Springer International Publishing, 2020.
37. Mahadevaiah G, Rv P, Bermejo I, Jaffray D, Dekker A, Wee L. Artificial intelligence-based clinical decision support in modern medical physics: Selection, acceptance, commissioning, and quality assurance. Med Phys. 2020 Jun;47(5):e228-e235.
38. Harvey HB, Gowda V. How the FDA Regulates AI. Acad Radiol. 2020 Jan;27(1):58-61.
39. Tandon D, Rajawat J. Present and future of artificial intelligence in dentistry. J Oral Biol Craniofac Res. 2020 Oct-Dec;10(4):391-396.
40. Hassani H, Andi PA, Ghodsi A, Norouzi K, Komendantova N, Unger S. Shaping the future of smart dentistry: From Artificial Intelligence (AI) to Intelligence Augmentation (IA). IoT. 2021;2(3):510-523.
38 Endodontic Practice US Volume 17 Number 1 CONTINUING EDUCATION
EP
Continuing Education Quiz
Clinical implementation and future of AI in endodontic dentistry
GLICK, ET AL.
1. AI is a broad term that generally refers to the ability for computers to perform tasks that typically require human intelligence; for example, viewing a dental X-ray and identifying interproximal caries.
a. True
b. False
2. ________ refers to the mathematical approach to accomplish this perceived human intelligence.
a. Neural learning
b. Machine learning
c. Database modeling
d. Natural Language Processing
3. _________ is based on a clinician providing the algorithm with a ground truth for labelled data.
a. A Receiver Operating Characteristic
b. The Convolutional Neural Network
c. Supervised learning
d. The Language-Specific Model
4. _________ is where the model learns without explicitly provided information to classify and can be accomplished through patterns within the data.
a. Unsupervised learning
b. Supervised learning
c. Neural Network Optimization
d. Predictive Outcome Recognition
5. AI has been applied in multiple facets for the treatment of endodontic practice such as determining ___________, implementing image guided robotic surgery, and other integrations of AI within hardware used for treatment purposes.
a. working lengths
b. assistive tools to navigate root morphology
c. optimal selection of force/torque during canal preparation
d. all of the above
6. AI presents an exciting tool to simulate human intelligence to help dentists achieve _________.
a. a higher quality of life
b. better decision-making capability
c. fewer postoperative complications
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 16 CE credits for only $149; call 866-579-9496, or visit https://endopracticeus.com/ subscribe/ to subscribe today.
n To receive credit: Go online to https://endopracticeus.com/continuingeducation/, click on the article, then click on the take quiz button, and enter your test answers.
AGD Code: 010
Date Published: March 18, 2024
Expiration Date: March 18, 2027
d. all of the above
7. Another issue that can affect AI is the imbalance of certain conditions like _______ that limit the number of instances for the algorithm to learn.
a. smaller dental offices
b. non-compliant patients
c. rare pathology
d. edentulous patients
8. For continuously learning algorithms, there is a potential risk that adaptive learning could __________.
a. introduce new errors
b. reduce reliable performance
c. add unnatural language
d. both a and b
9. AI behavior should be periodically monitored, and a set of welldefined metrics are needed to guide regularly scheduled testing.
a. True
b. False
10. ________ has become increasingly more stringent on this type of software that predicts and identifies medical/dental conditions.
a. Food and Drug Administration (FDA)
b. Environmental Protection Agency (EPA)
c. Consumer Products Safety Commission (CPSC)
d. Occupational Safety and Health Administration (OSHA)
To provide feedback on CE, please email us at education@medmarkmedia.com
Legal disclaimer: Course expires 3 years from date of publication. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
39 endopracticeus.com Volume 17 Number 1 CONTINUING EDUCATION
2 CE
CREDITS
Antibiotics in endodontics: a desktop reference
Dr. Joseph C. Stern discusses the benefits and drawbacks of prescribing antibiotics in endodontics
Introduction
Over the years, one of the biggest concerns with antibiotics has been their overuse. There have been many studies attesting to this. The Centers for Disease Control and Prevention (CDC) conservatively estimates that 47 million prescriptions for antibiotics (30% of all outpatient antibiotic prescriptions) are unnecessary.1-4 The result of this overuse is the development of microbial resistance. Antibiotics alter the natural balance of normal flora by attacking vulnerable organisms allowing resistant organisms to thrive and multiply. This overuse enables a greater quantity of our bacteria to become resistant to antibiotics over time.5 One of the ways to prevent this is with the very cautious use of antibiotics.
Regarding dental-related infections, antibiotics have limitations that should be understood before prescribing them.6-12 Without a blood supply in a necrotic and infected pulp, antibiotics have no access to the pulp space. They may only help to control the spread of the infection in the periapical area which is important in preventing the spread of infection beyond the fascial planes. Another point to be discussed is the importance of dental treatment as the primary way of combating dental infections rather than simply relying on antibiotic prescription. There are, however, times where antibiotics are indicated and should be prescribed.
Range of infection
Endodontic infections can range from being localized to life threatening. These infections are polymicrobial, characterized mostly by anaerobic bacteria and some facultative bacteria. Bacteria and their endotoxin by-products within the root canal produce a periradicular inflammatory response. With microbial invasion of periradicular tissues, an acute abscess and cellulitis may develop. The inflammatory response may give rise to a protective effect by isolating the infection to the periapical tissues and preventing it

Joseph C. Stern, DDS, is a Diplomate of the American Board of Endodontics. He is the Director of Endodontics at the Touro College of Dental Medicine and lectures frequently on the subject of clinical endodontics. He has lectured at many local county dental societies, the New Jersey Dental Association Annual Session in May 2019, and the Greater New York Dental Meeting in 2020. He maintains a private practice, Clifton Endodontics, in Clifton, New Jersey. He can be reached at jstern5819@gmail.com.
Disclosure: The author reports no conflicts of interest.

Educational aims and objectives
This self-instructional course for dentists aims to discuss the pros and cons of prescribing antibiotics for a range of endodontic procedures.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions by taking the quiz online at endopracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
• Recognize the statistics regarding antibiotic overprescribing.
• Realize how overprescribing may lead to antibiotic resistance.
• Identify types of endodontic infections, their causes, and detrimental effects.
Realize some reasons that antibiotics may not be effective in certain endodontic situations.
• Identify guidelines for prescribing or not prescribing antibiotics in endodontic practice.
• Realize prophylaxis guidelines and possible antibiotic regimens, when indicated. 2 CE CREDITS
from spreading systemically. However, it can also be very destructive to surrounding tissue and may become systemic.
Severe and life-threatening infections can develop beyond the local environment depending on the pathogenicity of the microorganisms involved and the resistance of the host. Clinical signs and symptoms of an infection are the result of damage to the tissues caused by the microbe and the inflammatory response produced by the host. The spread of infection and the inflammatory response will continue until the source of the irritation is
40 Endodontic Practice US Volume 17 Number 1 CONTINUING EDUCATION
removed. Antibiotics (and incision for drainage) can only assist in controlling the infection, but only removal of the source of the infection will ultimately lead to healing. Effective treatment of endodontic infections includes removal of the reservoir of infection by either endodontic treatment or tooth extraction.13-19
Occasionally, a local infection may suddenly spread systemically, due to a breakdown in the patient’s immune response, and become a life-threatening situation. Unless the dentist is reachable 24/7, it might be wise to prescribe antibiotics up front, to be taken only if systemic symptoms (pain, swelling, fever, etc.) develop.
Limitations
Patients often ask us, if I have an infection in my tooth, why do I need a root canal? Can’t I just take an antibiotic? We must be prepared to answer these questions in laymen’s terms, explaining the basics of root canal infections. Root canal infections are quite unique due to their isolated location. A root canal infection is a continuum of the carious process in which bacteria first invade the enamel and dentin and eventually make their way into the pulp. Bacteria inside the pulp create an inflammatory process which eventually leads to pulpal necrosis (destruction of the pulp tissue).
Unfortunately, the process doesn’t end there. As bacteria, and/or their endotoxins make their way through the apical foramen, they then trigger an inflammatory process (immune response) in the periapical tissues surrounding the root. This inflammatory response in the periapical tissues may give rise to a protective effect by walling off the infection in the periapical tissues and preventing it from spreading systemically. Eventually, with microbial invasion of periradicular tissues, an acute abscess and cellulitis may develop. This spread of infection can be very dangerous, even life threatening.
A common theme we speak of is: Location! Location! Location! A very unique component of root canal and periapical infections is their isolated nature and distance from an adequate blood supply. Herein lies the key as to why antibiotics don’t work to resolve root canal infections. Antibiotics travel via systemic circulation, while the root canal space and the body of a periapical lesion have very poor perfusion. Essentially, antibiotics have no circulatory pathway to enter the pulp. The “train” carrying antibiotics doesn’t “stop” at the root canal frequently enough, and thus, its inability to rid a root canal of its bacterial content. This begs the question of why we prescribe antibiotics at all? The answer is that it is the danger of a local root canal infection having the potential to spread systemically causing potentially life-threatening infections. In essence, antibiotics stand guard at the peripheral tissues to prevent the infection from spreading. Antibiotics are not prescribed to rid our body of a root canal infection but rather to aid our immune system in handling the infection in conjunction with root canal treatment.
Another reason antibiotics may be ineffective in removing root canal infections is because of the unique nature of these infections. The microbes in the canal are colonized in biofilm attached to the wall of the canal, and antibiotics don’t do well penetrating the powerful “fortresses” of the biofilm.20 Biofilm can be defined as a sessile multicellular microbial community
characterized by cells that are firmly attached to a surface and enmeshed in a self-produced matrix of extracellular polymeric substance (EPS), usually a polysaccharide. This structure allows the biofilm to firmly adhere to the dentinal walls, essentially like “bacteria stuck in glue.” Bacteria form complex communities that are very resistant to removal by disinfecting agents including the most powerful antibiotics. Bacteria form biofilms on the dentin walls inside the main root canal as well as in lateral ramifications, isthmuses, and even within the dentinal tubules themselves. In advanced stages of endodontic disease, they can also be found attached to the outer surface of the root apex.
The microbes can be extremely difficult to remove due to the many virulent factors they contain:
1. Biofilms can restrict the penetration of anti-microbial agents due to their sophisticated matrix and its neutralizing enzymes.
2. Bacteria in biofilms can enter a special stage called the “stationary phase” which allows them to survive in even the harshest environments, such as when they are under attack by antimicrobials. It also allows them to survive extended periods without the nutrients that are usually needed for survival.
3. Quorum sensing: bacteria living in biofilms have a very sophisticated form of communication. Think “iPhone for bacteria.” This form of communication is carried out by diffusible signal molecules or “auto-inducers,” which allow bacteria to communicate in a harmonious manner and survive and persist in harsh environments, such as the root canal.
4. Lateral gene transfer (LTG): Microbes in a biofilm exchange DNA, some of which transfer antibiotic resistance and generally enhance survival.
Because of the above-mentioned factors, it is prudent to be very selective with the use of antibiotics and understand their limitations. The key to treatment of these infections is dental intervention whether through pulpal debridement, incision and drainage, or tooth extraction when indicated.
Antibiotic guidelines21-23
Generally antibiotics are not prescribed for the following:
1. A patient with a diagnosis of pulpitis (irreversible or reversible) with or without apical periodontitis (pain to percussion caused by inflammation of the periapical tissues). Antibiotics are not indicated where the pulp is vital, even when severely inflamed. If the patient has signs and symptoms indicative of a vital but inflamed pulp, such as lingering pain to temperature or spontaneous pain caused by caries, a deep restoration, or a crack, the treatment of choice is root canal therapy, not antibiotics.
2. A patient with a diagnosis of pulp necrosis with symptomatic or asymptomatic apical periodontitis (periapical radiolucency present). This also includes the category of patients who have had previous endodontic treatment and present with a periapical radiolucency, with or without symptoms. The key is pain management and endodontic treatment. If immediate treatment or thorough instrumentation of the root canal is not possible, then
41 endopracticeus.com Volume 17 Number 1 CONTINUING EDUCATION
a “delayed prescription” can be implemented, where an antibiotic is prescribed to be taken only if the situation starts to deteriorate in terms of pain/swelling and systemic involvement. Many practitioners will prescribe antibiotics or a “delayed prescription” for an infected tooth whether immediate treatment is an option or not, as a precautionary measure.
3. A diagnosis of chronic apical abscess (sinus tract/fistula/ parulis). Endodontic intervention (or extraction if appropriate) is indicated.
Generally, antibiotics are indicated for the following:
1. A patient with a diagnosis of pulp necrosis with acute apical abscess (a necrotic and infected pulp that causes a localized swelling) if immediate treatment is not a possibility. However, if immediate endodontic intervention is an option, then a delayed prescription can be employed rather than initially placing the patient on an antibiotic.
Antibiotics are only an adjunct to treatments such as pulpal debridement, incision and drainage, or extraction
Table 1
Agent Instructions Dosage
PenicillinCan be used as an alternative to amoxicillin.
AmoxicillinStronger and more sustained serum levels than penicillin.
Augmentin (amoxicillin with clavulanic acid)
If the infection resists amoxicillin, then prescribe Augmentin.
ClindamycinSerious dental infections, but the patient is allergic to penicillin. (Clostridium difficile is a concern).
Azithromycin (Z-Pak) Serious dental infections, but the patient is allergic to penicillin. (Concern for causing cardiac arrhythmias).
Metronidazole (Flagyl)
Add to penicillin or amoxicillin if needed. Only effective against anaerobes.
Cephalexin (Keflex) Serious dental infections, but patient is allergic to penicillin (however if the patient has a history of anaphylaxis, angioedema, or hives with penicillin then azithromycin or clindamycin is indicated).
if appropriate. Many practitioners will prescribe antibiotics to be taken in all cases of acute abscesses as a precautionary measure.
2. A patient with a diagnosis of pulp necrosis with acute apical abscess and systemic involvement (swelling that is no longer localized). Systemic involvement includes one or more of these entities: evidence of lymph node involvement, facial space involvement, fever, or malaise. These are indicators that the infection is more widespread. Antibiotics are only an adjunct to treatments such as pulpal debridement, incision and drainage, or extraction if appropriate.
3. Generally, if after initiating root canal therapy the patient’s symptoms rapidly worsen in terms of pain and swelling, antibiotics should be considered.
4. Generally, if the patient is immunocompromised and being treated for an infected tooth, antibiotics should be considered to aid the patient’s immune system in resolving the infection.
Prophylaxis guidelines24-29
1. The main indications for antibiotic prophylaxis have been to prevent infective endocarditis (IE) and prosthetic joint implant infection (PJI).
Loading dose of 1,000 mg followed by 500 mg every 4-6 hours for 3-7 days (4 times a day)
Loading dose of 1,000 mg followed by 500 mg every 8 hours for 3-7 days (3 times a day) or 875 mg 2 times a day.
500/125 mg every 8 hours for 3-7 days (3 times a day)
Loading dose: 600 mg followed by 300 mg or 150 mg every 6 hours for 3-7 days (4 times a day)
Loading dose of 500 mg on day 1 followed by 4 days of 250 mg. (1 time a day)
Loading dose: 1,000 mg followed by 250 mg or 500 mg every 8 hours for 3-7 days. (3 times a day)
500 mg every 6 hours for 3-7 days (4 times a day)
2. Prophylaxis against IE is reasonable before dental procedures that involve manipulation of gingival tissue, manipulation of the periapical region of teeth, or perforation of the oral mucosa in patients with the following:
A. Prosthetic cardiac valves, including transcatheter-implanted prostheses and homografts.
B. Prosthetic material used for cardiac valve repair, such as annuloplasty rings and chords.
C. Previous history of IE.
D. Unrepaired cyanotic congenital heart disease or repaired congenital heart disease, with residual shunts or valvular regurgitation at the site of or adjacent to the site of a prosthetic patch or prosthetic device.
E. Cardiac transplant with valve regurgitation due to a structurally abnormal valve.
3. The risk of IE is highest in the first 6 months after a heart transplant because of endothelial disruption.
4. The regiment includes 2g of amoxicillin 30-60 minutes before the procedure. If the patient is allergic to penicillin, then one can use 2g of cephalexin, 600 mg of clindamycin, or 500 mg of azithromycin. If the dosage of antibiotic was inadvertently not administered before the procedure, it may be administered for up to 2 hours after the procedure.
5. For patients who require prophylaxis but are already taking antibiotics for another condition, select an antibiotic from a different class than the one the patient is already taking. For example, if the patient is taking amoxicillin, then select azithromycin or clarithromycin for prophylaxis.
6. In general, for patients with prosthetic joint implants, prophylactic antibiotics are not recommended prior to dental procedures to prevent prosthetic joint infection
42 Endodontic Practice US Volume 17 Number 1 CONTINUING EDUCATION
(PJI). In cases where antibiotics are deemed necessary, it is most appropriate that the orthopedic surgeon recommend the appropriate antibiotic regimen, and when reasonable, write the prescription.
7. If there is an increased medical risk, clinical recommendation should be integrated with the practitioner’s professional judgment and the patient’s needs and preferences. Consultation with the patient physician is prudent.
Recommended antibiotics (Table 1):
1. If the patient is not allergic to penicillin, then the recommended antibiotic is amoxicillin 500 mg 3 times a day. Penicillin 500 mg. 4 times a day can also be used.
2. If amoxicillin isn’t working, then either supplement with metronidazole 500 mg or switch patient to amoxicillin and clavulanate (Augmentin) 500/125 mg 3 times a day.
3. If the patient has a reported penicillin allergy but no history of anaphylaxis, angioedema, or hives with penicillin, ampicillin, or amoxicillin, then prescribe cephalexin 500 mg. If they do have a history of anaphylaxis, angioedema, or hives, then prescribe azithromycin 250 mg or clindamycin 300 mg. If this fails, then add metronidazole 500 mg.
4. The patient can stop the antibiotic after 3 days if the symptoms resolve instead of the usual 7-10 course.
Please note: The evidence based information in this article is not intended to substitute for a clinician’s expert judgment on a case-by-case basis.
REFERENCES
1. Fridkin SK, Cleveland AA, See I, Lynfield R. Emerging Infections Program as Surveillance for Antimicrobial Drug Resistance. Emerg Infect Dis. 2015 Sep;21(9):1578-1581.
2. Fleming-Dutra KE, Hersh AL, Shapiro DJ, Bartoces M, Enns EA, File TM Jr, Finkelstein JA, Gerber JS, Hyun DY, Linder JA, Lynfield R, Margolis DJ, May LS, Merenstein D, Metlay JP, Newland JG, Piccirillo JF, Roberts RM, Sanchez GV, Suda KJ, Thomas A, Woo TM, Zetts RM, Hicks LA. Prevalence of Inappropriate Antibiotic Prescriptions Among US Ambulatory Care Visits, 2010-2011. JAMA. 2016 May 3;315(17):1864-1873.
3. Cherry WR, Lee JY, Shugars DA, White RP Jr, Vann WF Jr. Antibiotic use for treating dental infections in children: a survey of dentists’ prescribing practices. J Am Dent Assoc. 2012 Jan;143(1):31-38.
4. Durkin MJ, Hsueh K, Sallah YH, Feng Q, Jafarzadeh SR, Munshi KD, Lockhart PB, Thornhill MH, Henderson RR, Fraser VJ; Centers for Disease Control and Prevention Epicenters. An evaluation of dental antibiotic prescribing practices in the United States. J Am Dent Assoc. 2017 Dec;148(12):878-886.e1.
5. Kim MK, Chuang SK, August M. Antibiotic Resistance in Severe Orofacial Infections. J Oral Maxillofac Surg. 2017 May;75(5):962-968.
6. Fouad AF, Rivera EM, Walton RE. Penicillin as a supplement in resolving the localized acute apical abscess. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996 May;81(5):590-595.
7. Walton RE, Chiappinelli J. Prophylactic penicillin: effect on posttreatment symptoms following root canal treatment of asymptomatic periapical pathosis. J Endod. 1993 Sep;19(9):466-470.
8. Pickenpaugh L, Reader A, Beck M, Meyers WJ, Peterson LJ. Effect of prophylactic amoxicillin on endodontic flare-up in asymptomatic, necrotic teeth. J Endod. 2001 Jan;27(1):53-56.
9. Pinheiro ET, Gomes BP, Ferraz CC, Teixeira FB, Zaia AA, Souza Filho FJ. Evaluation of root canal microorganisms isolated from teeth with endodontic failure and their antimicrobial susceptibility. Oral Microbiol Immunol. 2003 Apr;18(2):100-103.
10. Baumgartner JC, Xia T. Antibiotic susceptibility of bacteria associated with endodontic abscesses. J Endod. 2003 Jan;29(1):44-47.
11. Baumgartner JC. Microbiologic aspects of endodontic infections. J Calif Dent Assoc. 2004 Jun;32(6):459-468.
12. Baumgartner JC, Siqueira JF Jr, Xia T, Róças IN. Geographical differences in bacteria detected in endodontic infections using polymerase chain reaction. J Endod. 2004 Mar;30(3):141-144.
13. Ricucci D, Lin LM, Spångberg LS. Wound healing of apical tissues after root canal therapy: a long-term clinical, radiographic, and histopathologic observation study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009 Oct;108(4):609-621.
14. Ricucci D, Russo J, Rutberg M, Burleson JA, Spångberg LS. A prospective cohort study of endodontic treatments of 1,369 root canals: results after 5 years. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011 Dec;112(6):825-842.
15. Ricucci D, Siqueira JF Jr. Biofilms and apical periodontitis: study of prevalence and association with clinical and histopathologic findings. J Endod. 2010 Aug;36(8):1277-1288.
16. Márton IJ, Kiss C. Protective and destructive immune reactions in apical periodontitis. Oral Microbiol Immunol. 2000 Jun;15(3):139-150.
17. Nair PN. Apical periodontitis: a dynamic encounter between root canal infection and host response. Periodontol 2000. 1997 Feb;13:121-148.
18. Torabinejad M, Eby WC, Naidorf IJ. Inflammatory and immunological aspects of the pathogenesis of human periapical lesions. J Endod. 1985 Nov;11(11):479-488.
19. Tronstad L, Barnett F, Riso K, Slots J. Extraradicular endodontic infections. Endod Dent Traumatol. 1987 Apr;3(2):86-90.
20. Hargreaves KM, Goodis HE, Tay F, eds. Seltzer and Bender’s Dental Pulp, 2nd edition. Chicago: Quintessence Pub. Co., 2002.
21. Lockhart PB, Tampi MP, Abt E, Aminoshariae A, Durkin MJ, Fouad AF, Gopal P, Hatten BW, Kennedy E, Lang MS, Patton LL, Paumier T, Suda KJ, Pilcher L, Urquhart O, O’Brien KK, Carrasco-Labra A. Evidence-based clinical practice guideline on antibiotic use for the urgent management of pulpal- and periapical-related dental pain and intraoral swelling: A report from the American Dental Association. J Am Dent Assoc. 2019 Nov;150(11):906-921.e12.
22. AAE Position Statement: AAE Guidance on the Use of Systemic Antibiotics in Endodontics. J Endod. 2017 Sep;43(9):1409-1413.
23. Aminoshariae A, Kulild JC. Evidence-based recommendations for antibiotic usage to treat endodontic infections and pain: A systematic review of randomized controlled trials. J Am Dent Assoc. 2016 Mar;147(3):186-191.
24. Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Fleisher LA, Jneid H, Mack MJ, McLeod CJ, O’Gara PT, Rigolin VH, Sundt TM 3rd, Thompson A. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/ American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017 Jun 20;135(25):e1159-e1195.
25. American Association of Endodontists. AAE Guidance on Antibiotic Prophylaxis for Patients at Risk of Systemic Disease, 2017. https://www.aae.org/specialty/wp-content/ uploads/sites/2/2017/06/aae_antibiotic-prophylaxis.pdf (accessed January 16, 2024).
26. Sollecito TP, Abt E, Lockhart PB, Truelove E, Paumier TM, Tracy SL, Tampi M, Beltrán-Aguilar ED, Frantsve-Hawley J. The use of prophylactic antibiotics prior to dental procedures in patients with prosthetic joints: Evidence-based clinical practice guideline for dental practitioners--a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2015 Jan;146(1):11-16.e8.
27. American Dental Association–Appointed Members of the Expert Writing and Voting Panels Contributing to the Development of American Academy of Orthopedic Surgeons Appropriate Use Criteria. American Dental Association guidance for utilizing appropriate use criteria in the management of the care of patients with orthopedic implants undergoing dental procedures. J Am Dent Assoc. 2017 Feb;148(2):57-59.
28. Wilson W, Taubert KA, Gewitz M, Lockhart PB, Baddour LM, Levison M, Bolger A, Cabell CH, Takahashi M, Baltimore RS, Newburger JW, Strom BL, Tani LY, Gerber M, Bonow RO, Pallasch T, Shulman ST, Rowley AH, Burns JC, Ferrieri P, Gardner T, Goff D, Durack DT; American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee; American Heart Association Council on Cardiovascular Disease in the Young; American Heart Association Council on Clinical Cardiology; American Heart Association Council on Cardiovascular Surgery and Anesthesia; Quality of Care and Outcomes Research Interdisciplinary Working Group. Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation. 2007 Oct 9;116(15):1736-1754.
29. Wilson WR, Gewitz M, Lockhart PB, Bolger AF, DeSimone DC, Kazi DS, Couper DJ, Beaton A, Kilmartin C, Miro JM, Sable C, Jackson MA, Baddour LM; American Heart Association Young Hearts Rheumatic Fever, Endocarditis and Kawasaki Disease Committee of the Council on Lifelong Congenital Heart Disease and Heart Health in the Young; Council on Cardiovascular and Stroke Nursing; and the Council on Quality of Care and Outcomes Research. Prevention of Viridans Group Streptococcal Infective Endocarditis: A Scientific Statement From the American Heart Association. Circulation. 2021 May 18;143(20):e963-e978. Epub 2021 Apr 15.
43 endopracticeus.com Volume 17 Number 1 CONTINUING EDUCATION
EP
Continuing Education Quiz
Antibiotics in endodontics: a desktop reference STERN
1. The Centers for Disease Control and Prevention (CDC) conservatively estimates that 47 million prescriptions for antibiotics (_______ of all outpatient antibiotic prescriptions) are unnecessary.
a. 30%
b. 40%
c. 60%
d. 72%
2. Endodontic infections infections are polymicrobial, characterized mostly by ________.
a. anaerobic bacteria
b. some facultative bacteria
c. corynebacterium diphtheriae
d. both a and b
3. A very unique component of root canal and periapical infections is their ________.
a. isolated nature
b. distance from an adequate blood supply
c. excellent profusion
d. both a and b
4. Essentially, antibiotics have ________ to enter the pulp.
a. the best circulatory pathway
b. a direct circular pathway
c. no circulatory pathway
d. a unique way
5. Antibiotics are not prescribed to rid our body of a root canal infection but rather ________.
a. to aid our immune system in handling the infection in conjunction with root canal treatment
b. to give the patient more confidence in the clinician’s ability to prevent infection
c. to reduce the viral content in the root canal space
d. the bypass the patient’s natural immune system
6. can be defined as a sessile multicellular microbial community characterized by cells that are firmly attached to a surface and enmeshed in a self-produced matrix of extracellular polymeric substance (EPS), usually a polysaccharide.
a. Endotoxin bioproducts
b. Biofilm
c. Cellulitis
d. Antibiotics
7. If the patient has signs and symptoms indicative of a vital but inflamed
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 16 CE credits for only $149; call 866-579-9496, or visit https://endopracticeus.com/ subscribe/ to subscribe today.
n To receive credit: Go online to https://endopracticeus.com/continuingeducation/, click on the article, then click on the take quiz button, and enter your test answers.
AGD Code: 070
Date Published: March 18, 2024
Expiration Date: March 18, 2027
pulp, such as lingering pain to temperature or spontaneous pain caused by _______, the treatment of choice is root canal therapy, not antibiotics.
a. caries
b. a deep restoration
c. a crack
d. all of the above
8. Antibiotics are only an adjunct to treatments such as pulpal debridement, incision and drainage, or extraction if appropriate. Many practitioners will prescribe antibiotics to be taken in all cases of acute abscesses as a precautionary measure.
a. True
b. False
9. To prevent infective endocarditis and prosthetic joint infection, an appropriate antibiotic regimen should be administered. If the dosage of antibiotic was inadvertently not administered before the procedure, it may be administered for up to _______ after the procedure.
a. 2 hours
b. 3 hours
c. 24 hours
d. 48 hours
10. In cases where antibiotics are deemed necessary for patients with prosthetic joint implants, it is most appropriate that the ___________ recommend the appropriate antibiotic regimen, and when reasonable, write the prescription.
a. oral surgeon
b. general dentist
c. orthopedic surgeon
d. cardiologist
To provide feedback on CE, please email us at education@medmarkmedia.com
Legal disclaimer: Course expires 3 years from date of publication. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
44 Endodontic Practice US Volume 17 Number 1 CONTINUING EDUCATION
2 CE CREDITS
Odne – Swiss start-up transforming endo
At the upcoming AAE in Los Angeles, Odne will present its innovative technology platform for debridement and obturation to the endo specialist community for the first time. Odne™Clean, Odne™Fill, and Odne™Cure are expected to be game-changing developments providing significant advancement of the endodontic treatment workflow for endo specialists, their patients, and their referral base.
Swiss precision with strong roots in innovation and scientific excellence
Odne has its roots in a groundbreaking collaboration between two renowned Swiss institutions: the Swiss Federal Institutes of Technology in Lausanne and Zürich (EPFL & ETH). Founded in 2018, Odne’s journey began by licensing cutting-edge technology assets from these esteemed universities.
During the last 6 years, clinical application development focused on core challenges in endodontics, clinically as well as commercially. Driven by its mission — transforming endo with passion, scientific and clinical excellence, challenging status quo, accelerating practice building, and long-term tooth preservation — Odne has succeeded. After receiving FDA approval for Odne™Fill and Odne™Cure, the next exciting phase of Odne will start at AAE in Los Angeles, April 17-20, 2024 — US launch!
Listening well to the needs of endodontists and the patients and exploring needs and pain points are at the core of Odne’s DNA. Renowned specialists have been involved in requirements definition, usability, lab- and pre-clinical testing. To date, three clinical studies have started, partnering with University of Zürich, Istanbul Medipol University, and Universidade Federal Fluminense.
Transforming root canal treatment (RCT)
Modern endodontic therapy aims at preserving tooth structure within the root and the cervical region, taking on a restorative-driven approach. Long-term endodontic treatment outcome is no longer driven only by identifying the canals, instrumenta-


tion, and obturation of those canals, but by the complete reconstruction of the tooth allowing functional loading over time.
Odne strongly believes that root canal treatments (RCT) are transforming into root preservation therapy (RPT). With its innovations, Odne aims at supporting patient-friendly and economic treatment, minimizing postoperative pain, reducing chair time, increasing success rate, and delivering long-standing restorations.
Enabling root preservation therapy
(RPT) as a
practice builder
Patient comfort and patient marketing are one part of the practice-building challenge. Efficient treatment workflows for the endo specialist, especially training and collaborating with the referral base, are the other crucial part. As Odne’s solutions offer excellent price value and affordability, it enables the endo leader to standardize the treatment workflow within its referral base. Referred retreatments will become easier as the initial treatment preserves tooth structure. Removal of the obturation will become less complex. Transforming the practice network to RPT with Odne enables successful practice building.
Odne’s technology platform for debridement and obturation
Pain points of RCT are the highly technique-sensitive preparation of the root canal, bleach as the main irrigation and disinfection medium, and tedious obturation procedures. In addition, past innovations in endodontic devices often came at a prohibitive pricing.
Odne™Clean (FDA clearance pending) innovates root canal debridement introducing hydro-dynamic cavitation using saline as irrigation medium. Odne™Fill and Odne™Cure (both FDA cleared) are game-changers in root canal obturation. Odne™Fill is a light-curing, highly flowable, one material root canal filler that instantly photocures applying Odne™Cure micro laser curing.
45 endopracticeus.com Volume 17 Number 1 PRODUCT SPOTLIGHT
Odne’s product portfolio for root canal debridement and obturation
Odne™Clean handpiece and tip
Both technology platforms can be easily integrated in the existing workflows individually. Together, they enable root preservation therapy (RPT). RPT is increasing patient comfort through less surgical trauma/risk, which can boost your patient marketing. RPT using the Odne Solution is less complex to train and teach to your referral base and makes it easier to retreat complications.
Besides the core innovations in hydro-dynamic cavitation and light-curing hydrogel technology, the highly flexible application tips for Odne™Clean / Odne™Fill (190µm), and the optical fiber of Odne™Cure (200µm) are first of its kind in dental.
Odne™Clean, saline cavitation — minimally invasive endodontic debridement
Odne™Clean aims to establish a non-instrumented approach to RPT. A cleaning tip as thin as 190µm creates a hydro-dynamic cavitation cloud using physiologic saline solution inside the root canal. The cavitation jet removes debris inside the canals and tubules.

Based on current clinical protocol, infected and necrotic pulp tissue should be removed using barbed broach, and a glide path using manual or engine driven files of size ISO15.02 or ISO10.04 needs to be established. To freely move the Odne™Clean Tip, the root canal needs to have a minimum diameter of 190µm. Minimal shaping requirement is ISO 20.04 at working length. Depending on the clinical protocol, various cycles of Odne™Clean (30-60 sec.) are applied. Gold standard disinfection is reached with a final NaOCl rinse.
The minimal invasive approach of Odne™Clean preserves vital tooth structure, thereby reducing complications and the risk of potential structural failures of the tooth, over time. Limiting the use of aggressive disinfectants limits the risk of potential adverse reactions of the patient. Obviously, the periapical region and the soft tissue will react more favorably to saline than to bleach.
Odne™Fill, light-cured obturation — the first light-curing endodontic filler
Odne™Fill is the first FDA approved light-curing, injectable,


single-component endodontic material for root canal obturation. Odne™Fill is a highly stable hydrogel, a class of biomaterials known for their excellent biocompatibility. It forms a very tight interface with the hydrophilic dentin. Due to its water-like viscosity and the high hydrophilicity in its uncured state, it can reach the smallest endodontic structures.
After disinfection of the root canal, Odne™Fill is applied with the smallest dental cannula available (tip diameter of 190µm), filling the root canal gently from the apex. Odne™Fill is instantly curing once activated with the Odne™Cure micro laser. It is compatible with most prosthodontic materials and procedures for final restoration. Due to its pulp-like material properties, removal is hassle free, if necessary. With Odne™Fill, complex anatomic root structures (isthmuses, lateral canals, deltas, etc.) can be sealed simply, without any compaction needed.
Odne™Cure, high-precision laser curing — the thinnest dental light curing device
Odne™Cure is the micro laser-curing light to cure Odne™Fill. Equipped with the thinnest light conductor currently used in dental (220µm), Odne™Cure is applied inside the root canal. With the current curing protocol, Odne™Fill is cured in two steps: first, curing at working length -3 mm to -5 mm to seal above the apex. Second, curing above the root canal entry finalizes sealing the canal.
Odne Inc., USA — serving the US endodontic specialist market
To serve the US endodontic specialist market, Odne has recently founded Odne Inc, USA. The team of Odne is evolving, incorporating experienced and well-connected dental experts building training, service, marketing, and sales. Currently, the team is performing a Priority Access Program with renowned KOLs and US universities, to deepen the clinical experience and prepare to present Odne’s Technology Platform for debridement and obturation to the endo community at AAE 2024 in Los Angeles. Welcome Odne to the US.
46 Endodontic Practice US Volume 17 Number 1 PRODUCT SPOTLIGHT EP
This information was provided by Odne.
Odne™Fill Syringe (above). Odne™Fill Tip (left)
Light curing with OdneTMCure

Odne is Endo. Our innovations for debridement and obturation ease and accelerate minimally invasive endodontics. Preserving tooth structure. Inducing less trauma & risk. Transforming endo into a practice builder.
The first hydro-dynamic cavitation device using saline as main debridement medium1)

The first FDA cleared highly flowable, light-cured obturation material.

The first micro laser for light-curing inside the root canal.


www.odne.co 1) As of Feb 29th, 2024: FDA clearance for OdneClean is pending. OdneClean is not approved for clinical use in the US.
M-EA-0006-V1.0-ADV-EN-2403
min ISO 20.04 fluid hydrogel
curing complex shapes
Elevating your practice’s referral marketing: a comprehensive approach
Stacy Hill discusses establishing credibility and building long-term, genuine relationships with your referral network
In the realm of endodontic practice marketing, growth relies on incorporating these five essential components under the expansive marketing umbrella:
1. Website/SEO
2. Google reviews (Google Business Profile)
3. Social media
4. Print material
5. Referral marketing outreach
While not ranked in order of importance, consider this as a checklist to ensure a comprehensive approach. The bulk of time and financial resources needs to be allocated to Referral Marketing Outreach (No 5). Direct contact with the local dental community is the linchpin for exponential practice growth.
Before general dentists refer their patients to you, they must first KNOW, LIKE, and TRUST you. This is the North Star for both types of marketing strategies.
Referral
marketing strategies – two types
1. Referrer retention
A retention strategy, targeting existing referrers, proves cost-effective but falls short in addressing the inevitable churn rate. Churn rate occurs when referring doctors retire, relocate, keep procedures in-house, or move their referrals to another specialist. Focusing only on current referrers will inevitably lead to a contraction in your referral network.
2. Referrer acquisition
This is critical for sustainability and growth. It involves building relationships with new doctors, countering the churn rate, and ensuring a continuous influx of new referrals.
Strategic time management
To optimize efforts, focus on offices with the highest referral potential. Your practice management software, a valuable tool for data-driven marketing strategies, will aid in identifying emerging

Stacy Hill, a distinguished endodontic practice marketing specialist and the visionary founder of Endo Marketing Group, is dedicated to imparting cutting-edge marketing methodologies to endodontists and their teams through online training and coaching. Widely recognized as a sought-after speaker, she has delivered engaging lectures across the United States, focusing on dental specialty practice marketing. With 3 decades of invaluable marketing experience, including a transformative decade spent growing her husband’s endodontic practice, Stacy seamlessly combines her wealth of knowledge with passion for training, shaping her current role with precision and expertise.
Adoption Spectrum
referrers and shifts in referral patterns. Evaluating monthly and quarterly referral reports will help you monitor Adoption Spectrum movement within your referral network.
Monitor Adoption Spectrum movement
Watching the Adoption Spectrum movement within your referral network is the key to cultivating genuine, long-term relationships and retaining NEW referrers who continue to send patients.
• Awareness: If referring doctors are unaware of your practice, referrals will not materialize. Be present where it matters.
• Interest: Once aware, doctors seek information about you from mutual contacts, your website, social media, or your Google Business Profile.
• Trial: This is when the dentist moves from a cognitive state of being aware and informed to the emotional state of liking and hopefully preferring you.
• Adoption: This behavioral phase is when general dentists have adopted your practice as a regular referral option. Regular check-ins are crucial for relationship-building.
• Loyalty: In this phase, maintain regular communication to keep the entire office engaged.
Understanding the dynamic interplay between brand-building and strategic outreach is key. A robust brand establishes credibility, and referral marketing outreach serves as the driving force, propelling your practice to long-term success. This comprehensive approach guarantees not only survival but sustained growth in a competitive environment.
Enroll in a 45-minute on-demand marketing course tailored for endodontists (https://bit.ly/3T5mSA0). Discover effective techniques to enhance your reputation within your local dental community, foster long-term and genuine relationships, and establish a self-sustaining, data-driven marketing strategy. Leverage the resources already available at your practice to streamline these efforts, allowing you to focus on your expertise — patient care.
48 Endodontic Practice US Volume 17 Number 1 PRACTICE DEVELOPMENT
Endodontic Practice Marketing
RELEVANT
RELEVANT TRIAL TRIAL
HELPFUL
HELPFUL ADOPTION ADOPTION BE FRIENDLY BE FRIENDLY LOYALTY LOYALTY BE CONSISTENT BE CONSISTENT Hill, Stacy. Endo Marketing Group, Practice Marketing Adoption Spectrum. March 22, 2019. Image. https://EndoMarketingGroup.com EP
AWARENESS BE THERE BE THERE INTEREST INTEREST BE
BE
BE
BE

Sealing the deal on simpler root canals
ZenSeal™ Bioceramic Root Canal Sealer features high flowability and excellent sealability with zero shrinkage, while also reducing material waste per application
“Biocompatibility — it’s where the future of dentistry is going,” said Dr. Joseph Milholm, a practicing endodontist in Knoxville, Tennessee. Having experienced the challenge of residual moisture in the root canal before filling, he recently found solace in using Kerr’s ZenSeal™ Bioceramic Root Canal Sealer to seal the deal on his endodontic procedures.
“One of the main reasons I switched to using a bioceramic sealer is not having to worry if we didn’t get every ounce of moisture out of the canal before filling it, since the sealer is hydrophilic,” Dr. Milholm said. “With ZenSeal, even if there is still some moisture down the canal, we can ensure a good seal.”
Excellent sealing and biocompatibility
ZenSeal is a premixed, easy-to-use sealer that provides an optimal biocompatible environment for root canal tissues. Following the removal of infected pulp, it can be immediately inserted into the root canal using a convenient, singlesyringe delivery system with a disposable tip. Indicated for single cone or lateral condensation techniques, it adheres tightly to dentin and gutta percha with zero shrinkage.
“I think that ZenSeal checks off most of the boxes for what we want in a sealer,” said Dr. Milholm. “In my hands, it works exceptionally well.”
“After I have prepared and dried the canal, I thoroughly coat my cone with the sealer, push it down the canal and make it adhere to all the walls, place my cone, and seal it off at the orifice. Then, I use a plugger and pack it tight. It’s so quick and simple, and I feel confident it seals the canal well.”
Clinical and financial efficiency
Additionally, Dr. Milholm appreciates ZenSeal’s high flowability and radiopacity, as well as its effectiveness in reducing

Joseph Britton Milholm, DDS, is located in Chattanooga, Tennessee. He has 29 years of experience, and his specialties include endodontics and general dentistry. He graduated from the University of Alabama at Birmingham (UAB) in 1995, completed GPR at UAB in 1996, and received his Certificate in Endodontics from UAB in 1998. He started his practice in 1998. Dr. Milholm also is an Assistant Professor of Endodontics at Lincoln Memorial University College of Dental Medicine and practices at Fountain City Endodontics. He is now head of the Department of Endodontics at the Lincoln Memorial University (LMU) Dental School.

I
feel like I get more cases out of a full ZenSeal bioceramic syringe than a lot of the other sealers that I have used before.”
—
Dr. Joseph Milholm
waste per application. “The syringe tip’s design facilitates the sealer’s delivery into the canal without so much waste,” he added. “I feel like I get more cases out of a full ZenSeal bioceramic syringe than a lot of the other sealers that I have used before, and those cost savings are another major plus. It also cleans up much more easily than other products.” Dr. Milholm concluded, “I haven’t had any patients return to my office with adverse reactions to ZenSeal. This is just a fantastic product, especially as dentistry continues its shift toward biocompatibility.”
Make an appointment to speak with one of our Kerr Sales Specialists to learn about our NEW ZenSeal Bioceramic Root Canal Sealer, and try a sample. Visit https://go.kerrdental.com/ zenseal
50 Endodontic Practice US Volume 17 Number 1 PRODUCT PROFILE
This article was originally published
Dental Product
EP
This information was provided by Kerr Dental.
by
Shopper.
An Interconnected System elements™ Connect and Apex Connect
Dual Light Indicators With intuitive light indicators in both motor handpiece and the Apex file clip, you’ll have greater visibility for more confident shaping.
Patient Safety
The intuitive, easy-to-see smart light and audible indicators, as well as a large, bright viewing display alert you when you’re reaching the apex.
Portable Convenience
Easily move between operatories with this interconnected system; lightweight, ergonomic and cordless design.
AAE24



Shape with Confidence
Stop by Booth #519 and Get a Demo

elements™ Connect
Three motions in one motor
14 Settings Available-9 Kerr preset file settings, 1 reciprocating setting and 4 customizable settings.
Continuous Use-Comes with 2 removable and rechargeable batteries.

Apex Connect
Built-in Self Calibration that activates everytime the device is turned on.
Light and Audible Indicators for real-time working length information.
©2024 Kerr Corporation. All trademarks are property of Kerr Corporation. All Rights Reserved. MKT-23-0461 Rev 0
Freedom Day USA
Dr. Lou Shuman discusses how a lifetime of freedom can be repaid by giving a day for free
Every day, military men and women around the world are missing their families and risking their lives to protect our country. When they get back, despite their phenomenal service, they often quietly struggle to receive health and dental care. Eleven years ago, Dr. Robert Martino, CEO of Wilson Martino Dental, heard a touching testimonial about how much veterans endure to keep our country safe. He decided to show his appreciation in the best way he knew, by designating a day when his office would say thank you by providing free services to veterans. As the news spread about the incredible impact of his office’s day, the concept grew by leaps and bounds to become Freedom Day USA.
Over time, Freedom Day USA grew to having partners in every state with almost a million dollars in products and services donated. The concept was expanded so that non-dental businesses could partner with a dental team by donating door prizes or goods to be given at the dental office, or at their own location. Wendy Boyce, Vice President of Customer Relations for Wilson Martino Dental and Freedom Day USA National Director, notes that one local McDonald’s, whose franchise contains about 18 restaurants, gives veterans a free meal, as do Chick-fil-A and Honey Baked Ham. She says, “Our honored guests can eat hot dogs, and ice cream cones, all from our partner businesses for free. We have hair salons, manicure salons, a vision specialist and a chiropractor who provide services as well.”
Any company or practice, large or small, can help thank our military heroes. Vendors and large companies who support dental practices can extend an offer to a dental practice for free supplies or a service, such as one free lab fee. Boyce says, “We will communicate the offer to our participating dental providers, both local and national, and we connect them. Any company that provides Freedom Day USA support is included on our website, and all of the materials that we provide, as well as on our maps and social media.” She adds, “Many of our dental partners will print a flier to hand out to every patient who comes in the door that day with the names of companies who have partnered with them. That way participating companies get recognition for

Lou Shuman, DMD, CAGS, is the CEO of Cellerant Consulting Group, dentistry’s leading corporate incubator and accelerator bringing technologies into dentistry from all over the world. He is a venturer in-residence at Harvard’s i-Lab, co-founder of LightForce Orthodontics, founder of the Cellerant Best of Class Technology Awards, and just launched his third company, DSO Technology Solutions. He was selected in 2021 by Global Summits Institute as one of the World’s Top 100 Doctors.


whatever field they are in. If larger service or product providers want to offer services to dental offices, we can cultivate a flier offer that would go exclusively to Freedom Day dentists who are signed up for that year.”
Dr. Martino and his team realized that flexibility of scheduling would encourage more people to participate. Boyce explains, “The one-day restriction has been eliminated — businesses can
52 Endodontic Practice US Volume 17 Number 1 MILITARY MATTERS
Veteran patient at Cosmetic Dentists of Houston
Dr. John Wilfong at Wilson Martino Dental of Buckhannon
choose whatever day of the week works for them, do the whole week, pick one day, half a day, or even book one appointment for a military person, veteran, or family member.” She adds, “Our goal is to convey that Freedom Day is easy. Whatever you can do supports our mission.”
Any company or practice, large or small, can help thank our military heroes.
When a veteran comes in to get their teeth cleaned on Freedom Day, which to most people is not a big deal, it can change their perception of how people feel about them. Boyce continues. “It says to them, ‘you are heroes, and you should be treated that way.’” Besides the self-esteem issues, veterans also face obstacles to receiving medical and dental care. “Many veterans may not be eligible for full benefits, and some local VAs have very long waits. That’s the beauty of Freedom Day — to address their pressing issues immediately and hopefully get someone to a healthier state and in a positive atmosphere,” Boyce says.
Freedom Day USA in October 2023 was a huge success. Boyce says, “We definitely consider ourselves bounced back from the COVID

years, and in a steady growth pattern.” The 2023 event had 431 participants, doubling from the year before. Of the total, 106 dental offices across the US joined the appreciation event.
Joining Freedom Day USA is free-of-charge, and the process is simple. Once an office signs up, they are sent a digital media kit, complete with information, a planning guide, flyers, templates, and anything needed to plan a successful event. The templates are in electronic format so the office’s specific information can be entered easily. An enewsletter gives tips and information on creating a memorable and fun event. “We tailor all of our marketing items to their specific date, no matter what date they choose,” says Boyce.

The official date for 2024 Freedom Day USA is Thursday, October 10. This year, as a gift for participating, every dental team that signs up will receive an official Freedom Day USA custom scrub top with a unique Freedom Day print. More scrub tops are available, but one will be provided for free. There is no cost for signing up and no requirements about treatment provided. Boyce notes, “Our only request is that it is not an if/then offer — meaning, if you buy this, we will give you that because a true thank you is given freely from the heart from your practice.”
After 2023 Freedom Day, heartwarming stories came streaming in. Mequon Smile Design in Wisconsin helped a veteran celebrate his 100th birthday with dental services and enthusiastic congratulations. Dr. Martino’s schedule, in his West Virginia office, was full with a waiting list. Boyce said, “We found some pretty serious health conditions that were identified through Freedom Day screenings, so we saved some lives.” In North Carolina, Ballantyne Dentistry extended their offer to a full makeover for a patient, who now looks amazing. Practices receive thank you cards, and they create photo albums. Boyce says that team spirit is important and inspiring. “It is more impactful than anyone realizes. It feels so good that the whole team is giving back in appreciation for what those brave men and women have done for us. And the veterans turn around and appreciate right back. It’s a wonderful day.”
For more information, visit www.freedomdayusa.org/.
53 endopracticeus.com Volume 17 Number 1 MILITARY MATTERS
EP
Freedom Day became even more special when Mequon Smile Design in Wisconsin honored veteran Julian (pictured in the middle) on his 100th birthday and thanked him for his service
Veteran guest Daniel Hart at Wilson Martino Dental of Bridgeport
5 ways to help your practice reduce credit card processing fees
Matt Rej offers tips on how to mitigate the costs of accepting credit cards
Credit cards are convenient for patients and medical practices alike. It’s easy for dentists and specialists to collect payments immediately following an appointment in a way that their patients prefer. This helps keep accounts receivables low and simplifies the medical billing process.
While there’s no debating the convenience of card payments, many practices overlook the credit card processing fees eating into their bottom lines. Dental and specialty practices pay upwards of $7,500 to $12,000 or more on processing fees alone. These costs are often accepted at face value and typically rise over time.
The vast majority of medical practices can save money on credit card processing without switching processors or changing anything. There are five proven ways to reduce processing fees that can potentially save dentists and specialists tens of thousands each year.
1. Audit your statements
Take a look at your last three credit card statements. Credit card processors are notorious for adding extra fees and inflating bills in the hopes that these charges go overlooked. Line items for terminal fees, AVS fees, PCI compliance fees, IRS reporting fees, terminal fees, and gateway fees are all examples of inflated markups that don’t need to be included on the bill. Identifying and removing these unnecessary charges can instantly save you $2,500 to $4,000 annually.

2. Assess your contract
Beyond the extra charges, look for any inconsistencies from one statement to the next. If the statements are confusing and deceptive, there’s a chance your processor is trying to bury other hidden markups on your statements. It’s suspicious if the fees aren’t presented in a way that’s clear, logical, and easy to understand.

Matt Rej is the managing partner of Merchant Cost Consulting and has been since 2017. Located in Boston, Massachusetts, MCC has been exposing the payments industry since 2016 to help bring transparency to business to ensure they are on the most competitive pricing applicable to their needs. The typical cost savings MCC achieves its clients ranges from 20%-60% on the total fees they currently pay, often without the hassle of making any changes to their current setup. Matt is proficient in Interchange Optimization, Pin Debit Card Routing, Payment Processor Service Markup analysis, and MCC Interchange categorization.
Review the merchant agreement that you signed to start accepting credit cards. It’s a little bit easier to negotiate fees if the contract is nearing its expiration date. Processors don’t want to lose your business. They make money every single time a card is swiped, dipped, or tapped at your practice. Leveraging your contract expiration is a highly effective way to lower your fees.
It’s also worth comparing your contract terms against the statements you’ve audited. Some processors breach contracts by increasing rates or adding fees that weren’t part of the initial agreement. If your processor breached those terms, you’re entitled to compensation in the form of a refund for those overages.
3. Negotiate and push back
There are three components of credit card processing: interchange, assessments, and markups. Interchange fees and assessments are imposed at the card network level by Visa, Mastercard, Discover, and American Express. These are non-negotiable rates that must be paid to the card brand each time one of those cards gets used as a payment. Markups are charged by the processor, and those rates are completely negotiable.
It’s easier to negotiate these rates if you’re on an “interchange plus” pricing plan. This means that you pay the card network’s
54 Endodontic Practice US Volume 17 Number 1 FINANCIAL FOCUS
interchange “plus” the markups imposed by your processor. Everything other than the interchange fees and assessments can be negotiated. While processors are entitled to some fees for their role in facilitating the transaction, some of these markups are egregious and can often be cut in half.
4. Don’t switch processors
It’s a common misconception that switching processors will help save money on credit card processing. In reality, it’s usually more expensive. New processors will often ask to see what you’re currently paying and then undercut those rates to make their services seem more appealing. But then they inflate the processing rates by adding other markups to your statements. After a year or two, they’ll increase your rates, and you’ll end up paying more than you were with your old processor.
You’re much better off sticking with your current processor and just negotiating directly with them. If you aren’t getting anywhere in your negotiations, you can work directly with a merchant consultant to handle those conversations on your behalf. There’s no risk in going this route, as cost reduction firms aren’t compensated unless you save money.
5. Continue monitoring each statement
Even after you’ve successfully negotiated a reduction, you still need to make sure your statements have been adjusted appropriately. Unfortunately, many processors use deceptive tactics when dealing with merchants. So you can’t always take
While there’s no debating the convenience of card payments, many practices overlook the credit card processing fees eating into their bottom lines.
the word of a sales rep or customer service agent who promised a lower fee. Get everything in writing, and make sure those new rates are reflected on your next statement.
Furthermore, make sure that new hidden fees haven’t been added in place of the ones that were removed. Monthly monitoring is really the way to ensure that your negotiations have paid off, and it should be obvious that your total costs to process payments are lower. Rather than looking at just the fees, it’s often easier to calculate your “effective rate” as a more accurate representation of your average processing fees.1 This is a simple formula. Just divide the total amount that was deducted each month for processing by your total monthly sales. If this rate is higher or remains unchanged after your negotiations, then your processor is still doing something deceptive behind the scenes, and there’s more room to save money.
REFERENCE
1. O’Keefe C. Average Credit Card Processing Fees (2024). Merchant Cost Consulting. https://merchantcostconsulting.com/lower-credit-card-processing-fees/average-creditcard-merchant-fees/ (accessed January 16, 2024).
DocTalk Dental
LEARN through our interactive and captivating DocTalk Dental live interview series. DocTalk Dental is your source for thought leader interviews in endodontics. This series provides insightful and delightful conversations with top dental professionals. Each episode led by Lisa Moler, CEO and Founder of MedMark Media, takes a deep-dive into a different and intriguing area of dentistry.
• Simplifying Irrigation with Dr. Allen Ali Nasseh
• How To Leverage Your Dental Practice Real Estate
• Triton: All-In-One Irrigation Solution
• Demystifying Private Equity and SDSOs
WATCH NOW at https://endopracticeus.com/doctalk-dental/

55 endopracticeus.com Volume 17 Number 1 FINANCIAL FOCUS
EP
Connect. Be Seen. Grow. Succeed. | www.medmarkmedia.com
A collaborative shift
Dr. Michael Winick’s endodontic odyssey with Specialized Dental Partners
In the ever-evolving landscape of endodontics, stories emerge that transcend the routine narratives. Dr. Michael Winick, a seasoned endodontist, embarked on an unconventional path, entering endodontic residency at the age of 38, setting the stage for a remarkable career that found renewed vigor with Specialized Dental Partners (SDP).
From solo practitioner to partnership
His story begins with a unique twist — a late entry into endo school. This decision, while unconventional, laid the foundation for a successful solo practice in Canton, Ohio, opening in 2002. However, the trajectory of his career faced a pivotal juncture in 2021 when retirement loomed on the horizon.
The challenge of considering retirement at the peak of his professional stride prompted Dr. Winick to explore private equity-backed partnerships. He discovered SDP, and the encounter marked the inception of a transformative chapter in his practice. The decision to choose Specialized Dental Partners was influenced significantly by the qualities exhibited by the SDP team, such as their notable approachability and transparency at every level. These qualities set SDP apart, making it the preferred choice over other DSOs, as Dr. Winick valued the collaborative and supportive environment they provided throughout the transition and partnership journey. “Once I joined, I realized that it was more than just a retirement plan; it was going to be an exciting new chapter of practice,” Dr. Winick emphasized.
Operational transformations post-partnership
In 2021, formalizing the partnership marked a transformative phase for Dr. Winick’s practice. The shift brought not just a change in status but a reconfiguration of operations. Administrative responsibilities seamlessly shifted from Dr. Winick to the capable hands of the practice manager, Dodi Bachtel, and the adept team of business experts at Specialized Dental. This strategic move liberated Dr. Winick to dedicate his undivided


attention to patient care, a shift that significantly impacted the practice dynamics.
Engaging in Specialized Dental’s FLOW program, one of the many learning and development opportunities included with the SDP partnership, proved instrumental. Winick Endo experienced a surge in practice efficiency, a direct result of insights gained through the program. The ripple effect was evident in the increased daily patient intake and a discernible enhancement in the overall quality of patient care. Notably, Winick Endo grew 21% in 2023 over 2022. Best of all, they achieved that growth with no increase in staff or clinical days. They were working smarter, not harder.
Balancing professional and personal life
Dr. Winick’s story echoes practitioners’ sentiments, emphasizing work-life balance. Joining Specialized Dental Partners brought transformative change professionally and personally. “Once I became an endodontist, I was cruising along, but I worked in a silo. I viewed other endodontists in my area as my competitors. By partnering with Specialized Dental, I found my community and those competitors turned into collaborators, friends, and partners.”
Partnership with SDP is a journey that can bring efficiency, support, and community. Dr. Winick shows joining Specialized Dental Partners goes beyond a retirement plan — it’s a catalyst for professional and personal enrichment, harmonizing career success, and life outside the clinic.
To learn about partnership opportunities with Specialized Dental Partners, visit specializeddental.com.
56 Endodontic Practice US Volume 17 Number 1 ENDOSPECTIVE
Chair side with Dr. Michael Winick
Winick Endo’s Practice Manager, Dodi Bachtel, and patient EP



We’re proud to champion Dr. Posner and more than 300 elite dental specialists in our growing network. Since 2018, we’ve helped our partners focus on delivering exceptional patient care, while our business experts provide customized solutions to help streamline practice management. Find out how our powerhouse community of endodontists, periodontists, and oral and maxillofacial surgeons work together to champion your long-term prosperity.

Champion of Specialists Formerly US Endo Partners specializeddental.com Catch the full interview with Dr. Posner –Dr.
Partner from Bellevue Endodontic Associates | Bellevue, WA The future is bright!” me grow. to help a strong support team “I get to share a vision and a journey with highly engaged partners and
Lindsay Posner
PART OF THE ACE WORKFLOW
Everything you love about Brasseler USA’s minimally invasive XP-3D Shaper—now with an improved tip for optimal guidance and scouting.
✓ Transitions from an ISO# 15 to ISO# 30 within 1mm from the tip, functioning as a scouting and finishing file.
✓ Featuring our exclusive MaxWire® Technology, XP-3D Shaper+ adapts to the canal’s natural anatomy by expanding once exposed to body temperature.
✓ Adaptive Core™ Technology allows XP-3D’s smaller central core to move freely and adapt to the canal’s natural morphology.

SCAN QR CODE TO LEARN MORE &
Or visit www.XP-3D.com
A
Visit our website at BrasselerUSADental.com
To order call 800.841.4522 or fax 888.610.1937.


EP-04.24 ©2024 Brasseler USA. All rights reserved.
REQUEST
DEMO






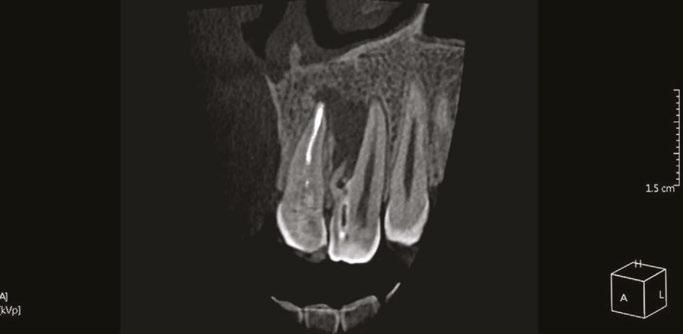








 Lisa Moler Founder/Publisher, MedMark Media
Lisa Moler Founder/Publisher, MedMark Media