Can your orthodontic practice survive a data breach incident?
Mark Pribish


Stem cells and the dynamic field of medicine, dentistry, and orthodontics

Dr. Amy B. Jackson
Dental infections: part 1 Wiyanna K. Bruck, PharmD, and Jessica Price
Partnerships — the key to building a successful practice
 Drs. Stuart Frost and Trevor Nichols
Drs. Stuart Frost and Trevor Nichols
1“ 1.25“ 1.75“ DRIVING THE FUTURE OF ORTHODONTICS READ MORE ON PAGE 8
Winter 2022 Vol 13 No 4 orthopracticeus.com PROMOTING EXCELLENCE IN ORTHODONTICS FAQs Special Section n 4 CE Credits Available in This Issue*

THE ULTIMATE EXPERIENCE TO SIMPLIFY YOUR MECHANICS Contact your Ormco Sales Representative or visit ormco.com/ultimahooks today. Introducing the Ultima™ Hook, the only re-positionable hook 1 , designed to save time for doctors who value performance while providing a healthier2 oral treatment option for their patients.* | Increased Performance | Reduced Chair Time | Designed for Patients MKT-22-1254 © 2022 Ormco Corporation 1 Using the Ultima™ Hook Repositioning Instrument. 2 When used as a stop. * Data on file.
Winter 2022 n Volume 13 Number 4
Editorial Advisors
Lisa Alvetro, DDS, MSD
Daniel Bills, DMD, MS
Robert E. Binder, DMD
S. Jay Bowman, DMD, MSD
Stanley Braun, DDS, MME, FACD
Gary P. Brigham, DDS, MSD
George J. Cisneros, DMD, MMSc
Jason B. Cope, DDS, PhD
Bradford N. Edgren, DDS, MS, FACD
Eric R. Gheewalla, DMD, BS
Dan Grauer, DDS, Morth, MS
Mark G. Hans, DDS, MSD
William (Bill) Harrell, Jr, DMD
John L. Hayes, DMD, MBA
Laurence Jerrold, DDS, JD, ABO
Marc S. Lemchen, DDS
Edward Y. Lin, DDS, MS
Thomas J. Marcel, DDS
Mark W. McDonough, DMD
Randall C. Moles, DDS, MS
Elliott M. Moskowitz, DDS, MSd, CDE
Rohit C.L. Sachdeva, BDS, M.dentSc
Gerald S. Samson, DDS
Margherita Santoro, DDS
Shalin R. Shah, DMD
Lou Shuman, DMD, CAGS
Scott A. Soderquist, DDS, MS
John Voudouris (Hon) DDS, DOrth, MScD
Neil M. Warshawsky, DDS, MS, PC
John White, DDS, MSD
Larry W. White, DDS, MSD, FACD

CE Quality Assurance Board
Bradford N. Edgren, DDS, MS, FACD

Fred Stewart Feld, DMD
Gregori M. Kurtzman, DDS, MAGD, FPFA, FACD, FADI, DICOI, DADIA
Justin D. Moody, DDS, DABOI, DICOI
Lisa Moler (Publisher)
Mali Schantz-Feld, MA, CDE (Managing Editor)
Lou Shuman, DMD, CAGS
© MedMark, LLC 2022. All rights reserved. The publisher’s written consent must be obtained before any part of this publication may be reproduced in any form whatsoever, including photocopies and information retrieval systems. While every care has been taken in the preparation of this magazine, the publisher cannot be held responsible for the accuracy of the information printed herein, or in any consequence arising from it. The views expressed herein are those of the author(s) and not necessarily the opinion of either Endodontic Practice US or the publisher.
ISSN number 2372-8396
INTRODUCTION
Orthodontists — in the human business
As a longtime observer as well as active participant in the field of orthodontics since 1982, I have had the luxury of watching, evaluating, and reacting to the invasion of orthodontics by a myriad of technological advances. Initially, the change from edgewise brackets to the preadjusted, preangulated appliances was a paradigm shift, especially for older practitioners who had been bending wire for decades when the straight-wire appliance entered the U.S. market.
A decade or so later along came computerized imaging and records storage, computerized cephalometric tracing programs, digital radiography, moving teeth with plastic aligners, temporary anchorage devices, and self-ligating brackets that actually gained traction with the practicing population of orthodontists. Surely, this period would prove to be the pinnacle of the introduction of technology into orthodontics. But not so fast.
In another short decade later, we were experiencing the introduction of 3D scanning, CBCT technology, 3D printing, both plastic and metal, and artificial intelligence into the field of dentistry and specifically orthodontics. Because of advances in bracket and wire technology, we were able to change our scheduling protocols and see the patients less frequently.
Along came COVID-19 with all of its disruptions just a few short years ago. We moved into technologies that allowed us to see our patients but not require a physical visit. Other technologies also entered into the orthodontic realm as well. Treatment planning with aligner therapy could now not only show the predicted positions of crowns with treatment, but the database had expanded enough so that now we can also predict root position with aligner therapy. We can treat cases with a new breed of fixed appliances that require no leveling. The teeth are directed to their final positions with the appliance without the traditional steps that we take with edgewise appliances. We are doing surgery first in selected cases, surgeries with aligner products, and also incorporating 3D printing into the rigid fixation devices for orthognathic cases.
Despite all of these advances, we still cannot replace one aspect of the provision of healthcare to our patients. The element that is irreplaceable is the human touch. No machine or piece of technology can replace a kind word, a pat on the back for a job well done, or a sympathetic ear when one of your young patients discusses a problem.
We are in a unique position to influence not only our younger patients but also our older patients. As much as we drive the idea of less contact with patients equating to practice efficiency, how do we put a price tag on a warm smile when patients enter our office, a congratulations when they accomplish a life goal, or reaffirmation that they can accomplish their life goals if the goals are reasonable and realistic, or even console them when they have a tragedy in their lives? These are all things to consider when we are trying to redirect our practices into a more technology-driven, less humanistic approach to our specialty. Embrace technology, and use it! But never forget, we are in the human business, and nothing can change that basic premise.
Everyone have a great 2023!
Dr.
1 orthopracticeus.com Volume 13 Number 4
Ricky E. Harrell, DMD, MA, is a 1979 graduate of the University of Alabama School of Dentistry. After serving 3 years as a general dentist in the Navajo Area Indian Health Service, he returned to The University of Alabama at Birmingham (UAB) and completed his orthodontic residency in 1984. After 22 years in the private practice of orthodontics in Westminster, Colorado, he entered into full-time orthodontic education at the University of Colorado in 2006. He became Program Director for the PG Orthodontic Residency at the Medical University of South Carolina from 2015 to 2017 and then came to Atlanta to assume the role of Program Director at Georgia School of Orthodontics in 2017 where he still holds that position.
Harrell is a life member of the American Dental Association and the American Association of Orthodontics. He is an ABO Diplomate and a Fellow of the American College of Dentists.


2 Orthodontic Practice US Volume 13 Number 4 TABLE OF CONTENTS
CONCEPTS Benefit of early Class II treatment — a treatise on validity of the 1998 Carolina randomized clinical trial
the Carolina Research papers on one- or
orthodontic treatment PUBLISHER’S PERSPECTIVE Telling the world about you Lisa Moler, Founder/CEO, MedMark Media 6 PRACTICE DEVELOPMENT Regain control over your practice: lower costs, eliminate supplychain issues, and increase customization Dr. Tom Shannon explains how in-house 3D-printed fixed appliances can help resolve common practice frustrations ...............................................................18 BOOK REVIEW Burstone’s Biomechanical Foundation of Clinical Orthodontics Kwangchul Choy, DDS, MS, PhD, 2022, Quintessence Publishing Co., www.quintpub.com ........... 22 FAQs SPECIAL SECTION Boyd Industries Market leader for orthodontic operatory equipment ............... 24 Brava by Brius™ Technologies Bringing transformative technology to orthodontics ........................................................ 25 Gaidge ..................................... 26 Specialty Appliances: Advances in orthodontics 27 8 12 COVER STORY Partnerships — the key to building a successful practice Drs. Stuart Frost and Trevor Nichols discuss how they make their orthodontic treatments more efficient, predictable, and differentiated from others in their market Cover image of Drs. Trevor Nichols and Stuart Frost courtesy of Spark™ Clear Aligners
ORTHODONTIC
Dr. John L. Hayes discusses the influence of
two-phase
that

SCHEDULE A DEMO TODAY
Track the Metrics
Matter Let Gaidge help you make smart, strategic decisions for your practice... all driven by data and insight.
CONTINUING EDUCATION Dental infections: help avoid antimicrobial resistance — part 1 Wiyanna K. Bruck, PharmD, and Jessica Price start their discussion on the judicious use of antibiotics in the dental practice

Adrienne Good, National Account Manager for Orthodontic Practice US, recaps Panthera’s memorable event

PRODUCT PROFILE The case for combination treatment Dr. Eric Wu explains how to improve patient satisfaction and profitability


Dr. Kyle Fagala offers insights on how to keep your practice in the spotlight 44
Kristin Tauras, JD, guides dental specialists through the legal elements
ORTHO PERSPECTIVE
Stem cells and the dynamic field of medicine, dentistry, and orthodontics


Dr. Amy B. Jackson discusses how stem cells from wisdom teeth can have promising medical benefits

4 Orthodontic Practice US Volume 13 Number 4 TABLE OF CONTENTS
your
..................................
CONTINUING EDUCATION Can
orthodontic practice survive a data breach incident? Mark Pribish offers facts and best practices on how to mitigate a cyberattack
28
.........................................................
33
EVENT RECAP Panthera Dental 10th Anniversary Celebration
..................................................
39
.....................................
...............................................................
40 PRODUCT PROFILE Smile Stream Solutions
42
MARKETING MOMENTUM 7 marketing musts for orthodontists in 2023
LEGAL MATTERS Navigating dental malpractice lawsuits — part 1
.......................................
46
.........................................................
Connect. Be Seen. Grow. Succeed. | www.medmarkmedia.com READ the latest industry news and business WATCH DocTalk Dental video interviews with KOLs LEARN through live and archived webinars RECEIVE news and event updates in your inbox by registering for our eNewsletter CONNECT with us on social media www.orthopracticeus.com *Paid subscribers can earn 4 continuing education credits per issue by passing the 2 CE article quizzes online at https://orthopracticeus.com/category/continuing-education/
48

Telling the world about you
Published by
Our worlds are so busy with our time consumed with improving clinically, professionally, and personally. We work hard and hopefully find the time to play hard. From my view as a publisher of four and soonto-be five dental publications, I see and hear about so much innovation going on in the dental community. Dentists are showing patients that dental health means better overall health, and there are so many ways to add technology, expand clinical options, and create your own new protocols and inventions that can change the face of your specialties. My team at MedMark is always searching for your stories — for your journeys, your successes, and even your speed bumps along the way. Entrepreneur Gary Vaynerchuk said, “Regardless of what you are trying to accomplish, you’ve got to tell the world about it.” I wholeheartedly agree. And that’s what we at MedMark Media have been doing over the past 17 years. We’ve been telling the world about you.
Publisher
Lisa Moler lmoler@medmarkmedia.com
Managing Editor
Mali Schantz-Feld, MA, CDE mali@medmarkmedia.com Tel: (727) 515-5118
Lisa Moler Founder/Publisher, MedMark Media
All of the new advancements in dental specialty fields are amazing — artificial intelligence (AI), virtual reality, 3D printing, robotics, the field of dental sleep medicine, braces and aligners that move teeth faster and more efficiently, and imaging in 2D and 3D that makes diagnostics more precise. Advances in endodontic materials such as bioceramics contribute significantly to that specialty’s incredible growth. Let’s not forget implants — according to iData Research, over 3 million dental implants are placed each year in the United States, and the U.S. market is expected to exceed $1.5 billion in 2027.
Here’s more good news! In this issue of Orthodontic Practice US, our Cover Story talks about partnerships and how having the right partner can help support the practice’s vision and maintain its leadership position. To differentiate their practice’s treatment options, Drs. Trevor Nichols and Stuart Frost turn to Ormco™, the Damon Ultima™ System, and Spark™ Clear Aligners. In our CE, cybersecurity expert Mark Pribish delves into how to identify and prevent cyberattacks on your practice. Our second CE is part 1 of a series discussing dental infections and use of antibiotics. Making the right decisions means finding out answers to the right questions! Check out our Special Section featuring responses to FAQs from Boyd Industries, Brius™, Gaidge, and Specialty Appliances.
Back to you — how can we help you tell the world about your innovations, techniques, and life-changing treatments? Our articles and advertisers show you what is possible and practice changing, and promises to help differentiate you from the rest. To change Gary Vaynerchuk’s quote just a bit: Regardless of what you are trying to accomplish, MedMark is here to help you tell the world about it.
To your best success,
Assistant Editor Elizabeth Romanek betty@medmarkmedia.com
National Account Manager Adrienne Good agood@medmarkmedia.com Tel: (623) 340-4373
Sales Assistant & Client Services Melissa Minnick melissa@medmarkmedia.com

Creative Director/Production Manager Amanda Culver amanda@medmarkmedia.com
Marketing & Digital Strategy Amzi Koury amzi@medmarkmedia.com
eMedia Coordinator Michelle Britzius emedia@medmarkmedia.com
Social Media Manager April Gutierrez socialmedia@medmarkmedia.com
Digital Marketing Assistant Hana Kahn support@medmarkmedia.com
Website Support Eileen Kane webmaster@medmarkmedia.com
MedMark, LLC
15720 N. Greenway-Hayden Loop #9 Scottsdale, AZ 85260
Lisa
Moler Founder/Publisher MedMark Media

Tel: (480) 621-8955 Toll-free: (866) 579-9496 www.medmarkmedia.com
www.orthopracticeus.com
Subscription Rate
1 year (4 issues) $149 https://orthopracticeus.com/subscribe/
6 Orthodontic Practice US Volume 13 Number 4 PUBLISHER’S PERSPECTIVE






BoydIndustries.com 727-471-5072 Scan the QR code to view our selection! Lean backand RELAX. Built to last. Built for you. Built by Boyd! Creating an office that is inviting to patients is important. We can help! From dental chairs to cabinetry, our products are reliable and visually attractive. Our equipment is comfortable, durable, and customizable. Let us help you create your dream office.
Partnerships — the key to building a successful practice
Drs. Stuart Frost and Trevor Nichols discuss how they make their orthodontic treatments more efficient, predictable, and differentiated from others in their market

Relationships help give life meaning and joy. Whether it’s family, friends, or coworkers, the quality of these relationships can have a significant impact on our happiness and can make life feel complete.
We, Drs. Nichols and Frost, are both twins. Growing up as a twin, we experienced the best of what relationships offer — someone to share a birthday with, someone with you on your first day of school, and even someone to share a physical appearance with! One of our favorite things about being a twin is how we learn to motivate each another and push each other toward greatness. The experience of being twins has taught us the importance of relationships and creating partnerships in life.
For this same reason, people rarely work entirely alone. When we collaborate with others and share ideas, we get inspired and get rid of what is not working. This mutual passion can create revolutionary work.
In our practice, we create many vital relationships and partnerships. For example, we hire team members who share and reflect our core values, mission, and vision for the practice. We also create essential relationships with other practitioners such as general dentists and other specialists. We trust these partnerships and rely on them for our success.
For an orthodontist, finding a partner who provides you with clinical freedom, invests in developing great products, and is easy to work with is vital. Since we went to school for 8 to 10-plus years to be orthodontists, we strive for autonomy to create a vision for our practice.

One of the most critical relationships is finding a partner who can supply the products needed to support our practice vision, ensuring we maintain our leadership position.
The clinical results and patient experience we provide are what drive our practice. This is what builds our reputation and
Trevor Nichols, DMD, MS, practices at Frost-Nichols Orthodontics in Mesa, Arizona. Dr. Nichols attended Arizona State University, where he completed a bachelor’s degree. He attended the Arizona School of Dentistry and Oral Health for his doctoral training. He also holds a certificate in Dental Public Health. In addition, Dr. Nichols completed specialty training in Orthodontics and Dentofacial Orthopedics, and gained a master’s degree while completing research on temporomandibular joint dysfunction.
Stuart Frost, DDS, is a recognized orthodontist, lecturer, educator, and author of “The Artist Orthodontist.” He is the owner of Frost Orthodontics in Mesa, Arizona, and received his dentistry degree from the University of Pacific and his orthodontics specialty certificate from the University of Rochester.
our brand. We all aim to create the best smiles and ultimate experience for each patient. When it comes to clinical results and creating beautiful smiles, we want to use products that make this process more efficient, more predictable, and most importantly, products that help us create a result that differentiates us in the market. For our practice, we partner with Ormco™, a onestop-shop solution for all our orthodontic needs, including the Damon Ultima™ System and Spark™ Clear Aligners.
8 Orthodontic Practice US Volume 13 Number 4 COVER STORY
Drs. Trevor Nichols and Stuart Frost
Dr. Trevor Nichols with a patient
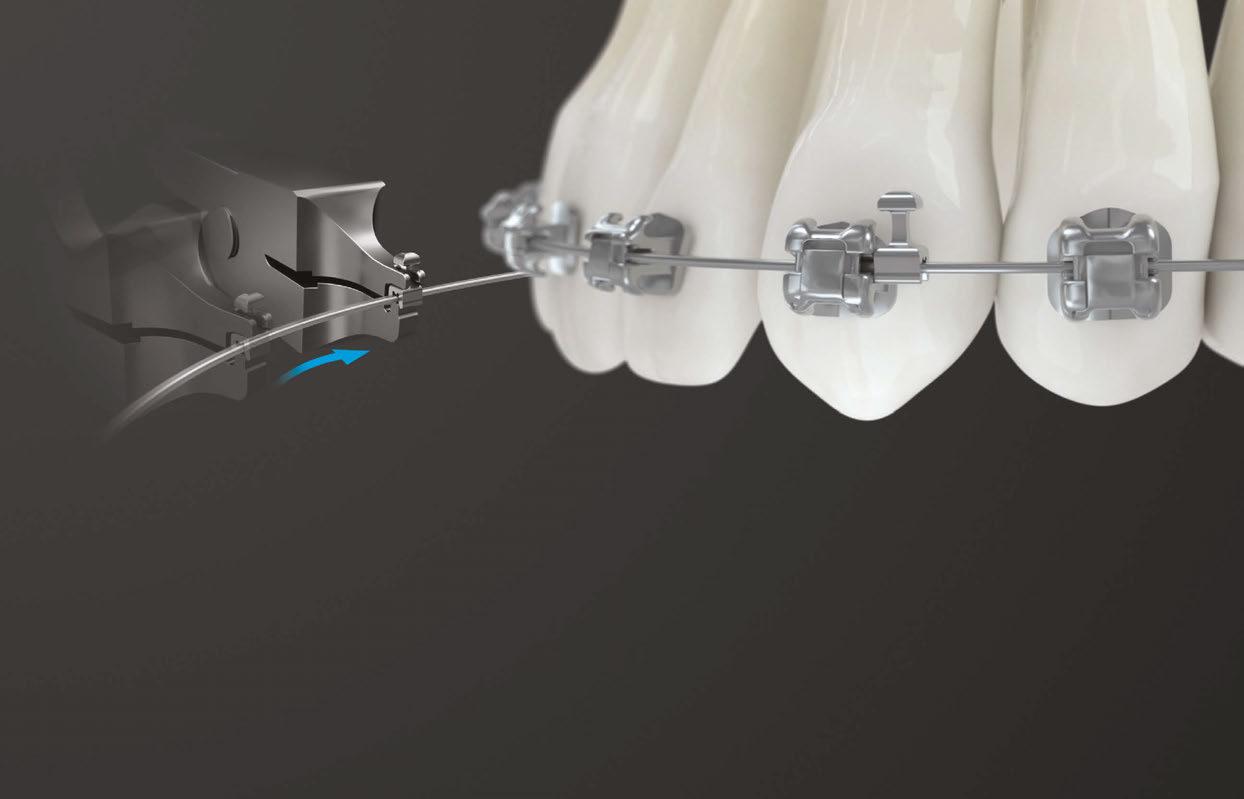
Damon Ultima™ System
The Damon Ultima™ System is an impressive system that combines PSL technology and precise finishing.*
One of the features that makes the Damon Ultima System unique is that it is designed with a round-sided rectangular wire and parallelogram-shaped slot to deliver engagement at vertical and horizontal contact points. Ultima has changed the way we practice because it is a full-expression orthodontic system designed for fewer wire bends throughout treatment for faster and more spot-on finishing.* No longer are we spending months of treatment time bending wire to detail the Frost Smile. Because of this, we have seen a significant decline in treatment times and the number of appointments since using Ultima. This has helped sustain our results in less time and created a better patient experience.
In addition to the new bracket, Ormco™ has a newly innovated hook that has helped solve some of our problems. The Ultima™ Hook is a repositionable1 hook explicitly developed for the Ultima wire. We love the hooks because they are preplaced on the wire, which saves us appointment time. They can be placed flush to the bracket, so the hooks can also act as a stop and prevent spaces from opening, and they hold extremely well for elastic use. We have found that these hooks are great because they no longer slide on the wire, helping provide better patient comfort and contributing to better oral hygiene.2
Case 1
Using the Ultima bracket, we have seen significant improvements, especially regarding practice efficiencies, with the number of appointments and treatment times improving dramatically. The following case provides an excellent example.

Melody came into the practice, never having had orthodontic treatment. She was looking for a solution that would provide her with the best results in the most efficient timeline. A case using older technology would have taken us approximately 18 months and about 12 visits. Half of the treatment time would be spent finishing wires, working to establish arch width, smile arc, and a variety of detail bends.
Melody presented with narrow arches and large buccal corridors, poor tooth shape, severe curve of Spee, and misaligned teeth. She was seeking ideal results and a shorter treatment time.
Using the Ultima bracket, Melody’s case was treated in just 10 months and 9 appointments. Melody was in final wires for less time and required significantly fewer detail bends to finish her case.
Spark™ Aligners
As we have worked for over 20 years to create the Frost Smile — a beautiful smile that flows from front to back, where each tooth introduces the next, has amazing arch width, smile arc, and incredible contours of both the teeth and the tissues — the next logical step was to create the same beautiful results with clear aligners. When using other aligner systems, we did not have the confidence or ability to create the same smiles we had created using brackets and wires. Since implementing Spark Aligners in our practice in 2018, our ability to create amaz-

Figure 2: Case 1

9 orthopracticeus.com Volume 13 Number 4 COVER STORY
Figure 1: Case 1
Dr. Stuart Frost with a patient
Figure 3: Case 2
Figure 4: Case 2
ing smiles with aligners has been incredible. We finally have the right tool to make Frost Smiles with aligners, and now our patients have the choice of treatment modality, knowing that the result will be the same.
Much of this is due to Spark’s innovation in aligner material. Spark’s TruGEN™ aligner material outperforms other aligner brands with greater sustained force retention and better surface contact area with the tooth.* In our experience, the contact surface area between the aligner and the tooth is a key factor driving aligner predictability. This has allowed us to create our famous arch width, smile arc, and strategic flow from anterior to posterior.
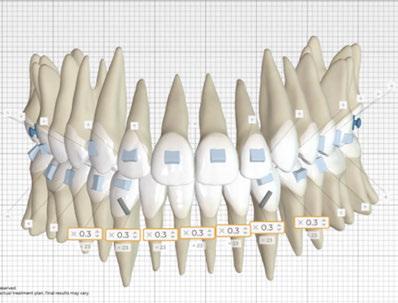
Spark provides unique case planning to give us flexibility, efficiency, and control. We use the root visualization tool with submitted CBCT DICOM files for accurate treatment planning and the posterior bite turbos for premolars and molars to assist with molar intrusion and gummy smile treatments just about every day. In addition, we use the TruGEN material for initial case treatment and TruGEN XR for refinements. The doctor portal has also helped us to optimize treatment planning and practice communications.
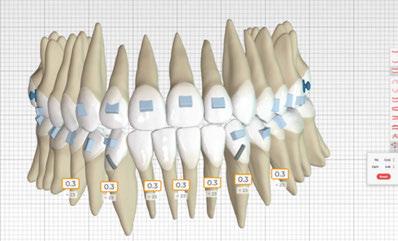
Another benefit that Spark offers that has changed the way we practice is the Approver Software. It was such an easy and welcomed transition from other software. We spend significantly less time going back and forth with technicians. Our time using the software to detail cases is much less. Truly, it has been the best fit for our practice and our patients. We have even switched some patients from previous aligner companies to Spark. Without exception, they have all preferred Spark aligners, and we have seen a massive reduction in treatment time and a huge decrease in refinements with better tracking.
Case 2
With Spark, we now have the confidence to treat a variety of complex case types with excellent results. Ashley’s case provides a good example of this. Her case is rather challenging when evaluated closely due to the maxillary cant, tipped-in posterior teeth, flat smile arc, and Class III occlusion.
Attachments were used to create smile arc, posterior bite turbos were used to tip the occlusal plane and intrude the upper right, and Class III elastics were used for corrections. Ashley was in treatment for 13 months and had six appointments.

Using Spark, we were able to level the cant, broaden her arches, establish a great smile arc, and correct the occlusion.

Conclusion
Relationships and partnerships are essential keys to building a successful practice. Choose a like-minded partner — Someone who will motivate you, and each will push the other toward greatness. Choose partners and products that offer clinical freedom for the practice. In our practice, the combination of the Damon Ultima System and Spark Aligners has allowed us to reach a higher level. We can now enrich more patients’ lives because we have increased control and efficiency, enabling us to serve more patients each year. The smiles we create are as beautiful as ever and are completed in fewer appointments and shorter treatment times.
OP
1. Using the Ultima™ Hook Repositioning Instrument.
2. When used as a stop.
* Data on file at Ormco™.
** Actual Spark and Damon Ultima patient images, which have not been altered. Patient results may vary. Images courtesy of Drs. Frost and Nichols.
10 Orthodontic Practice US Volume 13 Number 4 COVER STORY





Learn more at ormco.com/spark/r13-update Introducing Spark™ Aligners Release 13 TAKING TREATMENT PLANNING TO THE NEXT LEVEL SPARK TRUROOT™ CBCT FEATURE SPARK REAL TIME APPROVAL SPARK INTEGRATED HOOKS *Data on file. MKT-22-1588 *Data on file. THE FIRST TRUE FULL EXPRESSION SYSTEM Re-Engineered to Virtually Eliminate Play, for Faster, More Precise Finishing.* A Bracket That Works Hard, So You Don’t Have To. Visit ormco.com/ultima for more information.
Benefit of early Class II treatment — a treatise on validity of the 1998 Carolina randomized clinical trial
Dr. John L. Hayes discusses the influence of the Carolina Research papers on one- or two-phase orthodontic treatment

The purpose of this article is to evaluate the validity of the Carolina Research papers of 1997, 1998, and 2004.1,2,3 The Carolina Research was designed to answer the following questions: Should the approach for CL II care be “early treatment /phase 1 care — followed by a phase 2” or should it be “later care – 1 phase of care”?
In the end, the major conclusion of the Carolina Research follows:
We conclude that, for children with moderate to severe CL II problems, early treatment [a phase 1 of care] followed by later comprehensive treatment [a second phase of care] on average does not produce major differences in jaw relationship or dental occlusion [than waiting to start later—with 1 phase of care].2
Given some passage of time, the research conclusion came to be accepted as “all early treatment is a waste of time and money,” and some folks were stirred up enough to call for those who practiced “early treatment” to be pilloried.
The Carolina Research was very persuasive — enough to cause easy acceptance and marching orders. Why was it persuasive? Several reasons may be responsible for the “willing suspension of disbelief”:
1. Esteemed institutions were involved.
2. Esteemed prime movers were involved.
3. The research was touted as a true RCT (randomized clinical trial) with the reliability of a true RCT — “…the first ever RCT for orthodontic CL II research.”4
4. The research passed all the stringent peer-review hurdles. It should be fair to say that these papers did more to influence orthodontic diagnosis, treatment planning, and delivery of orthodontic care than any such research before or since — and
Figure 1: In search of the truth regarding two-phase versus one-phase orthodontic treatment. Which is best?
The reader of this article is promised a better understanding of:
1. Research biases — what they can be?
2. Some requirements for a true RCT — the closest thing to “science.”
3. How the Carolina Research fell short of a RCT due to biases resulting an invalid conclusion.
4. Which is better — a two-phase or one-phase orthodontic treatment?

not always in a good way, in the opinion of many. For the last quarter-century, the influence of these papers has been immeasurable — reaching beyond orthodontics.
When a true RCT has been accomplished — with a successful intervention — it is the most robust evidence for “science”; we are generally speaking of a medical RCT. 17 Some orthodontic research, although not meeting the requirements of a true RCT, has been referred to as “RCT research.” Scientists know that just because something is called an RCT does not make it so.
The conclusion of the referenced research was suspect from the outset because the research design and implementation were not consistent with a true RCT.5 The 1998 research methodology and conclusion, if placed on a validity scale of “science” at one end and “opinion” at the other end, would reside closer to the opinion end.
an orthodontist. He can be reached at jhayesortho@comcast.net.
An early misstep with the Carolina Research1,2,3 is evident from the basic research design: A CL II malocclusion is not a diagnosis, but rather — it is a symptom of some diagnosis. The research purpose apparently was to evaluate CL II symptoms
12 Orthodontic Practice US Volume 13 Number 4 ORTHODONTIC CONCEPTS
John L. Hayes, DMD, MBA, received his dental degree from the Boston University, H.M. Goldman School of Graduate Dentistry and his orthodontic certificate from the University of Pennsylvania, School of Dental Medicine, Orthodontic Department where he is a Clinical Associate. He continues to research and lecture on the advantages of early interceptive treatment and on the etiology of malocclusions. Dr. Hayes is in private practice in Williamsport, Pennsylvania, with his wife, Sharon, who is also






Transform Your Practice with TruDenta Request a Consultation Today! 855-770-4002 | Trudenta.com/doctors/ Our diagnostic technologies and FDA-cleared therapeutic procedures provide pain relief and rehabilitate force imbalances for new and existing patients with sleep apnea, chronic migraines and headaches, tinnitus, and other neck/jaw pain. Reap ROI With Your Investment Dental practices that provide TruDenta see nearly 389 percent in return on investment and $1,500 per hour for doctor chair time. Each drug-free treatment plan is tailored to address the individual patient’s symptoms, and includes the use of several tested technologies, including ultrasound, photobiomodulation, microcurrent, and muscle manipulation. As Seen On
inappropriately using a RCT as a kind of umbrella. RCTs are used to evaluate efficacy of an etiology. And symptoms are not etiologies. It is reasonable to consider a CL II, at least partially, as a symptom of “maxillary transverse deficiency” (a strong etiology theory… holding for decades now).6-14 The Carolina Research did not mention any possible CL II etiology.
In cases where the maxilla is too narrow in relationship to the mandibular skeletal transverse width, the mandible is caused to fit in a CL II retro position during growth. It is well-known that phase 1 care can improve the transverse by way of (nonsurgical) skeletal RPE expansion to create room enough for the mandible to grow anteriorly — given normal growth potential and early enough start (usually with help from an indexed Hawley of some type).13,14
The Carolina Research did not investigate, measure, or treat the deficient maxillary skeletal transverse dimension present with its CL II patients. The transverse dimension differential (maxillary transverse dimension as it relates to the mandibular transverse) is a “confounding variable,” and in this instance, it is also a “prognostic factor.”6,8,9,10,11 The Carolina Research did not address those biases, which in turn contributed to a non-evidential report. (Figures 2, 3, 4) Unfortunately, the Carolina study treated CL II symptoms only.
A RCT requires that we identify the etiology — treat the etiology — test the intervention (along with an untested control group), and if the intervention is effective — success!
The four definitions that follow are the helpful to understand the backbones of a true RCT: No. 1 The Scientific Method; No. 2 “Confounding” variable (the non-control of which would be a serious bias); No. 3 “Prognostic” factor or variable (the non-control of which would be a serious bias), and No. 4 “A Randomized Clinical Trial,” RCT.
No. 1 The Scientific Method
The regimen — 1. Formulate a hypothesis. 2. Gather data. 3. Analyze the data. 4. Then determine whether the findings support the hypothesis or not. Accept the hypothesis, or adjust the hypothesis, and repeat the process as necessary. “Nothing gets discovered without the Scientific Method” according to Sir Francis Bacon, (1561-1626). Therefore, Bacon would likely say that the answer to questions regarding early versus late CL II care would require the application of the scientific method.
No. 2 Confounding variables
The non-identification and non-control of confounding variables would be a serious bias. “Confounding bias is often referred to as a ‘mixing of effects’ wherein the effects of the exposure under study on a given outcome are mixed in with the effects of an additional factor (or set of factors) resulting in a distortion of the true relationship. In a clinical trial, this can happen when the distribution of a known prognostic factor differs between groups being compared.”15
For example, there are six varieties of CL II malocclusions, with possibly six different regimens to best treat each diagnosis; given that the patients were then treated in the Carolina study without regard to their specific CL II diagnosis, it would ensure some were treated less appropriately than others — introducing unwanted biases.18
Another example would be when the male and female data were homogenized as in the Carolina Research, the effects of earlier female skeletal maturity along with later male skeletal maturity caused age-sensitive data to be muddled — introducing unwanted biases.
No. 3 Prognostic factor (Figure 2)
Non-identification and non-control of any prognostic factor would create a serious bias. “The identification of and statistical planning for handling influential prognostic factors is an integral part of the planned analysis and hence should be set out in the protocol.”16
For example, if CL II situations were to be heavily influenced by the transverse skeletal harmony present with the maxilla as related to the mandible, a transverse deficiency would be at least partially prognostic (the etiology). Accordingly, the measurement of each patient’s skeletal transverse situation would be important. Some CL II patients are more transverse deficient than others; mildly deficient patient would be expected to respond to a reasonable regimen better that a severely deficient patient. The Carolina study had no idea which patients were which in the transverse skeletal arena (no handle on the prognostic factor), and thus, the data was muddled with biased results.
No. 4 Randomized clinical trial (Figures
3 and 4)
“(RCTs] remain the most robust research method available to find the real effect of an intervention, but a biased RCT [our emphasis] can lead to the adoption of a wasteful intervention and may even harm patients.”17
“In all likelihood, no matter how many variables one adjusts for, there will be residual confounding, possibly by factors that are unknown and cannot be measured.”16
Figure 2: Prognostic factor
•
identification of and statistical planning for handling influential prognostic factors is an integral part of the planned analysis and hence should be set out in the protocol.”16
Figure 3
The stringent requirements of a RCT create its “robustness” ... belief in the determination as science. Keys among the many RCT requirements are: 1. the determination of the etiology of the malady and 2. the intervention applied to the supposed etiology. The etiology is a “prognostic variable,” and it is also a “confounding variable.” If a RCT were to be designed using a particular intervention against some factor other than the etiology — it should not be considered a RCT17
14 Orthodontic Practice US Volume 13 Number 4 ORTHODONTIC CONCEPTS
• “A prognostic factor or variable is a patient characteristic that can predict that patient’s eventual response to an intervention.”
“The
Discussion of the Carolina Research
We do not believe that anything was done intentionally to present false information by the authors; however, the 1998 Carolina Research did not meet basic minimum standards to be called a true RCT — which it was touted to do on more than one occasion.4 The conclusion did not reach the level of “evidential” or “science” as promoted. The conclusion has been considered harmful to patients by some. Of the 12 RCT characteristics evaluated, the research only met one (prospective design) (Figure 4).
The first part of the two-part Carolina Research was the application of phase 1 care to one group while holding in abeyance a “symptom matching group” to be treated later in one phase for eventual comparison.2 It has been argued that the phase 1 methodology employed was a setup to place the worst foot forward and did not evaluate some of the most promising CL II regimens (such as maxillary expansion). The Carolina Research did evaluate both HG and Bionator; however, it should be reasonable to assume that the effectiveness of those regimens was effectively crippled because of the lack of adjunctive help from maxillary expansion.
Figure 4: RCT characteristics — a comparison
Identify confounding variables — (6 different CL IIs, etc.)7. No — confounding biases
No — not feasible with orthodontics bias
If the mandible is desired to grow into its CL I potential, the maxillary skeletal width needs to be wide enough to accommodate the mandible,11 and the patient needs to be young enough (notably for females).
The 1998 study conclusion has been seen by some as a detriment to young patients who have missed out on phase 1 care and missed out on lifelong advantages. The study has also been seen by some as a detriment to our colleagues — the oral surgeons whose patients may have experienced unexpected surgical relapses potentially caused by dental expansion. Dental transverse expansion is more common with later care. After orthognathic surgery, dental expansion tends to relapse and might be contributory to later surgical relapse.
There is no doubt that CL II correction is important. A fair question: How successful is late treatment CL II care? Successful long-term late treatment results are probably out there. One so-called success report revealed several case failures with excessive relapse.19 The failures and partial failures are likely related to failure to address the etiology. Accordingly, 1998 Carolina Research patients (either early or late treated) would have revealed even more CL II failures — had they been followed.
If the cause (or part of the cause) of a CL II malocclusion could be addressed early on, the results in the long term would be more stable.
Comparison of early with late treatment effectiveness
1. Anterior open bite (AOB). Late treatment with surgery or ortho, in addition to surgery, has not proven as effective as hoped. We could not find one case that was considered a success after looking over 50 AOB studies each with several subjects. In our experience, early treatment addressing etiology has opportunity for success.7
2. Impacted canines. Late treatment increases the likelihood for surgery and/or loss of teeth. Proper phase I care can help improve or avoid impactions.12
3. Poor facial growth. How effective is late treatment for poor facial growth? Late treatment is more frequently linked with orthognathic surgery. A transverse deficient maxilla is a prognostic factor for a CL II malocclusion and other skeletal problems. A transverse deficient maxilla also causes a transverse deficient nasal airway with related medical maladies.
4. Airway-related medical maladies. Early, nonsurgical RPE to help address maxillary skeletal transverse deficiency works best early on, as soon as the malady is diagnosed. This type of deformity may be first noticed by an orthodontist.
5. CL II correction. This pattern of poor growth can be improved by starting early enough to reduce distal pressure on the condyles by gaining accommodating skeletal maxillary width while encouraging the mandible into CL I with a Hawley bite plate, as one example of many.20 Patients are being successfully treated without surgery and with improved stability — a win-win.
6. Science. The recommendation of the Carolina study was that early intervention care was essentially wasteful in time and money compared to waiting for later treatment. That turned out to be closer to an opinion than science. The 1998 study on the benefit of early CL II treatment was not science because it was not a true RCT.
7. When to start. A parent’s preference (with either early intervention or later orthodontic care) plays the strongest role in starting. Trust in the family dentist and advice from an orthodontist can help tip the scale in one direction or another. It should be clear that both “later treatment” and “early intervention” are not yet supported by “science”
16 Orthodontic Practice US Volume 13 Number 4 ORTHODONTIC CONCEPTS
1.
1.
2.
2.
3.
3.
4.
4.
5.
5.
6.
7.
8.
9.
9.
10.
10.
11.
11.
12.
12.
A true RCT Carolina Research “RCT”
Scientific Method preceded with Pilot Study
No
Hypothesis confirmed with Pilot Study
No — no hypothesis stated
Prospective design
Yes
Randomized
No (age only); confounding biases
Controlled etiology severity
No (age only); confounding biases
Identify and treat Prognostic Factor/Etiology — (RPE)6. No — a prognostic bias
Selection biases considered — (M/F; maturity; appliances)8. No
Double-blind
Adjustments to intervention cell not allowed
No — intervention allowed biases
Female and males controlled
No, M/F combined — confounding biases
Female age 5-9 to start
No — selection bias (too old?)
(by way of a true RCT) — and that is OK given the multiple research constraints of such proof. In our opinion, a particular early treatment regimen has an edge in being eventually backed as “science.”6-12 A prognostic factor (etiology) for some malocclusions has been identified for decades now and has passed a pilot study followed by several thousand successful cases in one office. There are other reports; thus, a modified RCT could be planned. Numerous airway studies illustrate the important role an orthodontist can play early on with some airway-related medical maladies such as ADD, ADHD, and obstructive sleep apnea (OSA) among others.
OP
7. Hayes JL. A new regimen of phase I care applied to anterior open bite — 10 case studies: an etiology proposed by the strategy of triangulation. Orthodontic Practice US. 2012; 3(3):18-26.
8. Hayes JL. The Williamsport Orthodontic Study. 2005. A 10-year, phase-1 only study (abridged).
9. Hayes JL. Kennewick Man. Chapter 10, Orthodontics. The Scientific Investigation of an Ancient American Skeleton. TAMU Press 2014; 207-211.
10. Hayes JL. March 8, 2003. PAO Meeting, Philadelphia, PA. Presentation: A Clinical Approach to Identify Transverse Discrepancies.
11. Hayes JL. In search of improved skeletal transverse diagnosis. Part II: A new measurement technique used on 114 consecutive untreated patients. Orthodontic Practice US. 2010; 1(4):34-39.

12. Hayes JL. A new regimen of phase I care applied to potential canine impactions. Orthodontic Practice US. 2013; 4(3):44-51.
13. Lima AC, de Oliveira Ruellas AC. Spontaneous Correction of CL II Malocclusion After Rapid Palatal expansion. Angle Orthod. 2003;73(6):745-752.
REFERENCES
1. Tulloch, et al. Benefit of early Class II treatment: progress report of a two-phase randomized clinical trial. Am J Orthod Dentofacial Orthop. 1998;113(1):62-72.
2. Tulloch JF, Proffit WR, Phillips C. Influences on the outcome of early treatment for Class II malocclusions. Am J Orthod Dentofacial Orthop. 1997; 111(5):533-542.
3. Tulloch JF, Proffit WR, Phillips C. Outcomes in a 2-phase randomized clinical trial of early Class II treatment. Am J Orthod Dentofacial Orthop. 2004;125(6):657-667.
4. Proffit WR. Seminar. The world’s first gold standard orthodontic RCT research ever published: a randomized clinical trial. PAO Meeting (The Greenbrier) 1987. Presented at 50th Annual Penn Orthodontic Alumni Meeting (Philadelphia); 2003.
5. Hamilton DC. Critique of: Tulloch, et.al. Benefit of early Class II treatment: progress report or a two-phase randomized clinical trial. 1998. Presented at AAO National Meeting, Toronto, 2001; Tape 32B.
6. Hayes JL. The etiology of malocclusion and the scientific method. Orthodontic Practice US. 2020; 11(2):62-65.
14. Guest SS, McNamara JA Jr., Baccetti T, Franchi L. Improving CL II malocclusion as a side-effect of rapid maxillary expansion: A prospective clinical study. Am J Orthod Dentofacial Orthop. 2010;138(5):585-591.

15. Skelly AC, Dettori JR, Brodt ED. Assessing bias: the importance of considering confounding. Evid Based Spine-Care J. 2012;;3(1):9-12.
16. Berger VW, Sankoh AJ. Prognostic Variables in Clinical Trials. Methods and Applications of Statistics in Clinical Trials: Concepts, Principals, Trials, and Design. Wiley Online Library. Accessed November 3, 2022.
17. Bhide A, Shah PS, Acharya G. A simplified guide to randomized controlled trials. Acta Obstet Gynecol Scand. 2018; 97(4):380-387.
18. Moyers RE, Riolo ML, Guire KE,.Wainwright RL, Bookstein FL. Differential diagnosis of Class II malocclusions Part 1. Facial types associated with CL II malocclusions. Am J Orthod. 1980;78(5):477-494.
19. Fidler BC, Artun J, Joondeph DR, Little RM. Long-term stability of Angle CL II Division 1 malocclusions with successful occlusal result at end of active treatment. Angle Orthod. 1995;107(3):276-285.
20. Enlow DH, Hans MG. Essentials of Facial Growth. W.B. Saunders; 1996.
17
Volume 13 Number 4
orthopracticeus.com
ORTHODONTIC CONCEPTS
3 REASONS TO SUBSCRIBE • 16 CE credits available per year • 1 subscription, 2 formats – print and digital • 4 high-quality, clinically focused issues per year 3 SIMPLE WAYS TO SUBSCRIBE • Visit www.orthopracticeus.com • Email subscriptions@medmarkmedia.com • Call 1-866-579-9496 Orthodontic Practice US 1 year $149 / 1 year digital only $79
Regain control over your practice: lower costs, eliminate supply-chain issues, and increase customization
Dr. Tom Shannon explains how in-house 3D-printed fixed appliances can help resolve common practice frustrations


At our core, orthodontists are innovative problem-solvers. Think about it: Patients arrive at their initial visit, and we have a wide variety of treatment options for every imaginable clinical situation — you name it, we’ve seen it! Each patient requires his/her own unique combination, and the amazing chal-
Tom Shannon, DDS, MDS, is an early adopter of 3D printing. He has extensive experience in orthodontic simulation design, in-office application production, 3D-printed fixed appliances, and hybrid orthodontic treatments. A graduate of the University of Michigan and the University of Tennessee, Dr. Shannon is currently in private practice in southwest Michigan. He has published numerous papers on 3D printing and knows firsthand how it can revolutionize an orthodontic practice.
Disclosure: Dr. Shannon is cofounder and Chief Clinical Officer of Braces On Demand™.
lenge for orthodontists is looking at every mouth and figuring out how we can best utilize the tools and technology at our disposal to create the most functional and stable clinical outcomes.
But our love of problem-solving doesn’t end when the last patient goes home. As a busy orthodontist, I found myself with problems that wires and brackets couldn’t solve on their own — out-of-control variable costs, supply-chain problems, and the inability to innovate. These problems disrupted my practice, limited profit margins, and frustrated me and my staff members. I knew I wasn’t alone either — when we talked at conferences and networking events, I heard these same frustrations from other orthodontists.
On page 20 are some common frustrations of running an orthodontic practice and an explanation of how in-house 3D-printed fixed appliances can help you solve these issues while maximizing profits.
18 Orthodontic Practice US Volume 13 Number 4 PRACTICE DEVELOPMENT
Look, Mom! No Wires
The Fast, Hidden way to straighten teeth.
Not Braces. Not Aligners. Independent Movers™
Bringing Transformative Technology to Orthodontics. This patented biomechanical approach allows for independent and simultaneous movement and is hidden behind the teeth. Bespoke design leverages proprietary algorithms to pre-program the precise moment and force for each tooth of each patient. The result is effective, efficient and aesthetic treatment.

www.Brius.com
© 2022. Brius Technologies, Inc. All Rights Reserved.
Problem 1: out-of-control costs — how to maximize your profit margin
We all have our favorite products that we like to use — the company whose inventory we always have on hand. But as you know, keeping inventory in stock is incredibly expensive, and when buying bulk to maximize savings, we’re paying upfront for thousands of units of a product before we even use a single one. How many of us have drawers of inventory that will never get used and that might even get thrown away one day?
Powerful new 3D-printing software allows you to use your expertise as a practitioner, combined with the limitless customization of 3D printing.
shut down by COVID-19, leaving them to find another way to get the inventory they desperately needed.
As orthodontists we routinely provide the best treatment for healthy and functional smiles, but as small business owners, we also need to be concerned about our bottom line. Profit margins in orthodontics can be thin, and new systems and products often reduce those margins even more. Many of the variable costs we are paying are rapidly increasing such as the cost to pay and retain good staff. Increasing our profit margins means exploring how we can reduce other costs such as the products we use.
I first fell in love with 3D printing when creating models for fabricating clear aligners. Purchasing our practice’s first 3D printer was a big investment, but it also became a powerful tool. I loved the ability to innovate at the click of a button at a very low cost –- pennies on the dollar for the printer’s resin. I began to wonder how else I could use this innovative tool, and how it could improve my practice in other ways.
We live in a time of fantastic innovation in our field, but this innovation almost always comes with a higher overhead for the doctor. I wanted to create something that offered innovation and cost savings for orthodontists, allowing them to serve their patients better while increasing their profit margins.
I leveraged my knowledge of clinical orthodontics and sought out engineers who understood fixed-appliance design and 3D printing to help create custom software that would allow me to fabricate my own appliances in-house using a standard 3D printer and resin. This allowed me to print my own inventory in-house for incredible savings — from one-tenth to one-third of the cost of traditional products — and keep it stocked. But cost is just one consideration.
Problem 2: supply-chain issues — cut out the middle people
Here’s another scenario: You have a patient scheduled for an after-school appointment at 3:30 p.m., but there’s a problem. The appliance you need to treat the patient hasn’t arrived. You’ve checked the tracking on it 10 times, and it hasn’t even budged. So, your staff will have to call and cancel the appointment, frustrating the patient and parent and creating scheduling headaches for your staff, who now have an open hour to fill and a packed schedule to try to reschedule them.
Sound familiar? It was a common situation for many of us even before the pandemic overwhelmed our supply chains. Many orthodontists have been left scrambling as their favorite supplier was located in a part of the world that was completely
If you can create your own inventory in-house, your 3D printer solves the problem of always waiting on deliveries. As long as you keep track of which appliances you use most frequently, and will need in the coming weeks, you always have exactly what you want in stock — indefinitely.
In-house 3D printing completely eliminated the domino effect of not having the product I needed — no stressed staff, no frustrated patients, no convoluted schedule. It was a revolutionary fix for our practice!
By printing your own inventory, you also save on shipping costs and reduce your carbon footprint because in-house printed appliances don’t come with the excessive packaging of shipped products, meaning your office is cleaner and greener.
Problem 3: control — innovate and customize for better treatment outcomes
What’s your unique prescription? Because face it, we’re total nerds — and it’s the question we always ask when we meet another orthodontist. What tools do you like using and have consistently found to get the best outcome for your patients? For me, it’s .018 MBT with hooks on the 3’s, 4’s, and 5’s.
What if you could take these familiar and reliable tools and tweak them just a little bit? Combine different slot sizes and appliance architectures that could work more effectively together? Innovation at the push of a button without needing to carry higher levels of inventory.
Powerful new 3D-printing software allows you to use your expertise as a practitioner, combined with the limitless customization of 3D printing. It’s now easy to select the kind of bracket or other fixed appliance you want and customize it to your specifications, including size, slot type, slot size, prescription, hooks, type, prescription, and more, creating exactly what you like to use and what your patient requires.
The future is printed
I’m proud of the work I do every day with patients to improve their smiles, their oral function, and their quality of life. I’m sure you are too. And I’m equally proud of helping my fellow orthodontists to improve their practices and their bottom line while continuing to do the work they love. After all, as orthodontists we’re problem solvers, and I’m excited to continue working with other hardworking problem solvers in practices around the world to improve our profession for ourselves and our patients. OP
20 Orthodontic Practice US Volume 13 Number 4 PRACTICE DEVELOPMENT


goal
is to provide doctors with the absolute best tools. VISION is an end-to-end treatment planner made by doctors, for doctors. We have built VISION to keep the control in your hands, guaranteeing precision, and improving patient outcomes. TREATMENT PLANNING SOFTWARE YOU CAN SMILE ABOUT
See what's new at softsmile.com Our
at SoftSmile
Burstone’s Biomechanical Foundation of Clinical Orthodontics
 Kwangchul Choy, DDS, MS, PhD 2022, Quintessence Publishing Co. www.quintpub.com
Kwangchul Choy, DDS, MS, PhD 2022, Quintessence Publishing Co. www.quintpub.com
Whenever a classical textbook such as Biomechanical Foundation of Clinical Orthodontics reissues in a new edition, it returns to us in a new context. Dr. Burstone (1928-2015) is no longer here, and the book has taken a new title. Additionally, other changes have occurred based on reader feedback that have resulted in the re-creation of all the images for greater clarity, and video files with QR codes now accessible with smartphones or tablets. These videos illuminate and animate some of the topics to simplify readers’ understanding.
This book is the text par excellence for orthodontic biomechanics and should be the first book in every orthodontist’s library, for without the knowledge contained therein, clinicians will struggle to understand many of the iatrogenic creations that challenge and slow patient therapies.
Orthodontic technology continues to proceed — e.g., the 21st century has exploded with new procedures such as bone modification, distraction osteogenesis, temporary anchorage devices, new wire materials, and, of course, aligners. But despite what changes occur in therapies, none of them will supersede the need for a foundation in biomechanics described in this book. And that has special relevance as clinicians attempt to use aligners without such knowledge. Unfortunately, Burstone’s biomechanics are generally poorly understood and thus seldom taught in most orthodontic curricula. This new edition can remedy that intellectual deficit.
Orthodontic clinicians work in a dynamic environment that tests them daily and often severely. My own experience has reinforced the lesson that without a thorough knowledge and application of sound biomechanics that daily task becomes much harder and much less predictable, and readers of this book will discover cures for those lapses.
This new publication has eliminated two previous chapters without jeopardizing its central message, but it still approaches 9 lbs., so it isn’t a tome with which you want to snuggle in bed. Unlike a thrilling novel that readers refer to as “page turners,” this serious book is what I call a “page stopper” because you often need to carefully reread the text and then consider its application and compare the content with one’s own experience. And, finally, by solving the problems at the end of each chapter, readers will quickly learn if they completely understand the material.
Dentists by training and patient expectation are therapists, not diagnosticians, and that results in their being susceptible to new and promising therapies, which they can apply quickly without much thought. For example, one learns to use a new bracket system or incorporate a new Cl II corrector quickly without much effort or thought, whereas learning the lessons
of biomechanics can challenge and even discourage the finest technical practitioner. Additionally, clinicians are inundated with hyperbolic advertisements, endorsements of shills in the employment of manufacturers, and visiting sales representatives. The best antidote for such extravagant claims is to apply scientific biomechanical principles and apply a simple test: New techniques with more marketing than research should undergo scrutiny like Catholic saints — guilty until proven otherwise.
Frederick Crews once aptly said that “Fatigue with rational standards in one generation becomes the pathetic ignorance of them in the next.” Fortunately, Dr. Choy has kept the faith with Dr. Burstone’s rational standards and his intentions with this new edition, and it will continue to be a principal guide for orthodontists as they seek to provide the type of patient care envisioned and practiced by Dr. Burstone. My hope is that orthodontics never suffers fatigue with the biomechanical principles so carefully developed by Dr. Burstone and remembered here by Dr. Choy.
Readers will appreciate the care and quality Quintessence has rendered with this book — e.g., thick pages, excellent images, and a design that encourages readership and increases understanding.
OP
Review by Dr. Larry White.
22 Orthodontic Practice US Volume 13 Number 4 BOOK REVIEW
New Edition of Charles Burstone’s Bestseller
Burstone’s Biomechanical Foundation of Clinical Orthodontics, Second Edition

Kwangchul Choy
This textbook has taught thousands of orthodontists the importance of understanding biomechanics to ensure healthy, predictable movements in clinical practice, and this new edition will undoubtedly do the same for the new generations of students. Technology continues to advance in orthodontics, but no technology can replace a sound understanding of how the teeth move in their periodontal apparatus and how they can be pushed or pulled to get where they need to be. This book is the difference between an orthodontist who can move teeth and an orthodontist who can plan cases with predictability and achieve the sought-after results.
516 pp; 1,584 illus; ©2022; ISBN 978-0-86715-949-3 (B9493); US $190

US $190
CALL: (800) 621-0387 (toll free within US & Canada) • (630) 736-3600 (elsewhere) 11/22 FAX: (630) 736-3633 EMAIL: service@quintbook.com WEB: www.quintpub.com
QUINTESSENCE
PUBLISHING CO INC, 411 N Raddant Rd, Batavia, IL 60510
FA
Q SPECIAL SECTION
Boyd Industries

Market leader for orthodontic operatory equipment
Why is Boyd operatory equipment and cabinetry better than the competition?
As the market leader for orthodontic operatory equipment, Boyd is best known for its ideal design and customizable features combined with proven quality and reliability. The company’s orthodontic products are the industry standard having been time tested over the company’s history by thousands of orthodontists around the world.

Boyd designs and fabricates the widest variety of cabinetry options to fit the size, functionality, and style of your office. The cabinetry line of standard and custom designs sets the company apart from others in the orthodontic industry. The company’s designers can adapt standard configurations or design cabinetry completely unique.
Do Boyd products meet all FDA and regulatory requirements?
Yes, our equipment meets all required regulatory standards for compliance. These include IEC 60601 safety standard for medical/dental devices, CSA for Canadian, and CE for European. The FDA granted clearance of Boyd’s dental delivery units having issued the company a Premarket Notification or better known as a 510(k) for use.
As an internationally certified, ISO 13485:2016 company, Boyd goes through annual independent audits by the British Standards Institute to assure we meet FDA, ISO, and all other regulatory standards.
What makes Boyd unique for orthodontists?
We pride ourselves on providing our customers with the latest technology and innovations in orthodontics. Our operatory products are ergonomically designed to reduce fatigue experienced in running an active orthodontic office, while constructed using durable materials to provide dependable service.
Does Boyd offer financing options?
Boyd has a very competitive program for recent residency graduates and separating military members, offering them significant product discounts or favorable payment terms.
What is the lead time for receiving Boyd equipment, once I place an order?
Despite the volatility of today’s global supply chain, Boyd has been able to better manage its lead times because of the company’s U.S.-based factory and North American supply base. Boyd’s factory fabricates steel, plastic, upholstery, wood, and many other components used in its products. The capability to directly manage much of the product content internally allows the company to maintain lead times to under 8 weeks.
Where can I see Boyd equipment on display?
Boyd attends industry trade shows to display and demonstrate equipment. In addition to trade shows, Boyd has a product showroom at our headquarters in Clearwater, Florida.
Interested in learning more? Please call our sales team at (727) 471-5072, email us at sales@boydind.com, or scan the QR code for details.

24 Orthodontic Practice US Volume 13 Number 4 SPECIAL SECTION
Brava by Brius™ Technologies
Bringing transformative technology to orthodontics
Who is Brius™?
Brius Technologies is a forward-thinking innovation company dedicated to improving the orthodontic experience for both patient and orthodontist.
What is Brava™?
Brava by Brius is a completely new concept in orthodontic treatment — that of Independent Movers™. Brava is the only orthodontic system to provide simultaneous, independent tooth movement, a radical departure from traditional mechanics.
How is Brava different?
Brava is a fundamentally new way to move teeth — with Independent Movement. The movement of any tooth has little to no effect on any other tooth, so the reciprocal forces that cause unwanted side effects in conventional treatment and aligners are essentially nonexistent. Brava moves teeth independently, which results in highly effective and efficient treatment.

How does Brava work?
Brava leverages a digital workflow — digital scan, setup, and treatment plan approval by the orthodontist. Utilizing proprietary Brius Planner Software, precise force and moment are calculated for targeted tooth movement. Brava is then manufactured and delivered to the office.
The Brava system includes custom brackets loaded into digital bonding trays and Brava, which consists of an anchorage base and flexible NiTi arms that connect independently to each tooth via the custom bracket.
As teeth move, their reactive forces translate to Brava’s anchorage base, which then dissipate along the entire arch.
With clinically insignificant reactive forces, Brava’s Independent Mover technology puts each tooth on an independent path to its planned position.
What are Brava’s key features?
• Brava’s optimized biomechanics result in esthetically superior, personalized, convenient, and highly effective treatment.
• The entirety of Brava’s tooth movement is programmed into a NiTi device, active throughout the course of treatment.
• With Brava, there are no wires and no need to wait for larger archwires to start A/P correction as with traditional braces. With Brava’s Independent Mover Technology, A/P correction can be started from the outset of treatment, maximizing treatment efficiency.
• There is no limit to the types of cases Brava can treat.
To learn more about this exciting, technological revolution, visit www.brius.com.

FAQ SPECIAL SECTION
25 orthopracticeus.com Volume 13 Number 4 SPECIAL SECTION
The Brava™ Independent Mover™ System; Brius® Planner Software
Gaidge
FA
Q SPECIAL SECTION
How often do practices look at their data?
Many practices use Gaidge to look at their data every day — and it makes sense, given the critical business insights easily visible within the software. Looking at 80-plus orthodontic metrics and 35-plus key performance indicators can be transformative; it brings granular data to life and broadly illustrates the successes and downfalls often overlooked in manual analyses. Visually comprehensive data also allows orthodontic teams to set annual goals with an easy glance at monthly and quarterly trends.

When should a practice start using Gaidge?


Gaidge is extremely valuable for orthodontic businesses in every phase of the growth process, as it isn’t just limited to those with higher revenue. Every practice needs a clean, solid data foundation regardless of age. Brand-new practices can use Gaidge’s analytics to look for areas of improvement and opportunities for growth. With time, Gaidge compiles their historical data, so they can view a year-over-year (YOY) comparison.
How do I know how my practice is performing in comparison to other practices?
Gaidge not only compares the data of multi-location practices, but also showcases regional comparisons with built-in industry benchmarks. Together these features allow practices to compare themselves to regional counterparts and adjust where it’s needed.
What do you do with the data?
For an orthodontic practice to thrive in a competitive and often challenging market, it must be future-oriented and up-todate on its data. Gaidge provides access to valuable growth metrics, so practices can set and exceed goals. With this insight, orthodontic offices can measure their effectiveness by viewing every step in the patient’s journey from New Patient Adds to
Treatment Efficiency. These details are important because they reflect the business’s overall health and allow teams to move forward with a data-driven strategy for growth.
How do I best use Gaidge with my team?
Gaidge considers every aspect of an orthodontic practice, and running any business involves a clear understanding of its data. How else will practices know if they’re meeting their goals? Financial Coordinators can ditch their spreadsheets — which are time-consuming to update — to analyze revenue metrics like Productions, Collections, and A/R & Delinquency. With treatment efficiency tracking tools, doctors can strategically track patients’ treatment journeys, provide accurate treatment time estimates, and establish patient trust. Gaidge has dashboards for every role in your office to provide accountability and to ensure that your team isn’t spending valuable time manually pulling and analyzing data.
26 Orthodontic Practice US Volume 13 Number 4 SPECIAL SECTION
Scan the QR code to schedule a demo or visit www.gaidge.com/demo.
Advances in orthodontics:
3D-printed appliances
What technological advancements have had the greatest impact on orthodontic laboratories recently?
There have been many technological developments in orthodontic laboratories in the past 2 decades. Intraoral scanning has gone from being a limited-use item to the industry standard — facilitating substantial advancements in the laboratories. We now have 3D printers, 3D wire-bending machines, and CAD/CAM software to help with multiple areas of workflow and the digital design of complete appliances.
Are traditional and printed-metal appliances designed differently?
The designs are identical on permanent dentition. On mixed dentition, bonding pads to the lingual of the teeth can be used for added retention. For example, when fabricating a palatal expander for a patient with short clinical crowns, adding lingual bonding pads to the deciduous molars will provide more retention than lingual extensions.
What are the advantages of printed-metal bands and appliances?
The biggest advantage is the elimination of separator appointments. The bands are designed on the buccal and lingual of the clinical crowns and are attached only through the occlusal embrasures, making tooth separation unnecessary. Other advantages include improved fit as bands are designed to the scans, no blanching of the tissue, and easier delivery and removal.
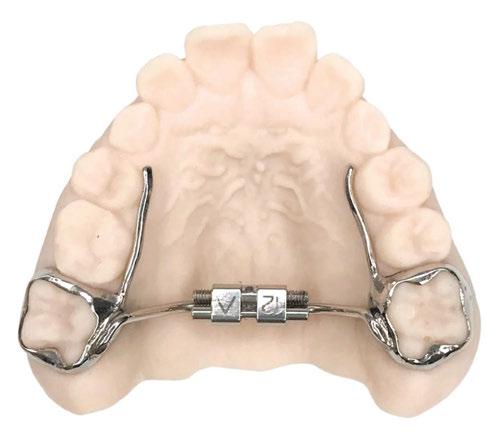
What is the bonding procedure for printed bands?
While the delivery of printed bands is similar to that of traditional bands, there are notable differences in the bonding protocol. The recommended procedure begins with etching the
areas to be bonded, which are bands and any bonding pads. Next, apply a bond enhancer, such as Assure®, and utilize Band-Lok® Plus adhesive. The areas to be etched and bonded are easily identified by the bands or bonding pad areas. Retention depends on the bond strength achieved during delivery.
Are printed bands stronger than traditional bands?
Traditional bands are made from stainless steel, while printed bands are generally made of cobalt-chromium, a stronger and more durable material. Cobalt-chromium can be printed as small as 0.004 inches, offering great versatility in appliance design.
Are there limitations on what appliances can be printed?

Currently, all metal appliances can either be fully printed or have traditionally bent wires attached to printed bands.

FAQ SPECIAL SECTION
27 orthopracticeus.com Volume 13 Number 4 SPECIAL SECTION
Visit us at www.specialtyappliances.com, or scan the
QR code.
Can your orthodontic practice survive a data breach incident?
Mark Pribish offers facts and best practices on how to mitigate a cyberattack


According to a June 2022 Aite-Novarica consumer report titled ”US Identity Theft: Adapting and Evolving,” identity theft has become so prevalent that it affected one-infour U.S. consumers in 2021 along with virtually every type of financial product and commercial platform including dental and orthodontics practices.1

Aite-Novarica Group is an advisory firm providing critical insights on technology, regulations, markets, and operations to hundreds of banks, insurers, payment providers, and investment firms — as well as the technology and service providers that support them. Aite-Novarica Group also released a July 2022 report titled Consumer Scams: Rising in Velocity and Sophistication that reported 34% of U.S. Consumers were Targeted by scams in 2021.2
According to the report, scams have become a regular part of our daily, digital lives with scammers using phishing (fraudulent emails), vishing (fraudulent phone calls and voice mail messages), smishing (fraudulent text messages), and social media to commit their scam tactics to fool victims and commit fraud.
As an orthodontic practice, you should be concerned about identity theft and consumer scam trends for both your practice and your customers. Why? Because of three major data breach incidents affecting the dental and orthodontics business sectors in the first half of 2022.
The first major data breach incident occurred in March. An article announced: “Data breach compromises over 1 million dental and orthodontic patients at a large Texas dental and orthodontics practice, including the sensitive information on over 1 million patients.” Jefferson Dental and Orthodontics (JDC) with 72 offices in Texas reported that hackers had copied documents stored on its servers in the summer of 2021. During this time, JDC discovered malware on its computers, which prompted the company to contract a third-party cybersecurity firm to work on the issue.3
The firm discovered the extent of the breach, which could affect just over 1 million patients, including clinical information,
Educational aims and objectives
This self-instructional course for dentists aims to identify the scope and adverse effects of identity theft and how to respond to a breach.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions by taking the quiz online at orthopracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
• Identify the prevalence of identity theft on dental practices.
• Define identity fraud scams.

• Recognize the ways that identity theft can happen in a business.
• Realize some preventative measures to avoid a cyberattack.
• Realize four best practices to help a dental practice mitigate exposure to data breach and identity theft events.
28 Orthodontic Practice US Volume 13 Number 4 CONTINUING EDUCATION
Mark Pribish is the Practice Leader for Identity Theft and Data Breach Solutions at Scottsdale, Arizona-based Vero, a CU Direct Company. He has authored hundreds of articles and is frequently interviewed by local and national media as an identity theft and data breach risk management expert. He is a member of the Identity Theft Resource Center Board of Directors and is a graduate of the University of Dayton.
2 CE CREDITS
Social Security numbers, driver’s license numbers, dates of birth, health insurance information, and financial information.
If this could happen to JDC, this can happen to any dental and orthodontics practice in the United States. Your practice needs to be prepared (for a data breach incident) or be prepared to lose (regarding fines, penalties, and lawsuits).
The second major data breach incident was in April when the American Dental Association (ADA) confirmed a cyberattack after a ransomware group claimed credit.4 Security researchers who have reviewed the leaked data say that it contains a variety of sensitive information, including W2 and other tax forms, financial spreadsheets, and information about private practices.
While the attack on the ADA itself is a major concern — this may just be the start of something more concerning — with follow-up attacks aimed directly at ADA member practices happening in future months.
The last data breach incident I will reference was reported in July in an article titled “Vendors Ransomware Attack Hits Over 600 Healthcare Clients”: “A ransomware attack on an accounts receivables management firm affects more than 650 covered entity clients, including dental practices, physician groups, and hospitals, resulting in one of the largest health data breaches involving a vendor so far this year.”5
Professional Finance Company (PFC), based in Greeley, Colorado, said in a statement “that on Feb. 26, it ‘detected and stopped a sophisticated ransomware attack’ involving an unauthorized third party accessing and disabling some of the firm’s computer systems.”
While PFC says the incident only affected data on the company’s systems, the vendor released a list of about 660 healthcare entity clients that were affected. Those entities were notified by PFC about the incident on May 5, the company’s statement says.
PFC reported that its investigation “found that files containing individuals’ personal information were accessed in the ransomware incident, including names, addresses, accounts receivable balance, and information regarding payments made to accounts. In some cases, affected information also includes date of birth, Social Security number, and health insurance and medical treatment information.”
According to the U.S. Department of Health and Human Services (HHS), medical identity theft is among the fastest-growing forms of identity theft in the United States.6
So, let’s turn back to identity theft when the 2022 Javelin Strategy Annual Identity Fraud Study found that identity theft and fraud losses totaled $52 billion and affected 42 million U.S. adults in 2021.7 The Javelin study also reported the following:
• 1 in 20 Americans were victims of fraud in 2021.
• The average per victim loss from traditional identity theft and fraud rose to $1,551.
• The average per victim loss from identity fraud scams was $1,029.
• The 2021 statistics show individuals and businesses are unprepared for the tactics criminals are deploying in our modern, digital-first world.
Since identity theft and fraud is constantly evolving, how does the 2022 Javelin Study reflecting 2021 statistics compare to the last two Javelin Studies in 2020 and 2019?
• In 2020, identity theft and fraud losses totaled $56 billion and affected 49 million U.S. adults.
• In 2019, identity theft and fraud losses totaled $16 billion and affected 14.4 million U.S. adults.
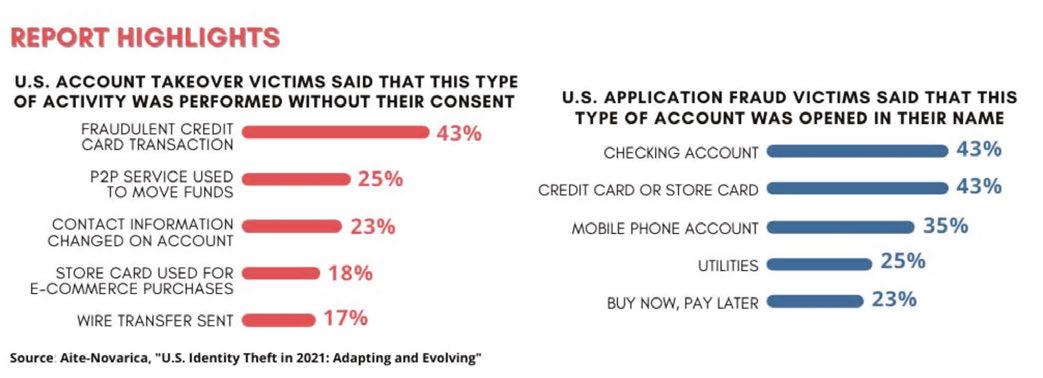
Javelin defines identity fraud as “the unauthorized use of another person’s personal information to achieve illicit financial gain. Identity fraud can range from simply using a stolen payment card account, to making a fraudulent purchase, to taking control of existing accounts or opening new accounts.”
In addition, Javelin defines identity fraud scams as “relatively easy to orchestrate and present an opportunity for criminals to bypass the fraud detection barriers maintained by financial services providers because they directly target the consumer.”
However, it’s not just about individuals and your orthodontic practice customers and employees — it’s also about your small to medium-size business (SMB). Most dental and orthodontic practices fall into the SMB category, and most SMBs are the new targets for hackers and the insider threat.
According to Chubb, one of the leading property and casualty insurance companies in the world, “the reputational costs of cyberattacks can ruin small and medium firms” in a report titled
29 orthopracticeus.com Volume 13 Number 4 CONTINUING EDUCATION
“Cyber Attack Inevitability: The Threat Small and Midsize Businesses Cannot Ignore.”8
Unfortunately, most small businesses, including orthodontic practices, continue to believe they are not targets for cyber and identity theft criminals based on their size and/or small databases of personally identifiable information (PII).
However, the reality of identity theft and data breach makes the threat landscape for small businesses a high-risk target for both cyber and identity theft criminals, along with the insider threat such as current and former employees, contractors, vendors, social engineering, and phishing.
The Chubb report stated that “the average price tag for a business to recover after a cyberattack is $400,000, which can be fatal for small and medium-size enterprises (SMEs).”
One of the reasons hackers and identity theft criminals are shifting their attention to smaller targets is that small businesses tend to lack information security and governance best practices compared to larger businesses.
When small- to medium-size businesses struggle to identify a data breach event and then struggle even more to report and respond to a breach, the total cost of the breach increases because of direct costs, indirect costs, and lost opportunity costs.
So, how can small businesses protect their organization?
The Chubb report concluded that “the majority of cyber incidents are preventable, as they mostly stem from human error or a simple lack of proper training [and Chubb] recommended [small businesses] take the following preventative measures:
1. Create a cyberattack response plan, and invest in the resources to ensure the plan can be executed.
2. Use a secure password manager to make it easier for employees to manage their credentials in a secure manner.
3. Educate employees about the risks of cybercrime and deploy software that can reduce social-engineering attacks such as phishing.
4. Install good antivirus software, and ensure it is always up-to-date.
5. Update operating systems and applications regularly to ensure they are supported by the manufacturer.
6. Protect networking activity with a secure router on your internal network and a virtual private network (VPN) externally.
7. Purchase a comprehensive cyber insurance policy.
In addition to the built-in loss mitigation services to reduce the risk of being targeted in the first place, a cyber insurance policy will likely include incident response services if an attack succeeds.
Small businesses need to recognize that hackers, identity theft criminals, and the insider threat are current and future risks.
Small businesses also need to accept responsibility in protecting their customer and employee information by increasing employee education, investing in new technology, and creating a formal data breach response and recovery plan.
Specific to your orthodontic practice, the FBI reported on an alarming rise in the cost of cyberattacks in its 2022 FBI Internet Crimes Report — and estimated losses to businesses to fraudulent activity at $6.9 billion led by phishing and business email compromises.9
Key points of the report included the following:
• Business email compromise complaints to the FBI in 2021 accounted for more than a third of all reported cyber losses.
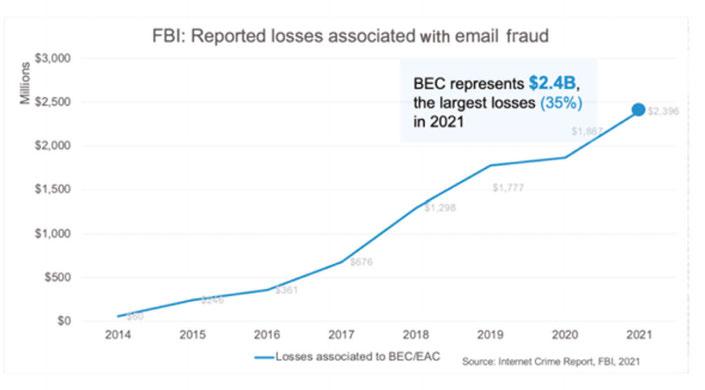
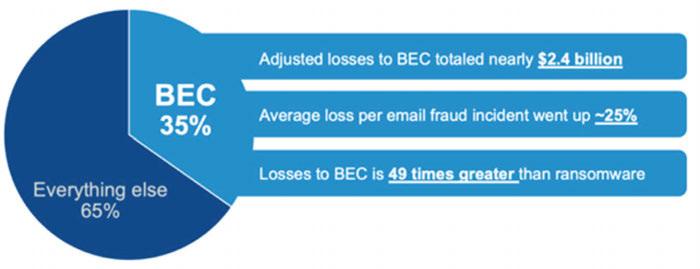
• Virtual meeting platforms represent a growing risk with access gained through BEC, spoofing, and deep fakes.
• Healthcare, financial services, and IT topped the list of business sectors hit by ransomware attacks.
According to the FBI’s Internet Crime Report for 2021, losses
30 Orthodontic Practice US Volume 13 Number 4 CONTINUING EDUCATION
from cyberattacks spiked 64% to $6.9 billion, the biggest increase since 2018.
Consistent with the trends identified in the FBI’s report on 2020 complaint levels, phishing and variants such as smishing and vishing were the leading threat vectors in 2021, rising 34% annually to nearly 324,000 incidents and racking up losses of $44.2 million.
One of the reasons hackers and identity theft criminals are shifting their attention to smaller targets is that small businesses tend to lack information security and governance best practices compared to larger businesses.
Business email compromise and email account compromise complaints were smaller in aggregate number than phishing but larger in impact. Nearly 20,000 BEC/ EAC complaints accounted for $2.4 billion in losses, slightly more than a third of the total losses tallied by the FBI across the full range of cyberattacks. (Note that the FBI includes some defrauded individuals’ transactions, known as EAC, in the predominantly business targeted BEC statistics.)
Overall, the FBI strongly encourages a heightened attention (and awareness) among businesses and consumers to an “urgent need” for cyber incident reporting to federal authorities. In addition to phishing and BEC, the threats tracked by the FBI include ransomware, tech support fraud, and identity theft — all of which grew in number.
To conclude, 43% of all cyberattacks target small business. Every small business, including dental and orthodontic practices, should implement information security and governance best practices.
The following four best practices will help your small business mitigate its exposure to data breach and identity theft events:
Best Practice No. 1 — Every dental office needs to understand how and where their technologies and systems comingle with the cybersecurity threat landscape. However, staying on top of all the security news and knowing the latest security trends is a time-consuming and challenging task. I recommend regularly reading Brian Krebs, who is the author of a daily blog covering cybersecurity, data breach, and cybercrime trends.10
Best Practice No. 2 Have a written information security and governance policy, and update this policy each year. Once complete, have every employee — even if your dental office has two to five employees — sign this information security policy document acknowledging that he/she has read, understands, and agrees to said policy. The National Institute of Standards and Technology has created a template document titled Small Business Information Security Fundamentals, which can help your dental practice create such a policy.11
Best Practice No. 3 Have a data breach risk management plan in place. The lack of cybersecurity preparedness, data breach planning, and employee privacy training have made dental offices a target for cybercriminals. The Federal Communication Commission (FCC) created a “Small Biz Cyber Planner” (https://www.fcc.gov/cyberplanner)12 to help small businesses create customized cybersecurity plans. Your dental practice can use this tool to create and save a custom cyber security plan.
Best Practice No. 4 Every dental office should consider having a cyber liability insurance policy, which can help protect
your business from cybercrime and a data breach incident. The CEOs and CIOs of Equifax and Target were not fired because they were hacked or breached; they were fired for their failed management response to their breach events. Cyber insurance can help your dental office be resilient and compromise ready. Talk to your insurance agent or broker about cyber insurance.
REFERENCES
1. Aite-Novarica consumer survey: Identity theft has become so prevalent that it affected one-in-four U.S. consumers in 2021, along with virtually every type of financial product, commercial platform, and government support. June 2022. https://www. prnewswire.com/news-releases/one-in-four-us-consumers-impacted-by-identitytheft-in-2021-aite-novarica-consumer-survey-finds-301562742.html#:~:text=Twenty%2Dfive%20percent%20of%20U.S.,to%20the%20COVID%2D19%20pandemic. Accessed November 2, 2022.
2. Aite-Novarica consumer survey: 34% of U.S. Consumers were targeted by scams in 2021, Aite-Novarica Group Consumer Survey Finds. July 2022. https://aite-novarica. com/34-us-consumers-were-targeted-scams-2021-aite-novarica-group-consumer-survey-finds#:~:text=Scams%20have%20become%20a%20regular,type%20of%20scam%20in%202021. Accessed November 2, 2022.
3. Data Breach Compromises Over 1 Million Dental Patients. March 23, 2022. https:// orthodonticproductsonline.com/practice-management/it/data-breach-compromisesover-1-million-dental-patients/. Accessed November 2, 2022.
4. American Dental Association confirms cyberattack after ransomware group claims credit. April 27, 2022. https://therecord.media/american-dental-association-cyberattack-black-basta/. Accessed November 2, 2022.
5. Vendor’s Ransomware Attack Hits Over 600 Healthcare Clients. July 5, 2022. https:// www.govinfosecurity.com/vendors-ransomware-attack-hits-over-600-healthcare-clients-a-19506. Accessed November 2, 2022.
6. U.S. Department of Health and Human Services — Office of Inspector General: Medical Identity Theft. https://oig.hhs.gov/fraud/consumer-alerts/medical-identity-theft/. Accessed November 2, 2022.
7. Identity Fraud Losses Total $52 Billion in 2021, Impacting 42 Million U.S. Adults – March 29, 2022 https://www.globenewswire.com/news-release/2022/03/29/2412099/0/en/ Identity-Fraud-Losses-Total-52-Billion-in-2021-Impacting-42-Million-U-S-Adults.html .Accessed November 2, 2022.
8. Chubb issues warning over potential cyberattacks against SMEs. February 20, 2019. https://www.insurancebusinessmag.com/nz/news/cyber/chubb-issues-warning-overpotential-cyberattacks-against-smes-159439.aspx Accessed November 2, 2022.
9. FBI Releases 2021 Internet Crime Report. March 29, 2022. https://www.ic3.gov/Media/ PDF/AnnualReport/2021_IC3Report.pdf Accessed November 2, 2022.
10. The Top 5 Cybersecurity Threats to Small Business in 2022. https://www.score.org/ resource/top-5-cybersecurity-threats-small-businesses-2022. Accessed November 2, 2022.
11. National Institute of Standards and Technology Small Business Information Security Fundamentals. https://www.govinfo.gov/content/pkg/GOVPUB-C13-7bad944538579 c44b5b3ba35f2fb8f13/pdf/GOVPUB-C13-7bad944538579c44b5b3ba35f2fb8f13. pdf. Accessed November 2, 2022.
12. Federal Communication Commission (FCC): Cyberplanner. https://www.fcc.gov/cyberplanner. Accessed November 2, 2022.
31 orthopracticeus.com Volume 13 Number 4 CONTINUING EDUCATION
OP
Continuing Education Quiz
Can your orthodontic practice survive a data breach incident? PRIBISH
1. According to a June 2022 Aite-Novarica consumer report titled, “US Identity Theft: Adapting and Evolving,” identity theft has become so prevalent that it affected ________ U.S. consumers in 2021 along with virtually every type of financial product and commercial platform, including dental and orthodontic practices.
a. one-in-four b. one-in-five c. one-in-six d. one-in-seven
2. Aite-Novarica Group also released a July 2022 report titled “Consumer Scams: Rising in Velocity and Sophistication” that reported ______ of U.S. consumers were targeted by scams in 2021.
a. 23% b. 34% c. 65% d. 72%
3. According to the report, scams have become a regular part of our daily, digital lives with scammers using ________ and social media to commit their scam tactics to fool victims and commit fraud.
a. phishing (fraudulent emails)
b. vishing (fraudulent phone calls and voice mail messages)
c. smishing (fraudulent text messages) d. all of the above
4. According to the U.S. Department of Health and Human Services (HHS), _______ is/are among the fastest-growing forms of identity theft in the United States.
a. click-bait b. pop-up ads c. medical identity theft d. telemarketing calls
5. One of the reasons hackers and identity theft criminals are shifting their attention to smaller targets is that small businesses ________. a. do not oversee employees who work on the computer as much b tend to lack information security and governance best practices compared to larger businesses c. tend to hire fewer computer-savvy employees d. do not expect to get hacked
6. The Chubb report concluded that “the majority of cyber incidents are preventable, as they mostly stem from _______.”
a. human error b. a simple lack of proper training
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 16 CE credits for only $149; call 866-579-9496, or visit https://orthopracticeus.com/subscribe/ to subscribe today.
n To receive credit: Go online to https://orthopracticeus.com/continuingeducation/, click on the article, then click on the take quiz button, and enter your test answers.
AGD Code: 550
Date Published: December 10, 2022
Expiration Date: December 10, 2025
c. intent to do harm d. both a and b
2 CE CREDITS
7. One preventative measure for a small business to take is to use a _______ to make it easier for employees to manage their credentials in a secure manner.
a. secure password manager b. handwritten list of passwords in a locked drawer c. common password for all password-protected applications d. a password in a disguised folder on the desktop
8. Small businesses also need to accept responsibility in protecting their customer and employee information by ________. a. increasing employee education b. investing in new technology c. creating a formal data breach response and recovery plan d. all of the above
9. One of the author’s best practices is to _________. a. have a discussion about the newest hacks at each weekly meeting b. send a memo to the staff that using social media in the office is prohibited c. have a written information security and governance policy, and update this policy each year d. none of the above
10. The Federal Communication Commission (FCC) created a “Small Biz Cyber Planner” to help small businesses create customized cybersecurity plans.
a. True b. False
To provide feedback on CE, please email us at education@medmarkmedia.com
Legal disclaimer: Course expires 3 years from date of publication. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
32 Orthodontic Practice US Volume 13 Number 4 CONTINUING EDUCATION
Dental infections: help avoid antimicrobial resistance — part 1
 Wiyanna K. Bruck, PharmD, and Jessica Price start their discussion
Wiyanna K. Bruck, PharmD, and Jessica Price start their discussion
on the judicious use of antibiotics in the dental practice
Introduction
Antibiotics are one of the greatest medical advances since their first introduction in the late 1920s. Alexander Fleming’s breakthrough discovery of penicillin paved the way for a domain of medicine that has enabled once deadly infections to be readily treatable.1
Excessive antibiotic use comes with steep consequences of real-time adverse effects; downstream antibiotics resistance (also referred to as collateral damage); and superinfections, such as Clostridioides difficile. Overuse and inappropriate use of antibiotics has led to an increased prevalence of resistance, which translates to limited effectiveness of antibiotics, increased healthcare cost, and rising mortality rates. Antibiotic resistance is recognized as a global health threat. According to the Centers for Disease Control and Prevention (CDC), approximately 2 million Americans are infected with resistant pathogens that result in 23,000 deaths annually.2 The CDC conservatively approximates that 30% of all outpatient antibiotic prescriptions written from 2010 to 2011 were unnecessary.3 If the previous statistic was applied to the 2020 CDC data for number of antibiotic prescriptions written by dental practitioners in the United States, 7.29 million antibiotic prescriptions would be deemed as inappropriate within that 1 year.4
Judicious antimicrobial prescribing is essential in all fields of healthcare, including dentistry.5-7 The 5Ds of antimicrobial stewardship is a popular concept that should be applied to the appropriate prescribing of antibiotics. The 5Ds, include the right Drug, Dose, Delivery route, Duration of therapy, and De-escala-
Wiyanna K. Bruck, PharmD, BCPS, BCIDP, BCPPS, is an assistant professor of Pharmacy Practice at South College School of Pharmacy as well as an Antimicrobial Stewardship and Emergency Medicine Clinical Pharmacist practicing at a community hospital. She teaches infectious diseases as well a pediatric pharmacotherapy to both pharmacy and physician assistant students. Dr. Bruck received her bachelor of science degree in biology, followed by a Doctorate of pharmacy degree, then completed a postgraduate pharmacy residency program at William Beaumont Hospital in Troy, Michigan. Her research interests include antimicrobial stewardship, infectious diseases, as well as food allergy awareness. Dr. Bruck is Boardcertified in pharmacotherapy, infectious diseases, and pediatrics.
Jessica Price is a Doctor of Pharmacy candidate at South College School of Pharmacy in Knoxville, Tennessee. She has a Bachelor of Arts degree in Advertising and Public Relations, with minors in Business and English Writing from the University of Central Florida. Price completed her post-baccalaureate track in Biology at Florida International University and at the University of Tennessee, Knoxville.
Educational aims and objectives
This self-instructional course for dentists aims to provide an overview of judicious use of antibiotics in the dental practice.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions by taking the quiz online at orthopracticeus.com to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:

• Identify bacterial pathogens implicated in dental infections.
• Identify antibiotic treatment for specific dental infections.
• Analyze how to determine the drug-of-choice for certain treatments.
Analyze prescribing indications related to duration of treatment.
• Recognize considerations related to the administration of medications for pediatric patients.
tion.8 Along with the concept of the 5Ds of optimal antimicrobial therapy, the CDC has constructed a Checklist for Antibiotic Prescribing in Dentistry (see Table 1), which serves as an excellent introduction to concepts that will be discussed in further detail.9
Bacterial pathogens implicated in dental infections
An odontogenic infection is a frequently encountered infection of the alveolus, jaws, or face that begins from a tooth or from its supporting structures. The most common cause of dental infections are dental caries, deep filling or failed root canal treatments, pericoronitis, and periodontal disease. The infection remains where it originates at the tooth or can spread into adjacent tissue or structures. The course of infection depends on several elements, including the virulence of the oral pathogens, the host resistance factors, and the surrounding anatomy.10
Determining the drug-of-choice for the treatment of odontogenic infections requires an understanding of which pathogens are implicated and whether antibiotics are truly necessary. Even when antibiotics are needed to treat dental infections, they might not be the first line therapy, but rather an adjunct after surgical drainage of an abscess, tissue debridement, or below the gum manipulation.
Bacteria that are frequently found in dental infections normally comprise the typical oral flora, which include a mixture of gram-positive streptococci (e.g., Streptococcus anginosus,
33 orthopracticeus.com Volume 13 Number 4 CONTINUING EDUCATION
2 CE CREDITS
Table 1: Checklist for antibiotic prescribing in dentistry
Pretreatment
• Correctly diagnose an oral bacterial infection.
• Consider therapeutic management interventions, which may be sufficient to control a localized oral bacterial infection.
• Weigh potential benefits and risk (i.e., toxicity, allergy, adverse effects, risk for Clostridium difficle infection) of antibiotics before prescribing.
• Prescribe antibiotics only for patients of record and only for bacterial infections you have been trained to treat. DO NOT prescribe antibiotics for oral viral infections, fungal infections, or ulcerations related to trauma or aphthae.
• Implement national antibiotic prophylaxis recommendations for medical concerns for which guidelines exist (e.g., cardiac defects).
• Assess patients’ medical history and conditions, pregnancy status, drug allergies, and potential for drug-drug interactions and adverse events, any of which may impact antibiotic selection.
Prescribing
• Ensure evidence-based antibiotic references are readily available during patient visits. AVOID prescribing based on non-evidence-based historical practices, patient demand, convenience, or pressure from colleagues.
• Make and document the diagnosis, treatment steps, and rationale for antibiotics (if prescribed) in the patient chart.
• Prescribe only when clinical signs and symptoms of a bacterial infection suggest systemic immune response, such as fever or malaise along with local oral swelling.
• Revise empiric antibiotic regimens on the basis of patient progress and, if needed, culture results.
• Use the most targeted (narrow-spectrum) antibiotic for the shortest duration possible (2 to 3 days after clinical signs and symptoms subside) for otherwise healthy patients.
• Discuss antibiotic use and prescribing protocols with referring specialists.
Patient Education
• Educate your patients to take antibiotics exactly as prescribed, take antibiotics only prescribed for them, and not to save antibiotics for future illness.
Staff Education
• Ensure staff members are trained in order to improve probability of patient adherence to antibiotic prescriptions .
Streptococcus mutans, Streptococcus intermedius group); anaerobic gram-negatives (e.g., Bacteroides spp, Prevotella spp., Fusobacterium); anaerobic gram-positives (e.g., Actinomyces spp., Peptostreptococci); and some rarer aerobic gram-negatives such as Eikenella corrodens. In general, the routinely used antibiotic agents (natural penicillin, aminopenicillin, penicillin combined with a β-lactamase inhibitor, and first-generation cephalosporins, tetracyclines, and macrolides) have good empiric coverage of the commonly implicated pathogens with the exception of coverage against anaerobic gram-negative bacilli.11-14 If there is a reason to suspect Prevotella species or other anaerobic gram-negative bacilli such as Fusobacterium or Bacteroides spp. that are positive for β lactamase (e.g., surveillance data suggest high prevalence), metronidazole is often added to the empiric coverage.5
Antibiotic treatment in dental infections
Pulpal pain, gingivitis, and periodontitis
Antibiotics are infrequently necessary for pulpal pain, gingivitis, and periodontitis. Irreversible pulpitis is characterized by acute and intense pain and is one of the most frequent reasons that patients seek emergency dental care. Antibiotics are not effective at treating pulpal pain, and treatment is not deemed appropriate if the patient has no signs of a spreading infection or systemic symptoms. Most important to note, inappropriate treatment of pulpal pain does not prevent the development of severe complications. Evidence suggests that combination therapy with nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen during meals and at bedtime is an effective way to manage pulpal pain.16 Aside from the removal of the tooth, the usual
approach in the management of pulpitis is relieving the pain by drilling the tooth and removing the inflamed pulp and cleaning the root canal. There is no proof of benefit with using analgesics and or antibiotics in irreversible pulpitis.
Most patients with gingivitis or periodontitis can be effectively treated with mechanical debridement or scaling and root planing (SRP) without the need of antibiotic therapy. In patients that lack a response to SRP alone and have few sites of disease, a onetime local delivery of topical antibiotic can be utilized (e.g., chlorhexidine 2.5 mg chip, doxycycline 10% gel, minocycline 1 mg microsphere, or tetracycline 12.7 mg fiber). In patients with refractory cases that have extensive disease or those with severe or aggressive disease, strong evidence suggests adjunctive systemic antibiotics. Obtaining a culture to guide therapy prior to initiation is strongly encouraged if feasible.17-19
Abscesses
Most dental abscesses are secondary to dental caries and, therefore, can largely be prevented when basic and consistent preventative oral health measures are followed. Dental infections are common, including suppurative infections (abscesses), but not all need to be treated with antibiotics. It is therefore important to elucidate the presence of regional or hematologic spread suggesting disseminated infection and distinguish local versus systemic signs and symptoms of infection.20
Additionally, the treatment of abscesses depend on the location. If the dental abscess is localized, incision and drainage (I&D) alone is usually sufficient for proper recovery. In these cases, the patient will have a better outcome with a procedural
34 Orthodontic Practice US Volume 13 Number 4 CONTINUING EDUCATION
I&D to obtain source control in comparison to the ineffective use of antibiotics alone. If the abscess is in the periapical region, treatment, including I&D, endodontic therapy, and adjunctive antibiotics are recommended.20-22 In patients who have severe systemic illness, in-patient treatment with intravenous antibiotics initially is generally justified.
If antibiotics are deemed necessary for either non-suppurative or suppurative odontogenic infections the agent selection is based on the coverage of oral typical oral pathogens. Historically, the drugs of choice were amoxicillin or penicillin V potassium. Although both agents were regarded as first line, amoxicillin was generally preferred due to having more robust gram-negative anaerobic coverage, less frequent dosing, ability to be taken on an empty stomach, and a lower incidence of gastrointestinal side effects.
However, some experts recommend additional coverage of β-lactamase producing Prevotella and Fusobacterium with amoxicillin/clavulanate or a historic agent combined with metronidazole. Cephalexin — a first-generation cephalosporin with similar gram-positive aerobic coverage as the historic first line agents but that lacks robust anaerobic activity — is the antibiotic of choice in those with a history of penicillin allergy without history of anaphylaxis, angioedema, or hives. In patients with a severe allergy to penicillin agents or other β-lactams, azithromycin or clindamycin can be prescribed. When deciding on an agent to use for dental infection, consider azithromycin has higher rates of gram-positive aerobic resistance and clindamycin
Table 2: Antibiotics for dental infections in adult patients15,20
substantially increases the risk of developing a Clostridioides difficile infection but has much more robust coverage of mouth flora with the exception of Eikenella. Therefore, the risks and benefits of treatment in patients with a severe β-lactam allergy should be weighed prior to prescribing an alternative agent.20-23 A summary of antibiotics used for dental infections in adult patients as well as red flags for progressing infection are available in Table 2.
Duration of treatment
If treatment is initiated for non-suppurative indications (e.g., gingivitis and periodontitis), antibiotic therapy is usually until oral lesions have healed and pain has subsided, typically 5 to 7 days. Antibiotic duration of therapy for suppurative infections is usually 3 to 7 days depending on clinical improvement. The implementation of follow-up for patients initiated on antibiotic therapy is of utmost importance. Dentists should reevaluate patients for improvement or lack thereof with an in-person visit, telehealth appointment, or follow-up phone call. In general, most patients can stop taking antibiotics after 24 hours of complete symptom resolution, irrespective of re-evaluation after 3 days. If patient symptoms do not improve with initial therapy, clinicians should consider broadening therapy by either adding metronidazole to first- line therapy or discontinuing initial therapy and beginning amoxicillin/clavulanate (both options are typically for a 7-day duration).23
With adequate source control, short antibiotic courses have been found to be effective. A prospective clinical study was
Antibiotic Dose Forms Usual Dosing
Gingivitis (streptococci [e.g., Streptococcus mutans), Actinomyces spp.])
amoxicillin 500 mg PO TID + metronidazole 250 – 500 mg PO BID/TID∆ OR
Common Side Effects
ampicillin/sulbactam 3 g IV Q6h OR
ceftriaxone 2 g IV every 24 hours + metronidazole 500 mg IV q8h Periodontitis (Aggregatibacter actinomycetemcomitans, Porphyromonas, Treponema, Prevotella)
Abscess (streptococci, Peptostreptococcus spp, Bacteroides, and other oral anaerobes [+ Pseudomonas and other gram-negative bacilli IF patient is immunocompromised])
amoxicillin/clavulanate 250 –500 mg PO BID/ TID or 875 mg PO BID¥
amoxicillin/ clavulanate 250 –500 mg PO BID/ TID or 875 mg PO BID¥
clindamycin 300 – 450 mg PO Q6h# OR doxycycline 100 mg PO BID OR azithromycin 500 mg PO Day 1 then 250 mg PO x 4 days
clindamycin 300 – 450 mg PO Q6h# OR moxifloxacin 400 mg PO daily* OR levofloxacin 750 mg PO daily + metronidazole 250 – 500 mg PO BID/TID∆
ampicillin/sulbactam 3 g IV Q6h OR aqueous penicillin G 2 – 4 million units + metronidazole 500 mg IV q8h OR
Piperacillin/tazobactam 4.5 g IV every 6 hours±
Red flags: might indicate spreading infection
Tachycardia, tachypnea, raised tongue/drooling, difficulty speaking, swallowing, breathing, lymphadenopathy, pyrexia, trismus, dehydration, hypotension, ↑ WBC, periorbital cellulitis
PO = oral, IV = intravenous; BID = twice daily; TID = three times daily; q6h = every 6 hours; WBC = white blood cell
¥ More expensive than amoxicillin, more gastrointestinal upset (mainly diarrhea), more broad coverage includes anaerobes and gram negative pathogens
∆ Add-on agent if Prevotella is suspected
# Considered 1st line in severe cases, those with penicillin/β-lactam allergy, or if anaerobes predominant, does NOT cover Eikenella
* Only consider in patients intolerant or allergic to penicillins/β-lactams/clindamycin
± Addition of agent with Pseudomonas aeruginosa and other gram-negative bacilli coverage if patient is immunocompromised
35 orthopracticeus.com Volume 13 Number 4
CONTINUING EDUCATION
Table 3: Antibiotics for dental infection in pediatric patients33-41
Antibiotic Dose FormsUsual Dosing Common Side EffectsComments
Amoxicillin (penicillin/ β-lactam antibiotic)
Amoxicillin/ Clavulanate (penicillin/ β-lactam- β-lactam inhibitor combination antibiotic)
Azithromycin (macrolide antibiotic)
Suspension, chewable tablet, tablet, capsule
Suspension, chewable tablet, tablet
Infants > 3 months of age < 40 kg: 25–45 mg/kg/day in divided doses every 12 hours (max 875 mg/dose)
Infants > 3 months of age: 25–45 mg/ kg/day in divided doses every 12 hours (max 875 mg/dose; dosed off the clavulanate component)
Nausea, vomiting, headache, diarrhea May take with or without food
Nausea, vomiting, diarrhea, diaper rash
Suspension, tablet, capsule, injectable
Cephalexin (1st generation cephalosporin/ β-lactam antibiotic)
Children ≥ 6 months up to 16 years old: 10 – 12 mg/kg on day 1 (max of 500 mg), followed by 5 – 6 mg/kg once daily x 4 days (max of 250 mg/day) [total duration of 5 days]
Headache, stomach pain or diarrhea, nausea, vomiting
Suspension, tablet, capsule
Clindamycin (lincomycin antibiotic)
Doxycycline (tetracycline antibiotic)
Metronidazole (nitroimidazole antimicrobial)
Suspension, capsule, injectable
Infants, children, and adolescents (mild–moderate infection): 25–50 mg/kg/day divided every 6 to 12 hours [max of 2 grams/day]) Severe infection: 75–100 mg/kg/day divided every 6–8 hours (max of 4 grams/day)
10–25 mg/kg/day in divided doses every 8 hours (max 450 mg/dose)
Methicillin resistant Staphylococcus aureus (MRSA) 30–40 mg/kg/day in divided doses every 6–8 hours
Nausea, vomiting, abdominal pain, diarrhea
With or without meals, w/meals increases absorption and decreases GI upset. ES needs to be taken with food. Use the lowest dose of clavulanate to decrease GI side effects
Option for patients with Type 1 allergy to penicillin or cephalosporin antibiotics; can cause cardiac arrhythmias in patients with preexisting cardiac conduction defects
Should not be used in those with a history of anaphylaxis, angioedema, or urticaria with penicillin agents
Stomach pain, diarrhea, nausea, vomiting, bad taste in mouth
Suspension, tablet, delayed release tablet, capsule, injectable
Suspension, tablet, extended release tablet, capsule, injectable
Children > 8 years old: 2.2 mg/kg/dose every 12 hours (max 100 mg/dose)
Children and adolescents (anaerobic skin and bone infections): 15–50 mg/ kg/day in divided doses 3 times daily (max of 2,250 mg/day)
Penicillin V potassium (penicillin/β-lactam antibiotic)
Liquid solution, tablet
Children and adolescents: 25–50 mg/ lg/day in divided doses every 6 hours (max of 2 grams/day)
performed over a 3-year period with the objective to evaluate shortened courses of antibiotics in the management of dentoalveolar abscesses. After abscess drainage, patients were treated with amoxicillin, erythromycin, or clindamycin. A robust 98.6% of the 759 patients had full resolution of symptoms at day three of treatment, and antibiotics were discontinued at that time. The study concluded that the duration of antibiotics in most patients with acute dentoalveolar infections can safely be 2 to 3 days, provided I&D has been performed.26
Antibiotic treatment — pediatric considerations
The administration of medications for pediatric patients is even more complex compared to adults because of the need to dose based on the child’s weight and take into consideration concerns that are not applicable to adults. Adverse reactions
Tooth discoloration, nausea, vomiting, diarrhea, lack of appetite
Black boxed warning: Clostridioides difficile-associated diarrhea; Option for patients with Type 1 allergy to penicillin and/or cephalosporin agents; no longer recommended for infective endocarditis prophylaxis
Administer with or without food (with food decreases stomach upset, but can also decrease absorption); take with fluid and remain in upright position to decrease throat irritation)
Constipation, diarrhea, stomach pain, stomach cramps, nausea, vomiting, metallic taste, headache, joint pain
Nausea, vomiting, abdominal pain, tongue discoloration, diarrhea
Black Boxed Warning: Carcinogenic in rats and mice, unnecessary use should be avoided; ingestion of alcohol as a beverage or an ingredient in medications or propylene glycol-containing products should be avoided
Should be taken on empty stomach for adequate absorption
caused by antibiotics are the most commonly reported reason for emergency department (ED) visits by those who are under the age of 18, which is represented by 140,000 ED visits each year specifically due to antibiotic adverse drug events.27
In addition, pediatric patients still have the same risks of side effects from antibiotics as adult patients, including the potential of increased resistance, allergic reactions, development of Clostridioides difficile infections, drug interactions, and common as well as rare side effects. Pediatric patients as young as 4 years old were found to harbor multidrug resistant bacteria in their mouths because of the overuse of antibiotics.28 Moreover, some antibiotics routinely used in adults have either not been studied in children or have demonstrated concern in animal models or in pediatric case reports. Tetracyclines and fluoroquinolones are two classes of antibiotics that are generally avoided in children.29
36 Orthodontic Practice US Volume 13 Number 4 CONTINUING EDUCATION
Tetracycline antibiotics (including doxycycline) may cause permanent tooth discoloration, enamel hypoplasia in developing teeth, and hyperpigmentation of the soft tissues. Because of the tooth and soft tissue related side effects of tetracyclines, their use is not recommended for pregnant women or children under the age of 8 years old. However, short-term (less than 21-day) use of doxycycline is advocated by the American Academy of Pediatrics as appropriate when benefits outweigh risks for certain infections due to the lack of evidence of the tooth discoloration side effect.30 Fluoroquinolone antibiotics appear at first glance to be an attractive choice since they are broad-spectrum agents, highly active in vitro against gram-positive and gram-negative pathogens, and are dosed only 1 to 2 times a day. However, these agents have numerous warnings associated with their use in patients of all ages as well as concerns related to increased possibility of musculoskeletal adverse effects in children.30 Fluoroquinolone (moxifloxacin) use within dentistry should be reserved for pediatric patients who are unable to take firstand-second line agents due to allergy or resistance.
When a dental clinician is considering antibiotic use in children, it is important as with adults to make sure that antibiotics are truly warranted.30-33 If caregivers are pressing for a prescription despite lack of evidence for necessity, it is wise to educate on the downstream negative effects. If antibiotics are considered appropriate, dosing and route of delivery should be taken into consideration as well as common and uncommon red flags for use in pediatrics (summarized in Table 3).33-41 Not only should the negative effects of antibiotics be discussed, but the prevention of dental caries with appropriate oral health maintenance should be reinforced.32
Summary
It is important to properly walk the fine line of treating infections that need to be managed with a short course of narrow spectrum antibiotics versus overprescribing antibiotics for either noninfectious indications or localized dental infections that don’t warrant antibiotics. With judicious use of antibiotics, dental practitioners can help curb the global threat of antibiotic resistance as well as avoid unnecessary side effects and increased cost for patients. Table 1 provides a summary of tools that can enable such practice.
Disclaimer
Clinician expertise in addition to evidence should be used when making treatment decisions for patients.
REFERENCES
1. Macfarlane G. Alexander Fleming: The Man and the Myth. Harvard University Press; 1984.
2. Centers for Disease Control and Prevention. Antibiotic Resistance Threats in the United States; 2013.
3. Fleming-Dutra KE, Hersh Al, Shapiro DJ, et al. Prevalence of inappropriate prescriptions among US ambulatory care visits, 2010-2011. JAMA. 2016;315(17):1864-1873.
4. Centers for Disease Control and Prevention. Outpatient Antibiotic Prescriptions – United States, 2020.
5. Fluent MT, Jacobsen PL, Hicks LA. Considerations for responsible antibiotic use in dentistry. J Am Dent Assoc. 206:147(8):683-686.
6. Durkin MJ, Hsueh K, Haddy Y, et al. An evaluation of dental antibiotic prescribing practices in the United States. J Am Dent Assoc. 2017:148(12):878-886
7. Ralph D, Azarpazhooh, Laghapur N, Suda KJ, Okunseri C. Role of dentists in prescribing opioid analgesics and antibiotics: an overview. Dent Clin North Am. 2018: 62(2):279-294.
8. Joseph J, Rovold KA. The role of carbapenems in the treatment of severe nosocomial infections. Expert Opin Pharmacother. 2008;9(4):561-574.
9. Centers for Disease Control and Prevention. Antibiotic Stewardship. https://www.cdc.gov/ oralhealth/infectioncontrol/faqs/antibiotic-stewardship.html. Accessed June 23, 2022.
10. Ogle OE. Odontogenic Infections. Dent Clin N Am. 2017(61):235-252.
11. Dental and Periodontal Infections. In: Ryan KJ. eds. Sherris & Ryan’s Medical Microbiology, 8th edition. McGraw Hill; 2022. https://accessmedicine.mhmedical.com/content.aspx?bookid=3107§ionid=260928993. Accessed June 23, 2022.
12. López-González E, Vitales-Noyola M, González-Amaro AM, et al. Aerobic and anaerobic microorganisms and antibiotic sensitivity of odontogenic maxillofacial infections. Odontology. 2019 107(3):409-417
13. Peterson LR, Thomson RB. Use of the clinical microbiology laboratory for the diagnosis and management of infectious diseases related to the oral cavity. Infect Dis Clin North Am. 1999;13(4):775-795
14. Brook I, Frazier EH, Gher ME. Microbiology of periapical abscesses and associated maxillary sinusitis. J Periodontol. 1996;67(6):608-610.
15. Tanner A, Stillman N. Oral and dental infections with anaerobic bacteria: clinical features, predominant pathogens, and treatment. Clin Infect Dis. 1993;16(suppl 4):S304-S309.
16. Moore PA, ZieglerKM, Lipman RD, et al. Benefits and harms associated with analgesic medications used in the management of acute dental pain: an overview of systemic reviews. J Am Dent Assoc. 2018; 149(4):256-265.
17. Santos RS, Macedo RF, Souza EA, et al. The use of systemic antibiotics in the treatment of refractory periodontitis: A systematic review. J Am Dent Assoc. 2016;147(7):577-585.
18. Gonzalez JR, Harnack L, Schmitt-Corsitto G, et al. A novel approach to the use of subgingival controlled-release chlorhexidine delivery in chronic periodontitis: a randomized clinical trial. J Periodontol. 2011;82(8):1131-1139.
19. Mylonas I. Antibiotic chemotherapy during pregnancy and lactation period: aspects for consideration. Arch Gynecol Obstet. 2011:283(1):7-18.
20. Robertson DP, Keys W, Rautemaa-Richardson R, et al. Management of severe acute dental infections. BMJ. 2015;350:h1300
21. Jaramillo A, Arce RM, Herrera D, et al. Clinical and microbiological characterization of periodontal abscesses. J Clin Periodontol. 2005;32(12):1213-1218.
22. Ahmad N, Abubaker AO, Laskin DM, Steffen D. The financial burden of hospitalization associated with odontogenic infections. J Oral Maxillofac Surg. 2013;71(4):656-658.
23. Shukairy MK, Burmeister C, Ko AB, Craig JR. Recognizing odontogenic sinusitis. A national survey of otolaryngology chief residents. Am J Otolaryngol. 2020;41(6):102635.
24. Jaworsky D, Reynolds S, Chow AW. Extracranial head and neck infections. Crit Care Clin. 2013;29(3):443-463.
25. Zawislak E, Nowak R. Odontogenic head and neck region infections requiring hospitalization: An 18-month retrospective analysis. BioMed Res Int. 2021;708763.
26. Martin MV, Longman LP, Hill JB, Hardy P. Acute dentoalveolar infections: an investigation of the duration of antibiotic therapy. Br Dent J. 1997;183(4):135-137.
27. Centers for Disease Control and Prevention. Antibiotic/Antimicrobial Resistance Threats in the Unites States, 2013.
28. Ready D, Bedi R, Spratt DA, Wilson M. Prevalence, proportions, and identities of antibiotic-resistance bacteria in oral microflora of healthy children. Micro Drug Resist. 2003;9(4):367-372.
29. Jackson MA, Schutze GE, Committee On Infectious Diseases. The Use of Systemic and Topical Fluoroquinolones. Pediatrics. 2016;138 (5):e20162706.
30. Committee on Infectious Diseases, American Academy of Pediatrics. Antimicrobial agents and related therapy, Section 4. In: Kimberlin DW, Barnett ED, Lynfield R, et al. eds. Red Book: 2021-2024 Report of the Committee on Infectious Diseases. 32nd ed. American Academy of Pediatrics; 2021.
31. Goel D, Geol GK, Chaudhary S, Jain D. Antibiotic prescriptions in pediatric dentistry: A review. J Family Med Prim Care. 2020; 9(2):473-480.
32. Fontana M, Karimbux NY, Cabezas C, Kim DM, Dragan IF. Dental Caries and Gingival and Periodontal Infections. In:. Pediatric Infectious Diseases: Essentials for Practice. Shah SS, Kemper AR, Ratner AJ (eds). McGraw Hill; 2019.
33. American Academy of Pediatric Dentistry. Use of antibiotic therapy for pediatric dental patients. The Reference Manual of Pediatric Dentistry. American Academy of Pediatric Dentistry; 2021. American Academy of Pediatric Dentistry. Useful medications for oral conditions. The Reference Manual of Pediatric Dentistry. American Academy of Pediatric Dentistry; 2019.
34. Amoxicillin. Pediatric and Neonatal Lexi-Drugs. Lexicomp. https://online.lexi/com Lexicomp; 2022. Accessed June 23, 2022.
35. Amoxicillin/Clavulanate. Pediatric and Neonatal Lexi-Drugs. Lexicomp Online. https:// online.lexi/com. Accessed June 23, 2022.
36. Azithromycin. Pediatric and Neonatal Lexi-Drugs. Lexicomp Online. . https://online.lexi/com. Lexicomp; 2022. Accessed June 23, 2022.
37. Cephalexin. Pediatric and Neonatal Lexi-Drugs. Lexicomp Online. https://online.lexi/com. Accessed June 23, 2022.
38. Clindamycin. Pediatric and Neonatal Lexi-Drugs. Lexicomp Online. https://online.lexi/com. Accessed June 23, 2022.
39. Doxycycline. Pediatric and Neonatal Lexi-Drugs. Lexicomp Online. https://online.lexi/com. Accessed June 23, 2022.
40. Metronidazole. Pediatric and Neonatal Lexi-Drugs. Lexicomp Online. https://online.lexi/com. Accessed June 23, 2022.
41. Penicillin V potassium. Pediatric and Neonatal Lexi-Drugs. Lexicomp Online. https://online. lexi/com. Accessed June 23, 2022.
37 orthopracticeus.com Volume 13 Number 4 CONTINUING EDUCATION
OP
Continuing Education Quiz
Dental infections: help avoid antimicrobial resistance — part 1 BRUCK/PRICE
1. Alexander Fleming’s breakthrough discovery of _________ paved the way for a domain of medicine that has enabled once deadly infections to be readily treatable.
a. penicillin b. cholera c. tetanus d. streptomycin
2. According to the Centers for Disease Control and Prevention (CDC), approximately _________ Americans are infected with resistant pathogens that result in 23,000 deaths annually.
a. 500,000 b. 1 million c. 2 million d. 3 million
3. The CDC conservatively approximates that ________ of all outpatient antibiotic prescriptions written from 2010 to 2011 were unnecessary.
a. 10% b. 30% c. 40% d. 50%
4. Even when antibiotics are needed to treat dental infections, they might not be the first line therapy, but rather an adjunct after ________.
a. surgical drainage of an abscess b. tissue debridement c. below the gum manipulation d. all of the above
5. ________ is/are characterized by acute and intense pain and is one of the most frequent reasons that patients seek emergency dental care.
a. Dental caries b. Irreversible pulpitis c. Pericoronitis d. Gram-positive streptococci
6. (When choosing an antibiotic for non-suppurative or suppurative odontogenic infections) Although both agents were regarded as first line, __________ was generally preferred due to having more robust gram-negative anaerobic coverage, less frequent dosing, ability to be taken on an empty stomach, and a lower incidence of gastrointestinal side effects.
a. penicillin V
b. cephalexin
c. amoxicillin
d. azithromycin
Each article is equivalent to two CE credits. Available only to paid subscribers. Free subscriptions do not qualify for the CE credits. Subscribe and receive up to 16 CE credits for only $149; call 866-579-9496, or visit https://orthopracticeus.com/ subscribe/ to subscribe today.
n To receive credit: Go online to https://orthopracticeus.com/continuingeducation/, click on the article, then click on the take quiz button, and enter your test answers.
AGD Code: 148
Date Published: December 10, 2022
Expiration Date: December 10, 2025
2 CE CREDITS
7. ______ — a first-generation cephalosporin with similar gram-positive aerobic coverage as the historic first line agents but that lacks robust anaerobic activity — is the antibiotic of choice in those with a history of penicillin allergy without history of anaphylaxis, angioedema, or hives.
a. Cephalexin b. Cefaclor c. Cefuroxime d. Ceftibuten
8. In patients with a severe allergy to penicillin agents or other β-lactams, _________ can be prescribed. a. azithromycin or clindamycin b. doxycycline and levoflaxin c. cefzil or tetracycline d. metronidazole or moxifloxacin
9. If treatment is initiated for non-suppurative indications (e.g., gingivitis and periodontitis), antibiotic therapy is usually until oral lesions have healed and pain has subsided, typically _______. a. 1 day b. 2 to 4 days c. 5 to 7 days d. 8 to 10 days
10. Tetracyclines and fluoroquinolones are two classes of antibiotics that are ________.
a. preferred for treatment of children b. generally avoided in children c. always recommended for use by pregnant women d. none of the above
To provide feedback on CE, please email us at education@medmarkmedia.com
Legal disclaimer: Course expires 3 years from date of publication. The CE provider uses reasonable care in selecting and providing accurate content. The CE provider, however, does not independently verify the content or materials. Any opinions expressed in the materials are those of the author and not the CE provider. The instructional materials are intended to supplement, but are not a substitute for, the knowledge, skills, expertise and judgement of a trained healthcare professional.
38 Orthodontic Practice US Volume 13 Number 4 CONTINUING EDUCATION
Panthera Dental 10th Anniversary Celebration



 Adrienne Good, National Account Manager for Orthodontic Practice US,
Adrienne Good, National Account Manager for Orthodontic Practice US,

Panthera Dental asked me to attend their 10th Anniversary Party and Master Cup Award Ceremony at their headquarters in Quebec City, in September this year. Over the years, I have been impressed with their versatility in the dental space, and I had to see this new facility in person. The owners, siblings Gabriel and Béatrice Robichaud, bring their own unique personalities to this more than 40,000 square foot building. From the bright distinct Panthera purple to the 1980s-themed game room, it seems like an awesome place to work. Esthetics aside, they considered efficiency and workflow when designing every detail of their headquarters. We even got to meet the hardest worker of all, their robot courier, Alfred. Everything is strategically set up with the end goal of your patients receiving their order within a quick timeline and with an exceptional quality product.
After a lovely tour, the top three winners of their Master Cup were announced. Panthera, in an effort to keep innovation with technology in dental alive, has a contest every year where globally, technicians compete by crafting a complete dental prosthesis. After mimosas and media interviews, the real fun began.
Guests arrived in the evening greeted by bartenders pouring drinks extending from aerial silk. The hors d’oeuvres were top notch, and the photo booth, along with their DJ playing throughout the night, were pure entertainment. The most memorable
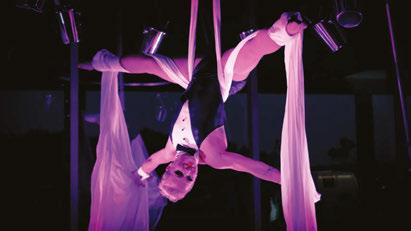
part of the night was when a school bus pulled up on the side of the building and took us to a small diner in downtown Quebec City. There, we got to try Quebec’s version of “diner food,” and network with colleagues from around the world.
I am not surprised Panthera’s party was a great success, because they put this kind of effort into everything they do. The quality in their work really shows, and I am fortunate to be able to witness the processes behind it all. Know that when you are purchasing a Panthera Dental product, whether it be esthetic, sleep, or implant related, you are supporting a wonderful bunch of people, a facility with the best technology, and most importantly, top notch quality you can pass down to your patients. OP
39 orthopracticeus.com Volume 13 Number 4 EVENT RECAP
recaps Panthera’s memorable event
The case for combination treatment
Dr. Eric Wu explains how to improve patient satisfaction and profitability
What is combination treatment?
Combination treatment is the use of two treatment modalities to achieve the best possible result in the shortest amount of time. Usually this means starting a patient in braces and then transitioning to clear aligners.
Why is combination treatment better?
Many prospective patients are interested in aligner-only therapy but often are not ideal candidates. When patients requiring extrusion, significant rotation, and/or posterior expansion present, here are your options:
1. Inform patients that they’re not a candidate, and recommend braces.
Eric Wu, DMD, received his Doctor of Medicine in Dentistry from the University of Pennsylvania; his Advanced General Dentistry degree from UCLA; and his Orthodontic degree from the University of Pittsburgh. He is adjunct Faculty at the University of Nevada, Las Vegas (UNLV) and Roseman University Orthodontics. He practices at Wu Orthodontics in Palo Alto, California, and Redwood Shores Orthodontics in Redwood City, California. He is a published author, inventor, and frequent speaker. Dr. Wu is passionate about clear aligner therapy innovation and additive manufacturing/3D printing, and has treated more than 4,000 patients with aligners.
Disclosure: Dr. Eric Wu serves as a key opinion leader and advisor to uLab Systems.

2. Attempt clear aligner treatment, anticipating a long case with multiple refinements.
3. Propose < 6 months in braces followed by clear aligners. By choosing option 3, you balance the patients’ wishes with the treatment requirements. The result is higher conversion rates, greater patient satisfaction, good clinical outcomes, and generally, shorter total treatment time. uSmile™ clear aligners are available on a pay-per-aligner basis with very rapid delivery from uLab Systems™, supporting the profitability and timing of these cases.
When to switch from fixed to clear aligners?
Start by planning any A/P corrections, significant expansion, extrusion, major torque, and significant rotations for the first, fixed phase of treatment. As soon as these major movements are accomplished, scan and transition the patient. Use aligners where they are undeniably superior — finishing, detailing, midline and tooth-size discrepancy management, and spacing correction.
Waiting until fixed appliances stall serves to only prolong treatment time and increase the total number of appointments.
How to price combination treatment?
You can offer combination treatment without modifying your fee scale. Pay-per-aligner lab fees — often just a few hundred dollars — are easily offset by the elimination of appointments.
40 Orthodontic Practice US Volume 13 Number 4 PRODUCT SPOTLIGHT
OP
Top
Reasons to

Design treatment plans or send cases to the uAssist™ service. Easily order uSmile™ aligners, request changes, or make changes yourself with a full suite of tools.
4 Pay-per-aligner pricing

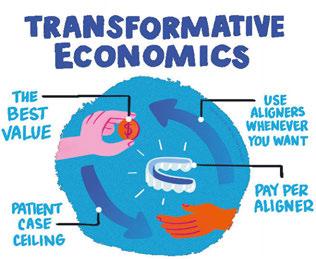


Finish cases with aligners, treat relapse and mild cases profitably, and scale your practice with minimal risk and no subscriptions.
2 Fast Delivery
Receive aligners 3-10 working days after order is accepted.


5 Flexibility
Order uSmile aligners or print in-office. Design plans yourself or send them to the uAssist service. Choose options like straight or scalloped trimlines.


customers
To learn more about uSmile aligners and the uDesign platform please call 866.900.8522 or visit ulabsystems.com
5
Switch Interested in a clear aligner provider that puts the power into the orthodontist’s hands? Here’s the top 5 reasons our
switched to uLab®... what’s yours?
1 No back-and-forth needed
3 Custom Branding Promote your practice with boxes featuring your logo, not ours. Customized pouches and aligner cases coming soon!
© 2022 uLab Systems, Inc. All Rights Reserved. uLab Systems,
and uSmile are trademarks and uDesign and
are registered trademarks of uLab Systems, Inc. MAR-0001073 Rev 1
uAssist, uView
uLab
Smile Stream Solutions

For the past 2 years, Smile Stream Solutions has remained true to both our strategic growth plan and our mission — to enhance the vitality of the orthodontic community through efficiency and savings in clinical supplies. In so doing, we have not only expanded our core product line of price-driven products, but also have developed a comprehensive aligner solution under the brand name of Stream Ligners. In addition, we have launched an entirely new business platform that addresses the premier market segment of traditional braces under the brand name of Genesis Orthodontics. These product and service developments, combined with our earlier acquisition of OrthoEssentials — a full-service provider of quality orthodontic supplies in its own right — now makes Smile Stream Solutions and its family of Stream Ligners, Genesis Orthodontics, and OrthoEssentials

dontic suppliers in the industry. Few other company’s offerings range from traditional braces to aligners within every price point and product category. What this means to single private


SMILE
SOLUTIONS
STREAM LIGNERS
increase your efficiencies and decrease your cost basis by single-sourcing most all of your products and essential services from one company.
Even better, Smile Stream Solutions also makes private labeling your brand possible. Between Stream Ligners’ private-label packages for your aligner treatment services and our Smile Print capabilities, we can apply your brand and logo to the packaging that your patients receive within your practice. We see this as a critical way to empower you and your brand within the community versus those of your service providers. Beyond all of that, however, is our newly released, patent-protected, innovative breakthrough tooth preparation formula Step-1 PumEtch. Step-1 PumEtch combines pumice and etchant into one single material and eliminates the need for slow-speed handpieces, pumice, prophy cups, and other redundant products and equipment while eliminating a step in your tooth preparation process for either bonding or sealant procedures.
These are challenging times for all of us, which is why you need a strategic supplying partner more than just a vendor. You need a company that can provide you with the quality you expect at a price you can accept. You need a comprehensive solution — Smile Stream Solutions. To learn more about how we can price quote, create a formulary, or bundle promotions together for you, visit us at smilestreamsolutions.com, or contact us directly at 1-720-689-1536.
This information was provided by Smile Stream Solutions.


42 Volume 13 Number 4 PRODUCT SPOTLIGHT
STREAM Your Efficient Clear Aligner Solution
A SMILE STREAM SOLUTIONS COMPANY SSENTIALS ORTHOE
Services
GENESIS ORTHODONTICS -Your Strategic Supplying Partner For Best-In-Class Products &
OP
Traditional Braces ~ Aligner Systems ~ Consultative Services



STEP-1 PumEtch More Effective Tooth Coverage Greater Application Control Reduces Chair Time, Procedural Steps, and Material Cost No Need for Prophy Cups or Paste Eliminates Slow Speed Handpieces Invented by board certified Orthodontist Dr. Frank Besson, DMD Patent Number: 8,033,829 The First Step in your Tooth Prep is the Only-1 you need Combines Pumice and Etch into one Solution Saves Time and Money smilestreamsolutions.com 720.689.1536 SOLUTIONS SMILE STREAM
7 marketing musts for orthodontists in 2023
 Dr. Kyle Fagala
Dr. Kyle Fagala

offers insights on how to keep your practice in the spotlight
Whatever industry you’re in, marketing can be a tough mountain to climb. But for orthodontic practice owners, there’s an added element of stress as you attempt to juggle a busy practice while implementing the latest and greatest in marketing and maintaining an active social media presence. We’re all looking for better ways to attract new patients and boost our conversion rate, and the good news is, there are several relatively simple tools for successfully advertising your orthodontic practice! Let’s take a look at some of my tried-and-true marketing tips that have helped us continue growing over the years.
1. Keep things simple with local signage
An analog solution in a digital world? Absolutely! Simple strategies like this one are often overlooked in favor of more technical methods, but signs and other printed materials will help increase your traffic with a one-time investment that will pay for itself over and over again. Connect with your community by identifying the high-traffic areas in town that your target demographic frequents — recreation centers, locally owned coffee shops, and YMCAs can be great places to start. Once you have a list of places in mind, roll in with well-designed posters, banners, flyers, and signs to get your name out there in a memorable way. Don’t forget to include your website URL, phone number, and even a QR code to increase the response rate.
2. Make your website more appealing
Your website is one of the most important tools in your marketing arsenal, with the potential to drive consultations and convert clients. Even if your current site is functional and attractive, it could probably do with a good once-over to ensure it’s working as well as it should be for your practice. There are a few things you can do to spruce up your site, starting with some shiny, new content. Even if you don’t think anyone is reading it, high-quality copy will boost your brand’s reputation, increase your authority as an industry expert, and help your website rank higher on Google.
You’ll also want several clear calls-to-action on your website. This could be a contact button, link to a free consultation, or an
invitation to connect virtually, but whatever it is, make it easy to find and easy to use. The same holds true for reviews or testimonials. Whether you post these in video or text form (or a combination of the two), a page or section of your homepage that’s dedicated to patients singing your praises will go a long way toward convincing potential patients to schedule a consultation.
3. Pay attention to your Google My Business listing
Aside from your website, your Google My Business listing page is one of your biggest assets. It’s essential that this tool is optimized to drive traffic to your business and improve your rankings. Fill out all the information possible, including your location, the services you offer, contact details, business hours, and so on. The more content Google has for your business, the less it has to guess, and the higher it will rank your site. Back this info up by listing your business everywhere you can using the exact same details — for example, Yelp, BBB, or Yellow Pages.
Don’t forget to post regularly on your Google My Business page. The more activity your business has, the more likely Google will rank it highly, and the more trustworthy its search engine algorithms will find you. This activity can (and should) include reviews. Research shows that most online shoppers use reviews to determine what products to buy and which services to use. Make it a habit to regularly ask former and current patients to leave honest reviews of their experience with your practice. Provide them with a link or QR code to make it easy, and steer clear of paid reviews as they can stand out like a sore thumb!
44 Orthodontic Practice US Volume 13 Number 4 MARKETING MOMENTUM
Kyle Fagala, DDS, MDS, is an orthodontist and cofounder of Neon Canvas, a digital marketing agency located in Memphis, TN. He hosts the podcast “The Digital Orthodontist: Live!” and runs a popular Facebook Group with the same name.
4. Keep relevant Facebook and Instagram ads running
Facebook and Instagram ads are the backbone of digital marketing, especially for local businesses. If you’re new to these ads or just want yours to be more compelling, you’ll want to start by creating high-quality photo and video ads to catch the eye of potential patients. Facebook’s Ad Manager is a helpful way to target the key demographic in your area. Feel like your ads need a little extra pizazz? Try creating a big giveaway to increase your brand’s publicity and drive additional traffic your way.
5. Add a few Google Ads to the mix, too
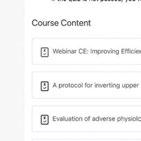

Once you’ve optimized your website and Google My Business Page, turn your attention to Google Ads. These can help spread your name and create fast traffic for major keywords. They’re also a quick way to get results as you continue building your search engine authority, but keep in mind that Google Ads can sometimes get a bit pricey, particularly when bidding on competitive keywords like “braces” or “Invisalign.”
6. Get social media-savvy
Successful online marketing revolves around regular content on social media. The key is to keep it as authentic, fresh, fun, and as original as possible. People have gotten pretty good at tuning out posts that feel forced or cliché, but quality content that comes across as fluid and natural is still a fantastic way to drum up interest in your practice.
While some orthodontists put a team member or outside source in charge of their social media, you don’t have to put in
endless hours for it to be effective. You can keep followers interested by posting regular shots of happy patients, showcasing your work with before-and-after images, taking viewers behind the scenes with fun videos, or getting in on the latest TikTok trends. Producing simple but engaging content like this will make you more relatable to your target audience and encourage them to contact you when they’re ready to begin their smile journey!
7. Take it back to the basics with email marketing Email marketing can be an extremely cost-effective way to remind potential patients that you haven’t forgotten about their interest in your practice. It’s also extremely easy to implement. Collect email addresses from people who visit your website, those who have signed up for a free consultation, or even former patients you want to check in on. You can send emails out in many forms, including those that greet new patients, special offers for new starts, happy birthday wishes, and other miscellaneous notes. If your practice management software doesn’t offering email blasts, and you’re looking for a service to do just that, MailChimp is a great, inexpensive option. With just a little bit of effort, you’ll be able to keep your books full at practically no cost to your practice.
If you’re looking to grow your orthodontic practice, these tips will set you up for success and help you smash all your marketing goals. To discover how each of them will work best for your practice, you’ll need to experiment with the basics and do some thinking that falls outside the box. Social media campaigns, printed materials, a revamped website — once you figure out what excites your target market, you’ve got a clear path toward success. OP

45 orthopracticeus.com Volume 13 Number 4 MARKETING MOMENTUM
FOCUSED on the content that matters to you EASILY find completed course certificates DISCOVER more topics with webinar courses ONE CLICK to your personal CE dashboard Not a member yet? Get started today at Orthopracticeus.com! www.orthopracticeus.com Explore Our Improved CE Dashboard
Navigating dental malpractice lawsuits — part 1
 Kristin Tauras, JD, guides dental specialists through the legal elements
Kristin Tauras, JD, guides dental specialists through the legal elements
Dental specialists are increasingly being sued for professional malpractice. As one plaintiff’s counsel explained, it is easier to get a dental specialist to settle than any other medical professionals these days. While most other medical professionals are aware that they are the target of lawsuits and have themselves been sued or see their colleagues getting sued, the same cannot be said for the dental profession. While not new, dental malpractice lawsuits are still a novelty to most in the profession. Dental specialists are unprepared for the havoc a lawsuit can cause in their practice, are embarrassed when they are sued, are less likely to tell colleagues that they have been sued or seek advice, and are more apt to settle quickly and quietly than fight what is oftentimes a defensible case.
The term dental specialist used throughout this article encompasses all dental and medical providers who treat diseases and problems of the teeth, gums, and jaw — including dentists, cosmetic dentists, pediatric dentists, prosthodontists, periodontists, endodontists, oral and maxillofacial surgeons, and orthodontists. This also encompasses the liability of the dental specialist’s staff — including dental hygienists, dental assistants, nurses, anesthesiologists, and other medical providers who assist with the dental treatment and potentially can be named in a dental malpractice lawsuit.
Proving professional malpractice
In every state, a patient may pursue a malpractice claim against a dental healthcare provider if the healthcare provider causes injury or death to the patient through a negligent act or omission. In dental treatment, professional malpractice is defined as any act or omission by a dental specialist, or someone under their direction, during the treatment of a patient that deviates from the accepted standard of care and causes harm to the patient.
To recover for alleged dental malpractice, the plaintiff must allege and prove that the dental specialist (or someone under his/her supervision) was negligent in the treatment of a patient,
Kristin Tauras, JD, is a partner in the law firm of McKenna Storer in Chicago, Illinois. She has a litigation practice in the areas of employment law, insurance coverage, and professional malpractice. McKenna Storer is a fullservice law firm providing legal services to individuals and small to midsize companies, including defending professional malpractice negligence lawsuits and Illinois Department of Professional Regulation investigation, as well as advising dental and medical professionals regarding business and employment matters.
and that the negligence caused harm to the patient. The elements may be broken down further:
• Duty of care owed by the dental specialist to the patient
• Breach of duty of care by the dental specialist
• Injury caused to the patient by the breach of duty of care by the dental specialist
• Damages to the patient
Duty of care
First, the plaintiff must establish that the dental specialist owed the patient a duty of care. This first element requires that there is a relationship between the dental specialist and the patient. Usually this element is easily proven through the use of medical records showing that the dental specialist treated the patient.
Other times though, the patient relationship falls within a gray area — for example, where the patient does not return for the treatment, the dental specialist declines or refuses to treat the patient for a dental issue, or the dental specialist refers the patient to someone else before the malpractice occurs.
It is also important to note that dental specialists are also liable in most states for those who work under their supervision with them and, in some cases, those to whom they refer cases. Just because the dental professional did not cause the injury, he/ she may still be liable for the acts of others. This includes their dental hygienist, nurse, or anesthesiologist.
46 Orthodontic Practice US Volume 13 Number 4 LEGAL MATTERS
LEGAL MATTERS
Breach of duty of care
Second, the plaintiff must establish a breach of duty of care. To do so, the plaintiff must establish the standard of care. The standard of care is a “reasonable person standard,” which is a legal fiction, created by laws, referencing a standard of care that all dental professionals in a similar situation and similar locale should follow. A breach of the standard of care occurs when the provider fails to act as a reasonably prudent and trained dental professional would under the same or similar circumstances when treating a patient. Both the standard of care and the breach of the standard of care must almost always be established through expert witnesses. The exception is where the breach is of such an obvious nature that the breach speaks for itself.
Breach of standard of care
Third, the breach of the standard of care must cause an injury. A plaintiff must prove that the healthcare provider caused the injury or made an existing condition worse by his/her action (or inaction). The patient must show a direct relationship between the alleged breach and the subsequent injury. This is known as “proximate cause.” The malpractice must proximately cause the injury suffered by the patient.
Damages
Fourth, there must be damages. Damages can be in the form of medical bills (the cost of medical treatment and corrective treatment), disfigurement, pain and suffering, loss of normal life, and economic losses (lost wages).
When dental errors result in permanent disability or death, family members may also, in most states, recover for the “loss of society” and/or wrongful death of the patient.
In rare cases, punitive damages may also be awarded. For this to occur, there must usually be malfeasance or malintent alleged.
Types of dental malpractice
Any deviation from the standard of care can constitute malpractice if it proximately causes a patient injury. There are an infinite number of ways dental practitioners can deviate from the standard of care. Examples of deviations from the standard of care that may result in a malpractice claim follow.
• Ignoring the current standards when recommending or pursuing a course of treatment.
• Improperly treating or failing to treat the dental condition.
• Failing to accurately diagnose an infection, lesion, cancer, periodontal disease, or other oral diseases.
• Causing an infection.
• Failing to adequately supervise employees under their direction or control.
• Improperly administering anesthesia that leads to complications such as brain damage or death.
• Causing nerve injuries that lead to complications such as neuropathy or paralysis.
• Causing damage to bone or soft tissue.
• Drilling too deeply, resulting in permanent injury to the tooth.
• Performing an improper extraction.
• Misaligning the teeth by improperly fitting fillings, crowns, or implants, resulting in issues with bite and speech.
• Using excessive force on patients.
• Recommending unnecessary dentures or failing to correctly fit dentures.
• Using improper instrumentation, improperly maintained instrumentation, or using outdated tools.
• Failing to consider a patient’s existing medical conditions, allergies, and physiology before treating the patient.
• Recommending and performing treatments that are not medically necessary.
• Failing to refer the patient to the proper dental specialist such as an oral surgeon or an endodontist.
• Failing to obtain informed consent and failing to explain the risks of the procedure to the patient in a manner and language in which the patient can understand.
Art of dentistry
Dental specialists are familiar with the term art of dentistry. Despite enormous advances in the practice of dentistry, the personal encounter between patient and physician remains the cornerstone of dental care. The dental professional becomes the diagnostic and therapeutic expert who applies the knowledge and skills of dentistry. It includes not only what is required for a diagnosis and healing, but also the ability to apply the generalized knowledge of dentistry to individual patients. Dental specialists should not allow the fear of a malpractice suit to hamper their judgment and their application of the art of dentistry, but they should be aware of the types of claims so they may make sure to protect themselves against a claim that they committed dental malpractice.
Best practice
Dental specialists should make sure they chart their thought processes, conversations with patients, and treatments thoroughly so that they may defend themselves against claims of malpractice.
The lack of charting is not listed as a basis of the typical allegation of negligence against a dental specialist, but lack of adequate charting may be a factor in a lawsuit against the dental specialist. A plaintiff’s counsel may argue that if it wasn’t charted, it didn’t happen; or if it wasn’t charted, it wasn’t considered. The failure to chart essential aspects of the patient’s care may lead to difficulties in defending the dental specialists’ reasons for their decisions and treatment.
While all dental specialists know that a substantial part of their treatment of a patient is the “art of dentistry,” taking into account the patients they see, their knowledge, training, and expertise, it makes it easier to defend their actions when these considerations are included in the chart.
OP
47 orthopracticeus.com Volume 13 Number 4
Dental specialists are unprepared for the havoc a lawsuit can cause in their practice. ...
Stem cells and the dynamic field of medicine, dentistry, and orthodontics
Dr. Amy B. Jackson discusses how stem cells from wisdom teeth can have promising medical benefits
When I was pregnant in 2004 with my first child, I was first introduced to the concept of banking cord blood. This is the process of a private company banking (or collecting) blood from a child’s umbilical cord at birth.
Like bone marrow, cord blood has scientifically shown to be impactful and effective in therapeutic transplants to treat a range of diseases, including leukemia, lymphoma, and various genetic disorders. The promising impacts don’t just come from the cord blood itself, but from the stem cells also contained in the detached umbilical cord. Those stem cells promised the potential to treat a broader range of conditions in the future.
At that time there were only 23 public cord blood banks and fewer than 65 hospitals throughout the country that were equipped to accept donations like these. Now, though, times have changed.
Presently, there are more than 450 cord blood banks worldwide. Cord blood is known to help treat nearly 80 unique conditions. It’s expanded beyond transplant medicine into areas of regenerative medicine in clinical research trials for conditions once thought untreatable such as autism, brain injuries, and certain types of cancer.
Stem cells also are potentially part of this process from a dental perspective with real, tangible benefits in the world of health and wellness. Stem cells are not only banked and preserved from umbilical cords. In fact, there are multiple ways to harvest these beneficial stem cells — even from wisdom teeth.
Harvesting dental stem cells can be as seamless as preserving stem cells collected from wisdom teeth during extractions. But how exactly does this work in practice, and what are the benefits of harvesting dental stem cells from wisdom teeth?
What exactly are stem cells?
Stem cells are often referred to as the body’s raw material — they’re cells from which all other cells with specialized functions are generated. Adult stem cells, also called somatic cells, are found
Amy B. Jackson, DDS, MS, is a Board-certified orthodontist in private practice for over 15 years and runs four practices in San Antonio, Texas. She began her dental career in Houston where she attended The University of Texas Health Science Center. During her time there, she was recognized by the UT Health Science Center with the Dental Public Health Award for community service and was awarded a Summer Research Fellowship from the AADR and the Barnard G. Sarnat Award in Craniofacial Biology from the IADR. Dr. Jackson continued her specialty training for orthodontics at The University of Texas where she completed a master’s degree through the periodontal department and was awarded the AAED’s research grant for her work with midpalatal implants.
Disclosure: Dr. Jackson is founder of Retainers for Life®

within the deep tissues of the human body (liver, heart, ovaries, muscles, testes, teeth, skin, and bones).
Stem cells, in general, have a variety of promising medical benefits for future treatments of a myriad of conditions. Stem cells acquired from dental tissue are no exception. Dental stem cells are found in the soft dental pulp of teeth and are a rich source of mesenchymal cells. These cells can be isolated when extracted, then preserved to be used later.
Wisdom teeth stem cell extraction: what to know
In the past after procedures like wisdom teeth extractions, those extra molars were disposed of. It’s only in the past several years we’ve learned how beneficial dental stem cells can be and further, how seamless acquiring and preserving those stem cells could be too. This procedure is the perfect opportunity to harvest those valuable soft dental tissues to derive the stem cells.
The ongoing demand for wisdom teeth surgery leaves plenty of opportunity for acquiring stem cells without any additional issues. These procedures are the perfect possibility for stem cell extraction, cryopreservation, and potential later use.
Dental stem cells
Stem cells — dental stem cells included — are known as precursor cells. That means they’re not just potent and viable raw materials; they’re capable of something called “self-renewal.” This means that like other stem cells, dental stem cells (when properly acquired and preserved) can regenerate and grow into cells — but not just dental cells.
Dental stem cells could grow into other types of specialized cells, like muscles, ligaments, bones, nerves, skin, and more. The benefits of extracting dental stem cells from wisdom teeth are varied and numerous.
When my youngest was born in 2009, we had planned to bank his cord blood. After a life- threatening delivery, his cord blood was destroyed. This renewed focus on preserving cells from wisdom teeth gives us one more chance to benefit from his young stem cells, making it possible for your children and grandchildren to benefit as well.
The present application of stem cell therapy or treatment is promising, and the future of it is even brighter. Scientists are always progressing in stem cell therapy research and may eventually be able to treat and/or cure conditions like arthritis, auto-immune diseases, pancreatic dysfunction, brain injuries, cognitive diseases, and beyond.
48 Orthodontic Practice US Volume 13 Number 4 ORTHO PERSPECTIVE
OP
“This is a fantastic curing light. It can cure at 3200 mW/cm2, the light feels great in the hand, and my team loves it. The light has curing timed modes for 2, 3, 4, 5, 6, etc. so there are lots of options to customize the light to your desired time. I don’t know of another light on the market that has this combination of features. I highly recommend this light with 5/5 stars!”



--- Dr. David Taylor | McAllen, TX
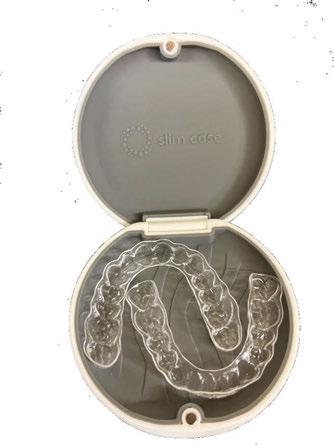





LEDEX MAX 120 curing light Introducing the Industry’s Most Advanced Curing Light... ALLURE ORTHO EXCLUSIVE! You Asked. We Listened. NEW!
WHAT DRS. ARE SAYING ONLY $425 ea. BUY 6 $375 BUY 3 $400 Can Cure All 20 Teeth in One Cycle! Ask About Our Mari’s List Discounts The AAO does not certify, guarantee, or warrant the products, services, or offerings provided by Allure Ortho. COME SEE US THIS WINTER! WOMEN
ORTHODONTICS
AZ
aligner holder SLIM CASE FREE Imprint on 10+ packs! -Ultra slim design -Fits in your pocket easily -Removable silicone inserts -Magnetic closure -E asy to use and clean - Also available with mirror Case Colors! ONLY $59 pack of 16 *One time set-up fee of $45 for imprint orders All of the Things You Love About the LEDEX Ultra (WL90) & So Much More We took your feedback and turned it into a curing light that will meet all of your office’s needs. New Rugged Design That’s Cavi Wipe Safe The sturdy body can be wiped down with cavicide and all other cleaning agents. You no longer have to worry about cracking or breaking. Improved Charging & Battery Functions Features a new convenient wireless inductive charging system as well as a new auto sleep mode for an extended life of the lithium battery.
Ortho
1-2 Second Cure
to 20 teeth
one cycle with a 1-2 second cure. Features
light examination mode,
it the perfect combination
curing and inspection
one light. Additional accessories
with 3 tip sizes offered.
WIPE SAFE
IN
JAN. 12-14 - PHOENIX,
AAO MID WINTER - BOOTH #300 JAN. 25-28 - LAS VEGAS, NV
Advanced
Functions with a
Cures up
in
a white
making
of
in
available
CAVI




 Drs. Stuart Frost and Trevor Nichols
Drs. Stuart Frost and Trevor Nichols

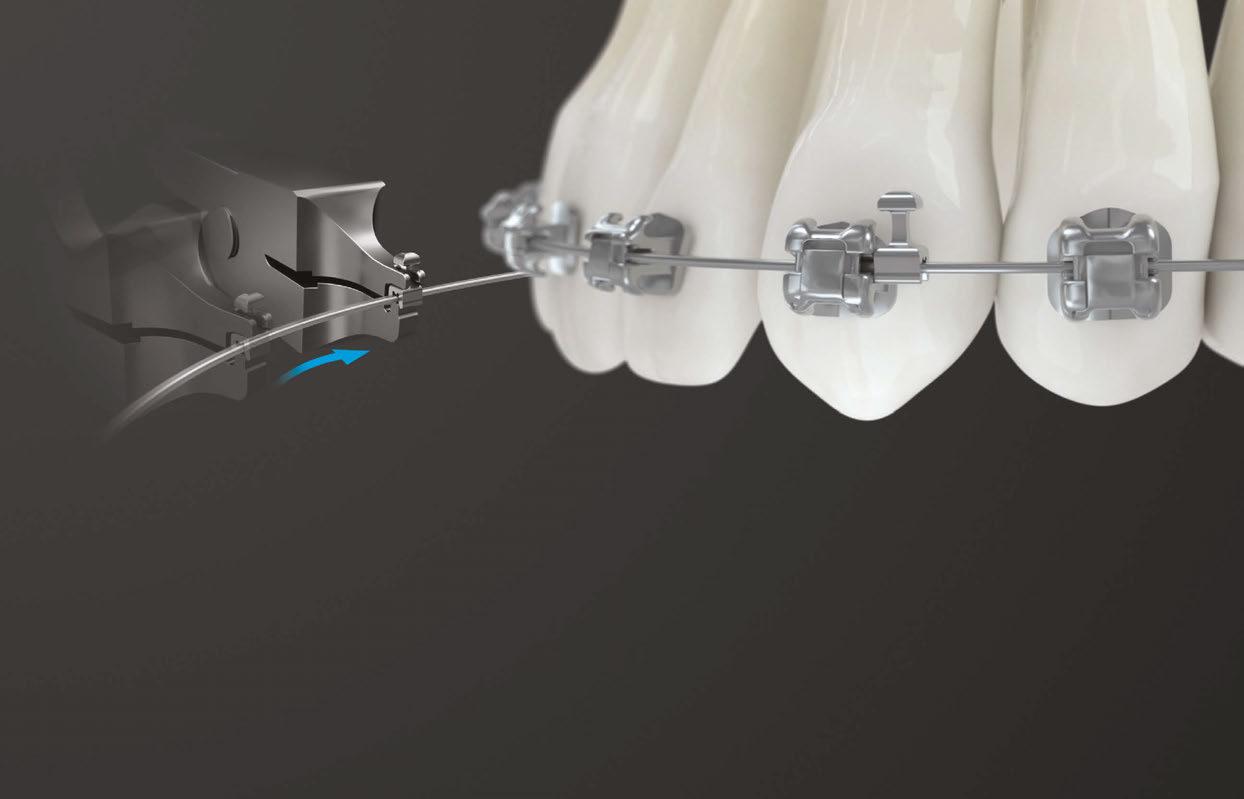





















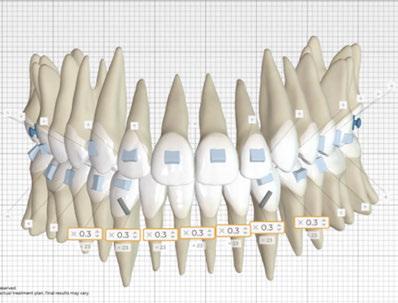
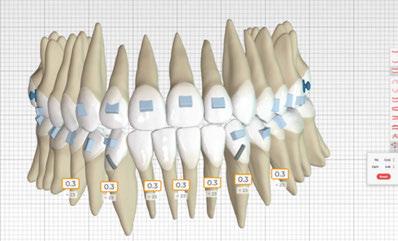






















 Kwangchul Choy, DDS, MS, PhD 2022, Quintessence Publishing Co. www.quintpub.com
Kwangchul Choy, DDS, MS, PhD 2022, Quintessence Publishing Co. www.quintpub.com










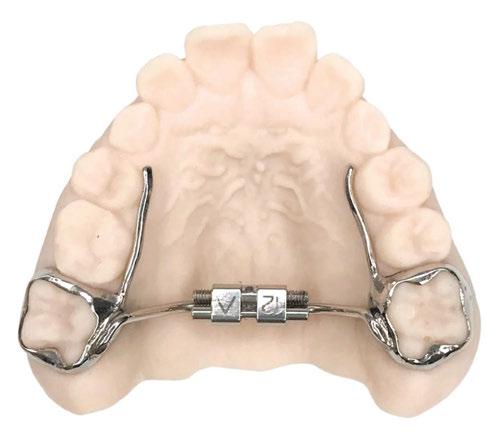






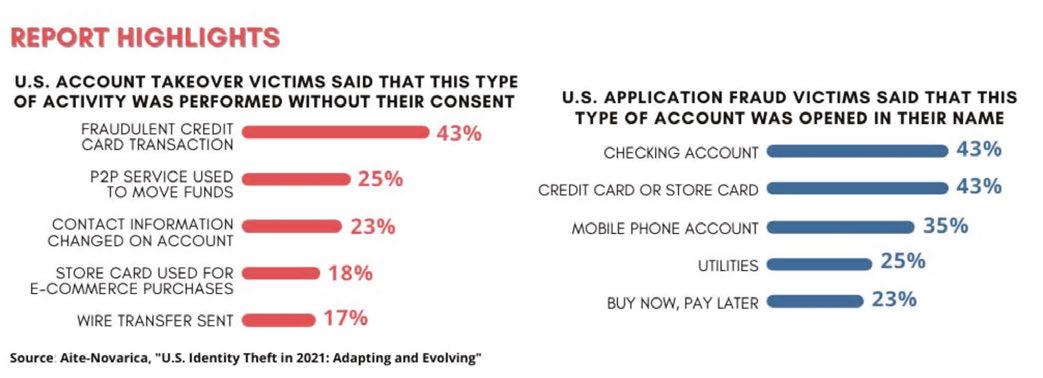
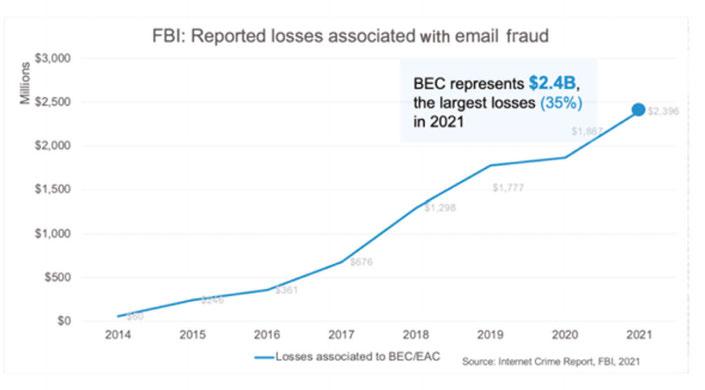
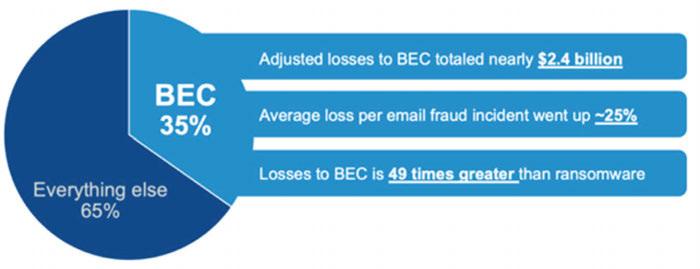
 Wiyanna K. Bruck, PharmD, and Jessica Price start their discussion
Wiyanna K. Bruck, PharmD, and Jessica Price start their discussion




 Adrienne Good, National Account Manager for Orthodontic Practice US,
Adrienne Good, National Account Manager for Orthodontic Practice US,



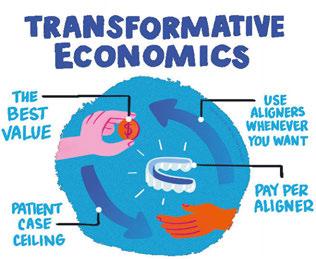













 Dr. Kyle Fagala
Dr. Kyle Fagala



 Kristin Tauras, JD, guides dental specialists through the legal elements
Kristin Tauras, JD, guides dental specialists through the legal elements