








His images are haunting which is an odd and harsh word for flowers to portray. Elusive like a Wednesday and catalytic like colors ought to taste, Maz Ghani’s photographs make the viewer look again with an unsettled curiosity.
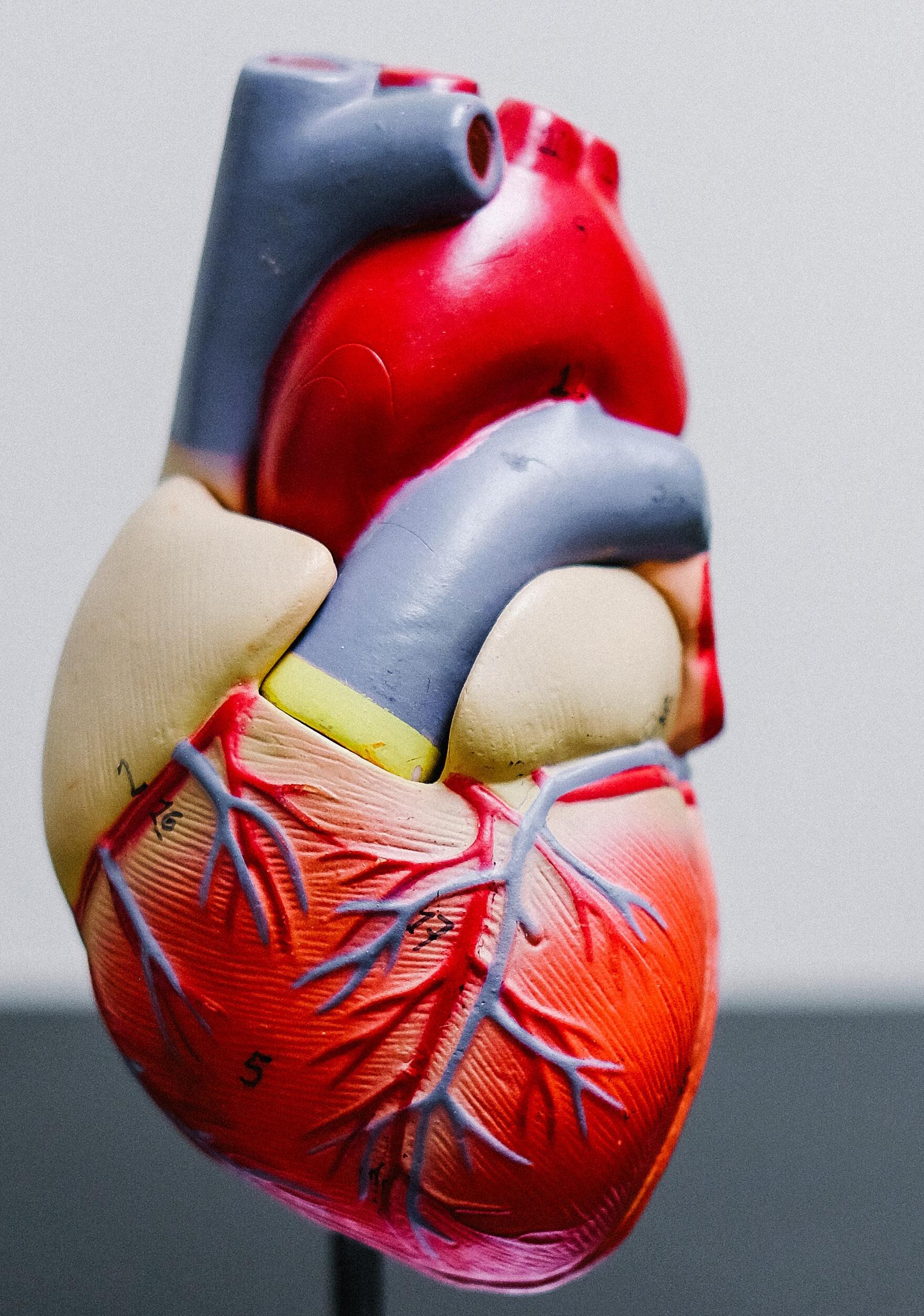
“My father was an accountant by trade but when he moved to Australia and Canada he worked in factories because that is what jobs he could get being a Middle Eastern foreigner. He did enjoy photography and he told me over and over to approach the world with curiosity,” Maz spoke of his upbringing and a father whose daring explorations defied being just secure or safe and risked shame. Maz Ghani would take his curiosity and his cultural pressures to succeed and enter the world of Medicine as a Radiologist. Still that end point is too flat a photograph. Maz’s life choices would layer onto itself like its’ own series of scanographs each speaking concertedly about arriving at a moment in his life with art at the helm.
“Some of them look almost three dimensional,” he admits quickly understanding something
that has to be admitted about his photographs, but he keeps a kind of reserve. Maz instinctually will not venture far into aggrandizing his own artistry. His art invites, lures, seduces the audience into conversations over their own curiosity.
“I love it when the spectator comes up and asks me about a photograph like whether the flowers are live or dried or if they are painted,” he engages. Remarkably and humbly, he keeps labels that might limit the natural organic expansiveness of his art or the decompression of his hobby at bay. He IS an artist and yet he takes care to be just a person enjoying a passion more fully each day sharing it if asked and approached.
I muse openly how I should compliment by attempting to capture someone who captures something while himself wandering life. Surprisingly, Maz Ghani says something that has grown clear in his life’s garden.
“I think I am still growing,” he reflects, and I know he is arriving at a center he has always had. I like that most about his garden.
“Do you see art in practicing
as a Radiologist?” I try to explore a parallelism thinking there is one.
“No, I keep it separate,” he covets as if one world cannot be allowed to taint the sanctity and reprieve of the other. “Work is very stressful,” he claims commonality with all physicians harboring the burden to help through knowledge and precision to elucidate. “By now I go through radiographic reads methodically. I am a perfectionist and I don’t want to miss anything. I don’t want to think I missed something and it harmed someone,” his voice trembles a bit with the gravity of admitting that fear out loud.
Immediately I think we in medicine have not understood something about Radiologists deeply enough. We have not seen the pressure to do no harm by missing an opportunity to discern something in an image that could help explain what may harm someone or what is harming someone. I feel immediately the weight Radiologists feel and I think that is the haunting air in the otherwise ethereal looking flowers. This elusive idea of awesome responsibility is the weight that conjures the need to run away after the job is done and seek ref-

uge in art.
Still I press, wanting to discover why a story of a Radiologist turned dramatic photographer seems too perfect. “Do you see any parallelisms between your photography and Radiology?” I reach unclear why the two seem akin but not exactly.
“No, I mean we don’t take the images in Radiology. We interpret them,” he reminds me. Suddenly, I
see it like a push of a button or a whisk through a gantry. The photo negative of Maz’s passion is his profession and the photo prints are of his hopes and safe guards.
It is suddenly both very dark in the reading room and very enlightened.
Maz Ghani is an expansive persona. He travels and explores permissibly curious to see things in ways that invite experiencing
and interpreting. He is aided and inspired by his parents (now deceased), his uncle, a constructively opinionated painter, his wife, a trained Forensic Pathologist and mother to his garden of subjects, and his son, a budding journalist and film artist. He is effusive like the sun on his own garden of supportive family and friends. “My wife has a beautiful garden and my son is an amazing artist but not because I think so but because others have said so,” he beams.
Come into Maz Ghani’s garden and get a little lost.
“I encourage everyone in Medicine to explore the arts. It’s so enriching and it gives rest and outlet and collaboration and conversation,” he beckons and mentors against burn out and the exhausting depletion of accountability and burden of sorrow in medicine.
I am already engulfed in the maze of Maz’ garden when he says this and I am surrounded by flowers photographed from the left, from the ground up, from a magical place suspended by faith and air. I think after a stroll I can go back to being responsible for answers. Beauty becomes our breath and girth to endure the bad shadows, lurking abnormalities shrouded in mystery, and the weight of unknowns and unexplained things.






If the last thing I wrote in the world had to be poignant I would argue that human persistent existence begs the possibility of constant renewing revolutions. We are at a spring board in a revolution given the global pandemic. This year is launching us forward and around and back again. It is near tangible the refreshed humanity and human joy within in it. There are resounding fundamental truths to hear.
Medicine and the practice of medicine is perfectly placed at the level of fundamental truth. Mortality begets illness and illness begets aid. Maz expresses perfectly two thoughts sharing the stress of weighty patient-focused care and the need for release by seeking har-
mony and art found within nature. In his broad and beautiful vantage, Maz calls to art those in medicine.
“Create something, even if nobody sees it,” he welcomes.
I asked Maz where he is heading in medicine and in art. “Nature provides us with abundant opportunities to explore and there is uplifting synergy when you collaborate with others,” he elaborates, “and I hope one day to open a gallery of sorts that has a curated gift shop, a garden for my wife’s creations and for others’ exploration and inspiration, and a space for conversation and creation. The destination I hope allows others to reconnect to nature.”
Maz is calling us all in medicine to remember our humanity and to
Dr. Maz Ghani was born in 1969 and moved to the US in 1995 after living in Australia and Canada. A Radiologist by training, Maz gained an interest in botanical photography several years ago while exploring his wife’s colorful gardens. He uses a combination of photography and scanography to compose the botanical layouts and is inspired by nature’s diversity. His works have been published in Travel and Leisure Magazine, Black and White Magazine along with an article “Art from the Garden” in Berkshire Magazine. His photos have been included in the SLO Museum of Art Juried Exhibition, Proud+ 2021 Juried Exhibition, the iMotif Juried Exhibition and the Contemporary Online Art Gallery.
STOCKISTS
Global Anthropologie.com
ArtfullyWalls.com
California
San Luis Obispo Botanical Garden gift shop, San Luis Obispo, CA Rhonda’s Relics, Arroyo Grande, CA Saatchi Art, Santa Monica, CA
Singapore
The Artling
PRINT/ONLINE MENTIONS
8/2022 “Your Best Shot,” Travel and Leisure Magazine, p. 180 5/2021 “Art from the Garden,” Berkshire Magazine, pp. 42-45 1/2021 Five photos published in Black and White Magazine (bandwmag.com)
use art to connect constantly with it. “Through the chaos of life, our lives are intertwined, braided by emotions and paths crossed, convoluted and complex,” he ponders.
If we are already caught in a riptide recycling our assets and aspirations, art is waiting and surviving the beating that becomes caring these days. Arming ourselves with art will find us all meandering some field of flowers extracting the clarity of our own calling.
I hope Maz builds this gallery and other physicians or professionals help and contribute, inadvertently or with violent intention. Through art and that photo negative exploration the fundamentals that elude us as the days grow long and weary will develop. ☤

AWARDS/HONORABLE MENTIONS
2/2020 Berkshire Magazine (Wild Places contest)
Honorable Mention - “Fleur du Sol”
Honorable Mention - “Busy in the Berkshires”
12/2019 Downtown Pittsfield Photography Contest
Honorable Mention - “Falling for Freedom”
12/2019 Contemporary Online Art Gallery (All Planet Earth competition)
Best in Show - “Standing Tall”
12/2019 Motif Collective (Symmetry contest)
Honorable Mention - “Shoe Heaven”

WANDERING DOWN THE GARDEN PATH
By Jean Robey, MD
THE FOUNDING STORY OF MD COACHES
By Rhonda Crowe, BSN, MBA
RAISING THE PHYSICIAN VOICE
By Randy Cook, MD
THOUGHTFULLY PRESENT
By Deb Roman, DO
THREE LESSONS FOR MEDICAL STUDENTS TODAY
By Rick Zollinger, MD
THE HOST OF RX FOR SUCCESS PODCAST
By Randy Cook, MD
COACHING QUIZ
By Mary Anna Rodabaugh, MD Coaches
PHYSICIAN PROFESSIONAL FULFILLMENT
By Deb Roman, DO
A MINUTE TO MINDFULNESS IN PRACTICE
By Dael Waxman, MD
By Dael Waxman, MD 02.
THE MINDFUL DOCTOR
THE RELATIONSHIP BETWEEN COACHING AND THE BUSINESS
By Desmond Bell, DPM, CWS
THE LEADER
By Desmond Bell, DPM, CWS THE LEGACY
By Rick Zollinger, MD
IT STARTED WITH A QUESTION
By Rhonda Crowe, BSN, MBA
INNOVATIVE WAY TO LICENSE MEDICAL GRADUATES
By Henna Sawhney, MD
ARTIFICIAL INTELLIGENCE
By Jean Robey, MD
TYPE ONE DIABETES
By Amanda Harrell, DO, Layla Harrell
FROM THE PUBLISHER CONFESSIONS FROM A RECOVERING MULTITASKER
By Marlene Wüst-Smith, MD



If you take one look at my credentials, you’ll see, I am not a doctor. But let me tell you, I have worked with many doctors for over 30 years. From the bedside to the boardroom, I’ve stood in front, behind, and alongside countless physicians.
When I began my career, I dove headfirst into nursing. I got my associates degree so I could get into clinical practice faster. Then, I went to get my bachelors. But the more I practiced, the more I realized medicine is not just clinical. It is a growing, thriving, evolving business. And I wanted to know more about the business side of medicine.
So back to school I went. After earning my Master of Business, I found my way to a corporate role in medicine. As I sat on the administrative side of healthcare, I made a few earth shattering discoveries. For example, in my last corporate role, I recruited, interviewed, hired, credentialed, and trained physicians in clinics across the country. It was a great way to make a significant impact, but ultimately, the impact was made on me.
I trained a variety of physicians who were from all different disciplines and specialty areas to know
how to properly do wound care. I’d say about 20% of those physicians really liked wound care. The remaining 80% were less enthused. That 80% lost their spark, their inner light, their joy for medicine.
This was a huge problem. A problem of epidemic proportions. And it wasn’t unique to wound care. This problem occurred across all specialties.
Physicians were burning out with nowhere to turn for support or coaching. Admitting a “problem” existed, is foreign for caregivers and physicians. Showing an ounce of vulnerability could cost them their professional credibility, career prospects, referrals, and other professional interactions. At least that is what history has demonstrated in the past. Our physicians are hardwired to think, feel, and internalize this unwritten professional rule. Vulnerability is self-perceived as a sign of weakness, even though it is anything but.
To learn more about Rhonda Crowe, BSN, MBA, go to https:// mymdcoaches.com/our-founder

Where do physicians go when they need someone to talk to? Family members? Friends? Peers?
Or no one at all.
I found myself at a crossroads. I could either reestablish myself into my nursing profession, or I could take everything I learned on both sides of practice and administration and change it. I wanted to do something to spearhead a global transition to wellbeing and… well…joy.
With this vision in mind, I set to work and MD Coaches was born. I created an organization dedicated to having physicians help other physicians work through those very specific challenges. I provided a resource for physicians to utilize to be a good physician leader. Today, MD Coaches is preparing, presenting, and providing thoughtful and expert resources to help physicians in need.
I always wanted to have a greater impact on healthcare in general. I just never imagined it would unfold in this manner. But I will admit, I am very grateful that it did. ☤
Sometimes I have to pinch myself when I think about all the things that I have seen over 44 years of medical practice and the number of things that have changed in healthcare. When I think about something as simple as the way we do operations, back in the beginning of my time as a surgeon, if we wanted to repair an abdominal aortic aneurysm, it would be through a massive abdominal incision, sometimes with two additional incisions in the groin. Nowadays, that operation is done through little more than a needle stick.
Indeed, the entire nature of healthcare delivery has changed dramatically over the years of my active practice and will continue to do so, likely at an ever-increasing pace. Many, in fact most, of these changes will be for the better. Who would want to return to the days of “exploratory” surgery, now that imaging techniques and directed tissue sampling can give us much more useful information than a dangerous and debilitating operation could provide just a few decades ago? On the other hand, some of these changes will be disturbing and disruptive. The intrusive oversight of payors and utilization police are only a couple of examples. These are the things we’ve already seen, and we can be certain there will be disruptive forces that we never anticipated.
I can now see retrospectively
that physicians began to buy into the false assumption that they were not properly equipped to understand business and therefore they should just step aside when there was a business decision to be made. The second big change is the ridiculous amounts of money that came into play and the healthcare landscape as a whole really got out of hand. If you look at the history of healthcare in America, many hospitals, particularly in the early to mid-20th century were operated by religious or other charitable groups. They were constructed for the benefit of the community. That was their sole purpose.
When did the shift start? Well, in the early 1970s, there began a divergence of priorities in healthcare where physicians tended to follow the path of quality of care, while ceding responsibility for revenue management to what was thought to be a more appropriate expert culture, i.e., the business school graduates. What we see now are hospital CEOs demanding salaries in the high six and even seven figure range, while nurses and other “round the clock” personnel are forced to work with too few staff and too few resources for too many hours and too little pay.
Nowadays, a lot of hospitals, are considered to be profit centers. If you want to make some money you can buy some stock. The financial pressure has caused a tremen -

dous change in the way hospitals and healthcare in general is administered. It has created quite a different feel, I think, to be a physician in the 21st century as opposed to when I started.
What has to be done? Well, three things.
First, physicians have to step up and say we are capable of and deserving of a voice in how medicine is delivered. Physicians are smart, intuitive, compassionate individuals. The business side of healthcare is in desperate need of their individual voices. The instant

the physician goes to work for someone other than the patient, the patient loses. Which is why it is paramount that physicians speak up and claim their rightful place at the business table. In my opinion, it is critically important for physicians to become more engaged in hospital management. To do so effectively, they will need to acquire some skills that were not taught in medical school. One place to look for help with such skills might be with either classroom or online business education courses. But more importantly, it’s crucial for physicians to question management and demand that institutions
put patient welfare at the top level of priority.
Ultimately, the good news is, we’re beginning to have a real conversation about how to elevate our system of healthcare to a level that we deserve, both as patients and practitioners. These conversations need to continue on a much larger scale.
When I first got into practice, many of the things I expected turned out to be entirely accurate. But the one thing that blew me out of the water was how much time physicians in the 1970’s and 1980’s spent battling with one another and fighting over turf instead of working together for a common purpose. For physicians to have a credible voice in the business of healthcare, they must stop fighting with each other. I don’t see quite the level of turf battling that I did 45 years ago, but part of the reason for that might be that so many physicians are now employed by hospitals or hospital systems. This is a serious problem that I believe is exacerbated by suffocating educational debt. If physicians must be employees, it is critical that they put forth a unified message with respect to patient advocacy.
Finally, physicians may need help finding their voice. When you’re battling debt, burnout, and bureaucratic processes, it can be easy to lose your voice and even your desire to stay in medicine. I’ve seen it happen time and again. The good news is that there are some relatively simple, easily accessible steps to deal with or, even better, head off these issues before they become bigger problems.
Professional coaching has been a highly popular and demonstrably effective method of dealing with the realities of the business
world for years. In much the same way that being a good student of business doesn’t guarantee being successful at business, the same is true of medicine. The challenges and realities of the practice environment are entirely different from the learning environment. Coaching affords a completely objective and unbiased advocate to help identify your strengths and weaknesses and to give you the space and the tools and the encouragement to perform at your best.
All of this puts me in mind of a favorite poet of mine. This one is from a much more recent era:
For the loser now Will be later to win
For the times they are a-changin’
Bob Dylan - 1964
It’s up to us to take control of the change. ☤

To learn more about Randy Cook, MD, go to https:// mymdcoaches.com/ourpodcast-host

L e t ' s G e t C o n n e c t e d f o r O u r L a t e s t N e w s & U p d a t e s
o n T w i t t e r @ C o a c h e s M D
o n F a c e b o o k f a c e b o o k . c o m / m d c o a c h e s l l c
o n Y o u t u b e y o u t u b e . c o m / m d c o a c h e s l l c 2 2 8 9
o n I n s t a g r a m @ m d c o a c h e s . l l c
o n L i n k e d I n / m d - c o a c h e s . l l c m y m d c o a c h e s . c o m

The children tried to cope, but at times, the best they could do was to go into a room and scream, sometimes for more than an hour, emerging exhausted and distant. They struggled to find comfort in play, unburdened by the weight of their experiences.
As a summer intern in a hospital for abused children, I hoped to get experience with a speech therapist on staff, but as I walked the halls after hours, and listened for the children, the depth of their suffering, and the response of the medical director moved me in a way that would change my direction.
I remember this physician as a smaller man, serious and determined, and when most of the staff had left the hospital for the day, I would find him in his office, sitting quietly, staring off into the dimly lit room, contemplating ways to reach these children and help them find peace.
It seems natural to want to cry for these kids, scream with them, pound our fists at the injustice and sheer cruelty of their experience, but this only further diminishes peace.
I looked to this physician for guidance. How do we help them heal? He taught me without words,
with glances and a timed touch of a child’s arm, with dedication to his art, seeking, listening and trusting in that which is innate and motivates our healing. He poured over charts, made endless calls to family members and other practitioners, and researched innovative treatments, but what I remember most was his time with the children.
When he was with the children, he was fully present, his eyes met theirs and they shared an unspoken, but profoundly clear connection, an acceptance that in itself was healing. Even the most withdrawn children seemed to watch
for him, and at times seek him out.
After a few months, I went home and informed my parents that I was going to medical school. I had experienced something that had changed me, and while I didn’t completely understand what it was at the time, I knew that it was profound. Many physicians share similar stories, highlighting the connection between physicians and patients as the primary motivation for their decision to train to practice medicine.
But as the medical field has changed over the past 30 years, the physician-patient relationship that inspires many of us to commit to this demanding profession has been influenced by increasing administrative duties, performance measures and regulation. When physicians are evaluated by the number of patients they see in a work day, and required to integrate often complicated and time consuming electronic medical records with expanded coding responsibilities, there is much less time and energy for relationships. Depersonalization of medicine results, with both physicians and patients aware that something integral to healthcare is missing.
Patients often express frustration with their inability to reach their physicians directly to discuss tests or diagnoses, the shortened time with their doctors during office visits and the absence of a shared journey as they face obstructions to health.
Physicians frequently express their dissatisfaction when the medical system does not prioritize their relationship with patients, and is not willing to dedicate resources to ensure that this aspect of care is protected. Patients share with me that they do not feel valued and respected, and physicians echo these frustrations.
In response, growing numbers of physicians, striving to negotiate these changes while continuing to meet their patients’ needs, are experiencing diminished health and well-being, and consequently, de -
creasing their hours and even leaving the medical field altogether.
When teaching a workshop to address physician burnout, I met an inspiring physician who despite frequent job changes and limited resources, always remained attentive to his relationship with his patients. We talked enthusiastically about the reasons that we love practicing medicine, the privilege of sharing our patients’ journeys and the ways that respectful, compassionate relationships with patients promote healing. We discussed the value of returning to a healthcare system rooted in the connection between a patient and a physician.
Healing takes time, time for the patients to unwind and share their stories, time for physicians to carefully listen and offer advice, and importantly, time to explore healing together.
Today, I integrate advanced training in integrative medicine, nutrition, mindful practice, meditation and yoga into my work. I founded Rediscovering Meaning in Our Work – a consulting and educational program with a focus on the well-being of physicians and medical school students. I am also a Cultivating Well-Being Coach and Consultant, offering services to physicians and other healthcare professionals who would like to work with a peer to explore the ways to ease stress, enhance well-being and engage in work that is meaningful and fulfilling. At a community level, I am actively involved in several initiatives to enhance equity and compassion in healthcare.
When I am not engaged in my work, I enjoy spending time with friends and family. You can often find me hiking in the mountains or relaxing in my backyard, enjoying the Boise sunshine as my dog Luca joyfully barks hello to neighbors who are passing by. ☤


Professional Achievements
• Medical School – Kirksville College of Osteopathic Medicine
• Residency – Family Practice –Mercy Suburban Hospital
• Board Certified in General Practice
• Founder of Rediscovering Meaning in Our Work
• Cultivating Well-Being Coach and Consultant
• Co-Founder of Idaho Physician Well-Being Action Collaborative
• Founder of Compassionate Communities Healthcare Movement
• Facilitator for the Compassionate Connections Community Healthcare Forum
• Assistant Professor of Family Medicine at the Idaho College of Osteopathic Medicine
• Executive Physician Coach with MD Coaches
To learn more about Deb Roman, DO, Physician Coach, go to
https://mymdcoaches.com/seniorexecutive-coach-d
As a physician, have you ever found yourself thinking,
“Well I wish they told me this was how it is.” The omnipresent “they” being your doctors and mentors in medical school. When you’ve reached double digits of years served, like me, you’ve encountered many highs and many lows. Sure, some of the challenges physicians faced were predictable, expected even. But there were so many challenges along the way that surprised me.
As a coach myself, I’m passionate about molding young minds and supporting the future of medicine. I know healthcare is continuously evolving, but the tried-andtrue traditions of medical practice are still rooted in these evolutions. Allow me to impart one of the bigger nuggets of wisdom I’ve learned throughout my career.
When I left residency, I was excited. But it didn’t take long for me to realize I knew nothing about the business of medicine. Sure, I knew bedside manner, patient care, charting, and how to ask for expert opinions. But the business side wasn’t taught. I bet your friends and colleagues who ventured into private practice, corporate healthcare, or even non-profit clinics, had
no idea what was involved politically. Because these nuances simply aren’t taught in medical school.
In today’s world, the word “politics,” carries a lot of meaning. That definition varies for everyone. But politics at its core, is really about people and relationships. Think about it, the inter-practice hierarchies, the physician schedules, committees, reports, EMRs, and cutthroat competition that is nearly bred into you…is all about politics.
Medical students are the best of the best. The cream of the crop, if you will. And whether you’re in your first year of medical school or you’re beginning your residency, I bet my best collection of golf clubs you cherish your autonomy. There is nothing wrong with that! But you have to learn how to work with people on the business side of medicine. As medicine becomes more corporate, the folks who teach young physicians may not be peer physicians, but administrators.
These teachers are still good people, but administrative goals and clinical goals differ sometimes. Despite the differences, administrators and physicians will always be colleagues. In healthcare politics, you have to learn early on how to manage your own expectations and the expectations of your superiors. Ask the right questions.
Don’t be afraid to seek clarity when things seem muddy. You are not expected to know everything on your first day of residency. Lean into learning.
As a young physician entering practice, I bet you are excited, energetic, and looking forward to your new world. One thing I have observed as I get older, is that young students seem to choose their specialty based on lifestyle or income. I’d say these are two very important factors, but the most important factor when it comes to choosing a specialty should be “do what you love.” When you do what you love, every day is filled with passion and excitement. And don’t worry if what you love changes over time, because it might!
You must learn how to tune out the “should” in your life. Your family, friends, peers, mentors, may all
weigh in on what specialty should be right for you. This decision is yours to make and yours alone. Seek council from those you trust but listen to your heart and follow your joy when you make your final decision. My advice is to always nurture your excitement. There may be days when that is the only thing that can help carry you through the day.
My father used to say to me, “don’t be freeze dried at 40, always learn new things.” By being a lifelong learner, you are constantly inviting new excitement and joy into your life. I may be retired from medical practice but I’m currently learning four languages, golfing, serving as a physician coach, and even making TikToks!
Ok, I get it. Becoming a doctor is tough. So much to consider. So many obstacles to overcome.
Such stress! When I think back on my career, I firmly believe coaching would have served me well as a young medical student and resident. Why? Well, coaching is having a trusted person listen to you and serve as a North Star when you need it. A coach is a sounding board for your fears and your expectations. A coach won’t give you solutions or diagnose your challenges. Instead, they will ask insightful questions that help you discover your own solutions.
As a coach, my last piece of advice is this: take a sabbatical every five years or so. Make it 100% non-medical. This will allow you time to recharge, redirect your energy, and relaunch. You will be absolutely amazed at how you can mentally turn back your own clock. The medical student and resident of today has a far better handle on self-care and mindfulness than my generation. But dare I say, this gen -
eration of medical students and residents could possibly benefit the most from having a physician coach on their side. Today, medicine moves at breakneck speed. What you learn today could change tomorrow. And the competition is fierce.
So, stay open minded and allow others to help you along your path.
Medicine is one of the most rewarding professions out there. Oh, to be in your shoes again. I would do it in a heartbeat! ☤
To learn more about Rick Zollinger, MD, go to https:// mymdcoaches.com/execu tive-physician-coach
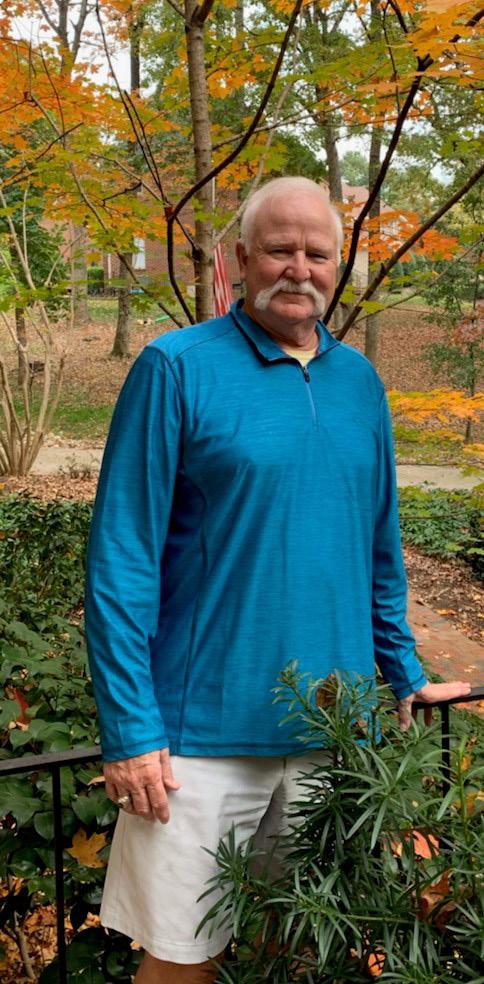
 Written by Randy Cook, MD
Written by Randy Cook, MD
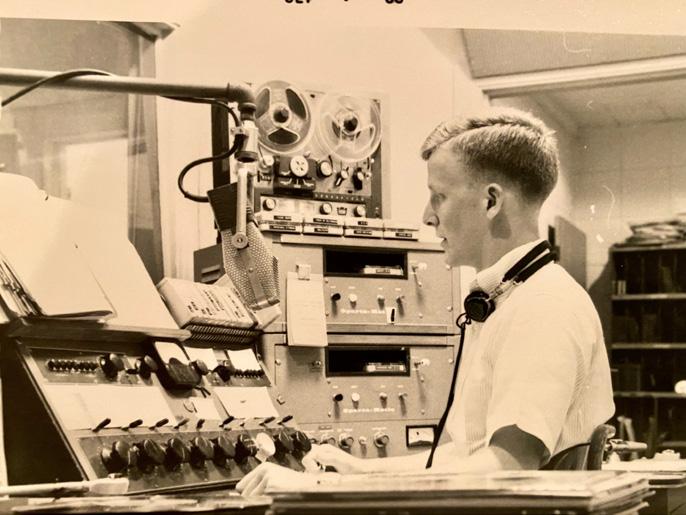
Believe it or not, by the time I got into my early teens, I was pretty sure that I was going to go to medical school. But when I turned 16, I had the opportunity to go to work in a small market radio station in East Central Alabama. I liked the work and it was a lot of fun for a lot of reasons. And briefly, I thought, “Well, maybe this might be something that I could do.”
I even had an interest in sports broadcasting, but I had the presence of mind to look around at other people in the business. And most of them, the great, great, great majority of them, were having a hard time making ends meet. So, I thought, “Well, this was a nice youthful endeavor, but now it’s time for me to get busy and get trained to do something that’ll make a living for me.”
I grew up in the small town south in an area similar to where I live now, and later moved to the big city of Birmingham to get my undergraduate education and also medical school. I got my MD at what is now the University of Alabama at Birmingham. And I knew early on that I wanted to go into surgery. I decided to do my residency at the Medical College of Georgia in Augusta for no other reason than I thought it would be a cool place to be. It’s kind of a smallish town as well, and I thought, “Gee, it might be nice to be able to go and see the Masters

golf tournament.”
Unlike a lot of really successful people, I have never been a long-term planner. When I entered my fifth year of residency, I really didn’t have a plan about what I was going to do. Fortunately for me,

one of the former surgery faculty members at the Medical College of Georgia had left about the time I started my chief residency. Within about six or eight weeks of his departure, he called me and said, “I’m in Clearwater, Florida. I’m in a place
where I’ve got more work than I can do, big multi-specialty group. The partners want me to bring on another surgeon right away and I can hold it down until you can get here if you can give me your commitment right now.” So that was it. That was how I lined up my first clinical practice.
I guess I kind of did things in reverse order. I started life in a gigantic multi-specialty group, but ultimately, I decided to move back home to Alabama. I joined a small surgical group, which dissolved after about five years. And then I found myself as a solo practitioner, during the last years of my surgical life. Then, after many years in surgical practice, I was asked by a hospital CEO to consider opening a wound care and hyperbaric medicine center for our hospital.
The timing was right. I needed to get off of emergency room call and was approaching an age when I knew my surgical skills would soon start to falter. So, I got really serious about it and embarked on a very intensive reeducation process. I got board certified in hyperbaric medicine. I got involved in management and got involved in wound care education. I even became involved with an organization to create an examination for certification of wound care physicians.
And that was what I did for the last years of my practice.
As I mentioned before, I’m not much of a planner. After just over a decade in the world of chronic wound care and hyperbaric medicine, I found myself spending more time fighting bureaucrats and administrators than fighting disease. I was 67 years old, and I hadn’t really intended to retire quite so early. I just got mad and quit. I didn’t have any plan other than to do what retired people do. But that wasn’t in the cards for me.
I had met Rhonda Crowe, founder, and CEO of MD Coaches, several years before. My wound
center was under management of a big company. I was on their teaching faculty for many years instructing healthcare professionals that were coming to learn how to be wound care specialists. So, Rhonda and I knew each other through that professional connection. I guess about seven or eight months before I made the decision that I was going to pull the plug on my practice, Rhonda called me out of the blue and said, “I’m starting this coaching company and I want to publicize it with a podcast. And I know you have a history in radio. Would you consider doing that?”
My response was, “Rhonda, do you know that my radio experience was concurrent with the invention of the vacuum tube?” She said, “Yeah, yeah, yeah, I know that, but this is what I want to do.” Rhonda was looking for physicians who would make qualified coaches. And she thought that if for no other reason, my 44 years of experience might qualify me for that.
Today I’m humbled to be the host of the Rx for Success Podcast and a physician coach with MD Coaches. To my surprise, we recently won the 2022 Columbus Podcast Awards, “Best Arts Podcast.” With four seasons and over 100 episodes, I have been able to share countless meaningful and inspirational stories along the way.
What a wild and fulfilling ride it has been so far! In my spare time you can find me spending quality time with my lovely wife and taking captivating photos of nature. ☤
Professional Achievements
· Medical School - University of Alabama, Birmingham
· Residency – Medical College of George, Augusta
· President of Medical Staff –Jackson Hospital, Montgomery Alabama
· Medical Director – Jackson Wound & Hyperbaric Medicine Center
· Fellow – American College of Surgeons and the Southeastern Surgical Congress
· Certified – American Board of Surgery
· Subspecialty Certified –Undersea and Hyperbaric Medicine
· Board of Directors – American Board of Wound Management
· Diplomat – American Board of Wound Management
· Physician Exam Co-chair –American Board of Wound Management
· Designated Medical Examiner –Federal Aviation Administration
· Podcast Host – Rx for Success
· Physician Coach – MD Coaches, LLC
To learn more about Rx for Success and view the full list of podcast episodes, visit https://rxforsuccesspodcast.com




 Randy and Jennifer Cook
Randy and Jennifer Cook
The physician experience is unique. Physicians are problem solvers, and rarely take the time to identify problems within their own lives because they are preoccupied with helping others. The bureaucratic idiosyncrasies of healthcare often fall on deaf ears outside the physician world. As pressures mount, emotional fatigue may set in. If you are a physician and are curious if you could benefit from physician coaching, take this short quiz. You will not regret it. Give yourself one point for every “yes” answer and subtract one point for every “no.”

Question 1: Do you have difficulty finding the right peer group to discuss career challenges with?
Question 2: Do you sometimes wish you could have a thoughtful discussion with an objective individual (or group) who understands exactly what you are going through as a physician?
Question 3: Have you considered a career change in the past year?
Question 4: Have you considered working toward a leadership position in the past year?
Question 5: Do you ever feel alone, burned out, exhausted, frustrated, or even apathetic about the healthcare system as a whole?
Question 6: Do you wish you loved healthcare now as much as you did when you first began your career journey?
Question 7: Do you feel like something might be missing from your personal fulfillment?
Question 8: Do you sometimes wish you could have a thoughtful discussion with an objective individual (or group) to celebrate accomplishments unique to healthcare professionals?
Question 9: Do you feel you could benefit from practical exercises to enhance your ability to have difficult conversations with patients, peers, and supervisors?
Question 10: Does anyone in your leadership team receive coaching of any kind?

If you scored between 7 and 10: Now is the time for physician coaching. You may be on the brink of transition and are seeking clarity on the path ahead.
If you scored between 3-6: Physician coaching is probably for you. You may just need a little nudge forward or perhaps need to role play a specific scenario to see a new perspective.
If you scored less than 3: We’d be lying if we said physician coaching wasn’t for you. If you scored less than 3, perhaps you don’t have a pressing need for coaching, but could use a sounding board to celebrate your achievements and plans for the future. ☤

Occasionally in life there are those moments of unutterable fulfillment which cannot be completely explained by those symbols called words. Their meanings can only be articulated by the inaudible language of the heart. - Martin Luther King Jr.
We each define and experience professional fulfillment in different ways. For me, as a family physician, relationships with patients and peers bring a sense of meaning and fulfillment to my work. One evening at about 9pm I received a call from Mary, an elderly woman who had been a patient for many years. She struggled with anxiety about her health, so I made every effort to return her calls quickly. When I received her call, I was tucked in bed with a high fever. I had contracted pneumonia and had been out of the office for a few days when my pager went off.
“Hi Mary, this is Dr. Roman. What’s going on?”
There was silence on the phone. After a few seconds, she responded:
“Dr. Roman, is that you? Oh my goodness, you are way more sick than I am. I want you to hang up this phone, get some tea and wrap yourself in a blanket. Don’t call me back until you feel better. You hear me? I will call to check on you tomorrow.“
As I cared for Mary, she cared
for me. These compassionate moments with patients fill me up. They give me energy for the long hours and many demands and challenges of medical practice.
My relationships with physician colleagues are equally fulfilling. Throughout my career, when I have encountered circumstances that challenge me, I have connected with peers. These relationships provide a stable foundation for open, non-judgmental conversations. They help me to make sense of my world and find my way forward.
The landscape of medicine has changed dramatically over the past few decades and the daily practice of medicine has been significantly altered. For many physicians, time with patients has been drastically reduced, making it difficult to cultivate strong, mutually respectful relationships. My colleagues and I no longer meet in the doctors lounge each evening while completing our hospital rounds after office hours. Many of us work in what has been described as “silos”

without the benefit of regular conversation with peers.
These changes in healthcare have prompted me to look more closely at the factors that enhance and diminish my level of professional fulfillment and identify specific ways to respond in alignment with my values.
A relatively new resource for physicians seeking fulfillment is professional coaching. In a 2019 study published in JAMA Internal Medicine, Mayo Clinic researchers reported that “Participants who received professional coaching had a significant reduction in emotional exhaustion and overall symptoms of burnout, as well as improvements in overall quality of life.” Individualized and group coaching are now available to physicians.
During group coaching, physicians come together in community with peers who share the physician experience to explore and address issues that are relevant and meaningful to them. The participants benefit from the support and insights of colleagues as pro -


fessional coaches (who are also physicians) facilitate.
The topics for each session are determined by the physician participants. Discussion topics may include the transition to new roles, misalignment between individual values and those of the physician’s employer, cultural biases, administrative/regulatory demands, interpersonal conflicts, disillusionment and other issues that are of interest to the physicians.
I am continually inspired by the insights, engagement and enthusiasm that arise during coaching sessions. Three foundational aspects of physician coaching contribute to meaningful and transformational experiences for physicians:
1. Respect for the unique experiences, creativity and resourcefulness of each physician participant. A coach can’t possibly know what another physician is experiencing or which factors will lead to an enhanced sense of meaning or fulfillment for that individual. Coaches cultivate a
non-judgmental space for exploration and encourage physician participants to identify these factors for themselves.
2. Integration of deep listening and reflective inquiry: Professional coaching differs from conventional coaching (in athletics, for example) where development of specific skills is the focus. Professional coaches do not advise, mentor or teach. Instead, experienced coaches actively listen, offer reflections and ask pertinent questions to allow participants to view situations from new perspectives and uncover possibilities that may not have been appreciated earlier. Active listening and reflective inquiry are also practiced by the participants.
3. Focus on forward movement: As insight and clarity emerge, physicians decide how they would like to integrate their new awareness moving forward. Many physicians share that when they determine for themselves how they would like to respond, their experience is meaningful,
sustainable and empowering.
At a time when there is a great deal of isolation and division in healthcare, and many physicians express that they do not feel heard, lack autonomy and have minimal control over factors that are significantly impacting their work, professional coaching provides a unique and valuable opportunity for physicians to access their capacity to choose and achieve changes that contribute to a greater sense of satisfaction and fulfillment.
Between stimulus and response there is a space. In that space is our power to choose our response. In our response lies our growth and our freedom.
- Viktor Frankl ☤To learn more about Deb Roman, DO, Physician Coach, go to https:// mymdcoaches.com/senior-executive-coach-d
You are seeing patient after patient and are one hour behind schedule. You were planning on taking Friday off but your colleague developed flu-like symptoms and now you have to step in to cover for her shift. You finally wind down for the day only to realize you still have at least two to three hours of charts to complete and records to check before officially signing off for the night. Sound familiar? These are the struggles that plague physicians everywhere. When working in such an other-focused profession, it can be hard to find time for yourself. In fact, you may even feel a touch of guilt if you spend time for self-care.
But I know you’ve heard it before. Check your own pulse first. Before running into the fray, you have to check your own pulse first. How can you do that in the middle of a busy day of medical work?
S.T.O.P.
You stop. No, I don’t mean quit, walk out, or run for the hills. There is a handy mnemonic that has been around for ages across many different disciplines. It is called STOP.

S – STOP.
The S simply means to stop, pause, cease action in the moment. You can use this when you are feeling emotionally triggered and when you want to autoreact to a situation. You can use this when you are feeling the effects of stress on the body. Maybe your chest feels tight or your shoulders have found their way up to your ears.
T – Take a Breath.
Take a deep breath in through your nose and slowly out through your mouth. This activates the parasympathetic system – which induces the relaxation response. Additionally, reconnecting with our breath can return our focus to the present moment, giving us a much-needed break from the anxieties of the future.
O – Observe.
Now it is time to observe what is going on within you. Check in with your body. Where do you feel tension. Is it better now than before you stopped what you were doing? What emotions are you feeling? Can you label them? What about their intensities? Can you determine just how intense the emotions you are feeling really are? Next, notice your body once more. Feel your feet touching the ground. Notice how you are sitting or standing.
P – Proceed.
You’ve stopped in the moment, taken a breath, and observed your body, emotions, and surroundings. While all the stress you are experiencing probably has not magically vanished, chances are, you are feeling less “fight or flight” than you were before you began this short exercise.
This can be done anywhere at just about any time. While it isn’t coaching, or even self-coaching, it is a tool for wellbeing you can use throughout the day. Our brains are programmed to auto-react for survival. This exercise slows down that programming so we can be present and intentional.
When my inbox is flooded with emails that demand my immediate attention and when I’m nervous about an upcoming presentation, I’ve used this mnemonic quite a few times myself. I think it is important to continue to find ways to add to your wellness toolkit.
An empty kettle doesn’t pour. Put your oxygen mask on first before helping your fellow passengers. And check your own pulse first. By continuing to practice this exercise, you can determine new ways to harness the power of mindfulness in your daily work and life. All it takes is a few moments and an open mind to give it a try. ☤

Toward the end of my residency, I didn’t know what to do next. It wasn’t full-time practice. I liked patient care but couldn’t see myself doing it full time. My advisor noticed I had a propensity for teaching and made a suggestion.
“I wonder if you’d be interested in a fellowship we have, and you can be chief resident of the family medicine residency at the same
time,” they told me. So, I did. I stayed as a fourth-year chief resident of the residency as well as did a faculty development fellowship in learning how to be a faculty member and learning how to teach. All while conducting full-service family medicine, as well. It was a great experience, but I yearned for more. I wanted to dig deeper into person-centered humanistic care.
Then one day I was in the library at the University of Arizona School of Medicine preparing for a talk I was going to give residents. I found an article I needed for my talk. As I perused the bound volume containing said article, I happened to open the book to a page containing a letter to the editor. The word “biopsychosocial,” caught my attention.
Naturally, I dove into research

on the term and discovered a fellowship at the University of Rochester on Psychosocial Medicine. I suppose this is a prime example of following your passions, because multiple doors opened. Turns out the University of Rochester had another fellowship on Family Systems Medicine. I applied for both. During my interview, the directors realized the two fellowships contained many similarities and decided to combine them into a single experience.
I was fascinated by everything.
I knew from this fellowship what I wanted to do was to bring that energy to education so I knew after the fellowship I was heading for an academic career – to teach about the very large overlap between mental health and primary care.
During my academic career, to further enhance my teaching and clinical care, I studied and received certification in Clinical Hypnosis, Mind/Body Medicine, and Mindfulness-based Stress Reduction.
As a physician and educator for over 35 years, I have experienced the joys of practice and teaching medicine but also the mental and emotional distress that can accompany it. This latter reality is unfortunately common in the med -
ical profession; as a result, since 2010, I have focused my attention on promoting well-being and preventing physician burnout. More recently, I decided to enhance my offerings beyond workshops and educational seminars, leading me to complete the Coaching Certificate Training at the Healthcare Coaching Institute in 2018.
In addition to coaching, I continue to teach family medicine residents, which allows me to remain even more connected to my clients’ realities. I am also experienced in physician leadership, mind/body medicine, and mindfulness-based stress reduction. I combine all of these experiences, practices, and framings to help medical professionals evaluate their goals, reconnect with their passions in healthcare, and achieve their personal and professional objectives.
Today you can find me speaking, coaching, and continuing to learn. When I am not deeply embedded in my work, I love traveling with my family, kayaking, and long-distance running. ☤

• Medical School – University of Kansas School of Medicine
• Residency – Family Medicine, University of Arizona, Tucson
• Chief Resident – Family Medicine, University of Arizona, Tucson
• Fellowship – Faculty Development, University of Arizona, Tucson
• Fellowship – Family Systems Medicine, University of Rochester
• Founder of Dael Waxman MD Coaching and Consulting
• Professor Emeritus of Family Medicine at Atrium Health in Charlotte, NC
• Physician Coach with MD Coaches ☤
To learn more about Dael Waxman, MD, visit https:// mymdcoaches.com/daelwaxman%2C-md
Ihad never heard the term “Life Coach” until a few years ago, and I must admit, it conjured up all kinds of mental images. Who needs a guy with a whistle around his neck, carrying a clipboard, yelling at someone as they do basic tasks, like making their bed, cleaning the house, or going to the supermarket? Personal trainers have been around for some time, helping “motivate” people with their fitness regimens, so I assumed a Life Coach was something similar, only beyond the walls of a gym. I did not think there would be much value for me, an independent problem solver who has never lacked motivation in completing tasks. I also figured that life coaches could be a good thing for someone who needs constant prodding, but also held the opinion that people who would seek out such a service, were looking for an easy fix or for someone to solve their problems.
Having grown up playing organized sports through high school and beyond, coaches represented the final authority. The coach shapes the team roster based on what they believe are the needs of the team, organizes practice, and makes the decisions on game day. The players have some accountability for sure, but their input is limited and in the final analysis, the coach gets much of either the credit or blame for the results.

That being stated, it is the coach who must bring out the best in his players and team. The coach is really a partner in the effort, and shares in the accountability. The coach, then, is really an Accountability Partner to each member of the team.
When I first learned about MD Coaches, I wasn’t sure what to think. I asked myself, why would doctors of all people need coaches? It seems contradictory in the sense that if any group of individuals could be classified as “Life Coaches,” it would be doctors and
therefore, the least in need of such a service. Again, using my own experiences as a barometer, I asked why would doctors need someone telling them what to do at this stage of their lives, especially if it is motivation they are lacking? Doctors are among the most highly competitive group of individuals, as the process to gain admission into medical school can sometimes be described as “cutthroat.”
What an eye-opening experience it has been for me over the past several years, as I have realized my first impressions of coach -

ing, especially the need among doctors, could not have been more inaccurate. I was recently asked a question regarding coaching, and it was when I heard the answer coming out of my mouth, that I realized most of my misconceptions were based on the name “Life Coach.”
I explained to the person who asked me the question that I thought the term mentor was a much more accurate term than coach. Mentoring, especially between peers, encompasses the type of relationship that doctors go through during their post-grad -
uate training and beyond. We are always learning from our peers and sharing our wisdom among our colleagues. This is part of the Hippocratic Oath and is one of the many incredible aspects of medicine, a career that encourages and expects sharing of knowledge that will benefit others. Mentors encourage, share, and listen. They assess and engage their peer in such a way that they promote problem solving through self-awareness and discovery. Coaching conjures up goal attainment that comes from an accountability partner, and while coaches can also be mentors, not all mentors can be Coaches. Coaches are employed to help identify, strategize, and progress toward goal attainment.
In uncertain times like the ones we are living in, it is no wonder we are seeing troubling symptoms among our peers in medicine. Physician burnout, general unhappiness, career changes, higher than average divorce rates, and suicide are just some examples that should set off an alarm, yet in a profession that demands putting others before self, if an alarm has gone off, it has blended in with lots of other background noise. The value of peer-to-peer coaching offers can be a lifeline. Ultimately, solutions come from within, but the process of identifying issues and solving problems with a coach can be invaluable.
There is no shortage of evidence supporting the benefits of coaching on the individual, but what about the bottom line? How can coaching positively impact the business of healthcare as a whole?
Improved communication flow: when colleagues learn inten -
tional listening skills, they subsequently sharpen communication skills in tandem. Many systemic problems begin with a lack of communication or a disconnection between expectations and reality. Coaching helps participants determine the best way to communicate their own needs while enhancing their own emotional intelligence for working alongside leaders and peers.
Employee retention: satisfied employees become loyal employees. When physicians feel understood, valued, heard, they are more likely to bring their best selves to work.
Right people, right seats: coaching is a highly beneficial way to help physicians determine their path to leadership positions. When you align interest, skillset, and vision with the candidate and the position, you set an enthusiastic path forward for both the physician and the organization.
Saves money: When you combine these benefits, there is a great chance the bottom line will see improvement due to lack of spending on recruiting new talent and addressing employee burnout on a case-by-case basis.
Over time, your purpose may change as you evolve, gain perspective, and grow through life experiences. Going back to basics when things get complicated can reduce background noise and the factors that lead to the stress and unfulfillment of a life without direction. And coaching can benefit not just the individual but the organization as a whole. ☤
To learn more about Desmond Bell, MD, visit https://mymdcoaches. com/epc-bell


Looking back, my career in medicine has spanned over 40 years, serving as a volunteer, an orderly and the past 25 years as a podiatric physician. What a career it has been, and currently is! Not from a boastful standpoint, but just in a collection of profound experiences that motivate me and inspire me daily.
I remember when I was a teenager, working as an orderly in a hospital in northern New Jersey. A patient on one of the med-surg floors was treated for a Stage IV sacral wound, and I would often assist the nurses during dressing changes. Dressing changes for this unfortunate patient were typically performed every shift, and the patient remained in the same hospital for more than a year before he finally died. I immensely enjoy providing wound care, and my favorite aspects include giving hope where previously there has been frustration and pain. Seeing someone regain independence and quality of life is a great reward, especially when amputation of a foot or leg was previously the only option offered. Naturally this joy led me to medical school.
I am a graduate of Tulane University, New Orleans, Louisiana. I graduated with a bachelor’s degree in Psychology. My thirst for knowledge was not sated, for I found myself in medical school shortly, thereafter. I received my Doctor of Podiatric Medicine Degree from the Temple University School of Podiatric Medicine in Philadelphia, Pennsylvania.

private practice that evolved into a free-standing wound center. Writing, lecturing, and immersing myself in the wound care community have allowed me to meet so many talented and kindred spirits who share the desire to continually improve outcomes and quality of life for our patients.
The most pivotal year of my career came during my first year of residency. I was working at the Department of Veterans Affairs Medical Center in Philadelphia. My time there led me to recognize the importance of wound care and limb preservation. An additional year of surgical training in Langhorne, PA at the Delaware Valley Medical Center and then a move to Florida in 1997 allowed me to further pursue my passion in wound care. I established my
Today I am the founder and president of The Save A Leg, Save a Life Foundation, a multi-disciplinary non-profit organization dedicated to reducing lower extremity amputations and improving would healing outcomes through education, evidence-based methodology, and community outreach. I also serve as the Chief Medical Officer of Omeza, a medtech and consumer healthcare company. I am also a physician coach with MD Coaches and a consultant with Arche Healthcare.
In 2022, I was named Difference Maker: Humanitarian by the Symposium on Advanced Wound Care. I was awarded the Frist Humanitarian Award by Specialty Hospital Jacksonville for 2009 and Memorial Hospital Jacksonville in 2018. ☤
Professional Achievements
· Medical School – Podiatric Medicine, Temple University School of Podiatric Medicine
· Chief Podiatric Resident–Department of Veteran Affairs Medical Center
· President and Co-Founder –Wound Summit Outreach, Inc
· Founder and President –Save A Leg, Save a Life Foundation
· Chief Medical OfficerOmeza
· Physician Coach with MD
To learn more about Desmond Bell, DPM, CWS, visit https:// mymdcoaches.com/epc-bell
Medicine was a huge part of my family. You may be aware of a little thing called Zollinger-Ellison Syndrome. Robert M. Zollinger and Edwin H. Ellison described two cases of a condition whereby patients developed severe, recurrent, multifocal ulcerative lesions of the proximal gastrointestinal tract. Well, Robert Zollinger was my uncle.
But my uncle wasn’t the only family member to go into medicine. My father, a mere nine years younger than my uncle, would find his own path to surgery. As a kid growing up, I just kind of thought that’s what you did for a living. It was all I ever knew.
When I went off to college, I started off as a chemistry major. I needed three more courses at the end of sophomore year, but I hated
chemistry. Naturally, I went to my advisor and asked what I could do differently. They told me I could take English, History or Political Science and graduate in four years. So, I picked English.
It wasn’t until my junior year when I got a taste of Comparative Anatomy, that my interest in medicine would grow by leaps and bounds. I’ll be honest. Those first few years of college I was flying around by the seat of my pants.
I tried to keep an open mind, but I always thought I was going to become a surgeon. The way I grew up, I knew what the lifestyle was. In fact, in those childhood days, I would sit on the anesthesiologist lap when my father did an appendectomy with the windows open in the OR. It was the 1950s.
As it turned out, I love obstetrics but I didn’t like gynecology. I loved delivering babies, but I also loved everything about the heart. I read Grey’s Anatomy cover to cover and highlighted its pages in yellow.I thought I could blend my love for obstetrics and cardiology together and become a pediatric cardiac surgeon. I didn’t quite make it to that specific career but looking back I can’t believe all the places my career has taken me.
When I was a fourth-year surgical resident, I rotated through cardiothoracic surgery at Ohio State University, where I met a guy from Akron, Ohio. He was our chief resident. Little did I know we’d eventu -
ally become friends and in a short time, he would be the reason I moved to Charlotte, North Carolina.
My wife’s family was from Durham, I ended up putting down roots in the beautiful city of Charlotte. I would go on to succeed in multiple practice settings as a single practitioner and for larger multi-specialty clinics and in group settings. I founded the Charlotte Cardiothoracic Surgical group and I served as an Assistant Clinical Professor of Surgery for the Department of Vascular Surgery at UNC Chapel Hill.
I loved teaching. The opportunity to positively influence and mold young minds excited me. Working with young people, if I had to do it over again, I would do more of it. It was very rewarding.
I was a sort of maverick physician in a way. As the hospitals and health systems started buying up physician groups, I got fed up with the system and I retired. After six months, one of the administrators who knew me beckoned me back into medicine. The hospital was starting a wound care center. I didn’t know much about wound care, but I was willing to learn. I had no earthly idea how complicated wound care was!
Turns out I ended up helping set up their first wound care and hyperbaric medicine center. It was exciting and fun because I got to do something where it wasn’t just oth -

er peers who did what I did. There were internists, infectious disease doctors, family physicians, cardio surgeons, and they were all doing wound care. You could talk about a complicated problem from all different perspectives. I really enjoyed that more than anything because it made me feel more a part of medicine than in my cocoon of cardio stuff.
Looking back with more than three decades of clinical moments in general, cardiovascular, thoracic surgery, and wound care, I could share stories with you for days. Today you can find me playing golf, traveling with my beautiful wife, inspiring the future of medicine on TikTok, and serving as a physician coach with MD Coaches. ☤
To learn more about Rick Zollinger, MD, go to https:// mymdcoaches.com/executive-physician-coach

When I was a little girl, about seven years old, my teacher gave our class an assignment to fill in the blanks to the following sentences:
When I grow up I want to be a ____. Some things I will do in my work are _____.
I remember my classmates and I having fun with the assignment. Paper, crayons, and pencils
became the tools with which we would use to declare our vocational missions. I don’t remember anyone struggling with the assignment or grappling with “finding their life’s purpose.”
As children do, we expressed truthfully and innocently what was in our hearts while finding joy as we did so. I proudly stated I wanted to be a nurse and knew my role
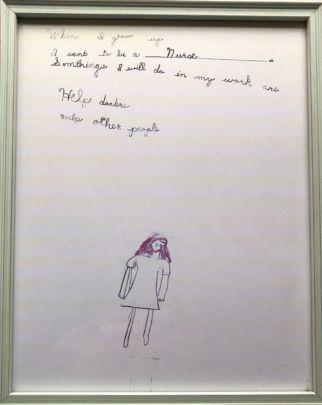
would be to help doctors help other people. I punctuated the offering with a hand-drawn picture of what I would look like in the nurse’s role, thus sowing a seed in my soul and plotting a course that would direct my steps, educational choices, and professional decisions into my adult years.
As I grew and pursued my learning through academic endeavors and life’s lessons, I made good on that promise and became a Registered Nurse. As wonderful and thorough as my nursing professors were, their preparation only provided me the opportunity to learn from the lessons awaiting me. You know, those real-life experiences my patients, colleagues and administrators offered. My experience as a nurse has afforded me the privilege to witness the heights and depths of the human condition. I’ve laughed, I’ve cried, I’ve worried, I’ve sighed in frustration and relief, and a myriad of other emotions with patients, family members and healthcare providers alike. The experiences have enriched my knowledge, my life and my soul; I am ever grateful for each one. I have fulfilled my mission to “help doctors help other people.”
In this most recent phase of my journey, I have observed the many challenges my physician colleagues have experienced with the ever-changing healthcare landscape. Physicians are relied upon to help develop and implement new methods of care delivery, increase quality of care, improve patient satisfaction, and reduce costs. All while spending less time with patients (what they are interested in most), more time with electronic health records (what they are interested in least), and many times being left out of the goal-setting/ problem- solving equation entirely.
These concerns have led to diminishing physician engagement and a silencing of their voices while adding to the ever-growing physician shortage through early retirement, changing career paths and decreasing medical school enrollments, all very real concerns for
the healthcare consumer.
With these thoughts and observations in mind, the meaning of my childhood declaration and drawing has changed. At this stage of my journey, it has a deeper meaning and representation within my work. I recommit to my childhood declaration with my work at MD Coaches.
Every day, my team of physician coaches and I strive to empower physicians to discover and actualize their vision of a fulfilling life. In doing so, I truly “help doctors help other people.” ☤



Professional Achievements
Registered Nurse
Clinical Staff Nurse
Six Sigma Green Belt Leadership Development Coach
Master’s in Business Administration
Founder and CEO, MD Coaches ☤
To learn more about Rhonda Crowe, BSN, MBA, go to https://mymdcoaches.com/ our-founder
Every year, thousands of qualified medical doctors are unable to advance to the next phase of their career after medical school graduation due to the bottleneck that is otherwise known as residency training3. In the most
recent residency application cycle (2021 - 2022), 11,532 medical graduates did not gain a residency position1. These are thousands of qualified medical doctors that are in a “limbo” period, meaning that they have their medical degree but

they have not completed the compulsory post-graduate training they so desperately need to obtain a full license to practice. This is not a new phenomenon because it happens every single year. Even this past year was no exception despite the global pandemic and an ongoing physician shortage that limits patient access to quality healthcare didn’t make
So what can these doctors do until they obtain a residency position? They can work as a medical assistant, research assistant, scribe, or find an observership where they are limited in practice and do far less than what is expected of a third-year medical student. Fortunately, there is a newer and lesser-known option that is far more suited to the skill sets of a doctor: obtain an assistant physician license.
I had the opportunity to get my license as an assistant physician in the state of Missouri and worked at both an urgent care and primary care clinic in this capacity. The scope of practice can be equated to the level of a nurse practitioner or physician assistant, where you have a collaborative practice with a board-certified physician to work under appropriate supervision. I was able to take histories, complete physical examinations, write/ sign medical notes, do procedures, and even prescribe medications. I was managing patients with both
acute illnesses (such as COVID-19) and chronic illnesses (diabetes mellitus, hypertension, etc.) so for the first time since graduating medical school in 2018, I was actually practicing medicine.
The particular clinics I worked at were in medically underserved and rural communities. There was a prerequisite 120 hours of directly observed training with your collaborating physician, after which it was up to your supervising physician to gauge the scope of your practice and what you would be comfortable to see independently. We had weekly didactics and case presentations to support our learning as one would in residency training. The urgent care clinics were also the only ones open 24/7 in the St. Louis area so a lot of patients would opt to be seen there rather than wait for hours in the emergency department. The primary care clinic I volunteered at had us taking care of patients with more complex conditions such as uncontrolled diabetes and hypertension; many did not have appropriate prior medical care or even health insurance. Our supervising physician also provided residency preparation like proofreading our personal statements and conducting mock residency interviews.
While the experience was not exactly equal to the rigor or breadth of residency, it gave me a chance to care for patients while also giving me the opportunity to enhance my residency application and connect with physicians that not only wrote strong LORs but also advocated on my behalf.
The eligibility requirements for this type of license is equivalent to that of residency: graduate from an accredited US or international medical school in good standing, completion of USMLE steps 1 and 2, ECFMG certification for Interna-
tional Medical Graduates (IMGs), and have not completed residency training. A few states have other requirements such as completion of the USMLE Step 3, proof of residence in that state, graduation from specific medical schools, or confirmation of employment prior to issuance of the license. It’s as simple as completing an application and providing supplemental documentation. Application review can take anywhere from a few days to a few months depending on the state.
These are the states that currently license medical school graduates to work under supervision2:
1. Missouri
2. Arizona
3. Florida
4. Washington
5. Arkansas
6. Utah
Due to the ongoing COVID-19 pandemic, several states issued temporary licenses to such individuals4. Illinois and New York are two examples of such states, but unfortunately those licenses have now expired.
More states have been joining the bandwagon; there are currently grassroot efforts to propose licensure in California, Colorado, Georgia, Oregon and Texas. The International Medical Graduate Assistance Act5 was also introduced to Congress in June 2022 to incentivize more states to provide licensure to unmatched medical graduates, particularly to those that are US citizens and legal residents that have graduated from a foreign medical school.
The greatest obstacle for these licenses is finding a collaborative physician. Due to the relative anonymity of this type of license, it has been difficult to find practice opportunities in the states listed above. As this movement continues to gain more traction though, it
is an innovative way for practicing physicians to support and teach the next generation of physicians while making a difference in their own communities.
Overall, these licenses are an easy way for medical graduates to work to the full capacity of one’s training, gain the meaningful skills needed to prepare for and succeed in residency and unite two generations of physicians to work together to increase access to care in communities of need.
Resources
1. NRMP Data 2022: https://www.nrmp.org/ wp-content/uploads/2022/05/2022-MainMatch-Results-and-Data_Final.pdf
2. Inside The Match Blog: https://www.insidethematch.com/medical-school-tips/ licensed-without-a-residency
3. DocWeighsIn Article: https://thedoctorweighsin.com/physician-training-shortage/
4. COVID-19 Temp Licensing by state: https://licensing.csg.org/covid-policy-responses/temporary-licensure/
5. International Medical Graduate Assistance Act 2022: https://adamsmith. house.gov/_cache/files/5/6/561877ace7c1-48ca-baf9-97d7cc0cfea1/AB2CD709015C63AC10C0323D0650FCE7.imgassistance-act-1-pager.pdf

https://www.asphysicians.org
To listen to “Redefining Success with Henna Sawhney”, an Rx for Success Podcast episode, go to: https://rxforsuccesspodcast.com/ LCM005


 Written by Jean Robey, MD
Written by Jean Robey, MD

She always comes in a puffy vest. Even in the summer she wears it.
“Your office gets so cold,” she giggles a complaint.
I tell her I am sorry I am late. She says I am not but I apologize every time because one time I was and I never want her to remember. She has lost weight and is thin. She lives alone in independent living, but “I still wash my own floors”, she declares. “I have a bucket and a rag and I do them all as well as the blinds. I’m getting slower but I do them. Others hire people. I do mine,” she swears.
“They should hire you,” I post the ad and she giggles a don’t-besilly back.
“Did you write your book yet?” she inquires when my back is away from her typing. Something about her asking is like a tsunami of realization ending in an eagle’s eye tracking and a slurp of a thick and perfectly comforting vanilla milk shake. Something of knowing she had decided at 87 to drive across the country to take her great grand kids to Six Flags by herself and drag them on a roller coaster with her makes me so proud she might ask me about MY guts. Some -
thing about her 92 now and wearing rouge lip stick and a perfect heart necklace I move to listen to her heart of hearts on a February 3 makes me mentally scurry and scour the internet for my writings to see if AI could read everything I have ever written and write a story no one could tell was not written by me but sounded like me.
Could AI take hold of medicine and humanity and cease in one week to invite and challenge the cathartic growth of writing?
Could I die never written my book but my book being written by someTHING assuming everything it found of me out there to assume my voice? So many things can kill humanity but the replaced artist digitized and plagiarized will be the furious death of cleaning our own floors on our frail hands and knees… and the blinds too.
Could AI know to apologize for a lateness that never happens to wall off the betrayal of one that did happen a decade ago?
Could AI know to touch a heart pendant and move it away to listen for the true beats that inspired the gift of love? Would it cheapen the epiphany that gold and stone is forever but the beats and winding down on a little loyal lady laughing while warm in her thoughtfully selected puffy jacket will one day cease to come in to see me?
Would I read everything with

Dr Irene Landaw is a graduate of the High School of Music and Art, SUNY at Purchase (BA), and Columbia University College of Physicians and Surgeons(MD).
She retired from Pediatric primary care at Kaiser Permanente in 2017 where she served as Immunization Champion and Chief of Physician Wellbeing.
suspicion and watch the world grow more hollowed out and stupid as young people never write for themselves nor subject themselves to the rigor of edits and the crucible of red ink negating their lesser voices to unearth the stronger one rising from knees scrubbing floors they call theirs? In a week’s time youth stops waiting for its’ future, stops allowing it to unfold having already decided the future is already written for them easily by AI. “It’s all been said,” they assume.
Somewhere is a capable young woman wanting to learn to derive the equations of quantum physics to marry it to music and make a quantum leap to something wholly human and extraordinarily brilliant for the chasm it should not have crossed having no graft point. She dies a little and tries less the time consuming errors for she hears AI solves her problem yesterdays ago in minutes.
“Oh,” she ponders, “the floors
She continues to serve on the Wellbeing Advisory Committee of her county medical society.
Dr Landaw trains medical teams in communication techniques around HPV vaccination for the American Cancer Society. She is enjoying her retirement from clinical medicine by nurturing her creative side with her trusted canine companion by her side.
She is an avid indoor and outdoor gardener, an ardent iPhone photographer and she also creates unique beaded jewelry (follow her on her Instagram @ Gemweaver and for custom pieces email her at RWB_ISL@ hotmail.com
are clean,” and schleps away the sloshy bucket and hangs a dry rag.
My lovely patient is waiting for my answer as I return to the room outside my flurry and fuss. I roll my chair over to face her and tear up.
“Not yet,” I confess, “ but I’m going to and I going to find a way to talk about you and say how you made it happen when everything threatened to steal the moment away from me. I was thinking the book could write itself these days but then what of you? How would AI know of you so exquisite a person who I have adored and admired and who has invited me to care for her?” I share my realization and she blushed a lover’s joy.
I love medicine. I love being a physician. Artificial intelligence will never take my love or lovers. Not even close. Come find me AI. Come scour the internet. You will always be my vague shadow at dusk and I your alluring master and muse barely unraveled but fully unattainable. ☤
 ARTIST SPOTLIGHT
ARTIST SPOTLIGHT
 Written by Amanda Harrell, DO
Written by Amanda Harrell, DO
When my now 14 year old daughter, Layla, was diagnosed with diabetes at the age of 8, I thought I had failed her. I, her physician mama, failed to see the many signs that were glaringly obvious now when I look back. I will never forget sitting with her in the children’s hospital with the insulin drip still running in her tiny veins. Hearing her little voice asking why this had happened to her, I would try not to tear up and tell her how brave she was.
When the attending and his many residents and fellows entered, I felt so incredibly embarrassed. Hearing them present her case, I would shrivel down into myself wondering how I missed the signs. “8 year old female presented with diabetic ketoacidosis. She had been experiencing increased hunger, thirst and urination along with weight loss prior to presentation and fell asleep in class today”.
The drive home from the hospital was long. She would stare almost longingly and sad outside the window. She would ask why
God would allow her to be sick. I would stumble through answering her many very grown up questions. Seeing her learn to inject insulin for the first time was hard for me. Knowing that she would have to do this for every single day for the rest of her life was even harder.
Everyone kept saying how lucky she was to have me because her doctor mom could handle it all. Man, what little I knew. What a steep learning curve. WHOA.
For the first several weeks, either my husband for I would stay up at night checking on her, finger sticking and fumbling through what the right steps would be with each and every finger poke. We would order scales and carb counting books, and download apps and join Facebook support groups. We would sit for what felt like an eternity before each and every meal trying to precisely count the carbs and dose her with the ongoing fear of what would happen if we miscalculated. We would accidentally dose to much and later have to force SO MUCH food and juice. We
would accidentally dose too little and stay up all night giving corrections. We would try to make life normal and arrange parent meetings with the schools and church and dance teachers. There was an incredible amount of coordinating that had to happen.
I felt like the biggest helicopter mom ever. Trying to allow your kid with a chronic illness to feel like everyone else is HARD. I want her to play sports, I want her to go to swimming parties, I want her to go to camps, I want her to eat whatever she wants whenever she wants and not have to pause before. I want her to not have to forgo the birthday cake at that party because she has her period and her blood sugar is through the roof (yeah, that happens). I want her to not have to sit out of dance class treating a blood sugar.
We, as physicians, see all of the many aspects of diabetes. We care for well controlled diabetics, but we also see the many complications of not managing the disease. We see vision loss, limb loss, poor
healing wounds, gastroparesis, and neuropathy. I tried so hard not to let those severe complications haunt me out of fear for what could happen to my baby girl. I tried not to think about all of the what ifs of diabetes. What if she overdoses accidentally and no one is there. What if her pump fails. What if her dexcom glitches and she doesn’t notice she is high all night long and goes into DKA in her sleep. The list goes on and on. The worries will eat you alive if you let them.
Having a kid with a chronic illness has taught me so much. I tell her all of the time that she makes me a better doctor. I would like to think I was empathetic to patients before, but I know I am definitely more aware what patients with chronic illnesses have to go through. The social, mental, and physical aspects of any chronic illness can be massive. I won’t even begin to touch on the cost of medications and equipment needed for those patients.
Over the years we have learned that we will always be learning. We will miss carb counts, pump sites will fail, her pump will fall off, insulin will accidentally be left in the sun too long, we will forget insulin when we travel states away, we will forget to dose, we will lose her pdm and so many other things will happen. What we have learned is to accept that is impossible to manage this disease perfectly. We will not get it right all of the time. We do have safeguards in place to keep those rarer life-threatening mistakes from occurring, but we give ourself grace on the daily chaotic nuances that can occur with diabetes.
Instead of living fearful of what could happen, we just live.

Below is Layla’s story. She was asked to write it for the local Children’s Miracle Network. It’s the kind of story that makes this physician mama so proud.

My Story, by Layla Harrell
I was the kid who jumped out of bed for school in the mornings, ready much earlier than needed, and excelled in school. Little third grade me was sitting in my school chair, my head pounding and my eyes drooping. I’ll never forget the day I fell asleep in class and the school nurse checked my blood sugar on a tiny little machine and it read HIGH.
My dad rushed me to meet mom at Freeman Health system. Long and bright halls lead me to a small room with a well-kept bed. The white sheets had a baby blue gown that my mom helped me change into. The doctors at Freeman worked quickly to help. I felt to cold sting of the IV needle going into my arm and I was so exhaust-
ed that I hardly flinched.
I remember having fluids given and labs drawn immediately. We knew now that I had diabetes, buy unfortunately I was in DKA, a life threatening complication of diabetes. They ended up having to get me into an ambulance to go to a Children’s Hospital in Kansas City. It was bigger inside than I had imagined. I woke up later, still in the vehicle.
When we got there, I got asked a lot of questions. Most of which my mother had to answer. I was told I couldn’t eat until my labs looked better, and I was crying because I was now starving. My labs finally got better around 2 am and they grabbed food for me. I could only eat the meat and cheese out of lunchables and I kept getting told to drink more water. Eventually, a doctor came in and introduced herself.
“Now, I’m going to say a lot of things you may not understand. But when I’m done, ask all the ques -
tions you have, got it?”
I nodded my head, happy to know what was happening, but also nervous, I never did like not understanding.
She told me I had something called Type One Diabetes. It was nothing I was at fault for, but it still happened. One of my organs had failed, and in doing so it failed to produce life-saving hormone. And for everyday for the rest of my life, I would have to get shots and stick my finger.
I remember taking a shot the very first time, the way it stung. Two weeks after my first hospitalization, I started poking my own finger, sometimes 8 times a day.
Thankfully I got a pump and a continuous glucose monitor which means way less sticks. I had to learn what a carbohydrate was and what insulin was. I had to learn to count carbs with literally every piece of food or drink I put in my mouth. I had to learn to give less insulin when I was swimming or playing with friends. I learned that I couldn’t eat some things when my blood sugar was too high. I had to learn to constantly monitor myself and think about diabetes before I do anything. Swim, bike ride, trampolines, dance, playing chase, all require extra attention because if my blood sugar dropped too low, I could die.
You read that right. Die. I learned that I had to take care of myself because I was at risk of being very sick if I didn’t. The anxiety and stressors alone of living with diabetes can cripple anyone. A simple common cold can cause my blood sugars to skyrocket. A growth spurt can wreak havoc on my numbers too. Having to explain to friends that they may need to give me a glucagon shot in case I pass out is terrifying.
There have been times my
pump failed or I missed the carb count on something leaving my numbers too high. This means my blood sugar was too high for dinner or whatever meal we would eat. I would either have to eat a zero carb meal or run laps around the back yard to bring it down so I could enjoy some Mac n cheese.
Some people think this is just a disease I got because I didn’t take care of myself. But I did, and I never asked for this, nor did I earn this. But no matter how many times people ask, yes, I can have sugar.
Diabetes is a really crummy disease. Given the right tools though, I have been able to realize it didn’t have to hold me back.
I have continued to dance competitively despite my diagnosis. I play guitar, and love acting in my school play. I was inducted into the national Junior Honor society last year, history is my most favorite subject. I love to write short stories, to read, and to sing at the top of my lungs. None of my classmates blink an eye now when I have to change my pump in class or my devices start to beep.
I used to be self conscious of my disease. Now, when someone asks what the device I wear on my arm does, I happily tell them.
I have been active in JDRF through having a a ONE walk team, and recently being a JDRF Gala ambassador for the Missouri/Kansas chapter. I think it’s important to raise awareness and help fund future research of T1D. Don’t get me wrong, I’ve had too many sleepless nights because of this disease, as I am sure to continue to have in the future. I just don’t want to choose to let diabetes to have control.
My mom tells me I can choose to either be a fountain or a drain.
I think this works for this disease. I can choose to pour into others who have T1D too! I have a little friend, about seven years old. Her name is Pearl. Sweetest little girl ever with an even sweeter smile. She got admitted to the hospital a bit over a year ago. Her little arms have marks from the cgm. And she freaks out when she goes low, almost in a panic. But she sees the brightness in it, making jokes about getting to eat candy in class. And calling me her diabetes sister. I love helping her pick new sites and learning to be even more brave than she already is.
Recently being awarded an alert dog through Children’s Miracle Network was a HUGE win for me. This dog will alert me of my highs and lows, which is huge when I sleep through my alarms, or when the technology fails. I am so excited to grow with my dog, Nico. He already feels like family.
My story is ongoing obviously. But what I do know is that while diabetes is a part of my story, it will not be the main character. It will not keep me from writing whatever story I want and achieving my dreams. ☤

This issue of Physician Outlook magazine has literally taken me several months to produce and get to the printer, and it is with a sense of relief and profound gratitude that I am finally able to put these words on paper. I recently had an epiphany during a session with my physician coach, Dr. Deb Roman. We were chatting about my life-long tendency to try to multi-task, and reflecting on how this strategy was no longer serving me when the lightbulb went off and I experienced my “a-ha moment.”
For many years I have resisted using the word "burnout" to describe my personal relationship with the career that I once adored and had always given me a sense of great fulfillment. For the first time in my adult life, I find myself living for the "day off,” craving time that is completely free from any and all patient care responsibilities.
I've been doctoring for more than three decades, and this is not how I ever expected to feel. I have ALWAYS been my happiest when I am one-on-one with a patient or a parent who needs my services. What, then, has changed?
Simply put, EHR’s have broken me. Electronic Health Records, particularly Epic Health Systems (known as “the Cadillac” of all EHRs) innately promotes and en-
courages its end users to dangerously multi-task.
Multi-tasking leads to decreased productivity and can contribute to or cause medical errors. When we are making eye contact with the keyboard and not our patient, we are missing important cues and information that could be relevant to a differential diagnosis. If we DON’T bring our computer/laptop into the exam room, we are often taking our work home with us at the end of the long workday or finishing our work on weekends. There is no beginning or end to our day. We lack boundaries. We start identifying with the time loop that plagues the Bill Murray character in the infamous 1993 “Groundhog Day” movie as he monotonously experiences the same day over and over again.
The decreased focus, cognitive overload, and unreimbursed time spent outside of regular work hours on administrative tasks is contributing to increased stress levels and leading to physician burnout.
As a profession, physicians are reporting rising levels of job
dissatisfaction and feelings of detachment from our work and our patients. Many doctors are looking for a way out of clinical medicine, and many (tragically) are committing or contemplating suicide.
Epic’s Hyperspace with its many screens, alerts, ever-elusive “refresh” buttons, Problem Lists, Diagnoses Tabs and “Tips of the Day” cause me to experience an extreme form of sensory overload. I sometimes talk (yell) in frustration at my computer screen, and I am often annoyed that the EHR isn’t “smart” enough to produce the test result or report I am searching for.
If the technology exists for Facebook, Instagram and Twitter to fill our personal social media feeds with eerily accurate targeted advertising, why hasn’t someone in the medical space taken the time to invent similar automations for Electronic Health Records? Why do we have to constantly confuse patients with After Visit Summaries that erroneously list medications as “discontinued” instead of fixing the glitchy Outside Medication Reconciliation process? Why isn’t the Newborn Metabolic Screen a hard-coded Epic-wide “Care Gap” for all children?
As a pediatrician with years of experience as a locum, I have had the “privilege” of working in many different hospitals and health systems, each with their own electronic medical records.
Epic is set up differently IN. EVERY. SINGLE. FACILITY, even at hospitals that are owned and operated by the same mega-health systems. In some EHRs it can literally take HOURS to find basic information that is relevant and necessary for safe and effective patient care. I call it “Easter Egg hunting.” All of the information is somewhere in the EHR; it’s just not in the same place twice. There is a steep learning curve with Epic’s software, and an absurd fascination with end-users being able to customize. Personally, I don’t want to re-invent the wheel or play in Epic’s “Playground.” I want meaningful interactions with my patients during the workday and quality time my family at home.
I am a life-long habitual serial multi-tasker in recovery.
I was raised thinking that I could do multiple things at once, and, more importantly, convinced that I could do them all well. I am smart, ambitious, passionate, engaging, and (once upon a time), I was efficient, task-oriented and organized. I knew how to delegate those tasks that could be assigned to others and I was able to effectively lead and motivate others to work as part of a team. I could do everything a man could do AND I also became a mother, the quintessential ultimate multi-tasker of all time.
The term “multi-task” was first coined in the 1940’s, but became popularized in 1960 by J.C.R. “Lick” Licklider, a brilliant mathematician, physicist and psychologist who

“I am a life-long habitual serial multi-tasker in recovery”
is commonly credited as being “the father of the internet.” Three years before I was born, Lick published his revolutionary paper entitled “Man Computer Symbiosis,” in which he foretold the eventual invention of real-time interactive computing. Licklider envisioned a future in which humans and computers would work together to solve complex problems.
In healthcare, the ideal symbiotic relationship would use “smart” Artificial Intelligence to scour and summarize a patient’s personal medical story, relevant family history, pertinent labs, specialist recommendations and other useful information. It would synthesize this information and present the end-user (the patient’s physician) with a succinct summary of the pertinent positives and negatives.
Licklider was a visionary ahead
of his time, and it would behoove all Hospital Administrators and Chief Informatics Officers to re-visit his groundbreaking tome, which argued that “Computers should be designed to work in a way that is intuitive and natural for humans, rather than forcing humans to adapt to the limitations of technology.”
(As for me, I will continue to work the steps towards recovery from my errant multi-tasking ways. I need to accept the things I cannot change, find the courage to change the things I can, and pray for the wisdom to know the difference.)
Dr. Marlene Wüst-Smith Publisher & Founder

Publisher: Marlene Wüst-Smith, MD Editor in Chief: Isabella Liberos, Marist ‘24 Managing Editors: Hannah Bushery, Marlene Wust-Smith, Jill Labecki VP of
Advertising: Pamela Ferman, VP of Operations and Digital Media Strategist: David Ramirez Director of Art and Production: Hannah Bushery Marketing/
Copyright Editor/Journalism/Social Media Interns: Dana Bushery, Madison M. Smith
Contributing Authors: Jean Robey, MD, Rhonda Crowe, BSN, MBA, Randy Cook, MD, Deb Roman, DO, Rick Zollinger, MD, Dael Waxman, MD, Desmond Bell, DPM, CWS, Amanda Harrell, DO, Layla Harrell, Henna Sawhney, MD, Mary Anna Rodabaugh, MD Coaches
Cover Art: Maz Ghani, MD
Published by “Physician Outlook Publishing” Editorial policy: Physician Outlook magazine is a national magazine dedicated to empowering physicians and their patients to improve the world of medicine together. Editorial decisions are based on the editor’s judgement of the quality of the writing, the timeliness of the content, and the potential interest to the readers of the Physician Outlook magazine. The magazine may publish articles dealing with controversial issues. The views expressed herein are of the authors and/or those interviewed, and may not reflect the official policy of the magazine. Physician Outlook neither agrees, nor disagrees with those ideas expressed, and no endorsement of those views should be inferred, unless specifically identified as officially endorsed by the magazine.
“Letters to the Editor” email: hello@physicianoutlook.com
Information on advertising, subscriptions, and job board email: hello@physicianoutlook.com
“Physician Outlook” is a registered trademark.
