

Early in your career as an Optometrist?
At Specsavers, we’re committed to helping you reach your potential.
We provide our optometrists with a solid career path and are focused on helping you achieve your professional goals.
With over 400 stores, you can find a Specsavers practice in a location that suits your preferences — from metropolitan to outer regional areas.
We also provide genuine career progression, from our graduate program all the way to partnership, supported with leadership and training through our Pathway programs.
Whether you’re looking for your first job, looking for new opportunities or ready to take that next step to partnership, at Specsavers you’re only limited by the scale of your own ambition. Go
spectrum-anz.com or contact us:

OMBUDSMAN REVIEWING AHPRA’S ‘VEXATIOUS COMPLAINTS’ FRAMEWORK

“If you want to ruin a doctor’s life, all you have to do is make a complaint against them and walk away. There will be no consequences against you. Certainly 90% of the time the doctor will be found to have done nothing wrong, but you will have ensured that that doctor has a year of utter misery.”
These were the comments of Australian Medication Association (AMA) spokesperson Dr Antonio Di Dio at a recent Senate Committee review of the Australian Health Practitioner Regulation Agency (Ahpra). It is an example of how vexatious patient complaints can affect practitioners, and was the impetus for Ahpra developing a special framework to deal with such complaints in December 2020.
Now, in 2023, the National Health Practitioner Ombudsman (NHPO) is reviewing Ahpra’s ‘Framework for identifying and dealing with
vexatious notifications’, examining its effectiveness and whether any unintended consequences have arisen.
Ahpra defines a vexatious complaint as one without substance, made with an intent to cause distress, detriment or harassment to a practitioner. It also notes they can come from anyone including patients, members of the public and other practitioners.
Australian Society of Ophthalmologists (ASO) president Dr Peter Sumich told Insight the organisation welcomed the NHPO’s ongoing independent review launched in June 2022.
“Vexatious complaints are hurtful to the practitioner involved and ultimately a waste of resources,” he said. “They detract from the validity of genuine scrutiny of the profession.”
Sumich said a small number of ASO
members have expressed concern about how heavily the framework is balanced in favour of the claimant, and how this has been used to suppress competition.
“These concerns are reflected in the AMA’s submission to the NHPO, a submission which the ASO supports,” he added.
In its submission, the AMA said the
general view of the medical profession is that handling of vexatious complaints – and the notification process broadly – must be improved. It said it was imperative Ahpra addresses growing distrust of the regulator among the profession – with minimising the impact of vexatious notifications being a key step in achieving this.
“The introduction of the framework does not mean that work by Ahpra on minimising the impact of and managing vexatious notifications is complete, instead it has been an important initial step,” AMA stated.
Referencing Dr Antonio Di Dio’s Senate Committee comments, the peak medical body said this speaks to one of the significant outstanding issues related to vexatious complaints where people can make a false complaint and face no repercussions
continued page 8
MEDICARE FRAUD REVIEW VINDICATES PROFESSION
An independent review into Medicare compliance has found no evidence of the $8 billion fraud quoted in media reports last year, instead finding that Medicare Benefits Schedule (MBS) compliance issues are overwhelmingly caused by the complexity of the system.
On 4 April, the Federal Government released the findings of a review by respected health economist Dr Pradeep Philip into Medicare Compliance and Integrity. It came in response to reports about the potential for widespread Medicare rorting and fraud.
Philip’s review found the overwhelming majority of health practitioners are well meaning and protective of Medicare, with there
being no evidence to support the $8 billion figure highlighted in some media reporting. The review found that the likely cost to Australian taxpayers is closer to $1.5 to $3 billion annually. But without action this figure could increase.
“A large part of the success and efficacy of Australia’s health system, to date, is due to this level of altruistic behaviour by health professionals. That said, my review highlights growing vulnerabilities and forces of change which could, in a short period of time, result in significant leakages, including fraud, in the system,” Philip, head of Deloitte Access Economics, said.
“It is my view that a significant part of the leakage in the Medicare payment system stems from
non-compliance errors rather than premeditated fraud. "
In a November 2022 Insight article, medical defence organisation Avant said optometrists have been reprimanded over the use of items that require patients to have been previously seen at the same practice as the providing optometrist, not at another practice within a corporate group.
Items 104 and 110, involving multiple specialities, have been a recent focus of the regulator. Concerns included poor record-keeping as well as a lack of evidence of a referral requesting a specialist consultation, inadequate communication of outcomes to the
continued page 8
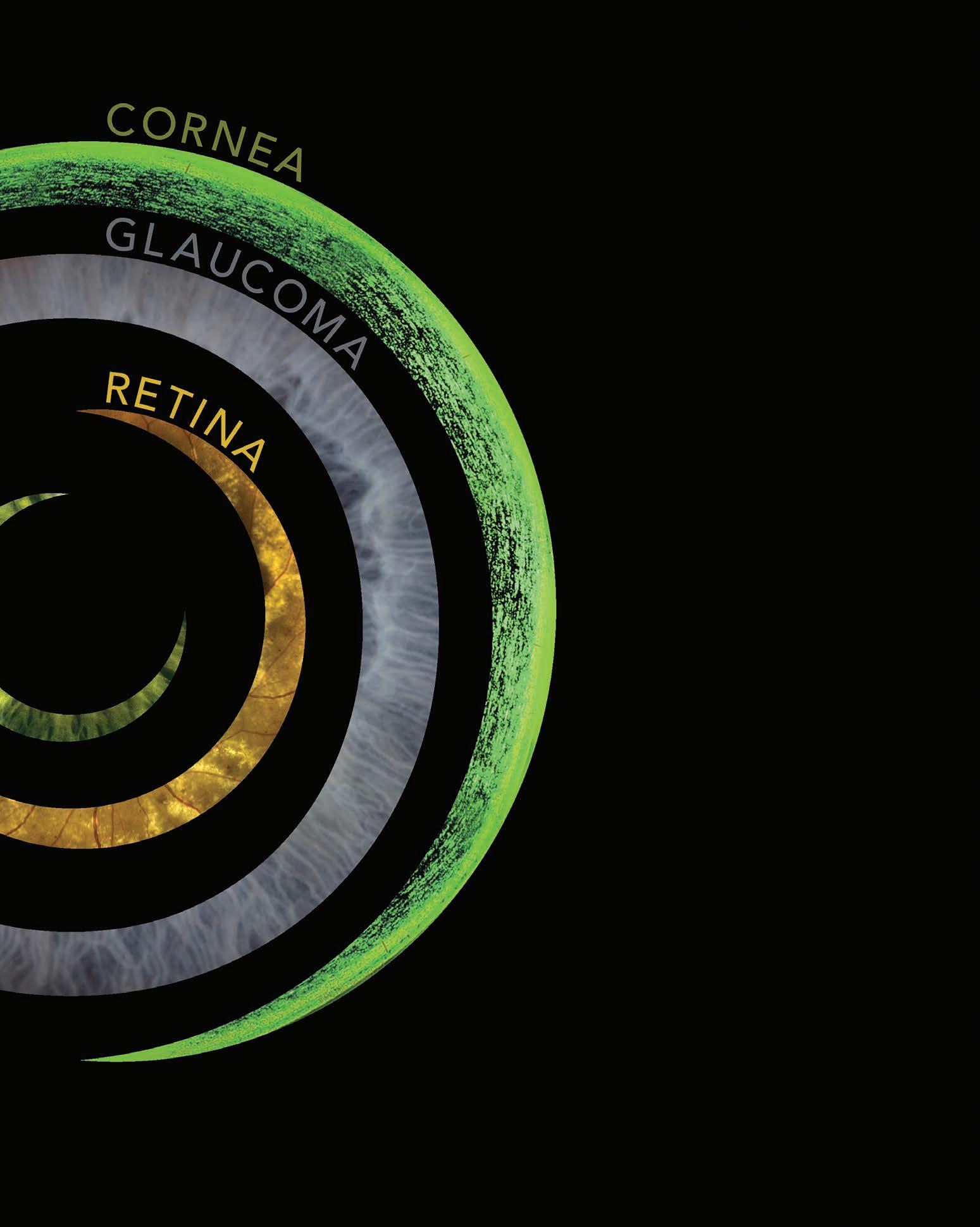
TRANSFORMATION
How integrated workflows – where devices talk to one another – and comprehensive data management solutions are reshaping the way ophthalmology care is offered in Australia in 2023.

Maximise your glaucoma workflow with ZEISS SLT.

Introducing ZEISS VISULAS green with SLT
Discover an efficient glaucoma treatment experience with the integrated SLT option on your VISULAS ® green laser from ZEISS.



• R otating aiming beam to accurately position on trabecular meshwork.
• C oaxial illumination of aiming and treatment beams.
• Fast SLT pattern application of 400μm delivered by 52 squared spots.
• D igital treatment report output to ZEISS FORUM.*
Early adopters of ZEISS SLT with VISULAS green laser are seeing immediate clinical benefits:
“SLT with the VISULAS green laser demonstrated clinically significant efficacy in terms of lowering IOP in eyes with POAG with about half of the treated eyes showing a 20% additional IOP reduction”1
zeiss.com/visulasgreen
Hear from the ZEISS SLT Experts:
AU: 1300 365 470 med.au@zeiss.com
IN THIS ISSUE
EDITORIAL
THE PRICE OF SAVING SIGHT
The macular disease community scored a decisive win last year when, during the federal election campaign, it secured a commitment from both political parties to remove the threat of a proposed 69% Medicare rebate cut for anti-VEGF intravitreal injections.


Overturning the controversial Medicare Review Taskforce plan was vital to ensuring patients would not skip these sight-saving treatments due to soaring out-of-pocket costs or long waits that would have ensued in an overwhelmed public system. But significant questions remain about what else can be done to help people persevere with eye injections, addressing issues like affordability and geographical access to treatment.
As part of its Macula Month campaign in May 2023, the Macular Disease Foundation Australia has released fresh insights from a PwC report it commissioned. A deep dive into the report can be found on page 27, revealing at least half of patients diagnosed with late-stage neovascular age-related macular degeneration (nAMD) will stop their anti-VEGF eye injection treatment within five years. And when they stop, significant vision loss can occur as early as the next three months.

The main reasons for skipping their appointments include the treatment burden, misconceptions about its benefit, personal financial cost, travel and comorbidities.

MDFA recognises this and has set out a three-pronged plan for modest taxpayer investments to improve health literacy, affordability and treatment access, which it says could lead to net savings in the order of billions of dollars over the next decade.

PROFITABLE PRACTICE
HEADLINE
Anti-VEGF is a miracle molecule that changed the game for nAMD patients who would have been resigned to a lifetime of severe vision loss 15 years ago. Although new approaches are lessening the burden by increasing treatment intervals, it’s clear more work needs to be done to lift treatment adherence; and it’s heartening to see optometry providers like Specsavers put this high on their agenda (page 24).
How the government responds is anyone’s guess, but it will be difficult to ignore MDFA’s plan when you think about the impact of a modest investment on individuals and the Australian economy.



Just as Insight went to print, the AIHW has released new eye health data for Aboriginal and Torres Strait Islander people. In its sixth report, it found: active trachoma prevalence in affected children aged 5-9 years fell from 15% in 2009 to 3.3% in 2021; 42% of Indigenous Australians who had a diabetes test also had an eye examination in 2019-20; and the age-standardised cataract surgery rate fell by 15% from
UPFRONT STAT
2018–19 to 2019–20. IN OTHER NEWS, Federal Health Minister Mr Mark Butler announced the latest recipients of the Medical Research Future Fund. The Centre for Eye Research Australia received $595,000 to develop of a photoreceptor regenerative therapy for blindness. Meanwhile, the University of Queensland was granted $1.3 million to progress home hearing and vision care to improve quality-of-life for people with dementia and their carers.

FINALLY, the Product Information (PI) for low dose atropine eye drop Eikance 0.01% has been updated. Supplied by Aspen Pharmacare Australia, the therapy is indicated to slow myopia progression in children aged from 4 to 14. When first approved, the TGA stated it should be supervised by a paediatric ophthalmologist. But on 9 March, the PI was updated, stating “treatment should be supervised by an eyecare professional”, acknowledging optometrists’ existing prescribing practices.
WEIRD
Researchers at Dartmouth College in the US have linked prosopagnosia (inability to recognise faces) with COVID-19. “Self-report survey data from 54 respondents with long COVID showed that a majority reported reductions in visual recognition and navigation abilities. It appears high-level visual impairments are not uncommon in people with long COVID,” they reported.
WONDERFUL
A protocol for treating dry eye in humans has been successfully adapted for horses. Horse and Hound reported a case of a horse who had persistent dry eye problems, including corneal ulcers, despite many treatments. An approach focusing on the meibomian glands using daily hot compresses, a lubricant, serum and topical antibiotic has delivered a long term solution.
WACKY
The person who sued high profile actor Gwyneth Paltrow is a retired army optometrist. Terry Sanderson sought $300,000, accusing Paltrow of crashing into him while skiing in Utah, causing injury. But Paltrow countersued for $1 and her legal costs, ultimately winning the case.
LET FOOD BE THY MEDICINE
A 30% reduction in dry eye risk has been found with each additional gram of omega 3 polyunsaturated fatty acids consumed each day. Page 35

WHAT'S ON
Complete calendar page 73.
NEXT MONTH MPIC 2023
21 MAY
Optometry NSW/ACT’s event at Luna Park, Sydney, is promising an optometry-led, face-to-face conference with affordable and clinically-relevant content by leading Australian and international experts.
vision@oaansw.com.au
10 JUNE
The second Myopia Progression in Children Conference, run by Dr Loren Rose’s Myopia Australia, invites eye health professionals to learn and interact with the latest research-proven methods.
info@myopiaaustralia.com.au
insightnews.com.au
Published by: 379 Docklands Drive, Docklands VIC 3008
T: 03 9690 8766 www.primecreative.com.au
Chief Operating Officer Christine Clancy christine.clancy@primecreative.com.au
Group Managing Editor Sarah Baker sarah.baker@primecreative.com.au
Editor Myles Hume myles.hume@primecreative.com.au
Journalist Rhiannon Bowman rhiannon.bowman@primecreative.com.au
Commissioning Editor, Healthcare Education Jeff Megahan Business Development Manager Luke Ronca luke.ronca@primecreative.com.au
Client Success Manager Salma Kennedy salma.kennedy@primecreative.com.au
Design Production Manager Michelle Weston michelle.weston@primecreative.com.au
Head of Design Blake Storey
Art Director Bea Barthelson Subscriptions
T: 03 9690 8766 subscriptions@primecreative.com.au
The Publisher reserves the right to alter or omit any article or advertisement submitted and requires indemnity from the advertisers and contributors against damages or liabilities that arise from material published. © Copyright – No part of this publication be reproduced, stored in a retrieval system or transmitted in any means electronic, mechanical, photocopying, recording or otherwise without the permission of the publisher.

'IT CONSTANTLY WEIGHED ON MY MIND'
continued from page 3
regardless of the impact on the doctor’s life.
“The ramifications of a vexatious notification can be mentally and financially damaging to doctors. The more serious the complaint, the more significant the impact on the life of the doctor. For example, a doctor cannot practise without a supervisor should the notification require a supervision order. This can take months to establish. As Ahpra is funded from registration fees, the fact that these doctors pay for the vexatious notification process and the resources it consumes adds to this injustice. The AMA would like to see improvements in the timeliness of managing all notifications, but vexatious notifications in particular.”
In 2017, Ahpra commissioned independent research that took the first international look at vexatious complaints. The report, ‘Reducing, identifying and managing vexatious complaints’, found vexatious complaints account for less than 1% of notifications, and that there is greater risk of people not reporting concerns than of people making truly vexatious complaints.
However, AMA was not convinced of this number.
“We would like to better understand the distinction between notifications that occur now that the framework has been in operation for 12 months,” its submission stated.
“Improving transparency on how vexatious
complaints are managed would improve how the profession views Ahpra and its processes. We need to see how the framework has changed behaviour and improved vexatious notification handling. We would like to see this as a driver to improve the framework. The AMA is committed to working with Ahpra to achieve this.”
A CASE STUDY
Recently, the Royal Australian College of General Practitioners (RACGP) warned that vexatious complaints are “out of control and damaging the morale of GPs across the nation”.
It comes following a poll of 1,290 doctors revealing that 80% of respondents were subjected to what they felt was a vexatious complaint.
“I’m glad to report we are making some headway,” RACGP president Dr Nicole Higgins said. “[Recently] I met with the chair of the Medical Board of Australia Dr Anne Tonkin and she advised that they now have a triage process in place for frivolous complaints to reduce the impact on the clinician. That is great news and I urge them to make sure that this process has an impact.”
RACGP vice president and Queensland chair Dr Bruce Willett outlined his own experience with a vexatious complaint in December 2021 arising from a patient who refused to wear a mask and then became abusive to front desk staff. He asked the
Ahpra's framework for identifying and dealing with vexatious notifications, outlines:
• principles and features of vexatious notifications
• the signific ant impacts of vexatious notifications
• potential indicators of vexatious notifications
• how to identify vexatious notifications, and
• what to do where there is a concern that a notification is vexatious.
“AS AHPRA IS FUNDED FROM REGISTRATION FEES, THE FACT THAT THESE DOCTORS PAY FOR THE VEXATIOUS NOTIFICATION PROCESS AND THE RESOURCES IT CONSUMES ADDS TO THIS INJUSTICE.”
AUSTRALIAN MEDICAL ASSOCIATION
patient to sit outside and noted that her behaviour was inappropriate.
“This patient put in a complaint that I had yelled at her, which was not true, and it took 10 months for the complaint to finally be dismissed without action,” he said.
“In that time, it took around 35 hours of writing reports and going back and forth with medical defence and having it constantly weigh on my mind during the working day and at night. Keep in mind that it was my first complaint in three-and-a-half decades of practising.”
The ASO told Insight that a draft report by the NHPO was due by the end of 2022, and a final report is earmarked for completion in early 2023.
“The ASO eagerly awaits the release of this final report and acknowledgement of revised mechanisms that will enable the framework to succeed,” Sumich said.
MEDICARE GROWTH NOT BASED ON CLEAR STRATEGY
continued from page 3
referring practitioner, and co-billing a consultation with a procedural service when the record did not support that a separate consultation was performed.
In his report, Philip said one could argue there is a significant amount of ‘fear’ of the compliance regime.
"Notwithstanding it is not as far reaching or effective as it could or should be in practice. But there is no room for complacency. Critical to addressing this is a recognition that the legislative basis for Medicare is fast becoming out-of-date, unable to reflect the changing health needs and modes of health service delivery in Australia.”
After conducting the review, Philip said it was clear Medicare had “grown organically over time” in response to
changing needs and government agendas, rather than based on clear strategy, changing demography, burden of disease and emerging therapeutics, models of care and technology.
“An unintended consequence of this growth over the last nearly 40 years is that there is no longer the same connection that there used to be between patient, the practitioner, and the payment,” he said.
“All these changes open the door for integrity and compliance risks.”
In highlighting Medicare’s “vulnerabilities”, Philip pointed to the changing nature of healthcare delivery that now encompasses: more than 6,000 Medicare items, many which are frequently updated; multidisciplinary teams for more complex cases bringing a broader range of healthcare professionals into the Medicare system remit, and where the biller isn’t always the service provider; and corporatisation of medicine where, increasingly, practitioners have less control over what is billed in their name.
Surprisingly, Philip said entities that run medical centres don't need to be registered for submitting Medicare claims and being paid by Medicare.
The review made 23 recommendations to the Federal Government.

MEMBERS TO VOTE ON OPTOMETRY AUSTRALIA’S INTEGRATION PLANS
Two southern state divisions of peak body Optometry Australia (OA) have announced plans for integration will soon be put to a vote, following months of discussions.
Last year, the boards of Optometry Victoria South Australia (OV/SA) and Optometry Tasmania (OTas) announced they had commenced discussions about a possible merger with Optometry Australia.
After continued discussions, rather than a total merge of the three organisations, OV/SA and OTas are now working towards operational integration with OA.
“The model under development will see each state board remaining as the respective representatives for Victorian, South Australian and Tasmanian members, with all services delivered by OA and monitored by the respective state board for its jurisdiction,” OA said.

Members of OV/SA and OTas will be asked to vote on the model in July and August respectively.
“The new model will see OA continuing to provide members nationally with access to
its full range of member services. The new, integrated structure will also deliver local member engagement, face-to-face CPD, advocacy and stakeholder engagement in Victoria, South Australia and Tasmania,” OA explained.
“No major assets of any organisation will be transferred initially, and services will be integrated and evolved over time to continue to maximise value for members. OA will have the resources and staff of both divisions in order to be able to deliver on the local services.”
The presidents of each organisation – Ms Elise Pocknee-Clem (OV/SA), Mr John Kingshott (OTas) and Dr Margaret Lam (OA) – recently issued a joint statement to members in Victoria, South Australia and Tasmania, outlining the intended benefits of the proposed integration.

These include:
• A strong and aligned strategic focus, more efficiently positioned to identify and prioritise critical issues affecting the sector.
• A more cohesive and effective advocacy
approach through a single voice.
Simplified governance, organisational and operational structure, enabling the organisation to streamline its decision-making processes, reduce duplication and create greater efficiencies.
Greater long-term financial stability and resources to fund future strategies and projects.
• Reducing confusion for the organisation’s external stakeholders, such as heads of ophthalmology and patient advocacy groups, enhancing its influence.

Currently, OV/SA and OTas teams are consulting with their members and seeking feedback on the proposal. Meanwhile, legal and financial due diligence is currently underway, as is the drafting of service and asset agreements.
The final decision on whether the integration occurs will rest with members of both OV/SA and OTas who will have the opportunity to vote on the proposed change. Should members vote yes, implementation is due to be completed by 1 November 2023.
Dr Margaret Lam, Optometry Australia.IN BRIEF
A RGOS ARRIVES
Alcon is releasing its new ocular biometer with image guidance in Australia and New Zealand after a more than year-long delay due to demand from overseas markets. According to the company, the Argos swept-source OCT biometer enables cataract surgeons to calculate the power for an IOLs and measure the relevant eye dimensions while achieving a higher measurement acquisition rates even in mature cataract cases. One study comparing Argos to another leading biometer reported higher acquisition rates for Argos (97.6% vs 92.6%) in 622 eyes. However, when concentrating on the 99 eyes with +4 grade dense cataracts Argos was shown to have better penetration, with 41% higher acquisition rates.
SURGERY WAIT TIMES
Vision 2020 Australia is campaigning for a reduction in waiting times for cataract surgery in NSW, which are the worst in the country, and an increase in sight saving eye injection treatment in the public hospital system. The Australian Institute of Health and Welfare Elective Surgery Waiting Times Report 2021-22 shows NSW has the longest median cataract wait time in Australia at 278 days, compared to the national median of 158 days, and well behind the best performing states Victoria and Queensland (84 days). Almost one in five people in NSW are waiting longer than 12 months before surgery in the public system.
SYNDROME TREATMENT
Two US-based optometrists have presented their new scientifically proven treatment for Visual Snow Syndrome, now published in the medical journal Frontiers in Neurology, at the Australasian College of Behavioural Optometrists conference. Dr Charles Shidlofsky and Dr Terry Tsang, who are associates of the Visual Snow Initiative that was founded to provide resources and hope to sufferers, told optometrists that while it is not a cure for the syndrome, it is the first physical treatment that has dramatically reduced the symptoms for all those involved in the research, results which have lasted for more than a year.
CALLS FOR OPTIMAL SCOPE ON WORLD OPTOMETRY DAY

Optometry Australia (OA) has harnessed the theme of World Optometry Day to urgently push for regulatory changes allowing optometrists to work to their full scope-of-practice, and highlight areas such as oral medications prescribing.
World Optometry Day is celebrated every year on 23 March to create awareness on the importance of eyecare, and to recognise the important contribution of optometrists in maintaining community eye health.
The World Council of Optometry’s (WCO) theme for 2023 is: ‘Expanding optometry’s role… the time is now!’. As part of this, WCO is seeking to “advocate for stronger global access to eyecare and ensure that optometrists around the world have the education and skills to thrive and contribute within their respective healthcare systems”.
In response to the annual awareness day’s 2023 theme, OA said that by making full use of Australia’s highly skilled optometry workforce, Australia can significantly enhance patient access to care and increase the efficiency of the eye health system.
OA president and Sydney optometrist Dr Margaret Lam said in Australia there are more than 6,000 registered and highly skilled optometrists who are well-distributed throughout metropolitan, regional and rural centres.
“However, we are not making optimal use of the full breadth of their skills,” she said.
“Optometry is a vital component of the healthcare system. Optometrists perform around 10 million eye checks annually and are appropriately the first point of contact for 80% of people with eye concerns. They diagnose, treat, manage and triage patients with eye disease, while bridging the gap in situations where timely care is not readily accessible.”
In order to reduce the burden of eye disease and its impact, Lam said there is a need for policy changes that will ensure optometrists’ skillsets are being maximised for the benefit of the community.
“For example, while Australian optometrists are unable to prescribe oral medications, their counterparts in developed countries, such as the UK, New Zealand and United States, have been doing so safely for many years. This supports a smoother patient journey and more timely access to needed treatment, particularly in the many regions of Australia
with limited access to GP or specialist care,” she said.
“We also need to ensure that we are utilising optometrists in eyecare pathways in the most effective way. This can be as simple as ensuring patients who can be treated by an optometrist in the community are referred to optometry rather than to the tertiary care system where costs are typically higher and wait times typically longer.”
According to OA, 90% of blindness and vision impairment is preventable or treatable with early detection, highlighting the important role of optometrists in maintaining community eye health.
More than 13 million Australians are reported to have one or more long-term eye conditions – with many undiagnosed cases – and nearly 85% of Australians with vision impairment are aged 50 or over.

‘‘We have an ageing population and a strained tertiary eyecare system. This is a recipe for poor outcomes, unless we act now to ensure we are utilising the skilled workforce we have, as well as we possibly can,” Lam said.
MORE OPTOMETRISTS NOT THE ANSWER
WCO president Professor Peter Hendicott, who is Australian, said optometry must recognise that solutions to the issues facing eyecare will not necessarily be attained by simply training more practitioners.
“We need to work smarter and more effectively. This will require us to develop future alternative models of the provision of eyecare by optometrists, aimed at improving equity, access, efficiency and outcomes,” he said.
“As a profession, we need to consider the inclusion of eyecare delivery by other practitioners, how they may work together with optometry, and how optometry can take a leading role in partnerships to develop models of delivery, training, leadership, and management of eyecare teams. We need also to consider the impact of current and future technology on the delivery of eyecare, and how these tools can be utilised by optometry, working with other eyecare professionals, to improve equity, access, and outcomes.”
Hendicott said the industry needed consider how the skills and competencies of optometry can be more widely used with health care systems.



COOPERVISION FURTHER EXPANDS PARAMETERS FOR MYDAY TORIC CONTACT LENSES
CooperVision has announced its latest parameter expansion for MyDay toric, increasing its current range by nearly 70% to 4,392 prescription options.
With the additional options, MyDay toric now matches the range of Biofinity toric to enable optometrists to fit the vast majority of their astigmatic patients with a silicone hydrogel 1-day lens.

The full range is now available across Australia and New Zealand, as of 20 March.
CooperVision professional services manager Mr Joe Tanner said the expanded range resolves previous limitations.
“We appreciate that optometrists want to be able to prescribe the best lens for each patient and not be limited by restrictions in the available parameters. For years, Biofinity toric
has set the standard for toric contact lenses, and optometrists have found tremendous utility from its comprehensive parameter range,” he said.
“This same range is now available with MyDay toric, ending the need for practitioners to prescribe a monthly lens when a daily disposable may be preferred."
CooperVision said its MyDay toric lenses combine the proven design features of Biofinity toric with the premium silicone hydrogel 1-day material of MyDay.
“Our outstanding toric technology, Optimised Toric Lens Geometry, provides uniform horizontal iso-thickness, a large toric optic zone, a smooth, continuous ballast and an optimised ballast toric design for a predictable, stable and
MYDAY TORIC WILL BE AVAILABLE IN THE FOLLOWING PRESCRIPTION OPTIONS:
(DS) Cylinders (DC) Axes
CONTAMINATED DROPS LINKED TO DEATHS
Three people have died, and a dozen people have experienced vision loss, including surgical removal of their eyes, due to a rare strain of highly drug-resistant bacteria that US authorities allege originated in a brand of artificial tears manufactured in India.
The latest update comes after the US Food and Drug Administration (FDA) issued an urgent product recall on 2 February 2023 for Global Pharma Healthcare and its artificial tears lubricant eye drops, distributed to US consumers as EzriCare Artificial Tears and Delsam Pharma Artificial Tears, due to possible contamination.
At the time of the recall, the outbreak
of carbapenem-resistant Pseudomonas aeruginosa – a rare strain of extensively drug-resistant bacteria that had never been found in the US previously – had affected 55 patients in 12 states. But as of 14 March, this was expanded to 68 patients in 16 states.
“Thirty-seven patients were linked to four healthcare facility clusters. Three people have died and there have been eight reports of vision loss and four reports of enucleation (surgical removal of eyeball),” the US Centers for Disease Control (CDC) said.
“Most patients reported using artificial tears. Patients reported over 10 different brands of artificial tears and some

comfortable fit,” the company said.
“In addition, the MyDay family of lenses features Aquaform Technology, which provides a unique combination of high oxygen permeability, a naturally wettable material, and optimum modulus for increased breathability and moisture in a soft, flexible lens.”

The material and design also provide for easy lens handling and there is a UV inhibitor which filters 86% of UVA and 97% of UVB rays, according to CooperVision.
To help streamline the fitting process and minimise chair time, CooperVision also offers the OptiExpert fitting app. The easy-to-use app includes a calculator which determines the recommended diagnostic lenses. A desktop version is also available.
AND ENUCLEATION
patients used multiple brands. EzriCare Artificial Tears, a preservative-free, over-the-counter product packaged in multidose bottles, was the brand most commonly reported.”
The CDC continued: “This was the only common artificial tears product identified across the four healthcare facility clusters.
Laboratory testing by CDC identified the presence of VIM-GES-CRPA (the bacterial strain) in opened EzriCare bottles from multiple lots; these bottles were collected from patients with and without eye infections and from two states. VIM-GES-CRPA recovered from opened products match the outbreak strain. Testing of unopened bottles of EzriCare Artificial Tears is ongoing."

RAYNER LAUNCHES RAYONE EMV TORIC IN AUSTRALIA

Rayner, the pioneering manufacturer and supplier of ophthalmic solutions for cataract and refractive surgery, has announced the launch of RayOne EMV Toric in Australia.
RayOne EMV Toric is the toric variant of Rayner’s popular RayOne EMV IOL that was developed in collaboration with world renowned Australian surgeon Professor Graham Barrett.
According to the company, its RayOne EMV platform features a truly non-diffractive optic that provides patients with up to 1.5 D1,4,6 of high-quality vision when used with an emmetropic target. Following excellent surgeon feedback for RayOne EMV’s monofocal levels of contrast sensitivity1, dysphotopsia2,5, and high levels of patient satisfaction3, RayOne EMV Toric has been designed to allow surgeons to correct from 0.5 D of corneal astigmatism with a wide selection of IOL plane cylinders.


Queenaland’s first commercial implanter of the RayOne EMV Toric IOL was Dr Graham Hay-Smith from Moreton Eye Group in Brisbane.
Commenting on the implantation of RayOne EMV Toric, he said: “I was impressed with the excellent patient outcomes I have had with RayOne EMV backed up with audit data.”
An audit of Hay-Smith’s initial RayOne EMV patient results showed:

• Excellent distance vision with no measurable compromise versus a standard monofocal.


• Useful near/intermediate vision for most patients with emmetropic targeting.
• Mini myopic group (mean target -0.49 D) maintain good UDVA: 0.1 LogMAR or better in 89% of patients.
• Mini-monovision group (0.75 D myopia) displayed an excellent range of vision: UDVA 0 LogMAR/better than N6 reading.


• Modest-monovision (i.e., 1.0 to 1.5 D of myopia) maintain UDVA and can give even better (and closer) near vision.

























Hay-Smith described the EMV as a forgiving lens that appears to provide excellent physiological vision with a significant improvement in intermediate
Experience The Difference
Meeting
and near vision, compared to standard IOLs. Overall, he has noted how happy patients are with the lens and been surprised by how much intermediate and near functional vision he is observing.
“These fantastic patient outcomes –coupled with my long-term confidence in rotational stability with the RayOne toric platform – made it an easy decision to implant the RayOne EMV Toric. I look forward to being able to provide the increased range and excellent quality of vision I’ve achieved with RayOne EMV to my astigmatic patients,’’ he said.
RayOne EMV Toric is available to order in Australia and has Prosthesis List Reimbursement from 1 March 2023.












REFERENCES
1. Ferreira TB. Comparison of visual outcomes of a monofocal, two enhanced monofocals and two extended depth of focus intraocular lenses. Presented at ESCRS 2022.
2. R ayOne EMV: First Clinical Results, Rayner. Oct 2020.

3. R ayner RayPRO, data on file.


















4. R ayner, data on file.
5. R ayner Peer2Peer webinar. May 2022.




6. R oyo, M. RayOne EMV and TECNIS Eyhance: A Comparative Clinical Defocus Curve. Data on file. 2021.







STUDY SHOWS REPEATED LOW-LEVEL RED LIGHT THERAPY SHORTENS AXIAL LENGTH

Three Australian institutions have been part of a study evaluating clinically significant axial length shortening among myopic children following repeated low-level red light therapy.
More than a quarter of children had axial length shortening greater than 0.05 mm following repeated low-level red light (RLRL) therapy, and the overall mean axial length change was -0.142 mm per year.
Researchers in the retrospective multicentre analysis involving the Centre for Eye Research Australia, Royal Victorian Eye and Ear Hospital, and University of Melbourne reviewed clinical data collected for myopic children aged 3-17 years who received RLRL therapy delivered by home-use desktop light device that emitted light at 650 nm for at least one year.
The clinical data included axial length, spherical equivalent refraction, and visual acuity measured at baseline and follow-up.
According to the abstract published in Ophthalmology and therapy, the primary outcomes were frequency of axial length shortening of greater than 0.05 mm, 0.10 mm, and 0.20 mm per year, and associated factors of axial length shortening per year.
A total of 434 myopic children with at least 12 months of follow-up data were included in the study.

The mean age of participants was 9.7 (2.6) years with spherical equivalent refraction of -3.74 (2.60) diopters.
There were 115 (26.50%), 76 (17.51%), and 20 (4.61%) children with axial length shortening based on cut-offs of 0.05 mm, 0.10 mm, and 0.20 mm per year, respectively.
In the multivariable model, axial length shortening was significantly associated with older baseline age, female gender, and longer baseline axial length or greater spherical equivalent refraction.
Among axial length shortened eyes, the mean axial length difference (standard deviation) was -0.142 (0.094) mm per year. Greater axial length shortening was observed among children who were younger and had longer baseline axial length.
GLAUCOMA COLLABORATION CELEBRATES 200TH CLINIC
The Glaucoma Collaborative Care (GCC) clinic, delivered by The Royal Victorian Eye and Ear Hospital (Eye and Ear) and the Australian College of Optometry (ACO), has celebrated its 200th clinic during World Glaucoma Week.
Originally serving as a pilot project between 2016-2017, the clinic was initiated by the Eye and Ear in response to rising glaucoma levels and aims to alleviate pressure on in-demand public health ophthalmologists and ensure appropriate care for patients.
The clinic provides diagnostic and ophthalmic review for low risk and glaucoma suspect patients from the Eye and Ear. The program has been developed for patient-centred, cost effective care. Its primary focus is on facilitating community-based follow-up when appropriate, while improving access to specialist hospital-based care for patients with diagnosed glaucoma who are at higher risk of disease progression.
Running fortnightly from the ACO’s Carlton clinic, the GCC clinic is said to be an example of how a team-based approach involving ophthalmologists, optometrists and orthoptists is integral to supporting positive eyecare outcomes.
Dr Catherine Green, head of the glaucoma clinic at the Eye and Ear, has advocated for the collaborative clinic since the start and believes its progressive
approach to care has made a difference to glaucoma patients.
“This shared care management of glaucoma patients has resulted in a more streamlined approach in the diagnosis and treatment of suitable patients,” she said.
The increasing prevalence of glaucoma is said to pose a major threat to the health and well-being of the community, as well as pressure on the public health service. Glaucoma Australia estimates 50% of the more than 300,000 Australians projected to have the condition are unaware they have it, risking significant vision loss.
Ms Janelle Scully, the ACO’s Ocular Disease Services lead optometrist, said the demand for public glaucoma services has been steadily rising due to Australia’s ageing population and increasing cost of living pressures.

“The collaborative clinic is uniquely positioned to offer patients access to suitable care while also easing the demand on Eye and Ear’s ophthalmology services. ACO Carlton is well-resourced to host the clinic and participate in the collaborative model of care which is so successfully demonstrated by this program,” she said.
During the past 20 years, the Eye and Ear has reported a 29% increase in surgical patients with glaucoma and estimates that across Australia glaucoma will increase to 379,000 in 2025 due in part to the identified aging population nationally.
IVERIC BIO REVEALS VISION LOSS REDUCTION DATA IN GA THERAPY
US biopharmaceutical company Iveric Bio has released new data for its avacincaptad pegol (ACP) therapy for geographic atrophy (GA), which showed up to a 59% risk reduction in rate of vision loss compared to sham treatment at 12 months.
In March, the company announced an exploratory time-to-event analysis from its GATHER clinical trial program evaluating reduction in vision loss with ACP 2 mg versus sham treatment.
GATHER1 and GATHER2 – both of which are randomised, double-masked, sham-controlled, multicentre Phase 3 clinical trials – were designed to evaluate the rate of lesion growth in patients with GA secondary to age-related macular degeneration.
ACP is an investigational drug currently under evaluation for safety and efficacy by the US FDA, which recently approved the country’s first GA therapy, SYFOVRE (pegcetacoplan injection), in February 2023.
ACP works as a complement C5 protein inhibitor, and is based on the theory that overactivity of the complement system and the C5 protein plays a critical role in the development and growth of scarring and vision loss associated with GA secondary to AMD.
By targeting C5, ACP has the potential to decrease activity of the complement system that causes the degeneration of retinal cells and potentially slow the progression of GA.
JILLIAN CAMPBELL TAKES REINS AT RICHARD LINDSAY & ASSOCIATES
Optometrist and business associate
Ms Jillian Campbell, 31, has taken over sole ownership of Richard Lindsay & Associates in Melbourne as the practice celebrates 25 years in business.
Campbell graduated from QUT in 2013 with a masters degree before moving to Victoria to join the Australian College of Optometry, which allowed her to focus on her areas of interest, particularly specialty contact lens fitting and ocular pathology.
She joined Richard Lindsay & Associates, part of the ProVision network, in 2015.
“It has always been my dream to own a practice. The transition from Richard to myself has eventuated naturally as I have been taking on more responsibility in the last seven years,” Campbell said.
“This is the kind of practice I’ve always wanted to own – full-scope, independent, and specialising in contact lenses.”
After being based in East Melbourne, opposite the Royal Victorian Eye and Ear Hospital, for 23 years, the practice had to relocate in October last year as the building it occupied was being demolished to make way for new apartments.
Campbell was directly involved in the process of finding a new location, and designing the new practice fit-out.

“We moved to Balwyn North, adjacent to the freeway exit, with plenty of onsite parking. Richard owns the building, so he is my landlord, and now my employee,” she said.
Campbell said Lindsay, who established Richard Lindsay & Associates in 1998, will continue working in the practice, which now employs four optometrists, and will continue to mentor her.

“Both Richard and Carly [practice manager], and ProVision, have been supportive with the transition. Phillip Fent, from Optometrist Business Brokers, and Craig Spiegel from Credabl, have also helped me broker the business transaction,” Campbell said.
Campbell has completed two postgraduate specialist certificates through The University of Melbourne and now works as a lecturer and clinical supervisor there. She has volunteered overseas in Vanuatu and India and previously worked with the Brien Holden Vision Institute.
AUSTRALIA SHINES IN ESSILORLUXOTTICA APAC BUSINESS IN 2022
OPSM and a record year for Sunglass Hut in Australia were standouts within EssilorLuxottica’s Asia-Pacific business in 2022, hich posted “comparable” revenue of €2.8 billion (AU$4.5 b) against the region’s 2021 performance.
Australia’s strong financial performance comes as the group announced a major renewable energy supply agreement as part of its plan to become carbon neutral in its direct operations by 2025.
In late February, EssilorLuxottica published its full 2022 financial results, with CEO Mr Francesco Milleri announcing record sales of €24.5 billion (AU$39.4 b), with a net profit of €2.2 billion (AU$3.5 b).
Asia-Pacific – EssilorLuxottica’s third biggest region after North America and EMEA – generated 7.2% more revenue in 2022 compared to 2021 at constant exchange rates (+11.8% at current exchange rates).
“The Direct to Consumer division grew mid-single digit at constant exchange rates driven by Australia, with a solid performance in OPSM and a record year for Sunglass Hut growing comparable-store sales by more than one third,” the company stated.
“Asia-Pacific posted comparable revenue … with Mainland China diluting the otherwise excellent performance of the region. Professional Solutions (wholesale
customers) was up high-single digit at constant exchange rates.
“All countries recorded strong growth except Mainland China, where the performance was strongly influenced by the COVID-19 circumstances present at different times during the year. However, despite the volatile environment, the demand for myopia management solutions in the country did not fade and Stellest recorded exponential growth more than doubling sales from the prior year.”
Milleri said in addition to record revenue, the company announced ground breaking product launches and delivered on its “promise of a strong, unified company in 2022”.
Meanwhile, EssilorLuxottica and ERG, a leading European producer of energy from renewable sources through its subsidiary ERG Power Generation, have signed a 12-year Power Purchase Agreement (PPA) for the supply of approximately 900 GWh of green energy between 2023-2034.
The agreement is based on the sale by ERG of approximately 75% of the energy produced by its Partinico-Monreale wind farm near Palermo, Italy.
For EssilorLuxottica, it marks an important step towards becoming carbon neutral in its direct operations (Scope 1 and 2 emissions) by 2025, starting with Europe by the end of the year.
KERING EYEWEAR ACQUIRES FRENCH MANUFACTURING FIRM
Kering Eyewear has signed an agreement to acquire 100% of the share capital of the French company UNT, Usinage & Nouvelles Technologies, to strengthen its position in the luxury eyewear industry.

Founded in 1989 in Eastern France, UNT is a described as a key player in the manufacturing of high-precision metal and mechanical components for the luxury eyewear sector.
Kering Eyewear, founded in 2014, itself is a major global player in the luxury segment. It is a division of the Kering Group and is responsible for 17 eyewear brands, including LINDBERG, Maui Jim, ZEAL Optics, as well as the houses brands Gucci, Cartier, Saint Laurent,

Bottega Veneta, Balenciaga and more. Many Kering brands are supplied in Australia through Sunshades Eyewear.
According to a statement, in addition to the acquisition of Manufacture Kering Eyewear in 2017 and the stake held in Trenti Industria Occhiali since 2019, the transaction represents another step in the industrial development strategy of Kering Eyewear.
UNT has been a longstanding business partner of Manufacture Kering Eyewear for the provision of its components. The transaction is subject to the clearance by the relevant competition authorities and is expected to be completed in the second quarter of 2023.
New
light adaptive lenses
Fades back to a fully clear lens indoors1 & reaches the half clear state in seconds2
Sensity Fast lenses are the fastest light adaptive lenses available*. They’re ideal for patients with busy lifestyles who move indoors and outdoors frequently.

— Convenient 2 in 1 solution: Sensity Fast lenses darken to a sunglass lens tint outdoors and fade back to fully clear prescription lenses indoors1
— Comfortable when using digital devices3: Modular Blue Light Control helps to control both outdoor and indoor blue light3
—
Provide 100% protection: against UV rays4
Available in 2 attractive colour options6: Grey and Brown
Ask your HOYA Sales Consultant about new Sensity Fast lenses.
For Sensity Fast performance details visit http://bit.ly/3HYtmeh.
recruiting and retaining staff CULTURAL FIT:

Attracting and screening suitable candidates is only one part of the employment process for eyecare practice owners. ProVision details how it is helping independents find the right fit for their business, and keep employees engaged in their roles.
When independent optometry practice manager and co-owner Mrs Lisa Summers needed to employ two new optical dispensers simultaneously, it created uncertainty and placed pressure on an already busy business. It’s a tale all too familiar to independents in a hot job market, so she didn’t hesitate to call Ms Samantha McEvoy, ProVision’s new dedicated recruitment specialist.
“We had employed an optical dispenser trainee last year under the Federal Government trainee subsidy program, but they decided it wasn’t for them, and a second optical dispenser wasn’t working out,” Summers, herself a qualified optical dispenser, says.
McEvoy advertised the two optical dispenser positions on offer at Insight Vision Care, the practice Summers co-owns with her brother and optometrist Mr Daniel Farrugia, in Werribee, screened applicants and provided them with a shortlist of suitable candidates.

Within a few short weeks of the positions being advertised, both roles were filled.
“Samantha’s involvement was a significant time-saver, especially given we’re short staffed. It can be difficult to find time to sort through applicants, and can be exasperating when some are not relevant,” Summers says.
Summers is at the coal face of an ongoing challenge facing the independent optometry scene. They’re balancing on a sharp ledge of managing people, and a business. Thankfully, her practice is part of the ProVision independent optometry network with around 450 practices. The organisation has acknowledged recruitment is a major challenge for its members, so has responded by employing in-house experts to support practices, providing relevant resources and flipping the script on the traditional hiring process.
Practice manager Mrs Naomi Arnold at Somerville & Merrin Optometrists in Toowoomba shared a similar experience earlier in the year. The practice was seeking a new casual staff member after its other casual employee left, leaving the business short.
“We spoke with ProVision about what we require in the role, and what we require in terms of our values,” she explains.
“I thought it was handled really well on their end. They did the initial phone interviews and provided me with a report that included the questions they asked, responses they got, and their overall view of the applicant, giving them a rating to indicate how well they thought they might fit in with us. Using this information, we then decided who we would interview face-to-face.”
HOW TO HIRE IN 2023
When hairdresser-turned-motivational speaker Ms Julie Cross spoke about resilience at ProVision’s national conference in 2022, it resonated with
members who share the common challenge of staffing their practices.
“I think we could all relate,” ProVision’s people and culture manager Ms Leanne Jackson, who was in the audience, says.
“We are all juggling a million things, and we’re all feeling pressures, be it financial, personal, or work/life balance. Julie talked about leveraging opportunity to face our challenges, and we all took away some practical insights.”
ProVision is not shying away from helping members face this challenge. It is boosting its optometry recruitment efforts on their behalf, after more than half (57%) identified staff recruitment and retention as their top challenge in a recent membership survey.
Jackson says finding the right person for a role, but more crucially, for a practice, is the number one industry challenge for independents. To assist, ProVision has partnered with Australian Retailers Association (ARA), and welcomed two new referral partners, Locumly and Eyecare Recruitment, to the network.
“We now have a dedicated recruitment specialist [Samantha McEvoy], which is a new resource for members introduced in November last year,” Jackson says. “We’ve always had an in-house recruitment service for our members, but we’ve never had a dedicated resource solely focused on this support. It’s a necessary process because it’s a very competitive space in a candidate-short market. I don’t think that has changed greatly in the last four months.”
Members in regional areas face an additional challenge: a shortage of candidates.
“Generally speaking, there aren’t as many candidates and everyone knows everyone in a regional area, making it more of a challenge. Cultural fit is also arguably more important in a small team,” Jackson says.
“If a small practice in a regional location advertises a position, and a local resident applies and doesn’t get a response, that can affect the brand and the future relationship with that practice. It’s vital to make sure we keep the candidate informed throughout the process of their application, and we’re very proactive with that.”
ProVision is also taking a fresh approach to the content and placement of job advertisements, regardless of whether it's for skilled or unskilled roles.
“We create a tailored job ad that is responsive to the market needs. Candidates are looking at what’s in it for them, as far as what is on offer from a prospective employer. They’re interested in knowing; What are the benefits of the role? What are the values the employer offers and aligns their employment offering to? And what does the job involve?” Jackson says.
“This approach switches the order of a traditional job posting from an employer’s perspective of ‘this is all about us’, then ‘this is the job’ and then ‘this is what we are looking for’. It’s about attraction. We’ve done a lot of work recently to attract a greater pool of candidates, and we’ve certainly seen an uptake on that.”
Placement of job ads also has a bearing. In November 2022, ProVision was advertising a lot more retail, entry-level roles, and the highest percentage of applicants were coming from job-search engines Indeed and Jora.
“Now we’ve got a 60/40 split of skilled to unskilled entry-level roles. We’re now recruiting for optometrists and optical dispensers that may have some experience and qualifications, so we’re seeing more of an uptake from candidates through Seek, LinkedIn, and other avenues,” Jackson says.
“We’ve tried to expand our candidate reach and support our members through a rigorous screening process – candidates get a star rating
room to improve our processes to help our members achieve greater placement success,” she says. “For the month of February this year, for example, we’ve helped to fill 10 roles which means that the referrals are the right fit for the practice and we’re partnering with our members to guide them through the employment process, end-to-end.”
HR SUPPORT AND EXPERTISE
Through the ARA, ProVision members have access to general employment law and HR advice, which goes hand-in-glove with RecruitPro, ProVision’s in-house program launched in 2021 to help members through the


“ProVision directly supports members through the screening and interviewing phase, and through our business coaches, and the ARA can assist with policy procedure, how to create a current employment contract, advice on how to handle difficult conversations, performance management, all the resources an employer needs during an employee’s
When a practice hires a new staff member, they are introduced to ProVision’s education platform, ProLearn, where they go through an onboarding program, and can access additional educational resources at their own pace and within their working hours.
“The platform is tailored to the role, so a retail assistant has different modules as opposed to an optometrist, for example. We also have an education calendar, which offers a plethora of education topics that range from entry level up to key training for leaders within optometry practices,”

“We’re also offering resilience training, which we’ve developed on the back of a resilience session presented by Julie Cross at our national conference last year which was one of the most highly valued sessions. Our ‘Reconnecting with Resilience’ program will take place in July this year.”
Jackson says there is something every month for everyone to access that complements the ProLearn platform. This helps with retention because people are learning, and they’re engaged.
As part of the company’s continuous improvement strategy, Jackson and her team are currently working on an internal initiative called ‘Wellness at
“Our goal is to roll it out to our members if it’s something they want to access or utilise within their own team,” she says.
“WE CREATE A TAILORED JOB AD THAT IS RESPONSIVE TO THE MARKET NEEDS. CANDIDATES ARE LOOKING AT WHAT’S IN IT FOR THEM, AS FAR AS WHAT IS ON OFFER FROM A PROSPECTIVE EMPLOYER.”
LEANNE JACKSON PROVISIONSomerville & Merrin Optometrists employs a large team across two practice locations in Toowoomba.
Myopia lens
TARGETS HORIZONAL MERIDIAN
Rodenstock
The physiology involved in myopia progression is fascinating when you consider it. In essence, when corrected with single vision lenses, light is focused accurately on the central retina, but by default light then focuses behind the retina in the periphery. For some children, the body wrestles to bring those peripheral rays into focus. It’s adapting with good intentions, but in reality causes a spiralling feedback loop that causes the eye to elongate, compromising its fragile structures.
Myopia is projected to affect every second person within 27 years. It’s a major problem, but not insurmountable. That’s because ophthalmic lens companies are developing specially designed lenses adopting the concept of “peripheral defocus” to arrest eye elongation. This non-invasive approach cleverly refracts light in the periphery so that it hits in front of the retina while ensuring sharp central vision.
In April 2023, Rodenstock became one of the latest companies to launch a myopia control spectacle lens. There are various lens designs available for myopia control. Some companies rely, for example, on concentric rings focusing on all quadrants of the peripheral retina – superior and inferior, as well as temporal and nasal. Rodenstock is tackling this by use of another design approach.
The company’s lens – named MyCon – is a peripheral defocus lens but differs due to its horizontally asymmetrical design. It has a central vision zone, which provides stable refraction around the optical centre, while the outer areas create a peripheral progression along the horizontal meridian –temporal and nasal.
The lens has three distinct zones:
• A central zone, where the optical power corresponds to the wearer’s nominal refraction.
• A temporal zone of progressively increasing power up to 2.5 D.
• A n asal zone of progressively increasing power up to 2.0 D.
It’s a unique design, but Rodenstock Australia national sales and professional services manager Ms Nicola Peaper says several studies have demonstrated asymmetry of the peripheral retinal refraction in myopia, influencing the patented design (German patent DE 10 2009 053 467 B4) of the MyCon lens.
A highly regarded study was conducted by Dr Anne Seidemann, part of Rodenstock’s R&D team, with Professor Frank Schaeffel, a renowned myopia researcher at Germany’s University of Tübingen. In 2002 they demonstrated peripheral refraction and assumed that peripheral eye length varies in different parts of the retina.
“Rodenstock looks to be new to myopia control, but we’ve been instrumental in a lot of myopia research in Europe for over 20 years, which is one of those little-known things,” Peaper says.
Another study, by Faria-Ribeiro et al in 2013, showed differences of asymmetries in peripheral refraction and eye shape for different refractive groups and progressive and non-progressive myopes.
“Looking at progressing myopes in that study, we can see their retina is significantly different compared to non-progressing myopes, but within the non-progressing group it’s also different nasally to temporally; you’ve got more hyperopia nasally in the progressing than the non-progressing group,” Peaper says.
“Another interesting finding from studies is that the nasal retina has more ganglion cells and more cones responsible for fine vision, implying a neuro-functional dominance of the nasal retina (Curcio et al., 1990; Curcio & Allen, 1990). There’s a school of thought that if you have a greater density of ganglion cells and cones, then you’re getting maybe more signals for eye growth in that area. At Rodenstock, we’re saying it’s important to look at the horizonal meridian at the retina in progressing myopia. Therefore, we are concentrating our efforts nasally and temporally.”
CLINICAL EFFECTIVENESS
While there isn’t a direct study of the MyCon lens, Rodenstock cites an independent clinical study by Tarutta et al conducted over five years (2012-2018) on a lens based in similar principles in children.

has launched a myopia control spectacle lens, adopting an asymmetrical defocus design covering the nasal and temporal zones.
The study monitored myopia progression of a group of 146 Caucasian boys and girls, with myopia varying between -1.00 and -6.00 D. Participants were divided into two groups with the same average age of 10.5 years.

The first experimental group consisted of 94 participants (aged 7-14 years) who used lenses based on the principles of MyCon lenses, while the second control group consisted of 52 participants (aged 8-14 years) who used normal single vision lenses.
The study was conducted by the Helmholtz National Medical Research Centre for Eye Diseases of the Russian Ministry of Health, with myopia progression (mean power and axial length) assessed after six months, 12-18 months, two years, three years, and four to five years from the start of lens wear.
“And the results show that the control group became 40% (spherical equivalent [D]) more myopic over five years,” Peaper says.
“In terms of axial length, eye elongation in the treatment group was reduced by up to 56% after two years and 35% after four to five years when compared to the control group.”
WHY IS TREATMENT IMPORTANT NOW?
Since announcing that Rodenstock will be offering a myopia control lens, Peaper has been overwhelmed, yet unsurprised, at the huge interest among Australian practitioners. After all, myopia control lens market penetration will likely pale in comparison to other products like progressive lenses.
But it ultimately comes down to the fact that optometrists now realise that single vision lenses are no longer an adequate response to progressing myopia.
While a standard minus single vision lens creates a divergence of light, forming a sharp image on the centre of the retina, it also projects light that is coming from the periphery behind the peripheral retina, which may trigger some children’s eyes to adapt and become excessively long, which increases myopia.
“If you are correcting using a spherical single vision lens, you are highly likely to induce very rapid eye growth, so we require a lens that focuses in the periphery in front of the retina. With Rodenstock’s MyCon lenses, it’s like thinking of a multifocal that starts with your distance script in the centre and then has progressive plus power horizontally to the outer edge. The nice thing is you still have your distance script vertically, so there’s a chance it’ll perhaps be easier to tolerate.”
It’s well documented myopia is one of the world’s biggest public health problems. This is because it’s predicated 50% of the world’s population will suffer from myopia by 2050, a staggering projection revealed by the Sydney-based Brien Holden Vision Institute in 2016.
Approximately 20% of children in Spain or Irish teenagers are affected,
reaching much higher prevalence of about 50% in Chinese urban teenagers to almost 90% in older Chinese urban teens. From 2006 to 2011, the myopia prevalence in Australia rose from 11.5% to 18.9%. Today, the rate for Australia and New Zealand is estimated to be 36%, with the forecast rate by 2050 an estimated 55%.
In myopia, there are aetiology, genetic, behavioural, gender and environmental factors at play. For example, it’s well documented that the Asian population is at greater risk, while a child with two myopic parents has a 35 to 60% risk of also being myopic. However, this risk is reduced (25-40%) when only one of the parents is myopic. Females are also at greater risk.
“What’s worrying is that if you take all of these elements into account, there shouldn’t be the rise in myopia that we’re seeing,” Peaper adds.
However, there are steps that families can take to protect their children, such as reducing near work activities and increasing outdoor time. Wildsoet et al in 2019 concluded at least 80 to 120 minutes outdoors had preventive effects against myopia development, with Sherwin et al in 2012 showing every additional one hour of outdoor time per week linked with a reduction in the risk of myopia by 2%.
In light of this evidence, Peaper says there’s a need to educate parents about the impact of near work activities and outdoor time, as well as interventions available that slow progression.
“When we’re talking about controlling myopia, one of the major things we should care about is the magical number of -5.00 D, the threshold of high myopia,” she says, noting while around 900 million people will suffer from high myopia in future.

“Once you hit that, you’re 20 times more likely to get a retinal detachment –and once you reach -7.00 D, you’re about 120 times more likely to get myopic maculopathy. In other words, in the worst case you can lose your central visual acuity and become blind. If we can prevent people from progressing beyond -5.00 D, then ethically, we have to try and do something.”
Furthermore, Australia is expected to have 4.1 million high myopes by 2050, unless myopia management is implemented universally. These forecasts highlight the scale of the problem that is facing eyecare professionals given Australia in 2020 had an estimated 1.1 million, and New Zealand over 200,000, high myopes.

DISPENSING THE LENS
Rodenstock MyCon lenses are available in index 1.5, 1.6, 1.67, and 1.74, which make the lenses both thinner and sleeker than many other myopia lenses on the market and well suited to high prescriptions.
Peaper says this is possible because the company grinds the lens on the back surface, rather than using moulds on the front surface. This also helps children who are potentially hesitant about wearing glasses because they are unhappy with the look.
According to Rodenstock, MyCon lenses are also well-suited for high prescriptions while also offering shock-resistance and high image quality. Practitioners can also choose the lens material to recommend to customers, with a wide range of available lens coatings available.
The adaption period is generally short, in a few cases up to two weeks.
“IF YOU ARE CORRECTING USING A SPHERICAL SINGLE VISION LENS, YOU ARE HIGHLY LIKELY TO INDUCE VERY RAPID EYE GROWTH.”
NICOLA PEAPER RODENSTOCK AUSTRALIA
‘WE CAN’T STAND BACK AND WATCH PATIENTS EXPERIENCE PREVENTABLE VISION LOSS’
One of the country’s largest optometry networks has teamed up with Macular Disease Foundation Australia in an Australian-first, supporting nAMD suspects to attend their first ophthalmology appointment and help with treatment adherence. With the pilot phase deemed a success, what’s next for the project?

For the past two years, Specsavers has worked with Macular Disease Foundation Australia (MDFA) to better understand and classify its patients with neovascular age-related macular degeneration (nAMD) through a pilot project involving 16 practices spread across Australia.



During the pilot project, the patients referred joined an intensive support journey, which included regular phone calls, emails, text messages and letters from MDFA’s patient education team.
Following the conclusion of the project, a number of key learnings emerged, including improved classifications of AMD, discussing diagnosis and support with patients, as well as observing the value patients felt when optometry and patient support services work together.
Specsavers optometry director Dr Ben Ashby was not surprised by the latter finding, having seen the value of Specsavers working together with several leading patient support groups across Australia for many years.
“Increasingly patients expect to be advised by their optometrist if they should engage with a patient support service such as MDFA,” he says.
“Often a diagnosis, or even a call to watch and monitor a condition, can leave a patient still processing the information, with questions coming to them after they’ve left the test room. That’s where the value of specialist support services come in, especially between appointments, where trained specialists can provide an extension of care to patients."
With a condition such as age-related macular degeneration, where symptoms can occur incredibly sudden and early intervention is crucial to saving sight, Ashby says it can be a lot for a patient to digest.
“Often many patients haven’t even heard of the condition before talking with their optometrist. Which is why it was so valuable through our partnership with MDFA, these patients had a specially trained educator contact them and so were able to have their questions answered and any issues or concerns raised,” he says.
“COLLABORATION WITH PATIENT SUPPORT BODIES IS ESSENTIAL FOR ANY HEALTH PROVIDER THAT WANTS TO BE AUTHENTICALLY PATIENT-CENTRED.”
DR BEN ASHBY SPECSAVERS ANZ
“This made them feel a lot more comfortable and led to them being more likely to continue with treatment or attend appointments they were feeling nervous about.”
Ashby continues: “Collaboration with patient support bodies is essential for any health provider that wants to be authentically patient-centred, because as we have learnt, between optometrists, ophthalmologists and other involved health professionals, patients often feel that they don’t know who is managing them. We’re all part of the eye health team, so we all need to work together for our patients. In the case of our pilot, having MDFA as the central and autonomous contact really helped patients understand they had a central port of call who could assist with anything they may be facing.”
MDFA CEO Dr Kathy Chapman agrees that the findings of the pilot showed the value of non-clinical support.

“Over the past two years we’ve invested in research to hear directly from people with macular disease, the people who care for them, and the people who treat them. Coupled with the experiences of our pilot with Specsavers, we are using this information to develop the very first patient support program for all people living with macular disease –based on their own needs and experiences,” she says.
“With partnerships like this one, patients know they are getting the very best of care whether they are in the clinic or at home.
“We know optometrists and ophthalmologists provide the highest quality of clinical care for patients; MDFA aims to be there for the rest, providing evidence-based support for how to live well with macular disease. Our focus will be on three pillars of support – social, emotional and practical – tailored to a person’s own situation. This partnership provides a 360-degree approach to patient care, striving to achieve the best health outcomes for our patients.”

NEXT STEPS
DR KATHY CHAPMAN MDFAFollowing on from the nAMD pilot project, Specsavers and MDFA are committed to continuing their partnership and focus on collaboration to enhance patient health outcomes.


Ashby says he is keen to take key learnings from the pilot and extend them to a wider base of patients with the disease.
“We’re now entering a phase where, through collaborating with MDFA, we will work toward further improving the health outcomes of more of our patients,” he says.
“As optometrists we can’t stand back and watch our patients experience vision loss that could have been prevented, we must do all we can to prevent vision loss. We are very fortunate to have similarly minded partners in Australia’s eye health industry and we look forward to working with them to change lives through better vision into th e future.”
by
For more information, speak to your local Rodenstock Account Manager.
“OPTOMETRISTS AND OPHTHALMOLOGISTS PROVIDE THE HIGHEST QUALITY OF CLINICAL CARE FOR PATIENTS; MDFA AIMS TO BE THERE FOR THE REST, PROVIDING EVIDENCE-BASED SUPPORT FOR HOW TO LIVE WELL WITH MACULAR DISEASE”



Persistence PAYS OFF
At least half of patients diagnosed with late-stage neovascular age-related macular degeneration (nAMD) will stop their anti-VEGF eye injection treatment within five years – and when they stop, significant vision loss can occur as early as the next three months.
This, combined with Australia’s ageing population, means that without additional investment by governments, the significant number of people who become permanently vision impaired and blind will severely impact the nation’s health and aged care systems, carers and patients in future, the Macular Disease Foundation Australia (MDFA) warns.
It’s a bleak outlook but one the MDFA is tackling head-on. It commissioned PwC to undertake an economic modelling report on the benefits to government, individuals and carers of increasing treatment persistence for people with nAMD.
The report, Investing to Save Sight: Health and Economic Benefits of Improving Macular Disease Treatment Persistence demonstrates that modest additional government investment to improve health literacy, improve affordability especially for those most in need, and improve access to treatment can all lead to net savings of billions of dollars to taxpayers over the next decade.
“The reality is, without action, the lives of many Australians will be devastated over the next decade, due to the increasing rates of avoidable vision loss and blindness from nAMD,” the MDFA says.
“Government investment now will mean substantial rewards in the future, not least of which would be enabling so many Australians to be able to continue to see their loved ones and lead independent lives.”
MAIN REASONS PATIENTS DISCONTINUE TREATMENT
It is forecast that 195,706 people will be diagnosed with nAMD by 2032, rising by almost 45,000 cases from 151,157 people in 2023 – less than a decade.
“This increase will already add to the cost burden to individuals and government of treating people with nAMD. When we factor in that approximately half of these people won’t stay on treatment and potentially go blind, the cost becomes both financial and personal,” the foundation says.
According to MDFA’s report, currently only 38% of the 156,000 Australian’s living with AMD receive anti-VEGF eye injection treatment, and treatment intervals currently range from four to 12 weeks. It describes five main reasons
why people find persisting with eye injections challenging:
1. The treatment can be a heavy burden, such as feeling fearful about the nature of eye injections
2. People don’t always perceive treatment will be beneficial
3. There are costs to being treated and patients can experience significant ongoing out-of-pocket costs
4. Travel requirements of getting to doctors’ appointments, including the need for someone to drive them to the appointments, as well not always having an eye specialist close to where they live
5. People with macular disease often have challenges in managing other medical conditions.
“We have estimated that of the 446,000 people with nAMD who will start treatment over the next decade, 267,000 will discontinue their eye injections. Tragically, more than 160,000 – that is more than half of those who stop their treatment – will progress to severe vision loss or blindness in a little less than a decade,” the MDFA predicts.
That equates to almost two in three people who start treatment between 2023 and 2032 will stop treatment and develop vision loss or blindness.
KEEP ON KEEPING ON
MDFA believes there are three key areas that can help patients stay on their treatment journey and reduce the health impacts of treatment discontinuation. These are:
1. Improved health literacy – providing education and support.
2. Improved affordability – removing cost barriers for those with low income.
3. Improved accessibility – making services more accessible in rural and remote locations.
“[We are talking about] pragmatic and modest improvements of between 10% and 25% of the treated population with net cost benefits to government to the tune of billions,” the organisation says.
A recent study cited in MDFA’s report found that treatment persistence increases when people with macular diseases are provided with tailored support

May is Macula Month. To mark 2023’s awareness campaign Macular Disease Foundation Australia reveals new insights into the health and economic benefits of investing in modest measures that encourage patients to persist with intravitreal injections.
IMPROVED AFFORDABILITY: FINANCIAL AND NON-FINANCIAL IMPACT SUMMARY, 2023-2032
Eliminating out-of-pocket costs for an additional 10% of people leads to an additional 5,000 patients continuing to receive treatment who would otherwise stop, saving the government $442 million and patients $241 million over the next decade.
SUMMARY OF FINANCIAL IMPACT FOR GOVERNMENT, SCENARIO SUMMARY, 2023- 2032
to assist their ongoing treatment and treatment planning.
In the study, patients receiving intravitreal injection were supported with a range of measures across various channels and included welcome packs, structured telephone calls from staff health professionals, and information booklets. MDFA provides these types of services through its My Eyes program.
“[We] have analysed providing a conservative estimate of 25% of the currently treated population with tailored tools and support measures to improve their health literacy surrounding nAMD. When compared to the costs of doing nothing, there would be significant gains in treatment persistence, with 22,000 fewer people losing their sight, and cost savings to government of $2.03 billion and savings to patients of $1.06 billion over the next decade,” the foundation says.
AFFORDABLE AND ACCESSIBLE
In Australia, approximately 62% of the population aged over 65 receive the age pension and their income is understood to be a minimum of $28,600 per year, and a maximum of $58,318 for individuals, according to MDFA’s report.
Set against this, intravitreal injection treatment is primarily provided in three outpatient settings; private ophthalmology clinic; public hospital; and bulk-billed private ophthalmology clinic.
“The out-of-pocket costs for private intravitreal injection treatment amount to approximately $1,900 per eye, per year, which makes it difficult for people who are on low incomes to commit to ongoing care. By helping a modest number of patients, this saves government hundreds of millions of dollars,” MDFA says.
“[PwC’s] economic modelling shows that eliminating out-of-pocket costs for an additional 10% of affected people leads to an additional 5,000 patients continuing to receive treatment who would otherwise stop therapy, which can save government $442 million and patients $241 million over the next decade.”
In addition to financial barriers to treatment, the MDFA, which supports macular disease patients and their carers, acknowledges the challenges in accessing treatment for people with nAMD who live in rural and remote communities.
Australian Government Department of Health and Aged Care data reveals most ophthalmologists (approximately 84%) are based in major cities; the remaining 16% service the 28% of Australians, or seven million people, who live in rural and remote communities.

“People with macular disease living in rural and remote areas face real struggles to commit to commencing intravitreal injection treatment and/or
to ongoing care,” MDFA’s report states. “Rural and remote patients requiring frequent injections – as frequently as once per month – can find this particularly challenging.”
In a separate report PwC prepared for MDFA in 2020, the corporate consultant mapped areas of unmet demand for treatment in Australia, where people living with nAMD have limited access to treatment – with travel times upwards of two hours or 100km – or no access at all.
“Our economic modelling analysed the impact of increasing treatment persistence in just 25% of the currently treated population. This was modelled on establishing treatment services in more accessible locations and reducing the travel burden where travel lengths exceed 100kms,” MDFA says.
“Increasing treatment persistence in 25% of current treatment recipients travelling long distances leads to an additional 22,000 patients continuing to receive treatment who would stop therapy, which can save government $2.11 billion and patients $1.12 billion over the next decade.”
PUTTING A PRICE ON SAVING SIGHT
Released to mark Macula Month this May, MDFA’s report illustrates how investments to achieve modest increases in treatment persistence can have huge health and cost benefits for government and patients with nAMD.
“Supporting just 22,000 more people to stay with their treatment through improved health literacy results in net savings to government of billions. Increasing accessibility for 22,000 more people who live in rural and remote areas can yield similar health benefits and cost savings,” MDFA concludes in its report.
“And providing eye injections at no cost to just one in 10 more people on treatment can save 5,000 people from losing their sight and save government nearly $450 million dollars over the next decade.”
While MDFA concedes that increasing treatment persistence would mean additional MBS and PBS costs in the short term, it says these costs will be substantially outweighed by the net cost benefit to patients, carers and government.
“We believe you can’t put a value on the heartbreaking impact of losing your sight to age-related macular degeneration, but thanks to this report, we can put a price on saving it.”
START WITH EXPERIENCE STAY WITH EFFICACY
*Over 15 years’ prescribing experience in Australia.1,2
Anti-VEGF with the broadest range of retinal indications registered on the ARTG1,4-6
†Demonstrated efficacy in treatment-naïve eyes with wet AMD (mean BCVA gain of 6.5 letters at 24 months).3
PBS Information: Authority required for the treatment of wet AMD, DME, BRVO, CRVO, PM or for the treatment of CNV secondary to causes other than wet AMD and PM. Refer to PBS Schedule for full Authority information. This product is not PBS listed for the treatment of PDR or ROP.

Use of this medicinal product in paediatric ROP patients is subject to additional monitoring in Australia. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse events at www.tga.gov.au/reporting-problems.
See approved Product Information before prescribing. For the most up to date Product Information go to https://www.novartis.com.au/products/healthcare-professionals/products Lucentis® (ranibizumab [rbe]). Indication: ♦Treatment of neovascular (wet) age-related macular degeneration (AMD). ♦Treatment of visual impairment due to diabetic macular oedema (DME). ♦Treatment of proliferative diabetic retinopathy (PDR) ♦The treatment of visual impairment due to choroidal neovascularisation. ♦Treatment of visual impairment due to choroidal neovascularisation (CNV) secondary to pathologic myopia (PM). ♦Treatment of visual impairment due to macular oedema secondary to retinal vein occlusion (RVO). ♦In preterm infants for the treatment of retinopathy of prematurity (ROP) with zone I (stage 1+, 2+, 3 or 3+), zone II (stage 3+) or AP-ROP (aggressive posterior ROP) disease. Dosage and administration: Complex dosage and administration – see full PI before prescribing. Contraindications: Hypersensitivity to product components, ♦active or suspected ocular or periocular infections ♦active intraocular inflammation (IOI). Precautions: ♦Intravitreal injections have been associated with endophthalmitis, IOI, rhegmatogenous retinal detachment, retinal tear, iatrogenic traumatic cataract and increased intraocular pressure (IOP). Proper aseptic injection techniques must be used. Review patients during the week following injection to permit early treatment if an infection occurs. ♦Transient increases in IOP have been seen within 60 minutes of injection of Lucentis. Sustained IOP increases have also been reported. IOP and perfusion of the optic nerve head must be monitored and managed appropriately. Patients should be reviewed for IOP rise pre-injection and 60 minutes post-injection. The dose should be withheld and treatment should not be resumed earlier than the next scheduled treatment in the event of an IOP of ≥30 mmHg ♦Bilateral use: limited data do not suggest an increased risk of systemic adverse events compared with unilateral treatment. ♦There is a potential risk of arterial thromboembolic events following intravitreal use of VEGF inhibitors. A numerically higher stroke rate was observed in patients treated with ranibizumab 0.5mg compared to ranibizumab 0.3mg or control, however, the differences were not statistically significant. Patients with known risk factors for stroke, including history of prior stroke or transient ischaemic attack, should be carefully evaluated by their physicians as to whether Lucentis treatment is appropriate and the benefit outweighs the potential risk. ♦As with all therapeutic proteins, there is a potential for immunogenicity with Lucentis. Since there is a potential for an increased systemic exposure in subjects with DME, an increased risk for developing hypersensitivity in this patient population cannot be excluded. Patients should be instructed to report if an IOI increases in severity, which may be a clinical sign attributable to intraocular antibody formation. ♦Risk factors associated with the development of a retinal pigment epithelial tear after anti-VEGF therapy for wet AMD include a large and/or high pigment epithelial retinal detachment. Caution should be used in patients with these risk factors for retinal pigment epithelial tears. ♦Lucentis should not be administered concurrently with other anti-VEGF medicinal products (systemic or ocular).♦Lucentis has not been studied in patients with concurrent eye conditions such as retinal detachment or macular hole. No formal interaction studies have been performed. ♦Limited experience with treatment of patients with prior episodes of RVO and of patients with ischemic branch RVO (BRVO) and central RVO (CRVO). In patients with RVO presenting with clinical signs of irreversible ischemic visual function loss, treatment is not recommended. ♦For indications other than ROP Lucentis is not recommended for use in children and adolescents. Long-term safety in preterm infants with ROP has been studied for two years and showed no new safety signals. Potential systemic suppression of VEGF cannot be excluded following intravitreal administration of ranibizumab in premature infants. ♦Patients who experience temporary visual disturbances following treatment must not drive or use machines until these subside. Pregnancy, lactation, females and males of reproductive potential ♦Pregnancy: Should be used with caution in women of child bearing potential in general, and during pregnancy in particular. ♦Lactation: As a precautionary measure, breast-feeding is not recommended during treatment with Lucentis. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for Lucentis and any potential adverse effects on the breastfed child from ranibizumab. ♦Females and males of reproductive potential: For women who wish to become pregnant and have been treated with ranibizumab, it is recommended to wait at least 3 months after the last dose of ranibizumab before conceiving a child; use of effective contraception is recommended for women of childbearing potential. Adverse effects: ♦Very common (≥10%): IOI, vitritis, vitreous detachment, retinal haemorrhage, visual disturbance, eye pain, vitreous floaters, conjunctival haemorrhage, eye irritation, foreign body sensation in eyes, lacrimation increased, blepharitis, dry eye, ocular hyperaemia, eye pruritus, IOP increased, nasopharyngitis, headache, arthralgia. ♦Common (1 to 10%): Retinal degeneration, retinal disorder, retinal detachment, retinal tear, detachment of the retinal pigment epithelium, retinal pigment epithelium tear, visual acuity reduced, vitreous haemorrhage, vitreous disorder, uveitis, iritis, iridocyclitis, cataract, cataract subcapsular, posterior capsule opacification, punctuate keratitis, corneal abrasion, anterior chamber flare, vision blurred, injection site haemorrhage, eye haemorrhage, conjunctivitis, conjunctivitis allergic, eye discharge, photopsia, photophobia, ocular discomfort, eyelid edema, eyelid pain, conjunctival hyperaemia, stroke, influenza, urinary tract infection*, anaemia, anxiety, cough, nausea, allergic reactions (rash, pruritus, urticaria, erythema). ♦Uncommon (0.1 to 1%): Blindness, endophthalmitis, hypopyon, hyphaema, keratopathy, iris adhesions, corneal deposits, corneal oedema, corneal striae, injection site pain, injection site irritation, abnormal sensation in eye, eyelid irritation. ♦Serious adverse events related to intravitreal injections include endophthalmitis, rhegmatogenous retinal detachment, retinal tear and iatrogenic traumatic cataract. ♦Post-marketing experience: Post-marketing safety profile of Lucentis remains in accord with the findings observed in clinical trial setting. *observed only in the DME population. Based on TGA approved Product Information dated 4 July 2022 (luc040722m). AMD, age-related macular degeneration; BCVA, best-corrected visual acuity; CNV, choroidal neovascularisation; DME, diabetic macular oedema; nAMD, neovascular age-related macular degeneration; Other CNV, choroidal neovascularisation due to causes other than nAMD or pathological myopia; PDR, proliferative diabetic retinopathy; PM, choroidal neovascularisation secondary to pathological myopia; ROP, retinopathy of prematurity; RVO, macular oedema secondary to retinal vein occlusion; VEGF, vascular endothelial growth factor.
References: 1. Lucentis Approved Product Information. 2. Australian Government. Services Australia Website. Available from medicarestatistics.humanservices.gov.au/statistics/pbs_item.jsp (report for the period January 2007 to October 2021; accessed February 2022). 3. Gillies MC et al. Ophthalmology 2020;127(2):198–210. 4. Eyelea Approved Product Information. 5. Beovu Approved Product Information. 6. Vabysmo Approved Product Information. Novartis Pharmaceuticals Australia Pty Limited. ABN 18 004 244 160. 54 Waterloo Road, Macquarie Park, NSW 2113. ®Registered Trademark. AU-23523. April 2023. NOLU29463M.
At the completion of this article, the reader should be able to improve management of patients with geographic atrophy (GA) ...
Including:
• Understand the importance of fully characterising GA lesions
• Know the role that identifying key lesion characteristics of GA plays in determining an individual’s risk of vision loss
• Understand what imaging modalities contribute to the detection and documentation of GA size, number and location of lesions
• Understand the importance of distinguishing geographic atrophy secondary to AMD from inherited retinal disease.
THE CHANGING FACE OF GEOGRAPHIC ATROPHY
Three Australian authorities in the field of retinal disease provide an overview of emerging therapies for the once-untreatable geographic atrophy (GA) and the changing role of optometry in the identification and documentation of the condition.



NOVEL THERAPIES FOR GEOGRAPHIC ATROPHY
Age-related macular degeneration (AMD) remains a leading cause of irreversible vision loss in Australia, with 14% of people over the age of 50 years showing signs of AMD, and 1% of people in this age group having late-stage disease.1 Worldwide, the prevalence of late-stage AMD increases significantly after the age of 75; 20% of people of European ancestry have late-stage AMD by 90 years. 2 Around half of those with late-stage disease will have geographic atrophy (GA),1 with estimates suggesting that approximately five million people have GA worldwide. 3
Until now, there has been no approved treatment to stop – or slow the progression of – GA. However, recently the USA Food and Drug Administration (FDA) approved pegcetacoplan (trade name Syfovre, Apellis Pharmaceuticals) for the treatment of GA secondary to AMD. 4
EFFICACY OF PEGCETACOPLAN
Pegcetacoplan is an inhibitor of C3, a protein critical to the complement pathway. Pegcetacoplan is administered by intravitreal injections monthly or every-other-month on an ongoing basis. The complement pathway is a key component of the innate immune system and is well-established as being implicated in AMD pathogenesis. 5 The FILLY (Phase 2),6 DERBY and OAKS (both Phase 3)7 randomised controlled trials have together shown that pegcetacoplan slows GA lesion growth.
The OAKS trial at 12 months showed a 21% reduction in lesion growth (measured by fundus autofluorescence (FAF) area) in the group treated with monthly pegcetacoplan compared to the sham group, and a 16% reduction in lesion growth in the group treated every-other-month, compared to sham.7 In a sub-analysis, the effect was greater for participants with extrafoveal lesions than those involving the fovea, with a 35% reduction compared to sham for monthly and 21% for every-other-month treatment at 12 months.
D ERBY narrowly missed reaching statistical significance between the treated and sham groups but the treatment effect trend was in the same direction. While treatment reduced the rate of
atrophic lesion growth, at 12 months there was no difference in visual acuity between treated and sham groups. Pegcetacoplan is expected to become available for use in the USA in the coming months. In light of that, approvals in other jurisdictions, including Australia, will be considered.
While pegcetacoplan is the first to market, there are several other novel interventions currently in late-stage clinical trials for GA (see section below), signalling that multiple treatments aiming to slow the progression of GA are likely to be just around the corner. These treatments are predicted to not only improve quality-of-life for patients, but will have an enormous impact on the day-to-day practice of eyecare practitioners. Optometrists and ophthalmologists need to be ready for this future. 8
HOW THE ADVENT OF NOVEL THERAPIES WILL CHANGE OPTOMETRY
With new treatments on the horizon for patients with GA, the clinical management of these patients is going to change dramatically. 8 Currently, people with early and intermediate AMD are principally seen by optometrists, rather than ophthalmologists. Current RANZCO referral guidelines9 and Optometry Australia’s chairside reference for the diagnosis and management of AMD10 indicate that those with GA should be reviewed 6-12 monthly by their optometrist
1. Centre for Eye Research Australia, Royal Victorian Eye and Ear Hospital, VIC 3002
2. Department of Surgery (Ophthalmology), University of Melbourne, VIC 3002
and management focuses on identifying and improving risk factors, counselling regarding home monitoring for symptoms of neovascular AMD (nAMD) and optimising spectacles and visual aids. Therefore, optometrists are often the first to detect the presence of GA and deliver this news to their patients. As such, the need to accurately diagnose GA is crucial, even more so now, if there is going to be a treatment available for GA secondary to AMD. It is vital to remember that there are other causes of atrophy and, as such, a need to differentiate them from GA, as treatments for GA will not be appropriate (or approved) for other causes of atrophy (see section below).
There is a need to fully characterise GA lesions, as lesion features will play an important role in deciding which, if any, treatment would be recommended. Unlike nAMD, where, in the vast majority of cases, anti-VEGF treatment is required in a timely manner, the decision to treat GA will be much more nuanced and taken on an individualised basis.

Year 1 Year 3 Year 5
Clinical management questions around who to treat, when to treat and which eye/s to treat are not straightforward and will require as much clinical information as possible on the lesion and its behaviour over time. 8 Since treatment aims to slow, but not stop, lesion progression, people being treated will need careful counselling with regard to their expectations of outcomes. Also, since there is no clinical measure that can be used to gauge early response to treatment, unlike when treating nAMD, the treatment cannot be as easily individualised and growth characteristics will be collected over the long term, with success measured as a change in rate of growth over an extended period.
GA often starts in the perifoveal region and enlarges to involve the fovea. This means that visual acuity is often normal despite the presence of GA. Hence, identifying key lesion characteristics, such as size, number of lesions and relationship to the fovea, will be important to help understand an individual’s risk of vision loss. In addition, the ability to determine an individual’s GA growth rate over a minimum period of 12 months will be a key factor for an ophthalmologist to consider when advising on the benefits and risks of treatment and deciding if and when to intervene.11
Hence, it is crucial that GA is documented by fundus images as soon as GA is diagnosed so that its characteristics over time can be captured. Both optical coherence tomography (OCT) and fundus autofluorescence (FAF) imaging are ideal for documenting GA size, number and location of lesions. They can also help identify high risk characteristics for progression such as particular FAF patterns and presence of reticular pseudodrusen (RPD).
As imaging equipment (OCT and FAF) have become widespread, optometrists are now well positioned to obtain the longitudinal imaging data that will be of critical importance in the clinical decision-making process for GA as treatments become available.
DEVELOPMENT OF GA SECONDARY TO AMD
GA has traditionally been defined on colour fundus photos (CFPs) as a sharply demarcated, pale (hypopigmented) lesion with a choroidal
vessel in its base (Figure 1A), often starting in the perifoveal region before expanding towards the fovea over time.12 However, FAF imaging has given us the ability to better delineate GA lesions. In FAF images of a healthy retina, there is a natural auto-fluorescent signal (white) from the RPE. Whereas in GA, the FAF signal is black where the RPE is missing with a sharply demarcated border to areas of relatively healthy RPE, making GA easier to detect on FAF images than CFP (Figure 1B).

Using FAF images is very useful when explaining the disease to patients and relatives as the non-functioning regions are black. FAF images are also well suited to showing how the lesions are changing over time to help understand the potential importance of intervention to slow progression towards the fovea (Figure 2).
Smaller GA lesions tend to grow slower than larger lesions (until they get very large) and extrafoveal and multifocal lesions have higher growth rates than foveal or unifocal lesions.13, 14 Progression towards the periphery is faster than towards the fovea,15 and progression is faster in
Optometrists will need to start a discussion on the possibility of treatment options and offer an ophthalmology referral for further treatment discussion. Including longitudinal imaging, especially FAF images, in referrals will be very useful to help determine individual progression rates and the relative merits of intervening.
THE IMPORTANCE OF DISTINGUISHING GA SECONDARY TO AMD FROM INHERITED RETINAL DISEASE

It is critical to determine if atrophy seen in the macula is GA secondary to AMD and not atrophy secondary to another condition, such as an inherited retinal disease (IRD). Macular dystrophies are the subset of IRDs that can mimic GA.
The dystrophy most often mistaken for AMD, with deposits that resemble drusen and atrophy that resemble GA, and in patients whose demographics fit with AMD, is Stargardt disease (caused by ABCA4 mutations in the vast majority), or more commonly its later onset form, fundus flavimaculatus.

“OPTOMETRISTS ARE OFTEN THE FIRST TO DETECT THE PRESENCE OF GEOGRAPHIC ATROPHY AND DELIVER THIS NEWS TO THEIR PATIENTS. AS SUCH, THE NEED TO ACCURATELY DIAGNOSE GA IS CRUCIAL, EVEN MORE SO NOW, IF THERE IS GOING TO BE A TREATMENT AVAILABLE FOR GA SECONDARY TO AMD.”
fellow eyes of those with GA.16 Banded and diffuse (particularly ‘diffuse-trickling’) FAF patterns suggest a faster rate of growth compared to those with no such FAF autofluorescence patterns.17 Furthermore, eyes with RPD have not only faster GA progression but the growth appears to be more towards the RPD.18-20 Regions with ellipsoid zone disruption on OCT may also predict the direction of GA progression. 21
INFORMED REFERRAL
Before recommending the commencement of GA treatment, information on GA size, lesion type, growth rate and direction and association with other biomarkers needs to be considered within the context of the patient age, visual acuities and quality-of-life issues.
Rarely, other diseases with dominantly inherited drusen can be mistaken for AMD such as Sorsby fundus dystrophy (caused by TIMP3 mutations) and familial dominant drusen (EFEMP1).
As Stargardt disease has autosomal recessive inheritance, patients usually do not have a family history of macular disease, so the possibility of an IRD needs to be kept in mind for all patients.
Imaging, especially with FAF, will be often the first clue that the disease is not typical of atrophy secondary to AMD. In Stargardt disease there are very sharply demarcated areas of atrophy, with very hyper autofluorescent linear flecks and no typical drusen. (Figure 3).
Due to their different aetiologies, potential treatments for AMD and IRD will be very different,
OTHER NEW GA DRUG THERAPIES ON THE HORIZON
The pathophysiology of AMD is complex, and as such there are many different treatment approaches being considered, including interventions to:
1. reduce oxidative stress
2. reduce toxic by-products by modulating the visual cycle
3. reduce inflammation by complement inhibition
4. take a neuroprotective approach
5. improve blood flow in the choroid
6. replace, repair or regenerate RPE cells and photoreceptors with cell-based therapies.
Several novel interventions are currently in late-stage clinical trials, most of which involve blocking the complement pathway. 22 Clinical trials in later-stage development that aim to block the complement cascade and are currently under way in Australia include C5 inhibitor (avacincaptad pegol, trade name Zimura, Iveric Bio), an antisense inhibitor of complement factor B (IONIS-FB-LRx, Ionis) and gene therapy (GT005, Gyroscope Therapeutics). Other complement pathway trials include ANX007 (Annexon), CB2782 (Catalyst), ALXN1720 (Alexion), HMR59 (Janssen) and Danicopan (Achillion), showing the immense interest from the pharmaceutical industry in this pathway.
Of particular note, the GATHER 2 trial, testing avacincaptad pegol met its primary 12 month endpoint23 and has filed its new drug application with the USA FDA. In addition, there are a number of later phase trials targeting non-complement pathways underway including ONL1204 (ONL Therapeutics), which targets Fragment Apoptosis Stimulator (Fas) pathways upstream of the death signalling and inflammatory pathways.
Not all these treatments are given via intravitreal injections, with some given orally or by subcutaneous injection, thereby offering the
opportunity to treat both eyes, but exposing the patient to potential systemic adverse effects. Gene therapy and cell-based therapies may require retinal surgery or potentially outpatient suprachoroidal or intravitreal delivery. A major benefit of gene or cell-based therapy is the possibility of a one-off treatment.
SUMMARY
It is likely that pegcetacoplan is only the first of what will eventually become multiple treatment options for patients with GA. Optometrists can assist by playing an active role in identifying patients with GA, introducing the topic of potential treatments and ensuring multimodal retinal imaging is undertaken to objectively document lesion progression.
REFERENCES:
1. Keel S, Xie J, Foreman J, et al. Prevalence of age-related macular degeneration in Australia: the Australian National Eye Health Survey. Jama Ophthalmol. 2017;135:1242-49.
2. R udnicka AR, Jarrar Z, Wormald R, et al. Age and gender variations in age-related macular degeneration prevalence in populations of European ancestry: a meta-analysis. Ophthalmology. 2012;119:571-80.
3. O wen CG, Jarrar Z, Wormald R, et al. The estimated prevalence and incidence of late stage age related macular degeneration in the UK. Br J Ophthalmol. 2012;96:752-56.
4. F DA approves SYFOVRETM (pegcetacoplan injection) as the first and only treatment for geographic atrophy (GA), a leading cause of blindness. https://investors.apellis.com/ news-releases/news-release-details/fda-approves-syfovretm-pegcetacoplan-injection-first-and-only. 17 February 2 023.
5. F leckenstein M, Keenan TDL, Guymer RH, et al. Age-related macular degeneration. Nat Rev Dis Primers. 2021;7:31.
6. L iao DS, Grossi FV, El Mehdi D, et al. Complement C3 inhibitor pegcetacoplan for geographic atrophy secondary to age-related macular degeneration: a randomized phase 2 trial. Ophthalmology. 2020;127:186-95.
7. G oldberg R, Heier JS, Wykoff CC, et al. Efficacy of intravitreal pegcetacoplan in patients with geographic atrophy (GA): 12-month results from the phase 3 OAKS and DERBY studies. Invest Ophthalmol Vis Sci. 2022;63:1500-00.
8. G uymer RH. Treating Geographic Atrophy–Are We Ready? A Call to Image. Ophthalmology Retina. 2023;7:1-3.
9. R ANZCO referral pathway for AMD management. https:// ranzco.edu/home/health-professionals/referral-pathway-for-amd-management/. 9 March 2023.
1 0. H art KM, Abbott C, Ly A, et al. Optometry Australia’s chairside reference for the diagnosis and management of age‐related macular degeneration. Clin Exp Optom. 2020;103:254-64.
11. S unness JS, Margalit E, Srikumaran D, et al. The long-term natural history of geographic atrophy from age-related macular degeneration: enlargement of atrophy and implications for interventional clinical trials. Ophthalmology. 2007;114:271-77.
12. B ird AC, Bressler NM, Bressler SB, et al. An international classification and grading system for age-related maculopathy and age-related macular degeneration. Surv Ophthalmol. 1995;39:367-74.
13. S chmitz-Valckenberg S, Sahel J-A, Danis R, et al. Natural history of geographic atrophy progression secondary to age-related macular degeneration (Geographic Atrophy Progression Study). Ophthalmology. 2016;123:361-68.
14. F leckenstein M, Mitchell P, Freund KB, et al. The progression of geographic atrophy secondary to age-related macular degeneration. Ophthalmology. 2018;125:369-90.
15. L indner M, Böker A, Mauschitz MM, et al. Directional kinetics of geographic atrophy progression in age-related macular degeneration with foveal sparing. Ophthalmology. 2015;122:1356-65.
16. F leckenstein M, Schmitz-Valckenberg S, Adrion C, et al. Progression of age-related geographic atrophy: role of the fellow eye. Invest Ophthalmol Vis Sci. 2011;52:6552-57.
17. H olz FG, Bindewald-Wittich A, Fleckenstein M, et al. Progression of geographic atrophy and impact of fundus autofluorescence patterns in age-related macular degeneration. Am J Ophthalmol. 2007;143:463-72. e2.

18. M arsiglia M, Boddu S, Bearelly S, et al. Association between geographic atrophy progression and reticular pseudodrusen in eyes with dry age-related macular degeneration. Invest Ophthalmol Vis Sci. 2013;54:7362-69.
19. W u Z, Fletcher EL, Kumar H, et al. Reticular pseudodrusen: a critical phenotype in age-related macular degeneration. 2021:101017.
With further treatment options under investigation, there remains a need to identify and refer patients with GA who may be suitable for pegcetacoplan, but also those interested in treatment trials to progress our knowledge of the treatment options.
All eyecare professionals are being called upon to help identify people with GA (and IRDs) and to refer them to clinical trial centres if they are interested in participating in research. With help and advocacy from the eyecare profession, we will continue to make headway towards improving the lives of those with this potentially devastating disease.
For further information regarding trials underway at CERA, visit the website (www.cera.org.au/ current-trials/) or contact the research team on: (03) 9929 8113 or amd-studies@cera.org.au (AMD referrals) or IRD@groups.unimelb.edu.au (IRD referrals).
20. T hiele S, Nadal J, Pfau M, et al. Prognostic value of intermediate age-related macular degeneration phenotypes for geographic atrophy progression. Br J Ophthalmol. 2021;105:239-45.
21. G iocanti-Auregan A, Tadayoni R, Fajnkuchen F, et al. Predictive value of outer retina en face OCT imaging for geographic atrophy progression. Invest Ophthalmol Vis Sci. 2015;56:8325-30.
22. L i H, Chintalapudi SR, Jablonski MM. Current drug and molecular therapies for the treatment of atrophic age-related macular degeneration: phase I to phase III clinical development. Expert Opin Investig Drugs. 2017;26:1103-14.
23. J affe GJ, Westby K, Csaky KG, et al. C5 inhibitor avacincaptad pegol for geographic atrophy due to age-related macular degeneration: a randomized pivotal phase 2/3 trial. 2021;128:576-86.
NOTE: Insight readers can scan the QR code or visit insightnews.com.au/cpd/ to access a link to this article to include in their own CPD log book.
so it is critical that both sets of patients are correctly differentiated.FIGURE 3: FAF images of an inherited retinal disease (Stargardt disease) showing areas of atrophy in the macula. Note that the patches of atrophy look similar to those seen in GA but the hyper autofluorescent linear flecks and absence of a typical drusen pattern help differentiate the diseases.
“WITH NEW TREATMENTS ON THE HORIZON FOR PATIENTS WITH GA, THE CLINICAL MANAGEMENT OF THESE PATIENTS IS GOING TO CHANGE DRAMATICALLY.”8
Relieve
NovaTears® acts as a lipid layer substitute and evaporative barrier for improved tear film stability and quality




Stabilises and thickens outer tear film
Allows replenishment of underlying water layer with natural tears

Assists regeneration of eye surface to a healthy state
months
6 opening shelf life after
Patented EyeSol® Technology
PBS Listed
A unique preservative-free eye lubricant utilising patented EyeSol® technology, specifically designed for the relief of evaporative dry eye disease

Clinically validated with significant improvement in signs and symptoms with Evaporative Dry Eye Disease and Meibomian Gland Dysfunction patients2,3
Spreads quickly and easily with longlasting effect

Warm silky feeling on eye – no blurring, stinging or burning
Small droplet size (4−5 x smaller than water-based drops) helps prevent spillover
Preservative, phosphate, water and surfactant free
STREAMLINED AUTHORITY CODE 6172
PBS Information: Authority Required (STREAMLINED): Severe dry eye syndrome in patients who are sensitive to preservatives in multi-dose eye drops.
minutes between using the other product and applying NovaTears®. NovaTears® should not be used in children under 18 years. NovaTears® should not be used while pregnant or breastfeeding. AFT Pharmaceuticals Pty Ltd, Sydney. ABN 29105636413.




At the completion of this article, the reader should be able to improve their managment of dry eye dis ease...
Including:
• Understand the impact of excipients, additives and non-nutritional components on ocular health
• Provide informed recommendations to patients with regards to their nutrition and their ocular surface health
• Understand the importance of the ratio of omega 3s to omega 6s
• Understand the role of the gut microbiome and where the research currently stands
DRY EYE DISEASE: ARE WE WHAT WE EAT?
Tear Film and Ocular Surface Society (TFOS) has published a report into the consequences of lifestyle choices on the ocular surface, including the impact of nutrition. A/Prof MARIA MARKOULLI, chair of the Nutrition Subcommittee, discusses the latest findings.
IMPACT OF DIET ON DRY EYE DISEASE?
We do not yet know what the optimal dietary intake needs to be to prevent and manage dry eye disease.

Diet can be looked at in terms of macronutrients (carbohydrates, lipids [also called ‘fats’] and proteins), micronutrients (vitamins and minerals) and hydration. In terms of macronutrients, there is some evidence that polyunsaturated fatty acids can help resolve dry eye-related inflammation.
FATS
The current hypothesis is that omega 3 in the diet might reduce the risk of dry eye disease and relieve its symptoms because of its known anti-inflammatory properties.
The ratio of omega 6 to 3 matters when it comes to our health. Omega 6 is found in food like corn, meat, poultry and eggs. Common sources of omega 3 are oily fish such as salmon, nuts and seeds. While modern Western diets typically boast an omega 6 to omega 3 ratio around 10 to 1, (sometimes as high as 30 to 1) the optimal ratio for health is less than 4 to 1.
In the Women’s Health Study of more than 32,000 women older than 45 years, a higher omega 6/ omega 3 ratio was associated with a significantly increased risk of dry eye disease; those consuming higher levels of omega 6 had a 2.5 times higher risk of developing dry eye than those who consumed the recommended ratio of less than 4 to 1.1 Additionally, a 30% reduction in dry eye risk was found with each additional gram of omega 3 polyunsaturated fatty acids consumed each day.1

There is limited evidence for the beneficial effects of extra virgin olive oil and primrose oil2 and there is only indirect evidence for other vegetable oils, sugars3 and artificial sweeteners.4
MICRONUTRIENTS
With regards to micronutrients, the major vitamins playing a role in ocular surface diseases include vitamin A, B12, C and D. Deficiency of vitamin A is the most frequent form of malnutrition that contributes to ocular disease.5,6 Of the minerals, the levels of selenium in tears have been found to be decreased in a dry eye model.7 One study reported a relationship between low levels of tear lactoferrin and the development of dry eye disease.8
HYDRATION
Based on the current limited studies, increased water intake has not been tied to improved dry eye or ocular surface outcomes. Increasing hydration has been associated with health benefits, such as increased skin hydration. With regards to the ocular surface, plasma osmolality and tear osmolarity have been shown to be strongly correlated. 9,10 No change in other clinical parameters has been reported.11,12 A population-based study investigating the association between both water intake and 24 hour urine volume found that neither were associated with a protective risk of dry eye.13
WHAT DO WE KNOW ABOUT EXCIPIENTS, ADDITIVES AND NON-NUTRITIONAL COMPONENTS?
Endocrine-disrupting chemicals
Endocrine-disrupting chemicals (EDCs) are substances in the environment (air, soil or water supply); food sources; personal care products and manufactured products that interfere with the normal function of the body’s endocrine system. EDCs are compounds that can bind to the hormone receptors of cells to activate – or block – the action of hormones, including sex hormones.
The main source of EDCs for humans is from ingestion or leaching from food containers or contamination during manufacturing or processing of foods. A systematic review concluded that there is growing evidence of these chemicals are changing the diversity of the gut microbiome.14
Further studies on the role of EDCs in ocular surface disease are clearly needed including any impact on the ocular microbiome. For example, it has been found that Bisphenol A (BPA) – one of the best known EDCs and the chemical used in the production of polycarbonate plastics such as eyewear, water bottles and epoxy coatings of some metal food cans and bottle tops – has the ability to bind to estrogen and has been shown to increase interferon-y and interleukin-17 in vitro in dendritic cells of patients with primary Sjögrens syndrome.15
Parabens
Parabens are a group of chemicals found in shampoos, makeup, toothpaste and shaving gels as well as food products like mayonnaise, salad dressings, and soft drinks. A 2020 study found significant positive correlations between dry eye signs and several parabens in the urine.16
Mercury
Mercury poisoning most commonly occurs via consumption of mercury-contaminated seafood. Increased tear osmolarity, tear cytokine tear levels and decreased subbasal corneal nerve morphology have been reported,17 and blood concentrations of mercury have been linked to dry eye symptoms.18,19
Alcohol
With regards to alcohol, two small studies have investigated the effect of a single event of alcohol intake, and found increased tear osmolarity, shortened tear breakup time and more ocular pain in the hours after alcohol consumption.20,21 A meta-analysis that included 10 studies found that alcohol was weakly associated with dry eye disease.22 There was no increased risk of dry eye seen in heavy drinkers.22
diet has been reported to be useful in chronic inflammatory diseases due to its anti-inflammatory properties. Given these properties, it might be expected to have benefits in treating dry eye disease. To that end, a higher adherence to a Mediterranean diet has been associated with a lower likelihood of developing primary Sjögrens syndrome.23 Another study randomised participants with Sjögrens to either a Mediterranean diet supplemented with extra virgin olive oil and nuts; or a hypocaloric Mediterranean diet and physical activity.24 In both groups, both the signs and symptoms of dry eye disease improved after six months, although more so in the group with exercise.24
When a systematic review within the report looked at the role of intentional food restriction such as occurs in religious fasting, bariatric surgery, short-term fasting, riboflavin depletion diet, anorexia nervosa and celiac disease, none of the studies were judged to be of high quality, most commonly due to the lack of masking and not reporting sample size calculations. ‘Mixed results’ were reported in relation to the effects of religious fasting, low certainty evidence for bariatric surgery and no clinical meaningful difference in anorexia nervosa.

CAN SUPPLEMENTS HELP WITH DRY EYE
Increased Schirmer scores and increased tear meniscus has been reported after caffeine In two large population-based studies, caffeine use was associated with a protective effect on dry eye but this protective effect was
not seen after correction for dry eye associated comorbidities, age and sex.25,26

Manuka Honey has been studied in and around the eye but less so as a dietary supplement. One double-masked randomised controlled trial found improved tear break-up time and Schirmer test scores;27 two studies found conflicting data on the impact of honey on allergic symptoms.28,29
Curcumin (the substance responsible for the golden colour in turmeric) has been found to inhibit oxidative stress, angiogenesis and inflammation. In humans, a curcumin combination taken for eight weeks improved signs and symptoms of dry eye disease.30
There are multiple reports of vitamin A improving dry eye symptoms.31
Although a deficiency in selenium has been associated with thyroid eye disease,32 a meta-analysis of two trials evaluating the efficacy of selenium supplementation for six to nine months in patients with Graves’ ophthalmopathy found no statistically significant difference in thyroid stimulating hormone receptor antibodies compared to placebo.33

Potentially the most studied dietary supplements relating to the ocular surface are omega 3 polyunsaturated fatty acids. When it comes to omega 3 supplements, results from clinical trials have had mixed results, often due to differences in study design.
A meta-analysis that investigated omega 3 versus placebo and included 17 randomised controlled trials with greater than 3,000 patients found that
COSMETICS UNIQUELY FOCUSED ON EYE HEALTH



You’re resilient, even in the worst times. But your eyes, not so much. Everyday they’re under assault. Atmospheric pollution, airborne toxins, blue light emissions, and yes, even your beauty choices, Èyes Are The Story brand is flipping the script with eye-conscious optocosmetics and skincare powered by eye science. These one-of-a-kind formulas are not only eye-safe, but eye-luxuriating.
We’ve blacklisted toxic ingredients found in mainstream cosmetics and skincare. Protect your eyes with a new line of optocosmetics and skincare created by leading innovators in the field of vision health, uniquely formulated for sensitive eyes, contact lens users, and sufferers of dry eye and digital eye strain.


omega 3 supplementation decreased dry eye symptoms and signs.34 We need future research to more clearly define who goes into these studies, to establish a set of core outcome measures, and to determine the optimal dose, composition and duration of supplementation necessary.
THE IMPACT OF THE GUT MICROBIOME AND ITS MODULATION
The gut microbiome seems to be ‘in vogue’. It has been linked to a range of systemic diseases, including autoimmune disease and depression. Its link to dry eye disease stems from the role it plays in the regulation of low-grade chronic inflammation.
Ecological shifts within the gut microbiome can induce imbalance or ‘dysbiosis’, which is associated with chronic disease. In dry eye disease, severe gut dysbiosis has been found to be significantly more prevalent in patients with Sjögren’s syndrome, compared to healthy controls.35 An obvious path to follow here is to explore whether modulation of the gut microbiome plays a role in treating dry eye disease.
Prebiotics boost the function of probiotics and other good bacteria, while probiotics include beneficial bacteria and can be obtained from fermented foods or commercial supplements. When a combination of prebiotics and probiotics was given to a group of people with dry eye disease for one month, when compared to a control group, the pro/prebiotic group was found to have an improvement in both the signs and symptoms of dry eye disease.36
In another double masked randomised controlled trial, 41 participants with dry eye were randomised to receive pro and prebiotics OR placebo.37 After four months, the average comfort score of the treatment group was significantly better compared to that of the controls.37 The field of modulating the gut microbiome as an intervention to treat dry eye disease is relatively in its infancy. More comprehensive investigations are needed on the proper dosage, duration, and formulation of these supplements.
DOES SYSTEMIC DISEASE AS A RESULT OF DIET ALSO IMPACT THE OCULAR SURFACE?
Many systemic disorders are affected by diet and nutrition. Moreover, systemic disorders may themselves further affect the body’s uptake, processing and distribution of nutrients.
Obesity has been linked to floppy eyelid syndrome, blepharoptosis and dry eye disease.38 Dyslipidaemia and hypertension have been similarly associated with dry eye disease,39 with two systematic reviews highlighting a positive
A meta-analysis of omega 3 versus placebo that included 17 randomised controlled found omega 3 supplementation decreased dry eye symptoms and signs.
correlation between dyslipidaemia and MGD.40 Metabolic syndrome has been reported to be associated with an increase in osmolarity of the tear film and symptoms, with a decrease in Schirmer and tear break up time, with similar results reported for prediabetes and diabetes,41 along with a decrease in corneal nerves and sensitivity.42
WHAT DO I TELL MY PATIENTS?
Good nutrition is clearly pivotal to good health. There is significant evidence that good nutrition also impacts the ocular surface. How exactly nutrition relates to each aspect of ocular surface health is, however, in its relative infancy. We as eyecare professionals need to consider the evidence prior to providing nutritional recommendations to patients with regards to their ocular surface health.
View the full report: Markoulli, M., Ahmad, S., Arcot, J., Arita, R., Benitez-del-Castillo, J., Caffery, B., Downie, L. E., Edwards, K., Flanagan, J., Labetoulle, M., Misra, S., Mrugacz, M., Singh, S., Sheppard, J., Vehof, J., Versura, P., Willcox, M. D. P., Ziemanski, J., & Wolffsohn, J. S. (2023). TFOS Lifestyle: Impact of nutrition on the ocular surface. Ocul Surf, (in press).
REFERENCES
1. M iljanovic B, Trivedi KA, Dana MR, Gilbard JP, Buring JE, Schaumberg DA. Relation between dietary n-3 and n-6 fatty acids and clinically diagnosed dry eye syndrome in women. Am J Clin Nutr 2005; 82(4): 887-93.
2. J albert I. Diet, nutraceuticals and the tear film. Exp Eye Res 2013; 117: 138-46.
3. B ray GA, Nielsen SJ, Popkin BM. Consumption of high-fructose corn syrup in beverages may play a role in the epidemic of obesity. Am J Clin Nutr 2004; 79(4): 537-43.
4. C hi L, Bian X, Gao B, et al. Effects of the Artificial Sweetener Neotame on the Gut Microbiome and Fecal Metabolites in Mice. Molecules 2018; 23(2): 367.
5. M arriott BP, Birt DF, Stalling VA, Yates AA. Present Knowledge in Nutrition: Basic Nutrition and Metabolism: Academic Press; 2020.
6. Tei M, Spurr-Michaud SJ, Tisdale AS, Gipson IK. Vitamin A deficiency alters the expression of mucin genes by the rat ocular surface epithelium. Invest Ophthalmol Vis Sci 2000; 41(1): 82-8.
7. H iguchi A, Inoue H, Kaneko Y, Oonishi E, Tsubota K. Selenium-binding lactoferrin is taken into corneal epithelial cells by a receptor and prevents corneal damage in dry eye model animals. Sci Rep 2016; 6: 36903.
8. S onobe H, Ogawa Y, Yamada K, et al. A novel and innovative paper-based analytical device for assessing tear lactoferrin of dry eye patients. Ocul Surf 2019; 17(1): 160-6.
9. Fortes MB, Diment BC, Di Felice U, et al. Tear fluid osmolarity as a potential marker of hydration status. Med Sci Sports Exerc 2011; 43(8): 1590-7.
10. Walsh NP, Fortes MB, Raymond-Barker P, et al. Is whole-body hydration an important consideration in dry eye? Invest Ophthalmol Vis Sci 2012; 53(10): 6622-7.


11. O sei KA, Ovenseri-Ogbomo G, Kyei S, Ntodie M. The effect of caffeine on tear secretion. Optom Vis Sci 2014; 91(2): 171-7.
12. M asmali AM, Alanazi SA, Alotaibi AG, Fagehi R, Abusharaha A, El-Hiti GA. The acute effect of a single dose of green tea on the quality and quantity of tears in normal eye subjects. Clin Ophthalmol 2019; 13: 605-10.
13. N guyen L, Magno MS, Utheim TP, Jansonius NM, Hammond CJ, Vehof J. The relationship between habitual water intake and dry eye disease. Acta Ophthalmol 2023; 101(1): 65-73.
14. M ousavi SE, Delgado-Saborit JM, Adivi A, Pauwels S, Godderis L. Air pollution and endocrine disruptors induce human microbiome imbalances: A systematic review of recent evidence and possible biological mechanisms. Sci Total Environ 2022; 816: 151654.
15. Wang J, She C, Li Z, et al. In vitro impact of bisphenol A on maturation and function of monocyte-derived dendritic cells in patients with primary Sjogren’s syndrome. Immunopharmacol Immunotoxicol 2020; 42(1): 28-36.
16. P ontelli RCN, Rocha BA, Garcia DM, et al. Endocrine disrupting chemicals associated with dry eye syndrome. Ocul Surf 2020; 18(3): 487-93.
17. Ca nadas P, Lantigua Y, Enriquez-de-Salamanca A, et al. Ocular Surface Pathology in Patients Suffering from Mercury Intoxication. Diagnostics (Basel) 2021; 11(8).
18. C hung SH, Myong JP. Are higher blood mercury levels associated with dry eye symptoms in adult Koreans? A population-based cross-sectional study. BMJ Open 2016; 6(4): e010985.
19. J ung SJ, Lee SH. Association between Three Heavy Metals and Dry Eye Disease in Korean Adults: Results of the Korean National Health and Nutrition Examination Survey. Korean J Ophthalmol 2019; 33(1): 26-35.
20. K im JH, Kim JH, Nam WH, et al. Oral alcohol administration disturbs tear film and ocular surface. Ophthalmology 2012; 119(5): 965-71.
21. S imsek C, Kojima T, Dogru M, et al. The Early Effects of Alcohol Consumption on Functional Visual Acuity, Tear Functions, and the Ocular Surface. Eye Contact Lens 2021; 47(1): 20-6.
22. You YS, Qu NB, Yu XN. Alcohol consumption and dry eye syndrome: a Meta-analysis. Int J Ophthalmol 2016; 9(10): 1487-92.
23. M achowicz A, Hall I, de Pablo P, et al. Mediterranean diet and risk of Sjogren’s syndrome. Clin Exp Rheumatol 2020; 38 Suppl 126(4): 216-21.
24. M olina-Leyva I, Molina-Leyva A, Riquelme-Gallego B, Cano-Ibanez N, Garcia-Molina L, Bueno-Cavanillas A. Effectiveness of Mediterranean Diet Implementation in Dry Eye Parameters: A Study of PREDIMED-PLUS Trial. Nutrients 2020; 12(5).
25. A rita R, Yanagi Y, Honda N, et al. Caffeine increases tear volume depending on polymorphisms within the adenosine A2a receptor gene and cytochrome P450 1A2. Ophthalmology 2012; 119(5): 972-8.
26. M agno MS, Utheim TP, Morthen MK, et al. The Relationship Between Caffeine Intake and Dry Eye Disease. Cornea 2023; 42(2): 186-93.
27. I noue S, Kawashima M, Hisamura R, et al. Clinical Evaluation of a Royal Jelly Supplementation for the Restoration of Dry Eye: A Prospective Randomized Double Blind Placebo Controlled Study and an Experimental Mouse Model. PLoS One 2017; 12(1): e0169069.
28. R ajan TV, Tennen H, Lindquist RL, Cohen L, Clive J. Effect of ingestion of honey on symptoms of rhinoconjunctivitis. Ann Allergy Asthma Immunol 2002; 88(2): 198-203.
29. S aarinen K, Jantunen J, Haahtela T. Birch pollen honey for birch pollen allergy--a randomized controlled pilot study. Int Arch Allergy Immunol 2011; 155(2): 160-6.
30. R adkar P, Lakshmanan PS, Mary JJ, Chaudhary S, Durairaj SK. A Novel Multi-Ingredient Supplement Reduces Inflammation of the Eye and Improves Production and Quality of Tears in Humans. Ophthalmol Ther 2021; 10(3): 581-99.
31. K im EC, Choi JS, Joo CK. A comparison of vitamin a and cyclosporine a 0.05% eye drops for treatment of dry eye syndrome. Am J Ophthalmol 2009; 147(2): 206-13 e3.
32. C ao J, Su Y, Chen Z, Ma C, Xiong W. The risk factors for Graves’ ophthalmopathy. Graefes Arch Clin Exp Ophthalmol 2022; 260(4): 1043-54.
33. Yu MG, Faltado A, Acampado LR. Efficacy of Selenium Supplementation on Autoantibody Titers in Graves’ Ophthalmopathy. Philippine Journal of Internal Medicine 2017; 55:1.
34. D ownie LE, Ng SM, Lindsley KB, Akpek EK. Omega-3 and omega-6 polyunsaturated fatty acids for dry eye disease. Cochrane Database Syst Rev 2019; 12(12): CD011016.

35. M andl T, Marsal J, Olsson P, Ohlsson B, Andreasson K. Severe intestinal dysbiosis is prevalent in primary Sjogren’s syndrome and is associated with systemic disease activity. Arthritis Res Ther 2017; 19 (1): 237.
36. C hisari G, Chisari EM, Francaviglia A, Chisari CG. The mixture of bifidobacterium associated with fructo-oligosaccharides reduces the damage of the ocular surface. Clin Ter 2 017; 168(3): e181-e5.
37. Tavakoli A, Markoulli M, Papas E, Flanagan J. The Impact of Probiotics and Prebiotics on Dry Eye Disease Signs and Symptoms. J Clin Med 2022; 11(16).
38. N etland PA, Sugrue SP, Albert DM, Shore JW. Histopathologic features of the floppy eyelid syndrome. Involvement of tarsal elastin. Ophthalmology 1994; 101(1): 174-81.
39. Vehof J, Snieder H, Jansonius N, Hammond CJ. Prevalence and risk factors of dry eye in 79,866 participants of the population-based Lifelines cohort study in the Netherlands. Ocul Surf 2021; 19: 83-93.
40. K uriakose RK, Braich PS. Dyslipidemia and its Association with Meibomian Gland Dysfunction: A Systematic Review. Int Ophthalmol 2018; 38(4): 1809-16.
41. E rdur SK, Aydin R, Ozsutcu M, et al. The Relationship between Metabolic Syndrome, Its Components, and Dry Eye: A Cross-Sectional Study. Curr Eye Res 2017; 42(8): 1115-7.
42. I ssar T, Tummanapalli SS, Borire AA, et al. Impact of the metabolic syndrome on peripheral nerve structure and function in type 2 diabetes. Eur J Neurol 2021; 28(6): 2074-82.
A WHOLE NEW APPROACH TO
dry eye care
InMode’s Envision platform transformed DR BRUCE DORNN’S practice beyond recognition, along with many other Canadian optometrists. Now the technology is available in Australia, presenting an opportunity for independents to offer a unique service patients can’t find anywhere else.
It’s no secret that dry eye services represent one of the key ways for independent optometry practices to differentiate their business. Many do so in the hope of improving their financial performance, but imagine if you could increase net profitability by half a million dollars.
That’s what happened for Dr Bruce Dornn – the principal optometrist at his full-scope independent practice in the Canadian province of Manitoba – after “a paradigm shift” in his dry eye practice centred on the use of a novel non-surgical technology platform.
The instrumentation by medical technology company InMode – and soon to be available in Australia – encompasses three elements designed for the eye:
bipolar radiofrequency (RF), intense pulse light (IPL), and minimally invasive fractional needling technology, which Dornn says has significantly elevated his approach to dry eye disease (DED) that was once built on artificial tears and prescription eye drops.
“We’ve completely shifted away from using a medical form of treatment –which is expensive in the long run, often comes with side effects and doesn’t have the best outcomes percentage wise – to now using a non-pharmaceutical treatment that rejuvenates the patient’s meibomian glands and helps them produce their own healthy tearfilm,” he explains.
“I’m now getting an 85-90% success rate in DED using this technology with patients paying $2,000 out-of-pocket for four treatments overall – but it’s a long-term, healthier solution. In turn, we’ve increased our profitability by half a million dollars, that’s net, not gross, so it’s had a major impact. I’ve been doing this for 20 years and we plateaued on revenue from spectacle sales, until we introduced the InMode Envision technology. Now, we’ve had a significant jump in what we can earn as a primary eyecare practice.”
InMode is a publicly listed company headquartered in Israel. Founded in 2008, it’s well known among plastic surgeons, gynaecologists, dermatologists and ENTs, but is a relative newcomer to the Australian eyecare market.
InMode Australia managing director Mr Dennis Cronje says RF technology is the genesis of InMode’s technology. RF is the basis of around 90% of its instruments and involves the selective and controlled rise in tissue temperature from a high frequency alternating current to heat the dermis skin layer, stimulating the production of collagen. The company’s portfolio also includes light-based energy and laser technologies, helping health professionals offer minimally invasive procedures and improve existing surgical procedures.
As one of its latest offerings, Cronje expects Envision will be of significant interest to independent Australian optometrists. It is described as a new in-office standard revolutionising ocular care procedures for meibomian gland dysfunction (MGD) and the symptoms of DED. The non-surgical ophthalmic platform features:
• Forma-I: bipolar RF – a thermal technology designed to deliver targeted bipolar RF energy to small delicate ocular zones, directly on the upper and lower lid, to address the symptoms of DED caused by MGD
• Lumecca-I: intense pulse light (IPL) – delivers precise spot-size IPL procedures to treat inflammatory conditions in smaller zones

• Morpheus8: minimally invasive fractional needling technology – a clinically proven fractional technology to treat tissue. RF energy is delivered to multiple depths through bipolar arrays of microneedles targeting the Fibro Septal Network (FSN) and results in localised heating for collagen stimulation, elastin production, and coagulation/tightening of tissue.
“Envision is the combination of RF energy but being able to deliver it bipolar that allows the user to apply it directly over the eye, very discreetly and effectively,” Cronje explains.
“The ability to then combine that with light-based energy to treat some of the other underlying ocular conditions, and then introducing Morpheus8 around the eyes, fits with a new direction we took as a company a few years ago to focus on medical conditions with an aesthetic side to them.”
WHERE ENVISION SHINES
Dornn says Envision’s small-size applicators – and precise depth control – allow for highly efficacious procedures in the small, more delicate subdermal layers of the periorbital region.
“Envision is a complete suite of devices perfectly suited for eyecare. It has been developed for use on eyelids, which is really important to understand because a lot of technology is great on thicker skin, but your eyelids are the thinnest skin on your body and you’ve got a cornea underneath that’s completely avascular, so if you’re applying too much energy, you’re going to have problems,” he says.
“Firstly, we have the Forma-I, featuring bipolar RF, which means I can do an RF procedure directly on top of an upper or lower eyelid with no shield. That’s a big deal. That’s saving me a lot of time in a busy clinic, and it’s very delegatable to ancillary staff.”
Forma-I is a thermal technology designed to deliver targeted bipolar radiofrequency energy to small delicate ocular zones, directly on the upper and lower lid, to address the symptoms of dry eye disease caused by meibomian gland dysfunction.
Secondly, in the Lumecca-I, Dornn says eyecare professionals have access to an IPL technology specially designed for use on eyelids. With a small spot size, the user can treat close and adjacent to the eyelash margin, which for some IPL models, can be difficult.
“Previously, that meant you had to be very careful – staying around 2 mm away from the lash margin – whereas now with the Lumecca-I, I can get right in on the lid margin. You can tell InMode has done the R&D and made devices that are very specific to eyecare – Envision is a complete departure from anything else.”
For Dornn, the third and final applicator – the Morpheus8 – is an indication of where optometry, at least in Canada, may head in future. He says the treatment could be used in the early stages of dermatochalasis (excess eyelid skin).
“Thereby avoiding a blepharoplasty later down the road – this is really appealing to my patients. Lots of people want to avoid surgeries, especially blepharoplasty which can be an uncomfortable procedure and cause other problems like severe dry eye.”
INTEGRATING THE PLATFORM INTO YOUR WORKFLOW
Dornn was an early adopter of the Envision system when he began using it four years ago. Today, he says the platform is used by around 150 Canadian optometry practices, with their US counterparts excited about its launch in their own country.
In his practice, DED is given equal consideration to other conditions like glaucoma and macular disease. It now means every adult patient is screened with meibography and a non-invasive tear breakup test (NIK-BUT).
Ultimately, there are two types of DED patients that visit the practice: those who are late-stage and symptomatic seeking immediate care; or those who are asymptomatic with early warning signs only identified through the screening process. Dornn’s practice has also dispelled the myth DED is a disease of the elderly, with issues such as increased screen time, blue light and lower blink rates bringing down the average age of his DED patient to 46 years.
“To me, it’s important to identify asymptomatic patients. I want to make a diagnosis early before they have symptoms or signs of damage. The outcomes are better and patients are happier,” he says.
“I show them the diagnostic images and illustrate how poorly they’re
Lumecca-I delivers precise spot-size IPL procedures to treat inflammatory conditions in smaller zones.
Morpheus8 is a minimally invasive fractional needling technology that results in localised heating for collagen stimulation, elastin production, and coagulation.
producing tears. I say we can wait a year, two years, but we’re going to lose some gland tissue, or we can treat this early and everyone’s going to be better off. Patients respond, they get it, and I have a lot of enrolment with this in my practice, I am extremely busy with this work.”
Integrating new technology into the practice workflow is a challenge for any practice, but Dornn has established a protocol that works well for him. He treats four to five DED patients per day that are slotted into his regular schedule, seeing up to 25 patients per week.

After being diagnosed, patients return for treatment. On that day, they are checked in by the practice staff, their eyelid skin is prepped, and the Forma-I procedure is performed by a non-clinical staff member – a significant cost saver for the practice.
Dornn then performs a manual gland expression, followed by Lumecca-I on the lids (when indicated).
“What people don’t realise is the majority of dry eye cases (85%) are really MGD – glands are blocked, and we need to unblock them. What’s so genius about the bipolar RF with the Forma-I machine is that it heats the gland very precisely 2 mm right into the dermis where the glands are. It’s far more effective than anything we’ve had before.”


In many cases, Dornn then combines treatments on the same day, starting with Forma-I bipolar RF followed by Lumecca-I IPL.
“I put a stainless steel shield on the patient’s eye and perform IPL on the upper and lower lids; when your glands get blocked, like any other part of your body, inflammation ensues. So bipolar RF (Forma-I) is treating the blockage, we’re heating and stimulating collagen growth and with the IPL I’m treating more superficially and trying to deal with the inflammation and any neovascular blood vessels. It’s the perfect combination.”


Patients usually receive four treatments each spaced one month apart. At $500 per treatment, dry eye care via the Envision platform is a major source of revenue for the practice. Dornn then builds on this by selling hot/cold compress kits, omega 3 supplements, skin care products and sunscreen for IPL patients.
“We provide everything they’re going to need for pre- and post-treatment, which really increases our bottom line,” he adds.
Although Envision could have a place in ophthalmology clinics, Dornn believes the platform adds the most value in primary eyecare clinics that are more focused on the ocular surface.
“Before I had the Envision platform, I’d never had an ophthalmologist refer a patient to me in 20 years of practice. Now I have oculoplastic surgeons referring to me, as well as rheumatologists with Sjogren’s and arthritic patients, and GPs with dry eye patients. Early adopters of this technology may find themselves getting busy quickly.”
NOTE: For Australian practices wanting to learn about how to integrate Envision into their practice, Dr Bruce Dornn has developed detailed training modules for optometrists and their staff: https://eyerevive.podia.com/
“I’VE BEEN DOING THIS FOR 20 YEARS AND WE PLATEAUED ON REVENUE FROM SPECTACLE SALES, UNTIL WE INTRODUCED THE INMODE ENVISION TECHNOLOGY.”
DR BRUCE DORNN DORNN EYE CARE
AT THE LEADING EDGE OF
dry eye disease
With dry eye disease (DED) affecting more than 700 million people globally, it is one of the most common pathologies in ophthalmic visits. Dry eye treatment is also a key consideration in many areas such as glaucoma, refractive and cataract surgeries, and contact lenses, among others.
Australians have seen a surge in dry eye prevalence, according to Optometry Australia, with more than 85% of the population estimated to have experienced it at some point. Of those affected, 55% only developed the condition after the pandemic in 2020 and almost one in five (18%) experience it frequently.
Associate Professor Laura Downie, research leader at Downie Laboratory – an anterior eye, clinical trials and research translation unit at The University of Melbourne – says there is increasing recognition DED is highly heterogenous in its clinical expression.
“As such, ‘dry eye disease’ might be considered as an umbrella term that describes clinical presentations with a spectrum of ocular surface symptoms and signs,” she says.
“Recognising its multifactorial nature, and that not all patients will have the same underlying pathology, we are witnessing the development of new, diverse treatments that are targeted towards subsets of dry eye patients.”
Downie says this includes drugs and devices aimed at resolving specific aetiological factors, including to improve meibum quality in meibomian gland dysfunction (MGD), augment lacrimal secretion in tear deficiency, and modulate specific inflammatory pathways for aqueous-deficient dry eye.
“From a diagnostic perspective, this means that accurately determining the subtype of dry eye is increasingly important to enable the prescription of more appropriate and targeted treatments for dry eye, and optimise patient health outcomes,” she says.

Downie, also director of Melbourne Cochrane Eyes and Vision Centre for Evidence-Based Vision Care, herself is leading a project to develop a revolutionary point-of-care diagnostic device. Named Acoustically-Driven Microfluidic Extensional Rheometry (ADMiER), it’s a first-of-its-kind device that will enable eyecare practitioners to take a patient’s tear-drop before immediately determining if the patient has DED and which sub-type.
LATEST TREATMENTS
New innovations in intense pulsed light (IPL) and prescription eye drops have dominated recent headlines in DED treatment in Australia.
One of the newest technologies is the Envision platform from medical technology company InMode. The system has been in use in Canada for some time now, but became available to Australian eyecare professionals in May 2023.
The platform (detailed on page 38) is unique due to its ability to offer precise depth control for procedures in the small, more delicate subdermal layers of the periorbital region, featuring three piece of technology.
Another major technology now available locally is the OptiLight IPL from Lumenis. Launched here in 2021, it’s the only light-based technology that is FDA approved and TGA listed for DED due to MGD.
Ellex/Quantel Medical, which is part of Lumibird Medical group, also joined the IPL fray for DED with its C.STIM IPL system, launched in Australia in 2022.
While IPL is making in-roads as one of the most effective treatments for more serious DED suffers, patient-applied therapy in the form of drops and lid hygiene remain the mainstay management options, but effectiveness depends on patient compliance.
For several years, Australian eyecare professionals watched with envy as their international counterparts accessed branded ciclosporin products, so it was a significant milestone when in March 2020 Cequa (ciclosporin 900 microgram/mL) was approved by the TGA.
The industry then scored another major win in October 2021 when another ciclosporin, Ikervis (0.1% ciclosporin), was listed on the Pharmaceutical Benefits Scheme.
Very recent results have provided real-world evidence supporting the effectiveness, tolerability, and safety profile of Ikervis for severe keratitis in DED. The PERSPECTIVE study results demonstrated significant improvement in corneal fluorescein staining (CFS) score from baseline at month 12, following Ikervis initiation in patients with severe keratitis in DED who remained insufficiently controlled despite treatment with artificial tears.
The development of new and diverse treatments for dry eye holds promise for the thousands of Australians living with the condition. Insight recaps the treatments breaking new ground, and asks some leading authorities about what the next wave of innovation might target.
The other major development in the prescription drug space was a regulatory change that allowed optometrists to prescribe Xiidra (lifitegrast) in November 2021. Under previous arrangements, lifitegrast could only be arranged through a medical practitioner, but with optometrists now allowed to prescribe, it’s hoped thousands more Australians can receive the medication without additional costs involving a GP or ophthalmologist.
LIFESTYLE
Research is also examining the influence of current lifestyle choices on the ocular surface. These include extended digital screen use, exposure to low humidity environments, as well as supplements, food, drink and apply to enhance their appearance.
Leading body the Tear Film and Ocular Surface Society (TFOS) recently published its reports on ‘A Lifestyle Epidemic: Ocular Surface Disease’. One of the reports within this workshop focused on the impact of nutrition.
UNSW’s Associate Professor Maria Markoulli is a TFOS Ambassador and chair of the Nutrition Subcommittee and discusses the latest findings in a CPD article on page 35, examining issues such as omega 6 to 3 ratios, benefits of the Mediterranean diet on the ocular surface, and what role the ‘in vogue’ gut microbiome might have.

She concluded: “There is significant evidence that good nutrition also impacts the ocular surface. How exactly nutrition relates to each aspect of ocular surface health is, however, in its relative infancy.”
EXPERTS AGREE
Professor Stephanie Watson, head of the Corneal Research Group at The University of Sydney’s Save Sight Institute, says because DED is multifactorial, patients suffer in a range of ways and with differing clinical patterns.
“What I find as the most interesting development in dry eye diagnostics is the range of ways to diagnose and classify dry eye disease types and severity. Validated questionnaires exist that patients can self-complete – for example, Ocular Comfort Index and Ocular Surface Disease Index –which can indicate dry eye and its severity,” Watson says.
“Then, following this, examination tools exist not only for the tear film – for example, inferometry, osmolality, meniscus height, non-invasive break up time – but also for the ocular surface and lids – for example, meibography, aesthesiometers.”
In Watson’s view, one of the most interesting developments is the ability to begin personalising DED treatments.
“For example, evaporative dry eye is now recognised as the most common type of dry eye in everyday clinical practice and treatments are emerging that will allow improved treatment of this dry eye type,” she says.


“The increasing availability of ‘safer’ anti-inflammatories has also been a major development; it is now possible to treat dry eye associated inflammation with therapeutics such as cyclosporins and lifitegrast.”
Watson says the ability to use data science is one of the most promising areas of research.
“EVAPORATIVE DRY EYE IS NOW RECOGNISED AS THE MOST COMMON TYPE OF DRY EYE IN EVERYDAY CLINICAL PRACTICE AND TREATMENTS ARE EMERGING THAT WILL ALLOW IMPROVED TREATMENT OF THIS DRY EYE TYPE.”
PROF STEPHANIE WATSON SAVE SIGHT INSTITUTE
“FROM A DIAGNOSTIC PERSPECTIVE, ACCURATELY DETERMINING THE SUBTYPE OF DRY EYE IS INCREASINGLY IMPORTANT TO ENABLE THE PRESCRIPTION OF MORE APPROPRIATE AND TARGETED TREATMENTS.”
DR LAURA DOWNIE THE UNIVERSITY OF MELBOURNE
“The Save Sight Dry Eye Registry is a tool that ophthalmologists and optometrists can use to follow their patients with dry eye, but it is also finding new aspects of dry eye natural history and treatment responses. The application of genetics in dry eye disease is emerging and it is an area that we will need to ‘watch this space’ on,” Watson says.
Clinical Australian optometrist Dr Leigh Plowman who founded the Dry Eye Directory, an online resource educating patients about dry eyes and connecting them with local clinics, is excited about Downie’s ADMiER

“ADMiER is an innovative way to diagnose and subtype dry eye disease. A small sample of the tear film is taken and put into a unit. The ADMiER device offers excellent sensitivity and specificity for diagnosing and subtyping dry
“DED prevalence has tripled in the last 10 years, according to Google Trends. Early diagnosis is important for helping patients to maintain quality-of-life and reduce dry eye disease progression.”
As a dry eye sufferer, Plowman is across the range of products available, having tried them himself, as well as his cumulated experience treating
“DED is multifactorial. It’s rare to have a treatment that can address multiple factors at once. However, Optilight (IPL) by Lumenis helps manage DED on multiple levels. In particular, I’ve found that it helps to switch on the meibomian glands. This helps to reduce evaporative dry eye. It also helps to reduce tear film hyperosmolarity, seal off eyelid telangiectasias, reduce inflammation, and control demodex and bacteria on the eyelids,” he says. Plowman is keeping a close watch on DED research, particularly into the causes of the condition.
“The better we understand the causes for dry eyes, the better we can manage the disease. Diagnostics for specific dry eye causes are in research – for example, Immunoglobulins. Soon we’ll be able to pinpoint causative factors via clinical tests similar to InflammaDry or Adenovirus
He is also excited about research into gut bacteria and the relationship with inflammatory DED, citing a review of evidence published by Watane et
“They found the gut has a balance of pro-inflammatory bacteria and anti-inflammatory bacteria. Ocular signs of gut dysbiosis can include reduced aqueous tear production, ocular surface inflammation, corneal staining and reduced goblet cell density,” he says.
“This research gives us an opportunity to talk with patients holistically about their dry eyes. Then support them to work with an Integrative or Functional Medical Doctor to improve their overall health. A patient of mine reported a significant improvement in her eyes and overall health by
Disclaimer: Dr Leigh Plowman is a consultant for Seqirus and Lumenis


THE ALL-IN-ONE SYSTANE COMPLETE – IN A PRESERVATIVE-FREE BOTTLE
Alcon has expanded its range of preservative-free eye drops with the addition of Systane COMPLETE PRESERVATIVE-FREE. This lubricating eye drop combines the all-in-one formulation of Systane COMPLETE with a multi-dose, preservative-free bottle.

Systane COMPLETE utilises Systane’s Intelligent Delivery system of HP-Guar and borate in combination with nano-lipid technology to support all layers of the tear film and relieve the symptoms of all types of dry eye (aqueous deficient, evaporative and mixed dry eye).
The bottle features patented PureFlow Technology, which is comprised of a one-way valve to ensure no contaminated liquid can be re-introduced into the container and a fine silicone membrane to filter returned air. 3 This eye drop is suitable for those with mild-moderate dry eye* in any of the sub-categories (ADDE, EDE or mixed)1,2 and it provides relief for all symptoms of dry eye for up to 8 hrs. 4
*recommendation based upon expected on-eye viscosity. References will appear in the online version and are available upon request.
Contact: visioncareorders.anz@alcon.com
RELIEVE AND PROTECT DRY EYES WITH NOVATEARS
It’s reported 85% of dry eye patients suffer from evaporative dry eye1 , so NovaTears can be recommended to relieve symptoms of excessive tear evaporation. NovaTears is a unique preservative-free eye lubricant using patented EyeSol technology that acts as a lipid layer substitute and evaporative barrier for improved tear film quality and stability.
According to AFT Pharmaceuticals, NovaTears spreads quickly and easily to consolidate the lipid layer, stabilising and thickening the outer tear film to allow replenishment of the underlying water layer with natural tears, and assisting regeneration of the eye’s surface to a healthy state.
NovaTears is preservative-, water-free, and can be used for six months after opening. A droplet size four to five times smaller than aqueous eye drops helps prevent spill over, and the warm silky feel with no stinging, burning or blurring aids patient

NovaTears is also clinically validated, showing significant improvement in signs and symptoms with evaporative dry eye disease and meibomian gland
Contact: receptionau@aftpharm.com
Dry eye products
OPTILIGHT A MUST-HAVE FOR DRY EYE CLINICS
Australian eyecare professionals wanting to elevate their dry eye management and treat inflammation can access the latest intense pulse light (IPL) from Lumenis. OptiLight is the only light-based technology that is FDA approved and TGA listed for the treatment of dry eye disease (DED) and meibomian gland dysfunction (MGD).
Lumenis, which pioneered IPL technology, secured US Food and Drug Administration (FDA) De Novo authorisation for OptiLight in 2021. The system is designed for a consistent, precise, and controlled light-based treatment for DED.

As the company’s newest IPL device for DED due to MGD, it became available to the Australian and New Zealand market in November 2021.

The multi-centre, double-blinded, randomised controlled FDA trial showed Lumenis IPL with patented Optimal Pulse Technology (OPT) significantly improved tear breakup time, meibum quality, and meibomian gland expressibility.
The clinical trial joins other studies of Lumenis’ IPL with OPT, that have shown the same results, as well as reduction of inflammatory markers. 2-5
References available upon request.
Contact: infoau@lumenis.com or 1800 586 364
VISCOTEARS GEL PF FOR LONGER TERM TREATMENT

Viscotears Gel PF is a preservative-free ophthalmic solution containing 0.2% carbomer which has a moistening and wetting effect on the eyes.
According to Bausch + Lomb (B+L), it improves the moistening of the ocular surface in the presence of dry eye sensation, burning or tiredness of the eyes, caused, for instance by watching television for a long time or extensive computer work, air from heating systems or air-conditioning.
As preservatives may result in ocular irritation, preservative-free products such as Viscotears Gel PF should be a preferred option for long-term treatments, B+L states. Viscotears Gel PF (preservative-free): 30 x 0.6g single-dose units are PBS-listed.
Always review product information before prescribing these medications. Product information is available on request from B+L. Contact: 1800 251 150.
Dry eye products
A REVOLUTIONARY ALTERNATIVE TO TREATING DRY EYE
Envision, by medical technology company InMode, is a new in-office standard revolutionising ocular care procedures for meibomian gland dysfunction (MGD) and the symptoms of dry eye (DED). This non-surgical platform, soon to become available to Australian eyecare professionals, features small-size applicators that can deliver precise heat and depth control for “highly efficacious procedures in the small, more delicate subdermal layers of the periorbital region”. The platform comprises:
• Forma-I: bipolar RF – a thermal technology designed to deliver targeted bipolar RF energy to small delicate ocular zones, directly on the upper and lower lid, to address the symptoms of DED caused by MGD
• Lumecca-I: intense pulse light (IPL) – delivers precise spot-size IPL procedures to treat inflammatory conditions in smaller zones


• Morpheus8: minimally invasive fractional needling technology – a clinically proven fractional technology to treat tissue. RF energy is delivered to multiple depths through bipolar arrays of microneedles targeting the Fibro Septal Network (FSN) and results in localised heating for collagen stimulation, elastin production, and coagulation/ tightening of tissue.
With Envision, practitioners deliver non-drug therapies to improve patient vision and quality-of-life. Turn to page 38 for an in-depth case study.
Contact: info@inmode.com.au
NEW DEVICE COMBATS GROWING MYOPIA AND DRY EYE CRISES
MYAH is Topcon Healthcare’s latest instrument for eye health practices wanting to strengthen their dry eye services.
ONE OF THE MOST COMPREHENSIVE DRY EYE ANALYSIS TOOLS AVAILABLE

The OCULUS Keratograph 5M, available through Designs For Vision, is an advanced Placido-based corneal topographer with a built-in real keratometer and a colour camera optimised for external imaging. It has established itself as one of the most comprehensive dry eye analysis tool available with the JENVIS Pro Dry Eye Report that supports objective grading for dry eye diagnosis.
The software enables the practitioner to find the cause of dry eye in an easy and reliable way with Screening, Comprehensive, DEWS 2 and Follow-up protocols, leading to an optimised workflow that saves time. The software is also customisable to suit the user’s preferences for imaging and documentation, and the easy-to-understand reports help to communicate the dry eye status to patients in an effective manner.
The Keratograph 5M is said to be a versatile device that excels not only in dry eye diagnostics, but also in the measurement of corneal topography and pupillometry.
Contact: orders@dfv.com.au
Exclusively distributed by Device Technologies in Australia and New Zealand since October, it is a versatile device providing the key tools for an evolving platform for dry eye management, as well as myopia management.
In dry eye, practitioners can conduct non-invasive tear break-up time, meibomian gland analysis, blink analysis, tear meniscus height analysis and real fluorescein imaging and video acquisition. The instrument is also said to be compact, simple to operate, and offers rapid capture.



“Myah is ideally suited to combat the growing crises of both myopia and dry eye disease. Its versatility and ease-of-use allows eyecare professionals to easily build a myopia service within their practice, educate patients on the implications of myopia and dry eye disease, manage their patients’ conditions, and grow their service offerings,” Topcon states. Contact: customers@device.com.au



Dry eye products
THE SYSTEMATIC APPROACH TO EYE LUBRICATION
HYLO-FORTE eye drops provide preservative-free relief for dry eyes through a unique multi-dose device, combining the comfort of a gel with the effect of a drop.

According to AFT Pharmaceuticals, the patented COMOD (COntinuous MOno Dose) application system protects the sodium hyaluronate solution from contaminated ambient air, ensuring the precise measured delivery of at least 300 sterile drops without the use of preservatives. This airless system also ensures use for up to six months after opening.
“The high concentration and quality of sodium hyaluronate in HYLO-FORTE results in a highly viscous solution for long-lasting, intensive and soothing relief of severe or chronic dry eye without vision impairment. HYLO-FORTE is suitable for use following surgery and can be used with contact lenses,” AFT states.

The company also says use of phosphate-containing eye preparations can result in damaging corneal calcification as a result of calcium phosphate precipitation in patients suffering pronounced corneal damage, and this can be avoided through the use of phosphate-free HYLO-FORTE.
Contact: receptionau@aftpharm.com
VISCOTEARS EYE GEL ‘FOR SORE, GRITTY AND DRY EYES’
Viscotears Eye Gel is a translucent, viscous gel containing 0.2% Carbomer which Bausch + Lomb (B+L) says provides soothing long-lasting relief for sore, gritty and dry eyes.
After instillation, Viscotears Eye Gel spreads rapidly and smoothly over the conjunctiva and cornea. Due to its physical properties, the eye gel binds water and forms a highly adhesive, translucent, lubricating, wetting, protective film on the surface of the eye with prolonged retention time which stabilises the tear film. The improvement in tear film stability is maintained for a period of up to six hours.
Viscotears Eye Gel is a long-lasting gel formulation which is suited for those who need extra protection, added night-time support, or prefer a heavier gel.
Viscotears Eye Gel 10g tube is PBS-listed.

Always review product information before prescribing these medications. Product information is available on request from B+L .
Contact: 1800 251 150
POTENTIAL TO DOUBLE YOUR REVENUE WITH THERMAEYE PLUS IN 2023
Thermaeye Plus is a described as a high quality IPL device designed and manufactured in Europe to exacting standards. The system delivers targeted fluence (energy) via a 650nm filter enabling the operator to treat with greater safety while retaining excellent efficacy.
A ONE-STOP-SHOP FOR PUNCTAL PLUGS
Device Technologies is the exclusive supplier of the CORZA Medical Punctal Plug range, comprising the EagleVision and Sharpoint ranges. For more than 40 years, EagleVision is said to offer the broadest range of treatment options designed to help relieve the discomfort associated with dry eye disease and improve patients’ quality-of-life. The patented punctal plug designs provide excellent fit, easy insertion and improved patient comport, according to Device Technologies.
Sharpoint UltraPlug punctal plugs are designed to offer long-term relief from dry eye symptoms and enable the eye to maintain more of its own natural tears. It’s available in both permanent and extended-wear, absorbable options, and aims to deliver the optimal balance of performance and patient comfort.
Contact: customers@device.com.au
The compact, portable easy-to-use device, available through OptiMed, features fractional pulsed technology and a water-cooled optical grade sapphire crystal delivery system providing epidermal cooling to reduce thermal spread and risk of burning. These features allow the operator to treat all skin types.



Throughout 2023, any orders placed for Thermaeye Plus will come with a complementary Xenon flash lamp including 30,000 free flashes to double the financial return for the practice. Approved customers can also take advantage of a 12-month interest-free and no repayments offer through Credabl finance.
Contact: 1300 657 720 (OptiMed Australia)
ONCE-DAILY IKERVIS® IN THE PERSPECTIVE STUDY: REAL-WORLD EVIDENCE OF IMPROVEMENT OF SEVERE KERATITIS IN DED * 1
*Significant improvements from baseline to Month 12 in mean CFS score (Oxford Grading Scale, P<0.0001).1
Find out more about the PERSPECTIVE study and how Ikervis® can help your patients at eyehealth.com.au


Ikervis® is indicated for the treatment of severe keratitis in adult patients with dry eye disease which has not improved despite treatment with tear substitutes.
PBS Information: Authority Required. Refer to PBS Schedule for full information.
Before prescribing IKERVIS ®, please review the Approved Product Information available from Seqirus Medical Information (1800 642 865) or www.seqirus.com.au/products
This medicinal product is subject to additional monitoring in Australia. This will allow quick identification of the new safety information. Healthcare professionals are asked to report any suspected adverse events www.tga.gov.au/reporting-problems.
MINIMUM PRODUCT INFORMATION: IKERVIS® (ciclosporin 0.1% ophthalmic emulsion). Indication: Treatment of severe keratitis in adult patients with dry eye disease which has not improved despite treatment with tear substitutes. Contraindications: Hypersensitivity to the active substance or any of the excipients; Ocular or peri-ocular malignancies or premalignant conditions; Active or suspected ocular or peri-ocular infection. Precautions: Any reversible underlying conditions, not associated with dry eye disease, should be treated prior to initiating IKERVIS ®; History of ocular herpes; Contact lenses should be removed before instillation of eye drops and re-inserted at wake-up time and careful monitoring of severe keratitis is recommended; Glaucoma – limited experience with IKERVIS®. Exercise caution especially with concomitant betablockers; Co-administration with eye drops containing corticosteroids may potentiate effects of IKERVIS® on the immune system; May affect host defences against local infection and malignancies. Use in Pregnancy (Category C): No data available; Not recommended in pregnancy unless the potential benefit to mother outweighs the potential risk to fetus. Use in Lactation: Insufficient information on breastfed infants; it is unlikely that sufficient amounts are present in breast milk. A decision must be made to discontinue either IKERVIS ® or breastfeeding during treatment. Use in Children: No data available. Interactions with other medicines: No data available. Adverse Effects: Common: erythema of eyelid; lacrimation increased; ocular hyperaemia; vision blurred; eyelid oedema; conjunctival hyperaemia; eye pruritus. Very common: eye pain, eye irritation. Dosage and administration: The recommended dose is one drop of IKERVIS ® once daily to be applied to the affected eye(s) at bedtime.



Dry eye products
AVENOVA SPRAY AN IDEAL DRY EYE SOLUTION


Eye lids are critical to the health of the ocular surface and susceptible to bacteria overpopulation, which can lead to redness and inflammation, as well as several chronic eye conditions. As an effective lid and lash anti-bacterial solution, Avenova has been clinically proven to help patients manage and relieve conditions like blepharitis, meibomian gland dysfunction (MGD), and dry eye.
The patented formula, available from Designs For Vision, uses pure 0.01% hypochlorous acid, which is a naturally occurring molecule produced by the human body to fight toxins and inflammation caused by bacteria. Avenova contains no harmful impurities like bleach, detergents or other surfactants, making it safe to use around the eyes. It is also gentle and soothing, causing no stinging or irritation for the patient. It comes packaged in a unique spray dispenser that controls the dose to the very last drop, making it convenient and precise.
Contact: orders@dfv.com.au
WHY DOCTORS RECOMMEND THE BRUDER EYELID CARE KIT
The Bruder Hygienic Eyelid Care Kit comes complete with everything needed for daily eye hygiene. Eyelid Wipes gently wipe away oil, dirt, pollen and other debris that can cause irritation and infection and are ideal for everyday use and hygiene on-the-go. Bruder Eyelid Spray is a safe and soothing way to reduce inflammation and harmful bacteria.
The kit, supplied by OptiMed, also includes the unique Bruder Eye compress with two-pad design and silver infused MediBeads that deliver soothing, extended moist heat to improve gland function and increase oil flow.
The treatment is designed to stabilise the tear film and maintain natural eye hydration to relieve the symptoms of dry eye, blepharitis and other eye conditions. Every pack includes detailed instructions for daily use to improve eye health.

Contact: 1300 657 720 (OptiMed Australia)
NEW REAL-WORLD EVIDENCE FOR CICLOSPORIN EYE DROP
TRIPLE ACTION TARGETS ALL LAYERS OF THE TEARFILM
Cationorm (cationic nanoemulsion) is a preservative-free, hydrating and lubricating emulsion eye drop which protects the eye surface, relieving the discomfort and irritation of persistent dry eye caused by prolonged use of contact lenses, or environmental conditions.1
Its triple action repairs the lipid layer to reduce evaporation by lubricating and stabilising the tear film, and restores the moisture balance in the muco-aqueous layer of the tear film. It also forms a barrier to lock in moisture, giving dry eyes the time they need to heal.2-5
Administered as one drop, up to four-times daily in the affected eye, Cationorm is suitable for use with contact lenses,6 and gentle enough to use every day.7

PBS information: Cationorm Multi Dose (10mL). Authority Required (STREAMLINED) 6172. Refer to PBS Schedule for full authority information. Cationorm (30 x 0.4mL) is not listed on the PBS. References available upon request. Learn more, visit Cationorm.com.au. Contact: orders@goodopticalservices.com.au.
Ikervis (ciclosporin 0.1% ophthalmic emulsion) is a once-daily ciclosporin eye drop helping break the cycle of inflammation in dry eye disease (DED).1-4 It is indicated for the treatment of severe keratitis in adults with DED insufficiently improved with artificial tears, and is listed on the PBS (authority required).

The recently published PERSPECTIVE study provided real-world evidence supporting the management of severe keratitis associated with DED with Ikervis, with significant improvements in corneal fluorescein staining (CFS) score from baseline over the 12-month treatment period (mean change, -1.42; p<0.0001).
By combining ciclosporin with positively charged nano-droplets, Ikervis is designed to prolong ciclosporin exposure on the ocular surface.1-3
The most common adverse events (AEs) are eye pain and irritation.1 Before prescribing, review the Product Information available from www.cslseqirus.com.au/products.
For more information on Ikervis, contact Seqirus Medical Information.
Contact: 1800 642 865 or aunz.medicalinformation@seqirus.com
Viscotears
Viscotears® Gel PF improves the moistening of the ocular surface in the presence of dry eye sensations, burning or tiredness of the eyes, caused for instance:

• by watching television for a long time
• extensive computer work
• dry air from air-conditioning or heating
Preservative free
Moistening and wetting effect1
®
Viscotears® Eye Gel provides soothing relief for sore, gritty dry eyes. Its long lasting gel formulation is suited for those who:

• need extra protection
• added nighttime support, or

• prefer a heavier gel
Maintains the tear film stability for a period of up to 6 hours2
Viscous gel for nighttime protection
For more information, contact your Bausch + Lomb Territory Manager or Bausch + Lomb Customer Service 1800 251 150





SELF-SUFFICIENT:
optometrist takes control of her career
A taste of indigenous eyecare in Central Australia left Flinders graduate ALEX COFFEY-OATES wanting more. It prompted her to set up her own small business, affording her the flexibility to work as she chooses.
Being on the same outback flight as a patient she referred to Darwin for urgent care stands out as one of the sliding doors moments in optometrist Ms Alex Coffey-Oates career.

Originally from Sydney, Coffey-Oates started studying biomedical science in New Zealand while on a working holiday before moving back to Australia where she completed a Master of Optometry at Flinders. While studying at Flinders, Coffey-Oates joined Specsavers in Norwood as a dispenser, then stayed for a further three years as an optometrist once she graduated.

The team and her experience while working at Specsavers Norwood helped to set her up with the skills, contacts and expertise to pursue her passion and set up her own small business, Allied Eyes, a locum optometry service specialising in rural and remote eyecare. Several moments have led to this point in her career, but one in particular stands out.
“There was a case in Arnhem Land where a patient with diabetes needed urgent care. He and one of his family members ended up on the same flight as me when I went back to Darwin. He was on the urgent flight to get to an ophthalmology appointment in Darwin to have laser treatment and intravitreal injections for diabetic retinopathy. That was a memorable, human moment,” Coffey-Oates says.
“It really showed the importance of having these visiting optometry services. If we had not been on that scheduled visit, this patient would very likely have ended up with extremely poor vision for the rest of his life. A lot of people think we go to these communities just to hand out glasses,
however there are countless vision saving moments we encounter. These moments can feel like true ‘right time, right place’ moments. In remote and very remote communities, those moments feel like they matter even more as our patients have no other options for eyecare without travelling enormous distances and being met with significant barriers – cultural, physical, emotional.”
By her own admission, Coffey-Oates has always wanted to work in Aboriginal and Torres Strait Islander eye health, and has been looking for opportunities to be involved, in addition to her full-time role at Specsavers.
“In 2022, Brien Holden Foundation and another organisation, called Community Eyecare, reached out to me to organise trips to Indigenous communities. It was additional work that I was doing on top of my full-time position at Specsavers. I loved it. It gave me an insight into how much work was available in that field. That then made me decide to shift away from my full-time role at Specsavers to make room for more of that type of work.”
Coffey-Oates’ involvement with Brien Holden Foundation and Community Eyecare stems back to her time at university.
“I got a scholarship during my final year at Flinders University to complete a placement with Brien Holden Foundation alongside their optometrist/NT clinic manager, Sarah Nicholls. We kept in touch. Sarah reached out again when she heard I was going to be in Darwin last year for the National Aboriginal and Torres Strait Islander Eye Health Conference (as announced by Optometry Australia due to me receiving a bursary to attend this event),” she explains.
“Ben Hamlyn, optometrist and owner of Community Eyecare and a

previous lecturer of mine, requested expressions of interest to provide outreach optometry service in SA via an online group of optometrists. He allowed me to join him for one of his trips to Pika Wiya Health Service in Port Augusta and then I began doing trips to APY Lands.”


While joining organisations like Brien Holden Foundation as a full-time employee was an option, to give herself maximum control over where she worked and when, Coffey-Oates decided to establish her own small business, Allied Eyes, leveraging self-employment lessons from her parent’s family-owned small business, while picking up additional work as a locum within Specsavers.
“I started the business in April 2022 as I was beginning to do some outreach work in Aboriginal communities, including APY Lands and Arnhem Land at the time. I wanted to achieve greater flexibility in my work schedule to facilitate travel and work in remote communities,” she says.
“In the coming months, I will be providing services to regional corporate practices and to remote Aboriginal communities in Central Australia. I plan to travel around the country and continue to provide eyecare to remote communities, as well as regional optometry clinics,” she says.

Although she hasn’t yet set up a business website for Allied Eyes, she is promoting her new business on social media and through word of mouth.

“A lot of people have reached out to me since I posted on LinkedIn that I’ve established Allied Eyes. My plan is to have a website that includes my availability so clinics can potentially book me,” she says.
“I bring all of my handheld equipment with me, the most important of which are my direct ophthalmoscope, binocular indirect ophthalmoscope, retinoscopy racks, 90D lens, diagnostic drops, and foreign body kit. Most clinics I attended have a slit lamp biomicroscope on site, for others the organisation I am working with brings one along with us.”
Gaining more experience each time she visits, Coffey-Oates is familiar with the ebb and flow of life in outreach communities.
“A lot of the focus in Indigenous communities is on screening for diabetic eye disease and dispensing basic glasses that make a huge difference to the people up there. Working in outreach communities certainly has its challenges. It’s very different to normal clinic life; there are no appointments – people just come into the clinic, or you drive around and find patients wherever, and see them. It’s very variable,” she says.
Coffey-Oates intends to share her clinical and travel experience on social media too, including the locations she visits, and interesting cases she encounters in the field.
“I plan to document these opportunities through social media to try to
encourage more optometrists to travel further out from the big cities and provide quality eyecare in these under serviced areas,” she says.
“I think there’s a big cultural shift happening in our generation in regard to work culture, with a much bigger focus on doing what you love and are passionate about, and creating a better work/life balance. For me, the best way to achieve this was to start my own locuming business where I am in full control of when and where I work.”
She continues: “I think a lot of people want flexible working arrangements where they can pursue other interests. They might be interested in working somewhere else for a few months, then returning to their regular role. The whole idea of part-time work being more of a standard rather than working full-time for your whole career.”
In coming months, Coffey-Oates and her husband, a physiotherapist, are planning to travel around Australia, combined with short bursts of work.

“For the next few months, I’ll be based in South Australia doing locum work in Central Australia, and then we’re heading off in June on a trip around the country. We’ll both locum along the way, and I’ll still fly into Central Australia for the Aboriginal community work,” Coffey-Oates says.
To keep informed of work available in Central Australia, Coffey-Oates stays in touch with Brien Holden Foundation and Community Eyecare.
“Brien Holden Foundation normally send out a list of dates they’re visiting outback communities and Community Eyecare have a spreadsheet; I add my name when I’m available, and they arrange the rest,” she says.
“It’s about getting that flexibility for myself to be able to do more of what I want to do. I want to have a mix of remote work, as well as rural or township-based work.”
“WORKING IN OUTREACH COMMUNITIES CERTAINLY HAS ITS CHALLENGES. IT’S VERY DIFFERENT TO NORMAL CLINIC LIFE; THERE ARE NO APPOINTMENTS.”
ALEX COFFEY-OATESBrien Holden Foundation sign at Laramba Health Clinic (Central Australia, NT). Room in Ramingining Community Health Service (Arnhem Land, NT) setup for delivering optometry clinics.

Happier staff, more time, and a safer, more enjoyable patient experience might sound like an eyecare utopia, however, developments in the digital healthcare space mean that many of these concepts already exist in several Australian ophthalmology clinics.


At the vanguard ofOPHTHALMOLOGY’S DIGITAL TRANSFORMATION
Sydney ophthalmologist Dr Peter Sumich can recall a time when the surgeon and patient were satisfied to simply complete a cataract surgery without complication. Today, patients expect this as a given, and are placing greater demands on their eye doctor to provide a refractive outcome optimised to their lifestyle.
For Sumich, this means there is greater need to closely inspect each data point for the patient work up, along with an expectation to have the patient actively involved in the IOL selection and planning of their surgery.
This trend means the traditional method at Hunter Street Eye Specialists –where staff collate volumes of data from print-outs and USB sticks to build a surgical plan – is no longer efficient and effective.
But, much of the redundant, manual work in Sumich’s practice has been eliminated after investing in ZEISS EQ Workplace, a cataract surgery planning solution developed by ZEISS which allows him to have biometry, other vital scans and a calculation platform all on a single display, with minimal manual data entry.

“With cataract and refractive surgery we are trying to pull together huge volumes of diagnostic data to make important and integrated decisions about
Sumich is the first to admit he is slow to change his habits, unless convinced otherwise. This shift towards digitalised workflows has seen IT infrastructure and support become a significant area of investment and focus for the practice.
“The saving on staff time has been tremendous. Frankly they love it as much as me. The biometry data from the IOLMaster is automatically populated into the networked – EQ Workplace, eliminating risks of transcription errors and making paper redundant,” he says.
“Topography, aberrometry and Hill RTC (still manual) are dragged and dropped into the additional data panels. ZEISS EQ Workplace includes the Barrett TK toric software which is my base formula and if needed I can manually add integrated Ks. All the other common formulas are there, although the Kane is notably absent.”
To use EQ Workplace to its full extent, the surgical plans can be stored on the cloud ensuring the surgeon can access them from the mobile device at multiple sites, including at the operating theatre. The patient’s work-up data in the cloud can link with ZEISS Callisto eye, a computer-assisted cataract surgery system.
EFFICIENT, MORE EFFECTIVE CLINICS
EQ Workplace is an example of how ZEISS is helping lead the digital transformation taking place in ophthalmology. It is achieving this through integrated workflows where devices talk to one another and comprehensive data management solutions.


By connecting devices, data and applications, the company has created an ecosystem helping eye doctors optimise the clinical management of their patients. Each ZEISS ophthalmic workflow can be broken into four distinct areas: 1. Assess & educate, 2. Plan, 3. Treat, 4. Check.
In the case of the Cataract Workflow, this could involve ZEISS IOLMaster biometry and the ZEISS Eyeguide Patient App (Assess & educate), ZEISS EQ Workplace and ZEISS Digital Ordering Platform (Plan), ZEISS OPMI Lumera 700 ophthalmic microscope, ZEISS Quatera 700 phaco system and the aspheric monofocal intraocular lens ZEISS CT Lucia 621 (Treat), and then a ZEISS slit lamp (Check).
According to ZEISS, the benefits derived from increasing developments in digital technologies are not limited to improvements in the treatment of cataracts. Significant advances in how huge volumes of data can be managed and analysed have created opportunities across the entire ophthalmological space.
In a recent expert interview about digital technology in ophthalmology, Mr Euan S. Thomson, PhD, president of ophthalmic devices & head of digital business unit at Carl Zeiss Meditec, says ophthalmology is an amazing environment where the eye is the window to the identification of so many different conditions.

“However, this is hard to do if you don’t embed tools like artificial intelligence into the environment. When you do it opens up many possibilities for patient management,” he says.
“There can be a huge number of variables associated with a patient and the more variables, the more data points you need to draw conclusions. However,

the number of patients that a physician can see during their entire career may not be enough to collect the needed data points to interpret some of those nuanced variables. If you aggregate the data and bring the data together on one platform you can then learn collectively.”

As this digital transformation accelerates, the ANZ market has recently seen the previously mentioned ZEISS Eyeguide Patient App being trialled. This app supports patients in their treatment journey allowing them to refer to information relevant to their upcoming cataract surgery, in turn, helping to reduce patient counselling time. The virtual coach tool also includes features such as pre- and post-operative checklists or eye drop notifications to improve compliance and overall experience.
Also in the pipeline, ZEISS has developed the Surgery Optimizer App that leverages artificial intelligence in surgical videos to enable surgical performance tracking, improvement and standardisation of surgical techniques.
ZEISS views the next 24 months “as an exciting time” as these product launches will see adoption of digital technologies gain further momentum among Australian and New Zealand surgeons.
“WITH CATARACT AND REFRACTIVE SURGERY WE ARE TRYING TO PULL TOGETHER HUGE VOLUMES OF DIAGNOSTIC DATA TO MAKE IMPORTANT AND INTEGRATED DECISIONS ABOUT REFRACTIVE TARGETS, LENS CHOICES AND EXCIMER LASER STRATEGIES.”
DR PETER SUMICH, OPHTHALMOLOGIST
Turning
OVER A NEW LEAF
Emerging Danish ophthalmic lasers company Norlase has developed a compact photocoagulator that’s a tenth the size of competing systems. Voice control and its ability to slot on to an existing slit lamp are among other features that led to A/Prof GEORGE KONG being one of the first to install the system in Australia.
Associate Professor George Kong’s private clinic, Mt Waverley Eye Surgeons in suburban Melbourne, was established five years ago, and geared towards his subspecialities in glaucoma and complex cataract. But the clinic also cares for a high number of retinal disease patients, many whom require laser treatment.
As one of the only Victorian ophthalmologists with a diode laser in his rooms, Kong had access to a highly effective therapy for his glaucoma patients delivering a wavelength of 810nm. While the laser could also be applied to retinal conditions such as retinal tears and holes, the system could be less efficient and comfortable in those cases. It is also less efficient in performing laser suture lysis for trabeculectomy procedures.
A green photocoagulator system was required, so he canvassed the market and sought the services of OptiMed Australia. The local ophthalmic equipment distributor had recently signed an agreement with emerging Danish ophthalmic device manufacturer Norlase to import its laser systems into Australia. It recommended Kong trial Norlase’s LEAF Green Laser System.
It wasn’t long before the manufacturer’s compact green photocoagulator was installed in his rooms.
“Several features attracted me to the Norlase LEAF, including its compact size (10 times smaller than existing systems). It also mounts directly to my pre-existing slit lamp and the alignment is very easy to adjust. For a small clinic, space is always at a premium, so it’s important to have equipment that doesn’t occupy too much room,” he says.
“The other thing that interests me is the option of performing subthreshold laser treatment, which I think will be increasingly used in the future in retinal conditions. Although this isn’t being adopted widely yet, having that option means I will be futureproofing my practice to potentially reduce some of the frequency of intravitreal injections for some macular conditions.”
For Kong, who became a RANZCO Fellow in 2016, it’s been interesting to see a newcomer like Norlase enter the ophthalmic lasers market.
While a new player, the company has originated from years of laser experience from within a prolific global laser manufacturer. The firm describes itself as a developer of next-generation laser solutions for retina and glaucoma that also work to improve practice efficiency, patient care, and convenience for ophthalmologists worldwide.
Mr Oliver Hvidt is a co-founder of Norlase, which started as a university research project, alongside high-tech entrepreneur Mr Peter Skovgaard who has a PhD in high-power semiconductor lasers and more than 20 years of experience in bringing photonics technology from research to market.
LEAF is one of three products developed by Norlase, which also produces ECHO, described as the world’s first ultra-portable pattern scanning laser, and LION, the first fully integrated, battery-powered laser indirect ophthalmoscope (LIO) and green laser.
According to OptiMed, the LEAF laser system is the size of a tablet or iPad, making it one of the most compact and versatile treatment additions to ophthalmic practices. Its sleek, smart design is said to be 10 times smaller than

Norlase had a major focus on developing a sleek, smart design, with the system 10 times smaller than existing lasers.
existing systems. It also features a built-in laser source which means there is no external fibre, eliminating one of the most common and costly service repair issues of laser photocoagulators.
Its size also means the system is portable so practitioners can easily share among multiple practices. Although Kong doesn’t expect to transport the system between his Mt Waverley and Box Hill clinics – the latter which is primarily focused on cataract – he says it’s nice to have this functionality for the future.

What he has been particularly impressed by, however, is Norlase’s use of industry-first speech recognition that allows for convenient control of laser parameters.
“It means I can control the machine to change the treatment power or treatment intervals while I’m doing the procedure, without having to stop and manually change those settings,” he explains.
“Treatment power is something that needs to be adjusted frequently in some cases, depending on the retinal reaction and also whether the patient has any discomfort. It can be awkward having to stop and change the power on the dial and then reapply the laser lens, but it’s much easier now with voice control – it’s a very useful function.”
FITTING LEAF INTO THE CLINICAL WORKFLOW
Since acquiring LEAF, Kong mainly used the system for laser retinopexy treatment of retinal tears, and holes. For his medical retinal colleague, Dr Rathika Kandasamy, who works in the practice, it also allows her to perform procedures like panretinal photocoagulation for proliferative diabetic eye disease.
Being able to provide an optimal laser therapy for retinal patients at Mt Waverley Eye Surgeons was important for Kong and Kandasamy.
The LEAF system promises to be a game-changer for more routine retinal procedures in the clinic, but, as outlined earlier, Kong is also excited about its capability to perform subthreshold laser procedures. This approach encompasses all types of laser treatment that show no visible signs or colour change of damage – as intended in retinal laser procedures – but still has a therapeutic effect through lower power.
“I’m quite excited about this treatment option. There are a few published papers on the treatment of central serous chorioretinopathy (CSC) with subthreshold laser,” he says.
“Increasingly, retinal subspecialties are looking at the use of this technology for these conditions and I think this is an ideal way to prepare my practice for the future, particularly with CSC patients. It is important to provide an effective treatment for macular conditions while keeping the risk of the procedure to a minimum.”
COMPELLING TECHNOLOGY AT A COMPELLING PRICE
While the Norlase LEAF system is designed to allow ophthalmologists to treat more patients while maximising practice space and providing greater quality of care and safety, another interesting aspect is its price point.


The company is selling the system at what it describes as a “compelling” rate, making it easier for clinics to expand into laser treatments.
“That’s another reason I ultimately went with this system – it comes at a reasonable price point as far as retinal lasers are concerned,” Kong says.
“A lot of clinics find it difficult to justify investing in a retinal laser because retinal conditions require laser less frequently than something like a YAG system (for capsulotomies). So having a good price point will likely allow me to get a get a return on investment earlier.”

Overall, Kong says it has been interesting to watch Norlase emerge as a new player with differentiated technology in the ophthalmic market. It’s a development that can only help improve the clinical performance of eye specialists and patient outcomes.

“Overall, I’ve been very happy with the LEAF system. It’s easy to use, the design is slick and compact, and the device controls using an intuitive touchscreen tablet have been straight-forward,” he says.
“Having voice control and speech recognition, as I say, it is quite a neat feature, and of course there is the foot pedal to control the actual treatment. All in all, it’s a great user experience, and the laser is very easy to control.”
"THE OTHER THING THAT INTERESTS ME IS THE OPTION OF PERFORMING SUBTHRESHOLD LASER TREATMENT, WHICH I THINK WILL BE INCREASINGLY USED IN THE FUTURE IN RETINAL CONDITIONS.”
A/PROF GEORGE KONG MT WAVERLEY EYE SURGEONSThe system features an intuitive touchscreen tablet, as well as speech recognition that allows for convenient control of laser parameters.
A microstent WITH MACRO RESULTS
It was important for the national health system, and indeed global ophthalmology, when Australia became the first global market to access the Hydrus Microstent. That was officially in 2018, but the minimally invasive glaucoma surgery (MIGS) device had been in use in Australia since 2013/14 when the manufacturer tested its real-world performance with a select group of local surgeons.
NSW glaucoma specialist Associate Professor Ashish Agar was part of that first wave of surgeons to implant the canal-based device for adult patients with primary open-angle glaucoma (POAG) almost 10 years ago.

“At the time it was the only device available to us as part of the new MIGS category, and I was lucky enough to be trained in-person by the bioengineer who designed the Hydrus Microstent,” Agar explains. “He travelled from the US to take me through my first list at Marsden Eye Specialists in western Sydney, which was in the very first week that the device was used in Australia. It was the most amazing introduction.”
Since then, the Hydrus Microstent (acquired by Alcon in 2022) has cemented its place as one of the most commonly used MIGS devices in Australia, in addition to the iStent system (Glaukos, first approved in 2015), and iTrack (Nova Eye Medical). Xen (Allergan, approved 2017) and Preserflo Microshunt (Glaukos, approved 2021) are part of another category Agar describes as MIBS or ‘minimally invasive bleb-forming surgery’ for later stage glaucoma.
Since their arrival, MIGS devices have come to occupy the middle ground of glaucoma treatment in Australia, addressing the gulf between first line therapies such as eye drops and selective laser trabeculoplasty (SLT) and more invasive interventions such as trabeculectomy and tube shunt surgery. Being a new type of medical technology, MIGS have navigated uncharted waters with the TGA, before eventually securing Medicare reimbursement as a standalone or combined treatment with cataract surgery.
In the case of the Hydrus Microstent, it is 8 mm in length, contoured to match the curvature of Schlemm’s canal, and made of nitinol –considered a highly biocompatible material. Using a gonioprism, the device is inserted through a clear corneal incision and guided through the trabecular meshwork into the canal. Once in position, it is advanced until the device has scaffolded approximately 90° of Schlemm’s canal, ensuring access to collector channels. Ultimately, the stent provides outflow pathways for aqueous, helping lower intraocular pressure (IOP) and reduce medication burden.


The device was developed by Californian firm Ivantis, which was acquired by Alcon in 2022 in a deal worth well over AU$600 million.
WHAT THE STUDIES SAY
Agar points to several reasons for the Hydrus Microstent’s success. The most notable is the robust data showing, among other findings, that it:
• I s consistent over time – critical when considering glaucoma is a long-term disease.
• S ignificantly lowers IOP with or without cataract surgery.
• R eal-world data matches that published in a randomised trial.
The HORIZON and SPECTRUM studies have been the most notable studies for Hydrus.
HORIZON is described as the largest prospective, randomised, controlled MIGS pivotal trial to date, while SPECTRUM is a global registry initiated in Australia to understand how it worked in the real world.
In HORIZON, Alcon says the device is the first and only MIGS implant to report clinical results from a pivotal trial at five years. included 556 patients at 38 centre from nine countries.
Importantly, it showed 66% of Hydrus Microstent patients remained medication-free at five years. The study has also demonstrated a relative reduction in incisional secondary surgical interventions (SSI) such as trabeculectomy, tube shunt and gel stent, for Hydrus Microstent patients compared to cataract surgery alone (2.4% in Hydrus+CS vs. 5.3% in CS only). 3 And the Hydrus group included a higher proportion of eyes with IOP of 18 mmHg or less without medications than the cataract surgery group.
More recently, the HORIZON results have shown the device lowers the rate of visual field loss by 47% versus cataract surgery alone. This finding was delivered in November 2021 by world renowned glaucoma specialist Dr Iqbal “Ike” Ahmed who said since the inception of MIGS, the narrative has been largely restricted to IOP lowering, medication reduction and invasive secondary surgery rates. However, the visual fields finding was important because there was now data indicating Hydrus is affecting the underlying disease itself. 4*
In terms of safety, the device has shown this over the long-term with comparable serious adverse rates reported vs cataract surgery alone. The five-year HORIZON data also showed “no clinical or statistically significant differences” in the key measure of endothelial cell loss from three to 60 months between the Hydrus and cataract surgery alone groups.1
For Agar, when he started using the Hydrus Microstent, safety was the most important consideration, given this was an entirely new field for glaucoma specialists.
The Hydrus Microstent, now owned by Alcon, has helped change the game when it comes to surgical options in glaucoma. A/Prof ASHISH AGAR reflects on the MIGS device’s past, present and future in Australia.
“IN THE OUTBACK, IT’S BEEN A GAME CHANGER TO PROVIDE AN OPTION THAT YOU CAN SAFELY DO IN A REMOTE AREA, WITH VERY LITTLE FOLLOW UP CARE REQUIRED.”
A/PROF ASHISH AGAR OPHTHALMOLOGISTThe Hydrus Microstent was recently acquired by Alcon.
“In the early days, we were very much still learning about it. Even though MIGS is considered an intermediate step that can be used frequently today, early on we didn’t want to take any risks, so at that stage, we were trialling it in patients who were running out of options,” he says.
“And when we had success in those patients, it gave us confidence to say ‘this is something that could make a difference – now, I’m going to start to use it more regularly’.”
Agar says he was also reassured when Hydrus’ manufacturer established the SPECTRUM registry, which was mandatory for all devices implanted early on.
“Every single Hydrus implanted in those early years was tracked in the SPECTRUM Global Registry, which was also granted ethics approval by RANZCO in 2014 and now involves almost 3,000 eyes from around 18 countries. That way we knew there was no way of hiding or trying to message the results, it was there for everyone to see. For me, that meant the highest possible level of monitoring, audit, and evidence collection. I thought that was a brave call from Ivantis at the time,” Agar says.
There’s also a third and important study involving the device. The COMPARE study was the first prospective, randomised, multicentre trial comparing Hydrus Microstent to two iStents Trabecular Micro Bypass implants without the confounding effect of cataract surgery (standalone). The study included 152 patients at 12 centers across 9 countries.
According to Alcon, key findings included: ~2x more Hydrus Microstent
patients were medication free compared to patients with two iStents at 12 months; mean medication reduction of 1.3 (52%) vs. 0.8 (30%) in the 2 iStents patients at 24 months; and at 24 months, Hydrus Microstent demonstrated a low incidence of secondary glaucoma surgery – none vs 9.1% in the two iStents group. 5
THE SURGICAL EXPERIENCE
Agar is “device-agnostic” when it comes to glaucoma surgical options. It ultimately comes down to the data and what’s best suited to the patient. While noting the effectiveness and safety of all MIGS devices are comparable, he says there are differences in the surgical experience for the ophthalmologist.
“When it comes to MIGS, I seem to have greater confidence in terms of effectiveness and reliability with the Hydrus stent. It differs from other techniques allowing me to titrate and adjust my technique until it’s just right. If it’s in a good position, you can easily tell, and if it’s not, you can dial it out and do it again. This can be done as many times as you need until you’re happy,” he explains.
“For me, that ability to adjust it on the operating table until you get it right is key.”
Alcon describes Hydrus as an “intuitive delivery system” that allows for a straightforward procedure with no need to target collector channels or implant multiple devices. 3

As such, Agar says the Hydrus Microstent has also benefitted patients as part of his outreach work in Broken Hill, a frontier mining town in the far west of New South Wales, more than 1,100km from Sydney. The first of these was in March 2018 when he performed the first Hydrus procedures outside a major metropolitan city, with four patients receiving the Hydrus Microstent at Broken Hill Base Hospital. At the time, he described it as “a boon for equity of access to specialist medical services for people living in the bush”.
Today, Agar still agrees with that assessment.
“These are places where patients can’t visit your rooms each week for follow up after trabeculectomy to have their sutures done etc. So in the outback, it’s been a game changer to provide an option that you can safely do in a remote area, with very little follow up care required.”
With the introduction of MIGS, Agar says glaucoma specialists can now offer surgical options at a much earlier stage in a patient’s journey, potentially avoiding a trabeculectomy or delaying it until absolutely necessary.
“It’s about getting better control over disease at an earlier point. What’s really changed is that it’s opened up so many more choices to consider for our patients, options we didn’t have before,” he says.
“Now, our ability to control IOP is much better and it means we’re moving to a different paradigm that Dr Ike Ahmed describes as: ‘surgical glaucoma, not as your last resort, but as an anytime resort'. You do it when the patient needs it, not when you’re too worried that nothing else is left."
NOTE: *Indications for Use: The Hydrus Microstent is intended for the reduction of intraocular pressure (IOP) in patients with primary open angle glaucoma (POAG) as a standalone treatment or in conjunction with cataract surgery.
REFERENCES:
1. A hmed I, et al; HORIZON Investigators. Long-term Outcomes from the HORIZON Randomized Trial for a Schlemm’s Canal Microstent in Combination Cataract and Glaucoma Surgery. https://www.aaojournal.org/article/S0161- 6420(22)00160-9/fulltext
2. S afety & Effectiveness Study of the Hydrus Microstent for Lowering IOP in Glaucoma Patients. ClinTrials.gov (NCT01539239)
3. S amuelson TW et al, A Schlemmm Canal Micorstent for Intraocular Pressure Reduction in Primary Open-Angle Glaucoma and Cataract: The HORIZON Study. Ophthalmol 2019;126: 29-37.
4. D r Ike Ahmed, November 2021, “New findings ‘alter forever how we think of MIGS’”. Accessed March 2023. www.insightnews.com.au/new-findings-alter-forever-how-we-think-of-migsdr-ike-ahmed/
5. A hmed et al.: A prospective randomized trial comparing Hydrus and iStent micro-invasive glaucoma surgery implants for standalone treatment of open-angle glaucoma: The COMPARE Study (Ophthalmology. 2020;127:52-61)
At her busy private clinic in Queensland, DR SONIA MOORTHY discusses the range of ophthalmic pharmaceuticals she uses to conduct comprehensive work-ups and procedures for her patient-base spanning several age brackets.
MAXIMISING
Minims
After growing up in Malaysia and studying medicine in the UK before eventually training and working as an ophthalmologist in three different medical systems, Dr Sonia Moorthy’s career has taken her to the Sunshine Coast where she established her private practice, EyeHub.

While focusing on more common areas like cataracts, pterygium, glaucoma and macular disorders, she also manages strabismus for adults and children. It’s the culmination of an extensive and varied ophthalmology traineeship that began at Sydney Eye Hospital in 2011, before pursuing paediatric and strabismus fellowships at Singapore’s National Eye Centre and the prestigious Moorfields Eye Hospital in London.
“In my career, I’ve had a worldly experience working in the UK, Australia and Singapore health systems, which was great exposure. When I returned to Australia in 2018 I worked in Cairns as an adult and paediatric ophthalmologist, but I wanted to work independently in a place where I could put some roots down for my family,” she says.
“That led to me establishing EyeHub in 2022 on the Sunshine Coast today where I see adults 70% of the time, and 30% children. My spiel is that I see ‘kids, lids and everything in between’, I very much enjoy diseases of the anterior segment – and so that is where a lot of my focus is.”
With this in mind, Moorthy’s clinic has a significant reliance on ophthalmic pharmaceuticals that allow her to conduct detailed patient work-ups, manage diseases and perform surgery. Products that work as a local anaesthesia, induce pupil dilation and staining the anterior segment are a vital, yet sometimes understated, part of the ophthalmologist’s toolkit.
To do this with confidence, eye clinics need to rely on manufacturers with scrupulous manufacturing practices, with the additional benefit of offering products that avoid preservative-related irritation ocular surface.
For EyeHub, the bulk of its eye health pharmaceutical range is sourced from Bausch + Lomb (B+L), with the company’s Minims range being a go-to in various diagnostic processes and pre-surgery preparation.
B+L’s Minims are used among eye specialists for three significant reasons: single-use, sterile ampules, and preservative-free. Sixteen products are available in the range, which is broken into five categories: Minims Miotics, Minims Mydriatics & Cycloplegics, Minims Local Anaesthetics, Minims Stains and Minims Other.
B+L’s pharmaceutical range in Australia also encompasses Diagnostics Strips (Fluorets 1 mg), Acetylcholine Chloride 20m / 2mL (Miochol-E: to
obtain complete miosis of the iris in seconds after placement of an IOL and in penetrating keratoplasty, iridectomy and other anterior segment surgery), and dry eye syndrome therapies Viscotears Eye Gel* 10g Tube and Viscotears Gel PF* 30 x 0.6g Single Dose Units.
For Moorthy, the reason B+L’s Minims have been commonly used in her practice comes down to the fact that the ocular surface is such a fragile entity.
“Considering the majority of patients we see are elderly, anything that minimises preservative contact with the eye, especially in the context of repeated procedures or repeated injections, is going to be beneficial to the patient,” she explains.
“Ultimately, I want to help afford better protection of the ocular surface, which is something that perhaps we underestimate. A lot of these patients may have co-existing dry eye disease – and repeated examinations with repeated drops, even with small quantities of preservatives, may have a long term impact.”
The most commonly used Minims in Moorthy’s clinic are:
• M inims Cyclopentolate Hydrochloride 0.5% & 1.0% Eye Drops (indication: to produce mydriasis and cycloplegia)
• M inims Oxybuprocaine Hydrochloride 0.4% (indication: to produce local anaesthesia in the eye for short opthalmological procedures)
• M inims Phenylephrine Hydrochloride 2.5% (indication: to dilate the pupil for diagnostic or therapeutic procedures)
• M inims Fluorescein Sodium 1.0% & 2.0% (indication: for staining the anterior segment of the eye and assessing the tear film integrity)
“Considering 30% of my patient base are children, I frequently use cycloplegic drops for cycloplegic refraction. In these exams, I would use Minims Cyclopentolate Hydrochloride 1.0% for anyone 12 months and above, and 0.5% under 12 months,” she says.

“The safety profile of this drug is good, but that’s only part of the picture, you don’t want to create any additional localised irritation arising from the drug. And that’s why Minims is such a helpful option for children.”

When it comes to dilation of her adult patients, Moorthy often uses Minims Phenylephrine Hydrochloride 2.5%. In patients with retinal issues who don’t dilate as easily, it affords her better visualisation of the fundus.
“I try to avoid cyclopentolate hydrochloride for routine dilation in adults because it tends to paralyse accommodation for too long, so that’s why phenylephrine hydrochloride 2.5% appeals. It also allows diagnostic differentiation of anterior segment inflammation, for example episcleritis versus scleritis,” she explains.
“However, intraoperatively is where it is most useful because phenylephrine allows additional splinting of the iris and pupil dilation in patients who have a floppy iris, which again is a very common scenario now in elderly patients.”
Moorthy believes one of the most versatile therapies in her toolkit is Minims Oxybuprocaine Hydrochloride 0.4%. In her clinical practice, it’s routinely used as a local anaesthesia in procedures such as anti-VEGF injections, conjunctival biopsies and cataract surgery.
“I have been performing topical cataract surgery routinely for around three

“WITH TOPICAL SURGERY, THE WHOLE POINT IS TO ALLOW FASTER VISUAL RECOVERY WITHOUT EPITHELIAL DEFECTS OR OCULAR SURFACE COMPROMISE – SO THAT’S WHERE OXYBUPROCAINE HYDROCHLORIDE REALLY SHINES.”
DR SONIA MOORTHY EYEHUB
Dr Sonia Moorthy’s most-used Bausch + Lomb pharmaceuticals are (from left) Minims Cyclopentolate Hydrochloride 0.5% & 1.0% Eye Drops, Minims Oxybuprocaine Hydrochloride 0.4%, Minims Phenylephrine Hydrochloride 2.5%, and Minims Fluorescein Sodium 1.0% & 2.0%.
years now, and I insist on pre-op prep with oxybuprocaine hydrochloride. In cataract surgery, you want the corneal surface to be as pristine as possible – and with topical surgery the whole point is to allow faster visual recovery without epithelial defects or ocular surface compromise – so that’s where oxybuprocaine hydrochloride really shines.”

The final most-common therapy used at EyeHub is Minims Fluorescein Sodium 2.0%.





Moorthy frequently uses the therapy in her paediatric patients with anterior segment problems, including blepharokeratoconjunctivitis, vernal keratoconjunctivitis and atopic keratoconjunctivitis. Although 2.0% is the higher dose, she finds it often dilutes with the tear film when the patient blinks.
“I find it provides good visualisation of the anterior segment structure, particularly follicles, limbal lesions and corneal epithelial defects, and it’s child-friendly because it doesn’t sting their eyes, which makes them more receptive during the consultation,” she says.

“Then inter-operatively, I use it during syringing and probing to establish nasolacrimal duct patency post successful probing.”
Overall, Moorthy says it’s vital to have access to preservative-free ophthalmic pharmaceuticals, particularly when patients may present with other pre-existing ocular surface conditions or concurrent preserved drop usage.
“In my practice, I’m very particular about maintaining the health of the ocular surface, and emphasise this in my approach to all patients, particularly the elderly” she explains.
“At the end of the day, it’s often a long-term relationship we are building with the patient. The presence of dry eye disease in general population is underestimated – and anything that I can do to minimise that burden on the patient, especially something as simple as this, is worth doing.”
NOTE: Always review product information before prescribing these medications. Product information is available on request from Bausch + Lomb on 1800 251 150. *PBS Listed

Material was prepared in March 2023 © 2023 Bausch & Lomb Incorporated. ®/TM are trademarks of Bausch & Lomb Incorporated or its affiliates. Bausch & Lomb (Australia) Pty Ltd. ABN 88 000 222 408. Level 2, 12 Help Street, Chatswood NSW 2067 Australia. (Ph 1800 251 150)
An optomap of Optos
In 1990 in the small Scottish city of Dunfermline, a 30-minute drive north of Edinburgh, five-year-old high myope Leif Anderson suffered a blinding retinal detachment. It was an event that would not only alter the course of his young life, but that of the ophthalmic imaging technology.
Leif’s father, Douglas, was perplexed. His son had regular eye examinations, but no one had picked it up with existing instrumentation. While he didn’t have any ophthalmic or academic experience, Douglas funnelled his experience as a healthcare product development expert into inventing a device that would ensure others with missed pathology in the retinal periphery did not face the same fate as his son.
Primarily he was concerned with scanning the peripheral retina of a young child without dilation, but discovered along the way that even adult retinal examinations needed improvement.
Two years later in 1992, Optos (called Zenoplan Ltd at the time, then Besca Ltd) was born, with the goal of producing a patient-friendly device to capture a much broader image of the retina than anything else in the market. Through this, Optos developed a device capable of ultra-widefield (UWF) high resolution digital images called optomap that capture approximately 82% and 200° of the retina, something the company says no other device can do in a single capture.
As Optos – whose Australian subsidiary is based in Adelaide – marks 30 years in business, it counts itself as a market leader in its field. It has progressively improved its technology over the decades to now offer four core imaging platforms – the Daytona, California, Monaco and Silverstone – with tens of thousands of devices installed globally helping millions of patients. Silverstone, launched in 2019, spearheads the Optos portfolio today. It’s unique because it is the only UWF retinal imaging device with integrated, UWF-guided swept-source OCT. It also takes a 200° single-capture optomap image in less than half a second and enables guided OCT scanning across the retina and into the far periphery.
The quality of Optos’ technology is such that the company has reported significant growth with record revenue of US$254 million (AU$385 m) in the year to March 2022, up 14%.

“We are proud of what Optos has achieved over the past three decades. We have remained true to Douglas’s core purpose of improving patient outcomes by providing the best imaging technology and so reduce the risk of sight loss,” Mr Rob Kennedy, CEO of Optos, says.
practices across Australia and the world, as well as in hospitals including the world’s leading teaching hospitals such as Great Ormond Street Hospital in London and Harvard Medical Center in Massachusetts.
Because the business has continued to invest significantly into research and development, it has continuously released new and improved versions of its UWF devices. For the year ended March 2022, it’s R&D budget amounted to US$18.6m, up more than 40% on the previous year.
This commitment to continual improvement has seen its early models such as the Plus 180 (first displayed at the American Academy of Ophthalmology in 1995) and the Panoramic 200 (launched at the American Academy of Optometry and the American Academy of Ophthalmology in 1999) morph into its current crop of devices, with the first of these, Daytona, launched in 2011.
Today, Optos says more than 2,000 published clinical studies show the long-term value of optomap imaging and OCT in diagnosis, treatment planning, and patient engagement. Some highlights include:
• optomap improves management of retinal detachments: one study showed the technology was equivalent to dilated fundus examination (DFE) when assessing rhegmatogenous retinal detachment (RRD) and was also consistent with intraoperative findings
• optomap improves clinic efficiency: a study conducted at a prominent research university found a 28-minute (33%) reduction in patient visit duration after implementing centralised optomap imaging
• optomap-guided OCT with Silverstone improves patient management: studies have shown this imaging impacts clinical decision making in 84% of cases, and 69% of cases had pathology only in the periphery while 31% had pathology in the central pole. In 38% of cases, optomap navigated SS-OCT
Beyond its superior retinal imaging technology, Optos has a rich history that all started with a father motivated to right an avoidable wrong that happened to his son.Optos founder Douglas Anderson (right) with his son Leif.
directly contributed to patient management plans (laser, injection or surgical treatment).
• optomap equivalent to Early Treatment Diabetic Retinopathy Study (ETDRS): The results of several studies comparing optomap images have indicated that there is substantial agreement with ETDRS 7-standard film photographs and dilated fundus examination in determining diabetic retinopathy severity.
THE OPTOS BUSINESS, HERE AND ABROAD
Optos has an intriguing history beyond the technology itself. Anderson, the company’s founder, met the late Queen Elizabeth in 2006 to receive the Order of the British Empire for his distinguished service to the sciences. Acquisitions have also formed part of the company’s journey, such as the 2011 takeover of Opko Instrumentation for its OCT technology.
More significantly, Optos itself was acquired in 2015 by Nikon, a Japanese company famous for cameras and binoculars. Bringing Optos into Nikon – in a £260 million (AU$470 m) deal – is part of the latter’s strategy to develop a global medical business.
Although Optos is now a division of Nikon, the Optos business employs more than 500 people in a variety of roles including R&D, manufacturing, clinical research and sales.
In Australasia, the business is headed up by managing director Mr Jason Martone. Optos Australia bases itself in Adelaide with employees serving all states and New Zealand. The technical support team takes care of installations and everything associated with product, with staff also selling and providing product training for eyecare professional customers.
The Optos AU NZ office provides support to Asia Pacific distributors of Optos devices. This includes customer service for APAC and the Middle East and parts of Africa, with additional functions such as orders coordination, technical support and shipments.
A major and recent addition to the Optos Australia business has been optometrist and Optometry Board of Australia board member Ms Renee Slunjski, who has taken on a newly created role as a regional product specialist.
Martone says Slunjski will play an important role in ongoing training, meaning customers can see first-hand how to integrate Optos systems into their practice.
“As an additional resource for customers, Renee will interact with internal and external customers, including optometrists, ophthalmologists, practice
TIMELINE
1990 – Fiv e-year-old Leif Anderson suffers a spontaneous retinal detachment. His father, Douglas, commits to develop an advanced retinal imaging system
1992 – Optos registered with the name Zenoplan Ltd which changed to Besca Ltd then became Optos Ltd
1995 – Plus 18 0 device first displayed at the American Academy of Ophthalmology
1998 – Panoramic 200 is granted a patent and approved for sale in Europe. US Headquarters opens
1999 – Panoramic 200 system launched at the American Academy of Optometry and the American Academy of Ophthalmology
2006 – Douglas Anders on receives the Order of the British Empire in recognition of his distinguished service to the sciences from Her Majesty Queen Elizabeth
2011 – D aytona system introduced. 30 millionth optomap patient imaged. Optos acquires Opko Instrumentation for OCT technology

2014
– California system revealed at the American Academy of Ophthalmology
2015 – Optos acquired by Nikon Corporation
2018 – Monaco s ystem launched
2019 – Silv erstone launched. Over 150 million patients imaged
2022 – Optos 30th Anniversary
personnel, product managers and the sales team,” he says.
“Renee will partner with the sales team to ensure that optometrists and ophthalmologists develop a thorough understanding of our optomap devices. She will take the lead in education: confirming the practice needs, running product demonstrations – both in person and virtual.”
Because Optos aims to be “the standard of care” for all optometrists and ophthalmologists, Martone says the company services a broad range of customers from small independent practices through to large groups, hospitals – and anyone else providing eyecare services.
Several factors make the technology a tantalising prospect for various practices types and sizes, particularly when it comes to workflow efficiency, ease-of-use and disease detection.
“optomap is the only UWF technology proven to improve practice flow. The technology has been proven to reduce patient visit time and improve practice flow and practice economics,” Martone explains.
“Optos UWF imaging is the best investment for increasing patient throughput and improving practice economics.”
In addition, optomap ultra-widefield (UWF) systems – said to be the only device offering single-capture UWF non-mydriatic images – have been shown to help doctors find more pathology. Martone cites a 2021 report that found 97% of optomap users reported finding unexpected pathology in the eyes of patients with no visual complaints.
“This means that Optos UWF imaging might be the eyecare professional’s most powerful tool in the fight to protect vision,” he says, adding that optomap imaging have been shown to improve treatment decisions.
“optomap UWF imaging is a proven tool for effective clinical decision making. Optos UWF technology is helping tens of thousands of eye doctors make better clinical decisions every day.
“optomap imaging is also enabling eyecare providers to see and document the retina with no face-to-face interaction; therefore it may help protect patients and staff by reducing the spread of airborne disease.”
With such a rich and varied history, Optos can count itself as an ophthalmic imaging powerhouse. But despite its global footprint, it’s remarkable to consider how the corporate firm has stuck to the guiding principles laid out by founder Douglas Anderson three decades ago. And with an aging population and more children suffering high myopia like Anderson’s son, Leif, the technology has potentially never been more relevant.
GLOBAL OPTICAL INDUSTRY descending Down Under
The combined O=MEGA23 and 4th World Congress of Optometry in Melbourne promises the biggest show in town come September. While optometry will be a major focus, organisers have released a program that will also be of value to the wider practice team.

It’s important to reinforce just how big a deal this year’s O=MEGA23 will be for the national optical sector. For the first time, Australia’s biggest eyecare and eyewear fair will combine with the fourth World Congress of Optometry (WCO4), creating the most credentialed and largest optometric clinical conference in the Southern Hemisphere.
The event (8-10 September in Melbourne) presents a rare chance to showcase Australian optometry on the world stage – and while a large portion of the show will be devoted to the profession, it’s also a vital opportunity to upskill front-of-house staff who play an essential role in running optical businesses across the country.
To acknowledge the importance of practice managers and optical dispensers, in particular, this year’s O=MEGA23/WCO4 will feature a Masterclass program, that will for the first time comprise two separate streams for each profession. Topics such as inventory management, succession planning and building a myopia specialty practice will feature in the practice manager’s stream, among others, while the optical dispensing stream will feature issues like lens and lifestyle needs for presbyopes, the emerging field of repeated low level red light therapy for myopia, and common dispensing myths and misconceptions, plus more. Fan favourites including top tips sessions will also be presented.
Ms Amanda Trotman, acting CEO of the Optical Distributors and Manufacturers Association (ODMA) which is running the event with Optometry Victoria South Australia (OV/SA), says it’s important to offer an event tailored to all functions within the practice, and not just optometry.
While in the past non-optometry staff may have attended O=MEGA for the trade show, offering an educational component for practice managers and dispensers ($50 per session) is aimed at improving business performance, particularly in the independent setting.
“In my prior career, the focus was helping small businesses improve their operations and profitability, and build a close-knit, well-oiled team,” she says.
“OV/SA is building a strong clinical program with CPD for optometrists at O=MEGA/WCO4. The clinical and the health side is crucial; it’s where everything stems from in terms of getting people into the practice. But most people purchase products like glasses after their consult, so ODMA is bringing its own educational element to the event that’s all about getting the rest of
the team trained and motivated to make the most of that opportunity for the business.”
Trotman says when practices invest in live event attendance for the wider team, it ensures they are up-to-date with the latest offerings. They’re also able to access cutting edge research, hear content specific to their role and understand how their contribution fits into the overall success of the practice.
“This is a valuable outcome that will provide a return on the investment made in both time and money to attend,” she explains.
“Time out of the day-to-day running of the business is not a luxury; it is a necessity to stay competitive in these challenging and fast-changing times. My love of live events is that you never know who you might meet or what you might
WHY YOU SHOULD ATTEND O=MEGA23/WCO4:
• Multiple s treams of exciting CPD compliant clinical content for optometrists
• Access to an array of national and international speakers
• Poster sessions with their authors available for discussion
• Mas terclass streams in Practice Management and Dispensing topics
• 9,000 sqm of quality suppliers in the trade fair displaying the latest product and service offerings
• Product demonstrations and promotions
• Soci al networking events
• Awards presentations
• O ptional social tours and industry relevant site visits
• The chance t o visit Melbourne and a conference centre that is a leader in sustainability

hear that could open up a whole new world of opportunity.”
Trotman says it is important for attendees to go into the conference with a plan. They must consider their key reasons to leverage the attendance and seek out people and content that fits that objective.
“Planning ahead is crucial, as well as making a personal time planner of what sessions you will attend, which suppliers you should meet and peers you can seek out – which is now easy with the wonderful invention of conference apps,” she explains.
“Reading speaker bios and considering a question or two you would love to ask that speaker and allocating time to seek them out is another great tip. Make a time and place to meet up with likeminded peers at social events and share ideas or even set a discussion topic in advance and hold your own small special interest group. You could brainstorm a challenge that others are no doubt also facing and will all have great input on. You could even request an organiser run certain panel sessions if you feel their agenda is missing some key topics.”
Trotman says the opportunity for practice staff to attend trade events should not be underestimated from a motivational point of view, helping build team comradery and shared experiences.
“All this contributes to employee retention and job satisfaction. Sharing learnings also provides marketing opportunities with your client base post the event and provides another source of engagement and an opportunity to further position your team as leaders in the optical field,” she says.
A SUSTAINABLE EVENT – ON MULTIPLE FRONTS
With an event the size of O=MEGA23/WCO4, it’s rare for an association group to run the entire event in-house, often requiring the services of a professional conference organiser (PCO).
With sustainability being a hot topic in the optical industry now and well into the future, it made sense for ODMA, OV/SA and the World Council of Optometry to partner with Arinex, a Melbourne- and Sydney-based full-service event management company that is Australia’s first PCO to obtain carbon neutral certification, achieving this in 2022.
Another major part of the puzzle is hosting the event at an environmentally-conscious venue, in the Melbourne Convention and Exhibition Centre (MCEC). The facility itself has committed to sustainability targets like eliminating single-use plastics and diverting 90% of waste from landfill by 2025, being 100% powered by renewable electricity by 2028 and reducing its net carbon emissions to zero by 2030.


To date, MCEC has:
• Between 2015 and 2019, reduced its carbon emissions by 22% per m2
• Installed 36 permanent ‘food cubes’, growing herbs, citrus and flowers to supply its menus
• Diverted 62% of all waste from landfill using 17 waste streams in 2018-19
• Installed an Energy Management System, resulting in 30% reduction in energy use since 2016
• In 2019, harvested over 3,100 kilolitres of rainwater and consumed 445 litres of water per m2
Trotman acknowledges events can generate a lot of waste and power consumption, so anything to minimise its environmental footprint is worthwhile, while bringing the issue to the attention of the industry.
The way Arinex runs its events means that all emissions from its activities as an event management company are offset. For O=MEGA23/WCO4, the company will also liaise with exhibitors and sponsors to provide ideas on how they can make small changes that assist the environment. This includes the materials used for signage through to the use of technology to substitute for printed materials, as well as using bags and giveaways made from recycled materials.
Trotman says the event has also made small changes like electronic submissions for abstracts, an app for the show program, and the use of lunch boxes with minimal packaging for delegates.
“The more we do, the better – and the more we bring it to people’s attention.
MASTERCLASSES LINE-UP
Practice Management Stream
• Personalities in practice – Emma Gillies, Purple Consulting
• AI and the future of lenses – Grant Hannaford, Hannaford Eyewear, UNSW
• 7 tips for practice management – Belinda Musitano, Eyes@ Optometry

• Succession planning – Mark Corduff, ProVision
• Building a m yopia specialty practice within a practice/Myopia management for children – Matt Oerding, Treehouse Eyes USA and Emma Gillies, Purple Consulting
• In ventory management to maximise profits – Kate Hall, ProVision
• Skills for trust based selling – Emma Gillies, Purple Consulting
Optical Dispensing Stream
• Practical lens dispensing – 5 skills you can’t do without – Steve Daras, TAFE NSW
• Final checking – The las t word on spectacle quality control –James Gibbins, ACOD
• Accurate measurements for dispensing (includes biomechanics)
– Steve Daras, TAFE NSW
• Myopia management for the optical dispenser – Grant Hannaford, Hannaford Eyewear, UNSW
• A dispens ers guide to understanding lens and lifestyle needs for patients with presbyopia – April Petrusma, ODA
• 5 common m yths or misconceptions to avoid when dispensing –Steve Daras, TAFE NSW
• Myopia control – repeated low level red light therapy – Jim Papas, Eyerising International
• Clinic al lens applications for paediatrics – Grant Hannaford, Hannaford Eyewear, UNSW
• Top 10 tips for quality dispensing – Steve Daras, TAFE NSW
NOTE: Draft at May 2023, subject to change.
From a sustainability point of view, we’ve focused on the suppliers and the venue we chose, but this year we are taking it a step further by building a new category into the Awards of Excellence program for exhibitors,” Trotman says.
The categories she’s referring to are the Sustainable Optical Products / Accessories or Business Processes. It’s designed as a broad category for businesses offering sustainable manufactured goods, and businesses that may have introduced environmentally initiatives that reduce things like packaging and freight.
“We’re encouraging all business that have done something in the sustainability space to make a submission – many are already doing great things, but often the industry doesn’t know and it’s worth highlighting that and celebrating all the great things our industry is doing,” Trotman says.
“At O=MEGA, we always have an award for the best custom booth and smallto medium booth, and this year we’ve added an award for the best “green booth” for exhibitors to think about how they can use more sustainable materials in their displays, focusing on reducing waste, recycling and reusing materials.”
“PLANNING AHEAD IS CRUCIAL, AS WELL AS MAKING A PERSONAL TIME PLANNER OF WHAT SESSIONS YOU WILL ATTEND, WHICH SUPPLIERS YOU SHOULD MEET AND PEERS YOU CAN SEEK OUT.”
AMANDATROTMAN ODMA
TIES Deepening
This year marked the first time since 2019 that Specsavers could hold its biannual Partner Seminar, in an event that offered a bit of everything for its hard-working ANZ store partners across optometry and audiology.

Around Specsavers 1,000 store partners and support team members across Australia and New Zealand gathered at the ICC in Sydney’s Darling Harbour in a jam-packed event featuring everything from business updates, networking opportunities, a Fred Hollows fundraising milestone and an appearance by Australian personalities Hamish Blake and Andy Lee.
Marking 15 years of business in Australia and New Zealand and five years of audiology, it recognised the impact store partners have made in their local communities, including the prevention of avoidable blindness and screening more than 2.5 million people for signs of hearing loss.
The full-day event, on Saturday 1 April, featured store partner panel discussions and business updates from Specsavers’ executive board members Mr Simon Hawkins, global strategy director, and Mr Peter
acclaimed futurologist Mr Magnus Lindkvist, and a Welcome to Country by Gadigal Elder, Uncle Allen Madden.
Specsavers ANZ managing director Mr Paul Bott said the event was a chance for Specsavers’ store partners from across Australia and New Zealand to get together to learn, network and celebrate the last few years of success.


“This year was the first time since 2019 that we were able to hold Partner Seminar, which was previously held biannually,” he said.
“It was fantastic to see old friends and colleagues reunited as well as initiate the hundreds of partners who have joined us since 2019. The energy and passion throughout the day filled me with so much excitement for the years ahead.”
During the day, there was a focus on learning and networking followed by an evening gala dinner where the recipients of the 2022 Specsavers Excellence Awards were announced. The 1,000 partners and support team staff sat down for a formal dinner and dance hosted by Hamish and Andy.

“The Specsavers Excellence Awards are our time to really celebrate the fantastic achievements within the partnership and the partners who are going above and beyond to look after their customers, their teams and their communities,” Bott said.
“There were so many fantastic examples of great partnerships and leaders that it was hard to narrow it down to finalists and overall winners. But in the end the winning stores’ passion, determination, dedication,

resilience, and unrelenting vision shone through.”





















The Excellence Awards recipients were:

• A NZ Best Place to Work – Specsavers Toowong, QLD
• A NZ Loved by Customers – Specsavers Mt Gambier, SA







• N Z Optics Store of the Year – Specsavers Dunedin
• AU Optics Store of the Year - Specsavers Strathpine
• N Z Audiology Business of the Year – Specsavers Whanganui & Palmerston North

• AU Audiology Business of the Year – Specsavers Werribee
This year’s Excellence Awards also included a raffle and auction which raised more than $120,000 for The Fred Hollows Foundation and was topped to $200,000 by Specsavers.



“We’re incredibly passionate about our partnership with The Fred Hollows Foundation in Australia and New Zealand and consider it an honour to have been alongside them as they’ve improved the eye health of Aboriginal and Torres Strait Islanders in Australia and restored and preserved sight in the Pacific. Our donation at Partnership Seminar allowed us to reach a milestone of $7 million to the foundation to date, which is something we are immensely proud of,” Bott added.

The Fred Hollows Foundation founding director, and Fred’s wife, Ms Gabi Hollows, attended the event and in her donation acceptance speech said: “Fred would have been so proud of what this partnership has achieved. He’d be proud to see how hard we’ve worked to continue his legacy and how tirelessly we’ve campaigned to end avoidable blindness. Thank you for all you’ve done over the past 11 years.”
In celebration of the partnership to date, a broach was presented to each store partner which featured The Fred Hollows Foundation’s logo and the words ‘I’m carrying on Fred’s vision’. The broaches will also be sent to all Specsavers store team members across Australia and New Zealand.
Optics Store of the Year NZ (Specsavers Dunedin): Andy Lee with retail partner Dominic Savill, optometrist partners Jennifer Robinson and Tianyuan Qu, dispensing partner Kim Bingham, general manager audiology Darrel Magna, and Hamish Blake. Australian personality Hamish Blake hosting the gala dinner for partners at ICC Sydney.

THE SPECTACLE PRESCRIPTION – MORE THAN JUST NUMBERS
IN PART 1 OF HER ARTICLE SERIES, ODA CEO APRIL PETRUSMA SAYS THE PRESCRIPTION OFFERS A WEALTH OF INFORMATION ABOUT THE PATIENT AND THEIR REQUIREMENTS, IF DECODED CORRECTLY BY THE OPTICAL DISPENSER.
APRIL PETRUSMA
“WHEN A PATIENT PRESENTS WITH AN OUTSIDE PRESCRIPTION OR THE HANDOVER DOESN’T RUN AS SMOOTHLY AS IT SHOULD, OUR PRESCRIPTION INTERPRETATION SUPER POWER COMES INTO PLAY.”
Not every patient that visits the practice will have a typical, easy-to-correct prescription. As dispensers, it’s our role to dissect the prescription prescribed by the optometrist or ophthalmologist, with the aim of finding the best possible solution to meet our patient’s lifestyle and visual needs. It requires a lot more than taking a few measurements and sending an order form to the lab.
On first inspection, the dispenser should be looking deeper than the numbers. This is where it is our job to stop and consider what the numbers on the prescription are actually telling us. We should be looking to identify ocular conditions, pre-empting potential problems with the aim of minimising risk factors, visualising appropriate lens and frame recommendations and planning any measurements that will be required.
In a perfect world the dispenser would have access to patient consultation notes or have a smooth interactive handover with the optometrist but unfortunately this isn’t always the case. When a patient presents with an outside prescription or the handover doesn’t run as smoothly as it should, our prescription interpretation super power comes into play. The prescription offers an enormous amount of information if we look at them closely enough. Whilst it may not be spelt out in words but rather encrypted through the numbers on the piece of paper, our unique skill set means we have the ability to uncover the patient’s ocular conditions.
It’s imperative we do this, as with most ocular conditions comes a range of potential problems that dispensers have a level of control over if identified and treated correctly.
If you follow these six steps when interpreting your prescription, you have the best chance of meeting your patient’s expectations and will keep them coming back for years to come. As soon as you pick up the prescription you should STOP and THINK:
1. What does the Optical Cross look like?
2. What Ocular Conditions can you see?
3. What Potential Problems could they cause?
4. What will be the best Lens Recommendations accordingly?
5. What Frames should you recommend based on the selected lenses?
6. What Measurements will be required?
Once you put these general principles in place, you can apply the same rules to any prescription. Below is a simple example to act as a refresher for those more experienced or as a guide for those that are newer to the profession.
A CASE STUDY
A skilled dispenser should always begin a dispense by visualising or drawing an optical cross. It shows the principal meridians of an astigmatic lens in the form of a simple diagram and helps us imagine what an astigmatic lens looks like through highlighting the principal powers. By starting here, we can easily note where any thickness will lie to aid in frame selection and can more easily identify the ocular conditions present to minimise potential problems and assist with lens recommendation.
Figure 1 demonstrates how the optical cross helps to identify the principal powers for each lens as well as the meridians in which they lie. This instantly starts guiding your thought process to recommendations but also allows you to easily identify the ocular conditions present.
In this case, we already know presbyopia is present due to the add in the prescription but the presence of plus (+) principal powers on both meridians in both lenses also tells us that the patient has a compound hyperopic astigmatism in both
eyes. We can also identify high ametropia which is ascertained by the high refractive powers that are evident. (The textbook definition for this is a prescription of plus (+) or minus (-) 6.00 dioptres or higher).
The first step is complete and we have easily identified the ocular conditions but why is this so important and what impact does it have from a dispensing point of view?
Unfortunately, when dealing with certain prescription types, particularly those that fall into the atypical category, there are all sorts of considerations and potential problems to think about. For high ametropia (which is just one example), we must consider more than the obvious issues of lens thickness, weight and an unattractive cosmetic appearance. There is also a need to consider:
• Chromatic aberrations
• Surface reflections
• Spectacle magnification
• Field of view limitations
• Ring scotoma
• Back vertex distance compensation
Part 2 of this series will cover the considerations required by the dispenser for each of the potential problems mentioned and will discuss actions that can be taken to improve outcomes.
ABOUT THE AUTHOR: APRIL PETRUSMA is the CEO of Optical Dispensers Australia and a Senior Lecturer at the Australasian College of Optical Dispensing. She is a qualified Optical Dispenser, RTO Trainer and Business Manager with a degree in Visual Communication.

A JOURNEY THROUGH BINOCULAR VISION DISORDERS
AFTER SPENDING 20 YEARS DEVELOPING AND EXPANDING HER KNOWLEDGE IN BINOCULAR VISION DISORDERS, ORTHOPTIST
TANIA STRAGA VENTURED OUT TO ESTABLISH A PRIVATE ORTHOPTIC PRACTICE IN ADELAIDE.
IUniversity, under the guidance of orthoptic greats including Zoran Georgievski, and Connie Koklanis.
I wanted to pursue a career in binocular vision and paediatric eye health care. I ventured west and was appointed to a graduate position at the Women’s and Children’s Hospital Adelaide. Though I faced a steep learning curve, I realised when I arrived that I had been right about pursuing my passion in binocular vision, and revelled in the constant challenge that disorders of binocular vision posed me.
and expanding my knowledge and expertise in this area, working in public and private practice, both in paediatric and adult strabismus management. In 2020, I decided to take the step of establishing a private orthoptic practice, Adelaide Eye Therapy.

Adelaide Eye Therapy has grown from a one orthoptist practice, to now having four orthoptists and an orientation and mobility instructor on staff. We offer comprehensive orthoptic rehabilitative care, including managing childhood conditions such as amblyopia, diagnosing and treating disorders of binocular vision affecting adults and children, visual field defects, and working with patients with low vision.
In recent years, we have expanded to provide treatment for accommodative and convergence dysfunction as a result of traumatic brain injury, whether as a result of concussion or more serious injury. Patients come to us with usually normal visual acuity, but significant symptoms of asthenopia or diplopia. They have often been referred by their optometrist or ophthalmologist, though increasingly patients are coming to us via word of mouth or a Google search.
As clinicians, we listen intently to a patient, and progress through a detailed assessment of vision. Based on our objective assessment and a patient’s specific symptoms, we diagnose and then treat a disorder of binocularity by guiding the patient with specific orthoptic exercises to strengthen their binocular function.
Patients work on set exercises at
the progress of someone with significant visual discomfort, improve their function over a period of time, to then be able to complete tasks that they had all but given up on being able to achieve.
Disorders of binocular vision are commonly undervalued. Patients can present with quite nondescript and vague symptoms, and if their acuity is normal but they are symptomatic, likely it’s their binocular function that needs further investigating and treating.
Fortunately, most optometrists and ophthalmologists are perceptive to referring patients when they suspect a disorder of binocular vision. Patients themselves often can’t pinpoint what it is about their vision that is uncomfortable, but they might report having difficulty with specific tasks, or with moving their eyes into a particular area of gaze.
They might report difficulty with depth perception, motion sensitivity, heachaches or dizziness. It is rare for someone to present with frank diplopia, and when they do, you can almost always diagnose the exact cause from specific questioning regarding their exact symptomology.
A disorder of binocular vision, whether constant diplopia or poor stereopsis, can be extremely debilitating to a person. It
Empowering people to regain strong binocularity is so rewarding – especially when they have walked into clinic with constant diplopia and are then fitted with a Fresnel prism that gives them back binocular vision and can get them back driving again.
As clinicians in eye health care, it is important that we all remember the importance of maintaining strong binocular function, and that we remember that vision is so much more than reading the bottom line on the chart. People with poor binocular vision or low vision in general, can usually benefit from guided orthoptic exercises, to improve and make the most of whatever level of vision they can achieve.
ABOUT THE AUTHOR: Tania Straga (BachOrth&OphtSc, GradDipGenetCounsell) is director of Adelaide Eye Therapy.

ORTHOPTICS AUSTRALIA strives for excellence in eye health care by promoting and advancing the discipline of orthoptics and by improving eye health care for patients in public hospitals, ophthalmology practices, and the wider community. Visit: orthoptics.org.au

“PATIENTS COME TO US WITH USUALLY NORMAL VISUAL ACUITY, BUT SIGNIFICANT SYMPTOMS OF ASTHENOPIA OR DIPLOPIA.”Orthoptist Tania Straga established Adelaide Eye Therapy in 2020.
GOING LIVE WITH YOUR NEW PRACTICE – PHASE 3
AS PART OF HER SERIES ON STARTING A PRACTICE – THE CRITICAL START-UP PHASE, KAREN CROUCH EXPLAINS THE THIRD AND FINAL COMPONENT TO ENSURE THE BUSINESS BEGINS ON THE RIGHT FOOT.
By now, you should have completed preliminary steps that ensure the practice will provide high quality healthcare from a demographically appropriate, selected location. You’ll also be confident that it will eventually return a reasonable profit for the effort and risk involved.
You’ve probably selected a descriptive, catchy practice name and administrative and clinical staff have been engaged under relevant employment contracts.
Essential technical equipment has been installed and telecommunications are in place along with fully functioning facilities for administrative, personal and clinical use. Of course, everything has already been tested under a comprehensive ‘test plan’ to ensure employees are familiar with their roles and use of equipment. Additionally, various manuals and reference documents have been created and are conveniently located whenever they need to be consulted.
Your website contains images of the practice, details of services and key clinicians. And other forms of marketing (local newspaper ads, letter box drops, perhaps even an opening day) have been identified.
Finally, the waiting/retail space is well equipped to welcome and accommodate the most important people of all – patients and families – and you are itching to provide best-in-class healthcare supported by a well-managed, efficient team of employees. And the telephones are ringing off the hook for appointments too.
This is the critical point from which all future successes will flow, provided prudent clinical, administrative, practice and business management ‘foundations’
have been thoughtfully established. While practitioners and support staff inevitably focus mainly on high quality healthcare, as they should, time consuming and complex administrative systems often receive less scrutiny.
And yet the structure and thoroughness of those very systems are the source of all information and knowledge, including details of the practice owners’ values and culture they wish to inculcate in the business – the organisation’s cornerstone. Examples of ‘foundation’ actions that support efficiently run practices are:
• Vision, mission and values: while these are sometimes briefly expressed, they should embody the essence of the business, reflecting values, principles and business goals of owners for employees to adhere to;

• Organisation chart: clearly defined roles and responsibilities including reporting lines, to enable employees to understand the practice’s ’chain of command’;
• Staff management (human resources): detailed job descriptions for every position, provided to each staff member, including measureable key performance indicators to support performance assessments and enable employees to appreciate key aspects of their jobs;
• Staff appraisals: consistently undertake programs to assess job performance and serve as a useful, periodical communication channel to promote staff relations with two-way feedback;
• Induction programs: carefully documented for each position, to ensure new employees are methodically introduced through training materials and job descriptions so they confirm understanding of their roles and expectations;
• Exit interviews: questionnaires from employees who leave the business to enable owners to gather useful feedback on positive or negative aspects of the practice;
• Rostering procedures: for larger practices with complex clinician attendance habits that must be supported by front desk staff. Short notice availability to cover unplanned absences is a necessary part of any back-up plan to ensure patients and clinicians are adequately supported;
• Policy & procedure manuals: These mission critical records, worthy of a full, separate article, are the ‘practice bible’ and should include instructions on all policies and procedures;
• Legal: details of WHS programs, other medico-legal compliance requirements including ‘case histories’ of incidents that may have occurred during daily operations, be they actual oversights/ errors or ‘near misses’, all of which should be included in group meetings, training or ‘work smarter’ planning sessions;
• Practice management operations:
- Supplier management program to ensure supplier relationships and cost effectiveness are optimised and that contracts are renewed on time or new suppliers explored;
- Regular budget monitoring and various performance targets diarised for review;
- Complaints registers to record patient issues from lodgement to resolution;
- Delegation schedules clearly defining authorities assigned to any staff, including dual authorisations where applicable e.g. payroll;
- Staff records should be securely stored, ideally in the hands of the owner/s. A sound practice is based on efficiently documented policies, procedures, reference documents and manuals – the foundation on which high quality front desk service supports healthcare administered by clinicians.
At a senior, management level, establishment of a well-documented clinical governance program will ensure cooperation and dispensing of highest quality, well co-ordinated, and consistent healthcare. For larger practices, establishment of a sound corporate governance framework is an important initiative to ensure meaningful and progressive oversight of the overall practice business.
ABOUT THE AUTHOR: KAREN CROUCH is Managing Director of Health Practice Creations Group, a company that assists with practice set-ups, administrative, legal and financial management of practices. Contact her on 0433 233 478, email kcrouch@hpcnsw.com.au or visit www.hpcgroup.com.au

KAREN CROUCH
“A SOUND PRACTICE IS BASED ON EFFICIENTLY DOCUMENTED POLICIES, PROCEDURES, REFERENCE DOCUMENTS AND MANUALS.”Establishing a vision, mission and values will provide guideposts for staff and what’s important to the practice.
SOAPBOX OPTOGENETICS IN OPHTHALMOLOGY
disadvantage is that they generally have slower kinetics than Type I opsins, and their regeneration relies upon cellular processes.
Alight to control the activity of neurons. In the context of vision restoration, optogenetics works by inserting the sequence for a light sensitive protein (opsin) into target cells, most commonly via a viral vector. This protein has the therapeutic effect of conferring light sensitivity to blind retina.
This therapeutic approach has implications for neurodegenerative diseases, with eye disease at the forefront of this field. In fact, in 2021 the first reported case of partial functional recovery after optogenetic therapy was in a patient with retinitis pigmentosa. Furthermore, positive results have recently been announced for the Phase II RESTORE study.
To understand optogenetics at a deeper level, it’s important to know the concept was initially conceived as a means of controlling neural circuits in the brain by expressing light-sensitive proteins in nerve cells via gene delivery (most commonly using adeno-associated viral vectors). These light-sensitive proteins can be from microbes (so-called Type I opsins) or animals (so-called Type II opsins).
Type I opsins act as both light detectors and as a conduit for ions. They are simple molecules: once activated by light – which converts their chromophore all-trans retinal to 13-cis retinal –they spontaneously return to their light-sensitive state. Type II opsins rely on second-messenger systems: this makes them sensitive (because of inherent second-messenger signal amplification). However, their
In the context of vision restoration, optogenetics is most commonly used to confer novel light sensitivity to either second-order (e.g. bipolar cells) or third-order (e.g. retinal ganglion cells) neurons in degenerate retina. This is generally achieved through intravitreal or sub-retinal delivery of adeno-associated virus carrying the sequence for an optogenetic protein. Optogenetics has also been used to restore light sensitivity to degenerate photoreceptors. The original experiments harnessing optogenetics concentrated on Type I opsins which were maximally sensitive to short-wavelength visible radiation.
However, when it comes to translating this approach into real-world therapies there are inherent problems.
First, the pre-receptoral ocular media strongly absorb these wavelengths. Second, the retinal illuminances required to activate optogenetic treated retinal neurons are close to the safety thresholds for light toxicity. These problems have been addressed through the identification and development of “red-shifted” high-sensitivity Type I opsins and partly through the harnessing of Type II opsins (e.g. the M-cone opsin).
At the Save Sight Institute in Sydney, our work is currently laboratory-based – using pre-clinical models, including a human retinal explant platform – to develop and assess new candidate opsins for vision restoration.
My group recently published in Scientific Reports on a new Type I opsin, bReaChES, which appears to offer some advantages over previously employed opsins (Optogenetic restoration of high sensitivity vision with bReaChES, a red-shifted channelrhodopsin. Sci Rep 12, 19312 [2022]). We have received funding to develop new approaches to address vision restoration in macular disorders from the Macular Disease Foundation Australia, and in inherited retinal disease (IRD) from the NHMRC.
Optogenetics is an attractive approach because it is ‘causative
mechanism agnostic’. That is, it should work for any condition resulting in outer retinal loss, but with preserved retinal ganglion cells (+/- the second-order neurons). This is important because more than 300 genes or loci have been reported in association with IRD – and Australia’s only approved ophthalmic gene therapy, voretigene neparvovec (Luxturna, Novartis), is available for just one of these diseases. Furthermore, around 30% of patients with IRD have no causative gene identified. Finally, nothing can currently restore lost vision in geographic atrophy.
At present, none of the optogenetic approaches investigated would be expected to confer “normal” vision. In some respects, it is fair to consider it a biological alternative to the “bionic” retina. However, the achievable resolution is likely to be superior to bionic retinae that have achieved regulatory approval to date (the best of which, in terms of visual acuity, was manufactured by RetinaAG).
Like any other new drug or therapy, optogenetic approaches must undergo the same rigorous development pipeline, including pre-clinical and Phase 1-3 clinical trials. Some approaches are currently undergoing evaluation in clinical trials. However, major obstacles with certain approaches are inherent insensitivity and lack of gain control/adaptation (which necessitates the use of stimulus goggles). Our lab plans to complete pre-clinical trials in the next year and a half before concentrating on translation to clinical trials in humans. Taking this step will require additional funding support.
Name: Professor Matthew Simunovic

Qualifications: MB Chir PhD FRANZCO
Primary place of work: University of Sydney, Sydney Eye Hospital, Sydney
Children’s Hospitals
Position: Professor of Ophthalmology & Visual Science, Senior VMO in Vitreoretinal Surgery
Location: Sydney
Years in profession: 15
IN SOME RESPECTS, IT IS FAIR TO CONSIDER [OPTOGENETICS] A BIOLOGICAL ALTERNATIVE TO THE 'BIONIC' RETINA.
2023 CALENDAR
MAY
ANZSRS MEETING
Melbourne, Australia
20 – 21 May ranzco.edu/events/2023
SUPER SATURDAY –OPTOMETRY NSW/ACT
Sydney, Australia
21 May
optometry.org.au/about-us/ our-organisation/optometry-nsw-act
NATIONAL ABORIGINAL AND TORRES STRAIT ISLANDER EYE HEALTH CONFERENCE
Sydney, Australia
24 – 26 May mspgh.unimelb.edu.au
JUNE
ASO EXPO 2023
Sydney, Australia
2 – 4 June asoeye.org
MYOPIA PROGRESSION IN CHILDREN CONFERENCE
Sydney, Australia
10 June myopiaaustralia.com.au
WORLD GLAUCOMA CONGRESS
Rome, Italy
28 June – 1 July worldglaucomacongress.org
JULY
AUSCRS 2023
Port Douglas, Australia
26 – 29 July auscrs.org.au/2023-conference
AUGUST
WORLD CONFERENCE ON OPHTHALMOLOGY & EYECARE
Rome, Italy
21 – 23 August eyecare.thepeopleevents.com
SEPTEMBER
ORTHOKERATOLOGY SOCIETY OF OCEANIA CONFERENCE
Gold Coast, Australia
1 – 3 September www.facebook.com/OrthoKSO/
O=MEGA23 & WORLD CONGRESS OF OPTOMETRY
Melbourne, Australia
8 – 10 September omega-event.org
EUROPEAN SOCIETY OF CATARACT & REFRACTIVE SURGEONS CONGRESS
Vienna, Austria
8 – 12 September congress.escrs.org/
SILMO PARIS
Paris, France
29 September – 2 October event.silmoparis.com/2023/en/
All Specsavers stores now with OCT
Exciting Optometrist opportunity – Specsavers
Hamilton CBD, NZ
Fantastic opportunity for an optometrist to join a fun team. Hamilton is a great location, in which you will see lots of pathology and paediatrics. You will be able to utilise some very exciting equipment including an OCT. This is a chance to really develop your skills, work in a very supportive team including 2 experienced optometrist partners and a great retail partner. So, if you want to know more about the further equipment and lucrative salary package, please reach out.
Optometrist Joint Venture Partnership Opportunity – Griffith, NSW
In the south – west of New South Wales, at the heart of the vast Murrumbidgee irrigation area is Griffith. With fertile land particularly well suited to vineyards, Griffith is a popular food and wine destination. There are more than a dozen wineries in the district with world famous names.
Specsavers Griffith is well positioned within Griffith Central Shopping Centre, attracting high volumes of foot traffic. The store opened in 2018, and contains 3 Optical testing rooms, a dedicated Audiology room, 5 dispense points, over 1100 frames on display and state of the art equipment including OCT and HVF analyser.
Locum opportunities in Western Australia
At Specsavers, we like to work with the most talented optometrists and give them what they need to thrive. This includes the provision of the highest quality equipment, ongoing enhancement of skills and access to industry leaders. Have you considered Locum Optometry: variety, travel and
the opportunity to expand your network? We have a number of vacancies across WA, and seeking optometrists who have a real passion to provide the best service to the WA people. With work available across the state why not reach out today for a confidential conversation on how we work.
Optometrist opportunities in Sydney
Due to exciting growth and several upcoming new stores and expansions, Specsavers has some great Optometrist opportunities available across Sydney. We offer flexible rosters to support work/ life balance with options for part-time or full-time work, we’ll give you access to the latest technology and equipment (including OCT in every store free for every patient) and we’ll pay you a competitive salary. We can also provide you with excellent opportunities for career development and progression – including pathway to Partnership, outreach opportunities and the chance to mentor new graduates.
Graduate program across Australia and New Zealand
Are you a final year student looking to secure your first role as a Graduate Optometrist? Specsavers have provided rock-solid career development paths for optometrists, offering great graduate packages and extraordinary patient-focused environments. By joining us as an optometrist, you can be certain you’ll have everything at your disposal to help improve health outcomes for your patients. If you like the idea of building your career and delivering patient-focused outcomes, then reach out
To list an event in our calendar email: myles.hume@primecreative.com.au
OCTOBER
RANZCO SCIENTIFIC CONGRESS
Perth, Australia
20 – 24 October ranzco.edu/events
ORTHOPTICS AUSTRALIA ANNUAL CONFERENCE
Perth, Australia
21 – 24 October orthoptics.org.au
NOVEMBER
SILMO INSTANBUL
Istanbul, Turkey
23 – 26 November silmoistanbul.com/en
DECEMBER
ASIA PACIFIC TELEOPHTHALMOLOGY SOCIETY CONGRESS
Pattaya, Thailand
2 – 3 December 2023.asiateleophth.org
In a few short years, Specsavers has achieved market leadership in Australia and New Zealand with more people choosing to have their eyes tested and buy their prescription eyewear from Specsavers than any other optometrist. To learn more about these roles, or to put your hand up for other roles as they emerge, please contact us today:
Joint Venture Partnership opportunities enquiries: Kimberley Forbes on +61 (0) 429 566 846 or E kimberley.forbes@specsavers.com
Australia Optometrist employment enquiries: Marie Stewart – Recruitment Consultant marie.stewart@specsavers.com or 0408 084 134
Locum employment enquiries: Matthew Cooney matthew.cooney@specsavers.com or 0447 276 483
New Zealand employment enquiries: Chris Rickard –Recruitment Consultant chris.rickard@specsavers.com or 0275 795 499
Graduate employment enquiries: apac.graduateteam@specsavers.com
People
ON THE MOVE
monthly bulletin to keep the Australian ophthalmic sector updated on new appointments and personnel changes, nationally and globally.
OPTOMETRIST BECOMES VISION 2020 AUSTRALIA BOARD MEMBER




Melbourne optometrist Murray Smith has been co-opted on to the Vision 2020 Australia Board following a recent nomination and selection process. As a past Director and President of both Optometry Australia and Optometry Victoria, and past director of Optometry Victoria South Australia, he has worked in most states and territories in Australia and spent five years as a lecturer and clinical supervisor/assessor in Papua New Guinea.
served at the company as CEO from 2010 to 2013. In total, he brings more than 25 years of leadership in healthcare, having served in president, CEO and chairman roles, among others, at several global pharmaceutical and health care companies, including Schering-Plough Corporation, Forest Laboratories Inc., Actavis plc, Allergan plc and The Beauty Health Company.

She says she is looking forward to using her optical expertise to offer ongoing assistance and service to her NSW customers. DO YOU HAVE CAREER NEWS TO SHARE?


on the role of CEO from Monday 27 March 2023. As Chief Medical Officer of the commission since 2021, and previously Clinical Director and Senior Medical Advisor from 2014, the commission said she was well positioned to lead at a time when the safety and quality of healthcare is a national priority. Duggan succeeds Adjunct Professor Debora Picone AO, who retired in September 2022 and was CEO from 2012.

EXPERIENCE OUTSTANDING CONTROL AND CLARITY†1-4
+6.0D to +14.5D Coming Soon!
Clareon® IOL with AutonoMe® is the first and only automated, disposable, pre-loaded delivery system. With its intuitive, ergonomic design, the AutonoMe® delivery system enables easy, single-handed control of IOL advancement and protects incisions as small as 2.2mm.1,5 Pre-loaded with the Clareon® IOL, the world’s most advanced optic† , delivering excellent clarity.†1-4,6,7


Available dioptre ranges:1,8
• Clareon® Toric IOL: +15.0D to +25.0D (T2-T6 in 0.5D steps)

• Clareon® IOL: +6.0D to +30.0D (in 0.5D steps)

STAY ON THE CUTTING EDGE WITH THE LATEST OPTICAL TECHNOLOGY

