Purpose of the Report:
The Penn Medicine State of Information Services report showcases key initiatives and activities from FY 2021-2023 performed by Penn Medicine Information Services, along with the combined efforts of our clinical, operational, and business partners.
By working together our health system was able to continue achieving maximum benefits and value from the health system’s investments. Industry insight, an innovative mentality, effective leadership, and organizational partnership are the elements that have been integral to successfully supporting Penn Medicine through a new, unprecedented era in healthcare. Our collective efforts applied in healthcare technology have delivered new tools and efficiencies that help provide our caregivers with the ability to continue to shape the future of medicine by transforming breakthrough science into exemplary patient care.
Our goal in Information Services is to support Penn Medicine’s mission and empower the larger healthcare technology industry by contributing as leaders, partners, and innovators. We also apply technology initiatives and outcomes that demonstrate our dedication to advance initiatives such as social determinates of health, health equity, and population health through our work, and support the local community through various outreach activities in the region.
Each day, our team is dedicated to the pursuit of using technology to achieve service excellence in patient care, education, and research. We continuously strive to design and deliver innovative, cutting-edge technology and services that enable us to offer unrivaled support to our caregivers and patients.
A Penn Medicine Information Services Publication https://www.pennmedicine.org/information-services/ Published
August 2023 The University of Pennsylvania Health System offers this publication for general informational purposes only. Penn Medicine, Philadelphia, PA 800-789-7366 © 2023 The Trustees of the University of Pennsylvania
on:
For centuries Penn Medicine has brought people together to advance excellence in clinical care, research, and education. The Information Services team plays a crucial role in how the institution creates and shares this knowledge, enriching the world’s understanding of health, disease, and treatment.
Increasingly, the intersection of technology and health care is transforming the way medicine is practiced to the benefit of both patients and providers. Thanks to Information Services, Penn Medicine is leading this charge.
Recent innovations are informing better ways to combat illness and speed cures; deliver superlative care; enhance the patient and provider experience; and develop strategies to secure the institution’s future amid a changing health care landscape. This progress also extends to strengthening student education and engagement.
As the home to the nation’s first chartered hospital, first school of medicine, and first teaching hospital, Penn Medicine has long served as a cradle of discovery. Its advances defined and shaped the field, and through the efforts of Information Science, the legacy continues. Now, as then, our potential is unlimited.
 J. Larry Jameson, MD, PhD
J. Larry Jameson, MD, PhD
 Kevin B. Mahoney Chief Executive Officer, University of Pennsylvania Health System
Kevin B. Mahoney Chief Executive Officer, University of Pennsylvania Health System

 Executive Vice President, University of Pennsylvania for the Health System Dean of the Ruth and Raymond Perelman Center for Advanced Medicine at the University of Pennsylvania, Robert G. Dunlop Professor of Medicine
Michael Restuccia Senior Vice President & Chief Information Officer, Penn Medicine
Executive Vice President, University of Pennsylvania for the Health System Dean of the Ruth and Raymond Perelman Center for Advanced Medicine at the University of Pennsylvania, Robert G. Dunlop Professor of Medicine
Michael Restuccia Senior Vice President & Chief Information Officer, Penn Medicine

I am so proud of the tireless efforts put forth by all Penn Medicine employees in advancing our mission and believe that teamwork and collaboration are the instrumental keys that propel Penn Medicine forward each day, toward shaping the future of medicine. I extend many thanks to our staff, partners, and caregivers for being the innovative and dedicated people who have created the integrated academic medical center that we are today.
Healthcare organizations are attempting to adjust to the new normal after experiencing more than three years of responding to the ongoing COVID-19 pandemic (compounded by the more recent omicron variant), hospital closures, clinical resignations, supply chain disruptions, escalating nursing costs, and medical reimbursement challenges.


































































































































































































































































Throughout these turbulent times, our Information Services team has engaged with operational leadership to ensure that advancements in research and patient care have continued to be the moniker in which our institution is viewed. Despite the adversity that has had both a global and lasting impact, the IS team relied on its core competencies to continuously enable the health system’s mission. These established competencies included:
1. Focusing on the concept of “team” and providing the needed flexibility to support one another. Whether our teammates were onsite or working remotely, supporting one another was paramount through these unchartered times.

2. Recognizing the challenging position of our front-line clinicians and rallying to support them in any way possible. Timely enhancements made to our applications, providing protective equipment for our desktop and clinical engineering teams to be there when needed, and developing a nationally recognized analytics package that guided our leadership team are just a few of the action steps taken by the IS department.
3. Communicating consistently with our teams to keep everyone well-informed of ongoing activities. Our IS newsletter, team huddles, The IS Hub employee portal, Morning Meetings with Mike, and the introduction of our virtual meeting collaboration platform, Penn Café, have all been instrumental in maintaining our team alignment and culture.
4. Leveraging the “inner good” in all our teammates, recognizing that enabling the mission of Penn Medicine is critical to the betterment of our community and personal livelihoods.


























































































































As time has shown us, no one can predict what the future will bring. The projects in this report reflect the collaborative team efforts, exemplified by the IS team and our operational partners, to deliver and exceed expectations, even in the most demanding situations.

IS DEPARTMENT PROGRAMS





















































An atmosphere of solidarity is fostered where our employees may attain professional growth, continual learning and personal enrichment while enjoying what they do. Programs such as: Employee Enrichment, We Care for Community Activities, Lunch and Learn are examples of the building blocks that create a supportive atmosphere among our colleagues to network and participate in initiatives which enhance us as individuals and as an IS community.
AWARDS
80























































































































































































































































































































THE PENN MEDICINE ORGANIZATION 6 CIO DIRECT REPORTS 7 ENABLING THE NEXT ERA OF WORLD CLASS HEALTHCARE THROUGH INNOVATION AND COMPASSION 8 PATIENT CARE Access to Care, Provision of Health Services, and Population Health Management 10 EDUCATION AND RESEARCH Penn Medicine enhances its status as a world leader in advancing medical science by continually improving the quality and impact of its research. 48 EMPOWERING TECHNOLOGIES These technologies and processes address the administrative infrastructure
and
infrastructure
58
support
physical
support.
78 BY THE NUMBERS 79
Penn Medicine is a leader in pursuing healthcare technology innovation and applying best practices toward delivering service excellence. Our leadership team adopts a progressive approach toward knowledge sharing and collaboration in the local, regional and national healthcare IT community. Healthcare IT committees, collaborative forums, conferences, published articles and speaking engagements are several ways in which we engage with others in the industry. Penn Medicine has also received multiple award recognitions for its accomplishments in implementing new, transformational IT initiatives. IN THE NEWS 81 GLOSSARY 82
Penn Medicine is committed to advancing knowledge and improving health through research and patient care to serve a changing world. Providing high-quality and family-centered care for our patients and the community is of the utmost importance, which is why Penn Medicine strives to advance innovations to improve the lives and health of all patients.
MISSON
At Penn Medicine, we are dedicated to discoveries that advance science, to outstanding patient care throughout the world, and to the education of physicians and scientists who carry on our legacy of excellence. We are a world-renowned academic medical center and strive to improve the health and well-being of people through research, education, clinical care, and community service. We are proud of our commitment to service and strive to use discovery and rigorous research to benefit our neighborhoods, our city, and our world. We embrace the opportunity to teach others, to learn from our partners, and to care for patients with skill and dignity.
HISTORY
Pennsylvania Hospital, part of Penn Medicine, is the nation’s first hospital, and was founded in 1751. The University of Pennsylvania opened its School of Medicine, the nation’s first, in 1765. And, the Hospital of the University of Pennsylvania was established in 1874 as the nation’s first teaching hospital. Read More Online
The stability of our mission and unwavering strategy are a cornerstone of our success. We focus on excellence and execution in everything we do, whether it is advanced medicine, scientific discovery, or community care. That stability is also evident in the longevity of our leadership and the tenure of our employees — that is very unique, and creates a genuine, collegial spirit across the institution.
Kevin B. Mahoney
Chief Executive Officer, University of Pennsylvania Health System






























Our people – our health care heroes, faculty, staff, students, and scientists – and our core mission – the integration of health, education, and research – will propel us forward and lead us to solutions.
J. Larry Jameson, MD, PhD
Executive Vice President, University of Pennsylvania for the Health System Dean of the Ruth and Raymond Perelman Center for Advanced Medicine at the University of Pennsylvania, Robert G. Dunlop Professor of Medicine
CORE VALUES
Excellence
We will strive for excellence through creativity and innovation.
Integrity
We will be truthful, equitable and committed to intellectual honesty.
Diversity
We will foster intellectual, racial, social and cultural diversity.
Professionalism
We will achieve the highest standards of professionalism through ethical behavior, collaboration, self-education and respect for all members of Penn Medicine.
Individual Opportunity
We support equal opportunity and individual creativity and innovation.
Teamwork and Collaboration
We will support each other and promote collaboration with our colleagues and thoughtful stewardship of University and Penn Medicine resources.
Tradition
We will learn from our history, take responsibility for the future and promote the unique nature of the Penn environment.
6
Penn Medicine’s core values define what we stand for as an organization and how we will continue the work of helping others that began here more than 240 years ago.
TOP ROW
Glen Fala
Associate CIO, Application Development
Gary Davidson
Senior Vice President/CIO Lancaster General Health
Julian Mihai
Chief Information Security Officer
John P. Donohue
Vice President of Information ServicesEntity Services
Paul J. Williams
Associate Vice President of Information Services Infrastructure Technology
BOTTOM ROW
Anna E. Schoenbaum Vice President of Information Services Applications and Digital Health
Michael Restuccia
Senior Vice President and Chief Information Officer

Maureen M. Hetu
Associate Vice President Information Services Operations
7
TO RIGHT
LEFT
EXEMPLARY INTEGRATED ACADEMIC MEDICAL CENTER
Penn Medicine is a world leader in all mission areas, harnessing education, and research to find new cures and make new medical discoveries. Our team leads in the use of informatics to catalyze discovery and integrate research and clinical care while also ensuring strong financial performance with balanced support across missions. The power of data science is used to advance biomedical research and care delivery, leading in first-in-human clinical trials of novel diagnostics and therapeutics. By using data to understand and respond to trends, Penn Medicine can help patients receive prompt and necessary treatment. Additionally, technology plays a crucial role in ensuring patient safety and delivering high-quality healthcare. Penn Medicine has built resilience in technology, infrastructure, security, and clinical applications, allowing for the development of innovative technologies that replace outdated practices and improve efficiency.
CONNECTING WITH PATIENT CENTERED CARE TECHNOLOGY

The approach to patient-centered care technology involves a unique integration of diverse medical technologies that connect clinicians with patients throughout the care continuum via interactive communication devices. This approach transforms the delivery of care and fosters cutting-edge medicine toward new medical innovations and advances. To achieve this, it is important to implement new technologies with interoperability and develop innovative tools and methods for discovery. By using technology to develop a patientcentered approach, the delivery of care can be transformed and result in new advances in medical technology.
Penn Medicine is shaping the future of medicine by providing a framework for future expansions to other hospitals and extending specialized care and expertise. This involves leveraging technologies such as mobility, AI technology, healthcare monitoring, robotic process automation, genomics, and research discoveries to achieve this goal. By using these technologies, Penn Medicine is wellequipped to meet the changing healthcare landscape and provide cutting-edge medical care to its patients.
ENHANCE ACCESS TO EXCEPTIONAL PATIENT CARE THROUGHOUT THE REGION AND CREATE AN OVERARCHING PHYSICIAN ORGANIZATION TO ENSURE COORDINATED PATIENT-CENTRIC CARE
The goal of enhancing access to exceptional patient care throughout the region is achieved by enabling an overarching clinician organization that ensures coordinated patient-centric care. Penn Medicine excels at the “Four Sites of Care,” which include our hospitals, outpatient clinics, virtual care, and homecare. The Pavilion is our most recent “hospital of the future” and represents one of the four sites of care that have increased Penn Medicine’s digital footprint by supporting the growth of the organization with the latest, state-ofthe-art technology. The framework for future expansions to other hospitals and the extension of specialized care and expertise is also supported.
Penn Medicine has also expanded patient care business models, including ACO and Penn Integrated Care, to address the rapid evolution of the healthcare landscape, including new partnerships among healthcare systems and payors, and affiliations among hospitals and physician groups to enhance access and coordination of care.

Providing continuous development of best practice processes helps streamline a patient’s efforts to access care and ensures that the care received is appropriate in terms of type, intensity, and location of care. Penn Medicine focuses on creating positive patient experiences that are of fundamental importance to our caregivers. Projects that enhance patient safety and satisfaction are a part of the patient-centered workflow, which aims to improve the patient experience and quality of care.
EMPATHY-DRIVEN WELL-BEING AND COMMUNITY SUPPORT
At Penn Medicine and within the Information Services team, we prioritized the well-being of our physicians, clinicians, and employees, recognizing the profound impact it has on healthcare delivery, work productivity, and emotional support. With a strong sense of empathy, we implemented various projects aimed at ensuring their safety and enhancing their overall health and well-being. As part of our commitment to safety, we launched COVID-19 initiatives such as COVID Watch, PennOpen Pass daily symptom and exposure screening, along with supporting safety measures like masking and gowning, and introduced appointment reminder and follow up texting communications. Our organization embraced technology to provide convenient and accessible healthcare through initiatives like Penn Medicine OnDemand telemedicine along with the expansion of online scheduling. Employee work flexibility was enabled through support for remote work (Microsoft Teams, Remote Access Portal). Also, employees’ physical safety in the hospitals and EDs was improved through implementing staff duress/safety systems.
Moreover, Information Services extends our support beyond the workplace, engaging in community outreach to address social determinants of health, health equity, and population health. The electronic health record incorporates the HelpFinder platform, which enables us to identify and assist those in need with medication delivery, transportation, food deserts, and support other essential needs. Additionally, our We Care program and humanity initiative further exemplify our commitment to supporting the community in meaningful ways. Through these comprehensive efforts, our department strives to foster a culture of empathy, ensuring the well-being and betterment of our employees, clinicians, and the communities we serve.
Access to Care begins the clinical encounter between the patient and Penn Medicine and its providers. Providing continuous development of best practice processes helps to streamline a patient’s efforts to receive care and ensures that the care received is appropriate in terms of type, intensity, and location of care. Providing patients with efficient access to care results in receiving the right care, at the right time, at the right location for the most appropriate cost.
Provision of Health Services expands care delivery beyond treatment of illness to prevention and wellness promotion to achieve optimal health status for individuals and populations. A person-centered and empowering approach to health care combines interrelationships among physical, mental, social, environmental, and spiritual dimensions of health and well-being. Interdisciplinary and inter-professional working relationships among practitioners’ support continuity and coordination in care while minimizing unnecessary variations in care using evidence-based guidelines and system-wide clinical protocols.
Population Health Management is the coordination of health services and the monitoring of health status across a well-defined population to improve clinical outcomes and manage financial outcomes. Population health management programs are the foundation of this process and can include care coordination, case management, disease management and health promotion, all based upon managing patient care and services to an evidence-based standard.
Technology Connects Parents and Hospitalized Infants in the Neonatal ICU at Princeton Medical Center

At Penn Medicine, creating positive patient experiences is of fundamental importance to our caregivers. Regarding the context of providing neonatal ICU care, we recognize that creating the opportunity to maintain meaningful connection between parents and their critically ill infant establishes significant comfort to the family.
Penn Medicine Princeton Medical Center installed cameras on individual beds in the neonatal intensive care unit (NICU) to provide 24/7 virtual access, enabling parents to keep ongoing connection to their baby during care. The implementation at Princeton completes a service offering that is now enterprise-wide throughout the health system, joining the other NICUs (Neonatal Intensive Care Unit) (Neonatal Intensive Care Unit) at our hospital facilities.
This state-of-the-art, HIPAA compliant, NICU camera system brings live-streaming video of the patient to family members anywhere, anytime, on any device. Livestreaming camera access may reduce stress and anxiety for parents with a child in intensive care, support bonding with their child when family members cannot be at the hospital and improve staff’s workflow efficiency.
To help enable the service, the IT team established secure access to an online webcam for parents and authorized representatives to view live stream video of their infant, while being treated in the NICU. A camera captures the face and torso of the assigned patient. An eSignature consent form enables the service, helping to benefit families with on-the-go access to their child with flexible viewing, the ability to replay video messages, and to be recognized as an integral member of the care team.

11
Patient Estimates Enable Price Transparency for Medical Services
The Centers for Medicare and Medicaid Services (CMS) issued a ruling, in January 2021, to improve price and quality transparency for “shoppable” healthcare services, such as an imaging study, laboratory service, or elective medical procedure. The legislation was enacted to enable patients to shop for the most effective, lowest-cost health care available. The regulation required hospitals to provide an online computer-friendly tool, displaying at least 300 services in a standardized format, to assist patients when shopping for a routine test or elective procedure.
Penn Medicine implemented the self-service estimates module in the EHR, allowing people to visit a userfriendly web-based price transparency tool. There, they could create an estimate informing them of payment expectations prior to the scheduled service or procedure. The module was built to provide patients with ‘out of pocket’ expenses that they may incur based on Penn Medicine’s verification of their current insurance benefits. Prior to implementing this feature, patients were directed to contact a Penn Medicine financial advocate to estimate pricing for an upcoming service or procedure. The financial advocate transcribed the patient’s information over the phone, generated the estimate in the EHR and then called the patient back with the estimated amount. By using the self-serve estimate module, patients could receive a personal, automated real-time estimate immediately after entering their information.
This functionality has improved the patient experience by offering patients clear, accessible, and easy to understand estimates and financial obligations. Patients have been empowered to make more informed decisions about their care and render payments in advance of services.

Penn Medicine Patient Experience Survey Expands to Lancaster General Hospital
The Penn Medicine Patient Experience team created a real time patient satisfaction survey platform (PMX Survey) to reach patients through text messages after having an ambulatory visit. This new survey tool resulted in much higher patient engagement with response rates of nearly 25%. Further, by receiving patient comments in near real time after a visit, the care team was enabled to receive immediate and targeted feedback as well as identify service improvement opportunities.
To fully achieve integrated access, a mechanism was developed to extract data from the PMX survey database that connected to both the LGH data warehouse and Penn Data Store. This enabled the consumers of the data at LGH to benefit from and incorporate survey feedback into care delivery. Previously, Lancaster General Hospital’s data warehouse did not have access to the PMX survey database, which prevented the entity from accessing patient experience reports and dashboards.
12 PATIENT ENGAGEMENT
Penn E-lert Intensive Care Monitoring Program Expands Enterprise-wide
One of the most essential technical components of the intensive care unit (ICU), is the continuous monitoring of patients’ vital parameters which has been shown to improve patient safety by reducing ventilator days, decreasing mortality, and reducing length of stay. Remote monitoring in the ICU is a viable option that provides the care team with unlimited access to critically ill patients across the ICUs (Intensive Care Unit) at Penn Medicine hospitals. This service allows for proactive identification of impending or evolving patient problems to effectively manage their care.
The Penn E-lert® electronic intensive care unit (eICU) monitoring system consists of real time clinical decision-making support and telemedicine technology to continuously monitor patients. The installation of the Penn E-lert® monitoring system is now available at all intensive care units, enterprise wide. The system offers 24/7 critical care monitoring and uses a fixed camera technology to monitor ICU patients remotely and document within the EHR. Penn E-lert® eICU is a state-of-the-art electronic intensive care system that provides an additional layer of expert medical and nursing support for critically ill patients. A primary benefit of the system is the clinical team’s immediate access to telemedicine specialty care consultants to assist in their clinical decision making based on an individual patient’s needs.
The Center for Connective Care manages this remote monitoring program, employing critical care registered nurses who perform consultations 24 hours a day, 7 days a week and critical care intensivists who perform consultations from 7:00pm-7:00am daily. Clinicians on the Penn E-lert® team are board certified Intensivists from the departments of trauma, anesthesia, pulmonary, neuro critical care, or emergency medicine.
Home Health Care Program Integrates Vitals Data into PennChart EHR

As part of Penn Medicine at Home’s telehealth program, patients have been using a monitoring device to measure their vitals so that essential information is reported and monitored by their caregivers. Previously, vitals data were manually entered by the caregiver during the home care visit on the remote home health web portal. Now, data is electronically captured and integrated from the patient’s device right into the electronic health record.
Information Services improved both the patient and caregiver experience by implementing an interface to send these patient demographics electronically between the system capturing the vitals and our PennChart EHR. The technology team implemented a results interface to communicate with our EHR. Print groups were configured to display patient and device reported vitals in the EHR remote client. Reports were also created to trend patient vitals information in the remote client so that the data could be viewed offline.
Vital signs were now able to be validated more efficiently, especially since they were transmitted in real- time and contained timestamps. The automated process also saved nurses from writing vital signs on a piece of paper, then re-entering them in the EHR. The interface also helped eliminate transcription errors that occurred when manually typing vitals. It additionally allowed vitals to be captured during times when a clinician was not visiting a patient or documenting an encounter.
13
Penn Medicine OnDemand (PMOD) Program Transitions Video Platform

The PMOD department was originally set up to perform telemedicine services with a video platform that Penn Medicine selected to integrate with our EHR. Once telemedicine gained mainstream adoption in healthcare, our EHR vendor established their own platform to support their client healthcare systems and facilities. Our technology team decided to switch solutions and prepare our users to transition platform support. New workflows were designed to use the application and system peripherals were also integrated. The technical team also determined where the video platform servers would be hosted, established licensing, and mapped out a maintenance schedule for continuous upgrades.
Due to these efforts, coordinated with our operational counterparts, Penn Medicine now has a validated and reliable long-term EHR integrated telemedicine solution implemented across the health system. A much-improved patient experience has also resulted from the new telemedicine technology. Patients were enabled to complete pre-check-in steps and connect to their video visit right from their myPennMedicine app. They no longer needed to search for email and text messages to find and connect to their appointment. Using this solution also allowed Penn Medicine providers to have a single platform to document their encounters and connect to their video visits. Another significant benefit achieved was that the servers became hosted by our EHR partner, which minimized maintenance work and potential challenges with troubleshooting issues between different integrated vendors.
Lancaster General Health Enables Telestroke Neurology Service
Lancaster General Health (LGH) developed the use of telestroke services to connect off-site stroke service providers to support overnight acute stroke management. LGH providers were able to remotely monitor patients and provide updated eHealth EHR consultation notes, using the Caregility platform. Integrating documentation and resulting orders improved the speed at which stroke patients could start lifesaving care. This allowed clinicians to assess the patient faster and start thrombolytic therapies to remove clots and restore perfusion to the brain.
Developing this new offering allowed for orders to be placed for testing, based on a more specific patient evaluation instead of following general protocols. Telestroke services enabled higher-level procedures to be performed, which historically would have required an on-site provider to monitor the outcome in person, rather than via remote monitoring. This program provided expedited services for LGH stroke patients and increased their recovery rate.
Information Services implemented carted mobile devices so that a remote stroke assessment could be made by a provider in the patient room. Complex clinical workflows were developed for LGH providers to coordinate care for stroke patients using mobile carts. LGH has used the technology more than 244 times since May of 2021 and has been able to drop its door to needle time from 51 minutes to 37 minutes.
14 MOBILE DIGITAL HEALTHCARE
Tele-Stroke Expansion Lends Help to Patients in Need of Specialized Care
Stroke is a time sensitive medical emergency that requires prompt evaluation and treatment. The “golden hour” after the onset of stroke symptoms is critical. Penn Medicine’s Telestroke Program is designed to provide urgent consultation to stroke patients at partner hospitals who need neurovascular specialists at the Comprehensive Stroke Center to provide specialized clinical expertise for severe, life threatening, or limiting conditions. This program helps stroke patients receive timely and appropriate care, irrespective of their location.
The Telestroke Program began by partnering with Shore Memorial Hospital, and then Grandview Hospital to develop a business model and new technology for patient care workflows. The team created a new workflow in the PennChart electronic health record to quickly register non-Penn Medicine patients, built tools for neurovascular specialists to conduct urgent telemedicine consults, and configured telemedicine carts to enable remote patient evaluations.
A new VPN tunnel was set up along with a new rapid server to enable physicians to facilitate faster, more accurate triage or hospital transfer decisions using advanced imaging artificial intelligence. The team trained providers at each organization on the new workflows and developed new reports for tracking tele-stroke consults.

The Penn Medicine neurovascular specialists provided numerous virtual consults and urgent telemedicine visits for patients, offering their clinical expertise and diagnostic skills. The service was supported by a unique integration of diverse medical technologies that connected physicians with patients across the care continuum with interactive communication devices. They helped with treatment and also transfers to the Comprehensive Stroke Center at HUP. Additionally, remote patient/device monitoring helped to streamline care delivery in tandem with the most widely used imaging software among physicians for stroke patient care, research, and clinical trials.
The Telestroke Program created a framework for future expansions to other hospitals and helped extend specialized care and expertise to some of the sickest patients in need of care for stroke and neurology related conditions. The program is a testament to the power of technology and collaboration in healthcare and demonstrates how telemedicine can be used to bridge the gap in medical access and improve patient outcomes.
15 MOBILE DIGITAL HEALTHCARE
Lab Collection Documentation Improved for HUP Phlebotomy Team

Phlebotomists at HUP handled a large, and continually growing volume of patients despite limited resources. An opportunity was seized to improve lab collection documentation to gain time efficiency for staff in processing online EHR documentation. Previously, it took at least a few minutes to sign on to the computer in each patient room and click multiple times to document each collection task. Also, if lab collection was not documented in a timely manner, the lab ordered time could have been pulled as a collected time, imposing safety risk.
To avert these issues, the phlebotomy team implemented an application to perform lab collection documentation at the patient’s bedside. Initial data indicated that the AM lab collection documentation improved significantly by about 26% within just a few months. “We feel that this application is the most efficient way to manage our draws within the Pavilion and HUP East” remarks Kara Eller, the manager of phlebotomy team. Now phlebotomy staff at all entities can more efficiently chart lab collection documentation as well as easily request lab label printing.
Using Mobile Applications for Inpatient Orders Helps Keep Physicians on the Go
Providers increasingly hoped to have a way to be able to place inpatient lab and medication orders using EHR integrated mobile apps and untether from stationary workstations, allowing them to improve clinical workflow and patient care. Members of our MForce mobile device program team and Information Services kept a close watch on the availability of an application version that would provide the desired functionality at Penn Medicine.
Once the application became available, the team conducted a pilot project to test the feature and assess its impact on clinical decision support. The results were positive, leading to a full roll out of the feature in June 2022. Since the initial launch, IS monitored the usage for mobile orders placed in hospital admissions and observed a steady increase in popularity. Initially starting with ~5200 orders placed in the 1st month, there were approximately 11,500 orders in the 3rd month of the project’s implementation. Over 25,000 inpatient mobile orders were placed within the first 6 months and volumes continue to grow!
16 MOBILE DIGITAL HEALTHCARE
Using a New, Modern UI Framework for Inpatient App Keeps Caregivers Rounding Efficiently

Carelign is a responsive web application used during inpatient rounding by a variety of caregivers at HUP, PPMC, and PAH hospitals to help maintain a patient’s care plan and manage handoffs between care teams. Carelign has been used weekly by over 4,000 residents, attendings, nurses, and other clinicians to help facilitate their rounding activity. Carelign was initially developed in 2014 using the JavaScript framework Angular.js.
Over the last few years, Angular.js was no longer supported and has been replaced by other, more modern frameworks. As a result, the Carelign user interface (UI) needed to be re-architected using a newer framework. Because Carelign can be launched from within our EHR, the new Carelign UI also needed to continue to support IE11, the browser that our EHR vendor uses when an application is launched in the sidebar; however, modern UI frameworks no longer supported IE 11 natively.
As a team, Application Development selected Vue.js as our preferred JavaScript framework. With the aid of a consultant, 6 application developers undertook learning Vue.js, redesigning key structures in the Carelign UI to better accommodate Vue.js, and then re-wrote the entire Carelign UI in Vue.js. The team also had to add in backwards compatibility with IE11, and perform an end-to-end test, covering all pathways within the UI. Re-writing Carelign on a new framework extended the life of the Carelign application for at least another 5 years.
TOTAL LOGINS TO CARELIGN DURING THE REPORT PERIOD
2,416,892 59% FROM PENNCHART
872,289 21% FROM DESKTOP
805,624 20% FROM MOBILE
4,094,805 TOTAL
17 MOBILE DIGITAL HEALTHCARE
Penn Medicine Welcomes Cedar Avenue Campus to the Health System

For many decades, Mercy Hospital’s West Philadelphia Campus had been an anchor health care institution providing essential services to its surrounding communities. When financial difficulties put the facility at risk of closure in fall 2020, Penn Medicine formed a partnership with Public Health Management Corporation, Children’s Hospital of Philadelphia, and Independence Blue Cross Blue Shield that allowed the healthcare system to maintain clinical operations at that location. Operating under the license of The Hospital of the University of Pennsylvania (HUP), Penn Medicine now provides emergency medicine and behavioral health services at this location. To make this move possible, the IT team partnered with HUP’s executive leadership and the departing health system and successfully replaced all technology associated with the needs of patient clinical care.
Over six months, the IT team worked diligently on a comprehensive plan to install Penn Medicine’s standard information technologies and systems. This effort included the deployment of over 100 health system applications, the training of over 650 new staff members and clinicians, the installation of new lab and pharmacy equipment, and the installation of a telemedicine support system. This project was unique because the team could not complete this work prior to the night of go-live. All information systems were replaced overnight, as the ownership of the building and services transitioned. The hospital remained open throughout the transition and continued to provide care to the community.
Because the transition to standard processes and computer systems was completed overnight, Penn Medicine was able to forgo a costly transitions services agreement, which resulted in notable cost savings for the health system. Extending our electronic health record, clinical imagining systems, human capital management systems, the use of Penn Medicine’s existing network infrastructure and telephony services allowed for reduced costs for licensing and professional services as well as considerable time and cost savings.
Penn Medicine Acquires Tower Health Transplant Institute, Expanding Access to World-Class Care
In December of 2021, Tower Health Transplant Institute and related transplant nephrology and hepatology practices transitioned to Penn Medicine. As part of the careful integration of both programs into the healthcare system, Tower Health transplant surgeries transitioned to the Penn Transplant Institute at the Hospital of the University of Pennsylvania in Philadelphia. The kidney and liver transplant programs were fully integrated with the Penn Transplant Institute, resulting in the Penn Medicine Regional Transplant program at Reading Hospital. The new regional transplant program has continued to provide high-quality patient screening and pre- and posttransplant kidney and liver care within central Pennsylvania.
Due to the acquisition, Penn Transplant Institute expanded to 4 locations, with a new location in Philadelphia on the Broad Street corridor. This transition required the replacement of all technologies with Penn Medicine supported devices. The IT team provided a robust infrastructure and hardware platform to support three clinical operations which allowed for the seamless transition to the Penn Medicine’s EHR application within a 4-month window.
18
Gastroenterology & Endoscopy Expands at Penn Presbyterian Medical Center

























































































































































































































































































































































Penn Presbyterian Medical Center’s Gastrointestinal/Endoscopy department outgrew its existing space and expanded its operation. The department relocated to a new space across the street from the Penn Medicine
University City building, moving both the clinic and outpatient endoscopy procedure unit. The new space included four procedure rooms and nine prep/recovery bays, allowing for some of the clinical space at PPMC to be redeployed for additional use. Numerous IT teams were involved in this successful expansion which resulted in increased patient procedure volumes.
Mobile 3D Mammography Screenings for At-Risk Residents in North and West Philadelphia

Penn Medicine partnered with Siemens to offer free breast cancer screenings to women in need, over the age of 40. This program provided a valuable service to underserved communities, addressing health disparities. A 54-foot-long mobile mammography unit featured the company’s MAMMOMAT Revelation digital mammography system, accredited by the American College of Radiology, and provided state-of-the-art mammography’s.
“Cancer disproportionately impacts lower socioeconomic groups and the medically underserved because they are unable to access cancer screening tests, and thus more likely to be diagnosed with late-stage cancer. This mobile mammography initiative is one of many efforts we have committed for engaging underserved communities with access to important healthcare resources and education.”
Carmen Guerra MD, Vice Chair of Diversity and Inclusion, Department of Medicine at University of Pennsylvania
The first engagement took place in mid-October 2021 during Breast Cancer Awareness Month at 21st Street and West Allegheny Avenue. The second event was held in June 2022, in partnership with the Church of Christian Compassion and its annual health street fair at 61st Street and Cedar Avenue. By bringing the mobile mammography unit to locations in Philadelphia, the program provided mammography services for women who may not have otherwise access to this type of care.
19 PATIENT CARE OUTCOMES
3D MAMMOGRAPHY
HUP Pavilion Elevates the Inpatient Patient Experience with Iris Careboard and Outside Door Displays

































































































































































































The vision behind designing the new patient Pavilion at HUP has been to create a state of the art ‘hospital of the future’. Included in this vision, from a technology approach, were two key components:
» Designing an electronic patient whiteboard, called Careboard, which replaced the physical whiteboard typically present in a patient room. The Careboard was developed to automatically update from our PennChart EHR with key information of interest to the patient and the patient’s family, including pictures and names of key members of the patient’s care team. The Careboard design was encompassed in part of a larger footwall monitor that also includes a television and countless other features.
» A touchscreen outside door display device was mounted outside each patient room to display key safety and precaution information for staff and visitors before entering.
Integrating the digital display of clinical systems to the staff was designed to improve patient care and provide a connection between the patient, the family, and the care providers of every specialty who entered the patient room. From the doctors and nurses to the therapist and social workers, to dietary and environmental service workers - all healthcare workers were integral to helping our patients feel part of the care team to manage their care and get well again. By integrating both the Careboard and outside door display with the EHR, patients and staff automatically received the latest information. Staff were also relieved of the onus of updating the whiteboard and of hanging/removing various safety signs outside the door of the patient’s room.
Working with the HUP technology and clinical committees, we identified the key pieces of patient data to be included on both the Careboard and outside door display. Then, working with our low-voltage integration partners, UPHS Application Development designed the mechanism for displaying the Careboard and outside door display—both web pages—on their respective devices. Application Development analysts further worked with the EHR team to acquire patient data needed for the Careboard or outside door display that they did not already have.
20 PATIENT CARE OUTCOMES
Unlike most web pages, the Careboard was designed with no input device. This meant that the ability to refresh it, to detect if it had become unresponsive, and to refresh it, each had to be built into the architecture of the web page and the device that controlled the footwall.
The outside door display would, however, have an input device—it is a touchscreen—so we were able to build into it two additional features: first, the ability to get more information about a selected icon by tapping on it, and second, the ability to put the device into “diagnostic mode” to assist with troubleshooting.

Clinicians began receiving real time information about the patient from the outside door display, which is also fed from the EHR. It replaced manual workflows indicating when a patient is in isolation, at risk of falling, or risk of seizures, among other vital information. It was also designed to inform a team member prior to entering the room if the patient has any communication challenges or needs assistance with activities like feeding. The outside door display was constructed to keep both the patients and clinicians safe from exposure to infectious diseases and harmful environmental conditions unique to each patient, like not bringing flowers into a room where a patient is neutropenic or latex balloons to a patient with a latex allergy.

Using technology to transform the delivery of care and develop a patient centered approach resulted in the ability to foster cutting edge medicine toward new medical innovations and advances. Automating the precautions and warnings using the outside door display has saved clinicians from manually hanging thousands of caution signs outside the rooms of patients since the HUP Pavilion opened.
Anecdotally, displaying the Careboard on the monitor facilitated discussion among the patient, patient’s family, and care team, providing valuable opportunities for education and feedback. Patients also reported increased satisfaction at knowing exactly who has just entered their room along with a certain “wow” factor that is apparent the first time anyone sees the system. The innovative technology engages the patient, which has been noted to improve patient experience and health outcomes.
21 PATIENT CARE OUTCOMES
OUTSIDE DOOR DISPLAY
Penn Genomics Results Portal Enables Genetic Counseling Sensitivity for Patients
The Application Development team implemented a web portal solution for the processing of genetic test results so that genetic counselors would receive exam results before being released to patients. Designing this technology workflow allowed genetic counselors to interpret the results first and plan their counseling approach appropriately for the patient expecting the results.
Genetic counselors signified the importance of creating the proper channel for delivery of information and counseling for patients learning their genetic test results. In some cases, these results which could confirm a lifelimiting diagnosis, were previously being released to patients without benefitting from this important expertise and opportunity for patients to be better advised as to the significance of the results.
At Home Colon Cancer Patient Screening Increases Patient Monitoring
Colon cancer screening is essential for early detection and treatment. Penn Medicine primary care and select specialty providers offer adult patients, who are over 45 years old and at average risk for colon cancer, the option to screen for the disease using at-home testing. The at-home test option uses DNA markers and blood in the stool to screen for colon cancer.
To expedite the submission and attainment of test results into a patient’s electronic health record, and to eliminate the need for in/out bound faxes, an IT team was formulated to develop an outbound orders interface and solicit result interfaces to support at home testing integration into the EHR. The project resulted in:
• The creation of a new interface/orders results anywhere (ORA), the first ever at Penn Medicine
• Re-purposing an existing EHR ambulatory order and configuring the order transmittal rule Partnering with Community Connect sites for integrated testing
• Partnering with Primary Care service line, GI and OB/GYN service lines
• Partnering with myPennMedicine to validate patient can receive the integrated results
• Integrating results to populate Health Maintenance topics. The results indicate a positive, negative, or inconclusive test result in the EHR
Transitioning from a manual process to an integrated workflow yielded the following benefits:
• Positive impact on patient care – faster processing, delivery and turnaround of results and integration with myPennMedicine
• Improved workflow for technicians and providers
• Reduced inefficiency and associate satisfaction
• Trackability of test kit workflow and completion metrics
• Elimination of 200+ weekly faxes
• Reduced time spent by staff sending and processing orders
The at home testing interface went live on December 7, 2021. Approximately 200 orders were placed electronically during the first week, with 9497 additional orders placed through the end of fiscal year 22. This development highlights the importance of colon screening and the critical role of technologies in enhancing the screening process.
22 PATIENT CARE OUTCOMES
LGH Launches Colorectal Cancer Detection Proactive Screening Program














































































































































































































































































































































































At LGH, a new colorectal cancer screening outreach campaign was made available to relevant patients. Technologists developed an automated, text-based, patient identification and cancer screening workflow which aligned with a patient’s birthday, for those 50 years old and above. The workflow was coordinated with colonoscopy referrals to various GI practices with automated FIT (fecal immunohistochemical testing) for those who declined colonoscopy. Document workflow for program support staff was also included. For patients enrolled in the FIT testing, automated reminder texts were sent out at specific intervals to encourage completion.
Program goals were set to improve the overall colorectal cancer screening rate and targeted improving health outcomes by detecting cancer earlier and increasing patient engagement toward their health. This project also sought to streamline current outreach methods and ease the burden from the individual practices by measuring screening completions in total and across key demographics to ensure that the program strategy was equitable.
There were more colonoscopy and FIT completions and clinical time for the staff was recouped due to this project. Employment of the campaign resulted in a 2% increase in patient engagement from 73% at go-live in August 2021 to 75% in May 2022 (1,500 additional patients screened in 9 months); exceeding the goal by a full percentage point.
New Addiction Medicine Services Help Patient Population Struggling with Substance Use
The LGH Behavioral Health Service Line created an Addiction Medicine program to improve access to evidenced based care for patients with opioid use disorder and other substance use disorders. Originally, this project was piloted to determine the need and assess the proof of concept, which led to additional rollout of regional sites that now support the broader community.
This addiction medicine division established the required processes for management and billing for the new practice sites. The addiction medicine providers and care management team have operated from a defined hub and spoke model of delivery in the areas and offices in which patient populations have been most comfortable.
The LGH eHealth team built out and deployed the substance use specific documentation tools, scheduling, and billing workflows to 35 departments spread across the primary care network to allow for improved access to care and to support regional care management delivery.










Establishing this addiction medicine program increased revenue through the creation of multiple regional practice locations which increased appointment availability. The additional departments also optimized billing for care management services delivered to patients served by both addition medicine providers and primary care providers. The referral process was optimized in support of more timely access to care for patients during the continuing opioid epidemic.

23 PATIENT CARE OUTCOMES
Colorectal cancer is preventable, if appropriate screening takes place.
Managing the Opioid Crisis Toward Better Healthcare Outcomes










Nationally, practice varies widely and opportunities to treat patients for Opioid Use Disorder (OUD) are missed due to difficulty identifying OUD patients, and not having a consistent workflow for initiating MOUD (Medications for Opioid Use Disorder) treatment among care providers. Substantial best practice evidence-to-practice gaps in treatment with medication for OUD existed.

Penn Medicine implemented an ED nurse driven triage screening protocol for OUD, wherein a positive screen triggers targeted electronic health record prompts to assess for withdrawal and initiate buprenorphine treatment.

An increase in positive OUD screen rate identified additional patients for ED triage screening and treatment protocol which led to increases in assessment and treatment with MOUDs. Protocols were designed to identify patients and prompt treatment, making treatment the default. These protocols show promise in increasing implementation of standard and consistent evidence-based treatment for Emergency Department OUD care.
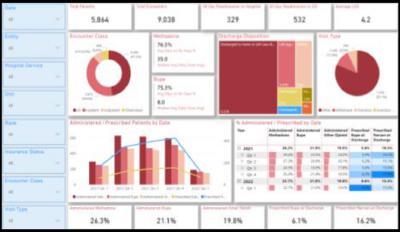
An Opioid Use Disorder dashboard was also developed to measure key quality metrics for OUD care; including use of evidence-based medication treatment, prescription of Naloxone for overdose prevention, and patientdirected discharges.


The OUD dashboard allowed measurement of outcome across Penn Medicine Emergency Department and hospitals to target opportunities for improvement and to measure progress in treating OUD patients. We could also identify equity issues, including racial and other disparities in outcomes. This tool became invaluable for targeting and tracking progress of new initiatives, including an addiction medicine consult service (piloting in 2023).
There is wide variability in a patient’s opioid needs after surgery, leading to a tendency to prescribe enough pills to cover the most severe anticipated needs. However, many patients end up with more opioid pills than needed which results in excess opioids in the community. An automated text messaging system was used to collect patients’ self-reported number of opioid pills taken after surgery. Eligible patients received automated text messages at specific days after the procedure asking a series of questions including pain intensity, number of opioid tablets used, and the number remaining. A recommendation to reduce the default number of pills was made and implemented. This keeps less unused prescribed pills in the community.
Patients who had lower pain scores at discharge and who were opioid naïve had lower post-op opioid consumption and were more likely to have pills left over. This information enabled the team to create nudges to prescribers and automated clinician feedback to encourage prescribing changes when appropriate.
Provider specific feedback was developed showing an individual’s prescribing metrics. The graphical view format provided straight forward comparison with target levels, their practice, and health system peers. Next generation guidelines will help clinicians make better prescribing decisions.
24 PATIENT CARE OUTCOMES
A Naloxone best practice alert was created and implemented to trigger when an opioid order overreaches a particular threshold. Co-prescribing Naloxone decreases risks of adverse events.
Patients that were prescribed opioids and met evidence-based criteria for increased risk of OIRD were listed for pharmacist triages to perform individual provider outreach for patients on the list – suggesting alternative analgesics, naloxone co-prescribing, sleep medicine consult/follow-up.
In addition to identifying patients at risk for OIRD and working with their attending providers, the technical development team added those patients to a co-prescribing best practice advisory that flag prior to discharge, created a workflow to ensure co-prescribing to the identified patients at risk for acetaminophen toxicity and updated order sets to provide the appropriate alternative.
Improving Hepatitis C Screening, Linking to Care During Hospitalization
The Center for Disease Control and Prevention and United States Preventative Services Task Force recommend one-time universal screening for hepatitis C for all adults over the age of eighteen. In addition, Pennsylvania law mandated hepatitis C screening for people born between 1945 and 1965. To improve hepatitis C screening, Penn Medicine implemented the automatic hepatitis C screening among previously unscreened patients who were born between 1945 and 1965, from the default order embedded into admission order set at HUP and PPMC. The Hepatitis Linkage Team was notified of all positive tests through a PennChart EHR mobile push notification. The team then followed up for test result disclosure, education, and among patients with hepatitis C viremia, linkage to curative treatment at timely manner.
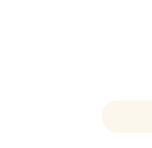
With this universal screening approach, 15,496 unique patients were screened between 9/2020-9/2022 and identified 164 patients with HCV (Hepatitis C virus) viremia status. The linkage group followed up with 126 patients and 39 patients underwent HCV treatment. Due to the multidisciplinary collaborative approach, we satisfied the Pennsylvania HCV screening and linkage mandate (2016 Act87), provided sustained increased HCV screening, and improved patient care quality.
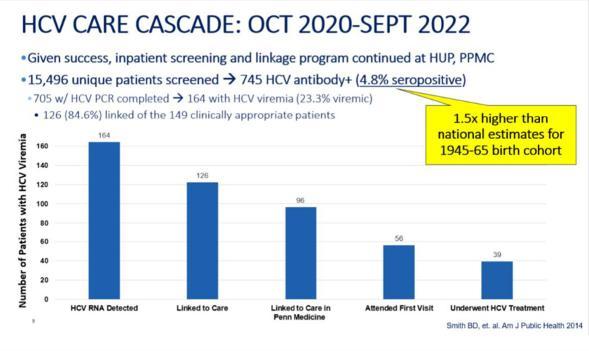
A universal ordering process was developed using an admission order set typically used for all patients upon hospitalization. The HCV order was auto populated for all patients born between 1945-1965 with no prior HCV testing in Penn Medicine and no report of HCV on their problem list. Clinicians could opt out of the testing if it were not clinically indicated from the order set. Additionally, the technical team embedded the EHR result, and documentation follow up process in PennChart, so the hepatitis C linkage group facilitated a treatment and follow-up care plan in a timely and effective way.
The new order approach contributed to an increase in HCV test completion by 31.8%. A total of 15,496 unique patients were screened from October 2020 to September 2022. There were 745 HCV antibody positive patient cases identified. 4.8% were seropositive cases which is 1.5 times higher than national estimates for the 1945-1965 cohort. Of 745 patients, 705 HCV PCR tests were completed and 164 were identified as HCV viremia (23.3%). The linkage team followed up with 126 (84.6%) patients for the next step of the plan. 39 patients underwent the HCV treatment. This universal ordering model and the linkage follow-up demonstrates support for continuity of patient care and engagement while being done efficiently.
25 PATIENT CARE OUTCOMES
LGH Implements Symptom Assessment and Management for Patient Oncology Program
LGH implemented a texting-based outreach system to help manage patient reported outcomes (PROs) during cancer treatment called SAM (Symptom Assessment & Management). This was accomplished by further automating the SAM interactions and directly integrating into the clinical workflow. LGH offered SAM to all Ann B. Barshinger Cancer Institute (ABBCI) patients to comply with CMS Oncology Care First program requirements. As cancer treatments have become more advanced and complex, follow up and monitoring from the clinical team became more difficult and frequent. Yet at the same time with this added complexity, the expectation emerged for a greater degree of proactive follow-up between visits, placing a large burden on the oncology nursing workforce. SAM has proven to be an effective way of reducing the growing number of outbound calls required to stay on top of the needs of high-risk patients. SAM has also been helpful in prioritizing nursing time towards those patients’ reporting issues and only those that required follow up from human nurses.
The implementation included the development of a texting algorithm on the Way to Health platform. The development of this framework supported future phases and included a pilot, implementing texting outreach to new patients in two of the four clinics, while phasing in existing patients and new patients over time. A later phase included an alternate outreach model—such as email and automated phone calls. Patients were seen prior to each cycle of medical treatment, in addition to treatment specific appointments. This texting program was stood up in parallel with the practice moving to a triage model where the patient would self-manage lowlevel treatment side effects from home and have access to a nurse triage team for assistance in more complex symptom management or as self-determined.
Cancer patients have been known to fight to survive both their disease and the side effects of treating it. In the turmoil of such uncertainty and physical and emotional challenges, patients have often held back from disclosing significant treatment side effects for fear that clinicians will alter or stop their life sustaining therapy. When combined with clinicians underestimating symptom severity, these factors not only contributed to lower quality of life for patients, but they have also driven increased health care expenditure through potentially unnecessary emergency room visits and hospitalizations. The implementation of SAM in Oncology significantly improved the clinical team’s ability to communicate with patients, control symptoms, reduce hospitalizations, and improve quality of life. The SAM tool has helped the clinical team achieve its primary goal of significantly reducing patients from going to the emergency room. Additionally, patients have reported high levels of satisfaction with using an AI-driven tool as an alternative to calling a clinician with basic questions.
Information Services provided extensive workflow analysis and documentation with the team for the oral and IV treatment pathways. The cancer, outpatient and patient portal teams completed build, testing, and training to support the clinical pathway changes, in addition to supporting the phone texting campaigns. After implementation, the team also modified the ADT feed to turn off/on Way to Health messaging when a patient is admitted/discharged, and automation of the enrollment step eliminating many incomplete enrollments.
Lancaster Community Gains Local Penn Fertility Care Clinic
A reproductive endocrinology and in-vitro fertilization (IVF) facility now serves the Lancaster General Health Suburban Outpatient Pavilion. Ambulatory eHealth integration ensures smooth patient integration of scheduling, clinical documentation, testing, and billing. The practice’s cryotanks and incubators house embryos and other high liability materials which are alarmed for temperature and liquid nitrogen level monitoring. Penn Fertility Care Lancaster General Health is also using a third-party application, as an assisted reproductive technology management system to manage the fertility information for all patients of the practice. This new clinic brings the entire IVF process—which includes egg retrieval, implantation, and storage to the Lancaster community. Patients no longer need to travel beyond their general region for this treatment.
26 PATIENT CARE OUTCOMES
Brachytherapy Radiology Oncology Services Refreshed to Provide Improved Experience
Brachytherapy is a critical procedure used in the treatment of cancer, and it is important to provide patients with a seamless and efficient experience. To this end, a brand-new procedure room was created in the Perelman Center for Advanced Medicine to provide brachytherapy procedures. Previously, these services were being performed in multiple phases and various procedure rooms or locations, causing a more cumbersome workflow for providers and staff. Due to this development, the services are now consolidated to provide a better patient experience.
By leveraging an existing interface, a new workflow was designed to allow brachytherapy procedures to be scheduled and performed in the newly renovated procedure room with all the appropriate medical equipment in one location. A new billing workflow was designed to streamline and improve billing workflows for technical and professional charges being performed for the procedures.

Patients now receive all phases of the brachytherapy procedure within one case, inside a newly renovated space. The new space provides a single location to receive the procedure, along with enhanced scheduling tools, and efficient billing.
New Order Panel Guides Evidence Based Ordering, Clinical Decision Support, and Interpretation
Penn Medicine’s Center for Evidence-based Practice (CEP) collaborated with the Antimicrobial Subcommittee, Sepsis Alliance, Critical Care Collaborative, and Pathology and Laboratory Medicine to establish evidence-based guidelines for inpatient procalcitonin (PCT) testing. This testing has been used to guide antibiotic discontinuation for sepsis or lower respiratory tract infection (LRTI). The guidelines provide recommendations on patient selection, testing frequency and timing, and result interpretation for ordering providers.
To improve provider ordering in the EHR, the previous inpatient PCT order was redesigned. PCT results now contained detailed guidance for serial PCT testing and antibiotic discontinuation based on indication and results for inpatient PCT orders. One order panel was created for use throughout the entire health system, carrying the same consistent clinical guidance.
By implementing evidence-based guidelines and a standardized ordering process, Penn Medicine has improved the quality of care for patients with sepsis or LRTI. Clinicians can now make more informed decisions regarding antibiotic use, which may ultimately lead to better patient outcomes and reduced healthcare costs.

27 PATIENT CARE OUTCOMES
High Sensitivity Troponin Project Leads to Significant Patient Care Outcomes

American Heart Association and American College of Cardiology 2021 guidelines indicate that, “high-sensitivity cardiac troponins (hs-cTn) are the preferred standard for establishing a biomarker diagnosis of acute myocardial infarction, allowing for more accurate detection and exclusion of myocardial injury” in the evaluation and diagnosis of chest pain or its angina equivalents. Two UPHS hospitals (LGH and CCH) were already using this biomarker, and the remaining 5 hospitals (PAH, PPMC, HUP, HUP Cedar, MCP) needed to be implemented.
Transitioning from conventional cardiac troponin to hs-cTn allows for earlier rule out while reducing rates of missed myocardial infarction. However, it can also be elevated in patients without ischemic disease. So, instead of relying on a single value and a reference range, proper use requires evaluation within the clinical context and interpretation of temporal changes (deltas) at set intervals relative to presentation. Patients without active ischemic disease can now be appropriately discharged with elevated troponins. Some of these will require follow up and others will be “incidental” and, thus, potentially seen in a wide range of outpatient practice settings.
This paradigm shift, both in workflow and interpretation, presents a large educational, logistical, and implementation challenge. In benchmarking with peers such as Duke, Mass General Brigham, and University of Texas Southwest, Penn Medicine learned that there were significant risks of diagnostic errors, inappropriate admissions, significant rise in cardiology consultation and unnecessary imaging, delayed discharges from the ED, and/or delayed outpatient follow-up.
An additional challenge with the launch at Penn Medicine was the variation in infrastructure. Hs-cTn is run on large analyzers in the core laboratories and not all laboratories have the same equipment. Harmonization of equipment would involve prohibitive large capital purchases and construction. The UPHS launch required a combination of types of hs-cTn biomarkers (Troponin T and I), each with the need for distinct interpretive guidance for each hospital depending on the analyzer in use.
The project was highly collaborative- engaging multiple physician disciplines, informatics experts, nursing leaders and operations leaders. It required interplay of clinical, laboratory, and informatics expertise. The physicians researched the existing algorithms, considering the different clinical workflows within the system. The team then worked with informatics experts to build the care path (the first one deployed at UPHS) and vetted the proposed workflow with different user groups, including every ED and many inpatient and outpatient users. Every potential user received targeted education on the impact to their area.
28 PATIENT CARE OUTCOMES
High sensitivity troponin is, by definition, a marker of early cardiac leak; it is expected to be elevated in disorders that elevate cardiac risk (cancer, diabetes, hypertension), which touches most providers in the system as potential impact (approximately 8000 individuals). Penn Medicine took the following implementation approach:
• Formed an interdisciplinary, enterprise-wide governance, eventually including 89 participants
• Designed algorithms for both I and T isoforms based upon research, embedded these in PennChart Care Path logic optimized for individual workflows through user collaboration as well as to the website for reference and links
• Coordinated the launch with all affected labs and analyzers
• Facilitated educational efforts:
• Provided five learning modules for users
• Created educational material such as tip sheets and eLearning
• Created a project hub (website) for FAQs and additional material links
• Numerous meetings with stakeholder groups to ensure education needs were met
• Coordinated communication plan for impacted groups, including newsletters, CMO office, the PM report, in addition to local messaging
• Supported a multidisciplinary command center for questions
• Created analytics dashboard for continuous monitoring
The initiative successfully went live on June 3rd, 2022 with an exceptionally smooth transition from the old assay to new high sensitivity troponin. Penn Medicine did not experience any reporting of diagnostic error, inappropriate admission, delaying discharge or increase in cardiology consultation. Patients with a chief complaint of CHEST PAIN have a 26% decrease in median percentage of observation dispositions. Of the patients with a chief complaint of CHEST PAIN or SHORTNESS of BREATH, 13% had an increase in median percentage of discharge disposition while there was a 17% decrease in median percentage of observation dispositions. Diagnosis of NSTEMI and STEMI increased for patients presenting with chief complaint of chest pain. Stable ED length of stay for patients presenting with chief complaint of chest pain despite unusually high boarding times.
Improving Sepsis Detection in Newborns Using EHR Neonatal Sepsis Risk Calculator
Early onset sepsis in neonates has long been established in the U.S. as a life-threatening condition. As a result, newborns have been screened for this risk after birth to take precautionary measures for detection. In the past, providers calculated a neonate’s risk of sepsis by manually entering data into a web calculator and copying the score back into the EHR. Caregivers sought a more automated tool, which appeared conveniently in workflows, to capture related data directly in our EHR. The hope was to leverage clinical documentation by generating an accurate score as soon as possible and begin therapy if it were needed.
The EHR application team developed a customized sepsis enhancement from a baseline feature in our EHR to meet our goals for more rapid scoring and automatic score recalculation. The team also designed the clinical decision follow-up recommendations to appear dynamically, depending on the reported values and the newborn presentation. The project team performed multiple proof of concept trials, enabling consistent calculation even when tested toward the event of less common, real-world scenarios. Additional performance adjustments were also applied to the design and testing, which improved run time.
Since the initial implementation in July 2021 through March 2023, the tool has auto calculated the sepsis risk score for 20,237 newborns. Patients and clinicians benefited from accurate scores and quick access, helping to expedite vital patient care. The benefits to clinical detection outcomes were so significant that our EHR partner decided to update their base application to match our new design so that all organizations could use a more featured, highly performant, research current calculator.
29 PATIENT CARE OUTCOMES
Clinical Trial Shows Effect of EHR Nudges to Increase Statin Prescribing

Statins reduce the risk of major adverse cardiovascular events, but less than half of Americans that meet guideline criteria for a statin are prescribed one. Effective statin therapy requires prescribing, acceptance, and adherence from patients and encouragement from clinicians. Barriers exist at both points, revealing opportunities to improve effective statin use.
A study team conducted a cluster randomized trial to evaluate the effect of nudges to clinicians, patients, or both on the initiation of statin prescriptions during primary care visits. These interventions were automated through the EHR, representing a scalable approach to nudge behavior. The clinician nudge included two components. First, clinicians received an active choice prompt by BPA (best practice advisory) which triggered when a clinician entered the order in the EHR. Second, clinicians received monthly peer comparison in the form of a 3-month rolling average of the percent of their eligible patients prescribed a statin and how that compared to peer clinicians at Penn Medicine.
Patient nudges were sent by text messages starting 4 days prior to their appointment, reminding patients of the upcoming appointment, and informing them of an important message about their heart health. Patients confirming their willingness to communicate by text were told: “Guidelines indicate you should be taking a statin to reduce the chance of a heart attack.” Patients were told “At Penn Medicine, it is standard of care to prescribe a statin to patients like you.” Patients were asked to reply “Y” if they were interested in taking a statin or reply “?” if they were unsure or had questions for the doctor. Patients replying “Y” were told to remember to discuss the statin during their visit and sent a link to a shared decision-making tool on statins. Patients replying were told to write down their questions or concerns and share them with their doctor at the visit. Patients were sent an additional message 15 minutes before their appointment time: “As a reminder, speak with your doctor about taking a statin medication to reduce your risk of a heart attack.”
The trial included 158 primary care clinicians from 28 primary care practice sites. During the intervention period, the sample included 4131 patients with a mean (SD) age of 65.5 years (10.5); 51.3% were male, 66.1% were white, 29.3% were Black, and 22.6% had Atherosclerotic cardiovascular disease. The primary outcome was initiation of a statin prescription by the end of the day of the primary care visit. A secondary outcome was whether a statin was dispensed by a pharmacy within 30 days of the visit.
In this pragmatic, cluster randomized trial, a clinician nudge alone, and when combined with a patient nudge significantly increased initiation of a statin prescription during primary care visits. Sending nudges to patients alone was not effective. These findings demonstrate the potential benefit and scalability of using nudges to change prescribing behavior through automated processes within the EHR.
30 PATIENT CARE OUTCOMES
New Clinical Workflow for Sepsis Improves Patient Care Treatment & Outcomes
Sepsis is a potentially life-threatening response to infection that has been known as a leading cause of death nationally. Prompt recognition, timely intervention, and adherence to evidence-based best practices have created well-established associations with improved outcomes and reduced mortality among patients with sepsis. Given its role in modern healthcare delivery, the electronic health record (EHR) provided a unique opportunity to impact clinical care in terms of sepsis response.
A team assembled to assess this need and found that more than 80% of sepsis patients came to Penn Medicine through ED admission, in need of more extensive care. Members from our sepsis alliance helped us design an extensive, multi-faceted sepsis EHR process to promote best practices, quality care through early recognition, and core measure compliance at critically relevant time intervals. A sepsis checklist was implemented to facilitate a new interdisciplinary care coordination process to guide providers and other clinicians through the first 18 hours of management of a patient in sepsis with organ dysfunction or septic shock. The intended goals of the sepsis checklist included:
1. Improving adherence to the 3 and 6-hour sepsis bundle
2. Improving adherence to the use of a problem list
3. Improving interdisciplinary team communication
4. Promoting seamless transitions of care
5. Improving patient outcomes related to sepsis
Upon ED admission, clinicians could see the sepsis treatment status promptly because this sepsis checklist opened automatically as a sidebar report. Due to the new clinical workflow, improved outcomes of septic shock patients quickly resulted from more consistent and timely application of evidence-based care and reduced practice variability. Care coordination from patients presenting with sepsis from the ED and transitioning to the inpatient setting was also a component of success toward promoting continuity of patient care.
Patient Medical Records Gain Electronic Sharing Through 21st Century Cures Act - Phase II
The 21st Century Cures Act required that healthcare providers and systems continually optimize patient’s medical record available to the patient and other healthcare providers electronically. By making data immediately available, the patient could better control their care while being supported with safe and efficient care delivery, especially if they needed to share their information among multiple healthcare sites.
A multi-disciplinary team worked with constituents to develop a deployment strategy that would meet the Act’s requirement while helping assure optimal patient care. The team assessed all the documents in the medical record and the various methodologies that would make them available to patients and clinicians. They evaluated the many complex types of interactions that occur at Penn Medicine, worked to assure patients that data was appropriately handled, and that the relationship between physician and patient remained optimal. The team also developed and delivered comprehensive education so that our clinicians were aware of the rule and its implications.
Patients now have access to most of their medical record and test results through their myPennMedicine portal. They have greater ability to make requests for their complete medical records and can send their health record data to personal health record apps. Other healthcare providers could access a patient’s record when they see that patient to assure safe and efficient continuity of care. In all cases, a patient’s privacy, and ability to control their data sharing has been maintained.
31 PATIENT CARE OUTCOMES
Cancer Registry Case Finder Application Brings More Efficient Reporting
For public health reasons, any healthcare center or office that diagnoses and/or treats oncology patients (including all hospitals, medical centers, MD offices, radiation oncology centers, hematology, and oncology centers, etc.) are required by law to annually report new cancer cases to a central or state cancer registry. Although Penn Medicine uses a commercial third-party vendor tool to collect and store our cancer registry data, we sought to determine how to cohesively identify, manage, and report on all the potential cancer cases from our large academic medical center.

Penn Medicine’s Abramson Cancer Center treats patients from among our six hospitals, many clinical departments and divisions, and has 75,000-100,000 related encounters as well as 30,000 - 35,000 unique patients related to the treatment or diagnosis of cancer each month. Since there was no suitable commercial solution for this problem, our technical experts conceived an in-house application to automate, organize, and manage this process. This has empowered users to identify which patients qualify efficiently and accurately for inclusion in the registry, transforming what was a manual, time-consuming, and resource intensive process. The department sought to use each manager’s time more effectively, instead of manually reviewing and reconciling many different spreadsheets and reading hundreds of e-mails a week related to the reconciliation process.
The Cancer Registry Case Finder (CRCF) was designed as a custom, homegrown, web-based application fully designed and built by the Penn Medicine Application Development - Database and Applications Group (DAG). All software used to build and maintain the CRCF is open-source, can be used with any major database, and uses the BSD-style and MIT licenses. This application is being used in our Cancer Service Line’s Cancer Registry which is an American College of Surgeons (ACOS) Commission on Cancer accredited program. The CRCF application is integrated with our EHR for source data and the cancer registry tool, allowing us to import and export to streamline our full abstraction process.
Case-finding is the first crucial piece in properly identifying reportable cancer cases to collect data on. Now, the application saves time in managing this data. The application provides:

• Real-time data reporting which decreases data delays
• Analytics to assess appropriate staffing
• Data quality improvement
• Data for research
32 PATIENT CARE OUTCOMES
One-Step Specimen Orders Improve Operating Room Specimen Tracking
It has been standard procedure for the operating room (OR) to send numerous specimens to pathology and microbiology for analysis. Tracking of specimens is very important to ensure that all specimens make it to the appropriate lab, minimizing risk of loss and allowing for appropriate evaluation to occur. However, nurses were not well equipped with an electronic mechanism for tracking these specimens with information such as the source, type, and specific tests. Our nurses were documenting intra-specimens using a non-order section of the electronic health record. They wanted the chance to track the specimens electronically from the OR to the pathology lab.
To sunset that workaround, the EHR Application Development team created a one-step specimen order section which interfaces the specimen orders to our lab vendor. The perioperative and pathology departments determined the specific specimen source, type, and tests which facilitated communication between departments. New label printers were ordered for each of the ORs at our hospital entities. By working with our end user services team, we configured these printers within our PennChart EHR to print specimen details onto a label and apply it to the OR specimen collected.
The specimens were tracked through PennChart and an interface message transmitted the specimen collection data to our lab partner. Specimens received in the lab were more efficiently scanned and documented appropriately. This electronic transmission replaced the previous workflow that was done completely on paper.
Now that specimen collection data is documented electronically, tracked, and transmitted through an interface, there has been a decrease in intra specimen errors. The new approach also provides an enterprise standard for how to document the specimen collection data.

New Hospital-wide Dietary System Enhances Patient Safety and Satisfaction
The Hospital of the University of Pennsylvania moved to a new hospital-wide dietary system to enhance service, quality, safety, usability, and system support. The new software included a Point of Sale (POS) system. Improvements included:
• Enhanced patient safety
• Enhanced patient satisfaction
• Full system support, that allows for system changes and settings configuration
33 PATIENT CARE OUTCOMES
Penn Medicine Moves to an Enterprise-wide Patient Flow Solution
In preparation for the opening of Penn Medicine’s newest hospital (the Pavilion), a new enterprise-wide patient flow model was designed, developed, and implemented that provided for the patient progression needs of relevant ambulatory practices and inpatient departments based on practice specific workflows, EHR build, testing, training, and on-site go-live support.
Following an analysis conducted by a core team comprised of nurse managers, IT subject matter experts and IT analysts to understand pre, intra, and postop area, it was determined that recent advancements in the functionality of our EHR’s patient progression module could support the patient progression workflows of ambulatory radiology practices and the inpatient perioperative workflows starting with the Hospital of the University of Pennsylvania and Penn Presbyterian Medical Center. As the staff were already using our EHR module that provides users with a more efficient way to improve operating room utilization, availability, and functionality for both inpatient and outpatient day surgery, the assessment also resulted in adoption of additional functionality within the module documentation and tools along with development of various status boards. The support staff made a full transition to new environmental service and transport modules. Benefits resulted in:
• Saving a significant amount of money each year by sunsetting the previous outdated system
• Increasing patient satisfaction by increasing transparency and eliminating confusion regarding a patient’s specific location within a department
• Reducing patient waiting time, inefficiencies, and reduced exam and clinic time with timestamps for every touchpoint both at the patient level and department level
• One application for surgical documentation and patient progression enhanced workflows
• Standardized processes for shared resources between the Hospital of the University of Pennsylvania and Penn Presbyterian Medical Center
• Ninety new configurable “Status Boards” were implemented to track the timely movement of patients for surgical cases and orchestration of staff and resources
e-Consents Launched for Ambulatory Departments
Transitioning from paper consents to electronic consents was part of the Ambulatory Practices Risk Reduction Initiative to reduce the risk of lost or incomplete consent forms and improve version management with quick and easy access to patient consents in the electronic health record.
The project’s initial phase included reviewing, standardizing, and revising all paper consents into patient-friendly language. The next phase was comprised of the technical consent build in the EHR, followed by the development of education and training materials on the new e-consent workflow by the EHR’s advanced clinical education team. Since go-live on 12/7/2021 over 1,834 consents have been built through fiscal year 2022.
Chester County Hospital Gets a Major Lab Software and Equipment Upgrade
To streamline the specimen labeling process and gain efficiencies with specimen collection workflow, existing lab software got a major upgrade at Chester County Hospital. Also, over three hundred and fifty new specimen label printers were deployed across all inpatient rooms. Printers were installed in the intensive care unit, medical surgery unit, emergency department, PeriOp’s pre/post procedure units, Pediatrics, and all women’s health units.
The installation and testing of all devices were completed without having to close any rooms at the hospital. Extensive lab and nurse training was integral to the success of the project. Initial results showed significant improvement in the turnaround time for specimen processing.
34
Penn Presbyterian Medical Center Trauma Unit Moves to Cloud-based Patient Monitoring System
Penn Medicine moved to a remote telemedicine intensive care (ICU) module for the Penn-Elert eICU patent monitoring system, used in the trauma unit at Penn Presbyterian Medical Center. The new system supports virtual patient observation for optimal care and staff productivity. The technology consists of wall mounted access point of care systems (APS) which contain high fidelity microphones and speakers, infrared lights for low light and night vision, and a high-definition camera.
The benefits of the system include:
• The availability of telemedicine consults for clinical decision making to aid in the care of the most vulnerable patients
• The activation of an enhanced rapid response system triggers an escalation of care to a higher-level of service in an urgent situation, precipitating a transfer to the critical care team
• Access to on-call specialists should the trauma physician need a patient consult
Radiation Oncology at Penn Medicine Princeton Health Migrates to an Enterprise Solution
In April 2022, the Radiation Oncology department at Penn Medicine Princeton Health migrated to two of Penn Medicine’s enterprise-wide applications:
• An oncology information system that supports medical and radiation oncology, including proton therapy

• A system to optimize a patient’s treatment plan based on a physician’s dose instructions, and information about the size, shape, and tumor location to be treated with radiation
The project included the implementation of all interfaces and archiving of data as determined by the IS team. The migration’s purpose was to improve workflow and efficiency and increase functionality for all shared models throughout the health system. The migration also included safety improvements and added components for radiation oncology business continuity.
Additional effort was needed to integrate a third system used by Radiation Oncology at Princeton health related to third-party professional billing. Charges were rerouted through a new VPN tunnel to bypass charging through the enterprises’ EHR. The benefit of performing this build additionally resulted in significant cost savings.
35 INTEGRATING AND UPDATING CORE SYSTEMS
Penn Medicine’s Gift of Life Organ Donation Program Integrates into the EHR
Penn Medicine’s Gift of Life program has long promoted organ donation and established advancements in the field through innovative clinical programs and novel research at Penn’s Transplant Institute. The move to integrate a patient’s discrete data from their EHR to the Gift of Life’s electronic medical record in real time, was integral in meeting the Transplant Institute’s goal to complete 10x’s the current transplant volume at Penn Medicine by spring 2022.

Penn Medicine was the first healthcare system to develop the ability to integrate patient data over the FHIRAPI model with the Gift of Life system. Thus, Penn Medicine was the beta site which required the core IT team to define the required end points to support the necessary discrete data points so the Gift of Life coordinators could assess a potential donor in real time.
Transitioning from a manual process to an integrated workflow yielded the following project benefits:
• Positive impact on patient care
• Improved workflow
• Reduced inefficiency and associate dis-satisfaction
IS Education Team Breaks Virtual Training Records
Penn Medicine’s education team exponentially increased technology learning throughout the health system in the past two years. The opening of the HUP Pavilion and the pandemic-related turnover in staff were two key factors for the significant increase that occurred in technology education. New staff hiring within Penn Medicine increased, causing a need for new EHR clinical classes.
Five records were broken in FY 2022, including total staff trained, total hours trained, and total classes held. Total learners trained by IS educators was 24,634; 11,696 of these were individual learners, the remaining attended more than one session. This was a 45% increase from the prior fiscal year. Total staff trained in virtual live sessions were 8,863 and total staff trained from e-learnings was 15,771. There were 1,562 classes taught and over 7,800 hours of education provided.
Penn Medicine has depended on our ability to protect the privacy and security of patient data and clinical systems that house it. Regarding privacy, inappropriate access to patient information, both accidental and intentional, can more than ever jeopardize patients’ trust in our institution. Regarding information security, while healthcare organizations have long been a target for hackers, threats have been increasing daily. As a result of these and other threats to our systems and data, we have enhanced our HIPAA education program.
To ensure that new hires completed HIPAA training before gaining EHR access, the education team instituted a new and effective process. The learning management system was reconfigured to match the time management system logic regarding manager oversite, resulting in all NPRs having an assigned manager. Full time employee compliance of completing HIPAA education in a timely manner increased to 94% and non-payrolled resources (NPR) compliance increased to 65%.
36 INTEGRATING AND UPDATING CORE SYSTEMS
Penn Medicine Automates Quality of Care Codes











To eliminate the mandatory, manual, and time-consuming process of submitting quality of care codes to insurance companies for performance improvement data, Penn Medicine implemented a technical system change in our EHR for code submission at the time of billing. The new automated procedure streamlined the metrics collection process to determine baselines and goals with all carriers.
Using quality of care codes at billing has eliminated the need to manually upload the data for the many incentive programs in which Penn Medicine participates. Capturing this data has helped to drive Healthcare Effectiveness Data and Information Set (HEDIS) performance improvements. Gaps in care have been more quickly identified as closed; which drove direct star rating improvements for the health care system. Coding for these services provided access to more accurate medical data which also helped Penn Medicine’s efforts to support our care plan through more targeted case management services.
Using the EHR to Tell a Patient’s Story


Penn Medicine implemented a new user interface tool in the EHR called Storyboard. The new display replaced the patient header and provides a quick overview to more easily access essential information in the patient’s story. Implementing Storyboard made it easier for Penn Medicine users to act on important patient related information in the electronic health record (EHR) using fewer clicks, mouse movements, and screen switches. It changed the way clinicians at Penn Medicine use the EHR. Storyboard took full advantage of modern widescreen monitors in a way that maximized information, presenting on one screen.
Before Penn Medicine implemented Storyboard, the ideas behind it were researched, developed, and tested for over seven years by more than 100 health care organizations. During that time, 1000 usability tests were conducted - involving clinical, revenue cycle, and access users. Storyboard was proven to streamline the user experience, allowing for a more patient centered workflow.
Storyboard provides users with a more tailored experience than in the past. In fact, there have been a variety of storyboards, each designed for a particular role, specialty, or context. At the same time, each storyboard’s content was designed to follow the same format, with basic information about a patient at the top, and specialized information at the bottom. Storyboard was also designed to provide users with options to view all information at once, or “hover to discover” over a section to see more detailed information as needed. To act, they just began to click from within Storyboard.
Benefits gained from this new design:
• Easier visibility of code status, allergies, admission date, and patient precautions
• Easier visibility of care team members, as hovering over Storyboard presented the team list
• Easier visibility of the patient’s primary family contacts
























































































































• Enabled ready access to the problem list in a way that was not possible before
















































































































































































































































• Eliminated need to regularly navigate to other sections of PennChart for essential information
• Gained key information more pronounced on the side of the screen, with added detail, at users’ fingertips.
Dr.
37 INTEGRATING AND UPDATING CORE SYSTEMS
“The major benefit is to have quick access to key data for clinical care without having to leave current activity such as note writing and order entry. The other major benefit is that the information is dynamically updated and only shown if available, or applicable to the patient.”
Kai Xu
Phoenixville Medical Associates Joins Penn Medicine
Penn Medicine embarked on a journey to incorporate Phoenixville Medical Associates (PMA) into the family of Penn Medicine clinical practices within the tri-county region. The 11 practices situated in Delaware, Montgomery, and Chester counties offer a host of clinical services, such as primary care, internal medicine, rheumatology, and sleep medicine with a total practice make-up of 44 providers, 122 staff, 11 clinical locations, 1 administrative location and 112 exam rooms. The addition of the Phoenixville Medical Practice Group is the largest expansion of Penn Medicine’s primary care network within recent history.
Before coming to Penn Medicine, Phoenixville Medical Associates were part of an accountable care organization (ACO). When integrating the practice group, the health system assumed ownership of the ACO membership, which required capturing specific data elements to maintain the affiliation. Working with our new ACO partner organization and PMMG leadership, Penn Medicine was able to establish four unique interfaces. Incorporating PMA into Penn Medicine opened new opportunities to participate in an ACO for the health system.
The transition of this new practice required the collaboration of many clinical and IT departments in the health system. During the implementation, the project team worked skillfully to migrate PMA, onto a host of Penn Medicine applications, a robust infrastructure and the ACO interfaces. One notable achievement was the conversion from 2 unique legacy electronic medical records onto the Penn Medicine’s electronic health record, within a 6-month period. All teams were presented with time constraints and rose to the challenge of completing the project with great success. Each location was outfitted with Penn Medicine’s Business Continuity Access application for critical access to medical records during any type of outage. The transition also included the activation of four interfaces to maintain the ACO and the electronic conversion from paper faxes, which significantly decreased paper consumption.
With expedited assistance from the networking team, a new network was deployed at each location. Included was new low voltage cabling, new data computing electronics, state of the art wireless networking, and environmental controls for each data closet. Working closely with the internet service provider, expedited delivery of internet services was quickly implemented. Most locations required the construction of a new data closet, which required close coordination with the construction team, low-voltage cabling contractor and the networking team.
Project benefits included:
• Coordination with operations and leadership which resulted in development of a program and toolkits for use on this and future implementations
• Established a regionalized approach for go-live support and deployment, the first of its kind at Penn Medicine to include local support staff
• Redesigned command center approach to accommodate multiple simultaneous activations, which provided improved transitional support for staff during the changeover
• Development of new EHR applications for 19 distinct departments using clinical workflows
• First of its kind rheumatology infusion workflow was developed for specific use in an ambulatory environment
• Deployment of over 5,000 devices, including PC’s, printers, and peripherals devices throughout 112 exam rooms leading to significant improvements in clinical workflows
• On-boarding of 167 employees by providing 2,500 hours of education to support informed and effective users
• Enhancement of on-time deliveries and lower overhead costs by using local warehousing for preequipment orders and deliveries
38 INTEGRATING AND UPDATING CORE SYSTEMS
Penn Medicine Partners Provide Services to the Underserved
Penn Medicine partnered with Public Health Management Corporation (PHMC) and the federal government to implement the PHMC Health Center on Cedar, a Federally Qualified Health Center (FQHC) located on 54th street in West Philadelphia. The PHMC Health Center on Cedar is staffed by clinicians from Penn Medicine’s department of family medicine and community health. This innovative public health campus provides community-informed, integrated care and social services to support individuals and families. The campus’ existing services include an emergency department and onsite inpatient and behavioral health services available through Penn Medicine.
To support this effort, the IT team at Penn Medicine installed state-of-the-art technology, including our networking and electronic heath record systems. Penn Medicine’s Public Health Campus on Cedar has improved the quality of life for the underserved patients of West Philadelphia. The preventative care provided is cost efficient and allows many patients to have access to affordable immunizations, mammograms, pap smears, health education, and other screenings. PHMC meets nationally accepted practice standards for managing chronic illnesses and reducing health disparities.
Services provided include:
• Primary care and preventive health care for adults and children

• Women’s health including regular OB/GYN care, and prenatal and postnatal care
• Behavioral health care
• Substance use disorder treatment
• Chronic disease management
• Social services support
EHR Upgrades Ensure the Latest Features and Functionalities
Each quarter, Epic Systems releases application improvements to their software. This is reflective of the vendor’s commitment to deliver consistent and continuous improvements for both clinical and revenue cycle applications. Information Services has also remained committed to implementing these application enhancements to benefit the health system.
ur organization’s EHR was upgraded in August 2020 and February 2021 to supply the latest functionality and feature enhancements. The upgrades also provided users with annual regulatory updates. The August 2020 upgrade improved employee satisfaction by implementing the first hybrid onsite and virtual approach to command center support and made 3,588 changes to EHR with minimal command center ticket volume.
Notable enhancements in the 2020 upgrade included new documentation options in the provider notes physical exam smart form, clinicians’ shortcuts to activities via patient lists, schedulable orders updated to “appointment requests,” appointment desk and work queues functionality updates, as well as enhancements to the Medicare Secondary Payer Questionnaire (MSPQ) that were instituted to allow for faster documentation. Additionally, clinicians were enabled to add a visit diagnosis from anywhere in an office visit using the taskbar.
Notable enhancements in the 2021 upgrade included the continued implementation of the first hybrid onsite and virtual approach to command center support. The team made 262 changes to the EHR with minimal command center ticket volume. Command center support closed in only 3 days; which resulted in a modified support model that efficiently closed tickets and minimized staffing allocations.
39 INTEGRATING AND UPDATING CORE SYSTEMS
PennChart Hardware Enhancements Support the Performance and Reliability Standards of EHR Upgrades
As part of Penn Medicine’s continuing effort to create the best user experience, the health system upgraded its version of EPIC over a two-year period in 2021 and 2022. In preparation for the upgrades, an evaluation was performed, determining that improvements to specific hardware and database requirements were needed to achieve performance and reliability standards.

The core IT team implemented updated hardware to accommodate additional capacity, licenses, and storage to support the upgrades for the most optimal performance and user experience. This activity required additional hardware to be purchased, provisioned, and installed to proactively mitigate any performance issues. Advance procurement of the hardware allowed for staging of the new hardware with the upgrades which minimized downtime during the EHR enhancements.
The result of the hardware upgrades reduced management and administration costs. Expensive legacy infrastructure was retired, and licensing consolidation efforts were completed to achieve economies of scale. Following the hardware upgrade, Penn Medicine’s electronic health record was successfully upgraded in support of EPIC’s latest functionality and feature enhancements, in addition to making annual regulatory updates.
HIM Data Mapping Improves Patient Care
One essential component of health IT interoperability and the improved care and efficiency it offers, is data mapping. Data mapping involves “matching” between a source and a target that enables software and systems to meaningfully exchange patient information, reimbursement claims, outcomes reporting, and other data.
Penn Medicine’s Health Information Management (HIM) team updated our point of origin table mapping process to ensure the accurate capture of the location of patient intake. Mapping plays a key role in moving data from setting to setting and use to use, from informing patient care to informing national policy decisions.
Early in 2022, our point of origin table mapping process needed updating to reflect the Centers for Medicare and Medicaid (CMS) current values and to accurately capture the location of patient intake for access areas at each hospital in the enterprise. Key changes included the removal of emergency values and defaults, requiring emergency department registrars to select the appropriate admission source/point of origin and the addition of new value added for home or work hospital billing.
• Point of origin accuracy improved metrics across the organization
• Identification of patients coming from a skilled nursing facility impacts other areas such as postacute care/episodes of care models
• Reduced inefficiency; consistency across all entities, including LGH
• Improved workflows for patient access, HIM, and coding
• Improved care quality and patient safety
40 INTEGRATING AND UPDATING CORE SYSTEMS
Advanced EHR Application Features Assist Caregivers with Improved Patient and Operational Workflows
Penn Medicine’s EHR partner, Epic, has continually enhanced and updated available features across all our licensed application modules. Epic’s ‘Honor Roll’ program has incentivized customers to adopt and use these features. Participating in this program allows us to deliver benefits related to new capabilities and be eligible to receive a reward from Epic when we have demonstrated that specific adoption requirements have been met.
A project team was assembled to engage all Epic EHR (PennChart) application teams and representation from the infrastructure and reporting teams. This team worked with their respective operational areas to review new feature adoption opportunities and Honor Roll program requirements.
Six Honor Roll program components were tracked and successfully met:

• Enterprise Data and Analytics
• Health Information Exchange
• Infrastructure Stability and Performance
• Patient Experience
• Population Health
• Staying Current
Enabling features included in these components and allowed the following benefits to be attained:
• Improvements in patient experience
• Faster release of test results in the patient portal
• Allowing patients to better manage appointments online
• Use of eCheck-in to reduce in-clinic wait times at registration
• Implementation of “Fast Pass” to give patients the opportunity for earlier appointment times
• Use of “Health Maintenance” reminders for annual screenings and wellness visits
• Workflow efficiency and system stability
• Implementation of image exchange to send and receive images with outside organizations
• Improvements in overall system performance, specifically note launching and ordering workflows
• Staying current with Epic version releases and enhancements
• Population Health
• Staying Current
By participating in this initiative, over 105 new enhancements were upgraded and implemented to the application version that allows us to remain current with Epic functionality. We also increased the response time for three heavily used workflows by an average of 40 points, allowing for better system performance. Lastly, we achieved Honor Roll Cum Laude status, which resulted in a reward from Epic.
41 INTEGRATING AND UPDATING CORE SYSTEMS
Penn Medicine at Home Implemented Electronic Visit Verification for Medicaid Claims

To automate documentation and ensure workplace compliance for Medicaid at home care services, Penn Medicine instituted a configurable mobile point-of-care field force management and Electronic Visit Verification (EVV) platform. The system electronically verifies the delivery dates and times of home services to the individuals needing these services and to the state aggregators. Medicaid claims are paid based on the submitted data, which affects reimbursement, patient safety, and satisfaction.
Cardiology Studies Respond More Readily with Remote Access Capability
The cardiology department’s multi-modality reading solution was upgraded to provide new feature enhancements, mapping solutions, and increase measurement options filing to our electronic health record application. Clinicians now have advanced remote capabilities to review studies at home to provide faster on-call results.
Penn Cardiology was able to upgrade the system at the Hospital of the University of Pennsylvania, Penn Presbyterian Medical Center, Pennsylvania Hospital, and a host of offsite ambulatory practices. Finally, later in the year, the inclusion of Chester County Hospital made the upgrade an enterprise-wide solution.
The technology team added servers to house the software, installed the testing environment, and the command center was operational for a week for support calls. Remote desktop software was installed onto designed PCs to allow staff to use upgraded remote capabilities.
Care Everywhere Image Exchange Helps Facilitate Patient Care
Image exchange helps clinicians visualize the care that patients receive at other organizations and helps with informing each respective caregiver’s part of the patient’s treatment plan. By exchanging documents and using reference-quality images, members of a patient’s care team from multiple health systems can see information like x-rays, EKGs, wound images, consents, and EMS run sheets in the patient’s chart. All this data provides an additional layer of detail, shared through health information exchange (HIE).
To facilitate this exchange at Penn Medicine, our PennChart EHR team enabled new technology to exchange image files with other organizations including consents, results, and radiology images (DICOM) through Epic’s Care Everywhere network. This technology development allowed clinicians at other facilities to have approved access to patient data, such as non-discrete information, and reference quality images for radiology and other imaging results.
Penn Medicine was one of the first Epic organizations in the region to go live with enabling Care Everywhere Image Exchange. The PennChart development team worked with clinical and business counterparts to acquire and install infrastructure, including support for share and retrieval of DICOM images with participating organizations. The team also developed education materials and communication to inform providers of the new information available for sharing through the EHR. Within just two hours of the initial go live, Penn Medicine retrieved 5 images and sent over 900, mostly to non-Epic organizations. Since 9/30/22 we have successfully retrieved 186,832 images.
42 INTEGRATING AND UPDATING CORE SYSTEMS
Connecting an Award-Winning Cancer Information Website to our Electronic Health Record

OncoLink is an award-winning cancer information website that was developed and based at Penn Medicine. OncoLink provides up to date, evidenced-based oncology patient education and survivorship care plans. With the implementation of this project, important patient education tools are now integrated into the EHR, which provides both patients and clinicians with the ability to use OncoLink for access to:
• The survivorship care plan builder and the treatment binder (patient education materials) via the dropdown menu
• The documents customizer feature, which allows for documents to be built and saved directly to the patient record, eliminating the need to exit the EHR, create and print OncoLink documents, and scan them into the patient’s chart.
• PDF documents, that once created, are available from the media tab in the chart and to patients in the My Documents section in myPennMedicine.
HTTPS://WWW.ONCOLINK.ORG/
The Information Services team partnered with the Penn OncoLink team and vendor to make this a reality. The IS Project Management Office guided the project through the discovery, security, and implementation. Multiple specialties within the Information Services team worked to enable integration of this application with the EHR for both clinicians (in PennChart) and patients (in MyPennMedicine), and developed a tool to be used for statistical analysis by the OncoLink team.
Benefits:
• Integration of OncoLink education materials and survivorship care plans into PennChart resulted in time savings for clinicians, and improved documentation of education provided, assuring documents are labeled and filed correctly
• Reduced the average time it takes to complete the process of generating and filing a survivorship care plan from 14 minutes to 2.5 minutes
• Integration eliminates the need for downloading and scanning and the potential to introduce errors
• The first year of this integration has resulted in the creation of over ten thousand education documents for oncology patients
43 INTEGRATING AND UPDATING CORE SYSTEMS
Post-Operative Staff Gain Immediate Access to Medications Administered During Bypass Surgery










































































































































































































































































































































































Medications given throughout cardiopulmonary bypass were historically documented in the perfusion chart in Penn Medicine’s perfusion and patient safety systems. The systems were designed to support a wide range of extracorporeal therapies, including ECMO. The medication chart existed in operating room documentation and was not readily accessible to physicians, advanced practice providers, pharmacists, and nurses post-operatively.
By integrating an incoming medication administration documentation interface from the perfusion system into the EHR’s read only section of the patient medication administration record (MAR), patient safety risk was mitigated. This type of interface was the first deployed for Penn Medicine and a first for the vendor interfacing administered medication to an electronic health record.



Perfusionists, anesthesiologists, pharmacists, and other providers from the Hospital of the University of Pennsylvania and Penn Presbyterian Medical Center collaborated on the selection of over 50 medications that were interfaced. Clinical staff who cared for patients post-operatively were enabled to view medications such as antibiotics and immunosuppressant administered to patients in the OR during cardiopulmonary bypass in the MAR. This is in addition to the usual location of the perfusion record. The achieved goal brought the information to a location in the EHR for a faster and easier view by clinical staff.
“Automated transfer of information from one part of the medical record to another is one of the implicit gifts of an electronic record. What many don’t realize, however, is that there are hundreds of medical devices and we’re slowly interfacing the most critical to the EHR. For example, an interface between the heart-lung bypass machine and PennChart has recently been completed and it both improves visibility about drugs administered in the operating room and cuts down on transcription errors. This is the result of a great collaboration between clinicians and information services experts.”
Dr. Bill Hanson
Penn Medicine at Home Expands Patient Outreach










Penn Medicine At Home offers a full range of health care needs from the comfort of home, or in a Penn Medicine hospice location. To expand the patient outreach program for Penn Medicine at Home patients, an interface was built between our EHR and the existing health engagement solution. Prior to the implementation, the workflow and business process for registering patients was manual and limited to a smaller set of home health patients. The previous process used EHR reports that needed to be manually executed daily, to determine the home health targeted audience. This process did not have automation for patient registration within the application as well as automated notification on status of upcoming patient’s scheduled appointments, appointment cancellations, and re-scheduled appointments for both ambulatory and home health patients.


To address these needs, the core IT team expanded the scope of the project to two interfaces to incorporate a scheduling interface that would include cancelled and re-scheduled appointments. Also, Penn Medicine at Home operational leadership determined that the additional custom report criteria would need to be expanded for daily home health census and discharge filings which resulted in additional accuracy to the daily patient engagement call list.
The new workflow benefits have increased patient satisfaction as the home health engagement program has become automated and scaled for the entire Penn Medicine at Home division. Also, the program has enhanced the quality of care. In addition, the elimination of manual processes has allowed home health resources to focus on patient care and patient well-being rather than manual tasks required to facilitate patient engagement workflow.

44 INTEGRATING AND UPDATING CORE SYSTEMS
Pulmonary Function Testing Results Move Directly into the EHR
Penn Medicine identified an opportunity to realize operational efficiencies by installing a new respiratory diagnostic system that follows the most up-to-date standards in pulmonary testing. It promotes higher levels of accuracy, is less intrusive, and less stressful for patients at the Hospital of the University of Pennsylvania and at the Perlman Center for Advanced Medicine. Once installed, the new system was integrated into our electronic health record that brought about the following benefits:
• Increased documentation in the EHR
• Reduced administrative burden - allowing pulmonologists to focus on clinical decision-making and patient consult
• Increased reviewing and reporting consistency
• Improved care quality and patient safety
Connecting Sleep Study Data to Penn Medicine’s EHR
Sleep study data was integrated into our electronic health record to maximize workflow efficiency for caregivers. The new interface was designed to ingest sleep lab reports and discrete data results. The project also included new hosting infrastructure changes and the addition of virtual machine servers to support the test environment. The legacy system required a server refresh along with alignments to the new test environment. The new observational results template was revised, along with updated flow sheets. Providers were enthusiastic to gain a more efficient system and an improved ability to focus on care management with this fully integrated process and additional result data visibility in the EHR.
Otorhinolaryngology Integrates their Inventory Management Software with the EHR
Penn Medicine identified an opportunity to reduce cost and improve operational efficiencies by integrating EHR demographics information to an inventory management software system for otorhinolaryngology and plastics, with the future ability to add dermatology and optical services.

The integration brought the following benefits:
• Eliminated the need for manual processing, resulting in better patient care
• Reduced patient waiting time
• Improved workflow, reduced inefficiencies, and increased user satisfaction
• This integrated inventory management software benefitted all departments using the software
• Optical and Dermatology requested department activation to join the integration channels
45 INTEGRATING AND UPDATING CORE SYSTEMS
Penn Medicine Pioneers the First Use of a Cutting-Edge Anesthesia Medication Injections System
Penn Medicine has pioneered the first use of a cutting-edge medication injections system with electronic health record interoperability in a clinical setting. Successful implementation of the IV bolus anesthesia medication injections system was introduced in the operating theaters at the Hospital of the University of Pennsylvania, Perelman Center for Advanced Medicine, and Pavilion facilities. The results of the IT implementation and clinical study informs future design improvement to the system, which is intended for widespread clinical use in the United States.
Since this was the first implementation of the EHR interfaces programmed into a production environment, our team completed a collaborative retrospective review of the technical implementation. This case study described implementation activities, outcomes, and the clinical impact of the project.
This implementation provided robust support for Penn Medicine’s hypothesis that anesthesia providers would find the technology helpful to enhance the quality of their medication management. It also identified several implementation recommendations that were broadly applicable to hospitals collaborating with vendors to implement new technologies having interoperability.

Radiation Oncology at Penn Medicine Princeton Health Moves to the EHR
Early in 2022 the radiation oncology department at Penn Medicine Princeton Health went live on the health system’s EHR with clinical documentation. This implementation required a system build and end-to-end testing and training. This direct connection to the electronic health record eliminated the use of a third-party system to perform hospital billing.
This project also introduced Penn Medicine’s new dictation application directly to the EHR for all Radiation Oncology patients. Use of the enterprise dictation system eliminated the previous carrier that had a turnaround time of up to 24 hours and required providers to manually add a progress note to the chart while waiting for transcription results. Use of the enterprise dictation system has enabled Princeton Health providers to dictate in the EHR in real time, improving the quality of the documentation and providing a significant cost savings to the health system by eliminating the need for double documentation.
46 INTEGRATING AND UPDATING CORE SYSTEMS
Good Shepard Penn Partners Opens Therapy and Fitness Facility
Good Shepard Penn Partners, the official therapy provider for Penn Medicine, opened a therapy and fitness facility at Pennsylvania Hospital. The renovated space on the 7th floor was successfully re-apportioned and equipped with printers and workstations to provide the required functionality within a rehabilitation space. Additionally, wireless access was realized throughout the location to provide Wi-Fi coverage as clinicians moved through the space with their laptops. Security cameras and a telecom system were also installed.
Therapy and fitness services include:
• Occupational Therapy

• Lymphedema Therapy
• Physical Therapy
• Pelvic Floor Therapy
• Hand Therapy
• Cancer-Related Fatigue
• Joint Replacement
• Shoulder Pain
• Spine (Neck and Back)
• Sports Performance
• Women’s Health (Pregnancy)
• Foot and Ankle Injuries
47 INTEGRATING AND UPDATING CORE SYSTEMS
The Perelman School of Medicine’s education programs develop the next generation of leaders in medicine and biomedical research. To attract the most qualified students and trainees, The School of Medicine and Penn Medicine Medical Group (PMMG) engage the most outstanding educators and researchers in teaching and training where educational relationships are fostered with the University and Penn Medicine network. We maintain and reward outstanding educators by providing an environment that promotes creativity and rewards teaching excellence. The Perelman School of Medicine, its faculty, and its alumni share a commitment to lifelong learning.





Penn Medicine enhances its status as a world leader in advancing medical science by continually improving the quality and impact of its research. The areas that Penn Medicine emphasizes are the fundamental mechanisms of biology and human disease; the translation of discoveries into novel approaches for the diagnosis, treatment, and prevention of disease; and the evaluation of medicine’s impact on the health of the public.

48
Center for Cellular Immunotherapies Gains Efficiency from New Technology Based Workflows

The Center for Cellular Immunotherapies (CCI) has interacted with many investigators in nearly all departments of the Perelman School of Medicine. Together, they have been translating novel immune-based therapies from bench to bedside. Because of their central position, they engaged with IS support in many areas to execute their fast-paced research initiative while maintaining accuracy, efficiency, and quality.
The Penn Medicine Lab Information Management Systems (LIMS) team partnered with CCI in multiple areas to support equipment maintenance, sample routing, and inventory management. The equipment capabilities ensured monthly calibration and maintenance were completed and documented for equipment used in creating product. From a quality standpoint, sample routing has been used to track samples and create a chain of custody throughout the process. Management of inventory ensured that materials were ordered and used correctly to avoid exhaustion, expiration, or supply waste.
By implementing several workflows into the lab system, benefits have been plentiful. The CCI team has increased productivity, collaboration, and communication by logging into a central location to complete all work. Dashboards of all workflows have provided the lab with top level details to address urgent needs first. Work orders were created to complete equipment calibration or maintenance. Samples were tracked with a full audit view and reporting capabilities. Full inventory tracking and barcoding prevented shortages or use of expired materials while providing traceability from initial source to final use. The capabilities provided by IS in using the enterprise LIMS system enabled high-quality research with reduced waste.
Penn Medicine Institute for Immunology Uses Tech to Advance Research Initiatives
An immune health project initiated at the onset of the COVID-19 pandemic and merged with the Penn Institute for Immunology (IFI) to form a key immunology core. Technology was needed to support this newly combined team with collaboration tools among key functions including the clinical research operations, the central processing unit, and partner investigators throughout Penn Medicine during this rapidly developing time in research and patient care.
Our laboratory information management systems (LIMS) and immune health teams adopted a strategy that would get COVID-19 sample tracking into our lab system quickly, with early deployments and further enhancements designed as other needs became more understood. Lab application expansions included calendaring of research collections and integration with a new iPhone app, named SpeciTracker, that was developed by the IS application development team. The app streamlined communication with the lab for research visits conducted in patients’ homes. In addition, billing integration with the iLab system was added for automated billable service reporting. Finally, the collaborative sharing of specimen inventory, participant data, and assay information through integration with the Pennsieve analytics platform was launched.
Through the nimble adoption of technology provided by IS, the immune health group has been able to gain high efficiency in sample processing and data tracking. Teamwork and communication have been the hallmarks of this partnership. An increase in data quality and a reduction in time spent on reporting through the new iLab and Pennsieve integrations with the lab system have allowed for higher throughput in the lab. Early adoption and continuous improvements have positioned the Penn Institute for Immunology as a group that thrives due to their willingness to leverage technology.
49 EDUCATION AND RESEARCH
Research Sample Collection Bolstered

The Penn Medicine Biobank (PMBB) collaborated with the IS team to increase its collection and storage of research samples by leveraging clinical workflows, systems, and barcodes. Integration with both our EHR and lab system was required to achieve this constructive collaboration.
The LIMS team and data analytics center (DAC) undertook development of new workflows within the lab information management system (LIMS) and new integrations between the LIMS and clinical systems. As a result, the PMBB team could scan existing EHR and lab labels on samples collected in clinical settings and link them to processed research samples within the lab system. These samples were then automatically linked back to the consented research participant.
Since the implementation, PMBB has added over 145,000 samples to the lab application as of June 30, 2022. These enhancements have allowed PMBB to easily receive and process more samples, enabling them to partner with Penn Medicine researchers to further their research goals.



Lancaster Community Supports Lead Abatement and Remediation Program
LGH took the initiative to provide community prevention, education, and remediation services to households of children with elevated blood lead levels and to aid secondary prevention resources in Lancaster County. Working with local government, the Community Health Services department coordinated lead hazard remediation and lead poisoning prevention education to child-occupied households in target communities. This increased lead poisoning awareness and decreased elevated lead levels across the pediatric community. Preventative services included blood lead screening, supporting the enforcement of local housing codes for lead abatement, and working with local government leaders to develop housing standards attracting private investment.
Data systems were integral in supporting lead case management, tracking the initiative’s impact. Through phone texting, Community Health Services provided communications methods to inform parents of lead screenings. Reports were created to track a child’s lead level and monitor until age six. Using the Efforts to Outcome Software (ETO), Community Health was able to measure the number of properties remediated, the number of children confirmed to live in a lead safe home, the number of children with lead levels screened, and the number of contracting jobs created. Resulting from the ETO software and the link of the eHealth medical record, between September 2021 and December 2022, there have been 1,606 program inquiries, with 200 home visits completed, and 153 lead remediated properties. This resulted in a community outreach of over 2,800 people.
50 EDUCATION AND
RESEARCH
CAR-T Program Available at the Ann B. Barshinger Cancer Institute
A team at Lancaster General Hospital developed a program to provide CAR-T services, at the Ann B. Barshinger Cancer Institute. This opportunity enabled Penn Medicine patients in the Lancaster region to receive this innovative treatment closer to their home. The team partnered with Novartis to gain site certification for use of their tisagenlecleucel (KYMRIAH) CAR-T product to treat patients with Diffuse Large B-Cell Lymphoma.
A CAR-T program leadership steering committee led the overall program approach, providing oversight to smaller working groups which included oncology, pharmacy, laboratory, blood bank, revenue cycle, quality, emergency services, critical care, project management, and information services. Groups worked hand in hand with the Penn Medicine Cellular Therapy team to develop future state workflows, create clinical documentation tools, and operational policies and procedures.
Chimeric Antigen Receptor (CAR)-T

cell therapy is an innovative cancer treatment that involves harvesting a patient’s own T-Cells and engineering them to find and kill cancer cells.
Use of EHR system foundation tools helped analysts create documentation tools for all staff involved in the patient’s CAR-T journey, to document directly into the EHR. This included CAR-T oncology treatment plans, a CAR-T checklist for coordinators to track their tasks, a CAR-T documentation template, order set to assist with CIBMTR reporting, flowsheets for infusion documentation, charge capture, as well as ED and critical care order sets to manage toxicity. The team also partnered with the New York Blood Bank who came and performed the leukapheresis cell harvesting procedure for our patients and subsequent cryopreservation of the cells as they made their way to Novartis for the engineering process.
Now, this life-saving CAR-T treatment has become available to patients in the south-central Pennsylvania region. The offering has been particularly helpful to these CAR-T patients who are also closely monitored for several weeks after their infusions, making the experience a game changer for them. The patients who signed up for the treatment would not have considered this therapy if they had had to do long-term travel to receive it. The team is hopeful to grow this program and offer more CAR-T treatments and extend to treat additional cancers in the future!
51 EDUCATION AND RESEARCH
Live Streaming from the Surgical Theater at Pennsylvania Hospital
COVID-19 restrictions brought about a new opportunity for live streaming from the surgical theater at Pennsylvania Hospital (PAH) so that medical students could view procedures remotely in real-time. Because the number of people allowed in the operating rooms was limited by COVID-19 regulations, PAH wanted to provide on-demand live stream of OR procedures for rotating students. The benefits afforded medical students’ real-time exposure to operations that was required as part of their surgical rotation.
To make OR procedure streaming happen, the IT team:
• Configured and installed encoders
• Set up remote access
• Enabled port activation in ORs
• Created AD accounts and added students
• Developed button on F5 portal
• Updated Service Desk scripts
• Created instructional/tip sheets
Perelman School of Medicine Website Design and Enhancements
The Penn Medicine IS Web Design team developed and launched 85 websites over this report period. Requests for new websites and features, as well as large-scale redesigns of existing websites for Perelman School of Medicine (PSOM) programs, labs, offices, and other organizations resulted in the creation of 47 new sites and 38 redesigns. The teams’ efforts included a major redesign of the website for the Executive Vice Dean, to incorporate additional research content and a new searchable/ filterable PSOM portrait collection.
Notable highlights included refining the interactive map for the Center for Global Health website to incorporate scholar data and PSOM programs and partnerships around the world. A new interactive timeline was developed to showcase the many achievements and milestones at the Department of Neurology over their 150year history.
The team also analyzed and remediated several older sites to ensure compliance with the University’s standards. Improvements were made to the image slideshow used on hundreds of sites to ensure accessibility. By using our content management system, new and improved websites were maintained for several hundred PSOM responsive entities, met the University’s web accessibility standards, and were fully editable.
52 EDUCATION AND RESEARCH
HTTPS://WWW.MED.UPENN.EDU/
Progression Dashboard Helps Navigate Radiology Patient Movement

With the implementation of our PennChart EHR’s patient progression module, the radiology department at HUP and PCAM needed a new mechanism for reporting on room utilization and patient movement. Over 20 reports became obsolete after transitioning from the previous system. Relying on this data was crucial to managing capacity and resource availability, preventing bottlenecks, and understanding other issues related to patient flow.
Instead of replacing each individual report, a dashboard was developed to provide one integrated view to meet the department’s reporting needs. The data was sourced from PennChart’s analytics reporting database to produce metrics related to census trends, wait times, room occupancies, and resource utilization.
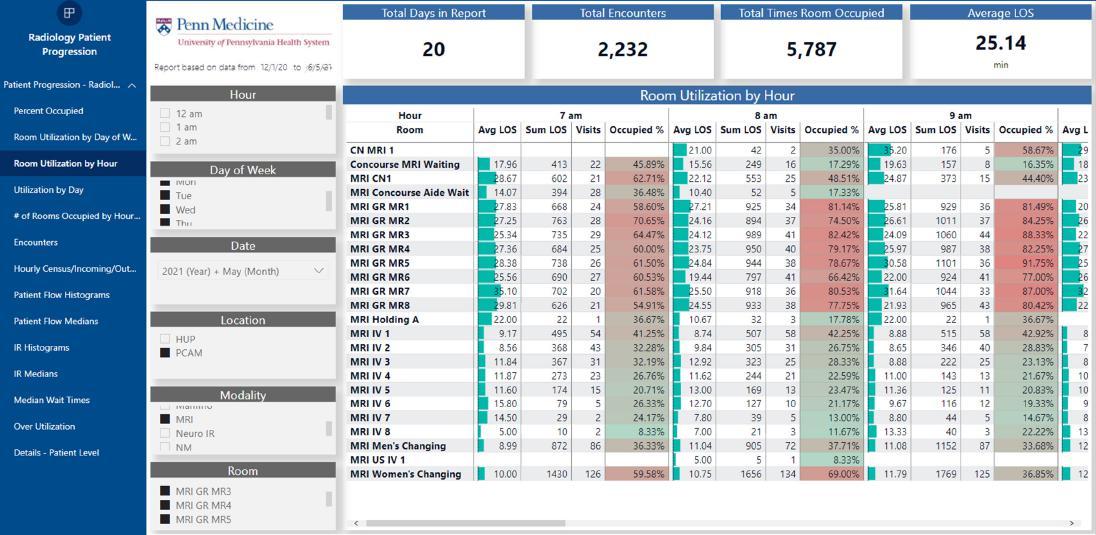
The dashboard did not just replace existing functionality, it expanded and provided improved information sought by our users. The previous reports were produced as static PDFs comprising many separate files. This old format allowed little opportunity for effective exploration and no means of drilling down and viewing the underlying data.
The dashboard data was designed to be broken down by modality, individual room, and resource and viewable by year, month, day-of-week, date, or even individual hour. The patient’s experience was reflected by metrics that tracked how much time was spent at each milestone of the visit from check-in to departure. In addition to summary data, exportable patient details were also available. Radiology administrators gained keen insight into where delays were happening, how to balance staffing and service availability, and when and what resources needed the most attention.
The dashboard became an insightful tool to help inform how to efficiently advance a patient through the stages of a radiology appointment, which improved the patient experience and quality of care.
53
Opioid Use Disorder Dashboard Helps Manage Population Health Outcomes
Deaths from opioid-related overdose continue to ravage many parts of our Nation. Philadelphia has one of the highest overdose death rates of any city in our country. The Penn Medicine Opioid Task Force launched a new strategic plan to significantly standardize and improve care for all and reduce opioid related harm.
The Opioid Use Disorder (OUD) analytics dashboard was created to enable Opioid task force members and clinical leaders across our hospital entities to track performance on key program measures as well as prioritize and target quality improvement initiatives.
Members from our data analytics center worked with our clinical partners to identify the metrics necessary and created a dashboard from the registry that was developed. The data was sourced from Caboodle and is our first dashboard using this source.
Migration to New Reporting Platform Enhances Data Analytics
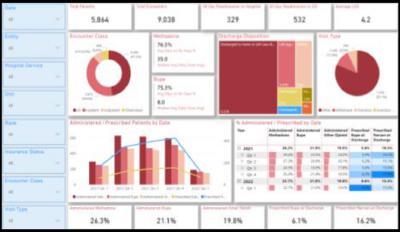
Penn Medicine’s EHR vendor has been supporting a specific integration platform for data analytics and reporting tools. To maintain the optimal compatibility for EHR reporting, our technical team transitioned to this platform and migrated approximately 16,000 reports. A phased approach was developed to assess report retirement as a first step; followed by the report migration among operational, financial, and clinical business functions.
Dedicated resources assessed report audit logs to classify reports for transition or deactivation. A threshold was also set to ensure that critical annual reports were identified. 7,000 reports not viewed over a 14-month period were retired. The 40% decrease in reports within our environment reduced support and maintenance from a time and cost perspective and improved system reporting performance.
Several benefits occurred because of this change:
• Cost savings resulted from eliminating previous annual maintenance fees
• Reduction in the number of supported reporting platforms
• Decreased number of reports by consolidating and eliminating unused reports


Analytics Pipeline Revised for Better Source Data Ingestion
Integrating multiple data sources such as applications, external partners, user generated/maintained, machine, etc., requires users to forage and gather data both independently and locally. By using a new cloud platform, the data sources are integrated together into one location. The platform scales dynamically to accommodate all types of our workloads; thereby providing cost-effective performance. In addition, added data storage capacity allows us to cost effectively store vast amounts of data while providing proper access.
The organization is running more efficiently with significant improvements in the lag time to begin analytics processes, due in part to a revamping of underperforming IS processes and technologies laden with technical workarounds. Reports are delivered on the first of the month more consistently and without intervention, meaning that operations processes relying on this data can be conducted days sooner. Processes and iterations can now be measured on a watch instead of a calendar.
54 BIG DATA ENABLES RESEARCH AND PATIENT CARE
OPIOID USE DISORDER (OUD) ANALYTICS DASHBOARD
Slicer Dicer Data Models Empowers Users with Information at their Fingertips
The data analytics center (DAC) continues to receive an increasing number of requests for new reports and report modifications to access data in our PennChart EHR. To alleviate high volume and duplicate requests, the DAC team makes the Slicer Dicer self-service reporting tool available to users. The following data models allow PennChart users to create their own analytics reports.
Inpatient Medications data model contains information about medication dispenses and workflows. Pharmacy managers can analyze where dispenses come from, how long they take to prepare, how well pharmacy staff follow preparation and checking policies, and other pertinent details. Dispensed medication component information can be investigated related to the components themselves, their usage, and ordering and verification circumstances. Managers can drill down on data to keep an eye on key performance indicators, such as adherence to approved protocols or verification that dispenses have been fully reconciled.
Outpatient Prescriptions provides data about outpatient medication orders, including opioid prescriptions. Physicians can use the data model to help spot trends and search for patients and medications that meet specified prescribing criteria. Clinic managers can monitor e-prescribing rates, dispensing practices, and opioid management habits across different providers and locations.
Outpatient Opioid Prescriptions unlocks information about opioid outpatient prescriptions, including medication orders both from clinics and on discharge from the emergency department or hospital. The data model helps users analyze prescribing trends and identify orders that do not follow clinical guidelines.
DRGs model has information related to the DRGs coded on hospital accounts, including associated metadata such as DRG weights and expected lengths of stay. Coding managers can look for trends in coding practice, investigate changes in case mix index (CMI), and search for DRGs meeting specified criteria.
Professional Billing specific information aids with insurance follow-up where managers can spot denial trends, search for denials meeting specified criteria, monitor outstanding denied dollars, and investigate the highest priority denial for each outstanding charge.
Imaging Recommendations Managers and radiologists can gain insight into the follow-up recommendations radiologists place, and whether those recommendations are being resolved. Using data to understand and respond to trends can help patients receive prompt and necessary treatment.
ED Encounters data model contains information about ED visits, including visits to urgent care departments. Emergency clinicians can query for trends and search for encounters that meet specified criteria. Department managers can use the data model to monitor patient throughput, order turnaround times, and provider productivity.
“SlicerDicer is a perfect bridge between these two analytics tools. It is great for getting an answer to a question quickly, particularly at the level of a larger population, or for analyzing how users are interacting with a BPA through the BPA data model. Those are the ways I typically use it most commonly.”
Jeffrey Tokazewski, MD
“SlicerDicer is unique in that it allows for filtering on sequential events! We used it to compare rates of patients with iron-deficiency anemia diagnoses within Philadelphia. We looked at patients with metastatic cancers to trend referrals to palliative care over time. We have used it to create a baseline for immunization rates for older adults.”
Robert Goodacre Senior Improvement Advisor Cancer Program

55 BIG DATA ENABLES RESEARCH AND PATIENT CARE
PROJECTS COMPLETED IN FY 2021-2023
» Interfaces were created for Penn Medicine hospital entities to send COVID-19 lab tests to HUP as a centralized location for processing.
» Automated scheduling of mental health appointments into PennChart EHR.
» Integration of ultrasound application to the Penn Medicine visiting nurses’ network, with the ability to retrieve the studies in the EHR.
» Operating rooms enabled for school of medicine residents to connect remotely, through a protected network, to access live stream procedures.
» Created Electronic MyPennMedicine Co-Pay & Insurance Verification: New features were introduced to permit co-pay submission and insurance verification via myPennMedicine.
» Designed Touchless Clinical Workflows: New department processes and related workflows were created to administer pre-visit communications and standard pre-visit COVID-19 screening alternatives for patients and their companions.
» Implemented e-visit functionality for Post Op Dermatology patients to submit an image and/or clinical questionnaire answerable by a physician within 24-48 hours. Increased patient access and patient/ provider satisfaction.

» Implemented new workflows to accommodate remote work which included RightFax, Enable OneDrive, Teams features etc.
» Enhanced Mobile EHR app to include patient COVID-19 status on all patient lists and headers for caregivers to easily reference.
» Designed appointment reminders for patients through the telecommunications system - using a solution to issue text-based appointment reminders to patients prior to their visit was successfully implemented.
» Patient self-scheduling was launched for targeted services (Cardiology, Ob-Gyn, Dermatology, Rehab, Orthopedics, Oral-Max, and pain services).
» Implemented new functionality to enable primary care flu shot self-scheduling.

» MyPennMedicine clinical questionnaires were designed to meet the needs of specific departmentsenabling remote processes, related workflows, and electronic submission of responses by patients prior to visits.
» Introduced patient screening interface for Penn Medicine at Home: Integration to deliver pre-visit COVID-19 screening results.
» Provided senior leadership and Infection Control department with timely reporting on COVID-19 exposures and quarantines for Penn Medicine staff.
» Provided electronic records and administration billing for vaccine series – including all COVID-19 vaccines and boosters as well as pediatric vaccines.
» Enhanced web-based clinical portal to support tracking COVID-19 tests and results from the lab system for Penn faculty, staff, and students. Established an interface for University of Pennsylvania Interventional Support Center to retrieve results near real-time.
56 BIG DATA ENABLES RESEARCH AND PATIENT CARE
Data Analytics Center Projects
PennOpen Pass Enhancements
PennOpen Pass was implemented as a daily symptom tracker to reduce the spread of COVID-19 across Penn Medicine and the University of Pennsylvania through daily COVID-19 screening of all employees, patients, visitors, contractors, and students.
» Met OSHA (Occupational Safety and Health Administration) and PA Department of Health regulations for daily COVID-19 screening for Penn Medicine employees.
» The PennOpen Pass dashboard was designed to aggregate the metrics of approximately 30,000 daily users to provide the data needed to help management and clinical staff better track compliance.
» The dashboard was actively used by management to view red passes issued and identify trends over time and to evaluate usage of the system as well.
» On average, this page was accessed 2,200 times per month. This information was key, not only to finding ways to improve the PennOpen Pass process, but also to provide easy access to the additional data gathered by the system.
19,504,869 SCREENINGS
126,734 SCREENINGS • DISTINCT USERS
18,760,836 GREEN PASSES
220,544 RED PASSES
46,715,320 SMS MESSAGES

405,008 INCOMING SMS MESSAGES
A mobile friendly daily screening tool that asks questions about an individual’s (staff, faculty, students, etc.) COVID-19 symptoms, exposures, and testing status. Based on the responses PennOpen Pass determines whether a person is cleared to come on site for the day (green pass) or whether they are not cleared to come on site (red pass). People can sign up for daily reminders via SMS text. The daily reminders contain a hyperlink that allows users to complete their daily screening via their smartphone or a computer. The collected data is used regularly to monitor trends in COVID-19 cases across Penn Medicine, and the University while they were using it.
57 BIG DATA ENABLES RESEARCH AND PATIENT CARE
COVID-19 and PUI Registry Updates
COVID-19 Positive Query Registry
COVID-19 Research Study Support
COVID-19 and ICU Dashboard with LOS (Length of Stay), vents, volumes
i2b2 infrastructure for COVID-19 multi-center studies
These technologies and processes address the administrative infrastructure support and physical infrastructure support that includes financial services, operations, human resources, managed care contracting, billing, materials management, and other administrative services. This enterprise-wide approach designs and implements product and service processes to achieve performance gains and decrease costs while optimizing resources.

58
The Pavilion has been one of the most detail focused and innovative projects undertaken at Penn Medicine. The state-of-the-art technology integrated within the Pavilion transforms the manner in which Penn Medicine provides patient care and experience through detailed organization and design. Innovation and technology were the primary focus when designing each and every wall in the hospital as the goal is to deliver the treatment of today and the medical advances of tomorrow. The following projects represent the technology built to support the Pavilion and transform the patient care experience using smart building integration.
Security camera system platform was designed with new IP based camera system including hardware, software, security operations center design and staff training.
Implemented over 55 employee time clocks throughout 1.5M square feet- determined placement, configured new low voltage wiring, programming and installation.
Implemented technology supporting cafeteria systems to include point of sale stations, 10 large format food menu selection display boards and ensured system security and auditing capability for transaction history for sales accuracy.
Installed an updated parking control system which secures payment, tracks vehicle flow, and establishes pay on foot capabilities on the 6 Pavilion parking garage levels.
Go-live readiness assessments and dress rehearsals were done to prepare for technology application transition, patient movement prep, and command center logistics.
Emergency department and inpatient hospital electronic health record workflow analysis, design, build, and testing were completed.
Imaging and modality integration was coordinated for vendor installation and configuration for the following clinical imaging equipment newly placed in, or moved to, the new Pavilion: Radiology PACS build, Cardiology PACS build, associated EHR build, connectivity testing, device testing and PACS / EHR integration testing. Device modalities included (Xray, CT, MRI, Ultrasound, etc.) and diagnostic reading/tech workstations
Application updates made to EHR modules OpTime, Cardiology and Radiology, supporting new innovative workflows and technology to support our clinicians in delivering exceptional care while improving the patient experience.
Implemented new equipment within the Pharmacies (robots and carousels) and Lab spaces (microscopes & IT devices).
Penn Medicine’s project management methodologies ensured the deployment was on time while adhering to high quality standards.

Installed new virtual enterprise level Nihon Kohden physiological monitoring system.
Automated vitals data capture and EHR recording for critical care patients, ICU and OR clinical computing hub
Deployment of clinical technology devices, including clinical engineering equipment.
Implemented robotic server and software technology for pharmacy operations and delivery of medications.
Introduced patient portal bedside module so patients and families can engage in their care through educational materials and by providing their lab results, vital signs, upcoming tests, and their health care team members.
Activated 120 patient rooms early, to provide extra capacity for anticipated surge in COVID-19 patients.
Deployed 65 iPads for patient use.
Technology infrastructure constructed for 3rd floor connector bridge from the Pavilion to Perelman Center for Advanced Medicine (PCAM). Relocated peri-operative waiting room to PCAM. Peri-operative area was expanded into the old waiting room with (10) new patient bays. The old per-operative area was used as the new pathway from PCAM and onto the Pavilion connector bridge.
New dermatology suite was built adjacent to the bridge area to coincide with connector bridge space.
Patient flow management application and care team tool was implemented.
Implemented a single enterprise information platform for managing content, increasing productivity and reducing cost.
Prepared billing and claims processes, ensuring continuity in charge method, and structure and coding processes to align with health system standards
HUP Pavilion - Revenue Cycle (HIM, EMPI) – Evaluation of HIM components for the Pavilion, ensuring the availability, accuracy and protection of clinical information needed to deliver healthcare services.
Designed new electronic patient white board display for patient rooms.
Implemented technology for nurse call system for patients to request help from their bed.
59 EXPANDING AND CHANGING THE PENN MEDICINE LANDSCAPE
Penn Medicine Opens the Largest Healthcare Equipment Sterilization Facility in the Country
Penn Medicine opened a new Interventional Support Center (ISC), the largest instrument processing and surgical supply preparation facility in the country. Located in Southwest Philadelphia, the ISC is the first facility of its kind in Pennsylvania. In this space, staff sterilize and package thousands of instruments each day in preparation for surgeries and procedures from basic scissors and clamps to advanced robotic instruments.
At nearly 110,000 square feet, the ISC was designed to process instruments from up to 200 surgical cases each day. Penn Medicine purchased the building in 2018 and built a physical plant to support the ISC’s operations. The ISC provides instrument processing services for the Hospital of the University of Pennsylvania, Pennsylvania Hospital, and the new Pavilion Hospital of the University of Pennsylvania, as well as three outpatient facilities: the Perelman Center, Penn Medicine Radnor, and the Tuttleman Center. The ISC was built to support additional Penn Medicine entities.
The opening of the ISC set a new standard for sterile instrument processing. It also marked a new approach from Penn Medicine. By moving processing operations from the traditional hospital setting to an offsite, dedicated facility, efficiency was increased in a high quality, cost effective way while keeping up with increasing demand. Plus, the ISC alleviated space at all clinical locations, providing room for hospital departments to expand their services.
In addition to providing hospital locations with much-needed real estate for patient care, consolidating these services off-site helped minimize any redundant equipment across the health system. The ISC itself was designed with a one-way forward flow approach that enables efficient instrument processing. The facility includes features that enhance sterilization efficiency, such as clean steam using reverse osmosis water. The ISC is a nearly dust-free facility - thanks to increased air changes and filtration. Airlocks throughout the building were also built to prevent cross-contamination of air between areas where dirty instruments are processed, and clean ones are repackaged.
The ISC team is made up of 140 employees from on-site instrument processing facilities at the Hospital of the University of Pennsylvania and Pennsylvania Hospital. In addition, 25 new employees were hired to staff the new building. The facility was created with ergonomic principles and employee well-being in mind, enabling a comfortable workspace for the ISC team members. All major equipment was designed for personalized adjustments for staff, such as height adjustable sinks and assembly tables.
To make this happen the IT team:
• Outfitted the new ISC building with all required IT hardware and implemented an enterprise-wide software instrument tracking system that was integrated with sterilizers, biological incubators, and an automated storage carousel system

• Standardized the instrument processing software system across the health system and integrated tracking software with our EHR, Penn Medicine’s human capital management solution software and Penn Medicine’s web-based tool for locating and viewing assets in realtime
• Established field service support for the service desk, and end-user-services

“Clean instruments are a crucial component of patient safety. Through centralized processing with state-of-the-art equipment, the ISC is an essential element behind Penn Medicine’s efforts to continue delivering high-quality, advanced patient care and safety,” said Phil Okala, Chief Operating Officer at the University of Pennsylvania Health System. “The ISC also stands as a unique, leading example for multi-hospital health systems looking to create improved processing systems and thoughtfully plan the best ways to maximize capacity for patient care.”

60 EXPANDING AND CHANGING THE PENN MEDICINE LANDSCAPE
Tracking Surgical Instruments at Penn Medicine Princeton Health Meets Enterprise Standards
To meet regulatory requirements, Penn Medicine Princeton Health implemented a surgical instrument management system to interface sterilizer data into the core instrument sterilization system. This implementation allowed for data values from the sterilizers to be transferred to the instrumentation sterilization parameters being documented in the system, consequently meeting the State of New Jersey requirements to monitor and maintain values for seven years.
The addition of the interface standardized the process throughout the enterprise and eliminated paper tracking which ended the need for dual documentation. It also linked patient information with the case trays, which allowed the tracking of trays to the patient level, improving patient safety.
Chester County Hospital Expands Emergency Services
Penn Medicine expanded its private room footprint in the emergency department and renovated legacy space to ensure a cosmetic and cohesive flow to the new emergency department space in the Pavilion at Chester County Hospital.
This three-phased project expanded the emergency department to include:

• Twenty-nine exam rooms
• Nine enhanced safety exam rooms
• Five nursing stations
• Three triage rooms
• Two resuscitation rooms
• Two trauma bays
Each phase took six months and included installation of new cabling infrastructure and deployment of new hardware. Chester County Hospital’s emergency department now provides increased access to emergency services for the community and benefits operationally from improved patient flow.
Gastroenterology and Endoscopy Expand Footprint
To meet the growing outpatient needs of the Gastroenterology/Endoscopy department, a new and spacious facility was designed and constructed on the west side of Penn Medicine University City. The new space was built having a common reception area for both Gastroenterology and Endoscopy, ten GI exam rooms, four endoscopy procedure rooms, twelve pre/post-procedure bays and provider touchdown/office space. The enterprisestandard, state-of-the-art monitoring platform was chosen for physiological monitoring – making it the first deployment on the Penn Presbyterian Medical Center campus.
At the same time, increased demand to accommodate a wider variety of procedures for inpatient Gastroenterology services necessitated the planning and deployment of four new operating rooms, designed specifically to meet the technical needs of the department. A new operating room was part of the Cupp Hematology-Oncology expansion at Penn Presbyterian Medical Center.
61 EXPANDING AND CHANGING THE PENN MEDICINE LANDSCAPE



62 EXPANDING AND CHANGING THE PENN MEDICINE LANDSCAPE REDC & FACILITY PROJECTS BY PHYSICAL LOCATIONS PENNSYLVANIA HUP 3600 CCB (CORP) PMUC HUP PAVILION RADNOR (KOP) CONSTITUTION PCAM 1800 RITTENHOUSE HEALTH PLAZA PAH WASHINGTON SQ 1608 WALNUT ST. PPMC PSOM 3400 CCB LGH CCH LANGHORNE, PA 10 2 4 5 2 1 1 1 2 1 1 42 NEW JERSEY CHERRY HILL, NJ MT. LAUREL, NJ VORHEES, NJ WOODBERRY, NJ PMPH 2 1 1 1 REDC & FACILITY PROJECTS BY TYPE 75 EXPANSIONS 18 TECHNOLOGY REFRESH REDC & FACILITY PROJECTS BY PHYSICAL LOCATIONS 19 RENOVATIONS 12 MOVES 4 CORPORATE SUPPORT PERELMAN SCHOOL OF MEDICINE PLANNING EXPANDED PATIENT ACCESS IMPROVED PATIENT SERVICES INCREASED PROVIDER EFFICIENCY WITHIN SOME SPECIALTIES ENHANCED PATIENT TIME SAVINGS/CONVENIENCE IMPROVED OVERALL PATIENT SATISFACTION IMPACTS *PPMG – Penn Physicians Medical Group | *CPUP - Clinical Practices of the University of Pennsylvania PPMG* PRACTICES GREW 71 to 85 PRACTICES FY20 to FY22 LGH* PRACTICES GREW 101 to 143 PRACTICES FY20 to FY22 IN PROJECTS FROM FY21/22 OVER FY19/20 INCREASED PHYSICAL REAL ESTATE 2 12 4 8 7 LANCASTER GENERAL HOSPITAL IMPLEMENTED A SUITE OF throughout the broader Lancaster community LGH ADDICTION MEDICINE SITES 43 HOSPITALS 73 MULTI-SPECIALTY OUTPATIENT (MSP) 6 CORPORATE LOCATIONS
Behind the Scenes - The Business of Keeping the Business Running
In the summer of 2020, Penn Medicine finance department staff were challenged to maintain social distancing guidelines at the 1500 Market Street office, while meeting the business needs of the healthcare system. The employee rotation schedule helped with social distancing, but employees working remotely had limited access to business systems. The recommendation was to outfit 700+ employees with new computers and modified workflows from a system’s perspective to perform their work remotely. To make that possible, a core IT team:
• Worked with the finance managers to identify required hardware to enable the team to work remotely
• Identified workflows that needed to be modified for remote work
• Implemented RightFax, enable OneDrive, reduce the need for printing
• Arranged for home delivery of equipment
• Setup a command center to transfer data from employee on-site desktops to new hardware
• Trained the employees on their modified workflows
The successful completion of these tasks allowed Penn Medicine’s finance division to work remotely. In turn, Penn Medicine was able to consolidate office space into three floors, reducing overall costs.

Hoteling Software Accommodates New Hybrid Work Environment
As part of Penn Medicine’s objective to support a hybrid work style and to efficiently manage real estate resources, a 12-week pilot of an office hoteling system was conducted in select Philadelphia locations. The pilot encompassed spaces at 1500 Market, the Pavilion, select areas at the Hospital of the University of Pennsylvania, and Human Resources at 3600 Civic Center Blvd. Workspaces that were a part of the pilot could be easily identified by the hoteling system label and QR code attached to the wayfinding (cube/office/room number/ name) plaque. A web portal or mobile app was used to select an available workspace from the system. Users were also able to coordinate with coworkers to reserve spaces together when they needed to collaborate in person.

The system proved to be useful in allowing users to reserve cubicles, offices, conference rooms, and other spaces rather than having fixed, permanent workspaces such as cubicles or offices assigned to them. During the pilot, the system was highly used in clinical facilities and user feedback was very favorable. It provided Real Estate Design and Construction with robust reporting for real estate planning and forecasting. The decision was made to adopt the system for production use and perform a phased implementation across Penn Medicine, expanding from the existing pilot locations.
The health system benefitted by gaining greater visibility into how office space could be used, and by whom. Some studies have shown that businesses could save about 30% on facilities costs from using hoteling. The expected benefit of the hoteling system was seen early on with a reduction in Penn Medicine’s real estate footprint and associated real estate cost. Employees were better able to find the types of workspaces and conference rooms they need when they need them.
63 RUNNING THE BUSINESS
PennforPeople Expands its Business Platform
PennforPeople entered the second phase of a five-year long program to move Penn Medicine from our previous business application platform to the next generation platform. With our initial phase that focused on human capital management completed, the goal of phase two was the implementation of state-of-the-art applications to replace disparate and paper-based workflows used to on-board employees and collect talent profile data –allowing this activity to be consolidated within PennforPeople.
After our kick-off of phase 2 of the PennforPeople expansion, it was determined that an additional system was required to ensure that Penn Medicine could implement the best possible candidate experience. So, a proactive recruiting system was added to build our career site and job application workflows.
The benefits that resulted from implementing this phase of the project:

• Enhancement and streamlining of the hiring and onboarding process by removing the need for 3rd party interfaces, thus eliminating the cost
• The elimination of manual paper-based processes from managers through PennforPeople
• Automation of the most time-consuming recruiting tasks, allowing recruiters to spend more time guiding and building relationships with candidates
• The streamlining of the offer letter creation process for our onboarding coordinator team

• Efficiencies to the candidate screening process by consolidating all human resource information into one system
• The immediate availability of employee documentation on resource records after candidates are hired
• The streamlining of workflows and the elimination of the manual licensing verification process for Penn Medicine recruiters, onboarding coordinators, managers, and candidates resulting from increased system functionality
Exit Interview Questionnaire Survey Created for HR Retention Program
In addition to the COVID-19 pandemic in 2021, Penn Medicine was impacted by the “Great Resignation”, as an elevated number of employees resigned. Penn Medicine’s leadership was interested in getting a better understanding of the reasoning behind employees exiting the health system. This initiative stemmed from the organization’s retention strategy that was created under Project Vital Advantage. Project Vital Advantage (PVA) was started as a system-wide project focused on recruitment, retention, compensation, work environment (including workplace safety), and workforce wellness and culture.
Application Development, in partnership with the HR department, created an exit survey that was sent to employees that recently resigned from the health system and employees that gave notice of resignation. The surveys were sent out as a post card with a QR code, which launched the survey when scanned. The survey was streamlined to consist of only 6 questions to ensure maximum adoption, with one question providing the employees the opportunity to have HR contact them for follow-up. A report was also built-in with the survey that allowed HR and leadership to view all submissions and track trends.
The information obtained from the surveys provided some valuable insights to leadership on some of the common reasons that employees were leaving. In addition, the organization was able to retain some personnel by following up with the employees that indicated they wanted to be contacted by HR. With the survey in place, the organization had a reportable and actionable source of information that they could use to ensure that Penn Medicine would be the place people want to stay and grow their careers.
64 RUNNING THE BUSINESS
Consolidated Retirement Plan Streamlines Employee Retirement Benefit
Before Penn Medicine consolidated its retirement plans with one of the most diversified financial companies in the United States, the health system was using three different vendors to manage employee retirement benefits enterprise-wide. With each vendor having different rules and requiring up to four interfaces each, the process was deemed too labor intensive to support administratively and technically.
Penn Medicine’s retirement department negotiated a contract with a single vendor and Information Services worked alongside them to build a revised enterprise processes that streamlined all administrative and technical support.
This combined effort resulted in:
• Efficient workflows, significantly decreasing staff support time
• A revised and simplified employee experience when accessing their retire account
• Lower administrative costs with the savings passed on to employees via lower account maintenance fees
Finance Capital Expenditure Request Process Reduces Work Burden
Over a decade ago, technology that handled the processing of capital expenditure requests allowed any staff to submit a request and lacked integrated data to handle routing and approvals. Data was manually gathered and updated behind the scenes by the finance capital budget team and approvals had to be manually re-entered into Lawson. Additionally, they managed all data and reporting through a local Microsoft Access database which required extensive manual work.
To alleviate this work burden, the IS team created a new technology solution that provided significant improvements by rewriting the process using standard Lawson development tools and integrating it within the system. The new process was designed to screen submitters by requiring them to log into Lawson and be authorized to submit requests. The review and approval processes were derived from information already set up in Lawson so that little effort is needed to enter or maintain this data. Routing to new approvers and sending back to prior users in the approval chain now had the same look and feel as other approval processes in Lawson, and action items were now managed using the same method as all other Lawson pending action items. Reporting became more automated and robust. Also, with the similar look and feel to other Lawson reporting, it allowed greater transparency in the process, and quicker turnaround to the requestor.
Most of the manual work previously performed by the finance capital budget team was replaced with built-in functionality to eliminate unnecessary work effort from staff resources. The team was furnished with power tools and reporting options that they did not previously have to do mass loads, data extraction, and ad hoc reporting. The new process was designed to be easily portable to the new PennforFSM (Penn for Finance Supply Chain Management) application, with additional features included, after implementation in June 2023.
65 RUNNING THE BUSINESS
Technology Based Patient Safety Reporting Now Enhanced


When reporting patient safety events related to technology, users previously had to submit two reports. One instance was entered into our application to report and track the safety issue, the other entry was made in the IS Service Desk system to address the technology issue. This reporting method was tedious and time-consuming for users, who were caregivers, focused on providing patient care.
Our IS department recognized the opportunity to alleviate the necessity for two entries into two different systems by combining the submissions into a single step. The IS operations team worked with the patient quality team’s system administrator to produce workable solutions. With support from our integration and networking groups, we modified the patient safety application to include an option to automatically generate a technology issue service ticket if the user selected it.
Upon making this update, an immediate increase occurred in reported technology-related safety events. Technology tickets were created, and optimization requests accumulated as well as benefits gained from system workflow issues were also addressed. User feedback was incredibly positive regarding this simplified submission process.
Technology Ticket Management Goes Mobile
It is no small task for an IS Service Desk team to consistently maintain superior customer service while responding to and triaging the high volume of incidents for a vast, highly complex health care organization. Among the ever-increasing demand for technology requests and fixes, key members of our application development and service desk teams recognized an opportunity to develop an iOS native app centered on ticket management. The concept was to design a mobile app that provided access to information about tickets, freeing the management team from being tethered to their workstations. Mobile access was attractive and helped to bring efficiency to the ticket management process, also allowing staff to track high-priority tickets without having to physically be at their desks.
The design team integrated multiple tasks into a single, cohesive experience by combining the ticket management functionality along with an existing approvals application to form a new iOS app. The necessary functionality was consolidated into this single application, along with increasing speed-to-market by leveraging the prior application’s infrastructure to avoid redundancy.
Since its introduction, the new ticket management app has been used daily by hundreds of staff members across IS. Staff can now perform approvals, and track tickets on their own time from the ease and comfort of their smart phone. Many staff have praised how the app has become a vital tool for their workflows by making tasks much more accessible and convenient.

66 RUNNING THE BUSINESS
Upgrades to Cost Accounting Aligns Services and Saves Time
Penn Medicine’s Financial Decision Support System (DSS) leverages data within Penn Medicine’s electronic health record to enhance financial processes and forecasts across the enterprise by transforming that data into knowledge, thus advancing financial decision support.
Early in 2022, the performance manager analytics application was upgraded. The application consolidated data from multiple systems into a single data model with useful pre-calculated metrics allowing cost accounting to perform sophisticated cost assignments while monitoring performance across patient populations and service lines. This upgrade allowed us to stay up to date with the latest product offerings, support, and available features.
To ensure stability, support organic growth, and provide ample capacity for future integrations, the team also migrated from physical servers to virtual servers. The upgrade and server migration resulted in improved run times of our monthly data extract by 40%, giving us more time to focus on new projects, optimizations, and enhancements. As part of the server migration, testing and development environments were built out to provide safe spaces for future needs and improvements to the existing data model. The Decision Support team has also been working with our partners in finance to enhance monthly processes and deliver useful data to support the organization’s goals.
Service Desk Thrives Using Quality Assurance Program
Penn Medicine’s technology support model grew more complex with the onset of the COVID-19 pandemic. As a segment of our workforce moved to function remotely, the Penn Medicine Service Desk expanded its program to service onsite and offsite staff, caregivers, and patients. Support for our patients involved not only support for the myPennMedicine patient portal, but also patients seeking to navigate general virus-related coordination around care. To ensure consistent service quality while also rapidly adapting to this new way of assisting our customers, the Service Desk implemented a new quality assurance (QA) program to optimize QA practices to continue providing world-class service.
This program was designed to be more comprehensive and work by using phone and screen recordings and analytics and ticket information to drive continuous improvement initiatives. Program essentials evaluated that the analyst verified the caller before discussing support needs. Agent soft skills were also monitored to gauge their demeanor when interacting with customers. Call management review was instituted to ensure that the analyst demonstrated call control and acted with appropriate responsiveness and urgency when warranted. Confirmation of issue resolution helped verify whether a customer’s issue was resolved and logged with the proper documentation.
Providing a superior customer service experience to our users translated into quicker resolution rates, allowing for positive patient experiences, and enabling our caregivers to return to meet our patients’ medical needs. Additionally, the new program improved analyst productivity and reduced the number of calls that needed to be re-routed or escalated. Monitoring customer service calls also helped to identify training opportunities for our analysts in situations that needed more coaching. The greatest result achieved was seeing an improvement in our first-call resolution rates.
67 RUNNING THE BUSINESS
Digitized Processes Brings Value, Supporting a “New Normal” Business Model

Since COVID-19 first struck in early 2020, the remote work model significantly increased, particularly among our corporate services. As a result, our health system needed to optimize business software to maintain office practices while enhancing business process flows through digital channels and mechanisms.
In fiscal year 2021, our IS finance team piloted services with DocuSign to determine if this software was viable in meeting administrative support goals. By FY22, the services had proved useful and created efficiencies that led to expansion of the pilot to other departments including our Office of General Counsel and Purchasing. We gained over 100 users and built the capacity to process over 20,000 electronic transactions annually! Using software technology and new electronic processes proved to be valuable in allowing us to maintain business continuity during the transition to a remote work environment for many departments while increasing operational efficiency.
SECURITY STRATEGY SETS THE STAGE FOR CYBER PROTECTION
As healthcare has become a prime target for cybercrime, it has become more important than ever that executive leaders, risk, and compliance practitioners, along with IT and cybersecurity personnel have a collective understanding of the potential impact that cyber risk can have - not just on the day-to-day operation, but to the very mission of our organization. To meet this problem head-on, Penn Medicine Cybersecurity program has established a clear set of objectives, and long-term goals, in support of our organization’s mission, as well as a 5-year plan of investments to guide our program enhancement over the following years. Having a strategy and roadmap in place aligns our stakeholders, resources, and investments so that all future projects and maturity enhancement initiative are effective, efficient, and support the long-term mission of the organization.
DECIDE ON RISK APPETITE
How do we facilitate informed risk decisions?
We provide the organization with accurate and actionable information about our cyber risk position, present courses of action, and record and track progress.
SECURE PARTNERS & WORKFORCE
How do we treat cyber risk that we cannot directly control?
We provide risk oversight and coordination among individuals, teams, and organizations outside of our cybersecurity program to help influence them to movie in alignment with our cyber risk decisions.
PREVENT CYBER INCIDENTS
How do we prevent cyber incidents that our reasonably preventable? We implement and operate security technology to prevent threats from disrupting our course, enrich our communities’ experience along the way, and promote operational excellence.
RESPOND TO ACTIVE THREATS
How do we respond to threats we cannot prevent?
We detect cyber threats, coordinate response, and test our defenses to quickly adapt to emerging hazards and safely and swiftly guide the organization back to normal operations after a cyber incident.
SECURE DIGITAL TRANSFORMATION
How do we integrate security into organizational evolution?
We engage with business partners to understand new journeys and provide security expertise to help chart new courses that integrate the latest advances in cybersecurity technology.

68 RUNNING THE BUSINESS
1 2 3 4 5
Medical Device Security is Improved through Network Enhancements

The Penn Medicine network was architected as a single network connecting all medical and non-medical devices across the health system. To provide more protection for our medical devices, a new strategic approach was taken to enhance the security of the Penn Medicine network. Access control measures were implemented to ensure that only known, authorized devices could gain access to the network. Separate partitioned network segments were set up for different categories of devices, such as medical, IT, facilities, and so on. Communications between different segments was restricted with controlled exceptions. Some segments, like medical devices, have the minimum access to the internet required for proper functionality (such as access to manufacturer’s maintenance sites). Network-wide monitoring for suspicious trafficking was implemented, and processes were developed to respond to any unusual or suspicious events on the network.
New standard processes were developed to require that all new devices go through a security risk assessment and provide a network profile describing the type of required network connectivity, connections to other Penn Medicine systems, and any connections outside of Penn Medicine before being placed on the network. Additionally, all existing medical devices (5,500+ low-risk medical devices, and 600+ high-risk medical devices) are being moved to the dedicated segment, with the majority having been completed. Penn Medicine worked with the device vendors to ensure that anti-virus software was installed on devices which could support it. A specialized network security tool was also evaluated on the medical devices segment at HUP and PCAM to assess the level of protection it may offer to medical devices that do not offer on-board protection or monitoring (such as anti-virus software).
Network access control was implemented universally across Penn Medicine, ensuring that only authorized devices can access the network. Standard tools and processes were put in place for network security incidents and event management, identifying external threats to the network and providing a playbook for responses to threats. The network was segmented at Penn Medicine’s hospitals and major medical facilities like Perelman Center for Advanced Medicine, Penn Medicine University City, Penn Medicine Rittenhouse, Penn Urgent Care South Philadelphia, and the Instrument Sterilization Center.
These activities have increased Penn Medicine’s ability to respond to threats, enhanced the ability to isolate and limit any threats that do enter the Penn Medicine network, and further protect Penn Medicine’s patient-facing medical devices from external attack.
Reduced Risk of Multi-Factor Authentication Unauthorized Access
Cybersecurity implemented new logic for new user account creation that limits our phone multi-factor authentication self-enrollment window, reducing the risk of unauthorized network access from a potential cyber attacker. The change was implemented without any disruption, using change management procedures that involved coordination with the Service Desk, enhancements to new employee orientation communication, and awareness campaign for existing users.
Due to the change, Cybersecurity significantly reduced the risk associated with the self-enrollment feature, while balancing the business need to allow for employment onboarding processes to complete. In short, enabling the business – securely.
69 RUNNING THE BUSINESS
Increased Threat Protection for UPHS Websites

The cybersecurity team worked with numerous web application owners to reconfigure all UPHS public websites and place them behind a layer of advanced defense against cyber-attacks, protecting the organizations’ digital presence, brand, and customer operations. The updates were executed through testing and change management procedures to prevent any disruption to users. Having this layer of defense in place has successfully prevented disruptions from coordinated website disruption attacks against large healthcare that were conducted by cyber-criminals in the first quarter of 2023.
24x7 Phishing Detection Becomes More Advanced
Penn Medicine has established a mature phishing detection, response, and awareness program. With the increased complexity of phishing attacks, and numbers on the rise, our IS security team realized that there was an opportunity to take our phishing detection and response capabilities to the next level, thus ensuring Penn Medicine had round the clock monitoring and response capabilities on reported phishing attempts.
Penn Medicine Cybersecurity recognized that phishing attacks were happening at an increased rate, were growing more dangerous, and needed round the clock monitoring on incoming email-based threats. While the in-house team could track the emails, the amount of time delegated to reviewing phishing emails was also increasing and taking time from other incident triage and management. To better protect the organization and provide timely response activities, Cybersecurity partnered with a 24x7 phishing detection and response service that rapidly receives, assesses, and remediates phishing attacks against Penn Medicine.
All corporate users, representing over 60,000 email accounts, are now able to report suspicious emails and within less than 30 minutes receive a response with the analysis and next steps. During this time, the cybersecurity monitoring team receives necessary information so that appropriate actions can be taken swiftly to protect the organization against emerging email campaign threats.
New Security Protections for Laptops and Off-site Computers
With the increased presence of a growing remote workforce, our cybersecurity team implemented a new security solution that protects Penn Medicine managed laptops, regardless of location – at home, on public Wi-Fi, or while traveling. The laptop internet security solution protects over 10,000 active Penn Medicine managed devices, with a continued effort and process in place to ensure that inactive devices are secured as they re-connect to Penn Medicine networks. By implementing these new protections, prevention and protection is enhanced against cyber criminals trying to deliver attacks through malicious websites.
Integration of Network Standardization for Princeton Hospital

Our enterprise Cybersecurity team worked with key IS teams to re-architect the Princeton network design to integrate with our centralized health system network. The team included the insertion of segmentation firewalls, redirection of all internet traffic through the Penn Medicine firewalls, and migration of legacy Princeton hosted resources to Penn Medicine hosted environments.
By creating the alignment with Princeton’s internet access, Penn Medicine maintained a standard security posture, logging, and monitoring capability. In addition, by bringing internet systems hosted within Princeton into the Penn Medicine environment, the same level of control and security were able to be applied, which greatly reduced the risk associated with a malicious attack.
70 RUNNING THE BUSINESS
Business Continuity Assessment is an Ongoing Process
Business continuity planning was developed to ensure the health system could provide ongoing patient care in an unplanned, catastrophic event. Assessing Penn Medicine’s comprehensive business continuity plan has been a continuous process, including periodic reviews of workflow resilience for applications and technology that is used in critical patient care-related areas.
To facilitate this effort, an enterprise-wide clinical care continuity workshop was conducted with senior clinical leadership from the inpatient and ambulatory care settings. Interviews were conducted across all six hospitals, six ambulatory sites, and three data centers to identify the high-level key workflows, applications, and technologies that power critical patient care activities. Additionally, because the business continuity plan crossed over multiple departments, an assessment was conducted against industry best practices for the crisis management and disaster recovery plans.
Based on the Information Systems Audit and Control Association specifications for Penn Medicine, a baseline was obtained to measure the level of maturity for staff awareness, operational processes, resiliency, and recoverability of key systems on the Capability Maturity Model. Once gaps were identified, priority projects were recommended to increase Penn Medicine’s posture in alignment with other academic medical centers. Recommended projects centered on improvements in process resilience, operational governance, and technology resilience. A three-year roadmap was presented to executive leadership for approval, funding, and resourcing for 2022. With a goal of doubling the maturity score, the following projects were selected:
• Relocate the Disaster Recovery Environment for Ensemble to a downtown datacenter
• Improve Citrix resiliency
• Replace aging Telemetry systems at PPMC
• Assess and improve resiliency / redundancy of third-party applications
• Implement a Configuration Management Database (CMDB)
• Conduct a Business Impact Analysis
Maturing Disaster Recovery Fortifies Business Continuity and Infrastructure Resilience
Early in 2021, Penn Medicine assessed the organization’s ability to provide technology that supports ongoing patient care in an unplanned, catastrophic event. In addition, work was done to determine the resilience of workflows, applications, and technology to provide continuity of care for critical patient care-related areas in the face of technical adversity. Led by the Penn Medicine Business Continuity Leadership Committee, IS and partnered services focused on work in two areas.
The first area of focus was the establishment of clinical care continuity workshops that included representation from clinical, IS, and business leadership with the goal of identifying high-level workflows, applications, processes, and technologies – key applications and technologies that power critical patient care activities. In parallel, the second area of focus was a business continuity and disaster recovery (BC/DR) current state assessment across 15 sites including hospitals, a diverse sample of clinics and outpatient centers, and 4 data centers.
In fall 2021, the work completed above resulted in two corresponding deliverables. The first focused on rationalizing and prioritizing the applications that power critical patient care activities. The second focused on presenting a gap analysis and recommendations for improvement of technical footprint (datacenters, infrastructural services). This information was used to help focus on datacenter rationalization and strategic planning toward meeting the organization’s needs.
71
Wireless Telemetry Monitors Bolster Rehabilitation Services
Penn Medicine replaced the health system’s physiological and telemetry monitors. The new telemetry monitors were installed at HUP and Ravdin 6, as part of a cutting-edge system that uses single to multi-parameter transmitters to provide the ideal tool set for an individual patient’s condition. An IT team was identified to upgrade the new telemetry monitors and incorporate wireless technology, which aligned with the department’s clinical workflow for transporting and monitoring mobile patients.
Benefits of this project included:
• New high-performance bedside/mobile system; comprehensive information that clinicians need, while helping to improve workflow in real time
• Lightweight transport monitors help protect patients, while seamlessly transmitting data into the EHR, leaving no gaps throughout the patient’s stay
• Continuous vital-sign surveillance to traditionally un-monitored, at-risk patients located in medical/ surgical units
• The interface between the telemetry system and the EHR allows us to seamlessly manage, share, and store neurology patient data, thereby improving workflow
Shared Clinical Mobile Devices Upgraded to a Single Platform


The Information Services Platform Engineering group had been supporting two mobile device management (MDM) systems simultaneously. To simplify support, and render immediate cost savings to Penn Medicine, one contract was eliminated by moving to an updated mobile device management system.
All clinical users were provided with detailed step-by-step self-service instructions to make changes to their mobile device. All mobile devices using the legacy system were moved to run under the new system, and the old system was decommissioned. The system now supports over twenty-six thousand mobile devices.
Enterprise-wide Data Center is Consolidated
Penn’s Medicine’s rapid growth resulted in the acquisition and development of twelve independent data centers used to house disaster recovery environments that protect primary data centers in an emergency. Because their growth had been organic and unplanned, they represented multiple inefficiencies to the health system.
Beginning in 2018, analysis of the current data center environment was accomplished. Physical and improved logical footprint designs were calculated by the data center staff and management. Considering the use of virtualization for most systems, and the ability to use high density network and server environments, the plan migrated into action to physically move high density data center systems into the least cost data center environments.
In addition to the retirement of aging systems, system updates and conversions to high density, new racks were also accomplished. As a result, in 2022, data centers evaluated as non-sustaining or too expensive were retired. Those centers that remained viable for future needs of the health system were improved by adding power, wide area network connections, and staff monitoring. Penn Medicine’s Brownstown data center, which supports Lancaster General Hospital, played a critical role in adjusting and improving overall data center efficiencies.
The consolidations resulted in lower building operations costs, a complete overhaul of the entire system’s unit maintenance, and increased data center support. In addition, all data centers housed at entities were removed, allowing for patient focused planning space.
72 INFRASTRUCTURE
Because Connection is Vital; Nurse Call Gets an Upgrade at HUP Cedar
In a hospital, communication between patients and caregivers is not plainly important, it is vital. The nurse call system acts as a lifeline, providing a secure, reliable platform that scales across the entire hospital. The new system at the Hospital of the University of Pennsylvania-Cedar was selected to replace the aging system in radiology, intensive care, and on the northwest wing’s third, fifth and sixth floors. To support this system, new data cabling was run and two tele-data rooms with new network switches were installed on the fifth and sixth floors. In addition to this, the HVAC and power in the existing tele-data rooms on the third floor were upgraded to bring this into compliance with Penn Medicine standards. The Hospital of the University of Pennsylvania-Cedar now has a reliable, state-of-the-art nurse call system that ensures patient safety and operational efficiency.
Penn Presbyterian Medical Center Upgrades to New Patient Bedside Monitors
Penn Medicine replaced all patient bedside monitors with a high-performance bedside system, throughout the enterprise. One hundred and three new patient bedside monitors were installed in the medical intensive care unit, the stepdown unit, and the critical medicine unit at Penn Presbyterian Medical Center. These new monitors track a patient’s vitals from arrival through discharge. The project team incorporated technology which aligned with the department’s clinical workflow.
The benefits Included:
• Seamless integration of data into PennChart EHR
• Migration to an enterprise standard patient monitoring solution
• Improved performance and reliability of hardware with an active service warranty
• Improved patient care by providing uninterrupted monitoring of patient vitals during patient transport from one unit to the other
• Patient’s information is combined into one patient file
• Increase security by having the patient monitor system run on a more secure operating system
Media Makeover: Audio & Visual Technology Refresh and Recycle Initiatives
The media technology and production team upgraded audio visual (AV) technology rich spaces throughout Penn Medicine and the School of Medicine campus to ensure continued standardization of AV technology across departments and entities. Media technology and production was constantly challenged with supply chain shortages, manufacturer device availability, and lead time push backs (specifically linked to semiconductor microchip manufacturing). The media team evaluated existing spaces that would benefit from being upgraded and found new areas to create. We updated meeting rooms, classrooms, and conference room spaces based on priority as well as the availability of AV technology hardware from various manufacturers.
Spaces were upgraded to provide additional access to Microsoft Teams, Zoom, and Blue Jeans video conferencing as well as soft codec conference call technologies. This helped provide virtual conferencing access to diverse user groups in clinical, research, and educational departments across the health system and campus. The operation and functionality of these AV rich technology spaces is uniform in terms of standards, functionality, and operation; allowing a consistent and user-friendly environment.
Spare and contingent AV equipment was being used in spaces that required video conferencing, video capturing, and video streaming technologies. Public spaces were being used at a greater volume and frequency with the expectation of accommodating a hybrid experience. This refresh program met all users’ expectations, despite the challenge of semiconductor microchip shortages due to the impact from the pademic.
73 INFRASTRUCTURE
Telecommunications Technologies Upgraded – Returned Significant Cost Benefits
Penn Medicine’s footprint of clinical practices and facilities has become quite expansive and continues to grow. As healthcare business support needs changed, our IS team recognized when opportunities arose to update equipment and technologies that modernized and enabled foundational business practices. Significant changes occurred to the actual administration of healthcare with the onset of the pandemic and continued to evolve with a significantly increased remote non-clinical workforce.
To elevate communication tools used to connect with our patients and serve a greater demand initiated through digital channels, IS designed a new, state of the art integrated call center by merging several independent clinical practices to a single number integrated service. A coordinated effort was also made to create a new station rollout plan, dialing plan, and new circuit delivery, supporting the new hospital Pavilion expansion and reconstruction. Lastly, in support of the expanding group of non-clinical workforce, a new unified Microsoft Teams Dialer solution was rolled out to remote staff. The actions taken by the telephony team resulted in both increased support efficiency, lower total cost of ownership and increased patient satisfaction.
The following highlights are noted below:
• Private clinical practices now fully supported under a centralized call center platform


• Patient satisfaction scores increased by integrating with a centralized call center, lowering call wait times and adding alternative call back feature

• New lower cost circuits and efficient phone routing plans; 30% reduction in circuit cost spend
• 25% increase in phone license quantity and future cost avoidance resulted from Pavilion construction activities and internal phone licensing auditing
• Added new Microsoft Teams dialer functionality as a new remote workforce telephony standard and support model. The new Teams dialer solution resulted in remote staff no longer having to use their own cell phone to make business-related calls. This new functionality is 50% lower in cost than previous solutions and provides a unified, all-in-one communications solution for the remote and hybrid workforce
These fundamental shifts taken to innovate new technologies from traditional communications means easily replaced outdated practices with new, impactful efficiencies.
74 INFRASTRUCTURE
Keeping the Lights On” is No Small Feat in Maintaining a Large Health System Infrastructure
Penn Medicine’s extensive fleet of computing devices is continuously maintained for optimal performance and tracked for age related hardware and operating system updates to remain in compliance with vendor support requirements. In terms of keeping the computing environment up to date, approximately 25,000 Penn Medicine computers were deployed with the latest Windows operating system. The platform engineering team also worked with members of each hospital entity to remotely upgrade the Citrix workstation environment to the latest release at a 99.8% success rate. Additionally, constant vigilance is applied to identify the most critical updates needed to remediate security vulnerabilities.
Amidst these run-and-maintain activities, a new request was presented to introduce the rollout of mobile devices in the hospital setting. Platform engineering staff worked with members of the new Pavilion’s patient experience team to deploy 500 iPads to be used by patients in their rooms with the goal of increasing their overall satisfaction.
The achievements gained by the platform engineering team have resulted in increased support efficiency, security compliance, and patient satisfaction. Key performance highlights during this reporting period include the following:
• Enhanced security from upgrading machines to receive monthly Microsoft security updates
• Developed a process to regularly upgrade endpoints to the most current supported build. Doing so ensured that no additional endpoints were on unsupported versions of Windows.
• The new Citrix workstation release included advancements in security and stability features and was updated for an upcoming EHR upgrade in 2022.

• By working collaboratively with various entities, the platform engineering team achieved faster upgrades times by 50% over previous upgrades.
• Patients began using the iPads at their bedside, laying the groundwork for these iPads to be used for additional pilots with further integration into the Pavilion patient rooms. Additional use cases assessed include designing a whiteboard app for non-verbal patients. Deployment of a room control application; Deployment of the EHR patient bedside application in coordination with our EHR vendor.
EHRs Need Infrastructure Upgrades and Expansions to Perform Optimally
Supporting and maintaining the growth of the electronic health record (EHR) through resilient infrastructure promotes a stable platform to support our clinical staff in providing world-class care for our patients. Continuous server and storage infrastructure upgrades provided more efficient, powerful, and cost-effective hardware. Operating system and database upgrades also continued to keep the EHR environment running effectively. As the PennChart EHR application teams continued to upgrade and enhance the application for increased functionality and user features, the EHR infrastructure team continued to provide associated growth to maintain and run on a stable infrastructure platform.
75 INFRASTRUCTURE
Maximizing Infrastructure Efficiencies through Upgrades, Expansion, Consolidation

Supporting Penn Medicine’s consumption of storage and compute services while looking for opportunities to drive down costs is not an easy feat given the system’s size, complexity, and distributed operational model. By maintaining annual asset life-cycle management, it ensured the continual influx of more efficient and costeffective infrastructure to support the growth of the organization. The expansion of the Brownstown data center with new, high-density pods helped add new systems and ongoing consolidation of systems and related infrastructure from Chester County Hospital to the Brownstown data center. Our infrastructure team also continued ongoing work within the new virtual server farm to eliminate older, less efficient technologies across the server, storage, and backup infrastructure. The culmination of these efforts continues to provide a resilient infrastructure for Penn Medicine and promotes the strategy of integrating while driving down cost to the organization.
Network Refresh and Expansions Brought Valuable Efficiencies to Users


As Penn Medicine expanded its service area with new practices and facilities, data usage grew exponentially. As a result, network infrastructure needed to be increased to accommodate the growth. Over 14,000 pieces of network equipment and thousands of miles of cabling required constant refresh to maintain stability, in addition to improving the user experience with our existing support staff.
The network team continually updated the technical environment and increased performance by incorporating advanced technologies and performance efficiencies through design think tank sessions. These improvements were used for new expansion projects such as the Pavilion at HUP and numerous practice acquisitions. They were also incorporated into refresh activities with users unaware of the transformations taking place, such as the replacement of the core fiber backbone that ties together all major locations in Penn Medicine. Other examples included a refresh of the small practice wide area network (WAN) and numerous switch refreshes and software upgrades across Penn Medicine.
The primary benefit that this work brought was an improved user experience. Design integration activities helped to improve user access between Perelman School of Medicine and health system resources. Backbone and WAN redesigns reduced bottlenecks and improved application performance. Redundant power systems and equipment reduced outages and red/blue switch designs reduced the impact of (and in some cases eliminated) outages associated with maintenance activities. By redesigning and renegotiating carrier contracts, Information Services was able to vastly increase network capacity while reducing and avoiding operating costs, adding up to almost $1M per year.
76 INFRASTRUCTURE
EHR System Access Enhancements for User Onboarding Process

The PennChart EHR Access-Onboarding request form is an enterprise application used to facilitate user access requests to PennChart (Health System’s EHR). Over the last few years there has been a significant increase in the number of employees needing user accounts in PennChart. This resulted in a backlog of access requests and an increase in the time needed for an employee to get an account configured. The organization needed to optimize the onboarding process to reduce process time.
The existing request form was revamped to include more comprehensive questions and additional branching logic, ensuring users were guided to provide only the information needed. In addition, the integration with the IT department’s ticketing system was revised to break out the account setup work into task that were automatically assigned to the teams that were responsible for that phase of the account creation, eliminating a manual triaging process.
With the enhancements made to the Access-Onboarding request form, PennChart analysts were provided all the details they needed to configure an account when the form was initially submitted. This eliminated some of the back-and-forth information gathering that was occurring prior to the enhancements. Combined with the automatic triaging of the tickets directly to the teams needed to configure an account, the overall time to grant user access requests was reduced. In addition to the reduced time, management gained more visibility into what stage a request was at in the onboarding process due to the account setup work being broken out into distinct tasks.
77 INFRASTRUCTURE
Virtual working environments have always been a common work setting option for Information Services departments serving hospital systems. As the number of Penn Medicine facilities has increased, so has the number of team members in the IS department. In the past few years, the Information Services Social Council (ISSC) had a goal of getting IS colleagues out of their remote locations and into the office to collaborate and make meaningful connections with their fellow colleagues. The routine of attending virtual meetings throughout a workday became the new normal for many employees, but, having the ability to step away from laptops and monitors, and put a name to a face remained crucial.
The social committee recognized this need; which resulted in creating a number of in-office collaboration opportunities which gave IS staff members the ability to establish and strengthen professional relationships. Many staff members emphasized how refreshing it was to see their colleagues in person rather through a computer screen. Here at Penn Medicine, a strong culture of collaboration and teamwork has been established to support employee enrichment and professional growth.
ACTIVITIES INCLUDED
» PENN MEDICINE IS ACTIVE CLUB RUNNING, BIKING, SWIMMING, WALKING
» PJS FOR CHOP PATIENTS
» COMPUTER MONITOR DONATION
» CARDS FOR VETERANS
» HEART WALK/BAKE SALE
» VENDOR SPONSORED LUNCHES
» PENN CAFE
» ADOPT A FAMILY
» BACK TO SCHOOL SUPPLIES
DRIVE
ISSC events have included sponsored lunches, physical activity sessions like running, biking, and walking, and community service opportunities. Penn Café was developed as a new addition designed for colleagues to connect with their peers in a virtual water cooler-like manner to chat about a topic of their choice. Each virtual “floor” in the café featured conversation topics like book recommendations, vacation ideas, new recipes, and more. A core team of individuals from the Information Services department also developed a new IS workplace collaboration site. Our “Information Services Hub-Plug into Your Workplace” portal was launched to connect and increase engagement among IS colleagues for both work and social connectedness. This new avenue of collaboration promoted a “one-stop-shop” for all workplace resources, departmental updates, and social collaboration at peoples’ fingertips.
WE CARE COMMUNITY ACTIVITY REWARDS EVERYONE
IN FY2021/2022 ACTIVITIES FOR THE WECARE PROGRAM (TOTAL RAISED $14,357.25):
$3,563
IS PENN MEDICINE HEART WALK
210BACKPACKS
BACK TO SCHOOL PROGRAM
CHOP 8 SOUTH HOLIDAY PAJAMAS $7,300 HOLIDAY ADOPT-A-FAMILY $3,493.95
Penn Medicine’s commitment to care for patients has extended far beyond the falls of our facilities. The WeCare program (Care= Community Activity Rewards Everyone) was created for IS team members to volunteer their time, skills, and knowledge toward a variety of community activities in support of the needs of our greater community. The program has allowed colleagues from Information Services to extend a helping hand to the communities that the health system serves. From philanthropic donations to local schools, gifts for families in need during the holiday season, and raising money to support non-profit organizations, colleagues have contributed in many regards. Since the program first began in 2010; it has grown exponentially in size as more colleagues have come together to achieve a common goal; care and support in the community. In 2021-2022, the WeCare program made a meaningful impact in the community through teamwork, dedication, and collaboration. In return, it improves employee morale and communication as well.
78
IS DEPARTMENT SUPPORTS
THE IS DEPARTMENT HAS OVER 250 PROJECTS ACTIVE AT ANY GIVEN TIME. THE PMO ACTIVATES AN AVERAGE OF 50 PROJECTS MONTHLY. ABOUT 40% OF IS PROJECTS ARE COMPLEX ENOUGH TO REQUIRE A DEDICATED PROJECT MANAGER FROM THE PROJECT MANAGEMENT OFFICE.
1.166 MILLION

10.7 MILLION
2,916 PMACS SUPPORTED LAPTOPS 307 OTHER NON-PRINTER DEVICES
1,137 PMACS PRINTERS


22,257 TOTAL RESOLVED TICKETS
DATA AND ANALYTICS
19 MILLION PENNCHART CARE EVERYWHERE RECORDS EXCHANGED WITH OTHER INSTITUTIONS
31 MILLION+ ADT TRANSACTIONS SENT TO HSX (OUR HEALTH SHARE EXCHANGED)







425 MILLION INTERFACE TRANSACTIONS PROCESSED PER MONTH










300 DATA ANALYTICS CENTER REQUESTS PER MONTH
8,000+ REPORTS & DASHBOARDS SUPPORTED BY THE DATA ANALYTICS CENTER (DAC)














































































































































































































































































































































































EMAILS
INFORMATION SERVICES PROCESSES PER DAY OPERATIONS PERFORMANCE BY THE NUMBERS
SPAM
TWO-FACTOR
DAILY
VPN CONNECTIONS (INCREASED DURING PANDEMIC)
MESSAGES BLOCKED MONTHLY 8 MILLION
AUTHENTICATIONS THIS YEAR 13,000
CONCURRENT REMOTE
378 EICU
MYPENNMEDICINE
RESEARCH 808
74 CLINICAL
NEW STUDIES NEW SUBJECTS NEW ACCOUNTS LIMS - NUMBER
RESEARCH
2.3 BILLION SECURITY LOGS REVIEWED PER DAY (SOC)
BEDS MONITORED 53,837
CALLS TO SERVICE DESK
83,203
TRIAL MANAGEMENT SYSTEM
OF
SAMPLES 683,827
*Numbers reported in the last 12-month period ending June 2022 or as of June 2022.
ETHERNET PORTS
SERVER
PSOM
TOTAL BY SUPPORTED ENTITIES UPHS PTP PRINCETON DXC
RESEARCH LGH (LPC,HPC) SOM CLIENT SERVICES GROUP (CSG) 3,243 PMACS SUPPORTED DESKTOPS
Penn Medicine’s Information Services leaders are focused on continuously developing industry-leading healthcare technology innovations and maintaining operations with the highest degree of efficiency, while providing superior customer service to our users. Significant efforts continue to be made at Penn Medicine, toward implementing and integrating advanced technology approaches that will shape the future of medicine. Leaders and subject matter experts in our Information Services department participate in local, regional, and national level speaking engagements and conferences, as well as publish articles to share their knowledge and wisdom with individuals throughout the Healthcare IT industry. Their insights contribute significantly toward promoting growth and awareness of trends and innovations shaping the industry. Penn Medicine is routinely recognized for achieving successful technology outcomes by being acknowledged through numerous awards and accolades. These awards and recognitions are reflective of Penn Medicine’s posture of being an ongoing leader in using healthcare technology to advance healthcare.




























































































































































































































































































































































































































































































































































































































































































































































































































































































































For additional information regarding these awards and more please visit: https://www.pennmedicine.org/information-services/about-us/awards-accolades Awards on this page are not in the order they where recieved by Penn Medicine Information Services.
Penn Medicine
Awards
Accolades 2021-2023 2023 HIMSS Level 7 The Leap Frog Group CHIME DIgital Health Most Wired Survey 2022 CHIME DIgital Health Most Wired Survey The Leap Frog Group 2021 CHIME Digital Health Most Wired Survey The Leap Frog Group
Lancaster General Hospital
and
JULIAN MIHAI HealthSystemCIO ENTERPRISE CYBERSECURITY

https://rb.gy/uu9jdh
















































































































































































ANNA SCHOENBAUM
WOMAN IN HEALTH IT AGILE PRACTICES





JOHN DONOHUE Healthcare Innovation
TRAILBLAZING TECHNOLOGIES


https://rb.gy/qv73zg
MAUREEN HETU HealthSystemCIO
REMOTE OR NOT, OUR TEAMS DELIVERED https://rb.gy/3c50gy














































































































































































































































































































































































































































































































































































































81
ABBCI
Ann B. Barshinger Cancer Institute
ACO
Accountable Care Organization
ACOS American College of Surgeons
APS
Access Point of Care Systems
AV
Audio Visual Technology
BC/DR Business Continuity and Disaster Recovery
BPA Best Practice Advisory
CAR Chimeric Antigen Receptor
CCH
Chester County Hospital
CCI
Center for Cellular Immunotherapies
CEP
Center for Evidence-based Practice
CIO
Chief Information Officer
CMDB
Configuration Management Database
CMO
Chief Medical Officer
CMS
Centers for Medicare and Medicaid Services
CRCF
Cancer Registry Case Finder
DAC
Data Analytics Center
DAG
Database & Applications Group
DICOM
Digital Imaging and Communications in Medicine
ECMO
Extracorporeal membrane oxygenation
ED
Emergency Department
EHR
Electronic Health Record
EMS
Emergency Medical Services
ETO
Efforts to Outcome Software
EUS
End User Service
EVV
Electronic Visit Verification
FDA
Food and Drug Administration
FIT
Fetal immunochemical test
FQHC
Federally Qualified Health Center
GI
Gastrointestinal
HCV
Hepatitis C virus
HEDIS
Healthcare Effectiveness Data and Information Set
HIE
Health Information Exchange
HIM
Health Information Management
HIPAA
Health Insurance Portability and Accountability Act of 1996
HUP
Hospital of the University of Pennsylvania
ICU
Intensive Care Unit
IS
Information Services
ISC
Interventional Support Center
ISSC
Information Services Social Council
IT
Information Technology
IVF
In-vitro fertilization
LCME
Liaison Committee for Medical Education
LGH
Lancaster General Hospital
82
LIMS
Laboratory Information Management Systems
LRTI
Lower respiratory tract infection
MAR
Medication Administration Record
MDM
Mobile Device Management
MOUD
Medication for Opioid Use Disorder
MPM myPennMedicine
MSPQ
Medicare Secondary Payer Questionnaire
NAC Network Access Control
NICU
Neonatal Intensive Care Unit
NPR
Non-payroll resources
NSTEMI
Non-ST- Elevation Myocardial Infraction
OB/GYN General Obstetrics and Gynecology
OR Operation Room
ORA Orders results anywhere
OUD
Opioid Use Disorder
P2PE
Point-to-Point Encryption
PaH
Pennsylvania Hospital
PAH
Pulmonary Arterial Hypertension
PCAM
Perelman Center for Advanced Medicine
PCI
Payment Card Industry
PCR
Polymerase Chain Reaction
PCT
Patient Care Technicians
PHMC
Public Health Management Corporation
PMA
Phoenixville Medical Associates
PMAH
Penn Medicine at Home
PMBB
Penn Medicine BioBank
PPMC
Penn Presbyterian Medical Center
PMMG
Penn Medicine Medical Group
PMPH
Penn Medicine Princeton Health
PMOD
Penn Medicine OnDemand
PMX Survey
Patient Experience Survey
POS
Point of sale
PTP
Philadelphia Tek Park
PVA
Project Vital Advantage
QA
Quality assurance
SAM
Symptom Assessment & Management
SOC
Security Operations Center
Telecom Telecommunications
TDR
Tele-data rooms
UPHS
University of Pennsylvania Health System
VOIP
Voice over IP Enterprise
VPN Virtual Private Network
WAF
Web Application Firewall
WAN
Wide Area Network
83




































































































































































































































































































 J. Larry Jameson, MD, PhD
J. Larry Jameson, MD, PhD
 Kevin B. Mahoney Chief Executive Officer, University of Pennsylvania Health System
Kevin B. Mahoney Chief Executive Officer, University of Pennsylvania Health System

 Executive Vice President, University of Pennsylvania for the Health System Dean of the Ruth and Raymond Perelman Center for Advanced Medicine at the University of Pennsylvania, Robert G. Dunlop Professor of Medicine
Michael Restuccia Senior Vice President & Chief Information Officer, Penn Medicine
Executive Vice President, University of Pennsylvania for the Health System Dean of the Ruth and Raymond Perelman Center for Advanced Medicine at the University of Pennsylvania, Robert G. Dunlop Professor of Medicine
Michael Restuccia Senior Vice President & Chief Information Officer, Penn Medicine