Finding his true






PHARMACEUTICALS, SURGICAL SUPPLIES, GRAFTING & EXCEPTIONAL SAVINGS
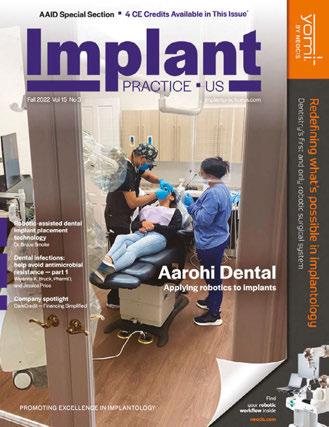
PROMOTING EXCELLENCE IN IMPLANTOLOGY FAQs Special Section n 4 CE Credits Available in This Issue* Winter
implantpracticeus.com
calling Dr. Alex Bachoura and his dental journey
2022 Vol 15 No 4
Communicating periodontal issues across dental implant platforms Drs. Stuart Segelnick and Mea A. Weinberg
Dental infections, part 2 — prophylaxis: help avoid antimicrobial resistance Wiyanna K. Bruck, PharmD, and Jessica Price Creating a memorable patient experience JoAn Majors



The leading Oral Surgery partnership group Our family of brands OS1partners.com I 305-206-7388 At OS1, we provide the resources needed to help you grow your practice. Our support will take the stress of practice management off your plate so you can focus on providing high-quality care to patients.
Editorial Advisors
Jeffrey Ganeles, DMD, FACD
Gregori M. Kurtzman, DDS
Jonathan Lack, DDS, CertPerio, FCDS

Samuel Lee, DDS
David Little, DDS
Ara Nazarian, DDS
Jay B. Reznick, DMD, MD
Steven Vorholt, DDS, FAAID, DABOI
Brian T. Young, DDS, MS
CE Quality Assurance Board
Bradford N. Edgren, DDS, MS, FACD

Fred Stewart Feld, DMD
Gregori M. Kurtzman, DDS, MAGD, FPFA, FACD, FADI, DICOI, DADIA
Justin D. Moody, DDS, DABOI, DICOI
Lisa Moler (Publisher)
Mali Schantz-Feld, MA, CDE (Managing Editor)
Lou Shuman, DMD, CAGS
© MedMark, LLC 2022. All rights reserved. The publisher’s written consent must be obtained before any part of this publication may be reproduced in any form whatsoever, including photocopies and information retrieval systems. While every care has been taken in the preparation of this magazine, the publisher cannot be held responsible for the accuracy of the information printed herein, or in any consequence arising from it. The views expressed herein are those of the author(s) and not necessarily the opinion of either Endodontic Practice US or the publisher.
ISSN number 2372-6245
The perfect smile
The first work by Leonardo Da Vinci that caught my attention was “The Skull c. 1489,” a sketch of the human skull. Frontal facing, sectioned in the midline with the left half showing the complete three-dimensional view and the right side showing a coronal section at the level of the mental foramen — the attention to detail is astonishing. The maxillary tooth in the coronal section is multirooted; the mandible is correctly sketched with an outer solid layer of cortical bone, while the inner layer is cavernous to depict medullary bone. The maxillary and frontal sinuses are accurately depicted. Its anatomical detail has withstood the test of time.
It’s as if Da Vinci were looking at a CBCT of a person and sketching the image on paper. But he wasn’t. In fact, his sketch predates CBCT technology by 500 years. So how did he do it? Was he merely a gifted artist? After all, his painting “The Mona Lisa” has been attributed the world’s most recognized smile.
Da Vinci was a gifted artist, but his true gifts surpassed taking pencil or brush to paper or canvas. His true gifts were rooted in his ability to observe his surroundings and develop a deep understanding of why things occur. Years of dissecting cadaver heads in the middle of the night in hospital basements deepened Da Vinci’s understanding of bony anatomy as well as inserting and attaching locations of facial muscles used in the process of smiling. His greatest gift, in my opinion, was his relentless pursuit of improvement. While there is no exact time frame for how long the “Mona Lisa” took to complete, in the biography, Leonardo Da Vinci, author Walter Isaacson states Da Vinci worked off and on this painting from 1503 to 1517 — 14 years for one work. A master unwilling to call his own work complete until he deems it perfect.
Observe. Innovate. Improve. As an oral surgeon committed to delivering optimal implant results to my patients, I use these three ideals to guide the continual evolution of my practice. Members of a patient’s dental implant team (restoring doctor, implant surgeon, dental laboratory technician) cannot be stagnant and unwilling to embrace at least some of the digital technology, which allows us to communicate more effectively, diagnose more completely, plan more precisely, and execute a treatment plan more accurately.
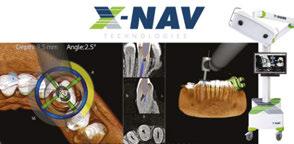
Da Vinci lived during the Renaissance, a period that saw a cultural rebirth of artistic, political, and economic ideals. Aren’t we, as oral health providers, living through a “Dental Renaissance”— a period when advancements in image acquisition (intraoral scanning, CBCT, digital photography, photogrammetry, facial scanning) and dental implant guided surgery (static guided surgery, dynamic navigation, robotic surgery) are allowing us to perform more complex dental implant procedures in a minimally invasive surgical manner to achieve more predictable, esthetic results than in any other time?
Leonardo Da Vinci would not recognize the world will live in today. Even with his fantastical imagination, he would probably not believe most of the creature comforts we have at our disposal. But what he would recognize and understand, what has not changed, and what should never change, is our pursuit of achieving the perfect smile for our patients.
Michael J. Hartman, DMD, MD
Michael J. Hartman, DMD, MD, completed his residency training in oral and maxillofacial surgery at the University of Maryland Medical Center in 2008. Dr. Hartman’s private practice — Hartman Oral & Maxillofacial Surgery — focuses on using cutting-edge technology to improve patient outcomes. He is also the president of Digital Provisionalization Technologies, specializing in provisional components using X-Guide® dental implant procedures.
1 implantpracticeus.com Volume 15 Number 4
Winter
n Volume 15 Number
INTRODUCTION
2022
4


2 Implant Practice US Volume 15 Number 4 TABLE OF CONTENTS CASE REPORT LOCATOR FIXED™ Attachment System
Xavier
Saab explains a new way to deliver fixed full-arch restorations utilizing traditional locator abutments and a new fixed attachment system
PERSPECTIVE Telling the world about you
Media 6 TECHNIQUE The benefits of “sticky” bone grafting with PRP
Garg
Gustavo
new formulation to predictably regenerate bone ......................... 15
Full-arch treatment using reverse concave neck implants to preserve crestal bone plus virtual planning through final prosthetics Drs.
achieving osseocompression and improving bone density during implant procedures .................... 18 FAQs SPECIAL SECTION Why are Boyd implant surgery chairs, carts, and cabinetry better than the competition? ........................................................ 24
FIXED™ Changing the edentulous landscape with LOCATOR FIXED ........................................................ 25 8 12 COVER STORY Finding his true calling
Dr.
E.
PUBLISHER’S
Lisa Moler, Founder/CEO, MedMark
Drs. Arun K.
and
Mugnolo discuss a
TECHNIQUE
Filip Ambrosio and Gregori M. Kurtzman discuss
LOCATOR
Renee Knight writes about Dr. Alex Bachoura and his dental journey Cover image of Dr. Alex Bachoura courtesy of PuraGraft.









4 Implant Practice US Volume 15 Number 4 TABLE OF CONTENTS
EDUCATION Dental infections, part 2 — prophylaxis: help avoid antimicrobial resistance
their discussion of concepts surrounding antibiotic prophylaxis
dentistry 31
DEVELOPMENT Creating a memorable patient experience JoAn
discusses working
a team toward case acceptance...................................... 36 EVENT RECAP Panthera Dental 10th Anniversary Celebration Adrienne Good, National Account Manager for Implant Practice US, recaps Panthera’s memorable event .................................................. 38 PRACTICE MANAGEMENT When medical insurance covers implant services Rose Nierman and Courtney Snow discuss common scenarios for medical reimbursement for implants ........................................... 40 Connect. Be Seen. Grow. Succeed. | www.medmarkmedia.com READ the latest industry news and business WATCH DocTalk Dental video interviews with KOLs LEARN through live and archived webinars RECEIVE news and event updates in your inbox by registering for our eNewsletter CONNECT with us on social media www.implantpracticeus.com 26 CONTINUING EDUCATION Communicating periodontal issues across dental implant platforms Drs. Stuart Segelnick and Mea A. Weinberg review typical challenges and management at the dental implant-abutment connection *Paid subscribers can earn 4 continuing education credits per issue by passing the 2 CE article quizzes online at https://implantpracticeus.com/category/continuing-education/
CONTINUING
Wiyanna K. Bruck, PharmD, and Jessica Price continue
in
PRACTICE
Majors
as
BONE GRAFTING PUTTY OSTEOSTIMULATIVE













NovaBone® is 100% synthetic, fully resorbable, and bioactive. Disposable uni-dose cartridges simplify dispensing of the graft, especially in hard-to-reach areas, thus facilitating minimally invasive techniques like ridge preservation and crestal-approach sinus lifts.








▼ NovaBone’s unique cartridge delivery system makes it an ideal choice for crestal sinus elevation. The 2.8 mm cannula attached to the cartridge is designed to fit directly into osteotomy. The hydraulic pressure created when the putty is being delivered to the site safely lifts the Schneiderian membrane.


Case
Step 1: An osteotomy is prepared to less than 1 mm from the sinus floor.
Step 2: An osteotome is then used to gently fracture the bone at the apex of the osteotomy.





Step 3: The cannula from the cartridge tip can be pressed against the surface of the bone, and the putty can then be injected into the area, resulting in membrane elevation with hydraulic pressure from the putty.

Step 4: An implant may then be placed in the augmented area.

To order, call
or go to osteogenics.com/NovaBone
1.888.796.1923
image courtesy of Dr. Philip M. Walton
1. Kotsakis GA, Mazor Z. A Simplified Approach to the Minimally Invasive Antral Membrane Elevation Technique Utilizing a Viscoelastic Medium for Hydraulic Sinus Floor Elevation. Oral
2. Mazor Z, Ioannou A, Venkataraman N, Kotsakis G, Kher U. Minimally Invasive Crestal Approach Technique for Sinus Elevation Utilizing
Cartridge Delivery
3. Mazor Z, Ioannou A, Venkataraman N, Kotsakis G. A
Sinus
Minimally Invasive Transcrestal Sinus Augmentation with
Cartridge System1,2,3
Kotsak
Maxillofac Surg. 2015 Mar;19(1):97-101.
a
System. Implant Practice. 2013;6(4):20-24.
Minimally Invasive
Augmentation Technique using a Novel Bone Graft Delivery System. Int J Oral Implantol Clin Res 2013;4(2):78-82.
NovaBone®
Impl
Telling the world about you
Our worlds are so busy with our time consumed with improving clinically, professionally, and personally. We work hard and hopefully find the time to play hard. From my view as a publisher of four and soon-to-be five dental publications, I see and hear about so much inno vation going on in the dental community. Dentists are show ing patients that dental health means better overall health, and there are so many ways to add technology, expand clinical options, and create your own new protocols and inventions that can change the face of your specialties. My team at MedMark is always searching for your stories — for your journeys, your successes, and even your speed bumps along the way. Entrepreneur Gary Vaynerchuk said, “Regard less of what you are trying to accomplish, you’ve got to tell the world about it.” I wholeheartedly agree. And that’s what we at MedMark Media have been doing over the past 17 years. We’ve been telling the world about you.
Published by Publisher
Lisa Moler lmoler@medmarkmedia.com
Managing Editor
Mali Schantz-Feld, MA, CDE mali@medmarkmedia.com Tel: (727) 515-5118
Assistant Editor
Moler Founder/Publisher, MedMark Media
Elizabeth Romanek betty@medmarkmedia.com
National Account Manager Adrienne Good agood@medmarkmedia.com Tel: (623) 340-4373
All of the new advancements in dental specialty fields are amazing — artificial intelligence (AI), virtual reality, 3D printing, robotics, the field of dental sleep medi cine, braces and aligners that move teeth faster and more efficiently, and imaging in 2D and 3D that makes diagnostics more precise. Advances in endodontic materials such as bioceramics contribute significantly to that specialty’s incredible growth. Let’s not forget implants — according to iData Research, over 3 million dental implants are placed each year in the United States, and the U.S. market is expected to exceed $1.5 billion in 2027.
Here’s more good news. In this issue of Implant Practice US, our Cover Story features Dr. Alex Bachoura, who operates five offices in the greater Houston area. With that many practices, he and his colleagues don’t have time for supply-chain constraints, so with PuraGraft as his distributor, he knows that he will be able to access all of the supplies that he needs to perform oral surgery. Our CE, written by Drs. Stuart Segelnick and Mea Weinberg, titled “Communicating periodontal issues across dental implant platforms,” explores common problems and manage ment at the dental implant-abutment connection. Part 2 of the CE by Wiyanna Bruck and Jessica Price titled “Dental infections, part 2 — prophylaxis: help avoid antimicrobial resistance” provides an overview of the cautious use of antibiotics in the dental office.
Back to you — how can we help you tell the world about your innovations, techniques, and life-changing treatments? Our articles and advertisers show you what is possible and practice changing, and promises to help differentiate you from the rest. To change Gary Vaynerchuk’s quote just a bit: Regardless of what you are trying to accomplish, MedMark is here to help you tell the world about it.
To your best success,
Lisa
Moler
Founder/Publisher
MedMark
Media
Sales Assistant & Client Services Melissa Minnick melissa@medmarkmedia.com

Creative Director/Production Manager

Amanda Culver amanda@medmarkmedia.com
Marketing & Digital Strategy Amzi Koury amzi@medmarkmedia.com
eMedia Coordinator Michelle Britzius emedia@medmarkmedia.com
Social Media Manager April Gutierrez socialmedia@medmarkmedia.com
Digital Marketing Assistant Hana Kahn support@medmarkmedia.com
Website Support Eileen Kane webmaster@medmarkmedia.com
MedMark, LLC
15720 N. Greenway-Hayden Loop #9 Scottsdale, AZ 85260
Tel: (480) 621-8955 Toll-free: (866) 579-9496 www.medmarkmedia.com
www.implantpracticeus.com
Subscription Rate
1 year (4 issues) $149 https://implantpracticeus.com/subscribe/
6 Implant Practice US Volume 15 Number 4 PUBLISHER’S PERSPECTIVE
Lisa
How to submit an article to Implant Practice US
Implant Practice US is a peer-reviewed, quarterly publication containing articles by leading authors from around the world. Implant Practice US is designed to be read by specialists in Periodontics, Oral Surgery, and Prosthodontics.
Submitting articles
Implant Practice US requires original, unpublished article submissions on implant topics, multidisciplinary dentistry, clinical cases, practice man agement, technology, clinical updates, literature reviews, and continuing education.
Typically, clinical articles and case studies range between 1,500 and 2,400 words. Authors can include up to 15 illustrations. Manuscripts should be double-spaced, and all pages should be numbered. Implant Practice US reserves the right to edit articles for clarity and style as well as for the limitations of space available.
Articles are classified as either clinical, continuing education, tech nology, or research reports. Clinical articles and continuing education arti cles typically include case presentations, technique reports, or literature reviews on a clinical topic. Research reports state the problem and the objective, describe the materials and methods (so they can be duplicated and their validity judged), report the results accurately and concisely, pro vide discussion of the findings, and offer conclusions that can be drawn from the research. Under a separate heading, research reports provide a statement of the research’s clinical implications and relevance to implant dentistry. Clinical and continuing education articles include an abstract of up to 250 words. Continuing education articles also include three to four educational aims and objectives, a short “expected outcomes” para graph, and a 10-question, multiple-choice quiz with the correct answers indicated. Questions and answers should be in the order of appearance in the text, and verbatim. Product trade names cited in the text must be accompanied by a generic term and include the manufacturer, city, and country in parentheses.
Additional items to include:
• Include full name, academic degrees, and institutional affiliations and locations
• If presented as part of a meeting, please state the name, date, and location of the meeting
• Sources of support in the form of grants, equipment, products, or drugs must be disclosed
• Full contact details for the corresponding author must be included
• Short author bio
• Author headshot
Pictures/images
Illustrations should be clearly identified, numbered in sequential order, and accompanied by a caption. Digital images must be high resolution, 300 dpi minimum, and at least 90 mm wide. We can accept digital images in all image formats (preferring .tif or jpeg).
Tables
Ensure that each table is cited in the text. Number tables consecutively, and provide a brief title and caption (if appropriate) for each.
References
References must appear in the text as numbered superscripts (not foot notes) and should be listed at the end of the article in their order of appear
ance in the text. The majority of references should be less than 10 years old. Provide inclusive page numbers, volume and issue numbers, date of publication, and all authors’ names. References should be submitted in American Medical Association style. For example:
Journals: (Print)
White LW. Pearls from Dr. Larry White. Int J Orthod Milwaukee. 2016;27(1):7-8. (Online)
Author(s). Article title. Journal Name. Year; vol(issue#):inclusive pages. URL. Accessed [date].
Or in the case of a book: Pedetta F. New Straight Wire. Quintessence Publishing; 2017.
Website:
Author or name of organization if no author is listed. Title or name of the organization if no title is provided. Name of website. URL. Accessed Month Day, Year. Example of Date: Accessed June 12, 2011.
Author’s name: (Single) (Multiple) Doe JF Doe JF, Roe JP
Permissions
Written permission must be obtained by the author for material that has been published in copyrighted material; this includes tables, figures, pictures, and quoted text that exceeds 150 words. Signed release forms are required for photographs of identifiable persons.
Disclosure of financial interest
Authors must disclose any financial interest they (or family members) have in products mentioned in their articles. They must also disclose any developmental or research relationships with companies that manufacture products by signing a “Conflict of Interest Declaration” form after their article is accepted. Any commercial or financial interest will be acknowl edged in the article.
Manuscript review
All clinical and continuing education manuscripts are peer-reviewed and accepted, accepted with modification, or rejected at the discretion of the editorial review board. Authors are responsible for meeting review board requirements for final approval and publication of manuscripts.
Proofing
Page proofs will be supplied to authors for corrections and/or final sign off. Changes should be limited to those that are essential for correctness and clarity.
Articles should be submitted to:
Mali Schantz-Feld, managing editor, at mali@medmarkmedia.com
Reprints/Extra issues
If reprints or additional issues are desired, they must be ordered from the publisher when the page proofs are reviewed by the authors. The pub lisher does not stock reprints; however, back issues can be purchased.
7 implantpracticeus.com Volume 15 Number 4 AUTHOR
GUIDELINES
Finding his true calling
Renee Knight writes about Dr. Alex Bachoura and his dental journey

Dr. Alex Bachoura is part of a successful oral and maxillofacial surgery group located in the greater Houston area. Here’s a look at his love for implant dentistry and how his group of five practices has over come the supply chain constraints that have impacted just about every industry over the past few years.
As a young high school student, Dr. Bachoura initially wanted to pursue a career as an aerospace engineer. Both his parents were engineers, so it just seemed natural to follow a similar path. He had an engineering mindset and an interest in the field, but the now oral surgeon dis covered he had a passion for dentistry at an unexpected place — the local jewelry store where he worked as a diamond setter.
His boss at the time, who didn’t have a background in dentistry, noticed Dr. Bachoura had a special talent. The high schooler not only loved working with his hands, but also clearly had an exceptional talent along with an impressive attention to detail. The jeweler suggested he look into dentistry as a career option rather than pursu ing aerospace engineering. So Dr. Bachoura did — and decided his boss was right — it became clear he was meant to take a different career path.
Dr. Bachoura found he loved the mechanical aspect of dentistry and knew he had the skills required to be suc cessful. “Believe it or not, there’s a lot of mechanics in the things we do. Like when we fix a jaw, it involves placing plates and screws. You have to understand the mechan ical aspects. It’s the same with placing dental implants,” Dr. Bachoura said. “For me, dentistry became a natural transition that allowed me to combine two things I really enjoy — mechanics and science. And there’s also the artistic element. You have to be good with your hands and know how to work with the materials. So, it all just came together.”
The road to oral surgery
Once he finished high school, Dr. Bachoura headed to the University of Southern California (USC) to earn his bachelor’s degree. He then went on to the USC School of Dentistry to obtain his DDS. That’s where Dr. Bachoura was first introduced to oral and maxillofacial surgery.
The school’s curriculum had a monthlong segment on oral surgery, and Dr. Bachoura was impressed with what he saw. He remembers watching the oral surgery team at USC repairing a jaw fracture using titanium plates and screws and knowing that was what he wanted to do. He
8 Implant Practice US Volume 15 Number 4 COVER STORY
Dr. Alex
practice by the numbers: 5 offices in the greater Houston area 7 full-time surgeons 60 employees 8,000 patients a year
Bachoura’s
picked it up quickly and decided his next step was to get the training he needed to practice oral surgery.
“I love the combination of the medical science and the mechanical/engineering aspect of what we do,” he said. “This is especially true when it comes to dental implants.”
After receiving his DDS in 2003, Dr. Bachoura moved on to the University of Texas Houston Medical School, graduating in 2007. He also completed an internship in General Surgery in Medicine and completed a 4-year oral and maxillofacial sur gery residency at the same institution as part of his training. He finished his residency in 2009 and has been a practicing oral surgeon ever since.
A look at his practice today
Dr. Bachoura is part of a five-office oral surgery group that has seven full-time surgeons and 60 employees. The practice serves more than 8,000 patients a year, both young and old, throughout the greater Houston area. The practices are full scope, with Dr. Bachoura and his colleagues performing wis dom teeth extractions, bone grafting procedures, facial trauma reconstructions, facial/dental tumor removal, and dental implant placement. His primary areas of interest include pathology, dentoalveolar surgery, dental implants, and maxillofacial trauma.
“I truly believe putting people out of pain and getting them back to productivity and normal, healthy lives are important,” Dr. Bachoura said. “I see patients from 2 years old all the way to 90-plus; at some point, every single human being will need some kind of oral surgical procedure. I feel like we are experts in the field of oral dental surgery.”
A focus on implants
Implant dentistry makes up 30% to 40% of the group’s busi ness, Dr. Bachoura said, and is one of the procedures he enjoys
performing most. He, of course, appreciates the mechanical aspect of surgically placing implants, as well as the challenges the cases present.
“For the most part, everything goes right, but when things go wrong, it can be pretty destructive. You really need to understand not just the surgical implant dentistry part, but how to salvage things when there’s an infection or another problem,” he said. “A lot of being an oral surgeon is having the capacity to deal with complex issues and bigger problems. I really enjoy the challenge of that.”
Over the years, Dr. Bachoura has seen a bit of a shift in implant dentistry, and one that’s for the better. General dentists who once restored only implants are now gaining the training and confi dence they need to start placing them, which has resulted in a boost for his practices.

“It means there’s a lot more awareness in the dental community of the benefit of implants,” he said. “They’re keeping more straightforward cases but sending the more complex cases they don’t have the skill set or knowledge to handle to oral surgeons, which has helped our business over the past few years.”
Overcoming supply chain issues
Like just about every business, dental practices have had to contend with supply chain constraints over the past few years, causing extra stress on doctors and their teams. That hasn’t been an issue for Dr. Bachoura and his colleagues, as the distributor they work with, PuraGraft, has done its part to ensure they have the products they need when they need them. PuraGraft carries a full line of grafting materials, pharmaceuticals, and all supplies necessary to perform oral surgery.
Get the details
To learn more about the PuraGraft products, including grafting materials, pharmaceuticals, and oral surgery sup plies, visit puragraft.com.

9 implantpracticeus.com Volume 15 Number 4 COVER STORY
Dr. Alex Bachoura treating a patient
Over the 8 years Dr. Bachoura and his team have worked with PuraGraft, they’ve gotten to know the team pretty well, espe cially their rep Drew Bailey, who Dr. Bachoura describes as personable and someone who really cares about his clients’ success. If he knows a product the offices use regularly will be on back order, he gives them a heads-up, so they can prepare. Unlike other practitioners he’s talked with, Dr. Bachoura and his colleagues are never left scrambling to find drugs or other products they need for surgery.
I love the fact that we have a personal relationship with them and can always pick up the phone and talk with a familiar person. If you need something, they go out of their way to make sure you get it. That’s why
had a long-lasting relationship.”
“They can foresee issues with supply chain interruptions, so we can stock up,” Dr. Bachoura said. “They’ll also give us alternatives; if they can’t get a particular drug we’ve been using, they’ll suggest another that does the same thing.”
Bailey and the team at PuraGraft not only have helped Dr. Bachoura navigate through supply chain interruptions, serving as a “crucial partner,” but also have offered exceptional customer service. And it helps that the company is local to Houston.
“When we order something, we get it the next day,” Dr. Bachoura said. “I love the fact that we have a personal relation ship with them and can always pick up the phone and talk with a familiar person. If you need something, they go out of their way to make sure you get it. That’s why we’ve had a long-lasting relationship.”
Pricing is also competitive, Dr. Bachoura said. Any time they find drugs from another source that are a little cheaper, PuraGraft almost always price matches.
Dr. Bachoura also appreciates the breadth of products the company offers; he said that the practice gets most everything they use on their patients from PuraGraft, including local anesthetics, IV drugs and antibiotics, bone-grafting materials, and biologic membranes. This makes purchas ing inventory more convenient, especially when you know the company will do what
it takes to ensure that you have access to the products you need. Certain IV antibiotics and biologic-grafting materials are among the products that have been difficult to find lately, Dr. Bachoura said, but the team at PuraGraft have worked their magic to deliver them.
“They’re very reliable,” he said. “We have never had any issues. And reliability is crucial in a world full of supply constraints.”
Life outside of dentistry
When Dr. Bachoura isn’t in the operatory performing complex surgeries, he likes to stay active. He spends a lot of time skiing, hiking, and running, and has even completed the Houston marathon several times. One of his favorite ways to spend his free time is restoring old vehicles, which is no surprise considering his interest in all things mechanical. He also recently started racing cars, a hobby that has helped him become an even better clinician.

“I love mechanical things,” he said. “I feel like racing cars gives me the opportunity to sharpen my skills and stay focused during operations.” IP

10 Implant Practice US Volume 15 Number 4 COVER STORY
Dr. Alex Bachoura getting ready for a race
we’ve



When quality and selection is what matters most, PuraGraft is the first choice for your oral surgery practice’s needs. Pharmaceuticals | Grafting | Surgical Supplies UNMATCHED SELECTION UNPARALLELED SERVICE SCAN HERE to download our catalog and order today PERSONALIZED SERVICE Receive an Account Manager and personalized shopping cart FREE, FAST DELIVERY Items shipped same day— no freight charges ONE-STOP SHOPPING Multiple product options to suit your needs and preferences www.puragraft.com I 877-540-3258
LOCATOR FIXED ™ Attachment System
Dr. Xavier E. Saab explains a new way to deliver fixed full-arch restorations utilizing traditional LOCATOR® abutments and a new fixed attachment system

Introduction
The treatment of edentulous arches with full-arch fixed dental prosthetics is the oldest form of restorations placed on root form endosseous implants as presented by Brånemark, et al., in 1977.1 Many different tech niques and philosophies of fixed full-arch restorations have been developed and described in the past 55 years, which include, but are not limited to, different types of restorative materials, implant numbers and angulations, management of the restorative space, healing protocols, and analog or digital workflows. Even though some of these variations of full-arch therapy may be clinically simpler to perform than others, the final prostheses usually require final insertion with prosthetic screws that make the prosthetic material easier to fracture and create the necessity to utilize materials to seal screw access holes. These issues increase the maintenance times and the potential for prosthetic complications throughout the life of the prostheses.

A.
Figures 1A and 1B: 1A. Pre-extraction records. Patient presented with periodontal con cerns and extensive decay. 1B. Six LOCATOR® Implants (Zest Dental Solutions) were placed in strategic positions for a future fixed-prosthesis option

A.
Imagine being able to design and build an FP-3 fullarch (fixed-detachable hybrid) prosthesis, utilizing the current techniques used to make a simple denture or overdenture. Imagine being able to deliver these pros theses with a single snap and perform maintenance and repair appointments without having to drill screw access covers, removing screws, choosing new screws, torqu ing the prosthesis, and resealing it after the required procedure.
B. B.
Figures 2A and 2B: 2A. A conventional prosthesis was fabricated with the intention to convert to a fixed prosthesis. 2B. LOCATOR FIXED housings were attached using intraoral pickup method and CHAIRSIDE Attachment Processing Material (Zest Dental Solutions)
This article presents a new, innovative, and simple technique to deliver fixed full-arch prostheses utilizing a proven and well-
Xavier E. Saab, DDS, MS, completed his residency and specialty training in Prosthodontics at The University of Texas Houston Health Science Center Dental Branch, where he received his Master of Science degree. Dr. Saab also completed residency rotation in the MD Anderson Cancer Center Department of Head and Neck Surgery. He serves as a Clinical Assistant Professor in the graduate program of the UTHHSC Dental Branch Department of Restorative Dentistry. Dr. Saab is highly renowned for lecturing and teaching continuing education to dentists around the world in Implant Dentistry and Prosthodontics.
Dr. Saab hails from a family of dental specialists and grew up assisting his father, a Periodontist. He completed his doctorate at the University of Guayaquil, Ecuador, as the valedictorian of his class and Magna Cum Laude graduate. Dr. Saab is an active member of the American College of Prosthodontists. He also trained at the Dawson Center for Advanced Dental Study. He enjoys treating senior patients, doing complete makeovers, and most of all, giving his patients their smiles back. In his free time, Dr. Saab enjoys reading and sculpting. Dr. Saab’s practice, Houston Prosthodontic Specialists, is located in the Memorial area of Houston, Texas.
Disclosure: Dr. Xavier Saab is a speaker and key opinion leader for Zest Dental Solutions.
known removable overdenture abutment (Zest LOCATOR®), with a new FDA-approved fixed prosthetic attachment (LOCA TOR FIXED™ Attachment System), while using traditional den ture fabrication procedures.
Patient background
Our patient presented with maxillary and mandibular ter minal dentitions. Different options were discussed with him for the replacement of his teeth, which included complete dentures, implant-retained overdentures, and fixed prostheses on implants. After considering the costs and benefits of each alternative, the patient decided to have all his remaining teeth removed and replaced with maxillary and mandibular implant-retained overdentures.
Initial treatment plan
Interim dentures were fabricated prior to the extractions. All remaining teeth were removed, alveoloplasty performed, and implants placed at the same appointment. The interim dentures were inserted immediately after surgery with a tissue-condi tioning reline material. The patient was allowed to heal for 4 months, then the implants were successfully tested for osse ointegration. LOCATOR abutments were selected and torqued as
12 Implant Practice US Volume 15 Number 4 CASE REPORT




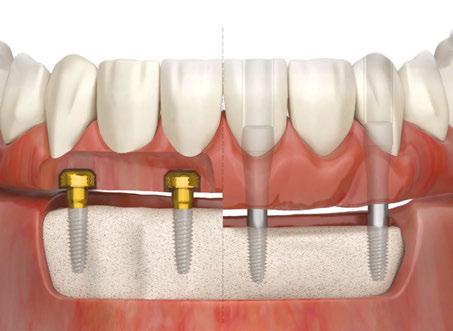
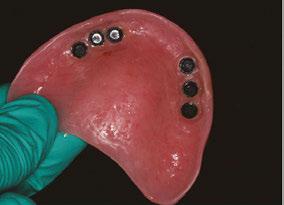
recommended by the manufacturer prior to beginning the definitive prosthetic treatment. Maxillary and man dibular implant-retained overdentures were fabricated using traditional indirect techniques. Both prostheses included metal frameworks for strength and long-term survival, and the LOCATOR housing was picked up chairside at the time of delivery.
Our patient reported to be very pleased with his new smile at the time of delivery. But after several adjustment appointments, he reported constant prob lems with his maxillary overdenture causing gagging and nausea after 1 or 2 hours of wearing his prosthesis. For over 1 year, he only wore his denture a few hours per day and at mealtimes, and he felt his quality of life had not improved since the time of extractions.

Revised treatment plan
We discussed the possibility of changing the type of prosthesis on the maxilla from removable to fixed. We explained to the patient the availability of a novel attachment system utilizing his existing LOCATOR abut ments, and he expressed excitement about the possibil ity. A new maxillary complete denture was fabricated around the LOCATOR abutment utilizing the indirect technique and conventional procedures. This time the denture did not have a metal-reinforcing framework since it will be converted into a fixed prosthesis.
Summary
Figures 3A and 3B: 3A. The prosthesis was trimmed and adjusted to eliminate the palate and flanges to convert into a fixed prosthesis. 3B. Processing inserts were replaced with LOCATOR FIXED (Zest Dental Solutions) inserts
For over 4 decades, the delivery of full-arch implant pros thetics has been a convoluted series of clinical and laboratory procedures that have made it challenging for the general prac titioner to make this therapy easily accessible to a great num ber of patients in need. The use of the traditional LOCATOR abutment with the LOCATOR FIXED Attachment System and
B. B. Implant Practice US 1 year $149 / 1 year digital only $79
Figures 4A and 4B: 4A. Before extractions and implants. 4B. After surgical procedures and prosthetic conversion into a fixed full-arch prosthesis

simple removable prosthetic techniques will make full-arch implant rehabilitation a more predictable and economical way to reach many underserved patients. It will allow more general dentists to grow personally and professionally. And it will make the hygiene, maintenance, and repair appointments simpler and more efficient for the general dental practice.
IP
REFERENCE
1. Brånemark PI, Hansson BO, Adell R, et al. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl.1977;16:1-132.
14 Implant Practice US Volume 15 Number 4 CASE REPORT
A. A. 3 REASONS TO SUBSCRIBE • 16 CE credits available per year • 1 subscription, 2 formats – print and digital • 4 high-quality, clinically focused issues per year 3 SIMPLE WAYS TO SUBSCRIBE • Visit www.implantpracticeus.com • Email subscriptions@medmarkmedia.com • Call 1-866-579-9496
The benefits of “sticky” bone grafting with PRP
Drs.
Arun K. Garg
and
Gustavo Mugnolo
discuss a new formulation to predictably regenerate bone

It has been more than 20 years since Drs. Arun Garg and Robert Marx developed the original formula for platelet-rich plasma (PRP), a vital wound-healing and regenerative agent that today is used by doctors in virtually every field of dentistry and medicine. In dentistry, the biologic assistance provided by PRP can facilitate bone healing under a range of implant-related procedures involving autogenous bone, allogeneic bone, syn thetic bone, and bone graft composites. This article describes a technique for using PRP in a unique formulation developed more recently by the authors to predictably regenerate bone and support implant placement without the need for autoge nous bone.
Sinus elevation bone grafting is a commonly performed pro cedure to increase maxillary bone height and width from the alveolar crest to the sinus floor for the support of one or more implants. Because of its osteogenic properties, autogenous bone remains the gold standard for this procedure and is the grafting material of choice for many surgeons.1,2 However, patients are often unwilling to accept this treatment method because of the added morbidity and potential complications associated with a second surgical procedure.
Bone allografts are obtained from human donors through tissue banks, accredited by the American Association of Tissue Banks, which screen, process, and store them under complete sterility.3,4 Allografts offer many advantages over autogenous bone grafts, including ready availability, avoidance of the need for a patient donor site, reduced time under anesthesia and in surgery, decreased blood loss, and fewer complications. Fresh allografts can be highly antigenic and generally are no longer used, but freezing or freeze-drying (lyophilizing) the bone sig nificantly reduces the antigenicity.5
The adjunctive use of liquid PRP to promote healing and increase bone volume has become a standard part of many
Arun K. Garg, DMD, completed his engineering and dental degrees at the University of Florida and completed his residency at the University of Miami/Jackson Memorial Hospital. Dr. Garg served as a full-time Professor of Surgery in the Division of Oral/Maxillofacial Surgery at the University Residency of Training Miami School of Medicine and as Director of the Program for 18 years.
Gustavo Mugnolo, DMD, PhD, MS, is a Board-certified oral surgeon who graduated first in his class from Cordoba National University in Argentina in 1990. In 1992, he completed a residency program in oral surgery at the Deutsche Clinic in Santiago, Chile. With a private practice limited to oral surgery and implant dentistry, he is regarded as a prominent oral surgeon in Argentina with a subspecialty in implants and related bone grafting
dental surgeons’ bone-grafting protocols, regardless of the graft ing material used. PRP contains growth factors that are believed to facilitate osteogenesis as well as cell adhesion molecules that enhance osteoconduction.6 A more recent application of PRP has been developed to exploit these benefits in a configuration that also takes advantage of the scaffolding properties of PRP’s fibrin component, which serves as a kind of intercellular high way that platelets creep along to form bone.

15 implantpracticeus.com Volume 15 Number 4 TECHNIQUE
Figure 1: Full-thickness flap raised to gain access to the lateral wall of the sinus (Two-stage sinus augmentation procedure using Garg sticky bone™)
Figure 2: The sinus membrane is detached to proper height from the medial wall of the sinus (Two-stage sinus augmentation procedure using Garg sticky bone™)
TECHNIQUE
This newer configuration, known variously as “Garg sticky bone™,” “sticky bone,” or “gummy bone,” is made by collecting the patient’s whole blood in a glass test tube and spinning it for an abbreviated cycle (about 3-4 minutes) to allow the com ponents to separate but not to fully clot. The result is a middle layer of concentrated platelets, leukocytes, and fibrin that is then used to hydrate particulated bone, in this case freeze-dried bone allograft (FDBA). After about 15 minutes, clotting will be com plete, and the result is “sticky bone.”
Excellent handling is the hallmark of Garg sticky bone™. Because it has the consistency of gummy bear candy, it can be easily molded into a surgical site and adapted to the shape of the bony defect. Furthermore, it maintains its 3D shape even after closure. The potency of sticky bone is excellent, providing approximately 5 times the baseline concentration of growth fac tors contained in whole blood.
Figure 4: The sinus cavity is completely grafted with Garg sticky bone until the material is flush with the level of the original lateral wall (Two-stage sinus augmentation procedure using Garg sticky bone™)
Garg sticky bone™ can be used effectively in place of liq uid PRP in sinus grafting, as shown in Figures 1 to 5. In this procedure, the lateral sinus wall is exposed via a broad-based, full-thickness mucoperiosteal flap, extending from the maxil lary tuberosity to a releasing incision in the canine fossa region. The flap should extend superiorly to just below the infraorbital foramen to provide access to the lateral wall of the sinus. A large oval finishing bur or diamond bur is used to create an oval hole in the lateral cortical bone for access to the sinus membrane. To preserve its integrity, the sinus membrane is directly reflected in a series of stages, beginning at the sinus floor — superiorly, anteriorly, and posteriorly around the edges of the oval entry — until the sinus membrane is completely elevated posteriorly to the tuberosity. PRP sticky bone is intro duced into the sinus to augment the alveolar ridge height. Note its excellent handling qualities. A PRP membrane can be used to close the oval window of the lateral sinus wall once the graft is in place.6
PRP’s growth factors enable the healing action of the end osteal osteoblasts and marrow stem cells that migrate from the bony sinus walls, while the allogeneic bone particles are bound by fibrin, fibronectin, and vitronectin, facilitating cell migration and bone regeneration. Using sticky bone in place of a standard bone graft makes this procedure easier and more predictable with accelerated healing.
IP
REFERENCES
1. Marx RE, Garg AK. Bone structure, metabolism, and physiology: its impact on denta limplantology. Implant Dent. 1998;7(4):267-276.
2. Marx RE, Armentano L, Olavarria A, Samaniego J. rhBMP-2/ACS grafts versus autogenous cancellous marrow grafts in large vertical defects of the maxilla: An unsponsored randomized open-label clinical trial. Int J Oral Maxillofac Implants. 2013;28(5):e243-e251.

3. Malinin T, Temple HT. Comparison of frozen and freeze-dried particulate bone allografts. Cryobiology. 2007;55(2):167-170.
4. Malinin TI, Carpenter EM, Temple HT. Particulate bone allograft incorporation in regen eration of osseous defects; importance of particle sizes. Open Orthop J. 2007;1:19-24.


Figure 5: The flap is then repositioned in place by means of tension-free single interrupted sutures (Two-stage sinus augmentation procedure using Garg sticky bone™)
5. Sheikh Z, Hamdan N, Ikeda Y, et al. Natural graft tissues and synthetic biomaterials for periodontal and alveolar bone reconstructive applications: a review. Biomater Res. 2017;21:9.
6. Garg AK. Autologous Blood Concentrates. 2nd ed. Quintessence Publishing; 2021.
16 Implant Practice US Volume 15 Number 4
Figure 3: The particulated FDBA graft material (OsteoLife Biomedical) is mixed with PRP to make Garg sticky bone (Two-stage sinus augmentation procedure using Garg sticky bone™)
Full-arch treatment using reverse concave neck implants to preserve crestal bone plus virtual planning through final prosthetics
Drs.
Filip Ambrosio and Gregori M. Kurtzman
discuss achieving osseocompression and improving bone density during implant procedures



Introduction
Full-arch implant prosthetics, referred to as “All-on-X,” have become a common option for treating either the edentulous arch or an arch that will be edentulous due to a failing remaining dentition. The goal typically is immediate provisionalization of the implants to provide a stable prosthesis during the integration phase and to not require the patient to wear a removal denture that may have minimal retention. With that in mind, selection of the implant would ideally utilize a design with deep aggressive threads. This will help to achieve osseocompression, thereby improving bone density around the implants when utilized in the less dense bone found in the maxilla. When employed in
Filip Ambrosio, DDS, MS, grew up in Rochester, New York, and attended college at the Rochester Institute of Technology. Next, he attended dental school at the University of Detroit, Mercy, completing his DDS degree in 2010. Dr. Ambrosio completed his education by earning a Master’s degree and Periodontal Surgery Certificate in 2017. Dr. Ambrosio is Board-certified with the American Board of Periodontics. He is also a member of the American Academy of Periodontology, the American Dental Association, the Seventh District Dental Society, and the New York State Dental Association’s peer review and quality assurance council. He has multiple publications in peer-reviewed journals and received the award for the most downloaded publication in 2018-2019 from the journal Clinical Advances in Periodontology.
Gregori M. Kurtzman, DDS, MAGD, FPFA, FACD, FIADFE, DICOI, DADIA, DIDIA, is in private general dental practice in Silver Spring, Maryland. He is a former Assistant Clinical Professor at University of Maryland in the department of Restorative Dentistry and Endodontics and a former AAID Implant Maxi-Course assistant program director at Howard University College of Dentistry. Dr. Kurtzman has lectured internationally on the topics of restorative dentistry, endodontics and implant surgery and prosthetics, removable and fixed prosthetics, and periodontics. Dr. Kurtzman has published over 800 articles globally, several ebooks, and textbook chapters. He has earned Fellowship in the AGD, American College of Dentists (ACD), International Congress of Oral Implantology (ICOI), Pierre Fauchard, ADI, Mastership in the AGD and ICOI and Diplomat status in the ICOI, American Dental Implant Association (ADIA), and International Dental Implant Association (IDIA). Dr. Kurtzman is a consultant and evaluator for multiple dental companies. He has been honored to be included in the “Top Leaders in Continuing Education” by Dentistry Today annually since 2006. Dr. Kurtzman can be reached at jdr_kurtzman@maryland-implants.com.
Disclosure: Drs. Ambrosio and Kurtzman report no financial interest in any of the companies mentioned in this article.
B A
1A. 1B. 2.
Figures 1A–2: 1A. The DSST generate a gentle and progressive vertical and horizontal bone compaction that enhances initial implant stability regardless of the bone type or quality. This preserves the vascularity of the osteotomy while maintaining the peri-implant marginal bone and soft-tissue. 1B. The ULT implant RCN (A) preserves a ring of marginal bone reducing stress on the crestal cortical bone. This prevents undesired vascular compression while preserving the peri-implant soft tissue. The platform switching (B), has a smaller diameter implant-abutment connection. This leaves space for the biologic width that limits bone resorption while stabilizing the soft tissue that ensures excellent papillary esthetics. The micro-grooves (A) provide mechan ical stimulus that helps preserve marginal bone, increase the surface area of the implant and the ability of an implant to resist axial loads. 2. The ULT implant bone platform switching preserves a ring of marginal bone reducing stress on the crestal cortical bone. This prevents undesired vascular compres sion while preserving the peri-implant soft tissue
the more dense bone of the mandible, the aggressive threads of the implant create a self-tapping effect, making insertion into the osteotomy easier. It is commonly accepted and supported by the literature that when insertion torque of 35 Ncm or greater is achieved, implants can be immediately loaded with a provi sional hybrid prosthesis during the initial healing and osseointe gration phase of treatment.1
A systematic review and meta-analysis of clinical success when higher insertion torque can be achieved showed no del eterious effect on implant survival rate or marginal bone loss.2 Overall implant survival has been reported up to 98% when the critical minimum insertion torque is achieved when immedi ately loading the provisional prosthetics.3,4 When four to eight implants are immediately loaded in the arch, and the accepted minimum insertion torque is achievable, a very high-clinical success has been reported.5,6
18 Implant Practice US Volume 15 Number 4 TECHNIQUE
TECHNIQUE
Selection of the implant
Selection of the implant may have an effect on the overall clinical success, especially when immediate loading is required. As previously mentioned, thread design on the implant has an effect on initial stability and is correlated to bone density at time of placement. The Ditron Ultimate Precision Implant (ULT™) is designed with double stressless sharp threads (DSST), which gen erate gentle progressive vertical and horizontal bone compaction upon insertion into the osteotomy (Figure 1A). This enhances initial implant stability regardless of the quality of bone present while preserving the bone vascularity.7
The authors recommend in lower density maxilla that the osteotomy diameter be underprepared so that the implant cre ates osseocompression, thereby densifying adjacent bone. For example, when the planned implant is 4.2 mm in diameter in Type III or IV bone (D3 or D4), the final drill diameter will be 3.2 mm drilled to the prescribed depth of the implant being placed. In Type I or II bone (D1 or D2), the final drill diameter utilized will be 3.8 mm In some instances, based on the bone type, the final drill may not go to depth. Additionally, the api cal aspect of the implant plays a factor on how the subsequent threads interact with the bone as the implant is threaded into the osteotomy. Helical apico-coronal slots (HACS) are present along
the length of the implant from below the micro-grooves to the apex. These slots help reduce resistance with the osseous walls of the osteotomy during insertion, allowing for collection of blood and bone chips from the osteotomy. These are drawn up, coating the surface of the implant, thereby creating a scaffold or matrix to accelerate osteoconduction during the initial phase of heal ing. The ULT implant has a cutting apex edge with progressive thread and sharp apical blades. Depending on the bone type and quality, this will act as a self-drilling, self-tapping feature to the implant design. The rounded apex itself improves ease of insertion, allowing mild directional refinement during the initial insertion of the implant into the osteotomy.
Maintenance of the crestal bone is important to the long-term success of the implant. Under function, the majority of loading occurs at the crestal portion of the implant.8 So, the thicker this bone is around the implant, the better the load handling and preservation of this critical bone over time. Frequently, the thin buccal crestal aspect of bone adjacent to the implant resorbs, which may contribute to soft tissue recession and resultant esthetic compromise. Given time, this may progress to peri-im plantitis and compromise the health of the implant. So, the thicker the bone is at crest on the buccal/palatal dimension and between implants or the implant and adjacent natural teeth, the easier it is to preserve that critical crestal bone long-term.9
With this in mind, the ULT implant is designed with a slight platform switch at bone level or slightly subcrestal upon place ment. But in addition, the reverse concave neck (RCN) provides what has been termed bone platform switching,10 a narrowed concave neck strategy to preserve additional marginal bone beyond the platform switch (Figure 1B). Enhanced bone volume at the cervical not only helps provide for greater resistance to bone resorption, but also reduces overall stress on the crestal cortex (Figure 2). Less titanium at the crest also helps to prevent removal of delicate marginal and subpapillary bone, providing the vascularity necessary for preservation of the peri-implant soft tissue.10
The combined strategy of platform switch and platform bone switch optimizes resistance to bone resorption, thereby stabiliz ing both hard and soft tissue elements.
Interestingly, the addition of microgrooves within the reverse concave neck provide a third bone preservation strategy, even

19 implantpracticeus.com Volume 15 Number 4
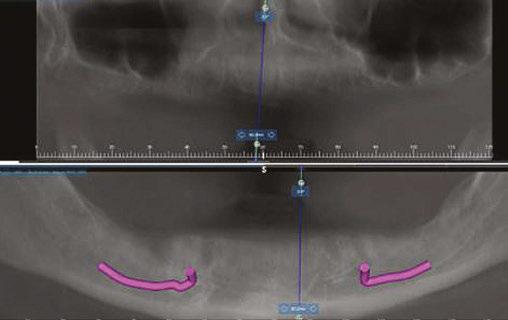
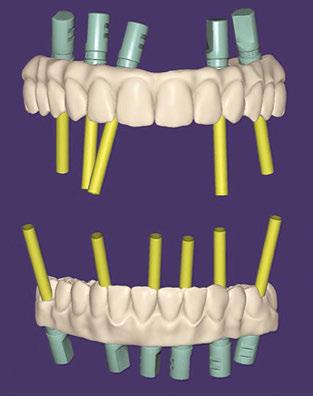
Figure 3: Preoperative panographic view of the maxillary and mandibular arches from the CBCT scan demonstrating anatomy that will impact implant placement
Figure 4: Extraoral scan of the full maxillary and man dibular dentures that patient presented with, which she was unable to wear due to a significant gag reflex
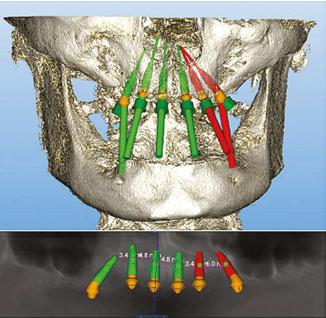
Figures 5A and 5B: Virtual planning of implant placement in the maxillary arch
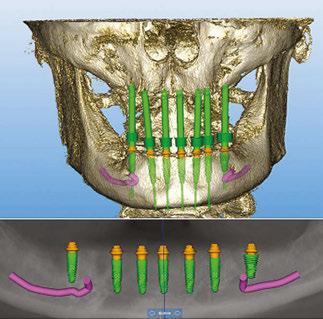
Figures 6A and 6B: Virtual planning of implant placement in the mandibular arch
TECHNIQUE
as it serves a favorable biome chanical purpose to increase implant surface area to reduce stress and promote maintenance of crestal bone under functional loading.11
Case report
A 49-year-old female patient presented with the chief complaint of her inabil ity to wear her current full maxillary and mandibular dentures due to a significant gagging reflex, indicating the dentures were delivered 2 years previously. She also expressed dissatisfaction with the current esthetics of the prosthesis and her smile. The patient’s general dentist had referred her for an implant consul tation. Her medical history was reviewed, and no significant health issues were disclosed.


Figures 7–9: 7. A printed replica of the scanned maxillary denture was fabricated as a surgical guide and a channel created to aid in placement in the arch. 8. White caps were placed in the implants and an impression taken of each arch using the patient’s current full dentures to get a rough VDO of the patient which were then scanned. 9. The virtual arches with white caps on the arches based on the scan of the implant impressions of the white caps utilizing the patient’s dentures as custom impression trays
x 11.5 mm), No. 11 (3.75 x 11.5 mm), and No. 14 (3.75 x 11.5 mm) (Figure 5B).
A CBCT scan was taken and panoramic views of the maxilla and mandible evaluated (Figure 3). Bilateral pneumatization of the maxillary sinus was noted, but adequate bone height was present between the premolars for implant placement to support an All-on-X hybrid prosthesis. In the mandibular arch, sufficient height was available between the mental foramen bilaterally and over the inferior alveolar nerve for implant placement to also sup port an All-on-X fixed hybrid prosthesis. A discussion was held with the patient that implants could be placed in both arches that would allow restoration with fixed prosthetics. Should sufficient insertion torque be achieved at the time of implant placement, a screw-retained hybrid provisional prosthesis would be placed and worn for several months during healing after which a final prosthesis would be fabricated. The patient would also be able to do a “trial-run” of the esthetics with the provisional prosthesis, with any requested modifications made when the final prosthesis was designed and fabricated. The treatment plan included six implants in each arch to support the planned hybrid prosthe ses. The patient was informed that reduction of the crestal bone would be required to achieve a flat ridge for adaptation of the prosthesis to the ridge as well as to provide adequate interarch space for the final prosthesis. The patient accepted the treatment plan. An intraoral scan of the arches was performed with Medit i500 (Medit Corp, Seoul, Korea) as well as the current complete arch maxillary and mandibular dentures (Figure 4). The patient was dismissed and scheduled for the surgical appointment.
The scans were imported into the planning software (Real GUIDE™, Allston, Massachusetts) and merged with the CBCT scan to allow implant planning. The maxillary arch was planned for implants at six sites, including tilted implants mesial to the maxillary sinus bilaterally to avoid the need for sinus augmen tation and allow more distal placement of the implant platform for a better anterior/posterior (A-P) spread (Figure 5A). ULT implants were planned as follows: No. 3 (3.75 x 11.5 mm), No. 6 (3.75 x 11.5 mm), No. 8 (3.75 x 11.5 mm), No. 9 (3.75
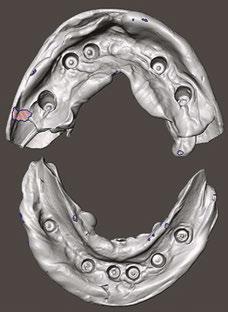
The mandibular arch was then planned for seven possi ble implants with the extra implant beyond what was initially planned should the short posterior implant on the patient’s left have less than ideal initial stability to provide better stability of the provisional prosthesis (Figure 6A). Ditron Dental ULT implants were planned as follows: No. 19 (3.75 x 11.5 mm), No. 20 (3.75 x 11.5 mm), No. 22 (3.75 x 11.5 mm), No. 24 (3.75 x 11.5 mm), No. 25 (3.75 x 11.5 mm), No. 27 (3.75 mm x 10 mm), and No. 30 (3.75 x 11.5 mm) (Figure 6B). A replica of the current dentures was fabricated to be used as a surgical guide, and the center of the replica was removed with a lab bur to create a zone for the implants to emerge to ensure they would be within the proper prosthetic zone (Figure 7).
The patient presented for surgery, and the consent form was reviewed and signed. IV sedation was initiated, and local anes thetic (2% Lidocaine with 1:100,000 epi) was administered in both arches. A crestal incision was made in the maxillary arch midcrest, and a full thickness flap was elevated to expose the buccal and palatal aspects of the ridge. Evaluation of the osseous ridge noted it was fairly flat, and reduction was deemed to be not necessary. The surgical guide was inserted and utilized to guide the location of the osteotomies. ULT implants were placed at the six planned sites: No. 3 (3.75 mm x 13 mm), No. 6 (3.75 mm x 10 mm), No. 8 (3.75 mm x 10 mm), No. 9 (3.75 mm x 11.5 mm), No. 11 (3.75 mm x 10 mm) and No. 14 (3.75 mm x 13 mm). Insertion torque of greater than 40 Ncm was achievable at five of the sites with site No. 10 being less than 30 Ncm and insuf ficient to support an immediate load. As sufficient A-P distance and adequate insertion torque was present utilizing the five other maxillary implants, it was decided to place an immediate provi sional hybrid prosthesis. Multi-unit abutments (MUAs) with the following angulations were placed: (No. 3 = 30 degrees, No. 6= 17 degrees, No. 8= 0 degrees, 11 = 17 degrees, and No. 14 = 30 degrees). The soft tissue was repositioned around the MUAs, and primary closure was achieved utilizing a continuous polylactic acid (PLA) suture.
20 Implant Practice US Volume 15 Number 4
TECHNIQUE
Figures 11 and 12: 11. Articulated virtual maxillary and mandibular provisional prostheses. 12. Panoramic view following implant placement, MUA attachment, and insertion of the provisional hybrid prostheses to document the initial clinical presence
A scalpel was then utilized to create a crestal incision in the mandible from the approximate first molar on the right to the approximate first molar on the left, and a full thickness flap was ele vated with identification of the mental nerve and its foramen bilaterally. As with the maxillary arch, the mandibular crestal bone was fairly flat, and ridge reduction was not needed. The surgical guide was inserted in the mandible and utilized to guide the location of the osteotomies. ULT implants were placed at six sites as: No. 20 (3.75 mm x 10mm), No. 22 (3.75 mm x 10m m), No. 24 (3.75 mm x 11.5 mm), No. 25 (3.75 mm x11.5 mm), No. 27 (3.75 mm x 10 mm) and No. 30 (3.75 mm x 10 mm). Insertion torque of greater than 40 Ncm was achievable at all of the sites. As sufficient adequate insertion torque was present, placement of an immediate provisional hybrid prosthesis was planned. MUAs with the following angulations were placed (No. 20 = 30 degrees, No. 22 = 0 degrees, No. 24 = 0 degrees, No. 25 = 0 degrees, No 27 = 0 degrees, and No. 30 = 0 degrees). The soft tissue was repositioned around the MUAs, and white protective caps were placed onto the MUAs. Primary closure was achieved, and a continuous PLA suture placed. The patients’ dentures were relieved to seat over the white caps, and a reline impression was taken with the two arches in occlusion to allow use of the current vertical dimension of occlusion (VDO) in the planned fabrication of the provisional hybrid restorations. The patient was dismissed and scheduled for postoperative check and suture removal in 2 weeks.

13 and 14: 13.
esthetics. 14. The maxillary


(Figure 10). The planned provisional hybrid prostheses were evaluated for esthetics and alignment of the midline in relation to the arches. The flange area was modified to convert the virtual prosthesis from a denture to a hybrid prosthesis (Figure 11). The virtual designed provisional hybrid prostheses were printed uti lizing Flexcera™ Smile resin (Desktop Health™, Newport Beach, California) with the EnvisionOne 3D printer (Desktop Health™).
The patient returned 2 weeks later to evaluate healing and for suture removal. She indicated general comfort during the initial healing period. Sutures were removed with slight bleeding noted related to the sutures, and soft tissue did not present with any significant inflammation. The printed immediate provisional prostheses were placed onto each arch and secured with the prosthetic screws to fixate them to the MUAs, and a panoramic radiograph was taken to verify seating of the prostheses and document the implants in relation to the anatomy (Figure 12). The occlusion on the provisional prostheses was checked and minor adjustments made intraorally for a more even occlusion upon occluding the arches. The patient was shown her provi sional smile and indicated that she was satisfied with the initial esthetics (Figure 13).
The tissue side of the impressions was scanned (Figure 8). The scan data was imported into the software (exocad), while the patient remained in the treatment operatory (Figure 9). Utilizing the planned implant positions, the information was merged, and analogs were added to the virtual models of the white protective cap scans. The scans of the current dentures with modifications to increase the VDO were added as well as projections for emergence of the screw access channels through the virtual prosthesis. The model was then removed virtually
The patient presented after 12 months of integration to initi ate fabrication of the final prostheses. A discussion occurred with the patient regarding the unloaded implant at site No. 10, where she expressed her anxiety regarding further surgery and asked if the case could be finalized on just the five implants in the arch as it “seemed” to be working with the provisional restoration. As the provisional was stable on the five implants and taking into account the patient’s desire not to have additional surgery to uncover the buried implant, the plan was modified to fabricate the prosthesis on the currently loaded implants in the maxilla. During further discussions with the patient regarding the esthet

21 implantpracticeus.com Volume 15 Number 4
Figures
View of the provisional hybrid prostheses inserted intraorally demonstrating natural
arch following removal of the provisional hybrid prosthesis
Figure 10: Virtual design of the provisional hybrid prostheses with the projection of the prosthetic screw access channels.
Figures 15-17: 15. The mandibular arch following removal of the provisional hybrid prosthesis. 16. The maxillary arch following insertion of the final monolithic zirconia hybrid prosthesis and sealing of the prosthetic screw access holes. 17. The mandibular arch following insertion of the final monolithic zirconia hybrid prosthesis and sealing of the screw access holes
ics of the provisional pros theses, she expressed that she wanted larger anterior teeth and that the current tooth shape was too rounded for her. She requested that a more square-shaped anterior tooth be used. That informa tion was communicated with the lab to modify the final prostheses. The lab modified the design virturally in the software and then milled the final monolithic zirconia hybrid prostheses for both arches.
Figures 18 and 19: 18. The patient smiling with the full-arch monolithic zirconia hybrid prostheses on the maxillary and mandibular arches. 19. Panorex of the final monolithic zirconia hybrid prostheses on the maxillary and mandibular arches
The patient returned for insertion of the final monolithic zirconia hybrid prostheses. The provisional restorations were removed, and minimal superficial inflammation was noted at the crestal top, which was felt to be due to the patient’s home care (Figures 14 and 15). Additional instruction on homecare under the prostheses would be given the patient at the end of the appointment after the final prostheses were inserted. The final monolithis zirconia hybrid prostheses were inserted, and the MUA prosthetic screws were hand tightened. A piece of teflon tape was placed into each screw access hole, and the hole was sealed with flowable composite (Figures 16 and 17). Occlusion was checked, and no adjustments were noted to be needed. After the patient was shown her teeth in a mirror, she expressed that she was more satisfied with the smile on the final prostheses. She said her smile appeared the way she remembered before the loss of her natural dentition (Figure 18). A panoramic radiograph was taken to document the final clinical results and verify com plete seating of the prostheses on the implants in both arches (Figure 19).
Conclusion
Implant treatment of the edentulous arch has challenges. Ide ally the plan is to immediately load the implant, which requires achieving implant insertion torque that is at or greater than the accepted value of 35 Ncm. Selection of the implant being uti lized plays a factor in achieving that desired insertion torque. The selected implant needs to have an aggressive thread to better engage the bony walls of the osteotomy and create osseocom pression in less dense bone to improve bone-to-implant contact (BIC) and initial implant stability.7 The platform switch and bone platform switching achieved with the reverse concave neck of
the Ditron Dental Ultimate Precision Implant permits added bone volume at the crestal aspect which is critical to maintain marginal bone, vascularity, and support for the peri-implant soft tissue under functional loading.

IP
REFERENCES
1. Alfadda SA, Chvartszaid D, Tulbah HI, Finer Y. Immediate versus conventional load ing of mandibular implant-supported fixed prostheses in edentulous patients: 10-year report of a randomised controlled trial. Int J Oral Implantol (Berl). 2019;12(4):431-446.
2. Lemos CAA, Verri FR, de Oliveira Neto OB, et al. Clinical effect of the high insertion torque on dental implants: A systematic review and meta-analysis. J Prosthet Dent. 2021;126(4):490-496.
3. Eckert SE, Hueler G, Sandler N, Elkattah R, McNeil DC. Immediately Loaded Fixed Full-Arch Implant-Retained Prosthesis: Clinical Analysis When Using a Moderate Inser tion Torque. Int J Oral Maxillofac Implants. 2019;34(3):737-744.
4. Caramês JMM, Marques DNDS, Caramês GB, Francisco HCO, Vieira FA. Implant Survival in Immediately Loaded Full-Arch Rehabilitations Following an Anatomical Classification System — A Retrospective Study in 1200 Edentulous Jaws. J Clin Med. 2021;10(21):5167.

5. Meloni SM, Tallarico M, Pisano M, Xhanari E, Canullo L. Immediate Loading of Fixed Complete Denture Prosthesis Supported by 4-8 Implants Placed Using Guided Surgery: A 5-Year Prospective Study on 66 Patients with 356 Implants. Clin Implant Dent Relat Res. 2017;19(1):195-206.
6. Slutzkey GS, Cohen O, Chaushu L, et al. Immediate Maxillary Full-Arch Rehabilita tion of Periodontal Patients with Terminal Dentition Using Tilted Implants and Bone Augmentation: A 5-Year Retrospective Cohort Study. J Clin Med. 2022;11(10):2902.
7. Greenberg A, Romanos GE. Effect of primary stability on short vs. conventional Ditron implants, Dept. of Perio Stony Brook University Poster Presentation AO; 2022
8. Oliveira H, Brizuela Velasco A, Ríos-Santos JV, et al. Effect of Different Implant Designs on Strain and Stress Distribution under Non-Axial Loading: A Three-Dimensional Finite Element Analysis. Int J Environ Res Public Health. 2020;17(13):4738.
9. Patil SM, Deshpande AS, Bhalerao RR, Metkari SB, Patil PM. A three-dimensional finite element analysis of the influence of varying implant crest module designs on the stress distribution to the bone. Dent Res J (Isfahan). 2019;16(3):145-152.
10. Carinci F, Brunelli G, Danza M. Platform Switching and Bone Platform Switching. J Oral Implant. 2009;35(5):245-250.


11. Yalçın M, Kaya B, Laçin N, Arı E. Three-Dimensional Finite Element Analysis of the Effect of Endosteal Implants with Different Macro Designs on Stress Distribution in Different Bone Qualities. Int J Oral Maxillofac Implants. 2019;34(3):e43–e50.

22 Implant Practice US Volume 15 Number 4
TECHNIQUE
RESORBABLE PERICARDIUM MEMBRANE


HIGHLY FLEXIBLE PROLONGED RESORPTION REMARKABLY
DURABLE
Exceptional Handling Properties

The OsteoFlex™ is easy to place and reposition. It has no memory and becomes highly flexible when hydrated. The membrane can adapt over grafted defect sites and be secured using our TriStar® screw system.
Can Be Stretched and Sutured
The OsteoFlex™ has a high tensile strength yielding a membrane with excellent resistance to suture pullout. Membrane can be used with our TriStar® tenting screw system to establish increased ridge height and width.
Naturally Extended Resorption
The OsteoFlex™ membrane achieves prolonged barrier function (over three months) while maintaining a naturally microporous collagen structure without any chemical crosslinkers ensuring optimal tissue integration.


www.impladentltd.com



Cross-Section View Surface View
Scan for references Remarkably Durable Highly Flexible
Call 800-526-9343 or Order Online at
FA Q SPECIAL SECTION
Why are Boyd implant surgery chairs, carts, and cabinetry better than the competition?
As the market leader for oral and dental implant surgery chairs and tables, Boyd equipment is best known for its ideal design combined with proven quality and reliability. The com pany’s dental surgery chairs are the industry standard for oral surgery, having been time tested over the company’s history during millions of surgical procedures.
To complement Boyd’s line of oral surgery chairs, the com pany offers a wide variety of mobile operatory carts designed to organize and store surgical items and devices. The carts are lightweight, easy to disinfect, and lockable with ergonomic handles to move between surgical suites.
Boyd designs and fabricates the widest variety of cabine try options to fit both the size, functionality, and style of your clinic. The cabinetry line of standard and custom designs sets the company apart from others in the dental implant industry. The company’s designers can adapt standard configurations or design cabinetry completely unique.
Do Boyd products meet all FDA and regulatory requirements?
Yes, our equipment meets all required regulatory standards for compliance. These include IEC 60601 safety standard for medical/dental devices, CSA for Canadian and CE for European.
As an internationally certified, ISO 13485:2016 company, Boyd goes through annual independent audits by British Stan dards Institute to assure it meets FDA, ISO, and all other regu latory standards.
What makes Boyd unique for Implant specialists?
We pride ourselves on providing our customers with the latest technology and innovations in Implant Dentistry. Our treatment chairs are ergonomically designed for dental implant procedures and can be configured specifically to the surgeons’ specifications.

Interested
Does Boyd offer financing options?
Boyd has a very competitive program for recent residency graduates and separating military members offering them signif icant product discounts or favorable payment terms.
What is the lead time for receiving Boyd equipment once I place an order?

Despite the volatility of today’s global supply chain, Boyd has been able to better manage its lead times because of the company’s U.S.-based factory and North American supply base. Boyd’s factory fabricates steel, plastic, upholstered wood, and many other components used in its products. The capability to directly manage much of the product content internally has allowed the company to maintain lead times to under 8 weeks.

Where can I see Boyd equipment on display?
Boyd attends industry trade shows to display and demon strate equipment. In addition to trade shows, Boyd has a prod uct showroom at our headquarters in Clearwater, Florida.
24 Implant Practice US Volume 15 Number 4 SPECIAL SECTION
in learning more? Please call our sales team at 727-471-5072, email us at sales@boydind.com for details, or scan the QR code.
LOCATOR FIXED
Changing the edentulous landscape with LOCATOR FIXED
Dr. John P. Poovey, DMD, DICOI, FADIA, FAAIP, is an early adopter of the LOCATOR FIXED full-arch solution from Zest Dental Solutions, the creator of the tried-and-true LOCATOR® attachment system. Having participated in the limited launch phases of the product rollout, Dr. Poovey has now focused on incorporating it into his daily patient treatment offerings.
Dr. Poovey addresses some key questions that clinicians are asking about the LOCATOR FIXED system from Zest.

How has LOCATOR FIXED changed your full arch patient offering?
Dr. Poovey: The biggest thing is that it creates a good middle ground where you have patients who have existing snap-ons, or you have patients who are interested in doing something fixed, but really are unable to come up with the price structure of a traditional fixed hybrid. So, what you are doing is capturing an untapped market of patients who really do not want to do a removable but cannot afford that pricier traditional fixed solu tion, or people who are in traditional snap-on overdentures and would like an alternative without starting from scratch.
Full-arch fixed prosthetics historically require more bone reduction and more complexity. In fact, prior to the introduc tion of LOCATOR FIXED, doctors who placed dental implants for overdentures with minimally invasive bone reduction were limited to overdentures, and if clinicians wanted to switch a patient from overdenture to fixed, they would essentially need to start all over again. LOCATOR FIXED has changed this paradigm.
When we talk with patients about snap-in overdentures, we explain to them that while it holds the denture in, it does not really change it from being a denture — it still walks and talks more like a denture. When we do a FIXED solution, they can experience a solution most like the teeth they used to have.
In fact, LOCATOR FIXED does not replace the traditional fixed hybrid screw-retained bridge; it is an additional offering that allows us to grow our practice by bringing in an untapped patient segment. At the end of the day, with LOCATOR FIXED, we are getting a higher level of case acceptance.
How can you use LOCATOR to build a full-arch practice and offer staged treatment planning?
Dr. Poovey: What’s great about LOCATOR FIXED is that it allows for treatment staging if you incorporate it up front. If we do a removable now, we can easily transition to FIXED later with the same implants and same LOCATOR abutments. Depending on the patient, I may need to place a couple more implants, but there is generally no bone reduction required. I just swap out the removable inserts and housings for LOCATOR FIXED. Just like that, the patient is converted from removable to FIXED.
How do you see LOCATOR FIXED changing the landscape for current and future edentulous patients?

Dr. Poovey: LOCATOR FIXED makes it much easier on both the patient and the dentist. The biggest thing is you can take patients in a removable appliance and easily move them into something FIXED. In doing so, you give them a permanent teeth-like solution.
Dr. Poovey: Traditionally, there has been a removable solu tion and then a costly fixed screw-retained solution, but noth ing in-between — until now. Historically, we did not have a solution to tap into that midrange market that wanted a perma nent tooth-like option but could not afford $30,000 per arch. They may be able to afford $12,000-$14,000 per arch, how ever. Now with LOCATOR FIXED, I can tap into that unserved patient population.
Dr. Poovey’s practice, JP Dental and Implant Center, has locations in Grand Junction and Glenwood Springs, Colorado. For more information on LOCATOR FIXED from Zest Dental Solutions, visit www.zestdent.com/locator-fixed.
FAQ SPECIAL SECTION

25 implantpracticeus.com Volume 15 Number 4 SPECIAL SECTION
™
Since offering LOCATOR FIXED in your practice, what benefits have you seen to the patients and practice?
Communicating periodontal issues across dental implant platforms
Drs. Stuart Segelnick and Mea A. Weinberg review typical challenges and management at the dental implant-abutment connection

Introduction
Dental implants have a record of long-term success with a cumulative survival rate of about 96% up to 10 years post-load ing.1,2 It is important to realize the various factors that can influ ence implant survival or failure. A higher rate of implant failure occurs in patients with a smoking history, hypertension without medication, and uncontrolled diabetes.3-5 In addition to systemic reasons, there are other properties of dental implants that could influence their long-term success, including crestal bone loss, placement of the platform at or below gingival margin, presence of excess cement from restoration cementation, presence of a microgap between the implant connector and the abutment, and non-submerged versus submerged implants. This article will review common problems and management at the dental implant-abutment connection.
Periodontal issues in implant failure
The first issue to consider is the location of the implant-abut ment connection (IAC) in regard to the bone level. This is important when considering that excessive marginal bone loss can result in implant failure.6,7 The question is whether there is a difference in success rates between having the platform placed below crestal bone (termed subcrestal implants), or at the level of bone (termed bone-level implants).6,8 There are mixed results regarding bone level placements that reduce marginal bone loss. Some articles found no difference if implants were placed at the level of bone or subcrestally.9,10,6 However, most articles, including a systematic review and meta-analysis article, found
Stuart
Northeastern Society of Periodontists
Second District Dental Society of New York SDDS Bulletin. Dr. Segelnick has co-edited five books on dentistry. He is a Diplomate of the American Board of Periodontology and the International Congress of Oral Implantologists. Dr. Segelnick is an Adjunct Clinical Professor at NYU Dentistry in the Department of Periodontology and Implant Dentistry.
Mea A. Weinberg, DMD, MSD, RPh, is a clinical professor in the Department of Periodontology and Implant Dentistry at New York University College of Dentistry. A Diplomate of the American Board of Periodontology, she has published many articles, chapters, and books on periodontics and pharmacology.

Educational aims and objectives
This self-instructional course for dentists aims to review com mon problems and management at the dental implant-abut ment connection.
Expected outcomes
Implant Practice US subscribers can answer the CE questions by taking the quiz online at implantpracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
• Understand how platform switching is important in pre serving crestal bone.
• Describe the microgap and its importance in implant failure.
• Describe how excessive cement around an implant crown can result in implant failure.
• Explain the role of keratinized tissue around the implant. Understand how non-keratinized mucosa around an implant can cause inflammation. Explain the oral hygiene process for implant care.
that subcrestal placement of implants is ideal because there is less chance for the implant to become exposed, thereby increas ing stability and reducing the risk of peri-implantitis.7,11 In the review article, it was concluded that recommendations are to place tissue level implants at the level of the crest and bone level implants subcrestally (Figure 1).12,13
Additionally, non-submerged implants stabilize the soft tis sue seal around the implant, preventing abutment movement that affects the soft tissue seal and thus preserving marginal bone.13 On the other hand, non-submerged implants cannot transfer stress or masticatory load as well as submerged implants (implants placed below the gingival margin), which can lead to marginal bone resorption.14 Non-submerged implants are ideal for immediate and early loading.
Standard platform implants that range in size from 3.5 mm to 4.2 mm in diameter are available in shorter lengths and narrower diameters, which is ideal for the anterior area. Wide platform implants are ideal for the posterior area; the sizes available are 4.5 mm to 6 mm. To prevent crestal bone loss, the question arises whether the abutment should be platform-matched, whereby the
26 Implant Practice US Volume 15 Number 4 CONTINUING EDUCATION
Segelnick, DDS, MS, is immediate past president of the American Association of Dental Editors and Journalists. He is editor of the
NESP Bulletin and the
2 CE CREDITS
abutment has the same diameter as the platform of the implant (Figure 2), or if the abutment should be platformed-switched (PLS), using a smaller diameter abutment on a larger diameter implant collar, mak ing the implant-abutment connection (IAC) more distinct (Figure 3).15 This type of connection shifts the perimeter of the IAC inward toward the central axis of the implant, allowing a thicker soft tissue cuff around the implant prosthesis, which is easier to maintain. Laz zara and Porter have hypothesized that shifting the IAC inward also shifts the inflammatory cell infiltrate inward and away from the crestal bone.16
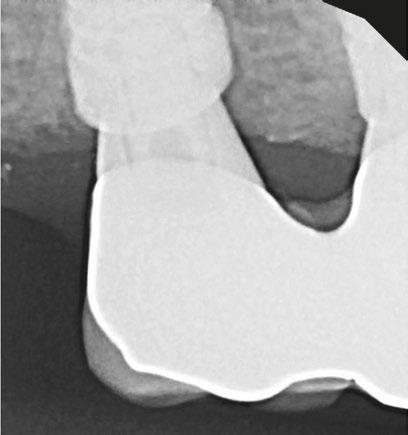
Platform switching, which was initially proposed by Gardner in 2005 and further described by Lazzara in 2006, is an IAC modification to control marginal bone loss (MBL) around an implant.16-18 Additionally, PLS is a process to improve long-term bone maintenance around implants as well as improved tissue response. A 2015 systematic review as well as the majority of more current articles conclude that the majority of clinical studies showed that there was significantly less mean MBL at implants with PLS versus platform-matching implant-abutment configuration.19,20 Mean crestal bone loss that was reported was 0.22 mm in platform-switched implants and 2.02 mm in nonplatform-switched implants. Also, the reduction of the abutment width by the platform circumferentially of 0.45 mm is sufficient to avoid peri-implant bone loss.15 Before placing implants, the surgeon should consider using platform-switching, which not only increases the distance between IAC and the crestal bone, but also increases the microgap to crestal bone distance and thus potentially preserving crestal bone.21
The microgap, the space between the implant and the abut ment, presents a reservoir of bacteria, and if in close proximity
to the bone, can result in peri-implantitis and bone loss.22 The bacteria adhere and proliferate in this gap causing an increase in inflammation around the IAC during soft tissue manipulation for the crown insertion and during function.22 Since there is no com plete seal at the IAC with any implant systems, it is ideal to have the smallest microgap between the implant and abutment and position it a distance from the outer perimeter of the implant. A pumping effect occurs when there is a larger microgap, allowing for bacterial movement inside and outside the connection during pressure changes as the restoration is loaded.6 A clinical review concluded that conical and mixed connections were better than implants with an external connector.22 An advantage of a onepiece implant is that there is no microgap; however, it must be cemented, and then there are possible problems with excess sub gingival cement that is not removed. Ideally, the smallest amount of bone loss that occurs around implants is when the microgap between the abutment and implant is placed 1–2 mm above the bone (supracrestally).6,23 Other studies have shown tissue level implants can be restored with a screw-retained crown.24 Differ ent studies found varied results relating the association of abut ment height and marginal bone loss. Long abutments showed less interproximal marginal bone resorption than shorter abut ments in screw-retained crowns and cement-retained crowns. It is speculated the decreased vertical height of the abutments

27 implantpracticeus.com Volume 15 Number 4 CONTINUING EDUCATION
Figure 1: Subcrestal placement of implant platform Figure 2: Platform is the same size as the abutment/crown screw down
The microgap, the space between the implant and the abutment, presents a reservoir of bacteria, and if in close proximity to the bone, can result in periimplantitis and bone loss.
would cause an encroachment on the supracrestal tissue attachment formation leading to an increase in bone loss around the implant.25,26
There are different implantabutment connection systems used to support a single or multiunit restoration with the purpose of reducing stress on the prosthetic component and on the bone-im plant interface and to provide good prosthetic stability.18 The platform may have an internal (internal hexagon, tri-lobe, and octagon) (Figure 4), conical (Morse taper), external (external hex), or tubein-tube connection.27 The internal connection is best to reduce bone loss and increase implant stability.6 The majority of articles concluded that dental implants with internal connections showed less MBL than implants with external connections, which was the result of platform switching.28,29 Moreover, abutment disconnection and reconnection multiple times were found to significantly cause marginal bone loss compared to implants with final abutment placement at the time of implant placement.30 Thus, it is recommended to limit the removal of the abutment once it is placed.
Levine, Present, and Wilson described complications with excess cement around dental implants, precisely at the resto ration-abutment connection. There are advantages and disadvantages of cement retention versus screw-retention crowns.31 Excessive remaining cement results in peri-implantitis which can lead to implant failure.32,33 Proper cementing technique is help ful to prevent excessive cement.34 Screw-retained restorations had 16.9% less inflammation than cemented restorations.35 One of the disadvantages of cement retention that can affect the IAC is the presence of excessive subgingival cement, and if the mar gins of the restorations were subgingival, particularly 2 mm or deeper, it made removal of excess cement difficult.36 Addition ally, the time after cementation to finding signs of peri-implant disease was from 6 weeks to 4 months but can be up to many years.36 It is recommended that the margin of a restoration be either supragingival or no more than 1.5 mm subgingival.31 Ideally, it is recommended to have the restoration-abutment connection far from the IAC to reduce marginal bone loss and not impede on the implants supracrestal tissue attachment (once known as biologic width).37


Most evidence supports that implants with non-keratinized tissue allow for more oral biofilm (plaque) accumulation, mar ginal tissue recession, marginal inflammation and patient dis comfort.38-41 One article found having < 2 mm of keratinized mucosa around an implant was a good indicator for future peri-implant disease.41
There are benefits in good oral biofilm control as well as regular professional maintenance visits in preventing periimplant disease.42 It is important to have the proper instruments such as plastic instruments or plastic sleeves on ultrasonic power scalers to prevent damage to the peri-implant tissues as well as the implant.44 Titanium or plastic brushes, curettes, scalers, and lasers have all been used effectively in oral biofilm removal. More recent professional oral hygiene recommendations to reduce peri-implant inflammation include use of glycine pow der air polishing and erythritol powder air polishing.45 Time must be taken to scale around implants due to the configuration of the restoration. When the emergence profile on a crown is ≥ 30 degrees and convex, it is more difficult to scale, thus increase the prevalence of peri-implantitis.46
Conclusion
There are many factors of the dental implant-abutment con nection that can influence periodontal issues. Management of these potential problems should be addressed when possible by placing the platform subcrestally, platform switching, using longer abutments to place the restorative margin closer to the gingival soft tissue margin, decreasing abutment disconnection and reconnection times, using screw-retained abutments, having adequate keratinized gingiva, and limiting bulbous prostheses. Including these factors in treatment planning can help reduce inflammation, marginal bone loss, and implant failure. Ulti mately, patients must be compliant with oral hygiene and mainte nance care to have better outcomes of implant success.
REFERENCES
1. Moraschini V, Poubel LADC, Ferreira VF, Barboza EDSP. Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: A systematic review. Int J Oral Maxillofac Surg. 2015; 44(3):377-388.
28 Implant Practice US Volume 15 Number 4 CONTINUING EDUCATION
Figure 3: Platform is larger than the abutment circumference
Figure 4: Internal hex implant. Photo by Ye Shi, BDS, MS IP
2. Howe MS, Keys W, Richards D. Long term (10-year) dental implant survival: A sys tematic review and sensitivity meta-analysis. J Dent. 2019:84:9-21.
3. Kasat V, Ladda R. Smoking and dental implants. J Int Soc Prev Community Dent. 2012;2(2):38-41.
4. Wu X, Al-Abedalla K, Eimar H, et al. Antihypertensive medications and the survival rate of osseointegrated dental implants: A cohort study. Clin Implant Dent Relat Res. 2016;18(6):1171-1182.
5. Wagner J, Spille JH, Wiltfang J, Naujokat H. Systematic review on diabetes mellitus and dental implants: an update. Int J Impl Dent. 2022;8(1).
6. Kowalski J, Lappinska B, Nissan J, Lukomaska Szymanska M. Factors influenc ing marginal bone loss around dental implants: a narrative review. Coatings. 2021;11(7):865.
7. Galindo-Moreno P, Catena A, Pérez-Sayáns, et al. Early marginal bone loss around dental implants to define success in implant dentistry: A retrospective study. Clin Implant Dent Relat Res. 2022; 24(5):630-642.
8. Esposito M. Impact of 0.5mm vs 1.5 mm subcrestal implant placement on marginal bone and aesthetics - 3-year results of a multicenter RCT. Clin Oral Implants Res. 2019;30(S19):31.
9. Nagarajan B, Murthay V, Lingstone D, Surendra MP, Jayaraman S. Evaluation of crestal bone loss around implants placed at equicrestal and subcrestal levels before loading: a prospective clinical study. J Clin Diagn Res. 2015;9(12): ZC47-ZC50.
10. Sargolzaie N, Zarch HH, Arab H, Koohestani T, Ramandi MF. Marginal bone loss around crestal or subcrestal dental implants: prospective clinical study. J Korean Assoc Oral Maxillofac Surg. 2022;30;48(3):159-166.
11. Chatterjee P, Shashikala R, Navneetham A. Comparative study of the crestal vs subcrestal placement of dental implants via radiographic and clinical evaluation. J Contemp Dent Pract. 2022;23(6):623-627.
12. Palacios-Garzón N, Velasco-Ortega E, López-López J. Bone Loss in Implants Placed at subcrestal and crestal level: A systematic review and seta-analysis. Materials (Basel). 2019; 12(1):154-173.
13. Saleh MHA, Ravidà A, Suárez-López del Amo, F, L GH, Asa´ad F, Wang HL. The effect of implant-abutment junction position on crestal bone loss: A systematic review and meta-analysis. Clin Implant Dent Relat Res. 2018;20(4):617-633.
14. Kim JC, Lee M, Yeo IL. Three interfaces of the dental implant system and their clini cal effects on hard and soft tissues. Mater Horiz. 2022;9(5):1387-1411.
15. Gupta S, Sabharwal R, Nazeer J, et al. Platform switching technique and crestal bone loss around the dental implants: A systematic review. Ann Afr Med. 2019;18(1):1-6.
16. Lazzara RJ, Porter SS. Platform switching: A new concept in implant dentistry for controlling postrestorative crestal bone levels. Int J Periodontics Restorative Dent. 2006;26(1):9-17.
17. Gardner DM. Platform switching as a means to achieving implant esthetics. N Y State Dent J. 2005;71(3):34-37.
18. Singla S, Kumar L, Rathee M. Know your implant connections. African Journal of Oral Health. 2018;6(2).
19. Strietzel FP, Neumann K, Hertel M. Impact of platform switching on marginal peri-implant bone-level changes. A systematic review and meta-analysis. Clin Oral Implantsl Res. 2015;26:342-358.
20. Tokgöz SE, Bilhan H. The influence of the implant abutment complex on mar ginal bone and peri-implant conditions: A retrospective study. J Adv Prosthodont. 2021;13(1):46-54.
21. Nayak R, Devanna R, Dharamsi AM, et al. Crestal bone loss around dental implants: platform switching vs platform matching – A retrospective study. J Contemp Dent Pract. 2018;19(5):574-578.
22. Lauritano D, Moreo G, Lucchese A, et al., The impact of implant-abutment connec tion on clinical outcomes and microbial colonization: a narrative review. Materials. 2020;13(5):1131.
23. Piattelli A, Vrespa G, Petrone G, et al. Role of the microgap between implant and abutment: A retrospective histologic evaluation in monkeys. J Periodontol. 2003;74(3):346-352.
24. Agustín-Panadero R, Bermúdez-Mulet I, Fernández-Estevan L, et al. Peri-Implant Behavior of Tissue Level Dental Implants with a Convergent Neck. Int J Environ Res Public Health. 2021; 18(10):5232.
25. Blanco J, Pico A, Caneiro L, Nóvoa L, et al., Effect of abutment height on interprox
imal implant bone level in the early healing: A randomized clinical trial. Clin Oral Implants Res. 2018;29(1):108-117.
26. Spinato S, Galindo-Moreno P, Bernardello F, Zaffe D. Minimum abutment height to eliminate bone loss: influence of implant neck design and platform switching. Int J Oral Maxillofac Implants. 2018;33(2):405-411.
27. Bittencourt ABBC, Neto CLMM, Penitente PA, et al. Comparison of the Morse Cone Connection with the Internal Hexagon and External Hexagon Connections Based on Microleakage - Review. Prague Med Rep. 2021;122(3):181-190.
28. de Medeiros RA, Pellizzer EP, Filho AJV, dos Santos DM, da Silva EVF et al. Eval uation of marginal bone loss of dental implants with internal or external connec tions and its association with other variables: A systematic review. J Prosthet Dent. 2016;116(4):501-506.
29. Kim DH, Kim HJ, Kin S, et al. Comparison of marginal bone loss between internaland external-connection dental implants in posterior areas without periodontal or peri-implant disease. J Periodontal Implant Sci. 2018;48(2):103-113.
30. Koutouzis T, Gholami F, Reynolds J, Lundgren T, Kotsakis GA. Abutment disconnec tion/reconnection affects peri-implant marginal bone levels: A meta-analysis. Int J Oral Maxillofac Implants. 2017;32(3):575-581.
31. Levine RA, Present S, Wilson Jr. TG. Complications with excess cement and dental implants: Diagnosis, recommendations and treatment of 7 clinical cases. Implant Realities. 2014;1:51-159.
32. Pesce P, Canullo L, Grusovin MG, et al. Systematic review of some prosthetic risk factors for periimplantitis. J Prosthet Dent. 2015;114(3):346-350.
33. Staubli N, Walter C, Schmidt JC, Weiger R, Zitzmann NU. Excess cement and the risk of periimplant disease – a systematic review. Clin Oral Implants Res. 2017; 28(10):1278-1290.
34. Reda R, Zanza A, Cicconetti A, et al. A systematic review of cementation techniques to minimize cement excess in cement—retained implant restorations. Methods Pro toc. 2022;5(1):9.
35. Agustín-Panadero R, Bustamante-Hernández N, Labaig-Rueda C, et al. Influence of biologically oriented preparation technique on peri-implant tissues; prospective randomized clinical trial with three-year follow-up. Part II: Soft tissues. J Clin Med. 2019;8:2223.
36. Linkevicius T, Vindasiute E, Puisys A, Peciuliene V. The influence of margin loca tion on the amount of undetected cement excess after delivery of cement-retained implant restorations. Clin Oral Implants Res. 2011;22(12):1379-1384.
37. Tokgöz SE, Bilhan H. The influence of the implant-abutment complex on mar ginal bone and peri-implant conditions: A retrospective study. J Adv Prosthodont. 2021;13(1):46-54.
38. Kungsadalpipob K, Supanimitkul K, Manopattanasoontorn S, et al. The lack of kera tinized mucosa is associated with poor peri-implant tissue health: a cross-sectional study. Int J Implant Dent. 2020;6(1):28.
39. Kamal, RK. Necessity of Keratinized Tissue Around Dental Implants to Maintain Peri-Implant Tissue Health: A Systematic Review. Dental Theses. 2018;33.
40. Saltz AE. Impact of keratinized mucosa in dental implant treatment. Decisions in Dentistry. 2020;6(8):40-44.
41. Grischke J, Karch A, Wenzlaff A, et al. Keratinized mucosa width is associated with severity of peri-implant mucositis. A cross-sectional study. Clin Oral Implants Res. 2019;30(5):457-465.
42. Cortellini S, Favril C, De Nutte M, Teughels, Quirynen M. Patient compliance as a risk factor for the outcome of implant treatment. Periodontology 2000. 2019; 81(1):209-225.
43. Gulati M, Govila V, Anand V, Anand B. Implant Maintenance: A Clinical Update. Int Sch Res Notices. 2014; 9:908534.
44. Baldi D, De Giorgis L, Menini M, Motta F, Colombo J. Efficacy of Instruments for Professional Oral Hygiene on Dental Implants: A Systematic Review. Appl Sci. 2022;12(1):26-44.
45. Tan SL, Grewal GK, Mohamed Nazari NS, Mohd-Dom TN, Baharuddin NA. Effi cacy of air polishing in comparison with hand instruments and/or power-driven instruments in supportive periodontal therapy and implant maintenance: a system atic review and meta-analysis. BMC Oral Health. 2022;22(1):85-102.
46. Yi Y, Koo KT, Schwarz F, Amara HB, Heo-SJ. Association of prosthetic features and periimplantitis: A cross-sectional study. J Clin Periodontol. 2020; 47(3):392-403.
29 implantpracticeus.com Volume 15 Number 4
CONTINUING EDUCATION
Continuing Education Quiz
Communicating periodontal issues across dental implant platforms
SEGELNICK/WEINBERG
1. Dental implants have a record of long-term success with a cumula tive survival rate of about ______ up to 10 years post-loading.
a. 82% b. 89% c. 96% d. 99%
2. A higher rate of implant failure occurs in patients with __________. a. a smoking history b. hypertension without medication c. uncontrolled diabetes d. all of the above
3. In addition to systemic reasons, dental implants’ long-term success could be influenced by crestal bone loss and placement of the plat form at or below gingival margin as well as __________.
a. presence of excess cement from restoration cementation b. presence of a microgap between the implant connector and the abutment c. nonsubmerged versus submerged implant d. all of the above
4. The ________, the space between the implant and the abutment, presents a reservoir of bacteria, and if in close proximity to the bone, can result in peri-implantitis and bone loss. a. microgap b. platform c. platform match d. none of the above
5. A _________ occurs when there is a larger microgap, allowing for bacterial movement inside and outside the connection during pres sure changes as the restoration is loaded. a. pressure gap b. pumping effect c. platform switch d. thicker soft tissue
6. Ideally, the smallest amount of bone loss that occurs around implants is when the microgap between the abutment and implant is placed _______ above the bone (supracrestally).
a. 1–2 mm
b. 3-4 mm
c. 5-6 mm d. 7-8 mm
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 16 CE credits for only $149; call 866-579-9496, or visit https://implantpracticeus.com/ subscribe/ to subscribe today.
n To receive credit: Go online to https://implantpracticeus.com/continuingeducation/, click on the article, then click on the take quiz button, and enter your test answers.
AGD Code: 490
Date Published: November 18, 2022 Expiration Date: November 18, 2025
2 CE CREDITS
7. Abutment disconnection and reconnection multiple times were found to significantly cause marginal bone loss compared to implants with final abutment placement at the time of implant placement. a. True b. False
8. Screw-retained restorations had _________ less inflammation than cemented restorations. a. 5.7% b. 16.9% c. 24% d. 45%
9. Additionally, the time after cementation to finding signs of periimplant disease was from __________. a. the day of placement up to 4 days after b. 1 week to a month after placement c. 6 weeks to 4 months but can be up to many years d. none of the above
10. When the emergence profile on a crown is _________ and con vex, it is more difficult to scale, thus increases the prevalence of peri-implantitis.
a. ≥ 10 degrees b. ≥ 30 degrees c. ≥ 40 degrees d. ≥ 50 degrees
To provide feedback on CE, please email us at education@medmarkmedia.com
Legal disclaimer: Course expires 3 years from date of publication. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
30 Implant Practice US Volume 15 Number 4 CONTINUING EDUCATION
Dental infections, part 2 — prophylaxis: help avoid antimicrobial resistance

Wiyanna
K. Bruck, PharmD,

and Jessica Price continue their discussion of concepts surrounding antibiotic prophylaxis in dentistry
Introduction
Use of antimicrobials in the field of dentistry is not limited to treating active dental infections. Many dentists prescribe antibiotics as a onetime dose prior to performing procedures. In fact, in the United States, general and specialty dentists are the third-highest prescribers of antibiotics in all outpatient settings.1 Moreover, looking at data from 2017 to 2019, it is estimated that somewhere between 30% to 85% of dental antibiotic prescriptions are “suboptimal or not indicated.”2-4 Appropriate use of antibiotics for prevention of infections surrounding dental procedures has received a lot of attention recently, which was illustrated by the American Dental Association (ADA) updating its antibiotic stewardship recommendations in the fall of 2020.5 It is well-known that antibiotics are one of the greatest medical advances that laid a foundation for an area of medicine, which has allowed once deadly infections to be readily treatable.6 However, excessive antibiotic use, even if it is just one dose, comes with consequences of side effects, antibiotic resistance, and superinfections like Clostridioides difficile.
Being attentive to appropriate antimicrobial prescribing is vital in all fields of healthcare, including dentistry, which is not limited to treatment, but also applies to antimicrobial prophylaxis.7,8 To aid in considering the threats of overusing antibiotics, but also being able to recognize when antibiotics are warranted, the Centers for Disease Control and Prevention (CDC) has constructed a Checklist for Antibiotic Prescribing in Dentistry (see
Wiyanna K. Bruck, PharmD, BCPS, BCIDP, BCPPS, is an assistant professor of Pharmacy Practice at South College School of Pharmacy as well as an Antimicrobial Stewardship and Emergency Medicine Clinical Pharmacist practicing at a community hospital. She teaches infectious diseases as well a pediatric pharmacotherapy to both pharmacy and physician assistant students. Dr. Bruck received her bachelor of science in biology, followed by a Doctorate of Pharmacy degree, and then completed a postgraduate pharmacy residency program at William Beaumont Hospital in Troy, Michigan. Her research interests include antimicrobial stewardship, infectious diseases, as well as food allergy awareness. Dr. Bruck is Boardcertified in pharmacotherapy, infectious diseases, and pediatrics.
Jessica Price is a Doctor of Pharmacy candidate at South College School of Pharmacy in Knoxville, Tennessee. She has a Bachelor of Arts degree in Advertising and Public Relations, with minors in Business and English Writing from the University of Central Florida. Price completed her post-baccalaureate track in Biology at Florida International University and at the University of Tennessee, Knoxville.
Educational aims and objectives
This self-instructional course for dentists aims to provide an overview of judicious use of antibiotics in the dental practice to avoid antimicrobial resistance.
Expected outcomes
Implant Practice US subscribers can answer the CE questions by taking the quiz online at implantpracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
• Observe some data regarding indications for appropriate use of antibiotics.
• Identify some ways to prevent transient bacteremia from dental procedures. Realize some published guidelines related to the preven tion of infective endocarditis.
• Recognize antibiotic prophylaxis in regard to prosthetic joint Infections.
• Identify some pediatric considerations in antimicrobial prophylaxis.
Table 1). This checklist serves as an excellent supplement to concepts surrounding antibiotic prophylaxis in dentistry that will be discussed in further detail.9
Prevention of transient bacteremia from dental procedures
There are antibiotic prophylaxis recommendations for two types of patients undergoing invasive dental procedures, which include those with heart conditions who may be at an increased risk of infective endocarditis and those with prosthetic joint(s) who may be predisposed to the development of a hematogenous infection at the site of the prosthetic(s). The oral cavity is colonized with numerous microorganisms that comprise between 300 to 600 species of bacteria, fungi, and protozoa. The rationale for antibiotic prophylaxis is to reduce or eliminate transient or intermittent bacteremia (bacteria in the bloodstream) caused by invasive dental procedures that might result in more severe infections for these high-risk patients.10 Theoretically, patients with certain conditions and/or a compromised immune system might not be able to mount an immune response adequate to clear intermittent bacteremia originating from their oral flora. However, the exact risk is unknown as transient bacteremia from everyday activities (e.g., brushing teeth, chewing) might pose
31 implantpracticeus.com Volume 15 Number 4 CONTINUING EDUCATION
2 CE CREDITS
Table 1: Checklist for antibiotic prescribing in dentistry
Pretreatment
• Correctly diagnose an oral bacterial infection.
• Consider therapeutic management interventions, which may be sufficient to control a localized oral bacterial infection.
• Weigh potential benefits and risk (i.e., toxicity, allergy, adverse effects, risk for Clostridioides difficile infection) of antibiotics before prescribing.
• Prescribe antibiotics only for patients of record and only for bacterial infections you have been trained to treat. DO NOT prescribe antibiotics for oral viral infections, fungal infections, or ulcerations related to trauma or aphthae.
• Implement national antibiotic prophylaxis recommendations for medical concerns for which guidelines exist (e.g., cardiac defects).
• Assess patients’ medical history and conditions, pregnancy status, drug allergies, and potential for drug-drug interactions and adverse events, any of which may impact antibiotic selection.
Prescribing
• Ensure evidence-based antibiotic references are readily available during patient visits. AVOID prescribing based on non-evidence-based historical practices, patient demand, convenience, or pressure from colleagues.
• Make and document the diagnosis, treatment steps, and rationale for antibiotics (if prescribed) in the patient chart.
• Prescribe only when clinical signs and symptoms of a bacterial infection suggest systemic immune response such as fever or malaise along with local oral swelling.
• Revise empiric antibiotic regimens on the basis of patient progress and, if needed, culture results.
• Use the most targeted (narrow-spectrum) antibiotic for the shortest duration possible (2 to 3 days after clinical signs and symptoms subside) for otherwise healthy patients.
• Discuss antibiotic use and prescribing protocols with referring specialists.
Patient Education
• Educate your patients to take antibiotics exactly as prescribed, take antibiotics only prescribed for them, and not save antibiotics for future illness.
Staff Education
• Ensure staff members are trained in order to improve probability of patient adherence to antibiotic prescriptions .
Reference: Printable checklist for antibiotic prescribing in dentistry available at: https://www.cdc.gov/oralhealth/infectioncontrol/faqs/antibiotic-stewardship.html
a higher risk for closed-spaced infections in these populations than transient bacteremia after a dental procedure in a patient without an active dental infection.11,13
Antibiotic prophylaxis: infective endocarditis
In 2008, the American Heart Association (AHA) published guidelines related to the prevention of infective endocarditis, which included guidance from the American Dental Associ ation (ADA).13 The first iteration of the guidelines were sup plemented with an updated scientific statement by the AHA in 2021.14,15 The scientific statement reaffirmed previous rec ommendations that prophylaxis is warranted in only a small subset of patients at highest risk of adverse outcomes. The recommendations consider the available evidence, weighing the benefits of preventing infective endocarditis with the risks, which include undue adverse effects as well as contribution to antimicrobial resistance. Moreover, these recommendations only apply to invasive dental procedures in which there is manipulation of the gingival tissue or periapical region of teeth, or perforation of the oral mucosa.16-18 The four broad categories of underlying conditions for which antimicrobial prophylaxis is advised are summarized in Table 2. The antibiotics suggested for use in those who are deemed to be at highest risk have empiric activity against the most common oral bacterial patho gens, most notably viridans group streptococci. The antibiotic regimen is chosen based on patients’ age, history of antibiotic allergy, and whether they can take oral medications (see Table
3). The antibiotic is given as a onetime by mouth dose 30 to 60 minutes prior to the invasive dental procedure; hence, prior to the dental appointment, patients would need to have a pre scription written with enough time to have it filled and admin istered. If the prescription is inadvertently not taken by patients before the procedure, then it can be given up to 2 hours after the procedure.19
One notable change in the 2021 AHA recommendations is that clindamycin has been removed from the options for pro phylaxis because it may cause more frequent and severe reac tions than other antibiotics used for prophylaxis.19 Clindamycin used to be the recommended prophylactic agent for patients with severe penicillin allergies. However, clindamycin has a listed a black box warning for Clostridioides difficile infection (CDI), which can be seen with onetime doses. The Minnesota Health Department found that patients were significantly more likely to have received a prescription for clindamycin in comparison to patients who received prescriptions from other non-dental providers. In this same study between the years of 2009 to 2015, it was found that 15% of patients with com munity-acquired CDI were treated by their dentist showing that a onetime prescription can produce undue downstream effects.20 The suggested alternatives for individuals unable to tolerate penicillin and β-lactam agents are azithromycin, clari thromycin, or doxycycline. If a patient has a non-IgE mediated allergy to penicillin or ampicillin, first- or second-generation cephalosporins can be chosen.19
32 Implant Practice US Volume 15 Number 4 CONTINUING EDUCATION
2:
• Transcatheter implanted prosthetic valves
• Annuloplasty, rings, or clips
• Left ventricular assist devices or implantable heart
Previous, relapse, or recurrent infective endocarditis
Congenital heart disease [CHD]
• Unrepaired cyanotic congenital CHD (including palliative shunts, conduits)
• Completely repaired defect with prosthetic material/device within 6 months after procedure
• Repaired CHD with residual defects at/or adjacent to the site of prosthetic material
• Surgical or transcatheter pulmonary artery valve or conduit placement
Antibiotic prophylaxis: prosthetic joint Infections
In contrast with antibiotic prophylaxis to prevent infective endocarditis, the ADA Council on Scientific Affairs concluded that “Evidence fails to demonstrate an association between dental procedures and prosthetic joint infections or any effectiveness for antibiotic prophylaxis.” Given this information in conjunction with the potential harm from antibiotic use, using antibiotics before dental procedures is not recommended to prevent prosthetic joint infections. Additional case control studies are needed to increase the level of certainty in the evidence to a level higher than moderate.21 Due to the paucity of available literature in this area, there may be individual scenarios when it is not apparent if antibiotic prophylaxis is indicated. In these cases, all patients, their risk of invasive infection due to oral pathogens after a dental procedure, as well as the risks and the benefits of antibiotic prophylaxis should be carefully weighed.21-26 However, the ADA guidelines cite that in cases where antibiotics are deemed necessary, it is most appropriate that the orthopedic surgeon recommend the appropriate antibiotic regimen and, when reasonable, write the prescription.
Pediatric considerations in antimicrobial prophylaxis
Pediatric dosing considerations for antimicrobial prophylaxis are also found in the AHA guidelines as seen in Table 3. Recommendations for pediatric patients are similar to adults with respect to empiric pathogen coverage, type of dental procedure warranting prophylaxis, and the use of a single oral prophylactic antibiotic dose. Clinicians should ensure the pediatric weightbased dose does not exceed a single adult dose.26 Pediatric patients are approached with less concrete guidance than adult patients, which has been described in separate documents. More discussion regarding pediatric patients with a compromised immune system who may be at an increased risk of complications of bacteremia are discussed in the Reference Manual of Pediatric Dentistry.16,27 In the Best Practice Report provided by the ADA Council on Scientific Affairs, it is mentioned that there is a lack of data to fully support antimicrobial prophylaxis as well
which high-risk patients should be considered for antimicrobial prophylaxis. Several additional conditions could also warrant prophylaxis for pediatric patients, including the following:
• immunosuppression secondary to human immunodeficiency virus (HIV)
• severe combined immunodeficiency (SCIDS)
• neutropenia
• cancer chemotherapy
• stem cell or solid organ transplantation
• history of head and neck radiotherapy
• autoimmune disease
• sickle cell anemia or other asplenia
• chronic high dose steroid use
• uncontrolled diabetes
• bisphosphonate therapy
• hemodialysis27
Additionally, if a patient undergoing an invasive dental procedure has a vascular shunt, a consultation with the child’s physician is warranted to guide the need for and selection of antibiotic prophylaxis.
Summary
It is not only imperative to be cautious with antibiotic overprescribing for the intended treatment of dental infections, but also equally important that careful consideration is taken prior to prescribing antibiotics for dental infection prophylaxis. Although prophylaxis is generally a onetime dose of antibiotics, there is still the potential for negative downstream effects of antimicrobial resistance and/or undue side effects. Table 1 provides a summary of tools that can be utilized to assist dental practitioners in curbing antimicrobial threats surrounding dental prophylaxis as well as dental infection treatment.
IP
REFERENCES
1. Durkin MJ, Hsueh K, Haddy Y, et al. An evaluation of dental antibiotic prescribing practices in the United States. J Am Dent Assoc. 2017;148(12):878-886.
2. Gross AE, Hanna D, Rowan SA, et al. Successful implementation of an antibiotic stewardship program in an academic medical practice. Open Forum Infect Dis. 2019;6(3): 1-6.
33 implantpracticeus.com Volume 15 Number 4 CONTINUING EDUCATION
Table
Underlying conditions for which antimicrobial prophylaxis is suggested (before certain dental procedures)19
Prosthetic cardiac valve or material
Cardiac transplant recipients who develop cardiac valvulopathy
Table 3: Single-dose antibiotics for prophylaxis prior to certain dental procedures: given 30 to 60 minutes prior to procedure19
Situation Antibiotic Single Dose for Adults
Able to take PO
Single Dose for Children¥
amoxicillin 2000 mg 50 mg/kg
Able to take PO, but allergic to penicillin or ampicillin cephalexin* 2000 mg 50 mg/kg
azithromycin 500 mg 15 mg/kg clarithromycin doxycycline 100 mg < 45 kg = 2.2 mg/kg > 45 kg = 100 mg
Unable to take PO (give agents IV or IM)ampicillin 2000 mg 50 mg/kg cefazolin∆» 1000 mg 50 mg/kg ceftriaxone∆» 1000 mg 50 mg/kg
IM = intramuscular; IV = intravenous; PO = oral
* Or other 1st or 2nd generation cephalosporin in equivalent adult or pediatric dosing
∆ Cephalosporins should not be used in patients with a history of anaphylaxis, angioedema, or urticaria with penicillin or ampicillin
» Allergic to penicillin or ampicillin and unable to take PO medications
¥ Pediatric weight-based dosing should NOT exceed adult single dose recommendations
3. Suda KJ, Henschel H, Patel MA, et al. Use of antibiotic prophylaxis for tooth extractions, dental implants, and periodontal surgical procedures. Open Forum Infect Dis. 2018;5(1): 1-5.
4. Loffler C, Bohmer F. The effect of interventions aiming to optimise the prescription of antibiotics in dental care: a systematic review. PLoS One. 2017:12(11):1-23.
5. American Dental Association. Oral health topics: Antibiotic prophylaxis prior to dental procedures. American Dental Association website. Last updated January 5, 2022. Available at: https://www.ada.org/resources/research/science-and-research-institute/ oral-health-topics/antibiotic-prophylaxis Accessed October 27, 2022.
6. Macfarlane G. Alexander Fleming: The Man and the Myth. Harvard University Press; 1984.
7. Fluent MT, Jacobsen PL, Hicks LA. Considerations for responsible antibiotic use in dentistry. J Am Dent Assoc. 2016;147(8):683-686.
8. Dana R, Azarpazhooh A, Laghapour N, Suda KJ, Okunseri C. Role of dentists in prescribing opioid analgesics and antibiotics: an overview. Dent Clin North Am. 2018;62(2):279-294.
9. Centers for Disease Control and Prevention. Printable Checklist for Antibiotic Prescribing in Dentistry: https://www.cdc.gov/oralhealth/infectioncontrol/faqs/antibiotic-stewardship.html. Accessed October 27, 2022.
10. American Dental Association. Oral health topics: Antibiotic prophylaxis prior to dental procedures. American Dental Association website. Last updated January 5, 2022. Available at: https://www.ada.org/resources/research/science-and-research-institute/ oral-health-topics/antibiotic-prophylaxis Accessed October 27, 2022.
11. Duval X, Leport C. Prophylaxis of infective endocarditis; current tendencies, continuing controversies. Lancet Infect Dis. 2008; 8:225-232.
12. Goff DA, Mangino JE, Glassman AH, et al. Review of guidelines for dental antibiotic prophylaxis for prevention of endocarditis and prosthetic joint infections and need for dental stewardship. Clin Infect Dis. 2020;71(2):455-462.
13. Wilson W, Taubert KA, Gewitz M, et al. Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. J Am Dent Assoc. 2008;139(suppl):3S-24S.
14. Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients with Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135(25): e1159-e1195.
15. Wilson WR, Gewitz M, Lockhart PB, et al. Prevention of Viridans Group Streptococcal
Infective Endocarditis: A Scientific Statement from the American Heart Association. Circulation. 2021;143:e963-e978.
16. Loyola-Rodriguez JP, Franco-Mrianda AF, Loyola-Leyva A, et al. Prevention of infective endocarditis and bacterial resistance to antibiotics: A brief review. Spec Care Dentist. 2019;39:603-609.
17. Goff DA, Mangino JE, Glassman AH, et al. Review of guidelines for dental antibiotic prophylaxis for prevention of endocarditis and prosthetic joint infections and need for dental stewardship. Clin Infect Dis. 2020;71(2):455-462.
18. Chen TT, Yeh YC, Chien KL, et al. Risk of infective endocarditis after dental treatments. Circulation. 2018; 138(4):356-363.
19. Thornhill MH, Dayer M, Lockhart PB, Prendergast B. Antibiotic prophylaxis of infective endocarditis. Curr Infect Dis Rep. 2017;19(2):9.
20. Bye M, Whitten T, Holzbauer S. Antibiotic Prescribing for Dental Procedures in Community-Associated Clostridium difficile cases, Minnesota, 2009-2015. Open Forum Infect Dis. 2017;4(Suppl 1):S1.
21. Sollecito TP, Abt E, Lockhart PB, et al. The use of prophylactic antibiotics prior to dental procedures in patients with prosthetic joints: Evidence-based clinical practice guideline for dental practitioners — a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2015;146(1):11-16 e8.
22. Watters W 3rd, Rethman MP, Hanson NB. Prevention of Orthopaedic Implant Infection in Patients Undergoing Dental Procedures: J Am Acad Orthop Surg. 2013;21(3): 180-189.
23. Rethman MP, Watters W,3rd, Abt E, et al. The American Academy of Orthopaedic Surgeons and the American Dental Association clinical practice guideline on the prevention of orthopaedic implant infection in patients undergoing dental procedures. J Bone Joint Surg Am. 2013;95(8):745-747.
24. Meyer DM. Providing clarity on evidence-based prophylactic guidelines for prosthetic joint infections. J Am Dent Assoc. 2015;146(1):3-5.
25. American Dental Association-Appointed Members of the Expert Writing and Voting Panels Contributing to the Development of American Academy of Orthopedic Surgeons Appropriate Use Criteria. American Dental Association guidance for utilizing appropriate use criteria in the management of the care of patients with orthopedic implants undergoing dental procedures. J Am Dent Assoc. 2017;148(2):57-59.
26. Quinn RH, Murray JN, Pezold R, Sevarino KS. The American Academy of Orthopaedic Surgeons Appropriate Use Criteria for the Management of Patients with Orthopaedic Implants Undergoing Dental Procedures. J Bone Joint Surg Am. 2017;99(2):161-163.
27. American Academy of Pediatric Dentistry. Antibiotic prophylaxis for dental patients at risk of infection. The Reference Manual of Pediatric Dentistry. American Academy of Pediatric Dentistry. 2019:416-421.
34 Implant Practice US Volume 15 Number 4 CONTINUING EDUCATION
Continuing Education Quiz
Dental infections, part 2 — prophylaxis: help avoid antimicrobial resistance BRUCK/PRICE
1. In the United States, general and specialty dentists are the _______ prescribers of antibiotics in all outpatient settings.
a. highest b. second highest c. third highest d. fourth highest
2. Looking at data from 2017 to 2019, it is estimated that somewhere between 30% to _________ of dental antibiotic prescriptions are “suboptimal or not indicated.”
a. 40% b. 60% c. 85% d. 92%
3. The oral cavity is colonized with numerous microorganisms that comprise between 300 to 600 species of _______. a. bacteria b. fungi c. protozoa d. all of the above
4. Regarding guidelines related to the prevention of infective endo carditis from the American Heart Association and American Dental Association, antibiotic prophylaxis is warranted ________. a. for every patient undergoing a dental procedure b. in only a small subset of patients at highest risk of adverse outcomes c. only for patients prone to joint infections d. only for patients who ask for it
5. One notable change in the 2021 AHA recommendations is that ______ has been removed from the options for prophylaxis because it may cause more frequent and severe reactions than other antibiot ics used for prophylaxis.
a. clindamycin b. penicillin c. azithromycin d. doxycycline
6. ____________ used to be the recommended prophylactic agent for patients with severe penicillin allergies.
a. Doxycycline b. Azithromycin c. Clindamycin d. Penicillin
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 16 CE credits for only $149; call 866-579-9496, or visit https://implantpracticeus.com/ subscribe/ to subscribe today.
n To receive credit: Go online to https://implantpracticeus.com/continuingeducation/, click on the article, then click on the take quiz button, and enter your test answers.
AGD Code: 010
Date Published: November 18, 2022 Expiration Date: November 18, 2025
2 CE CREDITS
7. If a patient has a non-IgE mediated allergy to penicillin or ampicillin, ________ can be chosen. a. first- or second-generation cephalosporins b. clarithromycin c. doxycycline d. levaquin
8. (Regarding prosthetic joint infections) The ADA guidelines cite that in cases where antibiotics are deemed necessary, it is most appropri ate that the ________ recommend the appropriate antibiotic regimen and, when reasonable, write the prescription. a. oral surgeon b. orthopedic surgeon c. orthodontist d. internist
9. When prescribing antibiotics for pediatric patients, clinicians should ensure the pediatric weight-based dose does not exceed a single adult dose. a. True b. False
10. As shown in Table 3, single-dose antibiotics for prophylaxis prior to certain dental procedures should be given _____ prior to procedure. a. 30 to 60 minutes b. 2 to 3 hours c. the night before d. the day before
To provide feedback on CE, please email us at education@medmarkmedia.com
Legal disclaimer: Course expires 3 years from date of publication. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
35 implantpracticeus.com Volume 15 Number 4 CONTINUING EDUCATION
Creating a memorable patient experience


JoAn Majors discusses working as a team toward case acceptance
Before we get too far into this article, let’s first agree that there is an exception to every rule. Let’s agree that you can find doctors who do their own presentations. Can we also agree that it is unlikely that doctors are answering their own phone for that onboarding process, prequalifying the patient (or family member) with outside financing if needed, or taking any initial necessary X-rays or scans? Then we can probably also agree that there could be hours of opportunity for a team member to preheat your mad skills or incredible personality, right? We’ve seen tremendous increases in case acceptance and a bet ter patient experience when your people function as a team.
Let’s take a moment to review how a patient is often onboarded in the practice(s). When those who answer the phone can function as marketing repre sentatives or advocates for your exceptional clinical skills and strengths, it is comforting for patients. It allows the patients to hear from someone who they perceive will not directly benefit financially from the treatment they may choose. In addition, having team members with the ability to ask simple yet open-ended questions before you see them gives you a window into their concerns or desires they might not share as quickly in the treatment room. White-
JoAn Majors, RDA, CSP®, CVP, is the content creation specialist and cofounder of The Soft Skills Institute, LLC, a National AGD PACE provider. She has earned a CSP — Certified Speaking Professional — the highest global designation for a professional speaker from the National Speakers Association — and is also a Certified Virtual Presenter. Published in over 25 magazines and newsletters, her first book on implants has trained thousands of implant teams. The only non-dentist faculty for the world-renowned Misch International Implant Institute for many years, she now offers her signature Soft Side of Implant Dentistry program privately to groups and study clubs. In addition, the Soft Skills Institute offers scalable and affordable online follow-up training to meet the needs of today’s busy providers and teams.
JoAn’s platform voice and writing voice are similar to her storytelling style. She is a member of multiple organizations and associations and serves on the advisory board for Dental Entrepreneur Women, aka DeW Magazine. An ambassador to select dental companies, she served as the Comprehensive Care Coordinator in her husband’s practice for over 2 decades. Finally, JoAn is an emcee when you need continuity and connection for your community as well as a speaking coach to those new to the business of speaking. To learn more or see her in action, visit www.joanmajors.com.
coat syndrome truly exists, and if your team can glean some insight to share in the morning huddle, it can be a game changer for the patient experience and case acceptance.
On the other hand, if you have team members on the phone who take only the essential information for an appointment, they need to be trained in customer service interaction skills. For instance, if we ask first about “the insurance,” we become the office about the insurance. If we take time to build rapport, we become the office about creating a relationship first. I’m talking about transactional questions versus transformational questions. The heart of the soft skills we teach factually increase case acceptance. It is much more complicated and more work for you to create rapport with basics than if you start by sharing something your team learned that you now can repeat to the patient. In that case, the patient feels as though you listened, which is much different than our counterparts in the medical community. The patient will often have a person on the phone, a receptionist for intake, a medical assistant, and even a doctor who all ask a similar version of this question: Now what are you here for today? You can choose how or if you want the patient experience to be memorable. This is the bedrock piece and the start of team case acceptance.
These are basic beginnings that move those key performance indicators (KPIs) in the direction you want when it comes to case
36 Implant Practice US Volume 15 Number 4 PRACTICE DEVELOPMENT
acceptance. I often hear people in our industry talk about revenue producers, and they rarely, if ever, mention the peo ple on the phone who quite frankly took the time to get them in the chair of a pro vider. I believe the people answering the phone are, in fact, revenue generators — or they are not! I’ve worked with groups and call centers with no idea how many patients they lost because of that initial call, and what was not asked. The few transformational questions should be first, not last, and honestly don’t generate yes or no answers. Again, if you want to be the practice about “the plan,” then keep asking those same mundane questions that miss almost 50% of callers from converting to patients. The numbers don’t lie, but the numbers of callers that don’t convert are rarely in the mix you measure.
I shared an article in Implant Practice US (2021), titled “I’m not the doctor but …”1 This is one of the tools in our toolbox to preheat the services the providers offer in a very general way. No pressure, no-nonsense, just information about what might be possible if prospective patients choose your practice. Understanding that the callers most often doesn’t have the same knowledge of dentistry allows us to lose the preconceived notion that we shouldn’t repeat the treatment opportunities for the patients. We are assuming (which could be problematic) that you have a morning huddle and make the time to share the little things that can make a big difference for these implant patients. Taking the time upfront keeps you from having to go fishing for facts when they arrive. Give patients who call ample time to build rapport or find someone else to answer your phone. You can’t afford not to if having the patients show up to your office matters in the end.
Another example of how we use a team to engage the patient in case acceptance is what we refer to as “overhear psychology.” Oddly enough, people often believe what they overhear more than what they are directly told. This is the art of having patients overhear something that can impact their deci sion or understanding of what is happening. In another article for Implant Practice US (2019), titled “Comfort, function, and beauty,”2 I shared how we ask patients to rate these in order of importance with their treatment options. Once the patient has marked a No. 1 on any of these, we take note and use this every time we can. Take, for example, a patient who marks “beauty” as No. 1. As a clinical assistant, while the doctor is doing the exam or reviewing the scan, I will ask several questions that are not directly for the patient, but you can bet he/she is listening to us. For example, I’d likely ask, “Dr. Wonderful, what is the esthetic opportunity for her/his treatment?” The doctor might reply, “you know JoAn, I think we can get a 9.5 on the esthetic outcome.” The patient’s ears perk up, and you’ll often see a smile, or the paitient might ask if it means he/she will finally have a beautiful smile.
After almost 4 decades in the industry, we’ve learned that if you have the support of your team when it comes to case accep
tance, the numbers go up. Period. This article isn’t for you if you do all the cases you present. It probably isn’t for you if you have someone reviewing all your incoming calls, and you know that you are converting all those shoppers to patients. Not for you if you take that personal nugget of information gleaned in the beginning and carry it into the conversation as if you were the one on the phone and heard it yourself. It really isn’t for you if you and everyone on your team learn in the morning huddle that Ms. Smith is a recent widow who took care of her husband with Alzheimer’s for almost 10 years and neglected her own care. She is ready to restore her smile, so she can get back to life in her church and community. She is even open to meeting someone to spend some time with, maybe even travel again. Oh, and by the way, we are not on her DD plan, and she understands that there will be a difference in our fees but feels as though this was a big difference in our phone call versus the others she has called on the plan. If this is the kind of data you are getting before you step into the room with the patient, you (and your team) likely already know how to use this data to have Ms. Smith feel as though she is in the right place, and can create instant rapport and the trust she needs to move forward.
The team can play a vital role in your ability to use those clinical skills and do more of the kind of dentistry you want. This only happens when intentional, measured, and transformational questions become second nature to you and your team. Today soft skills and the culture of your office matter more than ever in the delivery of care and the referral of other patients. If you think you need more marketing and new patients, first ensure you fully serve the ones calling and coming to your office at the highest level. If you aren’t adequately taking care of the ones you have, more patients aren’t the answer. You’ll have the front door open and the back door open at the same time. Tilman Fertitta wrote a book called Shut Up and Listen! He is an entrepreneur who owns many restaurants among other things, and he shared something in this book that I will never forget: “There are no spare customers.” While I realize that we call ours patients, cli ents, guests, and rarely customers, the concept is one you should think through. If all the people who call your office(s) could be your next best patients, are you and your team doing everything you can to serve them in an extraordinary way?
REFERENCES
1. Majors J. “I’m not the doctor but …” Implant Practice US. 2021;14(1):34-35.
2. Majors J. Comfort, function, and beauty. Implant Practice US. 2019;12(4):38-39.
37 implantpracticeus.com Volume 15 Number 4 PRACTICE DEVELOPMENT
IP
Today soft skills and the culture of your office matter more than ever in the delivery of care and the referral of other patients.
Panthera Dental 10th Anniversary Celebration




 National
National
Panthera Dental asked me to attend their 10th Anniversary Party and Master Cup Award Ceremony at their headquar ters in Quebec City, in September this year. Over the years, I have been impressed with their versatility in the dental space, and I had to see this new facility in person. The owners, siblings Gabriel and Béatrice Robichaud, bring their own unique person alities to this more than 40,000 square foot building. From the bright distinct Panthera purple to the 1980s-themed game room, it seems like an awesome place to work. Esthetics aside, they considered efficiency and workflow when designing every detail of their headquarters. We even got to meet the hardest worker of all, their robot courier, Alfred. Everything is strategically set up with the end goal of your patients receiving their order within a quick timeline and with an exceptional quality product.
After a lovely tour, the top three winners of their Master Cup were announced. Panthera, in an effort to keep innovation with technology in dental alive, has a contest every year where glob ally, technicians compete by crafting a complete dental prosthe sis. After mimosas and media interviews, the real fun began.
Guests arrived in the evening greeted by bartenders pouring drinks extending from aerial silk. The hors d’oeuvres were top notch, and the photo booth, along with their DJ playing through out the night, were pure entertainment. The most memorable
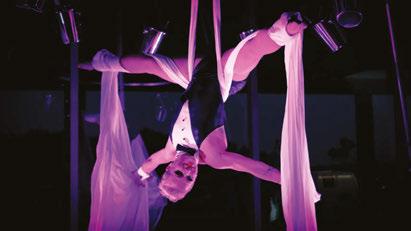
part of the night was when a school bus pulled up on the side of the building and took us to a small diner in downtown Quebec City. There, we got to try Quebec’s version of “diner food,” and network with colleagues from around the world.
I am not surprised Panthera’s party was a great success, because they put this kind of effort into everything they do. The quality in their work really shows, and I am fortunate to be able to witness the processes behind it all. Know that when you are purchasing a Panthera Dental product, whether it be esthetic, sleep, or implant related, you are supporting a won derful bunch of people, a facility with the best technology, and most importantly, top notch quality you can pass down to your patients.
IP
38 Implant Practice US Volume 15 Number 4 EVENT RECAP
Adrienne Good,
Account Manager for Implant Practice US, recaps Panthera’s memorable event
Zest Dental Solutions opens Global Education Center in Las Vegas

Zest Dental Solutions, manufacturer of the Zest LOCATOR® Family of FIXED and Removable Abutment Systems, including the Zest LOCATOR Implant System and provider of clinician-trusted dental materials and small equipment, is proud to announce the official opening of its state-of-the-art hands-on training center in Las Vegas, Nevada. The 10,000-square-foot Zest Dental Solu tions Global Education Center is poised to continue and elevate the tradition of comprehensive, relevant didactic and hands-on training that has become a staple for clinicians across the globe.
The Global Education Center features a unique immersive experience that is designed for real-world clinical educators to teach real-world dentistry in an incredible space dedicated to Zest and their partners. The center includes a private classroom for traditional presentations and hands-on training facility that together can seat large class sizes. The center also features the latest in audiovisual equipment, a dental treatment room to broadcast for clinically focused training programs, and a large banquet room for meals, parties, and interaction. Additionally, Zest implant and distribution partners, DSO and GPO custom ers, and laboratory partners have access to an exclusive space to host meetings and training courses on Zest-related projects.
To learn more, call 800-262-2310, or go to www.zest.com or www.zest.com/locator-fixed.
Shake up your idea of clean: SmartLite Pro EndoActivator™ endodontic activation system

Dentsply Sirona introduces the SmartLite Pro Endo Activator, an equipment solution designed for intracanal activation of irrigating fluids used for cleaning and disinfecting root canals. Designed for multidirectional movement, the SmartLite Pro EndoActivator uses elliptical motion and increased energy for effec tive irrigant activation. Activating irrigants can help produce a surface with more opened dentinal tubules, allowing for better obturation of lateral and accessory canals. SmartLite Pro EndoActivator Tips are available in three sizes, including a new Medium Long tip to better support longer file lengths. SmartLite Pro EndoActivator Tips are flexible, non-cutting medical grade plastic tips, which provide no ledging, transportation, enlargement, or shaping of the canal.
For more information, visit www.dentsplysirona.com.
Coming to the Dental DSO Space: endodontic training, personal wellness coaching, and advanced dental CE with direct mentorship
The AccessEndo Impact Academy (AEIA) is proud to launch their proven and intensive DSO-focused endodontic, personal wellness, and dental continuing education online program. The program features a specific, private, and uniquely branded edu cational web portal for each DSO client. The web portal includes:
• 35+ hours of comprehensive online endodontic CE including lecture and didactic training, clinical simula tion, live clinical case, and chairside learning and patient communication modules.
• 115+ hours of podcast-formatted CE covering endodon tic and specialty topics
• 15+ hours of personal wellness training via the “Power of One” program
• Monthly scheduled endodontic coaching calls
• Quarterly scheduled personal wellness coaching calls
• A la carte services
• A clinical endodontic case upload portal for specific end odontic case guidance/coaching
• A clinical endodontic and personal wellness question portal
For an AccessEndo Impact Academy program demo, please contact Dr. Richard Mounce (RichMounce@AccessEndo.org) to arrange an introduction by Zoom.
*All CE courses and coaching calls come with PACE AGD CE credits and certificates.
X-Guide Dynamic Navigation receives FDA 510(k) clearance to aid in minimally invasive endodontic procedures
X-Nav Technologies, LLC, creator of imageguided and robot-as sisted surgical products, announced that it has received clearance from the U.S. Food and Drug Administration to expand the use of its X-Guide® Dynamic Surgical Navigation system to aid dentists in delivering minimally invasive endodontic procedures. With X-Guide dynamic navigation, patients and dentists can now ben efit from more precise and minimally invasive access to tooth structures needing endodontic treatment – specifically, access to calcified canals and apicoectomies of affected teeth.
Combining 3D imaging with X-Guide navigation allows dentists to locate and access endodontic tooth structures more precisely, which is useful to:
• perform minimally invasive apicoectomy and root-end access
• achieve less invasive access and prep of calcified and hidden canals
• preserve tooth structure
• minimize damage to anatomical structures
• save time and potentially reduce intra-operative imaging
To read more, visit www.X-NavTech.com.
39 implantpracticeus.com Volume 15 Number 4 INDUSTRY NEWS
When medical insurance covers implant services
Rose Nierman and Courtney Snow
discuss common scenarios for medical reimbursement for implants
More than ever, patients are inquiring if their medical insurance will help cover the costs of implant services. The good news is there are situations where implant services and bone grafting are considered medical in nature rather than dental or cosmetic in nature! This is especially riv eting news knowing that dental benefits are remarkably limited.
The key to determining whether a case will be considered medically necessary is knowing the criteria medical insurers look for to offer medical reimbursement. Once you have verified specific medical plan benefits, use the correct ICD-10 diagnosis codes, and make your case with a narrative SOAP report to illus trate the medical necessity.
How can we distinguish between cases that might be consid ered medically necessary and cases that are not? Since insurance criteria vary, the most common scenarios where successful med ical reimbursement occurs are listed here.
Accidental injury/trauma, or misadventures of previous medical care
An example from a medical insurer’s coverage policy states implant services may be covered “when the procedure is intended primarily to improve/restore bodily function or to correct significant deformity resulting from accidental injury, trauma, or previous therapeutic process.” It is important to note that injuries from chewing and biting typically do not meet this requirement.
Tumors/cysts of the jaw
When removal of a tumor or cyst requires the removal of sound natural teeth, implant services to replace those teeth are commonly covered as a medical expense. Services that are

typically considered dental in nature are frequently regarded as medical when they are required to perform another medical in nature procedure.
Functional impairment
Functional impairment refers to difficulty or inability to com plete activities of daily living. Examples in the dental practice realm are patients unable to speak, swallow, or masticate properly. One medical insurer’s coverage policy states implant services may be covered when “the procedure is intended to correct defects and anomalies when they result in a functional impairment.”
Severe atrophy and inability to wear a prosthesis
A patient suffering from severe atrophy (bone height of less than 15 mm) who is also unable to tolerate or accommodate a dental prosthesis may also experience other issues as a result. An example from a medical insurer’s coverage policy states implant services may be covered when “trials of mandibular prosthesis have failed.” The policy clarifies these problems “may include, but are not limited to, malnutrition, persistent pain, gingival ulcerations, and/or mucosal hypertrophy due to instability and upper intestinal problems.”
Rose Nierman is the CEO of Nierman Practice Management (NPM) and creator of the DentalWriter Plus+ software. For over 30 years, Rose has taught dental practices successful & ethical medical billing through the iconic Successful Medical Insurance in Dentistry seminars.
Courtney Snow is the vice president and CE faculty member at NPM. Courtney has helped dental practices bill medical insurance for over 12 years using reliable education, support & software solutions. Contact Nierman Practice Management: contactus@dentalwriter.com or 800-879-6468.


Now that you know medical reimbursement for implant services is possible, the time is now to start collecting this infor mation from your patients. As you can see in the most common scenarios where medical reimbursement is successful for implant services, a thorough patient intake is crucial to determining the probability of the case being considered medical. This intake should include the patient’s chief complaints, systemic medical history, and symptoms that the patient is experiencing with a focus on problems arising from these issues. These problems may include previous trauma, malnutrition, pain, digestive issues, and functional impairments.
To be successful, it’s what you do upfront that counts! Ensure that you are gathering vital information. We encourage dental practices to have their patients complete Nierman Practice Man agement’s Medical Necessity Online Questionnaire to gather these imperative details before the evaluation.
40 Implant Practice US Volume 15 Number 4 PRACTICE MANAGEMENT
IP


























































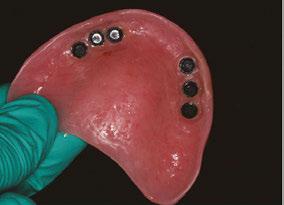






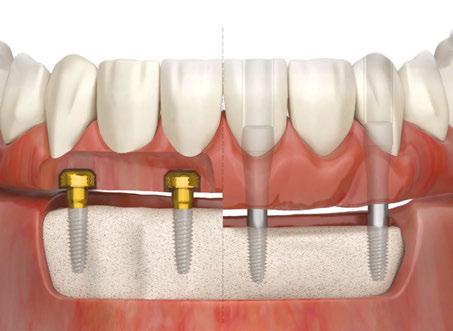







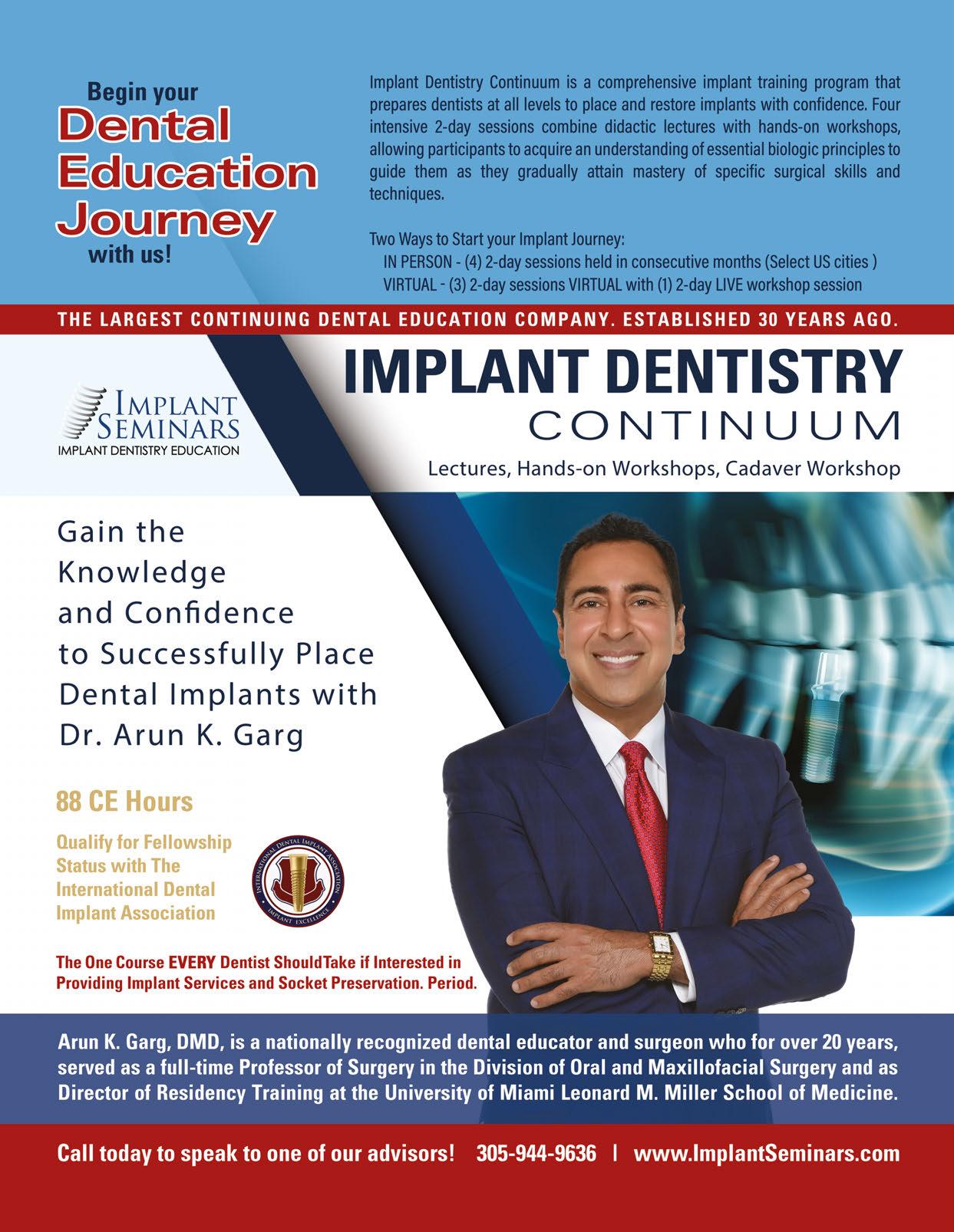



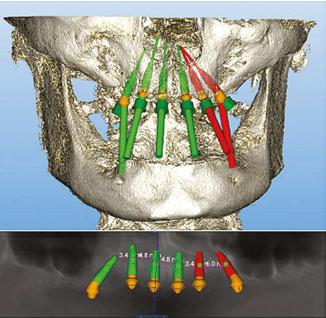
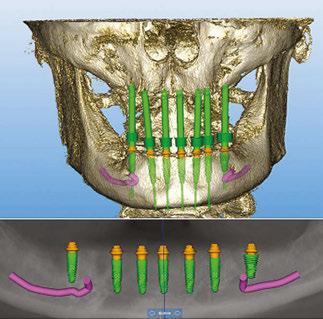
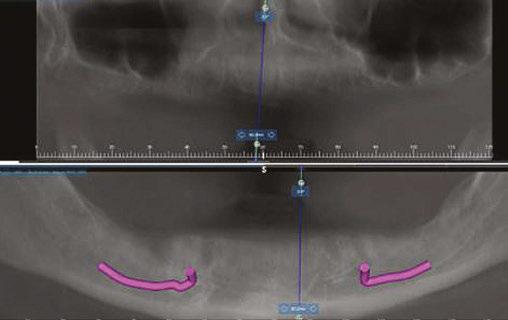



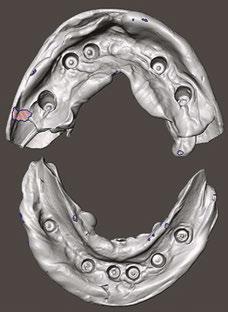



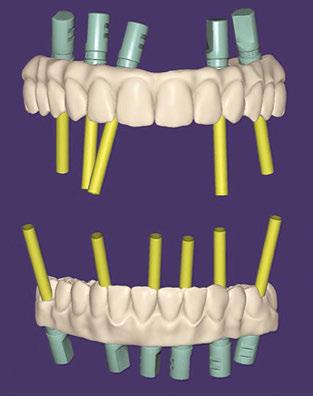





















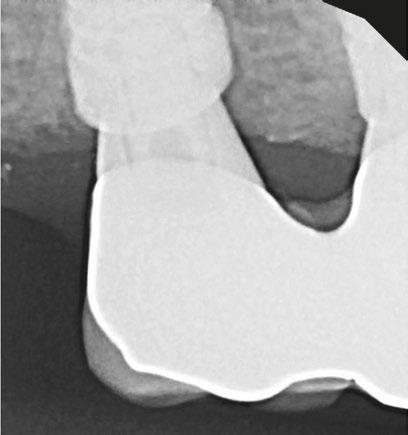











 National
National