4 minute read
Spatial resolution
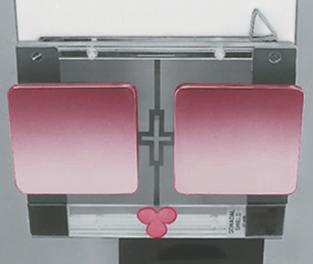
4. Upside-down focused grid Each grid is labeled to indicate the side that must be positioned to face the x-ray tube. The lead strips are tilted or focused to allow the x-ray beam to pass through unimpeded (if the SID is within the focal range and the grid is correctly placed). If the grid is positioned upside-down, the image will show severe cutoff (Fig. 1-131).
CR
Advertisement
Correctly centered grid Upside-down grid (results in grid cutoff or decreased density on both sides of image)
Summary of Contrast Factors Selection of the appropriate kV is a balance between optimal image contrast and lowest possible patient dose. A general rule states that the highest kV and the lowest mAs that yield sufficient diagnostic information should be used on each radiographic examination.* Close collimation and correct use of grids also ensure that the processed radiographic image displays optimal contrast.
sPATiAl ResolUTion Spatial resolution is defined as the recorded sharpness of structures on the image. Resolution on a radiographic image is demonstrated by the clarity or sharpness of fine structural lines and borders of tissues or structures on the image. Resolution is also known as detail, recorded detail, image sharpness, or definition. Resolution of film-screen images generally is measured and expressed as line pairs per millimeter (lp/mm), in which a line pair is seen as a single line and an interspace of equal width. The higher the line pair measure, the greater is the resolution; it is typically 5 to 6 lp/mm for general imaging. Lack of visible sharpness or resolution is known as blur or unsharpness.
Controlling Factors The optimal radiograph displays a sharp image, as listed under “Evaluation Criteria” for each position in this text. Resolution with film-screen imaging is controlled by geometric factors, the filmscreen system, and motion.
Fig. 1-131 Upside-down grid cutoff.
Large focal spot Small focal spot
Geometric Factors Geometric factors that control or influence resolution consist of focal spot size, siD, and object image receptor distance (oiD). The effect of OID is explained and illustrated in Fig. 1-137.
The use of the small focal spot results in less geometric unsharpness (see Fig. 1-132). To illustrate, a point source is used commonly as the source of x-rays in the x-ray tube; however, the actual source of x-rays is an area on the anode known as the focal spot. Most x-ray tubes exhibit dual focus; that is, they have two focal spots: large and small. Use of the small focal spot results in less unsharpness of the image, or an image with a decreased penumbra. A penumbra refers to the unsharp edges of objects in the projected image. However, even with the use of the small focal spot, some penumbra is present.
Larger focal spot (more penumbra) Small focal spot (less penumbra)
Fig. 1-132 Effect of focal spot size.
Film-Screen System With film-screen imaging systems, the filmscreen speed used for an examination affects the detail shown on the resultant film. A faster film-screen system allows shorter exposure times, which are helpful in preventing patient motion and reducing dose; however, the image is less sharp than when a slower system is used.
*Bushong S: Radiologic science for technologists, ed 9, St. Louis, 2009, Mosby.
Motion The greatest deterrent to image sharpness as related to positioning is motion. Two types of motion influence radiographic detail: voluntary and involuntary.
Voluntary motion is that which the patient can control. Motion from breathing or movement of body parts during exposure can be prevented or at least minimized by controlled breathing and patient immobilization. Support blocks, sandbags, or other immobilization devices can be used to reduce motion effectively. These devices are most effective for examination of upper or lower limbs, as will be demonstrated throughout this text.
Involuntary motion cannot be controlled by the patient at will. Therefore, involuntary motion, such as peristaltic action of abdominal organs, tremors, or chills, is more difficult, if not impossible, to control.
If motion unsharpness is apparent on the image, the technologist must determine whether this blurring or unsharpness is due to voluntary or involuntary motion. This determination is important because these two types of motion can be controlled in various ways.
Difference between voluntary and involuntary motion Voluntary motion is visualized as generalized blurring of linked structures, such as blurring of the thoracic bony and soft tissue structures as evident in Fig. 1-133. Voluntary motion can be minimized through the use of high mA and short exposure times. Increased patient cooperation is another factor that may contribute to decreased voluntary motion; a thorough explanation of the procedure and clear breathing instructions may prove helpful. involuntary motion is identified by localized unsharpness or blurring. This type of motion is less obvious but can be visualized on abdominal images as localized blurring of the edges of the bowel, with other bowel outlines appearing sharp (gas in the bowel appears as dark areas). Study Fig. 1-134 carefully to see this slight blurring in the left upper abdomen, indicated by arrows. The remaining edges of the bowel throughout the abdomen appear sharp. Fig. 1-133, by comparison, demonstrates overall blurring of the heart, ribs, and diaphragm. A clear explanation of the procedure by the technologist may aid in reducing voluntary motion; however, a decrease in exposure time with an associated increase in mA is the best and sometimes the only way to minimize motion unsharpness caused by involuntary motion.
Fig. 1-133 Voluntary motion (breathing and body motion)—blurring of entire chest and overall unsharpness.
Fig. 1-134 Involuntary motion (from peristaltic action)—localized blurring in upper left abdomen (arrows).
Summary of Spatial Resolution Factors Use of a small focal spot, an increase in siD, and a decrease in oiD result in less geometric unsharpness and increased resolution. Patient motion also affects image quality; short exposure times and increased patient cooperation help to minimize voluntary motion unsharpness. Involuntary motion unsharpness is controlled only by short exposure times.