The Preat workflow advantage
Dr. Carl J. Drago

AI in implant dentistry
Drs. Aaron Glick, Nicholas Tipton, Nisha Manila, and Jennifer Chang
Ailing and failing All-On-X cases and how to treat them
Dr. Dan Holtzclaw
Treating posterior mandibular atrophy using CAD/CAM subperiosteal implants
Drs. Mathieu Goudal and Cécil Bailly






Unlock Restorative Efficiency The Abutment Company Unlock Restorative Efficiency The Abutment Company
PROMOTING EXCELLENCE IN IMPLANTOLOGY
Digital Workflow / Guided Surgery n 4 CE Credits Available in This Issue* Spring 2024 Vol 17 No 1 implantpracticeus.com
Champion of Specialists


“I am no longer a lone wolf. I can now lean on an array of specialists from all over the country for help, advice, and friendship.”
Neil Zachs, DMD, MS Periodontist partner in Scottsdale, AZ
Strength in Numbers.
We’re proud to champion Dr. Zachs and more than 300 elite dental specialists and practice teams in our growing network. Since 2018, we’ve been helping our partners focus on delivering exceptional patient care, while our business experts help lessen the weight of practice management. Find out how our powerhouse community of periodontists, endodontists, and oral and maxillofacial surgeons work together to champion your long-term success.

Connect with our Partners
Spring 2024 n Volume 17 Number 1
Editorial Advisors
Jeffrey Ganeles, DMD, FACD
Gregori M. Kurtzman, DDS
Jonathan Lack, DDS, CertPerio, FCDS
Samuel Lee, DDS, DMSc
David Little, DDS
Brian McGue, DDS
Ara Nazarian, DDS
Jay B. Reznick, DMD, MD
Steven Vorholt, DDS, FAAID, DABOI
Brian T. Young, DDS, MS
CE Quality Assurance Board
Bradford N. Edgren, DDS, MS, FACD
Fred Stewart Feld, DMD
Gregori M. Kurtzman, DDS, MAGD, FPFA, FACD, FADI, DICOI, DADIA
Justin D. Moody, DDS, DABOI, DICOI
Lisa Moler (Publisher)
Mali Schantz-Feld, MA, CDE (Managing Editor)
Lou Shuman, DMD, CAGS
The war on edentulism
From the earliest years of my career, I have been committed to combating edentulism. During my dental school years, my focus shifted towards prosthetics and surgery. At The Ohio State University College of Dentistry (2009-2013), implantology discussions were superficial, lacking extensive training in surgical or prosthetic components. Implants seemed reserved for specialists, while general dentists were advised to stick to tasks like fillings. As an implantology educator, I consistently advise my mentees that implants are the backbone of the war on edentulism. I have realized that, almost always, an implant is the optimal solution for replacing a missing tooth. Learning how to replace missing teeth became crucial for enabling people to chew better, promoting healthier and happier lives. Without implants, our only fixed solution for missing teeth is a tooth-borne bridge. The absence of a terminal tooth raises the question — is suggesting a distal extension removable prosthesis the only viable option for a general dentist? We need to do better and provide fixed solutions for the edentulous or partially edentulous patient. Early in my practice, I embraced dental technology, a powerful yet often underutilized tool due to reservations about educational and financial investments. Postgraduate courses, fellowships, mentors, and the use of intraoral cameras, digital impressions, and CBCT made me comfortable enough to safely start placing routine dental implants. My journey began with fully surgically guided implant placements, impressing me with the accuracy and ease of the workflow, particularly in suitable cases (good bone, thick soft tissue, healthy patients, etc.). Providing the best option for restoring the partially edentulous patient was immensely gratifying. Subsequently, my journey delved into more complicated cases, aiming to offer more for my patients.
Recognizing the necessity to master various elements of surgery, periodontics, and prosthodontics, I explored socket preservation, guided bone/tissue regeneration, sinus augmentation, soft tissue grafting, and full-arch fixed solutions in traditional dental alveolar bone and remote anchorage.
The journey progressed from an analog workflow to a digital one. Our practice is now 99% digital with a fully functional in-house dental lab. We implement technology through 3D printing, milling (Zirconia, PMMA, titanium), custom abutments/implant restorations, removable dentures, implant-retained dentures, and implant-supported prosthetics such as full-arch fixed solutions.
Our practice targets individuals in need of full mouth rehabilitation with realistic expectations and psychological stability. Changing people’s lives is a source of great satisfaction, and they appreciate our work. While our primary goal is to save teeth whenever possible, it is crucial that if we have a patient in terminal dentition, fully or partially edentulous, we possess the training, education, and technology to provide a pathway back to optimal oral health with fixed implant solutions. I urge my colleagues to join the war on edentulism by leveraging the best surgical and prosthetic modalities available — implant-supported prosthetics.


Alex Smith, DDS, was raised in Bend, Oregon and pursued a degree in Human Physiology at the University of Oregon before earning his dental degree from The Ohio State University College of Dentistry. Following his academic journey, Dr. Smith dedicated 4 years to the U.S. Army Dental Corps, serving in Korea and at Ft. Bragg. A Dental XP Fellow and a member of both AAID and ABOI, Dr. Smith is committed to continuous learning and professional development. He also serves as a mentor at Implant Pathway, demonstrating his dedication to sharing knowledge and expertise within the dental community. Currently, as the owner of Dental Artistry Implants-Crowns-Veneers, Dr. Smith operates a DPO and actively seeks like-minded partner doctors to collaborate in the collective effort against edentulism. With aspirations to become a Diplomate at the ABOI, Dr. Smith remains passionate about advancing dental care and making a positive impact on patients’ oral health.
ISSN number 2372-6245
1 implantpracticeus.com Volume 17 Number 1 INTRODUCTION
© MedMark, LLC 2024. All rights reserved. The publisher’s written consent must be obtained before any part of this publication may be reproduced in any form whatsoever, including photocopies and information retrieval systems. While every care has been taken in the preparation of this magazine, the publisher cannot be held responsible for the accuracy of the information printed herein, or in any consequence arising from it. The views expressed herein are those of the author(s) and not necessarily the opinion of either Endodontic Practice US or the publisher.

COVER STORY
The Preat workflow advantage
Solving the complexities of restoring multiple implant interfaces while maintaining restorative consistency
Cover image of Dr. Carl J. Drago courtesy of Preat.
CASE STUDY

PUBLISHER’S PERSPECTIVE 2024 — appreci-8 your potential
Lisa Moler, Founder/CEO, MedMark Media............................... 5

EDUCATION SPOTLIGHT
The Pathway, supported by Affordable Care
Fostering a culture of clinical advancement .............................. 18 6
Treating posterior mandibular atrophy using CAD/CAM subperiosteal implants: clinical case and literature review
Drs. Mathieu Goudal and Cécile Bailly discuss a solution for managing atrophic posterior mandibular regions
2 Implant Practice US Volume 17 Number 1 TABLE OF CONTENTS
10



The Preat workflow advantage Dr.CarlJ.Drago AIinimplantdentistry Drs.AaronGlick,NicholasTipton, NishaManila,andJenniferChang Ailingandfailing All-On-X cases and how to treat them Dr.DanHoltzclaw Treatingposterior mandibularatrophy usingCAD/CAM DigitalWorkflow/GuidedSurgery n 4 CE CreditsAvailable inThis Issue* Spring2024 Vol17 No1 implantpracticeus.com PAGE 8 A30-year perspective on implant dentistry A conversation with Dr. David DiGiallorenzo IMPLANTOLOGY The use of photogrammetryforthe fabrication of full-arch immediateprostheses Dr.ChristopherR.Resnik Dental sedation: an overview Dr.BrianMcGue Treatmentofapatientwith trans-canineplacement ofadentalimplant Drs.DouglasD.Wrightand WilliamT.GoodwinII TradeshowSpecialSection n 4 CE CreditsAvailable inThis Issue* Fall2023 Vol16 No3 implantpracticeus.com 1 year print $149 1 year digital only $79 Connect. Be Seen. Grow. Succeed. | www.medmarkmedia.com Address the Implant Complexities You Face Everyday with... 3 EASY WAYS TO SUBSCRIBE VISIT www.implantpracticeus.com EMAIL subscriptions@medmarkmedia.com CALL 1.866.579.9496 SUBSCRIBERS BENEFIT FROM: 16 continuing education credits per year Clinical articles enhanced by high-quality photography Analysis of the latest groundbreaking developments in dentistry Real-life profiles of successful implant practices Technology reviews of the latest products Practice management advice on how to make implants more profitable Implant Practice US 4 Issues • • • • • • • • • • • • 16 CEUs







4 Implant Practice US Volume 17 Number 1 TABLE OF CONTENTS CONTINUING EDUCATION AI in implant dentistry: clinical implementation and considerations for use
Chang discuss the pros and cons of AI in the dental practice 20 INDUSTRY NEWS ...............................................................32 Connect. Be Seen. Grow. Succeed. | www.medmarkmedia.com READ the latest industry news and business WATCH DocTalk Dental video interviews with KOLs
through live and archived webinars
news and event updates in your inbox by registering for our eNewsletter CONNECT with us on social media www.implantpracticeus.com 26 CONTINUING EDUCATION Ailing and failing All-On-X cases and how to treat them Dr.
discusses some reasons for implant failure and a possible solution for certain types
subscribers can earn 4 continuing education credits per issue by passing the 2 CE article quizzes online at https://implantpracticeus.com/category/continuing-education/
Drs. Aaron Glick, Nicholas Tipton, Nisha Manila, and Jennifer
LEARN
RECEIVE
Dan Holtzclaw
*Paid
Published by

Publisher
Lisa Moler lmoler@medmarkmedia.com
Managing Editor
Mali Schantz-Feld, MA, CDE mali@medmarkmedia.com
Tel: (727) 515-5118
National Account Manager Adrienne Good agood@medmarkmedia.com
Tel: (623) 340-4373
Sales Assistant & Client Services
Melissa Minnick melissa@medmarkmedia.com
Creative Director/Production Manager
Amanda Culver amanda@medmarkmedia.com
Marketing & Digital Strategy Amzi Koury amzi@medmarkmedia.com
eMedia Coordinator
Michelle Britzius emedia@medmarkmedia.com
Social Media Manager
Felicia Vaughn felicia@medmarkmedia.com
Digital Marketing Assistant
Hana Kahn support@medmarkmedia.com
Website Support
Eileen Kane webmaster@medmarkmedia.com
MedMark, LLC
15720 N. Greenway-Hayden Loop #9 Scottsdale, AZ 85260
Tel: (480) 621-8955
Toll-free: (866) 579-9496 www.medmarkmedia.com
www.implantpracticeus.com
Subscription Rate
1 year (4 issues) $149
https://implantpracticeus.com/subscribe/
2024 — appreci-8 your potential
Numerology is the study of numbers that deal with their mystical meaning and effect on our lives. When you think of all of the numbers that surround us every day — our dates of birth, other special dates, births, anniversaries, and deaths of those near and dear to us, even your home address can have a deeper meaning. No better time to think about the power of numbers than this year. Add up the numbers in our new year, 2024, and the result is the number 8. Turn the number 8 on its side, and you get the infinity symbol — this year, you can harness the power of 8 — when opportunities to reach goals in our personal and private lives can be limitless.

A little numerology research on the number 8 shows that it represents the achiever and goal-reacher. The number symbolizes good sense, a powerful presence, and strong success drive. Balance is also a hallmark of the number 8, as reflected in its symmetrical shape that promotes stability, potential, and productivity. The number 8 is ruled by the planet Saturn (as is the zodiac sign, Capricorn). Traits of this planet are perseverance and ambition, so during 2024, our “8” year, we should strive to find our places as strong leaders ready to transform our plans and words into actions.
For this Spring 2024 issue, we want to help turn your plans into prosperity with our clinical articles and marketing expertise. With the growing implant market, clinicians need to be ready to treat patients who have a variety of implant platforms. Our cover story shows how Preat helps solve restorative implant mysteries to treat the expanding population of patients who need continued care. Our CE on AI in dentistry by Dr. Aaron Glick and colleagues, points out the pros and cons of having AI-based systems in the implant practice. In his CE, Dr. Dan Holtzclaw explores some reasons for implant failure in All-on-X cases and possible solutions.
What can you do to make the most of your “8” year? Keep achieving, be strategic, and fiercely tenacious. Be a leader, but listen to your team, and let them know that the most fulfilling achievements are the ones that you reach together. Give back when you can because the karma of the number 8 is connected to the infinite balance between success and gratitude. And remember like the balanced number 8, to make time for personal life, even while you pursue professional success. 2024 is the year to turn your potential into prosperity.
With appreci-8-tion for success in 2024,
Lisa Moler Founder/Publisher MedMark Media
5 implantpracticeus.com Volume 17 Number 1 PUBLISHER’S PERSPECTIVE
Lisa Moler Founder/Publisher, MedMark Media
The Preat workflow advantage
Solving the complexities of restoring multiple implant interfaces while maintaining restorative consistency
Introduction
The United States dental implant market size was worth $1.37 billion in 2022 and is projected to grow at a compound annual growth rate (CAGR) of 6.9% during the forecast period. The U.S. has had an increased need for dental restorations that replace missing teeth. Approximately ½ of the adults in the U.S. suffer from periodontal disease. Furthermore, the need for esthetic restoration of individual dental implants and increasing amounts of disposable income for adults over 50 years of age are indicators of an ever-increasing need for dental implants and restorations.
According to Elani, et al., there has been a large increase in the prevalence of dental implants, from 0.7% in 1999 to 2000 to 5.7% in 2015 to 2016.1 The largest absolute increase in prevalence (12.9%) was among individuals 65 to 74 years old, whereas the largest relative increase was ~1,000% among those 55 to 64 years old. There was an average covariate-adjusted increase in dental implant prevalence of 14% per year (95% CI, 11% to 18%). This study demonstrated that dental implant prevalence among U.S. adults with missing teeth substantially increased since 1999. Yet access to care overall is still low. Prevalence was consistently higher among more advantaged groups.
Over the last decade, technological advancements have played a considerable part in development of multiple industries. Dentistry is no different. From electronic recordkeeping and impressions or scans to treatment planning and producing restorations in-house, digital technology is having a significant impact on the industry.
Technological innovations have allowed dental practices improved access to new technologies that were previously too expensive. Developments in technology are helping to change dentistry by providing more efficient workflows, better treatment outcomes, and increased patient comfort.

Dr. Drago is an adjunct associate professor at Marquette University School of Dentistry where he teaches in the graduate prosthodontic program; he also lectures nationally and internationally and has published approximately 97 papers on various subjects in conventional and implant prosthodontics. He also has written five textbooks on dental implants and currently serves as the Clinical Science section editor for the Journal of Prosthodontics.

The changing implant environment
The realities of practicing implant dentistry today have vastly changed over the decades. In the 1980s, implant treatment was geared towards fully edentulous patients, and implant placement was primarily performed by oral and maxillofacial surgeons, while implant restorations were fabricated under the direction of prosthodontists. This was per the original Brånemark protocol.2
Times have changed:
1. Implants now are placed by restorative dentists, periodontists, and implantologists. Market research estimates that 31% of general practitioners in the U.S. placed implants in 2023. While the number of general practitioners placing implants is not projected to grow much over the next few years, those general dentists are expected to place more implants each.
2. Even with the advancement of implant-placing general dentists, specialists are still projected to place the majority of implants. Complex cases will still require an interdisciplinary team approach to ensure an optimal
6 Implant Practice US Volume 17 Number 1 COVER STORY
Carl J. Drago, DDS, MS, received his dental degree from The Ohio State University College of Dentistry and a Master’s Degree from the University of Texas Graduate School of Biomedical Sciences at San Antonio, Texas. Dr. Drago is also a Diplomate of the American Board of Prosthodontics, a Fellow in the American College of Prosthodontists and the American College of Dentists.
Carl J. Drago, DDS, MS
outcome. Communication will continue to be essential in the team approach.
3. As the dental implant landscape has matured over the decades, there is a growing population of patients with implants placed years ago that were never restored. This may be a dilemma as some implants have become obsolete, and restorative components are no longer available. Dentists may have trouble identifying a specific implant. There are several websites, including https://www.preat.com/ implant-identification, that will assist dentists in determining specific implants. Preat receives between 40 to 50 implant ID requests per day. The technicians can determine the specific implant and implant/abutment connection for dentists who submit a form on the website with the requisite information and will generally respond within 24 hours (or within 60 minutes for expedited requests). Preat will identify the implant as well as suggest instruments and products to assist with the treatment plan. Preat offers a convenient tool caddy called the Implant Buddy which includes prosthetic drivers for six common screw connections and reduces the complexity of restoring multiple implant systems.



4. In addition, there is a growing population of patients with existing restorations who need continued care. Aside from general hygiene and maintenance, these patients may need new restorations or may have lost additional teeth and need additional implants. Dentists should make an attempt to use the same or similar implant and implant/abutment connections to facilitate treatment. Attempts should be made to minimize implant component types (internal, conical, external hex, etc. connections) to decrease the potential for confusion and errors in selecting components.
5. Further complicating implant restoration is the continuous growth of dental implant systems available in the U.S. While market leaders introduce new designs, new companies are also entering the U.S. with their implant systems. According to the FDA 510(k) database, approximately 130 dental implant systems (from over 90 different companies) have been cleared by the FDA since 2019. This challenging environment makes finding ways to simplify the restoration of multiple implant systems more critical than ever. Open platform digital systems that allow the practice to standardize a process, instrumentation with common connections, and technical resources that possess holistic, rather than proprietary, knowledge of the implant landscape are all prime examples.
Digital dentistry
Digital dentistry means the use of digital instrumentation and processes for diagnostic and treatment processes. Digital formats


are used across all areas of practice, from equipment and scheduling to patient treatment and lab collaboration. Switching from analog to digital dentistry makes dental procedures more efficient and can improve treatment outcomes. Many dentists still use traditional processes such as conventional impressions and dental stone casts. Digital dentistry is quickly expanding as more digital tools become available, and dental practices look to meet changing patient demands.
7 implantpracticeus.com Volume 17 Number 1 COVER STORY
Astra TX Astra Tech EV BioHorizons® Internal 3i Certain® Dentsply Ankylos® Hiossen® ETIII Neoss® Neodent® Helix GM® Multi Unit MegaGen AnyRidge® Keystone TiLobe® Implant Direct Legacy™ NobelActive™ ConicalNobelBiocare™ Tri-LobeStraumann® BLXStraumann® Bone LevelStraumann® Tissue Leve Zimmer Screw-Vent®
Figure 1: This patient presented to the author with no other information. Using Preat’s implant identification service, the specific implant was identified and restored
Figure 2: Diagram of different implant/abutment connections. All require different restorative components
Figure 3: Screen shot of intraoral scan with scan bodies in place
Scan bodies are essential for the digital process. Scan bodies are recognized by intraoral scanners and provide the dental designer/laboratory technicians the exact location of the implant in CAD software used in designing a particular restoration. This includes the implant connection type, implant diameter, location of peri-implant soft tissues and adjacent teeth — information that was once mailed to the laboratory via an impression and written form — now sent electronically in seconds. Once received, the designer then has the ability to select the appropriate abutment in the CAD software.
Key considerations when choosing scan bodies include: material/surface, marking, and restorative flexibility. A titanium scan body with matte finish is ideal to allow seating verification by X-ray without reflection that will interfere with the intraoral scan. Clear marking on the scan body itself is helpful especially when working with multi-unit cases. Restorative flexibility will maximize efficiency both in the office and in the lab by allowing a single scan body design to be used for a full selection of restorative options — rather than requiring different scan bodies to be used and scanned for certain abutment options. The Preat titanium scan bodies, for instance, provide 18 implant-level abutment options per implant interface plus 9 different options for industry-standard multi-unit abutments.
The Preat workflow advantage
The Preat digital workflow was designed with simplicity and efficiency in mind for both the office and the lab. The features and restorative flexibility of the scan bodies make it easy to enter the workflow. In addition, Preat’s digital analogs and CAD library are designed to allow for easy digitization of traditional impressions.
The restorative flexibility combines a variety of abutment designs with compatibility for all major implant systems. This breadth is advantageous in managing the complexity of implant treatment over a patient’s lifetime.
Angulated screw channel
Preat ASC Titanium Bases utilize an angulated screw channel in certain restorative situations. This solution is beneficial in situations where a screw-retained restoration is desired, and implant placement and screw access channels compromise the ideal esthetic or functional outcomes. ASC Titanium Bases allow the screw channel to be angled up to 30° off-axis, thus directing the screw access hole to an optimal position. Available for both implant and multi-unit abutment level restorations, this improves esthetics for single crowns and helps simplify complex cases.
Abutment height versatility
Both the Verification Cylinders and the 9 mm tall ASC Titanium Bases can be reduced to 3 different heights, giving designers multiple restorative options while only needing to stock one component. The abutment is cut down to the correct height prior to luting the abutment to the milled or printed restoration. This is another example of the restorative flexibility that helps deliver the best restoration possible from a single scan body — not to mention an inventory advantage for those with an in-office lab.
Developments in technology are helping to change dentistry by providing more efficient workflows, better treatment outcomes, and increased patient comfort.


Best prosthetic solutions for patients
While every patient is different, patient expectations are to receive esthetic, functional restorations. The Preat workflow is about providing technicians and clinicians with the option to choose restorative components best suited for successful restorations. With the ever-evolving implant practice, the ability to treat patients with various implant types is now the expectation. Having a trusted multi-platform prosthetic partner is important in maintaining consistency and efficiency in today’s practice.
REFERENCES
1. Elani HW, Starr JR, Da Silva JD, Gallucci GO. Trends in Dental Implant Use in the U.S., 1999-2016, and Projections to 2026. J Dent Res. 2018 Dec;97(13):1424-1430.
2. Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981 Dec;10(6):387-416.
3. iData Research. U.S. Market Report Suite for Dental Implants and Final Abutments. https://idataresearch.com/?s=U.S.+Market+Report+Suite+for+Dental+Implants+and+Final+Abutments (Published March 2023).
8 Implant Practice US Volume 17 Number 1 COVER STORY
IP
Figure 4: Verification Cylinders and ASC Ti Bases height options available in CAD software
Figure 5: Preat patient-specific abutments
UNLOCK RESTORATIVE EFFICIENCY
Access a world of restorative possibilities with our smart workflow and open platform for all major implant systems.
A single intraoral scan gives the restorative team freedom to choose the best abutment for the case. Combined with broad implant compatibility, that means restoring implants with consistency, accuracy and efficiency.








 Single-Tooth Crown
Fixed Full Arch
Patient-Specific Solutions
Single-Tooth Crown
Fixed Full Arch
Patient-Specific Solutions
Request Preat on your Rx! Get Started with a Scan Body Today PREAT.COM • 800.232.7732
Bridge
Treating posterior mandibular atrophy using CAD/CAM subperiosteal implants: clinical case and literature review
Drs. Mathieu Goudal and Cécile Bailly discuss a solution for managing atrophic posterior mandibular regions
To this day, the dental implant rehabilitation of atrophic mandibular lateral regions remains a biological, temporal, and financial challenge. Thanks to CAD/CAM, titanium subperiosteal implants have become a viable alternative to conventional axial implants and bone regeneration.
Summary
Subperiosteal implants have a bad reputation due to outdated practices. The main drawbacks — lack of adjustment and biocompatibility — were corrected using CAD/CAM and titanium. New products have entered the market over the past few years. The CAD/CAM SUB Implant™ by Panthera Dental, developed in collaboration with Dr. Yvan Poitras, offers a solution in managing atrophic posterior mandibular regions.
History
First described by Dr. Gustav Dahl in 1940, subperiosteal implants allowed for fixed denture rehabilitation for complete or posterior edentulism (Class I).1 These implants were custom-made cobalt-chrome subperiosteal frames with transmucosal abutments to anchor implant-supported dentures. Made-to-measure implants were created using a direct bone impression after elevating large, full-thickness flaps. The frame was placed on the residual bone and stabilized using retaining screws, while possible adjustment defects were corrected through drilling or filling the space with bone substitute.2

Dr. Mathieu Goudal is a Doctor of Dental Surgery from the Faculty of Reims, France. He has an exclusive practice in Implantology, Surgery, and Periodontology AUI - Paris VII. Dr. Goudal has a University Diploma in Calcified Tissues, Biomaterials, and Implantology (INSERM) from the Faculty of Medicine of Angers (France), and a University Diploma in Surgery and Implant Prosthesis — Faculty of Odontology of Lyon (France). Dr. Goudal is also an International Team for Implantology (ITI) fellow, lead team member and study club director.

Dr. Cécile Bailly received her Doctor of Dental Surgery from Faculty of Odontology of Bordeaux (France).
Subperiosteal implants had a survival rate of 50% to 60% after 15 years with significant complication risks.3 The lack of osseointegration and the poor precision of the impression caused a lack of stability and adaptation of the metal frame and led to infection, inflammation, and bone resorption.4,5 These implants gradually became less popular and were replaced by endosseous implants, which were more reliable in the short and long term.6
Physiopathology of the mandible
However, in severe cases of atrophy, denture rehabilitation using axial implants can be very complex due to the loss of the alveolar bone. The alveolar bone exists solely for the dental organ, which is where this bone develops and grows. Teeth, the periodontal ligament, and the alveolar bone are therefore interdependent.
After edentulism, the labial alveolar bone will gradually decrease in height, density, and thickness. The loss of function of the alveolar bone and the stress it undergoes will cause resorption that begins in the periosteum, and bone apposition may decrease or even cease.7,8 If edentulism is not compensated, the alveolar bone will continue to undergo resorption and may even be lost completely. In the most serious cases of mandibular atrophy, basal bone loss can occur.
Conversely, an alveolar osteolysis caused by periodontitis leads to dental organ loss. Some bacteria involved in periodontal disease associated with unfavorable local and immune factors cause alveolar bone loss that leads to edentulism.9 In advanced stages, periodontitis can cause complete alveolar bone loss, even after edentulism.
This bone loss intensifies with age. The expression of homeogenes and hormones responsible for alveolar bone maintenance decreases with age, causing decalcification and bone destruction. Denture rehabilitation may be iatrogenic for the remaining bone, and wearing unstable and poorly adapted removable dentures may overload the alveolar bone, causing resorption as a defense mechanism. A failed implant rehabilitation may also increase the loss of residual bone volume.
Alveolar bone loss follows a predictable pattern represented by the Cawood physiopathological classification. This classification allows clinicians to choose the denture rehabilitation approach best suited to each situation.10 The edentulous mandible undergoes significant resorption and loses 40% to 60% of its height on average. At atrophic stages, the mandibular canal may be level with the alveolar ridge, compromising denture rehabilitation.11
10 Implant Practice US Volume 17 Number 1 CASE STUDY
Disclosure: Drs. Mathieu Goudal and Cécile Bailly are not compensated in any way by Panthera Dental.
Placing axial implants in severe cases of atrophy may require rearranging bone mass through guided bone regeneration, distraction osteogenesis, or crestal reconstruction through bone grafting.12-14 With these implant surgeries in atrophic areas, there are risks of hemorrhage and lesions to neighboring anatomical and nervous structures.
The results of mandibular bone volume reconstruction are fairly unpredictable, as the spongy bone is dense and the cortical bone is thick, thereby reducing blood flow and regenerative potential. It is a long, expensive technique that requires two surgeries with significant healing periods: one for crestal reconstruction and another for implant placement. Success depends heavily on the surgeon’s experience with the procedure.
For the rehabilitation of atrophic posterior mandibular regions, subperiosteal implants are an alternative worth exploring. Placing this implant is technically simpler for the surgeon and can be done in a single procedure with a shorter healing period.
Anatomy review and surgical approach
The mandible is characterized by the presence of the mandibular canal containing the inferior alveolar nerve, along with venous, arteries, and lymphatic vessels. This canal enters the mandible at its ramus through the mandibular foramen, runs through the body of the mandible, and exits through the mental foramen. The inferior alveolar nerve is the motor for the anterior belly of the digastric and the mylohyoid muscles. It also supplies sensation for mandibular teeth, the lower lip, and the chin. The pathway of the mandibular canal is variable and must undergo preoperative examination by analyzing a CBCT.
The lateral aspect of the posterior region of the mandible presents the external oblique ridge and is the insertion for the cutaneous muscles of the cheek. Its medial aspect is connected to the floor of the mouth formed by the mylohyoid and geniohyoid muscles, as well as the tongue. It presents the internal oblique ridge, the insertion point for the superior pharyngeal constrictor, the pterygomandibular ligament, and the mylohyoid muscle in continuity with the periosteum.
This area is adjacent to the submandibular and sublingual spaces, which are rich in neurovascular structures.
The submandibular space is characterized by the presence of the submandibular salivary gland, the hypoglossal nerve (XII, motor nerve of the tongue), the lingual nerve, the facial and lingual artery, and the facial and superior thyroid veins. The sublingual space, located between the floor of the mouth and the mylohyoid muscle, contains the sublingual salivary gland, the deep-lingual vein, the hypoglossal nerve (taste and tongue sensation, visceral motor of the salivary glands), and the submandibular duct15 (Figure 1).
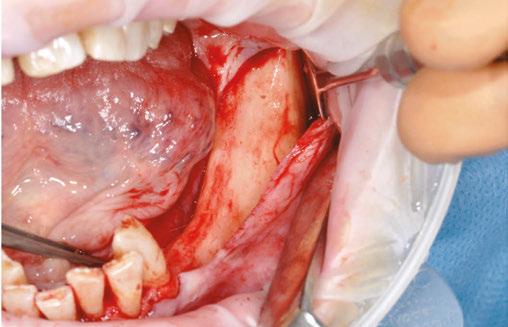
Surgery in the posterior region of the mandible is delicate due to the proximity of the sublingual and submandibular spaces and the presence of the inferior alveolar nerve. Two full-thickness flaps are reflected to access the underlying bone. The crestal incision needs to separate the residual keratinized gingiva in two equal vestibular and lingual portions. Posteriorly, the releasing incision must be made toward the anterior border of the mandibular ramus to avoid cutting the lingual nerve. Anteriorly, the vestibular incision must go around the mental foramen to preserve

the inferior alveolar nerve and extend toward the symphysis for laxity without a releasing incision.
During implant surgery on the posterior region of the mandible, two main priorities must be taken into account when elevating flaps: pushing back the sublingual space rich in neurovascular structures and avoiding damage to the mylohyoid muscle, which would lead to communication between the oral cavity and the submandibular space. This could lead to a hemorrhage obstructing the upper aerodigestive tract.16 Placing axial implants is limited in the atrophic posterior mandibular region due to the proximity of the inferior alveolar nerve in the body of the mandible and the risk of nerve injury it could cause.
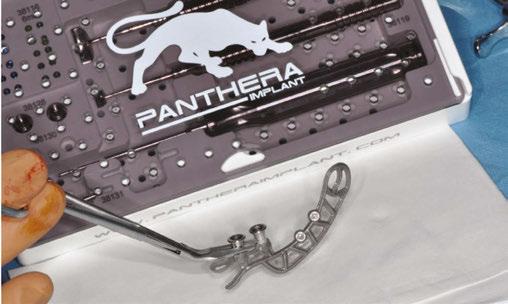
The Panthera SUB subperiosteal implant, shown below, is a viable treatment option in this situation. It is done in a single surgery: the proximity of the inferior alveolar nerve to the alveolar crest and the low bone volume available are not a contraindication.
Characteristics and design of the SUB implant
The Panthera SUB implant is produced by Panthera Dental (Québec) and was developed by Dr. Yvan Poitras (Québec).
Data collection is similar to that performed when planning axial implants:
• a CBCT
• a recording of the dental and mucosal surfaces
• a mock-up
The quality and precision of the CBCT are critical and the main factors determining how accurately the subperiosteal implant adapts to the bone surface. It is therefore necessary to optimize the dental X-ray equipment settings to obtain high-resolution images with enough contrast to visualize the bones in other structures. Moreover, a wide field allowing for a single pass of the molar zone to be implanted, the ipsilateral ramus posteriorly, and the symphyseal region up to the contralateral canine is a minimum requirement. Stitching (overlapping several “narrow-field” images) is strongly discouraged, given the risks of distortion. Finally, the data must be exported to the universal DICOM format.
A conventional physical impression that is later scanned by a laboratory scanner or a native digital image using an intraoral
11 implantpracticeus.com Volume 17 Number 1
CASE STUDY
Figure 1: Transverse section diagram passing through the submandibular space
camera allows for initial dental and mucosal surfaces to be recorded. The file must be exported to STL or PLY format.
A physical or digital mock-up must match up with the dental and mucosal surfaces. The surgeon and technician use the protocol with which they are most familiar (fully digital workflow, dual scan with radiopaque markers, etc.).
This data is recorded on the Panthera order platform. Using a simple step-bystep process, the clinician can indicate the number of teeth to be replaced, the desired position of the prosthetic platforms, etc. Once the order has been placed and the data sent, the dashboard can be used to track the progress of the work:
• confirmation of data receipt
• confirmation of data quality
• fusion of three-data layers
• implant design proposal
• validation by the surgeon
• implant production
• implant shipping

The combination of the following three characteristics achieve greater results for subperiosteal implants compared to traditional techniques:
• biocompatible material
• precise adjustment (CT scan, CAD/CAM, machining)
• rough surface
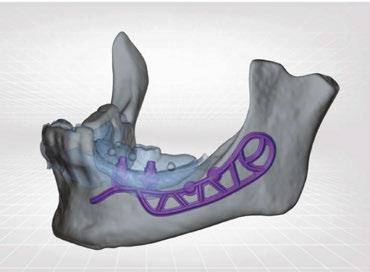
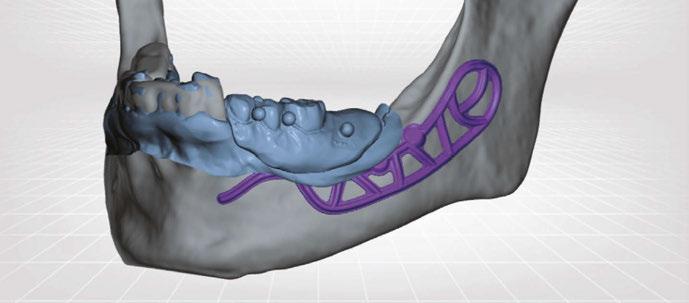
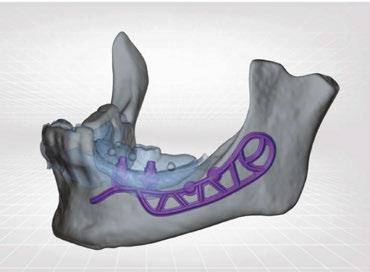
Panthera designers use proprietary software to perform a precise fusion of the three data types. The design is produced in-house according to the surgeon’s order and in accordance with the mock-up, all while following the same blueprint: In the vestibular region, the skeleton extends anteriorly by an arm going around the emergence of the inferior alveolar nerve, posteriorly by a loop up to the outer surface of the mandibular ramus. In the lingual region, the frame stops distally in vertical alignment with the most distal prosthetic platform and apically over the mylohyoid ridge. However, a loop extends the implant to the symphyseal region of the mandibular. Finally, the external oblique ridge, which is highly corticalized, is the anchoring location for osteosynthesis screws (Figures 2A and 2B).
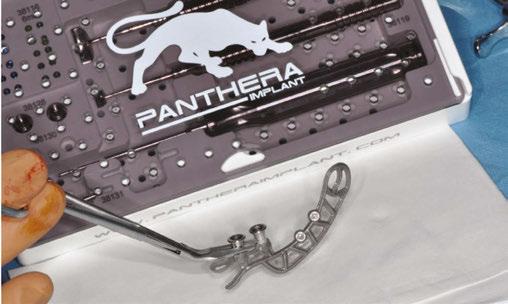
After validation by the surgeon, five-axis CNC milling machines with a precision of 5 μm (far superior to the acquisition of the CT scan) produce subperiosteal implants in disks made of Ti6Al4V ELI (Grade 23), a titanium-aluminum-vanadium alloy that is purer than the standard Ti6Al4V alloy. After machining, the surface in contact with the bone and the periosteum is sanded.

Clinical case and planning
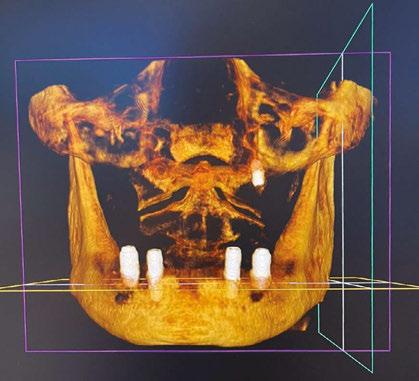
Our patient is consulting for pain in the right mandibular molar region and difficulty chewing (Figure 3).
Her history is quite common: discomfort, followed by a failure to wear the removable denture with a metal framework, and finally neglecting care for family reasons. At age 77, she is perfectly healthy enough for oral surgery. However, she would prefer


12 Implant Practice US Volume 17 Number 1
CASE STUDY
Figures 2A and 2B: Panthera Dental platform interface; vestibular (2A) and lingual (2B) views of the subperiosteal implant
Figure 3: Initial panoramic image
Figures 4A-4C: Visualization of the subperiosteal implant in relation to the mock-up




not to undergo long and complex implant treatment. Her request is first and foremost functional. Esthetics and price are secondary concerns. We therefore offer the following treatment plan: keep the malpositioned anterior mandibular teeth with only mild gingivitis, rehabilitate the left posterior mandibular region with a subperiosteal implant, extract molars 47 and 48, and reassess the best implant solution for this region after healing.
Given the initial anatomical situation (strong resorption, significant mobile soft tissue, blockage by the tongue, V-shaped mandible), a conventional impression with a CIT and a physical mock-up with radiopaque markers are preferred.
Data is exported to the Panthera platform, and we receive a design proposal within a few days. The visualization tools allow us to scroll freely in the three-dimensional reconstruction area. Each element (implant, mock-up, bone) can be viewed separately, hidden, made opaque or clear (Figures 2A, 2B, 4A, 4B, and 4C). The proposal is validated by the surgeon for the implant to be produced and shipped.
Once it is received, the implant is cleaned, decontaminated, and sterilized at the dental office.
Surgical procedure
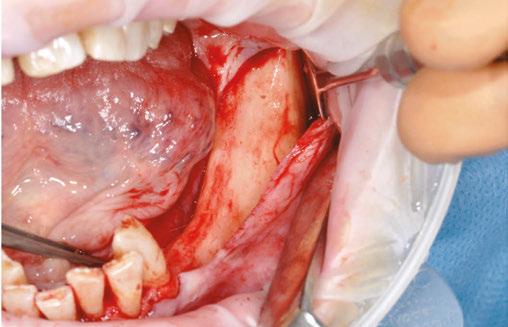
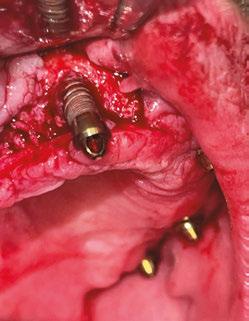
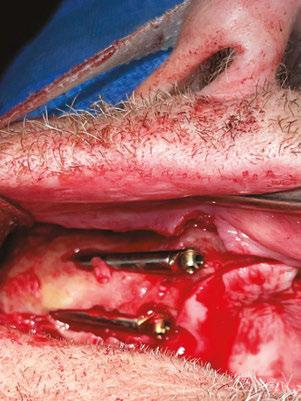
The procedure begins with local anesthesia at multiple points, vestibular and lingual, from the symphyseal region to the ascending ramus. However, an infiltration in the lingula of the mandible is not necessary. The incision is performed using the technique described above (Figures 5A and 5B).
It is imperative to carefully reflect a full-thickness flap following the periosteum. After reflection, an atraumatic periosteal expansion using a soft brush (Figure 6) will allow for the flaps to be repositioned without tension over the implant and bony surfaces at the end of the procedure.


13 implantpracticeus.com Volume 17 Number 1
CASE STUDY
Figures 8A-8D: Placing the subperiosteal implant and monitoring its adaptation
Figures 5A and 5B: 5A. Initial clinical view. 5B. Access flap
Figure 6: Periosteal expansion using a soft brush
Figure 7: Prehension of the subperiosteal implant
After the soft tissue is prepared, the bony surface is carefully cleaned. For easy insertion, the healing abutments are left in place, and the implant is held firmly with hemostatic forceps (Figure 7). The implant is inserted via distal translation in the direction of the angle of the mandible, then a mesio-anterior rotation. The surgeon must control the lack of mobility and the adaptation of the implant to the bony surface at all points (Figures 8A, 8B, 8C, and 8D).
To ensure the implant is stable during the osseointegration period, an osteosynthesis screw is placed in the prepared space (Figures 9A, 9B, 9C, and 9D).
The flaps are carefully repositioned and sutured without tension with Halsted and over-and-over sutures (Figures 10A and 10B).
Healing and osseointegration
Osseointegration takes 4 months to complete and occurs through two mechanisms:
1. First through direct contact of the bone with the rough titanium finish of the inner surface of the implant
2. Next through progressive bone apposition on the equally rough outer surface. In fact, the passive repositioning of the flap at the end of the procedure creates a space


between the periosteum (inner surface of the flap) and the implant placed over the bone where the blood clot will be trapped (Figure 11).17-19
The patient returns four months later for a clinical follow-up (Figures 12A and 12B) and X-rays (Figure 13).
The permanent dentures are then placed over a titanium frame processed by Panthera Dental and stratified in composite at the denture laboratory (Figures 14A-14C).
Literature review and success rate
We are at the stage where we can see if the survival rates of subperiosteal implants have improved compared to more common techniques such as mandibular grafts for implant rehabilitation of atrophic posterior mandibular regions. The systematic literature review below compares the clinical results of these two techniques and justifies the use of CAD/CAM subperiosteal implants.
Materials and method
The literature review was performed using the PRISMA protocol criteria. Searches took place in March 2021 using the PubMed, DOSS, Embase, and Cochrane databases, and it was split into two parts:





14 Implant Practice US Volume 17 Number 1
CASE STUDY
Figures 9A-9D: Screwing the drilling ancillary instrument to the location of the osteosynthesis screw (9A), drilling (9B), manually placing the screw in the initial drilling (9C and 9D)
Figures 10A and 10B: Clinical (10A) and radiological (10B) postoperative situation
Figure 11: Integrated subperiosteal implant (courtesy of Dr. Yvan Poitras, Québec)
CASE STUDY
1. A search focused on mandibular subperiosteal implants using the following keywords: “subperiosteal implant” and (“CAD/CAM” or “3D printing” or “direct metallaser sintering” or “additive manufacture”) and “dental




implantation, subperiosteal” [MeSH Terms] and “computer-aided design” [MeSH Terms].
2. A search focused on inlay bone grafts using the following keywords: “mandible” and “vertical ridge augmentation” and “sandwich osteotomy” OR “inlay bone graft” or “interpositional bone graft” and “alveolar ridge augmentation” [MeSH Terms] AND “mandible” and “alveolar bone atrophy” [MeSH Terms] and “bone grafting” [MeSH Terms] OR “mandibular osteotomy” [MeSH Terms].
Results
These searches found 30 articles meeting the selection criteria for this literature review: five on subperiosteal implants20–24 and 25 on inlay grafts.25–49 By analyzing the results, we can measure the implant survival rate (number of patients who did not lose any implants/total number of patients). Among the 86 patients who participated in studies on subperiosteal implants, three lost an implant due to recurring infections. The implant survival rate between 8 months to 3 years is 96.5%. For inlay grafts, implant survival depends on the success of the graft. Among the 345 patients who participated in studies, 28 grafts failed, and therefore no implants could be placed. Two studies did not specify the number of patients, but rather the number of implants when calculating the survival rate. The number of patients therefore decreases from 345 to 250. Among these patients, 19 lost one or more implants, for an implant survival rate of 92.5% between 8 months and 5 years.
Discussion
Analyzing these articles shows promising survival rates for the rehabilitation of atrophic posterior mandibular regions using subperiosteal implants. These articles are few, and their level of evidence is low. Most are clinical case reports with few patients (less than 100) with short-term follow-ups. Long-term clinical studies with a high level of evidence are required to reaffirm the true success of subperiosteal implants in a clinical setting.
A number of elements were unable to be assessed in this review, including the implant success rate, which is a better predictor of the long-term efficiency of implant-supported rehabilitation. However, the few prosthetic and biologic complications reported in the study seem to indicate high success rates for subperiosteal implants. Compared to inlay graft techniques, these implants have the advantage of requiring a single surgery with a short healing period and few postoperative and prosthetic complications, making them a reliable and promising alternative.


15 implantpracticeus.com Volume 17 Number 1
Figures 12A and 12B: Clinical postoperative situation after 4 months
Figure 13: Postoperative X-ray follow-up after 4 months
Figures 14A-14C: Permanent denture (14A and 14B), intraoral view (14C)
Conclusion
Thanks to CAD/CAM, Panthera SUB subperiosteal implants solve most issues encountered (lack of adjustment, two procedures, etc.) with their traditional counterparts. Moreover, using biocompatible titanium instead of cobalt-chrome allows for a true osseointegration of the implant. Finally, the literature tends to show good results with this technique in treating posterior mandibular edentulation.
REFERENCES
1. Silvestri KD, Carlotti AE. Subperiosteal implant: serving the dental profession for over 50 years. R I Dent J. 1995 Spring;28(1):11-13, 23.
2. Sconzo J. The complete mandibular subperiosteal implant: an overview of its evolution. J Oral Implantol. 1998;24(1):14-15.
3. Schou S, Pallesen L, Hjørting-Hansen E, Pedersen CS, Fibaek B. A 41-year history of a mandibular subperiosteal implant. Clin Oral Implants Res. 2000 Apr;11(2):171-178.
4. Bodine RL, Yanase RT, Bodine A. Forty years of experience with subperiosteal implant dentures in 41 edentulous patients. J Prosthet Dent. 1996 Jan;75(1):33-44.
5. Nguyen TM, Caruhel JB, Khonsari RH. A subperiosteal maxillary implant causing severe osteolysis. J Stomatol Oral Maxillofac Surg. 2018 Dec;119(6):523-525.
6. van Steenberghe D, Brånemark PI, Quirynen M, De Mars G, Naert I. The rehabilitation of oral defects by osseointegrated implants. J Clin Periodontol. 1991 Jul;18(6):488-493.
7. Nefussi JR. Le volume osseux résiduel après extraction dentaire est-il prédictible? (Is the residual bone volume after tooth extraction predictable?) In: Mise en place chirurgicale et gestion des tissus muqueux péri-implantaires. (In: Surgical implementation and management of peri-implant mucosal tissues) p. 102-21.
8. Nefussi JR. Biologie et physiologie du volume osseux implantable. (Biology and physiology of implant bone volume.) In: EMC. Elsevier Masson SAS. Paris; 2011. p. 1-12. Medecine buccale (Oral Medicine); vol. 28.
9. Hienz SA, Paliwal S, Ivanovski S. Mechanisms of Bone Resorption in Periodontitis. J Immunol Res. 2015;2015:615486.
10. Cawood JI, Howell RA. A classification of the edentulous jaws. Int J Oral Maxillofac Surg. 1988 Aug;17(4):232-236.
11. Pietrokovski J, Massler M. Alveolar ridge resorption following tooth extraction. J Prosthet Dent. 1967 Jan;17(1):21-27.
12. Urban IA, Nagursky H, Lozada JL. Horizontal ridge augmentation with a resorbable membrane and particulated autogenous bone with or without anorganic bovine bone-derived mineral: a prospective case series in 22 patients. Int J Oral Maxillofac Implants. 2011 Mar-Apr;26(2):404-414.
13. Guillaume B. Accroissement osseux préimplantaire par disjonction osseuse. (Pre-implantation bone growth by bone disjunction.) Inf Dent. 2004;86(1640).
14. Khoury F, Hanser T. Three-Dimensional Vertical Alveolar Ridge Augmentation in the Posterior Maxilla: A 10-year Clinical Study. Int J Oral Maxillofac Implants. 2019 Mar/Apr;34(2):471-480.
15. Laurentjoye M, Ella B, Caix P. La tête. (The Head) In: Anatomie tête et cou. (Head and Neck Anatomy) 2015e éd. Bordeaux: Bergeret; 2015. p. 3-101.
16. Coutant JC, Martin R, Huault L, Ella B. Chirurgie du lambeau lingual. (Lingual Flap Surgery.) Inf Dent. 24 avr 2019;(16/17):35-40.
17. Minichetti JC. Analysis of HA-coated subperiosteal implants. J Oral Implantol. 2003;29(3):111116; discussion 117-119.
18. Cohen DJ, Cheng A, Kahn A, Aviram M, Whitehead AJ, Hyzy SL, Clohessy RM, Boyan BD, Schwartz Z. Novel Osteogenic Ti-6Al-4V Device For Restoration Of Dental Function In Patients With Large Bone Deficiencies: Design, Development And Implementation. Sci Rep. 2016 Feb 8;6:20493.
19. Claffey N, Bashara H, O’Reilly P, Polyzois I. Evaluation of New Bone Formation and Osseointegration Around Subperiosteal Titanium Implants with Histometry and Nanoindentation. Int J Oral Maxillofac Implants. 2015 Sep-Oct;30(5):1004-10.
20. Cerea M, Dolcini GA. Custom-Made Direct Metal Laser Sintering Titanium Subperiosteal Implants: A Retrospective Clinical Study on 70 Patients. Biomed Res Int. 2018 May 28;2018:5420391.
21. Mangano C, Bianchi A, Mangano FG, Dana J, Colombo M, Solop I, Admakin O. Custom-made 3D printed subperiosteal titanium implants for the prosthetic restoration of the atrophic posterior mandible of elderly patients: a case series. 3D Print Med. 2020 Jan 8;6(1):1.
22. Cohen DJ, Cheng A, Kahn A, Aviram M, Whitehead AJ, Hyzy SL, Clohessy RM, Boyan BD, Schwartz Z. Novel Osteogenic Ti-6Al-4V Device For Restoration Of Dental Function In Patients With Large Bone Deficiencies: Design, Development And Implementation. Sci Rep. 2016 Feb 8;6:20493.
23. Oren D, Dror AA, Bramnik T, Sela E, Granot I, Srouji S. The power of three-dimensional printing technology in functional restoration of rare maxillomandibular deformity due to genetic disorder: a case report. J Med Case Reports. April 2021;15(1):197.
24. Gellrich NC, Zimmerer RM, Spalthoff S, Jehn P, Pott PC, Rana M, Rahlf B. A customised digitally engineered solution for fixed dental rehabilitation in severe bone deficiency: A new innovative line extension in implant dentistry. J Craniomaxillofac Surg. 2017 Oct;45(10):1632-1638.
25. Bolle C, Felice P, Barausse C, Pistilli V, Trullenque-Eriksson A, Esposito M. 4 mm long vs longer
implants in augmented bone in posterior atrophic jaws: 1-year post-loading results from a multicentre randomised controlled trial. Eur J Oral Implantol. 2018;11(1):31-47.
26. Esposito M, Cannizarro G, Soardi E, Pellegrino G, Pistilli R, Felice P. A 3-year post-loading report of a randomised controlled trial on the rehabilitation of posterior atrophic mandibles: short implants or longer implants in vertically augmented bone? Eur J Oral Implantol. 2011 Winter;4(4):301-311.
27. Felice P, Barausse C, Pistilli R, Ippolito DR, Esposito M. Five-year results from a randomised controlled trial comparing prostheses supported by 5-mm long implants or by longer implants in augmented bone in posterior atrophic edentulous jaws. Int J Oral Implant. 2019;12(1):25-37.
28. Felice P, Barausse C, Pistilli R, Ippolito DR, Esposito M. Five-year results from a randomised controlled trial comparing prostheses supported by 5-mm long implants or by longer implants in augmented bone in posterior atrophic edentulous jaws. Int J Oral Implantol (Berl). 2019;12(1):25-37.
29. Esposito M, Barausse C, Pistilli R, Piattelli M, Simone SD, Ippolito DR, Felice P. Posterior atrophic jaws rehabilitated with prostheses supported by 5 × 5 mm implants with a nanostructured calcium-incorporated titanium surface or by longer implants in augmented bone. Five-year results from a randomised controlled trial. Int J Oral Implantol Berl. 2019;12(1):39-54.
30. Esposito M, Pellegrino G, Pistilli R, Felice P. Rehabilitation of postrior atrophic edentulous jaws: prostheses supported by 5 mm short implants or by longer implants in augmented bone? One-year results from a pilot randomised clinical trial. Eur J Oral Implantol. 2011 Spring;4(1):21-30.
31. Felice P, Pellegrino G, Checchi L, Pistilli R, Esposito M. Vertical augmentation with interpositional blocks of anorganic bovine bone vs. 7-mm-long implants in posterior mandibles: 1-year results of a randomized clinical trial. Clin Oral Implants Res. 2010 Dec;21(12):1394-403.
32. Felice P, Marchetti C, Iezzi G, Piattelli A, Worthington H, Pellegrino G, Esposito M. Vertical ridge augmentation of the atrophic posterior mandible with interpositional bloc grafts: bone from the iliac crest vs. bovine anorganic bone. Clinical and histological results up to one year after loading from a randomized-controlled clinical trial. Clin Oral Implants Res. 2009 Dec;20(12):1386-1393.
33. Brandtner C, Borumandi F, Krenkel C, Gaggl A. A new technique for sandwich osteoplasty with interpositional bone grafts for fixation. Int J Oral Maxillofac Implants. 2014 Sep-Oct;29(5):1164-1169.
34. Geng YM, Zhou M, Parvini P, Scarlat S, Naujokat H, Abraha SM, Terheyden H. Sandwich osteotomy in atrophic mandibles: A retrospective study with a 2- to 144-month follow-up. Clin Oral Implants Res. 2019 Oct;30(10):1027-1037.
35. Marconcini S, Covani U, Giammarinaro E, Velasco-Ortega E, De Santis D, Alfonsi F, Barone A. Clinical Success of Dental Implants Placed in Posterior Mandible Augmented With Interpositional Block Graft: 3-Year Results From a Prospective Cohort Clinical Study. J Oral Maxillofac Surg. 2019 Feb;77(2):289-298.
36. Felice P, Pistilli R, Lizio G, Pellegrino G, Nisii A, Marchetti C. Inlay versus onlay iliac bone grafting in atrophic posterior mandible: a prospective controlled clinical trial for the comparison of two techniques. Clin Implant Dent Relat Res. 2009 Oct;11 Suppl 1:e69-82.
37. Laviv A, Jensen OT, Tarazi E, Casap N. Alveolar sandwich osteotomy in resorbed alveolar ridge for dental implants: a 4-year prospective study. J Oral Maxillofac Surg. 2014 Feb;72(2):292-303.
38. Bianchi A, Felice P, Lizio G, Marchetti C. Alveolar distraction osteogenesis versus inlay bone grafting in posterior mandibular atrophy: a prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008 Mar;105(3):282-292.
39. Esposito M, Grusovin MG, Felice P, Karatzopoulos G, Worthington HV, Coulthard P. Interventions for replacing missing teeth: horizontal and vertical bone augmentation techniques for dental implant treatment. Cochrane Database Syst Rev. 2009 Oct 7;2009(4):CD003607.
40. Starch-Jensen T, Nielsen HB. Sandwich osteotomy of the atrophic posterior mandible with interpositional autogenous bone block graft compared with bone substitute material: a systematic review and meta-analysis. Br J Oral Maxillofac Surg. 2020 Dec;58(10):e237-e247.
41. Esposito M, Grusovin MG, Felice P, Karatzopoulos G, Worthington HV, Coulthard P. The efficacy of horizontal and vertical bone augmentation procedures for dental implants - a Cochrane systematic review. Eur J Oral Implantol. 2009 Autumn;2(3):167-184.
42. Jensen OT. Alveolar segmental “sandwich” osteotomies for posterior edentulous mandibular sites for dental implants. J Oral Maxillofac Surg. 2006 Mar;64(3):471-475.
43. Pelo S, Boniello R, Moro A, Gasparini G, Amoroso PF. Augmentation of the atrophic edentulous mandible by a bilateral two-step osteotomy with autogenous bone graft to place osseointegrated dental implants. Int J Oral Maxillofac Surg. 2010 Mar;39(3):227-234.
44. Marchetti C, Trasarti S, Corinaldesi G, Felice P. Interpositional bone grafts in the posterior mandibular region: a report on six patients. Int J Periodontics Restorative Dent. 2007 Dec;27(6):547-55.
45. Sohn DS, Shin HI, Ahn MR, Lee JS. Piezoelectric vertical bone augmentation using the sandwich technique in an atrophic mandible and histomorphometric analysis of mineral allografts: a case report series. Int J Periodontics Restorative Dent. 2010 Aug;30(4):383-91.
46. Felice P, Iezzi G, Lizio G, Piattelli A, Marchetti C. Reconstruction of atrophied posterior mandible with inlay technique and mandibular ramus block graft for implant prosthetic rehabilitation. J Oral Maxillofac Surg. 2009 Feb;67(2):372-380.
47. Felice P, Piana L, Checchi L, Corvino V, Nannmark U, Piattelli M. Vertical ridge augmentation of an atrophic posterior mandible with an inlay technique and cancellous equine bone block: a case report. Int J Periodontics Restorative Dent. 2013 Mar-Apr;33(2):159-166.
48. Roccuzzo A, Marchese S, Worsaae N, Jensen SS. The sandwich osteotomy technique to treat vertical alveolar bone defects prior to implant placement: a systematic review. Clin Oral Investig. 2020 Mar;24(3):1073-1089.
49. Elnayef B, Monje A, Gargallo-Albiol J, Galindo-Moreno P, Wang HL, Hernández-Alfaro F. Vertical Ridge Augmentation in the Atrophic Mandible: A Systematic Review and Meta-Analysis. Int J Oral Maxillofac Implants. 2017 Mar/Apr;32(2):291-312.
16 Implant Practice US Volume 17 Number 1
CASE STUDY
IP

The Pathway, supported by Affordable Care
Fostering a culture of clinical advancement
Growing up on a ranch in western Nebraska, his family home for six generations, Dr. Justin Moody developed an appreciation for the work it takes to grow something from the ground up – literally. After dental school, he embarked on a successful career as an implantologist, growing multiple dental practices. He earned Fellow and Diplomate status in the International Congress of Oral Implantologists, Honored Fellow, Fellow and Associate Fellow status in the American Academy of Implant Dentistry, and was one of the youngest Diplomates in the American Board of Oral Implantology for which he is the President-Elect.
He also found his passion for continuing education. In 2016, Dr. Moody founded Implant Pathway, known today as The Pathway, a continuing education company, now supported by Affordable Care, the nation’s largest dental support organization (DSO) exclusively focused on tooth replacement. Based in Gilbert, Arizona, The Pathway recently expanded to a new 30,000-square-foot facility.
“The curriculum and vision for The Pathway came from the amazing dentists from whom I learned during my many years in dentistry,” shares Dr. Moody. “Now, I’m proud to call those dentists faculty members and mentors of The Pathway.”
“We offer a wide variety of dental CE courses covering a broad range of topics including live surgical implant training, complications, advanced implant solutions, CEREC, oral and IV sedation, and advanced restorations,” explains Dr. Moody. “Dentists from all over the country visit us to advance their skills.”

extensive implant experience, oral surgeons, periodontists, and prosthodontists.
“It’s an honor to be part of The Pathway’s faculty,” explains Dr. Holtzclaw, one of the world’s leaders in full arch implantology. A periodontist who specializes in complex cases utilizing pterygoid and zygomatic implants, traditional dental implant treatments, bone regeneration, and the treatment of periodontal disease, Dr. Holtzclaw has authored multiple implant textbooks including Pterygoid Implants: The Art and Science and Remote Anchorage Solutions for Severe Maxillary Atrophy: Zygomatic, Pterygoid, Transnasal, Piriform Rim, Nasopalatine, and Trans-Sinus Dental Implants.


He adds, “The faculty and mentors who become a part of The Pathway program are the very best dentists in our industry. Our focus and passion are on the dentists who have committed their time to learning and becoming the best version of themselves.”
One of the faculty trainers and mentors at The Pathway is Dr. Dan Holtzclaw, Chief Clinical Officer of the Advanced Dental Implant Center network, a rapidly growing supported dental network within Affordable Care, comprised of general dentists with
He adds, “Having access to a topnotch training facility is one of the many benefits to dentists who are part of the Advanced Dental Implant Center network. We are building an engaged doctor community through education and clinical advancement.”
He adds, “Serving as a faculty trainer and mentor at The Pathway allows me to give back to our industry and continue to advance our skills to benefit more patients.”
“Our courses serve dentists from private practice to small DSOs and large DSOs from across the U.S.,” shares Dr. Moody. “Our common goal is to join as a dental community, advance our skills, and help patients. Dr. Holtzclaw brings years of advanced experience with some of the most challenging implant patient cases. It’s not every day you can get access to a doctor of his caliber, and he’s so generous sharing his time and talent well beyond the training sessions.”
Visit thepathway.com to learn more about upcoming courses in 2024 including The Pathway Symposium scheduled for Sept. 26-28 in Arizona.
Scan the QR Code to learn about affiliation opportunities with the Advanced Dental Implant Center network. This information was provided by Affordable Care. IP

18 Implant Practice US Volume 17 Number 1 EDUCATION SPOTLIGHT
Dr. Dan Holtzclaw, Chief Clinical Officer of Advanced Dental Implant Center
Dr. Justin Moody, founder, The Pathway
Proud
- Dr. Dan Holtzclaw Chief Clinical Officer Advanced Dental


Scan the QR code or call us at: (888)537-2801 to learn about affiliation opportunities
Implant Center
serve DSO for ADVANCED DENTAL IMPLANT CENTER AN INVITATION for general dentists with extensive
experience, oral surgeons,
prosthodontists
We are attracting the very best general dentists with extensive implant experience, oral surgeons, periodontists and prosthodontists to affiliate with us and be a part of building something very special for patients and for doctors in our industry.
implant
periodontists and
to serve as the DSO for the Advanced Dental Implant Center network
TO JOIN OUR FAST GROWING NETWORK OF ADVANCED DENTAL IMPLANT PROVIDERS
NOW IS THE TIME
AI in implant dentistry: clinical implementation and considerations for use
Drs. Aaron Glick, Nicholas Tipton, Nisha Manila, and Jennifer Chang discuss the pros and cons of AI in
the dental practice
Introduction
Although artificial intelligence (AI) has been integrated in daily life, most are not aware that it has become an integral part

Aaron Glick, DDS, works in healthcare innovation and is on faculty at the University of Texas Health Science Center at Houston School of Dentistry and Sam Houston State University College of Osteopathic Medicine. He is a Diplomate of the ABDSM, faculty member of the AADSM Mastery Program, and holds fellowship credentials with Academy of General Dentistry and International Congress of Oral Implantology. He enjoys all technologies and has a background in software programming for neuroscience research at Brandeis University and Harvard University using 3D modeling, AI, and fMRI technologies. Dr. Glick has been published in medical and dental journals and lectures nationally on dental sleep medicine and digital/software technologies.

Nicholas Tipton, DDS, is a current periodontics resident at Texas A&M School of Dentistry in Dallas. He previously completed his DDS training at UTHealth School of Dentistry at Houston in 2023 and undergraduate degree at Texas A&M in College Station. Nicholas has many research and clinical interests including implantology, hard and soft tissue augmentation surgery, and implementation of AI within periodontics research. After residency, Nicholas plans to work within private practice and teach part-time.

Nisha Manila BDS, PhD, is an Associate Professor and Director of Oral and Maxillofacial Radiology at California Northstate University College of Dental Medicine. With a dental degree from India, and a Ph.D. in Oral Radiation Oncology from Tokyo Medical and Dental University, Japan, she completed Oral and Maxillofacial Radiology training at Texas A&M University. Dr. Manila is a fellow of the American College of Dentists, and her research interests include applications of AI in dentistry, CBCT imaging, and advanced diagnostic imaging modalities. Dr. Manila is an active member of several professional organizations.

Jennifer Chang DDS, MSD, is an assistant professor and program director in the Department of Periodontics at The University of Texas School of Dentistry at Houston. She completed her Doctor of Dental Surgery degree and 2 years of general practice residency in Taiwan. She obtained her Master of Science in Dentistry degree in periodontics from Indiana University School of Dentistry. Dr. Chang is a board-certified Diplomate in Periodontology and Dental Implant Surgery. She maintains a part-time practice at the school’s faculty group practice and in the greater Houston area. Her clinical and research interests focus on improving treatment options for periodontal/peri-implant disease.
Educational aims and objectives
This self-instructional course for dentists aims to identify how artificial intelligence (AI) works, as well as its advantages and disadvantages in the dental practice.
Expected outcomes
Implant Practice US subscribers can answer the CE questions by taking the quiz online at implantpracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
• Define AI and the evolving types of AI.
• Identify the basics of how the data is used in a clinical way by interacting with AI-enabled systems and machines.
• Recognize how AI systems are being used to improve aspects of the implant process.
• Realize some of the issues that need to be addressed to ensure patient safety, clinical success, and to safeguard the practice from legal complications.
of many aspects of modern life over the past few decades given the increased computing power, digitization of data, advances in algorithm, and improvements in accuracy. In fact, when a group of Americans were surveyed, over half were not able to identify that AI was the power behind wearable fitness trackers, automated chatbots, product recommendations, security cameras that identify unrecognized people, music playlist recommendations, and email services identifying spam messages.1 In dentistry, some of these same AI systems, such as chatbots, have been integrated for general office support and software automations. Other AI systems that are more dental-specific have also been used for approximately a decade. These include systems that automatically identify dental landmarks in CBCT,2 maxillary/mandibular segmentation from radiographic images,3 and digital reconstruction of tooth surfaces.4
Some examples of more current AI systems in dentistry are decision-support systems to aid clinicians in the diagnosis of caries and periodontal conditions, AI-enabled robotic surgeries, and creation of AI-generated dental restorations/appliances.5 Since AI is a tool, it can be used in multiple applications within the dental field, and as the algorithms advance in accessibility
20 Implant Practice US Volume 17 Number 1 CONTINUING EDUCATION
2 CE CREDITS
and accuracy, the amount of products with embedded AI likely will increase (Table 1). Therefore, it is important as a dental practitioner to understand the tools used, particularly if they can have a direct or indirect effect on patients.
How AI works
AI is a broad term that generally refers to the ability for computers to perform tasks that typically require human intelligence (Figure 1); for example, viewing a dental X-ray and identifying interproximal caries. Machine learning (ML) refers to the mathematical approach to accomplish this perceived human intelligence. These algorithms are programmed to take information and “learn” from these datasets. Since there are alternative methods for artificial intelligence, machine learning is considered a subset of the approaches to achieve artificial intelligence. Multiple types of algorithms can be programmed by the user. In one approach, a convolutional neural network (CNN) can feed a large dataset to identify the features that are most salient in a classification task. For instance, with multiple pictures of apples or cats, the neural network would be a mathematical model used to make the binary decision on if the currently presented image should be classified as an apple or cat. The CNN approach is typically selected for image operations since this algorithm is optimized to process images based on the extraction of spatial features.
Depending on the task to be performed, there are multiple types of models that are specific to optimizing for the type of data or output intended. For instance, chatbots require a textbased approach with grammatical rules built into sequences of words. Therefore, language-specific models would be used for text-based tasks, typically called natural language processing (NLP).
Further into the black box
While most dentists today don’t consider building custom AI products, there are products that will democratize the use of AI through no-coding technologies.6 Whether coding the algorithms or not, understanding the basics of how the data is used to derive a clinical decision/outcome is important since dentists are increasingly interacting with AI-enabled systems and machines.
When software manufacturers train an AI model, they require a large amount of data to process. In general, the full dataset is split into 3 distinct groups: 1) training set, 2) validation set, and 3) testing set (Figure 1). In a supervised model, a team of clinicians will label the full dataset. For instance, if the classification task is to automatically identify caries in bitewing radiographs, the clinician would identify areas of the radiographs with caries. These labeled radiographs serve as the “ground truth” for the algorithm. The bulk of the data is used in the training set to optimize the weights of the neural network identifying salient features of the categorized dataset. The model is then further optimized by using a validation dataset, where additional processes can improve the accuracy. The final step is to understand how accurate the fully trained AI model can perform on the similar dataset. Therefore, the testing dataset is then categorized by the trained model to provide an accuracy typically reported as a percentage of accurately categorized responses and Receiver
Table 1: Multifaceted uses of AI in dentistry
Dental specialtyUse case
Endodontics
Implant dentistry
Oral surgery
Orthodontics and pediatric dentistry
Pathology
Periodontics
Prosthodontics and restorative dentistry
Radiology
Non-clinical
• Identify root morphology, minor apical foramen
• Diagnosis of apical lesion, root fracture
• Risk of peri-implant diseases
• Surgical procedures
• Identification of anatomic features
• Screening and classification of oral cancer
• Cephalometric analysis
• Treatment needs and outcome evaluation
• Vertebral growth assessment
• Analyze histologic slides and cytologic specimens
• Clinical and radiographic assessment
• Immunologic and microbiologic analysis
• Caries detection
• Shade selection, tooth preparation, restoration design
• Radiographic mounting
• Caries detection, oral cancer diagnosis
• Patient education and engagement
• Dental research
• Practice management (i.e., HR and insurance automations, financial projections, scheduling chatbots)

Operating Characteristics (ROC) curve/area under the curve (AUC). The ROC curve and AUC offer additional details similar to the true positive rate and false positive rate. Ultimately, the
21 implantpracticeus.com Volume 17 Number 1 CONTINUING EDUCATION
Figure 1: Visualization of the distinction between terminology for artificial intelligence (AI), machine learning (ML), and Convolutional Neural Networks (CNN)
large dataset is trained, and the same isolated dataset is used to assess the accuracy in a non-clinical setting.
When building these algorithms, there are some additional key considerations as to how the algorithm uses data. In an oversimplification, an algorithm can be delineated as 1) supervised/unsupervised or 2) static/continuous learning. Supervised learning is based on a clinician providing the algorithm with a ground truth for labelled data, similar to the previous example. Unsupervised learning is where the model learns without explicitly provided information to classify and can be accomplished through patterns within the data. Static learning algorithms are the traditional type of AI, however, some current algorithms are designed to update and improve themselves based on additional data acquired during use.
AI in implant dentistry
AI is changing our daily lives and approaches to dentistry in general. In implant dentistry, AI has spurred innovations in automations, assistive technology, and predictive outcome recognition. There are multiple examples of AI systems being used to improve aspects of the implant process.

The first example is identification of the implant type in radiographs. The accuracy of these models was generally high and ranged from 91% to 98%.7 Another example of AI in implant dentistry is the prediction of osteointegration success, which depending on the study and model type used, was between 60% to 89%.7 Since a host of variables potentially dictates the success/failure of a placed implant, AI has the potential to identify surgical and host factors personalized to the specific case to predict later failure cases. Each implementation of AI uses different variables such as patient age, bone thickness, smoking, radiographic inputs, and implant placement location.
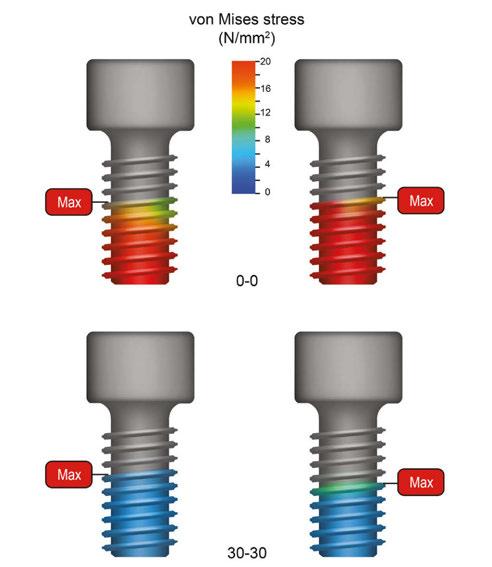
Optimization of implant design to reduce implant-bone interface stress is another example of using AI in dentistry. In these examples, an AI-generated implant body was tested based on simulated parameters.7 To generate the implants, some of the input parameters were implant length, diameter, porosity, and pitch of thread.
Additional examples are software features for implant planning such as generative tooth libraries and anatomical segmentations.5 Generally, automated, or near-automated steps during the process of implant planning in 3D digital space or fabrication of surgical stents are used to aid in the efficiency of the clinicians’ implant workflow.
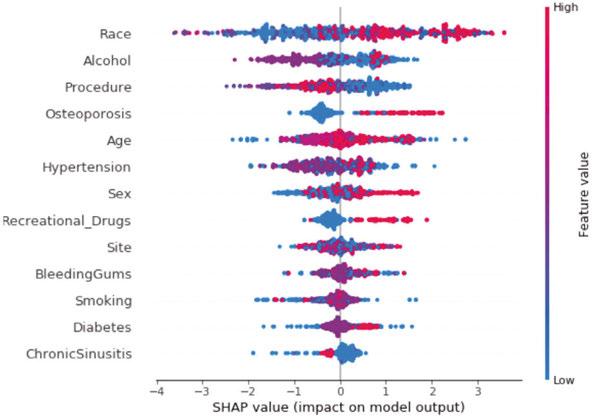
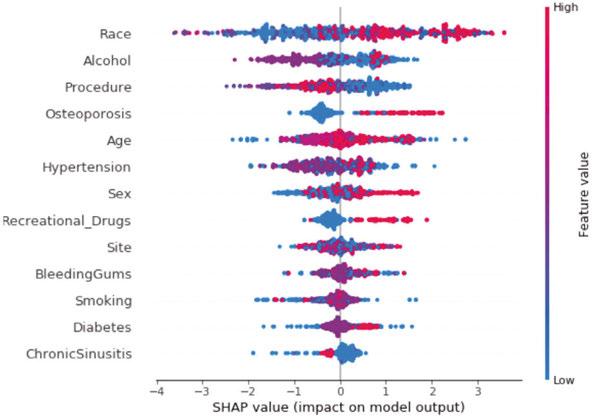
Lastly, AI can be used in the research of implant dentistry. In large datasets, there is potential to identify unknown patterns that could have clinical significance. In one research project conducted by the authors (JC, NT, AG), a Shapley Additive exPlanations (SHAP) analysis was performed, that allows explainable machine learning to measure the impact of each variable on the ultimate output of the model. In this case, a total of 205 patient
the outcome of peri-implantitis
records at the University of Texas Health Science Center at Houston School of Dentistry were used to determine the development of peri-implantitis, a risk factor for long-term implant health. Despite manually checking for data validation and accuracy for all patient records, the model found that race, osteoporosis, and recreational drugs were the most salient features of the model as a risk factor for peri-implantitis over other categories (Figure 3).
A light in the black box
AI presents an exciting tool to simulate human intelligence to help dentists achieve a higher quality of life, better decision-making capability, and fewer postoperative complications.8 However, despite these advances, AI in dentistry is in its infancy. On the horizon are more autonomous systems that do not require human input at the clinical stage within the AI algorithm. While a good understanding of the basics of AI is useful, the actual processes of most algorithms and datasets are not transparent to clinicians. Accuracy, trust, data stewardship, and equity/sustainability are concerns that clinicians and AI software manufacturers need to address to ensure patient safety, clinical success, and safeguarding from legal complications.
22 Implant Practice US Volume 17 Number 1 CONTINUING EDUCATION
Figure 2: Use of data with a supervised AI model
Figure 3: SHAP analysis on patient records showing colors for importance of each variable on the outcome of peri-implantitis. Red color means that it highly corresponded, and blue means that it did not correspond to peri-implantitis. The SHAP value relates to a positive or negative relationship to
Accuracy
The accuracy of an AI system is based on a predefined gold standard. Most clinical decision support tools are supervised algorithms and labeled by clinical dentists without histologic confirmation. Since the amount of data that is required to train the models is so large, it is impractical to build highly accurate datasets that are verified with high-quality standards. In fact, the sensitivity for dentists to detect interproximal caries in bitewings in dentin is low (.36),9 and provider agreement also is low (.4 kappa).10 Similar findings have been seen in other fields such as in periodontal conditions yet are task specific.11 While the quality of the dataset will likely not be transparent, the process for labeling the data as an important factor in the accuracy of the system could be stated by the manufacturer. Another issue that can affect AI is the imbalance of certain conditions like rare pathology that limit the number of instances for the algorithm to learn.
In implant dentistry, AI has spurred innovations in automations, assistive technology, and predictive outcome recognition.
What is the clinical accuracy of these AI models? Is the trained dataset similar to your patient population or data in your EHR? Most report accuracies on the original dataset that was used, yet the true accuracies with different datasets or after clinicians have interacted with the AI system remain limited, and independent testing remains even more limited. In fact, some studies have shown that when AI presents incorrect information, clinicians are more likely to be misled by this recommendation which could result in poor patient outcomes.11,12 Should incorrect guidance be provided by the AI system and patient harm occurs, the current legal climate would hold the clinician liable.13 Additionally, when the AI system is accurate, there are concerns of other biases and trust.
Trust
A human-computer interaction exists between the dentist and AI system that can affect the perception of clinical information and ultimately treatment performance and decision. Trust is a well-studied concept that is affected by many factors with transparency, reliability, and tangibility as some of the commonly cited values that apply most to human-computer interaction.14 Transparency is inherent in trust, and AI systems can be built to be explainable. While most traditional forms of AI suffer from the “the black box problem” (the inability for people to see how learning systems such as AI make their decisions), some offer detection strategies through computer vision,15 and others provide embeddings through natural language processing.16 Reliability offers a perception that the algorithm is making similar decisions in seemingly similar circumstances. For continuously learning algorithms, there is a potential risk that adaptive learning could introduce new errors and reduce reliable performance.17,18 Tangibility refers to the physical or virtual presence of the AI system and when it appears more real or anthropomorphic, which improves trust.19
Data stewardship
Machine learning sits at the intersection of big data and software algorithms. Given the need for large datasets to train
models, the data stewardship in regulated industries, especially dentistry, is important. Dental offices handle private data on patients within the electronic health records system, such as financial, demographic, disease state information, and other sensitive clinical information. With the digitization of records and equipment, the dental industry is a prime target for hackers and also lacks adequate knowledge about the prevention of these crimes.20 In fact, Henry Schein, a large distribution and software company with more than 23,000 employees and 1 million customers globally, halted operations due to a cybersecurity incident.21 Large, consolidated datasets with patient data are vulnerable to attacks. Additionally, generative AI that ingests data from multiple sources feeding back into the algorithm can pose a risk if patient data is used. For instance, divulging patient data on a generative AI platform to write patient notes more efficiently could put the dentist at risk of breaching HIPAA with patient data being used to continuously train the model. For example, Sarah Silverman is suing openAI and Meta over violations of her copyrighted book that surfaced when these platforms regurgitated substantial elements of her copyrighted materials.22
Equitability/Sustainability
The equitable treatment of patients is an ethical value upheld by the American Dental Association where all treatment decisions should be determined on the same basis as all other patients.23 As AI systems are built with human inputs, biases can be encoded into the model.24 In one example of this, Optum, a health service company, created an AI program to spot high-risk patients that should receive medical follow-up care. However, the follow-up care disproportionately identified white patients with 82% white and 18% black patients identified compared to an independent analysis finding that 53% white and 46% black patients should have been identified based on medical need. Before this error could be detected, the program had already been applied to 100 million patients.25 Additionally, the hardware that powers AI requires high energy and a large local ecological footprint.26 In fact, GPT3 took 1.287 gigawatt hours of electricity and 700,000 liters of clean freshwater.27
Implementation of AI systems
As manufacturers continue to release new and update current AI embedded technologies, dentists should be aware of how these tools operate and can potentially change patient care. Many dentists are likely to implement embedded AI technologies without fully realizing it since AI is commonly used as a tool to accomplish a task or optimize tasks, and most backend systems are not transparent to the user.
23 implantpracticeus.com Volume 17 Number 1
CONTINUING EDUCATION
In order to implement new technologies with AI into a dental office, technology acceptance and continual quality assurance should be a consideration. The primary factors for technology acceptance are perceived usefulness and perceived ease of use.28 Therefore, removing barriers to trust within the human-computer interaction can improve usage. Training with technology in a safe environment can build confidence and improve ease of use. Additionally, having a plan for continuous quality assurance with the use of AI can aid in patient safety given that the systems can change with updates or continuously learning models. AI behavior should be periodically monitored, and a set of well-defined metrics are needed to guide regularly scheduled testing.29
The U.S. government also functions to protect patients and dental offices’ implementation of AI through the FDA clearance process of software as a medical device. FDA has become increasingly more stringent on this type of software that predicts and identifies medical/dental conditions.30 As dentists expand their appetite for additional functionality of these software systems, there needs to be a balance between the regulatory burden and the ability to innovate.
Exciting future of AI in dentistry
With the digitization of dental records and radiographs, dentistry is an ideal profession to harness AI. Current applications of AI are already being implemented to change the workflow of dental offices and patient care. Despite risks of inaccuracies, human-computer mistrust, data security concerns, and inequities in applications, it is easy to imagine overcoming these obstacles as the perceived future benefits outweigh the risks.31 Healthcare in general is expected to see an increase in venture investments, as the value of AI in health is expected to grow from $4.9B in 2020 to $45.2B in 2026. Dentistry, however, is lacking in the amount and accuracy of data.32 To accelerate the advancement of AI, manufacturers need access to large, structured datasets that contain valid and reliable data. In fact, each of our practices holds valuable data that has the potential to improve the field.
REFERENCES
1. Kennedy B, Tyson A, Saks E. Public awareness of artificial intelligence in everyday activities. Pew Research Center. (Published February 15, 2023.) https://www.pewresearch.org/science/2023/02/15/public-awareness-of-artificial-intelligence-in-everyday-activities/. (Accessed: November 24, 2023.)
2. Cheng E, Chen J, Yang J, Deng H, Wu Y, Megalooikonomou V, Gable B, Ling H. Automatic Dent-landmark detection in 3-D CBCT dental volumes. Annu Int Conf IEEE Eng Med Biol Soc. 2011;2011:6204-6207.
3. El-Bialy A. Towards a Complete Computer Dental Treatment System. 2008 Cairo International Biomedical Engineering Conference, Cairo, Egypt. 2008:1-8.
4. Sporring J., Hommelhoff Jensen K. Bayes Reconstruction of Missing Teeth. J Math Imaging Vis. 2008;31:245–254.
5. Chang J, Glick A. Clinical implementation of artificial intelligence systems. J Greater Houston Dent Soc. 2023; 94(2):18-19.
6. Sundberg L, Holmström J. Democratizing artificial intelligence: How no-code AI can leverage machine learning operations. Business Horizons. 2023;66(6):777-778.
7. Revilla-León M, Gómez-Polo M, Vyas S, Barmak BA, Galluci GO, Att W, Krishnamurthy VR. Artificial intelligence applications in implant dentistry: A systematic review. J Prosthet Dent. 2023 Feb;129(2):293-300.
8. Nguyen TT, Larrivée N, Lee A, Bilaniuk O, Durand R. Use of Artificial Intelligence in Dentistry: Current Clinical Trends and Research Advances. J Can Dent Assoc. 2021 May;87:l7.
9. Schwendicke F, Tzschoppe M, Paris S. Radiographic caries detection: A systematic review and meta-analysis. J Dent. 2015 Aug;43(8):924-933. Epub 2015 Feb 24. Erra-
tum in: J Dent. 2021 Nov;114:103783.
10. Naitoh M, Yuasa H, Toyama M, Shiojima M, Nakamura M, Ushida M, Iida H, Hayashi M, Ariji E. Observer agreement in the detection of proximal caries with direct digital intraoral radiography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998 Jan;85(1):107-112.
11. Meusburger T, Wülk A, Kessler A, Heck K, Hickel R, Dujic H, Kühnisch J. The Detection of Dental Pathologies on Periapical Radiographs-Results from a Reliability Study. J Clin Med. 2023 Mar 13;12(6):2224.
12. Glick A, Clayton M, Angelov N, Chang J. Impact of explainable artificial intelligence assistance on clinical decision-making of novice dental clinicians. JAMIA Open. 2022 May 17;5(2):ooac031.
13. Gaube S, Suresh H, Raue M, Merritt A, Berkowitz SJ, Lermer E, Coughlin JF, Guttag JV, Colak E, Ghassemi M. Do as AI say: susceptibility in deployment of clinical decision-aids. NPJ Digit Med. 2021 Feb 19;4(1):31.
14. Maliha G, Gerke S, Cohen IG, Parikh RB. Artificial Intelligence and Liability in Medicine: Balancing Safety and Innovation. Milbank Q. 2021 Sep;99(3):629-647.
15. Glikson E, Williams Woolley A. Human trust in artificial intelligence: Review of empirical research. Academy of Management Annals. 2020;14.2: 627-660.
16. Meske C, Bunde E. “Transparency and trust in human-AI-interaction: The role of model-agnostic explanations in computer vision-based decision support.” Artificial Intelligence in HCI. First International Conference, AI-HCI 2020, Held as Part of the 22nd HCI International Conference, HCII 2020, Copenhagen, Denmark, July 19–24, 2020, Proceedings 22. Springer International Publishing, 2020.
17. Zini, JR, Awad M. On the explainability of natural language processing deep models. ACM Computing Surveys. 2022;55.5:1-31.
18. Vokinger KN, Feuerriegel S, Kesselheim AS. Continual learning in medical devices: FDA’s action plan and beyond. Lancet Digit Health. 2021 Jun;3(6):e337-e338.
19. Pianykh OS, Langs G, Dewey M, Enzmann DR, Herold CJ, Schoenberg SO, Brink JA. Continuous Learning AI in Radiology: Implementation Principles and Early Applications. Radiology. 2020 Oct;297(1):6-14.
20. Kim K, Bölling L, Haesler S, Bailenson, Bruder G, Welch G. Does a digital assistant need a body? The influence of visual embodiment and social behavior on the perception of intelligent virtual agents in AR. 2018 IEEE International Symposium on Mixed and Augmented Reality (ISMAR).
21. Melon E, Hernandez W. Cybersecurity in the dental healthcare sector: The need of knowledge for small practitioners. Issues in Information Systems. 2020;21(1):118-124.
22. Henry Schein. “Henry Schein provides information on cybersecurity incident.” [Press release]. Available at: https://investor.henryschein.com/news-releases/news-release-details/henry-schein-provides-information-cybersecurity-incident. (Accessed November 25, 2023).
23. Hayes, Carol Mullins, Generative Artificial Intelligence and Copyright: Both Sides of the Black Box (July 21, 2023). Available at SSRN: https://ssrn.com/abstract=4517799 or http://dx.doi.org/10.2139/ssrn.4517799. Accessed January 4, 2024.
24. American Dental Association. Principles of Ethics & Code of Professional Conduct. https://www.ada.org/-/media/project/ada-organization/ada/ada-org/files/about/ ada_code_of_ethics.pdf?rev=ba22edfdf1a646be9249fe2d870d7d31&hash=CCD76FCDC56D6F2CCBC46F1751F51B96. Accessed November 25, 2023.
25. Schönberger, Daniel. Artificial intelligence in healthcare: a critical analysis of the legal and ethical implications. International Journal of Law and Information Technology. 2019;27(2):171-203.
26. Obermeyer Z, Powers B, Vogeli C, Mullainathan S. Dissecting racial bias in an algorithm used to manage the health of populations. Science. 2019 Oct 25;366(6464):447-453.
27. Kopka A, Grashof N. Artificial intelligence: Catalyst or barrier on the path to sustainability? Technological Forecasting and Social Change. 2022;175:121318.
28. Baxter K, Schlesinger Y. Managing the risks of generative AI. Harvard Business Review. https://hbr.org/2023/06/managing-the-risks-of-generative-ai. (Accessed November 11, 2023).
29. Alhashmi SFS, Alshurideh M, Al Kurdi B, Salloum S. “A systematic review of the factors affecting the artificial intelligence implementation in the health care sector.” Proceedings of the International Conference on Artificial Intelligence and Computer Vision (AICV2020). Springer International Publishing, 2020.
30. Mahadevaiah G, Rv P, Bermejo I, Jaffray D, Dekker A, Wee L. Artificial intelligence-based clinical decision support in modern medical physics: Selection, acceptance, commissioning, and quality assurance. Med Phys. 2020 Jun;47(5):e228-e235.
31. Harvey HB, Gowda V. How the FDA Regulates AI. Acad Radiol. 2020 Jan;27(1):58-61.
32. Tandon D, Rajawat J. Present and future of artificial intelligence in dentistry. J Oral Biol Craniofac Res. 2020 Oct-Dec;10(4):391-396.
33. Hassani H, Andi PA, Ghodsi A, Norouzi K, Komendantova N, Unger S. Shaping the future of smart dentistry: From Artificial Intelligence (AI) to Intelligence Augmentation (IA). IoT. 2021;2(3):510-523.
24 Implant Practice US Volume 17 Number 1 CONTINUING EDUCATION
IP
Continuing Education Quiz
AI in implant dentistry: clinical implementation and considerations for use
GLICK, ET AL.
1. AI is a broad term that generally refers to the ability for computers to perform tasks that typically require human intelligence; for example, viewing a dental X-ray and identifying interproximal caries.
a. True
b. False
2. ________ refers to the mathematical approach to accomplish this perceived human intelligence.
a. Neural learning
b. Machine learning
c. Database modeling
d. Natural Language Processing
3. _________ is based on a clinician providing the algorithm with a ground truth for labelled data.
a. A Receiver Operating Characteristic
b. The Convolutional Neural Network
c. Supervised learning
d. The Language-Specific Model
4. _________ is where the model learns without explicitly provided information to classify and can be accomplished through patterns within the data.
a. Unsupervised learning
b. Supervised learning
c. Neural Network Optimization
d. Predictive Outcome Recognition
5. Each implementation of AI (for implant purposes) uses different variables such as patient age, ________ , and implant placement location.
a. bone thickness
b. smoking
c. radiographic inputs
d. all of the above
6 AI presents an exciting tool to simulate human intelligence to help dentists achieve _________.
a. a higher quality of life
b. better decision-making capability
c. fewer postoperative complications
d. all of the above
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 16 CE credits for only $149; call 866-579-9496, or visit https://implantpracticeus.com/ subscribe/ to subscribe today.
n To receive credit: Go online to https://implantpracticeus.com/continuingeducation/, click on the article, then click on the take quiz button, and enter your test answers.
AGD Code: 010
Date Published: March 1, 2024
Expiration Date: March 1, 2027
2 CE CREDITS
7. Another issue that can affect AI is the imbalance of certain conditions like __________ that limit the number of instances for the algorithm to learn.
a. smaller dental offices
b. non-compliant patients
c. rare pathology
d. edentulous patients
8. For continuously learning algorithms, there is a potential risk that adaptive learning could ________.
a. introduce new errors
b. reduce reliable performance
c. add unnatural language
d. both a and b
9. AI behavior should be periodically monitored, and a set of well-defined metrics are needed to guide regularly scheduled testing.
a. True
b. False
10. __________ has become increasingly more stringent on this type of software that predicts and identifies medical/dental conditions.
a. Food and Drug Administration (FDA)
b. Environmental Protection Agency (EPA)
c. Consumer Products Safety Commission (CPSC)
d. Occupational Safety and Health Administration (OSHA)
To provide feedback on CE, please email us at education@medmarkmedia.com Legal disclaimer: Course expires 3 years from date of publication. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
25 implantpracticeus.com Volume 17 Number 1 CONTINUING EDUCATION
Ailing and failing All-On-X cases and how to treat them
Dr.
Dan Holtzclaw discusses some reasons for implant failure and a possible solution for certain types
Introduction
Over the past 25 years, the All-On-X dental implant treatment protocol has revolutionized full-arch dental implant rehabilitation and, quite frankly, radically changed implant dentistry (Figure 1).1 For those of us old enough to remember, there once was a time when full-arch implant dentistry entailed a cornucopia of bone-grafting procedures which increased morbidity, pain, cost and treatment time for patients (Figure 2).2 It was not uncommon for patients to wait up to 2 years for restoration of their atrophic arches and/or undergo multiple bone grafting procedures only to later discover that they still did not have enough bone to adequately facilitate a full-arch implant-supported prosthetic. The All-On-X treatment protocol remedied this situation for many patients allowing for same-day immediate loading of dental arches sans bone augmentation in most cases.3 Early skeptics of this procedure have been heartily proven wrong with dental literature repeatedly showing high survival rates for All-On-X treatment.4,5 While the success of this procedure may encourage us to pat ourselves on the back as a profession, we should main-


Dan Holtzclaw, DDS, MS, is Chief Clinical Officer of Advanced Dental Implant Centers and Director of Fixed Arch Services at Affordable Care, LLC, Morrisville, North Carolina. He is a Diplomate of the American Board of Periodontology and Diplomate of the International Congress of Oral Implantologists. Dr. Holtzclaw has published over 60 articles in peer reviewed journals in addition to multiple textbooks. He served as the Editor-In-Chief of the Journal of Implant and Advanced Clinical Dentistry for 13 years in addition to serving as an editorial board member and/or editorial reviewer for several other dental journals.
Educational aims and objectives
This self-instructional course for dentists aims to discuss treatment techniques for ailing and failing All-On-X cases in the maxilla.
Expected outcomes
Implant Practice US subscribers can answer the CE questions by taking the quiz online at implantpracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
• Use published dental literature to ascertain the likelihood of All-On-X style dental implant treatment surviving over an extended period.
• Recognize signs of ailing All-On-X cases and know of options for treatment.
• Recognize reasons for failing All-On-X cases and know of remote anchorage options for treatment.
• Recognize that maintenance protocols play an important role in the long term health of All-On-X-style dental treatment, and why failure to adhere to such protocols can lead to prosthetic and implant complications.
• Recognize that the PATZi protocol offers a systematic algorithm for the treatment of failing All-ON-X cases with remote anchorage implants.
2 CE CREDITS
tain a discerning eye and consider how this treatment has held up over time.
The vast majority of All-On-X publications report data that encompasses 12-36 months6,7 with occasional studies extend-

26 Implant Practice US Volume 17 Number 1 CONTINUING EDUCATION
Figure 1: Panoramic radiograph of traditional All-On-X dental implant treatment in both the maxilla and mandible
Figure 2: Panoramic radiograph of patient treated with bilateral sinus lifts, various ridge augmentations, and multiple dental implants over a 2-year timeframe
ing to 5 years.4,8 In general, these studies report high success rates in the mid-to-upper 90 percentile range,3-8 but longer studies begin to show a decline in performance. With 10 years of follow-up, Karoussis, et al., documented a cumulative conventional dental implant survival rate in All-On-X treatment as low as 90.5%.9 A recently published study by de Araujo, et al., likewise documented 10-year cumulative survival rates for AllOn-X conventional dental implants at ~90%10 while Park, et al., found conventional dental implant survival rate at 89.08% in a mean follow-up of 12.6 years.11 As time stretches even further, Simonis, et al., documented a cumulative All-On-X conventional dental implant survival rate of 82.94% at 16 years.12 Finally, as we reach some of the longest reflective evaluations of this treatment, survival shows an even further decline.
In 2022, Vrielinck, et al., published a study evaluating over 20 years of All-On-X implant treatment.13 This study was somewhat unique in the fact that the patients in this study had AllOn-X treatment that used a combination of conventional and zygomatic dental implants. As remote anchorage implants were needed for the participants in this study, it is safe to assume that the maxillary arches involved were of a more atrophic nature. A total of 72 patients were evaluated, of whom 18% were smokers, 8.3% were bruxers, and 2.8% diabetic. The study population was nearly evenly split between male/female, and average age at treatment initiation was 57.8 years (range 31-78 years). With follow-up reaching nearly 22 years (mean 12.8 years, range 2.221.9 years), survival rates for conventional implants followed an early pattern that mirrored previously published dental literature with 95.3% at year 1 and 94.8% at year 2. As time extended, conventional implant survival dropped to 93.0% at 5 years and 90.5% at 10 years. While these findings show a consistent decline, All-On-X conventional implant survival is still above 90% and consistent with previously published studies.
Few All-On-X studies stretch beyond a decade of follow-up and this is where Vrielinck’s study becomes very interesting. At 15 years, All-On-X conventional implant survival dropped to 81.6%, and at 20 years, a precipitous decline to 67.7% was recorded. With the first decade of Vrielinck’s findings in this study paralleling previously published dental literature, it is logical to forecast that the survival rates for conventional All-On-X implants in other studies will likewise follow suit. Bearing this in mind, it is safe to assume that as a profession, we can anticipate seeing a deluge of ailing and falling All-On-X cases as time progresses.
Why do conventional dental implants fail over time with All-On-X treatment?
With multiple published studies showing consistent data, it is safe to conclude that ailing/failing dental implants are expected and “normal” as time extends from the initial date of All-On-X treatment. These studies were performed by different clinicians from all over the world using a variety of implant systems with diversity in both surgical and restorative protocols. This begs the question, with such a large number of clinicians showing congruent findings, why do conventional dental implants have an increase in failure rates over time in All-On-X treatment? The first culprit that comes to mind for many clinicians is that implant fail-
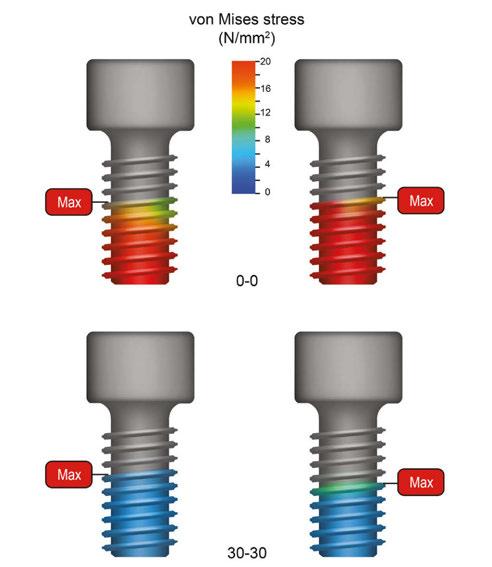
ure is a fault of the patient due to poor adherence to post-restorative maintenance. Published dental literature certainly supports the notion that failure to comply with maintenance protocols leads to poor outcomes over time. In dentate patients, tooth loss, and numbers of decayed, missing, and filled teeth (DMFT) have proven to be lower with high adherence to maintenance.14 Likewise, systematic literature reviews and meta-analyses have also shown that poor or irregular adherence to maintenance leads to decreased outcomes for dental implants.15,16 Is it fair, however, to completely blame dental implant issues on noncompliant patients? According to published literature, the answer to this is a resounding “No” as authors have noted, “…it must be stressed that even in the establishment of PIMT [peri-implant maintenance therapy], biologic complications might occur.”15
If dental implant complications and failures cannot be fully attributed to noncompliant maintenance, what are other means by which issues may occur? Summary and consensus statements from leading organizations such as the European Association of Osseointegration note that mechanical complications may occur in up to 39% of All-On-X restorations21 while other individual studies note long-term issues such as prosthetic screw loosening, multi-unit abutment loosening, and component/prosthetics fracture.17-20 Many of these issues are often correlated to cantilevers which are a hallmark of All-On-X treatment.17-22
All-On-X finite element analysis studies have consistently shown that longer prosthetic cantilevers produce increased stress values in peri-implant bone, abutments, prosthetic screws, and prosthetic frameworks (Figure 3).23,24 Regarding bone, this stress tends to concentrate at the implant platform adjacent to cantilevers, and overloading is associated with increased per-implant
27 implantpracticeus.com Volume 17 Number 1 CONTINUING EDUCATION
Figure 3: Finite element analysis shows longer cantilevers produce more stress in prosthetic screws (top) compared to shorter cantilevers which produce less stress (bottom)
bone loss.23-25 This bone loss often exposes dental implant threads, and long term studies up to 20 years have shown exposure to or beyond the second implant thread in nearly a quarter of fixtures.26 When the roughened surface of dental implants become exposed, bacterial adherence may increase should mucogingival recession occur. If this happens, the bacteria and endotoxin-laden surface of the implant elicits an immunologic host response that results in osteoclastic activity and bone destruction.27,28 Marginal bone loss at the neck of implants is also exacerbated by micromotion that may develop with loosened prosthetic and/or abutment screws.29
While it may be tempting to blame All-On-X implant issues on patient compliance with maintenance protocols, dental literature proves that this is a complex multifactorial issue and that complications may develop as a normal consequence of this treatment even under the most ideal circumstances.
How can clinicians deal with ailing/failing All-On-X cases?

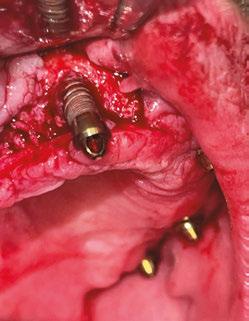

It can certainly be disconcerting when a patient has problems with their dental implants, especially in larger cases such as All-On-X treatment where failure of one fixture may lead to loss of the entire prosthesis. First and foremost, it is important to remember that dental literature unequivocally demonstrates that dental implants will have complications and fail.21,22,26,30 This is an indisputable fact. Over my decades of dental implant experience, I have had multiple complications/failures, and I will continue to have them. Anyone who thinks otherwise is deluding themselves and is not supported by published literature. When these problems occur, it is important to know treatment options available to either extend the life of the implants or replace them with suitable alternatives.
As noted earlier in this paper, one of the most common problems seen over time with All-On-X treatment is exposure of implant threads. If adequate amounts of keratinized gingiva are present, detoxification of exposed implant surfaces may be performed at maintenance visits, and the frequency of these visits may be increased. Patients should also be instructed to meticulously cleanse these areas at home. If minimal amounts of keratinized tissue are present, or if significant amount of implant thread exposure is noted, soft and hard tissue augmentation may be performed.31,32 In the maxilla specifically, a technique which I have been finding great success with is plasty of exposed implant threads with simultaneous tissue augmentation via pedicled connective tissue grafts (Figures 4-8).


28 Implant Practice US Volume 17 Number 1
CONTINUING EDUCATION
Figure 4 (left): Presurgical photo showing exposed implant threads at the neck of an implant used for traditional All-On-X dental implant treatment. Figure 5 (right): Intrasurgical photo showing bone loss and exposed implant threads on a conventional implant used for traditional All-On-X dental implant treatment
Figure 6 (left): Finishing burs are used to plasty implant threads and roughened surfaces, while polishing burs are used to achieve a smooth surface. The intent of this implantoplasty is to reduce the chances of bacterial endotoxin from adhering to exposed roughened implant surfaces. Figure 7 (right): A pedicled connective tissue graft is rotated from the palate around the plastied implant to cover the exposed implant surface and augment peri-implant keratinized gingiva
Figure 8: Mucogingival flap closure following implantoplasty and soft tissue augmentation of the exposed All-On-X dental implant threads
Implantoplasty is a clinical procedure in which a finishing bur is used to eliminate exposed implant threads to create a smooth surface, which is then polished with additional rotary instruments. This implant surface modification reduces bacterial endotoxin adherence, creating a more favorable peri-implant environment.33 When implantoplasty is combined with soft tissue grafting to improve gingival phenotype, long term favorable results can be achieved.34
While these techniques can extend the lifespan of ailing AllOn-X cases, instances of more significant bone loss or outright implant failure require different approaches. Firstly, the cause of implant failure should be considered, especially in cases of excessive cantilever, inadequate support, poor bone quality, etc. Second, the amount of residual bone remaining following planned implant removal needs to be adequate for not only replacement of the failed implant, but also to create favorable

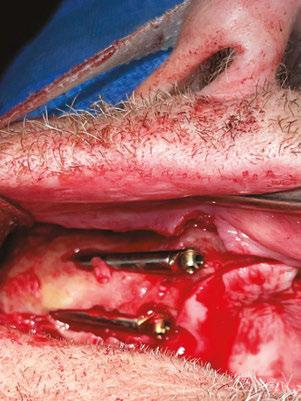
prosthetic support which prevents recurrence of failure. Often, preexisting maxillary atrophy combined with bone loss from failing implants necessitates placement of remote anchorage implants such as zygomatic, pterygoid, and transnasal fixtures.22 These highly specialized implants utilize dense type 1 bone for anchorage which does not atrophy with tooth loss.22 As such, these implants are ideal solutions for All-On-X patients who have experienced severe amounts of bone loss with failing implants.
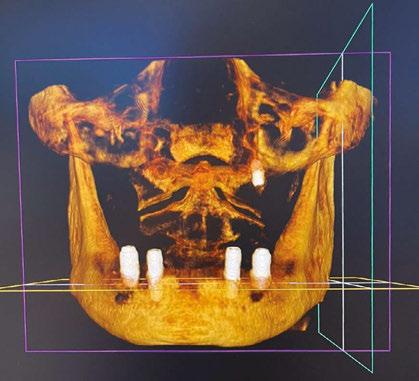
When determining which of these implants to use and where to place them, the PATZi protocol is a useful treatment algorithm which can guide the clinician.22,35 This protocol makes use of nearly all implant styles and may result in a near infinite combination of fixtures to treat virtually any condition of the maxilla. For example, Figures 9-13 document a case in which failing All-On-X treatment resulted in severe maxillary atrophy, and the PATZi protocol was used to rehabilitate the patient with a combination of pterygoid and quad-zygomatic implants. Without the option of remote anchorage treatment, this patient would need to endure multiple large bone grafting procedures entailing additional morbidity, cost, and time for the unguaranteed possibility of future implant treatment. Furthermore, the patient would need to forgo wearing a denture during much of the healing process to avoid putting pressure on the bone grafts. By using the PATZi protocol with pterygoid and quad-zygomatic implants, the patient was able to receive an immediately loaded fixed prosthetic without the need for bone grafting.


29 implantpracticeus.com Volume 17 Number 1
CONTINUING EDUCATION
Figure 9 (left): Presurgical photo of patient with failed maxillary All-On-X treatment. Figure 10 (right): Presurgical CBCT 3D rendering of patient from Figure 9 with failed maxillary All-On-X treatment
Figure 11: (left): Placement of two zygomatic implants in the right malar process of patient from Figures 9 and 10. Figure 12 (center): Postsurgical CBCT 3D rendering of patient from Figures 9-11 following placement of bilateral pterygoid and quad-zygomatic remote anchorage implants placed according to the PATZi protocol. Figure 13 (right): Postsurgical photo of patient from Figures 9-12 following restoration of remote anchorage dental implants used to remedy failing maxillary All-On-X treatment
Conclusion
The All-On-X treatment protocol has revolutionized dental implant treatment and now has 25 years of documentation to support its use. Like all treatment of biological systems such as the human body, complications will occur, and All-On-X procedures are no exception. Recent publications with long term follow-up of 20+ years have shown a verifiable trend of problems with conventional All-On-X dental implants that escalate with extended time. As the number of patients treated with All-On-X procedures has dramatically increased over the past decade, and these people continue to age, dental implant professionals will see an increased need to remedy these maladies. In addition to providing dental implant life extension measures such as implantoplasty for ailing All-On-X fixtures, remote anchorage techniques such as zygomatic and pterygoid implants will be required to rehabilitate cases with more severe problems. These remote-anchorage fixtures are highly complex surgical procedures and should only be attempted by clinicians with extensive training and experience with dental implants.
REFERENCES
1. Nobel Biocare. “Nobel Biocare awards Dr. Paulo Malo for 25 years of theAll-on-4® treatment concept.” Nobelbiocare.com. January, 16, 2023. www.nobelbiocare.com/en-int/news/ nobel-biocare-awards-dr-paulo-malo-for-25-years-of-the-all-on-4-treatment-concept.
2. Brånemark PI, Gröndahl K, Ohrnell LO, Nilsson P, Petruson B, Svensson B, Engstrand P, Nannmark U. Zygoma fixture in the management of advanced atrophy of the maxilla: technique and long-term results. Scand J Plast Reconstr Surg Hand Surg. 2004;38(2):70-85.
3. Maló P, Rangert B, Nobre M. “All-on-Four” immediate-function concept with Brånemark System implants for completely edentulous mandibles: a retrospective clinical study. Clin Implant Dent Relat Res. 2003;5 Suppl 1:2-9.
4. Maló P, Nobre Md, Lopes A. The rehabilitation of completely edentulous maxillae with different degrees of resorption with four or more immediately loaded implants: a 5-year retrospective study and a new classification. Eur J Oral Implantol. 2011 Autumn;4(3):227-243.
5. Maló P, de Araújo Nobre M, Lopes A, Ferro A, Nunes M. The All-on-4 concept for fullarch rehabilitation of the edentulous maxillae: A longitudinal study with 5-13 years of follow-up. Clin Implant Dent Relat Res. 2019 Aug;21(4):538-549.
6. Agliardi EL, Pozzi A, Stappert CF, Benzi R, Romeo D, Gherlone E. Immediate fixed rehabilitation of the edentulous maxilla: a prospective clinical and radiological study after 3 years of loading. Clin Implant Dent Relat Res. 2014 Apr;16(2):292-302.
7. Korsch M, Walther W, Hannig M, Bartols A. Evaluation of the surgical and prosthetic success of All-on-4 restorations: a retrospective cohort study of provisional vs. definitive immediate restorations. Int J Implant Dent. 2021 May 31;7(1):48.
8. Li S, Di P, Zhang Y, Lin Y. Immediate implant and rehabilitation based on All-on-4 concept in patients with generalized aggressive periodontitis: A medium-term prospective study. Clin Implant Dent Relat Res. 2017 Jun;19(3):559-571.
9. Karoussis IK, Salvi GE, Heitz-Mayfield LJ, Brägger U, Hämmerle CH, Lang NP. Longterm implant prognosis in patients with and without a history of chronic periodontitis: a 10-year prospective cohort study of the ITI Dental Implant System. Clin Oral Implants Res. 2003 Jun;14(3):329-339.
10. de Araújo Nobre M, Lopes A, Antunes E. The 10 Year Outcomes of Implants Inserted with Dehiscence or Fenestrations in the Rehabilitation of Completely Edentulous Jaws with the All-on-4 Concept. J Clin Med. 2022 Mar 31;11(7):1939.
11. Park WB, Han JY, Kang KL. Long-Term Comparison of Survival and Marginal Bone of Implants with and without Sinus Augmentation in Maxillary Molars within the Same Patients: A 5.8- to 22-Year Retrospective Study. J Clin Med. 2021 Mar 25;10(7):1360.
12. Simonis P, Dufour T, Tenenbaum H. Long-term implant survival and success: a 10-16year follow-up of non-submerged dental implants. Clin Oral Implants Res. 2010 Jul;21(7):772-777.
13. Vrielinck L, Moreno-Rabie C, Schepers S, Van Eyken P, Coucke W, Politis C. Peri-zygomatic infection associated with zygomatic implants: A retrospective longitudinal cohort study. Clin Oral Implants Res. 2022 Apr;33(4):405-412.
14. Adachi N, Sugimoto K, Shinada K. Association between tooth loss and adherence to oral maintenance in a dental clinic: A retrospective study of more than 20 years. Int J Dent Hyg. 2023 Aug 27.
15. Monje A, Aranda L, Diaz KT, Alarcón MA, Bagramian RA, Wang HL, Catena A. Impact of Maintenance Therapy for the Prevention of Peri-implant Diseases: A Systematic Review and Meta-analysis. J Dent Res. 2016 Apr;95(4):372-379.
16. Monje A, Wang HL, Nart J. Association of Preventive Maintenance Therapy Compliance and Peri-Implant Diseases: A Cross-Sectional Study. J Periodontol. 2017 Oct;88(10):1030-1041.
17. Maló P, Nobre Md, Lopes A. Immediate loading of ‘All-on-4’ maxillary prostheses using trans-sinus tilted implants without sinus bone grafting: a retrospective study reporting the 3-year outcome. Eur J Oral Implantol. 2013 Autumn;6(3):273-283.
18. Grandi T, Faustini F, Casotto F, Samarani R, Svezia L, Radano P. Immediate fixed rehabilitation of severe maxillary atrophies using trans-sinus tilted implants with or without sinus bone grafting: One-year results from a randomised controlled trial. Int J Oral Implantol (Berl). 2019;12(2):141-152.
19. Duarte LR, Filho HN, Francischone CE, Peredo LG, Brånemark PI. The establishment of a protocol for the total rehabilitation of atrophic maxillae employing four zygomatic fixtures in an immediate loading system--a 30-month clinical and radiographic follow-up. Clin Implant Dent Relat Res. 2007 Dec;9(4):186-196.
20. Hirsch JM, Ohrnell LO, Henry PJ, Andreasson L, Brånemark PI, Chiapasco M, Gynther G, Finne K, Higuchi KW, Isaksson S, Kahnberg KE, Malevez C, Neukam FW, Sevetz E, Urgell JP, Widmark G, Bolind P. A clinical evaluation of the Zygoma fixture: one year of follow-up at 16 clinics. J Oral Maxillofac Surg. 2004 Sep;62(9 Suppl 2):22-29
21. Hämmerle CHF, Cordaro L, Alccayhuaman KAA, Botticelli D, Esposito M, Colomina LE, Gil A, Gulje FL, Ioannidis A, Meijer H, Papageorgiou S, Raghoebar G, Romeo E, Renouard F, Storelli S, Torsello F, Wachtel H. Biomechanical aspects: Summary and consensus statements of group 4. The 5th EAO Consensus Conference 2018. Clin Oral Implants Res. 2018 Oct;29 Suppl 18:326-331.
22. Holtzclaw D. Remote Anchorage Solutions for Severe Maxillary Atrophy: Zygomatic, Pterygoid, Transnasal, Nasal Rim, Piriform Rim, Nasopalatine, and Trans-Sinus Dental Implants. Austin, Texas: Zygoma Partners; 2023.
23. Ozan O, Kurtulmus-Yilmaz S. Biomechanical Comparison of Different Implant Inclinations and Cantilever Lengths in All-on-4 Treatment Concept by Three-Dimensional Finite Element Analysis. Int J Oral Maxillofac Implants. 2018 Jan/Feb;33(1):64-71.
24. Saleh Saber F, Ghasemi S, Koodaryan R, Babaloo A, Abolfazli N. The Comparison of Stress Distribution with Different Implant Numbers and Inclination Angles In All-onfour and Conventional Methods in Maxilla: A Finite Element Analysis. J Dent Res Dent Clin Dent Prospects. 2015 Fall;9(4):246-253.
25. Di Fiore A, Montagner M, Sivolella S, Stellini E, Yilmaz B, Brunello G. Peri-Implant Bone Loss and Overload: A Systematic Review Focusing on Occlusal Analysis through Digital and Analogic Methods. J Clin Med. 2022 Aug 17;11(16):4812.
26. Ekelund JA, Lindquist LW, Carlsson GE, Jemt T. Implant treatment in the edentulous mandible: a prospective study on Brånemark system implants over more than 20 years. Int J Prosthodont. 2003 Nov-Dec;16(6):602-608.
27. Wu-Yuan CD, Eganhouse KJ, Keller JC, Walters KS. Oral bacterial attachment to titanium surfaces: a scanning electron microscopy study. J Oral Implantol. 1995;21(3):207-213.
28. Siddiqui DA, Jacob JJ, Fidai AB, Rodrigues DC. Biological characterization of surface-treated dental implant materials in contact with mammalian host and bacterial cells: titanium versus zirconia. RSC Adv. 2019 Oct 9;9(55):32097-32109.
29. Liu Y, Wang J. Influences of microgap and micromotion of implant-abutment interface on marginal bone loss around implant neck. Arch Oral Biol. 2017 Nov;83:153-160.
30. Cercadillo-Ibarguren I, Sánchez-Torres A, Figueiredo R, Schwarz F, Gay-Escoda C, Valmaseda-Castellón E. Immediately loaded implant-supported full-arches: Peri-implant status after 1-9years in a private practice. J Dent. 2017 Dec;67:72-76.
31. Mahn DH. Use of an Autogenous Connective Tissue Graft to Treat Peri-Implantitis With Gingival Recession Affecting an Implant Supporting an Overdenture. Clin Adv Periodontics. 2016 Nov;6(4):161-165.
32. Noelken R, Westphal L, Schiegnitz E, Al-Nawas B. Hard and soft tissue regeneration of severe peri-implantitis defects with the laser-assisted peri-implant defect regeneration technique: 3-year results. Int J Implant Dent. 2023 Feb 5;9(1):3.
33. Esteves Lima RP, Abreu LG, Belém FV, Pereira GHM, Brant RA, Costa FO. Is Implantoplasty Efficacious at Treating Peri-Implantitis? A Systematic Review and Meta-Analysis. J Oral Maxillofac Surg. 2021 Nov;79(11):2270-2279.
34. Rosen PS, Tarnow DP. Subcrestal Implantoplasty for Treating Peri-implantitis With Regenerative Care-How Deep Should Treatment Go? Compend Contin Educ Dent. 2023 Sep;44(8):440-446; quiz 447.
35. Holtzclaw D. Treatment of Severely Atrophic Maxillae using the PATZI Remote Anchorage Protocol: A Case Series. Impl Prac US. 2023;16(4):26-31; quiz 32.
30 Implant Practice US Volume 17 Number 1
CONTINUING EDUCATION
IP
Continuing Education Quiz
Ailing and failing All-On-X cases and how to treat them HOLTZCLAW
1. The vast majority of All-On-X publications report data that encompasses 12-36 months with occasional studies extending to 5 years. In general, these studies report high success rates in the mid-to-upper _________ range, but longer studies begin to show a decline in performance.
a. 50 percentile
b. 70 percentile
c. 80 percentile
d. 90 percentile
2. With multiple published studies showing consistent data, it is safe to conclude that ailing/failing dental implants ________ as time extends from the initial date of All-On-X treatment.
a. are expected and “normal”
b. are unusual
c. are very rare
d. have not been documented
3. In dentate patients, ________ has/have proven to be lower with high adherence to maintenance.
a. tooth loss
b. numbers of decayed and missing teeth
c. number of filled teeth
d. all of the above
4. Summary and consensus statements from leading organizations such as the European Association of Osseointegration note that mechanical complications may occur in up to ______ of All-On-X restorations while other individual studies note long-term issues such as prosthetic screw loosening, multi-unit abutment loosening, and component/prosthetics fracture.
a. 15%
b. 39%
c. 50%
d. 84%
5. All-On-X finite element analysis studies have consistently shown that longer prosthetic cantilevers produce increased stress values in _________ and prosthetic frameworks.
a. peri-implant bone
b. abutments
c. prosthetic screws
d. all of the above
6. Increased peri-implant bone loss (caused by stress that tends to concentrate at the implant platform adjacent to cantilevers) often exposes dental implant threads, and long term studies up to 20 years have shown exposure to or beyond the second implant thread in nearly _______ of fixtures.
a. a third
b. a quarter
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 16 CE credits for only $149; call 866-579-9496, or visit https://implantpracticeus.com/ subscribe/ to subscribe today.
n To receive credit:
Go online to https://implantpracticeus.com/continuingeducation/, click on the article, then click on the take quiz button, and enter your test answers.
AGD Code: 690
Date Published: March 1, 2024
Expiration Date: March 1, 2027
c. a half
d. three-quarters
2 CE CREDITS
7. ________, detoxification of exposed implant surfaces may be performed at maintenance visits, and the frequency of these visits may be increased.
a. If the cantilever is too long
b. If osteoclastic activity is suspected
c. If adequate amounts of keratinized gingiva are present
d. If a tissue graft was necessary
8. _______ is a clinical procedure in which a finishing bur is used to eliminate exposed implant threads to create a smooth surface, which is then polished with additional rotary instruments.
a. Detoxification
b. Implantoplasty
c. Remote anchorage modification
d. none of the above
9. Often, preexisting maxillary atrophy combined with bone loss from failing implants necessitates placement of remote anchorage implants such as zygomatic, pterygoid, and transnasal fixtures.
a. True
b. False
10. These highly specialized (remote anchorage) implants utilize dense ______ for anchorage which does not atrophy with tooth loss.
a. type 1 bone
b. type 2 bone
c. type 3 bone
d. type 4 bone
31 implantpracticeus.com Volume 17 Number 1 CONTINUING EDUCATION
To provide feedback on CE, please email us at education@medmarkmedia.com Legal disclaimer: Course expires 3 years from date of publication. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
Roland DGA and Straumann USA team up
Roland DGA’s DGSHAPE Americas Dental Business Group and Straumann USA are partnering to combine their collective talents and expertise to accelerate the awareness and acceptance of high-quality restorative solutions in the dental market. This new collaboration creates an exciting opportunity to provide world-class, full-service restorative solutions featuring Straumann’s implant solutions and DGSHAPE’s DWX Dental Milling Solutions. The partnership also enables Straumann USA to distribute Roland DGA’s state-of-the-art DGSHAPE DWX mills throughout the US and Canada.
To learn more about Roland DGA’s DGSHAPE dental solutions, visit https://www.rolanddga.com/products/dental/dwx-series. For more information on Straumann USA or its product line, visit www.straumann.com/us/en/dental-professionals.html.
DEXIS introduces AI-powered implant ecosystem
DEXIS™ announced the DEXIS digital ecosystem: an interconnected, AI-powered platform for digital implants — combining cutting-edge CBCT, intraoral scanning, diagnostics, and treatment planning. The ecosystem is designed to empower clinicians to manage each step of an implant case, from diagnosis to delivery, with one integrated tool set. With this prosthetic-driven implant system, clinicians can gain access to an open imaging platform, complete with diagnostics and treatment planning software, driven by Assisted Intelligence and tailored specifically for implant workflows. This user-friendly platform allows clinicians to efficiently organize, analyze, and plan cases while seamlessly collaborating with team members and partners. In late 2023, DEXIS launched the ORTHOPANTOMOGRAPH™
OP 3D™ LX, an advanced cone beam computed tomography technology that enhances 3D diagnostic capabilities with flexible FOV options and short scan times, boosting diagnostic confidence and supporting an evolving practice. After launching the OP 3D LX, DEXIS announced the release of an upgraded version of its intraoral scanning software — IS ScanFlow. Through guided workflows and the use of AI-powered tools, users can confidently navigate complex scanning situations and consistently acquire accurate data. A good example of this is the new full arch workflow, which assists users in obtaining scan data for full-mouth rehabilitations, providing step-by-step guidance throughout the process.
For more information, visit https://dexis.com/en-us.

Dentsply Sirona announces OSSIX Agile™ — a long-lasting pericardium membrane for bone and tissue regeneration
As the latest member of the OSSIX® family of solutions, OSSIX Agile™ is an innovative pericardium membrane, powered by GLYMATRIX®, scientifically proven to assure a long-lasting barrier effect and predictable results. The OSSIX® portfolio is designed to meet the challenges of bone and soft tissue regeneration, utilizing innovative technologies and materials to create reliable and resilient membranes. The pericardium membrane along with the GLYMATRIX® sugar cross-linking properties of OSSIX Agile™ provides longevity and biocompatibility, resulting in low host reactions and a long-lasting barrier effect. Meanwhile, the high-tensile force and tear resistance of pericardium raw material means that OSSIX Agile™ can be adjusted to fit various indications and techniques and can be fixated with tacks, sutures, or screws — potentially reducing overall chair time. The OSSIX® portfolio is designed to solve common regenerative challenges, offering clinical flexibility, predictable results, safety, and hassle-free handling, while allowing for soft and bone tissue regeneration.

For more information, visit https://www.dentsplysirona.com/ en-us/discover/discover-by-brand/ossix-agile.html.
Affordable Care CEO Gene Kirtser to retire

Affordable Care, LLC, has announced Chief Executive Officer Gene Kirtser’s retirement at the end of February 2024. Pete Bridgman will succeed Kirtser as the new Chief Executive Officer. Pete Bridgman is a veteran consumer healthcare and retail executive, having served most recently as Chief Executive Officer of Visionworks, the sixth largest optical retailer in the U.S., and as Chief Network Officer of VSP Vision, the second largest U.S. vision care company, following VSP’s acquisition of Visionworks in 2019. Prior to joining Visionworks, Bridgman previously served as President of Pearle Vision and President of LensCrafters – both brands under EssilorLuxottica, the world’s largest vision care company.
Affordable Care, LLC, is America’s largest dental support organization (DSO) focused on tooth replacement services. The company supports 440 affiliated dental practices, including Affordable Dentures & Implants, DDS Dentures + Implant Solutions, and Advanced Dental Implant Center, in 43 states by providing innovative, non-clinical business and administrative support services to assist affiliated dental practices in providing their patients with access to high-quality, affordable tooth replacement care.
For more information, visit affordablecare.com.
32 Implant Practice US Volume 17 Number 1 INDUSTRY NEWS
Pete Bridgman

and still practicing the way I wish to practice.”
stress
Dr. James Boyle, D.D.S., M.S. Susquehanna Oral & Maxillofacial Surgery 800 - 605 - 3437 | Specialty1partners.com #1 in Dental Services YOUR SPECIALTY IS OUR SPECIALTY . The Only Doctor-Founded, Doctor-Led Specialty Partnership Organization.
“Less














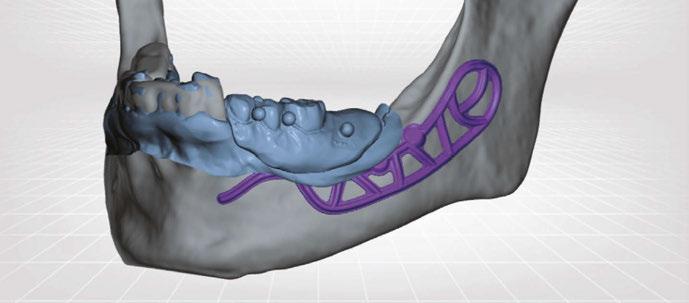

























 Single-Tooth Crown
Fixed Full Arch
Patient-Specific Solutions
Single-Tooth Crown
Fixed Full Arch
Patient-Specific Solutions