UNDER IMMENSE STRESS
Near-record levels of cataract patients are waiting more than a year for surgery.
RANGE
Stocking and selling the right mix of eyewear can reap major benefits for independents.

KERATOCONUS
Local projects tackling a disease that significantly deteriorates quality of life.
03
19
41
NOV 2022 INSIGHT NOVEMBER 2022 Front cover FAF.indd 1 4/10/2022 5:51:17 PM
SAY ‘I DO’ to your new Specsavers optometry business
with average annual sales of $3 million per store
with no upfront capital investment that guarantees a fortnightly pay cheque and five weeks annual leave delivers strong and sustainable profits that’s investing over $70 million in marketing every year where I can make a genuine impact on community eye health where community partnerships are real, enduring and worth millions of dollars every year
With a network of over 400 partner-owned stores producing average annual sales of $3 million each, Specsavers continues to have a growing impact on the Australian eye care landscape – and also on the lives and livelihoods of our current army of 800+ optometrists, dispensing and audiology professionals who have joined us as partners in their own stores. Profits are strong and sustainable, investment in technology is supporting ever improving health outcomes and our community partnerships are real and enduring with millions of dollars raised and distributed every year. So, if you are an ambitious optometrist, dispensing or optical retail professional keen to discover the benefits of a proven partnership model, talk to us today.
Visit spectrum-anz.com or contact Kimberley Forbes on +61 (0)429 566 846 or kimberley.forbes@specsavers.com.


that has uncertain store performance that requires personal bank borrowing to get started that doesn’t guarantee a regular salary that is a mix of partner-owned stores competing with company owned stores that under-invests in TV, radio and print marketing that is not committed to investing in OCT for every patient as part of standard eye care
where community ‘partnerships’ may not be as real as presented
‘I DO’ want to be an owner in a partnership
‘I DON’T’ want to be an owner in a group
NSW CATARACT PATIENTS WAITING MORE THAN 365 DAYS FOR SURGERY NEAR RECORD LEVELS
Despite a perception the Australian health system has moved past the worst of COVID-19, NSW public ophthalmology departments have never been under as much pressure, according to the Australian Society of Ophthalmologists (ASO), as new figures reveal near-record levels of cataract patients waiting more than a year for surgery.
The comments from ASO’s president Associate Professor Ashish Agar, who operates publicly at Sydney Eye Hospital and for the Prince of Wales Hospital’s outreach service in remote NSW, come in response to the latest Bureau of Health Information (BHI) statistics that also reveal which public eye departments are struggling to recover from
surgery shutdowns, creating greater inequity in the system.
“From the Federal Government down, there’s a myth that COVID’s over and therefore everything's back to normal,” Agar said.
“But the reality is the workforce has never been under more stress, more overworked, and more burnt out. In the early days, it was unusual for any of our staff to be off sick with COVID because we were protected, but that's now gone and so there's not a week that goes by without doctors and nurses being unwell. In some respects, the situation is actually worse than it ever was.”
The latest BHI figures from the April to June 2022 quarter shows only 64.2% of cataract surgeries were performed on time, a stark drop from the 93.1% rate at the
same time last year. The numbers were similar for all ophthalmology surgery categories in the state.
However, it’s important to note that between these reporting periods the Delta and Omicron COVID-19 strains caused intermittent elective surgery shutdowns in 2021/22, with
the NSW Government labelling January-March 2022 one of the most challenging quarters on record for surgery.
According to BHI, there were 98,625 patients on the total NSW elective surgery waiting list at the end of June, down 2.3% (2,286) from the end of March. At the end of the quarter, 18,748 patients had waited longer for elective surgery than clinically recommended, the highest of any quarter since BHI began reporting in 2010.

Cataract surgery was the biggest contributor to this, with 2,417 patients waiting longer than recommended (365 days in most cases). This was the highest
HUB AN ‘EXEMPLAR OF WHAT CAN BE ACHIEVED’
As Insight went to print, Lions Outback Vision (LOV) officially opened its new Kimberley Eye Hub in Broome, WA, a service that RANZCO says is a blueprint for others to follow in addressing inequitable access to eyecare in regional Australia.
The service, which was the brainchild of LOV founder Associate Professor Angus Turner, was officially opened on 3 October in a ceremony attended by Senator Patrick Dodson and Ms Divina D’Anna MLA. It will provide greater equity of eye health services and transform patient care in remote, regional and vulnerable Aboriginal communities across the North West comprising the Kimberley and
Pilbara regions.
The hub opened its doors in April 2021, but last month’s launch marked the completion of the second phase of building works, which was formerly the Kimberley Klub backpacker hostel. It was donated to LOV by the Wen Giving Foundation and Hawaiian Group and has since undergone a significant transformation, while retaining the distinctive façade of the hostel.
Ultimately, the facility will provide permanent specialised eye health services in Broome and outreach to 20 communities and five regional towns across the Kimberley. It includes a full-service eye clinic with state-of-the-art diagnostic
equipment, education and training spaces, a café and facilities for multi-disciplinary use by visiting specialists.
There are three resident LOV doctors, two resident optometrists and a number of other staff.
Turner, the McCusker director of LOV, said the model bridged geographical barriers. It will also build on the impressive work of LOV staff who, in 2021, treated more than 13,800 patients, including 3,000+ Aboriginal and Torres Strait Islander patients. Total treatments included 1,400 telehealth consultations and more than 900 eye surgeries.
RECOGNISING UVEAL MELANOMAS
To assist optometrists in early detection of uveal melanoma, Dr Lily Rolfe, Dr Daniel McKay and Dr Rod O’Day discuss the disease's epidemiology and introduce a scoring system to estimate malignancy and facilitate referrals (0.5 CPD).
 AUSTRALIA’S LEADING OPHTHALMIC MAGAZINE SINCE 1975
AUSTRALIA’S LEADING OPHTHALMIC MAGAZINE SINCE 1975
NOV 2022
continued page 8
There were 19,418 NSW patients ready for cataract surgery in the Apr-Jun 2022 quarter.
continued page 8
page 50






IN THIS ISSUE
EDITORIAL
A HERO DOING THEIR JOB
Often the most fulfilling work for eyecare professionals comes when a patient’s vision is restored or preserved. Think uncorrected refractive error, cataracts, glaucoma or macular disease. But the eyes can provide an early window into more sinister diseases lurking beneath and, increasingly, the role of the optometrist and ophthalmologist is extending into life-saving work.
As a health professional, what could be more satisfying than saving a life?
EYEWEAR SELECTION

The frames range can be a defining feature of independent practices, so it’s important to get right.
‘PODTHALMOLOGY’
Melbourne’s Dr Lana Del Porto is hosting a new thought-providing podcast for ophthalmologists.


KERATOCONUS CARE
Surendran Naidoo, an optometrist from Specsavers Dapto, can attest to this. He was recently awarded the company’s Dame Mary Perkins Award (page 32) after visual fields testing revealed a bitemporal hemianopia. Knowing this as a classic sign of a pituitary tumour, he urgently referred the patient who received surgery within days.
Despite earlier health complaints that now appear linked to the patient’s tumour, Naidoo found the root cause when other health professionals simply treated the symptoms. And the patient’s neurologist later remarked they were surprised she was still alive.

The rise of systemic diseases like diabetes and hypertension are another, more common, area where eyecare professionals are playing a vital role, helping patients address – and some cases reverse – their condition in the earlier stages.
Uveal melanoma also carries a mortality risk; as primary care providers, optometrists have a vital first-line role. And how this can be managed, and distinguished from benign conditions is detailed in a CPD article (page 50) co-authored by leading Melbourne ocular oncologist Dr Rod O’Day.

It’s thought almost 300 diseases can first be diagnosed by an optometrist, and the ability to image the retinal microvasculature with modernday equipment has become an important puzzle piece. But the technology is only as good as the eyecare professional interpreting the scan and, as this edition demonstrates, Australia should count itself lucky for a network of optometrists and ophthalmologists that prioritise continuous improvement and put patients first.
MYLES HUME Editor

25 28
BUDDING CAREER
Early-career G&M optometrists discuss what it’s like working with leading Australian professionals.
46
Dr Brendan Cronin explains how optometrists can nail their role in managing keratoconus (0.5 CPD).
19
FEATURES NOVEMBER 2022 07 UPFRONT 09 NEWS THIS MONTH 53 OPTICAL DISPENSING 54 ORTHOPTICS AUSTRALIA 55 MANAGEMENT 56 PEOPLE ON THE MOVE 57 CLASSIFIEDS/CALENDAR 58 SOAPBOX EVERY ISSUE INSIGHT November 2022 5








ZEISS AU: 1300 365 470 NZ: 0800 334 353 med.au@zeiss.com ZEISS CLARUS Colour. Clarity. Complete. Compromising image quality may leave some pathology unseen. The ZEISS CLARUS is the next generation fundus imaging system that provides true colour and high resolution in a 200 degree ultra-widefield image. www.zeiss.com/CLARUS Imaging ultra-wide without compromise. ZEISS HD Ultra-widefield Dry Age-related Macular Degeneration FAF-Green Geographic Atrophy FAF-Blue Proliferative Diabetic Retinopathy Fluorescein angiography Choroidal Nevus Red channel separation Proliferative Diabetic Retinopathy Green channel separation Retinal Nerve Fibre Layer Blue channel separation Carl Zeiss Pty Ltd, NSW 2113 AUSTRALIA. Carl Zeiss (NZ) Ltd, AUCKLAND 1026 NZ.
UPFRONT
Just as Insight went to print, LIONS EYE INSTITUTE published an Australian-first study showing ancestry may be a factor in the effectiveness of low-dose atropine for myopia. Overall, the study showed 0.01% atropine had a modest effect – slowing progression by 35%, and eye growth by 33%, after 18 months. But they were very effective in children of European descent – slowing myopia progression and eye growth by 50% in the first year. In children of mixed Asian-European and other non-Asian descent, the drops were even more effective, slowing myopia by 59% and eye growth by

n WEIRD
A new study, published in Psychology of Consciousness: Theory, Research, and Practice has revealed an unconscious tactic magicians may adopt to deceive their audiences. The researchers suggest magicians increase their blink rate when performing difficult tricks, which may encourage synchronised blinking in the audience, so spectators are more likely to miss deceptive actions.
n WONDERFUL
Guide Dogs Australia announced Coles Mackay in Queensland has taken out the honour of having the top fundraising coin Collection Dog in the country. The iconic Collection Dog at Coles has been changing lives for those who use the service, raising more than $800,000 nationally for Guide Dogs Australia in the last financial year.
n WACKY
A woman with an eye injury was airlifted out of Wee Waa, located in the New England region in NSW, after falling on a wine glass.
According to The Northern Daily Leader, the 42-year-old was airlifted on 24 September due to flooding in the area and the seriousness of her injury.
96%. But 0.01% atropine did not have an effect in children with solely an East/South Asian ancestry. The authors recommend these patients may require a higher dose of atropine.
IN OTHER NEWS, for the fourth consecutive year, Australian optometrists face a registration fee hike. The Optometry Board of Australia (OBA) announced the fee for 2022/23 will be $337. This represents a 3% increase on the 2021/22 fee ($327), which is “an increase limited to indexation”. The fee for optometrists whose principal place of practice is NSW, which are calculated by a separate authority, will remain at $323. “The board strives to keep fees low while ensuring they are set at a rate that allows us to realise our
STAT
READY FOR REFORM
vision and mission of keeping the public safe and retaining the community’s confidence and trust in optometrists,” OBA chair Mrs Judith Hannan said. FINALLY, EssilorLuxottica has launched a share buyback program, with plans to purchase up to 1.5 million shares, depending on market conditions, until 31 March 2023. The acquired shares will be awarded or transferred to employees and corporate directors of EssilorLuxottica and affiliated companies, particularly for profitsharing plans, bonus and performance share awards, stock option plans, and employee share ownership plans. The program reflected the group’s “confidence in its value creation and long-term prospects”, it said.
Published by: 379 Docklands Drive, Docklands VIC 3008 T: 03 9690 8766
www.primecreative.com.au
Chief Operating Officer Christine Clancy
christine.clancy@primecreative.com.au Group Managing Editor Sarah Baker sarah.baker@primecreative.com.au Editor Myles Hume myles.hume@primecreative.com.au Journalist Rhiannon Bowman rhiannon.bowman@primecreative.com.au Commissioning Editor, Healthcare Education
Jeff Megahan
Business Development Manager Luke Ronca
luke.ronca@primecreative.com.au
Client Success Manager Justine Nardone
justine.nardone@primecreative.com.au
Design Production Manager Michelle Weston
michelle.weston@primecreative.com.au
Art Director Blake Storey
WHAT’S ON
THIS MONTH APVRS 2022
18 – 20 NOVEMBER
The Asia-Pacific Vitreo-retina Society Congress in Taipei attracts leading vitreoretinal specialists from around the world to share their knowledge and experience.
NEXT MONTH OPHTHALMOLOGY INNOVATION SUMMIT
2 – 3 DECEMBER
Industry, clinical, and capital leaders will gather at the two-day event in San Deigo for the latest in anterior and posterior eye therapies. ois@healthegy.com
Graphic Design Michelle Weston, Kerry Pert, Louis Romero Subscriptions T: 03 9690 8766
subscriptions@primecreative.com.au
The Publisher reserves the right to alter or omit any article or advertisement submitted and requires indemnity from the advertisers and contributors against damages or liabilities that arise from material published.
© Copyright – No part of this publication be reproduced, stored in a retrieval system or transmitted in any means electronic, mechanical, photocopying, recording or otherwise without the permission of the publisher.

2022.apvrs.org Complete calendar page 57. insightnews.com.au
The Prostheses List contains 11,600 items and in 2019-20 more
than
3.1
million surgical devices
were provided at a cost of $2.1 billion. Page 38 INSIGHT November 2022 7
PUBLIC HOSPITAL EYE CLINIC CAPACITY IN DECLINE
number among all surgeries in the quarter, ballooning from just 76 patients a year ago.
And it’s the second highest number on record for cataract surgery. Since BHI records began in 2010, pre-pandemic the highest number of patients waiting longer than recommended peaked in 2015 at just 133 patients. Since COVID, it spiked to 1,954 in the April-June quarter in 2020, but was then whittled down to 76 patients in April-June 2021. Due to the 2021 lockdowns, it then spiked to a record high of 2,565 in the January-March 2022 quarter and dipped slightly to 2,417 in the latest April-June 2022 figures.
In terms of cataract surgeries performed on time, the Hunter New England Local Health District (LDH) was the best in AprilJune 2022 at 97.4%, while South Eastern Sydney achieved the lowest, with just 24.1% performed on time compared to 99.9% at the same time last year.
Agar said “unacceptably long” waitlists were already a problem in NSW prior to the pandemic, before COVID “knocked everything for six”.
To continue and catch up with surgeries, some hospitals outsourced surgeries to private hospitals, while others chose not to.
“You've got some centres, particularly out west, that managed to continue by using spare capacity in a private system
and then you've got other centres who refused to or shut up shop completely, creating this incredible gulf between what one health district was doing compared to the other, which has exacerbated the inequity,” Agar said.
“The other important point is these published figures hide the true scale of a problem, which is actually the waiting list to get on the waiting list. There is anywhere from a 12- to 18-month or more wait to get into a clinic to be then assessed for whether you're appropriate for surgery, before then going on a surgery waitlist of more than 12 months for many patients.
“Whatever these figures show for cataract surgery, add an extra year or two to everything that you're seeing – and then you'll start getting a true picture of what's happening.”
PUBLIC EYE SERVICE DECLINING
In response to the latest BHI figures, the Australian Medical Association (AMA)’s NSW branch said it was further proof the Federal Government needed to commit to a 50/50 funding split.
While funding was part of the solution, Agar said it needed to be well-directed, instead of desperate bids to be reelected, noting that surgery waitlists tended to open up six months out from a state election.
“At the core of it is a public ophthalmology presence. We’ve seen the
number of hospitals with public eye clinics reduce decade-on-decade for probably the last 30 years, so the public's access to free eyecare is going backwards,” he said.
“This is something that no government has managed to get their head around – and without that, there’s no solution.
Without a strong public system, the private system is left to pick up the pieces and the cost will be borne by those who can least afford it.”
AMA NSW president Dr Michael Bonning said it was good to see elective surgery activity was picking up. While fewer elective surgeries were performed than the historically high numbers a year earlier, NSW elective surgery activity in April-June 2022 was up 41.1% (15,649) compared with January-March 2022, when non-urgent surgery was suspended for a period.
“There is a need to address long elective surgery waitlists and we want to see the state adequately fund this work to be done in public hospitals, rather than outsourced to private hospitals,” he said.
Bonning added that the state must address the workforce shortages that are contributing widespread burnout among doctors.
“We know from member feedback that there are unprecedented levels of fatigue for doctors at all career stages. It is having a detrimental effect on doctors’ health and wellbeing and makes it more difficult to provide high quality patient care.” n
SERVICE HOPES TO ADD DAY SURGERY IN BROOME
exemplar of what can be achieved with vision, pragmatism and collaboration.
“The hub enables us to treat patients closer to home, and this accessibility is crucial in dealing with the challenges of remote eye health. People in isolated places like the North West have more blindness and complications from eye disease than in other places,” he said.
“In particular, Aboriginal and Torres Strait Islander people have more than three times the rates of blindness and 14 times the rates of vision loss from diabetes.”
Approximately 11% of the North West Aboriginal Islander population are vision impaired or blind, and 35% of this population have never had an eye exam.
RANZCO president Professor Nitin Verma described the service as an

“I had the pleasure of visiting Angus in May last year. It is amazing to see the progress he has made in such a short amount of time. The service brings the concept of equity of access to life – creating a hub for a population dispersed over our vast and sunburnt country,” he said.
“It is a model for others to follow and a blueprint for RANZCO as we bring Vision 2030 and beyond to fruition. Angus’ commitment to equity is commendable and it is a commitment shared by so many ophthalmologists across Australia and New Zealand. It is the collective vision of the college, and we are proud to support Angus and his team
on their endeavours.”
Turner said the development of the hub had also enabled the LOV team to put resources into prevention and education activities in communities. He said the next goal was to develop a day surgery in Broome, which would alleviate pressure on the Broome Hospital and enable more timely surgical and treatment interventions.
In addition to the Wen Giving Foundation and Hawaiian Group, the hub has been supported by the Western Australian and Federal governments, Kerry Stokes and Christine Simpson Stokes, McCusker Charitable Foundation, Channel 7 Telethon Trust, Fred Hollows Foundation, Rural Health West and industry partners including ZEISS, Alcon and Topcon. n

continued from page 3 continued from page 3
8 INSIGHT November 2022
“THESE PUBLISHED FIGURES HIDE THE TRUE SCALE OF A PROBLEM, WHICH IS ACTUALLY THE WAITING LIST TO GET ON THE WAITING LIST”
ASHISH AGAR, ASO
The Kimberley Eye Hub in Broome.
NEWS
n LASER OR SPECS?
LASIK eye surgery is more cost effective than some other forms of vision correction, a new study shows. A study of 1,050 people, conducted by a consortium of ophthalmologists and optometrists known as MyVision.org, found US consumers who require vision correction pay about US$500 (AU$778) annually for glasses, contact lenses, eye exams and insurance, equating to a US$31,000 (AU$48,200) cost over their lifetime. This is compared to about US$100 (AU$155) annually for those who have had LASIK surgery. “If they get LASIK, the surgery will pay for itself in a little more than 10 years,” the study noted, pointing out the average cost is around US$5,264 (AU$8,196) in America for LASIK.
n OPTOMETRY SCOPE
California’s Governor, Mr Gavin Newsom, vetoed a move that would have allowed optometrists in the state to perform ophthalmic laser procedures and administer eye injections. Assembly Bill 2236 was passed by a one-vote margin before Newsom stepped in. “This bill would authorise optometrists to perform ocular surgical procedures currently performed by ophthalmologists after completing specified education and training,” he said. "This bill would allow optometrists to perform advanced surgical procedures with less than one year of training. In comparison, physicians who perform these procedures must complete at least a threeyear residency program.”
n ANTI-VEGF UPDATE
Brolucizumab (Beovu) for nAMD in the real-world appears to be effective and safe, consistent with data from pivotal trials, a new study has found. Brolucizumab’s Phase 3 HAWK and HARRIER trials showed non-inferiority with aflibercept in visual acuity gains and 50% were maintained on a 12-weekly dosing interval through week 48, but it has been associated with infrequent events of intraocular inflammation, retinal vasculitis and retinal vascular occlusion in 2.1% of treated nAMD cases. The researchers conducted a systematic review of 26 studies involving a 2,907 brolucizumab eyes. “[Our] observations are in line with those from the pivotal trials in the brolucizumab development program. Physicians are likely to have gained increased awareness of how best to manage potential risks."
A/Prof Nicole Carnt, UNSW.

REUSABLE CONTACT LENSES MORE THAN TRIPLE RISK OF RARE EYE INFECTION
UNSW’s Scientia Associate Professor Nicole Carnt is the first-author of a new study showing wearers of reusable contact lenses are nearly four times as likely to develop a rare sight-threatening eye infection than daily disposable wearers.
The case control study, published in Ophthalmology and involving UCL and Moorfields researchers in London, also identified multiple factors that increase the risk of Acanthamoeba keratitis (AK) – including reusing lenses, wearing them overnight or in the shower – and highlighted “regulatory deficiencies” that mean online contact lens purchasers may not receive important educational information.
AK is one type of microbial keratitis (MK) that causes the cornea to become painful and inflamed. The most severely affected patients (a quarter of the total) end up with less than 25% of vision or become blind and face prolonged treatment. Overall, 25% require corneal transplants.
For the study, the researchers recruited more than 200 Moorfields Eye Hospital patients who completed a survey, including 83 people with AK, and compared them with 122 as part of a control group.
They found people who wore reusable soft contact lenses, such as monthlies, had 3.8 times the odds of developing AK, compared to people who wore daily disposables.
Showering with lenses increased AK likelihood by 3.3 times, while wearing lenses overnight increased them by 3.9 times. Among daily disposable wearers, reusing their lenses increased their infection risk. Having had a recent contact lens check with a health professional reduced the risk. With further analysis, the researchers estimated that 30-62% of cases in the UK, and potentially in many other countries, could be prevented if people switched from reusable to daily disposable lenses.
“Contact lenses are generally very safe but are associated with a small risk of microbial keratitis, most commonly caused by bacteria, and which is the only sight threatening complication of their use,” lead author Professor John Dart, from UCL Institute of Ophthalmology and Moorfields Eye Hospital NHS Foundation Trust, said.
“Given an estimated 300 million people
across the globe wear contact lenses, it's important people know how to minimise their risks for developing keratitis.”
Carnt, from the UNSW School of Optometry and Vision Science in Sydney, UCL Institute of Ophthalmology and Moorfields Eye Hospital, said previous studies had linked AK to wearing contact lenses in hot tubs, swimming pools or lakes.
“And here we have added showers to that list, underlining that exposure to any water when wearing lenses should be avoided. Public pools and coastal authorities could help reduce this risk by advising against swimming in contact lenses,” she said.
According to the researchers, contact lenses are medical devices so manufacturers are required to include information on safe use and risks.
However, manufacturers in the UK and European Union are reportedly using an exception to this requirement, reasoning wearers will have received this information and training from their prescriber.
“Now that lenses are available to consumers on the internet without professional involvement (20/85 in this study) in the UK and European Union – but not in the United States – many users may have no training or ongoing education in safe contact lens use,” the researchers reported.
“In the UK and European Union, and for soft lenses in the US, information on lens safety and risk avoidance recommendations is absent in lens packaging where the ‘do’s and don’t’s’ needed to reduce the risk of keratitis might be reinforced at each purchase.
"Instead, users are directed to access ‘Patient information/instruction for use’ guides on contact lens company websites or from their practitioner; these provide variable information about MK risks and risk avoidance.”
Dart said contact lens packaging should include information on lens safety and risk avoidance, even as simple as ‘no water’ stickers on each case.
“Basic contact lens hygiene measures can go a long way in avoiding infections, such as by thoroughly washing and drying hands before putting in lenses,” he said. n
IN BRIEF
INSIGHT November 2022 9
AUSTRALIAN GRANT HANNAFORD CROWNED INTERNATIONAL OPTICIAN OF THE YEAR
Prominent Australian optical industry figure Mr Grant Hannaford has been recognised as the 2022 International Optician of the Year at SILMO Paris.
Hannaford was one of only four finalists, including fellow Australian Ms April Petrusma, to be shortlisted for the award bestowed by the International Opticians Association (IOA) at SILMO.
The award, first given in 2018, recognises the importance of the optician in optical business and their role in the choice of optimum products for their clientele.
Hannaford’s wife and business partner, Ms Thao Hannaford, congratulated her husband on his award and thanked the IOA and SILMO Paris for providing the opportunity for opticians around the world to be recognised for their incredible work.
“His career in the optical industry spans over 27 years beginning as a practising dispensing optician, an aid worker recognised by the Australian Government, positions on industry boards past and present, a university lecturer to more recently a clinical researcher,” she said.
“I know I speak on behalf of Australia when I say we are incredibly proud of Grant who has become the bridge connecting optometry and optical
dispensing, creating a clinical practice model for the benefit of our patients so we may provide them with the best possible outcomes.”
The IOA said Hannaford, who is cofounder and director of the Academy of Advanced Ophthalmic Optics, has made Hannaford Eyewear the destination for leading edge innovation and excellence in clinical care for the Southern Highlands in Australia, as well as delivering optical dispensing training for optometrists at the University of New South Wales.
“Together with my wife, Thao, we have grown Hannaford Eyewear over the past 18 years from a single optometrist practice to a multi-practitioner location, quadrupling revenues in the process,” Hannaford said.
The IOA said the Hannaford’s had developed and mentored more than 50 staff in optometry, optical dispensing and administrative roles, a number whom now operate their own business as a result.
Hannaford Eyewear recently won the optometrist category in the 2022 Australian Small Business Champion Awards.

“Grant has also developed the Academy of Advanced Ophthalmic Optics where he has been a mentor, provided practitioner education on the implementation of advanced ophthalmic lenses and been recognised and accredited by the Optometry Board of Australia as an avenue for continuing education with General Optical Council accreditation forthcoming,” the IOA said.
IOA president Ms Fiona Anderson presented the 2022 International Optician of the Year award.
“I am delighted Grant has been awarded this prestigious award. He embodies an optician whose patients are at the heart of all that he does. A truly worthy winner and he deserves our hearty congratulations,” she said.
In addition to the title and certificate, Hannaford also received lifetime IOA membership and a trip to SILMO Paris 2023. n
FREMANTLE HOSPITAL OPENS NEW $5.5 MILLION PUBLIC OPHTHALMOLOGY UNIT

Fremantle has opened a new $5.5 million ophthalmology unit, bolstering one of the hospital’s busiest departments that sees almost 200 patients a day.
Outpatients began accessing eye services in the newly designed and built public ophthalmology facility on 20 September after it was shifted from another part of the hospital.
With more than 180 patients passing through its doors every day, ophthalmology is one of the busiest outpatient services at Fremantle Hospital.
According to the Western Australian Government, the new facility has been designed to suit the unique needs of the
service and its patients and paves the way for a major overhaul of mental health services at the site.

The ophthalmology unit was the final service to be relocated from 'V block' at Fremantle Hospital, which can now begin redevelopment works for the state government's new 40-bed mental health ward at the hospital.
The WA Government is investing $45.5 million to fund the 40-bed mental health redevelopment at Fremantle Hospital. This includes $5.5 million for the ophthalmology unit.
"This new state-of-the art ophthalmology unit will deliver modernised facilities
for patients of this busy and growing outpatient service,” WA Health Minister Ms Amber-Jade Sanderson said.
"The relocation of the clinic is also an important milestone in our $45.5 million redevelopment of mental health services at Fremantle Hospital as the last service to be moved so the expansion can begin."
The 40-bed mental health development will transform Fremantle Hospital into a mental health hub, significantly boosting the current 64-bed inpatient admission capacity and providing better access to expert care for patients with a mental illness in the south metropolitan region. n
NEWS 10 INSIGHT November 2022
Fremantle Hospital.
IOA president Fiona Anderson presenting Grant Hannaford with the award at SILMO Paris. Image: Thao Hannaford/Linkedin.
What’'s



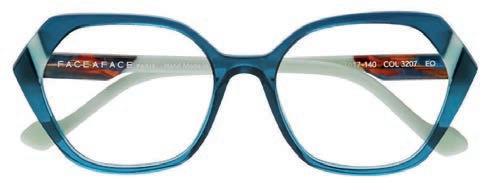


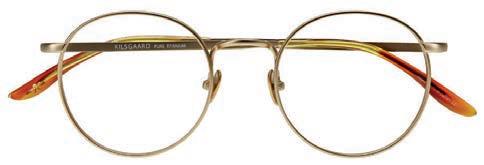




HOT Come with us as we explore this season’s gorgeous and colourful eyewear straight from France and Denmark. FACE A FACE PARIS - MEMFIS 2 9434 FACE A FACE PARIS - BOCCA SCULPT 2 0656 FACE A FACE PARIS - WITTY 2 3207 FACE A FACE PARIS - QUARTZ 2 4321 FACE A FACE PARIS - MERYL 2 8761 PRODESIGN DENMARK - HEXA 2 6345 PRODESIGN DENMARK - GAIL SPENCE ONE 9913 2721 KILSGAARD - TITANIUM 01 2021 WOOW - UPTOWN 1 1127 To view these models and more beautiful eyewear, visit www.eyesright.com.au
is aiming to understand what people know about gene technology through a survey led by Associate Professor Guei-Sheung Liu, principal investigator and head of the Genetic Engineering Research Unit.
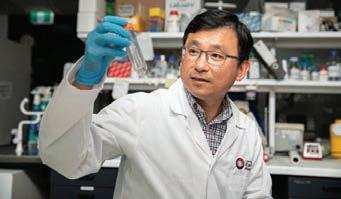
Liu and his team are interested in understanding the factors that influence people to undertake current and future gene therapies in order to inform the scientific community on how communication about future treatments should be delivered.
“It’s a little unusual for laboratory scientists to do this sort of research –we typically do work that is focused on understanding the biology of human cells,” Liu said.
“But now that we are introducing new technologies in treatments, we need to know how well the public understands these technologies and how they feel about it, so that we can think about introducing and integrating them into our healthcare system.”
Gene technology is opening the door to novel therapies for conditions that have previously been thought of as untreatable. Several gene therapies are already available to patients, but new, emerging technologies may transform how future treatments are developed.
“There has been a lot of development around traditional gene therapy over the last 10 years, with the aid of gene technology, particularly in eyecare, but little is known about what the public thinks about using gene technology to prevent, treat, or even diagnose disease,” Liu said.
“New therapies are being developed to repair the faulty genes, or replace them with working ones, to maintain cell function. We hope to have a clear understanding of what the public knows, and how they feel about it.” n
CHANGES TO MDFA RESEARCH GRANTS EVALUATION PROCESS
Macular Disease Foundation Australia (MDFA) has opened its 2023 research grant program, which will include a new Community Review Panel in the evaluation process for the first time.
MDFA made the announcement on World Sight Day 13 October, adding to the $5.1 million it has invested in 29 projects since the research grants program was launched in 2011.
Applications undergo peer review and rigorous evaluation based on the National Health and Medical Research Council (NHMRC) process. New to the 2023 evaluation process will be the Community Review Panel comprising of people living with a macular condition or directly supporting those with the disease.
As MDFA’s research program is funded through public donations, this change reflects the organisation’s desire to represent the voice of the macular disease community, recently-appointed CEO Dr Kathy Chapman said.

“Our research program exists because our community is deeply committed to advancing understanding of this disease,” she said.
“We hope that the Community Review Panel will contribute to the funding decisions through their lived experience, making the research we fund even more relevant to the needs of the community, as well as being scientifically rigorous.”
The Grant Family Fund – a legacy gift in honour of the late Faye Grant and her father Ronald Grant – will again offer a total pool of up to $100,000 for early-career researchers for “blue-sky” research.
Dr Anai Gonzalez Cordero, from the University of Sydney, was one of the first recipients. Her project aims to create a macula-containing organoid that could be used as a source of cells for replacement therapies and to test the efficacy of potential treatments.
“This type of blue-sky thinking is very hard to get funding for – it’s seen as highrisk,” she said. "But the Grant Family had a vision. They wanted to fund novel ideas. This sort of creativity and new ideas and research wouldn’t be funded otherwise.”
Applications close at 5pm (AEDT) 31 January 2023 before the successful applicants are announced in May 2023. n
HOYA Vision Care Australia and New Zealand has announced its most premium coatings will now be available on Nulux finished single vision lenses.
The company’s Diamond Finish coating will now be available standard with UV Control, at the current Diamond Finish price.
Full Control – HOYA’s four-in-one coating for everyday protection, including Diamond Finish, UV Control, BlueControl and Anti-Bacterial – will also be available on a wide range of HOYA Nulux single vision lenses.
“With the high levels of UV radiation we have in our part of the world, it’s particularly important for Australians and New Zealanders to have the front and back UV protection provided by UV Control,” HOYA Vision Care Australia and New Zealand managing director Mr Craig Chick said.

“And ever since we launched Full
Control, we’ve been asked by customers to have it available on Nulux stock lenses and now it is. Full Control overcomes the challenge of selling coatings as individual add-ons to patients who want the very best protection for their eyes.”
HOYA’s upgraded and expanded Nulux stock single vision range became available on 10 October 2022. n
12 INSIGHT November 2022
CERA SURVEY: WHAT INFLUENCES PEOPLE TO UNDERTAKE GENE THERAPY?
Centre for Eye Research Australia (CERA)
A/Prof Guei-Sheung Liu, head of the Genetic Engineering Research Unit at CERA. Image: Anna Carlile.
HOYA EXTENDS PREMIUM COATINGS TO NULUX SINGLE VISION RANGE
Full Control overcomes the challenge of selling coatings as individual add-ons.
Kathy Chapman, MDFA.
NEWS
Get Optos off your And into your practice
“We took out a leasing option on our optomap®. It’s easily paid for itself. It’s brought in new patients and has been a great practice builder. Patients are always amazed to look at their own eye in an optomap image! We only wish we’d got an optomap sooner…”

T: +61 8 8444 6500 Optos.com
Damon Ezekiel l Ezekiel Eyes
SPECSAVERS ANNOUNCES TOP OPTOMETRISTS AS PERKINS AWARD WINNERS FOR 2022
NSW-based Specsavers stores in Dubbo and Dapto, and the Hornby and Dunedin locations in New Zealand, were celebrated at the recent Specsavers Clinical Conference 2022, taking out the conference’s annual awards for clinical care and excellence.
This year’s Doug Perkins Medal winners were Ms Yvonne O’Sullivan, Mr Brian Thio and Ms Claire Curtin from Specsavers Dubbo, and Mr Lachlan Martin and Mr Hallie McCloy from Specsavers Hornby.
Specsavers ANZ head of clinical performance Mr Nick Gidas said the top 10 finalists represented the top 3% of practices in each country.
“The award is based on nationwide analysis using data collected through Specsavers clinical reporting. This information was combined with data from Specsavers’ patient feedback platform, as well as health outcome data from the Oculo electronic referral system,” he said.
“We were looking for practices that are leaders in delivering exceptional patient outcomes; that demonstrate a consistently outstanding patient
experience; that implement and improve store processes that deliver consistent quality eyecare; who are committed to accessible eye health and who lead a positive workplace and culture.”
The Dame Mary Perkins Medals were judged by leading industry professionals Diabetes Australia CEO Ms Justine Cain, The Fred Hollows Foundation CEO Mr Ian Wishart and Ms Pippa Martin, managing director of Glaucoma New Zealand. The awards were presented to two optometrists who stood out for going above and beyond in customer service, clinical care, clinical leadership or teamwork to benefit patient care.
They were Mr Surendran Naidoo, of Specsavers Dapto, and Ms Jennifer Robinson, from Specsavers Dunedin. Specsavers Dapto’s nomination was centred around the story of a patient who had a pituitary tumour detected in an eye test, leading to an urgent diagnosis and surgery that saved the patient’s life. More on this story can be found on page 34.
Similarly, Specsavers Dunedin’s
nomination involved a brain tumour detection and over and above follow up care for a young patient who required chemotherapy treatment.
It also described a day where Robinson, the award winner, saw an out-of-town farmer with a retinal detachment, requiring same day surgery. The farmer had come to Dunedin alone and had nowhere to park his ute and trailer while receiving the unexpected treatment which was causing him stress.
Robinson gave him her staff parking space until he had been given clearance to drive home so he could focus on recovery after surgery rather than city parking.
“All the nominees displayed incredible service for their patients and employed the values of Professor Fred Hollows,” Wishart said.
“They embodied kindness, compassion and integrity in their everyday lives. In the words of Fred himself, they truly demonstrate that ‘every eye is an eye,’ and ensure all people receive the care they deserve. Thank you for the opportunity to recognise their actions.” n
GLAUCOMA AUSTRALIA UNVEILS 2022 QUINLIVAN RESEARCH GRANT RECIPIENT

Glaucoma Australia and its patron Governor-General David Hurley have revealed the 2022 recipient of the charity’s ‘Quinlivan’ Research Grants Program.
This year’s research grant is awarded to Dr Owen Siggs, Associate Professor at the Garvan Institute of Medical Research, in his bid to develop a genomic risk stratification to improve glaucoma suspect triage in rural primary care.

Siggs said optometrists are often faced with difficult decisions regarding referral for a specialist glaucoma assessment. This is especially critical in a rural setting, where specialist glaucoma practitioners are in limited supply.
“Pinpointing individuals at highest risk of glaucoma blindness is a critical challenge, particularly for those in rural, regional, and remote areas where access to specialist care is limited,” he said.
“This study will test a new genetic risk prediction tool for glaucoma, to determine if it can help predict outcomes in glaucoma suspects presenting to rural optometry practices, with the ultimate aim of improving referral pathways for all glaucoma suspects.”
Siggs and his team will perform a world-first assessment of the utility of a glaucoma polygenic risk score to predict outcomes amongst glaucoma suspects assessed in a rural primary care setting.
“We hope the results of this study can be used to improve the ability of primary care practitioners to identify which glaucoma suspects require urgent referral to a specialist ophthalmology service, and which suspects can be monitored in a primary care setting,” he said.
“This could, in turn, improve the quality of treatment and monitoring for both high and low risk glaucoma suspects.”
Ultimately, Siggs hopes this research will play a key role in both increasing the rate of early detection as well as improving the treatment experience for people living with glaucoma. n
14 INSIGHT November 2022
Dr Owen Siggs, Garvan Institute of Medical Research.
Yvonne O’Sullivan, Specsavers Dubbo.
NEWS

NEW DATA ON MIYOSMART COMBINATION THERAPY WITH ATROPINE
Fresh insights into the effect of combination myopia treatment with the MiYOSMART defocus spectacle lens and low-dose atropine were presented at the recent International Myopia Conference (IMC) in The Netherlands.

Ophthalmic lens manufacturer HOYA Vision Care, a diamond sponsor of IMC held 4-7 September, hosted a myopia symposium where experts shared their latest findings of the clinical application of the MiYOSMART spectacle lens in myopia management.
Dr Andrea Lembo, of the University Hospital San Giuseppe Multimedica in Milan, Italy, shared the results of a clinical application of MiYOSMART in combination with 0.01% atropine drops in European myopic children and adolescents.
The results demonstrated that over one-year, axial elongation and myopia progression were reduced with maximum effect using the combination treatment, HOYA stated.
Meanwhile, Professor Hakan Kaymak from the Internationale Innovative Ophthalmochirurgie in Duesseldorf, Germany, presented the findings of his study on axial length growth under MiYOSMART treatment.
“The data of German children wearing the lens reconfirmed previous clinical study results” HOYA stated. “Further findings showed that children adapt very well to MiYOSMART spectacle lenses with no safety concerns even in combination with low-dose atropine.”
In addition, Professor Carly Lam, of The Hong Kong Polytechnic University, shared how myopia control effect may be influenced by baseline relative peripheral refraction (RPR) in children wearing the MiYOSMART spectacle lens with D.I.M.S. Technology. The results showed that myopia control effect was stronger in children with baseline hyperopic RPR than in children with baseline myopic RPR.
Since its launch in 2018, MiYOSMART is available in 28 markets, and became available in Australia and New Zealand in October 2020. n
AFLIBERCEPT 8MG TOUTED AS POTENTIAL STANDARD-OF-CARE
The drug company that produces Eylea (2mg aflibercept) has announced clinical trial results showing the anti-VEGF therapy can be delivered at a higher doses at longer intervals, with a similar safety profile.
"These pivotal aflibercept 8 mg trials demonstrated that nearly 90% of patients with diabetic macular edema (DME) and almost 80% of patients with wet age-related macular degeneration (wAMD) were able to maintain a 16-week dosing regimen," said Dr David Brown, director of research at Retina Consultants of Texas in the US and a trial investigator.
"These unprecedented durability data coupled with a safety profile consistent with that of Eylea support aflibercept 8 mg as a potential new standard-of-care in these diseases."
On 8 September, Regeneron Pharmaceuticals and Bayer announced the primary endpoints were met in two pivotal trials investigating novel aflibercept 8 mg with 12- and 16-week dosing regimens in patients with DME and wAMD. These were compared against an Eylea (2mg aflibercept) eight-week dosing regimen.
The PHOTON trial in DME and the PULSAR trial in wAMD both demonstrated that aflibercept 8 mg 12- and 16-week dosing regimens achieved non-inferiority in
Aflibercept 8 mg was consistent with the established safety profile of Eylea.
vision gains compared to the Eylea group.
In both trials, Regeneron/Bayer said there were no new safety signals for aflibercept 8 mg and Eylea, and no cases of retinal vasculitis, occlusive retinitis or endophthalmitis.
In these trials, the manufacturer reported the safety of aflibercept 8 mg was consistent with the established safety profile of Eylea. Regeneron and Bayer said they would now submit these data to regulatory authorities around the world.
Aflibercept 8 mg is being jointly developed by Regeneron and Bayer AG. In the US, Regeneron maintains exclusive rights to Eylea and aflibercept 8 mg. Bayer has licensed the exclusive marketing rights outside of the US, where the companies share equally the profits from sales of Eylea. n
Johnson & Johnson revealed clinical trial results of two investigational gene therapies at the American Academy of Ophthalmology (AAO) 2022 Annual Meeting.


The company’s pharmaceutical business, Janssen, reported the primary results from a Phase 1/2 study evaluating botaretigene sparoparvovec (formerly AAV-RPGR) for inherited retinal disease X-linked retinitis pigmentosa (XLRP) associated with the retinitis pigmentosa GTPase regulator (RPGR) gene.
It said the gene therapy was found to have an acceptable safety profile, and efficacy assessments in the proof-ofconcept study demonstrated encouraging improvements in retinal sensitivity, visual function and functional vision.

In a separate Phase 1 trial of investigational gene therapy JNJ-81201887
(JNJ-1887) for patients with geographic atrophy (GA), a late-stage and severe form of age-related macular degeneration (AMD), the company reported all three doses of the treatment met the primary endpoint for safety in adults.
In addition, the supportive efficacy measures, including evaluation of GA lesion growth rates, showed a continual decline in lesion growth over six-month increments. n
COMPANY 16 INSIGHT November 2022
Janssen comprises the pharmaceutical companies of Johnson & Johnson.
The event offered the latest insights to advance myopia management.
J&J GENE THERAPY PROGRAM UPDATES
INTRODUCING MERIDIAN LASERS
laser systems for Ophthalmology






Device Technologies are proud to partner with Meridian Medical to bring to market an innovative range of lasers to assist in treating retinal issues, cataract surgery and glaucoma.


With a long history of Swiss manufacturing and featuring a patented thermos electric cooling system, the Merilas laser range provides you with high-quality features to ensure longevity in your purchase.
The Merilas range is complimented by the MRQ YAG Laser system that fully integrates a YAG laser with a precision optics LED slit lamp. This is a flexible option for even the most space conscious practice.
AUS
NZ 0508 DEVICE
Innovative
DISCOVER the Meridian Laser range by scanning the QR
1300 DEVICE (338 423) customers@device.com.au www.device.com.au
(338 423) customers@device.co.nz www.device.co.nz

1800 637 654 @eyesrightoptical
MANAGING FRAMES SELECTION On rotation:
Selecting and maintaining a balanced range of frames can be a challenging part of managing an optometry practice. But it can also be rewarding in terms of remuneration and reputation if done right.

Sydney independent practice owner and founder of The Eye Piece
Mr Paul Lee enjoys hunting down the next new trend in eyewear. For Lee, it is not the frames per se, but the relationship with suppliers and customers, that is key to successfully stocking and selling the right mix.
Lee and his wife, Taeyon, opened their first practice in Chatswood in 2007 under their-then practice name Proview Optical. They have since sold this practice and now operate under The Eye Piece. They opened a practice in Sydney’s CBD in 2009, opened a second practice in the leafy suburb of Wahroonga in 2017 and a third in Balmain in late 2021.
“We knew the market we were going into when we started all our practices and how we would define ourselves as an upmarket boutique. We had numerous competitors when we opened our first practice in Chatswood, so we focused on targeting a niche market,” Lee says.
“We’re well-versed in eyewear brands and take a keen interest in eyewear fashion and certain brands. We look at the global market and what is trending in overseas shows, such as SILMO Paris and Milan and apply it locally.”

He says wearers are more conservative in Australia compared to Europe when it comes to choosing a pair of frames, but it’s valuable to know what trends are emerging.
“Our three practices [The Eye Piece] attract different demographics. Our CBD practice on Hunter Street attracts white collar professionals, such as lawyers and accountants, who tend to be conversative, whereas our recently opened Balmain practice attracts fashion-conscious younger couples.”
While knowing your patient demographic, what frames your local competition stocks, and the latest trends are staples of selecting your frame range, Lee says fostering reciprocal relationships with suppliers is key to getting ‘it’ right.
Testament to this is a unique retail space at The Eye Piece’s flagship CBD practice. Lee says it is the first optometry practice to execute a shopin-shop concept in Australia, housing collections from leading brands such as Chanel, Garrett Leight, Lindberg, Masunaga, Moscot, MYKITA and Oliver Peoples.

INSIGHT November 2022 19 RETAIL
Young Eyes Optometrists, in the Hilltops region of NSW, says stocking frames at multiple price points is a matter of necessity.
The Eye Piece's flagship Sydney CBD practice houses collections from leading brands.
“In our CBD practice, suppliers have a dedicated floor space, like a shop within a shop, to display their range. We borrowed this concept from high-end wristwatch boutiques and executed it in our CBD practice, which had the floor space to make it work,” Lee says.

“We knew which brands were strong, and we said to our suppliers, ‘We would love you to be part of it’. They invested in the idea, and it helped set a precedent for what The Eye Piece is about. Each brand effectively has their own ‘shop’ and it allows suppliers to go deep into their eyewear range.”
The CBD practice also has an in-house lab, which allows for a one-hour lens fitting service, as well as the latest digital dispensing aid – the visuREAL Master from HOYA.
But Lee doesn’t rely purely on a visually impressive range of frames on display, or fast turnaround, to drive retail sales. He also utilises marketing tools and frame rotation to attract new and retain existing patients.
“Patients research eyewear before they even set foot in our practice. We’ve had customers request fames they’ve seen on Sex and the City, for example. More recently we’ve been fielding questions about frames seen in Johnny Depp’s trial, so it is worth staying on top of trends in social media and pop culture,” Lee says.
Reiterating the importance of positive relationships with suppliers, Lee says The Eye Piece is currently among the country’s leading stockists for several eyewear brands such as Lindberg, which helps with Google searches.
Lee’s team also includes an in-house marketing specialist who analyses The Eye Piece website’s traffic on a weekly basis and uses social media to promote new collections.
“There is a ripple effect. If you have the right frame selection, patients appreciate what they walk out with. And once they walk out the door, they want to let other people know what their experience has been, through wordof-mouth, social media or Google reviews,” Lee says.
And if The Eye Piece doesn’t stock a particular frame a patient is looking for?
“We try to cater to requests as best we can. If it’s a frame from a brand we carry but don’t currently stock, we try to get it, we never say no.”
Lee says when it comes to brands, you need to know what works, stock up, and review and rotate stock frequently.
“If you take on a new brand, and it doesn’t sell, cut it loose,” he says. “You don’t want patients seeing the same stock still sitting there. You need to rotate. Say I order multiple similar frames but after a month, I’ve only sold a couple, leaving the majority still on the shelf. We would contact the supplier to rotate the remaining frames for different colours or different models in the same brand. Sometimes practices don't know that or do not get on top of their stock. Again, your relationship with your supplier is key to refresh branding,” he says.
Lee, who has been in the optical industry for 25 years and worked for corporations including Luxottica and Paris Miki before becoming an independent optometry business owner, says staff are also vital to a winning frame selection formula.

“When we opened our Balmain practice in December, we purposefully employed an experienced dispenser and optometrist who knows the market in Balmain. When we order stock in any of our practices, our team of optometrists and dispensers are all involved in choosing frames, because if they don’t like it, they won’t sell it. We empower them to choose,” Lee says.
“As an independent practice, we are grateful for the 15 years of support from our clients and suppliers. They have positioned and established us as to who we are now. All our dispensers and optometrists who have been with us from day one are on the floor actively helping with frame selection and dispensing. This provides a customer journey and our team makes our branding.”
DON’T TOLERATE AGED STOCK
At Young Eyes Optometrists in the Hilltops region of New South Wales, business manager Mr Simon Hobson says stocking frames at multiple price points is a matter of necessity, including budget frames that are strong and light for customers driven by function, to high-end fashion and bespoke frames.

Hobson is responsible for selecting Young Eyes’ frames range, with input from head dispenser Ms Melissa Oldfield, and as the practice is part of the ProVision network, using ProSupply and ProAccounts to manage supply.
“We select suppliers that have strong business-to-business connections. We need supply reliability – frames that are available for delivery direct to the lab – and ability to attend to breakages and warranty, and prefer access to best seller lists,” Hobson says.

20 INSIGHT November 2022 RETAIL
“YOU DON’T WANT PATIENTS SEEING THE SAME STOCK STILL SITTING THERE. YOU NEED TO ROTATE”
PAUL LEE THE EYE PIECE
The Eye Piece on Hunter Street in Sydney's CBD features a shop-in-shop concept inspired by wristwatch boutiques.
“We also use e-delivery of stock arrivals complete with frame parameters, barcodes and pricing direct into our point-of-sale. All the companies we deal with are able to provide modern e-commerce solutions.”
Given the practice’s regional location, Hobson accepts that it’s difficult for suppliers to present new ranges in person on a regular basis.
“We use the company website to review new stock. They may only come to our practice once or twice a year, but in-between, I need the company rep to make recommendations about stock. They need to have come to our practice initially because they need to get a feel for the type of business we are, but then they should be able to manage it with me with limited visitation,” he says.
“If you've got a range that's selling very well – particularly if it’s a high-end, bespoke material – it's important to get the new releases, so a good supplier rep will email me with some product photos that he or she thinks will work for our practice.”
Once Hobson and Oldfield agree to stock a range, they ask the supplier rep for advice on which model will best suit their patient demographic.
“The end decision is a combined recommendation from the supplier rep and our head dispenser,” Hobson says.
Young Eyes stocks best-selling models in at least two colours, and best-selling ranges are allocated two, three or up to four rows of display. “We go deep in the areas selling well,” Hobson explains. “We supply most frames direct supplier to the lab; best-selling frames will often sell several units a week.”
Hobson and Oldfield monitor sales reports regularly to ensure stock levels are adequate and they’re not holding onto individual units or ranges not performing.

“These are managed out of the system by our dispensers and the supplier rep. We actively manage out any aged stock. Even some ranges, through changes in design, will drop in popularity. We manage stock levels in that brand as appropriate and manage it out if required,” he says.
“If a range or an individual model is not performing, then you have to actively manage it because you cannot afford, in my opinion, to keep aged stock, and hang onto it thinking it's going to sell. You've either got to reprice it to a point where it does sell, consider packaging as a second pair, or work with your supplier partner to replace or rotate it with stock that will sell.”
Hobson says he monitors Young Eyes frames stock levels weekly, taking into consideration feedback from staff, to ensure the practice always keeps consistent levels of stock on the shelves.


“Occasionally we sell stock directly off the shelf for various reasons, such as it’s not available from the supplier to supply direct to the lab, or someone

“I TRY NOT TO DO STOCK ROTATIONS MORE THAN EVERY SIX MONTHS BECAUSE IT'S TIME-CONSUMING AND YOU DON'T WANT TO BE DOING IT TOO OFTEN”
SIMON HOBSON YOUNG EYES OPTOMETRISTS
comes in and wants to buy it there and then. When we replace units that have left our shelves, we refresh some units that aren’t selling.
“I personally try not to do stock rotations more than every six months because it's time-consuming and you don't want to be doing it too often. Hence, selection at the initial purchase is very important to try to get the stock right, which means using a supplier’s rep to give you advice, and your own sales team to tell you what they think will work.”
Although advice is welcome, Hobson says Young Eyes never puts a new range in store simply because a supplier’s rep recommends it.
“We ask supplier’s reps for a recommended new range, and then analyse if we have poor performing ranges at that price point. If we do, we then manage out the poor performing range and replace it with a new range,” Hobson says.
“If I am unsure about whether a range will work – and the supplier suggests it will – I will put it on display for six months and if it doesn’t sell, they take it back. If the supplier rep knows the range will sell, they should accept that arrangement.”
BELIEF AND CONFIDENCE OF PRACTICE STAFF
Independent optometry group Quinn & Co. Eyecare is experiencing a period of rapid growth, doubling in size from four practices to eight in a matter of months.
Co-owner Mrs Naomi Wajntraub has been overseeing the opening of four new locations since March, in addition to managing its existing practices in Ararat, Horsham, Stawell and Swan Hill.
Wajntraub, who has a business background and previously worked as an optical assistant, now manages the whole business.
“In March, we acquired our first metro practice, High On Vision in Kew, Melbourne. At the start of June, we acquired Eyecare Sunraysia in Mildura, which has two locations. And then in early July, we acquired Echuca Optical,” Wajntraub explains.

She says the main responsibility for selecting frames is assigned to the practice manager.
“We have a practice manager at each of our locations. However, we also like to get our dispensers and optometrists involved, if they happen to be free at the time,” Wajntraub says.
“We like to get the team involved because they're the ones selling the product, so they know what people are looking for. Perhaps they've struggled to find smaller frames for petite women, or really large sized frames for those with bigger heads. They know where the gaps lie and what we need to add to the range, so I prefer to give the teams the responsibility and fun task of selecting frames, insofar as deciding which
pieces they want within a set range.”
Quinn & Co. Eyecare positions itself as a premium practice, and therefore stocks a selection of high-end ranges at all its practices, but also takes into consideration the socio-economic status of its patient demographic.
“Some of the new practices that we've acquired haven't previously carried the more expensive ranges, so we're slowly introducing them into those practices. We probably have a few more high-end brands in our Kew practice, with Kew being an affluent area, whereas our regional locations stock more of a balance between affordable and high-end frames.”
Supplying frames to multiple new Quinn & Co. Eyecare practices in a short time frame hasn’t been a concern for Wajntraub because purchasing four established practices has also meant acquiring existing stock, which she has been managing with assistance from staff.
“They're established practices, so we have a good range of frames to begin with. If it's not the same stock as what we carry in our other practices, we spend a bit of time reviewing it, and speaking to the existing team who have continued on with us and asking them: ‘What have you found works? What brands do you like? What do you have people coming in asking for? Which ranges haven't sold well? Then working together with the team, we gradually cull certain ranges and then introduce new ones that have worked well in our other practices.”
Keeping stock current is high on the agenda for Wajntraub and her team of practice managers, with some suppliers standing out more than others for their rotation policy.
“Anything that is approaching nine months old, we like to rotate out when the reps visit. We have a number of different suppliers and they each work in different ways but we tend to favour working with those who are fantastic when it comes to helping us keep our ranges current and up-todate,” she says.
Eyes Right Optical national brands manager
When choosing a brand, ask:
• Does it suit your demographic?
• How often does the brand have new releases?
• Is the product stocked in Australia?
• Are there any minimums required to become a stockist?
• What is the brand's warranty process and percentage?
• What are the brand's marketing capabilities?
• Does the brand offer flexible rotations? 20:1, 10:1, 5:1, 3:1, 2:1, 1:1

Consider what the market-leaders are doing:
• They have amazing rapport with patients, reps and suppliers.
• They have a ‘narrow and deep’ brand strategy, meaning few brands and a large assortment in each brand.
• They have fewer suppliers, which means better supplier relations and less time spent doing/chasing paperwork, payments, credits etc.
• They hire passionate staff who can recognise patients’ needs and wants.
• They use data from usage reports and stock on hand to make informed buying decisions.
• They re-order their best sellers immediately
• They see their sales reps frequently to keep collections up-to-date and fresh.
• They involve staff in the buying process and incentivise staff to keep them engaged.
• They focus on dollars banked per dispense, not margin percentage.
22 INSIGHT November 2022
Lisa Wymond shares the following tips when considering frame selection:
Young Eyes Optometrists selects suppliers with strong busines-to-business connections.
RETAIL
W ith trade events effectively non-existent during COVID, Quinn & Co. Eyecare has relied on reps to showcase new ranges coming onto the Australian market and Wajntraub has listened to their advice on what is trending well. However, she says, the teams haven’t always been convinced about which new trends will appeal to customers.
“Different practice staff have certain beliefs about what will or won’t sell. A few years ago, round frames started coming back in fashion. I had team members in some of our regional practices saying, ‘No one is going to buy round frames here’ and they didn’t want to stock any round models. But we insisted. It's only when people try them on that they think, ‘I could wear a round frame – it actually looks good’,” Wajntraub says.
“It's the same with colour or more ‘out there’ styles. When we first introduced Face à Face, which is one of the Eyes Right Optical ranges, my team in Horsham, which is the first practice we introduced it into, thought that





they were never going to sell, because it had some quirky models and some really bright, beautiful colours. Now, it is one of our best sellers. Almost every person on our team has their own pair of Face à Face frames, or multiple, and they've just fallen in love with the brand. And so now they sell it without any issues. It comes down to their beliefs and confidence and their ability to understand the customer, their personality and what they want.” n
 Quinn & Co. Eyecare in Ararat is one of eight practices in the business, with stores in Horsham, Stawell, Swan Hill, Mildura and Echuca.
Quinn & Co. Eyecare in Ararat is one of eight practices in the business, with stores in Horsham, Stawell, Swan Hill, Mildura and Echuca.
“ANYTHING THAT IS APPROACHING NINE MONTHS OLD, WE LIKE TO ROTATE OUT WHEN THE REPS VISIT”
NAOMI
WAJNTRAUB QUINN & CO. EYECARE
BIOMETRIC INTELLIGENT GLASSES B.I.G. NORM™ Rodenstock is establishing a new lens calculation norm that ensures even more progressive lens users can experience the benefits of Biometric Intelligent Glasses.0% 100% Go to: rodenstock.com/bigvisionforall Follow: #BIGVISIONFORALL
Powerful technology for sustained intraocular pressure and medication reduction. Predictable outcomes from a truly tissue-sparing procedure. All on a proven platform with the most clinical evidence of any MIGS device.
Experience the latest evolution of the iStent® legacy of excellence in your practice.




iStent inject® W IMPORTANT SAFETY INFORMATION INDICATION FOR USE. The iStent inject® Trabecular Micro-Bypass System (Model G2-W) is intended to reduce intraocular pressure in adult patients diagnosed with mild to moderate primary open-angle glaucoma (POAG) currently treated with ocular hypotensive medication. The device can be implanted with or without cataract surgery. CONTRAINDICATIONS: The device is contraindicated for use in eyes with primary angle closure glaucoma, or secondary angle-closure glaucoma, including neovascular glaucoma, because the device would not be expected to work in such situations, and in patients with retrobulbar tumour, thyroid eye disease, Sturge-Weber Syndrome or any other type of condition that may cause elevated episcleral venous pressure. WARNINGS: This device has not been studied in patients with uveitic glaucoma. Patients should be informed that placement of the stents, without concomitant cataract surgery in phakic patients, can enhance the formation or progression of cataract. The surgeon should monitor the patient postoperatively for proper maintenance of intraocular pressure. iStent inject is MR-Conditional, meaning that the device is safe for use in a specified MRI environment under specified conditions; please see labelling for details. Physician training is required prior to use. Do not re-use the stent(s) or injector. ADVERSE EVENTS: Postoperative adverse events include but are not limited to: corneal complications including edema, opacification and decompensation, cataract formation (in phakic patients), posterior capsule opacification, stent obstruction, intraocular inflammation (nonpre existing), BCVA loss and IOP increase requiring management with oral or intravenous medications or surgical intervention. Please refer to Directions for Use for additional adverse event information. CAUTION: Please reference the Directions For Use labelling for a complete list of contraindications, warnings and adverse events.
AUSTRALIA PTY.
GLAUKOS
LTD. Suite 109/12 Corporate Drive • Heatherton VIC • 3202 • AUS • tel 03 9551 2220 • www.glaukos.com © 2022 Glaukos Corporation. Glaukos®, iStent®, iStent inject ® and iStent inject ® W are registered trademarks of Glaukos Corporation. Australian Sponsor: RQSolutions Pty Ltd / New Zealand Sponsor: Toomac. PM-AU-0208 *Based on units sold. GO FOR THE #1 MIGS DEVICE WORLDWIDE * POWERFUL PREDICTABLE PROVEN
OPPORTUNITIES ABOUND: Life as an earlycareer G&M optometrist

Much is made of George & Matilda Eyecare’s value proposition for optometrists later in their working life, but little is known about the wealth of opportunities for early career optometrists often working under the guidance of Australia’s leading practitioners.

Just four years after graduating, early career NSW optometrist Ms Antigone Kordas has experienced rapid career growth. Not only is she the principal optometrist at George & Matilda (G&M) Eyecare for Maroubra Optometrists, but she oversees appointments for the practice’s outback eyecare program and supervises final-year Deakin and UNSW optometry students.
On top of this, Kordas practises full-scope optometry, ranging from complex contact lens fittings, myopia control, dry eye disease and ocular health management. Through G&M, she’s even acquired a topographer from a local ophthalmologist so she can now start fitting rigid gas permeable (RGP) lenses from scratch and train for orthokeratology.
While she is one of those young optometrists with “exceptional natural ability”, according to her colleagues, she has found fulfilment in her career largely due to the opportunities provided by G&M and its community of experienced optometrist partners like Mr Kyriacos (Kyri) Mavrolefteros.
While the G&M network – now supporting over 100 communities across
Australia – doesn’t have a standardised graduate program, it customises the experience to each individual’s strengths and opportunities. Kordas is among a growing number of early career optometrists receiving a tailored experience that talks to their strengths, opportunities and interests while being mentored by some of Australia’s leading practitioners.
“Working within this particular practice has also given me the opportunity to experience outback optometry through Kyri, which is something very unique and I know I would not experience elsewhere,” Kordas says.

“Kyri from day one has been my number one advocate. Without him and his wife Katerina, I wouldn’t be the optometrist I am today. Working in a wellestablished practice had always been a main concern as a new graduate starting work for the first time, as I knew many patients would be hesitant to see someone younger and new. But Kyri never let his patients see it this way.
“He would always encourage them to see me and reassure them they were in good and very capable hands. Kyri often tells me of his joy when patients come to say hello and that it’s been great all these years but want to book an
INSIGHT November 2022 25 OPTOMETRY
Kyriacos Mavrolefteros (centre) and his optometrist wife Katerina (right), of George & Matilda Eyecare for Maroubra Optometrists, with early career practitioner Antigone Kordas (left) who is now the principal optometrist.
appointment with Antigone from now on. He has played an immense role as my mentor and shaped the way I practise today.”
Kordas’ optical career commenced in 2015 when she worked as an optical dispenser at a corporate store amid her first year of optometry studies. Then, in her penultimate year of study, she had a placement in Townsville at an independent practice, where her eyes were opened to the possibilities of independent practice.
Soon she was working at Maroubra Optometrists. A year later, Kyriacos and Katerina partnered with G&M.
“What I enjoy most about working for G&M is how they value every member of the work team, the role they play and especially their ‘patient-first’ approach,” Kordas says.
“As an optometrist, I have complete flexibility to help my patients in the best possible way, and there is a large emphasis for continuing education, with weekly meetings in areas of expertise within optometry such as myopia control, dry eye management, behavioural optometry and advanced contact lens fittings with some of the most experienced and knowledgeable optometrists within the industry.”

For Mavrolefteros, it’s important G&M continues to present opportunities for young optometrists to blossom, find their niche and pursue their passion in their profession.
“Our future is partly underpinned by our fostering and nurturing of young optometrists within the G&M family,” he says.
“Occasionally we come across some young optometrists, like Antigone, with exceptional natural ability to nurture/support younger colleagues. I am indebted to Antigone for capably supporting our work in the challenging outback optometry clinics from Walgett to Cobar and for fostering younger optometrists from UNSW and Deakin universities while they do their preceptorships in Maroubra and the NSW outback. She develops long lasting relationships with these students and is a source of support for our young colleagues upon graduation in the early stages of their careers.”
A TWO-WAY STREET
Mr Peter Park, who graduated from UNSW in 2020, was motivated to pursue an optometry career due to his experiences as a young myope. He was prescribed spectacles at the age of four in Korea, but the condition progressed until he was left wearing thick glasses due to limited clinical knowledge at the time.
Today, he’s an early career optometrist at G&M for theeyecarecompany in Top Ryde, working under the guidance of leading optometrist Dr Margaret Lam.

Similar to Kordas, Park began by optical dispensing, hired by Lam during the second year of his optometry studies.
“Throughout that time, Margaret and the team had taught me all the
technical aspects of being a dispenser. However, I learned the most not from information Margaret and the team had taught me, but rather from how they conducted themselves. Whatever the situation, they always had the patient’s best interests at heart and this was exhibited in every interaction,” he says.
“The term ‘work family’ was indeed very true throughout my time as a dispenser. I think it was these factors which ultimately led me in applying for a position as an optometrist in G&M in my final year.”
Now a fully-fledged optometrist within the practice, Park says three things stand out: the potential for growth and abundance of opportunity, stability in a time of instability and genuine relationships with team members and patients.
“The final year of optometry is a turbulent time, where placements, reports and patient examinations are required at a high level all whilst applying for potential graduate optometrist positions in the student’s spare time. Thanks to Margaret’s recommendation I was able to have an interview with Amelia Haywood, the regional manager for G&M, and was able to secure a graduate optometrist position. In a time of uncertainty, I was able to have my feet grounded which allowed me to focus my efforts on finishing university,” he explains.
“G&M have also allowed me to grow in the field of optometry. It was the platform from which I could pursue my passions in myopia control by mentoring me through fitting orthokeratology lenses and providing me with a store that fit that passion. Subsequently, I was able to have the opportunity to prescribe orthokeratology and full scope myopia management for my own patients and offer a variety of solutions to help with their eye needs.”
He adds: “Working under Margaret has been an honour as well as a privilege. Her level of professionalism and expertise in the field of optometry is exceptional and commitment to her patients and profession unparalleled.”
Lam says Park possesses “the trifecta” – warmth in his personality, a skill for developing rapport with patients through genuine care, and technical expertise and a meticulousness in professionalism.
She’s also learned a lot about becoming a mentor, explaining that clinical prowess does not always translate into strong teaching ability.
“It is far easier to learn from someone who is able to remember what it was like when they were first learning and remember the challenges you face at the beginning, than from someone who has mastered a skill but can’t remember the simple basics anymore,” she says.
“Mentoring requires extending empathy and patience, we need to understand we are all on a learning journey, albeit some are further along than others. It’s important this is done without any judgement and teaching is done patiently and gently. You can teach by showing someone all their mistakes and break them as a person, or you can highlight their strengths, and build on these to strengthen any areas for further improvement’.”
Lam adds it’s important to allow people to learn at the pace they’re capable of, not setting expectations to learn at your pace.
“For different skills, what I might learn slowly, you might pick up quickly, and vice versa, and if I’m able to be patient with supporting that learning journey for you, we all benefit. In our practices, we discuss case studies and there are lots of on-the-job learning experiences, and in our G&M learning community, we have discussion groups where everyone discusses patient case studies in a welcoming learning community. In a negative workspace where you don’t feel safe, very little growth occurs, so it’s critical to create a work environment where people feel they grow and learn backed by their team.”
FRESH IDEAS AND VIBRANCY A WELCOME ADDITION
Mr Andrew Salloum grew up Sydney’s southwest and become involved in optometry surrounded by family and friends who worked in healthcare. But his interest in regional practice was spurred by his optometry studies at Deakin in Waurn Ponds, in 2020, when he also worked as an optical assistant in nearby Geelong.
“I knew practising regionally would expose me to a large array of pathology which was particularly interesting to me. In a sense, Albion Park is a similar town to Geelong, considering they’re both about an hour away
26 INSIGHT November 2022 OPTOMETRY
Dr Margaret Lam (left) with early career optometrist Peter Park, at theeyecarecompany by G&M in Top Ryde, Sydney.
from the main city,” he says.
“Dirk den Dulk (optometrist partner at G&M for Partners in Vision, Albion Park) has a variety of interests and has developed such a large patient base which covers a large scope of optometry. This was enticing to me and is what ultimately led me to choose G&M in Albion Park for my three-month Clinical Residential Placement as part of my studies.”
At the time of writing, Salloum was G&M’s newest graduate, officially part of the practice for two months. During his placement, den Dulk’s style of mentoring allowed Salloum to independently develop his skills while addressing any concerns.
“I felt like this was important to my development and confidence as a budding optometrist. G&M Albion Park was the choice for me as I knew I’d be supported by the team,” he says.

“The most beneficial aspect G&M offers is their value for patient-centred care. G&M value clinical independence and allow me to practise and treat patients in the way I feel will be most effective, depending on each individual patient. As such, they give me the ability to take my time with patients without the pressure of KPIs, as the company understands the patient is a person and not a number. This allows me to enfranchise often marginalised groups in society. This G&M career pathway also offers me incredible mentorship, be it from Dirk and the Albion Park team, but also the support I get from G&M’s optometry services team.”
Den Dulk, who has now employed three Deakin graduates through G&M, says three-month student placements are a full time commitment between both parties. That union can feel like an eternity with a poor fit or pass quickly with a student like Salloum.
“It’s about making the student understand they have all the knowledge
but now require the skills to manage the patient through their optometric consult. Not only adequately testing, but compassionately fulfilling questions and concerns with a communication level that is both precise and understandable,” den Dulk explains.




“But I also learn lessons with every student. They present with fresh ideas and techniques and their understanding of technological and diagnostic advancements is current.

“I graduated 43 years ago, prior to the advanced technology and pharmacology that newly graduated optometrists have access to now. I feel uplifted by my experience with the new graduate optometrists. This generation are not only well-equipped with knowledge, but have greater clinical exposure before graduating. I am still enjoying my time with these young professionals – I love their passion and vibrancy for the vocation they have chosen and studied very hard for.” n
 Andrew Salloum began working at G&M for Partners in Vision, Albion Park, this year.
Andrew Salloum began working at G&M for Partners in Vision, Albion Park, this year.
Podthalmology:
DELVING INTO OPHTHALMOLOGY’S BIG ISSUES
The most pressing issues affecting Australian ophthalmology have been laid bare in the new Podthalmology podcast, hosted by Melbourne eye doctor DR LANA DEL PORTO. She discusses the philosophy behind the series, which includes guest appearances from leading cataract and refractive surgeons.
Have you considered auditing your cataract surgery performance, but struggled with getting started? And how deeply have you thought about the unconscious gender bias within your clinics, or whether increased uptake of presbyopia-correcting intraocular lenses (PC IOLs) is being driven by new technology or patient demand?
These thought-provoking topics – plus several more – are among the first episodes in a new podcast series called ‘Podthalmology’, hosted by Melbourne ophthalmologist Dr Lana Del Porto.

The podcast, released on 30 August, is sponsored by Alcon and produced by Bench To Bedside – an organisation focused on podcasts for Australian medical specialists dedicated to areas such as ophthalmology, oncology, haematology and rheumatology.
Podthalmology comprises five episodes where Del Porto delves into various industry hot topics with prominent Australian cataract and refractive surgeons. With three of the five guests being female, it has been endorsed with the RANZCO Women in Ophthalmology ‘tick’, achieving at least 35% female representation.
Del Porto is an accomplished ophthalmologist in her own right. Her training has taken her to the prestigious Moorfields Eye Hospital in London where she completed fellowships in neuro-ophthalmology and strabismus. Today, she is an associate at three private practices in Melbourne while heading up the neuroophthalmology unit at The Royal Victorian Eye and Ear Hospital (Eye and Ear) where she also teaches cataract and squint surgery.
She has an active social media presence
(Instagram: @drlanasurgeon) where she regularly posts ophthalmologyrelated content to raise the profile of the profession, which she believes is part of the reason she was approached to host Podthalmology.
“When I looked at the topics to be discussed in each of the five episodes, I was excited, thinking there’s certainly some controversy here and thoughtprovoking topics that would be of interest to our industry,” she says.
“In particular, there’s an episode about women in ophthalmology that focuses on unconscious gender bias, which was really interesting. There’s also an episode on presbyopia-correcting IOLs, which are the way of the future. I use them in 80-90% of my cataract patients. These subjects among others, are topical to our industry and many ophthalmologists want to hear about them.”
The five episodes include:
• Audits in ophthalmology – Dr Ben Connell, principal associate at Eye Surgery Associates in Melbourne.
• Patients and referrers – what they really want and why does it matter?
– Dr Armand Borovik, staff specialist at Prince of Wales Hospital, Sydney.
• Unconscious bias in medicine with a focus on ophthalmology – Dr Tanya Trinh, Sydney ophthalmologist and presenter of ‘Unconscious Gender Bias and How it Contributes to Imposter Phenomenon in Women’.
• Is new IOL technology driving broader use of PC IOLs or is a patient-centred approach to measuring outcomes making PC IOL use the new normal? – Associate Professor Smita Agarwal, Clinical Associate Professor at the Graduate
OPHTHALMOLOGY
Dr Lana Del Porto (left) interviews Dr Jacqueline Beltz for a new Australian ophthalmology podcast series.
28 INSIGHT November 2022
School of Medicine, University of Wollongong.
• Training: Next generation eye surgeons – Dr Jacqueline Beltz, staff specialist on the corneal unit at The Royal Victorian Eye and Ear Hospital.


For time-poor ophthalmologists, keeping on top of industry-specific developments can be tough, so Del Porto expects the podcast to resonate with her colleagues whether they be commuting, at the gym or in the garden.
Podthalmology’s arrival also comes amid a golden period for local podcasting, with 40% of the Australian population over 12-years-old now tuning in monthly for podcast content, significantly higher than pre-pandemic levels (22% in 2019), according to the latest Infinite Dial Australia report from Edison Research, commissioned by Commercial Radio Australia.
“Podthalmology is a great opportunity for Australian ophthalmologists to listen to familiar voices talking about concepts within the field they might not have given much thought to, which may improve their practice,” Del Porto adds, noting her own learnings from the experience professionally and in terms of digital audio production.
“It’s been a fascinating process. Each episode required background research to ensure I could engage with each of the guests on their topic of expertise. We provided the questions in advance and I tried to make the topics juicy for the audience, but I found that it’s also important to let the guest lead the discussion and for me to tailor my responses accordingly.”
OPHTHALMOLOGY-SPECIFIC CONTENT
The first Podthalmology episode (20min 33sec) was released on 30 August on the Bench To Bedside website – which requires listeners to provide their Ahpra registration number – where Del Porto interviews Connell from Eye Surgery Associates in Melbourne.
They discuss the importance of medical auditing and self-evaluation and helpful tools enabling surgeons to audit their own outcomes. Although this is mandated in specialities like vascular surgery, it isn’t in ophthalmology. But it can drastically improve performance.
In the episode, Del Porto discusses how an audit of her own cataract surgeries showed her prediction error for spherical outcomes was -0.14 D. Although she suspected surgery was resulting in patients being slightly myopic, having solid data helped her inform planning for future surgeries.

Connell discusses key barriers to uptake, including labour intensive data management, and some colleagues not seeing the benefits of auditing or adopting a belief their results are already good. He’s even heard a case of a specialist who thought the stress of knowing their outcomes would make them worse. However, he says most surgeons are motivated to know, but a lack of IT proficiency and specific platforms can make it challenging.
Reflecting on the episode, Del Porto says: “You're never going to improve your outcomes without knowing where your deficits are. As ophthalmologists we perform auditing better than some other specialties, but there is definitely room for improvement, so it’s important to encourage it.”
In the second episode, Del Porto speaks with Borovik about what patients and referrers want from ophthalmologists, focussing on research from Cerner Enviza (formerly Kantar Health).
“When an optometrist is referring for cataracts, they want a detailed letter back and want to know any post-operative complications. They want to be part of a holistic care of the patient, so that was an interesting point of discussion. It also disappoints them when the ophthalmologist sends the patient off for ready-made reading glasses from the pharmacy when they could be sent back to the optometrist for more stylish glasses that will fit them better and provide better vision,” she says.
“We also focused on patient expectations – and there was a post-operative simulation of what patients would see if they were given a monofocal lens versus an EDOF versus a multifocal lens. It was interesting to see, given that scenario, most patients wanted something that was going to correct their presbyopia. So I think the days of leaving everyone presbyopic after cataract surgery are over.”
In the third episode, Del Porto interviews Trinh who in 2020 presented a widely-viewed presentation at The Toronto Eye Review that can be accessed on YouTube. It was an analysis of the unconscious way both men and women exhibit subtle implicit bias on a daily basis and its impact on women.

“She’s got a lot of research to back her up, and your mind is blown once you watch her presentation – you don’t realise how insidious it is,” Del Porto says.
“We discuss how it's not just male patients who ask me – after I've consented them for cataract surgery – if I’m actually going to do the operation. We also cover unconscious gender bias in referrers, colleagues, people beneath and above you. We talked about a few of our experiences as well – it got deep and philosophical.”
In the episode on presbyopic-correcting IOLs, Del Porto and Agarwal question what is driving increased uptake – technological advances or patient demands to be spectacle-free?
“One feeds the other, doesn’t it? Patient demand requires the technology to keep up and move faster. But at the same time, technological advances are contributing to patients making these further demands,” Del Porto explains.
The fifth and final episode features Del Porto and Melbourne colleague Beltz discussing modern-day training of the next generation of ophthalmologists. With rapid advances occurring in the field, they say what’s learned as a trainee won’t necessarily sustain ophthalmologists throughout their career.
They argue that being a good learner is just as important as strong skill and technique.
Beltz is the founder of GENEYE in 2019, part of the Eye and Ear Education program. It focuses on integrating modern immersive educational techniques, high performance psychology and technologies such as virtual reality surgical simulation.

“There is a new teaching lab opening at the Eye and Ear soon, and Dr Beltz is really excited about that, but the point of the episode is that a good ophthalmologist will constantly be updating their skill set. Sometimes it's the trainee teaching the consultant, learning is not necessarily hierarchical; and that is how Dr Beltz has run things at her GENEYE conferences,” Del Porto says. n

INSIGHT November 2022 29
Podthalmology is available at benchtobedside.com.au
Podthalmology host: Dr Lana Del Porto.
Guest 2: Dr Armand Borovik, Prince of Wales Hospital, Sydney.
Guest 4: A/Prof Smita Agarwal, Graduate School of Medicine, University of Wollongong.
Guest 1: Dr Ben Connell, Eye Surgery Associates, Melbourne.
Guest 3: Dr Tanya Trinh, presenter of ‘Unconscious gender bias and how it contributes to imposter phenomenon in women’.
Guest 5: Dr Jacqueline Beltz, The Royal Victorian Eye and Ear Hospital Corneal Unit.
Overcoming
‘FRAGMENTED NATURE’ OF NZ DIABETIC RETINOPATHY SCREENING

RANZCO has launched a Position Statement on Diabetic Retinopathy and Diabetic Retinal Screening for New Zealand. It is calling for a national screening service that leverages AI technology, led by ophthalmologists overseeing RANZCO-accredited health providers.
In New Zealand, it is estimated that diabetes is present in 7% of the population, and prediabetes in 26%. Of those with diabetes, it’s estimated 20-25% have diabetic retinopathy (DR). The disease is a leading cause of sight loss in New Zealanders under 50. In 2018/19, the prevalence in Maori was 7.1% and in Pasifika peoples 11.2%. Maori were 1.85 times more likely to have diabetes compared to non-Maori (age- and gender-adjusted). Pasifika were 3.18 times more likely to have diabetes compared to non-Pasifka (age- and gender-adjusted).
At present, RANZCO says diabetic retinal screening across New Zealand is failing many patients because they are not engaged in the screening process. Hence, it has released a position statement to provide the country’s ophthalmologists and other New Zealand health professionals guidance on best practices for DR screening, management and treatment.
“Patients are also losing vision because early treatment was not available to them as they were not identified as needing it. This particularly affects Maori and Pasifika people,” the college says.
Because of the fractured nature of the current program, records and information about patients are not easily accessible or transferable. It also means people are “at grave risk” of missing out on screening when they move between centres.
Further, multiple local screening programs cause “unnecessary duplication” and there is significant variation between the patient pathways used by public health services. Some individual programs are also vulnerable to collapse if just one key individual becomes ill, goes on leave or resigns.
RANZCO’s position statement recommends a new focus on three key areas: the establishment of a national DR screening program, supported by a Telehealth IT support system integrated into the existing health IT ecosystem. This would be led by ophthalmology, which would provide clinical oversight and ensure the seamless integration of the screening program into existing eyecare services.
“Ideally, the screening program should allow patient feedback as this is very helpful in allowing the patient to understand their disease. For
instance, carrying out the screening in the optometry and GP setting, where the photographer is trained in the identification of eye disease, does allow this,” RANZCO states.
In the proposed model, culturally safe hubs would be led by ophthalmologists who oversee RANZCO-accredited eye health providers, community health advocates and GPs.
RANZCO says diabetic retinal screening across New Zealand is failing many patients, in its new position statement.
Having a single point of leadership provided by ophthalmology will: 1. Facilitate the close coordination of these satellite sites 2. Ensure that care across a region is equitable 3. Enable clear oversight and ongoing training and accreditation, thus ensuring that the highest clinical standards.

The advent of modern retinal cameras – capable of being used without needing to dilate patients – and improvements in both the size and cost, makes them easily transportable and accessible for many community centres, RANZCO states.
The hubs would also provide timely and accurate assessment of retinal images using artificial intelligence (AI) to diagnose and treat DR before vision is irreparably lost.
“The use of (AI) for the grading of diabetic retinopathy is current in a number of overseas screening programs, most notably in Singapore, known as Singapore Integrated Diabetic Retinopathy Program (SiDRP), and is being trialled in some centres in New Zealand,” RANZCO states.
“The use of AI to grade the retinal images significantly reduces the primary graders workload and enables the patient to be informed of the outcome of their retinal screening in real time at the point-of-care. The technology will allow our screening program to work smarter and more
30 INSIGHT November 2022 DIABETES
efficiently and increase opportunities for patients to understand their disease and make modifications as needed. There is broad support amongst existing screening programs to adopt AI technology; however, the accuracy, validity and client-responsiveness of AI technology need to be continually reviewed to ensure that it is fit-for-purpose.
“In particular, the specificity threshold needs to be set at an appropriate level to avoid a high number of false-positive referrals, which may overload an already-stretched secondary service.”
But even if AI assumes the bulk of the primary grading there will still be a need to have skilled personnel capable of auditing and verifying the grades. Although skilled, RANZCO points out these tasks can be repetitive and quickly become boring, risking human error.
“Many allied staff within ophthalmology departments and in the community, including nurses, technicians and optometrists are ideally placed to be trained via RANZCO training and accreditation processes, in the grading of retinal photographs,” the position statement says.
“Increasing the pool of people capable of grading the retinal images will ensure that these roles are more satisfying. In turn, this should aid retention of this vital workforce and safeguard the long-term viability of the screening services. RANZCO accredited staff, such as orthoptists, nurses, community health advocates, GPs or optometrists, can expertly discuss photographs on the spot with the patient who then can see and understand their disease.”
SMALL LOCAL WORKFORCE
To combat issues related to the “siloed nature” of the workforce, which rely heavily on individuals, RANZCO believes a national approach would enable support across regions to allow screening to continue, even if issues arise.
“We note that programs such as the one in Wellington, that include optometrists who have undergone further training specifically in DR screening and grading, and bi-monthly peer reviews attended by Wellington hospital ophthalmology registrars and a lead ophthalmologist, have successfully reduced this key person risk,” RANZCO states.
“A requirement for RANZCO training and certification of New Zealand eye health workforce including orthoptists, nurses, community health advocates, GPs and optometrists will build workforce capacity and ensure that best practice standards of care are maintained.”
NATIONAL DATABASE NEEDED
According to RANZCO, local screening providers face significant issues when trying to identify the appropriate people to screen within a given region. The need to involve GPs, social workers and Maori and Pasifika already in place in the community has been highlighted.




However, many of the most vulnerable – those at highest risk of disease – are often less engaged with primary healthcare.
“Maori and Pasifika also tend to have less secure housing and have been described as a vulnerable transient population which means that they move frequently, thus losing community connections and support networks,” RANZCO says.
“As a result, relying on individual primary care health practices to provide lists of those who need screening means that many of the most vulnerable will miss out on screening. Moreover, the current process is onerous for the primary provider and duplication errors are common as people move from provider to provider as their housing situation changes. A national database would facilitate the easy identification of all those who not only need retinal screening but also those who need support to manage their diabetes.” n

George
& Matilda Eyecare is currently recruiting Optometrist to join our team in Airlie Beach, Innisfail & Atherton. Reach out to our HR
Team at opportunities@georgeandmatilda.com.au
to
find
out more.
Is the warm weather and luxurious beaches of Far North Queensland calling you?
Bold ambitions:
WHERE TO NEXT FOR SPECSAVERS?
Specsavers continues to progress the optometry agenda in Australia, forging a new path into areas like glaucoma, diabetes and now AMD. And as ANZ director of optometry DR BEN ASHBY outlined in his SCC 2022 address, there is much more on the horizon.

Ahighlight of the Specsavers Clinical Conference (SCC) is the way in which it acknowledges the macro and micro elements that contribute to the success of its optometry business. Whether it’s the in-roads to now detect 87% of undiagnosed glaucoma in Australia, or the celebration of community optometrists who have detected potentially fatal tumours, SCC never fails to offer a rich program.
There’s also the tantalising glimpse into the rollout of new technology and career pathways, and hints at additional areas of focus: à la myopia management – not to mention the high calibre of CPD content on offer.
FIVE-YEAR AMBITIONS
Specsavers ANZ director of optometry Dr Ben Ashby kicked off proceedings of the 2022 virtual event (10-11 September), with a live broadcast produced at Specsavers’ support office based in Port Melbourne, Victoria, also known as ‘The G’ (Bunurong Country).
In 2020, Specsavers outlined its five-year ambitions – and SCC 2022 provided the halfway point of this plan.
In his update, Ashby outlined how the company was trending well towards its goal to achieve a 95% detection rate for avoidable blindness by 2025. With initiatives such as training provided by RANZCO fellows into stores and scanning every patient with OCT, he said Specsavers optometrists were now picking up 93% of avoidable blindness in the community.
“This is a genuinely world-leading outcome in eyecare,” he added. Ashby said Specsavers has other ambitions to support more optometrist partners into its business. Since 2020, there have been 135 new optometry partners in ANZ. And in terms of its goal to be “loved by every customer”, patient feedback from surveys has shown that 98% feel cared for.
“And of course, everything is not possible without our people and our ambition is to be a great place to work for all optometrists, and to support them to have fulfilling careers, and nothing shows this to be more true over the last 2.5 years with 500 graduating optometrists joining us, sharing our vison within our graduate program and beyond to change lives through better sight,” he said.
Ashby said Specsavers also has lofty goals around growth. With there being 10 million people across Australia and New Zealand who can’t access regular eyecare, Specsavers would like to open this up to an additional one million patients per year by 2025. The company has so far achieved this with 170,000 people (17% of the target). The numbers are lower than hoped due to the pandemic and forced shutdown on routine optometry for long periods.
“But in addition to the 170,000 people, there’s half a million patients that dropped out of eyecare during COVID that Specsavers optometrists have cleared the backlog for, so a massive thank you for all the work you’ve done because we all know that regular access to eyecare is what is drives out those avoidable blindness outcomes and help people see better and live better lives,” he said.
“It’s not a job done yet but we are at a very good place at the 2.5-year mark.”
DATA DEEP DIVE
During the past 12 months, Specsavers cared for 3,892,439 people, issuing and updating more than 2,538,735 prescriptions, with 415,347 of those for contact lenses.
Away from vision care, Specsavers has a well-documented initiative to tackle undetected glaucoma in Australia, which historical data shows is 50% undiagnosed in the community. As Ashby explained, the Specsavers
32 INSIGHT November 2022 EVENT
strategy is having a meaningful impact that started with detection of 10% of undiagnosed cases in Australia in 2017 to a remarkable 87% in 2022.
“Through diligently examining every patient’s OCT scan, following up with visual fields, working with Glaucoma Australia and referring them on to ophthalmology, we have now found 150,000 previously undetected glaucoma patients in the community; that is an enormous achievement, one I know other places in the world would love to replicate,” he said.
“And for a condition that, not too long ago, the Blue Mountains Eye Study reported there being 200,000 undiagnosed patients, Specsavers has now uncovered three-quarters of them.”
Ashby also acknowledged the Ashfield store, and optometrist Nada Pistilli, who found Specsavers’ 150,000th glaucoma patient. It was befitting of the store that is picking up glaucoma at the same rate as the community prevalence.
Another store was recognised for the impact it’s having in another disease area – diabetes. Optometrist partner Vincent Marzano, from Specsavers Albury, made the 500,000th patient registration to the KeepSight diabetes eye check reminder program in July, marking a major milestone.

“To think we started this program with Diabetes Australia and the Federal Department of Health in 2019, and have now made 500,000 registrations into the program, and more than half of patients with diabetes are returning to us year-after-year, shows KeepSight is working,” Ashby said.
“We started this program to take on the challenge against the leading cause of blindness in the working age – diabetes. The biggest risk factor for losing sight to diabetes is not being in regular eyecare, and the fact this first-of-a-kind eyecare program in Australia is delivering on outcomes and bringing patients consistently back into eyecare is an amazing achievement.”
Next, Ashby touched on Specsavers’ next major disease focus – AMD. It is running a pilot in 16 stores with the Macular Disease Foundation Australia, aimed at reducing the number of patients with wet AMD who stop receiving anti-VEGF intravitreal injections or attending eye health appointments. He highlighted the “terrifying stat” that around 30% of people drop out from this treatment pathway after one year in Australia, despite its sight-saving ability.
“This program is in its early days but delivering amazing outcomes in terms of protecting people’s sight, and we certainly hope to see this become bigger, at-scale across Australia and into New Zealand in future.”
In other statistics, Specsavers sought feedback from its optometrists and found 86% said it was a great place to work, up 10% on 2021. It’s also set to launch three new career pathways and now employs more than 1,000 optometrists.
Meanwhile, the company’s partnership with The Fred Hollows Foundation (FHF) has reached new heights, with $6 million raised (more than $5 million for FHF and almost $1 million for FHF NZ). On top of many other fundraising initiatives, 20 cents from each pair of glasses sold at participating stores helps support the foundation, which is then used to help build a stronger workforce of Aboriginal and Torres Strait Islanders in eye health, and improve eye health coverage across Australia.
LOOKING FORWARD
Ashby rounded off his SCC 2022 address with a glimpse of what’s to come at Specsavers.
“In the people space, we are launching new career pathways for optometrists working in our business, and technology changes that will provide a new way of looking at clinical images so that it’s easy to access the most important information,” he said.
“There will also be some Socrates (Specsavers’ patient management system) changes in Australia to make it easier to record eye health data and allow PBS prescribing through the platform. And in New Zealand, we are pleased to say we are finally integrating OCT into the Genysis platform as well, a change you’ve been waiting for, for some time.”
To improve the customer experience, Ashby said Specsavers’ clinical performance consultants will provide more training for clinical support teams such as new training for pre-testers to ensure there’s better information coming into the consultation, as well as a plethora of clinical tips around effective and efficient clinical decision making for optometrists.

“Finally, I want to acknowledge the amazing outcomes achieved in avoidable blindness already that have hugely benefited the older patients in our practices. Now we will apply that same focus to younger people in our stores,” Ashby said, hinting at a greater emphasis on myopia management.
“There’s a unique opportunity for children … new technology can help young myopes avoid avoidable blindness much sooner than previously, and we will be providing you more ranges of products and new training so you can impact younger people in our stores just as much you support the older people.” n
At SCC 2022, Specsavers also announced its highly anticipated Doug Perkins Medal and Dame Mary Perkins Award winners for 2022. More information on this can be found on page 14. Meanwhile, turn to page 34 for an in-depth article on the exceptional act of patient care that landed Mr Surendran Naidoo, from Specsavers Dapto, with his Dame Mary Perkins Award.
INSIGHT November 2022 33
Dr Ben Ashby, Specsavers ANZ director of optometry.
SCC host Ms Michelle Du (right) and Dr Loren Rose, of Macquarie University, whose presentation focused on myopia progression in children.
CAUTIONARY TALE
Optometrist life-threateninguncoverstumour
An Illawarra optometrist who detected a pituitary tumour, leading to an urgent diagnosis and surgery that saved the patient’s life, highlights the importance of listening to the patient, especially when they dismiss general health complaints as ‘unrelated’.
Mr Surendran (Suren) Naidoo from Specsavers Dapto was recently awarded Specsavers’ Dame Mary Perkins Award after a visual field test found a patient had a bitemporal hemianopia, a classic sign of pituitary tumour.
The award, introduced in 2021, is reserved for an optometrist within the network that has shown an exceptional act of patient care in the past 12 months – something Naidoo exhibited in spades when Mrs Kelly Pabis came to see him with a vision complaint.

Pabis, a mother with two children – one with special needs – and a partner, had been to Specsavers Dapto a few months prior but there was nothing obvious or unusual about her presentation.
“Her primary complaint at the time was mild double vision but I was not the optometrist that saw Kelly when she initially presented,” Naidoo says.
“I picked up the consultation three months later when she returned, saying that she felt something wasn't quite right with her vision and that her eyes weren't working together. She didn't mention it to me, but she told a staff member at reception that she missed a car in her visual field while driving. At the time she came to see me, she wasn't experiencing any double vision.”
After initial testing failed to provide a plausible explanation, Naidoo conducted a visual field test.
“I picked up what was very obviously a bitemporal hemianopia, but it was quite severe, it had crossed the midline and spread over to the other half. And there were quite a few errors on the visual field test,” he says.
“I said to her, ‘There are quite a few errors. I want to repeat the visual field test as soon as possible’. And she said, ‘Maybe I can come back in a couple
of weeks’, but I told her this could potentially be more urgent than that.”
Pabis returned the following morning. This time, the visual fields reliability was better. A bitemporal hemianopia was more clearly defined and demarcated. Now, Naidoo faced a dilemma.
“You don't want to scare the patient. I was very reluctant to tell her what I thought it was. But obviously I had to express the urgency of her situation, so I said to her ‘I'm hesitant to tell you what I suspect it is because it is not my area of expertise/speciality, but this has all the hallmarks and signs of a tumour of the pituitary gland’.”
He then questioned her further about other systemic symptoms and referred her to her GP with an urgent request for an MRI. To further complicate matters, the Specsavers Dapto store was about to close for three weeks for a planned expansion.
“During that time, we would have limited access to clinical records because we'd be working off site. I called Kelly and said, ‘We are closing for three weeks, and I'm particularly concerned about you. Have you seen your doctor yet? Because this is quite urgent’. She said ‘Well, actually,’ – she was very groggy when she spoke to me – ‘I've just come out of surgery’,” Naidoo recalls.
This was because – the day after seeing Naidoo – Pabis had an MRI and CT scan, returned home, and then received a call from Wollongong Hospital asking her to pack a bag and come immediately.
LISTEN IN
Naidoo has diagnosed serious conditions before, but not in Australia.
“I've lived and practised in a few countries. In England, we had a girl with an optic nerve tumour, which in that particular case was potentially life
34 INSIGHT November 2022 PROFILE
Specsavers optometrist Mr Surendran Naidoo (left) and patient Kelly Pabis who had a life-threatening tumour.
CT SCAN CONFIRMS TUMOUR
threatening. I have detected a couple of pituitary tumours in my time, but nothing in Australia until now,” he says.
Naidoo says Pabis’ CT scans (pictured opposite) revealed the tumour was about 2-2.5 times the size of an eye.

“It was, by my estimate, about five to seven centimetres in diameter, and it was very obvious on the scan that it had started bleeding into the sinuses, and that was why she started getting vision-related symptoms.”
Pabis had been experiencing other symptoms for years but never thought to mention them during an eye test, because she didn't think it was related to her eyesight, Naidoo says.
“She never mentioned the cortisone injections she was getting for joint pain,” he explains.
“According to Kelly, she had been seeing her GP since 2018, complaining of joint pains. The GP eventually diagnosed her with tendinitis. After doing multiple blood tests, they gave her cortisone injections every three months into her hands, elbows and feet just to keep the pain away because she had trouble walking and using her hands.”
It highlights the importance of taking a patient's history, but also the delicacy in asking certain questions that might draw out pertinent information.
“I ask patients if they have any health issues, and if they say no, I'll usually ask them if they have any other symptoms they can think of that they don't think maybe related to their eyes. Because I find that very often patients are experiencing systemic symptoms, but they don't think about it when you ask them,” Naidoo says.
“For example, I ask if they are taking any other medication, if they have any other symptoms they haven't mentioned. And they'll say, ‘I don't think my eyes have anything to do with that’. Some patients can get quite offended and aggressive, wondering why I’m asking these questions, thinking it’s got nothing to do with their eyes.”
Naidoo says that after surgery, Pabis said she felt numb, meaning the absence of aches and pains that had plagued her.
“All those pains in her joints and extremities vanished. It was only at the three-month check-up when everything was stable that the neurologist said to Kelly, ‘When you walked in, I had no idea how you were still alive’. Her tumour was that severe. Subsequently, Kelly came back to see me a few months later and we repeated her tests. Her vision, in terms of her prescription, hasn't changed very much but the bitemporal hemianopia has completely disappeared and her visual field is completely restored,” Naidoo says.
“That I found amazing because I've seen patients where it doesn't come back.”
His astute observations in Pabis’ case is something that comes with experience.
“It's a lesson to not just myself but other optometrists and even student optometrists that the case history never stops. After the patient comes in, it continues through the entire consultation and sometimes even subsequent consultations,” Naidoo says.
“I remember a lecturer of mine all those years ago telling us at university that when the patient walks into a room, nine out of 10 times they will indirectly tell you what's wrong with them. You just need to listen.”
THE PATIENT
Pabis can easily recall the sequence of events that turned a regular visit to the optometrist into an urgent surgical procedure, and the reassuring manner of the man who helped her navigate her way through.
“When Suren told me there's something pressing on my optic nerve, he wasn't an alarmist. He was just very straightforward, very calming, very assuring. He said, ‘You need to see your GP to get a referral for an MRI. And then they'll take it from there’.”
She got a GP appointment the following morning and was booked for an MRI in nearby Corrimal that afternoon. Midway through her MRI, Pabis was advised she also required a CT scan.
“At that point, I knew they'd found something because that wasn't ordered.” Pabis was given a copy of the scans and followed up with her GP the next day. “I read the scans. I saw what was there, but I didn't know what it meant.”
Her GP confirmed Naidoo’s suspicions and contacted a neurosurgeon. She soon received the call from Wollongong Hospital, advising her to pack a bag. Once admitted to hospital, Pabis was given hydrocortisone injections to reduce her blood pressure and blood sugar levels, in preparation for surgery.
“I was admitted on Wednesday night. They did their own MRIs and scans on Thursday, and I had to meet with the Ear, Nose and Throat team because they take the tumour out through the back of your nose. They removed a big chunk of my cartilage and took a chunk of fat from my thigh to make a plug in the back of my head,” she says.
TIME LAPSE
“I'm a very energetic person but back in 2018, I had no energy. I’d sleep for 12 hours and wake up exhausted. I went to the GP and underwent a range of tests,” Pabis recalls.
Unbeknown to her, the tumour was already wreaking havoc.
“In 2020/2021 I started getting very severe tendinitis. I was exercising and doing low impact things like aqua aerobics that don’t put a lot of strain on your body. But I was always getting tennis elbow, and nothing would heal. Painkillers wouldn't even take the pain away. So I was getting cortisone injections, which would help for three months, but then the pain would return.”
Now, nearly 12-months post-surgery, Pabis is pain free and her vision is stable.
“I'm lucky that I had Suren to explain what was happening. I'm assuming a lot of people wouldn't take that extra step and explain this is what these symptoms mean,” she says. n
INSIGHT November 2022 35
Kelly Pabis' CT scan showing the eyes (circled in blue) and the pituitary tumour (circled in red). The human eye is, on average, approximately 24mm, and the pituitary gland roughly 10mm. The tumour was 50-70mm. The optic nerves can be seen extending posteriorly from the middle of each eye (more visible on the right), with the medial and lateral recti muscles on each side. The optic nerves would meet at the optic chiasm which would be overlying the area where the tumour is shown in the scan, hence the effect on Pabis' visual field. The part of the scan circled green is a sagittal section which shows the vertical extent of the tumour, and the red line denotes the level at which the main scan was done.
SWISS-MADE LASERS DELIVERING PRECISE RESULTS
A favourable regulatory environment has ensured Australian ophthalmologists continued access to the latest ophthalmic laser technology. That privilege has become even greater after Meridian Medical Lasers signed a new distribution deal with Device Technologies Australia.
Over the years, Meridian laser technology has been available intermittently in Australia, with the oldest Meridian Nd:YAG in Australia (Microruptor V) installed in 1994 at the Sydney Eye Hospital where it continues to be used in supine treatments. There are several lasers more than 14 years old, and customers like Dr Vongphanit have reported being satisfied with their performance.
But since the beginning of 2022, the Merdian laser portfolio has become more widely available to Australian ophthalmologists, after the company signed a distribution deal with Device Technologies Australia (DTA). The agreement came after DTA discontinued the distribution of lasers from a competing manufacturer, opening the door for Meridian.


For more than a decade, a Swiss-made Nd:YAG laser has been the workhorse for comprehensive ophthalmologist Dr Jerry Vongphanit in his consulting room at Mona Vale Eye Centre in Sydney. But after 14 years of service, the system is being replaced to ensure the clinic can continue offering high level post-operative management of lens-based surgery and management of narrow anterior chamber angles.
Impressed with the quality construction and optics of his original system from Meridian Medical Lasers, Vongphanit has turned to the manufacturer again many years later seeking to implement its latest YAG laser technology – the MR Q (Micro-Ruptor and Q-switch) – into his busy clinic.
“I’ve found the new MR Q YAG laser is even easier to use. I can complete a capsulotomy within a minute, without the need for the capsulotomy contact lens for the majority of patients,” he says.
“The laser has a user-friendly interface and the power used to perform the treatment is more efficient. All this results in quicker turnover and happier patients. The variable offset feature also means I am less likely to pit the optic of the IOL with the newer laser. It’s also mounted on a mobile table, allowing easier treatment for patients who are wheelchair dependent.”
He adds: “A patient who had experienced the difference between the newer generation laser and older generation laser said the experience was much better with the newer laser. It was faster and we didn’t use a capsulotomy lens which made it less intimidating for them.”
Thun-headquartered Meridian has been an optical manufacturer since 1937, but the company turned heads on the ophthalmic laser scene in 1982 after teaming up with the renowned Professor Franz Fankhauser to release what it describes as the first commercially-available Nd:YAG laser, the Microruptor II, which is still used in medical offices today.
Since then – through proprietary innovations and acquisitions – it has gone on to develop a complete array of photo-disruptors (Nd:YAG), photo-coagulators (single-spot and multi-spot), and ablation lasers, offering therapeutic laser approaches for post-cataract, retinal disease, and glaucoma.
“We wanted to continue offering innovative laser solutions to the local ophthalmology market and Meridian with its Swiss-made laser technology was an ideal fit,” says Mr Angus Hatfield-Smith, product manager for ophthalmic diagnostics for DTA.
“So we worked out an agreement with Rick Behrens, Meridian Medical Lasers head of sales and marketing for Asia Pacific and Latin America, seeing DTA take over the sales and service for Australia and New Zealand with our team of around 40 staff focused on ophthalmology.”
The partnership has been a snug fit, with both Meridian and DTA having close ties with another Swiss medical device company, Haag-Streit, and the Meridian Meralis laser offering a good pairing combination with the HaagStreit slit lamp.
TECHNOLOGY THAT APPEALS TO AUSSIE EYE DOCTORS
The YAG laser being installed at Mona Vale Eye Centre, where Dr Vongphanit consults, is part of Meridian’s latest MR Q family, consisting of stand-alone Nd:YAG lasers that can be coupled with single-spot retinal
36 INSIGHT November 2022
LASERS
The Merilas 532nm shortpulse ophthalmic laser photocoagulator.
Meridian’s latest MR Q family, consisting of stand-alone Nd:YAG lasers, can be coupled with single-spot retinal lasers such as the Merilas, as pictured.
lasers such as the Merilas, described as a modern, solid, and reliable retinal laser, available in green and yellow wavelength.
Behrens, who has been with Meridian for more than two years after previously holding senior level sales roles at the Adelaide-based Ellex Medical Lasers (now part of Lumibird Group), says MR Q has become the company’s flagship device, replacing the Microruptor Nd:YAG.

And with the recent launch of the MR Q SLT at the European Society of Cataract and Refractive Surgeons in Milan in September 2022, this system is set to become its premier product.
“Our newest MR Q SLT will allow users to perform capsulotomies and SLT either on or off axis, at a competitive pricing. We want to help doctors to provide the right treatments without compromising the safety of their patients and preserving their financial position,” he says.
Behrens says Meridian has carved a reputation for providing reliable and solid lasers. They have the only approved Haag-Streit laser integration in the industry, meaning its Merilas laser becomes part of the slit-lamp through the slit lamp optical path, rather than an adaptor.
“We are sure this unique interaction with a leading slit lamp in Australia will be highly appealing to our Aussie doctors,” he says.
In addition to the laser technology itself, Behrens says there are many other features that make Meridian lasers an attractive option.
For example, its single-spot photocoagulators (Merilas range) are built using a robust aluminium housing, ensuring protection of the internal components, while the cavities are cooled by a propriety thermal electrical cooling system, eliminating the need for fans and noise, while remaining dust-free. To meet the strict quality requirements for multi-site photocoagulators, Meridian uses its own laser cavities encased in a robust and resistant material.
“We have some other unique features in our lasers,” Behrens adds.
“We can access each of our lasers remotely with minor help from the user. The distance in Australia complicates the work of the service engineers and the response may be delayed when the laser is in a remote location. Our remote service means customers, especially those away from the main cities, can be reassured Meridian and DTA will not leave them stranded without an immediate answer in the unlikely service event.
“Our Nd:YAG lasers also offer electronically controlled offset. One of the main complaints when performing a YAG treatment is lens pitting. This is often caused by the bad use of the offset. MR Q uses the relevant offset position for the capsulotomies and auto sets to ‘posterior 100’ as a default start, minimising the potential for human error.”
Many of these innovations are possible thanks to Meridian’s decision to vertically integrate with two European manufacturing facilities. This means its single-spot photocoagulators are made in Thun, Switzerland, where Meridian has its head office. The YAGs and multi-spot lasers are made in Slovenia, a high-tech country with significant German influence. And the multi-spot technology itself comes from Finland, a pioneer in pattern lasers.
The MR Q is mounted on a mobile table, making it easier for wheelchair dependent patients.

According to Behrens, Meridian is also working on developing a SRT (selective retinal treatment) system at Bern University with leading Swiss and German partners. This, he says, may offer a breakthrough age-related macular degeneration treatment, with live feedback on the response of the retina and the laser energy being delivered.
“We are also developing a series of late generation cavities for our lasers," he says.
Thanks to Australia’s regulatory environment, Behrens says local ophthalmologists have quick access to the technology, with laser selection driven by Medicare reimbursements that provide a privileged position among other countries.
The photodisruption market is dominated by dual action Nd:YAG, combined with SLT. He says this technology, launched in 2001 in Australia, has found its way as the “must have” laser platform in ophthalmology practices.
“The maturity and tenure of these lasers makes for a perfect replacement opportunity for newcomers,” he says.
“We know Australia is a tough market, I know first-hand the dominance of other brands. We are asking the doctors to give us the opportunity to bring a technically advanced device and allow themselves to treat with something new. My expectation from DTA is a strong commitment to the brand, and having a brand representative in the country should help their staff to engage with Meridian strongly.
“I have the utmost respect for DTA and its staff, I worked there, and I know how good they are when selling, servicing, and installing devices.” n
INSIGHT November 2022 37
“I CAN COMPLETE A CAPSULOTOMY WITHIN A MINUTE, WITHOUT THE NEED FOR THE CAPSULOTOMY CONTACT LENS FOR THE MAJORITY OF PATIENTS”
DR JERRY VONGPHANIT MONA VALE EYE CENTRE
REFORMING THE PROSTHESES LIST... one item at a time
To place downward pressure on private health premiums, a deal between Australian MedTech’s peak body and the Federal Government is expected to generate $900 million in savings in medical device costs for health funds. Will this be passed on to consumers, and do the reforms go far enough?
There’s no secret of the constant tension between the Australian medical technology (MedTech) industry and private health insurers (PHI): both blame each other for rising private health premiums. But some important developments have taken place in recent months affecting the way certain ophthalmic products like intraocular lenses (IOLs) are priced that ophthalmologists and their patients ought to know about.
The Federal Government has been keen to reform the Prostheses List (PL) – introduced and reviewed multiple times since 1985 – which is the way private hospitals and device companies know the exact price PHIs will pay for devices used in private surgery. The PL has grown in both size and complexity, now including more than 11,600 items.
In 2019-20, more than 3.1 million prostheses on the list were supplied at a cost – to private health insurers and policyholders – of approximately $2.1 billion. Ophthalmology prostheses – such as IOLs, glaucoma drainage devices, intraocular gases and artificial irises – account for around 5% of all benefits paid by health insurers.
Therefore, the Federal Government has invested $22 million over four years to introduce reforms that it hopes will push PL benefits closer to prices paid in the public system. As a result, it’s hoped the reforms will improve the affordability and value of PHI to Australians by keeping downward pressure on premiums, while still maintaining access to high quality medical devices.
But who is responsible for rising premiums is a contentious topic.
Last year health funds delivered what they described as the lowest average premium increase in 21 years, which was still 2.7%. Private Healthcare Australia (PHA) – which represents 20 registered health funds and collectively represents 97% of people covered by private health insurance – blames the MedTech industry due to the “inflated” prices
health funds pay for medical devices in Australia, especially compared to other countries.
But the Medical Technology Association of Australia (MTAA) – representing companies like Alcon, Bausch + Lomb, Device Technologies and Johnson & Johnson Vision – says it’s down to the multi-billion-dollar ‘management expenses’ that PHI’s pay for their own executive salaries, bonuses and expensive offices.
Either way, Australia’s MedTech industry has accepted it has a role to play in reducing PHI premiums and is working through a phased reduction of prostheses prices with the government through the PL reforms program.

In one of his final moves as Federal Health Minister, Mr Greg Hunt vowed to pave a smoother pathway towards the reforms that will be implemented by 2025.
Despite objections from the PHI industry that described it as “a lastminute pre-election deal” with big international MedTech companies, Hunt signed a Memorandum of Understanding (MoU) with MTAA on 17 March.
In essence, the four-year agreement outlines the Commonwealth’s iron clad commitments to the MedTech industry. The most important pertinent to the ophthalmic industry are:
• PL items will have their benefit levels reference priced by establishing the gap between the prices paid in public hospital system and the PL.
• PL devices priced less than 7% above the Weighted Average Price (price for prostheses in Australian public hospitals, as determined by the Independent Hospital Pricing Authority (IHPA)), would not be reduced.
38 INSIGHT November 2022 POLICY
• PL benefits for devices with a benefit more than 7% above the Weighted Average Price are to be reduced by: 40% of the difference on 1 July 2022; 20% of the difference on 1 July 2023; and 20% of the difference on 1 July 2024,
• However, PL device prices can not reduce below a 7% “floor”.
• No reductions to PL benefits are to occur in year four of the reforms, between 1 July 2025 and 30 June 2026, effectively providing a 20% private adjustment factor on the initial gap between the Weighted Average Price (public price) and the PL benefit.
The first price reductions have already come into effect on 1 July 2022. The public benchmarking was undertaken by IHPA, and its advice on the PL adjusted benefit amounts affected several ophthalmic items, according to government documents at the time of print.
For example, the benefit for viscoelastic (high molecular weight) was reduced from $65 to $58, while capsular tension rings dropped from $143 to $121 (simple) and $301 to $254 (complex). Others affected included foldable posterior chamber IOLs that included a microincision or edge modification element (i.e. foldable posterior chamber IOL with edge modification and aberration technology, toric >7 D, violet blue light filter is priced from $817 to $760).
In accordance with the MoU, these items, and others considered above the 7% price paid in public hospitals, would then be reduced another 20% of the difference in 2023 and then again in 2024.
Interestingly, intraocular fluids (viscoelastics) were originally slated for delisting by the health department entirely and to be funded by “alternative arrangements”. It didn’t go through with this after the ophthalmic sector advocated against the move, but the fact this was initially proposed compromised confidence in the PL reforms process for some groups.

TIME FOR HEALTH FUNDS TO STEP UP, SAYS MTAA
In signing the MoU with the Federal Government, MTAA was thankful for the certainty it provided, but was keen to highlight the “enormous sacrifices” the MedTech industry had made.
MTAA chair Mr Maurice Ben-Mayor was thankful for the agreement’s focus on recognising “the explicit distinction” between the public and private markets that still guarantees patient access and doctor choice. He was also thankful for former Minister Hunt’s decision to lead the reforms “away from abolishing the Prostheses List” and towards a process that would provide greater certainty for MedTech companies.
MTAA said the government’s measures would lead to significant cuts being passed on as savings to PHI companies by way of more than $900 million delivered by the MedTech industry. But it was important this trickled down to the consumer.
MTAA CEO Mr Ian Burgess said the total cuts incurred by the Australian MedTech industry of more than $2 billion over eight years, is in stark contrast to the $2.4 billion profits corporate health insurance companies have generated over the last two years.

“MTAA put forward the most comprehensive reforms to the PL, ever. Our industry understood the need for fit-for-purpose and effective reforms to the PL that could reduce premiums, while protecting the patient access and doctor choice guarantee of the PL,” Burgess told Insight
“The MoU was developed to clarify and set guardrails in an attempt to rectify the serious issues in the previous government’s proposed reforms. While the MoU still leaves significant challenges and didn’t address all of industry’s concerns, it made sensible and necessary changes to the former government’s previously announced reforms.
“MTAA fully expects corporate insurers to pass on the savings provided to them through MTAA’s four-year agreement to consumers, in full. Mechanisms should be put in place to ensure this occurs and consumers reap the benefit.”
MTAA believes that while these reforms will still place a significant burden on the MedTech industry, they’re far better than “the devastating changes the private health insurance industry had been lobbying for”, which it said could have seen doctor choice and patient access to medical devices severely restricted or even abolished.
At the time of signing the MoU (March 2022), Hunt said the government recognised the importance of providing predictability for the MedTech industry and the MoU set out a process to ensure a more seamless implementation of the reform arrangements. He said it would also ensure the commitment of the medical technology industry to see through the reforms.
“In particular, the MoU provides clarity to industry about how items on the list will be costed, setting in place a process to reduce the gap between the cost of medical devices in the public and private health sectors over three years,” he said.
BUT PRIVATE HEALTH INSURERS AREN’T IMPRESSED
Health fund peak body Private Healthcare Australia (PHA) believed the MoU amounted to a “watering down” of the PL reforms, and questioned whether the price reductions were enough.
In fact, PHA has called on the since-elected Albanese Government to reverse the Hunt-MTAA MoU that it says “locked in prices for medical devices in the private system 7-20% higher than public prices”.
PHA CEO Dr Rachel David said the deal would transfer an estimated $250-$400 million from Australians with PHI to medical device companies over the next four years.
According to PHA, Australian Prudential Regulation Authority (APRA) data over the past three years showed there was a 1.4% decrease in health fund benefits paid for in-hospital medical (MBS) services and a
PURPOSE OF THE PROSTHESES LIST REFORMS
n For Insurers – reduced expenditure on prostheses that may be passed on to privately insured patients through reduced private health insurance premiums.
n For Hospitals – assurance that any prostheses will be eligible for reimbursement through the PL arrangements.
n For Medical Device Companies – continued certainty around products eligible for reimbursement through the PL arrangements. Also, streamlined application and assessment pathways.
n For Clinicians – continued ability to choose the most appropriate prostheses for patients.
n For Privately Insured Patients – reduced private health insurance premiums. Plus, clarity around which prostheses are covered.
Source: Department of Health
INSIGHT November 2022 39
“MTAA EXPECTS CORPORATE INSURERS TO PASS ON THE SAVINGS PROVIDED TO THEM THROUGH MTAA’S FOUR-YEAR AGREEMENT TO CONSUMERS, IN FULL”
IAN BURGESS MEDICAL TECHNOLOGY ASSOCIATION OF AUSTRALIA
2.6% reduction in hospital episodes over the period.
But there had been a 4.3% increase in benefits paid for medical devices (prostheses) over the same period. This is in spite of the slowdown in surgery performed due to the COVID-19 pandemic. But MTAA said the numbers show insurers spent 4.2% less for medical devices compared to this time last year, despite procedure numbers recovering.
“The fact that medical device claims consistently continued to grow out of proportion to the number of procedures performed in hospitals during the COVID pandemic is evidence the pricing of medical devices in Australia’s private health sector is the single largest contributor to increasing PHI premiums,” David, of PHA, said.

She said the Albanese Government must prioritise medical device pricing reform in the upcoming Federal Budget so health funds can begin to offer premium relief to Australian families.
“Every single dollar saved by private health funds as the price of devices becomes fairer between the public and private systems will be sent back to members in the form of lower premiums. It will also save the budget around $100 million over the next four years,” said David.
“We cannot simply barrel down the path of the US health system which is facing 10% premium growth due to out-of-control health inflation.”
REMOVAL OF GENERAL USE ITEMS
A consequence of the work undertaken to clarify the PL scope has meant that hundreds of general use and consumable products have been identified for removal because they either do not meet the current criteria for listing or because they will not meet the new definition or listing criteria.
The Federal Government has made it clear this should not result in any additional out-of-pocket for consumers and has requested that insurers and private hospitals work together on an alternative funding agreement and to facilitate negotiations.
David, from PHA, said the removal of 400 ‘general and miscellaneous’ items from the PL was long overdue and will not impact patient care.
“Using a government price list to pay for consumable items like sponges, glues and staples is completely inefficient. Prices have been too high for too long and international medical device companies have profited at the expense of Australian consumers,” she said.
“These items remain wildly overpriced in Australia relative to other markets. The items will all be funded but not at five times market value. Suggesting that any health fund offering to roll up the funding for these consumable items into general contracting arrangements is refusing to fund the items is just mischievous.” n

“THE PRICING OF MEDICAL DEVICES IN AUSTRALIA’S PRIVATE HEALTH SECTOR IS THE SINGLE LARGEST CONTRIBUTOR TO INCREASING PHI PREMIUMS”
DR RACHEL DAVIID PRIVATE HEALTHCARE AUSTRALIA
POLICY
STRIVING FOR NEW HIGHS IN KERATOCONUS TREATMENT
Researchers behind a world-first Australian-built registry collating real-world data on current keratoconus treatment and patient outcomes, including quality-of-life markers, are hoping to add a novel stem cell treatment that can restore the cornea to its normal shape and size.

Based on studies in the early 1980s, keratoconus was estimated to affect one in every 2,000 people in the general population, according to Keratoconus Australia. Forty years on, it is thought to be as high as one in 750 people worldwide. A recent Australian study published in 2020 indicates a prevalence of 1 in 84 amongst 20-year-olds.

The variation, Keratoconus Australia notes, more likely reflects improved diagnostic techniques, rather than a rising incidence of this disease that new studies suggest affects quality-of-life more than other eye conditions.
Fortunately, treatment options have also evolved. Surgery, including corneal collagen crosslinking and less commonly intra-corneal rings, are feasible options, as well as the mainstay of treatment rigid contact lenses.
Now, medicine and engineering are combining to forge a multidisciplinary approach to finding a novel treatment that could potentially change the lives of those who are suffering from this progressive disease.
IT WORKS IN A TRIAL, BUT WHAT ABOUT THE REAL WORLD?
Professor Stephanie Watson OAM is head of the corneal unit at Sydney Eye Hospital, head of corneal research group at Save Sight Institute (SSI) and chair of Australian Vision Research as well as co-Deputy Director of Industry, Innovation and Commercialisation at Sydney Nano.

She was integral in establishing the Save Sight Keratoconus Registry in 2015, a world-first for keratoconus patients and clinicians. The registry
enables eyecare practitioners to benchmark their practice as everyday outcomes are tracked. Patients can also provide perspectives on their treatment via patient-reported outcomes questionnaires.
“I run a research program which has a number of facets; one of them is the Keratoconus Registry to immediately improve outcomes through providing clinicians with benchmarking and CPD points,” Watson says.
“We can track which treatments are being given to patients with keratoconus – as current treatments can have variable results, some treatments are good, and the evidence for some is still emerging.”
Corneal crosslinking is one treatment the registry is tracking.
INSIGHT November 2022 41
KERATOCONUS
An Australian study published in 2020 indicates keratoconus affects one in 84 20-year-olds.
“THE REGISTRY ALLOWS US TO SEE IF THE OUTCOMES IN THE REAL WORLD REFLECT WHAT HAS BEEN FOUND IN CLINICAL TRIALS”
PROF STEPHANIE WATSON SAVE SIGHT INSTITUTE
“Generally, crosslinking has good results, but it's been done in quite a number of different ways; there's a lot of innovation. For example, surgeons have started using oxygen within the crosslinking procedure. The registry allows us to see if the outcomes in the real world reflect what has been found in clinical trials,” she says.
“The registry is collecting data on the use of oxygen in crosslinking and we've just published a review of available evidence, so we can immediately find out what's going on with the current treatment.”
According to Watson, optometry plays a key role in keratoconus management, so an optometry module was added to the Save Sight Keratoconus Registry, allowing primary eyecare providers to track the outcomes of contact lens wear, considered a mainstay for restoring vision.
Watson says another facet her team is researching is quality-of-life, because a lot of measurements used to evaluate a patient’s condition don't always directly link to this.
“We're very much interested in that aspect. And that's why we work very closely with Keratoconus Australia, and patients with keratoconus, because we want the research to make meaningful changes to patients’ lives.”
Another closely related facet SSI researchers are investigating is the impact of keratoconus on mental health and wellbeing.
“For teenagers with keratoconus, when they're transitioning into adulthood, it can be distressing for them to know that their vision may decline. So that's another area that we’ve started to work on with the registry.”
Watson says while the treatments available can stop keratoconus getting worse, there isn’t any treatment that can make the cornea ‘normal’ again, and that’s where research is heading.
“We've started to investigate stem cells and cell-based therapies to try to change the cornea back to its normal shape,” she says.
“But to work with cells, we need to be able to harvest and transplant them. And to do that, we're looking at different materials and technologies, including nanotechnology.”
SSI has developed a preclinical model for keratoconus, which is ready for testing.

“We have pre-clinical models and a clinical trials unit at the Save Sight
Institute. So we've got the pathway to clinic ready; now we're refining the technology and hope to be able to bridge the translation gap,” Watson says.
“We want to develop treatments for the future. But we also need to look at current treatments and make sure they're safe and effective. That's why we cover both aspects in the corneal research program – tracking outcomes and developing treatments. Hopefully we'll be adding stem cell treatments to the registry and tracking the outcomes in future.”
APPLYING NANO-BIOENGINEERING TO KERATOCONUS CARE
Indian-born academic Dr Yogambha Ramaswamy was awarded a PhD in Biomedical Engineering from the University of Sydney and has been a recipient of the prestigious Vice-Chancellor’s Research Fellowship from UNSW and NHMRC Peter Doherty early career fellowship. She is currently a senior lecturer in the School of Biomedical Engineering at the University of Sydney.
Ramaswamy has a strong research experience in the area of biomaterials and tissue engineering. Her research work has led to the development of materials for tissue engineering applications and has had significant impact in advancing the knowledge in biomaterials and its translational potential.
She describes her involvement in keratoconus clinical research through meeting Professor Watson as serendipitous.
“I knew Stephanie briefly from my time at UNSW, however a chance meeting at the Sydney Nano Health forum last year gave us an opportunity to work together,” Ramaswamy says.
The pair got in touch towards the end of last year and, realising the synergy in their research expertise, conceptualised a project to apply their respective skills towards developing a novel solution for keratoconus treatment. In March, they secured seed funding through Sydney Nano Health, and have applied for further funding opportunities.
“I thought our multidisciplinary project was a novel way of integrating medicine and engineering by bringing together Stephanie’s clinical expertise in keratoconus treatment and my engineering experience in materials and nanotechnology,” Ramaswamy says.
The pair have also engaged other researchers, who are experts in in vivo models, stem cell biology and nanotechnology.
“I lead from engineering, and Stephanie leads from medicine. We feel that our research strengths and strategies can advance research in this area and lead towards clinical translation and potentially improve keratoconus treatment.”
Ramaswamy says there is a lot of global healthcare initiatives looking into nano bioengineering and applying it to various streams in tissue engineering including ophthalmology.
“There has been a lot of funding channelled into the global regenerative medicine and nano bioengineering market – which involves using materials, biomolecules, cells, and nanotechnology, to repair and restore damaged tissue, including ocular tissue – and it keeps increasing,” she says.
“As ophthalmology is dealing with soft tissue, polymer-based materials are considered to be appropriate, and you can integrate these materials with nanotechnology to improve and address diseases like keratoconus.”
She continues: “If you think of keratoconus, it is a progressive thinning and steepening of the cornea. Changes in corneal shape distort vision. When healthy stem cells become deficient, the regenerative capacity of these corneal stem cells is damaged.”
Ramaswamy says cellular therapy of the cornea is considered as a promising advanced therapeutic approach for corneal disease, including keratoconus.
“We want to see whether we can repair damaged corneas using tissue engineering approaches.”
42 INSIGHT November 2022
Figure 1: Topographic map of a cornea with keratoconus.
KERATOCONUS
In this project, Ramaswamy says the team will use a combination of stem cells, multi-functional nanomaterials, and polymer-based jelly-like hydrogel constructs that can help in the repair of the cornea.

“For corneal repair we want to increase the stemness of the cells to improve the stem cell quality and functionality, as well as their numbers.”
Watson and Ramaswamy believe that their nano-bioengineering platform comprising of polymers, stem cells and nanotechnology has the potential to achieve it.
“Stephanie led a clinical trial of a stem cell treatment that restored the cornea in limbal stem cell deficiency. But not all patients could be treated. We now want to see whether we can improve on stem cell numbers and quality using our multicomponent platform, and then transplant stem cells to the patient’s eye.”
Their project is currently lab-based but they are working towards a goal of clinical translation.
“We have applied for several funding grants and have a team who are helping us to advance our study. We have good support from scientific community who are really interested to see this work go forward.”
BRINGING QUALITY-OF-LIFE TO THE FORE
Nepal-trained optometrist Dr Himal Kandel travelled and studied extensively before accepting the position of Kornhauser Research Associate at SSI.
After graduating with a Master's in Public Health for Eye Care from the London School of Hygiene and Tropical Medicine at the University of London, Kandel then moved to Australia to pursue a PhD at Flinders University, focusing on the impact of refractive error on quality-of-life.
Immediately after completing his PhD, Kandel accepted his current research position at SSI.
Evaluating and improving quality-of-life has been a major focus of the Save Sight Keratoconus Registry.

“I am interested in looking at comprehensive patient outcomes. And here, we have the Save Sight registries, which track outcomes, including quality-of-life as well as other clinical outcomes,” he says.
Although SSI has produced quality-of-life research for eye conditions including age-related macular degeneration and diabetic macular oedema, Kandel is mainly focused on keratoconus. Because keratoconus is often diagnosed in adolescence, and is a progressively worsening condition, it affects patients for a lifetime.
He says the data shows that keratoconus patients have the worst
Minimum Product Information: XALATAN® (Latanoprost 50 μg/mL) Eye Drops. Indication: Reduction of intraocular pressure (IOP) in patients with open-angle glaucoma or ocular hypertension. Contraindications: Hypersensitivity to ingredients. Precautions: Change in eye colour due to increased iris pigmentation, heterochromia; eyelid skin darkening; eyelash and vellus hair changes; aphakia; pseudophakia; macular oedema; other types of glaucoma; contact lenses; severe or brittle asthma; herpetic keratitis; driving or using machines; elderly; children; lactation. Pregnancy: Category (B3) Interactions: other prostaglandins, thiomersal. See PI for details. Adverse Effects: Iris hyperpigmentation; eye irritation (burning, grittiness, itching, stinging and foreign body sensation); eyelash and vellus hair changes (increased length, thickness, pigmentation and number of eyelashes); mild to moderate ocular hyperaemia; punctate keratitis; punctate epithelial erosions; blepharitis; eye pain; excessive tearing; conjunctivitis; blurred vision; eyelid oedema, localised skin reaction on eyelids; myalgia, arthralgia; dizziness; headache; skin rash; eczema; bronchitis; upper respiratory tract infection; abnormal liver function. Uncommon: Iritis, uveitis; keratitis; macular oedema; photophobia; chest pain; asthma; dyspnoea. Rare: periorbital and lid changes resulting in deepening of the eyelid sulcus; corneal calcification. See PI for details and other AEs. Dosage and Administration: One eye drop in the affected eye(s) once daily. Other eye drops should be administered at least 5 minutes apart. (Based on PI dated 2 March 2021)

References: 1. NHMRC Guidelines for the screening, prognosis, diagnosis, management and prevention of glaucoma 2010 2. Australian Commission on Safety and Quality in Healthcare Active Ingredient Prescribing Guide - list of medicines for brand consideration December 2020
Aspen Australia includes Aspen Pharmacare Australia Pty Ltd (ABN 51 096 236 985) and Aspen Pharma Pty Ltd (ABN 88 004 118 594). All sales and marketing requests to: Aspen Pharmacare Pty Ltd, 34-36 Chandos Street, St Leonards NSW 2065. Tel: +61 2 8436 8300 Email: aspen@aspenpharmacare.com.au Web: www.aspenpharma. com.au Trademarks are owned by or licensed to the Aspen group of companies. © 2021 Aspen group of companies or its licensor. All
reserved. Prepared: June 2021 AF05768 ASP2528
“IF WE USE A PROTEIN MOLECULE THAT IS ALREADY FDA-APPROVED, OUR CLINICAL PATHWAY BECOMES A BIT MORE FEASIBLE AND LESS COMPLICATED"
DR YOGAMBHA RAMASWAMY UNIVERSITY OF SYDNEY
If clinically necessary for the treatment of your patient, prescribe by brand and disallow brand substitution2✔ A first choice for glaucoma management1
rights
Before prescribing please review Product Information available via www.aspenpharma.com.au/products or call 1300 659 646. PBS Information: Xalatan (latanoprost 0.005% eye drops, 2.5 mL) is listed on the PBS as antiglaucoma preparations and miotics.
THE NEED FOR EVALUATING PATIENT-REPORTED OUTCOMES IN ROUTINE CLINICAL PRACTICE
The Save Sight Registries at The University of Sydney found that visual acuity may not be the main factor in determining quality-oflife for people with keratoconus.
Using data from the world’s largest keratoconus registry, vision and quality-of-life were found to be only weakly connected.

The ground-breaking research has been published in the May/June issue of the Clinical and Experimental Ophthalmology journal, the official journal of RANZCO.
“Our research findings have important implications for everyday clinical practice as they show the need to measure the patient’s experience of the disease, not just visual acuity, in keratoconus. The patient experience (patient reported outcome) is needed to understand the impacts of keratoconus and its treatment as well as to make decisions on which treatments are needed,” Dr Himal Kandel, the paper’s lead author, said.
“Using patient reported outcomes in everyday practice can also improve communication between patients and clinicians with the end result being shared clinical decision making and improved quality of care.”
In this world-first large study, the researchers compared qualityof-life outcomes from 1,557 patients with keratoconus to those with retinal diseases – specifically age-related macular degeneration, retinal vein occlusion and diabetic macular oedema – in the Save Sight Registries international patient database.
The patients were recruited from 44 sites in Australia, Singapore, Italy, Bosnia and Herzegovina, Spain, and France.
The quality-of-life scores were collected using a validated questionnaire known as the Impact of Vision Impairment questionnaire which had questions on two domains: visual functioning and emotional.
Patients with keratoconus had lower quality-of-life scores, particularly emotional scores, than retinal diseases. Emotional issues had the greatest impact on keratoconus patients with severe disease. Overall, quality-of-life scores were lower in females with keratoconus than males.
Encouragingly, keratoconus patients who had undergone corneal crosslinking had better quality-of-life scores. This highlights the need for early diagnosis and treatment.
“Every day in the clinic, assessing quality-of-life in patients with keratoconus can guide treatment decisions. Our research shows that treatment should be aimed at optimising visual functioning and emotional wellbeing to improve quality-of-life and informs evidencebased resource allocations at the planning level,” Professor Watson, the senior author of the paper, said.

“Using the Save Sight Keratoconus Registry, patient reported outcomes collection can be easily incorporated into everyday clinical care. Patients with keratoconus can be reassured that clinicians have been made aware of the impact of their condition on their quality-of-life,” she said.
quality-of-life status compared to other eye conditions.
“Usually, people don't go blind because of keratoconus, meaning they may have quite good visual acuity compared to other eye conditions. But even though their visual acuity can be good, keratoconus can lead to severe quality-of-life impacts. This is the key message from our research because for policymaking or resource allocation, we have the option to consider visual acuity and vision impairment, but we don't consider quality-of-life impact,” Kandel says.
“The keratoconus patients may experience glare, distorted vision, dry eyes and tired eyes leading to poor quality vision. Similarly, they may have issues driving during the night, and difficulty working on the computer. The early age of onset and progressive and chronic nature of the disease may cause emotional stress. These issues may be more important in determining their quality of life than the ability to read letters in a visual acuity chart in a clinic.”

He continues: “Keratoconus patients may be considered to be doing well when we assess their vision only, I think our research highlights that we need to consider quality-of-life more comprehensively and how keratoconus is affecting day-to-day visual function along with other symptoms, and emotional well-being.”
Kandel says other studies performed at SSI using data from the registries have found that the quality-of-life scores are weakly correlated with clinical measures.
“That means it's really important to monitor how patients are doing with respect to quality-of-life, visual function and symptoms.”
He says gathering data on quality-of-life can be complex.
“If we don't use quality tools and methods, then we will not get quality results. We collect patient reported quality-of-life outcome data using validated questionnaires. When a patient comes to the clinic, they fill out the questionnaire during their waiting time and the data is uploaded

44 INSIGHT November 2022 KERATOCONUS
A Pentacam scan showing corneal steepening and thinning in an 18-year-old male with keratoconus.
“WE NEED TO CONSIDER QUALITY-OF-LIFE MORE COMPREHENSIVELY AND HOW KERATOCONUS IS AFFECTING DAY-TO-DAY VISUAL FUNCTION"
DR HIMAL KANDEL SAVE SIGHT INSTITUTE
automatically into the registry. We are then able to track quality-of-life outcomes with the registry. During the clinic, eyecare practitioners can look at the questionnaire scores, how it has improved or gotten worse, and researchers can study and compare the data,” Kandel explains.

Kandel presented the latest keratoconus quality-of-life research (see Side Bar) at KeraClub in August.


He says one of the questions he received from the audience –predominantly keratoconus patients – was regarding the mental health impact of keratoconus.
“We have recently started collecting data on the mental health of keratoconus patients. It is our next project – evaluating the mental health impact of keratoconus. We have added validated questions on mental health to the Save Sight Keratoconus Registry. We hope that our registry data will enable the mental health impacts of keratoconus to be understood, as the published evidence is conflicting,” Kandel says.


Kandel anticipates the study will support evidence that although keratoconus patients may have good visual acuity, they shouldn't be prioritised lower than other eye conditions because of the quality-of-life and mental health impact.


“Our team is the largest contributor in this area of research. The Keratoconus Registry data is really helping us to understand more about the impact of keratoconus. It is highlighting the importance of monitoring quality-of-life by eyecare practitioners in routine clinical practice. With the registry we can identify specific issues for a patient so that we can manage them, such as difficulty with computer work. Our research is really useful in finding out how patients’ lives can be improved.” n

Telephone: (02) 96437888 Toll Free: 1800804331 Email: sales@bocinstruments.com.au Website: www.bocinstruments.com.au Elevating eye health care with the touch of a button • New model – 80000 Scans/second & Wide Field Scans • Fully automated operation with a simple touch of a button • Easy as 1,2,3... enter patient information, position patient & touch to start • iScan vocally guides the patient through the entire scan process • Self-contained with small footprint – ideal for a range of clinical settings • Includes a full suite of Retina, Glaucoma, Cornea & Anterior Segment scans • Trend analysis with rate of change & significance AUTOMATED RETINAL IMAGING NFC-700 • Fully Automated with 3D Tracking, Auto focus and Auto Capture • Compact - integrated Tablet PC with HD touch screen, Win 10 OS • Sharp consistent HD Retinal and Anterior Eye imaging • Ten internal fixation targets for peripheral fundus capture • Enhanced connectivity – WiFi, USB, HDMI & Ether net • Image processing functions and remote viewing software Non-Mydriatic LED Retinal Camera Slit lamp photo of the left eye of a 21-year-old male patient with advanced keratoconus. Note the apical scarring and thinning. Image: Prof Stephanie Watson.
At the completion of this article, the reader should be able to improve keratoconus management.
Including:
• Understand the risk factors and symptoms for keratoconus
• Know how new technologies have improved keratoconus patient outcomes
• Understand the rationale behind updated keratoconus referral protocols
• Know the elements vital for an informed keratoconus referral
COLLABORATIVE CARE IN KERATOCONUS

Many ideas about keratoconus are changing. As DR BRENDAN CRONIN points out, there are new diagnosis and therapeutic technologies available, prompting changes in the optometrist’s role. Increasingly, keratoconus patients will rely on informed optometrists to notice and act on their symptoms early to ensure the best outcomes.

WHAT IS KERATOCONUS?
There have been profound changes in our diagnosis, understanding and treatment of keratoconus over a number of years. Improved diagnostics have enabled earlier detection and better estimates of the prevalence of keratoconus in the community. A better understanding of the pathophysiology of the disease has also led to a greater range of more effective treatments to alter its natural history.
Traditionally, in the Australian population, the rate of keratoconus was thought to have been around 1 in 2,000. More recent studies using corneal tomography and topography have demonstrated rates of keratoconus to be up to 1.2% of the population – or 1 in 84 people1; this takes the condition from being one that
was considered to be quite rare and not hugely relevant from a public health perspective to being one that is quite common.
Given the significant lifelong visual complications associated with keratoconus, there is an enormous public health benefit in early diagnosis and treatment. This requires a thorough understanding of the condition and excellent communication and collaboration between optometrists and ophthalmologists for ongoing patient care.
Keratoconus has traditionally been described as a non-inflammatory condition however, it is now widely accepted that it is an inflammatory disease.2 We understand that allergic eye disease and in particular, eye rubbing, is a very significant risk factor and can significantly
ABOUT THE AUTHOR: Dr Brendan Cronin
MBBS (Hons) DipOphthSci B.Com LLB FRANZCO Queensland Eye Clinic, South Brisbane, QLD Queensland Eye Clinic, Clayfield, QLD
exacerbate the condition. A family history of keratoconus is also one of the other major risk factors.3
Importantly, even subclinical keratoconus is a risk factor for offspring developing the disease. Given the documented high prevalence of the condition in the population, diagnosing even asymptomatic keratoconus in older patients has a significant public health benefit in that it will facilitate screening of other members of the family.
IDENTIFICATION AND DIAGNOSIS OF THE CONDITION
The hallmark symptoms of keratoconus along with the other corneal ectatic disorders are reduced visual acuity and increased sensitivity to light and glare, particularly flaring of lights at night.
Optometrists have always been very wellpositioned and particularly adept at identifying patients with these presenting symptoms along with a reduced best corrected spectacle
CLINICAL CPD HOURS This activity meets the OBA registration standards for CPD
LEARNING OBJECTIVES:CPD
Figure 1. Distorted mires seen on an autorefractor in keratoconus.
46 INSIGHT November 2022
acuity, particularly in the setting of increasing astigmatism, and identifying this as likely keratoconus. Clinical tricks such as the scissor reflex or the Charleaux/oil droplet sign on retinoscopy can be diagnostic of the condition.
In recent years more highly advanced diagnostic equipment has become much more commonplace in optometric practices. Even fairly basic equipment such as autorefractors can be beneficial in diagnosing the condition when patients still have a good best corrected visual acuity due to the presence of distorted mires on autorefraction machines (Figure 1). Obviously if there is a history of allergic eye disease, eye rubbing or a family history of keratoconus, this makes the index of suspicion that much higher, even in patients presenting with good vision.
The availability and reduced cost of topographers has been a game-changing development for the early diagnosis of keratoconus. Cheap but effective placido disc-based topographers are commonplace in optometric practices. As a result, a definitive diagnosis of keratoconus can be made in a primary care setting very early on in the disease. These days, many optometry practices also have tomography which can further document keratoconus by looking at the posterior elevations in corneal topography and also the characteristic corneal thinning that occurs in the disease.

Additionally, Some OCT machines now perform not only retinal OCT but also OCT-based topography, making this once very specialised and expensive diagnostic tool more readily available.
REFERRAL PATTERNS
Prior to the development of corneal cross-linking, referral to an ophthalmologist for a patient with keratoconus was only advantageous to either confirm the diagnosis or to offer surgery for visual rehabilitation of a patient intolerant of contact lenses. Because there are a range of treatments now available, referral patterns need to change accordingly. A delayed referral may have a profound difference in the long-term outcome for a patient and the treatments available to them.
CHILDREN
It is critical that children with a suspicion, or confirmed diagnosis, of keratoconus are referred urgently for review. Typically, the younger a patient is at presentation, the more aggressive the disease. In adolescence and young teenagers their best corrected acuity can plummet over a matter of weeks to a few months.4
While there are regional and interpersonal differences in what clinicians qualify as progression, the threshold for what is considered to be progression is generally considered to be significantly lower in patients who are younger. For example: if a patient has ever had an objective documentation of normal visual
acuity and then presents with reduced visual acuity and documented keratoconus, many clinicians would argue this is an adequate indication of progression.
In short, optometrists should not wait to document any type of refractive visual or topographic progression in children or adolescents with the condition. Referral should be made immediately on suspicion of the disease. The referring optometrist should include any previous visual acuity with the referral.
It is also vital to stop any eye rubbing and manage any allergic eye disease immediately in these young patients.
ADULTS
In adults, particularly those in their mid 20s and over, the requirement for referral can be divided into two broad groups. In the first group: those with a new diagnosis of keratoconus. These patients should all be referred for an opinion on treatments to halt the progression of the disease. In these cases, however, some type of objective documentation of their visual history is important. It is advantageous if referrals can include documentation of any refractive or topographic change over a period of time as this is required by Medicare to justify cross-linking.
In the second group are the large number of patients who will have stable keratoconus either due to their age or those who have potentially had cross-linking. If these patients have good visual acuity either in glasses or well-fitting contact lenses, there really is little need for them to be referred for ophthalmic assessment. If,
however, they have any reduction in their visual acuity or quality-of-life due to issues with wearing contact lenses, the availability of new treatments makes referral of these patients appropriate in the absence of progression of the disease.
CO-MANAGEMENT
Optometrists are crucial to the public health campaign to avoid both habitual and allergyrelated eye rubbing in adolescence to help reduce the incidence and progression of keratoconus. This applies to all patients who have any allergic eye disease but this is especially important for patients with keratoconus.
Typically, once a patient has been crosslinked, it will be their optometrist who follows them up annually for ongoing contact lenses or spectacles, so it is imperative that ocular allergies are being managed adequately on a long term basis. Diagnosing the condition in family members is another critical role in the primary care optometry setting to reduce the burden of disease.
Patients can still progress despite corneal cross-linking. Severe or rapid progression is quite rare but it is important to understand that, particularly in adolescents, there is a peak in the risk of progression around seven years after their initial collagen cross-linking procedure is performed. The reason for this is not entirely well understood but this is an important point to be aware of in the co-management of the condition.
As optometrists will often be the person primarily responsible for the visual rehabilitation
INSIGHT November 2022 47
Figure 2. CAIRS pre and post topography – The middle scan shows the topography pre-CAIRS, the left scan shows postCAIRS topography and the scan on the right is a map of the difference between the pre and post procedure topography. This demonstrates 20.2 dioptres of flattening one week after the procedure. The patient had five lines of improvement in best corrected visual acuity.
of the patient, either with glasses or contact lenses, they are very well positioned to monitor patients for progression of their disease and to recommend further treatment options that may be available.
NEW TECHNOLOGIES

It isn’t just the early diagnosis of keratoconus that has altered the course of the disease for many patients. New technologies exist both in the optometric and ophthalmic spheres to ensure people with keratoconus do not have to struggle with poor quality vision. These days, it is actually very rare for a patient to require a full thickness corneal transplant. There are numerous ways to avoid the long-term complications and morbidities associated with this procedure, although it is unfortunately sometimes still required.
On the simplest level, even spectacle technology has improved for keratoconus. Lenses can now be ground to incorporate wavefront measurements of the eye. This can minimise higher-order aberrations and improve spectacle visual acuity. Shaw lenses can also be used to minimise anisocoria when significant anisometropia exists.
Prescribing and dispensing these glasses requires specialised equipment that is not available in all optometry practices. It is important that optometrists are aware that referral to another optometrist with access to these lenses may be appropriate in mild cases.
CONTACT LENSES
New technology in contact lenses has improved the vision correction and comfort in contact lenses for keratoconus. While small diameter RGP lenses were the mainstay of visual rehabilitation for keratoconic patients for many years, the development of both wavefront contact lenses and other types of scleral lenses has made contact lenses much more comfortable for patients but it has also enabled optometrists to be able to fit much steeper and more ectatic corneas.
Corneoscleral topography and profilometry allows contact lenses to be made with customised landing angles and sagittal depths.
TAKE HOME
These extremely high levels of individualisation and customisation can facilitate the fitting of previously unfittable corneas so that even patients with very steep cones, other complex corneal ectasias, ocular surface conditions and decentred or mildly dehisced corneal grafts can achieve high quality vision with minimal higher order aberrations.
Unfortunately, not all patients will be able to tolerate or insert and remove contact lenses due to a variety of reasons. Thankfully developments in the surgical treatment of keratoconus have progressed in the same way that optometric treatments have. There are numerous routine procedures available that may assist in improving a patient’s topography and therefore their best corrected spectacle acuity.
PROCEDURES
Topography-guided cross-linking shows promise in providing a degree of corneal regularisation in patients. The advantage of this procedure is that a very wide range of corneas can be treated as no tissue is removed. There are very few corneas that can’t undergo this procedure, however it can also only provide a certain degree of topographic regularisation.
Topography-guided phototherapeutic keratectomy is a routine procedure for keratoconus. In this procedure, an excimer laser regularisation of the cornea is planned using the patient’s topography. Depending on the corneal thickness, the refraction, the topography and the higher-order aberrations, it may be possible to factor the patient’s refraction into the ablation profile, however generally these treatments are intended to improve a patient’s best corrected visual acuity, not to improve their uncorrected visual acuity. This is often combined with crosslinking, either due to the patient’s progression or to restore some of the corneal biomechanics that will be removed due to the stromal ablation.
Kerarings are a plastic insert that can be inserted into the cornea typically using a femtosecond laser to provide a mechanical regularisation of the corneal topography. While these can be very successful in some patients, a number of patients will experience issues due to the plastic insert.

CORNEAL ALLOGENIC INTRASTROMAL RING SEGMENTS (CAIRS)
A newer procedure, corneal allogenic intrastromal ring segments (CAIRS), shows great promise. In
the same way that Kerarings are inserted in a circular corneal pocket, CAIRS (Figure 2) uses non-viable corneal stromal tissue in exactly the same manner. This is performed as a routine day surgery procedure. CAIRS is currently undergoing rapid adoption around the world. The current three-year safety and efficacy data is very positive so hopefully longer term studies continue this trend.
Femtosecond laser assisted lamellar corneal grafting techniques are very much in their infancy but potentially show promise. Segments of lamellar corneal stromal tissue may be implanted into a patient’s cornea to thicken up very weak and/or thinned areas of the cornea and provide a resultant improvement in topography and best corrected visual acuity.
CONCLUSION
Collaborative care in keratoconus in Australia is very much alive and well. Optometrists, ophthalmologists and general practitioners currently enjoy an excellent working relationship for co-managing a wide variety of ocular diseases. It is important to ensure that all parties understand the developments in diagnostic and therapeutic technology that can alter the appropriate indications in the well-established referral framework that already exists. n
REFERENCES
1. Chan E , Et Al. Prevalence of Keratoconus Based on Scheimp flug Imaging: The Raine Study. Ophthalmology. 2021 Apr; 128 (4): 515-521.
2. Galvis V, Sherwin T, Tello A, Merayo J, Barrera R, Acera A. Keratoconus: an inflammatory disorder? Eye (Lond). 2015 Jul; 29 (7): 843-59.
3. Hashemi, Hassan MD Et al. The Prevalence and Risk Factors for Keratoconus: A Systematic Review and Meta-Analysis. Cornea. 2020 Feb; 39 (2): 263-270
4. Mukhtar S, Ambati BK . Pediatric keratoconus: a review of the literature. Int Ophthalmol. 2018 Oct; 38 (5): 2257-2266.
CPD NOTE: Insight readers can scan the QR code or visit insightnews.com.au/cpd/ to access a link to this article to include in their own CPD log book.
TIPS • Paediatric keratoconus can progress very rapidly – refer immediately and manage allergies and eye rubbing concurrently. • Consider referral for wavefront spectacles in very mild but symptomatic cases • New scleral contact lens designs may offer better vision and comfort than RGPs • There are numerous surgical options to achieve good vision in spectacles while still avoiding full thickness corneal transplantation 48 INSIGHT November 2022
Patients can still progress despite corneal cross-linking, but severe or rapid progression post-procedure is rare.
































See more, know more with more Insight Subscribe FREE and receive the latest news Insight is mobile and tablet friendlyFind jobs and advance your career with Insight’s Classifieds Get to know the newest products from suppliers across Australia Insight’s new website keeps you updated on the latest industry news and information. With a world-class responsive design, Insight is now accessible seamlessly on any device, 24/7. Sign-up FREE to our eNewsletters and industry reports delivered weekly straight to your inbox. www.insightnews.com.au
LEARNING OBJECTIVES:
At the completion of this article, the reader should be able to improve uveal melanoma management.
Including:
• Understand the risk factors and predisposing factors for uveal melanoma
• Identify where uveal melanomas are most likely to arise in clinical presentations
• Identify the symptoms of ocular melanomas
• Categorise lesions and provide informed referral to ophthalmological specialists
RECOGNISING AND CATEGORISING UVEAL MELANOMAS

Uveal melanoma can be difficult to diagnose – but treated, if caught early. To assist optometrists in early detection, the authors discuss the condition’s risk factors and epidemiology while introducing the MOLES acronym and scoring system to estimate risk of malignancy and facilitate informed referrals.

Uveal melanoma (UM) is a relatively rare disease with an estimated incidence of 4-6 per million per year globally; approximately 250 patients in all of Australia per year are diagnosed with UM.1 Although rare, it is the most common intraocular malignancy in adults and is associated with substantial morbidity and mortality.
Despite advances in the diagnosis and management of UM, metastatic disease develops in up to 67% of patients with the condition at 20 years.2 Median survival time is less than 12 months if this occurs.
Optometrists play a vital role for patients with UM through prompt recognition and referral of suspicious lesions.
In contrast to the rarity of UM, uveal naevi are very common, occurring in up to 6% of the adult Caucasian population in Australia.3

The majority of choroidal naevi detected incidentally in the community are benign and can be managed safely by optometrists.4 Biopsy of intraocular lesions carries a significant risk to patients, so the clinical and multimodal imaging features of uveal lesions are used to distinguish between a mole, or another benign condition, and a melanoma.
EPIDEMIOLOGY AND RISK FACTORS
A consideration of UM risk factors may be appropriate when assessing uveal lesions.
T Thickness >2mm (ultrasonography)
F Fluid subretinal (OCT)
S Symptoms – vision < 6/12
O Orange pigment –(autofluorescence)
M Melanoma hollowultrasonography
DIaM Diameter > 5mm
Table 1. Mnemonic summary of risk factors predictive of transformation of choroidal lesions.
UM most often affects males and Caucasian populations, and is rare in pigmented races.5-7 Unlike cutaneous melanoma, sunlight exposure has not been demonstrated to have a strong association with UM.8,9 Other predisposing factors include fair skin colour,5,7 lightly pigmented irides10 and a tendency to sunburn.11
DIFFERENTIAL DIAGNOSIS
Although the main differential diagnosis of UM is a benign naevus, there are many other potential diagnoses to consider, depending on the anatomical location of the lesion. For example: Choroidal: choroidal naevus, metastasis, osteoma and haemangioma; congenital hamartoma of the retinal pigment epithelium; eccentric disciform lesion (peripheral haemorrhagic chorioretinopathy); inflammatory lesion.
Iris: naevus; iris pigment epithelial cyst or adenoma; metastasis, leiomyoma; inflammatory lesion.
CLINICAL PRESENTATION
UM is often asymptomatic and detected on routine optometric examination. Approximately 90% of UMs arise from the choroid, while the ciliary body and iris only account for 6% and 4% of melanomas, respectively.2
CHOROIDAL MELANOMA
Although around 30% of choroidal melanomas are asymptomatic at diagnosis, presenting symptoms may include blurred vision, photopsia, floaters, visual field loss, pain or metamorphopsia.12 They may be pigmented, non-pigmented or a combination thereof.
The clinical features conferring a higher likelihood of the lesion being a melanoma (as well as an increased risk of growth and metastasis) are summarised by the mnemonic: ‘To Find Small Ocular Melanoma Doing Imaging’ (Table 1).13
However, this classification requires B-Scan ultrasound to determine the thickness of a tumour
CLINICAL CPD HOURS This activity meets the OBA registration standards for CPD
ABOUT THE AUTHORS:
Dr Lily Rolfe MD, BSc
Dr Daniel McKay MBBS, BComm, FRCPA, FRANZCO Ocular Oncology Clinic, The Royal Victorian Eye and Ear Hospital
Dr Rod O’Day MBBS, LLB, BSc, FRANZCO Ocular Oncology Clinic, The Royal Victorian Eye and Ear Hospital Centre for Eye Research Australia, The Royal Victorian Eye and Ear Hospital
CPD
50 INSIGHT November 2022
To
Find Small Ocular Melanoma Doing Imaging13
and ultrasonographic hollowness, which is not available to many non-specialist practitioners.
The MOLES scoring system is a sensitive tool developed to assist non-specialists in making referral and management decisions regarding pigmented choroidal lesions when more limited imaging techniques are available (Table 2).14 The MOLES scoring system may be used to categorise lesions as ‘common naevus’, ‘low-risk naevus’, ‘high-risk naevus’ or ‘probable melanoma'.
The MOLES protocol also suggests appropriate management based on scoring (Table 3).14 Nonpigmented (also known as amelanotic) choroidal lesions have a much broader differential diagnosis, including choroidal metastasis, and most should be referred to an ophthalmologist.
CILIARY BODY MELANOMA
Ciliary body melanomas have the worst prognosis of all UM, as their anatomical location impedes early diagnosis. These tumours are often diagnosed at a relatively advanced stage, with clinical features such as involvement of the visual axis, focal cataract, extraocular spread or progressive refractive disturbance.
SUPPORT SERVICES FOR PATIENTS
• Melanoma Patients Australia (MPA) is an independent, not-for-profit organisation dedicated to supporting and representing those affected by melanoma (melanomapatients.org.au).
• Cancer Australia was established by the Australian Government in 2006 to benefit all Australians affected by cancer, and their families and carers (canceraustralia.gob.au).
• Vision Australia is a not-for-profit organisation that is a leading national provider of blindness and low vision services in Australia (visionaustralia.org).
IRIS MELANOMA
Iris melanomas may be diagnosed de novo, or via documented growth of a pre-existing lesion. They are typically diagnosed at a relatively small size compared to choroidal melanoma. This appears to account for the relatively low overall mortality of iris melanoma.

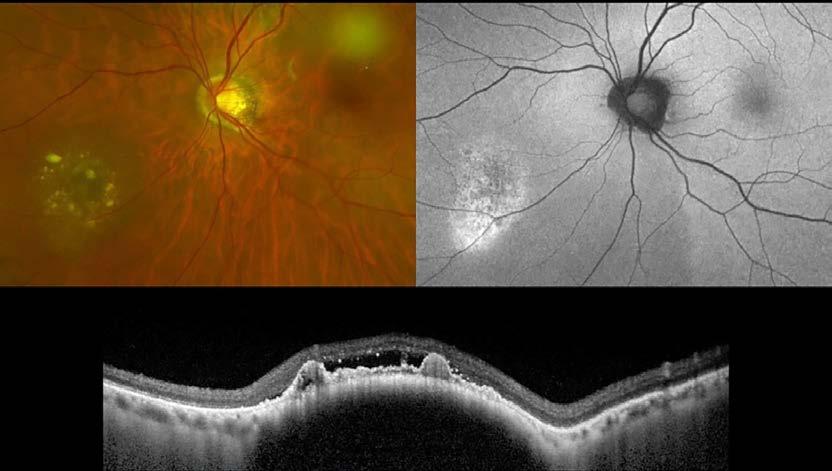
Estimating the risk of malignant transformation of an iris naevus may be assessed according to presence of risk factors summarised by the ABCDEF guide (Table 4).15
Other clinical features may include heterochromia, correctopia, secondary glaucoma, angle seeding and extraocular extension.16
The diagnosis of diffuse iris melanoma is difficult due to its flat, ill-defined growth pattern. Diffuse iris melanoma may present as acquired hyperchromic heterochromia iridis and ipsilateral glaucoma.17
MOLES scoring criteria14
Risk Factor Severity Score
Mushroom shape
Orange pigment
Absent 0 Unsure/early growth through RPE 1 Present 2
Absent 0 Unsure/trace (i.e. dusting) 1 Confluent clumps 2
Large size
Enlargement
Subretinal fluid
Thickness <1.0mm and diameter <3DD 0 Thickness 1.0-2.0mm and/or diameter 3-4DD 1 Thickness >2.0mm and/or diameter >4DD 2
None (or lesion not documented previously) 0 Unsure 1 Definite (i.e. confirmed with sequential imaging) 2
Absent 0 Trace (if minimal and detected only with OCT) 1 Definite (seen without OCT) 2
DD = disc diameter (=1.5mm); ignore thickness if this cannot be measured; assume SRF if unexplained visual loss
Table 2. MOLES scoring criteria.14
Figure 1. Low risk choroidal naevus with overlying drusen (visible between the retinal pigment epithelium (‘RPE’) and Bruch’s membrane on the OCT, bottom, as compared to lipofuscin which sits on the surface of the RPE (see OCT in Figure 2) and a pocket of subretinal fluid on OCT, bottom. It has no lipofuscin on its surface, which is best seen on fundus autofluorescence, top right. This lesion has a MOLES score of 1 (M0, O0, L0, E0, S1) and would have warranted a non-urgent referral to an ophthalmologist/ocular oncologist.
INSIGHT November 2022 51
Figure 2. Choroidal melanoma with overlying lipofuscin (visible on colour image as orange collections overlying the pigmented tumour, left, and fundus autofluorescence as hyper-autofluorescence collections in the same location, bottom right) and subretinal fluid (visible around the tumour on colour image, left, and on the surface of the tumour on OCT). This lesion has a MOLES score of 6 (M0, O2, L2, E0, S2) and would have warranted an urgent referral to an ophthalmologist/ ocular oncologist. Prompt diagnosis and treatment – most often with ruthenium plaque brachytherapy – may allow longterm retention of vision and also potentially prevent development of lethal mutations within the tumour.
Suggested Management
0 Common naevus Monitor in community with colour photography every 1-2 years.
1
≥
Probable
IMPACT OF IMAGING TECHNOLOGIES ON DETECTION AND REFERRAL
The increasing availability of wide-field fundus imaging technologies may facilitate the earlier detection of ciliary body and choroidal tumours, particularly peripheral lesions. High-resolution multimodal imaging including ultrasonography, fundus autofluorescence and OCT is central in evaluating choroidal lesions. Almost always, the diagnosis can be accurately made based on clinical history, examination and the imaging characteristics of a tumour – without the need for tumour biopsy, which carries a risk of complications and vision loss.
Iris lesion diagnosis may also be aided by imaging techniques such as anterior segment photography, anterior segment OCT and ultrasonography. Similarly, ciliary body lesions may be visualised with ultrasonography. These imaging modalities are used to measure tumour
Non-urgent referral to ophthalmologist/ocular oncologist for specialist investigation and imaging.

Urgent referral to ophthalmologist/ocular oncologist.
dimensions and evaluate for differential diagnoses based on typical imaging characteristics. Imaging modalities available to optometrists such as anterior segment or fundus photography and OCT are useful for diagnosing and monitoring lesions, and should be included in referrals to assist specialists in triaging.
Access to prior imaging is essential to determine if a lesion has grown or not and can be incredibly useful in informing management decisions, including facilitating early treatment of a melanoma. It is worthwhile doing a full set of imaging, with all modalities available to a clinician, at first diagnosis (colour imaging, OCT through the lesion, fundus autofluorescence, ultrasound, if available) and at follow-up visits to assess for growth or document change.
HOW TO PROVIDE AN INFORMED REFERRAL
In general, a uveal lesion showing any of the TFSOM-DiM or ABCDEF risk factors warrants referral to an ophthalmologist, ideally with a subspecialty interest in retina or ocular oncology. Documented growth of a previously diagnosed lesion – regardless of the presence of other risk factors – should also prompt referral. The urgency of referral depends on the level of suspicion and can be guided using the MOLES scoring system.
THE IMPORTANCE OF COLLABORATIVE CARE
REFERENCES
1. Kaliki S, Shields CL . Uveal melanoma: relatively rare but deadly cancer. Eye (Lond). 2017; 31 (2): 241-57.
2. Shields CL , Furuta M, Thangappan A, Nagori S, Mashayekhi A, Lally DR, et al. Metastasis of uveal melanoma millimeterby-millimeter in 8033 consecutive eyes. Arch Ophthalmol. 2009; 127 (8): 989-98.
3. Sumich P, Mitchell P, Wang JJ. Choroidal nevi in a white population: the Blue Mountains Eye Study. Arch Ophthalmol. 1998; 116 (5): 645-50.
4. Salehi O, van Wijngaarden P, Keel S, Foreman J, Dirani M, Damato B, et al. Estimating malignancy risk of melanocytic choroidal tumours detected in the Australian National Eye Health Survey. Clin Exp Optom. 2021; 104 (8): 854-8.
5. Hu DN, Yu GP, McCormick SA, Schneider S, Finger PT. Population-based incidence of uveal melanoma in various races and ethnic groups. Am J Ophthalmol. 2005; 140 (4): 612-7.
6. Singh AD, Topham A. Incidence of uveal melanoma in the United States: 1973-1997. Ophthalmology. 2003; 110 (5): 956-61.
7. Aronow ME , Topham AK, Singh AD. Uveal Melanoma: 5-Year Update on Incidence, Treatment, and Survival (SEER 19732013). Ocul Oncol Pathol. 2018; 4 (3): 145-51.
8. Singh AD, Rennie IG, Seregard S, Giblin M, McKenzie J. Sunlight exposure and pathogenesis of uveal melanoma. Surv Ophthalmol. 2004; 49 (4): 419-28.
9. Shah CP, Weis E, Lajous M, Shields JA, Shields CL. Intermittent and chronic ultraviolet light exposure and uveal melanoma: a meta-analysis. Ophthalmology. 2005; 112 (9):1599-607.
10. Saornil MA . Iris colour and uveal melanoma. Can J Ophthalmol. 2004; 39 (4): 448-52.
11. Weis E, Shah CP, Lajous M, Shields JA, Shields CL. The association between host susceptibility factors and uveal melanoma: a meta-analysis. Arch Ophthalmol. 2006; 124 (1): 54-60.
12. Damato EM, Damato BE . Detection and time to treatment of uveal melanoma in the United Kingdom: an evaluation of 2,384 patients. Ophthalmology. 2012; 119 (8): 1582-9.
TAKE
• The most common choroidal lesion detected in the community is a benign
Almost all of which can be safely diagnosed and managed by community optometrists with widely available imaging technology, including colour photography, OCT and fundus autofluorescence.
• The MOLES scoring system can be used to guide diagnosis and management
• Non-pigmented choroidal lesions should be referred to an ophthalmologist.
• Baseline imaging (colour photography, OCT and ultrasound if available) is crucial to establishing if a
has grown in the
Ocular oncologists – ophthalmologists whom have undergone fellowship training in management of ocular oncology patients – specialise in the diagnosis and management of UM. There are ocular oncologists in most of the states of Australia. Management of UM patients often requires involvement of radiation oncology teams in prescribing brachytherapy or stereotactic radiotherapy.
The involvement of other medical and surgical specialties is often required to treat metastatic disease. General practitioners coordinate care as well as monitor for evidence of metastasis through regular blood tests and imaging. Other allied health professionals such as ocularists create and fit prosthetic eyes, while cancer support services and psychologists provide support to patients in navigating psychosocial aspects of disease.
Caring for patients with UM requires multidisciplinary collaboration. The role of the optometrist is vital in the early detection of UM, hopefully enabling diagnosis in the early phases before metastasis occurs. n
13. Shields CL , Dalvin LA, Yu MD, Ancona-Lezama D, Di Nicola M, Williams BK, et al. CHOROIDAL NEVUS TRANSFORMATION INTO MELANOMA PER MILLIMETER INCREMENT IN THICKNESS USING MULTIMODAL IMAGING IN 2355 CASES: The 2019 Wendell L. Hughes Lecture. Retina. 2019; 39 (10): 1852-60.
14. Roelofs KA, O'Day R, Harby LA, Arora AK, Cohen VML, Sagoo MS, et al. The MOLES System for Planning Management of Melanocytic Choroidal Tumors: Is It Safe? Cancers (Basel). 2020; 12 (5).
15. Shields CL , Kaliki S, Hutchinson A, Nickerson S, Patel J, Kancherla S, et al. Iris nevus growth into melanoma: analysis of 1611 consecutive eyes: the ABCDEF guide. Ophthalmology. 2013; 120 (4): 766-72.
16. Henderson E , Margo CE. Iris melanoma. Arch Pathol Lab Med. 2008; 132 (2): 268-72.
17. Demirci H, Shields CL , Shields JA, Eagle RC, Jr., Honavar SG. Diffuse iris melanoma: a report of 25 cases. Ophthalmology. 2002; 109 (8): 1553-60.
CPD
NOTE: Insight readers can scan the QR code or visit insightnews.com.au/cpd/ to access a link to this article to include in their own CPD log book.
HOME POINTS
naevus.
decisions of pigmented choroidal lesions
mole
future. 52 INSIGHT November 2022 Table 4. Malignant risk factors for iris lesions.15 Malignant risk factors for iris lesions15 A Age (≤ 40 years old) B Blood – hyphaema C Clock hour – inferior D Diffuse configuration E Ectropion uveae F Feathery tumour margin Table 3. MOLES tumour categories and recommended management.14 MOLES tumour categories and recommended management14 MOLES Score
Low risk naevus
2 High risk naevus
3
melanoma
WHY DISSATISFIED CUSTOMERS ARE YOUR MOST IMPORTANT
Customer satisfaction has become more important than ever. The Australian optical industry is expanding at a rapid pace, meaning customers have increasingly more options at their fingertips to meet their optical needs.
If a customer has a positive experience they will share their experience with family, friends, and connections – all at no charge to your store. But what happens when they receive a product that isn’t performing to their expectations?
A study from Esteban Kolsky shows 13% of unhappy customers share their complaint with 15 or more people. Only one in 25 customers will share their complaint directly with you. Of that one in 25 who do share their frustrations, this is a chance to make amends. How you handle this can set your practice apart.
Having the ability to improve and influence customers’ vision is a responsibility optical dispensers should not take for granted. When something goes astray during the dispensing process, it can have a huge impact on the customers’ quality of life.
No two customers are the same. Each troubleshoot is going to present a unique structure of issues that we need to handle delicately. But how do we get the best outcome from unhappy customers?
The Trust Equation can help, see Figure 1. The goal is to build great relationships with your customers. The idea is to have high creditability, reliability and vulnerability and low selfishness. We can incorporate the Trust Equation into all interactions and troubleshooting by being open and transparent, caring about their story authentically, willing to take risks, dependable and focused on the customer’s objectives.

Listen to what they’re saying. It’s not you vs the customer – it’s you and the customer vs the issue. Take yourself out of the equation, each issue brought up from the customer is coming from a place of frustration. Sight is a huge factor in our daily lives and having spectacles that aren’t providing clear vision can be discouraging.
Figure 1 – The Trust Equation. Creditability refers to the words that we speak. Reliability refers to actions. Vulnerability refers to the security we feel when intrusting someone. Selfishness refers to focus. Is your focus on yourself or is your attention elsewhere? Credit: www.kevinsidebottom.com
When handling a troubleshoot, ask a mixture of open and closed questions like:
When and where are you experiencing these issues?
Do you need to hold your head at a certain angle to get clearer vision? Can you show me that position?
Can you describe how your workstation is set up?
Sometimes it can be difficult to grasp a customer’s full day-to-day activities in their spectacles at dispense. The more questions we ask, the better understanding we have to find a solution. Having a clear troubleshooting guideline in your store can greatly benefit your team members to resolving issues. It should address things such as:
Check the position of wear and go over the six key steps of final fitting. Horizontal alignment, pantoscopic angle, side width, side bow, length to bend and anatomical bend.
If the spectacles are ill-fitting, it can completely change the lens' performance.
Re-check the measurements. Have the heights and pupil distances been measured monocularly? Was back vertex distance, pantoscopic angle and frame wrap considered at the dispense?
Take time to observe how the customer moves as they speak. When they pick up something such as reading material or their glasses case, are they changing their direction of gaze or predominantly moving their head?
This can have a huge influence on the success of certain lens designs
such as progressives and bifocals, if the customer has not been properly coached on how to use the lens design.
By electing a designated team member instore to monitor and collate data, your store gets the opportunity to identify patterns and trends. If your store doesn’t already, it might be worth tracing the patterns and considering whether any are reoccurring? Starting a log of errors based on customer feedback and breaking it into relevant subsections is a great starting place. Over the span of a month or two your dedicated staff member can correlate where issues are occurring.
Highlighting this can result in better team training activities by individualising specific needs, rather than broad training. Training is best absorbed when it is interactive, educational, and engaging. Every mistake is a lesson that you can build from.
Remember customers pay close attention to our actions when they’re feeling distressed. The way you interact after their problem is resolved sets the stage for future encounters. It can be the difference between a loyal customer and losing one.
In fact, if your post-complaint actions are done successfully, the next time your customer talks about your business, they will reflect on the great level of service they received. n
ABOUT THE AUTHOR: NICOLE GRASSO is a trainer at the Australasian College of Optical Dispensing and works as a part-time optical dispenser for Specsavers on the Central Coast, NSW. She is a qualified optical dispenser (Certificate IV in 2017) and completed her Certificate IV in Training and Assessing in 2021.

NICOLE GRASSO “EACH TROUBLESHOOT IS GOING TO PRESENT A UNIQUE STRUCTURE OF ISSUES THAT WE NEED TO HANDLE DELICATELY”
TROUBLESHOOTS CAN BE A SPEEDHUMP IN OPTICAL DISPENSING AND TAKE TIME AWAY FROM THE SHOPFLOOR BUT, AS NICOLE GRASSO EXPLAINS, HOW YOU HANDLE COMPLAINTS CAN ULTIMATELY SET YOUR PRACTICE APART.
DISPENSING
INSIGHT November 2022 53
SIGHTS SET ON ASSISTIVE TECHNOLOGY POST-PANDEMIC MODE
We live in a world that is primarily setup for people who have full vision. So, how have people fared during a pandemic led by written or visual media reports and a world going socially tech savvy? It’s an interesting question to pose.
Industry leaders warned that the preCOVID world was not an accessible one for those with visual impairments. So, imagine navigating the world as a person who is blind or has low vision in the midst of a “social distancing, face-covering” mandate.
People who are vision impaired already experience loneliness at higher levels than the general population. They’re also more likely to suffer from depression and more likely to experience detrimental health outcomes as a result of self-isolation.
Adaptive technology, or the special versions of already existing technologies or tools that provide enhancements or different ways of interacting with the technology, is one way our community supports those who are blind or have low vision.
As orthoptists have more of a medical focus, specifically on diagnosis, treating and managing eye conditions, they frequently refer kids to Can:Do's allied health professionals for functional support.


This then allows us to take a holistic approach, exploring aspects of the child's daily interactions with activities and people in their natural environments.
Access to the right technology can make a real difference by increasing opportunities to learn whilst developing independence skills. The assistive adaptive technology service aims to support and meet the needs of the child and family by providing the tools necessary to interact with their surroundings.
Ultimately, the aim is to provide the child with independent and equal access to their visual environment. This means availability of resources and equipment they can trial in all environments they intend to use that aid.
After a couple years of a plateau in assistive technologies, some innovative technologies are now starting to have an impact.
SOME THINGS TO LOOK OUT FOR Be My Eyes (bemyeyes.com)
Be My Eyes allows blind people to call a pool of volunteers who have signed up as members to help 'be their eyes'. They use this for daily experiences such as asking what an expiry date is on food. Or, asking to help find something – for example, “I dropped my ‘xx’ can you see where it is for me?” Or, “I'm looking for ‘xx’ in the supermarket, can you tell me which of these it is?”.
DotPad (pad.dotincorp.com)
DotPad teamed with Apple to create a tablet that has 2,400 refreshable pins. It uses AI technology to process visual images and convert them into a tactile format.
I have been able to watch several blind people interact with DotPad and it is so beautiful to see the big smiles on their faces. For the first time they learned what the logos of different apps represented – for example, the mail app is an envelope.
Through DotPad, users are able to draw tactile shapes, read tactile shapes, and gather a visual understanding of representation of stock trends and graphs. They can also read multi-line refreshable
braille, allowing them to skim read and read more fluidly.
Historically, braille users would have only been able to get an understanding of this information via auditory descriptions, which can be quite exhaustive (imagine listening to graph descriptions).
This is likely going to be a game changer, especially in the education and paediatric space.
As we set course to come out of pandemic mode, we hope our community continues to embrace the assistive adaptive technologies available. n
ABOUT THE AUTHOR: ADRIANA SAPIO is Can:Do 4 Kids’ assistive adaptive technology specialist and a senior occupational therapist with a Graduate Certificate in Education (vision impairment). Can:Do 4Kids is South Australia’s oldest charitable service provider, offering vital therapy and support to children and young people who are blind, low vison, deaf or hard of hearing.
 ORTHOPTICS AUSTRALIA strives for excellence in eye health care by promoting and advancing the discipline of orthoptics and by improving eye health care for patients in public hospitals, ophthalmology practices, and the wider community Visit: orthoptics.org.au
ORTHOPTICS AUSTRALIA strives for excellence in eye health care by promoting and advancing the discipline of orthoptics and by improving eye health care for patients in public hospitals, ophthalmology practices, and the wider community Visit: orthoptics.org.au
AFTER A PLATEAU IN ASSISTIVE TECHNOLOGY DEVELOPMENT, SOME INNOVATIVE TECHNOLOGIES ARE NOW STARTING TO HAVE AN IMPACT, AS CAN:DO 4 KIDS’ ASSISTIVE ADAPTIVE TECHNOLOGY SPECIALIST ADRIANA SAPIO EXPLAINS.
54 INSIGHT November 2022
ADRIANA SAPIO
“ACCESS TO THE RIGHT TECHNOLOGY CAN MAKE A REAL DIFFERENCE BY INCREASING OPPORTUNITIES TO LEARN WHILST DEVELOPING INDEPENDENCE SKILLS”
Adriana Sapio says orthoptists frequently refer children to Can:Do 4 Kids for allied health professionals for functional support.
TIPS TO AVOID MEDICARE COMPLIANCE ISSUES
CASE STUDY
The optometrist was referred to the Professional Services Review (PSR) when Medicare records indicated an unusually high volume of daily services, including more than 30 services on more than 20 occasions.
The PSR remained concerned the optometrist had not always met the Medicare Benefits Schedule (MBS) item requirements for the services billed. They considered the optometrist’s medical records were inadequate, that not all services were clinically indicated, and clinical management was not always appropriate.
The optometrist was reprimanded and agreed to repay $80,000.
Tip 1. Understand the item number
As a provider, you are responsible for claims to Medicare made under your provider number. Be sure you are applying the correct MBS item numbers and that your consultation covers the elements required for you to charge that item number.
Descriptions can be nuanced so ensure you check the full item descriptor, understand the requirements and check for updates.
For example, optometrists have been reprimanded over the use of MBS items that require patients to have been previously seen at the same practice as the providing optometrist. The PSR has determined this means the patient must be seen at the same physical practice, not at another practice within a corporate group.
Check with the government email advice service AskMBS if you are unsure about how to use an item number.
Tip 2. Keep careful records
When you make a Medicare claim for a service, you must maintain an adequate and contemporaneous record that demonstrates the service was provided.
As in this case study, inadequate documentation can result in an audit finding the benefit for those services should not have been paid. The government will seek repayment of the full amount of the Medicare benefits paid for the service.
Your records need to identify the patient
and include a separate entry for each attendance by the patient for a service. Be sure to record enough details that explain why the service was needed, the clinical input you provided, and why the particular item number was billed.
Make sure your notes cover the:
• Reason for presentation and patient history
• Examinations or investigations
• Diagnosis (provisional or final)
• Management plan
• Time spent – if the item number has a minimum time component, make sure you record the time spent in the consultation. It is not enough just to select the item number for that consultation length.
Tip 3. Check all billings made under your provider number
You will be accountable for all services billed under your provider number and you are expected to make the decision about which item numbers to claim.
If administrative staff submit claims for you, make sure the process allows you to check and approve any claims billed under your number. If you are concerned your provider number may have been used to make incorrect claims, contact your professional indemnity insurer.
Claims can be audited after you have left your current practice, so keep a copy of all reports of claims submitted under your number in case any are ever questioned.
Tip 4. Keep up to date with peers and ask for feedback
Services billed must be clinically relevant. This is determined by what is acceptable to your peers, so it is important to keep in touch with peers and ensure your practice is in line with commonly accepted standards. You can ask practice staff to let you know if they think you have made a mistake.
Medicare reviews check for statistical outliers and anomalies. Being aware of your peers’ practices can help ensure your Medicare billing is consistent, or that you are aware of and can explain any differences. However, it is not a substitute for your own knowledge so always check the item numbers yourself.
Tip 5. Take special care to record referrals
Items 104 and 110 have been a recent focus of PSR reviews involving multiple specialities.
Concerns raised in relation to these item numbers included poor record-keeping as well as a lack of evidence of a referral requesting a specialist consultation, inadequate communication of outcomes to the referring practitioner, and co-billing a consultation with a procedural service when the record did not support that a separate consultation was performed.
CONCLUSION
The prospect of a Medicare audit can be daunting for practitioners. However, by following some principles of good practice, you will be better placed to avoid scrutiny of your billings or address any concerns. n

Disclaimer: This article is intended to provide commentary and general information. It does not constitute legal or employment advice. You should seek legal or other professional advice before relying on any content, and practise proper employment decision making with regard to the individual circumstances.
ABOUT THE AUTHOR: RUANNE BRELL BA LBB (Hons) is a senior legal advisor in the Advocacy, Education and Research team at Avant with almost 20 years’ experience in health and medical law.

FURTHER REFERENCES
1. Department of Health: AskMBS Email Advice Service
2. Avant resources: Medicare: what you need to know
A CASE STUDY INVOLVING AN OPTOMETRIST WHO REPAID $80,000 TO MEDICARE ILLUSTRATES SOME COMMON ERRORS THAT CAN CATCH PRACTITIONERS OUT. RUANNE BRELL OFFERS HER TOP TIPS TO MANAGE MEDICARE BILLINGS AND AVOID COMPLIANCE ISSUES.
RUANNE BRELL
"BY FOLLOWING SOME PRINCIPLES OF GOOD PRACTICE, YOU WILL BE BETTER PLACED TO AVOID SCRUTINY OF YOUR BILLINGS"
MANAGEMENT
INSIGHT November 2022 75
Items 104 and 110 have been a recent focus of reviews involving multiple specialities.
People ON THE MOVE
Insight's monthly bulletin to keep the Australian ophthalmic sector updated on new appointments and personnel changes, nationally and globally.
ORTHOPTIST TAKES ON ROLE IN ZEISS LASER BUSINESS


Stephanie Wang recently joined the ZEISS ANZ business in a national role as a Clinical Application Specialist covering the refractive laser portfolio. She has a Bachelor of Health Sciences, a Masters in Orthoptics and more than four years of experience working as a Clinical Orthoptist across various sub-specialities. According to ZEISS, this experience has helped her develop a strong understanding of both clinical workflows and the high quality of care necessary in the world of ophthalmology.
HOYA BOLSTERS QUEENSLAND PRESENCE WITH INTERNAL APPOINTMENT
Leighton Pratt is transitioning within HOYA to the role of Queensland Operations Manager. He is highly experienced in all facets of optics, as well as being a qualified optical mechanic and optical dispenser. Pratt will be supporting HOYA’s internal teams and working closely with safety customers in the Queensland region.

AUSTRALIAN COLLEGE OF OPTOMETRY PROMOTES EARLY CAREER OPTOMETRIST University of Melbourne optometry graduate Mina You has been appointed Manager Daily Operations at the Australian College of Optometry. She will be managing daily operations at the Carlton clinic by supporting optometrists, reception, and the dispensing team. You, who joined the ACO in 2020 as an optometrist, is also a current Clinical Supervisor and Chair of Optometrists Representation Group, and a committee member of Early Career Optometrists Victoria South Australia.

DESIGNS FOR VISION APPOINTS NEW TERRITORY MANAGER
Lorenzo Dio recently joined Designs For Vision as a Territory Manager for the diagnostics team. Lorenzo has previous experience in surgical sales and loan kits. His medical device career started off in the orthopaedic space with DePuy Synthes in Auckland, New Zealand, before making his way to Sydney. Lorenzo graduated from the University of Auckland with a BSc and MSc in Pharmacology – Drug Discovery & Development.
APAC APPOINTMENT FOR COOPERVISION SPECIALTY EYECARE




CooperVision Specialty EyeCare has named Weiwen Chen as Business Manager, Asia-Pacific. In this newly-created role, she will lead the organisation’s growth and category expansion across the region, with the exception of China, which is managed by a separate team. Chen was most recently a Consultant to Visioneering Technologies, where she led the company’s entry strategy into Asia.
TRIO LEADING DRY EYE EDUCATION INITIATIVE Prof James Wolffsohn is one of three global experts named as lead faculty for a new dry eye disease education initiative for optometrists run by the World Council of Optometry and Alcon. Wolffsohn, Head of the School of Optometry and Department of Audiology at Aston University, UK, will join Prof Jennifer Craig, Head the Ocular Surface Laboratory in the Department of Ophthalmology at the University of Auckland, and Prof Lyndon Jones, Director of the Centre for Ocular Research & Education at the University of Waterloo, Canada.
editor Myles Hume at myles.hume@primecreative.com.au to be featured.
CAREER 56 INSIGHT November 2022
Do
you have career news to share?
Email
2022 CALENDAR
NOVEMBER 2022
ASIA OPTOMETRIC CONGRESS & AEGEAN OPTOMETRIC CONFERENCE Kuala Lumpar, Malaysia 15 – 16 November asiaoptometriccongress.com/ 3rd-asia-optometric-congress
ASIA-PACIFIC VITREO-RETINA SOCIETY CONGRESS Taipei, Taiwan 18 – 20 November 2022.apvrs.org
JANUARY 2023
HONG KONG INTERNATIONAL OPTICAL FAIR Hong Kong 9 – 11 January event.hktdc.com
FEBRUARY 2023
MIDO Milan, Italy 4 – 6 February mido.com
ANZGS CONGRESS Queenstown, New Zealand 16 – 19 February anzgsconference.com
APAC ACADEMY OF OPHTHALMOLOGY CONGRESS Kuala Lumpur, Malaysia 23 – 26 February 2023.apaophth.org
100% OPTICAL London, UK 25 – 27 February 100percentoptical.com
MARCH 2023
CONGRESS ON CONTROVERSIES IN OPHTHALMOLOGY Lisbon, Portugal 24 – 25 March cophy.comtecmed.com
APRIL 2023
AUSTRALIAN VISION CONVENTION Gold Coast, Australia 1 – 2 April events@optometryqldnt.org.au
ARVO 2023 New Orleans, US 23 – 27 April arvo.org/annual-meeting
To list an event in our calendar email: myles.hume@primecreative.com.au
JUNE 2023
WORLD GLAUCOMA CONGRES Rome, Italy 28 June – 1 July worldglaucomacongress.org
SEPTEMBER 2023
O=MEGA23 & WORLD CONGRESS OF OPTOMETRY Melbourne, Australia 8 – 10 September omega-event.org
OCTOBER 2023
RANZCO SCIENTIFIC CONGRESS Perth, Australia 20 – 24 October ranzco.edu/events
across Australia and New Zealand and we have continued to develop our comprehensive two-year Graduate Program providing a support network and structured program to assist you in your development.
The Graduate Recruitment Team are currently looking for new graduates to join our teams in North QLD, NT, and WA, providing generous regional salary and relocation packages.
Optometrists can expect to earn in excess of $200k in Emerald & Rockhampton QLD! Interested in partnership? Why not try before you buy! Specsavers have two fantastic opportunities for Optometrists looking to take the next step in their careers. Emerald offers all the amenities of a big city alongside the relaxed lifestyle of a regional town. This rapidly growing small city is located in the Central Highlands region of Queensland. Alternatively, work across two stores in Rockhampton! Located on the east coast and on the Fitzroy River. Rockhampton Allenstown is a brand-new store located within the Stockland Rockhampton S/C. Social and welcoming teams to help you settle into the communities and relocation support available.
Highest package ever! $180,000 for the growing Mobile Optometrist Role
Specsavers is growing our community based Mobile Optometry Team Nationally, With home based locations in Newcastle, Perth & Melbourne along with longer term Fly in Fly out roles available. With an amazing $180,000 package on offer. You will experience a wide variety of cases, whilst being able to explore different regions of Australia. We are looking for someone who has the desire and flexibility to travel.
WA Locum Opportunities
Specsavers are looking for locum optometrists, we have several vacancies across WA and are seeking locums who have a real passion to provide the best service to our patients. We are offering $1,500 to any new locums who join and complete 38 hours through SRS before the 31st of January, we are also offering $1500 to anyone who refers a new locum. For locums interstate we can arrange and pay for your flights, accommodation and car hire for both regional and metro stores in WA.
In a few short years, Specsavers has achieved market leadership in Australia and New Zealand with more people choosing to have their eyes tested and buy their prescription eyewear from Specsavers than any other optometrist. To learn more about these roles, or to put your hand up for other roles as they emerge, please contact us today:
Joint Venture Partnership opportunities enquiries: Kimberley Forbes on +61 (0) 429 566 846 or E kimberley.forbes@specsavers.com
Australia Optometrist employment enquiries: Marie Stewart – Recruitment Consultant marie.stewart@specsavers.com or 0408 084 134
Locum employment enquiries: Cindy Marshall cindy.marshall@specsavers.com or 0450 609 872
New Zealand employment enquiries: Chris Rickard –Recruitment Consultant chris.rickard@specsavers.com or 0275 795
Graduate employment enquiries: apac.graduateteam@specsavers.com
SPECSAVERS – YOUR CAREER, NO LIMITS VISIT SPECTRUM-ANZ.COM SO LET’S TALK!
499
$20k refer a friend bonus up for grabs for Optometrists in WA! We offer flexible rosters to support work/life balance including full-time, part-time, fixed term or locum work, along with access to the latest equipment (including OCT in every store) and we’ll provide you with excellent opportunities for career development and progression – including pathway to Partnership. If your referral is placed or working before 31/01/23 you’ll both get $10k each for a full-time Optometrist or $1.5k each for a Locum optometrist. T&Cs apply. Graduate Recruitment Team are currently looking for new graduates Looking at starting your career with a dedicated mentor and graduate team to support you in your first steps? Specsavers are the largest employer of Graduate Optometrists
All Specsavers stores nowwith OCT
WHY SPORTING EYEWEAR MATTERS
BY DR GIZEM ASHRAF
When I was a medical student working at the Royal Victorian Eye and Ear Hospital (Eye and Ear) Emergency Department (ED) with Dr Rahul Chakrabarti and A/Prof Carmel Crock, we were shocked by the large number of patients who were presenting with sports-related eye injuries. However, when we searched the literature, we found that there were no recent large-scale studies in Australia assessing the characteristics of these injuries. To better understand the mechanism and pattern of eye injuries that occur during sporting activities, we performed our own sports-related eye trauma study.
We assessed cases of patients who presented to Eye and Ear ED between 2015 and 2020, examining various data including patient demographics, injury mechanism, injury characteristics and investigations and management performed. To our surprise, we found 1,793 cases of sports-related eye injury. Our results showed that sports-related eye trauma disproportionately impacts younger individuals with a mean patient age of 28 years and 30% of patients being paediatric. Over 80% of patients were male and winter was the most common season for presentations.
Soccer was the leading sport to cause injuries (18% of cases), followed by AFL (17% of cases) and basketball (12% of cases). These were also the top three
sports to cause injury in the paediatric population. The use of protective eyewear is not mandatory in any of these sports, likely contributing to the high number of presentations. In contrast, paintball, where the use of a face shield in Australia is mandatory, was the sport to cause the least number of eye injuries, contributing only 0.3% of cases.
The most common mechanisms of injury were a projectile object such as a ball (54% of cases), incidental body contact such as a finger or elbow (28% of cases) and sporting equipment such as a racket (6% of cases). The most common pathologies observed were hyphaema and traumatic uveitis, followed by commotio retinae, corneal injuries (such as abrasions and lacerations) and conjunctival injuries (such as subconjunctival haemorrhage). Only 27 patients were admitted to hospital and 26 patients required surgery. The most common sport contributing to surgical cases was AFL and the most common injury requiring surgery was globe rupture/ penetration. The most common non-surgical management was steroids and cycloplegics.
Multivariate logistic regression showed that the greatest risk of globe rupture or penetration was associated with martial arts, orbital blow-out fracture with skiing, hyphaema with squash, and retinal tears with foam dart projectiles. When planning targeted prevention strategies, it is not only important to consider the relative frequency of injuries caused by a specific sport, but also the relative severity of injuries caused by that sport.
Ocular injuries and their sequelae can predispose patients to long-term physical, psychosocial and healtheconomic impacts. The reduction of ocular injury requires a coordinated effort from the community including public health professionals, policy makers and role model athletes to encourage a safer sporting culture. Collingwood AFL player Mason Cox – who wears specially-made eyewear during matches after extensive surgery on both eyes – comes to mind as a sporting star that is helping to progress the conversation around safety eyewear in sport.

Although elimination of hazards remains the most effective way to prevent injuries, it is also important to educate children regarding hazard awareness and safe play, as well as encouraging the use of standardised protective eyewear. Not only is further research required to identify areas for intervention, but it is also important for us as health professionals to document whether there was use of protective eyewear so that we are able to examine the impact of the changes we make. n
Name: Dr Gizem Ashraf

Qualifications: BMedSci/MD
Organisations: Centre for Eye Research Australia, The Royal Victorian Eye and Ear Hospital
Position: Doctor Location: Melbourne, Australia Years in profession: 2
SOAPBOX
IN CONTRAST, PAINTBALL, WHERE THE USE OF A FACE SHIELD IN AUSTRALIA IS MANDATORY, WAS THE SPORT TO CAUSE THE LEAST NUMBER OF EYE INJURIES, CONTRIBUTING ONLY 0.3% OF CASES.
58 INSIGHT November 2022
Soccer was the leading sport to cause eye injuries in the study.






Innovative water-free mode of action Spreads quickly and easily on the lipid layer Lipid layer deficiency Apply NovaTears® NovaTears® is a unique preservative-free eye lubricant, which acts as a lipid layer substitute and evaporative barrier for improved tear film stability and quality. Clinically validated with significant improvement in signs and symptoms with Evaporative Dry Eye Disease and Meibomian Gland Dysfunction patients1,2 For Evaporative Dry Eye & Meibomian Gland Dysfunction NOVATEARS® OMEGA-3 AVAILABLE NOW* References: 1. Steven, Philipp, et al. “Semifluorinated Alkane Eye Drops for Treatment of Dry Eye Disease – A Prospective, Multicenter Noninterventional Study.” Journal of Ocular Pharmacology and Therapeutics 31 (8), 498-503 (2015). 2. Steven, Philipp, et al. “Semifluorinated Alkane Eye Drops for Treatment of Dry Eye Disease Due to Meibomian Gland Disease.” Journal of Ocular Pharmacology and Therapeutics. 33(9), 678-685 (2017). Sponsored by Novaliq GmbH. NovaTears ® Eye Drops (Perfluorohexyloctane 100% v/v, 3mL) are for the lubrication and relief of dry and irritated eyes. Do not use NovaTears ® with contact lenses. If using any other eye medication, allow at least 15 minutes between using the other product and applying NovaTears ®. NovaTears ® should not be used in children under 18 years. NovaTears ® should not be used while pregnant or breastfeeding. AFT Pharmaceuticals Pty Ltd, Sydney. ABN 29105636413. PBS Information: Authority Required (STREAMLINED): Severe dry eye syndrome in patients who are sensitive to preservatives in multi-dose eye drops. STREAMLINED AUTHORITY CODE 6172 – NovaTears® only *Please note: NovaTears ® + Omega-3 is not PBS listed PBS Listed For more information: 1800 238 742 www.aftpharm.com mydryeyes.com.au
SEE YOURSELF DOING WHAT YOU LOVE
At OPSM we invest in our people. Our Optometrists work with state-of-the-art technology, including Optos Daytona, Corneal Topographer, Visual Field, and OCT. As an optometrist, your success is enhanced by a number of great initiatives including financially supported clinical training, mentorship, peer learning communities, leadership programs and commercial development.
At OPSM, your career is limited only by the size of your dreams. We work with you to personalise a role based on your aspirations and support you in making the most of your career. We have amazing opportunities for Optometrists to join our team at OPSM across Australia and New Zealand.

MORE
US ON LINKEDIN
IN PAVING YOUR OWN PATH?
LEARN
OPSM.COM.AU/CAREERS VISIT
INTERESTED
PLEASE CONTACT OPTOMETRY.CAREERS@AU.LUXOTTICA.COM
WORKING AT OPSM MEANS YOU’RE PART OF SOMETHING BIGGER.





 AUSTRALIA’S LEADING OPHTHALMIC MAGAZINE SINCE 1975
AUSTRALIA’S LEADING OPHTHALMIC MAGAZINE SINCE 1975































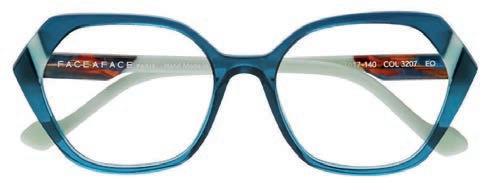


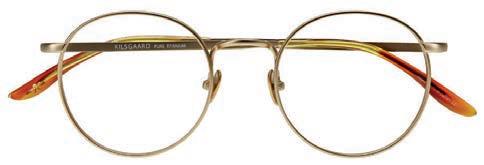



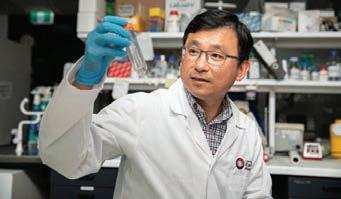































 Quinn & Co. Eyecare in Ararat is one of eight practices in the business, with stores in Horsham, Stawell, Swan Hill, Mildura and Echuca.
Quinn & Co. Eyecare in Ararat is one of eight practices in the business, with stores in Horsham, Stawell, Swan Hill, Mildura and Echuca.























































































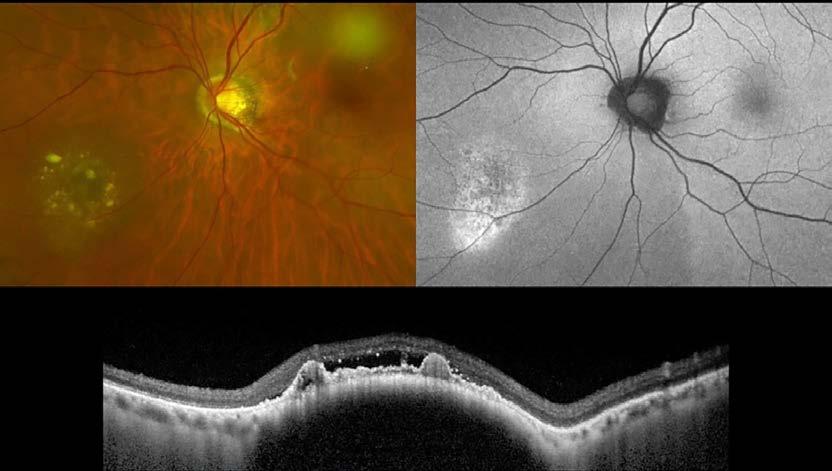




 ORTHOPTICS AUSTRALIA strives for excellence in eye health care by promoting and advancing the discipline of orthoptics and by improving eye health care for patients in public hospitals, ophthalmology practices, and the wider community Visit: orthoptics.org.au
ORTHOPTICS AUSTRALIA strives for excellence in eye health care by promoting and advancing the discipline of orthoptics and by improving eye health care for patients in public hospitals, ophthalmology practices, and the wider community Visit: orthoptics.org.au