What



What


We provide our optometrists with a solid career path and are focused on helping you achieve your professional goals.
With over 400 stores, you can find a Specsavers practice in a location that suits your preferences — from metropolitan to outer regional areas.
We also provide genuine career progression, from our graduate program all the way to partnership, supported with leadership and training through our Pathway programs.
Whether you’re looking for your first job, looking for new opportunities or ready to take that next step to partnership, at Specsavers you’re only limited by the scale of your own ambition. Go
spectrum-anz.com or contact us:

Optometry Australia (OA) is urging caution over potential changes to the way Ahpra uses its national database, with the regulator considering listing more information – such as a practitioner’s disciplinary history –which would be available to the public.
Optometry’s peak body is commenting on the regulator’s ‘Public consultation on a draft data strategy’, which will guide how it uses data it collects and holds on health practitioners, including optometrists and ophthalmologists.
OA has lodged a submission in response and, although not publicly available at the time of writing, it contains “a mixed, but generally positive response to the questions raised”.
Changes to the way the Australian Health Practitioner Regulation Agency (Ahpra) handles the public

register is potentially the most contentious part of the proposed new strategy.
Ahpra believes there may be value in making more information available on the public register, including things like additional qualifications, cultural safety training and authority to prescribe.
But it is also proposing listing a practitioner’s “regulatory action history”. According to Ahpra, the register doesn’t include previous registration or restriction information such as when a practitioner has previously been suspended, even where that information is in the public domain – such as in media reports.
“Optometry Australia understands and supports the need for the public to be able to access information to inform their healthcare choices. Notably, however, not all disciplinary
history would be objectively useful for this purpose and careful consideration of what disciplinary history is listed should be made,” OA interim CEO Ms Skye Cappuccio said.
“We also have some concerns about ongoing publication of disciplinary history – beyond what is required for intended protective effect of the regulatory action. The discussion
paper lists, and we would agree that there is ‘potential for detriment to their practice/reputation if restrictions they have met and no longer apply, remain on the register as historical records. Continuing to publish disciplinary history could have ongoing consequences for practitioners, beyond the intended protective effect of the regulatory action’.”
OA noted that from 2018, links to adverse tribunal decisions and court decisions are already published on a practitioner’s record on the national register.
“We understand that the links remain on the register – even if the sanctions imposed by that decision are no longer on the register – to ensure transparency for patients, potential patients and the public. Further
continued page 8
Ahead of the upcoming Federal Budget, Vision 2020 Australia is continuing to push federal policymakers to implement a nationwide vision screening plan the peak body has developed for all 3.5 to 5-year-old children.
The call forms part of a six-pronged submission from the body representing around 50 eye health member organisations, which is also advocating for investments to increase access to publicly funded sight-saving eyecare, end avoidable vision loss and blindness in Aboriginal and Torres Strait Islander communities and strengthen Australian eye research.
It's also calling for improved health systems in the Indo-Pacific and accessibility and inclusion for people
who are blind or have low vision.
As Insight reported in February, the Vision 2020 Australia National Framework for Vision Screening for 3.5 - 5-year-olds, published in November 2021, is based on the NSW Statewide Eyesight Preschool Screening Program (StEPS).
The organisation included its full framework in its Federal Budget submission, stating, if adopted, it would “provide an essential foundation for effective vision screening programs nationwide”.
“Vision 2020 Australia is requesting the Commonwealth and state governments adopt the framework and ensure implementation in each jurisdiction,” the organisation said.
“We know that vision loss has
life-long implications. In a study completed in 2016, Deloitte Access Economics found a 17-year-old living in Australia with a vision impairment received $53,916 less in real lifetime earnings than a person without vision impairment.
“Children’s vision screening programs in Australia have demonstrated good return on investment, decreasing blindness in children and outweighing associated health care costs. However, there is no consistent, national evidence-based approach to screening and in some jurisdictions, there is no screening at all, resulting in inconsistent outcomes for Australian children.”
The submission also urged the continued page 8
quality workmanship are the hallmarks of a relatively young European eyewear brand now available to Australian optical practices through Sunglass Collective. page 18


Discover an efficient glaucoma treatment experience with the integrated SLT option on your VISULAS ® green laser from ZEISS.


• R otating aiming beam to accurately position on trabecular meshwork.
• C oaxial illumination of aiming and treatment beams.
• Fast SLT pattern application of 400μm delivered by 52 squared spots.
• D igital treatment report output to ZEISS FORUM.*
Early adopters of ZEISS SLT with VISULAS green laser are seeing immediate clinical benefits:
“SLT with the VISULAS green laser demonstrated clinically significant efficacy in terms of lowering IOP in eyes with POAG with about half of the treated eyes showing a 20% additional IOP reduction”1
zeiss.com/visulasgreen
Hear from the ZEISS SLT Experts:
AU: 1300 365 470 med.au@zeiss.com

One of optometry’s great attractions is the many options to realise career fulfilment. For those with an entrepreneurial streak, practice ownership is a unique challenge – and there are countless examples of successful mum-and-dad-run optical businesses across Australia, or young partners making a fist of a profit-sharing arrangement within a corporate-style group.

Next to finance, one of the biggest barriers to ownership is business nous. The industry has long complained about graduates leaving university with all the clinical skills, but limited business knowledge. But this hasn’t curbed a desire among optometrists to seek out ownership opportunities. In fact, it's been heartening and surprising to hear of an uptick in young optometrists taking the plunge with greenfield practices in 2022, with more lining up to take over existing businesses.
The market conditions are ripe for ownership; many experienced independents who graduated in the 1970s are seeking succession through young optometrists, a transitional partnership or by selling to a group.
The great news for aspiring owners is that there are options due to the nature of the optometry business market today. It comes down to the level of control one ultimately wants over their business. For those seeking ultimate autonomy, independent ownership is one avenue, with optional support of organisations offering buying power and commercial assistance. Meanwhile, corporate-style groups can offer partnership opportunities taking care of all business functions, while sharing in the profits. The value proposition is nuanced – and readers can find some of the differences on pages 50-53.
Optometry has shown time and again it’s a resilient, stable sector. It therefore makes sense optometrists see the value in ownership/ partnership. Fortunately, the industry has stepped up to address the business skills knowledge gap. Many networks have formalised training programs that equip the next generation on matters like HR, finance, marketing and growth.



It’s a win-win, with the optometrist realising career fulfilment and each network ensuring its longevity –ultimately strengthening the profession.
MYLES HUME Editor



Just as Insight went to print, AUSTRALIA DAY HONOURS were presented to three people with links to the ophthalmic community. Fred Hollows Foundation members Ms Katrina Fanning and Ms Patricia Fiske were both recognised. Fanning was appointed an Officer in the Order of Australia (AO) while Fiske was awarded a Medal of the Order of Australia (OAM). Monash University Emeritus Professor Paul McMenamin – who specialises in the
structure and immunology of the eye –was also recognised a Member (AM) in the General Division. IN OTHER NEWS, the 54th RANZCO Congress is heading to Western Australia this year, with organisers announcing an altered program. “The jam-packed nature of congress is ensured with the event finishing a half-day sooner than usual. Many of you may have noticed that Tuesday is not as popular as the other days. The board have been monitoring this and have agreed to finish the Congress on the Monday afternoon” the college
said. The event is taking place 20-23 October 2023 in Perth. FINALLY, Bausch + Lomb has acquired intraocular lens (IOL) manufacturer AcuFocus. The company has developed breakthrough small aperture intraocular technology, including the IC-8 Apthera IOL, which was approved in the US in July 2022 as the first and only small aperture non-toric extended depth of focus IOL. Known as the IC-8 IOL in global markets, the IOL is available in select markets across Europe, as well as in Australia, New Zealand and Singapore.

Published by: 379 Docklands Drive, Docklands VIC 3008
T: 03 9690 8766 www.primecreative.com.au
Chief Operating Officer Christine Clancy christine.clancy@primecreative.com.au
Reindeer have been shown to change the colour of their tapetum lucidum – a mirror-like layer behind the retina –from gold streaked with turquoise, to a rich blue hue in winter. It’s thought this change occurs between summer and winter so they can maximise light absorption in the blue and below-blue colour wavelength during the long, dark winter twilight in countries like Norway.
This year the Australian Open held its first exhibition game of blind and low-vision tennis. Eight players took part, with matches involving an adapted foam ball rattling across the court. For those with no sight, up to three bounces are allowed on their side of the court. For those with low vision, one or two bounces are allowed depending on their sight classification.
Researchers from ETH Zurich have developed a new transparent gold nanocoating that harnesses sunlight to heat eyewear lenses, working to prevent fogging in humid conditions. The coating could potentially also be applied to car windshields, and its inventors have now applied for a patent for the technology.
Group Managing Editor Sarah Baker sarah.baker@primecreative.com.au
Editor Myles Hume myles.hume@primecreative.com.au
Journalist Rhiannon Bowman rhiannon.bowman@primecreative.com.au
Commissioning Editor, Healthcare Education Jeff Megahan Business Development Manager Luke Ronca luke.ronca@primecreative.com.au

Client Success Manager Salma Kennedy salma.kennedy@primecreative.com.au
Design Production Manager Michelle Weston michelle.weston@primecreative.com.au
Head of Design Blake Storey
Art Director Bea Barthelson Subscriptions
T: 03 9690 8766 subscriptions@primecreative.com.au
The Publisher reserves the right to alter or omit any article or advertisement submitted and requires indemnity from the advertisers and contributors against damages or liabilities that arise from material published. © Copyright – No part of this publication be reproduced, stored in a retrieval system or transmitted in any means electronic, mechanical, photocopying, recording or otherwise without the permission of the publisher.

continued from page 3
consultation between the regulator, peak bodies and patient groups may be required in this area to strike the right balance.”
Ahpra said there needed to be careful assessment, balancing competing interests of the public versus the practitioner’s career.
To highlight a flaw in the current approach, it presented a case study involving a medical practitioner in a rural local women’s health service with a history of ‘notifications’ involving female patients and inappropriate communication and poor approaches to consent and physical examination. Regulatory action was taken, including conditions for education, supervised practice and mentoring. Because the practitioner met these conditions, there is nothing on the public register to alert an employer or the public to their disciplinary history.
Subsequeently, a new patient learns about the practitioner's history from the local media, and was surprised not to see this reflected on the public register.
This therefore leaves the patient concerned about potential risks to themselves and questioning whether they should continue seeing the practitioner. Meanwhile, the practitioner feels they have met the conditions and it would be
detrimental to their career if the conditions were permanently displayed on the public register.
In response to making more information available like qualifications, prescribing authorisation and areas of special interest, Cappuccio said one of the objectives of the National Scheme was to facilitate public choice and access to healthcare provided by registered health practitioners.
“Optometry Australia believes the inclusion of additional information on the public register would assist patients in making informed decisions about their healthcare and would also help practitioners differentiate areas of professional interest and skills,” she said.
The second focus area of Ahpra’s strategy is its data sharing arrangements with other organisations.

The third area explores ways for the regulator to put its 10 years of regulatory data to greater use by using machine learning and advanced analytics. The body believes this could provide additional insights that could be combined with other sources to make its regulatory work more effective and efficient.
For example, in its registration processes, these technologies could help expedite applications, including from overseas-
qualified and registered practitioners.
And in notifications processes, advanced data analytics could review previous decisions and a range of predictive factors to then create new tools to triage higher risk matters, and manage increasing caseloads effectively.
Cappuccio said this could be “extremely important for patients and practitioners” as notifications continue to increase –up 6.5% last year to 10,800 across all registered health professions.
“And concerns remain over timeframes involved in dealing with these complaints. We would hope that this could be used to help improve efficiencies and processing times at Ahpra,” she said.

Overall, as a custodian of this data, Ahpra said it faced growing demand for both the data it makes public now through existing services, and what it could make available in the future, subject to privacy and confidentiality obligations.
“We recognise that while meeting the National Law and privacy requirements, there may be more opportunities to use and share some of the data we hold to give value to practitioners, the public and the broader health system, including improved public safety, practitioner regulation and workforce planning,” it stated.
continued from page 3
government to help enhance the eye health workforce and improve infrastructure for public access to eyecare. This included a pilot of a multi-disciplinary collaborative model for eye disease management focusing on providing timely and culturally appropriate healthcare in the right setting by an appropriate provider.
Additionally, it called for $2.5 million to pilot an eyecare specific electronic medical record system in a metropolitan and a regional public hospital to improve data collection and reduce wait times through improved assessment and collaborative triage.
“Vision 2020 Australia also calls for changes to MBS items 701, 703, 705 and 707 to make vision checks a requirement of chronic health checks. This would align with MBS item 715 for Aboriginal and Torres Strait Islander Peoples and the impacts on associated optometric MBS billing would be minimal
(0.7% increase on current billing rates).”
Meanwhile, the peak body highlighted Australia’s world class talent in vision and eye research. However, it said vision loss is not funded in either the first or second MRFF 10-year Investment Plan.
“Investment in eye health clinical trials and the translation of pre-clinical innovations provide a good return on investment, with every $1 spent returning a $10 economic gain (2009 figures).”
It called for a $150 million investment over 10 years to fund research through the establishment of a dedicated Eye Disease and Vision Loss Mission within the MRFF.
Aboriginal and Torres Strait Islander eye health was a major tenet of the submission, which Vision 2020 Australia said required $73.6 million for several initiatives.
One of them is an additional 12,300 outreach ophthalmology services through the Medical Outreach Indigenous Chronic
Disease Program (MOICDP), Eye and Ear Surgical Support Services (EESSS) and Rural Health Outreach Fund (RHOF). And enabling consultations, treatment (including cataract surgery) and follow-up care at regional and district hospitals to ensure Indigenous people receive ophthalmology services ($24.6 million over five years).
“Vision loss costs the Australian economy $27.6 billion annually. The main causes can be attributed to five preventable and/or readily treatable conditions,” Vision 2020 Australia stated.
“Failures in government policy and the impacts of the COVID-19 pandemic have led to growing wait lists for eyecare services and treatment which means key opportunities to prevent avoidable blindness are being missed. Addressing inequities in eyecare will help reduce health spending and free up resources, prevent conditions and injuries that cost us more in the long term.”
HOPE [ADVANCED ANALYTICS] COULD BE USED TO HELP IMPROVE EFFICIENCIES AND PROCESSING TIMES AT AHPRA”
SKYE CAPPUCCIO, OPTOMETRY AUSTRALIA



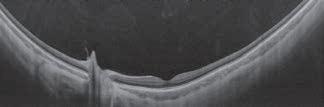
It has been described as one of the most unusual – and painful –corneal conditions in the field of optometric health, and it is currently on the rise in the Albury-Wodonga region.











Known as ‘Christmas Eye’, the condition results from a miniscule beetle causing the surface of the cornea to melt. It typically affects people during the holiday season in the hot, dry summer in South Eastern Australia between mid-November and late-February, Optometry Australia reports.


Wangaratta optometrist Mr Robert Holloway from Holloway Vision wrote an article explaining the condition and its management in Pharma in 2019. One of the practice’s patients had been affected three times in 10 years.
“The level of pain associated with Christmas Eye has achieved folkloric status. The hardy farming types, who make up a sizeable portion of the victims, shake their heads with sympathy when they hear of a friend or colleague who has been affected,” Holloway wrote.


He said the higher the pain level, the more likely the Christmas Eye presentation.
“Patients will often arrive cradling their head with their hand cupped over the affected eye. They are miserable and have often attended following an initial presentation at the local hospital emergency department.”


Holloway also suggested that the timeframe of the pain onset and corneal observation with fluorescein will provide further information to assist with the diagnosis.
More recently, optometrist Ms Kelly Gibbons from Wodonga Eyecare spoke to the ABC following a recent cluster of cases.
“Christmas Eye is essentially a really nasty cornea ulcer that happens at the front of the eye caused by a tiny beetle,” she said.
While a lack of physical evidence has made it difficult to identify the cause, a small hooded beetle from the Orthoperus species is
said to be most likely. As Holloway explained in Pharma , Orthoperus are known to carry the compound Pederin in their haemolymph which is released when the insect is crushed on the skin or eye.
“Pederin is a powerful inhibitor of protein biosynthesis and mitosis and is a known vesicant (blistering agent). With these properties, it is unsurprising that it has such a dramatic effect on the corneal epithelium,” he wrote.
Cases of ‘Christmas Eye’ usually involve the patient doing some sort of outdoor activity like gardening or mowing.











“There’s nearly always a history of them being outside mowing,” Gibbons told the ABC. “That there is something in the grass at that stage that has gotten into someone’s eye. But people don’t always remember something getting into the eye and certainly by the time I see the patient I can’t find anything.”
According to Optometry Australia, symptoms include excessive tears, an unpleasant response to natural light like burning, itching and redness of the eyes, as well as a headache and nausea.

Because of the damage done to the eye, Gibbons said treatment typically involves managing the pain and preventing infections until the surface of the cornea grows back again.

Patients will generally be prescribed anti-inflammatories and a bandage with a silicone hydrogel contact lens, and eye drops.
 ‘Christmas Eye’ can become more prevalent in Albury-Wodonga in summer months.
‘Christmas Eye’ can become more prevalent in Albury-Wodonga in summer months.
The US drug regulator has issued an alert to immediately halt use and importation of artificial tears eye drops – manufactured in India by Global Pharma Healthcare –that have been linked to permanent vision loss and one death. “FDA is collaborating with the Centres for Disease Control and state and local health departments to investigate a multistate outbreak involving a rare, extensively drug-resistant strain of Pseudomonas aeruginosa bacteria. As of January 31, 2023, CDC identified 55 patients in 12 states with infections that have been linked by epidemiologic and laboratory evidence to use of EzriCare Artificial Tears. Associated adverse events include hospitalisation, one death with bloodstream infection, and permanent vision loss from eye infections.”
South Korean ophthalmologists found a fungal endophthalmitis outbreak after cataract surgery was caused by contaminated viscoelastic material. The investigators, led by Dr Seong Woo Kim, from the Korea University Guro Hospital Department of Ophthalmology in Seoul, found that prompt intervention may improve the prognosis of fungal endophthalmitis caused by contaminated medical products. Fungal endophthalmitis is rare, occurring in 0.002% of cases in South Korea. The “unusual” outbreak developed in October 2020, which became a nationwide outbreak and was found to be associated with contaminated viscoelastic material, sodium hyaluronate, Optometry Times reported.
The National Boards and Ahpra are reviewing the current accreditation arrangements for the 2024–2029 period. The consultation ended 14 February. Ahpra’s accreditation activities involve two processes – program accreditation (performed by OCANZ for optometry) and practitioner assessment. “Program accreditation is the process of assessing whether a health practitioner education program and the education provider produce graduates who have the knowledge, skills and professional attributes to safely and competently practise,” the regulator said. “Practitioner assessment is the process of assessing whether an overseas-qualified practitioner has demonstrated the knowledge, clinical skills, and professional attributes.”

A new Federal Government program is expected to have “another profound effect” on optical dispensing training numbers in Australia – and is the first time in recent memory both the employer and employee receive a financial incentive for course enrolments.

The Australasian College of Optical Dispensing (ACOD) announced the “unexpected” news in early 2023, with employers able to access as much as $12,000 in wage subsidies over a two-year period – in addition to a one-off hiring incentive – while employees can receive thousands in training support payments for items such as laptops.
People who enrol into the Certificate IV in Optical Dispensing can access the incentives after the course was added to the Australian Apprenticeships Priority List Appendix A. The program acts as a replacement to the Boosting Apprenticeship Commencements (BAC) that was launched in a post-COVID recovery Federal Budget and led to a surge in optical dispensing training enrolments in 2021/22.
While the BAC closed to new enrolments on June 30, 2022, the Australian Apprenticeships Priority List Appendix A was launched on July 1, but was only available to selected accredited courses, excluding optical dispensing. However, ACOD director and senior trainer Mr James Gibbins said the list was revised in December 2022 with the Cert IV in Optical Dispensing now included, effective from Jan 1, 2023.
He understood that a small number of courses were removed due to low take up rates, and “an even smaller number of very
fortunate courses” were added due to a high take up rate in the BAC.
The new incentives and benefits include:
• B oth new entrant and existing worker trainees are eligible
• For employers – includes a 10% wage subsidy for two years, capped at $1,500 per quarter (up to $6,000 per year for two years, capped at $12,000)
• For employees – includes a training support payment capped at $5,000 for full time and $2,500 for part time, paid in four equal instalments of $625 over two years.
“Like the BAC, these payments are linked to enrolment and are not dependant on completion. If a student leaves the course for any reason, no refund of payments made to either employer or employee up till the point of leaving the course is required,” ACOD stated.
In addition, there have been amendments to the New Entrant hiring incentives, available to employers:
• Full time – two equal payments of $1,750 each are made at the six and 12 month mark ($3,500 in total)
• Part time – two equal payments of $875 each are made at the six and 12 month mark ($1,750 in total)


According to ACOD, unlike the previous new entrant hiring incentives, these payments are not dependant on course completion, only on enrolment.
While not as generous as the BAC program – which involved an annual wage subsidy of up to $28,000 for new or existing employees – Gibbins believed the latest new program would have another profound effect on enrolments throughout the optical industry.
“In particular, we have received widespread feedback from employers in recent years concerning employees reluctant to sign up to the course, sometimes because they are concerned about the incidental costs they will incur during their course – possibly like requiring a new computer,” he said.
“We believe the employee incentive will be extremely attractive to many optical assistants and will make the difference for many in choosing to enrol.


The number of people waiting for elective surgery is expected to reach more than 500,000 by 30 June this year if no action is taken by governments, the AMA has warned.

Australian Medical Association (AMA) president Professor Steve Robson said the AMA’s latest report, 'Addressing the elective surgery backlog', shows a system under enormous pressure and struggling to meet demand.
“Recently state premiers have talked about the dire state of the health system and the need for urgent action through National Cabinet – this report highlights a key part of the system that’s struggling,” Robson said.
“Our analysis shows hospitals can’t meet demand or the recommended timeframes for surgeries and it’s only going to get worse without intervention.”
He continued: “There’s currently an estimated elective surgery backlog of 306,281 patients nationally and this will grow to more than 500,000 by the end of the financial year if something isn’t done.”
Ophthalmology is not immune from the backlog, with data last year showing wait times for ophthalmic procedures increased by 6.5 weeks in 2020-21 compared to pre-pandemic levels and have more than doubled to 172 days for cataract surgery.
Robson said Australia needs a national
plan now to address the growing and increasingly critical backlog of elective surgeries, with an immediate injection of funds required.
“This plan needs to be funded by both states and territories and the federal government and backed by long-term funding commitments that deliver permanent expanded workforce and increased capacity to deliver services in our public hospital system,” he said.
The AMA’s analysis shows Victoria makes up the largest percentage of the backlog (134,950 patients, or 44% of the backlog) together with New South Wales (77,845 patients, or 25% of the backlog).
Queensland and Western Australia account for around 10% of the backlog each.
Hospitals were struggling to meet
community demand even before the COVID-19 pandemic and the pandemic had a significant impact on the number of elective surgeries performed in the last few years.
Robson said most of the backlog consisted of people who haven’t been added to the waiting list, and were likely waiting for an outpatient appointment with a specialist or had simply given up.
The AMA is calling for a new funding agreement between the state and territories and the Commonwealth that includes an upfront advance payment provided by the Commonwealth to support state and territory governments to expand their capacity (including workforce) to address the elective surgery backlog.
“This should reduce the backlog of hospital outpatient appointments (the hidden waiting list) by providing funding to state and territory governments or directly to health services to assist in expanding the number of public outpatient appointments,” Robson said.
“We also need to see data on waiting lists (including the hidden waiting list) reported more regularly and transparently across all jurisdictions to ensure the health system can be appropriately managed and patients are receiving the right care at the right time. This isn’t happening now.”
CooperVision is celebrating a significant milestone with its plastic neutrality initiative preventing the equivalent of more than 100 million plastic bottles from entering the oceans.
The company said the achievement has been accomplished in partnership with eyecare professionals, contact lens wearers, and Plastic Bank, which uses 1kg of plastic to equal 50 bottles.
CooperVision pioneered the plastic neutral model for the contact lens industry in 2021 and has continued to expand the scope of the global initiative, including into Australia and New Zealand in May 2022. Communities impacted rose from 171 in 2021 to 345 in 2022, according to Plastic Bank’s ‘impact dashboard’.

The contact lens manufacturer funds Plastic Bank’s collection, processing and
reuse of general ocean-bound plastic waste that is equal to the weight of the plastic contained in participating products across 27 countries throughout the Americas, Europe, and Asia-Pacific.
Mr Aldo Zucaro, senior director of corporate responsibility at CooperCompanies, said the company was thankful to the eyecare professionals and contact lens wearers who share CooperVision’s sustainability commitment.

“We couldn’t be more thankful to everyone who has helped this program become an absolute success. Each plastic neutral contact lens that is prescribed and worn makes a difference,” he said.
“Together, we’re making our oceans, our communities – and our future – better. We already have our sights set on the next 100 million.”
Beyond the positive impact on the environment, CooperVision’s plastic neutrality initiative benefits collection community members in more than 350 coastal communities who receive bonus payments through Plastic Bank for necessities such as groceries, cooking fuel, school tuition, and health insurance.
As a manufacturer of contact lenses, CooperVision is dedicated to reducing its environmental footprint, and its efforts extend beyond plastic neutrality.
The company has a track record of sustainable manufacturing and operations. It has developed best-in-class manufacturing processes resulting in award-winning conservation efforts in Puerto Rico and sustainability certifications in Puerto Rico, Costa Rica, Spain, the UK, and the US.
only one
Minims are the convenient, preservative-free range of single-dose pharmaceuticals. Single patient use to reduce the potential risk of cross-contamination.
Colour-coded packaging and individually marked for accurate selection.
Individually wrapped, ensuring sterility through to point of use.
For more information contact your Bausch + Lomb Territory Manager or Bausch + Lomb Customer service 1800 251 150
Always review product information before prescribing these medications. Product information is available on request from Bausch + Lomb on 1800 251 150.



A new study has revealed that Australia has the second longest healthcare waiting time in the OECD, with a median wait time of 84 days for cataract surgery and more than two thirds waiting over a month for a specialist appointment.
Health experts at NiceRx – which helps US patients access FDA-approved brand name medications from pharmaceutical companies – have revealed the countries with the highest and lowest healthcare expenditure, as well as those with the highest and lowest life expectancy and the longest and shortest healthcare waiting times.
For healthcare waiting times in Australia, it found:
• 14% of patients are waiting one day or more to hear back from a doctor.
• 39% of patients are waiting over a month for a specialist appointment.
• The median wait time for cataract surgery is 84 days.
• The median wait time for hip replacement surgery is 119 days.
• The median wait time for knee replacement surgery is 209 days. For cataract surgery, Australia ranked seventh for the longest wait time, with the list topped by Poland (246 days), and Italy performing the best (24 days). Further findings from the study revealed the US had the world’s highest healthcare expenditure per capita annually (US$12,318). This figure is over $US5,000 more than Germany, which has the second highest total. Australia’s ranked 11th at (US$5,627).
Hong Kong topped the list for life expectancy, averaging 85.29 years of age (82.38 male and 88.17 female). Australia ranked seventh at 83.94 years (82.08 male and 85.80 female). In comparison, Latvia has the shortest life expectancy in the world, averaging 75.73 years.
Norway has the longest healthcare waiting times of the countries profiled, with the country scoring a normalised waiting time score of 8.13. In comparison, Denmark has the shortest healthcare waiting times, with a score of 2.0/10.
Australians with diabetic macular oedema (DMO) or neovascular age-related macular degeneration (nAMD) now have access to Vabysmo under the PBS.
Minister for Health and Aged Care, Mr Mark Butler, announced on 1 January that Vabysmo (faricimab) will be listed on the Pharmaceutical Benefits Scheme (PBS) for the first time to treat both conditions.

Roche Australia announced in August last year that the Australian Therapeutic Goods Administration (TGA) had registered Vabysmo for the treatment of DMO and nAMD.
The therapy is administered by four initial four-weekly eye injections. Thereafter, Roche advises, the frequency of the ongoing injections will be determined by the treating ophthalmologist.
According to the Department of Health and Aged Care, last year more than 18,000 people with DMO and 62,000 people with nAMD accessed comparable treatments through the PBS.
Without the PBS subsidy, patients might pay more than $4,000 a year for treatment.
The announcement comes as the Albanese Government delivers on a election promise to make medicines cheaper for Australians.
As of 1 January, Australians will pay up to 29% less for their PBS prescriptions, with the maximum PBS co-payment dropping
For the first time in the 75-year history of the PBS, the co-payment for general scripts has fallen.
For a family relying on two or three medications, this can put as much as $450 back into their household budget, the department stated.
Since 1 July there has been additional funding approved for 61 new and amended listings on the PBS.
“The government has delivered on our commitment to cut the cost of medications for millions of Australians,” Butler said.
“Pharmacists have told me stories of their customers coming in with a handful of prescriptions asking for advice about which script they can go without, because they can’t afford to fill them all. Our cheaper medicines policy will make that choice redundant for millions of Australians.”
An Australian ophthalmologist is among a group of researchers behind a new study which identifies how to diagnose optic neuritis, a common cause of vision loss.

Associate Professor Clare Fraser from Save Sight Institute in Sydney, and London-based colleagues Dr Axel Petzold and Professor Gordon Plant, have developed diagnostic criteria that will help inform treatment options for patients with the condition.

Prior to the publication of their study, there has been no consensus on how to diagnose optic neuritis, inflammation in the optic nerve, making it challenging to provide timely treatment for conditions in which it is the first symptom.
“This is an important international collaboration, which expands our understanding and classification of all types of optic neuritis across the world,” Fraser said.
“We are hopeful that the criteria we have developed will lead to a consensus on how to design treatment trials for optic neuritis in the future.”
In the study, the researchers achieved a 95% expert consensus through a Delphi process to categorise the links between optic neuritis and other antibody mediated disorders including syndromes such as Neuromyelitis Optica, or Myelin Oligodendrocyte Glycoprotein Antibody-associated Disease, which are more common in patients of African and Asian origin.
1800 33 88 12

Facebook’s parent company Meta has acquired Luxexcel, the Netherlands-based creator of 3D printed lenses, marking the social media company’s latest move in the smart glasses market.
Founded in 2009, Luxexcel uses 3D printing to make prescription lenses for glasses. More recently, the company has focused its efforts on smart lenses, which can be printed with integrated technology like LCD displays and holographic film.
The acquisition was announced in late December 2022 and will enable Meta to produce prescription augmented reality (AR) glasses using lenses produced with Luxexcel’s proprietary 3D printing technology, VisionPlatform 7.

VisionPlatform 7 is technology-agnostic and integrates objects such as waveguides, holographic optical elements, and liquid crystal foils during the 3D printing process. The platform includes high-tech hardware, proprietary materials, and advanced software to create prescription smart eyewear on-demand.
Luxexcel won the ‘Augmented Reality & Virtual Reality’ category at the Prism Awards 2022 for VisionPlatform. The Prism Awards provide recognition to companies that are creating products that make a difference, solve problems, and improve life through photonics.
And in March 2022, the company co-developed a demonstrator of an AR prescription lens solution that enables OEMs to address users’ prescription requirements in their smart eyewear products. The product also allows them to make the lens thin, durable, and worn as fashion eyewear lenses.
In September 2021, Meta unveiled Ray-Ban Stories, smart glasses it produced with EssilorLuxottica, which went on to win prestigious design competitions.
A Meta spokesperson said the company was “excited that the Luxexcel team has joined Meta, deepening the existing partnership between the two companies”.

Following reports that Novartis is preparing to offload its ophthalmology business, the pharmaceutical giant’s CEO has responded saying it currently has “no intention” of taking such action. However, the company has outlined five core therapeutic areas that exclude eyecare.
Novartis CEO Mr Vas Narasimhan made the comments at the J.P. Morgan Healthcare Conference in San Francisco this month, according to Fierce Pharma, refuting a recent Bloomberg report that the company is weighing various options, including divestitures of ophthalmology and respiratory products.
At the same event, Novartis outlined its “New Novartis” strategy, as a pure-playinnovative medicines company that w ill prioritise five core therapeutic areas: cardiovascular, immunology, neuroscience, solid tumors and hematology.
This means it will focus on technology platforms, including gene therapy, cell therapy, radioligand therapy, targeted protein degradation and xRNA.
According to the report, compared with core focus areas, other assets will get fewer resources from a “relative prioritisation” standpoint, Narasimhan said.
While non-core assets may not get much attention in Novartis’ overall business, Narasimhan added “if something were to be a significant breakthrough ... we could build back up”.
Novartis’ ophthalmology unit – valued at US$5 billion (AU$7.5 billion) in some reports – has a significant presence in Australia and globally, with one of the first approved anti-VEGFs for macular disease, Lucentis (ranibizumab), available on the Pharmaceutical Benefits Scheme (PBS) since 2007.
The company subsequently developed the longer-acting (Beovu) which was listed on the PBS as a second-line anti-VEGF therapy for neovascular age-related macular degeneration in October 2021. Novartis’ gene therapy program also includes Australia’s first approved gene therapy, Luxturna (voretigene neparvovec), which became available from August 2020 for patients with inherited retinal disease caused by pathogenic biallelic RPE65 mutations. And in December 2021, the company announced the acquisition of Gyroscope Therapeutics, a UK-based company behind an investigational gene therapy, GT005, for geographic atrophy that is the focus of key clinical trials in Australia.
Glaukos announced positive results from a trial evaluating the safety of the surgical exchange procedure for its iDose TR (travoprost intraocular implant) for glaucoma.

The ophthalmic medical technology and pharmaceutical company revealed results of the multi-centre trial in subjects who had previously been administered an iDose TR in the Phase 2b clinical trial – referred to as the ‘exchange trial'.
Results from the exchange trial demonstrated a second administration of iDose TR and removal of the original iDose TR implant was safe and well-tolerated, with the second iDose TR demonstrating a favourable safety profile over a 12-month evaluation period.
Additionally, Glaukos reported that no person in the exchange trial exhibited a greater than 30% endothelial cell loss over the extended evaluation period of more than five years on average.
“We are pleased to clinically confirm the iDoseTR exchange procedure is safe and facile. We look forward to including these positive data in our upcoming NDA submission [with the US Food and Drug Administration] to further support the safety and tolerability of redosing iDose TR patients over time,” Mr Thomas Burns, Glaukos chairman and CEO, said.
“We continue to believe iDose TR can be a transformative novel technology able to fundamentally improve the treatment paradigm for patients with glaucoma.”

The often-cited 20-20-20 rule to avoid digital eye strain may not be an effective therapeutic intervention as previously thought, new research has revealed, and efforts should now focus on finding more optimal strategies to avoid the condition.

“Regular breaks are frequently recommended by clinicians to minimise digital eye strain,” Ms Sophia Johnson and Mr Mark Rosenfield, both of the SUNY College of Optometry, wrote in a study in Optometry and Vision Science
“The so-called 20-20-20 rule, whereby individuals are advised to fixate on an object at least 20 feet (6 m) away for at least 20 seconds every 20 minutes is widely cited. Unfortunately, there is relatively little peer-reviewed evidence to support this rule
Their investigation aimed to determine whether scheduled breaks are effective in reducing the adverse effects of digital device usage.
The use of digital devices has increased substantially in recent years across all age groups for both vocational and avocational purposes, with a wide range of proposed therapeutic and management options,


including optical, medical and ergonomic interventions.
The study involved 30 young people who performed a 40-minute, cognitively demanding reading task from a tablet computer. It required them to read random words and to identify which ones began with a specific letter chosen by the experimenter.
The task was undertaken on four separate occasions, with 20-second breaks being allowed every five, 10, 20 or 40 minutes, respectively. Both before and after each trial, subjects completed a questionnaire regarding ocular and visual symptoms experienced during the session.
Additionally, both reading speed and task accuracy was quantified during each trial.
The researchers found a significant
increase in post-task symptoms for all four trials, however, there was no significant effect of scheduled breaks on reported symptoms, reading speed or task accuracy.
“While widely cited as a treatment option, these results do not support the proposal of using 20-second scheduled breaks as a therapeutic intervention for digital eye strain,” Johnson and Rosenfield wrote.
“This is not entirely surprising, since there appears to be little or no existing evidence to support the use of the 20-20-20 rule to minimise symptoms. However, these findings should not be interpreted as evidence that taking breaks is not helpful.”
They said further studies should examine the effect of longer breaks at varying intervals to determine their effectiveness, rather than passively viewing a far target; for example standing up and moving around could also be beneficial.
“Given the very high – and apparently increasing – prevalence of discomfort associated with the almost universal use of digital screens, finding procedures to reduce the level of symptoms is essential,” they concluded.
All details matter when it comes to eyewear, but there is one element the duo behind Spanish brand KALEOS pay particular attention to in their designs: the shape.
“This is the most essential feature of a frame; it can change the perception of a face. The angles and the geometry involved are the essential elements to master the perfect shape,” KALEOS co-founders
Mr Juan Gassó and Ms Claudia Brotons say.
Having launched their collection at SILMO Paris in 2014, a serendipitous meeting has resulted in Australian company Sunglass Collective – owned and operated by the founding family of Eyes Right Optical – exclusively distributing the KALEOS range on Australian shores.
Mr Mark Wymond, CEO and managing director of Sunglass Collective, first learned about KALEOS last year.
“We were in Milan at MIDO in May 2022. We passed their stand and were immediately drawn to it; there was a large crowd, and the energy was amazing. We knew straight away that it was something we wanted to explore further,” he recalls.
“Upon visiting their stand, I discovered that the KALEOS export manager was someone I already knew, it was quite serendipitous really. She understood our business and was very eager to introduce us to Juan Gassó, KALEOS co-founder. Immediately there was a good connection and we felt comfortable.”
Wymond says that it was only after seeing the product that things got serious.
Located in the northwest of Barcelona and surrounded by mountains, KALEOS’ headquarters are set across three floors; the first is the showroom, the second is the main office and the third floor is the design and photography studio.
After supplying KALEOS eyewear for a matter of months, Wymond says the brand is already going from strength-to-strength. It promotes “creativity and individualism” for wearers, and practices are finding it has strong sell-through across demographics, especially attracting clientele in their 20s to 40s.

“The shapes are different yet very much on trend, there is nothing quite like it in the Australian market today,” he says.
Acknowledging the company’s focus on eyewear shape, the name KALEOS comes from the Greek word for “beautiful shape”.
“The concept of beauty plays an important role in all things KALEOS. A shape is always more than a shape; there is a concept behind it,” founders Gassó and Brotons say.
KALEOS uses predominantly acetate, and is said to work with high quality materials including Italian acetates and Italian lens companies.
“We are very demanding when it comes to the quality we require,” the duo add.
The company’s origins pre-date their debut at SILMO, to 2012. Gassó, now CEO, opened an optical store with the best curation of glasses and sunglasses brands. Alongside him from the start of this journey was Brotons, KALEOS’ creative director.
The pair met at university and have worked together ever since. Brotons, who has a fashion background, initially helped Gassó to differentiate his optical store in terms of product, image, and communication. Gassó, who has a background in business administration, has always had a particular interest in architecture and design.
They entered into the optics world without any prior knowledge, but were armed with a desire to merge their fashion-focused approach with a sector that has traditionally had a clinical and practical mindset.
According to the pair, while searching for brands to add to their portfolio, they continually found a lack of exciting curation in terms of frame shape.
An emphasis on shape and quality workmanship are the hallmarks of a relatively young European eyewear brand now available to Australian optical practices through Sunglass Collective.
blank sheet. This freedom played an important role in discovering the brand DNA, where the importance of shape and creative boldness has been a constant ever since.”
Their showroom served as a lab for their ideas and was an effective way to gain feedback from the final customer about the new ideas and prototypes they were developing.
Initially, the collection was designed solely for the KALEOS store, but following its success, Brotons and Gassó were determined to focus on selected wholesale distribution, making connections with suppliers like Sunglass Collective.


For Wymond, the KALEOS range has been the perfect addition to Sunglass Collective’s current portfolio of brands which include Serengeti Eyewear, Bolle and Morel Azur.
“With these brands we have something to offer consumers that are looking for technical, lifestyle, sport or application-based eyewear. KALEOS is the collection that allows us to promote creativity and individualism. With the range comprising both sunglass and optical frames, it all ties in well and our sales team have really embraced this,” he says.
“I wouldn’t say an emphasis on shapes is necessarily lacking in the market, but right now KALEOS are doing this as well as anyone else. It is absolutely their point-of-difference, but the colours are a huge drawcard too.”
Wymond says KALEOS’ wide appeal ultimately comes back to the shapes and the quality workmanship.
“The thing we love most about it is its broad appeal across
“THE SHAPES ARE DIFFERENT YET VERY MUCH ON TREND, THERE IS NOTHING QUITE LIKE IT IN THE AUSTRALIAN MARKET TODAY.” – MARK WYMOND, SUNGLASS COLLECTIVE
demographics. Whilst the typical wearer is someone looking for something a little more adventurous, it appeals equally to younger and more mature consumers,” he says.
“The recent release has also included a lot more men’s and unisex styles, and we are finding this to be the fastest growth area of the collection right now.”
Sunglass Collective launched KALEOS in August 2022, less than 12 months after meeting the company’s export manager in Milan.

Wymond says the uptake has been encouraging.
“It’s a collection that quickly captures people’s interest and this is reflected by the success it has experienced so far. Most pleasing though is the sell through; this demonstrates that the range resonates with practices and end users alike,” he says.
“It’s a rapidly growing range too. In November we released the KALEOS kid’s range, and in autumn we will see a very comprehensive spring-summer 2023 release. There is certainly a great deal to be excited about.”
Born and raised in the Netherlands, DR ED BOETS reached a turning point in his life and career. After nine years running his own practice, he wanted a change of pace and mapped out an alternative future in regional Australia.

In a bold and exciting move, Dutch-born ophthalmologist Dr Ed Boets left his well-established career in his homeland, deciding that his family’s future lay in Australia. He quickly began exploring employment options to fast-track his relocation.
The search led to a position with Vision Eye Institute (VEI) in Mackay – a Queensland region where ophthalmic services are in short supply and his expertise in glaucoma, cataract and strabismus would be put to good use.
As one of only four ophthalmologists in the area, his skills are vital to the community, but the shift to Mackay had much to offer Boets, 42-years-old at the time, his wife Sandra and their three children (two-, five-, and nine-years-old at the time).
“The lifestyle was certainly one of the selling points behind our move,” he recalls. “I’m fortunate to have beaches and national parks nearby where my family and I can go camping, and the Whitsunday Islands are only a two-hour drive north. It doesn’t get better than that.
“And, of course, the connection to wildlife is wonderful. I’m surrounded by wallabies, multiple bird species, bandicoots, bats and snakes. You can also spot whales and turtles along the coast. I never had this back in the Netherlands.”
The transition to a country lifestyle meant no longer dealing with the hustle and bustle of metropolitan living. It’s also kept his clinical skills sharp, which he expands on later in the article.
“Driving on country roads is much more relaxed than driving through the city’s peak hour traffic. Commuting to work takes me 20 minutes, and I only drive through three intersections with traffic lights. I much prefer this to the bumper-to-bumper metro traffic. Plus, the stunning country landscapes are beautiful to drive through,” he says.
Boets’ idyllic lifestyle was no simple feat to achieve. Relocating to Australia required what he described as an incredible level of support from VEI.
He felt fortunate. VEI took it upon itself to employ an agency that handled all the migration paperwork for his family and covered some of the costs for their emigration.
“My income was even guaranteed for one year,” he says. “They provided a reference to RANZCO, so I was able to gain fellowship without delay. The whole emigration process was a smooth success.”
Years later, VEI still provides Boets with the support required to navigate the challenges of regional healthcare.
“Vision Eye Institute takes away a lot of the noise around my work. One of the main issues encountered when working and living in a rural
area is access to resources. Vision Eye Institute willingly troubleshoots many of these issues so I can concentrate purely on practising medicine,” he says.
“For example, if I’m interested in some new equipment for the practice, they’ll help me do the sums and manage the whole process. There’s a lot of flexibility and they really listen. There’s a whole lot of knowledge that I can tap into – and it’s only a phone call away.”
Geographic spread, smaller populations, limited access to medical resources and the higher costs of delivering remote healthcare are some barriers that affect rural communities.
Boets notes that any form of vision loss can be problematic, given the lack of public transport in the region and the reliance on driving, highlighting the need for ophthalmology services to preserve the quality of life within rural communities.
Those who serve rural areas, like Boets, must be equipped to take on any case that enters their clinic using the tools at their disposal.
“Working in a remote location means abundant clinical variety compared to what my peers might see in an inner-city clinic,” he says.
“You really need to be versatile and resourceful when treating patients
with restricted adjunct services – your clinical skills and judgement are key. The decision to refer a patient to a large city for additional testing or medical opinion is not made lightly.
“And as one of only four ophthalmologists in the region, I have an endless stream of patients. Word-of-mouth recommendations are far more effective out here than an advertisement.”
Additionally, living and working in a rural location, where there is only a small group of doctors, Boets has found that it fosters a clinical community.
“The four ophthalmologists refer to each other for specific problems. Paediatric and strabismus patients are referred to me, while cases relating to retinal surgery, extensive eyelid surgery, cornea conditions or glaucoma are usually referred to the other doctors,” he says.
Resource shortages are one of the most clinically challenging aspects of working in a remote area. For Boets, this means restricted access to healthcare services and, in some cases, going without medical services entirely.
“We don’t have access to neurology and neurosurgery in Mackay. There are visiting specialists that travel from Townsville, but patients still have to wait for an appointment,” he explains.
“What I really lack in support is an orthoptist. A large portion of my patients are young kids and adults with strabismus. An orthoptist could have a full-time job in Mackay seeing pure orthoptic pathology.”
Boets says that’s not to say he is without the fundamental services and equipment: “Our clinic consists of six consulting rooms. Two rooms are used by the doctors, while the rest are for ancillary testing. We have a YAG and Argon laser, Humphrey Field Analyser, OCT and Pentacam, Optos and Lenstar, and A-scan.
“The latest phaco machines are available in the local day surgeries, but there is no excimer or femtosecond laser in Mackay, so we refer our patients requiring refractive surgery to our Vision Eye Institute colleagues in other locations.”
Essential medical services are also within arm’s reach.
“Day surgery is in the nearby facilities, and a pathology collection point and pharmacy are on the opposite side. Mater Hospital is located across the street, where we refer patients for x-rays and MRIs,” he says.
When Boets doesn’t have the equipment needed for testing, he refers patients to Brisbane (970km away) for diagnostic support.
“However, electrophysiological testing to examine the visual pathways requires patients to travel to a Sydney-based hospital,” he adds.
Even simple clinic appointments can pose a geographical challenge. He says some patients travel up to four hours or more for an appointment. If patients are unable to drive themselves, someone must accompany them for the day. But technology is helping overcome some geographic barriers.

“To ease the burden of travel, patients are co-managed locally by their optometrist and treated based on what their optometrist sees or by using pictures sent to our clinic via email,” he explains.

A nature enthusiast, Boets has taken it upon himself to care for the local wildlife, using his ophthalmological skills to tend to their eye injuries and helping them recover before releasing them back into the wild.
“I’m friends with wildlife carers, so animals are often brought to me to examine,” he says, noting that he treats injured koalas before releasing them back into bushland.

After moving to a foreign country, it’s an example of how Boets was determined to embrace the local community.
“Joining the rural fire brigade gave me a chance to volunteer and give back, and at the same time learn about land management – we have 13 acres on a hill ourselves. It also gave me a chance to discover more about the people in the region and visit places where you normally would not venture to,” he says.
Although rural ophthalmology has its challenges, the scenic locations, diverse clinical medicine and relaxed lifestyle are the ultimate payoffs for Boets’ move.
“The day-to-day variability and exposure to a range of cases have provided tremendous opportunities that aren’t available in metro areas. This, combined with working in close-knit communities, is why rural practise appeals to me.”
“AS ONE OF ONLY FOUR OPHTHALMOLOGISTS IN THE REGION, I HAVE AN ENDLESS STREAM OF PATIENTS.”
— DR ED BOETS, VISION EYE INSTITUTE MACKAYSurrounded by wildlife, Dr Ed Boets uses his ophthalmological skills to tend to animal eye injuries.







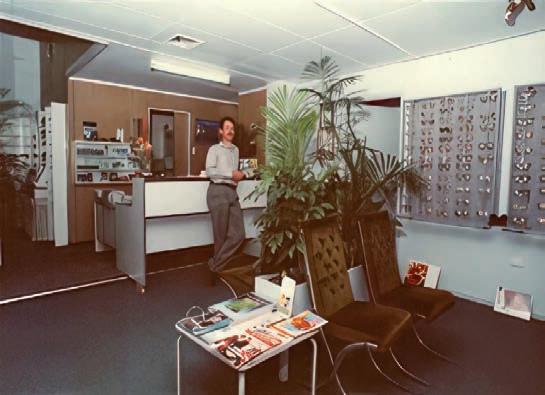
For Bernie Lanigan, making the most of unexpected opportunities has been a consistent theme of his optometric working life. Retiring after 43 years in 2022, he reflects on his career highlights, starting as a young Queensland graduate in the 1970s.
Ajob offer arising from his first – and only – interview initially lured optometrist Mr Bernie Lanigan to Townsville as a graduate in the late 1970s, working alongside Mr John Walcott.

“In those days, you could tender to regional and rural hospitals to supply spectacles and sight testing on a contractual basis. John, who had established a practice in Townsville, decided he would tender to a few hospitals to get some cash flow while his practice built up,” Lanigan recalls.
“Trouble was, he tendered to 17 hospitals and won all contracts against the incumbents, so he had to service them all. Some he had to turn around every four weeks, others every eight, but it meant he was on the road all the time. He ended up putting a locum in his own practice because he was on the road the whole time.”
Needing to recruit an employee, Walcott paid a visit to the-then Queensland Institute of Technology (QIT, now Queensland University of Technology), just as Lanigan was graduating at the end of 1978.
“He came down and sat in the clinic reception room at QIT and interviewed maybe seven or eight of us. I think he had seen me at a conference I’d attended as a student, and I got the job.”
“I remember the three things John told me at the interview: one, you work with me, not for me; two, call every patient by their first name, and three, don’t hang your degree on the wall until it’s 10 years old.”
Lanigan, originally from Brisbane, packed his bags and headed north, but he didn’t work in Walcott’s practice; instead, he started doing the hospital rounds.
“John worked in the practice, and I did the travelling. I didn’t even have permanent digs in Townsville until maybe six months in. I would stay in accommodation run by the Salvation Army two nights a week and then I’d be on the road for the rest of the time, driving west to Mount Isa, north to Cairns, south to Proserpine and Collinsville, visiting the hospitals there, and many in between,” he says.
It was in stark contrast to his workplace experience as a final year graduate student where he would have two hours with a patient alongside four or five other students performing a battery of tests.
“Whereas, on my first day in the hospital, I saw 28 patients – it was a bit of a culture shock. I had a trial frame, a trial set and a handheld ophthalmoscope – and that was it. I had to dispense as well. I had 15 minutes per patient, doing refraction, ophthalmoscopy – there was no time for binocular vision – and then dress them up in a frame. I was going the whole time,” he recalls.
When Lanigan returned to Townsville at the end of each week, after visiting any number of the 17 hospitals, he worked in Walcott’s practice on Saturday, made up spectacles on Sunday, and would be back on the road Monday.
“When the contract was up for renewal after 12 months, John and I got a bit wiser and decided we were going to charge the outlying hospitals a bit more,” he says.
“But once Trevor Henderson Optometry, the Brisbane-based group of practices at that time, realised there was someone up here tendering against them, they tendered and won them back the year after. Then we
tendered again the following year and got them back, but we did it more on our terms.”
When Lanigan was about 24 or 25 years of age, he and Walcott came to a business arrangement that would set the course of Lanigan’s career.
“John always said that I worked with him, not for him. He said, ‘Your qualifications are the same as my qualifications, so there’s no difference in status within the practice’.
“He said: ‘Buy in now as a partner, because it’ll cost you less to buy in now than if we build an empire and you have to buy in later’. So I became a business partner early on, which was crazy because I was still running around like a puppy with his tongue hanging out. I had no business sense,” Lanigan says.
Their business started to build. In addition to running the practice in Townsville’s CBD – then re-named Walcott and Lanigan – the pair also opened a suburban practice in Townsville, a regional practice in Bowen, two hours south of Townsville, and a part-time practice in Ayr, an hour south.
“I would service the practice in Bowen twice a week, covering 400kms there and back every Wednesday and Saturday. I did that for five or six years,” he says.
Looking back on it, Lanigan says he took opportunities as they presented.
“I’m not a planner, I tend to fall into opportunities, they just seem to envelop me. John was always the brains of the outfit in terms of business, and he would say we need to expand there, or we should look at that, so I’d go along for the ride. But I don’t know that I contributed a lot in moving the practices forward from a business point of view,” he says.
When they decided to dissolve their partnership after seven or eight years, Walcott bought Lanigan’s half of the Bowen and Ayr practices and kept the suburban practice in Townsville; Lanigan kept the CBD practice in Townsville, changing its name from Walcott and Lanigan, to Bernie Lanigan Optometrist.
He remained an independent optometrist for 40 years until he sold the practice 18 months ago to a corporate-style group.
“The price you pay as an independent is that you’re never really away from your practice. I’ve never had long service leave, for example. I think the longest I spent away from the practice in the 40 years was 18 days, so retirement is going to be interesting.”
Lanigan says he was fortunate too, in that Townsville’s CBD fell out of favour as a commercial centre, which worked to his advantage.
“Anyone who opened up a practice subsequently – or any of the retail-focused optometrists that came to Townsville – came to the suburbs, not to the CBD, so I ended up the only optometrist in the CBD,” he says.


“I ended up becoming a destination as opposed to having to rely on walk-ins. I always had reasonable foot traffic, but I was able to work more by appointment.”
Years later, having built a successful practice, Lanigan and his wife, who helped manage the business, started considering their retirement.
Unlike Walcott before him, Lanigan didn’t consider visiting QUT on a recruitment drive.
“I’ve never gone down the line of looking to employ another optometrist because I’d seen what heartache so many others have gone through,” he says.
“They’d get optometrists to come to Townsville, and none of them seem to want to buy into a practice or seem to have any commercial impetus. They just wanted to come and work and if they lasted 12 months, they lasted 12 months, and if not, someone could replace them. They didn’t look around as if Townsville was a place to come and live; it was only seen as the place to stage the beginning of a career.”
That tendency led Lanigan to believe his own practice would be difficult to sell.
“We believed there weren’t a lot of individuals out there, there weren’t a lot of independent people looking to buy a practice, and it may get to a point where we end up having to walk away from the practice. We’d almost resigned ourselves to that maybe six or seven years ago,” he says.
“Then, out of the blue, I had two phone calls; two large corporations came to me within a week and said, ‘Are you interested in selling?’. This is what I’m saying about opportunities; they seem to look for me rather than me go looking for them.”
“I REMEMBER THE THREE THINGS JOHN TOLD ME AT THE INTERVIEW: ONE, YOU WORK WITH ME, NOT FOR ME; TWO, CALL EVERY PATIENT BY THEIR FIRST NAME, AND THREE, DON’T HANG YOUR DEGREE ON THE WALL UNTIL IT’S 10 YEARS OLD.” — BERNIE
LANIGANBoth companies interested in Lanigan’s practice offered to look at his books.
“They both made an offer within pretty tight margins of each other. That gave me a solid indication of what my market value was going to be, so I didn’t even have to go out and price my practice.”
Lanigan and his wife declined both offers.
“It gave us some idea of what sort of figures we could generate if we wanted to give it four more years, so we did. And blow me down if one of the corporations didn’t come back to me three years later, still interested,” he says.
In that time, two independents also interested in purchasing the practice approached Lanigan, putting him in a strong negotiating position.
He ultimately reached an agreement on price, and terms and conditions, of the sale, remaining in the practice for a further 18 months as part of the deal.
Lanigan has now officially retired, having finished his 18-month term in November 2022.
Lanigan has seen many changes in the profession during his 40-year career.
Optometrists were not permitted to prescribe therapeutics when Lanigan started but later, when legislation was introduced, he decided not to pursue a qualification in prescribing therapeutics because, he says, he had such a good working relationship with the ophthalmologists in Townsville.
“I felt that there was an open relationship between GPs, ophthalmologists and optometrists in Townsville that I was able to co-manage rather than have to self-manage my patients,” he says.

Lanigan says one of the most significant changes that’s taken place in the years spanning his career is improvements in diagnostic technology.
When he was at university, a fundus camera would take Polaroid-style shots, and the practitioner needed to clip the Polaroid shot inside the file, to ensure it stayed intact.

“Tonometer readings also came out on facsimile paper and if you didn’t write them in the file, the readings would fade. And we didn’t have diagnostics in the early days, so we couldn’t dilate. But all that changed.”
Almost by accident, Lanigan became adept at fitting contact lenses for keratoconus patients. He was thrown into it because there was no one providing that treatment option in Townsville.
“I followed John Mountford through university, and often he would have a patient in Brisbane who would move to Townsville, and he’d asked me to monitor them for him. So, I fell into keratoconic contact lenses, and
then I had to move forward with the advances in technology, when it was never my intention to become a keratoconic contact lens practitioner,” he says.
“It became part of my practice because there was no one else doing it. It started building in its own right, because then I started getting referrals from ophthalmologists who were looking to have some of their patients fitted with RGPs. I would never classify myself as an expert, but it became an area of interest.”
He continues: “Again, little opportunities have thrown themselves my way. But I’ve always enjoyed the interactions with the patients.”
“When someone is buying your practice, they ask you what your KPIs are. I never had KPIs – the KPIs for me were patient outcomes. My aim was always to give them comfortable, useful vision, so we tended to work as problem solvers together, me and the patient, to find out where the problem exists, and design its resolution.”
With the average life expectancy at initial glaucoma diagnosis being up to 13 years, patients require a sustainable first line solution for a long-term condition. A study that altered the course of glaucoma management has presented new data reinforcing its initial findings.
The landmark Laser in Glaucoma and Ocular Hypertension (LiGHT) Trial – that ultimately recommended selective laser trabeculoplasty (SLT) as a first-line glaucoma intervention – has published six-year results further demonstrating the clinical effectiveness of the treatment.

“After six years of treatment and monitoring, SLT safely offers IOP control without the need for medical or surgical treatment in more than 70% of eyes with ocular hypertension (OHT) and open-angle glaucoma (OAG), while also demonstrating reduced progression rates and a reduced need for glaucoma and cataract surgery,” the study, published in Ophthalmology, said.
The original LiGHT study – published in The Lancet in 2019 and led by Professor Gus Gazzard, director of surgery at Moorfields Eye Hospital and Professor in Ophthalmology and Glaucoma Studies at UCL London – was a multicentre randomised controlled trial comparing initial treatment with SLT with initial treatment with IOP-lowering eye drops for treatment-naïve patients with OAG or OHT.
It reported that initial treatment of OHT or OAG with SLT is more cost-effective than initial treatment with contemporary IOP-lowering eye drops after three years, while also providing eye drop freedom to 74.2% of patients, a reduced number of glaucoma surgeries, and very low rates of adverse events.
Data from the original three-year trial also indicated eyes initially treated with SLT may demonstrate less frequent progression to more advanced stages of glaucoma, and a further analysis indicated that more eyes initially treated with topical medical therapy undergo rapid visual field progression compared with eyes initially treated with SLT.
The results prompted changes to international guidelines for glaucoma, with the European Glaucoma Society and the American Academy of Ophthalmology now listing SLT as an initial treatment for OAG and OHT
alongside medications, and the UK’s National Institute for Health and Care Excellence (NICE) recommending SLT as a first-line treatment.
Subsequently, the LiGHT trial was extended to six years “to provide longer-term, pragmatic treatment outcome data”, with the outcomes published in September 2022.

Now, this latest data – retaining 82% of the original 692 LiGHT participants – demonstrated SLT is a safe treatment for OAG and OHT, providing better long-term disease control than initial drop therapy, with reduced need for incisional glaucoma and cataract surgery over six years.
Patients within five UK settings who were treated initially with IOP-lowering eye drops switched to SLT to reduce medication load, to avoid increasing medication load, or to delay surgery.
Meanwhile, patients initially treated with SLT underwent a third and final SLT before escalating to IOP-lowering eye drops.
“Data after six years of treatment indicate statistically significant lower rates of disease progression and reduced need for glaucoma and cataract surgery for eyes initially treated with SLT,” the researchers stated.

“Drop-free IOP control and safety of SLT as a first-line treatment for OHT and OAG are confirmed after six years of careful, protocolised monitoring and treatment.
“SLT allowed successful drop-free IOP control in nearly 70% of the eyes after six years of treatment. This is reduced only slightly from 78% of eyes not needing topical therapy at three years and is an important outcome for long-term glaucoma and OHT management; of the initial SLT eyes that were free of drops, 90% underwent only one or two SLT treatments.”
The authors also concluded the safety profile of SLT “remains very good”, with no sight-threatening complications.
“Intraocular pressure rose > 5 mmHg from IOP before treatment in only 1% of treated eyes, and of these, only one eye needed treatment,” the wrote.
“Other adverse events were comparable between the two groups. Selective laser trabeculoplasty has been shown to be a safe alternative to eye drops in areas where advanced glaucoma is more common and where treatment resources and access to these are limited. The proven safety of SLT in such areas can transform glaucoma treatment rapidly and prevent sight loss.”
Glaucoma is a long-term condition requiring life-long treatment; average life expectancy at initial diagnosis of glaucoma is nine to 13 years, making the six-year data an important finding for a high priporation of patients.
The main limitations of SLT are that it cannot be used in all forms of glaucoma (specifically uveitic and angle closure glaucoma) and in more severe cases, it may be insufficient. The IOP lowering effects also wear off after time.
FEATURING:
PROFESSOR NICK RUMNEY

Senior Optometrist/Chairman





BBR Optometry, Hereford UK
Join Prof. Nick Rumney and host Jarrod Power as they explore the many facets of Myopia Management.
Released weekly, this 3-part mini-series will equip you with the knowledge and confidence to effectively introduce and ensure longevity and viability of your Myopia Management business.
Each episode has something for everyone, regardless of where you are on your Myopia Management journey.
EPISODE ONE
Why Myopia Management?

EPISODE TWO
Foundations Of Introducing Myopia Management To Your Practice.
EPISODE THREE
Optimising Your Established Myopia Management Practice.
SCAN THE QR CODE to REGISTER for your exclusive access.
Nulux iDentity V+ single vision lenses are personalised to your patient’s individual measurements, frame choice and wearing needs. They offer focused vision in all directions and superb visual performance over the entire lens.
The Nulux iDentity V+ lens design is highly recommended for patients:
• who want to have 360° visual comfort everywhere they look.
• who have higher prescriptions and struggle with peripheral distortions in standard single vision lenses.
• who feel limited in their frame selection due to lens thickness.
Ask your HOYA Sales Consultant about new Nulux iDentity V+ aspheric single vision lenses.

Glaucoma specialist and medical geneticist DR JANEY WIGGS revealed two new genes in juvenile early-onset glaucoma and dissected the value of polygenic risk scores when she delivered the Glaucoma Update Lecture at RANZCO's 53rd congress.
Contemporary glaucoma researchers are using a genetic approach to understand the mechanisms of glaucoma. This relies on the premise that the discovery and characterisation of genes that cause or contribute to glaucoma susceptibility will identify the molecular events causing disease and define the mechanisms that underlie disease development.
As Harvard Medical School Professor of Ophthalmology Dr Janey Wiggs explained to the audience at RANZCO’s Congress, using known genes for diagnostic genetic testing and pre symptomatic screening is critical for glaucoma patients to maximise their available sight, but further research is required.
“We’d like to be able to use genetics in the glaucoma clinic to determine people at high risk for disease, be able to identify people at early stages of disease when even conventional therapies are more effective, and to be able to develop therapeutic approaches based on risk,” she said. Genetic testing can be done for the genes currently known to cause early-onset forms of glaucoma.
“They’re caused by rare mutations with large biological effects and because of that, they occur in families. Traditionally, they were found using linkage analysis. Now, we use more modern techniques to find these genes using exome and genome sequencing, and currently we have 10 genes identified,” Wiggs said.

“There’s a real benefit to doing genetic testing for early-onset glaucoma. Using only genetic information, we can target surveillance and therapy to people in families who have the mutation. We can eliminate unnecessary surveillance of people in these families who don’t have the mutation, which is a great benefit to families,” Wiggs said.
To illustrate her point, Wiggs described the case of a mother-of-four who was diagnosed with glaucoma at approximately 40 years of age. She had surgery to control her intraocular pressure but was worried about her children’s risk. Wiggs’ lab did genetic testing on the mother, and found she carried the myocilin (MYOC) mutation, one of the 10 known early-onset glaucoma genes. They then tested all four children and found that the oldest son had the mutation and also had early evidence of disease as his intraocular pressure was slightly high, but his optic nerves were normal.
“We could initiate a surveillance plan for him and even potentially start
treating his pressure since we know he has this mutation. Her younger son also had the mutation but had no evidence of disease, so we could also initiate a surveillance plan for him. Her two daughters did not have mutation or evidence of disease; we could reassure them that their risk of disease development is no greater than that of the average population,” Wiggs said.
While families are appreciative of information about individual disease risk among their children and relatives, it’s not applicable to all families. Currently, the 10 known genes that cause early-onset glaucoma only account for disease in approximately 20% of patients.

“We really need to identify new genes and genetic causality that is responsible for the remaining individuals. Because these genes have been previously identified primarily in US or European Caucasian populations, we hypothesised that if we looked in other populations, we might be able to find additional genes for these early-onset conditions,” Wiggs said.

EFEMP1
Wiggs’ lab recruited 12 glaucoma-affected families (186 individuals) from the Philippines to test their hypothesis.
“We did whole exome sequencing where we sequence the entire coding region of the genome. We looked for mutations in genes that we already know cause these conditions and we found three families with MYOC mutations and one with a mutation in PAX6,” Wiggs explained.
“Then we applied the sequence data to a bioinformatics pipeline to identify DNA variants that are likely to contribute to disease. Interestingly, three of these families had mutations in a gene called EFEMP1 (also called Fibulin-3). These mutations affect important parts of the protein in terms of function.
They found that mutations that cause severe juvenile glaucoma cause increased intracellular protein retention, and that the extent that the protein is retained is correlated with disease severity.
“This work has led to an EFEMP1 genotype phenotype correlation, where we think there’s a correlation between how much protein is retained intracellularly and how severe the glaucoma is. The more that’s inside the cell, the more severe the disease,” she said.
“EFEMP1 is a new gene for juvenile glaucoma. Importantly, we have not seen these mutations in European Caucasian families. The absence
CYP1B1AR Cytochrome P450
LTPB2AR TGF beta signaling
Primary congenital glaucoma
TEK (TIE2) AD TEK/ANGPT signaling
ANGPT1AD TEK/ANGPT signaling
FOXC1 AD Transcription factor
Anterior segment dysgenesis
PITX2AD Transcription factor
PAX6AD Transcription factor, Aniridia
JOAG MYOCAD Extracellular matrix
Familial Normal tension OPTNAD Autophagy, ALS
TBK1AD Autophagy, ALS
Ten early-onset glaucoma genes have been identified.
of these mutations in those families suggests that doing this kind of work in other ethnicities and populations is important for detecting new disease-causing mutations.”
Studying families with different ethnic backgrounds, Wiggs’ team have also successfully identified Thrombospondin-1 (THBS1), a protein in the ocular anterior segment extracellular matrix, as another gene that causes early-onset glaucoma.
After first identifying a THBS1 mutation in a European Caucasian family in the US, Wiggs reached out to colleagues in the US and Australia, including Professor Jamie Craig at Flinders University, to expand her study.
“Jamie had two additional families that also had mutations in this gene that affected the same protein amino acid, which is an incredible result. We collaborated with a group at Boston Children’s Hospital and made a mutant mouse that had one of these mutations at this amino acid. The mouse also had elevated intraocular pressure, reduced outflow facility and reduced retinal ganglion cells, all consistent with a diagnosis of glaucoma,” Wiggs said.
“Interestingly, the mutant thrombospondin forms protein aggregates in the trabecular meshwork, the structure responsible for draining intraocular fluid. The thrombospondin mutation causes the protein to become unstable and form aggregates in the trabecular meshwork extracellular matrix causing disease. This was also confirmed looking at electron microscopy, showing that the thrombospondin formed these dense deposits in the trabecular meshwork.”
Wiggs said adding two new genes –EFEMP1 and THBS1 – to their repertoire of early-onset glaucoma genes will add to their ability to offer comprehensive genetic testing for affected families.
“It’s interesting too both genes are impacting the extracellular matrix. There are so many other proteins that we know of that function in the extracellular matrix
in the trabecular meshwork and that present interesting candidates also for similar phenotypes.”
One of the most significant problems with populations at risk for glaucoma is that there are many people in the population who have elevated intraocular pressure, but only a fraction of those will go on to develop damage to the optic nerve and be diagnosed with glaucoma, Wiggs said. “Compounding this issue is that we have some people who develop damage to the optic nerve without ever having elevated intraocular pressure. So, what kind of glaucoma screening tests can we develop that are clinically useful and also cost-effective?”
Wiggs believes the answer is genetics, which is more cost-effective than measuring intraocular pressure combined with OCT, or other measures of the optic nerve function, in glaucoma suspects.
“Unlike early-onset diseases where a single mutation is enough to cause disease, in the adult-onset cases, each individual genetic variant that contributes to disease has a small incremental effect, but in aggregate, the disease threshold can be reached,” she said.
“For the adult-onset diseases, it doesn’t make sense to test a single gene or a single DNA change, but instead to test a population for an array of genetic variants, that in aggregate can influence disease risk.”
This has given rise to the concept of the polygenic risk score (PRS): a measurement of genome-wide genetic risk. Individuals are scored based on the total number of risk alleles that they carry, and then analysed according to the population distribution.
“To develop this kind of opportunity for glaucoma, we – together with Professor David Mackey (Western Australia) and glaucoma genetic leaders around the world – formed the International Glaucoma Genetics Consortium that included all the datasets that were in our large genome-wide association study for primary open angle glaucoma,” Wiggs said.
Associate Professors Stuart MacGregor and Puya Gharahkhani from QIMR Berghofer Medical Research Institute in Brisbane led the genome-wide association study, which identified a total of 127 independent genomic loci.
“This is the kind of genetic data that we need to be able to develop these polygenic risk scores. Using this kind of genome-wide association study
Genetic testing and clinical management in a case study involving a mother-of-four who was diagnosed with glaucoma and was worried about her children’s risk.

Craig, MacGregor and colleagues performed a landmark study showing that people who were in the 90th percentile of a glaucoma PRS had a 15-times higher risk of developing glaucoma compared to people at the bottom of the distribution.
“That’s a phenomenal risk effect. They also showed that people in the highest genetic risk profile also develop disease at a much younger age – five to 10 years younger – than people in the lower genetic burden groups. They had thinner nerve fibre layer thickness, so more severe disease, and they also had a much greater need for incisional glaucoma surgery for treatment,” Wiggs said.
“The PRS for primary open angle glaucoma is a tremendous asset for risk stratification. We can find people who are at high genetic risk for earlier onset disease and treat them earlier and potentially more effectively.”
In a separate study, Wiggs’ team showed that patients who have a MYOC mutation – one of the mutations that cause early-onset glaucoma – and have a high genetic risk defined by the PRS, have higher disease prevalence and more severe disease than only having the MYOC gene.
Despite identifying two new early-onset glaucoma genes and applying polygenic risk stratification for increased surveillance and earlier treatment, Wiggs said more can be done.
“We still need a better understanding of the genetics
of early-onset glaucoma. Further gene discovery is important to be able to offer comprehensive genetic testing for individuals at risk,” Wiggs said.

Her team is involved in a large consortium project (ClinGen) to annotate all the known genes that can cause early-onset glaucoma and all the mutations in those genes. In Australia, this is an effort led by Dr Emmanuelle Souzeau at Flinders University.
“ClinGen represents a tremendous opportunity to understand known existing genetic contributions. We’re also involved in a large whole genome sequencing project with Professor Jaimie Craig to identify novel genes that cause these early-onset diseases. We’re also interested in the impact of polygenic risk and polygenic effects on these early-onset glaucoma diseases,” she said.
Wiggs said more work is needed to fully understand the clinical outcomes of polygenic risk for primary open angle glaucoma and other types of adult-onset glaucoma.
“We want to know about the clinical features that are associated with high polygenic risk, what factors can modify the polygenic risk score: people who have high polygenic risk and don’t develop disease – or people who have low polygenic risk and do develop disease –why is that? We also need to understand how polygenic risk affects risk of family members. What is the family risk of somebody who has a high polygenic risk score?,” Wiggs said.
PBS Information: Xalatan (latanoprost 0.005% eye drops, 2.5 mL) is listed on the PBS as antiglaucoma preparations and miotics.
Before prescribing please review Product Information available via www.aspenpharma.com.au/products or call 1300 659 646.
Minimum Product Information: XALATAN® (Latanoprost 50 μg/mL) Eye Drops. Indication: Reduction of intraocular pressure (IOP) in patients with open-angle glaucoma or ocular hypertension. Contraindications: Hypersensitivity to ingredients. Precautions: Change in eye colour due to increased iris pigmentation, heterochromia; eyelid skin darkening; eyelash and vellus hair changes; aphakia; pseudophakia; macular oedema; other types of glaucoma; contact lenses; severe or brittle asthma; herpetic keratitis; driving or using machines; elderly; children; lactation. Pregnancy: Category (B3) Interactions: other prostaglandins, thiomersal. See PI for details. Adverse Effects: Iris hyperpigmentation; eye irritation (burning, grittiness, itching, stinging and foreign body sensation); eyelash and vellus hair changes (increased length, thickness, pigmentation and number of eyelashes); mild to moderate ocular hyperaemia; punctate keratitis; punctate epithelial erosions; blepharitis; eye pain; excessive tearing; conjunctivitis; blurred vision; eyelid oedema, localised skin reaction on eyelids; myalgia, arthralgia; dizziness; headache; skin rash; eczema; bronchitis; upper respiratory tract infection; abnormal liver function. Uncommon: Iritis, uveitis; keratitis; macular oedema; photophobia; chest pain; asthma; dyspnoea. Rare: periorbital and lid changes resulting in deepening of the eyelid sulcus; corneal calcification. See PI for details and other AEs. Dosage and Administration: One eye drop in the affected eye(s) once daily. Other eye drops should be administered at least 5 minutes apart. (Based on PI dated 2 March 2021)

References: 1. NHMRC Guidelines for the screening, prognosis, diagnosis, management and prevention of glaucoma 2010 2. Australian Commission on Safety and Quality in Healthcare Active Ingredient Prescribing Guide - list of medicines for brand consideration December 2020
Aspen Australia includes Aspen Pharmacare Australia Pty Ltd (ABN 51 096 236 985) and Aspen Pharma Pty Ltd (ABN 88 004 118 594). All sales and marketing requests to: Aspen Pharmacare Pty Ltd, 34-36 Chandos Street, St Leonards NSW 2065. Tel: +61 2 8436 8300 Email: aspen@aspenpharmacare.com.au Web: www.aspenpharma. com.au Trademarks are owned by or licensed to the Aspen group of companies. © 2021 Aspen group of companies or its licensor. All rights reserved. Prepared: June 2021 AF05768 ASP2528
If clinically necessary for the treatment of your patient, prescribe by brand and disallow brand substitution
A first choice for glaucoma management
GENETIC TESTING FOR EARLY-ONSET GLAUCOMA. USING ONLY GENETIC INFORMATION, WE CAN TARGET SURVEILLANCE AND THERAPY TO PEOPLE IN FAMILIES WHO HAVE THE MUTATION.”
— DR JANEY WIGGS
condition could remain undiagnosed. We wanted to change that statistic and prevent future vision loss.”
In late 2016, Specsavers collaborated alongside industry partners to develop the RANZCO Referral pathway for Glaucoma Management. It also invested in a team to clinically support optometrists and integrated an e-referral platform into each practice’s patient management system. The initiation of e-referrals enabled the development of benchmark reporting, allowing ongoing measurement and assessment. Specsavers’ final step was rolling out OCT across its network and systematically using it as an additional test for early-stage and normal tension glaucoma.
“By the end of 2019, the provision of OCT was included in every eye test in every practice across the nation, an investment worth more than $40 million. As a result of Specsavers’ full glaucoma strategy, referrals increased and false positive referral rates reduced,” Ashby says.
“We have now detected 87% of undiagnosed glaucoma in Australia and alongside our similar strategies for other eye conditions, Specsavers optometrists are now picking up 93% of avoidable blindness in the community. False positive referrals have remained low.
“To some, celebrating that we’ve detected thousands of patients with glaucoma may seem insensitive, but this is something we are immensely proud of as these large numbers represent individual patients who now have more time and the opportunity to protect and preserve their sight.”
Following the integration of e-referrals into Specsavers’ patient management system, a simplified referral process to patient support body Glaucoma Australia was also developed.
This means at the time of specialist referral, patients may also give consent to be referred to Glaucoma Australia for additional support and ongoing care between appointments.
One such patient is Peter* from Queensland who was referred to Glaucoma Australia by his Specsavers optometrist last year.
Glaucoma Australia patient educator Ms Sapna Nand, an experienced orthoptist, says Peter was referred as a glaucoma suspect which enabled the support body’s education team to establish and maintain a relationship with him from the start of his glaucoma journey.
“To date, we have made four support calls over an eight-month period to Peter. After each call, detailed clinical notes are logged to ensure continuity of care. For Peter, as with most of Glaucoma Australia’s patients, these calls have played a significant role in offering him much-needed additional support,” Nand explains.
Specsavers has hit a major milestone in its efforts to find undetected glaucoma in Australia, ensuring patients now have more time and the opportunity to preserve their sight.


Optometry provider Specsavers Australia & New Zealand has announced its practices have now made more than 240,000 e-referrals for patients with suspected, new or existing glaucoma. Including more than 160,000 unique patients with the condition, the company says the figure is estimated to include 87% of glaucoma that was previously undiagnosed in Australia.
The glaucoma referral milestone is no surprise for ANZ director of optometry Dr Ben Ashby who says Specsavers has been on a preventative eye health journey to improving glaucoma detection and care for patients for the past six years.
“In 1996, the internationally regarded Blue Mountains Study calculated that 50% of an estimated 300,000 Australians over the age of 40 with glaucoma were undiagnosed, despite many attending routine eye tests,” he says.
“This trend was seen as normal amongst clinicians, but at Specsavers, we didn’t think it was fair that patients with a sight-threatening eye
“During Peter’s first call with our education team, he explained that he suffered from high levels of anxiety, bouts of depression and significant mobility issues which in turn made attending regular optometrist appointments and adhering to treatment difficult. We encouraged him to attend his optometrist appointments, explained the importance of eye drop adherence and suggested using an eye drop dispenser to assist with his difficulties.”
In the next two support calls, Nand says Glaucoma Australia continued to offer support and encouragement to Peter and by the fourth call there was significant improvement in his attitude both toward using his eye drops as well as his upcoming ophthalmic appointment.
“Peter’s high anxiety levels had reduced, and he had a more positive mindset about his condition. He also happily agreed to continued support calls to monitor his progress,” she adds.
Ashby says Peter’s story highlights the many challenges and obstacles faced by patients with glaucoma.
“It explains why Specsavers’ glaucoma strategy doesn’t just include increased detection rates but also includes a seamless specialist referral process and support body follow up care to ensure ongoing appointments are attended and treatment continues,” he says.
*Patient’s name changed due to privacy reasons
















At the completion of this article, the reader should be able to improve their management of patients with glaucoma.
Including:
• Refine their use of normative data base to reliably assess glaucoma
• Prioritis e the accumulation of data points in progression analysis before making therapeutic changes to treatment
• Recognise the impact of neurodegeneration in the assessment of glaucoma with visual fields

• Understand the role of laser iridotomy in the treatment of patients with angle closure glaucoma
A successful optometric practice in the 21st century depends on the clinical command of an ever-advancing range of diagnostic technology. While so much about glaucoma care is heading in the right direction, an over-reliance on technology and a lack of corroborating clinical evidence can lead to errors, DR JOSEPH SOWKA explains.

Glaucoma can be diagnosed by observations of characteristic changes in the optic disc and retinal nerve fibre layer, abnormalities in threshold perimetry, alterations in structure demonstrated on optical coherence tomography (OCT) and assessment of risk factors such as intraocular pressure (IOP) and family history of the disease. Diagnosing and managing patients with glaucoma can be a challenging task.
Therapeutic intervention, on the other hand, is generally straightforward; that is: reduction of IOP with medicines, lasers, and/or surgery. However, errors in diagnosis and therapeutics can make glaucoma management an arduous task. Take care not to make these common errors.
NUMBER 1: THE OCT IS WRONG
There are several issues in imaging that make OCT assessments for glaucoma very suspect and even misleading. A relatively limited normative database (against which the patient’s measurements are compared), signal quality, blinks and saccades, segmentation errors, media opacities, and an abnormal axial length can all contribute to induced false measurements on an OCT.1-3

When interpreting an OCT printout, ensure the quality score (as indicated for each specific proprietary device) has been met at a minimum. Look to see that there is proper illumination and clarity of focus and the optic disc image is properly centred with no missing data.
Inspect the scan for signs of eye movement. Look to see how the device has segmented the individual layers to ensure that no artificial errors have been introduced. Posterior vitreous detachments and other vitreal issues may confuse the device and make it seem that it is measuring tissue that really isn’t there.
Finally, if using any macular scans or ganglion cell analysis measurements, ensure that there is no concurrent macular disease. If there is, then do not use this potentially misleading information.
Most OCT printouts colour code results as to degree of statistical significance. Common coding
uses green to connote the patient’s measured data to be within 95% confidence interval, red to indicate when findings would occur normally in just 1% of the population, and yellow to indicate all intervening values with borderline significance.
In that, each OCT manufacturer employs a relatively limited normative data base to compare against. There commonly will be situations where a patient’s measured data falls outside the device’s normative data base, yet the patient may be completely healthy and normal. Just because a patient’s measured information falls outside the 99% level doesn’t mean that there is disease present. In this instance, much of the printout will be coded as abnormal in red, yet there is truly no disease present. This is commonly referred to as ‘Red Disease’.4
The use and overemphasis of imaging technology to the exclusion of additional clinical findings and assessment of risk will put patients in peril. All imaging technology must be interpreted in context with other clinical findings and when the
Service at the college’s eye institute. He was the program coordinator and supervisor for the Ocular Disease Residency. Sowka is also a founding member of both the Optometric Glaucoma Society and Optometric Retina Society. He is the founder and chair of the Neuro-Ophthalmic Disorders in Optometry Special Interest Group for the American Academy of Optometry, and a glaucoma diplomate of the American Academy of Optometry. He is a partner and co-owner of Optometric Education Consultants.
OCT results do not fit with known correlates of glaucoma, the results should be interpreted with caution.
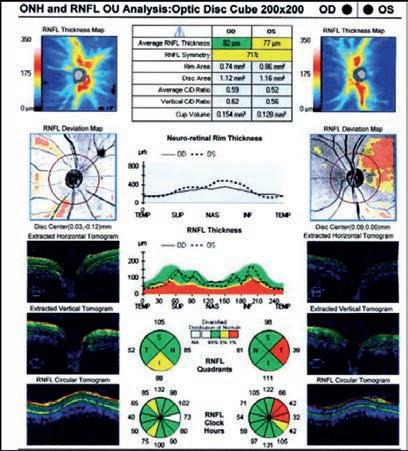
Similar to Red Disease discussed above, there may be instances where patient data may fall within the OCT normative confidence interval with results printed in green, yet have clinically, ophthalmoscopically visible damage to the retinal nerve fibre layer (RNFL) and functional loss on threshold perimetry. This commonly occurs when inspecting the Quadrant and Clock Hour Graphs on OCT. When the RNFL analysis is divided into four quadrants or 12 clock hours, it must be remembered that considerable area is being averaged to give these sector values.

A focal RNFL defect may be present ophthalmoscopically, but when averaged in with adjacent healthy tissue on OCT, the value may fall within the device’s normative data base.5 Thus, everything is printed in green, giving a false sense of security in an eye that truly has structural damage. Thus, it is important to weigh the OCT results against the optic disc photographs and clinical examination to ensure that ‘Green Disease’ is not missed.6
NUMBER 4: CHANGING THERAPY BASED UPON ONE BAD FINDING
IOP measurements and visual field results can be variable, especially when one considers patient compliance with medications and the psychophysical responses in threshold perimetry. Patients often overstate adherence to medical therapy. Even when not trying to be intentionally misleading, many patients may not correctly remember if they used their medication properly immediately before the examination. Medicines don’t fail overnight.
A medically-adherent patient will not have an IOP of 15 mm Hg on one visit and 30 mm Hg on the next visit due to medicine failure or progressing trabecular dysfunction. There will be a slow,
progressive upward drift of IOP in cases where medicines are failing to control IOP. Always insist at least two IOP readings above target (and preferably three) before making any therapeutic changes. Similarly, visual field changes occur frequently, but shouldn’t be considered progression unless the change is verified in a subsequent (and preferably two) visual field. Over 80% of abnormal visual fields noted in the Ocular Hypertension Treatment Study were not verified on repeat testing. Always look for a sustained decrease in visual field results before changing therapy.
Unless a patient presents with very high IOP (e.g., above 45 mm Hg) or has advanced disease (with loss of central visual acuity or relative afferent pupil defect in an eye), there is generally no need to rush to treat chronic open angle glaucoma. It’s beneficial to get several IOP readings (at least two and preferably three) before initiating treatment of any kind. At one visit, the patient may be exhibiting a peak IOP or a trough reading. Knowing the range is very important.

Similarly, one should never prematurely judge efficacy of treatment based upon the IOP reading immediately after initiation of therapy. Even if the first IOP measurement after initiating therapy isn’t impressively lowered, consider leaving therapy unchanged and check at least one more time before deciding if a medication is truly efficacious or not.
In the example in Figure 5, there was an abrupt IOP drop after the initiation of therapy. However, it is notable that there are several pre-treatment IOPs that are nearly identical to the post-treatment IOPs, indicating that the prescribed medication, while overall effective, doesn’t consistently give the robust pressure reduction initially seen.
One of the most insidious situations in eyecare occurs when a patient with glaucoma manifests a neurologic disease concurrently. While glaucoma causes arcuate visual field defects that respect the horizontal meridian and neurologic conditions cause hemianopic defects that respect the vertical meridian, such patterns can get lost
within the same patient.7,8
There are two ways to discern these differences. First, a glaucomatous visual field can be predicted by the optic disc and RNFL appearance. When the field loss is greater than expected and, often in an area not anticipated based upon the optic disc appearance, one should look for the neurogenicity by examining carefully both visual fields. Additionally, the Greyscale printout is exceptional at identifying visual field defects which respect the vertical meridian while the Pattern Deviation can be quite poor. Further, while glaucomatous and neurologic damage can occupy the same quadrant, neurological defects may actually manifest a deeper scotoma within a glaucomatous defect.
Figure 6 shows a 74-year-old woman previously diagnosed with glaucoma. She had optic nerve and RNFL damage consistent with glaucoma. However, observation of the Greyscale showed bitemporal visual field defects that respected the vertical meridian. The fields were repeated and the pattern persisted. Ultimately, she was diagnosed with a pituitary macroadenoma and scheduled for neurosurgical intervention.7
Figure 7 is a 65-year-old female also previously diagnosed with glaucoma. Her visual fields showed bilateral inferior defects. The left visual field matched extreme superior disc damage in that eye. In the right eye, her superior field defect matched optic disc and RNFL damage, but there was no structural abnormality to explain her inferior visual field loss. Most notable was the fact that the right inferior visual field defect stopped at the vertical meridian on the Greyscale in the right eye. While the left eye had a significant inferior arcuate scotoma, it was notable that the left inferior nasal defect was absolute and much deeper that the remainder of the field loss. This led to the observation that she had not only glaucomatous arcuate visual field defects, but also
a superimposed right inferior quadrantanopsia. Subsequent neuroimaging revealed an ischemic cerebral infarct.
In Figure 8, this 74-year-old woman presented with blurred vision. She is highly hyperopic (spherical equivalent of +5.00 diopters) and correctable to 6/19 OD and 6/6 OS with marked nuclear cataracts, right being worse than left. Her IOP is 30 mm Hg OD and 25 mm Hg OS. Gonioscopically, she is open to anterior trabecular meshwork nasally and temporally in both eyes with no visible angle structures in any other quadrants. Indentation gonioscopy demonstrates no peripheral anterior synechiae. Anterior segment OCT shows dramatically occludable angles. She was diagnosed with primary angle closure in each eye, prescribed bimatoprost 0.01% QHS OU and referred, not for laser iridotomy, but lens extraction. Upon surgical consultation, her IOP is lowered to 17 mm Hg OU and she underwent uncomplicated cataract extraction with resolution of her angle closure. This patient’s management is well supported by The Effectiveness in Angle Closure Glaucoma of Lens Extraction (EAGLE) study, which was a prospective, randomised clinical trial, indicating that lens removal is a viable option for chronic angle closure. It compared the safety and
Legend: OD=Green OS=Blue
FIGURE 5 (NUMBER 5): IOP curve before and after treatment initiation for glaucoma. Note that several pre-treatment IOPs were nearly identical to post-treatment IOPs, raising questions about the effectiveness of the chosen therapy.

effectiveness of laser iridotomy and subsequent medical therapy to clear lens extraction for patients with newly diagnosed chronic angle closure glaucoma. It was seen that patients undergoing phacoemulsification lens extraction needed far fewer IOP controlling meds than those undergoing iridotomy and had a comparatively insignificant need for additional trabeculectomy to control IOP.9
Figure 9 shows a 30-year-old woman with moderate hyperopia (+2.00 diopters spherical equivalent) and normal IOP (20 mm Hg OU) who has been diagnosed in 2018 with primary angle closure and had undergone laser iridotomy. While
the procedure was performed successfully, the status of her angles did not significantly change and she was subsequently diagnosed with plateau iris syndrome. At that point, the options suggested to her included chronic pilocarpine use, laser iridoplasty, and clear lens extraction, all of which were deemed poor choices for a young woman.
She had laboured under the admonition that she could never be dilated. In 2022, she presented for eyecare and had not been dilated for four years. After a discussion of risks and benefits, she was reappointed for an early morning dilation. She returned to the office throughout
For the treatment of primary open-angle glaucoma and ocular hypertension, Tango Reflex™ Neo incorporates Ellex’s proprietary Selective Laser Trabeculoplasty (SLT) technology providing superior energy control, a homogenous sharp-edged aiming beam and the industry’s fastest laser firing rate of up to 4Hz (four shots per second).


• Compliance with medication is key and can be extremely problematic1
• SLT takes compliance out of the patient’s hands and is a repeatable laser therapy2
• EGS Recommendation: SLT can be offered as a first-choice treatment for open angle glaucoma3
• Strength of Recommendation: Strong.
neurologic field is better appreciated on the Greyscale than on the Pattern Deviation.
the day for periodic evaluations until her dilation wore off. Throughout this time, her IOP never increased by more than 1 mm Hg in either eye. She was educated about signs and symptoms of acute angle closure and it was agreed that all future dilated examinations would follow a similar pattern.
It has come to light that possibly laser iridotomy may not be as necessary as once thought in patients with potentially occludable angles. A study performed in China examined 889 angle closure suspects where one eye received laser iridotomy and the other was observed without treatment. At 72 months, angle closure, as defined by IOP > 24 mm, development of at least one clock hour of peripheral anterior synechia, or an acute attack, was very infrequent. These endpoints occurred in 4.19 per 1000 treated eyes/yr and 7.97 per 1000 untreated eyes/yr (19 treated eyes and 36 untreated eyes). Acute angle closure occurred in only five untreated patients and one laser

iridotomy treated patient.
While prophylactic laser iridotomy statistically significantly reduced incidence of development of angle closure glaucoma, the authors determined that laser peripheral iridotomy was not justified.10 In a subsequent analysis of these patients followed over time, it was seen that the incidence of acute angle closure attacks after pharmacologic dilation was low even in this high-risk group and prophylactic laser iridotomy was not recommended.11
Glaucoma diagnosis and management can be quite challenging. It is important to be aware that there are common errors that can make management much more challenging. It behooves the careful practitioner to keep these possible errors in mind when diagnosing and treating patients with glaucoma.
an Y, Rettig S, Park SC, et al. Effects of circumpapillary retinal nerve fiber layer segmentation error correction on glaucoma diagnosis in myopic eyes. J Glaucoma. 2018 Nov;27(11):971-975.
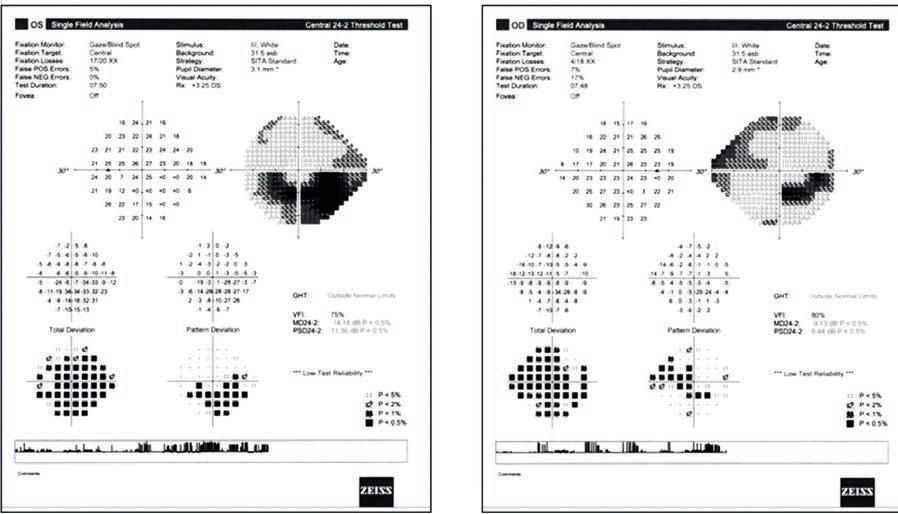
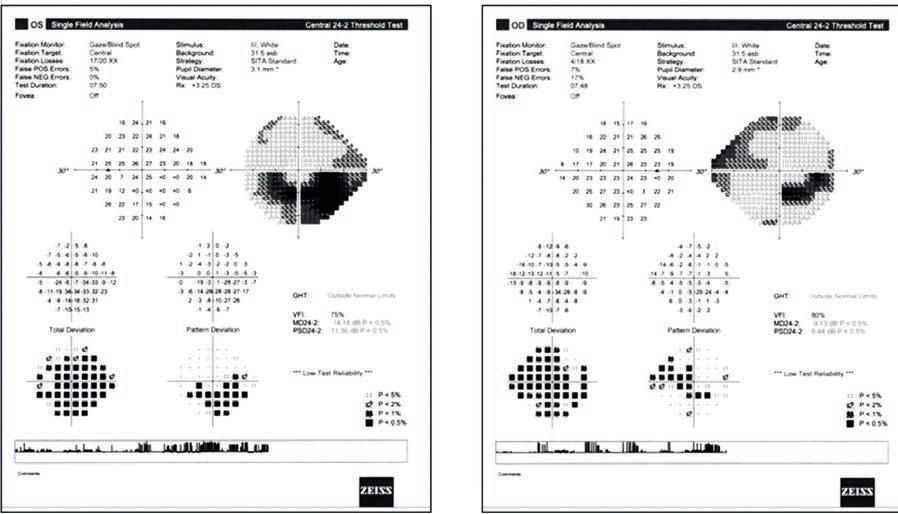
Giani A , Cigada M, Esmaili DD, et al. Artifacts in automatic retinal segmentation using different optical coherence tomography instruments. Retina. 2010 Apr;30(4):607-16.
Miki A , Kumoi M, Usui S, et al. Prevalence and Associated Factors of Segmentation Errors in the Peripapillary Retinal Nerve Fiber Layer and Macular Ganglion Cell Complex in Spectral-domain Optical Coherence Tomography Images. J Glaucoma. 2017 Nov;26(11):995-1000.
Chong GT, Lee RK. Glaucoma versus red disease: imaging and glaucoma diagnosis. Curr Opin Ophthalmol. 2012 Mar;23(2):79-88.
ang YH, Kim YY, Kim HK, Sohn YH. Agreement of retinal nerve fiber layer defect location between red-free fundus photography and cirrus HD-OCT maps. Curr Eye Res. 2014 Nov;39(11):1099yed MS, Margolis M, Lee RK. Green disease in optical coherence tomography diagnosis of glaucoma. Curr Opin Ophthalmol. 2017 Mar;28(2):139-153.
Thomas R , Shenoy K, Seshadri MS, et al. Visual field defects in non-functioning pituitary adenomas. Indian J Ophthalmol. 2002 Jun;50(2):127-30.


anaka K, Wada I, Suenaga T. Incongruous, incomplete, homonymous hemianopia due to an infarction localized to the lateral geniculate body. Rinsho Shinkeigaku. 2017 Oct 27;57(10):595-598.
9. Azuara-Blanco A, Burr JM, Cochran C, et al. Effectiveness in Angle-closure Glaucoma of Lens Extraction (EAGLE) Study Group. The effectiveness of early lens extraction with intraocular lens implantation for the treatment of primary angle-closure glaucoma (EAGLE):The Lancet. Volume 388, No. 10052, p1389–97.
10. He M, Jiang Y Huang S, Chang DS, Munoz B, Aung T, Foster PJ, Friedman DS. Laser peripheral iridotomy for the prevention of angle closure: a single-centre, randomised controlled trial. Lancet. 2019 Apr 20;393(10181):1609-18.
11. Friedman DS, Chang DS, Jiang Y, Huang S, Kim JA, Munoz B, Aung T, He M, Foster PJ. Acute Angle-Closure Attacks Are Uncommon in Primary Angle-Closure Suspects after Pharmacologic Mydriasis: The Zhongshan Angle-Closure Prevention Trial. Ophthalmol Glaucoma. 2022 May 11:S25894196(22)00082-5.









Powerful technology for sustained intraocular pressure and medication reduction. Predictable outcomes from a truly tissue-sparing procedure. All on a proven platform with the most clinical evidence of any MIGS device.
Experience the latest evolution of the iStent® legacy of excellence in your practice.

iStent inject® W IMPORTANT SAFETY INFORMATION
INDICATION FOR USE. The iStent inject® Trabecular Micro-Bypass System (Model G2-W) is intended to reduce intraocular pressure in adult patients diagnosed with mild to moderate primary open-angle glaucoma (POAG) currently treated with ocular hypotensive medication. The device can be implanted with or without cataract surgery. CONTRAINDICATIONS: The device is contraindicated for use in eyes with primary angle closure glaucoma, or secondary angle-closure glaucoma, including neovascular glaucoma, because the device would not be expected to work in such situations, and in patients with retrobulbar tumour, thyroid eye disease, Sturge-Weber Syndrome or any other type of condition that may cause elevated episcleral venous pressure. WARNINGS: This device has not been studied in patients with uveitic glaucoma. Patients should be informed that placement of the stents, without concomitant cataract surgery in phakic patients, can enhance the formation or progression of cataract. The surgeon should monitor the patient postoperatively for proper maintenance of intraocular pressure. iStent inject is MR-Conditional, meaning that the device is safe for use in a specified MRI environment under specified conditions; please see labelling for details. Physician training is required prior to use. Do not re-use the stent(s) or injector. ADVERSE EVENTS: Postoperative adverse events include but are not limited to: corneal complications including edema, opacification and decompensation, cataract formation (in phakic patients), posterior capsule opacification, stent obstruction, intraocular inflammation (nonpre existing), BCVA loss and IOP increase requiring management with oral or intravenous medications or surgical intervention. Please refer to Directions for Use for additional adverse event information. CAUTION: Please reference the Directions For Use labelling for a complete list of contraindications, warnings and adverse events.
At the completion of this article, the reader should be able to improve their glaucoma management.
Including:
• Understand the types of MIGS procedures
• Identify, and refer more confidently, the glaucoma patients suitable for MIGS procedures
• Understand the distinctions between MIGS procedures and MIBS procedures
• Provide pre-operative patient education and set patient expectations for minimally-invasive surgical interventions
• Review post-operative care protocols and complications
With the recent development of novel devices and surgical techniques, approaches to glaucoma management are changing. DR GEOFFREY CHAN and DR JONATHAN CHUNG-WAH-CHEONG discuss why it’s important for optometrists to consider minimally invasive glaucoma surgery, knowing which patients are best suited.
As principal primary eyecare providers, optometrists have an important role in glaucoma care as the initiators of a referral to ophthalmologists, flagging any potential requirements for escalation of glaucoma treatments and co-managing patients in shared-cared models of delivery.
Minimally invasive glaucoma surgery (MIGS) has been listed for use in conjunction with cataract surgery on the Medicare Benefits Schedule since November 2018, and as standalone procedures from May 2020. At the same time, the availability of minimally invasive bleb surgery (MIBS) devices has had rapid uptake in Australia. Generally defined, these are the surgeries that bypass the normal trabecular outflow pathway which are more akin in their mechanism of action to trabeculectomy.

As most optometrists know, it’s vital to stay informed of the advances in glaucoma treatment and to understand the differences between the surgical options available and the impact they can have on patient care. In this article, we hope to provide a helpful summary of the glaucoma surgical options
currently available. While not exhaustive, our
to traditional trabeculectomy and glaucoma drainage devices.
For any glaucoma surgery, it’s necessary for the patient to understand that the purpose of
MBBS (Hons) , MMedSc (UWA), PGCert Med Ed (University of
Lions Eye Institute, Nedlands, Western Australia, Australia
Centre for Ophthalmology and Visual Science, The University of Western Australia, Perth, Australia
Dr Jonathan Chung-Wah-Cheong


BSc (UWA), MD (UWA)

Lions Eye Institute, Nedlands, Western Australia, Australia
Department of Ophthalmology, Sir Charles Gairdner Hospital, Nedlands, Western Australia, Australia
any operation is to preserve their vision, and that any vision lost due to glaucoma cannot be restored.
All patients with glaucoma, suspected glaucoma or ocular hypertension require lifelong follow up to monitor for disease onset or progression. Required therapy should be tailored to the patient and their circumstances, with medical and surgical practice patterns for first-line treatment preferentially involving glaucoma medications or selective laser trabeculoplasty.
Historically, glaucoma surgery has been reserved only for cases of advanced or progressive disease, but that is changing. Increasingly, newer glaucoma surgical techniques with higher safety profiles are considered earlier in the patient’s treatment plan.

Trabeculectomy remains a standard of care in the surgical treatment of glaucoma. This procedure reduces intraocular pressure (IOP)
by the creation of a new outflow pathway for aqueous fluid to filter from the anterior chamber to the subconjunctival space. The pathway is a hole (sclerostomy) that is created under a partial thickness scleral flap, and hence is considered a ‘guarded fistula’.


One of the main advantages of a trabeculectomy is that it is proven to be a more effective way to lower IOP than both MIGS and MIBS devices.1 However, this does come at significantly increased risk of postoperative complications, as well as increased intraoperative time and postoperative recovery compared to micro-invasive techniques.
MIGS offers glaucoma patients the opportunity to have a single procedure that can decrease their medication burden, avoid the ocular surface complications caused by glaucoma eye drops and lower IOP with less risks compared to more invasive surgeries. In general terms, patients that would most benefit from MIGS are those with stable or mild-to-moderate stages of glaucoma, who may have issues with adherence to medication, concurrent cataracts or who are suffering from ocular surface disease caused by glaucoma medications.
As most MIGS procedures rely on visualisation of the iridocorneal angle

structures, it’s more appropriate as a treatment for open angle glaucoma. However in certain circumstances, MIGS can be combined with cataract surgery for treatment of angle closure glaucoma. For these cohorts, MIGS can help reduce the dependency on eye drops and maintain the lower IOP required for disease stabilisation.
With so many surgical options available, the main challenge is deciding which patients will benefit from surgery, what surgery is required and when should they have it. In patients with very high IOPs or advanced glaucoma, MIGS may not be as effective given their effect is limited by normal outflow resistance against episcleral venous pressure, and a more potent surgery that allows aqueous fluid to bypass conventional outflow may be required.
The alternatives to traditional trabeculectomy for these patients include MIBS devices –the PreserFlo MicroShunt and XEN Gel Stent are the main options in Australia – along with tube glaucoma drainage devices. THE IDEAL MIGS CANDIDATES

• P atients who have glaucoma and require cataract surgery
• P atient with glaucoma who are not compliant with medications
• P atients with glaucoma and compliant with medication but have disease progression
• P atients with glaucoma who are suffering from ocular surface disease
• P atients with advanced glaucoma who can’t have more invasive surgery
MIGS augments the conventional aqueous outflow pathway through the trabecular meshwork and into Schlemm’s canal, the physiological conduit of fluid that leads to collector channels and aqueous veins. The key feature of MIGS procedures is that they cause relatively minimal trauma or disruption to surrounding tissue. For patients, the development of MIGS means that they have access to earlier surgical interventions with the benefits of reduced postoperative recovery and perioperative morbidity compared to conventional glaucoma surgery. A helpful way to approach an understanding of MIGS procedures is to classify them based on their mechanisms of action. That is: devices which either stent, cut or dilate the trabecular meshwork or Schlemm’s canal tissue to achieve a reduction in intraocular pressure.
The trabecular meshwork bypass shunts (i Stent Inject W Trabecular Micro-Bypass Stent (Glaukos Corporation), Hydrus Microstent (Ivantis, Inc.)) are micro-bypass devices which increase aqueous outflow by allowing fluid to drain from the anterior chamber to Schlemm’s canal and bypass the trabecular meshwork (Figures 1A and 1B).

These devices are inserted via an ab-interno approach, meaning from ‘inside the eye’ through a small corneal incision.

2. Cut
A direct pathway for aqueous flow to S chlemm’s canal is created by cutting through the trabecular meshwork using various devices (Trabectome (NeoMedix Corporation), Kahook Dual Blade (New World Medical), Excimer Laser Trabeculostomy (AIDA, Glautec AG)) or techniques (gonioscopy-assisted transluminal trabeculotomy) via an a b-interno approach. 2
3. Dilate

Aqueous outflow through Schlemm’s c anal and distal collector channels can be enhanced by cannulation and dilation using certain device platforms (iTrack (Ellex Medical Pty Ltd.) and OMNI (Sight Sciences Inc.)). The iTrack canaloplasty microcatheter is a device used for catheterisation and pressurised viscodilation of Schlemm’s canal and can be performed ab-externo or ab-interno, whereas the OMNI Surgical System is performed via an ab-interno approach only. Both devices allow for treatment up to 360-degrees and may be performed in conjunction with trabeculotomy.
Patients should understand that the IOP-lowering effect of MIGS is relatively modest. The effects are limited by normal physiological outflow channels, and, as such, are generally recommended for patients with stable or mildly-progressive glaucoma.

This surgery is considered safe and can achieve a reduction in medication burden, but there are risks, including a period of postoperative elevated IOP, hyphema (bleeding), endophthalmitis (infection),
collection), bypassing the conventional outflow pathway altogether which allows drainage of aqueous directly into the subconjunctival space.
MIBS is more aggressive than MIGS, but generally considered less invasive than traditional glaucoma surgeries. There are two MIBS devices currently used in Australia: the XEN Glaucoma Treatment System (Allergan plc) and the PreserFlo MicroShunt (Santen Pharmaceutical Co). In general, the



inflammation and peripheral anterior synechiae which can then lead to stent occlusion. Also, poor positioning of stents can lead to later dislodgement or reduced effectiveness. 2
The term ‘MIBS’ is used to describe minimally invasive glaucoma devices that work slightly differently to the typical MIGS procedures. These devices target the subconjunctival space and form blebs (a ‘blister-like’ fluid
IOP-lowering effect of MIBS is greater than MIGS but lower than trabeculectomy.
The XEN Gel Stent was initially developed at the Lions Eye Institute in Perth. It’s composed of cross-linked porcine gelatin and the standardised size of the device, namely 6 mm length, helps regulate flow and reduces the risk of over drainage and post-operative hypotony.
The device is usually implanted through an ab-interno approach with minimal disruption
“FOR PATIENTS, THE DEVELOPMENT OF MIGS MEANS THAT THEY HAVE ACCESS TO EARLIER SURGICAL INTERVENTIONS WITH THE BENEFITS OF REDUCED POSTOPERATIVE RECOVERY AND PERIOPERATIVE MORBIDITY COMPARED TO CONVENTIONAL GLAUCOMA SURGERY.”
to the conjunctiva (Figure 3). The aim is for the device to form a posterior, low and diffuse bleb and is generally placed in the superonasal position. Due to its smaller 45 mm lumen size, postoperative needling to maintain stent flow may be a higher requirement for this implant. The IOP-lowering effect and safety profile are similar between the two MIBS devices.
The PreserFlo MicroShunt is composed of a biologically inert material and has been approved for use in Australia since February 2022. It is inserted via an ab-externo approach which requires dissection of the conjunctiva, allowing for the accurate placement of the device beneath the tenons plane.

Due to the 8.5 mm length of the device, the aqueous humour flow and bleb positions tend to be posterior and may be favorable for patient comfort (Figures 4, 5A and 5B).
In the pivotal trial performed by Baker et al which compared MicroShunt surgery to trabeculectomy, significantly less postoperative hypotony was noted with the PreserFlo Microshunt group (<6mmHg) within the early postoperative period (defined as the first three months following surgery), compared to traditional trabeculectomy and so this device may have particular advantages when used for patients at risk of hypotony (myopes, vitrectomised eyes). 3
Tube shunt surgery is another type of filtering surgery. These implants are characterised by
their larger tube lumen size and connecting plate, which allows for an increased surface area available for aqueous drainage (Figure 6). A scleral patch graft or other material is used to cover the tube and to minimise the risk of postoperative erosion through the conjunctival surface.
Given these devices are larger, require more invasive surgery and/or positioning underneath the recti muscles of the eye, tube shunts are generally reserved for patients who have either failed previous glaucoma surgery or at high risk of postoperative failure with a primary trabeculectomy/MIBS device.

Tube shunt surgery pressure stabilisation relies on the formation of a fibrous capsule, which occurs foiur to six weeks postoperatively, to regulate aqueous fluid outflow and may incorporate internal valve mechanisms to restrict flow. The Molteno tube (Molteno Ophthalmic Limited), Baerveldt tube (Johnson & Johnson Vision) and Ahmed Valve (New World Medical) are the more common devices used in Australia, and newer versions such as the Paul tube (Advanced Ophthalmic Innovations) are now available.
Similar to trabeculectomy, these surgeries require intensive post-operative follow-up to ensure desirable long-term outcomes. 4

It’s important that patients are followed up in the immediate post-operative period on a frequent basis after any glaucoma surgery. Patients undergoing less invasive MIGS surgery may be reviewed two-to-four weeks after their surgery, with trabeculectomy and MIBS patients requiring much more frequent and intensive postoperative review. This is generally required the day after the surgery and again at weeks one, two and four following the surgery. This reflects the faster recovery period following less invasive MIGS procedures.
Each surgery has its own complication profile, however the common complications, especially with MIBS, that the patient may be monitored for are: transient elevated IOP (spikes), low pressure (hypotony), wound leaks, choroidal effusions, shallow anterior chamber, suprachoroidal haemorrhage and infection (endophthalmitis or blebitis).
Antibiotic and steroid drops and/or topical non steroidal anti-inflammatories are typically prescribed following glaucoma surgery to reduce the risk of infection and to control inflammation during the healing phase. 5 The patient may be commenced on atropine or equivalent eyedrop to posteriorly rotate the ciliary body if deepening of the anterior chamber is required. For trabeculectomy and MIBS procedures, the patient’s usual glaucoma medications are typically ceased immediately following surgery and can gradually be recommenced depending on intraocular pressure outcomes following the surgery.
Post-operatively, a cause of surgical failure is obstruction of aqueous flow through the glaucoma drainage device with thickened and inflamed tenons tissue. A bleb needing procedure, to cut away fibroblastic scar tissue (typically augmented by an anti-mitotic agent such as 5-fluorouracil) may be performed over the weeks-months or even years downstream to the surgery to unblock the device.
Patients should be counselled about a reduction in best corrected visual acuity temporarily or permanently after glaucoma surgery. This may be largely related to inflammation and hyphaemia, which tends to settle over a few weeks. Patients are told to avoid bending over, lifting or straining after surgery which may increase the risk of haemorrhage.

“HAVING AN UNDERSTANDING OF THE VARIOUS GLAUCOMA SURGICAL PROCEDURES AVAILABLE WILL EMPOWER OPTOMETRISTS TO BEGIN PRE-OPERATIVE PATIENT EDUCATION”
Refraction changes are typically neutral with the implantation of MIGS devices, but can result in significant with-the-rule astigmatic changes stabilising at three months for glaucoma surgery requiring suture closure, such as trabeculectomy, PreserFlo microshunt and tube surgery. ‘Snuff-out’ of residual optic nerve function is rare but has been described in the literature, especially for patients with very end stage disease and preoperative split fixation. 6
Different surgeons have different preferences and may follow up patients at closer or longer intervals, depending on their progress and individual patient risk factors for the development of complications throughtout the postoperative phase.

MIGS and MIBS provides a new opportunity for early surgical intervention for patients with glaucoma which can result in sustained reduction in IOP, delay more invasive surgery, decrease in eye drops dependence and improvement to quality of life.
As adoption of MIGS/MIBS inevitably increases, co-management of glaucoma patients between optometrists and ophthalmologists will be pivotal to delivering safe, appropriate, and effective treatment
to patients. Having an understanding of the various glaucoma surgical procedures available will empower optometrists to begin pre-operative patient education, discuss patient concerns with ophthalmologists and be confident in identifying post-operative complications should they arise.
Continued open communication between optometrists and ophthalmologists is important in this ever evolving field to achieve our common goal of decreasing glaucoma-related blindness.


1. Marcos Parra MT, Salinas López JA, López Grau NS, Ceausescu AM, Pérez Santonja JJ. XEN implant device versus trabeculectomy, either alone or in combination with phacoemulsification, in open-angle glaucoma patients. Graefe’s Archive for Clinical and Experimental Ophthalmology. 2019 Aug;257(8):1741-50.


2. Wang J, Barton K. Overview of MIGS. In: Sng CCA, Barton K, editors. Minimally Invasive Glaucoma Surgery. Singapore: Springer; 2021. p. 1–10. Available from: https://doi. org/10.1007/978-981-15-5632-6_1
3. Baker ND, Barnebey HS, Moster MR, Stiles MC, Vold SD, Khatana AK, Flowers BE, Grover DS, Strouthidis NG, Panarelli JF, INN005 Study Group. Ab-Externo MicroShunt versus trabeculectomy in primary open-angle glaucoma: one-year results from a 2-year randomized, multicenter study. Ophthalmology. 2021 Dec 1;128(12):1710-21.
4. Gedde SJ, Schiffman JC, Feuer WJ, Herndon LW, Brandt JD, Budenz DL, Tube versus Trabeculectomy Study Group. Treatment outcomes in the Tube Versus Trabeculectomy (TVT) study after five years of follow-up. American journal of ophthalmology. 2012 May 1;153(5):789-803.
5. Almatlouh A, Bach-Holm D, Kessel L. Steroids and nonsteroidal anti-inflammatory drugs in the postoperative regime after trabeculectomy–which provides the better outcome? A systematic review and meta-analysis. Acta ophthalmologica. 2019 Mar;97(2):146-57.
6.
 Mohammadzadeh V Galian K, Martinyan J, Nouri-Mahdavi K. Vision Loss After Glaucoma Surgery: Progressive Macular Thinning as a Sign of Snuff-Out Phenomenon. Journal of Glaucoma. 2019 Jun 1;28(6):e99-102.
FIGURE 6. Anterior segment photo showing a Baerveldt tube within the sulcus plane.
NOTE: Insight readers can scan the QR code or visit insightnews.com.au/cpd/ to access a link to this article to include in their own CPD log book.
Mohammadzadeh V Galian K, Martinyan J, Nouri-Mahdavi K. Vision Loss After Glaucoma Surgery: Progressive Macular Thinning as a Sign of Snuff-Out Phenomenon. Journal of Glaucoma. 2019 Jun 1;28(6):e99-102.
FIGURE 6. Anterior segment photo showing a Baerveldt tube within the sulcus plane.
NOTE: Insight readers can scan the QR code or visit insightnews.com.au/cpd/ to access a link to this article to include in their own CPD log book.
Preservative-free and phosphate-free

Can be used for 6 months after opening
Compatible with contact lenses




At least 300 measured drops per pack, or 150 treatments (both eyes)
Delivered through the unique COMOD® multi-dose application system


Three on-the-go optometrists describe why they’ve chosen mobile optometry roles with Specsavers, and how it feeds into their future plans.
After three years rotating between 12 different stores in the Hunter Valley and Newcastle region as a Specsavers mobile optometrist in NSW, Ms Michelle Chau now has the breadth of experience and confidence to explore ownership opportunities.
Since graduating from UNSW in 2017, Chau accepted a graduate role with OPSM in Dubbo before supercharging her career with Specsavers in a mobile optometry role in the Newcastle region where has been exposed to various demographics, pathologies and store dynamics.
“The mobile optometry role was appealing because it was flexible and offered variety in terms of who I would be working with. I was originally planning to settle into one store, but three years later I’m still doing this role.”
Chau is part of a growing mobile optometry team, providing relief for Specsavers practices. It’s like a locum position but comes with a full-time contract and all the benefits of regular employees such as annual leave, birthday leave, CPD leave, and two free pairs of glasses a year.

Mobile optometrists, who can fetch generous six-figure salaries, support stores across the country, with some strategically located in locations including ACT, Newcastle and Perth where optometry resources are constrained. Others work in a ‘fly in fly out’ capacity and support regional locations to allow partners and employees to take leave or to provide support in stores where an ongoing resource is required.
Overall, the program – around in its current form since 2018 – has 28 positions across ANZ, with openings currently across Australia and New Zealand. It’s ideal for a confident optometrist who is comfortable with flexible working and an understanding family support system for those that travel away.
In her mobile optometrist role, Chau is typically rostered on five days a week and works in a different store every day.
“I have to be adaptable. I’m constantly meeting new staff. I drive up to about 50km from where I live in Newcastle. I did one week in Gladstone (Queensland) but that was rare, because there’s always demand in the Newcastle area.”
Rotating between a dozen stores, Chau notices the variation in patient demographics.
“If I’m working in a Newcastle CBD location, I see a lot more young, educated professionals. If I’m working in Cessnock in the Hunter Valley, I see six or seven patients with diabetes a day. I see a lot of foreign bodies when I work in Singleton and Cessnock, which are a lot closer to mining areas,” she says.
In 2022, Chau completed the Specsavers Pathway Program for aspiring store partners. She is exploring partnership opportunities, with several practices for sale in the Hunter Valley and Newcastle region.
A SPECSAVERS MOBILE OPTOMETRY CAREER – WHAT’S INVOLVED?
• Thr
• For ‘Fly in fly out’, Specsavers provide all travel (flights and car hire) and self-contained accommodation.

• Generally, Specsavers supports the needs of the mobile optometrist whether working away for three to four weeks at maximum capacity then a full week home resting, using time in lieu, or continuously travel from one location to the next, if preferred.
• Sta te-based roles, mobile optometrists work a 38-hour week across multiple stores in their vicinity with option to travel regionally if they wish to do so.

“I’ve been exposed to so many stores, I can see what works well, and I’d like to apply everything that I’ve learned to my own practice,” she explains.
“I’ve become friends with the directors and optometrists that work across the 12 stores I visit, so I’ll be able to get second, third, and fourth opinions on cases that I’m not sure about and lean on them for advice for operating the practice.”
This month Mr Anton Hong, who has been a full-time Specsavers mobile optometrist in Perth for more than a year, is moving to Adelaide to pursue a passion project. But his optometric skills will remain sharp in a part-time capacity.
“I’m relocating for a few reasons. Firstly, I run a YouTube channel about optometry – called Antonio the Optometrist – so I’m reducing my hours to develop this,” he says.


“Secondly, the time zone difference between Adelaide and New Zealand, where I’m from, won’t be as severe as in Perth, where it can be up to five hours, which makes it difficult to keep in touch with friends and family.”
Hong completed his optometry qualification at the University of Auckland in 2017. After graduating, he moved to Perth, and spent his first two years working at Specsavers. He then joined Bailey Nelson for the next two years, performing a floating store role. He returned to Specsavers to join the mobile optometry team.

“With a mobile role, it’s a new place every time and it’s problem solving on the spot, so it challenges you intellectually,” he says.

A keen golfer, Hong prefers driving to flying, so he can take his golf clubs.
“I only started playing golf recently, because I found while doing this role that I have the opportunity to check out so many different places, I might as well make the most of it.”

Most of his time in Perth – three weeks in a month – Hong was working in Specsavers city and metro stores, and living with optometry friends in a share house, including another mobile optometrist.
“It gave me a good insight. One of my housemates is now a Specsavers store director and another is about to become one, and because I have experience with different clinics, we discuss what works and what doesn’t and that helps them,” Hong says.
Every month or two, he travelled to rural areas where private specialists aren’t as abundant, testing his clinical and patient management skills to the limit. Bunbury, Busselton, and Albany, south of Perth, were locations he frequented, as well as up north at Geraldton, where he saw many mining industry patients with foreign bodies and dry eye.

“It’s sometimes a challenge – because I know that I won’t be in a certain clinic the next time – to fully manage a case. I have to ensure that by the time I’ve finished my shift, everything I can do, has to be done. I leave work knowing that I’ve given it my best.”
Hong hasn’t looked back since becoming a mobile optometrist.

“I don’t know if I could ever go back to just being in the one place,” he says. “Your clinical and communication skills have to be on point because you’re given 20 or 25 minutes with a patient to handle it from start to finish.”
His mobile optometrist experience sparked the idea of his YouTube project, which aims to provide straightforward explanations to certain eye diseases and how they’re managed.
“When seeing a patient, sometimes the knowledge gap is too large for optometrists to fully explain on the spot. If patients had access to resources, like my YouTube channel that allow them to understand certain concepts better, then they can get more out of the eye test.”
Exposure to more patients per day – and therefore, more pathology – was a strong drawcard for Adelaide-based Ms Katie Schneider to accept
“FULL TIME EMPLOYEE BENEFITS LIKE ANNUAL LEAVE ARE A BIG DRAWCARD. HOWEVER, THE JOB SECURITY THE ROLE PROVIDES IS PROBABLY THE MAIN BENEFIT.”
KATIE SCHNEIDERMichelle Chau enjoys her work-life balance, taking time to visit a vineyard in the Hunter Valley. Anton Hong has become a keen golfer.
a mobile optometry job. Like Hong, Schneider has been working as a mobile optometrist for over a year. She graduated from Flinders University in 2018 and started her career with Luxottica before joining Specsavers in June 2021.

The early-career optometrist typically alternates between metro and regional stores fortnightly, with her roster planned months in advance.
“It allows me to plan ahead and know where I’ll be. I’ve enjoyed the mix of being able to do locum-style work but also still being an employee. Full time employee benefits like annual leave are a big drawcard. However, the job security the role provides is probably the main benefit, as you are guaranteed 38 hours per week, compared to traditional locum work where the onus is on you to find work,” she says.
“I’ve done several regional placements in South Australia over the last year: Port Pirie and the Yorke Peninsula – including the Kadina and Minlaton stores – to Whyalla, Berri and the Riverland, and to
The New Standard in Visual Field Testing
V irtual Reality Visual Field device - incorporates complete Visual Field analysis.


Detailed progression analysis and the most versatile & efficient vision screening technology.
Latest technology provides the same reliability and reports as the “gold standard”.
Supplied complete with a Tablet PC –BlueTooth interface with the VF2000 NEO. Compact/Space-saving/Portable - can be used anywhere, no need for a darkened room.
Port Lincoln and Victor Harbor.”

She has also worked interstate, including Albany in WA, Emerald in Queensland, and more recently Lismore and Bega in NSW.
Schneider can see more than 20 patients a day in some locations, a significant change from her experience prior to joining Specsavers. Although Specsavers stores typically use the same software and equipment and operate similarly, she likes to be prepared for the unexpected and arrives early to her shifts to get a feel for the store.
“I see things that work well and areas that could be improved in different stores, and I’ve learned what sort of patient demographic I like treating. I’ve enjoyed a lot of regional placements where I’ve had more authority and have taken on more of the management than what I would in some of the city stores,” she explains.
Schneider has noticed a lot more patients with diabetes in regional areas.
“It depends on the region, but I’ve seen a lot more diabetic retinopathy and macular oedema,” she explains.
“In my second week of starting, I had a 16-year-old patient who had been hit in the eye with a soccer ball. She had a retinal tear and I had to refer her to an ophthalmologist in Adelaide, two-and-a-half hours away. I’ve referred patients with optic neuritis or papilledema for treatment, and removed a lot of foreign bodies, particularly metal, when working in regional areas. Often there are no hospitals nearby, so I’ve become a lot more confident with the Alger brush to remove them.
“Even treating uveitis or herpes simplex keratitis, because you don’t have ophthalmology nearby, you’ve got to take on more of that management yourself.”
Ph: 1800804331 Email: sales@bocinstruments.com.au
Active eye tracking –enhances reliability.


Full and Fast Thresholds VF Testing plus Neuro, Kinetic, Ptosis and Estermann tests
FDT Testing

Stereopsis
Visual Acuity and Contrast Sensitivity
Colour Testing (Ishihara, D15 and Advanced Colour Tests)
Eye Mobility and Strabismus

“THE MOBILE OPTOMETRY ROLE WAS APPEALING BECAUSE IT WAS FLEXIBLE AND OFFERED VARIETY IN TERMS OF WHO I WOULD BE WORKING WITH.”
Optometry ownership and partnership opportunities in Australia are many and varied, with each network offering a unique proposition in a competitive market. Corporate-owned stores, franchise models, joint venture partnerships, and independent groups are some of the options for practitioners seeking more from their career. What are their key differences, and similarities?
ProVision works to help optometrists find success as an independent, making starting, running, growing, and eventually selling, easier, plus more.
The network – with more than 450 practices – believes the future of eye health should be in the hands of people passionate about patients, care, and clinical expertise; and that Australians are better with optometrists spending more time with patients, not less.
“We exist to give this special kind of entrepreneur a competitive advantage and to make clinical expertise and freedom a growth business,” CEO Mr Tony Jones explains.
For owners, ProVision’s benefits include:
Buying power: Jones says members have the buying power across multiple product categories to match the biggest brands in the country, helping compete with choice and price. Depending on their level of membership, all practices have a degree of discretionary spend with non-appointed supplier partners, but there is an impressively high level of spend with supplier partners based on the trading terms negotiated by ProVision.
Business operations/coaching: ProVision has 30 years’ experience helping optometrists build businesses with systems and expertise to help their unique vision succeed. Leveraging departmental expertise for ongoing business coaching is an integral part of the value proposition – and this commercial assistance frees up optometrists to focus on clinical excellence.
Innovation: Jones says to remain competitive means doing things differently, so ProVision fast-tracks innovation, technology, and systems to be at the forefront of optometry.


Generating demand: Independents can compete against corporate marketing spend through targeted activity to attract new patients – critical to future growth.
Networking: Speaking to other optometrists with a familiar experience is comforting and reassuring. “It’s role models and inspiration, it’s validation and
education, and it’s a key value-add,” Jones adds.

For optometrists considering independent ownership, ProVision’s complimentary Associate Program provides information, tools and resources about the commercial aspects of practice ownership.

Members get exclusive notifications on practice sales and partnerships, often before they hit the market, while succession planning members are paired with Associate Members to discuss buying options.
For optometrists employed within a ProVision practice, the practice owner is the employer.
“Being part of an independent practice will benefit your career by exposing you to the benefits of clinical freedom along with the rewarding aspect of servicing a local community,” Jones says.
“You also benefit from education courses, market intelligence, supplier relationships, peer support, systems exposure, and a multitude of other learning opportunities.”
Specsavers’ purpose is to change lives through better sight and hearing; the company says it is number one for eye tests with more Australians and New Zealanders choosing the provider than any other optometrist.

For optometrists seeking ownership opportunities, it operates a joint venture partnership (JVP) model, with every store locally owned and led by the partners – usually an optometrist partner, retail partner and audiology partner. Partners are shareholders; in charge of the day-to-day running of the business and they receive the profits and enjoy capital growth.
Specsavers says its JVP model is unique to the industry, with the support offered allowing optometrists to focus 100% of their time in store on customers and the team, while Specsavers takes care of the rest. The model supports all back-of-house administration, finance support, business development, marketing, and people services.
“The benefit of the model for optometrists is the many opportunities on offer, based on an individual’s personal goals and interests. Working within our network provides opportunities to develop clinical and commercial expertise, setting its optometrists up for a successful career,” Mr Raj Sundarjee, director of professional recruitment, says.


“Specsavers optometrists have a high level of autonomy which enables them to explore and develop areas of interest or specialties that they are passionate about. We also have a wide range of spectacle and contact lenses that are exclusively available to our optometrists, which allows them to choose the best lens style and type for each individual patient.”
There are also several ways optometrists can develop their careers with Specsavers, with a view to becoming a store partner in the future.
For those starting their careers, the company offers the Graduate Program, a two-year personal and professional development program combining in-store experiences with external courses and events to build confidence and competence.
There’s also the Early Career Optometry program, a two-year program beyond the Graduate Program, providing opportunities for clinical courses to develop clinical skills in an area optometrists are passionate about. Optometrists can also explore non-clinical avenues.
Each team member is employed by their individual store, unless otherwise specified, such as those employed in the mobile optometry team (see more on page 49). This enables store partners and the team member to work together on personal and career development goals. Optometrists are supported by their store partners, as well as having access to professionals across all areas based in the national support office.
When an optometrist decides to pursue partnership, there’s the Specsavers Pathway Program, a specially designed development program equipping optometrists with the knowledge, leadership skills and business acumen to become a JVP in their own store.
George & Matilda (G&M) Eyecare exists to help the world see better, one person at a time by supporting and uniting local independents to build the best optometry community. For optometrists seeking ownership, the network offers its Partnership Model.

In the majority of its partnerships, G&M purchases the assets of the business and co-brands, building on the existing brand equity. The optometrist becomes a remunerated employee, and still shares in the profits for a fixed term, or can obtain shares in the business as another option.
All the while, G&M says it values clinical independence and doesn’t interfere with the way its partner optometrists care for patients. As a partner, G&M’s product team work alongside the optometrist to decide on product ranges supported by G&M data.
Initially in the start-up growth phase, the Partnership Model started with existing independents and some wanting to retire over time, but the network says it has always intended to be inclusive and build a meaningful connection between the forefathers of optometry and the next generation.
“We find this is a great way to pay respects to legacy and forward focus on the future while always improving the quality of patient care,” general manager of partnerships Ms Cassie Gersbach says.

“Now that we have grown to supporting 100-plus communities and some of our original partners are retiring, it opens the doors for optometrists to have a unique pathway and opportunity to our Buy in Model transitioning from the principal partner.”
Once the principal partners agreement ends and they retire, this allows for the next partner to join G&M and share in profits of the practice.

Instead of capital outlay and risks, time and expertise to manage all functions and expenses on their own, G&M provides support from
the ground up to enable “tried and adopted best practices, systems and platforms” for automation to provide ongoing support to grow the business.
“We have had success with some optometrists joining G&M as an employee first, until they are ready for partnership,” Gersbach says. “We have many discussions about career path and goals to identify what’s important to the individual and desired timeframes. Together we work towards those goals and seek for the ideal practice for the perfect fit.”
Eyecare Plus exists to help practice owners compete and succeed in a challenging market while practising their profession without restrictions. It focuses on enabling the optometrist to do what they do best, plus the benefit of commercial assistance.
As a branded, unbranded or co-branded practice, Eyecare Plus offers flexible and optional buying power, peer-to-peer sharing, clinical leadership as well as support, benchmarking, marketing and staff training –without compromising the practice’s independence.
For optometrists looking at independent practice ownership opportunities in the future, Eyecare Plus currently has metro and regional owners looking to transition their practices into safe hands. The organisation can assist prospective owners to find the right practice via confidential conversations.
Eyecare Plus positions itself as Australia’s largest branded group of independent optometrists. All practices are individually-owned and members run their businesses freely, so the freedom of choice is still there. The organisations says its combined strength gives it the opportunity to work with preferred suppliers for buying power, combined marketing, pooled resources, and more.

“Eyecare Plus members can utilise the strength of a large business, all while remaining free and independent. A point of difference is exclusive territories, this allows our members to discuss their business and share ideas, without concern that competing practice owners or staff are in the room,” national business development manager Mr Dylan Oblein says.
If an early-career optometrist joins an Eyecare Plus practice, it is in the capacity as an employee to one of the member owned practices.
“The individual would be joining a network of independent optometrists that spans across the entire country, giving them opportunities to be mentored by some of Australia’s best independent optometrists in either metro or regional locations,” Oblein says.




The EssilorLuxottica-owned OPSM and Laubman & Pank brands are synonymous with great eyecare, says the company’s general manager for retail ANZ Mr Matteo Accornero. From its first OPSM store in Macquarie St Sydney in 1932 to its current network of over 430 stores, the group’s core values have been to provide the best possible experience for its patients

Hence, more optometrists than before are joining EssilorLuxottica ANZ retail practices, which Accornero says is a testament to the unique set of
“We have a diverse network of over 50 passionate and influential managing optometrists who partner with the store manager to lead and support our store optometry team. We continue to invest in our people and introduce new “For our entrepreneurial optometrists we offer career progression opportunities supported by management and leadership training. For any practice owners-operators looking for a different path for the future of their optometry business or looking to retire, we would be pleased to discuss opportunities to continue the operation of their businesses and care of their customers, whilst providing a smooth transition for their staff and optometrists who wish to come on board as OPSM.”
Because optometry as a profession has changed, now more than ever, EssilorLuxottica says optometrists and graduates are looking for employers that listen and are adaptive to change. The company believes its success is a combination of investing in people and technology so that its optometrists can detect more pathology than a standard eye exam and provide the best vision solutions.
The organisation offers OPSM and Laubman & Pank optometrists a diverse range of experiences to ensure their continued professional success.
“Whether you want to be an amazing clinical optometrist or business leader, the opportunities are endless. All corporate optometrists are hired by our eyecare operations teams who are optometrists. They take the time in the interview process to understand your passion and interest and tailor opportunities to help support our optometrists career aspirations,” Accornero says.
“More opportunities, more choice and more time to practise full scope optometry are just some of the reasons more optometrists accelerate their career with OPSM and Laubman & Pank.”
During the past five years, EssilorLuxottica has invested over $500,000 in Luxottica Eyecare Development Award (LEDA) scholarships to support its optometrist’s professional development.
Matteo Accornero is the general manager of retail for EssilorLuxottica ANZ. OPSM Shepparton, in regional Victoria.Mr Tom Bennett had no intention of owning his own practice. In 2009, he and wife Alison, also an optometrist, were both working as employee optometrists in Townsville and weren’t planning on becoming small business owners. That all changed when a practice in nearby Charters Towers operating on a part-time basis came on the market.
Bennett, who had been working at The Optical Superstore in Townsville, says the practice in Charters Towers was appealing because it didn’t require a significant investment of time or money to take the keys.
“A rep told me there was a practice for sale. Because it was only open part-time, my wife and I were able to keep working in Townsville in our respective jobs, and travel to Charters Towers an hour-and-a-half away, taking turns in the practice,” he says.
Since taking ownership, they have joined the Eyecare Plus network, and the practice has grown organically from a part-time to a full-time operation.

“Because it was a small, part-time practice, it wasn’t a huge investment. We weren’t looking for a lifestyle change, it was just something on the side,” Bennett says.
Between them, Tom and Alison, who both graduated from QUT in 2004, had 10 years’ industry experience, working in independently and
corporately owned practices, when they purchased the practice. Although it might sound like they were dipping their toe into business ownership, Bennett says that wasn’t the case.
“If you had asked us when we moved to Townsville six months before we bought the practice, I would never have said we would become practice owners. It was never our intention. It was something that came up, and we thought about the fact that it only required one of us to work one day a week, and it wasn’t too expensive. We didn’t think it would change things too much.”
Nevertheless, 12 years and three children later, it is now operating as a full-time practice. Its growth happened organically, which Bennett puts down to a not-so-secret recipe.
“It’s an age-old formula: look after people and they will return. I think this is especially true in a country town like Charters Towers. The people are friendly and welcoming, so the longer we have been there, the busier we have become.”
Tom has also been prepared to go an extra mile for his patients, once booking a helicopter to fly to the practice when floods closed roads and bridges, cutting off all access to Charters Towers.
Now splitting all of their time between the Charters Towers practice and their young family, the Bennett’s enjoy the many benefits of independent ownership, including the freedom to make their own clinical and financial decisions.
“The control is in our hands. Both the decisions and the mistakes are ours – and we like that. We have the freedom to decide things like work schedules and holidays to fit in with our family life. You also do make mistakes, but you get to learn from these and use them to make improvements to your practice,” he says.
“I think probably the biggest benefit of independent optometry, is the satisfaction you derive from being committed to something that is yours. You’re building something that you’ve made a commitment to, and that has a deeper satisfaction. You can’t get that as an employed optometrist.”
As the Bennett’s have proven, you don’t need to necessarily have a long-term goal to become a practice owner in order to reap the benefits of independent ownership.

Whether it’s a long-held ambition, or an unexpected career move, the rewards of independent ownership are attainable to all, as two optometrists reveal.Tom and Alison Bennett organically grew Eyecare Plus Charters Towers from a part-time to a full-time practice.
"We never had a plan to become practice owners until it happened. You might think you’re not capable, but you are. You learn as you go."
When ownership of an outer suburban independent optometry practice transferred into the hands of Canadian-born optometrist Dr Geoff Demare in August 2022, an aspiration he’s held since he was 15-years-old was finally realised.

Optometry Sunbury and Vision for Children in Melbourne’s west is part of the ProVision network and has had three owners in its 36-year-history. Unusually, both former owners still work in the practice, alongside Demare, sharing their experiences and mentorship.


“I grew up on a 6,000-acre farm in Manitoba province in Canada. When my dad asked, ‘What do you want to do?’, I wasn’t sure. I shadowed my aunt and uncle who owned a pharmacy – that experience was all right, but not great – and then I sat-in with my local optometrist and thought, ‘this is pretty cool. Maybe I’ll go down this path’.”
After completing an undergraduate degree in science and microbiology at the University of Manitoba, Demare then moved to Australia where he furthered his studies, graduating with a Doctor of Optometry at The University of Melbourne in 2016.
He then joined an independent practice in Deniliquin in southern NSW. He stayed for three years, then accepted a succession-planning offer at Optometry Sunbury and Vision for Children, commencing in January 2020. He gradually transitioned from employee to owner, taking the reins from then-owner Mr Rod Baker seven months ago.
Demare has been overhauling practice management systems, and modernising its dispensing set-up.
“We recently purchased Rodenstock’s DNEye Scanner and adopted Rodenstock’s B.I.G. VISION lenses in the NORM and EXACT lines. We’re modernising our understanding of optical design principles and moving into clinical and biometric optics for patients. It’s proving to be a success, providing patients with great visual outcomes and allowing us to craft higher quality spectacles,” he says.
For Demare, one of the benefits of independent ownership is being able to build a health service that suits the needs of patients and takes them into account.
“They can tell us what they need, and we can then investigate how we can provide it. We launched a dry eye clinic as part of our practice in January [2023]. At the same time as purchasing a DNEye Scanner, we’ve made the investment in an Optilight from Lumenis as well.”
As practice owner, Demare says it was a very easy decision from a business perspective to establish a dedicated dry eye clinic at Optometry Sunbury and Vision for Children.

“Sunbury is undergoing a change in identity from a country town to an outer suburb. The nearest dry eye clinic of any description is 40km away. Dry eye is a significantly underserved area in healthcare, and we decided that was the direction we were going to go.”
One of the core tenants of the well-established practice is to serve the community, and Demare says being an independent owner lets him do that in several ways.
“We have frameworks of practice that help us to understand our patients’ needs and how we can address those needs. We have greater latitude to provide our patients with services that can fall outside both our framework and more traditional optometry frameworks,” Demare says.
“This approach also lets us develop referral sources and integrate with other allied health practitioners. For example, we’ve got physios that refer to us and vice versa. Being independent lets us connect with local healthcare practitioners that can continue to benefit patients not only here in our place, but in their practices as well.”
Owning his own practice has been a long-held ambition for Demare, and was a matter of when, not if.
When an opportunity came up in Sunbury, it ticked all the boxes.
“After moving from Melbourne to Deniliquin, my wife and I moved to settle near our family in Woodend. Taking a look at what opportunities were in the area, and wanting to have a semi-rural life, Sunbury is only a half-hour down the Calder Highway. I can take the train – the practice is a five-minute walk from the train station – or I can drive – it’s simple,” Demare says.
“For me, it presented an ideal lifestyle. One of the other benefits of owning an independent practice in a location of my choosing is it lets me live a lifestyle that that’s not too onerous. We get support through ProVision and networking opportunities with different practice owners. We see firsthand what other independent practice owners are doing and how their approaches help us.”
A father to five-year-old identical twins and a two-year-old, Demare says another benefit of being an independent owner is that he can be flexible with how he approaches his time spent on, and in, the business.
He believes anyone considering independent ownership would be well-served to take advantage of the learning opportunities early in their career.
“Take a moment to look outside of your consulting room to see how the business you’re working in functions on a day-to-day basis. Understand the processes going on around you from when the first staff member walks in the door until the last person is out.”
He also believes that successful practice ownership is not just about one person.
“Make sure you’ve got a group of good people around you to support you through all the ups and downs, because you can’t do it alone. I’m fortunate that my team is highly experienced; my staff all have a minimum of 10 years of experience in industry,” he explains.
“There’s no time like the present. There’s no good time for anything, best to just get started.”
“UNDERSTAND THE PROCESSES GOING ON AROUND YOU FROM WHEN THE FIRST STAFF MEMBER WALKS IN THE DOOR UNTIL THE LAST PERSON IS OUT.”
GEOFF DEMARE OPTOMETRY SUNBURY AND VISION FOR CHILDRENOptometry Sunbury and Vision for Children has had three owners in its 36-year-history.
Next month, the first biennial Optical Dispensers Australia Conference – created by dispensers for dispensers – will take place in Sydney as the organisation continues its push to raise the profile of the profession.


The event, taking place 28-29 April (Friday and Saturday) at the Sydney Masonic Centre, is an Australian-first with a two-day program complemented by a dedicated trade space, together with an evening recognising the achievements of outstanding dispensers and Certificate IV graduates.
The event marks a major milestone for Optical Dispensers Australia (ODA), an organisation that launched in January 2022 and now has a 1,700-plus strong subscriber network. The conference forms part of its goal to fulfil an unmet need around professional development and networking opportunities for the nation’s optical dispensing profession. ODA also exists to offer dispensing resources and support for employment and career matters, among other functions.
The conference will feature a line-up of Australian and international speakers and is open to the entire optical industry, including optometrists.
ODA CEO Ms April Petrusma describes it as unlike any other event in Australia.
“While it is open to everyone in the industry regardless of their level of expertise or experience, it has been created specifically with dispensers in mind. It is the only event of its kind catering purely towards the national optical dispensing profession,” she says.
“Opportunities for optical dispensers to grow their knowledge, upskill and continue their professional development have been sparse in our country for quite some time and, whilst there are various events throughout the year that dispensers can attend, very few, if any, have been designed with 100% dispensing-focused content.”
Despite only launching 14 months ago, ODA organised and hosted its first mini conference in September 2022. The response was positive and the ideal precursor for its first national event.
It released 50 tickets to the full-day event, held in Perth, which included lectures and practical sessions facilitated by industry experts to enhance professional development. The speaker line-up at the mini conference included Ms Nicola Peaper from Rodenstock Australia on improving lens performance, Mr Jack Layland from HOYA on dispensing safety glasses and Mr Cameron Bourke from Luxottica on frame styling. There was also presentations on contact lens dispensing.
“The mini conference sold out and the feedback from delegates unequivocally called for more events of its type,” Petrusma says.
An inaugural conference catering to the optical dispensing profession is the only event of its kind in Australia, and the first time a national medal for optical dispensing excellence will be bestowed.Optical Dispensers Australia’s first national conference will be held in Sydney in April. Optical Dispensers Australia’s mini conference in September 2022 in Perth was a sell out, and the perfect primer for its upcoming national event.
ODA has heeded those calls, with its marquee event in Sydney next month drawing wide industry support from companies including, HOYA, the Australasian College of Optical Dispensing, Hilco Vision, Human Ware, Younger Optics and Tokai Optical.
“With thanks to our sponsors, we have been able to make the biennial conference extremely affordable with a full two-day conference pass plus a ticket to the evening gala costing ODA members just $287,” Petrusma says.
“A broad range of topics will be covered with international and local speakers, including paediatric dispensing, troubleshooting progressives, low vision patients, understanding prism, polarisation, occupational dispensing, marketing in eyecare and more.”
A full list of speakers was yet to be released at the time of writing, but Petrusma says the topics will have broad appeal, keeping in mind the event is open to the entire optical industry.
“The ODA conference is not just appealing for dispensers, it is also a great way for optometrists to network and connect with dispensers and suppliers alike,” she says.
“With a trade area to engage with suppliers over breaks, and conference sessions covering topics that front-of-house staff are immersed in every day, it’s a great opportunity for optometrists to expand their own dispensing skills, better understand the role of their support staff and connect with the industry.”
The Optical Dispensers Australia Conference will also feature an inaugural awards ceremony, with winners to be announced at a gala evening on Friday 28 April.

Petrusma, who was one of four finalists in the Silmo IOA International Optician of the Year Award in 2022, understands the importance of recognition.

“The ODA National Excellence Awards honours outstanding optical dispensers across Australia and celebrates the vital contribution they make to the industry and the important role they play within the optical practice,” Petrusma says.
“With categories designed to recognise a variety of accomplishments, including the prestigious ‘National Medal for Optical Dispensing Excellence’, nominations are open to all ODA members and may be completed by the entrant themselves or a colleague.”
There are eight categories in the National Excellence Awards (see right) – and the judging panel consists of members of the ODA Advisory Board as well as representatives from its corporate partners, now numbering more than a dozen. Nominations close 31 March 2023.
The ODA Gala event includes a graduation ceremony for all industry members who have recently graduated from the Certificate IV in Optical Dispensing.
ODA was in the process of distributing invitations when Petrusma spoke with Insight
“At this stage we’re conservatively expecting about 60 graduates to attend. With the invites only going out [in late January], this is an estimate – but it will be the largest cohort to date,” she says.
ODA National Medal for Optical Dispensing Excellence
The winner of this prestigious award will be an outstanding, qualified optical dispenser who champions the profession. They will have excellent dispensing and communication skills, provide exemplary customer service and take immense pride in their role. They will show professionalism and advocacy for optical dispensing and will have evidence of their engagement in nurturing their own professional development.
Rookie of the Year Award
The winner will be a current student, trainee or recently qualified optical dispenser that has been in the profession for less than two years. It recognises dedication and drive for someone embarking on a career in optics. Entries are welcome from optical assistants and optical dispensers that possess ambition and enthusiasm towards their role. They will be able to provide evidence showing consistency in exceeding customer expectations and the positive contribution they make in the practice in which they work.
Outstanding Practice Owner Award
The winner will be a dispensing partner or owner of an optical practice that champions their role through empowering and leading their team, providing clinical excellence and delivering exceptional customer service. They will be able to provide evidence of innovation in their practice as well as patient satisfaction and positive team culture. As a qualified optical dispenser, they will exude professionalism and represent the profession in an enthusiastic manner.
CEO’s Member Dedication Award
The winner of this award will be an ODA member that excels in their role and takes pride in the profession and their own ongoing professional development. They will be an advocate that is able to show evidence of engagement within the profession and industry through active participation in networking, events or activities that enhance their knowledge and skills.
Role Model & Leadership Award
The winner of this award will be an optical dispenser that fulfills a leadership role within their practice. They may be a team leader, trainer, supervisor or practice manager that motivates and inspires others to be the best they can be. They will be able to provide evidence that shows they conduct themselves in a professional manner, demonstrate clear and concise communication skills guided by compassion, and empowers others to reach their highest potential.
Community Champion Award
The winner will be an optical dispenser or affiliate that demonstrates a positive impact on their local or wider community through participating in charitable work, supporting or implementing community initiatives or consistently going above and beyond their call of duty. They will be able to provide evidence of their community engagement or altruistic activities.
Sustainability Champion Award
The winner will be an optical dispenser or affiliate that possesses environmental awareness and participates in sustainable practices. They will be able to provide evidence showing their commitment to improving the environment through waste reduction, sustainable forward thinking and implementing ideas for a greener future whilst meeting the needs of their clients.
Support Services Dedication Award
The winner will be an optical dispenser or affiliate that provides a support service to retail optical practices. They may be a supplier representative, a customer service associate, a lab technician or may even be in a support office role. They will be able to provide evidence that demonstrates excellence in service, quality and nurturing relationships, all whilst exceeding their clients’ needs.
For more conference details, visit www.odamembers.com.au/ odaconference. More about the awards can be found at www.odamembers.com.au/odagala
“THE ODA CONFERENCE IS NOT JUST APPEALING FOR DISPENSERS, IT IS ALSO A GREAT WAY FOR OPTOMETRISTS TO NETWORK AND CONNECT WITH DISPENSERS AND SUPPLIERS ALIKE.”
— APRIL PETRUSMA, ODA CEO
Smokers can develop macular degeneration 5.5 years earlier than never smokers, and children exposed to second-hand smoke have been shown to have choroidal thinning. These are some of the headline statistics from a new World Health Organization summary into smoking and vision loss, developed with an Australian university.
The University of Newcastle, Australia has helped the World Health Organization (WHO) develop a new summary of evidence for eyecare professionals showing the association between tobacco use and vision loss.
The document – published late in 2022 – is the fifth in a series of 'Tobacco Knowledge Summaries' that ophthalmologists, optometrists and other eyecare professionals can use as an advocacy tool in the fight for tobacco control and prevention of tobacco-related adverse health effects.
The International Agency for the Prevention of Blindness also helped develop the resource, which focuses on the link between smoking and noncommunicable eye diseases including cataract, glaucoma and age-related macular degeneration (AMD).
“With a single breath, the hundreds of toxins in tobacco smoke begin damaging the lungs. These toxins then pass from the lungs to the bloodstream and to various organs throughout the body, including the eyes,” the summary stated.
“In addition to the impact of tobacco smoking on the development of eye disease in the user, tobacco smoke irritates the eyes and worsens dry eye syndrome in smokers and bystanders exposed to second-hand smoke, particularly among those who wear contact lenses.”
In AMD, smoking is said to be “the primary modifiable risk factor”. Tobacco smoking generates a local inflammatory response, and cigarette smoke is a strong oxidant. Furthermore, oxidative stress was found to be one of the primary mechanisms for smoking-related damage to retinal structures, contributing to the development and progression of AMD.
“[A meta] analysis found a fourfold increase in risk for neovascular AMD and a twofold-to-threefold increase in the risk of atrophic AMD associated with smoking,” the report said.
“Smokers also have a greater risk of developing AMD at a younger age. A study conducted in 2019 found that current smokers developed AMD 5.5 years earlier than never smokers, and 4.4 years earlier than ex-smokers.”
In terms of cataracts, one prospective cohort study (in 44,000 men) found current smokers of more than 15 cigarettes per day had a 42% increased risk of undergoing cataract extraction compared with never smokers.
“Studies have shown that smoking appears to generate free radicals, which raises the oxidative stress in the lens of the eye. This lowers the concentration of plasma in antioxidants, inhibiting their ability to discard damaged proteins. Cataracts develop when these proteins build up in the lens causing vision loss, and surgical removal of the cloudy lens and replacement with an artificial lens is the only option to restore vision,” the summary said.
Few studies have examined the relationship between tobacco and glaucoma in depth, indicating the need for further research before conclusions can be drawn. However, new evidence suggests that smoking may increase its incidence.
One study followed a cohort of smokers for 8.5 years, recording their smoking habits and recording the incidence of glaucoma. After controlling for potential confounders, current smokers were found to be at increased risk of developing glaucoma as compared with never smokers.
The report also delved into the impact of second-hand smoking, which is responsible for 1.2 million of the 8 million tobacco exposure related deaths each year.
In terms of eye health, it highlighted a study conducted at the University of Cambridge and University College London demonstrating that individuals who live with a smoker for at least five years are twice as likely to develop AMD as those who do not.
“[Another] study conducted at the Chinese University of Hong Kong Eye Centre in 2019 examined the impact of second-hand smoke on a cohort of children between six and eight years old, a third of whom had been exposed to second-hand smoke,” the summary said.
“Scientists measured the thickness of the choroid, which is the part of the eye that thins when exposed to tobacco smoke, and found that children who had been exposed to second-hand smoke experienced choroidal thinning of between 6 μm and 8 μm. This thinning can slow or completely stop choroidal blood flow, which leads to future vision loss associated with macular degeneration.”

According to the WHO, evidence of a potential relationship between e-cigarette use and visual impairment is evolving, but a recent population survey study in the US revealed that current e-cigarette users were at higher
odds of visual impairment compared with never e-cigarette users, independent of traditional cigarette use.
“A review of the impact of e-cigarette use on ocular health reported incidents of dry eye after e-cigarette use, as a result of disturbance in tear film stability. Dry eye is exacerbated by the voltage of the e-cigarette device during use, as higher voltage led to further aggravation of symptoms,” the summary said.

“This is mainly due to the increased concentration and release of toxins in the e-liquid, namely free radicals and aldehydes, at higher temperatures. Notably, flavours containing ethyl maltol and linalool may increase the production of free radicals which are harmful to the eyes. Minor traces of bilateral corneal staining have also been identified in e-cigarette users, as well as a decrease in ocular blood flow, altered retinal function and increased risk of developing eye cancer.”











As tobacco-related vision loss poses a significant health and socioeconomic burden, the WHO suggested strategies such as reducing the demand for tobacco and exposure to second-hand smoke, as well as helping tobacco users to quit, are key areas of action. Tobacco control advocacy campaigns should increase messaging around the risk of tobacco smoking and vision loss, as well as the risk of using novel and emerging nicotine and tobacco products.
“To reduce the demand for tobacco, governments are strongly encouraged to implement the measures laid out in the WHO Framework Convention on Tobacco Control, with a particular focus on the MPOWER measures for demand reduction,” the WHO stated.

“Raising taxes on tobacco products and banning the advertisement, promotion and sponsorship of tobacco products are critical to reducing the demand for tobacco. Given the effectiveness of smoke-free environments in protecting people from the harms of exposure to second-hand tobacco smoke, governments should continue to implement measures to create,
promote and enforce smoke-free environments.”
Although many of these practices exist in Australia, the WHO said this effort should include warning the general public about the harms of tobacco use through graphic health warnings on tobacco packs and mass-media campaigns, and ensuring the availability of tobacco-cessation services, including tobacco quitlines and integration of brief advice for tobacco cessation into the health system at all levels.




“Plain packaging on tobacco products is another effective strategy to reduce the demand for tobacco,” the summary said.



“To increase access to eyecare services for early detection and management of eyecare issues related to tobacco smoking, governments are strongly encouraged to implement the measures laid out in the WHO guide for action for integrated people-centred eyecare.”


























AS AN OPTICAL DISPENSER, EDDIE MOORE WANTED MORE FROM HIS CAREER, SO HE EQUIPPED HIMSELF WITH THE KNOWLEDGE AND SKILLS TO BECOME A PRACTICE OWNER. HERE’S WHAT HE LEARNED ALONG THE WAY.
Early in my career – after working at an independent practice and obtaining my Cert IV in optical dispensing – I secured a position with Baker, Payne and Webb (BPW) Optometrists in Port Macquarie, NSW. It was January 1995 and I was fortunate to work with an excellent optical dispenser, Ted Vogels. It presented an opportunity to learn new skills, but I wanted a more thorough education, so I started a bachelor of business part time while working full time at BPW.
It was a decision that altered the course of my career, seeing me ultimately become an optical dispenser practice owner. It’s also taught me many lessons that I hope to pass on to other dispensers with an entrepreneurial mindset.
In 2000 the practice manager took maternity leave and I successfully applied, staying in the role for five years. I was in charge of nine practices and it was a great training ground to running a business. I was with BPW for almost 11 years, but upon finishing my business degree, I had a young family and applied for graduate positions outside the optical industry. I wanted to further utilise my education.
Ultimately, we didn’t want to leave the area and my wife suggested an optometrist friend and I approach BPW
to purchase one of their two practices in Kempsey. Our families put everything on the line so failure couldn’t be contemplated.
Mr Ben Bailey and I negotiated the purchase of Masons Eyecare off BPW and started working for ourselves in January 2006, and remain business partners today.

KEY LESSONS
Because Ben was the incumbent optometrist since 1999, we were fortunate nothing changed for the patients, except for a new optical dispenser. It was Ben the optometrist, myself, and a receptionist. I had to quickly adapt to optical dispensing again while running a business. We were successful from the very first day.
We set the practice up as Pty Ltd and drew a wage as employees so we could focus on business growth while knowing we had a paycheck each week. This was one of the best decisions we made.
As a full-time optical dispenser, it was sometimes challenging wearing both hats as a business owner as well. But in some ways it was easier as I only had one practice to focus on, rather than nine.
My business degree has been invaluable and I’m not sure we would have been as successful had I not the skills in management – both financial and HR.
Ben and I clearly defined our roles at the beginning. He’s happy as an optometrist and while he has a keen interest in the running and success of the business, he didn’t want that to be his role. We therefore have defined roles and stay in our lanes, playing to our skills.
As we became more successful, I hired a trainee optical dispenser and a year later our receptionist retired so I hired another trainee optical dispenser. As we further grew, optometrist partner, Ms Naomi Keast, bought in and we hired another trainee optical dispenser.
Today, we have two full time optometrists and four full time optical dispensers although one is still training. We no longer have receptionists as I was keen to have everyone trained to cover all aspects of the business and the front-of-house can interchange with each other seamlessly as they all have the same skills.
If I have anything to offer prospective optical dispenser practice owners, it is only what worked for us. I am too risk averse to have bought a practice without an optometrist partner. Ben and I were already friends and had worked together so we knew what would work for us in a business relationship.

I don’t think being friends is necessary, but you must have similar goals – it would be untenable otherwise. That said, everyone has a different risk aversion and there are successful non-optometrist practice owners aplenty.
Having the skills of the business degree have been invaluable; in the early years, primarily the finance accounting aspects and, as we grew, the HR/people management skills. Having a young family and a wife that also worked, we had to be conscious of our time and I made sure everything was done.
We kept the name of the practice as it held weight in parochial country town and we didn’t think it necessary to have our names in the title of the business.
DREW A WAGE AS EMPLOYEES SO WE COULD FOCUS ON BUSINESS GROWTH WHILE KNOWING WE HAD A PAYCHECK EACH WEEK”ABOUT THE AUTHOR: Eddie Moore is a qualified optical dispenser and the part-owner of Masons Eyecare since 2006, a full-scope independent practice located in Kempsey, NSW.
AFTER BEGINNING HER ROLE AS AN ASSISTIVE TECHNOLOGY SPECIALIST AND ORTHOPTIST AT GUIDE DOGS VICTORIA IN 2021, JESS BUNSOY SHARES THE IMPORTANT ROLE ASSISTIVE TECHNOLOGIES AND OTHER AIDES PLAY.
ur loveable and iconic Guide Dogs are known across the country for their role in affording independence and companionship to people with low vision or blindness.

However, we find many people are unaware there’s more to our services than our beloved pups, with our broader suite of “non-dog” services now making up the majority of our work.
Services like Assistive Technology, Orthoptics, Occupational Therapy, and Orientation and Mobility are crucial to ensuring people with low vision or blindness build skills and live a life
After studying orthoptics at university, I knew I wanted to help people with low vision or blindness live more independently through technology. Like many others, I wasn’t aware Guide Dogs offered services that extended beyond dogs, but I now work with the organisation as an assistive technology (AT) specialist and orthoptist. In this role I help clients with everything from setting up an assistive technology device to establishing a way to work remotely, online shopping, studying, volunteering and everything in-between.
Assistive technology is one of our most popular and important offerings, partly
avoid, but largely because it offers such huge opportunities.
Historically, people with blindness or low vision used Braille to read, communicate and navigate daily life. Today, the number, and quality, of assistive technologies that are available is growing – from screen readers to applications on smartphones and TVs. And they’re helping give those with low vision or blindness an increased sense of autonomy, and the ability to carry out everyday tasks more easily.
But there are still gaps in accessibility, with cost often emerging as a barrier. Many of our clients will have funding providers, such as NDIS or HCP, and at Guide Dogs we provide supporting documentation to help clients secure that funding for necessary equipment. For those that don’t have funding options, we seek philanthropic support from donors to provide that equipment free of charge.
The technology is also quite diverse, so we’d like to see greater streamlining of the user experience to help support our clients picking up whatever device they need with ease. In a perfect world everything would have the option to be controlled by voice or gesture in the same way so it’s intuitive for the blind and low vision community.
We also still find some websites are not designed with screen reader users in mind. So, whilst, screen-readers are an amazing accessible technology, if a website is not accessible it can make navigation trickier for the individual.
We are advocating for these improvements and developments, but in the meantime helping people navigating these barriers is an incredibly important part of what we do – because realising the full impact
of technology can be life changing.
For one of my clients, Mr Simon Watharow, learning to use assistive technology has meant he can manage his own business in the wildlife rescue, and mental health support field, as well as his part-time work as a volunteer for Wildlife Victoria and Lifeline.

Simon said of his experience: “It’s been really helpful to have Jessica help me navigate and adapt different software to make it easier and more accessible for me to use. While technological developments have significantly improved in recent years, there’s still a long way to go when it comes to making software accessible. I regularly come across road bumps that need smoothing out, and Guide Dogs Assistive Tech services have really helped to improve my quality of life.”
At Guide Dogs Victoria we often rely on specialists to help us inform both our clients and the public about the services we offer. With that in mind, if you’re interested in finding out more about our broader services, assistive technology in particular, or chatting to us to get more specific information please visit our website.
With your help we hope to see more people come through our doors, or visit our website, so we can better support those living with low vision or blindness by opening up their world through technology.
To find out more or speak with a Guide Dogs Victoria vision specialist, visit: vic.guidedogs.com.au/
Email: info@guidedogsvictoria.com.au
Phone: 1800 804 805
ORTHOPTICS AUSTRALIA strives for excellence in eye health care by promoting and advancing the discipline of orthoptics and by improving eye health care for patients in public hospitals, ophthalmology practices, and the wider community. Visit: orthoptics.org.au

Practitioners engaged in group practices – or contractors, employees and licensees – often contemplate establishing their own practice at some point in their careers. It’s an exciting and rewarding prospect, but can be equally daunting as challenges arise.

KAREN CROUCH
“PRACTITIONERS SHOULD CARRY OUT A SELF-ANALYSIS AND BE CONFIDENT THEY HAVE THE APPETITE TO MAKE THE TRANSITION FROM HEALTHCARE PROVIDER TO BUSINESS OWNER”
Turning your mind to starting a clinic of your own often requires self-analysis and a mind shift. You’ll be going from predominantly a healthcare provider – with relatively limited responsibility for administration or people management – to managing business, people, suppliers and marketing, with responsibilities for good clinical and corporate governance in additional to your role as a healthcare provider.
Set-ups typically involve numerous tasks and may be daunting, requiring a significant time investment to oversee progress while making key decisions on items that practitioners have limited experience with.
And, of course, meticulously planned, overarching project management throughout the months-long implementation period is paramount.
Matters requiring personal experience or familiarity range from business planning, legal, premises selection, design, construction, finance, technology and communications, office and medical equipment and other matters such as signage, security, waste management, website (marketing) and recruitment of personnel (staff and clinical).
The new venture, properly orchestrated from start-up to ongoing management,
•
•
•
administrative, clinical, allied, contracts
• Plans: budget and monitoring, risk/contingency management, supplier management, staff induction and assessments, records management, policy and procedure manual, communication/effective meetings and (optional) board/owners’ management.
• Miscellaneous: Safe, toys & TV
ogo design & business documents
• Website & marketing
• Technology: Hardware and software
• Practice furniture
• Medical equipment/furniture/supplies
• Security
• Signage
• Telephone system
• Maintenance & other contracts
• Waste disposal
can be rewarding, provided plans are in place to ensure quality patient services while administrative and clinical “practice business” functions operate efficiently, cost effectively and in synergy with personal healthcare objectives of the owners. Once preliminaries have been completed to the practitioner’s satisfaction, several other start-up aspects of practice and business management come into play. Several of those, mentioned below, will be the subject of future articles in this three-part series.
Before deciding to start a practice, certain prerequisites are recommended:
• Business plan and feasibility study – a ‘road map’ of the owners’ plans for the venture, including financial analysis (staff, estimated patient volumes, revenue, expenses) to determine breakeven points and profitability (reward for owners’ endeavours). It will also support loan applications and ultimately provide a detailed budget for first-year operations and beyond;
• Business structure – essential for securing premises, finance and practice operations. Be careful not to miss the perfect premises due to absence of an appropriate business structure as the ‘entity’ is likely to purchase/ lease premises and apply for finance;
• Area/premises selection – while the business plan details pertinent aspects of practice goals, target patient segments, identification of the best physical premises requires demographic research of local statistics – age, ethnic makeup, income levels, demand, competition – to determine whether the planned services fit the
target area. Exploring site options and assessment is the next step. Legal aspects and negotiating skills play an important role in securing the best deals;
• Finance approval – the aforementioned feasibility study and business plan is required by financiers.
These actions will give aspiring new owners greater confidence in viability and likelihood of success, secure funding and ensure the new venture is afforded every opportunity to succeed.
SUMMARY
Practitioners should carry out a self-analysis and be confident they have the appetite to make the transition from healthcare provider to business owner and manager. Once you’ve got that mental shift in place, detailed, well thought-out plans will assist to establish a strong underpinning from which to launch the new clinic.
The myriad of requirements will ensure the practice is ready to go from day one. Success will hinge on selection of qualified, experienced suppliers and meticulous project planning to ensure tasks are performed in order, on time/budget, and in accordance with project plans.
Part 2 of this article will focus on how to implement basic business services – and contain references to the third part of this article series.
ABOUT THE AUTHOR: KAREN CROUCH is Managing Director of Health Practice Creations Group, a company that assists with practice set-ups, administrative, legal and financial management of practices. Email: kcrouch@ hpcnsw.com.au or website: www.hpcgroup.com.au

WHEN A PRACTITIONER TAKES THE PLUNGE TO ESTABLISH THEIR OWN PRACTICE, IT REQUIRES COURAGE AND A CRYSTAL-CLEAR PLAN, WRITES KAREN CROUCH.
(WHO) Lymphoma classification, VRL has been recognised as a lymphoma-type that arises in an immune privileged site, alongside CNSL and testicular lymphoma. In general, VRL patients have a poor prognosis, particularly if diagnosis is delayed.
PCL are low-grade B-cell lymphomas, that respond very well to low-dose radiotherapy. They are very similar to conjunctival low-grade B-cell lymphomas. However, PCL can be extensive leading to retinal detachment; as well as infiltrate other parts of the uvea, mimicking a diffuse melanoma, or even spread into extraocular tissues.
Iparts of the eye and show varied clinical manifestations, masquerading as many diseases; therefore, making the diagnosis is challenging.
Even when lymphoma is suspected, it can be difficult to confirm cytologically, because of the fragility of lymphoma cells. For these reasons, close cooperation between the ophthalmologist and pathologist is essential, particularly to optimise the information that can be obtained from these paucicellular samples.
Such collaboration requires the ophthalmologist to have a good understanding of intraocular lymphoma pathology and basic knowledge of the laboratory investigations required.
In the first part of this Soapbox, we describe the clinical manifestations of intraocular lymphomas. In the second section, we make recommendations for sample transport and outline briefly the tests undertaken for their diagnosis.
Essentially, intraocular lymphomas can be divided into: a) vitreoretinal lymphomas (VRL); b) primary choroidal lymphomas (PCL); c) secondary choroidal lymphomas. Rarer subtypes can occur as primary or secondary tumours in the iris; however, they will not be discussed here.
VRL are high-grade B-cell lymphomas that arise in the retina, with/without vitreous involvement. They typically are associated with central nervous system (CNS) disease, which can occur either concurrent or after the ocular disease.
In the new World Health Organization
Secondary choroidal lymphomas represent an intraocular manifestation of a systemic lymphoma. These typically occur in patients with advanced or relapsed Non-Hodgkin Lymphomas (NHL), with the subtypes varying considerably. The response to chemotherapy is dependent on the subtype of NHL.
LAB-BASED TESTING
Reaching the diagnosis of intraocular lymphoma requires good clinicopathological correlation. Communication between clinical and pathology lab teams is critical; particularly, it is important for the lab when the sample will be sent, avoiding late Friday afternoons, where possible.
Clinicians frequently-asked-questions concerns use of steroids prior to vitrectomy (best avoided) and the sample transport media of the vitrectomy or aspirate specimens.
We recommend a soft-fixative, such as CytoLyt or H.O.P.E. fixation, for both the undiluted and diluted samples. The cassette-washings should also be sent, as sometimes these contain the diagnostic cells.
The above-mentioned fixatives help maintain tumour cell integrity, and allow for same-day rapid cytospin preparations, and for most (if not all) laboratory tests (including molecular) to be undertaken.
Glutaraldehyde fixation should be avoided as it leads to poor quality DNA on extraction. Neutral buffered formalin for vitrectomy samples is not ideal as it requires wax-embedding, with the biopsied cells ‘settling’ at differing levels within the block. Numerous sections must then be undertaken to obtain a complete picture of the vitrectomy sample, often leaving insufficient material for essential molecular testing. However, it must be noted that
is visible as a tissue piece, then this should be sent in buffered formalin.
In addition to simple morphology stains, the main tests that are performed include immunohistochemistry (IHC), immunoglobulin chain rearrangement testing using polymerase chain reaction (IgH-PCR) and increasingly mutational gene analysis, e.g., MYD88.
The antibodies typically used in IHC include ones directed against: B-cells (CD79a, CD20 and PAX5), T-cells (CD3) and macrophages (CD68). Cells that are morphologically atypical and positive for a B-cell marker are highly suspicious of a B-cell lymphoma.

If these are within a vitrectomy sample and are medium-to-large in size, then this would speak for VRL. If these cells are smaller and the dominant population within a choroidal biopsy or aspiration, then this be suspicious of a primary choroidal lymphoma.
The molecular testing demonstrating either a monoclonal B-cell population and/or a MYD88 mutation (present in 70% of all VRL), steers diagnosis towards malignancy rather than inflammation. Integration of all findings is imperative to reach a definitive diagnosis.
NOTE: This article was co-authored by Dr Yamini Krishna, consultant histopathologist.
ABOUT THE AUTHOR

Qualifications: MBBS, PhD, FRCPath
Primary place of work: Liverpool Clinical
Laboratories and University of Liverpool
Position: Consultant Histopathologist and George Holt Chair of Pathology
Location: Liverpool, UK
Years in profession: 20 years
COMMUNICATION BETWEEN CLINICAL AND PATHOLOGY LAB TEAMS IS CRITICAL. IT IS IMPORTANT FOR THE LAB WHEN THE SAMPLE WILL BE SENT, AVOIDING LATE FRIDAY AFTERNOONS, WHERE POSSIBLE.
MARCH
ANZ CORNEA SOCIETY AND EYE BANK MEETING
Perth, Australia
9 – 10 March
rybooking.com/events landing/922238
WAVE 2023 – OPTOMETRY WA
Fremantle, Australia 18 – 19 March optometry.org.au/about-us/ our-organisation/optometry-wa/
CONGRESS ON CONTROVERSIES IN OPHTHALMOLOGY
Lisbon, Portugal
24 – 25 March cophy.comtecmed.com
APRIL
AUSTRALIAN VISION CONVENTION
Gold Coast, Australia
1 – 2 April events@optometryqldnt.org.au
SILMO SINGAPORE
Singapore 12 – 14 April www.silmosingapore.com
ARVO 2023
New Orleans, US 23 – 27 April arvo.org/annual-meeting
OPTICAL DISPENSERS AUSTRALIA CONFERENCE
Sydney, Australia 28 – 29 April odamembers.com.au/ odaconference
MAY
ANZSRS MEETING
Melbourne, Australia 20 – 21 May ranzco.edu/events/2023
SUPER SATURDAY –OPTOMETRY NSW/ACT
Sydney, Australia 21 May optometry.org.au/about-us/ our-organisation/optometry-nsw-act
NATIONAL ABORIGINAL AND TORRES STRAIT ISLANDER EYE HEALTH CONFERENCE
Sydney, Australia 24 – 26 May mspgh.unimelb.edu.au
JUNE
ASO EXPO 2023
Sydney, Australia 2 – 4 June asoeye.org
WORLD GLAUCOMA CONGRESS
Rome, Italy 28 June – 1 July worldglaucomacongress.org
JULY
AUSCRS 2023
Port Douglas, Australia 26 – 29 July auscrs.org.au/2023-conference
Specsavers have a fantastic opportunity on offer for an Optometrist looking to take the next step in their career. Join an established, market-leading brand with stateof-the-art equipment including OCT, at our brand-new store soon to open in Kings Meadows, Tasmania! King’s Meadows is a suburb in the south of Launceston, Tasmania. The suburb offers a central location and is only a short 10-minute drive from the city centre. It is a well-developed suburb with a greater number of shops than any other suburb within Launceston making it the largest commercial district in Launceston outside of the CBD.
Optometrist opportunity - Specsavers Karingal, VIC
A full-time Optometrist Opportunity is now available within the Specsavers Karingal store. This newly refurbished 6 test room store is decked out with fully automated, brand new equipment including phoropter, Tonoreff II and has 2 pre-test rooms, both of which have OCT machines. Work with a vibrant, committed, experienced and loyal team with a fantastic team culture. Free onsite car-parking is available and there is easy access to the peninsula link. The store are offering an attractive salary with a sign-on bonus of up to $20,000.
Interested in seeing Australia? $180,000 for the growing Mobile Optometrist Role
Specsavers is growing our community based Mobile Optometry Team Nationally, With home based locations in Perth & Melbourne along with longer term Fly in Fly out roles available. With an amazing $180,000 package on offer. You will experience a wide variety of cases, whilst being able to explore different regions
of Australia. We are looking for someone who has the desire and flexibility to travel.
Locuming in Western Australia Specsavers are looking for locum optometrists, we have several vacancies across WA and are seeking locums who have a real passion to provide the best service to our patients. We are offering $1500 to any new locums who join and complete 38 hours through SRS before the 31st of January, we are also offering $1500 to anyone who refers a new locum. For locums interstate we can arrange and pay for your flights, accommodation and car hire for both regional and metro stores in WA.
Interested in relocating to NZ?
Specsavers has a range of opportunities for NZ optometrists looking to return home. From North to South, we have fantastic opportunities for optometrists at all levels.
And as a Specsavers optometrist, you’ll have the chance to advance your skills and become part of a business that is focused on transforming eye health outcomes in New Zealand.
Be equipped with the latest ophthalmic equipment (including OCT in every store for use with every patient) and develop your clinical experience across a range of interesting conditions and an ever-growing patient base.
You’ll also have the support of an experienced dispensing and pre-testing team, the mentorship of store partners and access to an exemplary professional development program.
There’s no place like home – so if you’re ready to return, let us help you.
To list an event in our calendar email: myles.hume@primecreative.com.au
SEPTEMBER
ORTHOKERATOLOGY
SOCIETY OF OCEANIA CONFERENCE
Gold Coast, Australia
1 – 3 September www.facebook.com/OrthoKSO/
O=MEGA23 & WORLD CONGRESS OF OPTOMETRY
Melbourne, Australia
8 – 10 September omega-event.org
EUROPEAN SOCIETY OF CATARACT & REFRACTIVE SURGEONS CONGRESS
Vienna, Austria 8 – 12 September congress.escrs.org/
OCTOBER
RANZCO SCIENTIFIC CONGRESS
Perth, Australia 20 – 24 October ranzco.edu/events
In a few short years, Specsavers has achieved market leadership in Australia and New Zealand with more people choosing to have their eyes tested and buy their prescription eyewear from Specsavers than any other optometrist. To learn more about these roles, or to put your hand up for other roles as they emerge, please contact us today:
Joint Venture Partnership opportunities enquiries: Kimberley Forbes on +61 (0) 429 566 846 or E kimberley.forbes@specsavers.com
Australia Optometrist employment enquiries: Marie Stewart – Recruitment Consultant marie.stewart@specsavers.com or 0408 084 134
Locum employment enquiries: Matthew Cooney matthew.cooney@specsavers.com or 0447 276 483
New Zealand employment enquiries: Chris Rickard –Recruitment Consultant chris.rickard@specsavers.com or 0275 795 499
Graduate employment enquiries: apac.graduateteam@specsavers.com
monthly bulletin to keep the Australian ophthalmic sector updated on new appointments and personnel changes, nationally and globally.








Alcon® Toric IOLs allows you to correct even the smallest amount of astigmatism‡2-5

Most cataract surgery patients present with some level of corneal astigmatism.§6
The Alcon® Toric IOL portfolio, with cylinder powers from T2–T9, accommodate a wide range of astigmatic correction needs, from high to low. 2-5 Built on the heritage of the proven AcrySof ® platform, Alcon® Toric IOLs offer exceptional performance with outstanding refractive predictability7-10 and rotational stability7-10 for you and your patients.
