A Publication for Alumni and Friends of the University of Oklahoma College of Medicine
Transformative Gift Broadens Research at Stephenson Cancer Center New Program Creates Pathways to Medical School [ Fa l l / Wi n t e r 2019 ]
OU MEDICINE
As we prepare to enter a new decade, I am eager to share our college’s accomplishments with you and convey some of our goals for the years to come. This is an exciting time to be in medical education, and I am very proud of our faculty, students, residents and staff for their dedication to our mission each day. This past year has been an exciting one, as shown in the pages ahead. One of the highlights was our reaccreditation by the Liaison Committee on Medical Education (LCME), the accrediting body for all M.D.-granting programs in the United States and Canada. Although this process takes place every eight years, we spent two full years preparing for the LCME site visit in January. The outcome could not have been better – not only did the college maintain its full accreditation status, but the LCME added a rare distinction – accreditation with commendation, which signifies the college’s high level of performance. You’ll also read about our researchers’ significant progress and the ways their discoveries are being translated into promising new medical therapies. Our educators are creating new and innovative ways to prepare the physicians of tomorrow to practice medicine in an increasingly complex healthcare landscape. And our clinicians are transforming their patients’ lives every day with advanced technology and care.
Dean’s Message
In this edition of the magazine, we’ve also highlighted several ways in which philanthropic giving advances our mission. The power of the philanthropic gift is seen in a new $20 million donation to the Stephenson Cancer Center by Peggy and Charles Stephenson and the Stephenson Family Foundation. Their generosity will further cancer research endeavors, which ultimately provides our patients with new treatments and improved quality of life. To extend the impact of the gift, Stephenson Cancer Center is committed to raising another $20 million. Donations large and small will be crucial in meeting that goal. In another story, we highlight a $100,000 gift from the Wisdom Family Foundation toward translational research within the Oklahoma Center for Neuroscience. This donation will allow physicians and basic science researchers to collaborate on common areas of research interest, with the aim of moving discoveries more quickly from the bench to the bedside. You’ll also read about the 2019 presentation of the Harold Hamm International Prize for Biomedical Research in Diabetes. The prize, which comes with a $250,000 award, has been funded in perpetuity by Harold Hamm, the namesake of the Diabetes Center. His commitment to diabetes research is paving the way toward discoveries that will prevent, treat and cure diabetes. Many other philanthropic partners further the mission of the OU College of Medicine, including the Presbyterian Health Foundation, whose generosity helps our researchers initiate projects or advance them to the next level. We also are grateful for the ongoing support of the Children’s Hospital Foundation, whose endowments and direct support allow us to recruit and retain internationally recognized children’s physicians and scientists. We are very grateful for our philanthropic partners and all they do to help us improve the health and well-being of Oklahomans. Large or small, philanthropic gifts are transformational to our mission of patient care, research and medical education. I hope you enjoy this issue of the OU Medicine magazine and that 2020 brings you health and happiness.
John P. Zubialde, M.D. Executive Dean, OU College of Medicine
contents OU MEDICINE
University of Oklahoma College of Medicine
TABLE OF CONTENTS 4. College Reaccredited The OU College of Medicine earned full reaccreditation from the Liaison
Senior Vice President and Provost Jason Sanders, M.D., MBA
Committee on Medical Education, the body that accredits M.D.-granting
programs in the United States and Canada.
Executive Dean, College of Medicine John Zubialde, M.D.
18. CAR-T Offered
Executive Editor Jon Brightbill Associate Dean for Executive Affairs Assistant Vice President of Development, OU Health Sciences Center Stacey Maxon Editor/Feature Writer April Wilkerson
CAR-T therapy, which harness the body’s own cells to recognize cancer,
is now being offered in Oklahoma only at Stephenson Cancer Center.
Its initial use is for two different blood cancers, one affecting children and
the other affecting adults.
22. Behavioral Health Screening The Center on Child Abuse and Neglect, a program within the Section
of Developmental and Behavioral Pediatrics, partnered with the Oklahoma
Department of Human Services to develop and administer a child
behavioral health screener for children in state custody who are living
in foster homes.
12. Clinical Preparation OU Medicine is published twice a year by the OU College of Medicine. For more information or to submit news for the Class Notes section, contact:
To help students better adjust from their preclinical education into the
April Wilkerson, Editor oumedmag@ouhsc.edu (405) 271-2850
A team of researchers in the Department of Medicine discovered how
OU Medicine is online at www.oumedicine.com/magazine
36. PA Program Success
The University of Oklahoma, in compliance with all applicable federal and state laws and regulations, does not discriminate on the basis of race, color, national origin, sex, sexual orientation, genetic information, gender identity, gender expression, age, religion, disability, political beliefs or status as a veteran in any of its policies, practices or procedures. This includes, but is not limited to: admissions, employment, financial aid and educational services. Inquiries regarding non-discrimination policies may be directed to: Bobby J. Mason, University Equal Opportunity Officer and Title IX Coordinator, 405-325-3546, BJM@ou.edu, or visit http://www.ou.edu/eoo.html. Copies of this magazine were printed at no cost to the taxpayers of the State of Oklahoma. © 2019 University of Oklahoma
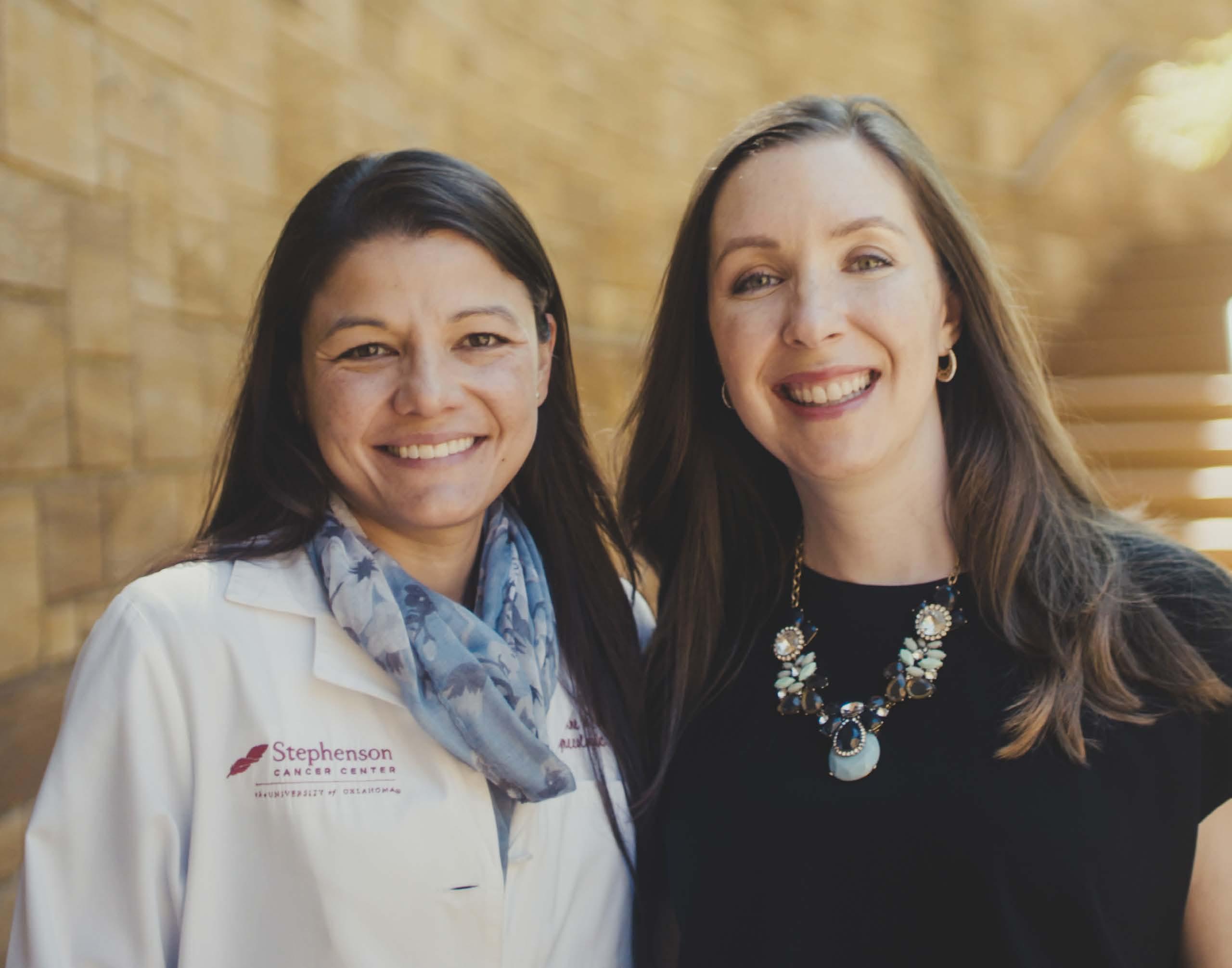
COVER PHOTO:
This fall, Peggy and Charles Stephenson (pictured left) and the Stephenson Family Foundation donated $20 million to the Stephenson Cancer Center. Patients like Susan Laurence, right, and her physician Debra Richardson, M.D., will benefit from the increased research made possible by the gift.
clerkships of their clinical years, the college created a course called
Clinical Transitions that prepares them to interact with patients.
35. Cancer Discovery
the muscle-wasting condition cachexia is triggered in patients with
pancreatic cancer.
The OU-TU School of Community Medicine graduated its 10th class of
physician assistants from a program that has grown in the depth and
breadth of educational experiences it offers.
38. Implicit Bias Internal medicine physician and educator Jabraan Pasha, M.D., has been
giving presentations on implicit bias to students, residents and faculty,
and to people outside healthcare around the nation and world.
46. Evening of Excellence Ophthalmology researcher Robert “Gene” Anderson, M.D., Ph.D., and
community leader David Harlow will be honored during the 2020
Evening of Excellence gala.
48. Alumni Day Alumni of the College of Medicine will gather on May 1 for a reunion
and to recognize the accomplishments of their peers.
The OU College of Medicine Alumni Association is now on Facebook. Like us at www.facebook.com/oucomalumni
Web Extras: Visit www.oumedicine.com/magazine for additional stories and photos about the OU College of Medicine.
VITAL SIG NS
College Accreditation Renewed by LCME On June 26, the OU College of Medicine learned it has maintained full accreditation status from the Liaison Committee on Medical Education, the body that accredits M.D.-granting programs in the United States and Canada. In addition to being compliant with all 12 LCME standards, the OU College of Medicine earned accreditation with commendation, a rare distinction signifying the high level of performance of the medical education program. Senior Associate Dean for Academic Affairs Christopher S. Candler, M.D., Ed.D., said the achievement was made possible by the hundreds of committed faculty, staff and students who diligently worked on many accreditation processes and tasks in preparation for the LCME site visit in January. “LCME accreditation ultimately serves the public good,” Candler said. “Full accreditation signifies that we are providing the highest level of education for our students and preparing them to be competent physicians. This accomplishment is the result of the many dedicated people within the College of Medicine.” In its exit survey report, the LCME team noted four areas of strength within the College of Medicine: • •
4
Educational and student affairs leaders at the college have been remarkably accessible and responsive to students at both campuses. The college has been highly successful in its efforts to
• •
recruit and retain Native American students and faculty members. The college has developed a comprehensive, objectives-driven medical education program that is effectively managed and is deeply appreciated by its students. The college has strengthened its efforts to eliminate student mistreatment, and data from the Association of American Medical Colleges Graduation Questionnaire indicate a dramatic improvement in student awareness of mistreatment policies and increased reporting of incidents. Independent Student Analysis data reflect extremely high levels of satisfaction with the policies for reporting, addressing and preventing mistreatment.
The College of Medicine did not receive any citations for non-compliance with standards. The LCME noted that it wants to monitor three areas: hospital-based resources for medical students; career advising services; and financial aid services. Preparation for the LCME accreditation process began more than two years ago with several required reports. The Data Collection Instrument is used to report college data, policies, procedures and practices that demonstrate compliance with LCME standards. A Self-Study Summary Report, developed by a Self-Study Task Force and several subcommittees, evaluated how well the college is doing in numerous areas based on information in the Data Collection Instrument.
[ Fa l l / Wi n t e r 2 019 ]
VITAL SIG NS
Students also completed an independent analysis of the college. “The LCME has always valued the perspective of students,” Candler said, “and it’s important to the LCME to have an unbiased view that’s free from any faculty or administrative influence. Students conduct their own independent survey that is separate from the rest of the self-study process.” Materials submitted to the LCME totaled more than 2,000 pages. The LCME examined the reports ahead of its January 27-30 site visit, an activity designed to verify and clarify the submitted information. To receive such high marks from a body that analyzes virtually every aspect of educational programs was gratifying, Candler said. “It was validating to know that all the hard work our faculty and staff have invested in our educational program was recognized by this kind of external rigorous process,” he said.
College Names Two Assistant Deans The OU College of Medicine has named faculty members Katie M. Smith, M.D., to the position of Assistant Dean for Student Affairs and Teresa Scordino, M.D., as Assistant Dean for Preclinical Curriculum. Smith, an OB-GYN, is filling a newly created position in the college’s administrative structure, created to enhance student services. She will serve in several functions, including medical student career/Match counseling sessions, activities and
Teresa Scordino, M.D.
programming. She will assist with medical student performance evaluations for a select proportion of senior medical students, and she will act as a student advocate, representing student interest and perspective at meetings and other venues. In the Department of Obstetrics and Gynecology, Smith is an associate professor and chief of the Section of Academic Generalists. She maintains a busy practice and has a special interest in lower genital tract disease and cervical cancer prevention, which has also been the focus of her clinical research and service on national committees. In 2015, she began serving as OB-GYN clerkship director. She also serves as co-chair for the Curriculum Evaluation Subcommittee. Scordino assumes a position previously held by Robert Blair, Ph.D., who retired. As Assistant Dean for Preclinical Curriculum, she will work with others to ensure the preclinical curriculum is developed, delivered and evaluated in accordance with college and university polices and standards. She will serve as chair of the Preclinical Curriculum Subcommittee and assist with the development, review and revision of academic policies and procedures. In addition, she will work with staff, faculty and administrators to develop innovative solutions and programs to address the needs and concerns of the undergraduate medical education program.
Katie M. Smith, M.D.
Scordino is associate director of hematopathology and the medical director of the clinical hematology, serology, urinalysis and Jimmy Everest Center laboratories for OU Medicine. She is the course director for the OU College of Allied Health’s pathology course and co-course director of the College of Medicine’s course on blood, hematopoiesis and lymphatics. She lectures to medical, allied health, nursing, physician assistant and dental students in seven courses across the OU Health Sciences Center, and she is involved in the education of pathology residents and hematology-oncology fellows. [ Fa l l / Wi n t e r 2 019 ]
5
VITAL SIG NS
Stephenson Cancer Center Director Robert Mannel, M.D., and Kris Gose, president of OU Medical Center, speak during a campus celebration of U.S. News & World Report rankings.
OU Medicine Receives High Rankings From U.S. News & World Report OU Medicine is the No. 1 ranked hospital system in Oklahoma, and its oncology program at Stephenson Cancer Center and OU Medical Center ranked in the Top 50 in the nation, in the 2019-2020 rankings released by U.S. News & World Report. This achievement makes OU Medicine, which includes OU Medical Center, Stephenson Cancer Center, The Children’s Hospital, OU Physicians, OU Medical Center Edmond and the OU Health Sciences Center, the only healthcare system in Oklahoma to currently hold a national ranking, and it marks the first time in state history that a cancer care program has earned a national ranking. For OU Medicine, the achievement comes a little over a year after becoming a locally owned, nonprofit healthcare system and a year after earning the prestigious National Cancer Institute designation at Stephenson Cancer Center, which is held by only 2% of cancer centers in the country.
6
“We are honored and inspired by the extraordinary dedication and skill of our physicians, nurses, researchers, healthcare professionals and support staff who bring their best to our patients every day, “ said Chuck Spicer, President and CEO of OU Medicine, Inc. “It is our privilege to serve the residents of Oklahoma by providing the most complex and specialized healthcare services that are only offered at OU Medicine.” U.S. News & World Report especially recognized OU Medicine for its breadth of medical specialties and physician expertise to treat the most complex diseases and conditions. In addition, the health system earned commendations for the highest performance possible in four specific areas: the specialty of ophthalmology and the treatment of chronic obstructive pulmonary disease and congestive heart failure, and colon cancer surgery.
[ Fa l l / Wi n t e r 2 019 ]
VITAL SIG NS
To generate hospital rankings, U.S. News & World Report evaluated nearly 5,000 hospitals nationwide. It assessed each hospital in 16 adult specialties, nine adult medical procedures or conditions and 10 pediatric specialties. OU Medicine broke into the coveted U.S. News & World Report national top 50 ranking for Best Cancer Hospitals by ranking No. 48 for 2019-2020. U.S. News and World Report started with an initial pool of 4,653 hospitals, then narrowed this list down to 900 top cancer programs nationwide for more in-depth analysis. In partnership with Stephenson Cancer Center at OU Medicine, the program was particularly recognized for its excellence in patient survival 30 days after a stay in the hospital, as well as the frequency that its patients are able to go directly home from the hospital rather than being sent to another facility for continued care. In addition, OU Medicine received a commendation for its volume of patients with high-risk cancers over three years. That recognition is especially relevant because higher patient volume is associated with better outcomes, according to research studies. “At Stephenson Cancer Center, we lead the nation in enrollment for clinical trials and offer the most cutting-edge and complex cancer treatments in the region. The National Cancer Institute designation we received last year is a testament to the excellent clinical research we are providing to our patients to ensure they are receiving the best cancer treatment available in the country. This additional recognition from U.S. News & World Report further confirms for Oklahomans that they can receive world-class cancer care right here at home,” said Robert Mannel, M.D., associate vice provost for cancer programs at OU Health Sciences Center and director of Stephenson Cancer Center at OU Medicine. OU Medicine’s cancer treatment program was also recognized for its use of advanced technologies, such as proton therapy and image-guided radiation therapy. For its holistic patient services, the cancer program received an excellent rating, which points to Stephenson Cancer Center’s Supportive Care program that provides pain management, palliative care, emotional and spiritual support, and more. U.S. News & World Report also highlighted Stephenson Cancer Center’s standing as a National Cancer Institutedesignated cancer center, offering the most comprehensive network of oncology physicians, a large clinical trials program and ongoing research. The rankings also noted the center’s certification by the Foundation for the Accreditation of Cellular Therapy, which certifies bone marrow and tissue transplantation programs. “As a comprehensive academic healthcare system, OU Medicine strives not only to offer the highest-quality care, but to engage in research that yields new treatments and to educate the healthcare professionals of tomorrow. The new rankings by the U.S. News & World Report confirms that OU Medicine is the leader in bringing the highest standard of treatment and compassionate care to patients in Oklahoma and in the region,” said Kris Wallace, president of OU Medical Center.
Surgeon General Jerome M. Adams, M.D., MPH, speaks at the OU Health Sciences Center during a visit this summer.
Surgeon General Visits Campus The Surgeon General of the United States, Jerome M. Adams, M.D., MPH, spoke to an audience of students, staff, clinicians and faculty members at the OU Health Sciences Center in August, describing his initiatives to improve the nation’s health. The high-profile visit served to underscore OU Medicine’s role as the state’s largest comprehensive academic health system. The “Nation’s Doctor,” Adams has an integral place in the advancement of national health priorities. As the surgeon general, Adams also holds the rank of Vice Admiral in the U.S. Public Health Service Commissioned Corps, overseeing operations of nearly 6,500 uniformed health officers serving 800 locations around the world. Adams has created several initiatives to address pressing issues in national health, including opioid use, oral health and the ways in which economic prosperity and national security are linked to community health. Adopting the motto, “Better health through better partnerships,” Adams is committed to strengthening relationships with members of the health community and establishing new partnerships among business leaders, faith-based organizations, professionals engaged in education and public safety as well as national security.
[ Fa l l / Wi n t e r 2 019 ]
7
VITAL SIG NS
During the bill signing for the Living Donor Protection Act, Oklahoma Gov. Kevin Stitt visits with a girl who received care at The Children’s Hospital at OU Medicine.
OU Medicine Plays Significant Role In New Legislation Protecting Organ Donors One of the most significant actions a person can take is to donate a kidney or other organ to a person who otherwise will eventually die without a transplant. That’s why it is especially important that a donor not face any additional hurdles to donating, such as denial of life insurance coverage. OU Medicine, along with the Oklahoma Hospital Association and the National Kidney Foundation, were instrumental in the Oklahoma Legislature’s passage of Senate Bill 704, the Living Donor Protection Act. The new law prevents insurers from denying or raising the rates of life insurance, disability insurance or long-term care insurance based solely on a person’s status as an organ donor. “There is a major need for organs, especially in Oklahoma, and this law removes a barrier for those who are making a huge decision about donating an organ,” said Greg Lewis, RN, director of Pediatric and Adult Dialysis at OU Medicine. Lewis led OU Medicine’s advocacy efforts at the state Capitol, joined by the Oklahoma Hospital Association, National Kidney Foundation, other Oklahoma transplant programs and LifeShare Transplant Donor Services of Oklahoma. A 2014 study by Johns Hopkins University showed that a quarter of living donors in the study faced discrimination when they tried to obtain or change their life insurance. The National
8
Kidney Foundation also hears regularly from donors who experienced premium changes or other restrictions on their insurance policies. “You can imagine what a disincentive it would be for a person who wants to donate a kidney, if they’re told they will not be insurable afterward,” said Alan Hawxby, M.D., surgical director of OU Medicine’s adult and pediatric kidney transplant programs and the designated living donor surgeon. “Chronic kidney disease is difficult to fight, so the more we can help facilitate a transplant, the better off the patient and donor will be.” Chronic kidney disease affects more than 30 million Americans. In Oklahoma, more than 21,000 Medicare patients have kidney disease, and 526 people are waiting for a kidney transplant. Although kidney dialysis keeps patients alive, it is not a long-term solution. “Last year, only 194 Oklahomans received a kidney transplant,” Lewis said. “Once a person is put on the transplant list, the average waiting time is three to seven years. The average life expectancy on dialysis is five to 10 years. The math is sobering. The clock is ticking for each and every one of those 526 patients on the waiting list. Everything we can do to encourage living donations saves lives.”
[ Fa l l / Wi n t e r 2 019 ]
VITAL SIG NS
is actually a statewide network of universities and colleges, as well as researchers from the Oklahoma Medical Research Foundation. Grant dollars not only advance existing research programs, but help to build a pipeline for the next generation of researchers and healthcare professionals through outreach to high school and college students. “This grant represents a continuum. It allows us to advance cutting-edge research and build a better pipeline for improving health and decreasing healthcare disparities in our state,” said Darrin Akins, Ph.D., director of the Oklahoma IDeA Network of Biomedical Research Excellence (OK-INBRE). “This grant enhances the number of students who go to college, choose a discipline in STEM (science, technology, engineering and math) and graduate with a STEM degree. Then we can mentor them as they go on to become health professionals or biomedical researchers,” said Akins, who is also a professor in the OU College of Medicine and associate director of education and training at the Stephenson Cancer Center. The Oklahoma State Regents for Higher Education are providing an additional $250,000 per year to support the program. The OU Health Sciences Center has successfully renewed the grant three times. Outcomes from previous grants show a significant return on investment. Achievements over the past five years include:
Darrin Akins, Ph.D.
OU Health Sciences Center Receives $18.7 Million Grant for Biomedical Research, Workforce Development The University of Oklahoma Health Sciences Center has received an $18.7 million grant from the National Institutes of Health to expand biomedical research for some of the most complex diseases and to develop the workforce to take that research into the future. The grant is from the NIH’s Institutional Development Award program (IDeA), whose aim is to broaden the geographic distribution of NIH funding. This grant specifically focuses on cancer, diabetes and the development of new medical devices and treatments for patients. While the OU Health Sciences Center leads the program, it
•
Because of successful investigations made possible by OK-INBRE funding, researchers were awarded six NIH R01 grants, considered the gold standard in research funding. They received 22 other federal agency awards and 116 state or foundation awards.
•
The OK-INBRE program provided $3 million in infrastructure development to its 17 partner institutions across Oklahoma, such as lab equipment and research opportunities for faculty and students.
•
Since its inception, OK-INBRE has facilitated summer hands-on research experiences at the OU Health Sciences Center and Oklahoma Medical Research Foundation for more than 500 students. Of those, 95 percent have gone on to earn a STEM degree, and 60 percent have continued to graduate or professional school.
•
The dean of the College of Mathematics and Science at the University of Central Oklahoma, Wei Chen, Ph.D., leveraged his OK-INBRE funding to earn an R01 award from the NIH, the first ever received by a regional university in Oklahoma.
• The OK-INBRE award, combined with additional grants generated by researchers over the past five years, has resulted in an $86 million economic impact to the state.
[ Fa l l / Wi n t e r 2 019 ]
9
VITAL SIG NS
Federal Grant Allows OU Health Sciences Center to Enhance Dementia Care Across Oklahoma The University of Oklahoma Health Sciences Center, working with partners across the state, has been awarded a $3.75 million federal grant to enhance the care and support of a growing group of Oklahomans – those who suffer from memory loss, Alzheimer’s disease and other types of dementia. According to the Alzheimer’s Association, 65,000 Oklahomans currently live with Alzheimer’s, and that number is expected to grow. An especially cruel disease with heartbreaking cognitive decline and no cure, Alzheimer’s requires a circle of support so that people with the disease can live as well as possible for as long as possible. The program established by the grant will focus on two overarching objectives: educating the current and future workforce to better care for people with dementia, and creating dementia-friendly health systems. Unfortunately, Oklahoma ranks near the bottom in several quality of life and health rankings for older adults. Lee Jennings, M.D., a geriatrician with the OU College of Medicine who is leading the grant, said she hopes the upcoming efforts will improve those numbers. “Dementia, particularly Alzheimer’s disease, is much more prevalent in older adults,” she said. “As the number of older Oklahomans increases, this disease will become more common. We don’t want people with Alzheimer’s and their caregivers to become isolated. We want communities and healthcare systems that are friendly to people with cognitive impairment and memory loss. We want people to thrive as long as they can, as best they can, with the support that they need.” The structure of the program is uniquely opposite of most academic grants. Rather than working solely with physicians and students on campus, the program will engage primary care clinics around the state, direct-care providers such as nursing home staff, organizations like the Alzheimer’s Association, and family members and caregivers of people with dementia. Most of the medical care for patients with dementia is provided by primary care clinics, but that only accounts for a short medical visit. That means families and other caregivers are taking care of loved ones the majority of the time. And because Oklahoma is largely a rural state with not enough primary care physicians, the need is great to increase support and knowledge for everyone helping a person with dementia. Hudson OU College of Public Health department chair Thomas Teasdale, who holds a doctorate in public health, is co-leading the program with Jennings. Through an existing partnership with the Oklahoma State Department of Health,
10
Lee Jennings, M.D.
Teasdale already works with the state’s 300-plus nursing homes, where 70 percent of residents live with some type of dementia. The grant also will allow him to enhance dementia care education for new audiences, including community health workers, in partnership with the Oklahoma City-County Health Department. Another partner agency, the Oklahoma Foundation for Medical Quality, will provide quality improvement consulting as the program evolves. Jennings and her team also will work with OKPRN, the Oklahoma Practice-Based Research/Resource Network, a large group of physicians who conduct ongoing research to improve the care they provide. In addition, the grant will allow OU dementia specialists to provide tele-consultations for rural physicians who might need help treating patients with complications. “We want to offer rural providers the expertise in our
[ Fa l l / Wi n t e r 2 019 ]
VITAL SIG NS
university setting. They may need new strategies for managing a patient’s neuropsychiatric symptoms or treating difficult diagnoses related to dementia,” Jennings said. The grant’s second objective – to create dementia-friendly health systems – covers everything from the physical layout of a clinic to the community resources that are available for people and their caregivers. Clinics can improve their environments by ensuring signs are understandable, exam tables are easy to use for older adults, and sensory aids like hearing amplifiers and large-print materials are available. A dementia-friendly practice also means both clinical providers and staff can connect patients and families with community resources where they live. Support groups, for both caregivers and the person living with dementia, are often crucial in helping people cope. They also can help reduce the stigma that is still associated with the disease. “We want to let people know that there are resources, and we don’t want caregivers to feel stigmatized,” Jennings said. “It can be isolating if caregivers don’t feel like they can go out into the community with their loved one. We want to help people live with dignity and be as independent as possible while they age with this disease.” The effort also extends to Oklahoma’s Native American tribes. The Choctaw Nation in particular is working not only within its own geriatric clinics, but beyond the healthcare setting to transportation access for people with dementia. “This grant and program would not be possible without our many community partners,” Jennings said. “We are putting these federal dollars to use in our communities throughout Oklahoma to improve the health and quality of life of people with memory loss, Alzheimer’s disease and other types of dementia.” This federal grant was awarded by the U.S. Department of Health and Human Services under the award number 1 U1QHP330820100.
Connect+Cure Gala Raises Record Amount for Diabetes Research Nearly a thousand people gathered for the 2019 Connect+Cure Gala on Oct. 22 to support Harold Hamm Diabetes Center and celebrate the progress being made toward a cure for diabetes. Now in its fifth year, the Connect+Cure Gala raised nearly $1.9 million, the most in the event’s history. In addition, more than $196,000 was raised to sponsor participants in Camp Blue Hawk, a residential camp program for children and teens, ages 9 to 17, with Type 1 diabetes.
“It was a pleasure to be in a room full of Oklahomans raising awareness of a pandemic and celebrating the achievements that bring us closer every day to our goal for a cure.” “It was a tremendous evening of celebrating the ongoing progress being made in finding a cure for diabetes,” said Harold Hamm, lifetime HHDC board member. “In addition to celebrating, we spent time educating and informing on the work we still have to do. The amount of money raised will make a significant impact on diabetes research, and I am as confident as ever that we will find a cure for diabetes right here at HHDC in Oklahoma.” Master of ceremonies for the evening was three-time World Series champion and Major League Baseball Hall of Fame manager Tony LaRussa. Grammy award-winning singer Trisha Yearwood provided the entertainment, performing both her hits and songs from her newest record. Guests also enjoyed a meal inspired by Yearwood’s recipes. The highlight of the evening was the presentation of the 2019 Harold Hamm International Prize for Biomedical Research in Diabetes, which comes with a $250,000 award. The honor was presented to Daniel J. Drucker, M.D., a professor of medicine at the Lunenfeld-Tanenbaum Research Institute, Mt. Sinai Hospital, University of Toronto in Ontario, Canada. Drucker’s discoveries have led to the development of two new treatments for Type 2 diabetes. “It was a pleasure to be in a room full of Oklahomans raising awareness of a pandemic and celebrating the achievements that bring us closer every day to our goal for a cure,” said Jed Friedman, Ph.D., director of HHDC and associate vice provost for diabetes programs. “One in three Oklahomans has Type 2 diabetes or is pre-diabetic, and our state ranks fourth in the nation for diabetes deaths. These numbers are tragic and unacceptable. Funds raised from Connect+Cure Gala will help us meet the goals of bringing talent, technology and teams to Oklahoma and help secure the future of HHDC in its efforts to prevent, treat and find the next cure for diabetes.”
[ Fa l l / Wi n t e r 2 019 ]
11
MEDICAL EDUCATION
Before entering their third year of medical school, students recite a reaffirmation of the oath they took at the beginning of their first year.
Clinical Transitions Course Guides Students Into Third Year of Medical School When it comes to transitions, the shift from the second year of medical school to the third is among the most significant. The first two preclinical years of medical education are heavy on lectures, studying and tests about organ systems of the body. In the third year, students are thrust into hospital wards and clinics with little preparation for the change in settings and expectations. Until now. A new course, called Clinical Transitions, was added to the curriculum last year in the week before students begin their third-year clerkship rotations. The course contains a multitude of information about everything – except medical knowledge. It ends with students taking a reaffirmation of the oath they recited at the beginning of medical school. “We wanted to give them a proper orientation to their third year with information that’s not as easy to pick up on their own,” said LaTasha Craig, M.D., professor of OB-GYN, who designed the course. “We talk to them about things like professionalism, implicit bias, death and dying, and working with diverse populations.” During the segment on professionalism, students hear from clerkship directors, residents and fourth-year medical students, each providing similar information but from different points of view. Students learn about the settings of various
12
clerkships, how to read the environment, what to do and when to ask questions. They also hear about interprofessionalism and their role on a healthcare team. “They will be working with nurses, pharmacists, dietitians, lactation consultants, social workers and more – all the people it takes to care for patients,” Craig said. “It’s so important to appreciate each other’s skills.” Learning how to work with diverse patient populations is another critical element of the course. This requires purposefully addressing implicit bias and how it may affect their care of patients as well as their work with families and caregivers. Students hear from faculty members about how to understand this bias and how to interact with patients across many different populations, whether in regard to ethnic, pediatric, geriatric or LGBTQ populations. Students also hear a lecture on death and dying. When they begin rounding on patients, students will inevitably face death, many of them for the first time. “We not only want to teach them how to care for a patient who is dying, but also how to speak with families and how to cope with witnessing death,” Craig said. “We don’t want students to become immune to the strong feelings that come with death, but they also need tools for working through it.”
[ Fa l l / Wi n t e r 2 019 ]
MEDICAL EDUCATION
his battle last October. His father talks to students about the compassionate care his son received, but also about some of the poor care that added to the despair his family was feeling. But the biggest impact of the talk is that students witnessed his grief and gained a better understanding of how their professional lives will be interwoven with families’ deepest loss and greatest joys. “We intentionally follow that with a reaffirmation of the oath that they took as first-year students,” Craig said. “It reminds them that they are about to begin experiencing the ultimate reason they began medical school: to care for patients.”
Student Participates in NIH Research Program OU College of Medicine student Annah Baykal was selected as one of 50 students nationwide to participate in the 20192020 National Institutes of Health Research Scholars Program. The yearlong research training program allows medical, dental and veterinary students to pause their university studies to live and conduct basic, clinical or translational research work on the NIH campus in Bethesda, Maryland. The scholars began their fellowship in July 2019. Baykal will resume her medical education in 2020 and will graduate with the Class of 2022.
LaTasha Craig, M.D., designed the Clinical Transitions course for medical students entering their third year.
Students are taught how take a focused patient history, followed by writing a concise, efficient note about the patient’s chief complaint. They also learn the importance of thinking about a patient’s differential diagnosis before they walk into a room. Faculty members created a clever acronym to help students remember – CCDIF, or the Chief Complaint Differential. In the afternoons, students then go to the college’s Clinical Skills Education and Testing Center, where they practice gowning and gloving, inserting IVs and other procedural skills they may perform. This hands-on training ensures they are ready to go on day one of rotations. One of the most powerful aspects of the Clinical Transitions course is a story shared by an Oklahoma physician who speaks not about his work, but from his perspective as a parent. A few years ago, his son, who was about to become a high school senior, was diagnosed with an aggressive form of acute myeloid leukemia. His father and his family sought care at hospitals in three states, but their son ultimately lost
Participants receive mentored training and will conduct research in areas that match their personal interests and research goals. For this class, interest in the fields of oncology and neurology was strong, with additional areas of robust interest in otolaryngology (research on causes of deafness and novel treatments for head and neck cancer), immunology, genetics, ophthalmology and urology. The training experience forms the core of the program and allows these future clinician-scientists to carry out research across the full spectrum of science in the interest of improving public health. The scholars work with an adviser who provides guidance on creating a career development plan and on selecting an NIH research mentor. Mentors are full-time NIH investigators with basic, clinical or translational research programs. Over the course of the academic year, students participate in courses, journal club seminars, a structured lecture series and clinical teaching rounds at the NIH Clinical Center. They also present their research to the NIH community and at national and international professional conferences. “The NIH Medical Research Scholars Program attracts the brightest talent from across the country. These scholars are the future leaders in American medicine,” said Thomas R. Burklow, M.D., director of the program.
[ Fa l l / Wi n t e r 2 019 ]
13
MEDICAL EDUCATION
College Aims to Boost Numbers of Primary Care Physicians from Diverse Backgrounds Oklahoma’s poor health outcomes are partly due to access to medical care: Of the state’s 77 counties, 76 have a shortage of primary care physicians. Seventy-three counties don’t have enough mental health professionals to care for the population. Those statistics, from the Oklahoma State Department of Health, may paint a discouraging picture, but the OU College of Medicine is determined to change those numbers, year by year. And the college has received new resources for the work: a $4.7 million grant from the U.S. Department of Health and Human Services. “We have a great need for primary care physicians in our state, particularly in rural areas, under-represented communities and tribes,” said Steven Crawford, M.D., Senior Associate Dean and Director of Healthcare Innovation and Policy. Crawford is leading the grant with James Herman, M.D., dean of the OU-TU School of Community Medicine on the Tulsa campus. The aim of the grant is two-fold: to recruit, retain and admit students from rural, tribal and medically under-represented areas, and to enhance the primary care experience among current medical students. Data shows that students from those groups who attend medical school and residency in Oklahoma are more likely to return to their communities to practice medicine. The ultimate goal is to reduce healthcare disparities among Oklahomans and raise the health of the state. The School of Community Medicine, the college’s branch campus in Tulsa, is a prime example of the need. The school was founded in 2008 in the wake of a city study that revealed a 14-year difference in life expectancy between people who live in north Tulsa and south Tulsa. When a person’s ZIP code largely dictates their health, change is needed. “Clinicians need to understand the needs of the people they are serving, to understand the facilitators of their health, to manage chronic disease, but also to understand the barriers to that for their patients,” said Frances Wen, Ph.D., an associate professor of family medicine on the Tulsa campus and a primary faculty participant in the grant. “Having personal and lived experience more fully informs a clinician’s approach to working with the people they serve.” The School of Community Medicine plans several experiences designed to help current students better understand the importance of primary care and perhaps choose it for their future careers. Two new courses, Lifestyle Medicine and Health Promotion I and II, have been added to the curriculum to further educate students about the roles of food and exercise in promoting better health for their patients. Two other courses, Health System Science in Practice I and II, teach
14
Recruiting, retaining and admitting students from diverse backgrounds is the aim of a new grant from the U.S. Department of Health and Human Services.
students skills needed to practice in the modern health system. They also take students on a deeper dive into the social determinants of health – understanding that their patients’ health is affected by what takes place in their families, neighborhoods, the community at large and healthcare systems. Students will put that knowledge into practice during the ongoing longitudinal care they provide at Bedlam Clinics, where people without health insurance receive treatment. Wen said partnerships also are being developed with the Creek Nation and Hillcrest Health System so that students can gain experience in their rural networks. “Despite everything a physician can do, if we can’t get patients access to healthcare, then we’re not going to be able to improve their quality of life,” Crawford said. “We need more primary care professionals so that we can focus on prevention – providing vaccines, mammograms, colonoscopies and other things that can prevent disease or discover it at its earliest stages.” However, to significantly increase Oklahoma’s number of primary care health professionals, the college must move upstream by interacting with students who are in middle and high school, mentoring those with interest and helping them clear hurdles to becoming a doctor. The new grant will expand several existing programs in the College of Medicine in which students come to campus to
[ Fa l l / Wi n t e r 2 019 ]
MEDICAL EDUCATION
interact with healthcare professionals and researchers. Programs like Club Scrubs and Mini Medical School have already seen success in sparking interest among young people. Robert Salinas, M.D., a family medicine physician and assistant dean for diversity, said the success of such programs hinges on supporting students for years along the pathway to medical school. “We believe that we can address the inequities in healthcare by bringing in students from diverse backgrounds – women, people from rural Oklahoma, the Latino and Hispanic communities, Native Americans, African-Americans and others who have traditionally been under-represented,” Salinas said. “Data suggests that if you bring in a more diverse workforce, you have better health outcomes. Those better outcomes may happen for a number of reasons – understanding the patient, culturally and linguistically, understanding their belief systems – but the overall goal is to bring in more students from around the state who want to go back and serve their communities, specifically in primary care.” Faculty from both campuses plan to reach out to primary care physicians in communities across the state to enlist them in mentoring young people who dream of becoming physicians or other healthcare providers. Doctors across Oklahoma are especially positioned to identify young people, perhaps their own patients, who are interested in medicine. “This grant asks us to be innovative and to create strategies – how do we reduce health disparities by bringing in students from under-represented groups who want to go back and serve their communities?,” Salinas said. “In what ways can we expose our current medical students to the importance of primary care? I believe this type of work is an institutional responsibility. As an academic health system, we have an obligation to provide leadership for the state.”
Brain Tumor Center in San Francisco in the laboratory of Shawn L. Hervey-Jumper, M.D. Almeida’s project focused on primary brain tumors in adult patients, who often lose the ability to speak, read or write. In particular, he explored tumor cells that affect the pathways controlling cognition in the brain. Findings from the study will lead to better understanding of the brain’s ability to repair and modify itself in response to brain tumors. “Understanding the pathophysiology of this disease is critical for developing the next generation of cutting-edge treatments,” he said. Almeida said he has long had a goal of becoming a physician-scientist. Working in an internationally recognized research laboratory is a significant opportunity on that path. “Improvements to medical care don’t occur in a vacuum,” he said. “Translational research has always been fundamentally important in bringing advancements from bench to bedside. For this reason, I find it fascinating to be involved in work that could potentially lead to novel treatment options and bring about tangible benefits.” Recipients of the AOA research fellowship are excellent students who want to increase their understanding of scholarly discovery, said Annie Moreau, M.D., associate professor in the Department of Ophthalmology and AOA councilor for the OU College of Medicine. “We are very proud of Nyle’s academic excellence and his enthusiasm for this research fellowship,” Moreau said. “He will no doubt be a wonderful physician who understands the value of research in providing the very best care for his patients.”
This project is supported by the Health Resources and Services Administration of the U.S. Department of Health and Human Services as part of an award totaling $4,704,476 with 10% financed with nongovernmental sources. The contents are those of the authors and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS or the U.S. Government.
AOA Awards Research Scholarship to Medical Student OU College of Medicine student Nyle C. Almeida, a member of the Class of 2022, spent the summer participating in a research fellowship made possible by a grant from the Alpha Omega Alpha medical honor society. Almeida was awarded the AOA’s 2019 Carolyn L. Kuckein Student Research Fellowship, which provides a $6,000 award for medical students to undertake a research project with an academic mentor. Almeida conducted his research at UCSF
Associate Dean for Student Affairs Mark Fergeson, M.D., presents a check to medical student Nyle C. Almeida for his participation in the AOA summer research fellowship.
[ Fa l l / Wi n t e r 2 019 ]
15
PATIENT CARE
A beam signed by numerous employees, accompanied by a tree and flags, is raised to the top of the new patient tower during a topping out ceremony on Nov. 6.
Topping Out Ceremony Marks Construction Milestone for New Patient Tower The largest hospital expansion project in Oklahoma history achieved a major construction milestone Nov. 6 as the OU Medicine patient tower reached its highest structural point. Under construction on the OU Medicine health campus and slated for opening late next year, the milestone was marked by celebration as the symbolic final beam was placed in the topping out ceremony. OU Medicine leaders, state and local dignitaries, employees and other guests heard remarks delivered by Jerome Loughridge, Oklahoma’s Secretary of Health and Mental Health, during the festivities. OU Medicine, Inc. CEO Chuck Spicer talked about the impact the new patient tower will make on Oklahoma’s healthcare and economics. “The tower represents not only state-of-the-art patient care, but is also creating new economic drive with statewide impact in this central Oklahoma hub of innovation, research, education and employment,” Spicer said. “Since 2018, OU Medicine has added 600 employees; as 2020 begins, an estimated
16
additional 100 full-time positions will become available.” Designed by Perkins and Will, the new patient tower will span 450,000 square feet over nine floors (eight of those above ground), with room to grow. This marks the first ground-up hospital construction project for OU Medicine since 1975. The current expansion will add 144 beds and 32 operating rooms to help support the needs of patients treated at Stephenson Cancer Center, those undergoing critical and complex surgical procedures, those with trauma-related injuries and more. “Often, the people we care for are here during times of great crisis in their lives,” said Kris Gose, OU Medical Center president. “Family space is a critical design element that you’ll see integrated in multiple ways. Patient rooms are bigger, with more space for visitors. Windows will offer views of the state Capitol or the city’s skyline. The space also will support efficiency of care with more room for doctors and nurses to function with ease.”
[ Fa l l / Wi n t e r 2 019 ]
PATIENT CARE
OU Medicine is the only comprehensive academic health system in the state, offering the widest range of medical and surgical services in the region. Skill, expertise, experience and talent all contribute to successful outcomes in any field of endeavor, said Ian Dunn, M.D., chair of the Department of Neurosurgery in the College of Medicine. “In every field, the craftsman, artisan or physician is capable of delivering a more satisfying product or experience when he or she has the best tools and the best-equipped environment in which to work,” Dunn said. “That’s what the new patient tower represents. Working as a team, we optimize our skills for the benefit of every patient who crosses the threshold of this center of health and healing.” The topping out ceremony can be traced to an ancient Scandinavian religious rite of placing a tree atop a new building to appease the tree-dwelling spirits displaced in its construction. As buildings became less timber-framed and more steel, the ceremony morphed into a tree or leafy branch being placed on the topmost beam, often with a flag tied to it. Today, in true Oklahoma fashion, a tree, the American flag and the Oklahoma state flag were placed with the final beam. The beam had been signed by many OU Medicine employees and guests at the topping out ceremony.
Elisa Crouse, M.D., associate dean for Graduate Medical Education at the OU College of Medicine, began working with architects early in the planning process to provide input about the particular needs of a hospital where residents and other learners are part of the healthcare team. The patient rooms will be larger than traditional rooms not only to accommodate an interprofessional team of healthcare providers and learners, but so that family members have ample space as well. “The rooms will be large enough for the team to come in and see the patient, but also to discuss their treatment with family, because one of our missions is to involve the patient and family in their own healthcare,” Crouse said. “The rooms will facilitate that with privacy so we can visit openly with patients and families.” On each patient care floor, there will be a conference room and three team rooms, where residents can discuss patient care issues as a group and participate in teaching sessions near patient rooms. At both ends of each floor, there will be smaller triangular spaces where an attending physician and residents can discuss something without having to walk back to a team room. “If they need to step out of the patient room to discuss something that furthers their learning, they don’t have to talk in the hallway where there’s less privacy,” Crouse said. “They can step into these spaces to discuss care issues, which allows the learning to happen in the clinical flow of rounding on patients. Later, they might go to a team room and pull up images or perform literature searches, and have in-depth discussions about appropriate care for different diseases or situations.” Another major feature is a large simulation center with two simulation rooms and several debriefing rooms. One simulation room is set up as an operating room suite, complete with anesthesiology booms and operating beds; the other room is more flexible so that it can be used by non-surgical specialties. Faculty will devise and oversee a variety of simulations designed to fine-tune residents’ skills and prepare for the unexpected. Simulations may include patient transports from the ER; patient handovers and related communication; interdisciplinary care; perioperative safety; and mock emergencies. Simulations can be videotaped, and the team can review them in debriefing rooms.
As seen from above, the new patient tower at OU Medical Center is taking shape, with plans to open in late 2020.
New Tower Designed With Trainees in Mind When OU Medicine’s new bed tower opens in 2020, it will have spaces that have been intentionally designed for trainees in a teaching hospital.
Of a more practical nature, there will be call rooms on each floor where residents and others can relax or take a nap as they are able during a long shift. Secure lockers will be incorporated into the new tower, as well as ample electrical outlets and USB ports to support a multitude of trainees who use mobile technologies to deliver patient care. “With the new bed tower, we’re not only growing our patient volume, but we’ve enhanced our educational space,” Crouse said. “It’s a wonderful opportunity for us and for all of our learners.”
[ Fa l l / Wi n t e r 2 019 ]
17
PATIENT CARE
Stephenson Cancer Center Offering CAR-T Immune Therapy A revolutionary new treatment that harnesses the body’s own immune cells to fight tumors is now being offered at the Stephenson Cancer Center at OU Medicine. Called CAR T-cell therapy, the treatment has been approved by the Food and Drug Administration and is being offered in Oklahoma only at the Stephenson Cancer Center. Its initial use is for two different blood cancers, one affecting children and the other affecting adults. “CAR-T is a major breakthrough for patients who have not improved with standard treatments,” said George Selby, M.D., director of the Stem Cell and Cellular Transplant Program at the Stephenson Cancer Center. “It is an immune therapy in which we’re harnessing our own cells to recognize cancer cells. That’s what a normal immune system does – it acts in a surveillance capacity so that when a malignant cell arises, it is killed by our immune system. CAR-T is a way of ‘rebooting’ the immune system when it has failed.” CAR-T initially will be used to treat advanced lymphomas in adults. In the coming months, physicians anticipate offering similar treatment for acute lymphoblastic lymphoma in children and young adults. In both cases, patients must have failed to respond to standard chemotherapy or stem cell transplant. CAR-T stands for Chimeric Antigen Receptor T-cell therapy. Patients being treated with CAR-T will first have their blood collected at the Oklahoma Blood Institute in a process that is similar to a typical blood donation. T cells, a type of white blood cells involved in immunity, are filtered out and the plasma and red cells are returned to the patient. The T cells are then sent to a company that injects them with the gene for a chimeric antigen receptor, which is known to bind itself to cancer cells and activate the T cell. This process allows the newly engineered T cells to recognize and attack cancer with remarkable efficiency. Once the CAR-T cells are generated, they are shipped back to the Stephenson Cancer Center and given to the patient through an IV, much like a blood transfusion. “Until the advent of CAR-T, if a patient’s tumor came back after a stem cell transplant, their options were very limited, if they existed at all,” Selby said. “This is a major breakthrough for those patients for whom standard treatment has not been successful.” Unlike other types of cancer therapies, CAR-T is a one-time treatment. The T cells remain in the body and, if the cancer
18
Adam Asch, M.D, deputy director of the Stephenson Cancer Center and chief of the Division of Medical Oncology and Hematology, speaks about the advent of CAR-T for patients with blood cancers.
comes back, the cells reactivate to attack the tumors. “These T cells go on to kill hundreds to thousands of tumor cells; the nickname for these cells is ‘serial killers,’” said Adam Asch, M.D, deputy director of the Stephenson Cancer Center and chief of the Division of Medical Oncology and Hematology. Using the immune system to fight cancer has been the holy grail for oncologists, Asch said. In recent years, basic science research has yielded important information about how the immune system functions and has identified targets that enhance the killing efficiency of T cells. CAR-T is especially exciting because of the excellent patient outcomes during clinical trials. “The research data that led to the approval of CAR-T has been extraordinary,” Asch said. “This therapy appears to be long-lasting in a high percentage of these patients.” CAR-T is incorporated into OU Medicine’s Stem Cell and Cellular Transplant Program, whose healthcare providers have received special training in the procedure and caring for patients. Selby provides leadership for the adult transplant program, joined by David Crawford, M.D., as head of the pediatric transplant group. With time, CAR-T’s use will only grow. Clinical trials are underway studying the effectiveness of CAR-T in treating other blood cancers, including multiple myeloma, as well as solid tumors. Another trial will study the effectiveness of CAR-T as compared to transplant; CAR-T potentially could
[ Fa l l / Wi n t e r 2 019 ]
PATIENT CARE
move ahead of transplant as a treatment because of its ability to use the patient’s own immune system rather than someone else’s. The Stephenson Cancer Center will be participating in several such clinical trials. CAR-T joins a growing collection of resources at Stephenson Cancer Center. Since earning National Cancer Institute designation last year, Stephenson is among the top 2% of cancer centers in the nation and is a leader in improving the level of care and quality of life of patients with cancer. “Our resources and personnel are unmatched because of NCI designation,” Selby said. “CAR-T is among the first of many good things to come out of NCI designation for the Stephenson Cancer Center.”
Thoracic Surgeons Offer Minimally Invasive Lung Cancer Surgery Kathy Shaw of Oklahoma City was less than six months out from treatment for breast cancer when she learned that she had nodule on a lobe of her lungs that was cancerous. It was more than she could bear to think about. She had just undergone a double mastectomy, chemotherapy and radiation, and the idea of undergoing another major surgery was disheartening. She was told that lung cancer surgery would involve a large incision, the spreading of her ribs to access the lungs and a lengthy hospital stay and recovery. “I went ahead and made the appointment for the surgery, but in my heart, I didn’t feel like I would go through with it,” she said. Instead, she began looking for another option. That search led her to thoracic surgeon J. Matthew Reinersman, M.D., an assistant professor in the Department of Surgery in the OU College of Medicine. Reinersman and his colleague Subrato J. Deb, M.D., are the only two surgeons in Oklahoma who specialize in a minimally invasive surgery for lung cancer called VATS – Video-Assisted Thoracoscopic Surgery. The surgery, which requires only three small incisions, removes the cancer while giving patients a much shorter hospital stay, less risk for complications and faster recovery. “I had the VATS surgery, and I went home after two days,” Shaw said. “I think I took one or two pain pills, but I didn’t experience what I would call real pain. Because of the procedure and Dr. Reinersman, my recovery has been pretty remarkable.” Reinersman has been performing VATS for patients with lung cancer since he arrived at the OU College of Medicine four
Kathy Shaw of Oklahoma City underwent VATS, a minimally invasive surgery.
years ago. Studies have shown VATS to result in outcomes that are just as good as those in a traditional, open surgery, but with all the benefits of a minimally invasive procedure. In the traditional procedure for removing cancers of the lung, surgeons make a large incision on the patient’s side and push apart the ribs to reach the lungs. This results in significant pain for the patient and a hospital stay of at least five to seven days, which then leads to greater risk of pneumonia, blood clots and infections. During VATS, Reinserman makes three small incisions to insert a tiny camera and his surgical instruments. The camera transmits images of the lungs onto a video screen to guide the surgery. Depending on the location of the cancer, he may remove a small part of the lobe, the entire lobe or more of the lung. Nearby lymph nodes also are dissected to ensure the cancer has not spread. “The advantage is that we can get patients out of the hospital as soon as one to three days after the procedure,” Reinersman said. “They have less pain, fewer side effects and can return to their normal activities faster.” The reduction of pain is a significant advantage of VATS. Patients having open surgery for lung cancer usually receive
[ Fa l l / Wi n t e r 2 019 ]
19
PATIENT CARE
an epidural catheter in their backs for pain control. Pain must be managed because patients need to be able to take deep breaths and cough to lower their risk of getting pneumonia – something they won’t do as well if they are hurting. Because VATS is minimally invasive, no epidural catheter is needed and pain is greatly minimized. Surgeons also use nerve blocks to provide long-acting pain control in the nerves that run along the ribs. “When I see my patients back in the clinic a couple of weeks after surgery, they’re usually taking little to no pain medicine and they’ve resumed doing most of the things they want to do. It’s really gratifying,” Reinersman said. Reinersman considers VATS for any patient with lung cancer, but the best candidates are those with Stage 1 or 2 cancer, he said. VATS is also preferable for patients who have borderline lung function because the procedure is easier for them to tolerate than an open surgery. In Shaw’s case, she has never been a smoker. About 20 percent of people diagnosed with lung cancer are non-smokers, Reinersman said. “That shows the importance of lung cancer screening and early diagnosis and treatment,” he said. “It’s not a death sentence. If we can catch it early, we can get them through it. We’ve done hundreds of VATS surgeries here.”
Many surgeons will use VATS for simple surgical procedures in the chest, but Reinersman and Deb are experts in its use for removing lung cancer, a more technically complicated surgery. The surgeons also are unique because they focus solely on surgeries of the chest and esophagus, whereas many cardiothoracic surgeons focus mostly on the heart. OU Medicine is also the only institution in Oklahoma that submits its lung cancer surgery data to the Society of Thoracic Surgeons General Thoracic Surgery Database, where it can be viewed by the public. OU Medicine’s two-star rating is equivalent to that of larger institutions like Mayo Clinic and M.D. Anderson.
Pediatric Surgeon Performs Lifesaving Surgery on Infant With Urological Condition Edmond residents Juan and Bibiana Rodriguez were excited to welcome their first child into the world and, after a normal pregnancy, their beautiful boy Simon was born. But only 12 days later, Simon began running a high fever and the Rodriguez family started a journey of surgery and medical care that was crucial to their son’s future. Initially, doctors thought Simon simply had a urinary tract infection, but it soon became apparent that something more was taking place. OU College of Medicine pediatric urologist Adam Rensing, M.D., diagnosed Simon with posterior urethral valves, a condition in which extra flaps of tissue, or valves, block the flow of urine so that it cannot leave the body in a normal way. The condition is serious because the baby’s bladder and kidneys can be damaged, sometimes to the point of renal failure. Posterior urethral valves is a congenital condition that is usually diagnosed during a prenatal ultrasound. However, for the Rodriguez family, the condition was not spotted during the pregnancy. Because the problem was diagnosed early, though, Rensing performed the surgery quickly. The procedure involves using a scope and a small blade to cut the tissue away so that the urine can flow and the bladder can empty more normally. Rensing compared the condition to the sail on a sailboat that catches the wind.
J. Matthew Reinersman, M.D., specializes in a minimally invasive surgery for lung cancer.
20
“When someone needs to pass urine out of the bladder, the valves fill up like a pair of sails and obstruct the flow of urine,” he said. “The valves are an abnormality that only serve as a blockage.”
[ Fa l l / Wi n t e r 2 019 ]
PATIENT CARE
“The No. 1 thing I tell families is that no matter how quickly we get to the patient and cut the valves, the changes to the bladder and kidneys are lifelong and need to be monitored closely, both by myself as a surgeon and by a nephrologist looking at the medical side of the urinary tract.”
Juan and Bibiana Rodriguez are pictured with their son Simon, who underwent a critical surgery performed by pediatric urology Adam Rensing, M.D.
The Rodriguez family said Rensing and his team have helped them understand and manage a frightening and difficult diagnosis. “Dr. Rensing is an incredible human being,” Bibiana said. “He is an amazing professional, and we feel like he’s become part of our family.” Although the surgery was lifesaving and corrected the immediate problem, posterior urethral valves usually causes problems for years to come. The problem begins in utero, when the baby’s bladder fights against the blockage. Because urine can’t get through the urethra, the bladder becomes distended and pushes up against the kidneys, which either don’t develop properly or become damaged. And because of the pressure on the bladder, the urine often flows back up into the kidneys, causing further problems. Even after the valves have been cut away, the bladder can change from a dynamic organ to a static, inflexible state, unable to fill and empty properly. “The No. 1 thing I tell families is that no matter how quickly we get to the patient and cut the valves, the changes to the bladder and kidneys are lifelong and need to be monitored closely, both by myself as a surgeon and by a nephrologist looking at the medical side of the urinary tract,” Rensing said. Simon is now over a year old, and Bibiana said she must insert a catheter three times a day and again just before he goes to bed. He also takes a low dose of daily antibiotics to ward off infections. The daily regimen can be challenging, she said. “It’s tough for us because I had to stop working – I cannot put him in a daycare,” Bibiana said. “When we do the cathing, we make sure we’re in a clean space and I wash my hands and Simon stays clean. We also make sure he eats healthy
foods so that his kidneys don’t have to work too hard. It’s a challenge, but I try to make him feel as normal as I can.” The Rodriguezes monitor Simon for a return of urinary tract infections, and they see an OU Medicine pediatric nephrologist regularly to assess his kidney function. There are no guarantees about how smooth or difficult the condition will be to manage as Simon grows up. Children born with the condition often wear diapers longer and need intermittent catheterizations to finish emptying the bladder because they have lost the sense of when they need to urinate. The condition can also affect quality of life as the child goes through adolescence and begins spending more time away from his parents. “With this condition, I’m working with the family to prepare them to handle everything,” Rensing said. “That’s why I think so highly of the Rodriguez family – they are the best parents you could ask for. They’re very on top of things, compliant with recommendations and are forthcoming with any issues they’re having, which is so important with pediatrics.” As new parents, the Rodriguez family gained the realization that they would do anything for their child, Bibiana said. That keeps her going during the ups and downs of managing Simon’s condition. “He’s a very happy boy,” she said. “He likes to explore everything and wants to know everything. I know there are no guarantees about his future quality of life, but we are adjusting and we are hopeful.”
[ Fa l l / Wi n t e r 2 019 ]
21
PATIENT CARE
been through abuse and neglect doesn’t automatically mean they need treatment. Some of our kids are really resilient and bounce back. We want to put less burden on our mental health system by identifying which children need services, rather than saying everyone needs it.” The screeners were geared toward children from birth to age 3 (and their caregivers) and children ages 4 to 17. For the younger group, caseworkers asked questions that assessed each child’s developmental milestones, such as ability to walk, roll over and say two-word sentences. For children age 4 to 17, the screener focused on four areas: inattention; externalizing behavior such as being defiant; internalizing behaviors such as withdrawal; and trauma responses.
Carisa C. Wilsie, Ph.D.
Center on Child Abuse and Neglect Partners with DHS to Develop Screening for Youth in Foster Care Children in custody of Oklahoma’s child welfare system may react in a multitude of ways to the abuse or neglect that sent them to a foster home. The Center on Child Abuse and Neglect (CCAN), a program within the University of Oklahoma College of Medicine, plays a significant role in identifying which children need treatment for their trauma and the types of services that will help them heal and build resilience. CCAN partnered with the Oklahoma Department of Human Services (DHS) to develop and administer a child behavioral health screener for children in state custody. The screener was designed for the prevention, early detection and treatment of behavioral and mental health difficulties. Questions on the screener assessed responses to trauma in children from birth to age 17. CCAN, in partnership with DHS staff, then trained DHS caseworkers, who visit each foster home monthly, to administer the screenings. The first iteration of the project, funded by a federal grant from the Children’s Bureau, saw 18,000 children screened multiple times over nearly three years, resulting in a treasure trove of data pointing to improved outcomes for both children and caregivers. “We wanted to identify kids early on and on a continuous basis,” said Carisa C. Wilsie, Ph.D., clinical assistant professor at CCAN. “Sometimes kids come into foster care and are fine during their first medical assessment. But it’s difficult to see the full picture of a child in one instant. Many children end up having problems later. At the same time, just because they’ve
22
When children received a score on the behavioral health screener that warranted a referral, they were connected with state services according to their age and needs. The results of that process were significant and positive, Wilsie said. The team accessed Medicaid data showing the types of treatments provided to children and the time frame they were provided during the study period. Of the children who needed treatment, 79% of them received services within 60 days. As children continued to receive screenings over time, those who were in treatment services saw their scores improve more quickly than those not in treatment, especially if they received evidence-based services. Children who were screened also had fewer foster home placements. “We thought that was really positive because it saves the state a lot of money in having to change placements, but it also means that we’re either getting kids reunited with their biological families quicker, or they’re getting on the adoption track quicker, which puts them in a permanent home situation sooner,” Wilsie said. Younger children in foster care also experienced successes. When caseworkers discovered that several children were regressing in their development milestones, their treatment revealed they had hearing impairments that no one knew about previously. In some cases, the problem was remedied by simply draining fluid from a child’s ears, allowing their speech and language development to improve. DHS caseworkers, too, reported the screener helped them better understand a child’s well-being, as well as looking at the behaviors of children through a “trauma lens” instead of viewing them as “bad kids.” In one instance, a child went from hiding under the covers in her bed to laughing and talking with her caseworker. DHS has now begun using the behavioral health screener with children who are in group homes and shelter care. Wilsie is serving as a consultant during the process and will guide the analysis of data as the screener continues to be used. “The value of the screening is not just that we got kids in services, but that we improved communication between caseworkers and foster parents,” she said. “They administered the screener more than 112,000 times in total, which meant ongoing conversations about the child’s needs and well-being.”
[ Fa l l / Wi n t e r 2 019 ]
PATIENT CARE
“I’m incredibly excited about this new facility,” said Morris Gessouroun, M.D., chair of the Department of Pediatrics at the OU College of Medicine. “It has been highly anticipated and will dramatically improve our capacity to care for the children of Oklahoma in need of these high-intensity and high-tech services. This pediatric ICU will be the most modern and technologically advanced PICU in the state, while at the same time being the most family-friendly of any such care facility in Oklahoma.” Housed on the sixth floor of The Children’s Hospital, the new PICU will have 34 non-cardiac intensive care unit beds, providing state-of-the-art care for seriously ill and injured kids up to 18 years of age. Previously, The Children’s Hospital had 13 non-cardiac intensive care unit beds and 12 cardiac intensive care unit beds. Renovations to those existing 25 PICU beds will begin in the near future, modernizing the existing area to become the cardiac intensive care unit, thereby increasing the total intensive care unit beds at The Children’s Hospital to 59. “Increased capacity means more patients receive the care they need from the most skilled providers with great depth of experience,” said Jon Hayes, president of The Children’s Hospital. “We struggled at times to be able to care for the many patients who needed our services. Now we are able to better fulfill our mission -- to take care of every child through our combined efforts.” Beyond superb patient care, the facility and its staff focus on family-centered care, providing support for the practical and emotional needs of family members. During construction, a family advisory council previewed the expansion and provided input based on first-hand experience. Amenities such as private bathrooms, separate sleeping areas and places to watch TV were among the recommendations.
A therapy dog from The Children’s Hospital helps with the ribbon cutting for the grand opening of the expanded Pediatric Intensive Care Unit.
The Children’s Hospital Completes PICU Expansion This summer, The Children’s Hospital held a grand opening celebration of its newly expanded Pediatric Intensive Care Unit (PICU). More than six years in the planning and implementation, the facility represents a $27.5 million investment in improving quality of care for children throughout Oklahoma and the surrounding region.
The PICU offers these services and features, among others: • 24/7 in-house, board-certified physicians with specific expertise in pediatric critical care medicine • PICU-trained physical and respiratory therapists • Family-centered approach to care includes private family spaces • Family spaces within patient rooms • Child life specialists with specific training for intensive care environments • Advanced technologies including: • Latest generation emergent extracorporeal membrane oxygenation (ECMO) • Renal replacement therapy • Bariatric rooms capable of providing care for obese patients • Isolation rooms for burn and immunocompromised patients.
[ Fa l l / Wi n t e r 2 019 ]
23
PATIENT CARE
Gynecologic oncologist Katherine Moxley, M.D., left, is pictured with her patient Tara Dominguez.
Cancer Survivor Encourages Other Survivors to Return to Those Things That Inspire Their Passions Tara Dominguez didn’t fit the profile, if there is one. She was young, with no personal or family history of cancer, and with none of the “usual” risk factors. The diagnosis – cervical cancer - was shocking. It was early in 2016, and a routine pap smear revealed an abnormal growth. A subsequent biopsy with Dominguez’ regular obstetrician-gynecologist determined cancer was present. “I asked where I should go for treatment – thinking I might be headed to Houston or New York. When I found out there was a cutting-edge cancer center right here in Oklahoma City, it really put my mind at ease,” Dominguez said. Her doctor referred her to Katherine Moxley, M.D., Stephenson Cancer Center gynecologic oncologist.
24
As a pharmacist, Dominguez had a healthcare background and her education was science-heavy. With that perspective, she familiarized herself with treatment guidelines. She understood the drugs and what therapy entailed. She asked myriad questions and gained a thorough understanding of what she was facing. “I got in to see Dr. Moxley right away. When I met her, she already had a plan and I was scheduled for surgery within a month,” Dominguez said. Dominguez had what was believed to be a fairly early-stage cervical cancer. According to Moxley, the imaging studies looked normal, but did not tell the whole story. Initially, surgery was the primary treatment, and in 85% of cases,
[ Fa l l / Wi n t e r 2 019 ]
PATIENT CARE
surgery would have been enough. Unfortunately, Dominguez defied these odds. Pathology identified high-risk characteristics requiring more aggressive treatment. Dominguez came to Moxley and Stephenson Cancer Center hoping to participate in a clinical trial that used less-aggressive treatment approaches aimed at preserving fertility. But from the beginning, her options began to dwindle. “We learned the tumor wasn’t confined to cervix,” Moxley said. “Chemotherapy combined with radiation became the next course of treatment, with radiation being the larger component.” Dominguez was no longer eligible for the fertility-sparing treatments she had hoped for, but became a candidate for a different trial focused on chemo radiation with chemotherapy. Newly married, Dominguez began to see one of her dreams – motherhood – slipping away. Moxley began to work through options that would enable Dominguez and her husband to become parents on the other side of treatment and recovery. Moxley said the physician’s primary goal for patients is to keep them whole, alive and undamaged. “So,” Moxley said, “the next question became, ‘How can we ensure your ability to have children?’ The answer took Donimguez through infertility treatments, and once they had viable embryos, she came back for surgery.” For Moxley, it felt as if each meeting was another occasion in which she had to deliver a new and different piece of bad news. “These findings were exceedingly uncommon, and it was astounding that they all happened to Tara. Repeatedly, I had to say, ‘…..but there’s something different, something more or something else.’” An avid runner before diagnosis, Dominguez competed in cross country events throughout high school. Later she started running 5Ks and 10Ks, then advanced to running a dozen or more half-marathons each year. Here too, Dominguez faced another significant loss in the life she had known. “After surgery I couldn’t run of course, but more than that, I was advised that radiation treatment would probably mean the end of running altogether,” Dominguez said. Now a cancer survivor, Dominguez also has become a runner again, thanks in large part to Moxley’s steadfast encouragement. Recovering from treatment, Dominguez and Moxley both completed the 2017 Go Girl Run. “Dr. Moxley stayed after the race to cross the finish line with me,” she said. “It was a new start to this new chapter, returning to being able to run.” Dominguez has completed five half-marathons this year. She participated in the Outpace Cancer Race 10K event on Oct. 6, with Moxley once again as her running partner.
“We seek to cure cancer, but also, enable individuals to return to those things that inspire their passions.”
to those things that inspire their passions,” Moxley said. Though the physician/patient relationship is first defined by professionalism, cancer treatment introduces a different dynamic. For Moxley and Dominguez, appointments were frequent and spanned an entire year. “Discussions about life and health are intensely personal. During that time, I came to know Tara as a person, as well as a patient. You can’t really treat someone for a long-term condition if you don’t know their lives,” Moxley said. “Cancer is like ‘slow trauma.’ You walk through it with the patient as an advocate.” As if experiencing a kind of mutual grace, the conversations seemed to follow a pattern with Moxley’s refrain, “I’m so sorry,” and Dominguez’ response, “Well, this is what we have before us, and I know you’re going to do the best thing for me.” Moxley described Dominguez as incredibly stoic and strong, meeting each new challenge with courage and determination. “Tara came through therapy beautifully, and her long-term prognosis is excellent. Aggressive treatment was crucial.” At Stephenson, Dominguez said she found one of the best treatment facilities in the nation. “I received the best care possible from amazing doctors – the best minds from across the country -- and incredible staff. All that, and not having to travel for treatment, having friends, family and a complete support network right here. … I already had obstacles in my mind, but these were no longer obstacles I had to cross.” Dominguez underwent chemotherapy and radiation treatment spanning nearly four months. She credits radiation oncologist Spencer Thompson, M.D., and his staff for making her feel so much at home and so confident of the care she received. Dominguez said her experience with cancer in some ways mirrors the effort of being a runner. “There are days you’re going to have setbacks, but you’ll also experience great joy and success.”
“We seek to cure cancer, but also, enable individuals to return [ Fa l l / Wi n t e r 2 019 ]
25
PATIENT CARE
Matthew Reinersman, M.D., is pictured with his patient Carla Prothro
Lung Cancer Survivor Gives Thanks With Every Step During Stephenson Cancer Center’s Outpace Cancer Event When Carla Prothro took part in the Outpace Cancer run/walk on Oct. 6, every step she took served as thanks for Stephenson Cancer Center physicians and nurses who gave her a second chance at life. Prothro, who lives in Tulsa, is among many patients, family, friends and employees who took part in the second Outpace
26
Cancer event, which raises money for cancer research and patient support at Stephenson Cancer Center. Prothro, who is a lung cancer survivor, said she was determined to fight against her Stage 4 cancer, and she credits thoracic surgeon Matthew Reinersman, M.D., with giving her the opportunity to win the battle. “The Outpace Cancer race gives me a chance to remember why I’m able to participate – because of the care I received at Stephenson Cancer Center and from Dr. Reinersman,” she said. Prothro’s journey with lung cancer began in March 2018, when she learned she had a tennis ball-sized tumor in the left upper lobe of her lung. Her determination to find the best care began by talking with her sister, who works at Mayo Clinic in Rochester, Minnesota. She received a second opinion from Mayo physicians, who recommended that she return to Oklahoma to see Reinersman, who completed his residency training at Mayo.
[ Fa l l / Wi n t e r 2 019 ]
PATIENT CARE
“I was fearful of the surgery; I’d never had surgery in my life. But I knew I was in very good hands, literally. I trusted everything Dr. Reinersman told me. And now I’m here and doing great. It’s been an incredible journey.” She did, and has never looked back. Prothro’s cancer was confirmed, but she also learned that it had spread to her right lung. Reinersman, working with her oncologist in Tulsa, created a treatment plan: She would undergo chemotherapy with immunotherapy, followed by radiation to the nodule on her right lung. Then she would have surgery to remove the cancer in her left lung. “Carla is very vibrant and strong – she is a fighter,” Reinersman said. “She wanted to do whatever it took to get rid of the cancer and beat it in any possible way that she could. I assured her that we would think outside the box. If patients are good candidates and in good shape, and they want to pursue aggressive treatment, we are going to figure out a way to help them.” Prothro made it through four months of chemotherapy and radiation, fueled by the belief that she was taking steps toward becoming cancer-free. When the day of the surgery arrived, she was nervous but determined to keep moving forward. “I was fearful of the surgery; I’d never had surgery in my life,” she said. “But I knew I was in very good hands, literally. I trusted everything Dr. Reinersman told me. And now I’m here and doing great. It’s been an incredible journey.” Prothro not only walked in Outpace Cancer, but she raised money and invited her family, who supported her along the way, to take steps alongside her. Each person participating and each dollar raised creates a brighter future for cancer patients, Reinersman said. “Cancer research may sound like a generic thing, but that’s the way we can really make a difference,” he said. “Research is the way we have been able to bring about new and exciting drugs and treatments that have really helped people.”
Participants in the Outpace Cancer race and walk begin the event, which weaves through the OU Health Sciences Center.
Stephenson Cancer Center Welcomes Hundreds to Outpace Cancer In October, Stephenson Cancer Center hosted its second Outpace Cancer race and walk. The event raises money for cancer research and to provide support for cancer patients and their families. This year, nearly 1,500 runners and walkers took part in 10k and 5k races and a 1-mile walk. The event raised $150,000.
[ Fa l l / Wi n t e r 2 019 ]
27
RESE ARCH
Peggy and Charles Stephenson, center, are joined by Stephenson Cancer Center Director Robert Mannel, M.D., left, and OU Interim President Joe Harroz during an announcement of the Stephensons’ new $20 million gift.
Stephenson Cancer Center Announces $20 Million Gift for Research Stephenson Cancer Center at OU Medicine announces a transformative $20 million gift from the Stephenson Family Foundation and Peggy and Charles Stephenson, the center’s namesakes and longtime supporters of the University of Oklahoma. The gift to the OU Foundation will expand the research mission of Stephenson Cancer Center. To extend the impact of the gift, Stephenson Cancer Center is committed to raising an additional $20 million, bringing a total of $40 million to discover new ways to prevent, diagnose and treat cancer. “Cancer is a malicious foe,” said Robert Mannel, M.D., director of Stephenson Cancer Center. “One in three women and one in two men in Oklahoma will be diagnosed with cancer during their lives. We are committed to providing tomorrow’s cancer care today through clinical trials, laboratory research and translational research. This gift from the Stephenson family will transform our research efforts.” The generosity of the Stephenson family will enhance research endeavors in a multitude of ways, including recruitment of new world-class scientists, the creation
28
of five new endowed chairs in cancer research and renovation of laboratory space with innovative features and technology. The gift also will further Stephenson Cancer Center’s pursuit of Comprehensive Status from the National Cancer Institute (NCI). In 2018, Stephenson achieved its position as Oklahoma’s only NCI-Designated Cancer Center, representing the top 2% of cancer centers in the United States. Comprehensive Status builds on that distinction with recognition for an added depth and breadth of research, as well as substantial collaboration between scientists across many types of cancers. “Peggy and Charles Stephenson are longtime generous supporters of the University of Oklahoma, and their latest gift will literally save lives,” said Joseph Harroz Jr., interim president of the University of Oklahoma. “Their generosity will have an amplifying impact on the research mission of Stephenson Cancer Center, creating opportunities for the discovery of breakthroughs in leading-edge cancer therapies. It’s because of the Stephensons and their vision for cancer care in Oklahoma that our state has the resources it does to
[ Fa l l / Wi n t e r 2 019 ]
RESE ARCH
provide the highest quality care for those afflicted with cancer. We are immensely grateful for their leadership in funding the acceleration of cancer research that will have a profound impact on our state.” Research plays a crucial role in the mission of Stephenson Cancer Center: to improve patient outcomes and reduce the burden of cancer for all Oklahomans. More than 130 Stephenson research members are engaged in over 250 investigations at the OU Health Sciences Center in Oklahoma City and on OU’s Norman campus. Standout areas of research include: cell signaling and the tumor microenvironment; cancer nanomedicine, bioengineering and imaging; cancer chemoprevention; tobacco research; and health disparities. The center is nationally recognized for disease-based research in gynecologic, pancreatic and gastrointestinal cancers. NCI-Designated Cancer Centers like Stephenson are able to accelerate their pace of discovery, thereby increasing the number of cancer survivors and enhancing their quality of life. A significant component of Stephenson Cancer Center’s research mission is its clinical trials program. Stephenson is one of 30 Lead Academic Participating Sites in NCI’s National Clinical Trials Network (NCTN). For the past two years, the center has ranked No. 1 among all cancer centers in the nation for the number of patients participating in clinical trials sponsored through NCTN. Stephenson is also home to the Oklahoma TSET Early-Phase Clinical Research Program, which provides access to a large portfolio of novel and targeted experimental therapies. New clinical trials are crucial because they can provide lifesaving treatment while paving the way toward newly approved drugs or new uses for existing drugs. The Stephenson family has been deeply affected by cancer during their lives. They have transformed those personal experiences into an opportunity for each patient and family at Stephenson Cancer Center to receive the best care available, informed by the latest research discoveries. “When we had the opportunity to give back in a way that would fight cancer, we knew that’s what we wanted to do,” the Stephensons said. “Our entire family is committed to helping the cancer center continue the pursuit of excellence. Research is crucial in creating more effective treatments for all types of cancers. Research excellence, combined with the care and compassion of everyone who works at the cancer center, is what makes it such a special place. We are grateful to help make a difference.” To donate and support Stephenson Cancer Center’s commitment to raising an additional $20 million in our fight against cancer, visit stephensoncancercenter.org/stephensongift.
Debra Richardson, M.D., is pictured with her patient Susan Laurence at the Stephenson Cancer Center.
Cutting-edge Treatment and Research Gives Patient Opportunity to Live Life to the Fullest In Susan Laurence’s battle against a highly aggressive form of uterine cancer, she has defied the odds and harnessed cutting-edge medical care to live life on her own terms. The ruthless reality of cancer is that it can steal a person’s hope and quality of life. For Laurence, that simply wasn’t an option. In 2015, Laurence arrived at Stephenson Cancer Center at OU Medicine after being diagnosed with uterine cancer. She learned that the cancer had metastasized to a lymph node and was poorly differentiated, which happens in less than 1% of patients and is very difficult to treat. In the four years since, she has undergone numerous treatments, seen the cancer spread to her spine and brain, lost the ability to walk and then relearned how, and today has stable disease thanks to a phase 1 clinical trial. “She is remarkable, and she has exceeded expectations,” said Debra Richardson, M.D., her current gynecologic oncologist at Stephenson Cancer Center. “I’m happy that treatment has allowed her to regain her life and do the things she enjoys, such as traveling the world. That’s the whole point of treatment – to be able to live life to the fullest.” When she first became a patient at Stephenson Cancer Center, Laurence’s gynecologic oncologist was Robert
[ Fa l l / Wi n t e r 2 019 ]
29
RESE ARCH
Mannel, M.D., director of the Cancer Center. He performed surgery, then she received radiation and chemotherapy on a National Cancer Institute clinical trial that was testing a particular combination. For about a year, she was fine, but in March 2017, she learned that her cancer had recurred. Mannel sent her tumor for testing, and the results were not favorable. She had numerous genetic mutations, whereas some cancers only have one or two. She also was found to have microsatellite instability – rather than correcting errors that occur in DNA replication, her cells were creating more mutations. The news kept getting worse. The cancer spread to her brain and to her spine, compressing the spinal cord. She suddenly lost the ability to walk. “I literally could not raise my feet to put one in front of the other,” said Laurence, an Edmond resident. “I got a motorized scooter.” After radiation to her spine and the brain lesion, the cancer shrunk and Laurence was able to move her legs and, with a lot of physical therapy, learned to walk again. “The side effect of losing my hair seemed silly in comparison,” she said. “I was alive and breathing and had tomorrow to look forward to. I was nursed into that feeling by all the loving, wonderful people around me.” Laurence soon learned she was a candidate for a phase 1 clinical trial, which tests drugs for the first time in humans. She was one of the first participants to receive an immunotherapy drug thought to be appropriate for cancer patients with numerous mutations like hers. The drug works by unmasking the cancer cells, which had been hiding, so that the body’s own immune system can recognize them as foreign and attack them. Laurence has now completed 21 cycles of the treatment, nearly two years’ worth, and goes to Stephenson Cancer Center every six weeks for a new infusion. While she is not in remission, her cancer has not progressed, and she has few side effects from the treatment. “It excites me to think that what doctors learn from my study might be somebody else’s future,” Laurence said. “There was no question that I wanted to be on the clinical trial. I’m OK knowing that something I’m living with may yield answers that are a salvation for somebody else.” Mannel said Laurence serves as a great example of why a National Cancer Institute-designated cancer center like Stephenson, with its breadth of research and clinical trials, is crucial to improving life expectancy and quality of life. Laurence is at the center of a team that strives to give her the best treatment options today while creating more possibilities for those who will one day walk in her shoes. “Battling cancer is a team approach,” Mannel said. “It’s about creating a supportive environment and providing opportunities for the patient to fight cancer. Susan is a great example of someone who has battled cancer with dignity and energy, as well as someone who is participating in a clinical trial not only for her own benefit, but for the ways it will help countless women in the future.”
30
Deepa Sathyaseelan, Ph.D.
Stephenson Cancer Researcher Awarded Large Grant To Study Role of Aging, Inflammation in Cancer and Other Diseases As part of normal aging, people build up inflammation in their bodies – not the acute kind that eliminates an infection, but a mild, persistent inflammation that creates a higher risk for age-related diseases like cancer, Type 2 diabetes and Alzheimer’s. A researcher at the Stephenson Cancer Center, Deepa Sathyaseelan, Ph.D., received a $1.6 million grant to further her investigations into the role of inflammation in both aging and age-related diseases like cancer. The grant is from the National Institute on Aging, a component of the National Institutes of Health. Sathyaseelan is focusing her research on necroptosis, a cell signaling pathway that causes inflammation. In previous studies, she discovered that with an increase in age comes an increase in necroptosis. Her hypothesis is that necroptosis leads to increased inflammation with age. With her new grant, she will try to block necroptosis to see whether it will reduce inflammation and whether that will have an effect on aging and age-related diseases. Her research is notable because it has major implications for both aging and cancer. “Aging and cancer are interrelated – you cannot separate them because aging is the biggest risk factor for most cancers,” she said. “Rather than targeting individual diseases, if we can learn how to positively affect or slow down aging, we
[ Fa l l / Wi n t e r 2 019 ]
RESE ARCH
may be able to have an overall preventive effect on diseases.” The beauty of Sathyaseelan’s study is that she may have some new drugs to test. Necroptosis also plays a major role in neurodegenerative diseases like Alzheimer’s, Parkinson’s and multiple sclerosis, and several drugs designed to treat those conditions are in clinical trials. If found to be successful, those drugs may also be effective for her studies, she said. Sathyaseelan also made an unplanned discovery that is particularly relevant to hepatocellular carcinoma, a type of liver cancer that is an example of an inflammation-related cancer. When she blocked necroptosis in her research model of hepatocellular carcinoma, the level of inflammation decreased. “That was a very exciting finding,” she said. “It’s a starting point for me to look more into the details of the role of necroptosis and inflammation in liver cancer.” Liver cancer is especially concerning in the United States, where it has risen dramatically since the late 1970s. Even though the major risk factor for liver cancer is chronic infection with hepatitis B and C, obesity and fatty liver disease are the likely causes behind the rise of liver cancer, Sathyaseelan said. And, as with other cancers, aging itself is a factor. By 2030, liver cancer is expected to be the third-leading type of cancer in the United States, she said. Research reported in this press release was supported by the National Institute on Aging of the National Institutes of Health under the award number 1R01AG059718-01A1. Sathyaseelan’s research also has been funded locally by the Presbyterian Health Foundation and the Oklahoma Center for the Advancement of Science and Technology.
Stephenson Cancer Center Physician Is Lead Author of Study Showing Drug Prolongs Life for Patients With Ovarian Cancer Women with ovarian cancer who have undergone four or more rounds of chemotherapy typically haven’t had much hope that another treatment option will lengthen their lives in a meaningful way. However, a new research study shows tremendous promise for a drug called niraparib to extend life when all options have been exhausted. Gynecologic oncologist Kathleen Moore, M.D., associate director of clinical research at the Stephenson Cancer Center, is the lead author for the study, which was published in The Lancet Oncology, the world’s leading cancer journal. The study reveals especially good news for patients with ovarian cancer who do not have a mutation of their BRCA gene, as well as those who have received multiple
chemotherapy treatments. Because the study showed a longer survival time for those patients, it lends support for an expansion of the use of niraparib, a PARP inhibitor that targets cancer cells without affecting normal cells. “This is another piece of the puzzle that helps our patients live longer,” Moore said. “There haven’t been a lot of studies done on patients without BRCA mutations who have received four, five, six or more lines of chemotherapy. That’s who this trial sought to study. Until we can cure patients, we are doing our best to find treatments that buy them meaningful periods of time, until we can provide them with the next effective line of therapy.” Because women with BRCA-associated cancers respond best to PARP inhibitors, they have been the most heavily studied group and led to the first indications for using the drugs in treating ovarian cancer. However, only about 25% of women with ovarian cancer have a BRCA mutation either in their tumor or blood, and there is a high unmet need for effective therapies for the 75% of women who do not have BRCA mutations, Moore said. Ironically, having a BRCA mutation means that the patient’s cancer will respond better to chemotherapy and to a PARP inhibitor like niraparib. Women with BRCA mutations have something called homologous recombination deficiency – which means that when their cancer cells make mistakes in the process of dividing, they have trouble repairing those mistakes. PARP inhibitors like niraparib make repairing those mistakes even harder, which equates to treatment being able to kill cancer cells more efficiently. However, women with BRCA mutations aren’t the only cancer patients who have homologous recombination deficiency. Up to 25% of women without a BRCA mutation can also develop the condition, meaning they, too, can benefit from taking a PARP inhibitor. The study further categorized patients into those who were resistant to platinum-based chemotherapy and those who showed some response to it. Among women who responded to their last chemotherapy treatment, 27% responded well to niraparib and averaged 9.2 months until the disease grew or spread. Participants in the study had an overall survival time of more than 20 months, which is quite remarkable in this late line of therapy, Moore said. “We don’t normally see response rates of more than 10% in women who have had four, five and six chemotherapy treatments,” she said. “So a 27% response, especially given that these were not all women with BRCA mutations, was a nice signal that these patients can still benefit from PARP inhibitor use.” Even among women whose cancers were resistant to their last chemotherapy treatment, niraparib still extended their lives. In that category, 33% of women benefited from the drug for at least four months. “Those additional months are important,” Moore said. “They are never enough, but several months of disease stabilization is better than none. They can get people to Christmas or to see a new grandchild or to another milestone. Then, if they
[ Fa l l / Wi n t e r 2 019 ]
31
RESE ARCH
are stabilized and feeling better, they might be able to take another drug or go on a clinical trial.” Research studies also are important for expanding the types of patients who can receive a drug like niraparib, Moore said. Per FDA regulations, the only way that women without a BRCA mutation can currently receive niraparib is to respond favorably to platinum-based chemotherapy, then go on the drug as maintenance. “We think this data supports the expansion of niraparib to be more inclusive of patients. PARP inhibitors work best in women with BRCA mutations, but they can still work well in women without the mutation. Niraparib really makes sense for a much broader population,” said Moore, who holds the Virginia Kerley Cade Endowed Chair in Cancer Developmental Therapeutics, funded by the Presbyterian Health Foundation.
OU Medicine Tobacco Cessation Researcher Receives Career-Launching Federal Grant A post-doctoral fellow at the Stephenson Cancer Center received a highly competitive federal grant that will launch her research career focused on using mobile technology for tobacco cessation. Emily Hébert, who holds a doctoral degree in public health, was awarded a K99 grant from the National Institute on Drug Abuse, part of the National Institutes of Health. She is completing her post-doctoral training at the Oklahoma Tobacco Research Center, a program of the Stephenson Cancer Center. Her research involves using smartphone technology to help people stop using tobacco. The K99 grant plays a key role for researchers as they transition from post-doctoral training to junior faculty member. In order to establish an independent research program, post-doctoral fellows must conduct preliminary research, then use the data from those studies to apply for larger federal awards. “The K99 award is a great opportunity,” Hébert said. “Most junior faculty are required to split their time across multiple projects and teaching. The K99 award guarantees that 75% of my time can be focused on my continued training and professional development, while I prepare and conduct a research study.” Hébert’s research focuses on using smartphones to understand the triggers that make people want to smoke, in order to automatically deliver tailored messages in real time to try to prevent them from lighting a cigarette. Thus far, most smoking cessation interventions have been based on group-level patterns of smoking lapse – when people are
32
Emily Hébert, DrPH
feeling stress, for example, they are more likely to smoke. But Hébert’s aim is to develop a personalized algorithm that identifies each person’s smoking triggers and automatically delivers messages only when they are needed. Hébert will spend the next two years exploring machine learning – the process by which computers use data to identify patterns. Through working with mentors on OU’s Norman campus and attending workshops and conferences, she will learn more about how machine learning can be integrated into her research. Her project involves sending short surveys via smartphones, several times a day, to research participants who want to stop smoking. Participants will be asked about their mood and environment, such as “Are you with any other smokers right now?” and “How strong is your craving to smoke?” The technology will then be used to “learn” how and when individuals are triggered to smoke. “This research will help us to identify patterns in each smoker’s behavior, then an algorithm will be used to determine the types of messages that should be delivered, and when they should be delivered, to try to prevent someone from smoking,” Hébert said. “Understanding machine learning also will enable me to use data from other technology, such as a person’s heart rate from a smartwatch or activity monitor, to indicate when smoking relapse is imminent. I believe these methods could be used to help tailor interventions that address other cancer risk factors, like obesity and physical inactivity.” During the second year of the grant, Hébert will begin interviewing for faculty positions. Once she secures a tenure-track faculty position, the next phase of her research career will begin: using machine learning to develop the actual smartphone-based smoking intervention.
[ Fa l l / Wi n t e r 2 019 ]
RESE ARCH
Michael Businelle, Ph.D., Hébert’s primary mentor on the study, said her research is part of a growing field that leverages technology to study and intervene in health risk factors and behaviors. “Dr. Hébert’s innovative project will contribute to this growing area of research while helping people to stop smoking and decrease their risk of developing cancer,” he said. The work of Hébert and other researchers at the Oklahoma Tobacco Research Center is supported by the Oklahoma Tobacco Settlement Endowment Trust. An endowment created by state voters in 2000 to improve the health of Oklahomans, TSET is dedicated to reducing the state’s leading causes of preventable death – cancer and cardiovascular disease – caused by tobacco use and obesity.
Interaction Between Genes, Lifestyle Could Point to Earlier Discovery of Diabetes The epidemic of Type 2 diabetes has taken a toll on thousands of Oklahomans, who often don’t know they have the disease until it has irreparably damaged their bodies. A researcher at Harold Hamm Diabetes Center is studying ways to predict who will get diabetes, so that physicians can intervene earlier. Dharambir Sanghera, Ph.D., received a $2.5 million grant from the National Institutes of Health to further her diabetes research, which aims to understand how a person’s genetic makeup interacts with lifestyle factors like poor diet and lack of exercise to lead to diabetes. Unlike diseases like cystic fibrosis, which is caused by a defect in one major gene, diabetes is caused by multiple genetic defects in combination with a person’s lifestyle, Sanghera said. Although people who are obese face a higher risk for diabetes, some people who are overweight never get the disease. Understanding why could hold the key to predicting, at an early stage, who is likely to get diabetes. “Diabetes is a devastating disease,” she said. “It can cause heart disease, stroke, hypertension, kidney failure, blindness and more. Our intent is to identify biomarkers that can be used to predict diabetes, then we can begin treating individuals who are at the highest risk.” Since the human genome was sequenced in the early 2000s, researchers have identified more than 100 genes that likely contribute in some way to diabetes, Sanghera said. However, very little is known about which of those genes play a role and to what extent. To illuminate that process, Sanghera is using a new approach called metabolomics. State-of-the-art technology will be used to create a snapshot of a person’s metabolomics profile, which will be combined with their lifestyle factors, to see if patterns come to light.
Dharambir Sanghera, Ph.D.
“In the human body, genes are the chemicals that produce proteins, and proteins determine whether a person has a disease like diabetes,” she said. “However, in diabetes, researchers are still trying to understand what happens in the process of genes creating proteins. With metabolomics, we can bridge the gap between genes and proteins and gain functional readouts of what is going on in our bodies.” In her research, Sanghera will profile more than 4,600 people, looking for genetic and metabolomics patterns that emerge, such as a chemical compound that consistently increases its response to insulin resistance. Because Sanghera’s team also knows each person’s lifestyle profile – what they eat, how much they exercise, stressors they face – the research is highly personalized. Sanghera’s research project is also unique because of the technology used, called mass spectrometry and gas chromatography. The technologies themselves are not new, but only in more recent years have they been able to read more than one sample at a time. A large number of samples is necessary to work toward a meaningful solution. “This technology is considered high throughput – they can read thousands of metabolites in one single sample,” she said. “If you’re looking at only 50 or 100 patients, you might find something interesting, but you have to have large data sets to discover something that might be applicable to patient care.” Sanghera predicts that in the future, physicians will order a genetic risk score test just as they order lab tests to check their patients’ cholesterol panel. She hopes her research helps to pave the way toward that reality and its potential to help people at risk for diabetes. “We are tackling this problem in multiple ways – we know that it’s not only genetics that causes diabetes, and it’s not only lifestyle. It’s their interaction, and that’s why it’s complicated,” she said. “Metabolomics is enabling us to sort it out and find solutions.”
[ Fa l l / Wi n t e r 2 019 ]
33
RESE ARCH
Research reported in this press release was supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under the award number 1R01DK118427-01A1. Sanghera leads the grant, working with collaborators Ravindranath Duggirala, Ph.D., and Harald Goring, Ph.D., at the University of Texas Rio Grande Valley. Sanghera’s research is also supported by the Presbyterian Health Foundation in Oklahoma City, which awarded a bridge grant that allowed her to earn the current NIH grant.
OU College of Medicine Researcher Discovers Gene Mutation That Contributes to Addiction In the field of addiction research, one question looms large: Why do some people face a higher risk than others for alcoholism and drug abuse? A researcher at the OU College of Medicine, William R. Lovallo, Ph.D., recently published one of the field’s few studies focused on how a person’s genes contribute to addiction. Lovallo’s research showed that a tiny genetic mutation can put people at higher risk for alcohol or drug addiction. His research was published in the world’s leading journal on alcoholism, Alcoholism: Clinical and Experimental Research. Many people ask whether addiction is caused by person’s genes or their family environment. The short answer is that it’s both. However, Lovallo’s research zeroes in on a specific gene and how it responds to a person’s environment. COMT is the name of a gene that helps the body manage dopamine, a chemical that is released when a person drinks alcohol or takes a drug like amphetamine. Lovallo’s research focused on a small mutation of COMT. What he discovered demonstrates the interplay between a person’s genetic makeup and adversity during childhood. People with this mutation of the COMT gene are more vulnerable to the effects of stress in their early lives, such as divorce or emotionally distant parents. That heightened vulnerability often leads to consumption of alcohol and drugs younger than age 15, which is one of the biggest independent predictors of addiction. “Early-life adversity doesn’t make everyone an alcoholic,” Lovallo said. “But this study showed that people with this genetic mutation are going to have a higher risk for addiction when they had a stressful life growing up.” Because the COMT gene is involved with how well dopamine works in the brain, the behavior of the genetic mutation is especially revealing. “This one random mutation makes a difference in how the COMT gene works fine in one person but not as well in
34
William R. Lovallo, Ph.D.
another person,” Lovallo said. “There is no such thing as a gene for addiction, but there are genes that respond to our environment in ways that put us at risk. You have to have the right combination to develop the risk factors.” Lovallo’s discovery is a top achievement in his 20 years of well-funded research in this area. As a senior research career scientist at the VA Medical Center, he has conducted studies on veterans with alcohol addiction. However, those studies, like many others, concentrated on people after they became addicted to a substance. He knew he wanted to shift his research toward understanding the causes of addiction and how to prevent it. “Many of us know people who drink alcohol moderately and never have any problems. And we know people who drink a little and then go down the path toward alcoholism,” he said. “What’s the difference between going down that path and not going down that path? Now we have a better understanding that it’s not just exposure to alcohol or drugs that leads to problems; there is a genetic component. “Addiction is a real health problem, and to be making progress toward understanding it is one of the most exciting and worthwhile things I’ve ever done,” he said. Lovallo, senior author on the study, is also a professor in the Department of Psychiatry and Behavioral Sciences in the OU College of Medicine. He published the research paper in collaboration with several other OU colleagues: Andrew J. Cohoon, Ph.D., from the Department of Psychiatry and Behavioral Sciences; Kristen H. Sorocco, Ph.D., from the Department of Geriatric Medicine; and Andrea S. Vincent, Ph.D., director of the Cognitive Science Research Center on the Norman campus. They had other collaborators at the University of Arkansas for Medical Sciences and the National Institute on Alcohol Abuse and Alcoholism.
[ Fa l l / Wi n t e r 2 019 ]
RESE ARCH
respond poorly to chemotherapy and radiation. OU College of Medicine researchers set out to learn more about why cachexia occurs, in order to give patients the best chance at fighting pancreatic cancer. The team focused on a protein called ZIP4, which they already knew is excessive in pancreatic cancer. In the new study, researchers discovered that ZIP4 is at the center of a communication that occurs between pancreatic cancer cells and muscle cells. During that communication, ZIP4 prompts the cancer cells to release two specific types of molecules and even sparks the opening of a pathway for their journey to the muscles. ZIP4 also does the equivalent of hailing a cab for the molecules – called an exosome -- which ferries them to the muscle cells, where they prompt cachexia to begin.
Courtney Houchen, M.D.
OU College of Medicine Researchers Discover Trigger for Muscle-Wasting Condition Associated With Pancreatic Cancer Among all major cancers, pancreatic cancer has the highest rate of death – 93% of patients die within five years of diagnosis.
“We think this discovery is significant because of its potential to be translated into a therapy for patients. If we can find a way to inhibit ZIP4, we hope to intervene much earlier with cachexia and help more patients become able to undergo surgery, when they previously would have been too weak. That also means they would respond better to chemotherapy and radiation, which would also increase the survival rate,” said Min Li, Ph.D., another lead author on the study, who holds the Virginia Kerley Cade Endowed Chair in Cancer Treatment. The OU College of Medicine research team, which includes both scientists and medical doctors from the Department of Medicine, leverages that collaboration for a quicker conversion of a laboratory finding into a patient treatment. Their next steps are to further study ZIP4 and to search for a way to hinder its role in triggering cachexia. “The way we have traditionally looked at cancer is that if you can just kill the cancer cells, then people will get better. But that’s not realistic – we have to address complications like cachexia to help people survive,” Houchen said. “Now we have the opportunity to look at potential targets for overcoming cachexia, which may then improve the treatment of pancreatic cancer and its devastating consequences.”
Treating the disease is difficult not only because the tumors spread quickly, but because of a muscle-wasting condition called cachexia that affects at least 80% of people with pancreatic cancer. However, a team of researchers from the OU College of Medicine has published a groundbreaking research study that reveals how cachexia is triggered, setting the stage for further studies on how to prevent it. The research was featured in the journal Gastroenterology, the leading publication in GI tract disease. “Pancreatic cancer is a very tough disease, and novel therapies like treating cachexia are the only way we’re going to make progress because the traditional approach of trying to destroy the tumor isn’t enough,” said Courtney Houchen, M.D., a senior author on the study. Although cachexia can occur in several types of cancers, it is especially prevalent in pancreatic cancer. Patients with cachexia experience a dramatic loss of muscle mass, usually accompanied by loss of appetite, weight loss and fatigue. Because cachexia takes such a toll on patients with pancreatic cancer, many cannot withstand surgery and they
Min Li, Ph.D.
[ Fa l l / Wi n t e r 2 019 ]
35
TULSA
PA program director Shannon Ijams, MPAS, PA-C, visits with students at the School of Community Medicine.
PA Program Graduates 10th Class In November, the OU-TU School of Community Medicine graduated its 10th class of physician assistants from a program that is distinctive for its broad and diverse approach to education. Traditional clinical and didactic experiences combine with unique learning opportunities, such as Lifestyle Medicine and Civil Mental Health Court, to equip PAs to help their patients with all the factors affecting health. From the first day of their careers, PA students are ready to care for the human beings in their exam rooms, not just their illnesses. “We want to produce highly trained, competent PAs who can engage with their patients in a compassionate way,” said program director Shannon Ijams, MPAS, PA-C. “Our hope is that by broadening our students’ understanding of what their patients may be going through, such as substance abuse or navigating the criminal justice system, they can help them with a non-judgmental, empathic approach.” PAs receive valuable clinical experience through PAL, the PA Longitudinal Clinic. It is part of the Bedlam Longitudinal Clinic
36
on campus, where medical students also care for patients who are underserved and uninsured. On their teams, PA students evaluate patients first, then work with a PA faculty member to determine the best care. Students also work alongside nursing, social work and pharmacy students to meet the entirety of their patients’ needs. “The PAL clinic empowers PA students to assume the role as a primary care provider for their patients, including ordering laboratory and radiological services, referring them for a mammogram or connecting them with community resources, like Family and Children’s Services for mental health issues,” Ijams said. “And because this is a year-long clinical experience, they care for patients when they return for follow-up appointments for their diabetes management, for example. This helps students learn that incredibly important skill of care management on a longitudinal level.” Through PA faculty members Bobby Bosse, MHS, PA-C, and Mark Perdue, MHS, PA-C, students also learn about the expanded use of technology in patient care – point-of-care
[ Fa l l / Wi n t e r 2 019 ]
TULSA
ultrasound. During the didactic portion of their education, students are taught how to examine patients using these handheld, pocket-sized devices. Soon, they will begin using them in the PAL clinic. The PA program’s clinical experiences are as robust as any, and students practice high-level procedures like intubation and lumbar punctures. PA students also undergo their six core clerkships alongside medical students, an uncommon feature among PA programs. That collaboration replicates how PAs and physicians will work together in practice after they graduate rather than learning it on the fly. What especially sets the PA program apart are the ways students come to understand the non-medical factors affecting a patient’s health. Ijams created an opportunity for PA students to collaborate with the First Step Male Diversion Program, a Tulsa program for men ages 18-25 who have non-violent charges. Instead of receiving a prison sentence, they can enter this program to receive intensive outpatient counseling, job training, mentoring and sober living. In addition, many men in the program are uninsured and lack access to primary care services; PA students will be among the teams providing that care. A related rotation, called Community Impact, takes students into the city to learn more about community resources. Students spend time at the Tulsa Day Center, a program for people who are homeless. At Little Light House, they work with children who are developmentally disabled, and at Clarehouse, they are exposed to end-of-life care. Students travel through Tulsa with a mobile clinic affiliated with the Mental Health Association of Oklahoma, seeing patients in their home environments. They also attend AA and Al-Anon meetings as well as a session of Civil Mental Health Court.
good health – the food we eat. During a Lifestyle Medicine course, students work with a registered dietitian faculty member and a professional chef to learn how to cook medically tailored, plant-based meals, complemented by lectures on how good food benefits patients with conditions like diabetes and high blood pressure. “It’s been fun to see how the course has impacted the students’ own food choices and how they function, and that creates the foundation for how they educate patients,” Ijams said. “As providers, we want our lives to model what we want for our patients.” The breadth and depth of PA education is paying off, and it has enhanced competency without compromising clinical skills, Ijams said. Since 2012, PA students have achieved a 100% pass rate on the Physician Assistant National Certifying Exam. Eighty percent of graduates stay in Oklahoma to practice clinically, and admission to the program is highly competitive – approximately 1,000 people compete for 24 spots each year. “Our goal is to keep graduating PAs in Oklahoma to meet the needs of our state,” she said. “Although we love to keep graduates in northeast Oklahoma, we want them to remain in the state where the needs are, which can include varied rural areas as well.”
“In the School of Community Medicine, we talk a lot about how the actual medical care we provide only makes up about 10 percent of a person’s well-being,” Ijams said. “When students look at the other parts of a patient’s life and the difficulties they have to navigate, they better understand how that affects health. As healthcare professionals, we may not be able to provide everything they need, but we can connect them to resources in the community where they can get that help.” The national Physician Assistant Education Association, through a grant from the Substance Abuse and Mental Health Services Administration, chose Tulsa’s PA program as one of 10 nationwide to develop a substance use disorder curriculum as part of a pilot program. Educating students more intentionally about substance abuse not only helps PAs understand how it affects patients’ health, but it fosters their ability to develop trust with patients and talk openly with them about possible substance problems. PAs also focus on approaches that are known to contribute to
As part of their Lifestyle Medicine course, PA students learn how to cook healthy food and its value for the patients they treat.
[ Fa l l / Wi n t e r 2 019 ]
37
TULSA
and obese don’t receive routine screenings as often as those who are not overweight or obese. Minority women, especially African-American and Hispanic women, are much more likely to die during or after childbirth than women who are not minorities. “Even when socioeconomic status and insurance payer status are equal, we know that these gaps still exist,” Pasha said. “So we know that a lot of it has to do with implicit bias.”
Jabraan Pasha, M.D., of the School of Community Medicine presents workshops on implicit bias to students, residents, faculty and many others beyond campus.
Physician-Educator Gives Implicit Bias Workshops on Campus and Beyond In healthcare, as in many areas of society, people take in mountains of information every day and often make decisions subconsciously without asking the conscious brain to weigh in. Many times, those decisions are sound and lead to good outcomes. But subconscious decision-making, by its nature, opens the door to implicit bias. Even though implicit bias occurs outside of a person’s awareness, it still drives decisions and affects outcomes. In the healthcare arena, that equates to health disparities. Internal medicine physician Jabraan Pasha, M.D., an assistant professor at the OU-TU School of Community Medicine, has immersed himself in the study of implicit bias and created a workshop that he presents locally and around the world. The key to dealing with implicit bias is understanding that no one is immune to it, he said. “Simply acknowledging that implicit bias is a reality for most of us is the first step,” Pasha said. “Implicit bias doesn’t have anything to do with our intentions, but the outcomes are the same no matter what the intentions are. There’s no way to protect against it if we don’t know it’s there.” In healthcare, implicit bias can be found in several well-documented ways. Women receive fewer necessary cardiac interventions than men do, Pasha said, because healthcare providers often don’t think their symptoms are associated with heart disease. African-American patients do not get their pain treated as aggressively as non-African-American patients. People who are overweight
38
Even though his workshop addresses a serious subject, Pasha said he strikes a lighthearted tone so that participants are more open to talking about their experiences. He also stresses that people must separate the feelings of guilt and shame from the idea of implicit bias. “Most healthcare providers want to provide good, unbiased care,” he said. “We don’t want to people to feel shameful about it because then they’re not going to face it. Once you remove that barrier, the acknowledgement and awareness piece becomes much easier.” During his presentations, Pasha talks about disparities not only in healthcare but in other high-stakes areas like criminal justice, employment and education. Participants share their experiences, both of being biased or experiencing bias. They also brainstorm and talk about methods of reducing implicit bias at both an individual and institutional level. Once the workshop is over, Pasha encourages participants to take online implicit bias association tests developed at Harvard. Multiple tests are offered in the areas of age, sexual orientation, race, religion, skin tone, disability and others. He also introduces the concept of how the tests work by having participants take an implicit association test about flowers and insects. The results are never surprising – most people have positive associations with flowers and negative for insects. Though simplified, the example sets the stage for a person to take the tests on their own. “Taking those tests can tell you that you have a propensity for bias toward certain groups,” he said. “It doesn’t necessarily mean that you have had discriminatory practices toward someone, but it tells you that you’re more likely to. That’s a good thing because it puts us on notice so that we can be more conscious about our thoughts and the decisions we make. It allows us to step back and say, ‘Am I making this decision based on enough information, or am I filling in the blanks and making this decision based on some biases that I have?’” Pasha teaches implicit bias to medical students going into their third year on both the Tulsa and Oklahoma City campus, as well as to PA students and in residency programs. He’s given the presentation to the Association of American Medical Colleges, the Royal College of Physicians and Surgeons of Canada, and to groups in Paris and Portugal. He has also presented the workshop to many organizations outside healthcare. “The good thing about the workshop is that it’s relevant to everyone,” he said. “I also believe that everyone should take the implicit association tests. It is important to not be too upset with what the results show. Stepping up and taking these tests say more about you as a person than the results.”
[ Fa l l / Wi n t e r 2 019 ]
TULSA
Patients also enjoy a good prognosis after robotic liver surgery because of Royall’s skills in performing more precise and advanced maneuvers than would be possible with laparoscopic surgery. “The robot allows me to have 360-degree range of motion, which lets me get around difficult areas and structures,” he said. “I can perform more delicate suturing, and I can do complex movements without any difficulty. We also remove lymph nodes from the area to make sure the cancer hasn’t spread, and the robot allows me to remove them safely while protecting sensitive blood vessels and organs in the area.” The robotic system provides additional tools to enhance the safety of the surgery. Three-dimensional imaging allows Royall to see where structures are in space. The robot also offers what is equivalent to X-ray vision – allowing him to see inside the liver and bile duct system.
Billy and Tereasa Mickle
“It allows me to quickly find the bile duct and blood vessels feeding the different parts of the liver,” he said. “I can make sure the ones that need to be protected are not injured during the surgery. It also helps to prevent leaks from areas like the bile duct.”
Tulsa Surgeon Brings Robotic Liver Cancer Surgery to Oklahoma
Royall finds it gratifying to provide a safer surgery that results in outcomes at least as good or better than traditional and laparoscopic surgery. His patients are grateful to have the option in Oklahoma.
Last spring was a discouraging time for Billy Mickle. He was diagnosed with liver cancer and his course of treatment seemed unsure.
“I was very blessed to have this surgery,” Mickle said. “I knew I was going to be alright.”
Then he was referred to Nelson Royall, M.D., a Tulsa-based OU Physicians surgeon who was the first to bring major robotic liver surgery to Oklahoma. Royall used the robot to perform minimally invasive surgery on Mickle, removing the left lobe of his liver, in which the cancer was confined, and sent him home only three days later. For Mickle, who lives in Sand Springs, Royall’s expertise was a godsend. The cancer had not spread, his small incisions healed quickly, and he’s back to his daily life. “Dr. Royall and his staff are just amazing,” Mickle said. “I give him the highest praise.” Royall brings a unique service to Oklahoma. He is one of only a handful of robotic liver and pancreas surgeons in the United States and is the first in Oklahoma to use the robot to perform surgery for liver and pancreatic cancer. He is fellowship-trained in surgery of the liver, bile duct and pancreas, bringing years of surgical oncology experience to patients in Oklahoma and around the region. With robotic liver surgery, patients bleed less, meaning they don’t require blood products or transfusions, Royall said. They face a lower risk for complications, leave the hospital faster, and recover more quickly than those who undergo traditional open surgeries. Incisions are 5 to 8 millimeters, which leads to less pain and scarring. In addition, the robot makes surgery possible for many patients who couldn’t tolerate open surgery or aren’t candidates for laparoscopic surgery because of other issues.
Nelson Royall, M.D.
[ Fa l l / Wi n t e r 2 019 ]
39
FACULT Y ACHIE VEMENTS
Frederick Miller, Ph.D., left, presents a preclinical award to Jason Wagner, M.D.
Educators Honored by Academy of Teaching Scholars Medical educators were celebrated during the Academy of Teaching Scholars Education Week this fall at the OU College of Medicine. The ATS was created in 2012 by former executive dean M. Dewayne Andrews, M.D., as a means to foster, recognize, celebrate and encourage excellence in teaching and scholarly pursuits. This year’s inductees into ATS are:
Faculty members: • • • • • • • •
40
Megan Peters, PT, DSc, PCS, Department of Pediatrics Jameca Price, M.D., MPH, MCR, Department of Obstetrics and Gynecology, Tulsa campus Alexander Raines, M.D., Department of Surgery Bruna Varalli-Claypool, MHS, PA-C, PA program, OKC campus Alisa Cross, M.D., Department of Surgery, OKC campus David Kelley, M.D., Department of Family Medicine, OKC campus Jo Elle Peterson, M.D., Department of Pathology, OKC campus Kathryn Klump, M.D., Department of Family Medicine, OKC campus
Associate Members: • • • • • •
Amanda Celii, M.D., Department of Surgery, OKC campus Stephen Clayton Jr., M.D., Department of Neurology, OKC campus Kelly Curran, M.D. MA, Department of Pediatrics, OKC campus Jeremy Johnson, M.D., Department of Surgery, OKC campus Amy Lee, M.D., Department of Pediatrics, OKC campus Aneesh Pakala, M.D., Department of Medicine, OKC campus
Trainee Members: • Elizabeth Douville, M.D., OKC pediatrics residency • Alessandra Landmann, M.D., OKC surgery residency • Paul McGaha II, M.D., OKC surgery residency Several faculty members also were honored with Dewayne Andrews Excellence in Teaching awards in the areas of preclinical, clinical, graduate medical education and PA education.
Preclinical Awards: • • •
Sanjay Bidichandani, MBBS, Ph.D., Department of Pediatrics, OKC campus Nancy Halliday, Ph.D., Department of Cell Biology, OKC campus Jason Wagner, M.D., Department of Radiological Sciences,
[ Fa l l / Wi n t e r 2 019 ]
FACULT Y ACHIE VEMENTS
OKC campus • Lori Whelan, M.D., Department of Emergency Medicine, Tulsa campus
Clinical Awards: • • • •
Christopher Czapla, M.D., Department of Psychiatry and Behavioral Sciences, OKC campus Cynthia Bradford, M.D., Department of Ophthalmology, OKC campus Houssein Youness, M.D., Department of Medicine, OKC campus John Laurent, M.D., Department of Psychiatry, Tulsa campus
Graduate Medical Education Awards: • • • •
Tammy Yanovitch, M.D., Department of Ophthalmology, OKC campus Vijaya Ekambaram, M.D., Department of Psychiatry and Behavioral Sciences, OKC campus Nelson Agudelo, M.D., Department of Medicine, OKC campus Emily Fitz, M.D., Department of Emergency Medicine, Tulsa
PA Faculty Awards: • Bruna Varalli-Claypool, MHS, PA-C, OKC campus • Vishal Mundra, M.D., Tulsa campus
Several grants for health education research were also presented. Recipients are: • • • • • •
LaTasha Craig, M.D., Department of Obstetrics and Gynecology, OKC campus Curtis Knoles, M.D., Department of Pediatrics, OKC campus Shauna Lawlis, M.D., Department of Pediatrics, OKC campus Frederick Miller, MS, Ph.D., PA program, OKC campus Mark Perdue, MHS, PA-C, Department of Family Medicine, Tulsa campus Bruna Varalli-Claypool, MHS, PA-C, PA program, OKC campus
Barbara L. Bonner, Ph.D.
Bonner Receives Lifetime Achievement Award Barbara L. Bonner, Ph.D., recently retired, tenured professor with the Department of Pediatrics, was awarded the Lifetime Achievement Award by the American Professional Society on the Abuse of Children. The award recognizes an individual for outstanding contributions to the field of child maltreatment. Bonner has achieved national and international prominence in the field of child abuse and neglect. She held the CMRI/Jean Gumerson Endowed Chair in Pediatrics, served as director of the Center on Child Abuse and Neglect and as associate director of OU Children’s Physicians Child Study Center. Under her direction since inception, the Center for Child Abuse and Neglect became a leading national academic-based center on child maltreatment. Partnering with many of the state’s major service systems, the center has collaboratively addressed research, training and clinical efforts.
Lisa Landrum, M.D., Ph.D., left, welcomes Jameca Price, M.D., MPH, MCR into the Academy of Teaching Scholars.
The impact of Bonner’s leadership and expertise in the field of child maltreatment exceeds state boundaries, influencing professional training and policy development on an international scale, including Sweden, Russia, India, Saudi Arabia and China, among others.
[ Fa l l / Wi n t e r 2 019 ]
41
FACULT Y ACHIE VEMENTS
him fine-tune the trial so that it would have the best chance of approval from the Food and Drug Administration. The workshop also included the input of patient advocates, who provided an important vantage point about the trial, such as how often patients would be required to come to the clinic, frequency of blood draws and number of treatments. The clinical trial will test the effectiveness of an existing immunotherapy medication, avelumab, combined with an investigational new drug. The new drug has already shown promise, by itself, in shrinking tumors in patients with ovarian cancer, Tripathi said. In his trial, the hope is that the new drug will work in concert with the immunotherapy drug to further stimulate the immune system to shrink and control the tumor cells in bladder cancer. The trial will be held at multiple sites around the United States, and Tripathi will serve as the national principal investigator over the entire trial.
Abhishek Tripathi, M.D.
Medical Oncologist Chosen for Clinical Trial Development Workshop A medical oncologist at Stephenson Cancer Center was one of only 25 faculty members in North America selected to attend a prestigious workshop in clinical trial development. The result is that Abhishek Tripathi, M.D., returned to Oklahoma with a fully vetted clinical trial that will soon begin enrolling patients to test a new combination drug therapy for the treatment of metastatic bladder cancer. Tripathi is an assistant professor in the Department of Medicine. The workshop was organized by the American Society of Clinical Oncology and the American Association for Cancer Research. To compete for a spot in the workshop, Tripathi developed his own clinical trial concept and secured funding to conduct it, a process that took a year. After a rigorous selection process, his was among the concepts chosen. The value of the workshop is that Tripathi worked with senior physicians, scientists and biostatisticians with decades of experience designing clinical trials. Their feedback helped
42
Debra Richardson, M.D.
Stephenson Cancer Center Physicians Earn Awards to Develop Clinical Trials for Uterine Cancer Patients Two gynecologic oncologists at Stephenson Cancer Center have earned national research awards to develop concepts
[ Fa l l / Wi n t e r 2 019 ]
FACULT Y ACHIE VEMENTS
for new clinical trials, with a particular focus on uterine cancer, a disease that is on the rise. Debra Richardson, M.D., was named a Scholar Investigator by the Gynecologic Oncology Group Foundation, one of 10 chosen nationwide. Camille Gunderson, M.D., was named one of 36 New Investigators by the GOG Foundation. Each receives a grant and stipend to support concept development of new clinical trials, travel to national meetings and service on committees within the GOG Foundation and NRG Oncology. Both are faculty members in the Department of Obstetrics and Gynecology. The aim of Richardson’s grant is to become the national principal investigator for a Phase 3 clinical trial. Her working concept focuses on treating uterine cancer with an existing form of chemotherapy and potentially adding a targeted drug to the regimen. Richardson’s grant also includes a mentoring component. She will be mentored by her colleague at Stephenson Cancer Center, Kathleen Moore, M.D., associate director for clinical research. Richardson, in turn, will mentor three of the new investigators. Gunderson, too, will be developing a clinical trial concept for a national proposal. Her niche in patient care is treating women with uterine cancer, one of the few cancers that is increasing in incidence and causing more deaths. For years, uterine cancer was not even in the top 10 causes of cancer deaths among women in the United States. Today, it is the fourth most common cancer diagnosed and the sixth most common cause of cancer death among U.S. women, according to the American Cancer Society.
Researchers Earn PHF Grants In July, researchers at the OU Health Sciences Center received 43 grants, totaling more than $2.7 million, from the Presbyterian Health Foundation, an Oklahoma City grant-making organization that supports biomedical research and education. PHF awards several different types of grants: bridge, seed, new investigator seed, equipment, team science, research support, symposium, and clinician scientist development. Since 2014, PHF has awarded nearly $16 million to OU Health Sciences Center researchers. With the help of that funding, researchers have secured more than $97.7 million in additional funding. Also this year, PHF partnered with Harold Hamm Diabetes Center to fund 11 grants totaling $1 million. PHF matched the Diabetes Center’s spending at 25%. This program also supports several types of grants.
Dale Bratzler, D.O., MPH
OU Medicine Enterprise Quality Officer Honored By Good Shepherd Clinic Good Shepherd Clinic in Oklahoma City presented its Hope Award to Dale Bratzler, D.O., MPH, OU Medicine enterprise quality officer, in recognition of his work as a clinic volunteer. To honor his legacy, the Hope Award will become an annual event in Bratzler’s name, with proceeds placed in the Dale Bratzler Endowment Fund. The Good Shepherd Clinic is a free, full-time clinic serving uninsured residents of the community. The clinic offers medical and dental services, provided by healthcare professionals who donate their time and skills to ensure that financial concerns do not become barriers to receiving care in a timely manner. Bratzler began volunteering at Good Shepherd in 2015, believing that healthcare should be available to all members of the community, beyond the emergency room and regardless of ability to pay. As a result of Bratzler’s persistence, the Unity Clinic will launch early in 2020. This initiative will use campus-wide, interprofessional teams of healthcare providers, faculty and students from the OU Health Sciences Center to provide patient care in partnership with Good Shepherd.
[ Fa l l / Wi n t e r 2 019 ]
43
FACULT Y ACHIE VEMENTS
Landrum also educated congressional members about a pending guideline within the Centers for Medicare and Medicaid Services. Called “step therapy,” it is problematic for patients, especially those fighting cancer, she said. The plan would require doctors to prescribe the least expensive drugs first, then prove patients had failed those therapies before advancing to a different, more expensive drug that is known to be more effective. “For example, I would be required to use cheaper anti-nausea medication first, knowing it would fail for my patients,” she said. “I understand that cost is a concern, but physicians have a significant amount of knowledge about which drugs a patient needs to manage nausea while undergoing specific chemotherapies. It’s cruel to make a patient take a less-effective drug. For some patients, their experience with chemo and nausea is so bad that they’re unwilling to even try again. That’s the kind of situations we risk encountering if physicians aren’t allowed to make the best choices for their patients.”
Urology Department Chair Elected to National Leadership Role
Michael Cookson, M.D., chair of the Department of Urology, was recently elected president of the Society of Urologic Oncology.
Lisa Landrum, M.D., Ph.D.
Cookson holds the Donald D. Albers Endowed Chair in urology, and he sees urologic cancer patients at Stephenson Cancer Center at OU Medicine. He was installed in his new role at the society’s annual meeting Dec. 3 in Washington, D.C., and will serve a one-year term.
Gynecologic Oncologist Honored for National Advocacy
Gynecologic oncologist Lisa Landrum, M.D., Ph.D., associate professor in the Department of Obstetrics and Gynecology, has been honored for her national advocacy work on behalf of her patients with gynecologic cancers. Landrum was presented the Ambassador Award from the Society of Gynecologic Oncology. As one of two winners across the United States, Landrum was recognized for educating Oklahoma’s congressional delegation about several issues of great importance to women who are fighting gynecologic cancers and the physicians who treat them. Landrum’s efforts began with a “Legislative Fly-In” organized by the Society of Gynecologic Oncology. Landrum joined her colleagues from around the nation in educating their congressional leaders and staff about several timely concerns. One was to encourage Oklahoma’s members of Congress to sponsor requests for more federal funding for gynecologic cancer clinical trials. In Oklahoma, gynecologic cancers affect a large number of women, and ovarian cancer is particularly difficult to treat.
44
“I am indeed honored to lead one of the most significant international organizations that advocates for urologic cancer care,” Cookson said. “SUO strives to bring together distinguished experts whose work is entirely or primarily focused on malignant diseases of the urinary tract that include prostate and bladder cancer. In this way, we harness our experience and expertise to conquer urologic cancers.” SUO offers members a forum for discussion, development and implementation of ideas to improve care for patients with malignant genitourinary diseases. Key objectives are to stimulate research and teaching in urologic oncology, disseminate principles of urologic oncology to the medical profession at large and to standardize fellowship training in urologic oncology. In addition, Cookson said SUO is spearheading efforts with the American Board of Urology to develop a new Focus Practice Designation in Urologic Oncology for those physicians immersed in the care of urologic cancer patients. “The goal of this initiative will be to allow patients to identify doctors who are experts in the field with the ultimate goal of improving patient outcomes for those diagnosed with prostate and urologic cancers,” he said.
[ Fa l l / Wi n t e r 2 019 ]
FACULT Y ACHIE VEMENTS
Stephenson Cancer Center Physician Proposes New Clinical Trial Concept for Ovarian Cancer A gynecologic oncologist at Stephenson Cancer Center recently presented her proposal to the National Cancer Institute to launch and lead a national Phase 1 clinical trial for the treatment of ovarian cancer.
Through a competitive process, Camille Gunderson, M.D., was named a project team member for the National Cancer Institute’s Cancer Therapy Evaluation Program. Her proposal is to test a combination of two drug therapies in patients whose ovarian cancer has recurred and is resistant to platinum-based chemotherapy. As the leader of a Phase 1 trial, Gunderson would test, for the first time in humans, a novel cancer agent that has already been approved for treatment of breast cancer, in combination with another cancer drug. “In a Phase 1 study, we’re primarily focusing on the safety of the combination of the drugs,” said Gunderson, an assistant professor in the Department of Obstetrics and Gynecology. “We’ll also be looking at how effective the combination is, as well as conducting both tumor and blood testing of how the drugs interact and are cleared from the body. This drug combination has already been evaluated in the laboratory and in animal models in multiple cancer types, including ovarian cancer, and holds great scientific rationale for also being effective in humans. In addition, we’ll be looking at whether subgroups of ovarian cancer patients may be more likely to benefit from the treatment than others.” If the trial is approved, Gunderson will serve as the national principal investigator, and the trial will be conducted at a number of cancer centers across the United States, including Stephenson Cancer Center.
Katherine Moxley, M.D.
Stephenson Cancer Center Physician Receives Award from National Cancer Institute
Gynecologic oncologist Katherine Moxley, M.D., associate professor in the Department of Obstetrics and Gynecology, is one of only 10 physician-scientists nationwide to receive a leadership award from the National Cancer Institute. This highly competitive honor – the NCI Cancer Clinical Investigator Team Leadership Award – recognizes Moxley’s efforts to improve the lives of people with cancer through leading NCI-funded clinical trials. The award acknowledges her leadership efforts at the Stephenson as well as with clinical trials collaborators throughout the United States.
Camille Gunderson, M.D.
The award comes with a monetary prize that she will use to develop a comprehensive precision medicine program at the Stephenson Cancer Center. The program will further the investigations of basic and translational scientists across OU and the Oklahoma Medical Research Foundation, specifically studying areas of cancer treatment for which effective drugs are lacking. [ Fa l l / Wi n t e r 2 019 ]
45
E VENING OF E XCELLENCE
Robert E. “Gene” Anderson, M.D., Ph.D.
Evening of Excellence Honoring Two at 2020 Gala A distinguished ophthalmology researcher and a leader of the community and finance sector will be honored during the 2020 Evening of Excellence.
Cross Research Professor, Professor of Ophthalmology and Professor of Cell Biology. In addition, he serves as interim chair of the Department of Cell Biology.
The dinner, sponsored by the OU College of Medicine Alumni Association to raise funds for research by junior investigators, will be held Jan. 23, 2020, at the National Cowboy and Western Heritage Museum. For information or tickets, contact Lindsey Manning at 405-271-2353 or Lindsey-Manning@ouhsc.edu.
He served as director of the Oklahoma Center for Neuroscience at the OU Health Sciences Center from 1995 to 1999, and from 1998 to 2007, he served as founding chair of the Department of Cell Biology. He also served as Director of Vision Research at the Dean McGee Eye Institute from 1998 through 2018. During his 25-year tenure on campus, Anderson has maintained an active research laboratory and has received more than $62 million in grant support from the National Institutes of Health, placing him among a handful of top investigators at the OU Health Sciences Center. In addition, he has received more than $6 million in non-NIH support. Among vision scientists in Departments of Ophthalmology in the United States, Anderson ranked second in the nation in NIH grant support in 2009 and third in the nation in 2010 and 2011.
The Dean’s Award for Distinguished Medical Service will be presented to Robert E. “Gene” Anderson, M.D., Ph.D., and the Dean’s Award for Distinguished Community Service will be presented to David Harlow. Robert E. “Gene” Anderson, M.D., Ph.D., serves in multiple capacities for the Dean McGee Eye Institute and the OU College of Medicine. Anderson arrived on campus in 1995, after serving in several faculty positions at Baylor College of Medicine in Houston, where he earned his medical degree in 1975. Prior to that, he had earned his bachelor’s, master’s and doctoral degrees at Texas A&M University in College Station, Texas. In 1968, he completed a post-doctoral fellowship at Oak Ridge Associated Universities in Oak Ridge, Tennessee. In the OU College of Medicine, he holds several professorships: James P. Luton Professor, George Lynn
46
Anderson’s research focuses on retinal degenerations and the roles of lipids and lipid metabolism in retinal structure and function. He has published more than 300 articles in high-impact journals. His contributions to the field are significant and include the importance of omega-3 fatty acids in the visual system, which led to the Food and Drug Administration’s inclusion of long-chain n-3 fatty acids in human infant formulas, and a landmark discovery regarding
[ Fa l l / Wi n t e r 2 019 ]
E VENING OF E XCELLENCE
“Dr. Anderson’s contributions to research in biomedical science have been truly monumental at every conceivable level.” the role of the insulin receptor in retinal photoreceptor cells. “Dr. Anderson’s contributions to research in biomedical science have been truly monumental at every conceivable level,” said Gregory Skuta, M.D., president and CEO of Dean McGee Eye Institute. “These achievements can be attributed to Dr. Anderson’s personal success in the scientific arena but also to his extraordinary skills as a leader, mentor and teacher.” Mentoring students and junior researchers has been a priority throughout Anderson’s career. Thus far, he has mentored 15 pre-doctoral students, 29 post-doctoral fellows and countless young faculty members, many of whom now have distinguished academic careers.
he was named regional executive and president of BancFirst Oklahoma City, and his responsibility grew to include the overall management and administration of BancFirst Corporation’s largest bank. In May 2017, he was named CEO of BancFirst Corporation. Harlow’s community board of director commitments include the Oklahoma City Innovation District, United Way of Central Oklahoma, Greater Oklahoma City Chamber of Commerce, Kirkpatrick Family Fund and YMCA of Greater Oklahoma City. He and his wife, Aimee, are parents to Kristina, age 23, and Will, age 21. Harlow serves as board chair for the Innovation District, of which the OU Health Sciences Center plays a crucial role. “We are grateful for David’s dedication to the Innovation District and his vision for increasing opportunities for entrepreneurship, innovation and community growth,” said Jason Sanders, M.D., MBA, senior vice president and provost of the OU Health Sciences Center. “He sees the tremendous potential of the Innovation District and is a leader in developing strategies for its success.” .
Anderson has held numerous leadership positions within his profession, including president of the International Society for Eye Research; vice president of the Association for Research in Vision and Ophthalmology; chair of the National Eye Institute’s Board of Scientific Counselors; and a member of scientific advisory panels for Research to Prevent Blindness, BrightFocus Foundation, and The Foundation Fighting Blindness. David Harlow, an Oklahoma City native, serves as CEO of BancFirst Corporation. With assets of $8.4 billion, BancFirst Corporation is parent to Oklahoma’s largest state-chartered bank with locations in over 50 Oklahoma communities. After receiving his bachelor of science degree in mechanical engineering from Southern Methodist University, Harlow returned to Oklahoma to earn his master of business administration degree from the University of Oklahoma. He began his career in the financial sector in 1986 with Liberty Bank and Trust, where he served as a loan administration officer. Eleven years later, he left Liberty as senior vice president and manager of the Metropolitan Lending Division. After two years as executive vice president of Dorchester Capital Corporation, Harlow joined the BancFirst organization in 1999, serving as executive vice president and manager of commercial banking for BancFirst Oklahoma City. In 2003,
David Harlow
[ Fa l l / Wi n t e r 2 019 ]
47
ALUMNI DAY
Alumni Association Reunion Day Set for May 1 Activities and honors for Alumni Reunion Day 2020 have been set, including five recipients of annual awards presented by the OU College of Medicine Alumni Association. Alumni Day will be May 1, 2020. Honorees are: • • • • •
Robert N. Cooke, M.D., Class of 1980 – Physician of the Year Award in Private Practice Woody Jenkins, M.D., Class of 1990 – Physician of the Year Award in Private Practice Bonnie Miller, M.D., Class of 1980 – Physician of the Year in Academic Medicine Award George Thompson, M.D., Class of 1970 – Physician of the Year in Academic Medicine Award Hanna Saadah, M.D. – Friend of Medicine Award.
Classes celebrating reunions will be: 1955, 1960, 1965, 1970, 1975, 1980, 1985, 1990, 1995, 2000, 2005, 2010 and 2015. For more information about Alumni Reunion Day 2020, contact OUCOMalumni@ouhsc.edu or 405-271-2300. Pictured on this page are the 2019 honorees: Bill McCurdy III, M.D., Class of 1964, Physician of the Year-Private Practice; Charles Pasque, M.D., Class of 1989, Physician of the Year-Academic Medicine; and Danny Cavett, OU Medicine chaplain, Friend of Medicine. In addition, alumni celebrating their 50th reunion received medals.
48
[ Fa l l / Wi n t e r 2 019 ]
ALUMNI DAY
As an Alumni Association, we can also play a role in supporting the leadership and initiatives of our Executive Dean, Dr. John Zubialde, whose vision for the College of Medicine is one that we’re proud to champion. I’m grateful for the role that the College of Medicine plays in my life and for the opportunity to lead the Alumni Association. I encourage you to stay connected to our college and to consider ways that you can interact with our alumni group. Sincerely, Jason Lees, M.D. President, Board of Trustees OU College of Medicine Alumni Association
In Memoriam Jason Lees, M.D.
Letter to Alumni Dear OU College of Medicine Alumni, No matter how long we have practiced medicine, most of us have fond memories of our medical school years. It was a time when we began learning the skills to become competent physicians and to further connect with our desire to change lives through the practice of medicine, all while developing lifelong friendships. As the new president of the OU College of Medicine Alumni Association, I wanted to take this opportunity to introduce myself and tell you more about my commitment to the OU College of Medicine. After graduating from the College of Medicine and completing my surgery residency on campus in 2005, I returned to be on faculty in 2006. Today I am a professor in the Department of Surgery, vice chair of academic affairs and director of the surgery residency program. Recognizing the lasting impact one can have in academic medicine and realizing that OU fulfills many missions within our state, I wanted to stay in academic medicine to help educate the next generation of physicians. I’ve had the pleasure of serving on the Alumni Association board of trustees since 2008 before assuming the president’s role this year. During my time on the board, its members have enhanced its structure and goals to better align with the college’s mission and to allow for greater alumni involvement. I’m grateful for the board’s contributions and enthusiasm for our future. Our alumni can be found practicing medicine not only across the nation, but in several countries around the globe. We also enjoy interacting with our medical students through STAT – Students Today, Alumni Tomorrow – and hope to increase our engagement with residents. We hope to create more ways to connect with each of you.
Robert Gastineau, ’50 M.D., Pittsburgh, Pennsylvania Melvin Hicks, ’49 M.D., Edmond, Oklahoma David Mackler, ’57 M.D., San Francisco, California Don Culwell, ’62 M.D., Payson, Arizona George Caldwell, ’79 M.D., Tulsa, Oklahoma Philip Morgan, ’51 M.D., Hattiesburg, Mississippi Frank Hirose, ’51 M.D., Sylmar, California John Gardner, ’59 M.D., Edmond, Oklahoma Buddy Lecrone, ’71 M.D., Edmond, Oklahoma Helen Hathaway, ’54 M.D., Denver, Colorado Joseph Frey, ’66 M.D., San Antonio, Texas Thomas Nicklas, ’62 M.D., Grove, Oklahoma William Baker, ’60 M.D., Norman, Oklahoma Charles Cathey, ’53 M.D., Oklahoma City Leonard Pendergraft, ’64 M.D., Joplin, Missouri Dick Morgan, ’69 M.D., 69 M.D., Overland Park, Kansas Holly Fouts, ’96 M.D., Bartlesville, Oklahoma Richard Wallrath, ’71 M.D., Bakersfield, California Charles Haunschild, ’61 M.D., Edmond, Oklahoma Charles Bollman, ’66 M.D., Osprey, Florida Thomas Finn, ’53 M.D., Oklahoma City R. Barton Carl, ’55 M.D., Edmond, Oklahoma Ted Fortmann, ’65 M.D., Kingston, Oklahoma Marvin Weisbard, ’65 M.D., Tucson, Oklahoma Jerry Morrow, ’63 M.D., Lake Worth, Florida David Neumann, ’68 M.D., Oklahoma City James Crump, ’55 M.D., Baton Rouge, Louisiana Earl Schoolar, ’64 M.D., Austin, Texas Bob Eaton, ’60 M.D., Edmond, Oklahoma Ronald Hempling, ’73 M.D., York, Pennsylvania Phillip Short, ’75 M.D., Denison, Texas James Braden, ’75 M.D., Crossville, Tennessee John Huser Jr., ’58 M.D., Weatherford, Oklahoma Bernard Lynn, ’56 M.D., Conroe, Texas Bruce Van Horn, ’65 M.D., Ada, Oklahoma Kenneth Whinery, ’55 M.D., Sayre, Oklahoma R. Timothy Coussons, ’63 M.D., Denver
[ Fa l l / Wi n t e r 2 019 ]
49
PHIL ANTHROPY
Peggy Wisdom, M.D., center, and her Wisdom Family Foundation donated $100,000 to the Oklahoma Center for Neuroscience for translational research. With her are Beverley Greenwood-Van Meerveld, Ph.D., director of OCNS, and Calin Prodan, M.D., assistant director of clinical research for OCNS.
Wisdom Family Foundation Makes Gift Toward Translational Research The Oklahoma Center for Neuroscience, an interprofessional organization at the OU Health Sciences Center, has received a $100,000 gift to facilitate translational research in the neurosciences. The donation comes from the Wisdom Family Foundation and recently retired OU and VA neurologist Peggy Wisdom, M.D., who continues her involvement in interprofessional activities on campus. The funds will be used to award seed grants to clinicians and scientists who collaborate on a research project. “OCNS has both clinician and research members, and our role is to facilitate conversations between them,” said Beverley Greenwood-Van Meerveld, Ph.D., director of OCNS and professor of physiology in the College of Medicine. “When we bring them together to discuss common areas of interest, there is greater potential that they will develop a collaboration and work together to treat human disease.” The concept of translational research is becoming increasingly important to healthcare. Scientists with Ph.D.s don’t always have the opportunity to interact with physicians and patients, nor do clinicians often interact with researchers. But when they begin talking about each person’s contribution to solving medical problems, their combined expertise sharpens their focus on the disease and potentially accelerates the pace toward discovering a new medical therapy. Identifying common areas of interest is the foundation of such partnerships. OCNS research focus areas include
50
neurodegenerative diseases, stress and anxiety disorders, stroke and cerebrovascular disease. “For example, a researcher and clinician might each have an interest in traumatic brain injury,” said Calin Prodan, M.D., assistant director of clinical research for OCNS and a professor of neurology. “The physician could explain things from a patient standpoint, such as the potential for memory loss, stroke and seizures. The researcher would talk about how those complications could be studied at the cellular or molecular level. The conversation is a constant back and forth between the bench and the bedside.” The Wisdom Family Foundation gift will be used to provide initial funding for projects that have been identified. Such seed grants are crucial because they allow a team to get a project off the ground. Once they obtain preliminary data, they can leverage those findings to apply for bigger state and national grants. Proposals for OCNS seed grants are externally reviewed and identifying elements removed so that the process is as fair. In addition, applications are fairly short and no biosketch is required, which benefits junior researchers who have fewer publications and funding on their CVs. Once collaborators have generated data from their projects, they are required to present their findings at a seminar. Because OCNS has members from all seven colleges at the
[ Fa l l / Wi n t e r 2 019 ]
PHIL ANTHROPY
OU Health Sciences Center, translational projects have the potential to be diverse. In addition to Ph.D./M.D. collaborations, partnerships might include physical therapists, dentists, pharmacists, nurses and others teamed with a basic science researcher. “The OCNS has consistently encouraged and cultivated interprofessional translational research collaboration among the basic science and clinician researchers at the OU Health Sciences Center,” Wisdom said. “The Wisdom Family Foundation is pleased to initiate an endowment to enhance the ability of OCNS to cultivate more interprofessional collaborations.”
Supporting the Basic Sciences
All medical discoveries start with an idea. A way to slow the progression of Alzheimer’s disease. A method of diagnosing cancer. A treatment for diabetes. Basic science research provides the foundation of knowledge from which future applied science develops. Understanding the complexities and mechanisms of the human body is fundamental to generating new ways to prevent, diagnose and treat disease. Basic science research is central to our mission at the OU College of Medicine. A solid core of researchers conduct investigations in our targeted areas of cancer, diabetes, neuroscience/vision and infectious diseases/immunology – areas with diseases that especially affect Oklahomans. Our researchers’ laboratory pursuits extend to many other conditions as well. Supporting research is an investment in health, both in the short term and for future discoveries. For information about how to make a gift to support research and medical discovery, contact the OU College of Medicine Office of Alumni and Development at 405-271-2300. [ Fa l l / Wi n t e r 2 019 ]
51
Top, OU Medical Center CEO Kris Gose speaks during the topping out ceremony for the new patient tower. At left, David Lee Gordon, M.D., chair of the Department of Neurology, signs the beam, which was flown to the top of the construction.
A Publication for Alumni and Friends of the University of Oklahoma College of Medicine