
23 minute read
ChaPTer 11 Cosmetic Dentistry
Chapter
11 Cosmetic Dentistry
Advertisement
Objectives Upon completion of this chapter, the reader should be able to identify and understand terms related to the following: 1. Definition of cosmetic dentistry and related areas. Define the meaning of cosmetic dentistry and the various applications in dentistry. 2. Smile makeover. Define a smile makeover, and describe the cosmetic procedures that can be completed to achieve it. 3. Tooth whitening. Cite reasons for tooth whitening and methods used to lighten tooth surfaces. 4. Tooth bonding and veneer application. Discuss the procedures used to repair, or alter size, shape, and color of teeth by bonding or veneer applications. 5. Cosmetic tooth restorations. Discuss the various types of cosmetic restorations, including inlays, onlays, and crowns. 6. Periodontal tissue surgery. Identify the different techniques used to correct damaged tissue and make an esthetic gum presentation. 7. Dental implants. Describe the assortment of dental implants and the use and necessity of implant dentistry. 8. Accelerated orthodontics. Discuss accelerated orthodontics to improve the adult smile and mouth occlusion.
Beyond maintenance and reconstruction of the oral cavity, the modern dental patient desires an esthetic appearance. People seek dental care to improve their looks and turn to their dentist for cosmetic restorations and esthetic correction of diseased tissues, stains, genetic imperfections, accidents, and other maladies of the mouth.
Although most cosmetic dentistry procedures can be completed by the dentist, some require a team consisting of the dentist and other dental personnel such as a prosthodontist, oral surgeon, periodontist, and dental laboratory
technician. Cosmetic techniques offered to improve patients’ esthetic appearance and restore or provide a functional use include tooth whitening, bonding, veneer application, cosmetic restorations, periodontal adjustment, implants, and tooth movement. Major repair and reconstruction of the mouth and facial structures are covered in Chapter 14, Oral and Maxillofacial Surgery.
Smile Makeover
The first thing that comes to mind in cosmetic dentistry is a beautiful smile. Two terms for cosmetic mouth dentistry are smile makeover, the desire for an esthetic appearance and full mouth reconstruction, the need for repair for maladies from birth, disease, or dental-health issues. Some of the needs and treatments used in cosmetic dentistry are: tooth appearance: darker, rough-surface, pitted teeth may receive bleaching, whitening, resin surface application, veneer coverings, or crowns. spacing and alignment: gaps (diastemas, dye-ah-STEE-mah) in front teeth, peg-shaped teeth, overlapping teeth, and out-of-line teeth may receive bonding, veneers, crowns, surgical frenectomies, and orthodontic care. smile harmony and balance: chipped teeth, gummy smiles, tooth length, and uneven papillae may receive bonding, surgical contouring, or gingival augmentation. missing and decayed teeth: may receive restorations, inlays, onlays, crowns, implants, bridges, or partial dentures. commercial smile enhancer: sometimes called “Hollywood Smile” has been developed for total cosmetic use. Snap-on Smile is a full arch covering that can be placed on and off the teeth by the patient to offer immediate good looks. In cases where no major disease or structural problems exist, the dentist will take an impression and send it to the laboratory where a flexible, beautified cover is prepared for the patient to use when the occasion calls for an improved appearance or as desired. No tooth constructive or curative dentistry is performed. It is the patient’s option when to wear the tooth covering. See Figure 11-1.


Figure 11-1
Snap-on Smile, a cosmetic enhancer that may be placed and removed by the patient
Tooth Whitening
The most common cosmetic procedure is the whitening or lightening of tooth surfaces. Aging, chemically stained teeth, such as the tetracycline brown band line, and genetic disposition are causes of intrinsic (in-TRIN-sick, from within) stain. Personal diet may cause teeth to look dark and unattractive with extrinsic (ex-TRIN-sick, from without) stain. Whitening or bleaching of teeth surfaces can be completed in the dental office, at home, or a combination. Bleaching of teeth, as defined by the FDA, is the whitening of teeth beyond their natural color, such as lessening of brown bands, while tooth whitening is the restoration of natural tooth color. At the start of the procedure, the patient’s present shade of tooth is photographed, recorded, and will be compared to the new shade after the lightening. Relevant terms to tooth whitening are: shade guide: handheld device with assorted and numbered tooth-shaded forms that are compared to the incisal two-thirds of the patient’s incisors (Figure 11-2). Color types and levels include the following: = Reddish brown: up to five variant levels = Reddish yellow: up to four variant levels = Gray: up to four variant levels = Greenish gray: up to four variant levels model impression: a reproduction of the patient’s teeth is made into a plaster/ stone study model. tray fabrication: a plastic or celluloid tray is made to fit the study model cast and will be used to carry and hold chemicals for lightening. gingival isolation: painting or covering the patient’s gingival areas with a liquid dam (mask) material to isolate the tissues from chemical damage; some
Figure 11-2
Shade guides are moistened and matched to the natural tooth to determine the color, which is recorded in the patient’s records.
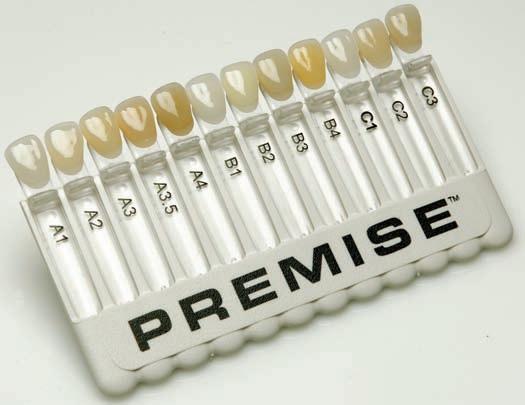
© Cengage Learning 2013
systems also use face drapes, foil intraoral liners, and/or cheek retractors for the patients’ protection, and provide protective glasses if about to use a curing lamp or laser setup. tooth bleaching: techniques and equipment vary according to the degree of lightening desired and the manufacturer’s recommendations and instructions that differ in chemical strengths and application methods. Some techniques may require additional home care, but the basic methods are: acid brush: 35% phosphoric acid solution applied to surfaces, particularly to tetracycline band lines on surfaces. The solution remains on the surface 15 seconds and then rinsed off; refreshened and reapplied up to three times as needed. tray method: gel-, or paste-filled tray placed into the mouth over cleaned tooth surfaces; gel may be activated by diode-laser handpiece or activated by curing light up to three times. gel application: a whitening gel containing a hydrogen peroxide or carbamide peroxide formula is applied directly to cleaned, isolated tooth surfaces, and may or may not be activated by bleaching, laser, or curing lights, as specified by the manufacturer; may be refreshed and reapplied as needed. laser activation: isolation of tissues, cleansing of tooth surfaces, and application of protective tissue covering and bleaching gel. Laser-light application for approximately an hour gives accelerated and more penetrating activation of the chemical gel material. Some patients are supplied DVD glasses for diversion during the wait. pen tip painting: some commercial manufacturers have developed a pen that may be purchased at the drug store and used at home to paint the surfaces for whiter teeth. The pens contain some peroxide/bleaching material and do lighten teeth, but not as many shades as claimed. tooth desensitization: following bleaching, a desensitizing liquid, paste, or gel applied to tooth surfaces seals dentin tubules to minimize discomfort and reduce shade relapse. Some formulas that also deter some sensitivity and remineralize the tooth include fluoride, calcium, and phosphate.
Following office lightening, the patient may be given a home tray and chemicals to complete the bleaching process. Assorted home bleach kits, strips, and gels are available, some from the dentist and others over the counter (OTC) at a local drugstore. Most contain a hydrogen peroxide or carbamide peroxide gel base that is placed in a tray, inserted in the mouth, and worn for a specified time, such as two to three hours, or overnight as directed. Professional whitening usually lasts a year provided that the patient monitors his or her diet and does not smoke, both of which darken the tooth surfaces.
Tooth Bonding and Veneer Application
Tooth bonding and veneer application are alternatives to tooth whitening, particularly if the tooth surfaces are excessively stained or have other irregularities such as open spaces, broken edges, pitted surfaces, and misshaped teeth.

Figure 11-3
A before and after example of tooth bonding

Courtesy of dentalcomposites.com/Paul R. Chalifoux, DDS
Tooth Bonding
Veneer
Tooth bonding involves applying a composite material that is mixed to a pliable dough form, applying it to a prepared tooth surface, and sculpting it into a tooth shape. The composite shade is chosen to match the existing tooth surface. The tooth is prepared by removing any present decay, followed by an abrasive roughening, and a gel etch. The surface is primed, the composite material is applied in layers, and the material is activated by a curing light. When shaped and finished, the composite is smoothed and polished (Figure 11-3).
In a veneer (veh-NEAR) application, a thin fabricated resin or porcelain cover is applied to the prepared tooth surface. Along with covering stained and affected teeth, the shape or color of the tooth may be altered. Depending on the severity and preparation needs of the teeth, veneers, also called laminates, can be applied using either of two methods: = Direct veneer application: methods that can usually be completed in one visit include: Similar to tooth bonding, a resin material is applied to tooth surfaces that have been roughened by air abrasion or rotary burs and wheels. The plastic material is cemented directly on the surface, and then smoothed and polished. Chair-side custom laminates can be made at the initial first visit with the use of a CAD/CAM technology. These laminates are prepared immediately, thereby eliminating the return second visit. Lumineers, Durathins, or other premanufactured, “no prep” veneer coatings can also be applied to facial tooth surfaces that need little or no surface removal (Figure 11-4).
Figure 11-4
Lumineers

= Indirect veneer application (requires two visits): At the first visit, the teeth are prepared by removing a small amount (0.5 mm to 1.0 mm) of enamel tissue. An impression is taken for fabrication of the porcelain veneers or laminates and sent to the laboratory. The dentist may or may not apply a temporary cover to last between visits. At the second visit, the teeth are cleaned, acid etched, and primed to receive the new laminates that are cemented on the tooth surface and light cured to set up. The porcelain veneers are cleaned and polished. Porcelain veneers usually are longer lasting and more expensive. See Figure 11-5 for an example of a before and after veneer application.


Figure 11-5
Veneer photos. Diastema of the central incisors has been eliminated by the application of veneer coverings.
Cosmetic Tooth Restorations
Tooth restorations are completed using materials that resemble enamel tissue. Older amalgam fillings can be replaced using composite material to give the whole mouth a natural look. Restorative procedures include: tooth restoration: prepared tooth receiving white composite restorative material, instead of metallic amalgam or gold; replacement of existing amalgam fillings with composite. inlay: a solid-casted or milled restoration, involving some occlusal and proximal surfaces, that is cemented into a tooth preparation. onlay: a solid-casted or milled restoration that covers some occlusal tooth cusp and side wall area and is cemented onto the prepared site. tooth crowns: covering the crown surfaces of the tooth with artificial coverings. The type of crown applied depends on the extent of the tooth repair and is named by the area involved: full crown: cast or milled restoration covering the entire crown area of a tooth (Figure 11-6). three-quarter crown: cast or milled restoration covering all surfaces except the facial view. porcelain fused to metal crown (PFM): full cast crown restoration with porcelain facing on exposed areas for cosmetic appearance. jacket crown: thin metal cover with a porcelain facing for an anterior tooth.
Multiple crowns or combination restorations involving larger areas of the mouth are united in dental bridgework. This area of reconstruction is covered in Chapter 19, Dental Laboratory Procedures. The construction of
Figure 11-6
Full crown
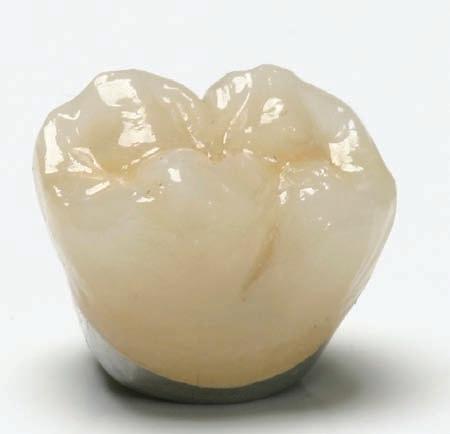
Courtesy of ROE Dental Lab
cast restorations will also be discussed in Chapter 19. Although many cast restorations are made with gold or precious metals and covered with porcelain or resin to present an esthetic appearance, a new system of chairside ceramic restoration construction has been developed for immediate cosmetic restoration: CAD/CAM systems (computer assisted design/computer assisted machine).
For example, the CEREC CAD/CAM system is made up of three parts, an acquisition unit, a milling machine, and a software system. The acquisition camera or wand surveys the tooth preparation that has been covered by a reflective powder and converts the pixel information to a 3D image on which the dentist designs the restoration (approximately 30 minutes). The acquired data is transferred to the office laboratory milling machine to carve the patient’s restoration out of a ceramic block (approximately 15 minutes). The dentist tests the fit, and then refines and polishes the restoration for bonding into the tooth preparation. The completed restoration is a solid ceramic block instead of a metal inlay, onlay, or crown with a porcelain esthetic covering. This method allows a one-trip restoration of tooth structure compared to other methods, where a provisional or temporary restoration must be prepared while the lab is fabricating the restoration.
Other systems work in the same manner, but imaging information may be sent from the camera capture in the patient’s mouth to a company software design center for digital interpretation and construction of a working model. The dentist may receive and use this model, or it may be sent to a commercial lab chosen by the dentist. Construction of the restoration is completed at the laboratory and sent to the dentist to be placed in the patient’s mouth. Meanwhile, the patient will wear a temporary coverage and return for the completion visit.
These CAD/CAM systems can complete a simple inlay or crown restoration as well as construct many pieces that are united into a bridge or whole arch reconstruction.
Periodontal Tissue Surgery
Periodontal plastic surgery, also termed mucogingival (myou-koh-JIN-jihvahl) surgery, can be performed as a treatment for diseased tissue or as a method to enhance the patient’s smile. Therapeutic periodontal treatment of gingival tissue will be discussed in Chapter 16, Periodontics, and Chapter 14, Oral and Maxillofacial Surgery. Esthetic gingival tissue surgery in cosmetic dentistry is used to either reduce or augment the gingiva as needed. Some examples and treatment of gingival cosmetic maladies are discussed next.
Gingival Reduction
In gingival reduction, excessive gingival tissue is removed by laser, periodontal knives, or bipolar electrosurgery. Depending on the case severity or the amount of tissue area involved, most gingival adjustments are completed with local anesthesia in a single visit. Occasionally, some bone reduction or augmentation


Figure 11-7
Before and after example of laser crown lengthening
Courtesy of Dr. Louis Poulos, http://www.drpoulosperio.com
may be required, which will require deeper anesthesia and surgical intervention. Reduction is used for the following: crown lengthening: exposing more tooth surface to eliminate a “gummy smile” (see Figure 11-7). gingival contouring: removing excessive tissue to obtain symmetry of the gingival crest. exposing unerupted teeth: removal of coronal tissue to expose tooth surface, such as slowly emerging mandibular third molars. enlarged labial frenum: condition where thick or enlarged labial frenum presents tissue growth between the mesial of central incisors, causing a space gap. A frenectomy (removal of excessive frenum tissue) will permit teeth to grow back together with minor tooth bracing.
Gingival Augmentation
Gingival augmentation builds up or reconstructs the gingiva to repair or replace tissue where needed. It involves the following: soft tissue grafting: transplanting mouth tissue from nearby gingival tissue or from the palate area to other sites. interdental papilla regeneration: replacing papilla tissue in intradental spaces. gingival recession: restoring the gingival crest to a natural height. pocket depth reduction: eliminating the pocket area and restoring the gingiva. exposed roots covering: replacing gingival tissue over exposed roots (Figure 11-8). ridge augmentation: building up gingiva and bone tissue in collapsed areas resulting from tooth extraction.


Figure 11-8
Tissue replacement for exposed cuspid root
Dental Implants
Dental implants are titanium fixtures that are surgically installed in the jawbone and used to stabilize or serve as an anchor for a tooth, an appliance, or a denture. They may be used as an alternative to a fixed bridge or in areas where tooth replacement requires stability. Placement of an implant often requires a team cooperation of several specialists, such as an oral surgeon, a prosthodontist, and perhaps a periodontist.
Implants are surgically installed and remain in place for three to six months while the appliance and bone unite in a process called osseointegration (oss-ee-oh-inn-teh-GRAY-shun = union of the bone with the implant device). They are then uncovered, and the artificial device is attached. Implants will be discussed more in Chapter 14, Oral and Maxillofacial Surgery, and Chapter 12, Prosthodontia. Terms related to implants are: root form implant—endosseous (en-DOSS-ee-us = within the alveolar bone): screw-type device that is screwed or cemented into the alveolar bone; used for a single tooth or post implant (Figure 11-9A and 11-9B). plate form implant: used for the narrow jawbone; flat-plate style. subperiosteal (sub-pear-ee-AHS-tee-al) implant: implant plate or frame extending through the jawbone, placed under the periodontium, and stabilized on the mandible bone. It is used when bone height or width is insufficient; rests on top of the bone. transosteal (trans-AHS-tee-al) implant: larger plate stabilized on the lower border of the mandibular bone with posts extending through the gingiva; used to anchor prostheses in difficult situations.
Crown (cement retained)
Abutment post
Implant
(A)
© Cengage Learning 2013 Courtesy of Imaging Sciences, Inc.

(B)
Figure 11-9
(A) Parts of implant with prosthesis; (B) radiograph showing implants in place
Accelerated Orthodontics
Malocclusion can present an unattractive smile, and the desire for a better cosmetic appearance may cause a patient to seek accelerated orthodontic treatment. Most orthodontic treatments require two years or more to complete, and many adults desire a quicker treatment method. With accelerated orthodontics, the task can be accomplished in three to nine months, with retainers to be worn another six months.
Accelerated Orthodontic Treatment
AOO treatment is a surgical orthodontic approach requiring a team of specialists trained in this procedure. It is a multiple-step process where the teeth are aligned and banded, sometimes after rectification (selective removal of interproximal tooth tissue of multiple teeth) that provides space for tooth movement. This slimming or narrowing of teeth eliminates the need for extraction. A week after banding, the patient’s gingiva is incised to expose the alveolar bone where a surgical drill places holes or removes bone tissue in the alveolar crest
to demineralize the bone, causing a condition called osteopenia (ahs-tee-ohPEE-nee-ah = lack of bone tissue). A bone graft material mixed with an antibiotic is placed on the site, and the gingiva is replaced and sutured into place.
While the bone is in a weakened stage, movement progresses rapidly. Return visits and banding readjustments are more frequent than with the normal orthodontic treatment, and retainers are worn for six months or so after the bands have been removed, allowing total remineralization to finish.
Other cosmetic applications for orthodontic treatment include the following: InvisalignTM: an orthodontic polyurethane tray method for tooth alignment using a series of clear, preformed, custom trays that apply pressure for tooth movement. Trays must be worn 20–22 hours per day, and when movement is finished, they must be worn at night. The trays are frequently changed (every two weeks) as movement or realignement occurs.
Some tooth surface-slimming adjustment may be made after the impression, X-rays, photos, and records are sent to the Invisalign lab for 3D model planning and tray fabrication. orthodontic enamoplasty: removing small amounts of enamel walls to acquire enough room to cause a slight correction movement; usually performed in a small area or trouble spot. lingual banding: placement of brackets and bands on the lingual tooth surfaces so they are not easily viewed.
More conventional methods of orthodontic treatment are discussed in Chapter 15, Orthodontics.
Review Exercises
Matching
Match the following words with their meanings. 1. full mouth makeover A. tooth stain from internal sources 2. inlay B. a thin resin or porcelain shell covering 3. transosteal implant C. protective gingival tissue covering when tooth bleaching 4. tooth whitening D. tooth stain from external sources 5. jacket crown E. lightening of teeth to natural color 6. osseointegration F. a cast restoration for a tooth cusp and proximal walls 7. tooth bleaching G. implant placed through the jawbone 8. onlay H. necessary repair for mouth maladies 9. intrinsic stain I. periodontal plastic surgery 10. root form implant J. anterior tooth metal covering with porcelain covering 11. mucogingival surgery K. casted cover on some occlusal surface and side walls 12. gingival augmentation L. union of bone with implant device 13. veneer M. lightening of tooth beyond the normal color 14. extrinsic stain N. a buildup of gingiva to replace tissue where needed 15. gingival isolation O. screw-type device inserted into the jawbone
Definitions
Using the selection given for each sentence, choose the best term to complete the definition. 1. A prepared restoration that is placed on a tooth prep involving some occlusal cusps and proximal wall is a: a. full crown b. jacket crown c. onlay d. inlay 2. Tooth whitening completed by the application of phosphoric acid is which method? a. acid brush b. tray application c. gel rub d. air polish 3. Which procedure is considered gingival augmentation? a. gingival contouring b. crown lengthening c. exposing root surfaces d. interdental papilla regeneration 4. Tooth stain from genetic, aging, or chemical enamel reactions is which type of stain? a. intrinsic b. extrinsic c. environmental d. regional 5. Tooth stain from diet, personal tooth care, and smoking is which type of stain? a. intrinsic b. extrinsic c. environmental d. regional 6. Implant placement would be considered proper treatment for which condition? a. missing tooth b. gummy smile c. fractured tooth edge d. full embrasure
7. The last step in office power tooth bleaching is: a. gel application b. desensitizing c. tray fabrication d. model impression 8. A tooth diastema (open gap) can be corrected using which technique? a. tooth bonding b. gingival augmentation c. acid etching d. tooth restoration
9. Invisalign is the term applied to which orthodontic procedure method? a. lingual banding b. clear bracket use c. customized tray d. metal braces 10. Which of the following is considered to be a laminate? a. implant post b. dental dam c. die pattern d. veneer 11. A cast restoration involving the entire tooth surface that is cemented onto the tooth preparation is called: a. inlay b. onlay c. full crown d. jacket crown 12. The FDA requires a whitening of tooth surface beyond the natural color to occur for: a. tooth whitening b. veneer placement c. tooth bleaching d. color tone 13. The method of applying gel whitening material directly to the tooth surfaces is termed: a. acid wash b. tray coverage c. strip placement d. gel application 14. Protection of the gingival tissue during the application of chemicals in power bleaching is completed by which method? a. liquid dam mask b. cotton roll application c. oral evacuation d. tooth bonding 15. An example of a alignment and spacing problem would be which of the following? a. chipped tooth b. peg-shaped lateral c. pitted tooth surface d. gummy smile 16. Soft tissue grafting is considered which type of periodontal surgery? a. gingival stabilization b. gingival reduction c. gingival desensitizing d. gingival augmentation 17. Which of the following implant devices is placed through the jawbone? a. root form implant b. plate form implant c. subperiosteal implant d. transosteal implant
18. Mouth impressions are taken for construction of which of the following: a. implant post b. tray fabrication c. brush well d. dental dam pattern 19. The demineralization and lessening of the alveolar bone in accelerated orthodontics creates a condition termed: a. osteogenesis b. osseointegration c. osteopenia d. osteoporitis 20. Which type of crown would be used mainly on anterior teeth? a. bracket crown b. jacket crown c. three-quarters crown d. full crown
Building Skills
Locate and define the prefix, root/combining form, and suffix (if present) in the following words. 1. mucogingival prefix ___________________ root/combining form ___________________ suffix ___________________ 2. endosseous prefix ___________________ root/combining form ___________________ suffix ___________________ 3. subperiosteal prefix ___________________ root/combining form ___________________ suffix ___________________ 4. osteopenia prefix ___________________ root/combining form ___________________ suffix ___________________ 5. orthodontic prefix ___________________ root/combining form ___________________ suffix ___________________
Fill In
Write the correct word in the blank space to complete each sentence. 1. The procedure of removing small amounts of enamel wall to permit orthdontic tooth movement is known as _________________________. 2. The union of bone with the titanium dental implant device is known as _________________. 3. A/an ____________________crown is a thin metal-casted restoration with a porcelain covering placed on an anterior tooth. 4. The orthodontic treatment method of moving teeth by using customized activation trays is known as _______________________________. 5. _______________________ is the term given to the surgical removal of gingiva to expose more enamel surface and reduce a “gummy” smile. 6. When power-bleaching teeth with chemicals, the gingiva is protected by _________________. 7. A/an _______________________ is taken to prepare a study model for fabrication of a bleaching tray. 8. A/an ________________________ is used to compare tooth colors and obtain the restoration color for a patient. 9. A dental implant is usually constructed using _______________________________ metal. 10. Another term for periodontal plastic surgery is _____________________surgery. 11. In the Invisalign tray treatment plan, the patient is required to wear the tray for __________________________ hours a day. 12. The white or tooth-colored material of choice used for an anterior restoration is
________________________________________. 13. A/an _____________________ implant is used for a patient with a narrow jawbone. 14. The placement of orthodontic bands on the back surfaces of the anterior teeth is termed _______________________ banding.
15. _____________________________ may be used to change the color and shape of the anterior teeth or to cover badly stained teeth. 16. A full-casted crown that is covered by a porcelain covering is known as a/an ________________________________ crown. 17. Repairing a chipped tooth by using a composite material in a dough consistency to build up the tooth surface is a process called tooth ________________________________________. 18. Another name for a dental veneer is a dental
________________________________________. 19. _____________________ stain is tooth stain caused by a diet of coffee, tea, and smoking. 20. ________________________ is a term applied to the condition of the alveolar bone after receiving the surgical bur treatment in accelerated orthodontics.
Word Use
Read the following sentences, and define the boldfaced words. 1. The last step of a tooth-whitening procedure is the tooth desensitization.
________________________________________
2. Certain medicines can cause intrinsic staining of newly forming teeth. ________________________________________ 3. Mrs. Swartz chose veneers to enhance the color and shape of her teeth. ________________________________________ 4. When matching tooth colors to a shade guide, the guide should be moist so that it reflects light like the natural tooth surfaces do. ________________________________________ 5. The assistant made an appointment for gingival augmentation for Mr. Peterson’s gum recession.
Audio List
This list contains selected new, important, or difficult terms from this chapter. You may use the list to review these terms and to practice pronouncing them correctly. When you work with the audio for this chapter, listen to the word, repeat it, and then place a checkmark in the box. Proceed to the next boxed word, and repeat the process.
augmentation (awg-men-TAY-shun) endosseous (en-DOSS-ee-us) extrinsic (ex-TRIN-sick) intrinsic (in-TRIN-sick) mucogingival (myou-koh-JIN-jah-vahl) osseointegration (oss-ee-oh-in-teh-GRAY-shun) osteogenic (oss-tee-oh-JEN-ic) osteopenia (ahs-tea-oh-PEE-nee-ah) subperiosteal (sub-pear-ee-AHS-tee-uhl) transosteal (trans-AHS-tee-al) veneer (va-NEAR)










