THE PANDEMIC PARADOX



Hudson College of Public Health 801 NE 13th St. Oklahoma City, OK 73104
https://publichealth.ouhsc.edu
Dean’s Office: (405) 271-2232 Student Services: (405) 271-2308
Heather Hollen Kyndall Wahkinney
June Frantz Hunt LEADERSHIP
Interim Dean Dale Bratzler, D.O., M.P.H.
Chair, Department of Biostatistics and Epidemiology Laura Beebe, Ph.D.
Chair, Department of Health Administration and Policy Dale Bratzler, D.O., MPH
Chair, Department of Health Promotion Sciences Neil Hann, M.P.H., C.H.E.S.
Chair, Department of Occupational and Environmental Health Margaret Phillips, Ph.D., C.I.H.
Associate Dean of Sovereignty, Equity, Diversity, and Inclusion
Lancer Stephens, Ph.D.
STAY CONNECTED
@OUPublicHealth
• Faculty Awards
• Alumni Awards
• Retirement Recognitions
Laying the Foundation for a Healthier Oklahoma
• Fascinating Feces: Searching for COVID-19 in community wastewater
• Bridging Public Health Across Sectors
• Particular Particles: Studying the movement of COVID-19 particles in the air
• A Beacon of Hope: Leading OU’s pandemic response

• Championing Community Health Workers in Oklahoma
A Renewed Focus on Sovereignty, Equity, Diversity, and Inclusion
• Covid-19 Student Research Highlights
• Meet the 2022-2023 Hudson College of Public Health Student Association
• 2022 Student Scholarships
• Class of 2022
The Key to Public Health: Interdisciplinary Collaboration
<< IMAGE LEFT: The toilet lab aerosol testing chamber on the fourth floor of the Hudson College of Public Health. Occupational and environmental health Professor Changjie Cai is still working on a creative name for the mannequin. To read about his aerosol research, see page 24.

This publication, printed by OU Printing and Mailing Services, is issued by the University of Oklahoma. 30 copies have been prepared and distributed at a cost of $____ to the taxpayers of the State of Oklahoma. The University of Oklahoma is an equal opportunity institution. www.ou.edu/eoo
Created by the Oklahoma Territorial Legislature in 1890, the University of Oklahoma is a doctoral degree-granting research university serving the educational, cultural, economic and health care needs of the state, region and nation. The Norman campus serves as home to all of the university’s academic programs except health-related fields. The OU Health Sciences Center, which is located in Oklahoma City, is one of only three comprehensive academic health centers in the nation with seven professional colleges. Both the Norman and Health Sciences Center campuses offer programs at the Schusterman Center, the site of OU-Tulsa. OU enrolls more than 31,000 students, has more than 2,500 full-time faculty members, and has 21 colleges offering 174 majors at the baccalaureate level, 191 majors at the master’s level, 86 majors at the doctoral level, 8 majors at the doctoral professional level, 9 undergraduate certificates, and 72 graduate certificates. The university’s total annual operating budget is $2.32 billion. The University of Oklahoma is an equal opportunity institution.
local health agencies. The center is also developing partnerships with community-based organizations and philanthropic groups across Oklahoma. Specifically, the center is emphasizing multidisciplinary, interprofessional, and multisector collaborations to improve health in our state.
This has been a year of fresh starts and new beginnings for many of us. In January, Dr. Gary Raskob became the interim senior vice president and provost at the University of Oklahoma Health Sciences Center. He was then confirmed for this position in September. As Dr. Raskob transitioned from his work at the Hudson College of Public Health, I was honored to be asked to step in as the interim dean. I recognize that this position comes with a great deal of opportunity and commitment, and I’m looking forward to leading the college during this critical time in public health.

Even though I’ve been in this role for a relatively short period, I’ve witnessed significant accomplishments from our incredible faculty and students over the past few months. Since the start of the pandemic, our college has been very busy helping with COVID-19 research and response efforts across Oklahoma. I am pleased that this issue of our magazine highlights a few of the many faculty members and students who have conducted groundbreaking research in the past two years.
As we apply the lessons learned during the pandemic, it is evident now more than ever that we must make significant investments in our public health infrastructure. The pandemic exposed an already eroded public health system and devastated the public health and health care workforces across the nation. Our college is committed to revitalizing the public health system and rebuilding these workforces in Oklahoma.
To accomplish this, we are expanding our public health pipeline programs that include practice-based education. In 2021, we established the Center for Public Health Practice, which is focused on strengthening and advancing existing partnerships with federal, state and
Another exciting development was the launch of the undergraduate degree in public health on the Norman campus in 2018. In collaboration with the Dodge Family College of Arts and Sciences, we introduced three degree tracks in public and community health. As of summer 2022, a total of 153 students have graduated across all three degree tracks. Each semester, an average of 450 students are enrolled across all public and community health courses. There are currently 222 majors across the three degree tracks. Our faculty and staff are excited to continue to grow the program and increase interest in public health among undergraduate students.
I’d also like to highlight the recent creation of the Sovereignty, Equity, Diversity, and Inclusion (SEDI) Office within the Hudson College of Public Health. Not only are these values a cornerstone of our academic health system, but they are also central to public health. The SEDI Office will build on our commitment to cultivating a welcoming environment for everyone by providing resources and support to faculty, staff, and students.
The headline of this issue—“The Pandemic Paradox”— refers to the paradox of increased public health awareness and financial support during the pandemic, while at the same time experiencing decreased trust in public health and a declining public health workforce. Needless to say, we learned a lot over the last two years. We came together as a global community to develop testing and vaccines with unprecedented speed and collaboration. Within our college, we quickly pivoted to remote learning and recognized the potential of this new platform to expand our reach. As the chief COVID-19 officer for the University of Oklahoma, I am proud of the exceptional work that we have accomplished across all three campuses throughout the pandemic.
At the Hudson College of Public Health, our faculty and researchers are on the cutting edge of transmission modeling, data collection, and disease surveillance. Yet, many of us witnessed firsthand the misinformation
You can find our graduates in positions all over the country, including positions that were instrumental in the pandemic response. Our college has a distinguished track record of excellence in education and public health. We have a broad array of training opportunities, and our programs are very costeffective. There are currently a lot of job opportunities for people with public health training.
that infected our communities and the resulting backlash against public health measures—like masking and vaccinations—in our state and throughout the nation. This was tough, and at times it felt like an uphill battle. However, we learned from our experiences. I’m a firm believer that we will recover public trust in our field and rebuild the public health workforce through education, innovation, and leadership.
As we look to the future, would like to thank you all for helping us continue to provide exemplary public health education to our undergraduate students in Norman and graduate students in Oklahoma City and Tulsa. We are grateful for the generosity of our current and past donors who realize investing in these talented students is an investment in the future of public health. Our college looks forward to continuing to provide enhanced training and exceptional research opportunities to students as we grow and strengthen the public health workforce.
Dr. Julie Stoner was born in 1972 in Garden City, Kansas. She realized early on that she enjoyed and excelled at mathematics, computing, and quantitative sciences. She earned a bachelor’s degree in mathematics and statistics from Kansas State University in 1995 and later earned a doctorate in biostatistics from the University of Washington. After receiving her Ph.D., Stoner moved to Omaha, Nebraska, where she worked as an assistant professor in biostatistics at the University of Nebraska Medical Center. In 2007 she was recruited to OUHSC, and she and her young family relocated to Oklahoma, where she served many roles, including professor of biostatistics, associate dean for research and chair of the Biostatistics and Epidemiology Department. She excelled not only because of her intellect and drive but also because of her heart for others.
The Julie A. Stoner Conference Room serves as a reminder of her outstanding contributions to each of the college’s missions of teaching, research, and public health service.


On April 7, 2022, Dr. Gary E. Raskob, senior vice president and provost, on behalf of the Hudson College of Public Health and the University of Oklahoma Health Sciences Center, formally dedicated the Department of Biostatistics and Epidemiology Conference Room in memory of Dr. Julie A. Stoner, a beloved colleague who lost her battle to cancer in 2020. The Julie A. Stoner Conference Room serves as a reminder of her outstanding contributions to each of the college’s missions of teaching, research, and public health service.
Stoner held the Edward E. and Helen T. Bartlett Chair in Public Health. She was recognized for her academic excellence as a Presidential Professor and a David Ross Boyd Professor. Stoner was passionate about improving collaborations between biostatisticians and clinical researchers across campus. She was a key contributor and core leader within the Clinical Translational Sciences initiative, and she led the impressive growth of research efforts within the Department of Biostatistics and Epidemiology. She significantly strengthened our partnerships with the other colleges, the Stephenson Cancer Center, and the Harold Hamm Diabetes Center.
“Julie was a very impactful, beloved member of our faculty and a great colleague during her esteemed academic career. But what we miss the most is her smile and laugh and how she led with humility and confidence. She was never too busy to listen and was sincere in her love for others. Julie treated everyone with respect. Oklahoma was very fortunate to have her here at the Hudson College of Public Health and OU Health Sciences Center,” said Laura Beebe, chair of the Department of Biostatistics and Epidemiology.
Hudson College of Public Health recognizes faculty for outstanding teaching, research, scholarly research, creative activity, and professional service to the college and university.
2022
Jessica Reese, Ph.D. Faculty Board Outstanding Teaching Award


Ganisher Davlyatov, Ph.D. Student Association Faculty Teaching Award


Sixia Chen, Ph.D. Provost’s Research Award
Jooyeon Hwang, Ph.D. Provost’s Research Award
Michael P. Anderson, Ph.D. Professor
Department of Biostatistics and Epidemiology
Sixia Chen, Ph.D. Associate Professor


Department of Biostatistics and Epidemiology
Evan L. Floyd, Ph.D. Associate Professor


Department of Occupational and Environmental Health
Jooyeon Hwang, Ph.D. Associate Professor


Department of Occupational and Environmental Health
Kai Ding, Ph.D. Presidential Professorship
Department of Biostatistics and Epidemiology
Tabitha Garwe, Ph.D. Presidential Professorship



Department of Biostatistics and Epidemiology
Recipients of this award must be a graduate of the Hudson College of Public Health (any program/department), must have demonstrated outstanding leadership related to their field, and must have achieved distinctive and notable accomplishments in at least one of the following: Professional/Career, Community Service, or University Service.
The Office of Alumni Affairs at the Hudson College of Public Health awards an annual Distinguished Alumni Award and Young Alumni Professional Achievement Award (under the age of 40) to outstanding alumni from each department within the college. Recipients of these prestigious awards are recognized for achieving professional and personal successes, and demonstrating exemplary service to their community and/or the university.
Department of Occupational and Environmental Health Kathleen Shaver, M.S. (’94)
Department of Health Promotion Sciences Brandie Combs, M.P.H. (’01)

Department of Biostatistics and Epidemiology CAPT Julie Erb-Alvarez, M.P.H. (’97)
Department of Occupational and Environmental Health Sara Greenlee, M.S. (’18)
Department of Health Promotion Sciences Sara King, M.P.H. (’15)
Department of Biostatistics and Epidemiology Juell Homco, Ph.D., M.P.H. (’19)
Department of Health Administration and Policy Casey Woods, M.H.A. (’11)
Read more about each of the 2021 awardees at https://publichealth.ouhsc.edu/Alumni/Distinguished-AlumniAward.
 Jessica Reese
Michael P.
Anderson
Ganisher Davlyatov
Evan L. Floyd
Sixia Chen
Kai Ding
Jooyeon Hwang
Tabitha Garwe
Kathleen Shaver Sara Greenlee
Brandie Combs Sara King
Julie Erb-Alvarez
Juell Homco
Casey Woods
Jessica Reese
Michael P.
Anderson
Ganisher Davlyatov
Evan L. Floyd
Sixia Chen
Kai Ding
Jooyeon Hwang
Tabitha Garwe
Kathleen Shaver Sara Greenlee
Brandie Combs Sara King
Julie Erb-Alvarez
Juell Homco
Casey Woods
On Jan. 27, 2003, Deanna Debus began her career at the Hudson College of Public Health when she was hired by Dean Elisa T. Lee as an administrative manager in the Center for American Indian Health Research. In 2005, Debus was hired as a staff accountant in the Office of the Dean. She was quickly promoted and became the Business Manager in 2005, Assistant Dean in 2010, and Associate dean of finance and administration in 2012.
Debus is married to her husband, Charlie.
Together they have seven children, 19 grandchildren, and one great-grandchild.
Outside of work, Debus is passionate about traveling, spending time with her family and being involved with the Benevolent and Protective Order of Elks, an American fraternal order that invests in communities through programs that help children grow up healthy and drug-free, meets the needs of today's veterans, and improves their quality of life.
In retirement, she plans to sit by her pool, visit the Caribbean Islands, and go on a Mediterranean cruise.



Carolyn Scott began her career at the University of Oklahoma Hudson College of Public Health on Nov. 5, 1975, in the Department of Human Ecology and Environmental Health. During this time, the department was located in a house on 14th street. Scott continued with the department through 2005, rising to the rank of administrative manager. Early in 2006, she moved to the Dean’s Office, where she worked as our business manager until 2022. Scott has been the backbone of our financial organization, consistently tackling multiple responsibilities. It may be surprising to know that Scott has served under eight deans.
Scott has been active in volunteer activities such as the Employee Liaison Council, Employee of the Month Committee, and serving on multiple Faculty Search Committees. Scott also has received numerous awards, including Employee of the Month in 1990, Distinguished Service Award in 1991, multiple Special Recognitions for Outstanding
Contributions to the Black Student Organization, the Student Appreciation Award for Dedicated Service in 1993, and Staff Senate Employee of the Month in 2002.
During her career at the Hudson College of Public Health, Scott achieved not only professional success but personal success. If you’ve ever been in Scott’s office, you know how much her family means to her. It’s evident by all of the photos that her life is centered around the importance of family. When she began in 1975, her oldest daughter (Twila) was only 6 months old. She and her husband of 42 years, Dennis, have two daughters, Twila and Chrishawna, and four grandchildren.

Scott is quite active in her church, Evangelistic Baptist Church of Christ, and enjoys traveling, spending time with family, sewing, and cooking.

Gary Cox, J.D., has served more than 50 years in public health practice in the state of Oklahoma, beginning his career in July 1969. Throughout his career, Cox served as former commissioner of the Oklahoma State Department of Health, director of the Tulsa Health Department for 40 years, and director of the Oklahoma City-County Health Department for 10 years.
Cox served as associate professor for 20 years and associate dean of public health practice at the University of Oklahoma Health Sciences Center Hudson College of Public Health since 2020. He served as chair of the Governor’s Joint Commission on Public Health and was a founding member of the Tulsa Community Health Foundation.
Cox is currently a member of the American Public Health Association and served as president of the Indian Nations Council of Governments General Assembly and had previously
served as a member of the Indian Nations Council of Governments Board of Directors.
Cox testified before the United States Senate Committee on appropriations regarding Homeland Security and Bioterrorism.
Cox works to achieve collective goals of public health education, health workforce development, and partnerships with governmental public health and community organizations. During the COVID-19 pandemic, Cox worked with the CDC Foundation on a grant to make vaccines and educational materials available to underserved communities. He served on the National Association of County and City Health Officials for more than 10 years, serving as president from 2008-2009. Cox is also a member of the Association of State and Territorial health Officials Alumni Society.
Gary is the recipient of two Governor’s Commendation Awards: the Oklahoma Champion of Health Award and the Oklahoma Public Health Association President’s Award.
 GARY COX AND NEIL HANN
GARY COX AND NEIL HANN

In the fall of 2020, health administration and policy Professor Gary Cox began exploring options for improving the pandemic response across Oklahoma. After months of discussions and planning, the Achieving a Healthy Oklahoma initiative was announced in November of 2021, with Cox taking the lead. The main focus of the initiative was to better understand how our state, as a whole, responded to COVID-19 and how that information could be used to improve the overall health of Oklahomans. This was a broad initiative that included stakeholders from the business, education, community engagement, and health care sectors.
“I was proud that the Hudson College of Public Health took an active role in bringing people together to discuss the pandemic,” says Cox. “Convening groups to talk about important health issues is one of the key strengths of public health.”
Cox initially assembled a group of Hudson College of Public Health faculty to provide professional insights and help guide the initiative. Health promotion sciences Professor Neil Hann was asked to help lead the initiative and conduct listening sessions in communities across the state.
“It’s been a good opportunity to look at our public health response to the pandemic,” says Hann. “I think we learned a lot of lessons about what went right and what went wrong.”
In addition to faculty guidance and support, Cox and his team also assembled a large steering committee of experts from various sectors across Oklahoma to

discuss the pandemic response and propose solutions to strengthen future health emergency responses. Improving health requires buy-in from people in public health and health care, as well as those working in education and with the economy. They are all interrelated, and if even one is missing, quality of life declines in communities. “To be successful, we had to bring as many partners, collaborators, and supporters to the table as we could,” says Cox. “It’s all about the collective impact, and it takes a broad coalition to really make a difference.”
Recognizing that education, business, community engagement, and health care are pillars of healthy communities, Cox mobilized leaders from each sector to participate in workgroups that provided sector-specific feedback to the Achieving a Healthy Oklahoma team. Everyone involved in this initiative was excited and engaged. “We convened a great group of folks that worked well together and made everything come together,” says Cox.
A big part of the initiative was collecting feedback from local communities about their pandemic experience.
“It’s easy to sit within the walls of the college, but it’s critical for us to get out into the communities to understand their concerns, thoughts, and suggestions related to public health,” emphasizes Hann. The Achieving a Healthy Oklahoma team conducted six regional listening sessions across Oklahoma in Duncan, Lawton, McAlester, Miami, Muskogee, and with the Southern Plains Tribal Health Board. When asked what his favorite part of the initiative was, Hann immediately replied that it was working with community partners. “I
– PROFESSOR NEIL HANNenjoyed going out to the communities for the listening sessions,” he says. “Every time you work with community partners, you learn something new.”
Hann highlights the importance of local communities and partners in public health practice. “I think it’s fair to say that improving public health starts at the local level,” says Hann. Cox and Hann ensured that local public
health partners were included in the initiative and had a way to voice their concerns and issues. “For me, the Achieving a Healthy Oklahoma initiative provided a good review of, and reminder about, the importance of community partners,” says Hann. The initiative was an opportunity to re-engage community partners so that the college can continue to work with them in the future to improve health on a statewide basis.
The Achieving a Healthy Oklahoma team developed a final report and recommendations based on feedback from a statewide survey, key informant interviews, listening sessions, workgroup meetings, and steering committee meetings. In addition to the final report, six policy recommendations were developed to address actions that state legislators can take to prepare Oklahoma to effectively respond to future health crises. One of the next key steps is encouraging Oklahoma legislators, political leaders, school boards, business leaders, health leaders, etc., to act on and implement the recommendations.
To learn more about the Achieving a Healthy Oklahoma initiative and read the final report, visit https://publichealth.ouhsc.edu/ Departments-Centers/Center-forPublic-Health-Practice/Achieving-aHealthy-Oklahoma
I want the center to be a voice for public health communication and to provide public health messages to our community partners that they can use.
The Achieving a Healthy Oklahoma initiative was housed in the newly created Center for Public Health Practice at the Hudson College of Public Health. Prior to his retirement in June of 2022, Cox was the director of the center. “The center is important because public health practice is important,” says Cox. After Cox’s retirement, Hann took over as the director. The hope is that the center will build upon the initiative by implementing several of the recommendations from the final report. One of the most significant recommendations is to rebuild the public health workforce. The pandemic highlighted the considerable need for public health workers and the severe shortage of those workers in our existing health care system.
The center will act as a hub for training and workforce development in Oklahoma. “There are a couple of different levels of public health training that are needed,” says Hann. “We have a number of individuals in the public health workforce who currently don’t have any official public health training.” One of the main goals of the center is to provide Public Health 101 training for those who are currently in the public health workforce but don’t have any formal public health training. Hann also hopes that the center will provide more advanced training to those who may want to continue their education with a master’s degree in public health or a certificate in population health, American Indian health, or social justice and inequity that the college currently provides.
Another recommendation that the center is focused on is improving and modernizing health-related data systems across Oklahoma. “I would love to see us be a data coordinator and help to facilitate discussions among those agencies and groups that have health data and would benefit from their data systems communicating with each other,” says Hann. Hann is specifically interested in making data more accessible to professionals, as well as the general public, who may want more information and data about current health trends. This could be provided via dashboards and similar types of technology that allow anyone to look at the data, understand what it’s saying, and make good health decisions based on the information.
PROFESSORnication and access to resources to create a better response for future pandemics,” says Hann. Cox and Hann both acknowledge that health is too important for people to be divided on trivial matters. “My hope is that folks will get back together and the state will begin the healing process and begin to embrace a new Oklahoma standard of helping and being kind to each other,” says Cox.
Hann is optimistic about the future of the Center for Public Health Practice and its ability to engage public health partners, community leaders, and tribal nations across the state. “I want to make sure the center remains engaged with our partners and committed to their continued involvement,” says Hann. This includes
utilizing partnerships to enhance training opportunities. “One thing I hope the center will be able to do is to help train the next generation of the public health workforce,” says Hann. “We will be actively engaged with the Oklahoma State Department of Health, local county health departments, the Oklahoma City-County Health Department, and the Tulsa Health Department.”
Even though Cox retired in June of 2022, he remains involved in the Hudson College of Public Health. “It was a pleasure working on this initiative and working with friends and colleagues across Oklahoma,” Cox says. “I hope it has laid the foundation for even better and bigger success going forward.”


We need to be proactive instead of reactive. This is a team effort, and the more people that we have involved, the better off we are.
– PROFESSOR GARY COXThe center will also work collaboratively with local public health partners to implement local solutions tailored to their specific community population. “One size doesn’t fit all, and that’s why I believe in community engagement so much,” says Hann. Every community is different and will improve its health by taking different approaches. “What might be effective in Guymon probably isn’t going to be effective in Poteau, Oklahoma,” says Hann. The center hopes to continue listening sessions with local health departments across the state. “Public health is all about relationships,” says Hann. “Once you have those community relationships built and strengthened, then you can see amazing things happen at the community level for public health improvement,” says Hann.
Cox and his team learned a lot about the pandemic through the Achieving a Healthy Oklahoma initiative. “We specifically heard about improving commu -
To keep up-to-date on the Center for Public Health Practice, visit https://publichealth.ouhsc.edu/Departments-Centers/Center-for-Public-Health-Practice.
I’m confident that we can improve health in Oklahoma. The way that we are going to do that is community by community, working with those partners and understanding what their local needs are.
–
NEIL HANN
Most people (other than parents of babies and toddlers) don’t think much about poop, but for epidemiology Professor Katrin Kuhn, poop is her passion. More specifically, analyzing wastewater samples for infectious diseases. Kuhn and her family moved from Denmark to Oklahoma in the middle of the COVID-19 pandemic. When she joined the faculty at the Hudson College of Public Health, she promptly dove into wastewater surveillance for COVID-19. “I was really lucky to find a team here who immediately invited me to be a part of their surveillance,” Kuhn says. In August of 2020, the team began looking for COVID-19 in wastewater from the OU Norman campus dorms. Shortly after, surveillance expanded to include sites in Oklahoma City, Tulsa, and Anadarko. The team currently samples from several locations in Oklahoma City, Tulsa, and Anadarko, including some dynamic sites that they can move around based on where cases are increasing or there is an outbreak of interest.
Kuhn recognizes the benefit of having a cross-disciplinary team that includes engineers, microbiologists, epidemiologists, and community health planners. She notes that the engineers are key in helping to determine the best locations for monitoring sites
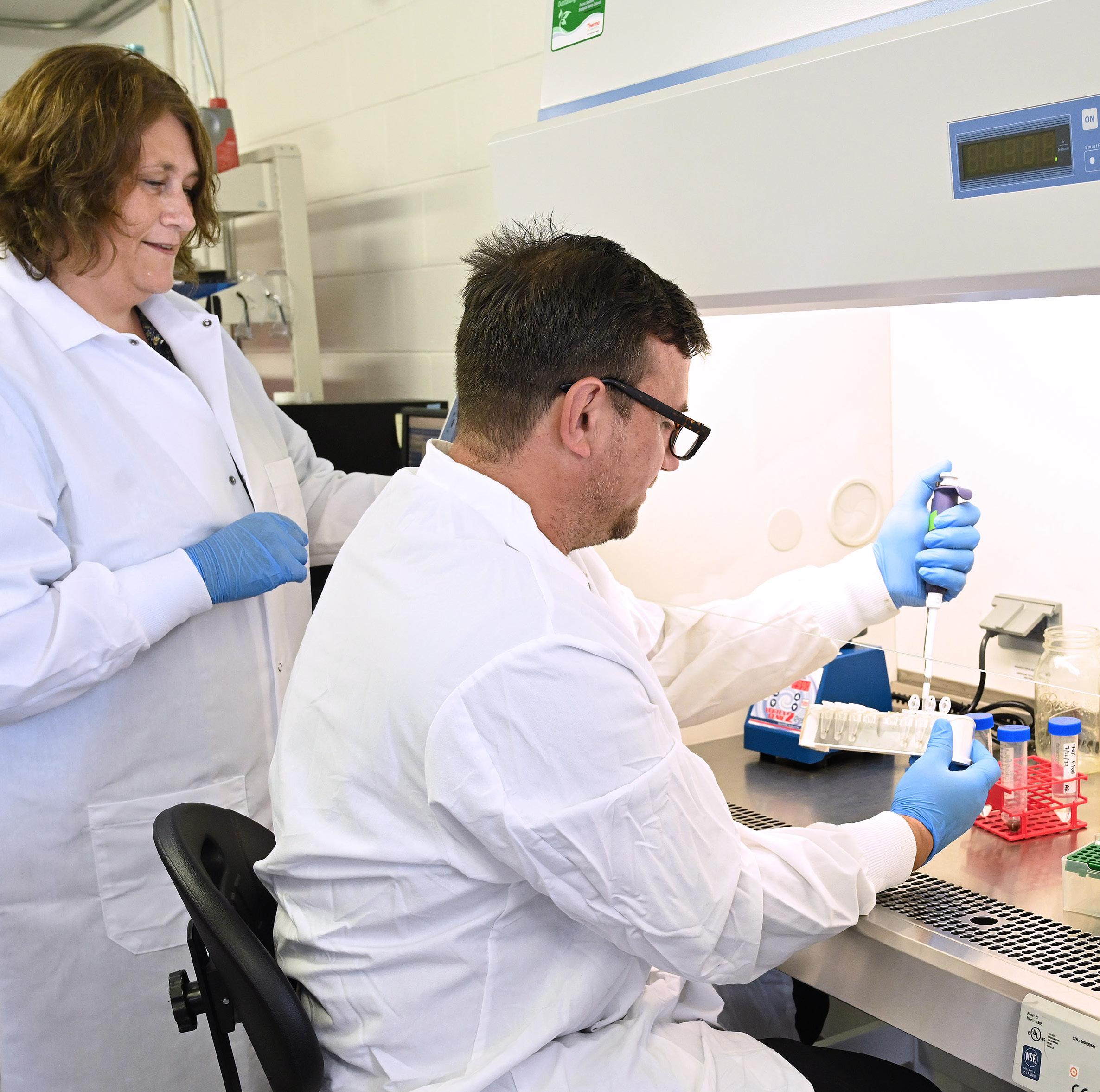
Dr. Kuhn supervising wastewater sample analysis in a George Lynn Cross Hall lab on the OU Norman campus.based on wastewater flow and population. “We don’t want to test in locations with too many factories and big businesses,” Kuhn says. “Those areas have completely different wastewater outputs than residential areas, and we want data (and poop) from where people are living.”
When asked how it works, Kuhn explained that the team uses a little machine with a hose that leads into the sewer system through a manhole. The machine collects sewage samples for 24 hours, and then someone from the team picks up the sample and drives it to the lab on the OU Norman campus. In the lab, the researchers purify the sample, extract the virus RNA [aka the genetic information], and test the sample using PCR analysis. The analysis determines if the virus is present in the sample and, if it is, how much of the virus is present. The team can also test for different variants, which allows them to quickly catch outbreaks from new variants.
is who's,” quips Kuhn. With wastewater surveillance, researchers capture data from an entire community, including the people who are infected but never go to the doctor or get tested. “It gives us a completely different picture of what the disease burden actually is,” says Kuhn. The hope is that wastewater surveillance will help public health researchers identify outbreaks in rural locations and areas with limited health care where people often don’t, or can’t, get tested by physicians.
When Kuhn and her team find high levels of COVID-19 (or another pathogen) in a sample, they immediately notify the corresponding local county health department. Health department employees can then go into the community and encourage testing, vaccinations, etc. Kuhn also mentioned that, early on when COVID-19 hospitalization rates were high, her team would notify local hospitals so the health care personnel would be prepared for a future influx of patients.
You might wonder why someone would want to study poop samples. Kuhn, who has worked in infectious disease surveillance for 15 years, has always been bothered by the fact that it takes so long to get surveillance data. “You are only getting the tip of the iceberg,” she says. “You only get the cases reported where people are ill enough that they go to the doctor, then the doctor has to order a sample, the sample has to be analyzed by a lab, they have to find the virus or bacteria in the sample, and finally the result has to be reported to the health department.” There are so many places in that process where a case could fall out and not be reported.
In many ways, wastewater surveillance is easier (and faster) than traditional surveillance measures. It doesn’t require taking individual samples from people to see what’s going on. “Obviously, I can’t tell whose poop
Kuhn sees wastewater testing as the backbone of future disease surveillance, and she hopes that eventually we will have sites in every community across the nation. “It’s a cheap, simple, and fast way to identify diseases in a community,” she says. The team recently signed an agreement with the Oklahoma State Department of Health to develop a statewide wastewater surveillance network. “We will have more than 40 locations that we’ll be monitoring, not only for COVID-19 but also to investigate how we can monitor for other diseases caused by foodborne and vector-borne pathogens,” notes Kuhn. The biggest issue that the team faces is working in rural areas where there isn’t an existing community wastewater system. An example of this is homes with septic tanks. This is something that the team is currently considering as they try to find a way to fit their surveillance into different types of sewage systems.

As an infectious disease epidemiologist, the pandemic proved to be beneficial for Kuhn and her research. “It was a fantastic oppor-
tunity for me to be able to set up the wastewater surveillance and learn how we can use this technology in the future with other diseases as well,’ she says. In many ways, Kuhn credits the pandemic with making the idea of wastewater surveillance more palatable to the general public.
When asked why she chose to study public health, Kuhn vividly recalls sitting in a master’s degree course at the London School of Hygiene and Tropical Medicine and hearing a lecture focused on the interplay between climate change and health in developing coun-
tries. “I kind of saw the light with that lecture, and I thought maybe this is something I could do with equations and predictions that could help people,” she says. Kuhn appreciates that her students could have a similar epiphany in the graduate courses that she teaches at the Hudson College of Public Health. In fact, several of her students have been involved in the wastewater surveillance research, and most have used their work as a basis for thesis or practicum projects. “The best part of the work I do is to see the students get excited about my research and experiences,” notes Kuhn. “It makes it all worthwhile.”
Bucket list item: Kuhn loves everything to do with water and the ocean. “I like to fish, so I want to go to Canada or Alaska and catch a salmon,” she says. “I also want to go to the Caribbean and catch some of the bigger fish there.”
Favorite thing about Oklahoma: “Everyone is so friendly,” says Kuhn. “Oklahoma is such a nice place, even though I had absolutely no idea and knew very little about the state when I first saw the faculty position here.”
Favorite food: Danish smørrebrød (pronounced smuhr-broht) sandwich. “We make a very nice one on black bread with shrimp, dill, mayo, and caviar,” declares Kuhn. Most surprising thing about Oklahoma: The food has been one of the biggest surprises. “We didn’t realize how many things you can actually fry,” she says. So far, Kuhn has tried fried pickles, fried green beans, and fried cheesecake. The huge trucks and cars here were also a surprise. “You don’t see big pickup trucks in Europe, so that’s been an eye-opener,” she says.
Favorite book: Kuhn has been a fan of Stephen King since she was 10 years old. “I know it’s not very academic, but I’m tired of reading academic books and manuscripts when I get home,” she comments.
“When need to relax, I get the newest book by Stephen King, and I just sit there and have a good time with it.”
Over the past two years, many of you have likely seen epidemiology Professor Aaron Wendelboe on the local news. His research on COVID-19 made him a popular guest to discuss updated case, hospitalization, and death counts—not just in Oklahoma, but also nationally and internationally. Participating in local and national interviews gave Wendelboe a chance to put some of his media training into practice. He notes that it’s not just about responding to the reviewer’s questions, it’s also about going into the interview prepared with the messages you want to emphasize and boiling them down to two or three points. “The key was delivering those points in a way that was confident but also humble enough to account for the fact that information was rapidly changing and being updated as we learned more about COVID-19,” he says. Rapidly changing information often made it difficult to predict what would happen next. “In the early days of the pandemic, I had to balance what we knew with what we didn’t know in a way that was helpful to the public, and it was certainly a challenge,” Wendelboe says.

As a Centers for Disease Control and Prevention-trained epidemiologist, Wendelboe has been preparing for a pandemic like this for his entire career. “My goal has always been to bridge applied and academic public health,” he says. It’s no surprise that he was asked to be the interim state epidemiologist in March of 2020 at the onset of the pandemic. During that time, Wendelboe helped to develop the Case and Contact Investigation Center at
the Oklahoma State Department of Health. This involved identifying a location, hiring thousands of people, setting up the IT infrastructure, and training supervisors and contact tracers—all while taking precautions to mitigate the spread of COVID-19. Wendelboe was also asked by the governor to develop a model that could help predict how COVID-19 might spread and impact Oklahomans in different parts of the state. He recognizes that this work with the OSDH was a great opportunity to bridge his academic research with practical applications. Wendelboe also credits this time for helping him to identify the most current pandemic-related issues and most common questions from the general public. “The issues and questions that were on people’s minds made it clear that there was a lot of misinformation and uncertainty about the disease,” he notes.
In an attempt to counter some of the misinformation and uncertainty about the COVID-19 vaccine, Wendelboe has given dozens of lectures and spoken at numerous town hall events across the state. “It’s difficult to know what impact the information we provided at these town hall meetings had on getting people immunized, but I hope that
Public health is special because it allows us to impact more people with fewer resources.
the information was helpful to people trying to make informed decisions for themselves and their loved ones,” he says. In addition to speaking with the general public, Wendelboe continued to lecture to his students in epidemiology courses at the Hudson College of Public Health. Specifically, he set aside time during classes to let students ask about COVID-19 or discuss epidemiological situations they had seen on the news. In many ways, the pandemic helped students contextualize epidemiology in a way that was relevant and interesting to them. “I used the COVID-19 vaccine as an example when our class talked about the difference between association and causation,” says Wendelboe. “We discussed how a researcher could find out whether the vaccines caused myocarditis [inflammation of the heart muscle], providing an opportunity for students to talk about the science and also discuss their preconceived ideas about vaccines and some of the political issues as well.”
Involving students in research is especially important to Wendelboe. Before there was a known case of COVID-19 in Oklahoma, he convened a group of five public health students to design a tabletop exercise for responding to an outbreak on campus. “I was really pleased with their work, and it was published in a peer-reviewed journal really early on,” notes Wendelboe. He also acknowledges the numerous students from the Hudson College of Public Health who served in many different roles at the OSDH over the course of the pandemic. Some of his students helped with epidemiological analyses, and others became supervisors with the Case and Contact Investigation Center. In fact, the template for the OSDH weekly epidemiologic summary was developed by a Hudson College of Public Health doctoral student. “In everything that I do, I try to
involve students to give them additional experience for their degree,” says Wendelboe.
In addition to his research at the college and with the OSDH, Wendelboe also works with community members and community-based organizations in the Oklahoma City metro area. During the pandemic, he aimed to better understand how different populations were impacted by COVID-19. Specifically, he wanted to know what services they needed for direct relief, as well as what services they needed to help with indirect impacts of the pandemic (e.g., access to food, transportation, and domestic violence support). One of the communities that Wendelboe worked with was a Marshallese community in Iowa. Initially, there were very few members who had received the COVID-19 vaccine. By working with trusted community leaders, Wendelboe and his team were able to increase the vaccination rate in the community from below 40% to over 80% in just a couple of months. Yet, not all of his experiences were this easy.
Wendelboe recalls an instance where he was working in an Oklahoma City metro community, and it took time to earn their trust. “They told me point blank that I look like a politician and that they didn’t really trust me,” he says.
“I wasn’t offended by that, but I bring it up to highlight that we need to develop community partnerships and work with organizations and people at different levels within communities.” One of the goals of this work is to help trusted community leaders become spokespeople for public health.
When asked what inspired him to study public health, Wendelboe recalls being a kid asking his science teacher, “How do we know that?” It wasn’t that he didn’t trust his teacher, but he had a keen desire to understand how we know things. “When I took my first epidemiology class in graduate school, I
realized that’s essentially what epidemiology is: trying to understand how we know what we know and quantifying our uncertainty,” says Wendelboe. Once he realized that it fit with his way of thinking, he shifted gears from pursuing a career in medicine to study-

ing public health and epidemiology. “Public health is a balance between addressing immediate needs and future needs,” he says. “Public health is special because it allows us to impact more people with fewer resources.”
Bucket list item: Scuba dive at the Great Barrier Reef in Australia. Favorite thing about Oklahoma: “I’m impressed by the great food that we have here,” Wendelboe says. “Big cities like to think they have a monopoly on ethnic cuisine, but I think the sushi, ramen, etc., in Oklahoma is just as good as what I’ve eaten in other places.”
Musical hobby: Wendelboe learned to play the guitar during the pandemic. “It provided an avenue for me to meditate and do something completely different from the scientific thinking and worries about COVID-19,” he says. When asked if he was in a band, he noted that he isn’t currently, but part of him would like to perform live.
Favorite book: “I’m a science fiction and fantasy nerd,” says Wendelboe. His favorite author is Brandon Sanderson, so he’s looking forward to the release of the fifth book in the Stormlight Archive series.
In the early days of the pandemic, I had to balance what we knew with what we didn't know in a way that was helpful to the public.DR. CHANGJIE CAI
For occupational and environmental health science Professor Changjie Cai, the pandemic provided a myriad of research opportunities to study the best ways to protect people in different environments. As an aerosol scientist, most of Cai’s work involves studying suspended solid and/or liquid particles in the air. From a stationary airplane fuselage (also used for pilot training) on the Oklahoma State University campus to an enclosed toilet chamber in his lab at the Hudson College of Public Health, Cai and his team are collecting air samples to test for the presence of particles that might contain COVID-19 and analyzing how particles move through different spaces. Dr. Cai’s studies are funded by U.S. Centers for Disease Control and Prevention, Presbyterian Health Foundation, and the National Aeronautics and Space Administration.
One of Cai’s many projects includes analyzing the dispersion of small airborne particles in aircraft cabins. His goal is to find ways to reduce exposure to airborne pathogens during air travel. Cai is particularly interested in submicrometer particles, a.k.a. particles that are smaller than a micrometer. (For reference, a single strand of hair is between 100 and 150 micrometers wide.) “The reason I’m interested in submicrometer particles is that those particles can stay in the air for much
longer than larger particles,” says Cai. For example, a previous study found that particles roughly 0.25-0.3 micrometers have the highest amount of COVID-19, and particles of this size can stay in the air for over three days without ventilation. For this project, Cai and his team aimed to develop an airflow controller for reducing particle concentrations. The first step was to analyze how different-sized particles moved throughout the aircraft cabin. In particular, they wanted to see how the aircraft ventilation system would impact particle distribution. Then the team looked at how different factors (e.g., the overhead seat fan, distance from the aerosol generation source, and seat direction) impacted the particle concentrations.
 COVID-19 FACULTY STORIES
COVID-19 FACULTY STORIES
Something that we can recommend for people who are traveling: turn on the fan to reduce the risk of exposure to not just COVID-19 but any kind of airborne disease.
“We’ve found some interesting results,” says Cai. For example, they noticed that ventilation was effective at reducing particles less than 0.5 micrometers in size. However, it wasn’t very effective for large particles. They also found that turning on the overhead seat fan and directing it towards the face (and, more importantly, breath) can help to reduce over 90% of the aerosol exposure. “That’s something that we can recommend for people who are traveling,” says Cai. “Turn on the fan to reduce the risk of exposure to not just COVID-19 but any kind of airborne disease.” Cai and his team also found that source control is very effective. When a single fan was turned on over the source, it helped to significantly reduce the distribution of the particles. The next step is to develop a lowcost airflow controller that would be placed in front of each seat. Essentially, this controller would capture the aerosols expelled from a person’s mouth or nose and move the air through a ventilation system, ensuring that the particles never have a chance to circulate in the aircraft and infect others.
If you can’t find Cai in the test aircraft, you might look for him in the toilet lab on the fourth floor of the Hudson College of Public Health. This lab is aptly called the toilet lab because it contains a large chamber with a flushing toilet. Previous studies in the chamber found that flushing the toilet generates numerous aerosol particles and large droplets, which are mostly caused by the bubble bursting and splashing as the water is sucked into the toilet. It’s important to study these particles and droplets because they can contain bacteria and viruses that become aerosolized and land on surfaces each time a toilet is flushed.
Unsurprisingly, different types of toilets can generate different amounts of particles—usually based on the water pressure. Cai and his team are looking at the different particle sizes created by flushing a commercial (flushometer-valve) toilet. This type of toilet is commonly found in commercial, industrial, and institutional restrooms (including hospitals). The aerosol measurement devices Cai and his team are using can measure a wide range of particle sizes, from 10 nanometers up to 20 micrometers, across 152 size bins. For reference, one nanometer is between two and 10 times bigger than the size of an atom.
Beyond simply measuring particle sizes, Cai and his team are also looking at ways to reduce the particles generated when the toilet is flushed. “Most institutional toilets don’t have a lid because lids can foster germ growth and are not easy to clean,” says Cai. However, this means that there is no barrier to keep particles from spewing into the air when someone flushes the toilet. To address this issue, Cai tested a temporary lid that acts as a blocker when a toilet is flushed, and he found a 50% reduction in aerosolized particles. He also observed that the lid was effective at reducing the number of droplets on nearby surfaces.
Next, Cai and his team used fluorescent dye to look at how the particles deposited on the bottom of the temporary lid. They discovered
most of the particles on the back part of the lid. However, they noted a large number of small particles escaped from the sides since the temporary lid wasn’t completely sealed. Cai hopes to improve the lid by using a filter and a small vacuum to capture these runaway particles. He notes that this type of device would be most useful to janitorial staff who clean toilets in health care environments with sick patients. It would also help protect nurses or others who might be exposed to particles deposited on surfaces or left floating in the air. “Our department mainly focuses on the occupational environment,” says Cai. “So, we are especially interested in protecting workers.”
Cai acknowledges the master’s and doctoral students who have participated in these projects and helped analyze the data. Several of his students have used the research for their thesis or dissertation work. Occupational and environmental health students have also co-authored articles with Cai for peer-reviewed publications and presented research findings at national and international conferences. Since many of Cai’s projects
are cross-disciplinary, his students have lots of opportunities to work with researchers from a variety of backgrounds and teams across the Health Sciences Center and OU Norman campuses.

When asked why he chose to study occupational health and environmental science, Cai notes his early interest in atmospheric science. “I was working with aerosols in the atmosphere and looking at how they impacted human health,” he says. At that time, Cai didn’t know about occupational and environmental health science. He laments that many people don’t know about this field. “Working environments impact almost every person at some point during their lives, so it’s important to make sure that working environments are safe and promote good health,” says Cai. He credits his doctoral advisor (Dr. Thomas Peter from the University of Iowa) for introducing him to aerosol exposure in occupational health science. Cai was immediately drawn to this field because he felt that he could directly help people reduce their risk of aerosol exposure.

Water hobbies: “I love swimming, boating, and fishing,” Cai comments. Yichun, his hometown in China, has natural springs and mountains. “When I first told my colleagues I was moving to Oklahoma, they felt like it was the middle of nowhere,” says Cai. “I really like it because there are a lot of lakes here.” Favorite board game: Cai is a fan of an Asian board game called Go. It’s a two-player game with the goal of occupying more territory than your opponent. “It’s considered one of the most complicated games in the world,” notes Cai. In 2016, developers created an artificial intelligence (AI) program that could defeat a human opponent. “I have a hard time envisioning AI defeating a human in this game,” he says. “It’s not just about calculations; there is an art and science to it as well.” Someday, Cai would like to test his Go skills with a match against the AI program.
Favorite food: BBQ lamb ribs. “I really enjoy cooking,” he says. “My wife, Dan, and my 1-year-old son, Ethan, are my biggest fans!”
In June of 2020, OU President Joseph Harroz, Jr. asked health administration Professor Dale Bratzler to be the chief COVID-19 officer for the University of Oklahoma. This was a time when the pandemic was ramping up, and different departments in different colleges on different campuses were trying to figure out how best to protect their faculty, staff, and students. Bratzler speculates he was asked to take the position in an effort to unite the three campuses (Norman, Oklahoma City, and Tulsa), each with its own set of educators and leaders. “President Harroz was quick to recognize the need for thoughtful policy implementation and unified messaging," states Bratzler. "We needed consistency and to be clear about what to prioritize." In his new position, Bratzler became a central hub for all pandemic-related recommendations. He would evaluate each one before sending it to President Harroz for approval and university-wide implementation.

Bratzler also recognized that recommendations and policies would differ between the campuses. For example, the policies on the Health Sciences Center campus (where patient care is involved) needed to be different from those on the Norman campus. Even though the pandemic has ebbed, the university continues to monitor all aspects—including the number of students infected, isolated, and quarantined. “On the HSC campus, we were vigilant about our workforce needs and
safety,” says Bratzler. “This included making sure that we had enough masks and gloves for our health care providers and students across the campus.”
Once vaccines became available in December of 2020, Bratzler and his team decided to utilize HSC students to help deliver as many COVID-19 vaccines as possible. The College of Pharmacy and the College of Nursing students had a head start since vaccination training was already built into their programs. However, the College of Medicine and the College of Dentistry programs had no formal training in delivering vaccines. “I pulled together a group working with student leadership on campus to put (literally) hundreds of our students through training on how to screen people for vaccination, draw and deliver the vaccine, and enter information for post-vaccine monitoring,” recalls Bratzler.
Within the first four months, nearly 50,000 COVID-19 vaccine doses were administered on the HSC campus. These clinics weren’t just for OU employees and students; they were focused on vaccinating the general public in the Oklahoma City metro area. In addition to events on the HSC campus, Bratzler and his team held multiple vaccination trainings and events on the Norman campus.
Bratzler is incredibly proud of how students were included in these events. In the Hudson College of Public Health, many students
helped administer the campus vaccine program; this included coordination, wayfinding, registration, and numerous other roles. Bratzler also acknowledges the university IT team’s excellent job building the screening tool. He credits the team for ensuring that vaccination data was automatically uploaded to the Oklahoma immunization registry.
According to Bratzler, one aspect of the chief COVID-19 officer role that surprised him the most was how he “became the big spokesperson for COVID-19 in the community.” Given that he was conducting weekly media briefings, it makes sense that he has been called the Dr. Fauci of OU. During these briefings, Bratzler discussed findings from the most recent medical literature to ensure that the general public was up-to-date on the pandemic. “I realized that part of this was to discredit some of the misinformation out there, so I made a point of always providing handouts to the press and including references for them to check my sources,” says Bratzler. He commends the OU Communica-

tions team for setting up the briefings with live stream and then sending the recording to the media afterward. “Reporters could participate in the live stream and text questions to the moderator,” Bratzler notes. “That kept the media from coming to the HSC campus and allowed us to maintain physical distancing.”
His news conference experiences also provided great examples for Bratzler to discuss in lectures with undergraduate students in Norman and graduate students in Oklahoma City. “It was so easy to teach some of the concepts of public health because the students were able to draw upon what was happening all around us,” Bratzler comments.
“Many of the basic public health concepts became real to them.”
When asked about the pandemic’s impact on the field of public health, Bratzler acknowledges that the general public has a greater awareness of public health right now. At the same time, he mentions the national shortage of public health workers. “I think we need
to use this opportunity to train more public health students and provide basic public health training in other programs [e.g., medicine and nursing],” says Bratzler. Due to the pandemic, there is substantial federal and private funding for public health programs and initiatives. However, history shows that this likely won’t last. “One thing that worries me a bit is something called the boom and bust funding of public health,” Bratzler reveals. “Right now, we are in a boom, but eventually, the pandemic will fade, and we will likely revert to budget cuts.”
Improving the data infrastructure in health care is critical to withstand the impending decline in funding. It’s no secret that the existing public health data infrastructure failed during the pandemic. Modernizing this infrastructure will include connecting public health data systems with other health systems to better predict and manage future outbreaks and pandemics. “This will require careful planning on how we take all of the different data sources and pull them together,” says Bratzler.
Bratzler also reminds us of the concept of the slow pandemic. Essentially, the slow pandemic refers to the chronic diseases (e.g., obesity, diabetes, and cancer) that kill Oklahomans daily. “Part of the reason I believe that Oklahoma had such a high mortality rate from COVID-19 was because of the unhealthiness of the population in our state,” says Bratzler. He emphasizes the importance of addressing chronic diseases and health equity issues across the state to ensure that
we are more prepared for pandemics in the future.
When asked why prospective students should consider studying at the Hudson College of Public Health, Bratzler notes the long track record of excellence in education and public health that the college has. As the only accredited public health program in Oklahoma, the college provides a variety of training options in biostatistics, epidemiology, health administration and policy, occupational and environmental health, and health promotion sciences. The college is currently working to enhance online education courses and certificate programs. “I would be pleased if every medical and nursing student at OU came out of their program with—at the very least—a basic certificate in public health,” says Bratzler. “ Public health knowledge is essential for health care providers to successfully respond to another major pandemic.”
When questioned why he chose to study public health, Bratzler recalls his early days as a physician working at a hospital in Tulsa. He was particularly interested in health care quality and practice guideline implementation. “I was questioning how we change the way that health care is delivered, and I realized that I needed additional training,” says Bratzler. In 1996, he earned a master’s degree in public health from OU. “I made many friends and connections, which is important in public health, and I utilized my skills in biostatistics and epidemiology to better understand and interpret data,” he says.
Bucket list item: Bratzler loves to travel and would like to travel more in the future. “I tend to prefer mountainous areas, so I would explore the Alps in northern Europe,” he says. Nature photography: Bratzler enjoys spending time in Alaska taking nature photos. “I have a big thing about capturing images of bears in the wild,” he mentions. Book recommendation: Most of what Bratzler reads is related to health care. “I’ve read piles of medical articles on COVID-19 over the past couple of years,” he says. His book recommendation is Patients Come Second, which the new CEO of OU Health suggested. “It seems counterintuitive,” Bratzler notes. “But the point is that you can’t improve the patient experience until the people within the organization are happy and enjoy what they do.” Woodworking hobby: Bratzler also enjoys woodworking and watching home construction shows on television. “My wife and I have completely rebuilt our barn, and I just really enjoy building things.”
Health promotion science Associate Professor Kerstin M. Reinschmidt is a trained medical anthropologist and has worked extensively with community health workers (CHWs) for the past 20 years. The American Public Health Association CHW Section defines a community health worker as “a frontline public health worker who is a trusted member of and/or has an unusually close understanding of the community served.” This trusted relationship makes CHWs intermediaries between community members and health/social services. Recently, Reinschmidt’s interests have expanded from CHW training and intervention to workforce development efforts.

Like many of us, Reinschmidt took note of the pandemic in March of 2020. “I was in Stillwater at an Oklahoma State University-led CHW forum just a couple of days before everything shut down,” recalls Reinschmidt. The timing was serendipitous since the forum was focused on creating awareness of the CHW workforce. Reinschmidt began thinking about how CHWs could be involved in the pandemic response. Since her previous work involved CHWs working with chronic diseases, Reinschmidt began researching CHWs working with infectious diseases. “I came across information about how CHWs have worked on Ebola prevention and control in African states,” says Reinschmidt. This reinforced that CHWs could be incredibly useful in helping to prevent and control COVID-19 in local communities.
During this time, Reinschmidt also attend-
ed numerous webinars hosted by CHWs to learn more about how they were helping with the COVID-19 response. This led to her first COVID-19 research project, where she compiled pandemic-related resources for CHWs. She presented this information at the 2021 Oklahoma Community Health Worker Forum Series. To watch the presentation, visit the Oklahoma Public Health Association (OPHA) YouTube channel link at www.youtube.com/ watch?v=wlWgF42AYVQ.
In order to learn more about CHW pandemic experiences and needs in Oklahoma, Reinschmidt talked to CHW members of the OPHA CHW Section and the OCCHD Wellness Now CHW Workgroup, both of which she co-founded. “I was interested in looking at what was going on at the community level with respect to COVID-19,” says Reinschmidt. “That’s what health promotion science is all about: working and collaborating with communities.” Reinschmidt notes that she observed a lot of top-down communication and messaging from the Centers for Disease Control and Prevention and the state and local health departments. She wondered if these messages were a one-size-fits-all approach or if they were being tailored for different communities. “I wanted to know if communities were receiving the messages, and if they were, did the messages make sense to them,” comments Reinschmidt.
Reinschmidt is also passionate about data reflecting the diversity among communities.
She notes that a lot of the data collected early on in the pandemic was missing information about racial and ethnic groups. “We need to know that information,” says Reinschmidt. She specifically recognizes the need to contextualize data that reflects the disproportionate burden of COVID-19 for different racial and ethnic groups. “We must acknowledge that some groups have a higher burden of COVID-19 because of the continued disparities related to social determinants of health,” says Reinschmidt. “This is important to take the stigma away.” Public health professionals and communicators need to work with community partners and directly involve them in public health messaging. “Community health workers are perfect for helping with this because their work is about reducing health disparities, supporting health equity, and helping with social justice,” states Reinschmidt.
In late 2020, Reinschmidt was asked by a group of colleagues to send out the CHW COVID-19 Impact Survey to community health workers across Oklahoma. “The survey specifically focused on what trainings
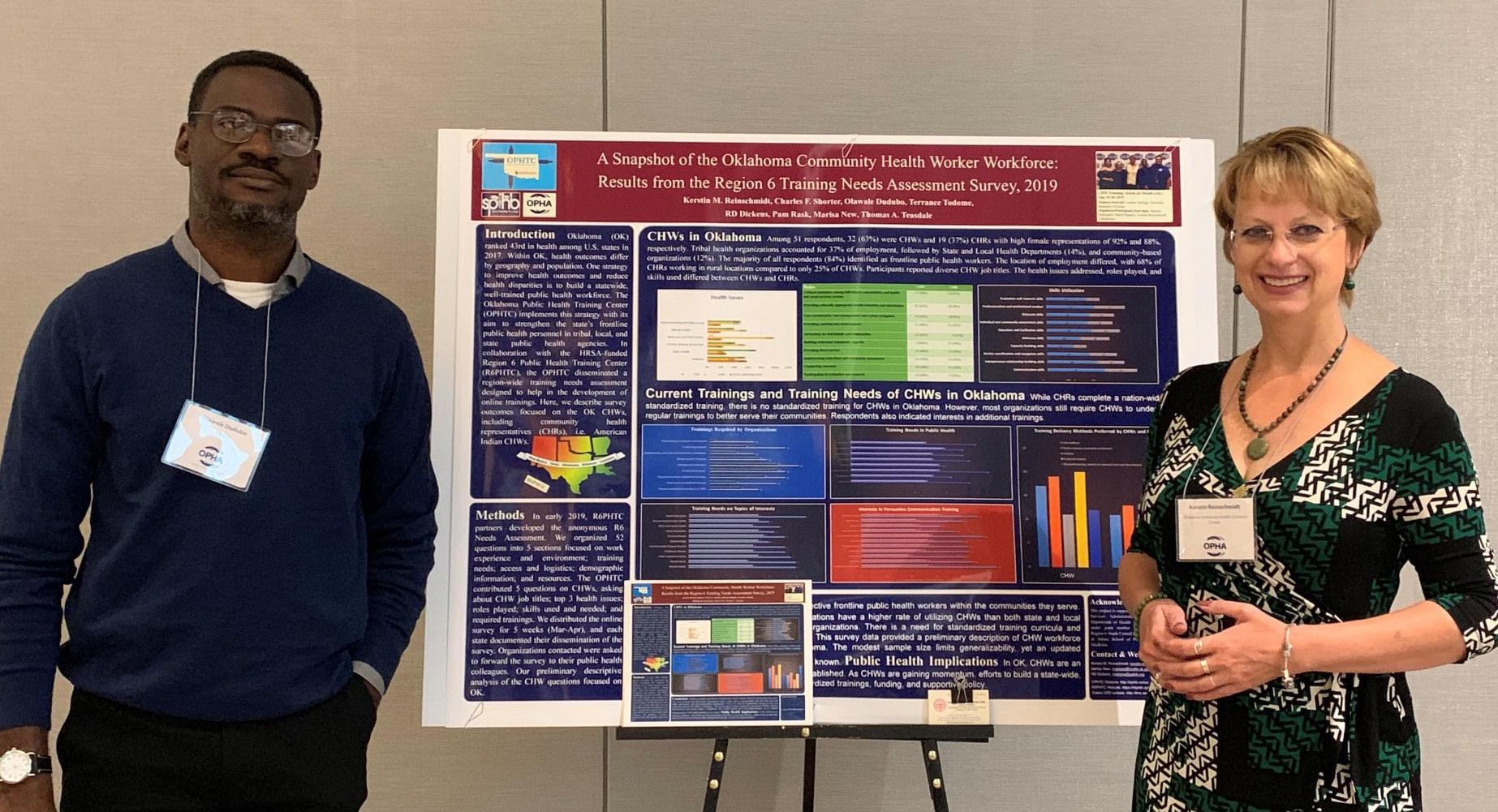
CHWs took during the pandemic and what trainings they need to better prepare for future public health emergencies,” she says. Reinschmidt worked with a BERD staff member and a biostatistics student to analyze the survey results. Unsurprisingly, she found that the pandemic impacted CHWs at the professional and personal level. At the start of the pandemic, CHWs were utilized as contact tracers, which pulled them out of their communities. “The direct contact with the population they serve was cut off, which was really bad because that’s at the core of what a frontline public health worker does,” says Reinschmidt. Many CHWs also had to balance continued needs in their communities (e.g., food, transportation, and chronic health care) with the added burden of COVID-19.
In 2021, Reinschmidt was asked to do a follow-up survey with CHWs that included questions about the recently approved vaccines. She worked with a colleague from OSU and a biostatistics student at the Hudson College of Public Health to organize a townhall and advisory board with CHWs to present the results from the first CHW COVID-19 Impact
Survey, and ask CHWs for recommendations and input on what additional information they wanted and/or needed to know. The responses were used to revise the survey before Reinschmidt distributed it. It’s important to note that CHWs from tribal nations were included in the townhall and survey distribution. The results from this follow-up survey indicated that CHWs felt that high-risk and disproportionally disadvantaged communities in Oklahoma weren’t being heard and didn’t have adequate access to necessary resources.
“The data from the two surveys is invaluable and super important because it highlights that this is a workforce that needs to be valued and supported,” says Reinschmidt. “The next step is to make our findings part of the
CHW Coalition work that I’m leading.” The final survey reports can be found on the Oklahoma Public Health Training Center website at https://ophtc.ouhsc.edu/Resources.
When discussing why she chose to study public health, Reinschmidt mentions her medical anthropology doctoral dissertation chair who had a background in public health and a master of public health degree. “I was impressed by the way he was able to apply medical anthropology with the added benefit of public health,” recalls Reinschmidt. This inspired her to pursue an M.P.H. program at the University of Arizona, the same semester that she graduated with her doctoral degree.
Bucket list item: “Being an anthropologist at heart, I want to travel the world,” says Reinschmidt. She enjoys seeing different countries and experiencing different cultures—especially in countries where she doesn’t know the language. “I speak English, Spanish, and German, so I get around pretty well in certain parts of the world,” she says.

Hometown: Reinschmidt grew up in Hanover, Germany. “That’s where they speak the best German,” she claims jokingly. “High German, the official language of Germany, is from this region.”
Favorite food: Reinschmidt loves Korean food. When her husband lived and worked in Korea, she visited him several times. “I love the taste of the food—especially the kimchi and garlic flavors,” she says. “It’s just awesome.” Book recommendation: Reinschmidt minored in American literature as a student in Germany. She is particularly fond of autobiographies. One book that she recommends to her students is Change Your World: The Science of Resilience and the True Path to Success by Michael Ungar. “We all need to be connected and supporting each other because that’s how we can be resilient,” says Reinschmidt. Dancing hobby: Reinschmidt has been Latin dancing for the last 20 years as a way to exercise, relax, and have fun. “When the pandemic hit, I stopped dancing because it’s a close contact activity,” laments Reinschmidt. In place of dancing, she and her husband started walking every day, and it quickly transitioned into running. Reinschmidt hopes to eventually return to dancing. “It’s still a very big part of me,” she says.
Dr. Reinschmidt showcasing her flamenco (sevillanas) dancing skills. Dr. Reinschmidt presenting her CHW research at the Oklahoma Public Health Association annual meeting.That's what health promotion science is all about: working and collaborating with communities.
 LANCER STEPHENS
LANCER STEPHENS
Creating an equitable, diverse, and inclusive environment is paramount to student, staff, and faculty experiences at the Hudson College of Public Health. With this in mind, past HCOPH Dean and new Senior Vice President and Provost Dr. Gary Raskob appointed Dr. Lancer Stephens, associate professor for health promotion sciences, as the associate dean for sovereignty, equity, diversity, and inclusion for the college. As a Native American tribal member, Stephens explained that it was important to him to include sovereignty in the title to acknowledge the strong relationship the college has with tribes and to be a constant reminder that we all have the right to be who we are without judgment or persecution.
This initiative includes faculty and students across the HCOPH. “I knew this initiative and developing its vision would require multiple sources of input, not just my own, to be successful,” says Stephens. His first call was to Dr. Deirdra “Dee” Terrell, associate professor, biostatistics and epidemiology, who has also worked in the area of diversity, equity, and inclusion for multiple years on local and national scales. “Dee and I have known each other since arriving on campus as doctoral students, and we have a relationship where we can speak freely and openly,” comments Stephens. “This is vital because a lot of ideas were discussed, and Dee helped to bring balance and focus.” Noting the extensive work being conducted, Dr. Bratzler, HCOPH interim dean, appointed Dr. Terrell as the SEDI faculty liaison to recognize her commitment to the students and the vision of the SEDI office.
In addition to the Faculty Liaison, the Hudson College of Public Health Student Association recently appointed Moriah Contino to be the SEDI and Interdisciplinary
Programs student liaison. The president of HCOPHSA, Whitney Kerr, is excited about the new position and the office. “When I heard that Dr. Stephens and Dr. Terrell were spearheading a SEDI office for our college I felt this was very important for the student association to connect with the office on a regular basis,” says Kerr. "I want all of our students to enjoy their time here and feel like the college is a safe space for their personal and professional growth.” Kerr aims to ensure that HCOPHSA is a resource for students and creates a learning environment where everyone feels welcome, respected, and supported.
The newly decorated SEDI office can be found on the first floor of the HCOPH in Room 156. This is a space where students, staff, and faculty within the college can go if they have an issue to discuss or are simply wanting to have a conversation and be heard. The plan is to have established weekly office hours with Stephens or Terrell. They are also looking into conducting routine listening sessions. The goal is to provide a safe space where anyone can go to talk or vent about relevant issues. Stephens mentions that this is something neither he nor Terrell had when they were students. “Just knowing that the space is there means a lot and can be a huge benefit,” says Stephens. “My hope is that no student ever comes in with a problem, but we are here to help if they do.”
Programs and policies can be developed without insight about whether they will impact everyone equally and fairly; as we’ve seen, unfortunately sometimes they do not. It’s extremely important for our public health students—and the eventual leaders they will become—to be able to look at programs and policies from different points of view to ensure that they are fair. I believe the classes here at the HCOPH and the SEDI initiative can help ensure that is the case.
The office also includes a library with books to help students see the world from other perspectives and develop leadership skills to empower everyone. “Any book that can help give a student a different perspective and build respectful relationships is a good book,” Stephens remarks. “If you go through life only looking through your own cultural lens, you’re missing a lot of the world. As public health professionals, connections to communities are paramount for our success, and the best way to connect is to go to that community and get involved.
Reading can help you prepare for this.” Students are encouraged to take books from the office, return them, or pass them along to others. If there are any books that you would like to see in the SEDI library, the office is currently accepting book donations.
“We want it to be known that this college is accepting and welcoming,” says Stephens. “Everyone should feel like a part of the SEDI office. It doesn’t matter where you come from or what your background is; all are invited.” The office is dedicated to helping students and giving them the tools to do incredible work going forward. To stay up-to-date with the SEDI office and SEDI initiatives, visit https://publichealth.ouhsc.edu/Diversity-Inclusion
Be who you are, and you will be accepted here.

worked at the CDC Foundation—attached to the Oklahoma State Department of Health—as a COVID-19 emergency relief epidemiologist and data analyst in the Acute Disease Service’s surveillance program. I analyzed state surveillance data in order to provide daily COVID-19 case counts and other surveillance reports, as well as worked to streamline disease reporting and improve analysis efforts at OSDH. If you saw the daily COVID-19 numbers, those actually came from me!

As a student, I helped organize and coordinate the Oklahoma branch of the Systematic Observation of Masking and Distancing in which we collected observational data in collaboration with an international research group headed by the Kaiser Permanente health system. These efforts were aimed at understanding how people in different areas reacted to risk, public health suggestions, and mandates concerning health behaviors such as mask wearing and physical distancing.

volunteered with OU Health in the early stages of vaccine distribution (January/February 2021) and entered COVID-19 patient vaccine data into the Oklahoma State Immunization system. This work contributed to a comprehensive effort to vaccinate over 25,000 of Oklahoma’s frontline workers and most vulnerable citizens. In addition to my volunteer work, I was part of the newly launched COVID-19 Committee in the Hudson College of Public Health.
I was also interviewed by News 9 for their Student Spotlight series to share my story of how the pandemic shaped my career and how it inspired me to pursue a graduate degree in public health, specifically epidemiology. (Link to news feature: www.news9.com/ story/60b8e1dd9b60d70baea43954/student-spotlight:-ou-graduateinspired-by-passion-for-public-health).


 Ozair Naqvi Ph.D.
Ozair Naqvi Ph.D.
I’m a former epidemiologist with the Acute Disease Service of the Oklahoma State Department of Health. I worked 24/7 on the state’s COVID-19 emergency response team for 16 straight months before beginning my PhD coursework at the Hudson College of Public Health. I’m now partnering with the Oklahoma Alliance for Healthy Families to share scientific information on everyday actions people can take to protect themselves and others from COVID-19 infection.
Example of a video I created: www.fb.watch/b_UrhkLcwf/
During the pandemic, I volunteered and conducted remote data entry for a variety of vaccine clinics. I was also a contact tracer for the Oklahoma City County Health Department. In 2021, founded the COVID-19 Committee—a student-led committee that recruits and connects OUHSC students across all seven colleges to COVID-19 projects and initiatives happening on campus and in Oklahoma. The C19C also recognizes student involvement in the fight to end the pandemic.

worked on two COVID-19related projects addressing vaccine hesitancy among underserved populations and long-term sequelae of SARS-CoV-2 (long-haul COVID-19). was also a graduate research assistant for Dr. Mary Williams, providing epidemiological and biostatistical support for Muscogee (Creek) Nation. In that role, assessed COVID-19 vaccine hesitancy and conducted community health needs assessments to examine the pandemic’s impact on this patient population.

My graduate thesis research focused on examining long-term consequences of COVID-19 among OU COVID-19 patients in Tulsa and Oklahoma City. This condition is defined by the World Health Organization as post-COVID-19 condition. My research aimed to better understand this condition in Oklahoma. The study was the first to estimate the prevalence of PCC in Oklahoma and examine demographic, clinical, and COVID-19 severity features that may predispose patients to develop PCC.
With the Unity Clinic in collaboration with the OU Health vaccination team, I was able to help with process improvement, quality, patient satisfaction, volunteer training, patient scheduling, and more. During my time as a volunteer (over 150 hours), I assisted in vaccinating over 50,000 Oklahomans.
I volunteered at the OU vaccination clinic in the spring of 2021. I also interned in the Emergency Preparedness and Response Services department at the Oklahoma State Department of Health) where I assisted in the coordination of ordering and distributing COVID-19 therapeutics and medications (monoclonals and antivirals) within the state. I was charged with revamping and revising the OSDH COVID-19 dashboard to aid researchers and other professionals in identifying past and present trends, as well as easily gathering relevant information to devise more meaningful and decisive interventions and preventative measures.
volunteered at the Manos Juntas clinic in Oklahoma City during the pandemic. We helped to educate patients about COVID-19 and offered them information on vaccine access and counseling. At this clinic, we did COVID-19 testing. The clinic also offered COVID-19 vaccines to patients at certain times throughout the year.
I worked at Oklahoma City County Health Department and put in roughly 290 hours doing contact tracing and COVID-19 case investigation. also volunteered with OUHSC vaccine events in the spring of 2021, where registered individuals to receive vaccines.
 Kara Cornell Master of Health Administration
Vaishnavi
Kara Cornell Master of Health Administration
Vaishnavi
 Whitney Kerr HCOPHSA President Epidemiology
Whitney Kerr HCOPHSA President Epidemiology


While working in clinical research after completing my M.S., experienced firsthand the impact that research can have on participants’ lives and the importance of the work that we do in participants’ experiences of health care. I got to know many of my research study participants on a personal level, and they trusted me with their stories and experiences of the health challenges they were facing. I feel like in epidemiology it’s easy to grow comfortable with working with numbers and get caught up in our scientific jargon and protocols; but there is a very human side to the work we do, especially when we work on projects collecting primary data by interacting with participants directly. It is of utmost importance to me to carry this perspective into my career and hopefully pass it on to students and trainees I work with one day. My experience working in clinical research has inspired me to pursue doctoral training in epidemiology with the goal of one day serving as a faculty member at an academic research institution and providing leadership in research as well as educating future research professionals.
Ozair Naqvi HCOPHSA Vice President Epidemiologywas always interested in pursuing a career in the health sciences realm, but in college, I read two books that changed me: The Great Influenza by John Barry, and The Next Pandemic by Ali Khan. Barry helped me find where I belonged: in public health; Dr. Khan showed me how to live in it: epidemiology. How could a yet undiscovered virus upend the entire world and kill millions? How heroic and awe-inspiring is the experience of entering the hot zone and saving lives by the thousands? When I think of epidemiologists, I think of giants like DA Henderson, who led the smallpox eradication program, the greatest medical achievement in human history. was inspired by this meticulous harnessing of data and medicine applied to populations to stop the spread of deadly diseases in their tracks. To me, this represented real, impactful change –the kind that I have longed to be a part of.
Malik HCOPHSA Secretary Health AdministrationI went to medical school in Pakistan; in order to obtain a license to practice as a general physician, I worked in a tertiary care hospital for one year. During that time, we had a Joint Commission International inspection and had many sessions on quality and quality improvement. I found health care quality to be exceptionally interesting and wanted to learn more about it.
 Angela Sharma HCOPHSA Treasurer Health Administration and Policy
Angela Sharma HCOPHSA Treasurer Health Administration and Policy


I had always been searching for my place in the field of health care and OU’s MHA program has really helped me find my place. Public health is a way to improve the health and well-being of other people and communities on an interprofessional and personal level. One of the most rewarding benefits for me in public health is knowing that I am making a lasting impression to improve society and access to care for my community.
April K. Lopez HCOPHSA Senator BiostatisticsWhen was an undergraduate student, I majored in biochemistry. I took my first public health class in my junior year of college and immensely enjoyed it. Public health filled in missing gaps when it came to health that I wanted to expand more on it.
 Patel HCOPHSA Senator Biostatistics
Patel HCOPHSA Senator Biostatistics
I chose to get a public health degree because I wanted to be in the medical/health care field, but science was not my best/favorite subject. Instead, I wanted to find a way to use my math skills, so got my bachelor’s degree in statistics. I later discovered biostatistics and thought it was the perfect combination and would be a great fit.
chose public health as my degree because I wanted to be involved in preventative care with a strong interest in chronic diseases. There are many factors that result in someone developing a long-term disease and figuring out how to eliminate contributing factors interests me. I also enjoy being surprised when the data shows something different than expected because not everything is as it seems when it comes to determinants of health.



When graduated high school, I received life-changing brain surgery. Although I was very lucky, the disparities in health care were made clear to me. The surgery changed my life in more ways than one. Not only did it change my health drastically, but it also changed my career path.
HCOPHSA Interdisciplinary Program and Education Liaison Interdisciplinary Public HealthWhen I was working as an intern physician during the COVID-19 pandemic, I got a chance to work with skilled public health professionals who were trying to develop different measures to curb the deadly pandemic. At that time, I understood the importance of public health field that as a physician I can treat a patient individually, but as a public health professional, I can study the trends and take adequate steps to prevent pandemics like COVID-19. I decided to pursue M.P.H. because I think that the having knowledge of clinical medicine and population medicine is essential to become a well-rounded physician.
Why did you choose to get a public health degree?
The Hudson College of Public Health is committed to preparing the next generation of leaders who promote the well-being of our families and communities.
In 2003, the Hudson College of Public Health had three scholarships to award.
This year, the college will award 35 scholarships of at least $2,500 to deserving students.
Each of these scholarships was created by generous donors and are named to honor them and their loved ones.
Scholarships provide not only critical financial resources to our students, but also invaluable encouragement that someone believes in their potential and wants to see them succeed.
While the incredible growth of donor-funded scholarships has helped dozens of students in recent years, today the college has the resources to provide scholarships to more than 20% of the talented students who apply with financial need.

Please join us in supporting our students as they work to protect and improve the health of the people of Oklahoma and beyond.
Receiving a scholarship made a great impact on my ability to pursue my educational goals. This incredible support helped reduce my financial burdens and provided muchneeded assistance to further carry me to the end of my educational career.
You have no idea what a true blessing it is to be a recipient of such generosity.
Madison Rhodes, 2021 MHA/JD Health Administration
AZIMI FAMILY SCHOLARSHIP
Toluwanimi Oni
Doctor of Philosophy, Occupational and Environmental Health, 2023
ROD AND SHIRLEY BRADLEY SCHOLARSHIP McKenzie Cowlbeck
Master of Public Health, Health Administration and Policy, 2023
EDWARD N. BRANDT JR. SCHOLARSHIP Anne Kapka
Master of Public Health, Epidemiology, 2023
EDWARD N. BRANDT JR. SCHOLARSHIP H. Gracie Pearcy
Master of Public Health, Health Promotion Sciences, 2023
DALE W. BRATZLER SCHOLARSHIP Demetria Aflleje
Master of Health Administration, Health Administration and Policy, 2023
BURNS-SCHAIFF SCHOLARSHIP Shweta Kulkarni Doctor of Philosophy, Epidemiology, 2024
CALVEY FAMILY SCHOLARSHIP Mary L. Williams Doctor of Philosophy, Epidemiology, 2024
RONALD L. COLEMAN SCHOLARSHIP David Bolade
Doctor of Philosophy, Occupational & Environmental Health, 2026
CONOCOPHILLIPS OCCUPATIONAL AND ENVIRONMENTAL HEALTH ENDOWED SCHOLARSHIP Peter Kim
Doctor of Philosophy, Occupational and Environmental Health, 2025
CONOCOPHILLIPS OCCUPATIONAL AND ENVIRONMENTAL HEALTH ENDOWED SCHOLARSHIP Mingze Zhu
Doctor of Philosophy, Occupational and Environmental Health, 2024
ROY B. DEAL JR. SCHOLARSHIP April Lopez
Master of Public Health, Biostatistics, 2023
DAVID J. FALCONE MEMORIAL SCHOLARSHIP Lauryn McAdam
Master of Health Administration, Health Administration and Policy, 2023
ROSETTA FISHER STUDENT SCHOLARSHIP (COPH ALUMNI ASSOCIATION)
Desmond Delk
Master of Public Health, Health Promotion Sciences, 2023
ROSETTA FISHER STUDENT SCHOLARSHIP (COPH ALUMNI ASSOCIATION)
Morgan Rom
Doctor of Philosophy, Health Promotion Sciences, 2024
JAMES N. GEORGE SCHOLARSHIP IN BIOSTATISTICS AND EPIDEMIOLOGY
Afsheen Hasan
Doctor of Philosophy, Epidemiology, 2022
EDMUND H. GLEASON SCHOLARSHIP
Quantonia "Queenie" Amado
Master of Health Administration, Health Administration and Policy, 2024
CLAUDIA GRIFFITH MEMORIAL SCHOLARSHIP
Abi Peters
Master of Science, Health Promotion Sciences, 2023
E. SCOTT, SUSIE, REGAN AND SHANNON HENLEY FAMILY ENDOWED SCHOLARSHIP
Bethanie Lor Master of Health Administration, Health Administration and Policy, 2024

HCOPH ADVISORY BOARD SCHOLARSHIP
John Webster
Master of Public Health, Epidemiology, 2023
HUDSON FAMILY SCHOLARSHIP
Marco Rayos
Master of Public Health, Epidemiology, 2023
BRENT HURD SCHOLARSHIP

Valentina Vasquez
Master of Health Administration, Health Administration and Policy, 2023
JOHNSON FAMILY SCHOLARSHIP
Bukunmi Akanji
Doctor of Philosophy, Occupational and Environmental Health, 2025
ROBERT W. KETNER SCHOLARSHIP
Madolyn Phillips
Master of Science, Industrial Hygiene, 2022 and Master of Public Health, Health Promotion Sciences, 2023
ELISA T. LEE SCHOLARSHIP
Anna Bailey
Master of Public Health, Biostatistics, 2023
DAN J. MACER SCHOLARSHIP
Pawan Acharya
Doctor of Philosophy, Epidemiology, 2023
DAN J. MACER SCHOLARSHIP
Osariemen "Osa" Omoregie
Doctor of Philosophy, Epidemiology, 2024
DAN J. MACER SCHOLARSHIP
Shannon Reeves
Doctor of Philosophy, Epidemiology, 2025
DAN J. MACER SCHOLARSHIP
Ozair Naqvi
Doctor of Philosophy, Epidemiology, 2025
OU GIVING DAY SCHOLARSHIP
Wyatt Montgomery
Master of Health Administration, Health Administration and Policy, 2023
GARY E. RASKOB SCHOLARSHIP
Araya Assfaw
Doctor of Philosophy, Health Promotion Sciences, 2023
DIANE E. RIGGERT SCHOLARSHIP
Robbie Massingill
Master of Public Health, Biostatistics, 2024
KATHLEEN A. SHAVER SCHOLARSHIP
Flor Ramirez Nunez
Master of Science, Environmental Health Sciences & Industrial Hygiene, 2023
JULIE A. STONER IN BIOSTATISTICS
Whitney Kerr
Doctor of Philosophy, Epidemiology, 2025
J.C. WATTS FAMILY HEALTH AND WELLNESS
SCHOLARSHIP
Jennifer Trejo Rojo
Master of Public Health, Health Promotion Sciences, 2023
The demand for public health professionals has never been greater.
On May 14, interim Dean Dale Bratzler, D.O., M.P.H., along with the Hudson College of Public Health faculty, conferred the degrees of more than 60 M.S., M.P.H., M.H.A., Ph.D. and B.P.H. public health students. The event was held at the National Cowboy and Western Heritage Museum and more than 500 family and friends were in attendance to celebrate the 2022 graduates.

Public Health graduates will go on to work in the very important fields of epidemiology, biostatistics, occupational safety, environmental health, industrial hygiene, health promotion, and health administration and policy.
“Throughout my time studying at the Hudson College of Public Health, the most important things I learned were to never stop asking questions and never rush learning experiences. While there will always be more for me to learn (both inside and outside of my discipline), professionally and personally, I have grown to realize that all learning processes are valuable opportunities that must be experienced with patience and diligence. Diligent, patient reflection and a posture of humility in all learning experiences will contribute to my goal of lifelong learning.”
Gabrielle “Gabbi” Westbrook M.P.H. in Health Administration and“I chose to study public health because I wanted to have a broader perspective of medicine. The BPH program has exceeded all of my expectations, and I believe it has prepared me in the best ways to continue pursuing my dream of becoming a physician.”
The public health realm has seemingly limitless facets throughout our existence. Without my Hudson College of Public Health team, I would be at sixes and sevens trying to traverse my way to success. Walking out of this degree with my OP tool bag, I feel confident to tackle a career defending all aspects of human health. What's really great is that I know all of my peers are in the same boat as me!
Adam Warren M.P.H. in Biostatistics
“Above all else, what I have taken away from my experience in earning my MPH at the Hudson College of Public Health is that virtually anything and everything can affect someone's health and well-being. It seems as though the lens through which I view these variables has simultaneously been broadened and refined. For that, I am forever grateful.”
Kenner Wignall M.P.H. in Health Promotion Science
“I am most looking forward to applying the knowledge and skills I have learned in the last two years to address various public health problems by improving access to health care and reducing disparities in our communities.”
Policy
Blakelee Eggleston Bachelor of Public Health Kavya Boyina M.P.H. in Epidemiology“I chose to study public health because it is the only degree that offered a holistic understanding of the complex workings of our health care system. This degree taught me how to be adaptable, resourceful, and—most importantly—empathetic. This is a skill I will carry with me through my entire career. I hope to use this skillset in my endeavors as a future physician at TCU School of Medicine and ultimately as a health care executive.”
I completed both my MS and PhD degrees in Biostatistics at the Hudson College of Public Health. I appreciate that the college maintains a supportive environment for international students. The generous support I received through college scholarships, graduate research work, and the Hudson Fellowship greatly eased my financial burden. I have gained solid professional training through course work and research experience of applied biostatistics in a variety of medical fields. Equipped with a strong academic background, I am ready to establish my career and finally make my dream come true.
Xi (Sophia) Chen Ph.D. in Biostatistics

 Winston Scambler Bachelor
Winston Scambler Bachelor
of Public Health

Oklahoma Pride: Working Together for the Well-Being of All Oklahomans was the brain-child of longtime business and civic leader Gene Rainbolt. Rainbolt and Dr. Gary E. Raskob (who served as the dean of the Hudson College of Public Health at the University of Oklahoma Health Sciences Center at the time) assembled a committee of subject-matter experts to determine the book’s discussion topics. Dr. Raskob was also the public health content advisor and editor. In a joint review, University of Oklahoma President Joseph Harroz Jr. and then-president of Oklahoma State University Burns Hargis heralded the book as a call to action to improve health across our state.

Use art and imagery to start a social conversation focused on Oklahoma’s greatest challenges around health and the critical relationships between health, education, and the economy. This idea inspired an innovative interdisciplinary collaboration between the Hudson College of Public Health and the School of Visual Arts within the OU Weitzenhoffer Family College of Fine Arts.
A book that combined the students’ artwork with public health expertise to create a profound and touching depiction of health outcomes and determinants using real-time statistics. Through the lens of art, the book’s collaborators hoped this visual storytelling would inspire the state’s leaders and citizens alike to work hand-in-hand to forge a healthier, more prosperous Oklahoma.
After the subject matter experts selected the main health indicators, OU art students used them as inspiration to produce hundreds of images and social media campaigns over several months. While the book starkly documents the facts regarding Oklahoma’s current state of health, the intent was not to criticize.
Jeffrey
Karen
Kelly
“The involvement of OU visual arts students made this book unique. As our next generation of leaders, today’s students will bear the consequences of these challenges, and viewing these issues from their perspective was a critical aspect of this project,” Rainbolt said.
“It was both a privilege and a pleasure to work on this book in partnership with a great community leader, Gene Rainbolt,” Raskob said.
Former Commissioner of Health Terry Cline, who also served as one of the book’s public health content advisers, explained the comprehensive approach to the project. “The basis for this book emphasizes the interlocking nature of three areas: health, education, and poverty,” Cline said. “It was important that the solutions outlined in the book avoided the all-too-common mistake of directing funds away from one area in an attempt to improve the other areas. This book offers a strategic, multi-year vision, informed by data to measure progress.”
This image dates back to 1928, when our building was completed. What is now the Hudson College of Public Health originated as the first College of Medicine building on the OU Health Sciences Center campus. It was one of the first buildings to make up what would eventually become the OUHSC. The College of Medicine building sat directly across the street from the University Hospital. Interestingly, Oklahoma City was chosen for this campus location due to its growing urban population and ability to support extensive medical facilities.
 Sharon Neuwald Consultant and former Chief of Staff and Director of Policy and Legislative Relations, Oklahoma Department of Human Services
Terry L. Cline, former Oklahoma Commissioner of Health
Dismukes, Director of Communications, Oklahoma Department of Mental Health and Substance Abuse Services
Diane Joy-Sisemore Senior Vice President, BancFirst
Hayes-Thuman, Professor of Art and Design, School of Visual Art, Weitzenhoffer Family College of Fine Arts at the University of Oklahoma
Dyer Fry former Editor and Publisher, The Oklahoman
James Tolbert Owner, Full Circle Bookstore (and Full Circle Press)
VaLauna Grissom Special Assistant, Hudson College of Public Health at the University of Oklahoma Health Sciences Center
Sharon Neuwald Consultant and former Chief of Staff and Director of Policy and Legislative Relations, Oklahoma Department of Human Services
Terry L. Cline, former Oklahoma Commissioner of Health
Dismukes, Director of Communications, Oklahoma Department of Mental Health and Substance Abuse Services
Diane Joy-Sisemore Senior Vice President, BancFirst
Hayes-Thuman, Professor of Art and Design, School of Visual Art, Weitzenhoffer Family College of Fine Arts at the University of Oklahoma
Dyer Fry former Editor and Publisher, The Oklahoman
James Tolbert Owner, Full Circle Bookstore (and Full Circle Press)
VaLauna Grissom Special Assistant, Hudson College of Public Health at the University of Oklahoma Health Sciences Center
NOWOver the past 100 years, our building—and its occupants—have changed a bit. In 1967, it became home to the University of Oklahoma College of Health. Twelve years later, the College of Health was divided into the College of Public Health and the College of Allied Health. After the split, the College of Public Health remained in the original building. In recognition of Dr. Leslie Hudson (alumni) and Clifford Hudson’s continual support and enduring commitment to public health in Oklahoma, the OU Board of Regents renamed the college the Hudson College of Public Health in 2018.
