








June 2023
As I write this Dean’s Message, we are welcoming the Class of 2027 to the OU College of Medicine. Earlier this year, we graduated the Class of 2023, a group that undertook their medical education almost entirely during the COVID-19 pandemic. This is an amazing time to be in academic medicine, and with each class we receive and send forth, I am excited to see the ways they will transform our profession.
This is also a bittersweet message for me because it is my last as dean of the college. Later this year, I will head into retirement, full of appreciation for the people I have worked with, the patients I have served, and for what we have been able to accomplish for the people of Oklahoma. Medicine is truly a wonderful discipline, and I have been privileged to spend much of my career at the OU College of Medicine.
In this issue of the magazine, you will read about many programs and activities that demonstrate why I take such pride in the college. In the medical education section is a story about our new Premier Medical Education Hub program — a revitalized opportunity for our students to undergo a one-month clinical rotation with a rural community hospital, clinic or tribal healthcare system. Students also immerse themselves in each community, meeting the people who call it home and taking part in their activities. I am excited about this program because it not only teaches students how to care for patients in rural settings, but it shows them just how integral physicians are in smaller communities. My hope is that the experience inspires the next generation of family physicians who want to serve in rural Oklahoma.
The research section of the magazine is full of exciting news about the innovative investigations taking place throughout the college. Our cover story is on the neonatal research endeavors in the Department of Pediatrics. Basic science, clinical and translational research is blossoming in the Section of Neonatal-Perinatal Medicine. A new laboratory infrastructure has been built at University Research Park, where shared space allows researchers to focus on their work rather than establishing their own labs. Our researchers are also gaining national prominence for their expertise in areas like necrotizing colitis and neonatal resuscitation.
Our clinical enterprise is strong and growing. In the patient care section, you will find a story about a new telehealth partnership between Oklahoma Children’s Hospital OU Health and Oklahoma City Public Schools. When students become sick while at school, they can be seen virtually by one of our providers, saving their families time and allowing them to get back to the classroom quicker. Other stories detail exciting announcements regarding OU Health Stephenson Cancer Center, including renewal of its National Cancer Institute designation, as well as a new partnership with Norman Regional.
In our section dedicated to the OU-TU School of Community Medicine, there is a story about an exciting initiative to support community college students who are interested in going to medical school. Too often, community college students do not have access to the same pre-med resources that are afforded to students at four-year universities. Yet many community college students are great candidates for medical school. Toward the end of the magazine, you will find information about alumni activities, the achievements of our faculty members and more.
I want to close by saying what a privilege it has been to serve the university and the state, including as dean of the College of Medicine these past five years. I am grateful for the many ways you have supported the college and the pride you take in our ultimate goal of improving the health and well-being of all Oklahomans. My heart is full of gratitude for what we have accomplished together.
John P. Zubialde, M.D. Executive Dean, OU College of Medicine
Senior Vice President and Provost, OU Health Sciences Center
Gary Raskob, Ph.D.
Executive Dean, College of Medicine
John Zubialde, M.D
Assistant Vice President of Development, OU Health Sciences Center
Stacey Maxon
Editor/Writer
April Wilkerson
Contributing Writer
Annelise Stephenson
Medicine is published by the OU College of Medicine. For more information, contact:
April Wilkerson, Editor april.wilkerson@ouhealth.com
Medicine is online at medicine.ouhsc.edu
The University of Oklahoma, in compliance with all applicable federal and state laws and regulations, does not discriminate on the basis of race, color, national origin, sex, sexual orientation, genetic information, gender identity, gender expression, age, religion, disability, political beliefs, or status as a veteran in any of its policies, practices, or procedures. This includes, but is not limited to: admissions, employment, financial aid, housing, services in educational programs or activities, or health care services that the University operates or provides.
Inquiries regarding non-discrimination policies may be directed to: Christine Taylor, University Equal Opportunity Officer and Title IX Coordinator, (405) 325-3546, christine.taylor@ou.edu , or visit ou.edu/eoo.html
Copies of this magazine were printed at no cost to the taxpayers of the state of Oklahoma.
© 2023 University of Oklahoma
COVER PHOTO:
Basic, clinical and translational neonatal research projects are growing and gaining momentum in the Section of Neonatal-Perinatal Medicine in the Department of Pediatrics.
04. National Academy of Medicine
Judith James, M.D., Ph.D., Associate Vice Provost for Clinical and Translational Science at the OU Health Sciences Center and a George Lynn Cross Research Professor and Professor of Medicine, was elected to the prestigious National Academy of Medicine.
08. New PA Program Director
Gary C. Pérez, DMSc, MPAS, PA-C, has been appointed program director and assistant professor for the Physician Associate Program at the OU College of Medicine.
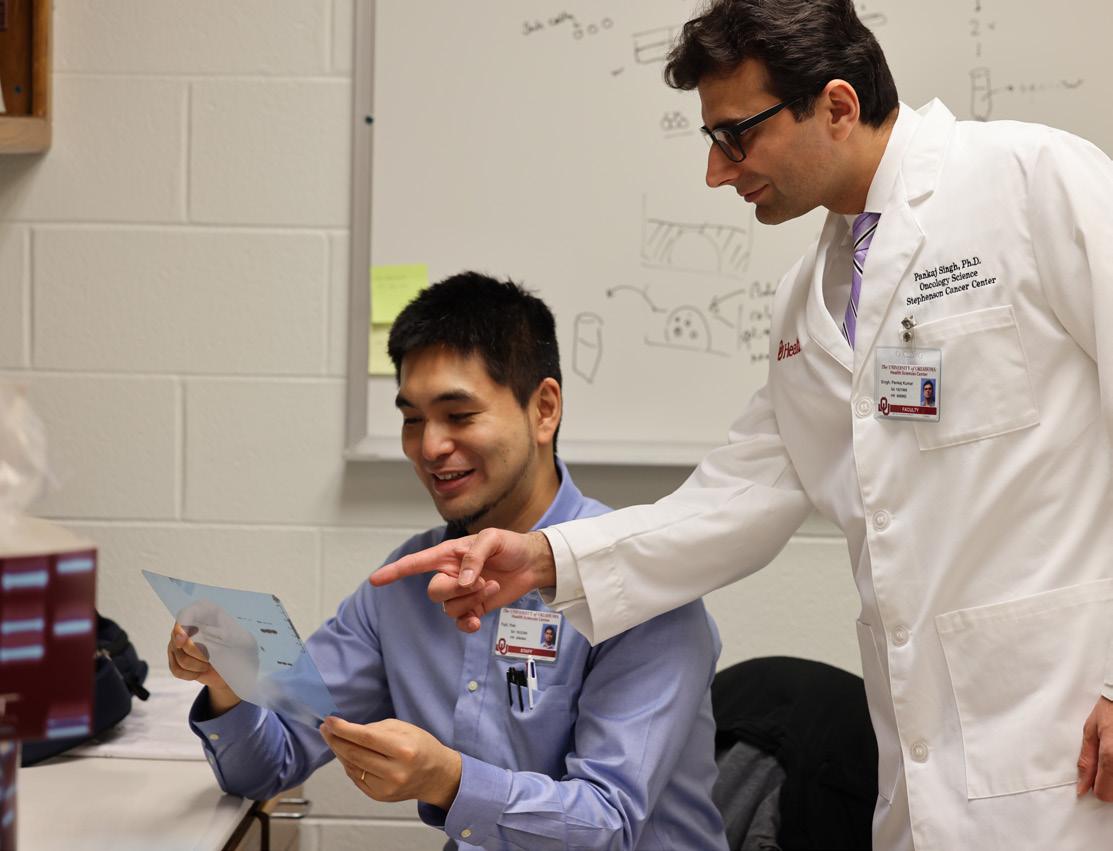
10. Oncology Science
Chair and Professor Pankaj K. Singh, Ph.D., is leading the development of the new Department of Oncology Science with the recruitment of faculty researchers and the creation of a doctoral program and a fellowship for clinicians.
27. Cancer Care in Norman
OU Health and Norman Regional are partnering to building a new cancer care facility at the Norman Regional Healthplex. The 50,000-square-foot facility will be named OU Health Stephenson Cancer Center at Norman Regional.
29. Telehealth at School
OU Health is partnering with Oklahoma City Public Schools to provide telehealth services so that children can be seen virtually for non-emergency illnesses while they are still at school.
36. Module Renamed
One of the college’s 10 study modules has been renamed for former U.S. Surgeon General Antonia Novello, M.D., MPH. The college’s chapter of the American Medical Women’s Association launched the initiative to rename modules to recognize underrepresented healthcare professionals.
37. Community Rotations
To allow third- and fourth-year medical students to experience medicine in community hospitals and clinics across Oklahoma, the College of Medicine has launched the Premier Medical Education Hub program.
43. Accelerating to Medical School
The OU-TU School of Community Medicine in Tulsa, along with the Tulsa Community College and the national nonprofit Health Professional Student Organization, launched the Undergraduate Medical Accelerator Program. The program provides resources to community college students from rural and underserved areas who are considering medical school.
51. Evening of Excellence
The Evening of Excellence gala, organized by the OU College of Medicine Alumni Association, honored a physician-researcher, a community leader, and a foundation during its annual event, which has raised $3.8 million for college researchers since it began 38 years ago.
The OU College of Medicine Alumni Association is on Facebook. Like us at www.facebook.com/oucomalumni
Judith A. James, M.D., Ph.D., Associate Vice Provost for Clinical and Translational Science at the OU Health Sciences Center and Professor of Medicine in the OU College of Medicine, has been elected to the National Academy of Medicine for her work in the field of autoimmunity and autoimmune disorders.
She is the first woman from an Oklahoma institution — and fifth overall Oklahoma-based scientist — to be selected for this prestigious honor, which is widely considered one of the highest honors in the fields of health and medicine.
James serves as director of the Oklahoma Clinical and Translational Science Institute at the OU Health Sciences Center. OCTSI is focused on building clinical and translational research infrastructure for the state, supporting the development of new and junior clinical investigators, and improving health and health outcomes for all Oklahomans. She is also chair of the Arthritis and Clinical Immunology Research Program and Vice President of Clinical Affairs at the Oklahoma Medical Research Foundation.
Election to the National Academy of Medicine recognizes individuals who have demonstrated outstanding professional achievement and commitment to service. The award is both nationally and internationally recognized.

James’ work has been cited as significantly advancing the understanding of how autoimmune diseases start and
how immune responses evolve. She has been studying the mechanism of lupus and has worked in understanding arthritis in Oklahoma tribal members, the early events of autoimmune diseases and launching prevention trials.
“I am extremely honored to be elected as a member of the National Academy of Medicine,” James said. “By studying these diseases that affect the lives of so many people and learning to understand them, we can work toward improving treatments and outcomes. I am also very committed to improving the health of all Oklahomans and building clinical and translational research in our state. I am very fortunate to work with so many faculty, staff and patients who are also committed to this same goal.”
Mary Beth Humphrey, M.D., Ph.D., a Professor of Medicine and Associate Dean for Research in the College of Medicine, said: “The election of Dr. James to the National Academy of Medicine is one of the highest honors a clinician-researcher can achieve and is based on her innovative autoimmune research that has been paradigmchanging, demonstrating exceptional service to national organizations and dedication to correct health disparities. We are proud that Dr. James was one of our first M.D.-Ph.D. students in the OU College of Medicine and chose to continue her career at the OU Health Sciences Center and at OMRF, leading the nation in autoimmune disease research.”
Two former OU College of Medicine executive deans, M. Dewayne Andrews, M.D., and Jerry Vannatta, M.D., were among the latest OU Regents’ Alumni Awards recipients.
Presented by the OU Board of Regents and the OU Alumni Association, the Regents’ Alumni Awards honor the important roles of OU alumni and supporters to the life of the university. A committee formed by the Alumni Association selects the award recipients from nominations made by alumni, friends and OU faculty and staff. Recipients receive a plaque, and their names are engraved on a permanent plaque in the Oklahoma Memorial Union.
Andrews, a 1970 graduate of the OU College of Medicine, retired from OU in 2017 after 40 years of service and leadership. He served for 15 years as executive dean of the OU College of Medicine, one of the longest-serving deans of a medical school in the United States.


He also served as the Vice President for Health Affairs for the OU Health Sciences Center. Under his leadership, the OU Health Sciences Center expanded research space, promoted a focus on interprofessional education and practice, and enlarged the impact of the clinical enterprise and the OU Health Sciences Center in the rapidly changing healthcare industry.
During his tenure, Andrews received numerous teaching, leadership and medical awards, including an honorary degree from OU, the university’s most prestigious honor. He also represented OU while serving as a national committee member to the American College of Physicians, American Medical Association, the Association of American Medical Colleges, the Liaison Committee on Medical Education and the National Commission on Certification of Physician Assistants.
In 2013, Andrews was inducted into the Oklahoma Higher Education Hall of Fame. In 2016, a new, nine-story academic tower for the OU College of Medicine was named in his honor.
Jerry Vannatta, M.D.
Vannatta, a 1975 graduate of the OU College of Medicine, is Professor Emeritus of Medical Humanities and David Ross Boyd Professor Emeritus of Medicine at the OU College of Medicine. He served many roles with the College of Medicine and the OU Health Sciences Center since joining the faculty in 1979 as an internal medicine physician.
In 1995, he was named Vice President for Health Affairs and Associate Provost of the OU Health Sciences Center. In 1996, he was named executive dean of the College of Medicine. While in those roles, he helped to lead the university’s negotiating team to create a new partnership for the teaching hospitals and to transform the faculty practice into OU Physicians.
Part of what makes Vannatta’s career and legacy so meaningful is his unique approach to the study and practice of medicine. He integrates humanistic values with a traditional scientific approach in the treatment of people. This trademark lens has earned him national recognition and has differentiated him as a medical practitioner and educator.
In 2016, Vannatta was inducted into the Oklahoma Higher Education Hall of Fame. He received an honorary doctorate from Oklahoma City University in the same year.
In 2021, Vannatta committed a $1 million gift to support the OU College of Medicine’s Academy of Teaching Scholars, a service organization that fosters excellence in teaching and health professions education. The gift will allow the academy to continue its important work of nurturing, recognizing and rewarding teaching excellence among the college’s faculty.
Hanna Abdallah Saadah, M.D., an emeritus professor of medicine at the OU College of Medicine, has been honored with the 2023 Stanton L. Young Master Teacher Award.

The honor, awarded since 1983, recognizes OU College of Medicine faculty members for excellence in teaching. It was established through an endowment made by the late Oklahoma City businessman Stanton L. Young. The award comes with a $15,000 cash prize, one of the largest in the nation for medical teaching excellence.
“Dr. Saadah has had a distinguished career in medicine, and he continues giving back to his profession by sharing his knowledge and experience with medical students,” said John P. Zubialde, M.D., executive dean of the OU College of Medicine. “Dr. Saadah is passionate about medical education and medical humanities, and he is widely respected by our students and faculty.”
Saadah is active as a volunteer faculty member, teaching medical students on the geriatrics selective rotation and leading preclinical ethics and humanities courses. In a nomination letter for the Stanton L. Young Master Teacher Award, a student wrote: “Dr. Saadah is the true definition of a master teacher. One of the things that makes him such a great teacher is his dedication to being a student himself. He has made it his mission to share as much knowledge as possible with his students, and it is beyond evident in his interactions with them.”
Another student said: “Dr. Saadah is still teaching and working with extremely high levels of efficiency at an age 15-plus years after other physicians choose to retire. He embodies everything a master teacher should be. If there were a picture
next to the dictionary definition of ‘master teacher,’ it would without a doubt be Dr. Saadah. I hope to be half the physician and teacher he is one day.”
Saadah earned his medical degree from the American University of Beirut and completed his residency in internal medicine and a fellowship in infectious diseases at the OU Health Sciences Center. He initiated the Adolescent Medicine Program at the OU Health Sciences Center in 1975 and directed it until 1977. During his career, his practice also has focused on internal medicine, headaches, psychopharmacology, infectious diseases, and sleep medicine. He continues to serve in an emeritus role at the OU Health Sciences Center and at the VA Medical Center.
He has made several medical discoveries during his career, including developing the occipital nerve block procedure for the treatment of headaches. He has published 31 scientific articles, 77 lay medical articles and more than 100 humanities articles. He also has published five poetry books, four novels and two books of short stories.
He is a fellow of the American College of Physicians and a member of the American Medical Association, American Society of Microbiology, Oklahoma County Medical Society, Oklahoma State Medical Association, American Pain Society and the Infectious Disease Society of America, among others.
He has been honored with numerous awards, including the 2019 Rhinehart Medical Service Award from the Oklahoma County Medical Society; the Aesculapian Award from the OU College of Medicine Class of 2019 for excellence in volunteer teaching; and the 2020 Friend of Medicine Award from the OU College of Medicine Alumni Association.

This spring, the OU College of Medicine presented the Patricia Price Browne Prize in Biomedical Ethics during Grand Rounds for the Department of Pediatrics. The 2023 recipient is Ezekiel J. Emanuel, M.D., Ph.D., Vice Provost for Global Initiatives and the Diane v.S. Levy and Robert M. Levy University Professor at the University of Pennsylvania Perelman School of Medicine.
The award is presented to a person who demonstrates high standards in the medical or professional ethics fields. The prize is named for an Oklahoma champion of women’s and children’s health, the late Patricia Price Browne. The honor comes with a $10,000 award.
Emanuel is an oncologist and world leader in health policy and bioethics. He is a special advisor to the director general of the World Health Organization, senior fellow at the Center for American Progress, and member of the Council on Foreign Relations. He was the founding chair of the Department of Bioethics at the National Institutes of Health and held that position until August 2011. From 2009 to 2011, he served as a special advisor on health policy to the director of the Office of Management and Budget and National Economic Council. In this role, he was instrumental in drafting the Affordable Care Act. Emanuel also served on the Biden-Harris Transition Covid Advisory Board.
Emanuel is the most widely cited bioethicist in history. He has over 350 publications and has written or edited 15 books. His publications include the books “Which Country Has the World’s Best Health Care?” (2020), “Prescription for the Future” (2017), “Reinventing American Health Care: How the Affordable Care Act Will Improve our Terribly Complex, Blatantly Unjust, Outrageously Expensive, Grossly Inefficient, Error Prone System” (2014) and “Brothers Emanuel: A Memoir of an American Family” (2013). In 2008, he published “Healthcare, Guaranteed: A Simple, Secure Solution for America,” which included his own recommendations for healthcare reform.

He has received numerous awards, including election to the Institute of Medicine of the National Academy of Science, the American Academy of Arts and Sciences, the Association of American Physicians, and the Royal College of Medicine. He has been named a Dan David Prize Laureate in Bioethics and is a recipient of the AMA-Burroughs Wellcome Leadership Award, the Public Service Award from the American Society of Clinical Oncology, Lifetime Achievement Award from the American Society of Bioethics and Humanities, the Robert Wood Johnson Foundation David E. Rogers Award, President’s Medal for Social Justice Roosevelt University, and the John Mendelsohn Award from the MD Anderson Cancer Center.
Emanuel is a graduate of Amherst College. He holds a master of science from Oxford University in Biochemistry and received his medical degree from Harvard Medical School and
his doctorate in political philosophy from Harvard University. During Grand Rounds, Emanuel gave the presentation, “Allocating Scarce Medical Resources: Lessons from COVID.” The award was presented following his lecture.
During his time on campus, he also visited with faculty, residents and students to discuss ethics in medicine.
The biennial OU Health Harold Hamm International Prize for Biomedical Research in Diabetes was awarded this year to Sir Stephen O’Rahilly, M.D., of the University of Cambridge for his investigations into the link between obesity and Type 2 diabetes.
The Hamm Prize recognizes and encourages lasting advances in the field of diabetes research. It is awarded to an individual who has either demonstrated lifelong contributions to the field or realized a singular advance, especially one that promotes curative potential. The honor includes a $250,000 award, the largest of its kind in the world.
O’Rahilly was selected for his research that linked a specific mechanism to the development of obesity. Obesity is considered the biggest risk factor for Type 2 diabetes; O’Rahilly’s clinical research defined specific molecular mechanisms and genes that are responsible for obesity.
“Obesity is caused by genetics, in part, and O’Rahilly has discovered some of these key genes that lead to actually understanding why obesity happens,” said Jed Friedman, Ph.D., director of OU Health Harold Hamm Diabetes Center. “It’s not just a disease of gluttony anymore; it’s a disease of genetics. His contributions to the field of diabetes have been immense, and we are really proud to have him as our prize winner.”
O’Rahilly leads one of the world’s largest institutes for metabolic research at the University of Cambridge. His findings have been recognized internationally, and in 2013, he was knighted for services to medical research, specifically in the area of diabetes.

“The Harold Hamm Prize is one of the most prestigious and distinguished awards a diabetes researcher can receive,” O’Rahilly said. “Its previous recipients are all giants in our field and it is a great honor to join their number. Research is clearly a team effort. I joyfully accept this prize on behalf of all the wonderful people with whom I have worked over nearly four decades in diabetes research, as we have strived to better understand the biology of this disorder and turn that knowledge into improved care for patients.”
The Hamm Prize, established in 2012, is named for Harold Hamm, chairman and chief executive officer of Continental Resources Inc. in Oklahoma City, which created an endowment to fund the prize in perpetuity. The winner of the Hamm Prize is chosen by a rotating jury of national and international leaders in diabetes research.
Last academic year, Gary C. Pérez, DMSc, MPAS, PA-C, was appointed program director and assistant professor for the Physician Associate Program at the OU College of Medicine.
Pérez enlisted in the U.S. Army after graduating from high school and served as an airborne combat medic with the 82nd Airborne Division. He graduated with honors from the U.S. Army Physician Assistant Program and received a bachelor of science with distinction from the Physician Associate Program at the OU Health Sciences Center.
He then served as the battalion surgeon for a light armored infantry battalion at Fort Hood in Texas; an armor battalion in Korea; and an airborne infantry battalion in the 82nd Airborne Division. He transferred to the U.S. Air Force and attended the USAF Orthopedic Surgery Residency for Physician Assistants. He finished his military career serving as Director of Medical Operations for the 720th Special Tactics Group, Air Force Special Operations Command.
Pérez earned a Master of Physician Assistant Studies (MPAS) from the University of Nebraska and a Doctor of Medical Science Degree (DMSc) from the University of Lynchburg in Virginia.
He began his career in PA education in 2014 as the founding clinical director for the Florida International University Herbert Wertheim College of Medicine Master in Physician Assistant Studies Program. He remained with the program until it achieved full accreditation. In 2019, he was appointed associate director of the University of Texas Medical Branch John Sealy School of Medicine Physician Assistant Studies Program.
He is a member of the American Academy of Physician Assistants, the Physician Assistant Education Association, the Oklahoma Academy of Physician Assistants, the Texas Academy of Physician Assistants, and the Texas Gulf Coast Physician Assistant Association.

OU College of Medicine researchers were among others across the OU Health Sciences Center who were awarded nearly $3 million in grants this summer from the Presbyterian Health Foundation (PHF), which supports Oklahoma’s biotechnology, medical research and education organizations.

The funds will support critical studies and equipment needs in areas such as diabetes, cancer, retinal disease, necrotizing colitis, tobacco use prevention and much more. PHF grants have played an important role in the advancement of research at the OU Health Sciences Center for many years.
“We greatly value the investments PHF has made into our research mission,” said Darrin Akins, Ph.D., Vice President for Research at the OU Health Sciences Center. “It allows our investigators to generate important data and submit competitive grant applications to national level programs. This funding is essential for enhancing our research capacity and infrastructure as we work toward being in the top tier among all academic health centers in the country.”
One of the newly funded studies in the OU College of Medicine focuses on inherited retinal disease, which affects approximately 2.7 million people around the world. Lea Bennett, Ph.D., a researcher in the Department of Ophthalmology, is leading a study that seeks to understand why genetic mutations cause blindness in people who have the condition. She is investigating the mutation of a specific gene through innovative laboratory assessments combined with an examination of human retinal tissue.
Another College of Medicine study seeks to increase prostate cancer screening among African American men. The study
is led by Jordan Neil, Ph.D., of the Department of Family and Preventive Medicine and member of the TSET Health Promotion Research Center at OU Health Stephenson Cancer Center.
Prostate cancer is the most diagnosed cancer in African American men and the second-leading cause of cancer-related deaths. In this project, Neil plans to develop and evaluate an app that will improve knowledge of prostate cancer risk and symptoms, as well as provide instructions for completing a prostate-specific antigen (PSA) test at home. Greater uptake of the PSA test may reduce the disproportionate burden of prostate cancer among African American men.
A study on bronchopulmonary dysplasia, a respiratory disease that can develop if a premature infant’s lungs did not develop fully in the womb, also was funded in PHF’s latest round of grants. The project is investigating an innovative therapy that aims to prevent the condition, thereby protecting the newborn from other problems that could develop, such as pulmonary hypertension, trouble feeding and learning difficulties. The study is led by Trent Tipple, M.D., chief of the Section of Neonatal-Perinatal Medicine in the Department of Pediatrics.
PHF primarily supports research and innovation taking place within the Oklahoma Health Center in Oklahoma City. Since PHF’s inception in 1985, it has awarded nearly $215 million in grants.
“We are incredibly proud of the top-notch research projects funded this cycle,” said PHF President Rick McCune. “Over the last 10 years, we’ve seen remarkable health discovery happening at the Oklahoma Health Center campus, all with the aim of improving the quality of healthcare available to all Oklahomans.”
The new Department of Oncology Science in the OU College of Medicine is gaining momentum with the recruitment of new faculty researchers and plans for the creation of a sought-after doctoral program and a fellowship for clinicians interested in research.

The work is led by founding chair and professor Pankaj K. Singh, Ph.D., who has a multifaceted vision for the department and its ultimate aim of improving care for patients with cancer. The department currently has four faculty members, with three others joining by the end of the summer and plans to add four more over the next five years. He is recruiting researchers with varied expertise, including cancer imaging, bioinformatics, cancer biology, biologic chemistry, multiomics, and health disparities. Singh also places a major emphasis on team science, translational research, and investigator-initiated clinical trials.

“The university already has a strong complement of cancer researchers and a strong clinical trials network. We want to further strengthen what is on campus and bring in new
expertise in selected areas,” he said. “This is a very exciting time for cancer research. Having the National Cancer InstituteDesignated Stephenson Cancer Center on campus has major implications for recruiting and for the work that we will do. We have the opportunity to achieve things that are innovative and transformative.”
The research team already holds millions of dollars in grants from the National Institutes of Health, including five R01 grants, considered the gold standard in awards, as well as a P01 grant to support broad, long-term research programs, and a U54
grant to fund the full range of research, from basic science to clinical research.
The department is beginning its work with a strong focus on pancreatic cancer. Kamiya Mehla, Ph.D., is studying novel immunotherapies against pancreatic cancer. She is also looking at how different immune cells program their metabolism and how that programming contributes to immune suppression. This year, her grant proposals to the NIH for an R01 grant and to the Department of Defense have been selected for funding.
Surendra Shukla, Ph.D., explores the epigentic mechanism of therapeutic resistance in gastrointestinal cancers, as well as designing novel strategies for overcoming therapy resistance. Jay Kim, Ph.D., is investigating the role of metabolic differences in tumor subtypes in order to identify precision medicine options. Singh’s research focuses on cancer metabolism, tumor-stromal interactions, and the kinds of mechanisms that tumor cells employ to develop resistance against chemotherapy.
Another focus for current faculty members is studying the metabolic basis of cachexia, a muscle-wasting disorder that affects the majority of patients with pancreatic cancer. Because their adipose tissue is being wasted, they are actively losing skeletal muscle mass, Singh said. That significantly diminishes quality of life to the point where many patients become bed-ridden.

“To be able to prevent some of the wasting, we are looking at the metabolites that are actively secreted and the effect that has on the skeletal muscles or the immune cells in the skeletal
muscles,” he said. “If we can better understand that, perhaps we can prevent muscle deterioration and help patients respond better to chemotherapy. When patients have better skeletal muscle mass, they can be eligible for higher doses of chemotherapy. More importantly, if they have good skeletal muscle mass, they can have a better quality of life and be able to participate in their daily activities.”
The department is also creating two core resources — a metabolomics core and a patient-derived xenograft and organoid core. The metabolomics core will allow researchers to profile cancer biofluids such as blood, plasma and urine as they search for markers for early detection of disease and potential new ways to target it. The patient-derived xenograft and organoid core will allow researchers to take different types of human cancer tissues and implant them into mice for research. These three-dimensional models of disease allow researchers to test human cells more effectively than traditional two-dimensional models of cell culture.
“Our goal is to provide every possible resource that is needed for faculty members to succeed.”
“There is a great need to understand tumors not just at the level of single cells, but also at the level of cellular heterogeneity,” Singh said. “There is an incredible amount of heterogeneity in tumors. Some tumors respond to some therapies, while others do not, so there is a need for understanding what that heterogeneity does and how it is critical for developing better therapeutic responses.”
Singh foresees much of the work taking place through collaborations, both within his department and with others across campus. Single investigator-driven projects are no longer the only way to ask research questions.
“As more and more high-throughput data sets are being made publicly available, now is the time for researchers to partner with experts in many different fields,” he said. “The pace of discovery has been so fast that it’s hard to keep up as a single investigator, and people are increasingly realizing that if they truly want to affect a disease, they cannot just look at it from a reductionist approach. They have to be willing to partner with other types of researchers and with clinicians who have an in-depth understanding of issues that arise in patients. They must partner with pathologists to understand the pathology of disease, with surgeons who understand surgical complications
and the need for better surgical margins, and with oncologists who are focused on getting the best therapies with fewer side effects.”
Singh also models a translational mindset in research projects. Advancing research through basic science is equally important, he said, but he encourages researchers to “put on their translational hat.” “We have to think about how the research questions we’re asking are truly related to what happens in tumors in patients. How is what I’m studying today going to affect the quality of life of patients someday?”
As he builds his department, Singh is simultaneously creating a mentoring structure for new faculty recruits at all levels. Each recruited candidate will have at least two dedicated mentors to help them grow their careers and become leaders on campus. Mentors will come from various cancer research programs on campus, as well as from other institutions across the United States. “Our goal is to provide every possible resource that is needed for them to succeed,” he said.
In parallel to the research mission of his department, Singh and his team are developing a Ph.D. program in oncology science, and he has welcomed several post-doctoral students. He is also working with various clinical departments to create a streamlined research fellowship program for clinicians who have an interest in cancer research. His education goals extend beyond campus as well. He plans to develop training programs for undergraduate college students interested in oncology science, and to initiate pipeline programs across the state to create a path to science for young people, especially those from minority communities.
As a longtime mentor himself, Singh knows that grants and publications would not be possible without the hard work of trainees. That’s why he wants to give them every tool possible for their careers.
“We will make strides in cancer research during my lifetime, but there will be some things that we cannot address and are beyond our reach,” he said. “Our next generation of investigators will be the ones to carry that forward.”
“This is a very exciting time for cancer research. Having the National Cancer Institute-Designated Stephenson Cancer Center on campus has major implications for recruiting and for the work that we will do. We have the opportunity achieve things that are innovative and transformative.”
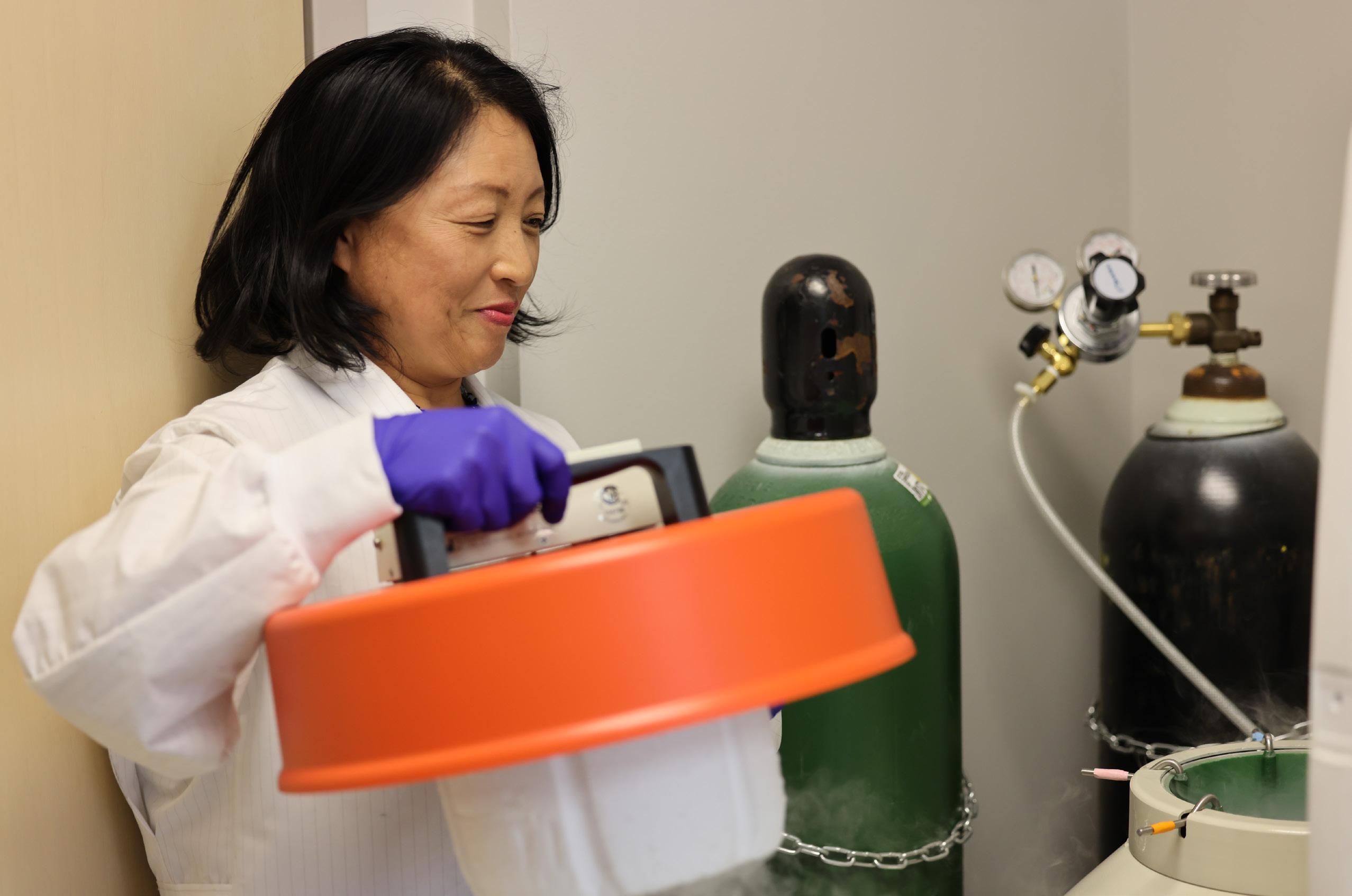
An average of 1,400 premature and sick newborns are treated each year by physicians in the Section of Neonatal-Perinatal Medicine in the Department of Pediatrics. A strong and growing research enterprise is woven through that clinical mission, allowing faculty members to think individually and collectively about how best to advance care for infants and their families.
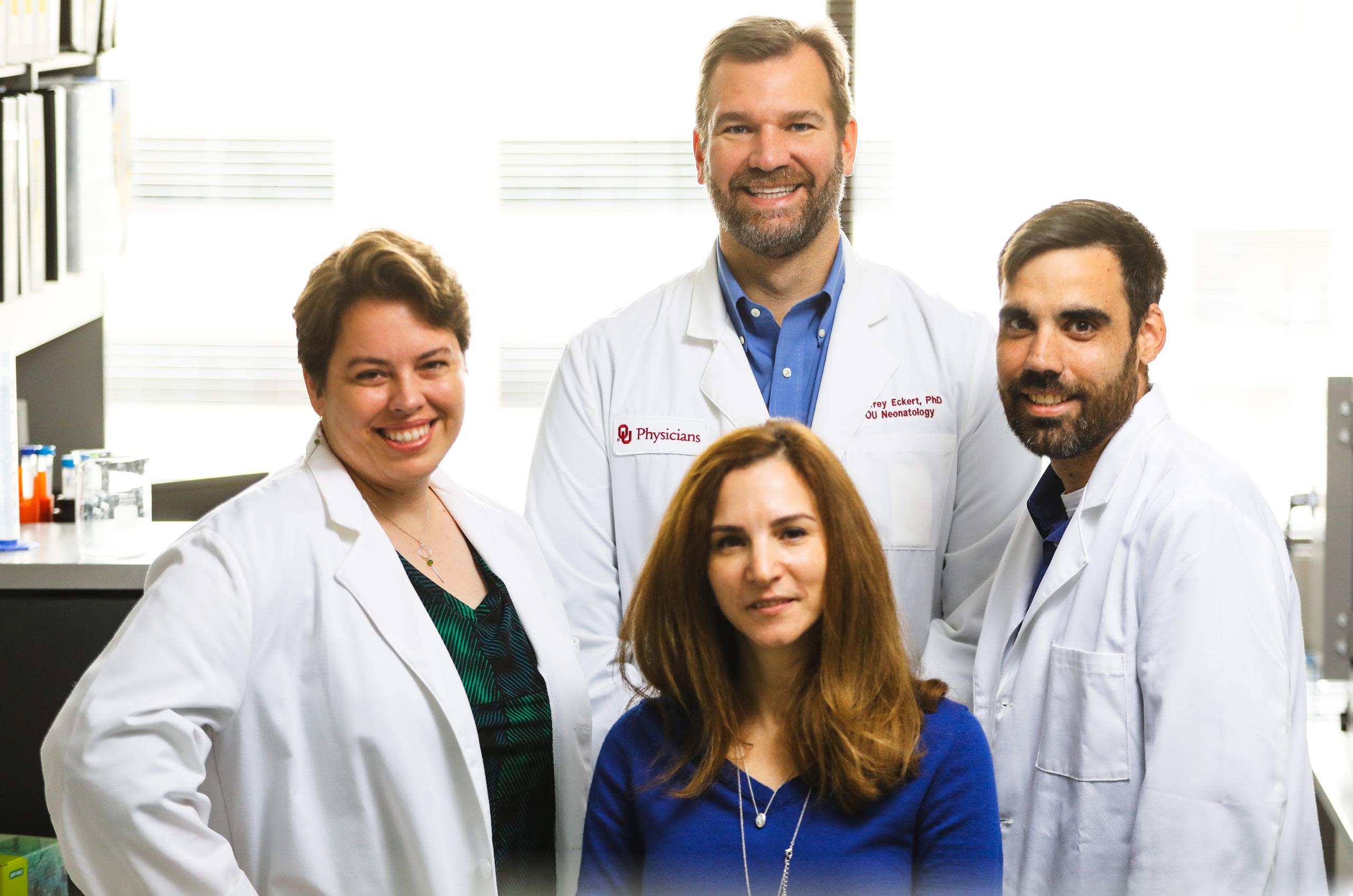
Trent Tipple, M.D., who arrived on campus four years ago as Chief of Neonatal-Perinatal Medicine, views his section’s research program as a Venn diagram, in which the overlapping circles are represented by researchers, clinician-scientists, and the development of junior faculty and trainees.
“The overlap of that Venn diagram becomes the identity of the research program,” said Tipple, who holds the CMRI Reba McEntire Endowed Research Chair in Pediatric Neonatology. “It’s been an effective way for us to have some early successes and competitive grant applications. We’re using it as a template from which to grow.”
The program is also developing a research laboratory infrastructure that looks different than it did in the past, when researchers essentially were given keys to their individual labs
and began the work of setting them up. Instead, the neonatal lab space is shared so that individual researchers can do their scientific work rather than worrying about what equipment to order and how much money they have to spend. The design is also beneficial for clinician-scientists, whose efforts to establish labs have always been challenged by clinical demands.

“Having an open, shared lab allows us to manage it in a shared way as well, which reduces the burden on each faculty member in terms of regulatory issues, budgeting, ordering, and management of personnel. It removes a lot of the barriers to them focusing on their science,” said Vitiello, who holds the CMRI Terrence L. Stull, M.D. Endowed Research Chair in Pediatrics.
In the Lab
The basic science component of neonatal research is relatively young. Vitiello has led the build-out of new lab space and the development of eight different research programs.

Investigations focus on the molecular basis of neonatal diseases seen in the NICU, including cardiopulmonary diseases such as bronchopulmonary dysplasia and persistent pulmonary hypertension; eye diseases such as retinopathy of prematurity; and diseases of the gut, specifically necrotizing enterocolitis (NEC).

The program has established service lines that are critical for researching the molecular origins of neonatal disease. One is the creation of a biorepository of samples from premature infants. Patient samples of urine, meconium, blood, plasma, DNA and other biological material are stored and available to researchers who are asking questions about specific diseases or processes.
The biorepository is also important for creating partnerships nationally. Two years ago, Oklahoma Children’s Hospital OU Health joined the Necrotizing Enterocolitis Society Biorepository to collaborate with other hospitals and academic medical centers around the nation. Samples in the biorepository are being used to investigate ways to prevent or better treat NEC, which primarily affects premature babies. In about 30% of cases, the infant dies, often hours or days after diagnosis. For preterm babies weighing 2 pounds or less, the risk of death is as high as 50%.
“There is a lot of potential in a multicenter collaboration that can conduct research using a large repository of human samples,” said Hala Chaaban, M.D., a leading NEC researcher in the section. “We hope that we can make a difference and eventually never have to see this disease again.” Chaaban recently received a $2 million grant from the National Institutes of Health to continue her investigations in how to prevent NEC, particularly focusing on the potential of human milk to protect against the disease’s development.
The center processes all breast milk and formula for the hospital, but embedded within it is the ability to conduct macro nutrient analysis to determine the composition of what is being fed to babies. That is especially important for promoting growth in premature babies.
“Sometimes what we think we’re feeding, especially when it comes to donor human milk, differs widely from what we’re actually feeding,” Tipple said. “It might mean that the milk for patient A is supplemented differently than what is fed to patient B. This allows us not only to deliver a higher level of clinical care, but to conduct research.”
The research program is also closely aligned with the new OU Health Center for Pregnancy and Newborn Health, which represents collaborations among scientists and physicians across campus. “Our work will strongly focus on two critical areas — the origin and progression of respiratory, intestinal, retinal and cardiac diseases in premature babies, and the impact of maternal and perinatal nutrition on newborn growth development. These factors greatly influence the course of health outcomes,” Vitiello said.
The clinical research team is also active, participating in 30 studies during the past two years alone. Areas of focus are telemedicine, resuscitation, hemodynamics, and nutrition, including a number of studies whose outcomes are likely to
change the standards of neonatal care. For the past seven years, clinical research was led by Edgardo Szyld, M.D.; upon his departure earlier this year, Chaaban has taken on the role of Director of Clinical and Translational Research.
Several resuscitation studies have led to improved care for preterm babies, whose life and health depend upon actions taken in the precious seconds and minutes after birth. For every 30-second delay in resuscitation, there is a 16% increase in the risk of death.
A team led by Birju Shah, M.D., MPH, MBA, developed a study that is investigating the effectiveness of CPAP (continuous positive airway pressure), the same technology used for sleep apnea, for late pre-term infants (born between 34 and 36 weeks) who are delivered through caesarean section. Babies born through c-section do not benefit from the process during vaginal delivery in which pressure on the newborn’s chest squeezes fluid out of the lungs and prepares it to take in air. Nor do those babies receive beneficial hormones from the mother, triggered during labor, that also help their lungs transition to breathing air.
“When the umbilical cord is clamped, there is a huge transition from a cardiorespiratory point of view,” Shah said. “The baby has been swimming in amniotic fluid, and all of a sudden, they have to breathe open air. This transition frequently does not happen normally for babies who are born by c-section, so we are proposing that prophylactically giving them air through CPAP will help them through this process. If we can do this in the delivery room, fewer babies will need to be admitted to the NICU.”
Shah and his team have also been instrumental in two studies — involving electrocardiogram (ECG) and laryngeal masks — that changed the standard of care for newborns and resulted in national and international attention. Laryngeal masks, which connect to an airway tube, are easily and quickly inserted. However, despite evidence showing their effectiveness in
Using electrocardiogram in the delivery room to measure a baby’s heart rate leads to improved outcomes for newborns, according to research led by neonatologist Birju
providing air, healthcare providers weren’t using them, Shah said. Laryngeal masks are a safe and effective alternative to intubation, especially if a physician is not immediately available to intubate a baby.

“If we lose the opportunity to ventilate babies in the first few minutes of life, the ‘golden minutes,’ then they may not get enough oxygen and blood flow to the brain,” he said. “If the brain is compromised, they can develop hypoxic ischemic encephalopathy and cerebral palsy. We published a study demonstrating that laryngeal masks are safe and effective, and we trained our team on their use.”

Similarly, a study that evaluated the use of ECG to measure a baby’s heart rate in the delivery room showed that it led to improved outcomes for newborns, including a lower rate of intubation. The theory behind using ECG to assess a baby’s heart rate is that it provides a more accurate measurement than humans can do with a stethoscope.
“In the highly stressful environment of a delivery room, sometimes you feel your own heart rate and you’re not subjectively assessing the baby’s heart rate,” Shah said.
“The ECG allows us to objectively assess the infant’s heart rate. A poor heart rate is the first indicator that a baby is not transitioning well. When we are able to objectively measure it, we will be more certain about whether we need to escalate an intervention, or if the baby is improving and we need to de-escalate the intervention and get the baby to the mother for the important skin-on-skin contact.”
One of the newest areas of clinical research growth is the hemodynamics program in the NICU, led by Marjorie Makoni, M.D. With a newly acquired echocardiogram instrument (ECHO), Makoni can measure the cardiac function of newborns in real time. Oklahoma Children’s Hospital is one of only a few hospitals in the United States that provides hemodynamic service in the NICU. At the same time she is providing this service, she is developing clinical and translational research projects.
Makoni is also using the ECHO for her research into better detection of pulmonary hypertension in newborns. Because many premature babies receive respiratory support for a
long period of time, they are at higher risk for developing pulmonary hypertension. “Dr. Makoni is developing translational research projects to evaluate markers for early detection of this pathology,” Tipple said. “If we can identify it earlier, we can take measures to prevent its progression.”
Tele-resuscitation, or the use of telemedicine to connect neonatologists with community hospital care teams during high-risk resuscitations, is another major focus for the section. Abhishek Makkar, M.D., leads the section’s telemedicine projects, which are proving to be highly effective and wellreceived by families and community hospitals alike.
As a regional referral center, Oklahoma Children’s Hospital provides a level 4 NICU, the highest level of care available, and receives more than 400 babies each year through emergency transport. To extend that level of care, the section’s neonatologists created a hybrid neonatology partnership in 2013 with Comanche County Memorial Hospital in Lawton, which has a level 2 NICU that cares for babies born at 32 weeks or more. OU Health neonatologists spend three days a week in Lawton caring for patients and cover the other four days through telemedicine.
Makkar and his colleagues published a study last year in the American Journal of Perinatology showing that the healthcare teams at both sites are pleased with the quality of care provided through telemedicine. Families, too, reported being well-informed about their child’s care and able to communicate routinely with neonatologists.

“Tele-resuscitation also allows families to stay close to the patient instead of driving an hour and a half to Oklahoma City,” Tipple said. “Participation of the family in the care of the babies has increased. Tele-resuscitation also saves money because critical care transports cost thousands of dollars for each trip. This effort is also important because it supports front-line providers in Oklahoma and enhances their ability to support their communities.”
Translational research projects are being advanced by several clinician-scientists, including Abhrajit Ganguly, M.D., who is studying the developmental differences between the lungs of preterm babies and the lungs of term babies. Using samples from the section’s biorepository, Ganguly grows cells from the preterm baby’s respiratory tract for analysis. “Later on in their childhood, preterm infants have more reactive airway disease, such as asthma, than term infants do,” Chaaban said. “Dr. Ganguly’s work is an example of why our biorepository is so important.”
Clinical research is also being advanced through Oklahoma Children’s Hospital’s participation in The Children’s Hospitals Neonatal Consortium (CHNC), a collaborative of North America’s leading children’s hospitals. By sharing data and pooling resources, they can improve care for critically ill infants and make discoveries that could not be accomplished by one hospital alone. Makkar is collaborating with several peer institutions on tele-resuscitation projects, and other researchers are developing projects in their areas of expertise, including NEC.
Many opportunities are ahead for the Section of NeonatalPerinatal Medicine. As part of an academic health center with seven colleges on the same campus, neonatology researchers are building interdisciplinary collaborations in which historically unrelated disciplines can apply their expertise to diseases of prematurity. The section is engaged with the “first 1,000 days” research focus of Harold Hamm Diabetes Center, and partnerships are being created with the Department of Nutritional Sciences in the College of Allied Health.
And even though the section is focused on the youngest babies, neonatology researchers have begun conversations with geroscience researchers who focus on the biology of aging. Being born prematurely is a state of health that appears to follow people over their lifespan. “We have gained a greater awareness in the past few years that prematurity is a lifelong disease,” Tipple said. “There are effects on lung function and other organs that reveal themselves sooner in the lives of people who were born prematurely or had a critical illness early in life. We’re just now starting to understand that.”
Tipple also envisions neonatal research playing a larger role in Oklahoma City’s Innovation District, an ecosystem of diverse sectors centered around the OU Health Sciences Center. Faculty members have undergone training in how to commercialize their discoveries, and a variety of tools are available to expand research beyond the traditional confines of a lab.
“We want to be thinking of discovery and innovation beyond earning grants and gathering data,” Tipple said. “We intentionally established our lab space in University Research Park, in close proximity to where investments are being made in the Innovation District. This is not how we’ve traditionally looked at research, but it is an exciting opportunity. At the end of the day, we are participating in many different projects because we want to make a difference for our patients and their families in Oklahoma and beyond. That is the driving force for all that we do.”
The news is rarely good for people diagnosed with glioblastoma, an aggressive brain cancer that is difficult to treat and rarely is cured. However, the prognosis is even worse for a subset of patients whose cancer-fighting immune cells are suppressed after radiation therapy.
But there is renewed hope in a study conducted in part by researchers in the OU College of Medicine, published in the journal Science Translational Medicine. The publication details their discovery of why some patients’ immune cells are suppressed during treatment, as well as the potential of certain drugs to reverse such immune suppression.
OU College of Medicine cancer biologist Dinesh Thotala, Ph.D., MBA, and Subhajit Ghosh, a post-doctoral fellow in his laboratory, began the research at their previous institution, Washington University School of Medicine in St. Louis, Missouri, where they collaborated with Jiayi Huang, M.D., an associate professor of radiation oncology and co-clinical director of the Brain Tumor Center at Siteman Cancer Center. They knew that nearly half of patients undergoing radiation therapy for glioblastoma develop lymphopenia, a suppression of the white blood cells that fight cancer. But they didn’t know why.
“The three of us began working to see if we could find the mechanism behind this lymphopenia phenomenon,” said Thotala, who is an associate professor and Director of Cancer Biology in the Department of Radiation Oncology. “This
suppression can last for six months to a year, and patients who develop lymphopenia are more likely to die sooner of a tumor recurrence.”
The team discovered that patients with lymphopenia have an increased level of myeloid-derived suppressor cells (MDSC) after radiation therapy, as compared to patients without lymphopenia. MDSCs — which can be called “bad” immune cells — suppress the body’s “good” cancer-fighting immune cells, thereby helping the tumor survive the effects of radiation therapy. The researchers made the discovery by analyzing blood samples from patients with glioblastoma and verified it with an animal model of the disease.
They took the research a step further by testing two different inhibitor drugs for their potential to prevent MDSCs from suppressing immune cells. The drugs, given during radiation therapy, were indeed successful, demonstrating they can prevent the development of lymphopenia and improve survival.
“This opens up a new horizon for treating glioblastoma better, at least for this subset of patients,” Huang said. “But we believe the drugs have to be given during radiation therapy because it’s the radiation that induces the production of MDSCs in some patients with glioblastoma, and that’s what is driving the lymphopenia and the resistance to treatment.”
The team’s discovery is distinct in cancer research because it represents a new way of understanding the relationship between the immune system and tumor resistance to treatment, Thotala said. Most studies focus on immune cell suppression within the tumor itself, not throughout the body, as Thotala and his colleagues are doing.
“What we have found is that MDSCs can suppress immune cells systemically — throughout the body — and not just in the tumor,” he said.
Much work remains in this area of research. The team tested only two of several possible drugs to inhibit MDSCs, but they are developing other clinical trials and working with pharmaceutical companies for further investigations. The process is complex and challenging because once MDSCs are inhibited, a person’s bone marrow can replenish them quickly.
Ghosh said the team’s recent findings also may be able to enhance cancer drugs other than chemotherapy and radiation, such as checkpoint inhibitors, commonly referred to as immunotherapy.
“While chemotherapy and radiation therapy work by attacking cancer cells directly, immunotherapy drugs work by stimulating the body’s own immune system to attack cancer cells, even after the treatment has ended,” Ghosh said. “However, immunotherapy has not worked well for glioblastoma and many other tumors, so it may be interesting to see if blocking MDSCs can make immunotherapy more effective.”

CAR T-cell therapy — a treatment in which a patient’s own immune cells are genetically modified to recognize and attack cancerous cells — is revolutionizing the care of people diagnosed with blood cancers. OU Health Stephenson Cancer Center took part in a global clinical trial that led to a change in the way oncologists use CAR T to treat an aggressive type of lymphoma. The results were published in the prestigious journal The Lancet.
CAR T was already approved as a third-line treatment for large B-cell lymphoma, the most common lymphoma in adults. In the clinical trial, CAR T was compared to the second-line standard of care — chemotherapy and stem cell transplant — in patients whose lymphoma either didn’t respond to the first round of chemotherapy or it returned quickly. The results showed CAR T to be the superior treatment because it more than doubled the time patients had before their cancer returned. That finding led the Food and Drug Administration to move up CAR T therapy to the second-line treatment.
“This trial has changed the way we treat patients with large B-cell lymphoma. We hope that by giving them CAR T earlier, they will fare better,” said hematologist-oncologist Sami Ibrahimi, M.D., who led Stephenson Cancer Center’s participation in the trial. “When lymphoma comes back after patients receive their first treatment, they typically don’t have a long survival time. We are always trying to improve outcomes for them.”

CAR T stands for Chimeric Antigen Receptor T-cell therapy. Patients being treated with CAR T first have their blood collected in a process similar to a typical blood donation. White blood cells (which include T cells) are filtered out and sent to a company that inserts the gene for a chimeric antigen receptor into the T cells. The chimeric antigen receptor then binds to cancer cells and activates the T cells. This process allows the newly engineered T cells to recognize and attack cancer with remarkable efficiency. Once the CAR T cells are generated, they are shipped back to Stephenson Cancer Center and given to the patient through an IV, much like a blood transfusion.
In Oklahoma, CAR T therapy is offered only at Stephenson Cancer Center, a National Cancer Institute-designated cancer center. It is part of the center’s growing transplant and cellular therapy program.
The clinical trial was held at 47 sites in the United States, Europe and Japan. Stephenson Cancer Center was among the top five enrollers of patients.
“We are grateful to the patients who were willing to participate in this clinical trial to try to get this promising treatment, but also to advance science for everyone,” said Ibrahimi, an assistant professor in the College of Medicine. “Our clinical trials team is also key to the success of a challenging trial like this. It takes an army to enroll that many patients and perform the required steps, and they put in a lot of hard effort to ensure a successful trial.”
“This trial has changed the way we treat patients with large B-cell lymphoma. We hope that by giving them CAR T earlier, they will fare better.”
Simply getting older is the primary risk factor for developing Alzheimer’s disease. There may not be a way to turn back time, but the research community increasingly recognizes that if the process of aging can be slowed, the onset of diseases like Alzheimer’s may be delayed as well. A recent publication by an OU College of Medicine researcher builds on that knowledge by illuminating the behavior of a pathogenic protein that accelerates aging in the brain.
The study comes from the laboratory of Veronica Galvan, Ph.D., professor and Donald W. Reynolds Endowed Chair of Aging Research in the Department of Biochemistry and Molecular Biology. In her study, published in the journal Nature Communications, she demonstrates just how damaging a protein called tau can be when it becomes pathogenic.
Tau plays an important role in healthy brain cells, but in the process of aging, tau can begin to “misfold” and take on a new formation that is pathogenic. Once it does, tau is transmitted from neuron to neuron until it has infiltrated the long neuronal chain that forms the electric circuit of the brain. In Galvan’s new study, she discovered an additional destructive step for tau — the protein is able to move into the nearby endothelial cells, which play a crucial role in the brain maintaining healthy blood flow.
“That was a surprise to us,” she said. “In the endothelial cell, tau triggers a process called senescence that is central to the biology of aging.”
When endothelial cells become senescent, they can’t do their jobs well anymore. They become highly inflammatory and damage surrounding cells, causing accelerated aging in the blood vessels of the brain. Senescence is also a precursor to atherosclerosis, which is a buildup of plaque in the arteries that obstructs blood flow.
“Even before you see any cognitive impairments, you have dramatic changes in blood flow in the brain. The brain is extraordinarily dependent on blood flow to get oxygen and glucose,” Galvan said. “Pathogenic tau is a cause of Alzheimer’s disease. That is important to understand because if we can remove pathogenic tau from the brain or block tauinduced endothelial cell senescence, then we may be able to prevent damage or restore brain function.”
In the same study, Galvan’s team tested whether a particular antibody could remove toxic tau from the brains of mice. The antibody, which was provided by a collaborating researcher, was able to restore about half of the mice’s brain function. The antibody is being prepared for clinical trials and will be further studied for its role in removing toxic tau.
“We were not able to completely restore function, but we were able to reduce the deficit by about half,” she said. “That was with only one course of treatment, so it could be improved.”
Galvan’s next step is to look for ways to block tau from entering endothelial cells. Her lab plans to perform genomewide genetic screens at the Center for Therapeutic Sciences at the OU Health Sciences Center to determine which genes allow pathogenic tau to enter the cells.
“Once we know which genes are involved, we can act from the other side — instead of trying to remove all of the tau, we can protect the cells by preventing the entry of tau,” she said. “Maybe there are drugs already available that can block tau, or perhaps we could develop a new drug at the Center for Therapeutic Sciences.”
Before arriving at the OU College of Medicine, Galvan worked at the University of Texas Health Science Center at San Antonio, where she played a pivotal role in advancing the drug rapamycin to clinical trials for the treatment of Alzheimer’s disease. The discovery of a drug like rapamycin that targets the rate of aging opened the door for researchers to deepen their studies into the biology of aging and its role in age-associated disease. The field of research is known as geroscience, a growing area of interest and federal funding.
“By targeting the rate of aging, we can, in principle, reduce the risk for a large variety of diseases,” Galvan said. “The idea is that we could help people maintain their health span, their healthy years of life. It would allow for what we call a compression of morbidity — people will still eventually develop health problems, but it would happen in a compressed amount of time and allow for a much longer span of health.”
Galvan is also director of the Oklahoma Nathan Shock Center of Excellence in the Basic Biology of Aging and co-director of the Center for Geroscience and Healthy Brain Aging at the OU Health Sciences Center. The first author for the new publication is Stacy Hussong, Ph.D., assistant professor of research in the Department of Biochemistry and Molecular Biology at the OU College of Medicine. Also serving as first author is Andy Banh, Ph.D., a medical student at the University of Texas Health San Antonio Long School of Medicine.
Oncologists treating patients who are living with both cancer and HIV have historically lacked scientific data about whether immunotherapy drugs will be effective. An OU College of Medicine researcher co-led a global study that revealed good news for this patient population.
The study analyzed the safety and effectiveness of immune checkpoint inhibitors, a type of immunotherapy that helps the body recognize and attack cancer cells, in patients diagnosed with both cancer and HIV. The results, published in the Journal of Clinical Oncology, show that immune checkpoint inhibitors are not harmful to people living with HIV and cancer and can successfully treat certain types of cancer. OU Health Stephenson Cancer Center was among 33 academic healthcare centers in North America, Europe and Australia that participated in the study.
“This study should give some level of confidence to clinicians who are treating patients living with HIV and cancer. They can use this data to guide discussions with their patients when considering immune checkpoint inhibitors. This will serve as a landmark paper in the field, given that little is known about immunotherapy among people with HIV and cancer,” said medical oncologist and hematology-oncology faculty member Abdul Rafeh Naqash, M.D., who led Stephenson Cancer Center’s participation in the study and was the overall lead investigator for the study.
The knowledge gap regarding immunotherapy for people living with HIV and cancer results from the long-term exclusion of this patient population from clinical trials. Because some people living with HIV have impaired immune systems, the scientific community typically has been concerned that they would not respond to immunotherapy or that the drugs would be toxic to them. Because that’s not the case, pharmaceutical companies and the National Cancer Institute should broaden their clinical trial criteria to include more people living with HIV if their CD4 count (a type of white blood cell) is within an acceptable range, Naqash said.
The data analyzed in the study came from patients whose physicians decided to prescribe immune checkpoint inhibitors despite a lack of robust evidence. Though it was not a randomized clinical trial, the study is sufficiently strong to warrant an increased use of immunotherapy, Naqash said. People living with HIV are at higher risk than people without HIV for developing various cancers for which immune checkpoint inhibitors are the standard of care. That includes lung cancer, which is the second-leading cause of cancer death among people living with HIV. If immune checkpoint inhibitors are not prescribed to treat cancers for which they are already approved as the standard of care, those patients would be receiving a substandard treatment.
Researchers studied data from patients with at least 10 different types of cancers. They analyzed several additional factors, including whether CD4 counts influence outcomes and side effects, as well as which tumors responded better to immune checkpoint inhibitors. Future publications detailing those findings are planned.
The study also underscored the importance of a multidisciplinary team treating patients living with HIV and cancer. Involving an infectious disease expert is especially important for monitoring the patient’s HIV viral count, watching for opportunistic infections, and ensuring compliance with antiretroviral drugs, Naqash said.

“We believe this study is a pivotal effort that will lead to further research in the HIV and oncology space to better inform treatment decisions for this patient population,” he said.
“This is the largest data set to date to be analyzed for these particular study questions across different tumor types. This study is also important because it represents the real-world population that we would see in the clinic. It provides a level of assurance that immune checkpoint inhibitors are broadly safe for people with HIV and have the potential to effectively treat several types of solid tumor cancers.”
“We believe this study is a pivotal effort that will lead to further research in the HIV and oncology space to better inform treatment decisions for this patient population.”
OU Health Stephenson Cancer Center at the OU Health Sciences Center has achieved renewal of its status as a National Cancer Institute-Designated Cancer Center. The accomplishment marks a milestone in the cancer center’s continued growth as a statewide cancer network that provides leadership in patient care, research, education and community outreach.
Stephenson Cancer Center is the only NCI-Designated Cancer Center in Oklahoma and one of only 72 such centers nationwide, representing the top 2% of cancer centers in the United States. NCI designation, which must be renewed every five years in a rigorous review process, acknowledges Stephenson Cancer Center’s ongoing excellence in all areas of its mission.
“Achieving renewal of our NCI designation is a tremendous accomplishment for Stephenson Cancer Center and for our advancements in research at OU,” said OU President Joseph Harroz Jr. “It confirms our commitment as a
research-intense university to conduct research that will lead to new treatment breakthroughs. This renewal is only the beginning. Stephenson Cancer Center is focused on bringing NCI-level care to all Oklahomans and helping to eliminate the burden of cancer in our state.”

“Achieving renewal of our NCI designation is a tremendous accomplishment for Stephenson Cancer Center and for our advancements in research at OU.”
Stephenson Cancer Center opened in 2011 and achieved NCI designation for the first time in 2018. Since then, Stephenson has grown significantly, attracting more than 100 highly skilled clinicians and researchers in the past decade alone and increasing research funding within the University of Oklahoma to $65 million annually. The cancer center is the largest and most comprehensive oncology practice in Oklahoma and commits significant resources to innovative research that drives new discoveries.
Nearly all NCI-designated cancer centers are a part of an academic healthcare system. Stephenson Cancer Center is a major clinical component of OU Health, the state’s only comprehensive academic healthcare system. The NCI designation is the gold standard for oncology research, placing the University of Oklahoma in an elite circle of oncology research centers while providing Oklahomans with some of the most innovative cancer therapies available in the country.
“As Oklahoma’s academic referral center, OU Health is committed to improving lives through healing and discovery by offering research-driven clinical care. No Oklahoman should have to leave the state for the care they need, and this NCI renewal affirms OU Health’s commitment to providing complex care here at home,” said OU Health President and CEO Richard P. Lofgren, M.D., MPH. “Stephenson is a key component of our academic healthcare system and plays an invaluable role in the health and well-being of Oklahomans.”
NCI designation is the highest federal rating a cancer center can achieve. Studies show that patients who receive care at an NCI-Designated Cancer Center can improve their survival rates by up to 25%. In Oklahoma, where 1 in 2 men and 1 in 3 women receive a cancer diagnosis during their lifetimes, Stephenson provides hope and healing to patients and their families.
Stephenson Cancer Center’s journey to NCI designation began in 2001, when the Oklahoma state Legislature passed bipartisan legislation mandating the creation of a statewide cancer network. Stephenson Cancer Center cares for patients through a multidisciplinary care model in which disease-site experts in surgery, medical oncology, radiation, pathology and other areas meet together to create individualized treatment plans. Stephenson also offers more clinical trials than any other center in Oklahoma, including the state’s only Phase I clinical trials program, which gives patients access to the newest early-stage investigational drugs. One in 5 patients at Stephenson is enrolled in a clinical trial.
“As an NCI-Designated Cancer Center, we have the resources to provide world-class treatments to our patients while offering the necessary support to providers, patients and our community to reduce the burden of cancer,” said Stephenson Cancer Center Director Robert Mannel, M.D., a professor of gynecologic oncology in the OU College of Medicine. “Because research underscores the care we provide, our clinicians and researchers often collaborate to seek answers to complex questions. Our emphasis on research creates an atmosphere where treatments are constantly being improved for the benefit of our patients.”
The Oklahoma Tobacco Settlement Endowment Trust (TSET) continues to play a crucial role in Stephenson Cancer Center’s research mission. TSET’s grants, funded through the state’s Master Settlement Agreement with the tobacco industry, support Phase I clinical trials, the recruitment of scientists, research grants to Oklahoma scientists, cancer screenings, and behavioral and tobacco cessation research in the state.
“It confirms our commitment as a research-intense university to conduct research that will lead to new treatment breakthroughs. This renewal is only the beginning. Stephenson Cancer Center is focused on bringing NCI-level care to all Oklahomans and helping to eliminate the burden of cancer in our state.”
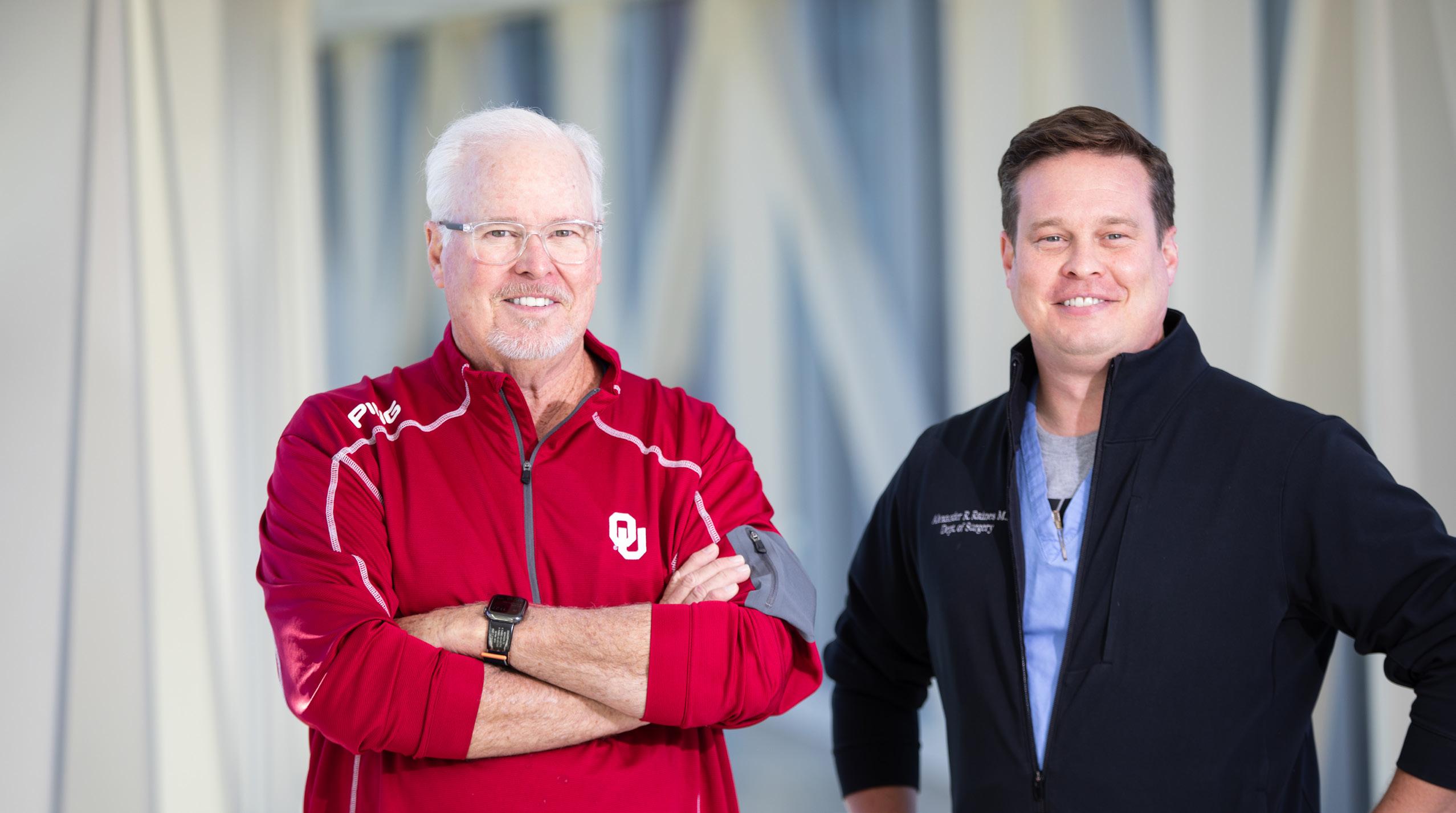
As a third-generation surgeon, OU Health general surgeon Alex Raines, M.D., was exposed to medicine from a young age and admired the role his father played in his patients’ lives. That admiration was reciprocated when his father, Ed Raines, M.D., arrived from out of state for a temporary surgery assignment and visited his son’s operating room for the first time.
Ed Raines was filled with pride upon seeing his son’s achievements and for the positive environment he has created for his patients, his trainees and the team surrounding him. In return, Alex was gratified by his colleagues’ warm welcome to the man who has given him the most valuable lessons in medicine and in life.
“I think the best part of that day was the phone call we had after the day was over,” said Alex, an associate professor in the Department of Surgery at the OU College of Medicine. “My dad said, ‘I’m really proud of your operating room because the culture was good and the team was awesome.’ That meant a lot to me because I know he knows the difference between a good operating room and a bad operating room. He wasn’t just being nice and being my dad. He walked into the operating room and felt a good culture.”
“It was also great to hear from students and residents and office staff about how great it was to work with my dad while he’s been here,” Alex said. “I’ve heard those things my whole life, but hearing them in my own hospital was really nice. It validates everything I’ve learned from him — that you create
an environment for patients to receive good care and for team members to feel valued.”
The majority of Ed Raines’ career has been in cardiothoracic surgery private practice in Nebraska. He is doing some regional work as a locum tenens, a Latin phrase that refers to a physician working temporarily in a practice that’s not his own. That work brought him to the OU Health Sciences Center for the first time.
Alex said the culture of his own operating room is directly tied to the lessons he learned from his father growing up. Alex distinctly remembers his father introducing him to one of his patients who was about to undergo a heart bypass. Calling her by name, Ed said, “She knows I’ve done thousands of these surgeries and have had really good outcomes. But she doesn’t care about those thousands that I’ve done. She cares about hers.”
“Patients aren’t numbers; they’re people. And while we do surgery every day, that might be the first surgery they’ve ever had.”
“That has stuck with me all these years,” Alex said. “Patients aren’t numbers; they’re people. And while we do surgery every day, that might be the first surgery they’ve ever had.”
“Growing up, I also remember being at school or in the mall and someone would stop me and say, ‘Is your dad Ed Raines?’ Then they would say, ‘He operated on my father’ or ‘He operated on my grandmother.’ I understood then how important those moments are in people’s lives. If a person has surgery, that is usually a milestone moment in their life. And we get to participate in that.”
Alex and his father both attended medical school at the University of Nebraska College of Medicine (as did Alex’s grandfather and uncle). When Alex was in his fourth year of medical school, he spent a one-month rotation in his father’s surgical practice, where he experienced an irony that he laughs about today. At the time, Ed was using robotics to perform some surgeries.
“I should have been in awe of this robot,” Alex said, “but instead I chastised my father for using it. I said, ‘Why are you using this big clunky machine? It’s expensive and it’s unnecessary.’ Fast-forward about 20 years, and now I’m using the robot and in fact have hung my clinical career on robotics because of the value it adds.”
The careers of father and son have taken a few other related, if unexpected, paths. When Ed was applying for residency, his top choice was the Mayo Clinic. He was so sure that was his destination that he almost bought a house there before it was official. As it turned out, his residency match was at the University of Utah Health, which ultimately was the best fit for him. Similarly, Alex had hoped to attend residency at the University of Utah as his father did, but he instead matched at the OU College of Medicine.
“In retrospect, OU should have been my No. 1 pick because this is exactly the culture I fit into and it’s a great program,” Alex said. “That’s been one of my most powerful lessons to relay to students: ‘Don’t hold on too tight to what you think the future is going to be.’”
Since finishing his residency and becoming a faculty member at the OU College of Medicine, Alex’s career has flourished, both as a surgeon and an educator. In addition to his busy surgical practice at OU Health Edmond Medical Center, he teaches medical students and residents. He serves as
co-director of the third-year medical student clerkship and as site director for surgery residency training at Edmond Medical Center.
Alex is so well-respected by his colleagues and his students and residents that he was awarded the Stanton L. Young Master Teacher Award by the OU College of Medicine. It is one of the largest awards in the nation for medical teaching excellence. He is also a member of the college’s Academy of Teaching Scholars, a group of faculty members who seek to improve medical education through scholarship.
Although he hadn’t planned on a career in academic medicine, Alex was drawn to education because it is ultimately another way of helping patients. “I can only operate on so many thousands of patients during my career, but every time I teach a student or resident and they take that into their careers, I’ve indirectly affected many more patients,” he said.
Beyond clinical skills, Alex is also passionate about teaching students and residents how to handle the emotional demands of being a surgeon. “You make connections with your patients. Bad outcomes will sometimes happen. It’s part of being a doctor,” he said. “You need to be able to navigate that not only with the patient but with yourself as well. I enjoy helping students with that emotional intelligence training.”
Seeing his son excel as both a surgeon and an educator is gratifying, Ed said, and he has done so by staying dedicated to his patients and the healthcare team that makes his success possible.
“Being from Nebraska, I used to say that’s what it means to be a Husker — you’re hard-working, you’re honest and you’re not cocky,” Ed said. “I think you can say the same thing about being a Sooner — it means you’re authentic and you treat people right.”

“Being from Nebraska, I used to say that’s what it means to be a Husker — you’re hard-working, you’re honest and you’re not cocky. I think you can say the same thing about being a Sooner — it means you’re authentic and you treat people right.”

A multidisciplinary team recently performed the first catheterbased mitral valve repair at OU Health University of Oklahoma Medical Center, broadening the options for patients with leaking mitral heart valves. The minimally invasive procedure eliminates many of the risks associated with open-heart mitral valve repair and allows many patients to go home the day after the procedure.
Usman Baber, M.D., Director of Interventional Cardiology and the Cardiac Catheterization Laboratory at OU Health and associate professor of medicine at the OU Health Sciences Center, said that for years, the only way to treat mitral valve leaks was with open-heart surgery, cutting through the patient’s sternum, and only if the patient was a suitable candidate. In some of those patients, the valve could be repaired, but others required a valve replacement. The minimally invasive MitraClip procedure can repair the valve without open-heart surgery.
The mitral valve is one of four valves in the heart that helps blood flow in the right direction, from the left atrium to the left ventricle. When it is leaking, a proportion of the blood that is supposed to go forward and deliver blood and oxygen to the body is instead going backward. Mitral valve disease occurs in approximately 3 % to 5% of the population and is increasing as the population ages in Oklahoma. Untreated, it can increase the risk of heart attack and stroke.
The MitraClip procedure is conducted under anesthesia, and physicians access the mitral valve with a catheter that is
guided through a vein in the leg up to the heart. The catheter carries a clip that is attached to the mitral valve, which helps it to close and restore normal blood flow to the heart. The success rate is high. The procedure takes about two hours, and patients’ symptoms, including fatigue and shortness of breath, improve almost immediately.
“When a patient has the MitraClip procedure, their symptoms improve, they’re less likely to be hospitalized with heart failure and they feel a lot better,” Baber said. “Typically, the patients getting this procedure are those who cannot endure openheart surgery, and we can now offer them a therapy to treat their condition, close to home. There is still a role for openheart surgery, but the catheter-based mitral valve repair is a complementary procedure that is of great benefit to many patients.”
The OU Health team conducting the MitraClip procedure involves a heart surgeon or interventional cardiologist, an echocardiographer working in real time, and an anesthesiologist.
“As an institution and a healthcare system we should be very proud of this new technology that we can now offer our patients with mitral valve disease,” Baber said. “This milestone is a testament to our team-based approach and our collective efforts, and it enhances our ability to take care of patients with complex cardiovascular disease.”
OU Health and Norman Regional are partnering to bring the highest level of cancer care to Norman by building a new cancer care facility, providing the expertise and convenience of Oklahoma’s only National Cancer Institute-Designated Cancer Center, OU Health Stephenson Cancer Center at the OU Health Sciences Center, to the residents of the south metro and south-central Oklahoma.
Located at the Norman Regional HealthPlex near I-35 and Tecumseh Road, the 50,000-square-foot facility will be named OU Health Stephenson Cancer Center at Norman Regional. The state-of-the-art facility will combine the full spectrum of medical oncology and radiation oncology services under one roof on the newly modernized Norman Regional HealthPlex campus. It will include two advanced linear accelerators to provide targeted and precise radiation therapy, as well as advanced diagnostic imaging services to improve detection and monitoring of treatment results. The facility is scheduled for completion in 2025.
“This is an exciting day for our two health systems as we join together to offer high-quality, research-driven cancer care to people in Norman and from across southern Oklahoma,” said Richard Lofgren, M.D., MPH, president and CEO of OU Health. “We are pleased to welcome Norman’s excellent oncologists to the OU Health team and to partner with them to provide National Cancer Institute-level care that is driven by research. This is a natural evolution for the long-standing relationship of our health systems.”
In January 2023, Stephenson Cancer Center assumed operations and management of Norman Regional’s existing medical oncology services at the Porter Medical Oncology Clinic. In 2025, with the opening of the new facility,

Stephenson will begin providing radiation oncology services in partnership with Norman Regional. This provides patients access to a larger range of expertise.
“Norman Regional has a long history of excellence in cancer care. Partnering with Stephenson Cancer Center will elevate those services in a variety of ways and allow patients to receive convenient care closer to their homes,” said Richie Splitt, president and CEO of Norman Regional Health System.
In addition to cancer treatments, patients in Norman will have access to other services offered through Stephenson Cancer Center, including clinical trials studying drugs for many types and stages of cancer. Phase I clinical trials, in which humans receive a drug for the first time, will continue to be offered only at Stephenson in Oklahoma City. However, with the opening of the new facility, patients can enroll in Phase II and III clinical trials and receive their care in Norman.
Norman Regional also will offer patients an expanded range of supportive care services through Stephenson Cancer Center. This includes counseling services specific to cancer patients, nutritional services to support the body through cancer treatment, palliative care to manage cancer-related symptoms, cancer rehabilitation to recover function, and much more.
“We are excited to extend the reach of Stephenson Cancer Center and bring these opportunities to patients in Norman and surrounding communities,” said Robert Mannel, M.D., director of OU Health Stephenson Cancer Center and professor of gynecologic oncology in the College of Medicine.
“This partnership represents Stephenson Cancer Center’s first opportunity to begin expanding into a statewide network for the residents of Oklahoma, which is the charge that the Oklahoma Legislature has given us. Stephenson Cancer Center is the state’s most comprehensive oncology practice, and we rank No. 1 among all cancer centers in the nation for the number of people participating in NCI-sponsored clinical trials. That means scientific breakthroughs are more readily translated into new treatment options that bring new hope to patients fighting cancer.”

When children in a behavioral health crisis are taken to an emergency room, they are often placed in small spaces that are not designed for safety or privacy, which can impede recovery and extend the hospital stay. That’s why three emergency rooms at Oklahoma Children’s Hospital OU Health have been renovated to create an environment that is conducive to healing and safety for patients and healthcare providers alike.
The new rooms feature LED lighting, peaceful sounds, and themes projected onto the walls. Children can play games on an interactive touchscreen wall and change the lighting and wall themes. Medical equipment is concealed behind a large door when not in use, and fixtures are tamper-resistant to protect patients at risk of harming themselves or others. The rooms are enclosed and situated near the nurse’s desk so they can be closely monitored while still offering privacy for patients.

“There is a pediatric behavioral health crisis at the moment, and parents can struggle with how to help their children and where to get help,” said OU Health pediatric psychiatrist Robyn Cowperthwaite, M.D., an assistant professor of
psychiatry and behavioral sciences in the OU College of Medicine. “The ambient rooms at Oklahoma Children’s Hospital are the first step in providing a safe place for children to de-escalate and start the healing process.”
The behavioral health rooms were created with funding from the U.S. Health Resources and Services Administration. “We are incredibly grateful for the support we have received from our federal delegation in procuring the specialized equipment for these rooms,” said Erin Walker, Associate Vice President of Operations for Oklahoma Children’s Hospital.
“We are incredibly grateful for the support we have received from our federal delegation in procuring the specialized equipment for these rooms. ”
To improve healthcare access for Oklahoma City children, OU Health is partnering with Oklahoma City Public Schools to provide school-based telehealth services.

OU Health’s secure telehealth devices are being placed in Oklahoma City Public Schools, beginning with a small pilot group and eventually expanding to all schools in the system. When a child is sick, the school nurse can request a telehealth appointment and the student typically will be scheduled to see a pediatrician the same day.
“When students have untreated health issues, it can lead to them missing school and experiencing academic struggles. Additionally, many parents are not easily able to leave work to take their child to the doctor during the day. The opportunity to ensure these young patients are able to receive healthcare
services in a timely manner is really exciting to us,” said Kathleen Combs, M.D., OU Health pediatrician and medical director of OU Health’s School-Based Telehealth Program. She also serves as an OU College of Medicine clinical faculty member.
Through telehealth, pediatricians may examine students who have a sore throat, congestion, nausea, ear pain, rash or a minor injury — a range of symptoms that are not emergencies but still should be seen by a physician. The telehealth device is equipped with a digital otoscope, stethoscope and handheld camera that the nurses navigates, allowing the pediatrician to perform the virtual exam. If a prescription is warranted, the pediatrician can send it to a pharmacy of the family’s choice.
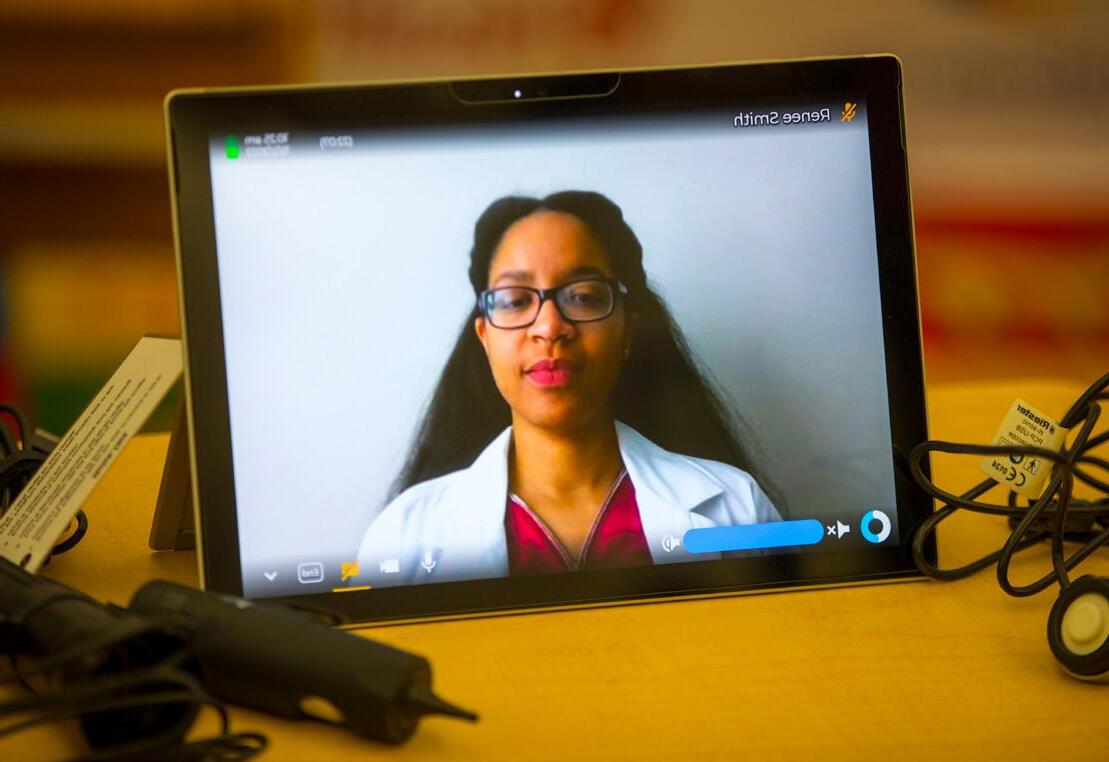
“In some cases, our school nurses are the only healthcare provider our students see regularly. The relationships they build with students and their families play a vital role in maintaining a safe and healthy learning environment for our students,” said Oklahoma City Public Schools Superintendent Sean McDaniel. “Offering telehealth through our partners at OU Health is a game-changer. It will allow our families to receive enhanced health services without having to take time off work to go to an outside clinic. We are thankful to OU Health for this critical partnership.”
Telehealth visits are provided regardless of the student’s insurance status. Eventually, OU Health plans to broaden telehealth services beyond sick visits to include maintenance of chronic conditions like asthma.
“As the state’s academic healthcare system, we believe it is our mission to provide healthcare that is accessible, timely, high-quality and affordable,” said OU Health President and CEO Richard Lofgren, M.D. “Our telehealth partnership with Oklahoma City Public Schools achieves that mission in many different ways. Ultimately, we want to play a role in providing children and families with the care they need and improving their health and well-being.”
The OU College of Medicine’s enrichment curriculum, designed to help students focus on the humanity of the patients they will be caring for, has grown larger with the addition of the course Social Justice in Medicine.
By focusing on the social determinants of health, the course gives medical students a real-life perspective on the disparities many of their patients face. Social determinants of health are the nonmedical factors that influence health, such as the environments where people live, work, learn, and spend social and leisure time. The Centers for Disease Control reports that communities with poor social determinants of health have a reduced quality of life and experience high levels of inequity.
“The numbers tell us that 80% of patient morbidity and mortality are influenced by their social determinants of health. That is astounding,” said course director Lin Goldston, Director of Operations and Administration for Academic Affairs in the college. “Therefore, socioeconomic status and social and physical environment factors have a greater impact than clinical care on health outcomes. These topics must be included in the education of future physicians.”
People may face systemic barriers when trying to access care for themselves and their families. Those barriers, often invisible, affect health outcomes, said Colleen Parrish, M.D., assistant professor of pediatrics and course director, assisted by patient care navigator and social work student Ana Bugarin.
“We want our students to understand that health isn’t just about the sickness,” Parrish said. “You can label someone as non-compliant, but if they aren’t taking their medication, they may be making decisions like, ‘Do I pay for food or do I pay for my meds?’ It’s easy to create that distance and mistrust in the system. This class helps students identify the inequalities that contribute to poor health outcomes.”
Students also go into the community to view inequity firsthand. Students participating in the course consider food insecurity, housing insecurity, adverse childhood experiences, trauma, and legislative advocacy, while also visiting with community partners to further the experience.
Medical student Sona Maan said she was prompted to take Social Justice in Medicine because her parents and her religion, Sikhism, modeled the importance of doing good for others. She developed an interest in the connection between social sciences and medicine that gave her a solid foundation for the experience.

“I picked this class because I want to be a better advocate for my patients. ... Now is the time to start learning how to best advocate for our future patients.”
“Social determinants of health is not a subject that many medical students are unaware of, but the specific activities we do in this course, such as touring the food bank and getting to meet community partners to learn about housing insecurity, is a very unique opportunity that I would not have otherwise been able to learn first-hand,” she said. “It is tremendously important to learn about the social determinants that impact our community directly and to be aware of the community resources available to be the best advocates for our patients in Oklahoma.”

Medical student Isha Jhingan reflected upon her own upbringing as she took the course. She was almost 8 years old when her family moved to the United States and had no vehicle. “We would go grocery shopping once a week and could only bring home what we could carry,” she said. “We had to hope our food would last until we could make our next trip to the store. Transport is such a huge issue for many people. Whether it’s buying fresh food or attending medical appointments, so many people are limited. We lived in the city, so at least we had buses, but for people living in rural areas and no access to transport, buying fresh food and accessing healthcare is very difficult.”
Understanding those barriers makes Jhingan passionate about patient advocacy, “I picked this class because I want to be a better advocate for my patients. This is going to be a useful skill regardless of the specialty I go into. Now is the time to start learning how to best advocate for our future patients.”
Social Justice in Medicine also allows students to begin thinking about how they can advocate through legislation and policy for changes that improve the welfare of their patients. Medical student Karanpreet Multani brings his passion for equity and justice to the work of removing barriers to good health.
“Justice is another principle of Sikhism that drew me to this subject — making sure that you fight injustice and you stand
up to things you know are wrong. In Sikhism, we are focused on equality — men and women are equal — and if you see inequities, you stand up for it. You have a responsibility to raise awareness and try your best to help,” he said.
Students in the course also gain awareness of resources that may help their patients, such as pointing them toward food pantries or crisis housing. “Understanding patients’ backgrounds and empathizing with their situation is so important,” Maan said. “When they’re having a tough time and are unable to afford groceries, that will directly impact their health and nutrition. Knowing the resources that are available to help them can make such a difference, and we can guide them to those resources to make their lives better.”
Social Justice in Medicine is part of an extensive roster enrichment courses. Others include Medical Reader’s Theater, The Art of Observation, Photography and Medicine, Literature and Medicine, and Philosophy and Medicine.
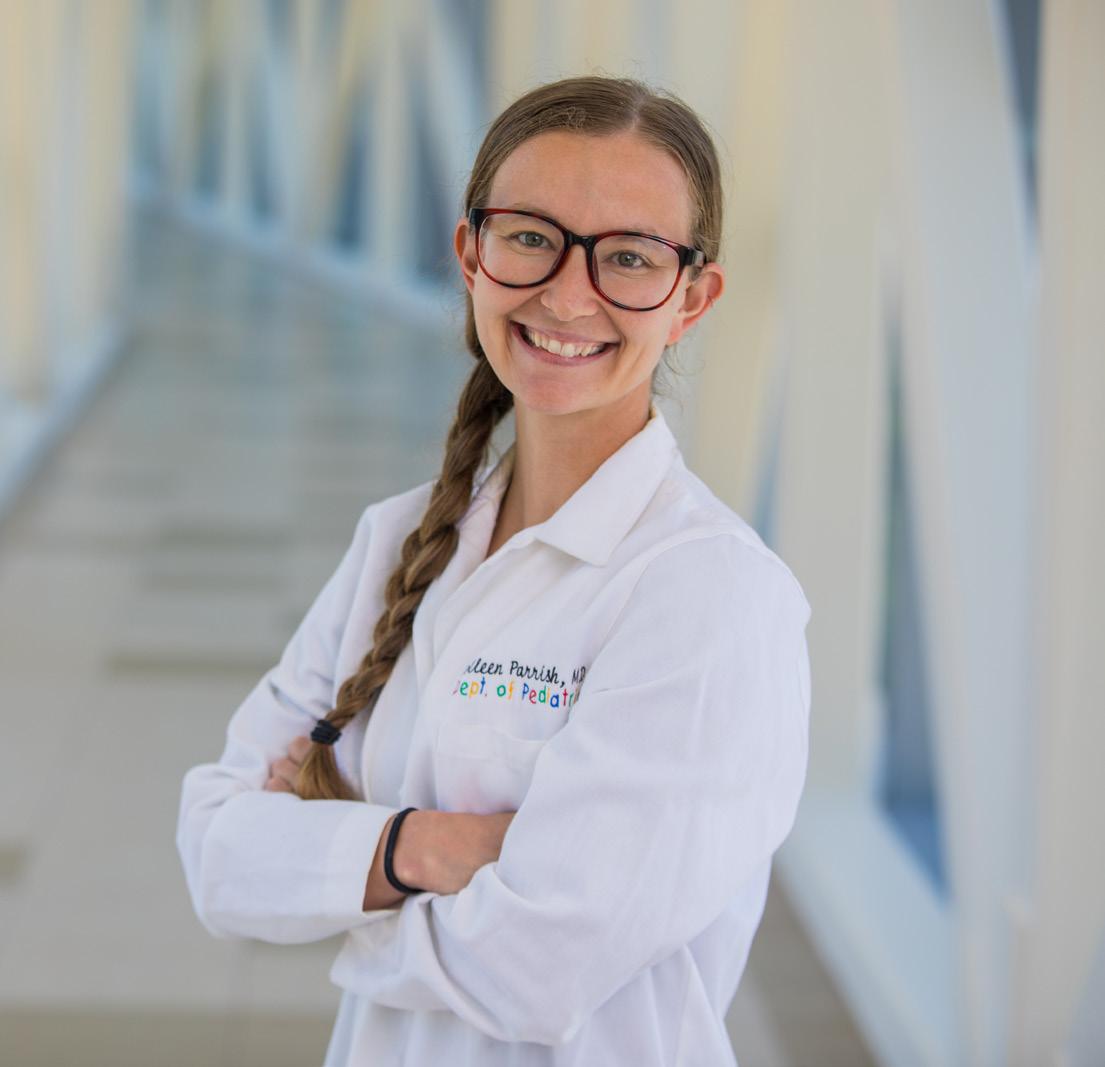
To increase diversity in the field of health-related sciences, OU Health Stephenson Cancer Center at the OU Health Sciences Center hosted its inaugural Diversity in Cancer Research Summer Internship last year. Ten Oklahoma college students from underrepresented groups took part in the program, during which they participated in research projects and engaged in activities that fostered problem-solving skills and innovation.
“Oklahoma is well known for having larger minority populations. The question is, how do we involve them and get them into the medical and biomedical field? If we can help them to become successful, the hope is that a good number of them will come back through the institution and be of benefit to their communities,” said one of the internship’s leaders, Rajagopal Ramesh, Ph.D., associate director for Education, Training and Career Enhancement at OU Health Stephenson Cancer Center and a professor of pathology in the OU College of Medicine.
While the program aims to advance diversity among cancer researchers, its effect on students was significant. Participants benefited from the program personally, and their experiences hold the potential to change communities. Eddy Bagaruka and Emily Battung came away from the internship inspired to make a difference in the lives of others.

Bagaruka studied biology with a pre-med emphasis at Oklahoma Christian University. He grew up in Rwanda and witnessed first-hand the ravages of war and a lack of access to healthcare. When Bagaruka was only 2 weeks old, his father was killed in the Rwandan genocide, leaving him and his siblings to be raised by their mother. No one in the family had gone to school, but Bagaruka’s mother encouraged him to pursue a medical career. His desire to be a change for good spurred him to help build houses for the elderly and to seek
medical training. For Bagaruka, the internship was not just about learning research skills, but how to improve himself through mentorship, constructive criticism and critical thinking.
Rwanda has limited access to healthcare and needs healthcare workers. Bagaruka has a passion to go into the medical field and aspires to serve minority groups in the United States and to train people in Rwanda so they can provide healthcare services to their communities.
“Healthcare has to be done in a team. I want to mobilize teams to educate minority groups who don’t realize what services are available to them, and to encourage them,” he said. “Many people in Rwanda do not have access to study, and I want to be able to teach others and to motivate them to do better.”
As a health and exercise science major and pre-med student at the University of Oklahoma, Battung was hesitant to apply for the internship because she felt that her application would not stand out. From Mexican and Filipino parents, Battung grew up in Texas and struggled with her cultural identity. Coming from two minority groups, she found it difficult to identify with either, which affected her confidence. Battung applied for the internship hoping to grow her research skills and to learn how to tackle scientific problems, but she walked away with much more.
“I have developed my communication skills, how to analyze, time management, and how important it is to keep trying. Hard work and determination pay off,” she said. Battung recognized that she was limiting herself and learned to push past her lack of confidence. “You are more than your racial identity,” she said. “It’s part of who I am, but it’s not all I am. This program has shown me that I want to be an inspiration and to tell young girls not to give up — if you fail the first time, then keep trying. Keep improving.”
The American Cancer Society’s Extramural Discovery Sciences department provided funding to support the participation of eight students in the internship. Private donors also supported the program.

Students on the Oklahoma City campus and at the OU-TU School of Community Medicine in Tulsa learned their residency matches in March.





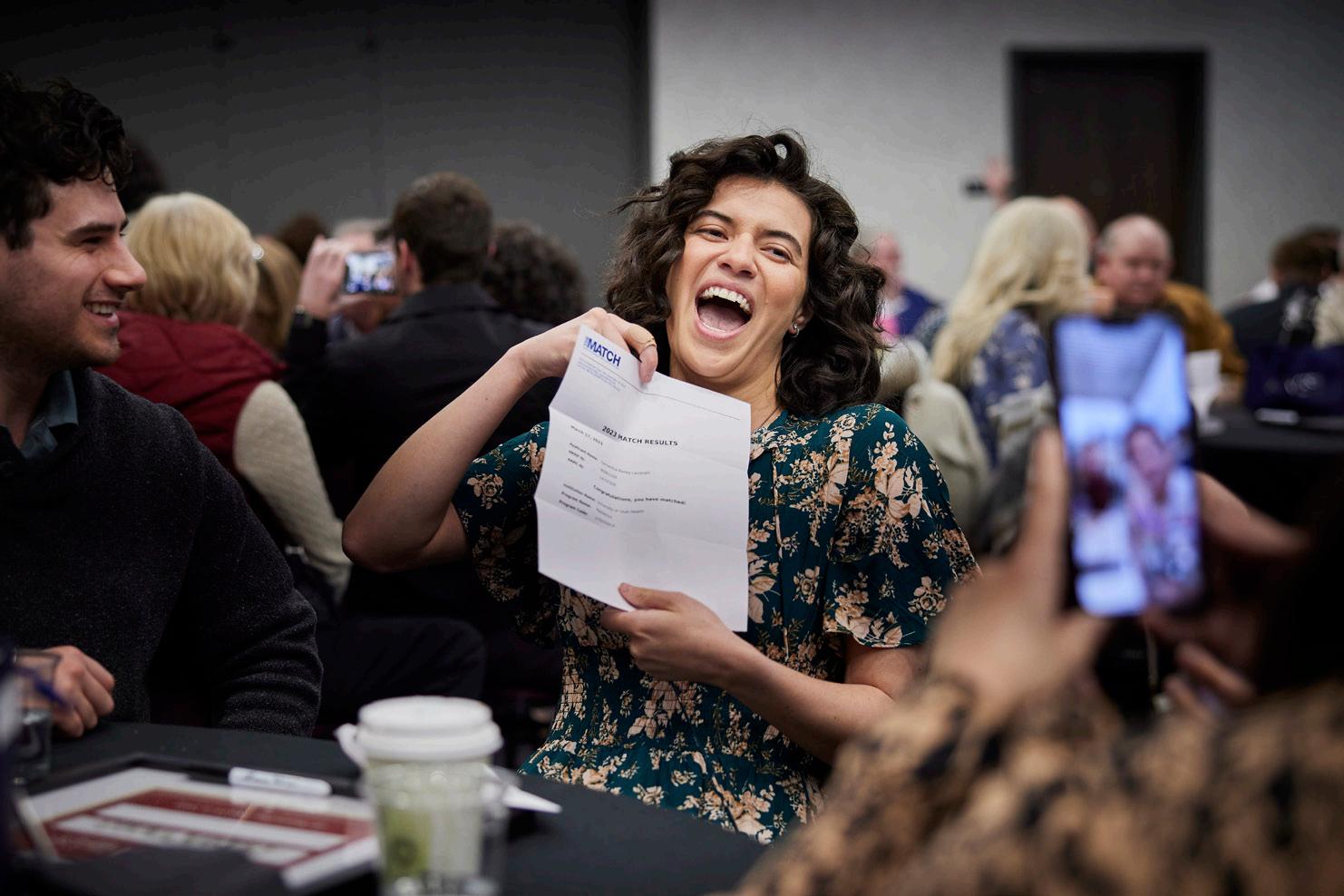

OU College of Medicine student Nate Cross credits his military experience with giving him the courage to answer his calling of becoming a doctor and conquering the challenges along the way.
The Navy veteran, husband and father of three was acknowledged for his pursuits in medicine and his military service by the Pat Tillman Foundation, which named him a 2022 Tillman Scholar – a recognition that comes with an average award of $10,000 per academic year and exclusive networking opportunities.
Despite the obstacles posed by embarking on a medical education during the pandemic, being a father and husband, and working a full-time job at the time of his decision to go back to school, Cross had faith in his abilities and that he could reach his goals, thanks to his military training.
“One of the biggest lessons I learned in the military was the importance of grit, perseverance and a strong network of support,” Cross said.
His decision to pursue medicine and leave a secure job as a warehouse and logistics supervisor required that he draw upon those lessons.
“I had a good job, good benefits; everything should’ve been perfect, but I was unsettled because I knew I wanted to be back in medicine,” he said.
Cross served as a Marine Corpsman in the Navy. It was through his training to provide field medicine in the military that he discovered his passion for connecting with patients.
“I know how important authentic human connection is,” Cross said. “As a physician, I hope to establish and maintain authentic relationships to better health outcomes, increase access to care and lower healthcare costs.”
Cross, who grew up in New Orleans, Louisiana, began his military career shortly after high school in the U.S. Navy Reserve as a Fleet Marine Corpsman.

He was enlisted for a total of eight years when he suffered a back injury that ended his time in the military in 2018. Still wanting to be of service, he began medical school at OU with hopes of becoming a family medicine doctor.
“My dream is to have a private family medicine practice in a rural setting,” Cross said. “Imagine the classic small-town doctor seen in media who treats patients of all ages and is able to form strong bonds with their community to help improve health outcomes.”
Cross earned a bachelor of business administration from the Michael F. Price College of Business and was admitted to the
OU College of Medicine in 2020. He expects to graduate in 2024.
Cross is the 13th OU student to be selected as a Tillman Scholar. Other OU Tillman Scholars have studied medicine, public health, education, law and biology.
The Tillman Foundation offers scholarships to U.S. service members, veterans or their spouses to help them pursue higher education and continue their service in the fields of healthcare, business, law, public service, STEM, education and the humanities.
It’s a highly selective scholarship, with no more than 60 recipients chosen per year from across the country since its inception in 2009.
Cross was chosen as member of the foundation’s 14th class in honor of the late Pat Tillman, who, as a professional football player in the National Football League, joined the U.S. Army and was killed in battle in 2004.
“I am beyond honored to have been selected as a Tillman Scholar, and I am still in a bit of disbelief about being chosen to join such a prestigious group of individuals,” Cross said.
“As a physician, I hope to establish and maintain authentic relationships to better health outcomes, increase access to care and lower healthcare costs.”
Preparation for medical school is a monumental task. The application preparation, financial obligations, a difficult admission exam, time commitment — all require extensive resources, which historically haven’t been afforded to underrepresented students.
However, through the OU College of Medicine’s OU MED REV UP! program, students are gaining the tools to successfully prepare for, apply and be accepted to medical school. REV UP!, a free six-month program for undergraduate students, began in 2021. It offers preparation for the Medical School Admission Test (MCAT), which normally costs thousands of dollars, as well as mentoring from a current medical student and a variety of workshops on how to be successful in medical school. The program is organized by the college’s Office of Diversity, Inclusion and Community Engagement and funded by the U.S. Health Resources and Services Administration.
One student who successfully leveraged the REV UP! experience to enter medical school is Prince Ohene-Nyako, whose family moved from Ghana to Norman when he was 3 years old. After earning a degree in health and exercise science at OU in 2020, he decided he wanted to pursue a career in medicine. He applied to medical school right after graduation, but wasn’t accepted. When he decided to try again, he became concerned about the costs of the MCAT preparation course, which he knew could help him succeed. That’s when he met Robert C. Salinas, M.D., the college’s Assistant Dean for Diversity, Inclusion, and Community Engagement.

“Dr. Salinas was so welcoming and wanted to help me get there,” Ohene-Nyako said. “When it was time, he encouraged me to apply for OU MED REVUP! and thankfully, I was accepted. I didn’t have the resources and guidance before then. The program made the most impact on my way to medical school — I needed to know what I should be studying and how I should be studying, rather than doing everything on my own.”
Ohene-Nyako will be the first physician in his family. He said the skills he learned from the program were life-changing. “It wasn’t just MCAT preparation that was so helpful. We learned about leadership building and soft skills building, which many of us had never had exposure to in our lives. Learning interview skills, like how to look somebody in the eye and clearly ‘sell yourself’ in a good way, is really underrated. We were taught so many skills such as financial commitments and study habits that will help in medical school and beyond — into residency and in sitting for board exams,” he said.
Another student who took part in REV UP!, Saramarie Azzun, said it prepared her well to take the MCAT. Azzun, who earned an undergraduate degree in neurobiology with a minor in African studies, began studying for the MCAT her sophomore year of college. But she lacked the funds to purchase a preparation course. When she was admitted into REV UP!, she found what she needed in the books, quizzes, flash cards and practice exams from Kaplan, a company that provides MCAT resources. REV UP! also offers resources from the Association of American Medical Colleges.
“The entire course was helpful but the one that helped me the most was the Kaplan resources and the fact that they were free, which alleviated my financial burden,” she said. “I went into the MCAT with a confidence I didn’t have prior to REV UP!”
Azzun is the youngest of four daughters to Nigerian parents who came to the United States before she was born. Azzun had dreamed of a career in veterinary medicine, but her family’s experience with mental health issues steered her toward medicine instead. She would like to become a family medicine physician.

“In Nigeria, there is a huge stigma attached to mental illness and this serves as a barrier to receiving treatment,” she said. “When I was in high school, I could see the socioeconomic symptoms associated with psychological disorders. As a physician I want to be able to acknowledge the stigma of mental illness and, eventually, I hope to dismantle it.”
Each year, REV UP! averages approximately 148 students who come from nearly 20 universities. Student ethnicities represented include African American, Hispanic, Native American and others.
“Our team has worked to create an innovative program that is open to helping all Oklahoma college students with limited financial resources achieve their dream of becoming a doctor,” said Salinas, himself a first-generation college student. “The collective effort is to help these students better prepare their application to increase their chances of matriculating into medical school and someday serving and addressing the healthcare needs of our communities.”
The OU College of Medicine has renamed one of its student modules for former U.S. Surgeon General Antonia Novello, M.D., MPH, who visited campus for the ceremony. Novello, who served as the 14th U.S. Surgeon General, was the first woman and the first Hispanic to hold the position.

Upon entering medical school, students are assigned to one of 10 on-campus study rooms known as modules, each of which is named for physicians of distinction. In 2019, student members of the college’s chapter of the American Medical Women’s Association recognized a lack of diversity among the roster. Working with the Office of Diversity, Inclusion and Community Engagement, the students launched an initiative to rename modules to celebrate underrepresented healthcare professionals.
“The renaming of the modules not only honors the pioneering work of physicians who came before us, but also serves to reflect the diversity within our own student body,” said medical student Merlyn Liando. “The OU College of Medicine strives to embody the virtues Dr. Novello has exemplified, not only as professionals but as individuals.”
Novello was chosen for the module renaming for her extensive service as a physician and public health advocate. A native of Puerto Rico, she earned both her bachelor’s and medical degree from the University of Puerto Rico. She then completed her internship and residency in nephrology at the University of Michigan Medical Center. She remained in Michigan for a fellowship in the Department of Internal Medicine, followed by a fellowship in the Department of Pediatrics at Georgetown University.
After two years in private pediatrics practice, Novello began working at the National Institute of Arthritis, Metabolism and Digestive Diseases of the National Institutes of Health. She held various positions at the NIH, rising to the job of deputy director of
the National Institute of Child Health and Human Development. She also served as coordinator for AIDS research.
During her years at the NIH, Novello earned a master of public health degree from the Johns Hopkins School of Hygiene and Public Health. She also made major contributions to the drafting and enactment of the Organ Transplantation Procurement Act of 1984 while assigned to the Senate Committee on Labor and Human Resources.
On March 9, 1990, Novello was sworn in as the U.S. Surgeon General, a position she held until 1993. During her tenure, she focused on the health of women, children and minorities, as well as on underage drinking, smoking and AIDS. She partnered with many organizations to promote immunization of children and childhood injury prevention efforts.
After her role as Surgeon General, Novello served as the United Nations Children’s Fund (UNICEF) Special Representative for Health and Nutrition. In 1999, she became Commissioner of Health for New York. In recent years, she has served as a spokesperson and public health advocate for COVID-19 vaccinations, and she continues efforts related to healthcare access, disease prevention, vaccination and education.
In her remarks during the renaming ceremony, Novello told students to maintain their humanistic passion for which they entered medicine. Medicine is becoming increasingly complex and technological, she said, but the doctor-patient bond must be preserved.
“We must continue to understand people’s lives, not just laboratory reports or the latest journal articles,” she said. “The reason doctors are still needed in addition to digital resources is that we are human beings dealing with human beings. As the best doctors have done, the patient — not just the illness — must remain our primary concern. When diagnosing and treating symptoms, we must consider the person’s experience.
“I urge you to keep up with all the new scientific discoveries, new political health policies and exploding technologies, but never forget the faces behind the data or the names behind the statistics. Remember, our patients will not care how much we know until they know how much we care. Medicine is still fundamentally a human endeavor.”

Third- and fourth-year medical students at the OU College of Medicine have a new opportunity to experience family medicine at community hospitals and clinics across Oklahoma and to immerse themselves in the daily life of those communities.
Last year, the college launched the Premier Medical Education Hub (PMEH) program, which allows medical students to choose a one-month clinical rotation at one of several approved sites. While there, students work alongside preceptor family physicians who train and mentor them in the care of patients. Outside of the clinic or hospital, students take part in activities like farmer’s markets and football game medical coverage to get a feel for the community and the people who call it home.
The effort has gotten off the ground through a multimilliondollar grant from the U.S. Department of Health and Human Services that created the TRU-OK initiative — an effort to recruit, mentor and admit medical students from tribal, rural and underserved areas of the state. Studies show that students from those areas who train in Oklahoma are more likely to establish their careers in the state, and they are more likely to choose primary care if they have a positive experience during their training.
Oklahoma faces a significant shortage of primary care physicians, particularly in tribal, rural and underserved areas. To maintain sufficient access to care, the state needs an
additional 451 primary care physicians by 2030, according to the Robert Graham Center, which advocates for family medicine in health policy decisions. Leaders of the OU College of Medicine say the PMEH program can help fill that need.
“The Premier Medical Education Hub program is a great example of how we can partner with community healthcare providers to create a valuable experience for our students,” said John Zubialde, M.D., executive dean of the OU College of Medicine. “Family physicians play a crucial role in the lives of the patients they treat and in the communities where they serve. With this program, our aim is to nurture interest among the next generation of physicians for patient care outside of urban areas. It is an area of medicine that is very rewarding for physician and patient alike.”
Thus far, three healthcare sites are serving as Premier Medical Education Hubs: Jackson County Memorial Hospital in Altus, the Chickasaw Nation in Ada, and the Oklahoma City Indian Clinic. Several more are in the works. Each hub site agrees to serve as a preceptor for up to five medical students each year.
Medical student Landon Hendrickson did his hub rotation at Jackson County Memorial Hospital in Altus, where he primarily worked in an outpatient family medicine clinic with Jamie Hockett, M.D., who graduated from the OU College of Medicine and completed her family medicine residency with OU. Jackson County Memorial Hospital is the sole provider for a population of 50,000, serving almost everyone in the county and portions of adjacent counties.
“We saw people with a wide variety of conditions, and I really learned how much rural communities rely on their primary care physicians to provide services that PCPs in bigger cities often refer to specialists,” Hendrickson said. “I learned so much about the challenges that patients in these communities face
when trying to access certain types of care, and I have a ton of respect for providers who serve these communities and daily overcome these obstacles.”
Outside of the clinic, Hendrickson became well-acquainted with many people and places in Altus. He made new friends and joined them for dinner in their homes or at local restaurants, and he was introduced to local high school talent by attending a musical theater production at the school. In just four weeks’ time, he grew to love the community and helping to care for local patients.
“Medical students can really benefit from doing a rural medicine rotation,” he said. “We need doctors who can advocate for resource allocation to rural areas, and learning in a rural setting humanizes the fight for rural communities. We definitely need providers in rural settings, and the experience makes me a lot more likely to serve these communities in the future.”
Hockett, a preceptor at Jackson County Memorial Hospital, said it’s important that students understand how to care for patients in rural settings, but also to get a feel for the relationships that develop as part of small-town medicine.

“I know my patients. I go to church with them, they teach my kids, they are my best friend’s parents, I see them every day at Walmart or the ball fields, and they live next door to me,” Hockett said. “This close relationship is unique to small-town medicine and helps me as a physician to help my patients that much more. Doctors are an integral part of the community in Altus, and that closeness is difficult to teach remotely. It must be felt while here in our town.”
Creating this opportunity required extensive work. Karla Finnell, Ph.D., a faculty member in the Hudson College of Public Health at the OU Health Sciences Center, joined family medicine colleagues in determining the benefits and
barriers to establishing the hub program. It became quickly clear, she said, that while physicians were interested in serving as preceptors, they also needed the support of their administration. Because many physicians are now employees of health systems, Finnell and her team conducted interviews with both physicians and health system leaders to understand how best to meet the needs of everyone involved.
“Physicians are interested in being preceptors because they want to give back to their profession and they’re stimulated by teaching. Administrators bring the perspective of someone managing an enterprise, but they also see the program as an opportunity to form relationships with students so that when they graduate, they may want to return to the community to practice,” Finnell said. “And everyone wanted efficiency in the process.”
Once issues had been addressed and best practices identified, the PMEH team created toolkits and checklists. The hub sites provide housing in the community for students. Physicians receive adjunct faculty appointments with the College of Medicine and continuing medical education credits. Hub rotations are currently optional for medical students. For third-year students who do the rotation, the credits count for the family medicine clerkship requirement. Fourth-year students can do the rotation as an elective.
Olivia Lust, D.O., a family physician and assistant professor in the OU College of Medicine, serves as a physician consultant and liaison for the PMEH program. She helps establish new hub sites and ensures the students’ experiences meet the college’s curriculum requirements. She is also available to visit with physicians if they have questions about how to teach students during a busy day of seeing patients. It can be a balancing act between mentoring students and incorporating them into the clinic workflow, Lust said.
“We talk about different ideas, whether it’s having the student shadow while the physician cares for the patient, or perhaps the student takes the patient’s history and does the physical exam while the physician acts as a scribe and proctor,” Lust said. “We also give them resources to hold ‘lunch and learns’ where the student reads up on a topic and you discuss it over lunch. We just want to give them ideas so that the student can have a good experience and take on responsibilities appropriate to their stage of training, but also that the process doesn’t slow down the clinic.”
Lust was drawn to family medicine during her own medical school years, when she completed rotations in East Texas. She loved the role of a physician in a small town, where they care for generations of the same family and see each other in the grocery store and at high school sporting events. Creating that experience for today’s students and preceptors is one of the joys of her work.
“Many physicians are passionate about teaching the next generation and showing their communities to students,” she said. “In turn, students get to see the importance of primary care in rural and tribal areas. I think their eyes are opened when they see all the things family physicians do and the roles they play in their communities.”
This fall, OU College of Medicine Executive Dean John Zubialde, M.D., begins retirement full of gratitude for his 32 years in academic medicine, starting as a faculty member in the Department of Family and Preventive Medicine and ending as leader of the 21-department college.

During his time on campus, Zubialde took part in several milestones for the college and campus, provided key leadership across the tripartite mission, and guided faculty, students and staff through a pandemic that changed the face of medicine.
“This has been a wonderful career, and I feel like I have worked with the best people on the planet,” Zubialde said. “We have great people who really care about our mission, our patients, our students, our researchers. I’m proud of what we have achieved. It has been transformative.”
Zubialde came to the OU College of Medicine via the military. He was serving as Chief of Family Medicine Services at the U.S. Air Force Clinic and Hospital at Tinker Air Force Base when he became acquainted with the college through his wife, Vickie Loemker, M.D., a fellow family medicine physician who joined the college. He was drawn to the people, as well as the faculty’s expertise in medical decision-making, one of only a few such groups nationally with such a focus at the time. In 1991, he became a general faculty member in the Department of Family and Preventive Medicine.
In 1994, he began his foray into graduate medical education as director of the family medicine residency program. After seven years in that role, he was named Associate Dean for Graduate Medical Education in the dean’s office, where for 15 years, he oversaw the college’s 60-plus residency and fellowship programs. It was a time of change for the Accreditation Council for Graduate Medical Education (ACGME), the body responsible for accrediting all graduate medical education training programs for physicians in the United States. It had transitioned from a time-based system to a competency-based curriculum and launched a milestones project to measure skills.
“It was a major mindset change in graduate medical education,” Zubialde said. “We were no longer following a set schedule, but we were understanding how residents learn, the critical competencies they needed to learn, and the time frame needed to achieve those competencies. Not only were we building new programs in the college, but we were transforming the way those programs worked. That was a great opportunity for leadership because it taught me how to
“This has been a wonderful career. We have great people who really care about our mission, our patients, our students, our researchers. I’m proud of what we have achieved. It has been transformative.”
After 15 years overseeing graduate medical education, Zubialde was named Senior Associate Dean for the college in 2015. In 2018, he was named interim executive dean of the College of Medicine, and the interim was removed the following year. In April 2019, he began serving as president of the OU Physicians faculty practice, taking it from 17 different departments into one comprehensively managed ambulatory and physician group.

Although he has been immersed in all of the college’s focus areas, he always considered education the core mission. During his various interactions with the college’s learners, he witnessed their passion not only for patient care, but for understanding the community and societal factors that shape health.
“I’m proud because I know our students will have a great impact on our future,” he said. “I often told students that medicine is not just about learning facts, but about taking those facts and applying them in tangible ways that make a difference. It’s also about the doctor-patient relationship. As technical as medicine can be today, it’s still all about the relationship.”
The college’s dedication to education is reflected in consistently high student satisfaction ratings, gleaned each year through a survey conducted by the Association of American Medical Colleges. The ratings are important because the college’s accrediting body, the Liaison Committee on Medical Education, places as much weight on student satisfaction scores as any other outcome, including standardized exam scores.
“High student satisfaction also points to the great job that our faculty do, day in and day out,” Zubialde said. “Our faculty members are not only excellent educators, but they spend time listening to our students and mentoring them. That dedication is apparent at both the undergraduate medical education and the graduate medical education levels.”
Zubialde also helped to welcome the advent of interprofessional education as a curricular requirement. Because the College of Medicine is one of seven colleges at the OU Health Sciences Center, interprofessional education is particularly robust. Students from the Zarrow School of Social Work on OU’s Norman campus are also part of a growing cadre of interprofessional activities. In addition to various oncampus learning opportunities, students care for patients as an interprofessional team at Oklahoma City’s free clinics, and they take an RV-sized “classroom on wheels” to communities throughout the state.
“I’m proud because I know our students will have a great impact on our future. I often told students that medicine is not just about learning facts, but about taking those facts and applying them in tangible ways that make a difference.”
“I have always told medical students that medicine is a team sport. They can’t do it by themselves. The people on their teams are just as important as they are, if not more important in many cases,” he said. “At the Health Sciences Center, we have a unique advantage in having so many health professional students in one area. They get to know each other while they’re in school so that when they’re in a practice environment, they understand how important those team members are.”
Faculty development also has been a major focus for Zubialde during his time as executive dean. A major avenue for that work is the of the Academy of Teaching Scholars, which was established more than a decade ago by then-Executive Dean Dewayne Andrews, M.D., to recognize and nurture teaching excellence. Zubialde led the expansion of the academy to become a faculty development arm.
“Through the work of dedicated leaders like Sheila Crow, Ph.D., Associate Dean for Faculty Affairs, and the generous support of people like former dean Jerry Vannatta, M.D., we have created a framework where faculty can help each other build their teaching skills, as well as guide junior faculty as they advance their careers,” he said.
Another area that has been gratifying to Zubialde is the college’s effort to increase the diversity of the student body and faculty. Through the Office of Diversity, Inclusion and Community Engagement, led by Robert Salinas, M.D., the college has created pipeline programs that attract and mentor young people who are interested in careers in medicine. With a grant from the U.S. Health Resources and Services Administration, the college has had a particular focus on youth from tribal, rural and underrepresented populations across Oklahoma.
Similarly, through the Diversity Alliance Task Force, led by Pam Allen, M.D., the college has taken important steps
toward recruiting and mentoring diverse clinical, research and teaching faculty members. “The more we are able to prepare students and faculty for understanding the needs of a diverse population, which includes every Oklahoman, the more successful we will be at improving healthcare and health outcomes,” Zubialde said.
With the arrival of COVID-19 in spring 2020, the College of Medicine, like all medical schools, faced unprecedented challenges. Very quickly, leaders and faculty came together as a team to determine the best way to care for patients, how to teach students when they couldn’t be in a clinical setting, how to create a high-quality hybrid environment, and much more. Students themselves rose to the occasion by organizing vaccination clinics on campus and around the state, and then vaccinating upwards of 70,000 Oklahomans.
“I’m really proud of how our faculty, students and staff came together during a very challenging time,” Zubialde said. “There was no recipe for how to do this. It shows the power of teamwork and of good relationships.”
The research mission of the College of Medicine also flourished during Zubialde’s time as executive dean. In recent years, researchers across the OU Health Sciences Center have earned an average of $150 million in extramural funding annually; in fiscal year 2020, they hit a record high of $188 million in grants, most of that going to College of Medicine investigators. Zubialde helped facilitate a thriving research enterprise, from basic science to clinical and translational projects, to dissemination and implementation research, helping practitioners “hard-wire” into their practices the discoveries that have been shown to improve lives.
Last year, the college added a new academic department solely dedicated to cancer research, the Department of Oncology Science, which has resulted in the recruitment of highly qualified researchers and an upcoming graduate program giving students the opportunity to pursue a doctoral degree in the field.
Zubialde conducted his own research projects during his career, focusing on topics such as care of the complex patient, health systems planning, and leadership development. “Discovery and innovation assure us there will be new solutions to health issues down the road,” Zubialde said. “I’m proud that our research mission drives the frontiers of medicine.”
He also lived out his own advice as a family medicine physician. In addition to seeing patients on campus, he served Oklahoma City’s underserved patient population as a volunteer provider at Good Shepherd Clinic for 25 years.
Although he is officially hanging up his white coat, Zubialde takes with him a trove of memories from his time furthering the mission of academic medicine.
“I couldn’t have been successful without working with such dedicated people,” he said. “I have considered my career a privilege.”

The Center for Integrative Research on Childhood Adversity (CIRCA) at the OSU Center for Health Sciences, which is served by the OU-TU School of Community Medicine Integrative Immunology Center as a core support center, was awarded $9.5 million from the National Institutes of Health to research Adverse Childhood Experiences (ACEs). The study is entering its second phase of research for which this grant will be used.
“The work of this research team and the support of this grant are a testament to what we can accomplish when we work together,” said Jim Sluss, Ph.D., OU-Tulsa interim president. “I have found it rewarding to serve on the grant’s internal advisory committee as we sought funding for this project as well as strengthened the ties between the institutions.”
ACEs, which include child abuse and neglect, parental mental illness, domestic violence, drug or alcohol abuse and divorce, affect more than 60% of Americans. It is estimated that ACEs cost North America more than $750 billion a year in preventable healthcare costs, as they are a leading cause of poor mental and physical health, substance use and other health-harming behaviors.
“This study into the effects and treatments of ACEs is valuable work that requires and deserves this important attention and support,” said Kent Teague, Ph.D., associate vice president for research at OU-Tulsa. “This study is also a template for how our two institutions can leverage their respective strengths to garner large federal grants that benefit the whole community.” Teague has worked closely with the study’s principal investigator and CIRCA Director Jennifer Hays-Grudo, Ph.D., as the entire team strives to make a difference in the lives of Oklahomans.
The first phase of the CIRCA study took place over five years and involved building the research infrastructure in northeast Oklahoma to support ACEs research. Phase one was awarded $11.3 million by NIH. This second phase will build on the infrastructure of the first by developing a center that supports researchers with mentoring and research core support in the study of the effects of ACEs and identifying more effective ways to prevent and treat them.
“The work of this research team and the support of this grant are a testament to what we can accomplish when we work together.”
Community college students who have the desire and skills to become physicians often don’t have access to the same premed resources offered at four-year universities. The OU-TU School of Community Medicine took part in a pilot program that aims to change that, not only in Tulsa, but nationwide.
Last year, the SCM partnered with Tulsa Community College (TCC) and the Health Professional Student Organization (HPSA) to hold the inaugural Undergraduate Medical Accelerator Program at TCC. HPSA, which was formed in 1983, is a national organization that supports students, regardless of their background, as they seek to become health professionals.
During the Undergraduate Medical Accelerator Program, TCC students heard presentations from HPSA leaders about prerequisites for medical school, admission requirements and extracurricular activities. SCM students visited with TCC students throughout the experience, giving first-hand advice about the path to medical school.
“This was a great opportunity for the School of Community Medicine to help pilot a program that provides resources to community college students who want to attend medical school,” said SCM Dean James Herman, M.D., who has served as a board member for HPSA. “We were excited to take part
in an innovative program that ultimately will help address the physician shortage in states like Oklahoma.”
Community colleges such as TCC are playing an increasingly larger role in the educational journey toward a bachelor’s degree, according to the 2019 National Survey of College Graduates. Among employed people who received their first bachelor’s degree before 2008, 48% had previously attended a community college. The number climbs to 52% of those who previously attended a community college and received their first bachelor’s degree between 2008 and 2017. The number who already earned an associate degree also increased from 19% to 25%.
Qualified pre-med students are attending community colleges, but often lack the resources to apply to medical school. The Undergraduate Medical Accelerator Program aims to close that gap.
“Community colleges don’t have pre-med advisement programs or pre-med clubs in the same way that four-year universities do,” said Meredith Talley, SCM Director of Student Services and Admissions. “So by the time a TCC student transfers to a four-year school, their peers have already had two years of working with pre-med advisors and talking to others about taking the MCAT (Medical School Admission Test). We hope to eliminate that information gap.”
SCM students who attended the Undergraduate Medical Accelerator Program played an important role by talking with TCC students one-on-one and sharing their experiences, such as how to gain the necessary job shadowing experience.

“Our medical students are great resources for prospective students,” Talley said. “Access to them is a big part of this program. They were able to visit in a setting that doesn’t feel intimidating.”
Students at community colleges also tend to be more diverse than those at universities. More first-generation college students attend community colleges, as do underrepresented populations. “As we look to diversify our healthcare workforce to make it look more like our population, community colleges are a place that we should be looking,” Talley said. “We know that physicians are more likely to practice medicine where they’re from, whether that be in an urban area in Tulsa or a rural area, so we need to support students from all different backgrounds and create pathways to help them get into medical school.”
Other community college students might be non-traditional, such as those who are taking classes as part of a career change, like TCC student Lily Robistow, who is switching from a teaching career to medicine and is a first-year medical student at SCM.

“Non-traditional students can look a lot of different ways,” Talley said. “It could be people who are changing careers like Lily, or it could also be someone who can’t attend a four-year university because of finances or a family situation, so they are picking up classes while working full-time.”
With two Undergraduate Medical Accelerator pilot programs in 2022, attendance and engagement doubled from the first to the second event. Eric Butson, TCC faculty member and co-organizer of the event, said students gained valuable

information about specific steps they need to take to apply to medical school, as well as the inspiration to get started.
“With these incredibly competitive medical school programs, students need to know the clock starts at the beginning of their college career, regardless of whether they start at a community college or a smaller four-year institution,” Butson said. “At TCC, we have developed this program to help bridge the gap for the success of our students and our community.”
HPSA aims to roll out the Undergraduate Medical Accelerator Program to additional community colleges in the future. The organization’s collaboration with TCC and SCM was a valuable first step to broadening the program across the nation.
“With the unwavering support of the OU-TU School of Community Medicine, our Undergraduate Medical Accelerator pilot program is breaking barriers and empowering community college students to pursue their medical dreams. Together, we’re rewriting the narrative of accessibility in healthcare education,” said Laura Turner, executive director of HPSA.
“Our Undergraduate Medical Accelerator pilot program is breaking barriers and empowering community college students to pursue their medical dreams.”
Each spring, OU College of Medicine students on the Oklahoma City campus and at the OU-TU School of Community Medicine in Tulsa honor faculty members with a variety of awards in recognition of their excellence in teaching.
The 2023 Edgar W. Young Lifetime Achievement Award was presented on the Oklahoma City campus to Teresa Scordino, M.D., Associate Dean for Student Affairs and faculty member in the Department of Pathology. The award recognizes longterm dedication to medical education.
On the Tulsa campus, Lauren Conway, D.O., received the 2023 Community Medicine Leader Award, given to a faculty or staff member who exemplifies the mission of the School of Community Medicine as evidenced by teaching, scholarship, community service, or significant service to the school or the Tulsa area. Conway is a child abuse pediatrician.
Medical school classes on both campuses also presented Aesculapian Awards. Honorees on the Oklahoma City campus were:
Class of 2026:
Aesculapian Award for excellence in teaching the preclinical sciences: Nancy Halliday, Ph.D., Department of Cell Biology
Class of 2025:
Aesculapian Award for excellence in teaching the preclinical sciences: Alexandra Regens, M.D., Department of Obstetrics and Gynecology

Class of 2024:
Aesculapian Award for excellence in teaching the clinical sciences: Marvin Williams, D.O., Department of Obstetrics and Gynecology

Aesculapian Award for excellence in teaching the thirdyear clerkship by house staff: Shana Usiukiewicz, M.D., Department of Medicine
Class of 2023:
Aesculapian Award for excellence in teaching the clinical sciences: Alexander Raines, M.D., Department of Surgery
Aesculapian Award for excellence in teaching the clinical sciences as volunteer faculty: Hanna Saadah, M.D., Department of Medicine
On the Tulsa campus, Aesculapians honorees were:
Class of 2026:
Aesculapian Award for excellence in teaching the preclinical sciences: Lori Garman, Ph.D., Department of Microbiology and Immunology
Class of 2025:
Aesculapian Award for excellence in teaching the preclinical sciences: Caleb Hurst, D.O., Department of Internal Medicine
Class of 2024:
Aesculapian Award for excellence in teaching the clinical sciences: Edward Cho, M.D., Department of Surgery
Class of 2023:
Aesculapian Award for excellence in teaching the clinical sciences: Kevin Smith, D.O., Department of Internal Medicine
The School of Community Medicine also awards Crimson Apple Awards to volunteer faculty and residents.
Crimson Apple Award for Volunteer Faculty: Robert Hauger, M.D., internal medicine
Crimson Apple Award for Residents: David Abraham, D.O., Department of Internal Medicine, and Pauli Whipple, D.O., Department of Surgery.
Each year, the OU College of Medicine recognizes excellence among faculty and residents with the presentation of the Leonard Tow Humanism in Medicine Award and the Lloyd Rader Award.
The Leonard Tow Humanism in Medicine Award, sponsored by the Arnold P. Gold Foundation, is given to a faculty member who demonstrates excellence in promoting scholarship, encouraging high standards of care, and integrity and commitment to compassionate care of patients and to the art and science of medical practice. Recipients of the award become members of the Gold Humanism Honor Society, an international organization with more than 20,000 members in training and practice.
This year’s recipient is Jad Kebbe, M.D., associate professor in the Department of Medicine. He is a pulmonary and critical care physician who specializes in advanced lung diseases, including interstitial lung diseases, pulmonary fibrosis and sarcoidosis. He is the director of Oklahoma’s first and only Interstitial Lung Diseases program.

In a letter of support for Kebbe, the writer said: “Many have observed and commended his skills in caring for patients who are facing their end of life due to irreversible conditions. Jad has developed a lifelong interest in palliative care and a deep respect for the worth of every human life. He treats people with kindness, compassion and dignity.”
The Lloyd Rader Award, named for the man who served as director of the Oklahoma Department of Human Services from 1951-1982, recognizes outstanding achievements in residency, both clinical care and research. This year, the Lloyd Rader Award was presented to two residents: Christie Buonpane, M.D., pediatric surgery, and Cynthia McClard, M.D., Ph.D., ophthalmology.
Buonpane has been active as a researcher, with five publications, seven abstracts and seven presentations. Those nominating her noted that she is an excellent teacher who is “highly responsible and kind,” “deeply invested in the wellbeing and experience of others,” and “diligent and able to identify potential problems before they arise.” Buonpane plans to go into academic practice at the University of Louisville.
McClard has had nine publications and three presentations. In nominations, McClard was described as an astute clinician, a consummate professional and “superwoman,” a devoted teacher dedicated to enhancing the skills of her students, and someone who is well-respected by peers and faculty. She is entering a vitreoretinal fellowship at Cincinnati Eye Institute.
“Many have observed and commended his skills in caring for patients who are facing their end of life due to irreversible conditions.
Jad has developed a lifelong interest in palliative care and a deep respect for the worth of every human life. He treats people with kindness, compassion and dignity.”
The Jerry Vannatta, M.D. Academy of Teaching Scholars (ATS), an organization that recognizes and fosters excellence in medical education at the OU College of Medicine, inducted new members and presented honors during its annual Education Week activities in fall 2022.

Awards are given to faculty members on both the Oklahoma City and Tulsa campuses in the areas of preclinical, clinical, and graduate medical education, as well as PA education. Recipients are nominated by students, faculty and colleagues. The awards, called the Dewayne Andrews, M.D., Excellence in Teaching Awards, are named for the former executive dean who founded the organization more than 10 years ago.
In the area of preclinical medical education, awards were presented to:
• Teresa Scordino, M.D., Department of Pathology, Oklahoma City
• Jo Elle Peterson, M.D., Department of Pathology, Oklahoma City
• Mary Moon, Ph.D., Department of Cell Biology, Oklahoma City
• Rob Jackson, Ph.D., Department of Family and Community Medicine, Tulsa
In clinical medical education, awards were presented to:
• Jarad Levin, M.D., Department of Dermatology, Oklahoma City
• Zain Ul Abideen Asad, M.D., Department of Medicine, Oklahoma City
• Joey Terracina, M.D., Department of Anesthesiology, Oklahoma City
• Jameca Price, M.D., Department of Obstetrics and Gynecology, Tulsa
Graduate medical education honors were presented to:


• Cindy McCloskey, M.D., Department of Pathology, Oklahoma City
• Kevin Watson, M.D., Department of Psychiatry and Behavioral Sciences, Oklahoma City
• Saleem Qureshi, M.D., Department of Medicine, Oklahoma City
• Brian Milman, M.D., Department of Emergency Medicine, Tulsa
In the PA program, awards were given to:

• Kenneth G. Foster, MBA, MHS, PA-C, Department of Family and Preventive Medicine/PA program, Oklahoma City
• Autumn Ackerman, MSPAS, PA-C, PA program, Tulsa
New full members welcomed into the ATS are:
• Seki A. Balogun, MBBS, Department of Medicine, Oklahoma City
• Michael W. Brand, Ph.D., Department of Psychiatry and Behavioral Sciences, Oklahoma City
• Tricia D. Gardner, J.D., Department of Pediatrics, Oklahoma City
• Zhamak Khorgami, M.D., Department of Surgery, Tulsa
• Andrew Liew, M.D., Department of Psychiatry, Tulsa
• Blake Wilson Porter, M.D., Department of Obstetrics and Gynecology, Oklahoma City
• Edgardo G. Szyld, M.D., Department of Pediatrics, Oklahoma City
New associate member inductees are:
• Krishna Mohan Baradhi, M.D., Department of Internal Medicine, Tulsa
• Laura M. Haws, M.D., Department of Pediatrics, Oklahoma City
• Alessandra Landmann, M.D., Department of Surgery, Oklahoma City
• Olivia Lust, D.O., Department of Family and Preventive Medicine, Oklahoma City
• Mary Moon, Ph.D., Department of Cell Biology, Oklahoma City
• Gary C. Perez, DMSc, PA-C, Department of Family and Preventive Medicine/PA program, Oklahoma City
• George Salem, M.D., Department of Medicine, Oklahoma City
New trainee members are:
• Maida Hafiz, M.D., Department of Medicine, Oklahoma City
• Patricia Pius, M.D., Department of Radiation Oncology, Oklahoma City
At the spring 2023 OU Health Sciences Center Faculty Awards Ceremony, several OU College of Medicine faculty members were honored with a variety of awards for their excellence in academic medicine.
Regents’ Awards:
Regents’ Awards for Superior Teaching
• Sanjay Bidichandani, MBBS, Ph.D., Department of Pediatrics, Oklahoma City campus
• Chris Brasel, Ph.D., Department of Family and Community Medicine, Tulsa campus

Regents’ Award for Superior Research and Creative/Scholarly Activity
• Lee Jennings, M.D., Department of Medicine, Oklahoma City campus
Regents’ Professorship
• Amanda Bogie, M.D., Department of Pediatrics

President’s Awards:
George Lynn Cross Research Professorship
• Kathleen Moore, M.D., Department of Obstetrics and Gynecology, Oklahoma City campus
Presidential Professorship
• Natarajan Aravindan, Ph.D., Department of Radiation Oncology, Oklahoma City campus
• Cindy McCloskey, M.D., Department of Pathology, Oklahoma City campus
• Dharambir Sanghera, Ph.D., Department of Pediatrics, Oklahoma City campus
Provost’s Awards:
Research-Junior Faculty (Basic Sciences Research)
• Kurt Zimmerman, Ph.D., Department of Medicine, Oklahoma City campus
• Elizabeth A. Wellberg, Ph.D., Department of Pathology, Oklahoma City campus
Research-Junior Faculty (Clinical/Translational Research)
• Andriy Yabluchanskiy, M.D., Ph.D., Department of Neurosurgery, Oklahoma City campus
Teaching-Early Career Faculty
• Brian Lich, M.D., Department of Medicine, Oklahoma City campus
• Nelson Ivan Agudelo Higuita, M.D., Department of Medicine, Oklahoma City campus
Priyabrata Mukherjee, Ph.D., a professor in the Department of Pathology, has been named a fellow of the American Association for the Advancement of Science, the world’s largest multidisciplinary scientific society.
Mukherjee’s research is centered at the interface between biology and materials science to address unmet challenges in human diseases. His laboratory is mostly funded by investigator-initiated research project grants from the National Institutes of Health. He currently has several multimillion-dollar R01 grants from the National Cancer Institute.
In addition, Mukherjee has been named an associate editor of Science Advances, a journal of the American Association for the Advancement of Science. He will serve in the biomedicine and life science section.

Christina Washington, M.D., assistant professor in the Department of Obstetrics and Gynecology, Section of Gynecology-Oncology, was selected for the Robert A. Winn Diversity in Clinical Trials Award Program, established by the Bristol Myers Squibb Foundation.

The program aims to increase diverse patient participation in clinical trials. Despite Black Americans representing 13%
of the U.S. population and Hispanics representing 16%, both groups make up a combined 7% of clinical trial participants. As a Winn Scholar, Washington will receive training in investigator-initiated and industry-sponsored clinical trials and in community outreach to facilitate underrepresented populations to participate in clinical trials.
Her project as a Winn Scholar is titled, “Building Bridges Between Community Leaders to Increase Involvement of Underrepresented Minorities in Clinical Trials.”
Neonatologist Marjorie Makoni, M.D., assistant professor in the Department of Pediatrics, Section of Neonatal-Perinatal Medicine, received the 2022 Community Health Partner Award from the Infant Mortality Alliance, an Oklahoma-based organization dedicated to reducing infant mortality in the African American community in Oklahoma County.
The award recognizes Makoni’s exceptional contributions to community health, focused on long-term impact and sustainability. In the award notification, Rebecca Faulkner, M.D., who chairs an Infant Mortality Alliance working group, said: “I have been deeply impressed with the impact that you are making in treating the most vulnerable infants as well as teaching about health disparities in order to create more aware and engaged physicians in our state. Your presence on the faculty of the OU College of Medicine creates space for students of color to see themselves reflected in positions of leadership, and the passion you bring to your practice sets a high standard for all your students and colleagues.”
The 38th annual Evening of Excellence gala, which honors healthcare and community leaders while raising funds to support research at the OU College of Medicine, honored three people this spring.
Evening of Excellence is organized by the OU College of Medicine Alumni Association. Since the event began, the alumni association has awarded over $3.8 million in grants to 167 researchers in the college.
This year’s honorees were Judith James, M.D., Ph.D., Dean’s Award for Distinguished Medical Service; Michael Cawley, Dean’s Award for Distinguished Community Service; and the Wisdom Family Foundation, Dean’s Award for a Distinguished Oklahoma Institution.

“This year’s honorees have truly made a difference in the lives of people in Oklahoma and beyond. I am thankful for their commitment to the College of Medicine and the OU Health Sciences Center. The Evening of Excellence provides a wonderful opportunity to honor leaders like these and to raise funds to further the careers of our researchers,” said John Zubialde, M.D., executive dean, OU College of Medicine.
A former recipient of an alumni association grant, Doris Benbrook, Ph.D., spoke about the importance of those early funds to her successful research career at the OU College of Medicine. She developed a new cancer drug, called OK-1, which is now being tested in humans for the first time at OU Health Stephenson Cancer Center. New drugs developed at an academic institution, without the aid of a pharmaceutical company, are rare.
“Thirty years ago, I received an $11,000 grant from the College of Medicine Alumni Association, and we’ve since transitioned that money into over $20 million for our research,” she said. “We’re hoping to change the way we treat cancer patients — to be able to effectively treat them without causing toxic side effects. The College of Medicine Alumni Association gave me that first step up that I needed. And, importantly, they are giving that step up to the next generation of researchers who will move on from here to develop new and extraordinary things.”
Following are the honorees’ bios.
Judith James, M.D., Ph.D.
James’ career extends across both the OU Health Sciences Center and the Oklahoma Medical Research Foundation. At the OU Health Sciences Center, she is Associate Vice Provost for Clinical and Translational Science, a George Lynn Cross Research Professor, and Professor of Medicine in the OU College of Medicine. At OMRF, she serves as Vice President of Clinical Affairs, chair of the Arthritis and Clinical Immunology Program, and holds the Lou Kerr Chair in Biomedical Research.
James’ research focuses on understanding the etiology and pathogenesis of lupus, Sjogren’s syndrome and related disorders; the evolution and pathogenic mechanisms of autoantibodies in systemic rheumatic disease; the interplay of genetic risk and environmental responses in systemic autoimmunity; and unique drivers of disease severity in Native American autoimmune rheumatic disease patients.
She has published more than 330 articles in peer-reviewed publications such as the New England Journal of Medicine, Nature Medicine, Journal of Experimental Medicine, and Arthritis and Rheumatology, and she has made seminal contributions to understanding how immune diseases start.
James’ research has been consistently funded by the National Institutes of Health since 1991, and she currently serves as the principal investigator for several large, multi-investigator grants funded by the NIH. At the OU Health Sciences Center, she leads the Oklahoma Clinical and Translational Science
Institute, which unites universities, nonprofit organizations, American Indian communities, public agencies and primary care providers in research focused on improving the health of all Oklahomans. The grant also helps junior investigators launch their biomedical research careers in Oklahoma; since the institute began, those previously unfunded scientists have brought more than $60 million in additional funding to the state. James oversees several other NIH-funded research programs at the local and national level, including the Autoimmunity Centers of Excellence, Accelerating Medicines Partnership in Autoimmune and Immune-Mediated Diseases, and the Rheumatic Disease Research Cores Centers.
She has been active as an educator throughout her career, mentoring more than 150 research trainees in her lab. Many have been rural students and tribal members, and nearly all have gone on to complete medical school, graduate school or both. Many now hold faculty positions across the nation while others practice medicine throughout Oklahoma.
James has also been active as a clinician. She is a boardcertified adult rheumatologist and sees patients at OMRF, the OU Health Sciences Center, and the Cherokee Nation.
She has been honored with numerous awards, most recently being elected to the prestigious National Academy of Medicine. She has received many other honors, including the U.S. government’s Presidential Early Career Award for Scientists and Engineers, the Dubois Award from the

American College of Rheumatology, the Evelyn V. Hess Award from the Lupus Foundation of America, the Distinguished Basic and Translational Scientist Award from the American College of Rheumatology, and the Stanley J. Korsmeyer Award from the American Society of Clinical Investigation.

She has held several leadership roles with the National Institute of Arthritis and Musculoskeletal and Skin Diseases, a component of the NIH, including her recent service as chair of the NIAMS Planning Committee and member of the NIAMS Scientific Advisory Council. She has served on multiple NIH advisory committees and chaired an NIH roundtable regarding preclinical autoimmunity. She also provided testimony supporting the NIH at the Nobel Laureates’ Hearing for the U.S. House Appropriations Subcommittee. She was elected secretary-treasurer of the American Society of Clinical Investigation, and she is a member of the Association of American Physicians.
A fifth-generation Oklahoman from Pond Creek, James was the first graduate of the OU College of Medicine’s M.D./Ph.D. program. She completed her internal medicine residency and rheumatology fellowship at the OU Health Sciences Center, as well as undergraduate, graduate and post-doctoral research training at OMRF.
Michael A. Cawley
Cawley, who was raised in the Oklahoma Panhandle community of Hooker, attended the University of Oklahoma,
where he received undergraduate degrees in economics and English literature, was a member of Beta Theta Pi fraternity, and earned a law degree. After completing a commitment to the U.S. Army, he and his wife, Betty Jane, moved to Ardmore, where he began practicing law. After a nearly 20-year legal career, Cawley became president, CEO and trustee of The Samuel Roberts Noble Foundation, Inc. in 1991. He retired from the Noble Foundation in 2012.
Throughout his life, Cawley has participated in many types of community service to his alma mater. He served as chair of the OU Board of Regents, which included membership on the integration steering committee that assisted with the creation of OU Health, the state’s first integrated academic health center. He was chairman of the OU Foundation Board of Trustees, chair of the OU Associates Council, and chair of fundraising efforts to complete the Jimmie Austin OU Golf Course and the Charlie Coe Teaching Center. He also served on the search committee that resulted in the hiring of Joe Castiglione as OU’s athletic director. He has been honored with a Regent’s Award from the university.
Cawley currently serves on the boards of several organizations, including the Merrick Foundation, Dean A. McGee Eye Institute, Dean A. McGee Eye Institute Foundation, the Oklahoma Medical Research Foundation and the State Fair of Oklahoma. He also serves on the Senior Trust Committee of BancFirst and the Investment Committee of the Oklahoma Arts Institute.
During his family’s time in Ardmore, from 1972 to 2020, Cawley was an elder and adult Sunday School teacher at his church; chairman of the Memorial Hospital of Southern Oklahoma (now Mercy Memorial Hospital); chairman of the Ardmore Development Authority; chairman of the Ardmore City Schools Enrichment Foundation; chairman of Oak Hall Episcopal School; and president of Dornick Hills Golf & Country Club.
He previously served in various capacities with the Oklahoma Heritage Association, Conference of Southwest Foundations, Noble Energy Inc., Noble Drilling Corporation, Panhandle Royalty Company, the Awards for Excellence Selection Commission for the Oklahoma Center for Nonprofits, the State Regents’ Task Force on the Future of Higher Education, and the Governor’s Task Force on the resolution of water rights litigation between the state of Oklahoma and the Choctaw and Chickasaw tribes.
Cawley and his wife, Betty Jane, moved to Oklahoma City in 2020. They have two children and eight grandchildren.

Since its founding in 2008, the Wisdom Family Foundation has supported healthcare, education, agriculture and the arts for people across Oklahoma.
The Wisdom Family Foundation was created in honor of the late C.W. and Grace Wisdom of Alva. The couple’s daughter, Peggy Wisdom, M.D., a 1972 graduate of the OU College of Medicine and professor emeritus of neurology, continues the family’s legacy through the foundation.
The foundation’s primary goal has been to develop and expand educational opportunities for students in northwest Oklahoma, the area of the Wisdom family’s roots. The foundation has been an ardent supporter of the arts, including the establishment of an endowed chair in art at Northwestern Oklahoma State University in Alva, as well as arts and humanities opportunities in the city of Alva.
In 2016, the foundation made a gift of $2.5 million to establish 10 endowed chairs at Northwestern Oklahoma State University in Alva to support the doctor of nursing practice program. The foundation also endowed a scholarship in the OU College of Medicine for students from five counties in northwestern Oklahoma who have been accepted to medical school.
The Wisdom Family Foundation’s support of programs at the OU Health Sciences Center has been extensive, including a major focus on interdisciplinary education, which teaches students from multiple health disciplines to deliver care as a team. Peggy Wisdom, with support from the foundation, was a leader in establishing the Health Sciences Center Interprofessional Collaboration in 2012. A core group of faculty members collaborated weekly to develop a curriculum for All Professions Day and EPIC (Empowering Patients Through Interprofessional Collaboration), both of which expose health profession students to team-building skills early in their education.
These efforts culminated in the establishment of the Office of Interdisciplinary Programs, which provides students and
faculty with a wide variety of interprofessional educational opportunities, clinical team-based experiences, and seed grants for interprofessional clinical and educational research projects.
In 2020, the Wisdom Family Foundation endowed the Nancy K. Hall Chair of Medical Education, which is currently held by Robert Salinas, M.D., to expand interprofessional activities for College of Medicine faculty, students and trainees. In 2022, the foundation funded the Neurology Simulation Program, which supports faculty members as they develop simulation projects to enhance neurologic education and improve patient care. The foundation also established an endowed fund to award residents in the Department of Neurology.
The foundation has supported many other programs and activities at the OU Health Sciences Center, including Blood and Thunder: Musings on the Art of Medicine, a humanities journal produced by medical students. The foundation has made generous donations to the College of Medicine’s scholarship campaign, which helps students with the growing costs associated with medical school.
In addition to leading her family’s foundation, Peggy Wisdom continues to teach the Neurology Doctoring Skills Course for neurology residents, and she is involved in interprofessional educational research on difficult conversations following neurologic emergencies.
Three physician graduates of the OU College of Medicine were honored during the 2023 Alumni Day activities.
E.N. Scott Samara, M.D., and Don L. Wilber, M.D., both were named Physician of the Year-Private Practice. Michael A. Weisz, M.D., was named Physician of the Year-Academic Medicine.
Following are their bios:
E.N. Scott Samara, M.D., is a kidney transplant surgeon with more than 50 years of medical practice in Oklahoma City, including many “firsts” in transplant history. He began his career with the OU College of Medicine in 1973. In 1986, the Integris Baptist Medical Center kidney transplant service was established under his leadership, and he continues to serve as the primary surgeon and surgical director for the kidney transplant division of the Nazih Zuhdi Transplant Institute.
Samara earned his medical degree from the OU College of Medicine in 1968. He completed his internship at what was then called University Hospital on the campus of the OU Health Sciences Center. He went on to complete two residencies at Wayne State University in Detroit, Michigan: general surgery from 1969 to 1970 and urology from 1970 to 1973.
Samara began his career in the Department of Urology at the OU College of Medicine as an assistant clinical professor. He became associate clinical professor in 1980 and full clinical professor in 1986. During his tenure at the OU Health Sciences Center, he was director of kidney transplantation from 1973 to 1980, chief of the kidney transplant section from 1980 to 2006 and chief of the pediatric transplant section from 1976 to 2007.
In 1980, Samara developed the Oklahoma Organ Retrieval System, the first organized organ procurement agency in Oklahoma. In 1986, he co-founded the Oklahoma Organ Sharing Network, which is now known as LifeShare of Oklahoma and is the procurement agency for the entire state.
Over the past five decades, he has played a leading role in several transplant achievements in Oklahoma and the United States, including:
• First living donor kidney transplant in Oklahoma, 1985
• First combined kidney/liver transplant in Oklahoma, 1994
• First combined kidney/pancreas transplant in Oklahoma, 1995
• First paired kidney donor transplant in Oklahoma, 2008
• First domino transplant in the United States (in conjunction with Baptist, John Hopkins, and Barnes Jewish hospitals) in which eight living donor kidney transplants were done in an 18-hour period, 2009
• First combined kidney/heart transplant, 2015
• First combined kidney/lung transplant, 2017
In 2000, Samara received the Lifetime Achievement Award from the National Kidney Foundation for his dedication to transplant development and organ donor achievements in Oklahoma. In 2019, he established the Samara Family Transplant Patient Assistance Fund, which, thus far, has helped 45 patients become listed on the United Network for Organ Sharing for kidney, liver, heart and lung transplantation.
He is a member of the medical honor society Alpha Omega Alpha, American Medical Association, Oklahoma State Medical Association, Oklahoma County Medical Society, Oklahoma State Urologic Society, American Urologic Society, American Society of Transplant Surgeons, American College of Surgeons, Society of University Urologists, American Association of Clinical Urologists and American Fertility Society. He is a founding member of the Urologic Society for Transplantation and Renal Surgery, a founding member and past president of the Oklahoma Transplantation Society and a past president of the Oklahoma Urologic Society.
In 2023, the OU College of Medicine Department of Urology honored Samara with the Pioneer in Urology for Lifetime Achievements Award.

Don L. Wilbur, M.D., has practiced pediatrics in Midwest City for more than 34 years. He graduated from the OU College of Medicine in 1978, followed by a pediatric residency at what was then called Oklahoma Children’s Memorial Hospital. After his residency, he joined the Oklahoma City Clinic in Midwest City as a pediatrician and has been a partner there since.
Wilber has been involved with the American Academy of Pediatrics as president of the Oklahoma chapter from 1990 to 1993; member of the Annual Chapter Forum Committee from 1991 to 1994; chairman of the National Nominating Committee from 2003 to 2006; and member of the Oklahoma chapter’s Executive Committee for 28 years. He has been Chief of Staff at Midwest City Hospital for five years and has served on the board of trustees for 12 years. He also has served as an alternate delegate for the American Medical Association.

Wilber has a special interest in vaccines and, for 20 years, has served as chair of the Vaccine Advisory Committee for the Oklahoma State Department of Health. From 2003 to 2007, he chaired the Federal Advisory Committee for Childhood Vaccines.
Wilber has been a preceptor for third-year medical students at the OU College of Medicine for 30 years and currently serves
on the OU College of Medicine Admissions Board. He also has served in various roles with the OU College of Medicine Alumni Association, most recently as president from 2017-2019.
He received the Champions of Health Award from the Oklahoma Caring Foundation in 2004 and was honored with an Aesculapian Award from the OU College of Medicine Class of 2013. He was named Teacher of the Year for the Department of Pediatrics for 2012-2013.
Outside of medicine, Wilber has coached 20 seasons of youth basketball, baseball and softball in the community. He has two children and six grandchildren.
Michael A. Weisz, M.D., is professor and chair of the Department of Internal Medicine at the OU-TU School of Community Medicine in Tulsa, where he also holds the C.S. Lewis Jr., M.D. Chair in Internal Medicine.
Weisz’s career in healthcare began in pharmacy. He earned a bachelor of science degree in pharmacy from OU-Tulsa in 1976 and worked for seven years as a hospital pharmacist at Hillcrest Medical Center. He then earned his medical degree from the OU College of Medicine in Tulsa in 1988 and completed a residency and chief residency in internal medicine at OU-Tulsa. He joined the faculty in 1991.
In addition to serving as chair of the Department of Internal Medicine, Weisz is medical director of the Simulation Center at OU-Tulsa (SCOUT). He teaches medical students in all four years of medical school on both the Tulsa and Oklahoma City campuses. His medical practice focuses on the care and management of patients with headache disorders.
Previously, Weisz served as program director of the internal medicine residency program and the director of the third-year internal medicine clerkship.

He has received numerous teaching awards and honors, including the Crimson Apple for Teaching Excellence, the Aesculapian Award, and the Stanton L. Young Master Teacher Award. He has also been honored with the Laureate Award and the Meritorious Service Award from the Oklahoma chapter of the American College of Physicians. He has served in many leadership positions, including president of the Tulsa County Medical Society and governor of the Oklahoma chapter of the American College of Physicians. In 2017, he was selected as a Master of the American College of Physicians, one of only 10 Oklahomans selected for the honor since the organization’s inception in 1923.
Weisz has been married to his spouse, Susan, for 48 years. They have three children: Gretchen, a middle-school Spanish teacher at Holland Hall in Tulsa; Kerry, a veterinarian in Austin; and Patrick, the Vice President of Guest Experience at the Tulsa Zoo. Weisz and his wife have five grandchildren, most recently twin boys born in November 2022.

Robert L. Alexander Jr., 1961 M.D., Muskogee, Oklahoma
Christine M. Avakoff Poochigian, 1976 M.D., Burlingame, California
Rex T. Baggett, 1962 M.D., Carson City, Nevada
Richard A. Baylor Jr., 1962 M.D., Champaign, Illinois
Samuel C. Bernhardt, 1960 M.D., Omega, Oklahoma
James G. Billingsley, 1955 M.D., Tacoma, Washington
Harlan J. Blackstone, 1979 M.D., Oklahoma City
Margaret Bonnell, 1969 M.D., Muskogee, Oklahoma
Michael J. Brantley, 1975 M.D., Lawton, Oklahoma
Ronald L. Brown, 1971 M.D., Wichita, Kansas
Robert A. Burton, 1978 M.D., Johnson City, Tennessee
Vaud A. Burton III, 1968 M.D., Oklahoma City
Robert P. Carter II, 1965 M.D., Odessa, Texas
Richard G. Chesler, 1985 M.D., Huber Heights, Ohio
Richard Crook, 1973 M.D., New York
Ralph W. Day, 1970 M.D., Lebanon, New Hampshire
Wesley A. Dickson, 2006 M.D., Oklahoma City
William E. Dieker, 1967 M.D., Tulsa, Oklahoma
John K. Earl, 1972 M.D., Tulsa, Oklahoma
Ronald C. Elkins, 1962 M.D., Oklahoma City
Charles C. Elliott, 1962 M.D., Sallisaw, Oklahoma
Charles L. Freede, 1945 M.D., Redondo Beach, California
Megan M. Fuzzell, 2018 M.D., Oklahoma City
B. Michael Hale, 1975 M.D., Tulia, Texas
William A. Hall, 1977 M.D., Muskogee, Oklahoma
James W. Hampton, 1956 M.D., Oklahoma City
Melvyn L. Harris, 1977 M.D., Oklahoma City
Allen Harrison, 1998 M.D., Siloam Springs, Arkansas
William L. Heinrichs, 1958 M.D., Stanford, California
Millard L. Henry, 1991 M.D., Oklahoma City
Royce A. Hinkle, 1963 M.D., Midwest City, Oklahoma
William E. Hoffmeister, 1958 M.D., Winter Park, Florida
Deborah L. Huff, 1984 M.D., Oklahoma City
Janna M. Journeycake, 1996 M.D., Oklahoma City
William E. Karnes, 1955 M.D., Oklahoma City
Mark A. Kelly, 1967 M.D., Tulsa, Oklahoma
Ronal D. Legako, 1966 M.D., Wellston, Oklahoma
Thomas N. Lynn, 1955 M.D., Oklahoma City
Laurence R. Mansur, 1968 M.D., Albuquerque, New Mexico
Jon M. McCauley, 1988 M.D., Yukon, Oklahoma
William E. McGuire, 1968 M.D., Midwest City, Oklahoma
James W. McLeod, M.D., 1972 M.D., Portsmouth, Virginia
Kelly D. Means, 1992 M.D., Lawton, Oklahoma
T. Richard Medlock, 1965 M.D., Tulsa, Oklahoma
Nicolaas L. Meiring, 1965 M.D., Oklahoma City
Robert W. Miles, 1972 M.D., Norman, Oklahoma
Jess E. Miller, 1947 M.D., Hollis, Oklahoma
Jennifer R. Montague, 2011 M.D., Tulsa, Oklahoma
William B. Nance Jr., 1973 M.D., Colorado Springs, Colorado
Robert R. Pavlu, 1965 M.D., Carrollton, Missouri
Gerald R. Reimer, 1963 M.D., Portland, Oregon
James A. Rodgers, 1976 M.D., Tulsa, Oklahoma
Ronald B. Saizow, 1980 M.D., Tulsa, Oklahoma
Wallace R. Sanders, 1956 M.D., Wichita Falls, Texas
Naebeal L. Shadid, 1967 M.D., Oklahoma City
William R. Smith, 1956 M.D., Enid, Oklahoma
James R. Snider, 1956 M.D., Fort Smith, Arkansas
Zachary P. Stamile, 2011 M.D., Oklahoma City
Michael J. Sullivan, 1972 M.D., Corpus Christi, Texas
Gilbert R. Teague, 1987 M.D., Tacoma, Washington
Kyle W. Toal, 1980 M.D., Oklahoma City
John D. Voiles, 1969 M.D., Fort Collins, Colorado
Kent H. Webb, 1983 M.D., Oklahoma City
Thomas L. Whitsett, 1962 M.D., Oklahoma City
William H. Yarborough, 1977 M.D., Tulsa, Oklahoma
Carroll L. Zahorsky, 1965 M.D., Dacoma, Oklahoma
laparoscopic node biopsy and perineal prostatectomy in Sydney, Australia.
Dr. Donat especially loved sharing his experience with OU College of Medicine residents and fellows, whom he taught for over 40 years. To recognize his dedication, the Department of Urology presented him its inaugural Pioneer in Urology award. “He was a great educator,” Anna said. “He never made people feel inferior about asking questions. He was a very personable teacher and took the time to illustrate and explain what he wanted people to know.”
Dr. Donat was also instrumental in the life and medical education of his niece, S. Machele Donat, M.D., who is now a urologic oncologist at Memorial Sloan Kettering Cancer Center in New York City. She also earned her medical degree from the OU College of Medicine and completed her residency on campus.
Anna and Paul Donat both attended John Marshall High School in Oklahoma City, though they didn’t know each other then. They first met in the 1970s, when Anna worked as a nurse and cared for his surgical patients in the hospital recovery room. One day he asked her if she would consider working at his medical practice, and she said yes.

During his 53-year medical career in Oklahoma, Paul Donat, M.D., was known for his skills as a urologist, for the kindness he showed his patients, and for his devotion to teaching the next generation of physicians. He also held a longtime dream of establishing an endowed chair in the Department of Urology at the OU College of Medicine, a vision that his wife, Anna, is turning into a reality.
Dr. Donat, who died in 2016, was a 1962 graduate of the OU College of Medicine, and he stayed on campus to complete his residency and fellowship. He was a founding member of Urology Associates in Oklahoma City. He also served in Vietnam as chief of urology at the 8th Field Hospital, earning a Bronze Star.
As his private practice got underway, he quickly earned a reputation as a skilled surgeon and a compassionate presence for his patients. “He loved his patients, and they loved him,” Anna said. “They were more than just patients — they were his family.”
Dr. Donat perfected the perineal prostatectomy to remove cancer of the prostate, performing more than 6,000 of the surgeries during his career. He researched the use of ultrasound for imaging the prostate and presented the results to Medicare, earning approval for its use. He also taught the first course on laparoscopic surgery in urology to Oklahoma residents and fellows. Because of his surgical reputation, he was asked to teach perineal surgery at M.D. Anderson and
In 2000, they married. Dr. Donat continued his practice for 14 more years. “Paul’s life was his family and medicine, and he loved it,” Anna said. “That’s why he kept working so long.”
Just six months after retirement, Dr. Donat was diagnosed with stomach cancer. Working with Department of Urology Chair Michael Cookson, M.D., Dr. Donat began the process of fulfilling his dream of creating an endowed chair. Although he died before it was established, he knew Anna would finish the effort. She has made significant gifts to fund the Dr. Paul Donat Chair.
“He would be thrilled to know that we are seeing it through to completion,” Anna said. “I see visions of it growing, and I hope it will benefit many, many people.”
Cookson called Dr. Donat a true pioneer in urologic surgery. “He was at the forefront of new surgical approaches to prostate and other urological cancers, and he was a gifted innovator in the field,” Cookson said. “However, perhaps one of his greatest achievements was passing his knowledge and expertise to other surgeons, including residents. And now, with the establishment of the endowed chair in his honor, the tradition will live on in perpetuity as OU Urology carries this forward. His ambition and commitment to excellence in patient care, coupled with cutting-edge advancements in minimally invasive surgery, are alive and well today. We are truly blessed and thankful to Dr. Paul Donat and his wife, Anna, for their kindness and generosity to the OU College of Medicine and the Department of Urology.”
University of Oklahoma College of Medicine

P.O. Box 26901
Oklahoma City, OK 73126-0901
Earlier this year, the Office of the Vice President for Research at the OU Health Sciences Center hosted a symposium and White Coat Ceremony for students in the M.D./Ph.D. program. Students received their white coats and heard from a variety of faculty, students and biotech industry speakers about their research and opportunities for clinician-scientists. The M.D./Ph.D. program is a cooperative venture between the OU Health Sciences Center and the Oklahoma Medical Research Foundation that allows students to earn their medical degree as well as a doctoral degree in one of five basic science programs in the OU College of Medicine. The dual-degree program is funded by the Presbyterian Health Foundation, a longtime supporter of research on campus. Students on the M.D./Ph.D. track are called PHF Scholars during their time in the program. Pictured is PHF Scholar Cameron Owens with Mary Beth Humphrey, M.D., Ph.D., Associate Dean for Research in the OU College of Medicine.