Guide to assessing candidacy for in-office pediatric sedation
Dr. Emily Knipper
Pediatric guided growth and development Patrick Kircher
The rationale for full coverage esthetic crowns: a case series
Dr. Patrick Ruck

Dr. Najia Usman


ENDOSEQUENCE ® BC PEDIATRIC PUTTY A new solution for your pediatric pulp needs from dentistry’s leader in bioceramic innovation. PROMOTING EXCELLENCE IN PEDIATRIC DENTISTRY Myofunctional Therapy / Lasers n Watch for Our Fall 2024 Issue Spring 2024 Vol 2 No 1 pediatricdentalpractice.com pediatricdentalpractice.com Using EndoSequence Root Repair Material for more predictable success




pulpdent.com/activademo

MERGING RESTORATIVE AND PREVENTIVE DENTISTRY
ACTIVA™ KIDS is an esthetic, BioACTIVE resin restorative that stimulates apatite formation and the natural remineralization process with release and recharge of calcium, phosphate and fluoride. It is an opaque white shade ideally suited for pediatric dentistry. Scan the QR code to schedule an in-person or virtual demo today.
Photos courtesy of Dr. Leon Katz
Embracing innovation
Pediatric dentistry has its foundation rooted in the profound understanding that a child's dental health odyssey molds their overall wellbeing for years to come. Pediatric dentists recognize the importance of staying at the forefront of developments and embracing new technologies and approaches. Our role transcends the clinical, as we guide children toward embracing lifelong habits that enshrine oral health as a paramount priority.
As the warm breezes of spring usher in a season of growth and renewal, we’re reminded of the cyclical journey of growth and transformation that influences all aspects of life. Within our profession, this season symbolizes a period of renewal, offering fresh perspectives and an ongoing commitment to enhancing our care for the youngest smiles in our communities.

With the increasing adoption of telemedicine and point-of-care diagnostics, we inch closer toward a future where pediatric dental care is accessible, convenient, compassionate, and tailored to the unique needs of every child.”
In this spirit of growth and renewal, we are thrilled to present our spring issue, brimming with latest insights, techniques, and discoveries that elevate our collective pursuit of excellence in pediatric dental care. Buckle up and prepare to be inspired, because this spring, we’re elevating your knowledge and skills to new heights!
Marilyn C. Sandor, DDS, MS, an experienced pediatric dentist based in Southwest Florida, is an innovative trailblazer. Since establishing her private practice, Naples Pediatric Dentistry, in 2001, she has distinguished herself as a clinical expert and innovative force. In 2009, Dr. Sandor introduced the globally acclaimed ZOOBY prophy angles, the first patented pediatricfocused dental prophylaxis angle, that prioritizes patient comfort and satisfaction.
Now, as the Founder and CEO of GoodCheckup Corporation, Dr. Sandor continues her commitment to enhancing dental care accessibility and equity. Through GoodCheckup, she has utilized cutting-edge technology to create innovative virtual care solutions for specialized dental services, eliminating geographical constraints and empowering dentists and patients. Dr. Sandor has earned widespread recognition, including nominations for the prestigious World’s Top 100 Doctors Award and the Denobi Award.
Dr. Sandor also is a passionate advocate for community welfare and a champion for diabetes research. She has also inspired positive change and transformation within the dental community and beyond through her role as a co-author of influential books such as Leadership - Changing the World from a Dental Chair and Alpha Dentistry volume 3: Paediatric Dentistry FAQ
GoodCheckup is a virtual care for dentistry platform designed to facilitate knowledge exchange and consultations enhanced by point-of-care diagnostics. Our app offers three cutting-edge platforms — GoodCheckup Doctor, Kids, and Caregiver. GoodCheckup Kids is a new mobile app for pediatric dentistry that connects you and your patients, quickly and easily. Provide quick offline dental screenings powered by AI to full video consultations and electronic prescriptions, and set yourself free with Your Office in Your Hand. For more information, visit www.goodcheckup.com.

Within these pages, you will find a curated collection of perspectives from renowned experts, exploring the latest developments transforming pediatric dental care. The issue is bursting with insights on myofunctional therapy and how it illuminates the complex relationship between orofacial muscle function and craniofacial development, advances in materials and equipment for conservative, precise treatments using biomimetic restoratives and cutting-edge diagnostics, strategies for caries management, incorporating lasers to perform precise, minimally invasive procedures with less discomfort and quicker healing, and advances in imaging modalities like digital radiography. Lastly, the potential of 3D printing for creating custom restorations, appliances, and surgical guides with unparalleled precision opens up new horizons in personalized patient care.
It also is crucial to recognize the profound impact of virtual care platforms, which signify a paradigm shift in how we deliver pediatric dental services. In line with the increasing adoption of telemedicine and point-of-care diagnostics across healthcare, these platforms enable dental professionals to provide remote consultations, track treatment progress, order and send prescription medications, provide preventative education, and receive customized care and diagnostic testing for an ever-expanding array of health markers, such as caries susceptibility and periodontal disease — all from the convenience of the patient's home. We inch closer toward a future where pediatric dental care is accessible, convenient, compassionate, and tailored to the unique needs of every child. As we embrace these digital technologies, let us never lose sight of the unique perspectives and emotional needs of our youngest patients and their families.
As you peruse the pages of this issue, we hope you will be inspired by the boundless potential that lies within the pediatric dental landscape. Here's to a spring filled with growth, inspiration, and the pursuit of excellence in patient-focused, integrated pediatric dental care starts.
1 pediatricdentalpractice.com Volume 2 Number 1 INTRODUCTION © MedMark, LLC 2024. All rights reserved. The publisher’s written consent must be obtained before any part of this publication may be reproduced in any form whatsoever, including photocopies and information retrieval systems. While every care has been taken in the preparation of this magazine, the publisher cannot be held responsible for the accuracy of the information printed herein, or in any consequence arising from it. The views expressed herein are those of the author(s) and not necessarily the opinion of either Pediatric Dental Practice US or the publisher.
Marilyn C. Sandor, DDS, MS
PD
Using EndoSequence Root Repair Material for more predictable success
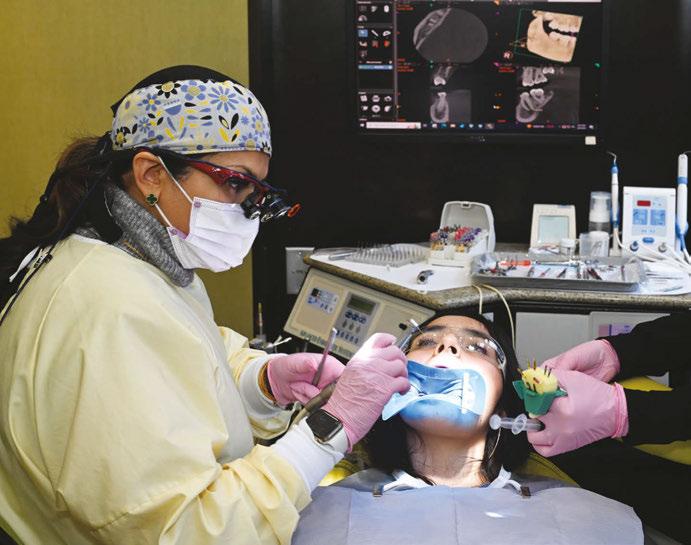
Dr. Najia Usman discussed working with biocompatible and bioactive materials from Brasseler USA
Cover image of Dr. Najia Usman courtesy of Brasseler USA.


Dr. Carla Cohn discusses her choice of restorative materials

Patrick Kircher, pediatric and airway specialist and founder of Nexus Dental Systems, takes an airway-centric approach to behaviors that can be misdiagnosed as ADD/ADHD
Dr. Emily Knipper offers a systems-based approach to in-office sedation
2 Pediatric Dental Practice US Volume 2 Number 1 TABLE OF CONTENTS
to assessing candidacy for in-office
EDUCATION Guide
pediatric sedation
PUBLISHER’S
6 CASE STUDY
PERSPECTIVE My Rx for summer Lisa Moler, Founder/CEO, MedMark Media...............................
Bioactive restorative selection in pediatric dentistry
15
PERSPECTIVE Pediatric
growth
PEDIATRIC
guided
and development
16 8 12 COVER STORY

More Procedures & Better Results
Perform a variety of soft-tissue procedures more e ciently with greater patient comfort and less healing time
Unbelievably A ordable Price
Only $3,495 many other soft-tissue diode lasers

Easy to Use
Wireless, lightweight, handheld design with an intuitive interface



































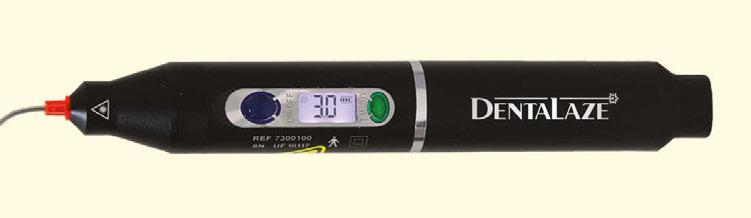
















Disposable Fiber Tips





















































































Laser Power & Battery E ciency


Saving time & preventing cross-contamination
New!
Delivers 3W constant and 5W pulsed power at 808nm & runs up to 45 minutes on a single charge
SNDL1-0823 Visit shofu.com Call 800.827.4638 Shofu Dental Corporation San Marcos CA 92078 Only $3495Order Today! To Purchase or Learn More scan QR Code NOW
CLINICAL


Treatment and delivery methods for myofunctional therapy
Nicole Cavalea, MS, discusses co-treatment goals of myofunctional therapy
CASE REPORT
The rationale for full coverage esthetic crowns: a case series
Beyond esthetics: Dr. Patrick Ruck discusses NuSmile® ZR Anterior Crowns as a long-term solution for complex pediatric dental cases 22
PRODUCT PROFILE
Harmonize™ restorative case study
Dr. Simona Cuevas discusses materials for direct restorative composite reconstruction ............ 28
TECHNOLOGY
Innovations in infant frenectomies
Dr. Lawrence Kotlow discusses how laser technology has influenced his practice............... 30
Published by

Publisher Lisa Moler lmoler@medmarkmedia.com
Managing Editor Mali Schantz-Feld, MA, CDE mali@medmarkmedia.com Tel: (727) 515-5118
National Account Manager
Adrienne Good agood@medmarkmedia.com Tel: (623) 340-4373
Sales Assistant & Client Services
Melissa Minnick melissa@medmarkmedia.com
Creative Director/Production Manager Amanda Culver amanda@medmarkmedia.com
Marketing & Digital Strategy Amzi Koury amzi@medmarkmedia.com
eMedia Coordinator
Michelle Britzius emedia@medmarkmedia.com
Social Media Manager Felicia Vaughn socialmedia@medmarkmedia.com
Website Support Eileen Kane webmaster@medmarkmedia.com
MedMark, LLC
15720 N. Greenway-Hayden Loop #9 Scottsdale, AZ 85260
Tel: (480) 621-8955
Toll-free: (866) 579-9496
HYGIENE PERSPECTIVE
Pediatric patients may need to use rinses more than adults
Kristin Goodfellow, RDH, discusses the importance of adding a mouthrinse to hygiene regimens .......................................... 26
PRODUCT PROFILE It’s 2024 y’all, and it’s time to stop using sticky varnish!
Joffree Bunleang applauds Profisil® as an innovation in flouride varnish ..............................32
www.medmarkmedia.com
www.pediatricdentalpractice.com
4 Pediatric Dental Practice US Volume 2 Number 1 TABLE OF CONTENTS
19

Early Airway Health Intervention HAS NEVER BEEN EASIER

DON’T WAIT TO START IMPROVING AIRWAY HEALTH FOR THE CHILDREN IN YOUR PRACTICE
“I have seen great improvement in my younger patients who use REMplenish Jr. You can see the difference in their facial structures, the way they swallow and their tongue posture. I can’t wait to see how it can help more kids improve their growth and development, airway, and sleep.”
Karindy Ong, MA, CCC-SLP, CFT


The REMplenish Myo-Nozzle provides myofunctional exercise simply by drinking water. There has never been an easier way to impact tongue posture, support nasal breathing and Improve sleep. Scan HERE to learn
Use code PEDIATRIC for 10% off your order
Try for 90 days risk free

www.REMasteredsleep.com
more:
My Rx for summer
How many times have you written prescriptions for your patients? Even after they leave your office, you strive to ease their pain, head off their infections, and get them back to healthy lives. I’m not a dentist, but I have played one for almost 20 years now! So, for this summer issue, it’s my turn to write a prescription – to encourage ongoing mental and physical health for our dedicated readers.
My Rx for a productive and rejuvenating summer
Vitamin D: Take some time to get out in the sun and soak up the relaxing rays! Change out of your scrubs and breathe some fresh air – and don’t forget your hat and sunscreen. You will return to work revitalized and ready to tackle any patient.
Get moving: Even if you don’t have time to get to the beach or take a longer vacation, exercise is one of the best ways to relieve tension and clear your mind. The CDC recommends 150 minutes of moderate-intensity physical activity per week. You don’t even need to join a gym – a daily walk will keep that blood flowing. Breaking the time up into 30 minutes a day for 5 days is very doable and can become a healthy habit.
and low on fats and sugars. But, as with all things under heaven, there is a time for ice cream and cake too (in moderation).
Build a trusted team, in and out of the office: Having support people to boost you when you are sad, and laugh with you when you are happy can make life a warmer, more welcoming place.
 Lisa Moler Founder/Publisher, MedMark Media
Lisa Moler Founder/Publisher, MedMark Media
Give your mind some thought: Every day, take some time for mindful thought or meditation. It doesn’t have to be the same time every day, or even done in the same way. Just pick a comfortable spot, close your eyes, breathe deeply, and focus on your breathing. Picture the beach, a mountain trail, or any spot that brings you peace. Taking a few minutes can reduce stress, ease frustration, and open the door to serenity.
Read, watch television, or listen to music: Having a way to unwind first thing in the morning or before bed can calm your mind and body.
Eat healthy, but give yourself a treat: We all know the drill – eat healthy fruits, vegetables and grains, go big on the protein
Forgive yourself! One of my main mantras throughout this journey of life is to give yourself a break. Everyone makes mistakes, and no matter what some people think, no one is perfect. Every mistake is an opportunity to learn from and grow.
Keep learning: Whether you are in the office or on vacation, take MedMark specialty publications with you! Keep learning new concepts so when you return to work, you can expand your patients’ options for care.
For our Cover Story, Dr. Najia Usman writes about her “aha moments” working with biocompatible and bioactive materials from Brasseler USA. In our Education column, Dr. Emily Knipper talks about the benefits and safety considerations for in-office sedation. In our Case Report, Dr. Patrick Ruck discusses how preformed pediatric zirconia crowns are becoming the treatment of choice for patients with high caries risk or diagnosis of severe early childhood caries. And Patrick Kirchner shares his perspective on the importance of collaboration between dentists and myofunctional therapists for comprehensive care and proper diagnosis of children with airway issues.
Even if your summer is busy with patients, there are plenty of ways to keep a healthy outlook on life. Journalist Charles Bowden once said, “Summertime is always the best of what might be.” Try a few of my Rx recommendations, and you will feel that endless summer in your hearts and minds for all future seasons.
To your best success,
Lisa Moler Founder/Publisher, MedMark Media




6 Pediatric Dental Practice US Volume 2 Number 1 PUBLISHER PERSPECTIVE
Don’t Miss the Next Issue of Sign up for your free subscription at https://pediatricdentalpractice.com and opt-in to our enewsletter to stay informed between issues. ENDOSEQUENCE A new solution for your pediatric pulp needs from dentistry’s leader in bioceramic innovation. PROMOTING EXCELLENCE IN PEDIATRIC DENTISTRY MyofunctionalTherapy/Lasers WatchforOurFall2024Issue Spring2024Vol2 No pediatricdentalpractice.com Using EndoSequence MaterialRootRepair for morepredictablesuccess Dr.NajiaUsman Guidetoassessing candidacyforin-office pediatricsedation Dr.EmilyKnipper Innovationsininfant frenectomies Dr.LawrenceKotlow Therationalforfull coverageesthetic crowns:acaseseries Dr.PatrickRuck
Why IDSO Partnership?
•Millions in Cash at Closing
•Full Autonomy in Clinical & Business
•Reduced Administration Burden
•Higher Reimbursement Rates
•Lower Costs in Clinical & Business
•Recruiting & Marketing Support
•Upside Gains in Retained Ownership
LPS vs. Do-It-Yourself & Small Advisors
•Six to Ten or More Bidders
•Highest EBITDA Calculation
•Full Knowledge of Risks & Rewards
• Most Tax Efficient Structures
•No Fee Unless the Transaction Closes
•Paid Only By Our Client, Not Both Sides
Large Practice Sales (LPS) is the largest transaction advisor to GP and specialty dental practices in the U.S. and completed over $1 Billion of Invisible Dental Support Organization (IDSO) partnerships in the last 24 months.
An IDSO partnership enables doctors to monetize 51-90% of their practice value with a silent partner for cash now at low tax rates. Doctors continue as owners leading their practice under the doctor’s brand, team, and FULL AUTONOMY for years or decades. Doctors gain the resources of a larger partner to grow faster, better, and more profitably to increase the value of their retained ownership.

-Dr. J.N., Maryland Achieved 12.2x EBITDA in 2023

HIGHEST VALUE
Large Practice Sales brings: MULTIPLE BIDDERS FOR THE
IN IDSO PARTNERSHIPS
844-7 734-8 8533 • MyP PedoValue.com • P PEDOUS@LargePracticeSales.com Get Your No-Cost, No-Obligation Practice Valuation.
“I never could have achieved this value or completed this deal without you. Thank you for everything.”
Visit Us at AAPD Booth #607
Using EndoSequence Root Repair Material for more predictable success
Dr. Najia Usman discussed working with biocompatible and bioactive materials from Brasseler USA
The evolution of my career as a self-proclaimed “Pediatric Endodontist” has been fortuitous. Having graduated from dental school in 1995 and then starting my residency in Portland, Oregon in 2000 meant that I would first be able to see the emergence of modern endodontics as we see it today. The new technology of apex locators, nickel-titanium files, and microscopes made my dental school undergraduate endodontic education seem outdated, but as they say, “You don’t know what you don’t know.” I remember my Chairman Dr. Craig Baumgartner handing me a small photographic film vial with a curious gray powder that I nicknamed “miracle mud.” This was MTA (Mineral Trioxide Aggregate) introduced by Mahmood Torabinejad in 1995 from Loma Linda that was being tested in labs and being given to endodontic residents around the country. It was comprised of tricalcium silicate, tricalcium aluminate, tricalcium oxide, and silicate oxide. Brought to market as ProRoot® by Dentsply, we used to mix it with our local anesthetic to a consistency that allowed the necessary handling properties for the task required. If it was a direct pulp cap, we needed it firm enough to plug into place. If we had a perforation, we needed it to flow and adapt to the defect, and if we needed to pack an open apex (apexification), we needed it to push it the length of the root but still stay put at the apex and not wash out.

Najia Usman, DDS, graduated from SUNY Buffalo in 1995. After completing a 1-year general practice residency at the Cleveland Clinic, she furthered her interest in endodontics by completing a 2-year endodontic residency at Oregon Health and Sciences University, Portland, Oregon in 2002. She was awarded her Diplomate status by the American Board of Endodontics in 2009. Dr. Usman has been in private practice since 2002. She is a clinical associate professor at the Case Western Reserve University School of Dental Medicine where she provides instruction to both dental students and graduate endodontic residents. She is a reviewer for the Journal of Endodontics and serves as chair of the American Association of Endodontics Public and Professional Relations Committee. Though she practices full-scope endodontics, she has cultivated an interest in the endodontic management in trauma, pediatrics, and resorptive lesions. She has organized and lectured in dental trauma symposiums. She has lectured and clinically taught dental students, endodontic and pediatric residents. She has lectured and conducted workshops internationally on topics such as endo-perio, atypical facial pain, regenerative endodontics, and pulpal injuries after orofacial trauma. Her study, “The Influence of Instrument Size on Debridement,” published in the Journal of Endodontics (Feb 2004, vol 30, 110-112) has been cited over 260 times. She is the proud mother of four children ages 18 to 28 and has been married to and shares a private multi-specialty practice with Dr. Faisal Quereshy, OMFS, for 29 years. They reside in Cleveland, Ohio.
Disclsoure: Dr. Najia Usman is a key opinion leader for Brasseler USA.

My first “ah-ha” moment came when I saw the closing of a long-standing large sinus tract on my pediatric 8-year-old patient, who after trauma presented with chief complaint of mobility, swelling, and likely a situation that looked hopeless. The biggest challenge with an open apex case is productive disinfection followed by creation of a long-lasting seal. Calcium hydroxide was used as the intracanal medicament between visits. Because it was not radiopaque, it was hard to gauge if it even made critical contact with the periradicular biofilm. I placed a CollaPlug® scaffold gingerly, visualizing with the microscope and then placed the MTA on the CollaPlug pillow taking several radiographs until I felt that I could see the MTA appear to encapsulate the irregularly shaped apex. Despite the visually satisfying post-op radiograph, I would come to see the amazing periapical healing complete with a rejuvenation of the periodontal ligament and concomitant osseous healing.
As we would review the current literature, terms like “biocompatible” and “bioinductive” were words that became associated with this new class of endodontics materials called bioceramics. Originally a purified version of Portland cement, this material was able to demonstrate fibroblast growth on top of its materials. The benefits of this new class of materials were rooted in its alkaline nature and ability to set in the presence of liquid “hydrophilic.” In addition, its excellent sealing properties made it a first choice for almost all complex endodontic applications.
We became very comfortable using it to heal our perforations. We changed from using our “ace in the hole” Super EBA® reinforced IRM in our retropreps following apical surgery to this
8 Pediatric Dental Practice US Volume 2 Number 1 COVER STORY
Dr. Najia Usman
new material. Despite the benefits though, we were now faced with the challenging handling properties of this material which quickly became a slurried mess when any blood came into our field. I remember Dr. Baumgartner remarking that if we could seal all of our canals with “this stuff” instead of gutta percha, “we would be on to something.”
I don’t remember the first time I actually used MTA for an apexogenesis in my private practice, but the circumstances were always the same. I would get a call regarding a fracture to a front tooth with a pulp exposure on an 8-year-old child. If I couldn’t see that child that day, I would instruct my referring dentist to gently cover the pulp exposure with GIC and refer to me ASAP. The protocol required removing a minimum of 2 mm of pulp tissue or until any bleeding stopped. I would use a diamond in a high speed with copious irrigation. Gently disinfecting with chlorohexidene and placing a saturated cotton pellet to assess healthy pulp was critical followed by placing a 2 mm thickness of MTA as a direct pulp cap. In those days, I would place a wet cotton pellet on top of the MTA and seal with Cavit™ per manufacturer’s recommendations. I would then bring the patient back to confirm set of the MTA, absence of symptoms, and do the definitive coronal restoration.


Whether it was a traumatic pulp exposure or a carious pulp exposure on an asymptomatic child with under developed roots, I was seeing consistent success. The patient was remaining asymptomatic because the pulp vitality and health was maintained. I was further rewarded with being able to see that beautiful dentin bridge that developed underneath the MTA protecting that healthy pulp as the root grew in length and closed.
With trauma protocols, we recall these patients quarterly for the first year prepared to intervene with traditional endodontic treatment anytime we see evidence of failure. We then see these patients annually for 5 years, or more often, until I am satisfied that the root growth is complete. Unfortunately, I was starting to see an ugly silver gray halo at the cervical margin as a result of the tooth erupting out of the alveolus as part of the normal growth of the child. All of a sudden, I was faced with another treatment challenge. Now I had to take out my minimalistic composite, remove MTA, and then remove tooth structure to facilitate non-vital bleaching. I remember being very frustrated that we were weakening tooth structure coronally after working so hard to grow the root. I also faced the possibility of damaging the pulp as we had to remove much of that 2 mm MTA cap.



Enter EndoSequence®. I remember my Brasseler rep coming to my office to fulfill my bur order. He asked me if I was familiar with this new bioceramic root repair material in a putty consistency. It has all the desirable qualities of my original MTA but also was the answer to my problems. Now there was a material which had amazing handling properties, did not require pre-mixing, and would bond to dentin because of its hydrophilic properties and very small particle size. A huge benefit was that it would not stain the dentin. At first being a purist, I was reluctant to change because I was so hooked on the benefits of my original MTA. I started using it first in my posterior apexogenesis cases where color was not a concern.

9 pediatricdentalpractice.com Volume 2 Number 1 COVER STORY
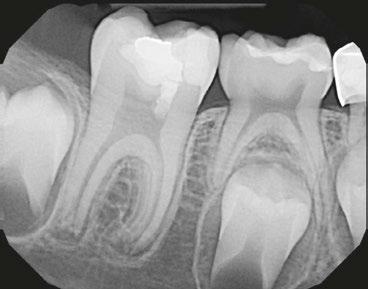
Figures 1 and 2: Example of staining from traditional MTA, non-vital bleaching after
Figure 3: Pre-op
Figures 4 and 5: Pulp cap
Figures 6: Apexogenesis

With a published success rate of >95%, Cvec pulpotomies or apexogenesis have become commonplace. Maybe it was my ability to manage children well or the fact that I was able to have consistent results, but my philosophy started to evolve from being reactive to trauma to being proactive. I would convert my referring dentists and pediatric dentists who would send me their “wait and watch” “well-intended” class 4 composites which ultimately became purulent disasters. I have now become the endodontist who lectures around the world about the benefits of placing a bioceramic root repair pulp cap even in a near pulp/ dentin (Ellis Class II) exposure with an open apex. Believe me, sometimes when I show periapical radiographs with an open apex and only dentin involvement, I get gasps on the mere suggestion of doing a Cvek. But from my vantage point, vital pulp therapy, which is defined as the art and science of maintaining the vitality of the pulp, is of great value. You see, I meet those patients who have been the recipients of conservative treatment. They are the patients who present with swelling, pain, or discoloration of their teeth. Depending on the age of injury, their apices may be open, and the prognosis even after treatment is far more questionable than if we had controlled the narrative from the beginning.
Armed with this new philosophy rooted in the satisfaction of hundreds of pediatric trauma patients over the last 20 years, I have been lecturing about regenerative endodontics of which vital pulp therapy is part of the treatment spectrum. While I have honed my skills and get consistent results, my mission is to equip pediatric dentists and general dentists to feel just as comfortable doing these procedures. One question I would consistently get from my pediatric residents was the concern about follow-up and the challenge of removing the cotton pellet and placing the definitive restoration. Typically in a pediatric residency, it is unlikely that they will see their patient again. One-year ago, my Brasseler rep provided a solution that has been a game changer in regenerative endodontics as a whole. EndoSequence has now created a liner in blue or white which bonds immediately to the EndoSequence RRM. It is a next-generation bioactive hybrid resin optimized for use with any of the bioceramic sealers and putty materials (BC RRM). What I love about these materials is the ease of dispensing and knowing that their performance is going to assure me of results without all the extra appointments. For years, pediatric dentists have maintained deciduous teeth in the mouth until natural exfoliation, by performing pulpoto-


mies. The pulpotomy can be defined as the surgical removal or amputation of the coronal pulp of the vital tooth. This step is followed by the placement of a medicament over the intact stump to fix, mummify, or stimulate repair of the remaining radicular pulp. Many materials have been used and investigated and they have differed with regards to biological compatibility, healing capabilities, mutagenicity, cytotoxicity, histological response, and carcinogenic potential. Though there historically have been many treatment approaches, most common is the Formocresol, ZOE pulpotomy.
MTA has shown high success rates clinically and radiographically, and it might offer the best immediate alternative to other medicaments. In the beginning of my career, I spent a small fortune on the original MTA, sold in packets that literally made it more costly than the price of gold. The EndoSequence BC RRM is the perfect material which now comes in cost-effective dispensing that makes it even more desirable. For someone with so many pediactric patients, I’m excited that they have recently launched their EndoSequence BC Pediatric Putty. It has all of the same bioceramic properies as their original BC RRM, including the easy-to-dispense delivery method, but now, it is available in standard and bulk packages at an extremely affordable cost. My hope is that my pediatric colleagues will use the new EndoSequence BC Pediatric Putty coupled with the liner to be able to manage traumatic and carious pulp exposures as well as the vital pulpotomies on deciduous teeth to create an antibacterial solution that is biocompatible and bioinductive, improving our patients’ smiles more predictably. PD
10 Pediatric Dental Practice US Volume 2 Number 1 COVER STORY
Figures 7 and 8: Recall 1 and 2
Figure 9: Recall 3
Figure 10: EndoSequence BC RRM
BC PEDIATRIC PUTTY ENDOSEQUENCE ®
A new solution for your pediatric pulp needs.
Works exceptionally well for pulpotomies while delivering the same advantages our bioceramic family is known for.
✓ Highly biocompatible and osteogenic for superior healing
✓ Bonds to dentin by leveraging the natural dentin moisture
✓ Antibacterial with a high alkaline pH
✓ Highly radiopaque and hydrophilic
✓ Ultra-small particle size for superior handling
✓ Use BC Pediatric Putty in conjunction with BC Liner™ to add a layer of protection over the putty


SCAN QR CODE TO LEARN MORE & REDEEM AN EXCLUSIVE OFFER
NEW! PDP-Spring.05.24 ©2024 Brasseler USA. All rights reserved. Visit our website at BrasselerUSADental.com To order call 800.841.4522 or fax 888.610.1937.

Guide to assessing candidacy for in-office pediatric sedation
Dr. Emily Knipper offers a systems-based approach to in-office sedation
Although most dental work can be completed without sedation, children may require sedation for the completion of dental work if they have severe anxiety, special needs that challenge cooperative ability, young age, and/or extensive treatment. For children requiring sedation, dentists are

Emily Knipper, MD, attended medical school at Wake Forest University in Winston-Salem, North Carolina. She completed a residency in Anesthesiology at the University of Virginia in Charlottesville, Virginia, and completed a fellowship in Pediatric Anesthesiology at Seattle Children’s Hospital. She and her family live in Charlotte, NC, and she provides in-office sedation for children having dental work in North Carolina and South Carolina.
Disclosure: Dr. Knipper is a partner of Pediatric Dental Anesthesia Associates.
faced with options regarding the type of sedation, who performs it, and the location of sedation. In-office IV sedation has the benefits of convenience for the dentist, staff, and patient, while the administration of IV medicine facilitates a predictable level of sedation. However, because of the potency of the medicines used and the in-office setting, selection of patients for this practice is key to ensuring safety. This article uses a systems-based approach to guide dentists in assessing a child’s candidacy for in-office sedation.
Neurological
A key consideration for assessing neurological pathology in this setting is to ask how a child’s neurological disease, if present, will affect his/her ability to recover from sedation in a timely and predictable manner. Neurological pathologies that
12 Pediatric Dental Practice US Volume 2 Number 1 EDUCATION

are associated with weakness, such as myasthenic syndromes, are poorly suited for the office setting, because weakness can necessitate assistance with breathing during recovery, and an in-office setting may not be equipped to handle this for extended periods of time.
Seizures are not infrequently seen in children. A history of a single febrile seizure in childhood will likely have little effect on a child having sedation, but a history of poorly controlled and/or frequent grand mal tonic-clonic seizures raises concerns about safety in a dental office. Practical questions to ask are if the child has ever received a “rescue medicine” for a seizure and the type and frequency of seizures.
Cardiovascular
Cardiovascular health is key for the safety of in-office sedation. When considering a child with congenital heart disease, the type of defect, what repair has been done, and whether or not any further surgery is planned are key. Children with simple congenital heart disease, such as small ventricular septal defects with left-to-right shunting, may be considered for in-office sedation, on a case by case basis and depending on their functional status. Children with more complicated disease, and particularly that which has necessitated repair, are often more safely taken care of in an operating room setting. Specifically, any sort of congenital heart disease necessitating the “single-ventricle pathway” for repair should not be taken care of in the office (i.e., hypoplastic left heart syndrome, double outlet right ventricle, tricuspid atresia, mitral atresia). Even in their “repaired” states, the physiology in these children is tenuous, and perturbations to fluid and oxygen status can lead to rapid deterioration. In general, if a heart surgery has been done, it is important to ask what repair was done for purposes of determining the need for prophylactic antibiotics, as well as the child’s functional status, and if there are any issues with heart arrhythmias, breathing, and nutrition. A recent echocardiogram is key, as it allows assessment of shunting, valvular pathology, and ventricular function.
Respiratory
When assessing respiratory pathology, it is important to consider how it affects a child’s everyday life. For instance, asthma that is poorly controlled and frequently flares should likely be better controlled before considering in-office sedation. Bron-
No matter the age, each child should receive a thorough evaluation and physical exam by an anesthesiology provider well-trained in pediatric pathology before being taken care of in an office setting, with ample time to assess any of the above conditions and to obtain records from specialists where applicable.”
chospasm or laryngospasm from reactive airways can quickly become life threatening. Obstructive sleep apnea is another pathology that affects a child’s everyday life and raises concerns about in-office care. Apnea or the need for supported ventilation during sedation can complicate care, prolonging recovery and increasing the chances of complications.
In-office sedation has the benefit of convenience and safety when careful consideration to patient selection is given. All body-systems are important in considering potential safety, but neurologic, cardiovascular, and respiratory concerns are frequently paramount. Of note, children with syndromes and any metabolic disorders (i.e., lysosomal storage disease, glycogen storage disease, mitochondrial disease), need to be carefully evaluated and are likely best taken care of in a hospital setting. Children who are at risk for aspiration due to delayed gastric emptying, severe acid reflux, or history of congenital defect (i.e., duodenal atresia as seen in Down Syndrome), should be identified and thoroughly evaluated.
Regarding age, no specific age cutoff has been delineated as unequivocally correlating with complications. However, individual anesthesia providers may vary in their facility with taking care of younger children, and providers with greater depth of pediatric training typically have more experience with younger children (i.e., under age 3 years old). Physiologic reserve is decreased in younger ages, making the margin for error in their care smaller. No matter the age, each child should receive a thorough evaluation and physical exam by an anesthesiology provider well-trained in pediatric pathology before being taken care of in an office setting, with ample time to assess any of the above conditions and to obtain records from specialists where applicable. Doing so preserves the safety of this unique and often convenient model of care. PD
14 Pediatric Dental Practice US Volume 2 Number 1
EDUCATION
Bioactive restorative selection in pediatric dentistry
Dr. Carla Cohn discusses her choice of restorative materials
Children should learn to practice oral hygiene from an early age, and dentists are specially trained to treat little ones and educate their parents on oral health care. Caries can develop as the primary teeth first begin to erupt, and maintaining healthy primary dentition is important for the growth and development of the arch, as well as the emotional well-being of the child.



The 5-year-old patient featured in this case study did not benefit from early oral care and had multiple carious lesions. Considering the young age, high caries risk, and the uncertainty of compliance with follow-up appointments, I wanted to restore and seal all teeth in one visit. One quadrant is shown in this case study. The carious lesion on tooth J (65) was cavitated and prepared, restored, and sealed. Tooth I (64) was non-carious and would only be sealed (Figure 1).
I chose Activa™ Kids Bioactive-Restorative and Activa Presto (Pulpdent) as restorative materials for this case because I have seen excellent clinical results over time with these bioactive materials. Continuous release and recharge of calcium, fluoride, and phosphate from these restoratives are beneficial in the fight against decay long into the future.
Choosing restoratives based on ease of use and the ability to work quickly was important in this case. All restorations were completed under general anesthesia in one appointment. There were wear facets on the occlusal surfaces of the molars, so it was important to use a material that would have some flexibility and resistance to fracture. The innovative composition of Activa Kids includes an elastomeric monomer or “rubberized” component that absorbs forces and was an ideal filling material. Activa Presto shares similar properties, and it was convenient to use as an occlusal surface sealant for this patient.
Tooth J (65) was prepared with a coarse tapered high-speed diamond bur allowing for some minor mechanical retention by incorporating minimal undercut in preparation. The occlusal

Dr. Carla Cohn is a general dentist devoted solely to the practice of dentistry for children. She owns and operates Kids Sleep Dentistry Winnipeg, a private practice at Western Surgery Centre in Canada. Dr. Cohn recently founded Lit Smile Academy, a continuing dental education company. With extensive teaching experience and numerous publications, she is recognized internationally for her contributions to continuing dental education.




surface of tooth I (64) was also lightly abraded with a diamond bur (Figure 2). The preparations were selectively etched with phosphoric acid, rinsed, and lightly dried (Figure 3). Bonding agent was applied to the entire occlusal surfaces of both teeth, air thinned, and light-cured (Figure 4).
Tooth J (65) was bulk-filled with Activa Kids. For this fast injection technique, I place the dispensing tip at the floor of the preparation and extrude the material without removing the tip until the preparation is completely filled (Figure 5). I like to do some minor manipulation of the filling material with hand instruments to create anatomy, as well as to ensure the material is flush with the surface of the preparation, and no air is trapped inside. Activa Kids is dual-cure, ideal for bulk filling, and can be cured with all lights. A thin topcoat of Activa Presto was placed as a sealant on the entire occlusal surface of teeth I and J (64 and 65) (Figure 6). Figure 7 shows the final clinical situation.
15 pediatricdentalpractice.com Volume 2 Number 1 CASE STUDY
This information was provided by Pulpdent.
PD
Figure 1 (left): Caries lesion on tooth J (65). Figure 2 (center): Preparation of tooth J (65) and abraded occlusal surface of tooth I (64). Figure 3 (right): Selective etch of enamel
Figure 4 (left): Bonding agent is applied to both teeth I and J (64 and 65). Figure 5 (right): The preparation is filled with ACTIVA Kids
Figure 6 (left): A thin topcoat of ACTIVA Presto is applied to the occlusal surfaces of teeth I and J (64, 65). Figure 7 (right): Final result
Pediatric guided growth and development
Patrick Kircher, pediatric and airway specialist and founder of Nexus Dental Systems, takes an airway-centric approach to behaviors that can be misdiagnosed as ADD/ADHD
In recent years, there has been a growing understanding of the intricate relationship between airway health and overall development in pediatric patients. Dentists who are already involved

Patrick Kircher founded National Dental Systems (NDS) in 2015 comprising a comprehensive medically necessary dental model including the diagnosis and treatment of Obstructive Sleep Apnea, DMSD, and associated symptoms. National Dental Systems acquired DreamSleep and TruDenta complementing what DreamSleep had in place with the ACSDD, medical reimbursement, and technology. Under his guidance, NDS experienced 100+% year-overyear growth and yielded 60% net margin leading to a highly profitable and scalable business. In 2020, NDS merged with Nexus Dental Systems to collaborate with industry leaders and provide more impactful services and solutions for the industry.
in airway treatment are well-aware of the significant impact of proper growth and development on children's long-term health and well-being. This article aims to shed light on the negative impacts of retractive nature of traditional orthodontics while emphasizing the benefits of early intervention, guides, and myofunctional therapy in promoting airway-centric development and preventing misdiagnosed cases of ADD/ADHD. We will explore the importance of adopting a holistic approach to pediatric care.
The airway-centric approach to pediatric development
The airway plays a crucial role in a child's overall health and development. Proper nasal breathing, sufficient oxygenation, and appropriate tongue posture are all essential for the normal growth of the face, jaws, and airway. Unfortunately, factors such as allergies,

16 Pediatric Dental Practice US Volume 2 Number 1 PEDIATRIC PERSPECTIVE

The Problem: Mouth breathing can lead to underdevelopment of the upper jaw and restricted forward growth of the lower jaw. This can cause crowding and restriction of the airway. Left untreated, the child may develop Sleep Disordered Breathing (SDB).
The Solution: Whole team education and training from Nexus.

Helping you grow healthy kids. Join us: nexusdentalsystems.com/pediatrics/

A Unique Approach to Saving Lives.
By identifying and addressing airway issues at an early stage, dentists can help prevent the need for more invasive treatments later in life.”
enlarged tonsils and adenoids, or structural abnormalities can compromise the airway, leading to mouth breathing and a cascade of adverse effects.
Negative impacts of retractive orthodontics without extractions
Retractive orthodontics, a common approach in traditional orthodontics, involves retracting the anterior teeth to correct malocclusion without extracting any teeth. While this approach may yield immediate esthetic improvements, it often fails to address the underlying causes of malocclusion, including airway issues. Studies have shown that retractive orthodontics can lead to narrowing of the upper arch, restricted nasal airflow, and compromised facial esthetics.
Furthermore, the consequences of retractive orthodontics extend beyond esthetics. These treatments can contribute to the development of a retrusive mandible, leading to a compromised airway and potential breathing difficulties. Additionally, they can exacerbate or create temporomandibular joint (TMJ) issues, facial pain, and sleep-disordered breathing in susceptible individuals.
Misdiagnosed ADD/ADHD: the impact of airway issues
A growing body of research suggests that airway issues can be misdiagnosed as Attention Deficit Disorder (ADD) or Attention Deficit Hyperactivity Disorder (ADHD) due to overlapping symptoms. Children with compromised airways often exhibit behavioral problems, poor attention span, hyperactivity, and difficulty concentrating, which are also characteristic of ADD/ADHD.
Statistics on misdiagnosis
According to a study published in the journal Sleep, up to 9 out of 10 children diagnosed with ADD/ADHD may have undiagnosed sleep-disordered breathing, often stemming from airway issues. The study further suggests that children with sleep-disordered breathing are 40%-100% more likely to exhibit symptoms

similar to ADD/ADHD. These statistics highlight the importance of considering airway health in the evaluation of behavioral issues, ensuring an accurate diagnosis and appropriate treatment.
Benefits of early intervention and guides
Early intervention is key to promoting optimal growth and development in children. By identifying and addressing airway issues at an early stage, dentists can help prevent the need for more invasive treatments later in life. Utilizing guides or functional appliances can guide the growth of the jaws and improve airway dimensions. Such interventions focus on encouraging proper nasal breathing, maintaining tongue posture, and enhancing facial development. Through this approach, children can achieve balanced facial esthetics, improved airway function, and reduced risks of sleep-disordered breathing.
The role of myofunctional therapy
Myofunctional therapy is a valuable adjunct to early intervention and guides in promoting proper oral function and myofacial balance. It involves exercises and techniques designed to encourage proper tongue posture and swallowing.
Collaboration between dentists and myofunctional therapists
Collaboration between dentists and myofunctional therapists is crucial for comprehensive care and optimal patient outcomes. Dentists who are already engaged in airway treatment can work closely with myofunctional therapists to develop integrated treatment plans. This collaboration allows for the identification and simultaneous treatment of airway-related issues, malocclusions, and orofacial muscle dysfunctions.
Together, dentists and myofunctional therapists can provide patients with a comprehensive approach that includes orthodontic interventions, expansion appliances, myofunctional exercises, and other appropriate therapies. This collaboration enhances the effectiveness of treatment, leading to improved airway function, craniofacial development, and overall oral health in pediatric patients.
18 Pediatric Dental Practice US Volume 2 Number 1 PEDIATRIC PERSPECTIVE
PD
Treatment and delivery methods for myofunctional therapy
Nicole Cavalea, MS, discusses co-treatment goals of myofunctional therapy
Orthodontists and pediatric dentists are often the first professionals to identify a patient’s abnormal patterning of the mouth and tongue, as these abnormalities interfere with the structural integrity of orthodontic treatment. A visual assessment of the following characteristics can indicate the need to co-treat with an orofacial myofunctional therapist:
• forward tongue protrusion during resting, speech, and/ or swallow
• open mouth posture
• weak lip seal
• postural changes to face
• open bite
• distorted speech
• jaw instability
• dark eye circles
• long face
• high, narrow palate
When a patient presents with a tongue thrust, the clinician will observe resting the tongue against the teeth, swallowing with the tongue pushing against the teeth, and making sounds (meant for placement on the alveolar palate) with tongue pressure against the teeth. Having a tongue thrust will apply pounds of pressure on the anterior teeth daily. This postural and functional imbalance may cause serious dental problems and greatly interfere with the efficiency of orthodontic treatment. If incorrect muscle patterning or swallowing has created a malocclusion, learning proper techniques to correct these imbalances

Nicole Cavalea, MS, is the founder of Strategies for Success, a speech-language pathology practice and myofunctional therapy clinic. She has worked in the field of communication disorders for 19 years. She received her MS degree in Speech and Language Pathology from San Jose State University. Cavalea has extensive expertise working with children of all ages in the assessment, treatment, and management of speech and language disorders, auditory processing delays, and myofunctional disorders. After incorporating myofunctional techniques into her practice, she began noticing her patients improving with quicker and more precise results, leading her to further her training in myofunctional disorders and treatment, and attending multiple intensive training courses from the Academy of Orofacial Myofunctional Therapy. Recent studies include an advanced course on breathing re-education, focusing on restoring adequate breathing in sleep apnea patients. Recently, Cavalea has expanded her practice nationwide through telepractice, and values and enjoys collaboration and cotreatment with multidisciplinary teams across the country. Nicole Cavalea can be reached at ncavalea@gmail.com.


19 pediatricdentalpractice.com Volume 2 Number 1 CLINICAL
Figure 1: Symptoms of apraxia
Figure 2: Child with expressive and receptive disorders
may prevent further damage as special orthodontic appliances or braces will be needed to reposition dental problems that have already occurred. If atypical swallowing is not corrected early, it can cause alterations in the development of the stomatognathic apparatus. Furthermore, the improper function of the tongue, in conjunction with dental malocclusion, will often lead to jaw instability, thus causing pain and headaches for the patient. For these reasons, myofunctional therapy is a useful adjunct treatment to orthodontics in subjects with myofunctional dysfunction.7
Obstructive sleep apnea (OSA) has become increasingly recognized as a notable health concern in children, given its consequences on behavior, function, and quality of life.
Two important factors in the correction of tongue-thrust swallowing are 1) growth and 2) orthodontic treatment to place the teeth in their proper positions and thus simplify proper tongue placement. However, growth and orthodontic treatment alone will not correct tongue-thrust swallowing. In correction therapy, the 22 muscles that are used in normal swallowing should be re-educated to eliminate the tongue-thrust swallowing habit in order for the patient to be able to unconsciously swallow in the correct manner.8
Therapy targeting a tongue thrust is aimed to strengthen, coordinate, and retrain the muscles involved in swallowing, resting posture, and speech. First, an assessment is used to deter-

mine the nature of the postural imbalances that are present and how they affect craniofacial development. Next, the patient is given a set of exercises to activate and strengthen the weakened muscles used incorrectly during swallow and involved in postural imbalances. Proper placement and precision are taught in regard to the function of swallowing. When swallowing correctly, the patient is instructed to voluntarily place the tongue against the roof of the mouth while bringing lips together and creating a suction to swallow. The patient is then taught correct resting posture and speech.
Lip exercises to strengthen the lip seal and to habituate a closed-mouth posture are elicited. The nature of therapy is to correct habitual use of the tongue while working on strengthening and patterning of the soft tissue involved. Treatment will last anywhere from 4 to 6 months with exercises and practice daily.
Improper oral resting posture of the tongue will have a negative influence of the oral cavity and airway. The anatomy of the upper airway in turn guides the growth and development of the nasomaxillary complex, mandible, temporomandibular joint, and ultimately, the occlusion of the teeth; thus, malocclusion and facial dysmorphism may be the result of compensation for a narrowed airway.5 Short lingual frenulum is a known factor in altering orofacial growth particularly impacting development of the maxilla due to the low placement of the tongue. It leads to the abnormal development of a high and narrow hard palate, and secondarily, mouth-breathing during sleep.4
Obstructive sleep apnea (OSA) has become increasingly recognized as a notable health concern in children, given its consequences on behavior, function, and quality of life. Statistically, 40% of children who suffer from sleep-disordered breathing (SDB) develop ADD, ADHD, and/or a learning disability. Additionally, children are diagnosed with SDB in the first 5 years of life, and left untreated, they are 60% more likely to require special needs education by age 8.1
20 Pediatric Dental Practice US Volume 2 Number 1 CLINICAL
Figure 3: Before treatment. Here, a tongue thrust is visible by the anterior tongue placement (pushing against teeth)
Figure 4: After 11 weeks of treatment. Noticeable postural changes after 11 weeks of a tonguethrust treatment protocol
Most children with OSA have difficulty breathing through the nose. Allergic rhinitis is the most commonly cited disease, followed by hypertrophy of the tonsils and adenoids.1 Orofacial and pharyngeal muscles are involved in important functions including breathing, with the vital role of maintaining airflow. Any upper airway (UA) obstruction may induce changes in neuromuscular function in order to ensure the passage of air. The most common consequence of UA obstruction is mouth breathing, a functional adaptation that may affect craniofacial growth and development during childhood. Another possible consequence is obstructive sleep apnea (OSA).1
Myofunctional treatment is aimed at correcting abnormal breathing patterns and muscular dysfunction that may impair upper airway patency.1 Adenotonsillectomy (T&A) and palatal expansion have established roles in the treatment of OSA after demonstrating considerable improvement related to adenoid or tonsillar hypertrophy, maxillary or mandibular deficiency, and orthodontic or craniofacial abnormalities. However, the implementation of other modalities such as myofacial re-education also plays a crucial role in the optimization of sleep-disordered breathing, as maladapted orofacial functions may be irreversible or present insufficient improvement even when their original cause is eliminated.1 If nasal breathing is not restored, despite short-term improvements after adenotonsillectomy, continued use of the oral breathing route may be associated with abnormal impacts on airway growth and possibly blunted neuromuscular responsiveness of airway tissues, both of which may predispose to the eventual return of upper airway collapse in later childhood or in the full blown syndrome of OSA in adulthood.2
Co-treatment goals of the myofunctional therapist follow: First, determine the nature of the postural imbalances that are present and how they affect craniofacial development and functional ability. Next, correct muscular imbalances of the lips, tongue, and jaw through exercises meant to re-pattern, coordinate, and strengthen these areas involved. Children with OSA were found to have relative impairments in orofacial functions and lesser muscular coordination.1 The therapist activates and strengthens the oral facial muscles of mastication to support the mandible and the genioglossus at night.
Approximately 30% of OSA patients have poor genioglossus muscle responsiveness to airway narrowing during sleep.6 The tongue muscles are trained to achieve palatal tongue rest position (aiding in correct tongue posture during rest, speech, and swallow). Proper placement and precision are taught in regard to the function of swallowing. When swallowing correctly, the patients are instructed to voluntarily place their tongue against the roof of the mouth while bringing lips together and creating a suction to swallow. Finally, correct nasal breathing, along with a proper resting oral posture, is established. Achieving proper nasal breathing will result in improving lung volume, increasing
nitric oxide through the body, improvement in sleep, and the reduction of allergies and illnesses.
To restore efficiency in breathing, first, the myofunctional therapist will educate patients on proper nasal/diaphragmatic breathing. Once coherence is established, they will learn a series of exercises that focus on the biomechanical and biochemical aspects of breathing. Biochemically, patients are instructed to breathe in a way that creates a desire for air (such as narrow, light breaths). This technique will decrease their sensitivity for CO2, therefore creating a larger threshold to eliminate sleep disturbances. Biomechanically, patients are instructed on ways to practice techniques that maximize breathing skills. For example, they learn deep, slow breathing through the nose where the air effectively expands the diaphragm. Treatment will last anywhere from 4 to 6 months, with exercises and practice daily.
Conclusion
Research indicates that successful treatment of functional postural abnormalities depends on the collaboration of multidisciplinary teams. Comprehensive management requires an integrated effort of the sleep physician, otolaryngologist, allergist, orthodontist, pediatric dentist, and myofunctional therapist.
Treatment of myofunctional therapy can be carried out in office or through telepractice (i.e., telemedicine or telehealth). Both modalities provide effective measures of intake, assessment, collaboration, and treatment for the patient.
Comprehensive management requires an integrated effort of the sleep physician, otolaryngologist, allergist, orthodontist, pediatric dentist, and myofunctional therapist.” PD
REFERENCES
1. De Felicio CM, da Silva Dias FV, Folha GA, et al. Orofacial motor functions in pediatric obstructive sleep apnea and implications for myofunctional therapy. Int J Pediatr Otorhinolaryngol. 2016;90:5-11.
2. Guilleminault C, Sullivan SS. Towards restoration of continuous nasal breathing as the ultimate treatment goal in pediatric obstructive sleep apnea. Enliven: Pediatr Neonatol Biol. 2014;1(1):001.
3. Huang YS, Guilleminault C. Pediatric obstructive sleep apnea and the critical role of oral-facial growth: Evidences. Front Neurol. 2012;3:184.
4. Huang YS, Quo S, Berkowski A, Guilleminault C. Short lingual frenulum and obstructive sleep apnea in children. Int J of Pediatr Res. 2015;1:1.
5. Moeller JL, Paskay LC, Gelb ML. Myofunctional therapy: a novel treatment of pediatric sleep-disordered breathing. Sleep Med Clin. 2014;9:235-243.
6. Osman AM, Carter JC, Carberry JC, Eckert DJ. Obstructive sleep apnea: current perspectives. Nat Sci Sleep. 2018;10:21-34
7. Saccomanno S, Antonini G, D’Altari L, et al. Patients treated with orthodontic-myofunctional therapeutic protocol. Eur J Paediatr Dent. 2012;13(3):241-243.
8. Straub WJ. Malfunction of the tongue. Am J Orthod. 1962;48(7):486-503.
21 pediatricdentalpractice.com Volume 2 Number 1 CLINICAL
The rationale for full coverage esthetic crowns: a case series
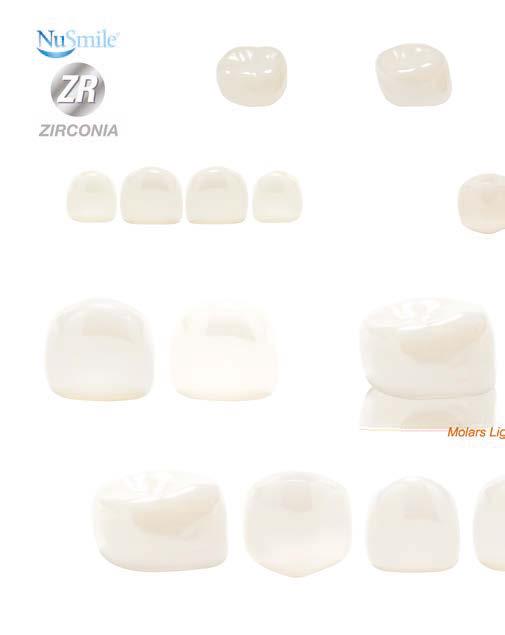
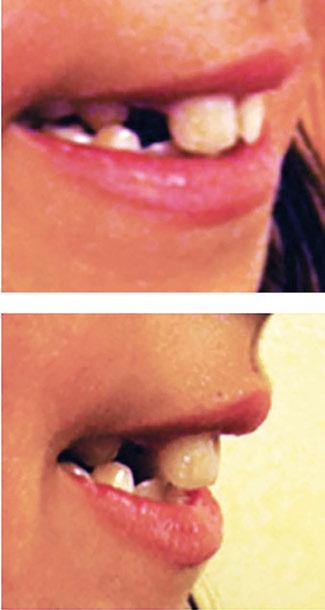
Beyond esthetics: Dr. Patrick Ruck discusses NuSmile® ZR Anterior Crowns as a long-term solution for complex pediatric dental cases
Background
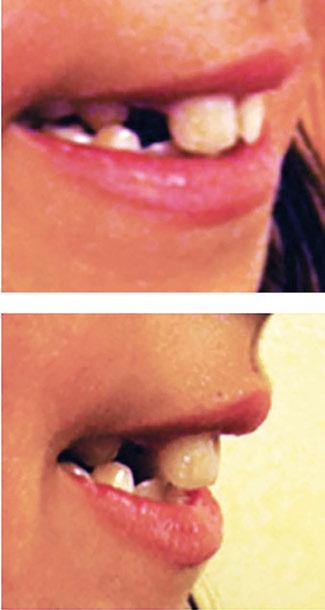
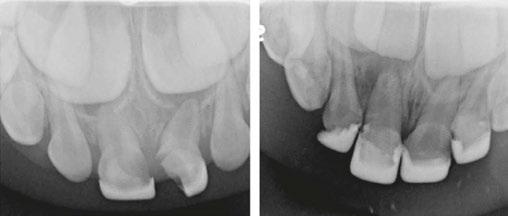
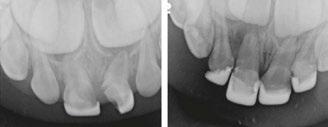
Several clinical solutions exist for primary anterior teeth with multisurface decay. Full coronal restoration of carious primary incisors may be indicated when caries is present on multiple surfaces, pulpal therapy is indicated, caries may be minor, but oral hygiene is very poor, or in a child with severe early childhood caries or a high caries risk diagnosis.1 Depending on the clinical scenario, a minimally invasive approach with the utilization of a high viscosity glass ionomer cement (HVGIC), with or without the combination of silver diamine fluoride (SDF) in a strip crown form, may pause the caries progression and provide an adequate clinical solution. Resin composite strip crowns have shown 80% retention rates and adequate parental satisfaction,1-4 although composite resin strip crowns have shown lower retention rates in teeth with decay involving three or more surfaces and particularly in children with a high caries risk4-6 (Figure 1). This could be from the continued high caries risk behaviors of the patient, as composite resin strip crowns in this population have shown to have increased inflamed marginal gingiva and gingival bleeding, increased plaque retention along the restoration, and loss of some restorative material.5,6
Alternatively, a resin-faced stainless steel crown provides a full coverage restoration with excellent retention.7 These crowns can serve as a full-coverage restoration with or without the resin facing, but the loss of resin facing can be a major esthetic concern for parents.7 Preformed pediatric zirconia crowns address many of the undesirable clinical outcomes of other restorative materials. Their biocompatibility, demonstration of excellent marginal gingival health, low plaque retention, high parental esthetic acceptance, and high survival probabilities make them an excellent clinical choice in the patient with severe early childhood caries.1,4,5,8-13
With parental interest increasing in esthetic treatment options for complex anterior caries, preformed pediatric zirconia crowns are becoming the treatment of choice for patients with a high caries risk or a severe early childhood caries diagnosis.14

Patrick Ruck, DDS, is an assistant professor at Cincinnati Children’s Hospital Medical Center. He can be reached at patrick.ruck@cchmc.org.
Disclosure: Dr. Patrick Ruck is a known opinion leader (KOL) for NuSmile.
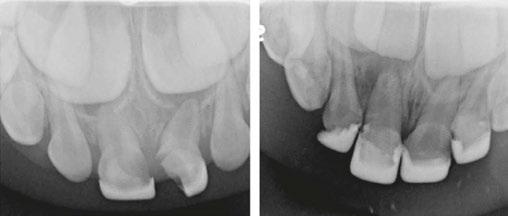


2: NuSmile® Anterior Zirconia crowns at 2-year follow up. Note the high amount of plaque accumulations along the untreated cuspid and existing stainless-steel crowns
This review discusses three clinical cases in which NuSmile® ZR (NuSmile, Houston, Texas) anterior pediatric zirconia crowns were the correct clinical decision in varying clinical scenarios.
Case 1
A 2-year-old male who received full mouth dental rehabilitation (FMDR) under general anesthesia presented for his 6-month recall at 2-year post FMDR. He had significant plaque accumulations with poor oral hygiene along his existing stainless-steel crowns (SSCs) and non-treated teeth. Additionally, the patient had gingival bleeding and gingival inflammation
22 Pediatric Dental Practice US Volume 2 Number 1 CASE REPORT
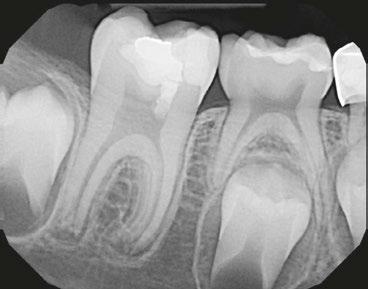
Figure 1: Occlusal films at recall visit in high caries risk patients showing loss of material and recurrent decay in composite resin strip crowns
Figure





























SPECIAL OFFER ZR ANTERIOR MASTER KIT $1,410.00 $1,269.00 Contains 56 Crowns $25.18 $22.60 Per Crown Call 713.861.0033 to claim your offer Promo Code: AMK2024 Offer valid until July 31, 2024 CLINICIAN'S #1 CHOICE WORLDWIDE FOR NATURALLY ESTHETIC ZIRCONIA CROWNS Call 713.861.0033 to claim your offer Promo Code: AMKM2024 Offer valid until July 31st, 2024
around these clinical sites. His anterior zirconia crowns showed healthy gingival margins with little-to-no plaque accumulations. This positive clinical finding is from the highly polished nature and biocompatibility of pediatric zirconia crowns. These restoration features limit plaque accumulations on the restoration and along the marginal gingiva, providing a localized positive aspect directly related to the choice of restorative material (Figure 2).
Case 2



A 3-year-old female presented with pulpal necrosis and abscess on #E and pulpal necrosis on #F. Extraction therapy or pulpectomy was offered. The family was highly motivated to retain #E and #F. The pulpectomy was performed with 0.02 K-Flex hand files, 3% NaOCl with a lateral vented needle, obturated with Vitapex (Neo Dental International Inc., Federal Way, Washington), a premixed paste of calcium hydroxide and iodoform. The access was filled with a HVGIC sealing the pulp therapy and increasing the clinical success by minimizing the potential for bacterial contamination. NuSmile ZR anterior crowns were selected as offering a full-coverage, esthetic, cemented restoration with no polymerization shrinkage when compared to a composite restoration. Crowns were cemented with NuSmile® BioCem (NuSmile, Houston, Texas). This is clinically beneficial as the provider would want to cement a restoration that provides limited microleakage minimizing the potential for bacterial contamination.15-17 At 6-month follow up, lesion healing had occurred with healthy gingival margins and no plaque accumulations (Figure 3).
Case 3

With parental interest increasing in esthetic treatment options for complex anterior caries, preformed pediatric zirconia crowns are becoming the treatment of choice for patients with a high caries risk or a severe early childhood caries diagnosis.”
A 4-year-old female presented with existing Silver Modified Atraumatic Restorative Technique (SMART) style restorations on #D, #E, #F, #G, and caries on other teeth. These anterior lesions

had been previously treated using SDF and covered with a HVGIC in a strip crown form. Though her lesions were stable from the clinical success of the SDF and HVGIC, these restorations were starting to fracture and demonstrate loss of material. The family wanted a more esthetic treatment option that would have a longer survivability. Additionally due to her high caries risk nature, a full coverage restoration with NuSmile® ZR anterior crowns were a more ideal solution in stabilizing her extensive decay pattern and covering staining from SDF therapy (Figure 4).

24 Pediatric Dental Practice US Volume 2 Number 1 CASE REPORT
Figure 3: NuSmile® ZR Crowns were selected as a cementable full coverage restoration. At 6-month recall, apical tissues were healed with excellent gingival health
Figure 4: SMART style restorations that were definitively restored with NuSmile® ZR Crowns as an esthetic option to cover SDF staining
Conclusion
There exist multiple treatment solutions, but NuSmile® ZR anterior crowns provide a highly biocompatible, long lasting, and esthetically pleasing restoration. This is an excellent clinical choice for the high caries risk patient with severe early childhood caries.
PD
REFERENCES
1. American Academy of Pediatric Dentistry. Pediatric restorative dentistry. The Reference Manual of Pediatric Dentistry. Chicago, Ill.: American Academy of Pediatric Dentistry; 2023:443-456.
2. Ram D, Fuks AB. Clinical performance of resin-bonded composite strip crowns in primary incisors: a retrospective study. Int J Paediatr Dent. 2006 Jan;16(1):49-54.
3. Kupietzky A, Waggoner WF, Galea J. The clinical and radiographic success of bonded resin composite strip crowns for primary incisors. Pediatr Dent. 2003 Nov-Dec;25(6):577-581.
4. Sharma M, Khatri A, Kalra N, Tyagi R. Comparison of parental satisfaction with strip crowns and primary anterior zirconia crowns in 3-5 years old children over 1 year. J Indian Soc Pedod Prev Dent. 2021 Oct-Dec;39(4):423-428.
5. Alaki SM, Abdulhadi BS, AbdElBaki MA, Alamoudi NM. Comparing zirconia to anterior strip crowns in primary anterior teeth in children: a randomized clinical trial. BMC Oral Health. 2020 Nov 10;20(1):313.
6. Amin M, Nouri MR, Hulland S, ElSalhy M, Azarpazhooh A. Success Rate of Treatments Provided for Early Childhood Caries under General Anesthesia: A Retrospective Cohort Study. Pediatr Dent. 2016;38(4):317-324.
7. Lopez-Loverich AM, Garcia MM, Donly KJ. Retrospective Study of Retention of Stain-
less Steel Crowns and Pre-veneered Crowns on Primary Anterior Teeth. Pediatr Dent. 2015 Nov-Dec;37(7):530-534.
8. Verma RK, Srilatha V, Patel S, Dithi C, Somaraj V, Vallabhaneni SK. Assessment of Parental Satisfaction with Various Aesthetic Crowns Among Children of Various Age Groups: An Original Research. J Pharm Bioallied Sci. 2023 Jul;15(Suppl 1):S196-S200.
9. Ajayakumar LP, Chowdhary N, Reddy VR, Chowdhary R. Use of Restorative Full Crowns Made with Zirconia in Children: A Systematic Review. Int J Clin Pediatr Dent. 2020 Sep-Oct;13(5):551-558.
10. Alrashdi M, Ardoin J, Liu JA. Zirconia crowns for children: A systematic review. Int J Paediatr Dent. 2022 Jan;32(1):66-81.
11. Vaghela LL, Patel MC, Bhatt RK, Patel CN, Joshi KR. Clinical Performance and Parental Satisfaction with Composite Strip Crown and Prefabricated Zirconia Crown for Primary Anterior Teeth: A Randomized Clinical Trial. J Contemp Dent Pract. 2021 Dec 1;22(12):1462-1470.
12. Holsinger DM, Wells MH, Scarbecz M, Donaldson M. Clinical Evaluation and Parental Satisfaction with Pediatric Zirconia Anterior Crowns. Pediatr Dent. 2016;38(3):192-197.
13. Seminario AL, Garcia M, Spiekerman C, Rajanbabu P, Donly KJ, Harbert P. Survival of Zirconia Crowns in Primary Maxillary Incisors at 12-, 24- and 36-Month Follow-Up. Pediatr Dent. 2019 Sep 15;41(5):385-390.
14. Gosnell ES, Thikkurissy S. Management of dental caries and esthetic issues in the pediatric patient. J Calif Dent Assoc. 2013 Aug;41(8):619-629.
15. Stepp P, Morrow BR, Wells M, Tipton DA, Garcia-Godoy F. Microleakage of Cements in Prefabricated Zirconia Crowns. Pediatr Dent. 2018 Mar 15;40(2):136-139.
16. Iampinitkul S, Chaijareenont P, Chinadet W, et al. Microleakage of luting cements in CAD/CAM pediatric zirconia crowns: An in vitro study, 05 February 2024, PREPRINT (Version 1) available at Research Square [https://doi.org/10.21203/rs.3.rs-3896630/v1]
17. Walia T, Brigi C, Ziadkhani MM, Khayat AA, Tabibzadeh Z. Retention Force of Glass Ionomer Based Luting Cements with Posterior Primary Zirconium Crowns - A Comparative in Vitro Study. J Clin Pediatr Dent. 2021 Oct 1;45(4):259-264.





25 pediatricdentalpractice.com Volume 2 Number 1 CASE REPORT
Connect. Be Seen. Grow. Succeed. | www.medmarkmedia.com READ the latest industry news and business RECEIVE news and event updates in your inbox by registering for our eNewsletter CONNECT with us on social media pediatricdentalpractice.com
Pediatric patients may need to use rinses more than adults
Kristin Goodfellow, RDH, discusses the importance of adding a mouthrinse to hygiene regimens
For both adults and children, brushing and flossing is not enough. Most patients do not do these steps well, and most of the time, they don’t floss at all. Children have limited dexterity and lack of ability to perform these steps, resulting in general poor hygiene and subsequent dental issues. Rinses are a frequently disregarded part of oral hygiene but can have a big impact on kids’ dental health. Recent studies have revealed the major benefits of rinsing which increases the urgency with which we need to recommend rinsing with the normal education of brushing and flossing.
Brushing and flossing obviously is important, but we know that even with years of education, adults still aren’t doing these steps well. If they did, 42.2% of adults at the age of 30 wouldn’t suffer from periodontal disease.1 To truly change this number, prevention has to start in childhood. A recent study by Listerine, which compared using a rinse to traditional flossing, showed that utilizing a rinse is more effective than brushing and flossing alone. “Individuals with lower levels of manual dexterity were shown to benefit from the addition of an essential oil mouthrinse to a regime of tooth brushing and flossing in this clinical trial. The addition of an essential oil mouthrinse improved interproximal gingival health and mitigated the manual dexterity variable.”2 Listerine is an over-the-counter rinse. Professional rinses like OraCare, have the ability to improve gingival health by 604%.3 It has the ability to reduce plaque, bacteria, and bleeding at a higher rate resulting in more effectiveness for patients. Incorporating a rinse at a young age can easily improve dental health and hopefully help young patients adopt better hygiene habits in years to come.


Kristin Goodfellow, RDH, practices in West Virginia where she has served as a preventative specialist for over 10 years. She completed her dental hygiene degree at Allegany College of Maryland and has also obtained a Bachelor of Arts Degree in Communication from West Virginia University. She is a soughtafter speaker who discusses the career paths and professional improvement of dental hygienists. She serves on Cellerant’s Best of Class Hygiene Board and is a Hygiene Liaison for several dental practices in her home state.
Disclosure: Kristin Goodfellow is the Chief Clinical Officer for OraCare, a national dental products company dedicated to increasing the standard of care in dentistry.
There are a number of factors, like decay, that put children at higher risk. Cavities are a common concern in children, primarily due to poor oral hygiene habits and a diet high in sugary foods and drinks. To truly aid in protecting children from cavities, ideally a layered approach works best. Obviously, trying to reduce sugars in their diet is recommended but can be extremely difficult for parents. I often hear parents saying, “But they don’t even eat a lot of candy,” not realizing that even healthy food choices like milk, fruit, and vegetables break down into sugars in the mouth that can cause decay. In order to help, we have to reduce s.mutans, the bacteria that causes decay. Rinses have the power to kill bacteria better at a higher level than toothpastes alone. A study titled “Antimicrobial Efficacy of Different Toothpastes and Mouthrinses,” found that using a rinse in combination with a triclosan toothpaste provides the highest benefit against s.mutans.4 That study utilized chlorhexidine. If you’re thinking that you’d never recommend chlorhexidine for long term use, because of side effects like staining or additional calculus build-up, I would agree. There are alternatives like OraCare, that have the same ability to kill bacteria, without those side effects, plus better compliance with children because of the better taste. Controlling bacteria is important for multiple oral issues. For example, gum disease, though less common in children than in adults, can happen, especially if good oral hygiene habits are not taught and maintained. Ultimately, we want to shape their
26 Pediatric Dental Practice US Volume 2 Number 1 HYGIENE PERSPECTIVE
habits early on to improve their oral health. We have to reduce bacterial factors like p.gingivalis in order to reduce the risk of disease. Rinses have the ability to do this, whereas few toothpastes provide this specific benefit. Therefore brushing alone is not going to provide our patients with the ability to circumvent the risks for gum disease. Some rinses work by minimizing the accumulation of bacteria and plaque along the gum line. A study recently conducted using OraCare showed a 255% reduction in plaque better than brushing alone, not only at the gumline but also interproximally.3 By incorporating mouthwash into their daily routine, children and their caregivers can take proactive steps to protect their gums and maintain healthy smiles for years to come.
As dental professionals, we want to recommend the most appropriate products for each patient based on their needs. For kids, there are typically options with vibrant colors and flavors but often the effectiveness can be lacking. We know that bacteria and plaque are major contributors to oral diseases, and this should be a focus of ours to disrupt. Look for products that have the ability to kill bacteria and break up biofilm. By giving the patients your professional recommendation on products, you can instill good habits while also providing them with more effectiveness in their oral hygiene routine to protect their dental health long term.
Mouthwashes are an essential addition to kids’ oral hygiene regimens, providing a host of advantages for their general and dental health. Since brushing and flossing have been proven to not be quite enough, mouthwash can help children to have healthy smiles. It provides extra cleansing power as well as defense against cavities and gum disease. It is our duty as dental experts to inform parents and other caregivers about the value of hygiene and to provide products that are suitable for each child’s specific needs. We can empower kids to take charge of their oral health and enjoy a lifetime of healthy smiles by establishing strong oral hygiene practices early on. The sooner we start the better the long-term outcome.
REFERENCES
1. Eke PI, Thornton-Evans GO, Wei L, Borgnakke WS, Dye BA, Genco RJ. Periodontitis in US Adults: National Health and Nutrition Examination Survey 2009-2014. J Am Dent Assoc. 2018 Jul;149(7):576-588.e6.
2. Milleman K, Milleman J, Bosma ML, McGuire JA, Sunkara A, DelSasso A, York T, Cecil AM. Role of Manual Dexterity on Mechanical and Chemotherapeutic Oral Hygiene Regimens. J Dent Hyg. 2022 Jun;96(3):35-45.
3. Reinhard Schuller. Clinical Efficacy and Safety Evaluation of OraCare Health Rinse in Adults on Plaque and Gingivitis in a Six-Week Model. Reinhard Schuller Consulting. 2023. Available upon request.
4. Prasanth M. Antimicrobial efficacy of different toothpastes and mouthrinses: an in vitro study. Dent Res J (Isfahan). 2011 Spring;8(2):85-94.





27 pediatricdentalpractice.com Volume 2 Number 1 HYGIENE PERSPECTIVE
PD Join Our Free Webinar! Emerging Laser Therapies: Unveiling the Promise of OraLase and BabyLase. Discover how gentle oral tissue releases can empower babies to thrive! June 27, 2024 I 5:00 PM PST Scan the QR code to learn more about the versatility of the Fotona LightWalker® and XPulse®! Register HERE! Speaker Dr. Tenholder
Harmonize™ restorative case study
Dr. Simona Cuevas
discusses materials for direct restorative composite reconstruction
Restorative dentists continue to challenge science to develop new dental composite materials that satisfy growing and varying clinical concerns. Many composites on the market today seem to meet what clinicians may be looking for, yet they seem to always fall short in one aspect or another.
Harmonize™, a nanohybrid universal composite from Kerr, seems to check all the boxes. This material demonstrates superb esthetics that is reinforced by ease of placement, strength, and longevity. Harmonize is infused with Adaptive Response Technology™ (nanoparticle filler network) as well as rheological modifiers resulting in better blending capabilities, enhanced structural integrity, and exceptional strength. Direct restorative composite reconstruction relies first and most importantly on the material used, and secondly on the quality of the clinician’s esthetic artistry and technique. The development of the following restorations follow a standard composite placement procedure.
Anterior case
The patient presented with a traumatic fracture of tooth No. 7. Due to my approach to extremely conservative dentistry, no bevel was placed (I prefer butt-joint margins on all my composite restorations), the fracture was etched (total etch technique), and OptiBond™ Universal by Kerr was used as the bonding agent (following the manufacturer’s instructions for use). Harmonize composite was then placed in a dentin shade (A3) as the lingual shelf and cured. The enamel shade (A1) was then layered on top and lightcured. The restoration was polished with ProGloss™ one-step polishers (Figures 1A and 1B).
Posterior cases



After amalgam removal, Harmonize composite was placed in a dentin shade (A3) as the lingual shelf and cured. The enamel shade (B2) was then layered on top, and posterior anatomy was sculpted prior to the final cure. After the final cure and occlusal adjustment, the composite was polished with a ProGloss polisher (Figures 2A and 2B).

Disclosure: Dr. Cuevas is a paid consultant of Kerr Corporation.



After amalgam removal and composite placement (Dentin A4, Enamel D2) following the exact same steps as previously described, I found it necessary to place some color modifiers (Kolor + Plus™ — Ochre by Kerr) inside the primary and secondary anatomy grooves in order to match this restoration to the rest of the patient’s stained dentition. This extra step made the restoration indistinguishable from the surrounding natural dentition in the patient’s mouth. The staining was followed by polish with a ProGloss polisher (Figures 3A and 3B).
This composite can create restorations that blend in seamlessly with the other teeth and are virtually indistinguishable from natural dentition. The addition of this new composite to clinicians’ arsenal will allow them to quickly complete durable and life-like restorations.
Disclaimer: The opinions expressed in this (article) are those of Dr. Cuevas. Kerr is a medical device manufacturer and does not dispense medical advice. Clinicians should use their own professional judgement in treating their patients. All registered trademarks are property of their respective owners.
28 Pediatric Dental Practice US Volume 2 Number 1 PRODUCT PROFILE
Simona Cuevas, DDS, received her dental degree from the University of Texas, San Antonio in 1995 and is the founder and CEO of The Institute of Esthetic Dentistry.
PD
Figures 1A and 1B: Anterior before and after images
Figures 2A and 2B: Posterior before and after images
Figures 3A and 3B: Posterior before and after images
SimpliShade ™



April 1 - June 30, 2024 | Promo Code: MMBF24
* Promotional goods must be of equal or lesser value and may not be combined with any other offers. Purchase must be made on one invoice between 4/1/24 and 6/30/24, unless otherwise noted. Redeem by 7/31/24. To receive your promotional goods, email or fax a copy of your authorized Kerr dealer invoice noting promo code MMBF24 and product(s) desired to: kerrpromo@kerrdental.com or FAX: 888.727.2614. Limit to 3 redemptions. Incomplete submissions will not be processed. Allow 8 weeks for delivery. Offers valid in the 50 United States only. Promotions are subject to change or cancellation without notice. Offer void if purchased product is returned. Note that you may have an obligation under federal, state or local law to reflect discounts on product given pursuant to this promotion on any cost report forms submitted to a federal or state government or private payer who provides reimbursement for that product.
1-800-KERR-123 | kerrdental.com ©2024 Kerr Corporation. All trademarks are property of Kerr Corporation. All Rights Reserved. MKT-24-0019 Rev 0
Case images courtesy of Dr. Kristin Fairbanks
BULK FILL
NEW!
it Takes
* SimpliShade Bulk Fill Flow
& BULK FILL FLOW Valid:
BUY 1, GET 1 FREE! *
One Shade is All
One Shade One Step An Easier Way to Bulk Fill
Scan Here to redeem offer Before After
Innovations in infant frenectomies
Dr. Lawrence Kotlow discusses how laser technology has influenced his practice
Frenectomies are having a moment. While the number of restricted tethered tongue and lip ties has remained constant, 77% of pediatric dentists report seeing an increase in frenectomy referrals in the past five years.1
After graduating high school in 1965, I went into pharmacy school because I wanted to do something in the health profession, but I wasn’t going to get into pre-med or pre-dent with my high school grades. So, I worked hard in pharmacy, and at the end of 3 years, I had all the requirements for dental school fulfilled. I got into dental school without an undergrad degree.
In dental school, I always intended to go into pediatric dentistry from the get-go. There was no question. I spent my high school years as a counselor in day camps working with young children. I always liked working with children, but I didn’t want to be a pediatrician. As a dentist, I try to be accessible to parents, so I give them my personal cell phone. If you have a newborn baby, you don’t want to wait 24 hours to get a call back from your doctor. You want to call back as soon as you can, so I don’t have an exchange. I don’t have anybody to cover for me. I have me, myself, and my team, and we take care of all the emergency calls from parents.

Dr. Lawrence Kotlow has been in private practice since 1974, serving the specialized needs of children. He is considered an expert in the world of restricted tethered oral tissue procedures (RTOTS), and is known throughout the country for his innovative techniques and lectures for some of the top dental societies and dental companies. Dr. Kotlow has lectured in Australia, Israel, Taiwan, Canada, England, France, and throughout the United States concerning pediatric dentistry and lasers, written over 35 articles, and authored chapters on pediatric dentistry and lasers for three laser textbooks. His 2016 book, SOS 4 TOTS: Exposing the Myths about Breastfeeding and Healing the Heartbreak to Make Breastfeeding a Joy, is a well-regarded resource for parents looking for information about how tongue and lip ties affect breastfeeding, dental development, and overall pediatric health. He completed board certification in the specialty of pediatric dentistry from the American Board of Pediatric Dentistry in 1980. He is one of only 18 dentists recognized by the Academy of Laser Dentistry to certify other dentists in standard proficiency to use lasers. Dr. Kotlow is a laser expert, having used many different lasers including erbium, diode, ND:YAG, and now Solea. Dr. Kotlow has been on the forefront of new technologies and continues to investigate and invest in any technology that will be of benefit to children. He attended the Albany College of Pharmacy, graduated from the SUNY Buffalo School of Dentistry, and completed his Pediatric Dental Residency at Cincinnati Children’s Hospital. Dr. Kotlow is a member of the American Dental Association, the New York State Dental Association, the International College of Dentists (Fellow), the Academy of Laser Dentistry (Achieved Mastership), the Third District Dental Society, the American Academy of Pediatric Dentistry (Fellow), the International Affiliation of Tongue-Tie Professionals, and the American Board of Pediatric Dentistry (Diplomate). Dr. Kotlow also became part of an exclusive group of dentists this year, when he was elected into the prestigious Pierre Fauchard Academy.



Dr. Kotlow uses his newly developed tongue guide during laser surgery to evaluate an infant for ankyloglossia. Right: Dr. Kotlow explains to a mother how to complete aftercare on her child to prevent the surgical site from healing back to its original form
When I graduated dental school, I would have older children coming in who had gone to speech therapy for three, four, five years. No one looked at their tongue as a potential source of their speech issues, even though it was attached to the tip of their jaw right behind the lower front teeth. So, I taught myself how to perform frenectomies. In those days, we’d use scalpels, and we had to use local anesthetics on everybody and suture everything. But you know what? We got good results.
Also in those days, I would see more patients with what we call nursing bottle syndrome, and all their front teeth would have decay. The only way we could save them would be by putting crowns on their front teeth. Now, if they had a tight upper lip tie, and we put the crowns on, the tissue wouldn’t heal right because
30 Pediatric Dental Practice US Volume 2 Number 1 TECHNOLOGY
Dr. Kotlow preparing to release restricted tethered oral tissues (RTOTs) in his surgical operatory
Left:
it was always pulling it away, so we started doing the lip ties. And when their teeth came in, they came in perfectly straight. It was rewarding because we could see these results. That’s why I feel like these procedures are so important.
Creating awareness for a life-changing procedure
In 1979, I wrote the first article about how the upper lip tie can affect tooth decay and the upper front teeth. That took a lot of effort to get published because people were not in tune with what I was doing, and they were saying it can’t happen. But it does happen. And now a lot of people understand why. Ultimately, what drives a parent to the office is their symptoms, or as I like to call them now, comorbidities — the baby’s and theirs — and how much it hurts. People want solutions that are proven to work, and I can demonstrate that frenectomies work. A lot of what we do is based on the fact that it works, that parents are happy, and that children develop normally. Parents who come back to me with their second or third or fourth child aren’t waiting around for a medical diagnosis. They come right to see me.
The biggest challenge to increasing awareness is getting medical professionals on board, so they see the value of frenectomies and start referring patients rather than discouraging them. I thought that once the physicians who were in practice 50 years ago stopped practicing, the new generation would see the results and understand the value. But that hasn’t happened yet. This knowledge has to get into medical schools. They have to understand how nursing works, and they have to understand that frenectomies are not a fad. Creating meaningful change is going to require getting into literature with peer-reviewed articles that they will accept and that they will publish.
Bringing relief to children and parents
Releasing restricted oral tissues can be a life-changing procedure for young patients and their parents. Here’s an example: It’s a Sunday night, I’m sitting watching football and I get a text message. It was a distraught mother whose baby was going to go under general anesthesia on Monday for an endoscopy because she had a distended belly. They’d run tons of genetic studies and could find nothing wrong with the child. So, she sent me some pictures, and I told her to cancel her appointment and see me the next day. The child’s lip and tongue were tied. We released it and in 24 hours, and all the symptoms were disappearing, giving the child and the mother significant relief and avoiding a more invasive procedure.
Over the years, technological advances, in particular the introduction of dental lasers, have transformed our ability to perform frenectomies. If we go back to when we used a scalpel to perform this procedure, we couldn’t do this on an infant because of the bleeding and difficulty to suture inside an infant’s mouth. Lasers have changed that.
In 2011, Convergent Dental came to me and said they’re developing a new 9.3-micron CO2 laser called the Solea® All-Tissue Dental Laser. And I told them I had five lasers and didn’t need another laser. But I listened to them, and a 1-hour conversation turned into 4 hours. I went to visit their facility in Massachusetts, and I worked with them to make sure the instrument would work on newborns and toddlers. Within a year, we

had a laser that really changed everything. Because now I have an all-tissue CO2 laser, with which we see little to no bleeding, and in the vast majority of patients, we don’t have to suture. Plus, we can get children in and out quickly. When I use a laser, if by chance the infant or toddler was to move, and I hit another piece of tissue, it turns white for a second, and then I just rub it, and it disappears. If that happens with a scalpel, I’d be putting sutures in. Lasers are precise instruments that allow dentists to precisely release soft tissue.
The combination of education, awareness, and technology adoption has made this procedure so much more accessible. I’ve lectured to over 5,000 dentists in the last 20 years, and in the past, I had patients fly in from around the world for treatment. Now, there are people all over the world who are performing this procedure. So, I think dentists, especially those who are open to using lasers and not scissors or scalpels, have learned the proper techniques, and education is on the rise as they hear me and other dentists speak about this technology and this procedure.
A dentist who bought a practice contacted me. The prior dentist had a laser, and he asked what he needed to do to use it. I said, leave it in the box and take a course. The Academy of Laser Dentistry provides proficiency courses and exams that will teach you the basics. If they want to do frenectomies, take my course or some of the other courses that are given by educated dentists. And ask your laser provider about the training and clinical support they provide for frenectomies and other procedures that can be performed with the device.
There are so many things we’re doing today that we didn’t do 50 years ago. In pediatric dentistry, if you’re good at performing frenectomies, you’re going to get many referrals. But you have to be prepared to be available. If you can’t do this job efficiently and you’re telling patients you’re going to see them in a month, that doesn’t work because they and their baby are experiencing pain and discomfort. That means you have to change your practice to make sure you’re there for your patients when they need you.
REFERENCE
1. Dhir S, Landau BP, Edemobi S, Meyer AK, Durr ML. Survey of Pediatric Otolaryngology Frenotomy Practice Patterns. Laryngoscope. 2022 Dec;132(12):2505-2512.
31 pediatricdentalpractice.com Volume 2 Number 1 TECHNOLOGY
PD
Dr. Kotlow and his hygienist complete an oral evaluation at a preventive checkup for a patient
It’s 2024 y’all, and it’s time to stop using sticky varnish!
Joffree Bunleang applauds Profisil® as an innovation in flouride varnish
Let’s roll out the red carpet for Profisil® — the MVPs of fluoride, the innovators of prevention and comfort!
Let’s just say this product is long overdue. Research on fluoride began way back in the 1900s, thanks to Fredrick McKay and Dr. G.V. Black. It wasn’t until the 1960s that we even started using fluoride gels and varnishes.1 Shame.2
Fast forward to present day. I feel as though I can speak for all of us and say we are feeling frustrated when we recommend fluoride to a patient with high risk for decay, and they decline merely because they do not like it. Their reasoning has nothing to do with cost and everything to do with how they simply just do not like “having fuzzy sweater teeth.”
As prevention specialists, our job is to educate our patients and allow them to make their own choices. Even when we mildly (or harshly!) disapprove of their decision, as professionals, we still honor it.
Friends and colleagues, if everything that I have mentioned thus far resonates with you, you are really going to enjoy what I am about to share with you!
I have discovered there is a new kid on the block! Allow me to introduce you to Kettenbach Dental! Kettenbach Dental has recently gifted the world of dentistry with Profisil, a new fluoride varnish. This is the fluoride of the future, an absolute game changer that belongs in all of our offices.

Let me tell you why this product is so amazing.
• Profisil contains no alcohol. Zero. Zilch. Nada. It matters because this means no more irritation to the gums, no more discomfort for patients, and a halt to patients asking “Is this supposed to sting my gums?”

• These guys have kept the options simple, yet covering all the bases with mint, berry, and they even make an unflavored varnish. So say goodbye to that foul taste we are all too familiar with.
• Until you try this product, you are just going to have to take my word for it. This varnish is like magic. It is so smooth, so silky; there is nothing sticky or gritty about it. You are probably wondering how can a varnish be smooth, silky, and leave patients with a clean prophy feeling? It’s simple — they don’t use colophony (rosin) aka the sticky sappy stuff. They use a silicone base which provides patients with a smooth feeling as opposed to that heavily hated fuzzy sweater feeling.
• This fluoride is here to help providers deliver the best level of care to their patients, and break the barrier of “I don’t like how my teeth feel with that sticky stuff.”
• Post-op instructions are simple. Don’t brush for 4 hours, no hot beverages, and no sticky foods.
Joffree Bunleang, co-founder of Hygiene Elevated, is dedicated to uplifting dental hygienists in her community. Through initiatives like the Hygiene Elevated Conversations and Innovations podcast and an apparel line, she brings joy and knowledge to the field. Her “Beyond Scaling” school presentation tour offers mentorship and practical advice to students. Known for her positivity and expertise, Joffree transforms hygiene departments and boosts productivity. Her guidance fosters growth and success in dental teams, while her approachability creates a collaborative atmosphere. As a hygiene consultant, she leads by example, inspiring excellence and empowerment in the dental community.
The clouds have parted, the sun is out, and the prayers of our predecessors have finally been answered! There is now a fluoride on the market that patients actually like! Join me and my team in the movement of no more fuzzy sweater teeth. Order direct by calling 877-532-2123 or visiting www.kettenbachusa.com.
REFERENCES
1. National Institute of Dental and Craniofacial Research. The Story of Flouridation. https://www.nidcr.nih.gov/health-info/fluoride/the-story-of-fluoridation#:~:text=Fluoride%20research%20had%20its%20beginnings,brown%20stains%20on%20 their%20teeth. Reviewed July 2018.
2. Seppä L. Fluoride varnishes in caries prevention. Med Princ Pract. 2004 NovDec;13(6):307-311. https://pubmed.ncbi.nlm.nih.gov/15467304/#:~:text=Abstract,time%20between%20fluoride%20and%20enamel. Accessed March 15, 2024.
This article was provided by Kettenbach USA.
32 Pediatric Dental Practice US Volume 2 Number 1 PRODUCT PROFILE
PD
Application of Profisil® fluoride varnish











































































































A NEW DIMENSION OF VARNISH GEL Keep the clean feeling with our New Fluoride Varnish Gel and Ultimate Protection Solution. Get patient pleased responses with grit and tacky free results. Contains no alcohol or colophony. Profisil®: easy and smooth application! Call today and see for yourself: 877-532-2123 TREATMENT OF DENTINAL HYPERSENSITIVITY S PROTECTED WITH PROFISIL ® FLUORIDE VAR NISH OHOLFREE LONAHTE ETHANOL ALCOHOLFREE LONAHTE EERFLOHOCLA ETHANOL ALCOHOLFREE LONAHTE EERFLOHOCLA ETHANOL ALCOHOLFREE LONAHTE EERFLOHOCLA ETHANOL ALCOHOLFREE LONAHTE EERFLOHOCLA0% % lAlcohol % ohol 100% FreeofEthanolAlcohol NEW NOW AVAILABLEALSOIN BULK PACKS!







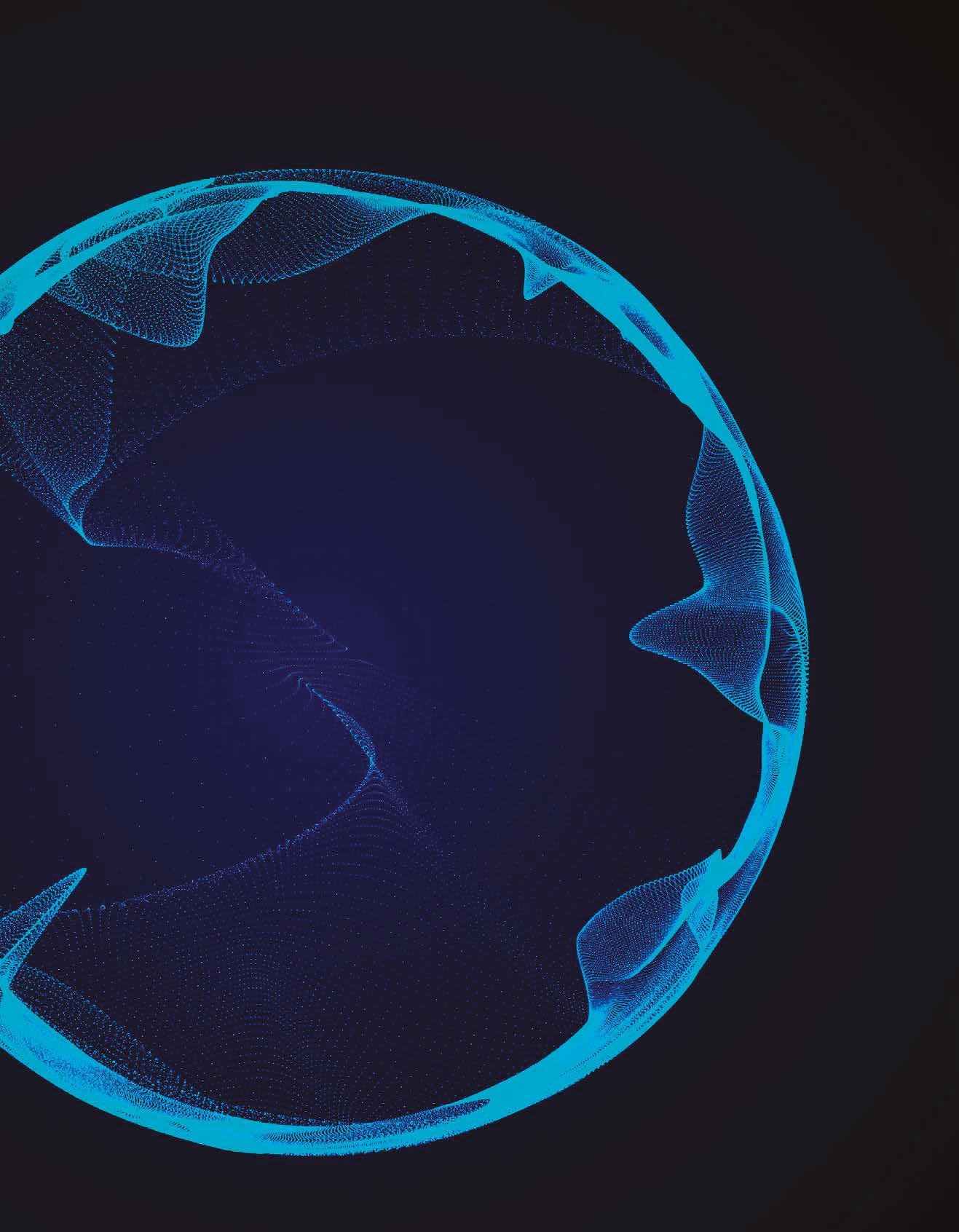

nusmile.com LEADING PEDIATRIC RESTORATIVE
SINCE 1991 -1991 Signature -2012 ZR & Try-In -2014 BioCem -2015 NeoMTA -2016 SSC -2019 ZR Permanent -2020 NeoPUTTY -2022 NeoLINER -2023 BioFlx -2023 Space Maintainer -2023 NuSmileTech
DENTISTRY










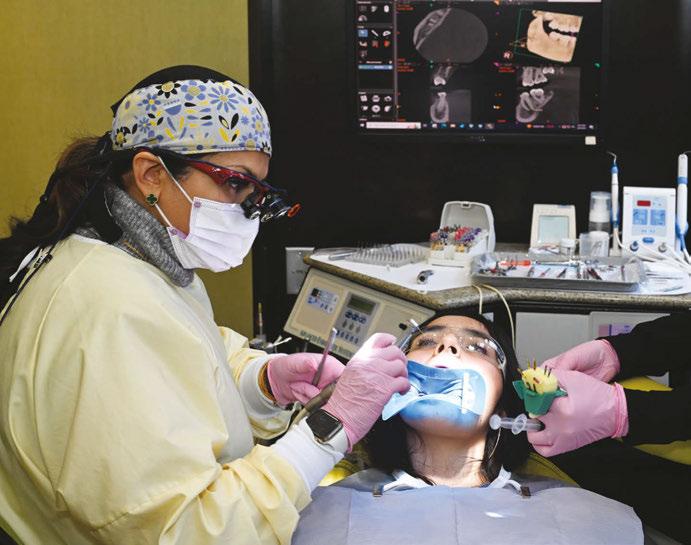











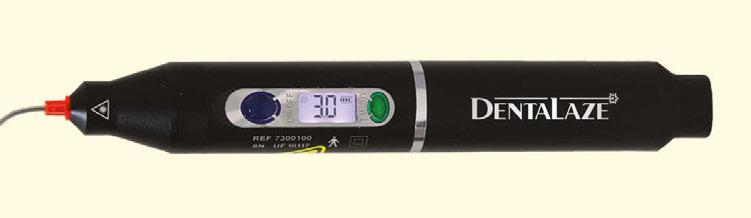





















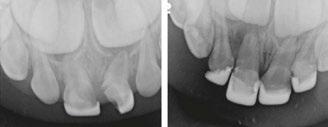





 Lisa Moler Founder/Publisher, MedMark Media
Lisa Moler Founder/Publisher, MedMark Media