A conversation with Dr. David DiGiallorenzo
The use of photogrammetry for the fabrication of full-arch immediate prostheses
Dr. Christopher R. Resnik
Dental sedation: an overview

Dr. Brian McGue
Treatment of a patient with trans-canine placement of a dental implant
Drs. Douglas D. Wright and William T. Goodwin II
1“ 1.25“ 10.875“ 1.75“ Th e Only Spec i al t y Par tne r sh i p O r gan iz at ion RE AD MO RE ON PAGE 8 FOUNDED AND LED BY DOCTORS.
A 30-year perspective on implant dentistry
PROMOTING EXCELLENCE IN IMPLANTOLOGY
Tradeshow Special Section n 4 CE Credits Available in This Issue* Fall 2023 Vol 16 No 3 implantpracticeus.com


Fall 2023 n Volume 16 Number 3
Editorial Advisors
Jeffrey Ganeles, DMD, FACD
Gregori M. Kurtzman, DDS
Jonathan Lack, DDS, CertPerio, FCDS
Samuel Lee, DDS
David Little, DDS
Brian McGue, DDS
Ara Nazarian, DDS
Jay B. Reznick, DMD, MD
Steven Vorholt, DDS, FAAID, DABOI
Brian T. Young, DDS, MS
CE Quality Assurance Board
Bradford N. Edgren, DDS, MS, FACD

Fred Stewart Feld, DMD
Gregori M. Kurtzman, DDS, MAGD, FPFA, FACD, FADI, DICOI, DADIA
Justin D. Moody, DDS, DABOI, DICOI
Lisa Moler (Publisher)
Mali Schantz-Feld, MA, CDE (Managing Editor)
Lou Shuman, DMD, CAGS
What is new in contemporary practice?
There have been tremendous advancements in existing technology and materials science. Diagnosis, treatment planning, and clinical therapeutics have become more accurate and efficient with the use of these tools. However, these advancements have not necessarily made the overall practice easier.
Immediate loading is not new. Throughout the 1960s and 1970s, blade implants were commonly placed, and they were routinely immediately loaded as they healed by fibrous integration. Personally, as soon as the ITI team launched the single-stage hollow basket implant, I embraced the concept of immediacy. I began utilizing single-stage protocols for immediate bridges, single implants, and full-arch cases as a routine part of my practice.
Scanning technology also has been in use. In the late 1980s and 1990s, we were already using hospital-based CT scans for implant cases during residency and private practice. Some of the significant changes include the addition of biologic modifiers. I have been using the BTI protocol for 15 years, developed by Dr. Eduardo Anitua, MD, DMD, which involves growth factors, drilling speed, autogenous recovery, and ridge expansion protocols. Additionally, the introduction of different laser wavelengths, such as LANAP, has revolutionized periodontal therapy by accelerating and modifying treatment. It allows for the treatment of advanced occlusal periodontitis that was previously difficult to address surgically. Full-mouth therapy can now be delivered without sutures or flapping, providing a conservative and repeatable treatment modality. Moreover, the use of surgical guides has evolved placement strategies, and pinhole placement options have become more common in various cases. The advent of CAD design has improved the tolerances between different parts and prostheses, although misfits still occur.
Many of the implant designs that are now considered standard of care were already available and being designed in the 1980s. Our colleagues in Europe were pioneering implants with specific biologic parameters, including reducing crestal bone loss through platform switching, achieving zero micro-gap for bacterial penetration and micro-movement, optimizing cell surface, and designing threads for optimal primary stability. As implant designs matured, macro-mechanical retention (primary stability) increased, micro-mechanical biologic healing (secondary stability or osseointegration) reduced to 12 weeks and then 8 weeks, and bone-to-implant contact approached 70%.
Globally, the dental profession has made tremendous strides in improving overall health outcomes. The periodontal research community has significantly advanced our understanding of the intricate relationship between oral inflammation and systemic inflammation. The connection is now clear, leaving no room for doubt. However, the U.S. has been slower in addressing critical health concerns such as the toxicity issues associated with the materials we use. Specific areas of concern include fluoridated water and metal alloys, which have been shown to disrupt cellular, electrical, and immune functions. As a result, I have observed an increase in sensitivities, neuralgias, unexplained pain, peri-implantitis, and implant failures.
US or the publisher.
ISSN number 2372-6245
David DiGiallorenzo, DMD, received his training at the University of Pennsylvania in the Department of Periodontics and Periodontal Prosthesis in the early 1990s. His training included prosthodontics, orthodontics, periodontics, and advanced oral reconstructive techniques, including oral implantology. He is in private practice in Collegeville and South Williamsport, Pennsylvania, focused on laser, esthetic and reconstructive periodontics, dental implantology, advanced reconstructive case management, immediate total tooth replacement, metal-free implantology, and TMJ. He is also focused on an integrative health-centered approach to health and wellness. He is a past clinical instructor at the University of Pennsylvania in the Department of Periodontics. He lectured both nationally and internationally at local and national meetings. He was a key opinion leader and consultant for DENTSPLY, Synthase, Keystone, OraPharma, and z-look zirconium implants.

1 implantpracticeus.com Volume 16 Number 3 INTRODUCTION
© MedMark, LLC 2023. All rights reserved. The publisher’s written consent must be obtained before any part of this publication may be reproduced in any form whatsoever, including photocopies and information retrieval systems. While every care has been taken in the preparation of this magazine, the publisher cannot be held responsible for the accuracy of the information printed herein, or in any consequence arising from it. The views expressed herein are those of the author(s) and not necessarily the opinion of either Endodontic Practice


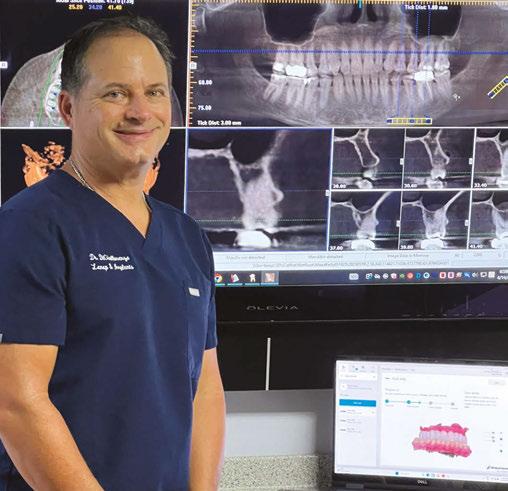
2 Implant Practice US Volume 16 Number 3 TABLE OF CONTENTS CASE REPORT Treatment of a patient with transcanine placement of a dental implant Drs. Douglas D. Wright and William T. Goodwin II treat a patient with multiple restorative challenges PUBLISHER’S PERSPECTIVE Staying informed and safe Lisa Moler, Founder/CEO, MedMark Media............................... 6 MARKETING MOMENTUM A good “NAP” is 1 of 3 ways to improve practice success Chad Erickson discusses how to generate more revenue from your local listings ........................ 18 TRADESHOW SPECIAL SECTION Advanced Dental Implant Center™........... 20 Elevate your dental implant practice with Boyd 21 Cool Jaw® hot/cold therapy ................................... 22 HighFive Healthcare .. 23 Specialty1 Partners ..... 24 Easily go from removable to FIXED with the Zest LOCATOR!............................. 25 8 12 COVER STORY A 30-year perspective on implant dentistry A conversation with Dr. David DiGiallorenzo Cover image of Dr. David DiGiallorenzo courtesy of Specialty1 Partners.
No New Abutment Required…
Now use LOCATOR Abutments for FIXED Full-Arch


Introducing a NEW flexible and accessible FIXED full-arch solution

LOCATOR Removable or FIXED... it's your choice.
Utilize patients' existing LOCATOR or newly placed abutments to transition from a removable overdenture to a FIXED, full-arch solution.
Offer staged treatment planning for your patients, removable today… FIXED tomorrow.

Give your patients the life they had with their permanent teeth with an affordable, permanent implant-secured solution.
A LOCATOR-proven alternative to the discomfort and pain associated with conventional dentures that feels more like permanent teeth.
Fixed Full Arch Choices
LOCATOR FIXED Conventional Fixed
Same Abutment, Reduced Chairtime, Less Bone Reduction… LOCATOR FIXED
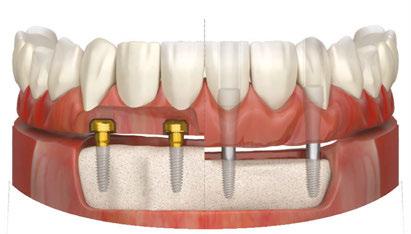
bit.ly/ImplantPractice_LOCFXD







4 Implant Practice US Volume 16 Number 3 TABLE OF CONTENTS CONTINUING EDUCATION Dental sedation: an overview Dr. Brian McGue discusses how sedation can affect patients and dentists 32 LEGAL MATTERS Reducing risks of malpractice claims Kristin Tauras, JD, offers direction on how to avoid a malpractice claim 36 PRODUCT PROFILE Boyd Industries The top choice for implant office equipment ....................................... 38 SERVICE PROFILE Advanced Dental Implant Center™ is powered by more than 50 years of proven experience ............................. 40 Connect. Be Seen. Grow. Succeed. | www.medmarkmedia.com READ the latest industry news and business WATCH DocTalk Dental video interviews with KOLs LEARN through live and archived webinars RECEIVE news and event updates in your inbox by registering for our eNewsletter CONNECT with us on social media www.implantpracticeus.com 26 CONTINUING EDUCATION The use of photogrammetry for the fabrication of full-arch immediate prostheses Dr. Christopher R. Resnik offers insight into improving the accuracy and efficiency of certain implant procedures using photogrammetry *Paid subscribers can earn 4 continuing education credits per issue by passing the 2 CE article quizzes online at https://implantpracticeus.com/category/continuing-education/
You handle the teeth.
At HighFive Healthcare, we’re passionate about the business of oral surgery. That’s why we partner with oral surgeons who are equally passionate about helping their patients. Our family of experts handle just about everything outside of dental implants, so you can focus on what you love and create your own tomorrow.

Learn more at high5health.com
Staying informed and safe
Recently, I saw a movie called “The Sound of Freedom,” the story of Tim Ballard, a federal agent who quits his job with the Department of Homeland Security to start his own independent team to rescue child trafficking victims. One of the movie’s executive producers is Tony Robbins. Tony has been a mentor and inspiration to me. The movie was emotional and moving for me, watching (as Tony describes on his website), “the harrowing experiences faced by victims of human trafficking and the relentless dedication of those fighting to dismantle these dark criminal networks, which continue to enslave millions of children globally each year.”
Human trafficking is not just a movie. The U.S. Department of Homeland Security (DHS) notes, “Every year, millions of men, women, and children are trafficked worldwide — including right here in the United States. It can happen in any community, and victims can be any age, race, gender, or nationality.” Violence, manipulation, false promises of well-paying jobs, and even the promise of romantic relationships can lead to imprisonment of these innocent, frightened victims. DHS adds, “Language barriers, fear of their traffickers, and/or fear of law enforcement frequently keep victims from seeking help, making human trafficking a hidden crime.”
At-risk victims may be hiding in plain sight. Dental professionals may not realize that patients who visit their offices may impacted by this terrible crime. Because of signs and symptoms of human trafficking, dentists may be able to help a victim of human trafficking during the course of the dental visit. Several states mandate that dentists need a human trafficking continuing education course to renew their licenses. In these courses, dentists learn details such as:
• Work-settings that may employ trafficking victims.
• Physical and psychological clues that the patient may be being trafficked.
• Some key words that the victim or perpetrator may say to the dentist to avoid being identified as a trafficking situation.
• Reasons why a victim may try to avoid being identified.
• Oral injuries that may indicate a trafficking victim.
• Resources for intervention specialists in human trafficking.
• What steps the clinician can take if the patient is identified as a trafficking victim.
The DHS says that in helping these victims, the healthcare professional also needs to pay careful attention to the safety of themselves and their teams. They warn, “Do not attempt to confront a suspected trafficker directly or alert a victim to any suspicions. It is up to law enforcement to investigate suspected cases of human trafficking.”
In our Cover Story, Dr. David DiGiallorenzo talks about his individualized approach to dentistry and how Specialty1 Partners has allowed him to benefit from the resources and support of a larger organization. In one of our two CEs, Dr. Christopher Resnik writes about how photogrammetry has improved accuracy and efficiency in the full-arch implant prosthesis workflow. Our Show Special Section features companies whose valuable products and services can enhance efficiency for your practice and patients.
In my Publisher’s Perspective column, I always share topics that are important to my growth not just as a publisher and entrepreneur, but also as a human being. Human trafficking is an outrageous and evil crime. Take a CE class on this topic to know warning signs and also to stay safe. Human trafficking “exists nationwide — in cities, suburbs, and rural towns — and possibly in your own community,” says DHS. Be aware, smart, and cautious — as you help patients to survive and thrive.
To your best success,
Lisa Moler Founder/Publisher, MedMark Media
Published by
Publisher
Lisa Moler lmoler@medmarkmedia.com
Managing Editor Mali Schantz-Feld, MA, CDE mali@medmarkmedia.com
Tel: (727) 515-5118
National Account Manager Adrienne Good agood@medmarkmedia.com
Tel: (623) 340-4373
Sales Assistant & Client Services Melissa Minnick melissa@medmarkmedia.com

Creative Director/Production Manager Amanda Culver amanda@medmarkmedia.com
Marketing & Digital Strategy Amzi Koury amzi@medmarkmedia.com
eMedia Coordinator
Michelle Britzius emedia@medmarkmedia.com
Social Media Manager April Gutierrez socialmedia@medmarkmedia.com
Digital Marketing Assistant Hana Kahn support@medmarkmedia.com
Website Support
Eileen Kane webmaster@medmarkmedia.com
MedMark, LLC

15720 N. Greenway-Hayden Loop #9 Scottsdale, AZ 85260
Tel: (480) 621-8955
Toll-free: (866) 579-9496 www.medmarkmedia.com
www.implantpracticeus.com
Subscription Rate
1 year (4 issues) $149
https://implantpracticeus.com/subscribe/
6 Implant Practice US Volume 16 Number 3 PUBLISHER’S PERSPECTIVE
Lisa Moler Founder/Publisher, MedMark Media
A 30-year perspective on implant dentistry

A conversation with Dr. David
DiGiallorenzo
How did you become involved with dentistry?
My father was a prosthodontist, and my uncle was one of seven lab technicians. Growing up in this dental environment, I had the privilege of witnessing the incredible talent of numerous academics and clinicians in the Philadelphia dental community. I eagerly took the opportunity to shadow many of them, which solidified my passion for the field.
How did you alter the traditional paradigm of dentistry?
Having a mother who advocated for health in the integrative space, I developed an understanding of environmental health, organic approaches, holistic, and alternative therapies as means to take control of one’s health. In my practice, we integrate reflexology during treatment, acupuncture, aromatherapy, massage, along with Biohealth IV and fat-soluble supplementation.
Furthermore, I aimed to improve efficiency and reduce treatment timelines for patients referred to our practice. We wanted them to return to their referring doctors as quickly as possible. Financial considerations also played a role, as my father used to say that when he received his patients back from the periodontist, they were tired and broke.
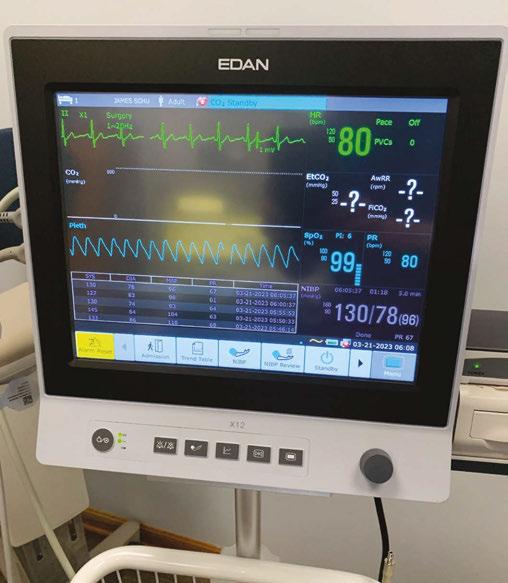
To adapt to these challenges, we performed minimal scaling in the practice and primarily focused on comprehensive fullmouth periodontal procedures under sedation. This approach was not common on the East Coast, but rather an evidence-based approach more prevalent on the West Coast. Single-visit conversions to implants and immediate implant placement were also key priorities early on in my practice. We established a daily practice of emergency immediate total tooth replacement.
How did you evolve your career and practice?
During my specialty program, I had the opportunity to practice general dentistry two evenings a week and on Saturdays. This allowed me to apply my advanced education to my patient population, which was incredibly beneficial. In 1989, I met my wife, who happened to be the daughter of an oral surgeon. She also had experience working within the field of dentistry.
After completing the periodontal program in 1995, we decided to open two offices in Pennsylvania focused on periodontics and implants. I briefly taught at Penn and then started working closely with several implant and periodontal therapeutic companies, providing education globally. I also had the opportunity to lecture at numerous society meetings and study clubs.
Therefore, my focus was primarily on private practice and education. The first 15 years of my practice coincided with the
golden age of implant dentistry and periodontics. During that time, most dentists had never restored implants, so we educated them on periodontal medicine, alveolar health, implant reconstruction, overdenture diagnosis and treatment, and the systemic manifestations of oral disease, occlusion, and diagnosis. Over the years, implants began to be treatment planned in general dentistry offices, which was a significant shift in the field.
How did you respond to this market shift?
In response to the market shift, we decided to start market-
8 Implant Practice US Volume 16 Number 3 COVER STORY
ing directly to consumers. We recognized an unmet need to save or replace teeth, and as periodontal specialists, we were well-positioned to deliver that message. Other providers were also actively doing direct-to-consumer marketing focused on implants to help educate consumers about this option.
Some practitioners were upset about the emergence of direct-to-consumer marketing, but we viewed it as an opportunity to increase overall awareness. Our goal was to position ourselves in the pipeline to direct these consumers to our practice through radio, TV, and the internet. We aimed to bridge the gap and ensure that we all spoke the same language, despite the competing needs and interests within the field.
How do you feel about specialist training?
The unique aspect of specialty education is that it allows you to spend 10,000 hours becoming an expert in your chosen specialty. It not only develops your clinical expertise but also equips you with the ability to handle adverse outcomes and diagnose and treat patients at a more sophisticated level. Specialty education still offers viable options, whether in academic or clinical settings, and consumers will continue to seek specialized care. While the cost of advanced education may be prohibitive, the return on investment is still significant.
How did implant dentistry evolve?
At that time, we still lacked crucial diagnostic information that would come later. We began recognizing challenges in the implant-to-implant relationship when placed in thin biotypes. Defining the microgap and understanding the biologic width around implants were ongoing areas of study. The clinical datasets and advancements in these areas would come later with Team Atlanta and Dr. Dennis Tarnow. It was truly a golden age of innovation in implant technology.
What is genuinely new in implant dentistry today?
Most of the advancements we see today, such as platform-switching designs, All-on-4 treatment planning, scanners, and CT scanning, have been with us for decades. However, these advancements have undergone generational improvements and refinements over time.
How has implantology changed over the past 30 years?
Over the past 3 decades, we have witnessed significant advancements in medical and dental imaging, guided surgery, digital planning, milling, and the use of adjunctive therapies like growth factors. These tools have become essential components of our toolbox, allowing us to provide better care once we have a proper diagnosis. However, the most notable change has been in the patients and the marketplace.
In my practice, the key to determining the best treatment options for each patient lies in comprehensive dental and medical diagnostics. Every patient receives a tailored approach based on their unique diagnosis. What has truly changed is our ability to deliver therapeutic options in a more timely and simplified manner. For instance, we can now often provide a full-arch fixed
All-on-6 solution in just four visits. This highlights the integral role of specialists in delivering predictable and efficient results. It’s important to remember that we are all held to the standard of care for our respective specialties.
Are we better off than before?
Presently, peri-implantitis affects approximately 50% of all implants, which has become a significant disease entity and a common concern in periodontal practices. Therefore, it is important to consider the maintenance of natural teeth as a viable option. Thus, the question arises — are we truly better off than before?
Currently, we are facing a crisis in commercialized dentistry with patients being sold treatment plans that do not meet acceptable diagnostic standards. Some practices and doctors are placing implants and undertaking complex treatment plans that exceed their skill set, resulting in poor outcomes. Patients who experience such negative outcomes share their dissatisfaction with others, distorting the perception of implant dentistry. Money and volume-driven paradigms have contributed to numerous adverse outcomes.
How has diagnosis changed in the past 30 years?

Dr. Morton Amsterdam always emphasized, “There can be only one diagnosis, but many treatment options. If we miss the diagnosis, our therapeutic endeavors become more prone to failure.” This statement remains critical today. While practitioners spend a significant amount of time refining techniques, it is essential to remember that expertise in a specific area requires approximately 10,000 hours. During specialty training, we spend 3 years studying and applying knowledge for around 60 hours per week.
However, the key to success still lies in proper diagnosis. Our literature has continuously evolved over the decades, providing critical information that must be firmly ingrained in our minds. In my approach, I start by examining the patient from the outside and work my way down to the dental level. Understanding the patient’s past dental history is crucial to avoid repeating past mistakes. Patient narratives also offer valuable insights for diagnosis. Additionally, we consider the medical history, vitamin D levels, inflammatory mediators, and sometimes conduct sensitivity testing for known materials.
We evaluate occlusion, angle classification, skeletal profile, periodontal health, caries, esthetics, phonetics, smile reveal, tis-
9 implantpracticeus.com Volume 16 Number 3 COVER STORY
sue biotype, previous failures, patient expectations, bone density, sinus health, joint health, alveolar health, endodontic diagnosis, and interproximal bone levels. We classify cases as perio, caries, or a combination thereof, as well as assess occlusion and neuromusculature. Patients with a history of cancer, Lyme disease, and other inflammatory conditions are candidates for zirconium implants, as metals can complicate the body’s electrical circuitry and induce inflammation.
Diagnosis is currently suffering in the implant world. There is a trend of edentulating patients and providing them with prosthetic periodontal biotypes. The idea that everyone is a candidate for All-on-4 treatment is questionable, especially when considering guided surgery. Mutilating a healthy gingival scaffolding and reducing the anterior maxilla’s healthy interproximal bone is not suitable for everyone. We have a higher responsibility to our patients.
How has the consumer marketplace changed over the past 30 years?
Over the past 3 decades, there have been notable changes in the consumer marketplace, largely influenced by the widespread use of the internet and digital technology. Patients now have easy access to information through search engines, leading to second opinions, misinformation, and a lack of loyalty to healthcare providers. Additionally, patients today prefer comprehensive solutions provided in a single location and have a strong desire for immediate results. They often seek treatment from commercialized vendors with varying levels of expertise, creating opportunities but also the need for careful evaluation when comparing different providers. It is crucial for dental professionals to resist an economic-based philosophy and avoid compromising on quality and patient care.
What are the largest differences between today’s patients and patients of 30 years ago?
One significant difference between today’s patients and those from 3 decades ago is the increased prevalence of medically compromised individuals. Chronic diseases such as diabetes, heart disease, Lyme disease, and immune disorders like lupus often coexist with periodontal disease and advanced caries in these patients. Furthermore, contemporary patients face higher levels of environmental cellular toxicity, endocrine disruptors, and metabolic disturbances. Circulating inflammatory mediators and cortisol levels are also elevated, which can negatively impact efficient healing and long-term homeostasis. Deficiencies in vitamins, trace minerals, micronutrients, and hormones further complicate the healing process, even in otherwise healthy individuals.
In light of the rampant occurrence of peri-implantitis and various health conditions, it is becoming increasingly common to recommend fixed perio-prostheses as an alternative to edentulation and implant-supported restorations. Traditional periodontal prosthesis and crown-and-bridge solutions regain relevance as a bail-out strategy when anterior implants fail in the esthetic zone. These fixed restorations offer a broader scope of treatment that helps control many variables contributing to functional and esthetic implant failures.
Are you concerned about the increasing presence of Dental Service Organizations (DSOs) in the dental market?

Yes, I am concerned about the widespread influence of general DSOs that prioritize high volume, low-cost implantology, and the use of mini-implants without proper consideration for patient care. What is particularly worrisome is that practitioners in these environments may lack the necessary expertise, often being recent graduates who are trained by sales representatives in a corporate setting.
One significant concern is the undue pressure placed on younger doctors to perform as many procedures as feasible within a limited timeframe. It is important to recognize that one cannot be an expert in all facets of dentistry. That’s why the specialty model remains crucial for our patients. By focusing on specialties, we ensure that patients receive the specialized care they require. This desire for specialists to grow and thrive was a contributing factor in my decision to join Specialty1 Partners.
Can you elaborate on the importance of expertise and experience in implant dentistry?
While we can teach anyone to perform a procedure, it is essential to understand that the diagnosis and management of complications come through expertise and experience. Only then can we effectively apply the technology and techniques available to us. It is the combination of knowledge, skill, and understanding that leads to successful outcomes in implant dentistry.
Are there any positive developments within the DSO landscape that you find promising?
I am genuinely excited about the emergence of specialty-focused partnership organizations, particularly partnerships that value the clinical autonomy of specialists and prioritize collaboration and partnership among their members. For specialists considering selling their practices, specialty-focused partnerships offer a more robust option that allows them to continue delivering specialized care while benefiting from the resources and support of a larger organization and, within some organizations such as Specialty1 Partners, retaining equity in the larger scalable entity. By working together and emphasizing the importance of specialized care, we can continue to provide the best possible outcomes for our patients. IP
10 Implant Practice US Volume 16 Number 3 COVER STORY

“It’s a partnership of specialists and we are all specialty strong.” - Partner Doctor (2022) 305 - 206 - 7388 | Specialty1partners.com YOUR SPECIALTY IS OUR SPECIALTY. The Only Doctor-Founded, Doctor-Led Specialty Partnership Organization. Visit us at booth #540
Treatment of a patient with trans-canine placement of a dental implant
 Drs. Douglas D. Wright and William T. Goodwin II treat a patient
Drs. Douglas D. Wright and William T. Goodwin II treat a patient
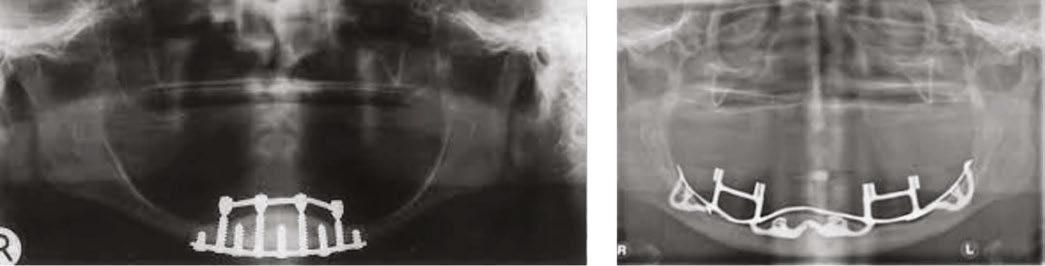
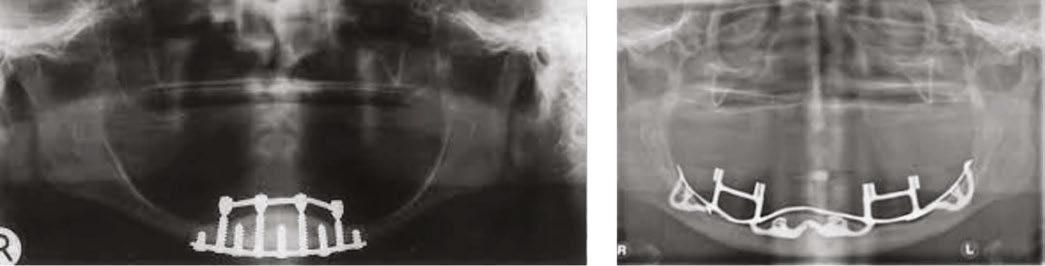
with multiple restorative challenges
The use of dental implants to replace missing teeth is causing a revolution in dental care. A dental student or dental resident in the 1970s learned about “new” techniques such as transmandibular staple-type implants1 or subperiosteal implants2 to support a removable overdenture (Figures 13A and 13B). These were invasive treatments that were confined to specialist’s practice. These early implant patients only enjoyed a moderate increase in comfort and function. This was a poor outcome for the time and expense involved.
These early techniques have been replaced by conventional periosteal implants or even mini dental implants. The more modern techniques can be provided by general dentists after some additional training. The reduction in cost and inconvenience opens dental implant treatment to an increasing number of patients.
A look at current trends provides additional insight. The American College of Prosthodontics website states 36 million Americans are completely edentulous; 120 million Americans are missing a single tooth, and 2.3 million single implant/tooth restorations were provided in 2019.1

Steady improvements in the science of implant dentistry have led to increased predictability of treatment with less invasive techniques. Improvements in implant dentistry, with the concurrent simplification in treatment techniques, have led to an explosion in the number of patients who desire restorations supported by dental implants. With this expectation of care from a growing number of qualified patients, some unique restorative challenges are being faced by dental professionals.
Some of the challenges a clinician faces can be studied in isolation on a case-by-case basis. For example, the decision whether to place a dental implant immediately after dental extraction or to wait until the extraction site heals is a narrow question that is relatively easy to study in a controlled clinical trial.
However in the day-to-day clinical practice, providers are often faced with multiple challenges in the same patient.
This is the presentation of the restoration of a 78-year-old male with multiple complicating factors.
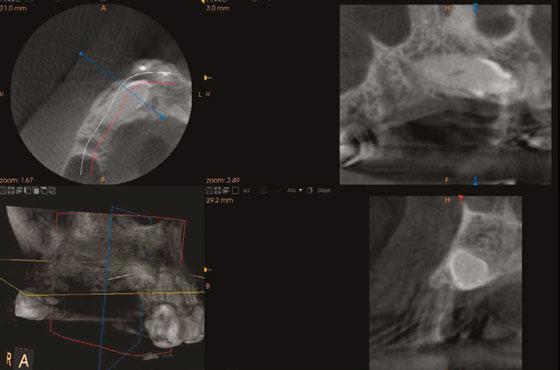
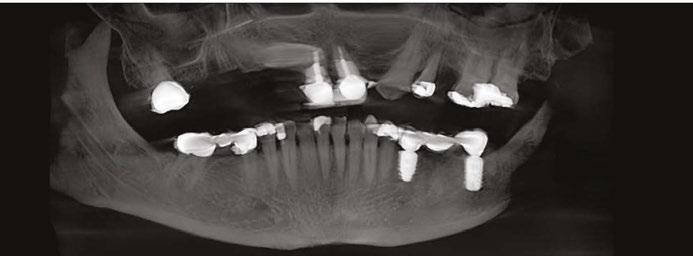
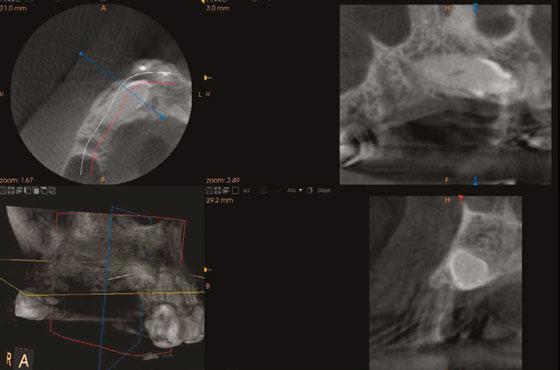
Mr. Z has a skeletal Class III malocclusion. He has never received orthodontic treatment. The CBCT shows tooth No. 6 is present but horizontally impacted (Figure 4).
Based on age of patient, health history, and presence of the impacted canine, the patient was sent to an oral surgeon for evaluation. The initial consultation asked the surgeon to consider removal of impacted tooth No. 6 and placement of bone graft as a prelude to restoring site 2-7 with an implant-supported fixed bridge (Figures
Close inspection of the CBCT shows tooth No. 6 is ankylosed. The oral surgeon indicated extraction of tooth No. 6 would require block resection of bone with the tooth. The resulting defect would have required extensive bone grafting
added time and cost to this case.
12 Implant Practice US Volume 16 Number 3 CASE REPORT
5 and 6).
and
Douglas D. Wright, DDS, is a general dentist in private practice in Staunton, Virginia.
William T. Goodwin II, DDS, is a maxillofacial surgeon in private practice in Harrisonburg, Virginia.
For questions about this article, please contact Dr. Wright at dominosign14@ gmail.com.
Figure 1: Pretreatment photo of patient. Note the extreme wear of mandibular incisors occurring from uncorrected malocclusion. Also note the contact between tooth Nos. 9 and 22 when the mandible moves to the right. This “canine guidance” was incorporated into the fixed-bridge design on the patient’s upper right side
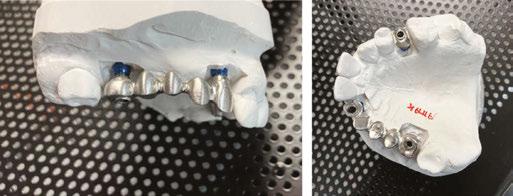
Figures 2 and 3: Metal framework at try-in appointment. Porcelain-fused-tometal was used to restore this case because of lack of interarch space
NON-CERAMIC & RESORBABLE BONE GRAFT



OsteoGen ® is a bioactive, non-ceramic & resorbable calcium phosphate crystal that is physicochemically and crystalographically similar to human cancellous mineral Ca5[PO4]3OH.1-6 The process of growing a crystal yields a unique Ca:P ratio that is NOT a ß-TCP and NOT a dense ceramic HA, nor is it a biphasic mixture of the two.

The OsteoGen® bioactive crystals and clusters control migration of connective tissue to form a strong bond with newly grown bone as the graft resorbs. The result is predictable bone formation for general grafting & use with implants.1-6

- $163.00
1.5g/3.0cc - $109.00
0.75g/1.5cc - $ 76.00
Buy 3 Vials and Save!

3.0g/6.0cc - $447.00
1.5g/3.0cc - $297.00
0.75g/1.5cc - $207.00
Scan for references

HYDROPHILIC CRYSTAL CLUSTER STRUCTURE
The crystallographic structure and geometry of a bone graft matters.
OsteoGen® non-ceramic crystal clusters intertwine to form a hydrophilic 3D matrix leading to the immediate absorption of blood flow. This is critical for the initiation of bone formation, early angiogenesis and bone bridging even across 8.0mm critical size defects.3-5
The x-ray reveals when sufficient bone has formed and the site is ready for implant placement. OsteoGen® non-ceramic crystals are radiolucent on the day of placement & radiopaque in ~4-6 months following crystal resorption and host bone formation.1-4
Contact 800-526-9343 or Shop Online at www.impladentltd.com
HYDROPHILIC CLUSTERS ® STRUCTURE BIOACTIVITY RADIOLUCENT TO RADIOPAQUE
JOIN US AS WE CELEBRATE NEARLY 40 YEARS OF OUR OSTEOGEN® BIOACTIVE RESORBABLE BONE GRAFTING CALCIUM APATITE CRYSTALS &
BIOACTIVE RESORBABLE
1. Ganz (2002) 2. Artzi (2003) 3. Valen (2002) 4. Spivak (1990) 5. Ricci (1992) 6. Jensen (1998) Radiographs courtesy of German Murias DDS, ABOI/ID RADIODENSITY VIALS 3.0g/6.0cc
Maxillary canines are the second most common tooth to be impacted in the oral cavity. Some studies indicate 4 patients in 1,000 have impacted canines.
Orthodontic care often includes managing impacted canines with the help of an oral surgeon and guided eruption.4

Unfortunately, not all impacted canines are treated using modern orthodontic techniques. Many patients with impacted canine teeth go through life without having the canines removed or moved into the dental arch. Over several decades, impacted canines can become ankylosed thus becoming extremely difficult teeth to extract.

When the need for a dental implant in the anterior maxilla arises, these impacted/ankylosed canines pose a unique challenge. In this case, removal of the ankylosed and impacted canine with a block resection leads to removal of bone where it is most needed.

Recent reports indicate dental implants can be placed directly through the impacted canine, eliminating the need for block resection and bone grafting.4,5
Histologically, trans-canine placement of a dental implant has similarities with the socket shield technique for preserving buccal contour when placing a dental implant in an area of limited buccal bone. Miltiadis demonstrated buccal bone growth 5 years after a dental implant was placed using the socket shield technique.6 In a recent review of this technique Ogawa7 presents over 283 cases of successful socket shield technique from the dental literature.

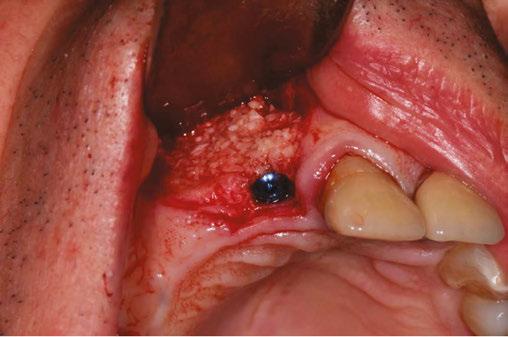
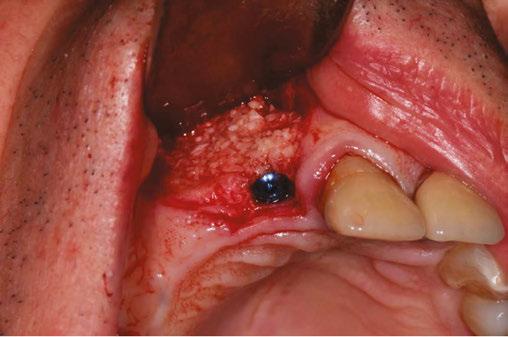
On the day of surgery, the patient had MegaGen AnyRidge® implants placed at the following sites under local anesthesia:
• Tooth No. 7: trans-canine placement of 4.0 mm x 13 mm
• Tooth No. 3: 5.0 mm x 7.0 mm with small crestal approach sinus graft
• Tooth No. 13: 4.0 mm x 10.0 mm implant
Retaining tooth No. 6 and placing the dental implant through the impacted and ankylosed tooth provided a new set of challenges. Keeping the ankylosed canine in place reduced the need for additional surgery; however, with the retention of the canine, insufficient interarch space would be available for a zirconia or resin-composite restoration. Because the interarch space was limited, a porcelainfused-to-metal restoration was used to complete the case.
To prevent isolated forces being placed on the new implantretained fixed bridge, modified anterior and “canine” guidance
14 Implant Practice US Volume 16 Number 3 CASE REPORT
Figures 7 and 8: Healing abutments in place
Figure 4: Pretreatment panoramic x-ray. Note position of maxillary right canine
Figures 5 and 6: Pretreatment CBCT scan with treatment planning software. Virtual implant placement at site 10 shows thin buccal bone. Buccal bone graft was provided at time of surgery
Figures 9 and 10: Porcelain-on-metal framework ready for delivery

was achieved by allowing the already established guidance between tooth Nos. 9 and 22 when the mandible moved to the patient’s right. The new bridge had occlusal forces balanced to the guidance provided by the contact in function between tooth Nos. 9 and 22 (Figure 1).
Restorative dentists often come up against multiple restorative challenges in a single patient. There are few reports of treating cases such as this with multiple challenges. Each individual restorative challenge can be reviewed in dental literature. Creative solutions can be offered to the patient based on clinical research, case reports, and well-established clinical practices (Figures 2, 3, 7, and 8).
In the 1970s and early 1980s, the surgery was extensive, painful, and the failure of these modalities was catastrophic for the patient. Photos like Figures 13A and 13B remind us how far the science and technology of implant treatment has come in a brief period. The best we can do for our patients is to put their interests first, offer clear choices, and provide evidence-based dental treatment (Figure 14).
REFERENCES
1. American College of Prosthodontists. https://www.gotoapro.org/facts-figures/. Accessed April 10, 2023.
Surg. 2002 Aug;60(8):851-857.
3. Beddis H, Lello S, Cunliffe J, Coulthard P. Subperiosteal implants. Br Dent J. 2012 Jan 13;212(1):4.

4. Cooke J, Wang HL. Canine impactions: incidence and management. Int J Periodontics Restorative Dent. 2006 Oct;26(5):483-491.

5. Smojver I, Katalinić I, Vuletić M, Stojić L, Gerbl D, Gabrić D. Guided Bilateral Transcanine Implant Placement and Implant-Supported Oral Rehabilitation in a Patient with Progressive Systemic Scleroderma. Case Rep Dent. 2021 Jul 13;2021:5576595.
6. Mitsias ME, Siormpas KD, Kotsakis GA, Ganz SD, Mangano C, Iezzi G. The Root Membrane Technique: Human Histologic Evidence after Five Years of Function. Biomed Res Int. 2017;2017:7269467.
7. Ogawa T, Sitalaksmi RM, Miyashita M, Maekawa K, Ryu M, Kimura-Ono A, Suganuma T, Kikutani T, Fujisawa M, Tamaki K, Kuboki T. Effectiveness of the socket shield technique in dental implant: A systematic review. J Prosthodont Res. 2022 Jan 11;66(1):12-18.
16 Implant Practice US Volume 16 Number 3 CASE REPORT IP
2. Paton G, Fuss J, Goss AN. The transmandibular implant: a 5- and 15-year single-center study. J Oral Maxillofac
Figure 14. Post implant placement. This CBCT shows implant at site 10 through the impacted canine. Implant at site 3 was placed right against the sinus floor
Figures 13A and 13B: 13A. Trans-mandibular dental implants. 13B. Subperiosteal implants
Figure 11: Surgical site on day of surgery
Figure 12: Implant placement of tooth No. 7 with buccal bone graft
Specialized is energized.
We were the first specialty DSO to champion endodontists and remain committed to the specialty—now, we’re expanding our impact and welcoming periodontists and oral surgeons to our community to revolutionize oral health care. Together, we’re delivering worldclass patient experiences and creating brighter tomorrows for all.


Welcome to the future of oral health care.
Energized care.
Elevate patient experiences with unparalleled support.

Energized excellence.
Advance oral health care with innovative technologies.
Energized connection.
Thrive in a community of growth-minded peers.

Energized future.
Secure your legacy while doing what you love.
specializeddental.com
Dr. Taylor Newman, Periodontist Cameo Dental Specialists Partner and believer since 2022
A good “NAP” is 1 of 3 ways to improve practice success
Chad Erickson discusses how to generate more revenue from your local listings
With an estimated 46% of all searches containing local terms such as “near me,” it’s clear that local search that contains more than just your name, address, and phone data (NAP) is more important than ever. If you aren’t optimizing your local search profiles to generate the newest business possible — and, therefore, the most revenue possible, you’re missing out on connecting with the people who conduct these searches. You also risk frustrating the people who are searching directly for your practice, as improperly maintained local search profiles often contain inaccurate information, which means more lost revenue from patients who choose not to work with you in favor of practices that are easier to get ahold of. Here are three easy ways to make your local search listings start (and continue) to generate more revenue.

1. Make inaccuracies your No. 1 enemy.
Inaccurate information on a local listing profile is incredibly frustrating. If you’ve encountered it, you know exactly how it feels. Driving to a business only to find out its hours are incorrect or their address is wrong is more than enough to cause potential patients to not want to do business with you. You might not have any inaccuracies in your online listings, but the thing that makes these such a problem is that they pop up so frequently. Whether through Google indexing new information about your practice, a suggestion from a user, or through data collected from thirdparty companies, the truth is that your online listings are subject to change at any time. The best way to avoid losing revenue through inaccurate listings is to audit your listings as frequently as possible. At the bare minimum, checking all of your directory listings at least once per month will help cut down on these incidents.
2. Work on optimizing your listings.
Once your listings are straightened out, it’s time to start optimizing them. That means adding information beyond the basics, like your name, address, and phone number (NAP). Google and other search engines utilize “relevance” as one of the search metrics to rank local search profiles, which measures how likely
Chad Erickson, VP Strategy and co-owner of MyAdvice, has been consulting clients on the best marketing strategies for their businesses since 1999. With a focus on both the internal and external aspects of effective marketing, he understands the complex aspects of owning and running a business. He has a proven record of raising capital, acquiring companies, and developing strategic alliances within the industry. He is also a faculty member for many top medical and dental conferences. For more information on local listings management, reviews, and digital marketing campaigns, visit myadvice.com.
your practice is to provide the service or product the searcher is looking for. Without complete profile information, it’s hard for search engines to tell precisely what your practice does. So adding this information can make a huge difference:
• Filling out the primary and secondary categories your business falls under
• Adding photos of your business
• Including all of the services you provide
• Including your business attributes and hours
• Any additional contact information like your social media and website links
• Regularly posting new photos and updates on your profile to show that your profile has active updates
3. Generate new reviews.
Reviews are massively important to local search. In fact, in a survey we conducted earlier this year, 57% of the practices we polled told us that generating new reviews had the most positive impact on their local search performance. They’re incredibly important to potential patients interested in your practice as well as search engines. That’s right, search engines are indexing your reviews! Another metric used by search engines to rank local search profiles is called “prominence,” and it consists of every mention of your business online. That includes your online reviews. Setting up an automated system to request reviews from your patients and making sure to respond to the reviews you do get goes a long way towards helping your local search profile generate more revenue. Make auditing your reviews a part of your local search audit system to avoid missing a review that needs a response.
18 Implant Practice US Volume 16 Number 3 MARKETING MOMENTUM
IP
How to submit an article to Implant Practice US
Implant Practice US is a peer-reviewed, quarterly publication containing articles by leading authors from around the world. Implant Practice US is designed to be read by specialists in Periodontics, Oral Surgery, and Prosthodontics.
Submitting articles
Implant Practice US requires original, unpublished article submissions on implant topics, multidisciplinary dentistry, clinical cases, practice management, technology, clinical updates, literature reviews, and continuing education.
Typically, clinical articles and case studies range between 1,500 and 2,400 words. Authors can include up to 15 illustrations. Manuscripts should be double-spaced, and all pages should be numbered. Implant Practice US reserves the right to edit articles for clarity and style as well as for the limitations of space available.
Articles are classified as either clinical, continuing education, technology, or research reports. Clinical articles and continuing education articles typically include case presentations, technique reports, or literature reviews on a clinical topic. Research reports state the problem and the objective, describe the materials and methods (so they can be duplicated and their validity judged), report the results accurately and concisely, provide discussion of the findings, and offer conclusions that can be drawn from the research. Under a separate heading, research reports provide a statement of the research’s clinical implications and relevance to implant dentistry. Clinical and continuing education articles include an abstract of up to 250 words. Continuing education articles also include three to four educational aims and objectives, a short “expected outcomes” paragraph, and a 10-question, multiple-choice quiz with the correct answers indicated. Questions and answers should be in the order of appearance in the text, and verbatim. Product trade names cited in the text must be accompanied by a generic term and include the manufacturer, city, and country in parentheses.
Additional items to include:
• Include full name, academic degrees, and institutional affiliations and locations
• If presented as part of a meeting, please state the name, date, and location of the meeting
• Sources of support in the form of grants, equipment, products, or drugs must be disclosed
• Full contact details for the corresponding author must be included
• Short author bio
• Author headshot
Pictures/images
Illustrations should be clearly identified, numbered in sequential order, and accompanied by a caption. Digital images must be high resolution, 300 dpi minimum, and at least 90 mm wide. We can accept digital images in all image formats (preferring .tif or jpeg).
Tables
Ensure that each table is cited in the text. Number tables consecutively, and provide a brief title and caption (if appropriate) for each.
References
References must appear in the text as numbered superscripts (not footnotes) and should be listed at the end of the article in their order of appear-
ance in the text. The majority of references should be less than 10 years old. Provide inclusive page numbers, volume and issue numbers, date of publication, and all authors’ names. References should be submitted in American Medical Association style. For example:
Journals:
(Print)
White LW. Pearls from Dr. Larry White. Int J Orthod Milwaukee. 2016;27(1):7-8.
(Online)
Author(s). Article title. Journal Name. Year; vol(issue#):inclusive pages. URL. Accessed [date].
Or in the case of a book: Pedetta F. New Straight Wire. Quintessence Publishing; 2017.
Website:
Author or name of organization if no author is listed. Title or name of the organization if no title is provided. Name of website. URL. Accessed Month Day, Year. Example of Date: Accessed June 12, 2011.
Author’s name: (Single) (Multiple)
Doe JF Doe JF, Roe JP
Permissions
Written permission must be obtained by the author for material that has been published in copyrighted material; this includes tables, figures, pictures, and quoted text that exceeds 150 words. Signed release forms are required for photographs of identifiable persons.
Disclosure of financial interest
Authors must disclose any financial interest they (or family members) have in products mentioned in their articles. They must also disclose any developmental or research relationships with companies that manufacture products by signing a “Conflict of Interest Declaration” form after their article is accepted. Any commercial or financial interest will be acknowledged in the article.
Manuscript review
All clinical and continuing education manuscripts are peer-reviewed and accepted, accepted with modification, or rejected at the discretion of the editorial review board. Authors are responsible for meeting review board requirements for final approval and publication of manuscripts.
Proofing
Page proofs will be supplied to authors for corrections and/or final sign off. Changes should be limited to those that are essential for correctness and clarity.
Articles should be submitted to:
Mali Schantz-Feld, managing editor, at mali@medmarkmedia.com
Reprints/Extra issues
If reprints or additional issues are desired, they must be ordered from the publisher when the page proofs are reviewed by the authors. The publisher does not stock reprints; however, back issues can be purchased.
19 implantpracticeus.com Volume 16 Number 3 AUTHOR GUIDELINES
Advanced Dental Implant Center™
As the nation’s largest Dental Support Organization (DSO) exclusively focused on tooth replacement services, Affordable Care expanded its support to the new Advanced Dental Implant Center (ADIC) network. Affiliated practices in the ADIC network provide comprehensive tooth replacement care with a focus on immediate fixed full-arch implant services.

Affordable Care, which provides business, operations, and clinical education support to more than 425 affiliated dental practices across 42 states, has a nearly 50-year history and proven track record in helping dental practices grow.
The ADIC network is comprised of general dentists with extensive implant experience, oral surgeons, periodontists, and prosthodontists with a high or growing volume of dental implant placement. These doctors have either rebranded
their practices to the ADIC name or chosen to maintain their existing brand name following affiliation with Affordable Care. Dr. Peyman Raissi affiliated his My New Smile Dental practice with Affordable Care as part of the ADIC network and continues to operate under the existing brand name. He explains, “Out of the different DSOs that were offering to affiliate with my practice, I felt Affordable Care had the best reputation. I had a blast building my practice from scratch, and grew it to a level where I felt it was important to have a solid support group to take care of everything in the office except the clinical care so I could practice what I love daily free of stress. I’m now part of something bigger, and ultimately, I’m very happy with my decision to affiliate with Affordable Care and to be a part of an excellent group of clinicians from across the nation.”

20 Implant Practice US Volume 16 Number 3 SPECIAL SECTION SHOW SPECIAL SECTION
Visit Affordable Care and Advanced Dental Implant Center at AAID Booth No. 103 Scan the QR code or call us at: (888) 537-2801 to learn about affiliation opportunities. Proud to serve as the DSO for the Advanced Dental Implant Center network An Open Invitation for general dentists with extensive implant experience, oral surgeons, periodontists and prosthodontists Now is the time to join our fast growing network of advanced dental implant providers. Leverage Affordable Care’s five decades of experience & proven track record in clinical education, business and operational support services to capture maximum value for your practice, invest in your legacy and focus on what matters most – transforming patient lives. Invest in your future. proud to serve as the DSO for ADVANCED DENTAL IMPLANT CENTER
Dr. Peyman Raissi
Elevate your dental implant practice with Boyd
Your unbeatable choice for operatory equipment
Are you ready to take your dental implant practice to the next level? Look no further than Boyd, the indisputable leader in dental implant operatory equipment. As the AAOMS 23 tradeshow kicks off, we invite you to visit Booth Number 1024 and discover why Boyd stands head and shoulders above the competition.
Boyd has been a pioneer in the dental industry, revolutionizing operatory equipment with cutting-edge technology and ergonomic design. Our state-of-the-art dental chairs, lights, and cabinetry are engineered to enhance efficiency and precision, ensuring seamless implant procedures and exceptional patient experiences.

Our equipment not only excels in technological superiority but also in craftsmanship, durability, and ease of maintenance. Built to withstand the rigors of a busy dental practice, our equipment saves you valuable time and resources. Moreover, our exceptional customer support and guarantee offers peace of mind for years to come.
Don’t settle for less when it comes to dental implant operatory equipment. Visit Booth Number 1024 at the AAOMS 23 tradeshow, and witness the Boyd advantage firsthand. Unleash the full potential of your practice, and deliver unmatched patient care with Boyd as your trusted partner. We look forward to meeting you there!
21 implantpracticeus.com Volume 16 Number 3 SPECIAL SECTION SHOW SPECIAL SECTION
Visit Boyd Industries at AAOMS Booth No. 1024 Visit us at AAOMS 2023 to see the latest Boyd innovations in Oral Surgery Products. Can’t make it to the show? Contact our Sales Team now about Boyd’s current show promotion. Find us at booth 1024 CONTACT SALES TEAM
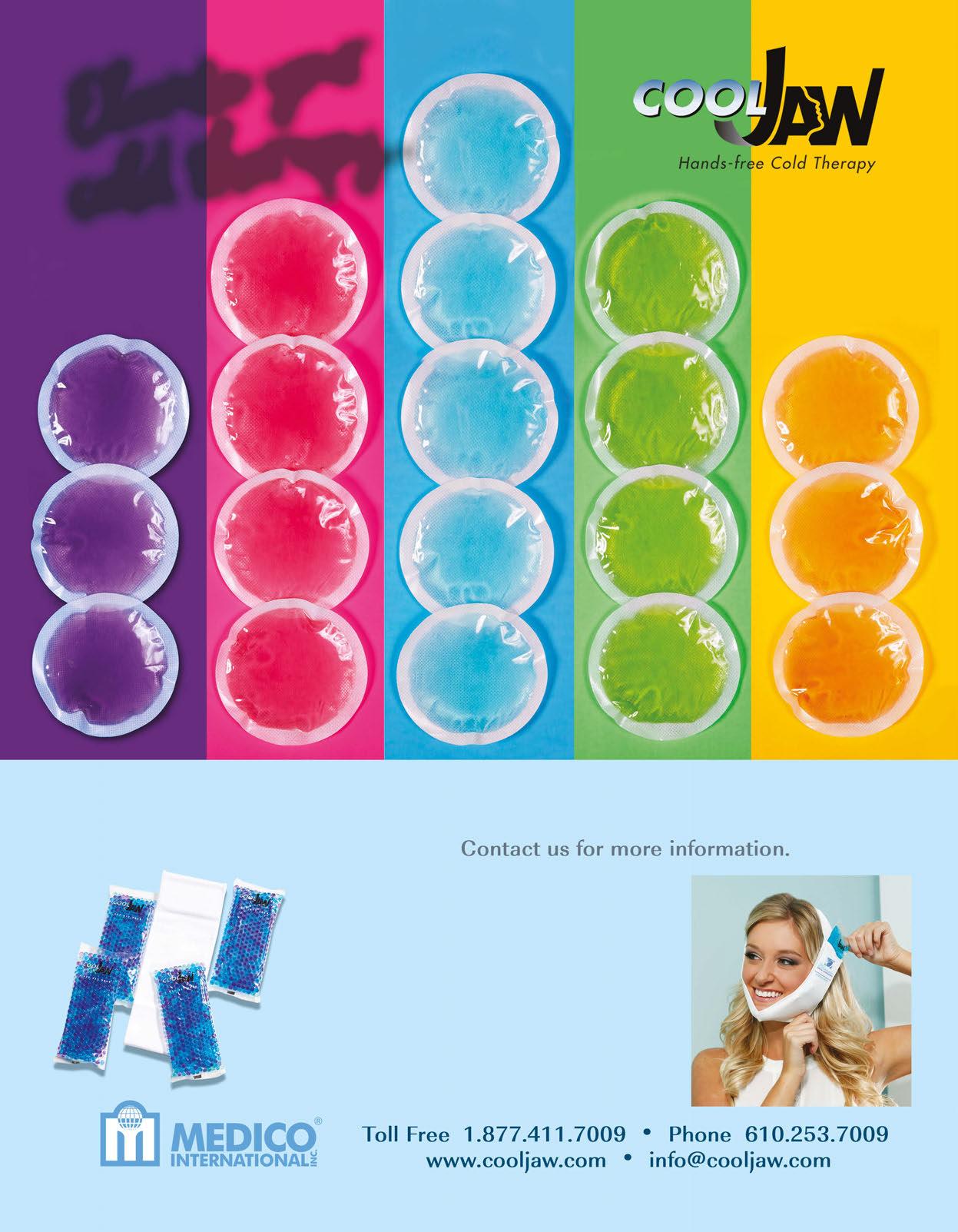
Cool Jaw ® hot/cold therapy
Cool Jaw® has paved the way to postoperative hot/cold therapy through the creation of our exclusive, hands-free patented designed wraps. The hands-free Cool Jaw system reduces postoperative swelling and discomfort and allows patients to recover in a convenient manner. Combine with our extensive variety of hot/cold gel packs to create a post-op recovery solution that best suits your patients.
Our Soft-Sided Round Gel packs are a convenient, post-op cold therapy option for after numerous procedures including implants and cosmetic injections such as Botox. These packs come in a variety of color options to match your office or simply add an element of fun to any procedure. Choose from bright solid colors as well as eye-catching glitters. These reusable gel packs are 4 inches in diameter and remain flexible when frozen, allowing for uniform cold therapy.

Take the Cool Jaw products to the next level, and add customization! Customization is a subtle, yet effective way to promote your practice and enhance your professional image.
Cool Jaw helps you to continue promoting your practice long after the surgery date.
Visit us at the booth, and ask for a free sample!

22 Implant Practice US Volume 16 Number 3 SPECIAL SECTION SHOW SPECIAL SECTION
Visit Cool Jaw at AAOMS Booth No. 1345 and AAID Booth No. 416
HighFive Healthcare

At HighFive Healthcare, we’re passionate about the business of oral surgery. That’s why we partner with oral surgeons who are equally passionate about helping their patients. With more than 60 years of healthcare experience, our diverse team of experts works hand-in-hand with our partners to streamline and optimize every aspect of practice operations. From recruiting, payroll, and human services, to IT services, data security, and customer relations, to branding, marketing, and office expansion, we take care of the business of teeth so our partners have more time to focus on what they do best. Our partnership contract is simple — take care of your patients, and we’ll handle the rest. While you continue to take care of patients, we can lift the burdens that come with the job of running a practice. Our unrivaled culture of fun and family puts you in the lead of a robust
team of experts ready to support you and the goals you have, not just for your practice, but for your life. Whether you’re after more family time, a larger office footprint, more efficient operations, or increased revenue, HighFive Healthcare is dedicated to helping our doctor partners create their own tomorrow!
Learn more at themonstertamers.com, and be sure to visit us at Booth No. 1440, Sept. 21–23 at the AAOMS Annual Meeting in San Diego.
23 implantpracticeus.com Volume 16 Number 3 SPECIAL SECTION SHOW SPECIAL SECTION
Visit HighFive Healthcare at AAOMS Booth No. 1440 The never-ending demands of business will see you now. RECRUITING | HUMAN RESOURCES | PAYROLL | ACCOUNTING | BRANDING & MARKETING | IT SERVICES | AND MORE themonstertamers.com
We take care of the business of teeth so our partners have more time to focus on what they do best. Our partnership contract is simple — take care of your patients, and we’ll handle the rest.
Specialty1 Partners
A dental surgical specialty organization founded by dental specialists
Specialty1 Partners is a leading provider of emergency and essential specialty surgical dental services, with a multi-site, multi-service, scalable platform positioned for growth. Operating across the country, Specialty1 Partners provides comprehensive business and operational support services to its endodontic, oral surgery, and periodontic practices. We partner with bestin-class dental surgical specialists nationally with the goal of greatly reducing their administrative burden, so they can spend more time at the heart of their practice — providing high quality dental care to patients.
Specialty1 Partners is the largest and preferred partnership group in the dental surgical specialty space. Our values help to
empower you and provide the framework to reach your professional goals with integrity and confidence.
Are you a specialty practice owner, resident, or skilled business/clinical professional exploring new career opportunities? We’d love to learn more about you and explore if we’re a good fit for what you’re looking for today or in the near future. Visit us at Booth 540, and let’s chat about joining our rapidly growing, doctor-focused organization.
24 Implant Practice US Volume 16 Number 3 SPECIAL SECTION SHOW SPECIAL SECTION
Visit Specialty1 Partners at AAOMS Booth No. 540 www.specialty1partners.com 305 - 206 - 7388 The Only Partnership Organization FOUNDED AND LED BY DOCTORS. Come see us at our booth!
It’s a partnership of
specialists,
and we are all specialty strong.” — Partner, Specialty1 Partners
Easily go from removable to FIXED with the Zest LOCATOR!

LOCATOR FIXED continues to turn heads among clinicians for its ease-of-use, simplicity, and effectiveness in delivering fixed, full-arch solutions to patients at an affordable price-point. The beauty of the latest LOCATOR-powered innovation from Zest Dental Solutions is all in the name — it uses the original LOCATOR abutment and workflow as the original removable LOCATOR attachment system to deliver a fixed prosthesis only removable by the clinician.

So what’s the difference? It’s all in the inserts and housings! Whereas the removable LOCATOR solution uses a flexible nylon insert and silver housing, the FIXED offering uses proprietary rigid inserts and a special gold housing.
With LOCATOR FIXED, you can easily convert a LOCATOR


removable overdenture into a permanent FIXED prosthesis without the need for any changes to the underlying LOCATOR abutments. You just need a minimum of four implants to begin the LOCATOR FIXED journey.








Dr. Gordon Christensen has become a notable fan of LOCATOR FIXED, labeling it as his fixed treatment of choice in Clinicians Report®. To download a free copy of the article, visit bit.ly/christensen_zest.
Visit Zest at the 2023 AAID Annual Meeting in Las Vegas, November 1-4, to learn more about LOCATOR FIXED as well as Regal GO, the new on-the-go oral care brush that helps maintain hygiene around and underneath fixed dentures.
To learn more about how LOCATOR FIXED works, visit bit.ly/howfixedworks.

25 implantpracticeus.com Volume 16 Number 3 SPECIAL SECTION SHOW SPECIAL SECTION
Visit Zest Dental Solutions at AAID Booth No. 313 SAME ABUTMENT. SAME WORKFLOW. REMOVABLE OR FIXED ONLY WITH ZEST LOCATOR ABUTMENTS LOCATOR Removable Overdentures LOCATOR FIXED Prosthesis TO FIXED FROM REMOVABLE USE THE SAME LOCATOR ABUTMENT FOR DIFFERENT OUTCOMES Flexible Removable insert: prosthesis removable by patient & clinician Rigid FIXED insert: prosthesis removable only by clinician
The use of photogrammetry for the fabrication of full-arch immediate prostheses
Dr. Christopher R. Resnik offers insight into improving the accuracy and efficiency of certain implant procedures using photogrammetry

Traditional chairside conversions for full-arch prostheses are time consuming and labor intensive. With the advent of digital technology in dentistry, there have been many advancements that have improved the accuracy and efficiency of the full-arch prosthesis process. Two such advancements include photogrammetry and 3D printing, which have been innovative in the digital work flow for full-arch implant prostheses.
Accuracy of full-arch implant prostheses
Obtaining an accurate representation of implant positioning is critical when fabricating full-arch prostheses. It is well established in implant dentistry that every step through the prosthetic process may lead to inherent error, resulting in an ill-fitting prosthesis. The long-term success of implant-supported prostheses is directly dependent on the accuracy of the records obtained in the prosthetic rehabilitation process.1,2 When a prosthesis exhibits passivity, there exists less stress and strain to the supporting implants. Inadequate fit of the implant prostheses may lead to excessive oblique loads, creating significant stress on the implants and their associated prosthetic connectors. While it is impossible to achieve 100% or total passivity, the goal is to reduce the marginal gap as much as possible. When evaluating prosthesis fit and accuracy, the literature has shown marginal errors up to 150 um to be clinically acceptable.3,4
Why photogrammetry?
In full-arch implant dentistry, obtaining an accurate representation of the implant positions is imperative to the fit and longterm success of the prosthesis. Conventional, open tray-splinted impressions (PVS, polyether) are still the most popular technique in the fabrication of full-arch prostheses. Although intraoral scanning has become very popular, complete arch scanning
Christopher R. Resnik, DMD, MDS, DICOI, is a prosthodontist in private practice in Winter Park, Florida. He completed his dental degree, prosthodontic residency, and master’s degree in oral implantology from the University of Pittsburgh School of Dental Medicine. He is a faculty member of the Resnik Implant Institute and holds associate faculty positions at the University of Pittsburgh Graduate Prosthodontic Program and Temple University Graduate Periodontics Program. He is a contributing author to multiple textbooks including Avoiding Complications in Oral Implantology, Misch’s Contemporary Implant Dentistry, and Dental Implant Prosthetics.
Educational aims and objectives
This self-instructional course for dentists aims to discuss the process of using photogrammetry for full-arch immediate prostheses during the implant process.
Expected outcomes
Implant Practice US subscribers can answer the CE questions by taking the quiz online at implantpracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
• Be informed about some history and research regarding photogrammetry.
• Realize the accuracy of full-arch implant prostheses over more traditional methods.
• Identify some benefits of photogrammetry.
• Realize the steps and technique involved in using photogrammetry in the implant process.
2 CE CREDITS
has been shown to exhibit a margin of error that may lead to prosthesis misfit. Many studies have shown acceptable accuracy with intraoral scanning for single implants;5-7 however, for fullarch implants, questionable results have been documented.8-10 With full-arch prostheses, intraoral scanning studies have shown marginal discrepancies greater than 150 um, which ultimately lead to future complications.11,12
Photogrammetry technology has been advocated to allow clinicians the ability to obtain reliable and accurate representations of dental implant positions digitally. In the past, the photogrammetry technology was first used in non-medical fields such as land navigation, car crash testing, and the development of ships and planes. In 1994, Lie and Jemt were the first to integrate this technology into the field of dentistry.13 In 2005, Ortorp, et al., introduced photogrammetry to implant dentistry with the discussion of the use of this technology in recording implant positions in comparison to conventional impression techniques.14
Kosago, et al., compared the accuracy between conventional splinted open-tray impressions, intraoral scans (i.e., with multiple intraoral scanning systems), and photogrammetry. They concluded that for complete arch implant impressions, photogrammetry had better accuracy and precision than any of the
26 Implant Practice US Volume 16 Number 3 CONTINUING EDUCATION
digital or conventional impression techniques.15 Also, a recent systematic review compared conventional impressions, intraoral scanning, and photogrammetry, concluding that photogrammetry is accurate for full-arch implant impressions.16
Advantages of photogrammetry in implant dentistry
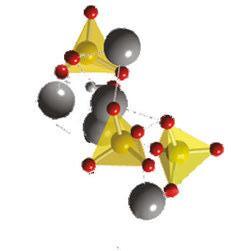
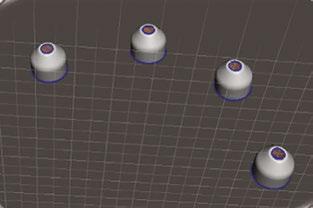
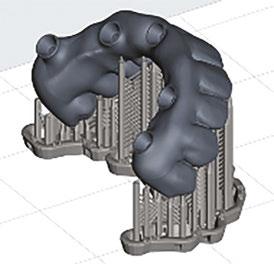
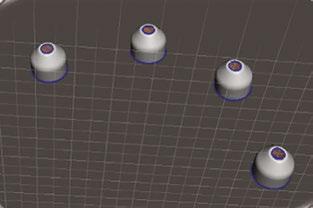
Photogrammetry technology may be used in implant dentistry to obtain accurate information with respect to recording three-dimensional implant positions for the fabrication of full-arch implant-supported prostheses. Through mathematical relations and stitching together 2-dimensional images, a 3-dimensional representation of the multiple implant positioning is created within an XYZ axis (Figure 1). Photogrammetry is the most precise and accurate digital method of recording the intraoral position of multiple implants. It is a technique for determining the geometrical properties of the imaged objects and their spatial arrangement from photographic images.

In comparison to conventional impression methods, photogrammetry is more efficient, faster, and provides greater patient satisfaction than conventional impression methods. With conventional impression methods, there exist many inherent patient factors which lead to inaccuracy. Material shrinkage, splinting material, implant angulation, impression material, patient movement, and intraoral conditions all alter the accuracy of the impression technique. With photogrammetry, these factors do not affect the accuracy as the record is being taken extraorally.
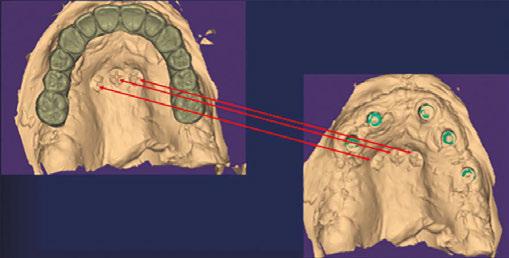
Although both are digital methods, photogrammetry technology is not the same as intraoral scanning. Photogrammetry scanning differs from traditional intraoral scanning in the acquisition and identification of its targets. During a photogrammetry scan, the targets and 3D position of the implant in the XYZ axis can be measured extraorally, from just one side. Therefore, the entire scan body is not required to pick up the implant location. In comparison with intraoral scanning (IO), IO accuracy is lost when measured between each of the scan bodies (Figure 2). Intraoral scanning must register the scan region (top 1/3 of scan body) to register implant positioning. Additionally, intraoral oral conditions (e.g., blood, saliva, soft tissue) and operator experience affect the accuracy of intraoral scanning.
Photogrammetry technique in implant dentistry
In implant dentistry today, there exist three different photogrammetry systems on the market — PICcamera (PICdental), iCam4D (iMetric4D), and MicronMapper (SIN Dental) (Figure 3). All photogrammetry units utilize the same basic techniques and workflow described below.

The photogrammetry technology allows the implant clinician to obtain three-dimensional (3D) coordinate measurements through
various photographic images, leading to a representation of the exact implant position. The photographic images utilize an extraoral receiver to record the geometric properties of objects and their spatial position.17 However, the only drawback of this system is that photogrammetry does not depict the soft tissues so a second STL file is required. With this workflow, the photogrammetry record will record the implant positioning within an XYZ axis, and an intraoral impression or scan is obtained to record the soft tissues. These scans will then be merged to create the patient’s prosthesis.
Step 1: Prior to placement of dental implants, the clinician must decide how to establish the correct and ideal tooth position as well as maintaining the patient’s vertical dimension of occlusion. This is a crucial step within the digital workflow to achieve accuracy. The following three methods can be utilized:
1. Use of fiduciary markers
Fiduciary markers can be used as an aide to relate the pre-and post-operative surgical data. Fiduciary markers are fixated within the oral cavity prior to surgery and remain in place until after the post-implant placement soft tissue record is obtained. Because of the constant position of the markers throughout the surgery, the merging of the pre- and post-surgical data can be completed. It is recommended to place a minimum of 2-3 fiduciary markers per arch. In the maxilla, the markers are most commonly placed in the palate, as this will not interfere with the actual surgical procedure. In the mandible, markers are generally positioned bilaterally in the retromolar pad area. The fiduciary marker surface should have a distinct marking (i.e., Phillips head) that can easily be recognized during an impression or scan. Tent screws are ideal to be used as fiduciary markers as they are stable when placed and easily depicted in the intraoral impression or scan. The vertical dimension is maintained by obtaining an accurate

27 implantpracticeus.com Volume 16 Number 3 CONTINUING EDUCATION
Figures 1 and 2: 1. Photogrammetry record for four implants registered within an XYZ axis (left). 2. Implant scan body examples. Inaccuracy occurs as the scanner moves between scan bodies, as well as when it is directed toward the gingival part of the scan body. Pink lines designate areas that intraoral scanner gets lost. Blue circle is the scan region of the scan body, the part the scanner must register to determine implant position (right)
Figures 3A-3B: 3A. iCam4D Photogrammetry System. 3B. Scan bodies (iCamBodies) inserted into the implants
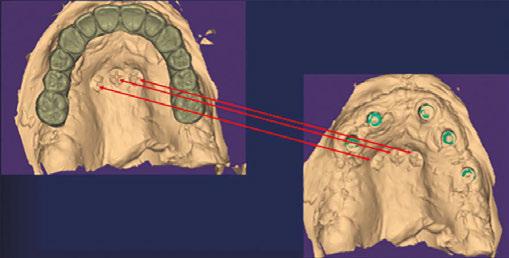
impression (i.e., PVS, polyether, or an intraoral scan) of the markers prior to and after surgery, as the fiduciary marker relates both data sets (Figures 4-6).
2. Selected abutment teeth
Another method to maintain the vertical dimension is to retain pre-determined abutment teeth throughout the surgery (Figure 7). Ideally, at least two teeth will be selected that will not interfere with the implant surgery. These teeth will remain in the arch until after the implant surgery, photogrammetry record, and soft tissue impression are obtained. After the records are completed, the teeth can then be extracted. By maintaining the selected teeth in the pre-and post- surgical impression (i.e., soft tissue impression with teeth and MUA healing caps), the two files can be merged together, thereby maintaining the vertical dimension.

3. Existing denture


The patient’s pre-existing or immediate denture can be used to help retain the vertical dimension. After implant placement and the photogrammetry recording, MUA healing caps will be placed on the implant abutments. A reline impression will then be taken with the patient’s denture (Figure 8). The denture will be scanned 360 degrees obtaining the soft tissue registration (from the reline impression), MUA healing cap positioning, and the denture tooth setup as well as bite registration. Within the CAD software, this will be imported as two separate files (i.e., preoperative wax-up and inverted soft-tissue scan). By inverting the intaglio of the denture scan, a soft tissue scan with the MUA healing caps is created. This scan can then be merged with the photogrammetry record, allowing the accurate position of the implants, soft tissue, and the patient’s denture tooth setup at the established vertical.
In summary, when restoring full-arch implants, three different records are needed:



1. Preoperative record
2. Photogrammetry record
3. Postoperative soft-tissue record (with MUA healing caps).
28 Implant Practice US Volume 16 Number 3 CONTINUING EDUCATION
Figures 4A-4B: 4A. Tent screws (fiduciary markers) placed prior to implant surgery. 4B. Impression obtained of tent screws
Figures 5A-5B: 5A. Post-implant placement with fiduciary markers still in place. 5B. Post-implant impression taken with MUA healing caps and fiduciary markers
Figure 6: Merging of the data between pre-op wax-up (left) and post-implant placement (right). The fiduciary markers are used to the merge the data as they are constant between both sets of data
Figure 7: Select teeth (i.e., red “X”) maintained during the implant surgery for relation of tooth position and vertical dimension. An intraoral impression or scan of patient’s soft tissue, MUA healing caps, and abutment teeth will be obtained and merged with the photogrammetry record and pre-op impression
Figure 8: Wash impression completed within patient’s denture registering soft tissue in relation to MUA healing caps. Bite registration also completed. Denture will then be scanned 360 degrees and uploaded to design software
These records are then exported into a design software (e.g., Exocad, 3Shape) where they will be merged to facilitate the design of an All-On-X prosthesis. All three of these methods can be utilized to align data to help record the vertical dimension as well as establish the ideal tooth position.

Step 2: Obtaining the photogrammetry scan
A. Scan body insertion

Photogrammetry scan bodies (e.g., PICtransfers, iCAM bodies, MicronMapper ScanBody) are specific to each photogrammetry system and are encoded with targets that allow the camera to transpose multiple images to determine the exact implant position. The scan bodies are inserted into multi-unit abutments of each implant, and verification X-rays are obtained to confirm seating of the scan bodies (i.e., most important for angled or deeper multi-units).

Once seating is confirmed, they must be oriented in a way to allow visualization of the maximum number of targets. This positioning increases the redundancy of the calculations as the photogrammetry record is being obtained (Figure 9).
B. Photogrammetry scan
The photogrammetry unit identifies the implant positioning from locating the targets on the photogrammetry scan body via an extraoral camera (Figure 10). The number of targets on the scan bodies, the type and number of cameras, and the method of obtaining images differs depending upon the photogrammetry systems (iCam4D, PicCamera, Micron Mapper).
The photogrammetry camera is positioned approximately 10 inches away from the scan bodies, at a maximum angle of 45 degrees (Figure 11). As the camera is rotated, images are continuously captured until the software verifies sufficient data has been obtained. During the scan, the software notifies the user when sufficient information has been recorded by demonstrating a color change in the scan body from red to green (Figure 12). Pictures are continuously obtained until enough intersections are created to record the exact position of the implants. This can generally be achieved in under 30 seconds.
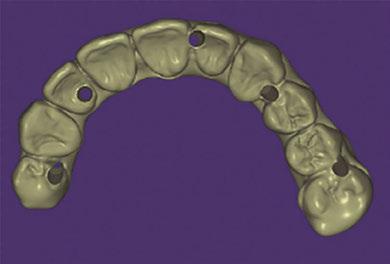
Step 3: Prosthesis fabrication
Once the photogrammetry scan is complete, a digital file extension (STL or XML file) is created that contains all the interrelated information on implant geometries, interfaces, healing abutments, and screws. This data can then be uploaded to CAD software to allow for digital alignment pairing and designing of the prosthesis.

All data sets are aligned within the CAD software (e.g., Exocad, 3Shape), and the patient’s immediate full-arch prosthesis is designed (Figure 13). The clinician has the option of designing and fabricating a prosthesis that inserts directly to the multi-unit abutment, without the use of a titanium cylinder or Ti-base (Figure 14). This is different from standard denture conversions and stackable surgical guides. With this, special abutment screws are utilized that have intimate fit within the prosthesis. All of these parameters are determined and specified within the design software.
After the prosthesis is designed, an “STL” file is sent to the 3D printer (Figure 15). This monolithic prosthesis can then be 3D-printed chairside for the patient in tooth-colored resin (Figure 16). Special characterization can be easily performed to optimize the esthetics prior to delivering the prosthesis. With this process, the patient is able to have an esthetic, passive fitting, immediate prosthesis (Figure 17).
29 implantpracticeus.com Volume 16 Number 3 CONTINUING EDUCATION
Figure 9: Photogrammetry scan bodies (iCamBodies) are inserted into the multi-unit abutments. They are positioned in a way to allow visualization of the maximum number of targets (i.e., white dots) extraorally
Figure 12: Example of the registration of the scan bodies on the designated software. Scan bodies will be highlighted green once adequate information is obtained
Figures 10 and 11: 10. Example of extraoral photogrammetry camera (iCam4D) (left). 11. Extraoral scanning of photogrammetry scan bodies. The camera will continuously record pictures as it is rotated, identifying the targets on the scan bodies (right)
prosthesis
CAD
Figure 14: Patient’s prosthesis can be designed and fabricated directly to the multi-unit
Special abutment screws, with digital libraries within the design software, will be used to retain the prosthesis in the mouth. Figure 15: “STL” file of a
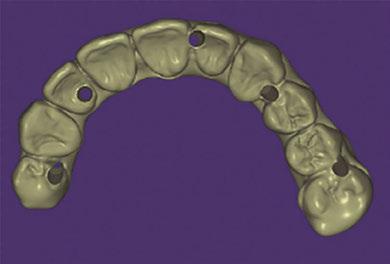
prosthesis in the printing software, with supports generated for printing. File will then be sent to printer for fabrication
Summary
The use of photogrammetry and 3D printing has given the implant clinician the opportunity to utilize an alternative full-arch prosthetic workflow option. A fully digital concept is now available for immediate loading procedures. Photogrammetry technology calculates the position and orientation of multiple implant interfaces quickly, efficiently, and accurately. It is the most accurate digital method to determine dental implant positioning for multiple implants, especially with full arch cases. Being able to create an instant digital file, many procedures and materials are eliminated, thereby reducing the possibility of error while saving time, reducing visits, and limiting patient discomfort.
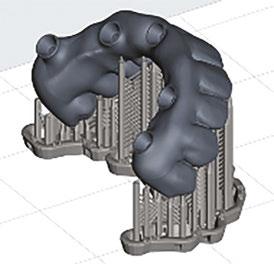
removed from the printer. Supports will be removed. Prosthesis will then undergo post-processing which includes gingival characterization to optimize the esthetics prior to delivering the prosthesis.

Figure
Diving into the digital workflow can be an overwhelming journey. Understanding the foundation of implant dentistry and the analog methods are still pivotal to applying these newer digital methods in implant dentistry. The Resnik Implant Institute, where I am a faculty member, has been implementing these digital methods in the surgical, prosthetic, and hands-on curriculum. Attendees receive didactic and hands-on training with photogrammetry and the digital workflow. Teaching these newer methods, as well as the foundation of implant dentistry, can help doctors understand and implement this technology in their practices.
REFERENCES
1. Abduo J, Judge RB. Implications of implant framework misfit: a systematic review of biomechanical sequelae. Int J Oral Maxillofac Implants. 2014 May-Jun;29(3):608-621.
2. Katsoulis J, Takeichi T, Sol Gaviria A, Peter L, Katsoulis K. Misfit of implant prostheses and its impact on clinical outcomes. Definition, assessment and a systematic review of the literature. Eur J Oral Implantol. 2017;10 Suppl 1:121-138.
3. Mizumoto RM, Yilmaz B, McGlumphy EA Jr, Seidt J, Johnston WM. Accuracy of different digital scanning techniques and scan bodies for complete-arch implant-supported prostheses. J Prosthet Dent. 2020 Jan;123(1):96-104.
4. Moslemion M, Payaminia L, Jalali H, Alikhasi M. Do Type and Shape of Scan Bodies Affect Accuracy and Time of Digital Implant Impressions? Eur J Prosthodont Restor Dent. 2020 Feb 27;28(1):18-27.
5. Wismeijer D, Joda T, Flügge T, Fokas G, Tahmaseb A, Bechelli D, Bohner L, Bornstein M, Burgoyne A, Caram S, Carmichael R, Chen CY, Coucke W, Derksen W, Donos N, El Kholy K, Evans C, Fehmer V, Fickl S, Fragola G, Gimenez Gonzales B, Gholami H, Hashim D, Hui Y, Kökat A, Vazouras K, Kühl S, Lanis A, Leesungbok R, van der Meer J,
Liu Z, Sato T, De Souza A, Scarfe WC, Tosta M, van Zyl P, Vach K, Vaughn V, Vucetic M, Wang P, Wen B, Wu V. Group 5 ITI Consensus Report: Digital technologies. Clin Oral Implants Res. 2018 Oct;29 Suppl 16:436-442.
6. Joda T, Katsoulis J, Brägger U. Clinical Fitting and Adjustment Time for Implant-Supported Crowns Comparing Digital and Conventional Workflows. Clin Implant Dent Relat Res. 2016 Oct;18(5):946-954.
7. Zhang Y, Tian J, Wei D, Di P, Lin Y. Quantitative clinical adjustment analysis of posterior single implant crown in a chairside digital workflow: A randomized controlled trial. Clin Oral Implants Res. 2019 Nov;30(11):1059-1066.
8. Kim KR, Seo KY, Kim S. Conventional open-tray impression versus intraoral digital scan for implant-level complete-arch impression. J Prosthet Dent. 2019 Dec;122(6):543-549.
9. Mizumoto RM, Yilmaz B, McGlumphy EA Jr, Seidt J, Johnston WM. Accuracy of different digital scanning techniques and scan bodies for complete-arch implant-supported prostheses. J Prosthet Dent. 2020 Jan;123(1):96-104.
10. Moslemion M, Payaminia L, Jalali H, Alikhasi M. Do Type and Shape of Scan Bodies Affect Accuracy and Time of Digital Implant Impressions? Eur J Prosthodont Restor Dent. 2020 Feb 27;28(1):18-27.
11. Wulfman C, Naveau A, Rignon-Bret C. Digital scanning for complete-arch implant-supported restorations: A systematic review. J Prosthet Dent. 2020 Aug;124(2):161-167.

12. Vandeweghe S, Vervack V, Dierens M, De Bruyn H. Accuracy of digital impressions of multiple dental implants: an in vitro study. Clin Oral Implants Res. 2017 Jun;28(6):648-653.
13. Lie A, Jemt T. Photogrammetric measurements of implant positions. Description of a technique to determine the fit between implants and superstructures. Clin Oral Implants Res. 1994 Mar;5(1):30-36.
14. Ortorp A, Jemt T, Bäck T. Photogrammetry and conventional impressions for recording implant positions: a comparative laboratory study. Clin Implant Dent Relat Res. 2005;7(1):43-50.
15. Kosago P, Ungurawasaporn C, Kukiattrakoon B. Comparison of the accuracy between conventional and various digital implant impressions for an implant-supported mandibular complete arch-fixed prosthesis: An in vitro study. J Prosthodont. 2022 Sep 9.

16. Hussein MO. Photogrammetry technology in implant dentistry: A systematic review. J Prosthet Dent. 2021 Nov 18:S0022-3913(21)00516-3.
17. Zhang YJ, Qian SJ, Lai HC, Shi JY. Accuracy of photogrammetric imaging versus conventional impressions for complete-arch implant-supported fixed dental prostheses: A comparative clinical study. J Prosthet Dent. 2021 Nov 11:S0022-3913(21)00567-9.
30 Implant Practice US Volume 16 Number 3 CONTINUING EDUCATION
IP
Figure 13: Design of patient’s
within
Software (Exocad).
abutment.
maxillary
16: Prosthesis
Figure 17: Final 3D-printed prosthesis
Continuing Education Quiz
The use of photogrammetry for the fabrication of full-arch immediate prostheses
1. When evaluating prosthesis fit and accuracy, the literature has shown marginal errors up to to be clinically acceptable.
a. 50 um
b. 100 um
c. 150 um
d. 200 um
2. In 2005, _________, introduced photogrammetry to implant dentistry with the discussion of the use of this technology in recording implant positions in comparison to conventional impression techniques.
a. Ortorp, et al.
b. Mizumoto, et al.
c. Wulfman, et al.
d. Vandeweghe, et al.
3. Kosago, et al, concluded that for complete arch implant impressions, photogrammetry had than any of the digital or conventional impression techniques.
a. less precision and accuracy
b. better accuracy and precision
c. more questionable results
d. more difficulty determining the geometrical properties of the imaged objects
4. With methods other than photogrammetry, material shrinkage, _________, patient movement, and intraoral conditions all alter the accuracy of the impression technique.
a. splinting material
b. implant angulation
c. impression material
d. all of the above
5. _______ can be used as an aide to relate the pre- and post-operative surgical data.
a. Geometric imaging
b. Open-tray impressions
c. Fiduciary markers
d. Healing caps
6. To maintain the vertical dimension, at least two pre-determined abutment teeth will be retained. These teeth will remain in the arch until after is/are obtained.
a. the implant surgery
b. the photogrammetry record
c. the soft tissue impression
d. all of the above
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 16 CE credits for only $149; call 866-579-9496, or visit https://implantpracticeus.com/ subscribe/ to subscribe today.
n To receive credit: Go online to https://implantpracticeus.com/continuingeducation/, click on the article, then click on the take quiz button, and enter your test answers.
AGD Code: 610
Date Published: August 21, 2023
Expiration Date: August 21, 2026
2 CE CREDITS
7. When the reline impression is taken with the patient’s denture, the denture will be scanned obtaining the soft tissue registration (from the reline impression), MUA healing cap positioning, and the denture tooth setup as well as bite registration.
a. 90 degrees
b. 180 degrees
c. 360 degrees
d. none of the above
8. Photogrammetry scan bodies (e.g., PICtransfers, iCAM bodies, MicronMapper ScanBody) are specific to each photogrammetry system and are encoded with targets that allow the camera to transpose multiple images to determine the exact implant position.
a. True
b. False
9. The number of targets on the scan bodies, the type and number of cameras, and the method of obtaining images is the same for all photogrammetry systems (iCam4D, PicCamera, Micron Mapper).
a. True
b. False
10. The photogrammetry camera is positioned approximately away from the scan bodies, at a maximum angle of 45 degrees.
a. 3 inches
b. 5 inches
c. 10 inches
d. 15 inches
To provide feedback on CE, please email us at
education@medmarkmedia.com
Legal disclaimer: Course expires 3 years from date of publication. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
31 implantpracticeus.com Volume 16 Number 3 CONTINUING EDUCATION
RESNIK
Dental sedation: an overview
Dr. Brian McGue discusses how sedation can affect patients and dentists

Sedation of dental patients is not a new concept. Dentists in the United States have been sedating patients for more than 150 years. In the mid-19th century, Horace Wells and William T.G. Morton were dentists who demonstrated that the perioperative use of sedation for dental procedures was beneficial.1 Wells attempted to demonstrate the use of inhaled nitrous oxide as a sedative for a dental extraction at the Massachusetts General Hospital in 1845. Though the sedation Wells performed was not deemed a success, Morton was very successful a year later, again at the Massachusetts General Hospital, while sedating a patient with ether.
At the beginning of the 20th century, sedation of patients for medical procedures became more widespread, and the medical specialty of anesthesiology was created. Technical advances coupled with scientific research and discoveries in pharmacology advanced sedation to become a safer and more predictable procedure. The overwhelming use of sedation, however, was in the field of medicine. Outside the widespread use of intravenous sedation by oral surgeons, dentists generally did not use sedation techniques beyond the use of nitrous oxide for very lightly inhaled anxiety control.
Dentists began to do more sedation in the 1990s when oral conscious sedation began to become popular.2 The use of an orally administered sedative pre- or peri-operatively became widespread for dentists to alleviate anxiety during dental procedures. The nature of current dental practice appears to be evolving to a more surgical focus with the accelerated use of implants. With this evolution, the use of sedation has become prevalent as dentists strive to make their patients more comfortable during these surgical procedures.
The increased use of sedation by dentists can be attributed to many factors. Some of these factors are obvious and some are not. This article will try to address some of these reasons.
Educational aims and objectives
This self-instructional course for dentists aims to discuss the benefits of using sedation in the dental practice.
Expected outcomes
Implant Practice US subscribers can answer the CE questions by taking the quiz online at implantpracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
• Realize some history of dental sedation.
• Identify reasons how dental sedation can increase patient comfort.
• Define antegrade amnesia from sedation and how this expands certain patients’ treatment options.
• Realize some reasons to decrease use of local anesthetic.
• Realize how using sedation can combat “compassion fatigue” in the dental office.
Why do we sedate patients?
Patient anxiety and comfort
Patient anxiety and comfort are the most obvious reasons for sedation. The American Dental Association estimates that 100 million Americans do not seek dental care.3 Severe debilitating fear of the dentist has been estimated to prevent 60 million people from entering a dental office. Sedation is a method for lowering this barrier and permits patients to receive dental treatment. If a dentist is attempting to build a patient base, this group of patients can be an aid in that endeavor.
Brian McGue, DDS, is a fulltime practicing general dentist with a private practice in Chesterton, Indiana. His practice has a comprehensive focus offering a variety of restorative and surgical treatments with an emphasis on full-mouth rehabilitation while using sedation for patient comfort. Dr. McGue and his wife, Susan, lecture on the topic of sedation and run hands-on workshops for dentists interested in incorporating oral and IV sedation into their practices at The Pathway in Tempe, Arizona (www.thepathway.com) and the 3-D Dentists facility in Raleigh, North Carolina, and Nashville, Tennessee (www.3ddentists.com). Together they have authored three textbook manuals on sedation. Dr. McGue is a fellow of the Academy of General Dentistry and a member of the American Dental Society of Anesthesiology, the International Anesthesia Research Society, and an educational member of the American Society of Anesthesiologists. Dr. McGue and Susan McGue can be reached at stayintheboxsedation@gmail.com.
Patients also have fear of specific dental procedures. The fear of some of these procedures can be understood. Third molar removals, implant procedures, multiple extractions, endodontic procedures, etc., can involve complex procedures, loud sounds, unpleasant sensations, and disconcerting instrumentation that can elevate a patient’s negative perceptions. However, the fear of some other procedures may not be as well understood by dental practitioners. From personal experience in my practice, two patients that we perform dental prophylaxis on every 6 months request sedation. Though many dental team members perceive receiving dental prophylaxis as a non-stressful, pleasant experience, there is a segment of the population that feels a sense of foreboding when they consider their routine dental prophylaxis.
Additionally, it may not be simply fear of a dental procedure that keeps a patient from seeking care — it may be the fear of sitting still for an extended length of time. Sitting in a dental chair with one’s mouth open for an extended time may be a source of stress for some people. Sedation helps with this because many of
32 Implant Practice US Volume 16 Number 3 CONTINUING EDUCATION
2 CE CREDITS
the sedation medications used in the dental office can cause the sensation of time compression. A 2-hour procedure can feel like a 15-minute procedure for a sedated patient.
Primum non nocere (First do no harm)
As health care providers, we have an ethical responsibility to not harm a patient. Iatrogenic injuries can occur in the dental office — most dental practitioners have inadvertently caused a minor injury to a patient. Nicking a tongue with a bur, retracting a patient’s cheek too aggressively, or having a tissue flap tear while reflecting are all examples of minor injuries that can occur but most likely do not have any long-term effects. Some injuries though are not obvious or even physical.
Mental trauma can occur from dental treatment. As mentioned before, dental procedures, even procedures that appear non-threatening, can create a lot of anxiety for patients. Most dentists can relate to having to manage an extremely fearful patient who had a previous negative dental experience. As dentists, it behooves us not to be the practitioner who created the negative experience that so traumatized a patient that he/she avoided dental care for years.
Anterograde amnesia
The primary class of medications used in sedation dentistry is benzodiazepines. Benzodiazepines are known to cause anterograde amnesia. Anterograde amnesia is the loss of memory of during the time the patient is under the influence of a certain medication. Patients simply don’t remember the procedure for which they were sedated. Many patients are happy with not having memory of the procedure. This type of patient arrives for the appointment, goes to “sleep,” and “wakes” up after the procedure is concluded. Almost all sedations done in dental offices are conscious sedations where the patient is awake and responsive so the patients are not asleep even though many think they were.
Anterograde amnesia can be a practice builder. If a patient has a painful tooth, and the dentist is able to sedate them, do an endodontic procedure, and a CAD/CAM crown during the sedation, the patient can emerge from the sedation with an asymptomatic white tooth. These patients will tell other potential patients about their positive experience and help build your practice.
Decreased use of local anesthetic
When we train dentists to perform sedations, we encourage the use of online services that check the patient’s own medications against the administered sedation medications for interactions and also the local anesthetics we are intending to use on the patients. Many of the attendees at our courses are surprised by the lack of interactions with sedation medications but are more astonished by the significantly higher number of interactions between the patient’s medications and the local anesthetics.
Many local anesthetics are vasoconstrictors and can cause an increase in heart rate and blood pressure. Physiologically, these changes can be detrimental to the patient and can precipitate a medical crisis. As dentists, one of our goals in treating patients is to try to reduce inherent risks for the patient. Sedation is one method of lowering how much local anesthetic we are required to use to properly anesthetize a patient for a procedure.
An article written by J.B. Murray in the Journal of Psychology in 19714 looked at decades of psychological research and was able to definitively conclude from his research that apprehensive patients have a lowered threshold of pain. In other words, a nervous patient will feel pain quicker and at lower stimulus levels then a non-anxious patient. As dentists, we already inherently know this. In the dental chair, it is the nervous patient that is harder to numb.
Prior to Murray’s article, there had already been connections made between the perception of pain and apprehension. In his 1960 book, Pyschophysiologic Approach in Medical Practice, William Schottstraedt5 theorized that pain and apprehension have a circular relationship. Pain causes apprehension, apprehension heightens one’s perception of pain, which then causes more apprehension.
If we can break the chain of apprehension through sedation, then we can lower the patient’s perception of pain, and thus, use less local anesthetic.
Higher quality of dentistry
Can the patient’s behavior negatively impact the quality of dentistry a dentist is trying to provide? As dentists, we all will answer “yes” to this question. We have all had the apprehensive patient who will not listen to our instructions, sit still during the procedure, and/or be overly dramatic when they perceive they’ve felt something.
By removing a patient’s negative behavior from the equation, the dental team can focus on the technical aspects of the procedure. One can equate this to placing an isolation device to get better visualization on the area we are treating. Another analogy

33 implantpracticeus.com Volume 16 Number 3 CONTINUING EDUCATION
Figure 1: Sedation can be part of any dental practice
is using a surgical guide to place an implant. The guide is just another tool we can pull off of our shelf in order to increase the level of the quality of dentistry we are providing. Similarly, sedation simply can be another tool to remove factors that may interfere with the quality of treatment.
Sedation enables the dental practitioner to perform and learn higher levels of dentistry

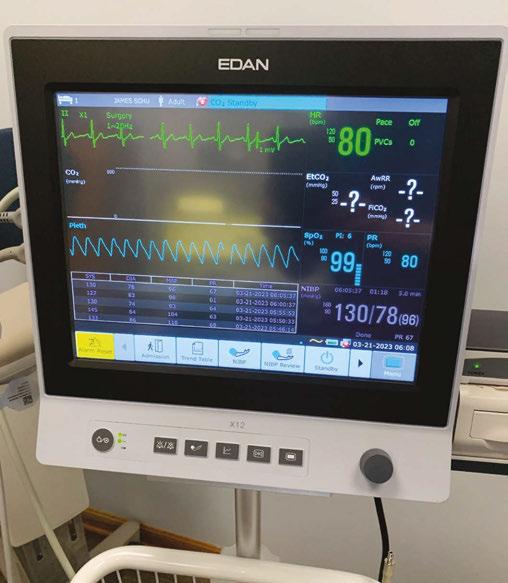
The profession of dentistry is unique and amazing. One of the reasons for this is the ability to continually expand and refine one’s clinical skills throughout a career. Very few professions are geared in this way. Continuing education courses offer a way to expand technical skills that can be honed with continued use of those new skills in practice.
Sedation is a tool that can be used in order to relax the patient, take their behavior out of the equation, and let the dental team focus on learning and refining these new skills. It has been said that “repetition is the moniker of learning.” Sedation is one way to have those early repetitions be in a lower stress environment for both the practitioner and the patient. This allows the dental team to focus on what they are learning in the early stages of their development.
Learning these higher levels of dental treatment is a win-win for both dentist and patient. For dentists, it can combat job burnout, promote long-term job satisfaction, and allow dentists to treat patients in a more comprehensive way. For patients, having the dentist able to perform higher levels of dentistry is advantageous because they can have most of their dental work done in one office and have more dentistry done in one appointment which helps them avoid multiple days off of work.
Compassion fatigue
Compassion fatigue is a clinical term that is applied to health care workers, educators, first responders, members of the clergy, and funeral home workers.6 For health care workers, there is a clear definition of compassion fatigue:
“The ‘cost of caring’ for others in emotional or physical pain. Defined as occupational burnout in conjunction with vicarious traumatic stress, which is caused by indirect exposure to stress. Finding emotional energy to calm and reassure apprehensive patients and maintain a confident demeanor while your patient is exhibiting fear or panic can be draining. The potential for negative energy transfer is substantial. Health care workers are generally very sympathetic and empathetic toward others. That is why they are in health care.”7
As dentists, we have all probably experience compassion fatigue at some point. I like to make the analogy that we all start the day with a large vat of compassion. Throughout the day, we ladle out compassion to whomever needs it. Eventually, toward the end of a long day at the dental office, the vat is dry. We leave the office and arrive home to our spouses, children, and/or pets, and many of them also want some love or compassion. Unfortunately, at this time of the day, the vat may be empty. Unchecked compassion fatigue can create burn-out, exhaustion, and mental illness.
Conclusion
Sedation can dramatically lower the amount of compassion a dental team has to ladle out because sedated patients are much less anxious.
Dentists have been sedating patients in their offices for a long time. In fact, in the early history of sedation and anesthesia, dentists were at the forefront of its development. In today’s modern dental practice, sedation has become widely used. For many dentists, it is a way to build a practice, expand their skills, and decrease their own stress level. The science of sedation will continue to evolve and most likely help to expand the options in the dental office.
REFERENCES
1. American Society of Dental Anesthesiologists. History. https://www.asda.org/ about-us-2/. Accessed April 17, 2023.
2. Donaldson M, Gizzarelli G, Chanpong B. Oral sedation: a primer on anxiolysis for the adult patient. Anesth Prog. 2007 Fall;54(3):118-128; quiz 129.
3. Beaton L, Freeman R, Humphris G. Why are people afraid of the dentist? Observations and explanations. Med Princ Pract. 2014;23(4):295-301.
4. Murray JB. Psychology of the pain experience. J Psychol. 1971 Jul;78(2d Half):193-206.
5. Schottstaedt, W. W. Psychophysiologic approach in medical practice. Chicago: The Year Book Publishers; 1960.
6. Cocker F, Joss N. Compassion Fatigue among Healthcare, Emergency and Community Service Workers: A Systematic Review. Int J Environ Res Public Health. 2016 Jun 22;13(6):618.
7. McGue, BC, Susan M. Oral Conscious Sedation. Stay in the Box Sedation [Course Manual]. 2021;(1), 4-5.
34 Implant Practice US Volume 16 Number 3 CONTINUING EDUCATION
IP
Figures 2A and 2B: 2A. Continuing education courses offer a way to expand technical skills. 2B. Dr. McGue and his wife, Sue, recently published a new Oral Conscious Sedation manual
Continuing Education Quiz
Dental sedation: an overview McGUE
1. In the mid-19th century, _____________ were dentists who demonstrated that the perioperative use of sedation for dental procedures was beneficial.
a. Horace Wells and William T.G. Morton
b. Ben Johnson and James Gutmann
c. Anton van Leeuwenhoek and Phillip Pfaff
d. Edwin Maynard and Edwin Truman
2. Severe debilitating fear of the dentist has been estimated to prevent ________ people from entering a dental office.
a. 500,000
b. 5 million
c. 60 million
d. 125 million
3. Third molar removals, implant procedures, multiple extractions, endodontic procedures, etc., can involve ________ and disconcerting instrumentation that can elevate a patient’s negative perceptions.
a. complex procedures
b. loud sounds
c. unpleasant sensations
d. all of the above
4. Dental procedures, even procedures that appear non-threatening, can create a lot of anxiety for patients.
a. True
b. False
5. ________ are known to cause anterograde amnesia.
a. Cepahlosporins
b. Benzodiazepines
c. Prilocaine
d. Pilocarpine
6. ________ is the loss of memory of during the time the patient is under the influence of a certain medication.
a. Transient Global Amnesia
b. Dissociative Amnesia
c. Anterograde Amnesia
d. Retrograde Amnesia
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 16 CE credits for only $149; call 866-579-9496, or visit https://implantpracticeus.com/ subscribe/ to subscribe today.
n To receive credit: Go online to https://implantpracticeus.com/continuingeducation/, click on the article, then click on the take quiz button, and enter your test answers.
AGD Code: 340
Date Published: August 21, 2023
Expiration Date: August 21, 2026
2 CE CREDITS
7. Many local anesthetics are vasoconstrictors and can cause an increase in heart rate and blood pressure.
a. True
b. False
8. A study by J.B. Murray in the Journal of Psychology noted that a nervous patient will feel pain ________ then a non-anxious patient.
a. quicker and at lower stimulus levels
b. more slowly and at lower stimulus levels
c. quicker and at higher stimulus levels
d. more slowly and higher stimulus levels
9. _________ is defined as occupational burnout in conjunction with vicarious traumatic stress, which is caused by indirect exposure to stress.
a. Traumatic Burnout Disorder
b. Dental Professional Stress Disorder
c. Compassion Fatigue
d. Emotional Energy Deficit Disorder
10. Sedation is a tool that can be used to __________.
a. relax the patient
b. take the patient’s behavior out of the equation
c. let the dental team focus learning and refining new skills
d. all of the above
To provide feedback on CE, please email us at education@medmarkmedia.com
Legal disclaimer: Course expires 3 years from date of publication. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
35 implantpracticeus.com Volume 16 Number 3 CONTINUING EDUCATION
Reducing risks of malpractice claims
Kristin
Tauras,
JD, offers direction on how to avoid a malpractice claim

It is impossible to avoid all lawsuits. As a defense attorney, we often tell our clients there is a low threshold for a malpractice suit to be filed against a professional. In Illinois and 32 states, all it takes to file a suit is the payment of a filing fee and the attachment of a certificate of merit by a health care provider in the field of dentistry. Eighteen states do not even require a certificate of merit. Nevertheless, there are things that a dental specialist can do to lessen the risk of being sued or, if sued, lessen the risk of a large adverse judgment.
Clearly communicate with your patient
Most patients are not well-versed in dental care and rely upon their dental specialist to tell them what they need to know. The dental professional has a duty to make sure the patient understands the treatment or procedure that is being proposed, and how the patient should continue to care for their condition once they are home. More importantly, they should want to provide the best care possible to the patient.
The communication should be patient-focused. Specialists who practice patient-focused communication know it is most important to practice the following behaviors:
• show respect and empathy
• listen attentively
• draw out and respond to their patients’ fears and concerns
• answer even the most difficult or emotion-laden questions honestly
• fully inform patients about their treatment options
• involve patients in the treatment decisions
• demonstrate sensitivity and respect for the patients’ social, familial, religious, cultural, and ethnic diversity. Dental specialists should explain the continuing treatment with the patient as well, including their at-home treatments. Patients need to understand why medicines or certain therapies or behaviors are being prescribed or discouraged, the proper dosing of pain medication and antibiotics, and why they should
take their pain medication and antibiotics. They should also take the time to explain why certain other OTC medications and/or alcohol may compromise their treatment. What may seem obvious to a dental specialist is not always obvious to their patients.
Take the time to know your patient
As a caveat to clearly communicating with the patient, it is essential that the dental specialists get to know their patients to provide the type of communication necessary to forge a positive relationship. Patients who have a long-standing positive relationship with their dental care providers rarely sue. If dental specialists and their staffs take the time to get to know their patients and develop a relationship with them, there is less likelihood that they will sue for something minor. Dental specialists may not avoid the larger suits, such as a permanent neuropathy or wrongful death case, but it may lessen the chance of being sued for something that is correctable.
Obtain informed consent
Prior to any dental procedure, the dental specialist should provide thorough information and obtain written informed consent. Informed consent is not simply a form that the patient signs. Informed consent includes:
• a verbal explanation of what the dental specialist intends to do
• why they intend to do it
• the risks of both doing the procedure and not doing the procedure.
36 Implant Practice US Volume 16 Number 3 LEGAL MATTERS
Kristin Tauras, JD, is a partner in the law firm of McKenna Storer in Chicago, Illinois. She has a litigation practice in the areas of employment law, insurance coverage, and professional malpractice. McKenna Storer is a fullservice law firm providing legal services to individuals and smallto-midsize companies, including defending professional malpractice negligence lawsuits and Illinois Department of Professional Regulation investigation, as well as advising dental and medical professionals regarding business and employment matters.
Alexandra Tauras, a biochemistry and molecular biology student on the premedicine track at the University of Iowa, assisted with drafting the article.
It also means that the dental professional should ask the patient if they have any questions and make sure they answer their questions thoroughly.
This information must be in both terms that are understandable to the patient and in a language that the patient understands. If the patient does not speak the same language as the dental specialist, a family member or outside interpreter should be brought in to assist with providing informed consent.
Be thorough in updating patient history
Missing or overlooking a problem is one of the most significant malpractice risks. A patient’s medical history is always evolving. At every appointment, the dental specialist should take the time to update the patient’s medical history, including changes in medical conditions, medications, and allergies. The update should include the patient’s history of smoking, drug and alcohol use when relevant. The dental specialist should also ask about other information that relates directly to the patient. For example, if the patient is going through an emotionally difficult time, this fact may impact whether a dental condition or pain is the result of a disease as opposed to stress.
Be thorough in examining and screening the patient
As a part of being thorough, the dental specialist should make cancer screening a part of every patient’s appointment. If there is something suspicious, the dental specialist should either perform a biopsy if they are qualified or send the patient for a follow up to a specialist that deals with oral cancers.
Dental specialists should also inform the patient of the need to follow up with their medical doctors when there are signs that the patient is potentially suffering from the following:
• Heart disease: Symptoms of gum disease (red, inflamed, bleeding gums) can affect the patient’s heart.
• Diabetes: Receding gums, dry mouth, bad breath, and loose teeth can be signs of diabetes.
• Osteoporosis: Bone loss may be due to osteoporosis.
• Cancer: Sores and growths can be signs of cancer
While dental professionals do not treat the underlying conditions, the conditions may impact the diagnosis and treatment of the patient, and they may be the first health care provider to notice the symptoms of these serious underlying diseases that, if caught early, could increase the chances of a positive outcome. The dental specialist should check for other medical conditions that may be evident in their exam of the patient and recommend that the patient follow up with their general practitioner or specialist.
Refer when appropriate
Dental specialists should refer, when necessary, especially where they are hesitant to do the treatment or know that there are other specialists better able to address the problems. Today, more
than ever, dentistry is specialized. Dental specialists should refer the patient to those specialists that are best equipped to address the patient’s dental condition.
Chart everything
Charting is the key to successfully defending a dental malpractice action. The dental specialist, or their office staff, should make a note on the chart of the following:
1. updating medical and social history
2. performing an oral exam
3. the patient’s complaints
4. the diagnosis
5. the tests and x-rays performed or captured
6. the treatment provided
7. the treatment postponed or referred, and the reason for that decision
8. informed consent
9. anything else significant in the treatment of the patient. Remember to err on the side of over-charting.
Follow up
Following up with the patient not only helps develop an excellent relationship with the patient, but it also provides valuable information on whether the course of treatment is working or whether there are additional problems that need to be addressed. Patients will often cancel the follow-up appointment or fail to show up because they think that they are better and do not want to waste the time or money, or think that the dental specialist made them worse. Either way, following up with the patient is advised because it permits the dental specialist the opportunity to develop good will with the patient and provides the opportunity to correct a reversible mistake or misdiagnosis.
Contact your malpractice attorney and/or malpractice carrier
When a patient is threatening to sue, or a suit has been filed, the dental specialist should immediately contact his/her attorney and/or malpractice insurance carrier. They are best equipped to assist in how to address the problem. Just as dental specialists deal with diseases of the teeth, jaw, or oral cavity, attorneys and insurance companies are well-versed in handling dental malpractice actions.
As stated above, a dental specialist may not be able to avoid every lawsuit, but they may be able to prevent some suits or lessen the liability when a suit is filed.
37 implantpracticeus.com Volume 16 Number 3 LEGAL MATTERS
IP
There are things that a dental specialist can do to lessen the risk of being sued or, if sued, lessen the risk of a large adverse judgment.
Boyd Industries
The top choice for implant office equipment
Boyd equipment leads the chairs and tables market for oral and dental implant surgery with its innovative designs, quality, and proven reliability. The company has set the standard, with its time-tested 65-plus year history enduring millions of surgical procedures. It is easy to see why Boyd’s customers remain loyal, purchasing for future endeavors.
Boyd designs and fabricates the largest variety of customizable operatory equipment and cabinetry options to fit the size, functionality, and style of any clinic. Our chairs are configurable to your ergonomic and design esthetic. The cabinetry line of standard and personalized designs sets Boyd apart from others in the dental implant industry by standardizing customizability. Boyd’s engineers and office design specialists will adapt standard configurations to create a design that meets your exact needs, created for your ideal work environment.
To complement Boyd’s line of oral surgery chairs, the company offers a wide variety of mobile operatory carts designed to organize and store surgical equipment and devices. The carts are light-weight, easy to disinfect, and lockable with ergonomic handles to move between surgical suites.
Boyd products meet FDA and regulatory requirements
Our equipment meets all required regulatory standards for compliance. These include IEC 60601 safety standards for medical/dental devices, CSA for Canadian, and CE for European.
Our products are unique for implant specialists

We are committed to providing our customers with the latest technological advancements and innovations in implant
dentistry. Our treatment chairs are ergonomically designed for dental implant procedures maximizing comfort for patients and efficiency for physicians. Equipment is configurable and can be specifically customized to the surgeons’ specifications.

Boyd’s financing option
Boyd has a very competitive program for recent residency graduates and separating military members, offering them significant product discounts or favorable payment terms.
Lead time for receiving Boyd equipment once orders are placed
Boyd Industries has been able to better manage its lead times because of the company’s U.S.-based factory and North American supply base. Boyd’s factory fabricates steel, plastic, upholstery, wood, and many other components used in its products. The capability to directly manage much of the product content internally has allowed the company to maintain lead times to under 8 weeks.
Want to see Boyd equipment in person?
Boyd attends industry trade shows to display and demonstrate a variety of customizable equipment and offers show discounts to attendees. In addition to trade shows, Boyd has a product showroom at our headquarters in Clearwater, Florida. Visit BoydIndustries.com for a custom quote, or to learn more, call our sales team at 727-471-5072. This information was provided by Boyd Industries.
IP
38 Implant Practice US Volume 16 Number 3 PRODUCT PROFILE
YOU DREAM WE BUILD IT!

BOYD INDUSTRIES’ SPECIALIZES IN DENTAL IMPLANT EQUIPMENT. PRIORITIZING PATIENT COMFORT AND PROVIDES PEACE OF MIND THROUGH INNOVATION AND EFFICIENCY.


SCAN TO FIND OUT HOW WE CAN BUILD YOUR DREAM

Advanced Dental Implant Center™ is powered by more than 50 years of proven experience
Founded in 1975, Affordable Care has been focused on a singular mission to help dentists expand patient access to high-quality tooth replacement care. Today, through Affordable Care’s growing Advanced Dental Implant Center (ADIC) network, that mission remains steadfast.
“We help doctors and dental practices grow to reach more patients,” explains Dr. Dan Holtzclaw, Chief Clinical Officer of the ADIC network. “We do this through cross-functional expertise and dedicated attention to doctors and their teams so they can truly focus on patient care.”
Affordable Care launched the ADIC network of practices last year. Since then, dentists from across the U.S. have chosen to affiliate their practices to leverage the business, operational, and clinical support provided by Affordable Care.
“I understand it’s a big decision,” shares Dr. Holtzclaw. “I was in the exact same place when choosing to sell my practice and affiliate with the ADIC network. I built and managed a successful fixed-arch clinic but was ready to expand to the next level professionally and explore more opportunities as an implant surgeon.”
Service through Centers of Excellence
As the nation’s largest Dental Support Organization (DSO) exclusively focused on tooth replacement services, Affordable Care supports more than 425 affiliated dental practices across 42 states. The support and services offered to ADIC network practices includes:
• Clinical: Clinical leaders and staff focus on building an engaged doctor community through education and advancement, including industry-leading CE training
• Laboratory: Dedicated team of experienced laboratory professionals focused on providing training and in-practice lab support
• Legal and Compliance: Team of legal experts with deep dental industry experience in legal affairs and regulatory compliance
• Information Technology: Advanced IT solutions including security and enterprise network support to handle day-to-day IT needs
• Finance: Accounting and financial management services to help maximize practice revenue
• HR/Recruiting: Dedicated team focused on recruitment to help attract and retain top talent and support day-today in-practice HR duties
• Marketing: In-house marketing team with a proven track record and access to decades of patient-driven data to increase brand awareness and patient flow for advanced implant providers

• Operations: Dedicated integration and operations team to help drive continued growth and efficiency
• Real Estate Management: Extensive experts in De Novo set up, site selection, and lease management to support new practice operations
• Research and Development: Multi-site clinical trial and pilot testing programs designed to advance the latest technologies in dentistry
• Staff Training and Development: Team of trainers focused on support and increasing the skills of dental practice staff
• Supply Chain: Founded the largest dental Group Purchasing Organization (GPO) in the U.S., known as Sevaredent Sourcing Solutions, to drive significant cost savings on clinic supplies and professional services
“We are looking for doctors who are at the top of their game,” explains Dr. Holtzclaw. “You have been successful for a reason. We don’t want to change what you have built, but rather enhance your practice through our proven experience and results. We help take both you and your practice to the next level, whatever your goals may be.”
Dr. Chris Epperson, managing dentist for Advanced Dental Implant Center of Phoenix, adds, “Within the network, there is this feeling of collaboration. To be among a group of doctors who care about your success is absolutely refreshing.”
Scan the QR Code or visit https:// affordablecare.com/affiliate to learn about affiliation opportunities.

40 Implant Practice US Volume 16 Number 3 SERVICE PROFILE
IP
This information was provided by Affordable Care.
ADIC network doctors join together for a networking event with Affordable Care leaders


Scan the QR code or call us at: (888) 537-2801 to learn about affiliation opportunities - Dr. Dan Holtzclaw Chief Clinical Officer Affordable Care’s Advanced Dental Implant Center Network We are attracting the very best general dentists with extensive implant experience, oral surgeons, periodontists and prosthodontists to affiliate with us and be a part of building something very special for patients and for doctors in our industry. serve DSO for ADVANCED DENTAL IMPLANT CENTER AN INVITATION for general dentists with extensive implant experience, oral surgeons, periodontists and prosthodontists Proud to serve as the DSO for the Advanced Dental Implant Center network NOW IS THE TIME TO JOIN OUR FAST GROWING NETWORK OF ADVANCED DENTAL IMPLANT PROVIDERS






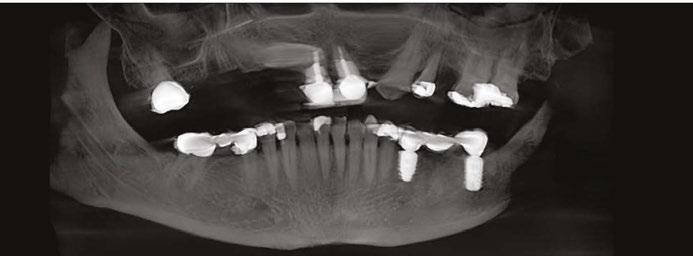






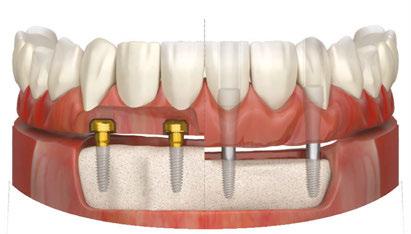






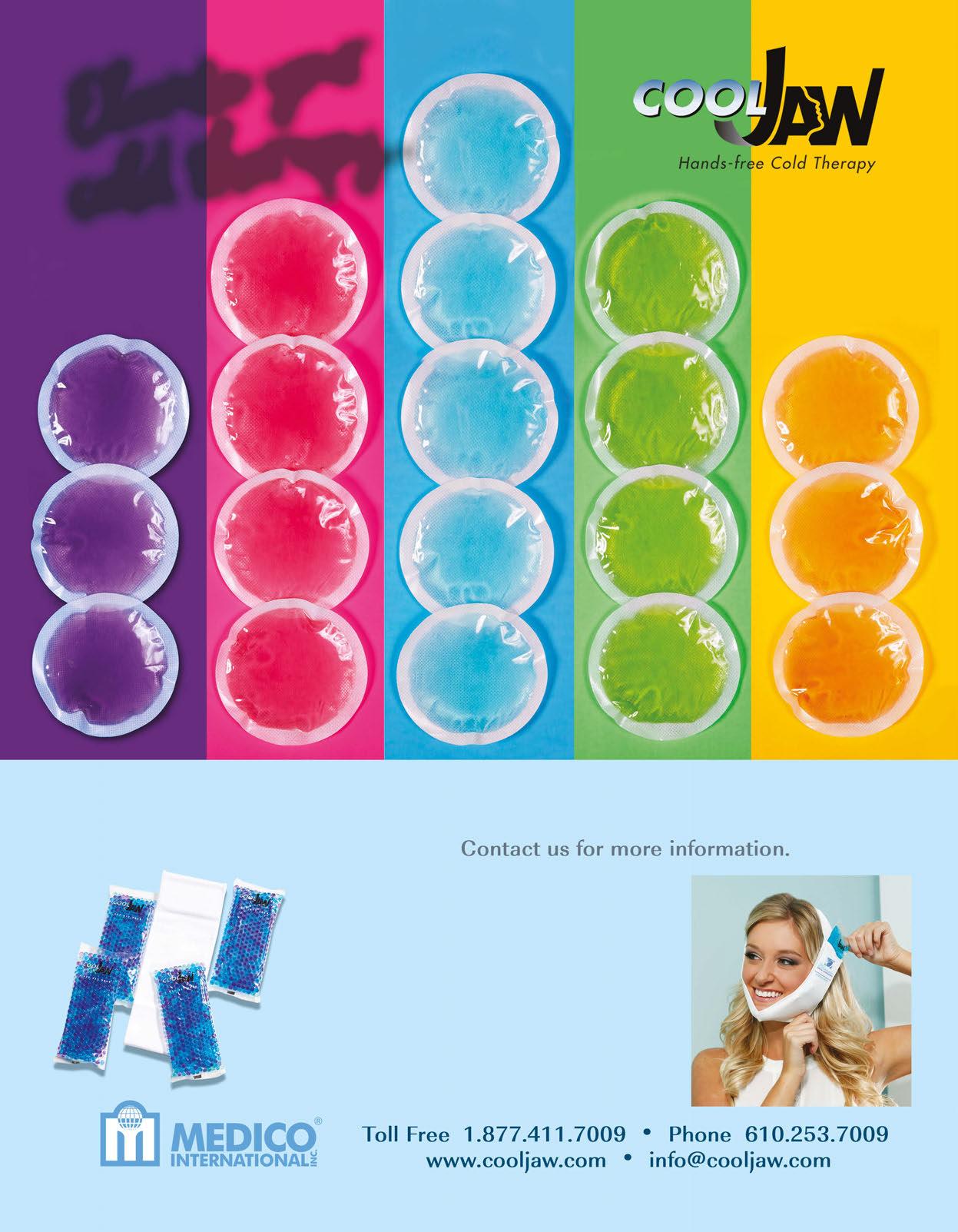

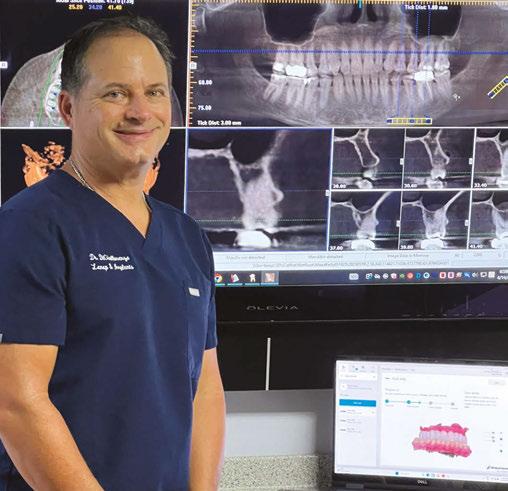



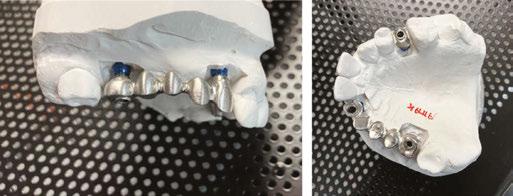 Drs. Douglas D. Wright and William T. Goodwin II treat a patient
Drs. Douglas D. Wright and William T. Goodwin II treat a patient