Pediatric dentists are the obvious ones to help children breathe, sleep, and prosper!

Dr. William M. Hang
Sleep-related breathing disorders during pregnancy
Dr. Steve Lamberg

Which one is the best?
Dr. Lauren Ballinger


Pediatric dentists are the obvious ones to help children breathe, sleep, and prosper!

Dr. William M. Hang
Sleep-related breathing disorders during pregnancy
Dr. Steve Lamberg

Which one is the best?
Dr. Lauren Ballinger

This inaugural edition of Pediatric Dental Practice US provides an opportunity for the creation of a fresh publication with a current perspective. Achieving continuous excellence in pediatric dentistry can be assured if new information for the pediatric dental practice is focused on our changing healthcare environment. We face a paradigm shift in all of healthcare. Artificial Intelligence, shifting social patient expectations, and corporate dentistry are just a few of many causes.
Parents will increasingly expect and value a great pediatric dentist. The direct marketing of aligners to children is a continuation of decades old marketing of toothpaste, toothbrushes, and so on. The tidal wave of information tugging and pulling on parents and children to buy the next best dental widget or technique provides an opportunity for dental professionals to lead.
As a specialist in orthodontics for over 40 years and a father of five children, I appreciate the meaningful difference pediatric specialists can make in our patient’s lives. A great pediatric-orthodontic team can become community leaders. They can make an enormous difference for both patients and our dental profession. A team approach is desired and respected by parents for being more comprehensive and professional. In a time of increasing pressure to focus on profitability, we can choose to balance our financial responsibilities with our oath to “do no harm” and desire to “do good.” Fortunately, we are not limited to a 60-second advertisement in the media.
As the first to see young children, the pediatric dentist often fulfills the role of screening children for existing and future
Anthony DeLuke, DDS, graduated Magna Cum Laude from the University of Buffalo School of Dental Medicine. He is dedicated to a comprehensive functional medical-dental approach to care with a focus on improving facial esthetics, smiles, and airway function. His creativity and passion for comprehensive functional orthodontics has resulted in his being awarded a U.S. patent on an orthodontic airway growth appliance. Patents are also pending for an additional orthodontic functional appliance and instrument for measuring facial growth. His palatal contoured expander design is used across the United States. He has influenced orthodontic teaching here and as far away as Japan. He and his high school sweetheart, Karen, have five children and 11 grandchildren. Dr. DeLuke aspires to help the greatest number of children and adults through sharing his experience with colleagues and parents. He is publishing, lecturing, and continuing to see patients in his mission.

problems. Their valuable advice, referrals, and care are critical. Abnormally delayed and less than normal facial skeletal growth is recognized as a primary underlying cause for the majority of patients with malocclusion. Early screening for facial growth problems will result in treatments which can reduce the eventual skeletal dysplasia and resulting malocclusion, sleep apnea, upper respiratory issues, and the esthetic disfiguring.
The orthodontist’s role is a resource for parents as well as a resource for the pediatric dentist. With digital records, the consult between the pediatric dentist and orthodontist can be collaborative. The orthodontist can assist the pediatric dentist in diagnosis and interceptive treatment planning as well as orthodontic care if the pediatric dentist chooses to deliver care.
The caregivers that dedicate themselves to children need innovative and creative outlooks. We are making decisions that will have an impact over our patients’ future dental and emotional health for likely 70 or 80 years. When reflecting back on my difficult choice of studying pediatric dentistry or orthodontics, I struggled but chose orthodontics. In hindsight, I still chose to treat children at a young age as an orthodontist knowing I wanted the best chance to improve growth.
I am excited to participate in the future of children’s health and to welcome this new publication as a forum for pediatric treatment. Children are not just smaller adults and need specialized care. Pediatric dentists need to develop techniques to make children comfortable in sometimes challenging situations. Orthodontists will partner with pediatric dentists to identify especially designed equipment and techniques for the oral health of children from infancy through the teen years. The future authors in this publication aspire to expand the horizons of specialists who care for the youngest in our society. Pediatric dentists are the “first dental caregiver” and can change the future of those who actually are the future.
Pediatric dentists are the “first dental caregiver” and can change the future of those who actually are the future.
Dr. William M. Hang explains why pediatric dentists should be leaders in airway health

with a case presentation from Dr. Paul
Dr. Francis Nasser, Jr. discusses the important role of military dentists and a special way to recognize their contribution to the field

Published by
Publisher Lisa Moler lmoler@medmarkmedia.com
Managing Editor Mali Schantz-Feld, MA, CDE mali@medmarkmedia.com
Tel: (727) 515-5118
Assistant Editor Elizabeth Romanek betty@medmarkmedia.com
National Account Manager Adrienne Good agood@medmarkmedia.com
Tel: (623) 340-4373
Sales Assistant & Client Services Melissa Minnick melissa@medmarkmedia.com
Creative Director/Production Manager Amanda Culver amanda@medmarkmedia.com
Marketing & Digital Strategy Amzi Koury amzi@medmarkmedia.com

eMedia Coordinator Michelle Britzius emedia@medmarkmedia.com
Social Media Manager

April Gutierrez socialmedia@medmarkmedia.com
Digital Marketing Assistant Hana Kahn support@medmarkmedia.com
Website Support
Eileen Kane webmaster@medmarkmedia.com
MedMark, LLC
15720 N. Greenway-Hayden Loop #9 Scottsdale, AZ 85260
Tel: (480) 621-8955
Toll-free: (866) 579-9496
www.medmarkmedia.com
www.pediatricdentalpractice.com
D4C Dental Brands is one of the largest dental support organizations (DSO) specializing in pediatric dentistry and orthodontics. We provide our network of doctors with the support and resources to continue focusing on high-quality care for their patients without the headache of administrative responsibilities.
We are strategically partnering with successful practices and hiring exceptional dentists that share common values and are passionate about working together to provide better healthcare to more children.

In my columns, I have always shared my thoughts on professional and personal success. I’ve shared MedMark Media’s triumphs, and in recent years searched with you for solutions to some very tough challenges. As always, I am so proud of MedMark Media’s publications and the team that has been the center of my life for so many years. With this column, I am thrilled to announce some amazing news. As of this writing, I just got notified that I am a 2023 Denobi Award nominee. This prestigious nomination is incredibly humbling and inspiring. The Denobi Awards recognize leaders in the dental industry worldwide — including, as the Denobi website notes, “clinicians, educators, brand leaders, students, administrative personnel, sales, advocates, speakers, and leading experts.” From the nominations, finalists include 10 individual winners, one dental team, and on individual that receives the esteemed Dr. Lou Shuman Denobi Pinnacle Achievement Award. Right now, as a nominee, I think back to the years when I ran MedMark out of my tiny condo. Step by step the company has grown into publishing of five magazines, many digital platforms, podcasts, webinars, and opportunities. Some have described me as a “go-getter,” but I like to define myself as a “goal-getter.”
inform and improve the practices of endodontists, implant specialists, orthodontists, and dental sleep medicine professionals, reaching clinicians that care for the youngest patients seems like a perfect fit into our coverage of dental care that spans a lifetime. In this issue of Pediatric Dental Practice US, our cover story introduces you to Dr. Amy Luedemann of Kidstown Dental. Her compassionate “whole child approach” is made possible by her expertise in pediatric laser dentistry and myofunctional therapy, along with many other steps in her comprehensive approach to children’s dental and overall health. In our Pediatric Perspective column, Dr. William M. Hang explains why pediatric dentists need to be leaders in airway health by recognizing and treating problems in children’s primary dentition.
Lisa Moler Founder/Publisher, MedMark MediaSpeaking of setting and reaching new goals, you all know that specialty dentistry is our focus and our passion. So some more good news is the debut this spring of our newest national publication, Pediatric Dental Practice US. Articles will focus on oral health from infancy through teens and offer pediatric dentists new insights on helping young patients. As we strive to


I struggled over whether to announce the Denobi Award nomination in my column. That humble voice in my head didn’t want to seem boastful. But, I know that my team, friends, readers, and advertisers would want to share in my excitement of this recognition. This is not just about me. I always try to encourage you all to take some chances, believe in yourself, and as inspirational author Norman Vincent Peale advises have a “humble but reasonable confidence in your own powers.” I also try to emphasize my philosophy of “know your worth.” It sure is a fantastic feeling when others realize your worth too.
To your best success,
Lisa Moler Founder/Publisher MedMark Media
































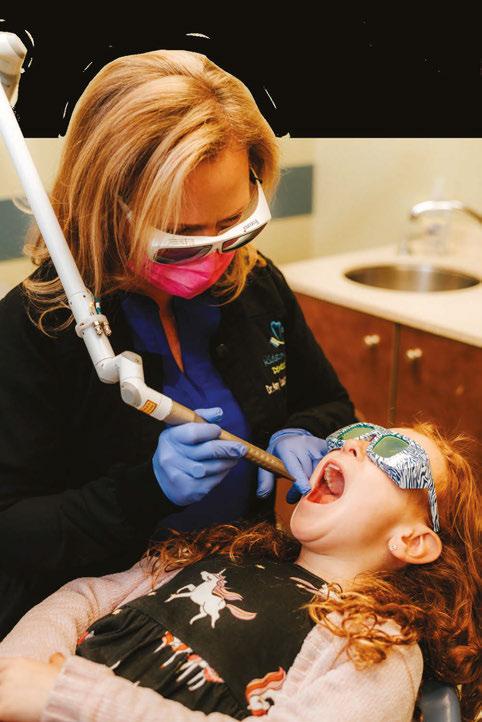
Kidstown Dental has become known for compassion and expertise in pediatric laser dentistry, frenectomies, myofunctional therapy, growth and development guidance as well as for a whole child, comprehensive approach to sleep and airway issues in children. Dr. Amy Luedemann and her team integrate the newest technologies with proven methodologies to create the best possible experience for children. Dr. Amy considers lasers to be the “key piece to achieving optimal results for our sweet patients and our business!”
Amy L. Luedemann, DDS, is a native Houstonian who has been involved in providing dental care since 1990. She started as a dental assistant and went on to put herself through school until she reached her ultimate goal of becoming a pediatric dentist, where her two loves – children and dentistry –come together every day.
In her practice of pediatric dentistry, Dr. Luedemann has become well known for her compassion and expertise in pediatric-laser dentistry, frenectomies, myofunctional therapy, MyoBrace, ALF as well as her comprehensive approach to sleep and airway issues in children. She has a passion for integrating technologies and methodologies to create the best possible environment and experience for each family and child in her care.
Dr. Amy was introduced to hard and soft tissue lasers in 2009, as an associate in a private pediatric dental practice, where she became passionate about doing “no-shot” laser dentistry. She said, “I am so passionate and believe in laser technology so much that if I were to be told that I could no longer practice without using lasers, I would simply rather not practice. I strongly rely on the precision, efficacy, and the high success rate, not to mention the gentleness for the patient that the LightWalker brings to my practice.”
Now, with 12 lasers between her home and office, Dr. Amy shares that the Fotona LightWalker laser has become one of her most leaned-on lasers. “It is so fast and so versatile — the best of both worlds.” Because the LightWalker laser has both an Nd: YAG and Erbium YAG, it can achieve deep soft tissue penetration and be minimally invasive, but also has fast, hard-tissue applications. The clinician is able to use the laser in lieu of a drill for dental decay. There is no direct contact with the tooth so no uncomfortable vibrations, and little-to-no heat with the Erbium YAG, so no need for anesthetic and no unnecessary heating damage to the nerve. Also, lack of friction and microfractures leads to better outcomes, improved comfort, and significantly less risk of recurrent decay. The wide range of applications includes operculectomy, gingival recontouring, pulpotomy, pulpectomy, frenectomy, shot-free laser-assisted extractions, and extensive healing applications via photobiomodulation and high-level laser interventions. She says, “The life-changing non-invasive laser treatments have really become my passion.”

A significant event impacted Dr. Amy deeply and changed her focus. A family brought their only young child, who previously had a mild sleep apnea diagnosis, for a simple checkup. Kidstown Dental’s comprehensive processes include an assessment of all patients for tongue tie and signs of sleep and airway issues. This child had an undiagnosed tongue tie, a known marker for sleep apnea. Shortly after this first visit, and before the child could get the help he needed, the child passed away from SIDS. This was so heartbreaking that she focused on helping children with these issues as early as possible and educating other healthcare providers. She’s been on the radio, podcasts, and is in process of writing her first book, all with the goal of widely sharing her knowledge. Dr. Amy also helped develop and co-teaches a comprehensive, advanced 2-day laser pediatric dental course 2 times per year in her practice to educate new laser users.


Newborn babies’ sleep issues often get chalked up to sleep regression, being fussy, or disliking sleeping on their back, but
often these are signs that are being missed, says Dr. Amy. Generally, when it comes to airway issues in kids, a pediatrician or ENT will only offer four options, none of which are root-cause solutions. The first option usually is to watch and wait. As a second option, if they are concerned, but the patient doesn’t yet qualify for surgery, they offer a steroid nasal spray to shrink the lymph tissues. This does not address why they are enlarged, and parents rightfully don’t want to keep their kids on steroids for long periods of time. The third option is cutting the tonsils and adenoids out, “to Roto-Rooter® the airway,” as Dr. Amy calls it. This also is not a root-cause solution, and often no one tells parents adenoids regrow frequently. Research shows that within 2 years, the relapse of sleep issues is extremely high. If the airway is small, it can still collapse on itself. The last option is a CPAP/BiPAP. In the long run, neither of these options addresses the whys. Why is the airway weak? Why are the lymph tissues enlarged? Why is the child underdeveloped in this way?
The airway is the space in front of the spine behind the jaws. If the child has underdeveloped jaws, the airway will also be underdeveloped and weak, more prone to breathing and sleep challenges over time. Feeling tired during the day, poor school performance, and ADHD are only some of the many symptoms of a child suffering from airway issues. Guiding the child’s growth from the youngest age possible is a root-cause solution. Dr. Amy shares that she prefers starting with a rootcause, non-invasive, healthy fifth option — a cutting-edge laser treatment that she has trademarked, called LAFTR, which stands for “laser assisted functional therapeutic release.” Using the specific, unique wavelength of laser energy that the Fotona Nd:YAG offers, LAFTR offers the deepest penetrating wavelength yet known. At targeted intensities in a specific sequence, it can accomplish a number of positive and healing effects. LAFTR is a “no-touch” laser procedure that releases tensions in the fascia
I strongly rely on the precision, efficacy, and the high success rate, not to mention the gentleness for the patient that the LightWalker brings to my practice.”
and activates idealized function of the cranial nerves, nervous system, fascia, and muscles. It also has a happy side effect of releasing endorphins, or feel-good hormones, and reliably puts the patient into “ventral vegas.” The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-regulation by Dr. Stephen Porges, explains how powerful of a tool that is!
Kidstown Dental often consults for “re-treat” on poorly done or reattached tongue ties. Dr. Amy shares a sweet email from a patient who had received a frenectomy in another practice with a laser that does not use water and works with heat. The family came to Dr. Amy months after the surgery, thinking they needed a second surgery because the child was still suffering with feeding, speech, and sleep. Dr. Amy did three of the non-surgical treatments of LAFTR paired with interdisciplinary bodywork and functional help, and they were able to achieve life-changing results without any further surgery. Now, he is 3 years old and is sleeping and eating normally and speaking in full sentences. Dr Amy shares, “Only a few years ago, this child would have likely ended up with multiple surgeries, increasing the risk of scar tissue, oral aversions, and trauma, and still end up in a variety of therapies, like speech and occupational therapy. I am so glad we can finally help families with this simple, elegant, yet powerful laser intervention.”
Dr. Amy explains how to avoid a surgery if the child has signs of tongue tie and even the look of a posterior tongue tie. “Sometimes a frenum can look short and tight, and the patient may present with a lot of tongue-tie symptoms, but it may not actually be a true physical restriction. LAFTR is a great tool to use for differential diagnosis, particularly of posterior tongue tie. For example, the genioglossus muscles are airway dilator muscles under the tongue, and the frenum lays just over these muscles with lots of fascia connected to and around it. When patients have an airway issue, their genioglossus muscles are going to be contracting to dilate that airway open, and the frenum will be necessarily shortened artificially. So a short frenum on the initial exam may be indicative of an airway challenge. When the patient’s frenum is cut, the body will generally form the new frenum to be just as short and tight as the previous frenum, and then it often gets classified as ‘reattached.’ But LAFTR instantly releases all the artificial tension in the fascia, making it supple, and sometimes the frenum will lengthen 2-3 times compared to how it appeared on initial exam. A true physical restriction of the lingual frenum doesn’t lengthen because the fibers of a true tongue tie are different from simple fascia in a normal frenum. This is why we use this tool prior to any non-reversible cutting procedures.”
As an innovator, Dr. Amy set up the third interdisciplinary clinic in the United States at Kidstown Dental, utilizing an osteopath and an internationally board-certified lactation consultant (IBCLC) in-house. When the frenum is obviously restricted, usually there is also restricted fascia in the floor of the mouth and all around the frenum restriction. If you don’t prepare the patient by releasing the extra “noise” or facial restrictions upstream and downstream of the physical restriction, you’ll likely have a more aggressive surgery, more potential for bleeding, pain, more contraction during healing, and more scarring. You will not only be
cutting the fibers of the frenum, you’ll be cutting fascia around it too to get the full range of motion. “Using the laser in the LAFTR protocol, which we do for every single frenectomy in 5 minutes, we are able to get the frenum clearly visible, releasing the other tensions non-surgically around it, for a faster, easier, more effective, and more comfortable frenectomy surgery.”
Dental visits can be painful, uncomfortable, and scary, with anesthetic injections and loud, vibrational drilling. Lasers make even comprehensive restorative dental needs much more comfortable. The laser allows earlier cavity detection and minimally invasive caries removal. When prepping a cavity, the laser enables you to gently remove the infected tooth structure quickly while effectively disinfecting it before restoring it. There is no smear layer filled with bacteria, no microfractures, and the nerve is not insulted by overheating it, all of which results in a significant decrease in the chance of leaving decay or recurrent decay.

Dr. Amy explains, “When I trained to use hard and soft tissue lasers, I was told that I could charge my patients more for using the laser technology by telling them for x amount I can do things the old fashioned shot/drill and fill way, or for an extra amount, I can do it with a laser with all of these benefits. That never made sense to me. Because of my own frightening childhood dental experiences, once I learned that doing dentistry for kids without shots and with lasers was a superior standard that gives superior outcomes, I could never go back to the old fashioned way. I invested in a hard tissue/soft tissue laser from day one, and I experienced double digit growth every year of my practice until the pandemic, even without marketing. I attribute it primarily to the community’s response to our use of lasers. Almost all of our referrals are from other healthcare providers or friends of current patients, who will drive or fly from long distances for the opportunity to have their children treated with lasers. Our 6th year of practice was a 55% growth year, which our financial advisor shared is extremely uncommon!“
She says, “You can reignite your passion and excitement for dentistry once you embark on laser dentistry. The choices are so endless!” PD
Dual Wavelength Nd:YAG and Er:YAG Laser

Faster recovery and minimal downtime
Little to no anesthesia needed
Avoid added stress due to injections
Comfortable and often painless
KEY TREATMENTS INCLUDE:
- Frenectomies
- No-shot cavity preps
- Airway enhancement
- Pulpotomies
- Extractions
- Photobiomodulation for faster healing
“Unlike a drill, with a laser, there is no direct contact with the tooth which means no uncomfortable vibrations, there is little to no heat with the Erbium YAG, so no need for anesthetic and no unnecessary heating damage to the nerve. There is no friction, no microfractures, all of which lends to better outcomes, improved comfort and significantly less risk of recurrent decay.“
To learn more about the versatile LightWalker:
Email marketing@fotona.org or chat with our team by scanning the QR code.



Did you know that very young children with reduced oxygen saturation during sleep can suffer from brain damage that can be irreversible?1 You might also be surprised to learn that these same children are more likely to have high blood pressure as adults.1
Breathing problems have been correlated with effects on overall health for more than 100 years.2 Journals from the late 1800s and early 1900s show that our profession realized that altered rest oral posture (which includes mouth breathing) caused changes to facial development and had an adverse effect on overall health. Very early treatment in the primary dentition was encouraged. Articles in respected journals discussed why and how to treat these problems orthodontically.3 Unfortunately, early voices advocating for the benefits of early treatment to establish nasal breathing were drowned out by a chorus of influencers who believed that dentists and orthodontists should focus exclusively on straightening teeth in adolescence. This is pretty much the current paradigm with a few exceptions.
The October 2017 ADA position statement4 recommending that dentists screen for airway issues brought sleep and breathing issues to our attention again. The White Paper from the AAO meeting on Airway and Orthodontics in January 2019, however, minimized the connection between orthodontics and airway. The late Dr. Christian Guilleminault had over 400 articles in the refereed literature and was arguably the most well-known name in the medical sleep arena until his death. He spoke at that AAO meeting but was not one of the authors of the White Paper the AAO published. He cited important medical reasons to recognize and treat airway problems as soon as they are recognized. He particularly cited the high incidence of breathing/sleep problems with premature babies and how waiting to treat them means accepting permanent damage to their health. The most recent AAO annual meeting in Orlando, Florida, featured 237 lectures with only five mentioning the word “airway” in the title. None of those specifically mentioned treatment of children in the primary dentition when many of the children Guilleminault referenced are first diagnosed with problems. If orthodontists are not recognizing and treating these problems in the primary dentition who is going to assume this responsibility?
William M. Hang, DDS, MSD, graduated at the top of his class from the University of Illinois College of Dentistry and the University of Minnesota Orthodontic program where he briefly taught orthodontics. He has been in private practice since 1975 and is currently practicing in Agoura Hills, California. Having been traditionally trained, he extracted teeth for crowding and often retracted the teeth. For the past 40 years, however, he has been a pioneer in nonretractive treatments to improve the airway in patients of all ages. He received a Lifetime Achievement Award from the American Academy of Physiological Medicine and Dentistry for his work.
Dr. Hang recently founded OrthO2Health™ to teach and mentor doctors about airway-healthy orthodontic treatments for all ages. His Early Childhood Health-Centered Orthodontic Mentorship™ focuses on treatments for children approximately age 10 and under with an emphasis on treating in the primary dentition. The Hang E.R.R.S.™ (Extraction Retraction Regret Syndrome™) Orthodontic Mentorship addresses treatments for teens and adults to optimize facial balance, TMJ health, and airway. Reversing previous orthodontic retraction, including reopening previous bicuspid extraction spaces or missing lateral incisor spaces and surgery, are also integral parts of this mentorship.
Disclosure: Dr. Hang practices Orthotropics® and has a mentorship in which he teaches other doctors the philosophy and technique of Orthotropics®
Orthodontists get little to no training in working with very young children and are not behaviorally the best trained professionals to deal with children in the primary dentition. Pediatric dentists are trained specifically to work with very young children and are the obvious group to assume a pivotal role in treating the airway pandemic which Guilleminault and others have described. Most pediatric dentists have well established referral patterns with pediatricians and are used to collaborating with that critical group in the medical profession. Clearly there is a gap between medicine and dentistry that should be bridged by the pediatric dentists. If they don’t act, who is left to help these very young children?
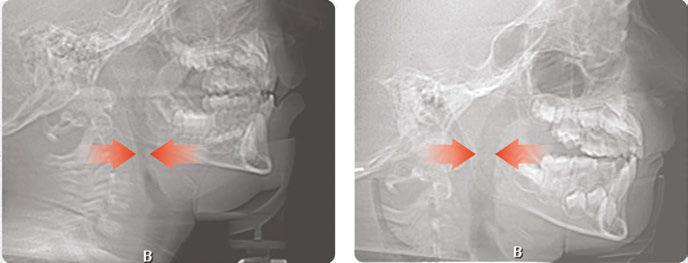
Over 10 years ago, we began Orthotropic® treatment for a 5 year, 3-month-old boy with a diagnosis of Pierre-Robin Sequence, Obstructive Sleep Apnea (OSA), and Failure to Thrive (Figure 1). With lack of forward development of the face com-
monly seen in Pierre-Robin patients, his airway was compromised, resulting in OSA. The Failure to Thrive diagnosis likely resulted from insufficient growth hormone being released during the deeper stages of sleep. This treatment began before any permanent teeth erupted. Our goal was to eliminate OSA.
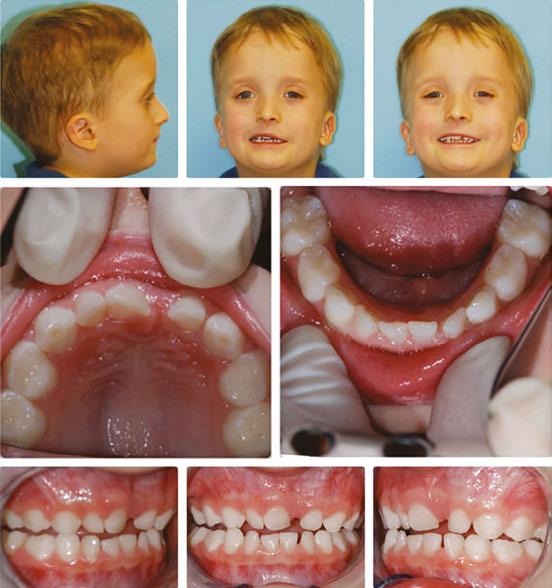
Orthotropics® uses removable appliances to laterally expand the upper arch while simultaneously advancing the upper anterior teeth to their proper place in the face. Then the mandible is developed forward. Orthotropics® is my preferred treatment in cases like this because it negates the head gear-effect producing better facial balance5 and also can result in substantial airway improvements (Figure 2).6
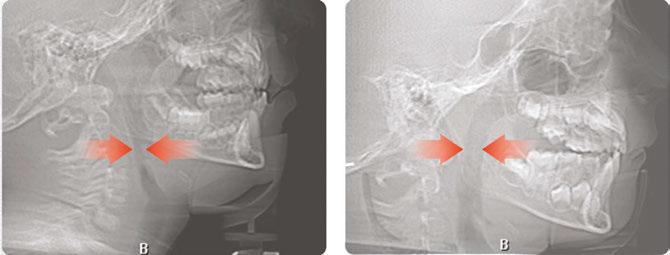
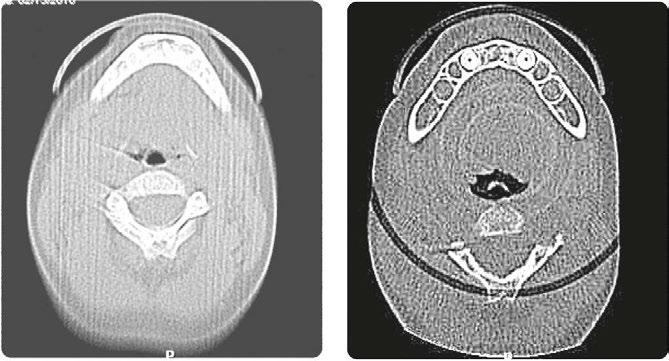
This young boy had great parental support and was very compliant during the treatment. A posttreatment sleep test showed no signs of sleep apnea.7 Failure to Thrive was also overcome. Now at 17 years old, this patient is 5 ft. 7in. tall and is still growing. I believe that improved breathing and sleep has resulted in an increase in HGH production which allowed him to resume normal growth. He’s an aggressive tennis player with a big smile and no return of his OSA (Figure 3). Thankfully, he’s an excellent student with no evidence of brain damage from his early OSA diagnosis.

I’ve had some orthodontists lament that they can’t get really young children to open their mouths for an
examination. The ironic thing is that airway problems can be recognized without the patient even opening the mouth! Lipapart posture, an accentuated cupid’s bow appearance of the upper lip, a flaccid rolled-out lower lip, crusty lips, mentalis muscle strain to close the lips, flat cheeks, narrow nostrils, forward head posture, or a tilted back forehead are common physical signs of an airway issue and all are obvious without having a child open the mouth. In reality, a properly taken medical history for children this age frequently raises suspicion about sleep/ breathing problems and doesn’t require having a child open the mouth. Pediatric dentists are the masters at getting kids to open their mouths and may be able to get an even more complete picture of a child’s dentofacial development as it relates to sleep/ breathing than other groups in the dental profession.
Dr. Stephen Sheldon, former director of the Sleep Medicine Center at Lurie Children’s Hospital in Chicago, says, “The identification of disordered sleep really rests on asking the right questions and being able to interpret the answers, and that really begins with all child healthcare professionals.”8 Pediatric dentists are in a perfect position to learn to recognize the signs and symptoms of these problems which can easily be incorporated into every pediatric dentist’s initial examination. If a patient like the one I’ve referenced in this article can be successfully treated, what about other children who may have other symptoms which indicate that they may not be sleeping and breathing well? They exist in virtually every dental practice that treats children.
Brain damage isn’t the only thing that may be prevented by treating the airway. Bedwetting often resolves after sleep and breathing issues are alleviated. Parents also report that there are fewer colds and ear infections, as well as calmer children who are better able to focus on tasks. According to a national 2016 survey, 6.1 million children are diagnosed with ADHD.9 Dr Sheldon says he doesn’t believe there is such a thing as ADHD. He believes it is always a sleep and breathing issue.10 If there are ways to treat this problem, does it make sense that we continue to have a growing percentage of our young children placed on Ritalin and other drugs for ADHD? Normalizing growth and eliminating possible negative effects of untreated sleep apnea should be at the top of the list of must-haves for our growing number of patients who present very early with symptoms of possible sleep and breathing problems. Waiting for permanent teeth to erupt to treat a health problem makes no more sense than waiting for growth to be complete before getting eyeglasses for a child with impaired vision.
My goal is to help others create better outcomes for our kids. I have treated patients as young as 3 years old and regularly treat in the primary dentition even though I have no special training in treating this age group. Highly motivated mothers can help people like me make treatment happen for their kids when they understand the consequences of failing to act. When it comes to sleep and breathing issues in children, I have seen a direct correlation between early treatment and better long-term outcomes.
James Nestor’s book, Breath, was No. 6 on the New York Times bestseller list and has been published in 32 languages. It has raised public awareness of the importance of nasal breathing and eliminating OSA for people of all ages as a primary health care goal. Helping young children to sleep and breathe well should be part of every pediatric dentist’s skill set. With Nestor’s
book and the ADA mandate, the stage has been set for the pediatric dentist to assume the lead in treating the airway.
With a new focus on sleep and airway health, a number of us are happy to share our experience about when and how to treat kids in the primary or early mixed dentition. Effectively treating this group almost always requires a team of other health care professionals working together. Dr Sheldon goes on to say, “If you identify the problem but can do nothing about it, then the need for identification becomes questionable, so the two cannot be done in isolation.”8 This means pediatric dentists not only need to recognize sleep and breathing problems, they need the skills to actually treat these children. Recognizing the symptoms and identifying the problem are the first steps. There are a number of approaches which can be effective in addressing the airway, and none are a panacea. I’ve had my successes and failures over the past 30 years as I’ve studied this problem. I’ve seen little movement in our profession to fund research to find better approaches. Doing nothing just because there isn’t a perfect answer for every case is not an ethical answer. It is ironic that 100-plus years ago orthodontists were treating these issues before OSA was even given a name, but such treatment disappeared as treatment to align teeth became commonplace. Hopefully the pediatric dental profession will embrace this public health issue, develop programs to train doctors in current treatment modalities, and fund research to find even better ways. Will the profession take the first step of recognizing more than tooth problems and help dentistry assume a pivotal role in starting children on a lifetime of airway health?
A number of pediatric dentists have already dedicated their practices to treating airway issues. Doing so has transformed their practices, increased their personal satisfaction, and improved the health of their patients. Can you envision you, your practice, and your patients benefitting from your airway awareness? There are people who have already blazed this trail, and we are happy to have you join us on this journey.
1. Harper RM, Kumar R, Ogren JA, Macey PM. Sleep-disordered breathing: effects on brain structure and function. Respir Physiol Neurobiol. 2013 Sep15;188(3):383-391.
2. Allen WH, Sedgwick WT. Civics and Health (1909). Boston: Athenaeum Press; 1909.
3. Philippe J. Who introduced early treatment to orthodontics? J Dentofacial Anom Orthod 2012;15:107. Available at: https://www.jdao-journal.org/articles/odfen/pdf/ 2012/01/odfen2012151p107.pdf Accessed January 3, 2023.
4. ADA House of Delegates; The Role of Dentistry in the Treatment of Sleep-Related Breathing Disorders. 2017.
5. Singh GD, Medina LE, Hang WM. Soft tissue facial changes using Biobloc appliances: geometric morphometrics. Int J of Orthod Milwaukee. 2009;20(2):29-34.
6. Singh GD, Garcia-Motta AV, Hang WM. Evaluation of the posterior airway space following Biobloc therapy: geometric morphometrics. Cranio. 2007;25(2):84-89.
7. Boyd KL, Sheldon SH. Sleep disorder breathing: a dental perspective. In: SH Sheldon, MH Kryger, R Ferber, D Gozal, eds. Principles and Practice of Pediatric Sleep Medicine, 2nd edition. London: Elsevier; 2012:275-280.
8. Diiulio R. Sleeping Like a Baby: Dr Stephen H. Sheldon’s Pediatric Sleep Medicine Practice. Sleep Review. Nov 2013. https://sleepreviewmag.com/sleep-treatments/therapy-devices/cpap-pap-devices/sleeping-like-a-baby-dr-stephen-h-sheldon-pediatricsleep-medicine-practice/. Accessed December 20, 2022.
9. National Survey of Children’s Health (NSCH) 2016: online and mail survey. https:// nschdata.org/browse/survey/. Accessed December 20, 2022.
10. Personal communication.
I recently sold my practice and am now spending more time teaching airway focused treatments to Pediatric Dentists, General Dentists, and Orthodontists.
Come learn how E.C.H.O. is empowering providers like you to treat kids under 10 - even in the primary dentition.
 Dr. Bill Hang
Dr. Bill Hang
Join us to learn how E.C.H.O. is helping providers like you treat kids under age 10 - and especially in the primary dentition




Designed for pediatric dentists, orthodontists, and general dentists who treat children
LEARN HOW T IDENTIFY DIAGNOSE & TREAT (OR REFER) AIRWAY PROBLEMS IN CHILDREN

Dr. Steve Lamberg discusses the impact of intervention on maternal and fetal health outcomes

Ample evidence exists showing Sleep-Related Breathing Disorders or SRBD, have a negative impact on maternal and fetal outcomes. A growing body of evidence reveals therapeutic intervention directed at SRBD creates positive health outcomes.
SRBD cover a spectrum of medical conditions ranging from Upper Airway Resistance Syndrome (UARS) through severe
Steve Lamberg, DDS, D.ABDSM, has been practicing comprehensive restorative dentistry in Northport, NY for 40 years. Always passionate about sleep and wellness, he became a Diplomate of the American Board of Dental Sleep Medicine in 2011 and has served on their board review faculty. He holds several patents, and is the inventor of the Lamberg SleepWell Appliance, which is FDA-cleared for the treatment of OSA. Dr. Lamberg also launched and serves as the director of the Pediatric and Adult Airway Network of New York (PAANNY), to provide a local platform where dentists, physicians, orofacial myologists, and other related professionals learn and collaborate on treatment patients of all ages. Additionally, Dr. Lamberg serves as a Scientific Advisor at the Kois Center in Seattle. His recently published book for the general public, Treat the Cause…Treat the Airway correlates many common medical conditions to airway and sleep and is available on Amazon.
Obstructive Sleep Apnea (OSA) and are frequently accompanied by the symptom of snoring. The prevalence of OSA ranges from 7.8% to 77.2% in adults aged 30-69 years.1 Among obese pregnant women, 15% to 20% have OSA, and this prevalence increases along with body mass index and in the presence of other comorbidities.2 These prevalence statistics in women are considered to be significantly underestimated due to gender-related differences in diagnosis resulting from women underreporting symptoms as well as an increased prevalence of UARS that does not meet the criteria to be OSA. Airway resistance even without a cortical arousal can upregulate the sympathetic nervous system and the hypothalamic-pituitary-adrenal axis causing a rise in blood pressure.3
A diagnosis of OSA as well as its key symptom of habitual snoring have been linked to hypertensive disorders of pregnancy, insulin resistance,4 gestational diabetes, and poor fetal outcomes. Habitual snoring means at least 3 nights/week, and pregnant women who are habitual snorers have a 2-fold greater risk of gestational hypertension relative to non-snorers, although it has also been shown that snoring onset during pregnancy has worse outcomes than if habitual snoring existed pre-pregnancy.5,6
During pregnancy as in menopause, women have an increased risk of SRBD attributable to changes in estrogen and progesterone as well as weight gain.7,8,9

Estrogen contributes to edema, vasodilation, and nasal congestion that could impact the upper airway by making it more collapsible, while progesterone enhances respiratory drive creating a “vacuum effect” and could contribute to airway collapse.2 SRBD during pregnancy increase the risk of hypertensive disorders of pregnancy (HDP), occurring in 1 of 10 pregnancies and are associated with significant maternal morbidity and mortality.10,11
The study, employing the United States Healthcare Cost and Utilization Project-National Inpatient Sample, examined 7,907,139 deliveries and found women diagnosed with OSA were at higher risk of having pregnancies with preeclampsia [odds ratio (OR) 2.2], eclampsia (OR 4.1), chorioamnionitis (OR 1.4), postpartum hemorrhage (OR 1.4), venous thromboembolisms (OR 2.7), and delivery by caesarean section (OR 2.1). Gestational diabetes as well as cardiovascular and respiratory complications were also more common among these women, as was maternal death, OR 4.2.12

Newborns of OSA mothers were at elevated risk of being premature, OR 1.3, and having congenital abnormalities, OR 2.3.12 The higher risk of congenital anomalies and resuscitation
at birth in neonates of mothers with OSA emphasizes the importance of identifying OSA in pregnant women and women of reproductive age.13
Fetal growth restriction was also more prevalent and is the basis of the Sleep Apnea and Fetal Growth Restriction study (SAFER). Fetal growth restriction (FGR), affecting 10% of all pregnancies, is a major contributor to fetal and neonatal morbidity and mortality with intrauterine, neonatal, and lifelong complications. While previous studies have reported an association between low birthweight and elevated blood pressure (BP) in adulthood, the recent Raine study14 explored the association between intrauterine fetal growth restriction from 1,440 women and BP of their adult offspring. Their data revealed evidence that restricted fetal growth was associated with significantly higher adult BP over two decades later that corresponded with a 10% higher risk of death due to heart disease and a 10% higher risk of stroke. This study further reinforces the importance of the early
A diagnosis of Sleep-Related Breathing Disorder has been linked to poor fetal outcomes.
intrauterine environment and its influence on adult BP. OSA has been hypothesized to be a modifiable risk factor for FGR.15,16
Premature birth is one that occurs before 37 weeks of gestation or having a low birth weight. The short-term and long-term effects of preterm birth (PTB) on a child’s physical and psychological growth and development have been a hot topic of interest. The brain, lungs, and eyes are the most susceptible organs, but facial bones and palate morphology may also be affected. The prevalence or PTB ranges from 0% to 10% in children, and 10% to 70% in children with low birth weight. Palates of premature infants have narrower and deeper forms compared to the palates of non-premature infants. Additionally the mandibular arches are less developed, and evidence shows that the lower the gestational age, the more the tooth development is delayed at age 9.17 Due to this, there is a greater risk of future malocclusion, difficulties in chewing or speaking, and esthetic problems.18 Malocclusion traits including crossbite, open bite, midline shift, open bite, spacing, and Angle’s Class 2, occurred significantly more often in early pre-term EPT (83.3%) and very pre-term VPT (73%) children, compared with full-term (51.2%) children. Deep bite was the most common malocclusion trait in the EPT and the VPT group. Higher orthodontic treatment need was found for the preterm children.19 Inadequate growth and development of the jaws compromises the airway and leads to compensations, which have consequences including orthodontic problems.
A normal physiological component of healthy pregnancy is fetal movement, which has been used both formally and informally as a marker of fetal well-being. Reductions in fetal movement accompanies complications such as fetal growth restriction. It has been hypothesized that SRBD may link preeclampsia with reduced fetal movement and that treatment of sleep-disordered breathing might improve fetal activity during sleep. A study by Blyton showed CPAP to be effective in improving fetal movements which suggests a pathogenic role for SRBD
in reduced fetal activity and possibly other poor fetal outcomes associated with preeclampsia.20
Fetal hiccups were reduced in women with preeclampsia and through intervention with CPAP were found to increase, providing intriguing evidence of the pathogenic connection of airway and fetal health.21 Fetal hiccups may be a manifestation of programmed isometric inspiratory muscle exercise in preparation for postnatal respiratory function.22
A scoping review of the literature with meta-analysis shows that maternal sleep events such as OSA, sleep disruption, and time spent in certain body positions, may have negative effects on the fetus, resulting in altered growth, gestational length, and even death.23 As SRBD are a prevalent risk factor of gestational cardiometabolic disease, they are a potential therapeutic target to reduce cardiometabolic morbidity.24
Robust literature demonstrates SRBD as a consistent, strong, and positive predictor of gestational hypertension and preeclampsia, similar to studies of SRBD and hypertension in non-pregnant adults. A systematic review reported OR 2.4 of pregnancy-related hypertension among women with habitual snoring or moderate-to-severe OSA.25
Therapeutic intervention has been shown to improve health outcomes in women. In a study of 11 women with preeclampsia and mild SDB, one night of CPAP reduced mean systolic (128 mmHg versus 146 mmHg ) and diastolic (73 mmHg versus 92 mmHg) blood pressure compared with a baseline night without treatment in the same women.26 In another study, for 12 women with preeclampsia, a single night of CPAP in the third trimester improved cardiac output and reduced peripheral vascular resistance, whereas no improvement occurred in a nontreated preeclampsia group.27 Larger sample sizes are needed to be powered to assess gestational outcomes. A phase III clinical trial is underway with 2,700 women to examine whether treating SDB in pregnancy reduces the risk of gestational hypertensive disease.28

Maternal sleep events such as OSA, sleep disruption, and time spent in certain body positions, may have negative effects on the fetus, resulting in altered growth, gestational length, and even death.
Given our current level of knowledge, pregnant women who have even mild sleep apnea should be treated for their SRBD. Questionnaires are an effective and efficient way to educate patients and screen for SRBD, treatment of which will benefit maternal and fetal outcomes while possibly serving to optimize craniofacial growth from infancy into adolescence and beyond. It is time to consider vigilance of maternal SRBD as the first step towards the earliest intervention to prevent SRBD along life’s journey from neonate to adult.
Screening and treatment of SRBD in pregnant women requires an interdisciplinary approach. Dentists can and do play an essential role in the multidisciplinary care of patients with certain sleep-related breathing disorders and are well positioned to identify patients, including pregnant women, at greater risk of SRBD. The American Dental Association encourages dentists to screen patients as part of a comprehensive medical and dental history to recognize symptoms such as daytime sleepiness,
1. Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MSM, Morrell MJ, Nunez CM, Patel SR, Penzel T, Pépin JL, Peppard PE, Sinha S, Tufik S, Valentine K, Malhotra A. Estimation of the global prevalence and burden of obstructive sleep apnea: a literature-based analysis. Lancet Respir Med. 2019;7(8):687–698.
2. Dominguez J E, Krystal A D, Habib A S. Obstructive sleep apnea in pregnant women: a review of pregnancy outcomes and an approach to management. Anesth Analg. 2018;127(5):1167–1177.
3. Lamberg S. Upper Airway Resistance Syndrome. Inside Dentistry. Jan 2021:60.
4. Sanapo L, Bublitz MH, Bai A, Mehta N, Messerlian GM, Catalano P, Bourjeily G. Association between sleep disordered breathing in early pregnancy and glucose metabolism. Sleep. 2022 Apr 11;45(4):zsab281.
5. O’Brien LM, Bullough AS, Owusu JT, Tremblay KA, Brincat CA, Chames MC, Kalbfleisch JD, Chervin RD. Pregnancy-onset habitual snoring, gestational hypertension, and preeclampsia: prospective cohort study. Am J Obstet Gynecol. 2012;207(6): 487. e1–487.e9
6. Li L, Zhao K, Hua J, Li S. Association between sleep-disordered breathing during pregnancy and maternal and fetal outcomes: an updated systematic review and meta-analysis. Front Neurol. 2018; 9:91.
7. Young T, Finn L, Austin D, Peterson A. Menopausal status and sleep-disordered breathing in the Wisconsin Sleep Cohort Study. Am J Respir Crit Care Med. 2003; 167(9):1181–1185.
8. Dunietz G L, Chervin R D, O’Brien LM. Sleep-disordered breathing during pregnancy: future implications for cardiovascular health. Obstet Gynecol Surv. 2014; 69(3):164–176.
9. Balserak BI. Sleep-disordered breathing in pregnancy. Breathe. 2015;11(4): 268–277.
10. Zhang J, Troendle J, Levine R. Risks of hypertensive disorders in the second pregnancy. Obstet Gynecol. 2000;95(4, Suppl 1): S77.
11. James PR, Nelson-Piercy C. Management of hypertension before, during, and after pregnancy. Heart. 2004;90(12):1499–1504.
12. Passarella E, Czuzoj-Shulman N, Abenhaim HA. Maternal and fetal outcomes in pregnancies with obstructive sleep apnea. J Perinat Med. 2021 Sep 15;49(9):1064-1070.0
13. Bourjeily G, Danilack VA, Bublitz MH, Muri J, Rosene-Montella K, Lipkind H. Maternal obstructive sleep apnea and neonatal birth outcomes in a population based sample. Sleep Med. 2020 Feb;66:233-240.
14. Yadav A, Beilin LJ, Huang RC, Vlaskovsky P, Newnham JP, White SW, Mori TA. The relationship between intrauterine foetal growth trajectories and blood pressure in young
snoring, or witnessed apneas and to evaluate risk factors such as obesity, retrognathia, age, and hypertension. Whenever a risk is determined, patients can be referred to appropriate physicians for sleep testing and diagnosis. Pregnant women should undergo serial monitoring with questionnaires as SRBD increases from the first to the third trimester. If the onset of SRBD occurs during pregnancy, sleep testing 3-6 months postpartum is recommended to evaluate if the SRBD has been resolved. When SRBD is diagnosed, there are many treatment options including CPAP and oral appliance therapy. Dentists with training in dental sleep medicine can fabricate a custom oral appliance to optimize the airway and breathing pattern. There are also simpler temporary appliances that can be fit and delivered at the first visit if necessary. Dentists and physicians can collaborate to enhance health outcomes of mother and fetus. We can even gift the expectant mother one of the many great books available to help her and her newborn along their way to optimal health.
adults. J Hypertens. 2022 Mar 1;40(3):478-489.
15. Chen YH, Kang JH, Lin CC, Wang IT, Keller JJ, Lin HC. Obstructive sleep apnea and the risk of adverse pregnancy outcomes. Am J Obstet Gynecol. 2012 Feb;206(2):136.e1-5.
16. Pamidi S, Pinto LM, Marc I, Benedetti A, Schwartzman K, Kimoff RJ. Maternal sleep-disordered breathing and adverse pregnancy outcomes: a systematic review and metaanalysis. Am J Obstet Gynecol. 2014 Jan;210(1):52.e1-52.e14.
17. Paulsson L, Arvini S, Bergström N, Klingberg G, Lindh C. The impact of premature birth on dental maturation in the permanent dentition. Clin Oral Investig. 2019 Feb;23(2): 855-861.
18. Oppitz LR, Gonçalves FM, Schneider NA, Arantes ACM, de Miranda BM, Guariza-Filho O, Johann ACBR, de Araujo CM, Camargo ES. Can preterm birth affect the palate morphology? A systematic review. Research, Society and Development, [S. l.], v. 10, n. 10, p. e107101018812, 2021.
19. Paulsson L, Söderfeldt B, Bondemark L. Malocclusion traits and orthodontic treatment needs in prematurely born children. Angle Orthod. 2008 Sep;78(5):786-92.
20. Blyton DM, Skilton MR, Edwards N, Hennessy A, Celermajer DS, Sullivan CE. Treatment of sleep disordered breathing reverses low fetal activity levels in preeclampsia. Sleep. 2013 Jan 1;36(1):15-21.
21. O’Brien LM. Positive airway pressure as a therapy for pre-eclampsia? Sleep. 2013; 36(1):5-6.
22. Kahrilas PJ, Shi G. Why do we hiccup? Gut. 1997;41:712-3.
23. Warland J, Dorrian J, Morrison JL, O’Brien LM. Maternal sleep during pregnancy and poor fetal outcomes: A scoping review of the literature with meta-analysis. Sleep Med Rev. 2018 Oct;41:197-219.
24. Laposky AD, Pemberton VL. Sleep-Disordered Breathing and Pregnancy-Related Cardiovascular Disease. J Womens Health (Larchmt). 2021 Feb;30(2):194-198.
25. Dunietz GL, Hao W, Shedden K, Holzman C, Chervin RD, Lisabeth LD, Treadwell MC, O’Brien LM. Maternal habitual snoring and blood pressure trajectories in pregnancy. J Clin Sleep Med. 2022 Jan 1;18(1):31-38.
26. Edwards N, Blyton DM, Kirjavainen T, Kesby GJ, Sullivan CE. Nasal continuous positive airway pressure reduces sleep-induced blood pressure increments in preeclampsia. Am J Respir Crit Care Med. 2000; 162:252–257.
27. Blyton DM, Sullivan CE, Edwards N. Reduced nocturnal cardiac output associated with preeclampsia is minimized with the use of nocturnal nasal CPAP. Sleep. 2004;27: 79–84.
28. ClinicalTrials.gov. Continuous positive airway pressure (CPAP) for sleep apnea in pregnancy (SLEEP) NCT03487185. 2018. Available at: https://clinicaltrials.gov/ct2/show/ NCT03487185 Accessed January 30, 2023.
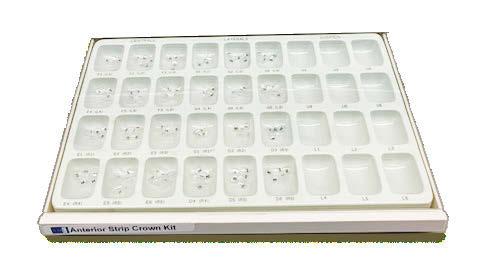
Cavity liners and indirect pulp capping (IDPC) materials have been used in dentistry for decades. The recent introduction of NuSmile’s NeoLINER™ LC now provides one of the most therapeutic, easy-to-use liners on the market! It is a light-cured MTA-modified bioactive material that is recommended for use as either a cavity liner or as an indirect pulp-capping material. For decades, calcium hydroxide was the most popular lining or indirect pulp-capping material, primarily because of its ability to stimulate reparative dentin. However, its solubility after placement was found to be a problem. Zinc oxide and eugenol, glass ionomers, and resin-modified glass ionomers have also been used as liners, bases, and IDPC materials, but each has shortcomings.
Liners are materials that are placed in thin layers over exposed dentin in the deepest portion of cavity preparations. They function to seal dentin tubules, prevent microleakage, provide some thermal insulation, and depending on the material used, stimulate the formation of reparative or tertiary dentin. Historically, indirect pulp-capping materials have been used when a thin layer of carious dentin remains after deep excavation with no exposure of the pulp and no clinical signs of irreversible pulpitis. In recent years, indirect pulp capping in pediatric dentistry has been utilized when larger amounts of carious tissue remain, but the caries can be sufficiently sealed from the oral environment with a full coverage restoration like a stainless steel or zirconia crown. The main goal of both liners and IDPC materials is to minimize inflammation, promote healing, and maintain vitality of the dental pulp. Indirect pulp capping materials may also demonstrate some bactericidal properties to kill any remaining bacteria that may remain.




The MTA in NuSmile’s NeoLINER LC provides a continuous high calcium release. This, in combination with a high pH, promotes hydroxyapatite formation and protects against hypersensitivity. The high pH also has bactericidal effects to reduce remaining bacteria. NeoLINER LC is packaged in a syringe with 27-gauge disposable tips that allow for precise and easy placement. Its viscosity ensures it will stay in the area where it is placed until it is cured with a curing light. NeoLINER LC is
William F. Waggoner, DDS, MS, is the founder and owner of Galaxy Smiles of Las Vegas, Pediatric Dental Care Associates, and Kids Dental Safari. He has been a pediatric dentist for nearly 40 years. He also serves as the Chief Dental Officer for NuSmile.
Paul Bahn, DMD, is a Diplomate of the American Board of Pediatric Dentistry and the American Board of Laser Surgery. He is a member of the American Academy of Pediatric Dentistry, the American Dental Association, the Parenteral Drug Association, the Philadelphia County Dental Society, and the Academy of Sports Dentistry.
moisture tolerant, has low water solubility, and is compatible with all etching, bonding, and resin restorative materials. It’s also radiopaque for easy postoperative assessment.
While it is an excellent liner and IDPC material, NeoLINER LC is not recommended for direct pulp capping because of its resin component which can act as an irritant. Any materials containing a resin can damage or kill pulpal tissue if placed in direct contact. If a pulpal exposure is realized, a resin-free MTA material such as NuSmile’s NeoMTA® 2 or NeoPUTTY® is recommended as a direct pulp-capping agent due to its exceptional biocompatibility. These MTA materials, which have a delayed set, may be covered with NeoLINER LC for placement of an immediate final restoration.
The versatility and handling properties of NuSmile’s NeoLINER LC make it a wonderful addition to the clinician’s restorative and pulpal therapy armamentarium.
This information was provided by NuSmile.
MTA MODIFIED LIGHT-CURE LINER/INDIRECT PULP CAP MATERIAL
Continuous high calcium release in combination with high pH promotes hydroxyapatite formation
Protects against hypersensitivity
Insoluble and moisture tolerant

1 g Kit +15 TIPS $42.00
Scan & shop
High pH has bactericidal affects to support healing
Precise, easy placement with command set
Compatible with all etching/bonding systems and dental restorative materials
4 g Kit +50 TIPS $135.00



High turnover, especially of administrative staff, is one of the biggest complaints I hear from doctors. Some doctors accept this as an industry standard and believe that everyone has this problem, and it is just a fact of life. However, I have some compelling statistics, research, and experience that say you don’t want to and don’t have to be victim of this industry standard.
We know that turnover is inconvenient and stressful, but do we know the monetary effects of turnover?
Josh Bersin of Deloitte Consulting estimates that the cost of losing one employee can cost up to 2 times that employee’s annual salary.1
Let’s do the math. Let’s say you have a front desk team member who is paid $30,000 annually. If it costs you 2 times his/ her annual salary, then it costs you $60,000 every time someone leaves. If you average three people leaving a year, you are spending $180,000 a year on turnover costs! In 5 years, you are spending almost a million dollars replacing administrative staff.
That’s a lot of money.
Before jumping into the three tips to help improve your employee retention in your practice, let’s talk about a wellknown company that has been able to do this despite industry standards — Starbucks.
The quick-service restaurant industry is another field with notably high turnover. Starbucks, however, has 120% less turnover than the average quick-service restaurant!2

Here’s the point: You don’t have to have high turnover just because it is standard in your industry.
In a national survey of 400 employees, 70% of the respondents said that training and development opportunities influenced their decision to stay at their job.3 Additionally, research shows that 40% of employees that don’t receive quality training and onboarding will leave within the first year.
Training makes your employees feel like they are developing and growing professionally. They see it as a perk of the job. Also, your team will feel like you are investing in them, believing in their ability to grow, and making them feel appreciated.
Fun fact: Starbucks consistently spends more money on training and development than they do on advertising.
According to a Harvard Business Review article, “The ability to visualize and articulate a possible future state of an organization or company has always been a vital component of successful leadership.”4
People want to feel like they are a part of something bigger than themselves, something important, and something worth sticking around for. If employees feel that they are just doing the same thing over and over every day with no goals or aspirations for the future, they will be significantly less engaged with their work and less inclined to stick around.
A vision for the future can also include a personal vision for one of your employees. For example, if you have great front desk team members, it is important to give them goals or ideas about where they can progress and grow within the company. Maybe one day they can be the front desk team leader, the marketing assistant, or can spearhead the annual events held at your practice. Opportunities for growth and development help retain top talent. People want to feel like you believe in their abilities. They want to look forward to something in the future.
According to Forbes, “People don’t leave bad jobs; they leave bad managers.”5
Here are a few things I’ve seen that make successful leaders who are respected by their team.
• Express appreciation, and say thank you! Tell your staff members they did a great job handling a difficult patient, thank them for coming in early, or tell them how much you appreciate everything they do to make your day run smoother. This simple act of gratitude can go a long way.
• Clearly communicate goals and expectations. If leaders want the team to be friendly to patients, they should communicate exactly what that looks like. If you don’t clearly
communicate, then the team may be confused or may think they are doing what you asked, but you get frustrated with them because they aren’t meeting expectations.
• Lead by example. Strong leaders should demonstrate the qualities that they ask for from their team. If the leader wants the team to be on time for meetings, the leader should be too.
• Be consistent. If managers implement a new system or protocol, they need to follow through with a system of accountability. If managers don’t consistently refer to the new system, teams think the managers just say things and move on. The next time they say something, teams don’t believe they have to do it. Not only that, but if there are employees who try to follow through, they will get frustrated that they are the only ones implementing the new system because other team members are just doing it their own way. This is a quick way to lose respect as a leader.
The key is to realize that your management team is an important part of the puzzle. A bad manager can create unnecessary turnover. Make sure you choose the right people to lead your teams and give them the necessary training and mentorship to be effective leaders who the team respects.
Let’s review the ways to reduce turnover:
1. Provide training opportunities.
2. Create a vision for the future.
3. Have quality leaders.
Just because it’s an industry standard to have high turnover, doesn’t mean you have to have high turnover too. Be intentional with keeping your good employees.
1. Bersin J. Employee Retention Now a Big Issue: Why the Tide Has Turned. LinkedIn. Available at: https://www.linkedin.com/pulse/20130816200159-131079-employeeretention-now-a-big-issue-why-the-tide-has-turned/. Accessed February 6, 2023.
2. Freeman L. Why Starbucks Is So Successful: 5 Must Have Ingredients. Addicted to Success. Available at: https://addicted-2success.com/startups/why-starbucks-is-so-successful-5-must-have-ingredients/. Accessed February 6, 2023.
3. Gutierrez K. Mind-blowing Statistics that Prove the Value of Employee Training and Development. Shift. Available at: https://www.shiftelearning.com/blog/statistics-value-of-employee-training-and-development. Accessed February 6, 2023.
4. Mayo T. The Importance of Vision. Harvard Business Review. Available at: https://hbr. org/2007/10/the-importance-of-vision. Accessed February 6, 2023.
5. Kelly J. People Don’t Leave Bad Jobs, They Leave Bad Bosses: Here’s How To Be A Better Manager To Maintain And Motivate Your Team. Forbes. Available at: https://www. forbes.com/sites/jackkelly/2019/11/22/people-dont-leave-bad-jobs-they-leave-badbosses-heres-how-to-be-a-better-manager-to-maintain-and-motivate-your-team/?sh=235cada922b9. Accessed February 6, 2023.
In a national survey of 400 employees, 70% of the respondents said that training and development opportunities influenced their decision to stay at their job.
Dr. Francis Nasser, Jr. discusses the important role of military dentists and a special way to recognize their contribution to the field
The Association of Army Dentistry (AAD) dedicated the Army Dentistry Monument on Friday, March 24, 2023, in a ceremony at the U.S. Army Medical Department (AMEDD) Museum in San Antonio, Texas. According to Dr Ronald Lambert (COL USA DC ret, Past President of the AAD), “The monument is a lasting tribute to all the soldiers, civilians, and spouses who have served and continue to serve in the Army Dental Care System in support of the U.S. Army and its military mission. The monument recognizes and honors the selfless contributions made by the diverse members of the Army Dental Care System and its key supporting components in the overall mission of Army Medicine.”
Founded in March 1911, the Army Dental Corps has a long and distinguished history of providing global dental services to soldiers and ensuring the readiness of the nation’s fighting forces. Even before 1911, the Army contracted dental surgeons to provide dental care to soldiers deployed to the new territories of a growing nation. The tradition of providing oral health services to soldiers wherever they are assigned continues to this day.
During World War II, more than 18,000 dentists served in uniform. It was during this time that the role of Army Dentistry expanded to include not only all levels of dental services, but also non-dental support and leadership. In the battle of Saipan in the Pacific, a Dental Corps Officer, Captain Ben Salomon, took command of the battalion aid station on the island. During an ensuing and desperate attack by enemy forces, CPT Salomon, also a skilled infantry soldier, heroically fought and defended the battalion aid station. He lost his life in the battle, but his gallantry and sacrifice did not go unrecorded. He was awarded the Medal of Honor posthumously, the only Army dentist to ever receive the nation’s highest military award. The image of Dr. Ben Salomon was used in the design of the dental officer sculptured in the monument.
Army Dentistry was firmly established as a permanent and essential element in preserving the readiness and fitness of the fighting force. During the conflicts in Korea and Vietnam, Army Dentistry continued to provide direct support to soldiers in the field of operations.
The Persian Gulf War brought the largest expansion of Reserve Dental Support in Army Dentistry. Over 220 reserve dental officers and 320 reserve enlisted soldiers were called up to support the mission. Overall, 121 dental officers served in the theater. The expanded use of reserve forces continued throughout the later conflicts in Iraq and Afghanistan.
Today the Army Dental Care System is a highly trained and integrated team of military officers, non-commissioned officers (NCO), enlisted soldiers, and government service (GS) civilians. The Army Dental Corps has 970 dentists in uniform and is augmented with 455 GS and contracted civilian dentists. There are 1,225 NCOs and enlisted soldiers and 2,300 civilians providing clinical and administrative support. All services and specialties of the dental profession are provided to the nation’s service members. In addition, Army Dentistry is a leader in the postgraduate education and specialty training of young dentists, and the advanced training of enlisted soldiers and civilians. The mission of the Army requires that Army Dentistry be prepared to support soldiers wherever they are deployed. Colonel Tom Goksel, DDS, MD, says, “The Army Dental Corps is the leader in expeditionary dentistry and sustainment of force readiness … the mission is to have a ready Dental Corps capable of delivering global dental services in order to sustain the readiness of the total military force.”
The Association of Army Dentistry is proud to keep the legacy of the Army Dental Corps alive and preserve its rich history, in order to inspire those who choose to serve and support the nation’s military men and women. The Army Dentistry Monument Dedication commemorates this unique contribution to the U.S. Army and the nation.




“In times of recession there are massive opportunities and fortunes to be made, so for new up-and-coming entrepreneurs, this is the time to go and start a business.” — Richard
Branson,founder of Virgin Records and the Virgin Group
I would echo Richard Branson’s sentiment as the greatest time to turn a dental practice into a dental business. It will require a focus beyond the dentistry you have to deliver.
More great companies and millionaires get created during recessions than in thriving economies. History will write that the COVID-19 pandemic was the triggering event that began the recession. It was also an incredible live test to see how businesses would respond through a crisis that had the ability to either break you like glass or sharpen you like a weapon. If all you learned was how to attain tax-free relief money but didn’t take any lessons about how your business, your people, or your patients responded, then you may still be at immense risk for what is to come.
In order to be a thriving success and not just a surviving mediocrity, you may have to abandon your natural instincts, avoid the herd mentality, escape your comfort zone, and embrace the contrarian approach to both business and finance. Fortunately for you, dentistry is proven and time-tested to be recession-resistant and crisis-proof (AIDS and COVID-19), and pediatric dentistry even more so because people still take care of their children and pets before themselves. However, when the economy contracts and layoffs happen and markets tank, you have to choose whether you are going to participate in the recessionary behaviors or reject them inside your business.
The average dental practice will contract and cut expenses. Now will be the best time in 40 years to be investing in your dental business for growth! When families’ pockets are being squeezed by inflation and layoffs in the household, it becomes
even more important to fight to get their attention for the dentistry their kids need. Since marketing is typically the first expense cut by most businesses, the cost decreases, and you can buy more patients’ attention for the same dollar spent — a reverse inflationary effect for your business. If the recession causes your existing patients to visit you less frequently, then you are certainly going to need some new patients. Prepare your business with cash for this opportunity as well as the opportunities to acquire failing or bailout practices during a recession. It will also be an employer’s market again for hiring talent that flees those practices to join yours if you are ready with cash to pay them and patients to keep them busy.
The recession is not the time to focus on thinning the profit and loss (P&L) of expenses, but rather to look where to invest in the P&L for revenue growth. It will be time to invest inside your business walls and not outside. Invest in marketing, hiring, and training to outpace the rest of your competitors, while they wait for the good times to come to them. A growing business with cash reserves during a recession is a great candidate for good deals on real estate ownership for your dental practice. Make sure your team at the office and your team of advisors are in complete alignment with your commitment to growth through the recession and into the next decade’s economic expansion.
Soft tissue surgical lasers have many advantages over traditional scalpel surgery, cryosurgery, and electrosurgery. However, not all lasers are equally efficient at both cutting the soft tissue and coagulating and hemostasis because light absorption in the soft tissue varies with wavelength.1-3 Some dental laser wavelengths (around 1,000 nm such as diodes and Nd:YAG) are efficient coagulators but inefficient scalpels since they are poorly absorbed by the soft tissue. Other dental laser wavelengths (around 3,000 nm such as Erbium lasers) are well absorbed by the water-rich soft tissue and are great at cutting but are not as efficient at coagulating and hemostasis. The 10,600 nm CO2 laser’s coagulation depth closely matches blood capillary diameters.2 The radiant energy of the CO2 laser is used directly to photo-thermally vaporize (cut, incise, ablate) and, at the same time, photo-thermally coagulate the soft tissues. The CO2 laser is a “What You See Is What You Get” surgical soft tissue laser with minimal collateral thermal effects that are sufficient for sealing blood vessels, lymphatics, and nerve endings; the surface bacteria are efficiently destroyed4 on incision/ablation margins. The modern flexible fiber CO2 lasers from LightScalpel, Inc. (Bothell, Washington) use scalpel-like ergonomic autoclavable handpiece (Figure 1) for (a) cutting, (b) ablation, and (c) photo-thermal hemostasis and coagulation. An important built-in
Martin Kaplan, DMD, completed his undergraduate degree at the University of Massachusetts and then attended Tufts University School of Dental Medicine. After earning his DMD degree, he completed a pediatric residency at Montefiore Hospital in New York. He is a member of American Academy of Pediatric Dentistry, Massachusetts Academy of Pediatric Dentistry, American Dental Association, Massachusetts Dental Society, Academy of Sports Dentistry, Massachusetts Breastfeeding Coalition, and Breastfeeding USA. When not practicing dentistry, Dr. Kaplan enjoys Ballroom Dancing and Karate in his spare time.
Peter Vitruk, PhD, is a founder of the American Laser Study Club and LightScalpel, Inc. in Bothell, Washington and a member of The Institute of Physics, London, UK. Dr. Vitruk can be reached at 1-866-589-2722, or pvitruk@lightscalpel.com.


safety feature is a sub-millimeter superficial depth of laser beam incision5 at low power settings (see Figure 1), which makes the CO2 laser a gentler and more forgiving tissue vaporization instrument in comparison with a scalpel, electro-surge, or hot glass diode surgery. Also quick switch from cutting to coagulation mode is enabled by simply defocusing the beam (laser beam fluence dropping below the ablation threshold of 3 Joules/cm2).2 For the CO2 laser, its excellent coagulation efficiency is due to the close match between the sub-100 µm photo-thermal coagulation depth2 and the oral soft tissue blood capillary diameters of approximately 20-40 µm.6

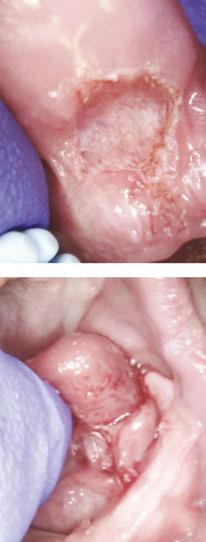
The enhanced hemostatic ability and precision of the CO2 laser is especially valuable in visible (esthetic) zones. The CO2 laser surgical removal of the tissue presented in Figures 2-8 illustrates excellent coagulation and hemostasis during soft tissue ablation.2
For example, Figures 2A-2C show the use of LightScalpel LS-1005 CO2 laser (2 watts SuperPulse Repeat Mode with F1-6 through F1-8 settings) for soft-tissue crown lengthening of the maxillary incisors and for labial frenum revision. Both procedures were performed during the same visit while the patient received local anesthesia. No sutures were placed. Figure 2 presents the self-correction of a rotated tooth No. 9 after frenum revision. Laser frenectomies in Figure 3 resulted in spontaneous closure of midline diastemas.
The CO2 laser accuracy is especially important for highly vascularized areas. For example, the 14-year-old patient in Figure 4 had a CO2 laser lingual frenectomy performed during which a sublingual vein was exposed and coagulated (sealed) with defo-
cused laser beam. As a result, no sutures were needed, and the surgical wound was left to heal by secondary intention.




Figure 5 summarizes the case of a 4-weekold bottle-fed baby, born at 8 lbs. 6 oz., not able to breastfeed and failing to gain weight during first 4 weeks of her life. The baby exhibited fussiness and gassiness post feeds and choked often during feeds. Oral exam revealed “wrinkled-looking” gingiva (possible sign of dehydration) and a restricted lip frenum that was corded, thick and tight, and an anterior, tight, calloused and short tongue-frenum causing a significant tongue mobility reduction (Figure 5A). Figure 5B illustrates the clean blood-free laser ablation. Release of tension and ability to flange the lip is now evident. At the 7-day follow-up (Figure 5C), the mother reported feeding times were more efficient, and baby’s weight gain was 1 lb. 11 oz. in the 7 days since surgery. At the 3-month follow-up, the baby now weighed 20 lbs. (9072 gm). There were no more feeding symptoms, and the baby was doing well. Unfortunately, the baby never returned to breastfeeding.

The CO2 laser is also an excellent tool to remove the excess soft tissue. Many pediatric patients require banding of molars, but an overlying operculum gets in the way of placing appliances on these teeth. Figure 6 presents the LightScalpel LS-1005 CO2 laser operculectomy (3 watts SuperPulse Repeat Mode F1-7) prior to band placement. Tissue hemostasis allows for banding to happen immediately after the CO2 laser procedure — bands were seated shortly after operculectomy was performed, in the same visit.


Figures 7-8 demonstrate a completely bloodless CO2 laser gingivectomy around the mandibular incisors in the orthodontic patient. CO2 laser gingivectomies, such as the ones presented in Figures 7-8, help improving the esthetics and oral health; they also allow for more ideal bracket placement and quicker treatment with less appointments.



Gaining access to an impacted tooth or teeth is often necessary in order to place orthodontic braces. With conventional scalpel surgery, many problems occur when placing brackets, such as sutures breaking before brackets are bonded. Brackets will not bond properly if enamel is wet due to bleeding. Clean, bloodless enamel is necessary for enamel acid etching and bonding of the composite resin. Using the

CO2 laser to expose an impacted tooth produces a dry surgical field, thus creating conditions required for immediate bracket bonding. The CO2 laser-assisted cuspid exposure procedure is shown in Figure 9. This quick CO2 laser treatment allows access for bracket placement, saving the patient months of waiting for the tooth to erupt on its own. The CO2 laser provides a clean, nonbleeding border. The CO2 laser straight and angled handpieces, illustrated in Figure 1, permit a convenient reach into areas that may be obstructed by braces. Once an impacted tooth is exposed by laser ablation, the bloodless surgical field is ready for the next step. The orthodontic traction hook can be bonded to the exposed enamel immediately after ablation during the same visit saving time for both the patient and clinician.
Studies have shown that there is a diminished risk of scarring and wound contraction associated with CO2 laser surgery.9
Laser-induced wounds heal with greater fibroblast proliferation, with young fibroblasts actively producing collagen. Laser wounds also have been reported to contain smaller amounts of myofibroblasts (cells responsible for wound contraction), compared to scalpel wounds.9 Secondary intention healing and lack of scarring are especially important for treating lesions located in esthetic/visible zones.
Patients report less postoperative pain and discomfort with laser surgery.9 The healing process associated with CO2 laser surgery is enhanced and less painful than with cryosurgery or electrosurgery.9
Figures 6A-6C: 6A. Pre-op view of operculum visible on mandibular 1st molar. The bands cannot be seated due to tissue interference. 6B. Immediately post-op view. Laser ablated the thick interfering tissue. Note lack of bleeding. 6C. Bands were seated properly and without discomfort during the same visit the operculectomy was performed


The many uses for a soft tissue CO2 laser in pediatric dentistry and orthodontics — e.g., gingivectomies, frenectomies, exposure of impacted teeth, and others — feature minimal blood loss and reduced discomfort for the patients. In comparison with other dental laser wavelengths (circa 1,000 nm for diode and Nd:YAG lasers and circa 3,000 nm for erbium lasers), the CO2 laser wavelength exhibits the least absorption rate by the stainless steel orthodontia hardware and the optimum coagulation depth closely matching gingival blood vessel diameters. The CO2 laser ablation depth can be controlled to a few tenths of a millimeter, which characterizes this wavelength as a safe and gentle soft tissue removal tool, while the sub-100 µm coagulation depth (significantly better than hot glass diodes)2,5 allows for enhanced, scar-free healing of highly vascular oral tissues secondary intention.5,9 The accuracy and precision of CO2 laser surgery are increased by the visibility of the surgical field not being obscured by bleeding.


Figures 7A-7C: 7A. Pre-op view. Gingival hyperplasia due to poor oral hygiene. 7B. Intra-op view with laser markings prior to incision. 7C. 2 weeks post-op view shows good tissue healing
1. Jacques SL. Optical properties of biological tissues: a review. Phys Med Biol. 2013;58(11):37-61.
2. Vitruk P. Oral Soft Tissue Laser Ablative & Coagulative Efficiencies Spectra. Implant Practice US. 2014;7(6):22-27.






3. Vogel A, Venugopalan V. Mechanisms of pulsed laser ablation of biological tissues. Chem Rev. 2003;103(2):577-644.
4. Cobb C, Vitruk P. Effectiveness of a Super Pulsed CO2 Laser for Removal of Biofilm from Three Different Types of Implant Surfaces: An In Vitro Study. Implant Practice US. 2015;8(3):14-20.
Figures 8A-8C: 8A. Pre-op view of thick hyperplastic gingiva. 8B. Immediate post-op view. Note excellent hemostasis. 8C. 2 weeks post-op view
5. Riek C, Vitruk P. Incision and Coagulation/Hemostasis Depth Control During CO2 Laser Lingual Frenectomy. Dent Sleep Practice. Spring 2018:32-38.

6. Yoshida S, Noguchi K, Imura K, Miwa Y, Sunohara M, Sato I. A morphological study of the blood vessels associated with periodontal probing depth in human gingival tissue. Okajimas Folia Anat Jpn. 2011;88(3):103-109.
7. Gama SK, De Araujo TM, Pinheiro AL. Benefits of the use of the CO2 laser in orthodontics. Lasers Med Sci. 2008; 23(4):459-465.

8. Wolfe WL, Zissis GJ. The Infrared Handbook. Office of Naval Research: Washington DC, 1985: 7-81.
Figures 9A-9C: 9A. Laser-marked outline of impacted tooth. 9B. Intra-op view of CO2 laser excision. 9C. Immediate post-op view of impacted tooth exposed to assist with eruption
9. Glazkova A, Vitruk P. CO2 Laser Surgery Post-Operative Pain and Healing: A Partial Literature Review. Dent Sleep Practice. Winter 2019:28-34.


Primitive cultures chewed on meat, tough gristle, nuts, seeds, bones, and raw vegetables — which was good exercise for the jaws and stimulated bone growth. Sadly, the modern processed diet requires little chewing effort.
Using a Myo Munchee promotes healthy development of facial muscle strength and encourages nasal breathing.
The original premise for the development of the Munchee was for gum health and oral hygiene — when it is chewed actively, there will be an increase in salivary flow, improved hygiene, as well as aerobics for the muscles of the jaw and face and improved periodontal blood flow. Over time, it became clear that there were many more benefits to be had from chewing a Munchee.
The benefits of chewing are far reaching, and more are being discovered all the time.
What we do know is:
• Chewing is involved in regulation and maintenance of bone growth.
• Chewing is the essential movement for optimal upper airway function to develop strength of the muscles involved in the complex process of swallowing.
• Chewing assists with eustachian tube and sinus drainage.
• Chewing develops the strength of muscles to ensure strength and stability of the TM joints.
• Chewing can reduce stress and is known to be neuro-calmative.
• Chewing contributes to better cognition.
• Chewing allows for the breakdown and absorption of foods more efficiently.
The Myo Munchee is made from flexible silicone giving it considerable elasticity. With its unique shape and many small prongs, it allows the jaws to comfortably rest in a Class 1 occlusal relationship.
Munchee benefits:
• oral hygiene
• myofunctional therapy tool
• myofunctional orthodontics
• pacifier replacement
• teething tool
• neuro-sensory tool
• special needs tool
We can have the greatest impact with the most ease — therefore early identification is essential. Malocclusions can be predicted from as young as 6 months and do not self-correct if left untreated. Malocclusions are often the root cause for many issues:
• speech and feeding
• dribbling and drooling
• ear infections
• mouth breathing and sleep disturbance
• postural instability and weakness
Babies can start using Myo Munchee Bebe anywhere from 5-8 months of age, depending on where the child is developmentally. When babies are bringing chew toys and hands to their mouth, they will be able to start engaging with the Bebe. Bebe creates awareness of the whole stomatognathic system. Over 1/3 of all sensory motor awareness is from the lower third of the face — lips/tongue and jaws. Bebe is suitable for children ages 5 months to 2 years old, and children over 2 years will be suited to the Myo Munchee Mini.
Conditions for use:
• oral hygiene
• low oral tone
• mouth breathing
• pacifier replacement

• teething
• dribbling/drooling
• fussy eater
• delayed speech
At the age of 6 months, the oral reflexes that have assisted with the breastfeeding and breathing mechanisms should be diminishing, and the chewing reflexes need to be activated and integrated. The Bebe is a great replacement to allow the age-appropriate activity of chewing to become more active rather than staying with sucking, which is the early mechanism for feeding.

The Mini is a fantastic tool to transition toddlers away from the pacifier and can be promoted to them as “the big kid’s paci.” Use the QR code for more information about the impacts of pacifiers.
Myo Munchees are available in sizes suitable for ages ranging from 6 months to adults.


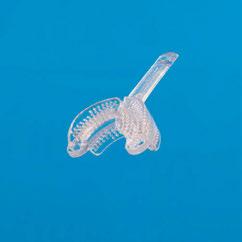


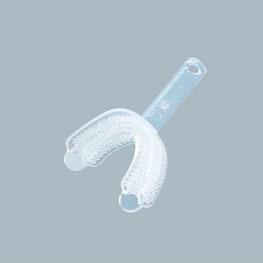
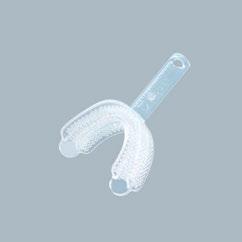


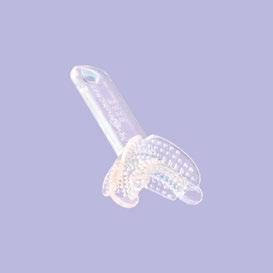
When I was pregnant in 2004 with my first child, I was first introduced to the concept of banking cord blood. This is the process of a private company banking (or collecting) blood from a child’s umbilical cord at birth.
Like bone marrow, cord blood has scientifically shown to be impactful and effective in therapeutic transplants to treat a range of diseases, including leukemia, lymphoma, and various genetic disorders. The promising impacts don’t just come from the cord blood itself, but from the stem cells also contained in the detached umbilical cord. Those stem cells promised the potential to treat a broader range of conditions in the future.
At that time there were only 23 public cord blood banks and fewer than 65 hospitals throughout the country that were equipped to accept donations like these. Now, though, times have changed.
Presently, there are more than 450 cord blood banks worldwide. Cord blood is known to help treat nearly 80 unique conditions. It’s expanded beyond transplant medicine into areas of regenerative medicine in clinical research trials for conditions once thought untreatable such as autism, brain injuries, and certain types of cancer.
Stem cells also are potentially part of this process from a dental perspective with real, tangible benefits in the world of health and wellness. Stem cells are not only banked and preserved from umbilical cords. In fact, there are multiple ways to harvest these beneficial stem cells — even from wisdom teeth.
Harvesting dental stem cells can be as seamless as preserving stem cells collected from wisdom teeth during extractions. But how exactly does this work in practice, and what are the benefits of harvesting dental stem cells from wisdom teeth?
Stem cells are often referred to as the body’s raw material — they’re cells from which all other cells with specialized functions are generated. Adult stem cells, also called somatic cells, are found
Amy B. Jackson, DDS, MS, is a Board-certified orthodontist in private practice for over 15 years and runs four practices in San Antonio, Texas. She began her dental career in Houston where she attended The University of Texas Health Science Center. During her time there, she was recognized by the UT Health Science Center with the Dental Public Health Award for community service and was awarded a Summer Research Fellowship from the AADR and the Barnard G. Sarnat Award in Craniofacial Biology from the IADR. Dr. Jackson continued her specialty training for orthodontics at The University of Texas where she completed a master’s degree through the periodontal department and was awarded the AAED’s research grant for her work with midpalatal implants.
Disclosure: Dr. Jackson is founder of Retainers for Life®

within the deep tissues of the human body (liver, heart, ovaries, muscles, testes, teeth, skin, and bones).
Stem cells, in general, have a variety of promising medical benefits for future treatments of a myriad of conditions. Stem cells acquired from dental tissue are no exception. Dental stem cells are found in the soft dental pulp of teeth and are a rich source of mesenchymal cells. These cells can be isolated when extracted, then preserved to be used later.
In the past after procedures like wisdom teeth extractions, those extra molars were disposed of. It’s only in the past several years we’ve learned how beneficial dental stem cells can be and further, how seamless acquiring and preserving those stem cells could be too. This procedure is the perfect opportunity to harvest those valuable soft dental tissues to derive the stem cells.
The ongoing demand for wisdom teeth surgery leaves plenty of opportunity for acquiring stem cells without any additional issues. These procedures are the perfect possibility for stem cell extraction, cryopreservation, and potential later use.
Stem cells — dental stem cells included — are known as precursor cells. That means they’re not just potent and viable raw materials; they’re capable of something called “self-renewal.” This means that like other stem cells, dental stem cells (when properly acquired and preserved) can regenerate and grow into cells — but not just dental cells.
Dental stem cells could grow into other types of specialized cells, like muscles, ligaments, bones, nerves, skin, and more. The benefits of extracting dental stem cells from wisdom teeth are varied and numerous.
When my youngest was born in 2009, we had planned to bank his cord blood. After a life-threatening delivery, his cord blood was destroyed. This renewed focus on preserving cells from wisdom teeth gives us one more chance to benefit from his young stem cells, making it possible for your children and grandchildren to benefit as well.
The present application of stem cell therapy or treatment is promising, and the future of it is even brighter. Scientists are always progressing in stem cell therapy research and may eventually be able to treat and/or cure conditions like arthritis, auto-immune diseases, pancreatic dysfunction, brain injuries, cognitive diseases, and beyond.


In September of 2022, an Invisible Dental Support Organization (IDSO) that focuses on Dental Trifectas partnering only with pediatric, orthodontic, and OMS practices, recapitalized at a new record value approaching $2 billion dollars. Large Practice Sales (LPS) partnered 110 practices with this unique IDSO in less than 36 months, and all of them achieved extraordinary gains on their retained ownership — some over 500%.
This recapitalization event has increased the value of larger pediatric practices nationally. LPS clients as young as 32 are now completing partnerships with IDSOs for the creation of long-term generational wealth, not just the high initial values in an IDSO partnership. Out of $612 million of LPS transactions in 2022, over $100 million were completed for doctors under 40. Some of the initial partnership values exceeded 400% of collections and 12x EBITDA.
IDSOs become a doctor’s silent partner by purchasing 51% to 90% of a practice for cash up front at today’s low tax rates. Doctors retain ownership in the balance and continue to lead the practice with their brand, team, and strategy for years or decades. Doctors retain full autonomy and freedom and are not micromanaged. They benefit from the resources of a large, silent partner including unique recruiting tools, enhanced marketing, admin burden reduction, lower costs, and higher reimbursement rates.
The Dental Trifecta IDSOs can achieve record values due to their internal organic growth rates far higher than typical IDSOs due to the creation of internal referral networks. Doctor partners in a Dental Trifecta IDSO are now able to monetize their patient referrals via their common ownership in the IDSO.
Captive referrals have been a part of the many ped/ortho IDSOs for many years. But the addition of OMS has multiplied referrals, growth rates, and IDSO values. Many ped/ortho IDSOs are now converting to Dental Trifectas by adding OMS partners. Several of the single specialty OMS and Ortho IDSOs are now eager to add the other two legs of the Dental Trifecta stool — pediatric practices are the most valuable piece of the puzzle.
Pediatric dentists are the biggest beneficiary of the Dental Trifecta “gold rush” as they are the gateway to all dentistry and the critical base of the Dental Trifecta. Practice values are achieving new records. A typical LPS pediatric client will have six to ten or more qualified bidders from which to choose their IDSO partner. More bidders equal higher values and broader choices in partnership for doctors.
Doctors partner with IDSOs for multiple reasons. Some are relieved to reduce the headaches of growing practice management challenges. Others are eager to monetize a part of their life’s work for millions in cash today to diversify their investment portfolios. Many doctors now understand that associates can no longer become a doctor’s long-term transition strategy. Today’s high practice values prevent associates from buying in to a practice under traditional models.
The multispecialty IDSOs are also eager bidders on pediatric practices nationally. Each of the dozens of well capitalized IDSOs has different support levels, initial values, and transaction structures. Doctors choose the IDSO partner that is the best fit for them both culturally, operationally, and financially. Pediatric specialists should understand all of their options.
Doctors can confidentially learn more about the IDSO opportunity and the value of their practice without cost or obligation. Contact LPS to schedule a discovery call to understand what is happening in your area today. Ultimately, larger practices will either join an IDSO or compete with many.

Iam frequently asked by colleagues interested in incorporating early airway-focused treatment into their practice, “Should I use Myobrace, Healthy Start, or some other myofunctional orthodontic ‘system?’” Nothing makes me happier or more excited for the future of our profession than knowing there are others wanting to learn how to treat littles with preventative dental sleep medicine.

Lauren Ballinger, DDS, is a board-certified pediatric dentist and a specialist in orofacial myology. She practices pediatric airway-focused dentistry in Western Massachusetts and is the founder of Good to Grow: Pediatric Dental Wellness, Airway, Grow and Sleep Solutions and The Nurture Frenectomy Center. Dr. Lauren founded The Endeavor Group: a global assembly of passionate health professionals promoting awareness of, and solutions for, optimal breathing and airway health for children under age 6. She is also the pediatric dental chapter leader for the AAPMD. Dr. Ballinger is a featured faculty member in The Pankey Institute’s Dental Sleep Medicine program, focusing on preventive dental sleep medicine for the pediatric dental population. She is forever grateful to her own children, Jack and Libby, who ignited her passion and motivated her pursuit of knowledge.
Rather than giving my personal recommendation on a specific system, I believe the best answer is found by asking yourself more questions. Do you understand WHY myofunctional orthodontic systems (oral trainers and appliances) work? Do you know what the goals of treatment are for these systems? Which patients are good candidates for this treatment approach? Answering these questions requires use of your own brain, rather than relying on a branded message. If you are willing to lean-in to the details, then I think any of these systems can be an excellent match for select patients.
After you’ve mastered the system details, there are patient-centered questions. What are their concerns and fears? Their dental and health goals? In pediatrics, it’s important to bring the child into the conversation in an age-appropriate way. They are the ones treating themselves, after all. Getting them curious and excited goes a long way in gaining their trust, acceptance, and compliance.
Having an understanding of anatomy and physiology, craniofacial growth and development, how behaviors and compensations come into play, and what internal (body) and external
(mind, environment) barriers your growing patient may face, are crucial to informing your treatment choices. Human variation requires more than one system, one appliance, one lab, or one treatment approach. The better you understand your patients, the more apparent it will become which “tool(s)” may be the most effective.
I am partial to Myobrace because that is what I am familiar with and have been using for almost 7 years; I am a certified provider. I like that Myobrace has a strong myofunctional educational platform that works in conjunction with their oral appliances and trainers. If you understand the science behind myofunctional therapy and how the appliances/trainers function as adjuncts, then it really doesn’t matter what system you use. You can think through these cases yourself, choose cases wisely, and know how to troubleshoot. On the other hand, I believe some of the other systems, such as Heathy Start, offer more direct guidance with case selection and treatment. This has benefits, especially for those new to these treatment options. Understanding why these systems help our patients is more important than which system you use.
Simply stated, these systems work on habits and muscles, not the teeth. They are functional appliances that can lead to better health, and as a “side benefit” also make the teeth straighter. These systems work via normalizing oral muscle function by way of re-patterning and correcting para-functional/dysfunctional orofacial muscle habits and establishing nasal breathing day and night. The younger we initiate treatment, the better we can help children untangle their poor habits and “grow-out” of the suboptimal growth patterns that put them at risk for sleep breathing disorders, including sleep apnea. Tooth and bite relationships begin to correct when the underlying causes of malocclusion and poor craniofacial growth are treated, e.g., incorrect muscle function, poor oral rest posture, and nasal disuse. These goals are universal; patient improvement is not, and progress requires time and support. If nasal breathing is not achieved in the first months of treatment, you should figure out why. Is it a compliance issue? Is it a structural issue? Do they need a referral to an ENT or allergist?
Any of these systems can produce aligned teeth, well developed faces, and healthier airways. Nasal breathing reduces inflammation in the nasal and posterior airways and improves blood gas balance. Your patients learn to keep their lips gently together at rest with the tongue in a supportive position in the palate, facilitating development of the maxillary arch. The facial muscles no longer need to assist with swallowing, reducing forces that cause downward and backward growth of the jaws, narrowing of the posterior airway, and stress to the TMJ. Breath-
ing is healthier and more efficient, restful sleep is more likely to be achieved, an overactive sympathetic nervous system begins to relax, pain patterns are reduced, and skeletal growth and dental development begin to normalize. The body returns to homeostasis. These appliances/trainers can also provide light forces that, in conjunction with improved muscle function, create some maxillary expansion and uprighting of mandibular teeth.
As impressive as the results can be, it is vital to understand the limitations of these systems. They are 100% reliant on patient compliance. Your job is to screen your patients, identify their goals for treatment, and offer a tool to help them. During therapy, our role is to monitor results and offer changes in course if the original treatment plan is not producing the desired outcome.
For example, while it is true that establishing nasal breathing can lead to reduced inflammation of the adenoids and/or tonsils, it is also true that they can be so obstructive that they are the barrier. In other words, can your patients breathe through their nose effectively and efficiently enough to be able to break through and find success in a myofunctional orthodontic program? Or are they stuck?
We want our patients to be successful and not get frustrated and give up. Sometimes, requiring a child to breathe through the nose, lips closed, with a rather large appliance in their mouth, is just too much to ask. Sometimes, it works like a charm. Recognizing the nuances and being able to think through WHY this treatment approach may be working well, or not so well, will produce clinical wisdom, improving your confidence. I cannot overstate the importance of remembering that every day a child is not breathing, sleeping, and growing well, is a day that they cannot get back. We must not waste precious time attempting to pound a square peg through a round hole. Change course if you need to. Adding a myofunctional component may be the key to making other therapies more successful.
Our young and growing patients who breathe through their nose both day and night, with harmony in their orofacial muscle function and proper oral rest posture, will grow-up healthier AND have better looking faces with straighter teeth. No matter which myofunctional orthodontic system(s) you use, as long as you understand WHY they work, choose your cases wisely, know what the potential barriers to treatment may be, when to refer for collaborative care, and that there is no such thing as a one-size-fits-all approach, then you can make a huge difference in a child’s life. AND have fun doing it. PD
Understanding why they help is more important than which system to use.
Pediatric Dental Practice US is a peer-reviewed, biannual publication containing articles by leading authors from around the world. Pediatric Dental Practice US is designed to be read by pediatric dentists and GPs performing pediatric dental techniques.
Pediatric Dental Practice US requires original, unpublished article submissions on pediatric topics, clinical cases, practice management, technology, clinical updates, literature reviews, and continuing education.
Typically, clinical articles and case studies range between 1,500 and 2,400 words. Authors can include up to 15 illustrations. Manuscripts should be double-spaced, and all pages should be numbered. Pediatric Dental Practice US reserves the right to edit articles for clarity and style as well as for the limitations of space available.
Articles are classified as either clinical, continuing education, technology, or research reports. Clinical articles and continuing education articles typically include case presentations, technique reports, or literature reviews on a clinical topic. Research reports state the problem and the objective, describe the materials and methods (so they can be duplicated and their validity judged), report the results accurately and concisely, provide discussion of the findings, and offer conclusions that can be drawn from the research. Under a separate heading, research reports provide a statement of the research’s clinical implications and relevance to pediatric dentistry. Clinical and continuing education articles include an abstract of up to 250 words. Continuing education articles also include three to four educational aims and objectives, a short “expected outcomes” paragraph, and a 10-question, multiple-choice quiz with the correct answers indicated. Questions and answers should be in the order of appearance in the text, and verbatim. Product trade names cited in the text must be accompanied by a generic term and include the manufacturer, city, and country in parentheses.
Additional items to include:
• Include full name, academic degrees, and institutional affiliations and locations
• If presented as part of a meeting, please state the name, date, and location of the meeting
• Sources of support in the form of grants, equipment, products, or drugs must be disclosed
• Full contact details for the corresponding author must be included
• Short author bio
• Author headshot
Illustrations should be clearly identified, numbered in sequential order, and accompanied by a caption. Digital images must be high resolution, 300 dpi minimum, and at least 90 mm wide. We can accept digital images in all image formats (preferring .tif or jpeg).
Ensure that each table is cited in the text. Number tables consecutively, and provide a brief title and caption (if appropriate) for each.
References must appear in the text as numbered superscripts (not footnotes) and should be listed at the end of the article in their order of appearance in the text. The majority of references should be less than 10 years
old. Provide inclusive page numbers, volume and issue numbers, date of publication, and all authors’ names. References should be submitted in American Medical Association style. For example:
Journals:
(Print)
White LW. Pearls from Dr. Larry White. Int J Orthod Milwaukee. 2016;27(1):7-8.
(Online)
Author(s). Article title. Journal Name. Year; vol(issue#):inclusive pages. URL. Accessed [date]. Or in the case of a book:
Pedetta F. New Straight Wire. Quintessence Publishing; 2017.
Website:
Author or name of organization if no author is listed. Title or name of the organization if no title is provided. Name of website. URL. Accessed Month Day, Year. Example of Date: Accessed June 12, 2011.
Author’s name:
(Single)
(Multiple)
Doe JF Doe JF, Roe JP
Written permission must be obtained by the author for material that has been published in copyrighted material; this includes tables, figures, pictures, and quoted text that exceeds 150 words. Signed release forms are required for photographs of identifiable persons.
Authors must disclose any financial interest they (or family members) have in products mentioned in their articles. They must also disclose any developmental or research relationships with companies that manufacture products by signing a “Conflict of Interest Declaration” form after their article is accepted. Any commercial or financial interest will be acknowledged in the article.
All clinical and continuing education manuscripts are peer-reviewed and accepted, accepted with modification, or rejected at the discretion of the editorial review board. Authors are responsible for meeting review board requirements for final approval and publication of manuscripts.
Page proofs will be supplied to authors for corrections and/or final sign off. Changes should be limited to those that are essential for correctness and clarity.
Mali Schantz-Feld, managing editor, at mali@medmarkmedia.com
If reprints or additional issues are desired, they must be ordered from the publisher when the page proofs are reviewed by the authors. The publisher does not stock reprints; however, back issues can be purchased.

You have decided to have a promotional video filmed for your practice. Great, right? Well, often the communication and coordination responsibilities of putting the video shoot together fall directly onto the front office staff. Maybe that’s the position you find yourself and your team in, and you’re not certain how to manage it all.
If you’ve not worked with a video production professional or company before, it can be a little nebulous and perhaps even a little intimidating. However, with a little insider information, you can make the process easy for your team, other dentist(s), and any patients you might have come in and participate.
Covering all aspects of working with a video crew is beyond the scope of this condensed article. However, one of the first questions the front office staff has is, “Who should we include in the video?” The answer isn’t as obvious as you might expect. The answer is, “Whomever you select, choose wisely.”
If you have team members who are beyond just being a little camera shy — they’re either terrified or ticked off about being on camera, so don’t force them. Adept videographers can do a lot to make people look and sound their best. However, there’s very little they can do to hide if someone is self-conscious or annoyed about being on camera. Choose team members who genuinely want to represent the practice in the video. If you have a larger office, it might not be necessary to include everyone in the video. In fact, trying to ensure that everyone gets into the video might be counterproductive and time-consuming.
An additional question routinely asked is, “What happens if we had a video filmed, but one or more dental team members are no longer with the practice?” It depends on their role in the video. For dental team members who are just featured in some of the non-speaking/action footage part of the video, (also called “bRoll” by video professionals), it’s not a big deal. However, if you had the team members being interviewed on camera, you
might need or want to remove them if they leave the practice. Therefore, be wary about asking the dental team to speak on camera. Most dental practices typically just have the dentist(s) speaking on camera — on a rare occasion a long-time office manager.
If you’re interested in having actual patients come in and help out with the video (either providing a video testimonial or just being in some of the bRoll), choose wisely.
Choose patients who are comfortable on camera, who love your practice, and who have the time to come in for an hour or so and participate. If you’re asking patients to provide a video testimonial, it may feel like an unnecessary step, but consider initially asking them, “What do you enjoy about the practice? What might you share about this practice on camera?” Your goal in asking them these questions is to learn ahead of time what they’ll say on camera and to get them to start thinking about what they’ll say.

All too often, well-intentioned patients blurt things out on camera like, “I love this practice because they are so cheap,” or “Dr. Smith is great because I can call him on his mobile phone over the weekend, and he responds!” Yikes, both statements might be true, but they should be kept on the DL and not included in the final edit of the video. Of course, statements like this can be easily edited out, but you want to ensure you don’t invest time in having a patient provide a testimonial that is bland, flat, or even one you can’t use.
Gently suggest to patients offering a testimonial that they do a little thinking about what they’ll say before the cameras start rolling — maybe even practice what they’ll say in front of a mirror or a friend/family member just a little bit. Patients, dentists, and just about everyone who haven’t been on camera sometimes assume that they can just “wing it.” And in truth, some can. However, for
most of us, doing a little preparation and visualizing what we’re going to say ahead of time will help tremendously.
You don’t need to give patients the third degree about what they’ll say on camera — let it come from their heart, but guiding them a little and helping to clarify what they’ll say might make a mediocre video testimonial a great one. Just asking them ahead of time, “What do you think you’ll share/say?” is enough to get them to do a little thinking before they get on camera, and that often results in a better testimonial.
If you do ask patients to appear on camera, ask them to sign a media release form. Yes, every patient who appears on camera should sign one of these forms. Your video professionals should provide you with one to hand out. If they don’t, ask for one. More important, provide these to patients before the day of the shoot so they have time to review, sign, and then return them via email. Having patients sign one of these forms right before they jump in front of a camera just adds a layer of stress, so it’s best to have them sign the form before the day of the shoot.
It’s important to note that if you don’t acquire signed media releases, anyone who is not an employee of the practice could potentially change their mind about being in the video long after it’s been uploaded and on your website. They can request that you remove them from the video, which means you’ll need to contact the video professionals and pay to have the video edited to delete the person who no longer wants to be in the video. Having non-employees sign a release form can help guard against this, so it’s worth the bother.
As a last note about who is and isn’t in your video, many practices don’t recruit actual patients to come in. Instead, they opt for friends and family members to pose as patients while bRoll footage is filmed. (No, they don’t ask friends and family members to provide fake patient testimonials.) Friends and family members usually are more willing to help, and they don’t often require any compensation! Nevertheless, it might be nice to provide anyone outside of the dental team with a gift card, free whitening, or some small token of appreciation for taking time out of their day to help you.
Bonus Tip: Consider bringing in a veggie/fruit plate or some doughnuts for people to nosh on while they are not on camera.
It usually takes a film crew about an hour or so to set up, so if you’re filming first thing in the morning, perhaps plan on having at least one person arrive an hour early to let the crew move their gear in and set up. Note: Expect the video crew to need 20-40 minutes to pack up their gear after the shoot has wrapped up.
Video crews typically have a lot of gear, so they must find a safe out-of-the-way place in the practice to store it. Before the video crew arrives, consider a lower-traffic area of the office where they could store their gear. Make certain there isn’t any printed/digital sensitive information (or valuables) laying about.
It might be tempting to squeeze a few patients in, perhaps schedule a patient or two, during the shoot, but it’s not recommended. You won’t be able to give your full attention to your patients or to your video crew, so outside of an emergency patient, avoid scheduling production during the video shoot.
If you are conducting interviews (often called “aRoll”) or patient testimonials, make sure you can mute the phone, background music, or anything else that might interfere with the audio recording. You might even consider making sure local landscapers aren’t working during the time of your video shoot. (Yes, this has happened to other practices.)
To make the best use of everyone’s time, ask the video crew to provide you with a schedule for the day. Ask them when you, the team, the doctor(s), and perhaps the patients need to be available. Review the schedule for the day, and make sure there aren’t large time windows when people are standing around doing nothing. Gently remind the video crew that you want to be respectful of everyone’s time, which means getting them in and out as efficiently as possible.
Make certain that everyone who is going to be on camera is aware of (and has agreed to) their start time and finish time. Nothing derails a video shoot more than someone showing up late, announcing they suddenly must leave early, or someone just not showing up at all. Ensuring everyone shows up on time is like oral care: “An ounce of prevention is worth a pound of cure,” so consider sending out gentle reminders a few days before as well as the day before the shoot so that everyone is aware of their responsibilities.
In working with a video crew, it’s important to recognize that they don’t know the details of your profession — most don’t “get” dental. To be fair, you might be unfamiliar with the video profession as well, so it’s important that you respect one another’s expertise, you communicate (even over communicate) so that everyone’s on the same page, and that you politely ask questions or raise concerns if they arise.

At the very least, consider at least one “pre-production” phone, Zoom, or in-person meeting so you can discuss your vision, logistics, etc. If it’s possible, ask if the video crew would be open to visiting the office before the day of filming to “scout” the location. The truth is, something always goes sideways during a video shoot, and that’s okay. An accomplished video crew will easily be able to manage any hiccups in the process. However, having discussed a plan of attack for the day before you begin filming will go a long way in reducing the likelihood that something will go sideways on you. Most offices have a morning huddle before the day begins — consider applying the same approach to having a video filmed for your practice.
In the end, the video crew and the dental team should have the same goal: to film a compelling promotional and/or educational video for the practice. Communicate, be honest (be open when you’re confused or need advice), and work together. Reprinted