Management of pre- and postoperative dental and surgical pain during the opioid crisis
Dr. Diana Bronstein
The importance of maintaining indoor air quality in dentistry

Drs. Tyler Orehek and Troy Roeder
Immediate loading of full-arch implants
Dr. Samantha Siranli with Tony Yoo and Shyun Oh

L OCATOR FIXED IS A GAME CHANGER! GO FROM REMOVABLE TO FIXED ... SAME ABUTMENT. SAME WORKFLOW. LEARN MORE INSIDE. ZESTDENT.COM
on FIXED Full-Arch
Focusing
discusses
PROMOTING EXCELLENCE IN IMPLANTOLOGY Digital Workflow n 4 CE Credits Available in This Issue* Spring 2023 Vol 16 No 1 implantpracticeus.com
Dr. Michael Scherer
establishing and growing an implantology practice
You handle the teeth.
At HighFive Healthcare, we’re passionate about the business of oral surgery. That’s why we partner with oral surgeons who are equally passionate about helping their patients. Our family of experts handle just about everything outside of dental implants, so you can focus on what you love and create your own tomorrow.

Learn more at high5health.com
Spring 2023 n Volume 16 Number 1
Editorial Advisors
Jeffrey Ganeles, DMD, FACD
Gregori M. Kurtzman, DDS
Jonathan Lack, DDS, CertPerio, FCDS
Samuel Lee, DDS
David Little, DDS
Ara Nazarian, DDS
Jay B. Reznick, DMD, MD
Steven Vorholt, DDS, FAAID, DABOI
Brian T. Young, DDS, MS
CE Quality Assurance Board
Bradford N. Edgren, DDS, MS, FACD


Fred Stewart Feld, DMD
Gregori M. Kurtzman, DDS, MAGD, FPFA, FACD, FADI, DICOI, DADIA
Justin D. Moody, DDS, DABOI, DICOI
Lisa Moler (Publisher)
Mali Schantz-Feld, MA, CDE (Managing Editor)
Lou Shuman, DMD, CAGS
Let us read you!
Implant Practice US has been dedicated to the field of implant dentistry for the past 15 years. So much has happened in the evolution of this remarkable invention — from early experiments of the infamous Dr. P. Brånemark to recent refinements in shape, materials, surfaces, and coatings, to promoting effective osseointegration and reducing post-implant infections. Innovations in this field are only limited by the resourcefulness, insight, and inventiveness of trailblazing dentists, inventors, and researchers.
© MedMark, LLC 2023. All rights reserved. The publisher’s written consent must be obtained before any part of this publication may be reproduced in any form whatsoever, including photocopies and information retrieval systems. While every care has been taken in the preparation of this magazine, the publisher cannot be held responsible for the accuracy of the information printed herein, or in any consequence arising from it. The views expressed herein are those of the author(s) and not necessarily the opinion of either Endodontic Practice US or the publisher.
ISSN number 2372-6245
The growth in the implant sector has been astonishing— according to the article “Trends in Dental Implants 2022” on the AAID website, more than 3 million implants were placed in the United States in 2019 before the COVID-19 pandemic. Now that offices have gotten back to work, it’s also time to get back to business. Globally, the dental implant market is expected to reach $13 billion this year. Demographics, consumer awareness, technology, and surgical and restorative advances continue to influence the expansive growth that is expected.
Mali Schantz-Feld Managing Editor
Technology is one key to keeping the specialty on a positive trajectory. Digital technologies, scanners, CAD/CAM, CBCT, lasers, and computer-guided surgery increase precision and accuracy in dental implant planning and placement. Advances in materials for implants lead to greater success in biocompatibility, osseointegration, and soft-tissue response. Implant shape and coatings can now even help to avoid infections such as peri-implantitis — an integral part of patients’ continued health after implant placement.
Even if you are skilled clinically, competition is literally just around the corner. A quick internet search of “Should I get a dental implant?” resulted in 84 million results — from “Are implants really necessary?” to “What type of dentists offer dental implants?” Unless you are marketing to potential patients in your area about what differentiates your practice, you are letting them wander around literally with their heads in the cloud. It’s imperative to establish a marketing plan that has their feet firmly planted on the ground — in your office, that is. Our experts can help with that too.
Implant Practice US speaks directly to the needs of your exclusive group, whether you are experienced or just starting in this niche. Our articles have helped myriad of dentists grow their practices and their skills over the years. To continue that vital collaboration, we depend on our author-dentists’ vision and knowledge to provide techniques and perspectives that increase successes and help mitigate failures in this constantly changing field. We welcome new authors who want to share their insights in our columns that include: case studies, step-by-step, clinical articles, laboratory-focused articles, practice management or development, and my favorite, peer-reviewed Continuing Education articles that garner 2 credits for our subscribers who pass a quiz.
If you want to be part of the cadre of implant-focused dentists who are advancing the field, call or email me to discuss your topics. We would be honored to help you spread your dental implant wisdom to our national readership.
Let 2023 be the year that your practice and your reputation as a dental implant leader thrive! Looking forward to hearing from you soon.
Mali Schantz-Feld Managing Editor
1 implantpracticeus.com Volume 16 Number 1 INTRODUCTION
from a grateful GOAL-getter Lisa
Founder/CEO,
Focusing on FIXED Full-Arch
Dr. Michael Scherer discusses establishing and growing an implantology practice, tips for doing more LOCATOR FIXED™ full-arch implantology cases, and treating patients for life

TECHNIQUE
Immediate loading of full-arch implants
Dr. Samantha Siranli teams up with dental lab technicians Tony Yoo and Shyun Oh to illustrate her fully digital protocol ...........
TECHNIQUE
Dental implant placement in a patient with cystic fibrosis utilizing Platelet Rich Fibrin (PRF)

Dr. Bart Silverman discusses a technique to promote osseointegration for patients with a respiratory disease
TECHNOLOGY
Fundamentals of lasers and dental implant placement
Dr. Todd J. Sheffler discusses how lasers can optimize patient comfort and improve clinical efficacy
2 Implant Practice US Volume 16 Number 1 TABLE OF CONTENTS
PUBLISHER’S PERSPECTIVE
Moler,
MedMark
6
Reflections
Media
16
20
STORY
8 12 COVER
Cover image of Dr. Michael Scherer courtesy of Zest Dental Solutions.


Dr. Diana Bronstein discusses protocols to reduce patient dependence on opioids for pain management





Dr. Francis Nasser, Jr. discusses the important role of military dentists and a special way to recognize their contribution 40


4 Implant Practice US Volume 16 Number 1 TABLE OF CONTENTS CONTINUING EDUCATION The importance of maintaining indoor air quality in dentistry Drs. Tyler Orehek and Troy Roeder discuss the reasons for maintaining diligent air quality standards in the office 30 MARKETING MOMENTUM Guide to having a video filmed for your practice Dental practice videographer Jeremy Tuber shares his expertise on the logistics of filming a promotional video .............................................................. 34 LEGAL MATTERS Anatomy of a dental malpractice action
Tauras, JD, defines the various complex parts of a malpractice claim 36 MILITARY MATTERS A commemoration of oral health services to soldiers
Kristin
Connect. Be Seen. Grow. Succeed. | www.medmarkmedia.com READ the latest industry news and business WATCH DocTalk Dental video interviews with KOLs LEARN through live and archived webinars RECEIVE news and event updates in your inbox by registering for our eNewsletter CONNECT with us on social media www.implantpracticeus.com 24 CONTINUING EDUCATION
of pre- and postoperative dental and surgical pain during the opioid crisis
Management
*Paid subscribers can earn 4 continuing education credits per issue by passing the 2 CE article quizzes online at https://implantpracticeus.com/category/continuing-education/

Reflections from a grateful GOAL-getter
In my columns, I have always shared my thoughts on professional and personal success. I’ve shared MedMark Media’s triumphs, and in recent years searched with you for solutions to some very tough challenges. As always, I am so proud of MedMark Media’s publications and the team that has been the center of my life for so many years. With this column, I am thrilled to announce some amazing news. As of this writing, I just got notified that I am a 2023 Denobi Award nominee. This prestigious nomination is incredibly humbling and inspiring. The Denobi Awards recognize leaders in the dental industry worldwide — including, as the Denobi website notes, “clinicians, educators, brand leaders, students, administrative personnel, sales, advocates, speakers, and leading experts.” From the nominations, finalists include 10 individual winners, one dental team, and on individual that receives the esteemed Dr. Lou Shuman Denobi Pinnacle Achievement Award. Right now, as a nominee, I think back to the years when I ran MedMark out of my tiny condo. Step by step the company has grown into publishing of five magazines, many digital platforms, podcasts, webinars, and opportunities. Some have described me as a “go-getter,” but I like to define myself as a “goal-getter.”
Speaking of setting and reaching new goals, you all know that specialty dentistry is our focus and our passion. So some more good news is the debut this spring of our newest national publication, Pediatric Dental Practice US. Articles will focus on oral health from infancy through teens and offer pediatric dentists new insights on helping young patients. As we strive to inform and improve the practices of endodontists, implant specialists, orthodontists, and dental sleep medicine professionals, reaching clinicians that care for the youngest patients seems like a perfect fit into our coverage of dental care that spans a lifetime.
In this issue of Implant Practice US, our cover story is a conversation with Dr. Michael Scherer who offers tips for growing your implant practice with LOCATOR FIXED™ full-arch cases. A CE by Dr. Diana Bronstein offers an overview of pain management that reduces dependence on opioids. A CE by Drs. Tyler Orehek and Troy Roeder discusses the importance of maintaining indoor air quality in dentistry. In our technique column, Dr. Samantha Siranli illustrates her fully digital protocol for immediate loading of full-arch implants.
I struggled over whether to announce the Denobi Award nomination in my column. That humble voice in my head didn’t want to seem boastful. But, I know that my team, friends, readers, and advertisers would want to share in my excitement of this recognition. This is not just about me. I always try to encourage you all to take some chances, believe in yourself, and as inspirational author Norman Vincent Peale advises have a “humble but reasonable confidence in your own powers.” I also try to emphasize my philosophy of “know your worth.” It sure is a fantastic feeling when others realize your worth too.
To your best success,
Lisa Moler Founder/Publisher MedMark Media
Published by Publisher
Lisa Moler lmoler@medmarkmedia.com
Managing Editor Mali Schantz-Feld, MA, CDE mali@medmarkmedia.com
Tel: (727) 515-5118
Assistant Editor Elizabeth Romanek betty@medmarkmedia.com
National Account Manager Adrienne Good agood@medmarkmedia.com
Tel: (623) 340-4373
Sales Assistant & Client Services
Melissa Minnick melissa@medmarkmedia.com
Creative Director/Production Manager

Amanda Culver amanda@medmarkmedia.com
Marketing & Digital Strategy
Amzi Koury amzi@medmarkmedia.com
eMedia Coordinator
Michelle Britzius emedia@medmarkmedia.com
Social Media Manager
April Gutierrez socialmedia@medmarkmedia.com

Digital Marketing Assistant Hana Kahn support@medmarkmedia.com
Website Support
Eileen Kane webmaster@medmarkmedia.com
MedMark, LLC
15720 N. Greenway-Hayden Loop #9 Scottsdale, AZ 85260
Tel: (480) 621-8955
Toll-free: (866) 579-9496 www.medmarkmedia.com
www.implantpracticeus.com
Subscription Rate 1 year (4 issues) $149
https://implantpracticeus.com/subscribe/
6 Implant Practice US Volume 16 Number 1 PUBLISHER’S PERSPECTIVE
Lisa Moler Founder/Publisher, MedMark Media
How to submit an article to Implant Practice US
Implant Practice US is a peer-reviewed, quarterly publication containing articles by leading authors from around the world. Implant Practice US is designed to be read by specialists in Periodontics, Oral Surgery, and Prosthodontics.
Submitting articles
Implant Practice US requires original, unpublished article submissions on implant topics, multidisciplinary dentistry, clinical cases, practice management, technology, clinical updates, literature reviews, and continuing education.
Typically, clinical articles and case studies range between 1,500 and 2,400 words. Authors can include up to 15 illustrations. Manuscripts should be double-spaced, and all pages should be numbered. Implant Practice US reserves the right to edit articles for clarity and style as well as for the limitations of space available.
Articles are classified as either clinical, continuing education, technology, or research reports. Clinical articles and continuing education articles typically include case presentations, technique reports, or literature reviews on a clinical topic. Research reports state the problem and the objective, describe the materials and methods (so they can be duplicated and their validity judged), report the results accurately and concisely, provide discussion of the findings, and offer conclusions that can be drawn from the research. Under a separate heading, research reports provide a statement of the research’s clinical implications and relevance to implant dentistry. Clinical and continuing education articles include an abstract of up to 250 words. Continuing education articles also include three to four educational aims and objectives, a short “expected outcomes” paragraph, and a 10-question, multiple-choice quiz with the correct answers indicated. Questions and answers should be in the order of appearance in the text, and verbatim. Product trade names cited in the text must be accompanied by a generic term and include the manufacturer, city, and country in parentheses.
Additional items to include:
• Include full name, academic degrees, and institutional affiliations and locations
• If presented as part of a meeting, please state the name, date, and location of the meeting
• Sources of support in the form of grants, equipment, products, or drugs must be disclosed
• Full contact details for the corresponding author must be included
• Short author bio
• Author headshot
Pictures/images
Illustrations should be clearly identified, numbered in sequential order, and accompanied by a caption. Digital images must be high resolution, 300 dpi minimum, and at least 90 mm wide. We can accept digital images in all image formats (preferring .tif or jpeg).
Tables
Ensure that each table is cited in the text. Number tables consecutively, and provide a brief title and caption (if appropriate) for each.
References
References must appear in the text as numbered superscripts (not footnotes) and should be listed at the end of the article in their order of appear-
ance in the text. The majority of references should be less than 10 years old. Provide inclusive page numbers, volume and issue numbers, date of publication, and all authors’ names. References should be submitted in American Medical Association style. For example:
Journals:
(Print)
White LW. Pearls from Dr. Larry White. Int J Orthod Milwaukee. 2016;27(1):7-8.
(Online)
Author(s). Article title. Journal Name. Year; vol(issue#):inclusive pages. URL. Accessed [date].
Or in the case of a book: Pedetta F. New Straight Wire. Quintessence Publishing; 2017.
Website:
Author or name of organization if no author is listed. Title or name of the organization if no title is provided. Name of website. URL. Accessed Month Day, Year. Example of Date: Accessed June 12, 2011.
Author’s name: (Single) (Multiple)
Doe JF Doe JF, Roe JP
Permissions
Written permission must be obtained by the author for material that has been published in copyrighted material; this includes tables, figures, pictures, and quoted text that exceeds 150 words. Signed release forms are required for photographs of identifiable persons.
Disclosure of financial interest
Authors must disclose any financial interest they (or family members) have in products mentioned in their articles. They must also disclose any developmental or research relationships with companies that manufacture products by signing a “Conflict of Interest Declaration” form after their article is accepted. Any commercial or financial interest will be acknowledged in the article.
Manuscript review
All clinical and continuing education manuscripts are peer-reviewed and accepted, accepted with modification, or rejected at the discretion of the editorial review board. Authors are responsible for meeting review board requirements for final approval and publication of manuscripts.
Proofing
Page proofs will be supplied to authors for corrections and/or final sign off. Changes should be limited to those that are essential for correctness and clarity.
Articles should be submitted to:
Mali Schantz-Feld, managing editor, at mali@medmarkmedia.com
Reprints/Extra issues
If reprints or additional issues are desired, they must be ordered from the publisher when the page proofs are reviewed by the authors. The publisher does not stock reprints; however, back issues can be purchased.
7 implantpracticeus.com Volume 16 Number 1 AUTHOR GUIDELINES
Focusing on FIXED Full-Arch
Dr. Michael Scherer discusses establishing and growing an implantology practice, tips for doing more LOCATOR FIXED™ full-arch implantology cases, and treating patients for life

How do you perform more fixed full-arch implant cases?
In the past 15 years of practicing, teaching, and doing research in dentistry, I have had so many wonderful opportunities to interact with clinicians from all over the country and world. Many clinicians want to know – “How do I grow an implant practice and do more cases?” That’s such a great question that has many avenues to discuss. I have grown my implant practice by focusing on a few key things. First, focusing on patients and communication skills; second, becoming experienced and credentialed in implant procedures, and finally, attending dental education courses to learn new techniques that allow me to distinguish myself within my community.
Start by investing in yourself and your teams! Focusing on patient communication skills is paramount since implant dentistry can be quite confusing for patients. The key items that I tend to address during appointments are lack of awareness in the procedures, the cost factor, and last but not least, the fear of going through the procedure.
Teamwork when managing the three factors starts on how patients learn about your office and creating awareness of your capabilities as a clinician. Simple and effective marketing strategies are the best, such as a well-constructed website, Google and social media local SEO rankings, patient reviews, star ratings, and search ranking. Ask patients to leave impactful reviews on focused procedures including using the key words that will help drive patients to learn about your office, such as “LOCATOR” or
Michael Scherer, DMD, MS, serves as the Chief Clinical Officer for Zest Dental Solutions, is an Assistant Clinical Professor at Loma Linda University, a Clinical Instructor at University of Nevada – Las Vegas, and maintains a successful practice limited to prosthodontics and implant dentistry in Sonora, California. He is a Diplomate of the American College of Prosthodontists and the American Board of Oral Implantology. He has published numerous articles, books, and in-person and online courses related to implant dentistry, clinical prosthodontics, and digital technology with a special emphasis on full-arch reconstruction. As an avid technology and computer hobbyist, Dr. Scherer’s involvement in digital dentistry has led him to develop and pioneer new approaches with restorative and surgical full-arch implantology, 3D printing workflows, CAD/CAM systems, and outside-of-the-box radiographic imaging and digital design concepts. Over the past 10 years, he has given over 360 presentations at dental conferences, main podium presentations, in-office training, and hands-on workshops. He has coached thousands of dentists around the world on how to integrate digital dentistry and implant dentistry from a high tech yet “wet-fingered, real-world” clinical perspective that makes his presentation style well-received by clinicians.
“FIXED implant bridge.” When patients reach out to the office either via phone or messaging, ensure your staff is well-trained to focus on those key words and making the consultation appointment process as easy as possible. Once they arrive at your office, ensure your entire staff, from front desk to dental assistants, are well-trained in communication and patient management. Creating touch points of awareness for the patient from the beginning of how they learn about the procedure until they are in your chair is key. Ensuring that patients are aware that fixed full-arch is an amazing option is a critical step to helping grow your implant practice.
How do you address costs and surgical fear?
Focusing on reasonable patient fees and addressing fear of the surgical procedures are regular and routine discussions one must have with patients in an implant practice. While tooth replacement of the failing dentition with standard tissue dentures is typically viewed as a necessary procedure, full-arch implant dentistry is often viewed as more elective than other options. Costs of implant procedures are important to consider — fixed full-arch procedures are typically 3 to 5 times higher than overdentures and substantially higher than standard dentures.
8 Implant Practice US Volume 16 Number 1 COVER STORY
Dr. Michael Scherer, Chief Clinical Officer at Zest Dental Solutions
Disclosure: Dr. Michael Scherer is the Chief Clinical Officer at Zest Dental Solutions.
I believe that the biggest competitor to a full-arch implantology practice is patients saying no to implant treatment and yes to denture adhesives! As clinicians, we tend to think our greatest challenge is the competition down the street; however, in my clinical practice, my goal is to focus less on competition from other clinicians and focus more on why patients are choosing less optimal alternatives. In our education courses, we address this goal through encouraging clinicians to study their expenses, evaluate their overhead, and focus on how they can leverage creative clinical workflows and new implant systems to help control ballooning patient fees. As a result, we can increase access to care for our patients and do more implant dentistry!
Tackling surgical fear of implant procedures is an aspect of an implant practice that we clinicians sometimes don’t spend enough time paying attention to. While it’s straightforward to control fear and pain during a surgical procedure with anesthetics and/or sedation protocols, growing an implant practice is often more focused on controlling the fear of the patient before the surgical procedure. Fear can be challenging to overcome as we have to dive into what is scary to the patient — is it fear of needles or simply fear of the unknown? I have found that fear of the unknown is often a bigger challenge than anything else related to the procedure. I often ask patients up front what concerns them and how I can help address those concerns. For example, many patients are concerned about invasiveness and bone-reduction procedures associated with fixed full-arch procedures. Expressing confidence, focusing on clear communication strategies on procedure risks, and having physical educational models and tools dramatically decrease fear of the procedure.
What are your new approaches to FIXED full arch?

Newer technologies and implant workflows are a driving force to help grow the implantology practice. My goal of new technologies is to help increase awareness of implant procedures, reduce the fear of the dental procedure, and to help control costs of clinical procedures by becoming more efficient.

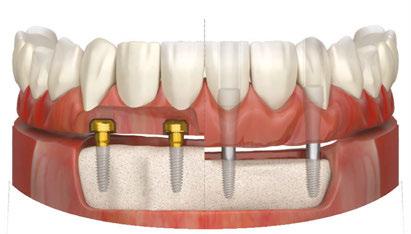
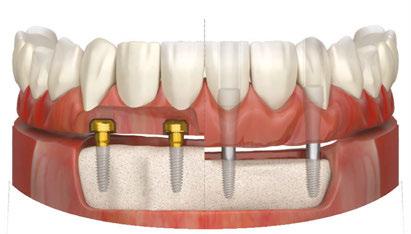
A new fixed full-arch system was introduced by Zest Dental Solutions called LOCATOR FIXED™. By using the same abutment as used in a removable overdenture, LOCATOR FIXED allows the clinician to easily and quickly convert from a removable overden-


ture into a full-arch fixed prosthesis simply by changing housings and inserts.1 LOCATOR FIXED utilizes a newly designed housing and insert pair that combines a super-strong snap-in style retentive mechanism together with a uniquely designed titanium housing that results in a prosthesis that is firmly attached to implants with no movement. Since the prosthesis is fabricated without screw channels that can weaken a prosthesis, patients can be restored with less prosthetic space requirements compared to traditional screw-retained bridges. Hygiene is also simplified because the snap-in-and-out mechanism allows for fixed function; however, rather than screw-retained bridges that take 20 to 30 minutes of clinician time to remove, removal of the LOCATOR FIXED prosthesis is done quickly by clinician and/or a dental auxiliary using a specialized removal tool. Clinical procedures of LOCATOR FIXED are fundamentally the same as that of overdentures including from the same impression techniques as overdentures to the same procedures to pick-up housings. Because clinicians can use removable clinical workflows with LOCATOR FIXED, it helps dramatically enhance simplicity of performing full-arch fixed procedures compared to that of screw-retained techniques. The combination of the simplicity
efficiency allows the clinician to keep the total cost of the procedure substantially lower than that of screw-retained restorations.
9 implantpracticeus.com Volume 16 Number 1 COVER STORY
and
Figure 1: A patient presents to the author’s dental practice with existing overdenture treatment performed several years prior
Figure 2: LOCATOR abutments were placed in strategic positions with future planning for FIXED prosthetics
A. B.
Figures 3A-3B: 3A. Digital impressions were made, and a new polymerbased prosthesis was fabricated. 3B. LOCATOR FIXED Housings were luted to the new prosthesis using CHAIRSIDE Attachment Processing Material. Processing spacers were changed to LOCATOR FIXED Inserts
LOCATOR FIXED was developed to aide clinicians who encounter patients who are concerned about rising costs of dental procedures, want to have flexibility of the prosthesis going from one option (fixed) to another (removable) quickly and easily, and to minimize fear of the procedure by minimizing bone reduction and invasiveness of the surgical procedure.
Tell us about the patient who converted from LOCATOR Overdenture to LOCATOR FIXED.


A 57-year-old female patient recently presented to my dental practice with the chief concern of, “Doctor, I love my overdenture, but I would like to change to permanent teeth!” The patient was treated by me several years ago, and she was happy with her overdenture; however, she always told me that she was interested in teeth that are more like her natural teeth. Her overdenture was treated with four LOCATOR abutments, and the prosthesis was completed with a metal framework-based acrylic overdenture prosthesis. She was worried because she was quoted our traditional screw-retained fee which was beyond her budget. While she was happy with her overdenture, she yearned for something more.
When I learned about LOCATOR FIXED, I instantly thought of this treatment option for this patient’s case. When performing her original treatment, the implants and abutments were placed in positions for an overdenture and with approximately 10 mm of prosthetic space from the top of the implant to the outside of the prosthesis. While her implants were placed in strategic positions to potentially upgrade her to a fixed prosthesis, the prosthetic space would have been a challenge for traditional screwretained prosthetics.2 Since it can be performed using prosthetic space requirements of traditional overdentures, she is a great candidate for fixed full-arch using LOCATOR FIXED. Finally, because the same LOCATOR abutment can be used for fixed and removable prosthetics, I could keep her costs much lower than my traditional screw-retained restorations. I presented this option to the patient, and she said yes to LOCATOR FIXED.
Digital impressions were made using LOCATOR Scan Bodies and of her existing prosthesis. The scan files were sent to a laboratory where a technician utilizes the scans to fabricate a fiber-composite polymer-reinforced PMMA arch restoration. The prosthesis was fabricated with recesses built into the intaglio of the prosthesis in the areas corresponding to the LOCATOR FIXED Housings. The patient returned to my office and placed the prosthesis onto the ridge, and the fit and occlusion was spot on. To keep my procedure simple and ensure passivity of the final prosthesis, I used CHAIRSIDE® Attachment Processing Material to lute the FIXED Housings to the new prosthesis using an intraoral pick-up technique with the patent biting lightly into occlusion while the resin polymerizes. After polymerization, the prosthesis was removed, polished, and occlusion and esthetics verified prior to final placement using the processing inserts that come with the FIXED Housings. The processing inserts were changed to definitive LOCATOR FIXED inserts and the prosthesis seated using finger pressure to engage the prosthesis.
I showed the patient her new smile, and instantly she began to tear up and said, “Doctor, wow, these teeth are so beautiful and SOLID! I can’t wait to eat with them!” I called her later and
she was thrilled beyond belief. She mentioned she can now eat anything — including nuts!
What is the favorite part of your implant practice?
An implantology-focused clinical practice is exciting, challenging, and absolutely rewarding in so many ways. Building the practice requires focusing on what matters the most — engagement with your patients, teams, and yourself. One key aspect of patient treatment is ensuring you choose treatment that allows you to be able to have flexibility for the patient at all touchpoints along their lives, from the beginning of their journey to when they are looking for something more. LOCATOR facilitates me as a clinician to be able to treat the patient for life!
REFERENCES
1. Scherer MD. Adapting the Digital Reference Denture Technique for Full-Arch Cases Using a Novel Fixed Attachment System. Compend Contin Educ Dent. 2022 Nov/ Dec;43(10):646-653.
2. Scherer MD. Planning full-arch reconstructions for today and tomorrow: implant overdentures and fixed restorations. Compendium eBook. Published September 2021.
10 Implant Practice US Volume 16 Number 1 COVER STORY
IP
Figure 4: The prosthesis was placed using finger pressure to completely engage the prosthesis with embedded housings onto the LOCATOR abutments. A radiograph was made to verify the adaptation of the prosthesis onto the abutments
Figure 5: Esthetics and occlusion were verified; the patient was thrilled with her new teeth
No New Abutment Required…
Now use LOCATOR Abutments for FIXED Full-Arch


Introducing a NEW flexible and accessible FIXED full-arch solution

LOCATOR Removable or FIXED... it's your choice.
Utilize patients' existing LOCATOR or newly placed abutments to transition from a removable overdenture to a FIXED, full-arch solution.
Offer staged treatment planning for your patients, removable today… FIXED tomorrow.

Give your patients the life they had with their permanent teeth with an affordable, permanent implant-secured solution.
A LOCATOR-proven alternative to the discomfort and pain associated with conventional dentures that feels more like permanent teeth.
Fixed Full Arch Choices
LOCATOR FIXED Conventional Fixed
Same Abutment, Reduced Chairtime, Less Bone Reduction… LOCATOR FIXED
bit.ly/ImplantPractice_LOCFXD
Dental implant placement in a patient with cystic fibrosis utilizing Platelet Rich Fibrin (PRF)
Dr. Bart Silverman discusses a technique to promote osseointegration for patients with a respiratory disease
Cystic fibrosis is a rare monogenic autosomal recessive genetic disease affecting around 75,000 people worldwide.1 The disease is typically diagnosed at birth and impacts Caucasians of northern European ancestry with an occurrence of 1 in 2,000-3,000 births, and occurs least often in Asian Americans with approximately 1 in 30,000 births.2 It is caused by passing a mutated gene for the cystic fibrosis transmembrane conductance regulator (CFTR) from both parents. The disease process is usually associated with respiratory failure. Patients typically have a life expectancy of approximately 2-30 years.3
Over the past few decades, with advances in pharmacological therapy, patients with cystic fibrosis have been living longer. With an increase in longevity, new long-term complications have arisen. This genetic disorder has been found to affect the pancreas, liver, kidneys, intestine, and bone. Osteopenia (low bone density) is present in up to 50% of all post-pubescent patients. Osteoporosis, a more significant form of bone weakening, is found in 10%-34% of all adult patients presenting with this disease.4 Cystic fibrosis has also been associated with limited Vitamin D absorption.5 A defi-
Bart Silverman, DMD, graduated from Fairleigh Dickinson University in 1982 Summa Cum Laude and received his Doctorate in Dental Medicine in 1986 from Fairleigh Dickinson Jr. School of Dentistry, where he was a member of the Omicron Kappa Upsilon Honor Society. He completed his Oral and Maxillofacial residency at Westchester County Medical Center in 1989 and was chief resident in his final year. He is in private practice limited to Oral and Maxillofacial Surgery in New City, New York and is a Diplomate of the American Board of Oral and Maxillofacial Surgery and the American Board of Oral Implantology. He has been lecturing in the field of implant dentistry for over 25 years. Dr. Silverman is an Attending Physician at Westchester County Medical Center, Department of Oral and Maxillofacial Surgery, a Clinical Associate Professor at New York Medical College, Adjunct Clinical Associate Professor Department of Oral and Maxillofacial Surgery at New York University School of Dentistry, and Surgical Director of NYU Post-graduate Continuing Education Dental Implant Program. He is also an Adjunct Clinical Associate Professor at Roseman School of Dentistry, Director of Roseman University Maxicourse in Implant Dentistry, Director BWS Dental Seminars, Faculty at Implant Pathways, and New York, Chicago, and Rutgers, Asia Dental Implant Maxicourses.

ciency in vitamin D absorption has been correlated with low bone density and poor bone healing.6 Low vitamin D levels have been correlated with an increased failure rate of bone grafts.7 The low vitamin D level and concomitant osteopenia/osteoporosis can make dental implant placement in areas of potential low bone density challenging in patients with cystic fibrosis.
Platelet rich fibrin is an autologous blood platelet-rich concentrate which has been shown to increase soft and hard tissue healing. It concentrates the patient’s platelets, fibrin, and growth factors.8 Platelets contain α-granules. The α-granules, in turn, contain growth factors that play a significant role in tissue healing. When platelets become activated and degranulate, the growth factors contained within the α-granules are released.9 The released growth factors provide parenchymal signaling for the recruitment of cytokines and stem cells into the surgical area.10 These stem cells differentiate into soft tissue and bone-forming cells. These recruited cells further bone regeneration.12 The placement of autogenous platelet concentrates in surgical areas has been shown to increase the rate of bone formation, bone density,13 and quality of the healed bone.14 Platelet concentration techniques may be used in compromised situations to aid in healing and possibly prepare an osseous site for future dental implant placement(s).
Clinical case report
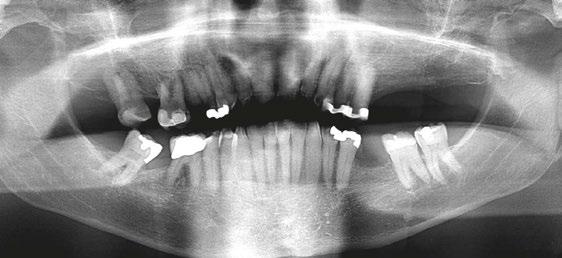
A 64-year-old male presented to the dental clinic for extraction of non-restorable maxillary left first, second, and third

12 Implant Practice US Volume 16 Number 1 TECHNIQUE
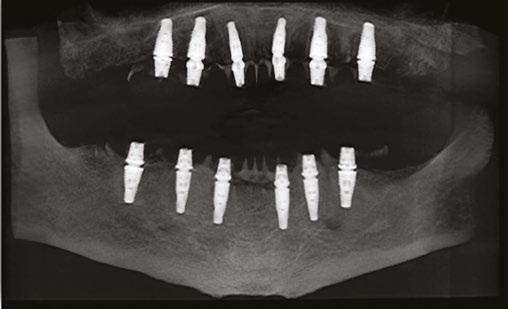
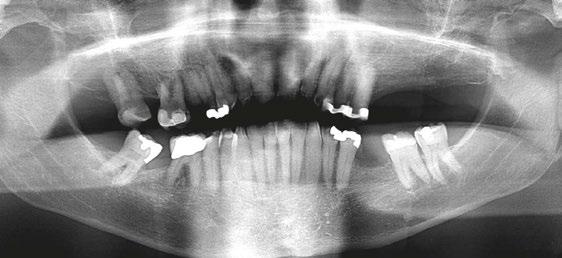
Figure 1: The patient’s panoramic radiograph upon initial consultation
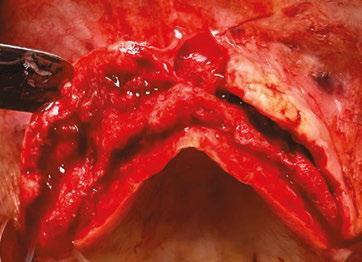
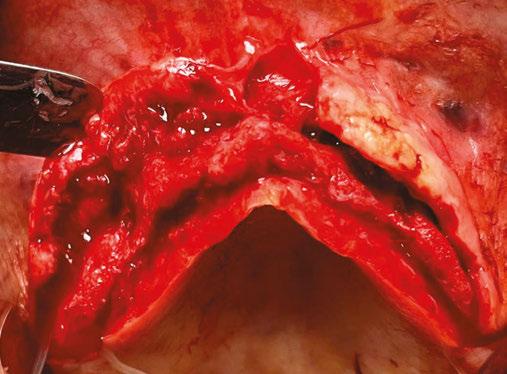
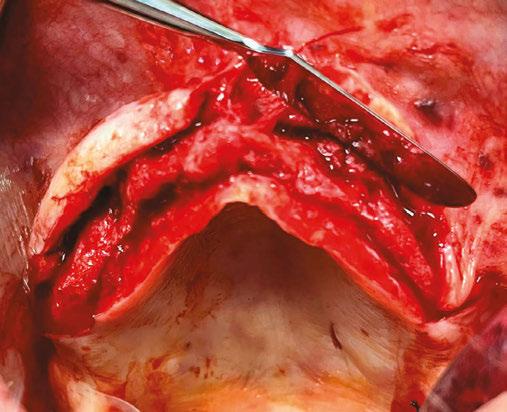
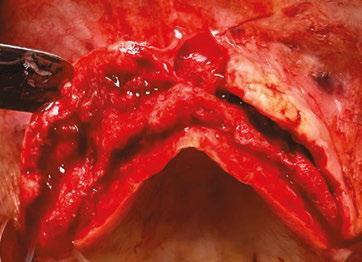
molars in January 2019. The past medical history was significant for cystic fibrosis and depression. He had an allergy to sulfa medications and was taking the following medications: Pulmozyme® (dornase alpha), testosterone, prednisone, and nifedipine. The patient presented with a chief complaint of “I didn’t think I was going to live this long with cystic fibrosis, but I did, and now I am ready to take care of my needs.” The clinical examination was significant for a grossly carious dentition in need of repair (Figure 1). After reviewing several options, it was decided to extract the non-restorable left maxillary first, second, and third molars and to restore the maxillary left first and second molars with fixed implant-retained restorations. With potential healing concerns secondary to his cystic fibrosis, the addition of platelet-rich fibrin (PRF) was discussed. The patient was taken to the surgical operatory where the blood pressure was taken, a pulse oximeter placed, and an IV was started using a 21-gauge butterfly catheter in the right antecubital fossa. PRF protocol was followed using Intraspin® centrifuge (BioHorizons; Birmingham, Alabama), and anesthesia was maintained thereafter using a balance technique. Maxillary left first, second, and third molars were surgically removed, and the resulting extraction sockets were curetted free of granulation tissue. PRF clots and membranes were prepared as described by Choukroun, et al.15 The PRF was mixed 50/50 with MinerOss® mineralized allograft cancellous bone particles (BioHorizons; Birmingham, Alabama) resulting in a “sticky bone preparation” that was placed in the maxillary left first and second molar sockets (Figure 2). Two PRF membranes were placed across the extraction sites (Figure 3), and 3-0 PTFE interrupted sutures were placed affording good wound apposition (Figure 4). Adequate soft tissue healing was observed at a 3-week postoperative check.



The patient returned a year later in December 2019 after receiving bilateral knee replacements. He wanted to fully recover and rehab from the knee reconstructive surgery before having his dental implants placed. A panoramic radiograph and CBCT were performed with Carestream CS9300 (Carestream

13 implantpracticeus.com Volume 16 Number 1 TECHNIQUE
Figure 5: Panoramic radiograph taken after healing of the grafted areas prior to implant placement
Figure 6: CBCT taken after healing of the grafted areas prior to implant placement
Figure 2: Placing the PRF and cortical cancellous bone preparation “sticky bone” into the extraction sockets
Figures 3 and 4: 3. Double-layer PRF membrane placed underneath the buccal and palatal flaps prior to closure. 4. 3-0 PTFE suture used to provide closure of the buccal and palatal flaps and stability of the PRF membrane. Notice here primary closure is not necessary. This technique will provide a large band of keratinized tissue for use during implant placement
Atlanta, Georgia) (Figures 5 and 6). The patient was taken to the oral surgical suite where a 23-gauge butterfly intravenous catheter was started in the right antecubital fossa, and anesthesia was maintained thereafter with a balance technique. A crestal incision was performed, and a full-thickness flap was reflected. Osteotomies were performed using appropriate drills. A BioHorizons Tapered Pro 4.2 mm x 12 mm implant was placed at tooth No. 14 position, and a BioHorizons Tapered Pro 5.2 mm x 10.5 mm implant was placed at tooth No. 15 area. Both implants were placed with greater than 35 ncm torque values (Figure 7). Gingival former healing collars were placed for single stage implant surgery. The wound was closed using interrupted sutures, and the patient was discharged in the care of a family member.
One can appreciate the decrease in bone density in the ungrafted posterior maxilla (Figure 8) and the moderately more dense appearance in the grafted site where the PRF graft changed the local topography (Figure 9). The implants have subsequently integrated, and the patient is waiting to return to the restorative dentist when “he feels comfortable returning to a dentist office post-COVID” for a planned splinted cement-retained restoration. In the posterior maxillary region, this restoration would allow a greater chance of success in the D3 bone.


Discussion
The life span of patients with cystic fibrosis has increased, and there is a tendency to see complications with organ systems other than just pulmonary. Problems with bone metabolism have been noted. With patients presenting for dental implants, clinicians must do what they can to increase the potential for osseointegration and successful outcomes. Autologous growth factors have been shown to improve bone healing.8,11,12 This case demonstrates the use of PRF in a medically compromised patient, one with cystic fibrosis, to change the bony landscape and provide a more predictable and enhanced outcome. This is one case supporting this theory, and more work needs to be performed in the future with these clinical situations.
REFERENCES
1. Fajac I, Wainwright C. New treatments targeting the basic defects in cystic fibrosis. Presse Med. 2017 Jun;46 (6 Pt 2): e165-e175. Epub.
2. Rafeeq MM, Murad HAS. Cystic fibrosis: current therapeutic targets and future approaches. J Transl Med. 2017;15(1):84.
3. Putman MS, Anabtawi A, Le T, Tangpricha V, Sermet-Gaudelus I. Cystic fibrosis bone disease treatment: current knowledge and future directions. J Cyst Fibros. 2019 Oct; 18 Suppl 2:S56-S65.
4. Chedevergne F, Sermet-Gaudelus I. Prevention of osteoporosis in cystic fibrosis. Curr Opin Pulm Med. 2019 Nov;25(6):660-665.
5. Hall WB, Sparks AA, Aris RM. Vitamin D deficiency in cystic fibrosis. Int J Endocrinol. 2010;2010:218691. Epub 2010 Jan 28.
6. Reid IR. Vitamin D effect on bone mineral density and fractures. Endocrinol Metab Clin North Am. 2017;46(4):935-945.
7. Choukroun J, Khoury G, Khoury F, Russe P, Testori T, Komiyama Y, Sammartino G, Palacci P, Tunali M, Choukroun E. Two neglected biologic risk factors in bone grafting and implantology: high low-density lipoprotein cholesterol and low serum vitamin D. J Oral Implantol. 2014 Feb;40(1):110-114.
8. Miron RJ, Zucchelli G, Pikos MA, Salama M, Lee S, Guillemette V, Fujioka-Kobayashi M, Bishara M, Zhang Y, Wang HL, Chandad F, Nacopoulos C, Simonpieri A, Aalam AA, Felice P, Sammartino G, Ghanaati S, Hernandez MA, Choukroun J. Use of platelet-rich fibrin in regenerative dentistry: a systematic review. Clin Oral Investig. 2017 Jul;21(6):1913-1927.
9. Marx RE. Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg. 2004;62(4):489-496.
10. Kang YH, Jeon SH, Park JY, Chung JH, Choung YH, Choung HW, Kim ES, Choung PH. Platelet-rich fibrin is a Bioscaffold and reservoir of growth factors for tissue regeneration. Tissue Eng Part A. 2011 Feb;17(3-4):349-59.
11. Srinivas B, Das P, Rana MM, Qureshi AQ, Vaidya KC, Ahmed Raziuddin SJ. Wound healing and bone regeneration in postextraction sockets with and without Platelet-rich Fibrin. Ann Maxillofac Surg. 2018 Jan-Jun;8(1):28-34.
12. Zhang Y, Ruan Z, Shen M, Tan L, Huang W, Wang L, Huang Y. Clinical effect of platelet-rich fibrin on the preservation of the alveolar ridge following tooth extraction. Exp Ther Med. 2018 Mar;15(3):2277-2286.
13. Marx RE, Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, Strauss JE, Georgeff KR. Platelet-rich plasma: Growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998 Jun;85(6):638-46.
14. Kang YH, Kang YH, Jeon SH, Park JY, Chung JH, Choung YH, Choung HW, Kim ES, Choung PH. Platelet-rich fibrin is a bioscaffold and reservoir of growth factors for tissue regeneration. Tissue Eng Part A. 2011 Feb;17(3-4):349-59.
15. Choukroun J, Adda F, Schoeffler C, Vervelle A. An opportunity in perio-implantology: The PRF. Implantodontie. 2001;42:55-62. IP

14 Implant Practice US Volume 16 Number 1 TECHNIQUE
Figure 7: Postoperative periapical radiograph immediately after implant placement
Figure 8: Notice the lack of bone density in the ungrafted maxillary left third molar socket
Figure 9: The PRF/cortical cancellous bone graft increased the density of the implant site as seen in the postoperative transaxial CBCT view
Available in Three Sizes



OSTEOGEN ® NON-CERAMIC BIOACTIVE CRYSTAL BONE GRAFT







T YPE I BOVINE ACHILLES TENDON COLLAGEN


At less than $50 per piece, the Impladent Ltd OsteoGen ® Bone Grafting Plug combines bone graft with a collagen plug to yield an easy and affordable way to clinically deliver bone graft for socket preservation and ridge maintenance, all without the need for a membrane!
Clinical Case Example


Clinical images courtesy of German Murias DDS, ABOI/ID


Tooth #15, set to be extracted.
Remove the entire pathologic periodontal ligament and flush socket twice. Use #6 carbide bur, make holes through the Lamina Dura to trabecular bone and establish Regional Acceleratory Phenomenon.
Insert Large or Slim sized OsteoGen® Bone Grafting Plugs and allow blood to absorb.



Two Slim OsteoGen® Plugs are in place. Suture over top of socket to contain Plug. Do not suture through Plug. No membrane is required.
OsteoGen® is a low density bone graft and the OsteoGen® Plugs will show radiolucent on the day of placement.




As the OsteoGen® crystals are resorbed and replaced by host bone, the site will become radiopaque.

The collagen promotes keratinized soft tissue coverage while the OsteoGen® crystals resorb to form solid bone. In this image, a core sample was retrieved.
Implant is placed. Note the histology showing mature osteocytes in lamellar bone formation. Some of the larger OsteoGen® crystals and clusters are slowly resorbing. Bioactivity is demonstrated by the high bone to crystal contact, absent of any fibrous tissue encapsulation.

® O NE S TEP B ONE G RAFTING S OLUTION F OR S OCKET P RESERVATION W ITHOUT T HE N EED F OR A M EMBRANE Contact 800-526-9343 or Shop Online at www.impladentltd.com Contact 800-526-9343 or Shop Online at www.impladentltd.com CALL TODAY OR SHOP ONLINE & USE CODE OGX808
1 2 3 7 8 9 4 5 6
10mm 20mm 6mm 25mm 15mm 20mm
1. Spivak, J Biomed. Mater Research, 1990; 2. Ricci, J Oral Maxillofacial Surgery, 1992; 3. Valen, J Oral Implantology, 2002.
Here For Product References
Here For Product Videos
Scan
Scan
Immediate loading of full-arch implants
Dr. Samantha Siranli teams up with dental lab technicians Tony Yoo and Shyun Oh to illustrate her fully digital protocol
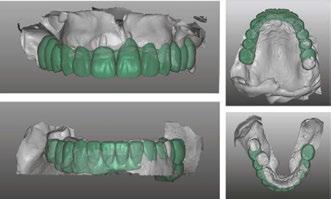
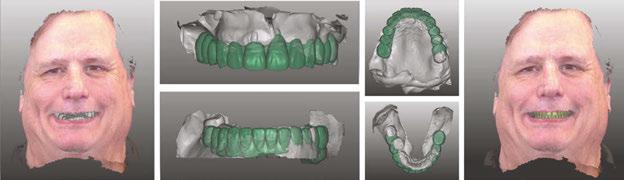
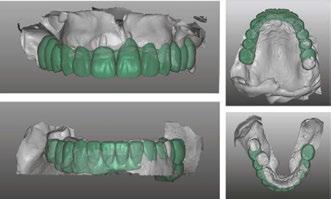
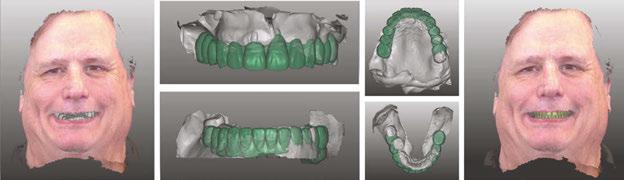
The protocol for immediate loading of fullarch implants includes the extraction of all non-salvageable teeth, implant placements, abutment placements, intraoral scans (Itero®) with scan bodies placed on the abutments, and in-house milling (Zirconzahn®) on the day of the surgery. The information referred to the esthetics, and vertical dimension is gathered with the extraoral 3D facial scans with Face Hunter software (Zirconzahn), 2D photographs, and intraoral scans prior to surgery. The day of extractions and implant surgery, abutments are placed and scanned, and initial designs are merged with anatomical landmarks. The polymethyl methacrylate (PMMA) prosthesis is milled in-house following the merging of the initial and post-implant placement digital scans and the design of the new teeth the day of the surgery.
Clinical step-by-step demonstration of the complete digital flow
Dr. Siranli starts by analyzing the patient’s facial esthetics to design a personalized smile and then combine 3D facial and dental scans (Figure 1).
Patient’s resting and smiling incisal display, vertical dimension of occlusion, and intraoral maximum intercuspation are evaluated clinically and through Face Hunter software (Zirconzahn®) prior to the surgery (Figures 2-4). A detailed smile design prescription gets created after this point. In this particular case presentation, the smile design prescription was:
• Bring the maxillary incisal edge down 8 mm.
• Bring the mandibular incisal edge down 4 mm.
Samantha Siranli, DMD, PhD, FACP, has been in practice for over 2 decades. She earned her dental degree from the University of Pittsburgh School of Dental Medicine and has completed several postgraduate programs in prosthodontics. She received a fellowship in implant dentistry at the University of Pittsburgh, completed her prosthodontics specialty at the Medical College of Georgia, is trained in advanced hospital dentistry, and obtained a PhD in research on dental implants. Dr. Siranli gained Board Certification (Diplomate) in Prosthodontics from the American Board of Prosthodontics and Diplomate status in Implantology from the American Board of Oral Implantology. She served as an associate professor, teaching and practicing implant dentistry and prosthodontics, at the University of Pittsburgh. Following that she was recruited to the Medical College of Georgia to teach esthetics, implant dentistry, and prosthodontics. Dr. Siranli has received numerous awards. She is the author of the book, Your Smile.

• Bring the mandibular bone level down 5 mm.
• Labiolingually, use mandibular anterior as a guidance.


• Open the vertical dimension of occlusion 6 mm.
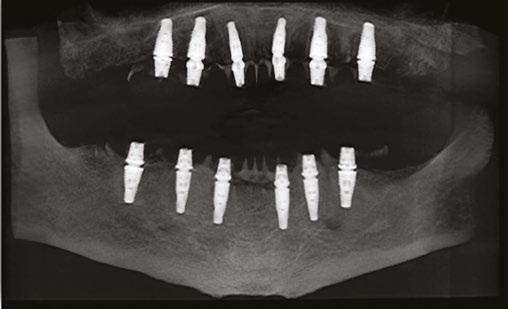
The day of the surgery, intraoral markers are placed, and intraoral scans are captured prior to surgery. The remaining teeth are extracted, implants and muti-unit abutments (Neodent®, Straumann) are placed (Figure 5), and abutment scan bodies

16 Implant Practice US Volume 16 Number 1 TECHNIQUE
Figure 1: Face Hunter 3D facial scans merged with intraoral scans. Green color represents the new digital design of the smile design
Figures 2-4: 2. Resting incisal display. 3. Smiling incisal display. 4. Maximum intercuspation
Figure 5: Implants, multi-unit abutments, and scan bodies placed
Figure 6: Post-surgery intraoral scans
Eliminate Airborne Threats
Air Quality Guard is a Clean Air System Designed for the Unique Challenges of Dental Practices



Air quality is CRITICAL to your practice. Contaminants are everywhere: Pathogens, Pollutants, Viruses, Bacteria & Fungi all threaten our air quality and quality of care.
Benefits of Air Quality Guard:
• Arm and ceiling intakes capture aerosols at the source and move them away from occupants
• Contaminated air is filtered through a 3 layer system, removing greater than 99.99% of all contaminants
• Reduces the spread of COVID-19 and reduces sick leave
• Negative pressure airflow cycle ensures that contaminants are captured before they can circulate
• Quietly and efficiently filters & replaces up to 100% of air with pure, clean air
• Power ful enough to replace all the air in the room every 7 minutes*
Pre-Filter Gas Phase Media Filter HEPA Filter Directional Airflow design
contaminants are removed at the source and replaced by fresh, clean air. Clean air returned to hallway Aerosols collected at source
ensures
on recommended system design principles. Customization may increase or decrease this value. Learn More and Request a Consultation Today! (800) 210-9768 | support@airqualityguard.com | www.airqualityguard.com
*Based
get connected. Intraoral scans are done again after the surgery (Figure 6), and pre- and post-surgery scans are overlapped to mill the PMMA teeth the day of the surgery. While I do own a 3D printer, I like milled PMMAs more since that provides more shade options with the lighter colors. I also find milled PMMAs are stronger than the printed PMMAs.
PMMA gets milled (Figure 7) and delivered the day of the surgery with a very passive fit (Figures 8 and 9).


I use this digital immediate-loading technique right after implant surgery for the temporary teeth to be fabricated on the same day of surgery. However, on some cases with the same technique, I can directly mill final teeth from zirconia right after the surgery as well. So, whether I place temporary or permanent teeth, the technique is the same. More often I fabricate temporary teeth because of the soft tissue changes following surgery during the healing time. I choose to delay the permanent teeth fabrication from zirconia the day of the surgery to give more time for soft tissue healing and settling. IP

18 Implant Practice US Volume 16 Number 1 TECHNIQUE
Figure 7: Milled PMMA
Figure 8: Inserted PMMA on the day of the surgery.
Figure 9: Patient’s pre- and postoperative pictures
Figure 10: Dr. Samantha Siranli (prosthodontist), Tony Yoo (CAD/CAM specialist), Shyun Oh (master ceramist)
Dr. Siranli starts by analyzing the patient’s facial esthetics to design a personalized smile and then combine 3D facial and dental scans.
New BONE-TITE™ — first supplement for dental implant patients

MediNiche, Inc. has introduced BONE-TITE, the first osseointegration support supplement for dental implant patients. BONE-TITE is an over-the-counter dietary supplement product developed in conjunction with prosthodontists, periodontists, and other dental professional experts in bone metabolism and bone growth for use with patients who may require nutritional insurance before and after dental implant procedures. BONETITE provides key vitamins, minerals, and nutrients known to be helpful for proper bone and soft tissue growth, repair, and overall health during implant osseointegration. The BONE-TITE formula is built around a “bone-building-complex” of key ingredients that are associated with benefits to help heal, repair, and strengthen alveolar bone structure. Formulation ingredients include Calcium, vitamins C, D-3, and K-1, and minerals Magnesium, Zinc, Manganese, Potassium, and Copper, and bone fortifying agents such as Ipriflavone, Bromelain, Boron, and L-Lysine. The osseointegration-specific components in BONE-TITE may be helpful for patients that, due to deficiencies or underlying health issues, may be susceptible to reduced osseointegration and implant failure and may require or benefit from specific nutritional support. Patients will obtain the product from a dental practice during implant procedure orientation or with doctor recommendation.
For more information visit www.bonetite.com, www.mediniche.com, or call toll-free 888-325-2395.
Curve Dental announces partnership with Dental Whale
Curve Dental, a cloud-based practice management solution for the dental industry, announced its partnership with Dental Whale®, practice solutions and learning provider. Curve Dental delivers an all-in-one practice management solution that makes everything easy — scheduling, billing, texting, patient engagement, imaging, charting, reports/dashboards, implementation, support, training, data conversion, and more. Through My Dental Whale™ Platform, clinicians and office staff have full control of their practice by streamlining access to essential business and marketing services, supply and equipment ordering, MasterClass training offering CE credits, and data intelligence. The partnership between these two companies makes it easier for practices to manage the clinical and operational side of their business while also saving money.
For more information on Dental Whale®, call 855-339-3740 or visit https://www.dentalwhale.com/, and for Curve Dental, visit www.curvedental.com, or call 1-888-910-HERO.
onDiem and ADAA announce partnership

Alisa Ulrey joins U.S. Oral Surgery Management as COO

U.S. Oral Surgery Management (USOSM), a specialty management services company that exclusively serves premier oral and maxillofacial surgeons, is proud to announce a new chief operations officer, Alisa Ulrey, a seasoned executive with more than 30 years of experience shaping two of the nation’s largest Fortune 500 companies, CVS Health and Target. As COO, Ulrey will oversee USOSM’s daily operations, design and implement business strategies, set company goals for performance and growth, and establish policies that promote company culture and vision.
For more information, visit https://www.usosm.com/.
onDiem has announced a strategic partnership with the American Dental Assistants Association (ADAA). At the core of this partnership is a mutual commitment to support dental assistants in thriving in their careers by providing access to resources, continuing education, and career development opportunities. This partnership will also aid practices in navigating dentistry’s nuanced and unprecedented staffing challenges. onDiem and the ADAA will work together to make onDiem’s Digital ID the trusted, single source of verification and credentialing to ensure safety and compliance across the industry. onDiem’s Digital ID streamlines navigating individual state boards for requirements and certifications for dental assistants — reducing risk and human resources.
onDiem’s staffing platform connects dental practices and dental professionals in all 50 states to meet real-time staffing needs. It is distinguished from other staffing platforms by offering employees, not contractors, for temporary shifts. They eliminate the burden of staffing compliance, so practices can focus on maximizing production and revenue. onDiem dental professionals enjoy healthcare benefits, employer-paid taxes, and insurance coverage, along with the ability to set their own work schedule and hourly rates. With a free account, dental professionals can look for temporary and permanent job opportunities, and practices can create posts for new temp shifts, search for professionals in their area, and communicate with candidates directly. For more information, visit https://hub.onDiem.com/.
19 implantpracticeus.com Volume 16 Number 1 INDUSTRY NEWS
Fundamentals of lasers and dental implant placement
Dr. Todd J. Sheffler discusses how lasers can optimize patient comfort and improve clinical efficacy

Failing dental implants are a significant concern for the implant dentist. No clinician places an implant with the expectation that is going to fail, yet the weighted mean prevalence of peri-implantitis is 22%.1 Various criteria for implant success or failure have been proposed over the last 40 years, starting in 1979.2 Consensus on the definition of success remains elusive. Regardless of the definition, optimizing the factors for implant success should be a priority when placing implants.
Many methods have been developed over the years to increase implant success. Implant manufacturers have manipulated designs of their implants for greater bone-to-implant contact (BIC). Manufacturers have developed new grafting materials and methods to increase implant success. New coating technologies have also been developed as well as new shapes and thread designs.
Dental laser companies have also made advances in the dental implant arena. Most of the early procedures involving lasers and implants focused on simple adjunct processes such as uncovering implants and hygiene maintenance around implants, i.e., laser pocket disinfection. After multiple laser manufacturers demonstrated the safety and success of laser pocket disinfection, research then switched to other implant-related procedures. As the incidence of failure grew, and no definitive treatment evolved, treating peri-implantitis via laser energy drew the attention of the entire
Todd J Sheffler, DDS, is a 1991 graduate of the Baltimore College of Dental Surgery/The University of Maryland School of Dentistry. After graduating, Dr. Sheffler completed a General Practice Residency at the Baltimore VA Medical Center, where he was trained in surgical techniques and implant placement.
In over 30 years of practice, Dr. Sheffler has immersed himself in the technology of dentistry, especially implant and laser technology. He lectures extensively on lasers and implant dentistry, while maintaining a large multiprovider office in Concord, New Hampshire.
Dr. Sheffler resides in the Lake Sunapee region of New Hampshire with his wife, a landscape architect. On weekends they can be found gardening together, on the many trails of the area or at the local antique store. They have two adult daughters, one a nurse at Dartmouth and one a professional equestrian in Florida.
industry. Nearly all laser manufacturers have published specific treatments to address peri-implantitis and implant mucositis.
I first incorporated dental lasers into my practice over 20 years ago. Throughout the years, I have purchased all types of dental lasers used in the United States. The goal has always been to optimize patient comfort with improving clinical efficacy. If a specific procedure does not benefit workflow or patient experience, it does not have a place in my practice. Using a laser “off-label” for applications similar to FDA-cleared uses requires a fundamental understanding of how each individual type of laser interacts with tissues.
As my experience with different lasers has deepened, I have incorporated specific benefits of each laser into my clinical workflow, increasing anesthesia-free restorations to reducing postoperative soreness. Leveraging this knowledge of laser physics, laser tissue interaction, and device specific parameters, I have adapted and evolved procedures to safely use lasers during implant placement and optimize the environment for implant success. Using this approach, we are seeing failure rates significantly lower than the industry average rates. Despite the increase in implant failures during the primary healing phase due to COVID exposure and elevated IL-6 levels currently being discussed, using a specific sequence of laser-based techniques during implant placement has improved success with this subset of patients as well.
Wavelengths, absorption, and physics — oh my!
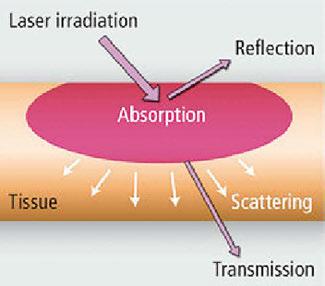
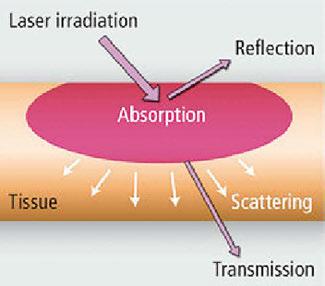
There are four different types of lasers commonly used today in dentistry — diode, erbium, CO2, and Nd:YAG. Each laser type represents a different wavelength, and each wavelength has its own absorption characteristics. I use all of these wavelengths in my practice. Laser light can be absorbed by tissue, reflected back, passed through tissue without absorption (transmission), or scattered in tissue (Figure 1). Diode and Nd:YAG wavelengths are absorbed in melanin and hemoglobin but pass through water and hydroxyapatite. Erbium and CO2 wavelengths are both absorbed in water and hydroxyapatite (Figure 2). Beyond wavelength, variable factors of each laser include pulse duration, length of pulse, spot size of beam, and energy density. One must understand these fundamentals of laser physics to

20 Implant Practice US Volume 16 Number 1 TECHNOLOGY
Figure 1: Laser reflection


1 year print $149 1 year digital only $79 Connect. Be Seen. Grow. Succeed. | www.medmarkmedia.com Address the Implant Complexities You Face Everyday with... 3 EASY WAYS TO SUBSCRIBE VISIT www.implantpracticeus.com EMAIL subscriptions@medmarkmedia.com CALL 1.866.579.9496 SUBSCRIBERS BENEFIT FROM: 16 continuing education credits per year Clinical articles enhanced by high-quality photography Analysis of the latest groundbreaking developments in dentistry Real-life profiles of successful implant practices Technology reviews of the latest products Practice management advice on how to make implants more profitable Implant Practice US 4 Issues • • • • • • • • • • • • 16 CEUs
understand the indications for lasers in surgery and accurately anticipate effects. This is critical when treating patients with various tissue types or on certain medications.
The most common dental laser is a diode laser, primarily due to price point. Diode lasers are electronic lasers where electrons are pumped through a p-n junction causing energy to be released as photons and operate in the 550-950 nm range. Diode lasers can be used in contact mode and non-contact mode. Diode lasers produce high heat and are absorbed in hemoglobin, melanin, water, and pigmented tissue. Most surgical procedures with a diode laser require an “initiated tip”; diodes do not have enough peak power on their own to efficiently cut tissue without initiation of the tip. Diode lasers are limited to soft tissue procedures.
Erbium lasers have a wavelength just under 3000 nm. These lasers are highly energy-efficient and accurate for photothermal ablation. Er:YAG has a 2940 nm wavelength and Er, Cr:YSSG is 2780 nm. While very similar, there is a difference in the water absorption between the two wavelengths. Overall, they behave in a comparable fashion. Their photothermal coagulation depths are significantly shorter than gingival blood vessel diameters. This makes erbium lasers great at cutting soft tissue but poor at coagulating.
CO2 lasers have gained popularity in the dental market in the past several years. CO2 lasers are primarily hard tissue lasers that function in the 10,600 nm wavelength. CO2 lasers are very efficient and exhibit excellent hemostasis as well as excellent tissue incision. CO2 lasers are ideal for incisional and excisional biopsies, frenectomies, gingivectomies, and for ablation and vaporization of leukoplakia and dysplasia.
Nd:YAG lasers are a near-infrared wavelength of 1064 nm. This wavelength is absorbed by pigment in the tissue, primarily hemoglobin and melanin. This wavelength can penetrate deeply into tissues, has excellent biostimulation properties, and can safely coagulate blood. Longer pulse duration settings can be used to stimulate fibrin formation. Nd:YAG lasers can be used for multiple soft tissue procedures such as periodontal treatments, gingivectomy, frenectomy, impression troughing, and biopsy.

Advantages of lasers in an implant practice
Lasers have several advantages over conventional surgical tools from patient perception to increased clinical convenience. No dental procedure starts without the consent of the patient. Before the patient can consent, they need to present into your office. We have found that highlighting technology in our marketing, including minimally invasive laser procedures, is an effective practice differentiator. Patients expect a certain level of technology. When we discuss laser treatment and indirectly show we have kept up with advances in the industry, patients exhibit a higher level of trust and acceptance. Indeed, both lasers and implants are perceived to be “fashionable treatments of modern dentistry.”
Clinically, lasers increase hemostasis, reduce damage to soft tissue resulting in less swelling and less postoperative pain for
patients, and are effective at decontamination. These clinical benefits translate into a better patient experience. Studies have reported that laser technology is more effective at eliminating bacteria compared to chemical products, another appealing benefit to our patient base.
The body of evidence for procedures throughout the lifespan of dental implants continues to support the usage of lasers around dental implants. Clinical papers by Kesler, Romanos, and Koren3 indicate the Er;Cr:YSGG laser can achieve osseointegration with less osseous tissue damage compared to conventional bur drilling in implant site preparation. Miller found laser ablation to be more effective at debridement around an implant compared to traditional acid wash.4 Misischia, et al., compare bacterial reduction of four lasers on titanium surfaces.5 Crippa, et al., discuss decontamination of infected or inflamed extraction sites via laser energy prior to immediate implant placements and the potential implications for long-term success.6 Kusek7 and Montoya-Salazar, et al.,8 presented cases of laser treatment with immediate implant placement, indicating shorter healing times than conventional methods.
Patient’s perspective
When your goal is to optimize patient comfort while improving clinical efficacy, getting patient feedback is essential. Patient-reported outcomes measures (PROMs) was one of the five major topics discussed at the 6th International Team for Implantology (ITI) conference. The consensus paper stressed that “understanding how patients respond to implant treatment is essential and that using PROMs can help clinicians in treatment planning.”
Over the last 20 years, I’ve placed thousands of dental implants. As my knowledge of laser physics expanded, I have utilized each laser to positively affect the implant site. What we have found in our practice is that patient acceptance rate is higher when incorporating laser procedures. Also, we are able to better control surgical variables and decrease healing times.
22 Implant Practice US Volume 16 Number 1 TECHNOLOGY
Figure 2: Laser absorption
Expanding the focus of dental lasers
When effective solutions are found to address critical issues, the focus shifts from triage to prevention. Laser manufacturers have addressed how to save ailing implants and how to keep them healthy. The next evolution for dental laser manufacturers and laser dentists including myself, is exploring how to increase successful osseointegration with higher rates of BIC. The solution might be laser-assisted implant placement.
Biolase has published a case report by demonstrating immediate placement with loading in the esthetic zone using the Er,Cr:YSSG wavelength.9 LightScalpel’s (CO2 10,6000 nm) published case report combines laser degranulation and bacterial reduction with manual debridement before implant placement.10 Millennium Dental (PerioLase MVP-7, 1064 wavelength) has a new protocol which looks promising, but is not yet published. I have been using an approach to laser-assisted implant placement that is showing very promising results. Patient feedback is extremely positive, and the short-term implant success rates are higher with this approach.
Optimizing laser-implant procedures
Laser-assisted implant placement in my office has made for more successful implant outcomes, created happier patients who refer more frequently, a stronger implant warranty, and a doctor with less stress. We continue to follow the success of implants placed using this technique, and hopefully in the near
future, I will be able to publish the details of my approach to laser-assisted implant placement.
REFERENCES
1. Derks J, Tomasi C. Peri-implant health and disease. A systematic review of current epidemiology. J Clin Periodontol. 2015 Apr;42 Suppl 16:S158-711.
2. Schnitman PA, Shulman LB. Recommendations of the consensus development conference on dental implants. J Am Dent Assoc. 1979 Mar;98(3):373-377.
3. Kesler G, Romanos G, Koren R. Use of Er:YAG laser to improve osseointegration of titanium alloy implants--a comparison of bone healing. Int J Oral Maxillofac Implants. 2006 May-Jun;21(3):375-379.
4. Miller RJ. Treatment of the contaminated implant surface using the Er,Cr:YSGG laser. Implant Dent. 2004 Jun;13(2):165-170.
5. Misischia WP, Xenoudi P, Yukna RA, Schurr MJ. Bacterial reduction effect of four different dental lasers on titanium surfaces in vitro. Lasers Med Sci. 2021 Oct;36(8):1759-1767.
6. Crippa R, Aiuto R, Dioguardi M, Peñarrocha-Diago M, Peñarrocha-Diago M, Angiero F. Laser Therapy for Infected Sites and Immediate Dental Implants in the Esthetic Zone: A Case Report and Review of Literature. Case Rep Dent. 2020 Jan 7;2020:2328398.
7. Kusek ER. Immediate implant placement into infected sites: bacterial studies of the Hydroacoustic effects of the YSGG laser. J Oral Implantol. 2011 Mar;37 Spec No:205-11.
8. Montoya-Salazar V, Castillo-Oyagüe R, Torres-Sánchez C, Lynch CD, Gutiérrez-Pérez JL, Torres-Lagares D. Outcome of single immediate implants placed in post-extraction infected and non-infected sites, restored with cemented crowns: a 3-year prospective study. J Dent. 2014 Jun;42(6):645-652.
9. Savion A. Laser-assisted surgery before implant placement: a clinical case report. J Laser Assisted Dent. 2022:24-30. https://savion-c.co.il/wp-content/uploads/2022/10/ LASER-ASSISTED-SURGERY.pdf. Accessed January 23, 2023.
10. Linden E, Vitruk P. Seeing the Light: SuperPulse 10.6 micrometers CO2 laser-assisted, closed flap treatment of peri-implantitis. Implant Practice US. 2015;8(4):30-34.
Do you know what you are paying for your patient financing?
Some patient financing companies calculate the administrative fees you pay based on the applicant’s creditworthiness. This not only adds ambiguity, it could also make your fees more costly. At LendingClub Patient Solutions, we are always transparent and straightforward. With us, your admin fee is based on the LOAN AMOUNT. We make sure you aren’t overpaying on fees.
The example below shows a savings of $2,250 by using LendingClub Patient Solutions on one case!
Register your practice with us today! Not only will your patients have access to a suite of payment plans, but you will also have the potential to save thousands of dollars in admin fees AND continue to start more cases.
“LendingClub” and the “LC” symbol, and “LendingClub Patient Solutions,” are trademarks of LendingClub Bank, N.A., Member FDIC, Equal Housing Lender (“LendingClub Bank”), a wholly-owned subsidiary of LendingClub Corporation, NMLS ID 167439. © 2023 LendingClub Bank. All rights reserved. Equal Housing Lender.
23 implantpracticeus.com Volume 16 Number 1 TECHNOLOGY
IP
Other
Provider Cost $998 3.99% admin fee As high as $3,248 Up to 12.99% admin fee
Financing Partners $25,000 Case Example
LendingClub Bank Installment Loan Call
Visit lendingclub.com/trypatientsolutions
844-366-6735
Management of pre- and postoperative dental and surgical pain during the opioid crisis
Dr. Diana Bronstein discusses protocols to reduce patient dependence on opioids for pain management
Introduction and background
The opioid crisis is a well-documented and reported current event which deserves attention and consideration when practicing daily patient care. With over 9.5 million Americans abusing prescription opioids in 2020 and over 2.7 million with an opioid use disorder, the U.S. Department of Health and Human Services has declared the misuse of opioids a public health emergency.2
Today’s clinicians are aware that the amount of peri- and postoperative opioid use for pain management and their intake duration following surgery are positively associated with chronic opioid use and addiction subsequently. It is one of the top contributors to this epidemic.3-5 The challenge is to reduce opioid use while maintaining adequate pain control.
Diana Bronstein, DDS, MS, MS, MS, has been a Clinical Professor, Associate Program Director and Faculty in the Department of Periodontology and at the Advanced Education of General Dentistry Department at Nova Southeastern University, College of Dental Medicine. She is double boarded as Diplomate by the American Board of Periodontology and Implant Dentistry (ABP) in Periodontology and Dental Implant Surgery, and she is a Diplomate and Fellow of the International Congress of Oral Implantologists (ICOI). Dr. Bronstein received her Specialty Certification in Periodontology and Oral Implantology from Temple University, Kornberg School of Dentistry, as well as a Master of Science degree in Oral Biology, where she was retained as an Adjunct Clinical Faculty at the graduate Periodontology and Oral Implantology Department for 3 years after graduation. Later, she earned a Master of Science degree in Medical Education and in Health Law from NSU. She has been a Pikos and Misch Resnik Institute faculty member and she co-authored the third and fourth edition of Misch’s and Resnik’s Contemporary Implant Dentistry volumes. Her numerous publications include research, clinical articles, as well as continuing education courses on surgical and nonsurgical periodontal and implant treatment with guided bone and tissue regeneration, chronic, aggressive, and acute disease as well as plastic periodontal surgery. Dr. Bronstein has actively practiced full-time and part-time for over 21 years in Europe and in the U.S. and is a member of the AAP, ABP, ADA, FDA, AO, Seattle Study Club, and ICOI. She is fluent in German, English, Russian and can communicate in French. Dr. Bronstein has a Diploma in Clinical Homeopathy which she practices upon patient request adjunctively to standard of care during her periodontal and surgical dental practice.
Dr. Bronstein acknowledges the time and effort of Research Assistant Samuel Rabins.
Disclosure: Dr. Bronstein reports that no financial or other interests exist for herself or her family members regarding StellaLife or any other brands mentioned in this article.
Educational aims and objectives
This self-instructional course for dentists aims to discuss how to manage pre- and postoperative oral surgery procedural pain in patients during the opioid epidemic.
Expected outcomes
Implant Practice US subscribers can answer the CE questions by taking the quiz online at implantpracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can: Realize the extent of the opioid crisis in the United States.
• Anticipate which cases will require analgesic intervention and to what extent.
Identify the best analgesia choices in individual patients dependent on patient history and procedure performed.
• Realize a variety of systemic, local, and topical prescriptions, chairside and OTC (over-the-counter) analgesia options for the patient and the practitioner.
2 CE CREDITS
This article will examine surgical procedures known to increase patients’ risk of developing chronic opioid use and propose protocols for better patient outcomes including reduction of dosage and duration of surgical procedure-related opioid use. Dose increases in both the postoperative inpatient and outpatient settings independently increase the risk of prolonged opioid use,3,6 including opioid naive patients.
Pain management modalities for surgical patients
Managing postoperative pain is an important part of the surgery that involves carefully weighing the risks and benefits since initial and progressive pain control plays a large role in a patient’s overall satisfaction with treatment. A patient experiencing too much pain leads to poor clinical outcomes, while providing access to more than the minimal necessary amount of opioids can initiate chronic dependency.7,8 The challenge is to judge the minimal effective dosage of opioids for adequate pain control successfully while it varies from patient to patient, making it difficult to assess their pain sensitivity objectively.9
24 Implant Practice US Volume 16 Number 1 CONTINUING EDUCATION
“One potential solution to this problem is the use of peripheral nerve blocks. Their use as a replacement for at least some percentage of opioid pain control during and after medical procedures has the potential to reduce opioid use, misuse, and dependency.” Current research suggests that using peripheral nerve block may present viable analgesia.1 According to Cardwell, et al., 2022, the use of pre-surgical peripheral nerve blocks significantly decreases opioid need not only after the procedure, but also in all facets of the surgical process. The most significant reduction in opioid consumption is seen in the first 1-3 days postop, and the patient who received peripheral nerve blocks in the study reported lower pain scores than the control group individuals. It is important to note that this reduction in opioid consumption did not negatively impact patient experience or increase their pain score levels. In fact, it has been shown that the “patients have significantly lower pain scores, higher overall satisfaction, and even prefer the use of blocks when compared to general anesthesia and opioids alone. However, utilization of peripheral nerve blocks is not ubiquitous” while this study produced evidence that peripheral nerve blocks are an effective tool for managing postoperative pain.
Another painful oral surgery sequela is post-extraction dry socket occurrence most often experienced by smokers and non-compliant patients. Dry socket is one of the most common postoperative complications after mandibular tooth extraction, characterized by severe pain and exposed bone. The usual palliative is irrigation of the socket to debride any food or foreign material and packing of the socket with medicated gel or paste to provide pain relief and allow normal wound healing.10
Studies have reported that dry socket pain starts 1–3 days after tooth extraction.17,18 The time it takes for the dry socket to heal varies depending on its severity, but usually, it ranges from 5 to 10 days.19

The management of dry socket has been less controversial18 than its etiology and prevention. Many authors agree that the primary objective is pain control until normal healing occurs as suggested by Fazakerley.16 Systemic analgesics or antibiotics
may be necessary or indicated.20 The use of intra-alveolar dressing materials is also suggested in the literature as local palliative treatment,21,22 although it is generally acknowledged that dressings delay the healing of the extraction socket.23
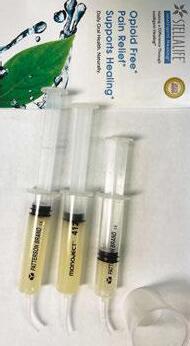
Another treatment modality of dry socket appears to be Platelet-Rich Fibrin (PRF). PRF is characterized by the slow polymerization during its preparation in the centrifuge that generates a fibrin network very similar to the natural one that enhances cell migration and proliferation.13 Choukroun, et al.,15 in France advocated the use of PRF, which is a second-generation platelet concentrate. PRF is a stringently autologous fibrin matrix. Dohan, et al.,14 suggested that PRF addition can correct destructive reactions in the natural process of healing of wound tissues, suggesting that PRF contributes to the immune regulatory mechanism. Choukroun, et al.,15 demonstrated a clinical example in which they used the PRF as a filling material in the extraction socket. There was a significant decrease in pain and the number of socket wall exposure by the third postoperative day; the pain had completely resolved and socket fully epithelialized by the tenth postoperative day. The use of PRF yielded promising results in terms of both pain reduction and improved wound healing which was comparable to the conventional Alveogyl (Septodont) dressing. It may be concluded that PRF is an effective modality for the management of dry socket.10
The studies confirmed that neovascularization and epithelial coverage of the extraction socket can be achieved with the use of PRF. PRF is a reservoir of platelets, leukocytes, cytokines, and growth factors. It is reported to allow the slow release of cytokines, transforming growth factor, platelet-derived growth factor, vascular endothelial growth factor, and epidermal growth factor, which play a vital role for angiogenesis, tissue healing, and cicatrization.14,15
There are further modalities of postoperative morbidity control. Many innovations have made their way into mainstream standard of care. One of the main challenges after extraction, especially postsurgical extractions of impacted 3rd molars, is pain control, and one of the treatments for pain control is low-

25 implantpracticeus.com Volume 16 Number 1 CONTINUING EDUCATION
Figures 1 and 2: 1. Irrigation syringe filled with StellaLife rinse to dispense to patients to use locally on surgical site on a cotton ball or rinse postoperatively. 2. StellaLife post-op kit recommended for patients to get before procedure and bring to appointment. Contains pre-and post-op rinse, gel, and spray
Figure 3: Post-op chairside application of StellaLife gel after second-stage implant uncover
level laser therapy (LLLT). The study by Santos, et al., 2020, aimed to assess the effectiveness of LLLT for pain control after extraction of lower third molars11 and concluded that LLLT within the parameters determined was effective in reducing the intensity of postoperative pain in third molar surgery, presenting the best results 48 and 72 hours after the procedure.


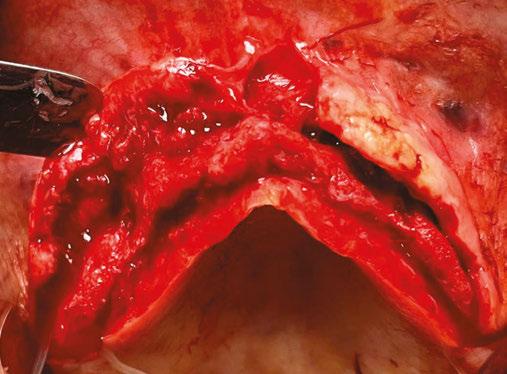
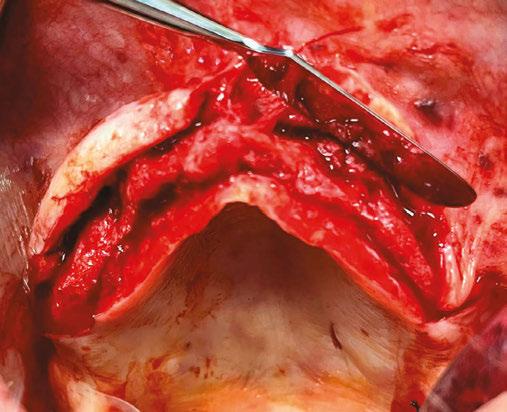
The application of LLLT can offer greater postoperative comfort and wellbeing to patients, functioning as both an inhibitor of the inflammatory process and a modulator. The working mechanism is by interference of the laser in biochemical and molecular levels, promoting the improvement of clinical signs and symptoms, considering that it stimulates endorphin release, inhibits nociceptive signals, and reduces pain proception. In addition, LLLT may reduce edema and hyperemia, accelerate the wound-healing process, and stimulate bone repair 51,52
With new modalities of pain management, there are also improved conventional pain medication protocols to provide today’s practitioners with evidence-based prescription framework. Since the efficacy and rapid onset of postsurgical oral pain relief are critical to improve clinical outcomes and reduce the risk of excessive dosing with analgesic drugs, another study by Cristalli, et al., 2021, compared analgesic effects of preoperative administration of paracetamol 500 mg plus codeine 30 mg in single-tablet and effervescent formulation to ibuprofen 400 mg, and placebo in the management of moderate to severe postoperative pain after mandibular third molar surgery 12
Within the limits of that study, over postoperative 3 days, a statistically significant intensity pain reduction and decreased rescue therapy consumption were recorded in the paracetamol-codeine group than to ibuprofen group. Nevertheless, lower pain intensity at 2 hours post-dose and longer time using rescue therapy was found in the ibuprofen group without statistical significance and without adverse events over the studied period.12,53
A critical property of antiseptic solutions is pain management, especially in terms of trying to limit opioid use. The U.S. opioid public health crisis due to over-prescribing, has subse-
26 Implant Practice US Volume 16 Number 1 CONTINUING EDUCATION
Figure 4: Preoperative maxillary ridge
Figure 5: Buccal and palatal full thickness flap retracted to visualize bilateral atrophic ridge.
Figure 6: Bilateral maxilary bone graft, secured with lasso technique and resorbable Ossix® membrane (OraPharma) for implant site development
Figure 7: Guided Bone Regeneration (GBR) procedure completed and sutured with chromic gut sutures continuous sling and secured with PTFE non-resorbable single interrupted sutures
quently created a drug overuse problem mostly affecting teenagers, leading to a dramatic increase in fatal overdoses.25
It has been more than 5 years since the Food and Drug Administration (FDA), National Institute of Drug Abuse (NIDA), National Institutes of Health (NIH), Drug Enforcement Agency (DEA), the Centers for Disease Control (CDC), and medical and dental organizations such as the American Medical Association (AMA), American Dental Association (ADA),26 and the American Association of Oral and Maxillofacial Surgeons (AAOMS) collectively declared a drastic need to combat their misuse.26,27,28,29,30
Since the mid-1990s, deaths from opioid overdose has more than quadrupled, which parallels the increase in opioid prescriptions written in dental and medical practices,31,32 which is why some countries have entirely banned opioid use in dental practice. In these areas, pain control appears to be manageable. Given that the surgical area is known prior to the procedure, pre-surgical analgesia can be implemented to help reduce the amount of opioid prescriptions in a private practice setting.33,34
Pain perception is initiated in the peripheral nervous system (PNS) before the central nervous systems (CNS) become involved, starting with nociceptors which transmit signals along small myelinated A and unmyelinated C fibers before synapsing in the dorsal horn of the spinal cord.35,37 Signals are then relayed through the thalamus and cortex via the spinothalamic tract of the spinal cord.36
Activity in the dorsal horn can be modulated by psychological factors.35 Active ingredients in StellaLife such as Aconitum, Gelsemium, and Ignatia have shown anxiolytic properties.40,42,43 Anxiolysis is critically important in dental pain management, since patients with anxiety or depression experience more pain from surgery.48 Post-operative pain occurs in two phases: an initial phase with acute pain at the point of noxious stimuli (or incision), and a second phase of prolonged, dull pain around the surgical area.35 The pain stimulus is initiated by inflammatory mediators released at the site of surgery.41,35 The objective of pre- and postoperative analgesia is to decrease inflammatory mediators post-surgery.35,45 Unlike conventional pain management regiments, minimizing postoperative pain with StellaLife® starts 3 days before the procedure. VEGA® Oral Care Recovery Kit by StellaLife has 16 active homeopathic ingredients including Arnica, chamomile, and Aconitum. In a study evaluating the mechanisms of Arnica montana flower methanol extract (AMME) in an arthritic rat model,47 the authors proved that AMME significantly reduced the amount of oxygen free-radicals and pro-inflammatory cytokines such as TNF-Į, IL-1, and IL-6, without the host exhibiting toxic side effects. Interestingly, when compared to the commonly utilized corticosteroid dexamethasone, AMME showed greater therapeutic efficacy in the study.50 Another ingredient in StellaLife is chamomile, which is commonly utilized for pain management due to its anti-inflammatory and anti-nociceptive properties.44,46 The mechanism of action is associated with its ability to inhibit pro-inflammatory cytokines such as TNF-Į, IL-1, IL-6 and IL-8,44 and by its COX inhibition, which is a main mediator of nociception and inflammation.46 Chamomile (Matricaria recutita), which has been used historically as a topical anesthetic, may also function as a selective cycloxege-
nase (COX)-2 inhibitor.46 It may have a synergistic effect when employed in combination with other non-steroidal anti-inflammatory drugs (NSAIDs), such as diclofenac.46 Chamomile has also been shown to reduce dose-dependent sodium channels, thus decreasing peripheral nerve excitability.39 The anxiolytic and anti-nociceptive mechanism of Aconitum works via blocking voltage-dependent sodium channels.49 It was used in ancient Chinese and Japanese medicine as an analgesic.38 In summary, many of the active ingredients in StellaLife exhibit known and proven anti-inflammatory and anti-nociceptive properties that aid in pain management. Pathways involved include the reduction of pro-inflammatory cytokines, COX inhibition, anxiolytics, and the blockade of neuronal sodium currents. While many of our patients report a soothing effect when using the StellaLife rinse and gel, more research is necessary to evaluate how these ingredients work synergistically to control pain by pre- and postoperative applications.
REFERENCES
1. Cardwell TW, Zabala V, Mineo J, Ochner CN. The Effects of Perioperative Peripheral Nerve Blocks on Peri- and Postoperative Opioid Use and Pain Management. Am Surg. 2022;88(12):2842–2850.
2. Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2020 national survey on drug use and health. Published October 2021. https://www.samhsa.gov/data/sites/ default/files/reports/rpt35325/NSDUHFFRPDFWHTMLFiles2020/2020NSDUHFFR1PDFW102121.pdf. Accessed January 6, 2023.

27 implantpracticeus.com Volume 16 Number 1 CONTINUING EDUCATION IP
3. Brummett CM, Waljee JF, Goesling J, Moser S, Lin P, Englesbe MJ, Bohnert ASB, Khe-
Figure 8: Surgeon during oral surgery procedure
terpal S, Nallamothu BK. New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults. JAMA Surg. 2017 Jun 21;152(6):e170504.
4. Clarke H, Soneji N, Ko DT, Yun L, Wijeysundera DN. Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ. 2014 Feb 11;348:g1251.
5. Sun EC, Darnall BD, Baker LC, Mackey S. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med. 2016;176(9):1286-1293.
6. Ruddell JH, Reid DBC, Shah KN, Shapiro BH, Akelman E, Cohen EM, Daniels AH. Larger Initial Opioid Prescriptions Following Total Joint Arthroplasty Are Associated with Greater Risk of Prolonged Use. J Bone Joint Surg Am. 2021 Jan 20;103(2):106-114.
7. Gan TJ. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res. 2017;10:2287-2298.
8. Demsey D, Carr NJ, Clarke H, Vipler S. Managing opioid addiction risk in plastic surgery during the perioperative period. Plast Reconstr Surg. 2017;140(4):613e-619e.
9. Younger J, McCue R, Mackey S. Pain outcomes: A brief review of instruments and techniques. Curr Pain Headache Rep. 2009;13(1):39-43.
10. Keshini MP, Shetty SK, Sundar S, Chandan SN, Manjula S. Assessment of Healing Using Alvogyl and Platelet Rich Fibrin in Patients with Dry Socket - An Evaluative Study. Ann Maxillofac Surg. 2020 Jul-Dec;10(2):320-324.
11. Santos PL, Marotto, AP, Zatta da Silva T, Bottura MP, Valencise M, Marques DO, Queiroz TP. Is Low-Level Laser Therapy Effective for Pain Control After the Surgical Removal of Unerupted Third Molars? A Randomized Trial. J Oral Maxillofac Surg. 2020 Feb;78(2): 184–189.
12. La Monaca G, Pranno N, Annibali S, Polimeni A, Pompa G, Vozza I, Cristalli MP. Comparative Analgesic Effects Of Single-Dose Preoperative Administration Of Paracetamol (Acetaminophen) 500 Mg Plus Codeine 30 Mg And Ibuprofen 400 Mg On Pain After Third Molar Surgery. J Evid Based Dent Pract. 2021 Dec;21(4):101611.
13. Al-Hamed FS, Tawfik MA, Abdelfadil E. Clinical effects of platelet rich fibrin (PRF) following surgical extraction of lower third molar. Saudi J Dent Res. 2017;8(1,2):19-25.
14. Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part II: platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006 Mar;101(3):e45-50.
15. Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, Dohan AJ, Mouhyi J, Dohan DM. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part IV: clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006 Mar;101(3):e56-60.
16. Fazakerley M, Field EA. Dry socket: a painful post-extraction complication (a review). Dent Update. 1991 Jan-Feb;18(1):31-34.
17. Fridrich KL, Olson RA. Alveolar osteitis following surgical removal of mandibular third molars. Anesth Prog. 1990 Jan-Feb;37(1):32-41.
18. Nitzan DW. On the genesis of “dry socket”. J Oral Maxillofac Surg. 1983 Nov;41(11): 706-710.
19. Blum IR. Contemporary views on dry socket (alveolar osteitis): a clinical appraisal of standardization, aetiopathogenesis and management: a critical review. Int J Oral Maxillofac Surg. 2002 Jun;31(3):309-317.
20. Heasman PA, Jacobs DJ. A clinical investigation into the incidence of dry socket. Br J Oral Maxillofac Surg. 1984 Apr;22(2):115-122.
21. Vezeau PJ. Dental extraction wound management: medicating postextraction sockets. J Oral Maxillofac Surg. 2000 May;58(5):531-537.
22. Swanson AE. A double-blind study on the effectiveness of tetracycline in reducing the incidence of fibrinolytic alveolitis. J Oral Maxillofac Surg. 1989 Feb;47(2):165-167.
23. Bloomer CR. Alveolar osteitis prevention by immediate placement of medicated packing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000 Sep;90(3):282-284.
24. Estrin NE, Romanos GE, Tatch W, Pikos M, Miron RJ. Biological Characterization, Properties, and Clinical Use of a Novel Homeopathic Antiseptic Oral Recovery Kit: A Narrative Review. Oral Health Prev Dent. 2022 Nov 30;20(1):485-499.
25. Rutkow L, Vernick JS. Emergency Legal Authority and the Opioid Crisis. N Engl J Med. 2017 Dec 28;377(26):2512-2514.
26. American Dental Association (ADA). American Dental Association announces new policy to combat opioid epidemic. 2018. https://www.prnewswire.com/news-releases/american-dental-association-announces-new-policy-to-combat-opioid-epidemic-300618928.html Accessed January 9, 2023.
27. Califf RM, Woodcock J, Ostroff S. A Proactive Response to Prescription Opioid Abuse. N Engl J Med. 2016 Apr 14;374(15):1480-1485.
28. Centers for Disease Control and Prevention. Opioid overdose: Understanding the epidemic. Centers for Disease Control and Prevention, US Department of Health and Human Services, 2017. Reviewed June 1, 2022.
29. Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic
Pain--United States, 2016. JAMA. 2016 Apr 19;315(15):1624-1645.
30. Hupp JR. Opioids: Combating Misuse While Properly Caring for Our Patients. J Oral Maxillofac Surg. 2019 Apr;77(4):669-670.
31. National Institute on Drug Abuse. Overdose death rates. National Institute on Drug Abuse, National Institutes of Health, 2017. Updated January 20, 2022.
32. Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in Drug and Opioid Overdose Deaths--United States, 2000-2014. MMWR Morb Mortal Wkly Rep. 2016 Jan 1;64(50-51):1378-1382.
33. Lee CYS, Suzuki JB. The efficacy of preemptive analgesia using a non-opioid alternative therapy regimen on postoperative analgesia following block bone graft surgery of the mandible: A prospective pilot study in pain management in response to the opioid epidemic. Clin J Pharmacol Pharmacother. 2019;1(2):1006.
34. Tatch W. Opioid Prescribing Can Be Reduced in Oral and Maxillofacial Surgery Practice. J Oral Maxillofac Surg. 2019 Sep;77(9):1771-1775
35. Gottschalk A, Smith DS. New concepts in acute pain therapy: preemptive analgesia. Am Fam Physician. 2001 May 15;63(10):1979-1984.
36. Gupta SC, Prasad S, Reuter S, Kannappan R, Yadav VR, Ravindran J, Hema PS, Chaturvedi MM, Nair M, Aggarwal BB. Modification of cysteine 179 of IkappaBalpha kinase by nimbolide leads to down-regulation of NF-kappaB-regulated cell survival and proliferative proteins and sensitization of tumor cells to chemotherapeutic agents. J Biol Chem. 2010 Nov 12;285(46):35406-35417.
37. Pogatzki-Zahn EM, Zahn PK. From preemptive to preventive analgesia. Curr Opin Anaesthesiol. 2006 Oct;19(5):551-555.
38. Ameri A. The effects of Aconitum alkaloids on the central nervous system. Prog Neurobiol. 1998 Oct;56(2):211-235.
39. Alves Ade M, Gonçalves JC, Cruz JS, Araújo DA. Evaluation of the sesquiterpene (-)-alpha-bisabolol as a novel peripheral nervous blocker. Neurosci Lett. 2010 Mar 12;472(1):11-15.
40. Bhat NP, Sairoz DC, Shetty A, Quadros L, Krishnan H, Bakthavatchalam P. Efficacy of Aconite and Ignatia as an anxiolytic-In vivo study. Int J Res Pharmaceut Sci. 2021;12(2):1484–1489.
41. Dahl JB, Kehlet H. Preventive analgesia. Curr Opin Anaesthesiol. 2011 Jun;24(3): 331-338.
42. Magnani P, Conforti A, Zanolin E, Marzotto M, Bellavite P. Dose-effect study of Gelsemium sempervirens in high dilutions on anxiety-related responses in mice. Psychopharmacology (Berl). 2010 Jul;210(4):533-545.
43. Marzotto M, Conforti A, Magnani P, Zanolin ME, Bellavite P. Effects of Ignatia amara in mouse behavioural models. Homeopathy. 2012 Jan;101(1):57-67.
44. McKay DL, Blumberg JB. A review of the bioactivity and potential health benefits of chamomile tea (Matricaria recutita L.). Phytother Res. 2006 Jul;20(7):519-530.
45. Ong CK, Lirk P, Seymour RA, Jenkins BJ. The efficacy of preemptive analgesia for acute postoperative pain management: a meta-analysis. Anesth Analg. 2005 Mar;100(3): 757-773.
46. Ortiz MI, Fernández-Martínez E, Soria-Jasso LE, Lucas-Gómez I, Villagómez-Ibarra R, González-García MP, Castañeda-Hernández G, Salinas-Caballero M. Isolation, identification and molecular docking as cyclooxygenase (COX) inhibitors of the main constituents of Matricaria chamomilla L. extract and its synergistic interaction with diclofenac on nociception and gastric damage in rats. Biomed Pharmacother. 2016 Mar;78:248-256.
47. Sharma S, Arif M, Nirala RK, Gupta R, Thakur SC. Cumulative therapeutic effects of phytochemicals in Arnica montana flower extract alleviated collagen-induced arthritis: inhibition of both pro-inflammatory mediators and oxidative stress. J Sci Food Agric. 2016 Mar 30;96(5):1500-1510.
48. Taenzer P, Melzack R, Jeans ME. Influence of psychological factors on postoperative pain, mood and analgesic requirements. Pain. 1986 Mar;24(3):331-342.
49. Wang CF, Gerner P, Wang SY, Wang GK. Bulleyaconitine A isolated from aconitum plant displays long-acting local anesthetic properties in vitro and in vivo. Anesthesiology. 2007 Jul;107(1):82-90.
50. Sharma SM, Anderson M, Schoop SR, Hudson JB. Bactericidal and anti-inflammatory properties of a standardized Echinacea extract (Echinaforce): dual actions against respiratory bacteria. Phytomedicine. 2010 Jul;17(8-9):563-568.
51. Karu T. High-tech helps to estimate cellular mechanisms of low power laser therapy. Lasers Surg Med. 2004;34(4):298-299.
52. Medrado AR, Pugliese LS, Reis SR, Andrade ZA. Influence of low level laser therapy on wound healing and its biological action upon myofibroblasts. Lasers Surg Med. 2003;32(3):239-244.
53. Bronstein D, Suzuki JB. Post Operative Pain Management During the Age of Opioid Crisis. Oral Health. https://www.oralhealthgroup.com/features/post-operative-painmanagement-during-the-age-of-opioid-crisis/ Accessed January 9, 2023.
28 Implant Practice US Volume 16 Number 1 CONTINUING EDUCATION
Continuing Education Quiz
Management of pre- and postoperative dental and surgical pain during the opioid crisis
BRONSTEIN
1. With over _______ Americans abusing prescription opioids in 2020 and over 2.7 million with an opioid use disorder, the U.S. Department of Health and Human Services has declared the misuse of opioids a public health emergency.
a. 3 million
b. 5.6 million
c. 9.5 million
d. 12 million
2. Dry socket is one of the most common postoperative complications after mandibular tooth extraction, characterized by ________.
a. severe pain
b. exposed bone
c. nausea
d. both a and b
3. The time it takes for the dry socket to heal varies depending on its severity, but usually, it ranges from ________.
a. 1 to 3 days
b. 5 to 10 days
c. 2 weeks to 1 month
d. 2 months to 3 months
4. ____________ is a reservoir of platelets, leukocytes, cytokines, and growth factors.
a. Platelet-rich fibrin
b. StellaLife
c. Guided bone regeneration
d. TNF-Į
5. The application of LLLT can offer greater postoperative comfort and wellbeing to patients, functioning as ________.
a. an inhibitor of the inflammatory process
b. a modulator
c. neuronal sodium
d. both and b
6. Since the mid-1990s, deaths from opioid overdose has more than ________, which parallels the increase in opioid prescriptions written in dental and medical practices, which is why some countries have entirely banned opioid use in dental practice.
a. doubled
b. tripled
c. quadrupled
d. quintupled
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 16 CE credits for only $149; call 866-579-9496, or visit https://implantpracticeus.com/ subscribe/ to subscribe today.
n To receive credit: Go online to https://implantpracticeus.com/continuingeducation/, click on the article, then click on the take quiz button, and enter your test answers.
AGD Code: 157
Date Published: February 28, 2023
Expiration Date: February 28, 2026
2 CE CREDITS
7. Pain perception is initiated in the peripheral nervous system (PNS) before the central nervous systems (CNS) become involved, starting with nociceptors which transmit signals along small myelinated A and unmyelinated C fibers before synapsing in the dorsal horn of the spinal cord.
a. True
b. False
8. The initial phase of postoperative pain starts with ________.
a. prolonged dull pain around the surgical area
b. acute pain at the point of noxious stimuli (or incision)
c. the bone graft
d. guided bone regeneration site
9. The objective of pre- and postoperative analgesia is to __________ inflammatory mediators post-surgery
a. intercept
b. increase
c. decrease
d. track
10. According to the article, _________ was used in ancient Chinese and Japanese medicine as an analgesic.
a. Aconitum
b. Arnica
c. Diclofenac
d. Matricaria recutita
To provide feedback on CE, please email us at
education@medmarkmedia.com
Legal disclaimer: Course expires 3 years from date of publication. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
29 implantpracticeus.com Volume 16 Number 1 CONTINUING EDUCATION
The importance of maintaining indoor air quality in dentistry



Drs. Tyler Orehek and Troy Roeder discuss the reasons for maintaining diligent air quality standards in the office
Three years into the Covid-19 pandemic, most industries and professions have undergone significant long-term changes. As more Americans resume their lives, each with a different definition of normalcy, all industries must adapt. New safety protocols, guidance, and equipment are the bare necessities for those looking to thrive in a post-pandemic world.
The dental industry is no stranger to these changes. A report from the National Library of Medicine explored how the industry must adapt to the challenges presented by the pandemic, namely through masking, sanitizing, and most importantly, indoor air purification.1 The prevalence of SARS-CoV-2, a highly contagious airborne virus, means that indoor air purification is crucial in any dental space. This is critical not only for patients who are unable to mask during cleanings and procedures, but for the dentists, hygienists, assistants, and office staff who spend hours of their days in these environments.
For dental offices, simply masking is not enough. During dental treatments, aerosols that may contain blood, saliva, oronasal secretions, microorganisms, filling particles, and tooth particles, are produced. Aerosols are created and spread through the air as a result of various devices used such as turbine handpieces, ultrasonic scalers, air and water syringes, polishing procedures, and surgical lasers. Given that most dental treatments involve the use of many of these instruments, the potential for viruses and infections to spread throughout a dental space is incredibly high.
Tyler Orehek, DC, MSc, CIEC, began his professional career in 2003, and he owned and operated a multidisciplinary practice in midtown Manhattan, serving as the primarycare physician and portal-of-entry healthcare practitioner, with a special emphasis on the treatment of pulmonary and neuromusculoskeletal conditions. Dr. Orehek has been an indoor air quality specialist since 2007. He is also a Council-Certified Indoor Environmental Consultant (CIEC), board-awarded by the American Council for Accredited Certification (ACAC).
Troy Roeder, DDS, is a general dentistry practitioner with over 30 years of experience based in Moline, Illinois. Dr. Roeder attended The University of Iowa, with studies in Biology and Chemistry, before completing his dental training at The University of Iowa College of Dentistry. Dr. Roeder’s dental practice provides both general and cosmetic dental treatments as well as orthodontics for teens and adults.
Disclosure: Dr. Orehek is the President of Airgle Corp., and Dr. Roeder employs Airgle air purification units at his dental practice.
Educational aims and objectives
This self-instructional course for dentists aims to discuss the importance of maintaining indoor air quality in dentistry.
Expected outcomes
Implant Practice US subscribers can answer the CE questions by taking the quiz online at implantpracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can: Identify the primary causes of airborne pathogens in dentistry.
• Recognize the role that dental tools play in spreading aerosols and airborne pathogens.
• View the most effective tools to combat aerosols and airborne pathogens.
• Identify various strategies that can be put in place to maintain air quality.
• Observe how air purification units work to eliminate aerosols and airborne pathogens.
2 CE CREDITS
A recent study demonstrated that saliva may have a significant role in the virus’ ability to spread through airborne transmission.2
A patient infected in the early stages of COVID-19, potentially before they’re even aware of the infection, could have high viral loads in their saliva, and cases with multiple symptoms often
30 Implant Practice US Volume 16 Number 1 CONTINUING EDUCATION
correlate with higher viral loads. These viruses can spread very far, quickly, and remain suspended in the air for very long periods of time.
Asymptomatic patients are also at risk of spreading high viral loads, as many can be unaware of their asymptomatic infection. Respiratory droplets are produced quickly, and heavier droplets can spread within 6 feet of the source in seconds. However, coughing and sneezing can produce even smaller droplets, which can linger in the air up to 20 feet from the source, hours after initially being produced and creating a hazardous environment for patients and dentists.3 Additionally, HVAC systems with poor specifications and efficiency can further contribute to the spread of such droplets.
Furthermore, dentists work in small, tight rooms, making it easy for infections to spread. This has forced the industry to become leaders in infection control in the past, and a similar opportunity presented itself over the past few years during the COVID-19 pandemic.
The pandemic forced dental practices to close for months in March 2020, providing yet another opportunity for the industry to reassess how to improve indoor air quality. For example, while high-volume evacuation (HVE) equipment is effective in sucking up aerosols, the smallest viral particles will often be able to escape, necessitating a more comprehensive solution. Alternative methods are required to improve air quality in dental offices, while also reducing the spread of airborne particles. The following are a few examples of the ways that the dental industry can prioritize indoor air quality, creating a safer environment for patients and practitioners alike.
Negative pressure rooms
One option for practices is to convert operatories into “negative pressure rooms,” which are typically found in hospitals. Designed to combat airborne infections, negative pressure rooms ideally undergo between six to 12 air changes per hour (ACH) and must have air pressure that is lower than the external air pressure. However, while negative pressure rooms protect those outside of the room, they do not provide additional protection to those inside. Additionally, this is a costly conversion, and out of reach for many practices.
HVAC and filtration
Another option is to modify existing HVAC systems, such as through adding high efficiency particulate air (HEPA) filtration. Unfortunately, older HVAC systems often use rudimentary filter stages and are also incapable of sustaining adequate air exchange. These systems are not as robust nor efficient in exchanging air as compared to stand-alone, medical-grade air purifiers, and the difference can be critical. One way to modify these systems is by incorporating UV light into existing HVAC systems, which works if microorganisms are consistently exposed to the UV light. However, this is far from a guarantee, and the modifications can be costly.
Oftentimes, HVAC systems are set to “auto” mode, which adversely affects indoor air quality as it turns off from time to time. This allows contaminants to remain in the air for longer periods of time. By switching the setting to “on,” HVAC systems can work more effectively, relatively speaking, by promoting constant air flow.
Medical grade air purification units
Ultimately, air purifiers are one of the most effective ways to improve indoor air quality. However, the quality and specifications are critical to examine when determining the kind of professional-grade air purifier to implement. While consumer-grade air purifiers are more economical, allowing numerous units to be installed throughout a practice, they are typically less effective than medical-grade air purification systems for a host of reasons. Lesser systems are often underpowered and have smaller cubic feet per minute (CFM) ratings compared to medical-grade purifiers. CFM represents how much air can be drawn into a system per minute. Dental operatories necessitate high CFM to be truly impactful. Additionally, consumer-grade purifiers cannot provide high ACH as compared to medical-grade systems. Lastly, many do not remove ultra-fine particles as small as the SARCoV-2 virus, which is incredibly small, with an average diameter of only 0.1 microns.
High efficiency, medical-grade air purification systems are one of the most effective ways to combat this issue. Standalone, medical-grade air purification systems are far more effective than HVAC systems in filtering out pollutants as well as airborne viruses, bacteria, and mold. Medical-grade purifiers have the highest rate of CFM, meaning they purify more of the air in the same amount of time as compared to other methods of purification. This helps mitigate the potential risk of transmission between doctors, patients, and other staff. Medical-grade purifiers effectively draw aerosolized particles away from operatories and trap them within its filter media. Studies have found that exposure to droplets and contaminants dropped 80% to 95% when air purifiers were used in dental offices.4
Air purification systems must be engineered to combat airborne pathogens (including CoV-2), ultra-fine particulates, and volatile organic compounds (VOCs). For example, Airgle air purification systems utilize a cleanroom-grade cHEPA filter with a capture threshold down to 0.003 microns, which is 100 times more discriminating than traditional HEPA, to capture the smallest of ultra-fine airborne particulates and microbial con-
31 implantpracticeus.com Volume 16 Number 1 CONTINUING EDUCATION
Air purification systems are the only solutions that have discriminating enough filtration, the necessary CFM of delivered air, and the vitally important air changes per hour, resulting in the cleanest possible air in the shortest amount of time.
taminants. Medical-grade purifiers also have more adept cubic feet per minute (CFM), a critical consideration for dental practices. As aerosols linger and remain suspended in operatories for longer periods of time, the risk for cross-contamination can increase exponentially.

An air purifier’s ability to contain airborne contaminants such as pathogens and mold, in addition to volatile organic compounds and ultra-fine particulates, is primarily determined by the type of filter used. An air purification system’s effectiveness is largely correlated to the quality, specifications, and integrity of the purification filter media used within a system.
Putting it into practice
When treating patients, it is critical to keep operating rooms as clean and safe as possible, with a focus on removing aerosols. Installing two medical-grade air purification systems, one at each side of the chair in the main operating room, can ensure a
healthy and safe space for patients. These units also incorporate germicidal UV lights and a high number of air changes per hour, ensuring that rooms are as clean and safe as possible for patients and staff.
While it was standard operating procedure to employ standard screening questions and take patient and staff temperatures when re-opening, patients were looking for more preventative measures. They wanted assurances that every action possible was being taken to make the air safe to breathe. Employing air purification units that filter out the smallest particles gave patients peace of mind when visiting the dental office. In fact, it would serve patients well to have high quality air purifiers in their own home and workplace.
Four main takeaways to highlight, both from personal experience and published studies on the matter:
1. The pandemic is here to stay. Americans are starting to return to their pre-pandemic lives, and many are looking for assurance that they’ll be safe from being exposed to CoV-2 when doing so.
2. Dental practices have a unique challenge. Operating rooms are small, tight areas, where potentially hazardous aerosols can linger for hours if not properly purified and ventilated. This is why dental practices are consistently leaders in public safety.
3. Not all methods of air purification are equal. HVAC systems are effective, but are often unable to combat the smallest of airborne particles like SARS-CoV-2. Consumer-grade air purification systems can be economical, but frequently do not possess the more discriminating filter media, nor the necessary CFM and ACH rates required to keep operatories as safe as possible. Negative pressure room conversions are also an option, but are often too costly for the average dental office to afford.
4. Medical-grade air purifiers are imperative. Air purification systems are the only solutions that have discriminating enough filtration, the necessary CFM of delivered air, and the vitally important air changes per hour, resulting in the cleanest possible air in the shortest amount of time. Purifiers are the most appropriate approach for targeting and capturing the SARS-CoV-2 virus.
The time is now for dental offices to make adjustments if they have not done so already, and medical-grade air purification is the best way to ensure safety for dentists and patients alike.
REFERENCES
32 Implant Practice US Volume 16 Number 1 CONTINUING EDUCATION
1. Ancuta G, Sandu D, Tatarciuc M, Luchian I. The Impact of the COVID-19 Pandemic on Dentistry and Dental Education: A Narrative Review. Int J Environ Res Public Health. 2022 Mar; 19(5):2537.
2. Carrouel F, Gadea E, Esparcieux A, Dimet J, Langlois ME, Perrier H, Dussart C, Bourgeois D. Saliva Quantification of SARS-CoV-2 in Real-Time PCR From Asymptomatic or Mild COVID-19 Adults. Front Microbiol. 2021; 12:786042.
3. Xie X, Li Y, Sun H, Liu L. Exhaled droplets due to talking and coughing. J R Soc Interface. 2009 Dec 6;6 Suppl 6(Suppl 6):S703-714.
IP
4. Chen C, Zhao B, Cui W, Dong L, An N, Ouyang X. The effectiveness of an air cleaner in controlling droplet/aerosol particle dispersion emitted from a patient’s mouth in the indoor environment of dental clinics. J R Soc Interface. 2010 Jul 6;7(48):1105-1118.
Operating rooms are small, tight areas, where potentially hazardous aerosols can linger for hours if not properly purified and ventilated.
Continuing Education Quiz
The importance of maintaining indoor air quality in dentistry
OREHEK/ROEDER
1. A report from the National Library of Medicine explored how the industry must adapt to the challenges presented by the pandemic, through ________.
a. masking
b. sanitizing
c. indoor air purification
d. all of the above
2. During dental treatments, aerosols that may contain __________, microorganisms, filling particles, and tooth particles are produced.
a. blood
b. saliva
c. oronasal secretions
d. all of the above
3. Aerosols are created and spread through the air as a result of various devices used such as turbine handpieces, ultrasonic scalers, air and water syringes, polishing procedures, and surgical lasers.
a. True
b. False
4. Respiratory droplets are produced quickly, and heavier droplets can spread within ________ of the source in seconds.
a. 6 feet
b. 10 feet
c. 12 feet
d. 14 feet
5. However, coughing and sneezing can produce even smaller droplets, which can linger in the air up to _________ from the source, hours after initially being produced and creating a hazardous environment for patients and dentists.
a. 20 feet
b. 30 feet
c. 35 feet
d. 40 feet
6. Designed to combat airborne infections, _____________ ideally undergo between six to 12 air changes per hour (ACH) and must have air pressure that is lower than the external air pressure.
a. positive pressure rooms
b. negative pressure rooms
c. high particulate rooms
d. auto-mode HVAC rooms
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 16 CE credits for only $149; call 866-579-9496, or visit https://implantpracticeus.com/ subscribe/ to subscribe today.
n To receive credit: Go online to https://implantpracticeus.com/continuingeducation/, click on the article, then click on the take quiz button, and enter your test answers.
AGD Code: 130
Date Published: February 28, 2023
Expiration Date: February 28, 2026
2 CE CREDITS
7. By switching the setting to ______, HVAC systems can work more effectively, relatively speaking, by promoting constant air flow.
a. “on”
b. “off”
c. “auto”
d “professional”
8. ___________ represents how much air can be drawn into a system per minute.
a. Pressure per minute (PPM)
b. High-volume evacuation per minute (HVEM)
c. Cubic feet per minute (CFM)
d. none of the above
9. Standalone, medical-grade air purification systems are far more effective than HVAC systems in filtering out pollutants as well as _________.
a. airborne viruses
b. bacteria
c. mold
d. all of the above
10. Studies have found that exposure to droplets and contaminants dropped when air purifiers were used in dental offices.
a. 25%-34%
b. 46%-53%
c. 65%-76%
d. 80%-95%
To provide feedback on CE, please email us at education@medmarkmedia.com
Legal disclaimer: Course expires 3 years from date of publication. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
33 implantpracticeus.com Volume 16 Number 1 CONTINUING EDUCATION
Guide to having a video filmed for your practice
Dental practice videographer Jeremy Tuber shares his expertise on the logistics of filming a promotional video

You have decided to have a promotional video filmed for your practice. Great, right? Well, often the communication and coordination responsibilities of putting the video shoot together fall directly onto the front office staff. Maybe that’s the position you find yourself and your team in, and you’re not certain how to manage it all.
If you’ve not worked with a video production professional or company before, it can be a little nebulous and perhaps even a little intimidating. However, with a little insider information, you can make the process easy for your team, other dentist(s), and any patients you might have come in and participate.
Covering all aspects of working with a video crew is beyond the scope of this condensed article. However, one of the first questions the front office staff has is, “Who should we include in the video?” The answer isn’t as obvious as you might expect. The answer is, “Whomever you select, choose wisely.”
Team members
If you have team members who are beyond just being a little camera shy — they’re either terrified or ticked off about being on camera, so don’t force them. Adept videographers can do a lot to make people look and sound their best. However, there’s very little they can do to hide if someone is self-conscious or annoyed about being on camera. Choose team members who genuinely want to represent the practice in the video. If you have a larger office, it might not be necessary to include everyone in the video. In fact, trying to ensure that everyone gets into the video might be counterproductive and time-consuming.
An additional question routinely asked is, “What happens if we had a video filmed, but one or more dental team members are no longer with the practice?” It depends on their role in the video. For dental team members who are just featured in some of the non-speaking/action footage part of the video, (also called “bRoll” by video professionals), it’s not a big deal. However, if you had the team members being interviewed on camera, you
might need or want to remove them if they leave the practice. Therefore, be wary about asking the dental team to speak on camera. Most dental practices typically just have the dentist(s) speaking on camera — on a rare occasion a long-time office manager.
Patients or “patient stand-ins”
If you’re interested in having actual patients come in and help out with the video (either providing a video testimonial or just being in some of the bRoll), choose wisely.
Choose patients who are comfortable on camera, who love your practice, and who have the time to come in for an hour or so and participate. If you’re asking patients to provide a video testimonial, it may feel like an unnecessary step, but consider initially asking them, “What do you enjoy about the practice? What might you share about this practice on camera?” Your goal in asking them these questions is to learn ahead of time what they’ll say on camera and to get them to start thinking about what they’ll say.

All too often, well-intentioned patients blurt things out on camera like, “I love this practice because they are so cheap,” or “Dr. Smith is great because I can call him on his mobile phone over the weekend, and he responds!” Yikes, both statements might be true, but they should be kept on the DL and not included in the final edit of the video. Of course, statements like this can be easily edited out, but you want to ensure you don’t invest time in having a patient provide a testimonial that is bland, flat, or even one you can’t use.
Gently suggest to patients offering a testimonial that they do a little thinking about what they’ll say before the cameras start rolling — maybe even practice what they’ll say in front of a mirror or a friend/family member just a little bit. Patients, dentists, and just about everyone who haven’t been on camera sometimes assume that they can just “wing it.” And in truth, some can. However, for
34 Implant Practice US Volume 16 Number 1 MARKETING MOMENTUM
Jeremy Tuber has served as the Arizona Dental Association’s Director of Marketing and Managing Editor since 2010. In 2014, he opened DDSvideo.com and has filmed more dental practice marketing videos in Arizona than anyone else in the state. He has filmed for Dentsply Sirona, ATSU/ASDOH, Diversity in Dentistry, AzDA, and is slated to film a PSA for the ADA in February 2023.
most of us, doing a little preparation and visualizing what we’re going to say ahead of time will help tremendously.
You don’t need to give patients the third degree about what they’ll say on camera — let it come from their heart, but guiding them a little and helping to clarify what they’ll say might make a mediocre video testimonial a great one. Just asking them ahead of time, “What do you think you’ll share/say?” is enough to get them to do a little thinking before they get on camera, and that often results in a better testimonial.
If you do ask patients to appear on camera, ask them to sign a media release form. Yes, every patient who appears on camera should sign one of these forms. Your video professionals should provide you with one to hand out. If they don’t, ask for one. More important, provide these to patients before the day of the shoot so they have time to review, sign, and then return them via email. Having patients sign one of these forms right before they jump in front of a camera just adds a layer of stress, so it’s best to have them sign the form before the day of the shoot.
It’s important to note that if you don’t acquire signed media releases, anyone who is not an employee of the practice could potentially change their mind about being in the video long after it’s been uploaded and on your website. They can request that you remove them from the video, which means you’ll need to contact the video professionals and pay to have the video edited to delete the person who no longer wants to be in the video. Having non-employees sign a release form can help guard against this, so it’s worth the bother.
As a last note about who is and isn’t in your video, many practices don’t recruit actual patients to come in. Instead, they opt for friends and family members to pose as patients while bRoll footage is filmed. (No, they don’t ask friends and family members to provide fake patient testimonials.) Friends and family members usually are more willing to help, and they don’t often require any compensation! Nevertheless, it might be nice to provide anyone outside of the dental team with a gift card, free whitening, or some small token of appreciation for taking time out of their day to help you.
Bonus Tip: Consider bringing in a veggie/fruit plate or some doughnuts for people to nosh on while they are not on camera.
Being prepared on the day of filming
It usually takes a film crew about an hour or so to set up, so if you’re filming first thing in the morning, perhaps plan on having at least one person arrive an hour early to let the crew move their gear in and set up. Note: Expect the video crew to need 20-40 minutes to pack up their gear after the shoot has wrapped up.
Video crews typically have a lot of gear, so they must find a safe out-of-the-way place in the practice to store it. Before the video crew arrives, consider a lower-traffic area of the office where they could store their gear. Make certain there isn’t any printed/digital sensitive information (or valuables) laying about.
It might be tempting to squeeze a few patients in, perhaps schedule a patient or two, during the shoot, but it’s not recommended. You won’t be able to give your full attention to your patients or to your video crew, so outside of an emergency patient, avoid scheduling production during the video shoot.
If you are conducting interviews (often called “aRoll”) or patient testimonials, make sure you can mute the phone, background music, or anything else that might interfere with the audio recording. You might even consider making sure local landscapers aren’t working during the time of your video shoot. (Yes, this has happened to other practices.)
To make the best use of everyone’s time, ask the video crew to provide you with a schedule for the day. Ask them when you, the team, the doctor(s), and perhaps the patients need to be available. Review the schedule for the day, and make sure there aren’t large time windows when people are standing around doing nothing. Gently remind the video crew that you want to be respectful of everyone’s time, which means getting them in and out as efficiently as possible.
Make certain that everyone who is going to be on camera is aware of (and has agreed to) their start time and finish time. Nothing derails a video shoot more than someone showing up late, announcing they suddenly must leave early, or someone just not showing up at all. Ensuring everyone shows up on time is like oral care: “An ounce of prevention is worth a pound of cure,” so consider sending out gentle reminders a few days before as well as the day before the shoot so that everyone is aware of their responsibilities.
In working with a video crew, it’s important to recognize that they don’t know the details of your profession — most don’t “get” dental. To be fair, you might be unfamiliar with the video profession as well, so it’s important that you respect one another’s expertise, you communicate (even over communicate) so that everyone’s on the same page, and that you politely ask questions or raise concerns if they arise.

At the very least, consider at least one “pre-production” phone, Zoom, or in-person meeting so you can discuss your vision, logistics, etc. If it’s possible, ask if the video crew would be open to visiting the office before the day of filming to “scout” the location. The truth is, something always goes sideways during a video shoot, and that’s okay. An accomplished video crew will easily be able to manage any hiccups in the process. However, having discussed a plan of attack for the day before you begin filming will go a long way in reducing the likelihood that something will go sideways on you. Most offices have a morning huddle before the day begins — consider applying the same approach to having a video filmed for your practice.
In the end, the video crew and the dental team should have the same goal: to film a compelling promotional and/or educational video for the practice. Communicate, be honest (be open when you’re confused or need advice), and work together. Reprinted with permission by
35 implantpracticeus.com Volume 16 Number 1 MARKETING MOMENTUM IP
Inscriptions, a publication of the Arizona Dental Association.
Anatomy of a dental malpractice action
Kristin Tauras, JD, defines the various complex parts of a malpractice claim
Today’s reality is that most dental and medical providers have a high probability of being sued. Below is a primer on the “anatomy” of a dental malpractice case. Lawsuits are controlled by state and federal law, but the basic anatomy of the lawsuit is the same in each state and follows the same general timeline.
The term used in the lawsuit may be “professional malpractice” or “dental malpractice,” but this article encompasses all professional negligence claims against dental specialists, including dentists, cosmetic dentists, pediatric dentists, prosthodontists, periodontists, endodontists, oral and maxillofacial surgeons, and orthodontists. It also encompasses the liability of the dental specialist(s) staff who assist with the dental treatment and may be named in the dental malpractice lawsuit, including dental hygienists, dental assistants, nurses, anesthesiologists, and other dental care providers.
Parties
There are at least two parties to a lawsuit: the plaintiff and the defendant.

The plaintiff is usually the patient or the parent/guardian of a minor patient. The lawsuit may be brought by the estate of a deceased or incapacitated plaintiff.
The primary defendant is the treating dental specialist, but there may be multiple defendants. Defendants may include any individual involved in the patient’s care and treatment leading up to and through the alleged malpractice event, including consulting dental specialists, nurses, radiologists, surgeons, dental hygienists, and even the medical malpractice insurance companies in some states. The lawsuit may also name the practice group, corporation, or limited liability company that employs the dental specialist(s).
Pleading stage
A dental malpractice lawsuit begins with a pleading or complaint that is filed with the court. It is the story the patient wants to tell the jury of what the dental specialist(s) did wrong and why the jury should award the patient money. The complaint must set forth that there was a patient and dental specialist(s) relationship, the dental specialist owed a duty of care to the patient, the den-
Kristin
tal specialist(s) violated the duty of care, and that the violation of the dental specialist(s) duty to the patient proximately caused the patient’s injuries, and the patient (or patient’s estate) suffered damages.
Twenty-eight states have the additional requirement to file a certificate of merit for a dental malpractice claim to move forward.
The complaint must be served on each defendant. The date of service of the complaint on the defendant governs the timing of when the defendant must respond to the complaint. The defendant typically has 21 to 28 days to respond to the complaint. The response may either be an answer to the complaint (admitting, denying, or claiming insufficient information with respect to the allegations), or a motion to dismiss the complaint for technical errors or substantive reasons why the dental professional is not liable.
The pleading stage is also where the defendant may want to file a third-party action against another entity to bring them into the suit. While most attorneys will advise against filing a thirdparty action against another dental treater so that they can bring a unified defense, there may be an occasion to file a third-party suit against the manufacturer of a faulty instrument that caused or contributed to the problem. Most dental malpractice claims do not have third-party actions.
Respondents in discovery
Some states allow for complaints to be filed against an individual, but not name the individual as a defendant. Called a Respondent in Discovery, these individuals are named for discovery purposes only. A Respondent in Discovery may be converted to a direct defendant so long as the plaintiff follows the rules of the state for converting the Respondent in Discovery to a proper party defendant.
Notifying the insurer
The dental specialist(s) must notify their insurance company at the time they know of a claim or are served with a lawsuit. Every insurance policy contains a duty to notify the insurance
36 Implant Practice US Volume 16 Number 1 LEGAL MATTERS
Tauras, JD, is a partner in the law firm of McKenna Storer in Chicago, Illinois. She has a litigation practice in the areas of employment law, insurance coverage, and professional malpractice. McKenna Storer is a fullservice law firm providing legal services to individuals and small-to-midsize companies, including defending professional malpractice negligence lawsuits and Illinois Department of Professional Regulation investigations, as well as advising dental and medical professionals regarding business and employment matters.
company upon learning of the potential claim when served with a lawsuit. If the dental specialist(s) fails to notify the insurance company, the insurer may refuse to defend and indemnify the claim.
Notice of the claim allows the insurance company to assign the dental specialist(s) an attorney, direct them on what records to keep, and how they should proceed. Some policies allow the dental specialist(s) to choose their own counsel.
Immediately retain documents and preserve evidence
Upon knowing of a claim and/or being served with a lawsuit, it is imperative that the dental specialist(s) retain all medical and dental records, notes, bills, x-rays or other imaging, correspondence with the patient, and machines used in the treatment of the patient, essentially “preserving” all evidence of the alleged malpractice. Your attorney and/or the insurance company will advise you what they need you to retain and send to them to defend the case as well. If you do not, or if you destroy relevant evidence, some states will allow a “spoliation of evidence” claim to be filed against you, which may include a putative finding of liability with just damages to be assessed.
Discovery stage
After the answer is filed or the motion to dismiss is resolved, the case will enter the discovery phase.
Discovery is broken down into three types: fact written discovery, fact oral discovery, and expert discovery.
Written discovery
All parties may issue written discovery against the other parties. Where there are multiple defendants, each plaintiff may issue discovery against each defendant, and each defendant may issue discovery against the plaintiff, as well as against each of the other defendants.
Written discovery is divided into four types: Interrogatories, Requests to Produce, Third-Party Subpoenas, and Requests to Admit.
Interrogatories are questions submitted to the other parties. The plaintiff’s Interrogatories to the defendant(s) will include requests for information such as the identity of all treaters (both dental and non-dental), dates of treatment, types of treatment, types of tests done prior to the treatment, cost of the treatment, and information regarding the insurance. The defendant(s) Interrogatories will include the basis for the negligence allegations, identify the claimed negligent treatment, damages (including alleged injury, days off work, cost of alleged repair or further treatment, as well as pain and suffering and disfigurement), and identity of witnesses.
The Requests to Produce are written requests for documents. The plaintiff’s Requests to Produce will usually include the patient’s dental records, bills, x-rays or other imaging, correspondence, as well as the office policies and procedures. The defendant’s Request to Produce will usually include the plaintiff’s dental and medical records, bills from additional treatment, and proof of damages such as time off work.
The parties may also issue Subpoenas to other entities not involved in the lawsuit, including other medical and dental treaters who have treated the patient both in the past and with respect to the claimed malpractice.
The parties may also issue Requests to Admit. These are statements that the parties must either admit or deny or set forth a reason they can neither admit nor deny the statements. Depending on the state law, these Requests to Admit may become binding on the parties at the time of trial.
Oral fact discovery
Discovery also includes non-expert testimony from the plaintiff, defendant(s), and any other fact witness.
The patient’s deposition is usually the first deposition taken in a case. If the patient is unable to testify, such as when the patient is a minor or the patient is disabled or deceased, the family members or next of kin who brought the lawsuit may testify about the patient’s treatment and injuries.
The defendant(s) depositions then take place. The defendant(s) include the dental specialist(s) sued in the case, as well as the other individuals in the office that took part in the care. The depositions of the defendant(s) usually center around the issues of informed consent, care provided to the patient, policies and procedures of the office, and the dental specialist(s) training and experience to perform the procedures that form the basis of the lawsuit.
After the defendant(s) depositions are taken, the parties will take the depositions of the other dental and medical treaters who have seen the patient.
Additional fact witness(es) depositions may also be taken. These fact witness(es) may include the office manager(s) to testify regarding bills and the office policies and procedures, and family members that can testify to the condition of the patient before and after the procedure.
Expert discovery
In all states, almost without exception, the plaintiff must have dental specialist(s) testify to the standard of care and whether the care deviated from that standard. While technically the defendant(s) may be qualified to testify to the standard of care and alleged deviation, standard of care experts are usually paid experts who evaluate the patient’s records and testify regarding their expertise. Expert testimony may be excused when it is readily apparent that malpractice occurred (such as inexcusably removing the wrong tooth) and that an expert’s testimony might be redundant. Many trials rise and fall on the strength of the dental specialist(s) expertise.
Other experts may also testify regarding damages, including financial experts who testify about the financial harm the plaintiff suffered because of the sub-standard care.
37 implantpracticeus.com Volume 16 Number 1 LEGAL MATTERS
Under most insurance policies, the dental specialist has the ultimate right to make all decisions regarding settlement.
Dispositive motions
Most states have a mechanism for filing a dispositive motion, such as a motion for summary judgment or summary decision, after the close of discovery. The dispositive motion requests that the judge review the law and the facts to see if there is an issue of fact that requires that the matter be tried. Usually, this motion is filed by the defendant(s), alleging that the plaintiff cannot prove a required element of their case.
Settlement
While settlement discussions can happen at any time during the case, most parties will engage in settlement discussions after the close of discovery or before the trial begins. In dental cases, there is the notion that the case is either in a “settlement posture” or a “trial posture.” Nevertheless, many cases do settle on the eve of trial. Under most insurance policies, the dental specialist(s) has the ultimate right to make all decisions regarding settlement.
Trial
Many dental malpractice cases go to trial. A trial date is usually set between 18 months to 36 months after the date the lawsuit was filed. The dental specialist(s) should sit at counsel’s table through the duration of the trial.
Professional malpractice trials are long, lasting a week or longer. The first day is usually a “pretrial conference.” The judge will attempt to settle the case and then rule to either admit or exclude evidence from trial (called the motions in limine), and review jury instructions.
Day 2 and Day 3 are spent with jury selection. Jury selection is heavily individualized by the judge who presides over the case. The judge may ask the jury questions or let the attorney ask the questions.
Once the jury is empaneled, the trial begins. The attorneys will give their opening statements, explaining to the jury what they believe the evidence will show. After that, the plaintiff will present their case in chief, and the defendant(s) will then present their case in chief.
At the end of the evidence phase, the judge will instruct the jury on the law, and the deliberation process begins. The jury will deliberate until either they reach a decision, or they inform the court that they are unable to reach a decision.
Motion to overturn the verdict or appeal
After the jury reaches its verdict, the jury foreman will read the verdict. This does not end the proceedings. The parties in all states have the right to file a motion to contest the jury verdict and/or file an appeal from the jury’s verdict.
If the jury verdict is affirmed by the appellate court, and the appellate process is exhausted, the matter ends. If the jury verdict is overturned by the judge and/or the appellate courts, then it is possible the matter will be retried.
Reporting
Some states require that any settlement or an adverse judgment be reported to the state licensing board. In that case, the dental specialist(s) should retain defense counsel to assist with the defense of the dental license. IP
Implant Practice US Webinars
LEARN about the lastest techniques and technology from industry leaders with our free live and archived educational webinars. Our online seminars are a convenient way to access great information and upskill. Check out our most recent webinars:
• Growing Your Practice with Robotics with host Dr. Leo Haydt
• 5 Ways to Decrease Overhead and Increase Productivity with host Dr. Jason Streeter
• Evolution of Implant Connections with host Dr. August de Oliveira
38 Implant Practice US Volume 16 Number 1 LEGAL MATTERS
WATCH NOW at https://implantpracticeus.com/webinars/ Connect. Be Seen. Grow. Succeed. | www.medmarkmedia.com
Panthera Dental to exhibit at IDS 2023
Panthera Dental, a global leader in CAD/CAM implant solutions and dental sleep appliance development, will exhibit for the first time at the International Dental Show (IDS) in March 2023. From March 14 to 18, the company will showcase innovative solutions, workflows, and more. Meet the team in Hall 1.2 at their 1,345 sq. ft./125 m² booth. Take part in Panthera’s live trainings, product launch, happy hours, and participate in a special Master Cup event hosted in partnership with VITA to celebrate past winners and participants.
For more information, visit www.pantheradental.com.
Dentsply Sirona’s Implant Solutions World Summit 2023
Registration is now open for Dentsply Sirona’s Implant Solutions World Summit 2023, taking place in Athens, Greece, from June 8 to 10, 2023. The congress will feature more than 40 international speakers, with inspiring main stage presentations, hands-on workshops, and break-out tracks on topics such as esthetics and the digital dentistry ecosystem. The Implant Solutions World Summit brings together professionals who are passionate about elevating the dental industry and improving the quality of implant treatments and care for patients. Attendees will be able to discover the latest innovations in implant solutions, including the EV Implant Family, digital dentistry, and bone regeneration. Attendees will learn about managing implant complications, the connections between systemic and oral health, maximizing esthetics, controlling risk factors, maintaining peri-implant health and also be able to visit an interactive exhibition and sign up for exciting master class workshops to learn more about Dentsply Sirona’s products, solutions, and workflows. The congress will take place at the InterContinental Athenaeum Athens hotel, close to Greece’s famous Acropolis.

For more information, visit www.dentsplysirona.com/ worldsummit.
DEXIS™ launches new DEXIS™ IS Intraoral Scanning Portfolio

The launch of the DEXIS IS (intraoral scanner) portfolio, a full suite of intraoral solutions, marks an important milestone for DEXIS, which now offers a full range of digital dental diagnostic systems that cover every stage of scanning. With a growing network of innovative software and award-winning scanners that seamlessly work together, DEXIS can now truly transform and simplify the day-to-day routine of dental practices everywhere. The DEXIS IS intraoral portfolio includes three levels of intraoral scanner: IS 3600, IS 3700, and IS 3800W, as well as the new IS Voyager, an all-in-one computer and trolley. From the entry level scanner, the IS 3600, to the recent Red Dot award-winner, the wireless IS 3800W, there is a DEXIS IS scanner to fit any type of practice and provide simpler, digitized workflows that enable better outcomes and improved patient experiences.
All intraoral scanners are paired with the latest IS ScanFlow v1.0.7 software update. IS ScanFlow enables accurate digital impression acquisition in a few straightforward steps. The software features expansive workflow capacity, an increase in scanning speed, and expanded processing options. IS ScanFlow also offers one-click export functionality to IS Connect, a secure online portal that makes it quick and easy for practices to transmit digital intraoral impression scans. IS Connect makes it easy to transfer both STL and rich DICOM 3D digital impression files – Making DEXIS IS a completely open system. Clinicians can easily communicate with their preferred manufacturer or lab partner, providing more flexibility.
For more information, visit http://www.dexis.com.
OraCare joins forces with TruBlu Direct in support of private practice dentistry
OraCare, provider of the award-winning OraCare Health Rinse, has announced a new partnership with TruBlu Direct. Effective immediately, TruBlu Direct member dental practices can now purchase OraCare products through the TruBlu Direct online marketplace. OraCare Health Rinse uses an activated chlorine dioxide formulation that destroys oral biofilm and pathogens, while eliminating the well-known issues associated with chlorhexidine rinses. It is the only rinse sold exclusively to dental professionals, supporting both an elevated standard of patient care and practice revenue growth. The product was selected as a Cellerant Best of Class Hygiene award-winning product in 2021 and 2022. The TruBlu Direct marketplace provides the benefits of purchasing at scale, otherwise only available to DSOs, to its independent member practices.
For information, visit https://www.oracareproducts.com/.
39 implantpracticeus.com Volume 16 Number 1 INDUSTRY NEWS
A commemoration of oral health services to soldiers
Dr. Francis Nasser, Jr. discusses the important role of military dentists and a special way to recognize their contribution to the field
The Association of Army Dentistry (AAD) dedicated the Army Dentistry Monument on Friday, March 24, 2023, in a ceremony at the U.S. Army Medical Department (AMEDD) Museum in San Antonio, Texas. According to Dr Ronald Lambert (COL USA DC ret, Past President of the AAD), “The monument is a lasting tribute to all the soldiers, civilians, and spouses who have served and continue to serve in the Army Dental Care System in support of the U.S. Army and its military mission. The monument recognizes and honors the selfless contributions made by the diverse members of the Army Dental Care System and its key supporting components in the overall mission of Army Medicine.”
Founded in March 1911, the Army Dental Corps has a long and distinguished history of providing global dental services to soldiers and ensuring the readiness of the nation’s fighting forces. Even before 1911, the Army contracted dental surgeons to provide dental care to soldiers deployed to the new territories of a growing nation. The tradition of providing oral health services to soldiers wherever they are assigned continues to this day.
During World War II, more than 18,000 dentists served in uniform. It was during this time that the role of Army Dentistry expanded to include not only all levels of dental services, but also non-dental support and leadership. In the battle of Saipan in the Pacific, a Dental Corps Officer, Captain Ben Salomon, took command of the battalion aid station on the island. During an ensuing and desperate attack by enemy forces, CPT Salomon, also a skilled infantry soldier, heroically fought and defended the battalion aid station. He lost his life in the battle, but his gallantry and sacrifice did not go unrecorded. He was awarded the Medal of Honor posthumously, the only Army dentist to ever receive the nation’s highest military award. The image of Dr. Ben Salomon was used in the design of the dental officer sculptured in the monument.
Army Dentistry was firmly established as a permanent and essential element in preserving the readiness and fitness of the fighting force. During the conflicts in Korea and Vietnam, Army Dentistry continued to provide direct support to soldiers in the field of operations.
The Persian Gulf War brought the largest expansion of Reserve Dental Support in Army Dentistry. Over 220 reserve dental officers and 320 reserve enlisted soldiers were called up to support the mission. Overall, 121 dental officers served in the theater. The expanded use of reserve forces continued throughout the later conflicts in Iraq and Afghanistan.
Today the Army Dental Care System is a highly trained and integrated team of military officers, non-commissioned officers (NCO), enlisted soldiers, and government service (GS) civilians. The Army Dental Corps has 970 dentists in uniform and is augmented with 455 GS and contracted civilian dentists. There are 1,225 NCOs and enlisted soldiers and 2,300 civilians providing clinical and administrative support. All services and specialties of the dental profession are provided to the nation’s service members. In addition, Army Dentistry is a leader in the postgraduate education and specialty training of young dentists, and the advanced training of enlisted soldiers and civilians. The mission of the Army requires that Army Dentistry be prepared to support soldiers wherever they are deployed. Colonel Tom Goksel, DDS, MD, says, “The Army Dental Corps is the leader in expeditionary dentistry and sustainment of force readiness … the mission is to have a ready Dental Corps capable of delivering global dental services in order to sustain the readiness of the total military force.”
The Association of Army Dentistry is proud to keep the legacy of the Army Dental Corps alive and preserve its rich history, in order to inspire those who choose to serve and support the nation’s military men and women. The Army Dentistry Monument Dedication commemorates this unique contribution to the U.S. Army and the nation.


40 Implant Practice US Volume 16 Number 1 MILITARY MATTERS
IP
Dr. Francis Nasser, Jr. is a retired Colonel in the U.S. Army Dental Corps and a current member of the Association of Army Dentistry Board of Directors.




The leading Oral Surgery partnership group Our family of brands OS1partners.com I 305-206-7388 At OS1, we provide the resources needed to help you grow your practice. Our support will take the stress of practice management off your plate so you can focus on providing high-quality care to patients.