


















As I reflect on my first year as Executive Dean of the University of Oklahoma College of Medicine, I am incredibly optimistic about the future of our institution. This year has been a whirlwind of activity, marked by significant milestones and inspiring moments that highlight our vibrant profession that, for us, is a calling.
An especially poignant experience of my tenure thus far was witnessing Match Day, a day of great anticipation and celebration as our students discovered where they will complete their medical residencies. This event is the culmination of years of rigorous training, dedication, and hard work. Seeing the look of joy on the faces of our students and sharing in their excitement reaffirmed my commitment to ensuring that our College of Medicine remains a beacon of excellence and a launchpad for future successes.
Similarly, leading the commencement ceremony was another very special occasion. It was moving to watch our graduates walk across the stage and receive their hoods, and seeing their excitement as they are ready to embark on their professional journeys. Not only was this event a testament to the exceptional education and training they have received here, but it also signified the unwavering support and guidance provided by our outstanding faculty and staff.
This summer, we welcomed a new class of medical and physician assistant students, as well as new residents across a variety of medical specialties. These individuals represent the future of healthcare, bringing with them fresh perspectives, boundless energy, and a commitment to advancing the field of medicine. It is our responsibility to provide them with the knowledge, skills, and clinical experiences they need to become compassionate, competent, and innovative healthcare leaders.
As I delve further into my role, I will share our developing strategic priorities as they sharpen. Of the many, one of my primary goals as dean is to foster a robust environment for research. The College of Medicine has a rich history of groundbreaking research, and I am committed to building upon this legacy. By expanding our research initiatives and securing additional funding, we can attract top-tier investigators and provide them with the resources they need to make significant life-altering contributions. Our focus will be on interdisciplinary collaboration, leveraging the diverse expertise within our institution to tackle some of society’s most pressing health challenges.
In addition to growing our research capabilities, attracting and retaining the best and brightest students and faculty will always be a top priority. The college is committed to providing a supportive and inclusive environment that nurtures talent and encourages professional growth. By investing in state-of-the-art facilities, cutting-edge technology, and comprehensive support services, we aim to create an academic and clinical environment that is second to none.
Our commitment to excellence extends beyond the classroom and the laboratory. We are also deeply invested in serving our community and addressing the healthcare needs of Oklahoma and beyond. Through our partnerships with OU Health, other local healthcare providers, community organizations, and policymakers, we strive to improve access to care, reduce health disparities, and promote overall well-being. Our students and faculty are actively involved in outreach initiatives, providing care to underserved populations and advocating for health equity.
As we move forward, I am inspired by the collective dedication and passion of our College of Medicine community. Together, we have the opportunity to shape the future of healthcare, to train the next generation of medical leaders, and to make a meaningful impact on the health and well-being of our society.
I am honored to serve as your dean and to work alongside such a talented and committed group of individuals. Thank you for your support and I look forward to all that we will achieve together in the coming years.

Ian F. Dunn, MD, FACS, FAANS, Executive Dean
The University of Oklahoma College of Medicine
President, The University of Oklahoma
Joseph Harroz, Jr.
Senior Vice President and Provost, OU Health Sciences
Gary E. Raskob, Ph.D.
Executive Dean, College of Medicine
Ian F. Dunn, M.D.
Contributing Writers
Edna Espino, OU Health
Kristen Hoadley, OU Foundation
Megan Louk, OU MarComm
Bonnie Rucker, OU MarComm
Annelise Stephenson, OU Health
Brady Trantham, OU MarComm
April Wilkerson, OU MarComm
the University of Oklahoma Office of Marketing and Communications on behalf of the OU College of Medicine. For more information, contact marcomm@ou.edu

Sometimes, on rare occasions, the dean of the University of Oklahoma’s College of Medicine finds some free time. The effort that comes with building off an already strong 125-year history to ensure that the future is even better requires a lot of work.
When Ian F. Dunn, M.D., FACS, FAAN does find those rare occasions, you might find him and his family at Mitch Park in Edmond. Located off West Covell Road between Santa Fe and Kelly Avenues, Mitch Park has 280 scenic acres of recreational ground and picnic areas perfect for relaxing and recuperating from heavy workloads and stressful workdays.
“It is just a great place to be together [with family],” said Dunn.
The area holds symbolic significance for Dunn and his family of five: his wife, Dr. Carolyn Kloek and their three children. In addition to being an outdoor sanctuary during the COVID-19 pandemic lockdowns, Mitch Park became a place where the Dunns developed a bonding tradition.
“First, I’m a bird guy, which is sort of nerdy. And I love taking my kids there. They are getting to an age where Dad isn’t so cool anymore, but deep down I still think they like going there with me.”
Finding time for recreation is more than recharging batteries for Dunn and his family. After spending most of his adult life in Boston attending Harvard, Dunn wanted to integrate in the region and community that his career path would lead him down.
“I love being a part of the OU community,” Dunn said. “Having been here for five and a half years, the culture at OU has created is special. The culture of service, belonging, leading in the state, region, and the world.
“It’s a really positive culture,” Dunn added.
Dunn’s father, Peter, was his first example of servant leadership, having served in the United States Air Force for 30 years. The family was stationed in England, when Dunn was born. They lived abroad for a period before moving to Virginia, where he received a job at the Pentagon.
The life of a military brat often begets its own set of advantages unique to the experience. Thanks to such a unique experience, some military children follow in their parent’s footsteps into the armed forces once they come of age. Dunn’s brother, Gavin, followed their father into the military, serving in the United States Naval Reserves. Dunn applies the principles of servant leadership to his passion for medicine and helping others.
“The military and medicine have a lot in common,” said Dunn. “Both are bound by a sense of service. My upbringing in the military informed my sense of service for others.”
This service mindset became Dunn’s fuel during his time at Harvard Medical School. After becoming a neurosurgery resident in Boston, Dunn found himself with a new opportunity. That’s where one of the other advantages of being a military brat came in handy – the ability to start anew in a different region or place.
In 2009, Dunn found himself in Little Rock, Arkansas to work with the Fellowship in Skull Base Neurosurgery with Dr. Ossama Al-Mefty, the world’s leader in this area. For a year, Dunn gained valuable experience and vital expertise. His time in Arkansas also provided the groundwork for what Dunn would be looking for later in his professional life.
“That was my favorite year of medical training,” said Dunn. “What appealed to me about Arkansas was the overall environment. The geographic features of one big medical system and the fact that the whole region looked to that system for leadership.”

Following his year-long stint in Arkansas, Dunn returned to Boston to become an associate professor of neurosurgery at Brigham and Women’s Hospital for the next eight years. His time in Arkansas still on his mind. Dunn longed for a leadership role like his experience in Little Rock, a hospital system that supported and served an entire state and region.
In 2018, Dunn realized this goal through an opportunity with OU Health Sciences. He accepted a role as the Harry Wilkins Professor of Neurosurgery. Quickly, Dunn saw the similarities between the OU Health system, which has a working and teaching hospital system in Oklahoma’s capital city, as well partnership sites across the state, and the one he served at in Arkansas. This was a health system that was here to serve the entire state and region – exactly what he was looking for.
“It’s that [remembering his time in Arkansas] times a thousand here,” Dunn said. “I think there’s something about being a part of a broader medical care system. For our research mission and medical mission all to be in Oklahoma City and Tulsa.
“The great thing about being here is, as the only big academic health system in the whole state, the chance to serve the whole region,” Dunn added.
Dunn has already had a successful first year as dean. One of Dunn’s passion projects within his leadership role at the College of Medicine is to address the state’s workforce shortage of highly skilled physicians. Dunn referenced that Oklahoma is 48th in active physicians per 100,000, population. To him, the answer is simple: the state needs to at least train and retain more doctors, nurses and other healthcare professionals. But Dunn knows that the answer to this challenge isn’t simple.
“We are just beginning to realize what our presence and participation means for health education in the state,” Dunn said. “There is a ton of work to do to improve the health outcomes for the state. We have an incredible legacy entering our 125th year, and the future has never been brighter.”
Dunn also aims to continue maximizing and supporting research within the health system in a way that “marries our clinical excellence with our research focus.”
“Research is a significant investment,” Dunn said. “I want to invest in our endeavors and our people to support our mission of service here.”
Already, plans are in place to ensure these challenges are met with success. To answer the call for more physicians in the state, the College of Medicine will compress the pre-clinical portion of students’ education to get them on the fast track to helping patients. This would be part of a new medicine curriculum, with the goal to increase the number of trained healthcare professionals and the chances of retaining them within the state.
Here in Oklahoma, Dunn has found the right environment to serve a community. Now, the University of Oklahoma’s College of Medicine has a leader to help propel the institution into a successful future.

In September, the University of Oklahoma Board of Regents approved an ambitious plan to incrementally increase enrollment in the Doctor of Medicine (MD) program in the College of Medicine by more than 40% over the next five years – a strategic initiative designed to address the critical demand for additional health care professionals in Oklahoma.
The plan will increase admissions to the program from 163 to 232 students while also adjusting the curriculum to support student wellness and promote further academic success. These enhancements will further OU’s contribution to Oklahoma’s physician workforce, which currently ranks No. 48 in the nation for the number of active physicians per capita.
“By expanding our Doctor of Medicine program, we are taking a decisive step toward addressing the evolving healthcare needs of our state,” said OU President Joseph Harroz Jr. “This will ensure we continue to educate a skilled and dedicated physician workforce, prepared to tackle the dynamic medical landscape of our communities.”
The expansion also directly addresses Oklahoma’s growing demand for high-quality medical care, driven by an aging physician workforce approaching retirement, a rising adult and elderly population and the expanding scope of medical conditions requiring specialized care. Notably, half of all physicians who graduate from OU practice in Oklahoma.
“By expanding our Doctor of Medicine program, we are taking a decisive step toward addressing the evolving healthcare needs of our state,” said OU President Joseph Harroz Jr. “This will ensure we continue to educate a skilled and dedicated physician workforce, prepared to tackle the dynamic medical landscape of our communities.”

“OU Health Sciences is pivotal in addressing Oklahoma’s workforce need by not only training a diverse range of healthcare professionals but also by driving innovation and leadership across our seven health professional colleges – allied health, dentistry, medicine, nursing, pharmacy, public health, and the health sciences graduate college,” said Gary E. Raskob, Ph.D., senior vice president and provost at OU Health Sciences. “Our graduates are exceptionally well-prepared to meet the state’s most pressing health challenges, ensuring that every community in Oklahoma has access to high-quality care.”
Also approved during the meeting was the creation of two pivotal new departments in the College of Medicine, including a new Department of Emergency Medicine and Department of Molecular Genetics and Genome Sciences.
The Department of Emergency Medicine will enable emergency room physicians to be trained in Oklahoma City at OU Health, Oklahoma’s only Level 1 trauma center, for the first time in more than 30 years. Emergency physicians will also be directly employed by OU Health for the first time in more than three decades, fostering greater integration and advancing clinical care, medical education and research.
The Department of Molecular Genetics and Genome Sciences will expand research capabilities at OUHSC in areas such as cancer genetics, epigenetics, genomic technology, artificial intelligence approaches to drug discovery and more, while contributing to OU’s goal of meeting benchmarks for Association of American Universities accreditation.
“The OU College of Medicine is a leader in innovative health research and medical education, driving advancements that shape the future of healthcare. As a key partner in the OU Health clinical enterprise, our faculty and residents are dedicated to delivering exceptional patient care and improving clinical outcomes through evidencebased practices and cutting-edge treatments.
“The OU College of Medicine is a leader in innovative health research and medical education, driving advancements that shape the future of healthcare,” said Ian F. Dunn, M.D., FACS, FAANS, executive dean of the OU College of Medicine. “As a key partner in the OU Health clinical enterprise, our faculty and residents are dedicated to delivering exceptional patient care and improving clinical outcomes through evidence-based practices and cutting-edge treatments. Our faculty are also engaged in groundbreaking research that not only addresses current challenges, but also paves the way for innovative treatments that will impact patient care for years to come.”
The Regents also approved the addition of a new Doctor of Philosophy in Cancer Biology, administered through the OU Health Sciences Graduate College. The new program will provide students with a specific background in cancer biology and translational research. According to the American Cancer Society, there are expected to be an estimated 24,450 new cases of cancer in Oklahoma in 2024, signifying the urgent need for additional cancer care and research in the state.
OU further reaffirmed its commitment to battling cancer in Oklahoma by announcing an expansion of OU Health Stephenson Cancer Center to Tulsa to improve health outcomes in Northeast Oklahoma. Read more about this imitative on page 25.

Physician associate students from the University of Oklahoma Health Sciences campus are embarking on three-month rotations in rural primary care clinics that integrate mental health services into their practices. The initiative aims to grow the PA workforce across rural Oklahoma and equip them with skills to address mental health concerns before patients ever leave the building.
Oklahoma has a significant shortage of both primary care and mental health providers, especially in rural parts of the state, where about 41% of the population lives. Because PAs are licensed to practice medicine with the supervision of a physician, they are uniquely positioned to extend the reach of medical care, and in Oklahoma, PAs can prescribe medications. In rural areas, primary care providers are often the first line of treatment for any type of health concern, making mental health care skills especially important.
“Our goal is to increase the number of trained PAs who choose to practice in rural areas of Oklahoma after they graduate. Right now, about 23% of PAs employed in Oklahoma practice in a rural setting, but studies show that when students are exposed to rural health care, they are more likely to practice there,” said Darlla Duniphin, interim director of the PA program and project director for the grant. “About 95% of our state is designated as a health professional shortage area, and PAs can help increase access to care.
“Our goal is to increase the number of trained PAs who choose to practice in rural areas of Oklahoma after they graduate. Right now, about 23% of PAs employed in Oklahoma practice in a rural setting, but studies show that when students are exposed to rural health care, they are more likely to practice there,”
“In addition, by training in a setting that integrates mental health with primary care, our students are learning the important role they can play in caring for their patients’ mental health. Too many times, a provider suggests that a patient seek mental health care or gives them a referral, but the patient never goes, and they fall through the cracks.”
The Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services awarded the OU Health Sciences campus in Oklahoma City a $2 million grant to create the rural rotation program. Much of the funds will help students pay for housing and meals in the rural communities where they stay during their training. To start, three Oklahoma health systems will host students for their rotations: the Okeene Municipal Hospital and Medical Clinic (Blaine County), the Iowa Tribe Perkins Family Clinic (Payne County), and the Health and Wellness Center (formerly Stigler Health and Wellness Center), which has a network of locations across eastern and southeastern Oklahoma.
Each site integrates mental health with primary care services. A primary care provider like a PA may treat a patient for both physical and mental health conditions, or may walk the patient down the hall to connect with a psychotherapist or other mental health practitioner.

Simply asking patients about their mood and energy level opens the door for them to talk about their concerns. “It’s important that we have these conversations with our patients because there is still stigma attached to mental health issues,” said Bruna Varalli-Claypool, co-leader of the grant and PA program faculty member. “It opens the door for them to talk about how they’re feeling. And sometimes they may come in thinking that they will be diagnosed with a migraine or an ulcer, but anxiety or depression are really causing their problems. We are building trust with them and taking care of the whole patient.”
In conjunction with the new clinical rotations, faculty have enhanced the PA curriculum’s instruction on mental health conditions, as well as substance abuse treatment, particularly regarding opioids, which remain a major problem in the state.
Even if PA students don’t ultimately practice medicine in a setting that integrates primary care with mental health care, they will be skilled in caring for both. PAs at OU Health Sciences are intentionally trained as generalists who understand the whole patient.
“We’re starting to understand and focus on the fact that mental health is a huge part of our physical health. Separation of the two doesn’t work. It’s incredibly important to prepare our students to have conversations about mental health with their patients,” said Mary Gowin, a co-leader of the grant and director of the Primary Care Health Policy Division in the OU College of Medicine.

In May, the College of Medicine announced the appointment Jason S. Lees, M.D., as the new associate dean of Graduate Medical Education (GME) and the college’s Designated Institutional Official (DIO). Lees brings a wealth of experience and a commitment to excellence in medical education, clinical practice, and research to this role.
“I am thrilled to welcome Dr. Jason Lees as the Associate Dean of Graduate Medical Education,” said Ian F. Dunn, M.D., FACS, FAANS, executive dean of the college. “His unwavering dedication to education, research, clinical excellence and leadership made him the ideal choice to lead our graduate medical education programs into the future.”
A native of Edmond, Lees is deeply rooted in the state of Oklahoma and has an impressive academic background. He graduated Magna Cum Laude with a Bachelor of Science in Zoology from the University of Oklahoma before earning his Doctor of Medicine degree from the OU College of Medicine. Following his medical education, Lees completed his residency in General Surgery at OU, where he was honored as the Lloyd Rader Outstanding Graduating Resident.
Lees furthered his training with a fellowship in trauma and surgical critical care at Jackson Memorial Hospital and the University of Miami. He then pursued a surgical education research fellowship through the Association of Surgical Education and Southern Illinois University.
“I am deeply committed to fostering a supportive learning environment where residents and fellows can thrive, and I look forward to working collaboratively with colleagues to uphold the highest standards of clinical medical education.”
Throughout his career, Lees has demonstrated a commitment to advancing medical education and clinical care. He has served as the program director of the General Surgery Residency program since 2012, overseeing its significant growth and achieving outstanding board passage rates. According to Dunn, Lees’ leadership has been instrumental in the success of the program, which has garnered national recognition.
“I am honored to have been named the associate dean of Graduate Medical Education at the OU College of Medicine,” said Lees. “I am deeply committed to fostering a supportive learning environment where residents and fellows can thrive, and I look forward to working collaboratively with colleagues to uphold the highest standards of clinical medical education.”
Lees’ appointment comes at a pivotal time for medical education, and his expertise will be invaluable as the College of Medicine continues to innovate and adapt to the evolving needs of healthcare professionals and patients.
“I am confident that in his new role, Dr. Lees will continue to champion excellence in graduate medical education, mentorship, and professional development for our residents and fellows. He will work closely with leaders across the College of Medicine to ensure the highest standards of training, equipping the next generation of physicians for unparalleled success,” said Dunn.

After a nationwide search, Michel Torbey, M.D., MBA, MPH, was named chair of the Department of Neurology at the College of Medicine, starting September 1. He also holds the Kathryn G. and Doss Owen Lynn, M.D. Chair in Neurology.
Torbey is a nationally recognized physician-scientist in neurology and neurocritical care. In addition to overseeing the academic and research missions of the Department of Neurology, he will serve as Clinical Service Chief of Neurology at OU Health.
“We are thrilled to have Dr. Torbey join the OU College of Medicine as the new chair of the Department of Neurology,” said Ian F. Dunn, M.D., executive dean of the college. “His addition marks a significant milestone for our institution as we continue our mission of excellence in health care, research and education. I am confident that, under his leadership, our neurology program will continue to see unprecedented growth, solidifying our position as a premier educational program and a regional leader in clinical care.”
Most recently, Torbey served as professor and chair of the Department of Neurology at the University of New Mexico. Under his leadership, UNM expanded specialized services in various areas, including child neurology, stroke, neurocritical care, epilepsy, multiple sclerosis, neuromuscular disorders and movement disorders. He also spearheaded significant growth in clinical services, research initiatives and educational programs within the neurology department. His strategic efforts led to a doubling in the department’s size, with a strong emphasis on program development and faculty recruitment.
Torbey’s impact extended beyond clinical growth, as he was pivotal in enhancing UNM’s research and education profile, overseeing the expansion of residency and fellowship programs, including those focused on stroke, epilepsy and neurocritical care.
Notably, he contributed to an increase in NIH funding, improved the department’s Blue Ridge Ranking and facilitated the establishment of key research centers such as an Alzheimer’s Disease Research Center and an NIH StrokeNet research hub.
“His addition marks a significant milestone for our institution as we continue our mission of excellence in health care, research and education. I am confident that, under his leadership, our neurology program will continue to see unprecedented growth, solidifying our position as a premier educational program and a regional leader in clinical care.”
Prior to his time at UNM, Torbey was a professor of neurology at the Ohio State University and held academic appointments at the Medical College of Wisconsin and Johns Hopkins. He is widely recognized for his groundbreaking research in stroke and neurocritical care, serving as principal investigator for the Southwestern Stroke Alliance Network, an NIHfunded stroke research network. He has also published more than 200 papers and presentations. He has held board of director positions in several national and international organizations. He is past president of the Neurocritical Care Society and council member of the Association for University Professors of Neurology.
“We are excited to welcome Dr. Torbey to Oklahoma to lead and continue to build a modern neurology services platform that improves the lives of Oklahomans,” said OU Health President and CEO Richard Lofgren, M.D., MPH. “As Oklahoma’s flagship academic health system, OU Health is developing destination programs so that no Oklahoman needs to leave the state for the highest level, research-driven specialty and subspecialty care.”

In August, the College of Medicine announced that Robert Katz, M.D., was named Chair of the Department of Pediatrics. In addition to overseeing the academic and research missions of the Department of Pediatrics, Katz will also serve as Clinical Service Chief of
Pediatrics at Oklahoma Children’s Hospital OU Health. In addition to his clinical responsibilities with OU Health.
Katz, a well-respected and longstanding leader at the academic health system, will helm the largest department at the College of Medicine, overseeing more than 200 faculty members across 16 divisions. He joined Oklahoma Children’s Hospital and the Department of Pediatrics in 2015 and has served as interim Chair of the department since October 2022.
During his tenure, the department has executed a strategic plan for research, and he has provided clarity, communication, transparency and leadership as OU Health throughout the integration of the clinics, hospitals and faculty practice.
“In getting to know Dr. Katz during this time, I have found his passion for the care of children – particularly those with pulmonary disorders in his area of expertise – to be profound and deeply rooted,” said Ian F. Dunn, M.D., FACS, FAANS, executive dean of the college. “I know he will continue delivering upon our mission of excellence in healthcare, research and education.”
Katz is a pediatric pulmonologist with expertise in asthma, bronchopulmonary dysplasia and the management of the child at home on a ventilator. Katz received his education at Case Western, Wayne State, the University of New Mexico, and Children’s National Medical Center in Washington, D.C. He has written in the areas of pediatric pulmonary and critical care, contributing manuscripts, chapters and an edited textbook to the literature.
“As the state’s comprehensive academic health system, we are committed to providing complex, life-altering care for Oklahomans. Dr. Katz embodies this mission with his years of unwavering dedication to the care of Oklahoma’s children,” said OU Health President and CEO Dr. Richard Lofgren, M.D., MPH, FACP.
“As the state’s comprehensive academic health system, we are committed to providing complex, life-altering care for Oklahomans. Dr. Katz embodies this mission with his years of unwavering dedication to the care of Oklahoma’s children.”
During his time at the University of New Mexico, Katz held various roles, including Director of the Pediatric ICU, Director of Pulmonary and Pediatric Critical Care, Chair of the Department of Pediatrics for eight years, and finally, Vice President of Clinical Affairs and Chief Operating Officer of the UNM Medical Group and Senior Associate Dean for Clinical Affairs at the UNM School of Medicine. Prior to UNM, he directed the Pediatric ICU at the University of Alberta in Edmonton.

Following a nationwide search, Andrew Jea, M.D., MBA, MHA, FACS, FAAP, has been named chair of the Department of Neurosurgery at the OU College of Medicine and clinical service chief at OU Health.
Jea is a nationally renowned pediatric neurosurgeon and physician scientist who has served OU Health as chief of pediatric neurosurgery since 2020. In his more than 20 years of experience, he has published extensively in the field of pediatric neurosurgery. At OU Health, he has been instrumental in the unprecedented growth in pediatric neurosurgery services at Oklahoma Children’s Hospital, with a focus on quality, safety, and program building.
Jea has served as vice chair of the department of neurosurgery at the College of Medicine; as the residency program director; and has served as interim chair of the department since March 1 after former chair Ian F. Dunn, M.D., FACS, FAANS, assumed the role of executive dean at the College of Medicine.
Jea began his career at Texas Children’s Hospital in Houston, after which he led the Section of Pediatric Neurosurgery at Riley Children’s Hospital at the University of Indiana.
“Through his career, Dr. Jea has built a significant reputation in pediatric spinal conditions in particular,” said Dunn. “He is a true ‘clinician-scholar’ and speaks and writes widely, having published over 250 papers in these areas. I made the decision to elevate him to the permanent role based on these credentials and based on his performance before and during his tenure as interim chair.”
Jea received his undergraduate degree at the University of Florida and earned his medical degree from the University of Miami, where he stayed and trained in neurosurgery in one of the most iconic departments in the field, completing his residency and fellowship training in orthopedic spine surgery there.
Jea is also a prominent member of national neurosurgical societies and is a member of the Society of Neurological Surgeons and the American Academy of Neurological Surgery. He has served on the editorial boards of Pediatrics, Operative Neurosurgery, and Journal of Neurosurgery: Pediatrics.
“Dr. Jea’s ongoing leadership in pediatric neurosurgery and his efforts in building world-class programs at OU Health are game changers for Oklahoma families. All Oklahomans should have access to world-class, innovative treatments right here at home.”
“Dr. Jea’s ongoing leadership in pediatric neurosurgery and his efforts in building world-class programs at OU Health are game changers for Oklahoma families,” said Richard Lofgren, M.D., MPH, FACP, president and CEO of OU Health. “All Oklahomans should have access to world-class, innovative treatments right here at home. As the state’s flagship academic health system, we’re committed to developing destination programs that blend groundbreaking research with specialized care, ensuring that even the most complex cases can be treated without having to leave the state.”

In January, the College of Medicine announced the appointment of Julia Busik, Ph.D., as chair of the newly combined Department of Biochemistry and Physiology. Busik also holds the prestigious Ed Miller Endowed Chair in Molecular Biology.
A distinguished scholar with an impressive academic background, Busik received her combined bachelor of science and master of science degrees from Novosibirsk State University in Russia, specializing in physiology and endocrinology. Afterward, she earned a scholarship from the Japan Society for the Promotion of Science and pursued her doctorate at the Graduate University for Advanced Studies at the National Institute for Physiological Sciences in Yokohama, Japan.
As a researcher, Busik has authored more than 80 papers in high-profile journals, establishing herself as a leading expert on the role of dyslipidemia in diabetic complications. Her ground-breaking work is supported by prominent awards from the National Institutes of Health, National Eye Institute, Juvenile Diabetes Research Foundation, and the American Diabetes Association.
In addition to her research contributions, Busik is actively involved in the scientific community, serving as an associate editor for Diabetologia, a peer-review journal for the European Association for the Study of Diabetes; Experimental Eye Research, a journal for the International Society for Eye Research; and Adler’s Physiology of the Eye, 12th edition. She is a Fellow of the Association for Research in Vision and Ophthalmology and has held leadership roles within the American Diabetes Association and the Annual Meeting Program Committee for ARVO.
“I am honored to lead the Department of Biochemistry and Physiology at the University of Oklahoma College of Medicine,” said Busik. “I look forward to collaborating with colleagues, students and the broader scientific community to make meaningful strides in building on our strength to advance understanding of biochemistry and molecular biology underpinning of normal physiology and pathophysiological processes. Together, we aim to foster innovation and excellence in both education and research.”
Busik’s outstanding achievements have been recognized with various awards, including the Junior Faculty Mentoring Award, Research Excellence Award and Distinguished Faculty Award from Michigan State University. She has also received the Distinguished Speaker Award from Gavin Herbert Eye Institute at the University of California, Irvine and The State University of New York at Buffalo, as well as the Reviewer of the Year Award for Diabetes Journal.
As chair, Busik has the added responsibility of leading the newly combined Department of Biochemistry and Physiology at the College of Medicine. Combining the two departments into one reflects a strategic and forward-thinking approach to scientific inquiry. Its formation will amplify the strength of existing programs and present an opportunity for tremendous growth for the department as a whole and each program individually.
Faculty in the new department are members of the Center for Gerosciences & Healthy Brain Aging, OU Health Harold Hamm Diabetes Center, Dean McGee Eye Institute and OU Health Stephenson Cancer Center. Current areas of strength in geroscience and aging research, vision and ophthalmology, diabetes and diabetic complication, cancer and structural biology have extensive synergies that will multiply combined strengths when brought into one unit. By integrating these areas of strength, the College of Medicine aims to create a collaborative environment that transcends traditional boundaries through the inherent interconnectedness of biochemistry and physiology.
“Our commitment to excellence remains unwavering as we embark on this integrated journey,” said Busik. “By uniting these departments, we strive to create a powerhouse of knowledge that will transform the existing areas of strength into cutting-edge research of tomorrow. I am confident that this strategic decision will lead to new discoveries, interdisciplinary breakthroughs and further development of the areas of emerging synergistic strengths across all research directions in the department.
“The areas of energy, mitochondria and lipid metabolism are gaining attention in each of the fields individually,” she added. “Combined in a strong new program, it will secure the department’s position as tomorrow’s leader in metabolic pathophysiology.”

Yuri Lansinger, M.D., associate professor with the Department of Orthopedic Surgery at the University of Oklahoma College of Medicine and a board-certified orthopedic surgeon specializing in hand surgery, received the prestigious Fulbright U.S. Scholar award for the 2024-2025 academic year.
The 10-month research award will help Lansinger connect with health care professionals in South Korea to compare the two different models of healthcare in U.S. and Korea to see if access to care, particularly, subspecialty care, lead to different patient outcomes in managing difficult nerve injuries of the upper extremity. She said it was surreal when she found out she received the Fulbright Scholar Award.
“I was delighted to hear that I was selected because it means a lot to me not just professionally but personally in terms of the opportunity that my family gets to experience together,” Lansinger said. “My family and I have been wanting to do this for a while and it’s actually coming into reality.”
Fulbright U.S. Scholars are faculty, researchers, administrators and established professionals teaching or conducting research in affiliation with institutes abroad. Fulbright Scholars engage in cutting-edge research and expand their professional networks, often continuing research collaborations started abroad and laying the groundwork for forging future partnerships between institutions.
Lansinger received a medical degree from Georgetown University School of Medicine in Washington, D.C., in 2007. Subsequently, she completed her Orthopedic Surgery Residency at the University of Pittsburgh medical center in 2012. In 2013, she pursued further specialized education and training in orthopedic hand surgery through a hand surgery fellowship at Integris Baptist Medical Center in Oklahoma City.
Lansinger said she hopes this Fulbright award will lead to further collaboration and partnership with OU and medical centers in South Korea.
“Under usual circumstances, if I were to practice out in community as a private practice hand surgeon, it would be difficult to take a year off to go somewhere abroad to do a research project,” Lansinger said. “Being at OU, from the department chair to my senior partner, they were all very supportive through the whole application process.”
She joins an alumni network of Fulbrighters that includes 62 Nobel Laureates, 89 Pulitzer Prize winners, 80 MacArthur Fellows, 41 heads of state or government and thousands of leaders across the private, public and non-profit sectors.

Nancy Halliday, Ph.D., a David Ross Boyd Professor in the Department of Cell Biology was named the OU College of Medicine’s 2024 Stanton L. Young Master Teacher.
Created by the late Stanton L. Young, and his wife, Barbara, the award is given to a truly inspiring teacher, one who goes beyond excellence in conveying knowledge, touching lives and changing attitudes. Master Teachers are respected for their professionalism, excellence in their discipline, and their strong personal involvement with students. They inspire by the example of their commitment as physicians and scientists and by their qualities as human beings. It comes with a $15,000 award.
Halliday, who also serves as the vice chair of education, is a member of the OU College of Medicine Academy of Teaching Scholars and has received the Outstanding Teacher Award for the college every year since 2018.
“Dr. Nancy Halliday’s dedication to education and her unwavering commitment to excellence embody the spirit of the Stanton L. Young Master Teacher Award,” said Ian F. Dunn, M.D., executive dean of the OU College of Medicine. “Her impact extends far beyond the classroom, shaping the future of medicine through her mentorship and inspiring leadership. We are proud to recognize her as the 2024 recipient of this prestigious honor.”
One student nomination praised Halliday, writing that she is “...kind beyond measure, passionate beyond compare, wise beyond words, and patient beyond time, but most importantly, she sees something wonderful in each of us.”
Another student wrote that Halliday “shaped my introduction to medical school and greatly influenced my love for learning medicine during that first semester, and I will always appreciate her for that.”
Halliday joined the College of Medicine faculty in 2010, where she is course director for the Human Structure course for MS1 students. She has been nominated numerous times for the Aesculapian Award for Excellence in Teaching the Basic Sciences and has been the recipient of that award four times over the past 12 years.
In 2020, she was awarded the Edgar W. Young Lifetime Achievement Award by the College of Medicine Student Council. She has also received several teaching awards across the OU Health Sciences campus, including the 2014 Regents’ Award for Superior Teaching and Outstanding PA Lecturer Award, and the 2018 Robert Magarian Faculty Award. Halliday was awarded the David Ross Boyd Professorship in 2018.
In addition to teaching the anatomical disciplines to first- and second-year medical students, she mentors MS4 students in an advanced anatomy elective. Halliday is also involved in the education of professional students across the OU Health Sciences campus.

Last September, Michael S. Cookson, M.D., professor and chair of the Department of Urology, was recognized by the University of Oklahoma as a recipient of the 2023 Regents’ Alumni Award during a ceremony on the OU Norman campus.
Regents’ Alumni Award honorees are chosen for their extraordinary dedication and service to the university. Cookson holds the Donald D. Albers Endowed Chair in Urology and also serves as the inaugural Chief Surgical Officer for OU Health Stephenson Cancer Center.
Cookson came to OU in 1980 on a small scholarship and was the first of his family to attend college. After earning a bachelor’s degree in journalism with honors in 1984, he was accepted into the OU College of Medicine, graduating in 1988. He completed his residency in urology at the University of Texas-San Antonio and then went on to complete a fellowship in Urologic Oncology at Memorial Sloan Kettering Cancer Center. After 15 years on the faculty of Vanderbilt University, he returned to his alma mater in 2013 to chair the Department of Urology and develop a prostate and urologic cancer team at OU Health Stephenson Cancer Center.
Nationally, he serves as a member of the American Urological Association and American Board of Urologists exam committees. He is also a member of the Society for Urologic Oncology and has developed a national benchmark in testing known as the Oncology Knowledge Assessment Examination. He is currently on the editorial board of the AUA Update Series and co-editor of Urology Times. He has served as chair of the AUA’s CPRC Guidelines Panel and vice chair of the American Urological Association/Society of Urological Oncologists Advanced Prostate Cancer Guidelines Panel.
Cookson has been internationally recognized for his outstanding contributions to the field of urologic oncology. He is one of 70 academic urologists nationally to be awarded membership in the prestigious American Association of Genitourinary Surgeons. An accomplished researcher and lecturer, he is the author of over 250 peer-reviewed journal publications and 34 textbook chapters.
Presented by the OU Board of Regents and OU Alumni Association, the Regent’s Alum ni Award celebrates the profound way OU alumni and supporters shape the university’s vibrant future. A committee formed by the Alumni Association reviews nominations submitted by alumni, friends and OU faculty and staff to select each year’s awardees. Recipients receive a commemorative plaque in recognition of their exceptional contributions, and their names are permanently inscribed on a plaque displayed in the historic Oklahoma Memorial Union.

Potential infection with Clostridioides difficle, or C. difficile, emerges as one of the most troubling risks during a hospital stay, particularly for people taking antibiotics or those with a weakened immune system.
Hospitalized patients with C. difficile, in addition to experiencing diarrhea, fever and nausea, also face a higher risk of reinfection and more dangerous problems like sepsis and irreparable damage to the colon. Although unsuccessful thus far, efforts to develop a vaccine to protect against C. difficile continue. And now, a surge of federal funding aims to bolster the science needed to create a more effective method of preventing these infections.
Researchers at the OU College of Medicine recently received a significant grant from the National Institutes of Health — $6.5 million over five years — to leverage a three-part approach to better understand how C. difficile often thwarts a person’s immune system.
Mark Lang, Ph.D., a Presbyterian Health Foundation Presidential Professor in the Department of Microbiology and Immunology in the College of Medicine, leads the work of the grant.
“Physicians see anywhere from 10 to 30 cases of C. difficile infections each month in the hospital, and it can be a major problem for patients with cancer, especially those who have had bone marrow radiation and a transplant, as well as other patients who are immune-compromised because of various conditions,” Lang said. “C. difficile can be treated, usually with an antibiotic, but that disrupts the healthy bacteria in the digestive tract and the patient is susceptible to reinfection. Each time a person is infected, the chance of reinfection is higher. We can knock C. difficile down, but we can’t knock it out.”

Researchers at the College of Medicine bring a wealth of experience and unique scientific methods to their three-pronged approach for better understanding C. difficile. Jimmy Ballard, Ph.D., George L. Cross Research Professor and chair of the Department of Microbiology and Immunology, leads one approach that uses the inactive C. difficile toxins that he created in his lab. Because he engineered the toxins to elicit an immune response to C. difficile, researchers can design studies that allow them to analyze the effects of the toxin during disease and following vaccination.
“The research community has gaps in knowledge about all the mechanisms by which C. difficile attacks its host, and how the bacterium affects the host’s immune response,” Lang said. “There have been several large clinical trials testing new vaccines that seemed promising, but ultimately too many people were still getting infected, and pharmaceutical companies stopped pursing the vaccines. It doesn’t matter how good a vaccine candidate is if the bacterium is doing something to limit its success.”
Lang’s contribution to the work of the grant focuses on the human immune response to C. difficile infection. In previous research, he profiled the entirety of the antibodies created in people who were infected with C. difficile and recovered. These antibodies, considered the body’s B cell “memory,” should protect against a reinfection of C. difficile, Lang said, but subsequent studies showed that the antibodies weren’t very good at remembering the bacteria when they returned, so reinfection could occur.
With funding from the new grant, Lang plans to recruit more volunteers, both healthy people and those who have recovered from a C. difficile infection, to create a more extensive profile of B cells and the antibodies they make. Somehow, C. difficile finds a way to limit a person’s immune response; understanding how immune suppression occurs marks a crucial step for developing a vaccine that prompts the body to make highly effective antibodies.
The third arm of the grant employs a different yet complementary type of research led by Maureen Cox, Ph.D., assistant professor in the Department of Microbiology and Immunology. She focuses on how the nervous system and the immune system intersect during an infection. C. difficile, like many bacteria and viruses, manipulates a person’s nervous system in various ways. Cox hypothesizes that C. difficile infections cause a profound depletion of the nerves in the gastrointestinal tract. Because the GI tract’s nerve cells play a role in fighting infection, having fewer such cells likely makes a person more susceptible to reinfection.
“This U19 grant is a clear recognition of Dr. Lang’s leadership in this field, and it further establishes the Department of Microbiology and Immunology as a hub for cutting-edge C. difficile research that will lead to new and effective vaccines against this serious human disease.”
“Our theory is that the people who lose the density of nerves in their GI tract are the ones who are going to relapse and see if susceptibility to C. difficile increases,” Cox said. “The research community also doesn’t yet know whether people are able to recover those nerves after infection. That means that future vaccines likely need to prevent C. difficile from damaging the nerve cells.”
The NIH funding for this work, called a U19 grant, brings together a team of researchers to target their joint efforts on C. difficile infection. Although researchers have made great strides in understanding how the bacterium behaves during infection, they need much more knowledge to create a vaccine that blocks all the ways it is able to evade the immune system.
“This U19 grant is a clear recognition of Dr. Lang’s leadership in this field, and it further establishes the Department of Microbiology and Immunology as a hub for cutting-edge C. difficile research that will lead to new and effective vaccines against this serious human disease,” Ballard said.

People who are diagnosed with head and neck cancer often receive a standard type of chemotherapy as part of their treatment. If they are exposed to secondhand smoke during chemotherapy — even if they have never smoked themselves — the treatment may be far less effective at killing cancer cells. That finding, considered the first of its kind, was revealed in a study recently published by researchers at the University of Oklahoma.
Tobacco use is a well-established risk factor for cancer and a signal of poor outcomes, especially if a person continues to smoke during treatment. However, researchers have understood much less about the effects of secondhand smoke on cancer treatment. Lurdes Queimado, M.D., Ph.D., a professor of otolaryngology at the OU College of Medicine, led the investigation into secondhand smoke exposure, which was published in the International Journal of Molecular Sciences. Her findings have major implications for cancer patients and the physicians who treat them.
“Head and neck cancer is the sixth most common cancer worldwide and is prevalent in Oklahoma, where we also have a high rate of smoking. This is the first time that researchers have examined the impact of secondhand smoke exposure on cancer patients and the mechanism of why it is happening. Our studies will continue, but we think it is important to raise awareness now that people who are exposed to secondhand smoke during treatment will likely have a worse prognosis,” said Queimado, who also directs the Tobacco Regulatory Science Lab in the TSET Health Promotion Research Center, a program of OU Health Stephenson Cancer Center.

Lurdes Queimado, M.D., Ph.D.
In her laboratory, Queimado and her team exposed head and neck cancer cells to secondhand smoke for 48 hours (a control group of cancer cells was not exposed to secondhand smoke). Simultaneously, the cells were treated with cisplatin, a chemotherapy drug commonly used to treat head and neck cancer. The findings were significant: Twice as much chemotherapy was needed to kill the cells than would have been necessary without exposure to secondhand smoke. In addition, the cancer cells that survived chemotherapy treatment were much more likely to replicate indefinitely.
“This was concerning to discover because not only was the effectiveness of the chemotherapy cut in half, but the cells that survived were able to divide and create huge colonies of cancer cells,” Queimado said. “If the chemotherapy can’t kill all the cancer, it will come back. And it will come back sooner because the cells are dividing so quickly. In addition, we cannot simply double the amount of chemotherapy we give to patients because it would be too toxic.”
Queimado and her team took the research a step further to understand how secondhand smoke decreases the effectiveness of chemotherapy. They found that secondhand smoke alters the expression of several proteins involved in drug resistance, effectively restricting chemotherapy’s ability to do its job.
“Cisplatin kills cancer cells by binding to their DNA and keeping the cells from dividing,” she said. “But if cisplatin can’t get into the cell, it’s not going to kill it. Essentially, there are doors to the cancer cells that control how cisplatin gets in and out. In the presence of secondhand smoke, there were fewer doors for cisplatin to enter, and there were many more doors for cisplatin to exit. So not only is less cisplatin getting into the cell, but more of it is leaving the cell before it has a chance to kill it.”
Greg Krempl, M.D., professor and chair of the Department of Otolaryngology – Head and Neck Surgery in the College of Medicine, said Queimado’s study broadens the importance smoking cessation during cancer treatment.
“For patients with tobacco-related cancers, smoking cessation has been shown to improve survival, so it is a part of comprehensive cancer treatment plans. This study provides novel data that would suggest including family members in the smoking cessation plan to reduce secondhand smoke exposure during chemotherapy for head and neck cancer may improve outcomes,” Krempl said.
According to tobacco use data, more than 20% of nonsmoking U.S. adults are exposed to secondhand smoke. Exposure is highest among Black people, those living in poverty, and children ages 3 to 11. Each year, secondhand smoke exposure causes more than 41,000 deaths among nonsmoking adults and 900 deaths in infants.
This new study points to the ongoing public health ramifications of both active smoking and exposure to secondhand smoke, said Balaji Sadhasivam, Ph.D., an assistant professor of occupational and environmental health at the OU Hudson College of Public Health. Sadhasivam was the lead author of the research publication.

“Even though this study was conducted in the laboratory, it closely mimics human exposure to secondhand smoke,” Sadhasivam said. “If cancer patients live with someone who smokes, it is important for them to avoid being exposed to smoke while they are being treated. We want to do everything we can to help people have better outcomes from their treatment.”
Cisplatin is the preferred type of chemotherapy for treating head and neck cancer, Queimado said, but physicians may want to consider another drug if they know their patients will be exposed to secondhand smoke during treatment. However, secondhand smoke exposure may affect other drugs, including non-cancer treatments.
“The proteins affected by secondhand smoke are not specific for cisplatin; they are involved in resistance to other drugs. We have not studied that yet, but it is likely that secondhand smoke decreases the effectiveness of several types of drugs.”
Patients with diabetes face a host of potential health problems as they work to manage the chronic disease. Still, one concern that seems to weigh heavily is the risk of losing their sight through a condition known as diabetic retinopathy.
Researchers at the University of Oklahoma and Memorial Sloan Kettering (MSK) Cancer Center are studying a new, revolutionary treatment for diabetic retinopathy that could change the prognosis for these patients. Julia Busik, Ph.D., professor and chair of the Department of Biochemistry and Physiology in the OU College of Medicine, in collaboration with Richard Kolesnick, M.D., of MSK Cancer Center, recently published a paper in the journal Cell Metabolism that details how anti-ceramide immunotherapy can address the root cause of the disease and stop progression toward blindness at an earlier stage than previous treatments.
“With the rise in diabetes, there’s a rise in complications. One-third of adults over age 40 with diabetes have retinopathy,” said Busik. “If left untreated, diabetic retinopathy can lead to blindness. Losing vision is one of the most feared complications for patients with diabetes.”

This blindness is caused by damage to the blood vessels leading to hemorrhaging and lipid build-ups. These start as dark spots in the field of view. If untreated, these can cause retinal detachment leading to blindness. There are currently two treatments for diabetic retinopathy, but both have serious health implications and are fairly invasive. One involves lasers that burn the vessels to stop the hemorrhaging; another involves injections directly into the eye that can stop the progression of the disease. According to Busik, these treatments, although effective at preventing blindness, can only be used at a very late stage of the disease. Moreover, not all patients respond to these treatments.
The researchers are working on an exciting new treatment that could address the root cause of diabetic retinopathy. Continuing research that she began at Michigan State University, Busik has taken a closer look at lipids, specifically lipid pathways in the retina of the eye, and how they are affected by diabetes. She and her team found that a certain, very damaging type of lipid, or ceramide, was present in the eyes of patients with diabetic retinopathy. In turn, they discovered that these ceramides, after stimulation by inflammatory cytokines, stick together into large domains that cause damaging inflammatory signals to cells in the eye. This causes cell death and the progression of diabetic retinopathy.
In collaboration with the Kolesnick laboratory at MSK Cancer Center, Busik’s team was then able to create an antibody against these lipids to prevent the ceramide buildup from happening and signaling the damage to healthy cells in the retina. The studies show great promise in animal and cell culture models.
Perhaps the most important advance from the current treatment is that it addresses the root cause of the disease, as opposed to late symptoms and stopping progression at the vision-threatening stage, explains Busik. It can also be administered systemically, so it does not have to be injected into the eye. Due to their invasive nature and safety concerns, currently available treatments are only used at very late stages of the disease when the vision is threatened.
“If we have this systemic safe treatment,” Busik said, “it could be given to a patient at a much earlier stage when they are just starting to progress, to make sure that they never get to that late stage.”

With a $5 million federal grant renewal, the University of Oklahoma is expanding the efforts of the Oklahoma Dementia Care Network. The program, which involves partners across the state, aims to improve health outcomes for people living with dementia and their caregivers through statewide geriatric workforce development.
Dementia is most often diagnosed in older adults, who face significant challenges in Oklahoma. In 2023, Oklahoma ranked 48th in the nation for early death among older adults, 46th for physical activity, 41st in experiencing mental distress and 40th in experiencing multiple chronic conditions. Only 35% of older adults live within Oklahoma’s two urban areas, leaving 65% many miles away from specialized geriatric care. By 2025, Oklahoma’s older adult population is estimated to exceed 750,000.
With the Oklahoma Dementia Care Network, OU is working to improve the quality of life for older adults through several primary objectives: helping staff at existing clinics and nursing homes become more skilled in caring for people with dementia; placing current OU nursing, medicine and social work students in rural clinics and nursing homes for training; and providing support and resources to people with dementia and their caregivers.
“We have a great opportunity to support and grow the geriatric workforce in Oklahoma,” said Lee Jennings, M.D., an OU Health geriatrician and associate professor of geriatrics in the OU College of Medicine. “Our frail older adults, particularly those with cognitive impairment who have difficulty navigating their own health care tasks, are vulnerable and at risk.” Jennings is leading the grant work through the primary grant recipient, the OU College of Medicine. Other collaborating colleges include the Hudson College of Public Health and the Fran and Earl Ziegler College of Nursing on OU’s Health Sciences campus, and the Zarrow School of Social Work on OU’s Norman campus.
The Oklahoma Dementia Care Network was established five years ago with the initial federal grant awarded by the Health Resources and Services Administration of the U.S. Department of Health and Human Services. A Stakeholder’s Advisory Council was established with 77 members from 26 different community, state, tribal and academic partners across Oklahoma.
The network’s achievements over the past five years include training 1,578 nursing home direct-care workers in dementia-specific care; supporting 10 primary care clinics and nine nursing homes as they achieved national AgeFriendly Health System recognition; training 586 family caregivers; creating a dementia training program for community health workers; and delivering aging- and dementia-sensitivity training annually to over 330 health profession students at OU.
In this second iteration of the grant, that work continues, but with a larger focus on tribal, rural and medically underserved areas, each of which significantly overlaps the others in Oklahoma. OU nursing, medicine and social work students will train at several rural nursing homes, a federally qualified health center, and several tribal health facilities, learning skills that are both evidence-based and culturally relevant. Notably, the students learn how to care for older patients as an interdisciplinary team rather than siloed health professionals.

“The students get to see how their individual disciplines work together to improve the care of the patient,” Jennings said. “There may be a medical or prescribing issue that the physician is managing, and the nurse may be thinking about how the patient can carry out their daily activities at home. The social worker may be thinking about community resources that could be utilized or how the patient’s social determinants of health are impacting care. When students feel like they’re part of a valuable team that is making a difference, that’s very fulfilling. And we hope by exposing our students to the care of older adults, they will consider it for their own future careers.”
The need for additional nursing home care providers is especially great in Oklahoma. OU College of Nursing students will have several additional opportunities to immerse themselves in geriatric care. For example, students in the Bachelor of Science in Nursing program will participate in eight-week clinical rotations at a rural nursing home. In addition, nursing home and dementia care topics will be integrated into the curriculums used by students seeking bachelor’s, master’s and doctoral nursing practice degrees.
“This curriculum’s focus on geriatric care is consistent with the College of Nursing’s strategic goal of creating and maintaining innovative programs and partnerships that accelerate the development of nurses who exemplify excellence in practice. The college has been involved in geriatric care since 1995 through its case management practice and through its recognition as a Reynolds Center of Geriatric Nursing Excellence,” said Melissa Craft, Ph.D., interim dean of the OU College of Nursing.
Another new initiative involves working with nursing homes to create career advancement opportunities for certified nursing assistants. The training required for CNAs in Oklahoma is 75 hours, and the median annual salary is only $16 an hour. Turnover tends to be high in nursing homes, but a career ladder could start to change that. Grant leaders plan to create a new apprenticeship program in collaboration with the OU College of Nursing, Oklahoma’s Career Technology Centers, and the Oklahoma State Department of Health to help qualified CNAs advance their training to LPN (licensed practical nurse) and then to the level of BSN (bachelor of science in nursing).
The Oklahoma Dementia Care Network also prioritizes caregiver support. Through in-person and virtual classes, caregivers and other supportive care workers learn tools to care for their loved ones and themselves during times of stress and grief.
“Dementia management is different from the management of other diseases because you really have to engage caregivers,” Jennings said. “As the disease progresses, the person needs more and more support, not just for their dementia, but for other areas of their health. If they don’t take their medications for heart disease, for example, they’re at risk for their heart problems getting worse. They may end up being hospitalized for reasons not directly related to dementia.
“The work of the Oklahoma Dementia Care Network is exciting because we are trying to expand access to high-quality dementia care by growing our workforce, as well as making health care overall more age-friendly and dementia-friendly,” she added. “The work is very fulfilling, and we have the opportunity to make a difference in the lives of older adults and those who care for them.”

Newly published research in The Lancet Oncology lays the foundation for many patients with head and neck cancers to be treated with tailored therapies that are less invasive and to avoid major, potentially debilitating surgeries.
This step toward a major shift in practice is prompted by new imaging guidelines established in the study. As a result, imaging techniques like CT, PET and MRI can be better utilized to determine the aggressiveness of the cancer and point patients toward radiation therapy instead of surgery in certain cases. Christina Henson, M.D., a University of Oklahoma faculty member, is the lead author of the pivotal study, which involved head and neck cancer experts from 29 countries around the world.
“The impetus for the study is that today, approximately 80% of head and neck cancers are associated with an HPV infection rather than smoking and tobacco use,” said Henson, an OU Health radiation oncologist and associate professor in the OU College of Medicine.
“Because HPV-related head and neck cancers respond much better to treatment than tobacco-related cancers do, many patients can undergo minimally invasive surgeries or receive radiation treatment. Such ‘organ-sparing’ therapies will keep them from a complex surgery in which they might lose their voice box or part of their tongue.”
For appropriate therapy to occur, however, the oncology team needs to determine whether the patient has an extranodal extension – when the cancer has grown outside the lymph nodes and into surrounding tissue. Extranodal extension signals an aggressive type of cancer that requires radiation therapy and chemotherapy rather than surgery.
If a patient undergoes surgery and extranodal extension is found in the lymph nodes that are removed, the patient then needs radiation and chemotherapy after surgery – three separate forms of treatment with three separate sets of side effects. For this reason, the oncology team tries to avoid surgery on patients with extranodal extension because they are better treated with radiation and chemotherapy. If physicians had a way of identifying extranodal extension through an imaging test prior to

surgery, patients could avoid unnecessary surgical procedures and go straight to radiation and chemotherapy. The new imaging guidelines will fill that gap in knowledge.
“Until now, there have been no criteria by which to interpret the presence or absence of extranodal extension on imaging,” Henson said. “Radiologists have seen what they believe to be extranodal extension, but they have been hesitant to call it as such because there have been no criteria to follow. But now we have established guidelines that will give radiologists confidence to make that call so that patients can be appropriately treated.”
Henson, who often sees patients along with surgeons, said people would be relieved if told they will be treated with two forms of treatment rather than three, with equivalent outcomes and fewer side effects.
“Radiation therapy certainly has its own side effects, but it is significant to provide a treatment that will save people from having issues with their swallowing and their voice down the road,” she said.
The research was conducted according to the Delphi consensus in which questions were presented to experts for their feedback on the details of defining and identifying extranodal extension. Questions that didn’t result in agreement were revisited until all nuances had been addressed.
Now that the guidelines have been published, Henson and the study team are taking the next steps toward incorporating them into practice. Radiologists are familiarizing themselves with the guidelines and testing the new approach to continue establishing its reliability. The results of that effort will also be published.
In addition, a related study is ongoing to determine which imaging techniques are most accurate for identifying extranodal extension. Thus far, Henson said, a combination of CT and MRI scans appear to provide the highest accuracy.
The guidelines also will likely be used to inform the next edition of staging protocols for head and neck cancers, Henson said. Head and neck cancer staging criteria were last updated in 2018.
This study was part of a series of four articles published in the current edition of The Lancet Oncology. Another study followed the same Delphi process to refine existing guidelines that pathologists follow for interpreting extranodal extension. The remaining two studies established a common “language” for defining and measuring recurrent/metastatic head and neck cancers and curative head and neck cancers. The results are especially important for future clinical trials.
“Both of the last two studies were looking at endpoint definitions – for example, when there is a clinical trial, what is it measuring and how is survival defined? It is crucial to have standardized definitions of endpoints we’re using in clinical trials so that when we use a term, we are all meaning the same thing,” Henson said.

In April, the OU Health Stephenson Cancer Center announced its expansion to the University of Oklahoma-Tulsa, marking a significant milestone in providing access to research-driven cancer care to northeastern Oklahoma residents. As the state’s sole National Cancer Institute (NCI)-designated cancer center, Stephenson Cancer Center’s expansion will offer local patients unparalleled access to advanced cancer treatments and hundreds of innovative clinical trials for multiple cancers.
“This is a landmark day for OU Health Stephenson Cancer Center and the state of Oklahoma,” said OU President Joseph Harroz Jr. “As part of Oklahoma’s flagship academic health center, Stephenson Cancer Center’s mission is to reduce the burden of cancer across our state. This expansion brings local access to people in Tulsa and surrounding communities who can receive the best research-driven cancer care while staying close to their families and support systems. Statistics show that patients receiving care at NCI-designated cancer centers have up to 25% improved survival one year after diagnosis. That is the level of care we want to make accessible to all Oklahomans.”
Stephenson Cancer Center providers are now seeing patients and conducting clinical trials in Tulsa. Plans are also in motion to build a state-of-the-art facility at OU-Tulsa, extending the most advanced, research-driven cancer care and life-saving clinical trials exclusively offered at Stephenson Cancer Center to the people of northeastern Oklahoma.
Although the state’s cancer incidence overall is below the national average, Oklahoma ranks fourth in the nation for cancerrelated deaths with nearly 23,000 new cases diagnosed annually. The cancer mortality rates in northeast Oklahoma are some of the highest in the state, and over the next ten years, the forecasted need for outpatient cancer care is expected to increase by 13% in northeast Oklahoma. Many of these cancers are complex, rare or resistant to traditional therapies where clinical trials can provide life-saving care. Despite these statistics, people living in northeastern Oklahoma have the lowest participation rates in clinical trials at Stephenson Cancer Center, underscoring the need for the expanded access to comprehensive cancer care that the expansion to Tulsa will provide.

Robert Mannel, M.D., director of Stephenson Cancer Center, emphasized the importance of regional hubs in providing highquality care and clinical trials to urban and rural populations. “Our goal is to eliminate the barriers to accessing top-tier cancer care,” he said. “This commitment to Tulsa is crucial in our mission to serve all Oklahomans.”
Stephenson Cancer Center’s multidisciplinary approach to cancer care places patients at the forefront, offering a wide range of resources and support services. With about 300 active clinical trials and the state’s only Phase 1 Clinical Trials Program, the center is at the frontline of cancer research and treatment innovation.
“Healthcare shouldn’t be an ‘away game.’ We know care makes the greatest impact when you are able to remain in your community,” said OU Health President and CEO Richard P. Lofgren, M.D., MPH. “As the flagship academic health system, we have a responsibility to the citizens of our state to offer life-saving specialty and sub-specialty care. No Oklahoman should have to leave the state to get the care they need, and this expansion brings us closer to this goal.”
The expansion of the Cancer Center to Tulsa is facilitated by a robust public-private partnership involving key stakeholders. It includes an initial $50 million appropriation by the legislature from the American Rescue Plan Act and the state General Revenue Fund to the University Hospitals Authority and Trust (UHAT).
“We are excited to be building this state-of-the-art facility in Tulsa in furtherance of UHAT’s mission to support the clinical, research and educational missions of OU Health and the University of Oklahoma,” said G. Rainey Williams, board chairman of UHAT and OU Health.
Moreover, substantial contributions from Peggy and Charles Stephenson, the Cherokee Nation and other anticipated gifts underscore the collaborative endeavor aimed at enhancing cancer care in northeastern Oklahoma.
The expansion to Tulsa continues a long-held goal for the Cancer Center’s namesakes, Peggy and Charles Stephenson. Their support led to the opening of Stephenson Cancer Center in Oklahoma City in 2011, and their ongoing dedication has paved the way for the same in Tulsa.
“Peggy and I are grateful to be a part of the effort to bring the best treatment and clinical trials to Tulsa,” Charles Stephenson said. “People are cared for in a very compassionate and professional way at Stephenson Cancer Center, and that is what we want to bring to northeastern Oklahoma.”
“I am proud to stand alongside OU Health Stephenson Cancer Center as they expand their services to Tulsa, bringing muchneeded cancer care closer to our Cherokee citizens and all northeastern Oklahoma residents,” said Principal Chief of the Cherokee Nation Chuck Hoskin Jr. “Through this partnership and other health investments, we are making a generational stride in improving the health of our citizens.”
An innovative new field of research holds the promise for pediatric cardiologists and heart surgeons to predict the future structural integrity of a child’s heart valves so they can perform the best possible surgery today.
At the University of Oklahoma, a pediatric heart surgeon and cardiologist are collaborating with a biomedical engineer in a type of research that few in the nation are doing. By leveraging the expertise and technology of their respective fields, they are creating computational models to help them more fully understand the intricacies of individual hearts. Whereas traditional imaging techniques like echocardiogram provide a picture of the heart in motion, a computational model offers a simulated view of the shape of the valves, possible weak spots, the blood moving through the valves, and potential surgical steps to prevent future problems.
“This is truly translational medicine,” said OU Health pediatric heart surgeon Harold Burkhart, M.D., who is also a professor and chief of cardiovascular and thoracic surgery in the OU College of Medicine.

“Because of our multidisciplinary collaboration, we have the knowledge together to create a computational model that goes beyond what we are able to see with both 2D and 3D echocardiogram. It allows us to go a step further and visualize the heart as it would be in real life with the characteristics of each individual,” Burkhart said. “With that understanding, we can test what would happen if we put a stitch here or tighten a valve there — does it put too much stress on the valve, or does it address the problem? It can potentially give us a lot more direction before we even go into the operating room.”
The research group began their studies with hypoplastic left heart syndrome, a severe birth defect in which the left side of a baby’s heart does not form correctly and cannot pump blood well, leaving the right side of the heart to pump blood to the lungs and the rest of the body. Without a set of three of open-heart surgeries to repair the defect, the condition is often fatal. While continuing those studies, they are now developing computational models for atrioventricular canal defect, sometimes called a hole in the heart, because the baby is born with a hole in the wall separating the heart’s chambers.
“Because of our multidisciplinary collaboration, we have the knowledge together to create a computational model that goes beyond what we are able to see with both 2D and 3D echocardiogram. It allows us to go a step further and visualize the heart as it would be in real life with the characteristics of each individual.”
While surgeries for both conditions are often successful, children sometimes face a risk of reoperation in the future because of leaky valves, Burkhart said. In hypoplastic left heart syndrome, about 25% of patients have leaky valves by the time they are in preschool. Babies with atrioventricular canal defect sometimes experience valve leakage six months to two years after the initial surgical repair, for reasons that are not yet understood. Follow-up surgeries are about half as successful as the original procedure, and if the repair can’t be made, the child may need a mechanical heart valve, which comes with its own set of risks and complications.

During surgery, when the heart is stopped and on a bypass machine, it lays flat and doesn’t maintain its structure as it would if it were pumping blood. Surgeons employ techniques to inflate the valves to improve their view, but heart surgery is time-limited and allows for no trial and error. If a computational model can predict which areas of the heart valves could become problematic, surgeons may be able to take steps to prevent that leakage in the future.
“Even with 3D echocardiogram, it’s hard to see the finer details of the valves,” said OU Health cardiologist Arshid Mir, M.D., an associate professor of pediatric cardiology in the OU College of Medicine. “Most heart valves are like Pringle chips — they are more angular and have high and low points. We want to learn about these valves and try to predict which valves, right at birth, would have a risk of becoming leaky when the child is between 1 and 5 years old, so that we can try to address them surgically at the time of the first repair.”
“What we are doing is moving toward personalized medicine,” Mir added. “How do we think about each patient differently rather than thinking of a condition as a single disease? What is unique about this child’s anatomy that makes him at higher risk for reoperations? This is the way we will be thinking about these diseases as we head into the future.”
Burkhart and Mir work with Chung-Hao Lee, Ph.D., a former OU biomedical engineering researcher now at the University of California, Riverside. He builds computational models that draw from the fields of physics, fluid dynamics, geometry and bioengineering to create something that hasn’t existed before. Burkhart and Mir provide 2D and 3D echocardiograms of patients enrolled in the studies for the calibration of the models and for model prediction. They will continue to gather data from patients at multiple time points over the next several years.
“What we are doing is moving toward personalized medicine. How do we think about each patient differently rather than thinking of a condition as a single disease? What is unique about this child’s anatomy that makes him at higher risk for reoperations? This is the way we will be thinking about these diseases as we head into the future.”
“Through this image-based computational model, we want to provide the missing information — which patients will have valve dysfunction,” Lee said. “If we can better understand which valves have weak spots and may start leaking, surgeons may plan their surgeries differently and cardiologists may want to monitor or follow the patient more closely after surgery.”
Thus far, the research team has published about 10 papers on their computational modeling for hypoplastic left heart syndrome and recently published a paper on atrioventricular canal defect in the Annals of Biomedical Engineering.

In May, experts at OU Health completed the state’s first liver transplant for a particularly challenging and oftentimes deadly form of a bile duct cancer known as cholangiocarcinoma. This achievement not only places OU Health among the few elite programs in the country that treat bile duct cancers with transplantation but also brings immense relief to Oklahomans who no longer must leave the state to receive this life-saving treatment.
Before this first transplant at OU Health, patients traveled to centers several hundred miles away for a transplant to address hilar cholangiocarcinoma. Hilar cholangiocarcinoma – bile duct cancer that occurs where the ducts exit the liver – is one of the most lethal cancers and among the hardest to treat. The overall five-year survival for those diagnosed with this disease is less than 10%. Historically, the only chance at a cure is to surgically remove part of the organ.
Only 20 to 30% of patients are eligible for a surgical option due to how aggressive and advanced the cancer can be at the time of diagnosis. For the few patients who are candidates for surgery, the complex operation requires removing up to 70% of the liver, resulting in a high risk of morbidity and mortality. The procedure is only performed at a few high-volume centers with expertise and resources for complex hepatobiliary surgery, which now includes OU Health.
The patient at OU Health was first treated with a complex regimen of preoperative chemotherapy and radiation, said OU Health Stephenson Cancer Center surgical oncologist Ajay Jain, M.D., FACS, core medical director for Stephenson Cancer Center and professor of surgery and chief of the Division of Surgical Oncology in the Department of Surgery at the OU College of Medicine. Jain also serves as Oklahoma State Chair for the American College of Surgeons Commission on Cancer.
However, Jain recognized that a liver transplant would offer the highest chance of success and thanks to OU Health’s ability to perform a liver transplant for this complicated disease, the patient now has a higher chance of long-term survival.

Cholangiocarcinoma is a type of cancer affecting the bile ducts carrying the digestive fluid bile from the liver to the gallbladder and small intestine. It typically occurs in individuals over the age of 50, though it can occur at any age.
Because of its aggressive nature, cholangiocarcinoma is often diagnosed when the cancer is advanced, making successful treatment difficult to achieve.
“Only 20 to 30% of patients with this cancer will be able to receive surgical treatment options because the disease is silent, and when it gets diagnosed, most patients will be at an advanced state where surgical resections or transplants are not possible,” said OU Health Transplant Institute surgeon Narendra Reddy Battula, MBBS, MRCS, M.D., FRCS, assistant professor in the Division of Transplant Surgery in the Department of Surgery at the OU College of Medicine.
“The transplant technique for bile duct cancers differs from liver transplant done for liver failure or liver cell-based cancer. When we do routine liver transplants, we disconnect the bile ducts. But when we treat bile duct cancer, we need to do an extensive removal of the bile duct, which joins the liver to the bowels near the pancreas. We must make sure no cancer has spread beyond the liver.”
In the late 1990s, Mayo Clinic began the first clinical trials to assess the use of liver transplantation as a treatment for hilar cholangiocarcinoma. Over several years and multiple clinical trials, data has shown that patients who undergo successful transplants have five-year survival rates of 65 to 68%, and 10-year survival rates reaching up to 60%. This marks a significant improvement compared to the usual 10% five-year survival rate associated with the diagnosis.
Despite the improved survival rates, only roughly 20 programs in the country offer transplantation for cholangiocarcinoma. This limitation stems from the demanding nature of the procedure which requires specialized, multidisciplinary expertise from various fields, including interventional radiology, advanced gastrointestinal, medical oncology, radiation oncology, hepatobiliary surgery, transplant surgery, and transplant medicine, to name a few.
“OU Health now performs more than 50 traditional liver transplants a year, and because of the expertise at Stephenson Cancer Center and our outstanding transplant program at OU Health already doing some of the most complicated transplants in the country, we felt we could start doing liver transplants for cholangiocarcinoma,” said Jain. “This transplant was the first one of its kind done in the state.”
Battula and his colleague, transplant surgeon Maheswaran Pitchaimuthu, MBBS, MRCS (Edin.), FRCS (Eng.), assistant professor in the Division of Transplant Surgery in the Department of Surgery at the OU College of Medicine, worked alongside a team of medical oncologists, radiation oncologists and transplant hepatologists to implement diagnostic, chemotherapy and radiation protocols needed for this innovative treatment.
Other key medical professions included Stephenson Cancer Center oncologists Hassan Hatoum, M.D., Ryan Nipp, M.D., MPH, and Susanna Ulahannan, M.D., MMed, as well as radiation oncologists Andrea Johnston, M.D., and Christopher Bozarth, M.D.; advanced endoscopy specialist Amir Rumman, M.D., and transplant hepatologists Abdul M. Oseini, M.D., MSc and Sidra Ahsan, M.D.
“All these patients were being referred to other centers out of state to be considered for transplant, and we had to question ourselves as to why we weren’t offering this,” Battula said. “We have an amazing cancer center and an amazing transplant center here. It’s a huge emotional burden for the patient and their families to be far away in an unfamiliar environment. We have all the components, and now we are the only center in the state who can offer this type of liver transplant.”

In a groundbreaking achievement, Oklahoma Children’s Hospital OU Health has performed the world’s first Deep Brain Stimulation (DBS) procedure utilizing a mini robot in a pediatric patient, resulting in immediate improvement in motor function the child did not have prior.
DBS, a surgical technique involving the implantation of electrodes into specific brain regions, has traditionally been used to treat movement disorders like Parkinson’s disease, essential tremor and dystonia. This procedure has been performed robotically in pediatric patients using other platforms; however, this is the first time it has been performed using the Medtronic Stealth Autoguide mini robot. The use of robotics enhances the surgical precision and safety of the procedure while also unlocking new possibilities for improved patient outcomes.
Karleigh Fry, an 8-year-old patient also cared for by Bethany Children’s Health Center, was diagnosed with rapid-onset primary dystonia, a movement disorder that causes the muscles to react involuntarily. Initially Karleigh was paralyzed and could not eat, walk or even sit up on her own. Despite many different medications, she recovered only a bit, but had at times self-injurious dystonia.

Andrew Jea, M.D., MBA, MHA, FACS, FAAP
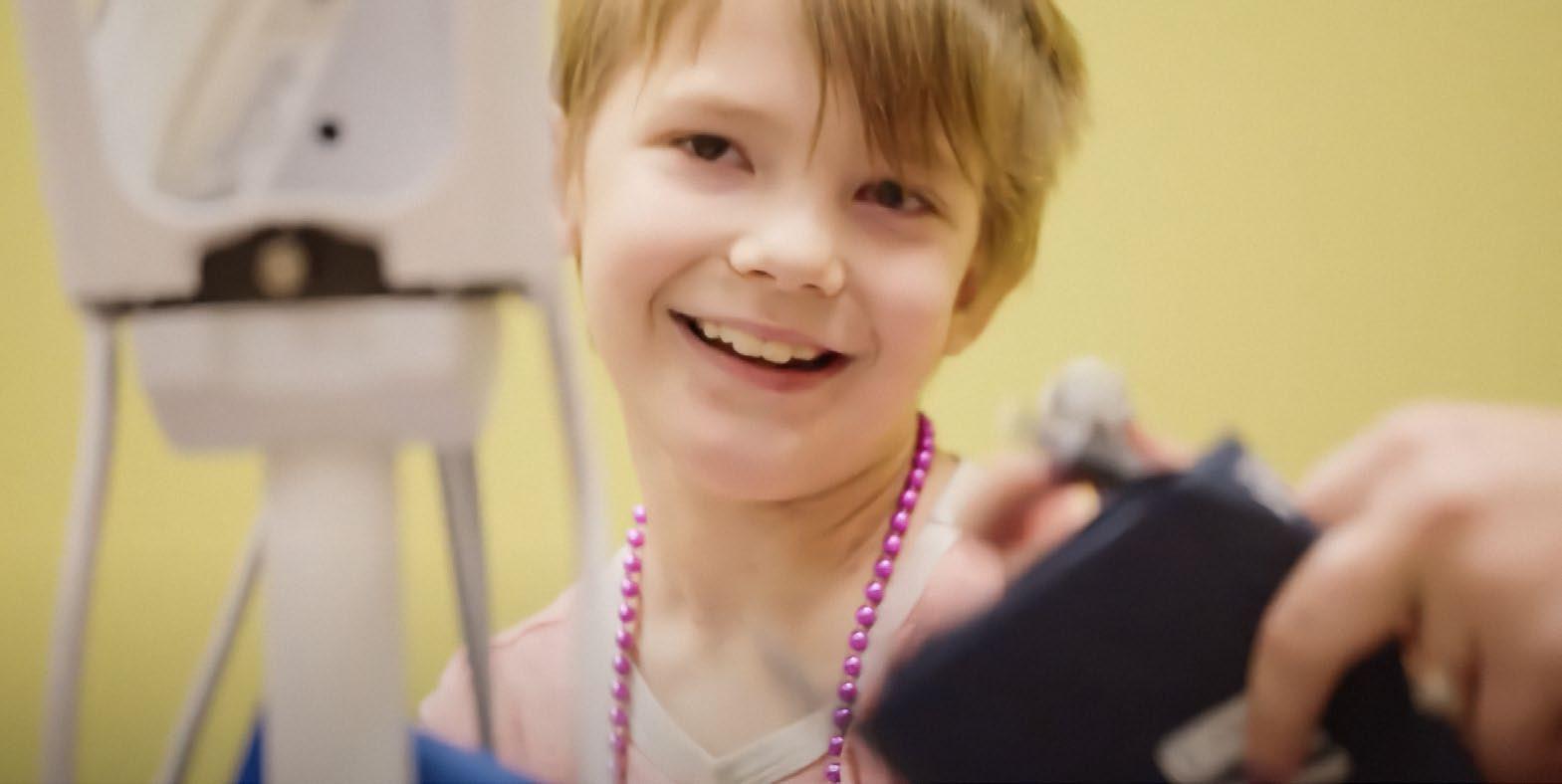
“This marked the global debut of using a robot from our operating rooms to perform DBS in a child, setting a precedent not only in Oklahoma but also across the United States and worldwide,” said Andrew, Jea, M.D., chair of the Department of Neurosurgery at the OU College of Medicine and clinical service chief at OU Health.
Following her groundbreaking surgery at Oklahoma Children’s Hospital, Karleigh’s postoperative care was seamlessly continued at Bethany Children’s Health Center, an innovative leader in the field of pediatric rehabilitation and 24-hour complex care and the only inpatient pediatric rehabilitation facility in Oklahoma.
“This marked the global debut of using a robot from our operating rooms to perform DBS in a child, setting a precedent not only in Oklahoma but also across the United States and worldwide.”
When the neurostimulator was activated after the procedure, Karleigh was able to lower and relax her arms within minutes, something she was unable to do prior. Her movements are becoming more controllable, and her verbalization has shown improvement as well. “Her arms used to lock up to the point we would put socks on her hands because she would scratch her neck,” said Karleigh’s mother, Trisha Fry. “There’s definitely been some improvements, even from the moment they turned it on. She is even using her voice a little bit more, and we can make out some of her words. I think she’s going to have a great future for sure.”
The successful world-first outlines the benefits of destination specialty and subspecialty programs that academic health systems can deploy and optimal results to improve the quality of pediatric patient care in Oklahoma and beyond.

OU Health is spearheading a first-of-its-kind initiative to bring Ukrainian surgeons to the United States for training in facial plastic surgery reconstruction. The training is designed to address the urgent demand for specialized surgeons capable of treating severe war-related facial and neck injuries in Ukraine by offering hands-on instruction and use of innovative technology.
Working with the American Academy of Facial Plastic and Reconstructive Surgery, OU Health facial plastic and reconstructive surgeon Mark Mims, M.D., assistant professor in the Department of Otolaryngology–Head and Neck Surgery at the OU College of Medicine, has led the initiative to develop an academic-based educational observership in head and neck reconstruction for foreign Ukrainian surgeons. Mims specializes in surgical and nonsurgical cosmetic and reconstructive techniques of the face, head, and neck.

Operation Ukraine is offered multiple times a year and includes both observation of techniques in the operating room as well as hands-on experience in the Clinical Skills Education and Testing Center lab on the OU Health Sciences campus. In addition, visiting surgeons are provided with tools needed to begin training other surgeons in Ukraine.
OU Health is the only academic medical center in the U.S. providing this type of advanced training. Since the beginning of 2023, OU Health has hosted three groups of surgeons from three different cities in Ukraine. The latest Winter 2024 cohort arrived in February and was comprised of four military surgeons who staff some of the busiest tertiary referral centers for the Ukrainian military in Kyiv and L’viv.
“A lot of our patients require reconstructive surgery and microvascular surgery to recover from all the wounds after the huge mine blast injury or gunshots,” said Mykola Sinyuk, M.D., one of the visiting Ukrainian surgeons from Lviv Military Hospital.

Guided by OU Health’s multidisciplinary team, Ukrainian surgeons spend a month acquiring the skills necessary to treat both civilian and military casualties. They receive comprehensive training in various surgical specialties including plastics; oral and maxillofacial surgery; ear, nose, and throat services (ENT); and oculoplastics. Additionally, the Winter 2024 cohort of Ukrainian surgeons were gifted Ohana One Smart Glasses with live-streaming capabilities that will allow for year-round mentor mentee relationships and consultation on active cases abroad.
The Smart Glasses provide portable high-quality viewing capabilities that allow Ukrainian surgeons to perform complex surgeries in their home country while getting real-time guidance and support from OU Health surgeons. Because the smart glasses are compact, they are easily shared with colleagues, not limiting their use to just one location or operating room.
“We are breaking barriers to advancing surgical education in low-middle-income-countries (LMICs) though technology partners such as TeleVU and NGO partners such as Dr. Mims and Operation Ukraine at OU Health,” said Marchelle Sellers, executive director of Ohana One Surgical Aid & Education. “We are continuously inspired by the innovation and dedication of surgeons such as Dr. Mims, who commit their time and energy to providing mentorship and surgical support to countries that need it the most. We look forward to this opportunity in advancing access to remote surgical training in the Ukraine, ultimately improving the standard of patient care.”

Since the onset of the conflict in Ukraine in February 2022, over 14,000 civilians and numerous soldiers have suffered debilitating head and neck injuries, predominantly from explosive-type weapons. However, the number of Ukrainian surgeons trained to manage such complex reconstructions falls short, leaving many patients with severe deformities and difficulties in eating, drinking, talking, and facial movements.
“The ultimate goal for Operation Ukraine Health is to allow the Ukrainian surgeons to train their own future generations,” Mims said. “Once we have a base cohort there that knows how to do these techniques, then they will be able to train other surgeons and hopefully we can fade into the background and let Ukrainians take care of Ukrainians.”
The training and the Ohana One Smart Glasses prove to be invaluable to the success of Ukrainian surgeons.
“It’s really important for us as physicians to reach out to our colleagues in other countries who may have a need to offer whatever aid we can so they can better take care of their patients,” Mims said. “This is part of our mission as physicians, and also part of our mission at OU Health in order to take better care of patients not only here in Oklahoma, but also all around the world.”
Operation Ukraine is 100% funded by generous donors. Other organizations, including Kerecis and Razom for Ukraine, have also facilitated the effort.
In March, students on the Oklahoma City campus and at the OU-TU School of Community Medicine in Tulsa participated in Match Day. Match Day is where medical students across the nation find out where they will be completing their residency program.


















In May, the OU College of Medicine graduated 146 medical students. Commencement ceremonies were held in Norman and Tulsa in celebration of the Class of 2024, marking the culmination of four years of dedication, perseverance, and academic rigor. Families, faculty, and friends gathered to witness this significant milestone as the graduates transitioned from students to physicians.
Ian Dunn, MD, executive dean of the College of Medicine, led the ceremonies, delivering a heartfelt message to the graduates. In his address, Dunn acknowledged the extraordinary challenges the students faced, especially in light of the global pandemic, and commended them for their resilience and adaptability. He emphasized the importance of compassionate and ethical care and lifelong learning in throughout their medical careers.







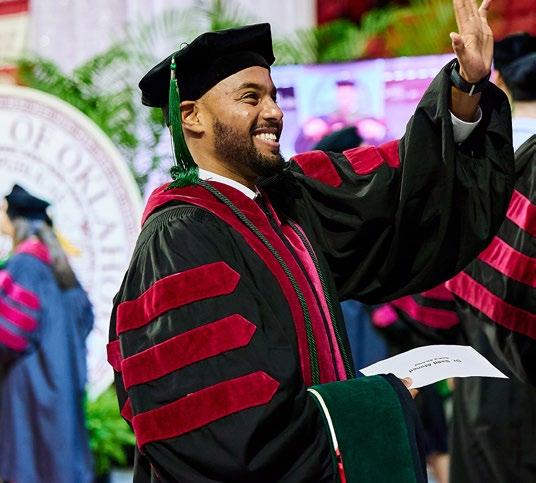







In August, the OU College of Medicine welcomed its newest medical and physicians associate classes. Students were welcomed into their respective programs with a white coat ceremony. Ceremonies took place on both the Oklahoma City campus and in Tulsa for students at the OU-TU School of Community Medicine.
“The White Coat Ceremony marks a pivotal moment in the journey of our health sciences students,” said Gary E. Raskob, Ph.D., Senior Vice President and Provost at the University of Oklahoma Health Sciences Center. “It serves as a reminder of the sacred trust between healthcare professionals and their patients.”

















Last fall, it was announced that the University of Oklahoma will receive $16 million over four years from the Health Resources and Services Administration of the U.S. Department of Health and Human Services to recruit, retain, and graduate medical students from Tribal, rural and medically underserved communities in Oklahoma, with the goal that those students will go on to practice in their home communities.
The initiative, “The Tribal, Rural, and Medically Underserved Communities in Oklahoma Pathways Program” or TRU-OK, is jointly administered between the University of Oklahoma College of Medicine on the OU Health Sciences campus in Oklahoma City and the OU-TU School of Community Medicine in Tulsa.
“This award will enable OU Health Sciences to greatly expand our recruitment of medical students from Tribal and rural Oklahoma for the benefit of Oklahomans and will be a significant step in our efforts to reduce health disparities across the state,” said Senior Vice President and Provost of OU Health Sciences Gary E. Raskob, Ph.D.
Jim Barrett, M.D., CAQ-Sports Medicine, Edith Kinney Gaylord Presidential Professor and Family Medicine Chair at the OU College of Medicine, is the principal investigator of the grant.
“We are thrilled about this grant and are excited to partner with communities across Oklahoma,” said Barrett. “One of the unique aspects of this grant is that it is focused on enhancing medical student education by creating curricula that emphasizes how primary care can improve the health of all Oklahomans, particularly those in underserved and rural locations. I believe that through our amazing partnerships we will be able to highlight the power of primary care for future and current medical students and build the primary care workforce for our state.”
Mary Gowin, Ph.D., MPH, an associate professor in the Department of Family and Preventive Medicine, OU College of Medicine, and co-investigator for the project, says the grant will help fill a significant need for primary care medical services in underserved areas of the state.

“We rank 47th in the nation in terms of primary care access, and we have two counties in the whole state that are not classified as primary care health profession shortage areas, so really, this is so vital,” Gowin said. “Approximately 41% of our Oklahoma population lives in rural cities and towns. We also have the largest number of federally recognized tribes at 38, and Tribal land makes up about 43% of the state’s landmass. Having primary care in these areas is vital to the health and economic well-being of our state.”
“Some of our counties, or areas within an urban county, are being underserved because all the health care is concentrated around a few hospitals or health systems,” added Frances K. Wen, Ph.D., co-investigator, professor and director of research for the Department of Family and Community Medicine, OU-TU School of Community Medicine.
To increase the primary care workforce in TRU-OK areas, the project team plans to address barriers students face to entering medical school. The initiative will create an online pre-medical program to give students a broad range of tools and resources to support their application to medical school, such as study materials and interview preparation resources.
“The pre-medical program is a brand new effort that will significantly help people who are interested in going into medical school,” Erin Ellis, TRU-OK program manager, said. “For someone who’s perhaps gone to college, gotten a bachelor’s degree, but decides later in life they want to go to medical school, this is going to be a perfect opportunity for them to be able to get all of the information and the coursework required to go back to school.”
“Some of the students who come from Tribal, rural, and underserved communities are first-generation college students, let alone first-generation entering into a health professional school,” Wen added. “They may discover later on in their trajectory that this is something that they’re really interested in and excited about, and the pre-medical program allows them to explore and prepare themselves for a career in medicine.”
The project also supports financial need through scholarships for students from Tribal, rural, and medically underserved communities to attend medical school at OU. Other avenues of financial support include stipends for participation in primary care research experiences and travel to primary care conferences.
The team is also working with several academic, Tribal, and hospital partners to facilitate expanded opportunities for students to gain experience in primary care, social determinants of health, vulnerable populations, and trauma-informed care, as well as opportunities to do rotations and clerkships and electives in underserved areas across Oklahoma.
“We have already been closely partnering with the Muscogee Creek Nation, Chickasaw Nation, Hillcrest HealthCare Systems and Jackson County Memorial Hospital, and we plan to continue and expand those relationships,” said Gowin. “In addition, we have brought on new partners (Integris Health, SSM Health, Variety Care, Southwestern Oklahoma State University, and Langston University). We’re very excited about building that network up and having strong relationships with our partners who provide care or education in these areas.”
This broad partner network supports outreach and training opportunities spanning TRU-OK communities and is a key to the project’s success.
“The School of Community Medicine is proud to be a major participant in this new HRSA grant project,” OU-TU School of Community Medicine Dean James M. Herman M.D., MSPH, said. “We look forward to expanding our tribal and health system partnerships as we continue to bring talented new medical students, physician assistant students, and resident physicians in numerous specialties from many communities in Oklahoma and beyond to our school.”
“We just love that the acronym TRU-OK is able to really reflect what we feel, which is that this is truly for Oklahoma, and we feel really proud of being able to be a part of a program that’s aimed at helping all of Oklahoma,” Gowin said.
The first published evidence from humans that semaglutide specifically reduces the symptoms of Alcohol Use Disorder (AUD) has been published in The Journal of Clinical Psychiatry and details a recent collaboration between clinicians and scientists at the OU-TU School of Community Medicine and Oklahoma State University Center for Health Sciences. The paper outlines the outcomes of six patients who received semaglutide during treatment for weight loss, demonstrating a significant and noteworthy decrease in their Alcohol Use Disorders Identification Test (AUDIT) scores.

The paper is titled “Significant Decrease in Alcohol Use Disorder Symptoms Secondary to Semaglutide Therapy for Weight Loss: A Case Series.” This collaboration has the potential to impact the lives of individuals struggling with Alcohol Use Disorder.
Semaglutide has made headlines recently as an FDA-approved drug for the treatment of diabetes under the name Ozempic, and weight loss under the name Wegovy. Recently, attention has turned to the possibility that semaglutide may have broader applications, including its potential impact on addictive behaviors such as reducing drug craving and alcohol consumption. Pre-clinical research in rodents and monkeys has demonstrated that semaglutide is associated with marked decreases in drug and alcohol consumption, and many patients taking the drug for diabetes and weight loss report significant reductions in the urge to drink alcohol.
“This research marks a significant step forward in our understanding of the potential therapeutic applications of semaglutide in the field of addiction medicine,” said the lead author, Jesse Richards, DO, FACP, director of Obesity Medicine and assistant professor of Medicine at OU-TU School of Community Medicine.
Kyle Simmons, Ph.D, the paper’s senior author and professor of Pharmacology & Physiology at OSU-Center for Health Sciences noted that this case series evidence paves the way for gold-standard placebo-controlled clinical trials such as the one he is currently conducting in Tulsa at the OSU Hardesty Center for Clinical Research and Neuroscience.
Called STAR (Semaglutide Therapy for Alcohol Reduction), the clinical trial is funded by the Hardesty Family Foundation and OSU-CHS. A sister study is also currently underway in Baltimore funded by the National Institute on Drug Abuse (NIDA).
“This is an example of what can happen when our two R-1 research institutions in Oklahoma collaborate,” said Simmons. “With the publication of this case series in the Journal of Clinical Psychiatry, the stage is set for future clinical trials, such as the STAR studies, which can definitively tell us whether semaglutide is safe and effective for treatment of alcohol use disorder.”
The researchers emphasized the need for further investigation through larger, controlled studies to validate and expand upon these initial findings. Until the results of future placebo-controlled clinical trials are available, the authors believe that healthcare providers should point patients toward established behavioral treatments and medications that have been validated by the FDA for alcohol use disorder.
Semaglutide Treatment and Alcohol Use Disorder: The study reveals a marked reduction in Alcohol Use Disorder Identification Test (AUDIT) scores in all six patients who received semaglutide treatment in the course of pharmacotherapy for weight loss. The results suggest a potential role for this medication in the management of Alcohol Use Disorder.
Implications for Future Research: The findings open new avenues for future research into the use of glucagon-like peptide-1 medications, such as semaglutide, in the treatment of addictive behaviors.
Collaborative Research Model: This collaboration between The University of Oklahoma School of Community Medicine and Oklahoma State University Center for Health Sciences is an example of the potential when clinicians and scientists collaborate to explore innovative solutions to complex health care challenges.

Research at the University of Oklahoma, in collaboration with The University of Tulsa, has resulted in a new method of screening for sleep disorders in children. The tool, the first of its kind, allows health professionals to assess children for multiple sleep problems at once, resulting in a quicker evaluation and more targeted treatment recommendations.
The research that created the tool, called a structured clinical interview, was published recently in the journal Behavioral Sleep Medicine. The publication details the effectiveness of the interview questions across several types of sleep disorders, which often have overlapping symptoms but can require distinct treatments.
“Sleep problems can be common in kids, but we have not had a means of getting a comprehensive view of what is going on with their sleep,” said child and adolescent psychiatrist Tara Buck, M.D., an associate professor in the OU School of Community Medicine in Tulsa. “It takes time to go through all the individual disorders to narrow down what’s going on. This structured clinical interview allows us to screen for the most common sleep problems at once and gain a better idea of how to treat them.”
Development of the structured clinical interview was led by Mollie Rischard, Ph.D., a post-doctoral fellow in the Department of Psychiatry at the OU School of Community Medicine. The project also served as the dissertation topic for her doctoral studies at The University of Tulsa. She started with the adult comprehensive assessment for sleep disorders, which already existed, and began the meticulous work of adapting it for children. After several iterations, input from clinical experts, and ensuring it aligned with criteria in the Diagnostic and Statistical Manual (the authoritative guide for diagnosing mental disorders), it was tested in a clinical trial. Results showed it to be an effective tool.
The gold standard for diagnosing sleep disorders is a sleep study, in which a child spends the night in a sleep lab connected to sensors that measure the quality of sleep. However, sleep studies are expensive and may not be needed in every instance, Rischard said.

“Sleep apnea, for example, is a medical problem that must be diagnosed through a sleep study, but before we make costly referrals and ask families to undergo a sleep study, we want to be as sure as we can that it’s necessary,” she said. “There are a lot of overlapping symptoms among sleep disorders, where a child has difficulty falling asleep and staying asleep, so it’s important to determine what is driving the problems. They may have restless leg syndrome or a disruption in their circadian rhythm. Having a better understanding will give us a better sense of how to treat it. Cognitive behavioral therapy can be effective for several sleep disorders.
“We advocate for targeting sleep problems because there’s such a high degree of daytime impairment when kids don’t sleep well,” Rischard added. “It’s not just excessive daytime sleepiness, but we often see a paradox where kids can appear hyperactive and may be misdiagnosed with something like ADHD. Many sleep disorders are very treatable because we make behavioral changes that can produce quick improvements. And if you start sleeping better, you genuinely feel better.”
The need for a comprehensive structured clinical interview for pediatric sleep disorders grew out of a related research collaboration between OU and TU: a clinical trial studying a new cognitive behavioral treatment for youth with nightmares. Lisa Cromer, Ph.D., a professor of psychology at TU and a volunteer child psychiatry faculty member at OU-Tulsa, led development of the treatment because of a growing recognition in the field that nightmares should be addressed as a singular problem rather than a symptom of another problem. The new structured clinical interview helps identify children who have nightmare disorders.
“There is growing evidence that nightmares are a signal for very serious mental health problems, in particular suicidal ideation and behavior,” Cromer said. “Another big risk factor for suicidality is impulsivity, and we know that people are better able to control impulses when they’ve been sleeping well.”
Cromer’s cognitive behavioral treatment incorporates relaxation strategies, stress management, sleep behaviors, and visualization to change the structure of dreams. Parents are involved in the treatment process as well. Data from the trial, though ongoing, show a promising decrease in suicidal thinking among children with nightmares after they’ve received the treatment. Cromer and Buck plan to publish the results of their study soon.
“It’s not just excessive daytime sleepiness, but we often see a paradox where kids can appear hyperactive and may be misdiagnosed with something like ADHD. Many sleep disorders are very treatable because we make behavioral changes that can produce quick improvements. And if you start sleeping better, you genuinely feel better.”
“In the past, we’ve seen nightmares as a symptom of other conditions, and we thought there wasn’t much we could do,” Buck said. “We might try to treat their PTSD or anxiety and hope that the nightmares got better. But now there are treatments to empower kids to reduce or eliminate their nightmares. It’s a paradigm shift for both families and health professionals.”

The OU-TU School of Community Medicine’s Culinary Medicine Program recently unveiled a new teaching kitchen, a dynamic space designed to address an urgent gap in modern healthcare: the intersection of food and health. With chronic conditions like diabetes, hypertension, and heart disease on the rise, many of these issues trace back to poor dietary habits. The solution, while simple, has been long overlooked: food as medicine.
Food is an essential part of one’s overall health, and everyday choices profoundly shape not just our bodies but our minds and wellbeing. Despite its importance, medical professionals receive little training on how nutrition can be used as a powerful tool for both preventing and managing chronic diseases. The Culinary Medicine Program, launched in 2018 as a joint initiative between the OU-TU School of Community Medicine and the OU Hudson College of Public Health, is changing that.
The program addresses an urgent need: the standard American diet, high in salt, sugar, and unhealthy fats, is a major contributor to chronic conditions like obesity, diabetes, and heart disease. Research shows that over 80% of U.S. healthcare costs stem from lifestyle-related factors, including poor nutrition. By teaching participants how to cook with whole, minimally processed ingredients, the Culinary Medicine Program provides practical solutions to improve dietary habits and overall health. The kitchen also promotes mindful eating and the joy of preparing food, encouraging a deeper connection between food and wellbeing.

Leading the teaching kitchen is Chef Valarie P. Carter, MPH, CPH, CHE, an Oklahoma native with extensive experience in both public health and culinary arts. Chef Carter earned her MPH from the OU Hudson College of Public Health and an A.A. in Culinary Arts from the Art Institute of Atlanta. She brings a unique perspective, blending her passion for nutrition with hands-on cooking instruction, to teach future healthcare providers how to incorporate food as a central component of patient care.
As the Culinary Medicine Program continues to grow, it aims to reshape how healthcare professionals and communities approach nutrition. The new teaching kitchen serves as a hub for learning how to use food as a powerful tool for health, prevention, and healing—making it clear that food can indeed be medicine.

Min Li, Ph.D., George Lynn Cross Research Professor of Medicine, Surgery and Cell Biology in the University of Oklahoma College of Medicine at the OU Health Sciences Center, is currently serving as president of the American Pancreatic Association, with his term beginning last November.
The American Pancreatic Association (APA) is the largest professional organization for physicians and researchers specializing in pancreatic diseases. Recognizing that progress in understanding, diagnosing and treating pancreatic diseases requires multidisciplinary analysis, the APA encompasses multiple disciplines, including surgery, medical oncology, gastroenterology, radiation oncology, pathology, and basic science research. The APA also works closely with non-profit organizations to raise funding for pancreatic cancer research.
“Serving as president of the APA is a huge honor for me, and it is a recognition of our work on pancreatic cancer research,” Li said. “I am thrilled about the opportunity to serve this amazing organization and to help people suffering from devastating diseases. I hope to carry on the legacy from past presidents of APA, to work with other leaders in the field to raise more awareness for pancreatic cancer research and treatment nationwide and internationally, and to expand the APA family. Our mission is to foster clinical and basic science research needed to cure diseases of the pancreas and to train the next generation of pancreatologists.”
At the OU College of Medicine, Li has been awarded a significant amount of federal funding for his research on pancreatic cancer and continues to advance the field with his investigations. He has published articles for several consecutive years in leading journals on gastrointestinal tract disease, including PNAS, EMBO Molecular Medicine, Gastroenterology, Cancer Research, and Clinical Cancer Research.
Several publications have focused on the protein ZIP4, which transports zinc throughout the body. Each study has focused on a different role for ZIP4, which serves as a “master switch” for several things to occur in pancreatic cancer.
Last year year, Li published two research articles in Gastroenterology. In the first paper, Li analyzed the behavior of two different types of RNA — circular RNAs and microRNAs. He found that a specific circular RNA can control the growth of pancreatic cancer cells by “sponging,” or binding to, a specific type of microRNA. This process is the same for cachexia, a muscle-wasting condition that affects at least 80% of people with pancreatic cancer.
In the second paper, Li and his colleagues discovered that a particular metabolic enzyme could increase the intake of nutrients to tumor cells and promote muscle wasting. Li’s research group is the first to discover the behavior of these two RNAs and the metabolic enzyme in pancreatic cancer. The findings are important because once the mechanism of a behavior is understood, it could serve as a target for treating the cancer.
Li also holds the Virginia Kerley Cade Endowed Chair in Cancer Treatment in the OU College of Medicine. In addition, he serves as Associate Director for Global Oncology for OU Health Stephenson Cancer Center at the University of Oklahoma.
Jerry Jaboin M.D., Ph.D., M.B.A.

The world’s largest society for radiation oncology professionals recently voted to confer upon Jerry Jaboin M.D., Ph.D., M.B.A., the chair of the Department of Radiation Oncology at the University of Oklahoma’s College of Medicine, the designation of Fellow of the American Society for Radiation Oncology (FASTRO). Jaboin received the FASTRO designation at an awards ceremony in Washington, D.C., on Tuesday, October 1, during ASTRO’s 66th Annual Meeting.
Jaboin mentioned his gratefulness for being recognized as a peer to a distinguished society. The recognition, he feels, can accelerate other opportunities for national and international visibility. His work has been heightened by working at the Stephenson Cancer Center due to its reputation for being “pound for pound the number one clinical trials institution in the country.”
“What this affords me is the ability to sponsor other likeminded faculty and trainees’ greater access to opportunities within ASTRO,” said Jaboin. “It is a true pleasure to be a member of this team”
Awarded annually since 2006, the ASTRO Fellows program recognizes individuals who have made significant contributions to radiation oncology through research, education, patient care and service to the field. Since its inception, the FASTRO designation has been awarded to just 498 of ASTRO’s 10,000 members worldwide. The 2024 class is the largest since the inaugural Fellows were named nearly two decades ago.
“Dr. Jaboin, a physician at OU’s Stephenson Cancer Center, joins an elite group of just 48 physicians and medical physicists who are recognized this year for their far-reaching contributions to the field of radiation oncology and their progress in advancing cancer research, education, and patient care,” said Jeff M. Michalski, M.D., M.B.A. and chair of the ASTRO Board of Directors. “Congratulations to Dr. Jaboin for achieving the designation of ASTRO Fellow.”
Jaboin completed his graduate work as one of the inaugural students within the NIH Graduate Partnerships Program as an individual member of Howard University from 1996 until 2004. He then worked as a radiation oncology resident, and American Board of Radiology Holman Fellow at Vanderbilt University from 2006-10. Before arriving at OU Health Sciences in Nov. 2021, he was a professor and vice chair of the Department of Radiation Medicine at Oregon Health and Science University in Portland.
“Dr. Jerry Jaboin’s recognition as a Fellow of the American Society for Radiation Oncology is a testament to his exceptional dedication and expertise in the field of radiation oncology,” said Ian F. Dunn, MD, FACS, FAANS, executive dean for the OU College of Medicine. “This prestigious honor not only highlights Dr. Jaboin’s significant contributions to cancer care and research but also underscores the caliber of faculty at the OU College of Medicine.
“We are proud to have such distinguished professionals leading the way in advancing medical science and patient care,” continued Dunn.

OU College of Medicine researcher Paul L. DeAngelis, Ph.D., has been awarded the President’s Innovator Award by the Society for Glycobiology.
DeAngelis, a President’s Associates Presidential Professor in the Department of Biochemistry and Physiology, has dedicated his career to glycobiology, a field that explores the structures and functions of sugars. He has a particular focus on the biology of glycosaminoglycans, which are important complex carbohydrates that participate in many biological processes and are highly relevant for the discovery of new drugs.
DeAngelis has written 94 research publications and 14 review articles and book chapters, and his work has been issued 48 U.S. patents and 99 foreign patents. His innovative technologies have been licensed to multiple pharmaceutical and biotechnology companies, including four Oklahoma City-based companies that he founded and for which he has served as chief scientist and director. They are Caisson Biotech, LLC, Hyalose, LLC, Heparinex, LLC, and Choncept, LLC.
Among his notable achievements, his research on heparosan (HEP, a naturally occurring sugar polymer) led to the development of the HEPtune drug delivery platform. The technology has been used to link HEP to biologic drugs such as insulin to extend their duration of action in the body, ultimately improving drug delivery. The same technology has been used to enhance coagulation proteins for their role in blood clotting, as well as growth factors, which are natural molecules that control cell division, growth and repair. DeAngelis also developed methods for synthesizing heparin, a naturally occurring glycosaminoglycan that is one of the most frequently used drugs in hospitals. Synthetic heparin provides several advantages over biological sources of the drug.
In addition to his work with HEP and heparin, he has had a long-standing interest in the biology and biosynthesis of hyaluronic acid, a naturally occurring glycosaminoglycan found throughout the body’s connective tissue. His research in this area has been leveraged to develop technologies used in the production of biomaterials, drugs and other substances involved in chemical reactions.
DeAngelis has received numerous awards during his career. He was elected a Fellow of the National Academy of Inventors in 2013 and received the Oklahoma Bioscience Association Innovation Award in 2014. He also received the Rooster Award for scientific achievement for synthetic hyaluronic acid in 2007 from the International Society for Hyaluronan Sciences.
His career with the OU College of Medicine began in 1994. He earned his bachelor’s degree from Harvard University, followed by his doctorate from the University of California Irvine. He then completed a postdoctoral fellowship at the University of Texas in Galveston.

Britta Ostermeyer, M.D., MBA, chair of the Department of Psychiatry and Behavioral Sciences in the University of Oklahoma College of Medicine at OU Health Sciences, was recently honored by the American Academy of Psychiatry and the Law (AAPL) for her service to the organization and dedication to forensic psychiatry, a field at the intersection of mental illness and the law.
AAPL presented the Outstanding Service Award, called a Red AAPL, to Ostermeyer at its annual meeting in Chicago. Ostermeyer has been a member of AAPL since 2001 and has served as a councilor and as vice president. She currently serves as treasurer, board member, co-chair of the membership committee and fundraising committee chair for the AAPL foundation. She is also the co-chair of the Rappeport Fellowship Committee, a position she has held for 12 years.
The Rappeport Fellowship Award is given annually to six senior medical residents in the United States who have an interest in forensic psychiatry. In 2001, Ostermeyer herself received the award, which sparked her interest in forensic psychiatry. Under the mentorship of a senior forensic psychiatrist, she immersed herself in the field and completed a fellowship at Case Western Reserve University in Cleveland, Ohio, one of the nation’s leading academic institutions for forensic psychiatry. The Rappeport Fellowship Award is named for Jonas Rappeport, M.D., who founded AAPL in 1969. It is the largest organization of forensic psychiatrists with 2,000 members from around the world.
As a board-certified forensic psychiatrist, Ostermeyer serves as an expert in civil, criminal and administrative cases in Oklahoma. She provides evaluations for competency to stand trial cases, insanity defenses, competency to be executed cases and others.
Ostermeyer also works closely with her neuropsychology colleagues in the department, who provide cognitive evaluations for licensing boards, such as those for attorneys, physicians, nurses and airline pilots, when cognitive impairment is suspected. The OU Department of Psychiatry and Behavioral Sciences offers a post-doctoral training program in clinical neuropsychology, one of the most established in the country, having graduated its first resident in 1979.
“In forensic cases, we’re not in the role of treater, and the person evaluated is not in the role of patient,” she said. “Our role is to be neutral and to find the truth. We are proud to provide this service to the community and the state.”


Each Spring, OU College of Medicine students on the Oklahoma City campus and at the OU-TU School of Community Medicine in Tulsa honor faculty members with a variety of awards in recognition of their excellence in teaching.
The 2024 Edgar W. Young Lifetime Achievement Award was presented on the Oklahoma City campus to Mark Fergeson, M.D. This award recognizes long-term dedication to medical education.
On the Tulsa campus, Blake Lesselroth, M.D., received the 2024 Community Medicine Leader Award, given to a faculty or staff member who exemplifies the mission of the School of Community Medicine as evidenced by teaching, scholarship, community service, or significant service to the school or Tulsa area.
Medical school classes on both campuses also presented Aesculapian Awards.
Honorees on the Oklahoma City campus were:
Class of 2027
• Frederick C. Miller, Ph.D., Department of Family and Preventative Medicine, Department of Cell Biology.
Class of 2026
• Jo Elle Peterson, M.D., Department of Pathology.
Class of 2025
• Brian Lich, M.D., Department of Medicine.
• MacKenzie Senogles, M.D., Department of Obstetrics and Gynecology.
Class of 2024
• Salar Faiazi, M.D., Department of Internal Medicine.
• Ambreen Rahman, M.D., Department of Psychiatry and Behavioral Sciences.
On the Tulsa campus, Aesculapian awardees were:
Class of 2027
• Robert Jackson, Ph.D., Department of Cell Biology, Department of Family and Community Medicine.
Class of 2026
• Michael Weisz, M.D., Department of Internal Medicine.
Class of 2025
• Prashanth Iyer, M.D., Department of Vascular Surgery.
Class of 2024
• Monica Henning, M.D., Department of Obstetrics & Gynecology.
The School of Community Medicine also awards Crimson Apple Awards to volunteer faculty and residents.
Crimson Apple Award for Volunteer Faculty
• Todd Dunaway, M.D., Department of Neurology Crimson Apple Award for Residents
• Arad Abadi, M.D., Department of Vascular Surgery Garrett Snell, DO, Department of Obstetrics and Gynecology

Each year, the OU College of Medicine recognizes excellence among faculty and residents with the presentation of the Leonard Tow Humanism in Medicine Award and the Lloyd Rader Award.
The Leonard Tow Humanism in Medicine Award, sponsored by the Arnold P. Gold Foundation, is given to a faculty member who demonstrates excellence in promoting scholarship, encouraging high standards of care, and integrity and commitment to compassionate care of patients and to the art and science of medical practice. Recipients of the award become members of the Golden Humanism Honor Society, an international organization with more than 20,000 members in training and practice.
This year’s recipient is Brian K. Firestone, M.D., clinical associate professor in the Department of Ophthalmology and ocular oncologist and pathologist at the Dean McGee Eye Institute. He is the only fellowship-trained ocular oncologist and pathologist in Oklahoma. He has specific interest and expertise in caring for patients with tumors in or around the eye and performs microscopic evaluation of eyerelated biopsies and tissue.
The Lloyd Rader Award, named for the man who served as director of the Oklahoma Department of Human Services from 1951-1982, recognizes outstanding achievements in residency, both clinical and research. This year, the Lloyd Rader Award was presented to Jena Deitrick, M.D., urology.
Deitrick was widely regarded by faculty as one of the strongest residents the Department of Urology has seen in years. During her residency, she participated in 5 research projects and was invited to showcase results at regional and national professional meetings. In a letter of support, Deitrick was described as patient and kind and the type of individual who goes out of their way to make others feel valued.
Deitrick is currently an attending urologist at Mercy Hospital in Oklahoma City.

The Jerry Vannatta, M.D., Academy of Teaching Scholars, an organization that recognizes and fosters excellence in medical education at the OU College of Medicine, inducted new members and presented honors during its annual Education Week activities in fall 2024.
Awards are presented to faculty members on both the Oklahoma City and Tulsa campuses in the areas of preclinical, clinical, and graduate medical education, as well as physician associate education. Recipients are nominated by students, faculty and colleagues. The awards, called the Dewayne Andrews, M.D., Excellence in Teaching Awards, are named for the former executive dean who founded the organization more than a decade ago.
In the area of preclinical medical education, awards were presented to:
• Andrei Belousov, PhD, Department of Biochemistry and Physiology, Oklahoma City
• Amir Butt, MD, MPH, Department of Anesthesiology, Oklahoma City
• Lori Garman, PhD, Department of Microbiology and Immunology, Oklahoma City
• Mike Weisz, MD, Department of Internal Medicine, Tulsa
In clinical education, awards were presented to:
• Jeremy Haney, MD, Department of Anesthesiology, Oklahoma City
• Erin Nicole Jorgensen, MD, Department of General Obstetrics and Gynecology, Tulsa
• Kathryn Kramer, MD, Department of Obstetrics and Gynecology Academic Generalists, Oklahoma City
• Margaret Lee, MD, Department of Psychiatry and Behavioral Sciences, Oklahoma City
Graduate Medical Education awards were presented to:
• Brandon Koenigsknecht, MD, Department of Emergency Medicine, Tulsa
• Olivia Lust, DO, Department of Family Medicine, Oklahoma City
• Cody Thomas, MD, Department of Pathology and Hematopathology, Oklahoma City
• Frank Clifford Wood, MD, Department of Surgery, Section of Acute Care Surgery, Oklahoma City
In the PA program, awards were presented to:
• Jeremy Paysnoe, MHS, PA-C, Department of Family Medicine, Physician Assistant Program, Tulsa
• Christine Vo, MD, FASA, Department of Anesthesiology, Oklahoma City
At the Spring 2024 OU Health Sciences Faculty Awards Ceremony, several OU College of Medicine faculty members were honored with a variety of awards for their excellence in academic medicine.
President’s Awards

David Ross Boyd Professorship
Michael Cookson, M.D., Department of Urology, Oklahoma City

Provost’s Awards


President’s Associates
Presidential Professor
Resham Bhattacharya, Ph.D., Department of Obstetrics and Gynecology, Oklahoma City


George Lynn Cross Research Professorship
Priyabrata Mukherjee, Ph.D., Department of Pathology, Oklahoma City
Edith Kinney Gaylord Presidential Professor
Catherine Hunter, M.D., Department of Surgery, Oklahoma City
Research – Junior Faculty (Basic Sciences)
Stefano Tarantini, Ph.D., Department of Neurosurgery, Oklahoma City

Research – Senior Faculty (Clinical/Translational Research)
Jeanie Tryggestad, M.D., Department of Pediatrics, Oklahoma City
Teaching Award – Senior Faculty
Dominic Frimberger, M.D., Department of Urology, Oklahoma City

The 39th annual Evening of Excellence gala, which honors healthcare and community leaders while raising funds to support research at the OU College of Medicine, honored three people earlier this year.
Evening of Excellence is organized by the OU College of Medicine Alumni Association. Since the event began, the alumni association has awarded more than $3.9 million in grants to 170 researchers in the college.

This year, Harold Burkhart, M.D., was named the recipient of the Dean’s Award for Distinguished Medical Service; Rachel and David Holt were presented with the Dean’s Award for Distinguished Community Service; and the Presbyterian Health Foundation was presented the Dean’s Award for a Distinguished Oklahoma Institution.
Following are the honorees’ bios.
Harold Burkhart, M.D.
Since he arrived at the University of Oklahoma 10 years ago, Harold M. Burkhart, M.D., has transformed a small pediatric heart surgery program into a high-volume, nationally recognized program serving the children of Oklahoma and beyond.
Burkhart earned his medical degree at the James H. Quillen College of Medicine at East Tennessee University, followed by his residency in general surgery at Indiana University. He then completed a three-year fellowship in cardiothoracic surgery at Mayo Clinic in Rochester, Minnesota, and a oneyear advanced fellowship in pediatric heart surgery at the Hospital for Sick Children in Toronto.
His first heart surgical practice was at the University of Iowa, followed by practices in pediatric and adult heart


surgery and cardiac transplant at the Mayo Clinic, where he also directed the residency program. After seven years at Mayo, he accepted an offer to build the pediatric heart surgery program at the OU Health Sciences Center. At the time, the majority of Oklahoma children needing heart surgery were being sent out of state for care. Burkhart quickly built a program that would allow children to receive the highest quality care without leaving the state and the support of family and friends.
Within a few years, OU’s pediatric heart surgery program grew in patient volume to one of the top one-third in the country. In parallel, the pediatric cardiology group grew, almost tripling in size. A large pediatric intensive care group of providers is dedicated to the care of cardiac patients, and a new 25-bed cardiac ICU was constructed. Currently underway is the development of a pediatric heart transplant program.
This type of complex, congenital pediatric heart surgery and related care is available nowhere else in the state. Outcomes have been excellent — the OU program has had better results than 90% of other programs across the country. For the past two years, the U.S. News & World Report has named OU’s pediatric cardiology and heart surgery programs among the top 50 in the nation.
As part of an academic health system, Burkhart has been active as an educator and a researcher. Residents and fellows are engaged in multidisciplinary patient rounds and conferences, learning alongside some of the best health care providers in the nation. As a researcher, Burkhart has published 261 peer-reviewed articles, including serving as lead author for the first publication in the world about stem cell therapy for hypoplastic left heart syndrome, a groundbreaking effort in collaboration with Mayo Clinic.
Burkhart has multiple academic titles within the OU College of Medicine, including division chief of Cardiovascular and Thoracic Surgery, and he holds the CHF/Brandon Weeden Endowed Chair in Pediatric Cardiac Surgery and the Paul H. and Doris Eaton Travis Chair in Thoracic Surgery. He previously served as acting CEO of OU Health, the clinical partner of the OU Health Sciences Center. At Oklahoma Children’s Hospital OU Health, he is the medical director of Pediatric Cardiovascular Surgical Services and chief of Pediatric Cardiothoracic Surgery.

As a couple and individually, David and Rachel Holt are dedicated to making a difference in the lives of people in Oklahoma City and across the state. David is the mayor of Oklahoma City and the dean of the Oklahoma City University School of Law, and Rachel is the president and CEO of the United Way of Central Oklahoma. They married in 2003 and have two children, George and Margaret.
Rachel Canuso Holt became president and CEO of the United Way of Central Oklahoma on Nov.1, 2023.
Rachel previously served from 2020-2023 as the executive director of the Office of Juvenile Affairs (OJA), Oklahoma’s juvenile justice agency. She spent seven total years at OJA, where she also held the titles of chief operating officer and general counsel. Prior to her tenure at OJA, she served as an assistant attorney general and an assistant district attorney.
In her 11 years of state service in juvenile justice, Rachel witnessed firsthand the importance of community resources and the vital role played by United Way Partner Agencies in central Oklahoma. As an advocate supporting the wellbeing of Oklahoma families and children, Rachel’s role at United Way continues her life’s work supporting Oklahomans who are vulnerable and in need of help.
Rachel is a graduate of the George Washington University and the University of Oklahoma College of Law. She is a native of Philadelphia.
David Holt is the 38th mayor of Oklahoma City and the 14th dean of the Oklahoma City University School of Law. Previously, he served in the Oklahoma Senate for eight years. He is a licensed attorney and spent nine years with Hall Capital in Oklahoma City. Prior to that work, he served in staff positions in the White House, the Office of the U.S. House Speaker, as chief of staff to his predecessor, Mayor Mick Cornett, and in the offices of several state and federal officials.
David was elected mayor of Oklahoma City in 2018 and was re-elected in 2022. His leadership theme of “One OKC” has led to remarkable accomplishments for the city. His achievements include the development and overwhelming passage of two major initiatives: MAPS 4, an ambitious, $1.1 billion package passed in 2019 that includes 16 quality-of-life projects; and his effort in 2023 to “Keep OKC Big League,” which secured a new arena for the city and a commitment from the Thunder of the NBA to remain in Oklahoma City for another 30 years.
He received a Bachelor of Arts degree from the George Washington University and his juris doctorate from Oklahoma City University School of Law. David is a member of the Osage Nation and is Oklahoma City’s first Native American mayor. He was recently named one of TIME’s “100 Next” and will serve as the president of the United States Conference of Mayors in 2025-2026. He is the author of two books about Oklahoma City’s history.
Since its inception, Presbyterian Health Foundation (PHF) has been a major supporter of biomedical research, medical education and health innovation, awarding more than $215 million in grants and investments to researchers at OU Health Sciences, the Oklahoma Medical Research Foundation and


other health initiatives. To date, the awards made to OUHSC and OMRF researchers have assisted them in securing over $550 million in extramural funding.
PHF was established in 1985 with proceeds from the sale of Presbyterian Hospital in Oklahoma. Soon after, PHF built a worldclass research park along Lincoln Avenue consisting of 770,000 square feet of laboratory, research and office space. The complex of buildings, now owned by the University of Oklahoma and called University Research Park, meets a critical need for researchers and plays an important role in the development of the bioscience industry in Oklahoma.
Since 2014, when PHF refocused its funding on biomedical research, it has awarded nearly $29 million to researchers across the OU Health Sciences campus, directly resulting in those researchers securing $293 million in extramural grant funding. The overall return on investment is $9.16 for every dollar of PHF grants to OU Health Sciences researchers.
PHF awards several types of grants. Seed grants help researchers gain preliminary data that they use to apply for larger grants, and bridge funding supports researchers between external grant funding periods. PHF grants also support team science projects, early-career physician-scientists, equipment needs, symposiums, and several other areas. With the arrival of the COVID-19 pandemic in 2020, PHF funded researchers who were studying the virus, its implications on health, and vaccines to prevent it.
For more than 20 years, PHF has been a strong supporter of the M.D./Ph.D. program, a partnership between the OU College of Medicine, the Health Sciences Graduate College, and OMRF. Since 2000, PHF has invested and committed more than $10 million to the program. Students, who earn both medical degrees and doctorates, are called PHF Scholars.
PHF’s support of basic science in Oklahoma has the potential to catalyze economic growth, enhance educational opportunities, improve healthcare outcomes, and contribute to the overall well-being and cultural richness of the state. It positions Oklahoma as a hub for innovation and scientific excellence, with benefits extending to various sectors of society.
Tom R. Gray, III, is chair of the board of directors, and Rick McCune is president of PHF and a board member. The board of directors plays a pivotal role in guiding strategic initiatives and is comprised of individuals with diverse expertise and a shared commitment to health care advancements. Likewise, the staff takes pride in being part of an organization that is actively contributing to the acceleration of scientific discoveries with the potential to transform health care outcomes.
By continuing to focus on locally relevant issues, PHF plays a central role in the tangible improvements in health care outcomes for the people of Oklahoma.

Three physician graduates of the OU College of Medicine were honored during the 2024 Alumni Day activities. Darius Maggi, M.D., was named Physician of the Year for Private Practice. Dwight Reynolds, M.D., was named Physician of the Year for Academic Medicine. Lynn Mitchell, M.D., MPH, was presented with the Friend of Medicine Award

Darius R. Maggi, M.D., began his medical career as a small-town Oklahoma physician. He went on to build a large practice as an obstetrician gynecologist in Denison, Texas, where he served for more than 20 years.
In 2004, he founded the West Africa Fistula Foundation to provide women with access to education, resources and medical treatment to address obstetrical fistula – a severely debilitating consequence of extended labor that occurs in women who need a caesarean delivery but do not have access to proper medical care. Since 2000, Maggi has participated in nearly 60 volunteer physician trips to Africa, primarily Sierra Leone, and has performed this procedure hundreds of times.
Over the past few years, Maggi and the West Africa Fistula Foundation team have created the West Africa Village for Children to provide comprehensive medical care, housing and education for children in dire need, many of them disabled, blind or abandoned. To learn more about this important work, please visitwestafricafistulafoundation.org and westafricavillageforchildren.org.
Maggi graduated from the University of Oklahoma College of Medicine in 1974. He completed an internship at St. Johns Hospital in Tulsa, followed by residency at Charity Hospital in New Orleans. He is a diplomat and fellow for the American College of Obstetrics and Gynecology, as well as a member of the Texas Medical Association. Maggi served as a member of the board of directors for the American Bank of Texas, Thelma Braun Foundation, Youth in Action and Texas Conservative Coalition Reserve Institute for Health Care Reform. He also was the director of Texans for Lawsuit Reform and has been recognized as one of the best doctors in the Dallas-Fort Worth area.
Maggi published the first paper ever to provide evidence-based outcomes on obstetrical fistula repairs in the International Journal of Obstetric Trauma. In 2016, he published “Basta! A Doctor’s Story of Giving Back,” a book detailing the inspiration behind his career and the work performed by the West Africa Fistula Foundation.
Maggi has three children and seven grandchildren. He and his wife, Karen, reside in Southlake, Texas.

Dwight Reynolds, M.D., was born in Guam and lived there for several years before moving to his father’s home state of Oklahoma. He completed his undergraduate education at the University of Oklahoma before completing his medical degree at OU in 1974. His internal medicine residency and cardiovascular diseases fellowship were done at the University of Alabama-Birmingham where he spent a year on the UAB faculty before returning to OUHSC as faculty.
Over the years on faculty at OU he was promoted to a tenured professor of medicine and in 2015 was honored with a Regents Professorship. He served as program director for the cardiovascular diseases fellowship at OUHSC for 13 years, was the vice chief of the cardiovascular section for 8 years and then served as chief of the cardiovascular section for 25 years before becoming professor emeritus in 2023. He now works clinically and assists on some administrative projects.
Reynolds is a board-certified internist and cardiologist. His career at the University of Oklahoma has been clinically focused on the development and evolution of cardiac implantable electronic devices such as pacemakers, implantable defibrillators and the management of patients and their complex diseases.
His professional organization involvement has been significant. Reynolds served as the president of the Heart Rhythm Society, the principal international organization of heart rhythm professional expert electrophysiologists based in Washington, D.C., the largest cardiovascular subspecialty organization in the world. In addition to his presidency and other roles within the Heart Rhythm Society, he served for several years on the board of trustees of that organization.
He also has served the American College of Cardiology on several national committees and served as Oklahoma’s American College of Cardiology chapter president. He has also been involved in the American Heart Association serving as the local chapter president as well as on the board of trustees.
Reynolds recently served as president of the Association of Professors of Cardiology, the national organization of chiefs of cardiology from universities around the U.S.
Reynolds has been married to his wife, Sheila, for almost four decades. He has six children and six grandchildren. While he has enjoyed golf and hunting in years past, his principal and almost life-long hobby is fly-fishing. While he enjoys the sport in Oklahoma, his passion is fishing for trout in the rivers and streams of Montana, where he and his family have a cabin.

Lynn Mitchell, M.D., MPH, has served as the chief medical officer for Oklahoma Complete Health since November 2021. Prior to this role, Mitchell was the chief medical officer/chief wellness officer for OU Physicians and associate dean for clinical practice at the University of Oklahoma College of Medicine. Her interests include preventive care and public health, patient-centric care, innovative healthcare delivery models, provider well-being and healthcare financing.
From 1995 to 2010, she held a variety of roles with the Oklahoma Health Care Authority, including serving as the state Medicaid director from 2000 to 2010. Mitchell has extensive experience with health systems and assessments of healthcare outcomes. She has been deeply involved with healthcare policies at the state and federal levels.
Mitchell received training from the Medicaid Leadership Institute at Robert Wood Johnson Foundation with the Center for Health Care Strategies. She currently serves as volunteer faculty at the University of Oklahoma Health Sciences.
Mitchell is a graduate of the OU College of Medicine and completed residency training in family medicine and occupational/ preventive medicine at OU Health Sciences. She also earned a master’s in public health with an emphasis in epidemiology and biostatistics from OU. She is a member of the American Medical Association, Oklahoma State Medical Association, Oklahoma County Medical Association, American Academy of Family Physicians and Oklahoma Academy of Family Physicians.
Mitchell and her husband, Barry, have three children and four grandchildren. Between her children and their spouses, five out of the six have a health-related degree from OU, including three medical degrees, one in social work and one in healthcare administration.
Anthony Alvarado M.D., Class of 1970, Kirkland, WA
Delmar Caldwell M.D., Class of 1961, Folsom, LA
John Caughron M.D., Class of 1960, Bethesda, MD
John Chaffin, M.D., Class of 1975, Oklahoma City, OK
Jeffrey Collins M.D., Class of 1967, Port Townsend, WA
David Confer M.D., Class of 1971, Tulsa, OK
Norvell Coots M.D., Class of 1989, Laytonsville, MD
Thomas Douthit M.D., Class of 1954, Kingwood, TX
David Eakin M.D., Class of 1965, Tulsa, OK
Craig Ferris M.D., Class of 1983, Russellville, AR
Donald Garrett M.D., Class of 1968, Norman, OK
Edgar Gedosh, M.D., Class of 1960, Fort Smith, AR
Lawrence Green M.D., Class of 1969, Evanston, IL
Stephen Haas M.D., Class of 1965, Washington DC
Joseph Hargis M.D., Class of 1972, Edmond, OK
James Hart M.D., Class of 1968, Livingston, TX
Bob Herrin M.D., Class of 1955, Marshall, TX
Horace Hewett, M.D., Class of 1957, Norman, OK
Stephen Lindsey M.D., Class of 1979, Norman, OK
Anthony Loehr M.D., Class of 1971, Bixby, OK
George Markert M.D., Class of 1960, Tulsa, OK
Joni McClain M.D., Class of 1983, Oklahoma City, OK
William McCreight M.D., Class of 1973, Oklahoma City, OK
Leroy Milton M.D., Class of 1959, McAlester, OK
Richard Morris M.D., Class of 1966, Virginia Beach, VA
Rickey Nagy M.D., Class of 1978, Kansas City, MO
Byron Niebruegge M.D., Class of 1966, Plano, TX
Syed Sarosh Nizami, M.D., Class of 2011, Denton, TX
Susan O’Brien M.D., Class of 1978, Tulsa, OK
Ronald Peterson M.D., Class of 1977, Manchester, WA
Marilyn Porter M.D., Class of 1956, Oklahoma City, OK
Helen Ramey M.D., Class of 1960, Cedar Park, TX
Robert Rock M.D., Class of 1958, Austin, TX
Stephen Rodgers M.D., Class of 1970, Edinburg, VA
Walter Stark, Jr. M.D., Class of 1967, Longboat Key, FL
Stephen Vernier M.D., Class of 1993, Yukon, OK
Gregory Williams M.D., Class of 1974, Tulsa, OK
Robert Zumwalt M.D., Class of 1953, Norman, OK
