WWW.PHYSICIANOUTLOOK.COM PUBLICATION DEDICATED SOLELY TO PHYSICIANS AND THEIR PATIENTS Cover Artist Lucie Mitchell, DO 2022: THE YEAR WE START ANEW VOLUME 12 | 2022 PHYSICIAN OUTLOOK MAGAZINE

Securities offered through Fortress Private Ledger, LLC. Member FINRA/SIPC Investing involves risks, and investment decisions should be based on your own goals, time horizon, and tolerance for risk. The return and principal value of investments will fluctuate as market conditions change. When sold, investments may be worth more or less than their original cost.
The Thorny Rose
CARING FOR THE PATIENT WITH INVISIBLE ILLNESS
Written by Marlene Wüst-Smith, M.D.
As physicians, it is humbly satisfying when we are able to utilize our training and expertise to adeptly diagnose, treat and sometimes even cure those who come to us with a particular malady. Many of us have the unique privilege of caring for many different types of patients.
Some of us are drawn to specialties where the diagnoses and required interventions are obvious. Think of the Orthopedic Surgeon who takes care of patients with skeletal trauma, or the dermatologist who is able to help a patient get rid of a disfiguring skin condition.
As a pediatrician I am part of a group of professional ‘gardeners’ who are drawn to care for the tiniest forms of life, helping them to survive the elements and thrive in a complexly orchestrated but sometimes quite harsh ecosystem. An ecosystem that can unwittingly threaten their survival and ability to blossom into beautiful flowers.

Perhaps the most challenging type of patient to treat is the individual who appears to look completely “perfect” on the outside, but who is afflicted with a condition that is invisible to the outside world.
This issue of Physician Outlook Magazine is dedicated to those pa -
“It is only with the heart that one can see rightly. What is essential is invisible to the eye.”
-Antoine de Saint-Exupery
tients who suffer in silence, who are often misunderstood, judged or ignored.
This world of invisible illness, where those afflicted often self-identify as “Spoonies” (a term famously coined in 2003 by a patient blogger with lupus), is a growing universe and one in which physicians receive very little training.
Throughout this issue, you will read stories authored by doctors, patients and other professionals who are living with invisible illnesses, helping loved ones with unseeable maladies, or treating patients who are suffering invisibly.
Dr. Adam Harrison , a British doctor, lawyer and coach, sheds light on the lasting effects of chronic work place bullying.
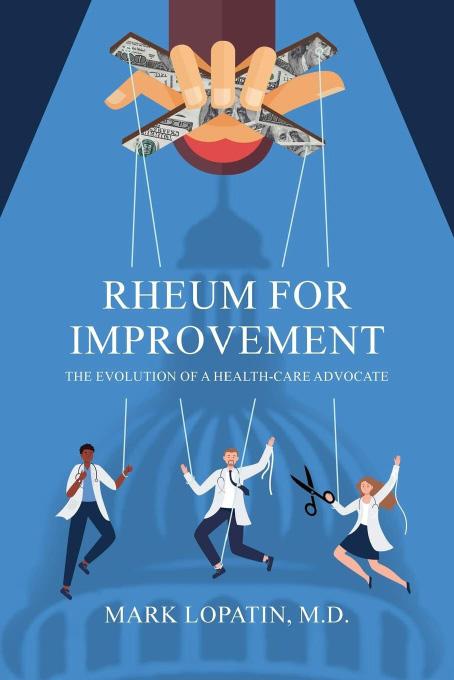
Dr. Mark Lopatin, a recently retired rheumatologist and author of “Rheum for Improvement” discusses the dangers of assuming that patients with fibromyalgia and other forms of chronic pain have issues that are “all in their head.”
Charles Bens, PhD points out the importance of assessing immune markers when treating patients with invisible illnesses. Traditional labwork can often be normal but there are ways to optimize nutrition to improve symptoms.
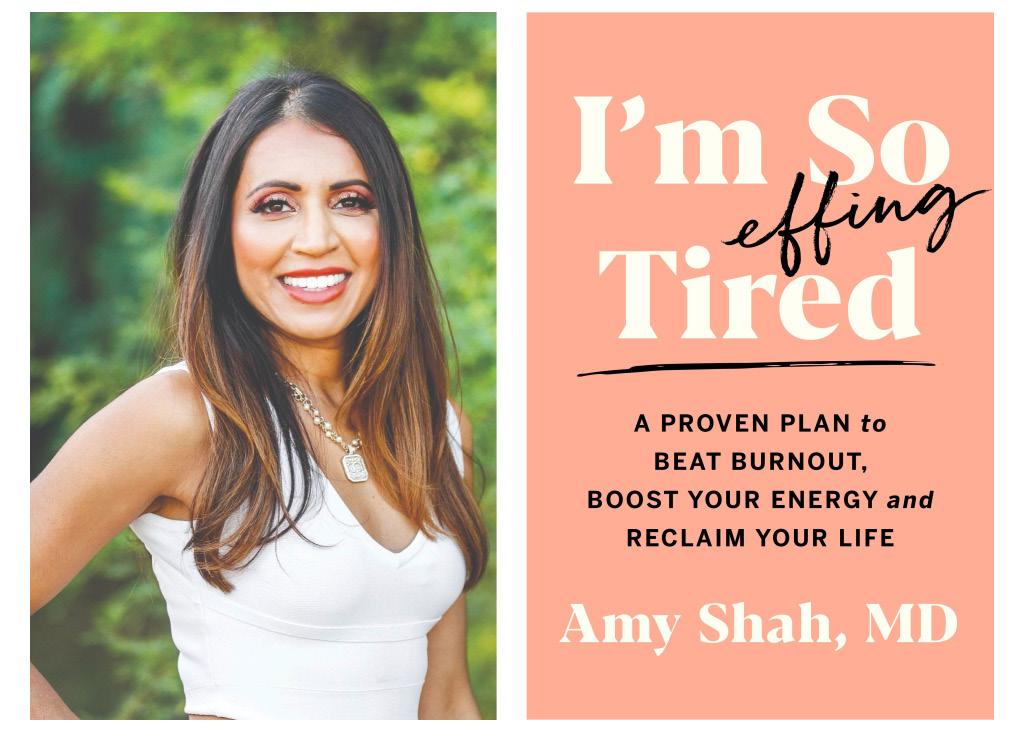
An interview with Dr. Amy Shah provides a glimpse into the world
FROM THE PUBLISHER IMAGE BY LUCIE MITCHEL, DO
4 | 2022 VOLUME 12
of the microbiome and the groundbreaking work being done in that medical field.
Dr. James Harris Jr. (in a prequel to a memoir he is writing) reveals what it was like growing up with a crack-addicted father. Adverse Childhood Events are prevalent in many who suffer silently, but this surgeon is living proof that it is possible to overcome even the most devastating experiences.
Dr. Laura Fortner ’s article on litigation stress discusses the many lasting physical and emotional effects that occur when a physician is accused of malpractice.
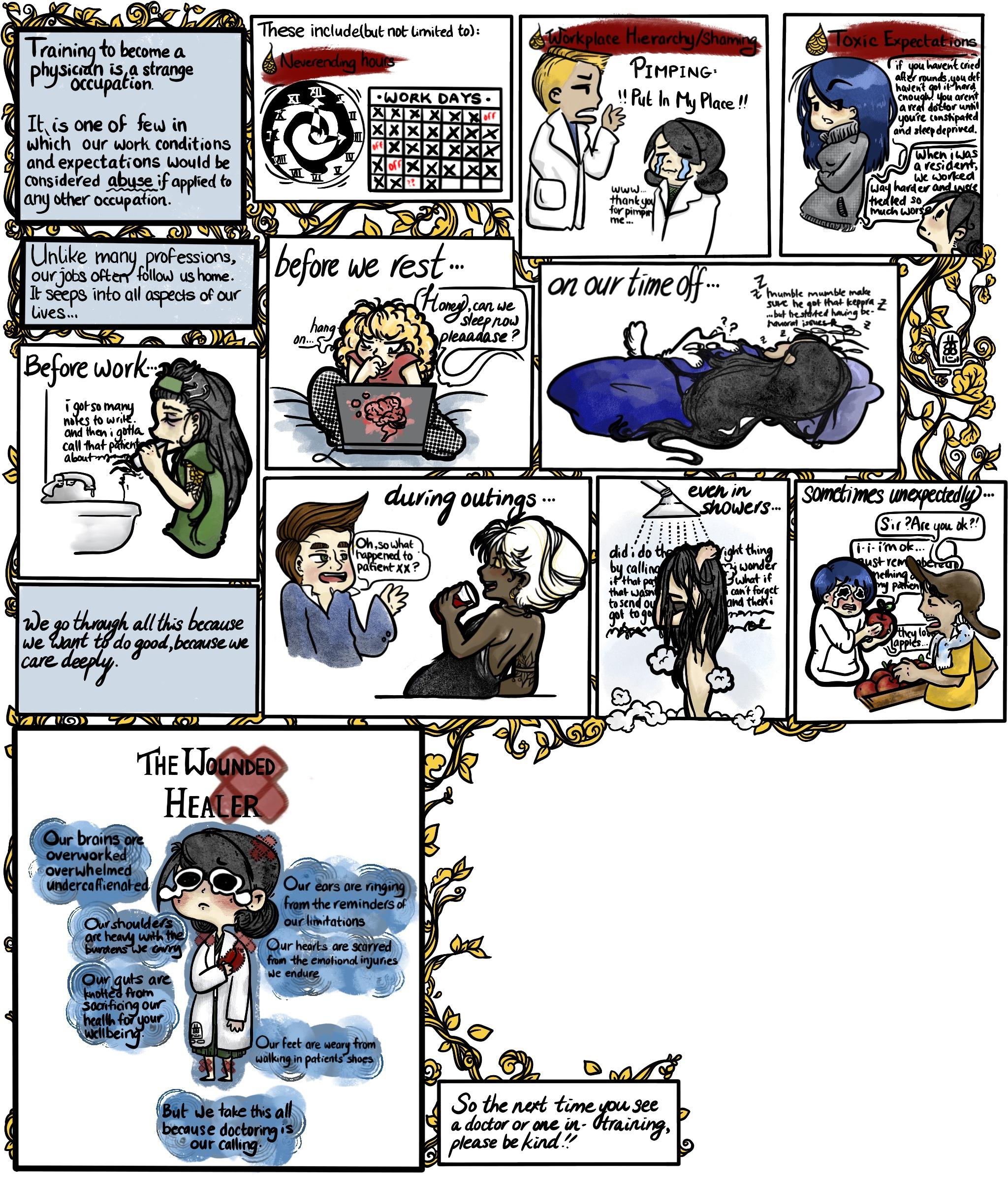
Dr. Nita Chen brings the world of art to medicine with her full page comic. It is no easy task becoming a doctor and this cartoon demonstrates that in a relatable way.
This issue features an update about the practice of “Chronically (Ch)ill” former orthopedic surgery resident-turned-physiatrist, Dr. Alissa Zingman , who, after years of being told she was a hypochondriac, was finally diagnosed with Ehlers-Danlos Syndrome. She is the founder of a unique integrative multi-specialty practice that is dedicated to the treatment of patients with EDS and other hypermobility syndromes.
Sometimes necessity becomes the mother of invention, and Terry Wilcox , co-founder and the Executive Director of Patients Rising Now, writes about how the COVID-19 pandemic, which has given rise to a cohort of virus survivors afflicted with “long-COVID,” may actually help to shed some much needed light on the plight of those with biopsychosocial illnesses, particularly persons of color, whose medical needs have traditionally been ignored to a greater extent when compared with white counterparts.
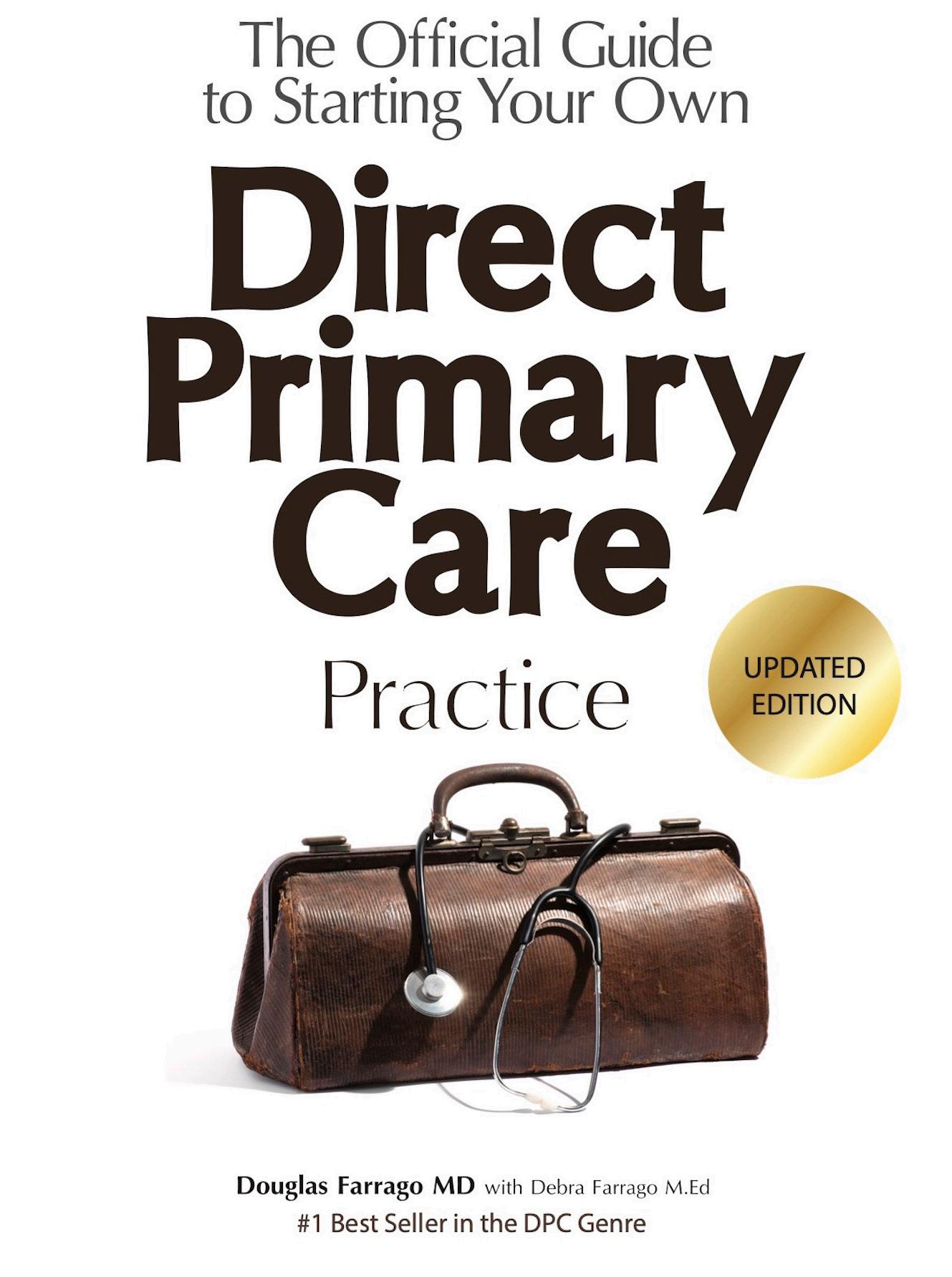
Christy Gupton and Liz Antaya of Mitigate Partners bring awareness to some of the “outside of the box” work being done by those in the Benefits Management industry. Direct primary and specialty care models ARE appropriate for patients with chronic illnesses, and can save
employers and patients significant money, AND often compensate physician-led care teams better than the traditional very expensive bureacracy-laden BUCAH insurance products so prevalent in the marketplace.
Dr. George “Jeep” Naum and Jill Labecki both wrote about what it is like to love family members with livi invisible burdens. Their stories are inspirational for families who may be struggling.
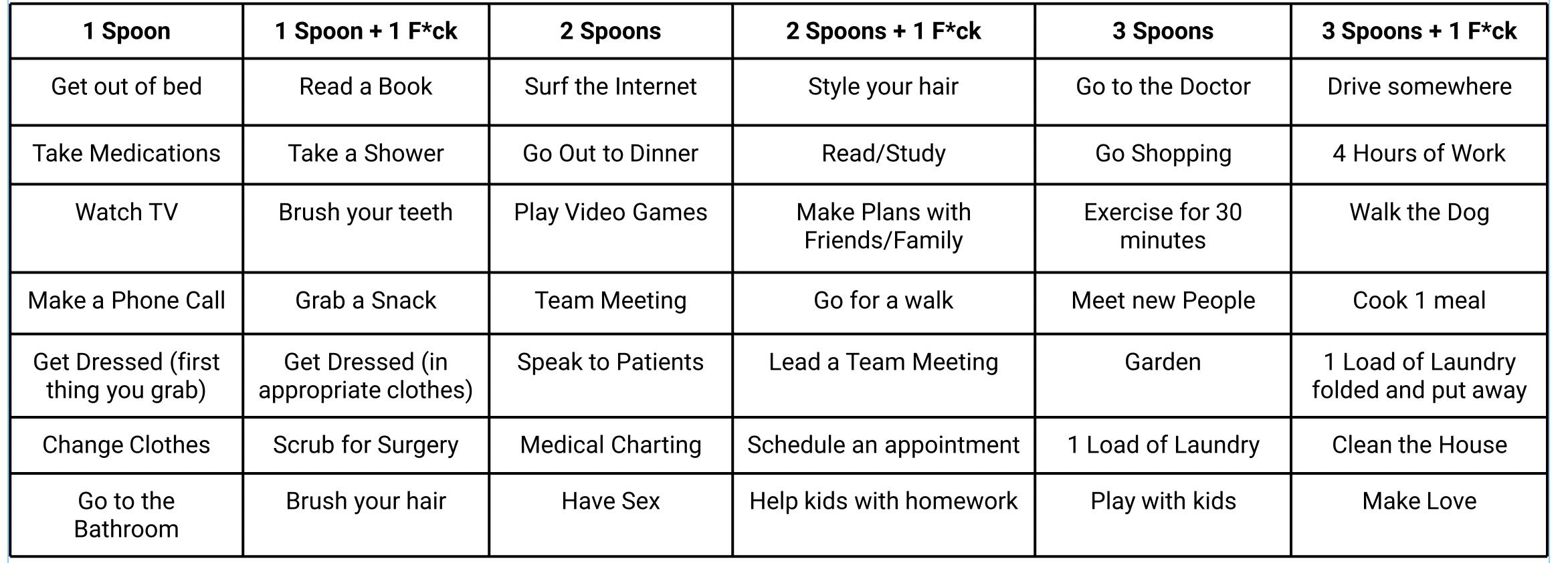
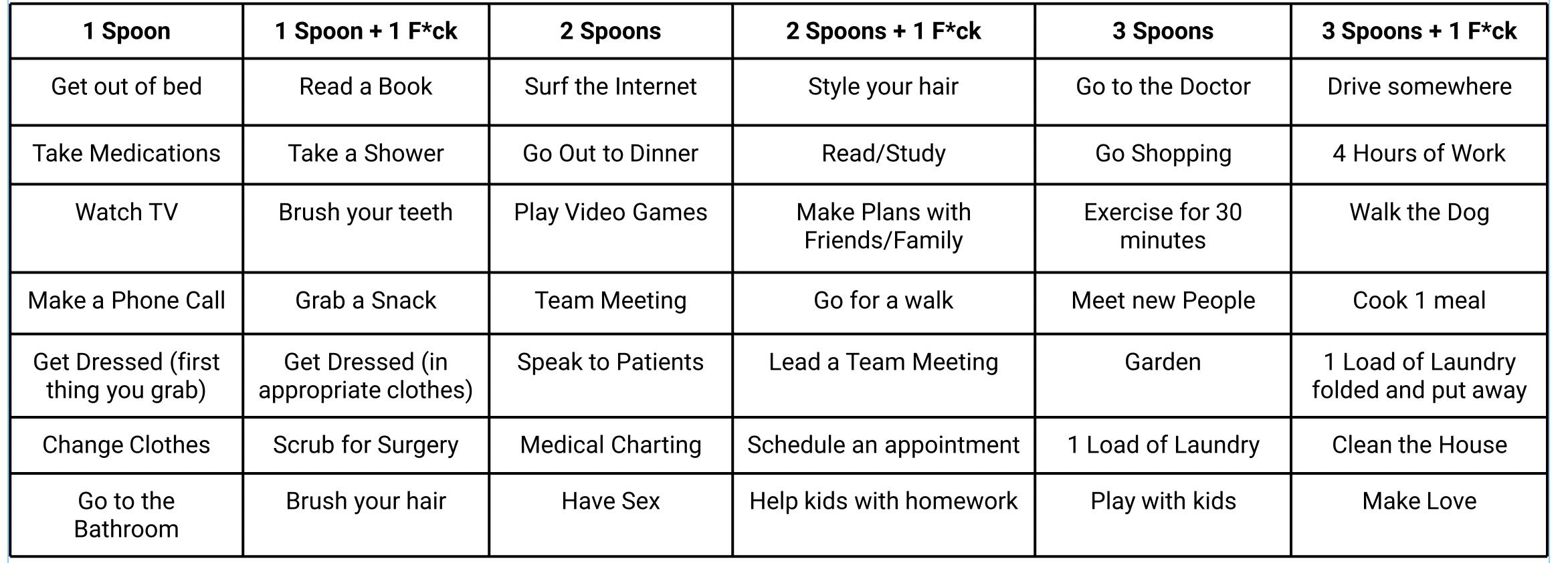
Roxanne Bruce, MBA, DrBA has led several support groups for the National Multiple Sclerosis Society, and published a book that helps patients effectively communicate their symptoms and challenges with their doctors. She challenges readers to schedule a week of their lives as if they had a chronic illness, following the guidelines of “Spoons” and “F*cks” to help better understand what it is like to live with a chronic, unseeable illness.
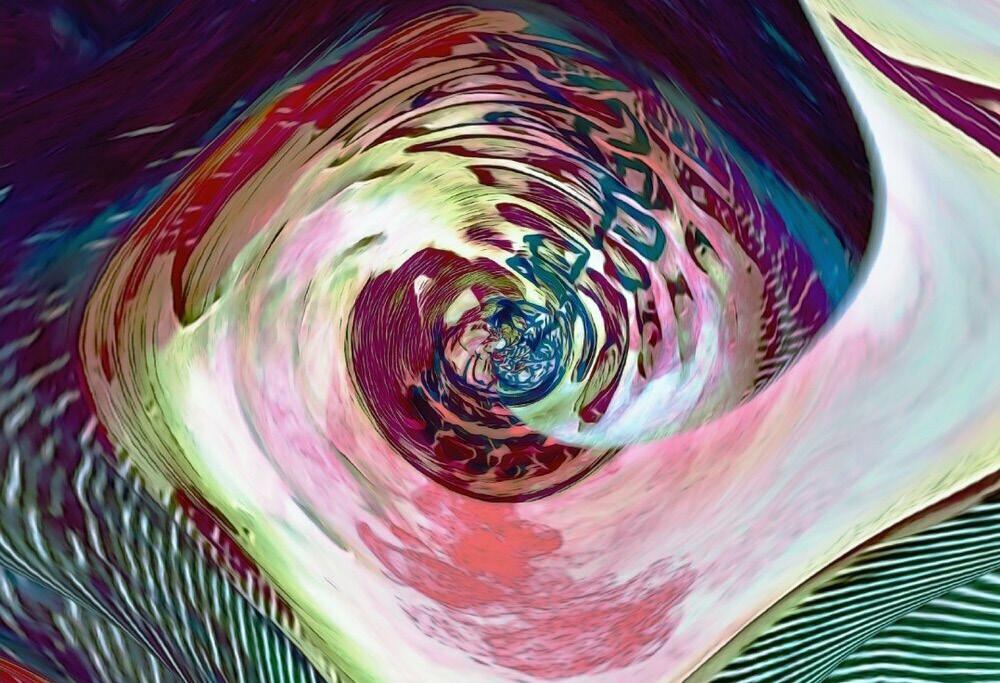
Back and neck pain are common amongst patients with chronic illnesses. The beautiful art on the cover and throughout this issue are the creations of Dr. Lucie Mitchell, who creates unbelievably beautiful images using abstract spine photography.
As I read through the articles featured in this issue I am reminded of one of my favorite books as a child, “Le Petit Prince,” written by Antoine de Sainte-Exupery. This famous parable, (which is more of a cautionary tale for adults than a children’s story) tells the story of a Little Prince who leaves his tiny asteroid planet because of the vain demands of a beautiful but thorny rose with whom he develops a caretaker relationship.
Patients with chronic, unseeable illnesses are much like the beautiful rose who depends on the protection of her thorns and a glass jar to survive.
As a physician I can relate to the Little Prince’s decision to leave the rose, and his yearning to return to her after exploring the universe and realizing that it was a mistake for his soul to have left his beloved rose, despite her “silly games” and neediness.

The reality is that our chronic patients NEED us, and we need them.
All of us involved in healthcare (physicians, patients, and all of the providers who make up care teams) have fallen victims to unfair rules that are being played in the healthcare space. The Corporate Practice of Medicine has made us all become unwitting players in a game that leaves us unfulfilled, and like the Prince, looking for answers.
Joining forces with others outside of medicine to help make visible the rules of the game is one of my callings through Physician Outlook Magazine.
I encourage all reader to share their voyages as we continue to help “Take Back Medicine One Issue at a Time.” ☤
Dr. Marlene Wüst-Smith Publisher & Founder
WWW.PHYSICIANOUTLOOK.COM | 5
PHOTO BY DREAMSTIME

6 | 2022 VOLUME 12
04. 08. 10.
12.
14.
15.
16.
FROM THE PUBLISHER THE THORNY ROSE
By Marlene Wüst-Smith, MD
THE INVISIBLE CONSEQUENCES
By Adam Harrison, MD
INVISIBLE NO MORE
By Terry Wilcox
IT’S ALL IN YOUR HEAD
By Mark Lopatin, MD
SPOONS & F*CKS
By Roxanne Bruce, MBA, DrBA
LIVING INVISIBLY
Could You Get Through The Week With An Invisible Illness?
CENTURY OLD PHARMACY BRINGS BACK “HOUSE CALLS”
By Cristy Gupton
HOW TO MITIGATE HEALTHCARE COSTS FOR EMPLOYEES WITH CHRONIC CONDITIONS
By Liz Antaya
TOP TEN IMMUNE SYSTEM MEASURES
By Dr. Charles Bens, PhD


FIGHT INVISIBLE ILLNESS
By Eden Courville
INVISIBLE SCARS
By James Harris Jr.,
LITIGATION STRESS
By Laura Fortner, MD
THE WOUNDED HEALER
By Nita Chen, MD
DESIGNED TO BE INVISIBLE spooniethreads.com
MEET DR. ALISSA ZINGMAN, MD, MPH
By Danielle Hartnett
SARCOIDOSIS AWARENESS
By Jill Labecki
CHOOSE LOVE
By George “Jeep” Naum, MD
WHEN MEDICINE IS THE FAMILY BUSINESS
By Chris Gure
IS IT AN ILLUSION?
By Roxanne Bruce, PhD, DrBA
20. 22. 25. 26. 29. 30. 32. 34. 38. 40.
2022 | VOL. 10 CONTENTS PHYSICIAN OUTLOOK MAGAZINE BY LUCIE MITCHELL, DO BY LUCIE MITCHELL, DO
17. 18.

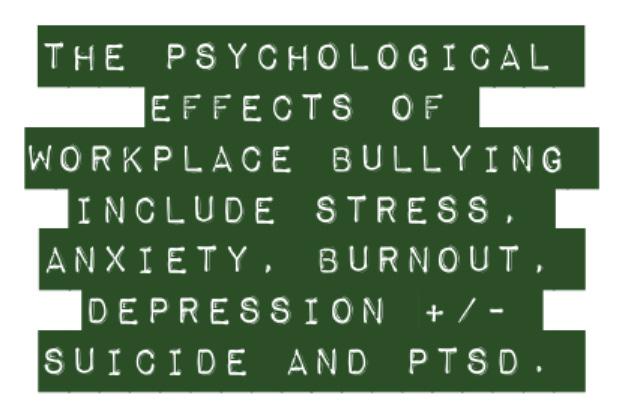
The Invisible Consequences
LIVING WITH THE PHYSICAL EFFECTS OF WORK PLACE BULLYING
Written by Adam Harrison, MD
8 | 2022 VOLUME 12
When I was a teenager I experienced some bullying at my all-boys school. Aside from the usual almost-to-be-expected name-calling, ridiculing and shaming, which upset me, but that, in the main, I was able to brush off, I was also physically assaulted and required stitches to my right pinna.
So, when I left school and, indeed when I left medical school, my notion of what bullying was really only included its physical manifestations and name-calling. Then I joined the world of work and experienced workplace bullying at the hands of my medical seniors, and my field of vision as to what bullying could involve expanded beyond those common two forms.
As you would expect, when I was working as a trainee surgeon, there was no name-calling in the schoolyard sense of the term, but there were comments like: which only served to magnify my already burgeoning feeling of imposter phenomenon.
But there were also the mor*e subtle, less overt forms of work-




place bullying, like gaslighting, ostracisation and passive aggression, sometimes done one-to-one so as not to alert colleagues.
Added to these were the more specific work-related types of bullying, which included (but aren’t limited to) withholding praise, excessively or unjustly criticising you, withholding training opportunities from you, undermining your decisions, over-monitoring your work or setting unrealistic goals, deadlines or work load for you.
Why is this relevant to an article on the invisible consequences of bullying though?
Because all of those types of bullying in the workplace, whether physical or psychological, direct or indirect, overt or covert, can all lead to the same health-related consequences which often go unnoticed by others due to physicians mostly being ‘high-functioning’ patients i.e. they can hide their symptoms or persuade their managers / colleagues that they are fine.
In fact, according to a 2013 survey conducted by the US-based Workplace Bullying Institute (WBI), ‘The Toll of Workplace Bullying on
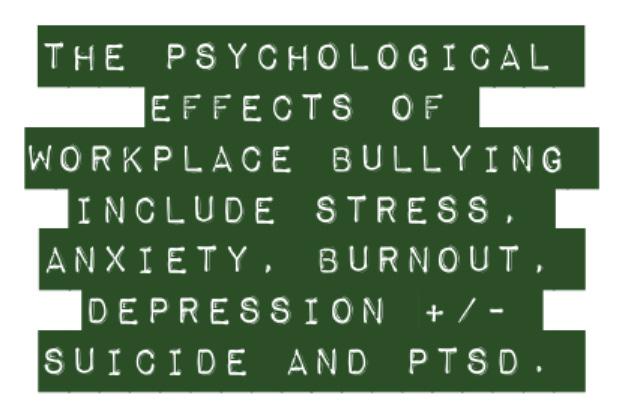
Employee Health’, of the 516 respondents, 63% had been treated by a licensed mental health professional for work-related symptoms and 49% of the respondents reported having been diagnosed with depression as a result of being bullied.
In the same WBI employee health survey, 71% of the 516 respondents reported having been treated by a doctor for work-related physical health symptoms, some of which e.g. high blood pressure /irritable bowel syndrome/ fibromyalgia / headaches etc., can again be hidden by physicians who don’t want their colleagues to know about their illnesses.
For those victims targeted over a long period of time, repeatedly high stress levels can persistently elevate hormones like cortisol, leading to conditions like type-2 diabetes, and chronically high levels of inflammatory proteins can cause long-term inflammatory conditions as well as cancers.
To conclude, regardless of the mode of bullying employed by the perpetrator, the effect on the target’s physical and/or mental health can be the same and often goes unseen. It is also, very sadly, the case, that some of the conditions suffered by the target can be fatal e.g. death by suicide, myocardial infarctions and cancers. ☤
The most common physical health-related conditions:
• High blood pressure
• Heart palpitations
• Ischaemic heart disease
• Type-2 diabetes mellitus
• Irritable bowel syndrome (IBS)
• Fibromyalgia
• Migraine and tension headaches
• Sleep disturbances
• Loss of concentration / memory
• Types of cancer

General types of Work Place Bullying:
• Verbal / physical aggression, hostility, shouting, threats or intimidation e.g. fist-shaking / finger-pointing
• Uncontrolled anger or tantrums
• Public criticism, shaming or berating
• Discriminating against / harassing people
• Gas-lighting
• Ostracizing / excluding /socially isolating people (aka ‘silent treatment’)
• Mobbing
• Gossiping / spreading rumors about people
• Personal attack of a person’s private life and/or personal attributes
• Passive aggression or extreme sarcasm
• Offensive jokes
WWW.PHYSICIANOUTLOOK.COM | 9
Invisible No More
RISING LONG COVID-19 CASES HELP “SPOONIE” CONCERNS BECOME MAINSTREAM
Written by Terry Wilcox
According to a recent study in the New England Journal of Medicine, between 10 and 30 percent of Americans who contracted Covid-19 will experience debilitating long Covid symptoms, such as fatigue, joint pain, shortness of breath, brain fog, sleep problems, headache, dizziness, depression, and loss of smell and taste.
The study’s authors conservatively estimate that 15 million Americans, whose average age is 40, will suffer from these invisible long Covid ailments in the months and years ahead. They conclude: “Long Covid is likely to cast a long

shadow on our health care system and economic recovery.”
With this vast influx of chronic disease patients, “spoon theory” is more relevant than ever. Coined by lupus patient Christine Miserandino in 2003, spoon theory describes the predicament facing patients suffering from rare conditions that are regularly ignored or downplayed by broader society, including the medical community.
Christine uses spoons as a metaphor to describe the toll these painful conditions take on patients, who are regularly told by their family, friends, colleagues, and even doctors,
“You don’t look sick.”
A collection of spoons are used to represent the amount of energy these patients have to perform their daily activities. While healthy people generally have near-limitless energy to complete their daily work, chores, hobbies, and family commitments, patients with rare and chronic diseases only have a finite amount—a limited number of spoons. Each task they perform expends a unit of energy, represented by handing over one of their spoons.
When their spoons run out, these patients cannot do additional activities without threatening the next day’s supply—i.e., without
10 | 2022 VOLUME 12

burning out and flaring up their conditions. In addition to long Covid and lupus, invisible illnesses can include fibromyalgia, migraines, rheumatoid arthritis, back pain, and numerous autoimmune disorders. These patients are referred to as “spoonies.”
Patients with these invisible illnesses often have difficulty receiving appropriate care. “Some of the disregard can be attributed to the fact that long Covid has disproportionately affected women,” write the NEJM authors in a sentiment that can be expanded to cover all spoonie conditions. “Our medical system has a long history of minimizing women’s symptoms and
dismissing or misdiagnosing their conditions as psychological.
Women of color with long Covid, in particular, have been disbelieved and denied tests that their white counterparts have received.”
Consider the typical challenges spoonies face. Bianca from Wyoming was diagnosed with fibromyalgia in 2019 after almost a year and a half of chronic pain, fatigue, and brain fog.
Yet her doctor refused to give her specialist referrals until a psychiatrist confirmed that her symptoms were not psychological. Her doctor also denied her access to a pain clinic because he thought that
she wasn’t in enough pain to attend since she continued to work.
“Because my illnesses are invisible, I am often questioned, denied medical care, and gaslit by providers,” says Bianca. “I appear young and in good shape, so it is difficult for medical providers to take me seriously when I explain how I am feeling.”
Dianne from Connecticut suffers from migraines and has experienced the stigma spoonies often encounter. She explains how people frequently tell her, “You don’t look sick” or “C’mon, it’s just a headache.” They downplay her symptoms by recommending that she take a couple of Advils or even simply drink more water. She has had significant difficulty explaining how her migraines are far more severe than headaches and not all in her head.
Minorities often have an even more difficult time accessing treatment for their invisible illnesses. For instance, Isabel Mavrides-Calderon from New York has faced significant bias from the medical establishment while trying to get treatment for her spinal injury. “I learned that doctors don’t respond as positively to my immigrant mother with a Spanish accent or me, a young Latina girl, but they do respond to my white-passing father, a man.”
It is difficult for healthy people to sympathize with the daily struggle facing those with invisible illnesses. Spoon theory helps explain the pain and burdens they encounter. As the number of spoonies is set to skyrocket with the nascent long Covid epidemic, now is the time for the healthcare community to commit to finally treating them appropriately.
Doing so can arm this growing patient population with more spoons to dramatically improve their daily lives. ☤
WWW.PHYSICIANOUTLOOK.COM | 11
IMAGE BY LUCIE MITCHEL,
DO
IT’S ALL IN YOUR HEAD
THERE’S “RHEUM” FOR IMPROVEMENT
Written by Mark Lopatin, MD

How often have those words been said to patients when a doctor cannot identify the etiology of their complaints? In my world of rheumatology, it typically occurs when a patient complains of widespread pain, and most commonly when they suffer from fibromyalgia.
Fibromyalgia is a poorly understood condition characterized by wide spread pain, fatigue, non-restorative sleep and specific tender points on physical exam. Lab studies and x-rays are negative and there really aren’t any obvious objective findings to identify the etiology of the
pain. Patients with this condition are therefore commonly dismissed.
However pain by definition is not an objective phenomenon. Pain is currently defined by the International Association for the Study of Pain as an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.1 Pain is in part a learned experience and must be viewed through the filter of a patient’s prior biological, psychological, and social experien- ces.
As an example, when a patient had a tummy ache as a child, did their parent coddle them and put
them to bed, or did the parent tell them to toughen up and go to school anyway.
Each of us has a multitude of lifetime experiences related to pain or discomfort. The way in which we experience pain is in part a function of those prior experiences.
In general, pain serves as an alarm system that serves to protect us from further injury. Under normal circumstances, there is some type of tissue damage which results in a pain signal being sent to the brain. Examples would include a laceration or a sprained ankle. The pain warns us to protect the damaged area until
12 | 2022 VOLUME 12
IMAGE BY LUCIE MITCHEL, DO
it heals. When it does heal, the pain resolves.
However, that assumes that our pain system is functioning properly. Consider the analogy of a fire alarm. It makes a loud unpleasant sound in the presence of a fire that warns us to leave the building. Suppose however that there is a short circuit in the alarm system, such that the alarm rings even though there is no fire. We escape the building and call the fire department, but they find no fire.
That is all well and good, but if there is a short circuit in the system, the alarm may ring over and over again, if not continuously. What happens if the fire department tells us that since there was no fire, we must have imagined that the alarm actually rang, without considering the possibility that maybe the alarm is not working properly.
One of our basic human needs is the need to be validated. Being told by a physician that we are imagining symptoms can be harmful. In my entire 31 year career, I only met one patient who I felt was lying to me about being in pain and that was because he made it clear to me that he wanted to avoid work.
Some physicians will discount the problem by saying that it is strictly an emotional issue. Maybe so, but that does not make the symptoms any less valid. There are numerous examples of emotional issues producing physical symptoms. Tension headache and stress ulcer immediately come to mind.
I often use the example of blushing, where an emotional stimulus produces embarrassment, which results in the physical response of dilation of the blood vessels in the face.
It should be noted that many patients with fibromyalgia do have underlying emotional issues with a much higher percentage of having been molested or abused as a child.²,³,4
But pain and fibromyalgia are not strictly subjective entities. Research has shown objective evidence of physiologic changes in patients with fibromyalgia. For example, Substance P is a chemical mediator of
pain. Studies have shown increased levels of Substance P in the spinal fluid of patients with fibromyalga5 as well as other neurochemical changes in the hypothalamic- pituitary- adrenocortical axis and the sympathetic nervous system that modulate our perceptions of pain.6
Another example involves functional MRI’s of the brain. Functional magnetic resonance imaging uses magnetic resonance imaging to measure changes in blood flow that take place in an active part of the brain.7
As an example, if you give a subject a meal, and then do a functional MRI, the parts of the brain that deal with digestion will light up. If you stimulate a patient sexually, the parts of the brain that deal with sexual responses will light up. If you inflict pain on a subject, the parts of the brain that deal with pain processing will light up. Functional MRI studies done in patients with fibromyalgia reveal evidence of augmented pain processing.8 9 The main issue in all of this is the arrogance of some physicians who assume that if they cannot find an objective etiology for a symptom, then the symptom does not exist. There is a big difference between saying “I cannot find the reason for your symptom” as opposed to “I cannot find the reason for your symptom, therefore the symptom does not exist.”
The latter statement is harmful to patients. I had one young fibromyalgia patient who told me that another doctor had patted her on the head and stated to her, “There, there dear. There is nothing really wrong with you. You just need to get yourself pregnant.” This kind of attitude is harmful to patients and should be condemned. As physicians, we cannot always diagnose our patients. We cannot always cure them or relieve their symptoms. No shame in that. However, we can always validate them and it is incumbent upon us to do so. For a number of patients with fibro- myalgia, that may be all they need.
That is the very least we can do and we fail in our role as a physician if we choose not to do so. ☤
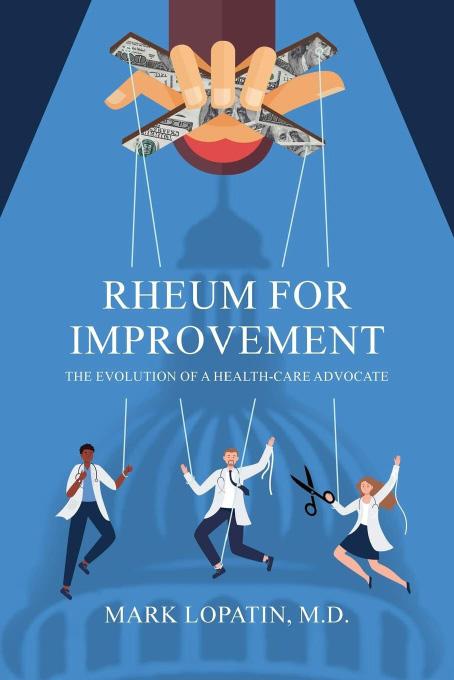
Reviews from Amazon:
“This book gives patients and the medical profession an honest and personal account of a journey in Health Care advocacy. You will not only learn why your healthcare is so expensive and complicated, You will be inspired to do something about it!!
Dr. Marion Mass
“I got a real insight to Dr Mark Lopatin’s views on the health care system then and now, kudos Definitely glad I read this book I am now sharing with others!”
Wendy Stahler
AVAILABLE ON AMAZON
1 - IASP Announces Revised Definition of Pain, July 16, 2020. https://www.iasp-pain.org/publications/iasp-news/iasp-announces-revised-definition-of-pain/
2 - Chandan, JS, et al, “The Association Between Exposure to Childhood Maltreatment and the Subsequent Development of Funtional, Somatic, and Visceral Pain Syndromes.EClinicalMedicine, June 1, 2020. https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(20)30136-X/fulltext
3 - Wexler, M, MS, “Mistreated Children More Apt to Develop Fibromyalgia Later in Life, Study Finds”Fibromyalgia News Today, Aug 4, 2020. https://fibromyalgianewstoday.com/2020/08/04/ study-links-childhood-mistreatment-with-increased-fibromyalgia-risk/
4 - Kaleycheva, N et al, “The role of lifetime stressors in adult fibromyalgia: systematic review and meta-analysis of case-control studies”, Cambridge Universtiy Press, Feb 19, 2021, https:// www.cambridge.org/core/journals/psychological-medicine/ article/role-of-lifetime-stressors-in-adult-fibromyalgia-systematic-review-and-metaanalysis-of-casecontrol-studies/5329C49CDEF274DD931A544514EC4E8A
5 - Russell, IJ, MD et al, “Elevated cerebrospinal fluid levels of substance P in patients with the fibromyalgia syndrome”, Arthritis Rheum Nov 1994. https://pubmed.ncbi.nlm.nih.gov/7526868/
6 - Boomershine CS, MD, “Fibromyalgia”, Medscape, Sep 14, 2021. https://emedicine.medscape.com/article/329838-overview#a2
7 - Magnetic Resonance, Functional (fMRI) – Brain, RadiologyInfo.org For Patients, https://www.radiologyinfo.org/en/info/ fmribrain#:~:text=MRI%20does%20not%20use%20radiation,active%20part%20of%20the%20brain.
8 - Gracely RH, et al. “Functional magnetic resonance imaging evidence of augmented pain processing in fibromyalgia”,Arthritis Rheum. 2002 May. 46(5):1333-43. https://onlinelibrary.wiley.com/ doi/epdf/10.1002/art.10225
9 - Holzman, DC,“fMRICan Help Diagnose Fibromyalgia”, The Rheumatologist, Mar 20, 2017. https://www.the-rheumatologist.org/ article/fmri-can-help-diagnose-fibromyalgia/
WWW.PHYSICIANOUTLOOK.COM | 13
Spoons and F*cks
TOOLS FOR COPING
Written by Roxanne Bruce, MBA, DrBA
Christine Miserandino created the spoon theory to help explain her invisible illness to the world. It has changed the way thousands of people explain their illnesses. You are given an allotment of spoons which stand in for energy. When your spoons run out, you have no more energy to do things throughout the day. If you try to force extra energy, you often end up removing spoons from the next day, leaving you depleted.
A few authors have doubled down on the Spoon Theory by adding F*cks. You see, some days you have enough spoons to do the things that you want to do, but you have no f*cks to give. When that happens things might get done but you don’t care about them.
More often you have f*cks, but no spoons. You end up caring too much, and are

physically unable to do all the things that you care to do. F*cks without spoons can leave you feeling depressed, and worthless, even though you aren’t.
A f*cks but no spoons day is often followed by a day with no f*cks and no spoons. Nothing gets done on these days. You have no energy to do the things, and no f*cks to care about them. Sometimes this results in a surplus of f*cks and spoons later in the week, but not always on the same day.
There are rare, and extraordinary days when you have both spoons and f*cks. These days leave you feeling like a superhero because you can both do the things you want to do and you care about doing them. I want to encourage everyone to try their hand at the exercise on the next page.
ROXANNE’S BOOK “MY BEST DAY JOURNAL” IS AVAILABLE ON AMAZON
IMAGE BY LUCIE MITCHEL, DO 14 | 2022 VOLUME 12
Living Invisibly
COULD YOU GET THROUGH THE WEEK WITH AN INVISIBLE ILLNESS?
Plan out your week based on Spoons and F*cks! You can use the charts below to accomplish your goals. To be more accurate, you will want to plan your week as if you have 1 good day, 2 bad days, and 4 average days. On a good day you can use 14 spoons and 5 f*cks, on an average day you can use 12 spoons and 2 f*cks, on a bad day you get 4 spoons and 0 f*cks. Remember that if an activity that you are doing requires spoons and f*cks, but you don’t have enough spoons and/or f*cks, you can attempt the activity. You can use extra spoons/f*cks for something special, but you must subtract them from the next days’ rations. You can indeed use up your entire weeks’ spoons and f*cks in one day, leaving you with 0 spoons and 0 f*cks for the rest of the week.

My Best Day Journal was featured by the National Multiple Sclerosis Society and readers have this to say about the book.
“Amazingly easy for the user and yet detailed enough for your doctors. Best aid out there for people who are active in their own medical health. Perfect for anyone who has a serious medical condition or multiple illnesses! ~ Amazon Customer
“This book is a gift for anyone trying to sort through multiple symptoms and medications, for people looking for answers or trying to live with chronic or progressing conditions. I wish everyone knew about this tool.” ~ P. Thomas
WWW.PHYSICIANOUTLOOK.COM | 15
IN TIMES OF COVID
Century Old Pharmacy Brings Back “House Calls”
Written by Cristy Gupton, President of Custom Benefits Solutions+ Mitigate Partner serving North and South Carolina

Moose Pharmacy has been serving residents in the Charlotte area for more than 100 years. At the height of the COVID-19 pandemic, they did something for employees no one expected. They brought back the doctor “house calls” that were so common in the 1930’s.
A board certified family medicine doctor answers a telemedicine hotline that pharmacy employees can call 24/7. If that doctor needs additional information, they dispatch a mobile unit to the employee’s home. In 2020, it saved sick employees the stress of leaving home to find care and risk ex-
posure to COVID-19. Two years later, the house calls are still in place, helping Moose Pharmacy employees avoid costly urgent care or ER encounter.
I’ll never forget brainstorming with Joe Moose, who is carrying on the Moose family legacy, which now spans five generations.
To embed this extra layer in their telehealth benefits, we created the toll-free hotline for employees to call in and speak to a family medicine doctor within minutes. If the physician feels diagnostic testing or imaging is needed, they dispatch a mobile unit to that employee’s home. Even
when it turns out to be less serious than expected, it’s worth it. Prescriptions can be called in immediately and the medicines are delivered right to the employee’s door. Helping these 100+ employees feel connected and build resilience, most of the time the prescriptions delivered came directly from the pharmacy location where that employee works.
They are a tight-knit group and beloved in the Charlotte suburbs where they serve residents from 7 pharmacy locations. Working with Joe, I learned Moose’s employees have earned “community hero” status. Why? Because they’ve been taking care of many families for multiple generations!
We looked at different scenarios and options to make sure we got this right. Nothing was too “old-school” or too “out there” for us. As a small business owner, Joe wasn’t just worried about his employees and customers. He felt a huge weight of responsibility – how to keep Moose Pharmacy going amid a global pandemic. It’s the family business started by his great grandfather, A.W. Moose, in 1882.
Joe is the fourth generation of his family to run it. I feel privileged to have a job where I can help make sure he’s not the last. It’s what we do as health benefit managers. We help people.
Ninety percent of the time, it’s a grueling, thankless job in this broken healthcare system. My work with Moose Pharmacy, and others like it in North and South Carolina, remind me that I am doing my part to fix a broken healthcare system, badly in need of repair. ☤
About Mitigate Partners:
Mitigate Partners specialize in cost containment and risk management, with more than 29 benefit consulting firms and brokerages in every region of the nation. To find the the Mitigate Partner nearest you, visit www.mitigatepartners. com
16 | 2022 VOLUME 12
HOW TO MITIGATE
Healthcare Costs for Employees with Chronic Conditions
Written by Liz Antaya
Many employees on corporate health plans rarely use their benefits. Other unfortunate individuals, however, suffer from chronic illnesses like diabetes, heart disease, or Lupus, and tell a different story. The health plan these employees utilize can mean the difference between living life to its fullest, just muddling along, or worse! It can also mean the difference between financial solvency or medical bankruptcy.
For employees managing a chronic illness on a traditional BUCAH (Blues, United, Cigna, Aetna and Humana) health plan, the biggest concern likely becomes the Out-of-Pocket Maximum (OPM) exposure, because they will most likely hit it each year, up to a maximum of $8,700 in 2022. This happens because they have no one in their corner ensuring that they are getting the right quality care, at the right place, at the right time, and lastly, at the right price and because of rising deductibles, co-pays and co-insurance calculated off egregiously inflated bills, this adds up quickly.
An employee managing a chronic illness on a FairCo$t Health Plan
that Mitigate Partners constructs and oversees, however, has a whole different experience. Some of the “bricks” in the house that we build for a high-value, actively managed, employer-built health plan are the following:
Direct Primary Care (DPC) is the foundation of the plan where a member selects a DPC doctor and has 24/7 access to the services provided. There is a true and “direct” doctor/patient relationship that is established that harkens back to Dr. Marcus Welby and the good old days. It is estimated that a DPC provider can handle 70-85% of the medical needs of any patient, including one struggling with an on-going illness that needs monitoring.
Cost and Quality Guidance and Navigation is a crucial component in managing cost and improving health outcomes for patients by making sure that if care is needed outside of the DPC model that they are pointed to providers and specialists of the highest possible quality with the best possible outcomes. Consequently, the misdiagnosis, infection rates, re -
admission rates, complications and, logically, the costs, all come down when the quality of care goes up.
Pharmacy Benefit Managers (PBMs) that are transparent and pass-through will commit to “passing through” all discounts and rebates to the plan sponsor ensuring they get the best possible price on needed medications. The DPC can also ensure on a personal level that the patient stays compliant with any prescribed and necessary medications.
Defined Benefit Pricing Strategies ensure that the employee and the plan are paying a fair and agreed upon price before the service is rendered. Depending on the employer, other “bricks” or risk mitigation strategies might also be included, like Medical Bill Review, Direct Contracting, Active Data Mining, Telehealth, Second Opinions, Centers of Excellence, Onsite Clinics, or carve-outs for Joint Replacements or Transplants. All these strategies can help alleviate the financial burden of managing a chronic illness while providing a higher quality of care and a more personalized care experience.
WWW.PHYSICIANOUTLOOK.COM | 17
☤
IMAGE BY GERD ALTMANN

TOP TEN
Immune System Measures
Written by Dr. Charles Bens, PhD Founder of Healthy at Work
18 | 2022 VOLUME 12
Having a strong immune system is the number one factor in determining if someone will succumb to the coronavirus, cancer, or any chronic illness. Not experiencing frequent colds and flu is one possible measure of this strength, but there is a much better and more scientific way to make this determination. Getting the best blood, urine, and cellular energy tests will provide a much more accurate measure of the strength of any person’s immune system. Here is a list of some of the best measurement tools for this immune system analysis:
1. Omega 3/6 ratio - This blood test measures the ratio of omega 3 to omega 6 fatty acids in the body. Omega 3 is anti-inflammatory, while omega 6 is inflammatory. Too much omega 6 means the body is vulnerable to illnesses such as cancer, flu response and other chronic illnesses.
Good ratio: 2.1 - 3.1.
2. Vitamin D3 - Vitamin D3 controls hundreds more genetic predispositions than any other nutrient or drug. High levels in the blood are proven to dramatically reduce the risk of cancer and viral infections, including the Coronavirus.
Desired levels are 50-90 ng/mL.
3. Vitamin C - Vitamin C is a powerful antioxidant with the proven ability to prevent and effectively treat many cancers, heart disease, and many viruses, including the Coronavirus. Good blood levels are 400 micromol/L.
4. Co-enzyme Q10 - CoQ10 increases energy production in the mitochondria of our cells, and provides antioxidant protection for the nucleus of our cells, which contains our DNA. Energy levels are crucial for organs such as the liver, pancreas, kidneys, lungs and the heart. Diseases such as Parkinson’s, cancer, kidney disease and heart disease have been effectively treated. Good level 0.8-1.5 vng/mL.
5. C-reactive protein - CRP is the measure of inflammation in the

body. Inflammation is caused by the presentence of toxins, too much fat in the body, poor nutrition and injuries. It is a warning sign for the development of heart disease, cancer, brain disease and much more. Good level is less than 1mg/L.
6. 8-OHgD (deoxyguanosine - This urine test measures the accumulated oxidative stress and DNA damage in our cells. DNA damage is caused by toxins, viruses and other pathogens. High 8-OHgD levels are an indication that the body is vulnerable to diseases such as cancer and heart disease. Levels in males: 29.6+/-24.5 ng/mg, and females: 43.9+/- 42.1 ng/mg creatinine.
7. GGT test - The Gamma-Glutamyl Transpeptidase Test is a measure of how well your liver is functioning. The liver is the body’s primary detoxification organ. If it is not functioning properly something is wrong, and should be corrected. Normal levels are 0-30 IU/L.
8. GlycoMark - Sugar is public enemy number one in our body. The best measure of sugar’s presence and behavior in our body is the GlycoMark test. This test measures all aspects of sugar influence including after meal glucose spikes. A safe level is 10-31 ug/mL.
9. Lymphocytes - Lymphocytes represent up to 40% of the white blood cells in our body, and are crucial to the immune system defense mechanism. Levels increase in the presence of infections, including viral infections. Blood cancer and autoimmune diseases also cause levels of lymphocytes to increase. Normal safe levels are 1000-3000/ ml.
10. Homocysteine - This test measures the levels of vitamin B6, B12 and folate in the body. These three nutrients are crucial to the development of hormones and neurotransmitters. Low levels lead to inflammation and the development of many chronic illnesses.
Best range 5.0-7.0 mmol/L.
There are other good tests such as the Glutathione (GSH) test, but it is very expensive. Electrodermal Screening (EDS) is another good test that measures energy output in the mitochondria of our cells. It is also expensive, but could be used if the scores on the above ten tests point to an immune system challenge. This test panel can be an excellent starting point for anyone searching for strategies for becoming healthier. Healthy at Work-Sarasota, FL - March 6, 2020
WWW.PHYSICIANOUTLOOK.COM | 19
☤
Fight Invisible Illness
WITH THE MICROBIOME
Written by Eden Courville
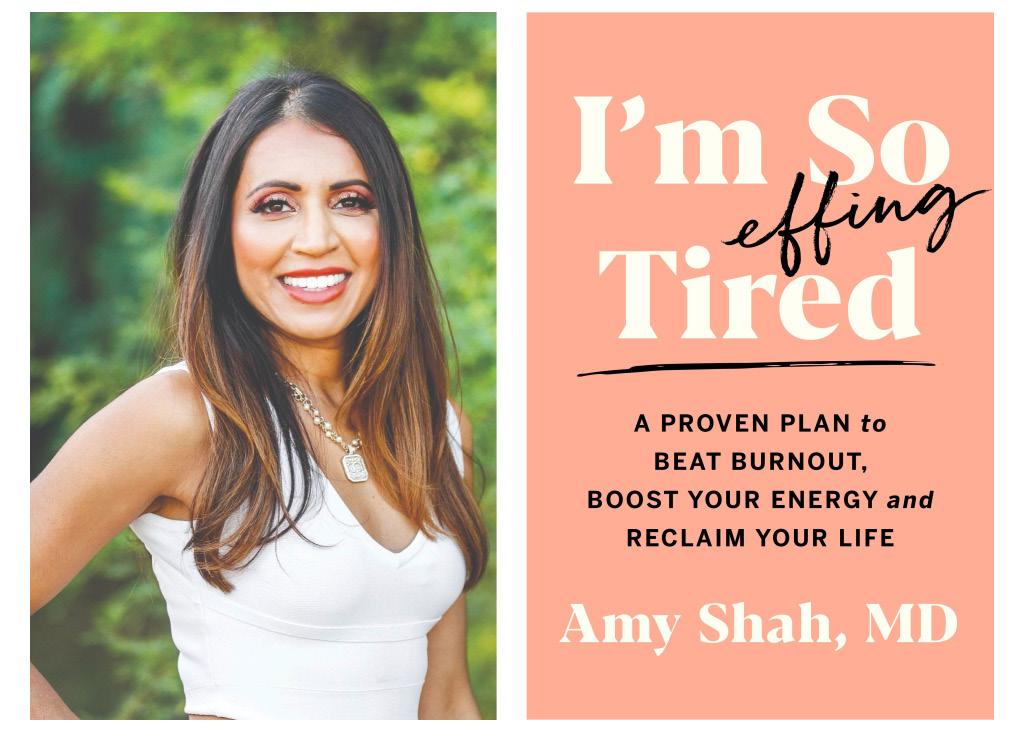
Dr. Amy Shah is a double board-certified MD who specializes in food allergies, hormones, and gut health. She graduated from Cornell University with a degree in Nutrition. She has also received training from Cornell, Harvard, and Columbia University. Her focus on nutritional help has led her to assist others to better their health. Some of these techniques involve healing inflammation, assist
with digestion, and heal food sensitivities. She is also an advocate and expert on intermittent fasting for women. Dr. Shah has been named one of mindbodygreen.com’s Top 100 Women in Wellness to Watch in 2015. She has also been named in Phoenix Top Doctor’s magazine five years in a row starting in 2017. Her book, I’m so Effing Tired, is a guide to health improvement, and was published March 2nd, 2021.
1. What inspired you to write your first book, I’m So Effing Tired?
“My own experience with fatigue, health problems, and burn- out! I was in a place where I didn’t feel good every day -- either I was bloated, fatigued, or had a headache - I had trouble concentrating.”
2. How were you able to manage to balance the hard work it took to be named in the Top Doc list for 5 consecutive
20 | 2022 VOLUME 12
years by Phoenix Magazine, while also being a wife and a mother? Was maintaining the balance between work and family as hard as it looks?
“Yes, it is as hard if not harder than it looks. I have a lot of help. I have clear boundaries, but I struggle just like the rest of us. I wrote my book to give others a little framework in case they were struggling as well.”
3. In your book, you address that creating a better diet routine and trying intermittent fasting helps with increasing energy. Does this also help with other things like weight loss and self-control?
“Yes, it improves your gut health which in turn improves your energy. The type of intermittent fasting I love to talk about is really called time restricted eating in the literature. What I argue is that if you sync to your circadian rhythms, our inner clock, with our actions like sleeping and eating - we will achieve better health. We are not meant to eat late into the night. When we identify better sleep routines, we should also identify better eating habits as well as the quality and timing. Simple acts like getting morning natural light and having an early night have immense effects on burnt out in individuals like physicians.”
4. How does your gut health affect one’s entire mood and energy?
“The gut microbiome is directly connected with your brain. There are multiple pathways where the gut bacteria and your own cells communicate with the brain giving it signals to be more happy or energized. The microbiome also has a large effect on our hormones which, as most women know, regulates so much of their mood, energy, weight, and overall well-being. Focusing on improving gut health is one of the most underused strategies to get more energy an improved mood.”
5. When you are feeling stressed, what is your go-to exercise?
“This would definitely be a nature-based movement. Being in direct natural light and surrounding yourself in nature is a calming restorative activity.”
6. How do you think this would help women from all over? Is each person different when trying to relieve their stress?
“Although it’s individual, nature-based workout is almost always restorative. We have natural Circadian Rhythms and wiring through our eyes and our brain, that cause us to feel calm in the presence of nature. Yoga, Tai Chi, and other meditative exercises are also really great and can give people a restorative stress relieving movement.”
7. Do you plan on writing other books? If so, what do you plan on talking about?
“Yes! I am writing one now. This one is going to be about the wirings of our brain towards food. Such a fascinating subject and an area that has really been tapped in by large food manufacturers yet the general public and even doctors don’t know this information.”
8. Outside of being an author and a doctor, do you have any hobbies?
“I have so many, too many some would say! First and foremost, I am a very active person - usually getting 1-2 workouts in, yoga, outdoor walking, hiking -- you name it. Besides movement and nature, I also love to read, and spend time with my family. If I have a few hours off I will be reading and working out for a few hours. I’m also really obsessed with Nutrition and Healthy Foods, so you’ll probably catch me at a farmers’ market. Of course, time with my family doing any of these things would be my ideal day.”
9. What inspired you to become a medical doctor?
“I went into medicine as a way to strengthen my nutrition knowledge and help others. There are so many inspirational people in my life - like my dad who was such a hard-working immigrant who felt you should work hard for your passions.”
10. How do you hope to inspire others?
“I hope that it is my actions more than my words. Inspiration comes from seeing people live out their ideals.”
11. What is the best piece of advice that you have either given or received for women with burnout issues?
“The best piece of advice I wish I knew earlier:
There is a moment in your life where you stop caring about what other people think of you, or if you’re included or accepted. That’s when you know your self-work is paying off. What matters is your health, doing good work, having peace, and surrounding yourself with positive people.” ☤
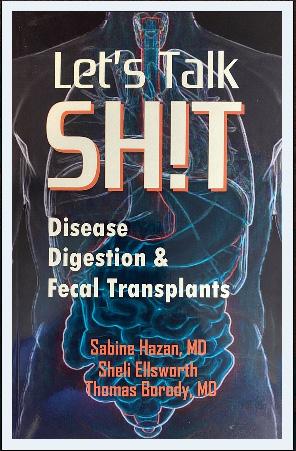
Let’s Talk Sh!t is a humorous, easy to digest explanation of gastrointestinal disorders, their current treatments, as well as next generation hope for heart disease, obesity, autism, Alzheimer’s, and more. From constipation to cancer, research indicates that our unique microbiomes may be the basis for future advances in health and wellness.

WWW.PHYSICIANOUTLOOK.COM | 21
“Desperation is an understatement when it comes to describing people who are hooked on crack.”

Invisible Scars
Written by James Harris Jr., MD, FACS
CRACK
22 | 2022 VOLUME 12
When I dream or have nightmares, I still find myself there. My house was the one about halfway down the street with the big mulberry tree. I am forever trapped within its cracked white walls which were filled with roach eggs and an underbelly beneath the house crawlspace which was shared with all the rats.
The berries from outside were tracked in by those who frequented our home, leaving stains in the 70’s shag carpet that over time looked like they were part of the pattern. In my room, with my door closed, I was never afraid. I had a nail that was driven halfway through the door frame which was then bent in the shape of an “L.”
I could twist the nail from side to side as a way of locking it. I thought I was a genius when I came up with that. It kept out the crazy people that frequented and lived in my home. Most of the crazy people were my family. The only one that was sane in my young eyes was mama.
My room was right next to the bathroom where they would smoke crack. When I was between the ages of seven to thirteen, my father, my uncle, one of my aunts, and multiple “family friends” would use that bathroom as their sanctuary. Crack has a musky, sweet odor, one that could probably be mistaken for incense by the layperson; I was able to identify this smell by the time I was nine.
The back wall of the closet in my room was thin and made up the other side of the bathroom wall. There were once nails that had been hammered through this wall to hold up various pictures over the years. After these pictures came down, along with the nails, the holes remained. From these holes I was able to watch them.
The glass crack pipe was the popular choice of smoking, but some would fall back on other various contraptions, I assume because they lost their pipe while on one of their delusional rampages. Considering the depth of their drug-induced insanity at times, the ingenuity always surprised me. It was like watching that old television show MacGyver: an old
soda can, a toilet paper roll with some tin foil, you name it, give them the resources and they would make it into a crack pipe.
Desperation is an understatement when it comes to describing people who are hooked on crack. Some of their makeshift pipes would get so hot they burned their lips. So strange to watch it happen.
They would react to the pain when the scorching hot pipe touched their lips, but then go straight back to it for another hit. Once they got that rock, it was going to get smoked.
Some acted stranger than others when they smoked crack. Most could try to act normal as an attempt to not let mama know what they were doing. Mama and my aunt Pat were the only ones that didn’t use. My father was by far the worst. At baseline, my father was already paranoid, but when he was using, you knew it.
Over 300 pounds, pacing the floor, drenched in sweat, opening and closing doors, locking and unlocking windows. Even if I was in my room with the door closed, I could tell what was going on by the frantic sounds of his footsteps throughout the house. The weight of each step reverberated through the baseboards enough to wake me from sleep, afraid there was an intruder that broke in or that we were being raided by the police.
On multiple occasions, I would try to keep him from going outside when he was high. I wanted to protect myself from the embarrassment of the neighborhood kids seeing him in his “cracked out” state. One time, when I was around 9 years old, I thought I could use all my strength to keep that 300+ pound man in the house by force, I obviously was mistaken.
I grabbed his arm by the elbow when he reached for the front door. I was met with a quick glance through eyes that didn’t seem to recognize who I was. It wasn’t my dad, but a monster who somehow stole my voice like in one of my nightmares where I was unable to scream. My mouth opened, but the sound remained trapped in my lungs making my chest feel like it was about to explode.
I was thrown on the couch, unable to even exhale. My muscles involuntarily tightened as I curled into a ball, preparing to be hit. My father had never struck me, but everything in the moment seemed as though this man with the empty unrecognizing eyes was not my father.
The crack was like rabies to his mind. I was facing Stephen King’s Cujo in the form of a man. Instead of feeling the impact of a fist, I felt his hands going down to my waist. He started to burr his huge hand into my pockets.
His fingers felt like multiple little mice had entered my pocket and were looking for some other way to escape.
I didn’t initially understand what was happening, but my fear immediately transformed into anger which broke my paralysis. My scream finally escaped as a young boys shrill which could probably not be distinguished from that of a girls. He was not phased by my screams.
He pulled my front pockets inside out. His focus then shifted as his eyes showed a feeling of hope. He picked at a white ball of lint in my pocket and closely inspected it. He held me down with one hand while the other raised the potential crack rock up to the light of the window in his field of view.
As I screamed helplessly on the couch, mama came from behind him, swinging a frying pan, yelling at him to get out. I think she may have struck him at least one time because he quickly retreated out the front door in the way that an injured bear, shot by a hunter, would scurry off into the woods. A couple years passed before seeing him again. ☤

24 | 2022 VOLUME 12
Litigation Stress
THE INVISIBLE ILLNESS
Written by Laura Fortner, MD

Aknock at my door was so unexpected after the holidays. So myself and my 3 little ones in tow answered. It was a sheriff and he was delivering a summons. “You are served.” I was in complete shock.
It was hard to hold back the tears. My kids were confused as to what was happening and all I could muster was to get them in front of the TV so I could slip away and sob. I was being sued for medical malpractice and the emotional distress was real.
First, it was anger. How could this happen? I have sacrificed my whole life in service to others. Missing my kids’ first steps, family events, funerals, weddings, and so many other important events because my patients needed me. All I could think was that this shouldn’t be happening.
Reading the summons made things worse. The legalese and wording was alien to me. The words like “negligence” and others bordered on the line of emotional abuse. I could feel the anger rise up in me. My chest tightening, my heart racing and my stomach in knots.
Fear enveloped me. What would this mean for my career? Would my insurance rates go so high I couldn’t practice anymore? Would my income go down? What about my reputation? What would my colleagues think?
Then the shame. That painful feeling of humiliation. I must not be good enough. If I got sued then this must mean I may not be as good as I thought I was, while ignoring all the other countless patients that have written me thank you notes for how I helped them.
This is litigation stress.
The invisible illness.
This is widespread in our medical profession. 95% of us get litigation stress, but no one is talking about it. We are told by our lawyers we can’t, and this is the death of us. The feelings of anger, fear, negative self image, shame, self doubt, isolation, and helplessness are real. We mix up who we are with what we do and this is a deep moral injury to us. It shakes us to our core. And this can literally go on for years.
The stats are that 75% of us will be sued if we are in a low risk specialty and that 99% of us will be in a high risk specialty if we practice until age 65.
One would think then this is normal. We should expect to get sued in our profession. And our lawyers and others say It’s just about money and don’t take it personally. Even though these statements seem logical, it does not change the emotional reaction of what we experience. Many of us never get over it. Many of us walk around still in pain from it years later.
When I got sued I went through all the emotional reactions and it took me several years to get help. I was resistant at first. I went to therapy and I also did EMDR. These worked temporarily.
What helped me the most was hiring a life coach and learning tools on how to manage my thoughts about the lawsuit. This was work that helped me find peace of mind now no matter the outcome of the case. It helped me manage pain and suffering. It helped me find JOY again which had been zapped out of me and it helped me love medicine again. ☤
WWW.PHYSICIANOUTLOOK.COM | 25
Written by Nita Chen, MD
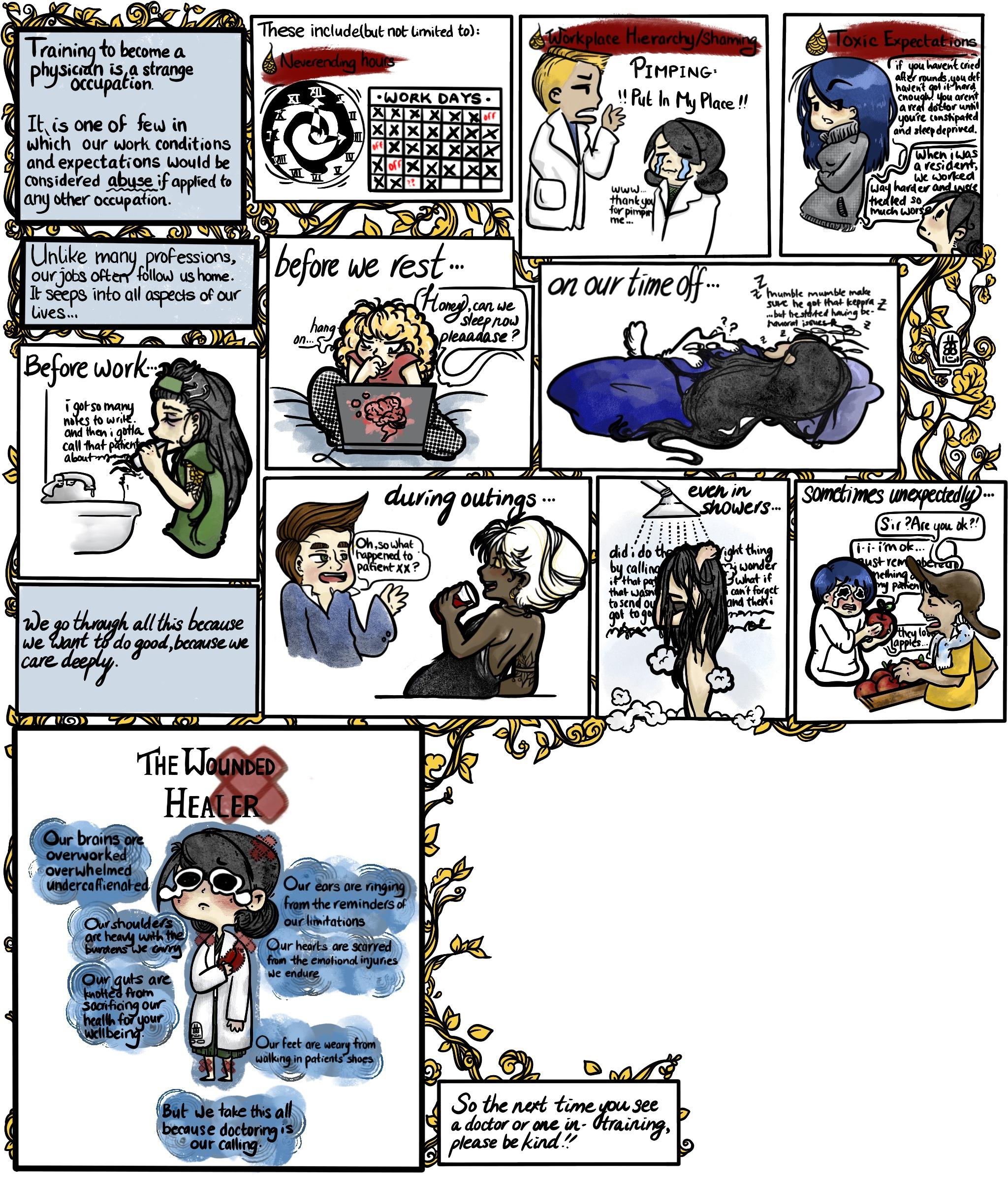

PandasAnatomyShop Medical art with a floral spin Gainesville, Florida
Wounded
The
Healer
CREATED BY NITA CHEN, MD 26 | 2022 VOLUME 12
THE STRANGE LIFE OF PHYSICIANS-IN-TRAINING
Reserve your seat for July 2023
WWW.PHYSICIANOUTLOOK.COM | 27
Fire Department Coffee

I was a Damage Controlman in the Navy which is the rate that trains the ship in firefighting and works to maintain the firefighting equipment. I was always fascinated by medicine. When I got out of the Navy, Rockford Fire hired me and trained me as a paramedic. I memorized my SMO’s, Standing Medical Orders, front and back so that I could make quick and confident decisions in the field.
I always thought if someone was calling us to help them in a medical emergency, I wanted to do everything possible to help. The medical field can sometimes require you to think fast with little time to decide. It’s an opportunity to help someone in what can be the scariest time in their life, from the first responders to the ongoing care. I’m thankful for all those who answer the call to take care of someone and do their best to give the person the best chance for a positive outcome that could


16 | 2022 VOLUME 10
RAISE A MUG FOR OUR FELLOW FIREFIGHTERS
Fire Dept. Co ee gives back to help sick and injured firefighters.
Each small batch of Fire Department Co ee is freshly roasted in the
U.S.A.
FIREDEPTCOFFEE.COM
Enjoy our range of roasts, from our family to yours.
RAISE A MUG FOR OUR FELLOW FIREFIGHTERS
Fire Dept. Co ee gives back to help sick and injured firefighters.
Each small batch of Fire Department Co ee is freshly roasted in the U.S.A.
FIREDEPTCOFFEE.COM HIGH-QUALITY, HANDCRAFTED COFFEE, RUN BY FIREFIGHTERS. 28 | 2022 VOLUME 12
Enjoy our range of roasts, from our family to yours.
Designed to Be Invisible
Aconversation with a distraught parent led to Spoonie Threads’ first product: a 3-layer g-tube pad. The mother’s fears of her child pulling out a newly placed gastrostomy tube button also inspired the second product, an adaptive baby bodysuit to keep curious little fingers away, while providing access to parents. After seeing the lack of adequate adaptive clothing, Dr. Julie Sanchez co-founded Spoonie Threads in 2015

for children and adults with disabilities or chronic illnesses. Dr. Sanchez has been practicing for over two decades as a Pediatric Surgeon. She treats infants, children, and adolescents with various issues, including liver disease, intestinal blockages, congenital abnormalities, and more.
Spoonie Threads products are designed with her medical insights to keep customers feeling stylish, comfortable, and clean throughout the day. The name “Spoonie Threads” references Christine Miserandino’s “Spoon Theory”. Spoon Theory imagines that every person has a limited number of spoons, or units of energy, and every task - getting dressed, eating a meal - costs one spoon. A chronically ill person might run out of spoons before lunchtime, while a healthy person may still have spoons leftover at the end of the day. Spoonie Threads products have many uses: ostomy care, diabetes care, post - surgical recovery, breastfeeding, tube and port care, and more.

Spoonie Threads sells pajamas, bodysuits, and adaptive shirts designed to allow easy access to ports and other medical devices — without the indignity of having to remove clothing. Ostomy covers keep bag leaks from staining clothing and come in a range of colors, playful prints, and funny sayings. Soft - stretch belts hold insulin pumps, and waistbands provide gentle support for ostomies, feeding tubes, abdominal surgeries, and more. Soft sleeves support diabetes devices, and PICC lines. Spoonie Threads strives to create happiness, spread optimism and simplify life for those with chronic illnesses or disabilities. ☤
For more information, visit spooniethreads.com

WWW.PHYSICIANOUTLOOK.COM | 29
Meet Dr. Alissa Zingman, MD, MPH
FOUNDER AND CEO OF P.R.I.S.M.
Written by Danielle Hartnett
Dr. Alissa Zingman, MD, MPH has created an innovative practice, P.R.I.S.M., that is a model for care for ALL types of invisible illnesses.
P.R.I.S.M. has become a “must visit” destination for many patients with connective tissue disorders, particularly Ehlers-Danlos Syndrome, because of the excellent comprehensive care provided.
Physician Outlook Magazine was one of the firs national publications to take notice of Dr. Zingman and her practice when she was featured as the “Chronically ch(Ill)” rockstar that she is. Since then, she has received well-deserved national attention by People Magazine, The Guardian, The Washington Post, and many others. She continues to make strides to reshape the face of medicine as we know it., particularly for patients with chronic, rare “invisible” illnesses.
“I knew it was coming [COVID-19] and I was able to sort of plan for a little bit “ Zingman admits, as she breaks down the precautions that her background in Public Health prepared her for. Like all things Alissa seems to do, it was comprehensive and well thought out.
The amount of information that she was able to convey in 40 minutes, information sitting on the top of her head, organized in thoroughly descriptive chunks that she lists in a verbal outline of care and connections to caring. Information that has been compiled by her, and her colleagues, gleaned from specialists, coordinated with physicians and physician adjacent practices, all available to her patients and colleagues through her
practice, P.R.I.S.M., a true labor of devotion, and need.
Need
That is what lead to the part of our interview that was most enlightening to Alissa’s character. I asked her to tell me something that she wants to get out there to other physicians: to set the tone for what she is dealing with and how they can have a better understanding of themselves in this system.
“My advice to other physicians is, to do what you feel called to do. Don’t allow external forces to make you pick a mold to fit yourself into. If you have something that you are passionate about, find a way that you can fill a need doing that. If you are competing for patients, that means that you haven’t found your niche. There are
If you are competing for patients, that means that you haven’t found your niche.
so many unmet needs for patients. None of us should be competing for patients. Find a void that you will derive satisfaction from filling, and do that.” Dr. Zingman responded.
The idea is that physicians should stop competing for patients, and stop the competition for care. It will force the field of medicine to reevaluate itself, which will force the insurance and pharmaceutical companies, forcing them to re-structure themselves from the current 20-minute drive-thru set up.
Alissa clarified that physicians don’t have to find something uncommon to specialize in.
Finding an unaddressed part of a common illness and addressing that in a novel way is just as important. “Look at the community that we live in. What are the unmet needs of that community? What of those needs “lights your fire,”and go do that.” Zingman states.
“My waitlist is over 4 years long. I have never advertised what I do. I have never taken out an ad. It’s all word of mouth. It’s all based on need.”
Currently, physicians and patients are not in control of healthcare. Practices exist as Rheumatology, Neurology, Internal Medicine, etc. There are no Multiple Sclerosis Practices with a Psychiatrist, Neurology, and Primary care specializing in Multiple Sclerosis. But, Why not? Wouldn’t that make so much more sense?
P.R.I.S.M. is an EDS and Connective Tissue disorder practice that has structured itself around multiple specialists and doctors to treat a primary disorder. It allows the practice to specialize to the patients’ needs. P.R.I.S.M. is unique because it looked at this disease and the needs of its patients, and created the practice base on the results of the needs assessment. The main purpose of Dr. Zingman’s practice is to look at the needs and fill that gap between what is needed and what is available.
There are not enough places that are coordinating care, creating plans with patients, and creating a framework for how those patients can gain access to that care. That is what Alis-
30 | 2022 VOLUME 12

sa’s practice is doing. The change is based on the need. A business model that caters to the needs of a particular illness and which is obviously thriving while helping patients.
“I never intended my practice to be over 90% EDS patients.” Dr. Zingman clarifies.
“I enjoy taking care of dancers and athletes. I would do that again. I don’t plan to spend my entire carrier focusing on EDS, I never intended to do that. That is just how my schedule filled. The need was there. I also take care of patients with rheumatologic issues, those who have other complex conditions, including those who have had multiple surgeries, as well as those recovering from motor vehicle accidents.”
It was with that admonition that Alissa revealed the most telling statement of our interview: “I want to personally be completely irrelevant in 10 years.”
“What I have created is a training facility. I have trained a large number of individuals. Nobody needs ME. The number of people flying from California, England, Europe, to see me...that is outrageous. First of all, it excludes a tremendous number of people from getting care. Second of all, even if you have resources, that shouldn’t be necessary.
“My hope is that in 10 years I will have created enough educational materials, raised awareness, that I can sit in my pool and relax. “
Dr. Zingman is still trying to figure out what steps are needed to make sure that the type of coordinated, comprehensive care that P.R.I.S.M. provides to those who suffer from hypermobility and other “zebra” conditions becomes broadly available to ALL of the patients that need it.
“I like being a teacher and a doctor. The idea of having more locations and staff doesn’t appeal to me. I am not going to do that.”
Ideally she would like to develop a training institute that offers continuing medical education and hands-on training to a variety of different medical professionals or for P.R.I.S.M. to become a consultant group for other practices.
All of her hard work, all of her addressing needs and her vision and passion have finally found a culmination: The Ehlers-Danlos Syndrome Research Foundation. EDSRF is a 501c3 foundation that is funded by friends and patients sympathetic to the lack of research on the disease.
The foundation has several studies underway. One of the re -
“I want to personally be completely irrelevant in 10 years.”
search studies has already been submitted for publication. “I think that the reality is, that you don’t even know all the problems in EDS, or the most common presenting symptoms. We don’t know how much better they can get. From what I have been told by others who work with EDS patients, patients get a lot better at P.R.I.S.M. than they do at any other facility.”
Dr. Zingman wants to be able to provide data to her patients and colleagues, and the foundation helps to fund the necessary research studies that need to be conducted to document the progress being made at P.R.I.S.M. The EDSRF helps to ensure that scientific principles are being followed through well-designed research studies, and demonstrates to insurance companies and colleagues that the business model, practice and approach are working in quantifiable ways.
“I am very grateful for my MPH from Hopkins,” Zingman often mentions the invaluable help that her Public Health background has allowed. “Public Health gave me tools I wouldn’t have known I needed. I really think that if more physicians were given the opportunity for a true Public Health Educations background, we wouldn’t have a lot of the problems we are having in our communities, and physicians would have more control over what is going on in medicine. That would be a lot better for the community.“
“I didn’t want any of this. I wanted to work 3 days per week and live a low-key life.” She knows better than anyone what it is like to live with a chronic illness, and is building a practice that can fluorish without her physical presence.
She won’t stop until her goals are reached. She is one of the few people in this world actively trying to make herself expendable, and she seems happy to do so. ☤
WWW.PHYSICIANOUTLOOK.COM | 31
Sarcoidosis Awareness
NO TWO CASES ALIKE
Written by Jill Labecki
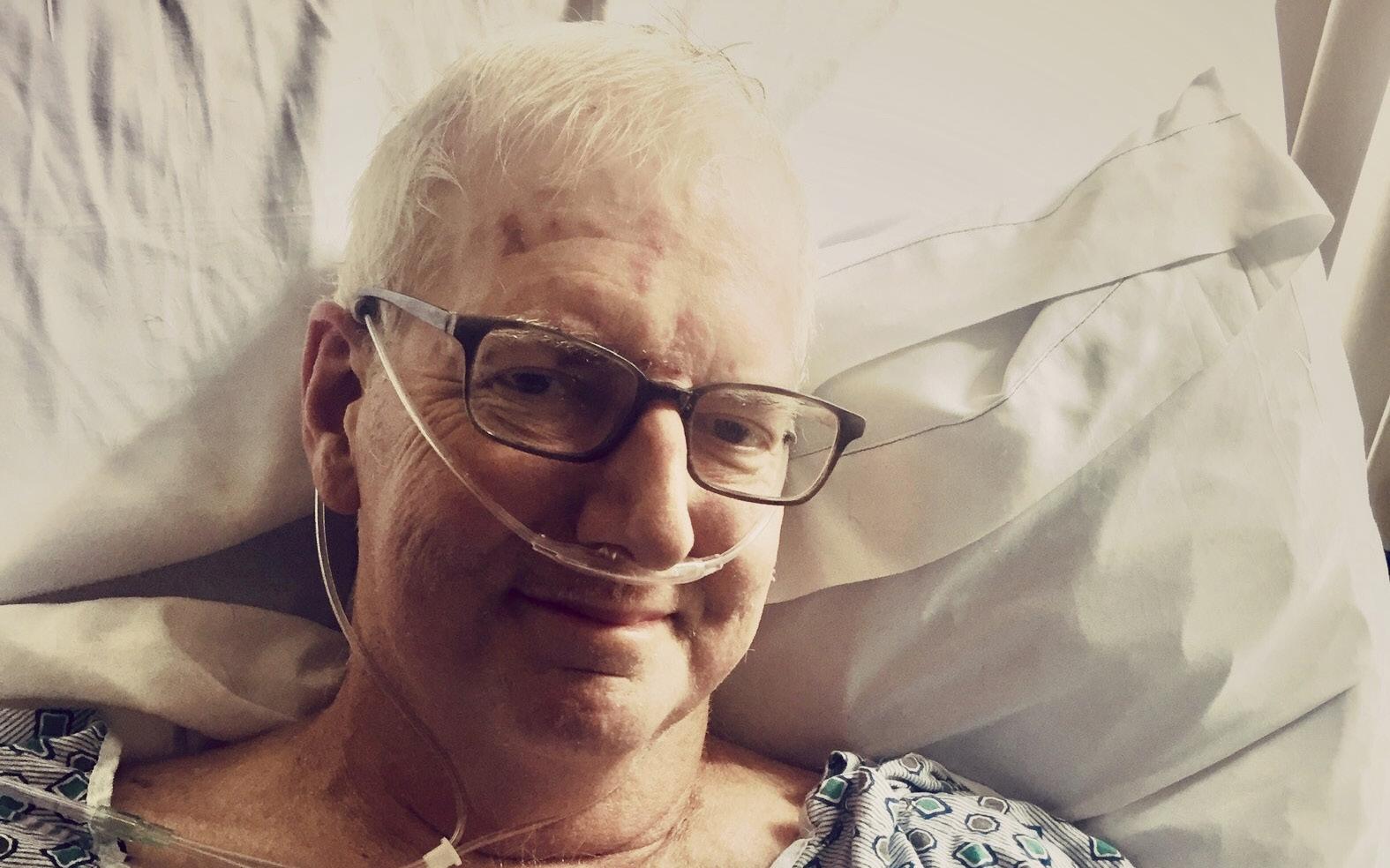
Don’t let a lack of resources and knowledge affect your patients and their families.
Sarcoidosis is often referred to as the “Snowflake Disease” because patients present with many different symptoms; no two cases are alike. Some symptoms of sarcoidosis often mimic those of other diseases.
This makes diagnosis of this rare disease very challenging. It can affect multiple organs in the body, causing inflammation and growth of granulomas. Like most autoimmune
diseases, the exact cause and what triggers this abnormal response in unknown. Although it is controllable with corticosteroids and immunosuppressants (which can slow the growth of the granulomas), the sad truth is that the disease has only palliative treatments.
Sarcoidosis is incurable.
In 2009 my dad was diagnosed with Sarcoidosis. His symptoms started after recovering from open heart surgery. The shortness of
breath, fatigue, and mild chronic coughing was presumed to be part of recovering from this major surgery. This went on for many months before eventually, a chest Xray showed densities in his lungs.
My parents lived in a very rural town in northern Pennsylvania. My Dad’s PCP ordered loads of tests. The doctor ordered every bloodwork panel he could, to try to figure out what was going on. Dad had multiple CT’s and PET Scans that did not give a clear answer either way.
32 | 2022 VOLUME 12
Was it pneumonia? Was it pulmonary nodules? Was it cancer?
At the time of my dad’s surgery, I had been working in healthcare as a CT technologist for 15 years. Even though I understood the process of putting the pieces of all the results together to (hopefully) come to a diagnosis, it was still frustrating for me to wait for results. I saw the frustration in my dad too. He felt sick and feared what could be wrong.
Dad started getting fluid in his lungs and had to be transferred to a hospital near Pittsburgh. After a thoracentesis, the pulmonologist decided to do a bronchoscopy and biopsy the densities. This biopsy showed it was thankfully NOT CANCER! BUT it did show granulomas. My dad was officially diagnosed with Sarcoidosis.
Dad was sent back home and told to follow up with his PCP. Since Sarcoidosis is rare and challenging, he was referred to a specialist at Cleveland Clinic. He was started on Methotrexate and Prednisone to stop the inflammation. The thing with Sarcoidosis is that it is completely possible to live a normal life with little to no symptoms if it isn’t “active”. If Sarcoidosis becomes “active” the granulomas form faster and can spread to other organs in the body.
In 2014, my dad became sick with a nasty cold that turned into pneumonia. The Sarcoidosis became active. An increase in granulomas caused atelectasis in his lungs. From that day forward, he would need to be on oxygen. The disease now seemed to progress faster, presenting new and complicated symptoms.
Weekly bloodwork showed low RBC, so dad was referred to an oncologist that treated him for MDS (“pre-leukemia”). A bone marrow biopsy revealed the sarcoidosis was now in his bones and bone marrow. He developed debilitating back pains from the granulomas in his bones. It was so hard to see this strong, active man now confined to his chair, on oxygen and constantly in pain.
Dad’s daily life became more difficult. He could only walk, hunched over, with a walker or cane. The tubing from the constant oxygen he required followed him everywhere he went. It was his “lifeline”. The most that he got out of his chair was to go to appointments and his occasional trips to see family. Every day at work I witness the frustration of my patients who physically can’t do the things they want or need to do, they feel useless. I was now seeing those same feelings in my dad.
The last 3 months of his life were spent in a Pittsburgh hospital. The medical team had determined that he had a blood infection. Someone with a healthy immune system could have easily fought off the infection, but with this disease it was causing Dad to spike fevers. He was possibly becoming septic. They treated him with very powerful antibiotics. We were hopeful they would get rid of the infection, and we could possibly get him on the lung transplant list.
The first time they put him on Bipap, the resident said Dad told her to “just keep him going”. Dad fought so hard for so long, I could tell his body was growing weary. He eventually went into respiratory failure, and the medical team wanted to intubate. We knew he wouldn’t want to live like that.
Comfort Measures Only.
We were all able to say our goodbyes on March 12, 2017 and the next day he passed away in the ambulance on his way back home. From what our family experienced, there is an extreme lack of knowledge and resources when it comes to sarcoidosis and how to properly treat it. This was especially true in the rural area where they lived. With every symptom he developed the medical team would say “must be from the sarcoidosis” since they couldn’t figure it out.
I want to encourage medical professionals to investigate the multiple research sites that offer up to date information on this rare and completed disease. (Foundation for Sarcoidosis Research and Bernie Mac Foundation). ☤
WWW.PHYSICIANOUTLOOK.COM | 33
Choose Love
WHEN YOUR SOULMATE IS SUFFERING
Written by George “Jeep” Naum, MD
My wife Vanessa and I celebrated our 31st year together this year, and she lives with a chronic illness. Living with a spouse who has a chronic illness is very challenging. You may think that it’s easy for me because I’m a doctor, but at times, it can be a long and difficult journey. I certainly have a better understanding of what it is like to live with someone with a chronic illness, but I went a step further.
I made a decision to love her. You see, feelings are flighty. A decision to love is a commitment to love and be loved unconditionally. Feelings come and go, but love requires an active choice. A decision that allows for the possibility of pain but also includes the certainty of hope.

Let’s explore how a decision to love can provide the container, safe space, if you will, for those of us living with someone who has a chronic illness.
Vanessa contracted Rheumatic Fever at the age of 11, and about six months later, Fibromyalgia-like symptoms started. Unfortunately, it would take another fifteen years while we were dating to be correctly diagnosed. I was in the midst of a rheumatology rotation, and my preceptor diagnosed a patient we were seeing. Unfortunately, the patient’s symptoms sounded all too familiar. It’s as if I was listening to Vanessa. She managed her symptoms well with Advil. However, it was not until pregnancy and postpartum that her symptoms exacerbated.
These are some of the questions she and patients like her would ask:
Do you know what it feels like going through most of your life not knowing why you feel the way you do?
Do you know what it feels like to go from doctor to doctor and hear them say ‘what you’re feeling is all in your head,’ ‘not real,’ or ‘I’m sorry, I can’t help you? Yet, much worse, blame it on depression, a midlife crisis, an early change of life
Do you know what it feels like to have family and friends sigh and roll their eyes because your symptoms are frustrating them? They don’t seem to understand why you feel the way you do and may think you are attention-seeking and ruining their plans on purpose?
Do you know what it feels like to have your self-esteem decimated, your
34 | 2022 VOLUME 12

self-confidence beaten and battered, intrusive thoughts that tell you you’re useless, the problem is yours, and you’re responsible for it?
Previously called fibrositis and often confused with many other similar diagnoses, Fibromyalgia has been around for decades. It is a diagnosis that includes a constellation of symptoms, including, but not limited to, severe pain that waxes and wanes and transiently spreads to various areas of the body. In addition, the pain can be incapacitating. Notable associated symptoms include severe and often incapacitating fatigue as well as cognitive dysfunction that Vanessa and I “affectionately“ refer to as “Fibro Fog.“
Some form of trauma initiates the ideology of fibromyalgia. In Vanessa’s case, the trauma was an
infection. The traumatic event sets up a widespread pain phenomenon much too overwhelming and too difficult for the brain to respond to. This response to these stimuli is called the “wind up phenomenon.”
Wind up is a frequency-dependent increase in the excitability of spinal cord neurons evoked by electrical stimulation of afferent C-fibres. The brain “gives up“ and sends a response to areas of the body that weren’t directly affected by the initial injury. Patients experience widespread and diffuse bodily pain. Distraction caused by pain often leads to fatigue, cognitive dysfunction, depression, and more.
A key point is the acceptance by all involved as well as the spouse, family, etc. that it is indeed a real diagnosis. It is critical for the patient who is suffering to know they are
accepted for who they are. Without support from a spouse or significant other, long-term improvement may be significantly and adversely affected.
Another key is acceptance by the patient themselves of their own illness. Vanessa still suffers from feeling like a victim at times and understandably so; however, she has long ago accepted her illness and the limitations that it causes her especially when the weather changes.
In combination with a defiant will to persevere and succeed, Vanessa has achieved much in her life including an MBA, but most important to me is the fact she has been an incredible life partner. Were there times that I was frustrated by working a very hard day and coming home to my wife, who was having an unproductive day? I would be lying if I didn’t say the answer was yes. However, I made the decision to love and understand her for the good of Vanessa and our family.
You see, Vanessa did not choose to be afflicted with this illness. I knew full well that the self-flagellation and mental and emotional pain she would put herself through was already too much, and whatever I would say would be an unnecessary dagger to the heart.
As colleagues, I urge you to offer love, support, and empathize to chronically ill spouses and family members. It takes a decision to love, persistence, compassion, and lots of love. Vanessa is in a much better place and manages her illness very well. Our marriage not only survives, but thrives, and is better because of my decision to love her no matter what. ☤
WWW.PHYSICIANOUTLOOK.COM | 35
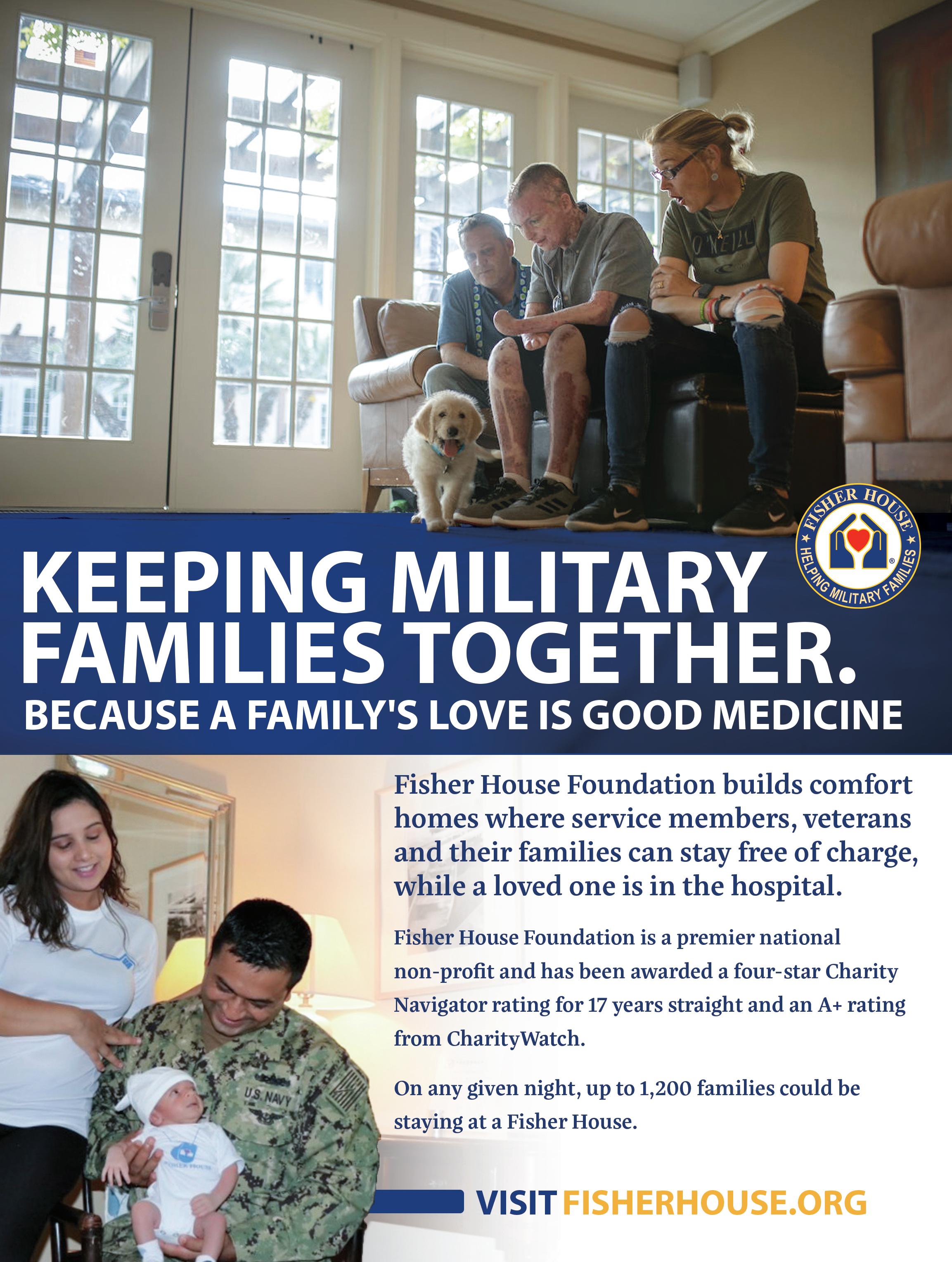

WWW.PHYSICIANOUTLOOK.COM | 37
When Medicine is the Family Business
PROPER TAX PLANNING REDUCED A PHYSICIAN FAMILY’S TAX BILL BY ALMOST 50%
Written by Chris Gure

As financial advisors, one of our main goals is to help ALL clients, especially physicians, make sure they are saving enough for retirement. For physicians who are employed (the vast majority of them) we help to make sure that they are contributing the maximum allowable amount to an Employer-Sponsored Retirement Account, typically a 401(k).
I n 2022, most physicians are currently full-time employees of large hospital systems, but there are a growing number of doctors and other “medical families” who are getting tired of “working for the man.” They are venturing back into traditional private or group practices, starting their own Direct Primary or Specialty Care practices, and some are becoming entrepreneurs and pursuing “side-hustles. When physicians own their own business -
es, saving for retirement can becomes a little more complicated, but our role as advisors is to help break things down so they are simpler, compliant with tax code and which allows families to achieve true financial health.
ALL IN THE FAMILY
W e have had the opportunity to work with physician clients who employ their family members within their practice and for marketing purposes, billing and for other practice-related job duties. Not only have they all been able to pitch in to make the practice successful, but with our help they were able to take advantage of some pretty significant advantageous tax benefits.
When the second-round of stimulus checks were being distributed in 2022 there were some medical residents and fellows (but few At -
tending Physicians) who were eligible to receive them.
Using a family of four as an example of a household who was eligible to receive a stimulus check of $5,600 for those with an Annual Gross Income (AGI) of under $150,000 (after maxing out 401ks, HSAs, etc) we use the example of the fictional Jones family. Dr. Jones is a Family Practitioner, and her husband is the office manager.
Family Medicine LLC distributes $225,000 to the Jones Family annually. Mr. Jones handles the operations of the business. Dr. Jones provides all medical care, and their two children provide marketing support.
**This scenario is based on a real example where a physician client’s children are paid models and their photos are used in the marketing materials of the clinic.**
A Financial Planner from For -
38 | 2022 VOLUME 12
tress Physicians manages the Family Medicine LLC 401(k) Plan for the business and the four participants referenced above. Since they are all eligible based on the plan’s governing documents and are all receiving reasonable compensation for their duties, they all were able to contribute to the 401K plan. Setting up financial plans can take significant attention to detail and research to ensure compliance with state and federal tax regulations (not to imply that it is brain surgery!). As with ANY tax strategy, we urge clients to consult with their tax preparers/ accountants as well as their attorneys to ensure that all the “T’s” are crossed and “I’s” are dotted.
E ach of the four members of the Jones family was able to contribute their individual allowable $19,500 maximum 2021 employee contribution, which totaled $78,000. They also jointly contributed the allowable maximum of $7,000 into a family Health Savings Account. Here is where the benefits of holistic financial planning really started to compound.
As you will recall from this scenario, Family Medicine LLC has been distributing $225,000 to the family in the form of income. This is noticeably over the $150,000 AGI limit that made a family eligible for the second round of stimulus checks.
With the planning that Fortress assisted them with, they were able to “max out” their contributions into their 401(k)s and HSA accounts, which resulted in an $85,000 decrease their income from $225,000 to $140,000. This, in turn, made them eligible to receive that stimulus check…that was an additional $5,600 in the family’s pockets thanks to effective planning.
The Jones family recently added a new member to their family when they adopted a one year old. This baby is ALSO following in his older siblings’ footsteps and is modeling, and has proven to be quite effective in marketing the practice to families with younger infants and toddlers. Family Medicine LLC is planning on using the $5600 stimu -
lus check and an additional $400 to pay the baby a $6000 annual salary ,,
By paying this new member of the family an annual $6000 bonus for marketing expenses for the next 18 years and investing the money into their Roth IRA (which is also allowed) they will be contributing $108,000 over that child’s lifetime. Assuming an 8% annualized rate of return, this baby would have over $5,000,000 in this tax-free retirement account by the time they retire (age 60) from these contributions alone! ☤
TO SUMMARIZE:
Before Planning:
Taxable Household Income:

Total Income taxes (Estimated Based on NC)
After Planning:
Taxable Household Income:
Retirement Plan Contributions:
HSA Contributions:
Total Income Taxes (Estimated Based on NC)
$225,000 Roughly $60,000
$140.000 $78,000 $7,000 Roughly $30,000
This is just an example and values are estimated to help express the point that proper tax planning is a crucial part of any financial plan. As with any tax strategy, we urge you to contact your tax preparer/accountant as well as your attorney for any legal advice.
WHAT'S ON YOUR MIND?
We’ll be sharing tidbits of wisdom like this with Physician Outlook subscriber every two weeks, along with deeper dives for our private clients every month or so.
Please send us your questions and topics of interest and reach out to us via email, and follow us on SubStack.
WWW.PHYSICIANOUTLOOK.COM | 39
PHYSICIANS BY THE NUMBERS: 42 Physician Households as Clients $680,000 Average Household Income Average Age 44 $3.25 Million Net Worth 29% Average Savings Rate Securities and Investment Advisory Services offered through Fortress Private Ledger, LLC. Member FINRA/SIPC
FORTRESS
Is it an illusion?
VISUAL AIDS IN MEDICINE
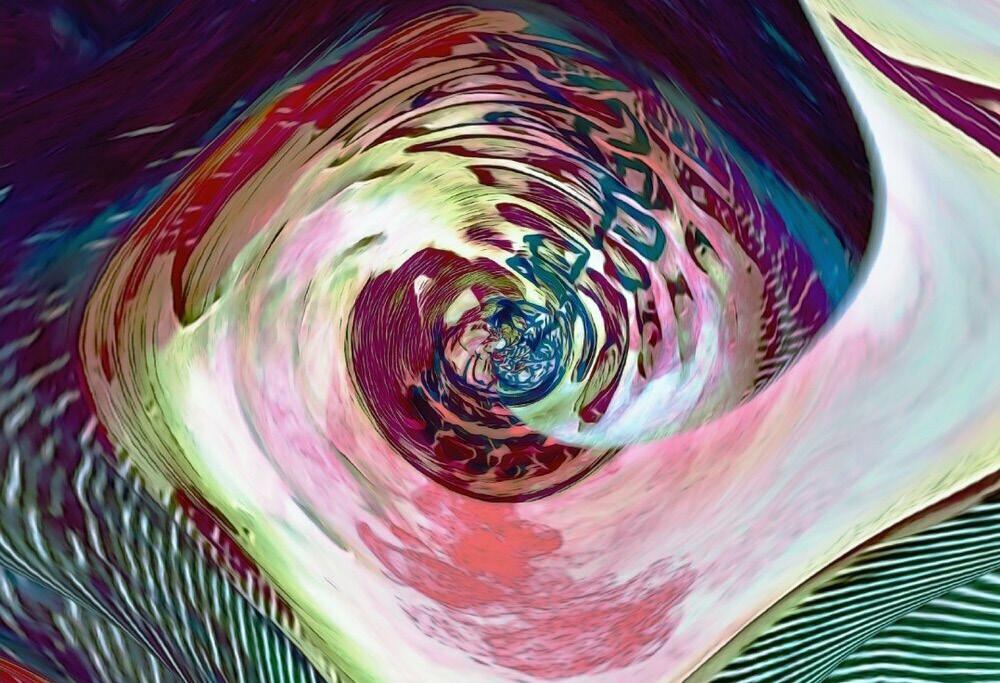
Visual aids have long been used in medicine (particularly in the fields of neurology and psychiatry) to help understand the inner workings of the brain. They are used to study the synaptic connections that recreate, ignore or establish inferred realities.
Most people are unable to accurately identify the midpoint of the stylized arrows that comprise the Müller-Lyer test. Some
Written by Roxanne Bruce, PhD, DrBA BY LUCIE MITCHELL, DO
are unable to “see” both the vase and profile silhouettes in the famous black and white optical illusions. The test for color-blindness requires persons to identify a “hidden” number in the center of an image made up of different-colored pastel dots, and the “ink blot” Rorschach test has long been used to assess patients with anxiety, depression and psychosis. How one interprets a work of art can
also tell us alot about our neural pathways.
This abstract work of art titled “Mind Games” was created by physician artist Dr Lucie Mitchell using an image of one of her own cervical vertebrae. It represents the games our brains play when we become pre-occupied with unrelenting thoughts and worries. Unable to rest, we become bleary-eyed and unable to focus on the days ahead.
☤
40 | 2022 VOLUME 12
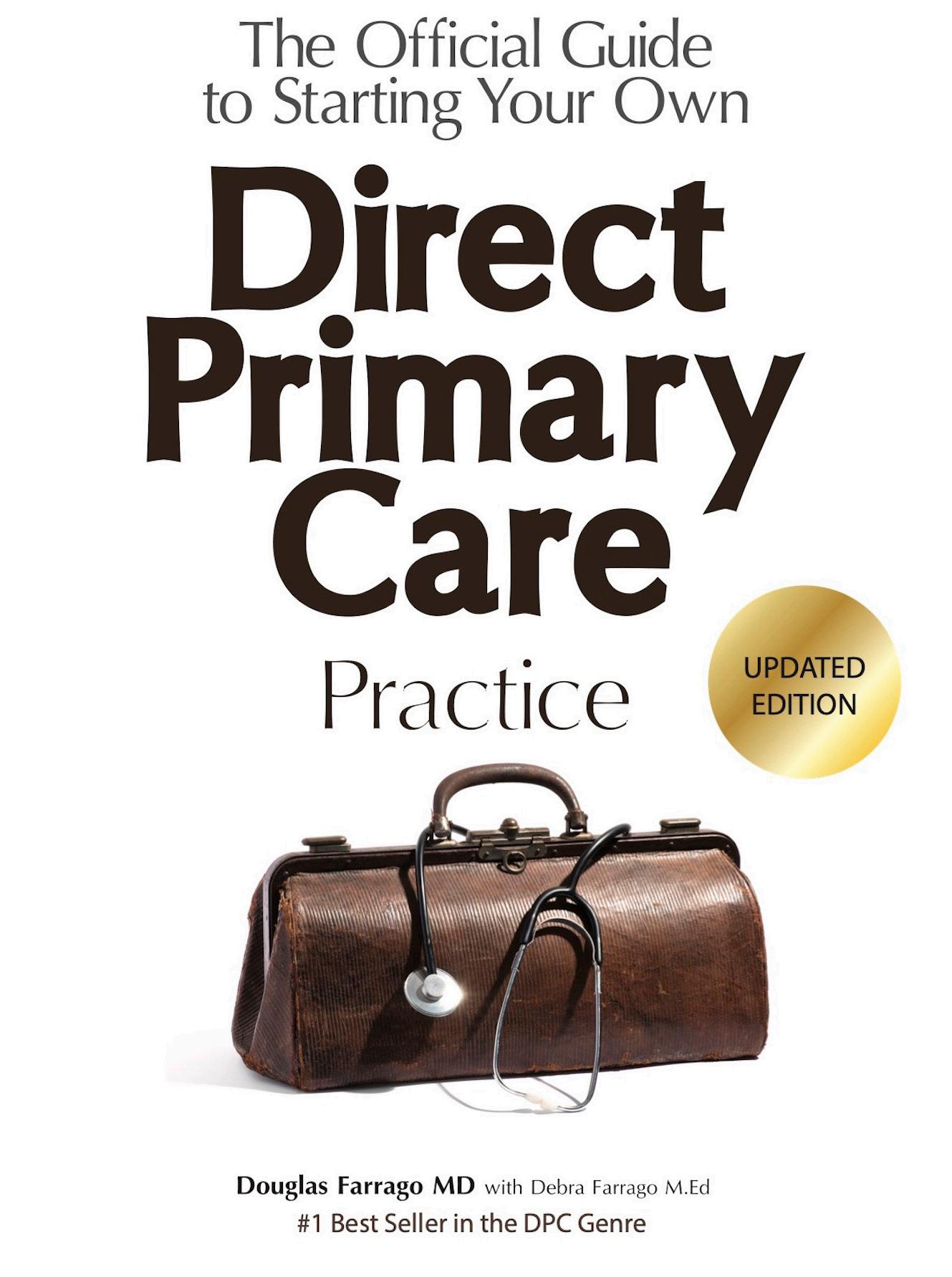
WWW.PHYSICIANOUTLOOK.COM | 41
Coffee with a Mission
I’m not a veteran and I always make that clear.
Dad was the youngest of 16 - 14 boys, 2 girls. 3 of the boys served in WWI and my uncle Perce was awarded a Silver Star for action in France with the USA 77th Division. 5 siblings served in WWII, my dad with the Marines who spent 20+ months in the Pacific. 1, uncle Dink fought in both wars and ran into his son while landing under fire in Okinawa, who was also a USN CB.
I had my right eye removed at age 7, and so couldn’t serve in uniform. I ended up trading green coffee on Wall Street, lived in Brasil for several years and then came back and was the CEO of a Brasilian Agr Group’s global HQ which happened to be down the block from the US Marines’ MCRD HQ on Long Island, NY. I befriended the Marines there and did what I could to support them and their families and when I retired from trading in 2005 (and never having an opportunity to serve as my family had) I went to them and asked for help to get a deployment to Iraq.
In 2008 at age 55, I deployed to Iraq as part of the OIF LOGCAP (logistical support mission) and then volunteered to forward deploy and was sent to FOB Warrior, Kirkuk. It was there, see ing first had what a great job our men and women do - and in such miserable conditions - that the idea for Military Java Group was born.
That’s me on a very rare day off - ergo the shorts - LOL!
~ Matt Phillips, Founder/President of Jarhead Java



Share a mug. Support a cause. And, we’ll donate 50% of our profits to the Semper Fi & America’s Fund to assist our wounded heroes. Great coffee for a great cause. Find our family of high-quality coffee products at MilitaryJavaGroup.com, MCX, DeCA, and Amazon. MP1129_Share a Mug 5x6.indd 1 2/10/22 5:06 PM 42 | 2022 VOLUME 12


Publisher: Marlene Wüst-Smith, MD Editor in Chief: Alicia Roselli Managing Editor: Roxanne Bruce, MBA, DrBA VP of Advertising: Pamela Ferman Director of Art and Production: Tobias Sarrio Marketing/Copyright Editor/Journalism/Social Media Interns: Elizabeth Egan, Hannah Bushery, Dana Bushery, Madison M. Smith, Cindy Huang
Contributing Authors: Marlene Wüst-Smith, MD, Adam Harrison, MD, Terry Wilcox, Mark Lopatin, MD, Roxanne Bruce, MBA, DrBA, Cristy Gupton, Dr. Charles Bens, Eden Courville, James Harris Jr., MD, FACS, Laura Fortner, MD, Danielle Hartnett, Jill Labecki, George “Jeep” Naum, MD, Chris Gure
Cover Art:
Published by “Physician Outlook Publishing” Editorial policy: Physician Outlook magazine is a national magazine dedicated to empowering physicians and their patients to improve the world of medicine together. Editorial decisions are based on the editor’s judgement of the quality of the writing, the timeliness of the content, and the potential interest to the readers of the Physician Outlook magazine. The magazine may publish articles dealing with controversial issues. The views expressed herein are of the authors and/or those interviewed, and may not reflect the official policy of the magazine. Physician Outlook neither agrees, nor disagrees with those ideas expressed, and no endorsement of those views should be inferred, unless specifically identified as officially endorsed by the magazine.
“Letters to the Editor” email: hello@physicianoutlook.com
Information on advertising, subscriptions, and job board email: hello@physicianoutlook.com
“Physician Outlook” is a registered trademark.
WWW.PHYSICIANOUTLOOK.COM | 43






SUBMIT YOUR ART
SUBSCRIBE

SUBMIT AN ARTICLE

ISSN 2768-6019