EYEWEAR TARIFF FIGHT CONTINUES

After a rejected appeal, ODMA is to lobby the government over the controversial ABF decision
NAILING YOUR MARKETING STRATEGY
With the end-of-year rush in full swing, independents offer their key marketing pearls
CONSIDERING A COUNTRY CAREER?
How RANZCO is addressing workforce maldistribution with more regional opportunities
03
29
46
SINCE 1975 DEC 2022 YOUNG OPTOMETRISTS TAKE HARD ROAD TO PRACTICE OWNERSHIP BOLD AMBITION
AUSTRALIA’S LEADING OPHTHALMIC MAGAZINE
COVER STORY

Business ownership on your horizon? Ready for a new challenge in 2023? We’re looking for the next generation of ambitious and dedicated optometrists to join us as partners. We’ve announced a number of new locations that form part of our ongoing plan to provide even greater access to eye care services across both Australia and New Zealand. If business ownership is on your future career agenda, now is the time to position yourself for a role at Specsavers. Go to spectrum-anz.com or contact contact Kimberley Forbes on +61 (0)429 566 846 or kimberley.forbes@specsavers.com
OPTOMETRY AUSTRALIA WEIGHS INTO PROPOSED CHANGES TO ENGLISH LANGUAGE STANDARDS
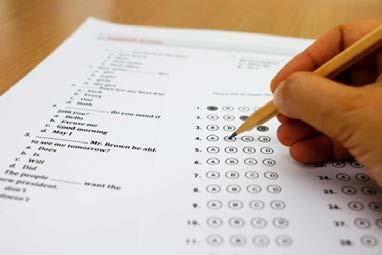
Optometry Australia (OA) has suggested changes to Ahpra’s newly proposed English language skills (ELS) registration standards, drawing attention to issues such as parental leave breaks and difficulties for practitioners who attended English-speaking schools but in “unrecognised” countries.
The regulator sets requirements for English language skills ensuring optometrists and other registered health practitioners can provide safe care and communicate effectively in English.
But the Australian Health Practitioner Regulation Agency (Ahpra) is now proposing changes to this standard “where real improvements have been identified to align with available evidence, clarify processes, reduce duplication, streamline and remove unnecessary information and address
gaps in content”. One significant proposal would see South Africa removed from the list of Englishspeaking “recognised countries”, which typically offer a smoother path to registration if practitioners have completed their education and qualifications there.
Ahpra also considered making Hong Kong, Malaysia or Singapore recognised countries, but could not find sufficient evidence to do so.
If South Africa is removed, the remaining recognised countries would be Australia, Canada, New Zealand, the Republic of Ireland, UK and US.
“The research showed that qualifications across the professions are offered in South Africa at multiple institutions, which in some cases, have different entry requirements,” Ahpra stated.
If practitioners haven’t completed their education in English, they can sit an English language test to demonstrate proficiency.
“Many of these requirements are substantially below the equivalent Australian entry level ELS requirements and some have no English minimum requirements for entry.”
In its submission, OA agreed with most of the proposals, but suggested some changes of its own.
There are currently four pathways for practitioners to meet the ELS standards. The most common is the Combined Education Pathway for applicants who have completed both their qualification and some secondary schooling in English in a recognised English-speaking country.
Another is the Extended Education Pathway (to be renamed the Advanced Education Pathway) developed to capture applicants who have completed a qualification for registration in the profession, and have undertaken advanced education in English in a recognised country – but who have not completed their schooling in English in a recognised country.
ODMA VOWS TO CONTINUE TARIFF CONCESSION FIGHT
The Optical Distributors and Manufacturers Association (ODMA) has appointed a regulatory consultant as it seeks to lobby the government for a reversal of an Australian Border Force decision that wiped a 5% tariff concession on acetate frames, increasing importation costs on eyewear from Europe.
It comes after Australia’s border authority refused an appeal by ODMA for a review of a decision, backdated to 13 May 2022, that ultimately overturned a Tariff Concession Order (TCO) on plastic frames that ODMA instigated around 20 years ago.
TCOs are an Australian Government revenue concession
that exists where there are no known Australian manufacturers of goods that are substitutable for imported goods. The original TCO meant importers of acetate frames were exempt from paying a 5% duty rate in Australia. But that privilege has now ended after Port Macquariebased Optex Australia notified the ABF that it produces acetate eyewear in Australia.
The move has hit importers of European eyewear the hardest because Australia doesn’t have a free trade agreement with the continent yet.
ODMA consulted with the industry and lodged an appeal to the Customs Delegate for the revocation approval to be reviewed, but was
advised in September that it was unsuccessful.
“Border Force found the limited manufacturing capability of Optex quite acceptable in its original decision. Border Force deemed that Optex Australia was producing, in their view, substitutable goods that are produced in Australia and that Optex Australia were prepared to accept an order to supply,” ODMA stated.
“It was deemed there was no requirement for Optex Australia to be supplying a certain volume, and given this, as feared, the appeal avenue did not turn out to be a successful one. This is of course an unfortunate outcome given the work
WHAT MADE HEADLINES IN 2022?
From major practice acquisitions and high-profile personnel appointments, to new product launches for myopia and macular disease, 2022 marked another prosperous year for the ophthalmic sector.

DEC 2022
AUSTRALIA’S LEADING OPHTHALMIC MAGAZINE SINCE 1975
continued page 8
continued page 8
page 50


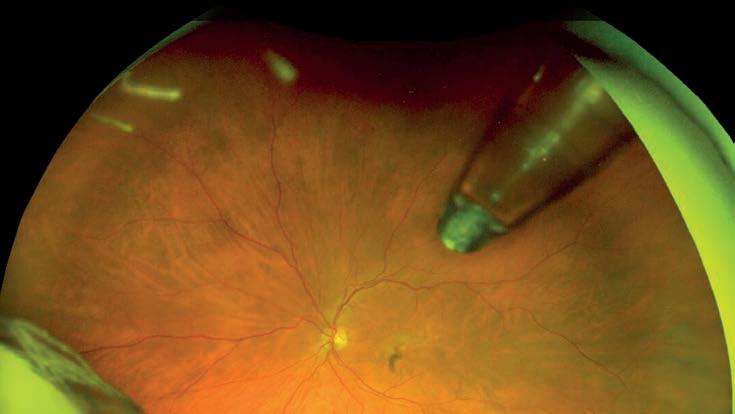
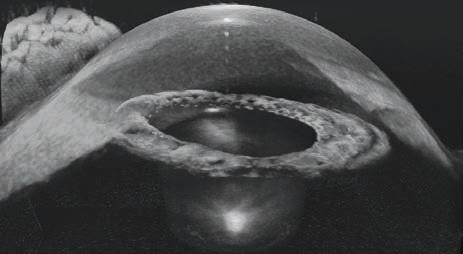
Introducing a new experience in phaco. Our answer to your phaco efficiency demands: • Z EISS patented QUATTRO Pump ® • D igitally integrated surgical workflow • A utomated Ultrasound Power on Demand Contact your local ZEISS representative for more information or to book a demonstration. ZEISS QUATERA 700 NEW! ZEISS AU: 1300 365 470 NZ: 0800 334 353 med.au@zeiss.com Carl Zeiss Pty Ltd, NSW 2113 AUSTRALIA. Carl Zeiss (NZ) Ltd, AUCKLAND 1026 NZ.
IN THIS ISSUE
18 BUDDING BUSINESS
Two early career optometrists discuss their journey to set up a greenfield practice in Melbourne.

42 OUT ON YOUR OWN
What does it take to establish a private ophthalmology clinic in Australia?


SALES STRATEGY

Tips to ensure independent optometrists capitalise on the busy December period.
WANTED: REGIONAL EYE DOCTORS

The tendency of ophthalmologists to settle in metropolitan centres – meaning access to eyecare can differ greatly depending on the patient’s postcode – remains a major sticking point for the sector, but a recent push to incentivise more of the workforce into regional areas is heartening.
The maldistribution is best demonstrated in data showing only 16% of ophthalmologists practise in non-urban locations, despite 29% of the Australian population being regionally based. Of ophthalmologists who trained and graduated between 2013-16, 90% now reside in urban areas.
Thankfully work is being done to fix this imbalance, with RANZCO highlighting the issue in its Vision 2030 and beyond initiative.
The college is aware ophthalmologists with a regional background are 2.7 times more likely to settle in regional Australia, but just 9.3% have a regional background at present.
This important insight has seen the college increase trainees with a regional background (around 40% in the past two to three years) and in February it will begin the new Regional Enhanced Training Network (RETN – see page 46).
The major differences between the RETN and existing networks are that trainees will complete their entire five-year vocational training program with the RETN, with two-thirds of their time spent in regional Australian areas like Darwin, Shepparton, Wagga Wagga, Tamworth and Orange.
COUNTRY CAREER
Attracting new-age eye doctors into the regions to address workforce maldistribution.
These strategies have been evidenced as powerful tools in sustainably addressing workforce maldistribution. And regional training posts offer boarder and deeper surgical experience with more opportunities to follow patients throughout, contrasting with the experience in big-city teaching hospitals with subspecialty clinics.
The same logic applies when they become fullyfledged 'generalist' eye doctors in the regions. It's positive to see RANZCO has made major strides to address workforce maldistribution, heeding on the advice from a 2018 government report.
But as the college points out, this is only part of the puzzle. Policymakers also need to come to the party and strengthen the country's public ophthalmology service where next-gen ophthalmologists are taught. Without this, regional patients may not get the care they deserve.
 MYLES HUME Editor
MYLES HUME Editor
29
46
FEATURES DECEMBER 2022 07 UPFRONT 09 NEWS THIS MONTH 53 OPTICAL DISPENSING 54 ORTHOPTICS AUSTRALIA 55 MANAGEMENT 56 PEOPLE ON THE MOVE 57 CLASSIFIEDS/CALENDAR 58 SOAPBOX EVERY ISSUE INSIGHT December 2022 5

1800 637 654 @eyesrightoptical
UPFRONT
Just as Insight went to print, SMS HEALTHCARE, a major Australian eye surgery provider, expanded into Darlinghurst and Brookvale. The latest deal with Sydney Eye Clinic follows SMS' acquisition of Queensland-based LASERSIGHT earlier this year. Sydney Eye Clinic founding partner Dr Ilan Sebban said finding the right partner to progress and maintain the clinic’s reputation played a key role in the decision to join SMS.
n WEIRD
A Harvard University neuroscientist has come under fire for her work that removes newborn monkeys from their mothers before suturing their eyelids shut to understand how the primate brain processes faces. The studies have been labelled as cruel and unethical by primatologists and animal rights activists, but some neuroscientists say it’s crucial for understanding human vision, Science.org reported.
n WONDERFUL
Fire and Rescue NSW has joined forces with Guide Dogs to deliver a specialised fire safety education program for children with low vision or blindness. The program includes practical demonstrations and workshops for children, conducted by firefighters at the Emergency Services Academy in Orchard Hills in Sydney’s west.
n WACKY
A US ophthalmologist who filmed herself removing 23 contact lenses from a patient who slept with them in has watched her video go viral. The patient complained of a foreign body sensation after neglecting her eye health due to the stress of a family event. The video was viewed on social media more than one million times.
IN OTHER NEWS, Specsavers has raised more than $1 million for The Fred Hollows Foundation in Australia in 2022. Since the partnership began in 2011, the optometry network has generated $5 million for the foundation.

"The funds generously donated by Specsavers go towards two areas: building a strong workforce of Aboriginal and Torres Strait Islander people in the eye health sector and strengthening the capability and coverage of eyecare around Australia," Fred Hollows CEO Mr Ian Wishart said.
FINALLY, I nsight has formed a partnership with Optical Dispensers Australia (ODA). In addition to regular ODA news updates and features, in 2023, Insight will introduce bi-monthly ODA Member Profiles to promote a career in optical dispensing.
“ODA is committed to growing and highlighting the optical dispensing profession across Australia, and we are honoured to forge an ever-growing and strengthening optical community together with our new partner Insight,” ODA CEO Ms April Petrusma said.
Published by: 379 Docklands Drive, Docklands VIC 3008
T: 03 9690 8766
www.primecreative.com.au
Chief Operating Officer
Christine Clancy
christine.clancy@primecreative.com.au
Group Managing Editor
Sarah Baker
sarah.baker@primecreative.com.au Editor
Myles Hume myles.hume@primecreative.com.au Journalist Rhiannon Bowman
rhiannon.bowman@primecreative.com.au
Commissioning Editor, Healthcare Education
Jeff Megahan
Business Development Manager
Luke Ronca
luke.ronca@primecreative.com.au
Client Success Manager
Salma Kennedy
salma.kennedy@primecreative.com.au
Design Production Manager
Michelle Weston
SIGHT-SAVING THERAPIES

michelle.weston@primecreative.com.au
Art Director
Blake Storey
Graphic Design
Michelle Weston, Kerry Pert, Louis Romero
Subscriptions
T: 03 9690 8766
subscriptions@primecreative.com.au

The Publisher reserves the right to alter or omit any article or advertisement submitted and requires indemnity from the advertisers and contributors against damages or liabilities that arise from material published.
© Copyright – No part of this publication be reproduced, stored in a retrieval system or transmitted in any means electronic, mechanical, photocopying, recording or otherwise without the permission of the publisher.
WHAT’S ON NEXT MONTH OPTI MUNICH 13 – 15 JANUARY Taking place in Germany, the event is a platform for product premieres from international market leaders and startups alike. contact@ghm.de THIS MONTH OPHTHALMOLOGY INNOVATION SUMMIT 2 – 3 DECEMBER Industry, clinical, and capital leaders will gather at this two-day event in San Deigo for the latest in anterior and posterior therapies. ois@healthegy.com Complete calendar page 57. insightnews.com.au STAT
There is a “linear relationship” between visual acuity improvement and the number of anti-VEGF injections for AMD patients, particularly between four and 10 injections in the first year. Page 39. INSIGHT December 2022 7
PATHWAY 'COULD BE OPEN TO EXPLOITATION'
While Ahpra said most proposed changes will have minimal impact, changes to the Extended Education Pathway would be the “exception”. It’s intending to strengthen this by requiring applicants to have completed at least six years in total of (full-time equivalent) education solely in English in a recognised country. This needs to include their qualifications, and advanced education at a degree level or higher requiring students to read, write, listen to and speak English.
Ahpra would also set a maximum of two-year break between the person’s qualifications and advanced education. The last period of education must have been completed no more than two years before applying for registration.
“The researchers found that the Extended Education Pathway could be open to exploitation and was lenient compared with like countries,” Ahpra stated.

“There are more changes proposed to this pathway to address the issues highlighted in the review and to strengthen the robustness of this pathway. Although this may mean a small number of applicants would no longer meet this pathway and would need to use the Test Pathway, this will assure boards of an applicant’s adequate level of English and subsequent protection of the public.”
OA suggested a rewording of this to “a maximum of two years break in this period of obtaining your qualification and the advanced education will be accepted”.
“The reasoning for this request is that many potential applicants have children at this period in their life and often take six to 12 months off, which has previously ruled out many (otherwise safe) applicants from being able to use this pathway,” OA said.
“If Ahpra considers a two year break between the periods of education acceptable, then logically a pause of the same duration elsewhere in the period carries identical (low) risk.”
In the current Test Pathway – for applicants who have not completed their qualification and/or secondary schooling in a recognised country, meaning they must pass an English language test – Ahpra currently allows practitioners to combine test results from two sittings within six months, but is proposing to extend this period to 12 months.
OA agreed with this move, stating: “It provides additional flexibility for applicants without adding any significant risk for the regulator. Some applicants have noted difficulty in being able to take the tests on dates offered by providers (or difficulty if they miss a test date due to illness etc) and a greater time window would provide more flexibility in being able to take a second test.”
OA also suggested Ahpra consider the impact on practitioners who have completed their education in English-speaking international schools, but unrecognised countries.
“We understand the need to make the standard as simple as possible and that it cannot cover every possible scenario,” OA said. “However, a situation that has been
PROPOSED CHANGES TO ENGLISH LANGUAGE STANDARD FOR OPTOMETRISTS
• Clearer naming of the pathways in the standard
• Renaming the current ‘Primary Pathway’ to the ‘School Pathway’ to have a clear differentiation between the pathway and primary education
• Strengthening and renaming the Extended Education Pathway to the Advanced Education Pathway
• Aligning with Department of Home Affairs requirements by removing South Africa from the recognised country list
• Adding the Cambridge C1 advanced and C2 proficiency tests to the accepted English language tests
• Reorganising content to make the sequence more logical
• Minor changes to improve wording and expression
• More active and personal language, making the ELS standard speak more directly to practitioners where appropriate
flagged to us on quite a few occasions is where an applicant has completed all of their primary and secondary schooling at expat/international schools in unrecognised countries where 100% of classes are taught in English. We have seen that there is currently no flexibility for these applicants but flag this for consideration,” OA said.
The fourth and final Primary Language Pathway (to be renamed the School Education Pathway) is used by a third of applicants. It captures applicants who have completed all primary and secondary education in recognised country and their tertiary qualification in English – but not in a recognised country. n
HOPES FOR EUROPEAN FREE TRADE AGREEMENT
to date to avoid this current situation the industry faces, and whilst Border Force’s due process has been followed, we do not feel a bigger picture has been considered in this decision and that this potentially inflationary outcome has come at a bad economic time for all involved.”
As a result, ODMA urged eyewear importers to ensure they have a Declaration of Origin (DOO) to clearly state goods originating out of those countries where Australia has a free trade agreement so a duty is not wrongfully applied.
It also urged suppliers to ensure their order data can be split between metal
frames and plastic frames to reduce instances of tariffs being applied to a whole invoice when it should only apply to part. The TCO for metal frames remains in place.
ODMA said it would continue to pursue the matter and has appointed a regulatory consultant to help prepare correspondence to relevant ministers and government departments.
The organisation is also urging eyewear business owners to submit letters to ODMA to evidence the impact of the revoked TCO.
“I can then ensure that examples are referred to as we now go forward and put our case to government that this was not a common-sense application of the law,”
ODMA acting CEO Ms Amanda Trotman said.
“And whilst I will take the [regulatory consultant’s] advice on what we include, I have offered to pass on any supporting statements I receive that contains evidence of the impact, especially on Australian businesses, employees and consumers.
“We will continue to fight the decision made on the industry’s behalf, I will continue to update ODMA members via bulletins as I have updates and I will ensure we keep across the developing European Free Trade agreement to hopefully share how that will mitigate the effects of this recent TCO revocation we would hope some time in 2023.” n
continued from page 3 continued from page 3
8 INSIGHT December 2022
NEWS
Amanda Trotman, ODMA.
n O=MEGA23 UPDATE
Organisers for O=MEGA23 and the 4th World Congress of Optometry (WCO4), to be held in Melbourne from 8 – 10 September 2023, have confirmed Dr Susan Cotter as a keynote speaker for the event. She is a USbased optometrist in paediatric optometry and a professor at the Southern California College of Optometry at Marshal B Ketchum University. Cotter’s primary research interests include clinical management strategies for amblyopia, strabismus, convergence insufficiency, and childhood refractive error. Optometry Victoria South Australia CEO Ms Ilsa Hampton said securing Cotter was "a major coup" for the event.
n GLAUCOMA CAMPAIGN
Following its successful launch last year, Glaucoma Australia (GA)’s fundraising initiative, the 7 Sights Challenge, will return in March 2023. The initiative encourages Australians to get out and about on their own or as part of a team to capture seven pictures – whether they walk, paddle, run, swim or ride – to remind them their sight is precious while raising much-needed funds for glaucoma research, early detection programs and critical support services. “The 7 Sights Challenge is asking all Australians to join the mission to raise vital dollars for glaucoma research and patient support programs. Anyone can develop glaucoma and the risk increases with age. By the age of 40, about one in 200 Australians will be diagnosed with glaucoma,” CEO Richard Wylie said.
n FLOOD RELIEF
The Victorian Eyecare Service (VES), which provides subsidised glasses and contact lenses to Pensioner and Health Care cardholders, Aboriginal and Torres Strait Islander people, and refugees, has been replacing glasses or contact lenses acquired through VES or the Victorian Aboriginal Spectacles Subsidy Scheme (VASSS) which have been lost or damaged in the recent Victorian floods. The natural disaster plagued areas in northern towns such as Echuca in October following heavy rainfall, which also affected towns in NSW and Tasmania. The VES will cover the patient contribution so the individual incurs no cost where a standard frame is selected. Patients who needed replacement optical appliances were urged to visit an Australian College of Optometry clinic or participating optometrist.
Fred Hollows hopes new funding will help close the eye health gap for Indigenous Australians. Image: Michael Amendolia.
FEDERAL BUDGET 2022-23 EYE HEALTH HIGHLIGHTS
PBS script cost cuts for patients, a bolstered First Nations health workforce and a focus on driving more health workers into the regions are among the most pertinent announcements for the ophthalmic sector from the 2022/23 Federal Budget.
On 25 October, Federal Health Minister Mr Mark Butler unveiled a package that would spend $104 billion on health, $30.6 billion on aged care, and $633 million on sport, totalling $135 billion, up 5.7% on last year.
The centrepiece of the health budget is $2.9 billion “to strengthen Medicare that will address a decade of cuts and neglect in general practice and primary care”. The government hopes this will reaffirm the scheme as the cornerstone of the Australian health system and take the pressure off overloaded hospitals.
Patients who use the Pharmaceutical Benefits Scheme (PBS) to access therapies for glaucoma, macular degeneration, dry eye and other eye diseases can expect their maximum co-payments to drop from $42.50 to $30, at a cost of $787 million to the taxpayer, from 1 January 2023.

“The maximum cost to general patients for PBS medications has doubled since 2000. These high costs meant that close to one million people delayed or did not fill their medications in 2019–20,” the government said, noting this is the first price drop in the scheme’s 75-year history.
While there were no announcements specific to Indigenous eye health, the government is investing $314 million toward First Nations health outcomes. Specifically, it will deliver improved infrastructure, including new and expanded Indigenous health clinics in locations with high and growing First Nations populations ($164 million).
The First Nations Health Workers Traineeship Program ($54 million), led by the National Aboriginal Community Controlled Health Organisation (NACCHO), will train up to 500 First Nations health workers.
Overall, The Fred Hollows Foundation has welcomed $1.2 billion in practical measures to close the
gap for Aboriginal and Torres Strait Islander people.
“We are hopeful this will help us address the gap in eye health as Aboriginal and Torres Strait Islander people are still three times more likely to be blind or vision impaired than other Australians,” CEO Mr Ian Wishart said.
Elsewhere, the 2022/23 Budget will address health workforce shortages particularly beyond Australia’s capital cities, making new investments in preventive health and improving mental health support.
The $185 million Rural Workforce package will attract, support and retain more doctors and allied health professionals into regional and rural communities, including new funding for the successful Innovative Models of Care program ($24.7 million).
More health workers will also be eligible for salary support through the Workforce Incentive Program ($29.4m).
The government is also delivering 480,000 fee-free TAFE and community-based vocational education places over four years. As a first step, the government is entering a $1 billion agreement with the states and territories to provide 180,000 places in 2023.
This agreement will prioritise training for students that traditionally face barriers to work and study, including women facing economic equality issues, and target industries with severe skill shortages.
Independent eye clinics haven’t been immune from the impacts of recent flooding and COVID lockdowns. For impacted businesses, the government is providing $15 million to extend the tailored small business mental health and financial counselling programs, NewAccess for Small Business Owners and the Small Business Debt Helpline.
“These programs have assisted many small businesses through the challenges of COVID-19 and recent natural disasters,” the government stated. n
IN BRIEF
INSIGHT December 2022 9
TWO NEW DIRECTORS ELECTED TO ODMA BOARD
Two prominent members of the optical industry, Ms Gail Giordani and Ms Jacque Katsieris, have been named as new Optical Distributors and Manufacturers Association (ODMA) board directors, bolstering female representation on the board.

Giordani, head of ZEISS Vision Care in Australia and New Zealand, and Katsieris, who co-founded ProOptics in 2009, join the current ODMA board of directors comprising chair Mr Robert Sparkes (OptiMed), Mr Mark Altman (Device Technologies), Mr Daniel Burgess (CooperVision), Mr Craig Chick (HOYA), Mr Lionel Minter (MIMO), Mr Sean Rosenberg (Frames Etcetera) and Mr Brad Saffin (Marchon).
The pair were elected to fill two vacancies following the resignation of one director, and the passing of director Mr Richard Grills in July 2022. They will serve on the ODMA board for the 12-month period up to the 2023 Annual General Meeting, when all the seats on the board will be open to nomination and election.
Giordani began her career at ZEISS South Africa in 1999 as a member of the microscopy division focusing on the market development. In 2014, she
was appointed managing director of Carl Zeiss, responsible for medical technology, industrial quality and research and consumer products business in sub–Saharan Africa.
Later that year, she took over as managing director of Carl Zeiss Vision, responsible for the Vision Care business in South Africa. Then, in March 2021, she was transferred to Australia to head the Zeiss Vision Care business for Australia and New Zealand.
“She brings international market
development experience across multiple industries and an emerging market perspective on the optical industry,” ODMA said.
Katsieris also started her optical career in 1999 at Tower Optics/Jonathan Sceats Eyewear, learning each aspect of the optical business from design and development of eyewear brands such as RM Williams and Deborah Hutton, to importing collections such as Tommy Hilfiger.
During her time at Tower Optics, Katsieris organised the successful ‘Manage Your Own Practice’ series of training events. Leveraging her business relationships with Sola, CooperVision and BOC, she arranged this free training series throughout Australia for independent practices.
In 2009, Katsieris and Mr Raymond Kessler co-founded ProOptics, distributing both high-end and lifestyle collections as well as design and development of proprietary brands for Australian fashion labels.
“Jacque has a reputation for her close relationships with her customers and this insight into the day-to-day workings of optical practices gives her an opportunity to deliver what they need,” ODMA said. n

EYEQ OPTOMETRISTS AND NATIONAL OPTICAL CARE
END STRATEGIC ALLIANCE
EyeQ Optometrists and National Optical Care (NOC) are parting ways next month, ending a two-year alliance.
The decision means there will now be 25 EyeQ practices, and 21 NOC practices.
The companies have confirmed that their current strategic business alliance, which commenced in November 2020, is reaching the end of its initial two-year term.
Their agreement was originally conceived during COVID, with a goal to support mutual growth plans and explore business opportunities, leveraging both financial and operational resources of each entity.
In an announcement on 20
October, EyeQ and NOC said their alliance proved very successful with numerous business innovations and strong practice growth achieved for each company.
“With these goals completed and the worst of COVID now behind us, EyeQ and NOC have decided the time is right to separately focus on the development of their own respective practice communities,” they said.

In line with the decision, Mr Jason Gowie will be leaving his role as joint CEO of EyeQ and NOC to take up a non-executive director role with NOC, with Mr Tomas Steenackers taking the helm at NOC.
Mr Ray Fortescue will resume operational responsibility of EyeQ,
within his current role as executive chairman, while Ms Lily Wegrzynowski will return to an EyeQ focus as general manager of optometry and people. n
NEWS 10 INSIGHT December 2022
Jason Gowie (left), of National Optical Care, and Ray Fortescue, of EyeQ Optometrists.
Gail Giordani, of ZEISS Vision Care (left) and Jacque Katsieris, of ProOptics.

Essilor® Stellest™ lenses slow down myopia progression by 67% on average*, compared to single vision lenses, when worn 12 hours a day. Essilor® Stellest™ lenses slow down myopia progression by 67% on average* #1 SPECTACLE LENSES WORLDWIDE(1) ESSILOR® *Compared to single vision lenses, when worn by children at least 12 hours every day. Bao, J., Huang, Y., Li, X., Yang, A., Zhou, F., Wu, J., Wang, C., Li, Y., Lim, E.W., Spiegel, D.P., Drobe, B., Chen, H., 2022. Spectacle Lenses With Aspherical Lenslets for Myopia Control vs Single-Vision Spectacle Lenses: A Randomized Clinical Trial. JAMA Ophthalmol. 140(5), 472–478. https://doi.org/10.1001/jamaophthalmol.2022.0401. 1. Euromonitor, Eyewear 2021 Edition; Essilor International SA Company; Retail Value Sales at RSP.
DRUG TO PREVENT CONE CELL LOSS IN INHERITED RETINAL DISEASE SHOWS PROMISE
The Lions Eye Institute (LEI) is investigating the therapeutic potential of a novel drug, GSK-J4, to protect cone cells in a specific type of inherited retinal disease known as achromatopsia, or total colour blindness.
Led by Dr Livia Carvalho at the LEI’s Retinal Genomics and Therapy research group, a large part of the research is focused on how to preserve cone-mediated vision.Cone cells are integral for most vision, including colour and bright light vision. Without cone cells functioning properly, people may struggle to perform tasks such as reading, driving and recognising faces.
In a recently published study, PhD candidate Ms Annie Miller delved into epigenetics, which looks at genetic changes to the way a cell works without a altering the DNA. Epigenetic changes can be the addition or removal of certain chemical groups to the DNA itself, or to a special molecule called a histone. Histones are essential proteins that help to tightly compact DNA in the cell, allowing each cell to store almost two metres of DNA.

The study included scientists from Germany and Switzerland, as well as local contributors from The University of Western Australia and Murdoch University.
According to the LEI, they used a disease model of achromatopsia and found epigenetic changes to a specific type of histone, which appears to contribute to the death of the cone cells in this disease.
“When the team targeted this change with a drug called GSK-J4, they found if they continually administer the drug into the cone cells, they could prevent the death of these cones,” LEI said.
“Currently, it is not possible to provide continuous release of a drug in a patient’s retina, however, large strides are being made in the field. To further research into the treatment potential of GSK-J4, the team is currently investigating exciting nanoparticle approaches to provide this drug to a patient’s retina continuously, and also testing if GSK-J4 can protect cones in other models of inherited retinal disease such as retinitis pigmentosa.” n
lens is based on Essilor’s H.A.L.T technology.
NEW SPECTACLE-BASED MYOPIA CONTROL APPROACH LAUNCHES
Australian and New Zealand eyecare professionals (ECPs) now have access to a new myopia control treatment, with EssilorLuxottica ANZ launching Essilor Stellest lenses.
The spectacle-lens based intervention, introduced in October, are designed to correct vision and slow myopia progression. According to the company, clinical trial results show that after two years, Essilor Stellest lenses slow myopia progression by 67% on average, compared to single vision lenses, when worn 12 hours a day.
According to the company, the lens incorporates H.A.L.T technology and involves the constellation of 1,021 lenslets spread on 11 rings designed to create a volume of signal that slows elongation of the eye. Based on scientific publications, EssilorLuxottica said its R&D experts concluded that a volume of signal has a stronger effect on the slowing down of myopia progression than a surface signal.
“The aspherical lenslet design and their arrangement create this targeted effect of volume of non-focused light in front of the
retina, following its shape,” the company said in a statement.
“In children, whose eyes are still developing, this volume of signal helps keep the eye elongation process in check.”
Essilor Stellest lenses are specially designed for children and suitable for a variety of paediatric frames. In addition to customer partner launch events, EssilorLuxottica is offering education and in-store assets and demonstration tools to support optometrists to introduce the lens with patients.
OptiMed, which formed a joint-venture with Essilor in 2019, will have technicians available for support with Essilor instruments such as the Myopia Expert 700 designed to support practitioners with myopia management.
“While current results are based on children from eight- to 13-years-old, Essilor Stellest lenses can be recommended to children as young as six and up to 16-years-old, upon the decision of the optometrist,” the company stated. n


VIDEO ON APPLYING EYE DROPS REITERATES WORLD SIGHT DAY MESSAGE

The Royal Victorian Eye and Ear Hospital (Eye and Ear) has partnered with the World Association of Eye Hospitals (WAEH) to produce a new animated eye drops application video.
They hope the new instructional video conveys this year’s World Sight Day theme, Love Your Eyes, to patients living with eye disease.
Co-funded by WAEH and the Nelken Trust, the video forms a patient eye drop education package to be used globally to teach a standardised technique for clinicians and patients – with the aim to improve compliance and health literacy.
Chair of the WAEH executive board Ms Cathy Kowalewski is encouraging all eye health professionals to share it with their patients.
“WAEH is proud to have developed a practical, patient-centred resource that will benefit the eye healthcare of patients globally. It has specifically been animated to allow for translation into
The video has been animated to allow for translation into any language.
any language,” she said.
The Royal Victorian Eye and Ear Hospital led the project in collaboration with the Wilmer Eye Center, John Hopkins, Baltimore USA; Moorfield’s Eye Hospital, NHS Foundation, London UK; Rotterdam Eye Hospital, Netherlands; Bascom Palmer Eye Institute, University of Miami, USA; Aravind Eye Care, India and Singapore National Eye Centre, Singapore. n
12 INSIGHT December 2022
Dr Livia Carvalho, of LEI’s Retinal Genomics and Therapy research group.
NEWS
The
9/10
children prefer MiSight® 1 day to glasses





Proven by 7 years of clinical data to significantly slow myopic progression with no rebound effect

Supported by the Brilliant Futures™ myopia management program
Further information at childmyopia.com and coopervision.net.au / coopervision.co.nz
*95-100% of children expressed a preference for contact lenses over glasses at each visit over 36 months. †’How much do you like wearing your contact lenses?’ 87/97 (90%) Top box ‘I like contact lenses the best’ Subjective response at 60 months. ‡Compared to a single-vision, 1-day lens over a three-year period; rate of progression maintained out to 6 years. On average, there was no indication that accumulated treatment effect gained following 3 or 6 years of MiSight® 1 day wear was lost during a 12-month cessation study in children aged 8-15 at initiation of treatment. Instead, eye growth reverted to expected, age average myopic progression rates. References: 1. Sulley A et al. Wearer experience and subjective responses with dual focus compared to spherical, single vision soft contact lenses in children during a 3-year clinical trial. AAO 2019 Poster Presentation. 2. CooperVision® data on file, 2019. 3. Chamberlain P et al. A 3-year randomized clinical trial of MiSight® lenses for myopia control. Optom Vis Sci 2019;96:556–567. 4. Chamberlain P et al. Myopia Progression in Children wearing Dual-Focus Contact Lenses: 6-year findings. Optom Vis Sci 2020;97(E-abstract):200038. 5. Chamberlain P et al. Myopia progression on cessation of Dual-Focus contact lens wear: MiSight 1 day 7 year findings. Optom Vis Sci 2021;98:E-abstract 210049.
6. Hammond D et al. Myopia Control Treatment Gains are Retained after Termination of Dual-focus Contact Lens Wear with no Evidence of a Rebound Effect. Optom Vis Sci 2021;98:E-abstract 215130. For instructions for use refer to https://coopervision.net.au/patient-instruction. MiSight®, Brilliant Futures™ and CooperVision® are registered trademarks of the Cooper Companies, Inc. and its subsidiaries. EMVCOO0841 ©2022 CooperVision.
1,2*†
UP
-10.00D
TO
HAILS CONGRESS 'REUNION BUZZ' RANZCO
Australian ophthalmology’s marquee event returned after three years, with the college ringing in governance changes and launching its comprehensive strategy to address eye health inequity across the country.
The 2022 RANZCO Congress took place in Brisbane, with the college hailing the success of its first hybrid event that also marked the beginning of several governance changes and launch of the Vision 2030 and beyond initiative.


The congress, held at the Brisbane Convention & Exhibition Centre from Friday 28 October to Tuesday 1 November, welcomed more than 1,700 in-person delegates who enjoyed a rich content program and trade exhibition.

“The energy levels were exceptional and created a reunion buzz that lasted from Friday through to Tuesday,” the college stated.
“As RANZCO’s first foray into hybrid congress, those watching remotely were able to join live-streamed plenary sessions.”
RANZCO’s new Vision 2030 and beyond project outlines the strategic direction and goals for the college to advocate for, and enable, equitable access to eye healthcare services across Australia.
Outgoing RANZCO president Professor Nitin Verma provided an overview of the strategy and key focus areas. It has been developed by a steering committee in consultation with multiple stakeholders over an 18-month period. And it is the result of targeted and public consultations, informed by contributions from many stakeholders including federal and state governments, peak bodies representing patients and professions, NGOs involved in eye health services, and many others.
At the launch, Verma acknowledged Dr Kristin Bell for her work as clinical lead in developing the strategy. Vision 2030 and beyond focuses on six key areas: service delivery, workforce and training, Aboriginal and
Torres Strait Islander healthcare, preventative healthcare, sustainability and global eye health.
Regarding workforce, Verma said a healthy ophthalmology workforce was dependent on a healthy public ophthalmology service right across Australia "because this is where most specialist training does and should continue to occur".
“For a sustainable workforce into the future, we need more training positions in public hospitals,” he said.
He said that RANZCO had increased the proportion of trainees with a regional background, is actively working to increase regional training posts, and has inaugurated a national Regionally Enhanced Training Network (RETN), where the trainee is regionally-based for 60% or more of their training. Two trainees have been selected for NSW Northern pathway and Victoria pathway to commence in 2023 (see more on page 46).
Noting that existing public ophthalmology services across Australia are overwhelmed, with long waits, Verma said “we need to advocate for more public ophthalmology services, particularly in rural, remote and outer urban areas, where comprehensive ophthalmology services are delivered to meet population needs”.
Going forward, the implementation of the strategy will be driven by a steering committee led by Verma working with committee chairs
14 INSIGHT December 2022 EVENTS
Professor Nitin Verma handing the RANZCO presidency to Dr Grant Raymond (left).
The Vision 2030 and beyond plenary session, featuring a high-powered panel (from left) Dr Shweta Kaushik, A/Prof Angus Turner, Dr Kristin Bell, Dr Justin Mora, A/Prof Ashish Agar, co-chairs Dr Grant Raymond and Prof Peter McCluskey, and Prof Nitin Verma.
The congress hosted more than 70 exhibitors over 100 booth spaces.
Associate Professor Ashish Agar, Associate Professor Angus Turner, Dr Shweta Kaushik, Dr Justin Mora and Dr Jesse Gale who also served as panellists at the launch.
Vision 2030 and beyond is described as a “living document” that will be regularly reviewed and updated as the college engages stakeholders and achieves the desired outcomes.
Dr Grant Raymond, who co-chaired the launch session with Professor Peter McCluskey (now RANZCO president and vice president, respectively) advised that the development of a strategy for New Zealand is underway with Mora as clinical lead.
COUNCIL ELECTIONS
In other major activities at the congress, the RANZCO Council met on Friday 28 October when three directors and a new vice president were elected on to the 11-strong RANZCO Board.
Incumbent director Dr Clare Fraser was elected for a second term. Dr Peter Hadden and Dr Sonia Yuen were elected to two other available director positions. Hadden is the current New Zealand branch chair while Yuen is an oculoplastics and paediatric ophthalmologist from Brisbane.

RANZCO’s censor-in-chief is also a director. As Dr Justin Mora’s term in the role ended at the congress, Dr Andrew Thompson replaced him on the board. Thompson has been heavily involved with RANZCO’s exam and education committees and also hails from New Zealand.
Meanwhile, current director, McCluskey, was elected as vice president. This came after Dr Grant Raymond was elevated to the role of RANZCO president, in a triple presidential handover at the congress dinner that saw Associate Professor Heather Mack (2018-2022) handover to Professor Nitin Verma (2020-2022), then to Raymond (2022-2024). The next congress will be held 20-24 October 2023 in Perth. n


n
2022 TRAINERS OF EXCELLENCE
n
n
n
n
n Dr Tim Henderson AM – SA
n Dr Weng Chan – SA
Dr Harry Bradshaw – NZ
Dr Svetlana Cherepanoff – Prince of Wales, NSW
Dr Krishna Tumuluri – Sydney Eye Hospital, NSW
Dr Anthony Fong – QLD
A/Prof Anne Brooks AM – VIC
Dr Lynn Gordon (pictured) was the keynote speaker of the Women in Ophthalmology luncheon, with Prof Helen Danesh-Meyer as chair and Dr Robyn Troutbeck as deputy.
Future-ready: PROVISION INDEPENDENTS CONVERGE FOR NATIONAL CONFERENCE
Independent optometry is in good hands if ProVision’s National Conference is any indication. The event returned in October with a record turn-out and all-star speaker line up. Insight reports on the main highlights.

‘L
ook forward’ was the theme of this year’s ProVision National Conference – and the program lived up this promise, bringing some of the country’s most entrepreneurial eyecare professionals under one roof to understand how they can galvanise the future of Australian independent optometry.

The biennial event – held at the Pullman Melbourne Albert Park on 21-23 October – attracted a record attendance of more than 470 delegates, an indication of the industry’s desire to reconnect after three years in the COVID wilderness (the last conference was Adelaide 2020).

“Having risen to the challenges of the last few years, delegates were ready to engage, learn and network once again,” ProVision acting CEO Mr Tony Jones said. “The majority of attendees were ProVision optometrists and practice staff but this was complemented by over 60 supplier partner representatives and a small number of non-members on the back of ProVision’s first industry-wide invitation.”
Following the conference, Jones said there was optimism and positivity around the future of independent optometry across the ProVision network. The organisation exists to help position practices for future strength, whether that’s by increasing patient relevance or helping them be competitive and profitable in a competitive market.
“Member feedback at the conference was overwhelmingly positive –reinforcing that our current value proposition reflects the needs of members, and that our business services and key initiatives help support the ProVision mission,” Jones said.
“The conference theme was Look Forward and the key objectives were to help members be more future-focused by considering services and resources that help to future-proof their practice. The future in terms of growth opportunities has never been stronger for independents as patients seek out a more customised experience.”
KEY HIGHLIGHTS
Delegates enjoyed an impressive list of keynote speakers such as 2022 Australian of the Year, retired wheelchair tennis legend and disability advocate Mr Dylan Alcott, but the agenda also included three workshops presented by both internal and external subject matter experts, focusing on topics such as succession planning and optimising the practice website for patient acquisition.
Alcott closed the conference and discussed the need to address opportunities for inclusivity in the workplace and broader community. Paraplegic soon after birth, he recalled tough moments growing up, particularly when he discovered he was being excluded because his friends were too shy to discuss his needs, not because he was different.
“When I started talking about my disability more, it normalised it for everyone else,” he said, noting that it was from this point that he began to realise his purpose – to ensure people with a disability enjoy the life they deserve and to break down the stigma.
“The hardest challenge is not the lack of accessibility, it’s the lack of expectation of what people think you can do. Ask questions, put in a bit of effort, listen, and learn from your consumers about what they need, and you’ll change their lives.”
In one of the Future Focussed Workshops, ProVision business services manager Mr Mark Corduff and and Synstrat director Mr David Collins outlined the most crucial factors when it comes to succession planning. With 85 ProVision Associates looking at a future in independent ownership, they emphasised the importance of meeting certain criteria to make the business an attractive proposition.
They also said it was important to start planning five to 10 years out from retirement, and refer to ProVision’s Succession Planning Checklist to understand where they sit.
16 INSIGHT December 2022 EVENTS
ProVision's Leanne Jackson (L), Adrian Hunt, Tony Jones, Sarah O’Connor and Andrew Parker.
The conference included a trade fair for supplier partners.
Collins also introduced the financial considerations for practice owners and insight into how practices are valued. There are factors that can improve a valuation outcome and maximise their price over a three-year journey.

Another Future Focused workshop focused on digital marketing and was presented by Mr Jonah David and Mr Russ Lazarus from EyeCarePro, an international digital marketing company solely focused on optometry businesses that recently formed a strategic alliance with ProVision. Part of its service involves revamping and managing websites, SEO and PPC and monthly digital campaigns for ProVision members.
performance, quality and content of the practice’s webpage. It’s also important
awareness, as well as weekly posts to complement practice-generated content. The balance of engagement should be around 80% educational, and 20% promotional.
Regarding Google Ads, they advised an ad spend of $500 and the need to allow three months before considering its return on investment.
Elsewhere, award-winning marketer Ms Katrina McCarter offered an intriguing presentation on understanding Gen Y & Z consumers, which have differing needs.

Among the most important considerations for Gen Y customers (26 to 41 years) were: a mobile-first marketing strategy, prefer content such as blogs, videos and articles over traditional marketing, consider businesses’ values in their purchasing decision, and seek out fun shopping experiences.
For Gen Z (10-25 years), practices should understand: they’re hyperconnected and can filter content quickly, prefer social media over traditional media especially platforms like TikTok and BeReal, are risk adverse compared to other generations, trust brands featuring real customers in their ads (start working out how to engage customers to photograph themselves wearing your glasses and tagging your business), and they’re incredibly purpose-driven.
Other key speakers included Mr Keith Abraham on the importance of setting goals that provide a clear focus and motivate employees, while Ms Julie Cross spoke about the need for positive energy stating that, like physical muscles, emotional muscles need to be exercised by reframing poor experiences to be equipped for life’s challenges.
ProVision’s next conference will be held in Perth in 2024.
“By all accounts there is a buzz already and we expect it to build on the patronage and engagement of our recent Look Forward conference in Melbourne,” Jones, acting ProVision CEO, added. n
Australian of the Year 2022
Dylan Alcott was a keynote speaker.
DIY-approach
PAYS OFF FOR EARLY CAREER OPTOMETRIST-BUSINESS OWNERS
Locked down in separate states, not even closed borders could prevent COVID-era Deakin optometry graduates DR ALISHA SHASTRI and DR EBRU EFEM from pursuing their plan to open their own practice.
After graduating from Deakin University in mid-2020, optometrist Dr Alisha Shastri returned to her home state of South Australia and joined a corporate practice while her classmate Dr Ebru Efem worked in an independent practice in Melbourne.
As their careers progressed and experience grew, it sparked an idea: what would it be like to manage their own practice?
“We started thinking about what we wanted to bring in terms of patient care and eye health, and fashion in eyewear. We wanted to make sure both elements were shown through the branding of the business. We were aware this was something we needed to get right from the beginning,” Shastri says.
The duo began considering their options, including buying an existing business, or establishing a greenfield practice, with support from independent optometry network ProVision.
The pair joined ProVision as part of the free ProVision Associate Program which pairs optometrists launching their own independent practice with an experienced professional who can share valuable first-hand industry knowledge, act as a sounding board and a trusted advisor and ultimately enhance new business owner’s chances of success.
“We went through the process of evaluating what’s out there, and we looked at a couple of practices that were selling. That pathway does come with a lot of pros, including an established patient database,” Shastri says.
“But we thought for us to really implement our ideas, starting fresh was the way to go. We put in the time and effort – there’s a lot that goes into something like this. But it was one of the best journeys we could have gone on and I would do it again in a heartbeat because there was plenty of fun and learnings along the way.”
Once they decided to open a greenfield practice, choosing a location presented the next hurdle. Shastri was based in Adelaide; Efem, also a qualified orthoptist, was in Melbourne. Which city should they choose?
“We went back and forth on that idea, weighing up which was going to be best. We thought Melbourne provided the greatest opportunity for growth of a new practice. It became obvious both of us knew we wanted to be there,” Shastri says.
With Shastri stuck in Adelaide due to lockdowns, Efem, in locked down Melbourne, started investigating commercial properties within a 5km radius of her home.
The pair found their preferred location in Greenvale Shopping Centre in Melbourne’s north.
“The area we’ve selected has never had an optometry practice,” Efem explains. “Greenvale is expanding with new housing and development of schools and infrastructure, and there’s lots of new families coming into the area. We thought there was a great opportunity for us to be part of the community and provide a service that didn’t exist here.”
GETTING STARTED
Shastri and Efem negotiated a lease directly with Greenvale Shopping Centre management.
“We went to them with the idea of opening an optometry practice, and they loved it. They were supportive and encouraging – and agreed it was what the area needed,” Efem says.

They then created a list of more than 200 potential business names and whittled it down to one – iOptical.
Next, they turned their attention to securing finance and acquiring equipment, which had to be conducted online because of COVID restrictions.
“We spoke to a range of suppliers on Zoom, so we couldn’t see the equipment properly or even have a play around with it, but we trusted ourselves and our suppliers,” Shastri says.
“We also spoke to banks, created a business plan and estimated cash flow,
18 INSIGHT December 2022 PROFILE
Two Deakin graduates opened greenfield practice iOptical in Melbourne in May 2022.
but sought advice to ensure it was up to standard.”
Their practice fit-out was organised through the connections of the shopping centre’s management.
“Our interior designer was fantastic and worked well with us even though they had never done an optometry practice fit-out. They had designed several other retail stores, including a few in Chadstone Shopping Centre,” Efem says.
“They knew what they were doing but there are extra things to consider when creating a healthcare and retail space, such as the right lighting. So, it was a collaborative journey.”
Shastri and Efem were confident in selecting a range of frames for iOptical, but found it was difficult not to overspend in this area.
“We had a geographic report given to us by Greenvale Shopping Centre management, so we know who is in the area, their occupation, and median income,” Efem says.
“Frames selection was one area that we knew we shouldn’t sacrifice. We knew we needed to stock the major eyewear brands because people in the area were purchasing big-name eyewear brands from optometry practices in the surrounding suburbs. We wanted to make sure we catered to them. We had to be careful which brands we brought in and be mindful of our budget.”
“It’s the one area we were concerned we went over-budget with, but it’s paid off,” Shastri adds. “We also didn’t work too far from this area in our previous jobs. We would see people from this area come in. We were able to observe, to see what they were wanting and what they were buying. We took that into consideration when opening in the area, too.”
Being familiar with some local faces has helped build a patient database, and their location in the shopping centre has attracted several walk-ins.
“We literally started from zero. Even when we were building and the hoarding was still up, people would come in and talk to us if we were around, or occasionally sit at the cafe across from the practice, and people got to know us,” Efem says.
“I think people are very open to supporting their locals. We had one guy come in and say, ‘I want to support local, I want to give you a go’. We didn’t even have the shelves up yet, but he booked an appointment with us. I think it’s that sense of community.”
“Right now, we’re getting people walking in, they’re curious to see what’s around,” Shastri adds. “They’re wanting to get their eyes tested or know that it’s time for them to get it done and they would prefer to drive three minutes rather than 15 minutes, so it’s a convenient spot for a lot of people in the area.”
While the practice’s bright frontage draws in passing foot traffic, the pair have also invested in an online marketing presence, with their branding, website and social media managed by a Melbourne digital marketing agency.
point of meeting local GPs and ophthalmologists.
“We’re very lucky because we have a GP clinic just outside where we are. We went in and introduced ourselves, similarly to other local GP clinics. We met a lot of the doctors in the clinic too. It was nice to introduce ourselves in person, so they know who they’re referring their patients to and vice versa,” Efem says.
“We also met with local specialists. We wanted to explain what we do, what service we can offer, what technology we have, so they know they can refer to us. We might be new, but we’re here to stay, and we’re here to help as well,” Shastri adds.
COMMITTING TIME AND EFFORT
Shastri and Efem began planning iOptical in the beginning of 2021 – while both working as fulltime optometrists in other practices – with the intention of opening in November the same year, but COVID delayed their plans. They opened in May 2022.



“But it gave us those extra few months, which helped us in the planning,” Efem says.
“We would go to work then come home and then work until midnight on iOptical, essentially having two jobs at that point. But you’ve got to be willing to put in the time and effort because not everything comes easily. We really worked hard to get to where we are,” Shastri adds.
They both transitioned out of their employee positions only a few weeks before opening iOptical.
They both now work in iOptical five to six days a week (Efem also works one day a week in ophthalmology at The Royal Children’s Hospital) and employ two dispensing staff; one part-time and one casual.
“At a time when there weren’t a lot of dispensers looking for new jobs or wanting to move, we were lucky in getting two people who had over 10 years’ experience in the industry,” Shastri says.
Six months into practice ownership, Shastri and Efem put their early success down to commitment and ongoing support.
“It’s all about having the right people around you, people who also believe in you, especially during those hard times of starting your own business during COVID,” Efem says.
“And even now, every day we feel like there’s always something new to learn, or there’s always something new to grow with. I think that’s the beauty of it too – we’re both very open to growth and innovation in the business, wanting to make sure that we’re keeping up-to-date,” Shastri says.
“Now, we have to think about the future of the business. We’ve engaged a business coach through ProVision to make sure that we’re ticking all the boxes, and we’re on the right path when it comes to not just thinking about now, but what the business is going to look like in the next five years,” Efem says. n
INSIGHT December 2022 19
Dr Ebru Efem (left) says purchasing equipment was made more challenging by COVID restrictions.
Dr Alisha Shastri and her business partner gave a lot of consideration to their frame’s selection.



www.icare-world.com iCare is a registered trademark of ICARE FINLAND OY. CENTERVUE S.P.A., ICARE USA INC. and ICARE FINLAND OY are parts of REVENIO GROUP and represent the brand iCare. + Fast and easy IOP self-measurement taken in supine, reclined or sitting positions + Smart light guide for correct positioning +Comprehensive insights into IOP fluctuations and peaks +Monitor treatment efficacy and adherence + Engages patients in glaucoma management More information: info@icare-world.com ICARE-HOME2-AD-TA023-249-EN-1.1-AUS iCare HOME2 24-hour at home tonometry NOW AVAILABLE AT shop.glaucoma.org.au
2022/23Summer showcase
In the wake of numerous product launches in recent months, Insight is bringing together a host of Australia’s leading suppliers to showcase their 2022/23 releases.
Over the next four pages, eyecare professionals will discover the latest in ophthalmic lens technology, including premium coatings and myopia control interventions.
New equipment, such as ophthalmic lasers, OCT machines and tonometers, are also featured, along with the latest eyewear designs out of Europe.


THE
COOPERVISION MAKES ALL ONE-DAY CONTACT LENSES PLASTIC NEUTRAL

To provide an easy way for optometrists and their patients to be more sustainable, CooperVision has made its one-day contact lenses distributed in Australia and New Zealand plastic neutral.1,2 The initiative is made possible through a global partnership with Plastic Bank, a social enterprise that builds ethical recycling ecosystems in coastal communities.
For every box of CooperVision one-day contact lenses distributed in Australia and New Zealand, CooperVision purchases credits that fund the collection and recycling of ocean-bound plastic, that is equal to the weight of the plastic used in its one-day contact lenses, the blister and the outer carton packaging.2
According to the company, Plastic Bank collectors in the coastal communities receive a premium for the materials they collect, helping to provide basic family necessities such as groceries, school fees, and health insurance.
References available upon request.
Email: hello@au.coopervision.com
LENSES WITH AN X-TRA CLEAN FINISH
According to Rodenstock, to achieve the best performance from a spectacle lens it is important to have a high-quality finish with excellent anti-reflection properties. However, dirt tends to be more visible with the minimal reflections from an antireflection coating, and can be annoying for the spectacle wearer.

With the X-tra Clean Finish, Rodenstock says it has set a new standard in ophthalmic optics.
“The extremely smooth surface means that dirt hardly sticks – and if the lens does get dirty, the dirt can be easily removed without leaving any streaks or residue on the lens,” the company says.
According to Rodenstock, an independent market research study carried out by market research agency with face-to-face interviews with spectacle wearers age 40-70 years showed:
1. After cleaning the lenses with X-tra Clean Finish, 100% perceive them as absolutely clean without residue

2. 93% state that lenses with X-tra Clean Finish are easier to clean than their current lenses due to the smoothness of the lenses.
Added to the Rodenstock current Solitaire 2 family of coatings, which have UV back surface protection and a three-year manufacturer’s warranty, X-tra clean coat could be the answer to patient antireflection coating objections, the company says.
Email: optics@ rodenstock.com.au
THE ULTRA-COMPACT, WIRELESS GREEN LASER SYSTEM

The next generation LEAF laser system is the size of a tablet or iPad, making it one of the most compact and versatile treatment additions to ophthalmic practices, exclusive Australian distributor OptiMed says. Its sleek, smart design is 10 times smaller than existing systems, mounts directly on to any slit lamp and is portable so practitioners can easily share among multiple practices. Industry-first speech recognition allows convenient control of laser parameters and, with no external fiber, it eliminates the need for counter space, reducing the risk of damage, mechanical breakdown and disruptive service repairs.
“The Norlase LEAF Laser System allows you to treat more patients while maximising practice space and providing greater quality of care and safety. It comes at a compelling price to make it easy for you to expand your practice with laser treatment,” OptiMed says.
Norlase is a Danish company with exceptional design craft. While a new player, it has originated from years of laser experience from within a prolific global laser manufacturer.
Email: sales@optimed.com.au
SUNGLASS COLLECTIVE INTRODUCES LATEST FROM FASHION-FORWARD SPANISH BRAND
Sunglass Collective is presenting the latest offering from the fashion-forward Spanish brand, KALEOS. Shape, geometry, colour. A homage to details and silent luxury. Frames to see and be seen. Between oversized shapes, reinterpreted cat-eye sunglasses, and the panto shapes, there is a frame and sunglass for everyone.

“The inspirations behind this sun collection were a wide range of things but there is one we should mention, the intriguing and avant-garde world of Bauhaus. A strong pop of colour appears occasionally, creating the perfect balance with our range of classic tones,” Sunglass Collective states.
“RIDGEWAY is the perfect bold sunglass for people who desire luxury handmade sunglasses made to make a statement. Expert craftsmanship and construction details are seen all-over. RIDGEWAY is created using only the highest quality materials. Your new favourite sunglasses are here and they add a classic touch to any look.”
Email: sales@sunglassco.com.au
22 INSIGHT December 2022 Summer showcase 2022 2023 2021
NEW MYOPIA INTERVENTION LAUNCHES IN ANZ

Essilor Stellest lenses designed to slow myopia progression in children are now available in Australia and New Zealand. According to the company, clinical trial results show that after two years, Essilor Stellest lenses slow myopia progression by 67% on average, compared to single vision lenses, when worn 12 hours a day.1


The lens incorporates what is described as H.A.L.T2 technology that involves the constellation of 1,021 lenslets spread on 11 rings designed to create a volume of signal that slows elongation of the eye. Based on scientific publications, EssilorLuxottica says its R&D experts concluded that a volume of signal has a stronger effect on the slowing of myopia progression than a surface signal.
“The aspherical lenslet design and their arrangement create this targeted effect of volume of non-focused light in front of the retina, following its shape,” the company says. “In children, whose eyes are still developing, this volume of signal helps keep the eye elongation process in check.”
References available upon request.

Email: marketing@essilor.com.au
A NEW GENERATION OF ASPHERIC
IOL
The new CT LUCIA 621P/PY represents a new generation of aspheric IOL from ZEISS, applied on a monofocal hydrophobic C-loop platform. It offers consistent visual outcomes*, excellent stability and intuitive injector handling.


CT LUCIA 621P/PY IOLs, with ZEISS optic features, are designed to compensate for potential decentration and lens misalignments. Reducing the risk of decentration allows the ophthalmologist more time to focus on their patients and their needs.
According to the company, the architecture of the IOL enables very stable positioning in the capsular bag for consistent and excellent performance.
The CT LUCIA 621P/PY comes in an optimised fully preloaded injector system for an easy and intuitive cataract workflow.


*data on file with ZEISS
Email: info.au@zeiss.com
Summer showcase 2022 2023
HP-OCT OFFERS ‘PARTICULAR ADVANTAGES IN THE ANTERIOR SEGMENT’
Cylite is an Australian-based company developing the next generation of diagnostic OCTs for optometry and ophthalmology. The company’s Hyperparallel OCT (HP-OCT) is a world-first, capturing accurate volumetric data of the eye, with particular advantages in the anterior segment.
“Scanning at an industry-leading 302,400 A-scans per second, the technology simultaneously images across a wide area of the eye with minimal motion artefacts, allowing the production of highly accurate and repeatable elevation and curvature maps, as well as accurate analytics to enable clinicians to make more informed decisions for better patient outcomes,” Cylite states.
According to the company, in one scan, the HP-OCT captures a full 3D image of the anterior segment, which can be used for personalised contact lens fitting, as well as a full set of biometric measurements, including axial length, for use in myopia management. The same volumetric imaging technique can also be applied to the posterior segment to produce excellent volumetric retinal images.

Website: info@cyliteoptics.com
SELF-TONOMETER OFFERS 24HOUR IOP MONITORING
iCare HOME2 is described as an innovative self-tonometer, offering comprehensive insights into IOP fluctuations and peaks, as well as adding significant value to treatment decisions and assessments.
The device, available to patients now at Glaucoma Australia, enables clinicians to optimise care, monitor treatment efficacy and customise individual management for their patients, with all data accessible via cloud software.

“The difference between readings we obtain in the office and the data from the iCare HOME is like the difference between a single snapshot and a continuous movie of a patient’s daily life,” remarked renowned Canadian glaucoma specialist Dr Ike K. Ahmed.
For patients, iCare HOME2 is said to provide peace of mind and may help improve adherence to medication. It is described as easy-to-use, with the same gentle and accurate rebound technology as other iCare tonometers, and no anaesthesia or eye drops required.
Email: homesupportau@icare-world.com
RACE EMBODIES PRODESIGN

DENMARK DNA
Eyes Right Optical is presenting the latest release from ProDesign Denmark. RACE is described as a true ProDesign frame and the very definition of what the eyewear maker does best.
According to Eyes Right, it features specially fitted shapes with easy-to-wear fronts and a thin, yet powerful colour detail starting from the end-piece and running along the temple.
“The colourful temple tips, metal milling and tip cuts are neatly aligned and serves as proof that careful craftsmanship has been utilised in this design,” the company states.
“It’s sporty, yet subtle and provides great variation in sizes. Stocked in Australia for your convenience, ProDesign Denmark is the versatile best-selling collection that will complement your practice.”
Email: sales@eyesright.com.au
TOKAI OPTICAL EXPLOITING NEUROSCIENCE IN LATEST PROGRESSIVE DESIGN
Tokai Optical is set to debut the progressive lens brand NEURO SELECT in Australia, offering customised lenses for people enjoying diversifying activities and lifestyles.
According to the company, the high-specification progressive lens exploits cutting-edge neuroscience and is selected by the brain, according to the person and their lifestyle. The lenses have been developed in collaboration with the National Institute for Physiological Sciences of the National Institutes of Natural Sciences, assessing how images appear in the brain and evaluating the clearness of the peripheral areas of lens.
NEURO SELECT features a unique basic design that introduces three types of technology: N-style Binocular Link Design, Variable Zone Control, and Dedicated Multi Optima System, to all grades.
“N-style Binocular Link Design is the key technology for NEURO SELECT, which verifies the effects of lenses with the aid of neuroscience using magnetoencephalography and approximates the vision of both eyes,” Tokai stated.

“In addition, NEURO SELECT offers Variable Zone Control to Daily, Town and Home to meet the needs of lifestyle and purpose.”
Other than the standard high-quality premium coatings, various functional coatings are available in the NEURO SELECT range.
Email: toa.orders@tokaiopt.co.jp
24 INSIGHT December 2022 Summer showcase 2022 2023































more, know more with more Insight Subscribe FREE and receive the latest news Insight is mobile and tablet friendly Find jobs and advance your career with Insight’s Classifieds Get to know the newest products from suppliers across Australia Insight’s new website keeps you updated on the latest industry news and information. With a world-class responsive design, Insight is now accessible seamlessly on any device, 24/7. Sign-up FREE to our eNewsletters and industry reports delivered weekly straight to your inbox. www.insightnews.com.au
See
At
completion
article,
Including:
• Understand why measurement of axial length is integral to the emerging standard of care in myopia management
• Be aware of the demographic and cultural confounders in myopia research
• Develop a more methodological approach to the use of atropine doses in myopia management
• Determine patient conditions that encourage a more tailoredapproach to myopia management
MYOPIA MANAGEMENT: CUSTOMISING PROTOCOLS FOR OPTIMAL OUTCOMES
LOREN
sociodemographic profile.
Although there has been a considerable amount of progress in childhood myopia research in recent years – understanding how myopia occurs in children, its progression and useful intervention strategies – there still remains a considerable amount of confusion regarding the best protocol for management.

Admittedly, the number of articles published monthly on myopia causes and interventions can be overwhelming. This expansion of information has led to confusion about the best treatment for myopia progression in children.
One of the common issues is how to measure myopia progression in children. Traditionally, optometrists use the diopter progression to measure how much the eye has progressive myopia with the increase in dioptres. Most studies and publications measure the fast progression of myopia in children as half a dioptre per year.1-3 This is a measurement of the actual change power of the lens needed to improve vision to the macular of the eye. The accuracy of this method required cycloplegia

given a child’s ability to accommodate significantly.
However, the more objective, accurate and reproducible measure of progression is axial length (AL) growth, best measured with interferometry.4,5 Interferometry gives us a very accurate non-contact method of measuring how the actual length of the eye changes, hence myopia progression in childhood.
The AL is the underlying cause relating high myopia to pathological myopia in adulthood. It has become the standard in research studies and is quickly becoming the standard of care in clinical practice. Historical data suggested an average childhood AL growth of 0.1 mm per six months.6,7 An analysis of average axial change in Europe is variable with age, with greater progression in under nine years.8 There is also an ethnic difference with greater progression noted in the Asian population (average of 0.30 mm/year).9-11 The common conversion is -0.5 dioptre per year equates to 0.2 mm elongation per year.4
Figure 1. Haag-Streit Lenstar Myopia software highlights titrating progression and early treatment to prevent high myopia in a patient. Atropine 0.01% initiated after second visit date (06.12.16). Dosage changed after a year to 0.05% atropine (17.06.20). The patient’s final spherical equivalent refraction at 16 years old was RE: -6.75; LE: -7.5.
progression is the question of what atropine dosage to start with when treatment is initiated – and how to progress in a treatment algorithm. In fact, there is a surprising variability of the initial doses of atropine drops used by clinicians when they commence their myopia management treatments in children.
It is not uncommon to hear and see patients starting their first dose of low-dose atropine at 0.05%, while some clinicians will start on 0.025% and others on 0.01%. The source of this confusion is the recent studies showing the efficacy of atropine to be dose-related. The stronger the dose, the more the powerful the effect on retarding axial elongation, which is the aim of myopia intervention.
There is no debate that the stronger the dose of the atropine, the more the effect. However, equal attention needs to be made to the fact
26 INSIGHT December 2022
In the rush to establish effective myopia control strategies, many eyecare professionals may be too reliant on rigid treatment protocols that fail to observe specific patient needs. DR
ROSE says an effective plan addresses the patient’s unique physiology, culture and
the
of this
the reader should be able to align their clinical protocols more closely to a best-practice approach to myopia intervention
CLINICAL CPD HOURS
This activity meets the OBA
registration standards for CPD
LEARNING
CPD
OBJECTIVES:
that the stronger the dose of the atropine, the more likely the patient will be affected by the side effects. These side effects include blur, glare, and rebound when we stop the drops too early.
‘CONFOUNDING’ PATIENT DEMOGRAPHICS
Taking a step back, the basis of these doses follows the three-year Low-Concentration Atropine for Myopia Progression (LAMP) studies conducted by researchers from the Chinese University of Hong Kong.9,12,13 Collectively, the LAMP Studies directly compared low concentrations of atropine (0.05%, 0.025% and 0.01%) and ultimately concluded that atropine 0.05% appears to work best over three years to control axial elongation.
However, the study left a vital question unanswered: How do these concentrations perform in other patient demographics?
Simply put, the LAMP Studies are based on an Asian population and may have ethnic and lifestyle confounders. The study was based on four to 12-year-olds in Hong Kong. We know that the Asian population generally experiences myopic progression faster than those in Western populations. In a population study in Australia, myopia in the Asian cohort progressed faster than myopia in the Caucasian cohort. However, the Asian cohort did not progress as fast as the Asian counterparts in Asian studies.14 These observations suggest that besides ethnicity, there are other contributors to myopia progression in these Asian studies. These may be different cultural environments, such as time spent outside and doing near work, which are known as ‘confounders’.15-17
GEOGRAPHY AND LIFESTYLE
Additionally, there are concerns that lighter irises (more common in Australia) are more likely to experience the side effect profile of higher doses of atropine, and may not tolerate the higher doses due to blur and glare, especially in Australian children who have better light-exposure compared to some Asian countries.18 Higher atropine concentrations have greater side effects of dilation and cycloplegia, which are tolerated best by dark irises.

Tolerating outdoor time is important as part of the strategy to reduce the risk of myopia progression,19 especially in the Australian sun. Finally, an American study showed that in doses of more than atropine 0.02%, children were more likely to experience the side effects profile of atropine.20
Therefore, atropine 0.025% dose has limited benefit on axial growth but a similar side effect profile (as 0.05%), especially in lighter eyes. Given the dose consideration in the Australian context, a more methodological approach to atropine doses should be considered.
BEST PRACTICE APPROACH TO MYOPIA INTERVENTION IN AUSTRALIA
In keeping with this theory, we need to understand our children’s needs. There should be a best-
practice approach to myopia intervention, including atropine drops, that accommodates the specific conditions found in this specific population.
It is important that myopic children are diagnosed early and monitored for fast growth. Interferometry provides high accuracy and ease of use in children to monitor the progression of axial growth. As myopia prevalence and incidence are predicted to increase, such tools will be invaluable in optometry practices. The use of interferometry helps to monitor change precisely, so if a patient is a fast progressor (>0.1 mm/6 months), then atropine can be initiated and interferometry can be used to monitor the response in the next six months.
In some children, axial elongation progresses very slowly and they may not benefit from an intervention such as atropine. In such cases, the favoured approach would entail a discussion about lifestyle with less near-work, increased time in natural light and monitor for change.
On the other hand, the sequential approach is the best and safest for children who are considered to be fast progressors. As with any medication, the lowest clinically significant dose should be the first prescribed as part of the treatment algorithm. Ultimately, a sequential approach to treatment, including dose concentration, allows for monitoring of treatment effects and side effects.
ATROPINE 0.01%
The lowest dose of atropine known to be effective should be the first dose in treating myopia progression. Apart from the ATOM and LAMP studies, the effect and benefit of atropine 0.01% have been widely established.2,4,21,22
This research includes an Australian-based study which resulted in a mean 50% reduction of axial progression in fast progressors based on the
If low dose atropine is tolerated but does not have enough of the desired effect to control myopia growth, Dr Loren Rose’s approach is to titrate the dose.
profile is similar to 0.025%, but the greater efficacy of 0.05%. I schedule regular review intervals at six months to reassess the axial growth with each intervention.
I feel it is also important to ensure that the patient and their family can report and intervene earlier if they feel that glare and/or blur are significantly a problem. I also feel it’s important to educate patients and their families that stopping a higher dose without follow-up can lead to a higher chance of a rebound, and explain how the rebound may undo some of the good work that atropine is done for them.
CONTRAINDICATIONS
The best practice and management of myopia will continue to evolve as more research helps us find new ways of intervening in the axial length growth of the eye. However, it is important to remember
previous six months of axial growth, and this effect was sustained during the two years follow-up.4
Recently, the 0.01% dose of atropine has been TGA-approved and is available in sterile, preservative-free, single-dose formulation (EIKANCE 0.01%). The approval is for myopic children ages four to 14 years with progression greater than one dioptre/year. It is useful to consider measuring the axial length greater than 0.1 mm/6 months or 0.2 mm in one year.
MY CLINICAL ATROPINE PROTOCOL
My practice is to titrate the dose if the low dose is tolerated but does not have enough of the desired effect to control myopia growth. The next dose is usually atropine 0.05%, given that the side effect
that these new therapies are done safely and monitored.
One of the safety measures is the correlation between axial length and dioptre change. If the dioptre change does not match axial growth, other causes of perceived myopia progression may exist. These conditions include keratoconus and spherophakia, which may contraindicate the use of atropine. Additionally, some syndromic causes of high myopia, including connective tissue diseases, also contraindicate the use of atropine.
THE BIGGER PICTURE
Patient education is vital to understand that atropine therapy has side effects and, importantly, rebound. Therefore, treatment and cessation must
INSIGHT December 2022 27
"THERE IS NO DEBATE THAT THE STRONGER THE DOSE OF THE ATROPINE, THE MORE THE EFFECT. HOWEVER, EQUAL ATTENTION NEEDS TO BE MADE TO THE FACT THAT THE STRONGER THE DOSE OF THE ATROPINE, THE MORE LIKELY THE PATIENT WILL BE AFFECTED BY THE SIDE EFFECTS" – DR LOREN ROSE
be monitored for at least six months to a year.
Alongside lifestyle, suggestions must be made to ensure the best treatment response. Near-work of all forms, including reading and screen time, has an undesired effect of increasing myopia progression and natural light has the desired effect of retarding progression.
Talking about 'screen and green' time as an adjuvant to any intervention for myopia management is important. As in any medical treatment/intervention, the use of lifestyle to achieve the maximum effect is universal. Patient and parent education needs to include the bigger picture of myopia, where increasing myopia means not just thicker glasses but the bigger issue of progression to high myopia and potentially pathological myopia that can cause significant sight-threatening eye diseases in adult life. n
REFERENCES
1. Cheng D, Schmid KL, Woo GC, Drobe B. Randomized trial of effect of bifocal and prismatic bifocal spectacles on myopic progression: two-year results. Arch Ophthalmol. 2010;128(1):12-19.
2. Sacchi M, Serafino M, Villani E , et al. Efficacy of atropine 0.01% for the treatment of childhood myopia in European patients. Acta Ophthalmol. 2019;97(8):e1136-e1140.
3. Wu PC, Yang YH, Fang PC. The long-term results of using low-concentration atropine eye drops for controlling myopia progression in schoolchildren. J Ocul Pharmacol Ther. 2011;27(5):461-466.
4. Rose LVT, Schulz AM, Graham SL. Use baseline axial length measurements in myopic patients to predict the control of myopia with and without atropine 0.01. PloS one. 2021;16(7):e0254061.
5. Wolffsohn JS, Kollbaum PS, Berntsen DA, et al. IMI - Clinical Myopia Control Trials and Instrumentation Report. Invest Ophthalmol Vis Sci. 2019;60(3):M132-M160.
6. Chua WH, Balakrishnan V, Chan YH, et al. Atropine for the treatment of childhood myopia. Ophthalmology. 2006;113(12):2285-2291.
7. Hou W, Norton TT, Hyman L, Gwiazda J, Group C. Axial Elon gation in Myopic Children and its Association With Myopia Progression in the Correction of Myopia Evaluation Trial. Eye Contact Lens. 2018;44(4):248-259.
8. Tideman JWL, Polling JR, Vingerling JR, et al. Axial length growth and the risk of developing myopia in European chil dren. Acta Ophthalmol. 2018;96(3):301-309.
9. Yam JC, Li FF, Zhang X, et al. Two-Year Clinical Trial of the Low-Concentration Atropine for Myopia Progression (LAMP) Study: Phase 2 Report. Ophthalmology. 2019.
12. Yam JC, Zhang XJ, Zhang Y, et al. Three-Year Clinical Trial of Low-Concentration Atropine for Myopia Progression (LAMP) Study: Continued Versus Washout: Phase 3 Report. Ophthal mology. 2022;129(3):308-321.
13. Yam JC, Jiang Y, Tang SM, et al. Low-Concentration Atropine for Myopia Progression (LAMP) Study: A Randomized, Dou ble-Blinded, Placebo-Controlled Trial of 0.05%, 0.025%, and 0.01% Atropine Eye Drops in Myopia Control. Ophthalmolo gy. 2019;126(1):113-124.
14 Ip JM, Huynh SC, Robaei D, et al. Ethnic differences in the impact of parental myopia: findings from a population-based study of 12-year-old Australian children. Invest Ophthalmol Vis Sci. 2007;48(6):2520-2528.
15. French AN, Morgan IG, Burlutsky G, Mitchell P, Rose KA. Prevalence and 5- to 6-year incidence and progression of myopia and hyperopia in Australian schoolchildren. Ophthal mology. 2013;120(7):1482-1491.
16. Morgan IG, French AN, Ashby RS, et al. The epidemics of myopia: Aetiology and prevention. Prog Retin Eye Res. 2018;62:134-149.
17. Morgan IG, Wu PC, Ostrin LA, et al. IMI Risk Factors for Myopia. Invest Ophthalmol Vis Sci. 2021;62(5):3.
18. Rose KA, Morgan IG, Ip J, et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008;115(8):1279-1285.
19. Lingham G, Yazar S, Lucas RM, et al. Time spent outdoors in childhood is associated with reduced risk of myopia as an adult. Sci Rep. 2021;11(1):6337.

20. Cooper J, Eisenberg N, Schulman E, Wang FM. Maximum atropine dose without clinical signs or symptoms. Optom Vis Sci. 2013;90(12):1467-1472.
NOTE: Insight readers can scan the QR code or visit insightnews.com.au/cpd/ to access a link to this article to include in their own CPD log book.

10. Wei SF, Li SM, Liu L, et al. Sleep Duration, Bedtime, and My opia Progression in a 4-Year Follow-up of Chinese Children: The Anyang Childhood Eye Study. Invest Ophthalmol Vis Sci. 2020;61(3):37.




11. Yi S, Huang Y, Yu SZ, Chen XJ, Yi H, Zeng XL. Therapeutic effect of atropine 1% in children with low myopia. J AAPOS. 2015;19(5):426-429.
21. Tsai HR, Chen TL, Wang JH, Huang HK, Chiu CJ. Is 0.01% Atropine an Effective and Safe Treatment for Myopic Chil dren? A Systemic Review and Meta-Analysis. J Clin Med. 2021;10(17).
22. Zhao Y, Feng K, Liu RB, et al. Atropine 0.01% eye drops slow myopia progression: a systematic review and Meta-analysis. Int J Ophthalmol. 2019;12(8):1337-1343.
CPD
George & Matilda Eyecare is currently recruiting Optometrist to join our team in Airlie Beach, Innisfail & Atherton. Reach out to our HR Team at opportunities@georgeandmatilda.com.au to find out more. Is the warm weather and luxurious beaches of Far North Queensland calling you?
Back-to-school and beyond:
BUILDING AN EFFECTIVE MARKETING
STRATEGY
With the end-of-year health fund rush in full swing, and back-to-school around the corner, planning an effective marketing strategy is best approached with a coordinated year-long view, industry insiders say.

For Somerville & Merrin Optometrists, part of the ProVision network in Toowoomba, their end-of-year campaign is their biggest for the entire year.
“End-of-year health fund related communications gives us the highest return on investment compared to any other campaign. Planning for end-of-year campaigns begins in August, or early September,” optical dispenser Mrs Danielle Bauer says.
Bauer has worked in the business for 16 of its 23 years and is stock and marketing manager across its two practice locations.
About eight years ago, she was asked to manage social media content, but her responsibilities have grown to now include implementing marketing campaigns, with support from ProVision’s headquarters.
Rather than bombard patients with marketing-related offers, Somerville & Merrin are specific in their communications.
“We use our software and database to tailor our end-of-year communications so that we are only targeting the people that will get value from the campaign. For this campaign, that would include people who have a calendar year health fund, that have visited in the last four years, they’ve purchased glasses before, but they haven’t
bought anything this year,” Bauer explains.
“We start rolling this out at the end of September or very early October with mail-out communications to that target group and follow up with email and text messages throughout November and December.
“Some of our early October messages to this group of patients is along the lines of ‘Avoid the December rush. Come in early to use your health fund benefits’, because it just gets busier and busier in December. We always have detailed target groups, to ensure we’re contacting the people who will find the information useful.”
Bauer says Somerville & Merrin’s initial end-of-year communications are relatively general and information-based, followed by an incentive to visit the practice before the end of the year.
“Initially, our communications are broadly suggestive. For example, ‘We noticed you haven’t used your health fund? Do you have benefits to use? These are some options for you’. Or we might say, ‘Perhaps you would like a spare pair? Do you want to update your look? Do you need a work-related digital eyewear solution?’,” she says.
The practice also leverages offers from frame and lens suppliers. Its main lens lab will typically offer a discount on a second pair of
INSIGHT December 2022 29 MARKETING
lenses purchased for the same person on the same day, allowing the practice to pass this saving on to their patients.
Bauer says the notion or suggestion of a ‘second pair’ is better received by patients when you can impart information about the various options and benefits.
“You might give them options for digital eyewear – obviously there’s a lot of information available now about blue light reduction – and the eye health implications of using digital devices. You might ask, ‘Do you need contact lenses for sport? Are you outside a lot? Are you protecting your eyes with sunglasses?’. It’s about getting to know your patients and giving them tailored information as to why you would suggest a second pair.”
Alongside patient-focused communications, managing stock is an integral component of end-of-year campaigns, Bauer explains.
“We do have to stock up over that end-of-year timeframe because we want our patients to be able to see something new and fresh. It’s a point-of-difference for us. In most cases, we won’t order a same frame twice. We might get the same frame in a different colour, perhaps, but rarely will we have exactly the same frame on the shelf. Once it’s sold, it’s sold,” she says.
In addition to launching an end-of-year campaign in October, Somerville & Merrin roll out a Summer sunglasses promotion in November through to January, followed by a back-to-school campaign.
“Somerville & Merrin has two behavioural optometrists who work with children and vision development. Our kids’ range is our biggest push throughout January. Usually, we roll out back-to-school after Christmas because as a mum with three kids, I know that time between school finishing and Christmas, nothing is going to get done,” Bauer says.
The practice’s back-to-school promotion is generally about raising awareness. If kids are starting school for the first time, it advises parents to give their children the best start to their schooling life. Two pairs are always recommended to kids, especially if they only have to wear them in the classroom.

“They need to have a pair they can keep at school, and a pair at home for homework or any screen time. That type of information goes out at the end of December, throughout January and into the beginning of the school year.”
The success of each campaign comes down to planning.
“The industry as a whole gets really, really busy by the end of October, November, December,” Bauer explains.
“All of this [marketing] has to be planned in August, September. We don’t have the time or manpower to be figuring it out at the start of December. It’s important for us to have a cohesive plan of how it all fits in, when it comes out, and how we market it in store and digitally via our social media and website.
“Everything that we do as a starting point comes from ProVision. They give us an outline of a marketing plan we can follow, then we add in our own campaigns and our individual flair. It’s also important to ensure everything is cohesive, including consistent imagery from our window displays to our social media and other digital marketing, to what people are seeing on their mail-outs or emails.”
According to Bauer, consistent point-of-sale and communication at each touch point means patients will be familiar with the campaign before entering the practices and beginning conversations.
‘LIKE GOING TO THE GYM’
ProVision’s national retail operations manager, Ms Kate Hall, whose role encompasses supporting practices like Somerville & Merrin Optometrists, says ideally a practice will have a marketing plan for the full year, not just for end-of-year.


“This way, you have a strategy with a schedule of marketing activities to provide you with a high-level view of where you’d like to be and how you’re going to get there,” she says.
“It is a little like going to the gym. You can go to the gym and wing it and get a workout or you can have a program that is designed for you to get the best workout and results. Same amount of time and effort goes in; however, it is not about the effort – it’s about doing the right things in the right combination.”
Hall says members who have a well organised and executed marketing plan have achieved sustained growth.
“An effective marketing plan enables them to take a targeted and cost-effective approach to drive increased revenue and return on investment, rather than the far too common and wasteful ‘spray and pray’ approach,” she says.
“Once you have a plan, it is about executing it across all forms of marketing, both internal with your current patients through patient communications and attracting new patients through media/social media, window displays and community networking.”
She says maximising the potential of a promotional plan comes down to a focus on the “3 P’s”, people, product, and process.
“Educate the entire team around the philosophy of a holistic lifestyle eyewear approach to provide the best patient care. Ensure they understand the rules and regulations around health funds and feel comfortable in having these discussions with patients by understanding your patients and asking understanding questions,” Hall recommends.
“WE USE OUR SOFTWARE AND DATABASE TO TAILOR OUR ENDOF-YEAR COMMUNICATIONS SO THAT WE ARE ONLY TARGETING THE PEOPLE THAT WILL GET VALUE FROM THE CAMPAIGN”
30 INSIGHT December 2022 MARKETING
DANIELLE BAUER SOMERVILLE & MERRIN OPTOMETRISTS
Somerville & Merrin Optometrists’ practice in Toowoomba’s The Range Shopping Centre.
She also advises having a process in place to help team members maximise this time of year and always have the right range and product on show.
“The most important aspect to communication is understanding the lifestyle needs of your patients and ensuring that you and the team are asking the right questions. Your clients don’t know what they don’t know. They rely on you, the vision care expert, to explain what they need and why. Practices that do this well achieve between 20-25% second pair percentage all year round. It also helps a patient identify why they need to come in and use their health fund,” Hall says.
TIME-LIMITED INCENTIVES
Optometrist and practice owner Ms Emma Slinger acquired Eyecare Plus Karalee, in a rural residential suburb of Ipswich, nine years ago and earlier this year, acquired an existing practice a 30-minutes away, re-branding it Eyecare Plus Acacia Ridge.
She is directly involved in practice marketing.
“I have a marketing assistant, who I bounce ideas off, but her main role is to essentially work with Eyecare Plus’ marketing team to organise campaigns,” Slinger says.
While her marketing approach at Karalee is fine-tuned, Acacia Ridge is a work-in-progress, as the practice had no computerised records when Slinger took over in April 2022. It’s only 47sqm, has had two previous owners in the past 50 years, and several patients are aged in their 70s and 80s.
“Nothing had been done to the practice. It was dying out basically – it wasn’t getting enough new patients to survive,” Slinger says.
“It was a very old practice that only had paper records. You could call it a ‘patient database’ of sorts, but not one that was easily usable in terms of marketing, because I couldn’t even send a bulk letter out to patients.”
Slinger immediately invested in installing computers and upgrading ophthalmic equipment and started the time-consuming process of digitising existing patient records. She is essentially starting from scratch in terms of communications to patients, including referrals, appointment reminders, and marketing messages.

The previous practice owners’ recalls were still done in a binder book.
“We went through the strenuous task of sorting patient files into those that are too old and need shredding, and then files within the last seven years we needed to keep. We then separated those into two batches. One is patients that hadn’t been in the last three or four years; we’ve put those aside, stored in alphabetical order, ready to use when they come back. And then the rest we made a database by manually creating a spreadsheet of their names and addresses.”
“Unfortunately, the previous owners didn’t record who was a health fund member and who wasn’t, and which health fund they’re with.
That’s an important part because otherwise you come to the end of the year, and you can’t pick those people out.”
Meanwhile, operating for nearly a decade in Karalee has honed Slinger’s end-of-year marketing tactics, including targeting messages to specific demographics.
“We send targeted marketing collateral to health fund patients at our Karalee practice, particularly between October and December. I think you’ve got to be more specific with your message. If you’re trying to target everyone, you’re going to get no one,” Slinger says.
“We start planning our ‘use it or lose it’ optical benefits marketing in August, ready to be launched at the start of October. We start off with a direct mail out to patients with a strictly time limited voucher for glasses.”
Slinger has learnt from past experience that patient incentives need to have an expiry date.
“A few years ago, we would send out a voucher that was valid until the end of December. But we’d get patients that weren’t necessarily responding to the voucher, they were just due to come in in December anyway and already had the voucher, so we were giving almost unnecessary discounts away,” she explains.
“We decided that the only discount we would give is at the start of our campaign. That meant that patients who came in on 31 December weren’t getting a discount. They paid full price, but they were responding to our second messages. Basically, we do an email and SMS campaigns, which get increasingly more urgent in messaging. The last one goes out two weeks before the end of December.”

Patients are required to make a minimum purchase of $300 in order to redeem the voucher, and it can’t be used with other deals or offers. Slinger is also testing the waters of a marketing campaign geared towards summer holidays.
A RECORD 14.26 MILLION AUSTRALIANS NOW WITH PRIVATE HEALTH INSURANCE
n According to the Australian Prudential Regulation Authority (APRA), optical is the second largest area of expenditure (behind dental) by private health insurers under general treatment (extras) cover. One in six (17%) of ancillary claims expenditure annually by private health insurers are for optical or eyecare.
n Optical is also the second highest modality or allied health treatment service type that private health funds pay for, making up 13% of total allied health treatment services paid by private health funds on an annual basis, according to APRA data.
n APRA’s data also shows health funds currently collectively pay over $919 million each year in member benefits for optical or eyecare services, covering over 11.7 million services annually. The average health fund benefit paid per optical service is currently around $78.
n As at 30 June 2022, more than 14.26 million Australians (55.2% of the Australian population) were covered by a general treatment policy with optical or eyecare coverage.
n APRA data for the year ended June 2022 revealed that claims by private health insurance members overall were at 96% of pre-COVID 19 claiming levels.
n Over the recent June 2022 quarter, optical services claimed by private health insurance members slightly exceeded pre-COVID 19 claiming levels over the June 2019 quarter.
“IT IS NOT ABOUT THE EFFORT – IT’S ABOUT DOING THE RIGHT THINGS IN THE RIGHT COMBINATION”
INSIGHT December 2022 31
KATE HALL PROVISION
“We have dabbled in that, but haven’t found it as effective. Every year we’ve been tweaking this process and it’s getting better, so we’re focusing on getting that right.”
She doesn’t run a back-to-school campaign – but does promote it on social media.

“Parents don’t seem to respond to the back-to-school messaging. We might send an email, but there’s no sales campaign attached to it. We find the first three weeks of February, when kids are going back to school, are quiet. I don’t know if it’s because parents are transitioning into school or it’s all too much to get back into school,” Slinger says.


“We have social media accounts for both practices – although Acacia Ridge doesn’t have anyone following it yet. We use a combination of material Eyecare Plus supplies, as they have quarterly marketing campaigns and back-to-school is usually one of those – we will use those social media tiles. We also do a lot of window displays as part of our marketing,” Slinger says.

CREATING A SENSE OF URGENCY
For practice owners like Slinger, Eyecare Plus marketing manager Ms Isobel Bishop and marketing coordinator Ms Kimberly Paas create and coordinate a range of different marketing activities, in addition to the Eyecare Plus national campaigns.

“We generally try to provide end-to-end marketing support for
our members. We work closely with them to ensure each practice’s marketing plan targets their specific patient demographic. That’s the benefit of being independent; we can help them individually on a local level,” Bishop says.
Bishop and Paas highlight that both the end-of-year ‘use it or lose it’ and back-to-school campaigns are time sensitive, and therefore approach them with that in mind.
“With the local ‘use it or lose it’ campaigns, our goal is to create a sense of urgency within the message of the campaign. That rolls out into the New Year as well, while everyone is on holidays and school holidays. We tap into that sense of needing to take action and then seamlessly flow into the back-to-school campaign,” Paas says.
“We’re definitely looking to create a sense of urgency for patients around the importance of their eye health – it’s not something to put off, particularly for young children and helping them with their education and returning to school. It’s also important we use key facts and statistics to help push that messaging,” Bishop explains.
In the first quarter of the year, Eyecare Plus national office provides a back-to-school campaign for practices that see many paediatric patients and there’s also a standard New Year campaign practices can implement – or both.
“We provide the messaging and digital assets and point-of-sale material for a quarterly campaign. Members can also request additional customised material that, for example, highlights key stats relevant to their patient base, or if they’re focusing on myopia in their patient demographic we can do that as well.”
Incentives like a time-sensitive voucher can help to create a sense of urgency, and maximise sales early on, before the busy retail rush in December, Bishop and Paas say.
“Our advice is to make sure that you have not just one or two marketing campaigns locked away in your calendar, but really try to prepare a year-long marketing strategy. An organised quarterly campaign will allow for a steady stream of patients rather than trying to deal with the rush of ‘use it or lose it,’ Bishop says.
“If you have marketing strategies in place year-round, then you’ll tend to see a more steady stream. What type of local quarterly campaign is very specific to individual practices. Some members focus on myopia or dry eye because that’s most relevant to their patient demographic. Otherwise, you can do something as simple as general eye health awareness. Nationally, we focused on specialty lenses in our last quarter.”
Bishop says practices can work with suppliers to create in-store sale events but that alone won’t sustain a practice year-round.
“You need to have some sort of backbone to your marketing strategy throughout each quarter and on top of that, include additional once-off in-store special sale events sales,” she says. n
“WE START PLANNING OUR ‘USE IT OR LOSE IT’ OPTICAL BENEFITS MARKETING IN AUGUST, READY TO BE LAUNCHED AT THE START OF OCTOBER”
EMMA SLINGER EYECARE PLUS PRACTICE OWNER
“WE WORK CLOSELY WITH [MEMBERS] TO ENSURE EACH PRACTICE’S MARKETING PLAN TARGETS THEIR SPECIFIC PATIENT DEMOGRAPHIC”
32 INSIGHT December 2022 MARKETING
ISOBEL BISHOP EYECARE PLUS
Eyecare Plus’ end-of-year marketing campaign.
compatible Why OPTOMETRY AND AUDIOLOGY ARE
At the largest optical event in the UK in 2018, audiology companies invited to attend were asked why optometry and audiology are a good fit and how optometry practitioners could integrate hearing services into their practice.
Mr Steven Ross, then business development manager of hearing care solutions company, Sonova, said optometry and audiology service similar demographics.
“The reason optometry and audiology should meet is because they share the same customer base: 97% of over 65-year-olds need some form of vision correction; 73% of 70-year-olds need some form of hearing correction,” Ross told Optometry Today
He said integrating audiology into an existing optometry practice was relatively straight forward.
“You’ve already got the premises, you’ve got the front-of-house staff, you’ve already got the customers. One of the hard things is to get a database. You’ve already got it. The cost to start up is minimal,” Ross said.
“The key thing is trying to find the right person that fits the business needs. A lot of opticians, especially independents, differentiate themselves by customer service. If they go into partnership with someone, they’ve got to really find that person who has the same values and beliefs as them.”
Closer to home, a few months before the UK conference, Specsavers launched audiology services into a handful of existing optometry practices in
Australia – that number has now grown to 238 out of 356 Australian stores. Meanwhile, one independent practitioner has achieved the rare career feat of becoming dually-qualified in optometry and audiology.
Insight spoke to both to understand the challenges and benefits of this approach, as well as to Australia’s only hospital that provides eye and ear care.
A FAMILY AFFAIR
An unassuming principal owner of an independent practice with two locations in Melbourne holds a unique place in the profession: he is one of few, if not the only, in Australia who is a qualified optometrist and audiologist.

Mr Lachlan Smith is owner, director, principal audiologist and optometrist at Smith Eye and Ear Solutions (formerly Anthony Smith Optometrist), Melbourne’s first combined optometry and audiology practice, located in Moonee Ponds and Camberwell Junction.
Smith first graduated with a Masters in audiology from the University of Queensland and worked in Cairns for two years, before returning to his home state of Victoria.
He wanted to work in his own practice, ultimately incorporating audiology into his father’s established optometry practice in Moonee Ponds.
“Dad came to me with the idea. He knew Boots and Specsavers in the UK had successfully integrated both services into one business, so it was not completely unprecedented. His optometry clinic of 35 years was well-
INSIGHT December 2022 33 BUSINESS
Since 1863, audiology and optometry have been intwined in the Australian healthcare system to some degree. In the modern practice era, they are providing a complimentary service and means to attract and retain patients. And as Insight discovers, the cost of entry may not be as high as some think.
LACHLAN SMITH SMITH EYE AND EAR SOLUTIONS
established and had a loyal patient base, so thought it could work well,” he says.
“After adding an audiology service to Dad’s optometry clinic, I then started studying optometry, completing a Masters from Deakin University. When Dad retired, I bought the business, and now perform eye and ear consultations in both the Moonee Ponds and Camberwell Junction practices.”
Optometry is second nature in Smith’s family; he is supported by his sister, who is a part time optometrist in the business, plus additional support staff. Until recently, Smith Eye and Ear Solutions operated a third practice in Caulfield, but it closed during COVID-19.

“On an average day, I might see eight audiology patients and two or three optometry patients. I have separate rooms at both clinics (Moonee Ponds and Camberwell Junction) and move back and forth between rooms throughout the day,” he says.
“It generally works well. Audiology consultations typically take longer, as there is more conversation, counselling and communication involved, and case history takes longer. Conversations with audiology patients can also draw out issues with their eyes and vision.
“The association between hearing and vision issues increase as patients get older, they go hand-in-hand. Patients are often a little surprised that I’m qualified in both fields but recognise the convenience of that, as a logical progression. It often pops up in conversation with patients that I’m dually qualified and they will remark ‘I could just come here’ for both their hearing and vision needs.”
Smith says his combined skills are particularly convenient for patients in rural areas, where it’s hard to get consistent services. He provides audiology and optometry services to Indigenous communities in northwest Queensland, funded through Check-up, a state government agency, and is chief audiologist at Hearing Choices, an organisation connecting independent audiologists.
From a business perspective, he says combining audiology and optometry services capitalises on the cost of leasing premises.
“In terms of physical space, audiology consulting rooms don’t need to be big, and optometry equipment is not huge, so you can make it work, not only in terms of rent, but administration staff too. They can perform dual administrative tasks.”
Smith says unlike optometry’s retail component, where showcasing a range of frames is de rigueur, audiology doesn’t require practitioners to have stock on hand, as hearing aids are typically custom-made and ordered as needed.
In this regard, Smith says the biggest advantage is being an independent practice and having the freedom to choose suppliers.
“A lot of audiology clinics are owned by hearing aid companies, which means they only sell a particular type of hearing aid. It also means their advice can be compromised by financial dividends.”
Unlike in the eyecare sector, where ophthalmologists are prohibited from owning an optometry clinic, Smith says the same is not true in audiology,
where ear, nose and throat (ENT) surgeons can and do own audiology clinics.
For example, ENTs own Neurosensory, a chain of 24 audiology clinics across Queensland, New South Wales, Victoria and Tasmania.
But regardless of ownership, it’s patient trust that trumps all else, Smith says.
“Some clinics in the past have tried and failed to combine optometry and audiology services. One network in particular had 30 clinics nation-wide, but it wasn’t a success and the reason for that, I believe, is trust,” he explains.
“If you’re incorporating audiology into an existing optometry clinic, and the patient is seeing a different clinician every time, they don’t develop a rapport. Generally speaking, audiology patients need to be seen more regularly than optometry patients, so if their regular practitioner changes, there needs to be a good reason for that.”
CHANGING MINDS

To some extent, particularly in the UK, optometry and audiology are established bedfellows, with Specsavers and Boots both offering hearing care and eyecare under one roof, the former for at least 18 years.
The concept is newer here. Specsavers launched audiology services in existing optometry practices in Australia at the end of 2017, and in 2019 in New Zealand.
Specsavers ANZ chief audiology officer Mr Nick Taylor, a qualified audiologist with more than 20 years’ experience, has been an integral part of the integration.
“Why introduce audiology to optometry?” English-born Taylor, who previously worked at Specsavers in the UK, asks rhetorically. “Our customers want convenience, they want more than one service in one place, not separate appointments in separate locations. The convenience of both services under one roof is a big driver.
“In the UK, the majority of audiology services are provided by the National Health Service (NHS), so patients had to go to hospitals to receive audiology services, when they’re much happier to go to an optical store for their hearing care. That’s the origins of the UK model.”
Taylor, who has been in Australia for five years, says it’s important to emphasise to the public that Specsavers optometrists are not providing hearing care – it’s provided by qualified, experienced audiologists, a professional discipline in its own right.
“Because Specsavers is established in optics, it makes more sense to build audiology into optometry stores. We’re a trusted brand,” he says, with the firm this year being recognised in both optometry and hearing services

“CONVERSATIONS WITH AUDIOLOGY PATIENTS CAN ALSO DRAW OUT ISSUES WITH THEIR EYES AND VISION”
34 INSIGHT December 2022 BUSINESS
Hearing aids today are sophisticated and discreet.
NICK TAYLOR SPECSAVERS
The hospital delivers more than half of Victoria’s public eye surgery and all of Victoria’s public cochlear implants.
“Hearing and vision impairment are strongly age-related. With an ageing population that is living longer, the prevalence of sensory loss associated with hearing and vision loss remain key health issues, particularly for Aboriginal and Torres Strait Islander peoples. From that perspective alone, along with potential synergies for research, it makes sense for services to be co-located,” Gardner says.
He says it is also well known that hearing impairment can be associated with a greater risk of cognitive decline in the elderly, so optimising both eye and ear care is extremely important, especially within an ageing population.


“I think we all want to age well as a society.”
categories in Reader’s Digest magazine’s most trusted brands consumer survey.
“Our ambition is to have audiology services in all our optometry stores, everywhere. Out of our existing 356 optometry stores, 238 offer audiology services. Over the next three years, we will aim for all Specsavers stores to offer optometry and audiology services,” Taylor says.
He says the decision of which stores offer audiology services largely comes down to physical capacity to fit a dedicated soundproof and soundtreated audiology consulting room fitted with the latest testing equipment. Taylor adds that nothing specialist is required for front-of-house, as practices can utilise existing staff to welcome patients, and there is little or no retail space required for hearing solutions.
If a patient needs hearing aids as a result of a hearing loss assessment, they are custom ordered for the individual patient, who then receives a full fitting.
“Unlike spectacles, we don’t have stock on display. Generally speaking, people start losing their hearing in their mid-20s, but it’s a slow deterioration, which people begin to notice in their late 50s or early 60s. Many people think hearing aids are not fashionable, often referred to as ‘beige bananas’, but actually they are more sophisticated and discreet than ever before,” he says.
While Specsavers audiologists on occasion have refer patients to ear, nose and throat (ENT) consultants, Taylor says there is not a referral system in audiology equivalent to Oculo in the eyecare space.
He says the biggest challenge is to educate Australians that Specsavers provides eye and ear care.
“Specsavers’ name is synonymous with ‘specs’ and eyes. It’s a process to educate people that optometrists are not providing hearing tests – we employ fully qualified audiologists. We’re offering convenience and customer service,” he says.

While Specsavers is active in the eye health space in Australia, involved in programs like KeepSight that is aiming to prevent vision loss to diabetes, it is at the very early stages of hearing care awareness, taking part in Tradies National Health Month for the past two years which, amongst other health risks, promotes protection against hearing loss caused by excessive workplace noise.
CROSS-POLLINATION

The Royal Victorian Eye and Ear Hospital is Australia’s only specialist eye, ear, nose and throat hospital, and the origins of that, says CEO Mr Brendon Gardner, dates back to 1863.

“The Eye and Ear founder, Andrew Sexton Grey, started work at St Mark’s Ophthalmic Hospital and Dispensary for Diseases of the Eye and Ear in Dublin. After he moved to Melbourne, he set up the first iteration of the Eye and Ear in 1863 with one bed, treating eye and ear diseases for underprivileged people in Melbourne,” he explains.
“From those humble beginnings the Eye and Ear has grown to become an internationally recognised leader in clinical service delivery, teaching, and research in both ophthalmology and otolaryngology and the largest public provider of ophthalmology and ENT services in Victoria.”
Integrating eye and ear care in a clinical setting like a hospital also brings other advantages, including opportunities for doctors to cross-pollinate ideas across their different specialities and collaborate in the research domain.
“We cross-pollinate regularly in Emergency Departments. From a medical perspective, I understand that some conditions such as orbital cellulitis, where there is an abscess pressing on the eye, is co-managed by ophthalmology and ENT, as the underlying problem is often a sinus infection which can cause vision loss if not rapidly treated,” Gardner says.
“We also cross-pollinate with emergency medicine, as many eye and ENT emergencies are seen in general Emergency Departments. We train 28 emergency registrars per year from Victoria’s general Emergency Departments on assessment and treatment of eye and ENT emergencies.”
Breakthrough innovations like the cochlear implant are also filtering through to new vision solutions for people with blindness and vision impairment.
In 2012 the bionic eye was born – led by the Centre for Eye Research Australia, the Bionics Institute, the University of Melbourne, the University of New South Wales in a collaboration as Bionic Vision Australia, with the Eye and Ear as the clinical partner – paving the way for vision loss innovation in Australia.
Fast-forward to 2021, with the completion of second-generation trials, participants can now use the device to perform everyday activities in and out of the home. Associate Professor Penelope Allen, the Eye and Ear’s Head of the Vitreoretinal Unit and Principal Investigator at CERA leads this research.
“The hospital was instrumental in preparing for the first-in-human surgeries, and in the postoperative care of the participating patients,” Gardner says.
“When developing the surgical approach, the trial saw a unique collaboration between eye surgeons and ENT surgeons. In particular, Professor Robert Briggs and his extensive experience with cochlear implants made this collaboration successful.”
Gardner adds there is also collaboration between ENT surgeons with ophthalmologists, in particular the oculo-plastic surgeons, for the management of certain conditions such as nasolacrimal obstruction and thyroid eye disease. n
“THE PREVALENCE OF SENSORY LOSS ASSOCIATED WITH HEARING AND VISION LOSS REMAIN KEY HEALTH ISSUES”
BRENDON GARDNER ROYAL VICTORIAN EYE AND EAR HOSPITAL
“BECAUSE SPECSAVERS IS ESTABLISHED IN OPTICS, IT MAKES MORE SENSE TO BUILD AUDIOLOGY INTO OPTOMETRY STORES”
INSIGHT December 2022 35
BRINGING TELEHEALTH AND AI INTO REAL-WORLD PRACTICE
Telehealth and artificial intelligence hold the key to breaking down some of the biggest eye health inequities in Australia. But the sector needs to find ways for real-world implementation, says DR ANGUS TURNER.
The tyranny of distance in Australia – and the subsequent eye health disparities for rural and remote communities – was the focus of Dr Angus Turner’s presentation at SCC 2022 that offered new solutions by way of technology. Could optical dispensers play a role in eye disease telehealth consultations, and what impact could artificial intelligence (AI) have in addressing diabetic eye disease detection rates in outback communities?
These questions were posed in his discussion entitled ‘Integrating telemedicine and artificial intelligence into eyecare services’, where he outlined the real-world efficiencies brought about by telehealth consultations in eyecare. This technology is applied in regional and rural Western Australia where he founded the Lions Outback Vision outreach program.
Before going into his points, it’s important to define telehealth in eyecare. The current MBS reimbursement, introduced in 2015, for a telehealth consultation requires the optometrist and patient to be present together while an ophthalmologist participates via online video technology.
These MBS items are restricted to patients who are in ‘telehealth eligible’ areas which is non-metropolitan and outside a 15km radius from the treating ophthalmologist. This restricts use to those outside metropolitan areas, unless they are providing care in an aged care facility or for Aboriginal patients.
Turner started by outlining the slow traditional pathway to the ophthalmology clinic where a GP or optometrist writes a referral letter with the patient often waiting a long time to be seen in the tertiary eye clinic. This is exacerbated in regional and remote areas where the number of fulltime ophthalmologists per 100,000 people is much lower than in metro areas.
However, he said telehealth helps to expediate this pathway. Optometry practices are much more accessible for regional communities, with the optometrist able to perform the necessary tests and image acquisition. With these results in hand and the patient present, they can then schedule a video call with the specialist who then guides the diagnosis and treatment plan.
Highlighting the benefits brought about by telehealth, Turner said it provides patient-centric management; they’re able to view the images being discussed and reasons for diagnosis. It also formalises a medical record and makes it easier to follow through with what was discussed. Importantly, it makes specialist care more accessible, while creating patient retention for local optometry practices.
In addition to convenience for the patient, telehealth has been shown in peer-review papers to drive better eye health outcomes, including a halving the wait time for cataract surgery, a 10 times increase in access for Aboriginal people when an on-call service was introduced and high patient

36 INSIGHT December 2022 SCC 2022
Dr Angus Turner, founder of Lions Outback Vision, assessing a scan on the ZEISS Clarus ultra widefield retinal camera at the new Northwest Hub in Kimberley, WA.
satisfaction. A systematic review also showed outcomes were equal or better with telehealth compared to regular specialist care, it improves surgeon efficiency and eliminates duplication, and reduces and eliminates pre- and post-op visits.
“So what cases can we use telehealth for?” Turner asked.
“It turns out the bread and butter of surgeons’ work, which is cataract, pterygium and various laser treatments, can all be expediated through telehealth because with good OCT scans, fundus images (if possible, depending on the cataract grade), and exam of eye, there is no point waiting for that clinical appointment with a specialist,” he said.
“It’s also useful for any aspect of optometry that carriers a risk outside their comfort zone, and you can talk to the specialist about anything through telehealth, it’s a great upskilling tool (disease process, acute management, contraindications), and certain cases require collaborative care by law (glaucoma and progressive cases), so we need to chat about those anyway and this process makes it easy.”
He said telehealth can also be used for systemic associations, and for talking through the case history with the guidance of the specialist, as well as discussing straight-forward surgical and procedural plans and direct bookings such as cataract, intravitreal injection, curettage, YAG peripheral iridotomy and capsulotomy.
BARRIERS TO UPTAKE AND FUTURE PROSPECTS
While telehealth works well when executed correctly, Turner acknowledged it’s not always straight forward getting the optometrist, specialist and patient on the same call at the same time, especially if one is running late.

“A certain amount of rhythm needs to be established between the two healthcare practitioners to understand how the process works so one isn’t left waiting with the patient, so logistics is the key; it takes some goodwill, a bit of practice and understanding of rhythm.”
In terms of the future prospects for telehealth in optometry, Turner said there was a need to discuss dispenser and optometric assistant driven opportunities, so optometrists can provide reports and imaging, but not have to be present for all tasks. It also offers opportunities for more comanagement and efficiency, especially in regional areas.
In a trial that was granted ethics approval and coincidentally conducted as COVID forced border closers, Turner said they tested telephone-based and hospital-based telehealth, which both hinged on the importance of a good optometry assessment.
In telephone-based telehealth, the patient was assessed at the nearest optometrist. If they lived hours away, the ophthalmologist would then receive the clinical information via the Oculo referral system, and then phone the patient at home.
Dr Angus Turner speaks with optometrist Dr Alex Craig and a patient in a telehealth appointment.
“And that way the patient doesn’t have to come all way back to sit in the specialist’s rooms again. They might also have visual impairment and find the landline is more useful, so it worked quite well for certain patients,” Turner said, also noting the difficulties the visually impaired have with videoconferencing and travel.
The hospital-based telehealth concept put to work ophthalmic equipment such as OCTs, visual fields, and biometry machines that are located in public hospitals, but used infrequently by visiting specialists. In this case, an optometrist was able to run a clinic in the hospital and conduct work-ups for surgery.
“In the end, the outcomes showed that a third (28%) of patients were able to be discharged completely by telehealth, another third (35%) were sent for specialist review (laser or injection/face-to-face clinic), a quarter (25%) needed surgery booked directly, and 12% could be followed up and plan developed via telehealth,” Turner said.
“As you can see, telehealth halves the amount of work a specialist has to do in person or face-to-face – and that’s got to be worth something when there is a low workforce.”
AI IN EYE HEALTH
Another major technological puzzle piece to overcome distance barriers to care is AI. Turner’s presentation focused on applying the technology to diabetic eye disease, which his team’s recent study found affected Aboriginal people more than non-Aboriginal.
“We thought diabetic retinopathy affected Aboriginal people as much as non-Aboriginal, but a recent systematic review showed that’s actually not the case; we knew there was a higher prevalence, but we didn’t know retinopathy was more worse or severe,” he said.

Turner said many patients were not getting recommended screening checks, with data showing 28% haven’t been checked in the Kimberley region. This added impetus for new ways to make it easier for patients to receive a screening grade on the spot.
Lions Outback Vision is conducting projects to address this in Australia collaborating with Google, the Centre for Eye Research Australia (CERA) and Eyetelligence, and Topcon and Thirona, applying their deep learning systems (DLSs) in this space.
With the Google technology, Turner said they wanted to validate this in a large group of Aboriginal people in an urban setting (Perth), using 1,682 retinal images from 864 diabetic patients. It was compared against findings from retinal specialists, including a three-person adjudication
INSIGHT December 2022 37
Lions Eye Institute managing director Prof Bill Morgan (from left), A/Prof Angus Turner, Patrick Dodson and Divina D’Anna at the Kimberley Eye Hub opening in October. Image: Sarah Landro.
panel as a reference standard, and was shown to be significantly more sensitive (98%) compared to human graders (96%) for more than mild DR and vision-threatening DR, with a slight drop in specificity (95%) vs human graders (96%).
The system was also applied to diabetic macular oedema, which brought in OCT scans alongside fundus images, combining of multiple datasets from around the world. It was shown to have non-inferior sensitivity and higher specificity than human graders.
Turner then provided an update on a second DLS: the CERAEyetelligence system developed by Professor Mingguang He. Using a different algorithm, it showed overall referrable retinopathy was found in 96.9% of patients and 87.7% specificity. However, a subgroup analysis saw the specificity reduced to 70% in Aboriginal patients for various possible reasons.
The final DLS (Topcon-Thirona) has been installed in five clinics in various clinical settings, including the Lions Outback Vision Van, optometry and an Aboriginal medical service.
“These machines are a fantastic tool taking a colour photo and OCT at same time. With the first 100 eyes compared to retinal specialists, two eyes had incorrect diagnosis and 80% had the correct diagnosis if the probably score of that disease was more than 50%,” Turner said.
“At the moment, this is all research, however Thirona and Eyetelligence are TGA-approved and can be used in Australia. But how to incorporate them into our flow to ensure patients get a point-of-care test is a current area of focus for real world implementation.
“The future is bright if Aboriginal health workers can have a traffic light system to grade their diabetes, and tell the patient they are fine at the moment and see you in one year, or you need a referral let’s talk to a
specialist right now about what that means, that will be very beneficial.”
NORTHWEST HUB UPDATE
Turner also provided an update on the Northwest Hub, the first permanent eye clinic in the sparse Kimberley region based in Broome.
Lions Outback Vision (LOV) has transformed a former backpacker accommodation into a new eyecare facility, featuring at least two resident ophthalmologists available for 24-hour emergency support including retinal surgery.
The second phase of the facility opened in October, with the service to feature a hub-and-spoke model servicing six towns through outreach services, while providing access to ophthalmology and telehealth clinics, seminar rooms and open space for community diabetic health education. The new part will also house an area for optometry education, research facilities and a café.
The facility has been made possible through philanthropic donations from Wen Giving/Hawaiian, the Federal Government, Zeiss, Topcon, Alcon, Novartis, Fred Hollows and Australian Capital Equity. A $4.7 million Western Australian Government investment will help to employ the eye health workforce.
Turner also touched on the new University of WA optometry school that will soon begin turning out its first graduates with a cohort spending a term of regional practice at the new Kimberley Hub.
“WA rural still has lowest access to optometry in Australia, according to recent 2020 stats, so we need to do something about that maldistribution. This optometry school will be sending students to Broome and Geraldton so it will be giving them a taste of country practice and some will say they want to do this rest of my life, so we look forward to this in future.” n
B.I.G. NORM™
BIOMETRIC INTELLIGENT GLASSES

100%


Rodenstock is establishing a new lens calculation norm that ensures even more progressive lens users can experience the benefits of Biometric Intelligent Glasses.
Go to: rodenstock.com/bigvisionforall
Follow: #BIGVISIONFORALL
SCC 2022
0%
THE LATEST AMD THERAPIES? Are we ready for
The treatment landscape for wet and dry age-related macular degeneration is undergoing a seismic shift. CERA’s head of macular research PROF ROBYN GUYMER discussed this at SCC 2022, as well as challenges that need to be overcome so Australian eyecare professionals are equipped for new therapies when they reach our shores.

Since ranibizumab (brand name: Lucentis) was listed on the Australian Pharmaceutical Benefits Scheme (PBS) in 2007, anti-VEGF therapies have been regarded as a turning point for patients with neovascular age-related macular degeneration (nAMD), and associated macular diseases. And this was bolstered with the arrival of aflibercept (brand name: Eylea) in 2012, with Australia being just the second country in the world to introduce the therapy.
While these anti-VEGFs have been the mainstay for well over a decade, they aren’t perfect, leaving the door open for newer, longer-acting therapies that overcome the treatment burden so often associated with patient drop out, as well as other issues like macular scarring or fibrosis.
This rapidly evolving field was the focus of Professor Robyn Guymer’s intriguing presentation at the recent Specsavers Clinical Conference (SCC). The Centre for Eye Research Australia (CERA)’s deputy director and head of macular research outlined why it is such an “exciting time” for patients with either form of late-stage AMD, with a new treatment for nAMD pending PBS listing in Australia and the first approved therapy for geographic atrophy (GA), or dry AMD, most likely just around the corner.
While this is a promising time for patients, Guymer described how it poses new challenges for Australian eyecare professionals when it comes to defining disease and deciding who will most benefit from new therapies. Also, the true benefits of the newer therapies won’t be fully known until more real-world data is available.
LONGER-ACTING THERAPIES AND BEYOND
Beginning with nAMD, Guymer explained why there’s still a major unmet need, despite the game-changing nature of the existing suite of anti-VEGF therapies.
Highlighting the real-world outcomes from America based on 50,000 eyes, she demonstrated how a significant proportion of patients were receiving fewer than the desired number (approximately seven) of intravitreal injections in the first year (Figure 1), a trend that exists around the world.
She said this mattered because data from the same population showed a “linear relationship” between visual acuity (VA) improvement and the number of injections, particularly between four and 10 injections in the first year (Figure 2). At the lower end of the range, patients with five or fewer injections in year one generally lost vision.
Additionally, in the real world after one year of treatment, Guymer
pointed to a long-term UK study over 10 years showing that even if vision is improved in the first one to two years, vision still declines gradually over time. A similar trend was also shown in a Denmark study with 4,678 treatment naïve eyes.
“When we looked at the (Save Sight Institute) Fight Retinal Blindness! Registry, which essentially started in Australia and New Zealand and has now spread internationally, using real world cohort data from 3,192 patients with nAMD treated in routine eye clinics between 2007 and 2015, we developed a model to predict vision for the rest of someone’s lifetime after starting anti-VEGF treatment, which averages around 11 years," she said.
“Even with optimal dosing frequencies, we estimated 12% would retain driving VA at time of death and an estimated 15% retained reading VA in at least one eye. Maybe you could say that is terrific news because before these treatments virtually no one ended up with this sort of vision with nAMD, but on the other hand, given such good treatments now, why is it that we cannot preserve reasonably good vision until death in more people?”
Guymer said questions remain whether the industry can do better with longer-acting therapies to reduce under-treatment, as well as therapies that do more than just block VEGF. Another major unmet need was vision loss due to scarring, or fibrosis, and atrophy, which no treatment addresses yet.
Enter faricimab (brand name: Vabysmo), a treatment approved in Australia in 2022, and now recommended for PBS listing. According to its
INSIGHT December 2022 39 SCC 2022
Prof Robyn Guymer, Centre for Eye Research Australia head of macular research.
Figure 1 - Histogram showing a nearly normal distribution of nAMD patient eyes stratified by number of anti-VEGF injections received in the first year of treatment. The median number of anti-VEGF injections received in the first year of treatment was seven.
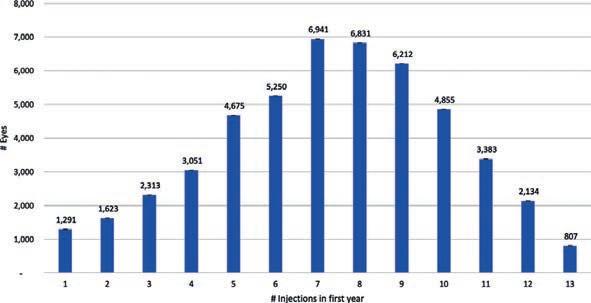
Credit: Ciulla et al. Ophthalmology Retina 2020;4:19-30.
manufacturer, it is administered by four initial four-weekly injections, but thereafter, the frequency will be determined by the treating physician up to 16 weeks apart.
According to Guymer, the therapy’s point-of-difference is its anti-VEGF effect combined with an anti-Ang-2 component – the latter thought to have an important role in vascular instability and inflammation – potentially reducing fibrosis.
In the Phase 3 TENAYA and LUCERNE trials, Vabysmo patients were treated every eight, 12 or 16 weeks and compared to Eylea every eight weeks. Non-inferior vision gains were demonstrated in all Vabysmo groups. However, the studies did not extend the Eylea control arms beyond eight weeks, so it didn’t present a true head-to-head comparison, Guymer added.
“After 48 weeks, the studies showed 80% of faricimab patients could be treated every 12 weeks or longer and 45% could be treated every 16 weeks,” she said, noting that subsequent two-year data had shown that – even though vision was declining in both groups – a large proportion of Vabysmo patients can be kept on 12 weekly treatment (14.7%) and 16 weekly treatment (63.1%), which was 77.8% combined.
“So it might be possible to let more patients go longer with this new drug compared to Eylea, but it wasn’t a true comparison, so we will have to wait until real world use of this drug to see if we can get this proportion of people truly out to three or four monthly treatment. And we will need to wait for longer term outcomes to see if there is less fibrosis and atrophy and thus better longer term vision.”
SLOW RELEASE THERAPY SHOWS PROMISE
Another therapy seeking to overcome the treatment burden barrier is a refillable port delivery system (PDS) implanted in the eye that slowly releases ranibizumab. The brand name is Susvimo PDS and while it has been granted approval in the US, it is still under review in other jurisdictions, including Australia (turn to page 58 to read A/Prof Anthony Kwan's Soapbox article on trialling this treatment at the Queensland Eye Institute).
Guymer said the aim of this reservoir-like treatment implanted in the sclera is to increase treatment intervals even further, possibly out to six months, however safety challenges remain.
“Phase 3 trials, only conducted in America, have been completed comparing this long-acting device with monthly ranibizumab and the primary objective was to see whether the six-month refill was equivalent to monthly ranibizumab,” Guymer said.
“After an initial drop in vision due to the surgery, they found vision picked up and there was equivalency between these treatments. There’s a Phase
Figure 2 - There appears to be a linear relationship between mean letters gained and mean number of anti-VEGF injections, between four and 10 injections over the first year of treatment, after which the relationship plateaus. At the lower range, those patient eyes that received four or fewer anti-VEGF injections in one year generally lost vision at one year. Credit: Ciulla et al. Ophthalmology Retina 2020;4:19-30.

3b study still going on outside America and Australia is part of that.”
Guymer pointed to significant safety concerns due to it being surgically implanted and, as such, there are strict protocols for surgeons to follow to reduce any surgical complications.
Findings of ocular adverse events of special interest were reported in 19% of the PDS 24 weekly arm, and 6% in monthly ranibizumab.
In the PDS arm:
• 1.6% endophthalmitis cases
• 0.8% retinal detachment
• 5.2% vitreous haemorrhage
• 2.4% conjunctival erosions
• 2% conjunctival retractions
Most adverse events occurred within one month of implantation.
“As you can see, there are some safety concerns, particularly around conjunctival erosion and retraction, which isn’t ideal as the conjunctiva should be covering the device,” Guymer said.
“We need to think about surgical safely and long-term implant safety and a question remains as to how we should best monitor these people who potentially only need treatment every six months?
“Do we want to see them more often, and if so, maybe they’d be better with a longer acting drug, so there’s work to do to determine where this might fit into our treatment armamentarium. But there is some thought that if we can home-monitor these patients, we can stop them coming in to be checked. For example, vision monitoring at home is available with certain apps and at-home OCT might be applicable here.”
DAWN OF A NEW ERA FOR GEOGRAPHIC ATROPHY
In the other late form of AMD, geographic atrophy (GA), patients have had little hope with no approved therapies yet. But Guymer said there are several late-stage novel therapies that, once approved, will pose different challenges and opportunities compared to anti-VEGFs for nAMD.
“When we have the first treatment approved for GA, it’s going to completely change the lives of patients, but also yours and mine as eyecare professionals,” she said.
“We will need to determine who to treat, when to treat, which treatment and whether it should be done in one or both eyes; these are just some of the questions we haven’t addressed as a community yet.
“It’s going to be different to nAMD where we treat almost anyone. It’s unlikely we will be able to individualise treatment – there will not be judging whether someone receives four or 16 weekly treatment because there isn’t
40 INSIGHT December 2022 SCC 2022
Figure 3 - Retinal scans of a 95-year-old female presenting 6/18 with choroidal neovascularisation (top) before sustaining fibrosis/scaring post-treatment (bottom). Five years later, despite a great response to anti-VEGF long term, visual acuity was not maintained due to atrophy and fibrosis caused by current treatment approaches.
much to measure in trying to slow the growth of patches of atrophy. It is more likely going to be a forever treatment for everyone and many people with GA have few or no symptoms early on, so how you ‘sell’ this therapy to the patient will present challenges.”
To start with, Guymer said optometrists will be required to distinguish between GA and inherited retinal disease (IRD) – both can present similarly on scans but treatments under development for these conditions differ drastically.
“Fundus autofluorescence has come into its own for GA. It seemed to be a technique looking for a reason, but it’s now a great way to look at growth of atrophy over time. One plea I’d make to the eyecare community internationally is to start taking images so we can obtain baseline images to determine growth rates – that’s going to be crucial when starting to talk to people about treatment,” she said.
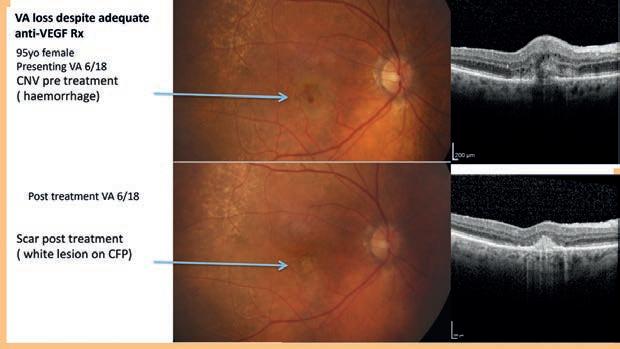
According to Guymer, one of the great challenges with GA is that researchers still don’t precisely know its cause, but they have identified some of the likely pathways involved. This has led to investigational therapies that target and regulate the complement system to suppress inflammation.
One late-stage therapy adopting this approach is by Apellis Pharmaceuticals and its therapy pegcetacoplan, which is being trialled at sites in Australia.
Guymer pointed to the completed Phase 3 OAKS and DERBY studies involving 1,258 participants across 200 global sites. Patients in the treatment group were given either monthly or every-other-monthly pegcetacoplan, with the aim of slowing growth of the GA area. Secondary endpoints – reported at 24 months – include functional outcomes such as best corrected visual acuity, low luminance visual acuity, reading speed and microperimetry.
“The OAKS study showed a statistically significant overall slowing of GA growth across the whole pegcetacoplan group and if you look at patients who had extrafoveal lesions – where it tends to grow faster – the therapy seemed to have a bigger impact,” she explained.
“Unfortunately, the DERBY study did not reach significance in its primary endpoint and there was little difference in growth rate overall, but when they looked at extrafoveal lesions there was a significant difference in one of the arms.”
However, at 18 months, both studies reached significant slowing in lesion growth and then, more recently in September 2022 at EURETINA, 24-month data showed there was significant slowing in both trials.
“As you can appreciate this isn’t a miracle in a sense that we haven’t

Figure 4 - Pegcetacoplan, which could be one of the first therapies approved for geographic atrophy, showed clinically meaningful reductions in GA lesion growth from baseline out to two years.
cured the disease, but given we don’t have a treatment, anything that’s stopping that growth, especially extrafoveal lesions getting to the fovea, is a good thing,” Guymer said.
“Apellis is awaiting an outcome in the US in late 2022 and, if successful, the rest of the world including Australia will apply for approval shortly afterwards."
NEW HOPE WITH GENE THERAPIES
Other companies are also targeting the complement system, but in different ways for GA.
Guymer said one novel method is the Complement Factor B anti sense program using RNA technology, which targets treatment in the liver, meaning it can be delivered subcutaneously. This would offer the opportunity to treat both eyes simultaneously with a systemic treatment, while offering the ability to self-treat at home.
But a one-off treatment could be even more advantageous and this is where gene therapies come in. CERA is a trial site for a therapy developed by Gyroscope Therapeutics (acquired by Novartis in February 2022) called GT005, with Dr Tom Edwards the first to deliver the therapy locally at The Royal Victorian Eye and Ear Hospital in 2021.
“With this therapy, they’re hoping to augment Complement Factor I which will down regulate the alternative complement pathway,” Guymer said.
“Originally, this therapy was designed for people only with a mutation in a particular gene with very low levels Complement Factor I, but now they’ve found it’s probably useful for anyone with a complement-based genotype, which is 95% of patients with GA, so now enrolment is almost open to anyone with GA.”
To find suitable candidates, Guymer said CERA has been involved in the TELESCOPE study, a community-based genetic screening study designed to identify people with GA. It involves 12 optometry practices in Victoria who have been recruiting GA patients for the GT005 trial.
“We are trying to grow a network of optometrists to help recruit patients for ongoing GA studies,” she added.
In conclusion, Guymer said the pathophysiology of GA is complex and most therapeutic approaches are trying to slow growth rates, particularly by targeting the complement system.
“Once treatments are approved, these patients will need regular intravitreal injections, but this won’t be the final mode of delivery – it can’t. There’s a huge number of people with GA who, in early stages, don’t have much in the way of symptoms, so we will need longer acting therapies and perhaps this is where gene therapies can help.” n
INSIGHT December 2022 41
SECRETS TO SETTING UP AN ophthalmology practice
Whether it's their first year in business or decades down the track, Insight speaks to those who know what is involved in establishing an ophthalmology practice, and where to turn for advice.
Despite being in the early stages of his ophthalmology career, Dr Jonathan Kam is well versed in the challenges of setting up his own ophthalmology clinic, having learnt through experience what works, and what doesn’t.
His keen observation skills and business acumen have helped guide his newest venture, Inner East Eye Surgeons, a clinic he has recently established with colleagues Dr Nicholas Cheng and Dr William Tao, at the Epworth Eastern’s recently built 14-storey East Wing Tower in Box Hill.

“Being able to build our clinic at Epworth Eastern has offered many advantages. The quality of the fit out and level of infrastructure is very high, and we are in close proximity to a lot of other specialists in other fields. It also has allowed us to connect with the Eastern Clinical Research Unit and get involved in research trials to help progress medicine,” he says.

“We felt that being in an area which we live close to – and have also grown up in – and associating ourselves with the hospital would put us in good stead to establish ourselves.”
Each of the ophthalmologists completed a fellowship in a different subspeciality, so together they can provide a comprehensive range of ophthalmology services. Dr Cheng completed his fellowship in retinal
disease and uveitis and Dr Tao completed fellowships in glaucoma and paediatric ophthalmology, while Dr Kam did a fellowship in complex cataract surgery.
Kam says he and his partners considered purchasing a bricks-andmortar house converted into a medical clinic, common in the profession, but found that the capital investment for that was not something they were keen to take on at this stage in their career.
They rent their purpose-built suite and the three-way partnership means each own a third of the practice.
“I’ve always wanted to start my own practice, although this is actually the second practice I’ve started,” Kam says, adding that it’s the first for Cheng and Tao, who he has known since they were in medical school.
“WHAT I’M DISCOVERING … IS THAT YOU DO HAVE TO LEARN SKILLS OUTSIDE OF MEDICINE, AND THERE ARE MANY AVENUES TO LEARN”
42 INSIGHT December 2022 ENTERPRISE
DR JONATHAN KAM INNER EAST EYE SURGEONS
Dr Jonathan Kam recently opened Inner East Eye Surgeons with two colleagues at the Epworth Eastern’s recently built 14-storey East Wing Tower in Box Hill, Melbourne.
He started his first practice immediately after finishing his training, four years ago.
“I started in a close-by suburb renting two rooms in a commercial retail space which was set up as a health hub. It was doing well but when the pandemic hit, a lot of the health hub tenants moved out. The owners of the health hub decided to close because they couldn’t run their business anymore,” Kam explains.
Forced to move out of necessity, only two years after establishing his practice, Kam relocated his practice to Doncaster Eye Centre, a wellknown clinic with 12 ophthalmologists.
“One of the reasons why I joined Doncaster Eye Centre was because I had trained under their doctors, who are all very good; they knew me and they felt that I would fit into their practice well,” Kam says.
“Doncaster Eye Centre was where I learned economies of scale firsthand. You can do bigger things with more people.
After running my practice by myself as a solo clinic – at the health hub – I realised that there are things that you can’t do as one person that are much more possible with three doctors.
“It also means you don’t have to shoulder all the costs yourself and you can hire enough staff to provide a good service. That’s ultimately why we [Kam, Cheng and Tao] came up with this plan of three doctors in a medical suite that didn’t have a large capital investment required, but enough that we could buy quality equipment, and have a quality fit out.”
Kam says his business acumen has mostly developed through observation. When working in different locations, he has taken mental note of what works well – and what doesn’t.
“I enjoy learning different skills and that’s what attracted me to running a clinic. I thought, wouldn’t it be great if I could put a clinic together that had the best elements of all that I’ve learned along the way,” he says.
“I also read a lot of books. When it comes to finance and negotiation skills, I learn from books. There’s a great book called Never Split the Difference by an FBI negotiator [Chris Voss], which I found insightful. “What I’m discovering, with the clinic that we have established [Inner East Eye Surgeons] is that you do have to learn skills outside of medicine, and there are many avenues to learn.”
Kam believes that if you want to evolve the practice of medicine, you must adapt with the times, including the path to establishing your own clinic.
“For a young doctor to buy a big property nowadays, it’s very hard. And when you take on a lot of risk and debt as a doctor, I feel that it can affect your stress levels and your decision making. You want your patient care to come first.”
Setting up Inner East Eye Surgeons in consulting suites connected to a private hospital allows him to execute his vision at a level he wouldn’t be able to achieve without collaboration.


“The practice is set up to provide a level of care to patients in a way
that I always wanted to. I know I have the knowledge and skills but then having the setting, tools and staff to help me is also what I need to practise in the way that I need.”
When it came to purchasing equipment for Inner East Eye Surgeons, Kam, Cheng and Tao were guided by quality and cost.
“We wanted reliable instrumentation that is modern and is latest technology. I’m a ‘details’ person, so I look at the specs, and the cost. We bought the best of what each company can offer. For example, we bought Ellex lasers because it’s what we’re familiar with and it’s Australian-made. We bought Haag-Streit because it’s the gold standard of slit lamps. I felt that buying from each supplier means you know that you’ve bought what is needed, rather than getting roped into a package deal.”
“Together our goal is to work as a team to provide up-to-date and individualised patient care.”

POINT OF DIFFERENCE
Ophthalmologist Dr Louise Robinson established Coastal Eye Surgeons at Hope Island on the Gold Coast in September last year, soon after completing her fellowship. “I always wanted to own my own practice, or be in a partnership,” she says.
Perhaps unlike many of her peers, Robinson has a business background. She has corporate finance and accounting degrees and was working in banking before returning to university to study medicine and finally, ophthalmology.
Her first step towards attaining the goal of practice ownership was narrowing down a preferred location where she was going to be happy living and working.
It was difficult to decide between Sydney and the Gold Coast, she says.
“I did my training in Sydney and had colleagues and professional support there. On the other hand, I had family and had grown up on the Gold Coast.
“To set up a practice, I needed a point of difference which I determined was my sub-specialty and location. I needed to find a location where a need was evident. Once I established the area, I needed to find a suitable premise. I did a lot of research myself to find a location.”
Around that time, Robinson attended a conference run by The Private Practice, a Sydney-based company that provides health professionals with business and financial resources which are tailored to different stages of their careers.
DR LOUISE ROBINSON COASTAL EYE SURGEONS
“The conference covered different aspects of starting a healthcare business, such as practice design, advertising, website, as well as business structures, insurance, income protection amongst many other topics,” she says.
Once she found a suitable site, Robinson contacted a property consultant who negotiated the lease.
“TO SET UP A PRACTICE, I NEEDED A POINT OF DIFFERENCE WHICH I DETERMINED WAS MY SUB-SPECIALTY AND LOCATION”
INSIGHT December 2022 43
Gordon Eye Surgery in northern Sydney.
“The area my clinic, Coastal Eye Surgeons, is located is predominantly residentially zoned on Hope Island (north of Southport). The area has many privately secured communities, retirement villages and there is very little commercial space available. I found a new commercial development – the building is three years old – and my clinic is part of the Professional Suites that includes a GP, cardiologist, physiotherapist and allied health.”
Robinson’s site was a 146m2 shell that required interior construction and installation, including consulting rooms and a surgical room for minor procedures.
Through The Private Practice, Robinson was put in contact with the Health Business Network’s founding director, Mr Russell Lee, who specialises in medical practice growth and strategy.
“He assisted me in all areas of the business set-up from finding a finance broker to setting up computer and phone software and recruiting staff. I chose a local architect firm who had experience in setting up ophthalmology clinics, which was invaluable, as they understood the equipment requirements, size and patient flows that work,” she says.
“The business developer was on site every week, overseeing construction, ensuring the builders followed the architect’s design. Once construction was complete, I had to choose equipment and software, a task you want to do only once and do it well. Software had to be ‘cradle to grave’ and paperless; from booking appointments, letter generation to billing and accounting.”
But it wasn’t all smooth sailing, as the COVID pandemic disrupted Robinson’s plans.
“I found the site after completing my fellowship, and not long after attending The Private Practice conference, it was all put on hold. Thankfully I hadn’t signed the lease prior to the beginning of the ‘lock down’. The lease was signed in March 2021, and the design and build was a six-month work in progress,” she says.
While Robinson is the sole owner of her clinic and works fulltime, her business development manager, who oversaw the construction, continues to oversee the clinic’s business operations, accounts and staff.
“He is like a remote practice manager. He manages staff contracts, he does the financial figures, and we sit down on a quarterly basis and go through the accounts.”
Since Robinson has achieved her goal of owning a business, RANZCO has subsequentially created resources that can help ophthalmologists in the transition from training to Fellowship.
Robinson is also doing her part to support her peers. She is a member of RANZCO’s Younger Fellows’ Advisory Group.
“I represent Queensland-based Younger Fellows in RANZCO. We have a collegiate meeting every quarter where we welcome Younger Fellows and provide them with support around working in private practice.”
Coastal Eye Surgeons celebrated its first anniversary in September this year.
“It is a challenging, daunting, yet rewarding experience setting up a
practice by yourself, but worth it. I wanted to create a work environment which was modern and relaxed, somewhere that my staff and I enjoy working, which in turn is enjoyed by the patients.”
THREE-FOLD GROWTH IN THREE DECADES
Orthoptist-turned-business manager Ms Donna Glenn manages a large privately owned ophthalmology clinic in Australia which will celebrate 30 years in business next year.
Gordon Eye Surgery, north of Sydney, has 18 ophthalmologists, plus other specialists including a neurologist and an immunologist, and a satellite practice in Lane Cove, which opened in 2016.
“I originally trained and worked as an orthoptist and then moved to consulting in accreditation and quality management for practices and day surgeries giving me insights into the running of practices, so practice management then became a logical progression,” Glenn says.
Glenn was practice manager of Gordon Eye Surgery for nine years, changing into a business management role for the last six years overseeing both locations.

She is also a former RANZCO Practice Managers committee member and is now chair of RANZCO Professional Standards committee and is also a NSW representative of the Australian Association of Practice Management.

She can’t overstate the importance of ‘doing your research’ before selecting a location.
“Understanding the demographic of the area where you are setting up an ophthalmology clinic is vital to success, including the age and socioeconomic demographic, and looking at what other services are in the area,” Glenn says.
Deciding how to financially structure a clinic is as important as finding a suitable location, she says.
“Getting this correct at the outset is important and will save time, money and stress in the long term.
“Think about how to run the clinic, how to fund the project, how to structure it, whether to rent or buy in your preferred location. Getting it right is so important. Think of setting the business up with a mindset of how you would exit the business is important. Think about scenarios, what happens if you want to sell the business, what happens if you want to add a business partner, and so on.”
Glenn says a small group of ophthalmologists own Gordon Eye Surgery, and her role involves working with those owners, who are also clinicians at the clinic, and working with the practice manager to ensure the clinic provides exceptional service.
Over the past 15 years, the clinic has expanded – outgrowing its previous location – and a new business manager role was created for Glenn to oversee its growth.
“Gordon Eye Surgery is now three times the size of what it was, as our capacity has increased three-fold. It was started by two ophthalmologists


“UNDERSTANDING THE DEMOGRAPHIC OF THE AREA WHERE YOU ARE SETTING UP AN OPHTHALMOLOGY CLINIC IS VITAL TO SUCCESS”
DONNA GLENN GORDON EYE SURGERY
“WE’RE ALSO ANSWERING THE BIG QUESTION: ‘ARE YOU READY TO TRANSFORM AND TAKE CHARGE OF HOW YOU PRACTICE?’”
44 INSIGHT December 2022 ENTERPRISE
ANDREW CHAMBERS RANZCO
30 years ago, and both are still working at the clinic today,” she says.
“The success of the practice is their mindset and the cultural tone they have set. They have stayed true to their clinical ethos despite the practices growth.”
As business manager, she oversees a practice manager, clinical manager and administration manager, 15 administrative staff and 10-12 clinic staff, including nurses and orthoptists.
“Day-to-day, my role has involved managing moving locations as we needed more space which included looking for a new location for our satellite practice negotiating ownership of the location – as in not leasing – plus managing finances and compliance such as Medicare and HR, managing capital purchases such as equipment, and maintaining relationships with our 18 ophthalmologists,” Glenn says.
Three years ago, Glenn gave a presentation ‘Do you need a practice manager?’ to RANZCO Younger Fellows, which has now been incorporated into a RANZCO CPD business modules.
As chair of the RANZCO Professional Standards Committee, Glenn oversees management of the nucleus program available to RANZCO Fellows and says it provides many tools that are useful for setting up a practice including a set of templates for governance.
“Technology and equipment are major investments. Data storage and networking are becoming major considerations for practice management. Ophthalmology is the second most expensive specialty other than radiology, according to the AMA. We rely on technology dayto-day,” Glenn says.


“We are fortunate to have a practice manager at Gordon Eye Surgery that has a keen interest and understanding in technology management which is a resource that is very valuable in a practice.”
“Technology is expensive yet necessary in our business the importance is that it is used to create efficiencies and improved clinical decisions.”
ANSWERING THE BIG QUESTION
RANZCO acknowledges that while many Younger Fellows work in the private setting, most do not feel they had adequate exposure on how to start or join a private practice during training.
A demand to know more about the business elements of private practice was the driving force for RANZCO’s learning content coordinator Mr Andrew Chambers to develop a set of modules.
Younger Fellow Ms Tanya Karaconji completed a research project on readiness for private practice as part of RANZCO’s 2018-2019 Leadership Development Program, finishing in 2019. It was the impetus for RANZCO to launch the Business Skills Workshop the same year. This has been on pause in 2020-2022 due to COVID but the content helped inform the online pathway that Chambers developed.
“I am building a set of professional development learning modules around practice set-up and management for Younger Fellows (or any fellow) who want to move into this setting,” Chambers says.
“The first module in the pathway is about learning about basic business development skills, similar to an MBA student, and thinking through the various factors behind this important decision. The other modules will then become more specific to the skills needed.”
Chambers says RANZCO has deliberately used the phrase ‘setting up a new practice’ rather than ‘consulting rooms’, mainly due to the large number of factors that ophthalmologists need to consider.
“We ask them to reflect a lot on their motivations to ensure they are making a good decision or set of decisions,” he says.
“In the first module, the primary skills and knowledge areas we will focus on are all related to learning the basics of practice set-up and planning a new venture.”
This includes understanding the basics of business analysis as it
applies to practice set-up, performing business analysis in order to make a business plan, and structuring practices for better collaborative work practices and management.
“We’re also answering the big question: ‘Are you ready to transform and take charge of how you practice?’,” Chambers says.
“We included several business models, frameworks, and skills that relate directly to practice set-up/planning, business planning, and practice sustainability which we believe they [fellows] would find useful.”
Recommendations on ways to collaborate and network with others are also provided, although it is self-paced.
Chambers says the second module, currently being developed, is more practical and covers what fellows need in order to set up a viable practice.
“Step by step, this includes the premises, ophthalmic equipment and fit-outs, registrations, merchant services, practice systems and software, basics of staff, recruitment and HR, marketing basics, financing considerations, insurances, asset protection and superannuation.”
The first module in the learning pathway was launched to members in May this year. n
INSIGHT December 2022 45
Inner East Eye Surgeons invested in a ZEISS IOLMaster700, and has made a point of acquiring the best technology from several suppliers.
Dr Nicholas Cheng (left), Dr Jonathan Kam and Dr William Tao rent a purpose-built suite and the three-way partnership means each own a third of the practice.
Country care:
ATTRACTING MORE OPHTHALMOLOGISTS
The geographic maldistribution of ophthalmologists in Australia is a long-standing issue contributing to eyecare inequity for residents with a regional postcode. Insight talks to regionally-based ophthalmologists and investigates what is being done to fix the issue.


When Dr Kong-Chan (KC) Tang was an ophthalmology trainee in the mid-1990s, all he had ever known was the bright lights of Sydney. But an opportunity arose to spend a year in Orange under Dr Henry Liu, in a move that altered the trajectory of his career.

Almost 30 years later he remains there practising solo at his Midwest Ophthalmology clinic, a situation he wouldn’t have considered if it wasn’t for the exposure he had during his training. It also helped that – after completing his training in 1998 – a position in Orange was waiting for Tang whose wife had a country background.
“I was very fortunate, particularly these days we find it difficult to attract people to areas like Orange because the doctor’s partner and their professional commitments also come into the decision, so it isn’t always possible to make the stars align,” he says.
“To practise in the country, you also need to have broad-based knowledge. When we advertise for locums, many say they don’t see glaucoma patients or kids etc, but I have a paediatric clinic, I do squint surgery, completed my fellowship in retina and even perform the odd glaucoma operation, so you have to be well-trained to be confident to work in the country.”
Part of the problem, according to Tang, is that trainees get into teaching hospitals where fellows oversee their own ophthalmic sub-speciality such as glaucoma, retina and paediatrics. As a result, trainees may not get the hands on experience required to feel equipped for regional practise.
There’s also the issue of succession. Tang, like many regional ophthalmologists, is in his 60s and acutely aware of the need to entice the next generation. In Orange there are two other full-time ophthalmologists with another splitting their time between Dubbo and Orange.
“We’re getting a fellow, a fourth-year trainee, for the first time next year who will come to the area with some funding, which is great because we have been scratching our heads to attract people here,” he says.
“But ultimately I think the fact I had done some prior work in Orange opened my eyes to what’s possible in regional areas, and that’s why it’s
important the college tries to expand the network of rural positions to give people that exposure."
HOW RANZCO IS RESPONDING
Fortunately, RANZCO is across many of the issues Tang raises, and has new, evidence-based initiatives to bolster the regional ophthalmology workforce.
The imbalance of urban versus regional/rural eye doctors was laid bare in a 2018 Department of Health ophthalmology workforce report confirming 84% work in big cities (category 1 in the Medical Monash Model [MMM] –a spectrum that extends to MMM7 to determine if a location is city, rural, remote or very remote). That means some 16% of ophthalmologists work in regional areas, which is insufficient for the 29% of the Australian population that lives regionally.
In this 2018 report, based on 2015 data, ophthalmology was considered
46 INSIGHT December 2022 WORKFORCE
“IT’S IMPORTANT THE COLLEGE TRIES TO EXPAND THE NETWORK OF RURAL POSITIONS TO GIVE PEOPLE THAT EXPOSURE"
DR KC TANG ORANGE, NSW
TO THE REGIONS
RANZCO’s own analysis has also shown that of the ophthalmologists who trained and graduated between 2013 and 2016, 90% reside in urban areas. This aligns with the 2018 report that found 85% of trainees are located in major cities (MMM1), with 9% in MMM2, 3% in MMM3 and 1% each in MMM6 and MMM7.
The report recommended an increased intake of trainees to counter the predicted undersupply of ophthalmologists in 2030 of three per year from 2019 – compounding.
But it had a particular focus on regionally-focused initiatives for RANZCO.
This included several steps including formalised training of additional supervisors, particularly in regional, rural and remote settings, as well as potential mechanisms to address maldistribution such as preferential selection of trainees with a rural background, or who have undertaken rural placements as a medical student, or worked as a junior doctor in a rural area.
It was also recommended trainees undertake at least six months training in a regional, rural or remote area and/or experience working within an Indigenous health service and that final fellowship assessment demonstrates fellows can practise the full scope of ophthalmology across Australia.

For several years, Dr Justin Mora, who finished a six-year term as RANZCO’s censor-in-chief in November 2022, and Tasmanian ophthalmologist, Dr Kristin Bell, have been working behind the scenes to bring many of these recommendations to fruition.
Mora tells Insight many factors contribute towards ophthalmologists choosing to practise in capital cities. One is that RANZCO trainees typically don’t get on to the course until they are around 30-years-old. This is because, after leaving medical school, they can spend up to four-and-a-half years trying to bolster their CVs with experience and training.
Ophthalmology is a highly competitive speciality among trainees, with around 135 applications each year for around 32 positions across Australia and New Zealand. In previous years, the ophthalmology trainee selection process has rewarded those with the best academic record and experience. At a minimum, all have done a mandatory two-year internship out of medical school, usually followed by one year of ophthalmic experience.
6 and density of ophthalmology
The ophthalmology workforce is located throughout Australia, but typically concentrated in metropolitan areas (84% MMM1). Source: Ophthalmology –Australia’s Future Health Workforce report, 2018.
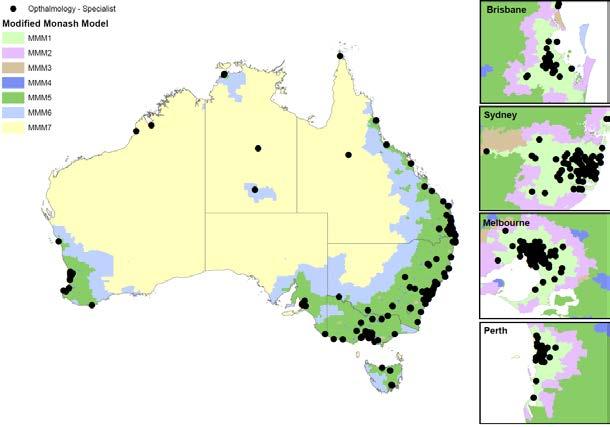
Some then go even further to stand out.
“There was one particular year where out of 32 new entrants, we had 18 Master’s degrees and four PhDs. And of course, that adds time to people’s post-medical school experience,” Mora explains.
“By the time you’re 30-years-old, if you’ve spent all that time in an urban environment and have a spouse or partner, it gets harder to leave that lifestyle to go work in a regional area. A lot of trainees also have young families by the time they qualify, and they’re worried about schooling.”
While RANZCO is attempting to address this issue by enticing younger medical school graduates through different selection pathways, Mora and Bell have been focusing on two key areas, as highlighted by the 2018 workforce report, to strengthen the regional workforce at the trainee level. These are:
1. A greater emphasis on accepting trainees with a regional background and First Nations applicants
2. The establishment of RANZCO’s Regionally Enhanced Training Network (RETN), which will commence its first rotation in February 2023.
At the same time, RANZCO is also advocating for more training positions in public hospitals, stating that a healthy workforce is dependent on a healthy public ophthalmology service right across Australia because this is where most specialist training does and should continue to occur.
“We have repeatable data from our workforce surveys that tell us that people from regional backgrounds proved to be 2.7 times more likely to end up practising regionally, either living regionally or doing outreach regionally,” Mora says, noting that only 9.3% of RANZCO fellows had a regional background in 2017.
“Therefore, we had the evidence to give higher priority to people from regional areas. That has proven successful. The way the system works is RANZCO creates a shortlist based on objective criteria, and then the hospital networks put their selection criteria around it.”
As a result, more than 40% of trainees during the past two to three years have a regional background.
Mora says RANZCO has been addressing concerns about the level of training too.
He points to a trend during the past 20-30 years where graduates increasingly subspecialise in their final year, potentially impacting their confidence to work regionally where ophthalmologists need to be generalists.
7
INSIGHT December 2022 47
“We’re trying to address that as part of our curriculum review where we’ve refocused our attention on creating general ophthalmologists. And as Figure
The MMM is a classification system that better categorises metropolitan, regional, rural and remote areas according to both geographical remoteness and town size. The system was developed to recognise the challenges in attracting health professionals to more remote and smaller communities. MMM1 indicates major cities and progresses to MMM7, which indicates very remote Australia. As can be seen in the map below, the ophthalmology workforce is located throughout Australia, but typically concentrated in metropolitan areas (84 per cent in MMM1).
Figure 6: Ophthalmology workforce (clinicians) by Modified Monash Model
Source: NHWDS, Medical Practitioner 2016
Source: NHWDS, Medical Practitioner 2016.
graduates, an impending critical shortage of paediatric ophthalmologists and a lack of funded training positions in the public sector.
“If they pass, they can go into a subspecialty year, and if they haven’t, then they have to do more general ophthalmology in their final year.”
GREATER REGIONAL EXPOSURE
Kicking off in February 2023, the Regionally Enhanced Training Network (RETN) is a new Australia-wide training network RANZCO has developed that will ultimately see trainees on the program spend 60% or more of their time in regional Australia.


RANZCO has proposed four pathways: the Top End Pathway, Northern Victorian Pathway, Northwest NSW Pathway, and Western NSW Pathway. The first two RETN trainees are set to commence in February 2023.
Each takes five years to complete with the ‘first foundation year’ spent in a regional centre public hospital setting, the ‘second consolidation year’ in a regional private practice or public hospital, the ‘third subspeciality year’ in a major city, and the ‘extension and challenge’ final two years based regionally in a comprehensive practice, including care for Aboriginal and/or Torres Strait Islander patients.
For example, the Northern Victorian Pathway is: Year 1: Geelong, Year 2: Albury- Wodonga, Year 3: Melbourne, Year 4: Shepparton, Year 5: Shepparton.
According to RANZCO, the major differences between the RETN and existing networks are that trainees will complete their entire five-year vocational training program with the RETN, and trainees will complete an increased proportion of their training in regional Australia.
“Dr Kristin Bell’s projections are that we could see 10 rotations within the next 10 years, which is ambitious but possible with appropriate funding. This would equate to 40 trainees – that’s a lot when you consider we take around 35 across Australia and New Zealand each year, with around 25 in Australia alone,” Mora says.

“That’s potentially another eight people per year just in the regionallyenhanced scheme, so that would have a major impact.”
Mora says it has been a long and arduous process to establish RETN, which demonstrates RANZCO’s leadership among the medical colleges. As the trainee progresses through RETN, RANZCO is required to work out a bespoke funding model due to the various ways regional ophthalmology training is provided in Australia.
A mixed model of funding for the RETN training posts is used consisting of a combination of conversion of existing unaccredited registrar positions to accredited positions, the Federal Government’s Specialist Training Program (STP – more detail on this below), and State Health Services funded positions. It’s also important to note the funding covers each training ‘post’ so each position is filled each year to ensure continuity of regional service provision, and the funding doesn’t necessarily move with the trainee.
“The funding of RETN encompasses not just the salary for the trainee, but also access to cases, funding of surgical cases and clinics, accommodation, teaching money, transportation back-and-forth and so on. It’s a significant package and it all has been accounted for – we can’t set up an under-funded program,” he says.
Mora says Bell has been influential in bringing the complex RETN to life, twisting arms to make it happen, including commitments from state governments. Both state and commonwealth health departments are keen to deliver regionally enhanced specialist training programs, however, with the health dollar under pressure and the complex interplay in health funding between the state and the commonwealth and within each state health department, navigating this complex funding environment has been challenging and remains so.
“It’s been gratifying in the last 12 months to see things start to gel. We’ve been pursuing this during the past three to four years and it felt like it was falling on deaf ears,” Mora says.
“And then with RANZCO’s Vision 2030 and beyond project – which highlighted the need for more ophthalmologists overall, regional ophthalmologists, First Nations ophthalmologists, and presented the many issues as a package – suddenly, federal and state governments have been spurred into action. They’ve realised how serious we are about addressing this issue.”
According to RANZCO, regional posts have a lot to offer trainees. They provide broad comprehensive ophthalmology clinical experience with increased opportunities to follow each patient through the course of their presenting problem. This contrasts with the patient journey in big city teaching hospitals, where patients are typically funnelled into subspecialty clinics. Regional terms typically offer trainees a wider range of surgical training.
The primary aim of the RETN is to train well-rounded ophthalmologists who have the skills and confidence to practise comprehensive ophthalmology post-fellowship in any area.
The college says it’s designed so that trainees can develop a solid foundation of knowledge and clinical and surgical skills which they then build on over the initial three years, culminating in them taking the RANZCO Advanced Clinical Examinations (RACE) at the beginning of their fourth year of training.
In the final fourth and fifth years, Mora says RETN is deliberately designed so the trainee spends two continuous years in the same regional area.
“That’s in the hope they will become embedded in the local community and encourage them to continue working there once qualified,” he says, noting that RANZCO can’t ultimately dictate where RETN trainees go.
FLAWS IN SPECIALIST TRAINING PROGRAM
RANZCO’s RETN wouldn’t be achievable without in-part funding from the Federal Government’s STP; especially the Integrated Rural Pipeline Funding (IRTP) part of the STP which allows for in-part funding of urban posts for regionally enhanced trainees.
STP was introduced in 2010 to support medical training positions outside of traditional metropolitan teaching hospitals. The latest extension of this,
48 INSIGHT December 2022 WORKFORCE
“PEOPLE FROM REGIONAL BACKGROUNDS PROVED TO BE 2.7 TIMES MORE LIKELY TO END UP PRACTISING REGIONALLY”
DR JUSTIN MORA RANZCO
Regional centres like Wagga Wagga, in NSW, face a shortage of ophthalmologists if younger eye doctors aren’t encouraged to move to the town.
announced in March 2022, will see $708 million spent from 2022 to 2025 to fund 920 full-time equivalent places annually, with at least 50% of training occurring in regional, rural and remote locations or private settings.
To help cover the annual salary of trainee specialists, STP provides RANZCO and other medical colleges with $105,000 per full-time equivalent position, an additional $25,000 Rural Support Loading allowance for training positions in regional, rural and remote areas, and a Private Infrastructure and Clinical Supervision allowance of $30,000 for training positions in a private sector setting.
However, STP funding does not fully cover the cost of a state health funded Local Hospital Network (LHN) employing the trainee but does cover a large proportion of the costs. There is an expectation from the Federal Government from the state health departments will also contribute. The challenge is to get a commitment from LHN to employ the registrar and cover any additional costs.
The main drawback of STP and STP-IRTP funding is that the program works on three- to four-year funding cycles and can’t guarantee what will be available in the following five- to 10-year period. This presents a challenge in medium to long term workforce planning but RANZCO has been told it is unlikely to change in the foreseeable future.
Mora notes: “We need more certainty – we need to know if we’re setting up a training program for five years, that it’s covered for the entire time span. The way STP is designed means funding is rotated every four years, so there are no guarantees.”
However, the Federal Government, as well as several state health departments, have indicated their support of the RETN and communicated that existing funding is likely to be continued and further development of the program supported. This gives RANZCO the confidence to further develop and extend the RETN.
WHAT IT’S REALLY LIKE TO PRACTISE REGIONALLY
Dr Christopher Bailey, who has been practising in Wagga Wagga for 28 years, is aware of the RETN and other schemes to encourage more trainees to settle regionally. While he’s supportive of the idea, he believes it’s important RANZCO selects trainees that will stick with the spirit of the program.
“When I was trying to get on to the ophthalmology training program 30 years ago, some people would say they intended to work in the country and so they got picked, but now they’re working in the eastern suburbs of Sydney,” he recalls.

“You can’t dictate where people go at the end of the day, but it will perhaps get people to strongly consider a career in the regions.”
Originally from Sydney’s west, as a trainee Bailey was destined to head overseas for a fellowship. But the funding fell through, and a call went out
“When you work in the regions, the first thing you notice is the amount of work coming your way, you’ll hit the ground running – and no one’s going to be unhappy if you take away some of their work,” he explains.
“In Wagga, we’re at the point now where we could easily help someone who wants to sub-specialise. One of the other ophthalmologists here subspecialises in oculoplastics and if someone arrived and said I’d like to do glaucoma, we’d ask them when can you start? And we also have a retinal surgeon 100km away.


“When registrars come on rotation, some say they didn’t realise that things were so good away from the city. They don’t have to travel an hour to get 15km; it takes me seven minutes to get to work. The housing prices are much lower and you can get 60 acres of land 10km out of town, if that’s what you want to do.”
Fellow Wagga Wagga ophthalmologist Dr Brent Skippen, the previously mentioned oculoplastic surgeon, believes the main barriers to a regional ophthalmology career are the fact many have family in Sydney, or a perception that a city job is more prestigious.
In terms of ways RANZCO could incentivise young eye specialists into the regions, he supports moves to prioritise rurally born doctors, those with rural families and those rurally educated. During training, he said more registrar training could be performed in the country with six- and 12-month rotations, rather than rotate every three months.
“Post-training, we could encourage more rural locum placements for junior specialists – this might convince some to change course posttraining and relocate to a regional practice,” he said.
In the early stages of his career, Skippen was a junior doctor at St Vincent’s Hospital, a smaller city hospital that had a similar feel to a large rural hospital. Wagga was the rural secondment on several occasions. He’s also worked for Médecins Sans Frontieres in Armenia, and in regional Australian areas such as Goulburn (student) and Armidale, Wagga and Lismore (doctor). He completed his oculoplastic fellowship in the UK and
He met his wife – a Wagga local – in Sydney, before getting married in the regional NSW town and deciding it was the best place to raise their family.
He’s found his career is well balanced between general ophthalmology training and subspeciality training (oculoplastics).
“In terms of fulfilment from regional practice, clinically I have great patients and close collaboration with likeminded colleagues. Teachingwise, I’m an Associate Professor with the UNSW clinical school and senior lecturer with University of Notre Dame rural clinical school, and in research, I maintain close ties with an Italian colleague (mentor), and we are able to generate research and publications and mentor UNSW students.
“I’m also only a 10-minute drive from home – on five acres – to
INSIGHT December 2022 49
“IN WAGGA, WE’RE AT THE POINT NOW WHERE WE COULD EASILY HELP SOMEONE WHO WANTS TO SUB-SPECIALISE”
DR CHRISTOPHER BAILEY WAGGA WAGGA, NSW
“POST-TRAINING, WE COULD ENCOURAGE MORE RURAL LOCUM PLACEMENTS FOR JUNIOR SPECIALISTS”
DR BRENT SKIPPEN WAGGA WAGGA, NSW
The return of in-person events marked a highpoint in 2022, alongside remarkable individual achievements. There were also major advances in diagnostic equipment and therapies for myopia and macular disease.
With COVID-19 largely in the rear vision mirror, 2022's running theme was "a return to normality", with major product launches, business deals, personnel changes and breakthrough product launches shaping some of the biggest moments in the Australian ophthalmic sector.


KEY BUSINESS HIGHLIGHTS
In a deal finalised in February this year, ASX-listed Healthia acquired the eight-practice business LensPro Optometrists, securing its largest optometry acquisition since its 2020 takeover of The Optical Company. The acquisition increased Healthia’s optical practice tally to 53, with LensPro helping expand its reach in southeast Queensland and northern NSW.
George & Matilda Eyecare welcomed several practices into the fold too, with the largest being Rolfe Optometry Group’s nine practices in New South Wales. Albany Creek Optometrists and Aspley Optical House, both in Brisbane, Optometrist Menai in Sydney, and Peter Baker Optical in Caringbah, NSW also joined the network.
In August, Vision Eye Institute announced it is expanding its existing laser service to South Australia, offering refractive surgery options including LASIK, ASLA/PRK and refractive lens exchange through its partnership with Eye Surgeons SA.
In the same month, Lions Eye Institute opened a state-of-the-art clinic in Midland, WA, ensuring people in Perth’s eastern corridor have access to high quality eye health services. While it had operated a clinic in the area for more than six years, its new purpose-built facility provides the
Also in WA, Fremantle Hospital opened a $5.5 million ophthalmology unit, bolstering one of the hospital’s busiest departments that sees almost 200 patients a day.
Private health provider SMS Healthcare made significant in-roads into the ophthalmology market in 2022, adding to its 14 clinics with the addition of three Queensland LASERSIGHT clinics and two clinics operating under the LASERSIGHT banner in Victoria and Tasmania. Then in October, it added two clinics with the acquisition of Dr Ilan Sebban’s Sydney Eye Clinic.
EyeQ Optometrists and National Optical Care (NOC) agreed to part ways in November, ending a two-year strategic alliance. Originally conceived during COVID, with a goal to support mutual growth plans, their disbanding means there will now be 25 EyeQ practices, and 21 NOC practices.
In the eyewear space, Kering Eyewear – a global company whose portfolio comprises Gucci, Cartier, Saint Laurent and other luxury brands, distributed in Australia by Sydney firm Sunshades Eyewear – acquired Maui Jim.


And EssilorLuxottica-owned OPSM – an iconic Australian optometry brand – celebrated 90 years in business in October.
KEY DECISIONS AND POLICIES
In a move that sent shockwaves through the industry in July, Port Macquariebased frames manufacturer, Optex Australia, successfully sought the removal of a 5% tariff concession enjoyed by acetate eyewear importers. Gazetted by the Australian Border Force (ABF), the move caught local wholesalers off
50 INSIGHT December 2022
2022
2022 REVIEW
OPSM celebrated 90 years in business.
ODMA's OSHOW returned in Sydney to much fanfare.
Charles Hornor, who bought Specsavers to ANZ, departed after 16 years.
A 20-year tariff concession on acetate eyewear was controversially removed.
guard, which has increased the cost of acetate eyewear imports from Europe.


ODMA sought a review of the decision, which was denied by ABF, so it is now planning to lobby at the government level. Watch this space.
Regulation was in the spotlight at various times throughout the year, beginning with the medical technology sector raising concerns in April over Prostheses List (PL) reforms. In the end, peak body the Medical Technology Association of Australia signed an agreement with the Federal Government that will see a staged reduction in the prices paid in the private system for some medical devices, to align them with prices paid in the public system, hopefully generating around $900 million in cost cuts for private health insurance policyholders.
In August, OA raised concerns about the agility of the national registration and accreditation system as part of its submission to a Senate inquiry into the way the Australian Health Practitioner Regulation Agency (Ahpra) handles registrations and complaints. OA took aim at the time it takes for Ahpra to respond to serious complaints like sexual misconduct, while also taking issue with tightened CPD requirements making it harder for optometrists to obtain exemptions while on parental leave.


Ahpra again made headlines in September when it announced a clampdown on rogue medical practitioners using the title ‘cosmetic surgeon’ by introducing an endorsement process to establish minimum qualifications. The decision was cautiously welcomed by ophthalmologists and oculoplastic surgeons, but details remain unclear on how the endorsement process will work.
Overseas, the optometry regulator in New Zealand approved a major scope-of-practice change allowing the profession to perform ophthalmic laser surgery, dismissing ophthalmology objections regarding safety and lost training opportunities for registrars. The policy came into effect on 1 July.

PEOPLE AND LEADERSHIP
In a standout moment for the industry on the international stage, prominent Australian optical industry figure Mr Grant Hannaford was named the 2022 International Optician of the Year at SILMO Paris. Hannaford was one of only four finalists, including fellow Australian Ms April Petrusma, to be shortlisted for the International Opticians Association award.
Locally, the profession also shone with three ophthalmologists – Professor Graham Barrett, Dr David Moore and Professor Stephanie Watson – and optometrist Mr Geoffrey Fitzpatrick recognised in the 2022 Queen’s Birthday Honours. In addition, ophthalmologists Dr James La Nauze and Dr Stephen Godfrey were recognised in the 2022 Australia Day Honours.


In business, Alcon announced two new appointments in January to lead the company’s Asia Pacific (APAC) operations. Mr Chintan Desai joined as the vice president of Alcon’s surgical business in APAC, while Ms Stephanie Waugh, previously vice president and global head of ocular health, was appointed vice president of vision care for the region.
EssilorLuxottica’s unification strategy took shape on local shores, with Mr Marco Caccini appointed to lead the new EssilorLuxottica Wholesale business for Australia and New Zealand in March. Two further key internal appointments included Mr Stephen Locke stepping into the role of VP – optical channel, leading the frames and lenses sales team, and Ms Larissa Brander leading wholesale marketing.
Meanwhile, one of the founding partners of Specsavers in Australia and New Zealand, Mr Charles Hornor, announced his departure after 16 years, in search of downtime and new challenges.
The eyecare sector welcomed several new CEOs in 2022; Cylite’s vice president of sales and marketing, Ms Kylee Hall, was promoted to CEO in April; Mr Mark Carmichael commenced as RANZCO CEO in May, Mr Richard Wylie commenced as Glaucoma Australia CEO in July, the same month Dr Kathy Chapman commenced as Macular Disease Foundation Australia CEO.

On the flipside, Optometry Australia CEO Ms Lyn Brodie, Vision 2020 Australia CEO Ms Patricia Sparrow and ProVision CEO Ms Frances Mirabelli each announced their resignation this year, with Mr Tony Jones stepping up as acting CEO at ProVision.
OCTOBER
JUNE
Four industry professionals, including Prof Graham Barrett, recognised in Queen’s Birthday honours.
SEPTEMBER
Ahpra announces clampdown on cosmetic surgeons, welcomed by oculoplastic specialists.
INSIGHT December 2022 51
RANZCO Congress returns in Brisbane.
JULY
NZ optometry regulator allows sector to perform ophthalmic laser procedures.
FEBRUARY Healthia acquired LensPro Optometrists.
MARCH
MTAA signs MoU agreement with Federal Gov over Prostheses List reforms.
MAY
Major optical trade show OSHOW returns in Sydney.
The profession lost four well-known individuals this year, with the passing of prominent NSW ophthalmologist and father-of-two Dr Con Moshegov (aged 59); Optical Distributors and Manufacturers Association (ODMA) board member and optical industry stalwart Mr Richard Grills (aged 80); South Australian optometrist Mr Ronald Fieldhouse (aged 97); and past Optometry Australia president Professor Brian Layland (aged 92).
THERAPIES AND EQUIPMENT
After much anticipation, EssilorLuxottica ANZ launched its Essilor Stellest lenses for myopia management in October. This followed CooperVision’s announcement that its MiSight 1 day contact lenses are now available in higher prescriptions, while Device Technologies and HOYA formed a strategic alliance to promote greater use of biometry in myopia management.
Elsewhere in the myopia space, the Therapeutic Goods Administration (TGA) approved EIKANCE 0.01% in March, Australia’s first low-dose atropine eye drop for myopia progression in children and young teenagers.
In another major approval, the TGA registered Vabysmo (faricimab) for neovascular age-related macular degeneration (nAMD) and diabetic macular oedema (DMO). Vabysmo, administered by four initial four-weekly eye injections, joins an expanding list of approved anti-VEGF therapies for macular disease in Australia, which currently comprises Eylea (aflibercept), Lucentis (ranibizumab) and, more recently, Beovu (brolucizumab). Lucentis was also granted its seventh indication, this time for retinopathy of prematurity (ROP), making it the first anti-VEGF approval for the rare disease affecting premature infants.
Also on the horizon in macular disease, Australian biopharmaceutical company Opthea made a major leap towards bringing its therapy OPT302 to market after securing AU$245 million in funding from a major global investment firm. OPT-302 is a VEGF-C/D ‘trap’ inhibitor that Opthea is combining with ranibizumab or 2.0 mg aflibercept for nAMD in trials.
OPHTHALMIC SURGERY
Associate Professor Anthony Kwan performed Queensland’s first surgery for nAMD with an anti-VEGF port delivery system (PDS) that is approved in the US and may have regulatory clearance in Australia soon. Kwan operated on the first patient in Queensland – and 14th in Australia with Sydney-based Professor Adrian Fung performing the country’s first – with the therapy that slowly releases anti-VEGF medication within the eye (over 24 to 36 weeks). Surgeons’ ability to perform glaucoma canaloplasty procedures took a step forward this year when Nova Eye Medical launched the iTrack Advance in April, building on the company’s proprietary iTrack device released in 2008. The main feature is an easy-to-use handpiece, in the hope that the procedure can be performed by a wider group of surgeons.
Vision Eye Institute’s Associate Professor Michael Lawless became the first
year. It uses the VISUMAX 800, the newest generation of ZEISS femtosecond lasers.
In another ‘first’, Australian ophthalmology network PersonalEYES, with 10 surgery clinics in NSW and ACT, offered a breakthrough method of measuring and combining data to generate a multi-dimensional model of the eye for more precise laser eye treatment, after installing Alcon’s Innoveyes system.
KEY EVENTS AND TRADE SHOWS
Almost three years since its last major event, ODMA hosted a successful of OSHOW22 in May and hinted that it could become a permanent biennial fixture for Sydney. The optical trade fair attracted around 1,100 industry professionals who capitalised on the opportunity to view the latest releases from more than 70 suppliers across 130 booths.
Similarly, the long and weary return to an in-person RANZCO Scientific Congress came to an end in October/November, as the college put three years of disruption behind it to deliver the 53rd congress as a hybrid event at the Brisbane Exhibition and Events Centre. The event, which welcomed more than 1,700 in-person delegates, also marked several new governance changes for the college with Dr Grant Raymond elected president, Dr Andrew Thompson censor-in-chief, Dr Peter Hadden and Dr Sonia Yuen as new board directors and Dr Clare Fraser elected for a second board term.
Meanwhile, registration opened for an event taking place next year that is being hailed as the largest optometric clinical conference and trade show in the Southern Hemisphere.
O=MEGA23, in partnership with the 4th World Congress of Optometry, will be held in Melbourne in September 2023, following a partnership between ODMA, Optometry Victoria South Australia and the World Council of Optometry (WCO). The joint event is expected to attract more than 2,000 eyecare professionals.

WORKFORCE
At the beginning of the year, when the nation was still at the mercy of the COVID pandemic, Victorian ophthalmologist Dr Anton van Heerden voiced his criticism of the state government’s month-long ban on non-urgent elective surgery, as cataract patients sat at home with deteriorating quality-of-life while day surgeries remained empty ready to operate.
At the time of writing, Portland District Hospital in regional Victoria was yet to find a replacement for ophthalmologist Dr Robert Harvey, who resigned this year after the hospital turned down his request for a contractual change that would have seen him become a visiting medical officer (VMO), allowing him to seek and train a successor.
His departure – with no obvious successor in sight – has created uncertainty for 150 patients on his surgical waitlist and thousands more attending regular clinics at PDH for chronic eye conditions.
The difficulties in finding ophthalmologists to work in regional areas is not limited to Victoria.
Further north, Tamworth native and mother-of-two, ophthalmologist Dr Phoebe Moore, recalled the events that led to her returning from Bristol, UK, to her hometown alongside her father Dr David Moore, which was facing a critical shortage of ophthalmologists.
Tamworth’s ophthalmology situation has since become a flashpoint in a push for policy change around how the government determines areas of workforce shortage. n

52 INSIGHT December 2022
2022 REVIEW
Dale Rolfe’s nine-practice optometry group joined George & Matilda this year.
Dr Phoebe Moore returned to Tamworth to practise alongside her father, helping to relieve an ophthalmology workforce shortage in the area.
BIG TIPS FOR LITTLE FACES – PART 1
 CASSIDY
CASSIDY
Paediatric patients require certain dispensing techniques and a different approach for their little faces. But too often they are treated the same as adults, resulting in inappropriate outcomes. In this two-part series, I’ll reiterate the importance of paying extra attention with this group.
COMMUNICATING
The way you approach a paediatric dispense will set the tone. It’s important to include the child in the discussions and speak in a way they understand. Squat or kneel at eye level, use eye contact and body language so the child feels at ease.
It’s common to be treading a fine line communicating with both the child and guardian. Normally, their needs and wants differ. For example, it’s more likely the child will be more concerned with the colour, shape and brand while the parent may be looking more at functionality, cost and warranties. Prioritising what’s most important can be tricky, but remember a child won’t wear uncomfortable glasses, or specs they don’t like.
In addition, you may come across dominant parents. If they use phrases such as: “Mum and dad are the ones that need to like the frame as we are the ones looking at you”, or “we are the ones paying for it, you have to wear it”, then you may need to have a quiet word reminding them of the need for the child to be involved and happy with the final choice. We want to remain respectful and professional when doing this, ensuring the parents are on board, and not contradicting them in front of the child.
FRAMES
It pays to be mindful of a few points when choosing frames specifically for kids.
Firstly, if it’s their first pair, they may still be processing the news and react in several ways. Some older children or teens may see specs as an accessory in today’s culture, but others may understandably be upset and anxious about being teased. We need to avoid negative stigma around glasses and try and make the process fun and enjoyable, keeping in mind it may simply take time for them to come to terms with it.
For first-time wearers, it’s likely they won’t have a strong preconceived idea
about their image. Therefore, encourage trying on what fits them, allowing them to experience a range of styles. We can use phrases like: “that looks cool” or “does this go in the good pile or the bad pile?”. Use relatable and age-appropriate language. Specifically, the frame fit for children requires utmost attention. It’s important not only that the frame can support the lenses and prescription, but that it’s comfortable. A child won’t want to wear a frame otherwise.
In years gone by, kids frames were simply small adult frames. Today, we have frames much more appropriate to children’s faces. Remember their anatomy is still growing. Younger children will not have a developed bridge. That means we want frames with low crest heights, larger frontal angle, larger splay and flatter pantoscopic angle. Often we will require nose pads, or some ability in adjusting the bridge.
The temples should also be paid special attention. An inappropriate dispense occurs when a frame is chosen where the temple tip is behind the ear, and the metal part of the arm is sitting on the child’s ear. This would be difficult to adjust, and cause pain, discomfort and slipping of the frame. A good frame characteristic would be the ability to shorten the temple tips.
Durability is an important factor for
paediatric dispenses too such as spring hinges. Most frames for children are typically a metal frame. We should be ensuring these meet the previous requirements, and don’t have sharp edges that could injure them if struck with a ball. Titanium or a flexible metal are the ideal metal materials for kids. Something to avoid is demonstrating the flexibility of a frame to the child. This can could encourage them to bend, and possibly break the frame.
Finally, we should not be dispensing frames that the child will “grow into”. Having wider frames means they can be knocked off, affects the lens choice, increases aberrations, thickness and weight. It also impacts the basic fit of the frame, and typically kids won’t want to wear oversized frames.
Part two of this series will cover lenses and measurements when dispensing for children, and a few pointers on how to approach collection time. n
 ELIZABETH
ELIZABETH
“WE WANT FRAMES WITH LOW CREST HEIGHTS, LARGER FRONTAL ANGLE, LARGER SPLAY AND FLATTER PANTOSCOPIC ANGLE”
DISPENSING FOR CHILDREN CAN BE A CHALLENGING – AND EQUALLY REWARDING – PART OF THE JOB. ACOD TRAINER ELIZABETH CASSIDY OUTLINES WHERE EXTRA CARE IS REQUIRED FOR THESE PATIENTS.
ABOUT THE AUTHOR: ELIZABETH CASSIDY who started working in optics in 2015, is an optical trainer and compliance officer for the Australasian College of Optical Dispensing (ACOD). She has completed a Cert IV in optical dispensing and a Cert IV in Teaching and Assessing. She has worked at numerous practices across Australia, as a senior dispenser and training other staff.
DISPENSING INSIGHT December 2022 53
The needs of the child and parent can differ when it comes to selecting frames.
NEW PRESIDENT TO OVERSEE THREE-YEAR STRATEGIC PLAN
Orthoptics Australia (OA) held its 78th Annual Conference in Brisbane on the 29-30 October 2022. The highly successful event, run concurrently with the RANZCO Congress, saw a return to in-person meetings for the organisation and marks an important re-focusing on the future following the disruption of the COVID-19 pandemic.
Following the OA Annual General Meeting (AGM) on the 29 October 2022, annual conference delegates welcomed myself as the newly elected president of the organisation.
As an orthoptist, senior academic and researcher in the Discipline of Orthoptics, Graduate School of Health at the University of Technology Sydney, I come to the role with a strong connection to the profession, and understanding of OA operations, having held positions within the organisation at both state and federal level for over a decade, including the role of OA vice president for the last three years.


I replace Ms Jane Schuller who had been OA president since the latter part of 2019, and who on stepping down will remain a member of the OA Board.
During this period, OA had successfully transitioned to a new governance structure as an association incorporated under the Commonwealth Corporations Act. However, the subsequent emergence of COVID-19 brought with it numerous other unpredicted challenges.
Jane’s leadership of OA during the pandemic was exceptional. She provided clear and supportive communication to members during a time of uncertainty and was integral in directing the organisation through challenges as they arose – an achievement for which Jane was awarded the Zoran Georgievski medal for service to the profession.
The OA Annual General Meeting was also the launch for OA’s new 2023 – 2026 Strategic Plan, following an extensive consultative process.
The OA Board worked with member
for all communities across Australia at the heart of OA’s activities over the next three years.
Four key priorities were set out in the plan that emphasise connecting, strengthening, promoting and growing.

Our strategic priorities are about building a stronger orthoptic profession and connecting more broadly with the sector and the community to advocate
University
ORTHOPTICS AUSTRALIA strives for excellence in eye health care by promoting and advancing the discipline of orthoptics and by improving eye health care for patients in public hospitals, ophthalmology practices, and the wider community Visit: orthoptics.org.au
of Technology Sydney, and has held state and federal level positions within Orthoptics Australia over the past decade, including the role of vice president.
A NEW THREE-YEAR STRATEGIC PLAN ADOPTED BY ORTHOPTICS AUSTRALIA EMPHASISES CONNECTING, STRENGTHENING, PROMOTING AND GROWING, WRITES NEWLY ELECTED PRESIDENT DR AMANDA FRENCH.
54 INSIGHT December 2022
AMANDA FRENCH
“OUR STRATEGIC PRIORITIES ARE ABOUT BUILDING A STRONGER ORTHOPTIC PROFESSION AND CONNECTING MORE BROADLY WITH THE SECTOR AND THE COMMUNITY”
Dr Amanda French (right) with outgoing Orthoptics Australia president Ms Jane Schuller.
THE UPSIDE OF COVID
IMPROVED COMMUNICATION, COOPERATION, SELF-CARE AND TECHNOLOGY WERE JUST SOME OF THE BENEFITS TO COME OUT OF THE PANDEMIC, WRITES KAREN CROUCH.
Undoubtedly, COVID and its variants were a devastating pandemic and a curse on mankind, including serious adverse impacts on every aspect of modern life – health, financial, economical, psychological/mental and business, among others.
welcome was the increased attention and care for aged folks although, given the disease’s deadly impact on the elderly, many were infected and even died before a more reliable defence could be developed.
PRACTICES
KAREN CROUCH
However, given the strength and resilience of the human spirit, it was converted to achieve many improvements in various aspects of our day-to-day lives which I refer to as “Good COVID”. In this article, I will revisit some valuable derived benefits –even though they were forced on society.
COMMUNICATION & COOPERATION
Federal, state and all levels of government constantly kept in touch through technology-driven, audio visual conferences to promulgate disease management, reporting and healthcare standards. There were inevitable disagreements under our federation style of democracy which affords each state and territory decision making rights over their federal counterparts, resulting in differences of opinion e.g. border closures. Regardless, the overall intention of controlling the pandemic was never so unanimous.
Cooperation between authorities and individuals was never more universal despite several protests and strongly expressed views of opponents to vaccines. Compliance with health mandates (mask wearing, hand washing, isolation and lockdowns etc) was remarkable as each one was onerous or required strict discipline. More than ever, it generated increased concern about each other, encouraging more frequent use of the caring “are you OK?” practise. Most
And boy didn’t all practice staff apply the basic rules of ‘effective meeting’ management (communication/ cooperation)? These are worth revisiting to ensure the efforts are maintained as the age-old habit of some healthcare practices holding meetings for social, rather than health-related outcomes, were discontinued as a result of new COVID-related pressures.
I was once requested to outline what makes for an effective meeting. With experience of practice meetings and staff cooperation, we identified the following components:
• Improve communication and decision making;
• Exchange experiences, information and knowledge;
• ‘Work smarter’ (research) forums;
• Implement decisions effectively; and
• Corporate governance reasons.
Some meetings for social purposes are conducted on an informal basis, for business/relationship development purposes. Generally, content is less structured, albeit well planned beforehand. We asked meeting groups the following questions, based on the general principles of effective meetings:
• Do meetings have a pre-circulated agenda? – indicates a ‘purpose’ for the meeting;
• Is a chairperson or leader appointed? –evidence that there will be a ‘controller’ to focus attendees on agenda items under discussion, assign actions to specific individuals where necessary, and ‘watch the clock’ so items are not deferred or left undecided;
Are desired outcomes or decision options understood? – where applicable, this ensures participants are aware that a decision is required for certain discussion items;
Are meetings properly ‘time planned’? – suggests thought has been given to adequacy of time required to do justice to each topic;
• Is relevant pre-reading circulated? – where an item warrants it, prereading affords attendees an opportunity to prepare and contribute more meaningfully, also evidencing thoroughness of the meeting coordinator;
• Are self-assessment ‘meeting evaluations’ conducted? – means by which teams strive to improve meeting quality and outcomes; and
• Are minutes (including resolutions) and Action Items documented and distributed? – provides continuity and implementation of resolutions when minutes are tabled at subsequent meetings.
Staff, clinicians and principals found the exercise highly beneficial, injecting meaningful structure and achievementoriented content into meetings, without introducing excessive bureaucracy.
Noted, while meetings are a useful form of communication, decision making and planning, the other extreme is too many – meetings for the sake of meetings. A decision that could be made relatively easily by circulated email might only require a meeting if parties involved cannot reach agreement on a proposal.

CONCLUSION
Through these effective staff gatherings we all learnt how to protect ourselves through constantly updated information broadcasts about the latest health requirements, such as lockdowns and vaccines.
Overall, while we may wish to never revisit another pandemic like COVID, let’s be positive-minded while continuing to be alert and vigilant, looking back on the valuable benefits we derived from this nasty experience. It’s made us much stronger for analysing it, developing solutions and deriving many personal and business-wide practices to live with it. n
ABOUT THE AUTHOR: KAREN CROUCH is Managing Director of Health Practice Creations, a company that assists with practice set ups, administrative, legal, business and financial management. Contact Karen on 0433 233 478 e-mail kcrouch@hpcnsw.com.au or visit www.hpcgroup.com.au.

MANAGEMENT
“A DECISION THAT COULD BE MADE RELATIVELY EASILY BY CIRCULATED EMAIL MIGHT ONLY REQUIRE A MEETING IF PARTIES INVOLVED CANNOT REACH AGREEMENT”
INSIGHT December 2022 55
COVID forced businesses to embrace technology for effective meetings.
People ON THE MOVE
ophthalmologist in China and then most recently as a ophthalmology specialty fellowship, at the prestigious West China University of Medical Science. She hopes to place a strong focus on providing professional








at
2020 Australia CEO Ms Patricia Sparrow is departing to return to the aged care sector. She has accepted a new role as CEO of Council on the Ageing, Australia’s national peak body for older Australians. Prior to joining Vision 2020, she was CEO of Aged and Community Services Australia for five years. Sparrow commenced as Vision 2020 Australia CEO in September 2021, leading the development of a new ambitious strategic plan, including a refreshed policy
CAREER 56 INSIGHT December 2022
Consultants SA. He was previously RANZCO's VicePresident, with Prof Peter McCluskey now elected to
Abbott, Phillips and Becton Dickinson, Roche Diagnostics and Biorad Laboratories. Most recently, she held the role of General Manager for Abbott’s Structural Heart franchise.
Email editor Myles Hume at myles.hume@primecreative.com.au to be featured.
Insight's monthly bulletin to keep the Australian ophthalmic sector updated on new appointments and personnel changes, nationally and globally.
JANUARY 2023
HONG KONG INTERNATIONAL OPTICAL FAIR
Hong Kong 9 – 11 January event.hktdc.com
FEBRUARY
MIDO Milan, Italy 4 – 6 February mido.com
2023
MARCH 2023
ANZ CORNEA SOCIETY AND EYE BANK MEETING Perth, Australia 9 – 10 March rybooking.com/events landing/922238
CONGRESS ON CONTROVERSIES IN OPHTHALMOLOGY Lisbon, Portugal 24 – 25 March cophy.comtecmed.com
ARVO 2023 New Orleans, US 23 – 27 April arvo.org/annual-meeting
MAY 2023
ANZSRS MEETING Melbourne, Australia 20 – 21 May ranzco.edu/events/2023
JUNE 2023
ANZGS CONGRESS
Queenstown, New Zealand 16 – 19 February anzgsconference.com
APAC ACADEMY OF OPHTHALMOLOGY CONGRESS
Kuala Lumpur, Malaysia 23 – 26 February 2023.apaophth.org
SPECSAVERS
Locum Opportunities in SA
APRIL 2023
AUSTRALIAN VISION CONVENTION Gold Coast, Australia 1 – 2 April events@optometryqldnt.org.au
ASO EXPO 2023 Sydney, Australia 2 – 4 June asoeye.org
WORLD GLAUCOMA CONGRES Rome, Italy 28 June – 1 July worldglaucomacongress.org
To list an event in our calendar email: myles.hume@primecreative.com.au
JULY 2023
AUSCRS 2023
Port Douglas, Australia 26 – 29 July auscrs.org.au/2023-conference
SEPTEMBER 2023
O=MEGA23 & WORLD CONGRESS OF OPTOMETRY Melbourne, Australia 8 – 10 September omega-event.org
OCTOBER 2023
RANZCO SCIENTIFIC CONGRESS Perth, Australia 20 – 24 October ranzco.edu/events
Specsavers are seeking locums who have a real passion to provide the best service to our patients in metro and regional South Australia. If you’re flying in from interstate all flights, accommodation and car hire will be provided and booked for you. We currently have many locum days available across the state from November through to the new year and onward with the opportunity to fill your diary or just pick up the odd day. If your optometry goal is to improve the health of every Australian, please contact Matthew on 0447 276 483 or matthew.cooney@specsavers.com.
Interested in relocating to NZ?
Specsavers has a range of opportunities for NZ optometrists looking to return home. From North to South, we have fantastic opportunities for optometrists at all levels.
And as a Specsavers optometrist, you’ll have the chance to advance your skills and become part of a business that is focused on transforming eye health outcomes in New Zealand.
Be equipped with the latest ophthalmic equipment (including OCT in every store for use with every patient) and develop your clinical experience across a range of interesting conditions and an ever-growing patient base.
You’ll also have the support of an experienced dispensing and pre-testing team, the mentorship of store partners and access to an exemplary professional development program. There’s no place like home – so if you’re ready to return, let us help you.
Optometrist Joint Venture Partnership opportunity- Cessnock, NSW
The store is situated in the Cessnock Plaza, opened in 2009, is equipped with 2 Optical test rooms, 4 dispense desks, over 1000 frame display, 1 pre-test room and a dedicated VF room, and state of the art equipment including OCT. Within the next two decades Cessnock is expected to be among the fastest growing areas in NSW. Opportunity for an expansion into a 3-test room practice with a dedicated Audiology room. Located in the Hunter Region of New South Wales, Cessnock lies 40km west of Newcastle and provides easy access to the Hunter Valley, Australia’s oldest and internationally acclaimed wine region.
Optometrist opportunities across NSW
Due to exciting growth and several upcoming expansions, Specsavers has great Optometrist opportunities available across NSW with both metro and regional locations on offer. We offer flexible rosters to support work/life balance with options for part-time or full-time work, we’ll give you access to the latest technology and equipment (including OCT in every store) and we’ll pay you a competitive salary. We can also provide you with excellent opportunities for career development and progression – including pathway to Partnership.
Highest package ever! $180,000 for the growing Mobile Optometrist Role Specsavers is growing our community based Mobile Optometry Team Nationally, With home based locations in Newcastle, Perth & Melbourne along with longer term Fly in Fly out roles available. With an amazing $180,000 package on offer. You will experience a wide variety of cases, whilst being able to explore different regions of Australia. We are looking for someone who has the desire and flexibility to travel.
SO LET’S TALK!
In a few short years, Specsavers has achieved market leadership in Australia and New Zealand with more people choosing to have their eyes tested and buy their prescription eyewear from Specsavers than any other optometrist. To learn more about these roles, or to put your hand up for other roles as they emerge, please contact us today:
Joint Venture Partnership opportunities enquiries: Kimberley Forbes on +61 (0) 429 566 846 or E kimberley.forbes@specsavers.com
Australia Optometrist employment enquiries: Marie Stewart – Recruitment Consultant marie.stewart@specsavers.com or 0408 084 134
Locum employment enquiries: Cindy Marshall cindy.marshall@specsavers.com or 0450 609 872
New Zealand employment enquiries: Chris Rickard –Recruitment Consultant chris.rickard@specsavers.com or 0275 795 499
Graduate employment enquiries: apac.graduateteam@specsavers.com
2023 CALENDAR
– YOUR CAREER, NO LIMITS VISIT SPECTRUM-ANZ.COM
All
stores now
Specsavers
with OCT
PORT DELIVERY SYSTEM FOR NEOVASCULAR AMD
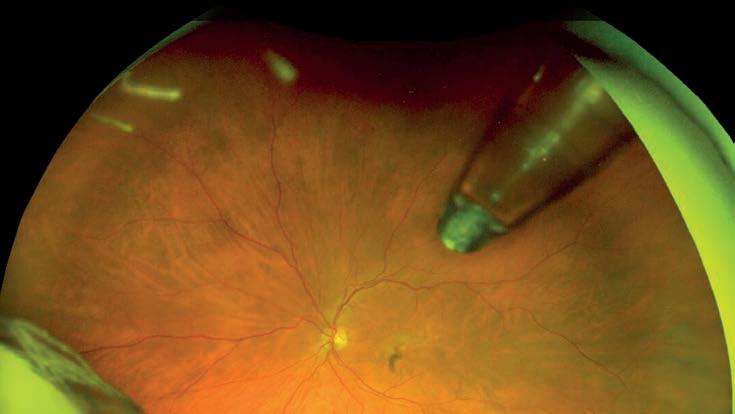
PDS filled every 24 visual outcomes to monthly ranibizumab year. It showed 98% of the PDS group didn’t need additional treatment, and was well tolerated. The PDS’ main issue is it’s a new device implanted with a new surgical technique. It’s associated with an increased risk of potential complications (similar to the first IOL implantation or glaucoma tube surgery). Possible complications for PDS include vitreous haemorrhage, conjunctival erosion or retraction, endophthalmitis, rhegmatogenous retinal detachment, and septum dislodgement. It’s comforting to know these rates appear to be trending down due to a combination of improving techniques and experience.
approach over existing treatments first PBS-listed 15 years ago1, alternative anti-VEGF agents and drugs are being explored. But still regular anti-VEGF injections – every four months in the best cases – remain the gold standard.
In October 2021, the US approved a new, first-of-its-kind, treatment device for nAMD, namely the Port Delivery System (PDS), delivering a customised formulation of ranibizumab.2 The approval was based on the Phase 3 ARCHWAY randomised controlled trial.3 The PDS is a permanent, refillable implant surgically inserted via the pars plana into the vitreous cavity and buried under the conjunctiva. The device is pre-filled with a specific ranibizumab concentration (100 mg/ml) which diffuses slowly and continually into the vitreous gel, maintaining a therapeutic level of anti-VEGF. The device will need to be refilled at a specific interval in an office or clinicbased refill-exchange procedure. It has a controlled release element at one end, letting ranibizumab diffuse into the vitreous cavity, and an extra-scleral flange encasing a silicone septum at the other end where the refill occurs. This therapy aims to replace regular injections, with refills occurring up to twice per year.
The two-year, Phase 3 ARCHWAY study compared the PDS to monthly ranibizumab injections in recently diagnosed nAMD (previously treated with intravitreal anti-VEGF therapy for up to nine months). It demonstrated a
Based on these encouraging results, a new study, Velodrome (a Phase 3b, global, multicentre, randomised, visual-assessormasked study), is assessing the efficacy, safety, and pharmacokinetics of the PDS with ranibizumab 100 mg/mL delivered every 36 weeks compared with 24 weeks. It aims to recruit over 440 nAMD patients worldwide. The first patient in Australia (and first outside the US) was under the care of A/Prof Adrian Fung in Sydney, and the implant procedure was performed in July 2021. Many new trial sites are now recruiting across Australia. More recently, the first patient was enrolled on trial by A/ Prof Fred Chen in WA.
In July 2022, the first patient underwent the procedure at our site, the Queensland Eye Institute. All sites are carefully selected to ensure they have the necessary clinical expertise, personnel, and equipment support. A strict inclusion and exclusion criteria is followed for participants to ensure patient safety. The surgeons are specially trained via online seminars and courses to ensure they’re familiar with the device and implantation procedure. Surgical steps are meticulously explained – with regards to the importance of tissue (conjunctiva and tenon) handling – to reduce the risk of postoperative implant exposure, haemostasis to minimise vitreous haemorrhage risk, and precise measurement of the sclerotomy to ensure a snug fit for the device. Surgeons used model eyes to practise the technique prior to the implantation date. There is a Global Surgical Device Liaison from the trial company on site to supervise and to maximise outcomes. Our patient was enrolled after four injection doses
and a failure to extend the injection interval. He underwent the implantation procedure uneventfully in July. He responded favourably and provided the nAMD remains under control, the refill-exchange will take place in 2023. Patients recruited across Australia is approaching 30, but due to the recently reported complication of septum dislodgement, there is a pause to this trial and all PDS implantation.
Due to its complication rate, PDS isn’t suitable for all needing intravitreal injections for nAMD, but will add to the treatment armamentarium for a certain patient subgroup, for example, those needing short injection intervals. The PDS is perhaps the first new treatment providing a paradigm shift in nAMD management. On the horizon, there are other potential treatments, including molecules with dual actions or gene therapy.4 The future of the nAMD management is exciting and forever changing. n
NOTE: References will appear in the online version of this article.
Name: A/Prof Anthony Kwan
Qualifications: MBCHB, MD (London), FRCOphth (UK), FRANZCO Organisations: Queensland Eye Institute, Mater Hospital Brisbane, and the University of Queensland Position: Director of Vitreoretinal Service (QEI), Senior Staff Specialist and consultant vitreoretinal surgeon Location: Brisbane. Years in profession: 30, clinical practice and research.

SOAPBOX
THE PORT DELIVERY SSYSTEM FILLED EVERY 24 WEEKS HAD NON-INFERIOR VISUAL OUTCOMES TO MONTHLY RANIBIZUMAB OVER ONE YEAR.
58 INSIGHT December 2022
A widefield angle retinal scan showing the Port Delivery System in the eye.
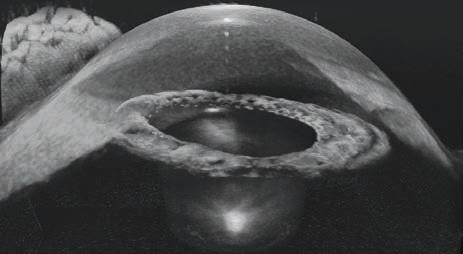


Are you an influential optometrist who wants to take the next step in their career? We are looking for strong people leaders, passionate optometrists with a business drive to lead our Western Australia stores. The role of the Managing Optometrist is to lead, coach & develop our in store optometry team, and build strong partnerships with the store team to deliver great eyecare. You will also participate in special projects to support our state eyecare team. It is a fantastic personal and professional development step and you will have the opportunity to accelerate your career!

This fantastic opportunity is available in the following locations: • Mandurah • Joondalup • Perth • Morley • Rockingham • And more! ACCELERATE YOUR CAREER WITH OUR MANAGING OPTOMETRIST OPPORTUNITIES. TAKE YOUR EYECARE CAREER TO THE NEXT LEVEL! WANT TO KNOW MORE ABOUT THE OPPORTUNITY? PLEASE CONTACT OPTOMETRY.CAREERS@AU.LUXOTTICA.COM LEARN MORE OPSM.COM.AU/CAREERS VISIT US ON LINKEDIN










 MYLES HUME Editor
MYLES HUME Editor



















































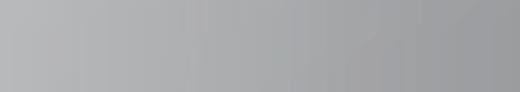



















































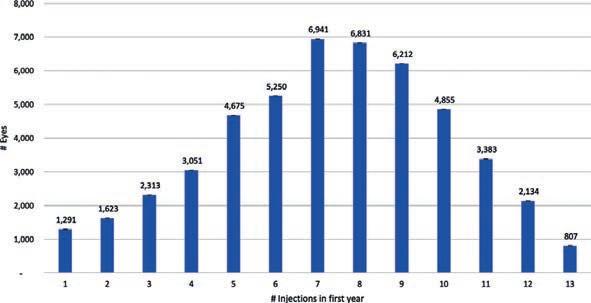

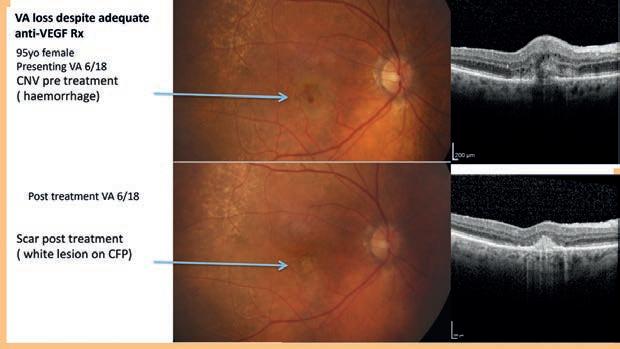


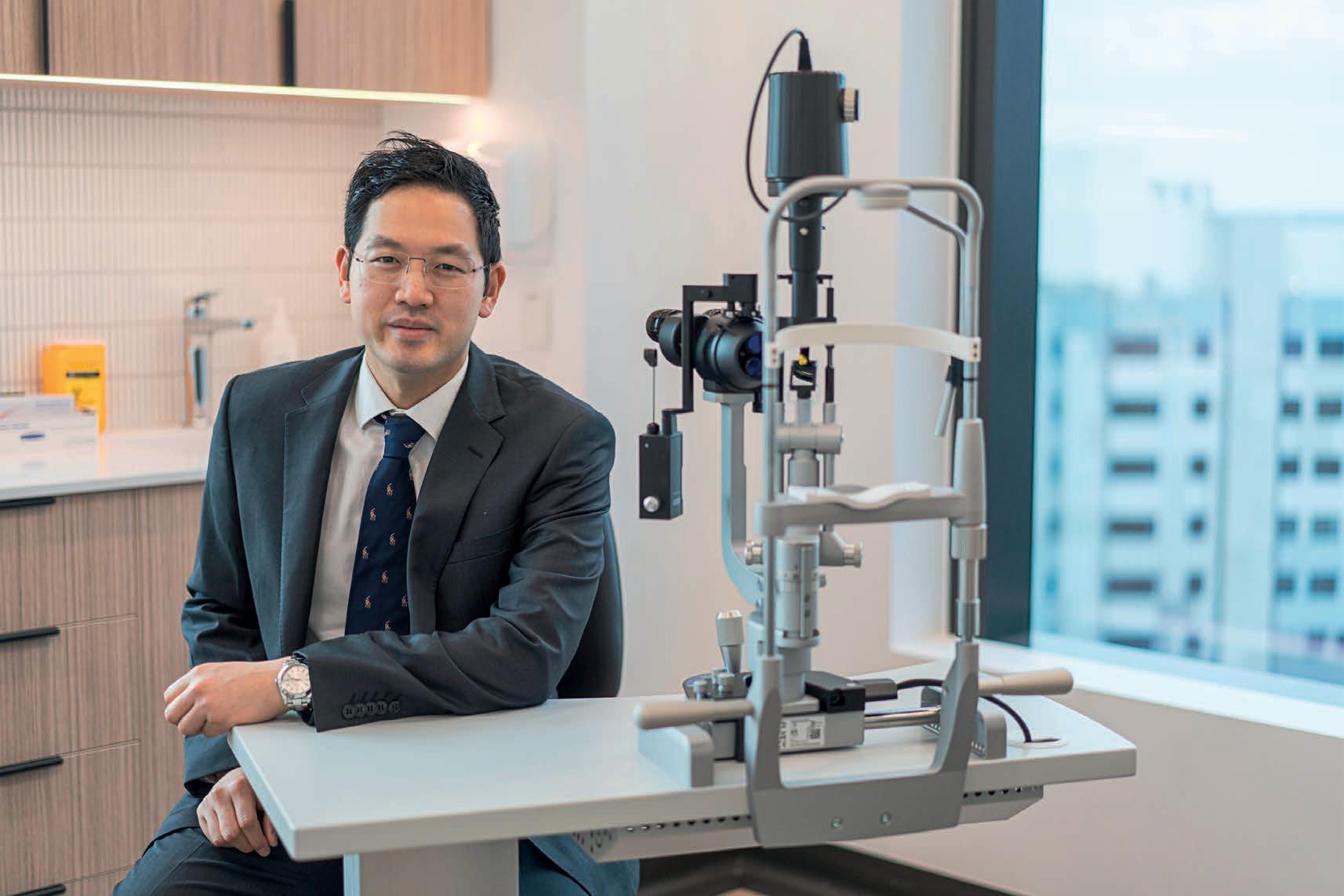










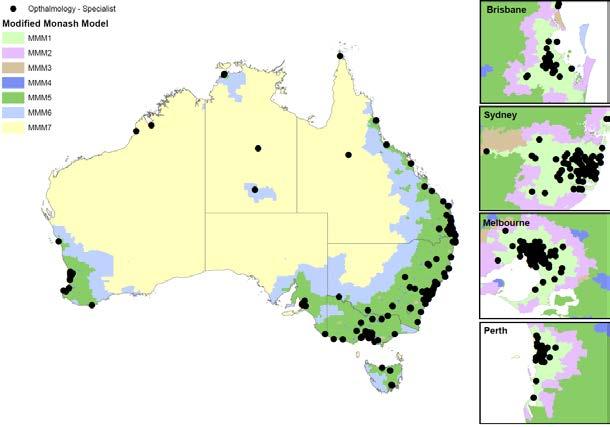

















 CASSIDY
CASSIDY
 ELIZABETH
ELIZABETH