You’d look good in Specsavers
Ranked as one of Australia’s Best Workplaces for 2023.



Ahpra beefs up investigations team amid a dramatic rise in ‘boundary violations’ 25
SEXUAL MISCONDUCT CRACKDOWN
DEMOGRAPHIC DIFFERENCES IN MYOPIA
Where public and private clinics differ when managing young myopes in Australia
49
SHOPPING CENTRE vs THE HIGH STREET Which location is better when establishing a new optometry practice?
03
SEPT 2023
AUSTRALIA’S LEADING OPHTHALMIC MAGAZINE SINCE 1975


Are you an analytical person? You’d look good in Specsavers If, like Tasneem, you love the idea of a career where you’ll use the latest technology, like OCT, to help improve people’s lives, you’ll shine at Specsavers. www.spectrum-anz.com Tasneem
Optometrist
GREATER TRANSPARENCY IN PRACTITIONER SEXUAL MISCONDUCT CRACKDOWN
The health industry watchdog has finalised its Data Strategy dictating for the next five years what practitioner information will be publicly available, including past disciplinary action. Although contentious, the regulator says there has been widespread support for more transparency around serious historical offences, including sexual misconduct.
It comes as the Australian Health Practitioner Regulation Agency (Ahpra) beefed up its specialist investigations staff headcount by 10 as it works to deal with a dramatic rise in ‘boundary violations’ where practitioners have blurred professional and personal relationships with patients or demonstrated unethical behaviour of a criminal or sexual nature.
On 18 July, Ahpra published its ‘Data Strategy 2023-2028’ after
an extensive public consultation that included submissions from Optometry Australia and the Australian Society of Ophthalmologists.
A major proposal was to publish “regulatory action history”. According to Ahpra, the register doesn’t include previous registration or restriction information such as when a practitioner has been suspended, even where that information is in the public domain – such as in media reports.
Although Ahpra doesn’t have a published final report, it will gradually release information about its work to implement the strategy. The regulator noted “different opinions” in the 109 submissions about what information should be included in the public register, but said many health industry organisations supported “a risk-based approach to publishing
registered health practitioners’ disciplinary history”.
“In particular, many submissions supported the publication of serious historical offences, including sexual misconduct,” the regulator said. Sexual boundaries cases have become a top priority for Ahpra in recent times. It has publicly stated a willingness to publish more information on the public register
about practitioners with a history of professional misconduct of a exual nature.
Currently, the register is limited to publishing links to tribunal decisions and court outcomes on a practitioner’s record on the national register, a move implemented in 2018. “In support of this work, health ministers have committed to taking urgent action to ensure there is greater transparency for patients around a practitioner’s regulatory history,” Ahpra stated. Meanwhile, Ahpra’s increased scrutiny of sexual misconduct in the healthcare system has led to sustained jump in reports to authorities as well as the number of practitioners facing regulatory action to protect the public.
continued page 8
DISPENSER WAGES IN SPOTLIGHT AMID AWARDS INCREASE
Optical dispensers and other front-of-house staff being paid award minimum wages have received a pay rise, however a new industry survey shows practice support staff are increasingly been paid above minimum rates.
As part of the Annual Wage Review 2022-23, the Fair Work Commission increased the national minimum wage to $882.80 per week or $23.23 per hour while award minimum wages increased by 5.75%, effective 1 July 2023.
Optical Dispensers Australia CEO Ms April Petrusma said it was becoming more common for employers to pay optical dispensers above the award –with employers recognising the need for long term employee retention.

But the award wage rise was good news for staff currently being paid under the General Retail Industry Award or the Health Professionals and Support Services Award – currently the two awards being applied across optometry practices for support staff.
Petrusma said it had become increasingly difficult to hire support staff in recent years, with some employers recognising this and offering attractive salary packages, with training opportunities and career longevity.
“If this was to become the norm, the optical dispensing profession would become more attractive to career seekers which would incentivise more people into joining the industry,” she said.
In December 2022, ODA undertook a small survey of 130 practice support staff on behalf of Eyecare Recruitment. The findings indicated a lack of consistency across pay structures but highlighted what appears to be a rising percentage of employees being paid above award rates.
• 34% were being paid between $45,000-$55,000
• 32 % were being paid between $56,000-$65,000
• 34% were being paid between $66,000-$96,000 +
“When considering a salary package, the employer really should consider the role the employee is undertaking and the tasks they perform. The renumeration should be consistent
continued page 8
LET THERE BE LIGHT
With the mental health of optometrists in the spotlight, Shonit Jagmohan takes Insight on a tour through his Melbourne practice to show the many mood-boosting improvements he has made to the consulting room. page 20

SEPT 2023
AUSTRALIA’S LEADING OPHTHALMIC MAGAZINE SINCE 1975
A boundary violation blurs professionalpersonal relationships with patients.
Introducing Vizo-PF Dorzolatim
Preservative-Free Eye Drops
The only preservative-free Glaucoma eye drop treatment in a multi-dose bottle
MINIMUM PRODUCT INFORMATION
Before prescribing, please review the full product information at www.aftpharm.com/prescription/vizo-pf-dorzolatim.
Indications:
Treatment of elevated intraocular pressure (IOP) in patients with ocular hypertension or open-angle glaucoma when concomitant therapy is appropriate.
Contraindications:
Reactive airway disease, bronchial asthma or a history of bronchial asthma, or severe chronic obstructive pulmonary disease; sinus bradycardia, sinoatrial block, second or third degree atrioventricular block, overt cardiac failure, cardiogenic shock; hypersensitivity to any component of this product.
Precautions:
Adverse reactions found with systemic administration of beta-blockers may occur with topical administration.
Cardio-respiratory reactions; vascular disorders should be treated with caution; masking of hypoglycemic symptoms in patients with diabetes mellitus; masking of thyrotoxicosis; surgical anesthesia; immunology and hypersensitivity, the dorzolamide component is a sulfonamide; concomitant therapy with carbonic anhydrase inhibitors; not been studied in patients with acute angle-closure glaucoma; choroidal detachment has been reported; increased potential for developing corneal oedema in patients with low endothelial cell counts; beta-adrenergic blockade has been reported to increase muscle weakness; patients should be advised to seek their physician’s advice if they develop an intercurrent ocular condition or any ocular reactions; Dorzolamide/timolol 2%/0.5% has not been studied in people wearing contact lenses; not been studied in patients with hepatic impairment; not been studied in patients with severe renal impairment (CrCl < 30 millilitre/min); for use in the elderly and paediatric use,
see full Product Information (PI).

Pregnancy Category C, (see full PI). A decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Interactions with other medicines:
See Contraindications and full PI; specific drug interaction studies have not been performed with Vizo-PF Dorzolatim. The potential exists for additive effects and production of hypotension and/or marked bradycardia with timolol maleate; disturbances have been reported with oral carbonic anhydrase inhibitors; mydriasis resulting from concomitant use of timolol maleate and adrenaline has been reported.
Adverse effects:
Most frequently reported adverse effects were: ocular burning and stinging, taste perversion, corneal erosion, conjunctival injection, blurred vision, tearing, and ocular itching; urolithiasis was reported rarely; others (see full PI). May affect some patients’ ability to drive and/or operate machinery.
Dosage:
One drop in the affected eye(s) two times daily; when substituting for another ophthalmic antiglaucoma agent(s), discontinue the other agent(s) after proper dosing on one day, and start Vizo-PF Dorzolatim on the next day. If another topical ophthalmic agent is being used, the other agent should be administered at least ten minutes apart; efficacy in paediatric patients has not been established (for more information regarding safety in paediatric patients ≥ 2 and < 6 years of age, see full PI).

To avoid contamination of the solution, keep the container tightly closed, do not let the dropper tip touch any surface.
Unopened bottle: Store below 25°C. Protect from heat. Opened bottle: Store below 25°C. Discard contents 4 weeks after opening the bottle. Protect from heat.
Dorzolamide (as HCI) 20 mg/mL, Timolol (as maleate) 5mg/mL
P R ESER VATI V E FREE P R ESER VATI V E FREE AFT Pharmaceuticals Pty Ltd, 113 Wicks Road, North Ryde, NSW 2113. Phone: 1800 238 742. ABN 29105636413. Date material prepared: July 2023
PLASTIC WASTE HELPS REDUCE
PBS Information: Restricted benefit. Treatment of elevated intraocular pressure (IOP) in patients with ocular hypertension or open-angle glaucoma when concomitant therapy is appropriate.
IN THIS ISSUE
It’s interesting talking to my office colleagues about their optometry experiences to gain a snapshot of how the general public views the profession.
Just recently, one colleague lauded their optometrist for spotting bilateral optic swelling, leading to a diagnosis at the root of previously unexplained health issues. On the other hand, others liken the optometrist to the dentist – and have been put off by ‘hard sell’ tactics with eyewear. One person who plays night tennis under lights has never been offered trial contact lenses before.
18 49
SOCIAL CONSCIENCE
How Seekers Optical became the first independent globally to secure B Corp status.

LOCATION, LOCATION
Will a practice achieve more success located in the high street or a shopping centre?


31 54
MYOPIA MATTERS
Melbourne's Dr Philip Cheng on why it’s important to remember adult myopes progress too.

DATA SCIENTIST
With the nation’s largest optometry dataset, Pamela Tse is privy to the industry's big issues.
Personally, I enjoy the experience. Recently my optometrist informed me of a significant incomplete blink, potentially causing dry eye with contact lens wear. I was also hellbent on a pair of round-shaped frames I saw at the practice 18 months earlier, and the dispenser was generous to order this back in for me to try and, ultimately, buy. With an updated script in premium lenses, my vision is great and I’m liking my new look. A great experience all round.
In this issue, we detail the many other wonderful things practices are doing to enrich the patient experience.
Sydney independent Mr Daniel Tracton is one example. He started seeing an accountant who couldn’t adapt to progressives for 30 years, instead owning three pairs of specs for each distance. Tracton recommended a special design from Tokai Optical that worked, with the patient so happy they purchased two subsequent pairs.
Further south, in Melbourne, Seekers Optical has become the first single independent globally to receive B Corp certification. Achieving this status means the socially-conscious practice chooses long-term investments over quick wins (i.e. 20% discount for lenses in an existing frame), an approach that is sure to make patients seek out their services and feel valued when they leave.
We also speak to data scientist Ms Pamela Tse who searches for correlations and patterns in the huge Specsavers dataset. Many of her insights are helping inform the company’s eyecare strategy that is picking up diseases like glaucoma at rates never seen before – changing lives.

This issue is a microcosm of the many great things happening in our industry and shows the long term value created (for all) when patients are placed at the centre of every decision.
Editor
INSIGHT September 2023 5
MYLES HUME
FEATURES SEPTEMBER 2023 07 UPFRONT 09 NEWS THIS MONTH 65 OPTICAL DISPENSING 66 ORTHOPTICS AUSTRALIA 67 MANAGEMENT 68 SOAPBOX 69 CLASSIFIEDS/CALENDAR 70 PEOPLE ON THE MOVE EVERY ISSUE
EDITORIAL
AVOID
THE QUICK WIN
All you need to master myopia management
OCULUS Myopia Master® combines the most important parameters to make Myopia Management easier than ever. It measures refraction, axial length and keratometry in one stylish unit, backed by a comprehensive myopia software suite. Utilising the latest Brien Holden Vision Institute data, you can create personalised reports detailing current myopia status and the likely outcome in adulthood, plus track the progress of any treatments prescribed. These BHVI data sets, with diverse strata of age, gender and ethnicity, improve modelling in a wider patient cohort and enhance parent counselling – giving you confidence without compromise.

EXCLUSIVELY powered by data from Brien Holden Vision Institute Get


T 1800 225 307
E enquiries@dfv.com.au dfv.com.au

DV1390-0723
in
touch
UPFRONT
As Insight went to print, VISION HOSPITAL GROUP revealed expansion plans with the a ddition of Boroondara Day Surgery in Hawthorn, Victoria, taking the number of day surgeries operating under the banner to 11. CEO Ms Amanda Cranage said the site is being refurbished and expected to be open in September 2023. "Boroondara Day Surgery expands our offering in Melbourne, with patients now able to access a range of
WEIRD
University of Ottawa researchers have revealed an injectable biomaterial activated by pulses of low-energy blue light has "tremendous potential" for on-the-spot repair to the cornea. Guided by biomimetic design, the researchers’ compelling results show that a novel light-activated material can be used to effectively reshape and thicken damaged corneal tissue, promoting healing and recovery.
WONDERFUL
Samsung Electronics has announced the addition of SeeColors mode on its 2023 TV and monitor lineup. The newly added accessibility feature provides various colour settings based on degrees and types of colour vision deficiency, offering an improved viewing experience. The feature adjusts red, green and blue levels to ensure viewers can easily distinguish colours on the screen depending on their degree or type of colour vision deficiency.
WACKY
A new study published in PLOS Biology shows that the shape of objects could be perceived via vision and touch. The inferolateral occipitotemporal cortex selectively encodes object shape even in people who become blind from a very early age, suggesting that the brain is organised to execute a given function regardless of input senses.
day procedures at five locations across the city," she said. IN OTHER NEWS, Optometry Australia has appointed Mr Ramy Aziz to its national board. Bringing blue-chip financial expertise to the table, Aziz was the former CEO of ASX Ltd, with experience in the finance, strategy, risk and governance sectors. He has a keen interest in healthcare. "We are delighted to welcome Ramy to the national board. Optometry Australia will benefit greatly from his invaluable skills in treasury, governance and general business
acumen," OA president Dr Margaret Lam said. FINALLY, a six-month pilot optometry role at the Women’s and Children’s Hospital in Adelaide to reduce the current long waiting periods for paediatric tertiary eyecare has been extended for a further six months. Early-career optometrist Ms Claire Ong, who began in the pilot role in January 2023, said the project has highlighted how important paediatric ophthalmology services are in South Australia and the benefits of multidisciplinary care.
insightnews.com.au
Published by: 379 Docklands Drive, Docklands VIC 3008
T: 03 9690 8766 www.primecreative.com.au
Chief Operating Officer Christine Clancy christine.clancy@primecreative.com.au
Group Managing Editor Sarah Baker sarah.baker@primecreative.com.au
Editor Myles Hume myles.hume@primecreative.com.au
Journalist Rhiannon Bowman rhiannon.bowman@primecreative.com.au
Commissioning Editor, Healthcare Education Jeff Megahan Business Development Manager Luke Ronca luke.ronca@primecreative.com.au
Client Success Manager Salma Kennedy salma.kennedy@primecreative.com.au
A VOICE IN EYECARE
Around 42% of Indigenous Australians who had a diabetes test also had an eye examination in 2019-20. Page 57

WHAT'S ON
Complete calendar page 69.
8-10 SEPTEMBER
Australia's biggest optical fair and the Southern Hemisphere’s largest optometry clinical conference runs alongside the 4th World Congress of Optometry.
omega-event.org
20-23 OCTOBER
Registration is now open for the 54th RANZCO Congress, taking place at Perth Convention and Exhibition Centre.
ranzco.edu/events
Design Production Manager Michelle Weston michelle.weston@primecreative.com.au
Head of Design Blake Storey
Art Director Bea Barthelson Subscriptions
T: 03 9690 8766 subscriptions@primecreative.com.au
The Publisher reserves the right to alter or omit any article or advertisement submitted and requires indemnity from the advertisers and contributors against damages or liabilities that arise from material published. © Copyright – No part of this publication be reproduced, stored in a retrieval system or transmitted in any means electronic, mechanical, photocopying, recording or otherwise without the permission of the publisher.

INSIGHT September 2023 7
MONTH RANZCO CONGRESS
NEXT
THIS MONTH O=MEGA23/WCO4
STAT
'WE WANT TO HEAR ALL MATTERS – BIG AND SMALL'
continued from page 3
New data reveals 841 allegations of ‘boundary violations’, including sexual misconduct, were made to Ahpra in 2022-23, with the allegations relating to 728 registered health practitioners. As a result, Ahpra has increased its specialist investigations staff headcount by 10.
The latest complaint figures are 50% higher than the number of reports two years ago, when Ahpra introduced new complaint categories as part of wider measures to stamp out sexism, sexual harassment or gendered violence in healthcare. This year’s complaints also follow on from a record 925 boundary violation allegations received last year.
Across the 16 professions, medical practitioners, which covers ophthalmologists, remain the most complained about with 359 followed by 215 complaints about nurses and 120 about psychologists. There has also been a steady rise in complaints about physiotherapists, with 33 sexual boundary notifications relating to that profession in 2022-23.
Optometry has consistently had one of the lowest complaint rates, with just nine alleged boundary breaches since 2012-13.
Generally, Ahpra said the types of complaints range from inappropriate or sexualised remarks, intimate touching of a patient without consent, personal relationships where there is an imbalance of power, to aggressive sexual, criminal offending.
Ahpra CEO Mr Martin Fletcher said this underlined the importance of a continued push to better support patients speaking

up, and the regulator’s investment in an increased number of specialist investigators and support services. The sector has been critical of the way in which Ahpra handles complaints, particularly the length of investigations.
“Greater reporting provides greater opportunity to act. When we are told of instances where practitioners are failing to behave ethically and professionally, we have opportunities to respond,” Fletcher said.
MORE INVESTIGATORS
Fletcher said increasing the number of staff dealing with these matters means Ahpra can reduce investigation times and reach an outcome quicker.
"More specialist investigators and social workers are being deployed to support people who are reporting their experiences with Ahpra," he said.
With the bolstered Ahpra specialist investigation team, this will grow the unit’s capacity by another 13.5% over the next year, on top of increased investment in resources and training since the team’s inception in 2018.
Ahpra has also expanded its Notifier Support Service led by social workers which provides support and help to victims and survivors navigate the regulatory and tribunal process. The NSS pilot program has reportedly met a significant need, receiving 278 referrals since its commencement in September 2021.
More than 850,000 health practitioners are registered in Australia and fewer than 2% have a notification made relating to their practice or behaviour for any reasons each year.
“INCREASING THE NUMBER OF TEAM MEMBERS DEALING WITH THESE MATTERS MEANS WE CAN REDUCE INVESTIGATION TIMES AND REACH AN OUTCOME QUICKER.”
MARTIN FLETCHER, AHPRA
More than 1,000 boundary violation complaints were dealt with across the financial year, with a record 114 referred to independent tribunals for disciplinary action. A further 239 resulted in regulatory actions such as restricted practice, education or cautions.
Ms Christine Gee has been close to this work for many years as one of the founding members of the Medical Board of Australia’s specialist committee, established in 2017. She has seen the changes in approach to these cases as well as the change in the public conversation about sexual misconduct in health settings.
“The whole system has been improved and strengthened. Any hint of departure from appropriate professional boundaries is escalated quickly,” she said.
“The committee has zero tolerance for sexual misconduct, and we will recommend immediate action to place strict conditions or temporarily suspend a practitioner if we’re concerned about risk to the public while we investigate. It is so encouraging to see more patients reaching out each year to tell us about their experiences, as difficult as it is for victims to share their stories.”
An investigator in the Ahpra specialist investigation unit, trained to respond to these matters and support complainants as the one direct contact with the body, said: “It’s about creating a safe space to tell these stories. Some of them are hard to hear, but all are important to report. We want to hear the big and small matters, because sometimes the small ones lead us to identifying bigger problems.”
HIGHER WAGES TO NEGATE WORKFORCE SQUEEZE
continued from page 3
with their level of experience, skill set and job requirements,” Petrusma said, noting that ODA plans to run a broader survey in future.
“Qualified optical dispensers and practice managers that are performing tasks above and beyond the minimum – such as frame buying, edging and fitting, looking after accounts, troubleshoot dispensing etc –should not be paid at a minimum rate and certainly should not be defined as performing ‘general retail’ duties.”
Petrusma said employers also needed to consider that on average in Australia, the cost to recruit and hire a new employee currently hovers around $23,000, according to the HR
Industry Benchmark Survey Australia and New Zealand.
“Therefore, it becomes quite obvious that a well-paid, rewarded optical dispenser will not only bring revenue into the practice, but in the long term, will essentially cost less than having to re-hire and re-train new team members.”
For practice staff already being paid above award wage rates, the 5.75% does not apply to them. It only applies to those being paid the minimum required by law.
Petrusma noted there is no single award named for optical dispensers and optical assistants in Australia. It is up to the employer to determine the most relevant (General Retail Industry Award or the Health Professionals
and Support Services Award) to match the employee's role and nominate it in the contract of employment.
“The general stance of ODA and the wider industry is to follow the advice set by Optometry Australia in relation to award coverage for support staff employed within optometry practices both in a retail and practice setting,” she said.
“During a meeting between Optometry Australia and the Fair Work Ombudsman in 2019, they were quite firm in their position that optometry practice support staff should be provided coverage under the Health Professionals and Support Services Award or above.”

8 INSIGHT September 2023
April Petrusma, ODA.
NEWS
EYERISING MYOPIA MANAGEMENT DEVICE FIRST TO BE GRANTED TGA APPROVAL FOR HOME-USE RED-LIGHT THERAPY

Medtech company Eyerising International has announced its myopia management device – based on repeated low-level red-light (RLRL) technology that can be used at home – has been approved by the Australian Therapeutic Goods Administration (TGA).

The approval adds to existing regulatory clearances for the Eyerising Myopia Management Device from the Conformité Européene (CE) in the European Union, Medicines and Healthcare Products Regulatory Agency (MHRA) in the UK, Medsafe in New Zealand, the National Medical Products Administration (NMPA) in China, as well as in Turkey.
Eyerising is currently preparing for Food and Drug Administration (FDA) approval in the US and has submitted approvals for the Singapore, Malaysia and India markets.

The Eyerising Myopia Management Device is described as a world-first technology to safely and easily treat myopia – and can be readily used at home.
Eyerising International CEO Mr Paul Cooke said the device is a safe, affordable, and proven technology. It treats myopia using RLRL that has been clinically proven to control myopia progression.
“The TGA has recognised the safety and performance of the device – the first evidence-based red-light therapy with demonstrated ability to effectively and safely control the progression of childhood myopia with potential life-long benefits in avoiding later eye disease,” he said.
The company has finalised distribution licenses with sales already taking place












in Japan, New Zealand and Turkey. It is targeting a minimum roll out in 10 countries by the end of December 2023.












According to Eyerising International, the Eyerising Myopia Management Device can sustainably improve the way the eye functions through improved blood flow to thicken the choroidal layer of the eye wall in turn reducing eye elongation and myopia progression.
A recent study of RLRL for myopia control in children achieved 87.7% efficacy with no significant side effects, the company stated. The Eyerising Myopia Management Device is based on the work of Professor Mingguang He, a world-renowned ophthalmologist and myopia expert.
Eyerising said it is already in widespread use overseas with significant growing global market potential as myopia increases across populations including students. At current rates of progression, it is anticipated that one in two people globally will be myopic by 2050, with nearly 10% at risk of high myopia.








 The Eyerising Myopia Management Device.
The Eyerising Myopia Management Device.
IN BRIEF
SLT STUDY
In a world first, ophthalmology experts at Flinders University will trial early intervention selective laser trabeculoplasty (SLT) in high risk glaucoma patients. Chief investigator Professor Jamie Craig has been awarded more than $1.7 million for the project. It will use SLT – shown to slow disease progression by lowering intraocular pressure – and will determine its effectiveness and suitability as an early intervention to prevent the onset of visual loss. After receiving SLT, participants will be monitored twice a year over a two-year period. “We have developed a tool that can identify individuals who are deemed at high risk of losing their vision from glaucoma, however there is still a major gap between identifying them and how they may be safely treated,” Craig said. “Insights from this trial will have immediate implications for the monitoring and treatment of high-risk glaucoma patients."
KODAK LICENSE
EssilorLuxottica and Eastman Kodak Company have signed a worldwide license agreement granting EssilorLuxottica the exclusive right to use the Kodak registered trademarks for products and services in connection with its business. Effective 1 January 2024, the deal is an evolution of the multi-year licensing agreement with Kodak currently in place. Now, EssilorLuxottica will continue to develop, manufacture, and distribute optical products and services featuring the Kodak brand indefinitely. “Kodak is an iconic brand rich in innovation and trusted by tens of millions of consumers around the world. We are pleased to make this substantial and permanent addition to our brand portfolio and are looking forward to leveraging our innovation capabilities and distribution network to create new opportunities for the brand," said Mr Paul
du Saillant,
deputy CEO of EssilorLuxottica.
KERING PROFITS
Kering Group has reported that global revenues for its luxury Kering Eyewear business for the first six months of 2023 hit a record €869 million (AU$1.4 billion), an increase of 51% (compared to sales of €591 in the prior year’s first half). The company noted “the significant contribution of Maui Jim”, which it acquired October 2022. Kering Eyewear’s overall sales were up 16% on a comparable basis. In the second fiscal quarter, the business reported sales rose 58% and generated a sustained sales growth of 21% on a comparable basis. The house produces eyewear for Gucci, Cartier, Saint Laurent and other luxury brands. In Australia, the Kering portfolio is distributed by privately-owned Sydney firm Sunshades Eyewear.
NEW ACUTE OPHTHALMOLOGY SERVICE OPENS IN VICTORIA
The Royal Victorian Eye and Ear Hospital (Eye and Ear) has opened its new Acute Ophthalmology Service (AOS) clinic after relocating from Level 5 to the ground floor.

The hospital said the move strategically places the AOS clinic, equipped with 10 consulting rooms, in close proximity to the Emergency Department.
“The co-location of these services will facilitate seamless coordination and collaboration between teams, resulting in improved patient care and streamlined treatment for individuals,” the Eye and Ear said.
The move is part of a redevelopment project, with the Eye and Ear working closely with the Department of Health to enhance its facilities to better serve the community.
The hospital's executive director of operations and chief nurse officer, Ms Leanne Turner, officially opened the new clinic on 17 July.
“As we stand here in this delightful new and modern space, I am filled with a sense of excitement and anticipation for the great patient outcomes that await us. It is a testament to what can be achieved when we work together towards a common goal,” she said.
Earlier in July, the Eye and Ear operationalised its Short Stay Unit (SSU) within the Emergency Department, a move which aligns the hospital with the Department of Health’s vision of emergency care for Victoria.
“The SSU comprises four 24-hour beds, allowing us to offer designated care for patients who require short-term treatment and monitoring. This unit offers increased comfort, improved monitoring and care,” it said.
Established in 1863, the Eye and Ear is Melbourne’s third oldest hospital and Australia’s only specialist eye, ear, nose and throat hospital. It sees more than 250,000 patients in a typical year.
VISION ON KOORNANG TAKES HOME INAUGURAL LOCAL BUSINESS AWARD
Independent optometry practice Vision on Koornang in Carnegie has beaten 56 businesses to be named overall winner of Glen Eira City Council’s first annual Business of the Year Awards, as well as taking out the Professions and Service Business category.

The practice is co-owned by optometrists Mr Daniel Duldig and Ms Clare Campitelli and is part of the ProVision network.
For the awards, businesses were judged against set criteria, including environmental sustainability practices, future plans, diversity and customer service, and manufacturing practices.
Campitelli applied to the awards on behalf of the practice, which also employs a full-time dispenser and two part-time optical assistants.
“Thirty-four years in business is a significant achievement. The practice has such longevity that we now see the children
and in some cases grandchildren of some original patients. Vision on Koornang has doubled in turnover in the past 12 years,” Campitelli said.
“We adopt sustainable practices where we can. We have started to stock environmentally sustainable frames and will continue to add more ranges as these become available. We also have a recycling program for soft contact lenses and packaging. We have reduced paper usage by 50% over the past five years and plan to be paper neutral in five years’ time."
Campitelli is completing a certificate in visual rehabilitation for people with mild traumatic brain injuries.
“We plan to add an additional consultation room to provide vision care to more people in need. Our vision therapy sector of the business is small, but we plan to add a vision therapist to our staff in 2024 as we grow this side of the business,” Campitelli said.

10 INSIGHT September 2023 NEWS
Daniel Duldig and Clare Campitelli, Vision on Koornang.
One of 10 new consultation rooms in the Acute Ophthalmology Service clinic. Image: Thomas Elia.



PREMIUM HYDROPHOBIC IOL with PUre Refractive Optics (PRO) TEchnology For your daily range of vision © 2023 Bausch & Lomb Incorporated. ®/TM denote trademarks of Bausch & Lomb Incorporated and its affiliates. Bausch & Lomb (Australia) Pty Ltd. ABN 88 000 222 408. Level 2, 12 Help Street, Chatswood NSW 2067 Australia. (Ph 1800 251 150) New Zealand Distributor: Toomac Ophthalmic. 32D Poland Road, Glenfield 0627 Auckland New Zealand (Ph 0508 443 5347) LUX.0005.AU.23 For more information please contact your Bausch + Lomb Territory Manager, Customer Service at Customer.Service@bausch.com or scan the code to receive a call back.
SMITH OPTICS AUSTRALIA AND CR LABS FORM NEW SUN LENS PARTNERSHIP
SMITH Optics Australia, in conjunction with Safilo Australia, is forming a world-first partnership with Melbourne’s CR Labs for the production and supply of Smith ChromaPop prescription sunglasses.
Launching on 1 August 2023, the joint commercial initiative is exclusively available in the Australian market.
SMITH – a global leader in eyewear and headwear protection since 1965 and headquartered in Portland, Oregon – is best known for its market share in snow goggles and helmets. The brand has recently taken a significant strong hold in the outdoor, water and cycling eyewear channels, particularly with the launch of ChromaPop proprietary lens technology, which the company says offers wearers sharpness and contrast of colours.
ChromaPop lenses are designed to filter light at two specific wavelengths, eliminating “colour confusion” for the brain, and ultimately recognising true colour
faster, regardless of lens tint.
“We are excited to bring ChromaPop sun lens technology to prescription eyewear and are thrilled to be able to do it with a local company,” Safilo senior director Mr David Pearson said.
“CR Labs is a testament to Australian manufacturing, and we believe the combination of leading technology and quality local surfacing, coating and fitting capabilities will make SMITH ChromaPop sunglasses a leader in the Australian market.”
CR Labs, located in Melbourne, is the first external lab, globally, to be authorised to produce ChromaPop prescription lenses, after completing a rigorous production testing and qualification process.
According to Safilo, CR Labs’ commitment to innovation, quality and customer service, makes the partnership a natural fit for SMITH which shares similar values.
MEMBERS VOTE ‘YES’
Optometry Victoria South Australia (OV/ SA) members have voted in favour of an operational integration with Optometry Australia (OA).

OV/SA CEO Ilsa Hampton and president Ms Elise Pocknee-Clem announced at a General Meeting held on 18 July that 86% of members voted in favour of the move.
More than 88% of members also voted in favour of the proposed modifications to OV/ SA’s constitution.
Pocknee-Clem said the change will deliver a multitude of benefits to members, brought about by increased efficiencies and alignment.
“The new model means that members will still have an OV/SA board made up of local members, however, our team and resources will move across to OA so that they can fully integrate member services into their day-to-day work, including state leads for Victoria and South Australia,” she said.
“OA will continue to provide all members nationally with access to its full range of member services. These arrangements will be carefully monitored via a Services Agreement that we will have with OA.”
The vote follows an announcement last year that the boards of OV/SA and Optometry Tasmania had commenced discussions about a possible integration with

TO INTEGRATION
Optometry Australia.
Optometry Tasmania members were expected to vote on the model in August.
“The model under development will see each state board remaining as the respective representatives for Victorian, South Australian and Tasmanian members, with all services delivered by OA and monitored by the respective state board for its jurisdiction,” OA said last year.
The organisation said the new model will see OA continuing to provide members nationally with access to its full range of member services.
“The new, integrated structure will also deliver local member engagement, face-to-face CPD, advocacy and stakeholder engagement in Victoria, South Australia and Tasmania,” OA explained.

“No major assets of any organisation will be transferred initially, and services will be integrated and evolved over time to continue to maximise value for members. OA will have the resources and staff of both divisions in order to be able to deliver on the local services.”
Should Optometry Tasmania members also vote yes, implementation is due to be completed by 1 November 2023.
CR Labs will supply the complete SMITH ChromaPop sunglass through independent optical practices, available in a range of SMITH sunglass designs matched with five ChromaPop lens colours, covering outdoor activities and light conditions.
“Our mission has always been to help Australians see better through cutting edge technologies, high quality products and trustful relationships,” CR Labs CEO Mr Adam Fletcher said.
“The partnership with SMITH fits all those criteria and we believe will provide superior quality outdoor vision, exceptional value for money, and meet the expanding and changing needs of prescription sunglass eyewear.”
The program will be backed by a patient marketing and education campaign, including the support of local SMITH athletes Ms Molly Picklum (surfing) and Ms

12 INSIGHT September 2023 NEWS
The deals centres on SMITH ChromaPop lenses.
John Bartlett (from left), Cassandra Haines, Timothy Lo, Ilsa Hampton.
Ilsa Hampton (from left), Flora Hui, Andrew Metha (back), Anne Weymouth, Theo Charalambous.
Lyn Hsieh (from left), Ilsa Hampton, Joe Chakman.


SEE YOU AT OMEGA23!
SPECSAVERS ANNOUNCES JUDGES FOR 2023 DAME MARY PERKINS AWARD
NEW ICARE TONOMETER DESIGNED FOR FASTER AND EASIER IOP MEASUREMENTS

The new iCare IC200 tonometer, distributed in Australia by Designs for Vision (DFV), features an innovative upgrade that aims to enhance the process of measuring intraocular pressure (IOP) by providing faster, more comfortable, and efficient examinations.
patients while ensuring accurate IOP measurements,” DFV said.

Specsavers has unveiled its panel of judges who will recognise an optometrist who has delivered an exceptional act of patient care in the Dame Mary Perkins Award 2023.
The judges – Ms Skye Cappuccio, CEO of Optometry Australia, Ms Carly Iles, CEO of Vision 2020 Australia, and Mr John Mulka, chair of Eye Health Aotearoa and chief executive of Blind Low Vision NZ – bring together a wealth of knowledge, expertise, and experience from across Australia and New Zealand.
The Dame Mary Perkins Award recognises the positive impact Specsavers’ optometrists have on their patient’s life, whether it’s a lifestyle improvement through vision correction or a sight-saving act.
Iles said that while the awards have traditionally been won by optometrists who have saved the life or sight of their patients, she is keen to celebrate optometrists who deliver exceptional eyecare services to everyday patients.

“Dame Mary Perkins is well known for providing exceptional patient care. It is these traits I will be looking for in the nominees for the Dame Mary Perkins Award – someone who consistently puts patients first and goes above and beyond to deliver quality patient care and/or support to the local community,” Iles said.
Similarly, Mulka said that often the unsung heroes are the optometrists who are able to build trust and rapport with their patients, leading them to be more likely to return for timely eyecare services and adhere to any treatments they may require.

“Optometrists play a vital role in the prevention of avoidable vision loss. I’m very much looking forward to hearing the stories of optometrists who are going above and beyond to support their patients in protecting their sight and selecting the 2023 winners of these awards,” he said.

Cappuccio commended Specsavers for celebrating its optometrists in this way and is looking forward to reading the nominations put forward.
The Quick Measure feature of the IC200 reduces the number of required measurements from the standard six to only two or three rapid individual measurements. As a result, the test time is significantly shortened, saving valuable time for both eyecare professionals and patients, DFV said.
“This new method offers a quicker alternative without compromising the accuracy and precision necessary for reliable IOP measurements.”
Central to the ground-breaking enhancement is iCare’s patented rebound technology, which has established the iCare tonometer as a trusted choice worldwide.
“This technology eliminates the need for traditional methods such as air puffs or anaesthetic drops. As a non-invasive and comfortable examination method, it enhances the overall experience for
With iCare IC200, IOP measuring is fast, reliable and repeatable, with readings displayed in mmHg to one decimal point. The local distributor said faster and fewer individual measurements makes the Quick Measure feature ideal for the most challenging patients.
“This further augments the iCare IC200 and its versatility in accommodating patients in different positions. Whether supine, reclined, or seated, the iCare IC200 tonometer can effectively measure IOP, making it accessible to a wider range of patients,” DFV said.
Quick Measure represents a significant innovation in the tonometry experience, benefiting both eyecare professionals and patients. By combining rapid measurements with the performance of the iCare IC200, practitioners can optimise their workflow while maintaining the accuracy and reproducibility of results that iCare is renowned for.
iCare is the original developer of rebound technology for handheld tonometers.
RODENSTOCK INTRODUCES LAMBDA LENS TECHNOLOGY
Rodenstock has launched its new Lambda lens technology, resulting in high precision, contrast-optimised sunglasses.
The lens manufacturer said the lower-contrast colours create "a truly natural colour feel".
“While the mid-contrast colours offer a good balance between contrast and natural colour feel, the high-contrast colours create a warmer colour feel and a high level of contrast,” it said.
In addition, contrast is created by ensuring that less blue light is let through the lens.
“Due to its short wavelength, a large share of scattered light is blue light. Since scattered light carries no visual information, blue light reduces vision sharpness. By minimising the amount of blue light that’s let through the lens, our Lambda lens technology sunglass lenses
provide sharper vision,” Rodenstock said. Furthermore, the company said, in sunny situations, sunglass lenses based on Lambda lens technology help reduce glare by blocking reflected light, further increasing vision sharpness.

14 INSIGHT September 2023 NEWS
Frame R3338C Smoky Grey Dusty Honey Grey CONTRAST CONTRAST 95 25 MORE DETAILS.
The new Lambda Lens Technology enhances colours and contrast in our sunglasses, creating a better, more detailed vision for all. Find the right fit for your vision with our Colour Contrast Index. Exact biometric lenses from your experts
SHARPER VISION.
Rodenstock’s new Lambda lens technology ensures less blue light is let through the lens.
The new iCare IC200.
Carly Iles (from left), John Mulka and Skye Cappuccio.




1
IOL MANUFACTURER RELEASES NEW PROMs PLATFORM
B+L ACQUIRING JOHNSON & JOHNSON'S BLINK EYE DROPS
Global eye health company Bausch + Lomb will purchase the Blink product line of eye and contact lens drops from Johnson & Johnson Vision for US$106 million (AU$155 m).

After a separate bid to acquire the Xiidra prescription dry eye drug from Novartis, B+L says the latest deal is part of a strategy to focus on over-the-counter (OTC) consumer eyecare products.
IOL manufacturer Rayner has launched its latest RayPRO digital innovation that seeks to solve a much-needed gap within the global ophthalmic standard of care – patient-reported outcomes measures (PROMs) in cataract surgery.

The online, cloud-based platform is designed to save chair time by collecting clinically validated PROMs autonomously via email. According to Rayner, it tracks patients’ long-term recovery over a three-year period with minimal input from the clinical staff and maximum value added to the patient pathway.
PROMs have emerged as an ideal tool for ophthalmologists to understand whether they are giving patients the vision they want, and how they are faring after discharge. Within clinical trials, PROMs are routinely collected, but outside of controlled environments, their collection can be the exception rather than the rule (Field, Holmes, & Newell, 2019).
According to Rayner, the ophthalmic sector has acknowledged that existing post-operative standards of care and clinical measurements such as visual acuity testing do not always reflect the patient’s experience or the impact of the disease on the patient’s life (Denniston, Kyte, & Burr, 2014). The lack of adherence within clinical routines to collecting PROMs data has been highlighted by many to be down to the lack of time or staff during established check-ups post-operatively.
Rayner’s device-agnostic RayPRO can be used with all IOL makes and models, providing clinical staff powerful data read-out on true lens performance, powered by real-time patient feedback.
Thew company’s latest iteration of RayPRO will launch in September 2023 and offers surgeons “a powerful comparison view”, where they will be able to segment individual lenses and compare their performance over a long-term three-year period, in real-time from patient feedback.
“There’s a growing need for relieving the symptoms of dry eyes and dry contact lenses, and OTC products are often the first option consumers choose,” said Mr John Ferris, B+L’s executive vice president of consumer.
“The addition of Blink expands our robust portfolio of OTC eyecare brands, enabling us to provide more choices for consumers and eyecare professionals.”
The Blink range consists of various eye drops and contact lens rewetting drops that are designed to provide immediate and long-lasting symptom relief. The products that are part of the acquisition include:
• B link Tears Lubricating Eye Drops
• B link Tears Preservative Free Lubricating Eye Drops
• B link GelTears Lubricating Eye Drops
• B link Triple Care Lubricating Eye Drops
• B link Contacts Lubricating Eye Drops
• B link-N-Clean Lens Drops
For the deal, B+L will acquire the Blink product line for US$106 million (AU$161 m) with cash on hand.
In the previously Xiidra deal, B+L will acquire the therapy from Novartis for up to US$2.5 billion (AU$3.6 b). Xiidra (lifitegrast ophthalmic solution) 5% can be prescribed by Australian eyecare professionals, and is a non-steroid eye drop for signs and symptoms of dry eye focusing on inflammation.
The acquisitions are set to complement B+L’s existing dry eye portfolio that includes consumer eye and contact lens drops, as well as its pharmaceutica business.
EARLY ADOPTERS GIVE VERDICT ON MELBOURNE-MADE HP-OCT
As the launch of Cylite’s highly anticipated HP-OCT approaches, the company is putting the final touches on the instrument’s accompanying software – Cylite Focus.
The latest version will be shown for the first time at the Orthokeratology Society of Oceania (1-3 September, Gold Coast) and O=MEGA23/WCO4 (8-10 September, Melbourne) conferences.
The Melbourne manufacturer said that although the main factor that sets the HP-OCT apart is its unique optical design to capture true volume images, the Focus software will be the main medium through which users will interact with the device.
“As such, it is extremely important to the operation of the instrument and the resulting analysis of the generated images,” Cylite said.
The company has put significant thought and effort into the software design to optimise its clinical utility and
the user experience. “Since the HP-OCT is so flexible, the designers have carefully considered how to transition seamlessly between a broad range of applications ranging from traditional OCT to corneal topography,” it said.

“Our efforts seem to have paid off. We’ve been pleased to have received positive feedback about the software from a number of our early users. Common feedback has been that the auto-alignment of the capture software makes scanning simple and that the software is both intuitive and easy to navigate. Additionally, users have responded positively to its modern, dark design, which we think adds to the overall cutting-edge feel of the device.”
The software development is 100% home-grown, using the expertise of a team of Australian designers, user-experience experts and skilled software engineers, Cylite said.
16 INSIGHT September 2023
COMPANY
Cylite's Focus software features a modern, dark design.
The Blink range consists of various eye drops and contact lens rewetting drops.
The RayPRO dashboard is designed to be user friendly for cataract surgeons.
EYE DROPS TWICE AS EFFECTIVE AS INJECTIONS IN RETINAL VEIN OCCLUSION – STUDY

A new study suggests eye drops developed by Columbia University researchers could be a more effective – and comfortable –therapy for retinal vein occlusion (RVO).
Standard therapy involves intravitreal anti-VEGF injection; this approach improves vision but patients with retinal damage due to impaired blood flow often have poor outcomes, the researchers noted.
Dr Carol Troy, professor of pathology and cell biology and neurology at Columbia University, said there’s an opportunity to help more people with the disease, which affects up to 2% of people aged over 40, and is a leading cause of blindness worldwide.
“Anti-VEGF therapy has helped a lot of people with RVO, but the fear factor –having to get a needle in the eye – causes many people to delay treatment, which can lead to retinal damage,” she said.
The study found that an experimental eye drop treatment was twice as effective as the standard injection therapy at reducing swelling and improving blood flow within the retina of mice with RVO. The eye drops also prevented neurons (photoreceptors) in the retina from deteriorating and preserved visual function over time, whereas the standard injections had no effect on either.
The eye drops contain an experimental drug that blocks caspase-9, an enzyme that triggers cell death, and was found by Troy’s lab to be overactive in blood vessels injured by RVO. Dr Maria Avrutsky, the study’s first author, conducted the research as a postdoc in the Troy lab.
“We think the eye drops improve the health of blood vessels in the retina, which then decreases the toxic signaling that damages the retina’s neurons and leads to vision loss,” she said.
Future studies are aimed at preparing to test the eye drops in human clinical trials and identifying additional therapeutic targets.
“Finding the root cause of RVO is the holy grail, but if we can at least provide better symptomatic relief that doesn’t distress patients, it would be a really good start,” Troy said.
DISCOVERY MAY ACCELERATE NEW APPROACH TO GLAUCOMA
International research led by QIMR Berghofer has found hundreds of new genes linked to a person’s risk of developing glaucoma, including key genetic targets that could, for the first time, pave the way for treatments that prevent the retinal damage that causes blindness.
The findings, from the largest-ever global genetic study of the degenerative eye disease, have been published in the prestigious journal Nature Genetics
The research significantly advances academia’s understanding of the genetics of glaucoma, building on a previous 2021 study to identify another 185 previously unknown genes linked to glaucoma risk, bringing the total number to 312 genes.
Lead researcher and internationally-recognised genetic epidemiologist Professor Stuart MacGregor, who heads QIMR Berghofer’s Statistical Genetics Laboratory, said the discoveries could rapidly accelerate a new approach to treatment.
“Existing treatments focus only on lowering eye pressure. The dream has always been to find a way to make the retina itself stronger so it can withstand the build-up of pressure and prevent the damage that causes permanent blindness,” MacGregor said. “Our findings are really
exciting because for the first time we’ve discovered the set of genes that could be targeted to induce this ‘neuro-protection’ in the retinal cells. We’ve also identified existing drugs that could be used on those genetic targets. This could rapidly advance effective treatment to finally prevent retina and optic nerve damage.”
Repurposing drugs has many benefits including faster translation of research findings into treatments for patients because the drugs have already been proven safe in humans.
The researchers are hoping to collect more data to increase the accuracy of their genetic prediction tool and find even more genes linked to glaucoma risk.
More than 5,000 Australians have already volunteered to take part in the QIMR Berghofer Genetics of Glaucoma study, but the researchers are appealing for more participants.
“We’re urging Australians who have a personal or family history of the disease to sign up to the QIMR Berghofer Genetics of Glaucoma study. We particularly encourage people aged 50 to 65 who don’t have glaucoma currently but who have a close relative (parent, sibling) with the disease to sign up,” MacGregor said.
AUSTRALIAN RESEARCHERS REDEFINE IMMUNE CELL LANDSCAPE IN HUMAN EYE

University of Melbourne researchers have discovered that the sentinels guarding the healthy human cornea from pathogens and inflammation are T cells, and not another type of immune cells, as previously thought.
The discovery, published in the Proceedings of the National Academy of Sciences journal, redefines current understanding in the field and builds on previous research published by the team in 2022 in Cell Reports showing T cells protect the eye against virus infection in mice.
The research team led by Professor Laura Downie and Dr Holly Chinnery from the Department of Optometry and Vision Sciences, and Professor Scott Mueller, from the Department of Microbiology and Immunology at the Doherty Institute, developed a new imaging technique as part of their investigation.
Mueller said knowledge of the various immune cell types in the human cornea
is important for establishing the eye’s protective mechanisms.
“We were able to discover that a significant number of cells at the surface of the healthy cornea are actually T cells,” he said. “Until now, these cells were mistakenly classified as dendritic cells based on static imaging. This completely changes the current dogma in the field that only dendritic cells are present in the healthy cornea.”
Downie added: “Using our non-invasive imaging approach, which we term Functional In Vivo Confocal Microscopy (Fun-IVCM), we have been able to see that these T cells move around quickly and interact with other cells and nerves in the outermost layer of the cornea,” she said.
“We also captured different cell dynamics in response to contact lens wear and in allergic eye disease, and quantified how these behaviours are modulated by drug treatments.
INSIGHT September 2023 17 RESEARCH
A/Prof Laura Downie, University of Melbourne.
A/Prof Puya Gharahkhani and Prof Stuart MacGregor, QIMR Berghofer. The eye drops prevented photoreceptors from deteriorating.
‘B Corp’ OPTOMETRIST BLAZES TRAIL
The co-owners of a greenfield Melbourne practice that opened in 2020 explain how they became the first and only optometrist in Australia – and the first single independent practice in the world – to achieve B Corp certification.

least a year,” O’Donnell, who was integral in getting the accreditation over the line, says.
The same kind of thinking applies to consumers: they prefer purchasing products from certified B Corporations, or ‘B Corps’. That was the case for co-director, optometrist Dr Jayson Stone, who originally learned about certified B Corps through a now-favourite clothing brand of his, Patagonia.
B Corps are businesses that meet high standards of social and environmental performance, accountability, and transparency. A not-for-profit movement, B Corps “envision a better economic system where businesses can benefit people, communities, and the planet”, the official website explains. Businesses who obtain the sought-after label also “choose long-term investments over quick wins, and measure their success based on the positive impact they create”.
B Corp is a growing movement, and there are now more than 7,000 certified businesses spanning across more than 161 industries; more than 560 are based in Australia and New Zealand.
Stone wanted Seekers in Gertrude Street – an iconic strip in the trendy inner Melbourne suburb of Fitzroy – to be one of them.
“I’d always envisaged owning my own practice at some point. I wanted Seekers to benefit everybody who was involved in it – us, as owners, but also our team members, patients and customers, and the environment,” he says.
“Gone are the days where you can simply say to customers, ‘We’re sustainable, we do this, and we do that’ without having to prove it. For us, B Corp is a way to formalise our credentials, and demonstrate to our customers we’re actually doing it, we’re meeting stringent standards.”
TESTED IN EVERY DIRECTION
The process for Seekers to be B Corp certified has taken over 12 months.
“You can’t apply to become a B Corp until you’ve been operating for at
“You’ve got to measure your positive impact on community, employees, environment, governance, and customers and meet requirements across each of those five standards. You need to respond to set questions, tailored to your sector, and your business impact model – demonstrating how you’re trying to make a difference, essentially,” he says.
Seekers was assessed in the retail pathway, as a health and wellness business model. The first step in the process involved completing a points-based online self-assessment, which allocated an impact score. The B Lab verification team then reviewed and verified Stone and O’Donnell’s self-assessment.
“It took a couple of months to complete the initial self-assessment because there’s hundreds of questions to answer and you need to

18 INSIGHT September 2023 BUSINESS
Dr Jayson Stone (from left), Kenny Chua and Kye O’Donnell, of Seekers Optical in Gertrude Street, Fitzroy, Melbourne. Image: Tailor Agency.
Through TerraCycle, Seekers Optical patients can recycle contact lenses and blister packs. Image: Tailor Agency.
understand how their question applies to optometry,” O’Donnell, who is also Seekers’ lab manager and technician, says.
The verification process took longer, with wait times of over six months due to the popularity of B Corp certification.
“There’s a lot of global organisations wanting to become a B Corp so you’re placed in a queue. We had to wait about nine months for them to verify our self-assessment. We were then assigned an analyst, who requested documentary evidence to support our self-assessment and asked additional questions,” O’Donnell says.
“We worked with three different analysts, including one solely for a quality assurance step, but it’s all been online through B Lab’s online assessment tool.”
As part of the health and wellbeing business impact model, Stone and O’Donnell had to demonstrate how they’re providing long-term benefits to their customers.
“We had to provide peer reviewed journal articles as evidence that routine examinations and early detection results in better outcomes for our patients, and we had to show how we support that,” Stone says.
“The fact that we do OCT scans on every patient, for example, is a way of demonstrating that we’re providing long-term care for them.”
SEEKERS’ SUSTAINABLE PRACTICES
Stone, who became an optical dispenser in 2003 before completing his training as an optometrist in 2016, and O’Donnell have one employee – retail manager and buyer, Mr Kenny Chua. Seekers is also part of Eyebenefit, an optical buying group for independent owner-operated optical stores. They stock high quality ethically made frames, including plant-based acetates, and titanium metal frames, for their strength and durability.

“We encourage our patients to re-use their existing frames as part of our re-use, re-lens, re-cycle program. We offer a 20% discount off any lenses put into an existing frame, because it’s sustainable. That’s the reason why we sell master crafted frames, because they have longer life expectancy,” Stone says.

“We’ve also teamed up with TerraCycle, so patients can recycle contact lenses, and blister packs. They take home a satchel made from a plant-based material and fill it with their used contact lenses and blister packs, and when they purchase a new supply of contact lenses, they bring in the satchel and we empty it into our TerraCycle box. We also recycle display lenses from spectacle frames, and patients’ used lenses when they replace the lenses in their existing frames.”
To meet B Lab’s high standards of governance, Stone and O’Donnell had to engage lawyers to amend their constitution.
“It’s about transparency and making sure the public knows who is behind the organisation and that it is independently owned. It’s about transparency for employees as well, keeping them constantly informed about business performance, and financial status. For example, we have a monthly KPI report that gets circulated amongst the team,” O’Donnell says.
“There was a legal change we had to make to our constitution, as directors, to be legally required to balance profits against community, environmental, sustainability, and ethical business objectives.”
Stone and O’Donnell donate $1,000 each quarter to a chosen charity, and have done so since day one of opening their practice, equating to about $12,000 in total.
“We began with choosing a charity ourselves and made a donation but now, each quarter, when patients are collecting their glasses, we offer
them the option to vote between three charities, and whichever gets the most votes, we donate to. We’ve now donated to more than 12 charities,” Stone says.
“When patients come in to collect their glasses, we let them know which charity received the donation. We also encourage patients to offer suggestions of which charities to support the following quarter.”
Some charities they’ve supported have been local, including the Victorian Aboriginal Health Service based in Fitzroy, others have been optometry focused, such as the Outback Vision mobile clinic in Western Australia, and some have supported women’s reproductive choices and the LGBTIQ+ community.
To maintain their B Corp status, Stone and O’Donnell will have to repeat the assessment process once every three years – but that has its benefits, O’Donnell says.
“Going through the process has helped us achieve more than we would have on our own accord. Doing it again might shed light on different areas to improve in the future,” he says.
And there’s another incentive: “Some consumers will opt for B Corp practices, or only purchase from B Corp businesses. Up until this point, there hasn’t been a B Corp optometry option in Australia. Our certification is published on the B Corp directory, including our assessment scores,” Stone says.
“Some employees prefer to work for B Corporations, and we prefer to deal with them. For example, we bank with Bank Australia, which is a B Corp, and get our toilet paper from Who Gives a Crap.”
INSIGHT September 2023 19
“SOME CONSUMERS WILL OPT FOR B CORP PRACTICES, OR ONLY PURCHASE FROM B CORP BUSINESSES. UP UNTIL THIS POINT, THERE HASN’T BEEN A B CORP OPTOMETRY OPTION IN AUSTRALIA.”
DR JAYSON STONE SEEKERS OPTICAL
Seekers stocks quality, ethically made frames, including plant-based acetates, and titanium metal frames. Image: Matt Chandorkar.
THE WAY Lighting
The discovery of a window in his consultation room, hidden behind an in-built cupboard, was a revelation for optometrist SHONIT JAGMOHAN that got him thinking about what other mood-boosting improvements he can make to his Melbourne practice.



It only takes 11 seconds for Mr Shonit Jagmohan’s consultation room to transition from natural light to complete darkness, but it has made a world of difference to his mental health and wellbeing.
With a simple touch of a button on his mini iPad, he can activate an electronic block-out blind and pre-set modes of lighting, so the transition is seamless for patients and provides ideal testing conditions for the optometrist.
For Jagmohan, having a window allowing natural light and fresh air in his consultation room has made a significant difference to his mental health, a subject he says the profession needs to keep discussing. The cumulative effect of a career in artificial light and bland consulting rooms is just one factor that make optometry a challenging career for some.
“I have read about the impact poor mental wellbeing has had on our industry, especially given the last couple of years with the pandemic, and lockdown. It is horrifying to read the statistics, to know so many optometrists have been struggling, but it is also somewhat comforting to know we are not alone,” he says.
“As a profession, it is something that we don’t often talk about, but we are all impacted in one way or another, and it was exacerbated during the pandemic with Melbourne being the most locked-down city.”
A pre-COVID survey of 505 registered practising Australian optometrists in mid-November 2019 revealed that 31% were experiencing moderate to severe psychological distress, with similar findings for depression and anxiety. One in four were also experiencing moderate to extremely severe stress.
The survey, led by the Queensland University of Technology (QUT) School of Optometry and Vision Science head Professor Sharon Bentley, also demonstrated a prevalence of high burnout, as indicated by exhaustion (56% of respondents), cynicism (57%) and professional efficacy (23%).
Mid-COVID, in perhaps the most comprehensive data on the psychological impact so far, Optometry Australia (OA) also surveyed 3,290 optometrists during the month of April 2020 to provide a snapshot of optometrists’ mental state. It indicated 88% of optometrists were ‘travelling ok’, which OA said is an indication of the sector’s resilience, but it meant 12% were struggling.
“Shining a light on mental health and having it in the forefront of our
20 INSIGHT September 2023
PROFILE
“IT HAS BEEN A GAME CHANGER, AS AN OPTOMETRIST, TO HAVE NATURAL LIGHT AND FRESH AIR.”
SHONIT JAGMOHAN VISION CAMBERWELL
Tones, texture and a sense of space in the newly renovated rooms at Vision Camberwell provide an environment for optimal mental health.
minds is important,” Jagmohan says. “Many of us have been there, and need support from our friends, families, but also our working community as well. Over the last few years, I personally have found the pandemic extremely difficult. I needed to find a way to support my mental health to be able to maintain my resilience and still be the best practitioner for my patients.”
To address this, practice owners Jagmohan and his wife, Sharon, decided to renovate their two consulting rooms at Vision Camberwell in Melbourne’s inner east during the pandemic.



Established in 1951, the practice has been in its current premises on Burke Road, Camberwell for 34 years. Jagmohan joined the practice in 2016 and became a managing partner in 2017 as part of a succession plan with then-owner Associate Professor Richard Vojlay. Jagmohan and Sharon, who manages the practice’s finances, purchased the practice from Vojlay in 2020.
It was the impetus to create an environment that was better for Jagmohan’s mental health long-term.
“The driver for wanting to renovate the consulting rooms is what we already know about mental health and Vitamin D – it’s accepted knowledge that natural light and exposure to outdoors are good for our mental health,” he says.
“If you’re stuck indoors without natural light, without fresh air – as optometrists tend to be – it can be a driver for reduced mental health. I’ve got patients who are radiologists who can 100% relate.”
Before joining Vision Camberwell in 2016, Jagmohan spent two years working in Queensland; when he moved to Melbourne, he noticed the onset of the ‘winter blues’.
“It impacts people differently. I’m a Kiwi of Fijian-Indian descent – it impacted me more than Sharon, who is Australian-European. When I moved to Melbourne, I was making a conscious effort during winter to manage my exposure to light,” he says.
Jagmohan and Sharon first spoke to their electrician – who is also a patient – about lighting options for the practice, such as installing globes that emit UV light, to promote better health when working indoors for long hours.
“As a practitioner with an interest in myopia management, I know we need to spend two hours outdoors a day, we know natural light is good for us. How do I support that, given my profession is an indoor profession that’s often associated with darkness? That’s when we thought about installing a window and electronic blinds,” he says.
Their electrician introduced them to an interior designer who specialises in creating spaces that boost mental health. She met with Jagmohan and his wife and joined Jagmohan during a patient consultation.
“She watched me do a consult to see my workflow, and what I needed in terms of adaptive lighting. As optometrists, we’re sitting, we’re standing, we’re washing our hands, we’re getting saline, we’re getting fluorescein, we’re getting behind a slit lamp, dimming lights, we’re constantly moving, so we also wanted to make sure the space was efficient. She also interviewed me to see what kinds of colours and textures resonated for me,” he says.
They then emptied the consultation room, removing all equipment and several built-in cupboards, to get a full sense of the space they were working with.
“When we pulled everything out, we discovered an old window, which was completely boarded up and covered with cupboards, looking out on to a disused courtyard. We thought, ‘this changes everything’.”
Given the practice is a commercial property and the building is over 125 years old, they had to seek approval to install a new, functioning window, but it was well worth it, Jagmohan says.
“I have fresh air when I want it and we created a small garden outside my window in the courtyard. It has been a game changer, as an optometrist,
to have natural light and fresh air,” he says.
“Removing overhead cupboards has helped by not having a lot of clutter around my head space, and we installed a large mirror – again to create a sense of space.”
They changed the room layout, installed textured wallpaper, replaced the carpet with new flooring in natural wood tones, and Jagmohan selected artwork for the walls, including a large photo above his desk of a monk watching a sunrise at Angkor Wat, a temple in Cambodia.
They also renovated a second, smaller consultation room.
“It’s hard to believe I spent six years in a windowless room. It’s only now that I’ve got this different space, with natural light and fresh air that I’ve been fortunate to create, that I realise it’s more conducive to me being at my best. I don’t know how I survived before,” he says.
“I think we don’t realise the impact being inside a windowless dark room can have on us. It doesn’t mean everyone can change their lighting or colour scheme – a lot of practices are in shopping centres – but if someone is thinking of doing something new, they might read this and factor in how their choice of lighting, tones and textures can affect their mental health, more than they considered before.”
INSIGHT September 2023 21
The brightness and tone of overhead lighting can be changed and a block-out blind activated in settings on a mini iPad.
A second, smaller consultation room was also renovated, with the layout mirroring the main consultation room.
TRACING THE
contaminated EYE DROP SAGA
The FDA and Centers for Disease Control issued an urgent product recall on 2 February 2023 for Global Pharma Healthcare and its artificial tears lubricant eye drops, distributed to US consumers as EzriCare Artificial Tears and Delsam Pharma Artificial Tears, due to possible contamination. But as it turns out, tainted bottles had been causing problems long before then.
Recently in Antimicrobial Agents and Chemotherapy, an interdisciplinary group of researchers and physicians in Cleveland, Ohio, describe a c ase of a 72-year-old female from November 2022 that helped expose the mysterious source of the outbreak at the time.
According to a report in the American Society of Microbiology (ASM), P. aeruginosa is a pathogenic, gram-negative bacterium that’s resistant to treatment with most antibiotics. It can cause swimmer’s ear – a painful infection of the outer ear canal – and more serious conditions, especially in people with compromised immune systems.

But the case in Cleveland was unusual, stated Dr Morgan Morelli, the study’s first author and an infectious disease fellow at University Hospitals Cleveland Medical Center.
“I’ve never recovered it from an eye,” she told the ASM. Because P. aeruginosa isn’t usually found in eye infections, she said, finding the right diagnosis was a challenge. “It required a lot of thinking and digging to figure out what was going on. And we never thought it was related to a global manufacturing issue.”
The elderly woman in this case presented to an outpatient eye clinic with unilateral vision loss. She was found to have a large corneal ulcer with hypopyon. She was referred to the hospital’s emergency department where she was evaluated by ophthalmologists. They cultured the infection, prescribed a combination of strong antibiotic eye drops, and sent her home. But the next day, the eye was worse, prompting a referral to a corneal specialist.
The patient had noticed a yellow discharge on her pillow, and she hadn’t been swimming: “We wondered if she’d accidentally touched something, or there was some freak accident, to explain the infection,” Morelli said.
At that point, Morelli said her case was referred to microbiologists and infectious disease experts at the hospital. Infectious disease specialist Dr Scott Fulton asked the patient’s husband to bring in her eye drops for testing. A sample from the patient was sent to the lab of Dr Robert Bonomo, an expert in gram-negative, drug-resistant bacteria at Case Western Reserve University School of Medicine.
The outbreak of a lethal drug-resistant bacteria strain linked to an eye drop manufacturing breakdown is one of the biggest health stories in 2023. A report from the American Society of Microbiology details how this complicated case came to light.
In February 2023, the ophthalmic sector was on high alert as a contaminated artificial tears brand was linked to a host of serious adverse reports in the US. The latest update from the US Food and Drug Administration stated 14 patients had suffered vision loss, an additional four required enucleation (surgical removal of the eye), and four deaths.

In total, 81 infected patients have been identified in 18 states. Authorities allege the outbreak originated from contaminated artificial tears manufactured in India. The infections have been caused by carbapenem-resistant P seudomonas aeruginosa – a rare strain of extensively drug-resistant bacteria that had never been found in the US previously. Multidrug-resistant bacteria like this have been labelled “one of the most concerning threats in modern medicine”.
Then, Morelli said, the pieces came together. Bonomo’s lab identified a P. aeruginosa isolate that matched genetic material found in the EzriCare artificial tear eye drops she’d been using. Then researchers connected the eye infection to the contaminated drops.
Because the bacteria was resistant to any antibiotics that could be delivered via the eye, this was problematic for the patient’s treatment plan. She was prescribed a strong antibiotic, intravenous cefiderocol, that has some activity against gram-negative bacterium, as well as two other topical antibiotics, polymyxin B ophthalmic solution and doxycycline. The injury to her eye improved, Morelli told ASM, but it’s unclear whether the patient will ever regain total vision.
According to the case study, the patient was discharged from hospital after two weeks and continued with the treatment regime. She had complete resolution of the hypopyon with improvement in the epithelial defect. However, two months after her initial presentation, she developed low intraocular pressure and was found to have choroidal detachment. At the time of publication, the vision potential in the eye remains poor, given the extent of her injuries.
Since issuing the warning in February, the CDC has identified infectious cases due to P. aeruginosa as early as autumn 2022.
Morelli said people may still have the contaminated eye drops on the shelf at home, but she hoped ophthalmologists and optometrists who may be the first physicians to see future patients with this infection will know what to look for.
22 INSIGHT September 2023
REPORT
Four Americans have required enucleation and four deaths have occurred from patients who used the eye drop brand in question.
Grow revenue
for your practice with
optomap ®

optomap has been shown to enhance pathology detection, disease management and to improve practice revenue.
Our expectation was to image between 4-5 patients a day, we’ve easily exceeded that. We often see up to 15 patients a day!
Michael Wicks l Wicks Eyecare


We took out a leasing option on our optomap. It easily paid for itself. We only wish we’d got an optomap sooner.
Damon Ezekiel l Ezekiel Eyes
T: +61 8 8444 6500 | Optos.com Contact Optos to learn about the additional benefits of implementing optomap in your practice.
The first age-related myopia management solution from ZEISS.

ZEISS MyoCare lenses with two designs for specific age groups


• C.A.R.E® Technology creating alternating defocus and correction zones in a ring-like pattern.
• ClearFocus design ensuring clarity of vision in all directions of gaze whilst effectively managing myopia progression.
• Available in a wide range of materials and indices.
Scan to watch

Managing myopia IN A PUBLIC HEALTH SETTING
Managing myopia in children can be a different ball game in a public-facing clinic, opposed to those in a corporate, networked or independently-owned practice, new research shows.

New data on how managing children with myopia in a public health setting differs to a private optometry clinic has not yet been formally published, but those attending O=MEGA23 will be the first to know.
Australian College of Optometry’s lead optometrist in paediatric services, Ms Zeinab Fakih, is presenting the research in her lecture entitled: ‘Implementing a myopia control clinic in a public health optometry setting.’
At the highly anticipated conference and trade fair, Fakih aims to describe the challenges, limitations and outcomes of implementing a myopia control clinic in a public health setting.
“At the core of the Australian College of Optometry is its public service mission to provide clinical care to people from diverse cultural and socio-economic backgrounds,” she says.
Due to its not-for-profit status, Fakih says, the ACO’s myopia clinic is a unique setting for the provision of myopia control.
“We know that health literacy is a key determinant to compliance and ultimately success in applying evidence-based treatments in medicine.
“I THINK BIOMETRY DEFINITELY ALTERS HOW WE MANAGE PATIENTS AND HOW WE ADAPT TREATMENT –THAT’S PROBABLY THE FUNDAMENTAL DIFFERENCE BETWEEN MANAGING MYOPIA IN A PUBLIC HEALTH SETTING VERSUS PRIVATE.” DR ROHAN HUGHES QUT MYOPIA CONTROL CLINIC



This principle certainly extends to myopia control,” she says.
“At O=MEGA, I will be presenting data looking at how the management of children with myopia looks different in a public health setting compared to a private optometry clinic.”
Given the ACO’s diverse patient base, Fakih and her team looked at determinants and trends in recommendations, and perceived barriers, to treatment decision-making and compliance by ACO clinicians.
“We showed that clinicians often face barriers to the initiation of myopia control and compliance including lower socio-economic background, costs, and frequency of follow-up appointments,” she says.
Summarising what her team has noted in their review of myopia control
INSIGHT September 2023 25
MYOPIA
COST COMPARISON
Australian researchers Tim Fricke, Professor Serge Resnikoff, Dr Nina Tahhan and Professor Mingguang He are among seven authors of a study on establishing a method to estimate the effect of antimyopia management options on lifetime cost of myopia.
The study led by Brien Holden Vision Institute was published in the British Journal of Ophthalmology in March 2022.
Using examples in Australia and China, the authors demonstrate a process for modelling lifetime costs of traditional myopia management (TMM = full, single-vision correction) and active myopia management (AMM) options with clinically meaningful treatment efficacy. AMM included low-dose atropine, antimyopia spectacles, antimyopia multifocal soft contact lenses and orthokeratology.
Myopia care costs were collected from published sources and key informants. Refractive and ocular health decisions were based on standard clinical protocols that responded to the speed of progression, level of myopia, and associated risks of pathology and vision impairment.
“We used the progressions, costs, protocols and risks to estimate and compare lifetime cost of myopia under each scenario and tested the effect of 0%, 3% and 5% annual discounting, where discounting adjusts future costs to 2020 value,” the authors explained.

Lifetime cost of traditional myopia management with 3% discounting
at the ACO, Fakih says one of the most pressing findings is the apparent trend for eye drops over contact lenses.
“Contact lens options, both soft contact lenses and orthokeratology, were not recommended as commonly at the ACO compared with private practice. We inferred this was due to the requirement for multiple initial visits, increased maintenance requirements at home, and certainly cost was a big barrier,” she says.
“We found that atropine 0.05% was the most commonly prescribed myopia control option as cost was more easily spread across the year with monthly drop purchases.”
She says the study highlights the need for targeted frameworks when managing children with myopia from low socio-economic backgrounds.
“Compliance differed across patients and closer reviews were implemented when compliance was seen to be a barrier for continued control.”
As a public clinic, with clinical research capacity, the ACO is currently involved in a multicentre trial looking into the effectiveness of repeated low level red light therapy (RLRL).

Fakih says preliminary results from the research “supports findings of the very promising” effects of RLRL in myopia control found in ‘Effect of repeated low level red light therapy for myopia control in children: a multicentre randomised trial’, published in 2022 by Yu Jiang et al.
“Embedding research into a public myopia clinic is very exciting. From August, the ACO will expand its clinic research in the field as it commences a real-world study of RLRL. It’s hoped that findings of the research will help shape the way RLRL therapy is rolled out into mainstream myopia control clinics in the future,” she says.
LIMITED HUMAN RESOURCES
With the challenges of managing children with myopia in a public health setting, Dr Pauline Kang understands how saving time and money – in terms of the mode of treatment and chair time – can be a motivating factor for families.
Kang, who coordinates the Myopia Control Clinic at the UNSW Optometry Clinic, says limited resources can be another challenge. “Paediatric myopia management is likely to be ongoing for several years, and depending on the type of treatment you prescribe, you may need to see a child for multiple visits. With any clinic, particularly those in a public health setting, human resources can be quite limited. To be able to manage children already on treatment, and new children coming on
was US$7,437 in Australia and US$8,006 in China. The lowest lifetime cost options with 3% discounting were antimyopia spectacles (US$7,280) in Australia and low-dose atropine (US$4,453) in China.
They found the additional early costs of active myopia management (AMM) options are substantially balanced across a lifetime by reduced refractive progression, simpler corrective lenses, fewer lens replacements, reduced risk of eye disease and vision loss, and reduced management of myopia complications. The cheapest lifetime cost of all scenarios tested was low-dose atropine in China, regardless of discount level.
The authors also noted that specialty contact lenses represent a significant step in commitment and cost for a family who otherwise intended to wear spectacles, but a relatively small step for a family who intended to pursue regular contact lenses regardless of any AMM option. However, they acknowledged the limitations of their methodology.
“In reality, clinicians make adaptive, iterative decisions based on evidence and observation. They are likely to change management as cases evolve, potentially to a different AMM if rapid myopia progression continues with the first option, or ceasing intervention if progression drops below an acceptable threshold,” the authors wrote.
“The rigidity of our assumptions is a sensibly conservative modelling approach, increasing our estimated cost of AMM options compared with TMM.”
26 INSIGHT September 2023 MYOPIA
Dr Rohan Hughes and Dr Emily Pieterse in Queensland University of Technology’s Myopia Control Clinic.
board, that’s one of the problems we encountered,” she says.
“Appointments would get booked months in advance, because we had to manage children that we had already seen but we also had a lot of new patients who wanted to come, but we didn’t have the capacity to be able to see them.”
Some contact lens treatments, such as soft contact lenses or orthokeratology, can potentially require the patient to attend five to 10 appointments in the space of a year, Kang says.

“You see them for the baseline, they come back for the lens fitting, teaching them how to insert and remove the lens, if the lenses don’t fit properly then they have to come back again. It requires a number of visits and once treatment is established, you may see them every three months at first, and then on a six-monthly basis. The time and resources available to be able to see patients for all those visits is a significant challenge.”
By comparison, atropine is much less demanding on chair time and clinic resources.
“As long as there’s no contraindications, any allergies to any of the components of the drug, as long as they don’t have serious side effects – and you wouldn’t typically expect any because the concentration is so low – then it’s relatively straightforward,” Kang says.
“Once they start atropine treatment, you might see them early on to make sure they’re compliant, no adverse effects, understanding how everything works, then you might not see them for another three or six months.”
Atropine can also be a go-to treatment for children as young as five-years-old whose parents might not be comfortable with their child being prescribed contact lenses.

“Atropine is a simple-to-apply treatment that works for most patients
and it’s easy to get – we’ve got the commercially available 0.01% option, although other concentrations are increasingly used,” Kang adds.
Newer, emerging treatments, such as RLRL therapy, are yet to be imbedded in public health, but online forums are discussing the latest treatment, which can be administered in-clinic and at-home.

“Repeated low level red light therapy is still quite new and we’re trying to understand the safety of repeated exposure to low level red light for children,” Kang says.
In early August, Eyerising International Pty Ltd announced TGA approval of its Eyerising Myopia Management Device, a world-first technology based on RLRL. The company says it's "a safe, affordable, and proven technology" that can sustainably improve the way the eye functions through improved blood flow to thicken the choroidal layer of the eye wall, in turn, reducing eye elongation and myopia progression. A recent study of RLRL for myopia control in children achieved 87.7%

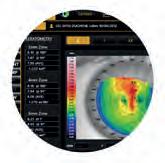



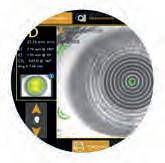
THE MYOPIA EXPERT 700 MEASURES AXIAL LENGTH , ENABLING NON-INVASIVE AND ACCURATE MONITORING WITHOUT ANY NEED FOR CYCLOPLEGIA FOR
EXPERT Select patient and acquisition mode 4 EASY STEPS Align patient and adjust automated chinrest Follow alignment guides to focus and trigger to start Review patient progression Available exclusively from OptiMed. For more information call 1300 657 720 or visit optimed.com.au MAKES YOUR PRACTICE PERFECT
COMPLETE MYOPIA CARE LOOK TO THE
“WITH ANY CLINIC, PARTICULARLY THOSE IN A PUBLIC HEALTH SETTING, HUMAN RESOURCES CAN BE QUITE LIMITED. TO BE ABLE TO MANAGE CHILDREN ALREADY ON TREATMENT, AND NEW CHILDREN COMING ON BOARD, THAT’S ONE OF THE PROBLEMS WE ENCOUNTERED.”
DR PAULINE KANG UNSW MYOPIA CONTROL CLINIC
efficacy with no significant side effects, the company reports.
“The TGA has recognised the safety and performance of the device – the first evidence-based red-light therapy with demonstrated ability to effectively and safely control the progression of childhood myopia with potential life-long benefits in avoiding later eye disease," Eyerising International CEO Mr Paul Cooke says.
Further, a recent study involving Melbourne institutions reviewed clinical data for myopic children aged 3-17 years who received RLRL delivered by a home-use desktop light device emitting light at 650 nm for at least one year. More than a quarter had axial length shortening greater than 0.05 mm following RLRL, and the overall mean axial length change was -0.142 mm per year.
“I’ve read in optometry forums on Facebook where some optometrists are discussing the option to lend out RLRL devices to patients for in-home treatment, which in a public health clinic we might also need to consider, and may need to have multiple devices, if they want the option to lend them out,” Kang says.
While she is unsure of the unit cost of RLRL devices, she didn’t think it would be a barrier to access.
“If anything, I would argue public health settings have more financial resources to purchase new equipment. For example, our university has access to funding opportunities and because we’re a teaching facility as well, we try to get the latest equipment to educate students. We have the latest ocular biometers, whereas many private clinics don’t because they do cost a lot,” she says.
In the past, Kang says, patients have come from as far as Canberra and Campbelltown to access the services at UNSW’s Myopia Control Clinic, but this is becoming less common as more private practices are implementing myopia management.
“When myopia management was still in its infancy, and practitioners weren’t as confident about doing it themselves, we would manage a lot of children together, particularly for their initial visits when they started
treatment,” Kang says. “Instead of them having to travel to us for a 15-minute appointment, we would ask them to go to the referring optometrist to get their vision or pressure checked, to make it more manageable for them, and reduce the demand on us.”
ACCESS TO MODERN EQUIPMENT
Like UNSW, Queensland University of Technology’s Myopia Control Clinic also has “the latest and greatest” equipment, allowing final-year students to more thoroughly assess and monitor myopia progression and effective treatment, Dr Rohan Hughes says.
“Our clinic operates on a referral basis. Optometrists in the community can refer patients, or if patients come to our paediatric clinic, they can be referred to the myopia clinic as well,” he says.
Hughes began clinically supervising students in QUT’s Myopia Control Clinic in 2017 while undertaking a PhD, and now jointly co-ordinates the clinic with its founder, Dr Emily Pieterse.
Pieterse initiated, developed and implemented the Myopia Control Clinic within the QUT Optometry Clinic in 2016 when she was completing her PhD studies.
According to Optometry Australia, it was the first such clinic established in an Australian university, and the evidence-based clinical procedures and myopia management guidelines developed by Pieterse have since been adopted by other universities when integrating myopia control into their clinical training.

“We’ve got the ability to monitor axial length, which is becoming more common in private optometry clinics, but up until the last 12 to 18 months, ophthalmology clinics and our university clinics were the only clinics that had access to biometry,” Hughes says.
Echoing one of the barriers to myopia control in a public health setting Kang described, Hughes says it’s not possible to assess patients and implement strategies immediately.
“We’ve been able to monitor myopia progression more closely using
28 INSIGHT September 2023 MYOPIA
Zeinab Fakih, lead optometrist of paediatric services, in a consult in the Australian College of Optometry’s Myopia Clinic.
biometry but in saying that, it’s not like a private optometry clinic where patients can just call and book an appointment – there’s months of wait time between when we get a referral and when we’re able to see that patient because of limited availability and resources in the clinic.”
While QUT’s Myopia Control Clinic offers the full scope of evidence-based myopia control treatments – including atropine, soft contact lenses, orthokeratology, and spectacle lenses – one treatment is more common. “We are probably in a similar situation to the Australia College of Optometry, in that we prescribe quite a lot of atropine. From parents’ point of view, it’s definitely viewed as an easier treatment to manage, but it’s also seen as the less expensive of the four treatment options, when comparing upfront costs,” Hughes says.
For patients who are using atropine drops as their sole treatment, Hughes says most would be using spectacles, most likely single vision.
“With the low concentration formulations, our experience is that




most children tolerate the side effects well such that they don’t require anything more than multifocal or anti-fatigue spectacles, although we strongly encourage sun protection – either sunglasses or photochromatic lenses,” he says.

Frame and lenses start at around $150 for basic single vision lenses through the QUT clinic. In Queensland, single vision spectacles are available at no charge through the Medical Aids Subsidy Scheme (MASS) Spectacle Supply Scheme, but eligibility is restricted to pension and health care card holders.
“Orthokeratology is our most popular treatment secondary to atropine, probably because our clinic offers lower cost orthokeratology compared to private practice – our low comparative cost is only because students undertake the contact lens fitting, overseen by qualified optometrists. We therefore don’t charge the same as what community optometry is charging so we have quite a lot of patients using orthokeratology.”
A fifth treatment option – RLRL therapy – is not available at the QUT clinic, yet. While treatment compliance at QUT’s clinic isn’t dramatically more or less than in community practice, and patients are managed much the same as in community practice, one observation stands apart.
“We probably make different management decisions at times because of the fact that we have access to ocular biometry. Often, we’ll have a patient come back, they’ve had no refractive change, but their axial length has increased, which might trigger a change in treatment strategy, as opposed to if it was in community optometry without biometry, where they might be told to come back in another six months,” Hughes says.
“I think biometry definitely alters how we manage patients and how we adapt treatment – that’s probably the fundamental difference between managing myopia in a public health setting versus private.”

Natalie Beardsworth Paediatric Optometrist +64 27 9037 160 beardsworthreadingchart.com a GREAT addition to every optometrist’s toolkit Accurate and easy to use Page 1 text for readers Page 2 single letters, numbers and pictures for non readers Simple children’s story with repetition, familiar themes and colourful characters for context Easy vocabulary comprising of the “first 100 sight words” Child friendly Comic Sans font from size N32 to N4 Calibrated for use at 30cm and laminated $99 NZD for 1 chart $249 NZD for 3 charts P&P in NZ $4.80 P&P in AUS $6.30
“WE KNOW THAT HEALTH LITERACY IS A KEY DETERMINANT TO COMPLIANCE AND ULTIMATELY SUCCESS IN APPLYING EVIDENCE-BASED TREATMENTS IN MEDICINE. THIS PRINCIPLE CERTAINLY EXTENDS TO MYOPIA CONTROL.”
ZEINAB FAKIH ACO MYOPIA CLINIC
Confidence through evidence.
That’s MiYOSMART.
MiYOSMART, the smart way to manage myopia in children.
Evidence is key to providing myopic children with clinically proven solutions at a critical time.1 We’ve conducted extensive research worldwide to provide you with an evidence-based solution, with the answers you need in your everyday clinical practice.
Feel confident in your clinical practice, with MIYOSMART
The D.I.M.S. Technology used in MiYOSMART spectacle lenses stems from the widely-accepted peripheral hyperopic defocus theory5, 6

Sustained efficacy with no rebound effects7, 8
High patient acceptance, 9 tolerance9 and easy adaptation10
Tested in children of different ethnicities and age groups8, 10
Improved outcomes in combination treatment with atropine12, 13
Awards and endorsements from credible associations, institutions and international experts15-18
Over 25 publications are available on MiYOSMART spectacle lenses, learn more by scanning the QR code!
1-18 For reference details visit https://bit.ly/3rRecC4
At the completion of this article, the reader should be able to align their clinical protocols more closely to a best-practice approach to myopia intervention…
Including:
• Understand why axial length measurement is the gold standard for myopia management
• Understand the rationale and significance of accurate baseline measurements of refraction, keratometry, corneal topography and axial length in managing an adult with myopia
• Assess the treatment options for adults with myopia progression
WHEN MYOPIA PROGRESSES IN ADULTS
What needs to be done when an adult presents with myopia? If the progression is due to axial elongation, many of the same treatments prescribed to children apply. As PHILIP CHENG explains, the higher vision demands of adults means objective, reliable metrics are key along with a proactive management plan.
Many of us come across these patients regularly in our practices: adults attending with complaints about their distance vision; patients of adult age being diagnosed with myopia for the first time; and those with myopia who continue show progression. It’s long been thought that children’s eyes stop growing and therefore should stop progressing by the time they turn 18. Is that true?
As our knowledge on myopia as an eye condition continues to expand with increasing research, it is becoming clearer that myopia may, in fact, continue to progress for patients well into the 20s. While genetics play a role in myopia development, the impact of the visual environment cannot be underestimated.
It’s well-established that in children, myopia onset and progression due to lifestyle changes during the COVID-19 pandemic increased. This has been confirmed by a recent review and meta-analysis of studies in relation to myopia progression during COVID vs pre-COVID.1 The myopic shifts observed is likely due to children spending less time outdoors, remote learning and increased screen time and near work.
A retrospective study on young adults with a mean age of 22.5 years found a statistically significant increase in myopia between pre-COVID and two years after the pandemic, 2 indicating that myopia progression in adulthood can occur from changes in lifestyle as well.
ABOUT THE AUTHOR:
Philip Cheng
B Optom (Melb) Therapeutics Endorsement
FIAOMC — Fellow of the International Academy of Orthokeratology & Myopia Control Committee board member, Orthokeratology Society of Oceania
Eyecare Concepts – Myopia Clinic, Melbourne

Recently, findings from the Raine Study conducted on a cohort of adults in Western Australia found that more than one third of the subjects had myopia progression of 0.50D or more between 20 and 28 years of age. 3 The study found that myopia onset also occurred in one of seven people who did not have myopia at age 20; women have a faster rate of myopia progression than men and higher risk of myopia onset as adults; and tertiary education, starting full-time work and digital device use are possible causes for myopic progression in adults in their 20s.
Further, the study is among the first to confirm that axial elongation occurs in adults with myopia progression by an average of 0.2 mm growth in the third decade of life – and as much as 1 mm in some subjects.
The implications of these findings are profound: myopia progression in adults cannot be assumed to be from accommodation or lenticular changes. When axial elongation is occurring in our adult patients, conversations need to be initiated to proactively managing the progression and reduce the ocular health risks – just as we would when a child presents with myopia.
COMPREHENSIVE ADULT MYOPIA EYE ASSESSMENT
A myopia management assessment for any patient, child or adult, should start with a comprehensive vision and eye health examination. It’s important to measure refraction as accurately as possible, which might involve the use of cycloplegics. Although autorefractors are commonplace and handy as a starting point, care should be taken when

INSIGHT September 2023 31
CLINICAL CPD HOURS This activity meets the OBA registration standards for CPD 0.75
CPD – MYOPIA
LEARNING OBJECTIVES:
Figure 1. Zeiss IOLMaster 500 optical biometer measuring axial length in an adult patient.
using autorefraction results. It’s also easy to over-minus a patient’s refraction subjectively, which affects interpretation of progression. Retinoscopy and binocular refraction can assist in determining an accurate refraction, aiming for the least-minus result for clear distance acuity. High myopia patients can be particularly challenging to refract, from the effects of vertex distance. Checking habitual acuity through existing spectacles and a quick over-refraction with flipper lenses can be a helpful guide to check that the new refraction makes sense.
THE GOLD STANDARD IN MYOPIA MANAGEMENT
Refraction is the sum of all the optical components of the eye and its length. A myopic shift in refraction can be due to different factors, such as changes in corneal curvature, crystalline lens density, accommodation and axial length.
As interventions for myopia management are aimed at primarily slowing axial length changes, baseline axial length is arguably the most important measurement. Indeed, the ability to accurately measure axial length with optical biometry is the gold standard in myopia management. Axial length is an objective, repeatable and reliable metric to monitor axial elongation in myopia progression. Optical biometry is about eight to 10 times more sensitive at detecting and tracking progression

than subjective refraction, and measurements unaffected by accommodation. Practitioners can use axial length changes to validate changes found in subjective refraction, where 0.1 mm increase in axial length approximately correlates to a 0.25D myopic shift.
Ocular health is an important part of an adult myopia eye assessment. Any level of myopia increases the lifetime risks of ocular diseases, such as glaucoma, myopic maculopathy, retinal tears, retinal detachment and cataract. Although high myopia carries the highest risks of ocular complications, even low and moderate myopia have considerable risks. 4
Axial length also provides an indication an individual’s ocular health risks, as the risk of visual impairment is strongly related to eyes with longer axial length regardless of the refractive error. Eyes with axial length greater than 26 mm have a 25% lifetime risk of uncorrectable visual impairment, rising to a staggering 90% for eyes longer than 30 mm. 5
Assessment and documentation of the optic discs and maculas, using retinal imaging and optical coherence tomography (OCT) may reveal subtle structural changes and help to assess changes over time. Patients with high myopia should have regular dilated fundus examination to check the health of their peripheral retina. Ultra widefield (UWF) imaging such as optomap, which can capture a 200-degree wide retinal image in a single
shot, can be a very useful tool for screening and documenting peripheral retinal changes, such as asymptomatic atrophic holes and lattice degeneration, in patients with myopia and high myopia.
Adults with myopia seeking advice for myopia management are generally concerned about their eye health. Many present with already high myopia, worried about vision loss and hoping their myopia progression can be stopped. Providing great care means having the tools to look after these patients to the best of our ability, while giving them comfort and reassurance of their ocular health. Striving for the highest level of clinical care, our myopia clinic is equipped with a comprehensive suite of diagnostic technologies including the ZEISS IOLMaster and OCULUS Myopia Master optical biometers, OCT, visual fields, corneal topographers, Pentacam and Optos California UWF imaging.
ADULT MYOPIA PROGRESSION TREATMENT
While there are gaps in our knowledge in managing adult myopia progression, the same treatments that we prescribe for children could potentially apply, providing that progression is due to axial elongation which these interventions help modulate. These interventions include peripheral defocus spectacle lenses, dual-focus or multifocal contact lenses, orthokeratology (orthok),
32 INSIGHT September 2023 Requires no drugs treatment e cacy Up to
87.7%
CPD – MYOPIA
Figure 2. High myopia adult orthok axial map with a Medmont corneal topographer.
atropine and combination therapy. There are different considerations when prescribing these treatments to an adult compared to a child; it’s important to consider quality of vision as well as treatment effectiveness, due to the higher visual demands of an adult.
SPECTACLE LENSES FOR ADULT MYOPIA
There has been a rise in new spectacle lens designs marketed for myopia management in the recent times. Two of these, with robust data from randomised controlled trials involving children, 6,7 are the HOYA MiyoSmart defocus incorporated multiple segments (DIMS) and Essilor Stellest highly aspherical lenslet (HAL) lenses.
In adults, we need to consider whether the optics of these defocus spectacle lenses may affect distance visual acuity, contrast sensitivity and glare sensitivity. A German study 8 evaluating traffic safety of DIMS lenses on a group of 12 young adults (age 24-45) found that lenses did not show visual impairment that would be relevant to road safety and concluded the lenses to be safe for driving. (MiyoSmart and Stellest lenses are currently limited to polycarbonate material (1.59 index), limiting their use in high myopia prescriptions where lens thickness and cosmesis may be an important factor).
CONTACT LENSES FOR ADULT MYOPIA
Many adults with myopia already wear contact lenses and may prefer contact lenses over glasses. For those who are progressing, a switch from a single vision (SV) lens to a centre-distance multifocal design may be beneficial. The BLINK study 9 demonstrated a dose-response where a higher add power (+2.50D) was more effective than a medium add power (+1.50D).
Care should be taken to advise patients of the difference in quality of vision if they

ORTHOKERATOLOGY FOR ADULT MYOPIA

Orthok is an option for adults who wish to enjoy the freedom of not needing to wear glasses or contact lenses in the daytime. Suitable adult candidates for orthok are those with low- to-moderate myopia, regular sleeping patterns, good compliance to wearing their lenses and hygiene, and flexible with some slight variation in vision from day-to-day. Some adults may consider orthok as an alternative to refractive surgery, or have intolerance to dryness from soft lenses,
are currently wearing SV lenses. The consideration in prescribing these lenses to adults is the impact on distance acuity with the higher add powers. The aim is to give highest tolerable add power; if +2.50D add is too difficult to wear, reducing the add to a more tolerable level (+2.00D or +1.50D) might be necessary. Distance acuity may also be improved by increasing the distance spherical power by -0.50D to offset the effect of the add power.
or have heard about orthok for myopia management. Managing patient expectations is vital for successfully fitting an adult with orthok; patients should be advised that they are likely to experience halos and starburst effects at night, and reduced contrast sensitivity in low light situations as the pupils enlarge. These visual effects are related to the higher-order aberrations induced in the corneal reshaping process and increases with the amount of myopia correction; they
Repeated Low-Level Red-Light Therapy Advanced myopia control made early, easy, and more effective * Jiang, Yu, et al. “Effect of repeated low-level red-light therapy for myopia control in children: a multicenter randomized controlled trial.” Ophthalmology 129.5 (2022): 509-519. No known significant side e ects Adjunct to existing therapy Requires no contact lenses Requires no drugs Requires no injections Suitable for children as young as 3 y/o Easy use, high loyal >80% COMPLIANCE treatment e cacy Up to 87.7% No known significant side e ects Adjunct to existing therapy Requires no contact lenses Requires no drugs Requires no injections Suitable for children as young as 3 y/o Easy use, high loyal >80% COMPLIANCE treatment e cacy Up to 87.7% No known significant side e ects Adjunct to existing therapy Requires no contact lenses Requires no injections Suitable for children as young as 3 y/o Easy use, high loyal >80% COMPLIANCE treatment 87.7% * NOW AVAILABLE IN AUSTRALIA (ARTG No: 41275) To learn more, please visit us at OMEGA23 8-10 Sept: booth B12
“WHEN AXIAL ELONGATION IS OCCURRING IN OUR ADULT PATIENTS, CONVERSATIONS NEED TO BE INITIATED TO PROACTIVELY MANAGING THE PROGRESSION AND REDUCE THE OCULAR HEALTH RISKS – JUST AS WE WOULD WHEN A CHILD PRESENTS WITH MYOPIA.”
also occur in laser refractive surgery.
Orthok is a highly effective treatment in slowing axial elongation in children. Recent work in orthok research has suggested that customising lenses with smaller back optic zone diameters (BOZD) may enhance the therapeutic effect in retarding axial elongation compared to conventional designs.10 However, such an aggressive myopia control orthok design could be difficult for an adult to adapt to. Adult orthok lenses are generally designed with larger BOZD of 6 mm or greater to enlarge the central treatment zone and reduce the effects of night halos.
For an adult proceeding with orthok with myopia management in mind, there should be lens design considerations for myopia control as well as providing satisfactory quality of vision for the patient’s lifestyle and visual tasks. Adults with near esophoria and accommodative lag may also benefit from the exophoric shift and improved binocular vision that OK lenses can provide, compared to single vision contact lenses.11
ATROPINE

Low-dose atropine is less often used for adults, the mild cycloplegic effect of atropine
is likely to be more pronounced for an adult with less active accommodation than a child, making the stronger, more effective doses (0.025-0.05%) more difficult to tolerate. For adults who may be interested in trying low-dose atropine, the commercially available Eikance 0.01% could be a starting point to assess tolerance.
CASE STUDY 1
A 22-year-old woman was referred for management of her adult myopia progression. The referral letter reported that “her prescription had steadily increased over the years and in the last 12 months, she has had more than -1.00D myopic shift in her left eye”. Her refraction was reported as R -6.00/-2.75x11 and L -6.75/-2.75x167, while her current glasses measured R -5.50/-2.75x6 L -5.50/-2.75x163. She alternates between her single-vision glasses and monthly-replacement soft contact lenses.
A cycloplegic examination was performed, finding a refraction of R -6.00/-2.75x6 and L -6.50/-2.75x160. Her axial length measured R 24.78 mm L 25.07 mm with the IOLMaster 500 optical biometer. She has steeper-than-average corneas, with keratometry readings of R 7.38 mm and L 7.34 mm along the flat meridian. Corneal topography is part of our initial assessment for myopia management, both to assess for patient suitability for orthokeratology and also as a screening for keratoconus. Given this patient’s moderate astigmatism and steep corneas, it was important to exclude the possibility of corneal ectasia
causing her refractive changes. Her corneal topography showed regular, with-the-rule corneal astigmatism not suggestive of keratoconus. Her ocular health examination was unremarkable.

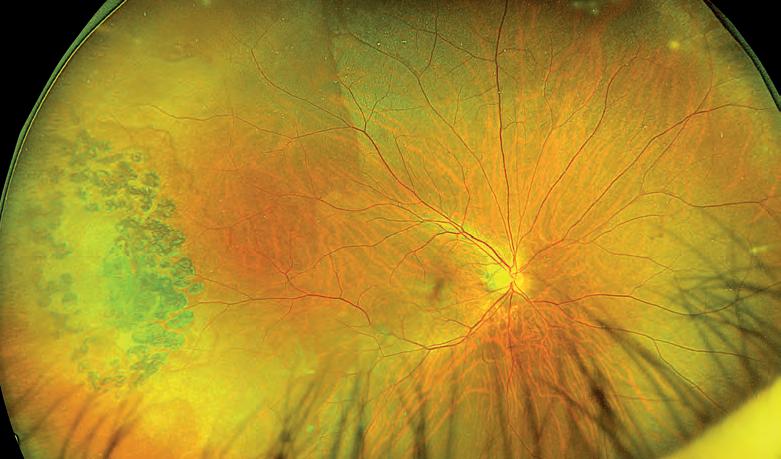
The patient was concerned about her myopia and was keen to explore options to slow her progression. We discussed management options including spectacle lenses, soft contact lenses and orthok. While orthok is a possibility, it could be a challenging fit and as a patient was already a happy soft lens wearer, we decided to start intervention with multifocal contact lenses. She was fitted with CooperVision Biofinity Multifocal toric lenses, centre-distance design with a +2.00D add. After three weeks, she had adapted well to her lenses and felt comfortable with her corrected vision of R 6/6 L 6/7.
After 12 months of treatment with multifocal contact lenses, her myopia had not progressed. She reported good compliance wearing her lenses daily, although she needed lubricating eye drops for end-of-day dry eye symptoms. Her subjective refraction was stable, and her axial length of R 24.81 mm L 25.05 mm confirmed no axial elongation in the past year. She was pleased with the result and was happy to continue myopia management wearing multifocal contact lenses.
CASE STUDY 2
A 21-year-old university medical student from regional NSW booked into our clinic for orthokeratology assessment. With concerns for her high myopia, she had been researching myopia management options for herself. She started wearing glasses from age eight and had year-by-year progression. She previously tried multifocal contact lenses but stopped due to dry eye. Her refraction measured R -5.50 and L -6.25/-0.25x45, axial length R 24.64 mm L 24.95 mm and keratometry readings R 7.54 mm L 7.50 mm and relatively spherical corneas on topography.
Following her detailed myopia assessment, we discussed her options for adult myopia management. While she understood that her myopia may not progress as quickly as it did when she was younger, she wanted to be proactive to prevent further deterioration of her vision. She was particularly interested in orthok for the benefit of myopia control as well as being free from wearing glasses or daytime contact lenses. It was important to advise her of vision expectations of
34 INSIGHT September 2023 CPD – MYOPIA
Figure 3. An Optos ultra widefield scan revealing retinal pathology in high myopia.
Figure 4. Adult orthokeratology lens with fluorescein pattern.
“ANY LEVEL OF MYOPIA INCREASES THE LIFETIME RISKS OF OCULAR DISEASES, SUCH AS GLAUCOMA, MYOPIC MACULOPATHY, RETINAL TEARS, RETINAL DETACHMENT AND CATARACT.”
orthokeratology for her high myopia: the likelihood of night halos from aberrations, the need for good sleeping patterns and lens hygiene. And, with her long travel distance from the clinic, she had to understand that multiple visits for her ongoing reviews would be required, particularly in the first few months of starting orthok treatment. With her informed consent, we proceeded to start her on orthok, using custom-designed EyeSpace Forge OK lenses.
She stayed overnight in Melbourne for her orthok lens fitting and day one review, then attended subsequent reviews at three weeks and at three months. She has been very happy with her treatment; she wears her lenses nightly for seven to eight hours, enjoys full correction of her myopia and unaided VA of 6/6 R&L. Her corneas are healthy, without any staining. She reported no issues with halos at night and her eyes feel more comfortable than she wore soft daytime lenses. Although it is too early to assess progression at this point, her axial length measured R 24.53 mm L 24.88 mm at three months and will be reviewed again four months later.
CONCLUSION





There is now sufficient evidence that myopia onset and progression can occur
in adulthood. Just as myopia management in children is important and is gradually moving towards being a standard of care in optometry, we should not forget about the adults with myopia who may also progress. Establishing an accurate baseline with reliable refraction, keratometry, corneal topography and axial length will help with clinical decision making in managing an adult with myopia.
Management options should be guided by patient expectations, visual demands, lifestyle and personal preferences. Patient education of the lifelong risks of myopia and regular comprehensive ocular health examination are important aspects of managing adult patients whether they are still progressing or stable in their myopia.
REFERENCES:
1. Li M, Xu L, Tan CS, Lanca C, Foo LL, Sabanayagam C, Saw SM. Systematic Review and Meta-Analysis on the Impact of COVID-19 Pandemic-Related Lifestyle on Myopia. Asia Pac J Ophthalmol (Phila). 2022 Sep 1; 11 (5): 470-480.
2. Kohmarn T, Srisurattanamethakul N, Watcharapalakorn A, Poyomtip T, Poolsanam C. Outbreak of COVID-19-Related Myopia Progression in Adults: A Preliminary Study. Clin Optom (Auckl). 2022 Aug 4;14:125-131.
3. Lee SS, Mackey DA. Prevalence and Risk Factors of Myopia in Young Adults: Review of Findings From the Raine Study. Front Public Health. 2022 Apr 27;10:861044. doi: 10.3389/ fpubh.2022.861044.
4. H aarman AEG, Enthoven CA, Tideman JWL, Tedja MS, Verhoeven VJM, Klaver CCW. The Complications of Myopia: A Review and Meta-Analysis. Invest Ophthalmol Vis Sci. 2020 Apr 9; 61 (4): 49.
5. Tideman JW, Snabel MC, Tedja MS, van Rijn GA, Wong KT, Kuijpers RW, Vingerling JR, Hofman A, Buitendijk GH, Keunen JE, Boon CJ, Geerards AJ, Luyten GP, Verhoeven VJ, Klaver CC. Association of Axial Length With Risk of Uncorrectable Visual Impairment for Europeans With Myopia. JAMA Ophthalmol. 2016 Dec 1; 134 (12): 1355-1363.
6. L am CS, Tang WC, Lee PH, Zhang HY, Qi H, Hasegawa K, To CH. Myopia control effect of defocus incorporated multiple segments (DIMS) spectacle lens in Chinese children: results of a 3-year follow-up study. Br J Ophthalmol. 2022 Aug;106(8):1110-1114.
7. B ao J, Yang A, Huang Y, Li X, Pan Y, Ding C, Lim EW, Zheng J, Spiegel DP, Drobe B, Lu F, Chen H. One-year myopia control efficacy of spectacle lenses with aspherical lenslets. Br J Ophthalmol. 2022 Aug;106(8):1171-1176.
8. K aymak H, Mattern AI, Graff B, Neller K, Langenbucher A, Seitz B, Schwahn H. Safety of DIMS Spectacle Lenses and Atropine as Combination Therapy for Myopia Progression. Klin Monbl Augenheilkd. 2022 Oct; 239 (10): 1197-1205.

9. Walline JJ, Walker MK, Mutti DO, et al. Effect of High Add Power, Medium Add Power, or Single-Vision Contact Lenses on Myopia Progression in Children: The BLINK Randomized Clinical Trial. JAMA. 2020; 324 (6): 571-580. doi:10.1001/jama.2020.10834
10. G uo B, Cheung SW, Kojima R, Cho P. One-year results of the Variation of Orthokeratology Lens Treatment Zone (VOLTZ) Study: a prospective randomised clinical trial. Ophthalmic Physiol Opt. 2021 Jul; 41 (4): 702-714. doi: 10.1111/opo.12834. Epub 2021 May 15. PMID: 33991112; PMCID: PMC8251614.
NOTE: Insight readers can scan the QR code or visit insightnews.com.au/cpd/ to access a link to this article to include in their own CPD log book.

11. G ifford K, Gifford P, Hendicott PL, Schmid KL. Near binocular visual function in young adult orthokeratology versus soft contact lens wearers. Cont Lens Anterior Eye. 2017 Jun; 40 (3): 184-189. doi: 10.1016/j.clae.2017.01.003. Epub 2017 Feb 16. PMID: 28215499.




PBS Information: Xalatan (latanoprost 0.005% eye drops, 2.5 mL) is listed on the PBS as antiglaucoma preparations and miotics.


Before prescribing please review Product Information available via www.aspenpharma.com.au/products or call 1300 659 646.




Minimum Product Information: XALATAN® (Latanoprost 50 µg/mL) Eye Drops. Indication: Reduction of intraocular pressure (IOP) in patients with open-angle glaucoma or ocular hypertension. Contraindications: Hypersensitivity to ingredients. Precautions: Change in eye colour due to increased iris pigmentation; heterochromia; eyelid skin darkening; reversible eyelash and vellus hair changes; macular oedema often associated with aphakia / pseudoaphakia; other types of glaucoma; contact lenses; severe or brittle asthma; herpetic keratitis; driving or using machines – transient blurry vision; elderly: no data; children: do not use, no data; lactation- metabolites present in breast milk, risk / benefit. Pregnancy: Category (B3) Interactions: other prostaglandins, thiomersal. See PI for details. Adverse Effects: Eye Disorders: blurred vision, burning, conjunctivitis, excessive tearing, eye pain, foreign body sensation, hyperaemia, iris hyperpigmentation, itching, punctate epithelial erosions, grittiness, stinging, eyelash and vellus hair changes, punctate keratitis, blepharitis, eyelid oedema, localised skin reaction on eyelids; Systemic: bronchitis, upper respiratory tract infection, eczema, rash, urinary tract disorder, abnormal liver function, myalgia, arthralgia, dizziness, headache, rash, chest pain, asthma, dyspnoea . See PI for details and other AEs. Dosage and Administration: One eye drop in the affected eye(s) once daily. Other eye drops should be administered at least 5 minutes apart.

References: 1. Clinical Practice Guide for the Diagnosis and Management of Open Angle Glaucoma. Optometry Australia 2020 2. Australian Commission on Safety and Quality in Healthcare Active Ingredient Prescribing Guide - list of medicines for brand consideration December 2022
Aspen Australia includes Aspen Pharmacare Australia Pty Ltd (ABN 51 096 236 985) and Aspen Pharma Pty Ltd (ABN 88 004 118 594). All sales and marketing requests to: Aspen Pharmacare Pty Ltd, 34-36 Chandos Street, St Leonards NSW 2065. Tel: +61 2 8436 8300 Email: aspen@aspenpharmacare.com.au Web: www.aspenpharma.com.au Trademarks are owned by or licensed to the Aspen group of companies. © 2023 Aspen group of companies or its licensor. All rights reserved. Prepared: July 2023 AU-LAT-072023-07653



✔
If clinically necessary for the treatment of your patient, prescribe by brand and disallow brand substitution
2
A first choice for glaucoma management1
MYOPIA Management Lenses
for Young Patients
MyoEase MyOnic
Uses multi-pinhole micro-transparent lens defocus design.

Micro-transparent pinhole defocus area
Helps correct myopia at the fovea while simultaneously defocusing the peripheral hyperopia.

SV Zone diameter 10mm
Positive Defocus Zone radius 10mm max positive defocus +2.00 to +3.00 D
Constant Power Zone for an easier adaptation on ocular movements
Central optical zoom
*Available in 1.56, 1.60, 1.67, and 1.74.
*Available in
Envision the Possibilities
1.50, 1.53, 1.56, 1.59, 1.60, 1.67, 1.74 www.opticare.com.au
Envision the Possibilities
QR code to learn more about our Myopia Control Lenses and other premium products. 1800 251 852 info@opticare.com.au 8-10 SEPT MELBOURNE
US AT
Scan this
VISIT
At the completion of this article, the reader should have a better understanding of the role of outdoor light exposure in myopia management...
Including:
• Will have reviewed the evidence on outdoor exposure as a protective factor against myopia
• Understand the critical role of light intensity, rather than the absence of near-work, in myopia
• Have reviewed RANZCO’s recommendation of two or more hours a day (with UV protection) for optimum daily outdoor light exposure to decrease myopia incidence
‘GREEN TIME VS SCREEN TIME’: THE FIRST STEP IN MYOPIA MANAGEMENT

Eyecare professionals increasingly find themselves in a bind. Time spent outdoors slows myopia progression, but too much UV light poses a danger to their eye health. Dr LOREN ROSE summarises the evidence on the role of increased lux visible light and the recommendations developed by RANZCO to navigate this set of circumstances.
WHAT IS THE IMPACT OF MYOPIA?

Myopia is an increasingly prevalent eye disorder, with its incidence expected to reach 52% by 2050 worldwide.1,2 It is predicted that one billion people worldwide will have high myopia with refractive errors ³ -6.0D and axial lengths of 26 mm. As this prediction becomes a reality, high myopia will be the leading cause of permanent blindness worldwide. The sightthreatening complications of pathological myopia include retinal detachment, neovascular membrane secondary to myopic macular degeneration, glaucoma, and pre-senile cataract. 3,4
DOES FAMILY HISTORY PLAY A PART?
It has been established that genetics contribute to myopia development, and it is associated with increased risk with increased family history. 5 Large genetic studies have identified hundreds of genetic loci which carry information from how large the eye is to how fast it will grow to even how susceptible it is to environmental influences affecting myopia progression. Genetic studies have implicated light-induced signalling as a driver for refractive error. 6
KEY QUESTIONS
Which environmental elements are protective? Which are risk factors for myopia development? International studies show that outdoor exposure is a protective factor against myopia.
Environmental influences such as sunlight exposure and near work are implicated in the development and rate of myopia progression in many animal models and epidemiological studies. 3,6-10 A meta-analysis and systemic review established that the incidence of myopia decreases with increased time spent outdoors in hours per week.7
Furthermore, increasing the time children play outdoors reduces myopia progression.11 It has been shown that the incidence of myopia can be reduced by increasing the time six-year-old children spend outdoors by 40 minutes a day.12
The combination of time spent outdoors, education levels, and near work that contributes to the prevalence of myopia can confound each other in studies.13-15 For example, children who spend more than two hours per day at ‘cram school’ (coaching centres after school) attendance have
an increased incidence of myopia, which may be due to the reduced time spent outdoors or the increased time doing near activities or both.16
In 2007, the Orinda Longitudinal Study of Myopia reported the longitudinal evidence of a protective association between more time spent outdoors and a reduced risk of myopia onset in elementary school children in northern California.17 The risk of developing myopia in a high family history was reduced from 60% to 20% by spending at least 14 hours per week outdoors.

More recently, public health policy overseas has again highlighted the protective effect of natural light exposure on myopia prevalence. In 2020, the Tian Tian 120 project was published. In Taiwan, children were exposed to 120 minutes a day of outdoor time during school hours. The Taiwan trend of nine years of increasing prevalence of at least one eye of 20/25 or worse from 35% in 2001 to 50% in 2011 was reversed to 46% in 2015.18
Rose K et al19 analysed outdoor activity compared with near work and concluded that light intensity rather than the absence of near work was the critical factor. Sunlight contains the wavelengths of visible light and the shorter ultraviolet wavelengths known to cause eye and skin diseases.
INSIGHT September 2023 37
CLINICAL CPD HOURS This activity meets the OBA registration standards for CPD 0.75
LEARNING OBJECTIVES:
CPD – MYOPIA
Replacing screen time with more outdoor time is an important first step when intervening in progressing myopia cases.
ROLE OF OPTOMETRISTS AND EYE HEALTH PROFESSIONALS
• Empower families in their decision-making and lifestyle choices as the first step toward myopia control/management:
• Dis cuss “less screens and more green” on the first consultation. As already outlined, outdoor light reduced both the prevalence in pre-myopes and the progression (if significant time is spent outside).
• Encourage the family by highlighting benefits, that even family history risk is “reversed” in longitudinal studies.
• Encourage making outdoor play a routine for children from a young age, including sports that help maintain the outdoor requirement for myopia control.

What is the impact of UV light exposure versus bright light in protecting against myopia?
Although many studies are still ongoing, it is known from well-designed animal studies, including on rhesus monkeys, 20 chicks21 and tree shrews22, that UV light is not critical for the regulation of ocular growth. UV-free lighting systems were used to inhibit scleral growth rates experimentally.
Karouta and Ashby noted that UV exposure does not underlie the ability of bright light to retard the development of deprivation-myopia or the ability of bright light to maintain normal untreated eyes in a hyperopic state23,24 Instead, their data indicate that the ability of light to retard the development of deprivation myopia is driven by intensity-dependent increases in retinal dopamine release. 21
Furthermore, they noted that broadening the spectral output of the lighting system to include UV output was unlikely to induce an even greater protective effect against the development of myopia, as the development of deprivation myopia can be abolished in rhesus monkeys at 20,000 lux 20 and chicks at 40,000 lux of bright light alone. 25 Hammond et al 26 compared UV-free light to illuminance-matched UV-containing light and found no difference in modifying the emmetropisation process in myopia animal models.
Indoors, light is typically between 50 lux in a home27 to 320-500 lux in an office. 27,28 Outdoors, there is a huge increase from 20,000 lux on a cloudy day to 100,000 lux in direct sunlight. Hence, even if there were additional slowing in myopia from UV exposure, the increased risk of UV-related blinding eye diseases seems unnecessary.
Ho CL et al,11 in their meta-analysis of the dose-response relationship between outdoor exposure and myopia indicators, found that more than 120 minutes of daily outdoor light exposure decreased myopia incidence by 50%, spherical equivalent refraction by 32.9% and axial elongation by 24.9% for Asian children aged 4-14 years. Furthermore, less than 40 minutes outdoors daily is associated with more rapid axial length progression. 29 Hence, at least two to three hours of outdoor activity should be encouraged with UV-protecting eyewear d uring childhood.
Who is the audience?
Public awareness of the increasing incidence and lifelong visual complications of myopia is currently limited. Parental understanding of the causes and health risks of myopia is poor, and parents/caregivers may be nonchalant regarding myopia in their child. Increasing public awareness is obviously important in improving myopia control.
Rodenstock’s ColorMatic® 3 lenses change from clear to dark and fade back to clear again 30% faster than the previous generation – making them our fastest photochromic lenses ever.
For more information, speak to your Rodenstock Account Manager.

Frame R3338C
with Biometric
CPD – MYOPIA
INTRODUCING COLORMATIC® 3: THE NEW GENERATION OF COLORMATIC®
Available
Intelligent Glasses
What messaging is needed to highlight risks and benefits?
In recommending children increase outdoor time, a child’s subsequent risk of skin cancer and UV-related eye diseases, including periorbital skin cancers, 30 ocular surface tumours including limbal squamous cell carcinomas, 31 pterygium, 32 cortical cataracts 33-35 and increased risk of age-related macular degeneration 34 must be balanced with their risk of myopia. 36

Children have the least naturally-developed protection against UVR; 80% of UV eye exposure occurs before a child turns 18. 37 It has been demonstrated that 30% of children 9-11 years show UV damage to their eyes using UV fluorescence photography. By 12-15 years of age, 80% of children had damage detected using UV fluorescence, but even more alarmingly, 30% had clinically evident pingueculae or pterygium. 38
This result was again demonstrated by Kempen JH et al, 39 who showed that areas with the highest prevalence of skin cancers had the lowest levels of myopia by using the data from the Beaver Dam, Rotterdam, the Blue Mountains Eye Studies and the Melbourne Vision Impairment Project. Therefore, the degree of UV damage to the eye correlates with the degree of high lux light.
The presence of pterygium has been associated with reduced axial length measurements. Only 1.8% of patients with axial lengths greater than 26 mm have pterygia compared to 51.4% of pterygia patients with axial lengths less than 23 mm in the same population group. 40 Although UV light is not the protective component of sunlight for limiting myopia, it is simultaneously present with the bright lux of light from the sun when people are outdoors.
By increasing the exposure of the paediatric eye to an increased lux of visible light and limiting exposure to UV radiation, it is possible to limit both UV-related ocular diseases and myopia. With the protective benefit of high lux visible light to reduce myopia and by excluding the damaging impact of the invisible UVR on the eye with maximally protective sunglasses, both these silent epidemics can be combated simultaneously.

RANZCO RECOMMENDATIONS
RANZCO’s policy is to optimise exposure to outdoor light while protecting from UV light to reduce skin malignancy (recognising that periorbital skin cancers account for 5-10% of all skin cancers that occur in the body). 41,42 Importantly, based on the evidence, RANZCO recommends maintaining exposure to sufficient high-intensity sunlight to minimise myopia progression.
Therefore, as the standard setters in ophthalmology, and with a vision to stop preventable blindness, RANZCO recommends two or more hours a day with UV protection to the skin and ocular surface to limit the progress of myopia while protecting against the risk of cancer.
REFERENCES:
1. H olden, B.A., et al., Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology, 2016. 123(5): p. 1036-42.
2. The impact of Myopia and High Myopia. 2017, World Health Organization p. 5.
3. F litcroft, D.I., The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res, 2012. 31(6): p. 622-60.
4. H aarman, A.E.G., et al., The Complications of Myopia: A Review and Meta-Analysis. Invest Ophthalmol Vis Sci, 2020. 61(4): p. 49.
5. Tedja, M.S., et al., IMI - Myopia Genetics Report. Invest Ophthalmol Vis Sci, 2019. 60(3): p. M89-M105.
6. Tedja, M.S., et al., Genome-wide association meta-analysis highlights light-induced signaling as a driver for refractive error. Nat Genet, 2018. 50(6): p. 834-848.
7. X iong, S., et al., Time spent in outdoor activities in relation to myopia prevention and control: a meta-analysis and systematic review. Acta Ophthalmol, 2017. 95(6): p. 551-566.
8. M utti, D.O., Hereditary and environmental contributions to emmetropization and myopia. Optom Vis Sci, 2010. 87(4): p. 255-9.
9. G oldschmidt, E. and N. Jacobsen, Genetic and environmental effects on myopia development and progression. Eye (Lond), 2014. 28(2): p. 126-33.
10. R ose, K.A., A.N. French, and I.G. Morgan, Environmental Factors and Myopia: Paradoxes and Prospects for Prevention. Asia Pac J Ophthalmol (Phila), 2016. 5(6): p. 403-410.
11. H o, C.L., W.F. Wu, and Y.M. Liou, Dose-Response Relationship of Outdoor Exposure and Myopia Indicators: A Systematic Review and Meta-Analysis of Various Research Methods. Int J Environ Res Public Health, 2019. 16(14).
12. H e, M., et al., Effect of Time Spent Outdoors at School on the Development of Myopia Among Children in China: A Randomized Clinical Trial. JAMA, 2015. 314(11): p. 1142-8.
13. M organ, I.G. and K.A. Rose, Myopia and international educational performance. Ophthalmic Physiol Opt, 2013. 33(3): p. 329-38.
14. E nthoven, C.A., et al., The impact of computer use on myopia development in childhood: The Generation R study. Prev Med, 2020. 132: p. 105988.
15. W illiams, K.M., et al., Increasing Prevalence of Myopia in Europe and the Impact of Education. Ophthalmology, 2015. 122(7): p. 1489-97.
16. Ku, P.W., et al., The Associations between Near Visual Activity and Incident Myopia in Children: A Nationwide 4-Year Follow-up Study. Ophthalmology, 2019. 126(2): p. 214-220.
17. J ones, L.A., et al., Parental history of myopia, sports and outdoor activities, and future myopia. Invest Ophthalmol Vis Sci, 2007. 48(8): p. 3524-32.
18. Wu, P.C., et al., Increased Time Outdoors Is Followed by Reversal of the Long-Term Trend to Reduced Visual Acuity in Taiwan Primary School Students. Ophthalmology, 2020. 127(11): p. 1462-1469.
19. R ose, K.A., et al., Outdoor activity reduces the prevalence of myopia in children. Ophthalmology, 2008. 115(8): p. 1279-85.
20. S mith, E.L., 3rd, L.F. Hung, and J. Huang, Protective effects of high ambient lighting on the development of form-deprivation myopia in rhesus monkeys. Invest Ophthalmol Vis Sci, 2012. 53(1): p. 421-8.
21. A shby, R.S. and F. Schaeffel, The effect of bright light on lens compensation in chicks. Invest Ophthalmol Vis Sci, 2010. 51(10): p. 5247-53.
22. N orton, T.T. and J.T. Siegwart, Jr., Light levels, refractive development, and myopia--a speculative review. Exp Eye Res, 2013. 114: p. 48-57.
23. K arouta, C. and R. Ashby, Author Response: Light Levels and the Development of Deprivation Myopia. Invest Ophthalmol Vis Sci, 2016. 57(3): p. 825.
24. K arouta, C. and R.S. Ashby, Correlation between light levels and the development of deprivation myopia. Invest Ophthalmol Vis Sci, 2014. 56(1): p. 299-309.
25. G alvis, V., A. Tello, and M.M. Parra, Light Levels and the Development of Deprivation Myopia. Invest Ophthalmol Vis Sci, 2016. 57(3): p. 824.
26. H ammond, D.S. and C.F. Wildsoet, Compensation to positive as well as negative lenses can occur in chicks reared in bright UV lighting. Vision Res, 2012. 67: p. 44-50.
27. P ears, A., STRATEGIC STUDY OF HOUSEHOLD ENERGY AND GREENHOUSE ISSUES A REPORT FOR ENVIRONMENT AUSTRALIA. 1998.
28. A dministration, U.S.D.o.L.-O.S.a.H., Illumination - 1926.56, in Occupational Health and Environmental Controls. 2009.
29. R ead, S.A., M.J. Collins, and S.J. Vincent, Light Exposure and Eye Growth in Childhood. Invest Ophthalmol Vis Sci, 2015. 56(11): p. 6779-87.
30. M oran, J.M. and P.O. Phelps, Periocular skin cancer: Diagnosis and management. Dis Mon, 2020. 66(10): p. 101046.
31. C ook, B.E., Jr. and G.B. Bartley, Epidemiologic characteristics and clinical course of patients with malignant eyelid tumors in an incidence cohort in Olmsted County, Minnesota. Ophthalmology, 1999. 106(4): p. 746-50.
32. L ee, G.A. and L.W. Hirst, Retrospective study of ocular surface squamous neoplasia. Aust N Z J Ophthalmol, 1997. 25(4): p. 269-76.
33. M oran, D.J. and F.C. Hollows, Pterygium and ultraviolet radiation: a positive correlation. Br J Ophthalmol, 1984. 68(5): p. 343-6.
34. S liney, D.H., Physical factors in cataractogenesis: ambient ultraviolet radiation and temperature. Invest Ophthalmol Vis Sci, 1986. 27(5): p. 781-90.
35. S liney, D.H., Ocular exposure to environmental light and ultraviolet--the impact of lid opening and sky conditions. Dev Ophthalmol, 1997. 27: p. 63-75.
36. S liney, D.H., Ocular injury due to light toxicity. Int Ophthalmol Clin, 1988. 28(3): p. 246-50.
37. W HO. Protecting Children From Ultraviolet Radiation - archived 11 December 2009. 2009 [cited 2020 24th April]; Available from: https://www.who.int/uv/resources/archives/fs261/en/.
38. O oi, J.L., et al., Ultraviolet fluorescence photography to detect early sun damage in the eyes of school-aged children. Am J Ophthalmol, 2006. 141(2): p. 294-8.
39. Kempen, J.H., et al., The prevalence of refractive errors among adults in the United States, Western Europe, and Australia. Arch Ophthalmol, 2004. 122(4): p. 495-505.
40. P an, C.W., et al., The Impact of Parental Rural-to-urban Migration on Children’s Refractive Error in Rural China: A Propensity Score Matching Analysis. Ophthalmic Epidemiol, 2020. 27(1): p. 39-44.
41. H oel, D.G., et al., The risks and benefits of sun exposure 2016. Dermatoendocrinol, 2016. 8(1): p. e1248325.
42. A lfredsson, L., et al., Insufficient Sun Exposure Has Become a Real Public Health Problem. Int J Environ Res Public Health, 2020. 17(14).
NOTE: Insight readers can scan the QR code or visit insightnews.com.au/cpd/ to access a link to this article to include in their own CPD log book.
INSIGHT September 2023 39
Protective sunglasses are a key tool in helping children get enough outdoor light exposure, safely.


This medicinal product is subject to additional monitoring in Australia. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse events at https://www.tga.gov.au/reporting-problems. Aspen Australia includes Aspen Pharmacare Australia Pty Ltd (ABN 51 096 236 985) and Aspen Pharma Pty Ltd (ABN 88 004 118 594). All sales and marketing requests to: Aspen Pharmacare Pty Ltd, 34-36 Chandos Street, St Leonards NSW 2065. Tel: +61 2 8436 8300 Email: aspen@aspenpharmacare.com.au Web: www.aspenpharma.com.au Trademarks are owned by or licensed to the Aspen group of companies. © 2023 Aspen group of companies or its licensor. All rights reserved. Prepared July 2023. AU-ATR-072023-07585. ASPPH3029. PBS Information: This product is not listed on the PBS. *P-value not available (ATOM 1&2 studies, placebo was a historical control from ATOM 1).ATOM 2 study data available for 5 years with 1 year washout after 24 months.3 EIKANCE 0.01% eye drops (atropine sulfate monohydrate 0.01%) is indicated as a treatment to slow the progression of myopia in children aged from 4 to 14 years. Atropine treatment may be initiated in children when myopia progresses ≥ –1.0 diopter (D) per year.1 Scan to review full Product Information and to order samples, or call 1300 659 646. References: 1. Approved EIKANCE Product Information, 14 March 2023. 2. Chua WH et al. Ophthalmology 2006;113:2285–91. 3. Chia A et al. Ophthalmology 2016;123:391–9. SLOW MYOPIA PROGRESSION BY UP TO 60% WITH ATROPINE 0.01% EYE DROPS AT 2 YEARS COMPARED TO PLACEBO *1-3
A JEWEL IN THE CROWN Myopia
CooperVision’s MiSight 1 day changed the game when it became widely available to Australian practitioners in 2016 for myopia management. Since then, the contact lens has gained even greater acceptance thanks to robust clinical data, a daily disposable replacement schedule, adaptability and expanded power range.
There are two distinct moments in Ms Melody She’s life which led to her being an optometrist and proponent of soft contact lenses for myopia control.


Myopic in her childhood – progressing from -0.50D to -4.00D within three short years – she will never forget the personal transformation she experienced when fitted with contact lenses for the first time as a young teenager, overcoming confidence issues she had with spectacle wear.

While her contact lenses didn’t treat the root cause of her myopia at the time, it motivated her to pursue an optometry career where she experienced another life altering moment. That was in 2015 at the landmark BHVI-World Health Organization meeting in Sydney where agreement was reached on a series of statements, definitions and priorities for myopia. There, she also learned of CooperVision’s MiSight 1 day contact lens with a myopia control indication that would become widely available to Australian eyecare professionals a year later, in 2016.
For She – an optometrist at 1001 Optical Top Ryde, Sydney – it represented a full-circle moment. Not only was there a soft contact lens to correct the shortsighted vision and improve the confidence of myopes in her care, but now there was a clinically proven option that could slow progression.
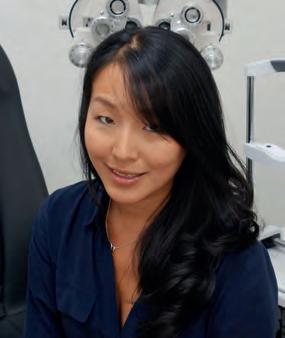
“At the time, we were using multifocal and bifocal spectacles and some off-label multifocal distance centre contact lenses, but when I heard about this option, I couldn’t wait to get my hands on it, and today I continue to
prescribe it regularly in my practice,” she says.
“We had all these methods to slow myopia, but we didn’t really know how to decide who would benefit from each treatment, and so I set about upskilling myself to learn about each modality. Today, when caring for patients, it’s all about them choosing an option that’s backed by clinical data, works best for them in terms of budget, and what the child will enjoy wearing to ensure consistent wear.”
MiSight 1 day firmly fits this brief for many of She’s patients. But one of the biggest factors for optometrists is the robust clinical data behind the contact lens. MiSight 1 day is at the centre of the world’s longest continuous
“CONTACT LENSES DRAMATICALLY IMPROVE QUALITY-OF-LIFE FOR KIDS, THEIR CONFIDENCE, THEIR SPORTING ABILITY, AND ALSO THEIR ACADEMIC ABILITY AND SELF-PERCEPTION.”
INSIGHT September 2023 41
JESSICA CHI EYETECH OPTOMETRISTS
MYOPIA
running soft contact lens clinical trial for myopia control that is now out to seven years.
This was pivotal to CooperVision securing highly sought-after FDA approval in the US in 2019, with the lens gaining even greater acceptance among the eyecare community. This was bolstered again when CooperVision expanded the power range, making it available to patients with higher prescriptions.

Practitioners are confident in prescribing MiSight 1 day thanks to a key piece of three-year data showing the lens slowed myopia progression by 59% as measured by mean cycloplegic spherical equivalent and 52% with respect to mean axial elongation of the eye.
After six years, 23% of eyes prescribed MiSight 1 day at the study’s initiation displayed a total refractive change of less than -0.25D (spherical equivalent), which could be considered clinically stable. The same study also suggested that while intervention at an early age is optimal, commencing treatment at an older age could similarly slow the rate of myopia progression.
And the latest seven-year findings showed no evidence of myopia control rebound in children 12 months after treatment ended.

In She’s own practice, many of her patients have responded well to MiSight 1 day, something she has quantified through monitoring their refraction and axial elongation with an optical biometer.
“For some patients, their myopia has completely stopped progressing, or remained stable for a long time. Just recently, I saw a child who progressed significantly from -0.50D to -2.00D within a year. That was in 2021, and now in 2023 after being prescribed MiSight 1 day and 0.025% atropine, one eye has remained exactly the same and the other has increased by -0.25D – I thought that was a pretty amazing result.”
IDEAL PATIENT CANDIDATES
Melbourne optometrist Ms Jessica Chi offers nearly the full gamut of myopia control options and – as Victorian president of the Cornea & Contact Lens Society of Australia since 2014 and a former national president of the society – is well-versed in the nuances of each approach. In fact, the location she now owns, Eyetech Optometrists in Carlton, was the first in Victoria to offer orthokeratology (orthok) in 1991 (before her time).
Speaking from a purely myopia control point of view, she says contact lens options offer benefits over other modalities because they remain unaffected by gaze angles, meaning the lens treatment zone is correctly positioned throughout the entire wear period.
“In my experience, compliance, an important factor, tends to be better with soft lenses and orthok because it’s not as easy for children to take them in and out,” she adds.
Myopia control is also a personal topic for Chi who grew up as a young myope with limited, if any, treatment options. When discussing interventions with parents today, she considers the uniqueness of each case.
“Every patient is different. Firstly, it’s about understanding the patient and the parents and their motivations. I’m a big believer and advocate of contact lenses for kids, but only if they are ready for it. There have been many studies showing that contact lenses dramatically improve quality-of-life
for kids, their confidence, their sporting ability, and also their academic ability and self-perception. I can vouch for this because I was shy and introverted as a child, but once I received contact lenses it gave me a lot more confidence.”
If contact lenses are preferred, Chi also considers the patient’s ocular surface, any corneal irregularities and checks for high astigmatism, which may limit their access to a soft contact lens option. If the patient is a low myope seeking contact lenses, then MiSight 1 day or other soft contact lenses might be suggested for optimal peripheral blur because in orthok the optometrist can only blur the periphery as much as they correct the centre.
“A benefit of MiSight is that it’s relatively easy-to-prescribe for the optometrist, and comfortable right away for the patient,” she says.
Studies have shown children are generally more compliant than anticipated, Chi says, because they are accustomed to following instructions, attending follow-up appointments and are supervised by their parents. Reinforcing this, Professor Mark Bullimore’s 2017 review on the safety of soft contact lenses in children found the incidence of corneal infiltrative events in children is no higher than in adults and, in eight- to 11-year olds, it may be markedly lower.
“We do find parents who are cautious of sending their kids to school with something in their eyes and would prefer the controlled home environment of orthok use, but the studies have shown the safest form of contact lens wear is daily disposable lenses,” Chi explains. “And although the risk of infection with orthok is very low, eye infections can still be devastating. I explain this to parents and we talk together with the child about the best option. There’s no right or wrong, but you’re never really prescribing just for the child, it’s the whole family.”
She, from 1001 Optical, agrees – adding that it’s important children are not only motivated to free themselves of spectacle wear, but are committed to learning how to handle contact lenses – and remaining compliant with this.

“When they start putting something on the eye, they need to maintain good habits. It also requires more follow up and education around eye health and outlining the importance of coming to see us immediately if there’s a potential issue. I always remind them there’s a level of responsibility, and most of the children understand that – they just want to get away from wearing glasses,” she says.
Back in Chi’s practice, MiSight 1 day patients are typically reviewed every six months, but more frequently if progressing more than expected. Contact lens interventions in the right patient have proven to be successful, with many showing no progression. In those who show fast progression, they tend to spend a lot of time indoors and read on devices in the dark. Some will wear their soft contact lenses throughout the day and take them out when reading at home after school. For maximal treatment effect, this is something she advises them against.
While the treatment effect of myopia interventions is arguably the biggest consideration, questions around cost are often a close second –especially in families with more than one myope. Chi says it varies across the board, but if a contact lens option is preferred, she discusses the initial upfront investment of orthok (with ongoing costs for lens solutions etc),

42 INSIGHT September 2023 MYOPIA
“I TELL PARENTS OFTEN THAT MOST OF MY KIDS DO BETTER THAN WHAT THE STUDIES ARE SAYING … I HAVEN’T HAD ANY CHILD THAT’S PROGRESSED MORE THAN -0.50D IN A YEAR.”
ASHLEY TUCKER US OPTOMETRIST
CooperVision’s MiSight 1 day contact lens became widely available to Australian eyecare professionals in 2016.
alongside the continuous nature of a soft contact lens option.
Further, Chi and She are unanimous in their appreciation of CooperVision expanding the parameters of MiSight 1 Day, which was previously only available up to -6.00D, leaving them to rely on alternative soft contact lens designs above this prescription.

But the new expanded range covers -0.25D to -10.00D (0.50D steps after -6.00D) – which means that MiSight 1 day now covers 99.97% of prescriptions for Asian children, and 99.97% for Caucasian children – who have myopia and less than 1.00D of astigmatism.
A GAME-CHANGER IN THE US
US optometrist Dr Ashley Tucker used to lose a lot of patients who required myopia management. Either they weren’t prepared for orthok, or it would be hard for parents to grasp the off-label use of a distance centre soft multifocal lens that was originally designed for presbyopia.
But since MiSight 1 day became available in the US Spring of 2020, it has helped fill a major gap in her practice, now becoming the primary mode of management at her practice, Bellaire Family Eye Care in Houston Texas.


“It changed everything here in the US, especially for my practice," Tucker tells Insight. "It took off because it’s an FDA-approved option; parents love there is something that has research and plenty of science behind it. Orthok had that similar buzz because it was so different and unique, but a soft contact lens option opened the door for a lot of patients who were afraid to wear hard contact lenses, or whose parents were worried about that remodelling of their child’s cornea.
“MiSight 1 day has made contact lens wear and myopia management so much more accessible.”
There are many pieces of data that Tucker appreciates about MiSight 1 day: “But I love the stat that there’s no rebound effect,” she says.
“All the time, I talk about the six-year mark where about 25% of patients didn’t progress at all – that’s pretty remarkable. It may not seem like a lot but that is a huge amount of kids that didn’t progress at all in the lens and I love telling parents that stat. It’s been a game-changer for some parents, who need that information and don’t want to just take your word for it.”
Tucker has three-plus years of clinical information of how MiSight is performing in her own patients. The sample is growing, but out of the 15 or so children involved from the beginning, very few have progressed at all.
“The majority of my patients are in that 25% that didn’t progress. I tell parents often that most of my kids do better than what the studies are saying, but you don’t want to over promise and under deliver. I haven’t had any child that’s progressed more than -0.50D in a year,” she explains.
“The fact that most kids adapt to it well is also something that I talk about. Parents don’t think their kids can wear contact lenses and that it’s going to bother them, but the truth is, most kids adapt just fine. It’s really the parents holding them back – if only they allow the child to be released into my care to show them how to use and care for the lens.”
Melody She, optometrist at 1001 Optical Top Ryde, Sydney, says consistent wear associated with soft contact lenses makes them suited for myopia control.
Tokai Optical’s Neuro Select range of progressive lenses use neuroscience principles to minimise distortion.
Developed by Tokai Optical, a Japanese company specialising in ophthalmic lenses, in collaboration with NTT Data Institute of Management Consulting, the lens harnesses neuroscience to achieve a progressive lens where any distortion is not recognised by the brain. It has succeeded, particularly for patients who suffer from vertigo or vestibular issues, patients with complex prescriptions, or slightly impaired vision as a result of cataract, glaucoma, or macular degeneration.
Mr Justin Chiang, general manager of Tokai’s Australian base, says the Neuro Select range overcomes a previous challenge with progressive lenses, but is a product not yet well known to the general public.
“Progressive lenses have a structure in which the magnification is progressively changed within a single lens, which results in the characteristic swaying, distortion, and blurring,” he says.
“This leads to a sense of discomfort for the wearer, and in principle, it is impossible to eliminate this distortion. Therefore, the eternal theme for most lens developers has focused on how to develop progressive lenses with minimal discomfort.”
For Tokai Optical’s R&D department, a breakthrough came from an unexpected source, when it learned a brewery was researching the relationship between brain waves and the evaluation of taste.
“Tokai Optical R&D contacted NTT Data Institute of Management Consulting, which had overseen EEG (electroencephalogram)

LENSES
measurement in the brewery’s research program. From there, a system for the joint development of a neuroscience spectacle lenses was started,” Chiang says.
The result was a progressive lens with good merchantability, high quality, and brand power.
“Essentially, Neuro Select progressive lenses are the result of a collaboration between Tokai Optical and NTT Data for applied neuroscience, using brain wave measurement to quantify the sensitivity of subconscious feelings and sensations stimulated by the brain,” he says.
Chiang acknowledges it is impossible to eliminate distortion from progressive lenses but using neuroscience, it is possible to drive the distortion to a level where the brain does not care or is not aware.
After several years of research and development, Tokai Optical released the neuroscience ophthalmic lens to the market, but it didn’t stop there. It has evolved further, with Tokai embarking on joint research with the National Institute for Physiological Sciences (NIPS).
“The new Neuro Select progressive lens product was developed in response to recent changes in visual lifestyles, such as the spread of large-screen TVs, smartphones, and tablet devices. Based on the neuroscience principle, Tokai Optical continues to imply the latest technology available into the design,” Chiang says.


For optimum comfort, patients select from three lifestyle situations – daily, town or home – and from six lens grades, ranging from 3 (basic grade back-surface progressive lens) to 9X (super premium grade double-sided progressive lens).
‘Daily’ provides a clear field of vision when driving or playing sport, ‘Town’ provides a comfortable field of vision during shopping or business errands, and ‘Home’ provides a wide, deep field of vision in the office and at home.



FEWER NEEDLES IN THE HAYSTACK
Chiang says Tokai Optical’s neuroscience ophthalmic lenses are a major breakthrough in the field of eyewear.
“By using neuroscience principles, Tokai Optical has been able to develop lenses that are both comfortable and effective. These lenses offer a new level of visual performance, and they are sure to be a popular choice for people who want the best possible vision,” Chiang says.
Tracton agrees.
“There’s been many upgrades in the technology of progressive lenses since they were first commercialised. As each new iteration hits the market, you get vast improvements in the reduction of peripheral distortion, which has been the bugbear of progressive lens wear and has caused issues with adaptation and visual comfort,” he says.
“Over the last few years, freeform progressives have really improved in technology, and this new neuroscience mode of design has really improved adaptation times – the patient adapts quicker, whether they be an existing or a new progressive lens wearer.”
Tracton says there has always been a certain percentage of the population that hasn’t been able to adapt to progressives, such as his accountant patient.
“Finding a solution for a patient who can’t adapt to progressives is like trying to find a needle in a haystack, until this newer technology from Tokai. It’s a good lens for patients with complex prescriptions, oblique astigmatism, prism, high astigmatism, high myopia, hyperopia or combinations thereof,” Tracton says.
He says harnessing neuroscience technology in progressive lens design is a revolution for patients who suffer from vertigo or vestibular issues, who in the past have found wearing progressive lenses problematic.
“There’s been a lot of R&D that’s gone into this product, which has utilised previous generation technology of freeform progressives to improve even further on that technology to reduce peripheral distortion, and more smooth progression from distance to near zones,” Tracton says.
For Tracton, Neuro Select adds another string to the bow in Tokai’s selection of lenses. He and his wife Michelle, the practice operations manager and optical dispenser, toured the Tokai factory in Okazaki in Japan a few years before the pandemic and were impressed with the quality control, lab facilities, R&D and the attention to detail.
“When we set up our practice in Bondi Junction two years ago, our brief was to make the practice stand apart and provide a unique clinical and service philosophy. We wanted to provide the best service and products to the community. Tokai fit the brief for us,” he says.
Tracton Optometrists receive and generate a large volume of referrals to and from some of Sydney’s leading ophthalmologists and believe it is essential to provide premium products for these patients and provide the best clinical outcome for their needs, which at times are highly complex.

“We use a large volume of 1.76 Tokai product in our practice in both single vision and progressives. It is the thinnest resin lens on the planet, available in very few optical outlets. We have become a destination for challenging prismatic correction, and many of our optometry and ophthalmology colleagues refer to us for this mode of optical correction,” Tracton says.
“We have found our patients adapt successfully and quickly to the Neuro Select progressives. Tokai’s specialised coatings and tints are also top tier, enabling us to offer lens specialisations when suitable.”
The practice also has an onsite lens laboratory, which Tracton embedded as a competitive point-of-difference and to enable the practice to provide good service time and quality control.
“We can provide one-hour service with Tokai product we keep in stock. This is very useful, with patients coming in needing spectacles urgently, rather than waiting two to three weeks in the busy periods. We have developed personal relationships with the Tokai team, and they all go above and beyond for those jobs that need extra attention and urgency.”
INSIGHT September 2023 45
Patients can select their preferred lifestyle from three options.
Lenses
THAT OUTLAST THEIR PRESCRIPTION
Anti-reflective coatings now do much more than the name suggests. HOYA is one lens lab focusing on properties that promote greater durability and scratch resistance, culminating in a new flagship coating offering the clarity modern day spectacle wearers expect from their lenses.
There is a list of key demands patients have when they are prescribed a new pair of premium lenses. Clarity of vision is the top priority, but they also want a lens that withstands the rigours of everyday life, and remains in a similar condition to the day they picked up their spectacles from the practice.
Increasingly, patients also want to avoid the need to clean lenses constantly, put up with scratches or feel conscious about reflections. According to lens manufacturer HOYA, a premium lens doesn’t only set itself apart by the material or design, but requires a high quality coating that elevates the wearing experience and acts as the ‘finishing touch’.
The most well-known of HOYA’s lens coatings in the Australian market has been its flagship Diamond Finish coating, which has been gradually upgraded over the last decade. But the company will soon discontinue this and replace it with its most advanced coating to date, Hi-Vision Meiryo Diamond.
It’s a big deal for the company to launch a new flagship coating, considering the success of Diamond Finish, but HOYA is confident it has delivered tangible improvements. In fact, Hi-Vision Meiryo Diamond is being marketed with some eye-catching statements that HOYA says it has validated through a new testing regime more rigorous than industry standards.
The new Hi-Vision Meiryo Diamond coating will be available from October 2023 and a key feature of HOYA’s presence at O=MEGA23/ WCO4 in Melbourne (8-10 September). According to the company, it offers:
• S uperior clarity that lasts longer
• U p to 2.5 times better scratch resistance than other market leading lens coatings.
• S tays easy-to-clean up to five times longer than other market leading lens coatings.
• E xceptional clarity due to 56% lower reflectance than other market leading lens coatings.
“Hi-Vision Meiryo Diamond is HOYA’s best new coating that provides exceptional clarity and long-lasting benefits due to its low reflective properties, extreme scratch resistance and what we have found to have unmatched durability,” says HOYA Lens Australia national training and development manager Mr Ulli Hentschel.
“This coating is ideal for consumers who prioritise high-quality and long-lasting clarity over short-term cost savings. It allows patients to protect their valuable lenses from anything that life throws their way, with surface lens protection which extends the lifetime of the lenses.”

The name ‘Meiryo’ was derived from the Japanese word for ‘clarity’. It is both a reference to HOYA’s Japanese origins and a nod to the technological qualities of the coating. The name ‘Meiryo Diamond’ stands for long-lasting durability and superior clarity, and allows HOYA to continue to benefit from the brand equity it has built with the Diamond Finish coating.
ADVANTAGES FOR INDEPENDENT PRACTICES
HOYA’s own research shows that for 96% of patients, clarity of vision is a key reason for choosing their glasses, and 80% of patients are willing to spend more for high quality lenses that provide clarity. This represents a clear opportunity for independent optometry practices.
But Hentschel says patients don’t want to only be able to see clearly when they leave the store – they want high-quality, durable lenses that last.
“Our previous flagship Diamond Finish coating achieved global success and was one of the most premium coatings on the market. It was upgraded over the years, but when developing a new flagship coating in Hi-Vision Meiryo Diamond our R&D team were keen to deliver something that is quite different to what we had before, and led the market in several ways,” he says.
“Some key advantages for the eyecare professional include confidence in recommending the best lens protection available through innovation and technology. We also want patients to be so satisfied with the lens they received, they return to the practice seeking the same lens, but with an updated prescription. In turn, happy patients will refer their friends and family, helping build the practice’s reputation on quality and value.”
There are many key qualities of the Hi-Vision Meiryo Diamond coating. These include: 100% UV protection on the front surface and extra protection on the back, scratch resistant surface lens protection that extends the lifetime of the lenses, anti-reflective properties for clarity of vision and better aesthetics, dirt repellent and easy-to-clean, water repellent for optimal vision in rain or condensation, and enhanced contrast and glare reduction during the day and at night.
When it comes to the lens clarity and lower reflectance, a key feature with Hi-Vision Meiryo Diamond is a new subtle reflex colour.
The dominant wavelength is different from HOYA’s standard green, but
46 INSIGHT September 2023
LENSES
is light blue, instead. There is a very low luminous reflection, which the company says is 56% lower than the previous generations and lower than other market leading lens coatings. This will also lead to better aesthetics for the wearer due to less “mirror effect” of the lens surfaces.
HOW HOYA TESTED THE COATING
When it comes to the value proposition of Hi-Vision Meiryo Diamond, HOYA sums it up with the phrase: “Clarity that lasts”, or in other words, lenses that outlast their prescription.
That means a major emphasis on scratch resistance, durability and easy-to-clean properties.
The company has achieved this with its advanced multi-layer technology involving what it describes as a “super-resistant” hydrophobic layer that prevents water stains, and an anti-static layer that repels dust and dirt.
But with all of that said, how can eyecare professionals and patients be confident the lens will last as HOYA has intended?
To address this, HOYA set out to develop the LongLife Index evaluation method. This new regime is a measure of the performance and durability of anti-reflective lens coatings and comprises five tests that the company says are more rigorous than industry standards.

“The LongLife Index was developed and adopted by HOYA as a working standard. Passing the rigorous and severe tests gives us the confidence that the coating is of the highest quality and is able to endure extreme conditions and various lifestyles,” Hentschel adds.
Hi-Vision Meiryo Diamond was subjected to the test – in addition to two other HOYA coatings and five coatings from competing lens companies – and compared.
The five tests include:
Droplet test – this assess how easy lenses are to clean and their water resistance. For this test, lenses are wiped with paper up to 10,000 times, then water droplets are used to measure how much hydrophobic coating remains. The shape of the droplets on the surface determines the amount of hydrophobic coating left behind, and thus how slippery the lenses are and how easy they are to clean. The more spherical the droplet, the more hydrophobic coating is present; the flatter the droplet, the less hydrophobic coating present.
Sandpit test (HOYA Bayer value) – this is a well-known test for resistance to abrasion. Lenses are placed in a ‘sandpit’ full of gravel and are shaken vigorously 800 times. The lenses are then analysed for transparency and the Hoya Bayer value is calculated.
Steel wool test – to quantify resistance to harsh scratches, HOYA used carbon steel wool brushed on the lens surface. The test uses weights up to 2.5kg to apply pressure onto the steel wool, which moves side-to-side 40 times (20 cycles) across the lens surface. The lenses are then analysed for scratches under artificial lighting.
Oven test – testing for heat resistance, the lenses are subjected to temperatures exceeding 95°C in a laboratory-graded oven.
The temperature is gradually increased until the cracking point of the coating.
Extreme weather test - the lenses are put into a machine called a QUV a ccelerated weathering tester. This tests the lenses by exposing them to cycles of UV light and moisture at elevated temperatures – similar to the harsh equatorial climate. The remainder of coating is measured every week up to a total of four weeks. This is combined with a cross hatch test to reveal peeling from the lens surface.
Overall, HOYA says Hi-Vision Meiryo Diamond was superior or equal on almost every measure (visual clarity, durability of cleanability, durability, scratch resistance, thermal resistance, resistance to peeling).
"Our testing shows that we can bring our coating to market with confidence that it performs better than major competitors overall, which we hope will underpin long-term practitioner-patient relationships," Hentschel says.

“Our aim with this coating is for patients to feel excited and feel good about how they look in their glasses, not only when they first put them on, but after days, weeks, months and even years of wearing them, because the true test is time.
“We want to save them time and allow them to live worry-free so they can enjoy life without the need for constant maintenance.”

INSIGHT September 2023 47
“THIS COATING IS IDEAL FOR CONSUMERS WHO PRIORITISE HIGH-QUALITY AND LONG-LASTING CLARITY OVER SHORT-TERM COST SAVINGS.”
ULLI HENTSCHEL HOYA LENS AUSTRALIA
HOYA’s LongLife Index evaluation method measures the performance and durability of anti-reflective lens coatings and comprises five key tests.
Are you a futurefocused person?

You’d look good in Specsavers
If, like Sophia, you love the idea of a fulfilling career in optometry, helping improve people’s vision, you’ll shine at Specsavers. join.specsavers.com/au/find-a-job

Sophia
Early Career
Optometrist
TRADE OFF SHOPPING CENTRE THE HIGH STREET VS
Location is crucial for any new optometry business. Shopping centres and the high street are the two main options, with each offering differences in leasing arrangements, fit out requirements, foot traffic and marketing that entrepreneurial eyecare professionals may need to account for.

Optometrist Mr Brett Parsons knows better than most that lease renewals are an inevitable and uncomfortable part of running a practice. With a mix of locations across eastern Melbourne, it requires a nuanced approach with each landlord to ensure he gets the best outcome for the business.
Parsons is the longest-serving current partner of Harris Blake & Parsons Optometrists (HBP), an independent optometry business with a high street practice in Croydon, two practices within medical centres in Yarram and Healesville, and its flagship store in Eastland shopping centre, Ringwood.
Having diversity across practice locations has served the business well since its inception in 1958, and means Parsons and his business partners are well-versed in the pros and cons of high street vs shopping centre practice locations. Taking into account matters like leasing arrangements, fit out requirements, capturing foot traffic and marketing, he’s learned valuable lessons that other entrepreneurial optometrists might want to keep in mind when determining the location of their new practice.
For instance, HBP is a foundation tenant of Eastland when it was developed 58 years ago and, alongside Myer, is the only continuous leaseholder in the mall. One would think the practice has earned some loyalty, but in reality the landlord-tenant relationship remains business-like.
“Location is important in any scenario – and there’s a cost to a good position,” he says, noting that practice owners need to be assertive tenants, especially in shopping centres.

“Shopping centres tend now to have a separate corporate leasing specialist area that’s quite intentionally separate from day-to-day arrangements with the centre manager, which means they can be purposely more hard-nosed about offers. Whereas, with your local agent or high street landlord, the person you’re working with is often the one
that does the deal with you, so it’s a more personal relationship.”
In a shopping centre, he says traders need to come to the negotiation table having done their homework. Finding out what other tenants are paying, investigating the market rate high street rent, and taking note of empty shops in the centre can all help the business to leverage a better agreement.
Ultimately, for HBP occupancy costs per square meter are much cheaper in its high street location, with less hoops to jump through in general. In the shopping centre, there’s usually other requirements such as refitting every five years or so (at a higher cost than a high street refit), rules around opening hours and generally higher bills to pay. But there are many up sides too, especially if the practice is located near major retailers like Woolworths and Myer.
“You need to be aware of traffic zones, and we have been in this corridor for a long time and know it’s one of the best,” he says.
There’s also many other factors that can influence the performance of a practice depending on its location. With this in mind, three business-savvy Australian optical industry figures sit down with Insight in an effort to get to the bottom of which location is better: the shopping centre or the high street?
BUDGETS, LEASING, RENT
As one of the masterminds behind Specsavers’ entrance into the Australian and New Zealand market in 2008, Mr Charles Hornor has been involved with a spectrum of landlords over the years – and notes there are some fundamental figures to be aware of before committing to a practice acquisition or establishing a greenfield optometry business.
After leaving Specsavers in 2022 after 16 years, he’s now a director at the new Chemist Warehouse-backed venture, Optometrist Warehouse, which recently opened its first practice on Glenferrie Rd in Malvern, Melbourne, with plans for a national rollout.

INSIGHT September 2023 49
BUSINESS
Hornor says some basic metrics to run a profitable optometry business include: occupancy costs (rent, bills, etc) not exceeding 10% of total sales/revenue, and staffing costs, including the nominated salary of the owner, not exceeding 30% of revenue.

“Of course, these percentages will decrease as volume goes up, but these are some important benchmarks to remind yourself of, especially if you’re setting up a new store as an independent or as anyone else to be honest. If you’re not hitting these, then you’re probably not going to be making a profit,” he says.
When it comes to rent and leasing costs, Hornor says there are several ways practices can set themselves up for success in the negotiation phase, but there are some key differences between how this happens with a high street landlord and a shopping centre.
A “three by three” lease is ideal to negotiate in a high street scenario, he says, meaning the practice has an initial three-year term that has the option to be extended another two times, if the tenant wishes, equating
lease, but I think you want to be careful not to overdo it. And indeed, you might have expanded and need more room to grow, which isn’t ideal if you’re stuck with a lease,” he says.
“In a shopping centre, the landlord will readily help you to expand into a larger premises, but if you’ve got a private landlord on the strip and you want to break the lease, then they will be seeking rent from you until they’ve found a new tenant unless they have agreed a clear break clause in your lease at the outset.”
According to Mr Mark Corduff, business services manager at the ProVision independent optometry network, practices renting in the high street typically pay a market rate, while those in shopping centres generally pay a percentage of their turnover. This commonly translates to a much higher rent in shopping centres.

“For high street locations, it’s much easier to ascertain what the rent might be. When I negotiate rents for ProVision members, I’ll complete a market review on the area and call the agents to find out what the current going rate is per square metre. It’s quite simple, whereas in a shopping centre they are privy to your turnover, and you essentially pay your rent based on your occupancy cost – there’s also other costs involved,” he says.
At ProVision, which supports 450 independents across the country, Corduff supports members with their business endeavours to improve their profitability and the value of their businesses. Property and leasing are a major part of this, and he often advises members negotiating commercial lease terms to optimise their outcomes.
Around 15-20% of ProVision’s practices are in shopping centres, with the majority on the high street, and a small percentage embedded in medical centres.
Typically, he says a shopping centre lease is five years, but after this initial term they may offer shorter terms, and they generally don’t provide options, which can make it challenging for a practice to formulate longer term plans.
“Often when you look at a shopping centre lease there’ll be a requirement to make upgrades to your fit out. Recently, we’ve seen some of these requirements passed on to members – and they have been expensive. Often at this point, they don’t contribute financially

50 INSIGHT September 2023
Harris Blake & Parsons Optometrists partners (from left) Dina Anastas, Brett Parsons, and Linda Harwood.
Harris Blake & Parsons Optometrists, which operates across four Victorian locations, has established its flagship in Eastland shopping centre, Ringwood.
towards it. Generally speaking, that means after one or two lease terms, there’ll be another significant investment to make, whereas in a strip, you have the flexibility to update and do what you want when you’re ready,” he says.
A nother clause to be vigilant of is exclusivity in a shopping centre. This is particularly important for independents who can suffer if the centre is over-indexed with optometry practices, or if a corporate store moves in nearby.
There are also other outgoing costs in shopping centres that Corduff says practices needs to be aware of. For instance, ideally one needs to avoid paying for the lights and air conditioning when they are closed while other shops like supermarkets are open. There’s usually a marketing levy of around 5% of the base rent baked into the contract.
“With the marketing levy, you really need to be knocking on the door of the centre to make sure that you’re maximising that otherwise it’s just a lost expense,” Corduff says.
“It’s also important to remember at the end of each lease term, there’ll be a market review and we are typically seeing the increases come in lower in shopping strips than shopping centres at the moment.
“Overall, we spell out the importance of maintaining a favourable business relationship with landlords, which can be challenging sometimes, but can go a long way to ensuring stability and optimal commercial outcomes for practice.”
FIT OUTS AND EXPANSION
The practice fit-out is another area where there are significant differences for new practice owners.

Hornor says in the high street, optometry businesses effectively have carte blanche with their practice design, configuration and shopfront. In

“IN THE SHOPPING CENTRE, A CUSTOMER MAY SHOP AROUND IF THEY HAVEN’T MADE A LONG TERM CHOICE ABOUT THE OPTOMETRIST THEY SEE. THAT HONES EVERYONE’S COMPETITIVE INSTINCTS … BUT THAT’S PROBABLY WHY IT BECOMES MORE OF A RETAIL THAN A HEALTHCARE PROMOTION.”
 CHARLES HORNOR OPTOMETRIST
CHARLES HORNOR OPTOMETRIST
WAREHOUSE
a shopping centre, however, there are standards that the landlord will require to be met, covering all sorts of areas like the quality of fixtures and fitting, all the way through to the look and feel of the premises.

“On the flipside, it can be helpful because it means you’ve got that quality built-in, it’s a really good solid way of making sure you’re fit-for-purpose in the marketplace because that’s what shopping centres demand,” he says.
While there’s more flexibility in the high street, Corduff says it does require approval from the landlord, it’s generally much easier and comes in at a lower cost compared with a shopping centre.
A key challenge in shopping centres is that fitouts can only be conducted outside of regular operating hours, but the centre usually works to accommodate that. If negotiated well, shopping centres may also contribute to the initial fit out (but not subsequent renovations), anywhere from six to 12 months of the base rent as a benchmark.
“They can also guide you through the process and will have preferred shop fitters and designers available to use,” Corduff adds.
When it comes to expanding or relocating a practice, Corduff agrees that a shopping centre can facilitate this more easily. In the high street, a practice may need to wait until the shop next door becomes available to knock a wall out, and/or seek an entirely new location and landlord.
In saying that, shopping centres have the power to dictate where the practice will be located, which can be daunting if the practice is placed in a less favourable position, away from the big retailers or tucked away near the car park.
“After the term expires, or even mid-term, if they look at relocating a practice, they will typically financially incentivise you to do that – but this takes careful negotiation," HE SAYS.

"In the shopping strip, there’ll often be a demolition clause or another clause that allows the landlord to enact that and you could potentially have nowhere to go. So, it’s always about understanding that you’re leasing the space and it’s not forever, and you need to always keep in the back of your mind what your options might be if anything ever turned untoward.”
FOOT TRAFFIC
Given the notably higher occupancy costs, potentially less stability and restrictions around opening hours and even marketing activities, it may prompt one to ask why a practice would set up in a shopping centre?
Hornor says the key benefit is that shopping centres are a destination where people intend to shop. They also tend to be unaffected by weather events. In fact, people often seek refuge in shopping centres to escape intense heat, wind or heavy rain. This means that ‘no shows’
are often lower in shopping centre environments. For high street practice, this means they need to be prepared to capture foot traffic that comes in off the street, and local area marketing such as flyers and promotions need to be optimised. Flyers can be more challenging in a shopping centre and will require approval and a fee if it’s to be done outside the shop perimeter.
“On the high street, practices need to hone their short term recalls. You’ve got to follow people up, make sure they come in – whether you’re capturing them off the street or at home once they’re part of your customer database,” he says.
“In the shopping centre, a customer may shop around if they haven’t made a long term choice about the optometrist they see. That hones everyone’s competitive instincts, and that’s really important, but that’s probably why it becomes more of a retail than a healthcare p romotion. On the high street, you can really make the most of your healthcare credentials.”
Although high street businesses may need to consider seasonal factors, Corduff says practices can reap the rewards if they choose their location carefully. Since COVID, ProVision has recognised a significant shift in consumers preferring to shop on the locally.
“When you’re looking at opening on a strip, I always keep a close eye on accessibility. Parking is important as well as visibility – also being able to precinct yourself near other health services to benefit from similar types of customers or patients walking past.”
In saying that, Corduff says there are ProVision practices that perform very well in shopping centres: “You’ve got to know your numbers and be really focused on growing your business.
“These practices understand their target market. You need to be
52 INSIGHT September 2023
BUSINESS
High street landlords can see value in the longevity of a lease and more personable, while shopping centres can be more business-like in their approach.
maximising the fact that customers would go to that centre anyway. They have the luxury of ticking off the bakery, chemist, supermarket and optometrist in one hit. It’s a nice warm environment and a relatively seamless experience.”
SALEABILITY AND OWNERSHIP



At the other end of the business lifecycle, Corduff says the location can also influence the practice’s saleability. High street practices are more favourable to this for several reasons.

“Typically, because they’ve got a lower occupancy cost. If you’re looking to sell your practice in a shopping centre, you want to make sure that your base rent is as low as possible and there are no incentives tacked on. Often when they are offering a lease term, shopping centres will say the rent is $100,000 for example, but we’re going to provide you with an ‘incentive’ of$25,000 a year to bring it down to $75,000. When someone’s purchasing that, the bank will look at that and say the rent is $100,000, so you want to prepare and ensure that you’ve negotiated well so that it’s in a good place to sell.”

The best-case scenario would be for the practice to eventually purchase the premises if the landlord is seeking to sell.
Many independents have this arrangement.
“A lot of optometrists purchase a premises and manage it through their super fund or purchase it outright so they are then benefiting from the additional income that comes as a result of that – you can control the rent etc. Whenever we’ve had practices sell with the business owner as the landlord, it’s a far more seamless process.”
THE VERDICT


All in all, Parsons, from HBP Optometrists, says there are ups and downsides to each location, and none is better than the other. Although his high street practice in Croydon is more cost effective to run, it can occasionally be impacted by the vagaries of the weather, meaning patients will seek the comfort and convenience of a shopping centre.
On the up side, it means HBP has all its bases covered, with the diversity of the business serving it well.

















“It also makes things interesting from a business and professional perspective. They’re all slightly different challenges, slightly different patients with different needs. But the variety keeps things interesting,” he says.





“The way you run a business, your professional care and quality service, builds your patient base. When convenience comes into it – and certainly shopping centres offer this – you’re building a bigger business within for several reasons. We’ve got plenty of opposition, so for us, it’s a case of doing what we do really well and not trying to be all things to all people.
“My advice when looking at where to establish your practice would be that you’ve got to balance your risk and reward and sometimes take a bit of a risk for that reward.”




“WE SPELL OUT THE IMPORTANCE OF MAINTAINING A FAVOURABLE BUSINESS RELATIONSHIP WITH LANDLORDS, WHICH ... CAN GO A LONG WAY TO ENSURING STABILITY AND OPTIMAL COMMERCIAL OUTCOMES FOR PRACTICE.”
MARK CORDUFF PROVISION
THE NUMBERS DON'T LIE
Data has become one of the sharpest tools to inform the clinical and commercial aspects of optometry businesses in 2023. Insight sits down with data scientist PAMELA TSE at Australia’s largest optometry provider to understand how she brings numbers to life.
Assumption, intuition and anecdote used to be the way optometry businesses informed their strategies. But when it comes to multi-million-dollar technology rollouts, reporting on Medicare utilisation to prevent vision loss and making a meaningful dent in undetected eye disease rates, there is only one tool that guarantees results – data.

Since arriving on the Australian optometry scene in 2008, Specsavers has been advancing the local eyecare agenda on several fronts, using swathes of data that are interpreted to drive macro and micro clinical decisions, commercial initiatives, its trademark marketing campaigns, and much more.
In fact, it’s thought the company holds the largest optometry dataset in Australia, and one of the biggest and most robust globally. It tracks every single point of 4.5 million patient journeys per year, accounting for around 42% of all optometry appointments in Australia.
At the company’s ANZ support office in Port Melbourne, Ms Pamela Tse has the important role of filtering through the data collected from thousands of appointments held daily across Specsavers’ 385 stores across Australia. As the in-house optometry data consultant for almost four years, she is tasked with turning these into actionable insights that gives full visibility around how many clinical components of the business are performing.
After initially wanting to pursue a career in physiotherapy before eventually studying economics, accounting and statistics at university, the role is ideally suited to her.
“I’ve always had an ability to see patterns in numbers. I wouldn’t say I’m special, but I’m different in that way; in fact, I can still remember my grandma’s phone number today,” she says.
“To help people perform their job better and help manifest the good health outcomes we’re seeing every day at Specsavers is a privilege for me. The care and nurture I had back when I wanted to be a physio has now translated into reading numbers and telling optometrists you are doing exactly what you need to do, you are treating your patients exactly how we want you to. It’s also been phenomenal to see with programs like KeepSight how system change can create behavioural change and deliver better patient outcomes.”
Tse works closely alongside Dr Joe Paul, head of professional services for Specsavers ANZ. He says in a previous era the industry was content to assume it was doing a good job.
“And for the most part we were, but to practise optometry in 2023 it’s incredibly important to be informed by the data,” he says. “It lets us answer the big questions and make real tangible changes that are driven by an understanding of what the current situation is, and what it needs to be. It informs all decisions we make; there’s nothing we do in the optometry team that isn’t measured, tracked and based on a quantifiable problem.”
Paul says one of the most powerful examples of a data-informed strategy is the OCT roll out to all Specsavers stores in Australia and New Zealand. The world-first initiative to use a Topcon Maestro Fully Automated OCT/Fundus Camera in the standard eye exam was a $40 million-plus investment.
“I believe this was one of the best examples of a data-driven intervention not only in optometry, but healthcare, in the past 10 years,” Paul says.
“There was a problem that 50% of glaucoma was undiagnosed in the community. As an industry, we weren’t tracking how many of our patients were being referred. We started to track this and found that the referral rate was less than the population prevalence of glaucoma, so clearly there was an issue."
Specsavers put OCT into a handful of practices, looked at 150,000 patient journeys and suddenly saw that by implementing OCT systematically alongside the RANZCO referral pathways for glaucoma and the accompanying training and support for optometrists, it was referring glaucoma twice as often, much closer to the population prevalence.
“This is a great example of using data to find a problem, measure the problem, put an intervention in place, and measure the outcome – and even though it was a small group of patients at the time, it very clearly worked," Paul says.
"That then informed the much larger strategy of store partners investing in an OCT machine at every practice to be used free-of-charge on every patient. The data supported this because we showed a measurable outcome for patients and a major improvement in detection of glaucoma across the country.”
Specsavers has now seen 175,000 unique glaucoma patients during
54 INSIGHT September 2023
DATA MANAGEMENT
the past five years, and with ongoing monitoring can confidently say it is detecting glaucoma at the estimated national prevalence rate.
REAL TIME INDUSTRY INSIGHTS
To make data a central component to an operation at scale, a lot of work needs to occur in the backend to ensure it can be optimised for use.
At Specsavers, this has involved a lot of work to standardise the data being collected. The company has set up automated systems that pre-populate data straight from the measurement device and into the optometrist’s clinical records/Socrates practice management system, eliminating wasted time and the potential of transcription errors with manual data input.
The data then flows onwards to the data engineering team, being de-identified and ready for use by Tse, the IT team and other departments for reporting purposes and to obtain high level insights.
Tse says across all industries there are questions about the reliability of data and whether it’s ready for use.
“Over time we have identified opportunities to improve the quality of our data; we are in a privileged position of having a team that has put processes in place so that we can collect data in a more uniform way. We find it is a lot more reliable and user friendly, which helps immensely with interpretation and eventually making informed decisions for the business,” she says.
Paul says one of the major benefits of the Specsavers dataset is its ability to provide insights in real time. This is because the metrics are automatically refreshed every week, painting an up-to-date picture of the national optometry landscape. If referral rates, for example, are below expected, it may be a sign that a certain system or process is breaking down.
It also means optometrists at the coalface get almost immediate feedback and support on their clinical performance. Several years ago, Specsavers introduced clinical benchmark reports that are provided regularly to each store.
“This represents the closing of the loop in our data strategy,” Paul says. “It’s all well and good to have this data, but it offers the most value for optometrists on the ground who can get visibility of the fantastic job they’re doing, while using that to continuously improve. That’s why every week we send a pack of reports to all stores detailing their clinical benchmark performance. For example, how many patients are being referred for glaucoma, and are they doing that at national prevalence rates? It’s in the hands of the people who need it the most, regularly.”
Another powerful example of the value of the Specsavers dataset was in 2020-21 during the height of the COVID-19 pandemic. At the time, routine optometric care was off-limits for weeks, if not months, in some states.
In her role, Tse had become accustomed to counting down to milestones at the time such as the 100,000 th glaucoma patient or the 500,000 th KeepSight registration – often drilling into the data to celebrate the optometrist who helped achieve this.

But her work took on a more serious tone during the lockdowns. It was a fascinating period to track as a data scientist, but equally alarming when it became clear how many people with potentially blinding eye disease were
missing essential follow up appointments.
“It was not a project that we embarked on on-purpose, but we had to because of the massive dataset that we have and the number of patients we see every day,” she says.
“Seeing that significant number of appointments drop off, and then come back with a big uplift in volume of urgent referrals was something we’d never seen before. It was concerning, but having these statistics was incredibly helpful for us to tell the industry exactly what was needed on the ground.”
Paul agrees, adding that the Specsavers dataset was crucial when it came to the industry banding together, including Optometry Australia and its various state branches, to advocate to keep primary eyecare services operational to some degree.


Some headline stats from the initial shutdown showed 600,000 fewer optometry Medicare patient services from March-April 2020 compared with the same months in 2019. In the first week of the March 2020 lockdown, Specsavers saw a 91% patient drop compared with the same week-long period a year earlier. And over a two-month period, 25,208 Specsavers patients that likely had eye conditions requiring specialist attention did not attend their appointments.

“It’s another really good example of having a real-time view of what’s happening across different states and territories and our ability to highlight problems and talk with the industry,” Paul says.
“When governments were considering new lockdowns, using our data we were able to show what happened to eye health in previous lockdowns. That meant we were able to more effectively lobby governments to at least consider the impact that those restrictions would have on avoidable blindness detection.”
INSIGHT September 2023 55
“DATA INFORMS ALL DECISIONS WE MAKE; THERE’S NOTHING WE DO IN THE OPTOMETRY TEAM THAT ISN’T MEASURED, TRACKED AND BASED ON A QUANTIFIABLE PROBLEM.”
DR JOE PAUL SPECSAVERS ANZ
Pamela Tse has been the in-house optometry data consultant for Specsavers ANZ for almost four years.
HOW DATA WILL SHAPE OPTOMETRY’S FUTURE

Tse doesn’t only analyse internal Specsavers data. She provides insights on Medicare utilisation and census figures. Many of her findings are also made public both in trade media publications such as Insight, as well as on Specsavers’ own HealthHub data website (www.healthhub-anz.com) and in conferences and events, in a bid to influence the national eye health agenda,
and prompt other optometry providers to evaluate their care models.
Paul says this approach is starting to positively impact the industry – and there is increasing appetite for a national optometry dataset, something that Optometry Australia is currently working on, and is supported by Specsavers.

“With the number of patients Specsavers sees each year, we can confidently extrapolate from that to understand the wider industry, but it’d be great if we didn’t have to. When issues like Medicare reviews come up like they did a few years ago, it’s much more powerful if we can, as a whole industry, demonstrate why funding shouldn’t be cut, or where extra funding is needed,” he says.
“Once we can get to that level, it becomes much easier for us to talk to governments, stakeholders and other funders about the challenges we face.”
Paul says it’s clear the important role that Tse plays within Specsavers ANZ. Other networks are following suit, with more data scientists joining the industry.
“Pamela is very unique among people that work in our industry. Optometrists are very good at caring for patients and doing things on an individual level, but seeing the bigger picture, pulling together large datasets, and picking out trends most wouldn’t notice, I think you’d be hard-pressed to find someone as good as her. That’s why she has been behind highlighting many of the fascinating stories that we’ve been talking about over the past few years,” Paul says.
“We’re fortunate to sit in this position to look at millions and millions of patient journeys every year. It’s never something I thought I’d end up doing in my career but I’m incredibly glad I am here because having that visibility of the big issues in our industry – and the fantastic work of every optometrist in our stores to help uncover the potential solutions and address these challenges – is a privilege.”
Fast, error free Toric calculations. Get in touch with us today for a free trial. Web: www.schulteholt.com Email: team@schulteholt.com Schulte Holt Technology
Revolutionising CATARACT TECHNOLOGY
DATA MANAGEMENT
Specsavers has invested in automated systems that pre-populate data from measurement devices into the practice management system. This is then de-identified and used for statistical analysis.
Eye health and the Voice
FIXING A LEAKY PIPE
Retired Professor Hugh Taylor, a strong proponent of the Voice, says his five decades spent working on eye health in Indigenous communities shows the need for a permanent Voice to Parliament.
Early in his career, after completing his ophthalmology training, Taylor was appointed assistant director of the National Trachoma and Eye Health Program led by Professor Fred Hollows. At the time, the program found the rate of blindness in Indigenous Australians was 10 times higher than in non-Indigenous Australians.
In 2008, he established the Indigenous Eye Health Unit (IEHU) in the Melbourne School of Population and Global Health, whose aim was to end avoidable blindness and vision loss and close the gap for vision.
Taylor likened the care pathway for Indigenous patients to a ‘leaky pipe with many cracks and gaps where people would fall out of the system’.
Working closely with communities and leaders, the IEHU launched the Roadmap to Close the Gap for Vision in 2012, and established 64 regional groups nationwide to coordinate and provide eyecare; two-thirds of those are Indigenous-led.
“Overall, our work has achieved real improvements in eyecare provision that are now reported each year by the Australian Institute of Health and Welfare,” Taylor wrote in an opinion piece on the University of Melbourne’s multi-media platform, Pursuit
“The gap for blindness has been halved and the rates of eye exams or cataract surgery increased three-fold.”

He says this success involved many people but would have been impossible without strong Indigenous community advice, support and leadership.
“An independent review of this work highlighted the importance of allyship, the need for cultural safety, and the development, strengthening and support of Indigenous leadership. This showed the importance of putting Indigenous eye health into Indigenous hands,” he wrote.
Taylor says the value of community consultation and leadership was made clear during NACCHO’s handling of COVID.
“We have to listen to and support Indigenous communities and leadership. That is why the Voice is so important. It is clear that decisions for First Nations people need to be made with them, not for them.”
In recent months, many organisations and associations in the eyecare sector have publicly shared their support for the Uluru Statement from the Heart and its call for a Voice to Parliament.
This includes, but is not limited to, the Indigenous Eye Health Unit (IEHU) in The University of Melbourne, Australian College of Optometry (ACO), the National Aboriginal Community Controlled Health Organisation (NACCHO), Orthoptics Australia, Royal Australian and New Zealand College of Ophthalmologists (RANZCO), Fred Hollows Foundation and Vision 2020 Australia.
A referendum on the Voice to Parliament, taking place this year, will ask voters to approve an alteration to the Australian Constitution, creating the Aboriginal and Torres Strait Islander Voice (an independent and permanent advisory body) to represent Indigenous Australians to the parliament and federal government on matters of Indigenous affairs – including their health. For Mitchell Anjou, it’s a cause close to his heart. An optometrist and self-described ‘white fella’, Anjou is Associate Professor and now Director of IEHU in the University of Melbourne’s School of Population and Global Health, and sits on several eye health advisory boards.
He wears a ‘vote Yes’ badge on his lapel and actively encourages conversations about the Voice at every opportunity. He and his colleagues have also been proactive in encouraging eyecare-affiliated organisations, including the IEHU, to adopt a public position supporting a Voice, Treaty, and Truth.
“I think eyecare can potentially be improved by a Voice to Parliament and certainly by the sector supporting our Aboriginal colleagues in advancing their self-determination,” he says.
As a sector, Anjou says eye health has made progress which, in his words, is not exemplary but is demonstrable, and evidenced through the Australian Institute of Health and Welfare (AIHW) reporting.
“There’s been significant changes over the last decade showing improvement in the number of eyecare services provided, improvement in
INSIGHT September 2023 57
POLICY
With the Voice to Parliament referendum expected to be held sometime between October and December 2023, Insight asks what would a ‘yes’ vote mean for Indigenous eye health.
Prof Hugh Taylor has spent decades working with Aboriginal and Torres Strait Islander-led organisations to reduce avoidable blindness. Image: University of Melbourne.
KEY STRATEGIES NEEDED TO IMPROVE EYE HEALTH
A workshop discussion of First Nations people working in First Nations Eye Health, held at the National Aboriginal Torres Strait Islander Eye Health Conference 2022, identified key strategies needed to improve eye health care outcomes for First Nations people. Below are some of the visions for the Aboriginal and Torres Strait Islander eye health sector in 2030:
• R adical change in eye health education for communities, led by First Nations people.
• Every child in Australia by age five has had a comprehensive eye health examination.

• E quitable access to eye health services regardless of location. Patient led technology driven eye health care.
• B etter health outcomes through Aboriginal and Torres Strait Islander co-designed pathways.
• C hallenging concepts such as ‘remote’, ‘overcrowding’ and ‘capacity building’.
• Every product or process seen through a First Nations lens.
• S oftware and technology processes to revolutionise eyecare service delivery.
• O ur choice, our vision through a national peak body for Aboriginal and Torres Strait Islander Eye Health.
Excerpt from Vision 2030 report
access to subsidised spectacle schemes, improvement in screening rates for people with diabetes, support for screening in primary health care and improvement in surgery rates for Aboriginal and Torres Strait Islander people,” he says.

The 2008 National Indigenous Eye Health Survey (NIEHS) and 2016 National Eye Health Survey (NEHS) confirmed the gap, or inequity, in eye health and that Aboriginal and Torres Strait Islander people are three times more likely to have vision impairment or be blind than other Australians.
“There’s another survey being conducted at the moment – the data probably won’t be available until 2024 or 2025 – but we are hoping that it shows a further improvement or reduction in the relative rates of vision loss and blindness between Aboriginal people and non-Aboriginal people,” Anjou says.
According to the latest Ahpra data, Anjou says, there are 12 Aboriginal and/ or Torres Strait Islander registered optometrists out of 6,000, and only one ophthalmologist, which is well below population parity.
IN FIRST NATIONS HANDS
A consistent outcome from evaluating IEHU’s Roadmap to Close the Gap for Vision through 2019 to 2021, conducted by two independent consultants, has been that Indigenous eye health needs to be in Indigenous hands.
“There is a recurring message around supporting self-determination, supporting leadership, and supporting greater involvement of Aboriginal people in Aboriginal and Torres Strait Islander eye health,” Anjou says.
As a result, the IEHU has continued to shift its internal structures to reflect this approach.

“The IEHU Advisory Board now has a majority of Aboriginal and Torres Strait Islander people on it. Our chair, Aunty Pat Anderson, and deputy chair, Karl Briscoe, are First Nations people. Half our staff are Aboriginal and Torres Strait Islander, and since the retirement of Professor Hugh Taylor in 2022 we
also had opportunity to establish a leadership group that has a majority of Aboriginal and Torres Strait Islander people.”
Anjou says the IEHU team are also encouraging regional stakeholder groups in the eye health sector to have Indigenous leadership and Indigenous voices ‘front and centre’, and supporting organisations in the sector to implement Reconciliation Action Plans.
“A genuine question for the sector is how to elevate Indigenous voices, and provide space for Indigenous leaders to propose an opinion or view or express their thoughts around an issue, which is what the Voice to Parliament is proposing. In the case of the eye health sector, organisations need to listen to what Indigenous people say in a meaningful and real way,” he says.
“I see Aboriginal voice as being a key objective to be introduced into the agencies and the way the eyecare sector operates.”
Leading the way, an Aboriginal and Torres Strait Islander reference group, established originally for an IEHU project, has morphed into the National Experts Group for Aboriginal and Torres Strait Islander Eye Health (NEGATSIEH) which, in turn, has provided the leadership of the National Aboriginal and Torres Strait Islander Eye Health Conference for the last two years.
NEGATSIEH has since supported the establishment of the First Nations Eye Health Alliance (FNEHA) and released Vision 2030, a report which details, from the perspective of Aboriginal and Torres Strait Islander eye health professionals, the vision and future efforts needed to eliminate avoidable vision loss and blindness in Aboriginal and Torres Strait communities by 2030.
“This is Aboriginal and Torres Strait Islander people who are involved in eye health coming together and forming organisations where they can provide important voice and leadership into what is happening in the eyecare sector. We white fellas need to get out of the way and find a meaningful role as allies,” Anjou says.
“If the referendum is successful, I hope that eyecare is able to reflect the change of empowering Aboriginal people to have genuine voice into how the eyecare sector works and operates.”
IN THE FIELD
In May this year, Dr Josephine Li attended the National Aboriginal and Torres Strait Islander Eye Health Conference in Western Sydney with Anjou and Professor Hugh Taylor, and about 240 delegates from across Australia. The trio participated in a session at the conference to talk about the yes vote, and how it could impact medical practice, and how to improve the quality of health care for people in the Indigenous community.
Li, a qualified optometrist, is general manager of Victorian Eyecare Service (VES) and outreach programs at the Australian College of Optometry (ACO), based in Melbourne.
“I think it is a very important step for Aboriginal communities to have a representation in the parliament, which could potentially address a range of issues,” she says.
“If the yes vote is successful, I think there will be more people from Indigenous communities willing to come forward and contribute to their community. I think there’ll be more people trying to raise awareness of
58 INSIGHT September 2023 POLICY
“THERE IS A RECURRING MESSAGE AROUND SUPPORTING SELFDETERMINATION, SUPPORTING LEADERSHIP, AND SUPPORTING GREATER INVOLVEMENT OF ABORIGINAL PEOPLE IN ABORIGINAL AND TORRES STRAIT ISLANDER EYE HEALTH.”
A/PROF
MITCHELL ANJOU INDIGENOUS EYE HEALTH UNIT
The Vision 2030 report details, from the perspective of Aboriginal and Torres Strait Islander eye health professionals, the vision and future efforts needed to eliminate avoidable vision loss and blindness in Aboriginal and Torres Strait communities by 2030.
eyecare or healthcare and it can help us to close the gap, maybe using a different approach,” Li says.
The ACO receives funding from the Victorian Department of Health to run the Victorian Eyecare Service (VES), and within it, the Victorian Aboriginal Spectacles Subsidy Scheme (VASSS).
Through the VASSS program, Aboriginal and/or Torres Strait Islander communities in Victoria are eligible to obtain spectacles for a co-payment of $10.
“That applies to all our Australian College of Optometry branches, including our seven metro clinics, plus our main clinic in Carlton. We also have visiting optometrists conducting eye tests at the Victorian Aboriginal Health Service in Fitzroy twice a week,” Li says.

In addition, the ACO receives Australian Government Rural Workforce Agency Victoria (RWAV) funding to provide outreach eyecare services to metropolitan and rural health centres for Indigenous communities.
BY THE NUMBERS
The prevalence of trachoma in school aged children is trending in the right direction – that is, down – according to the Australian Institute of Health and Welfare’s (AIHW) latest annual eye health data for Aboriginal and Torres Strait Islander people.
In the sixth annual report to update the eye health measures for Aboriginal and Torres Strait Islander people, Eye health measures for Aboriginal and Torres Strait Islander people 2022 includes information on the prevalence of eye health conditions, diagnosis and treatment services, the eye health workforce and outreach services.
It found:
T he prevalence of active trachoma in children aged 5-9 in at-risk communities fell from 15% in 2009 to 3.3% in 2021
• Around 42% of Indigenous Australians who had a diabetes test also had an eye examination in 2019-20

• T he age-standardised cataract surgery rate for Indigenous Australians fell by 15% from 2018–19 to 2019–20

• I n 2019–20, the median waiting time for cataract surgery was 130 days for Indigenous Australians.
“On top of that we have over 30 rural private optometry practices that have signed up for VASSS, so that allows people living in rural communities to access the scheme.”
The ACO also hosts students from varies universities for outreach and Indigenous eyecare placement. This allows early exposure to future optometrists to be ready to practice under different cultural settings.

“The ACO has also adopted a Reconciliation Action Plan, and has one Indigenous staff member who is working in the optical dispenser lab,” Li says.

Wyndham Clinic Day Surgery offers you • 2 theatres and large recovery areas • We are located just 20mins from the Westgate Bridge • Ex RVEEH clinical staff with high volume capacity • Very competitive uninsured rates
Easy access and great value parking for patients
Centurion Phaco system with active sentry technology
MIGS, Trabeculectomy, Strabismus, Pterygium and Ocuplastic Wyndham Clinic Private Hospital 242A Hoppers Lane Werribee VIC 3030 Phone: (03) 9731 6646 Fax: (03) 9748 7057 Sally Bebawy Business Development Manager Phone: 0421 713 747 Email: sbebawy@wyndham.clinic Web: www.wyndhamclinic.com.au/ophthalmology Contact us today to discuss opportunities. Secure your private theatre list now - Monday to Friday.
•
•
•
“I THINK IT IS A VERY IMPORTANT STEP FOR ABORIGINAL COMMUNITIES TO HAVE A REPRESENTATION IN THE PARLIAMENT, WHICH COULD POTENTIALLY ADDRESS A RANGE OF ISSUES.”
DR JOSEPHINE LI AUSTRALIAN COLLEGE OF OPTOMETRY
CAN GENDER PARITY IN EYE HEALTH LEADERSHIP
reduce inequities?
Women comprise 70% of the global healthcare workforce but occupy less than a quarter of the most influential leadership positions, equating to a major missed opportunity to improve eye health, a new analysis reveals.
The global health sector will continue to lose out on women’s talent and perspectives unless measures are taken to accelerate towards equal representation in senior leadership positions.
This is the view of Australian-registered charity The Fred Hollows Foundation, which has put its thought-provoking hypotheses to the test in a new report entitled: ‘Women deliver eye health: Let’s reframe who leads it.’
The specific hypothesis centers on the of parity for women in leadership positions and what this would unlock for eye health services and outcomes.
Although not an academic review, the report is an attempt to draw out some key lessons and experiences from other sectors and organisations, acting as an invitation to consider how the eye health sector can go about enacting change.
A cornerstone of the report is a World Health Organization (WHO) statistic showing that women comprise 70% of the global healthcare workforce but occupied less than a quarter of the most influential leadership positions (figure 1).
“It’s clear that women are being excluded from leadership positions in global health – having more women in positions of power will generate better public health outcomes for women and girls,” Fred Hollows global advocacy executive director Ms Jennifer Gersbeck says.
The Fred Hollows report shows that an estimated US$12 trillion (AU$18 t) could be added to global output by 2025 if the gender gap was closed in both the workforce and leadership.
Key barriers to overcome include: less investment in women’s mentoring, workplace bullying and sexual harassment, perpetuating norms and gender stereotypes, gender pay gap and discrimination.
“Global health is losing out on the talent, skills and perspectives of women,” Gersbeck says.
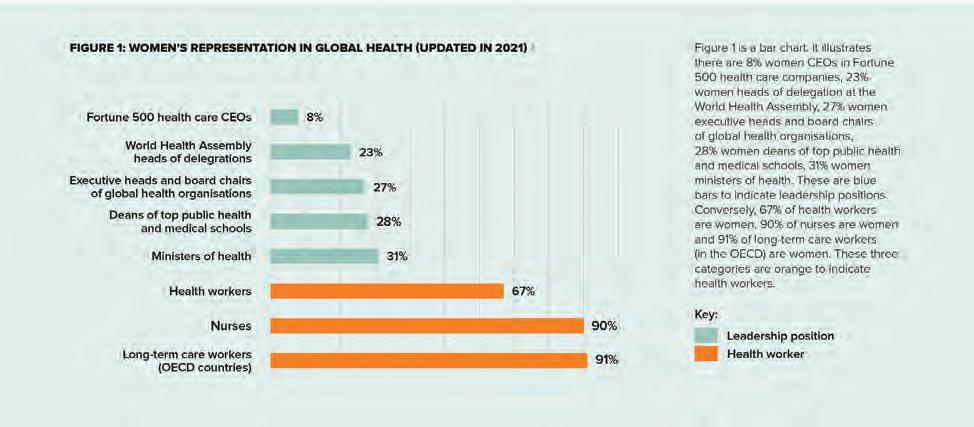
“If these barriers are removed, women leaders can significantly expand the global health agenda and give greater priority to issues that affect women and girls. Enabling equal representation supports diverse decision-making and services that better reflect the needs of the entire population.”

Gersbeck says women and girls accounted for 55% of the world’s blind and vision impaired.
“The Fred Hollows Foundation believes that achieving gender parity in eye health leadership will help reduce inequities in eye health.”
THIRD OF EYE HEALTH ORGANISATIONS HAVE FEMALE BOSS
In global health, it is estimated that women contribute more than US$3 trillion annually to international health systems. According to Fred Hollows, this
contribution is markedly undervalued because women in health tend to be clustered into lower status, low paid and often unpaid roles (like nursing, midwifery or social care roles).
“Women do not have equal participation in health leadership or decisionmaking,” the foundation states.
“A seminal 2019 report by the WHO titled ‘Delivered by Women, Led by Men’, with research conducted by the Gender Equity Hub (GEH) co-chaired by WHO and Women in Global Health, found that women occupy almost 70% of the global health workforce but hold only 25% of senior roles. This is consistent across all levels of leadership, from international organisations to the community or local level.”
Further, evidence from the ‘2021 Global Health 50/50 Report’ offers a glimpse into what is happening in the private sector where there is a “slow crawl” towards gender parity in leadership.
“In 2018 health organisations had an average of 29% women CEOs or executive directors, which increased to 31% in 2021. This trend is worse in low- and middle-income country settings,” the report says.
“In 2018, boards in global health comprised only 20% women – this has increased to 26% in 2021. There is senior management team (SMT) parity in only 36% of global health organisations, and board parity in less than one third of organisations. The public sector closely mirrors this trend.”
Meanwhile, the number of women leading ministries of health shows it is
60 INSIGHT September 2023
WORKFORCE
FIGURE 1: WOMEN'S REPRESENTATION IN GLOBAL HEALTH (UPDATED IN 2021)7
FIGURE 1: The status quo of the 70:25 ‘pyramid’ in 2021 where women comprise the majority of health care workers (orange bars) but hold few senior leadership positions across international health institutions and governing bodies (blue bars).
the highest area for women’s leadership at 31% but varies significantly based on geography and context. In the regions of Southeast Asia, Western Pacific, and Eastern Mediterranean it is relatively low, while in Europe, Africa and the Pan American regions, women head more than 30% of health ministries. At the WHO itself, women account for under 10% of the 34 executive board members.
Drilling down into the performance of eye health organisations, the Fred Hollows report says the International Agency for the Prevention of Blindness (IAPB) has been tracking women’s leadership representation since 2020 through its annual gender equity in eye health survey.

The survey is limited – reaching 90 organisations in eye health – but presents some useful insights including: in 2021 31% of organisations surveyed had board member parity and 32% had a female CEO. This is higher than the ‘2021 Global Health 50/50’ finding (29%). The IAPB found that 56% of eye health organisations surveyed have parity or almost parity in SMT leadership – notably higher than outside of eye health (36%).
BARRIERS TO ENTRY
The gender gap in leadership amounts to a systemic issue, according to Fred Hollows.
This includes “deep-rooted, historical power structures of medicine, hospitals and health systems and the ‘glass ceiling’ effect, that creates a preferential opportunity for men to be leaders and occupy influential roles in the sector”.
According to the foundation, this establishes a power dynamic that enables men and disempowers women.
“Still, there is no shortage of women in the age cohorts that typically feed into leadership,” the report says.
“As the Closing the Leadership Gap paper notes, ‘the problem is not a shortage of women entering the leadership pipeline, rather a blockage in the pipeline which stops women entering leadership in equal numbers as men’. Women face many visible and invisible barriers along the pipeline to leadership not just at the final hurdle (glass ceiling). This is referred to as a ‘leaking pipeline’.”
IMPLICATIONS FOR EYE HEALTH
Overall, the foundation believes achieving equal representation in positions of power across health will support more diverse voices making decisions around system design, resource spend and policy change which leads to systems and services that better reflect the needs of the entire population. This creates role models for the next generation of future women leaders. The implications for eye health include:
Better access to services: Fred Hollows says the gender split suffering preventable blindness is 55% women and 45% men. This is due to several factors, including women living longer, women and girls not being prioritised
in access to services especially in low- and middle-income countries, women facing higher barriers to services (such as breastfeeding, rearing young children, cultural constraints). Research has also shown that decisions in healthcare have led to conditions primarily affecting women being understudied and underfunded historically.

Buy by achieving gender parity in leadership, the foundation says this could help increase attention to these diseases and conditions – including vision loss which disproportionately affects women – ensuring more equal access to resources.



More inclusive service design and delivery: A lack of women leaders in eye health sees negative impacts on the service design process, including limited considerations for data disaggregated by sex or services catered to meet women’s specific requirements.
More representation and role models: Fred Hollows points to a lack of female leaders across leading eye health organisations including international non-governmental organisations, multilaterals, academic institutions, publishing/editing houses, global institutions and bodies etc. It is also important to consider diversity, geographic, cultural and ethnic representation in leadership.
WHERE TO FROM HERE?
“This initial research and evidence-gathering gives confidence that the hypothesis holds true,” Fred Hollows concludes in its report.
“Achieving equal representation in positions of power across health, and in sectors outside of health, matters. It supports more diverse voices making decisions around system design, resource spend and policy change. It creates role models for the next generation of future women leaders. The gender gap in health can only be closed by addressing systemic barriers to women’s leadership. Changing policy and practice in any sector is hard. Tackling systemic barriers to equality is not an overnight job and this is beyond one institution or organisation’s capacity to change.”
INSIGHT September 2023 61
AND SERVICES THAT BETTER REFLECT THE NEEDS OF THE ENTIRE POPULATION.”
JENNIFER GERSBECK FRED HOLLOWS FOUNDATION
Women and girls account for 55% of the world’s blind and vision impaired.
THE PERKS OF A REGIONAL OPTOMETRY CAREER
For RESHMA SETH, working in a metro optometry setting was busy and diverse, but working as a regional optometrist provides a sense of community, both inside and outside of the clinic – and she hasn’t looked back.

George & Matilda Eyecare (G&M) optometrist Ms Reshma Seth is well-acquainted with differences in regional vs metro optometry, but for her a regional career comes out trumps every time. Perhaps this is why she has remained in the Mid-North Coast town of Forster, NSW, since arriving there 19 years ago.
Seth started her career in Sydney after graduating from the UNSW optometry school but wanted to escape the fast-paced nature of her work in search of an opportunity offering a greater sense of community and fresh clinical challenges.
After moving regionally in 2004, today she works as an optometrist at George & Matilda Eyecare for Rolfe Optometrists, Forster, part of the nine-practice strong Rolfe Optometry Group that joined G&M in August 2022.

“I didn’t want somewhere too isolated as I have friends and family in metro areas. Some of the other key attributes I looked for when relocating included having well-equipped rooms, a good team with knowledgeable dispensers and a shared view of delivering quality eyecare,” she says.
“Working in metro optometry was busy and diverse. When I worked in Sydney, the cross-section of patients and concerns was quite different to what I have experienced since moving. Regional optometry provides a sense of community, both inside and outside of work. I’ve had three generations of a family as patients and usually get to see a lot of familiar faces.”
She continues: “The demographic is quite different and so I deal with a different set of concerns and prescriptions. Although I have enjoyed working in both types of practice, I really do like the sense of community in regional practices.”
Since joining 12 months ago from a different practice in Forster, Seth has enjoyed working at George & Matilda for Rolfe Optometrists in Forster and interacting with the community from a “beautiful” location. It also helps that the rooms are well-equipped, with a widefield digital camera, OCT, and dry eye assessment and management technology such as an intense pulsed light (IPL) machine.
“Dry eye disease is prevalent in my patient demographic and I am looking forward to increasing my knowledge base in this area,” Seth, who also became therapeutically endorsed in 2016, says.
“Forster is a perfect location for me; it is stunning geographically without being too isolated from more metro areas. I get to live in an area surrounded by wonderful beaches, lakes and national parks. It’s away from the hustle and bustle of cities whilst being close enough to friends and family in Newcastle and Sydney.”
After working regionally for many years, Seth has appreciated what G&M has been able to offer for her career. Importantly, the support team has ensured a smooth transition into the G&M network, allowing staff to focus on their daily roles and responsibilities.
“I have a wonderful team of dispensers and optometrists and it’s great to have colleagues with whom I can confer and collaborate with for specific patient needs,” she says.
“The leadership team is approachable and accessible, any help needed is just a phone call away. George & Matilda have an ethos of putting patients first and being deeply embedded in the community. These are my core values in my work, so it is important to me that this is an inherent part of the company’s values.”
62 INSIGHT September 2023
CAREER
The practice team at George & Matilda Eyecare for Rolfe Optometrists, Forster.
Reshma Seth has lived and worked in Forster, on the Mid-North Coast of NSW, for almost two decades.
Missed eye exams
CONTRIBUTE TO 100,000 HOSPITALISATIONS ANNUALLY
Skipping eye exams and other crucial health checks for people with type 2 diabetes may be costing the Australian health system more than $2 billion a year, new research reveals.
Mr Linden Moffatt understands as well anyone the need for a health system that is geared towards supporting people with diabetes to live well and prevent disease-related complications while protecting the health system.
As someone with diabetes, it can be hard to keep on top of the spectrum of regular health checks, but as part of his diabetes management he receives reminders from the KeepSight automatic eye check reminder system, and regularly sees an optometrist.
“I know many individuals who have been affected by diabetes-related eye disease and I’ve witnessed first-hand the effect these conditions have on their lives, their confidence,” he says. “I encourage everyone to have their eyes monitored and tested. An early detection can be the difference between keeping and losing your vision.”
He’s right. Missed health checks and reduced access to routine healthcare for people living with type 2 diabetes in particular could be costing the Australian health system around $2.3 billion per annum. New modelling from Diabetes Australia, based on US research, found that the cost impact of people in Australia living with type 2 diabetes not receiving recommended care was around AU$3,564 per person per annum.
An estimated 50% of Australians living with type 2 diabetes are not accessing a range of recommended diabetes health checks that help to prevent and manage diabetes-related complications including checks for diabetes management, cholesterol, kidneys, feet and their eyes.
Missed health checks contribute to the increased prevalence of diabetes-related hospitalisations and complications. Annually this includes:
• 100,000 hospitalisations for eye complications
• 710,000 admissions to hospital for dialysis
• 256,000 admissions to hospital for other kidney-related conditions
• 19,000 diabetes-related emergency admissions
• 5,163 amputations
This results in extra costs to the health system, with an increased prevalence of diabetes-related complications, many of which are preventable, Diabetes Australia states.


The organisations says this is why it is important to pinpoint the blockages and gaps in the current system that are making it harder for people living with type 2 diabetes to access optimum care. KeepSight is an example of how the ophthalmic sector has responded to this challenge.
Ms Taryn Black, director of the KeepSight diabetes eye check reminder
program, says in addition to the impact of missed eye health checks on the economy, it was also a significant, but unnecessary, risk for the individual.
“We know that regular eye checks and early intervention can prevent more than 90% of vision loss for people with diabetes. Quite simply, regular checks save sight,” she says.
KeepSight was developed specifically to address this issue by sending people reminders when they are due for an eye check. Run by Diabetes Australia and now in its fourth year, the program’s goal is to ensure all Australians with diabetes are receiving regular eye checks. It’s backed by a public/private partnership with the Federal Government and Specsavers.
Diabetes Australia Group CEO Ms Justine Cain says diabetes is complex and can lead to a range of debilitating and costly complications, many that could be prevented or delayed by ensuring people receive timely and appropriate medical care.

“One of the challenges with Australia’s healthcare system is that it has been orientated towards treating people when they are sick and unwell, rather than preventing issues before they develop,” Cain says.
“For people with diabetes, this means we need to ensure people can easily access the routine health checks which can detect problems like vision loss early when it is most treatable.
“That’s why we are strong supporters of the Federal Government’s Strengthening Medicare process which will create a health system that better meets the needs of people living with chronic conditions such as diabetes.”
On the back of National Diabetes Week in July 2023, Diabetes Australia is working with people living with diabetes to document their experience to inform the Australian Government’s Parliamentary Inquiry into Diabetes.
“We’re hoping to amplify the voice of people with diabetes who understand the reality of living with diabetes better than anyone to ensure this inquiry focusses on the priorities that will change the future,” Cain said.
“We need to have a health system that is geared towards supporting people living with diabetes to live well and prevent diabetes-related complications and protect our health system.”
INSIGHT September 2023 63
DIABETES
“ONE OF THE CHALLENGES WITH AUSTRALIA’S HEALTHCARE SYSTEM IS THAT IT HAS BEEN ORIENTATED TOWARDS TREATING PEOPLE WHEN THEY ARE SICK AND UNWELL, RATHER THAN PREVENTING ISSUES BEFORE THEY DEVELOP.”
JUSTINE CAIN DIABETES AUSTRALIA
Almost 1.3 million Australians have type 2 diabetes, representing 85-90% of all cases.
































See more, know more with more Insight Subscribe FREE and receive the latest news Insight is mobile and tablet friendly Find jobs and advance your career with Insight’s Classifieds Get to know the newest products from suppliers across Australia Insight’s new website keeps you updated on the latest industry news and information. With a world-class responsive design, Insight is now accessible seamlessly on any device, 24/7. Sign-up FREE to our eNewsletters and industry reports delivered weekly straight to your inbox. www.insightnews.com.au
DISPENSERS CAN BE LIFELONG LEARNERS TOO
Despite there being no formal requirement in Australia for dispensers to attain and maintain CPD points, unlike our optometrists, it is in our own and our patients’ best interest to stay on top of our personal and professional development and continue with a student outlook of always learning. There are numerous reasons why we should – and ways in which we can – continue with our development even once we are formally qualified and regardless of our varying lengths of service. The key objective of CPD is to ensure that our skills and knowledge are always up-to-date in a constantly developing industry.
Notably, the new industry body, Optical Dispensers Australia (ODA) of which I am an advisory board member, is bridging this gap between educational content and dispensers seeking professional development by hosting regular webinars and occasional in-person events. For ODA members, a currency certificate will be distributed to those that have completed 10 CPD points each calendar year. On top of the educational benefits of the program, the currency certificate is a great addition to present to a future or current employer to show relevancy and up to date knowledge in the industry.
WHERE CPD COUNTS
One important reason why CPD is crucial for optical dispensers is so that we can stay on top of advances in technologies and research in the industry. No two practices offer the same services and to be able to answer our patients’ questions about a wide range of possible care and
treatment options would be beneficial, ensuring we are providing the best and most accurate information available. For example, many patients will look for advice and information on dry eye treatments. Even if your practice does not offer dedicated dry eye clinics or specialist treatments such as IPL, it would reflect positively on your skills and your practice if you were able to discuss confidently with your patients and direct them appropriately.
CPD is also very important for dispensers when it comes to broadening knowledge of lens advances and new approaches to dispensing. Depending on the type of practice that you work in, your exposure to the vast range of options may be limited to the core options that your practice offers.

Some practices will order from numerous lens suppliers based on their customer needs or preferences, while others will have a more limited catalogue they pull from, generally of the most common lens types more broadly used. This can lead to knowledge gaps around what is available in the industry vs what is available in said practice.
You will be able to find a range of readily available information on lens styles available from the various suppliers and by looking at ODA’s CPD webinar calendar for upcoming online presentations.
CPD events and opportunities can come in many different formats, whether it be through trade shows, webinars, lens supplier trainings, frame suppliers’ information events and conferences.

All of these are great opportunities for dispensers to network with peers and to expand professional relationships. It would also be reasonable to assume that job seekers looking for a new opportunity would be looked on favourably by employers if they are proactive in their professional development. As your career progresses, the work you have put into expanding your network may also broaden your access or visibility to future job opportunities.
CPD can also help to build confidence for an optical dispenser. As technical skills and knowledge develop, we become much more comfortable in our interactions with our patients and confident in our abilities to provide them with an appliance that will fulfil their optical need. Our now expanded network means we have peers that we can look to for support, advice or suggestions in relation to those tricky dispenses and likewise provide that support in return.
In summary, though the types of CPD are varied i.e. structured or self-directed, the benefits for optical dispensers ourselves and, in turn, our patients cannot be underestimated. The development of new skills and knowledge ensures that we are providing the best possible care for our patients and staying up to date on trends and advances in our industry.
DISPENSING INSIGHT September 2023 65
The first national Optical Dispensers Australia conference in Sydney in April 2023 was an ideal chance for dispensers to gain up-to-date product and technical knowledge.
“JOB SEEKERS LOOKING FOR A NEW OPPORTUNITY WOULD BE LOOKED ON FAVOURABLY BY EMPLOYERS IF THEY ARE PROACTIVE IN THEIR PROFESSIONAL DEVELOPMENT.”
ABOUT THE AUTHOR: CATHERINE LEETCH is a qualified optical dispenser and practice manager at Eyescan in Melbourne. She is also an Advisory Board Member for Optical Dispensers Australia.
EVEN THOUGH PROFESSIONAL DEVELOPMENT IS NOT A MANDATORY REQUIREMENT FOR THE MODERN-DAY OPTICAL DISPENSER, THERE ARE SEVERAL OPPORTUNITIES TO UPSKILL AND SET THEMSELVES APART, SAYS CATHERINE LEETCH.
FRAMEWORK FOR VISION PROBLEMS AFTER STROKE
ARE NOT TYPICALLY PART OF THE CORE STROKE MULTI-DISCIPLINARY TEAM IN AUSTRALIA –BUT THEY SHOULD BE, ARGUES SHANELLE SORBELLO.
While the Stroke Foundation’s Australian Clinical Guidelines for Stroke Management1 strives to improve stroke care practices across the country, there remains an alarming gap in current guidelines with respect to eye-related rehabilitation.

Lack of guidance in eye-related stroke care in Australia indicates its provision is not standardised and unlikely to attract the resources and attention given to other stroke related deficits.
Recommendations from the Stroke Foundation Acute Stroke Services
Framework2 omits mention of eyecare specialists in the multidisciplinary stroke team and their presence in stroke or rehabilitation facilities is undocumented.
The 2017 Orthoptics Australia Workforce Survey3 found 21 orthoptists working in a rehabilitation setting, while 38 identified clinical neuro-ophthalmology as their main area of employment.
In 2020, NSW Health reported that 37 orthoptists were employed in 9 out of 15 local health districts.4 This suggests that unlike other countries with locally trained orthoptists, such as those within the UK, orthoptists are not typically part of the core stroke multi-disciplinary team in Australia.
In addition, few NSW public hospitals having on-site ophthalmic services (6%).5 With only two hospital eye clinics outside Sydney, this indicates that patients with stroke-related eye deficits in rural and remote regions are likely at even greater disadvantage.
As part of the Pathway Research for Eye Care in Stroke (PRECiS) study, I conducted a scoping review of current post-stroke vision care in Australia.6 This revealed limited Australian research, with no published protocols or pathways to support provision of eyecare for stroke survivors in Australia.
Most evidence is from the UK and Europe. In 2019, a UK study showed that 85% of stroke health professionals utilised post-stroke vision care protocols.7 This is the likely result of a growing UK evidence-base, inclusion of eye specific information in stroke guidelines8 and naming orthoptists as necessary members of the stroke team, with orthoptic assessment considered the gold-standard and proving to address gaps in provision of vision rehabilitation.9,10,11
Utilisation of evidence-based vision screening tools for stroke survivors
administered by non-eyecare professionals, also facilitates prompt identification of eye conditions.9,12,13,14
The PRECiS study used surveys and interviews with stroke survivors and stroke health professionals to capture their experience of current vision care practices.
The overwhelming majority of health professionals reported that they did not have protocols or care plans for eye problems following stroke.
Stroke survivors reported issues such as significant delays in initial vision assessment and diagnosis, poor provision of information on eye conditions and available support services, with a generalised lack of short-term management and onward referral.
The PRECiS study consequently developed the NSW Post-stroke Vision Care Framework (NSW-PVCF) consisting of 43 best practice statements and a diagrammatic care pathway, in agreement with stakeholders.
The NSW-PVCF is a considerable expansion to the current eye-related Australian national and state-based stroke guidelines.1,15,16 Stroke clinical care pathways have previously shown improvement in multidisciplinary care provision, reduced length of hospital stays, and health costs17 highlighting potential benefit to the health system and stroke survivors.
The NSW-PCVF was developed in
consideration of the unique characteristics and challenges presented within the context of Australian healthcare. However, the strategies employed in this framework may be transferrable to other countries looking to overcome challenges in delivering equitable, high-quality healthcare in regions where there are sparse populations,18 geographically diverse communities, and proportionately to countries in UK and Europe, relatively small, ageing and stroke affected populations.19
Acknowledgements: The PRECiS study was undertaken as a doctoral project by Shanelle Sorbello at the University of Technology Sydney under the supervision of Professor Kathryn Rose (Primary Supervisor), Dr Amanda French and Professor Fiona Rowe.
References will be available online.

ABOUT THE AUTHOR: SHANELLE SORBELLO holds a PhD in Orthoptics at the University of Technology Sydney and is currently teaching in the Masters of Orthoptics course at UTS.

ORTHOPTICS AUSTRALIA strives for excellence in eye health care by promoting and advancing the discipline of orthoptics and by improving eye health care for patients in public hospitals, ophthalmology practices, and the wider community. Visit: orthoptics.org.au

66 INSIGHT September 2023
ORTHOPTISTS
“STROKE SURVIVORS REPORTED ISSUES SUCH AS SIGNIFICANT DELAYS IN INITIAL VISION ASSESSMENT AND DIAGNOSIS.”
Recommendations from the Stroke Foundation Acute Stroke Services Framework omits mention of eyecare specialists in the multidisciplinary stroke team.
CYBER RISK VIGILANCE IN HEALTHCARE
IN RECENT YEARS, CYBERCRIMES TARGETING U.S. OPTOMETRY PRACTICES HAVE EXPOSED PERSONAL HEALTH AND FINANCIAL INFORMATION OF MILLIONS OF PATIENTS. DO YOU KNOW HOW ROBUST YOUR DATA SECURITY SYSTEMS ARE?
he Office of the Australian Information Commissioner noted a 41% increase in breaches caused by malicious and criminal attacks in its most recent report, to December 2022. The Australian Cyber Security Centre received 76,000 reports of cybercrime in 2021-22, according to its annual cyber threat report July 2021 to June 2022. That is one report every seven minutes.
Health data is attractive to cyber criminals and practices may experience attacks designed to expose patient healthcare and financial records and/or demand ransom payments.
As well as the risk to patient privacy and reputation, breaches may cripple practice operations, as an Avant member discovered after a ransomware attack: “All our records, all our appointments, all our contacts, all our address books are on the computer system which meant that we had no data at all. We didn’t have … billing information or any links to our health funds. We did have backups and we thought that was a good thing to do. Unfortunately, it turns out that the links to the backups were not secure and so the backups were infected as well.”
PROTECTING YOUR PRACTICE SYSTEMS AND REDUCING RISK
1. Establish a culture in your practice that takes cyber security seriously
No organisation is too small to be vulnerable to cyber breaches and your system may be connected to other systems including suppliers, hospitals or government. If you connect to the My Health Record, you are required to comply with legislated security requirements.
Malicious attacks often involve an element of human error, so training staff to be cyber security aware can help reduce your risk. Make sure staff understand and follow information security practices, such as using strong passwords, and thinking before you click on links.
Consider also taking out cyber insurance to cover the risks to your practice.
See the links in the online version of this article for a range of resources to assist including information guides, eLearning
If practice owners suspect a breach, immediately seek help because it may have occurred days or weeks earlier.
2. Make sure your security measures are up-to-date
Criminals take advantage of system vulnerabilities. Keep your systems up-to-date and use anti-virus and ad-blocking software. Apply security patches regularly and allow automatic updates from the manufacturer. Password security can be strengthened by using two factor authentication. Secure your backups.
An IT expert can undertake a security audit or risk assessment to test potential threats to your systems, including any devices that connect to your practice network.
3. Review your information handling practices
Review how you handle patient information including the information you collect, how you use that information, and how you store it. Also consider what information you need to share with suppliers such as eyewear and device manufacturers, and share only what is necessary.
Make sure your processes set out how long you need to keep information, and what you do with information when it is no longer needed.
Australian privacy law says you must destroy or permanently de-identify information collected for a specific purpose when you no longer need it for
that purpose. However, in the case of health records, there are requirements regarding how long these must be kept and when and how they can be destroyed.
Avant members have told us patients contacted them after the Optus and Medibank breaches asking for all their records to be deleted. If you receive such a request, you may still be legally required to keep records even for former patients so seek advice if you are unsure.

4. Seek help if you have a cyber security incident
Call for help as you immediately become aware of an incident as your system may have been breached days or weeks earlier. Contact the Australian Cyber Security Hotline, your IT service provider or your insurer for further advice and assistance.
If patient data has been compromised you may have mandatory notification requirements under the Notifiable Data Breach scheme.
If you connect to the My Health Record system and there has been a potential compromise of that system, you are required to notify the Australian Digital Health Agency.
ABOUT THE AUTHOR: GEORGIE HAYSOM BSc LLB (Hons) LLM (Bioethics) GAICD, is the General Manager Advocacy Education and Research at Avant.

MANAGEMENT INSIGHT September 2023 67
“NO ORGANISATION IS TOO SMALL TO BE VULNERABLE TO CYBER BREACHES AND YOUR SYSTEM MAY BE CONNECTED TO OTHER SYSTEMS INCLUDING SUPPLIERS, HOSPITALS OR GOVERNMENT.”
ACCESSING DONOR EYES FOR EYE RESEARCH
provide the tissue, while others provide as gratis.
While this process seems straightforward, in Australia – as elsewhere in the world – access to deceased research donation is limited. This is because the donation system has been established to support transplantation, with research demand emerging as an area of secondary need. There are several key reasons for research donation access limitations:
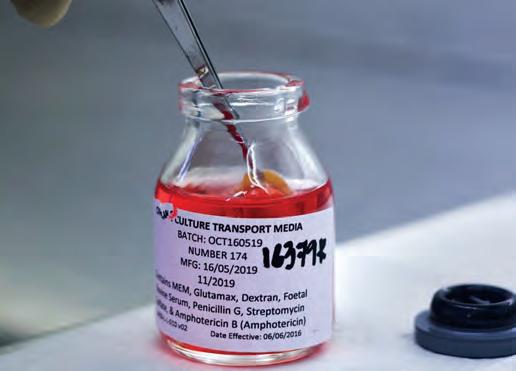 BY HEATHER MACHIN
BY HEATHER MACHIN
For many researchers who are investigating the eye, access to end-of-life (deceased) donated eyes is paramount. Despite this, researchers who seek deceased human eye donations for their projects may not be prepared for the barriers they may face.
In Australia, access to deceased eye donations for research is through an eye or tissue bank.
There are five banks that manage this in Australia, located in Adelaide, Brisbane, Perth, Melbourne, and Sydney.
They work with Donatelife and the Australian Commonwealth Government’s Organ and Tissue Authority to recover and allocate tissue for transplantation, training, and research.

While each bank operates slightly differently, they generally work with end-of-life donation agencies and hospital and mortuary staff to identify deceased donors, discuss donation with the donor’s family, and then consent and recover the donation.
They then allocate the donation to research groups with ethics approval, and approval by their bank.
Some banks require researchers to reimburse them for all or part of the costs they incurred to recover and
1. T he health system (Medicare/ private health insurance) reimburses the banks only when the donation is transplanted. This means most banks, unless they are reimbursed, do not have the resources to recover additional quantities of donations for research unless the research team reimburses them.
2. T he public donation awareness programs, the donation system and end-of-life conversation focuses predominantly on transplantation. Therefore, donors and families have not had the chance to receive information about becoming a research donor, and in turn have to make the decision at the point-of-donation.
3 I n Australia, researchers have historically received eye donations as gratis. They have not had to budget and therefore do not have the resources ready to reimburse the bank.
4. D emand from Australian researchers has increased in the last five years, meaning the few donations that are available must now stretch across more research projects.
5. A s researchers now require access to ‘big data’, individual research projects are now seeking greater quantities of donations. These are often above the ability of the current system. Collectively, this means researchers, regardless of obtaining ethics and bank approval to receive tissue, do not receive access to enough donations in their expected time frame.
This means some researchers may have to amend their research protocol timeline and/or design.
While addressing system-wide issues will take some time, researchers who need access to deceased human eye donations can help improve their access to tissue long term by connecting with their nearest bank before submitting grants and ethics applications.
This will allow the bank to provide practical guidance on how to access donations to prepare the research team for any challenges ahead. Lastly, everyone can help share forward the importance of becoming an end-of-life donor for transplantation, training and research, and register themselves on the Australian Donatelife Register at: www.donatelife.gov.a/register-donor-today.
NOTE: Find a local eye bank: ebaanz. org/about-us/#Eye-Bank-Members
Further reading: Machin H, Brown K, Sutton G, Baird P. Ocular Tissue for Research in Australia: Strategies for Potential Research Utility of Surplus and Transplant-Ineligible Deceased Donations. Translational Vision Science and Technology. April 2020, Vol.9, 4. doi: doi.org/10.1167/tvst.9.5.4
Name: Heather Machin
Qualifications: RN MBA PhD
Primary place of work: The Lions Eye Donation Service and Corneal Research
Unit, Centre for Eye Research Australia
Position: CERA Biobank Lead, Senior
Project Manager
Location: Melbourne
Years in profession: 21
68 INSIGHT September 2023 SOAPBOX
THE DONATION SYSTEM HAS BEEN ESTABLISHED TO SUPPORT TRANSPLANTATION, WITH RESEARCH DEMAND EMERGING AS AN AREA OF SECONDARY NEED.
The latest 2021 data shows there were 1,472 deceased eye donors.
2023 CALENDAR
SEPTEMBER
ORTHOKERATOLOGY SOCIETY OF OCEANIA CONFERENCE
Gold Coast, Australia
1 – 3 September
www.facebook.com/OrthoKSO/
O=MEGA23 & WORLD CONGRESS OF OPTOMETRY
Melbourne, Australia
8 – 10 September omega-event.org
EUROPEAN SOCIETY OF CATARACT & REFRACTIVE SURGEONS CONGRESS
Vienna, Austria
8 – 12 September congress.escrs.org/
INTERNATIONAL VISION EXPO WEST
Las Vegas, US
14 – 17 September west.visionexpo.com
NEURO-OPHTHALMOLOGY SOCIETY OF AUSTRALIA CONFERENCE
Adelaide, Australia 21 – 22 September (training day to be held 23 – 24 September) nosa.net.au/2023-meeting
SILMO PARIS
Paris, France 29 September – 2 October event.silmoparis.com/2023/en/
OCTOBER
RANZCO SCIENTIFIC CONGRESS
Perth, Australia 20 – 23 October ranzco.edu/events
ORTHOPTICS AUSTRALIA ANNUAL CONFERENCE
Perth, Australia 21 – 24 October orthoptics.org.au
EYECARE PLUS BOOTCAMP AND AGM
Sydney, Australia 27 – 28 October y.safier@eyecareplus.com.au
NOVEMBER
HONG KONG INTERNATIONAL OPTIC FAIR
Hong Kong 8 – 10 November hktdc.com/event/hkopticalfair/en
SILMO INSTANBUL
Istanbul, Turkey 23 – 26 November silmoistanbul.com/en
DECEMBER
ASIA PACIFIC TELEOPHTHALMOLOGY SOCIETY CONGRESS
Pattaya, Thailand
2 – 3 December 2023.asiateleophth.org
All Specsavers stores now with OCT
$40k Sign-on bonus
To list an event in our calendar email: myles.hume@primecreative.com.au
THE 16TH CONGRESS OF THE ASIA-PACIFIC VITREO-RETINA SOCIETY (APVRS) 2023
Hong Kong
8 – 10 December 2023.apvrs.org
JANUARY 2024
SKI CONFERENCES FOR EYECARE PRACTITIONERS
San Vigilio, Italy
13 – 20 January skiconf.com
FEBRUARY 2024
MIDO EYEWEAR SHOW Milan, Italy
3 – 5 February mido.com
MARCH 2024
SKI CONFERENCES FOR EYECARE PRACTITIONERS
Furano, Japan
3 – 10 March skiconf.com
Optometrist
opportunities
in Regional Australia
Although 2023 has been a challenging year across the world, Specsavers continues to show steady growth, with 11 new stores already opened this year and more to come. This growth is creating more opportunities for patient focused optometrists to join us. We offer flexible rosters to support work/life balance, access to the latest technology (including OCT in every store free for every patient) and extremely attractive salaries – with $40k sign-on bonuses in selected locations. We will provide you with excellent opportunities for career development – including Pathway to Partnership, outreach opportunities and the chance to mentor new graduates. Join us now!
Optometrist opportunity –
Specsavers New Plymouth, NZ
Seeking a talented optometrist to join our extraordinary team at Specsavers New Plymouth. We offer cutting-edge technology, a friendly environment, and a commitment to professional growth. Embrace the breathtaking
beauty of the region and enjoy a perfect work-life balance. Explore stunning coastal views and immerse yourself in a vibrant arts scene. Don’t miss this incredible opportunity to be part of Specsavers New Plymouth. Apply now and unlock a rewarding journey in one of New Zealand’s most spectacular locations.
Optometrist Joint Venture Partnership Opportunity –Devonport, TAS
Specsavers are currently on the lookout for a passionate Optometrist who understands what it takes to lead a team, to join as a Joint Venture Partner at our established store in Devonport, Tasmania. Devonport is a beautiful coastal city located on the northwest coast of Tasmania, the city is surrounded by natural beauty, rich history and vibrant culture. Devonport is a captivating city that provides a warm and welcoming atmosphere with plenty happening throughout the year.
Locum opportunity at Canberra
As weekday opportunities in metro Sydney are not as plentiful, we encourage locums to look
further out. We have great opportunities throughout the rest of the year to secure block locum work in the ACT. With all your accommodation, flights, and car hire covered, now is the time to explore the nation’s capital and fill up your diary supporting multiple stores across the CBD Graduate Opportunities in Tasmania and regional Queensland
The Specsavers Graduate Recruitment Team have a number of exciting opportunities available across regional QLD & Tasmania. Whether it be for a new challenge, or starting a new lifestyle – a move to regional Australia could be your first step in an rewarding career.
Specsavers are the largest employer of Graduate Optometrists throughout Australia and New Zealand, and we have continued to develop our comprehensive two-year Graduate Program which provides newly qualified optometrists with a dedicated in-store mentor and structured program.
In a few short years, Specsavers has achieved market leadership in Australia and New Zealand with more people choosing to have their eyes tested and buy their prescription eyewear from Specsavers than any other optometrist. To learn more about these roles, or to put your hand up for other roles as they emerge, please contact us today:
Joint Venture Partnership opportunities enquiries: Kimberley Forbes on +61 (0) 429 566 846 or E kimberley.forbes@specsavers.com
Australia Optometrist employment enquiries: Marie Stewart – Recruitment Consultant marie.stewart@specsavers.com or 0408 084 134
Locum employment enquiries: Matthew Cooney matthew.cooney@specsavers.com or 0447 276 483
New Zealand employment enquiries: Chris Rickard –Recruitment Consultant chris.rickard@specsavers.com or 0275 795 499
Graduate employment enquiries: apac.graduateteam@specsavers.com
Specsavers YOUR CAREER, NO LIMITS Visit spectrum-anz.com
TALK!
LET’S
People
ON THE MOVE
monthly bulletin keeps the Australian ophthalmic sector updated on new appointments and personnel changes, nationally and globally.


up collaborative care and supporting optometrists to practise to full scope. Yapp commenced in his new role in early August 2023, while also continuing in his current role as the Head of Clinical Operations and Teaching at the Centre for Eye Health (CFEH). He joined CFEH at its inception in 2009.






EMAIL EDITOR MYLES HUME AT MYLES.HUME@PRIMECREATIVE.COM.AU TO BE FEATURED.
CAREER
70 INSIGHT September 2023

©2023 Alcon Laboratories Pty Ltd. AUS: 1800 224 153; Auckland NZ: 0800 101 106. ANZ-VC-2300022 Restock your Alcon trial lenses in a clicks few Download MyAlcon FitSCAN to get started.

CUSTOMISE YOUR
TO YOUR
Join the OPSM team. We have the scale and resources to help you personalise your position and choose your career path based on your goals. Accelerate your career aspirations with OPSM. Visit opsm.com.au/careers today.
ROLE
CAREER ASPIRATIONS

























































 The Eyerising Myopia Management Device.
The Eyerising Myopia Management Device.
























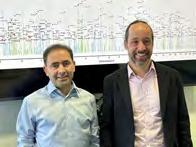

























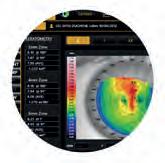






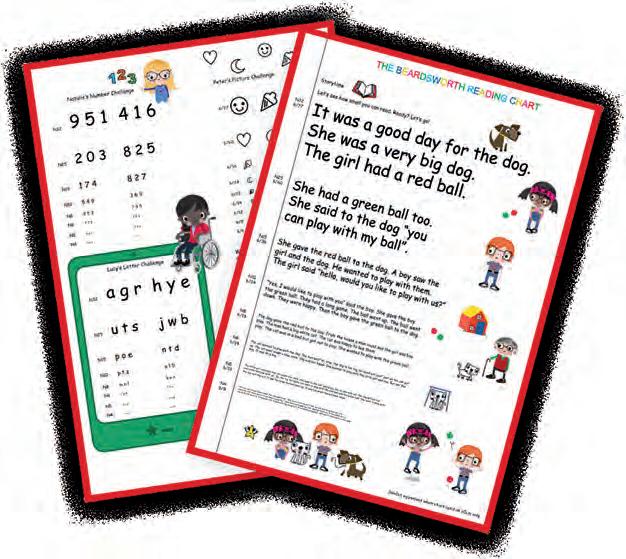









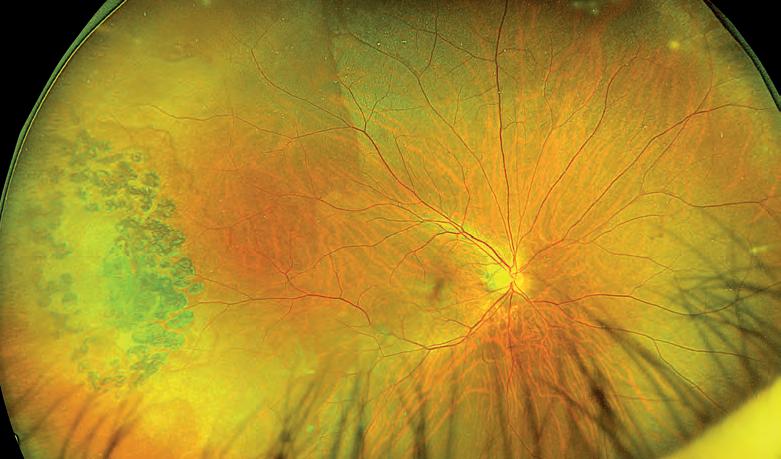


























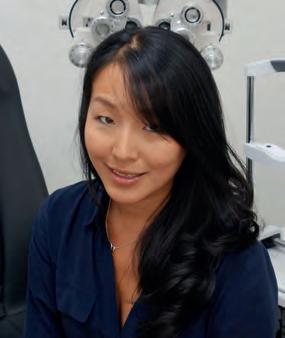






















































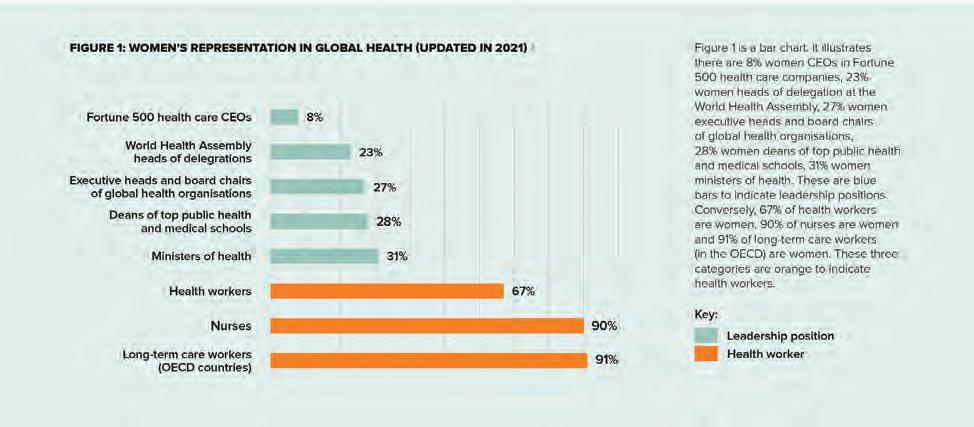






































 BY HEATHER MACHIN
BY HEATHER MACHIN