



WWW.PHYSICIANOUTLOOK.COM PUBLICATION DEDICATED SOLELY TO PHYSICIANS AND THEIR PATIENTS 2023: THE YEAR WE SET OURSELVES FREE VOLUME 16 | 2023 COVER ARTIST: KATELYN HANSON, DO


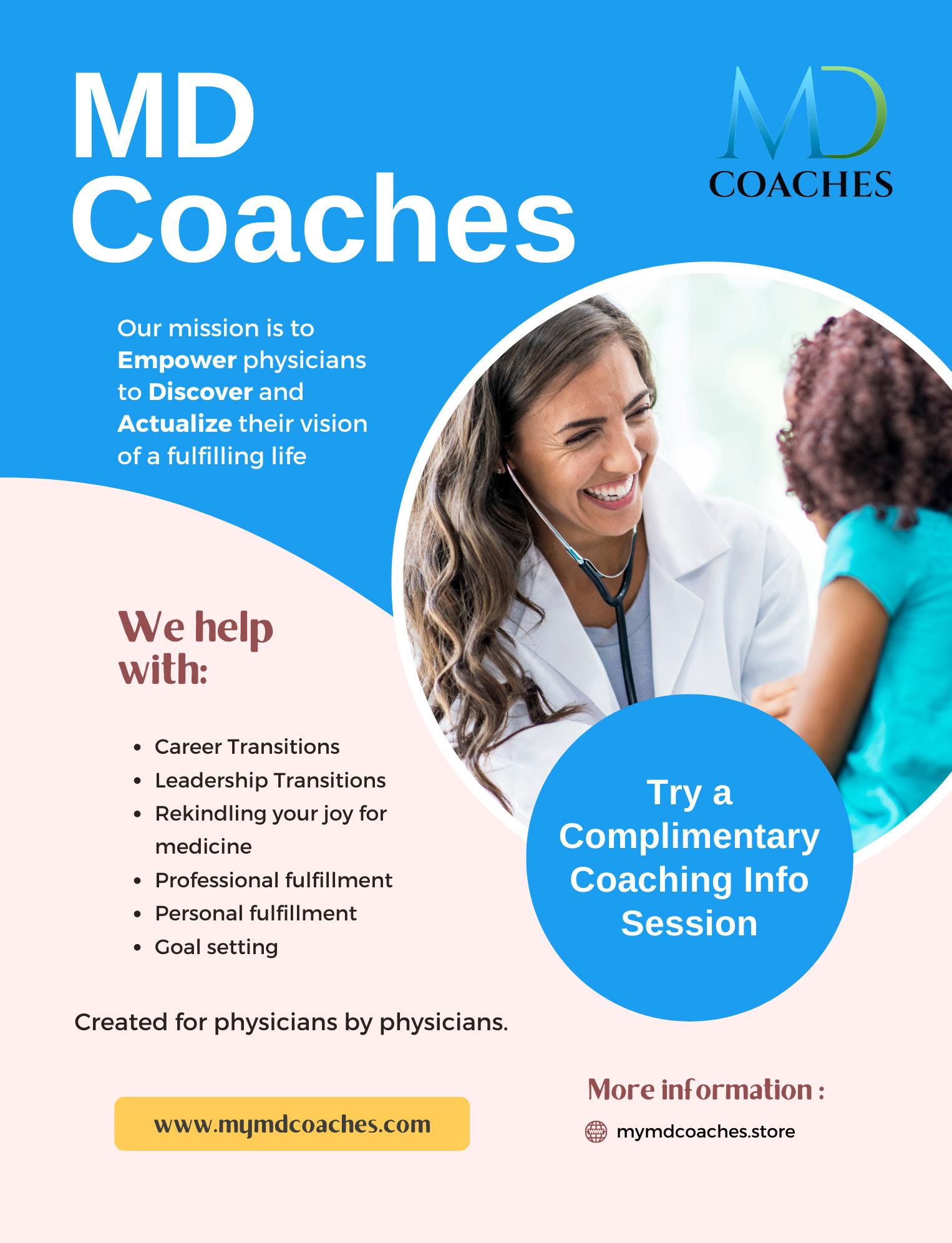
4 - W E E K G R O U P C O A C H I N G C O H O R T

P r e p a r e f o r M a t c h I n t e r v i e w s
L e a r n h o w t o h i g h l i g h t a n d a r t i c u l a t e y o r u u n i q u e v a l u e t o t h e w o r l d o f m e d i c i n e i n a
4 - w e e k g r o u p c o a c h i n g c o h o r t a n d 1 i n d i v i d u a l c o a c h i n g s e s s i o n l e d b y M D
C o a c h e s
C o n n e c t w i t h O t h e r s
C o n n e c t w i t h l i k e - m i n d e d i n d i v i d u a l s i n a s a f e v i r t u a l e n v i o r n m e n t L e a r n f r o m o n e a n o t h e r a n d b u i l d l a s t i n g f r i e n d s h i p s
M o v e F o r w a r d
W i t h n e w i n s i g h t s a n d c o a c h i n g t o o l s , m o v e f o r w a r d w i t h a p l a n t h a t a l i g n s w i t h y o u r v a l u e s a n d s t r e n g t h s



M D C o a c h e s a n d A m e r i c a n S o c i e t y o f P h y s i c i a n s B R O U G H T T O Y O U B Y REGISTER TODAY MDCOACHES.STORE $475 *Special discount for ASP Members
DR. CARMEN ANGLES: THE BACKBONE OF RESILIENCE
By Alicia Roselli
ROBIN ARZÓN: STRONG LIKE HER MOTHER Spotlight on Robin Arzón, by Physician Outlook Team
IS THE PHYSICIAN STETHOSCOPE OBSOLETE?
By Scott Abramson,
MD
SPEAK UP
By Roxanne Bruce,
MBA, DrBA
HUGE ADVANCES IN MENTAL HEALTH ACCESS FOR YOUR PATIENTS
By Amy Mickle,
MS Ed. LPC and LMHC
PATIENT ADVOCATES LIKE DARLA S. BELL ARE MORE IMPORTANT THAN EVER
By Terry Wilcox,
Executive Director of Patients Rising
VIA COLORI CHALK ART FESTIVAL
By Marlene Morales Tollett, MD
WHY THIS PEDIATRICIAN DECIDED TO WRITE BOOKS
By Dr. Robert Saul, MD
THE PUBLIC HEALTH CRISIS OF CHILD SEX TRAFFICKING
By
Ann Di Maio, MD
LINES ON STEAKS
By Isabella Libreros, Editor-in-Chief
I AM NOT A DOCTOR... NOR DO I PLAY ONE ON TV
Spotlight on Jason Littlefield, M.Ed. by Physician Outlook Team
THE MEMORIAL
By Gregory Jasani, MD
REBUILDING TRUST IN MEDICINE
By Physician Outlook Team
LIVING WITH COVID-19: THE LATEST PANDEMIC
By Ana Paula Velez, MD
FEMALE INCONTINENCE: AWARENESS NEEDED
By Samantha Pulliam, MD
HANSON’S ANATOMY: THE COLORFUL JOURNEY OF A VISUAL LEARNER IN MEDICINE
By Katelyn Hanson, DO
MAGMA
By Claire Unis, MD
WE ARE... GOING TO BE A DOCTOR!
Spotlight on Jackson Kollasch, Lewis Katz School of Medicine Class of 2027
A PERSONAL RETROSPECTIVE IN THREE PARTS
By Susan J. Baumgaertel, MD

ARTWORK: Head Vessels by Katelyn Hanson, DO
04. 07. 09. 10. 12. 14. 16. 18. 20. 2023 | VOL. 16 CONTENTS PHYSICIAN OUTLOOK MAGAZINE 23. 24. 28. 30. 32. 35. 38. 40. 42. 44.



Dr. Carmen Angles: The Backbone of Resilience
Written by Alicia Roselli
For as long as I can remember, I’ve been surrounded by the smartest, strongest and most resourceful, persistent bunch - the women in my life. In the beginning, I didn’t have much choice - as the saying goes, you can’t pick your family. But as I matured and was able to choose the friends that become family, strong women were abundantly represented.
Right away, Dr. Angles struck me as a woman I would want in my tribe. Her accomplishments and story are inspiring to say the least,
but it was her humble demeanor and sense of gratitude for all the support she received on her journey that impressed me the most.
PO: You are a Cuban refugeewhen did you leave and what was it like growing up in Cuba?
Dr. Angles described her childhood as “magical.” Her grandfather owned sugar cane plantations, or “colonias de caña” in Spanish. They were privileged, living a lavish lifestyle that included service staff, a beach house and farms. Fidel
Castro’s Cuban revolution turned their world upside down. She and her family became outcasts, referred to as “gusanos” or worms, a term used by Castro for any reactionary, counter-revolutionary (sane) person.
In the height of the cold war, after the failed Bay of Pigs Invasion, her family was forced out of Cuba. The Freedom Flights program, operating from 1965-1973, transported over 300,000 Cubans to Florida. Dr. Angles, then almost 14, her parents and one of two brothers were among them. Imagine the heart wrenching decision to leave their eldest son behind...Castro wanted the 17 year old engineering student for his own army and did not authorize his departure.
Dr. Angles recalled what the pilot told his passengers as they left Cuban airspace - “You are now country-less. You are no longer Cuban citizens and you have no cit-
Photo credit: @RobinNYC
4 | 2023 VOLUME 16
Photo credit: @RobinNYC

izenship anywhere.” Not exactly empathetic words of encouragement to people facing what was likely the scariest moment of their lives.
PO: What challenges did you face in the U.S.?
Subsequent to their arrival in Florida from Cuba, Dr. Angles’ family settled in Philadelphia, where they had relatives able to help them get established. When asked about the challenges she and her family faced, I braced myself for a litany of hardships. What I got instead was an earful about the wonderful, supportive people who helped them succeed. After the Cuban Revolution, many Cuban exiles arrived in Philadelphia between 1959 and 1965. Some connected directly with family and friends already in Philadelphia and others relocated from Florida. Many from this wave of Cubans created social and cultural groups that are still active in promoting solidarity and Cuban culture. El Club Cubano and Club Banence were two prominent groups at the time that provided support to Dr. Angles and her family. This phenomenon of Cuban exiles arriving in the US, surviving and thriving with help from fellow Cubans was a commonplace occurrence in multiple other cities such as in Rochester, NY.
One of the biggest challenges for Dr. Angles was the language barrier and overall approach to refugee integration into US schools.
Our school systems often struggle with placement for refugees, having little objective data on which to base decisions and having few resources to effectively evaluate student competency in the face of language barriers. Dr. Angles entered US schools as a high school sophomore, an age where the aptitude to learn new languages tips from effortless to monumental. Early on, she was pigeon-holed into a vocational track. Thanks to an empathetic classmate Ana Lopez, also a Cuban refugee who advocated on Dr Angles’ behalf to their school Principal, Dr. Angles was eventually accepted into the academic track. She went to summer school for ESL - English as a Second Language, to help pull up her grades sufficiently to qualify. Dr. Angles credited the quality programming on PBS as being key to her learning the English language, highlighting Sesame Street’s word of the day and the “easier to follow because it’s slow” dialog in documentaries.
PO: What inspired you to become a doctor?
Dr. Angles was intrinsically motivated to excel in school, it was in her blood. There was no question that she would go to college - it was simply expected. She was interested in the sciences, and wanted to start earning a living as soon as possible, not only for herself but for her parents who had sacrificed so much for their children. Dr. Angles considered a career in physical therapy, but missed the deadline to apply to the program. A simple question from her ASPIRA counselor who later became husband… why not a physician? She switched to premed at Penn State (with a dual major in health administration as a plan B), and was accepted to both Temple and Harvard
Medical Schools. With the help of loans available to Cuban refugees, the promise of US citizenship within 5 years the only debt, Dr. Angles graduated from Temple with a degree in Physiatry and Rehabilitation Medicine.
PO: What does a typical day look like for a physical medicine and rehabilitation specialist? What are the nuances that make it different?
In a nutshell, go big or go home is the theme here. Dr. Angles works at MossRehab, now part of Jefferson Health, where she runs a comprehensive, in-patient rehabilitation unit that handles highly complex cases and employs some of the most medically challenging techniques in practice today. Patients’ rehabilitation needs can stem from trauma, accidents, burns, cancer and organ transplants just to name a few. She enjoys the challenge of in-depth specialization in innovative technology including robotics, interventional physiatry, injections, nerve blocks, electro diagnostics among others.
Patients are typically in her care for at least 14 days at the in-patient unit. Dr. Angles finds that really getting to know her patients and their families during their extensive and intense treatment is one of the most rewarding
WHAT IS A PHYSIATRIST?
Physical Medicine and Rehabilitation (PM&R) physicians, also known as physiatrists, treat a wide variety of medical conditions affecting the brain, spinal cord, nerves, bones, joints, ligaments, muscles, and tendons. By taking the whole body into account, they are able to accurately pinpoint problems and enhance performance without surgery.
WWW.PHYSICIANOUTLOOK.COM | 5

aspects of her practice. Her busiest days are at the musculoskeletal clinic, where she sees those same patients after discharge for follow-up care. It’s this continuity that helps ensure all patients receive the best care possible and Dr. Angles has the latitude to determine the course and length of follow-up required.
PO: What are your interests outside of medicine?
Outside of medicine, Dr. Angles starts her busiest days with a Peloton class, taught by none other than her own daughter. It was her daughter Robin Arzón that inspired Dr. Angles’ interest in fitness. After a traumatic assault, Arzón needed a path to healing and her journey into the world of fitness began with running in 2009. She later inspired her mother to do the same with a surprise family enrollment in a Turkey Trot. Dr. Angles could only walk for most of the race, and finished near last. Running was not “a thing” among Latinos of her time. Now she keeps up with her badass Peloton instructor and enjoys 5K runs. Her daughter is the 2x New York Times

bestselling author of Shut Up And Run and Strong Mama, and she welcomed her second baby, Atlas Sage Arzón-Butler on Sunday, July 16. As Vice President of Fitness Programming and Head Instructor at Peloton, her life’s mission is to “redefine, reform, and rethink possibility through movement.”
PO: What are your hopes for the future of medicine?
Dr. Angles’ answer was plain and simple, but powerful - access to affordable, quality healthcare for every person without demographic bias. It brought to mind Maslow’s hierarchy of human needs - health is at the foundation, just one step up from food and water. Dr. Angles’ desire is to see all of our citizens cared for, closing the gaps that exist based on the zip code one lives in. Her desire is for healthcare to be equitable and effective in preventing the chronic diseases that bring patients to her unit. Depriving one of quality healthcare is equivalent to depriving one of food and water.
At the close of our interview, Dr. Angles was reflective and gratefulgrateful to have found a rewarding
niche in medicine where the joys of healing outweigh the burnout afflicting many physicians today.
Dr. Angles is a fellow of the American Academy of Physical Medicine and Rehabilitation, and a member of the American Congress of Rehabilitation Medicine. She has teaching appointments at Thomas Jefferson Medical College and Temple University School of Medicine.
Resources
1. https://www.hsp.org/sites/default/files/legacy_files/migrated/latinophiladelphiaataglance.pdf
2. ASPIRA, Inc. of Pennsylvania was formed in 1969 and primarily serves the North Philadelphia community, which has the third-largest Puerto Rican population outside of Puerto Rico. To address the low academic attainment of youth in Philadelphia, ASPIRA began its hallmark Leadership Development program in 1969, which is still active in several schools today. <https://www.aspirapa.org/apps/ pages/index.jsp?uREC_ID=1415468&type=d&pREC_ID=1585802>
3. https://www.robinarzon.com/ about
☤
Photo credit: @RobinNYC
6 | 2023 VOLUME 16
Photo credit: @RobinNYC
Robin Arzón: Strong Like Her Mother
Written by Physician Outlook Team
“I am my mother’s daughter. My spine is stronger because of her.”-Robin Arzón
Robin Arzón is well known to many because of her commitment to and passion for fitness. She has many physician “fan-girls” (our publisher/editor included) who came together as a community virtually and in-person when they discovered Peloton™, “ The Doc Mom’s Bike to Nowhere,” that quite literally became the lifeline for many in the healthcare world (pre and post-pandemic).
What many DON’T know is that Robin is the strong daughter of a “bad-ass” female physician, Dr. Carmen Angles, who bravely immigrated to the United States from Cuba as a teenager without knowing a word of English. Dr. Angles taught her daughters Robin and Margaret Arzón from an early age how to reap resilience and tenacity. She instilled in them the ability to stand firm in their own space, impervious to ignorance, yet open to compassion and acceptance.
Dr. Angles taught herself English by watching Sesame Street on PBS, setting an example of resilience and determination for both of her daughters. Now in her 70s, Dr. Angles continues to work as a fulltime practicing Physiatrist at the world-famous MossRehab Hospital (part of the Einstein Healthcare Network and Jefferson Health) outside of Philadelphia, a testa -

ment to her unwavering strength and dedication.
The Apple Does Not Fall Far from The Tree
Robin Arzón, a type 1 diabetic who was diagnosed in her early 30s (in spite of her very healthy lifestyle), has overcome many personal challenges fearlessly by embracing wellness and the lessons imparted to her by her upbringing. Her journey of empowerment began after a near-death traumatic event, where she discovered the healing power of movement. One of her mantras is that “Movement is Medicine,” which echoes her mother’s lifework as a physician who specializes in Physical Medicine and Rehabilitation. Arzón’s struggles ignited a passion for running and endurance challenges that changed the course of her life, and that of many others.
Arzón’s pursuit of athletic excellence led her to become an avid ultra-marathon runner, including a remarkable feat of running five marathons in five days to support Multiple Sclerosis research
Through these physical challenges, Robin has continuously pushed the boundaries of human capability, redefining what is possible through movement.
Beyond her physical achievements, Robin Arzón believes in the importance of mental strength. She imparts her wisdom through a sought-after MasterClass on Mental Strength, empowering participants to transform their inner critic into a powerful inner advocate, unlocking their full potential in all aspects of life.
Robin’s influence extends far beyond the fitness realm. She is a renowned keynote speaker and collaborator, leaving a lasting im-
Photo credit: @RobinNYC



pact on audiences at prestigious events for Fortune 500 companies such as Google, Facebook, and Verizon. Her unapologetic and inspirational ethos seamlessly intertwines wellness, lifestyle, and fashion, earning her influential partnerships and collaborations.
Not only does Robin empower adults through her books Shut Up and Run (released in June 2016), and an inspirational Empowerment Journal called Welcome Hustler (September 2023), she also uniquely fosters empowerment and a love of movement and play through her children’s books. Her first book, Strong Mama, (released in January
of 2022 following the birth of her daughter Athena Amelia in March of 2021) teaches the importance of self-care for new mothers and the healing power of movement. Following her commitment to empowering the younger generation, she released her second children’s book, Strong Baby, in February of 2023. In the summer of 2023, following the birth of son Atlas Sage, she released an innovative line of bilingual children’s toys through Tomy called Bebé Fuerte.
Robin Arzón’s exceptional journey has garnered significant recognition. She was honored on Fortune Magazine’s esteemed “40 Under
40” list in 2020, solidifying her position as one of the most influential people of her generation. In 2021, Glamour Magazine bestowed upon her the “Daring to Disrupt” Award, recognizing her bold contributions to empowerment and wellness.
Her legacy of empowerment and resilience continues to inspire countless individuals worldwide. From her academic excellence as an undergraduate at New York University and Villanova University School of Law, graduating magna cum laude, to her expertise in various fitness disciplines, holding multiple certifications, including RRCA certified running coach, NASM certified personal trainer, Schwinn spin instructor, certified Pilates instructor, and specialized training in Pre/Post Natal fitness, Robin Arzón continues to redefine possibilities through movement.
As the Vice President of Fitness Programming and Head Instructor at Peloton™, Robin’s life’s mission revolves around transforming lives through sweat and inspiring others to embrace limitless possibilities through movement, fearlessly pioneering wellness, and empowerment. Her journey exemplifies the incredible potential of the human spirit, and she remains an unwavering beacon of strength and inspiration for people around the world.
One of the most heartwarming aspects of Robin’s journey is how she inspired her previously non-exercising Latino mother to participate in a “Turkey Trot,” which has since become a beloved Thanksgiving tradition for ALL members of the Angles-Arzón-Butler families.
Robin’s impact extends beyond her own life, touching the lives of her loved ones, who now share in the joy of fitness and togetherness.☤
ARTWORK: Spinal by Katelyn Hanson, DO
Photo credit: @RobinNYC
Photo credit: @RobinNYC @BrianKingNYC
Is the Physician Stethoscope Obsolete?
Written by Scott Abramson, MD
“ Is there a doctor on the plane?”
These were the words that struck me with instantaneous and profound terror.
I was flying Delta Airlines, San Francisco to Atlanta a while ago when I heard this announcement. I have been retired from my neurology practice for almost four years now. But when no one else answered the call, I realized I was the guy.
So, I sashayed to the back of the plane where a middle-aged Filipino woman was lying on the floor, panting for breath.
I quickly got a medical history from her daughter. (Later in the flight, the daughter began to have similar symptoms as her mom… but that’s another story). I did my “routine” initial assessment. I accurately concluded that this situation was essentially a case of hyperventilation-anxiety. However, since all the other passengers were gazing back toward us with intense interest, and since the flight attendant was hovering over me with such helpful concern, I figured I might as well entertain them all as I reveled in my doctor role. Then in my best Marcus Welby voice, I turned to the flight attendant and asked for the Delta Airlines medical bag. Ever so helpful, the flight attendant handed me a stethoscope. I patiently and


very professionally applied it upon my new patient. I heard nothing of concern; in fact, I heard nothing much at all, (but I never could hear much from this part of the exam anyway, hence I became a neurologist.) But this did not prevent me from proceeding with my “thorough” examination, listening carefully to the chest and the heart and even the abdomen with that invaluable instrument of inquiry.
I must confess: Even though I heard nothing much, I was feeling pretty damn important wielding that stethoscope. All eyes of the passengers were upon me, and doggone, if I was not feeling like some sort of medical hero. Not only was I giving care to this distressed lady, but I was preventing Delta from making an emergency landing that would have inconvenienced a few hundred of my fellow passengers. Again, like I said, stethoscope in hand, I was beginning to enjoy all the attention. I began to relish (what I fantasized was) my fellow passengers’ silent admiration of my doctoring skills.
Until:
The flight attendant, with a concerned and puzzled expression, quietly asked me the following question:
“Excuse me doctor,” she whispered, “but shouldn’t you put the stethoscope in your ears?”
Oops. Major oops.
Double Major Oops.
My cover was just blown!
And I was looking so darn good!☤
Addendum #1: Actually, it didn’t turn out so bad. Delta took my name and address. A few weeks later they sent me a box of See’s candies for my “volunteer assistance.”
Addendum #2: Memo to my physician colleagues: If you, my colleagues, are ever traveling by plane and an emergency call goes out for a doctor, please remember to connect the ear tubes of the stethoscope to the EARS! (Frankly, it’s just a better look!)
Speak Up
Written by Roxanne Bruce, MBA, DrBA

Not everyone reacts the same way to an injury/illness, and physicians have the difficult task of interpreting a patient’s response in real time during a potentially life-threatening event. I must remind myself of this every time I seek medical attention. You see, the simple fact is… I do not have a “normal” pain response. If my pain is mild to moderate, I am probably cracking jokes, telling stories, laughing, and generally ignoring it. If my pain is severe, then I am usually quiet and focusing inward. I am probably not your average patient!
There have been several big events that showed me just how different I was and served as a training moment for the doctors who cared for me.
Situation 1:
I was in a bad automobile accident. The vehicle I was riding in hit a bridge pillar head on. I was crushed in the backseat between the roof and the seat. I argued with the ambulance drivers asking that they save my Subway meatball sandwich. At the hospital, I argued with the nurse that I did not want a tube put down my throat. The plastic surgeon on call had to rush to the hospital because my face had been mangled. When he arrived in the room, he didn’t realize and was not told that I was awake.
He started manipulating the skin on my face to get a better look at my skull and jaw bones. I did not react well because I was awake and
had not been given any pain medication. The medical professionals had assumed that since I wasn’t crying, yelling, acting like I was dying, or begging for pain medication that I was not with them mentally. I was very much with them and focused on dealing with the excruciating pain by meditating.
I still have nightmares from this event, and regularly dream of fighting with doctors and nurses, telling them no and having them treat me anyway. The medical professionals were doing what they had to do to keep me alive.
Situation 2:
I presented to the emergency room complaining of stomach pain
10 | 2023 VOLUME 16
and an inability to go to the bathroom. I had a history of bowl issues (due to surgery from the auto accident and multiple sclerosis). The doctor seeing me in the ER did a physical exam and sent me home with instructions to drink more water and try an over-the-counter medication. Since I was cracking jokes, they didn’t take me seriously.
Later that afternoon, the pain became unbearable. I returned to the emergency room requesting more help. Another physical exam and this time the doctor listened more carefully and decided to run an x-ray. It wasn’t long after the x-ray happened that I was admitted to the hospital and met with a surgeon. My intestines had shut down completely and since this had happened multiple times before, the doctor wasn’t confident that we could get them going again. I was warned that I may have to live with a colostomy bag if they didn’t regain function.
Over hours of treatment, IV’s and enemas, as well as medications to stimulate movement I joked with nurses and tried to stay positive. By the end of the day, I was begging for something for pain, to which they responded it would just make it harder to go. To this day I must take my medical records with me to the ER when my intestines decide to shut down. Since my reaction to pain isn’t what they are expecting, they ignore the severity of what I am experiencing or write me off as faking it. I do not have a colostomy bag yet but have learned what it feels like as the intestines are shutting down and have a plan in place to deal with it.
Situation 3:
I was on disease modifying therapy #5 to try and treat my multiple sclerosis. I had allergic reactions to 1-4 with the worst of them leaving me bed ridden for a few days. Upon receiving medication #5, I was instructed by the nurse and doctor how to administer the medication and that I may experience mild site reactions. They went on to say that
hives would be normal and not to worry, so when the hives appeared during the first injection I didn’t worry.
Fast forward 2 weeks and I was covered head to toe in hives. With every injection they got worse. It was immediate! From the moment I started injecting, the skin swelled into large bumps that were painful and itchy. I couldn’t take it any longer! I had called several times on the phone with no solutions, so I went to the doctor’s office. I couldn’t believe that it should be this uncomfortable or that the hives should last this long. When I walked to the front desk at the doctor’s office, they didn’t check me in. The nurse came out, took one look at me, and sent me to the Emergency Room. I was having a horrible allergic reaction to the medication and it was becoming a dangerous situation.
What I hope you learn from my experiences…
Patients, know what is normal for your body. If something seems wrong, it very well could be. Make sure that you have good written notes, explain yourself clearly, bring another person with you to help describe the situation. If you can’t do it on your own, seek help. My book My Best Day Journal was recognized by the National MS Society as a great way to communicate with your physician. It is modeled after the journal that I carry to help describe my conditions and what has worked in the past. But more than anything else, if the doctor you are sitting with is refusing to hear you, find another doctor.
Doctors, every patient is an individual and it will be important to listen to exactly what the patient is saying. Don’t immediately write something off because it is on the warning label of a medication, or because their behavior isn’t what you would expect. Your job, as a doctor, is incredibly difficult. You are expected to know a little about everything and a lot about a few things and use that information to diag -
nose at the drop of the hat. Do not be afraid to ask your patient more questions. Give them a tool (book or journal) to work on at home to help you understand what they are living with. You and your patient are a team!
In the end, there is never a one size fits all way to handle medical emergencies.
Every doctor is different, and every patient is different. We all need to advocate for the best outcome for everyone involved. Mistakes can happen, side effects can occur, and things aren’t always as they seem.

WWW.PHYSICIANOUTLOOK.COM | 11
☤
HUGE Advances in Mental Health Access for Your Patients
 Written by Amy Mickle, MS Ed. LPC and LMHC
Written by Amy Mickle, MS Ed. LPC and LMHC
Hip, hip hooray…more help is on the way…!!
Most of us would agree that we are in a national mental health crisis. Now more than ever communities are suffering from all time high levels of depression and anxiety (including suicidality) while at the same time our nation is witnessing a shortage of mental health professionals and services. It is not unusual for our patients to wait 4-5 months to see a psychiatrist or 2-3 months to see a therapist. When folks are in need of mental health interventions, this wait time is extremely painful which can cause an increase risk in additional emotional and psychological decompensation.
There are many causal and correlational factors to blame for this social service deficit such as: collateral damage from the Covid pandemic and a low workforce of professionals. The need for counseling is so much greater presently due to: the by-products of social media, higher unemployment, social stressors such as an increase in bullying, political distress, recent police brutality, human trafficking,
substance abuse and immigration related issues.
So, that’s the bad news... but wait...there is good news that should help you help your patients.
Beginning January 1, 2024, 225,000 new highly qualified mental health practitioners will finally be granted access into the Medicare system.
President Joe Biden signed the Omnibus Mental Health Access Improvement Act 2021 also referred to as S.828 and HR 432. The new law is P.L.: 117-328 allows Licensed Professional Counselors (LPC), Licensed Mental Health Counselors (LMHC) along with their cousins Licensed Marriage and Family Therapists (MFT) to serve as mental health providers. This is a big, big deal! Variations of this bill have been in discussion in the House and Senate for the last decade. In addition, the Centers for Medicare and Medicaid have not updated their policy since 1989. The Center has released the 2023 Physician Fee Schedule final note which expands
the role of counselors within the program to provide mental health and substance abuse services to those who qualify as being over 65 or meeting criteria for a permanent disability.
To understand the magnitude of this opportunity, it may be helpful to understand the historical background. To date, only Licensed Clinical Social Workers (LCSW) have been able to directly bill Medicare for the provision of mental health services. Licensed mental
12 | 2023 VOLUME 16
health counselors and marriage and family therapists have had to work directly under a physician (a doctor had to literally be on site) and had to bill as “incident to” under the MD which was very difficult for many clinicians and agencies. While the new entourage of professionals will continue to work under the general supervision of the physician, the clinician can provide services independently.
To make this clearer, let’s use an analogy using mid-level medical providers. So, a social worker is to a nurse practitioner as a professional counselor is to a physician assistant. While the training and scope of practice is very similar, the degree of autonomy is very different. A quick look at the program differences gives a glimpse of why there is such a discrepancy between the two disciplines. The social work professional community has always had preferential access for many years. Professional counselors, on the other hand, did not. In the 1960’s the mental health profession actually “shot itself in the foot” as educational programs were not standardized across the board. For example, some of us may have been sitting in a circle singing “Kum-ba-yah” and another was running a free style T-Groups. Then, in 1981, arrived CACREP (Council for Accreditation of Counseling and Related Educational Programs) which ensured that all graduate counseling programs were teaching the same standardized coursework of excellence. With this, the counseling field finally started to earn professional
respect. That said, there are some pedagogical differences in the mental health counseling versus the social work disciplines. As a general rule, the Counseling discipline focuses on micro counseling skills with the underlying goal of empowering clients to take control of their lives with an internal locus of control. The Social Work profession, on the other hand, tends to take a more global or macro-approach and focus on case management and social justice in referring clients to the appropriate social services that would help meet their needs as a more external locus of control. At the same time, Marriage and Family Therapy focuses on the dynamics of the family system and personal relationships.
Also, another contributing factor to the discrepancy in access to mental health professionals is the fact that historically the social work profession has had a very strong lobbyist representation in Washington, while the professional counseling and marriage and family therapy profession have not. The National Association of Social Workers (NASW) movement has had strong advocacy in the national government since the 1960’s yet the MHC and MFT movement has only been more highly represented in the last several decades.
Additionally, in preparation for the great in-pouring, the national government along with Medicare had to be prepared to “pay out” more funds to providers once potential clients were given access to MHCs and MFT. Thus, with the new law, licensed mental health professionals will be able to provide services to outpatient clinics, hospice programs and rural and underserved geographical and social areas. Unfortunately, at this time, mental health care in nursing home facilities will not be included
in this new law.
The bottom line here is that with the new legislation is a win-win for clients, programs and mental health providers. The obstacles to access have been significantly removed.
Assuming that the average therapist maintains a caseload of 50 clients (which is a very low estimate), this would mean that over 1 million additional clients could be served. Now, medical providers will have more options to refer Medicare qualifying patients for assessment and treatment than ever before.
Thank you to all the advocates, law makers and professionals who made this much needed and very overdue law a reality!☤


Amy Mickle, MS Ed. LPC and LMHC works as an independent contractor and consultant providing clinical supervision to mental health counselors seeking licensure.
Patient Advocates Like Darla S. Bell Are More Important Than Ever
Written by Terry Wilcox, Executive Director of Patients Rising
There’s perhaps never been a more critical time for patients and caregivers to make their voices heard about healthcare policy. Pending legislation in Congress would significantly impact the rare and chronic disease community if passed. That’s why compelling advocates like Darla S. Bell, who recently won the Free2Care coalition’s inaugural Dan Weber patient advocacy award, are more important than ever.
Darla amplifies the voices of patients with rare and chronic diseases who often feel powerless to overcome the enormous healthcare barriers facing them.
She has a chronic condition requiring a specialty medication, so she knows firsthand the hurdles patients face. She is a leading advocate against the use of Copay Accumulator Adjustment Programs (CAAPs), which are becoming prevalent in health plans across the country.
CAAPs forbid copay assistance from counting toward patients’ deductibles. Copay assistance is a vital financial lifeline from drug -
makers for countless patients who otherwise can’t afford their medications. By not allowing copay assistance to apply to deductibles, CAAPs force patients to pay for the total cost of their prescription drugs mid-year when their copay assistance runs out. CAAPs impose a financial burden that’s insurmountable for some patients while allowing health plans to double-dip, earning twice as much pre-deductible revenue.

CAAPs are part of a growing trend of healthcare cost-shifting onto the backs of patients. They disproportionately hurt the sickest and most vulnerable people in society whose medication needs are most pressing.
Darla has led the charge against the proliferation of CAAPs. She fought back personally when they were adopted by her health plan, threatening her access. She wrote an op-ed in the Austin American-Statesman educating the public about their pernicious rise, and advocated for Texas state legis -
lators to pass legislation banning them.
Darla shows that patients can help change American healthcare for the better. Voices like hers are needed now to inform pending policy changes affecting patients. For instance, the U.S. Senate recently passed an infrastructure bill delaying a prescription drug rebate rule that could significantly reduce medication prices for patients. The rule requires middlemen in the drug supply chain to pass along rebate discounts they receive from
14 | 2023 VOLUME 16

manufacturers directly to patients at the prescription counter. Given that these rebates often make up around half the price of a drug, ensuring they reach the hands of patients who need them would significantly reduce costs and help those struggling to pay for medicines.
Congress is also considering separate legislation that would implement government price-setting on medications for Medicare plans. According to the nonpartisan Congressional Budget Office, such
ARTWORK: ODE TO INTERNAL MEDICINE
Katelyn Hanson, DO
price-setting would result in between 21 and 59 fewer medicines brought to market. This outcome is unacceptable for those with rare and chronic diseases who depend on the prescription drug pipeline of new medications to save their lives and livelihoods. The best hope for patients and caregivers like Dorothea Lantz from Miami, whose son has a rare disease known as Prader-Willi syndrome, is a breakthrough medication. Price-setting would make such new treatments less likely.
By following Darla’s lead and telling their stories, patients can influence these bills and other proposals affecting them. It’s easy for patients to feel like they have no voice at all, but in reality, their compelling stories are the most potent form of advocacy. They have more impact than research papers or “expert” advice ever could. Stories connect with people on a far more profound and emotional level than any other form of communication.
A good place for patients to begin their advocacy journey is by simply telling their stories to their elected representatives, whose contact information can easily be found online. Patients can also enroll in Patients Rising’s Advocacy Master Class, of which Darla is a graduate, to learn additional tips and tactics to influence the healthcare debate.
Those impacted most by healthcare policy should be front and center when these policies are shaped. Darla shows patients how this advocacy can be done. Patients need an army of Darla Bells to fight back against healthcare trends that threaten their care. Her story can convince more patients to join the fray.

Terry Wilcox is the executive director of Patients Rising.
WWW.PHYSICIANOUTLOOK.COM | 15
☤
by

Via Colorli Chalk Art Festiva l
Written by Marlene Morales Tollett, MD
16 | 2023 VOLUME 16

Art has always been my creative outlet and my greatest therapy. I was fortunate enough to find and connect with a group of local female physician artists on Facebook, and that is how I came to meet Vy Mui, MD, a psychiatrist and lover of all things arts and crafts. She approached me about participating in Via Colori Houston, a chalk art festival benefiting The Institute for Spirituality and Health. As a watercolor artist, the idea of working with a new medium on a huge and unfamiliar scale was daunting to me. However, she assured me that we could gather a group of fellow physician artists to pitch in and help.
I found an image online by Gerd Altmann—an eye with a globe of the world replacing the iris. As an ophthalmologist, this anatomy naturally appealed to me and felt
familiar. Moreover, I thought it was just such a beautiful image that could be interpreted in so many different ways. Stephanie Fong, MD, who practices internal medicine and pediatrics, suggested adding the quote,
“Choose to see the world through grateful eyes and it will never look the same again.”
It worked out perfectly and became a message that could uplift people after a challenging couple of years.
I collaborated with these women to figure out how to execute this large art piece on a 10-foot by 10foot square of pavement. We superimposed a grid over the image and then recreated a similar grid on the pavement. This allowed us
to transfer the drawing square by square. I sketched it, and a few other female physicians came to help fill in and shade with pastels. Dana Kober, MD, a child psychiatrist who was involved with the project, said, “Much of my clinic day involves individual work. Creating art as a team was rewarding, and I’m still feeling joyful.” Drs. Mollie Gordon, Shruti Varadarajan, and Kathy Nguyen were also part of the team.
Together, we were able to create a beautiful, colorful piece that drew so much attention by those attending the festival. We were pleased with the positive reactions we received. We love collaborating on art projects and hope to do more in the future. In fact, we have been discussing the possibility of entering the Art Car Parade in Houston next year if we can find a sponsor.☤
WWW.PHYSICIANOUTLOOK.COM | 17
Why This Pediatrician Decided to Write Books
Written by Dr. Robert Saul, MD

Pediatrics is a great medical specialty. Its impact on its practitioners and on patients and their families can be long lasting. For me, the impact has been enormous. I have felt that I have a tremendous responsibility to children and their families. The practice of pediatrics has made me a better person. Parents seek medical care and trusted counsel from a respected health care provider with the following abilities— to listen, to diagnose, to provide care, to empathize, to be trusted, to prescribe, to recommend, and to treat their patients like one of their own. While pediatricians do not use holy water in their interactions, they do invest an incredible amount of professional experience and emotional energy as they engage in a partnership with their families.
I have always marveled at how my pediatric colleagues refer to their patients as “my children.” Initially, I found that to be a bit presumptuous. Families bring their
children to the pediatrician for medical care, not to cede control of them to the doctor. But now I understand the derivation of the rationale. A physician actively engaged in the medical care of their pediatric patients really does (or at least should) invest their physical, mental, and emotional energy into the care of these children. Their patients effectively become “their children.” Years later when these children grow up and have their own children, pediatricians have the real privilege of seeing and often caring for this next generation. The pride in this continuing relationship can be as palpable as the pride that pediatricians who are grandparents have in their own grandchildren.
It is in this latter spirit that I have written a series of books (listed below)—to provide a legacy of thoughts and suggestions that could potentially have a positive lasting impact for—
My children. My two sons are well into adulthood, and I am so
proud of their advocacy for others and their realization of their responsibilities to seek out and help others. Their empathy for others has shone bright and will continue in the years ahead.
My granddaughters. These young ladies, truly my children’s children, will hopefully heed the messages of their parents and carry the beacon forward. I am proud to light the flame.
My patients. Pediatricians often consider their patients their own children. Parents place great trust in pediatric care givers, and in turn, these caregivers do treat their patients like their own children. I have always treated my patients as I would want my own children to be treated, medically and emotionally. So, it is not a stretch for me to say that my writings were directed at my patients (“my children”) and their children to come (“my children’s children”). I have hoped that these writings provide some guidance in the years ahead.
All children. Lastly, my career
18 | 2023 VOLUME 16
has had many facets – young pediatrician who was deeply committed to excellence in diagnosis and treatment, young medical geneticist excited by the new practice of clinical genetics and its burgeoning science, middle age pediatrician realizing the need for a greater role in community advocacy, middle age medical geneticist providing genetic education guidance for my pediatric colleagues, and senior pediatrician coming full circle to provide administrative support for my fellow pediatricians engaged in pediatric training and to directly provide clinical care to a very special group of patients and families – children with complex health care needs. And, during this last period, I also realized that the vital role of advocating for children, of advocating on behalf of families and of advocating for community improvement is never done.
I must be the voice for all children wherever and whenever I can.
So, my writings are also aimed to support all children, not those even under my direct care. I also consider them to be “my children’s children” (the children and their subsequent offspring, the next generation).
I’d like to think that if I have been successful, I can thank my mother and pay her the ultimate tribute. The ultimate tribute for a parental job well-done is the internalization of positive values from one’s parent(s). They can make a difference in the lives of children for years to come. And I hope that is what has occurred with my books.
My mother was a remarkable woman. She was extremely dedicated to her two sons. My parents divorced when I was around 10 years of age. While we were a family of means based on the wealth of my mother’s parents, my mother had no substantive emotional support from her family and
had to deal with issues of spousal alcoholism and my father’s propensity to verbal and physical abuse all on her own. Her ability to essentially strike out independently and to empathize with, care for, and genuinely love virtually everyone she met was indeed remarkable. I’d like to think that the values that I espouse now are those of my mother. But I didn’t know it at the time.
My mother was always engaged in her community and genuinely cared for her fellow citizens and for the life of the community. My mother wrote a significant journal entry (Chapter 2, My Children’s Children: Raising Young Citizens in the Age of Columbine) during the turbulent 1960s with the Vietnam War and the assassination of Martin Luther King Jr. as the backdrop. She was called to action from the events of the day.
It appears that the events of Columbine in 1999 were a similar call to action for me. Since 1999, I have been on a journey, suggesting ways to raise young citizens in the years after Columbine or “the age of Columbine.” Events and powers beyond my control have beckoned me to act on behalf of others. I have welcomed the challenge.
These books are for parents who like my mother want to raise their children the right way—to be good parents and raise good citizens. So, I hope to provide a framework that can help guide parents in the raising and nurturing of their children. Healthy children (physically, mentally, educationally, financially and socially) are good citizens. Healthy children are our future. Oh—and, thank you, Mom.☤
Books
MY CHILDREN’S CHILDREN: RAISING YOUNG CITIZENS IN THE AGE OF COLUMBINE [2013]
ALL ABOUT CHILDREN (children’s book and illustrated by Jan Yalich Betts) [2017]
THINKING DEVELOPMENTALLY: NURTURING WELLNESS IN CHILDHOOD TO PROMOTE LIFELONG HEALTH (co-authored with Dr. Andrew Garner, published by the American Academy of Pediatrics) [2018]
CONSCIOUS PARENTING: USING THE PARENTAL AWARENESS THRESHOLD [2020]
References:
Saul, R. (2023, January 24). Why this pediatrician decided to write books. SoMeDocs: Doctors on Social Media. https://doctorsonsocialmedia.com/this-pediatrician-decided-to-write-books/

The Public Health Crisis of Child Sex Trafficking
Written by Ann Di Maio, MD

In 2000, President Clinton signed into law, the Trafficking Victims Protection Act (TVPA). It defined sex trafficking as the recruitment, harboring, transportation, provision, obtaining, patronizing or solicitation of a person for the purpose of a commercial sex act induced by force, fraud or coercion or in which the person induced to perform such act has not attained 18 years of age. It clearly established that minors can not be willing participants in commercial sex acts such as prostitution. The TVPA defined every aspect of sex trafficking and propelled it into the public consciousness. It gave law enforcement the ability to vigorously investigate these crimes and prosecutors the opportunity to bring these predators to justice.
Yet 20 years later, sex trafficking is still a billion-dollar business with more than 4.5 million victims worldwide with 2 million being children. In the United States, it is estimated there are 200,000 to 300,000 child sex trafficking victims alone.
I became involved in caring for child sex trafficking victims in 2014 when I was working in St. Louis Missouri. At the time, I was an attending in the Pediatric

Emergency Department at Cardinal Glennon Children’s Hospital. I am both a Pediatric Emergency Medicine and Child Protection Physician so have expertise in caring for children who are victims of physical and sexual trauma. St Louis is a hub for Sex Trafficking. In 2014, the
city was ranked 15th in the country. It is currently ranked 10th. The reasons are many. It has an international airport, intersecting highways, three military bases in close proximity to the city, successful sports teams, convention centers, and strip clubs. These attract tran -
20 | 2023 VOLUME 16
sient men looking for sex. It was estimated at that time there were 1,000 victims of sex trafficking in a city of 300 ,000. In 2021, over 300 victims of human trafficking were rescued in Missouri. Over 200 were sex trafficking victims and half of those were children.
As part of our duties in the ED, we would perform “Fit for Confinement Examinations” for the St Louis Metropolitan Police
trafficking. They were just getting simple physical exams, cleared of any acute life-threatening illnesses and then being sent to their facilities. It became clear we were not providing these children with appropriate and adequate care. They needed more than just a simple physical exam.
During this time, The St. Louis Metropolitan Police Department was training all their officers on

Department. These were medical clearance exams on adolescents who were taken into state custody before being placed in residential facilities. They were remanded for placement for various reasons, one being “prostitution”. But they were not prostitutes but victims of sex
how to recognize and respond to sex trafficking victims, child and adult. After discussion with the lead social worker in the ED, we asked permission from the St. Louis PD if we could attend the training and they graciously agreed. It was eye opening. The course
educated us on how to recognize victims. What factors put them at risk, how the traffickers selected their victims, manipulated, brutalized and controlled them. They explained to us why victims do not come forward and how hard it is to escape. One speaker also enlightened us on the poor medical care these victims receive despite presenting to hospitals for treatment. She explained how they often go unrecognized as trafficking victims, and this represents missed opportunities for rescue.
After this training it became obvious, we needed to establish a program in St. Louis that would address all the medical needs of child sex trafficking victims. A program that would provide both acute medical intervention and comprehensive ongoing medical care. I decided that care should be delivered at my hospital. We would be their medical home providing acute care, routine and preventive care as well as ensuring any needed subspecialty care. These exams would be delivered in an environment where the victim felt safe, protected, not judged. She would be the focus, heard, and believed. In addition to medical care, we would also interface with other agencies including Children’s Division, Law Enforcement, Circuit Attorney’s Office, FBI, Homeland Security, and assist in arranging other needed services including placement, drug counseling etc. I presented the idea to the hospital, and it was approved. Next, I approached the St. Louis Metropolitan Police Department. They were familiar with our hospital and staff as we always had a strong working relationship in the past. They enthusiastically supported the idea and agreed to partner with us.
The next step was to form a team and delineate responsibili -
ARTWORK: Pediatrics by Katelyn Hanson, DO

ties. I would be responsible for performing all the acute and follow-up exams as well as providing for all their medical needs. The acute exams would be performed in the ED since it is open 24/7, is fully staffed with nurses, social workers and has the ability to perform laboratory studies and administer any needed treatment. Follow up exams were performed in my clinic. If I was unavailable, one of the ED attendings would perform the acute exam. The ED social workers would perform a cursory forensic interview. They were all trained by the Lead ED Social worker on how to interview a trafficking victim in a non-traumatic manner with a script prepared by the St. Louis Metropolitan Police Department. The Lead ED social worker would interface with Law Enforcement, CPS and any other agencies. Finally, we had a Child Protection Nurse who performed all the follow up duties; checking the labs, arranging appointments and calling to check on the condition of the patient.
Next, I developed a Clinical Practice Guideline. This outlined the assessment and management of suspected victims of trafficking. It was a comprehensive aid and helped health care practitioners every step along the way from recognizing a victim, interviewing them, ensuring their safety, assessment and medical management, obtaining resources &, interfacing with other agencies, safe placement
etc. Finally, it guided a healthcare professional on what to do if the patient did not disclose and advised them on how to remain an advocate for the patient informing them they can return to the ED anytime if their situation should change
Our program was successful. Detectives began bringing in victims. They did not act seasoned like criminals but just victimized children. They were not aggressive or angry. They were quiet, cooperative, almost passive. They welcomed the care and the attention. Often, they were tired and hungry. Their clothes were worn and dirty. They asked for simple items such as a comb or Vaseline for their lips. We noted other similarities. They were female, young in their early teens, had a prior involvement with Children’s Division, disclosed exchanging sex for money, drug use, being assaulted, prior history of STI’s, and even being involved in criminal activity including selling drugs or carrying weapons for their boyfriends.
In addition to providing medical care, our team served as a resource for education and training of medical personnel and the community. We lectured extensively to doctors, nurses and community groups. We shared our CPG with other institutions and even met with politicians who were interested in enacting legislation to prevent trafficking and aid victims.
Child sex trafficking is a public health crisis. It impacts all communities urban, suburban and rural. While some children are at higher risk, any child can be victimized.
As health care professionals, it is our responsibility to advocate for these victims. We must have the knowledge to recognize them, learn how to respond appropriately to their vast medical and social needs and do so in a compassionate manner. We must establish an environment where the victim feels safe to disclose, be heard and believed so they may seek care on their own. This means hospitals must create a comprehensive program with a multi-disciplinary team to coordinate the care these victims so richly deserve and desperately need.☤
ARTWORK: The Bony Pelvis by Katelyn Hanson, DO
Lines On Steaks
Written by Isabella Libreros, Editor-in-Chief

In a realm of mysteries, and a little girl making jokes,
My journey began. With cracks and quivers, an enigma unplanned, Years of searching, elusive as a wisp, My little duck-like walk, a puzzle to resist.
Through countless doors, I wandered with care, Doctors and opinions, their hands in the air, X-rays and questions, all seeking the why, The secret held tight, evading each try.
A needle, a puncture, Revealing the truth, the cause to elate, An inward pelvis, the root of my ache, A quest for relief, a decision to make.
At seventeen years, the surgeon’s embrace, To mend my hips, to claim back my space, Minutes before, on the surgical bed, A trembling heart, a tear that I shed.
A needle’s touch, my world went askew, The spinal embrace, my spirit subdued, A moment of weakness, a tear in my eye, As the nurse held me tight.
I woke to a vision, enshrouded in white, From hips to my toes, bound in bandages tight, A mummy I seemed, confusion did grow, Laparoscopy’s truth, I came to know.
The night was a torment, sleepless I lay, Excruciating pain, my constant dismay,
Days merged with pain, nights danced with sorrow,
Through writing, books, and tears, my soul found its consort.
My body transformed, unrecognizable and new, Swollen and tender, strength it withdrew, Learning to walk, like an infant I stood, Step by step, I reclaimed what once was.
Through trials of pain, my resilience was tried, Physical therapy, my grandma, a guide for each stride,
With strength I emerged, the pain easing away, My bones found their grace, the cracks did decay.
In the journey’s midst, a moment of dread, A meal on my table, my panic widespread, The lines on my steak, a vision so stark, Scars of the surgery, haunting like a mark.
An odd association, my brain’s trick of fear, A month without meat, as my mind steered clear, But days turned to weeks, weeks into months, My body rebuilt.
The pain found its solace, a distant refrain, No more cracking sound.
Now, scars are my story, A tale to behold, The lines on steaks, Don’t haunt me anymore.☤
WWW.PHYSICIANOUTLOOK.COM | 23
I am Not a Doctor... Nor Do I Play One on TV
SPOTLIGHT ON JASON LITTLEFIELD, M.ED
Written
by Physician Outlook Team

Jason Littlefield, M.Ed., is an Educator by training and a Social and Emotional Learning (SEL) Specialist. In the first of a series of thought-provoking articles written for Physician Outlook Magazine,
Littlefield discusses the importance of physicians (really ALL healthcare workers) understanding the role of social and emotional learning and the value of using SEL as a framework when interacting
ARTWORK: RENAL E-BOOK STUDY
GUIDE by Katelyn Hanson, DO
with one another, especially with our patients, for whom we have taken the “Primum Non-Nocere” oath of doing no harm.
24 | 2023 VOLUME 16
WHAT IS “SEL”?
SEL is an acronym that is widely used in the world of Education, but not one familiar to most healthcare professionals.
In a nutshell, Social and Emotional Learning is a developmental process through which humans learn skills that support healthy development and relationships. To be considered “Socially and Emotionally Competent” learners must be taught and master skills in the following areas:
Self-awareness
Self-management
Social awareness
Responsible decision-making
Relationship-building
SEL skills include goal setting, stress management, team building, and perspective-taking. He finds that the intense focus on diversity, equity, and Inclusion and the accompanying indoctrination is counterproductive and can potentially be harmful to humanity and to individuals’ well-being.
There is abundant research that indicates that social and emotional learning creates individuals who are more likely to achieve the goals that they set for themselves. Socially and emotionally competent learners also report higher levels of happiness, an objective sense of well-being, good overall physical health, as well as positive life outcomes. They are less likely to report career or personal life “burn-out.” Perhaps most important in the field of Medicine is that when SEL is intentionally embedded as part of a curriculum or patient/peer education, it can also serve as a powerful tool for prevention and helps to foster resilience.
Littlefield worries that the current emphasis on ideology that blindly promotes DEI undermines the very tenets of social and emotional learning, and could actually make our world LESS diverse, equitable, inclusive, and fair by undermining the importance of our individual and collective humanity.
The Hippocratic Oath emphasizes providing the best possible care to patients without bias or discrimination. An ideology that prioritizes certain identity groups over others can have the unintended consequence of causing potential conflict with this commitment, as we may feel pressured to consider identity factors when making medical decisions.
Littlefield gained a unique perspective and insight into the patient-doctor relationship and the new “woke” healthcare system after he became the primary caregiver for his aging medically-frail father. He highlights the need to re-humanize medicine and presents Empowered Humanity Theory (EHT) as a potential framework for positive change. EHT is a set of attitudes and practices that DECREASES the human capacity for prejudice and INCREASES and STRENGTHENS the neural pathways that are linked to our psychological well-being.
Littlefield offers strategies for self-care, patient care, and a way to TRULY defend the Hippocratic Oath, while still acknowledging that we have a long way to go in a society that has historically been marginalizing and ostracizing to many of our fellow humans.
Doctors and other healthcare professionals face unique challenges in these times of cultural upheaval, and one of the most difficult to navigate is that it is not currently socially acceptable to
voice opinions that differ from the prescribed teachings.
Littlefield advocates for using social and emotional learning techniques to find balance and inner dignity.
Incorporating social and emotional learning techniques will allow us to confront changes (and our patients) courageously.
The results of using EHT can be contagious and as team leaders, we will immediately reap the benefits by modeling positive interactions for ALL members of our healthcare teams. By treating the patient in front of us as the human that they are (without having to worry about the color of their skin, the language they are speaking, the zip code that they come from, or the insurance (or lack thereof) that they carry, we give that patient much needed human dignity and respect.
Systemic disparities in healthcare DO exist. We need to strike a balance between fostering a diverse and inclusive healthcare environment while simultaneously upholding the Hippocratic Oath’s core principles.
Littlefield became worried and upset when he realized that a very divisive ideology was being inculcated not just in his own field of Education, but into the fabric of almost EVERY discipline, including Medicine. He feels that a culture that prioritizes “the group” above an individual and that person’s amazing individual humanity has the potential to promote prejudice, shame, and resentment in the long run. As a society, he feels, we must be wary of any politically-driven ideology that promotes “groupthink” and reinforces dangerous stereotypes.☤
WWW.PHYSICIANOUTLOOK.COM | 25

ARTWORK: NEUROLOGY E-BOOK
STUDY GUIDE by Katelyn Hanson, DO
Littlefield is the Executive Director of EmpowerED Pathways, co-founder of Free Black Thought (whose slogan is “Black thought varies as widely as black individuals”), and also serves as a Board Member for the Institute of Liberal Values (a consortium of organizations that have joined together to advance liberalism, promoting the
classical liberal values of reason and freedom for the common benefit of all humanity).
To learn more about Jason Littlefield and his nuanced recommendations for re-humanizing Medicine, please go online to www. PhysicianOutlook.com and read “I Am Not A Doctor…Nor Do I Play One on TV.”

26 | 2023 VOLUME 16
The Memorial
A short story written by Gregory Jasani, MD
To read the full story go to physicianoutlook.com
”The Memorial” is a futuristic short story about a retired physician, as he accompanies his eight-year-old grandson Danny to the Healthcare Hero Memorial in Washington, D.C. The memorial commemorates healthcare workers who battled the COVID-19 pandemic. Despite his personal reluctance and painful memories, the physician agrees to visit the memorial.
Throughout their journey to the memorial, the physician reflects on his experiences during the pandemic and his struggles as a healthcare worker. He remembers the challenges, the constant threat of the virus, and the emotional toll it took on him. As they approach the memorial, he engages in conversations with Danny about the pandemic, explaining its impact, the role of healthcare workers, and the significance of vaccines.
The story underscores the challenges faced by healthcare workers and the intergenerational bond between the physician and his grandson.
My alarm goes off, though I don’t really need it. I haven’t really slept at all. Today is going to be hard and I know it. Every fiber in me is begging me not to get up, to just stay in bed and come up with some excuse why I can’t go. It would be easy enough; nobody asks too many questions when a man in his late
sixties says he doesn’t feel up to something. My knee has been bothering me a lot lately, and there promises to be a decent amount of walking. Maybe that could be my excuse? As much as I want to skip out, though, I know I have to go. My grandson wants to go, and how can I tell him no? I’m his grandpa; doesn’t that mean I am legally required to bend to every whim and fantasy he has? Plus, the creeping thought is always in the back of my mind that in the not-too-distant future he will be a teenager and probably want nothing to do with me. I have to take advantage while he still thinks I’m cool, if kids his age even use the word “cool” anymore. Still, of all of the adventures he could have chosen to take us on, why oh why did it have to be this? Of all the places to go and things to see on God’s green earth, Danny wants to go to the Healthcare Hero Memorial.
“Can’t you take him?” I asked Monte, Danny’s dad and my eldest son.
“He asked for you, Dad,” Monte replied to me. “Also,” he continued, “it wouldn’t be the same if I took him”.
That was true. Monte, perhaps as a result of all of the holidays I had missed, ran about as far away from the healthcare field as he could. I didn’t stop him; in fact, I encouraged it. Being a physician was soul-crushing. Monte, smartly, went into law. He is a lawyer at a successful tax law firm. He has never missed Christmas dinner. In
the 18 years that Monte lived under my roof, I had missed 6.
“You know there’s a reason I haven’t gone to that place!” I snapped back.
“I know, Dad,” Monte calmly replied. “You don’t have to take him. I wouldn’t blame you. But I am not telling Danny. If you don’t want to go, then you have to look Danny in the eyes and tell him yourself. If you can do that, then you are a stronger man than I.” Monte knew I wasn’t a stronger man than him. Especially not when it came to Danny.
“What are you drinking, Grandpa?”
Danny asks as I take a swig from my mug.
“Just some coffee Danny,” I reply. “Coffee makes grandpa run.” My coffee addiction is the result of a career spent absolutely wrecking my circadian rhythm. Day shifts, night shifts and all variations in between. At the height of my career, I drank four cups a day. I became so habituated to it that I could drink a big cup of Joe, then immediately go pass out in bed. Honestly, as with many, lesshealthy addictions, it became less about the stimulating effect and more about not crashing. I have since weaned myself down to 2 cups a day, but I’m pretty sure if I tried to ever go below that, the cumulative caffeine withdrawal would kill me. When I’m on my way out and can no longer swallow, somebody please run some coffee through my IV.

“Are you excited to see the

memorial?” Danny asks me, snapping me out of my musings on life, death and coffee.
I turn slightly to look back at him. He is sitting in the back seat, still quite a few years away from being old enough to ride shotgun, looking up at me with the big, blue eyes that he clearly got from his mother. I want to tell him how I really feel. I want to yell, “Hell no I’m not and the only reason I’m doing this is because I was too chicken-shit to tell you no!” But, of course, I say none of this. Partially
because his father would kill me if I introduced my eight-year-old grandson to the word “shit”. But also because how can I look my sweet, innocent grandson in the eyes, my grandson who wanted to spend his Saturday with me instead of watching cartoons, and say any of that. So I lie.
“Of course Danny. I’ve wanted to see it for a long time,” I say to him. I turn away as I finish the sentence. I don’t want my face to betray anything.☤
Dr. Gregory Jasani is a dedicated emergency medicine physician based in Maryland, where he currently serves as an Assistant Professor of Emergency Medicine at the University of Maryland School of Medicine. Dr. Jasani is passionate about teaching and research and possesses a special interest in administration, Emergency Medical Services (EMS), and disaster preparedness and response. He earned his Bachelor’s degree in Political Science and Government with a minor in Theology from Georgetown University, and he completed his Medical School education at The George Washington University.
Beyond his professional commitments, Dr. Jasani finds joy in various pursuits, including running, reading, scuba diving, playing the bass, and cherishing moments with his beloved wife and son. When asked about his choice to pursue his residency at the University of Maryland School of Medicine, his response was, “My wife did…sometimes the couples match works really well!”
Read Dr. Jasani’s full short story at physicianoutlook.com.
Sources:
https://www.linkedin.com/in/ gregory-jasani-2b31a525a/
https://em.umaryland.edu/ profiles/resident/2050/
 Image created with AI
Image created with AI
Rebuilding Trust in Medicine
THE CHALLENGE OF OUR TIMES
Written
by Physician Outlook Team, adapted from the Editorial “The Medical Establishment Past Reflections and Hope for our Future” written by Dr.
Chaminie
Wheeler, Pediatrician. (Lehigh County Health and Medicine Magazine, Summer 2022.)

Trust is a fundamental pillar in the field of medicine.
However, in recent times, we have witnessed a growing loss of trust in the medical system. This loss of trust has been exacerbated by the COVID-19 pandemic, which has had a significant impact on our lives, not only in terms of lives lost but also in the policies implemented to combat the pandemic and the global challenges it has posed. It is time to reflect on this situation and explore ways to rebuild trust in medicine.
Over the past two years, we have witnessed the devastation caused by COVID-19. Millions of
lives have been lost worldwide, and the policies implemented to contain the virus have generated controversies and challenges. In addition to the direct effects of the virus, there has also been an increase in mental health problems in the population. According to the National Alliance on Mental Illness, 21% of adults in the United States experienced mental illness in 2020. Furthermore, suicide has become the second leading cause of death in individuals aged 10 to 34. These statistics are alarming and compel us to reflect on how we have reached this point.
Amidst this situation, a phe -
nomenon called “disinformation” has emerged. It refers to ideas that are questioned and labeled as false or misleading information. It is concerning to see how disinformation has spread and how it has affected trust in medicine and healthcare experts. We wonder if the censorship and suppression of ideas contrary to established norms have stifled our freedoms and hindered the scientific process.
Science, as defined in the Oxford dictionary, is the systematic study of the structure and behavior of the physical and natural world through observation and experimentation. Discord, which arises when two parties disagree, is a fundamental element in scientific advancement. Challenging accepted ideas and subjecting them to rigorous testing and debates is essential to arrive at the truth and continue progressing.
But to better understand how the lack of scientific discord can impact medical progress, we can analyze two historical cases. The first is that of Dr. Ignaz Semmelweis, who challenged conventional ideas about handwashing in the 19th century. Despite his findings showing a significant reduction in mortality in childbirth, he was rejected, and his ideas were ignored by the medical community of the time. Only after his death, his work was recognized, and his legacy was honored.
The second example is that of Dr. Andrew Taylor Still, who founded Osteopathic Medicine. Dr. Still questioned conventional medical practices and sought more natural and holistic approaches to patient care. Despite the successful results he achieved, he faced exclusion and numerous difficulties. However, his perseverance and
30 | 2023 VOLUME 16
IMAGE: JC Gellidon, UNSPLASH

dedication to a more humane and patient-centered medicine eventually led to the recognition of his work and the establishment of Osteopathic Medicine as a legitimate medical discipline.
These historical examples teach us the importance of allowing and fostering scientific discord in the field of medicine. We must be willing to challenge established ideas and subject them to rigorous scrutiny. Additionally, we must be humble and acknowledge our mistakes when we make them. Only through this process of questioning and learning can we move forward and rebuild trust in medicine.
Another crucial aspect in regaining trust in medicine is financial transparency. It is important for patients to know where their money truly goes and how it is distributed within the healthcare system. Currently, less than 7.5% of the revenue generated in the healthcare system in the United States goes towards physician income. This raises the question: What happens to the other 92.5% of the revenue? Patients deserve access to this information and
an understanding of how their resources are being utilized.
Lack of financial transparency in the healthcare system can also result in hidden costs for patients. For example, the cost of a chest X-ray can vary significantly depending on whether the patient has health insurance or not. This lack of cost clarity creates mistrust and necessitates the promotion of transparency in this aspect.
Furthermore, the lack of medical autonomy is another factor that affects trust in medicine. Often, medical decisions are conditioned by insurance company policies and the availability of covered medications. This limits the ability of physicians to provide the best possible care to their patients and can generate frustration for both doctors and patients. It is essential to regain medical autonomy and allow physicians to make decisions based on the individual needs of their patients.
In conclusion, rebuilding trust in the field of medicine requires several important steps. We must foster scientific discord, allowing ideas to be challenged and subject-
ed to rigorous scrutiny. Additionally, promoting financial transparency is crucial, providing patients with clear information on how their resources are being utilized. Lastly, we must regain medical autonomy and allow physicians to make decisions based on the individual needs of their patients.
In this era of medical and technological advancements, it is crucial to rebuild trust in medicine. Together, we can work towards improving medical practice and ensuring that patients receive the best possible care.
It is time to come together and build a healthcare system based on trust, where the health and well-being of patients are always the utmost priority.☤
References:
From Lehigh County Health & Medicine Summer 2022by Hoffmann Publishing Group. (2022, June 11). The Medical Establishment. issuu. https://issuu.com/nhgi/docs/lchm_summer22_issuu/s/16064897
Living with Covid-19
THE LATEST PANDEMIC
Written by Ana Paula Velez, MD
Since the creation of the Earth, bacteria, fungi, and viruses have been part of nature. Humans have been able to coexist and adapt to these organisms, even using them to treat potential infections and manufacture vaccines. Examples of the wide use of these organisms include the discovery of penicillin by Alexander Fleming (1), fecal transplants to treat Clostridium difficile (2), the use of adenovirus vectors for gene cancer treatment and vaccines (3), and the use of bacteriophages to treat multidrug-resistant organisms (4).
Approximately every century, the world population suffers from a severe lethal pandemic. These pandemics usually last 2 to 3 years. Eventually, the microorganism becomes less virulent, vaccines and medications are developed, and the human body acquires immunity against the new pathogen.
On January 30, 2020, the World Health Organization declared an outbreak of a novel Coronavi -
rus-19 (COVID-19) that originated in Wuhan, China, a public health emergency of international concern (5). Multiple unanswered questions about the novel virus shook the world. Questions about the transmission rate, fatality rate, treatment options, and possible vaccine development had to be answered immediately. Human behavior drastically changed, and social isolation became the norm worldwide. Unfortunately, the necessary changes in human behavior introduced to lessen the propagation of the virus resulted in significant negative economic, social, and emotional impacts. Additionally, managing other chronic health illnesses, such as diabetes mellitus, hypertension, chronic kidney disease, heart disease, obesity, and psychiatric disorders, became more challenging, resulting in devastating consequences.
Eventually, several COVID-19 treatment options became available for outpatient and inpatient management (6), and multiple

vaccines were developed to acquire passive immunity (7). Today, three years after the pandemic, and after more than 103 million cases of COVID-19 and over 1.1 million deaths in the United States, managing this lethal infection has finally changed the prognosis of COVID-19 since the start of the pandemic. The development of vaccines is attributed as the most significant impact leading to a reduction in mortality. Thanks to the new developments in treatment and vaccines, humans have returned to a semi-normal lifestyle with everyday social interactions.
Finally, COVID-19 has been added to the innumerable list of pandemic infections that have affected humankind, making us aware once again that the battle against infectious diseases is endless.
This will not be the last pandemic, but humans have, once again, survived, adapted, and learned to live with one of the most lethal pathogens ever encountered.
Hopefully, the lessons learned will persist until the next pandemic comes...☤

32 | 2023 VOLUME 16
With a background as an accomplished artist, Dr. Ana Velez holds positions as an Associate Professor at the University of South Florida and an Infectious Diseases physician, who has practiced at Moffitt Cancer Center with immunocompromised patients since 2007. While she explores a diverse range of artistic styles, her preference lies in depicting the microorganisms she encounters daily in her healthcare practice. Through her art, she skillfully conveys the complexity and beauty present in some of the most formidable pathogens. Driven by a fusion of vivid hues and subtle tones, her paintings effectively capture the essence of fungi, bacteria, and viruses.

WWW.PHYSICIANOUTLOOK.COM | 33

ARTWORK: FEMALE FORM 5 by Katelyn Hanson, DO
Female Incontinence: Awareness Needed
Written by By Samantha Pulliam, MD
Women’s health has a long history of being sidelined. Federal law only required the National Institutes for Health (NIH) to require grant recipients to include both men and women in clinical studies in 1994. Women’s health research accounted for 10.8% of the NIH budget in fiscal year 2020.
Women’s health issues, especially those cloaked in embarrassment, are uniquely at risk of being overlooked or ignored.
Urinary (UI) and fecal incontinence (FI) are among the conditions for which shame keeps women from speaking with their physicians about bothersome symptoms, which contributes to today’s grim reality: the adult diaper market now exceeds the market for baby diapers.
I believe this is wrong, particularly when easy, at-home treatment exists.
UI and FI are common progressive disorders that desperately deserve more attention. Vastly undertreated, they are the most prevalent pelvic floor disorders that women experience. UI affects 78 million and FI affects 12 million women in the U.S. alone. Globally, the numbers are in the hundreds of millions. The theme for this year’s
Women’s Health Week is “Women’s Health, Whole Health: Prevention, Care and Wellbeing.” I believe continence is core to a woman’s well-being, and annual screening should be part of a woman’s annual wellness appointment regardless of age.
The impact of untreated pelvic floor disorders
Incontinence affects women disproportionately. Beyond the staggering prevalence numbers, pelvic floor disorders negatively impact women’s psychosocial and emotional wellbeing and are associated with increased economic burden, decreased physical activity, and functional decline. Among older women, UI is a major risk factor for falls, hospitalization, nursing home admission, and dependance on a caregiver. Women with UI experience faster and greater degrees of physical decline when compared to women who are continent. They score lower on physical performance tests and show significant declines in muscle mass. Research shows that women with UI may reduce physical activity or stop exercising to manage symptoms, which can lead to functional decline and even worsen UI symptoms over time.
Women rarely seek treatment. It is estimated that as few as 25% of women with UI seek care and

of those who are care-seeking, many have had symptoms for six years or more. When queried, many women indicate they did not know treatment was available, they prioritized other issues, and their healthcare provider did not ask directly about these symptoms. Individual- and institutional-level barriers have been documented as limiting factors in care-seeking and participation in treatment. All the while, prevalence of pelvic floor disorders continues to increase in the population, sufficient to regard it as a population-level health concern.
First-line treatment: promise and perils
The first-line treatment for UI and FI is pelvic floor muscle training (PFMT). Clinicians often encourage women to access PFMT by doing “Kegels.” However, data show few women do them correctly or consistently enough to effectively reduce symptoms. This contributes to healthcare providers’ reticence to recommend first-line therapy, leaving many women living with leaks.
The pandemic accelerated the availability and adoption of telemedicine and digital health, which have favorably shifted how treatment can be accessed. Thanks to devices, wearables and apps, many can now receive treatment in the
WWW.PHYSICIANOUTLOOK.COM | 35
environment that’s most comfortable, the home. Pelvic floor health has benefitted. Today, women can perform PFMT at home using a mobile phone app paired with a medical device, supporting correct and consistent PFMT. While there are many pelvic floor strengtheners, very few support the rigorous data that women’s health deserves and allows clinicians to remain engaged in treatment. Level-one evidence shows pelvic floor muscle training is most effective when performed under the supervision of a skilled healthcare provider, which suggests that pelvic floor muscle strengtheners that require a prescription have the best chance for symptom relief.
The advent of digital health and telemedicine has made firstline treatment practical and accessible to a large group of women, regardless of location. However, awareness and discussion must occur before women can access treatment. The open-access manuscript and infographic, “Female Urinary Incontinence Evidence-Based Treatment Pathway: An Infographic for Shared Decision-Making,” seeks to increase access first line therapy by packaging evidence-based guidelines for UI screening and treatment in a graphical, easy to access format for use by clinicians on the frontlines of women’s health. Professional organizations and health systems may also find it valuable for clinician and member education. The infographic depicts female UI risk factors, influences on care-seeking, screening and evaluation. It also includes a stepwise treatment approach, for which there is broad international and multidisciplinary agreement. It synthesizes current evidenced-based literature as well as multiple UI screening guidelines, position statements, and associat-

ed references from the American College of Obstetricians and Gynecologists, the Women’s Preventive Services Initiative, American Academy of Family Physicians, American College of Physicians, the Society of Urodynamics and Female Urology, the American Urological Association, and the American Urogynecologic Society.
Incontinence is common but it’s not normal
Incontinence can have significant negative impacts on women’s lives. The uncertainty and unpredictability that come with UI and FI can affect women’s mental health, quality of life and relationships. Women may limit their physical activity or social engagements, experience feelings of isolation and distress and/or experience problems with intimacy.
Presently, 62% of adult women live with bladder leaks, and this is expected to rise due in large part to the size of the aging demographic and the national obesity epidemic, both of which are associated with increased risk of UI. I believe UI is an important health condition that warrants screening and treatment.

Level I evidence supports PFMT effectiveness and describes this intervention as most effective when performed under the supervision of a skilled HCP (supervised PFMT/sPFMT) for a period of at least 12 weeks. Digital health tools allow clinicians to treat more women effectively while allowing treatment to take place where it’s most convenient, at home. Women’s Health Week offers an opportunity to remove the veil of shame that keep women from discussing their symptoms with their providers. While incontinence is common, it is not normal. Effective treatment is available and accessible. In some instances, treatment is covered by insurance. No woman should be left feeling that adult diapers are her only solution.
From policy makers to families to individuals, all of us have a responsibility to prioritize women’s health.
Women’s Health Week is an excellent first step.☤
36 | 2023 VOLUME 16
Image created with AI

ARTWORK: CARDIO E-BOOK STUDY
GUIDE by Katelyn Hanson, DO
WWW.PHYSICIANOUTLOOK.COM | 37
Hanson’s Anatomy
THE COLORFUL JOURNERY OF A VISUAL LEARNER IN MEDICINE
Written by Katelyn Hanson, DO
Istarted college at seventeen, knowing I wanted to be a doctor.
I’m originally from Portsmouth, New Hampshire, but I yearned to explore a place vastly different than where I grew up, and that’s how I ended up at Tulane University, in New Orleans, Louisiana. New Orleans is a bright, bold, and loud place, and I thrived there. As I studied, I was inspired by those bright bold colors of the city, and began DRAWING to reflect what I saw around me. I incorporated those colors into my notes for my premed classes; benzene rings with vibrant reds and blues, biochemical pathways with neon pinks and oranges, and physics schematics in the gold, purple, and green of Mardi Gras. It was during that time that I realized I was a visual learner, and that my brain studied best through drawing.
I returned to New England to study medicine, and found the curriculum so much more difficult to engage with than my time as an undergraduate. I couldn’t figure out how to study. I would attend lectures and try desperately to scribble down notes as the professors taught, but couldn’t seem to retain any of the information in front of me. I had the hardest time studying human anatomy; listening to descriptions of the human body wasn’t enough for me to understand it. I then decided to re -

turn to my roots, to the method of learning that had worked so well for me in the past. I stopped going to lectures, and instead would spend hours and hours at the library, pouring over books and at-
lases and creating my own bright and bold images that represented the subject matter. And with that, Hanson’s Anatomy was born.
I regained my love of learning, and I began to excel in my course -
38 | 2023 VOLUME 16
work. I continued to create and began to share my work on social media. Through these online platforms, I met thousands of other students who, like me, realized that they too best learned through visual mediums.
Traditional medical school education is not for everyone, and by introducing my method of visual learning with the world, many others sent me messages saying my work inspired them to start learning through artwork as well.
During my clinical years in medical school, once I had passed my first two steps of the USMLE (United States Medical Licensing Examination), I began to paint. I took anatomical concepts that I had spent the previous two years meticulously drawing, and began to express them with acrylics on canvas. I rekindled my love of art and my love of anatomy, and continued to share my work with a wide reaching audience online.
After medical school I entered a dual residency program in Emergency Medicine and Internal Medicine in Philadelphia, PA. While I found myself with much less free time for creating than I had previously known, my co-residents and co-workers were incredibly supportive of my way of learning, and of my art. It was during this time that my husband and I self-published my book, Hanson’s Anatomy, The Complete Book, and began to sell online. The book consisted of all of the notes I had made during my time in medical school to study for the USMLE, and it became wildly successful. Again, I found myself meeting people from all over the world who could relate to visual note taking, and who were inspired

by my work. During my time in residency I also began to experiment with painting portraits as well as more abstract images of the human body.
I stayed in Philadelphia for an additional year to complete a fellowship in Critical Care Medicine, where I had found my niche. I had worked through the pandemic in an extremely busy ICU, and I found that I loved the acuity, the procedures, and relationships with patients and families that I could build during a patient’s stay in our unit. Critical Care Medicine encompassed the things I loved
ARTWORK: HEENT E-BOOK STUDY GUIDE by Katelyn Hanson, DO
about both Emergency Medicine and Internal Medicine, and with the support of my mentors and my colleagues I developed my passion for the specialty.
I just moved back to my home town of Portsmouth, New Hampshire, to begin a career as an Attending Physician. I’m excited for this next chapter, to teach new residents about my specialty, to continue to share my style of visual learning with new students, and to get back to the drawing board myself, to create new work.☤
WWW.PHYSICIANOUTLOOK.COM | 39
Iam perched alongside resting volcanoes, gazing down pine-covered, arid hillsides into a valley where there are meadows and houses, roads and cars. I know this vista like an old friend. Like me she shows signs of wear, fine creases where before the topography was smooth and unbroken like innocent skin. I do not notice. Mountain breath on my face, I recognize the puffs of cumulus now appearing as a premonition of thunderstorms gathering, but these are typical here. They will pass.
How many times have I sought perspective by scrambling to this vantage point, lungs straining in the thin air, my unease pushed into my legs as they pump, step after step, over rocks and pumice and roots? How many stories have I brought here, worried over in my mind like stones in the stream until they should smooth out?
Today feels different.
I am no longer an angst-filled adolescent, pitting my independence against the desire for love. Long ago I decided on my career, severed ties with toxic relationships, chose to move away, reconciled my yearning to move back. I am happily married and have typ -
Magma
Written by Claire Unis, MD
ical maternal anxieties about my children, but today’s pilgrimage isn’t about me.
Gaze flowing over the rock faces as they change color, dark plum to gray to cream and speckled with green, I remember how I yearned to see the world in black and white. I so admired the friends who did not hesitate in anything, decisions at the ready, confidence to spare. Their self-assurance beckoned me like fire, singed me in the end. A warning. A lifetime of introspection brings me back to this same vantage. To think I used to look for conflict so I could form an opinion about it, testing my morals and knowledge of world affairs and measuring my self-worth, a bit, on how articulately I could defend my position. That wasn’t me, I realize now. That was who I thought I should be. An aspiration, like a constellation, with points of brilliance but a picture you had to squint to imagine was actually there.
And now? I built my life on the handholds and footholds I knew would hold, steps of surety in a trail that could be slippery. I had no heart for politics. I cared deeplysometimes too deeply - and found my way to a career in which this
was more a boon than a liability. I loved to solve problems. I loathed capitalism. I am a doctor for many reasons but perhaps chief among them, because all the signposts pointed the same way.
Near where I sit there is an earthquake fault. You can stand on the edge and look down into the crevasse, imagining the magma that bubbles many layers underneath your feet, threatening to rend this half of the world from the other, a stone’s throw away. The valley shows no such sign of distress from this vantage, but anyone who has grown up around dormant volcanoes knows the tumble and shudder of this unpredictable venting, a pointed reminder: nothing is certain.
I did not guess at the depth of the fissures that threaten civilized society. Like the houses below me, in a fertile valley with a rim of solid-appearing mountains around them, I thought I had found my forever home.
With science as bedrock and a constant trickle of knowledge, medicine seemed protected from the whimsy of political fire.
40 | 2023 VOLUME 16


Most volcanoes erupt in a cycle of hundreds or thousands of years - and not in our lifetimes. The number of buildings below me testify that no one expects this one to blow. But it is hard to ignore the rumblings of magical thinking over science, of fear over evidence, of narcissism over communal welfare, bluster over nuanced thought. Tectonic plates are shifting. What I see now, taking in the granite thrusts and rolling mountainsides, is not just forest and trees, but the paths lava has taken - may take again - as it makes its way down from the mountaintop.☤
Claire Unis MD MFA is a pediatrician and author of a memoir about drawing on diverse experiences in the process of becoming a doctor, titled Balance, Pedal, Breathe: A Journey through Medical School. She facilitates writing workshops, narrative medicine sessions, and discussions of literature for her medical group in northern California. Her writing has appeared in Intima, East Iowa Review, Awakenings Review, and The Examined Life. Find her at www. claireunis.net, or on social media, @literaryartinmedicine.
Image created with AI
WE ARE... going to be a Doctor!
FROM A PENN STATE NITTANY LION TO A TEMPLE UNIVERSITY HOOTER OWL
Spotlight on future physician Jackson Kollasch, Lewis Katz School of Medicine Class of 2027

Jackson graduated from Penn State University Main Campus in 2022. In his 4 years of studies, he achieved a Master of Public Health in Community and Behavioral Health, a B.S. in Biobehavioral Health, a Minor in Global Health, and a Graduate Certificate in Global Health. As a member of the prestigious Penn State Blue Band for all four years of his undergraduate education, the future Dr. Kollasch will be starting his M.D. journey at Temple University Lewis Katz School of Medicine in August of 2023.
Jackson’s preliminary plans are to pursue a residency in Hematology/Oncology, although he is aware that this may change over the next 4 years. He has spent his gap year working as a medical scribe at the UPMC Hillman Cancer Center in York, PA under the direction of Dr. Gunning-Carter. Here, he learned more about the
importance of patient-provider interactions as well as the impact that environmental factors such as travel, socioeconomic status, and access to resources can have on a patient’s prognosis. Jackson is passionate about addressing disparities in healthcare, which fueled his selection of Temple University as his place of study. He is excited to work with a diverse population of patients and gain valuable experience at a Level 1 Trauma Center.
Through his undergraduate career, Jackson has been focused on achieving a holistic perspective on healthcare and Public Health. While the COVID-19 pandemic halted plans to work with Public Health organizations in South Africa, he was able to work as an intern with Church World Service providing support and fulfilling basic needs of refugees living in Lancaster County, PA. Being exposed to the marginalized experience of healthcare strengthened his passion for becoming a better advocate for all patients, emphasizing the importance of respect in the examination room.
Jackson believes that the future of medicine is full of empathy, advocacy, and passion.
As time marches forward, we discover new ways to treat and advocate for patients. And, while the
science remains steadfast, the art of Doctoring evolves.
The following two excerpts are from Jackson’s essay on the Russian-Ukraine conflict’s effect on global food insecurity.
Wars and conflicts between countries have been known to result in mass displacements of people. This leads to an increased food demand yet a decreased food supply. In addition to having decreased access to food, this causes steep increases in food prices at local markets (IFPRI, 2015). This is seen with some of the displacements and attacks that have occurred in this conflict. Currently, Russia and Ukraine make up 30% of the global exports of wheat (McFarlane et. al., 2022). Due to both of them being in conflict, their efforts are being placed elsewhere. Additionally, when areas with plants and workers who contribute to wheat exports are attacked, this decreases the capacity at which the country can export this good. This is a concerning aspect of the conflict because of the already worsening climate crisis that is currently affecting wheat exports.
One of the most important takeaways I’ve learned from my public health graduate research, is that children are not as autonomous as we may think they are. When you are designing a health intervention or providing a service that serves children, it can get difficult due to
42 | 2023 VOLUME 16

their lack of autonomy. Children often do not have control of their schedules, they cannot effectively transport themselves, and, most importantly, they cannot provide for themselves. Children have access to the food that is given to them, which makes them the most vulnerable when it comes to food insecurity. With the Russia-Ukraine conflict decreasing wheat exports, the already malnourished children will be even more disadvantaged.
UNICEF has emphasized the vulnerability of children in the Middle East and North Africa because, in some countries, 90% of the food they eat is from exports, and chil -
dren already don’t receive adequate nutrition. This conflict will only exacerbate this disparity. Aside from these speculated outcomes, we are already seeing countries that are experiencing higher rates of food insecurity due to the ongoing war.☤
Read Jackson’s full essay at physicianoutlook.com.
A Personal Retrospective in Three Parts
 Written by Susan J. Baumgaertel, MD
Written by Susan J. Baumgaertel, MD
At the end of a year and the beginning of another, emotions tend to run high.
Whether it be the loss of a loved one or the tangled web of interactions with relatives; an unexpected illness or travel plan glitches; wonderful moments to cherish or joyful connections – all are wrapped up like presents topped with emotional bows.
The opening and unraveling part often takes courage and creativity.
This is a series of three short vignettes involving emotions and circumstance, fitting for the changing of seasons and passing of time.
Part One: Empathy
A couple of years ago, during a previously unusual snowstorm in Seattle, I was carefully driving home from work in sub-freezing temperatures. I had seen many patients who braved dangerous travel that day to get medical care from me, and was feeling satisfied that I was able to be of help.
On my snow route home, I got off the main road to stop and wait for a light to turn green before crossing the overpass to get to the icy side streets that led to my home just a mile away.
A man was holding a cardboard
sign with a scrawled plea for help. He had a coat on, hood up, partly protected from the dense snow that was blowing everywhere.
As he approached my car, I hastily grabbed a $20 bill from my purse and rolled my window down, the sudden icy cold wind rushing into my warm car. His face lit up when he saw my gesture, and he came close by.
I held out my offering. He reached out and our fingers touched for a brief moment. He was not wearing gloves, and I had taken mine off to get into my wallet.
My breathing stopped as I saw his hands. All ten fingers were shriveled and had turned black.
I looked up at his face and our eyes met. That moment seemed like an eternity but it only lasted a few seconds. His expression of thanks was almost imperceptible.
Our interaction was abruptly halted as the light turned green and I had to drive on.
I turned onto the overpass and drove two blocks further. I then pulled over, knowing that I was risking getting stuck as I pulled off the road into deeper snow next to the hidden curb.
My tears flowed and I couldn’t stop crying long enough to continue driving. I could only think of the next 24 hours in this man’s life, hoping that someone would find
him if he fell or lay down.
I hoped that he would be taken by ambulance to Harborview ER, our region’s Level 1 trauma center. I thought of the amputations that needed to happen. I wondered if he would get subsequent care.
I am still moved by the vivid memory of our fingers touching for that brief moment.
Our eyes meeting.
The contrast in circumstances.
Food, water, and shelter are essential for human life.
And,
Empathy.
Part Two: Joy
I never thought I’d be a Navy mom.
Never, in even my wildest dreams.
My daughter is now serving as an officer in the US Navy, and I couldn’t be more proud!
For Christmas this year we paid for pricey plane tickets to fly her home for 10 days. She sent screenshots of her itinerary through Atlanta to Seattle, with a return trip via Detroit.
As always seems to happen every end-of-year, a lot of tasks get scrunched together. I was balancing the books for my new business, seeing a final few patients before my vacation, and thinking about last-minute gifts, which seems to be my usual modus operandi.
Mixed into the final frenzied weeks I had a number of personal medical appointments, blood tests, diagnostic imaging, and consultations. My daughter was following along via texts and was hoping my upcoming weekend – the one prior to her arrival –would be restful.
I was finally able to make time for the Christmas tree outing (see Part Three for the story!) and she laughed at the naked tree picture I texted. I hoped I would have time to decorate before she came.
Two days before her arrival I had finally finished decorating the tree, hanging up the stockings, arranging holiday cards, and taking pictures to eventually text her. She called and I dashed to get my phone which was in another room.
She said, “Go check the front porch, there is a present for you.”
I eagerly opened the door.
Nothing.
Well, it wouldn’t be the first time a delivery service marked a package as delivered when they hadn’t yet arrived.
I went back inside, still on the phone, and said there was nothing there.
She said, “Go look again.”
And there she was – running on the sidewalk, still on her phone with a huge smile, up our steep sets of stairs in a flash and into my arms for the biggest hug ever!
Two days early.
The perfect present.
I couldn’t stop crying, Tears of joy.
Part Three: Humor
Have you ever noticed the frequency of certain numbers, letters or words?

ARTWORK: There’s No Box That Could Contain You by Joanna Cranston,
MD
“I created this piece to reflect my own journey from surgeon to artist, and to give other physicians hope that they can be fully themselves, not just one facet of themseves.”
Dr. Joanna Cranston Is a general surgeon by training and a U.S. Army Veteran. She left clinical practice in 2021 to found Words of Hope Designs, where she creates hand lettered art with messages of hope. She enjoys the freedom of not trying to fit in one particuar box, and wants other physicians to experience this freedom as well. She lives in Tennessee with her three children, and loves hiking, thunderstorms, and coffee.

Sometimes I find it fun to notice alliteration in everyday events – often afterwards. Or, maybe by focusing on something, I see more of it? Our brains are truly wondrous.
In the past almost thirty years of being a physician, many of my patients and most of my staff called me “Dr. B.” Saying “B” is so much easier than pronouncing my last name!
Along the way, I’ve learned a few B words from my daughter who is in her twenties.
I gifted her my 2004 Honda CRV that she promptly named Beatrice. Beatrice is still doing well, now past 100,000 miles.
My late beloved rescue cat came pre-named: Buttercup – yes, named after Robin Wright’s character Buttercup from The Princess Bride.
Apparently I have a bougie car – and here I thought cars in that category would be BMWs , Mercedes et al (I have an Audi Q3).
I have learned that a Navy ship, an iffy hotel and my body all can be described as busted.
Okay, I have never named my car but we do call that rather large spider in the corner of our garage Brad.
I have just recently learned that bussin refers to food that is so f*ckin good.
What is really fun is when some of these words all come together in one place – like when I went to get our Christmas tree this year.
I arrived alone at Donna’s Trees, set up in the side parking lot of a nearby golf driving range and nine hole course. I was the only one there, browsing around looking at trees.
When did they get so expensive? I typically go for a seven foot Noble fir, but they were all in the $220+ price range.
I was drawn to a certain tree, but it didn’t look so great. A number of branches had tips that were dried and less-than-green.
The friendly farmer-type young man approached and asked me if I had picked out my tree. I said yes, but he then said, “You don’t sound so sure.”
I explained that I didn’t have my assistant with me and this was the first time in a while I had picked out a tree by myself. I explained that my assistant was in the US Navy and was coming home for Christmas.
He quickly became more attentive and then asked if I wanted him to hold out a specific tree to take a better look. I pointed to the one and he took it for a twirl.
I said, “It looks busted .” He said, “Well, sometimes the trees on the edge of the orchard don’t do so well.”
I asked if he’d cut me a deal. Without hesitation he offered me $80 off. I felt like this one was about to go to the wood chipper soon, but I said yes.
He happily cut the end and trimmed a few straggling lower branches, and then asked which car was mine. I said that my previous car – now named Beatrice – was the tree car but, since I no longer owned it, I wanted the tree loaded up on top of my Audi.
He chuckled and told me about three “kids” buying a tree earlier that day using their parent’s bougie car – I think it was a BMW. We then wondered why a certain generation names their cars.
I told him I didn’t name my car but we had a spider in our garage named Brad. We then had a funny discussion about spiders. He made sure to put the tree in the “shaker” to shake out the old needles – I told him I appreciat-
ed him shaking out the spiders.
Once home, I lugged the tree up our steep front stairs (yay core and upper arm strength!) and settled the tree into the tree holder in the living room. My husband asked me if they were out of trees – cue the story of the busted tree that was $80 off.
I later told this story to my daughter who had a good laugh, and was amazed I had used my new vocabulary!
She subsequently made The Best Lemon Cookies which were definitely bussin
I smiled as I stood in our kitchen, looking through the window at my bird bath with the juncos taking turns bathing.
A whimsical week, À bientôt!
~ Dr. B☤




Publisher: Marlene Wüst-Smith, MD Editor-in-Chief: Isabella Libreros, Marist ‘24 Managing Editors: Hannah Bushery, Marlene Wust-Smith, Jill Labecki VP of Advertising: Pamela Ferman, VP of Operations and Digital Media Strategist: David Ramirez Director of Art and Production: Hannah Bushery Marketing/
Copyright Editor/Journalism/Social Media Intern: Madison M. Smith
Contributing Authors: Alicia Roselli, Scott Abramson, MD, Roxanne Bruce, MBA, DrBA, Amy Mickle, MS Ed. LPC and LMHC, Terry Wilcox, Executive Director of Patients Rising, Marlene Morales Tollett, MD, Ann Di Maio, MD, Isabella Libreros, Editor-in-Chief, Jason Littlefield, M.ED, Gregory Jasani, MD, Ana Paula Velez, MD, Samantha Pullman, MD, Katelyn Hanson, DO, Claire Unis, MD, Jackson Kollasch, Lewis Katz School of Medicine Class of 2027, Physician Outlook Team
Cover Art: Katelyn Hanson, DO
Published by “Physician Outlook Publishing” Editorial policy: Physician Outlook magazine is a national magazine dedicated to empowering physicians and their patients to improve the world of medicine together. Editorial decisions are based on the editor’s judgement of the quality of the writing, the timeliness of the content, and the potential interest to the readers of the Physician Outlook magazine. The magazine may publish articles dealing with controversial issues. The views expressed herein are of the authors and/or those interviewed, and may not reflect the official policy of the magazine. Physician Outlook neither agrees, nor disagrees with those ideas expressed, and no endorsement of those views should be inferred, unless specifically identified as officially endorsed by the magazine.
“Letters to the Editor” email: hello@physicianoutlook.com
Information on advertising, subscriptions, and job board email: hello@physicianoutlook.com
“Physician Outlook” is a registered trademark.
WWW.PHYSICIANOUTLOOK.COM | 47



Cover Artist: Katelyn Hanson, DO
Dr. Katelyn Hanson is a passionate and talented emergency physician affiliated with Portsmouth Regional Hospital in Portsmouth, New Hampshire. After high school, she pursued her education at Tulane University in New Orleans, where she double-majored in Cellular and Molecular Biology and Spanish. Upon returning to New England for medical school, Dr. Hanson discovered a wonderful way to blend her appreciation for vibrant colors and art with her fascination for science and the human body. To follow her journey and explore her artwork, you can visit her website hansonsanatomy.com and follow her on Instagram @hansonsanatomy.
Impressed by her unique approach to combining art and medicine, Physician Outlook Magazine decided to collaborate with Dr. Hanson to showcase her extraordinary artwork, allowing a wider audience to appreciate her story and the beauty and significance of art in the medical field.


























 Written by Amy Mickle, MS Ed. LPC and LMHC
Written by Amy Mickle, MS Ed. LPC and LMHC

















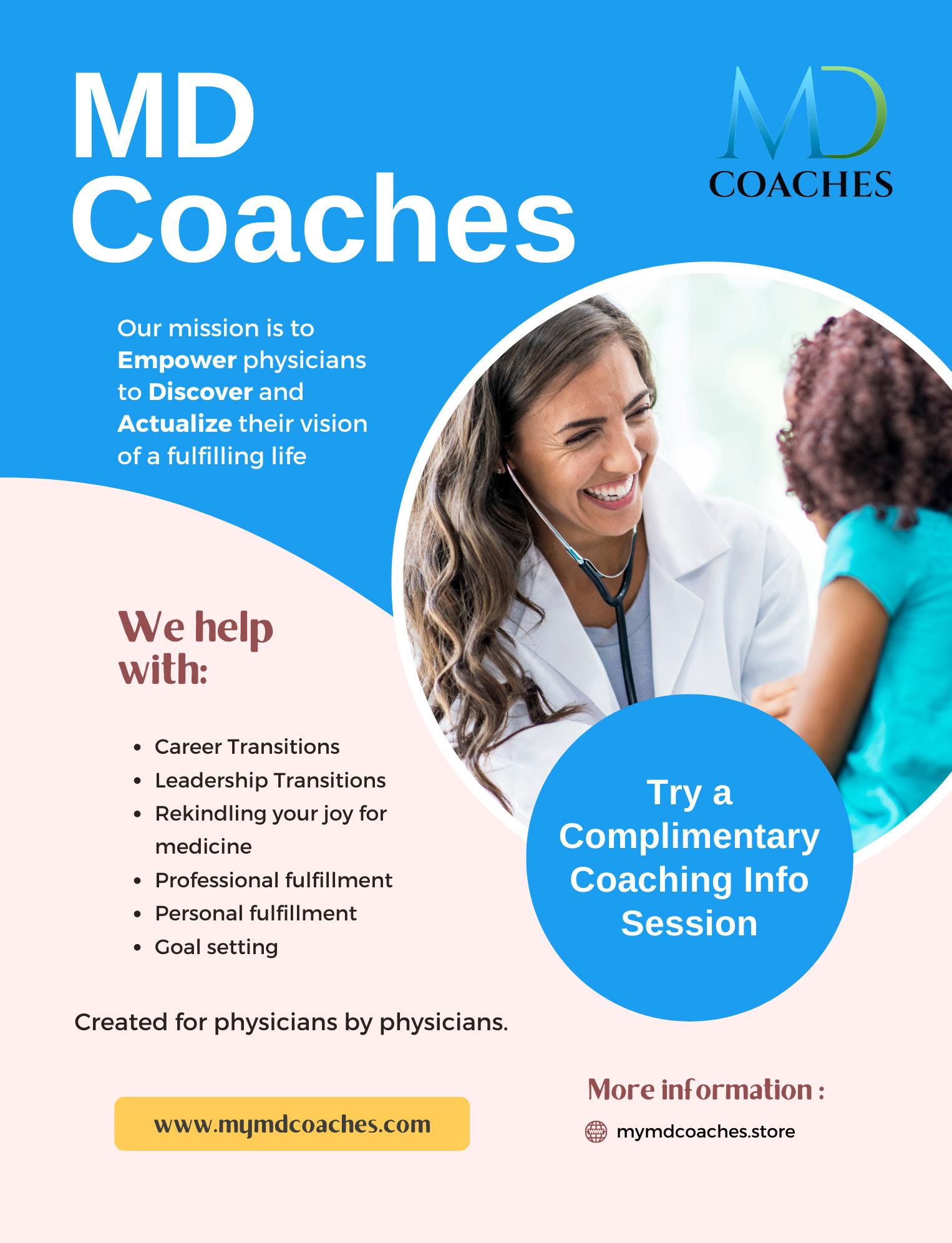


 Image created with AI
Image created with AI
















 Written by Susan J. Baumgaertel, MD
Written by Susan J. Baumgaertel, MD








