Advanced Stroke Care at Monument Health

Terminating Patients for Disruptive Behavior
Community Health Workers: A Developing SD Workforce
Sanford Breaks New Ground in Orthopedics
Dr. Jae Kim & Dr. Lien Diep


Dr. Jae Kim & Dr. Lien Diep

Congratulations to the Heart and Vascular Institute.

In its first year participating in the American Heart Association’s Get With The Guidelines®-AFib Registry, the Heart and Vascular Institute achieved the Silver Award, the highest possible first-year award.

For the 11th straight year, the American College of Cardiology presented the NCDR Chest Pain–MI Registry Platinum Performance Achievement Award to Monument Health, which is one of only 240 hospitals nationwide to receive the honor this year.
The Cardiovascular Surgery Program achieved a rating of 2 out of 3 stars from The Society of Thoracic Surgeons. The Society of Thoracic Surgeons is a national leader in health care transparency and accountability. Participation in the STS National Database is a crucial investment for quality improvement.
PAGE 6 | [SPONSORED]
Community Health Workers: A Developing Workforce in South Dakota

They may be new in SD, but in other states, CHWs have already been successfully integrated into the patient care team for decades.
Exclusive online articles, Celebration for the MED team, local DAISY Award winners, & Make-A-Wish sets a bold goal
With a new hybrid OR, new technology, and a new specialist, Monument Health takes big strides closer to becoming the Black Hills’ first Comprehensive Stroke Center.
PAGE 12 | [SPONSORED]
Breaking Ground on the Future of Orthopedic and Surgical Care Sanford begins construction on a new orthopedic hospital in Sioux Falls.
PAGE 14 | NEWS & NOTES
New providers, awards, certifications, and mergers in area healthcare
PAGE 19 | USD School of Health Sciences Success Spotlight: Kristi “Cricket” Palmer
■ By Dennis Boyle
Expert advice from COPIC on important considerations when managing this delicate situation.
Welcome to the November issue of MED Magazine, your premier source for healthcare community news in the South Dakota tri-state region.
In this issue...Stroke care is advancing in the Black Hilks. We introduce you to the team and the technology behind Mon ument Health's comprehensuve new stroke program.
We also have features on the value of community health workers and Sanford's new orthopedic hospital. Plus, the experts at COPIC have advice on terminating your relationship with a disruptive patient.
And just in case you've missed any local healthcare headlines this fall, we have them all for you in our jam packed News & Notes section.
We take pride in every issue of this publication and we are honored by your continued support and readership!
All the Best, —Alex and Steff
PS—Be sure to join the VIP list at MidwestMedicalEdition.com to stay up to date between issues.
Publisher / MED MAGAZINE, LLC Sioux Falls, South Dakota
Vice President Sales & Marketing STEFFANIE LISTON-HOLTROP
Editor in Chief / ALEX STRAUSS
Staff Writer / KIM LEE
Graphic Design / CORBO DESIGN
Web Design / SAMPSON HOUSE
Digital Media Director / ALYSSA MCGINNIS
STEFFANIE LISTON-HOLTROP VP Sales & Marketing 605-366-1479 Steff@MidwestMedicalEdition.com
ALEX STRAUSS Editor in Chief 605-759-3295 Alex@ MidwestMedicalEdition.com
WEBSITE MidwestMedicalEdition.com
MAILING ADDRESS PO Box 90646, Sioux Falls, SD 57109
ISSUE DUE
JAN/FEB Dec 10
MARCH Feb 10
APRIL/MAY March 10
JUNE May 10
JULY/AUG June 10
SEP/OCT August 10
NOVEMBER Oct 10
Nov 10
Editorial contributions due November 5 Ads due November 10
The Emergency Department Provider Toolkit is an interactive guide for hospital staff and administrators. It includes strategies and best practices for screening and diagnosis, referral to treatment, safe prescribing, and community resources in an ED setting.
The toolkit was designed for both urban and rural hospitals and features an easy-to-use decision tree, and evidence-based clinical and educational resources.
Quick access to OUD information can help ED providers identify patient risk, diagnose, and provide treatment and education for patients and their families.

Explore the toolkit today!
For technical support contact the South Dakota Association of Healthcare Organizations (SDAHO) at 605-789-7531 or 605-789-4995 and ask to speak with a Clinical Improvement Consultant.
NU17CE924994-01-01, funded by
for Disease
Department of Health and Human Services.
Opioid use disorder (OUD) is a life-threatening disease.
Department providers can play a critically important role in improving patient outcomes and supporting a patient’s path to recovery.
(CHWs) may be a new and devel oping profession in South Dakota but in many other states, CHWs have been successfully inte grated into the patient care team for decades. CHWs play an integral role in expanding com munity access to health care, often working within interdisciplinary teams of health care professionals, including medical providers, nurses, and social workers.
The American Public Health Association defines a CHW as “a frontline public health worker who is a trusted member of and/or has an unusu ally close understanding of the community served.” This trusted relationship allows them to connect patients to the care they need, assess barriers to health and mitigate some of the social determinants of health gaps.
In the past year, more than 115 CHWs have been hired and trained in South Dakota. As the CHW profession continues to grow across the state, clinics, hospitals, and nonprofit entities are hiring individuals and training them in these positions within their organizations to bridge the gap between communities and the health and social services systems.

Monument Health recently launched a CHW program, hiring and training three CHWs in Rapid City and one in Spearfish. The CHWs partner with Ambulatory Case Managers at the Rapid City primary care clinic and the Family Medicine Residency Clinic to identify patients who would benefit from the involvement of a CHW. Proven outcomes of CHW programs include fewer trips to the Emergency Room and more preventative and maintenance care for diseases like diabetes, hypertension and mental health. CHWs also address and overcome barriers related to patients’ Social Determinants of Health needs.
“What’s so exciting about this approach is that CHWs meet the patients where they are. It could be their home, the homeless shelter or wherever,” said Shelly Roy, Associate CNO of Nursing Professional Practice, who implemented the CHW program at Monument Health. “By going to them, we’re able to learn more about them and develop a relationship to help get what they need on their health care journey.”
South Dakota is fortunate to be just one of a handful of states that currently has fee-for-service reimbursement for CHW services through Medic aid. This reimbursement will help to sustain these developing positions across South Dakota.
In South Dakota, the Community Health Worker Collaborative of South Dakota (CHWSD) leads CHW awareness and workforce develop ment through support from the South Dakota Department of Health. More information about CHWs, Medicaid reimbursement, and the developing workforce can be found by accessing www.chwsd.org. ❖
L to R: LaRissa Claymore, Adonica Little, Madeline Sitting Holy and Denisse Chavez are Monument Health’s first Community Health Workers.



Accessing a certified Sexual Assault Nurse Examiner (SANE) in rural regions of the country can be nearly impossible. Virtual SANE exams can offer improved clinical care while safeguarding evidence for future use.
With the recent release of a new report detailing the horrific toll of the nation’s overdose and death epidem ic, the American Medical Association (AMA) is calling for an all-hands approach to help save lives.
A new report shows South Dakota has the highest share of adults over 60 with the zoster vaccination. At 55.10 percent, SD’s rate is 2.1 times higher than the state with the lowest percentage of zoster vaccination, which is Mississippi. Minnesota did well in several other vaccines, as did Iowa.
Learn more about eSANE in this exclusive online article.

MED’s team recently met to celebrate the expansion of the company’s digital news service into North Dakota and Nebraska. Thanks to the readership and the support of our digital sponsors and advertisers, more than 11,000 digital subscribers now receive state-specific news from MED twice a month, in addition to the 5,000+ readers of MED Magazine. Thanks!
See what they’re proposing and get a link to the full report on the website.
You’ll find a link to the full report on our website.
The following nurses recently received DAISY Awards for extraordinary nursing from their institutions.


 Highlighting content and opportunities available exclusively at MidwestMedicalEdition.com
Highlighting content and opportunities available exclusively at MidwestMedicalEdition.com
Make-A-Wish South Dakota & Montana granted 81 wishes to children with life-threatening illnesses this fiscal year. While that number is still not quite up to pre-pandemic levels, CEO Sue Salter says the organization is excited to be heading firmly in the right direction again.


We never stopped granting wishes, but the kind of wishes we were granting changed dramat ically. Prior to the pandemic, close to 80 percent of wishes involved travel. But we had an entire year (2021) where there was no plane travel allowed. So we saw a change to things like shopping sprees. We still have a moratorium on international travel.
Tell us about the impact survey conducted last year by MAW
SS: This was a survey of medical providers, wish alumni, and wish parents. One of the most exciting findings is that 100 percent of medical providers reported that the wish experience improved both a child’s and their own emotional wellbeing. It has been an especially trying few years for healthcare workers. But we experience joy when we see other people having their burdens lifted and that includes providers.
MED: Is there evidence that a wish can impact a child’s physical as well as their emotional wellbeing?
SS: Yes! In that same survey, 9 out of 10 medical providers said that a wish increased compliance with treatment. The same number observed that the wish experience had a positive impact on a child’s physical wellbeing and overall quality of life. By giving them something to look forward to, it can renew their strength to fight their illness. In fact, 8 out of 10 providers said that they believed a wish to be a necessary part of a child’s journey.
MED: What are Make-A-Wish South Dakota & Montana’s goals going forward?


SS: Our strategic vision for the future includes a goal of granting 650 wishes in a five-year period. That includes a goal of 115 wishes in the current fiscal year, which started September 1. One of the most important things we plan to do to achieve that vision is to hire a full-time medical outreach and intake manager to help us build and strengthen relationships with our medical com munity partners. We are really looking forward to granting the wish of every eligible child in Montana and South Dakota.
FOLLOW US! Facebook.com/medmagazinesd Linkedin.com/company/midwestmedicaledition




Scan the QR code on this page or visit MidwestMedical Edition.com TO JOIN THE VIP LIST.



 DR. JAE KIM & DR. LIEN DIEP
BY ALEX STRAUSS
DR. JAE KIM & DR. LIEN DIEP
BY ALEX STRAUSS
But where stroke is concerned, Diep says ‘time is brain’. Millions of brain cells may be lost for every minute of impeded blood flow. Diep and her colleagues are deter mined to save brain cells and lives by taking stroke care at Monument to the next level. They are building a com prehensive stroke program to advance and coordinate care from the earliest stages of diagnosis to rehabilitation and recovery.
“Before I came, everyone was working independently,” says Dr. Diep. “What we needed was to bring them together in a more cohesive way. The stroke program does not belong to neurologists only. I came here to help connect the dots.”
One critical step on the path to a comprehensive stroke program in the Black Hills was the addition of interven tional neurologist Jae Kim, MD. Dr. Kim moved from Sioux Falls to Rapid City last spring to join the Monument Health Neurology and Rehabilitation Clinic. He is an interventional neurovascular specialist who performs clot retrievals, aneurysm care, and a broad range of interventions for blocked and ruptured blood vessels in the brain.
“I have been working with Monument Health on a referral basis for several years,” says Dr. Kim. “What I noticed over the last couple of years is that the number of patients who need neurointerventions has been increasing. But there was a lack of specialty care West River. I came to Monument because I saw what they were creating and I wanted to be part of that growth.”
“My goal was always to have neurointervention here, but I knew there needed to be certain things in place first,” says Dr. Diep. “We worked with the cardiologists to help bring in CT perfusion and we negotiated with the radiol ogists to get biplane cineangiography for our new hybrid operating room. Things came together over time. When I felt we had the right pieces in place, that’s when I reached out to bring Dr. Kim here.”
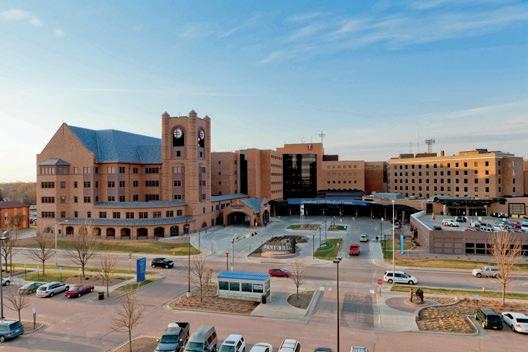
Rapid City Hospital’s new hybrid operating room is an advanced procedural space that combines a traditional operating room with an image-guided interventional suite.
Dr. Kim says it can streamline workflows and provide a safe experience for patients.
“If something like an aneurysm happens while we are doing angiography and we decide we need neurosur gical expertise, instead of the patient having to be transferred to another OR, the neurosurgeon can come to our hybrid room and transform it from an IR room to an OR room,” says Dr. Kim. “It is a very important piece of the puzzle.”
The room is home to a state-of-the art biplane cine angiography system which produces sophisticated real-time, three-dimensional imaging of vessels deeps in the head and neck. The biplane represents a significant leap forward in allowing physicians to diagnose neuro logical abnormalities and treat them with minimally invasive endovascular procedures.
“We have some dramatic stories thanks to this equip ment,” says Dr. Diep. “ We had an 85-year-old farmer come in with an occlusion. He was out working and he just dropped. Even TPA could not fix that. But 45 minutes after Dr. Kim got to him, he was walking again.”
The hospital will soon also have access to rapid AI software that will allow Dr. Kim to diagnose an occlusion in a patient at a referring hospital within seconds of a CT scan, potentially expediting the transfer of patients who need thrombectomy.
While the program is not yet certified by the Joint Commission as a Comprehensive Stroke Center, they are well on their way.
The hospital is carefully tracking metrics to show an improvement in the time it takes to open occluded vessels. They will also need to establish a dedicated neurointensive care unit and bring in a second neurointerventionalist. Dr. Diep says it is all in the works.
“We have all the pieces in place and I am confident that we are going to get there,” says Dr. Diep, who is anxious to spread the word about the program’s capabilities to referring physicians throughout the Black Hills
“My protocol is, if people need help, bring them over here,” she says. “Don’t wait. Let us decide if it’s a stroke. We don’t want to deny saving lives.” ❖
“ There was a lack of specialty care West River. I came to Monument because I saw what they were creating and I wanted to be part of that growth and have more impact.”
TO THE TUNE OF 205,000 SQUARE FEET, Sanford Health is growing its ability to provide the best in orthopedic care. A $160 million orthopedic and surgical services expansion broke ground in June with an anticipated opening date set for the fall of 2025.

“Our patients are going to be impacted by the advances in technology and technique,” said Joshua Crabtree, MD, president of Sanford Clinic in Sioux Falls. “We’re committed to taking care of people here.”
The new hospital will include 161,000 square feet of new space and 44,000 square feet of remodeled space for housing technology solutions that advance therapy, treatment, surgery and recovery. All of this will live to the south of the Sanford Children’s Hospital and to the west of the surgical tower on the main Sanford Health campus in Sioux Falls, South Dakota.
“This investment elevates an already high-quality, high-performing service into a program that more strongly aligns with advances in technology and expectations of both physicians and patients,” said Paul Hanson, pres ident of Sanford Health Sioux Falls.
Designed collaboratively by physi cians, staff, administrators and patients, the hospital will have 12 new
operating rooms, 35 additional prep and recovery rooms, and 56 medical suites. Because outpatient surgeries continue to increase, the medical suites will be designed to give patients and their families a comfortable place to stay before or after a procedure, with the assurance that supportive care is just around the corner.
“The addition of these medical suites is a testament to how far we’ve advanced recovery, drastically decreasing the length of stay for total joint procedures from four overnights to same-day discharges in many cases,” said Mike Wilde, MD, vice
president and medical officer for the Sioux Falls region.
With shorter recovery times, in just weeks many patients today are taking steps to get back into the activities they love.
“Maybe that’s playing outside with the grandkids, getting back on a bike or working on that golf swing,” said Dr. Wilde. “While we can’t guarantee their golf game will improve, we can help them ease back into their stride.”
Hanson emphasizes that the field of orthopedics and sports medicine care today is all about “getting people back to life as it should be.”
Meanwhile, more operating rooms will allow for more patients and providers too.
“We can expand our services and recruitment efforts into communities that maybe we don’t have a strong presence in today, but we will tomor row,” he said.
When the orthopedic hospital opens, it will transform how both current and future physicians deliver care —from how they treat conditions to how they further research and education.
“We’re in the fifth year of our orthopedics residency program, and this building is going to make that program even more competitive,” said Kristofer Kimber, MD, an orthopedic surgeon at Sanford Health. Tech nology additions to the hospital will include cutting-edge surgical spaces and an intraoperative MRI machine,
which will provide near real-time imaging during procedures.
“Enhanced care doesn’t come without enhanced technology,” said Kimber.
The hospital’s groundbreaking creates an exciting new chapter for Sanford Health Sioux Falls, which has been caring for patients in the community for almost 130 years.

“A foundation has been built throughout the years by visionary Sanford staff, physicians and commu nity leaders that empowered us to
create an organization to meet the needs of those we serve where they are now and in the future,” Hanson explains.
Patients were at the heart of the decision to build the hospital — to provide more people with the highest quality of care and latest treatments.

“The Sanford Orthopedic Hospital is going to change the game —for those we serve and for those we work alongside,” Hanson said. “We wholeheartedly welcome that responsibility.”
Expanding orthopedic and
surgical services in Sioux Falls will also enhance access for patients across the region.
“We want to make sure that we are providing top-notch health care no matter what your zip code is,” said Dr. Crabtree. “I think when we put a building like this in place and we make a commitment like this, it solidifies our intention to be the premier rural health care provider in the country.”
To learn more, visit sanfordhealth.org.
Avera is one of four recipients nationwide to receive the Rural Maternity and Obstetrics Management Strategies Program funding, otherwise known as RMOMS, from the federal Health Resources and Services Administration. The grant provides $4 million over four years to increase access to obstetrics services and improve outcomes such as preterm labor, low birthweight, infant mortality and more in South Dakota. RMOMS-SD will implement remote patient monitoring and telehealth, coordination between different aspects of OB care and existing resources, ensuring access to statewide wraparound services, and a social determinants of health screening program.

Matthew A. Barker, MD, FACOG, with Avera Medical Group Urogynecology in Sioux Falls, has been elected Director at Large of the 2023 American Urogynecologic Society Board of Directors. His three-year term as Director continues 2023 – 2025. Dr. Barker is Director of Female Pelvic Medicine and Reconstructive Surgery at Avera McKennan Hospital.
Jami Kortan, a PA at Monument Health Spearfish Clinic, has received a Clinical Excellence Award. She was nominated by a colleague. The Monument Health Physician Operations Group established this award in 2022 as a way to recognize the commitment to excellence physicians and providers show their patients.

Laboratories at Monument Health Orthopedic and Specialty Hospital and Monument Health Rapid City Urgent Care have received the COLA Laboratory Excellence Award. COLA is a leading national laboratory accreditor, whose program and standards enable clinical laboratories and staff to meet U.S.
Clinical Laboratory Improvement Amendments and other regulatory requirements. The Excellence Award is awarded to only 11 percent of surveyed labs.
Bhaskar Purushottam, MD, FACC, FSCAI, FSVMB, an Interventional Cardiologist at Monument Health Heart and Vascular Institute, has published a research study in Vascular Health and Risk Management The study concludes that femoropopliteal arteries experienced a low rate of target lesion revascularization at a one-year follow up when treated by a Jetstream Atherectomy followed by paclitaxel-coated balloons, with a significant reduction in bailout stenting following vessel prepping with the Jetstream.

Monument Health Rapid City Hospital has received the Stryker Gold Environ mental Excellence Award in recognition of sustain ability efforts. To earn this award, Monument Health caregivers identified and recycled 13 tons of single-use medical equipment. Ultrasonic scalpels, ligatures, EP catheters and ECG leads were recycled and sent to Stryker Sustainability Solutions for reprocessing and remanufacturing, rather than going to a landfill. Once recaptured items are processed or remanufactured and quality tested, they may be repurchased at lower costs resulting in savings and reduced waste. By working with Stryker and commit ting to purchasing recycled materials, Monument Health saved more than $426,000 in 2022.
Monument Health Heart and Vascular Institute is the first healthcare system in South Dakota and among the first in the nation to introduce a new technology that allows for greater precision and greater success in treating atrial fibrillation. Octaray is an advanced high-density mapping catheter used for diagnosing complex arrhythmias in the heart. This technology provides improved clarity in high-density maps which enables optimal accuracy and efficiency for Monument Health’s electrophysiologists as they perform mapping procedures.
ERICA DEBOER Sanford Health’s chief nursing officer, Erica DeBoer, RN, MA, CCRN-K, CNL, gave the keynote presentation at the 39th annual National Oncology Conference of the Association of Community Cancer Centers in Palm Beach, Florida in October. She focused on Sanford’s efforts to deploy a data-driven approach to managing clinical workforce scheduling and staffing needs. The organization has been working toward automating schedules for the past several years, and this year, began partnering with Flexwise with the goal of implementing a more flexible staffing model.

Sanford Health researcher Kurt Warnhoff, PhD, has received a $2 million grant for his work on the biology of the molybdenum cofactor (Moco). The rare disease, known as molybdenum cofactor deficiency (MoCD), is a lethal condition that causes brain dysfunction that worsens over time. Dr. Warnoff’s proposed research program will define fundamental pathways that govern Moco biology and may suggest new therapeutic strategies to treat rare and common diseases where Moco and Moco-mediated metabolism are disturbed.

Sanford USD Medical Center and clinics has attained Magnet recognition from The American Nurses Credentialing Center’s Magnet Recognition Program® for the fifth straight time, one of only 40 hospitals to do so. Magnet recognition is the gold standard for nursing excellence and is a factor when the public judges healthcare organizations. Research demonstrates that Magnet-recognized hospitals have higher job satisfaction among nurses as well as higher patient satisfaction and better outcomes.
Sanford USD Medical Center has been recognized as a top performer in the 2022 Bernard A. Birnbaum, MD, Quality Leadership Ranking by Vizient, Inc.
Sanford USD Medical Center is one of about 10% of participating Vizient members in the large, specialized complex care medical center cohort for demonstrating excellence in delivering high-quality care on the Vizient Quality and Accountability Study, which has been conducted annually since 2005. The ranking measured performance on the quality of patient care in six areas: safety, mortality, effective ness, efficiency, patient centeredness and equity.
Sanford Health recently reopened the newly-renovated Sioux Empire Medical Museum on the lower level of the Sanford USD Medical Center. The Sioux Empire Medical Museum opened in 1975 as South Dakota’s first medical museum and remains the state’s only to this day. It closed temporarily in recent years for the remodel. Now, visitors will be taken through the history of nursing through video, photos, historical medical equipment, uniforms, and panels of information. One of the highlights of the museum is an Iron Lung.

Sanford Health Plan’s one year-old Medicare Advantage plan, Align powered by Sanford Health Plan, is expanding to 38 new counties in Iowa, Minnesota, North Dakota and South Dakota for the 2023 plan year. Enrollment is open through December 7th.
Hy-Vee/Sanford Legends for Kids is donating back a record $290,000 to local youth sports organizations following this year’s Legends events. This year’s total pushes the amount donated since 2005 to $3.135 million. This year, 2,200 kids attended the free clinics, 900 athletes attended the Legends Football Camp (a new record), and there were 456 participants at the Legends Golf Tournament. The $290,000 will support the Legends scholarship program ($40,000), the Legends Foundation for Youth Grant Program ($190,000) and the Folds of Honor Foundation ($60,000).
on the 60,000 square foot Sanford Virtual Care Center in Sioux Falls. The Sanford Virtual Care Center will feature dedicated clinician workspaces equipped with the latest telemedicine technology to offer a variety of service lines, including on-demand urgent care, behavioral health care and primary care. The building will also house innovation, education and research initiatives to advance digital healthcare and workforce solutions for the future.
MercyOne and the city of Moville, Iowa plan to construct a new building to house a primary care location and therapy area. Construction on the 10,000 square foot, $3.5 million facility is expected to begin in the spring and will be located off Highway 20. Once complete, MercyOne will lease the first floor of the facility to replace the current MercyOne Moville Family Medicine clinic.
CNOS and a wellness center will occupy the second floor.

The Iowa Hospital Association honored several MercyOne colleagues from across the state at its 2022 Annual Meeting held at the Community Choice Credit Union Convention Center in October. Seven MercyOne employees from across the state of Iowa were recognized with “Hospital Heroes” awards, including:
Michelle Arensdorf, RN, MercyOne Dubuque Medical Center
Michele Dikkers, DO, Guttenberg Municipal Hospital & Clinic
David Eilers, MercyOne Central Iowa
Diane Probasco, BSN, RN, RN-BC, MercyOne Central Iowa
• Kelly Richards, DNP, RN, MercyOne Northeast Iowa
• Douglas Summerfield, MD, MPH, MercyOne North Iowa Medical Center
• Larry Volz, MD, MercyOne Siouxland Medical Center/ Midlands Clinic

The IHA is a nonprofit trade association of 119 hospital and health system members headquartered in Des Moines.
MercyOne became a full member of Michigan-based Trinity Health System, based in Livonia, Michigan, in September. Trinity Health is one of the largest not-for-profit Catholic health systems. The news follows an April announcement that Trinity Health signed an agreement with CommonSpirit Health to acquire all facilities and assets of Iowa-based MercyOne, including Home Care, Hospice, and Infusion locations. Since the agreement was announced on April 19, plans have been underway to complete the integration including regulatory filings and other steps necessary to finalize the agreement.
Sarkisian has joined specialty gastroenterology, hepatology and obesity disorders. Originally from San Diego, California Dr. Sarkisian moved to New York City for medical training, obtaining his medical degree at Weill Cornell Medical College. He completed both his residency in internal medicine and fellowship in Gastroenterology and Hepatology at Tulane. During his fellowship, he obtained a board certification in Obesity Medicine. Dr. Sarkisian’s clinic is located at the South Sioux City Riverview location in South Sioux City, Nebraska.
CNOS recently broke ground on their new 6500-square-foot Imaging Center, expanding their offering of CT and MRI services to Siouxland patients. The CNOS Imaging Center expansion is another step to continue enhancing the healthcare services provided to the Siouxland Community and beyond. The cutting edge hardware and software will be ready for patient use in January 2023.
UnityPoint Health has been named to the 2022 Forbes “America’s Best Employers By State” list in all three states of its footprint –Iowa, Illinois and Wisconsin. The fourth annual Forbes list, compiled in partnership with market research company Statista, anonymously surveyed 70,000 Americans working for businesses with at least 500 employees to come up with the state-bystate rankings. Fair pay, safe working conditions, inclusive culture, remote work benefits and diversity initiatives were amongst the criteria used for this year’s Forbes’ rankings. Less than 275 hospitals and health systems nationwide were named to this year’s list.

Orthopedic surgeons at UnityPoint Health—Trinity Regional Medical Center have begun using new technology which aims to improve outcomes for orthopedic patients. The new Robotic Surgical Assistant (ROSA) can help with the precision and fitting in hip and knee replacement surgeries. Recently, TRMC was recognized as the first hospital in Iowa to receive the DNV Hip and Knee Replacement Program Certifica tion, which validates the hospital’s excellence across the spectrum of hip and knee replacement care.

Dr. Ashlesha Kaushik, the Pediatric Infectious Disease Medical Director and a physician with UnityPoint Health – Sioux City, has been named a 2022 Immunization Emerging Leader by the National Conference for Immunization Coalitions and Partnerships (NCICP). Dr. Kaushik was one of six individuals recognized by NCICP for outstanding leader ship, innovation, and collabora tion in immunizations. NCICP, which is sponsored by Immunize. org and Voices for Vaccines, is the only conference dedicated to collaboration and partnership to improve immunization update, educate our communities, and prevent the spread of disease.

RAS has gained the trust of over 300+ healthcare facilities in the Midwest building a reputation as a thought leader in the work comp insurance industry.



KNOW HEALTHCARE
HEALTHCARE FACILITIES INSURED
Crystal Drayer, MD, has joined the team at UnityPoint Clinic General Surgery. Dr. Drayer received her medical degree from the Wayne State University School of Medicine in Detroit, Michigan. She is also a fellow of the American College of Surgeons and is board eligible in General Surgery. Most recently, Dr. Drayer worked at Sparrow Hospital in Lansing, Michigan, where she was General Surgery Resident Physician. She has an interest in all aspects of general surgery particularly hernia repair and laparoscopic abdominal cases like appendectomies and colectomies.
St. Luke’s College–UnityPoint Health has added a new, full-time Accelerated Bachelor of Science in Nursing program (ABSN) for students interested in becoming a Registered Nurse.




Located on the campus of UnityPoint Health –St. Luke’s hospital in Sioux City, the St. Luke’s College ABSN was developed as a response to the changes in health care and the increased need for nurses and nurse leaders. The tri-state area of Iowa, Nebraska, and South Dakota have all identified the need for additional nurses. The first semester begins in January.
Interventional radiologist Khalil Yousef, MD, has joined UnityPoint Health–St. Luke’s. Dr. Yousef received both his BS and his medical degree from the American University of Beirut in Lebanon. He completed a surgery/ENT internship and residency at the American University of Beirut Medical Center, a burn surgery fellowship at Vanderbilt, a radiology residency at New York Medical College, and a vascular and interventional radiology fellowship at Mayo Clinic in Rochester, Minnesota. He is a board-certified interventional radiologist and is a member of the Society of Interven tional Radiology. He brings 23 years of experience in interventional radiology to the Siouxland community.

Prairie Lakes Healthcare System recently welcomed Physician Assistant, Kahley Meyer and Nurse Practitioner, Travis Erickson to the cardiology Meyer earned her degree in Physician Assistant Studies from MCPHS University in Worcester, Massachusetts. Erickson is a Brookings native who earned his BSN at SDSU, where he also received his Doctor of Nursing Practice –Family Nurse Practitioner.

Dr. Aaron Pickrel has joined PLHS as a hospitalist. Dr. Pickrel grew up in Watertown and is returning to Prairie Lakes Healthcare System where he was a Telemetry Technician from 2013 – 2015. He received his medical degree from Edward Via College of Osteopathic Medicine in Spartanburg, South Carolina and completed his Internal Medicine Residency at the Abbott Northwestern Hospital in Minneapolis.


Josh Dahl is the new Director of Facilities He replaces Rick Masloski upon his retirement after ten years. Dahl joined Prairie Lakes in 2015 as a Certified Maintenance Technician, was promoted to Maintenance Supervisor, and spent the last 3 years mentoring under Masloski’s supervision. He plans, directs, supervises, and evaluates the infrastructure and physical plant management at PLHS.

Board-Certified Interventional Cardiolo gist, Ravi Kalaga, MD, has joined PLHS’s team of heart specialists. Dr. Kalaga received his MD from the University of Health Sciences, Andhra Medical College in Visakhapatnam, India and completed his internal medicine residency at the University of Nebraska Medical Center in Omaha. He is fellowship trained in cardiovascular medicine from Bridgeport Hospital, Yale University School of Medicine in Bridgeport, Connecticut, and his fellowship in Interventional Cardiology was completed at the University of Arkansas for Medical Sciences in Little Rock.
Kristi Palmer, known to her friends as "Cricket", is one of those rare students who came into the School of Health Sciences master's program in Addiction Counseling & Prevention with decades of experience in the field.
For 20 years of her 28-year military career, Palmer worked in the South Dakota National Guard's Drug Demand Reduction (DDR) program, teaching students across the region about the dangers of drug and alcohol abuse and addiction.

“Once I retired from the military in 2017, I decided I wanted to take the next step and get a master's degree in Addiction Counseling & Prevention,” says Palmer. “It had been 30 years since I was an undergrad, so it was a huge decision to make.”
Palmer says she was drawn to USD's program because of the depth of knowledge and experience among the professors, the diversity of students in the program, and the emphasis on prevention as well as addiction.
“Many places only focus on addiction, but the School of Health Sciences brings in the prevention aspect, too, which is so important,” says Palmer. "Prevention is really my first passion so that was one of the most appealing things about the program for me."
Another appealing feature of USD's program was the opportunity to add a concentration in co-occurring disorders, which Palmer did.
“There is always a reason why people are drinking and drugging,” says Palmer, whose current job as an Alcohol and Drug Control Officer with the South Dakota National Guard is part of a larger psychological health program which includes things like suicidie prevention and resiliency.
“We know that these things often occur together," says Palmer. "The fact that USD addresses that just adds to the strength of the program.”
Prairie Lakes Healthcare System recently welcomed PT Todd Hodenfield and OT Chelsea Hodenfield to the Rehab and Therapy Services team. Chelsea Hodenfield grew up in Sioux Falls and earned her MS in Occupational Therapy from USD. Todd Hodenfield grew up in North Dakota and earned his Doctor of Physical Therapy from the University of North Dakota in Grand Forks. He later completed an Orthopaedic Physical Therapy Residency with Evidence in Motion. He is a Board-Certified Clinical Specialist in Orthopaedic Physical Therapy.

The CDC has highlighted South Dakota for its accomplishments on the Project Firstline program. Out of 50 states, just 5 states were spotlighted in the national CDC report, and South Dakota was the only state recognized for its efforts in marketing and promotion of the program.
Project Firstline is a national CDC collaborative to educate and train healthcare workers on infectious disease prevention. The SD Foundation for Medical Care leads the Project Firstline program in South Dakota, in partnership with the CDC and the SD Department of Health.
Brookings Health System has expanded its rehabilitative services to now include hand therapy. Occupational Therapist Sara Lutz, MSOTR/L, will treat patients with conditions that affect their upper extremity, including the hand, wrist, elbow and shoulder. Some conditions of the hand and arm system Lutz will treat include tendonitis, injuries and fractures, arthritis, trigger finger, carpal tunnel syndrome and rotator cuff repairs. Lutz holds a master’s degree in occupational therapy from The University of Mary in Bismarck.
of their birth to help them through the labor and delivery process. It’s hoped that choosing a doula ahead of time will allow them to establish a relationship with that person before the birth. Doulas provide continuous labor support during childbirth and assist mothers and their partners with emotional and physical needs during and after the birth.

Want to go deeper? Read the full versions of these and other recent news items on our website.
Brookings Health System has partnered with the South Dakota Board of Nursing to offer a clinical enrichment program for nursing students. The clinical enrichment program runs for 10 weeks and offers nursing students the opportunity to continue learning the practice of nursing outside their formal education. Selected candidates will perform tasks of direct and indirect patient care under their nurse preceptor’s guidance.

Internal medicine physician Rebecca Runge, MD, has joined the Huron Regional Medical Center (HRMC) medical staff. A native of Wessington, Dr. Runge completed her medical training at the USD Sanford School of Medicine in Vermillion and completed her residency at USD Sanford School of Medicine in Sioux Falls.


Rachel HaighBlume has joined HRMC as director of information services.

Haigh-Blume holds both an Associate of Science in Business Management and a Bachelor of Science in Respiratory Care from Dakota State University in Madison. She completed an MS in Healthcare Administration from Capella University in Minneapolis. Currently, Haigh-Blume is enrolled in a data analytics program through Career Foundry. She will coordinate IS related activities for the hospital and HRMC Physicians Clinic.
majors in health professional disciplines, including dental hygiene, nursing, social work, addiction counseling and prevention, medical laboratory science, physician assistant studies, public health and health sciences. Attached to the Andrew E. Lee Memorial Medicine and Science building, the building also provides more opportunities for health sciences and medical students to work together.

The Sioux Falls VA Health Care System recently received the Most Improved in Outpatient Experience Award for fiscal year 2021 at the VA’s Patient Experience Symposium in Washington, DC. The award recognizes the SFVAHCS for having the most improved patient satisfaction scores across the Veterans Health Administration’s primary care outpatient clinics during the 2021 fiscal year. Sioux Falls had an improvement from 72.6% to 83.5%, an increase of 10.9%.

In partnership with South Dakota State University (SDSU), Huron Regional Medical Center and Northern Plains Health Network affiliate hospitals in Madison and Brookings have received a grant of over $1.5 million from the Health Resources and Services Administration. The money will fund BREATHE-SD, which aims to bring respiratory therapy education and public health opportunities to rural facilities and the communities they serve. Grant funds will be utilized to hire additional training staff and purchase equipment to give students hands-on experience.


A 35-year-old patient “no showed” for her appointment for the third time in a year. Your office has a firm policy of termination after three missed appointments (with out proper notification to office staff). You have clearly discussed this policy with the patient at two previous visits with no apparent change or good explanation for her nonadherence. You decide to discharge her.
A 60-year-old patient is openly frustrated in the office waiting area. Previously, he was involved in a couple of incidents where he was abusive and threatening to the front desk staff. During this latest encounter, he loudly muttered that he is going to bring a gun to his next visit. You decide to discharge him.
These two case studies provide examples of situations where there is a question about how to terminate the provider-patient rela tionship. In the practice of medicine, there are several situations where the patient relationship has deteriorated to the point where ter minating the relationship is a relevant option.
In these cases, it is vital to end the relationship in an appropriate manner. The relationship itself is voluntary, so ending it may be appropriate, but it is necessary to proceed properly to avoid a claim of abandonment. Ending the provider-patient relationship typically revolves around situations that include:
• Patient nonadherence
• No shows to appointments
• Bill nonpayment
• Abuse and/or threatening behavior
Before getting to the point of termination, providers should make an effort to repair the relationship, partic ularly when it involves nonadherent conduct or financial issues. Other more extreme situations, such as threats of violence, may call for quicker action in terminating the relationship.
When you decide to discharge the patient there are a number of issues to consider:
ABANDONMENT Allegations of abandonment are the most serious consideration and the one most likely to be considered by your state medical licensing board. The patient must be in a stable condition. You must give adequate notice and be available for emergency care, generally for 30 days. Records should not be withheld and should be expeditiously provided to the next clini cian, even if there are monies owed. Examples of situations that may require longer times before termi nation include a hospitalized patient, a patient in late pregnancy, an immediate post-operative patient, or someone receiving chemotherapy. In these situations, it may be necessary to arrange for further care.
DISCRIMINATION Termination may not be based upon gender, race, religion, disability, ethnic origin, national origin, or age. Disability status can be complex and contentious.
CONTRACT ISSUES Be cautious when terminating patients who are members of managed care plans. Your contracts with health plans might specify the manner of termination with a member patient. This is especially true if the method of payment is capitation. Plans might need notification of the reason for termination to prevent allegations of dismissing a patient because he or she is “too expensive to treat.” The patient might also have different time constraints for the health plan to complete reassignment to a new physician. Medicaid has a spe cific process for termination of Medicaid patients, and health care professionals need to consult their pro vider participation agreement for details.









At Sanford Health, our team is committed to providing your patients with care close to where they live, work and play. Our ear, nose and throat specialists deliver the most advanced procedures and treatments for:
Chronic ear issues, including recurrent infections
Deviated nasal septum
Head and neck cancer treatment

Hearing and balance treatment



Pediatric cleft lip and palate reconstruction


Sinus issues
Sleep apnea treatment
Tonsil and adenoid