4 minute read
Pregnant patient
Summary of Rules for Specific Area Shielding Proper specific area shielding is a challenge for each technologist because its use requires additional time and equipment. However, the importance of protecting radiosensitive organs and the gonads from unnecessary radiation should be sufficient motivation to encourage consistent practice of the following three rules for gonadal shielding: 1. gonadal shielding should be considered for all patients. A common policy of many imaging facilities directs the use of specific area shielding for all children and adults of reproductive age; however, the best practice is to shield the radiosensitive tissues outside the anatomy of interest for all patients. 2. Placement of gonadal shielding is necessary when the organ of concern lays within or near (2 inches [5 cm]) the primary beam, unless such shielding obscures essential diagnostic information. 3. Accurate beam collimation and careful positioning is essential. Specific area shielding is an important additional protective measure but no substitute for accurate collimation.
Pregnant Patient
Advertisement
All women of childbearing age should be screened for possibility of pregnancy before an x-ray examination. This concern is particularly critical during the first 2 months of pregnancy, when the fetus is most sensitive to radiation and the mother may not yet be aware of the pregnancy. Posters or signs (Figs. 1-185 and 1-186) should be prominently displayed in examination rooms and waiting room areas, reminding the patient to inform the technologist of any known or potential pregnancy.
If the patient indicates that she is pregnant or may be pregnant, the technologist should consult the radiologist before proceeding with the examination. If the mother’s health is at risk and clear indications for an imaging study exist, the examination should not be denied or delayed because of the pregnancy. Radiation protection practices already described, especially careful collimation, should be used.
For examinations of body parts above the diaphragm or below the hips, the scattered dose to the fetus is very low, and the examination may proceed normally. For examinations in which the fetus is in the direct beam and the estimated fetal dose is less than 10 mGy (1 rad), the radiation dose should be kept as low as possible consistent with obtaining the desired diagnostic information. Shielding of the abdomen and pelvis with a lead apron should be considered. Limiting the number of views should be considered. For examinations in which the fetus is in the direct beam and the estimated fetal dose is greater than 10 mGy (1 rad), the radiologist and referring physician should discuss other options such as sonography and MRI that can provide the needed information.
If the x-ray imaging procedure is deemed appropriate, the patient should be informed of the risks and benefits of the procedure. The clinician responsible for the care of the patient should document in the medical record that the test is indicated for the management of the patient.
In the past, the 10-day or lMP rule (last menstrual period) was applied to prevent exposure to the embryo/fetus early in pregnancy, when the pregnancy is not known. This rule stated that all radiologic examinations involving the pelvis and lower abdomen should be scheduled during the first 10 days following the onset of menstruation because conception will not have occurred during this period. Currently, this rule is considered obsolete because the potential harm associated with canceling essential x-ray procedures may greatly exceed the risk of the fetal radiation dose.
The following examinations deliver a dose of less than 10 mGy (1 rad) to the embryo/fetus: • Extremities • Chest • Skull • Thoracic spine • Head CT • Chest CT
The following examinations have the potential to deliver a dose of more than 10 mGy (1 rad) to the fetus and embryo: • Lumbar spine series • Fluoroscopic procedures (abdomen) • Abdomen or pelvis with three or more views • Scoliosis: full series • CT abdomen • CT pelvis
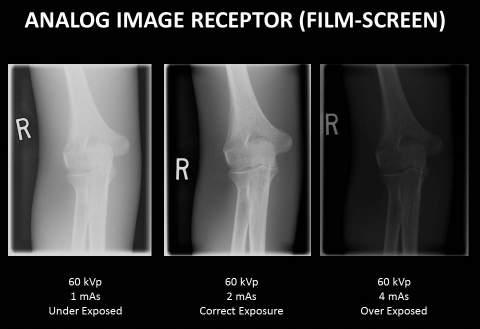
Optimum Speed
As a general guideline, the highest speed film-screen combination that results in diagnostically acceptable radiographs is desirable to manage patient dose. The presence of the screen does result in some loss of spatial resolution and becomes more pronounced as the speed is increased. The radiologist must balance the reduction in patient exposure with the potential loss of detail in the resultant image. A common practice is to select a slow 100-speed (detail) screen with tabletop procedures, such as upper and lower limbs, when a grid is not used and spatial detail is important. A 400-speed screen is commonly preferred for larger body parts when grids and higher exposure techniques are required. For other applications, a 200-speed screen may be preferred. Departmental protocol generally indicates the film-screen combination for each procedure. This is not a decision that is usually made by individual technologists.
Digital imaging systems have essentially replaced film-screen for most radiographic applications. These digital receptors are more sensitive than film-screen and have the potential to reduce patient dose greatly. In addition, their wide dynamic range results in fewer repeated “films.” Automatic exposure control (AEC) for digital systems is usually set at an exposure indicator level that produces images with an acceptable level of noise. However, the technologist may adjust the AEC density control to change the effective system speed. The wide dynamic range of digital receptors enables this variation in dose, while still producing a quality image (although noise becomes more pronounced as the dose is reduced). Because the FPD-TFT is often integrated into the radiographic unit, the variable speed option is readily available to customize the speed for each imaging protocol.
Fig. 1-185 Warning sign. (Courtesy St. Joseph’s Hospital, Phoenix, AZ.)