Advanced systems to enhance your practice and patient engagement

HOYA HUB
HOYA Consultation Centre 360
HOYA Digital Fitting
HOYA visuReal Master AI
HOYA Order Centre
QUESTIONS OVER RED TAPE CUTTING
Will medical colleges need to relinquish the vetting of overseas-trained specialists?
OPERATING IN A LOW PRESSURE ENVIRONMENT
New tech allows NSW surgeon to perform cataract surgery at near-physiological IOP levels
HEALTHY EATING FOR HEALTHY EYES
New Australian nutrition guidelines for AMD and the concept of 'food synergy'
03
28
36
LEADING OPHTHALMIC MAGAZINE SINCE 1975 MAY 2024
AUSTRALIA’S


Are you looking to develop your career? You’d look good in Specsavers If you’re looking for a company that prioritises career growth through tailored development programs like our Graduate, Early Career Optometry, and Pathway initiatives, you’ll shine at Specsavers. spectrum-anz.com/careers-at-specsavers/
QUESTIONS OVER COLLEGE’S GATEKEEPER ROLE FOR OVERSEASTRAINED OPHTHALMOLOGISTS
The Australian Society of Ophthalmologists (ASO) is “strongly opposed to the emerging indications” that the Federal Government may remove the power of RANZCO and other medical colleges when vetting and approving overseas-trained specialists to practise in Australia. The call comes as the government considered 28 recommendations from the ‘Independent review of Australia’s regulatory settings relating to overseas health practitioners’ – conducted by Ms Robyn Kruk – aiming to remove “unnecessary regulatory barriers” faced by internationally qualified health professionals. It’s hoped cutting red tape will make Australia a more attractive destination for foreign health professionals and alleviate workforce pressures, leading to better healthcare for the population.
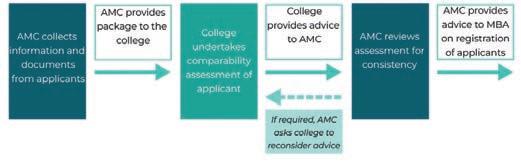
During the consultation phase, RANZCO said it could not endorse a proposed transition of equivalence assessments for specialist international medical graduates (SIMGs) from the medical colleges to the Australian Medical Council (AMC). A 2018 workforce report shows 12 ophthalmology SIMGs join the workforce annually.
The college said this represented a major move away from qualified assessors who are the recognised clinical experts in their field, and instead called for colleges to streamline their own assessments as a better, faster and cheaper method to ensure the community interests were served.
Kruk’s review found these medical college assessments were costly, with varying fees and processing time frames. It was noted some

and play a key role in the individual comparability assessment.
Since then, Kruk’s final report has emerged with slight wording changes. It stated the immediate focus should be on streamlining processes, removing duplication and providing greater support for specialist comparability assessments to ensure more timely decision making and consistent outcomes.
colleges only review applications for SIMG recognition at specific times throughout the year.
To address these issues, the interim report proposed transitioning the “determinative part” of comparability assessments from the specialist medical colleges to the AMC to drive greater consistency in performance and outcomes and reduce costs. Colleges would retain expertise
“However, should outcomes fall short of workforce needs within ministerially agreed timelines, the review recommends that centralising comparability assessment with the AMC, in full or in part, remains as an appropriate escalation strategy available to health ministers,” the report noted.
“A transition to the AMC would be a means of providing support to
‘NUISANCE TARIFFS’ TWIST IN EYEWEAR IMPORTS SAGA
The Optical Distributors and Manufacturers Association (ODMA) is re-energised in its fight to abolish tari s imposed on European eyewear imports after news the government is reviewing “nuisance tari s” hindering Australian businesses.
ODMA said after exhausting several avenues, it had now written to the Treasury Department to ask that optical products be included in the list of nuisance tari s.
This comes after “a legislative technicality penalised our industry and its consumers without providing any broader benefit”, resulting in a 5% border tax hike for eyewear imports into Australia from any country without a free trade agreement (FTA).
On 11 March 2024, the Federal Government revealed plans to abolish around 500 nuisance tari s to boost productivity, reduce compliance costs for businesses and ease the cost of living for Australians.
“We consider that these [optical] tari s are consistent with the description of the treasurer, the Hon. Dr Jim Chalmers MP when he stated, ‘Australian workers and businesses are not protected by these tari s, but they still have to navigate the red tape involved and bear the costs of complying with the tari regime’,”
ODMA stated.
“These tari s do nothing but increase costs to businesses and consumers and achieve no benefit
for local manufacturing.”
The saga began on 7 July 2022 when the Australian Border Force (ABF) revoked a tari concession order (TCO) for plastic spectacle frames that had been in place since 2003, with retrospective e ect from 13 May 2022. Months later, this was extended to metal frames, meaning that all eyewear imports into Australia from the European Union (EU) and other places without a FTA were subject to the border tax.
ODMA said the TCOs had been in place for decades given Australia’s “essentially non-existent domestic manufacturing capabilities in our sector”.
However, the ABF’s decision

AUSTRALIA’S LEADING OPHTHALMIC MAGAZINE SINCE 1975 MAY 2024
page
continued
8
Cutting red tape could make Australia more attractive for overseas trained practitioners. Image: Inside Creative House/Shutterstock.com.
continued page 8 page 18

AU: 1300 365 470

CIRRUS 6000
At 100,000 scans per second, ZEISS CIRRUS 6000 is the next-generation OCT delivering high-speed image capture with wider field of view and HD imaging detail.
Maximise patient throughput with performance OCT, proven analytics and patient-first design.
ZEISS
med.au@zeiss.com Carl Zeiss Pty Ltd, NSW 2113 AUSTRALIA. zeiss.com/CIRRUS6000
high-performance OCT.
ZEISS
Make every second count with

IN THIS ISSUE
FEATURES

Scoring runs
An independent network’s sophisticated marketing strategy capable of targeting individuals in postcodes.


Macula Month
20 31 23 47
The latest therapies, diagnostics and treatment protocols for macular disease in Australia.
Solid ground
A new scheme that’s providing more direction for early career optometrists across the country.

Topical subject
Exploring the best dosage and treatment duration of ciclosporin in dry eye disease (0.5 CPD).
A

Imagine a future where a patient asks their ophthalmologist for hawk-like visual acuity – eight times more powerful than humans – dialled in on demand. Or even crazier, the ability to hack the retina so one can simultaneously read text messages while driving down the freeway, giving each task equal attention.
It’s di cult to grasp, but the pathway is clear for Dr E.J. Chichilnisky, a Professor of Neurosurgery and Ophthalmology at Stanford University, who recently discussed his leading e orts to restore sight to the blind and o er visual augmentation for sighted people on one of the world’s (and mine) favourite podcasts, Huberman Lab.
In this fascinating discussion (episode 168), Dr Chichilnisky applauds the work of various ‘bionic eye’ projects allowing blind people to see blobs and flashes, or even a window on a dark wall. But none of these remotely resemble natural vision, and he believes much of the science has been left on the table. He says scientists have known for years dead photoreceptor cells – leading to conditions like macular degeneration and retinitis pigmentosa – can be bypassed with an implant delivering electrical signals to the deeper retinal ganglion cells that then send visual signals to the brain, creating crude visual gains.
But Dr Chichilnisky says these e orts fail to harness 20-odd retinal cell types that, in healthy eyes, deliver an organised yet complex pattern of electrical activity to the brain. With what’s currently known, he believes it’s possible to build a retinal implant that can recognise the distinct cell types and stimulate them independently before creating a coherent visual signal to the brain, resembling human vision. Theoretically, if the cell types operate independently – which Dr Chichilnisky believes they are – then it could be possible to manipulate them so humans can see multiple things at once, or augment their vision in ways never thought possible.
While the prospect of super-human vision is tantalising, it’s likely those with retinal vision impairment will benefit first if such technology is ever realised, with the Elon Musks of the world to follow shortly after.
As Australia marks Macula Month, the prospect of highly accurate bionic eyes is exciting for a patient cohort that has benefitted from many technology leaps (see pages 31-45), and will continue to do so for years to come.
MYLES HUME Editor
INSIGHT May 2024 5
MAY 2024 07 UPFRONT 09 NEWS THIS MONTH 72 OPTICAL DISPENSING 73 ORTHOPTICS AUSTRALIA 74 MANAGEMENT 75 SOAPBOX 76 CLASSIFIEDS/CALENDAR 78 PEOPLE ON THE MOVE EVERY ISSUE
MACULAR
MIRACLE EDITORIAL





























NOW AVAILABLE FOR ASTIGMATISM

Just as Insight went to print, GLAUCOMA AUSTRALIA has welcomed journalist and Seven News Melbourne newsreader Mr Mike Amor as an o cial ambassador. He joins Mr Kirk Pengilly from Australian rock band INXS and Seven TV personality Mr David Koch, as ambassadors of the organisation. Amor was first diagnosed with the disease in his 20s but required emergency surgery after it almost took his sight five years ago. As an ambassador, he hopes to raise awareness of the importance of eye health, in particular glaucoma, and to encourage Australians to get their
UPFRONT STAT
WEIRD
A group at Columbia Engineering in New York has unveiled Emo, a robot integrated with high-resolution cameras within the pupil of each eye, enabling it to make eye contact for more “life-like” interactions. The researchers have called this “revolutionary” in human-robot interactions because robots have become adept at verbal communication, while their nonverbal communication skills have lagged.
WONDERFUL
Five famous paintings, including works by Sandro Botticelli and Thomas Gainsborough, were changed to show the visual experience of individuals with glaucoma. Displayed at London’s National Gallery, these pieces feature blurred edges and omitted details, o ering insight into the reality of the millions a ected by glaucoma.
WACKY
A research team in Korea has explored a potential treatment for blindness-causing retinal detachment – using viscous seaweed. The slick surface of seaweed is attributed to alginate, a mucilaginous substance. The researchers created a hydrogel from alginate and successfully implanted it in animal models to prevent the recurrence of retinal detachment.
eyes checked. IN OTHER NEWS, Deakin University and its optometry school have joined Vision 2020 Australia as the peak body’s newest member. With a duration of three-and-a-half years over 10 consecutive trimesters, Deakin’s optometry course is described as Australia’s only accelerated Bachelor of Vision Science/Master of Optometry course. According to Vision 2020, the course was the first optometry curriculum in Australia to be built on a backbone of ‘problem-based learning’, and the first optometry program in Australia to mandate a full trimester (13-weeks) of rural placements. The optometry course celebrated its 10-year milestone this year,
and has graduated 651 students. FINALLY, EssilorLuxottica and the World Council of Optometry have teamed up to raise awareness of presbyopia and the ageing eye and will establish standards of care for eyecare professionals to follow. Currently, there are an estimated 2.1 billion people worldwide with presbyopia. Due to the ageing population, this number is expected to reach four billion (approximately 40% of the world’s population) by 2050. The program will feature insights from several international experts in the field, to build the standard of care resolution and bring the latest research and evidence in easily accessible educational.

Treatment dropout
Around 20% of Australians with nAMD quit treatment within a year, with 50% discontinuing eye injections within five years. Page 31.
WHAT'S ON
Australia’s boutique optical trade event returns to Sydney’s Hordern Pavilion, featuring education, awards, eyewear releases and new technology. events@odma.com.au
1 – 2 June
Complete calendar page 76.
An opportunity to come together with ophthalmology peers for the latest in best practice, knowledge and cutting-edge medical technology. sandra@asoeye.org
Published by:
379 Docklands Drive, Docklands VIC 3008 T: 03 9690 8766
www.primecreative.com.au
Chief Operating O cer
Christine Clancy christine.clancy@primecreative.com.au
Group Managing Editor
Sarah Baker sarah.baker@primecreative.com.au
Editor
Myles Hume myles.hume@primecreative.com.au
Journalist
April Hawksworth april.hawksworth@primecreative.com.au Commissioning Editor, Healthcare Education
Je Megahan
Business Development Manager Luke Ronca luke.ronca@primecreative.com.au
Client Success Manager
Salma Kennedy salma.kennedy@primecreative.com.au
Design Production Manager
Michelle Weston michelle.weston@primecreative.com.au
Head of Design
Blake Storey
Art Director
Bea Barthelson
Subscriptions T: 03 9690 8766 subscriptions@primecreative.com.au
The Publisher reserves the right to alter or omit any article or advertisement submitted and requires indemnity from the advertisers and contributors against damages or liabilities that arise from material published. © Copyright –No part of this publication can be reproduced, stored in a retrieval system or transmitted in any means electronic, mechanical, photocopying, recording or otherwise without the permission of the publisher.
INSIGHT May 2024 7
NEXT
month ASO SKILLS EXPO 2024
THIS month OSHOW24
17 – 18 May
insightnews.com.au
Image: Mikhailov Studio/stock.adobe.com.
ASO EXPRESSES CONCERNS TO HEALTH MINISTER
continued from page 3
colleges that would retain responsibility for individual assessments of an SIMG’s comparability, while also providing an opportunity to drive greater consistency, and create a process and governance structure consistent with best practice regulatory outcomes.”
But the ASO said it still wasn’t clear how this would take shape. It was opposed to removing the “vital, longstanding, and proven role of medical colleges in maintaining high – and most importantly – safe standards of specialist education and training”.
In November 2023, the ASO wrote to Health Minister Mr Mark Butler to express its concerns and advocate against recommendations from the Kruk Review.
“This also included addressing concerns regarding other recent ministerial recommendations that aim to take greater control of medical colleges and their role assessing international graduates and training post accreditation,” the organisation told Insight
“The ASO has received no response to this letter of grave concern.”
It is the understanding of the ASO that the Federal Government has since accepted recommendations from the Kruk Review, but the body said there has been little discussion or engagement around how it may look in practise.
The Medical Board of Australia will host the first meeting of the Specialist IMG Pathways Review Advisory Group on Monday 22 April 2024.
ASO President Dr Peter Sumich said he was eagerly awaiting this roundtable
meeting “and the opportunity to learn more in detail about any changes being proposed to vetting and approving overseas-trained medical professionals”.
In its earlier submission, RANZCO said it had already simplified its application process for SIMGs and worked to assure quality through the same assessment methods used for RANZCO trainees, an established dual pathway for New Zealand applicants.
The college has also been trialling a pilot in Australia leading to full fellowship via work based and final on-site assessments. This was in response to the need for a more flexible and e cient approach to ‘area of need’ demands.
But transitioning equivalence assessments to the AMC would completely change the underlying framework that has formed the basis for SIMG clinical competency assessment, RANZCO stated, noting this was based upon the highest level of peer reviewed expertise and experience built up over decades.
Expedited pathways
Kruk said only applicants with qualifications, skills and experience from a small number of countries and professions were eligible for expedited pathways to practise in Australia. Applicants entering via these pathways experience a quicker journey, pay less and need to meet fewer requirements. However, medical specialists do not have access to expedited registration pathways, meaning it can take years to be registered. GPs report spending two years navigating the system and incurring more than $33,000 in costs. Under the changes, international
(final report).
medical graduates who are eligible for expedited pathways would save $7,700, and would be expected to result in more health practitioners choosing Australia.
Overall, Kruk said feedback from overseas-trained practitioners was the end-to-end journey was complex, costly and slow. Applicants need to deal with several regulators, often supplying the same information multiple times.
Applicants also report the assessments and regulatory processes were often di cult, with requirements that are unclear, onerous and lack transparency, and result in inconsistent outcomes.
Despite being valuable to the Australian health system, the report noted that practitioners who specialise can face particularly high barriers.
“Unlike graduates with recent exam experience, many struggle to demonstrate they meet the required standard. Almost half feel their prior professional and clinical experience is insu ciently recognised. For those who come, many need to work in more junior roles and receive lower pay for an initial period. Too often, applicants report the process makes them feel undervalued, disrespected and even demeaned.”
TARIFF NOW PLACES MAJOR BURDEN ON EYEWEAR SUPPLIERS
continued from page 3
was made following an application from a small, boutique, luxury Australian eyewear manufacturer operating from regional NSW.
“We understand the production capacity of this manufacturer to be in the low thousands,” ODMA said.
“ODMA filed an appeal against the ABF decision on 5 August 2022. However, that appeal was rejected on 15 September 2022.”
The e ect of revoking the TCO means the $4 billion optical dispensing and eyewear industry – which ODMA estimated sells more than five million frames each year – is now faced with a 5% tari on millions of frames imported annually.
“This decision has, after decades of nil tari s for the industry, increased costs for retailers and consumers, unnecessarily exacerbated cost of living pressures on the millions of Australians who use optical products and contributed to the upward pressure on inflation,” ODMA CEO Ms Amanda Trotman's letter said.
“The decision has also created significant additional red tape and uncertainly for our members who are now faced with further administrative burdens when determining which products and countries the tari applies to. We are aware of a number of instances where this has resulted in members needing to spend time changing paperwork

and challenging incorrect tari charges.”
ODMA’s letter intended to show that removing the tari s would return the longstanding policy position and ensure Australian companies no longer faced the recent increased compliance and costs.
“Given the unfortunate delay in progressing the EU-FTA – which we were hopeful would be a solution to these nuisance tari s – were the tari s [we propose] not removed as part of this process, Australian businesses would essentially be encouraged, by virtue of government policy, to preference Chinese-made goods over those from European countries,” Trotman said.
8 INSIGHT May 2024
Amanda Trotman, ODMA. Image: ODMA.
NEWS
A proposed model of the AMC's involvement to test the comparability of overseas trained specialists. It’s hoped such a move would improve the efficiency, timeliness and transparency of assessment processes. Source: Kruk Review
OPTOMETRY AUSTRALIA PROGRAM TO RECOGNISE EXPERTISE AND BOOST COLLABORATIVE CARE
Optometry Australia (OA) has established an Advanced Practice Recognition (APR) program aiming to recognise and credential optometrists with demonstrated expertise in particular clinical areas, starting with glaucoma management.
OA said this is in adherence to its ‘preferred future’ for optometry in 2040 and hopes that advanced practice recognition will also strengthen collaborative care. The peak body envisages a future where advanced practitioners will attract interprofessional referrals for complex cases from fellow optometrists, while working closely with ophthalmologists and other specialities.
With easy identification through OA’s register, collaboration will reportedly become seamless, leading to enhanced patient outcomes through multidisciplinary approaches.
APR o ers optometrists an alternative career aspiration and a clear pathway for career progression, making it easier to break through the profession’s ‘ceiling e ect’. This ensures that talent within the optometry field
is nurtured and retained, contributing to a vibrant and dynamic workforce.
“We believe that the APR program positions optometry to adapt to evolving healthcare landscapes, in close alignment with the forward-looking strategy of optometry in 2040. Recognising the importance of robust governance and structure, OA has undertaken thorough due diligence in developing the program to date,” the peak body said.
An Advanced Practice Oversight Committee (APOC) has been established to ensure the program’s integrity and e ectiveness from inception. A Clinical Advisory Committee (CAC) has also been set up, comprising experienced practitioners tasked with defining competencies and experiential criteria for glaucoma management – OA’s first clinical area of excellence.
“OA is committed to fostering a culture of inclusivity, continuous learning and professional growth within the profession, and with the CAC’s support, will develop



dedicated resources to support clinicians in developing advanced skills, ensuring equal opportunity for both seasoned professionals and recent graduates,” OA said.
OA CEO Ms Skye Cappuccio added: “By recognising advanced skills, fostering career progression, and enhancing collaborative care, the APR program not only benefits individual practitioners but should also help ensure timely patient access to needed care.”
Optometry Australia intends to launch a pilot version of the APR program in mid-2024 before inviting members to apply for APR in glaucoma management; after which programs for other clinical areas of interest will be developed.



 The program will start by recognising glaucoma management expertise. Image: rh2010/stock. adobe.com.
The program will start by recognising glaucoma management expertise. Image: rh2010/stock. adobe.com.
IN BRIEF
CYBER THREATS
Optometrists are urged to enhance data protection measures amid rising cyber-crime threats targeting healthcare, as revealed by National Australia Bank (NAB). NAB's research highlights healthcare as one of the top five industries under cyber-attack, with 21% of health service businesses a ected. NAB said malware and ransomware attacks are prevalent, especially among small to medium enterprises (SMEs). NAB emphasises continuous review of systems and protocols to safeguard business and client data. To counter cyber threats, NAB suggests implementing security measures such as Australian Cyber Security Centre Essential Eight, automatic updates, and employee education.
OSHOW AWARDS
Optical Distributors and Manufacturers Association (ODMA) is debuting an awards program that will focus on frames. The awards program, open to all ODMA members, will honour excellence and innovation within the optical industry and “highlight the remarkable achievements of products”. All entries will be displayed at O-SHOW 24, from 17-18 May at the Hordern Pavillion, Sydney, with winners announced during the Friday networking event from 5pm. CEO Ms Amanda Trotman said the awards “aim to spotlight the significant contribution that frames make to the comfort, eyecare, and visual appeal provided to its wearers” and present a unique opportunity to celebrate the optical industry’s fashionable, fun, and creative dimension, by emphasising frames. Award categories will include most outstanding newly released frame RRP under AU$300 and most outstanding newly released frame AU$330 and over with judging occurring via a ‘people’s choice’ approach.
OPTOS MILESTONE
Retinal imaging technology company Optos has achieved a dual milestone of more than 25,000 devices installed worldwide, and a collection of 2,500 clinical and peer-reviewed studies spanning 235 disease states. CEO Mr Robert Kennedy said it demonstrated the more than 30 years of positive impact the company has had on the standard of retinal imaging technology. “The ongoing growth and recognition of the robust body of clinical research e orts underscores the dedication of our team to continue improving patient outcomes and driving development in ophthalmic care,” he said. “We extend our sincerest gratitude to our customers for their continued trust and support. Their feedback and partnership are invaluable as we strive to make retinal imaging more patient-friendly and accessible while empowering clinicians to deliver exceptional care.”
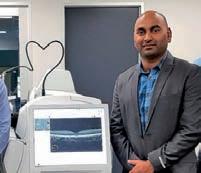
GEORGE & MATILDA EYECARE EXPANDS PROFESSIONAL SERVICES TEAM
George & Matilda Eyecare (G&M) has expanded its professional services team substantially, with five optometrists taking on the responsibility to upskill and drive evidence-based best practice across the network.
During the past six months, G&M has gone from one professional services manager to five.
The professional services managers are:
• Anthony Sargeant – Queensland and NSW Mid North Coast
• Michael Angelos – NSW North
• Shazaan Khambiye – NSW South
• Alem Catic – Victoria, South Australia and Western Australia
• Tristan Gutteridge – Tasmania.
Each report to G&M chief operating o cer Mr Matt Bradford while continuing to work as optometrists, with time allocated during the week for professional services support.
Bradford said providing education, support, and engagement for G&M’s optometrists was crucial. He added that the professional services team is comprised

of optometrists experienced in delivering quality clinical care and educational content to their peers.
"In addition to grassroots optometrist support, they deliver educational content ranging from myopia management strategies, to embracing the latest in eyecare technology, driving evidence-based best practice within our optometry team."
Bradford said given the rapid growth of the network, G&M acknowledged support, continuous education, communication frequency and collegiality were important factors in building a sustainable optometry network.
OPTOMETRY AUSTRALIA DEVELOPING SUSTAINABILITY ROADMAP

Optometry Australia (OA) has commissioned a sustainability roadmap to target waste, carbon, and eco-awareness challenges within the optometry sector, and chart a new course towards a more sustainable future for eyecare.
Director of optometry advancement, Ms Sarah Davies, said this commitment was one of the key objectives of OA’s 2021-24 shared strategic plan.
“Optometry Australia is committed to exploring and developing initiatives in response to emerging evidence on the impact of climate change, specifically on optometry and eye health,” Davies said.
“Australia’s health sector, including optometry, has a role in both climate change mitigation and adaptation, and in reducing its overall environmental impacts, which is why we partnered with sustainability agency Edge Impact to commission the sustainability roadmap.”
The roadmap identifies environmental targets and action issues that are important
for the eye health sector, while drawing insights from extensive sector research, carbon footprint and waste audits, stakeholder interviews and focus groups.
It identifies three key environmental ‘hotspot’ areas within the optometry sector that need to be addressed, including waste, carbon and sustainability knowledge.
The roadmap proposes four action levers for change including collaboration with key stakeholder groups, creating future-fit spaces, proactive purchasing and empowering people to increase their knowledge in this space.
“Optometry Australia will seek to collaborate with colleagues across the eye health sector, as well as those working in the broader climate action and health space such as the climate and health alliance, to ensure our work is aligned, and coordinated with other e orts,” she said.
More information about these initiatives will be shared with members via OA’s communication channels throughout 2024.

10 INSIGHT May 2024
Alem Catic (from left), Anthony Sargeant, Shazaan Khambiye, Tristan Gutteridge and Michael Angelos. Image: George & Matilda Eyecare.
NEWS
Sarah Davies, Optometry Australia. Image: Optometry Australia.












































© 2024 Bausch & Lomb Incorporated. ®/TM denote trademarks of Bausch & Lomb Incorporated and its a liates. Bausch & Lomb (Australia) Pty Ltd. ABN 88 000 222 408. Level 2, 12 Help Street, Chatswood NSW 2067 Australia. (Ph 1800 251 150) New Zealand Distributor: Toomac Ophthalmic. 32D Poland Road, Glenfield 0627 Auckland New Zealand (Ph 0508 443 5347) EVA.0001.AU.24 For more information contact your Bausch + Lomb Territory Manager or Customer Service 1800 251 150 References: 1. enVista Directions for Use. 2. Data on File. Bausch+Lomb Inc. Exceptional performance. Without compromise. Aberration-free optic1 | Glistening-free performance1,2 | Predictable outcomes1 ENVISTA IS NOW PRELOADED
RODENSTOCK EXPANDS GLAZING LAB NETWORK WITH TASMANIA SITE
Rodenstock has expanded its edging and fitting laboratory network into Tasmania, shortly after opening sites in Melbourne and Brisbane.
Up until last year, the ophthalmic lens manufacturer’s only fitting lab was in Sydney, but the company’s German headquarters has made a significant investment in Australia to improve turnaround times and enhance customer service to its independent optical practice customers.


THE OPTICAL COMPANY ACQUIRES ADELAIDE EYE CARE
The Optical Company (TOC) has acquired all three Adelaide Eyecare (AEC) optometry practices, taking its practice network to 60 locations.
With its first acquisition of 2024, the TOC network now comprises The Optical Co, Kevin Paisley Optometrists, LensPro, The Eye Place, Stacey & Stacey Optometrists, Optical Warehouse and the nib Eye Care Centres. The company also acquired Kosmac & Clemens and Vision Eye Health in 2023.
The move follows other high level changes after TOC’s parent company Healthia – an allied health group – was acquired in December 2023 by private markets investment firm Pacific Equity Partners. TOC remains as the Eyes & Ears division of Healthia.
and wife optometry duo Mr René Malingré and Ms Liz Capper, assuming leadership of the company in 2003.
“We have proudly upheld the traditions of the original business, not only by advancing diagnostic technology and personalised optical dispensing but also by continuing our strong history of contact lens expertise,” Malingré said.
“Focused on maintaining a high standard of care and nurturing the skills of our great team of optometrists, we are thrilled to have joined The Optical Company. We are excited to have found an alignment with The Optical Company to strengthen our legacy and expand the business.”
Rodenstock’s Tasmania lab, in George Street, Launceston, commenced operations in January 2024. The company purchased an existing glazing lab known as Slama Optical, operated by Mr David Slama. As part of the transition, he has also joined Rodenstock and they will continue the business together.
“It is a great opportunity for Slama Optical to be partnered with a well renowned lens manufacturer and still provide a local, high quality service to Tasmania. It is a perfect match,” Rodenstock Australia general manager Mr Tim McCann said.
The Melbourne lab, which opened in 2023, is centrally located in Mount Waverly within a spread of Rodenstock customers with easy courier access.
Meanwhile, Rodenstock’s Brisbane lab came after the owners of independent lens fitting firm C&S Optical – which provided a service for some of the major lens manufacturers – were seeking a partnership, so Rodenstock Australia acquired the business and its experienced employees.
“The new laboratories create opportunities to improve Rodenstock’s service and distribution capabilities, reducing delivery times, o ering greater flexibility and responsiveness to meet the practice’s needs, and ensuring more reliable timing and quality delivery of your orders,” he said.
“Local fitting services also reduce freight costs for practices and reduce transit times for frames going to and from the lab. Stock lens services are particularly fast with local turnaround.”
E ective 29 February 2024, TOC has purchased AEC practices situated at Mawsons Lakes, Blackwood and Westbourne Park.
AEC was founded in 1982, with husband
Mr Aaron Kangisser, COO of TOC, said an independent spirit and focus on optometry care defined the AEC practices, which aligned with the existing network.
“It’s a privilege to have the opportunity to work with René, Liz and the practice teams as we work together on AEC’s next phase of growth,” he said.
MOREL REBRANDS COLLECTIONS TO SIMPLIFY AND INCREASE VISIBILITY
Popular independent eyewear company MOREL has restructured its collections as part of a long-term strategy to drive greater awareness, visibility, and growth of the label.
Now available through MOREL Australasia – operated by Mr Mark and Ms Lisa Wymond – MOREL has rebranded its eight di erent brands (Marius, Nomad, Öga, Koali, Lightec, Azur, 1880, Marius MOREL) to bring them under the brand names, M Classic, M MOREL and MOREL.
According to a statement, the spirit of the previous collections will be retained and will now be in three segmentations: an a ordable designer collection (M CLASSIC), a core business collection (M MOREL), and an ‘authentic style’ collection (MOREL).

Lisa Wymond said the move would result in a wider choice of product for independent practices and their patients.
“Benefits to the practices include a larger collection to choose from that covers multiple di erent looks and price points. This means practices cover more product o erings within the three collections, resulting in less time spent
with multiple reps to cover those same product categories and less time spent on paperwork,” she said.
“Practices can expect the same fantastic quality design driven product that they are familiar with from MOREL and high level of customer service that they are used to from MOREL Australasia.”

12 INSIGHT May 2024
The company acquired Slama Optical operated by David Slama (pictured). Image: Rodenstock.
Aaron Kangisser, The Optical Company. Image: TOC.
NEWS
At SILMO Paris, Francis Morel (from left), Amelie Morel, Lisa and Mark Wymond, and Jerome Morel. Image: MOREL Australasia.









FACE A FACE PARIS - NOCHI 1 2703 - EYES RIGHT OPTICAL FACE A FACE PARIS - NINNA 1 8031 - EYES RIGHT OPTICAL FACE A FACE PARIS - NOCHI 2 4176 - EYES RIGHT OPTICAL FACE A FACE PARIS - ZAIKU 1 4174 - EYES RIGHT OPTICAL FACE A FACE PARIS - ZAIKU 2 6591 - EYES RIGHT OPTICAL FACE A FACE PARIS - HALOS 1 1472 - EYES RIGHT OPTICAL FACE A FACE PARIS - HALOS 2 2045 - EYES RIGHT OPTICAL What’s Hot!
SAFILO CONFIDENT DESPITE 2023 HEADWINDS
Safilo Group CEO
Mr Angelo Trocchia remains optimistic after “a complex” 2023 for the global eyewear company challenged by a weakened North America market and a 60% revenue hit after EssilorLuxottica’s acquisition of the GrandVision optical chain in Europe.

Meanwhile, the group’s Asia Pacific sales increased to €59.9 million (AU$99 m), up 9.1% at constant exchange rates and 3.9% at current exchange rates, compared to €57.7 million (AU$95 m) recorded in 2022.
The group’s sales were down 2.3% at constant exchange rates and 4.8% at current exchange rates compared to 2022.
“In a complex year like 2023, in which a tense and unstable geopolitical and macroeconomic environment added to our direct challenges, it was particularly important for us to achieve a level of revenue very close to the strong performance recorded in 2022, when growth, compared to pre-pandemic 2019, was +12%,” he said.
“North America continued to be a ected by the prudent attitude of the main eyewear distribution channels and by an unfavourable sun season, while in Europe the incredible job of our teams allowed us to e ectively o set the decline of the business in the former GrandVision chains, further demonstrating the resilience of our group.”
In 2023, Safilo also reviewed its industrial footprint with a brand portfolio that was “no longer aligned with the know-how present”. Trocchia acknowledged the early renewal of licenses for Kate Spade, Tommy Hilfiger, BOSS and HUGO. The group signed new agreements with Etro and Stuart Weitzman.
“This was a very important achievement for us, which sits alongside the solid and long-lasting growth of our home brands, an almost unique portfolio in the industry, which, in 2023, at approximately 44% of our sales, progressed on our target of representing over 50% by 2027,” he said.
RAYNER CONTINUES SUSTAINABILITY PUSH WITH PACKAGING UPDATE
Cataract surgery product manufacturer
Rayner has introduced its latest packaging updated to reduce its carbon footprint, fulfil its environmental goals, and to improve ease-of-use for customers.
According to the company, the new packaging will include:
• Replacing traditional paper instructions for use (IFU) documents with a QR code to enable downloading of the relevant eIFU instead, which will result in the elimination of 35 tonnes of paper every year.

• Switching from a plastic tray and lid container to a pouch, resulting in an 83% reduction in single-use plastic packaging waste.
• A 30% reduction in energy usage due to changes to the manufacturing process.
• Updates to the carton to improve tamper-proofing and robustness during transport.
Rayner said these improvements contribute to its ESG goals for 2024, following the company’s recent recognition as being in the top 17% of companies in the 2023 EcoVadis ratings.
EcoVadis is an internationally recognised assessment platform that rates businesses’ sustainability
based on four key categories: environmental impact, labor, and human rights standards, ethics, and procurement practices.
“Environmental responsibility is important at Rayner,” Mr Tim Clover, Rayner CEO, said.
“With easier-to-use cartons, vastly reduced plastic packaging waste, the removal of paper IFU leaflets and lower energy manufacturing processes, we’re making strides to develop not only a better experience for our customers, but a reduced environmental impact too.”


“We look to 2024 with confidence, hoping that both our challenges and the opportunities arising from the continuous growth of our portfolio of home brands and core licenses will find their place in a more stable international scenario.”
CR LABS LAUNCHES MULTIFOCAL LENS
Independent ophthalmic lens supplier
CR Labs has launched Australis Easy, a multifocal lens the company says represents a breakthrough in lens design, o ering “unparalleled adaptability, a ordability, and ease of dispensing”.
As the latest addition to its Australis portfolio of premium freeform lenses, the lens manufacturer said the Australis Easy had been developed with world-leading technology to provide “superb visual performance in all viewing areas”.
The lens technology is said to combine both hard and soft design elements into one seamless solution that supports a smooth transition for wearers when switching or upgrading from
He added that it’s important to recognise the e ect the company’s actions have on the environment and to take action where possible to mitigate the impact of cataract surgery. previous designs.
According to CR, the lens supports the wearer’s accommodative ability to focus at di erent distances while reducing swim e ect caused by lateral image distortion.
Mr Adam Fletcher, CR CEO, said: “This lens represents a fusion of cutting-edge technology and user-centric design, providing wearers with a hassle-free experience at an a ordable price point.”
Australis Easy joins the Australis VR and Australis AllDay lenses to complete the comprehensive Australis Series With CR positioning Australis Easy as the “good” solution, Australis AllDay as the “better”, and Australis VR as the “best”, wearers now have access to several options tailored to their needs.
14 INSIGHT May 2024
Updates to the carton to improve tamper-proofing and robustness during transport. Image: Rayner.
Australis Easy supports accomm -odative focus at different distances while reducing swim effect. Image: CR Labs.
NEWS
Angelo Trocchia, Safilo. Image: Safilo.

DISCOVER phaco’s most advanced control centre *, at your fingertips *Based on the range of features available for the Centurion Active Sentry System that are not available with other devices curr ently on the market. © 2024 Alcon Inc. Alcon Laboratories (Australia) Pty Ltd ABN 88 000 740 830 Phone 1300 224 153 New Zealand: Phone 0800 101 106. ALC2075 01/24 ANZ-CNT-2200005.
STUDY: CHILDREN WITH MYOPIA SUFFER FROM SLEEP DISTURBANCES
Research by Flinders University experts has found that myopia may be linked to poor sleep in children.
The study, published in Sleep, looked at di erences in melatonin timing and output, sleep characteristics and cognitive function in 26 myopic and 14 non-myopic children aged between eight and 15 years.
“Our study found myopic children have both lower nocturnal melatonin output and delayed melatonin circadian timing compared to normal-sighted children,” said Dr Ranjay Chakraborty, Associate Professor of Optometry at Flinders University.
“We also observed delays in short-sighted children’s sleep and wake-up time as well as poor and reduced sleep among this myopic group.”
Good sleep is beneficial for a child’s eye development and exposure to daylight is connected to melatonin, dopamine and other regulators which can help circadian patterns, the study authors said.
Emeritus Professor of Psychology and sleep expert Dr Leon Lack said further evidence that myopic children have disturbances in their sleep and melatonin circadian rhythms paves the way for more treatments and management strategies.
“We would recommend children increase their morning light exposure to outdoor sunlight or enhanced indoor lighting,” he said.
“Further research could investigate ways to stop or at least reduce the development of myopia – or prevent it from developing –would be immense clinical importance.”
While prescription glasses or contact lenses are usually used to manage the symptoms, myopia is said to be the leading cause of vision impairment and a major cause of blindness – a challenge for the World Health Organization’s global initiative for the elimination of avoidable blindness.
The researchers recommend that a larger study in future could assess the long-term relationship between systemic melatonin and myopia.
RESEARCHERS WORK ON IMPLANTING SOLAR PANELS INTO THE RETINA
University of New South Wales (UNSW) engineers are examining ways that solar panels can be implanted in the human retina to restore sight.

Dr Udo Roemer, who specialises in solar panel technology, is in the early stages of researching how solar technology can be used to convert light entering the eye into electricity, bypassing the damaged photoreceptors to transmit visual information to the brain.
“It has long been thought that biomedical implants in the retina could stand in for the damaged photoreceptors. One way to do it is to use electrodes to create voltage pulse that may enable people to see a tiny spot,” Roemer said.
“There have already been trials with this technology. But the problem with this is they require wires going into the eye, which is a complicated procedure.”
The concept entails a tiny solar panel attached to the eye that converts light into the electric impulse that the brain uses to create visual fields. The panel would be naturally self-powered and portable, without requiring cables and wires into the eye.
Roemer is focusing on semiconductor materials such as gallium arsenide and gallium indium phosphide, as its properties are easier to tune as opposed to

Dr Lyndon Jones says its a potential a game changer for corneal wound healing. Image: CORE.
silicone-based devices.
“In order to stimulate neurons, you need a higher voltage than what you get from one solar cell,” Roemer said.
“If you imagine photoreceptors being pixels, then we really need three solar cells to create enough voltage to send to the brain. So, we’re looking at how we can stack them, one on top of the other, to achieve this.”
Roemer said the technology is in the proof-of-concept stage and is still a way down the track before it will be implantable in the retinas with degenerative eye diseases.
“So far we’ve successfully put two solar cells on top of each other in the lab on a large area – about 1cm2, which has got some good results,” he said.
CONTACT LENS MATERIAL COULD RELEASE DRUGS AS NEEDED
A cross-disciplinary University of Waterloo team has developed a new contact lens material that could act as a bandage for corneal wounds while releasing drugs in a controlled manner to help the eye heal faster.
“It’s a targeted-release drug delivery system that is responsive to the body,” said Dr Lyndon Jones, a professor at the Centre for Ocular Research & Education (CORE) in Canada. “The more injured you are, the more drug gets delivered, which is unique and potentially a game changer.”
Collagen is a protein naturally found in the eye that’s also often involved in the wound healing process – however, it’s considered too weak for a contact lens material. The
researchers found a way to transform a collagen derivative into a biomaterial 10 times stronger. One unique property of collagen-based materials is they degrade when exposed to an enzyme called matrix metalloproteinase-9.
“These enzymes are very special because they’re involved in wound healing, and when you have a wound, they’re released in greater quantity,” said Dr Chau-Minh Phan, also involved in the project. “If you have a material that can be degraded in the presence of this enzyme, and we add a drug to this material, we can engineer it so it releases the drug in a way that is proportional to the amount of enzymes present at the wound.”

16 INSIGHT May 2024
Dr Ranjay Chakraborty, Flinders University. Image: Flinders University.
The solar panels would be naturally self-powered, without wires into the eye. Image: francescosgura/ stock.adobe.com
NEWS
HOYA Consultation Centre (HCC360): Enhance consultations with seamless personalised service

HCC360 is an innovative application designed to be used in practice to help guide patients through the vision consultation journey.
HCC360 supports your business by:
• Demonstrating the differences and benefits of progressive, occupational and single vision lenses, in an easy-to-understand and tangible way
• Displaying interactive and relatable simulations of various lens designs, coatings and treatments, explaining the necessity and advantages of supplementary vision solutions
• Featuring a vision profile questionnaire to recommend a personalised lens design that is tailored to your patient’s lifestyle
• Offering customisable branding and messaging to represent your practice and brand
Fast track the digitalisation of your practice today.
To learn more about HOYA Consultation Centre, please contact your HOYA Sales Consultant or call 1800 500 971.
Beneficiary to benefactor
For Mr Sylvester Prasad, the generosity of several Australian benefactors meant he could bridge vision care gaps within his Fijian community with his new optical dispensing certification. Grateful for the opportunity, he is working hard to pay this goodwill forward.
He covered his travel costs to New Zealand while the course fees were covered by ACOD and Hansen. He completed four workshops of four days each and was able to finish the course in December 2023.
The certificate, according to Gibbins, equipped Prasad with the expertise required to deliver the level of care his community needed.
“He’s a far more confident optical dispenser. Optical services are extremely limited in Fiji. So not only can he work in his commercial practice much more successfully, he can also work in their volunteer aid work that he’s been doing for years there. He’s far more confident in his village outreach as well,” Gibbins says.
Prasad’s gratitude and motivation to complete the course was driven by his desire to service the eyecare needs of and provide clarity to the people of Fiji.
“Without being an optical dispenser, I wouldn’t be able to do the mobile clinic and couldn’t help all the people I am helping now. And so, I’m really thankful for the sponsors. I do believe that without their help, I wouldn’t have achieved much of this yet,” Prasad says.
Gibbins adds: “He was delightful in class, incredibly dedicated to his studies, and polite, quiet, courteous, extremely appreciative and hardworking.”


Armed with a certificate in electronic engineering, Mr Sylvester Prasad’s initial exposure to eyecare was a camera installation in an optometry clinic in Ba, Fiji.
This would become a regular occurrence where he would accumulate valuable knowledge of the industry through his technician work, while simultaneously managing his sugarcane farm.
During his time as a technician, he saw a necessity for eyecare services in the local area and, wanting to contribute to the health outcomes of the community, he asked the manager of the clinic if he could take on additional responsibility.
“The people in the local area were su ering with their eye health and they didn’t know what to do about it. So, I wanted to get more heavily involved,”
Prasad says. “There’s a lot of people out here who aren’t aware of what’s going to happen when their eyesight fails them.”
Within a year, he went from completing patient registrations to voluntarily conducting visual field testing, where he then received an o er from Opticare Eye Center in Western Lautoka as a dispensing technician in 2019. As part of his work at the practice, Prasad conducts mobile clinic services, where he travels to isolated villages and localities, screens for visual acuity, and conducts refractions.
It’s been a worthwhile venture, but Prasad knew he could have an even greater impact with more formalised optical training.
Mr Mark Hansen, an optometrist from Orange in NSW who had supported aid work in Fiji, heard about Prasad through colleagues, and recommended he was sponsored to complete the Cert IV in Optical Dispensing at the Australasian College of Optical Dispensing (ACOD).
Prasad received an o er to enrol from Mr James Gibbins, director and senior trainer at ACOD, with the college sponsoring 50% of the course fees, and Hansen the remaining 50%, marking the first student sponsorship made by the college.
With his course set to begin in 2020, COVID delayed Prasad’s ability to attend workshops, so it wasn’t until 2022 that he was able to fulfil the requirements of his certificate.
A vital part of the training experience is graduating alongside one’s peers. To fund Prasad’s graduation in December 2023, Gibbins searched for sponsors, and Specsavers agreed to cover his out-of-pocket expenses. This included for him to attend the adjoining three-day conference which was embedded as an event at the graduation.
Hansen contributed $500 and an anonymous donor contributed $200 as well, which allowed for Prasad’s wife, Kitty, to attend.
“It was such a thrilling moment for me to know that everything was being taken care of,” Prasad says.
GOODWILL ON A LARGE SCALE
Wielding his new Certificate IV in Optical Dispensing, Prasad is now playing an integral role in Optical Dispensers Australia (ODA) upcoming aid trip to Viti Levu, Fiji in July 2024.
The aid trip will comprise a team of 12, including two optometrists and 10 optical dispensers. ODA will coordinate large village outreach, specifically targeting isolated villages being targeted with donated frames and lenses.
Visual screening and refractions will be conducted, and then full prescription spectacles fabricated in Lautoka and sent back to the communities.
Prasad wants to help his people be more engaged in this space, so he has been raising awareness of the Cert IV to his peers so they can give back to their local community in the same way.
“There are at least two or three students enrolled in the course, that are working in the clinic right now,” Prasad says.
Despite being the first and only sponsorship by ACOD, Gibbins says he hopes this won’t be the last.

18 INSIGHT May 2024 PROFILE
Image: Sylvester Prasad.
James Gibbins (far right), Sylvester Prasad (third from left) and his wife, Kitty Prasad (second from left) at the ACOD graduation in Nelson, New Zealand, 2023.
The sponsorship means that Sylvester Prasad can provide vision care to the people of Fiji.
Image:
ACOD.

















Free delivery* on your first order. Enter code FREEDELIVERY at checkout. Offer ends 31/5/24. For more information visit device.com.au/deviceonline 3,000+ OPHTHALMIC PRODUCTS ON DEVICE ONLINE SCAN THE QR CODE TO LEARN MORE *T&Cs apply. Device Online is for access and use by Australian Healthcare Professionals only.






The modern-day optometry marketing strategy
As the largest branded group of independent optometrists in Australia, Eyecare Plus is leveraging its position to capitalise on a sophisticated marketing strategy that can be targeted all the way down to individuals in certain postcodes – and it’s scoring major runs for participating practices.
Picture yourself in this patient scenario. You turn on your smart TV to watch your favourite show on demand after putting the kids to bed. An advertisement for an independent optometrist in your community plays and – realising you haven’t been for an eye check for a while – you watch the ad. Later, before heading to bed, you check Facebook and see another ad for the same optometry brand, and it happens again while using Instagram and Google the next day.
Throughout the week, the notion of a new pair of spectacles is enticing. It’s been a few years. You Google the optometry network in question and a nearby practice is listed at the top of your search and you make an online booking for the following week. Post-appointment, you’re so satisfied with the service and eyewear, you become a patient for life and tell your family and friends.
For many individual independents, this sophisticated, multifaceted approach to patient acquisition is only attainable with a large investment. But this is a strategy that Eyecare Plus – an independent optometry group with 120 practices – has been employing with great e ect for the past three years.
The decision to invest more in digital marketing marks a major shift for the

network that once relied heavily on direct mail and traditional marketing techniques such as print media, yellow pages, radio and free-to-air
TV. By adopting a digital strategy, Eyecare Plus advertisements can be geo-targeted into specific communities and to certain patient groups.
In 2023 alone, the network generated and tracked close to 5,000 patient appointments from this new approach.
“The way I explain it is that you’re no longer buying ad space during a show or in a publication in an attempt to reach patients. You’re purchasing ad space in front of a target audience across multiple platforms,” Eyecare
20 INSIGHT May 2024 BUSINESS
Image: Ground Picture/Shutterstock.com & Eyecare Plus.
YouTube advertising, here featuring optometrist member Soojin Nam, forms part of the Eyecare Plus’ digital marketing strategy.
Eyecare Plus Bundoora optometrist Jean Walters in an on demand TV campaign.

“The way I explain it is that you’re no longer buying ad space during a show or in a publication in an attempt to reach patients. You’re purchasing ad space in front of a target audience across multiple platforms.”
Philip Rose Eyecare Plus
Plus general manager Mr Philip Rose says.
“There’s an enormous opportunity for our group to go further down this road because it solves the problem of how we can make consistent, highly e ective all-year-round advertising a ordable for our independent member optometrist.”
The way Eyecare Plus structures its membership means independent practices at the local level can leverage regional and national advertising strategies like this. This is because a significant number of practices are branded or co-branded (Eyecare Plus is the largest branded group of independent optometrists in Australia) that allows them to share in marketing costs while unifying under one banner.
Another important element is its exclusive territories model. In other words, you won’t find two Eyecare Plus practices in the same community. While this means its optometrists can freely share intel with one another, it also allows Eyecare Plus to ‘turn on’ ads and promotions for certain geographies because each practice chooses the campaigns it participates in.
Beyond Eyecare Plus brand awareness, Rose says frame, lens and contact lens suppliers are also capitalising on this new way of advertising to the consumer.
For example, if there’s a promotion on an eyewear brand in-store, the frames supplier can tap into Eyecare Plus’ geo-targeted advertising know-how. If a consumer clicks on the promotion, it takes them to a page with Eyecare Plus practices participating in the promotion.
“Suppliers can present a frame or lens o er specifically to the local communities of the participating Eyecare Pus practices, in a measurable and unified manner,” he says.
“With a supplier campaign they may tell us the target audience is a male aged 30 to 50 and interested in sport, so they’re the people who then have the promotion presented to them via our digital marketing. If one of our practices doesn’t stock the product, then that’s not a problem, the ad simply won’t show in their area. The common Eyecare Plus brand allows us to send out a single message to all relevant locations in a targeted fashion, rather than relying on good luck.”
THE INNER WORKINGS
While Eyecare Plus can help individual practices with their marketing campaigns and collateral through its own internal experts – which it calls Marketing Plus – for the more technical digital advertising work it has engaged two external agencies.
According to Rose, the biggest barrier to entry for traditional advertising on free-to-air TV in metropolitan areas has always been the cost of campaigns because this covers large geographic areas, such as the greater Sydney or Melbourne regions. However, by using on demand TV, Eyecare Plus can reduce the cost by narrowing the target to specific postcodes and demographics.
“People are realising more and more that they can catch-up on their favourite shows when their own schedule allows, as opposed to watching

live as it airs on traditional TV broadcasting,” he says.
As such, the optometry network is advertising on all the major platforms, including 7Plus, 9Now, Network 10, SBS On Demand, Kayo, Foxtel and YouTube.
“This is because we’re purchasing the audience and not the ad space on the show,” Rose says. “Hardly anyone watches free-to-air TV in Europe –it’s all on demand, and it’s now here in Australia and growing in a big way,” he says.
“Our practices right now are getting cost e ective TV ads. That’s why there’s so much satisfaction among our members; the money they are spending for the qualified eyeballs on our ads in their area isn’t something they have been able to access before.”
Once the end-user engages with the Eyecare Plus advertisement via on demand TV, Rose likens it to leaving a trail of breadcrumbs. They are tracked, and additional Eyecare Plus advertisements are displayed to that person on Meta-owned social media channels Facebook and Instagram, as well as Google Ads.
In the marketing industry, this method is known as “retargeting” which allows businesses to place their advertising before people who have previously engaged with its advertising or website. Retargeting o ers an opportunity to recapture potential leads or customers.
“It’s multifaceted, you have to bring together these threads to make your digital marketing strategy complete. For an individual to do this from a time and money perspective is very di cult. They have to be committed to their marketing budget,” Rose says.
Under its digital strategy, branded and co-branded Eyecare Plus practices are now a ording consistent Facebook and Instagram advertising in their local communities.
“We are achieving great value for money for our members. Of course, if we had a bigger budget we could do more and hammer home even more messaging, but for our group at this point it’s su cient and scoring runs for us,” Rose says.
“We’re often receiving patient feedback, ‘I saw your ad and I was compelled to come in’. The new patient ratio in our practices is also a key indicator and we’re also tracking interactions on our website, by phone call, and through our online appointment booking.”
INSIGHT May 2024 21
An example of an Eyecare Plus advertisement shown on social media to a targeted audience.




















POWERFUL PREDICTABLE PROVEN


















Experience the latest evolution of the iStent® legacy of excellence in your practice.
iStent inject® W IMPORTANT SAFETY INFORMATION




Powerful technology for sustained intraocular pressure and medication reduction. Predictable outcomes from a truly tissue-sparing procedure. All on a proven platform with the most clinical evidence of any MIGS device.



INDICATION FOR USE. The iStent inject® Trabecular Micro-Bypass System (Model G2-W) is intended to reduce intraocular pressure in adult patients diagnosed with mild to moderate primary open-angle glaucoma (POAG) currently treated with ocular hypotensive medication. The device can be implanted with or without cataract surgery. CONTRAINDICATIONS: The device is contraindicated for use in eyes with primary angle closure glaucoma, or secondary angle-closure glaucoma, including neovascular glaucoma, because the device would not be expected to work in such situations, and in patients with retrobulbar tumour, thyroid eye disease, Sturge-Weber Syndrome or any other type of condition that may cause elevated episcleral venous pressure. WARNINGS: This device has not been studied in patients with uveitic glaucoma. Patients should be informed that placement of the stents, without concomitant cataract surgery in phakic patients, can enhance the formation or progression of cataract. The surgeon should monitor the patient postoperatively for proper maintenance of intraocular pressure. iStent inject is MR-Conditional, meaning that the device is safe for use in a specified MRI environment under specified conditions; please see labelling for details. Physician training is required prior to use. Do not re-use the stent(s) or injector. ADVERSE EVENTS: Postoperative adverse events include but are not limited to: corneal complications including edema, opacification and decompensation, cataract formation (in phakic patients), posterior capsule opacification, stent obstruction, intraocular inflammation (nonpre existing), BCVA loss and IOP increase requiring management with oral or intravenous medications or surgical intervention. Please refer to Directions for Use for additional adverse event information. CAUTION: Please reference the Directions For Use labelling for a complete list of contraindications, warnings and adverse events.
GLAUKOS AUSTRALIA PTY. LTD. Suite 109/12 Corporate Drive • Heatherton VIC • 3202 • AUS • tel 03 9551 2220 • www.glaukos.com © 2022 Glaukos Corporation. Glaukos®, iStent®, iStent inject ® and iStent inject ® W are registered trademarks of Glaukos Corporation. Australian Sponsor: RQSolutions Pty Ltd / New Zealand Sponsor: Toomac. PM-AU-0208 *Based on units sold. GO FOR THE #1 MIGS DEVICE WORLDWIDE *
Supporting the early career optometrist
After receiving feedback there needed to be development opportunities beyond its initial two-year Graduate Program, Specsavers responded in 2023 by rolling out a new scheme that’s providing more direction for its early career optometrists.
After speaking to Dr Edmund Tong for a few moments, the conviction in his voice immediately indicates this is a driven individual. Even before he began working as a fully-fledged graduate optometrist, he had his sights on one thing – store partnership – and has achieved this in his fourth year out of university at Specsavers Devonport, Tasmania.
Today, he is still considered an early career optometrist, but the career development opportunities within Specsavers have allowed him to accelerate towards his goal, now running a team of around 20 people alongside optical dispensing partner Ms Anafa Fok Chak.
“I knew I wanted to pursue store partnership since I started working for Specsavers as an optical assistant in 2017. Even during my graduate optometry interview in 2021, one of my questions to my bosses then was how soon can I work towards store partnership?” he says.
In the first two years, Tong benefitted from Specsavers’ Graduate Program that provides stability in such a delicate moment in an optometrist’s professional life. At the other end of the spectrum, he’s also gained important knowledge from the Pathway Program equipping aspiring business owners with the acumen they need for joint venture partnership within the network.
But in recent years Specsavers spotted an important opportunity to ensure optometrists still only part-way through their career – but after relinquishing the security of the Graduate Program – could continue to develop their skills and experience.
That’s why in 2023 the company launched the Early Career Optometrists (ECO) Program. As part of the initiative, third- and fourth-year Specsavers optometrists receive a monthly newsletter where they can choose from various development opportunities. These include clinical opportunities, voluntary work, and upskilling courses, as

"A key part of the success of the program is the strong relationships built with each individual optometrist, thereby understanding their needs and helping to support them in the best way.”
Cindy Nguyen Specsavers head of professional development



well as non-clinical opportunities such as financial advice and information. Networking events and mentoring are also important components of the initiative.
For Tong, the ECO Program was a key steppingstone on the way to store partnership. He rates one-on-one meetings with Ms Cindy Nguyen, head of professional development at Specsavers ANZ, as one of the most crucial elements.
“With the ECO Program, there are several events and opportunities to serve your clinical skills or further your financial acumen skills,” he says. “Mine was a little di erent purely because I wanted to develop my leadership skills for store partnership. Cindy gave me the encouragement and a tailored recommendation advising if that’s what I wanted, then I needed to lead an initiative in store, or if I wanted to be seen more highly by my peers then I needed to run a CPD event.”
Tong got to work. He set up an in store project to better link recommendations to a patient’s lifestyle, further increasing his leadership and commercial skills. Within a matter of months, he went from being an optometrist at Specsavers Waurn Ponds, Torquay and Belmont (operated by the same partners) to store partner at Devonport, commencing in March 2024.
“I can’t praise the value of those one-on-one meetings enough because it maps a path forward. I already knew where I wanted to go, I just needed someone to fill in the gaps for me,” he says.
“For early career optometrists to have the ECO Program, it’s fantastic because now optometrists don’t have to head into the world of optometry without any formalised support. They have somewhere to turn to when they need it. Retention is so important and having this structured program means that optometrists can have an even greater reason and cause to stay with Specsavers because they know someone cares about their development.”
ELIMINATING BLIND SPOTS
In the years after joining Specsavers in 2021, like any graduate, Ms Alvia Faiza’s priority was to build her clinical abilities. This was going well, but there was one patient group that always made her nervous – children. “Children’s testing can be more objective. You can’t always rely on
INSIGHT May 2024 23 CAREER
Dr Edmund Tong recently became a partner at Specsavers Devonport, Tasmania.
Specsavers.
Images:
care.



about maintaining good eye health is such a big part of what we do,” she says.
“If I can upskill through the ECO Program this year and go out to the wider communities through outreach work, I’d get a lot of fulfilment out of that. It makes the biggest di erence because patients understand the importance of regular eye checks; you don’t lose them to follow up.”
A SEAT ON THE ECO ADVISORY COMMITTEE
Altru Festival is an event for Australia’s homeless youth and disadvantaged. At the 2023 event in Brisbane’s West End, volunteers manned booths o ering haircuts, laundry services, nutritional advice and other essentials.
Specsavers was also there, with its optometrists providing basic eye screening, advice and even referrals. One of those optometrists was Ms Brie Tsang who spied the opportunity via the ECO Program.
“We handed out glasses to several presbyopes. We also came across cases of suspected astigmatism, and even a patient who had a suspicious looking lesion (basal cell carcinoma) on their eyelid, so we informed them it would be best to see an optometrist in store for a thorough test,” she says.
“We also handed out vouchers for free pairs of glasses, educated patients about our bulkbilled eye tests, and included detailed written referrals. It was a rewarding experience and I think a lot of people appreciated seeing us there.”
When Specsavers first announced the ECO Program in 2023, Tsang knew she wanted to be part of the ECO Advisory Committee to help shape the program and provide opportunities to co-present at Specsavers events.
answers from the parent and child,” says Faiza, who practises at both Specsavers Maroubra and Eastgardens, NSW.
“It’s all about ruling out serious causes, but there’s also di erent norms to consider. There’s much closer follow up and it’s their development years, so it’s more consequential for their vision later in life. Managing amblyopia is also important because up until the age of seven or eight, it’s very di cult to treat and regain vision.”
As part of the ECO Program, early career Specsavers optometrists can access the Australian College of Optometry’s Advanced Certificate in Children’s Vision. It’s a six-month program with CPD hours attached and covers abnormal binocular vision, paediatric amblyopia, strabismus, nystagmus, vision therapy, learning related vision problems, myopia control and paediatric ocular disease.
Realising this was an area she wanted to develop, Faiza signed up and now has more confidence when presented with a paediatric case, seeing children, as well as teenagers with myopia management.
“Having the support of the ECO Program introduces you to opportunities you might not have sought out otherwise,” she says.
Faiza realised in her high school years that optometry was the career for her while she sat in a Specsavers waiting room. It’s perhaps unsurprising this culminated in her employment there, but the network’s structured approach to career development was a major drawcard, alongside its clinical approach to optometry.
After completing two years under the highly structured Graduate Program, Faiza says the ECO Program is about exploring potential special interests and upskilling in those areas.
In another opportunity born out of the program, she conducted voluntary work at a Diabetes Australia conference where people with the condition could speak to her and other Specsavers optometrists on the booth about the implications for their eye health. This experience has fuelled a desire to influence beyond the consulting room, and emphasised the importance of programs such as KeepSight.
“Now that I’m in my fourth year, I’ve seen that community education
But 2023 was significant for other reasons too. After starting her career at Specsavers Maroochydore on the Sunshine Coast – a store she went to with another optometrist from her Queensland University of Technology cohort as part of the company’s ‘go with a friend’ initiative – she moved back to Brisbane where she purchased her first home.
The company managed to secure her a role at its Indooroopilly location. Such a big change can be exciting and unsettling, but she’s found stability through mentorship within the ECO Program.
“The opportunity for one-on-one meetings with the professional development team to let them know how I was going has been incredibly helpful, especially after relocating. And the support o ce was very accommodating in finding a store that’s now just 15 minutes from my home,” she says.
“At this point in time, I’m not so much looking at partnership, it’s more about settling in to be the best clinical optometrist I can, furthering my clinical development opportunities, continuing to network and do the best that I can on the ECO Committee.”
Now in her second year of the ECO Program, Tsang is keen to explore other opportunities, potentially through paediatric and glaucoma courses with the ACO. A key benefit of the ECO program is a $3,000 allowance and elected day o to pursue for continued professional development (CPD).

“Retention is so important and having this structured program means that optometrists can have an even greater reason and cause to stay with Specsavers because they know someone cares about their development.”
Dr Edmund Tong Specsavers Devonport
24 INSIGHT May 2024 CAREER
Alvia Faiza, of Specsavers Maroubra and Eastgardens, NSW, has leveraged the ECO Program to upskill in paediatric

“It’s exciting because we’re still developing the ECO Program, so there may be even more opportunities in future,” she says.
ECO PROGRAM – IN A NUTSHELL
The Specsavers Early Career Optometry (ECO) Program was rolled out in 2023 and is a two-year development program for third- and fourth-year optometrists within the network. It is described as a holistic program o ering clinical and non-clinical development opportunities to optometrists, allowing them to tailor their own personal and professional growth with the support of their store partners.
The program was born out of feedback from store partners and other optometrists at Specsavers for the need for more development opportunities beyond the initial Graduate Program.
As part of the ECO Program, Specsavers optometrists receive the ECO Newsletter monthly, where di erent development opportunities are sourced and shared. These opportunities include clinical opportunities like working with The Fred Hollows Foundation on outreach, Diabetes Australia and upskilling with the Australian College of Optometry, as well as non-clinical development opportunities like information on buying a house with CommBank and financial well-being advice from Victoria Devine, which is an extension of Specsavers' new ‘WeCare’ program, designed to help take care of employee’s emotional, physical, financial and social wellbeing, both inside and outside of work.
In 2023, 28 di erent opportunities were shared with ECO optometrists.
“A key part of the success of the program is the strong relationships built with each individual optometrist, thereby understanding their needs and helping to support them in the best way,” Specsavers head of professional development Cindy Nguyen says.
“This is solidified with ECO social and networking events throughout the year, where the sense of community is strengthened. This year, we have welcomed our second cohort of the ECOs, and we plan on expanding the opportunities o ered to them and also set up career development pathways for our ECO optometrists entering their second year.”

















“The great thing about working at Specsavers is there are many career pathways – everyone has di erent plans and goals and that’s OK. At the end of the day, the business is here to support us regardless of what direction we choose. You’re never alone and there’s such a great team culture and dynamic, and incredible support systems we can always refer back to.” If clinically necessary for the treatment of your patient, prescribe




PBS Information: Xalatan (latanoprost 0.005% eye drops, 2.5 mL) is listed on the PBS as antiglaucoma preparations and miotics.
Before prescribing please review Product Information available via www.aspenpharma.com.au/products or call 1300 659 646.
Minimum Product Information: XALATAN® (Latanoprost 50 µg/mL) Eye Drops. Indication: Reduction of intraocular pressure (IOP) in patients with open-angle glaucoma or ocular hypertension. Contraindications: Hypersensitivity to ingredients. Precautions: Change in eye colour due to increased iris pigmentation; heterochromia; eyelid skin darkening; reversible eyelash and vellus hair changes; macular oedema often associated with aphakia / pseudoaphakia; other types of glaucoma; contact lenses; severe or brittle asthma; herpetic keratitis; driving or using machines – transient blurry vision; elderly: no data; children: do not use, no data; lactation- metabolites present in breast milk, risk / benefit. Pregnancy: Category (B3) Interactions: other prostaglandins, thiomersal. See PI for details. Adverse Effects: Eye Disorders: blurred vision, burning, conjunctivitis, excessive tearing, eye pain, foreign body sensation, hyperaemia, iris hyperpigmentation, itching, punctate epithelial erosions, grittiness, stinging, eyelash and vellus hair changes, punctate keratitis, blepharitis, eyelid oedema, localised skin reaction on eyelids; Systemic: bronchitis, upper respiratory tract infection, eczema, rash, urinary tract disorder, abnormal liver function, myalgia, arthralgia, dizziness, headache, rash, chest pain, asthma, dyspnoea . See PI for details and other AEs. Dosage and Administration: One eye drop in the affected eye(s) once daily. Other eye drops should be administered at least 5 minutes apart.
References: 1. Clinical Practice Guide for the Diagnosis and Management of Open Angle Glaucoma. Optometry Australia 2020 2. Australian Commission on Safety and Quality in Healthcare Active Ingredient Prescribing Guide - list of medicines for brand consideration December 2022
Aspen Australia includes Aspen Pharmacare Australia Pty Ltd (ABN 51 096 236 985) and Aspen Pharma Pty Ltd (ABN 88 004 118 594). All sales and marketing requests to: Aspen Pharmacare Pty Ltd, 34-36 Chandos Street, St Leonards NSW 2065. Tel: +61 2 8436 8300 Email: aspen@aspenpharmacare.com.au Web: www.aspenpharma.com.au Trademarks are owned by or licensed to the Aspen group of companies. © 2023 Aspen group of companies or its licensor. All rights reserved. Prepared: July 2023 AU-LAT-072023-07653
by brand and disallow brand substitution2 ✔ A first choice for glaucoma management1
Brie Tsang, of Specsavers Indooroopilly, Queensland, is on the ECO Advisory Committee, helping to shape the program.
Your Professional Dry Eye Assistant
Objective grading scales
All results at a glance
Comprehensive screening
Monitor treatment progress






OCULUS Keratograph 5M advanced corneal topographer with JENVIS Pro Dry Eye Report.
Dry eye management has never been this easy. The comprehensive analysis supports objective grading for diagnosis of dry eye disease, with an optimised workflow to save time. All results are summarised and presented in a patient friendly report. Get in touch 1800 225 307 enquiries@dfv.com.au dfv.com.au

Keratograph 5M

Proven Dry Eye Solutions








Optimel
Antibacterial Manuka honey drops, gel and eyelid cream





Oasis
Punctum plugs


Form Fit, Soft Plug Silicone & Extended Duration

Avenova


Eye lid treatment with Pure Hypochlorous Acid




Tea Tree Cleanser
Eye-Eco Tea-Tree facial cleansers






I-LID ‘N LASH
Range of lid and lash cleansing wipes




Eye-Eco Masks & shields
Dry eye heat masks and night-time seals


All the treatment options you need for patients with mild, moderate and severe dry eye disease.
DV1427-0224

A low pressure approach to cataract surgery
The latest phaco technology from Alcon is allowing Australian ophthalmologists to perform cataract surgery at near-physiological intraocular pressure levels. By effectively halving her target pressure, A/PROF SMITA AGARWAL says this is offering benefits to surgeons and patients.
Each day, NSW ophthalmologist Associate Professor Smita Agarwal sees first-hand how cataract surgery has entered the era of optimisation. Aside from premium intraocular lens (IOL) technologies, patients are demanding a more comfortable surgical experience and quicker recovery times. In one recent case, she implanted an IOL in a medical professional seeking to return to work the next day.
“Modern-day patients not only want quality vision, but they also want it as fast as possible. The patient in this case did go back to work and saw 50 patients the next day,” she says.
“These are the kind of requests we are dealing with today, and often we’re implanting multifocal, premium lenses. Patients don’t want blurred vision for a week as it used to be in the past due to corneal swelling. They don’t have the patience or time for that today.”
For Dr Agarwal in recent years, the use of near-physiological intraocular pressure (IOP) has been one of the key leaps in her cataract surgery approach. She has gone from operating at an average of 55 mmHg to as low as 22 mmHg, helping to protect the delicate intraocular structures in her patients’ eyes while maintaining normal anatomic relationships.
In addition to greater safety and surgical e ciency, she’s seen marked improvements in intraoperative patient comfort and post-operative recovery. And importantly, she’s been able to preserve a happy and safe working space between the corneal endothelium and posterior capsule.
The key piece of technology behind this change has been the Active Sentry Handpiece from Alcon launched in 2019. The phaco technology is used on the company’s Centurion Vision System and together they o er automatic, real-time surge reduction support to improve safety, consistency and control for cataract surgeons.
Alcon says the Active Sentry Handpiece is the first and only phaco handpiece with an integrated fluidics pressure sensor. Dr Agarwal says this crucial design feature means IOP is e ectively detected at the eye, making it highly responsive to fluctuations in IOP. This gives her the confidence to operate at a near-physiological IOP, providing an elevated experience for her patients.
Today, Dr Agarwal performs surgery with the Active Sentry Handpiece at her own day surgery she opened in 2023, Victoria Street Private Hospital, and at Nowra Private Hospital. She consults out of her rooms in Wollongong, Nowra and Warilla as part of Wollongong Eye Specialists.
“With previous technology, the fluidics pressure sensors were not in the handpiece, and pressure alterations at the tip of the phaco probe travelled to a sensor located inside the cassette at the speed of sound which caused delayed response in adjusting fluidics. In the gravity system the delay was measured by the length of the tube – at least 1.2 metres from the BSS (balanced salt solution) to the fluidic management system in addition to 1.2 metres from the fluidic management system to the patient’s eye. Eye surgery doesn’t have much of a threshold, things happen in a matter of milliseconds,” she says.
“It’s a smart move putting the sensors in the handpiece. Because of this, the moment the pressure reduces, there are pressure plates that compress on the BSS bag to increase the inflow of the BSS to maintain the chamber stability. There is no time lag. Surgery is becoming easier to perform with technology like this. As surgeons, we take the credit but it’s the machines driving the safety and e ciency of surgeries these days.”
A TRIP DOWN PHACO LANE
Prior to arriving in Australia in the early 2000s, Dr Agarwal remembers her ophthalmology training in India in the mid-1990s when it would take her professor up to an hour to set up the phaco machine. Thankfully, the technology has progressed since then, with several iterations along the way.
By the late 1990s, the Legacy system (Alcon) was introduced to the market which Dr Agarwal briefly used during her training days. It had longitudinal ultrasound which caused clogging of phaco tip hence the need for increased fluid pressure.
Then in 2003, the Infiniti gravity based fluid infusion system was released but it still needed a lot of fluid and it was not uncommon to need a second bottle of BSS. These passive infusion systems caused more corneal oedema due to increased fluid use.
Next in 2008, torsional ultrasound represented "a game changer" as it caused less clogging of the phaco tip and the chances of surge reduced hence chamber stability became better.
Then, in 2013 Alcon launched the Centurion Vision System.
“I remember talking to Alcon and saying, ‘Well I’m very happy with Infiniti, how much better can it get?’. And they said, ‘no, you need to it try
28 INSIGHT May 2024 CATARACT
Images: Alcon.
Alcon says its Active Sentry Handpiece is the only phaco handpiece with an integrated fluidics pressure sensor.
to believe it’. We bought three Centurions at the same time in the area because the phaco equipment here was getting out of date, and it was so good. It brought us Active Fluidics which means the infusion is no longer gravity based, but is based on compression plates, improving surge and chamber stability.
“But at that time, we didn’t have the Active Sentry Handpiece, which was later released in 2019. The way it is able to maintain the chamber volume fluidics – with the pressure sensor in the handpiece – means there is a reduced risk of endothelial damage, or posterior capsular tear due to sudden shallowing. With reductions in surge and less fluid usage, we are also noticing eyes are much clearer. There’s less inflammation and visual recovery is faster.”
She adds: “Good is only good until something better is introduced and that’s what we are noticing with phaco technology evolution."
When she first started using the Active Sentry Handpiece, initially Dr Agarwal’s IOPs went from 55 mmHg to 40 mmHg. Although it was only a small drop, she did feel patients were recovering faster, but didn’t pay it a lot of attention. Progressively, she dropped her IOP to 30 mmHg, 25 mmHg and is now operating at 22 mmHg, and has experienced no compromise in her surgical performance.
“In fact, the chamber was maintained. My Alcon rep asked if I felt any di erence, and I said, look if I didn’t say anything, that means I didn’t feel anything, and that’s a good result,” she says.
“I would say to other surgeons, by adopting this technology the benefits are far greater – and there is no learning curve because it is done in such a safe and e cient way that you don’t even notice the di erence during surgery. Where you will notice the di erence, however, is in the first week, in terms of faster recover times and less inflammation.”
WHY HIGH IOP IS NO LONGER PALATABLE
Today, Dr Agarwal’s 22 mmHg cataract surgery IOP is a far cry from an earlier era of ophthalmology when operating at 80-110 mmHg was acceptable practice.
Back then, high IOP values maintained adequate chamber stability at e cient aspiration flow and vacuum and helped to compensate for dynamic pressure losses and chamber shallowing resulting from flow out of the eye. As such, surgeons perhaps weren’t as worried about the potential consequences of high IOPs, but instead were more concerned about complications mid-surgery.
Dr Agarwal says poor fitting tips, tubings and larger incisions all led to greater egress of intraocular fluid, and therefore the need for higher IOPs.
“But high IOP causes reduced blood supply to the retina and optic nerve. Energy consumption and dissipation is higher, and hence, more intraocular inflammation post-operatively. It can also cause endothelial cell loss which we are noticing in our study, and increased corneal swelling day one,” she says. “There can also be pain intraoperatively when there is a sudden increase in pressure. We noticed sometimes in

“It’s a smart move putting the sensors in the handpiece. Because of this, the moment the pressure reduces, there are pressure plates that compress on the BSS bag to increase the inflow of the BSS to maintain the chamber stability. There is no time lag.”
A/Prof Smita Agarwal Wollongong ophthalmologist
The handpiece is used on the Centurion Vision System and together they offer real-time surge reduction support to improve safety, consistency and control.



high myopic eyes where the chambers are deep, patients can feel pain in the eye on sudden irrigation in the eye. So, we are now creating greater patient comfort by lowering the IOP.”
As alluded to, Dr Agarwal is now collecting data to understand how the combined Centurion Vision System and Active Sentry Handpiece is improving outcomes. She is comparing its performance at the Victoria Street Private Hospital with the Centurion Vision System at Shellharbour public hospital where phaco is performed with a di erent handpiece.
On each participant, she is gathering their pre-operative baseline visual acuity, corneal thickness, central foveal thickness and corneal endothelial cell count, and comparing this seven days post-surgery. From this, she hopes to compare the performance of the Active Sentry and non-Active Sentry handpieces.
“The early data shows that the endothelial cell loss is significantly less when using the Active Sentry Handpiece, which makes sense,” she says.
“Because the chamber is maintained there is probably less energy hitting the corneal endothelium. Sometimes even if we feel that the chamber is maintained, there are subtle di erences we don’t visualise that are probably causing more endothelial cell loss without the Active Sentry Handpiece.”
While impressed with the current level of phaco innovation, Dr Agarwal says the future may lie in artificial intelligence o ering customised lens options and surgical settings based on the individual’s anatomy. Whether a patient has glaucoma, a compromised retinal vasculature due to diabetes or other vascular events, then the ideal IOP could be tailored for that patient.
“Or based on the patient’s corneal endothelial cell count, artificial intelligence could indicate the ideal pressure and fluidics to avoid any damage and improve outcomes post-operatively,” she says.
“It could be about customising the settings rather than having to use the same for each patient that enters the operating theatre.”
INSIGHT May 2024 29





Get Optos off your wish list and into your practice




9 modalities provide additional retinal visualisation*


2500 studies demonstrate clinical value and practice efficiency*



Patients choose to pay for Optos imaging ≥ 80% of the time*




Do future you a favour

©2024Optos. All rights reserved. Optos®, optos® and optomap® are registered trademarks of Optos plc.
Macular disease report 2024

The Australian eyecare sector is challenging the idea that vision loss with age is inevitable. This, combined with cutting-edge research from world-renowned experts, promising therapies, and ongoing efforts to enhance patient outcomes, position the country as a global leader in the fight against macular disease.


The notion that vision loss is an inevitable product of ageing is outdated, according to Macular Disease Foundation Australia (MDFA) CEO Dr Kathy Chapman.
Indeed, addressing the increasing prevalence of macular disease as the population ages is one the sector’s greatest challenges, but shaking the stigma that vision loss is a forgone conclusion as we age is a challenge of equal proportions.
“We do know that if people can be detected early and be monitored and get on to the right treatment pathway, vision loss doesn’t have to be the case,” Dr Chapman says.
To drive this mindset, a key focus of the peak body’s ongoing and upcoming initiatives is to equip an increasing number of people with macular disease with accurate and relevant information about their disease. Dr Chapman says more widespread early diagnosis provides a hopeful outlook for disease management.
This can be attributed to technological advancements and to optometry adopting some of the responsibility of disease detection (which would have typically occurred at the level of the ophthalmologist). Now, more practices are incorporating OCT into their daily workflows.
“A lot of optometry practices have new technology and capabilities which allow them to see those signs and symptoms to refer people on early. I think that’s an exciting development,” Dr Chapman says.
ON THE FUTURE OF MACULAR DISEASE
MDFA’s strategic priorities include community awareness, support services, advocacy, and funding research e orts to combat macular disease. Dr Chapman cites ongoing Social Impact Surveys as a significant area of investment for MDFA that are directed to people with various forms of macular disease.
“Our Social Impact Surveys are the largest snapshot of people living with macular disease in Australia,” Dr Chapman says. “We’re giving patients a chance to share their main areas of concern.
“This is a really important piece of research for MDFA because it helps us understand the bigger issues at a systemic level, what we should be advocating for, and how we can design our support programs to really answer people’s concerns.”
Beginning in 2021, each survey has a particular focus, with the most recent survey in 2023 exploring mental wellbeing. The results from this survey helped inform the formation of MDFA’s new My Eyes service being launched in May 2024.

My Eyes – the latest support and care initiative of MDFA – is a free service tailored to patients’ diagnoses. Piloted since October 2023, it serves as a safety net for patients in between clinic visits. As part of the service, MDFA personalises information based on disease stage, individual anxiety levels, and severity of vision loss, with a commitment to maintain contact over an extended period.
“It’s a way of being able to keep in touch with people in between their clinic visits with their eye health professional,” Dr Chapman says. “Rather than thinking they’re just calling us once or that we will provide as much information as possible, we tailor our support and stay in touch with people for a 12-to-18-month period.”
The forthcoming 2024 Social Impact Survey is focusing on the cost of treatments – a major barrier to treatment uptake and compliance in neovascular age-related macular degeneration (nAMD).
It has been demonstrated 20% of patients who begin their anti-VEGF intravitreal injections withdraw from treatment in their first year, and 50% withdraw by the fifth year.
“Cost and being able to be treated close to home are the two biggest reasons why people drop out,” Dr Chapman says.
With the results of the survey, MDFA has been able to direct attention to the federal and state governments to lobby for greater access to ophthalmology services in public outpatient settings.
“About 80% of people who require the intravitreal injections receive them in private ophthalmologist rooms and only about 20% of them are able to access them through public hospital outpatient clinics,” Dr Chapman says.
“We’ve talked to the government about looking at practice incentives to increase access to more bulk billed services, particularly for aged care

Image: Kathy Chapman.
“We do know that if people can be detected early and be monitored and get on to the right treatment pathway, vision loss doesn’t have to be the case.”
Dr
Kathy Chapman
MDFA
INSIGHT May 2024 31 MACULAR DISEASE
Image:
Marti Bug Catcher/shutterstock.com


UPDATED AMD REFERRAL GUIDELINES
RANZCO’s Referral Pathway for AMD Management has been updated as Australia gears up for the first approved treatments for GA.
“With the era of treatment for GA upon us, it is imperative that we review our current management of the disease and update it accordingly so that it is fit for purpose. As such we specifically updated the section in the guidelines for GA,” said Australian macular disease expert Professor Robyn Guymer AM who has been instrumental in developing the guidelines since they were released eight years ago.

Two GA therapies are now approved in the US, but no therapy has yet been cleared for Australia.
Apellis’ pegcetacoplan injection created history as the first approved GA therapy in the US in February 2023 under the name Syfovre. Dr Guymer said regulatory evaluation is under way for this therapy with a TGA-targeted decision date in 2024. Meanwhile, avacincaptad pegol (ACP) intravitreal solution received FDA clearance in August 2023 under the brand name Izervay, and according to Dr Guymer, Astellas Pharma Australia is planning on submitting the treatment to the TGA for regulatory assessment.
The initial AMD referral guidelines, led by Dr Guymer, head of macula research at CERA, were devised in 2016 by the RANZCO AMD guideline working group. The panel has since reconvened to update the guidelines which now reflect the appropriate counselling of a patient with GA and potential treatment options.
“GA is one of two late forms of AMD, which until now has remained untreatable. With the approval of these new treatments – and several more in advanced stages of clinical trials – this has prompted a change to the AMD referral guidelines,” Dr Guymer said.
Along with stakeholders such as Optometry Australia and MDFA the new guidelines have been developed and approved by RANZCO.
“Not everyone with GA will be interested to learn about these new advances, but everyone should be given the opportunity to consider them,” Dr Guymer said.
In the original guidelines regarding GA, they recommended optometrists explain the disease to patients, identify and improve risk factors, recommend use of an Amsler grid, optimise spectacles, refer to low vision support services as appropriate, and review them in six to 12 months, depending on individual needs.
Now, the guidelines advise patients to be non-urgently referred to an ophthalmologist if they are interested in a potential GA treatment or to learn more about the treatments to enable them to make an informed decision.
“It may not be currently possible for public patients to be referred to see an ophthalmologist, as outpatient clinics in public hospitals have limited ability to see GA patients,” Dr Guymer said.
“However, when treatments become available on the PBS this is likely to change with more access to treatment becoming available.”
pensioners. We’re also advocating for helping people with the cost of travel for treatment because if you live in a country area, you tend to have further to travel and more to pay,” Dr Chapman says.
Much of the discussions between MDFA and the government involve a long-term look at the economic benefits of increasing funding in this space. The foundation recently compiled an economic modelling report entitled ‘Investing to Save Sight: Health and Economic Benefits of Improving Macular Disease Treatment Resistant’.
“It was amazing to find that over a decade – and if we could get just 25% more people staying on their treatment course – the government could save up to $2 billion,” Dr Chapman says.
“Stopping people from going blind and accruing all the extra health and aged care costs as a result means that it is vital for government to be investing now.”
As part of Macula Month, MDFA is also launching updated nutrition guidelines for people with macular disease. The organisation completed a systematic review of all the published evidence on the association between diet and macular disease (more information is available on page 36).
“Fish, as well as a variety of fruits and vegetables, are all very beneficial parts of an eye-healthy diet,” Dr Chapman notes, with the research also uncovering disease risk factors such as alcohol – now reinforced in MDFA’s messaging.
Looking ahead, Dr Chapman would like to see greater referrals to MDFA to capture the largest possible patient base. As the foundation bridges the gap between clinic visits, it provides much-needed social support absent from traditional diagnosis and treatment regimes.
“We often hear people saying, ‘I wish I’d known about Macular Disease Foundation earlier’,” she says.
“MDFA is helping people live with the condition; the foundation wants to be here to help people live with the disease and to really enjoy the best quality-of-life with ongoing information and support.”
LEADING THE CHARGE
Associate Professor Anthony Kwan works at the Queensland Eye Institute (QEI) and Mater Hospital in Brisbane. As a retinal specialist, AMD is a staple of his day-to-day work life.
He works closely with the MDFA on its medical and research committees, helps the organisation award grants to new prospective treatments, and guides patient support groups to optimise service delivery.
Dr Kwan places Australia at the forefront of macular disease developments due to the availability of treatments and clinical trials, and in terms of patient outcomes. As one example, Australia is a proven leader in vision preservation shown in the Fight Retinal Blindness! (FRB!) digital database.
The adoption of treat and extend regimens – involving progressive
32 INSIGHT May 2024 MACULAR DISEASE
The MDFA’s Social Impact Surveys are the largest snapshot of people living with macular disease in Australia, which the foundation uses to craft tailored social support services.
Prof Robyn Guymer, CERA.
Andrey_Popov/shutterstock.com
Image: Anna Carlile/CERA. Image:
extension of treatment intervals up to 16 weeks – can be attributed to these better outcomes, according to Dr Kwan.
“With a treat and extend regime, patients’ results are likely to be better than treating as needed. Here, vision is more likely to be maintained if they adhere to the treatment,” Dr Kwan says.
The first approved macular disease therapies are reaching maturity – with anti-VEGF intravitreal treatments first entering the scene in 2007 (Lucentis) followed by Eylea in 2012. For several years, these have remained as the main treatment options for nAMD. More recently, Vabysmo (Faricimab) has entered the market and has given specialists more choice in the management of diabetes-related macular oedema (DMO) and nAMD.
While these treatments are still considered the gold-standard, the therapies have their drawbacks. In particular, treatments are not once-o , with patients requiring frequent, ongoing injections. This, coupled with the cost of private ophthalmology services, results in a significant dropout rate.
With treatment options available for nAMD, diabetic retinopathy and vein occlusion, attention is now turning to the other late form of AMD, geographic atrophy (GA).
So far, only two therapies have been approved for GA in the US – Syfovre by Apellis and Izervay by Iveric Bio – both in 2023. While both drug companies intend to bring their therapies to Australia (Syfovre has been submitted for TGA approval with Izervay following suit shortly), Dr Kwan says it is unclear when or if they will become available.

“These drugs are not approved in Australia, partly because there are some limitations,” he says. “They’ve been shown to slow down the progression of degeneration involved in geographic atrophy but that doesn’t necessarily improve the patient’s visual function. The other consideration is the long-term safety of these new treatments. So that’s why I believe the government has to carefully consider approving and funding these treatments.”
Image: Anthony Kwan.
“With a treat and extend regime, patients’ results are likely to be better than treating as needed. Here, vision is more likely to be maintained if they adhere to the treatment.”
A/Prof Anthony Kwan
Queensland Eye Institute
Dr Kwan, alongside the MDFA, lobbies individual state governments to improve treatment availability – as delivery of service di ers between states,
Dr Kwan points to NSW and the ACT who have not signed up for the Pharmaceutical Reform Agreement which means they do not have access to the pharmaceutical benefit scheme (PBS). That is, PBS subsidised medicines are not readily available in public clinics in these states and territories.
To overcome non-compliance of treatment, Dr Kwan says there are clinical trials for orally delivered agents that will hopefully have similar e cacy to intravitreal injections.
One example is the investigational drug danicopan – an oral complement factor inhibitor. It is currently in Phase 2 clinical trials, led by Professor Robyn Guymer at the Centre for Eye Research Australia (CERA), to test its e ectiveness in slowing GA and asses its safety profile.
Elsewhere, the Port Delivery System designed for prolonged delivery
Advanced LayR technology adds multifunctional performance layers to our Biometric Intelligent Glasses, enhancing vision clarity by tackling obstacles like lens reflections, dust, dirt, scratches, UV light, and artificial blue light. In fact, 82% of spectacle wearers report seeing more clearly because of the technology.*



ALL-NEW LAYR TECHNOLOGY MULTIPLE LAYERS. MULTIPLE FUNCTIONS. CLEARER VISION. Learn about all the benefits at www.rodenstock.com
Frame R7136 A
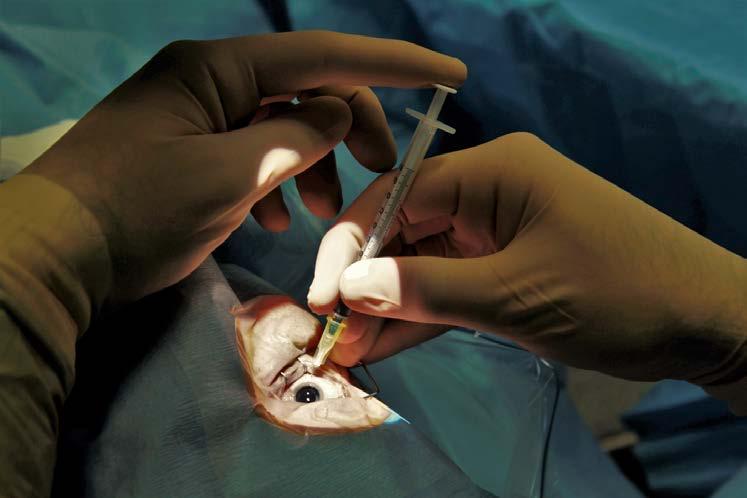
of ranibizumab is being assessed in Phase 3 clinical trials. This system is surgically implanted into the eye and then requires an annual or biannual top-up which is considered more e cient than the current delivery of therapy each month or two.
Additionally, there is a new UNSW-developed molecule – called BT2 – that could be administered via an eye drop for nAMD. This is being commercialised by clinical-stage Australian biotechnology company Filamon Limited which hopes to have the therapy in clinical use within three years.
On the research horizon, Dr Kwan is hopeful for gene therapy to lead the charge, despite the discontinuing of the GT005 gene therapy clinical trial for GA last year.
“This would involve injecting the gene product for anti-VEGF therapy for nAMD into the back of the eye, where it would behave as an ‘intraocular factory’ and continuously produce the drug,” he says.
ELEVATING THE TREATMENT LANDSCAPE
Professor Mark Gillies, director of the Macula Research Group (MRG) at the University of Sydney, says treatment outcomes from the clinical trials of therapies approved in the US for GA only serve to delay vision loss.
“Roughly, with two years of monthly injections, you defer vision loss that was going to happen in two years, to three years. That’s currently the major benefit that patients can expect – which isn’t amazing,” he says.
Dr Gillies says patients are not aware that the rate of expansion of their macular atrophy has been slowed, as treatments delay vision loss but do not improve vision. This may act as a driver for non-compliance.
To restore vision lost from macular atrophy, he says researchers are working to transplant retinal pigment epithelium and photoreceptors. Although still in early stages and not yet achieved, many groups around the world are working on it with Dr Gillies hoping there will be progress in the foreseeable future.
“There’s a lot of work in this area that will hopefully continue to develop and produce outcomes over the next few years, but at the moment, that’s not something that we can do with atrophic AMD,” he says.
Dr Gillies says the new generation of nAMD therapeutics – which includes Beovu by Novartis – are designed to be more potent than their predecessors and therefore last longer with increased intervals between injections.
“Beovu certainly appeared stronger than previous agents, but it had a higher rate of causing inflammation inside the eye, so it is only used occasionally for eyes that are very di cult to control with other agents,” Dr Gillies says.
Furthermore, in January 2023, Roche’s Vabysmo became the first TGA-registered bispecific antibody approved for the eye in Australia. It specifically recognises and blocks the activity of proteins known as angiopoietin-2 and vascular endothelial growth factor A, and joins an expanding list of approved anti-VEGF therapies for macular disease in Australia.
The other new VEGF inhibitor, high-dose Eylea, has recently been approved in the US and Europe. It has four times the dose (8mg instead of 2mg) of the original Eylea formulation that was released 10 years ago.
The FRB! Project – developed by Dr Gillies at the Save Sight Institute – has tracked real world outcomes of therapeutic outcomes. The project recently found that 40% of eyes with nAMD lesions that could not be inactivated by other VEGF inhibitors became inactive after introduced to Vabysmo when treatment intervals were lengthened by approximately three weeks. This occurred 12 months after switching to the new treatment.
Despite this e ectiveness, Dr Gillies says that further research is required to determine whether the new treatments are associated with greater risks of intraocular inflammation than are found with existing agents. And even if they last longer – with some treatments administered every five or six months – it is believed that injections need to be continued indefinitely which is expensive for the government to fund.
Another significant development in this space, according to Dr Gillies, are projects focusing on macular telangiectasia type 2 (MacTel). The disease is sometimes mistaken for AMD due to similar symptoms and clinical signs, however, there is currently no available treatment.
Dr Gillies was the chief investigator of two major randomised Phase 3 clinical trials for NT-501, a treatment for MacTel. In study A the therapy, developed by Neurotech Pharmaceuticals, reduced the rate of expansion of atrophy by approximately 55%, and by around 30% in study B.
The drug is delivered through an implantable device which secretes ciliary neutrophic factor (CNTF) with controlled, long-term delivery. An implant that was removed from an eye after 15 years was found to still secrete the drug.
“It’s a real one and done procedure. MacTel currently doesn’t have any other treatment – so that’s a big breakthrough,” Dr Gillies says.
Furthermore, his research extends to defining the anatomy of the macula – what he describes as an ambiguous segment of the eye – to understand why it develops MacTel in particular, but also AMD and DMO.
As part of this, Dr Gillies says his team are among the first to grow and study human maculas from eyes donated for corneal transplantation ex vivo (in a culture chamber).
“Even though you get some disease in the peripheral retina, they’re much more focused in the central macula and that has a much greater e ect on the patient as this is where the central vision is,” Dr Gillies says.
“There’s not a lot of research known about why the macula is so di erent. Everyone knows it’s anatomically di erent, but not of the biochemical and physiological di erences which make it so susceptible to getting the diseases.”


“There’s not a lot of research known about why the macula is so different. Everyone knows it’s anatomically different, but not of the biochemical and physiological differences which make it so susceptible [to disease].”
Prof Mark Gillies University of Sydney
34 INSIGHT May 2024 MACULAR DISEASE
Image: Mark Gillies.
Image: kerale/shutterstock.com
Around 20% of Australians with nAMD quit treatment within a year, with 50% discontinuing eye injections within five.
GEOGRAPHIC ATROPHY
WE CAN’T WAITAND SEE
Geographic atrophy (GA) is a relentless disease and is associated with irreversible vision loss.1-4
At Apellis, our goal is to bring to market a treatment for this debilitating disease.
To learn more about GA and its impact, scan here
Vision impairment due to geographic atrophy may vary.


References: 1. Boyer DS, et al. Retina. 2017;37(5):819-835. 2. Lindblad AS, et al. Arch Ophthalmol. 2009;127(9):1168-1174. 3. Holz FG, et al. Ophthalmology. 2014;121(5):1079-1091. 4. Sunness JS, et al. Ophthalmology. 2007;114(2):271-277.
Apellis Australia Pty Ltd, L3, 141 Camberwell Rd. Hawthorn East, VIC, 3123 ABN 87 600 316 612 | March 2024 | AU-GA-2400016


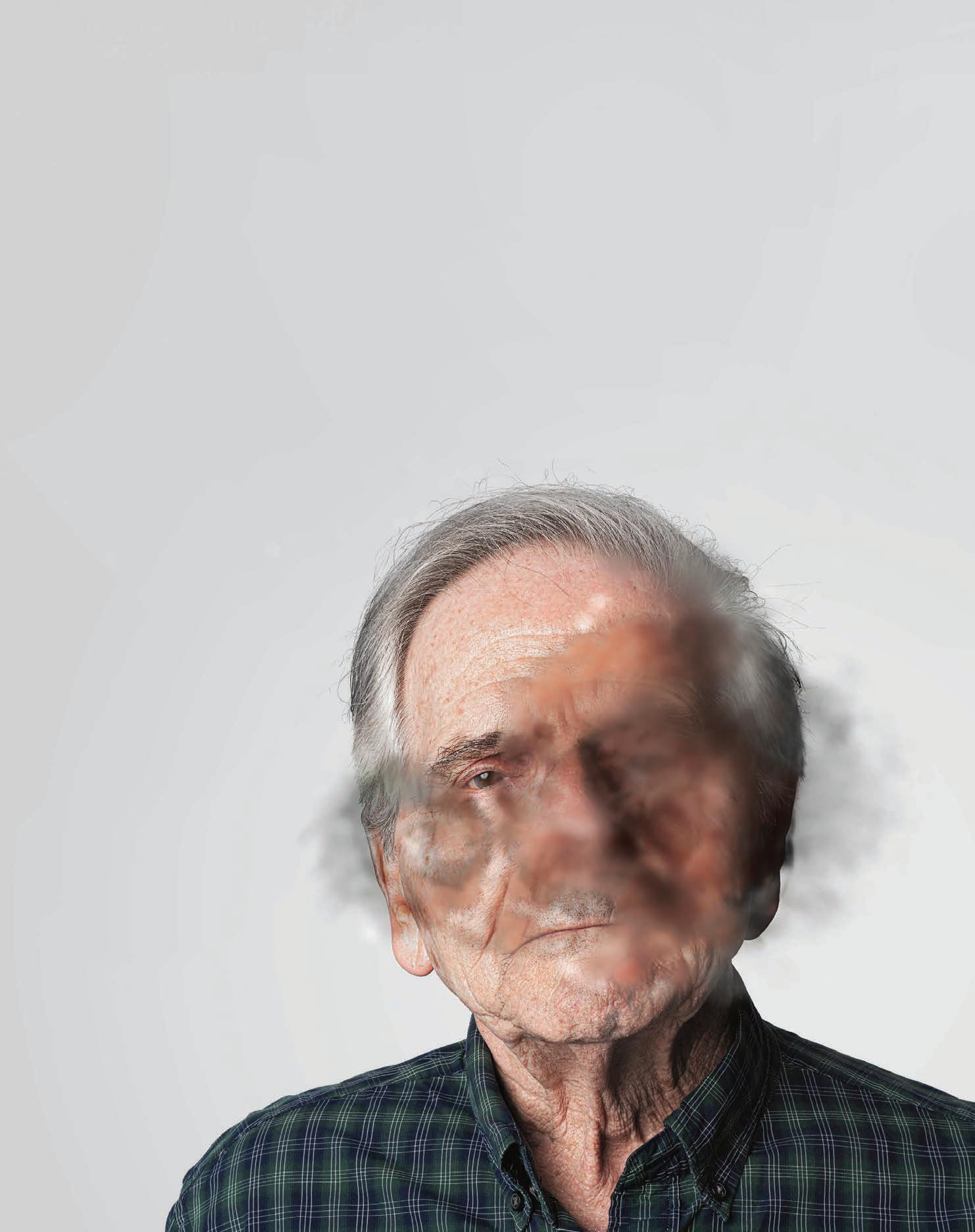
Healthy eating for healthy eyes




People


Eoften turn to supplements or superfoods to ward off macular disease or prevent its progression, but new Australian nutritional guidelines suggest the concept of ‘food synergy’ might be more effective. So what is the ideal macular disease diet?
ye healthcare professionals often advise their patients on diet. In fact, a survey of Australian optometrists found two-thirds of practitioners regularly discuss the impact of diet on eye diseases, and 91% routinely recommend nutritional supplements to age-related macular degeneration (AMD) patients. Given the emphasis on positive eating habits, it’s perhaps surprising there are currently no o cial nutrition guidelines for AMD.
But there is a clear need for evidence-based dietary information, according to Macular Disease Foundation Australia (MDFA), which has worked with homegrown academics to provide key insights into the type of eating patterns that reduce the likelihood – and even protect against – AMD.
In May 2024, as part of its Macula Month awareness campaign, MDFA is launching updated Nutrition Guidelines for AMD. The organisation recently conducted a systematic review evaluating the strength of the evidence for dietary patterns, foods, nutrients and supplements to prevent AMD and/or slow its progression.
According to MDFA, randomised controlled trials (RCTs) have reported the e cacy of multi-antioxidant supplements in reducing the risk of late AMD. An association between certain antioxidant-rich foods and fish in lowering the risk of AMD was first noted in epidemiological research in the 1990s. Meanwhile, the high intakes of vegetables, fruit, fish and plant-based proteins in traditional Mediterranean and Asian-style diets have also been associated with lower incidence of AMD.
MDFA’s updated nutrition recommendations are based on the first systematic review of all published systematic reviews investigating dietary patterns, food, nutrients, nutrition supplements and AMD, performed in association with the University of Sydney. The organisation’s CEO Dr Kathy Chapman holds a PhD in public health nutrition and began her career as a dietitian.
To develop the guidelines, systematic reviews were included if they investigated an association between any diet, food, macronutrients, micronutrients and/or dietary supplements and AMD (early, intermediate, late, atrophic and/or neovascular) in adults.
Interpreting the large number of published studies linking di erent eating patterns and food groups is a big undertaking and required MDFA to analyse both observational study designs and RCTs. Observational studies – like cohort studies – follow up large numbers of people in the population over time and help to inform associations with eating patterns and individual foods. RCTs also help to understand if nutrition supplements taken in capsule form are e ective. From 575 studies identified in the literature search, 21 systematic literature reviews were identified for analysis.
Chapman says healthy eating can help prevent age-related macular degeneration (AMD) by providing a wide range of potentially protective antioxidants like omega-3 fatty acids, lutein, zeaxanthin, vitamins C and E, and zinc.
“Eating patterns that boost consumption of these nutrients protect against oxidative stress, inflammation, and cellular damage in the eyes, reducing the risk of developing AMD or slowing its progression. It’s important that a healthy, macula-friendly diet be an integral part of both prevention and treatment for AMD,” she says.
“A key finding we found in our study is that it is important to consider overall eating patterns rather than focussing on single nutrients and foods. People often try to improve their diets with nutrient supplements or so-called ‘super-foods’, but more and more studies are pointing to the benefits of an overall healthy eating pattern with a wide variety of plant-based foods.”
‘Food synergy’, the combined action of food constituents on overall health, is an important message MDFA wants practitioners and the broader
36 INSIGHT May 2024 MACULAR DISEASE
Image: Evgeny Atamanenko/Shutterstock.com.
macular disease community to take note of.
Studying foods consumed regularly together may demonstrate an enhanced e ect on health, compared to studying foods or nutrients in isolation. MDFA says this might explain why Mediterranean and Asian-style eating patterns were consistently linked to a lower risk of developing – and slowing progression of – AMD while the evidence was less certain for a high intake of individual foods and nutrients.
Mediterranean and Asian-style diets both include a high intake of fresh fruit and vegetables, fish, nuts, and seeds, with little meat and dairy. While Asian-style diets have a high intake of rice, soy products and other plant-based foods, the Mediterranean diet is based on regular use of olive oil and cereal products. Both feature a high intake of fish, foods rich in omega-3 fatty acids, and antioxidants – foods with the strongest protective associations.
In MDFA’s study, omega-3 polyunsaturated fatty acids and fish consumption were frequently reported to protect against AMD.
Foods rich in lutein and zeaxanthin, like dark green leafy vegetables (such as kale and spinach), broccoli, peas, corn and eggs, are likely associated with reduced risk of developing or progressing to late AMD. Multi-antioxidant supplements were associated with delaying progression of AMD, but not preventing it.
According to MDFA, new evidence shows that more than one standard alcoholic drink was likely associated with higher risk of developing early AMD. High meat consumption – especially red and processed meat – was also associated with a probable increased risk of developing early AMD. MDFA says its findings indicate that following a Mediterranean diet may protect against both early and late AMD, while adherence to an Asian-style diet may delay the progression of late AMD. The research has shown inflammation plays a role in the development of chronic conditions like AMD.

A Mediterranean diet has been linked to lower levels of oxidative stress biomarkers. This may be due to the antioxidant and anti-inflammatory properties of fruit, vegetables, and fish.
“As part of our Macula Month awareness program, we urge all eye health professional to encourage their patients to follow eye-healthy diets,” Chapman says.
“Nutritional information is crucial for holistic patient care as it impacts physical health, mental well-being, and overall quality-of-life. Understanding dietary needs helps manage chronic conditions, like AMD, and supports recovery from illnesses, enhances energy levels, promotes mental clarity, and contributes to emotional wellbeing, leading to comprehensive and e ective healthcare outcomes.”
NOTE: For a copy of MDFA’s updated Nutrition Guidelines for AMD, visit www.mdfoundation.com.au.








Image: monticello/Shutterstock.com.
MDFA’s findings indicate that following a Mediterranean diet may protect against both early and late AMD.












Optometry's role in macular disease patient support
Optometrists have an opportunity to maximise care for their patients after they depart the consulting room thanks to patient support bodies who follow up with crucial details about their disease, practical advice and psychosocial support. A recent partnership between a major optometry network and Macular Disease Foundation Australia is exemplifying this.
When patients are diagnosed with a form of macular disease, often it’s their first time hearing of the condition. It can be a discombobulating diagnosis and between optometrists, ophthalmologists and other health professionals, patients report sometimes feeling unsure of who’s actually managing them.
Accurate information about their condition can be hard to come by too. The experience can lead to patient disengagement – a harmful move when you consider that for neovascular age-related macular degeneration (nAMD – the most aggressive and sight-threatening version of AMD) there are e ective treatments that can work to restore people’s sight while preserving their vision.

Macular diseases, including AMD, represent a significant public health
“MDFA is a great resource for educating patients as they have online and in person education for patients, carers and optometrists, as well as support programs for patients and family.”
Maddy Balson
Specsavers Elsternwick
concern globally. In Australia alone1 one in seven people over the age of 50 have some evidence of age-related macular degeneration (1.5 million Australians), and around 17% of those will experience vision impairment. Almost 15% of Australians aged over 80 have vision loss or blindness from age-related macular degeneration.
Positively, unlike previous generations, more patients are accessing eye tests than ever before. With more patients in regular eyecare, optometrists can detect conditions earlier and refer for diagnosis and treatment, preventing unnecessary vision loss. Despite this however, the statistics are still alarming for patients. For the 156,0902 Australians who currently have nAMD, an estimated 20% will stop treatment in their first year and 50% will stop their eye injections in the first five years. 3 A further 22% are lost to follow-up, not attending their prescribed specialist and optometrist appointments.4
Dr Ben Ashby, clinical services director at Specsavers ANZ, says with this in mind, it is imperative that optometrists lean on their patient support body partners to ensure patients are receiving as much information and support as possible when caring for patients with macular disease.
“We know that patients often have many questions, concerns and problems after they leave an eye test consultation, and those who are directed to receive additional support and information from trusted patient support bodies are more likely to adhere to treatment and attend future appointments, helping to prevent vision loss in the long term,” he says.
“It is our goal, as providers of eyecare, to do all we can to set our patients up for success so that any eye conditions are e ectively managed, and their vision is protected for many years to come.”
INSIGHT May 2024 39 MACULAR DISEASE
Images: Specsavers.
'MY EYES' PROGRAM BORN OUT OF FINDINGS FROM SOCIAL IMPACT SURVEYS
This Macula Month in May 2024, Macular Disease Foundation Australia (MDFA) is launching My Eyes, Australia’s first evidenced-based free support service for people living with age-related macular degeneration (AMD).
MDFA has spent more than three years working with people living with macular disease and trusted healthcare professionals to develop My Eyes. This service will provide people living with AMD, and their carers, with tailored health information, practical tips, and emotional support for up to 18 months.
Like all patient-support programs, the organisation says there had to be a reason for the investment of time and money. The feedback MDFA received from its 2020 and 2023 'Social Impact Surveys' continued to reinforce the need for comprehensive, supportive, and holistic care for people living with macular disease, especially considering the number of people experiencing mental health issues and reduced quality-of-life.
Further studies showed that only 56% of macular disease patients could recall their diagnosis when they left their clinical appointment, and only 45% recalled receiving an explanation of what may happen to their vision in the future.1 MDFA states clinical care is only part of the care equation –what a patient does in between their visits is also important.
“The burden of macular disease and vision loss can significantly impact an individual’s emotional well-being and quality-of-life, extending its e ects to those around them. Rates of depression in individuals with AMD are significantly higher than in the general older population, and according to recent studies, depression rates in AMD patients are comparable to those in individuals with other chronic and disabling diseases,2 MDFA says.
“AMD presents unique challenges. The uncertainty surrounding future vision changes, whether sudden or gradual, leads to heightened anxiety and feelings of hopelessness.3 This makes coping with AMD particularly di cult compared to other eye conditions.”3
More than 10% of people interviewed in MDFA’s Social Impact Survey said they had been diagnosed with a mental health problem, with one in five receiving support for their mental wellbeing. The My Eyes service is designed to include emotional support to address this unmet need for many people living with AMD.
According to MDFA, peer support and improved health literacy play a crucial role in alleviating emotional distress associated with AMD. These strategies can not only decrease emotional distress but also enhance self-e cacy and activity levels.4 As part of the My Eyes service, patients can opt-in to connect with others living with macular disease either face-to-face, online or over the phone.
MDFA says its peer support programs have already yielded excellent results with volunteer-led peer groups being run in every state in Australia, and more than 160 people engaged nationally.
“The My Eyes service will continue to empower people living with AMD by involving them in decision-making processes regarding their care, leading to improved treatment adherence and better health outcomes for the macular disease community,” MDFA says.
Patients can be connected to to My Eyes via Oculo or, visit www.mdfoundation.com.au/ refer-to-myeyes
REFERENCES:
“THE MY EYES PROGRAM HELPED A LOT AS I DIDN’T KNOW MUCH ABOUT MY MACULAR DISEASE. IT GUIDED ME A LOT WITH TIPS ON WHAT TO DO AND IMPLEMENT; I’VE RECOMMENDED IT TO A COUPLE OF OTHER PEOPLE. I LOVE TALKING TO THE MDFA STAFF, THEY FEEL LIKE ALL MY FRIENDS AND THE PHONE CALLS HELP ME A LOT EMOTIONALLY.”
MY EYES COMMUNITY MEMBER
1. Clinton, S., Hoad, G., Bloomfield, P. et al. Comparing views of patients and eye care professionals on the information provided on age-related macular degeneration and diabetic macular oedema. Eye (2024). DOI: 10.1038/s41433-024-02939-z.
2. Casten R, Rovner B. Depression in Age-Related Macular Degeneration. J Vis Impair Blind. 2008;102(10):591-599. PMID: 20011131; PMCID: PMC2792986.
3. Cimarolli VR, Casten RJ, Rovner BW, Heyl V, Sörensen S, Horowitz A. Anxiety and depression in patients with advanced macular degeneration: current perspectives. Clin Ophthalmol. 2015 Dec 30;10:55-63. doi: 10.2147/OPTH.S80489. PMID: 26766899; PMCID: PMC4699633.
4. Bradley, P., Mitchell, J., & Bradley, C. (2005, September). Peer support for people newly diagnosed with macular degeneration: a pilot study. In International Congress Series (Vol. 1282, pp. 211-215). Elsevier.
SPECSAVERS AND MDFA
Dr Ashby says Specsavers is working with Macular Disease Foundation Australia (MDFA) and to date its main focuses have been:
• Improving the referral rates of consenting patients to receive support from MDFA
• Assisting MDFA with the perspectives, feedback and opinions of optometrists to assist with improvements for how they support patients
• Helping to build awareness of MDFA from within its optometrist and patient network.
“In 2022, Specsavers and MDFA launched a pilot that targeted patients with nAMD and aimed to achieve these goals,” Dr Ashby says.
“The pilot involved 16 practices from around Australia who identified and referred patients with nAMD at levels consistent with the prevalence rates that were also seen in Australia’s National Eye Health Survey (0.24% of the population have been shown to have nAMD). 5 A further 100-plus patients with other macular diseases were also referred from the practices, and these patients went on to receive support and resources also.”
Specsavers Elsternwick optometrist Ms Maddy Balson says MDFA is an organisation that can be trusted to support both patients and optometrists to reduce the impact and burden of macular diseases.
“They have resources for optometrists which we use regularly, including an Amsler grid, which I often get my patients to use weekly to detect any changes in the macula between visits,” she says.
“MDFA is a great resource for educating patients as they have online and in person education for patients, carers and optometrists, as well as support programs for patients and family. MDFA also funds extensive research to further advance macular disease detection and treatment outcomes.”
Dr Kathy Chapman, CEO of MDFA, says the Specsavers nAMD pilot led to many insights and learnings that were used to inform MDFA’s new patient support program, My Eyes.
“MDFA values our collaboration with Specsavers and optometrists to improve the visual outcomes of people living with macular disease,” she says.
“Working closely with the Specsavers network of practices across Australia, the nAMD pilot allowed us to communicate with a pool of patients and optometrists, gaining valuable insights and data on di erent and improved ways of supporting optometrists with the right information, but also importantly supporting patients to live better with their macular disease. It helped feed into the development of our newly launched patient support program.”
MDFA’S
NEW MY EYES PROGRAM
O cially launched this Macula Month (May 2024), My Eyes is Australia’s first, free, national, macular disease patient support program and has been designed for people with newly diagnosed or existing AMD.
Dr Chapman says the service has been developed following extensive research involving people with macular diseases, their carers, and ophthalmologists, as well as the learnings from the nAMD Specsavers pilot.
“Feedback from patients and carers revealed a desire for more practical and emotional support throughout the treatment and disease journey, beyond what they might receive in their visits with health professionals,” she says.
My Eyes provides three main areas of support tailored to a patient’s level of vision, diagnosis and current perceptions about their wellbeing: disease information, practical support and psychosocial support.
“We launched the program as a pilot in November 2023, and have been pleased to see the positive feedback from patients and their optometrists already coming in,” Dr Chapman says.
One patient involved in the My Eyes service shares how the My Eyes
40 INSIGHT May 2024 MACULAR DISEASE
Program helped him better manage his AMD.
“I am pleased to be part of the My Eyes program, having struggled with age-related macular degeneration. Initially I was lacking accurate information, and the information I received from various sources was often misleading and incorrect. It wasn’t until I visited an optometrist for a glasses check that I was introduced to the My Eyes service provided by the MDFA organisation,” he says.
“I discovered the service through MDFA and found their assistance invaluable. The MDFA team provided clear and accurate information, helping me understand my condition and manage it e ectively. Grateful for the free and quality support, I appreciate the comprehensive knowledge gained through the My Eyes program.”
Any optometrists who wish to refer patients to MDFA’s My Eyes program can do so via Oculo or on the MDFA website: www.mdfoundation.com.au/ refer-to-us/.
LOOKING AHEAD
Dr Ashby says the the Specsavers-MDFA partnership has been aimed at improving outcomes and quality-of-life for people a ected by macular diseases.

“Specsavers encourages more optometrists to connect their patients with macular disease to MDFA. Optometrists need to make the most of the care that is available for patients after they leave the testing room, as patient support bodies such as MDFA can help to follow up on patients’ practical and clinical needs, as well as address their psychosocial well-being,” he says.
“Moving forward, continued collaboration with MDFA and other patient support bodies will be instrumental in advancing optometry care and transforming the lives of individuals living with eye conditions.”
REFERENCES:
1. https://www.mdfoundation.com.au/about-macular-disease/age-related-macular-degeneration/amd-overview/
2. amazonaws.com/s3fs-public/Deloitte_Eyes_on_the_ Future_Report_web.pdf
3. Pharmaceutical Benefits Advisory Committee – Drug Utilisation Sub Committee (2018). Ranibizumab and Aflibercept: Analysis of Use for AMD, DMO, BRVO and CRVO. Accessed www.pbs.gov.au/pbs/industry/listing/ participants/public-release-docs/2018-05/ ranibizumab_and_ aflibercept__analysis_of_use_for_amd%2C_dmo%2C_b.
4. Obeid A et al (2018). Loss to follow-up among patients with neovascular age-related macular degeneration who received intravitreal anti-vascular endothelial growth factor injections. JAMA Ophthalmol. 2018;136(11):1251-1259.
5. Foreman, J., Keel, S. et all. 2016. The National Eye Health Survey 2016. As published https:// www.vision2020australia.org.au/wp-content/uploads/2019/06/National-Eye-Health-Survey_Full-Report_FINAL.pdf

Transforming retinal photocoagulation
— effectively, efficiently
Integre Pro Scan™ combines multi-color photocoagulation with a precise computercontrolled pattern scanning laser in an ergonomically advanced all-in-one laser/slit lamp design. Whether positioning focal treatment in the macular area, or performing PRP in the periphery, Integre Pro Scan™ provides a comprehensive pattern and wavelength choice to cover all retinal pathologies.
With Integre Pro Scan™, the following wavelength configurations are available:
• Yellow-red configuration (561 nm and 670 nm)
• Green configuration (532 nm)
• Yellow configuration (561 nm)
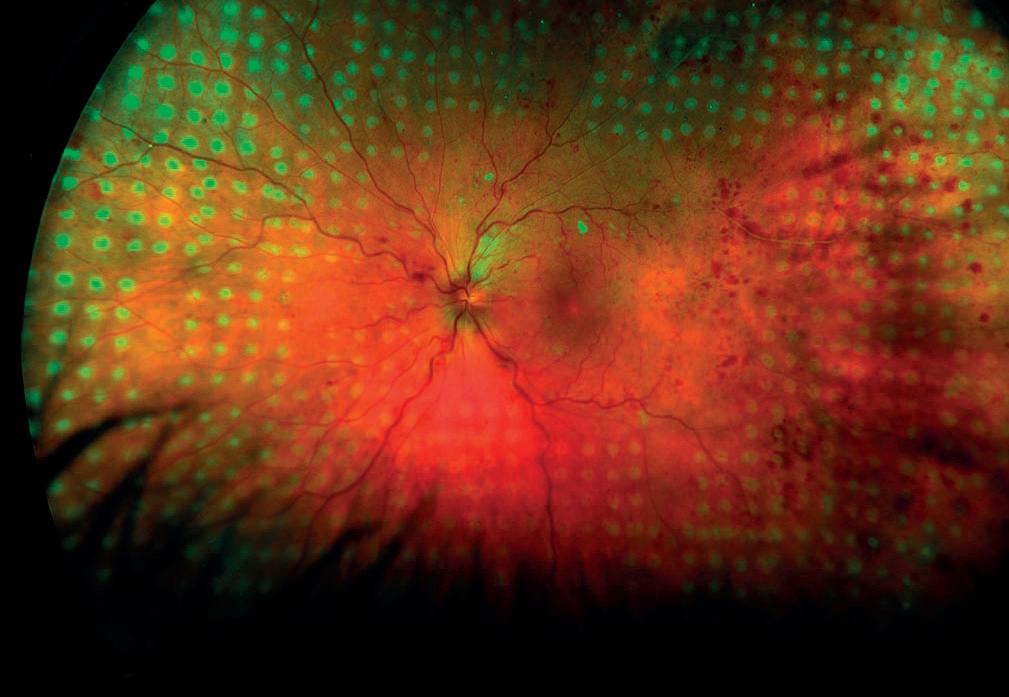
Its proprietary dual-mode laser cavity delivers uniform energy distribution across the full spot diameter, eliminating hotspots and achieving optimal, homogenous burns. It’s a key feature that means you can achieve consistent, predictable treatment outcomes across a broad range of pathologies.
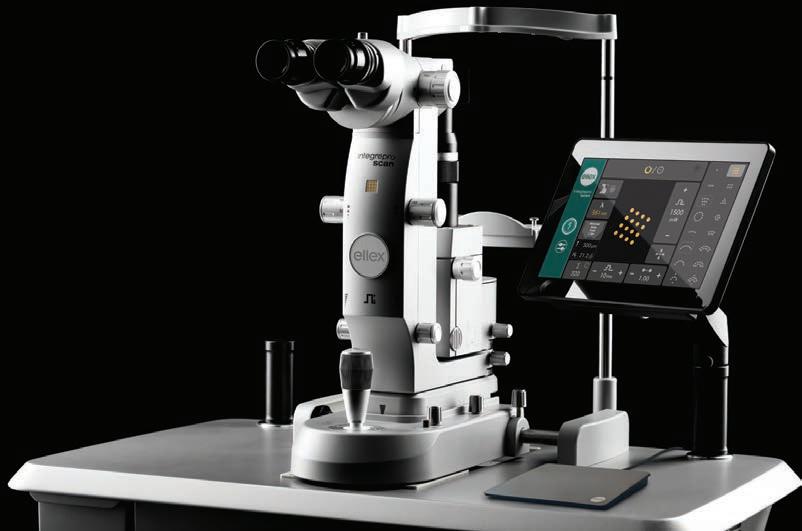
Contact us: salesadmin@ellex.com
| Tel.: +61 8 7074 8200 | ellex.com
Image: Inside Creative House/Shutterstock.com.
My Eyes is the first national macular disease patient support program for people with newly diagnosed or existing AMD.
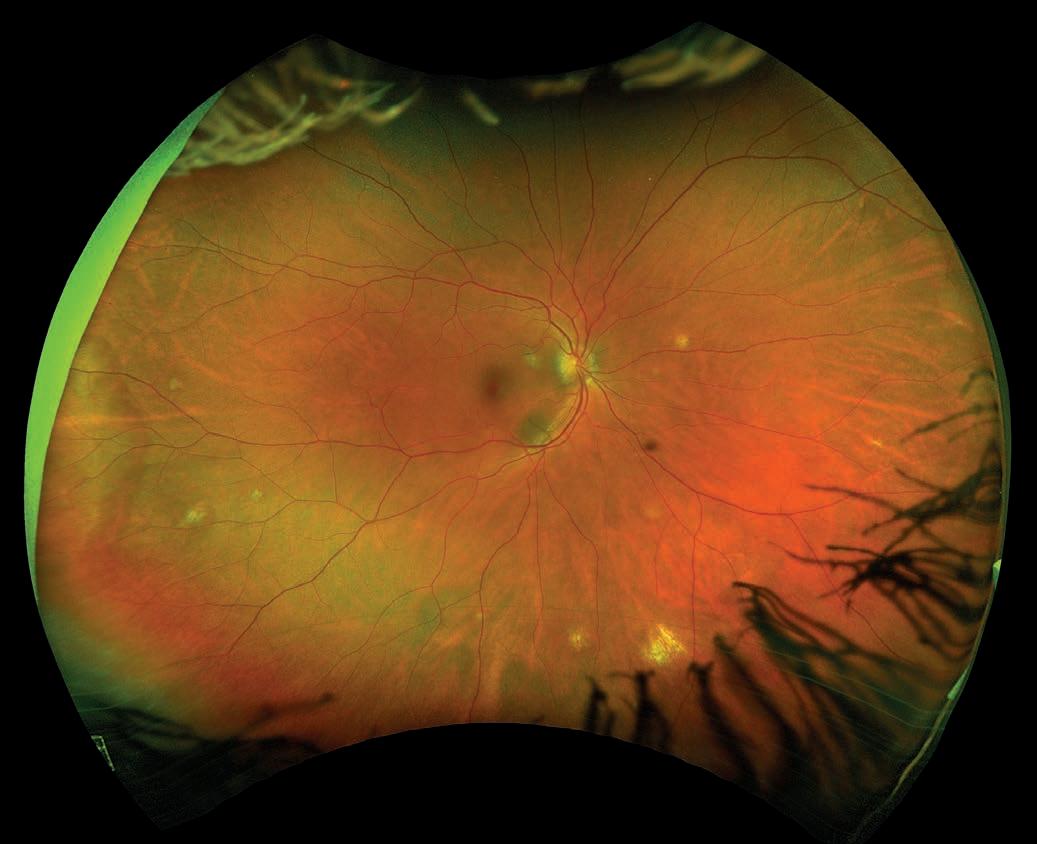
Ultra-widefield, ultra results
Ultra-widefield retinal imaging has become so crucial to the clinics that have adopted the technology, they can’t picture practising without it. Two Australian ophthalmologists discuss how their investments in Optos technology has transformed their care.
Regardless of how excellent an ophthalmologist might be at their craft, Canberra retinal subspecialist and cataract surgeon Dr Richard Barry struggles to see how any of his peers could practise today without an ultra-widefield (UWF) retinal camera. In fact, in the not-too-distant future, he believes physically looking into the back of an eye will become redundant in most cases.
As the principal of Blink Eye Clinic – specialising in premium cataract surgery, macular and vitreoretinal surgery and medical retina – Dr Barry says an ultra-widefield camera plays a central role in his practice from a disease diagnosis and management perspective.
But his most recent investment – Optos California – is also o ering major advantages in terms of practice e ciency, patient education and documentation. He’s been so impressed with the technology that he’s now considering investing in Optos’ latest instrument – Silverstone, the only model with integrated swept-source OCT (SS-OCT) – which will allow his clinic to screen retinal pathology even more e ectively in the periphery.
“From my point of view, it’s a standard of care to have an ultra-widefield device – and Optos is the gold standard in its field,” he says. “For any clinic that doesn’t use ultra-widefield imaging I believe it would be di cult to provide the same quality of service. Having ultra-widefield imaging for most patients on each visit to compare is necessary in my practice – it’s a lot of

data to collect, but it’s incredibly useful and makes the consultation so much easier and faster.
“It doesn’t matter how experienced and skilled you are, you can’t consistently achieve this level of data by looking into someone’s eye through a lens or indirect ophthalmoscope and using written documentation.”
The reason Dr Barry, among an increasing number of Australian ophthalmologists and optometrists, has turned to California and other Optos devices (Monaco and Silverstone) comes down to their optomap images capturing approximately 82% and 200° of the retina – something the company says no other device can do in a single shot. Optos has expanded its technology now with nine imaging modalities available across all its platforms, including the recent addition of optomap colour red, green blue laser (rgb), natural colour and blue fundus autofluorescence.
Since acquiring the device, Dr Barry has noticed much greater use of fluorescein angiography (FA) especially in retinal vascular disease and uveitis. This is largely due to the ease that sta can acquire the image, as well as the quality and ultra-widefield obtained.
“We were performing FA on another device previously, and while it’s a great device, the image quality was sometimes poor and required me to search around in the periphery to show sta exactly what I wanted. Whereas now we utilise FA much more because it’s fast, e cient, ultra-widefield and provides an excellent quality image on the California,” he says.
Dr Barry says the technology is creating other e ciencies in the practice, especially when it comes to scan acquisition performed by triage sta –captured in less than 0.5 of a second – and documenting findings at scale over long periods.
“Some key benefits of having an ultra-widefield in your practice are legal and medical documentation and interaction with patients. It’s much more e ective than having to draw diagrams and write extensive notes that can be di cult to re-interpret six months, 12 months or two years later versus an actual photograph,” he says.
“In terms of patients, it provides them insight and ownership into how they’re going to be managed, rather than providing a script for an eye drop and saying ‘I’ll see you in six months’ without an understanding of their disease. When you actually show them an optomap image, it’s more engaging and makes consulting that much more enjoyable. Plus, the patients are very impressed – they feel like they’re receiving a great service.” Patients are happy for another reason too. California and other Optos devices eliminate the need for pupil dilation. This provides a more frictionless practice workflow – and a more convenient experience for those who may need to drive or return to work after the consultation.
LEFT: A red-green retinal scan of uveitis taken with the California device.
42 INSIGHT April 2024 MACULAR DISEASE
ABOVE: A fluorescein angiography image of the same disease.
Images: Optos.
Interestingly, when Blink Eye Clinic first trialled the California and compared it with its pre-existing ultra-widefield device, sta initially thought they would prefer what they were familiar with. But after adapting to a new process that requires the patient to position their head before a green circle appears to confirm the image can be captured, it didn’t take long before Optos became their technology of choice.
“It was an adjustment, but then over time sta found the Optos to be much better because it’s fast and convenient. We still have the previous ultra-widefield machine in our clinic, but the California is now used the majority of the time,” Barry adds.
Now that he’s had the chance to appreciate the impact the California on the clinic, Dr Barry says he is considering investing in the Silverstone that has the added functionality of SS-OCT that will be useful as a screening tool for lesions in the peripheral retina. For more detailed diagnostics, he has a separate, standalone OCT that he will continue to use.
“If you’re looking at breaks, schisis, detachments, choroidal nevi, or retinal lesions like CHRPE (congenital hypertrophy of the retinal pigment epithelium) for example, it’s useful to have the SS-OCT feature because currently we need to switch to a separate OCT device to then scan around in the periphery of the retina. So having this technology will create even more e ciencies,” he says.
MAJOR WORKFLOW EFFICIENCIES
For Dr Simon Chen, the ability to diagnose before even seeing the patient in many cases is one of the great benefits of investing in Optos ultra-widefield technology.
As a retinal and cataract surgeon at Vision Eye Institute in Sydney (across Bondi Junction, Chatswood and Drummoyne) with a busy workload, being able to delegate image acquisition to orthoptic sta and have a large optomap image immediately available on his consulting room monitor is a major time saver.
“Just recently, I had a classic case of a patient presenting with flashing lights and floaters where the Optos clearly demonstrated a macula-on retinal detachment. So even before seeing the patient, I already knew the correct diagnosis and that the patient would require urgent retinal detachment surgery. This enabled me to focus the consultation on education and preparing the patient for surgery,” he says.
“And similarly, in patients with diabetic retinopathy, often we can see very clearly from the optomap image what’s occurring.”
Dr Chen was a relatively early adopter of Optos ultra-widefield and now has three California models installed. His first Optos unit was installed in 2012. “
This was early on when there wasn’t much of this technology around. I had no intention to acquire an Optos device but a company rep talked me into trialling one, which I did for a couple of weeks. I found it so useful, particularly for patients with small pupils that couldn’t dilate properly. There’s no question you can often get a better view with the optomap image than you can by examining the patient, especially when the view of the

“Even before seeing the patient, I already knew the correct diagnosis and that the patient would require urgent retinal detachment surgery. This enabled me to focus the consultation on education and preparing the patient for surgery.”
Dr Simon Chen Vision Eye Institute


retina is obscured by conditions such as vitreous haemorrhage or cataract,” he says.
“By the end of the trial period, I had become spoiled by the benefits of using the Optos technology and it had become an important part of my routine clinical workflow so I have been using it ever since.”
From a clinical perspective, he says the California shines in enabling clinical monitoring of pathology in the peripheral retina such as choroidal nevi because these lesions would be very di cult to image otherwise.
“The Optos is often the best way to monitor patients with peripheral retinal pathology to see whether there have been any changes between visits,” he says.
“It’s also useful for assessing the peripheral retina for retinal tears, lattice degeneration and retinal detachments. This is particularly relevant in myopes who are at increased risk of retina detachment, so it facilitates discussions with the patient.”
Optos – and its autofluorescence imaging modality – has also found its place in monitoring geographic atrophy. It’s thought this could become even more relevant with the first approved therapies for this disease expected in the near future in Australia.
“The fundus autofluorescence feature is a great way to assess progression of this disease” Dr Chen says.
“It’s also a simple way of educating patients because it shows black patches where there’s atrophy in the macula, and over time, if those areas enlarge, it’s quite obvious on the optomap image. It makes it easy for patients to understand and visualise the progression of their condition.”
Echoing Dr Barry’s comments in terms of pathology documentation, Dr Chen says by performing optomap scans on each new patient, he can document evidence of the patient’s retinal health at various points in time.
“Even if someone is undergoing straight-forward cataract surgery and has no retinal problems, a baseline image is helpful because if problems arise post-surgery – for example a retinal detachment a few months later –patients can question whether something was missed earlier on,” he says.
“But if you’re able to bring up their optomap scan, you’re able to show they had normal-looking retinas beforehand, which allows them to understand what’s occurred is something new.”
INSIGHT April 2024 43
Dr Richard Barry says the Optos California model has created several workflow efficiencies at his clinic in Canberra.
Image: Dr Simon Chen.
Image: Blink Eye Clinic.





EIDON combines the best features of scanning laser ophthalmoscopy systems with standard fundus imaging to redefine retinal imaging standards.

How this is breaking diagnostic boundariesoptometrist
For optometrist MARTIN ROBINSON, iCare’s EIDON fundus camera has supercharged his practice and is an example of superior ergonomics, top-tier imaging quality, and the advantages of ultra-widefield imaging.
At Martin’s Eyecare in Tasmania, Mr Martin Robinson’s investment in iCare’s EIDON fundus camera has elevated his practice to new heights. The imaging modality has played a crucial role in life-saving diagnoses and has seamlessly integrated into his suite of instruments.
A curious case that might not have been diagnosed without the EIDON retinal camera is a naevus melanoma. Thanks to its autofluorescence feature, it can di erentiate between an amelanotic melanoma by fluorescing, and a non-melanotic nevus that will not fluoresce.
“We've been able to accurately diagnose melanomas in something that are not easily observable – and is outside the range of our OCT – and have then referred those away to an ophthalmologist and then to an oncologist,” Robinson says. “It’s a lifesaving investigation.”
Robinson first experienced the imaging modality at an O=MEGA conference on the Designs For Vision (DFV) booth. There, he was given a textbook featuring traditional images from retinal cameras, OCT scans, and EIDON images for various diseases.
“I thought it was amazing and I was really impressed because at that stage I had an older non-mydriatic fundus camera which I’d had for several years and bought secondhand,” he says.
“I wanted something better, more current and integrated, and with the same footprint as my existing camera.”
For Robinson, the EIDON was ergonomic and integrated seamlessly into his existing workflow. In a practice limited by space constraints, the device slotted right in.
He also sought a refined imaging modality that could cater to the high volume of diabetic patients he sees. Identifying retinal detachments and tears are also important but constitute a fraction of his patient base.
“I was seeking something that was superior for diagnosing early diabetic changes – and that's where the EIDON kicks butt because its clarity and resolution are o -the-charts-amazing for diabetes,” Robinson says.
REDEFINING IMAGING STANDARDS
EIDON, distributed by DFV in Australia, is described as the first TrueColor Confocal system that combines the best features of scanning laser ophthalmoscopy (SLO) systems with those of standard fundus imaging to redefine retinal imaging standards.
Image: Martin Robinson.




“I was seeking something that was superior for diagnosing early diabetic changes – and that's where the EIDON kicks butt because its clarity and resolution are off-the-chartsamazing for diabetes.”
Martin
Robinson Martin’s Eyecare
44 INSIGHT May 2024 MACULAR DISEASE
Robinson uses the imaging modality on most of his patients, while the other optometrist in his practice opts to use it for patients with small pupils and ones with cataract or vitreous opacities that make internal viewing di cult.
The confocal imaging, which can work with pupils as small as 2.5mm without the need for dilation, is reported to be superior to conventional fundus photography, with Robinson describing it as having the ability to “cut through scatter like a hot knife through butter”.
The imaging modality can pick up on micro aneurysms that Robinson has not been able to see using traditional methods such as a normal fundus camera or through slit lamp fundoscopy.
In Martin’s Eyecare, he has opted for the ultra-widefield module – which can be attached to all EIDON models, including retrofitting of many older units – and has been invaluable for detecting early diabetic changes and signs of pathologies that start to appear in the periphery.
With diabetic patients, Robinson completes a three shot horizontal mosaic where he takes three photos in one sequence for one eye – one with the eye looking straight ahead, one looking temporal, and one looking nasal. The EIDON then stitches the images together to produce an image of about 200 degrees across, with that resolution extending all the way to the periphery.
“This means I've got an excellent view of any diabetic change happening centrally within the arcades and in the periphery as well,” Robinson says.
Following the scan, he exports high-resolution PDF files direct from the viewing program where he can then discuss and interpret the results with patients. He also attaches the images for triage or for a full referral – with the higher quality images meaning a better outcome for his patients.
“I get communications back from my virtual retinal specialists saying, ‘That's some amazing imaging camera that you've got – there's no doubt about the diagnosis’,” he says.
“I'm not referring people away for an opinion if I don't need to, and I can look after them and review them in-house, which is more cost e ective for the patient and more time e ective for the ophthalmologists.”
EIDON also features Flicker technology that compares a current image of an eye to an historic one. The technology can then overlay them, with the ability to flicker repeatedly between one another to monitor structural changes.
“I can check the nerve and see if there's any changes to the cup. I can see if there's any vascular changes around the nerve. I can look at the macula and see if there are changes,” Robinson says.
“So, it's an incredibly e ective communication tool to show the patients how much the eye has changed.”
For example, EIDON’s ability to cut through media opacities such as those associated with asteroid hyalosis and cataracts has enabled Robinson to make life-altering diagnoses.
“In asteroid hyalosis, when the optometrist looks inside, they see these asteroids that are drifting inside the vitreous. Trying to look at it manually with a slit lamp or a traditional camera, all you see is white because it reflects the light you're shining into the eye and you can't see through them,” Robinson says.
“I’ve been referring patients along for cataracts, for example, with asteroid hyalosis. I’ve been sending images of the retina, and the surgeons are grateful as it provides a superior fundus view.”
He says that sending images that have cut through the asteroid hyalosis, gives the surgeon more confidence they can give the right advice to the patient.
Beyond its imaging capabilities, machine upkeep is simple and streamlined, according to Robinson, with service updates occurring virtually and remote and without disruption to the workflow.
“I just make sure I have the right settings on the camera, and I'll leave it on overnight. Diagnostics are run and then the system is updated remotely


– which is great,” he says. “I come in the morning and it's running the new software – it's seamless.”
In terms of equipment fault, Robinson says DFV were quick to loan him a camera until his could be fixed. Acknowledging these issues are inevitable with the computerisation of most equipment nowadays, he was impressed with the response.
“I didn't have any worries for that – I had a camera, and I didn't have any downtime,” he says.
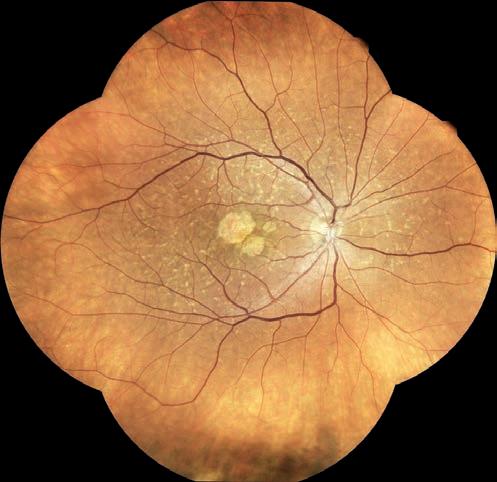
INSIGHT May 2024 45
FROM TOP: With the EIDON ultra-widefield module it is possible to increase the field of view up to 200 degrees, which helps to detect signs of pathologies that start to appear in the periphery; Retinal vein occlusion; Stargardt disease.
Images: Designs For Vision.
LEARNING OBJECTIVES:
At the completion of this article, the reader should be able to improve their management of dry eye disease (DED) ...
Including:
• Understand the role of inflammation in DED and the use of topical anti-inflammatory drops like ciclosporin A (CsA) in managing the condition
• Understand the challenges in prescribing CsA, the varying formulations, dosages and treatment durations, as well as patient compliance and potential side e ects.
• Be familiar with the findings from clinical trials regarding CsA dosage, treatment duration, and comparative e ectiveness with other treatment options for DED.
Practical evidence for treating moderateto-severe dry eye with ciclosporin
Despite the promise of ciclosporin A in dry eye disease, many eyecare professionals find themselves navigating a maze of varying concentrations, formulations and dosing regimens. DR NGOZI CHIDI-EGBOKA and PROF STEPHANIE WATSON examine the literature on its effectiveness in relieving symptoms and explore the best dosage and treatment duration.
Dry eye disease (DED) is a chronic inflammatory condition of the ocular surface a ecting one in five people globally and increasing in incidence as the population ages and by lifestyle and environmental conditions change.
Dry eye diagnosis is based on the patient exhibiting a series of sensitive inflammatory thresholds characterised by loss of ocular surface homeostasis including symptoms and clinical signs such as ocular surface disease index (OSDI) ≥13, Schirmer < 10mm/5min, tear breakup time <10 seconds, positive corneal and/or conjunctival staining, poor meibomian gland secretion and expressibility, fast tear evaporation and increased tear osmolarity.1
Dry eye may be caused by and/or exacerbated by several factors including allergy (Figure 1), ocular rosacea, contact lens wear, pterygium, uncorrected refractive error, ocular surgery, blepharitis (Figure 2), dysregulation of the immune system (autoimmune disease), hormonal changes, medication use and other systemic disease triggers.
DRY EYE AND INFLAMMATION
Inhibiting the chronic inflammatory cycle and rebuilding ocular surface homeostasis imbalance is a key goal for DED treatment. A range of studies have investigated and reported the use of topical anti-inflammatory drops such as corticosteroids and/or ciclosporin A (CsA) in DED management.2,3 Long-term use of corticosteroids may lead to the risk of ocular hypertension, glaucoma, or cataract.4
Topical CsA has been widely used as an immunomodulatory therapy targeted to: inhibit apoptosis or programmed cell death in the ocular surface epithelium; prevent the activation of T-cells; and reduce the chronic cycle of inflammatory cell infiltrates in the lacrimal gland, which may increase tear production.5 CsA is


OD MPH PhD, FNCO FAAO
Corneal Research Group

Save Sight Institute, Faculty of Medicine and Health
The University of Sydney
Professor Stephanie Watson OAM Bsc(Med), MBBS, PhD, FRANZCO, FARVO, GAICD
Corneal Research Group
Save Sight Institute, Faculty of Medicine and Health
The University of Sydney
recommended for long-term management of dry eye syndrome as it has no systemic adverse e ect.
TOPICAL CICLOSPORIN
The US Food and Drug Administration (FDA) approved the first CsA ophthalmic emulsion Restasis (CsA 0.05%, Allergan Inc, Irvine, CA, USA) in 2002 and the second, Cequa (CsA 0.09%, Sun Pharma, Cranbury, NJ, USA), was approved in 2018. The indication for both emulsions was mainly for improved tear production in clinical cases of ocular surface inflammation associated with moderate to severe dry eye disease.
Apart from Restasis and Cequa, there are five other commercial CsA products available globally including Ikervis (CsA 0.1%), TJ Cyporin (CsA 0.05%), Clacier (CsA 0.05%), Zirun (CsA 0.05%) and CyclASol (CsA 0.1%) made available by new technologies and formulations to improve CsA delivery systems and partly due to the low bioavailability of Restasis.2
Treatment of ocular surface inflammatory conditions using topical ciclosporin formulations compounded by pharmacists have also proven to be therapeutically useful.6 The relatively recent emergence of these preparations in the
market has led clinicians to seek evidence for their use and for researchers to understand their therapeutic potential.7
Available products in Australia are CsA 0.1% and CsA 0.09%. Topical CsA 0.1% (Ikervis, CSL Seqirus (Australia) Pty Ltd) is the first ciclosporin to be PBS-listed in Australia which became available from 1 October 2021 as prescription-only medicine, with optometrists and ophthalmologists exclusively eligible to prescribe. CsA 0.09% (Cequa, Sun Pharma ANZ Pty Ltd) became PBS-listed in Australia from 1 June 2023 also as prescription-only medicine. Both CsA 0.1% and 0.09% are approved for use in adults for treatment of moderate to severe DED and ocular surface inflammation associated with severe keratitis. Treatment may be used in combination with artificial tears.
PRESCRIBING INDICATIONS FOR DED
Evidence from randomised clinical trials (RCTs) on the use of topical CsA has mostly included moderate-to-severe cases of DED and has supported the US FDA’s approved indications for use.2,3,8,9,10 Some studies have shown that patients with mild DED may also benefit from early intervention with CsA treatment which may
Images: Save Sight Institute. INSIGHT May 2024 47
CLINICAL CPD HOURS This activity meets the OBA registration standards for CPD
CPD DRY EYE
Figure 1. Inverted upper lid showing a conjunctival papillary reaction in a patient with allergic conjunctivitis and dry eye.

reduce the progression of DED severity.
In Australia, the current Pharmaceutical Benefits Scheme (PBS) guideline for prescribing CsA states that the patient should undergo an initial treatment phase for up to 180 days and must exhibit corneal fluorescein staining (CFS) Grade of 4 at treatment initiation using the Oxford scale or equivalent (Figure 3) and an ocular surface disease index (OSDI) score of ≥ 23. In addition, the ocular surface condition must be inadequately controlled by monotherapy with a preserva-
tive-free artificial tear substitute. Simultaneous treatment with a preservative-free artificial tear substitute is strongly indicated. The PBS recommendation for continuing treatment with CsA after the initial treatment phase is dependent on patient receiving subsidised treatment and requires an improvement in corneal fluorescein staining by ≥ 3 grades and OSDI score by ≥30% from baseline (i.e., before initial treatment).
Given that symptoms and signs of DED often do not correlate, determining severity for treatment
selection based on DED subtype classification features is strongly recommended by the TFOS DEWS II management and therapy report. The features suggested to identify include deficient meibomian gland features (meibomian gland orifice plugging, lid margin vascularity, secretion Grade 8-12, expressibility Grade of 2 and a meshwork or wave flow lipid pattern) and low tear volume (between ≤ 5 mm/5min to < 10mm/5min).4
Tear film inferometry is an a supplementary test that may support a diagnosis of evaporative dry eye (Figure 4). In cases of aqueous tear deficiency, consideration should be given to whether the patient has underlying Sjogren’s disease by consulting with a rheumatologist as concurrent systemic treatments maybe indicated in such patients.
WHAT CLINICAL TRIALS SAY ABOUT TREATMENT DOSAGE
Numerous clinical trials have been performed to assess the e ectiveness and safety of the various CsA formulations for dry eye and other ocular surface diseases. For DED, CsA has been used in varying concentrations and dosage including 0.05%, 0.08%, 0.09%, 0.1%, 0.2%, 0.5% and 2%. The most-frequently reported dose of CsA 0.05% was one drop instilled twice a day in each eye. Evidence from several published studies


CPD DRY EYE
CONTACTYOURSAFILOREPRESENTATIVE TOVIEWTHECOLLECTIONTODAY au.customerservice@safilo.com|1800252016
Figure 2. Anterior blepharitis in a patient with dry eye disease.

showed significant improvements in DED symptoms and signs (improved tear breakup time and reduced corneal fluorescein staining) with twice-daily drops treatment of CsA 0.05%.
Treatment with twice-daily drops of CsA 0.05% was also reported to have a higher e cacy in terms of patient responder rate compared to vehicle or AT alone for DED treatment. 2,3 Other topical CsA including CsA 0.1% and CsA 0.09% have demonstrated similar treatment e ect and superior responder rate compared to vehicle. 8-10
The post-surgical management of ocular surface inflammation or dry eye with twice-daily drops of CsA 0.05% also showed better e cacy for improvement in symptoms and clinical signs including, tear stability, tear secretion, and tear osmolarity compared to antibiotics and steroid twice-daily drops in post-refractive surgery.11
Conflicting evidence on CsA dosage has also been reported. Four-times-daily drops treatment with CsA has been reported to produce a more rapid clinical response, especially for patients with persistent symptoms despite prolonged treatment with twice-daily drops treatment. Though other studies reported better treatment e ect with four-times-daily drop of artificial tears over twice-daily drop of CsA 0.05% treatment12 and vice versa.13
In more severe DED, frequent CsA dosing beyond twice-daily use or additional use of antihistamines, mast-cell inhibitors (artificial tears), or topical corticosteroid may provide faster relief from symptoms and clinical signs.14 Use of increased concentrations of CsA have not been proven to have any therapeutic benefits, but there is increased likelihood of stinging and other side e ects when higher CsA concentrations are used. Topical CsA concentrations from 0.05% to 0.1% have yielded better balance between e cacy and side e ects.15 Increasing the daily dose of topical CsA has not been linked to systemic side e ects given that there is insignificant systemic adsorption of the drug after topical application to the eye. Optimal dosing for CsA is yet to be established. Evidence from RCTs has supported the current prescribing indications for the CsA formulations. Evidence is also emerging on variations on these dosage regimes.
THE APPROPRIATE LENGTH OF TREATMENT
Improvement in outcome following twice-daily drops with CsA 0.05% for patients with moderate DED usually occurs in four to 12 weeks following the start of treatment and may take three to six months to e ectively relieve symptoms. Once daily drops of CsA 0.1% also showed similar timeline to improvement e ect in particular reduced ocular surface staining within four weeks and maintained up to 24-weeks treatment duration. 8,9 The delay in symptom relief is thought to occur because CsA does not deactivate
previously activated T-cells, but rather prevents new T-cell activation.
After treatment has been commenced, there is evidence that relapse of DED may occur following 12-months of treatment cessation.16 In some severe cases of DED or Sjögren's syndrome associated DED, treatment may be continued for an extended period of time, or sometimes indefinite to prevent relapse.
Overall, there is no universal consensus with regard to CsA treatment e ect timeline. Evidence based on clinical studies was that CsA of di erent concentrations may require several weeks of treatment to show an e ect. Further studies are needed to confirm if there is added advantage of indefinite treatment.
EVIDENCE ON TREATMENT OUTCOMES
Randomised clinical trials have compared the e cacy of CsA with no treatment, placebo or with other topical treatment options including artificial tears, and other topical anti-inflammatory eye drops. The treatment e ect of commercially-available CsA formulations globally was compared by meta-analysis and CsA 0.05% concentration (Restasis) was ranked most e ective for reduced DED symptoms.2 Other formulations of CsA 0.05% (Zirun and TJ Cyporin) also demonstrated higher e cacy in improving tear secretion and
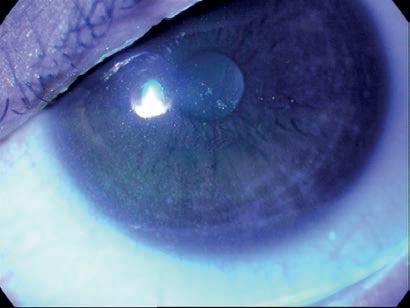

“OVERALL, THERE IS NO UNIVERSAL CONSENSUS WITH REGARD TO CSA TREATMENT EFFECT TIMELINE.”
tear breakup time compared to CsA 0.1% or placebo.2 The risk of reporting bias in the studies included in the meta-analysis was considered low. A Cochrane review reported inconsistent results on the e ect of di erent CsA concentrations on DED symptoms and clinical sign changes including on tear secretion, tear breakup time and corneal fluorescein staining.3 Although the Cochrane review reported greater improvement in conjunctival goblet cell density with CsA 0.05% compared to artificial tears or vehicle as demonstrated by two studies, the certainty of evidence was low.
In other studies, more frequent dosing of artificial tears – up to four or five times daily drops – was reported to have a better e ect over CsA 0.05% in improving tear film function.2,3 One study also reported better treatment e ect with topical steroid drops over CsA 0.05% in improving tear film function. Studies that compared CsA 0.05% to CsA 0.1%, CsA 0.08% or 0.1% to fluorometholone, reported no di erence in treatment e ect on symptoms.
Overall, the majority of studies have reported better e ect of reduced DED symptoms and ocular surface inflammation staining scores with CsA treatment compared to artificial tears (AT) alone or vehicle.2,3
CHALLENGES IN PRESCRIBING
A low risk of poor patient compliance is evident in the literature. Discontinuation or dropout from the clinical trials due to treatment related adverse events, especially stinging, upon CsA drop instillation was low in published studies. No serious side e ects from topical CsA were found in most of the existing studies.
The common treatment-related complaints of side e ects were mild-to-moderate ocular stinging, ocular burning and blurred vision. These adverse events were not significantly di erent between CsA treatment and other treatment comparators. The events were mostly found to have resolved within the clinical trial period, requiring no further observation beyond the trial duration.
Upon CsA prescription, patients should be warned about the possibility of side e ects such as burning, stinging upon instillation, and conjunctival redness. They should also be re-assured that there are no threats to vision if side e ects are encountered, since they typically resolve as the ocular surface improves. Clinical guideline recommendations are that prescribing short-term topical steroids, not more than two to four weeks prior to starting CsA 0.05% (Restasis Allergan, Irvine, CA) may decrease the associated burning and stinging associated with the drops.17
INSIGHT May 2024 49
Figure 4. Tear film interferometry in dry eye disease.
Figure 3. Corneal staining with fluorescein viewed with Cobalt blue light on the slit lamp in dry eye disease.
Caution must be exercised when using topical steroids due to potential adverse e ect of raising intraocular pressure, causing cataracts and the risk of infection.
THE BIGPICTURE
Prescribing trends based on evidence from published clinical studies show that twice-daily drops of CsA is likely to be e ective for DED treatment. Significant changes from baseline have been seen on outcomes within 12-weeks of initiating treatment. Most studies found CsA 0.05% to be e ective and with higher responder rates compared to other CsA concentrations or topical treatment alternatives.
CsA 0.05% demonstrated consistent improvement in treatment e ect on DED symptoms and ocular surface staining. Frequent CsA dosing of more than twice-daily drops or concomitant use with antihistamines, mast-cell inhibitors (artificial tears), or topical corticosteroid may not show more e cacy of faster symptoms and clinical signs relief. Topical CsA may be better than vehicle or AT alone for managing symptoms and common clinical signs of DED. The e ect of CsA treatment on tear function and other DED clinical signs may be somewhat disproportionate. Treatment-related adverse events with CsA treatment are mostly mild. There is relatively low
risk of lack of patient compliance to treatment. There was low-to-moderate certainty of evidence on the superior e ect of CsA compared to vehicle, AT, or other topical treatment alternatives for DED. All published trials were short-term and did not assess whether CsA has longer-term (over one year) disease-modifying e ects, thus limiting the ability of clinicians to make informed decisions regarding the use of CsA for DED treatment; and importantly, being that DED is a chronic disorder requiring long-term therapy in most patients. Future longer-term studies are needed to confirm or validate available evidence. Work is also needed to develop a framework of practical guidelines for the use of topical CsA. Moreover, there is a need to consolidate all available evidence and provide recommendations that will enhance appropriate clinical practices for the safe use of CsA for DED treatment.

NOTE: Insight readers can scan the QR code or visit insightnews.com.au/cpd/ to access a link to this article to include in their own CPD log book.
REFERENCES:
1. Wol sohn JS, Arita R, Chalmers R, et al. TFOS DEWS II Diagnostic Methodology report. The Ocular Surface. 2017;15(3):539-574.
2. Gao D, Da Z, Yang K, Shi Y. Comparison of seven cyclosporine A formulations for dry eye disease: A systematic review and network meta-analysis. Front Pharmacol. 2022;13:882803.
3. De Paiva CS, Pflugfelder SC, Ng SM, Akpek EK. Topical cyclosporine A therapy for dry eye syndrome. Cochrane Database of Systematic Reviews. 2019(9).
4. Jones L, Downie LE, Korb D, et al. TFOS DEWS II management and therapy report. The ocular surface. 2017;15(3):575-628.
5. Periman LM, Mah FS, Karpecki PM. A Review of the Mechanism of Action of Cyclosporine A: The Role of Cyclosporine A in Dry Eye Disease and Recent Formulation Developments. Clinical Ophthalmology. 2020;14(null):4187-4200.
6. Donnenfeld E, Pflugfelder SC. Topical Ophthalmic Cyclosporine: Pharmacology and Clinical Uses. Survey of Ophthalmology. 2009;54(3):321-338.
7. González-López JJ, López-Alcalde J, Morcillo Laiz R, Fernández Buenaga R, Rebolleda Fernández G. Topical cyclosporine for atopic keratoconjunctivitis. Cochrane Database Syst Rev. 2012(9):Cd009078.
8. Baudouin C, Figueiredo FC, Messmer EM, et al. A randomized study of the e cacy and safety of 0.1% cyclosporine A cationic emulsion in treatment of moderate to severe dry eye. European journal of ophthalmology. 2017;27(5):520-530.
9. Leonardi A, Van Setten G, Amrane M, et al. E cacy and safety of 0.1% cyclosporine A cationic emulsion in the treatment of severe dry eye disease: a multicenter randomized trial. Eur J Ophthalmol. 2016;26(4):287-296.
10. Goldberg DF, Malhotra RP, Schechter BA, Justice A, Weiss SL, Sheppard JD. A phase 3, randomized, double-masked study of OTX-101 ophthalmic solution 0.09% in the treatment of dry eye disease. Ophthalmology. 2019;126(9):1230-1237.
11. Kang KW, Kim HK. E cacy of Topical Cyclosporine in Mild Dry Eye Patients Having Refractive Surgery. Journal of the Korean Ophthalmological Society. 2014;55(12):1752-1757.
12. Altiparmak UE, Acar DE, Ozer PA, et al. Topical cyclosporine A for the dry eye findings of thyroid orbitopathy patients. Eye. 2010;24(6):1044-1050.
13. ElShazly IY, Morsy MH, Bekhit AA, Ramadan AA, Mossallam EF. Topical cyclosporine A for the treatment of dry eye: a randomized clinical study. Delta Journal of Ophthalmology. 2021;22(3):165.
14. Utine CA, Stern M, Akpek EK. Clinical review: topical ophthalmic use of cyclosporin A. Ocular Immunology and Inflammation. 2010;18(5):352-361.
15. Stevenson D, Tauber J, Reis BL. E cacy and safety of cyclosporin A ophthalmic emulsion in the treatment of moderate-to-severe dry eye disease: a dose-ranging, randomized trial. The Cyclosporin A Phase 2 Study Group. Ophthalmology. 2000;107(5):967-974.
16. Rao SN. Reversibility of dry eye deceleration after topical cyclosporine 0.05% withdrawal. J Ocul Pharmacol Ther. 2011;27(6):603-609.
17. Foulks GN, Forstot SL, Donshik PC, et al. Clinical guidelines for management of dry eye associated with Sjögren disease. Ocul Surf. 2015;13(2):118-132.




























Instant relief in a blink of
Convenient spray that works on closed eyelids
Contains liposomes to refresh and moisturise dry and tired eyes




Do your patients need relief from dry eyes? MURINE® provides a preservative free range of eye care products MURINE® Dry eyes For focused & hydrated eyes Triple benefit formula o ers: Long-lasting dry eye relief Lubrication Protection from further moisture loss
mist
refreshed
revitalised eyes
MURINE® Eye
For
&
an eye
ZADITEN® also available for allergy eyes symptoms For enquiries email: hcp@carepharma.com.au or register to hcp.carepharma.com.au/register ALWAYS READ THE LABEL AND FOLLOW THE DIRECTIONS FOR USE
CPD DRY EYE


Are you aspiring to become a business owner in the future? You’d look good in Specsavers If you’re looking for a company where your optometry career can thrive, supported by training and development programs designed to guide you towards owning your own store, you’ll shine at Specsavers. spectrum-anz.com/careers-at-specsavers/















Dry Eyes? Restore the tear film with every










blink® Intensive Tears


Long lasting relief from the feeling of dry, tired eyes. An advanced lubricating eye drop specially formulated to provide protection and comfort for the eyes that are dry, irritated or uncomfortable.
• With hyaluronic acid
• May be used with contact lenses










blink® Intensive Tears PLUS
A thicker, more viscous advanced lubricating eye drop formulation that adapts to your dry eye needs and provides long lasting relief.
• Specially formulated for enhanced ocular comfort
• Recommended for both day and night use
• With hyaluronic acid
• For Moderate to Severe Dry Eye
For more information contact your Bausch + Lomb Territory Manager or Bausch + Lomb Customer service 1800 251 150
Material was prepared in February 2024 © 2024 Bausch & Lomb Incorporated. ®/TM are trademarks of Bausch & Lomb Incorporated or its a liates. Bausch & Lomb (Australia) Pty Ltd. ABN 88 000 222 408. Level 2, 12 Help Street, Chatswood NSW 2067 Australia. (Ph 1800 251 150) BTLD.0001.AU.24
LEARNING OBJECTIVES:
At the completion of this article, the reader should be able to improve their diagnosis and management of dry eye disease (DED) ...
Including:
• Review the implications of the definition of dry eye as a multifactorial disease.
• Be aware of the prevalence of asymptomatic dry eye.
• Recognise the importance of comprehensive diagnostic procedures for DED.
Exposing the underlying factors contributing to dry eye
Dry eye is entering an era where thorough assessment with innovative technology is essential to disease management. Optometrist JOSEPH
NAZARIAN draws on recent case reports to demonstrate how the ZEISS ATLAS 500 enhances dry eye detection and treatment, particularly in asymptomatic patients.
It has been seven years since the Tear Film & Ocular Surface Society (TFOS) Dry Eye Workshop (DEWS) II defined dry eye as ‘a multifactorial disease.’*1 In the intervening years, most optometrists have come to recognise the diverse array of contributing factors to dry eye disease (DED) and acknowledge that detecting and measuring them is essential for developing treatment plans for their patients.
It’s an important recognition to make. The prevalence of DED is reported to be in the range of 5-15% of the Australian population,2 and it is one of the leading causes of patient visits to eyecare providers in Australia today. Bottom line: it’s the foremost medical condition driving patients to consult with eyecare professionals and is expected to continue to grow in prevalence.
However, dry eye is rarely straight-forward. Successful management of a multifactorial disease requires multifactorial approaches – approaches that can address the specific factors relevant to each patient. For dry eye, informed diagnostic procedures include careful history taking and examination and specific tests.
Symptoms of burning sensation, dryness, and stickiness are, of course, the most prevalent among dry eye patients. However, the percentage of patients with asymptomatic dry eye can be significant. As a 2023 study in the International Journal of Environmental Research and Public Health reported, up to 24% of patients were found to have asymptomatic dry eye.3 The disparity between what the patients report, and clinical findings, has been reported by other researchers as well. Nichols et al have discussed a lack of correlation between signs and symptoms of dry eye and have suggested that it probably varies with patients’ awareness and sensitivity toward the symptoms.4
As research continues to endorse the complexity of DED, three things have emerged which are essential for optometrists to embrace to ensure they are providing the best treatment of the condition.
1. Embrace the complexity

Only by understanding the central complexity of dry eye can optometrists develop more e ective treatment plans tailored to each patient's specific needs. At the same time, recognising dry eye as multifactorial encourages optometrists to stay up-to-date with the latest technological advances and treatment options.
2. Embrace patient education
It’s vital that optometrists commit to ongoing education and communication with patients. Despite the fact that eyecare professionals have, in the last decade, benefited from extensive leaps in the understanding of dry eye, patients' comprehension of the condition significantly trails behind. For that reason, optometrists are in a unique position to empower their patients to actively participate in their treatment and achieve improved outcomes.
3. Embrace emerging technology
Due to the complexity of DED, detection, diagnosis, and treatment remain a considerable challenge for many eyecare professionals. Frequently, patients experience an overlap of disease aetiologies, coupled with fluctuating signs and symptoms over time. There is a need to adopt the newest advances in technology to assess and analyse multiple components of the ocular surface.
The ZEISS ATLAS 500 topographer, introduced in September 2023 at the O=MEGA23 trade fair in Melbourne, is one such advancement. It o ers a variety of tests and clinical indicators, enabling optometrists to compare and observe key metrics, leading to informed diagnoses and tailored treatment solutions.
One of the key features of the ZEISS ATLAS 500 is its ability to provide a comprehensive dry eye report. The report includes detailed information on various parameters such as meibography, which calculates the area of loss; ocular redness, graded by the Nathan Efron scale; tear meniscus
ABOUT
THE AUTHOR:
Joseph Nazarian B.Optom., M,Sc(Optom.) (UNSW)
height; tear film break-up time; and the Ocular Surface Disease Index (OSDI) questionnaire. Additionally, the ZEISS ATLAS 500 can optionally input osmolarity data. In the clinic, it provides a clear, systematic approach to dry eye management which benefits clinical workflow, education and patient outcomes.
IN THE CLINIC
Because of its quick-to-capture, step-by-step guidelines, comprehensive analytics and a simple report generation feature, our patients are routinely screened with the ZEISS ATLAS 500 for DED as part of a comprehensive ocular assessment.
A pair of reports have been provided to illustrate how the ZEISS ATLAS 500 has been integrated into eye assessments at Nazarian Optometrists, providing a comprehensive evaluation of symptoms and enhancing the detection and treatment of dry eye of two patients who presented asymptomatically to the practice.
Case 1: Moderate evaporative dry eye
Patient NG is a 56-year-old female who presented for an annual eye examination. She had no complaints regarding her visual acuity or ocular surface health. Upon routine assessment, her unaided visual acuity was 6/6 in both eyes with unremarkable intraocular pressures (16 mmHg in both eyes), OCT and undilated ultra-widefield fundus imaging.
For a comprehensive ocular surface assessment using the ZEISS ATLAS 500, a detailed meibography and ocular redness examination was conducted. The meiboscale reported a third degree loss of area in the right eye, while a second degree in
INSIGHT May 2024 55
CPD DRY EYE
CLINICAL
CPD HOURS This activity meets the OBA registration standards for CPD
Image: Joseph Nazarian.
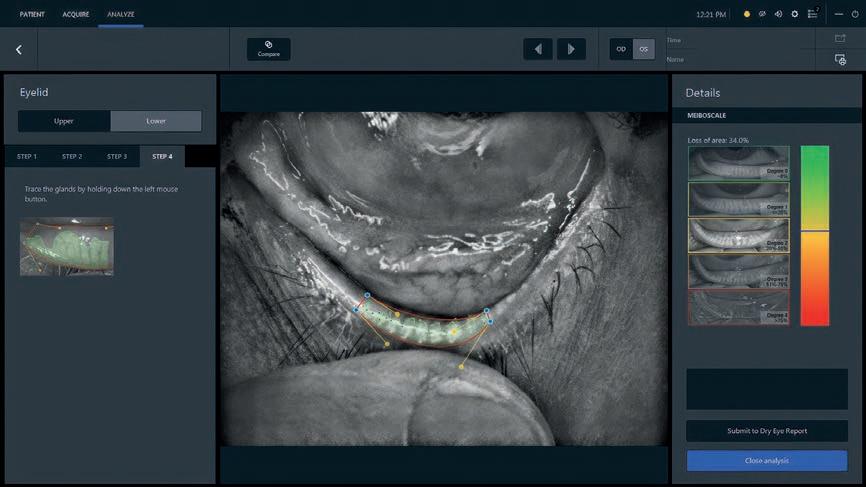
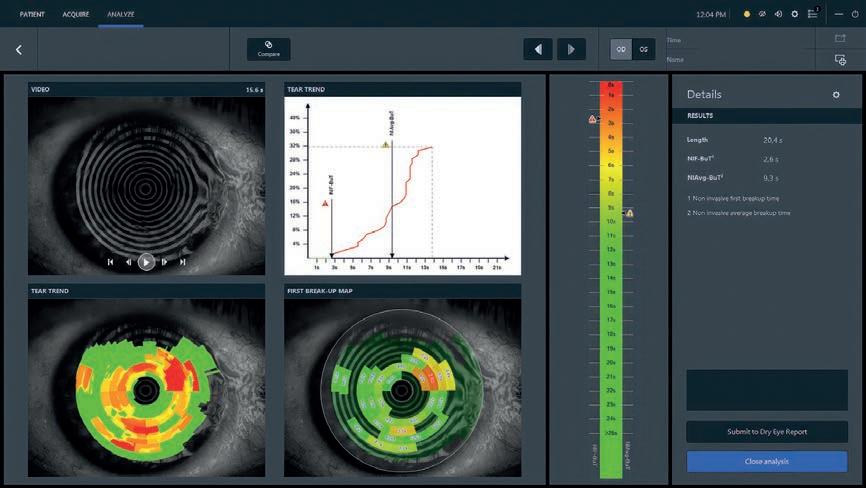
the left eye (56.2% and 47.9%, respectively). Efron grading indicated ocular redness of the conjunctiva on the right eye to be Grade 2 and Grade 3 for the left (see Figure 1A).
In the right eye, non-invasive first tear film break-up time (NIF-BuT) recorded 2.6 seconds and the non-invasive average break-up time (NIAvg-BuT) was 9.3 (see figure 1B). Her left eye demonstrated a NIF-BuT of 6.6 seconds and NIAvg-BuT of 12.4. Additionally, both tear meniscuses were unremarkable.
The dry eye report agglomerated each component of NG’s ocular surface assessment and was able to concisely display the right and left eye deficiencies in meibomian gland area, conjunctival redness, and tear film break-up time.
From this information, we were able to diagnose her with moderate evaporative DED. The patient was advised of environmental factors that may exacerbate her dry eye including air conditioning, smoking and digital device use. She was also advised of lid hygiene by way of hot compresses and tear film supplements, including liposomal sprays in the event that symptoms of blurred vision or gritty foreign body sensations commence.
Case 2: Evaporative and aqueous deficient DEDs
Patient MG is a 68-year-old female who attended her optometry annual review with no notable changes in her vision since her last visit and no symptoms of dry eye. Her unaided visual acuity was unchanged at 6/7.5 in both eyes with each recording intraocular pressures of 15 mmHg. A further comprehensive posterior check of the macula and optic disc, through OCT, was also found to be unremarkable.
The ATLAS 500 was utilised for a full ocular surface health check. Ocular redness was determined to be a Grade 3 for the right conjunctiva and Grade 2 on the left. Meibomian gland loss in the right eye was 33.6% (classified as a Grade 2) with the left eye analysis also demonstrating a 35.3% loss (Grade 2, see Figure 2A). Tear meniscus height for the right eye (0.22 mm) was within normal limits (i.e >0.2 mm), however, the left eye registered a deficit at 0.19 mm. This reduction in tear meniscus height was measured without instilling fluorescein or any form of pharmacological drops. NIF-BuT for the right eye was documented at 3.6 seconds with 1.1 seconds in the left.
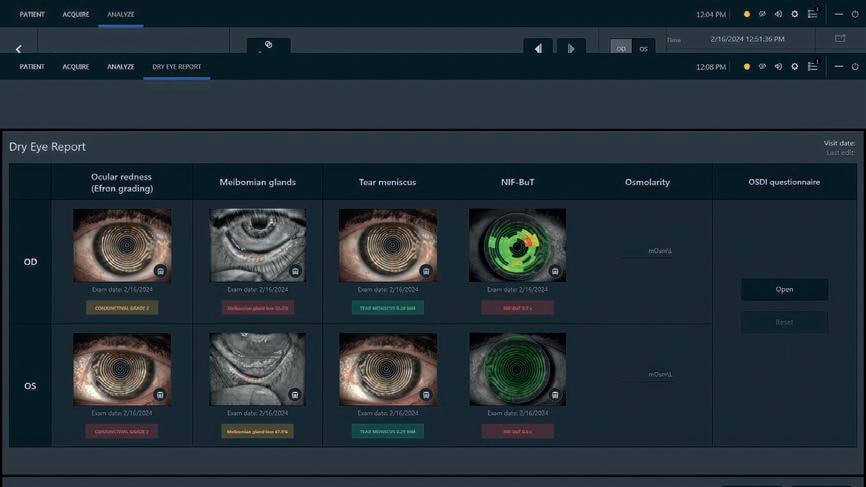
The dry eye report is a clear visual representation of ocular surface health, allowing practitioners the ability to have a quick glance at summarised patient data. The ATLAS 500 also allows the examiner to perform the Ocular Surface Disease Index (OSDI) questionnaire directly using the software, rather than printing multiple pages and manually tallying up scores.
Patient MG was diagnosed with a combination of evaporative and aqueous deficient DEDs. This
56 INSIGHT May 2024 CPD DRY EYE
Figure 1A. Meibography of patient NG’s left lower eyelid with onscreen grading scale marking meibomian gland loss.
Images: Joseph Nazarian.
Figure 1B. Tear film break up time analysis of the right eye with colour graded scale of severity.
Figure 1C. Comprehensive dry eye report indicating overall ocular surface health with summaries of each component.
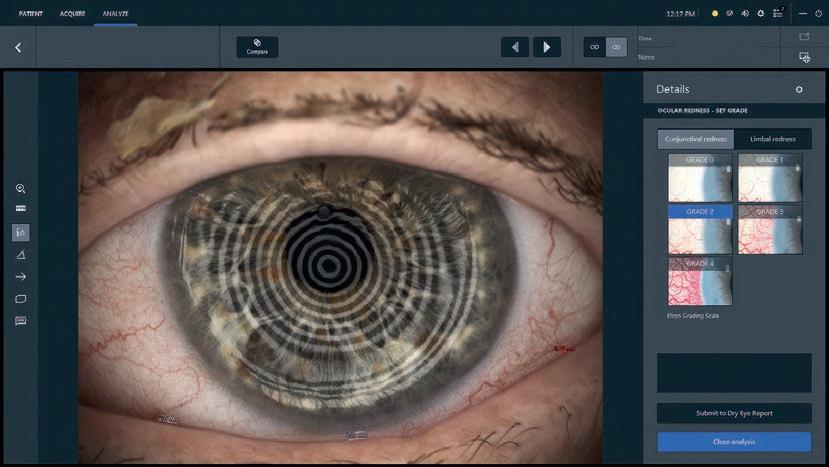
was found to be moderate to severe. Similar to treatment advice for Case 1, a thorough explanation was given to MG on the possible causes of her dry eye and similar lid hygiene and tear supplement education were intensively discussed. She was provided relevant ocular lubricants and will be reviewed in a further three months’ time for a comparative assessment.
It is widely understood that many patients do not routinely present to an eyecare professional describing the feeling of ‘dryness’ or ‘discomfort’ unless prompted. This means that the ability to identify asymptomatic dry eye patients is important within eyecare to prevent further exacerbation of symptoms and ocular surface damage. From this article, both Case 1 and Case 2 demonstrate patients who fit within the asymptomatic group of DED, as they did not verbally express any overt clinical features.
CONCLUSION
The ZEISS ATLAS 500 was found to be a great tool in the evaluation of ocular surface disease. Further to the information provided in the above cases, this device provides an additional section to document the patient’s osmolarity, although this requires manual input and must be captured by a separate device. At Nazarian Optometry, we do not have access to an osmolarity measuring tool, and so, this information was not included in the cases above.
Despite the intricacies of the data captured, quantified, analysed, and presented on the screen, I have found the ZEISS ATLAS 500 requires minimal training through its on-screen prompts and guides. This makes it quite easy to integrate into any clinical workflow and the ideal time saving solution for clinical sta . With optimisation for a seamless integration into the ZEISS medical ecosystem, the ZEISS ATLAS 500 allows existing FORUM users additional connectivity benefits, including dry eye PDF report generation to view all key patient
TEAR TREND
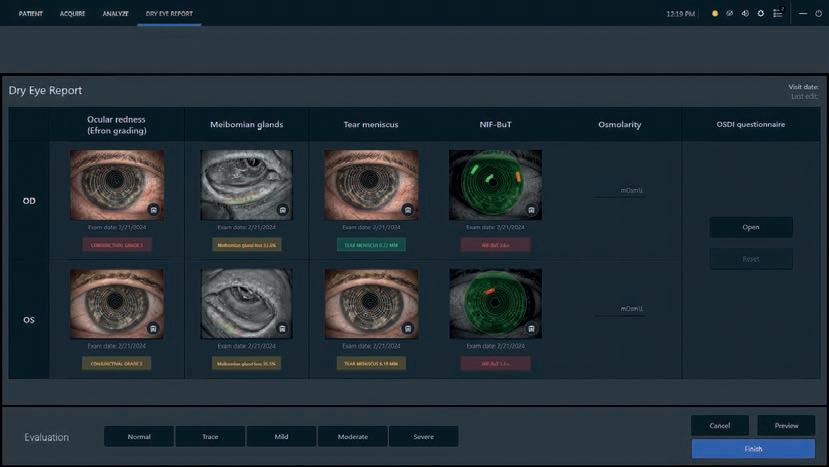
information anywhere in the practice.
By providing a wide range of measurements and analysis tools, the ZEISS ATLAS 500 empowers optometrists to better understand the underlying factors contributing to DED. This, in turn, allows them to develop more e ective treatment plans tailored to each patient's unique needs, ultimately improving patient outcomes. This could further be applied to the management of cataract pre- and post-operatively while allowing an ophthalmologist to choose an appropriate IOL without being hindered by inconsistent readings due to DED. At Nazarian optometry, sta are embracing complexity, education and technology for the best treatment and management of this multifactorial and complex disease.
* Full quote as published in the published in The Ocular Surface journal in 2017: ‘a multifactorial disease of the ocular surface characterised by a loss of homeostasis of the tear film, and accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities play etiological roles.’
REFERENCES:
1. Craig JP, Nelson JD, Azar DT, et al. TFOS DEWS II report executive summary. The Ocular Surface. 2017; 15 (4): 802-812.
2. Chia EM, Mitchell P, Rochtchina E, Lee AJ, Maroun R, Wang JJ. Prevalence and associations of dry eye syndrome in an older population: the Blue Mountains Eye Study. Clin Exp Ophthalmol. 2003; 31 (3): 229-32.
3. Wróbel-Dudzińska D, Osial N, Stępień PW, Gorecka A, Żarnowski T. Prevalence of dry eye symptoms and associated risk factors among university students in Poland. International Journal of Environmental Research and Public Health. 2023 Jan 11; 20 (2): 1313. doi:10.3390/ijerph20021313
4. Nichols KK, Nichols JJ, Mitchell GL. The lack of association between signs and symptoms in patients with DED. Cornea. 2004; 23: 762–70.

NOTE: Insight readers can scan the QR code or visit insightnews.com.au/cpd/ to access a link to this article to include in their own CPD log book.
INSIGHT May 2024 57
Figure 2B. Right eye tear trend graph indicating 1% of loss at 3.6 seconds (NIF-BuT).
Figure 2A. Measured tear meniscus height of the left eye with conjunctival redness grading of 2.
NIF-BuT NI Avg-BuT 0s 1s 2s 3s 4s 5s 6s 7s 8s9s 10s 11s 12s 13s 14s 15s 16s 17s 18s 1% 2% 3% 4% 5% 6% 7% 8% 9% 10%
Figure 2C. Dry eye report as displayed in software demonstrating intuitive results and ideal for patient education.

SLOW MYOPIA PROGRESSION









This medicinal product is subject to additional monitoring in Australia. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected


Aspen Australia includes Aspen Pharmacare Australia Pty Ltd (ABN 51 096 236 985) and Aspen Pharma Pty Ltd (ABN 88 004 118 594). All sales and marketing requests to: Aspen Pharmacare Pty Ltd, 34-36 Chandos Street, St Leonards NSW 2065. Tel: +61 2 8436 8300 Email: aspen@aspenpharmacare.com.au Web: www.aspenpharma.com.au Trademarks are owned by or licensed to the Aspen group of companies. © 2023 Aspen group of companies or its licensor. All rights reserved. Prepared July 2023. AU-ATR-072023-07585. ASPPH3029. PBS Information: This product is not listed on the PBS. *P-value not available (ATOM 1&2 studies, placebo was a historical control from ATOM 1).ATOM 2 study data available for 5 years with 1 year washout after 24 months.3 EIKANCE 0.01% eye drops (atropine sulfate monohydrate 0.01%) is indicated as a treatment to slow the progression of myopia in children aged from 4 to 14 years. Atropine treatment may be initiated in children when myopia progresses ≥ –1.0 diopter (D) per year.1
to review full Product Information and to order samples,
call 1300 659 646. References: 1. Approved EIKANCE Product Information, 14 March 2023. 2. Chua WH et al. Ophthalmology 2006;113:2285–91. 3. Chia A et al. Ophthalmology 2016;123:391–9.
adverse events at https://www.tga.gov.au/reporting-problems.
Scan
or
BY UP TO 60% WITH ATROPINE 0.01% EYE DROPS AT 2 YEARS
TO PLACEBO *1-3
COMPARED
Stable tearfilm,
predicable results
Identifying and addressing dry eye disease is one of the most important steps before anterior segment surgery. DR AVENELL CHEW lays out his protocol and the lubricants he uses to pave the way for a predictable outcome.
As an adopter of sophisticated refractive laser techniques and intraocular lenses (IOLs), Western Australian ophthalmologist Dr Avenell Chew is constantly on the lookout for any factors that may influence the final refractive outcome.
“I’m of the opinion that if you’re going to have surgery in the eye, especially for cataract, that it should be a one-time thing and treated as a single opportunity to obtain the vision patients are seeking,” says Dr Chew, who practises at WA Laser Eye Centre alongside managing director and principal surgeon Associate Professor Robert Paul.
Dr Avenell Chew says regular use of artificial tears are crucial in the weeks leading up to refractive and cataract surgery.

“The expectations of patients following laser refractive procedures is high and reasonably so given that they usually already have excellent best corrected acuities. The key determinants in their satisfaction with the surgery are the refractive outcome and their experience of any pain or discomfort peri-operatively.”
Armed with fellowship training in cornea and external eye diseases (Birmingham & Midland Eye Centre, UK), Dr Chew is well acquainted with dry eye disease (DED) and its ability to determine cataract and refractive surgery outcomes. That’s why preservative-free artificial tears, such as Viscotears (active ingredient carbomer [polyacrylic acid]) from Bausch + Lomb, have been a key tool for optimising his patients’ ocular surface in the weeks leading up to surgery.
For instance, precise topography, tonometry and biometric measurements are prerequisites for cataract surgical planning, and the eventual post-operative visual performance. They require – as the first refractive component of the eye – an intact, healthy pre-corneal tear film. However, suboptimal tearfilm quality is a common issue. Gupta et al., in a prospective case series of 120 cataract patients in the US, reported 80% had at least one abnormal tear film measurement parameter.1
“DED is also especially significant among people seeking laser refractive surgery, many of whom have been wearing contact lenses already because they don’t want to wear glasses,” Dr Chew says.
“And by virtue of wearing contact lenses, that tends to disturb the tear film and chronic contact lens wear can impair corneal sensation too. Pre-operatively it’s a priority for me to address any DED because the better you treat it at this stage, the fewer problems you’re going to face down the line. Ultimately your outcomes are only as good as your measurements.”
In the case of cataract surgery, Chew says an unstable tearfilm can result in significant changes to the degree of astigmatism measured pre-operatively; not only the amplitude of the astigmatism, but even the axis can change.
“If you’re implanting a lens on completely the wrong axis, then patients can potentially end worse o than pre-operatively," he adds.
For refractive patients, DED can create variability during the pre-operative

subjective refraction, creating delays and potential uncertainty leading into the procedure. “If I’ve identified significant DED pre-operatively, I’m asking patients to optimise their tearfilm with something like Viscotears, as well as additional agents depending on the aetiology of their DED, for at least four to six weeks before their measurements are taken,” he says.
“I’m very open with patients that how religious they are with the treatment will determine the accuracy of their result.”
If he’s prescribing artificial tears, Dr Chew makes a point to recommend Viscotears Gel PF. The preservative-free nature of the drop avoids any potential for toxicity prior to the surgery, given the frequency of their use. To reinforce this, Jee et al., investigated the e ects of preservatives on DED after cataract surgery by randomising 80 patients to receive either post-operative preservative-free eye drops, or drops containing preservatives. Two months after surgery, those receiving preservative-free drops had better tear break up times, goblet cell counts, Schirmer I test, corneal fluorescein staining and Ocular Surface Disease Index questionnaire scores. 2
For Dr Chew, Viscotears is an eye drop he’s used extensively, particularly during his fellowship in the UK. This is due to positive experiences among his patients, good therapeutic e ects, and the fact it’s manufactured by a well-established company.
While lubricants play a key role in the lead up to surgery, they play an equally important part thereafter. All of Dr Chew’s refractive patients are prescribed the lubricant for several weeks post-surgery.
“The act of corneal refractive surgery results in injury to the corneal nerves and that reduces the reflex tear production of the eye. That means everyone’s going to have reduced tear production post-operatively, and some dry eye, so it’s imperative to prescribe a lubricant post-operatively,” he says.
“This is usually for four to six weeks, but even beyond that it can take three to six months. Studies show that for the vast majority of people, corneal sensitivity returns to preoperative levels by about six months.”
NOTE: References available upon request.
INSIGHT May 2024 59 DRY EYE
Image: WA Laser Eye Centre.
Viscotears Gel PF, from Bausch + Lomb, is preservative-free, helping to avoid potential toxicity prior to surgery. Image: Bausch + Lomb.




Empowering tomorrow’s optometrists
Through a combination of professional development opportunities, expansive support networks, and exposure to cutting-edge technologies, EssilorLuxottica’s Graduate Program is offering new optometrists a platform to become confident and capable practitioners.
Pursuing a career in healthcare requires some degree of altruism: People do not choose these careers lightly, and so finding an employer that aligns with the level of care they want to deliver is an important requirement for many of today’s graduates.
Growing up, Mr Vusa Bhebhe was always encouraged to volunteer, so goodwill was high on his checklist for potential employers. EssilorLux ottica’s charitable work through the OneSight Foundation– delivered locally and globally – piqued his interest. He’s also been impressed by the structured approach of the company’s Graduate Program o ering a smooth transition into becoming an optometrist at its OPSM and Laubman & Pank stores after completing university.
“The commitment to help people around the world to ‘see more and be more’ through the OneSight EssilorLuxottica Foundation stuck out to me,” he says.
A Queensland University of Technology (QUT) 2023 graduate, Bhebhe has spent his initial months in the workforce at the OPSM store in Garden City, Perth. He has since discovered the opportunities for professional development within the network are boundless, alongside potential career pathways.
Bhebhe is among 70 graduates new to the network this year who were all welcomed into the industry with the EyeLaunch induction event – a key moment to kickstart the graduate journey. It’s all part of the company’s Graduate Program, one of its major drawcards to attract new optometrists to the network with opportunities for personal and professional growth, networking, ongoing clinical and leadership education, and participation in outreach clinics.

is delivering.
For Bhebhe, the first year of the Graduate Program is designed to sculpt confident, and capable optometrists with the second year focused on developing special interests and finding growth opportunities.
Working for OPSM, Bhebhe says the company has been quick to build his confidence and begin refining his clinical skills through the high volume of patients that come through the store.
“In my first seven weeks, I have seen almost 200 patients. I think it’s just given me the opportunity to gain that confidence in my early career,” he says.
As part of the program, each graduate is assigned a mentor. Bhebhe says
FAMILIAR TERRITORY
Transitioning into the workforce from university can be daunting. For QUT graduate Mr Zichun (William) Wang, it was EssilorLuxottica’s support for those wanting to pursue a regional career and prior experience with the network that influenced his decision to o cially join the company and its Graduate Program.
Currently, Wang is practising at Cairns Smithfield OPSM, but spent
60 INSIGHT May 2024 CAREERS
William Wang, OPSM Smithfield.
several years working as a casual optical dispenser throughout university with Laubman & Pank in Mt Gravatt, Brisbane.
“My experience as a casual dispenser in Laubman & Pank really helped a lot because I worked with a lovely team. Everyone’s so nice, and I really enjoyed the clientele base there,” Wang says.
To consolidate his decision and ensure he wasn’t taking a blind leap, Wang could visit his preferred locations and hear directly from the team.
“I was able to talk to the store managers, the dispensing team and also the optometrist working there to ask them about the store,” he says.
For Wang, the safety net of having a mentor optometrist within arm’s reach gives him the assurance he can grow into the best practitioner he can be.
“From day one, my mentor set me up for success and o ered to sit in with me. I can ask them straight away about anything I was unsure of –it’s great,” he says.
AN INDUSTRY STEPPING STONE
To provide its graduates a peek into the future, equip them with foundational knowledge, and help them ease into the workforce, EssilorLuxottica holds an annual EyeLaunch induction event.

The company’s senior manager eyecare operations for ANZ, Ms Sephora Miao, says EyeLaunch marks the start of a graduate’s optometry career with the company.
“This year’s induction brought together all our graduate optometrists across Australia and New Zealand for three exhilarating days of learning and connecting,” she says.
At EyeLaunch this year on 4-6 March, 70 graduates from across the country were welcomed into the network where they were familiarised with the premium brands they can find within the network and to connect with industry leaders and representatives.
In addition to educational sessions, the event allowed Bhebhe, Wang and their fellow graduates to connect with new colleagues and reconnect their peers from university. Social activities were incorporated throughout, including the welcome evening on the first day at the company’s support o ce in North Sydney, as well as a harbour cruise on the second day.
“It was a good way to bring us all together. Some of us had only practised for a few weeks; others for about a month or a little longer. And it allowed us to be able to come together and share our experiences and touch base with each other,” Bhebhe says.
The event featured presentations from leaders within the company who were once in the graduates’ shoes and who could speak on the various pathways and growth opportunities available within the company.
“EyeLaunch is a fantastic opportunity for graduates to connect with peers across ANZ and their support network, from senior leadership to HR to EssilorLuxottica's innovative learning platform, Leonardo Education, and uncover the boundless opportunities for personal and professional growth in EssilorLuxottica,” Miao says.
Wang adds: “The event went above and beyond the optometry career

“The commitment to help people around the world to ‘see more and be more’ through the OneSight EssilorLuxottica Foundation stuck out to me."
“With a large network of talent and a myriad of resources to leverage, we have the ability to support every graduate in finding their path towards success.”
and gave an expanded view on the variety of career pathways available
“You can also join the Onesight EssilorLuxottica Foundation to deliver eyecare to communities that have di culty accessing eyecare services.
ENDLESS OPPORTUNITIES
Miao says what makes the Graduate Program so attractive to new optometrists is its responsiveness and relevance to modern-day demands on optometry.
“Optometry is continuing to evolve as a profession and today’s graduates are looking for employers who are attentive, progressive and invested in their success,” she says.
“This year, it was pleasing to see increased interest to practice in regional settings from graduates wanting to broaden their impact.”
The Graduate Program o ers a diverse range of experiences to present graduates with every opportunity for personal and professional growth, whether they want to pursue clinical optometry or business leadership.
“Having access to diverse opportunities and a rich support network are some of the reasons graduates choose to start their careers with EssilorLuxottica,” Miao says.
The program has been curated to reflect the latest developments within the industry, which ensures graduates stay ahead of the curve.
Indeed, EssilorLuxottica can support its next generation of optometrists before they even graduate. Each year, the company o ers numerous clinical placements, allowing students to refine their clinical skills with the guidance of experienced optometry mentors.
For some, the company provides opportunities to kickstart their careers within the OPSM or Laubman & Pank networks as optical dispensers or through the cadetship program, where successful candidates receive a guaranteed regional position upon graduation.
Following EyeLaunch, graduates are o ered numerous avenues for personal and professional growth. This includes networking opportunities, access to the company’s vast library of complimentary CPD and leadership modules through Leonardo, key opinion leader programs, opportunities to take part in outreach clinics with the OneSight Foundation, and many more.
The company’s ultimate goal is to help each graduate find their success, regardless of the opportunities they pursue.
“Our eyecare leadership team considers several critical questions at key graduate milestones: Do they have a particular area of interest? Are they interested in exploring opportunities outside their home store, or interstate? Do they aspire to develop towards a leadership role?” Miao says.
Vusa Bhebhe OPSM Garden
City
“With a large network of talent and a myriad of resources to leverage, we have the ability to support every graduate in finding their path towards success.”
INSIGHT May 2024 61
Images: EssilorLuxottica.
Sephora Miao EssilorLuxottica









©2023 Alcon Laboratories Pty Ltd. AUS: 1800 224 153; Auckland NZ: 0800 101 106. ANZ-VC-2300022 Restock your Alcon trial lenses in a clicks few Download MyAlcon FitSCAN to get started.

Revolutionising tomorrow:
the cutting-edge of gene therapy

From the beginning of the genetic revolution when the double helix DNA model was first described in the 1950s, to recoding our genetic makeup, medicine has taken strides that were once unfathomable by treating disease at the crux –and ophthalmology is at the forefront.

Globally, medicine is transitioning towards genetically tailored therapeutic options. Gene therapy interventions have exploded on to the clinical landscape with its potential to treat disease on the genome level.
This radical shift has seen rapid market expansion, with Australia welcoming its first approved ophthalmic gene therapy, Luxturna, in 2020 and an unprecedented number of programs entering clinical trial stages here and abroad.
Insight provides a snapshot of the Australian gene therapy landscape and shines a light on the current research focus in this space and its projection.
ONE SIZE FITS ALL
Although the current pipeline is robust, and advancing rapidly, many of the therapies are highly targeted for rare genetic diseases, culminating in multiple programs that stand to benefit a small proportion of patients.
Associate Professor at the University of Melbourne and Centre for Eye Research Australia (CERA), Dr Lauren Ayton, believes the infrequency of these genetic mutations among patient cohorts means the future of gene therapy will see a shift from specific, highly targeted therapies, to broad spectrum genetic approaches.
With its large socio-economic impact, Dr Ayton has dedicated her work to therapeutic interventions in this space with a particular focus on inherited retinal diseases (IRDs). This refers to 300 di erent known genes that can cause degenerative eye disease, which collectively are the most common cause of blindness in working-aged Australians.
At CERA, Dr Ayton says it begins with identifying candidates for gene therapy through genetic screening.
Her group has a natural history registry called VENTURE which involves enrolling people with an IRD with the goal of learning more about these conditions in preparation for the oncoming stream of gene therapies. The team collects clinical data on their disease pathophysiology and o ers them genetic testing where possible.
The clinical trials are a collaboration between CERA, the University of Melbourne, and the Royal Victorian Eye and Ear Hospital.
“We almost see it as our central research pillar,” Dr Ayton says, noting the VENTURE program facilitates gene therapy research by collecting patient samples and generating stem cells to learn more about disease. “It’s like an

ecosystem of research into IRD, allowing us to learn more about the disease process, but also how the conditions impact on people’s quality-of-life.”
IRDs are a target for current gene therapies due to their monogeneity. That is,

RESEARCH
Image: Livinskiy/stock.adobe.com.
Dr Lauren Ayton and the VENTURE team at CERA.
Image: Anna
Carlile/CERA.
GENE THERAPY PIPELINE AND THEIR LAUNCH YEAR 1
Drug
Luxturna IRD (RPE65)
GS030 Retinitis pigmentosa
Laruparetigene zosaparvovecRetinitis pigmentosa
Botaretigene sparoparvovecRetinitis pigmentosa
RGX314 DMEWetAMD
OCU400 Retinitis pigmentosa

Intraoccular injection (once) 2017 (TGA – 2020)
Spark Therapeutics, Inc / Novartis APPROVED
Intraoccular injection (once) 2024 (Projected)GenSight Biologics
Intraoccular injection (once) 2025 (Projected) Beacon Therapeutics
Intraoccular injection (once) 2025 (Projected) Johnson&Johnson/ MeiraGTx
Intraoccular injection (once) 2026 (Projected) AbbVie/RegenxBio
Intraoccular injection (once) 2026 (Projected) Ocugen
disease – is a significant limitation in gene therapy development. As there are so many potential target genes, the costs of developing individualised therapies are excessive. Gene-agnostic therapeutic approaches target pathways, as opposed to genetic factors, are thereby broadening the benefits to a larger cohort of IRD patients.
“What I’m most excited about is what we call the gene-agnostic treatments. That involves using gene therapy or potentially stem cells to treat patients, no matter what their gene is,” Dr Ayton says.
“That’s what I’m looking forward to: being able to o er these treatments to everyone, rather than just a smaller cohort.”
Gene therapy delivery methods include traditional mechanisms such as viral vectors, the most common of these being the adeno-associated virus (AVV). Dr Ayton says this has now extended to novel methods, including nanoparticles of metal such as gold, and liposomes.
“We don’t know what is going to be best for patients now. So, I think it’s important that we keep supporting the di erent therapies that are out there. It’s a very exciting time for people with IRDs, who have not had the opportunity to access treatments before,” Dr Ayton says. “But we do need to temper the excitement with knowledge of the significant challenges that the research field faces.”
One such barrier in gene therapy trial programs is the small sample sizes available to researchers. This is due to the rarity of IRDs, but to compensate for this – and amass a larger patient cohort – CERA is part of an international consortium called the Foundation for Fighting Blindness. Here, with informed patient consent, it shares data internationally to increase patient numbers for a particular disease subset.
For Dr Ayton, the future lies in advanced genetic testing to map out disease.
“We’re starting to get more involved in research into the genetics of these conditions, led in large part by my colleague Dr Ceecee Britten-Jones and our
Phase 1/2
Phase 2/3
Phase 3
Phase 3
Phase 3
1.CVS Health Gene Therapy Report Q1 2024 - Q4 2026
colleagues at the Ocular Genetics Clinic, Royal Victorian Eye and Ear Hospital. “We’re trying to learn more about the unknown. We’re hoping that learning more about the causes of these diseases will then lead to other opportunities for new treatments as well.”
Patients can be referred for the VENTURE registry at IRD@groups.unimelb. edu.au
SWITCHING IT UP
In the works at CERA is SwitchGene therapy for diabetic retinopathy. Led by Dr Ayton’s colleague, Associate Professor Guei-Sheung (Rick) Liu, SwitchGene has been in development for the last five years and is currently in the preclinical phase. The therapy uses a novel mechanism of action that selectively inhibits vascular endothelial growth factor (VEGF) in a controlled manner. This is opposed to continual suppression o ered by conventional gene therapies.
Some diseases require lifetime treatment, but for other diseases constant activation of certain genes can be harmful. For example, indefinite activation of anti-angiogenesis genes can result in adverse e ects such as hemorrhage, clots in the arteries (with resultant stroke or heart attack), hypertension, and impaired wound healing.
To circumvent this, SwitchGene involves a single intravitreal delivery of the necessary gene to the back of the eye. Then, the gene is activated when required through administration of eye drops.
“Conventional gene therapy continually neutralises VEGF, thereby significantly reducing VEGF in the back of the eye. This might have some negative e ects and impact the normal capillary vessels in the retina,” Dr Liu says.
“We have to remember that VEGF is an important growth factor for maintaining vascular integrity and homeostasis in the retinal tissue as well. So, in the long term, this may also damage the retina.”
Relative to conventional gene therapies, Dr Liu says SwitchGene o ers a potentially improved safety profile.
“Our idea was to create a gene therapy that was in control. We control when we need it activated and silenced,” he says.
The therapy could also work to alleviate some healthcare burdens, with the potential for patients to self-administer the drops without the need for a specialist.
“SwitchGene can save a lot of costs because you don’t need to administer intravitreal injections once a month as is the case with existing anti-VEGF therapies. The eye drops are also a cheap formulation so it would be a ordable to patients.”
It is di cult for eye drops carrying larger drug molecules, such as anti-VEGF drugs, to penetrate the cornea for entry into the back of the eye. Therefore, existing anti-VEGF drugs require frequent intravitreal injections by a retinal specialist. Instead, Dr Liu’s team performs a single intravitreal injection that delivers the gene therapy into the back of the eye. The molecule used to activate the gene therapy – which is relatively smaller – is a good candidate for administration by eye drops.
64 INSIGHT May 2024 RESEARCH
Disease ROA Approval date (FDA) Company Development phase
Dr Rick Liu’s lab is working on SwitchGene therapy for diabetic retinopathy which selectively inhibits VEGF.
Image: Mathew Lynn/CERA.
Currently, the eye drops are e ective for two days with Dr Liu hoping to extend the e cacy for up to a week.
To advance the therapy further, Dr Liu’s team want to titrate the therapeutic via the eye drops to suit the individual’s needs. Because everyone presents with di erent degrees of disease and progression, a dose that’s e ective for one person won’t necessarily be e ective for another.
“For example, when a patient goes to see an ophthalmologist, and they’re diagnosed with very early-stage disease, the surgeon can then recommend administration of a lower dose of eye drops after the gene therapy,” Dr Liu says. “And if a patient presents with more severe disease, we’ll recommend a higher dose to induce acute activation.”
Another promising development in gene therapy is the mRNA retinal delivery method. Dr Liu’s lab is also exploring the delivery of gene editing therapy in mRNA form for treating IRDs. This approach works by using mRNA to direct the retinal cells to make a gene editing protein using its natural machinery and correct the error genetic code.
Once its corrected, there is no need for further treatment intervention. Although this gene editing technology has entered clinical trials for metabolic disorders, delivery into the retina is a challenge.
Since gene editing therapy only requires transient expression of the editing machinery in the retina, an mRNA form of the treatment makes it a viable option.
“This way, you will carry the genetic correction your entire life. You won’t need to worry how long the treatment will last and what sort of side e ects they may cause by the delivered gene,” Dr Liu says.
“The disease is essentially being cured.”
THE FUTURE IS BRIGHT FOR RNA
Associate Professor Fred Chen, of Lions Eye Institute (LEI), is developing a precision RNA therapeutic for patients with IRDs.

“I think there’s a tremendous future in this approach because many mutations causing inherited retinal diseases affect how RNA molecules are processed. Since the molecule stays in the cells for a long time, retreatment can be given over several months if not years.”
A/Prof Fred Chen Lions Eye Institute
He primarily works with antisense oligonucleotides, which are advantageous over traditional viral method delivery methods due to a lower chance of inducing an immune response.
These molecules bind to RNA as opposed to DNA, reducing the risk of genotoxicity because the molecule can’t integrate into the genome.
He says that RNA precision therapy shines an optimistic light on the future of gene therapy.
“I think there’s a tremendous future in this approach because many mutations causing inherited retinal diseases a ect how RNA molecules are processed. Since the molecule stays in the cells for a long time, retreatment can be given over several months if not years,” Dr Chen says.
“The other advantage of antisense oligonucleotides is that it can allow very fine tuning of the expression of the gene. Whereas with gene replacement therapy, we have no control over the dosage that each cell receives. The over production of certain proteins in the retina may also be detrimental.”
VP-001, an antisense oligonucleotide, has progressed to clinical trial stages













Available exclusively from OptiMed. For more information call 1300 657 720 or visit optimed.com.au MAKES YOUR PRACTICE PERFECT
TO TREAT DRY EYES AND
THE LATEST IN IPL INNOVATION SAFE | EFFECTIVE | ALL SKIN TYPES See us at the O-Show. Booth Equipment 03
TARGETED ENERGY
INFLAMMATION
Image: Fred Chen.


“We were paving the way, so that now means that there’s a pathway established of how to do this in ocular gene therapies. And that makes it easier for everybody else to come through.”
Professor John Grigg
The University of Sydney
“For example, rather than looking at visual acuity, we can look at retinal thickness, atrophy area, number of cells and cell density, and the size of blind spots,” Dr Chen says.
“Despite visual acuity being the most commonly-adopted endpoint for any eye treatment, most inherited retinal diseases patients would tell me that their visual acuity has not changed in decades and so we really cannot use that parameter as a measure of successful treatment.”
Some gene therapies have failed to receive approval, despite demonstrating clinical e cacy, due to nonsensical endpoint criteria which are not suitable for diseases that progress over decades, Dr Chen says.
“With diseases that take decades to progress, it’s not feasible to use visual acuity as an endpoint.”

and is a joint venture company between LEI and PYC Therapeutics. The therapy targets retinitis pigmentosa type 11, a monogenic, dominantly inherited, severe and progressive blinding disease.
“That product is now in Phase 1 trials in the US. Once these patients complete the trial, the FDA will examine the clinical and laboratory data to ensure that there are no safety concerns. If there are no issues, Phase 2 trial will commence shortly,” Dr Chen says.
He says regulatory hurdles are necessary to ensure safety for patients but this slows the approval process. Pre-clinical development through to market approval can take 10 to 15 years, which some of these patients do not have.
“As more of these gene therapies are commercialised and approved, the regulatory process for bringing these treatments to the clinic will become faster and easier."
He adds: "The traditional model of doing large, randomised controlled trials is not feasible for a lot of these patients simply because there aren’t enough patients to participate in these trials. There’s a steep learning curve even within the regulatory agency for adopting a di erent approach to streamline the approval process of these personalised treatments.”
Dr Chen says the biggest hurdle his lab faces is predicting and measuring disease progression. Particularly for diseases that progress slowly over decades, clinical trials may have to be conducted over many years to demonstrate e cacy.
Traditionally, when therapies come to market, there is a post-marketing surveillance program to ensure the e cacy observed in clinical trials are also replicated in the real-world. This is a dynamic process whereby the treatment’s safety and e cacy are constantly being monitored.
The aim of many of these therapies is to slow down or stop disease progression, which is di cult to quantify. The FDA usually wants to see improvements in visual acuity in ophthalmic clinical trials, which is not always a viable endpoint due to the nature of the diseases.
Dr Chen says that, as a result of the slow change in traditional endpoints such as visual acuity, there is an emphasis on implementation of surrogate biomarkers using high-resolution cellular imaging, which is a refined way to measure retinal cell integrity and ascertain the degree of disease progression in a matter of months as opposed to years.
THE DEVIL’S IN THE GENETIC DETAILS
Professor John Grigg is a clinical and experimental ophthalmology specialist at the University of Sydney and is a member of the Eye Genetics Research Unit led by Professor Robyn Jamieson at the Children’s Medical Research Institute and Save Sight Institute.
His principal role is in genotype-phenotype correlations, developing outcome measures for clinical trials and overseeing those clinical trials. He says this role is essential in mobilising the development of genetic therapies.
Additionally, Jamieson’s work – which highlights that clinical genetics underpins everything – determines whether gene replacement, editing or silencing is required. In her role as head of the Eye Genetics Research Unit, Jamieson oversees the development of new therapies, investigating inconclusive genetic results and identifying patients for clinical trials.
A key figure in the Australian gene therapy landscape, Dr Grigg along with Jamieson, Professor Matthew Simunovic and Dr Gaurav Bhardwaj, were among the team to first deliver the Luxturna therapy; the first prescription gene therapy to help improve functional vision in patients with IRD.
Luxturna – a subretinal injection used to treat patients with IRD caused by RPE65 mutations and the first genetic therapy for inherited blinding eye conditions – gained FDA approval in 2017 and TGA approval in 2020. It e ectively established the regulatory framework in Australia for future gene therapies to adhere to. Since its approval in Australia, 10 patients with mutations in RPE65 have been treated with Luxturna with another six patients being worked up for the therapy.
In the lead-up to its approval, a gene and cell therapy working group - Ocular Gene and Cell Therapies Australia (OGCTA) - comprising 16 primary members was established. The group brought clinical and molecular genetics together with ophthalmology, vitreoretinal surgery, orthoptics and nursing. The team ensured all the regulatory infrastructure was in place and that Luxturna complied with the gene regulatory agency.
“The OGCTA team, chaired by Jamieson, provides an excellent collaborative environment to bring together the clinical geneticists, molecular scientists and ophthalmologists to optimise the care for IRD patients. With Luxturna, we were paving the way, so that now means there’s a pathway established of how to do this in ocular gene therapies which makes it easier for everybody else to come through,” Dr Grigg says.
Dr Grigg says a notable challenge in administering this therapy is health equity. He says that although specialised IRD ophthalmic and genetic services exist in each state, the funding models are outdated. Since IRDs are now the most common cause of blind registrations in Australia, Dr Grigg says the IRD workforce needs genetic counselling and orthoptic and ophthalmology enhancement to ensure a ected individuals receive timely care.
“A federated disease registry process will ensure each state has their own disease registry that adheres to local governance systems and comes together to form a national dataset,” he says.
According to Dr Grigg, Australia boasts a good clinical trial and regulatory environment, which will hopefully attract the next generation of gene therapies. This provides hope to patients that they will receive the latest clinical care.
66 INSIGHT May 2024 RESEARCH
Image: Fred Chen.
Clear progression of Stargardt disease despite stability of visual acuity due to sparing of the fovea (centre point of the retina) by the atrophy (dark patches in the centre).
Image: John Grigg.

LAUNCHING JUNE 2024











Hearing Practitioner Australia is the only dedicated business-to-business publication for the nation’s hearing industry. Established out of a desire for premium, local and independent content for audiologists, audiometrists, otolaryngologists/ENTs and other Australian hearing professionals, HPA brings industry-specific reporting and analysis, in addition to the latest in news, business, products, policy, and research, plus more.








FOR MORE INFORMATION CONTACT Luke Ronca | luke.ronca@primecreative.com.au | 0402 718 081 SCAN TO SIGN UP TO THE HPA E-NEWSLETTER
Innovative Myo-freeform technology that o ers the next generation of managing childhood myopia.

Central viewing zone
Allows for clear and sharp vision for enhanced comfort, all the while sustaining a harmonious equilibrium with the treatment zone.
Peripheral treatment zone
O ers a more optimal and targeted treatment option as it takes into consideration the asymmetry of the back of the eye.*
Reading addition
Helps to relax the eyes when performing near-work tasks. The smooth transition enhances comfortability and improves compliance.
Remarkably thinner
Slim and aesthetically pleasing appearance.
hub.crlabs.au/myome-ecp
Myo-freeform technology meets myopia management
*Faria-Ribeiro, M., Queirós, A., Lopes-Ferreira, D., Jorge, J. and González-Méijome, J.M., 2013. Peripheral refraction and retinal contour in stable and progressive myopia. Optometry and Vision Science, 90(1), pp.9-15.




Optical Dispensing’s night nights
The very best of Australian optical dispensing was on display at the Melbourne Town Hall for the Optical Dispensers Australia Gala evening. Insight was there to cover some key updates and the national awards program.
The Optical Dispensers Australia (ODA) Gala headed to Melbourne in 2024 where the industry was reminded of the critical role they play in the ophthalmic ecosystem and were left inspired by South Australian eyewear designer Mr Peter Coombs whose unique pieces have featured in private collections globally, including that of Sir Elton John.
The event took place on Friday 1 March 2024 at the Melbourne Town Hall and welcomed 157 attendees for a black tie evening – held a little over two years since ODA was first established as Australia’s new peak body for the optical dispensing profession.

A feature of the gala was the ODA National Excellence Awards honouring the country’s most outstanding optical dispensers and celebrating the contribution they make to the industry and within their workplaces. This year’s recipients featured some incredible stories of selflessness (see on the following page).
Alongside this, the event included the Australasian College of Optical Dispensing (ACOD) graduation ceremony where 37 of this year’s 156 graduating cohort were present to receive their Cert IV in Optical Dispensing.
A highlight of the evening was Coombs – the guest of honour who describes himself as a designer, jeweller and metalsmith. He took attendees on a journey through his career that started in 1985 with his first pair of spectacles while studying for a Bachelor of Design at The University of South Australia, leading to a 30-year exploration of innovative methods to form and colour all sorts of precious and refractive metals into eyewear.
Acknowledging his pieces aren’t for everyone, he sees his eyewear as “jewellery for the face”; all pieces have limited availability with some one-o designs as a result of private commissions. He has even worked with Elton John since the 1980s on eyewear designs, and had his frames feature in movies, including one starring Daniel Radcli e (not for a Harry Potter movie).


As such, his eyewear has been recognised with international design awards in Japan and Australia, and has appeared in museums and private collections globally.

Also among the keynote speakers were Mr Adam Fletcher who recalled the journey from working in his father’s lens lab during school holidays to now running that business – CR Labs – considered one of, if not the, leading independent optical lens manufacturer in Australia. Attendees also heard from Dr Ben Ashby, clinical services director at Specsavers ANZ, who reiterated the vital contributions of optical dispensers now and into the future, especially with the rise of myopia management.
ODA CEO Ms April Petrusma echoed these sentiments in her address where she outlined the work ODA was doing to raise the profile of the industry through online professional development, in-person events and advocacy. This included ODA partnering with Optometry WA to incorporate a dispensing stream at the WAVE Conference for the first time in March 2024, and an aid trip in July where 12 ODA members will
INSIGHT May 2024 69 EVENT
Prime Creative Media.
Images:
Peter Coombs explaining the eyewear he designed worn by actor Daniel Radcliffe in a movie.
ODA CEO April Petrusma addressing the 157 gala attendees.
ODA NATIONAL EXCELLENCE AWARDS
2024 RECIPIENTS
Rookie of the Year – Astrid O’Connor from Quinn and Co. Eyecare in Horsham, Victoria
O’Connor has made a remarkable impact on her team in the short time she has been part of it, taking on many responsibilities in the practice well beyond the call of duty while excelling in her Cert IV studies with ACOD. Despite her workload, she continues to exceed expectations in the primary roles of dispensing, administration, and reception duties. Her presence fosters a sense of camaraderie and warmth, contributing to a supportive and uplifting workplace atmosphere for all.
CEO’s Member Dedication Award – Raymond Moses from RM Optical Dispensary in Merrylands, NSW
Moses takes pride in his role as an optical dispenser and professional development. He is a wonderful advocate for continuing education and is constantly striving to better himself by seeking new knowledge and engaging in learning opportunities. Even as a business owner, it is not unusual to see him at one of ODA’s CPD events and in 2023 he was a recipient of an ODA Currency Certificate for achieving 10 ODA CPD points for the year.


Outstanding Practice Owner Award – Lucija Valentic from Base Curve Optical in Sandringham, Victoria Valentic has been an optical dispenser for 15 years, and is a small business owner that prioritises integrity and accountability in delivering what she promises to clients. She shows respect when dealing with patients and embodies the core characteristics of the ultimate professional. Valentic demonstrates a high level of competence and knowledge in optical dispensing and eyecare, is conscientiousness in running her business, and continues to upskill through training and development opportunities.
Role Model & Leadership Award – Kayla White from Quinn and Co. Eyecare in Horsham, Victoria


White is a qualified optical dispenser that has been recognised by her workplace to have such exceptional skills that a specialised role has been created for her to travel to other practices and provide training to both new and experienced dispensers. Her wealth of experience and dedication to sharing knowledge benefits her team members across all locations. Recently, White spent several hours collaborating with other healthcare professionals to identify the most effective ways to assist and support patients who do not speak English, exemplifying her dedication to inclusive care. She has motivated optical assistants to pursue the optical dispensing course by sharing the valuable skills and knowledge she has acquired through her own experience.
Community Champion Award – Brett Willis from Friendlies Eyecare in Claremont Western Australia




This special award recognises the acts of someone that has gone above and beyond their call of duty. Willis is a practice owner that has been training for a 700 km ride with a charity called Ride for Youth. The charity raises funds for youth mental health and suicide support. The ride took place over four days beginning 19 March. To add to this, Willis is known for acts of selflessness. Not too long ago he assisted someone who urgently needed replacement spectacles, by making a last minute dash to the international airport to make the delivery moments before they boarded the plane.
ODA National Medal for Optical Dispensing Excellence – Joshua Oronce-Simpson from Spex in the City Eyewear & Cooper and Lourie East Victoria Park, Western Australia
Oronce-Simpson, the winner of this prestigious award, not only works full time as a qualified optical dispenser in practice but also owns his own mobile optical dispensing business. He shows professionalism by respecting others whether it be colleagues or patients and displays a strong work ethic being diligent, dedicated, and focused on his responsibilities. He has a drive for exceeding patient expectations that is supported by his ongoing search for new personal development opportunities. He takes every opportunity to attend CPD events, ranging from international and local trade fairs to ODA webinars and workshops.

TOP: Attendees were entertained thanks to a wide variety of speakers, awards and the ACOD graduation ceremony.
ABOVE: ODA National Excellence Awards recipients who were present to accept their awards were (from left) Lucija Valentic (Outstanding Practice Owner Award), Astrid O’Connor (Rookie of the Year), Joshua Oronce-Simpson (ODA National Medal for Optical Dispensing Excellence) and Kayla White (Role Model & Leadership Award), with ODA CEO April Petrusma (back right).
provide vision screening, eye education, optical dispensing and spectacle servicing to isolated villages and communities within the Fiji islands.
“ODA is here to provide opportunities to network, grow and develop at any stage of your career,” she said.
“There really is no greater gift than sight and as an optical dispenser, you personally play a role in the visual outcomes of every single person you serve inside or outside of your workplace.
“Your skills and abilities should never be undervalued as even the smallest action can change someone’s life. You are not just another cog in the wheel in the business in which you work, you have a super-power and provide something very special with your vast skill set and immense amount of knowledge.”
70 INSIGHT May 2024 EVENT


































See more, know more with more Insight Subscribe FREE and receive the latest news Insight is mobile and tablet friendly Find jobs and advance your career with Insight’s Classifieds Get to know the newest products from suppliers across Australia Insight’s new website keeps you updated on the latest industry news and information. With a world-class responsive design, Insight is now accessible seamlessly on any device, 24/7. Sign-up FREE to our eNewsletters and industry reports delivered weekly straight to your inbox. www.insightnews.com.au
‘MEET THEM WHERE THEY ARE AT’
Creating diversity in the way one interacts with patients can be one of the sharpest tools in the optical dispenser's kit, creating satisfied and lifelong patients, writes

CUES THAT YOU USE TO FLAG A SENSORY NEED, AND DO YOU KNOW HOW YOU COULD DIVERSIFY YOUR SERVICE TO ACCOMMODATE THIS?”
FSARAH THOMPSON

ew would doubt the significance of optical dispensers within a practice. As I have moved through my years of dispensing, I’ve experienced various demographics, products, patients, and colleagues who all operate on di erent levels and in their own ways. Which brings me to the focus of this column: diversity within our practice. One of my mentors for the past four years talks about the importance of ‘meeting people where they are at’. This relates to every individual who walks through the door regardless of their status or background. It encompasses what you o er, how you o er it, and your relationship and retention of that patient. The way optical dispensers work in one practice will be di erent to the next given the values and business goals unique to each store. But the way in which we target our patients, and ‘meet them where they are at’ is essential. No one wants to feel like a transaction, and we must remember that because we dispense eyewear all day long, it doesn’t mean the patient is going to understand the terminology we use with our colleagues. Our product knowledge is essential, but so is the ability to explain it in di erent ways. Some people are going to want to know all about it, while others won’t care for it as much. Everyone is going to have their own needs, their own story, and it’s on us to put it all together. But how do you create diversity within the practice? Well, diversify your customer service.
There are a lot of ‘people skills’ and empathy required for those you are dispensing to. We must consider more than just someone’s refractive needs before we start showing them frames. Be it an aged pensioner with a small budget in mind who needs a new frame and progressive lenses, or a professional in the peak of their career who wants cutting-edge technology in lenses with a high-end frame. The way you engage with each of these patients is going to be di erent, but also the same. For example, you spend the same amount of time and e ort into your dispense with both cases, regardless of how much money you take from them. You also
make both feel good about the frames they choose and understand the lenses you’re recommending.
What’s di erent is the lens design you o er and the frames you suggest which is all price based. Maybe you leave the anti-reflection coating o the older persons glasses despite your KPI, or what you believe to be better. Catering for your demographic is what’s important because you are respecting their needs. We have a huge impact on quality-of-life when it comes to enabling our customers to see the world around them, we must achieve this within their means.
People’s personality types will determine the way in which you dispense; the frames, the way you engage with them and even the way you take your measurements. Society has come a long way with neurodiversity for example. What are the cues that you use to flag a sensory need, and do you know how you could diversify your service to accommodate this? Thinking on your feet and outside the box is your biggest saviour here. If we are meeting these people on their level, you are going to deliver a service that resonates with them, which makes the process more enjoyable, memorable and is more likely to create better retention. Maybe you don’t use your whizzbang measuring tool and revert to old school marking
up, or even take them into a quiet space or outside while they can process their options. What about cultural di erences? Are you aware of any marketing material for those with culturally and linguistically diverse (CALD) backgrounds? Are you aware of di erent cultures most prevalent in your area and the most respectful way to engage with them? Location. It goes without saying country living is vastly di erent to city life, and so are the people you’re typically looking after. Their mannerisms, the way they engage with you, their values and what is important to them is going to di er. Not to mention access to di erent services and, for example, where the nearest ophthalmologist is. Understanding this as a factor is going to help you show empathy and build rapport.Optical dispensers are essential to any optometry business, so it’s vital to diversify our skills and abilities to create a client-centred approach. While diversity is a huge topic and I’ve just touched the surface, if only you consider how to ‘meet people where they are at’ in a better way, we are on the road to improving our service as optical dispensers.
ABOUT THE AUTHOR: Sarah Thompson is the practice manager at Wills Street Eyecare, advisory board member of Optical Dispensers Australia as of 2024 and assessor for the Australasian College of optical Dispensing.
72 INSIGHT May 2024 OPTICAL DISPENSING
Sarah Thompson is the practice manager at Wills Street Eyecare in Bendigo, Victoria.
Images: Sarah Thompson.

ORTHOPTICLED CLINICS IN PRIVATE PRACTICE
Orthoptist RAFAL AL-QASEER describes how collaboration with ophthalmologists in orthoptic-led clinics ensures the best patient outcomes.

"OVERALL, ORTHOPTICLED CLINICS ELEVATE THE STANDARD OF CARE AND EMPHASISE PRECISION, COLLABORATION, AND PATIENTCEN TREDNESS IN THE FIELD OF EYE HEALTH.”
Igraduated from the Master of Orthoptics course at the University of Technology Sydney (UTS) in 2020, and have since been working across all three Marsden Eye Specialists locations (Castle Hill, Parramatta and Penrith).
At Marsden Eye Specialists, various orthoptic-led clinics provide specialised care to our patients including paediatric and strabismic, myopia control, dry eye, keratoconus progression monitoring, and refractive screening. Currently, I oversee the paediatric and strabismic clinic, as well as the myopia control clinic under the guidance of Dr Ross Fitzsimons, an expert in strabismus and refractive surgery. In private practices, time constraints often hinder the ability to conduct thorough orthoptic examinations. This is where orthoptic-led clinics prove invaluable. The clinics’ role extend beyond routine assessments and – in collaboration with ophthalmologists – involve a nuanced approach to identifying and managing vision disorders with precision.
Consider a scenario where a patient reports intermittent diplopia with prior visits to di erent practices yielding no diagnosis. A standard examination reveals a 2-dioptre esophoria. In our orthoptic clinic, prolonged occlusion and prism adaptation tests, which take up to 1.5 hours, reveal an undetected 32-dioptre esotropia. Similarly, a patient with vertical diplopia finds no relief from prisms. However, a detailed orthoptic exam using the synoptophore reveals that the main issue is subjective torsion in down gaze, hence prisms will not help. Such cases underscore the crucial role of orthoptic-led clinics in uncovering latent issues. The results also guide surgeons towards e ective treatments and surpass the limitations of conventional examinations. Orthoptists also play a crucial role in paediatric eye health. Children diagnosed with amblyopia at Marsden Eye Specialists are referred to our orthoptic clinic for tailored management, ensuring seamless collaboration with referring ophthalmologists. The same happens with the myopia control clinic, where patients are referred to the orthoptic clinic to closely monitor their results while they are on low dose atropine or other treatments.
Orthoptic-led clinics provide comprehensive care across various eye conditions.

Conducting orthoptic assessments for paediatric patients demands clinicians with exceptional communication and counselling skills. These capabilities are pivotal in establishing a rapport with both the young patients and their families. Through e ective communication, orthoptists can provide precise information that reassures families and provides the best possible outcome for the patient.
In our refractive orthoptic-led clinic, orthoptists conduct comprehensive 60-minute assessments – including contact lens trials where suitable – to determine the best outcomes for our patients. Given the complexity of these cases, a brief 10- or 15-minute consultation may not cover all necessary aspects. Therefore, multiple visits are often required to explore di erent options, such as monovision, to ensure a tailored and e ective approach to vision correction.
The dry eye clinic involves detailed testing which identifies the cause and type of dry eyes. The orthoptist then prescribes a home management regime and performs appropriate in clinic treatments.
Similarly, in our keratoconus progression monitoring clinic, patients undergo corneal topography and refractive assessments, with ophthalmologists reviewing the findings to inform ongoing care plans. This clinic also encompasses collagen cross-linking procedures which heavily involve the orthoptist.
The implementation of orthoptic-led

clinics within private practice settings – exemplified by the comprehensive approach at Marsden Eye Specialists –represents a significant advancement in eyecare. These specialised clinics address the limitations of time-constrained conventional examinations. Through the employment of thorough assessments and specialised tests, orthoptists can collaborate closely with ophthalmologists to uncover latent issues and provide nuanced management strategies. The role of orthoptists extends beyond clinical duties to include patient education and support to ensures individuals understand their conditions and treatment options. Through their dedication and expertise, orthoptists contribute significantly to improving patient outcomes and enhancing the quality of eyecare services in private practice and hospital settings. Overall, orthoptic-led clinics elevate the standard of care and emphasise precision, collaboration, and patient-centredness in the field of eye health.
ABOUT THE AUTHOR: Rafal Al-Qaseer graduated from UTS with a Master of Orthoptics in 2020. She has paediatric and strabismic special interests and practises at Marsden Eye Specialists in Sydney.
ORTHOPTICS AUSTRALIA is the national peak body representing orthoptists in Australia. OA’s Vision is to support orthoptists to provide excellence and equity in eye health care. Visit: orthoptics.org.au
INSIGHT May 2024 73
RAFAL ALQASEER
Images: Rafal Al-Qaseer.
MAKE MEETINGS GREAT AGAIN
KAREN CROUCH’S firm was once asked to sit in on a practice’s meetings and offer guidance on how staff can extract more from these interactions. Here’s what she found.

While meetings are often loathed for being time-consuming and unproductive, executing them well is pivotal for collaboration and organisational success. And there are many techniques to ensure meetings – not just one-on-one meetings but formal o ce forums – bring value to the practice.
"WHERE AN ITEM WARRANTS IT, PREREADING AFFORDS ATTENDEES AN OPPORTUNITY TO PREPARE AND CONTRIBUTE MORE MEANINGFULLY.”
E ective communication is essential to developing a well-coordinated, team-focused environment. Conducting e ective meetings – whether for educational or practice management purposes or general team building – is a key to maximise the e ective communication e ort.
Practices sometimes pride themselves on strong interpersonal communication based on the number of meetings. However, upon closer inspection, it’s clear they often lack the more important factors – quality and results.
Our firm was once requested to assess the e ectiveness of a particular practice’s meetings to enrich the quality and ‘achievement value’ of these gatherings, improving decision making, and promulgating meeting resolutions including enactment of the decisions. Practice meetings were conducted between various job families: administration, clinicians and principals. Most felt the level of communication within the practice was high. However, most interviewees agreed that decisions were not always clear, or communicated e ectively despite ample debate about the issues in point. This resulted in poor implementation of meeting resolutions. With sta cooperation and input, we

defined the following attributes of an e ective meeting:
• Ensure a planned ‘agenda’ to impart a clear understanding of subject matter and target outcomes
• Improve communication and decision making
• Exchange experiences, information and knowledge between participants
• ‘Work smarter’ (research) forums
• Implement decisions e ectively including post-implementation reviews to assess success
• Complement and potentially improve corporate governance.
Some meetings for social purposes –such as Christmas party planning – were conducted on an informal basis, mainly for o ce planning purposes and for business/relationship development e orts. Generally, content was less structured, albeit well planned beforehand. Such gatherings were obviously more relaxed and did not require much structuring or deeper review.
We asked meeting groups the following questions, based on the general principles of e ective meetings:
• Do meetings have a pre-circulated agenda? – this indicates a purpose for the meeting and provides participants with subject matter they may investigate for debate or presentment
• Is a chair or leader appointed? –evidence there will be a ‘controller’ to focus attendees on agenda items under discussion, assign actions to specific individuals where necessary, and ‘watch the clock’ so items are not left undecided.
The importance of formally deferring items (developing a ‘Deferred Items’ list) that may not have been discussed due to time delays or excessive discussion was highlighted to ensure they are carried forward to the next meeting
• Are desired outcomes or decision options understood? – where applicable, this ensures participants are aware a decision is required for certain discussion items and sta should be prepared to voice personal views on various topics
• Are meetings properly ‘time planned’?
– this suggests thought has been given to adequacy of time required to do
justice to each topic by ‘guesstimating’ approximate amount of time required to do address each agenda item
• Is relevant pre-reading circulated? –where an item warrants it, pre-reading a ords attendees an opportunity to prepare and contribute more meaningfully, also evidencing thoroughness of the meeting coordinator
• Are self-assessment ‘meeting evaluations’ conducted? – means by which teams strive to improve meeting quality and outcomes, such as valuable ‘feedback’ for the chair or meeting leader;
• Are minutes (including agreed resolutions) and ‘Action Items’ documented and distributed? – this provides continuity and implementation of resolutions when minutes are tabled at subsequent meetings. Of course, such minutes should be reviewed and accepted by the meeting leader to ensure they are an accurate reflection of the group’s discussions. Matters that may have been discussed casually, and even agreed, after the meeting should not be recorded in minutes but held over for the agenda of the next formal meeting. Sta , clinicians and principals found the exercise beneficial, injecting meaningful structure and achievement-oriented content into meetings, without introducing excessive bureaucracy. As an aside, we also suggested occasional (not just customary annual) rotation of meeting leaders to spread valuable experience. While meetings are a useful form of communication, decision making and planning, the other extreme is too many meetings; meetings for the sake of meetings (refer the infamous John Cleese skit, ‘Meetings, meetings, bloody meetings”). A decision that could be made easily by circulated email might only require a meeting if parties involved cannot reach agreement on a proposal or the matter is su ciently important to deserve holding a formal meeting.
ABOUT THE AUTHOR: Karen Crouch is managing director of Health Practice Creations Group, a company that assists with practice set ups, administrative, legal and financial management of practices. Contact her on 0433 233 478, kcrouch@hpcnsw.com.au or visit, www.hpcgroup.com.au.
74 INSIGHT May 2024 MANAGEMENT
KAREN CROUCH
BELOW: It’s quality and results of meetings, rather than the number of meetings, that ultimately counts, says Karen Crouch.
Image: Karen Crouch.
Image: Jacob Lund/Shutterstock.com.
SOAPBOX
COULD OUR SPIRAL LENS REVOLUTIONISE OPTICS?
 BY LAURENT GALINIER
BY LAURENT GALINIER
Progressive spectacle lenses, di ractive intraocular lenses and multifocal contact lenses are the standard methods for many people to see at di erent focal points as they go about their day, but what if a whole new spiral lens concept could negate the shortcomings in these designs?
The ‘spiral diopter’ lens is a cross-discipline innovation involving myself, founder and director of Spiral SAS, and Dr Bertrand Simon and his team at the Photonics, Numerical and Nanosciences Laboratory (LP2N), a joint research unit between the Institut d’Optique Graduate School, the University of Bordeaux and the CNRS in France.
The spiral design essentially causes light to spin, like water going down a drain. This phenomenon – known as an optical vortex – creates multiple clear focus points, which allow the lens to provide clear focus at di erent distances. Optical vortices have the ability to “autofocus” depending on their spinning amplitude. Our lens also incorporates the elements necessary to make an optical vortex directly into its surface; this is a thriving field of research, but our method simplifies the process, marking a significant advancement in the field of optics.
Crucially, unlike existing multifocal lens designs, our lens performs well under a wide range of light conditions and maintains multifocality regardless
of the size of the pupil. The main drawback of multifocal or progressive lenses is that the optical power is distributed according to particular zones of the optical surface (for example, in concentric zones for multifocal contact lenses). Consequently, the opening or closing of the iris means that not all zones are necessarily involved in a loss of multifocality.
With our lens, the distribution takes place over the entire surface, thanks to spiralisation. For potential implant users or people with age-related farsightedness, we believe it could provide consistently clear vision, potentially revolutionising ophthalmology.

The spiral lenses are manufactured by reshaping the surface of a polymer to create the spiral optical vortex design. This process involves a numerical lathe and a precise manipulation of the material to generate the desired optical properties that allow for multi-focusing capabilities and continuous clear vision. We recently described this work in the journal Optica. The lens was validated by using it to image a digital ‘E’, much like those used on an optometrist’s light-up board. The image quality remained satisfactory regardless of the aperture size used. We also discovered that the optical vortices could be modified by adjusting the topological charge, which is essentially the number of windings around the optical axis.
So far, studies to validate the performance of the spiral lenses have shown promising results in early volunteer trials. Volunteers experienced noticeable improvements in visual acuity at various distances and lighting conditions. We are now working to better understand the unique optical vortices produced by the lens. We then plan to perform systematic trials of the lens’ ability to correct vision in people to comprehensively establish its performance and advantages in real-world conditions. Further research is ongoing to explore the potential applications in correcting accommodation defects, myopia, hypermetropia, and potentially
addressing other ocular aberrations like astigmatism.
In addition, we are exploring applying the concept to prescription spectacles.
All in all, we believe our new lens could significantly improve people’s depth of vision under changing lighting conditions. Further into the future, this technology might also lead to advancements in wearable devices and remote sensing systems for drones or self-driving cars, which could make them more reliable and e cient.
There’s also potential in compact imaging technologies. It could streamline the design and function of these systems while o ering a way to accomplish imaging at various depths without additional optical elements. These capabilities, coupled with the lens’ multifocal properties, o er a powerful tool for depth perception in advanced imaging applications.
Name: Laurent Galinier
Affiliations: Spiral SAS
Location: Caen, France
Years in optical industry: 35
CRUCIALLY, UNLIKE EXISTING MULTIFOCAL LENS DESIGNS, OUR LENS PERFORMS WELL UNDER A WIDE RANGE OF LIGHT CONDITIONS.
INSIGHT May 2024 75
By harnessing the phenomenon of optical vortex, this creates multiple clear focus points Images: LP2N.
CALENDAR EVENTS
To list an event in our calendar email: myles.hume@primecreative.com.au

MAY 2024
SQUINT CLUB MEETING 2024
Melbourne, Australia
3 – 4 May ranzco.edu/events
ARVO 2024
Washington, US 5 – 9 May arvo.org
OSHOW24
Sydney, Australia 17 – 18 May o-show.com.au
SUPER SUNDAY 2024
Sydney, Australia
19 May (immediately after OSHOW24) vision@oaansw.com.au
JUNE 2024
AUSTRALIAN SOCIETY OF OPHTHALMOLOGISTS EXPO 2024
Sydney, Australia
1 – 2 June asoeye.org
THE ART OF OCULAR IMAGING (AOI) CONFERENCE 2024
Sydney, Australia 8 – 9 June artofocularimaging.com.au
GENEYE 2024
Melbourne, Australia 19 – 21 June geneye.org.au
JULY 2024
NORTH QUEENSLAND VISION CONFERENCE 2024
Cairns, Australia 6 – 7 July optometryqldnt.org.au/nqv
AUSCRS 2024
Hamilton Island, Australia 24 – 27 July auscrs.org.au
AUGUST
2024
EUROSCOLE AUSTRALIA
Melbourne, Australia 3 – 4 August euroscole.com
OPHTHALMOLOGY UPDATES!
Sydney, Australia 24 – 25 August ophthalmologyupdates.com

PROVISION NATIONAL CONFERENCE Perth, Australia 30 August – 1 September icmsmeetings.eventsair.com/provision-2024
SEPTEMBER 2024
SPECSAVERS CLINICAL CONFERENCE (SCC) 2024
Gold Coast, Australia 14 – 15 September specsaversclinicalconference.com.au
NOVEMBER 2024
RANZCO CONGRESS 2024
Adelaide, Australia 1 – 4 November ranzco2024.com

76 INSIGHT May 2024
returning bigger
2024, including a line up of interstate and international speakers. Image: Specsavers. Image: Ophthalmology Updates! Image: ProVision. Independent optometry network ProVision is taking its biennial national event to Perth in 2024.
The Specsavers Clinical Conference is being held on the Gold Coast in September 2024. Ophthalmology
Updates! is
in
CHANGING LIVES THROUGH
BETTER SIGHT AND HEARING

Years within the business: 6 (3 as an optometrist)
SPECSAVERS STORIES: ISHMEEN
WHY DID YOU PURSUE AN OPTOMETRY CAREER?
Optometry seemed appealing as it would allow me to study anatomy and optics while also contributing towards a healthcare career post my studies. The more practicals we did in the five-year degree at University of Auckland, the more I enjoyed honing my skills and I looked forward to one day doing it out in the community where I could make a di erence.
HOW DID YOU COME TO WORK AT SPECSAVERS?
I joined Specsavers as an optical assistant in 2017 where I worked part time in Auckland and studied optometry full time. I graduated in 2020 and continued working with Specsavers as I knew it was the perfect fit for me. I was familiar with the model and I knew I could contribute my skills to the community on a larger scale with the help of a strong and supportive team.
WHAT WAS YOUR FIRST ROLE WITHIN THE BUSINESS?
I started at Specsavers Dunedin as a graduate optometrist. I slowly built my skillset of knowledge and expertise in community optometry by seeing multiple patients daily and managing varying pathologies.
WHAT GROWTH OPPORTUNITIES HAVE PRESENTED THEMSELVES?
Since then, I’ve present remotely online in multiple guest lectures to optometry students and new graduates in New Zealand, as well as for nurses studying optometry in Papua New Guinea. I completed a project as part of my two-year graduate program that would improve the visual field test performances in our store as well as encouraging ongoing learning among team members.
Specsavers
LET’S TALK!
In a few short years, Specsavers has achieved market leadership in Australia and New Zealand with more people choosing to have their eyes tested and buy their prescription eyewear from Specsavers than any other optometrist. To learn more about these roles, or to put your hand up for other roles as they emerge, please contact us today:
Joint Venture Partnership opportunities enquiries: Carly Parkinsonon +61 (0) 478 201 057 or carly.parkinson@specsavers.com
Australia employment enquiries: Marie Stewart – Recruitment Consultant marie.stewart@specsavers.com or 0408 084 134
Locum employment enquiries: Matthew Cooney matthew.cooney@specsavers.com or 0447 276 483
New Zealand employment enquiries: Chris Rickard –Recruitment Consultant chris.rickard@specsavers.com or 0275 795 499
Graduate employment enquiries: apac.graduateteam@specsavers.com
I joined the Early Career Optometrists Program in my third year which has encouraged me to continue my development and, by doing so, I participated in outreach work with The Fred Hollows Foundation in 2023. The ECO group has also launched CPD events, extra allowance to take further educational courses and webinars on financial literacy which has been useful.
CAN YOU OUTLINE YOUR TOP CAREER HIGHLIGHTS SINCE JOINING SPECSAVERS?
My top highlight would be spending 1.5 weeks in Fiji training nurses to improve their refraction skills and community screening with Fred Hollows in August 2023. I was grateful to share my skills and knowledge of optometry. I got the chance to interact with nurses and patients from di erent backgrounds which highlighted the barriers of access in rural healthcare. Some challenges included language and equipment barriers. I enjoyed embracing these issues because it got me out of my comfort zone and helped improve my skills in areas I would not have done so usually in my day-to-day practise. It was my first time in Fiji, so I loved learning about a new culture and being in a new environment applying my skills. I would love to partner with the foundation again in future to continue learning and contributing more to these communities.
WHAT EXCITES YOU MOST ABOUT TURNING UP FOR WORK EACH DAY?
The great team I work with and interacting with new people from di erent walks of life. I feel better about my day knowing I have been able to help improve their sight or help solve any issues they have related to my expertise.
ALL SPECSAVERS STORES NOW WITH OCT
Optometrist Joint Venture Partnership Opportunity – Swan Hill, VIC
We are currently on the lookout for expressions of interest for an Optometrist to join Specsavers as a Joint Venture Partner in our brand-new store opening in Swan Hill, Victoria.
Swan Hill is a vibrant city in Victoria’s northwest that blends regional charm with urban convenience. Situated along the picturesque Murray River, the city boasts stunning riverfront views, fresh produce, and a warm climate. With an array of outdoor recreational activities, cultural attractions, and a welcoming community – Swan Hill has something to o er everyone!
$20k bonus to refer a friend to join Specsavers in regional QLD!
Specsavers are expanding our Optometry team in QLD’s far north. Home to rainforests, beaches, markets and a vast array of great cafes, bars and restaurants along with access to the Great Barrier Reef, there is something to suit everyone. If you think Specsavers is a great place to work and you know someone who believes in providing best value eye care, exceeding customer’s expectations and who would like to be part of our mission to change lives through better sight then you could earn up to $20k by simply providing a name.
Optometrist opportunity – Specsavers Dunedin, NZ
Seeking two optometrists to join our extraordinary team at Specsavers Dunedin, our Specsavers’ store of the year in NZ. O ering cutting-edge technology, a friendly environment, and a commitment to professional growth. Embrace the breathtaking beauty of the region and enjoy a perfect work-life balance. Don’t miss this incredible optometrist opportunity to go with a friend and be part of Specsavers.
Graduate Opportunities
The Specsavers ‘Early Bird Package’ which o ers our highest sign on bonus yet is now live! For select opportunities across ANZ, final year optometry students will be eligible for a $30,000 sign on bonus when they sign an employment contract before June 30 2024.
At Specsavers you will have access to cutting edge technology, and be part of the driving force bringing Optometry into the forefront of the healthcare industry.
Regional Locum Opportunities
Are you an experienced optometrist looking for an exciting opportunity? From September onwards Specsavers Darwin, NT are seeking dedicated locum optometrist. Whether you’re seeking short-term assignments or longer-term placements, we have flexible locum opportunities to suit your schedule and preferences. We o er competitive rates along with flights, car hire and accommodation ensuring that your skills and expertise are valued and rewarded.
YOUR CAREER, NO LIMITS Visit spectrum-anz.com
DHALIWAL
People on e move


myself and my patients. I will continue my public VMO (visiting medical officer) positions at Westmead Children's Hospital and Bankstown Hospital and continue my education/research roles at Macquarie University and the University of Canberra,” she said. Rose was previously an Associate at PersonalEYES. She ceased working at the Canberra clinic in December and Burwood and City clinics most recently.

FRED HOLLOWS ESTABLISHES TOWNSVILLE
The Fred Hollows Foundation has welcomed Country Director Vincent Bin Dol, a proud Torres Strait Islander, to take the helm of its Indigenous Australia Program. government and in non-government organisations with a career spanning 31 years working with Aboriginal and Torres Strait Islander Peoples.
“My approach to working with Aboriginal and Torres Strait Islander communities is through co-design, and having genuine conversations so we get it right the first time. Only then can we design capacity strengthening models that improve the eye health needs of our Aboriginal and Torres Strait Islander community,” he said.

Tanya Morris has been appointed as the Program Manager for the Fred Hollows Foundation Indigenous Australia Program. She is a proud descendant of the Bar-Barrum people from the Atherton Tablelands
“With a background in nursing and more extensively in public health, I have channelled my passion into addressing the health disparities prevalent in rural and remote areas, particularly among Indigenous populations. I recognise the disparities and barriers that exist in accessing quality healthcare, particularly for our Aboriginal and Torres Strait

Fiona Muller has joined CR Labs as the newest
With more than a decade of experience in optics and in optical retail in both the corporate and independent space, she offers a wealth of industry knowledge and insight for CR’s partners.
In her spare time, Muller pursues photography and is a fan of both rugby union and league. “We’re excited to have Fiona as part of our growing team,” CR said.
 Ms
Ms
DO YOU HAVE CAREER NEWS TO SHARE? Email editor Myles Hume at myles.hume@primecreative.com.au to be featured CAREER Image: HOYA. Image: Fred
Foundation. Image:
Hollows
Dr Loren Rose. Image: Fred
Hollows Foundation.
Image: CR Labs. Image:
78 INSIGHT May 2024
WCO.
INSIGHT'S MONTHLY BULLETIN TO KEEP THE AUSTRALIAN OPHTHALMIC SECTOR UPDATED ON NEW APPOINTMENTS AND PERSONNEL CHANGES, NATIONALLY AND GLOBALLY.


A perfect fit1 for your patient’s ablation profile

Just like the most refined haute couture, each wavelight plus procedure is fully tailored.1
InnovEyes™ Sightmap measures the unique optical system using biometry, tomography and wavefront.2
Innovative ray tracing methods create a personalised 3D model of the eye,1 used to plan a truly unique treatment with excellent visual outcomes.*3






The next generation in Refractive Surgery.
*3 months post-op; n=212 eyes.

References: 1. Mrochen M, Bueler M, Donitzky C, Seiler T. Optical ray tracing for the calculation of optimized corneal ablation profiles in refractive treatment planning. J Refract Surg. 2008;24:S446-S451. 2. InnovEyes Sightmap Diagnostic Device User Manual 1089. 3. Alcon data on file, 2021. RFP911-P001 Postmarket Study of Outcomes from WaveLight EX500 InnovEyes – V-RIM-0063613. For indications, contraindications and warnings please refer to the relevant product’s instruction for use. WaveLight Plus is the alternative equivalent trade name for INNOVEYE treatments. © 2023 Alcon Laboratories Pty Ltd. AUS: 1800 224 153; Auckland NZ: 0800 101 106. ALC2054f. 12/23 ANZ-IVE-2300002.


CHOOSE TO SPECIALISE IN THE FIELD YOU LOVE
Join the home of some of the best optometrists in the business. With our experience and support, we offer the freedom to practice full-scope optometry or choose a specific area of interest.
Accelerate your career aspirations with OPSM. Visit opsm.com.au/careers today.







































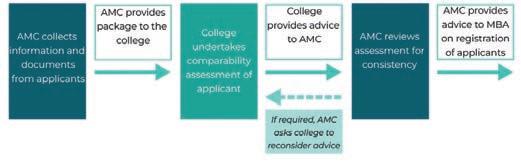







 The program will start by recognising glaucoma management expertise. Image: rh2010/stock. adobe.com.
The program will start by recognising glaucoma management expertise. Image: rh2010/stock. adobe.com.































































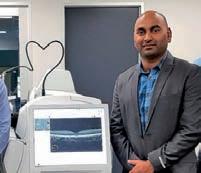

















































































































































































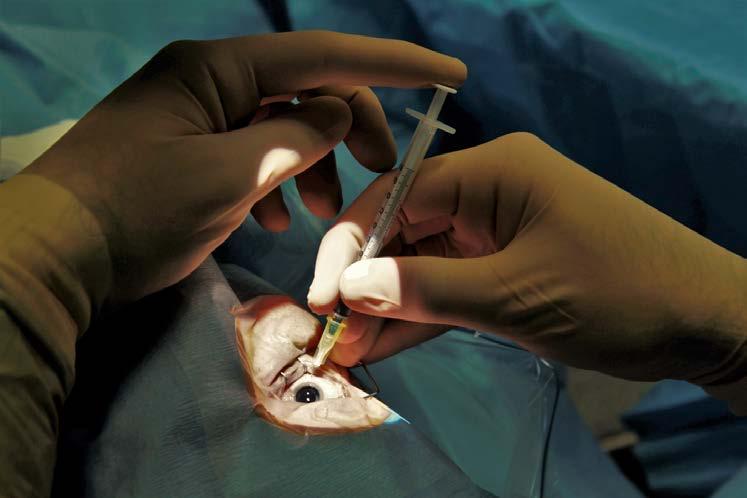





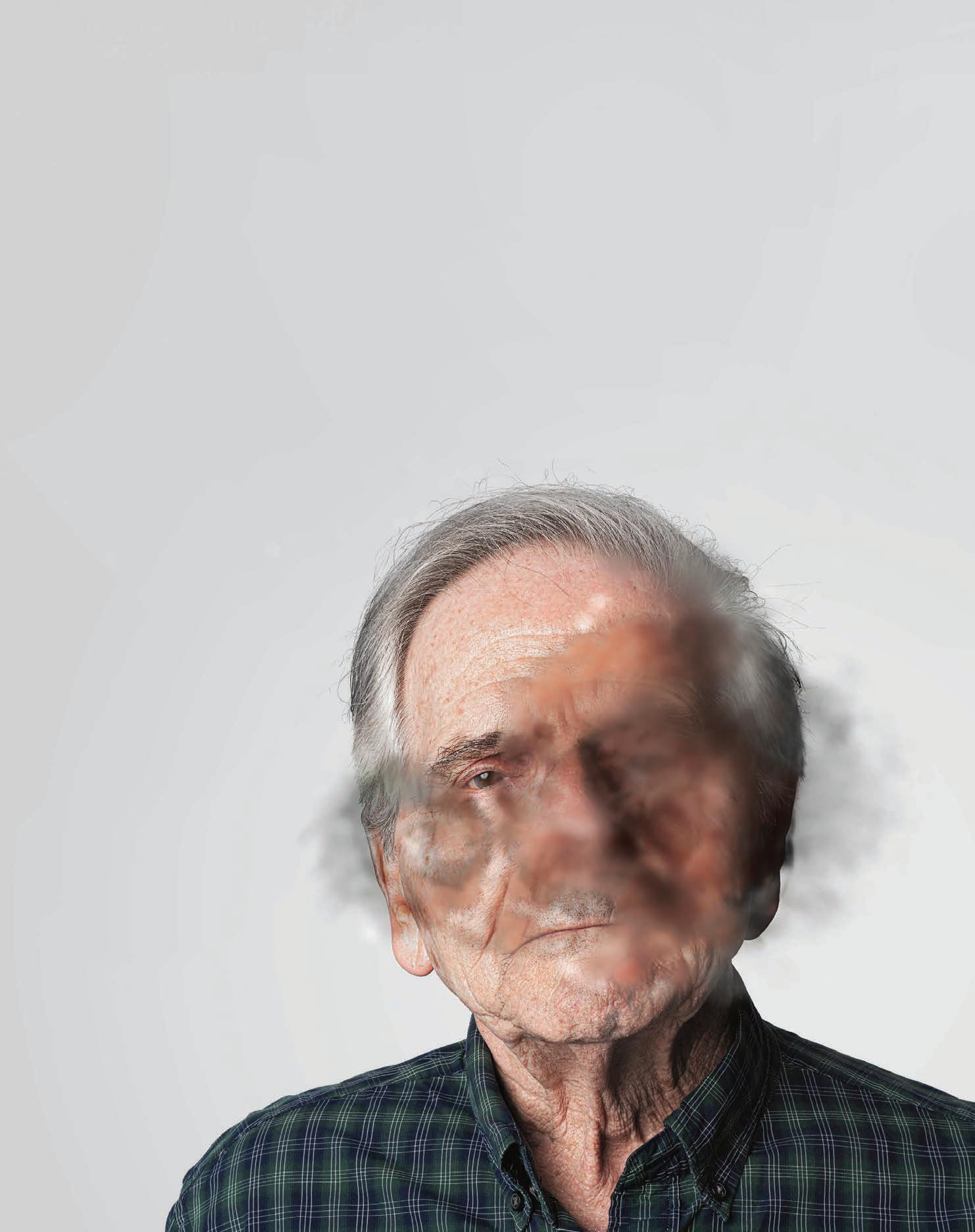
























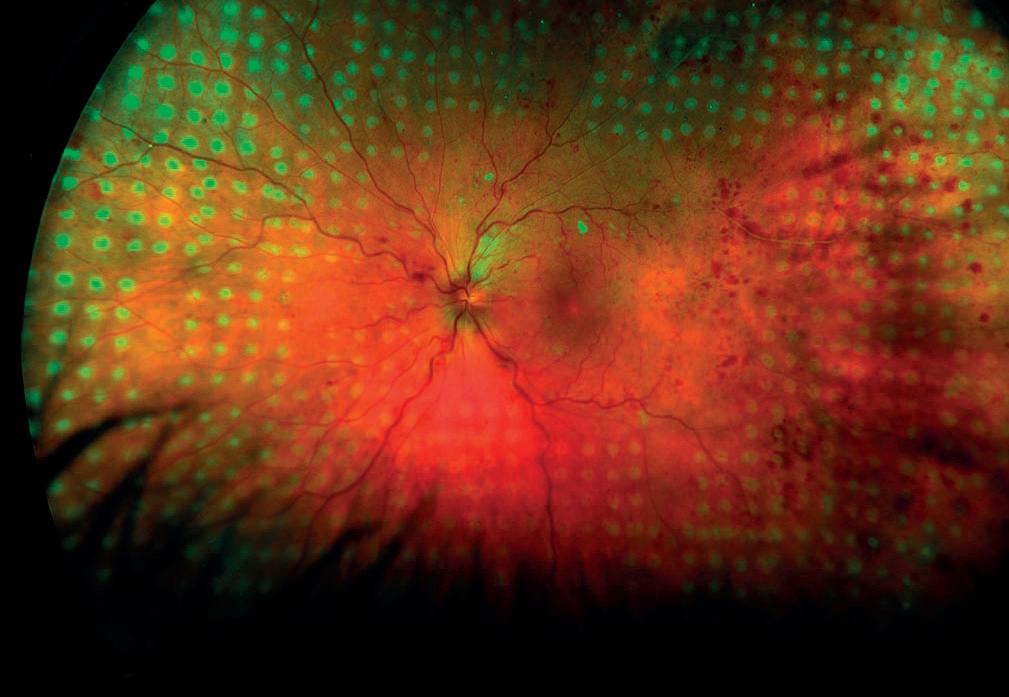
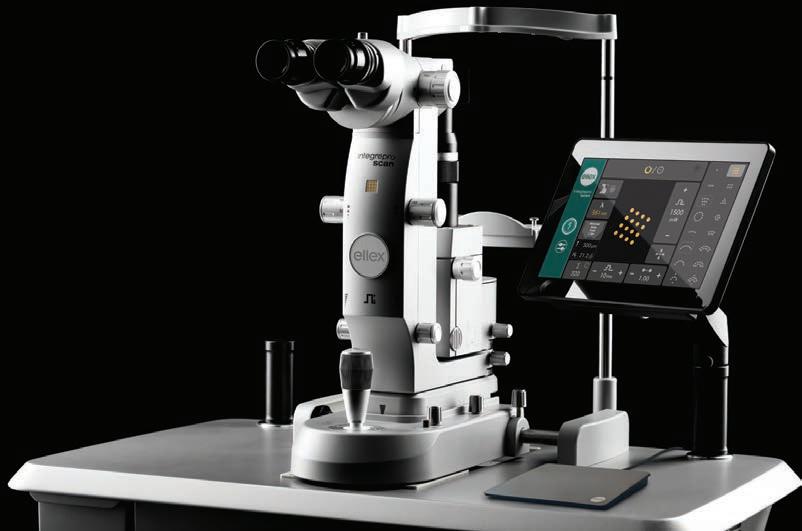
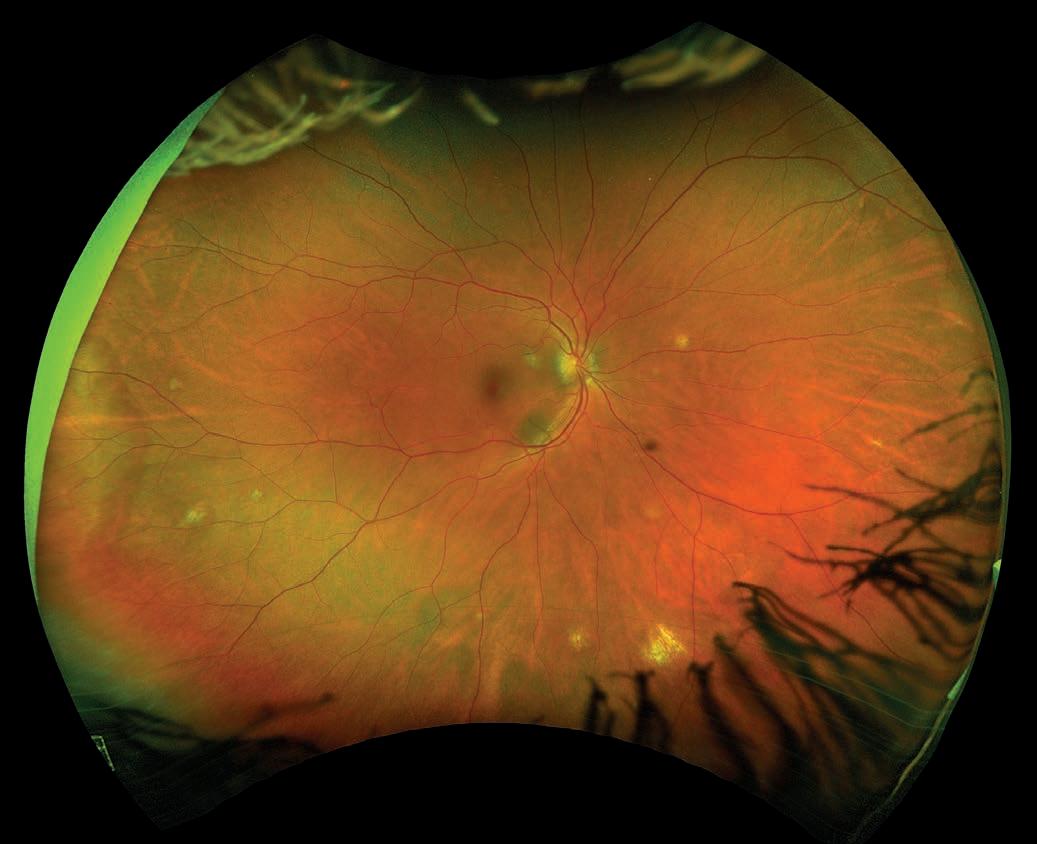














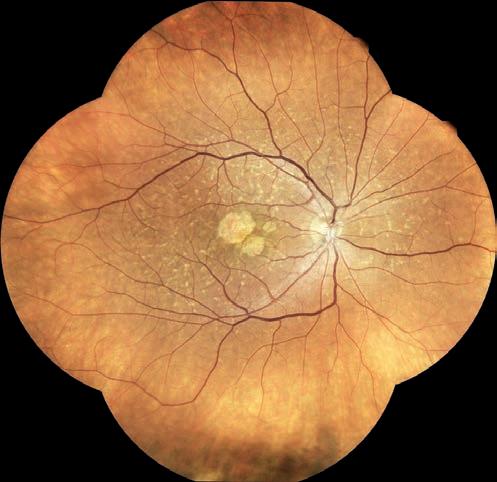







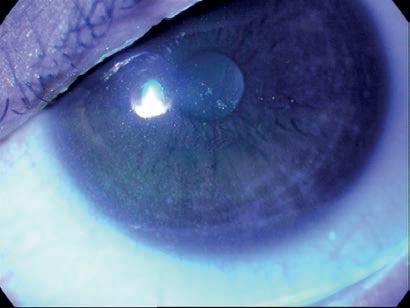
































































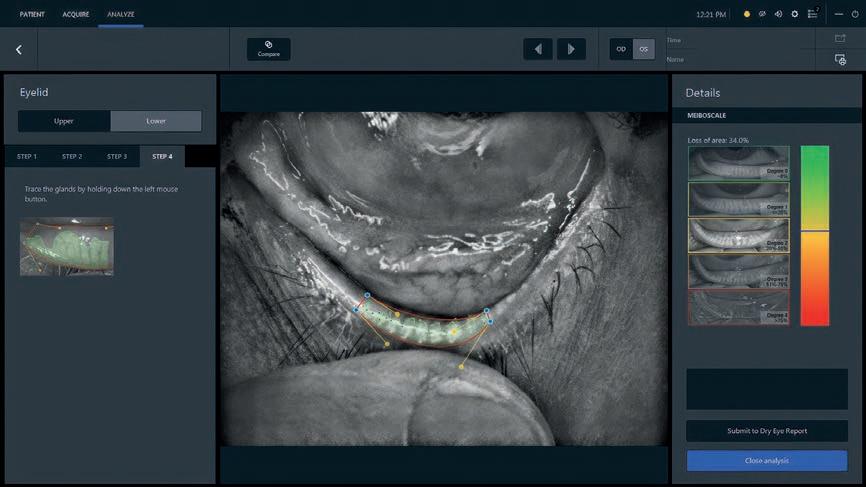
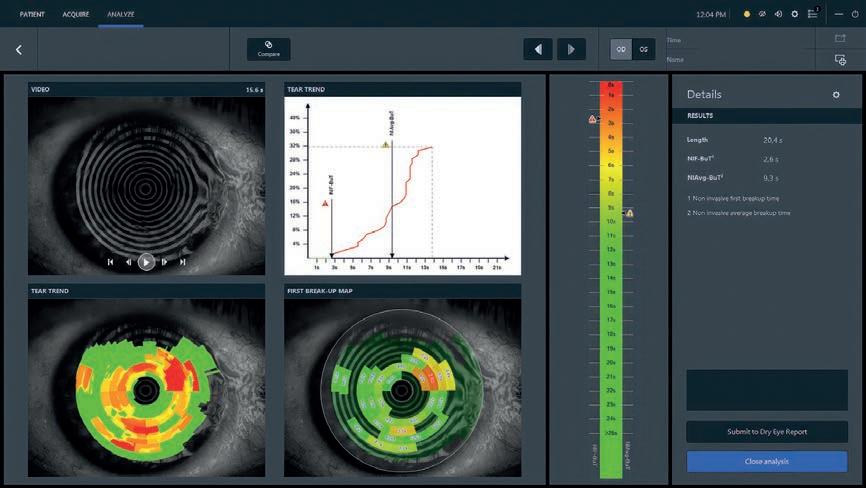
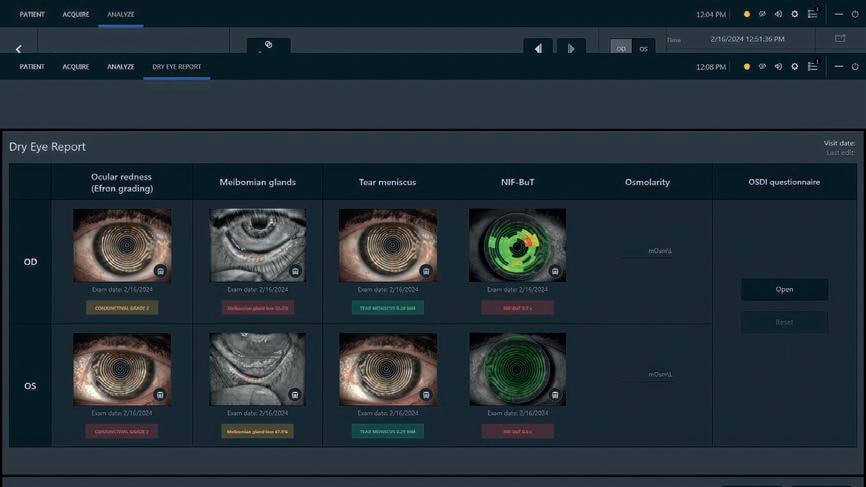
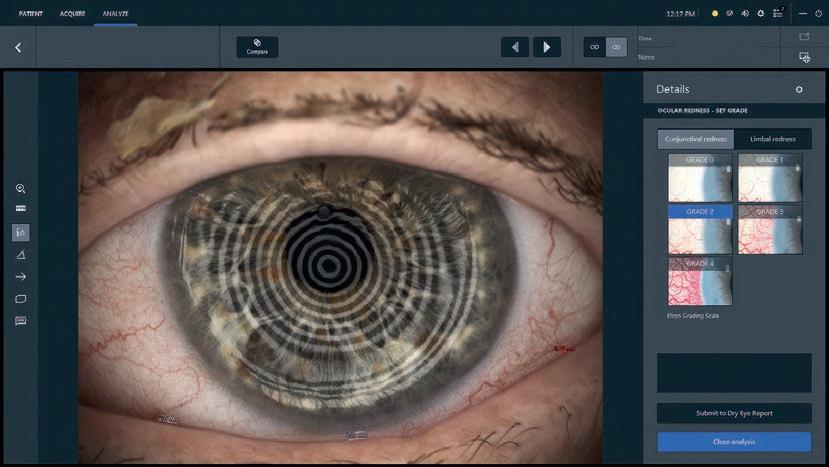
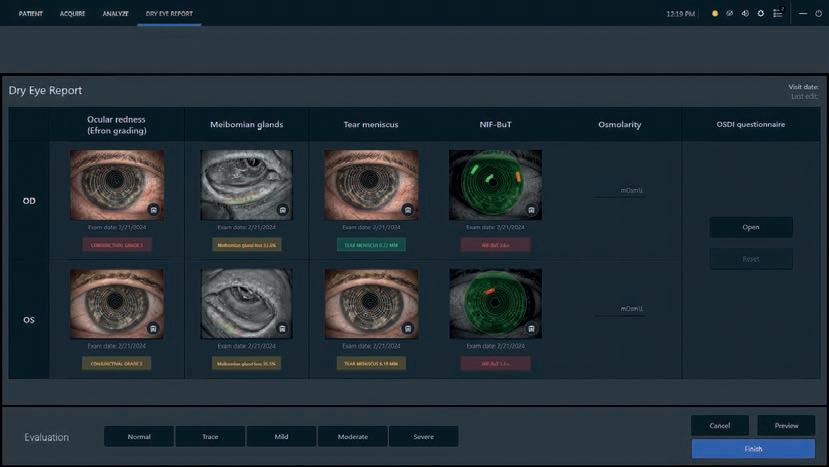





























































































































 BY LAURENT GALINIER
BY LAURENT GALINIER










 Ms
Ms