DUAL
How


DUAL
How

If you love the idea of a fulfilling career in optometry, where you’ll have access to the latest technology and be part of a business that’s focused on advancing your career, you’ll shine at Specsavers.


The trust and confidence that Australian eyecare professionals have in their regulator have taken a hit, according to a survey of practitioner sentiments and perceptions of the Australian Health Practitioner Regulation Agency (Ahpra) and the National Boards.
The latest results – a snapshot from 2021 – show that while above the average of all health disciplines, the level of trust optometrists had in the Optometry Board of Australia (OBA) were the lowest since the surveys began in 2018. Meanwhile, for medical practitioners including ophthalmologists, trust levels were significantly low in the Medical Board of Australia (MBA), at 38%.
The survey reflected the full spectrum of views towards the OBA, with some feeling it is a trustworthy, open and honest organisation that supports the sector, while others
questioned the body’s understanding of the modern-day optometrist and the relevance of the CPD program.
Meanwhile, Australian Society of Ophthalmologists (ASO) president Dr Peter Sumich says trust in the MBA is being undermined by its bureaucratic approach, and the way doctor’s reputations are affected during the complaints process.
Ahpra, the OBA and MBA released these “reputational insights” in late June 2023, which will inform their work to improve engagement with regulated health professions, with the aim of improving trust and confidence in the National Registration and Accreditation Scheme.
The reports provide results from an anonymous survey conducted in late 2021 of a random sample of registered health practitioners. There were 14,670 responses from practitioners across all regulated
health professions, including 776 optometrists and 1,059 doctors.
As the survey was voluntary, Ahpra warns the sample from some professions may not be representative of the whole profession. In addition, the survey responses reveal the differing roles of National Boards, Ahpra and professional associations are not well understood, so caution is needed

when considering the results.
In total, around 5% of optometrists who responded to the survey have had a complaint about them made to the OBA, and 40% have been audited to check their compliance with mandatory registration standards. Around 65% of optometry respondents viewed the OBA in a positive light, a decrease compared to 2020 but a higher rate than in earlier years. Optometrists also perceived their board significantly more positively than sentiments toward boards on average (54%). However, 64% of optometrists indicated that they had trust in the OBA, a 13% decrease from 2020 and the lowest rate of trust recorded in the four years since these surveys began. Confidence also dropped to
continued page 8
A new report commissioned by the private health insurance (PHI) industry states Australia is paying more for medical devices used in surgery than many other developed countries. In 2022, prices on the Prostheses List (PL) were reportedly 67% higher than those in New Zealand for 25 common devices.
However, the MedTech industry’s peak body – representing some of Australia’s main ophthalmic device suppliers – says the data shows a continued decline in what health funds are paying for medical devices, largely due to a March 2022 deal signed with the previous government committing to a phased reduction in prices paid for PL devices.
Mandala Australia’s report –instigated by Private Healthcare
Australia (PHA) representing 20 health funds – says Australia is paying some of the highest prices globally for medical devices through the PL.
For a selection of 46 frequently used devices, the report said Australia paid more compared to the UK, New Zealand, France and Germany. The UK pays 71% of what Australia does, France less than half, and Germany around 22%.
“Australia’s relatively distant geography and small market size have been used to justify expensive prices, but countries that are similarly distant from international manufacturers such as New Zealand pay less for their medical devices, despite having an even smaller market size than Australia,” the report said.
“In 2022, prices on the PL were 67% higher than those in New Zealand for 25 common devices (including IOLs). Given an overall expected price reduction of 13% by 2024 through adjustments to the list, Australia’s PL will still be up to 46% more expensive than New Zealand for this selection of devices.”
The government has been keen to reform the PL and better align prices in the private system with those paid in public hospitals – and comparable international markets.
Before leaving power, former Federal Health Minister Mr Greg Hunt signed a Memorandum of Understanding (MoU) with the Medical Technology Association of Australia (MTAA), the continued page 8
to now manage business -to-business relationships with private health insurers for EssilorLuxottica. As part of the leadership team, she is also helping shape the company's eyecare agenda.



A comment from Vision Eye Institute’s national medical director Dr Lewis Levitz in Insight’s July 2023 issue got me thinking about an often-underrated part of the eyecare professional’s repertoire: communication skills.

In the context of intraocular lenses, he explained the importance of investing time to discuss options and the compromises inherent in each design – keeping in mind that the patient regards a pre-operative educational talk as a ‘discussion’, while that same discussion afterwards an ‘excuse’.
All you need to know to maximise your attendance at O=MEGA23/WCO4.
Levitz’s wise words can be applied across all professions within our public-facing sector, and may prompt one to consider how they can sharpen their communication and other soft skills. Afterall, if the patient doesn’t understand, how are they expected to become invested and satisfied with their eyecare?
In 2019, an Optometry Board of Australia analysis showed over a seven-year period that communication was a key theme of optometry patient complaints. A major issue was communicating realistic expectations and limitations of new spectacle and contact lens scripts, to combat a widespread belief there is no adaptation period.

In this issue on page 61, we delve into the spectrum of soft skills required to perform optimal eyecare, taking into account additional factors like body language, decision-making, problem-solving and time-management. Three credentialled Australian eyecare professionals share thought-provoking tips on how they approach cases, demonstrating how to seize key moments with patients through their non-clinical skills.
Locum optometrists can be a lifesaver, but only if they are set up for success (0.5 CPD).
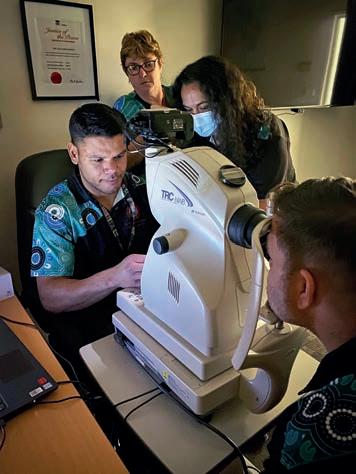
A new ophthalmology project is helping overcome eyecare access issues in regional NSW.


Coincidentally, many Australian ECPs are about to upgrade their clinical skills. In September 2023, O=MEGA23 is combining with the 4th World Congress of Optometry, putting our national industry on the global stage. Ahead of the event in Melbourne, this edition features a comprehensive guide to some of the key sessions, as well as products making their first appearance on the trade floor (page 40).
With a clinical program focusing on many of optometry’s hot topics, and sessions tailored for practice managers and dispensers, it’s also exciting to see an agenda catering for the entire practice team. As part of our committment to growing the industry and organisations within it, the Insight team will be there in full force and looks forward to seeing you there.



UPFRONT
Just as Insight went to print, WESTERN EYE SPECIALISTS , consulting across three locations, announced a partnership with Vision Eye Institute to create the largest private ophthalmology clinic in Melbourne. “[Vision Eye Institute’s] focus on excellence in patient care and integrity in their clinical and business practices aligns perfectly with our core values ... This shared focus will allow us to deliver even more exceptional care,” Western Eye Specialists founder
WEIRD
New findings in colour vision research imply that humans can perceive a greater range of blue tones than monkeys do. “Distinct connections found in the human retina may indicate recent evolutionary adaptations for sending enhanced colour vision signals from the eye to the brain,” Proceedings of the National Academy of Sciences reported.
A domiciliary optometrist has seen 1,300 patients during a three-day eye camp that she established in Kenya. Kejal Shah, who works for Specsavers Home Visits in the UK, travelled to Kenya with hundreds of pairs of glasses donated by her patients and was expecting to see 600 people, according to Optometry Today. However, demand exceeded her expectations, with patients queuing from 5am each day.
Australian UFC fighter Justin Tafa suffered one of the worse ‘eye pokes’ in the combat sport’s history in June. His opponent Austen Lane accidentally stuck a finger in his eye, causing the fight to stop. It’s not yet known if he will regain full vision. “I thought my eyeball had been ripped out, honestly. The first thing I was thinking was, ‘Can I see my kids again?’. I just hope it’s not really bad damage.”
Dr John McKenzie said. IN OTHER NEWS, international research led by Brisbane's QIMR Berghofer has found hundreds of new genes linked to a person’s glaucoma risk. “Existing treatments focus only on lowering eye pressure. The dream has always been to find a way to make the retina itself stronger so it can withstand the build-up of pressure,” lead researcher Professor Stuart MacGregor said. “For the first time we’ve discovered the set of genes that could be targeted to induce this ‘neuro-protection’ in retinal cells. We’ve
also identified existing drugs that could be used on those genetic targets."
FINALLY, results of a global survey on cataract revealed Australia is among the lowest in the world for patients having a lens discussion with their surgeon prior to cataract surgery. Misconceptions about cataract surgery also remain, highlighting the need to educate patients aged 50-plus on the procedure and options. The findings were part the '2023 Alcon Eye On Cataract Survey' in support of Cataract Awareness Month in June 2023.
insightnews.com.au
Published by: 379 Docklands Drive, Docklands VIC 3008
T: 03 9690 8766 www.primecreative.com.au
Chief Operating Officer Christine Clancy christine.clancy@primecreative.com.au
Group Managing Editor Sarah Baker sarah.baker@primecreative.com.au
Editor Myles Hume myles.hume@primecreative.com.au
Journalist Rhiannon Bowman rhiannon.bowman@primecreative.com.au
Commissioning Editor, Healthcare Education Jeff Megahan Business Development Manager Luke Ronca luke.ronca@primecreative.com.au
Client Success Manager Salma Kennedy salma.kennedy@primecreative.com.au
Design Production Manager Michelle Weston michelle.weston@primecreative.com.au


WHAT'S ON
THIS
MONTH
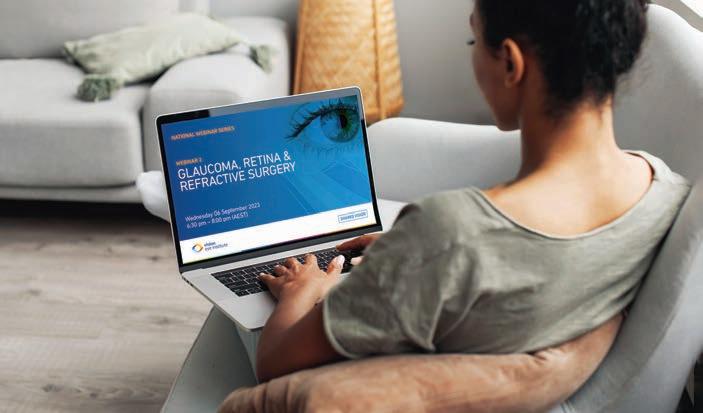
Taking place at Fullerton Hotel, Sydney, the conference is an ideal chance for eye doctors to brush up on common subspecialty topics. ophthalmologyupdates.com
Complete calendar page 89.
NEXT MONTH O=MEGA23/WCO4
8-10 SEPTEMBER
Head of Design Blake Storey
Art Director Bea Barthelson Subscriptions
T: 03 9690 8766 subscriptions@primecreative.com.au
The Publisher reserves the right to alter or omit any article or advertisement submitted and requires indemnity from the advertisers and contributors against damages or liabilities that arise from material published. © Copyright – No part of this publication be reproduced, stored in a retrieval system or transmitted in any means electronic, mechanical, photocopying, recording or otherwise without the permission of the publisher.

continued from page 3
66%, which, while 7% lower than the 2020 result, is not inconsistent with previous years’ rates.
“Despite the reductions, these findings were still significantly higher compared to the average trust and confidence reported across all practitioners,” the OBA report found.
When looking across all Ahpra-regulated professions, 52% of practitioners reported trust and confidence in their National Board, representing an 11% decline in trust and a 4% decline in confidence from 2020. As with sentiment toward Ahpra, despite a slight decline, practitioner perceptions of the boards in the latest survey are still more positive than in the 2018 survey, though the decline in trust remains notable.
Practitioners were also asked to rate the level of support they received from Ahpra and the National Boards to maintain or improve their professional practice. When combined, 40% of optometrists rated the support received favourably, 32% rated the support as fair, and 19% rated this negatively. The remaining 10% selected ‘I don’t know’.
“These values are similar to data collected in 2020,” the OBA report stated. “Nevertheless, optometrists remained slightly more likely to rate the support they received positively as compared to the other practitioner groups in the combined sample.”
Medical practitioners, including ophthalmologists, held much harsher views of Ahpra and the MBA. Almost a quarter of doctor respondents have had a complaint
about them made to the regulator, and 8% audited for registration compliance.
Less than half (41%) of respondents viewed the MBA in a positive light. On average, medical practitioners perceived the board significantly less positively compared to practitioner sentiments toward boards overall.
Only 38% of respondents indicated that they had trust in the MBA, a 13% decrease from 2020 values. Confidence in the MBA also declined to 40%.
“Both trust and confidence in the board have declined since the first survey in 2018. Levels of trust and confidence were significantly lower compared to the average across all practitioners,” the MBA report stated.
Sumich, ophthalmologist and president of the ASO, said the Medical Board used to be simple, effective and cheap, with each state having their own board whose job was to register eligible medical practitioners.
“There was an investigatory function and a disputes process. The colleges policed the good and bad on their turf,” he said.
“Then along came Ahpra and the National Law. Depending on your politics, it could be seen as a neat tie up of the many state bodies or a grand socialist plan to nationalise medicine, under the control of bureaucrats and politicians. The Ahpra fees are now 10 times greater than the previous state registration bodies. It has become an organ attempting to justify its own existence and funding and seeking ever greater control over the profession.”
Nowadays, he said investigations of practitioners tended “to occur in backwards fashion to that of natural justice”.
Examples of optometrist quotes and trust in the OBA:
• “ Their goals of furthering the optometry profession and supporting optometrists nationwide are supported by their actions.”
• “ They have been very informative throughout all of COVID and been very supportive.”
• “I feel it is a trustworthy, open and honest organisation.”
• “It ensures all practitioners are well supported throughout their career.”
• “I agree with the standards they have agreed upon and upheld.”
• “ They strive to better our profession to increase patient care.”
Examples of optometrist quotes and distrust in the OBA:
• “Bureaucratic and self-serving, in it for themselves rather than the profession.”
• “Run by the powers that be rather than the normal everyday practitioner.”
• “ They have no idea of how hard it is for allied health professionals to make a living and keep increasing the unpaid work demands by unrealistic CPD and reflective writing requirements that are not helpful. Where is the evidence that this level of requirement improves patient safety?”
• “ They do not actively represent the entire profession, I have felt let down by their leadership in the past when support was needed.”
Note: Because the free text questions were not mandatory, some professions had less responses and limited quotes. This was the case for distrust in the OBA, so Ahpra urged caution against making inferences from these comments.
Source: 2021 Practitioner perceptions of Ahpra and the National Boards Supplementary report prepared for the Optometry Board of Australia
“A vexatious accusation may be made without any proven foundation, and the long delay in investigation and dismissal of the complaint has caused at least half a dozen suicides by emotionally affected medical practitioners. Having your name listed on a website as an impaired, restricted or investigated practitioner is devastating,” he said.
continued from page 3
latter acknowledging it had a role to play in reducing private health premiums.
The document provides clarity about how items on the PL will gradually reduce in price, establishing a process to reduce the gap between the cost of medical devices in the public and private sectors over three years. The multi-year reforms are anticipated to deliver savings of $900 million for PHIs to pass on to consumers.
But PHA said this “last-minute MOU” effectively put a 7-20% surcharge on medical devices for private patients. The body is calling for the current government to
review the agreement.
Recently, however, MTAA CEO Mr Ian Burgess said the data showed PL reforms were continuing to deliver significant savings to health insurers, which now total more than $2.1 billion since 2017.

“What we are seeing is a continued decline in the benefit levels for medical devices, delivered by the MedTech industry, but which are yet to be passed on to consumers by corporate health insurers in full,” Burgess said.
“Despite the increase in utilisation, Australian Prudential Regulation Authority’s data shows that the total benefits paid for medical devices dropped by 8.9% in March 2023, compared
to December 2022 – a clear result of the ongoing reforms to the Prostheses List.
“The MedTech industry is continuing to play its part to help ease cost-of-living pressures for Australians, it’s well time a mechanism was introduced by government to compel corporate insurers to pass on the savings, delivered by our industry, to consumers.”
Additional data PHA provided, from a separate 2022 report, shows the higher cost Australians can occasionally pay for IOLs. For one premium IOL, the Australian price was $934, while in South Africa it was $322, Germany $516, Sweden $765, Austria $960 and Italy $1,133.
Over 200 eye drops sold online in the US have been identified to have potential safety issues and have been reported to the FDA. Not-for-profit group the Dry Eye Foundation discovered the products – across 62 brands – the majority of which were packaged exclusively for sale in a country other than the US. Many are advertised as preservative-free but are pictured in bottles designed only for preserved eye drops. More than 60 individual products have been found on Amazon.
“Raising awareness about the safety hazards of purchasing eye drops online has become our top priority for 2023. In 2022 we were worried about three incorrectly packaged biologic eye drops. Then came the Ezricare tragedy earlier this year, which increased our sense of urgency," said Dry Eye Foundation executive director Ms Rebecca Petris, referring to the alleged contaminated artificial tears brand that has been linked to three deaths and 12 cases of vision loss, including enucleation.
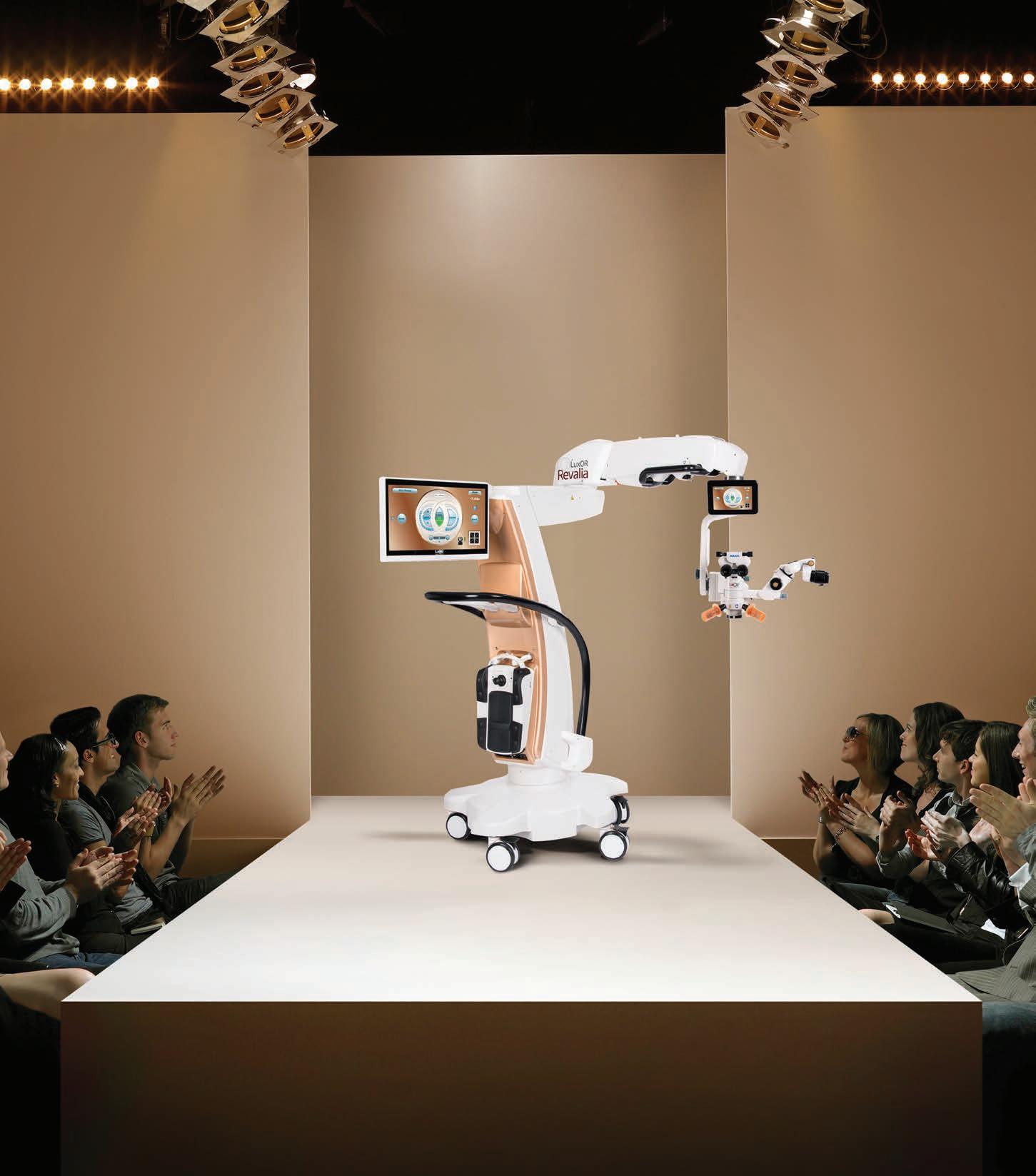
Using artificial intelligence combined with an understanding of consumer lifestyles, EssilorLuxottica has developed its best overall progressive lens, Varilux XR series. The lens – available in Australia from 1 July 2023 –represents the latest advance in the Varilux brand, which originated in 1959 and boasts around 70 patents. The group has gathered more than one million pieces of data to develop what is describes as a “breakthrough behavioural modelling system” that predicts how presbyope individuals will look at objects around them. “The insights we established from data collected from customer orders, real life wearer tests, in store measurements and physiological models are exclusive to EssilorLuxottica. Thanks to the digital twinning technology, we can now establish a visual behaviour profile for every single prescription and provide the first eye-responsive lens that respects the natural behaviour of the eye,” Mr Norbert Gorny, the group's co-chief operating officer, said.
Vision Australia has made a submission to a Federal Government public consultation supporting the proposed introduction of an Acoustic Vehicle Alerting System (AVAS) to electric vehicles. When travelling at low speeds, electric vehicles can be hard for pedestrians to hear, proving risky for the blind and low vision community, the organisation said. “Specifically, [the government] is determining whether to adopt United Nations Regulation 138/01 as a new Australian Design Rule in electric cars. If mandated, the AVAS could save lives and avoid thousands of injuries.” Through the National Road Safety Action Plan 2023-25, the government is committed to mandating AVAS for electric vehicles, subject to the outcomes of an impact analysis process. At this stage, the government is proposing to introduce AVAS only for light electric vehicle classes.
Ten eye health care professionals were recognised in the King’s Birthday Honours this year, including the late Mr Richard Grills, a prominent member of the Australian ophthalmic community.

Grills – a former director of ODMA and founder of Designs For Vision – passed away in July 2022, but was posthumously awarded Member (AM) in the General Division for significant service to community eye health, and to the ophthalmic optics industry.
In ophthalmology, clinical associate professor at The University of Sydney, Andrew Chang (AM), was recognised for significant service to ophthalmology and retinal surgery as a clinician and educator.
Chang is a consultant ophthalmologist and the head of ophthalmology at the Sydney Eye Hospital and the medical director of Sydney Retina Clinic and Day Surgery, among other appointments.


Distinguished professor Justine Smith (AM), from the College of Medicine and Public Health at Flinders University, was recognised for significant service to ophthalmology, particularly research and education. Smith is an internationally recognised expert in the causes, effects and treatment of uveitis. Her work extends to infection by parasites and viruses, and ocular cancers. She is also executive vice-president of the Association for Research in Vision and Ophthalmology.
Meanwhile, Dr Brett O’Donnell was awarded a Medal (OAM) in the General Division for service to ophthalmology. O’Donnell is a dedicated oculoplastic reconstructive and cosmetic surgeon at St Vincent’s Private Hospital Sydney and Mater Hospital, North Sydney.
In optometry, Scientia Professor Fiona Stapleton was awarded Officer (AO) in the General Division for distinguished service to optometry as a researcher, mentor and role model, to tertiary education, and to national and international organisations. She is currently president of the International Society for Contact Lens Research and holds numerous memberships and executive affiliations with scientific organisations.
Conjoint professor Arthur Ho (AM) was recognised for significant service to optometry as a researcher, designer and educator. He is currently the chief scientist innovation officer at the Brien Holden Vision Institute (BHVI), in addition to an appointment as Visiting Professorial Fellow at the School
of Optometry and Vision Science, UNSW.
Dr Margaret Crowley (AM), who joined the board of the Lions Eye Institute in 2016, received her honour for significant service to community health, and to people with low vision. She has held senior executive positions in state and national governments, universities, and the not-for-profit sector – including 15 years as CEO of the Association for the Blind of WA. CERA research fellow and clinical orthoptist Dr Sandra Staffieri (AO) was acknowledged for distinguished service to medicine as an orthoptist and vision researcher, and to paediatric ophthalmology. Her research is focused on hereditary eye diseases, including congenital glaucoma, congenital cataract, eye movement disorders and retinoblastoma.
Epidemiologist and former optometrist, Scientia Professor Rebecca Ivers (AM), head of the School of Population Health at UNSW, was recognised for significant service to community health through injury prevention research and education.
Professor Alice Pébay (AM) from The University of Melbourne was awarded for her significant service to science, particularly through stem cell and neuroscience research. Pébay is investigating genetic diseases of the eye, many of which have no intervention or cure.

Australia faces a $4.3 billion economic hit from the impact of glaucoma by 2025 unless the Federal Government invests now in initiatives that work to improve patient compliance, according to Glaucoma Australia.
The nation’s peak body for glaucoma patients commissioned a new report revealing that the costs of early intervention in glaucoma “is a drop in the ocean” when compared with the significant long-term burden premature blindness places on the health system and National Disability Insurance Scheme (NDIS).
According to economic consulting firm Evaluate, who conducted the analysis, the demand will accelerate further in the next few years with the aging population, which will see the cost to the community rise from $1.9 billion to $4.3 billion.
“Glaucoma is known as the ‘thief of sight’ as it robs a person of their vision with such stealth that patients often don’t know they have this insidious disease until it’s too late. It’s important that governments understand that saving sight is also good for the economy – it can save billions,” Glaucoma Australia CEO Mr Richard Wylie said.
“The major focus has to be on early
diagnosis and supporting patients to stick with their treatment regimen long-term, because there is no way to reverse the vision loss caused by glaucoma. We can slow it down, but we cannot ‘cure’ it.”
The report acknowledged there were several costs for ongoing treatment, including prescribed medicines, surgical procedures, acute hospitalisation, treatment for hip fractures from falls (10x more likely for people living with glaucoma), as well as the significant costs associated with long-term disability support payments, carer costs and early entry into aged care.
However, this far outstrips the cost of investing in greater awareness, early identification of ‘at risk’ patients and making Glaucoma Australia’s Patient Support Program more widely available, the report concluded.
Glaucoma Australia’s Patient Support Program already has more than 23,000 patients on its database – increasing at a rate of about 300 a month. The program provides ongoing support via clinical educators who are available to patients five days a week.
“Being able to see is one of life’s
greatest gifts, yet so many people are at risk of preventable blindness, due to a lack of awareness about the disease and the importance of treatment adherence,” Wylie said.
A recent survey showed 85% of patients who take part in Glaucoma Australia’s Patient Support Program adhere to their prescribed treatments, and 91% attend their recommended appointments – both important indicators for management success.
In addition, the number of patients who frequently felt anxious about their glaucoma fell from 44% to 20% after receiving education and support through the program.
“Glaucoma Australia has been able to achieve all of this without any support from state or federal governments. But with demand growing rapidly at the rate of up to 300 new patients a month seeking our help, we now need to ask for support from Canberra,” Wylie said.
“There is such an exciting opportunity to make a big difference if we identify people early, and if we support them properly, we can get superior health outcomes, and save the health budgets billions.”

A new University of South Australia (UniSA) study has revealed that rural experience could be the key factor in increasing the number of health workers in Australia’s rural and remote communities.

Examining the work locations of UniSA health graduates, researchers found that nearly half of the new rural allied health workforce in 2020 originated from metropolitan areas, with 88% completing a rural placement during their studies.
Significantly, 25 graduates from the same cohort moved from metro employment to rural practice within two years of graduation; most of these graduates (76%) had done a rural placement.
In Australia, around 7 million people – or 28% of the population – live in rural and remote areas. Despite having greater medical needs, these communities face severe health workforce shortages, with
eye health being a key issue.
UniSA Department of Rural Health researcher Dr Lee Puah said understanding the connection between rural placements and rural practice is vital for addressing workforce shortages.
“This type of research can help us understand and plan future placements to help address the maldistribution of the workforce,” Puah said.
“Our study found that rural placements were fundamental in attracting allied health professionals to rural areas, both after graduation and beyond as they provide a taste of the rural work environment.”
The study assessed 264 students who had completed podiatry, occupational therapy, or physiotherapy at UniSA in 2019. After graduation, 40 were practising in rural areas, with 26 remaining in rural practice two years later – a 65% retention rate. Interestingly, by 2022, 25 city-based allied health
(76% had done a rural placement and 20% had rural origins).
Puah said the experience and insights gained through the rural placement programs prove critical for securing allied health workers in rural and remote areas.
“Addressing the health workforce shortage in rural and remote communities is a challenge, though a rural placement program may be part of the solution.”
Specsavers recently hosted an industry-first, cross sector collaborative meeting for patient support bodies across Australia and New Zealand.

Attended by Glaucoma Australia, Glaucoma NZ, Vision Australia, Macular Disease Foundation Australia (MDFA), Diabetes Australia and Specsavers, the event aimed to strengthen relationships and build a more collaborative community of patient-centred eye health professionals and services across Australia and New Zealand.
With some attendees meeting each other for the first time, the event saw participants present information on their organisation, their patient support journey and the successes and challenges they face in delivering day-to-day care.
Dr Kathy Chapman, MDFA CEO, said the day was an ideal opportunity to listen and understand more about what each player in the patient support sector does.
“Thanks to Specsavers for bringing all the eye health organisations together. The open discussion showed where we have similar strengths and where we have different but often complementary offerings available for patients,” she said.
“I came away seeing lots of potential to
better collaborate and complement each other’s work, especially because we were able to share similar challenges such as how do we increase referrals so that more people are aware of our valuable services. The more we as eye health organisations and optometrists know about the services out there, the better equipped we are to help people living with
eye health issues maintain their sight and improve their quality of life.”
Mr Richard Wylie, Glaucoma Australia CEO, agreed, stating that all organisations in the eye health sector want better health outcomes for their community.
“Therefore, formalising a time to meet and explore opportunities to collaborate made perfect sense,” he said.
Specsavers ANZ optometry director Dr Ben Ashby said that while many connections were made, the goal of the event was to take the first step in establishing a network where new strategies could be devised to benefit patients and the eye health sector in future.
“As the largest provider of optometric services in both Australia and New Zealand, we see firsthand the impact of patient support bodies in positively engaging with relevant patients outside the testing room,” he said.
“We hold direct relationships with these organisations, so it made sense for us to bring them all together. Our next steps are to hold a follow up workshop before the end of the year, where we will brainstorm and plot out exactly what we could do together that could lead to enhanced health outcomes for more patients.”


Eyecare Plus has launched a ‘Catch-up TV’ campaign promoting its ‘locals caring for locals’ brand positioning – and the early results are promising for members, the group said.
‘ Catch Up TV’, officially known as Broadcaster Video on Demand (BVOD), is an internet-based platform that makes free to air television advertising accessible to smaller businesses.
According to Eyecare Plus, the biggest barrier to entry for advertising on freeto-air-television in metropolitan areas has always been the cost of campaigns because traditional free-to-air-television covers large geographic areas, such as the greater Sydney or Melbourne regions.
However, with BVOD, businesses like
Eyecare Plus – with 123 independently owned optometry practices – can reduce the cost by narrowing the target to specific postcodes and demographics.
“Eyecare Plus is the largest branded group of independent optometrists in Australia and sharing the cost of marketing is a key strategic advantage for us, and Catch-Up TV makes television advertising accessible for all our members,” Eyecare Plus chairman Mr Martin Gregory.
“This campaign has delivered great early results, and while it is impossible to measure precisely, we have seen an additional 1,000 appointments booked online since the start of the campaign, with over 500,000 completed views per month,” he said.
The eyecare group said the media
market has been greatly fragmented by the internet, and there is no longer a dominant mass medium like free-toair-television once was, but that doesn’t mean people are watching less television. In fact, it said, more video is being consumed on screens than before, but the options for how programs are consumed are now much greater – from streaming services and YouTube, to the various on demand ‘Catch-up TV’ channels as well as traditional television.
“Importantly, this campaign is designed as a brand building exercise that seeks to reinforce our ‘locals caring for locals’ positioning in the market. It is not a discount driven ‘call to action’ campaign so we can expect the return on investment in our brand to grow through time,” Gregory said.


Children and young people who are blind or have low vision and their families are set to benefit from a refreshed service approach from Vision Australia.
The leading blindness and low vision service provider has launched its new Life Ready program, developed by Vision Australia’s expert paediatric team. Tailored services and programs are delivered by Vision Australia’s paediatric specialists, in collaboration with educators, health professionals and other key figures in the lives of children and young people.
Vision Australia research shows 24% of Australians who are blind or have low vision are in fulltime employment, making Life Ready – and its ethos of early intervention – vital.
“Much of what we learn in life is through what we see, so children who are blind or have low vision need to gather information about their world in different ways,” Mr Ron Hooton, Vision Australia CEO, said.

“Life Ready will equip children and young people with the support and skills needed to build strong foundations for life and put them on the path to meaningful long-term employment.”
Core to Life Ready is supporting participants to develop nine internationally recognised life skills.
“The skills include practical things such as learning to use assistive technology, sensory efficiency, developing orientation and mobility skills, and strengthening independent living skills. They also include concepts such as career education, building social skills and understanding self-determination,” Hooton said.
“Extensive research has shown equipping children and young people who are blind or have low vision with these skills helps them overcome the challenges blindness or low vision can present to participating in wider society, whether that is at school, in the workplace or in social settings.”
More information about the Life Ready program can be found at www. visionaustralia.org/services/find-services/ children. To refer people to Vision Australia, visit www.visionaustralia.org/healthcare-professionals/refer-patient-form
Macular Disease Foundation Australia (MDFA) has awarded more than $700,000 in research funding to six projects building the macular disease knowledge bank.
The organisation awarded grants worth $560,000 for three projects examining atrophic age-related macular degeneration, also known as geographic atrophy, for which there are no currently approved treatments in Australia.
“Geographic atrophy is a significant cause of vision loss and blindness in Australia and has many unanswered research questions. One project includes a stem-cell derived modelling of geographic atrophy, and the second will address hyperspectral imaging for detecting and monitoring geographic atrophy,” MDFA said.
An additional $150,000 will fund three new early-career researchers undertaking innovative ‘blue sky’ research into macular disease, made possible by a bequest made in memory of the late Faye Grant.

Their research will seek deeper insights into sight-threatening diabetic macular ischaemia, enhanced diagnostic approaches to reduce misdiagnosis of macular disease, and an evaluation of high-density lipoprotein levels that might identify people with high-risk phenotypes of age-related macular degeneration.
The function of mitochondria, the
energy-producing centres in cells, are the focus of research by second-time funding recipient Dr Gerald Liew of the Westmead Institute for Medical Research, University of Sydney, and first-time recipient Dr Grace Lidgerwood of the Centre for Eye Research Australia, University of Melbourne, whose work builds upon previous research funded by MDFA.
Joining MDFA’s Expert Review Panel and International Peer Reviewers in the 2023 grant selection process was a new Community Review Panel comprising people caring for or living with macular disease.
MDFA CEO Dr Kathy Chapman said including the Community Review Panel ensured the macular disease community remained at the centre of its work. The latest funding round brings MDFA’s commitment to macular disease research to $5.8 million across 35 projects since 2011.

Macquarie University ophthalmology researchers have discovered a link between the protein neuroserpin and glaucoma and have subsequently developed a gene therapy technique.
Professor Stuart Graham, head of ophthalmology and vision science at Macquarie Medical School, is leading the team with vision neurobiologist Associate Professor Vivek Gupta and vision scientist Dr Nitin Chitranshi.
“Other researchers have linked changes in neuroserpin to stroke and neurodegenerative disorders like Alzheimer’s and Parkinson’s diseases, but our work is the first to relate it to glaucoma,” Gupta said.
“Cells naturally break down and

are recycled in the body, but when neuroserpin is absent, this process speeds up in the retina. Essentially, the body begins to eat away at the retinal ganglion cells and the optic nerve,” he said. After testing in mouse models, the team is preparing for further testing of an enhanced gene and will commence new trials shortly.
Graham said glaucoma is a complex disorder: “For this reason, our gene therapy is unlikely to be a silver bullet for all glaucoma, but we have great hopes that it will become a valuable part of treatment for use in conjunction with other therapies, making the nerve cells more resistant to damage.”

























We care about your patients, team, goals, succession, and legacy


















Meeting our team & partners will help you make the right decision Proudly













A Sydney research team has found the total estimated lifetime cost per person with an inherited retinal disease (IRD) is $5.2 million, with societal costs such as government support and lost income for people with impaired sight and their families accounting for 87% of this figure.
The study was published in the Medical Journal of Australia in June by a 10-strong team of academics, including Professor John Grigg and Professor Robyn Jamieson, from the Children’s Medical Research Institute, Save Sight Institute and the University of Sydney, Sydney, as well as lead author Dr Deborah Schofield from the Centre for Economic Impacts of Genomic Medicine at Macquarie University.
They used microsimulation modelling to estimate the healthcare and societal costs of IRDs in Australia, which involved interviews of people with IRDs and their carers and spouses over a set period.
After 94 people and 30 carers completed study surveys, the total estimated lifetime cost was $5.2 million per person with an IRD, of which 87% were societal and 13% healthcare costs.
The three highest cost items were lost income for people with IRDs ($1.4 million), lost income for their carers and spouses ($1.1 million), and social spending by the Australian Government. Overall, the estimated total annual cost of IRDs in Australia was $781 million to $1.56 billion.
“Given that 87% of the overall costs were societal, largely related to lower rates of employment for both patients and carers and their greater need for social support, it is crucial that societal costs are considered by cost-effectiveness evaluations of future IRD i nterventions, including genomic testing and targeted therapies,” the researchers concluded.
“The increasing loss of income across life reflects the impact of IRDs on employment and career op portunities.”
Women are significantly more likely than men to present with recurrent ocular toxoplasmosis, a study involving Flinders University has found.
Professor Justine Smith, from College of Medicine and Public Health at Flinders, was a joint senior author of ‘Impact of gender on clinical features and outcomes of ocular toxoplasmosis’ published in British Journal of Ophthalmology

The observational study involved 262 patients (139 women and 123 men) who presented to a tertiary referral uveitis service in Ribeirão Preto, Brazil, with serological and clinical evidence of ocular toxoplasmosis.
According to Smith and her fellow researchers, which also included Flinders University medical student Ms Matilda Lyons, approximately equal numbers of women and men had active versus inactive ocular toxoplasmosis.
In both women and men, most infections were remotely acquired.
Men were significantly more likely to present with primary active disease than women (24.4% versus 12.9%). Conversely, women were significantly

more likely to present with recurrent active disease than men (36.0% versus 28.5%).
According to the study’s results, one toxoplasmic retinal lesion was observed in more male eyes than female eyes (50.4% versus 35.3%), while women’s eyes were more likely to have multiple lesions than men’s eyes (54.7% versus 39.8%).
Lesions in women’s eyes were significantly more likely to occur at the posterior pole compared with those in men’s eyes (56.1% versus 39.8%). Measures of vision were similar for women and men.

“There were no significant differences in measures of visual acuity, ocular complications, and occurrence and timing of reactivations between the genders,” the authors noted.
They concluded that ocular toxoplasmosis has equivalent outcomes in women and men, with clinical differences in the form and type of disease, as well as characteristics of the retinal lesion.
Up to a quarter of Americans with diabetes are estimated to have some form of diabetic retinopathy (DR), according to a new study in JAMA Ophthalmology
The study, led by Ms Elizabeth Lundeen from the US Centers for Disease Control and Prevention Division of Diabetes Translation, set out to understand the 2021 US prevalence of DR and vision-threatening DR.
The study team estimated that 9.6 million people in the US – 26% of those with diabetes – had DR and 1.84 million people – 5% of those with diabetes – had vision-threatening diabetic retinopathy.
“There was marked variation in prevalence across states and the number of people living with diabetes-related eye disease grew substantially since prevalence was last estimated in 2004,” the
It’s estimated 37.3 million people in the US have diabetes, representing 11.3% of the population.

research team noted in the study.
“ The US prevalence of diabetes-related eye disease remains high and may grow in the coming decades due to the increasing burden of diabetes among youth and adults.”
DR is a common microvascular complication of diabetes.
No matter what life throws at you, HOYA’s Hi-Vision Meiryo Diamond lens coating provides superior clarity that lasts: featuring exceptionally low reflectance plus strong protection from scratches, smudges, UV, and glare.
To learn more about Hi-Vision Meiryo Diamond lens coating contact your HOYA Sales Consultant or call 1800 500 971.

Prescription dry eye drug Xiidra is changing hands, with ophthalmic giant Novartis signing a deal to sell the therapy to Bausch + Lomb (B+L) for up to US$2.5 billion (AU$3.6 b). It forms part of a new direction for Novartis, which is selling off its ‘front the eye’ drug portfolio.

Xiidra (lifitegrast ophthalmic solution) 5% can be prescribed by Australian eyecare professionals and is a non-steroid eye drop for signs and symptoms of dry eye disease (DED) focusing on inflammation.
“This acquisition is a prime example of our strategy in action, as it provides needed scale for the company and transforms our pharmaceuticals business by making us a leader in ocular surface diseases,” said Mr Brent Saunders, B+L chairman and CEO.
“The deal is also expected to accelerate margin expansion through a larger mix of pharmaceutical products in our portfolio, provide strong and immediate earnings accretion and presents a clear path to deleverage, making it financially compelling.”
Xiidra is expected to complement B+L’s existing dry eye portfolio that includes consumer eye and contact lens drops, as well as its pharmaceutical business that features MIEBO (perfluorohexyloctane ophthalmic solution), recently approved by the FDA as the first and only eye drop for DED that directly targets tear evaporation.
As part of the deal, B+L will also acquire libvatrep, an investigational compound for chronic ocular surface pain, and AcuStream technology, an investigational device with the potential of precise dosing and accurate delivery of certain topical drops.
By divesting ‘front of eye’ ophthalmology assets to B+L, Novartis chief strategy and growth officer Mr Ronny Gal said the move would enhance the company’s focus on innovative medicines to alleviate society’s greatest disease burdens, including the ophthalmic gene therapy Luxturna.
“Our ongoing portfolio refinement enables us to best deploy our scientific expertise and resources towards priority programs and therapeutic areas, while remaining open to opportunistic development for additional high impact conditions leveraging our advanced technology platforms,” he said.
“We believe B+L has the capabilities, scale and commitment to continue the work of Novartis in delivering and developing [these] much needed therapies."
Chemist Warehouse-backed Optometrist Warehouse has signed a Memorandum of Understanding (MoU) to collaborate on a study focused on the effectiveness of artificial intelligence (AI) in screening diabetic retinopathy (DR).

The collaboration – with Singapore-based healthcare technology company EyRIS – will leverage EyRIS’s AI algorithms and Optometrist Warehouse expertise with links to the extensive network of Chemist Warehouse pharmacies across Australia to demonstrate the efficacy and efficiency of AI in identifying patients at risk and facilitating early intervention.
EyRIS CEO Mr Lai Teik Kin said the company was thrilled to partner with Optometrist Warehouse.
“By harnessing the power of AI, we can revolutionise diabetic retinopathy screening, ensuring early detection and timely treatment for patients. Our technology has the potential to transform healthcare delivery, saving lives and reducing healthcare costs.”
Mr Peter Larsen, managing director of Optometrist Warehouse – whose
mission is to transform health outcomes by systematically connecting pharmacy with optometry – said it recognises the transformative impact of AI in medicine.
“We are proud to collaborate with EyRIS to explore the possibilities of AI in diabetic retinopathy screening. This study aligns with our mission to improve healthcare outcomes for all Australians. By leveraging EyRIS’s AI expertise, we can enhance the accessibility and affordability of early screening, thereby empowering patients and healthcare providers alike,” Larsen said.
The companies said the collaboration underscores their commitment to leverage technological advancements to improve healthcare.
The potential benefits of AI-driven DR screening include reducing the burden on healthcare systems, minimising unnecessary referrals, and enabling targeted interventions, ultimately improving patient outcomes, they said.
The study will span 36 months and involve a large sample size of diabetic patients across Australia.

EssilorLuxottica has announced a new exclusive license agreement to design, manufacture, and distribute Jimmy Choo Eyewear globally.
The deal will be effective from January 1, 2024, the day after Jim Choo’s pre-existing agreement with Italian eyewear company Safilo ends.
EssilorLuxottica will produce Jimmy Choo Eyewear until December 31, 2028, with an automatic renewal option of an additional five years. The first collection between the companies will be available on the market from Q1 2024, with all collections to be developed under Jimmy Choo creative director Ms Sandra Choi.
“We are excited to embark on this new journey with Jimmy Choo, a pioneer in the art of celebrity styling and the global luxury business,” Mr Francesco Milleri, chairman and CEO of EssilorLuxottica said.
“Together, we will design innovative
luxury eyewear collections that will embody the best of the brand’s artistic vision and signature glamour. In turn, our collaboration will further strengthen the high-luxury segment in the eyewear category.”
Ms Hannah Colman, CEO at Jimmy Choo, said: “We are thrilled to be partnering with EssilorLuxottica combining our shared expertise in accessories and eyewear categories to bring to life the essence of Jimmy Choo’s glamorous and c onfident aesthetic.”






















New Zealand is aiming to deliver 3,500 more cataract surgeries as part of a new nationally consistent threshold that removes “the postcode lottery” that has denied some New Zealanders access to the life-changing procedure, the government has announced.
In the recent budget, Minister of Health Dr Ayesha Verrall said $118 million was allocated to reduce wait lists and standardise access to healthcare, including cataract surgery.
“Ophthalmologists and patients across the country have been calling for consistency around life-improving cataract surgery and the revised threshold I’m announcing responds to that,” she said.
“For decades, the former District Health Boards (DHBs) used a point system that had wildly differing thresholds for access to cataract surgery – largely varying from 46 to 61 points. A score of 46 represents mildly reduced vision. A score of 61 represents poor vision and meant that the person could no longer legally drive.”
In Auckland and Waitematā, for example, patients become eligible for cataract surgery with a score of 46. But in Canterbury and Southern, people needed a score of 61.
That variation represented the worst of what’s become widely known as "post code health", Verrall said.
“In a first under the new health system there will be a nationally consistent score of a maximum of 46 in order to access surgery, opening up eligibility for approximately 3,500 more surgeries,” she said.

“A score of 46 means patients with mildly reduced vision as a result of cataracts will have much earlier access to surgery, improving their quality of life considerably.”
New Zealand's public health agency will work with referrers to identify who will be eligible for surgery under the new score and ensure they have timely access to the procedure.

system.

build on this revised cataract surgery threshold as a model to improve other waitlists into the future.”






Although the news was widely welcomed, ophthalmologists have raised concerns about whether public hospitals would be able to cope with increased demand.

To cater for this, the government is implementing initiatives such as outsourcing to other providers and ophthalmologists, as well as improving productivity through innovative models of care, and improving theatre efficiency.
“Hospitals will probably need to allocate some resources just to cataracts, which in a stretched service might reduce access to other types of eye surgery,” Dr Jesse Gale told Radio NZ on behalf of RANZCO.
He said the plan to outsource some operations to private ophthalmologists could be effective as long as the price was right.
But he wasn’t sure how the government was going to improve productivity when all public hospitals were already working hard to be efficient.

In seven short years, George & Matilda Eyecare (G&M) has built an expansive network alongside high-powered Australian optometrists. Much of its success comes down to a desire to innovate not only in technology, but its operating model. The latest – and most intriguing – way it is doing this is the addition of a new allied health stream.
Globally, audiology has emerged as an ideal adjunct sensory service in optometry practices. Able to operate out of the same premises and serve the same patient base, the model can be executed at scale, and is well-established in overseas markets like the UK. The concept has been gaining traction in Australia too where the number of people with hearing impairment is expected to double to 7.8 million people by 2060.
Supporting over 100 Australian communities, G&M has seized this opportunity to elevate the patient experience by becoming one of Australia’s newest audiology providers, seeking to offer a service beyond industry norms.
The rollout began in May 2023 via a pilot at George & Matilda Eyecare for Antonello Palmisani Optometrist, the company’s Leichhardt practice in Sydney, coinciding with a relocation of the practice and new fit out.
G&M’s foray into audiology is being underpinned by two key appointments with Mr Ant Hudson, G&M’s new general manager of audiology, and Ms Roshni Joseph, clinical audiologist at Leichhardt, who are responsible for devising the company’s audiology blueprint.

In Hudson, G&M has someone with rare, high-level experience across optometry and audiology. Prior to coming on board, he was the national sales and operations director for Audika, responsible for leading the clinical teams across more than 300 hearing care clinics in Australia (Audika is part of the Demant Group, one of the largest global manufacturers within the hearing care industry). In eyecare, he also spent six years with Luxottica as vice president of optical, leading the OPSM and Laubman & Pank optical teams across Australia and New Zealand.
He says integrating audiology into an optometry network makes sense, being able to leverage the pre-existing premises, front-of-house staff, and patient base. In terms of goodwill and trust, much of the legwork has already been done.
“Our G&M practices proudly have long-standing and strong relationships with our patients, having provided outstanding care to them for decades. Our patients trust our optometrists and dispensing teams and have high levels

of confidence in the optical services which we provide,” he says.
“Our practices now have an opportunity to provide more holistic care to our patients, by adding audiology services. Providing both optical and audiology services will increase our leadership standing within our local communities as we continue to place the health and wellbeing of our patients first and foremost.”
Starting with a guiding characteristic of “patient first” care at G&M and a blank canvass, Hudson has been excited by the opportunity to re-imagine how the future of Australian audiology may appear.
“We will have several key differences compared to what else is offered in the industry. A great example of this will be the introduction of cerumen management (ear wax removal) as an additional service available in our practice, rather than sending patients away to their GPs to have excessive ear wax removed. This is not a standard service within the industry,” he explains.
“Being proudly Australian, we are an alternative to the corporates from abroad. We are locally owned, managed and operated, and taking insights from our ‘patient first’ experience through optical digital imaging, we will show every patient what is happening inside their ears, through the use of video otoscopy in every practice. This also currently isn’t a standard practice within the industry.”
Given that audiology will be added to an existing optical business model, Hudson says G&M can offer highly competitive pricing by industry standards.
“Our ambition is to help patients get the best possible solutions for their hearing. In addition to very competitive hearing aid prices, if patients choose to purchase rechargeable hearing aids from us, we will provide them with a free charger for their hearing aids. Most of the industry charge a fee of up to $500 for a charger,” he says.
“We are that confident in our pricing that we will guarantee a price match on any identical hearing aids supplied from another physical practice or clinic.”
While the Leichhardt practice will be the template for a comprehensive audiology service at other G&M practices in future, the rollout may not look the same across the board.
In Leichhardt for example, G&M has built a fully soundproof testing room. By soundproofing the entire room, this has removed the need for patients to be placed inside “the old claustrophobic sound booth” during their hearing assessments, Hudson says.
Audiology is presenting as a new way for existing optometry practices to elevate their service. This trend hasn’t been lost on the decision makers at George & Matilda Eyecare, which has now completed its first audiology integration in Sydney.Optometrist Antonello Palmisani (right) and audiologist Roshni Joseph in the newly fitted Leichhardt practice.
“Ideally, we are looking to provide the full audiology service within an existing practice, however in some instances, we may not have sufficient space to provide a ‘patient first’ experience. In these instances, we will be looking to complete initial hearing screenings with our patients and then if required refer our patients to our closet practice, which provides the full audiology services,” he says.

THE AUDIOLOGY OPPORTUNITY
Globally, Hudson says it’s accepted that audiology and optometry can co-exist,


join was Ms Roshni Joseph, who Hudson knew from Audika. Wanting to pop the “clinical bubble” of her previous role, she was equally nervous and excited to join the new venture.
With a background in behavioural therapy before moving into audiology 6.5 years ago, she has relished the chance to help shape a new audiology program.
“Being able to develop procedures and protocols so that we can deliver a high level of care – and an easier way of accessing it privately – is one of the biggest reasons I was keen to take on the role,” she says. “At this early stage, there’s
“AUDIOLOGY SERVICES ARE NOW IN THE OPTICAL SPACE AND THEY ARE HERE TO STAY. WE HAVE AN OPPORTUNITY TO EMBRACE THE CHANGE AND PROVIDE AN EVEN GREATER LEVEL OF CARE TO OUR PATIENTS.”
ANT HUDSON GEORGE & MATILDAThe practice has served the Leichhardt community for 23 years in NSW.
future, we are also looking at a scanner to take impressions of people’s ears when they need hearing aids, which will speed up that process.”
For optometrist Mr Antonello Palmisani, who has served the Leichhardt community for 23 years, the opportunity to add audiology to the practice came as he sought to leave the practice’s shopping centre location, in search of a new high street premises.

The move into audiology made sense to him, with there being many parallels between optometry and audiology, including the vestibular ocular reflex which shares the cranial nerve (and keeps people steady and balanced even though
the eyes and head are moving), as well as the fact that vision and hearing are the two most important senses for survival.
The aging population is also important to both sectors.
“My practice already has a significant following, so if people in that age group come in, or someone has any concerns, I can now provide this extra service. But more importantly, it’s the type of service; the audiology care here is unbelievable, so that was important for me, to maintain a high standard of care.”
A major part of G&M’s value proposition for independents who join its network has been its ability to provide comprehensive back-end office support, as well as access to technology and operational data insights – all while protecting the optometrist’s clinical freedom. Palmisani says this was a wise strategic decision by G&M, and the addition of audiology is another shrewd move.


“Providing two essential services under the one roof makes sense. People won’t perhaps visit an audiology practice randomly on the street, but people do to browse eyewear, so having this opportunity to explore any concerns they may have with their hearing in a familiar, safe environment works well.”
Palmisani says there are no plans to impose the audiology service on optical patients when they visit. He prefers word-of-mouth marketing and many patients have become aware of the service purely because it is written on the shopfront.
While it’s early days, Hudson says G&M is delighted with the way patients are responding to the additional care within the Leichhardt practice.
“We are very fortunate to be working with some fantastic supply partners and continue to seek out best practices from across the globe, with the ambition to continue to raise the bar in ‘patient first’ care within the Australian audiology industry,” he says.
“Audiology services are now in the optical space and they are here to stay. We have an opportunity to embrace the change and provide an even greater level of care to our patients.”
G&M has built a fully soundproof testing room, removing the need for patients to be placed in a booth during hearing assessments.Leader in hand-held Fundus Imaging

Expanded 50 degree field of view



Sleek moder n design
Versatile and compact
Clear Fundus & Anterior Eye imaging
High resolution q uality display screen
Autofocus and AutoExposure
Integrated image quality analysis
9 Internal fixation points for Peripheral imaging
WLAN or USB connectivity


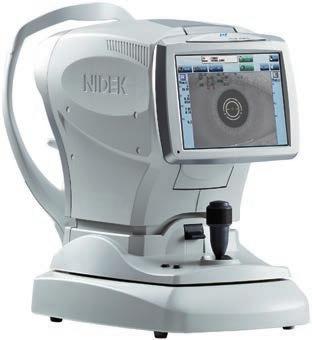
For Myopia management – predict and monitor the progression of myopia.












Simple operation with 3D Auto tracking and Auto shot.
Myopia risk evaluation can be monitored and assessed against typical AL growth rates.
The MV-1 software presents trend reports influenced by treatment and patient behaviour.
Virtual Reality Visual F ield device - incorporates complete Visual Field analysis.
Detailed progression analysis and t he most versatile & efficient vision screening t echnology.





Latest technology provides the same reliability and reports as the “gold standard”.
Supplied complete with a Tablet PC - BlueTooth interface with the VF2000 NEO.
Compact/Space-saving/Portable - can be used anywhere, no need for a darkened room.
Active eye tracking – enhances reliability.























Full and Fast Thresholds VF Testing plus Neuro, Kinetic, Ptosis and Esterman tests
FDT Testing
Stereopsis
Visual Acuity and Contrast Sensitivity
Colour Testing
(Ishihara, D15 and Advanced Colour Tests)
Eye Mobility and Strabismus
Ms Kirby Phillips had the mindset of most other graduates when she began her optometry career at OPSM Maroochydore in 2019: to become a highly effective clinician that improved the lives of her patients. But within four short years, her role at EssilorLuxottica has transformed into something far beyond what she imagined.

For starters, she has swapped out the consulting room in sunny Queensland for the group’s Australasian head office in North Sydney – and rather than building rapport with patients, she is now managing business-to-business relationships with private health insurance companies and educating policyholders on eye health.
In her new position as the EssilorLuxottica health funds relationship manager ANZ, she is also helping shape the company’s strategy for the region as part of the senior leadership team. Her appointment – in March 2023 – is part of a deeper commitment within the business to elevate OPSM and Laubman & Pank optometrists into more influential roles beyond the consulting room.



Mr Carl James, senior vice president of store operations ANZ for EssilorLuxottica, is helping drive this change, saying that the company has upped its investment within the eyecare team.
“Recently, we made the decision that our optometrists should be recruited by optometrists, managed by optometrists and developed by optometrists. In turn, we are seeing an expanded scope of responsibility among our optometrists, and it’s working with more optometrists joining us than ever before,” he says.



“We’re proud that we’ve now got a much more diverse representation of optometrists at the senior leadership level. It demonstrates our commitment to eyecare in Australia and New Zealand because we’ve now got around 10% of our senior leadership group who were clinicians. This means they’re

“Today, I take many of those problem-solving skills to my role working with the different health funds that EssilorLuxottica has partnered with. This involves nurturing the relationship and developing special offers for their members that health funds, in turn, make known to their members through communications. It also involves written clinical content for eye health awareness issues such as diabetes to help educate their members about the importance of regular eye tests.”
For Phillips, it has been a rapid rise through the ranks. Three years after graduating, she was promoted to the position of area eyecare manager for the Queensland North region. In this capacity, she acted as a “work coach”, helping set up optometrists for success whether it be navigating complex clinical cases, or ensuring their practices and equipment are fully functional, among other responsibilities.
But her big break came when she recently presented before EssilorLuxottica ANZ executives. Phillips was approached to join the company’s Accelerate Program that develops "high potential people" within the business. The course culminated in her taking part in a group business pitch on why EssilorLuxottica should have a greater presence in the metaverse.
Having impressed the executive team with her presentation, a few weeks later Kirby was mapping out her future within the business with James, leading to her recent promotion.
As is the case for many optometrists early in their career, Phillips wasn’t initially aware of the breadth of non-clinical opportunities for optometrists in Australia. During her studies, she thought the options were mainly limited to the consulting room or lecturing at universities. What she has come to appreciate is the number of transferrable skills her optometric experience has provided.
“Explaining complex clinical issues to a lay person is something that we do as optometrists all the time, and that’s a skill that I have been able to apply in this role speaking to health funds and their members,” she says.
“Having experience in the clinical environment also gives me exposure to many different departments within the business. For example, people
Many people pursue an optometry career to improve the lives of patients, while others seek a work-life balance, safe work environment and stable employment. There are also opportunities to move into leadership and influence the eyecare agenda.EssilorLuxottica ANZ’s head office in North Sydney, overlooking Darling Harbour where many optometrists hold leadership positions. Kirby Phillips was recently promoted as EssilorLuxottica health funds relationship manager ANZ.
in operations will have a concept and ask whether it could be feasible in our stores. EssilorLuxottica also gave me a scholarship to complete the Australian College of Optometry’s Certificate in Public Health and Leadership in Eye Care, which speaks to the role that optometrists play as leaders in the practice. Being an optometrist, we are that source of truth for patients and a reference point in the practice, so being a person people can go to has helped when transferring into the support office where we’re often looking for solutions to different problems or problems that don’t even exist yet.”
For James, the role of senior vice president of store operations for EssilorLuxottica ANZ is one that involves oversight of many functions: eyecare (arguably the most critical), franchising and business development, retail operations and services, store excellence (lens capability and dispensing), customer service, and project management (to deploy technology initiatives), and operational analytics, all come under his remit.
As a trained optometrist, he’s also helping advocate for and inspiring the next generation of EssilorLuxottica optometrists with an entrepreneurial streak. When optometrists graduate, at this early stage, their focus is often on passing their course, getting through their first year and learning to become a great optometrist.
“In my role, I’m lucky to meet each new graduate. We bring them together once a year and I get the opportunity to talk to them particularly about my career journey, and many are surprised at what those opportunities are and what’s available to them outside the consulting room,” he says.
“Over the last couple of years, I’ve noticed a much greater desire among the new graduate cohort to have those discussions. When they realise those opportunities exist, the very next question is: ‘What do I need to do to get there?’. There’s been a shift from new graduates being 100% focused on becoming great clinical optometrists to now realising there’s a bigger world out there and other roles they can perform with their skillsets.”
To understand the leadership options within EssilorLuxottica, James says it’s important to understand the career paths on offer.
The majority of optometrists are on a pure clinical path delivering community eyecare. However, those seeking to influence beyond the
consulting room can start out by joining advisory panels for areas such as contact lenses, the eyecare strategy, and myopia management.
From there, EssilorLuxottica has around 50 managing optometrists in ANZ who work in larger locations alongside the store manager, in both a clinical and non-clinical capacity, to ensure those practices are maximising customer outcomes.
“This is an opportunity for optometrists to start developing more commercial acumen and become more involved more in the day-to-day running of the store. This role can be performed store-based, with 80-90% of their time consulting.”
From there, the company offers various “field-based roles”, which are the traditional succession path for optometrists – showing commercial or strategic aptitude – to move into leadership roles. This involves the area eyecare manager team, of which there are 11, and five professional services manager roles, and an eyecare country manager in New Zealand.

“This team is responsible for the recruitment, engagement, development and performance management. They essentially work full time with individual optometrists on improving their skills, ensuring they’re engaged and getting the development they want, while also supporting the commercial outcomes of the organisation. This is often the gateway to more senior roles in the organisation for optometrists.”
Today, the company has several recent examples of optometrists moving into leadership roles, including:
• Elizabeth Kodari, state director optical NSW/ACT
• Lucas Lister, retail projects senior manager
• S ephora Miao, senior manager of eyecare operations
• Astha Rai, professional services manager NSW/ACT (relocated from NZ)
• H ayley Gobell, professional services manager, SA
• Daniel Rezaeian, customer relationship management analyst
• N ina Chai, optometry engagement manager
James says the company is proud to have more optometrists influencing the eyecare agenda. Many of those have been identified through the Accelerate Program, the 12-month course that is available not only to emerging optometrists, but also dispensers, store managers, marketing managers, and more.
“The fundamental commonality across each of these examples is that they’re not just great clinical optometrists, but they also possess the necessary soft skills,” he says.
“Beyond that, they have an aptitude for leadership, a growth mindset and a strategic mindset. Communication skills are an absolute must, and in an organisation of our size, the ability to build and maintain relationships is key. A lot of these people are now working with important stakeholders in Milan, Paris or the US, so the ability to build those relationships – face-to-face as well as over a Teams meeting or email – is critical.”
Born as a triplet, Ms Tegan Matheson learned from a young age the fine art of maximising different personalities and strengths within teams. It’s an attribute


“AS
TEGAN
AN OPTOMETRIST, IT’S MORE FACE-TO-FACE AND DEALING WITH THINGS ON A GRASSROOTS LEVEL, WHICH IS EQUALLY AS HARD, BUT IN THIS ROLE I’M ABLE TO DRIVE CHANGE ON A BIGGER SCALE.”
MATHESON COUNTRY EYECARE MANAGER NZCARL JAMES SENIOR VICE PRESIDENT OF STORE OPERATIONS

Similar to Phillips, it’s a quick elevation after graduating in 2017, but Matheson’s relationship with the company began nine years earlier in 2014 as an optical dispenser. During her placement as an optometry student, she upskilled in orthokeratology (orthok) and intense pulsed light (IPL) therapy for dry eye, which she completed upon graduating. By this point, her consults were also as long as well-established optometrists within the group. In other words, she was an eager and rising talent.

Matheson is also passionate about supporting other optometrists and has helped many develop their skills in the premium eyecare space. She then moved into regional relief work which took her stores across Victoria and Tasmania and tested the robustness of her clinical skills.
This saw her become the area eyecare manager for Victoria and Tasmania, which was the ideal introduction into the commercial aspect
of optometry practices. Then, in March 2023, she started overseeing the eyecare operations for New Zealand, comprising around 50 practices.
“I say yes to every opportunity that comes my way, and I love a challenge. It’s been nice to bring a different leadership style to the role. I believe you can still lead with empathy, and we are getting really good results.”
In her current role, Matheson oversees OPSM’s eyecare strategy in New Zealand, with two area eyecare managers reporting to her, as well as six managing optometrists. In addition, she is leading myopia control for EssilorLuxottica Australia and New Zealand – leveraging her skills in orthok and with the new Essilor Stellest spectacle lens – and will continue offering her time to the OneSight EssilorLuxottica Foundation that runs clinics for disadvantaged communities.
“One of the biggest differences in this role is the scope of responsibility, whether that’s running engagement events, having an active role in recruitment and analysing store data,” she says.
“As an optometrist, it’s more face-to-face and dealing with things on a grassroots level, which is equally as hard, but in this role I’m able to drive change on a bigger scale. In saying that I do love being an optometrist, so every time I visit a store, I try perform testing and offer support in the clinical space. And when I attend OneSight clinics, we can see up to 200 people a day, which keeps my clinical skills up to scratch.”
She adds: “I think it’s great the company is building an internal talent pipeline of optometrists. Being able to go into a store and still answer the phone, or do basic repair, makes you relatable as a leader. Your clinical experience makes you aware of the grassroots issues; if you don’t understand these, how are you meant to implement change? It’s inspiring for younger optometrists, or any optometrists, knowing there are opportunities to use and elevate their strengths outside the consultation room if they wish to go down this path within EssilorLuxottica.”
Just 24 per cent of people who are blind or have low vision in Australia are in fulltime employment, a statistic that drove the development of the new Life Ready Program.


The program is designed for children aged 0-25 because starting early gives children time to acquire skill, learn strategies and build a level of self-belief to manage future obstacles.
Founded upon internationally recognised curriculum to deliver best practice, evidence-based solutions, access technology, and expert guidance to help paediatric patients develop the skills and confidence to achieve true meaningful participation and life-long employment.
1300 84 74 66
“WE’RE PROUD THAT WE’VE NOW GOT A MUCH MORE DIVERSE REPRESENTATION OF OPTOMETRISTS AT THE SENIOR LEADERSHIP LEVEL. IT DEMONSTRATES OUR COMMITMENT TO EYECARE IN AUSTRALIA AND NEW ZEALAND.”
ANZ
iCare EIDON presents a more colour-balanced retinal image with greater richness allowing for improved discriminative power and diagnostic accuracy, providing a precise documentation of retinal structures.1

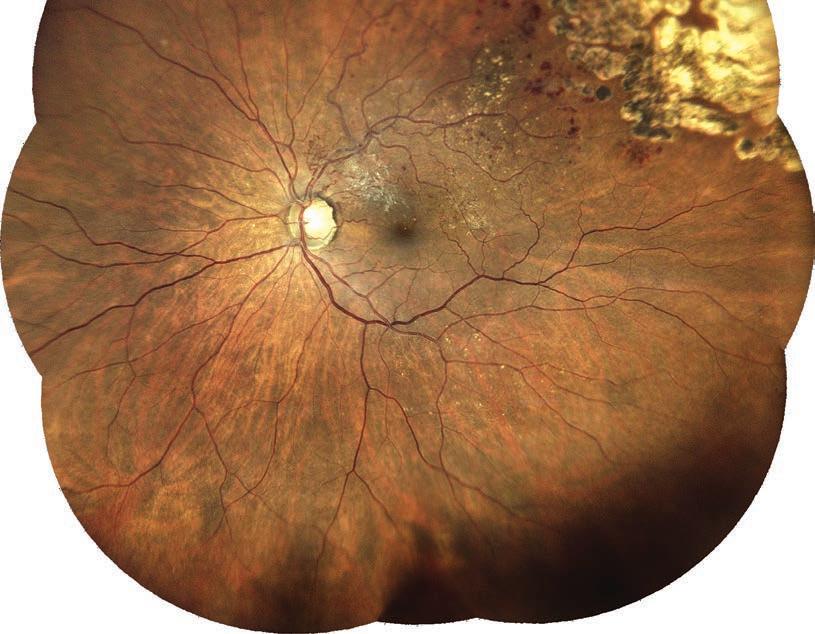

iCare Tonometers are fast and reliable tools designed to help in the process of detecting and monitoring glaucoma. They are easy to use, and measurements do not require anesthetic drops or calibration.

+ 20 years of experience in versatile clinical tonometers. Suitable for patients of all ages and even for post-surgical applications.
+ Over 200 clinical studies and white papers confirm the reliability and reproducibility of the measurements.
+ 200 degrees positional freedom with the iCare IC200 tonometer.
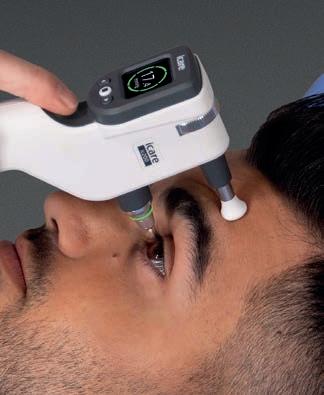
Enhanced image quality revealing details invisible to others1

Since 2002, the Pentacam has revolutionised examination of the total cornea and anterior segment, with detailed 3D imaging and extensive normative analyses.

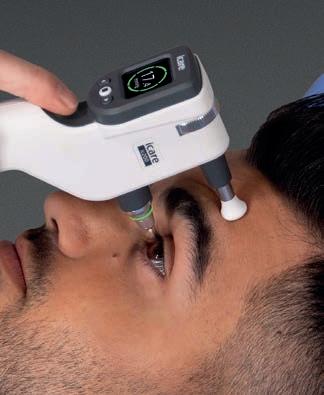
Offering complete anterior eye segment screening in a matter of seconds, all models of the Pentacam® family provides a comprehensive range of in-depth analysis and reporting to suit the needs of your practice.
OCULUS Myopia Master® combines the most important parameters to make Myopia Management easier than ever. It measures refraction, axial length and keratometry in one stylish unit, backed by the most comprehensive myopia software suite.
Utilising the latest Brien Holden Vision Institute data, you can create personalised reports detailing current myopia status and the likely outcome in adulthood, plus track the progress of any treatments prescribed.
These BHVI data sets, with diverse strata of age, gender and ethnicity, improve modelling in a wider patient cohort and enhance parent counselling – giving you confidence without compromise.

T 1800 225 307
E enquiries@dfv.com.au
dfv.com.au
In September 2023, the doors will open on the largest optometric event in the region when O=MEGA23 combines with the 4th World Congress of Optometry. Insight details some of the most thought-provoking sessions, and speaks to practice owners about their motivation for attending.
The rare combination of a national and international optical event has presented organisers of O=MEGA23 and the 4th World Congress of Optometry (O=MEGA23/WCO4) with a unique opportunity to create a program that will be of value to the full gamut of the optical sector – with the benefits of attendance to prolong for years after.



Event partners Optometry Victoria South Australia (OV/SA), the Optical Distributors and Manufacturers Association (ODMA) and the World Council of Optometry (WCO) have poured many months into jointly planning Australia’s biggest eyecare and eyewear fair with the most credentialed and largest optometric clinical conference in the Southern Hemisphere.
The event (8-10 September in Melbourne) presents a chance to showcase Australian optometry on the world stage – as well as shine a light on the importance of practice managers and optical dispensers. To that end, this year’s O=MEGA23/WCO4 will feature a Masterclass program that will for the first time comprise two separate streams for each profession.

As the weeks countdown to the official opening with a traditional Welcome to Country, Ms Amanda Trotman – who stepped in as ODMA’s acting CEO midway through the planning stages and has since been appointed permanent CEO – says the dynamic event is an opportunity that comes around rarely.
“Time is running out to secure your space at this unique event opportunity and to plan ahead so that you really make an investment that will reap rewards for you and your team well into the future,” she says.
“Join in as the industry comes together and ensure you don’t suffer from the fear of missing out.”
Trotman expects the trade fair will be a bustling space, with 85 exhibitors on the trade floor.
“At the trade fair you will discover cutting-edge brands and the latest
technology and innovations presented to you by the experts that can explain how to use their offering to enhance your practice and profits,” she says.
Ms Belinda Musitano, qualified optical dispenser and director of three practices in Western Australia, is travelling to Melbourne with two of her staff to attend the event.


“As a practice owner, I invest in my staff (and myself) attending events such as O=MEGA for a number of reasons. It boosts motivation and enthusiasm in their job, bringing them home full of new ideas that can be implemented in store,” she says.
“It also breaks the everyday routine of ‘this is how we do it’ and challenges us to change our thoughts and patterns around how we practise, how to be more innovative and offer a point-of-difference. Events such as O=MEGA also give us the exposure to new equipment, brands and meeting new people. I personally always come back with a notebook of many areas I would like to introduce to make our patients' experience in my practices the best they can be.”
PRACTICE“I INVEST IN MY STAFF (AND MYSELF) ATTENDING EVENTS SUCH AS O=MEGA FOR SEVERAL REASONS. IT BOOSTS MOTIVATION AND ENTHUSIASM, BRINGING THEM HOME FULL OF NEW IDEAS THAT CAN BE IMPLEMENTED IN STORE.”
BELINDA MUSITANO
OWNER
Optometry practice owner Mr Jim Papas, who established eyeclarity in Sunbury in 1986 and who is presenting a Masterclass at the event, says he can attest to the value of attending O=MEGA23/WCO4 for three days of world-class education.

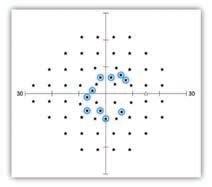
“The clinical conference offers up-to-date clinical content that is essential for providing the best possible care to our patients. And the trade fair provides a unique opportunity to see the latest equipment and treatments all in one place, saving you time and money,” he says.



“This is an opportunity to connect with your peers and stay up-to-date with the latest developments in eyecare. This is the premier event for the global eyecare community and not to be missed.”
ODMA, OV/SA and WCO invited two internationally renowned keynote speakers who will each deliver multiple presentations throughout the clinical conference.
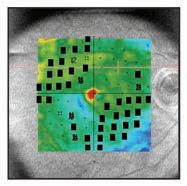
“We are delighted to confirm Professor James Wolffsohn and Professor Susan Cotter as our keynote speakers,” Trotman says.
OV/SA CEO Ms Ilsa Hampton is excited about the event: “Susan and James lead the clinical program which has more streams than ever, features both international and local speakers, and given the event is on the global stage in partnership with the 4th World Congress of Optometry, incorporates the latest research and the opportunity for real sharing of ideas from a world of optical experience.”
WCO managing director Ms Alyssa Callaghan says it is a great time to get the optometric community together after COVID lockdowns forced the event to be postponed from 2021.
“We are delighted to have such a strong combined program with O=MEGA, and know that members of the international community are looking forward to connecting with their colleagues Down Under.”
In addition to the clinical conference program, there are streams of Masterclasses with dispensing and practice management topics. In the Trade Fair Knowledge Area, there will be short, sharp tips and techniques sessions provided free-of-charge, plus there are the exhibitors providing in-depth demos on their booths.

“No matter what the practice or what stage of their career attendees are at, they cannot fail to learn and be inspired by this year’s content,” Trotman adds.

Prof JAMES WOLFFSOHN, a Professor of Optometry at Aston University since 2000 and a popular figure on the ophthalmic speaker circuit, is presenting on topics ranging from digital eye strain to procedures for dry eye management and the power of consensus.

“How many hours have you spent on a digital device already today?” Wolffsohn asks
“Reports suggest between 33% and 97% of the population get eye strain when immersed in a digital environment based on current questionnaires, but is this just a manifestation
His presentation on digital eye strain will address how best to define digital eye strain; what the current thinking is on the mechanisms of eye strain in digital environments; and what management strategies are supported by scientific evidence.
“Do marketed therapies such as blue light blocking help? The Tear Film & Ocular Surface Society (TFOS) Lifestyle reports has recently explored the evidence base on this topic, which will be presented at O=MEGA23,” he says.
Wolffsohn, who is head of the School of Optometry and head of the Department of Audiology at Aston, will also speak about changing procedures for dry eye management.
“TFOS DEWS II established a new consensus definition for dry
eye and derived a diagnosis based on symptoms, using one of two established questionnaires, and homeostasis loss signs including non-invasive breakup time, osmolarity and ocular surface staining, in 2017,” he says.
“Management could only be presented in stages due to the lack of comparative trials. However, time has moved on, so what evidence do we have that should influence our choice of artificial tears and in-office therapies such as intense pulsed light therapy or photobiomodulation?” he asks, hinting at the content of his presentation.
Wolffsohn’s third presentation, titled The Power of Consensus, will show delegates how consensus reports are developed and how they can be utilised.
“In practice there can be a conflict between clinical intuition, based on experience, and the need for standardisation, based on research evidence. Where should there be latitude and when is there need for prescriptive practice? Using a series of examples, this topic will be explored along with highlighting new resources in the optometry field that can be easily accessed to enhance practice standards,” he says.
Dr SUSAN COTTER is president of the American Academy of Optometry, co-chair of the Paediatric Eye Disease Investigator Group, and a Professor of Optometry at Marshall B. Ketchum University. Among the topics she’s discussing is whether correcting refractive error can change a child’s life trajectory.

“Moderate hyperopia left uncorrected in preschool years may have long-term ramifications, and not just with aspects of visual function such as visual acuity, stereoacuity, and eye alignment,” she says.
“The VIP-HIP research group found that many of these children perform worse on tests of early literacy, sustained attention, visual-motor integration, and visual perception. Optometrists and ophthalmologists need to pay more attention to these children because research suggests that when undetected or left uncorrected, moderate hyperopia in young children could have a significant adverse effect on academic and economic opportunities throughout life.”
In a separate lecture, Cotter will be discussing the risks and rewards of overminus lens treatment for intermittent exotropia (IXT).
“I describe the results from the recent Pediatric Eye Disease Investigator Group (PEDIG) randomised clinical trial of children with IXT that evaluated the effectiveness of overminus lenses for improving distance control of their IXT as ‘good news and bad news’,” she says.
“The good news was that the overminus lens group had significantly better IXT control at distance when assessed in their overminus glasses after 12 months of treatment compared with the


children in the non-overminus glasses control group. The bad news I will save for the presentation.”
Lastly, Cotter is broaching the subject of ChatGPT in eyecare. A study published in JAMA Ophthalmology this year found the artificial intelligence (AI) tool answered less than half of the questions correctly in an exam resource commonly used by trainees preparing for ophthalmology certification.
“From patient consultations and educational resources to research and diagnostic support, ChatGPT has the potential to revolutionise the way eyecare professionals interact with their patients and enhance the quality of care provided,” Cotter says.
Her presentation will delve into the advantages and challenges of integrating ChatGPT into eyecare practices.
“Implementing ChatGPT in eyecare presents unique challenges, because there are potential pitfalls, biases, and uncertainties associated with its use in medical contexts,” she says.
“One must consider the ethical considerations related to patient privacy, informed consent, and the responsibility of human oversight when utilising ChatGPT in eyecare practice. While ChatGPT’s potential to enhance patient care is enormous, its limitations are not trivial. The question is, how can we maximise the benefits while mitigating the risks of ChatGPT integration into the eyecare practice?”
Australian optometrist JIM PAPAS will discuss his involvement with the world’s first red light therapy to manage myopia at ho me
In the Masterclass Dispensing Stream, Mr Jim Papas will share his experience and observations on repeated low-level red-light therapy for myopia control. In addition to managing eyeclarity, Papas is also clinical director of Eyerising International.
The Melbourne-based med-tech company launched Myproclear, described as the world’s first red light therapy to manage myopia at home, at the Asia Pacific Academy of Ophthalmology Congress e arlier this year.

“Repeated low-level red-light therapy is an emerging treatment; early evidence shows it is close to 90% effective in arresting myopia progression, shortens axial length in almost 25% of children, with minimal rebound effect if treatment is stopped, and very safe to use,” Papas says.
“This is an at-home treatment which is done three minutes twice a day, four hours apart, five days per week, usually done before and after school and we have shown there is a high compliance rate.” Papas’ masterclass session will elaborate more on its effectiveness, axial length recovery and the business model to allow an understanding of the treatment’s effectiveness.
Australian-based 2022 International Optician of the Year GRANT HANNAFORD will be discussing artificial intelligence (AI) and the future of lenses.

“Ophthalmic optics has long been an area in which developments in computational techniques have found rapid applications. My presentation (in the Practice Management Stream) will examine core concepts and techniques in the application of big data to models implementing machine learning and artificial intelligence,” he says.
“From a foundation of linear regression and iterative
models, I’ll discuss general cases which demonstrate a common pathway used in machine learning. This process is then developed in the context firstly of lens design optimisation, then postural integration into lens design, and the incorporation of large biometric data sets into normative sets for the application of biometric data to lens designs.”
Hannaford’s masterclass will also discuss some of the risks contained in the implementation of machine learning in lens design, and some of the legal and ethical framework surrounding these techniques and applications.
Rodenstock’s ColorMatic® 3 lenses change from clear to dark and fade back to clear again 30% faster than the previous generation – making them our fastest photochromic lenses ever.

For more information, speak to your Rodenstock Account Manager.
Available with Biometric Intelligent Glasses
KATE HALL, the national retail operations manager for the independent optometry network ProVision, will feature in the Practice Management Stream on inventory management to maximise profits.
“Managing stock efficiently is paramount for the success of optometry practices, and there are four compelling reasons why it should be a top priority,” Hall says. “First and foremost, it allows practitioners to control their spend, ensuring that financial resources are allocated wisely. By optimising stock levels, practitioners can avoid unnecessary expenses and make better purchasing decisions.
“Secondly, effective stock management directly impacts sales and conversion rates. Having the right products in stock at the right time not only satisfies patient needs but also improves their overall experience. This, in turn, leads to increased sales and customer satisfaction.”
Hall says another vital aspect of managing stock effectively is streamlining cash flow.
“By managing stock effectively, optometry practices can ensure that their
cash flow remains consistent and healthy. Unnecessary stock holding ties up capital that could be invested elsewhere, so finding the right balance is crucial,” she says.
“Managing stock with a strategic approach directly contributes to growing profitability. By refining inventory management practises, practitioners can decrease stock holdings, improve product offerings, and make smarter buying decisions, ultimately boosting profitability.”
Hall will be sharing practical strategies specifically tailored for optometry practices.

“We’ll dive into topics such as leveraging supplier partnerships, reducing aged inventory, creating a comprehensive range and buying plan, and simplifying ordering processes," she says.
“The goal is to equip optometry practitioners with the knowledge and tools they need to optimise their stock management processes, ultimately elevating their practice’s profitability.”
MARK CORDUFF, business services manager at ProVision, will also present in the Practice Management Stream discussing the key components to an effective exit strategy.
With a significant number of practice owners nationally planning their retirement, Corduff’s role at ProVision includes assisting owners plan, then execute, their succession plans.
“There are a number of different options available to practice owners. At O=MEGA23, I will be presenting the key considerations owners should be looking at
FRIDAY 8 SEPTEMBER
Practice Management Stream
• Personalities in practice
Emma Gillies, Purple Consulting
• AI and the future of lenses
Grant Hannaford AAOO, Hannaford Eyewear, UNSW
• 7 tips for practice management
Belinda Musitano, Eyes@Optometry
• Succession planning
Mark Corduff, ProVision
Dispensing S tream
• Practical lens dispensing – 5 skills you can’t do without
Steve Daras, TAFE NSW
• Final checking – the las t word on spectacle quality control
James Gibbins, ACOD
• Accurate measurements for dispensing
Steve Daras, TAFE NSW
• Myopia management for the optical dispenser
Grant Hannaford AAOO, Hannaford Eyewear, UNSW
SATURDAY 9 SEPTEMBER
Practice Management Stream
• Building a m yopia specialty practice within a practice / Myopia management for children
Matt Oerding, Treehouse Eyes USA, and Emma Gillies, Purple Consulting
• AI and the future of lenses
Grant Hannaford, Hannaford Eyewear, UNSW
• 7 tips for practice management

Belinda Musitano, Eyes@Optometry

• Succession planning
Corduff, ProVision
• In ventory management to maximise profits
Kate Hall, ProVision
so they can successfully retire, ensure their patients receive the same care in the future, as well as maximising a return on their investment,” he says.
“Expect insightful information on what needs to be prepared in a lead up to a sale, how to attract potential buyers, how a practice is valued and who you need on your side to support you through the process. The aim of the presentation is that the audience walk away informed, with some tools to start a successful plan of their own.”
Dispensing S tream
• A dispens er's guide to understanding lens and lifestyle needs for patients with presbyopia
April Petrusma, Optical Dispensers Australia
• 5 common m yths or misconceptions to avoid when dispensing
Steve Daras, TAFE NSW
• Myopia control – repeated low level red light therapy
Jim Papas, Eyerising International
• Clinic al lens applications for paediatrics
Grant Hannaford, Hannaford Eyewear, UNSW
• Top 10 tips for quality dispensing
Steve Daras, TAFE NSW
SUNDAY 10 SEPTEMBER
Practice Management Stream
• Skills for trust-based selling
Emma Gillies, Purple Consulting
• AI and the future of lenses
Grant Hannaford AAOO, Hannaford Eyewear, UNSW
• In ventory management to maximise profits
Kate Hall, ProVision
Dispensing S tream
• Myopia management for the optical dispenser
Grant Hannaford AAOO, Hannaford Eyewear, UNSW
• A dispens er's guide to understanding lens and lifestyle needs for patients with presbyopia
April Petrusma, Optical Dispensers Australia
• Accurate measurements for dispensing
Steve Daras, TAFE NSW
NOTE: Masterclasses can be bought in addition to the conference, or on their own for those wishing to only attend Masterclass workshops. They run alongside the Clinical Conference with Practice Management and Dispensing streams. There are some 4pm and 5pm sessions for those only able to attend outside business hours.



Oral options: what our patients can put in their mouths to help their dry dye
Adele Jefferies
Matthews Eyecare, Cornea and Contact Lens Society of New Zealand, New Zealand Association of Optometrists
9-10am
Learning objectives
• Unders tand the current benefits, risks and prescribing recommendations of oral medications in the management of dry eye disease in Australia and New Zealand
• Unders tand how some lifestyle habits can impact signs and symptoms of dry eye disease
• Unders tand the current evidence surrounding nutrition, including essential fatty acids, and its impact on dry eye disease
Unanswered questions in myopia management
Myopia management
Kate Gifford 1 and Paul Gifford 2
1 Myopia Profile Pty Ltd, Queensland University of Technology
With abstracts from 26 countries, the clinical program for O=MEGA23/WCO4 has been curated to offer a broad base of subjects for delegates to choose a personalised schedule for their areas of interest.
The latest research and insights will be presented in various forms: keynote presentations, full lectures, short paper presentations, dedicated sponsor sessions and poster sessions. For optometrists, sessions will be accredited for continuing professional development (CPD) hours/points.
Insight has canvassed the program and listed
Friday 8 September
What can corneal immune cells and sensory nerves tell us about eye and systemic health?
Anterior eye and oral medication
Laura Downie 1 and Holly Chinnery 1
1The University of Melbourne
10.30-11.30am
Learning Objectives
• Des cribe the immune cell subtypes in the cornea, and how these cells are important for maintaining the health of the ocular surface and for deriving therapeutic effects
• Appreciate how corneal in vivo confocal microscopy can be used as a non-invasive tool that provides unique insight into eye and systemic disease, and the use of different therapies
• Unders tand the bidirectional interaction between corneal immune cells and sensory nerves, and how this interplay can be leveraged to develop new therapies to treat corneal disease
Combination of low-dose atropine and optical myopia control methods in children with myopia progression
Myopia management
Joanna Przeździecka-Dołyk 1, Aleksandra Danielska 2
1 Ophthalmology Clinical Centre SPEKTRUM, Wrocław
University of Science and Technology, Polish Society of Ophthalmologists
2 Ophthalmology Clinical Centre SPEKTRUM
below some oral presentations taking place at the Melbourne Convention and Exhibition Centre that might be of interest to Australian optometrists, covering many hot topics in the industry right now.

Note: the program is subject to change. For updates, refer to the conference website: www.omega-event.org
1:30-2:30pm
Learning Objectives
• The proper diagnosis including the cycloplegic refraction and binocular vision changes and proper structured approach enables better compliance of the children and their guardians to the proposed treatment as well good treatment results
Computer vision syndrome: do blue-light filtering lenses (and other therapies) help?
Other
Andrew Anderson 1, Laura Downie 2
1 Dept of Optometry and Vision Sciences, The University of Melbourne
2 The University of Melbourne
9-10am
Learning Objectives
• Quan titively appreciate how much blue light is emitted from electronic screens, and how this relates to emissions from natural light sources and to safety guidelines regarding blue light exposure
• Unders tand what recent randomised controlled trials say about whether blue-filtering spectacle lenses are effective in treating computer vision syndrome
• Appreciate what a recent review of the randomised controlled trial evidence says about the efficacy of various other therapies (e.g. the use visual hygiene protocols, and of oral supplements) for alleviating computer vision syndrome
2 Myopia Profile Pty Ltd, University of New South Wales, Sydney
9-10am
Learning Objectives
• Explain the general evidence-base for myopia management interventions based on age and refraction
• Dis cuss approaches in understanding comparative efficacy of myopia control treatments
• De termine what represents a successful long-term outcome in childhood myopia management
Prevalence of myopia amongst children presenting to optometrists in Australia and New Zealand
Myopia management
Joseph Paul 1, Pamela Tse1, Duchesne Markham 1 and Ben Ashby 1
1 Optometry Department, Specsavers Australia and New Zealand

11:30am-12:30pm
Learning Objectives
• Iden tify trends in the prevalence of myopia in patients who presented to a cohort of optometric practices in Australia and New Zealand
• Unders tand the prevalence of myopia in Australia and New Zealand in a global context
Effects of short-term wear of myopia control spectacle lens on binocular functions of myopic children
Paediatric binocular
Fatin Nur Najwa Norazman 1, Bariah Mohd-Ali 2, Mizhanim Mohamad Shahimin 2 and Norliza Mohamad Fadzil 2
1 Universiti Kebangsaan Malaysia; Universiti Teknologi MARA
2 Universiti Kebangsaan Malaysia
11.30am-12.30pm
Learning Objectives
• To investigate visual function changes following short-term wear of DIMS lenses among myopic children
Dr Kate and Dr Paul Gifford will seek to answer many of the unanswered questions in myopia management.

o determine accommodation function changes following short-term wear of DIMS lenses among o determine vergence function changes following short-term wear of DIMS lenses among myopic
Learnings from implementing a myopia control clinic in a public health optometry setting
tify barriers to myopia control in a public health tand the need for a targeted framework when managing children with myopia from a low socioeconomic background
Migraine: what’s optometry got to do with it?
Systemic disease

Bao Nguyen
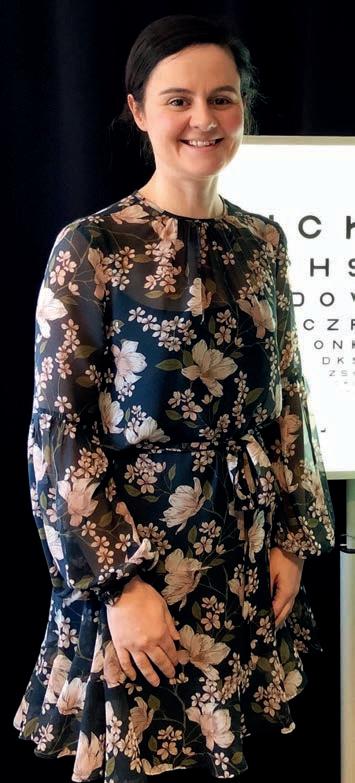
The University of Melbourne
2.30-3.30pm
Learning objectives
ecognise migraine, based on symptomatology w the clinical vision tests that might be confounded by migraine eciate how optometrists and other eyecare professionals can play an important role in the management of migraine
Strategies to promote mental wellbeing and avoid burnout in optometry
Other
Lis a Jansen
University of Western Australia
9-10am
Learning Objectives
• Summaris e the factors that lead to burnout in optometry
• Outline e vidence-based strategies to improve mental health and wellbeing
Implementation and scalability of shared care models for chronic eye disease: a realist assessment informed by health system stakeholders in Finland, the UK, and Australia
Public health
Lisa Keay 1, Belinda Ford 2, Blake Angell 2, Hueiming Liu 2 and Andrew White 3
1 Optometry Australia, Association for Research in Vision and Ophthalmology


2 The George Institute for Global Health
3 Sydney University
9-10am
Learning Objectives
• Unders tand the importance of local context in implementing new models of care
• Learn about key determinants of successful implementation and scalability
• Apply thes e concepts to current challenges in eyecare delivery
Building paediatric eyecare capability via project echo tele-mentoring in Australia
Professional Practice (ethics, communication skills and evidence into practice)
Melinda Toomey 1

Lisa Keay 1, Ann Webber 2 and Kerrie Ren 1
1 University of New South Wales
2 Optometry Australia, American Academy of Optometry (FAAO)
2:30-3:30pm
Learning Objectives
• Unders tand current paediatric eyecare knowledge gaps experienced by optometrists
cribe the challenges, limitations and outcomes of implementing a myopia control clinic in a public
• Dis cuss the importance of education in skill development to increase resilience
• Explain the factors in workplace culture and design that impact professional satisfaction
• Unders tand how Project ECHO tele-mentoring program can improve practitioner capabilities
• Unders tand the benefits of engaging in tele-mentoring programs for both practitioners and patients.
ABOVE, LEFT TO RIGHT: The University of Melbourne’s A/Prof Laura Downie, and Prof Lisa Keay, head of the UNSW optometry school



















Disclaimer: Exhibitors featured in this section are partners of Insight magazine. This was created independently, and does not represent the exhaustive list of O=MEGA23 exhibitors.
O=MEGA23 will be a significant occasion for Melbourne-based medical technology company Cylite which will announce the worldwide launch of its HP-OCT. The company is inviting conference attendees to visit its exhibit to see the ground-breaking technology in person.
Featuring industry-leading scanning speeds of over 300,000 scans per second, this Australian designed and manufactured OCT scans the eye with 1,008 simultaneous and parallel beamlets in a series of snapshot captures, which effectively neutralises eye motion artefacts for each snapshot, and in doing so, produces true-volume 3D images of the anterior and posterior segments, as well as axial length.
According to Cylite, this opens the HP-OCT to a broad range of applications, such as corneal topography, advanced contact lens fitting (including orthok and scleral lenses), myopia management and retinal imaging.
As a result, the HP-OCT combines the functionality of several devices into a single, space-saving and cost-effective instrument.
STAND:
As a Diamond sponsor of O=MEGA23/WCO4, HOYA will be holding a myopia symposium at 10am Sunday 10 September, a “must attend” event for all practitioners seeking the latest findings and insights.
The HOYA trade stand will showcase its latest services, equipment and soon-to-bereleased products, including a lens coating and two new premium progressive lenses. The new Hi-Vision Meiryo Diamond coating is HOYA’s most advanced premium coating yet. Compared to major competitors’ best coating, it is said to provide 56% lower reflectance, up to 2.5x better scratch resistance, lasts up to 5x longer and provides 100% UV protection.
Meanwhile, HOYA says its new Hoyalux iD LifeStyle 4 is easy for wearers to adapt to, and is also easy to prescribe. With three design variants tuned to patients’ daily activities, it considers today’s digital lifestyle by introducing HOYA 3D Binocular Vision technology. It also comes with two additional corridor lengths.
The Hoyalux iD MySelf Profile progressive provides an elevated visual performance, combined with a fuss-free consultation process. This lens is made for a digital world and makes customisation easy with five pre-defined design variants.


STAND: G6
EssilorLuxottica ANZ will showcase its premium lens, frame, and instrument offerings, while also introducing new brands and products to the market.

The group will occupy a significant space which will combine EssilorLuxottica’s expertise in lens technology and eyewear manufacturing. The trade fair booth will reflect the group’s ambition to support eyecare professionals and grow the optical industry in Australia and New Zealand.
“As an industry leader, being innovative means providing the market with a drive to move forward by supporting partners and patients with the latest products and services. The goal is to bring this to life at O=MEGA23 via an immersive and engaging experience,” the company says.
“This will include the latest breakthrough innovations of the group including Varilux XR series, the Vision-R 800 phoropter which offers continuous power changes in 0.01 D increments, reinventing refraction, Stellest and the new Ray-Ban Reverse.”
Essilor, a leading vision care brand of EssilorLuxottica, will take the opportunity to officially launch its latest generation of Varilux progressive lens – the Varilux XR series. This is described as the first eye-responsive progressive lens, enabling progressive addition lens wearers to benefit from instant sharpness, even in motion.
During the World Congress of Optometry, Mr Sebastien Fricker, head of the lens design team for Essilor International R&D, will discuss recent advances in progressive addition lens design. Essilor will also present during the conference on myopia management. EssilorLuxottica Clinical Conference program sessions will be on Friday 8 September and Sunday 10 September at 2.30pm. The booth will also have a dedicated space for the eyewear brands within its portfolio to highlight upcoming trends and products across Ray-Ban, Oakley, Versace, Prada and a new brand for the group, Swarovski.
STAND: D1, D2, E1 AND E2


ZEISS will highlight the ZEISS Optometry Workflow at O=MEGA23. This portfolio of solutions is focused on the core objective of making the early detection of eye disease and management of progression more straightforward. Visitors to the booth will be able to experience how the diagnostic devices, including CIRRUS OCT and CLARUS fundus camera, integrate seamlessly with ZEISS FORUM to give a full picture of patients’ eye health.
ZEISS MyoCare lenses (pictured) will also be showcased. These lenses are the first age-related myopia management solution from ZEISS. The design adopts annular cylindrical microstructures to induce simultaneous competing myopic defocus on the peripheral retina to slow down the progression of myopia. The C.A.R.E technology incorporates alternating defocus and correction zones expanding towards the periphery of the lens. Due to the eyes moving behind the spectacle lens and with a focus on optimal wearability and efficacy, an optimised freeform back surface helps to minimise hyperopic defocus. The design variants are: ZEISS MyoCare available to children younger than 10 years; and ZEISS MyoCare S available to children 10 years and older.
STAND: F6


The Eyes Right Optical stand will be a hive of activity, featuring the latest from FACE À FACE, and unleashing three new brands to join its portfolio. For the new season, FACE À FACE designers continue to explore the Memphis movement with four surprising and impertinent designs starring in a playful, poetic collection. ASHOKA (pictured) are highly feminine, glamorous sunglasses offer a sharp, vibrant tribute to Ettore Sottsass’ work: zany, exaggerated but perfectly balanced.

Eyes Right Optical will also launch the latest eyewear collections by William Morris London and Charles Stone, new brands it is now supplying in Australia and New Zealand. Playing with the theme of London’s iconic transport systems, this new release plays with the England capital’s inspired colours in fluid shapes and styles. Made with sustainable biodegradable Mazzuchelli acetate, and thanks to the smooth thin lines all over the frame, the lightness of this model makes for a super comfortable wear.
The Eyes Right Optical stand will also features a new high-end sustainability collection, Project Green, featured in detail on page 54.
STAND: A10 & B5
Optical Dispensers Australia (ODA) is Australia’s peak body providing support, resources and development opportunities for optical dispensers and their affiliates right across the country. The organisation aims to enhance the profile of the optical dispensing profession while creating a community for members to network, grow and feel supported. Offering three tiers of membership (Qualified, Affiliate and Student), ODA provides valuable content for all members, regardless of their level of experience.

With access to an ever-growing list of exclusive perks, members can engage in a comprehensive online CPD program, gain discounted tickets for ODA conferences and events, enjoy use of the online optical calculators, access HR support, take advantage of a dispensing troubleshooting forum and more.
With more than 2,000 subscribers in its network, ODA is committed to seeing the optical dispensing profession reach its full potential. Created by dispensers for dispensers, the organisation says there is no better time to invest in an optical career.
STAND: A14

On the Rodenstock Australia exhibition there will be a focus on the streamlined patient journey, along with demonstrations of its premium products and latest instrumentation.
A major feature will be CNXT smart, a software solution that seamlessly connects Rodenstock measuring devices such as the DNEye Scanner and ImpressionIST tower, with the practice’s PC, laptops or tablets, as well as the practice’s management software (including WinFit and Optomate). The system is designed to reduce time and manual imput for database maintenance.
CNXT Select will also be on display. The program allows practices to showcase different lens types and to create an individual design for the patient.

“Visit the Rodenstock stand and find out about latest offers and programs and how Rodenstock can help the patient journey in your practice,” the company says.
STAND: G6
PRECISION1 for Astigmatism contact lenses will be a focus of the Alcon Vision Care booth at O=MEGA23. The lens is designed to meet the needs of the mainstream patients, who want long lasting comfort, even at 16 hours1,8-9 with great stability, according to Alcon2†*

PRECISION1 features two unique technologies:
SMARTSURFACE TECHNOLOGY – A permanent, microthin layer of moisture on the lens surface that exceeds 80% water.3 Alcon says this helps provide longer-lasting lens surface moisture stability†4-6 and a more stable tear film.
PRECISION BALANCE 8|4 – A proven lens design that provides the on-eye stability astigmats need for consistent vision.7
Note: Always follow the directions for use. References available upon request.
†Based on lens movement, centration, and rotation at initial fitting.
*Based on 98.7% of eyes with lens oscillation with blink of ≤5° while wearing PRECISION1™ for Astigmatism contact lenses
STAND: J6

Spanish eyewear brand KALEOS will be a highlight on the Sunglass Collective booth, alongside the latest lightweight model from Bollé.
KALEOS has a philosophy that despite age, everyone should enjoy beautiful eyewear. Crewe C3 by KALEOS KIDS (pictured) embodies this, and is easily dispensed to adults with small faces. Crewe has handmade cream tortoiseshell acetate with white acetate highlights and “gorgeous lilac temple tips”, including 100% UV protective lenses and a back surface anti-reflective coating.
Meanwhile, KALEOS’ goal to find beauty in various shapes is evident in Grayson C3, handmade made from Mazzuchelli acetate. With its high contrast colours and unique tri acetate lamination, this piece will capture attention.
Bollé’s new ultra-light frameless model, Icarus, will also be on display. Crafted from a TR90 frame and impact resistant lenses, it’s described as “23 grams of pure performance”. Icarus is available with Phantom photochromic lenses, and Volt+, a revolutionary high contrast polarised lens. Other features include anti-fog and anti-Scratch treatments, hydrophobic coating and available on Bollé’s RX program with a script range of +6.00 to -8.00.
The CooperVision exhibit will showcase the MiSight 1 day Starter Kit – designed to help patients effectively learn how to use their contact lenses and have fun while learning.
The MiSight 1 day Starter Kit includes essential information on MiSight 1 day contact lenses for myopia control and quick tips on application and removal via a QR code to ensure patients become confident with their new contact lenses.
The kit comes in a zip-up case and includes a getting-started booklet, paper soap, handball, and hand mirror. The kits are free to order with any new MiSight 1 day trial lenses.

“Simply call our customer service team on 1800 655 480 to place your order or come and visit us at O=MEGA,” the company says.
“If you have any questions about the MiSight 1 day Starter Kit or any other CooperVision products, please get in touch with your CooperVision business development manager.”
STAND: C8

Device Technologies (DT) and Topcon will showcase the latest hardware and software innovations together at O=MEGA23.
DT – the local distributor of Topcon hardware – and Topcon Healthcare Solutions, which oversees its own Topcon Harmony software in Australia, will showcase their unique end-to-end solution for eye health practices.
Specifically, the popular Topcon Maestro2 OCT will be on display, along with Topcon’s refractive ecosystem that works to seamlessly integrate several pieces of equipment involved in the patient eye test. Meanwhile, delegates can also get a glimpse of Topcon Harmony, a web-based data management application that works to connect all ophthalmic imaging devices regardless of the manufacturer.
DT will also be showcasing its two myopia management solutions offering axial length measurement: the Topcon MYAH, and the HaagStreit-manufactured Lenstar Myopia.
STAND: F1
BOC Instruments will be displaying an extensive range of ophthalmic equipment for the various equipment requirements of eyecare professionals.
The distributor’s latest products include the new VF2000 NEO Virtual Reality portable visual field analyser and the new Nidek AL-Scan M optical biometer for myopia management.
It also has several OCT and fundus camera options, including the Aurora hand-held fundus camera, which is versatile and portable while the NFC-600/700 models provide complete automation with exquisite image detail, BOC states.


For dry eye diagnosis and management, BOC supplies a range of SBM products. It is possible to upgrade most slit lamps for digital imaging and with a further upgrade option for comprehensive dry eye diagnostics at an affordable price.
“We look forward to demonstrating these exciting products,” national sales executive Mr Robin Lanesman says.
STAND: E3
A feature on the OptiMed stand will be the Essilor Vision-R 700 phoropter, incorporating an exclusive breakthrough optical module. According to the distributor, which will be exhibiting alongside EssilorLuxottica, the system provides excellent patient experience during refraction and eliminates the feeling of failing a test.
Optometry practices using the technology have been able to make the refraction more memorable, offering a modern, compact design and silent lens change.

Because there’s no need for superposition of lenses compared with traditional phoropters, OptiMed says the patient has a more natural field of vision and is more comfortable without the effect of tunnel vision.
With this technology, the patient now has the option to report they see “no difference” or “doesn’t know which option is better”. The smart tests use this information to give accurate results, meaning the guessing game is eliminated, and patient confidence reassured. Thanks to the shorter process, patients also experience less visual fatigue by providing fewer direct answers.
Finally, the Vision-R 700 offers an efficient and detailed comparison function, where multiple different scripts and scenarios can be compared at the click of a button.
Eyecare professionals seeking to elevate their dry eye services can visit the Lumibird Medical exhibit and learn more about its premium intense pulsed light (IPL) device, C.STIM.

O=MEGA23 will also mark the Australian launch of a new diagnostic device, enabling the company to offer customers a premium dry eye suite of solutions for their practice.
C.STIM is described as an easy-to-use, ergonomically designed system with intuitive software, adaptable for any clinic or practice set-up, specifically for the treatment of dry eye disease.
“This intense pulsed light device operating in the 610-1200 nanometre wavelength, is designed to treat meibomian gland dysfunction, significantly reduce the viscous cycle of chronic inflammation, and decrease demodex folliculorum in skin phototypes I through V,” the company says.
“Unlike other devices, C-STIM uses a flash-lamp water-cooling system to guarantee homogenous energy throughout the treatment process to maximise patient comfort.”
STAND: I6


ZEISS MyoCare lenses with two designs for specific age groups


• C.A.R.E® Technology creating alternating defocus and correction zones in a ring-like pattern.
• ClearFocus design ensuring clarity of vision in all directions of gaze whilst effectively managing myopia progression.
• Available in a wide range of materials and indices.
Scan to watch


Whether it’s an optometry student searching for their first placement, or a seasoned optometrist looking to launch, grow or sell their own practice, ProVision has it covered.
At O=MEGA23, the ProVision team is encouraging delegates to learn about Australia’s largest network of independent optometrists.
Public presentations on the hour will help:
• Unlock the full power of business systems to increase practice efficiencies
• Attract and retain talented staff using proven recruitment tools
• Take the first step towards being your own boss
Attendees also get the chance to explore ProVision’s exclusive member systems including ProAccounts, ProSupply, ProMarket and ProLearn. And with the ProVision team on deck, it is a great opportunity for optometrists to talk about their unique practice needs, like succession planning and profitability.
STAND: H4
Optometrists and dispensers with business ownership in mind can visit the Eyecare Plus stand to understand the value it can generate for independent practices.

The network provides business support and marketing services to more than 120 clinically-focused independent, full-scope optometry practices throughout Australia.
Owned by its members, Eyecare Plus offers three membership options; branded and co-branded which include an exclusive territory, as well as unbranded. All three have access to professional marketing campaigns, media planning, benchmarking, buying group benefits, business advice, conferences and workshops, staff training and many other services.
Cost of Eyecare Plus membership can be covered by the extensive marketing support and the purchasing bonuses it offers members.
“We also provide assistance to optometrists and dispensers who are looking to establish their own practice.
If you are looking to buy, or sell, an optometry practice, contact us,” general manager Mr Philip Rose says.
Tokai Optical’s NeuroSelect progressive will feature prominently on its booth. The lens is the result of a collaboration between Tokai Optical, NTT DATA, the National Institute for Physiological Sciences, and the Consortium for Applied Neuroscience, using brain wave measurements to quantify the sensitivity of subconscious feelings and sensations stimulated from the brain.
With key design features such as Binocular Link Design, Variable Zone Control, and Dedicated Multi Optima Zone, Tokai says the result is a progressive lens that provides single vision-like comfort. The peripheral sway and distortion are eliminated so the wearer can enjoy clear, comfortable vision no matter which direction they look.


“Tokai NeuroSelect offers a variety of lifestyle selections to suit wearers’ needs and purposes. Whether you need lenses for day-to-day use, intermediate vision enhancement, or close vision focus, Tokai NeuroSelect has a lens that will meet your needs,” the company says.
The full range of Tokai NeuroSelect lenses also offers Neuro Individual Design, taking into account the frame shape, as well as other parameters such as pantoscopic tilt, vertex distance, and wrap angle etc.
STAND: I5
Opticare, a leading Australian optical lab for more than three decades, is exhibiting at O=MEGA23. Delegates can expect to see the launch of new freeform lenses, developed through German technology and produced in-house by the company’s team of lens experts. Myopia management and a whole new range of specialty lenses will be the focus this year.
Opticare will also showcase its sought-after consulting and diagnostic equipment, including the Huvitz HOCT-1/1F (above) and the Visionix VX650 (below).

According to the company, the Huvitz HOCT-1/1F combines a full-colour fundus camera, PC, and OCT in one powerhouse tool. It provides high-speed scanning and delivers high-resolution images, making extensive examination and instant diagnostic results possible.

The Visionix VX 650, meanwhile, combines an aberrometer, a fundus camera, and other essential technologies to monitor anterior and posterior segments in a single device. From cornea to retina, it detects major defects and pathologies, including diabetic retinopathy.
Attendees should also look out for more information about Opticare’s upcoming software service.
STAND: A9
STAND: A12
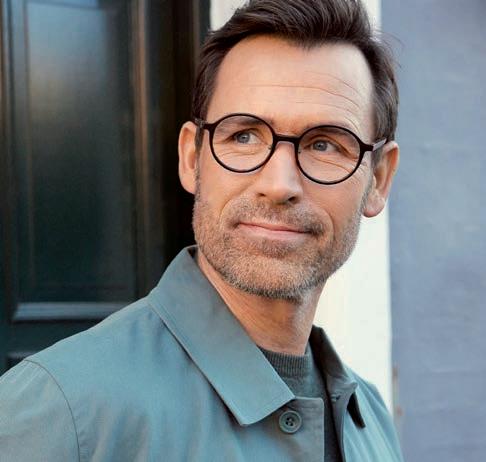
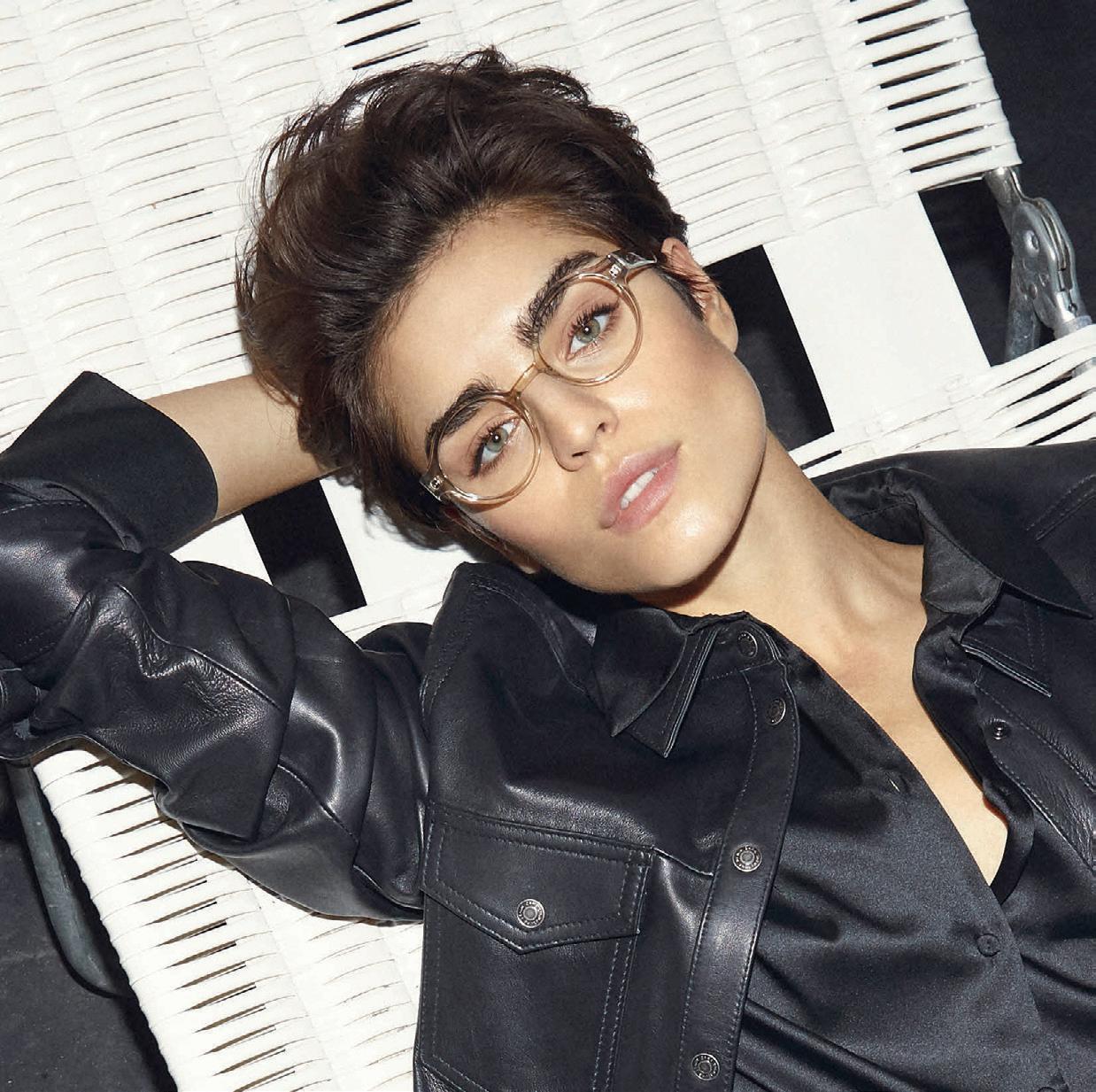







Designs For Vision will feature a range of technology on its stand, starting with two key devices from OCULUS.
The OCULUS Pentacam AXL Wave (left), described as the established gold standard in anterior segment tomography, is the first device to combine Scheimpflug tomography with optical biometry, objective refraction, wavefront aberrometry, and retroillumination. According to the company, its detailed analysis modules also make it an indispensable tool for detection of corneal diseases, spectacle prescriptions, contact lens fitting and myopia management.

The DFV booth will also feature the OCULUS Myopia Master (right) which measures three key parameters – refraction, axial length and keratometry – to help make myopia management easier and more reliable. It is the only device to incorporate the latest BHVI data for estimating future myopia progression, enabling personalised reports detailing a child’s current myopia status and their likely outcome in adulthood.
Finally, the iCare EIDON Ultra Widefield (centre) ushers in a new era with the power of TrueColor Confocal Technology. With 200o coverage of the retina, rich detail, and natural colours, the EIDON is said to provide a significant advantage in early detection and monitoring of
Eyecare professionals can learn more about AFT Pharmaceuticals’ preservative-free, over-the-counter eye drop range for dry eye on the trade floor. Two major products within its portfolio are NovaTears and its HYLO range. With 85% of dry eye patients estimated to suffer from evaporative dry eye, NovaTears can be recommended to relieve symptoms of excessive tear evaporation. It is a unique preservative-free eye lubricant using patented EyeSol technology that acts as a lipid layer substitute and evaporative barrier for improved tear film quality and stability.
AFT says NovaTears is also clinically validated, showing significant improvement in signs and symptoms with evaporative dry eye disease and meibomian gland dysfunction patients.
Meanwhile, preservative-free HYLO-FRESH (sodium K hyaluronate 0.1% w/v, 10mL), delivers lubrication for dry eyes of moderate or medium severity, while the more viscous HYLO-FORTE (0.2% sodium hyaluronate w/v, 10mL) is ideal for the treatment of severe or chronic dry eye.
HYLO drops provide a systematic approach to dry eye treatment through the unique COMOD (COntinuous MOno Dose) application system, delivering at least 300 sterile drops per bottle. Both can be used with all contact lenses, are suitable for post-surgery use, and are phosphate-free.
STAND: G7
retinal pathologies. With its automated imaging process that captures images even through media opacities and small pupils, DFV says it is a must-have in any practice.
STAND: B2

AVANTI has been an iconic Australian eyewear brand since 1982 – and will be a major feature on the Modstyle stand. This season, AVANTI focuses on vibrant colour, including colourful men’s frames.
One of these is KAL. KAL (pictured), a sporty look for the modern man with high contrast neon colours on an easy-to-wear, modern and light weight stainless steel frame.
KAL is described as "a must have this season" for patients looking for something exciting and different.
STAND: C4
At O=MEGA23, Optos will show why an investment in ultra-widefield technology could be the differentiator practices are seeking.
The company’s devices produce ultra-widefield optomap images of approximately 82% or 200 degrees of the retina, something it says no other device is capable of doing in a single capture.

With the support of more than 2,000 peer reviewed clinical studies, optomap is said to be the only clinically-validated, ultra-widefield retinal imaging technology in the industry.

“Our products enable eyecare professionals to detect, monitor, and effectively treat more retinal pathology thus saving sight,” Optos says.
“Throughout O=MEGA 2023 we will host training sessions aimed at customers wanting to understand Optos Advance software. The sessions are hosted by Renee Slunjski, an Optos Regional Product Specialist and qualified optometrist.”
STAND: C6


1 2 3
● Improved tear film quality
● Better meibum quality and expression
● Reduction in patient symptoms and neuropathic pain relief

● Reduced inflammatory markers in tears
● Maximising patient comfort through a flash-lamp water-cooling system to guarantee homogenous energy throughout the treatment process, which maximises patient comfort

● Regulated Pulse Train for safety and effectiveness, resulting in less inflammatory reaction and no thermal damage
● Unique Stim-ULITM (Uniform Light Intensity) technology that offers the best combination of clinical efficacy and patient comfort with a perfectly homogenous spatial distribution of energy








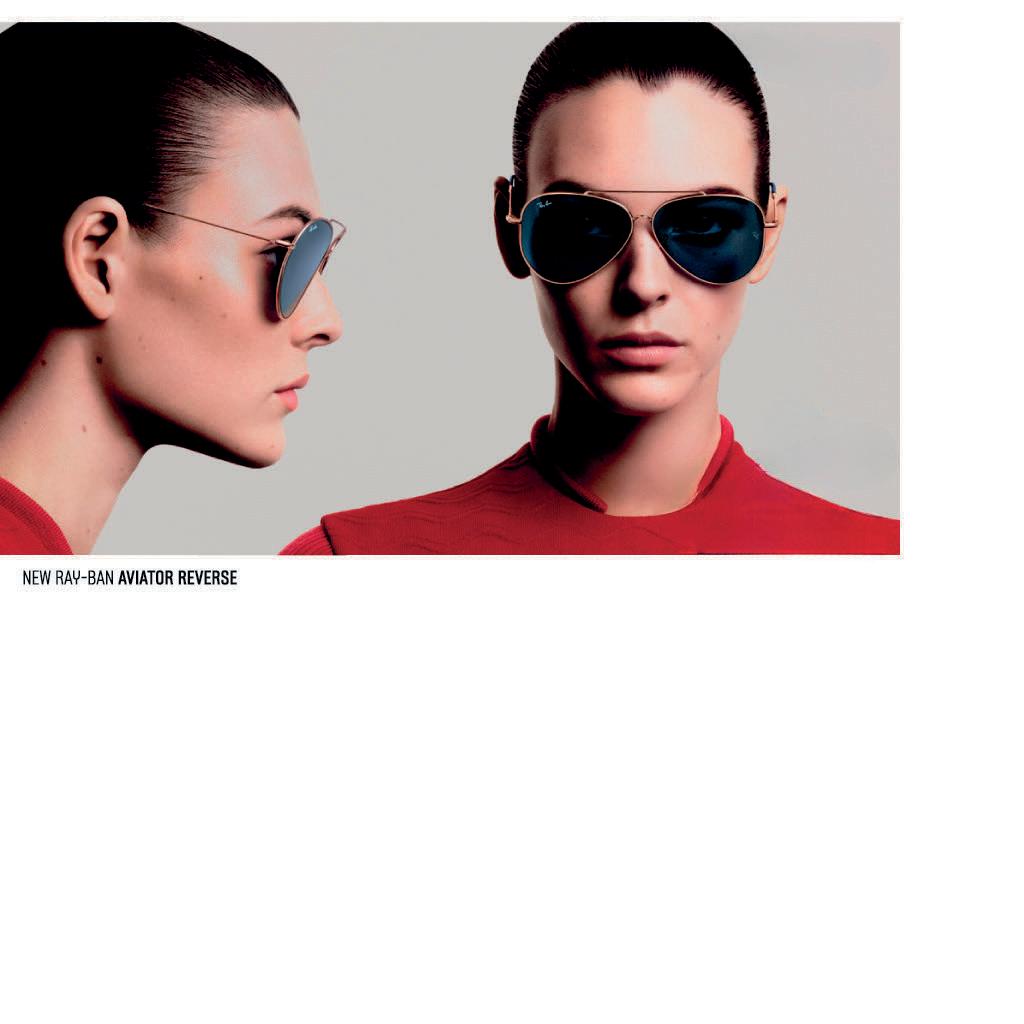

A high-end sustainability collection and the return of iconic British eyewear label William Morris are latest brands to join the Eyes Right Optical stable, providing independent optical practices with more possibilities to separate their business from the bunch.
Wthe biggest and boldest circle is often drawn around an ODMA trade event. This year it’s O=MEGA23, which presents not only as a chance to build key business connections with independent optical practices, but an opportunity to make a splash with new collections.
Two new additions to the company’s portfolio will feature prominently on the Eyes Right Optical stand for different reasons.
The first of these collections is Project Green, a new range of sustainable eyewear that has set out to satisfy environmentally-conscious practices – and end consumers – with high quality bio-acetates, compostable demo lenses and a market leading hinge design.
The other collection to feature at O=MEGA23 – combining with the 4th World Congress of Optometry 8-10 September in Melbourne – is the well-established British brand William Morris, which is returning to the Eyes Right Optical fold after being acquired by Design Eyewear Group in September 2022. The Charles Stone eyewear brand is also included in this new deal.
Wymond says these latest additions complement the Eyes Right Optical portfolio that includes brands such as FACE À FACE, WOOW and ProDesign. They fit within the framework of supplying high quality, designed-focused fashionable eyewear to mid- to high-end independent optical practices, or the top-end of a budget conscious store.

In Project Green, Wymond says there is an opportunity to fulfil an unmet need. While sustainable eyewear collections exist, he believes major improvements can be made to capture other parts of the market.
“Project Green has been created as a high-end, environmentally-friend ly collection that doesn’t compromise on quality, style, look, or feel. This collection aims to be more like the Tesla of sustainable eyewear, rather than the Prius,” he says.
“It has been designed to have an eco-friendly feel that uses bio acetates from world-leading Mazzucchelli acetates, as well as other high-end eyewear material providers from around the world. It also features bio demo lenses that break down under compost conditions. They also come in a reconstituted leather case.”
The new brand, launching worldwide in September 2023, features about 30 models and 120 SKUs, which are predominantly feminine in style, but there are several men’s designs too.
According to Wymond, some hallmarks of the collection include earthy tones, contemporary shapes, and attention to detail. One of the key features is a collaboration with Visottica Comotec, a global leader in customised components for frames. Project Green will feature the company’s patented 2D hinge that allows up and down movement of the temples, and a higher resistance to bending than traditional flex hinges.
For Eyes Right Optical, launching a new sustainable collection fits with the company’s own focus of minimising its environmental footprint – something it initiated long before it became mainstream.
For example, the electricity bill for its premises in Scoresby, Victoria, is less than $500 per quarter thanks to solar panels sprawled across its roof. The company also uses hybrid cars, actively composts and recycles and even has a veggie garden. Other moves include a shift towards 100% compostable courier bags, and the development of a Sustainable and Ethical Practices Policy in 2020 that also includes the practices of its own suppliers.
It all forms part of a wider trend in the optical sector whereby more suppliers and eyecare providers are moving to sustainable practices to align with consumer expectations.



“Even though we have been implementing all these initiatives, we’ve found there is a real appetite for an environmentally friendlyeyewear collection –and that’s why we’ve gone about sourcing this new product, Project Green,” Wymond says.
“There’s definite demand for it. I feel people want to do the right thing and act sustainably, but they don’t want to compromise on quality or style. So that’s the opportunity we see with this collection.”
“PROJECT GREEN HAS BEEN CREATED AS A HIGH-END, ENVIRONMENTALLY-FRIENDLY COLLECTION THAT DOESN’T COMPROMISE ON QUALITY, STYLE, LOOK, OR FEEL.”
MARK WYMOND EYES RIGHT OPTICALProject Green is a new high-end sustainability brand to join the Eyes Right Optical portfolio.
The introduction of William Morris, founded in 1996 by Mr Robert William Morris, represents a ‘full circle’ moment for the Wymond family. Eyes Right Optical held the local distribution for William Morris in the early 2000s when it was owned and operated by Mark’s parents Mrs Gaye and Mr David Wymond. This marked its arrival on the Australian market, but in more recent years a different distributor held the rights here.
In a major development in September 2022, Danish company Design Eyewear Group – which develops and markets iconic eyewear brands – signed a deal to acquire William Morris London. The agreement incorporates the William Morris sub collections London and Black Label and, separately, Charles Stone New York, a standalone brand launched in 2013.


With Eyes Right Optical being a long-term partner and exclusive Australia and New Zealand supplier of Design Eyewear Group brands, this means William Morris and Charles Stone will join its portfolio from 1 August 2023 and will be on display at O=MEGA23.
Inspired by original London and New York styles, the acquisition complements the existing brands on offer by Design Eyewear Group and Eyes Right Optical, which includes four Danish (ProDesign, Kilsgaard, Inface and Nifties) and three French labels (Face a Face, WOOW and Alium).
“We’re delighted to take the collection back on. We’ve been watching the progression and development of William Morris London from afar and have been impressed with the direction Robert has taken it. When Design Eyewear Group took it on and wanted us to take on the distributorship, we were delighted to accept,” Wymond says.
“We’re excited by the London-look of the collections with striking shapes and bold style. Robert’s style and flare is unique, and I feel it’s a good price point for the level of quality.”
The William Morris London deal with Design Eyewear Group will see Morris continue in the new setup as the senior brand ambassador. In this
role, he will ensure that both customers and employees worldwide gain an insight into the company’s DNA and the British design philosophy, while ensuring the design style is continued and developed for all brands under the William Morris London portfolio.
Mr Lars Flyvholm, CEO of Design Eyewear Group, says the acquisition is being seen as an opportunity by Morris to grow and develop the William Morris brands further in all markets.
“Design Eyewear Group strives to have a portfolio of designer brands keeping true to their identity … we feel it was a perfect fit adding on a UK design brand, expanding the choice for our opticians worldwide,” he says.
“The Australian market is very important for these brands. Being one of our biggest markets already, bringing the William Morris brands to a level of how our other brands are performing is very exciting. From a design and marketing point of view, the very clear British identity will bring a lot of awareness and appreciation among Australian customers.”
Flyvholm thanked Frames Etc who has supported the establishment of the William Morris brand in the Australian market for several years, however, it makes sense to switch Eyes Right Optical who Design Eyewear Group has a 20-year-plus relationship with.
“Eyes Right Optical has successfully grown the business for the brands of Design Eyewear Group year-after-year via strong communication and exceptional customer service. At Design Eyewear Group we always look for the best synergies to provide the best service to our customers so the choice to change the distribution was part of that,” Flyvholm says.
Morris is delighted that William Morris London is now joining forces with Eyes Right Optical and Design Eyewear Group.
“I’m very proud of the development William Morris London has undergone since it all began more than 25 years ago,” he says. “I’m also convinced that Design Eyewear Group is the right partner to grow the company further through their global sales network, which was launched almost 50 years ago when ProDesign was founded in Aarhus in 1973.”
With OCT machines now considered essential in modern optometric practice, practitioners are seeking devices that offer multiple functions helping save money and space. The REVO OCT fits this description and has found a home in several independent practices across Australia.
Sydney optometrist Dr Jim Kokkinakis can usually rely on his instincts to make a split-second decision on new technology investments, but when it came to his OCT machine earlier this year it was something he agonised over for months.

On one hand, there was his existing system from a reputable manufacturer that had many years of crucial patient data and statistical analysis, but the service contracts and reliability of the machine left him unsatisfied. On the other, he was considering the REVO OCT, from Polish manufacturer Optopol, which performs the standard functions optometrists come to expect from an OCT, plus advantages in anterior segment imaging for his scleral contact lens work, and more.
Kokkinakis was at a crossroads. Should he relinquish the data that enabled him to track his patients’ macular and optic nerve changes for up to 10 years in favour of the functionality of a new system, or stay with what he knew.
“Normally I see an instrument and know right away whether I’ll buy it or not. But in this case, it took me many months because there was a lot to consider. Everyone’s got different preferences – the individual maybe cannot forego the historical database and I can understand that – but in the end I chose functionality,” he says.
“It means I’ve effectively got to now rebuild a new database, but at the end of the day, I don’t want to be prevented from obtaining better equipment because of an issue like that. It was the best decision for my practice going forward.”
Earlier this year, Kokkinakis installed the REVO FC 130 model, the most advanced of Optopol’s five OCTs in the REVO range, available in Australia through distributor OptiMed. At his business – The Eye Practice in Sydney’s CBD – it’s the sixth OCT upgrade over the decades.
According to Optopol, the REVO OCT is an all-in-one device eyecare professionals can use in several ways. This includes high quality OCT imaging (with up to 130 000 A-scan/sec scanning speeds) and OCT-A. What makes it unique is a full colour fundus camera (12.3 megapixels), and the ability to
combine simultaneous OCT and fundus images.
It also comes with optional ‘modules’, such as T-OCT which provides detailed corneal curvature maps, and True Net Curvature information (ideal for specialised contact lens practitioners like Kokkinakis). This module provides axial maps, tangential maps, total power map, height maps, epithelium and corneal thickness maps.
There’s also a B-OCT module for biometry for myopia management and intraocular lens calculation, capturing axial length, central cornea thickness, anterior chamber depth, lens thickness, pupil size, and white to white.
“It’s an instrument that can be used in so many ways, it’s unbelievable,” Kokkinakis says.
“I do a lot of scleral contact lens work (around 25% of total workload), and from that perspective the REVO shone because we can scan and view a much bigger portion and see how the cornea and contact lens are interacting in a far more accurate way – that was one of the tipping points when deciding which OCT to purchase.”
Kokkinakis says the fundus camera is also something he hasn’t experienced with an OCT, and he’s been impressed by Optopol’s ability to innovate a built-in anterior lens allowing the user to perform anterior segment imaging without installing an additional lens or forehead adapter.
According to Optopol, it means practitioners can display the whole anterior segment using a radial scan to view 18mm wide and 6mm deep for various angles. This is a standard feature in each of the five REVO models.
“I also do a lot of keratoconus management these days and with keratoconus being a contraindication for laser surgery, we’re able to perform screening with the REVO using topography and corneal thickness. The system then combines these to give you a risk factor for keratoconus,” he says.
“It takes a matter of seconds and next thing you know, you’ve got data overload. At the end of the day, you can’t have too much data; if you’ve got it, you can use it.”
When Kokkinakis was canvassing the market for a new OCT, he trialled around four options before landing on the REVO. Workflow is a major consideration for him. When patients enter his rooms, each undergo three initial tests: an ultra-wide field Optos scan, intraocular pressure tonometry test, and then a REVO OCT scan that assesses their optic nerve, macula and screens for corneal irregularities.
“For me, it’s important a device is easy-to-use and can be delegated to other staff, and delegated with confidence. I found this was the case with the REVO OCT which my staff could use well with a short period of training,” he says.


Merimbula Vision, located on the coast of southern NSW, opened eight years ago as a greenfield independent. With no patient base and trading history, along with fitout costs, it was a leap of faith to invest heavily in technology early on.
“But the reality is that we simply could not practise the way we wanted to and our patients needed us to, without it,” principal optometrist Mr Bayd Rosenbaum says.
The practice opted for a REVO Copernicus, an earlier model, which remains in the practice today and hasn’t required any technical assistance over the years which vouches for the design build. Initially Rosenbaum sought an OCT so he could confidently monitor his patients’ macula.
“To meet the needs of our patients, their GPs, and the ophthalmologists we were referring to and co-managing with, we simply had to be confident in our detection of wet age-related macular degeneration and diabetic macular oedema, along with many other conditions, of course, and get our referrals correct and accurate,” he says.
“When looking at the different machines available we considered the additional features of each and how they might benefit us. The REVO unit at the time was one of few machines to have an anterior function for pachymetry and contact lens fitting, a widefield lens for angles, and an option for biometry for axial length measurements. These features added to our diagnostic
capabilities and met needs that were missing from the practice at the time.”
Today, the REVO OCT remains crucial to Merimbula Vision’s glaucoma detection and co-management, and provides confidence in macular disease.
Rosenbaum was surprised initially how often what he thought was a simple hyperopic shift was in reality a vitreo-macular traction.
“It has come in handy for assessing clearance in rigid contact lenses and for axial length measurement in myopia control. Patients like to see the anterior scans of their cataracts or IOLs, and I like to monitor the cornea scans for oedema in our cataract surgery aftercare regime,” he says.
“But when you ask where it shines the most, I would have to say as a regional optometrist it is the ability to send the images we capture to the ophthalmologists we are referring to for an opinion on the urgency of a referral or when reporting back to them following treatment that they have done.”

In terms of the OCT’s functionality, ease-of-use is also a standout.
“It has an automatic capture function so the imaging can be performed by anyone in the practice,” Rosenbaum says. “The instrument gives instructions to the patient to follow such as where to look and when not to blink. I have found the software that allows you to monitor for progression to be reliable and easy to use.”
Optometrist father-daughter combo Mr Gavin Boneham and Ms Sarah Boneham operate across two distinct practices. Boneham Peters Optometrist, known as a destination for boutique frames, and Boneham Optometrist Sydney CBD (Eyecare Plus) that is more well known for its rigid contact lens work. Both practices function with an Optopol REVO as their OCT machine. It serves each practice in slightly different ways, with Boneham Peters Optometrist relying mostly on its OCT functionality and biometry, while Boneham Optometrist Sydney CBD uses it for this, as well as its anterior imaging for scleral contact lens fitting.
After relocating in 2017, Boneham Peters Optometrist sought an OCT upgrade in 2019 and chose the REVO for several reasons. One of those was for axial length measurements for myopia management, as well as the ability to add modules for different functions in future, such as topography.


“The servicing was also very reasonable, and when it comes to upgrades, we don’t have to necessarily upgrade the entire machine each time,” Sarah Boneham says.
“It’s also easy-to-use and customise; I’ve used a lot of different OCTs in my time, but I’m able to use this one in particular to get far peripherally to look at different lesions. I use it to see if there’s a retinal tear sometimes or show a patient how their tear appears. I’m able to do that effectively on this machine, whereas I’ve tried it on others and can’t really obtain it as easily.
“During the decision process, we were provided papers assessing the validity of the biometry and OCT modules which gave us the confidence to go ahead. All in all, it’s been a great investment for our practice.”
“I DO A LOT OF SCLERAL CONTACT LENS WORK AND FROM THAT PERSPECTIVE THE REVO SHONE BECAUSE WE CAN SCAN AND VIEW A MUCH BIGGER PORTION AND SEE HOW THE CORNEA AND CONTACT LENS ARE INTERACTING IN A FAR MORE ACCURATE WAY.”
JIM KOKKINAKIS THE EYE PRACTICEREVO offers quality OCT imaging and OCT-A, but a full colour fundus camera makes it unique, along with modules for myopia management and scleral contact lens fitting. The REVO T-OCT module is ideal for advanced contact lens practitioners, providing axial maps, tangential maps, total power maps, height maps, epithelium and corneal thickness maps.

At Looking Smart Optometrists in Pelican Waters on Queensland’s Sunshine Coast, patients undergo a comprehensive pre-test before being seen by one of the practice’s three optometrists. It’s helped build the practice’s reputation as an adopter of modern technology, but for optometrist and director Dr David O’Neill the process was creating a problem.
“We provide a full pre-test which involves a Topcon TRK-2P 4-in-1, OCT, widefield imaging with a DRSMini, and visual field test. This is done before the patients see our optometrists,” O’Neill says.
“But now that we have grown to three optometrists and 75 patients daily, the field test was creating a bottleneck. We have been using two existing visual field devices – but their testing time is 12 minutes for a threshold and six minutes for a screening.”
They were minutes he couldn’t spare.
O’Neill knew he needed to resolve this workflow issue, and upgrading the equipment to speed up the visual field testing process seemed the obvious solution. He purchased the VF2000 Neo from a US medical equipment manufacturer, exclusively distributed in Australia by BOC Instruments.
While he acknowledges it is unconventional to perform visual fields on all patients, he says Looking Smart Optometrists is “always on the precipice of the future”.
“We only do ‘screening’ field tests on patients over 50 which we do not charge to Medicare. We pick up one patient every one to two months who is having or has had a stroke or brain tumour,” he says.
“We believe in testing to see what is wrong rather than test when you see what is wrong. We do not charge the patient for this.”
The same philosophy applies to OCT imaging.
“I would personally pick up two to four patients with a sight threatening condition that would have been missed by conventual testing. We have provided OCT for free since 2012, one of the first in the country. We have only just replaced our machine after 11 years and a total of more than 500,000 scans,” O’Neill says.
But testing takes time. While he concedes that six minutes of field tests is excessive, he argues it saves six to 12 patient lives a year per optometrist,
“Those six minutes are invaluable to those we diagnose. I would say to each patient, ‘Is six minutes – or one minute on the VR goggles – worth the potential of saving your life?’.
“This week alone I have picked up a cystoid macular oedema treated with Acular, which saved the patient’s vision 10 weeks post cataract surgery, a glaucoma with completely normal eyes, and a case of wet macular degeneration which had no visible symptoms, but I got the patient into anti-VEGF injections on the same day, avoiding long term vision loss.”
O’Neill says this adds up to hundreds of patients yearly whose vision or life he is saving.
“The $60.00 per consultation Medicare rebate we receive is hardly sufficient for this task, but I can sleep at night knowing that I have done the best for my patients and in the fact that I am unlikely to receive a phone call because I missed something,” O’Neill says.
“I could not afford to do this in an individual practice, with staffing costs, but when the independent optometrists can band together to provide excellent healthcare, we can excel.”
When it came to deciding about which visual fields device to purchase, one model stood out.
“We could have purchased a more advanced field tester from our existing supplier, which has faster test times, but requires annual maintenance which I think is around $1,100 per year. Instead we opted for the VF2000 Neo,” he says.
“A full threshold takes five minutes, and the machine gives full verbal instructions to the patient. For a screening, it takes under a minute and does an Easterman for driving assessments.”
Mr Robin Lanesman, national sales executive at BOC Instruments, says the company only recently started supplying the VF2000 Neo to its Australian customers. O’Neill is one of the first to receive it.
The new compact, sophisticated, Bluetooth-connected portable visual field analyser has been designed to replace bulky conventional devices.
An innovation from Micro Medical Devices in the US, the VF2000 Neo broadens the clinical scope beyond offering reliable visual field testing. According to the manufacturer, the VF2000 Neo virtual reality visual field device incorporates complete visual field analysis and progression, with versatile and efficient vision screening technology in a compact portable device.
Equipped with the latest internal optics, the VF2000 Neo can quickly run visual field protocols and a variety of added self-guided vision tests in full-colour 4K-resolution.
Significant growth in patient numbers at DR DAVID O’NEILL’s independently-owned optometry practice on the Sunshine Coast has created a bottleneck when conducting visual field testing, leading him to find a speedier solution.The VF2000 Neo virtual reality visual field analyser.
“It is designed to improve every aspect of patient testing from patient experience and clinical results to practice efficiency without compromising the accuracy of results,” Lanesman says.
“AI virtual assistance guides the patient and enables communication in multiple languages. Active eye tracking ensures enhanced accuracy, and testing pauses when a patient loses fixation or closes their eyes, and alerts the patient.”

The VF2000 Neo provides multiple visual field tests including full and fast threshold visual fields, Frequency doubling technology (FDT) perimetry, neuro, kinetic, ptosis and Esterman tests.
The the device also includes an option to select bilateral fixation, meaning a non-fixating eye can be tested without issues.
“This technology provides the same reliable standard of visual field analysis and is Gold Standard Visual Field compliant with identical report format,” Lanesman says.
“Furthermore, it offers a broad range of additional tests such as visual acuity, contrast sensitivity, colour testing – including Ishihara, D15 and advanced colour tests – stereopsis testing, eye mobility and strabismus, with more in development.”
The VF2000 Neo is supplied with a tablet PC and uses Bluetooth interface between tablet and device, and does not require WiFi for testing. Test results are stored and accessed from the tablet and automatically uploaded to the cloud, and can therefore be retrieved on any PC through Micro Medical Devices online portal (micromedinc.com).
“Compact, space saving and extremely portable, the VF2000 Neo can be used anywhere. It provides a far more comfortable and relaxed experience, an eye patch is not required as occlusion is done digitally, and no dedicated space nor a darkened room is needed,” Lanesman s ays.
O’Neill, who began training as an optical dispenser in 1996 at OPSM, went on to study optometry at Queensland University of Technology, graduating in 2001.
He gained experience working in locations ranging from Cairns to Southport, including at Precision Eyewear in Wynnum and Premier Optique (now Specsavers) in Maleny before opening his own practice in 2006.

At the time of writing, O’Neill had only been using the VF2000 Neo for a few short weeks, and had yet to discover if it held all the answers to his problems.
“Questions remain, such as how is the battery life of the machine? We will know more when we can run it with more patients. It can operate plugged in, but I would prefer wireless if it can last the 60 tests daily,” he says.
A few weeks later, he had an answer:
“The tester goes several days without needing a recharge, now we have used it continuously.”
He says the ease-of-use was one of the features that drew him to the VF2000 Neo.
“When the patient is doing the test, it monitors eye position and warns them to look in the centre rather than relying on an operator or the blind spot analysis,” O’Neill says. “You just need to start and stop the machine.”
“The web interface allows easy viewing in any consultation room, and we have thought of sharing this with ophthalmologists when we co-manage glaucoma to save them from repeating fields. It is also easier for entry of patient data with a regular keyboard.”
O’Neill has also used the device’s strabismus settings, which have been useful, he says, in calculating prism in patients, similar to a synoptophore.
“This does it in a fraction of the time. The VF2000 Neo can also be utilised in other areas, like acuity and visual training, but we are not using it for this.”
“To be honest, we are too busy doing what we do. I really need another two optometrists, as we are severely short staffed. I keep taking on other optometrist’s client lists as they retire. We already serve up to 50,000 patients and will possibly double that number in the future. Our practice is 30% larger than 12 months ago, and the growth of business is causing a problem of having too many patients to look after,” O’Neill says.
“I do my best to only hire the best optometrists. I want those who want to continue their career. My goal is to teach them what I can, but for them to go forth as better optometrists than myself and to strive to greater heights in the community. I am proud of the people who have worked here, and they are incredible optometrists who are a credit to the profession.”

How do you put nervous patients at ease? How do you set aside your own bias and assumptions to make a balanced, informed, well-considered clinical decision? Insight explores why soft skills are arguably as important as clinical skills for optometrists.

Albert Einstein’s philosophy, ‘If you can’t explain it simply, you don’t understand it well enough’, holds an important lesson for communicating with patients, Specsavers head of clinical performance Mr Nick Gidas says.
Gidas is passionate about developing optometrists’ soft skills and spoke about effective communication at Specsavers Clinical Conference last year.
“As optometrists, we can have all the clinical knowledge required, but unless we’re able to impart that knowledge in a way that has meaning for our patients, we’re probably not going to get the best health outcome or give our patient the best experience,” he says.
“Taking it a step further, effective communication is not only when the information is received and understood, but understood well enough, where that person can relay that information to another person. That’s when we truly know that it’s been understood.”
Communication is a skill and – like any clinical skill – for it to perform at its best consistently, requires training and development. It is one skill among a host of soft skills optometrists can deploy in what is predominantly a people-facing profession, to ensure patients receive optimum care, and keep returning.
Poorly performing soft skills that fall short of the mark can have negative repercussions.
According to Specsavers data collated over the past three years, overwhelmingly 98% of patients feel cared for. However, in those rare circumstances where they don’t, it is communication that is most commonly identified as the cause.

Gidas highlights two negative outcomes of ineffective communication.
“The first is wasted time. If we think about those important moments where optometrists are discussing the patient’s case history, results, management plan, recommendations, or transferring care as part of a handover, when we’re ineffective in those moments, we’re adding time because we’re creating confusion, and indecision,” he says.
“As a result, the patient may not have time to go through the dispensing process, or we inconvenience them by asking them to come back on another day.”
The second major impact of ineffective communication is emotional.
“When we’re ineffective in those moments, we are the ones leading that conversation that creates confusion and indecision. Our patients may be prescribed a product that may not turn out favourably or they may need to come back for a remake. Worse still, they may decide they don’t trust us, and not come back for future health care they need.”
In his 27 years as a practising optometrist and the last seven in a clinical performance support role, Gidas has had conversations with thousands of optometrists and patients.
“I can honestly say that no two conversations have been the same, and that’s simply because no two people are the same. I’ve had to adjust what I’ve said and how I’ve said it many times, so the person I’m communicating with is able to receive that information the first time and understand it.
“As optometrists, our purpose is to improve the quality of life of every patient that we see, whether we do that through early disease detection and management, through education or a product recommendation, or referral to a specialist or a support group. We are delivering information
that we need our patient to receive and to understand.”
He continues: “Anything that blocks that from happening is what we need to be accountable for. In our profession, perhaps the biggest block is our language. These are words that are comfortable and familiar to us in the way we say and hear them, but that’s because it’s part of our everyday language. For our patients, they aren’t as familiar, and for some it may be the first time they’re hearing about an eye health condition or a prescription. We need to ensure we’re finding ways to communicate that are relatable and understandable.”
Discussing a patient’s history is a case in point.
“Commonly what I hear are words and phrases like, ‘How’s your distance? How’s your reading? Is this for a routine test?’. Unless we’re following up these questions by asking our patients, ‘What does distance mean for you? What does reading mean?’, then we’re not communicating effectively,” he says.
“If our purpose is to improve the quality of life of every patient, it stands to reason that our line of inquiry through case history should be about understanding the patient’s lifestyle and their barriers to good vision.”
He says to develop effective communication as a skill, optometrists need to understand the attributes that make an effective communicator.
“One of the strengths of an effective communicator is being a good listener. If we can grasp this, it’s going to help us communicate and consult more effectively, because that’s what helps you navigate through conversations. It helps you be in the moment, answer questions, tackle challenges, and provide the right guidance and advice,” Gidas says.
“The other major strength is remembering it is not about you – it is about your patients. You have to remove your assumptions and provide relevant information in a way that your patients can understand.”
When taking a patient’s case history, Gidas recommends asking lifestyle-oriented questions, such as: ‘Where is it important for you to have cl ear, comfortable vision?’, ‘What activity were you performing when you experienced eye strain?’ – and listening to what patients say.
“This approach means the patient is always receiving the message in a way that matters to them, but not necessarily the way you think it best sounds,” he says.
One of the most common challenges optometrists encounter is how to best communicate with a patient who has a weak prescription, or minor change to an existing prescription, where the optometrist is not able to easily demonstrate a noticeable change in acuity.
“There is a fear of upsell because the patient is not able to read any additional letters on a distance or reading chart,” Gidas says, adding he has been asked how to handle this type of situation numerous times in his role at Specsavers.

“Generally, in those instances, the optometrist transfers responsibility to the patient with words such as ‘It’s up to you; it’s only a small change’ without any other information.
“But, if we’ve asked the right questions and listened to the response, then those patients we can help with only minor changes in prescription
will give us that information when they tell us their story in their own words – words like ‘fatigue’, ‘eyestrain’ and ‘blur’.”
Effective communication is a two-way street, Gidas says, and devoting time to developing the skill of communication has immense benefits.
“Getting it right more consistently the first time does save time, which is valuable for the patient, and it saves emotions, because we give them a great outcome more consistently. It encourages that patient to self-care, which is important for future outcomes, and it builds relationships because in that moment, your patient feels like they’re the most important person in that time with you.”
Paediatric optometrist Ms Soojin Nam relies on her interpersonal skills to set the tone when welcoming new patients into her practice.

“Some children can be quite frightened or apprehensive about getting their eyes tested, especially if it’s their first time. Being able to create rapport early on and as quickly as possible to put those little patients at ease – I think that’s a real skill that can only be beneficial,” she says.
“It starts from the moment they come into the practice. I tell my paediatric patients, ‘I’m so excited you’re here to see me today. We’re going to have so much fun during the eye test’. Even something as little as that sets the tone for the rest of the eye test.”
Nam is part owner of three Eyecare Plus practices, and sole owner of an additional three Eyecare Plus practices, all located in Sydney.


“I graduated in 2000 and started my first practice in 2001 after winning a Shell LiveWIRE business competition. As part of the award, I was incredibly fortunate to receive a year’s worth of professional PR to grow the business,” she says.
Over time, as opportunities presented themselves, Nam slowly increased the number of practices she owned. She says every stage of business growth requires a different set of management and leadership skills, but soft skills are applicable at any stage.
“There are a number of soft skills you need in the workplace, but in an optometry practice there are certain ones that really come to the fore, most notably interpersonal skills, communication skills, decision-making and problem-solving ability, and time-management skills,” she says.
When dealing with parents who might be concerned about their children’s vision problems, Nam draws on her empathy and ability to communicate with parents in a calm, professional manner, to ease their concerns.
“If it’s an adult patient and they genuinely have a visual concern that’s causing them stress, one of the biggest assets I have in my practice is time. As an independent optometrist, I’m not under time constraints – it’s not one of my KPIs. That changes the way I approach the patient’s visual
needs because I’m focused on solving their presenting concerns. If I feel they need more time with me, I simply book them in. I always go with the adage that people don’t care how much you know, until they know how much you care.”
Although Nam has a certain degree of liberty to spend more time with patients as needed, sometimes the decision-making process can stump her, and she leans on her networking skills to seek answers, be it clinical or business.
“When it comes to making decisions, the more experience you have, the more it’s going to be beneficial, and that only comes with time. I’m certainly not afraid to ask for help and saying ‘I don’t know’. Making good decisions comes down to your experience, intuition and logic and seeking out as much information as you possibly can. When you’re making clinical decisions, you really want to have the largest, widest range of problem-solving solutions in your toolkit to be able to solve the patient’s visual problems.”
Managing teams across six practices, Nam says soft skills not only apply to how she interacts with patients, but staff too, to help create a harmonious workplace environment.

“Communication and teamwork in many organisations are often an area that can pose a challenge. If communication is not free flowing and open, then it’s most likely the cause of perceived difficulties. If a patient has a positive experience with a dispenser but are then disappointed with the optometrist, the whole thing was a failure for them, and vice versa, if they have a negative experience with reception staff, but have an amazing experience with the optometrist – it really takes the entire process to deliver the service the way it’s meant to be delivered.”
When she purchased her first practice, Nam remembers being told “having more than one practice is very difficult and not many can manage more than two or three”.
Nam was motivated early in her career to challenge the status quo. “One practice was manageable, three was definitely the most challenging, six is when it became a lot easier because you have the economy of scale. My skill set, as a business manager, had to adapt at every stage. Managing three employees is a completely different experience to managing 50,” she says.
As the former head optometrist of the established practice theeyecarecompany, now part of the George & Matilda Eyecare network, Dr M argaret Lam understands that establishing rapport helps understand patient’s health and medical needs, as well as their occupation and lifestyle needs.
“Patients benefit from strong interpersonal skills from their optometrists. In the context of optometrists communicating with their patients in close physical proximity, one patient’s definition of ‘comfortable personal space’ may vary widely to another, so it is very important to read subtle social cues from a patient,” says Lam, who recently started a new role as the head optometrist of 1001 Optical in Bondi.

While showing warmth and openness to welcome a patient, she advises looking for subtle cues to help patients feel comfortable, so they feel confident sharing their personal history.
“All the simple things are important, such as an optometrist maintaining appropriate non-verbal and verbal communication cues, maintaining appropriate eye contact, adopting a friendly, warm manner, speaking in a communication style that makes your patient comfortable, listening actively to your patient’s concerns, avoiding medical jargon, expressing complex concepts to patients in a way that is simple and easily understandable, and showing sincere interest in their overall health and well-being, all these soft skills are critically important,” she says.
Lam, who is also national president of peak body, Optometry Australia, says optometrists can use open-ended questions to encourage patients to share more information about their symptoms, medical history, and lifestyle.

“Starting with open-ended questions before seeking clarification, and then leading them to arrive organically at management solutions that work for a patient will help to keep the patient aligned with you on your recommendations for their eyecare.”
“Then, at the beginning of an eye exam, when you’re ready to examine a patient’s eyes, setting a clear plan and expectations for the eye test in the patient’s mind is also very important, as the patient takes away the sense that their eye test was thorough, methodical and purposeful, and attentive to their needs. Doing this gives the patient structure and aligns you and your patient’s expectations, and allows a patient to feel you’ve met and even exceeded their expectations for their eye exam,” she says.
“For example, once you understand what vision-related concerns your patient has after taking their history, it is worthwhile – at the start of the eye exam – to explain your goals for what can be tested and achieved in their eye exam. You can discuss what their expected outcomes will be, and what they should expect from you as far as what type of advice and management plan you will share at the end of their consultation.”
Before any decision making takes place, Lam recommends optometrists seek clarification and confirmation that they understand what the patient has shared with them, to minimise any misunderstandings.
“It is good practice to summarise the information you have gathered to

“ONE OF THE STRENGTHS OF AN EFFECTIVE COMMUNICATOR IS BEING A GOOD LISTENER. IF WE CAN GRASP THIS, IT’S GOING TO HELP US COMMUNICATE AND CONSULT MORE EFFECTIVELY.”
NICK GIDAS SPECSAVERS
ensure you have correctly understood the patient’s concerns. Clarifying with the patient can reduce any potential misunderstandings.”
It is important that it feels like a consultative decision when assessing if the patient will be comfortable adhering to the management plan being offered, Lam says.

“Explaining next steps that they will need to follow in their vision and eye management plan are also helpful. Professor Charles McMonnies has published excellent research showing that writing down your recommended management plan for a patient results in double the number of patients complying with an optometrist’s recommendations for their eye health management and advice.”
The onus is also on the practitioner to ensure all their health recommendations are in line with the most up-to-date advice they can provide their patients at the time of the eye exam.

“We’re fortunate to be in a field where improvements in clinical care, and thanks to the ever-expanding body of ongoing research, improvements in standards of what is best practice for patients is expanding quickly. We’ve seen an increase in accessibility to subspecialty expertise, with strengthened close working relationships with ophthalmology, and close collaboration with general practitioners and allied health care practitioners,” Lam says.
“All of these changes improve patient outcomes considerably, when we are all working together closely for a patient’s best interests. In the event a patient has a condition that is extremely time sensitive, this can be the difference between a patient losing their vision or retaining it.”

“Having a science and health background, optometrists rely heavily on evidence-based practice to guide their health care recommendations. We consider the patient’s individual needs, values, and preferences, find an appropriate solution compassionate with the patient’s needs,
a nd a solution that we try and ensure the patient is on board with accepting. We explain potential outcomes in order so that we can help a patient take preventative steps to protect their own vision or eye health,” Lam says.

As a practitioner with more than 22 years clinical experience, and 20 years business experience, Lam believes soft skills in optometry are as important as the technical and clinical skills of an optometrist.
“Cultivating those soft skills, including qualities such as compassion, empathy, resilience, and adaptability, are important to provide the best care possible for our patients. Optometrists should also work collaboratively with other healthcare professionals, embrace diversity and inclusivity, and maintain professionalism at all times, as ultimately, this enhances a patient’s ability to follow the advice of their eyecare professional and improve a patient’s long-term vision and eye health outcomes.”

New research shows a significant number of adults in the US are interested in purchasing both contact lenses and glasses, representing a largely untapped ‘dual wear’ growth opportunity for the eyecare community. Could the same opportunity await Australian optometry practices?
Do you wear contact lenses or glasses? It’s a question the Contact Lens Institute (CLI) in Washington, DC, says positions the two methods of vision correction as an “either or” proposition – when the real choice lies in having the ability to pick between the two at any given moment.

It’s the reason why CLI recently surveyed more than 2,000 prescription vision-corrected Americans, asking them a wide range of questions about what they use to improve their vision, what drove their choices, and how their preferences may vary based on other factors in their lives.
Among respondents, 70.6% reported using only glasses while 5.7% reported using only contact lenses (allowing for glasses as emergency backup only). About one in four (23.6%) shared they were dual wearers, alternating between contact lenses and glasses, for various reasons.
The report found almost one in five glasses-only wearers (18%) are ‘very interested’ in contact lenses, and the same percentage of contact lens-only wearers are ‘very interested’ in glasses. In total, this represents an unrealised prescribing opportunity for more than one-third of all patients in the US.
You read that right: untapped demand for dual wear among current glasses and contact lens wearers in the US is more than one in three patients (36%).
According to the report, titled Double Duty: The Patient & Practice Potential of Dual Contact Lens & Glasses Wear, 75% of glasses wearers reported that contact lenses were not discussed at their most recent appointment, although such a conversation would help at least one in five of them strongly consider wear.
Likewise, 45% of contact lens wearers report that glasses were not discussed during their most recent exam; where that did occur, more than half of the conversations were about backup options.
“Seizing the opportunity requires a simple but largely underutilised approach from the eyecare community: having a conversation,” the report’s authors note.
It’s a simple conversation that often helps Australian optometrist Dr Alem Catic gauge his patient’s interest in, and awareness of, the benefits of having a pair of glasses and contact lenses.
Catic, an optometrist at Wood & Associates Optometrists by George & Matilda Eyecare in Essendon in Melbourne’s north, says he gained a lot of experience in discussing and prescribing dual options to patients under the guidance of business owner Mr Graeme Wood.
“I don’t assume what patients want,” Catic says. “I don’t presume they only want glasses. If they wear glasses, I may ask when they wear them and if they say they wear their glasses for everything except swimming, then I’ll ask: ‘Have you thought about trying contact lenses?’.
“It’s about asking questions, questions, questions.”
Another question Catic often asks helps draw out a reason why a patient may not have tried contact lenses.
“It’s a little unusual but I ask patients if they feel wearing contacts is unsafe, in terms of the risk of infection. I ask, ‘Do you think they’re safe for you, or are you worried about something?’,” Catic says.
If safety is a concern, he explains their evidence-based safety profile, before suggesting the patient try a pair in-store – complimentary, without any obligation or pressure.
At this point in the conversation, Catic drills down into their lifestyle, asking patients about their occupation, whether they play sport, their hobbies or activities, and where or what occasions they may like to wear contacts.
“Some patients who haven’t thought about wearing contacts before may
say they’d like to wear them for special occasions or to play tennis once a week. I then explain the different types of modalities – daily, fortnightly, monthly, and multifocals. Some patients are visibly nervous or hesitant, so I offer to insert a pair to wear while they’re looking at spectacle frames,” he says.
He finds patients are often willing to try them in the safe confines of a practice where they don’t have to handle the lenses themselves.
“I explain that I don’t need to teach them then and there how to insert or remove them. I say, ‘Just wear them while you’re in the practice and when you’re done, I’ll take them out and you’re free to leave’,” he explains.
“More than half of the patients who agree to try contacts while in the practice then ask for a follow-up appointment so I can teach them how to insert and remove contacts and how to take care of them.”
According to Double Duty, identifying situational wear (as Catic does) can increase consumers’ consideration of embracing both contact lenses and glasses.
Among dual wearers in the US, 60% prefer glasses when working from home, 81% say they are likely to choose contact lenses for fitness/sports
activities. Yet among glasses-only wearers who discussed contact lenses during their last eye exam, their application for sports and fitness were only raised 9% of the time.
CLI noted that dual wearers overwhelmingly like the ability to choose their own path. About eight in 10 dual wear respondents agreed that having choice is a powerful benefit, including feeling their best in different situations, accounting for how their eyes felt every day, choosing their own look, and having more control over their vision.
“Patients want options. Why not give them the opportunity with dual wear?,” CLI’s report suggests.
Catic’s approach of offering patients trial contact lenses is one of several actions that practices can implement to help patients experience the benefit of dual wear, according to Double Duty

“The largely overlooked importance of trial stands out within the research. Among glasses-only wearers, contact lens trials are largely underutilised,” the authors wrote.
Nearly one in three (32%) of the glasses-only patient population said that a free trial would increase their consideration. Yet among the subset who reported that contact lenses were discussed at their most recent exam, only 10% were subsequently offered trials of any type.
About one in five (21%) said they have not tried contact lenses in more than 11 years.
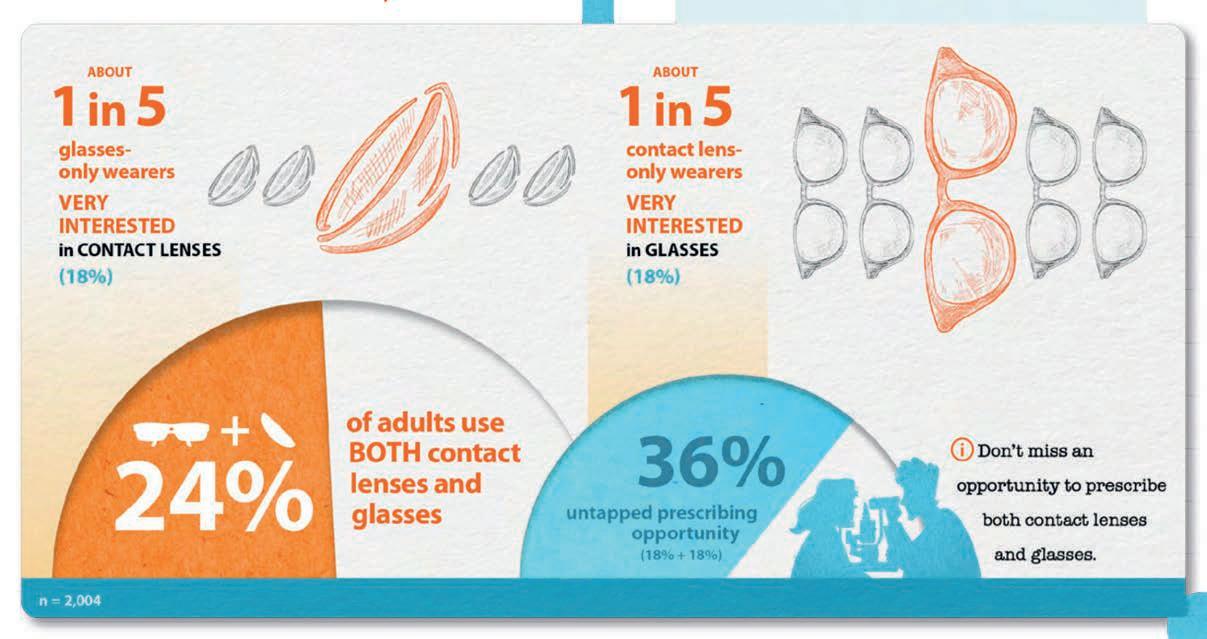

“Suggesting trial for the first time – the all-important conversation – and offering former wearers to re-experience more advanced contact lens designs and materials has a strong potential for success,” the report said.
The CLI survey results also show that, unlike their glasses-only counterparts, contact lens-only wearers are looking at cost when considering dual wear.
Catic says cost can be a difficult topic to navigate.
“I begin that conversation by talking with the patient about the modality that best suits their needs. For example, I explain that dailies range from $90 to $150, if the patient is only intending to wear them on certain occasions, one or two hours a week. I always discuss pricing and also explain that I’m going to give them a few free trial lenses to try before they commit,” he says.
“DAILY DISPOSABLES HAVE BEEN A BIG GAME CHANGER FOR PART-TIME WEAR BECAUSE IT’S AN AFFORDABLE WAY FOR PATIENTS TO USE CONTACTS FOR WEEKEND WEAR, SPECIAL OCCASIONS OR SPORT.”
ANDREW BOWDEN ENVISION OPTICAL
Wood & Associates Optometrists doesn’t charge a fee for fitting contacts because, Catic says, it has found that patients are then less inclined to
“I let them know that if they buy a box of 90 but they’re only going to wear them once a week, they will get nearly two years’ worth of wear. It’s still cost effective, just to have that second option. I generally find that women are more inclined to purchase a box of contacts for occasional wear.”
Catic explains to his patients that if they feel like they want to wear contacts more frequently, he has different options available, including fortnightly or monthly contacts.
“If cost is an issue, I explain that monthly or fortnightly contact lenses are cheaper per wear, so they can wear them more often. Some patients, after wearing daily's occasionally for three months, come back and say they’d like to wear them more often. They’ve come to realise how good they are as backup or as a second option of wear,” he says.

On the flip side, Catic, who is also G&M Eyecare professional services manager for Victoria, South Australia and Western Australia, says having a conversation with contact-only wearers about trying glasses can be challenging.

“It’s all about educating them. I tend to explain that while it’s fantastic that they’re compliant in wearing their contact lenses, things can go wrong. I might say, ‘If you get an infection tomorrow, how are you going to see?’ and it starts a discussion about considering the merits of a cost-effective pair of glasses,” he says.
“If a contact lens patient is in their 30s, and their vision is stable, I explain that they may get five or six year’s wear from a pair of glasses. I also recommend to patients who wear contacts to purchase a pair of non-prescription sunglasses. Although contacts have UV protection built in, they don’t protect the conjunctiva or the rest of the lid anatomy. Sunglasses offer added protection, helping to prevent melanomas and pterygium, or Surfer’s Eye, from developing.”
Unlike Catic’s patients, when contact lens-only wearers in the US had a conversation about glasses with their eyecare practitioner, only one in three reported being offered the chance to look at glasses in the practice. In addition to talking with patients about the benefits of dual wear, Catic says front-of-house staff have an important role to play in the
“It could be as simple as saying, ‘I see you’ve come in for an eye test. Did you bring your contact lenses?’ and if the patient says ‘I don’t wear contacts’ staff can respond, ‘Why don’t you talk to the optometrist? Or do you have any questions for us?’. Front-of-house are important for easing into that conversation and building a rapport with the patients.”
For independent optometrist Mr Andrew Bowden, prescribing glasses in companion with contact lenses, and vice versa, is not rocket science – it’s a matter of investing time.
Bowden, part of the ProVision network, owns two practices in Queensland, Envision Optical in Tweed Heads and Burleigh Waters, the latter recently undergoing an extensive renovation and fit out. He has a special interest in complex contact lens fitting and diagnosing and managing dry eye disease.


“My whole approach is educating patients about their vision, including any problems with their vision, and the possible solutions, including explaining to the patient all their options, if their prescription is available in glasses, sunglasses and contact lenses,” he says.
“Daily disposables have been a big game changer for part-time wear because it’s an affordable way for patients to use contacts for weekend wear, special occasions or sport.”
Bowden prescribes a lot of multifocal contact lens solutions to his adult patients.
“As a consequence, there’s a little bit of upfront time involved, and I charge for that, but the success rate is a lot higher because I spend a little bit more time showing them what’s possible,” he says.
“There’s an element to getting the right prescription balance because it’s not a direct translation from glasses into multifocal contacts, so I need to try a few different lens options. Once I get that good visual balance, I start running them through the foundational basics of how to manage contact lenses correctly, so I’m setting them up for success.”
Bowden always schedules a follow-up appointment for new contact lens wearers.
“That’s what really gets solid results,” he adds. “Spending a little bit more time at the start, asking lifestyle-related questions, discussing all the options, explaining what’s available in their prescription, fitting trial lenses, booking in a follow-up, all leads to more lasting success.”
He spends time on the foundations of wearing contact because he wants patients to feel comfortable taking the lenses in and out before they leave the practice.
“You’re going to have a higher success rate long-term with patients who don’t feel overwhelmed by it.”
Bowden also spends time explaining the benefits of having a pair of prescription spectacles on hand as an alternative to contact lenses.
“I might say, ‘If you get an infection, you need something to wear because you’re at the level of prescription where you’re not able to drive without vision correction,” he says.
“I explain to my contact lens patients that it’s wise to have an option to avoid over-wearing their contacts. I say, ‘If you’re home on Saturday for a few hours, wear your glasses around the house, and then pop your contacts in to go out’. I use the term ‘credits in the bank’ for long term success, rather than them developing an allergic reaction to contact lenses because of over-wear.
“It’s as simple as talking about it. It’s not rocket science.”
If, like Jessica, you love the idea of a job where you get to help people change their lives through improved vision and hearing, you’ll shine at Specsavers. join.specsavers.com/au/find-a-job

Relieve
NovaTears® acts as a lipid layer substitute and evaporative barrier for improved tear film stability and quality


Stabilises and thickens outer tear film
Allows replenishment of underlying water layer with natural tears


Assists regeneration of eye surface to a healthy state
months
6 opening shelf life after
Patented EyeSol® Technology
PBS Listed
A unique preservative-free eye lubricant utilising patented EyeSol® technology, specifically designed for the relief of evaporative dry eye disease
Clinically validated with significant improvement in signs and symptoms with Evaporative Dry Eye Disease and Meibomian Gland Dysfunction patients2,3
Spreads quickly and easily with longlasting effect

Warm silky feeling on eye – no blurring, stinging or burning
Small droplet size (4−5 x smaller than water-based drops) helps prevent spillover
Preservative, phosphate, water and surfactant free
STREAMLINED AUTHORITY CODE 6172
PBS Information: Authority Required (STREAMLINED): Severe dry eye syndrome in patients who are sensitive to preservatives in multi-dose eye drops.
minutes between using the other product and applying NovaTears®. NovaTears® should not be used in children under 18 years. NovaTears® should not be used while pregnant or breastfeeding. AFT Pharmaceuticals Pty Ltd, Sydney. ABN 29105636413.

At the completion of this article, the reader should be able to prepare their practice for a locum optometrist ...
Including:
• Know the equipment necessary for a successful locum
• Develop strategies to facilitate seamless locum experiences
• Review the trading structure options and tax obligations of a locum
• Understand the importance of thorough record keeping
• Know what to include in patient notes to practice optometrists, and why
It takes two to locum: the visiting optometrists and the resident practitioner. As ANDY SHAO points out in this non-clinical CPD article, some preparation by both parties can make the experience gratifying and successful for all.
My name is Andy Shao and I am a mobile optometrist for Specsavers based in Perth, Western Australia. I’ve been in my current role for the past year and a half, and my position has given me the opportunity to enhance not only my clinical knowledge and skill, but also my understanding of myself as a clinician-at-work, as well as my personal life outside of work.

The experience of being a mobile optometrist for Specsavers is similar to that of a locum.
We are expected to work in different clinical settings almost daily and our workdays can vary greatly – every clinic has its own intricacies and ways of operating. Because of this, it’s important to be adaptive and well-prepared for anything the day can throw at you.
This includes having all the necessary equipment with you:
• A lger brush and foreign body remover, especially in regional settings where there is less accessibility to care and higher incidence of foreign body injuries.
• A msler grids or access to printable templates. Less accessibility to ophthalmology care means more responsibility on the patient to monitor for any progression which may require further investigation or treatment, and more importantly, on you as the clinician to give the patient the appropriate advice and care to allow for best outcomes.
Travelling to different clinics almost daily means meeting a lot of new colleagues and forming and building these relationships in the short amount of time you are there.
Due to these time restrictions, your actions and behaviour will have a greater impact on their impression of you, especially during your first meeting.

Reputation is critical to being a mobile optometrist or locum, as you are your own ‘brand’ and employers look not only at your clinical skills and performance, but also in your ability to work smoothly within the team.
• B e punctual and attend morning team huddles. This can make a great impression on team members, as it shows your willingness to participate and work with the team. This also gives you sufficient time for the team to show you the layout of the practice and their way of managing their diary and clinic etc, as well as answering any questions you have before starting the day.
• B e proactive and help the team when possible. This piece of advice is especially relevant today, as from my experience, most practices are short on staff and will often be running on a skeleton crew especially if there are last-minute illnesses. This may include doing your own pre-testing as well as taking the patient to start frame-styling if no dispensers are available for a handover.
Being often in new clinical settings will mean you don’t have the pre-existing rapport with colleagues and this needs to be built at the
time. Often this can lead to more difficulty in effective communication, especially when handing over a patient.
As every patient’s visual needs are unique, it is essential to gather the relevant information to formulate the best and most appropriate recommendations for their needs. As optometrists we are familiar with building trust and relationships with the patient over the

Members of Specsavers’ mobile optometry team provide relief for Specsavers practices. And although it’s a lot like a locum position, these positions come with full-time contracts and benefits such as sick leave and annual leave.

Being a locum can be rewarding or frustrating. You have the power to make it successful, but it does take some preparation and planning. First off, there are a number of financial requirements when working as a locum that don’t apply when you’re a full- or part-time employee (you won’t receive sick leave, holiday leave, carer's leave, superannuation or other employee benefits).
Locums are also at the mercy of the needs of business, which can fluctuate depending on the location you are working for.
The best advice I can give any optometrist considering establishing themselves as a locum is: get more advice. There are a lot of legal and financial requirements involved in setting yourself up, but consulting with an accountant who specialises in taxes can help lower the barriers.
Locums operate under ‘sole trader’ or ‘company’ trading structures. As a sole trader you don’t have to register a business name, as you can use your own personal name. As a sole trader you can also use your individual tax file number (TFN). However, you’ll need to manage your own superannuation, payroll tax and insurance.
For a sole trader, ensuring you have the right insurance coverage is very important.
A sole trader owns all the business assets and
course of the consult, so we can recommend and deliver the best health and visual outcomes for the patient. However, sometimes this is not as easily communicated to the dispenser during a handover, especially when working in a new or foreign environment without the established relationship between the optometrist and the dispenser.
It’s important to make sure the patient understands our recommendations and address any concerns they may have prior to the handover; this allows the patient to have a better understanding of what to expect from the coming discussion with the dispenser and leaves less room for uncertainty in both parties.
During the handover, it is important to check in for any final questions the patient may have, or offering assurances and demonstrating that the patient’s concerns have been actively addressed during the consult. It is also important to communicate to the dispenser any relevant details of the management plan, which may include a specific recall period or the need to book in for additional testing or review.
Sometimes it may be helpful to highlight or
is responsible for all the liabilities of the business. Liability is unlimited, it can include your personal assets, including any assets you share with another person, such as a jointly-owned home or money in a joint bank account.
Usually, a company has members (shareholders) who own the company and directors who run it. But an independent contractor can set up a ‘one-person company’ with a sole director and member. While ‘companies’ have limited liability, ‘directors’ can be personally liable. Regardless of your status, insurance is required.
GST
The provision of optometric locum services is a taxable supply for the purposes of Goods and Services Tax (GST). If you anticipate that in a year
write any additional notes on the patient board which may go unattended, especially in a busy clinic where another colleague might take over during the dispensing process. This reduces the risk of incomplete care or management for the patient.
Thorough and effective record keeping is essential as a mobile optometrist or locum, especially if you are working only for one day at that specific location and won’t be returning in the near future.
This becomes especially important in the case of ocular emergencies or acute conditions which require therapeutic management, such as keratitis or uveitis. I’ve worked in clinics where I was the only therapeutically-endorsed optometrist, so I had the responsibility of providing appropriate care for the patient as well as giving the next optometrist clear notes for review.
Sometimes it is helpful to take an anterior slit lamp photo with your phone and either give the photo to the patient to show the next
you would earn more than $75,000 from being a locum, you have to register for GST. (In order to register for GST you will also need an ABN). You can register for GST and a range of other requirements depending on your tradingstructure, through the Australian Taxation Office (www.ato.gov.au/Business).

If you are providing locum services as a sole trader, you are responsible for your own superannuation arrangements. This is also important to remember when you are setting a pay rate for a locum assignment – remember to include your superannuation rate in your expenses.
optometrist or securely store the photo on the computer or patient file. Having access to a photographic view of their condition is often much more helpful than trying to describe their signs, which can lead to confusion or uncertainty.
In other cases where immediate review is not necessary, it’s important to write effective notes to allow best patient care. Make your notes easy to understand for the next optometrist. Include a clear management plan and an appropriate recall period, as well as communicating these to the patient and front staff if necessary.
If you are an optometrist partner/owner of your own business considering a locum, there are a number of points to consider.
Good communication with the locum prior to their shift is essential. It builds the relationship prior to meeting them, especially if it’s their first time working at the practice. Remember to provide the locum with a contact number, in case they require any assistance during their shift and
giving them the necessary information to set up their provider number for the practice such as ABN and contact details for the practice, and any other useful information which can assist with their travel and finding the practice. This may include information about any dedicated staff parking areas or alternative arrangements for parking, which is especially useful if the practice is based within a shopping mall or in an area with limited parking options.
Informing the team about the locum’s upcoming shift and delegating the clinic coordinator/manager or another staff member to greet and show them around the practice once they arrive is very helpful in settling them in, as well as discussing other details they should be aware of. Inviting the locum to the morning team huddle can also help them settle in as any concerns can be easily addressed before opening for the day.
Often times, different practices will have different equipment and machines available, as well as specialised care the clinic may be responsible for. Before booking the locum in, it may be beneficial to check with them any specialty cases they are comfortable seeing and if there are certain demographics or conditions they may struggle with. This may include complex contact lens fits and
Keeping an open channel of communication before their shift can reduce the risk of any incompatibilities or difficulties they may face on the day with certain specialty care.
This may also apply for busy clinics running on shorter testing time, as some locums may not be comfortable working a 20-minute clinic and may require or request for longer test times. Therefore, it is important to check with the locum beforehand when booking them in to make sure they are comfortable with the set testing time. It may be appropriate to block out some admin time for them to catch up or write referral letters and reports if the clinic is expected to be very busy in the day. This may be done either during the day or towards the end of their shift depending on the practice’s preference.
Checking availability of locums and booking them in advance can save stress during busy periods of trade. This may be dependent on location as some cities and areas have a larger pool of locums and mobile optometrists available, whereas smaller cities and regional towns may struggle to find cover on short notice.
In Perth, there is a significant shortage of locums during the year so planning ahead and checking for optometry cover well in advance
is recommended, even more so for remote areas where locums may have to be flown from interstate.
Being a locum isn’t for everyone, but I can honestly say there is really nothing quite like it. Whether you choose to be a Specsavers mobile optometrist or to locum, the experience offers travel and the flexibility to make lifestyle choices that a permanent role may not allow.
For the optometrists who employ locums, it’s important to be clear with them – and yourself – about your expectations around productivity, clinical testing and staff support.
For the locum, it’s important to understand that ‘work’ is an important part of the acclaimed ‘work-life’ balance that the experience of being a locum affords. Ultimately, although being a locum offers a lot of freedom, it’s based on your ability to keep and stay organised – with your patient notes, with your handover notes and with your finances. If you are a self-starter that can do this and stay flexible, I can almost guarantee you will enjoy your time as a locum.


The October 2023 issue will feature the Insight Dry Eye Directory, Australia’s most comprehensive source for dry eye care.
Back by popular demand, this all-in-one resource is a valuable purchasing guide for practices, showcasing available Therapies and Diagnostics in Australia. It will also feature a comprehensive list of dedicated Dry Eye Clinics.
It’s FREE and EASY for you to list your products or services.
If you operate a dry eye clinic, or are a supplier of dry eye products, scan the QR code to organise you listing, or visit insightnews.com.au/dry-eye-directory-2023
Scan HERE to arrange your listing.

To amplify your product via advertising, contact Insight BDM Luke Ronca: 0402 718 081 or luke.ronca@primecreative.com.au
www.insightnews.com.au

At the completion of this article, the reader should be able to improve their management of dry eye disease ...
Including:
• Define hyaluronic acid and its use in dry eye treatment
• Review the TFOS DEWS II stepped-approach to the management of dry eye
• C o nsider the clinical utility of Systane HYDRATION
UD Lubricant Eye Drops and where they fit in the management of dry eye symptoms
Artificial tears have been a mainstay dry eye treatment, but as manufacturers bring new products to market it can be challenging for optometrists to remain abreast of the best-performing therapies. MARTIN ROBINSON explains why hyaluronic acid is considered a lubricant with desired properties and performance.

At my recent dry eye workshop series at the AVC conference, I was a little surprised at the prevalence of some outdated treatments recommended in response to poll questions I presented. The treatment suggestions improved rapidly as I outlined the logical reasons why I offer somewhat different treatments. This give and take, to me, showed the power of historical cognitive biases. We can, and often do, automatically prescribe a treatment based on knowledge that we learned years or even decades ago. It’s something I think we’re all guilty of at times. In a rushed clinic, we fall prey to a snap diagnosis and treatment path, which can sometimes be based on old knowledge, especially in what was once considered a dry topic such as dry eye disease (DED).
When I see a patient for an initial consultation, I always ask them what eye drops they’ve had prescribed in the past, which worked and which did not. Commonly, I hear eye drops listed that I have not used for many years, drops that I stopped prescribing as evidence emerged of inferior performance compared to newer generation products. I see that as further evidence of historical cognitive bias at play; we prescribe what we were taught was the ideal eye drop for the symptoms. But what if that education was five or 10 years ago?
One of the aims of self-directed learning plans is to identify areas of knowledge deficit and plan to upskill these fields. However, what if we feel confident in our own knowledge? We may then choose to study another topic and carry on confidently using our historical wisdom. I feel this is why I still read reports from referring optometrists that state: “I prescribed lid scrubs with baby shampoo.” Considered appropriate practice 20 years ago, baby shampoo was
explicitly mentioned in The Tear Film and Ocular Surface Society Dry Eye Workshop II (TFOS DEWS II) reports. They pointed out that baby shampoos are pro-inflammatory,1 and obviously baby shampoos were not designed for application to the eyes. There are far better products for cleaning eyes of blepharitis today.
Hyaluronic acid (HA) is an ingredient present in several currently-available eye drops in Australia and New Zealand. I believe there’s enough evidence to support changing your own historical cognitive biases, whatever they may be, and to consider prescribing HA-containing lubricating eye drops more frequently.
What is HA? My patients recognise it as an essential ingredient in ‘youth restoring’ face creams and makeup. HA, or hyaluronan, has an important function in the body – in fact, our connective tissue, skin, intervertebral discs, joints and nerve tissue, the vitreous and cornea – all contain HA.
Although the cornea is avascular, hyaluronic
acid occurs in the intercellular spaces. One of its roles is to supply nutrients and dispose of metabolic products. Additionally, it is thought to play a part in such processes as cell differentiation, cell renewal and wound healing. 2 It was first used as a viscoelastic for vitreous surgery in 1969, 3 first discussed as a DED treatment in 1982 and first appeared as a commercial eye drop in 1987. One of the most important characteristics of HA is the ability to be produced in a low osmolarity or hypotonic form. 4
There are dozens of eye drops containing HA available around the world, some single ingredient, some with multiple ingredients.
A recent meta-analysis was published comparing HA-containing eye drops to non-HA eye drops. There were statistically significant improvements found in several key areas, but not always superior to other artificial tears (ATs): 4
• H A eye drops significantly improved Schirmer test scores, compared with non-HA eye drops (p<0.05)
• Tear Breakup Time (TBUT) after using HA improved significantly versus saline (p<0.05) and was similar to that of ATs
• C orneal fluorescein staining scores after using HA eye drops was similar to that of ATs
• T he HA group showed similar improvements in OSDI scores to the non-HA group
STEP 1:
• Education regarding the condition, its management, treatment and prognosis
• M odification of local environment
• Educ ation regarding potential dietary modifications (including oral essential fatty acid supplementation)
• Id entification and potential modification/elimination of offending systemic and topical medications
• O cular lubricants of various types (if MGD is present, then consider lipid-containing supplements)
• Li d hygiene and warm compresses of various types
STEP 2:
If above options are inadequate consider:
• Non-preserved ocular lubricants to minimise preservative-induced toxicity
• Tea tree oil treatment for Demodex (if present)
• Te ar cons ervation
- Punctal occlusion
- Moisture chamber spectacles/goggles
• O vernight treatments (such as ointment or moisture chamber devices)
• In -office, physical heating and expression of the meibomian glands (including
• D evice-assisted therapies, such as LipiFlow
• In -office intense pulsed light therapy for MGD
• Pres cription drugs to manage DED
• Topic al antibiotic or antibiotic/steroid combination applied to the lid margins for anterior blepharitis (if present)
- Topical corticosteroid (limited-duration)
- Topical secretagogues
- Topical non-glucocorticoid immunomodulatory drugs (such as cyclosporine)
- Topical LFA-1 antagonist drugs (such as lifitegrast)
- Oral macrolide or tetracycline antibiotics
STEP 3:
If above options are inadequate consider:
• Oral secretagogues
• Autologous/allogeneic serum eye drops
• Therapeutic contact lens options
• So ft bandage lenses
• Rigid s cleral lenses
STEP 4:
If above options are inadequate consider:
• Topical corticosteroid for longer duration
• Amnio tic membrane grafts
• Surgical punctal occlusion
• Other surgical approaches (eg tarsorrhaphy, salivary gland transplantation)
HYALURONIC ACID VS AUTOLOGOUS
HUMAN SERUM EYE DROPS
Some studies stand out as very interesting. In a small-scale study, high-molecular-weight HA was explored as an alternative to autologous human serum eye drops, (ASED). 5 ASED treatment has been identified as a stage 3 treatment in TFOS DEWS-II.1
High-molecular-weight HA was found to be an acceptable alternative to ASED, with 50% of the participants continuing with the HA drops after the study. Another small, randomised, double-blind study examined using HA to dilute ASED. 6 The HA dilution was stable compared to the original preparation in all
areas. The exciting findings were significant improvements in TBUT (p = 0.03), fluorescein and rose Bengal staining (p = 0.02) and corneal/conjunctival cell squamous metaplasia levels (p = 0.008) in the HA dilution group.
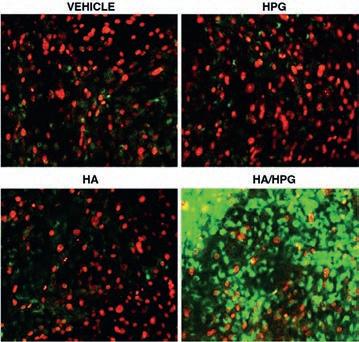
Does this mean we should start considering HA as a stage 3 treatment, as per TFOS DEWS II? 1 More appropriate perhaps to consider it as stage 2, along with non-preserved drops? (Table 1).
There are limitations in studies of all designs and although research findings can be
exciting and surprising, they may not always reflect what practitioners find in clinic.
In my experience, HA eye drops are superior to other ATs in nearly every case where I prescribe them. I choose which patients to prescribe them to, based on the signs and symptoms. If patients report burning and stinging, this often indicates the presence of a higher osmolarity tear film, TFOS DEWS II mentions hyperosmolarity as being a common finding in DED. Stinging or burning are the most common symptoms reported in my DED patients. Prescribing low osmolarity eye drops, containing HA, makes sense in the presence of hyperosmolarity.
Sjögren’s syndrome patients treated with hypotonic HA had greater symptom reduction, improved TBUT and showed reduced staining.7 Is this why I find them so successful? There is yet to be a study specifically looking at stinging and burning symptoms, but I’d like to see one looking at the role of HA in treating symptoms of stinging and burning.
One of the most exciting developments are the multi-ingredient HA drops emerging over the past few years. For many years, I’ve been reading papers and attended lectures discussing these new eye drops. Some amazing claims have been made with some, at first glance, showing statistically significant results, but sometimes they compare eye drops that are not similar. 8 So, caution should be practised when only reading the conclusions of publications, and not looking at the study details.
In vitro studies are often the first line experiment, done ‘in glass’, or more easily understandable, as cells outside their normal environment. An in vitro study was published in 2015 by Rekha Rangarajan et al 9 that looked at the effect of a pairing of hyaluronic acid/ hydroxypropyl guar (HP/HPG), currently available as Systane HYDRATION Lubricant Eye Drops. The results were encouraging in multiple areas when the HA/HPG combination
was compared to both HPG and HA alone.
Protection and maintenance of hydration from desiccation was statistically greater with HA/HPG compared to either HPG or HA alone (p<0.01). Testing the cells for fluorescein permeability showed significantly better cell and barrier protection after induced trauma with HA/HPG compared to either HPG or HA alone (p≤0.01). Interestingly, when surface friction was assessed in an artificial blink, all three reduced friction compared to saline, and HA/HPG was significantly superior to HA alone (p = 0.02). With results like these it is enough to get excited about the duality of HA/HPG, even if this was an in vitro study.
It is no surprise that we have seen several eye drop offerings launched locally with multiple ingredients and containing HA, from many suppliers with offerings in the dry eye space. Thinking of patient care in multiple demographics, these products are now available in a variety of cost brackets, meaning fewer people will be disadvantaged by cost as a factor. There are even PBS options following the appropriate criteria. The current offerings of preservative-free options in bottles that can be used for 90 days is more affordable than single use vials. Eye drop bottles are becoming easier to use for patients with poor dexterity and arthritis in their fingers and hands. Having a variety of product designs with the same ingredients is an advantage as it allows more of the population to access an eye drop that works, supplied in a product design that they find easy to use.
Clinically, I experience greater success with Systane HYDRATION UD Lubricant Eye Drops and a lipid/aqueous combination drop over HA alone – in a similar way to the TFOS DEWS
sound achievable.
Admittedly, you cannot expect a single drop to solve all your patients’ symptoms. As per the TFOS DEWS II definition of dry eye as a ‘multifactorial’ condition,1 so too we should consider and treat any signs of B.E.I.S.T.O. found.10 (‘BEISTO’ is a concept first coined by dry eye pioneer Dr Laura Periman. That is: Bugs/Bacteria, Enzymes, Inflammation, Statis, Temperature and Obstruction. When a sign of any of these BEISTO impediments is found, a different treatment pathway is required).
REFERENCES:
1. J ones, L., Downie, L. E., Korb, D., Benitez-Del-Castillo, J. M., Dana, R., Deng, S. X., Dong, P. N., Geerling, G., Hida, R. Y., Liu, Y., Seo, K. Y., Tauber, J., Wakamatsu, T. H., Xu, J., Wolffsohn, J. S., & Craig, J. P. (2017). TFOS DEWS II Management and Therapy Report. The ocular surface, 15(3), 575–628. https:// doi.org/10.1016/j.jtos.2017.05.006
2. Tammi, R. and M. Tammi, Hyaluronan in the Epidermis. Glycoforum 1998
3. H ynnekleiv L, Magno M, Vernhardsdottir RR, Moschowits E, Tønseth KA, Dartt DA, Vehof J, Utheim TP. Hyaluronic acid in the treatment of dry eye disease. Acta Ophthalmol. 2022 Dec; 100 (8): 844-860. doi: 10.1111/aos.15159. Epub 2022 May 5. PMID: 35514082; PMCID: PMC9790727.
4. Yang YJ, Lee WY, Kim YJ, Hong YP. A Meta-Analysis of the Efficacy of Hyaluronic Acid Eye Drops for the Treatment of Dry Eye Syndrome. Int J Environ Res Public Health. 2021 Mar 1; 18 (5): 2383. doi: 10.3390/ijerph18052383. PMID: 33804439; PMCID: PMC7967738.
II stepped approach to management of dry eye,1 I use HA as a first line drop, then I upgrade to multi-ingredient Systane HYDRATION
UD Lubricant Eye Drops or a lipid/aqueous combination drop as a second tier drop when needed for more moderate dry eye, especially when staining does not reduce adequately with HA alone, or when a patient complains that their current HA drop does not help enough.
I see a superior reduction in staining with Systane HYDRATION UD Lubricant Eye Drops and patients report a greater reduction in their symptoms. My prescribed schedule with Systane HYDRATION UD Lubricant Eye Drops is tiered depending on severity, starting at three times a day, or at breakfast lunch and dinner. Increasing to five to six times a day for more severe cases, which I often describe as ‘almost every time you eat or boil the kettle,’ making it
Prescribe the most suitable lubricant eye drop that the patient can afford, but don’t assume what they can afford, so ask them. If a patient is attentive to environmental concerns, discuss the ways companies are tackling plastic waste globally, discuss the differences in waste with unit dose vs multi-use bottles. If your patient has arthritis or weak hands, give them a sample bottle/vial, and see if they can use them successfully.
Eye drops are an essential part of most treatment strategies. It is no longer appropriate to offer our patients a variety bag of eye drops and ask them to see which one works best. The real world presents other challenges for eye drops, environmental waste, cost of supply and ease of use, so discuss these issues with your patients. As optometrists, we should prescribe the eye drops which will best address the clinical signs and symptoms of our patients.
The evidence is sound that HA is a lubricant with desired properties and performance. The mixing of HA with other active ingredients has broad reaching implications that we are only just starting to explore.
5. R ia Beck, Oliver Stachs, Anita Koschmieder, Wolfgang G.K. Mueller-Lierheim, Sabine Peschel, Gysbert-Botho van Setten; Hyaluronic Acid as an Alternative to Autologous Human Serum Eye Drops: Initial Clinical Results with High-Molecular-Weight Hyaluronic Acid Eye Drops. Case Rep Ophthalmol 3 September 2019; 10 (2): 244–255. https://doi. org/10.1159/000501712
6. L ópez-García JS, García-Lozano I, Rivas L, Ramírez N, Raposo R, Méndez MT. Autologous serum eye drops diluted with sodium hyaluronate: clinical and experimental comparative study. Acta Ophthalmol. 2014 Feb;92(1):e22-9. doi: 10.1111/aos.12167. Epub 2013 Jul 26. PMID: 23890196.
7. A ragona P, Di Stefano G, Ferreri F, Spinella R, Stilo A. Sodium hyaluronate eye drops of different osmolarity for the treatment of dry eye in Sjögren’s syndrome patients. Br J Ophthalmol. 2002 Aug;86(8):879-84. doi: 10.1136/bjo.86.8.879. PMID: 12140209; PMCID: PMC1771217.
8. P into-Bonilla JC, Del Olmo-Jimeno A, Llovet-Osuna F, Hernández-Galilea E. A randomized crossover study comparing trehalose/hyaluronate eyedrops and standard treatment: patient satisfaction in the treatment of dry eye syndrome. Ther Clin Risk Manag. 2015 Apr 13;11:595-603. doi: 10.2147/TCRM.S77091. PMID: 25926736; PMCID: PMC4403513.
9. R angarajan R, Kraybill B, Ogundele A, Ketelson HA. Effects of a Hyaluronic Acid/Hydroxypropyl Guar Artificial Tear Solution on Protection, Recovery, and Lubricity in Models of Corneal Epithelium. J Ocul Pharmacol Ther. 2015 Oct; 31 (8): 491-7. doi: 10.1089/jop.2014.0164. Epub 2015 Jun 11. PMID: 26067908; PMCID: PMC4599388.
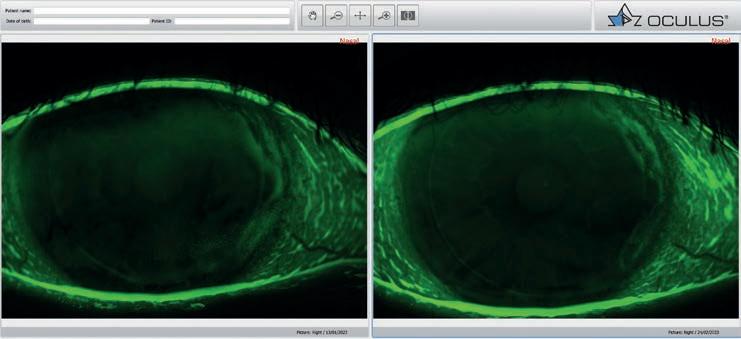
10. R obinson, M. Dry eye – a multifactorial approach to a multifactorial disease. Available: https://www.insightnews. com.au/dry-eye-a-multifactorial-approach-to-a-multifactorial-disease/ Accessed: 05/06/2023
NOTE: Insight readers can scan the QR code or visit insightnews.com.au/cpd/ to access a link to this article to include in their own CPD log book.
“IN MY EXPERIENCE, HYALURONIC ACID EYE DROPS ARE SUPERIOR TO OTHER ARTIFICIAL TEARS IN NEARLY EVERY CASE WHERE I PRESCRIBE THEM.”
Since graduating 3.5 years ago, Ms Tram Nguyen has worked as a clinical orthoptist at Vision Eye Institute (VEI) Chatswood, Sydney. Alongside her core duties, she’s been involved in pharmaceutical trials as a clinical technician, whetting her appetite to pursue her own research project. But she faced a common challenge: finding the time, funding and guidance to get started.
Phacovitrectomy – combining cataract surgery with vitrectomy – was an area that she was particularly interested in investigating, so when the ophthalmology research-dedicated Future Vision Foundation (FVF) launched its inaugural round of funding in 2022, it provided the ideal chance to conduct a study of her own.
“Our project seeks to understand the phacovitrectomy patient and how we may be able improve pre- and post-operative information, discussion and general experience. Even if it is a subset of the ophthalmic surgery population, I believe this will make a difference,” she says.
“Patient protocols and processes have been studied across cataract surgery in general however there has been little to understand the patient journey within the combined procedure, which is increasingly an option.”
Nguyen says cataract surgery is a common procedure where clinicians can mostly focus on great visual outcomes, particularly with modern IOLs.
“Patients expect this but those with pre-existing retinal conditions are often restricted to the potential visual outcome post-surgery. This is an important discussion and providing the most appropriate information, and feedback, to the phacovitrectomy patient is essential to match expectations to possible outcomes to avoid disappointment.”
Projects like this – with potential real-world applications – are vital to address some of the biggest issues in eyecare, and are the motivation behind FVF, a new body launched by Vision Eye Institute (VEI) providing another avenue to support ophthalmic research.
In 2021, Australia’s largest private ophthalmology provider established the not-for-profit that features a board of prominent ophthalmic researchers and industry professionals, supporting the research efforts of VEI staff and associated clinicians or researchers. This includes those with little-to-no formal research experience but who are keen to improve diagnosis, treatments and/or healthcare experiences for patients with eye conditions.
Nguyen’s phacovitrectomy project was among 12 recipients awarded grants in FVF’s first funding round in 2022, which also included other intriguing
studies such as the performance of EDOF IOLs with glaucoma surgical devices, why keratoconus patients suddenly progress long after cross-linking, and the role of music in reducing anxiety prior to refractive surgery.
FVF is now assessing applicants for the second round of funding for 2023, expected to be announced in July.
Nguyen is conducting the study with fellow clinical orthoptist Ms Opal Mai, and Dr Simon Chen, VEI Chatswood’s primary retinal surgeon. She says phacovitrectomy may offer several potential benefits such as faster visual recovery and possible reduction of complications – compared to separate surgeries – reduced costs and improved patient convenience.
“The team at VEI have helped guide me with respect to project development, understanding existing research options and how we may be able to optimise the practical outcomes of the research for our patients,” Nguyen says.



“Conducting the project within the VEI clinics has also allowed me to reach out across the clinics which potentially expands the sample. The FVF funding has helped me in a way where I can dedicate time to focus on doing the project, working outside of work hours and providing the flexibility to develop the project further.”
Participating in research and developing her own research idea was not something Nguyen expected upon graduating. However, she says FVF and the supporting environment has allowed her to develop the project.
“This is really important for a young researcher,” she says. “These opportunities can develop your own skills and interest and ultimately may be beneficial for patients and the community.”
Many clinicians possess real-world solutions that would elevate the greater ophthalmic sector, but there have been few avenues to test their theories in a proper research environment. The Future Vision Foundation seeks to bridge this gap.
“THE FVF FUNDING HAS HELPED ME IN A WAY WHERE I CAN DEDICATE TIME TO FOCUS ON DOING THE PROJECT, WORKING OUTSIDE OF WORK HOURS AND PROVIDING THE FLEXIBILITY TO DEVELOP THE PROJECT FURTHER.”
TRAM NGUYEN ORTHOPTIST
Dr Christopher Hodge is the clinical research coordinator at VEI, and was appointed chair of the FVF Advisory Committee that helps FVF applicants like Nguyen refine their proposals to ensure their relevance and maximum impact.
While larger studies seek lucrative grants from bodies such as the National Health and Medical Research Council (NHMRC), he says the FVF seeks to bridge the gap for smaller ophthalmic projects with more practical objectives.

“There are many good clinicians with great ideas to improve our industry, but they don’t necessarily have the time to go down the full postgraduate research pathway,” he says.
“They may also not understand what’s required to progress their ideas in a research context. If we’re able to facilitate that with the support of the Future Vision Foundation while they’re still performing their clinical duties, then we’re providing the chance to elevate ophthalmology as a whole.”
While many applications in the first-round cohort had links to well-established researchers, the FVF aims to support emerging researchers and those new to the academic field. It’s not limited to ophthalmologists and orthoptists either, with grants supporting optometrists, allied health nurses and administrative staff.
A key function of FVF’s Advisory Committee is to provide feedback to the FVF Board comprising several prominent ophthalmic industry professionals, including UNSW’s Professor Fiona Stapleton, Mr Tim Grant, an executive with broad experience in the ophthalmic sector, former long-serving senior manager of ZEISS Mr Joe Redner, and ophthalmologist Associate Professor Tim Roberts (chair).
“It’s a highly impressive board, and from a research perspective they have unimpeachable credentials,” Hodge says.
“We also have industry representatives who offer a different perspective. In addition to making decisions around which projects are successful, they’re also there to provide feedback on how we can evolve the foundation – their experience and knowledge has helped significantly.”
The FVF will soon announce the recipients of its second round, using criteria based on current NHMRC guidelines. Hodge says there were around 18 applications this year, with projects focusing on topics such as optimised protocols around post-operative patient care, the role of computation to improve imaging and diagnosis, and the potential impact of microplastics in the eye.
A little more than half of these are expected to become successful 2023 recipients.
For people struck by corneal endothelial pathologies from injury, inflammation, infection, or diseases like Fuch’s dystrophy, there’s sometimes only one option: surgery involving donated corneal tissue. The problems is, there’s a shortage globally, but imagine if patients could overcome this with a man-made biomaterial.
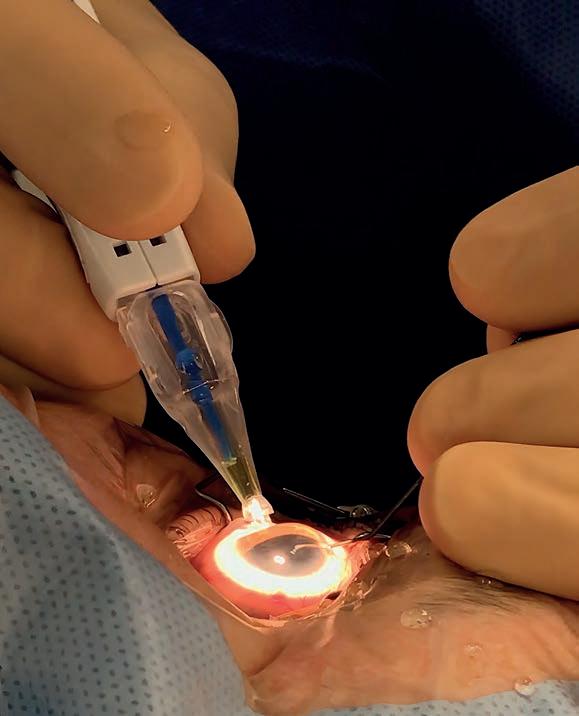
It might sound like a concept from an ophthalmological era decades from now, but a team of scientists, clinicians and orthoptists in Sydney are bringing this concept to life, assisted by FVF support.

In essence, they are investigating the use of surgically discarded lens capsule discs as a platform to grow primary corneal endothelial cells obtained from donors. The resulting construct will then be compared to a normal corneal endothelium and tested for its potential as a substrate for clinical and surgical use.
If successful, it could ease demand on eye banks globally, including Australia which receives around 1,400 donations a year for around 2,400 corneal transplants.
Postdoctoral researcher Dr Sheng Hua, from the University of Sydney, has been involved in the study. So far, support from the FVF – as well as the NSW Organ Tissue Donation Service – has enabled the use of discarded lens capsules to generate a bioengineered corneal endothelial layer. This layer is exhibiting favourable endothelial characteristics, relative physical properties – such as thickness, size, and mechanical strength –
and excellent optical clarity. Currently, the product is awaiting testing in a mock-surgery trial by surgeons.
“Human donor tissues are a valuable and limited resource, particularly in the context of corneal transplantation, which is currently considered the gold standard of care. The current practice relies on accessing end-of-life (deceased) donations of corneal tissue, which are retrieved, prepared, and provided to surgeons through Australian eye banks. Unfortunately, there is a global shortage of donors, with 53% of the world’s population lacking direct access to the required tissue,” Hua says.
“Our project focuses on developing alternative approaches that utilise surgically discarded tissue for clinical applications. For instance, we explore the use of such tissue as surgical materials for endokeratoplasty.
“Additionally, we will develop bioinks containing human type I and IV collagen using our patented formulae, which will be derived from discarded stromal and lens capsules. Bioinks have the potential for treating ocular tissue wounds, including those in the cornea, retina, or brain. The combination of this bioink and the novel corneal endothelium will enable the exploration of advanced cornea prototypes for in vitro testing.”
Supporting Hua in the study is the Save Sight Institute’s Professor Gerard Sutton, a VEI ophthalmologist and renowned cataract surgeon, the University of Sydney’s Dr Jingjing You, orthoptist Ms Michelle Phung and Hodge.
Hua says support from the FVF has provided resources that are otherwise difficult to obtain. Bioengineering research on human tissue faces particular challenges, including the production cost of biomaterials, biocompatibility issues, and the need to achieve optimal physical properties.
“The availability of biocompatible tissues resolves half of these challenges, simplifying and streamlining subsequent research. It is remarkable that these valuable (FVF) resources can be utilised for research, and I am hopeful that they will be applied for greater medical purposes in the future,” he says.

“THE COMBINATION OF THIS BIOINK AND THE NOVEL CORNEAL ENDOTHELIUM WILL ENABLE THE EXPLORATION OF ADVANCED CORNEA PROTOTYPES FOR IN VITRO TESTING.”
DR SHENG HUA POSTDOCTORAL RESEARCHERSupport from the Future Vision Foundation may help improve the phacovitrectomy patient experience.
When an ophthalmologist and a hospital director floated the idea of establishing a visiting eye health service at Griffith Base Hospital – a six hour drive west of Sydney – little did they know that 24 months later their initiative would be nominated by the hospital staff for a NSW Government Murrumbidgee Local Health District (MLHD) Excellence Award.
At a ceremony in Wagga Wagga in June, ‘Saving Sight is our Vision’ was named winner of MLHD’s Keeping People Healthy Award, one of 15 award categories.
At the time, MLHD CEO Ms Jill Ludford said it was rewarding to see the number of activities happening across the district with sincere efforts to support First Nations communities.
“Improving access to eyecare services through the delivery of high quality, sustainable, affordable, regular and culturally sensitive eye services has been Griffith Ophthalmology’s focus."

Led by Associate Professor Geoffrey Painter, one of the founders of Gordon Eye Surgery and a director of Foresight Australia, and colleague Dr Dominic McCall, a group of mostly Sydney-based ophthalmologists visit Griffith Base Hospital every four weeks to see and operate on patients from the Western MLHD. In addition, Foresight has sponsored two training courses to upskill employees from the Griffith Aboriginal Medical Service.
“The project started with A/Prof Painter, and Kerrie Legg, hospital director and director of nursing at Chatswood Private Hospital with support from Foresight Australia and Turramurra Rotary," McCall says. "For close to a decade, under the auspices of charity organisations Foresight Australia and Open Heart International, we were part of a team that used to go to the Philippines every year on outreach trips – until COVID prevented it."
Like many organisations during the COVID pandemic, Foresight Australia turned inwards, so that the team could pivot to providing outreach in NSW, particularly in Aboriginal health. Painter and Legg, whose extensive nursing career led to specialising in ophthalmology, visited Griffith Base Hospital in June 2021 to begin negotiations on how to provide support.
Providing specialist medical services in regional NSW has always been challenging. In 2021, RANZCO made a submission to the NSW Government parliamentary inquiry into health outcomes and access to health and hospital services in rural, regional and remote NSW, noting that 80% of permanent visual loss can be prevented through timely access to appropriate eye treatment.
“Southwestern NSW was identified as an area of need by NSW Health, and our group was asked to assist. This coincided with the well-deserved retirement of the local ophthalmologist in Griffith,” McCall says.
With extensive support from Griffith Base Hospital management and the MLHD, the retiring ophthalmologist’s equipment was purchased, and the Griffith Base Hospital Ophthalmology Department was established, with the service commencing at the beginning of 2022.
“Our department now supports the routine eye health needs of the Western MLHD including towns such as Lake Cargelligo and Hay. It is supported by emergency and specialist ophthalmic services in Wagga Wagga (a two-hour drive), and Albury (a three-hour drive) which have well-established ophthalmic services delivering very high levels of care for their communities which commonly spans many hundreds of kilometres,” McCall says.
The partnership between Griffith Base Hospital and the Griffith Ophthalmology Project was to deliver three goals in line with the MLHD strategic goals:
• Provide short term assistance to reduce the cataract surgery waiting list for the Western MLHD at Griffith Base Hospital.
• Provide long term sustainable ophthalmic care for the Western MLHD based at Griffith Base Hospital.
• Develop an effective ophthalmic outreach program for the Indigenous people of the Western MLHD. The team have been gradually increasing their workload to achieve
An ophthalmology project set up at Griffith Base Hospital in NSW to improve access to eyecare services for Indigenous and non-Indigenous people living in the Western Murrumbidgee Local Health District has hit the ground running and with further support can strengthen its delivery of eyecare to the region.
The surgical wait list has been dramatically reduced and the clinic is working hard to reduce the waiting time for routine clinic appointments.
“We’ve been going four-weekly, sometimes more regularly, depending on need. We usually have two or three consultant ophthalmologists each visit. Additionally, Chatswood Private Hospital provides a registrar and Gordon Eye Surgery provides an orthoptist. Interested Resident Medical Officers and medical students join the team from time-to-time. A majority of consultants are from Gordon Eye Surgery at the moment, but some are from different practices throughout Sydney, and one from Melbourne. We are hoping to expand this to other practices in the future,” McCall says.
The team typically take an-hour-and-a-half flight, arriving on a Sunday evening and leaving on Wednesday afternoon or evening.
“We spend about three days every four weeks in Griffith operating and seeing an increasing number of patients. We are looking to expand the service to every two weeks, but the limiting factor at the moment is staffing, unfortunately,” he says.
“We’ve been privileged to have local administration staff that have been trained to work in high volume outpatient clinics and a local assistant in nursing (AIN) who has been helping us in the clinic. The clinic could not survive a day without their tireless efforts. I’m looking to upskill local clinical staff to make the service more sustainable from a local perspective.”
The team has also met with local optometrists who are supporting the eye department by providing a valuable triage and co-management of patients for referral and are keen to provide support.
“As the workload increases, especially as the Indigenous screening project increases referrals, we’ll need even more staff. If we can’t employ local staff, we’ll need to find people who are willing to go out there on a semi regular basis – we’re talking about orthoptists, optometrists, registrars and consultant ophthalmologists, everyone is an important part of making it sustainable long term.”
Amid the four-weekly clinics, the team have also been working with the Griffith Aboriginal Medical Service to get screening programs off the ground in more remote locations for both Indigenous and non-indigenous patients in more remote communities, McCall explains.
“While it is satisfying, from a personal perspective, to go out and see communities in regional areas, logistically it’s much better having people that are trained, that know the community, who can screen for significant eye disease locally and then refer them to a centralised service,” he says.
“So far we have done two teaching symposia for the Griffith Aboriginal Medical Service on how to screen for vision, intraocular pressures, cataract, and diabetic retinopathy. There is a retinal camera at a couple of their clinics for the detection of diabetic retinopathy and we have been teaching how to implement a screening program, as well as teaching general eye pathology and what to look out for.”
Further training courses for local Aboriginal healthcare workers from the Griffith Aboriginal Medical Service and Griffith Base Hospital as well as nurses and doctors from these organisations are planned for the near
In addition, the team is establishing referral pathways so patients at the more distant clinics can be seen in Griffith, reducing cost and travel
“That’s the key. By providing a comprehensive eyecare service in Griffith it prevents people from having to travel excessive distances for routine eyecare. It’s a long way when patients are travelling two or three hours just to get to Griffith, and then it’s another two hours to get to Wagga, the next regional centre, if our service didn’t exist,” McCall says.
A/Prof Painter says it was therefore with great pride for the team that the Griffith Base Hospital staff nominated the project for an MLHD Excellence
“It was even more pleasing that the project won the award. It is a recognition of all the hard work that Griffith Base Hospital staff, the project members and the sponsoring organisations have put into establishing and running a Griffith Base Hospital ophthalmology department,” he says.
At the commencement of the program in March 2022 there were 123 patients on the waitlist for ophthalmic surgery with an average wait time of 131 days.
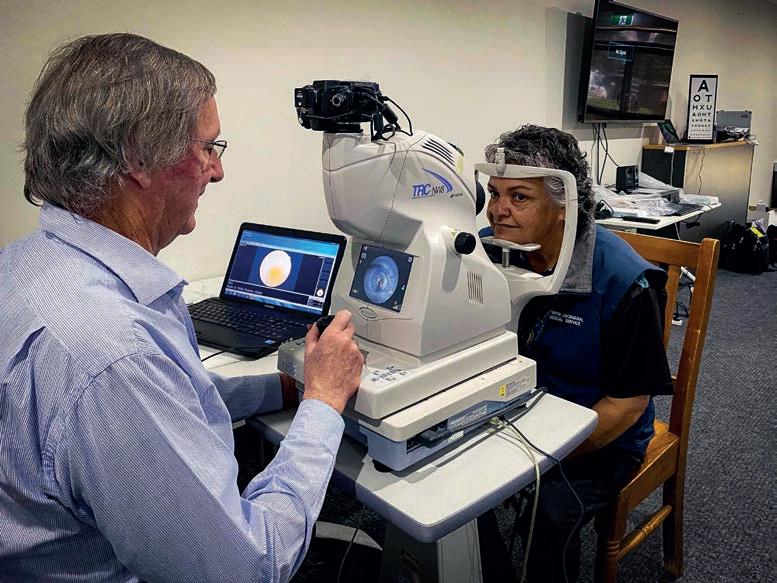
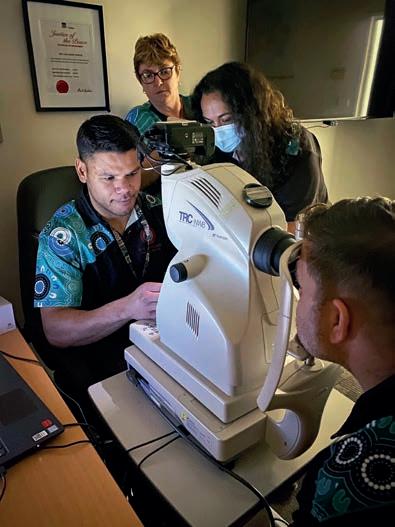
As at March 2023, the program had 10 patients on the waitlist, signalling a significant reduction in wait times. There have been 13 public clinics conducted in the 12 months resulting in 1,796 consultations for an average of 138 consultations per four-week visit. Approximately 8% of these patients identified as Indigenous.
While the data shows what impact the clinic has had in the 12 months it has been operating, McCall says the anecdotal evidence is even more compelling.
“The patients often tell us how appreciative they are that they don’t have to travel further for ophthalmic care and family members don’t have to take time off work to drive them there,” he says.
Being a public hospital ophthalmology clinic, the team has been invited to contribute to the development of the State-wide Referral Criteria (SRC) for NSW Health specialist outpatient services.
Facilitated by the NSW Ministry of Health in partnership with the Agency for Clinical Innovation, the project's aim is to facilitate safe, timely and effective referral and prioritisation of patients requiring access to NSW Health specialist outpatient services. SRC are intended to support patients and referring health professionals when issuing referrals as well as NSW Health specialist outpatient services at the point of screening and triage.

“BY PROVIDING A COMPREHENSIVE EYECARE SERVICE IN GRIFFITH IT PREVENTS PEOPLE FROM HAVING TO TRAVEL EXCESSIVE DISTANCES FOR ROUTINE EYECARE”
DR DOMINIC MCCALL OPHTHALMOLOGIST


The biggest eye care and eyewear fair in Australia combines with the most credentialed and largest annual optometry Clinical Conference in the Southern Hemisphere - the 2023 program will run in partnership with the 4th World Congress of Optometry in an exciting international event that should not be missed.


A series on non-clinical Masterclasses will run concurrently with the event’s clinical conference program. This year’s masterclasses will be hosting 2 streams; Practice Management and Dispensing.

Spaces are limited so secure your spot in your preferred stream today, and plan on some after session hours exploration of Melbourne’s laneways. www.omega-event.org/masterclasses
omega-event@arinex.com.au www.omega-event.org
1. What initially attracted you to a career in optical dispensing, and how did you enter the profession?
My interest started when I landed a gap year job working for the local ophthalmologists in town – and what an exposure that was. In just over 12 months I was exposed to a range of ocular health conditions and emergencies all requiring treatment and management. Being involved in minor procedures and observing in theatre was a real eye-opener. I then went off to university to study a Bachelor of Education majoring in Health and PE and a sub-major in Social Work, which I graduated from. In my first year at university I was asked to come and work for what was then a budget eyewear store, but now OPSM. Fast forward 14 years and I’m working in an independent practice as practice manager and senior optical dispenser.
2. What are your main career highlights?
My most recent career highlight is attending the ODA conference in Sydney along with my graduation ceremony and excellence awards. Not only did I officially graduate, but I was awarded the National Excellence Award for Role Model and Leadership. Other highlights include being able to follow a child’s journey from initial presentation, frame selection to putting lenses in front of their eyes and seeing their reaction of taking in the world around them clearly for the first time, which is often their parents. That’s special. I remember when I first edged blanks into a frame, that was certainly a good feeling too. Even just creating a positive experience for patients through individualising care is an awesome feeling. In hindsight, had I not taken my gap year working at the ophthalmologists, I wouldn’t have continued in the industry or be in the position I am today.
3. What are your strengths as a dispenser and what excites you about your job?
A big part of being an optical dispenser that can be overlooked is understanding personalities and how that is going to impact a frame choice. I love allowing a patient to feel understood with

the frames I suggest in their selection process. Whether that be conservative or bold. Patients love my attention to detail and style advice. I am honest and patients actively show appreciation for this. I love throwing a curve ball in there to empower people to feel confident in expressing themselves, whether they take it, or it plants the seed for next time.
4. If you could go back and provide advice to yourself at the beginning of your career, what would you say?

Say yes to any opportunity. Whether it be a lab tour, attending conferences or workshops or even being involved in the frame buying process with reps if you’re with an independent. The industry within optical dispensing is so broad. Most definitely though, advocate for yourself and complete the Cert IV in Optical Dispensing.
5. What do you see as the key opportunities and challenges facing the future of optical dispensing in Australia?
Optical dispensers within a practice are vital. Recognition of our role, and the knowledge and continued learning that is necessary to do our job well, is so important. Credibility for the work we do has traditionally been overlooked. With continued learning and compulsory CPD point structure to maintain qualification, it is a great opportunity for both industry recognition, and credibility for the roles we play. ODA has a fantastic educational program whereby subscribers obtain CPD points for each webinar they attend, which is a fantastic way to build
At Will Street Eyecare, Sarah Thompson likes the patient to feel understood with the frames she suggests.




knowledge and skills that are current and relevant. This is a great step forward.
6. How do you ensure your skills and knowledge stay up to date in such a fast-moving industry?
I am a member of ODA which is a great starting point to access current recourses within the industry. I attend workshops run by ProVision and talk regularly with sales reps about frame trends, and with lens companies about design updates or new releases. I actively read Insight and ask questions around medical advancements, technology, or studies to build on my understanding. I network and collaborate with other optical dispensers and practice managers where we share ideas, knowledge and support one another.
7. Why did you become a member of Optical Dispensers Australia, and what value do you see in the organisation?

ODA has begun to pave the way for optical dispensers in recognition and credibility. I became a member once I completed my Cert IV to keep up to date with knowledge and gain access to some great resources and learning opportunities.
8. What would you say to others thinking of joining Optical Dispensers Australia?
It’s a no brainer – you will gain access to a wealth of support, resources and opportunity to attend their next conference where you will have exposure to so many industry experts to learn from and network with. Go for it!



















RODENSTOCK’S NICOLA PEAPER DISCUSSES WHY DISPENSERS SHOULD TAKE THE OPPORTUNITY TO EDUCATE PATIENTS ON TINT COLOURS AND THEIR APPLICATIONS WHILE ACCOUNTING FOR THEIR PREFERRED COLOUR CHOICE.
When we talk about ‘dispensing a tint’ we usually think along the lines of tints for medical purposes such as migraine relief or improving vision for macular degeneration sufferers. As practitioners, however, we should always take the opportunity to discuss the benefits of different tint colours and intensities even if the spectacles are simple sunglasses. Most tints supplied in Australia – be they photochromic, polarised or simple plastic lens tints –are grey. Whilst this may often give the best colour rendering as it removes wavelengths across the visual light spectrum, it may not always be the most suitable for specific tasks and hobbies. The opportunity should be taken to discuss different colours and their usage whilst still taking into account the patient’s idea of their preferred colour.
The ideal sunglass lens should provide protection from glare whilst improving contrast. Scattered light increases glare and, due to its short wavelength, a large share of scattered light is in the blue part of the spectrum. As scattered light carries no useful visual information it can be said that blue light reduces visual sharpness affecting both contrast and depth of vision. To absorb blue light, a complementary colour is necessary. Complementary colours to blue are yellow, orange, and red. However, whilst these colours will give the best levels of contrast, they are not aesthetically appealing and for this reason brown and amber tints tend to be used for good contrast in a fashion frame.
As it is often difficult to explain the difference between individual lens colours, and why one colour should be chosen over another, a colour contrast index (Figure 1)
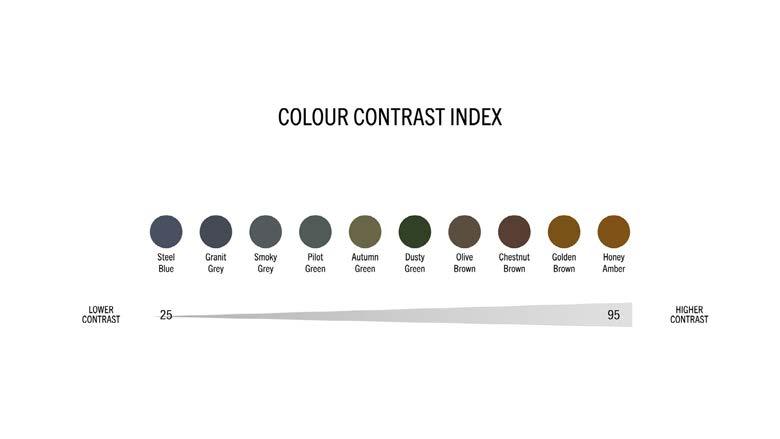
is useful. This is from Rodenstock Lambda Lens Technology which has been used to develop a scale with values describing the level of contrast provided by the different lens colours of the Rodenstock tint portfolio. These calculated values are based on, among other aspects, the ratio between the amount of red light and the amount of blue light let through the lens. This method is used, rather than percentages, to give an intuitive order to the colours. If purely percentages were used, the grey, green and brown lenses would be clustered together and the amber lens would be much further up the index. Using the index and general tint samples is a discussion that can be had to highlight two simple criteria for the spectacle wearer to consider:
1. W hat contrast level feels right?
2. W hat colour feel is right for me? Colour feel is important as, whilst u nderstanding levels of contrast, patients may still have a fixed view on what tint colour is ‘comfortable’ for them. Talking about the implications to vision of each colour allows the patient
to at least make an informed choice. If sunglasses are going to be worn during sports and hobbies, a more detailed conversation needs to take place. As mentioned, the red, orange and yellow tints may not be aesthetically pleasing but may be far safer for certain sports such as skiing or mountain biking where good contrast and depth perception are essential.
Rodenstock, within its Lambda Technology, has three contrast tints. These tints are in specific colours and transmissions, making them suitable for certain sports and weather conditions.
• D ynamic Yellow. This yellow tint will only block about 15% of light but all of that will be of the blue wavelengths. Effectively it brightens the surroundings making contours and details in the landscape more visible to the wearer. This tint is highly suitable for skiing or mountain biking in foggy or cloudy conditions.
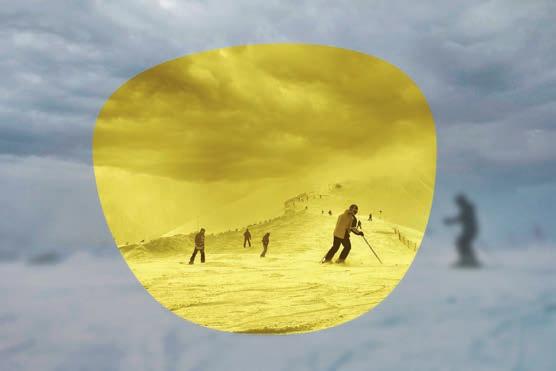
• D ynamic Orange. This 40% tint is a suitable choice for bright conditions, such as a reflective snow field, but with an overcast sky or little direct sunlight.
• D ynamic Red. This lens increases contrast whilst significantly reducing glare as it is an 80% absorption tint. Suitable for changing but mostly sunny conditions.

With its introduction of a colour contrast index and contrast tints, Rodenstock has created a clear way to explain and highlight the benefits of various tint solutions.
ABOUT THE AUTHOR: NICOLA PEAPER is the National Professional Services Manager for Rodenstock Australia. She spent 20 years working as an optometrist in the UK, and for the past 17 years she has worked within the lens manufacturing industry.

NICOLA PEAPER
"RED, ORANGE AND YELLOW TINTS MAY NOT BE AESTHETICALLY PLEASING BUT MAY BE FAR SAFER FOR CERTAIN SPORTS SUCH AS SKIING OR MOUNTAIN BIKING.”FIGURE 1: A colour contrast index can be useful to explain the difference between individual lens colours.

Ihave been an orthoptist for 15 years. I have managed a clinical team across three different sites in South Australia and run private and public orthoptic clinics in the neuro-ophthalmology department at the Royal Adelaide Hospital.
After 14 years working as a clinicallyfocused orthoptist, in March 2022, I took on the added challenge of developing and managing a surgical team. This represented a move away from my clinical role at Eyemedics, to manage eye health in a different way.
Surgical waiting lists are always inevitable. Ideally no patient is on a wait list for longer than 365 days. But keeping waitlists under 12 months post COVID and in regional and remote Australia brings additional challenges.
Working with 12 doctors’ operating lists at 11 different locations with a small team of three staff, including myself, we have risen to the challenge of managing 45 surgical waitlists a month across public and private health services.
Orthoptists are well practised in delivering a multidisciplinary approach. I liaise with a broad range of health professionals including optometrists, ophthalmologists, ophthalmic assistants and nurses every day to deliver excellence in eye healthcare.
My ability to apply this multidisciplinary approach to an operating list has meant I can effectively engage stakeholders across multiple hospitals and focus on the common goal of ensuring our patients are operated on in a timely manner.
Across Australia elective surgeries were suspended through the COVID period. Even the relatively short suspension in South Australia has had a massive flow-on effect and adding to patient backlog.
Hospitals are short staffed (like many sectors post COVID) and surgery lists are routinely shorter than pre COVID. COVID restrictions also lead to higher numbers of staff taking sick leave and patients having to reschedule surgeries.
Each aspect has further compounded the issue of surgery waitlists. We have seen an increase in Category 1 and 2 cataract patients requiring surgery within three to six months, only pushing the Category 3 patients further down the list. It feels like a case of one step forward and three steps back.

We manage public waiting lists across country South Australia in Wallaroo, Port Lincoln, Clare and Victor Harbor. Managing waitlists in regional and remote areas of Australia has additional challenges of access to services, long travel distances for staff and
Eyemedics manage public waiting lists across country South Australia in Wallaroo, Port Lincoln, Clare and Victor Harbor.
patients, impacts of weather, and health infrastructure. These challenges add more complexity to an already intricate task.
Increasingly patients are choosing to self-fund their surgery to avoid lengthy public hospital waitlists. This is a substantial financial cost at a time of increased cost of living pressures, adding additional financial strain on patients.
Employing a multidisciplinary approach is to bring together healthcare professionals from different fields in order to determine optimum treatment for patients.
Initial conversations to get the list moving is an important starting point. I’ve slowly been meeting and discussing the requirements with necessary management and key stakeholders.
My role as an orthoptist and having a clinical background has been extremely beneficial in having those conversations with executive directors of medical services, nurse unit managers and elective surgery strategy coordinators to get our ideas heard and potentially put into action.
I am thankful for the relationships I have started to develop at all locations, where we need to not only work together but also understand the limitations we all face in our corresponding workplaces. This complex role is only possible with the commitment of many managers, doctors, orthoptists and surgical teams.
The conversation about surgical waitlists, post COVID, is a critical one. The healthcare system must acknowledge that we are facing problematic public wait times for surgery and work together to make it better.
ABOUT THE AUTHOR: SHANDELL WISHART is a senior orthoptist at Eyemedics in South Australia, and has been working for the company since graduating with honours in 2007 from LaTrobe University in Melbourne.

ORTHOPTICS AUSTRALIA strives for excellence in eye health care by promoting and advancing the discipline of orthoptics and by improving eye health care for patients in public hospitals, ophthalmology practices, and the wider community. Visit: orthoptics.org.au

THE CONVERSATION ABOUT SURGICAL WAITLISTS POST-COVID IS A CRITICAL ONE, WRITES SHANDELL WISHART, AN ORTHOPTIST WHO HAS TAKEN ON A NEW CAREER CHALLENGE MANAGING SURGICAL LISTS FOR SOUTH AUSTRALIAN DOCTORS.
SHANDELL WISHART
“INCREASINGLY PATIENTS ARE CHOOSING TO SELF-FUND THEIR SURGERY TO AVOID LENGTHY PUBLIC HOSPITAL WAITLISTS.”
In a three-part series earlier this year, I described the phased approach to starting a practice. With this in mind, it’s an appropriate time to review one of the essential foundation documents that practices depend on for reference, training and more.
A Policy and Procedures (P&P) Manual should ideally be completed as part of the start-up process, preferably prior to opening the practice to the public. A thoroughly documented manual, detailing various policies of the practice and the manner in which they are to be executed procedurally, is not only a vital reference guide but is often viewed as the “practice bible”.
This important manual should also provide protection against litigation claims and complaints from patients, staff or external parties as they are a reflection of the practice’s normal operating processes and procedures which should be favourably viewed by a court, insurer, or workers’ compensation authority.

It is also important to ensure operating success by regulating personnel performance so that procedures are carried out accurately, consistently and efficiently, in accordance with the P&P Manual.
Apart from its usefulness as a training tool for new staff, it also serves as an authoritative point of arbitration in situations where staff have differing opinions on operational matters. Such situations should also highlight any unclear directions which deserve attention to ensure clarity.
In summary, a comprehensively documented and regularly updated P&P Manual will serve the following purposes:
• Reference point: new or existing staff may verify or clarify correct procedures from time to time;
• Risk management: provides evidence of documented instructions and training that staff are given, a defence against claims that the employer may be liable for acts and/or omissions by administrative and/or clinical employees;
• Induction: a training tool for new staff to absorb the policies and procedures of the practice and also understand the owner’s principles and preferred culture;
• Practice performance: to determine whether the most efficient systems are employed and whether periodical amendments – such as alignment with recent regulations – are deserving;
• Staff appraisals: provides benchmarks and service standards by which staff performance may be measured when conducting appraisals and/or salary reviews;
• Professional standards: regular reviews and updates will ensure the highest standards within the practice and compliance with any recent regulatory requirements.
In compiling a P&P Manual, it is comprised of two parts:
• Policies which dictate the manner in which practice operations and business administration should be framed to meet the owner’s aspirations to develop a particular culture and reputation; and
• Procedures by which various policies and healthcare practices will be executed. While the procedural aspects are adequately covered above, it is appropriate to focus on the base aspect of how and who should develop policies – a sort of “policy on policies”. In this standalone section of the P&P Manual, the following matters deserve inclusion:
• Employees, administrative or clinical, who are authorised to dictate ‘policy’ as distinct from administrative procedures. This section will logically include a Delegation Schedule listing relevant staff by name or title (including ‘standby’ delegations to cover possible staff absences or vacancies);
• The nature and extent of areas in which a delegated employee may frame a
particular policy and whether it requires confirmation by a senior employee. Suggested actions to execute the newly dictated policy, including carefully project managed implementation, may be entrusted to a different individual/team for actual execution and ultimate confirmation that the overall process represents a practical action.
Responsibility for compiling the P&P Manual and regularly updating it usually rests with the practice manager (and a clinician for clinical matters) who should be familiar with the overall process and capable of documenting one as a critical ‘practice start up’ action. Additionally, other clinical staff will need to be involved in preparation of policies and procedures such as ophthalmologists, orthoptists and nurses laying the ground for development of a meaningful clinical governance structure.
Finally, the P&P Manual should be readily accessible to all staff and not one of those reference folders that accumulate dust on a backroom shelf. Periodical reviews, typically organised by a practice manager, will ensure the contents are current and in accordance with latest regulations and best practice management and healthcare aspirations of the owner.
ABOUT THE AUTHOR: KAREN CROUCH is the Managing Director of Health Practice Creations Group, a company that assists with practice set ups and the administrative, legal and financial management of a practice. Contact Karen email kcrouch@hpcnsw.com.au or visit, www.hpcgroup.com.au.

OFTEN REFERRED TO AS THE ‘PRACTICE BIBLE’, THE POLICIES & PROCEDURES MANUAL SHOULD BE READILY ACCESSIBLE AND NOT A REFERENCE DOCUMENT THAT ACCUMULATES DUST ON A BACKROOM SHELF, WRITES KAREN CROUCH.
KAREN CROUCH
“THIS IMPORTANT MANUAL SHOULD ALSO PROVIDE PROTECTION AGAINST LITIGATION CLAIMS AND COMPLAINTS FROM PATIENTS, STAFF OR EXTERNAL PARTIES.”All staff, from the clinician to the receptionist, should be familiar with the practice’s Policies & Procedures Manual.
patient population, with a relatively small group of experienced surgeons. In addition, the high cost of clinical trials means that the follow up window is usually short relative to an individual patient’s journey with glaucoma. While RCTs provide the gold standard of what is achievable under such controlled conditions, there is now ample evidence to show that outcomes in the “real world” are generally not as good as that shown
In contrast, registries usually do not exclude any patients from data collection, and they are very cost effective for providing longer term outcomes than clinical trials can usually provide. They therefore provide additional information as to how different treatments perform in a real-world patient population, as opposed to the highly controlled environment of a
As new technologies are released to market, such data gives an excellent opportunity to compare safety and efficacy outcomes with more established technologies. The importance of this is unscored by the CyPass experience where a minimally invasive glaucoma surgery (MIGS) device was withdrawn from market because of safety concerns that only became evident after five years of follow up.
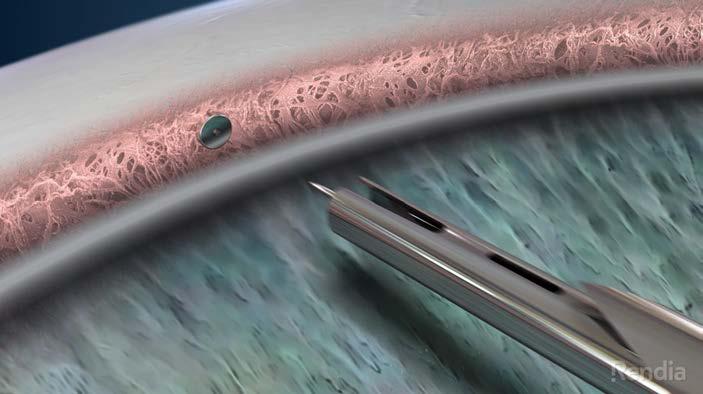
introduced to market with the hope of trying to improve patient safety while still achieving adequate intraocular pressure (IOP) reductions.
New technologies invariably take time to mature, and some will be proven over time to have superior safety, efficacy, or value in particular patient populations. Unless there is a systemic process for evaluating outcomes, there is the potential that patients are not receiving the best possible available care.
Randomised controlled trials (RCTs) provide high level evidence
Fight Glaucoma Blindness! (FGB) is one such registry that we, at the Save Sight Institute, set up to follow the outcomes of a range of glaucoma surgeries. Many surgeons are interested in auditing their outcomes to see whether they are doing a good job. We made this task easier by developing a web-based application to easily capture the data and provide an in-built statistical analysis that allows comparison of results with other surgeons.
On top of this audit role, the aggregated data is then available for publication of large data sets. Currently, FGB is tracking more than 2,500 iStent inject surgeries, 600 Xen implants, as well as large numbers of more traditional
One of the biggest limitations in being able to scale registry data is the ongoing requirement for data entry. Minimising data entry was at the forefront when designing FGB and its sister registries, but it remains a significant barrier to scale. The Save Sight Registries group is actively involved in integrating the registries with electronic medical records. The ultimate goal is single point data entry, where data entered in the electronic medical record is automatically populated into the registry software. Our data is maturing to the point where we can now provide clinicians with a good understanding of what outcomes they can achieve in different patient populations with different surgeries. As we scale the project, we hope to incorporate audit of outcomes as part of routine clinical practice. Such a tool provides rapid feedback to clinicians as to how particular surgeries are performing and help select the best possible procedure for each individual patient.
Save Sight Registry modules track outcomes in a number of different subspecialty areas, and the platform allows audit of outcomes at no cost to the user. For more information or to request access for the glaucoma, retina, corneal or any other module, visit: savesightregistries.org
Name: Associate Professor Mitchell Lawlor

Qualifications: BMed MMed
FRANZCO PhD
Affiliations: Save Sight Institute
Location: Sydney
Years in industry: 8
THERE IS NOW AMPLE EVIDENCE TO SHOW THAT OUTCOMES IN THE “REAL WORLD” ARE GENERALLY NOT AS GOOD AS THAT SHOWN IN CLINICAL TRIALS.The Fight Glaucoma Blindness! Registry is tracking more than 2,500 iStent inject surgeries.
AUGUST
TASMANIA LIFESTYLE CONGRESS (TLC)
Hobart, Tasmania
5 – 6 August
taslifestylecongress.com.au
WORLD CONFERENCE ON OPHTHALMOLOGY & EYECARE
Rome, Italy
21 – 23 August
eyecare.thepeopleevents.com
OPHTHALMOLOGY UPDATES!
Sydney, Australia
26– 27 August
ophthalmologyupdates.com
SEPTEMBER
ORTHOKERATOLOGY SOCIETY OF OCEANIA CONFERENCE
Gold Coast, Australia
1 – 3 September
www.facebook.com/OrthoKSO/
O=MEGA23 & WORLD CONGRESS OF OPTOMETRY
Melbourne, Australia 8 – 10 September omega-event.org
EUROPEAN SOCIETY OF CATARACT & REFRACTIVE SURGEONS CONGRESS
Vienna, Austria 8 – 12 September congress.escrs.org/
INTERNATIONAL VISION EXPO WEST
Las Vegas, US 14 – 17 September west.visionexpo.com
NEURO-OPHTHALMOLOGY SOCIETY OF AUSTRALIA CONFERENCE
Adelaide, Australia
21 – 22 September (training day to be held 23 – 24 September) nosa.net.au/2023-meeting
SILMO PARIS
Paris, France 29 September – 2 October event.silmoparis.com/2023/en/
OCTOBER
RANZCO SCIENTIFIC CONGRESS
Perth, Australia 20 – 24 October ranzco.edu/events
ORTHOPTICS AUSTRALIA ANNUAL CONFERENCE
Perth, Australia 21 – 24 October orthoptics.org.au
EYECARE PLUS BOOTCAMP AND AGM
Sydney, Australia 27 – 28 October y.safier@eyecareplus.com.au
NOVEMBER
HONG KONG INTERNATIONAL OPTIC FAIR
Hong Kong 8 – 10 November hktdc.com/event/hkopticalfair/en
To list an event in our calendar email: myles.hume@primecreative.com.au
SILMO INSTANBUL
Istanbul, Turkey 23 – 26 November silmoistanbul.com/en
ASIA PACIFIC TELEOPHTHALMOLOGY SOCIETY CONGRESS
Pattaya, Thailand 2 – 3 December 2023.asiateleophth.org
THE 16TH CONGRESS OF THE ASIA-PACIFIC VITREO-RETINA SOCIETY (APVRS) 2023
Hong Kong 8 – 10 December 2023.apvrs.org
FEBRUARY 2024
MIDO EYEWEAR SHOW
Milan, Italy
3 – 5 February mido.com
Specsavers have a fantastic opportunity for an Optometrist looking to accelerate their career by owning and working within our Noosa store. This is a unique opportunity as we are converting an existing store with an established database of loyal customers. Noosa is at the northern end of the Sunshine Coast, a diverse region between Brisbane and Fraser Island, extending from coastal towns to hinterland. If you are seeking a laid-back beachside culture, look no further than the Sunshine Coast.
Specsavers Berri offering up to $184,000 package
Specsavers Berri is looking for a passionate and dedicated full-time Optometrist to join their supportive and welcoming team. Berri is situated on the banks of the Murray River and is the perfect regional town to explore and experience. Work in a 2 test-room store with market leading equipment including OCT for every patient. Enjoy excellent
opportunities for further career development and progression. An extremely attractive salary package is on offer of up to $184k.
Seeking a talented optometrist to join our extraordinary team at Specsavers New Plymouth. We offer cuttingedge technology, a friendly environment, and a commitment to professional growth. Embrace the breathtaking beauty of the region and enjoy a perfect work-life balance. Explore stunning coastal views and immerse yourself in a vibrant arts scene. Don’t miss this incredible opportunity to be part of Specsavers New Plymouth. Apply now and unlock a rewarding journey in one of New Zealand’s most spectacular locations.
The Specsavers Graduate Recruitment Team are currently looking for graduates to join our stores around Tasmania.
Available with our ‘Go with a Friend’ bonus, along with a generous regional salary and relocation package.
Specsavers are the largest employer of Graduate Optometrists across Australia and New Zealand, and we have continued to develop our comprehensive two-year Graduate Program which provides a newly qualified optometrist with a dedicated in-store mentor, a support network, and structured program to assist with your development.
Locum opportunity at Berri, SA
Specsavers have a fantastic opportunity available at our Berri store. This newly expanded store can offer locum block bookings of a few weeks to a few months at a time with all flights, car hire and accommodation provided and booked for you. Berri provides a beautiful regional location within a three-hour drive from the busy city life in Adelaide.
In a few short years, Specsavers has achieved market leadership in Australia and New Zealand with more people choosing to have their eyes tested and buy their prescription eyewear from Specsavers than any other optometrist. To learn more about these roles, or to put your hand up for other roles as they emerge, please contact us today:
Joint Venture Partnership opportunities enquiries: Kimberley Forbes on +61 (0) 429 566 846 or E kimberley.forbes@specsavers.com
Australia Optometrist employment enquiries: Marie Stewart – Recruitment Consultant marie.stewart@specsavers.com or 0408 084 134
Locum employment enquiries: Matthew Cooney matthew.cooney@specsavers.com or 0447 276 483
New Zealand employment enquiries: Chris Rickard –Recruitment Consultant chris.rickard@specsavers.com or 0275 795 499
Graduate employment enquiries: apac.graduateteam@specsavers.com
Insight's monthly bulletin to keep the Australian ophthalmic sector updated on new appointments and personnel changes, nationally and globally.




technology as key deliverables that supports the everyday of our client-facing teams,” said Mr esley Coote, Healthia’s Group Managing Director and



previous roles at the ACO include Head of Paediatric Services (1998-2007), Manager of Professional Development & Membership (2006-2007) and Director of Specialty & Community Services (2010-2012).
analysis, retinal substructure assessment, advanced retinal imaging technologies, and vision restoration approaches. Sadda has been a member of ARVO for several years, and served on the Board of Trustees for the past three years. His term will commence May 2024 at the conclusion of ARVO’s 2024 annual meeting.

DO YOU HAVE CAREER NEWS TO SHARE?
EMAIL EDITOR MYLES HUME AT MYLES.HUME@PRIMECREATIVE.COM.AU TO BE FEATURED.
The rst and only MIGS device to report clinical results from a pivotal trial at 5 years.1,2
1. Ahmed I, et al; HORIZON Investigators. Long-term Outcomes from the HORIZON Randomized Trial for a Schlemm’s Canal Microstent in Combination Cataract and Glaucoma Surgery. https://www.aaojournal.org/article/S0161-6420(22)00160-9/fulltext

2. Safety & Effectiveness Study of the Hydrus Microstent for Lowering IOP in Glaucoma Patients. ClinTrials.gov (NCT01539239)
Please refer to product direction for use for list of indications, contraindications and warnings. © 2023 Alcon Inc. Alcon Laboratories (Australia) Pty. Ltd. ABN 88 000 740 830. Phone: 1800 224 153. Auckland, New Zealand NZBN 9429047030480 Phone: 0800 809 189. ANZ-HDM-2300010

To be the world leader in environmentally friendly eyewear and help the environment.
Focused on environmental rejuvenation, Project Green creates high-end, environmentally-friendly eyewear that doesn’t compromise on quality, style, look, or feel. We focus on providing environmentally conscious eyewear for the patient who appreciates luxury eyewear and wants to reduce their impact on the earth.
Mazzucchelli biodegradable acetates
Biodegradable demo lenses
Finest quality Italian hinges
Reconstituted leather cases
Biodegradable packaging
For every frame purchased, we donate to an environmentally focused charity. This year we have chosen to plant one tree for every frame purchased through ONE TREE PLANTED. Project Green is an environmental rejuvenation movement.


• Are solar powered! In 2011 we installed 116 solar panels on the roof of our warehouse. These solar panels provide majority of the power to our large warehouse and offices.
• Our sales reps have hybrid cars to reduce their carbon foot print.
• Have a vegetable garden and fruit trees at our head office! See below for a photo of our Managing Director Mark Wymond and National Brands Manager Lisa Wymond in our vegetable garden with a fresh carrot harvest.

• Have LED lighting throughout the office and warehouse to reduce our carbon footprint
• Consolidate our shipments from our suppliers. This means less packaging, lower transport costs and reduced carbon foot print
• Use compostable courier bags for our deliveries
• Donate usable discontinued product to the Australian College of Optical Dispensing and various charities, so it doesn’t end up in land fill!
• Recycle any unusable eyewear via our Terracycle ‘Eyewear - Zero waste’ box
• Electronically invoice to save paper and reduce the carbon footprint of postal deliveries
• Re-use returned bubble wrap and boxes
• Recycle our cardboard, paper and plastic waste.