WOMEN'S HEALTH AND MEDICAL RESEARCH




Supporting women's health and medical research is, an obvious thing to do. It is crucial for Australia; it is imperative for our home life, our work, our play as well as the ongoing viability and sustainability of our nation. It is not about one gender being more important or valuable than another, it is about recognising differences and then providing equity and access.
Unfortunately, we see bias surrounding women’s health and medical research throughout the health and medical research ecosystem. At the workforce end there is overwhelming evidence that women face systemic challenges in the STEM workforce and beyond, which negatively impacts their engagement, experiences, and opportunities for career progression. Monash University found that women only make up approximately 17% of leadership positions, such as senior scientists in Australia.
At the funding end of the ecosystem, Professor Anne Kelso found that between 2019 and 2021, male applicants received about 35% more investigator grants from the NHMRC and 67% more total funding (about $95 million extra per year) than female applicants.
It therefore seemed obvious that this bias would flow onto the health and medical research, and clinical sections of the pipeline. This view is supported by the fact that the article for the “Last Word” was written by The Hon Ged Kearney MP, Assistant Minister for Health and Aged Care, sharing her views on the “deeply entrenched bias against women in the health system”.
I was deeply honoured when she invited me to join her and other health and medical research leaders on the National Women’s Health Advisory Council, whose role is to provide strategic advice to government on improving Australia’s health system for women and girls.
And yet I was also saddened that we are still having this conversation in 2023! Supporting women's health and medical research is vital to outcomes for the National Women’s Health Advisory Council, because if we don’t commence change at the research stage then nothing will change further along the health and medical research pipeline.
In this edition of INSPIRE we were delighted by how many diverse and informative articles we received from you, sharing your stories of women inspired health and medical research. The Victor Chang Institute and the Australian Centre for Heart Heath both contributed wonderful articles
about Spontaneous coronary artery dissection (SCAD), which is responsible for causing one quarter of all heart attacks in women under the age of 50!
Read about how the Garvan Medical Research Institute and Calvary are using innovative technology and reviving previous research to find answers to treating various types of breast and ovarian cancers. Learn more about research that is taking place at Curtin University around improving the understanding of menstrual health for young women. Explore the complimentary work being done by the University of Queensland and the University of Newcastle to understand menstrual disorders in adolescents, which is being mapped in a longitudinal study on Australian women’s health.
Read about community lead initiatives for migrant and refugee women’s sexual and reproductive health needs in Western Sydney. See the advances that are being undertaken in reproductive health from uterus transplantation to the potential to develop a prognostic test to guide personalised treatment. Finally read from members The George Institute about and gender politics in women’s health and medical research. Be inspired by the stores of advancing women’s health care from Monash University and female led research from the RACP.
Our members were again truly generous in sharing their “INSPIRE-ing” work that is being done to help shine much needed light on women’s health and medical research. We hope that you, like us, are in awe of the work that is being done to improve the lives of the women in our lives; our mothers, wives, sisters, daughters, friends and colleagues.
Best wishes
Nadia and your Research Australia Team














14 How 57,000 women are shaping health policy in Australia UNIVERSITY OF NEWCASTLE


16
Is my period ‘normal’?
UNIVERSITY OF QUEENSLAND
Publisher Research Australia Ltd
Art Direction
Matthew Ware p +61 403 844 763 e matt@objktive.com
For Advertising enquiries please contact the Research Australia office on p 02 9295 8546 or e admin@researchaustralia.org researchaustralia.org
INSPIRE ONLINE issuu.com/researchaustralia
INSPIRE is a publication of Research Australia Ltd ABN 28 095 324 379 384 Victoria Street Darlinghurst NSW 2010
Who can submit articles?
Any current member of Research Australia who would like to share a relevant story that affects their organisation including, philanthropic donations and their outcomes, research findings, and any other related health and medical research topic that affects the Australian population.
Submission guidelines & deadlines
For information regarding how to submit and publishing deadlines visit the Research Australia website
Disclaimer
26 UNIVERSITY OF WESTERN AUSTRALIA
The longer-term effects of IVF on offspring from childhood to adolescence


28
Development of a national program to prevent harmful early births
UNIVERSITY OF WESTERN AUSTRALIA
36 Mapping migrant and refugee women’s sexual and reproductive health needs.
WESTERN UNIVERSITY
38
Building Bridges for Health: Advancing Women’s Sexual and Reproductive health
UNIVERSITY OF ADELAIDE
The opinions expressed in INSPIRE do not necessarily represent the views of Research Australia. Whilst every effort has been made to ensure accuracy, no responsibility can be accepted by Research Australia for omissions, typographical or inaccuracies that may have taken place after publication. All rights reserved.
The editorial material published in INSPIRE is copyright. No part of the editorial contents may be reproduced or copied in any form without the prior permission from Research Australia. © Research Australia 2020.
40 Simple low-dose aspirin may boost ovarian cancer survival
QIMR
 My Twitter : @chriskere CHRISTOPHE KEREBEL CHRISTOPHE KEREBEL My Twitter : @chriskere
My Twitter : @chriskere CHRISTOPHE KEREBEL CHRISTOPHE KEREBEL My Twitter : @chriskere


















At its August 2023 meeting, the Health Economics Roundtable focused on the role of health economics in health system reform, with a particular exploration of the Medicare system in this context. The meeting heard from Mr Simon Cotterell, First Assistant Secretary Department of Health and Aged Care on the current Medicare reforms, Professor Tony Scott and Dr Susan Mendez from Monash University on research into Medicare and Dr Pradeep Philip and Ms Sruthi Srikanthan on the findings of the independent review into Medicare Integrity and Compliance. These thought-provoking presentations prompted discussion about the need for accessible data sources, the value of a coordinated, unified approach to advocacy and the opportunities for health economics to contribute to this landscape of significant reform.
Research Australia continues to use our Health Economics Roundtable as a forum for collaboration, discussion, and advice, to advance the unique role for health economics research in driving the development of evidence-based policy and programs that deliver better health and a more effective and efficient health system. The next Health Economics Roundtable will be held in 2024.
The Research Australia University Roundtable on 30 August was hosted by the University of the Sunshine Coast (USC) at Sunshine Coast Health Institute (SCHI).

The program commenced with a tour of the SCHI led by SCHI Operation manager Clare Hanlon and accompanied by USC’s Professor Rob Harvey. This was followed by lunch in the Boardroom where the group was joined by Professor Ross Young, DVCRI, at USC, and guest presenter Professor Scott Bell, CEO at the Translation Research Institute.
The formal proceedings commenced after lunch with those unable to attend in person joining the meeting virtually. 24 universities were represented, and the meeting was chaired by Professor Russell Gruen, Dean of the ANU College of Health and Medicine. The two main topics for the day were ‘researchers engaging with the Health system’ which commenced with a presentation by Professor Bell, and ‘Researchers engaging with Government’, opening with a presentation from former Health Minister and now University of Melbourne Honorary Enterprise Professor Greg Hunt.
Nadia Leven, Research Australia CEO & Managing Director, with Mr Simon Cotterell, First Assistant Secretary Department of Health and Aged Care.

On 26 August, Research Australia held a very well attended function at QIMR Berghofer – Queensland’s oldest medical research institute - on Unlocking the Economic Potential of Queensland Health Innovation. Professor Fabienne Mackay, Director and CEO of QIMR Berghofer, hosted Research Australia as we gathered together around 80 Research Australia members, key government officials and economists to discuss the amazing growth in health and medical research in Queensland over the last 25 years and its economic impact going forward.
The event acknowledged the role of Queensland Government programs such as Smart State and Advance Queensland and also the very generous donors to the Queensland HMR sector over many years, such as Clive Berghofer and Chuck Feeney, in funding both infrastructure and research.
A panel comprising Dr Julie White, Executive Director of Health Innovation at Queensland Health; Senior VicePresident of Vaxxas Ltd Mike Junger and CEO of QIMR Berghofer Prof Fabienne Mackay, gave the audience

some interesting insights.
The audience heard that the Queensland Biomedical 10-year Roadmap and Action Plan’s aim of a globally competitive Asia-Pacific biomedical hub would see the sector’s export value in Queensland worth $477 million by 2027, with an annual gross value added to the economy of $2.11 billion.

Following this panel, the audience heard from a health economist and two health and medical research business founders on how Queensland is monetising research, to the point where manufacturing, at 15.3% annually, is now the state’s largest single economic output.
Finally, Member for Stretton James Martin MP, who was representing the Queensland Health Minister Shannon Fentiman, spoke on behalf of the State Government, recognising the great contribution to both the economy and population health of the Queensland Health and Medical Research community, and recognised that the financial contributions of government and philanthropy were also essential in continuing growth in the sector.
Mr James Martin MP, Member for Stretton, Professor Fabienne Mackay, QIMR Berghofer CEO, and Nadia Levin, CEO and Managing Director Research Australia CHRISTOPHE KEREBEL CHRISTOPHE KEREBEL CHRISTOPHE KEREBELIt’s also the most common cause of heart attack associated with pregnancy and generally affects women who are otherwise fit and healthy.
Scientists at the Victor Chang Cardiac Research Institute are finally honing in on what drives this disease and are leading Australia’s first research program into SCAD.


Spontaneous coronary artery dissection (SCAD) is a serious condition, mainly occurring in women, when a tear forms in one of the blood vessels of the heart. This can

It used to be considered a rare disease. But spontaneous coronary artery dissection or SCAD is now known to cause around a quarter of all heart attacks in women under the age of 50.Left to Right: Dr Christine Lucas, Dr Nicole Bryce, Dr Kathryn Wolhuter, Professor Jason Kovacic
slow or block blood flow to the heart, leading to a heart attack.
Many people who develop SCAD are otherwise fit and healthy. Unlike traditional heart attacks, SCAD is not associated with a plaque build-up and a blockage of the arteries.
Scientists at the Victor Chang Cardiac Research Institute are part of an international team that has recently published research in Nature Genetics showing there are at least 16 genes associated with SCAD, with one gene called PHACTR1 thought to be a key driver.
By examining data from nearly 2000 patients, they discovered the genes involved in causing SCAD are mainly implicated in forming the matrix or scaffolding around the cells forming coronary arteries, as well as a gene involved in blood clotting. A deficiency in this clotting factor is thought to increase the likelihood of a spontaneous bleed into the artery wall, which reduces blood flow as it expands and leads to a SCAD heart attack.

“We have performed the largest study to date aimed at understanding the genetic basis of SCAD, discovering multiple genetic regions that confer susceptibility to SCAD,” said Associate Professor Eleni Giannoulatou, who together with Professor Bob Graham and Professor Jason Kovacic led the Australian arm of the study.
Professor Kovacic, Executive Director of the Victor Chang Cardiac Research Institute, said: “SCAD is still a relatively little-known disease, but it has a huge impact and is behind a quarter of all heart attacks in women under the age of 50. We now have a much clearer picture of the genetic risk of SCAD and how it is related to other cardiovascular diseases. Understanding these mechanisms should lead to new approaches to its management and treatment.”
Professor Kovacic’s team is leading research into the gene called PHACTR1 which has been identified as having one of the strongest genetic associations with SCAD.
It is hoped that by better understanding the function of the PHACTR1 gene, researchers at the Institute may be able to uncover how to control the gene to treat and potentially prevent SCAD from occurring in the first place.

In addition, the researchers are the first research team outside of the USA to join the iSCAD Registry – the International SCAD registry - a global collaboration of researchers and patients investigating the features and pathophysiology of SCAD.
The iSCAD Registry contains the medical history of 1271 SCAD patients – who until now were all from the United States. Australian patients can now contribute their data to shed more light on this disease.
The Institute has been invited to play a key role as the Australian contingent of the first international randomised, controlled trial of SCAD management (the APT-SCAD trial) involving over 2,500 SCAD survivors from 190 centres in 10 countries. This trial will test if moderate - as compared to intensive - blood thinning treatment improves outcomes and reduces major adverse cardiovascular events, including bleeding and recurrences, in SCAD patients.
If successful, the Institute will be the coordinator of the Australian arm of this study, which will involve 200 SCAD patients.
The result of this application will be announced by late 2023.
Professor Bob Graham
Professor Graham heads the Institute’s Molecular Cardiology Department and is the former Executive Director of the Institute. He was also recently appointed Vice President of the Australian Academy of Science and Secretary of Biological Sciences. His research for many years has focused on molecular cardiology, with emphasis on circulatory control mechanisms, hypertension, receptor signalling and cardiac hypertrophy. More recently, his work has focused on cardiac regeneration, cardioprotection, and SCAD. He is the author of over 300 peer-reviewed papers that have received over 20,000 citations.
Professor Jason Kovacic
Professor Kovacic is the Executive Director of the Victor Chang Cardiac Research Institute and Adjunct Professor at the University of Western Australia. In parallel with his vital ongoing research to define new ways to prevent and treat vascular disease, Prof Kovacic is a practicing clinical cardiologist at St Vincent’s Hospital, Sydney, specialising in vascular disease and blockages of the heart arteries.
Professor Kovacic has authored numerous scientific and clinical papers on heart and vascular disease and serves on several NIH committees. He has a particular interest in unraveling the pathobiology of the vascular diseases - fibromuscular dysplasia, and SCAD.
He is also President-Elect of the Australian Cardiovascular Alliance.
Author: Professor Jason Kovacic,
ExecutiveDirector of the Victor Chang Cardiac Research Institute
Spontaneous coronary artery dissection (SCAD) is a non-atherosclerotic cause of acute myocardial infarction (AMI) that occurs from a bleed into a coronary vessel wall causing obstruction of blood flow to the heart1. SCAD is an increasingly recognised cause of heart attack in younger women with few traditional cardiac risk factors. Approximately 90% of SCADs occur in women. SCAD accounts for up to 35% of AMIs in women aged under 501 and is the most common cause of pregnancy-related AMI2. Hospital readmission and event recurrence are more common post-SCAD compared to typical AMI3
SCAD carries significant psychological burden, including shock, uncertainty, isolation and anxiety 4 The stressfulness of SCAD has been attributed to its unpredictability, sudden onset, relative rarity, and high reevent rate1,3. Despite these major impacts, prior to 2020, very little research focussed specifically on emotional and psychosocial aspects of SCAD.

The Australian Centre for Heart Health (ACHH) and the Victor Chang Cardiac Research Institute (VCCRI) began their collaborative partnership in April 2020, following discussions of their shared concerns regarding the
paucity of published literature on psychosocial impacts of SCAD. Since that time, the two organisations have jointly undertaken four inter-related projects, using both qualitative and quantitative methods, with the aim of understanding and addressing psychosocial needs of Australian SCAD survivors.
The partnership between ACHH and VCCRI is very productive, as the Victor Chang team has expertise in identification and management of SCAD, while the ACHH team has expertise in psychosocial research and intervention.
Study 1: SCAD Focus Group Study. Our first study used a qualitative approach to explore experiences of SCAD survivors, specifically highlighting the nature of their stresses and concerns as well as their support needs 4. Thirty participants from the VCCRI database of SCAD survivors (n=27 women) who had their SCAD in the previous 12 months participated in one of seven focus groups. The overarching theme that emerged and dominated all other sub-themes was ‘lack of information about SCAD’. Participants commented that many health professionals had never heard of SCAD, often causing major distress and frustration. Many emotional impacts were identified, including confusion and uncertainty, shock and disbelief, fear and anxiety, loss and grief, and isolation and abandonment. Participants also identified the need for a facilitated support group to assist in their SCAD recovery, and to be able to share their own stories, hear others’ experiences, and feel supported in their journey. Findings of this study were published in PLoS One4.
Study 2: SCAD vs. Non-SCAD AMI Comparative Study. Using data from an earlier study of 162 AMI patients that we had conducted in 2020-2021, we compared anxiety, depression and distress levels in people with SCAD (n=35;22%) and non-SCAD AMI (n=127; 78%). We found a significantly larger proportion of SCAD AMI patients were classified as depressed, anxious or distressed compared to non-SCAD AMI patients. After controlling for other common factors associated with post-event mental health issues, having a SCAD AMI was a significant and unique predictor of anxiety, depression and distress post-event. This work was published in the Journal of Cardiopulmonary Rehabilitation and Prevention5
Study 3. SCAD Online Survey. Building on the findings of the SCAD Focus Group study, our third study aimed to quantify experiences, concerns and psychosocial wellbeing of SCAD survivors. SCAD survivors enrolled in the VCCRI Genetics Study were invited to complete an online questionnaire exploring a range of psychosocial issues, such as SCAD-specific distress, anxiety, depression, resilience, identity, quality of life, and social
support. A total of 310 participants completed the questionnaire, representing a 72% response rate from the 433 SCAD survivors invited to participate. We are currently analysing this data and look forward to presenting findings in due course.
Study 4. SCAD Online Support Program. study arose from the findings of studies 1 and 2 and aimed to address issues and concerns facing SCAD survivors, and to support their emotional recovery after SCAD. With funding from a National Heart Foundation Vanguard Grant, this project involves development and pilot-testing of a SCAD-specific group-based online support program. We developed the program in January and February 2023, began trialling it in March, and will complete this study in December 2023. The program uses the principles of Acceptance and Commitment Therapy (ACT), an evidence-based approach to support psychosocial wellbeing. The 4-week program, which involves 4 weekly sessions of 1.5 hours conducted over Zoom, has now been delivered five times over the trial period. Programs are facilitated by a health psychologist with co-facilitation from a SCAD survivor. Four programs have been delivered to women only, while one program has been for men only. The program is being evaluated by assessing changes in participants’ emotional wellbeing after program participation.
Through this collaboration and series of interrelated projects, we are understanding more about psychosocial issues associated with SCAD and have become wellequipped to support the emotional and psychosocial recovery of this particularly vulnerable and previously under-researched group of patients. According to project lead Dr Barbara Murphy, “this productive collaboration between ACHH and VCCRI has enabled us to better understand the psychological experiences and unmet needs of SCAD survivors and to develop and trial innovative programs to support them in their psychosocial recovery”. This program of research has provided an important foundation to enable us to continue to support Australian SCAD survivors in the future.
Authors: Dr Michelle Rogerson1, Dr Stephanie Hesselson2 , Dr Siiri Iismaa PhD2,3 , Dr Rosemary Higgins1, Mr Michael Le Grande1, Professor Robert Graham2,3 , Professor Alun Jackson, PhD1,4 , Dr Barbara Murphy PhD1,4


1 Australian Centre for Heart Health, Melbourne, Australia.
2 Victor Chang Cardiac Research Institute, Sydney, Australia
3 St Vincent’s Clinical School, University of New South Wales, Sydney, Australia
4 Melbourne School of Psychological Sciences, University of Melbourne, Australia


and housing and residential care for older women, among others.
The ALSWH collects data about the physical and mental health of more than 57,000 participants across four age cohorts: those born between 1921-26, 1946-51, 197378 and 1989-95. Regular surveys also capture insights on a broad range of health factors including the use of health services, health behaviours, risk factors, sociodemographic factors and more.
This year, the study’s oldest active participants are turning 102, giving researchers unprecedented insights into issues that affect women throughout their lifespan.
Professor Deb Loxton from the University of Newcastle and her counterpart, Professor Gita Mishra from The University of Queensland are the directors of the Australian Longitudinal Study on Women’s Health (or ALSWH). Diving into some of the most pertinent issues facing women across all ages, the ALSWH offers the most comprehensive databank of information about women’s health in the country.
Established in 1996, the ALSWH has tackled issues such as the lifelong health implications of violence and abuse, mental health, the impact of multiple chronic conditions,
Professor Deb Loxton, Director of the ALSWH program at the University of Newcastle, says the unprecedented size and scope of the study has enabled researchers to gain unmatched access into the issues facing women of all ages.
“By analysing such a broad demographic over such a long span of time, our research teams have and will continue to obtain crucial data that is vital in shaping the future of women’s health policy,” adds Professor Mishra.Study data from the ALSWH is linked with data from national administrative datasets such as the Medicare Benefits Schedule, Pharmaceutical Benefits Scheme, National Death Index, and Aged Care. It also links to state and

Researchers from the University of Newcastle and the University of Queensland have created the largest and longestrunning women’s health study in Australian history – and its findings are shaping policy and practice at the state, national and international levels.
territory datasets including hospital admissions, perinatal data, and cancer registries.
These datasets serve as a platform for evaluating policies and strategies such as perinatal mental health screening, access to psychological services, health assessments and medication use.
Findings have contributed to policies and guidelines aimed at improving Australian women’s health, wellbeing and access to health services, including the National Women’s Health Strategy 2020-M2030, the perinatal mental health guidelines of 2017, and a vast array of other foremost policies and guidelines.

The recently released National Plan to End Violence against Women and Children 2022-2032 was heavily influenced by data gathered through the ALSWH.
“We were especially pleased to see that the plan acknowledged the long-term impacts of violence and recognised that the ALSWH was the first study to examine health impacts of domestic violence using longitudinal data,’ Professor Loxton explained.
ALSWH also makes regular submissions to government inquiries, including a recent inquiry into traumatic birthing and reproductive healthcare. Additionally, the collaboration contributes to special reports on topics including the lifetime impact of abuse and the significance of global and domestic emergencies, including bushfires and the COVID-19 pandemic.
ALSWH collaborators stretch across the globe, with more than 650 collaborators from countries including Sweden, the United Kingdom, the Netherlands, Japan, the United States of America, Switzerland and Argentina.
To support the sharing of new knowledge and knowledge translation, survey information is freely available to collaborating researchers on the project’s website, as are links to nearly 1,000 scientific publications that leveraged ALSWH data.

Earlier this year, both Professor Loxton and her ALSWH counterpart at the University of Queensland, Professor Gita Mishra, were invited to join the Australian Government’s new National Women’s Health Advisory Council experts from women’s health organisations, consumer groups and peak bodies. issues such as for women in priority populations, diversifying medical research, and training and education.
“I am honoured to be in the company of such distinguished experts,” Professor Loxton said of her appointment. “It’s an incredible privilege to work alongside such passionate and accomplished advocates for women’s health.“
“I may be one of 16 Council members, but I will take the experiences of 57,000 women who have been part of the Australian Longitudinal Study on Women’s Health with me into the each of the Council meetings. I feel an enormous responsibility to represent them and their needs.”

Author: In addition to her role with the ALSWH, Professor Loxton is the Director of the University of Newcastle’s Centre for Women’s Health Research and Director of the Women’s Health Research Program at the Hunter Medical Research Institute, which focuses on the impacts of violence against women, its Worldwide Wellness of Mothers and Babies program, and healthy ageing.


Adolescents suffering through menstrual disorders and pelvic pain without treatment or support are at risk of life-long disadvantage. The University of Queensland’s Professor Gita Mishra is driving research to better understand the origins of pelvic pain and menstrual disorders, and empower Australian teens.
For adolescent girls, menstrual disorders (irregular, heavy, or painful periods) and noncyclic pelvic pain are both incredibly common and incredibly disruptive.
A recent Australian study indicates that as many as 1 in 3 female students report missing school due to menstrual symptoms, and for 1 in 10, this happened every cycle.1 The majority of these girls felt menstruation had an impact on their performance in tests and assignments, and reduced their participation in sports and physical activity.
“The potential long-term health, educational, and socioeconomic implications are troubling, particularly if this early disadvantage is further compounded by a delayed diagnosis of endometriosis, PCOS, or fibroids,” says Professor Gita Mishra, Director of the Australian Women and Girls’ Health Research Centre at UQ.
“It’s not unusual for adolescents to experience irregular menstrual cycles or heavy periods as their bodies settle into a rhythm. It is perhaps because of this normalisation, that there are some key knowledge gaps,” says Professor Mishra.
There is very little epidemiological evidence on the causes of menstrual disorders and pelvic pain in adolescents. The search for answers is challenging. It requires reliable information on the risk factors that girls may be exposed to during adolescence and early childhood, such as nutrition, exercise, weight, drugs, alcohol, tobacco, experiences of violence, and socioeconomic factors.
These same factors, and many more, can also have an
1 Armour M, Ferfolja T, Curry C, Hyman MS, Parry K, Chalmers KJ, et al. the prevalence and educational impact of pelvic and menstrual pain in Australia: A national online survey of 4202 young women aged 13-25 years. J Pediatr Adolesc Gynecol. 2020;33(5):511-8.

impact on child development at critical points in utero and even in the years before pregnancy, known as the preconception period.

As part of the Centre’s portfolio of projects, Professor Mishra leads a multidisciplinary team investigating the maternal and early life origins of adolescent menstrual disorders and pelvic pain and the impact on teens. She is also the UQ-based Director of the Study on Women’s Health (ALSWH), a large national cohort study that is uniquely positioned to meet the research challenges ahead.
As the largest and longest-running women’s health study conducted in Australia, ALSWH has delivered insights into the prevalence and impacts of menstrual disorders and informed a range of Federal and State Government policies including the National Women’s Health Strategy 2020-2030.
The often-cited statistic that 1 in 9 Australian women are diagnosed with endometriosis comes from the ALSWH cohort born between 1973-78. These women have participated in ALSWH’s comprehensive health and wellness surveys since 1996, when they were aged 18-23. Now, their female children are set to join the study as part of a 5-year project funded by the National Health and Medical Research Council (NHMRC).
This new intergenerational study will draw on more than 25 years of health and wellbeing data from mothers in the ALSWH and pair it with information from teens about their health, their menstrual symptoms, and the impact it has on their day-to-day lives. The team aims to support clinicians with resources that will inform clinical advice on the prevention and management of menstrual disorders in teens.
The current National Women’s Health Strategy 2020-2030 takes a life course approach that identifies adolescence as a critical period for education and awareness around reproductive health and building confidence in and relationships with primary health care providers.
“And with good reason; less than 30% of girls seek help from a doctor, despite the high prevalence of period pain2,” Professor Mishra says.
“The vast majority of young women are unwilling to speak to a staff member about menstruation despite saying that their pain keeps them from school or hinders their performance on exams.”
A large focus of this project will be translating findings into co-designed resources that will empower adolescent girls,
2 14. Li AD, Bellis EK, Girling JE, Jayasinghe YL, Grover SR, Marino JL, et al. Unmet needs and experiences of adolescent girls with heavy menstrual bleeding and dysmenorrhea: A qualitative study.J Pediatr Adolesc Gynecol. 2020;33(3):278-84.their families and educators to understand what is normal, and when to seek help.

Professor Mishra is well aware that achieving a meaningful impact is impossible without collaborative links between health professionals and women’s health community and advocacy groups.
“The 2018 Australian Government-funded National Action Plan for Endometriosis was a world first and it created a foundation for the future, through capacity building, collaboration, and community engagement, and it’s a model that is benefitting all areas of women’s health research,” says Professor Mishra.

This project brings together members of the Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG), the Royal Australian College of General Practitioners (RACGP), The Pelvic Pain Foundation of Australia (PPFA), and advocacy and community QENDO. Professor Mishra also sits on the National Women’s Health Advisory Council along with Professor Deborah Loxton, (ALSWH Director at the University of Newcastle).
The Department of Health and Aged Care has established the council to address medical misogyny and provide practical advice on implementing the National Women’s Health Strategy 2020-2030.
Research is progressing rapidly with work on these topics now covered extensively in the recent publication of the 2nd edition of a key textbook in the field, A Life Course Approach to Women Health (2023, Oxford University Press), on which Professor Mishra is chief editor.
Looking to the future, she is eager to showcase Australia’s progress on the world stage.
Author: Professor Gita Mishra is internationally recognized for her expertise in epidemiology and women’s health across the life course, especially her research on the links between reproductive characteristics, from menarche to menopause, and non-communicable diseases, such as diabetes and cardiovascular disease. She is the Director of the UQ-based Australian Women and Girls’ Health Research Centre, the Australian Longitudinal Study on Women’s Health at UQ, and the Centre of Research Excellence in Women and Non-Communicable Diseases. She is the Scientific President of the 2025 World Congress on Endometriosis in Sydney, an event that will bring together clinicians, researchers, and patients to discuss the latest advances in the field and to progress the translation of findings into real-world improvements in women’s health and wellbeing.
Prof Gita MishraFor adolescent girls, menstrual disorders (irregular, heavy, or painful periods) and non-cyclic pelvic pain are both incredibly common and incredibly disruptive.




Health literacy, as defined by the World Health Organization, refers to a person’s ability to access, understand, and utilize health-related information effectively to maintain good health. Ovulatory menstrual health literacy, specifically, encompasses the knowledge and skills needed to maintain personal health in relation to the cycle, which involves understanding the connection between ovulation and menstruation, and actively engaging with healthcare providers as needed.

Ovulatory menstrual health literacy is important for several reasons. Firstly, menstruation is a natural biological process that affects approximately half of the world’s
reproductively mature population, and lasting for about 40 years of life. Secondly, the cycle features strongly in a woman’s life journey from menarche to menopause and the fertility events in-between. Even though it is so significant, the cycle is often burdened by negative stereotypes and stigma, impacting both physical and mental health. Finally, the cycle serves as an indicator of overall health. However, distressing challenges such as painful periods, heavy bleeding, irregular cycles and mood disturbances occur with adolescents. Ovulatory menstrual health literacy offers the possibility of restoring good health by cooperating with the menstrual cycle to proactively manage these challenges under suitable medical supervision.
Research indicated that many young women lack adequate ovulatory menstrual health literacy, even though
it is so important. In response to this knowledge gap, efforts have been made to improve menstrual health education. Often though, initiatives address singleissue menstrual rather than providing a comprehensive understanding of the cycle itself, and consequently tend to have a deficit-oriented approach to menstrual health education.
My Vital Cycles® was developed in response to the improvements needed in menstrual health education. This whole-school program aims to empower girls by equipping them with scientifically sound knowledge about the cycle and the skills to manage it. For example, by understanding ovulation as the key driver of the cycle, girls learn to distinguish between different types of bleeds. This is important for when doctors ask the simple question of “when was your last period?”. Furthermore, the program adopts a holistic approach, taking into account the girls’ emotional and social contexts, to deepen an understanding of their bodies and health. This is part of its strength-based approach, which emphasizes the positive aspects of the cycle instead of focusing solely on problems and deficiencies.


A trial was conducted to evaluate the effectiveness of My Vital Cycles® in one single-sex school in Perth Western Australia, and the results were promising. The 94 participants showed improved ovulatory menstrual health literacy, along with an increased confidence in discussing cycle patterns with healthcare providers. Furthermore, the program challenged common beliefs that period pain and mood disturbances are normal. Having engaged with the program, participants also reported improvements in their mood concerns. This positive change could be attributed
to several factors. Firstly, the program encouraged girls to observe the unfolding of their cycle, and understand what it signified in terms of body functionality. One theory is that the body is perceived as a site of self-becoming which enlarges an understanding of the body and its capacities. This may have contributed to improved body image and self-appreciation. Secondly, the program promoted a positive view of self as unique, built competencies to recognize personal cycle patterns, and fostered individual agency.
My Vital Cycles® presents promising evidence of improving ovulatory menstrual health literacy among adolescent girls. This strengths-based program not only enhances self-understanding and agency but also contributes to improved mood. Future research could explore the long-term retention of knowledge and the application of the program in different settings. Ultimately, empowering young women with comprehensive ovulatory menstrual health literacy may lead to their improved overall health, well-being, and self-confidence as they navigate the reproductive years ahead.
This research was supported with the Australian Government Research Training Program Scholarship (grant CHESSN8617438119), Curtin Medical School 2020 Pilot Study Award, and the Western Australian Institute for Educational Research – Fogarty Foundation Postgraduate Award 2020.
 Author: Felicity Roux, PhD candidate and Research Officer M+Th, Curtin Medical School
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
Author: Felicity Roux, PhD candidate and Research Officer M+Th, Curtin Medical School
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
Murdoch Children’s Research Institute is working to improve women’s health in the first two decades after having a baby, and better understand common conditions like endometriosis, period and pelvic pain.

Murdoch Children’s is well known for longitudinal studies – including the Mothers’ and Young People’s Study, a nearly 20-year study of 1,507 first-time mothers and their first-born children.
The study, which has been funded by National Health and Medical Research Council (NHMRC) since 2003, focuses on women’s health over the first two decades after becoming a mother – and it has dispelled many myths about women’s physical and mental health and recovery after childbirth.
Lead Researcher and Intergenerational Health Group Leader Professor Stephanie Brown said, “The findings show that many physical health problems such as incontinence and backpain experienced for the firsttime during pregnancy or after childbirth have long term consequences for women’s health and wellbeing across the life course.
“The study was also one of the first to demonstrate the extent to which women’s physical and mental health are linked, identifying the need for strategies promoting women’s mental health after childbirth to also focus on healing and recovery from common physical health issues,” she said.
Professor Brown and her team also found that depression was more common five to ten years after having a first child than at any stage in the first 12 months postpartum, which suggests that the need for mental health support is even greater as children grow up.
Researchers have also found that one in three women and their children were exposed to physical or psychological partner violence in the first decade after the study children were born, so another major focus of the study is the impact of family violence on women and children’s health.

Ten years after the birth of their first child, women who had experienced recent partner violence were three-five times more likely to be experiencing depression, anxiety or Post-Traumatic Stress Disorder (PTSD) symptoms and increased risks of cardio-vascular disease and chronic pain, while their children were two-three times more likely to have a probable psychiatric diagnosis.
“Despite these profound impacts on their health, women are often reluctant to discuss family violence with health professionals,” Professor Brown said. “Our findings suggest that only around one in three women experiencing partner violence disclose this to a GP, psychologist or other health professional.”
Professor Brown said she hoped the research would help strengthen the capacity of health services to identify and respond to women and families whose lives are affected by this global public health issue.
Murdoch Children’s researchers are also working to improve the care and management of period and pelvic
pain and endometriosis, a condition where tissue similar to the lining of the uterus grows outside the uterus.
Endometriosis affects about one in every 10 Australians who menstruate and is associated with infertility and chronic pelvic pain. There are no symptoms that are specific to endometriosis and at least half of those who have surgery to try to investigate pain will have no signs of the condition found.
The LongSTEPPP Project aims to explore factors associated with pain, quality of life, mental health and health utilisation, to better understand the educational and management strategies required to help ensure that young people’s lives are not ruined by period and pelvic pain.
The project, led by Professor Sonia Grover and coordinated by Dr Courtney Munro, is recruiting more than 3,000 young Australians between 10-18 years via social media, GPs, private gynaecologists and 11 hospitals nationally, who experience period or pelvic pain and endometriosis and have been referred to a gynaecologist.
The research builds on preliminary findings that show the care of young people by adolescent gynaecologists results in lower surgical intervention rates, achieves good control of symptoms and has positive long-term outcomes with lower than-expected infertility and endometriosis rates when followed up 10 years later.

Professor Grover said the project was the first of its kind due to its focus on young people, leading to the possibility of prevention of endometriosis-related problems through early control of menstrual issues and pelvic pain.
“There is limited education to ensure young people seek help for their period problems,” she said. “Young people often report that their symptoms are ignored or normalised, and many will experience years of pain before it’s acknowledged and their pain treated. Evidence suggests that recurrent severe period pain predisposes people to chronic pelvic pain.
“Most young people who have periods will experience some pain,” Professor Grover said. “For others, the pain and associated symptoms they experience will stop them from doing everyday activities and will affect their quality of life and mental health.”
Professor Grover believes the research could provide insights into the optimal management of period and pelvic pain that could help prevent chronic pain and endometriosis.
With these projects, Murdoch Children’s aims to promote positive health outcomes for women across the lifespan and from all walks of life.
This article was supplied by MCRI.
Data collected by the National Endometriosis Clinical and Scientific Trials (NECST) Registry participants demonstrates lower levels of quality of life compared with peer counterparts without disease.
Endometriosis is a common yet under-recognised chronic inflammatory disease. It affects 176 million women, trans and gender diverse people globally 1 equating to more than 830,000 women and girls in Australia2
Painful periods, chronic pelvic pain, abnormal menstrual bleeding, and infertility are the most common symptoms of endometriosis. Diagnostic delay of endometriosis remains prolonged, between 6 to 8 years.3 It has been estimated that in Australia, the cost burden of endometriosis on patient’s and society is over $9.7 billion per year.4
The National Endometriosis Clinical and Scientific Trials (NECST) Registry is a nationally coordinated clinical database – collecting and tracking diagnostic, treatment and quality of life (QoL) data for people with endometriosis. It is a key outcome of the research
priority area of the Australian Government’s National Action Plan for Endometriosis (NAPE7) and is part of a national collaborative project by Australian clinicians, researchers and patient advocates; the NECST Network, also an Australian Government initiative. A principal outcome is the production of consistent, prospective data on endometriosis to determine healthcare changes and reduce data duplication across health services in Australia.5
To assess the current impact of endometriosis on the QoL of women, trans and gender diverse people with endometriosis, the NECST Registry was interrogated at multiple time points.

We recruited participants through hospitals, specialist private clinics, and the general community via social media.
Consenting participants answer questionnaires and providing personal details, clinical presentation and medical history data, and patient-reported outcome measures (PROMs) using the validated tools of the Euroqol (EQ)-5D and Endometriosis Health Profile (EHP)30. Participants are followed up at 6-months, 12-months and annually thereafter, capturing any changes to their symptoms and management and to complete the EQ-5D and EHP-30.
Of 1401 registered participants to-date, ages range from 18–66 (mean of 35) years and the most common presenting symptom for clinical review is dysmenorrhoea (43%), followed by other types of pelvic pain (15%). From those that had a diagnosis of endometriosis (91%), the most common method of diagnosis was via laparoscopy, (80%), followed by imaging (ultrasound/MRI/CT scan), (12%), with symptom-based diagnosis accounting for the fewest registrants (5%), with 3% recording they experienced no endometriosis symptoms.
Participants recorded they started experiencing endometriosis symptoms from as young as 8 years, and as old as 47, with 18 years being the average age of endometriosis symptom onset.
The most common medical therapy was pain medication (60%), followed by hormonal therapy (44%), allied health and complementary modalities (43%) of which the most common were physiotherapy (n=105/414) and acupuncture (n=71/414).
Currently, 320 participants have matched baseline and 6-months data and 45 have matched EQ-5D data to 12-months. Overall, NECST Registry participants reported lower levels of QoL (mean=0.69, SD=0.23) compared to the general female population (mean=0.91; SD=0.14),9 p<0.001. Additional analyses demonstrate age at first menstruation ≤11 years had EQ-5D scores significantly and consistently lower at follow-up compared to 1215 and 16+ years (p=0.004). Participants that recorded they had previous surgery at baseline vs those that had no surgery or were unsure, had similar EQ-5D scores at baseline, however, by the 12-month follow up, there was significantly higher EQ-5D scores for those that had previous endometriosis surgery at baseline (p=0.003). Those 51+ (vs ≤50) years at recruitment had significantly higher EQ-5D scores and remained higher at all timepoints (p=0.005).
These preliminary findings demonstrate that there is a significant impact of endometriosis on quality of life. This is consistent with previous research demonstrating the negative impact of endometriosis on all aspects of the person’s lives 6,7,8 . Novel data from the NECST registry suggests that the impact of endometriosis to QoL may be predicted by certain baseline characteristics, such as younger age at menarche and a history of previous surgery for endometriosis. These results also provide supportive evidence that as individuals age, QoL is improved.
Next steps in the data analyses will be to further explore the impact of QoL on endometriosis patients and determine the efficacy of medical and surgical options and how they relate to symptom outcomes, recurrence, and the need for reintervention. These outcomes will help to better inform patients and healthcare providers the likelihood of success of a treatment and the likely need for additional treatment(s).
References for this article can be provided upon request. Graphic created with BioRender.com

Authors: Cecilia H. M. Ng1, 2 (Research Manager) and Jason A. Abbott1,2 (Research Group Lead)
Institute/organisation affiliations
1 School of Clinical Medicine, Medicine and Health, Discipline of Women’s Health, University of New South Wales, Sydney, Australia
2 Gynaecological Research and Clinical Evaluation (GRACE) Unit, Royal Hospital for Women and University of New South Wales, Sydney, Australia
CHRISTOPHE KEREBEL CHRISTOPHE KEREBEL CHRISTOPHE KEREBEL
Over 10 million children have been born subsequent to assisted reproductive technologies (ART) globally (1), and approximately 2.5 million ART cycles are performed annually. However, despite these figures the longer-term health outcome of the children born subsequent to ART is unclear. The short-term outcomes suggest some potential early life predictors of disease in later life(2-4). Such as, an increase in blood pressure, adiposity, vascular dysfunction, and unfavourable lipid and glucose profiles (5). Although, more recent studies are less conclusive (6-9). However, studies performed on adolescents are scarce. Importantly, several studies have reported differences between ART conceived and naturally conceived offspring with regard
to mental health outcomes, reporting a potential higher prevalence of depression, autism spectrum disorder attention-deficit disorder, and behavioural differences (1012). Furthermore, conflicting reports exist as to whether asthma and allergies are more prevalent in ART offspring (13, 14). In view of these potential concerns the author (RH) established the Growing Up Healthy Study (GUHS) (15), to study the health outcomes of adolescents and young adults born from ART in Western Australia prior to 2001, comparing them to a birth cohort (Raine cohort) (16), demonstrated to be representative of the wider Western Australian population, and replicating the same detailed adolescent clinical assessments. This paper provides an overview of the findings from this study.
In our GUHS study 163 ART of offspring at 17 years of age replicated the assessments previously completed by the 1,457 Raine study at a similar age (17). After adjustment for cofounders, we demonstrated that the ART offspring females had a lower BMI, thinner skinfolds and less subcutaneous fat, than Raine participants, whereas males were not significantly different. ART offspring had a narrower waist circumference than their naturally conceived counterparts, with no differences in their serum metabolic indices, homeostatic model assessment for insulin resistance, the presence of fatty liver, blood pressure or heart rate, providing reassuring data in cardiometabolic measures for boys and girls in adolescence (17).
At 14 years of age, 152 participants in the GUHS Study undertook detailed respiratory questionnaires and spirometry, a metacholine challenge test to attempt to evoke a bronchial response, skin prick tests for allergy, and questionnaires for food allergies (14). No differences were detected in the prevalence of current asthma; indeed lung volumes were larger in the ART adolescents, and bronchial hyper-responsiveness was less prevalent. Although, allergic rhinoconjunctivitis (hay fever) rates were higher in the ART cohort, food allergies were more prevalent, and more adolescents had a positive skin prick test, than the 1,845 naturally conceived Raine Study participants who underwent assessment (14).

The thyroid function of 181 offspring of ART within the GUHS, was compared to 1,359 naturally conceived children in the Raine Study at aged 14 and 20 years of age (18). The mean concentrations of thyroid stimulating hormone (TSH) were similar between the two groups, while free triiodothyronine (fT3) concentration was lower, and the mean free thyroxine (fT4) higher, but both were increased at 20 years of age in comparison to the naturally conceived comparison group, although all measures were within the normal range. Furthermore, the prevalence of thyroid autoimmunity did not differ between cohorts at both ages, and no differences in the prevalence

of subclinical and overt hypo- and hyperthyroidism. Furthermore, thyroid function did not differ between the offspring of fresh and frozen embryo transfers (18).


In the GUHS the behaviour and mental health parameters of 160 adolescents conceived after ART were compared to 1,351 spontaneously conceived adolescents at 14 and 17 years of age (19), adjusting for relevant confounders. At both 14 and 17 years of age, ART conceived adolescents demonstrated less externalising behaviour (delinquent and aggressive behaviour), which was concordant with their parents’ reports. At both 14 and 17 years of age there were no differences in internalising behaviour (withdrawn behaviour, somatic complaints, anxiety and depression) between the two groups. However, at 14 years of age ART offspring had a higher incidence of clinical depression (12.6% vs. 8.5%), although these differences were not detected at 17 years. On further analysis of the Raine Study participants we confirmed an association of adolescent depression with parental subfertility, as those adolescents born in the Raine cohort to subfertile (nonART) parents showed higher rates of clinical depression than those born to fertile parents at 14 years of age (13.7% vs. 6.9%), raising the possibility that any differences may be environmental and not related to ART per se (19).
The evidence about long-term health of children conceived through ART is reassuring. However, the rapid changes over time in ART treatments performed, limit the generalisability and significance of long-term findings, and further studies are essential.
Authors: R. J. Hart 1,2, , L. A. Wijs 1 .
1 Division of Obstetrics and Gynaecology, University of Western Australia, Perth, WA, Australia, 6008;
2 City Fertility & Fertility Specialists of Western Australia, Bethesda Hospital, 25 Queenslea Drive, Claremont, WA 6010, Australia
A world-first national program is currently underway across Australia designed to safely lower the rate of preterm and early term births. Early successes suggest this prevention program will likely save lives, prevent lifelong disabilities and improve childhood educational outcomes.
Discovering how to safely prevent preterm and early term birth should be one of the highest priorities in health care. Preterm birth, defined as birth before 37 completed weeks of pregnancy, is the single greatest cause of death in young children and a major contributor to life-long disabilities. Eight percent of Australian children are born preterm, and in First Nations Australians the rate is nearly double. Over recent years, however, we have come to learn that for many children the fetal brain and other organs are not fully mature until 39 weeks gestation, leading to the 14 day period between 37 weeks and 38 weeks and 6 days now being defined as “early term”. Being born in the early term period substantially increases the risk of learning and

behavioural problems at school age. There has been a progressive increase in the number of early term births, with one in three Australian children now born in this 14 day window. This increase in early birth is believed to be a significant contributor to the rise in behavioural disorders observed in our classrooms. Many of these early births are unnecessary and can be safely delayed.
In 2014, Western Australia hosted a whole-of-state, wholeof-population program designed to safely reduce the rate of preterm birth. The change package included education of healthcare personnel and the general public, improved use of prenatal ultrasound imaging, and medication that had been shown to be effective in the presence of certain risk factors. Leadership of the program was based in the UWA Division of Obstetrics and Gynaecology. The strategies adopted had followed several decades of discovery research at UWA, combined with findings from other Australian and overseas research programs.
In the first year following introduction of the initiative, the rate of preterm birth state-wide fell by 7.6% and in the major tertiary-level hospital by 20%. This was the world’s first successful whole-of-population multi-faceted preterm birth prevention program and showed that such an approach can be effective.
With support from a NHMRC Partnership Grant administered by UWA, the Australian Preterm Birth Prevention Alliance was established in June 2018 enabling the WA program to be rolled-out nationally (www. pretermalliance.com.au). Early success was seen in some states but not others. In the ACT and Tasmania, preterm births fell by 10% and 20% respectively. The early term rate in the ACT was reduced by 34%.
These findings taught us the strategies can be clinically effective, but population-based success at a national level would require addition of a new approach to implementation and with more funding.
The Australian Preterm Birth Prevention Alliance was then awarded $13.7 million in the May 2021 Commonwealth Budget providing the support necessary to expand the program. Leadership of the Alliance and the National Program has continued to be based in the UWA Division of Obstetrics and Gynaecology with Professor John Newnham as Chair and Professor Jonathan Morris from University of Sydney as Deputy Chair. Strong partnerships have been developed with Women’s Healthcare Australasia (WHA) led by their CEO Dr Barbara Vernon, the Institute for Healthcare Improvement (IHI) led by their Vice-President Lisa McKenzie, and each of Australia’s
eight jurisdictional health departments. The administering institution is the Women and Infants Research Foundation.

In order to rapidly and safely improve clinical practice, the National Program has embraced the field of Improvement Science and adopted the IHI Breakthrough Collaborative methodology. The partnerships established to achieve this goal bring together near-real time clinical data from our hospitals, software to enable rapid sharing of data and improvement strategies, and inclusion of the full range of necessary healthcare disciplines and consumer groups.
The clinical program is based on the original strategies but also includes emphasis on continuity of care models and First Nations women. Sixty hospitals are formally included in the program encompassing about 55% of Australian births, although the elements of the change package are available to all our nation’s healthcare facilities. The methodology is based on education, empowerment of clinical leaders in each site to tailor the implementation for their own clinical environment, face-to-face meetings and on-line sharing of improvement data.
At the time of writing, the Collaborative is half-way through its 16 month timeframe. The program is proving highly effective with strong evidence of improvement in clinical practice. There is every reason to hope the program is on-track to achieve its goal of safely reducing the rate of preterm and early term birth by 20% or more.

This Australian story provides an example of discovery research being implemented effectively in one geographic region and then rolled-out nationally. The signs are very positive that our nation will be the world’s first to safely and strategically lower the rate of untimely early birth, preventing death and disability and improving the health and wellbeing of our next generation.
Author: Professor John Newnham AM is Professor of Obstetrics at The University of Western Australia and Chair of the Australian Preterm Birth Prevention Alliance and the National Collaborative. He was the 2020 Senior Australian of the Year.
The process of human reproduction starts with an egg that is fertilized by a sperm to form an embryo. However, it can still take around a week until the embryo nestles comfortably into the lining of the mother’s uterus, through a process called implantation.
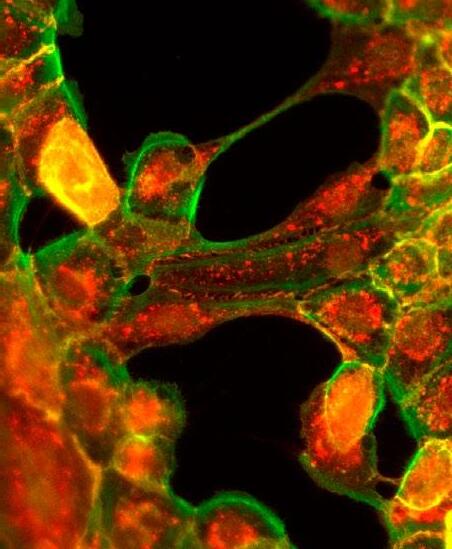
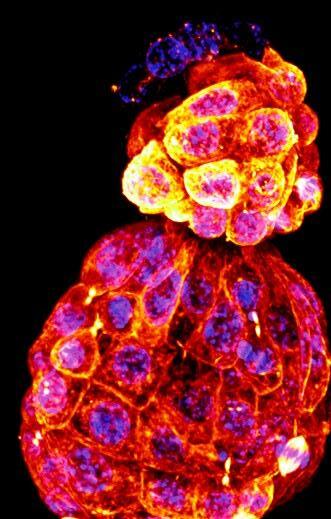 Image of a hatching mammalian embryo, ready to implant into the uterus of the mother.
Captured by Dr. Jessica Greaney, Zenker Lab, Australian Regenerative Medicine Institute, Monash University.
Image of a hatching mammalian embryo, ready to implant into the uterus of the mother.
Captured by Dr. Jessica Greaney, Zenker Lab, Australian Regenerative Medicine Institute, Monash University.
Successful implantation signals the beginning of a pregnancy and triggers the production of hormones that are detected by pregnancy tests.
Until now, scientists have been largely in the dark about the early events prior to implantation. A new study 1 published, led by Dr. Jennifer Zenker at the Australian Regenerative Medicine Institute within Monash University, has found that the biological decisions of individual cells within the embryo can significantly influence the journey to pregnancy.
Prior to implantation, the embryo undergoes a mesmerizing journey, travelling down the fallopian tube to reach the uterus. At the same time, the embryo transitions from a single cell to a complex structure comprising more than one hundred cells.
All the while, each cell within the embryo is making vital decisions that guide their fate, such as whether it will form the embryo or if it will instead make up the placenta. Work by the Zenker Lab sheds light on these mysterious biological processes through the painstaking process of recording live movies of developing embryos.
What is unique about these movies is that Dr. Zenker and her team are able to identify specific components within cells of the embryo, such as proteins and nucleic acids (e.g. DNA and RNA), to understand whether these guide the decision making process or even go on to endow cells to carry out their essential functions during pregnancy. Remarkably, these movies are filmed in real time, while living embryos are delicately housed in a viewing chamber.
Already, work from the Zenker lab has helped fertility experts and researchers in this field to better understand how embryo health at the level of individual cells influences a successful pregnancy. Here are three of their main findings:
1 Cells of the early embryo have highly organised internal scaffolds. Inside each cell of the embryo is a complex network of internal scaffolding known as the “microtubule cytoskeleton”. This scaffolding is not only key for giving embryonic cells their shape, but Dr. Zenker’s research is among the first accounts to prove that the microtubule network is highly organised during early mammalian embryogenesis2,3,4

1 Hawdon, A. et al., Apicobasal RNA asymmetries regulate cell fate in the early mouse embryo. Nature Communications, 2023. 14(1): p. 2909.
2 Zenker, J. et al., A microtubule-organizing center directing intracellular transport in the early mouse embryo. Science, 2017. 357(6354): p. 925-928.
3 Zenker, J. et al., Expanding Actin Rings Zipper the Mouse Embryo for Blastocyst Formation. Cell, 2018. 173(3): p. 776-791.e17.
4 Hawdon A. et al., Microtubule-dependent subcellular organisation of pluripotent cells. Development, 2021; 148(20):dev199909
This has been a significant breakthrough because, until this research, the microtubule cytoskeleton was widely regarded as disorganised. Furthermore, contrary to the textbook view that microtubules radiate symmetrically from the centre to the periphery of a cell, Dr. Zenker discovered that microtubules grow in a highly organised way through a previously undiscovered structure they named “interphase bridges” . The discovery of interphase bridges has led to new directions for research into the way cells of the preimplantation embryo can be monitored and studied.
2 Each cell of the early embryo influences their own destiny by organising their belongings, including their RNA. Following from their discovery of the microtubule network within cells of the early embryo, the Zenker Lab has recently discovered that Ribonucleic acid (RNA), typically recognized as an information facsimile transcribed from the DNA blueprint of the cell, is deliberately transported along the internal microtubule network of ‘roads’ that lead to different locations within the cell1. Hitchhiking on special ‘taxis’, known as lysosomes, different subtypes of RNA, including rRNAs, mRNAs and tRNAs, are distributed across opposing ends of each cell. Notably, this distribution of RNA subtypes guides the fate of cells as the embryo grows.
3 Advances in microscopy will transform fertility research and lead to improvements in IVF. The novel microscopy techniques pioneered by teams including the Zenker lab have been vital to study embryo quality non-invasively2,5,6. By shining a light on how the internal organisation of cells of the early embryo affects its health, the Zenker lab aims to develop improved methods to monitor embryos cultured in vitro, and find ways to keep embryos healthy for use in assisted reproduction.
5 Greaney, J. et al., Spatiotemporal subcellular manipulation of the microtubule cytoskeleton in the living preimplantation mouse embryo using photostatins. Journal of Visualised Experiments, 2021; (177).doi :10.3791/63290
6 Zenker J., Traffic lights on early embryo development help understand cell pluripotency. Research Features, 2023
Authors: Dr. Jennifer Zenker is a Research Group Leader at the Australian Regenerative Medicine Institute (ARMI), Monash University (Melbourne). Dr. Julian Heng is Founder and Director of Remotely Consulting (Australia), a company that provides manuscript and research editing services as well as strategic guidance to life scientists.

Oocyte in vitro maturation (IVM) is a variation on IVF which eliminates most or all of the hormones used in IVF, significantly reducing patient burden and cost. A new and improved version of IVM is now being offered to some infertile and cancer patients in Sydney.
Infertility affects 1 in 6 couples globally. Assisted reproductive technologies, like in vitro fertilisation (IVF), are enormously important medical procedures for society, bringing joy to millions of parents around the world. However, while effective for some couples, 4 out of 5 couples are unsuccessful when trying to conceive a baby using IVF treatment. IVF is also an invasive procedure and some women do not tolerate the hormones associated with the procedure well. This is especially the case for women with polycystic ovarian syndrome (PCOS), who are particularly sensitive to the hormones used in IVF
treatment. IVF is also expensive – it is a major financial burden on patients and on the Australian Medicare budget which provides generous subsidies for IVF treatment.
A second area where assisted reproductive technologies are important is for fertility preservation for patients diagnosed with cancer. These patients commonly face urgent life-saving, but potentially fertility-destroying, chemotherapy and/or radiotherapy, and if possible it is preferable to freeze eggs or sperm prior to their cancer treatment. For women, egg freezing is possible but requires ~1 week of hormone stimulation similar to an IVF cycle. However, unfortunately, in many cases an egg freeze is not possible; either because patients do not have ready access to an IVF clinic, the urgency of their cancer treatment does not permit enough time for a stimulation cycle and egg freeze, they have an estrogen sensitive cancer (e.g. estrogen receptor positive breast cancer), or they are too young for the procedure. For these cancer patients an alternative to an IVF-like stimulation cycle is needed.
There are many causes of infertility and as such there are many different approaches to infertility treatment. A variation on IVF is oocyte in vitro maturation (IVM). This is a reproductive treatment that requires patients to have only 2-3 days of hormone treatment (as opposed to the
8-14 days of hormones required for IVF). It may even be possible to eliminate the use of hormones altogether with IVM. Hence, IVM is far less burdensome on patients than IVF. As the treatment is much shorter and without the adverse effects of high oestrogen levels including no risk of ovarian hyperstimulation syndrome, patients do not require the frequent blood tests and ultrasound monitoring needed for IVF. The total cycle costs are about half that of IVF mainly due to less hormone use. Using IVM, eggs are deliberately collected in an immature state from the ovaries and matured for 1-2 days in the lab. Thereafter the procedure is identical to IVF. IVM is safe for mothers and babies and is classified as a routine, non-experimental procedure.

Given these clear advantages to patients of IVM, why isn’t IVM the treatment of choice for infertility treatment? There are two main reasons. Firstly, IVM has a lower overall success rate than IVF in terms of cumulative live birth rate per cycle (41% for IVM, 55% for IVF). This matters as patients, doctors and clinics generally all place a high value on success rates. Secondly, only about 10-15% of infertile patients are suitable candidates for IVM, due to the need for a high number of eggs collected for IVM to be successful. Hence, IVM is best suited to patients with PCOS. IVM is currently not suitable for poor prognosis patients including women of advancing reproductive
age, e.g. >38 years. As such, IVM has not been widely practiced in Australia and NZ, with only one clinic in Perth performing it routinely.


Until recently improvements in IVM practice had stagnated for decades. In the meantime, major new advances were occurring behind the scenes in animal egg biology research. Professors Robert Gilchrist from UNSW Sydney and Johan Smitz from Brussels, Belgium, and others, made a concerted effort to take these advances from the animal research lab to the clinic; a “bench-to-bedside” research effort.
This major research endeavour over a number of decades focused on using the new knowledge of how an egg matures in vivo, to attempt to mimic these natural processes using new in vitro technologies. This led to new, more efficient ways of performing IVM in the laboratory. These ideas then progressed to pre-clinical and then clinical trials in Brussels and Saigon, demonstrating clinical safety and efficacy. Recently, Gilchrist and Professor William Ledger from UNSW have established this new IVM procedure for clinical use at the Royal Hospital for Women in Randwick, Sydney. IVM is now being used to treat women with infertility, especially PCOS women, and women and girls with cancer requiring urgent fertility preservation.

 Professor Robert B. Gilchrist
Professor Robert B. Gilchrist
In 2014 a proof-of concept was established for uterine transplant with the birth of a healthy baby boy after a uterine transplant (UTx) (1) in Gothenberg Sweden.
Prior to the development of UTx the condition uterine factor infertility (UFI) was largely untreatable. There are several different causes of UFI. It may be due to uterine absence (surgical/ congenital) or a uterine defect (anatomic/functional).
It is estimated that the prevalence of UFI is approximately 20,000 women of childbearing age in a total population of 100 million (3). Hysterectomy in women of reproductive age is an unintended consequence but may occasionally be required due to symptoms of fibroids or following surgery for cervical/endometrial cancer or atonic uterine bleeding. Congenital uterine absence is seen in the Mayer-Rokitansky-Küster-Hauser syndrome (MRKH), a condition with uterine absence and upper vaginal aplasia
in a female with normal karyotype and normal secondary sex characteristics (4). Congenital causes of AUFI are also seen in women with uterine malformations, such as hypoplastic uterus, unicornuate uterus, or bicornuate uterus, which are associated with repeated pregnancy loss (5). Acquired uterine conditions, such as extensive adenomyosis and severe intrauterine adhesions may also cause UFI (5).
The inspiration for the Swedish team’s longstanding research in animal and human trials commenced in Adelaide Australia whilst Professor Mats Brannstrom was undertaking a gynaecological oncology fellowship in 1999. Subsequent systematic animal research occurred over a decade, involving rodents, domestic species, and non-
human primates, resulting in the first clinical UTx trial being launched in 2013, with a live donor, and a baby born the following year.

Altruistic gestational surrogacy for genetic motherhood, can provide genetic and legal motherhood (after adoption from surrogate). Although available in Australia, for ethical, religious and/or legal reasons this becomes exceeding difficult for many couples seeking this treatment.
Our first case was performed in January 2023. Prior to surgery, medical, transplant and psychological screening of the participants and in-vitro fertilisation is performed, with cryostorage of a minimum of 5 blastocysts. The first recipient was a 30-year-old woman who lost her uterus to a post-partum hysterectomy following an obstructed labour. The donor was her mother who had 2 normal vaginal deliveries. The donor surgery took 9 hours 54 minutes, and the recipient surgery took 6 hours and 12 minutes.



Immunosuppression in the recipient commenced on the day of surgery and continues throughout the time that the uterus remains in place. Cervical biopsies are taken to monitor for signs of rejection following the Swedish protocol. The patient had her first period 33 days after surgery and the first embryo transfer 3 months after surgery, which was successful. She has had reassuring nuchal translucency scan at 13 weeks, and a normal foetal anomaly scan at 18 weeks gestation (Figure A).
Uterus transplantation is the first available treatment for UFI. As a consequence of meticulous research preparations, the initial clinical introduction of UTx in 2013 resulted in several births that occurred during 2014-2017. Multiple new trials are underway in all continents. Uterus transplantation should stay at this experimental stage for several years to allow time to optimize the procedure further and to ensure that the procedure is safe, including any long-term medical and psychological effects, for the donor, recipient, partner of recipient and future children.
Author: Dr Rebecca Deans1,2
1 School of Clinical Medicine, Medicine and Health, Discipline of Women’s Health, University of New South Wales, Sydney, Australia
2 Gynaecological Research and Clinical Evaluation (GRACE) Unit, Royal Hospital for Women and University of New South Wales, Sydney, Australia
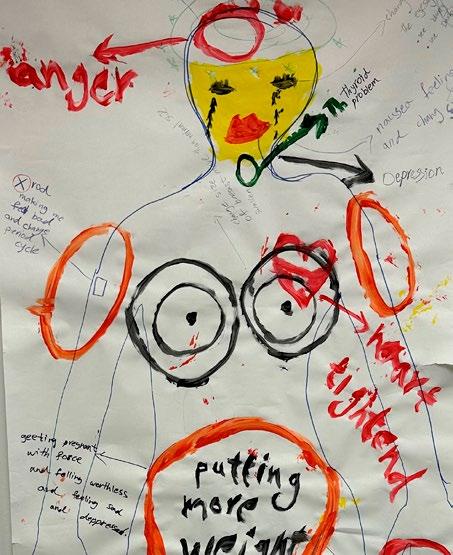
Image of foetus following UTx pregnancy at foetal anomaly scan Dr Rebecca DeansThe use of community co-design and artsbased research is shedding new perspectives on the sexual and reproductive health needs of migrant and refugee women in Australia.
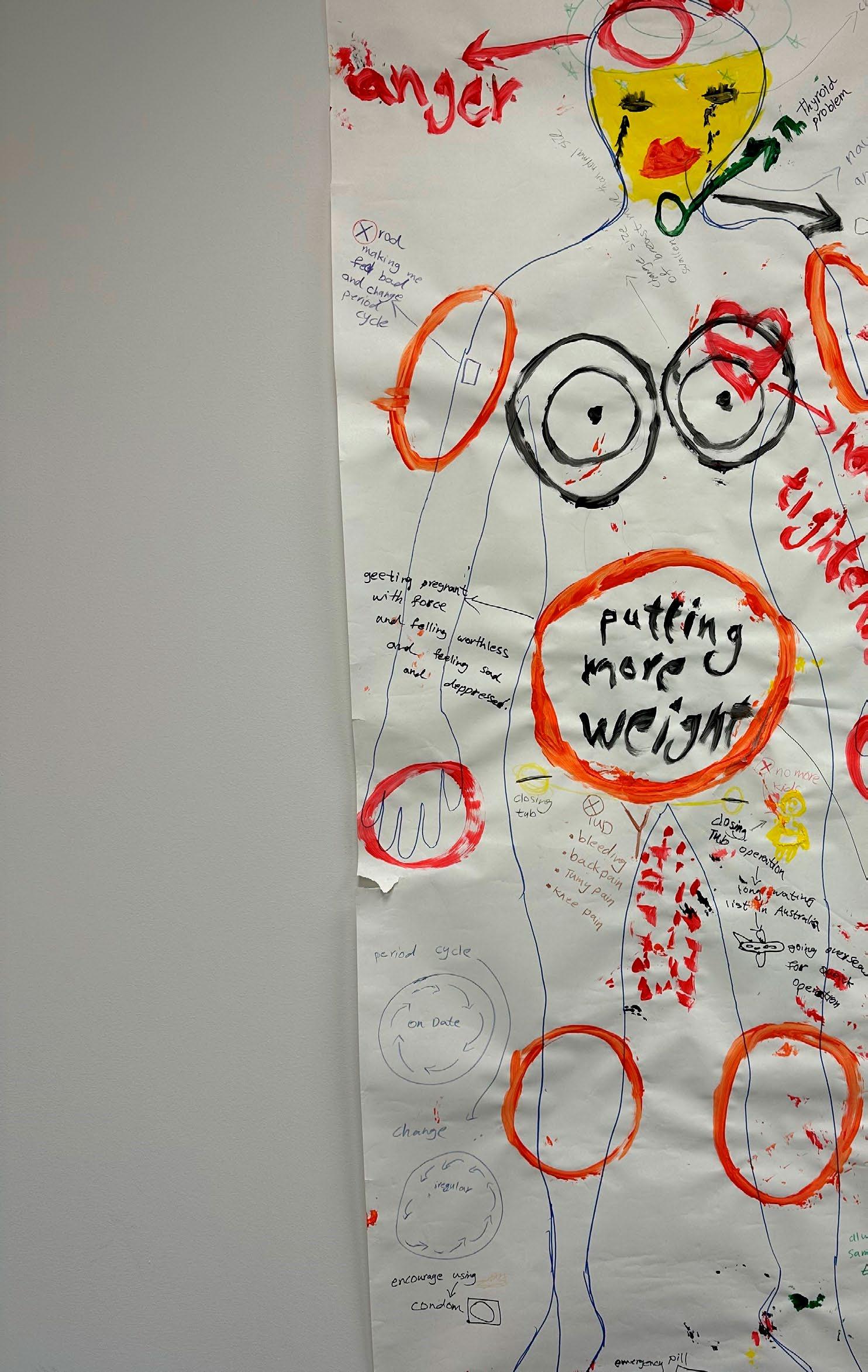 An example of a body map exploring fertility management with an Iraqi community knowledge holder.
An example of a body map exploring fertility management with an Iraqi community knowledge holder.
Sexual and reproductive health is a vital component of physical and psychological wellbeing, with utilisation of sexual health services associated with good quality of life and mental health. However, culturally and linguistically diverse (CALD) migrant and refugee women in Australia experience poorer sexual and reproductive health outcomes compared to Australian-born women and report difficulties accessing culturally appropriate healthcare services and information.
Despite these inequities, the glaring absence into the sexual health needs of migrant and refugee women in Australia was the impetus for action for a team of researchers at the Translational Health Research Institute (THRI) at Western Sydney University (Professor Jane Ussher, Professor Janette Perz, Dr Alexandra Hawkey and Dr Rosalie Power).
Led by Professor Jane Ussher, in one of the biggest studies globally, our Australian Research Council (ARC) Linkage Grant found migrant women in both Australia and Canada experienced significant shame and silencing around their sexual and reproductive bodies.
One-hundred and sixty-nine migrant and refugee women, across eight different cultural backgrounds shared how this had implications for sexual health knowledge, behaviour, and use of health services across the reproductive lifespan. For instance, many women described limited knowledge of menarche and menopause, experienced difficulties in addressing and negotiating sexual pain, and frequently did not attend healthcare services for contraception or to undertake recommended cervical cancer screening1
To address these issues, this body of work directly contributed to the development of the first set of evaluated recommendations for healthcare professionals in Australia working with migrant and refugee women in the field of sexual and reproductive health2
Low levels of cervical screening among migrant and refugee women found in our ARC study and changes in the National Cervical Screening Program was the driving force behind our Ainsworth Fund study to explore “blue sky” possibilities for cervical screening health promotion. This study demonstrated the feasibility and effectiveness of co-designed and culturally tailored “health forums” with women from African and Middle Eastern backgrounds. Integrating cervical cancer screening information with broader women’s health topics, the inclusion of creative activities selected by each community (e.g. Zumba), alongside practical support like childcare, encouraged attendance. The facilitation by community health workers allowed for language and cultural sensitivity, while
1 https://link.springer.com/article/10.1007/s10508-016-0898-9
2 https://www.westernsydney.edu.au/__data/assets/pdf_ file/0020/1225334/SRH_CALD_Report.pdf
professional co-facilitators supported the accuracy of the information shared.
The initiative’s success hinged on flexibility in timing, content co-design specific to each community, and balancing insider understanding with expert knowledge. Participants described feeling enlightened and empowered, with many expressing interest in further sessions and a strong desire to share the knowledge within their communities
International and Australian research indicates that migrant and refugee women are less likely to utilize effective contraception methods, leading to higher rates of abortion and unintended pregnancies, with significant health, social, and financial consequences. While we know that factors such as limited health literacy, cultural norms, religious objections, misconceptions, and gender roles potentially impact migrant and refugee women’s use of contraception, significant gaps in our knowledge still exist.
Recognising this, team member Dr Alexandra Hawkey has successfully obtained an NHMRC Emerging Leadership (L1) Research Fellowship grant to delve deeper into migrant and refugee women’s perceptions and experiences of fertility management. Informed by reproductive justice and intersectionality theories, this project is utilising the innovative arts-based method of body mapping (See image of body map) and qualitative interviews to explore under-researched areas including experiences of hormonal contraception side-effects, abortion and emergency contraception, and reproductive coercion.

With community co-design informing each stage of the research process, the outcomes of this study aim to address fertility management health literacy and health service support needs through the development and evaluation of a culturally tailored multilingual contraception hub. An interactive knowledge translation exhibition for community members and healthcare professionals, and recommendations for health promotion and healthcare provision will also increase opportunities for sexual and reproductive health and wellbeing among Australia’s most marginalised communities.
Exploring sensitive research topics in non-traditional and empowering ways, as well as recognising migrant women as leaders and experts in their sexual and reproductive health forms the basis of all research and translational outcomes within the team at Western. Together with our community partners and bi-cultural co-researchers, our vision is to foster an environment where migrant and refugee women’s voices are heard, and sexual and reproductive healthcare and information needs are met in accessible and culturally meaningful ways. Addressing migrant and refugee women’s sexual and reproductive health is pivotal to achieving gender, health, and social equity.
3 https://bmcwomenshealth.biomedcentral.com/articles/10.1186/ s12905-022-01936-2

Within my comprehensive program of research work, I focus on the Reproductive, Maternal, Newborn, Child, and Adolescent Health (RMNCAH) continuum of care.
My program comprises diverse research initiatives, encompassing evidence synthesis, evidence gap mapping, priority research exercises, and an active engagement strategy involving stakeholders and vulnerable populations.
With a focus on adolescents and young women, my approach employs rigorous analysis, stakeholder engagement, and innovative program design to enhance sexual and reproductive health outcomes.
By bridging knowledge gaps, my goal is to drive meaningful improvements in the health of vulnerable populations, particularly adolescents and young women, where comprehensive research is lacking. My core research focus centres on addressing research gaps in

sexual and reproductive health, but my vision extends to encompass preconception care, an often-overlooked area. By expanding into the preconception phase, I aim to illuminate a crucial domain that significantly shapes the future health trajectories of women and potential offspring. Furthermore, my strategy is acutely attuned to the distinct needs of marginalised groups such as migrants, refugees, and disadvantaged communities from developing nations. Their complexities, spanning cultural barriers to healthcare access, are pivotal to my research approach. By dedicating attention to these populations, I ensure that the interventions I develop are tailored to their unique circumstances.
Integral to my methodology is the use of an evidence gap map – a strategic tool that systematically identifies research voids in the field. This serves as a navigational guide, grounding interventions in robust research and evidence. However, my research transcends mere identification.

Through engagement with stakeholders like consumers, experts, and policymakers, I ensure a comprehensive perspective that informs research prioritisation, amplifying effectiveness and real-world relevance. Central to my approach is involving the population my research aims to benefit – adolescents and young women. Employing participatory intervention design, I empower them to shape initiatives addressing their distinctive challenges in sexual and reproductive health.
The convergence of these efforts – spanning evidence gap mapping, stakeholder engagement, addressing preconception care, and focusing on vulnerable populations – underscores a unified objective: to enhance understanding and drive effective interventions for the sexual and reproductive health of adolescents and young women.
By meticulously identifying research gaps and involving both experts and the target population, I am paving the way for impactful change. My work contributes to a comprehensive understanding of the challenges and opportunities within this critical domain, offering a roadmap for evidence-based interventions that can significantly enhance the lives of vulnerable populations. One pivotal aspect of my program focuses on contributing to the United Nations’ Sustainable Development Goals (SDGs) by empowering women to take control of their health and wellbeing. My program of work involves equipping women with financial knowledge and skills to enhance their autonomy and decision-making abilities, thereby fostering greater control over their health-related choices.
Recognising the interplay between economic empowerment and health outcomes, this initiative contributes to multiple SDGs, including gender equality, poverty reduction, and good health and wellbeing.
Furthermore, my program is exploring the critical issue of climate change and its impact on women’s health and pregnancy outcomes. Through thorough investigation and
analysis, we seek to uncover the nuanced ways climate change disproportionately affects women, particularly in vulnerable regions. This research informs strategies that mitigate risks and protect women’s health, reinforcing our commitment to SDGs related to climate action and maternal health.
Aligned with rapid technological progress, my research capitalises on cutting-edge tools like machine learning and artificial intelligence (AI) to address pressing issues. My collaborative and multidisciplinary team leverages AI to understand women’s postpartum mental health, extracting valuable insights for designing targeted interventions that promote mental wellbeing. This AI-driven approach mirrors our dedication to innovative methodologies aligning with the evolving scientific landscape.
In summation, my research approach transcends traditional boundaries, actively engaging stakeholders, vulnerable populations, and the broader healthcare landscape. Through a multifaceted strategy, I tackle gaps in sexual and reproductive health research for adolescents and young women, incorporating preconception care and focusing on marginalised populations.
This holistic effort is a testament to my commitment to advancing understanding and catalysing positive change in this vital field. As we collectively strive for improved sexual and reproductive health outcomes, my work serves as a bridge connecting research, intervention, and the needs of the populations it serves.

My research program also serves as a dynamic platform for women’s empowerment, where financial literacy, climate resilience, and advanced technologies converge to create impactful change. Through these multi-pronged efforts, we are not only advancing the SDGs but also ushering in a new era of research that harnesses the potential of AI to revolutionise the understanding and promotion of women’s health on a global scale.
Author: Dr Zohra Lassi, Associate Professor and NHMRC Emerging Leader (EL2) Fellow Robinson Research Institute and School of Public Health University of Adelaide

Ovarian cancer is Australia’s deadliest gynaecological cancer. It is difficult to detect so women are often diagnosed in the advanced stages of disease when treatment options are limited.
Anew study by QIMR Berghofer researchers offers hope that affordable and readily available low dose aspirin may improve ovarian cancer survival rates.
Professor Penny Webb knew from talking to women with ovarian cancer that they often want to know if there was anything they can do to help beat the disease or to prevent it from returning.
The head of QIMR Berghofer’s Gynaecological Cancers Group set up the world-first Ovarian Cancer Prognosis and Lifestyle (OPAL) study in 2012, leading a team of researchers trying to find out whether lifestyle choices may help to improve survival rates and quality of life for women with ovarian cancer.
More than 900 Australian women newly-diagnosed with ovarian cancer signed up to the OPAL study, which was funded by the National Health and Medical Research Council of Australia. The factors investigated included diet, physical activity and common medicines. As part of the information gathered, the women were asked how often they used aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs) in the 12 months before their diagnosis and in the first-year post-diagnosis.
Using data from the OPAL Study, the QIMR Berghofer team has found that simple low-dose aspirin may improve ovarian cancer survival.

Lead researcher Dr Azam Majidi said the study found that women who reported taking NSAIDs at least four days a week in the 12 months before or after diagnosis, lived longer on average than occasional or non-users. Most of the frequent users were taking daily low-dose aspirin.
“Our findings suggest that frequent NSAID use might improve survival for women with ovarian cancer, regardless of whether they start taking the drugs before or after diagnosis,” Dr Majidi said.
“We found the difference would translate to an average of an extra 2.5 months’ survival in the five years postdiagnosis. While this might not sound like a lot, it is significant for ovarian cancer. The disease is often diagnosed at an advanced stage when the prognosis is poor, and treatment options are limited.”

Ovarian cancer can be hard to detect and usually isn’t discovered until stages three or four, when the five-year survival rate is just 29 per cent. It claims the lives of almost 1,000 Australians each year and is the sixth most common cause of cancer death in Australian women.
Up to 80 per cent of women experience recurrence of the cancer after treatment. However, the QIMR Berghofer
study suggested that in those who frequently used NSAIDs, the cancer did not come back as quickly.
“One of the exciting things about these results is that lowdose aspirin is affordable and relatively safe for use at a population-wide level,” Dr Majidi said. However, she also stressed that aspirin is not safe for everyone so women should not start taking it without consulting their doctor.
“While more targeted and advanced treatments show great promise, at the moment they are very expensive and not accessible to everyone – especially in poorer countries. The findings suggest low-dose aspirin may help improve survival rates while researchers continue to search for better therapies.
“More research including clinical trials is needed to confirm whether these drugs can improve survival for women affected by this terrible disease,” Dr Majidi said.
The study is not the first to suggest a link between NSAIDs and ovarian cancer survival. However, some previous studies may have been affected by methodological problems, which this latest research sought to address. The results have been published in the Journal of the National Cancer Institute.

Professor Penny Webb said it was important to recognise the vital contribution of the OPAL study participants to the research that could help other patients in the future.
“This work would not have been possible without the 958 women with ovarian cancer who willingly took part in the OPAL study and the support given by their clinicians across Australia.
“We know that the way women with ovarian cancer respond to treatment and their outcomes can be very different which suggests there are other factors that are important in determining survival. Our aim is to be able to provide advice for women diagnosed with ovarian cancer about lifestyle changes that may help them,” Professor Webb said.
Author: Dr Azam Majidi is an epidemiologist and cancer researcher in the Gynaecological Cancers Group at QIMR Berghofer
Microscopy showing triple-negative breast cancer cells’ proteins (in red and green) that allow them to stick together and maintain their structure.
 Felix Kohane PhD Student Garvan
Associate Professor Christine Chaffer
Felix Kohane PhD Student Garvan
Associate Professor Christine Chaffer
Triple-negative breast cancer, diagnosed in around 2,500 Australian women per year, is one of the most aggressive forms of breast malignancy.
These tumours, lacking receptors for estrogen and progesterone, do not respond to the hormonal treatments that benefit other breast cancer subtypes. With limited therapeutic options, patients often face chemotherapyresistant cancer that recurs after initial therapy as incurable metastatic disease. This ability of triple-negative cells to evade standard treatments makes the cancer difficult to eradicate.
At the Garvan Institute of Medical Research in Sydney, my lab is focusing on an innovative approach to ‘stategate’ triple-negative breast cancer cells, trapping them in a vulnerable state. This potentially opens the door to more effective therapies, not just for triple-negative breast cancer but possibly for other stubborn cancers too.

Over the past 15 years, the landscape of cancer treatment has undergone a remarkable transformation. In the early stages of oncology, the primary focus was on complete eradication of cancer cells with aggressive treatments such as surgery, radiotherapy, and chemotherapy. This ‘scorched earth’ strategy was based on the belief that cancer was a static entity, a mass of rogue cells to be annihilated.
However, our understanding of cancer’s intricate nature has evolved, revealing it as a complex, dynamic disease. We’ve come to realise that cancer isn’t just a mass of identical cells, but a complex, heterogeneous population with an uncanny ability to adapt and evolve in response to their environment, including treatment pressures. This phenomenon, termed ‘plasticity’, allows cancer cells to evade the immune system, survive treatment onslaughts, and disseminate through the body.
In my lab we investigate how plasticity enables some triple-negative breast cancer cells to endure treatment and spawn lethal metastatic growths. Our goal is to develop innovative treatment strategies as well as ways to predict which patients will respond poorly to standard regimens, necessitating additional interventions upfront.
Based on our insights into cancer cell plasticity, we’ve discovered a promising mechanism to ‘state-gate’ triple-negative breast cancer cells, locking them into a vulnerable state. This radically different approach seeks to control their ability to change, to adapt, and ultimately, to resist treatment – or, as we’ve come to think of it, trying to ‘catch a shapeshifter’. By doing so, we aim to make existing therapies more effective, instead of continually searching for new, more powerful drugs.
So, how do we achieve this state-gating? The key lies in understanding the mechanisms that drive cancer cell plasticity. We’re employing a combination of cutting-edge genomic techniques, machine learning algorithms, and experimental models to comprehend the genetic and environmental factors that cause these cells to change their state.
Our research reveals that the androgen receptor, which responds to male hormones, is one crucial signalling mechanism that enables triple-negative cancer cells to switch identity. By using drugs to block this receptor, the shape-shifting process gets halted. Cells remain trapped in a state sensitive to chemotherapy, enabling more complete tumour destruction.

We now have a clinical trial underway at The Kinghorn Cancer Centre to evaluate state-gating therapy for triplenegative breast cancer patients. This trial, called 4CAST, represents the first attempt to therapeutically exploit plasticity dynamics in the disease. The trial revolves around an experimental drug, seviteronel. This drug works like a master switch, jamming the androgen receptors that tell triple-negative breast cancer cells to adapt against chemotherapy. It’s early days, but we’re hopeful that our approach will boost the efficacy of chemotherapy in these patients. If successful, seviteronel could be on its way to a larger safety study within a year.
Androgen signalling is also relevant in other malignancies such as prostate cancer. Furthermore, brain cancer, lung cancer, pancreatic cancer, melanoma, and leukaemia also exhibit high cellular plasticity, with specific signalling pathways yet to be discovered. The state-gating concept could have wider applicability and open a world of treatment possibilities.
Our state-gating work is part of a watershed moment in oncology research, where with an enriched understanding of tumour heterogeneity, cancer treatment is being redefined. As we continue to explore the promise of stategating, we’re approaching a future in which our treatments are not just stronger, but smarter, offering a glimmer of hope in the relentless pursuit of better treatments, and ultimately, cures for cancer.
Author: Associate Professor Christine Chaffer is head of the Cancer Cell Plasticity Lab at the Garvan Institute of Medical Research and a Conjoint Associate Professor at St Vincent’s Clinical School, Faculty of Medicine and Health, UNSW Sydney.
How a radical rethink of cancer’s identity helps to pin down its evasive tactics with ‘state-gating’ therapy.CHRISTOPHE KEREBEL CHRISTOPHE KEREBEL CHRISTOPHE KEREBEL My Twitter : @chriskere
How the study of antiparasitic compounds for the livestock industry led to the unexpected discovery of a breast cancer armoury.

Composite microscopy image showing the selective killing of breast cancer cells while having no effect on normal breast cells.
(a) Untreated breast cancer cells. (b) Breast cancer cells treated with one of our breast cancer selective molecules (NAP-6, 24 h) showing cell death. (c) Untreated normal breast cells. (d) Normal breast cells treated with NAP-6.
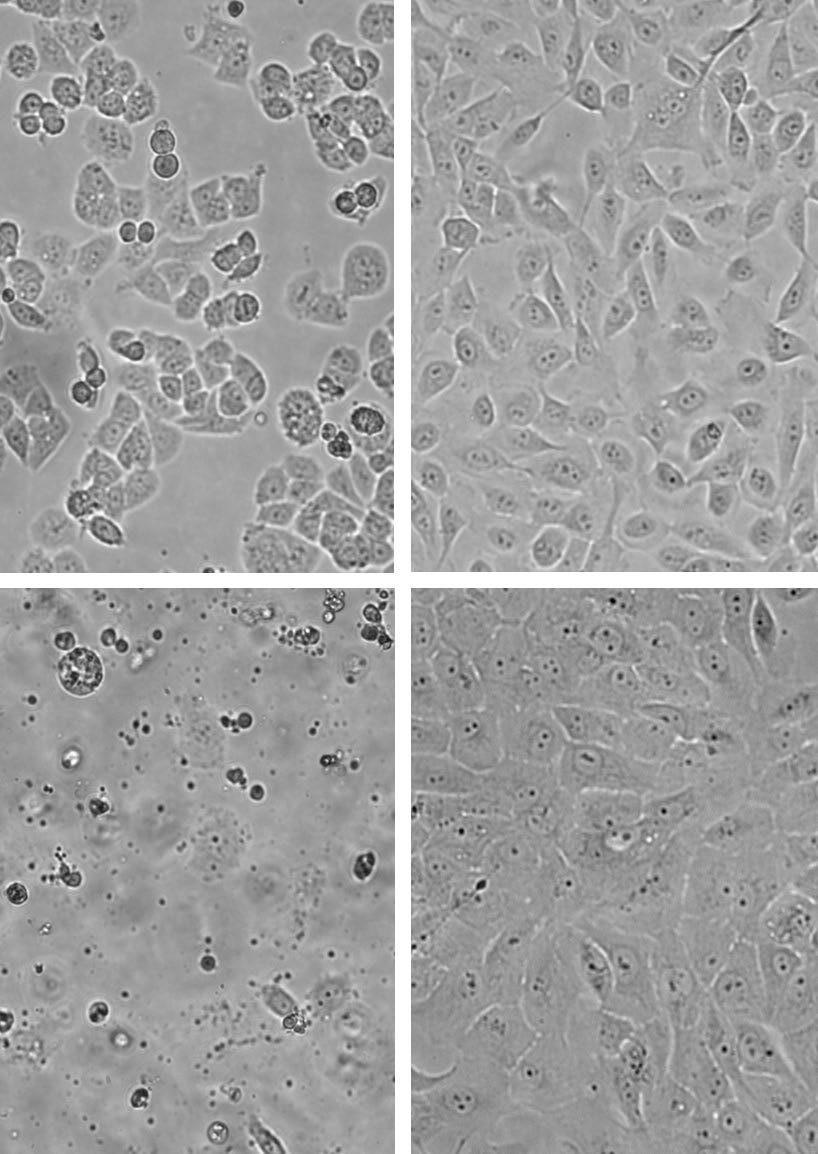 Associate Professor Jennette Sakoff in the laboratory.
Associate Professor Jennette Sakoff in the laboratory.
Some 14 years ago, Associate Professor Jennette Sakoff, Calvary Mater Newcastle’s (CMN) Medical Oncology Experimental Therapeutics Group head, made an unusual discovery.
A colleague at the University of Newcastle was developing anti-parasitic compounds for the meat and livestock industry, and A/Prof Sakoff assisted by screening the compounds to determine whether they were detrimental to human cells. What she and her team unexpectedly found was that the compounds were killing certain populations of breast cancer cell lines very well.
“My colleague decided they didn’t like the compounds for their own purpose, but I couldn’t ignore what I was seeing down the microscope,” A/Prof Sakoff said.
“Their trash became our treasure, and I needed to find out why these compounds were so selectively targeting and killing our breast cancer cell lines.”
“Sometimes you see drugs or compounds that work twice as well in one cell type or tumour type, but this was one thousand times better at killing these cells. The selectivity was phenomenal.”
The team set about investigating how and why this compound was working so effectively. Was it targeting the estrogen receptor? Was it targeting the enzymes that make estrogen? The answer was a resounding no.
“We did find an anomaly in the cell cycle analysis process; specifically how the DNA was being metabolised,” she said.


For years the Mater team sent molecules all around the world looking for answers, conducting further biology testing, however they struggled to make progress. A/Prof Sakoff continued researching to find literature that might point the team in the right direction.
“We came across literature about the aryl hydrocarbon receptor pathway, which is the pathway that the body metabolises aryl hydrocarbons, or what we might know as environmental toxic substances,” she said.
“When you have the right chemical pathway in the first instance, aryl hydrocarbons are metabolised into nasty, DNA-interactive compounds that can form cancers. Our molecules were binding to this DNA, stopping them from replicating and killing them.”
After years of further research, the team now plays with the chemical composition of molecules to produce a compound targeted to kill breast cancer cells without harming the healthy ones. As an extension of this, the team has switched focus to other cancers largely induced by environmental factors, including pancreatic and bladder cancers.
“There are thousands of molecules that we inhale (some of which come from cigarette smoke or car
exhausts for example) and that turn on and bind to this aryl hydrocarbon receptor pathway and turn nasty,” she explained.
“The great thing is our team has found five molecules that bind to this pathway, inhibit it and turn it off like a unique chemical switch. Simply speaking, this can translate to potential drugs to treat cancer.”
According to A/Prof Sakoff, the United States Food and Drug Administration has fast-tracked the exploration of similar molecules in the treatment of bladder cancer, however none have been translated into clinical use at this stage.
“Our molecules will not replace treatments, but they may eventually be used as an additional option for chemotherapy and you always want more than one molecule in your armoury,” she said.
In recognising these findings, the support of the late Naomi Keir, a former breast cancer patient at Calvary Mater Newcastle, her family and friends, as well as the organisers of the annual Boobs Bubbles and Breakfast fundraiser, must be acknowledged. Without them, this important work to date would not have been possible.
“As scientists, we rarely get out into the real world and you never really see your work translate, but Naomi was always so interested in what we were doing
“She couldn’t participate in the science side, but along with her family, friends and other community groups, has contributed enormously to the funding aspect, which is so greatly appreciated.”
A/Prof Sakoff explained it was a “no brainer” to publish her team’s findings to further the development of treating cancer.
“People often ask if me if I think there will ever be a cure for cancer and my reply is no, because as long as we are living in an environment that harms us, we can’t escape it.
“But if we can understand the biology better, we can continually look at ways of treating and targeting it better, and that is what we are trying to achieve.”
The initial study can be found in the Molecular Pharmacology journal
Author: Associate Professor Jennette Sakoff (PhD, Chief Hospital Scientist, Medical Oncology).
A/Prof Sakoff is the Chairperson of the Calvary Mater Newcastle Research Development and Engagement Committee and also holds a senior conjoint appointment at the University of Newcastle.
Breast cancer remains one of the greatest threats to women’s health worldwide.
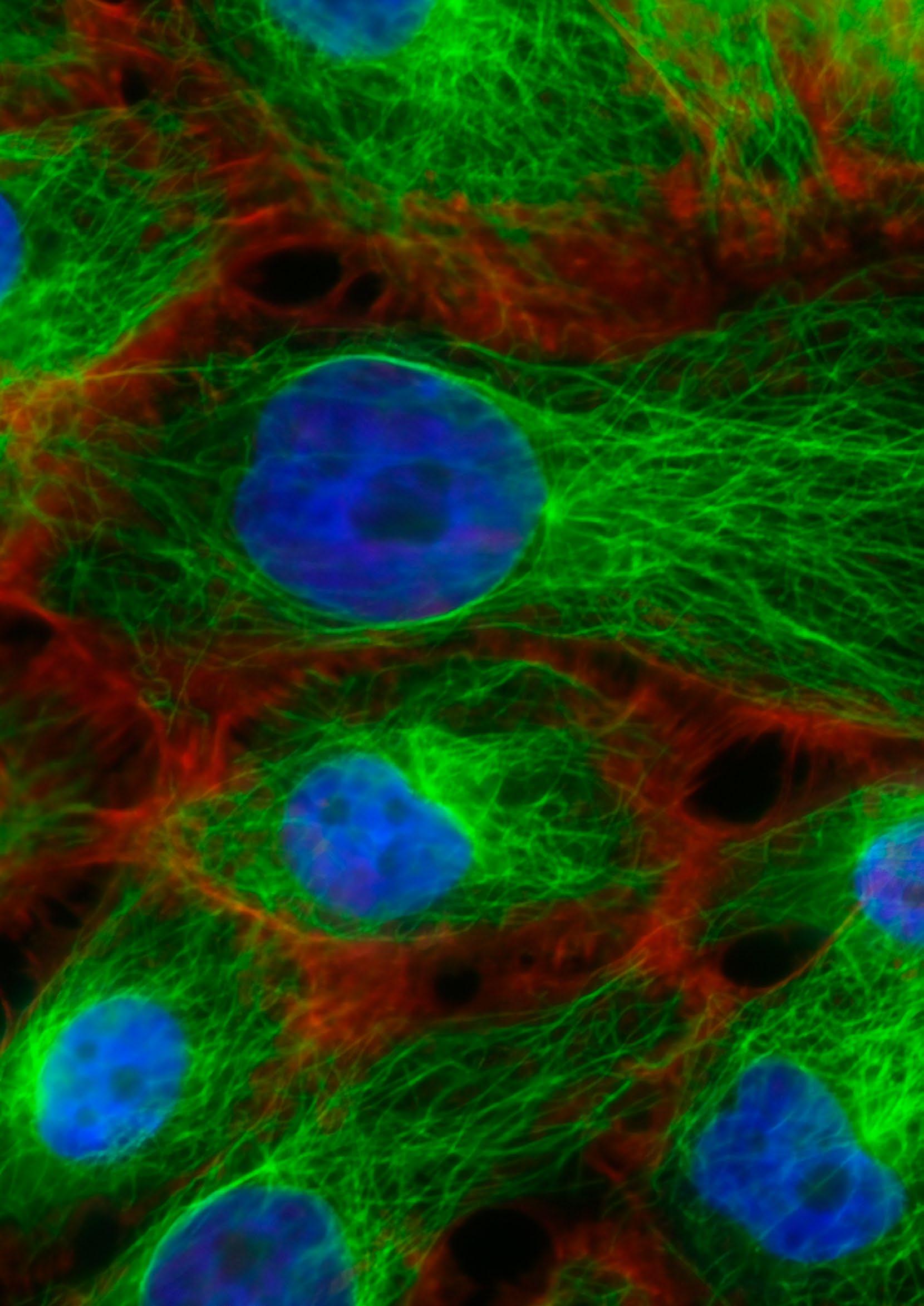
While treatment advances have saved countless lives, more than 500,000 are still tragically lost to this disease every year. Associate Professor Liz Caldon’s team at the Garvan Institute of Medical Research is dedicated to exploring strategies to reduce its deadly toll.
Cancer is known for its fast, uncontrolled growth. But my group studies some of the slowest growing cancer cells, which can gradually accumulate without detection for years after treatment. Over my 15 years as a breast cancer researcher, I’ve become particularly interested in this phenomenon, called late recurrence.
I focus specifically on estrogen receptor-positive (ER+) cancers, which make up about 70% of all breast cancer cases. These cancers have receptors for estrogen, meaning they can be treated with endocrine therapy to block hormone receptors, preventing the estrogen from stimulating cancer cell growth. The trouble is that five, 10 or even 20 years after successful treatment, in approximately 25% of patients, cancer cells will re-emerge. These recurring cells are more aggressive and elusive than ever, the tumours confounding oncologists. They don’t match typical models – they’re often slow growing rather than highly proliferative. And they lack some of the clear prognostic indicators present in other breast cancers. Finding a way to prevent or treat these late recurring ER+ tumours would greatly reduce breast cancer mortality.
In this work we are focusing on a high need target group, women at risk of recurrence. These patients live in fear of their cancer returning. They are taking many long-term preventative treatments, often with adverse side effects, without knowing if they are needed or if they will even work.
Advanced metastatic breast cancer is difficult to study in patients. We don’t have tests to identify which patients will get a late recurrence, and targeted therapies are not developed to treat these recurring cancers. In my lab, my team and I have made it our mission to illuminate how and why these cells hide in the shadows, resisting therapy, only to later cause chronic disease. We’ve pioneered new models mimicking late recurrence in the lab – a vital tool for studying the progression of this disease. What we’ve found is that endocrine therapy allows some cancer cells to avoid therapy through very slow proliferation, a resistant state where they avoid death, and this allows disease to slowly accumulate until it is no longer treatable.
We’ve also found a potential key to preventing late recurrence. These persisting cancer cells seem to rely heavily on Rac1 signalling pathways to survive and spread. Specifically, they use a protein called P-Rex1 to hyperactivate Rac1 signals within the cells.
Rac1 is a protein that helps control cell movement and growth. P-Rex1 is like the accelerator pedal that revs up Rac1 activity in the cancer cells. This enables the cells

to keep growing and migrating even when treated with therapy. The good news is that this reliance on Rac1 signals appears to be an Achilles heel we can exploit. There are existing drugs, called Rac inhibitors, that can block these Rac1 cell signals. In our cell and animal models, we saw that these Rac inhibitor drugs could effectively stop the growth and spread of individual recurring cancer cells that had this activated P-Rex1/Rac1 pathway.

Our next focus is further testing to bring this promising discovery one step closer to the clinic. My team is now repurposing an experimental drug to act as a Rac inhibitor in advanced breast cancer treatment. By working closely with clinicians, we hope to take this treatment from bench to bedside here in Australia. We see a future where breast cancer patients are routinely screened to discern who could benefit most from Rac-inhibitory drugs as a treatment. There are certainly challenges ahead, but right now the momentum is palpable. We’ve assembled key elements –cutting-edge tools, accurate modelling, clinical connections – to translate discoveries into real outcomes. Through persistent research, we are uncovering the intricate mechanisms behind breast cancer’s late recurrence.
Ultimately, this work only moves forward thanks to the generosity of our funders and community. Their support empowers our team to push the boundaries of research and care. Together, we are writing a future where groundbreaking science translates into longer, richer lives.
Author: Associate Professor Liz Caldon is head of the Replication and Genome Stability Group at the Garvan Institute of Medical Research and a Conjoint Associate Professor at St Vincent’s Clinical School, Faculty of Medicine and
 Health, UNSW Sydney
Health, UNSW Sydney

Ovarian cancer has non-specific symptoms and no screening test; therefore, it is commonly diagnosed at an advanced stage, when it has already spread. Less than 40% of women with advanced stage disease will survive for five years after diagnosis.
The treatment options for patients diagnosed with ovarian cancer are limited, and most patients receive standard chemotherapy. Identifying women who respond poorly to
Combining large scale international research and input from consumers with lived experience, to advance personalised treatment for ovarian cancer patients.Research Assistants, Annie Bui and Christine McCaffrey, working in the Molecular Oncology group laboratory at UNSW Sydney.
current standard treatments, and finding more effective treatments for this group, will improve prognosis. Unlike other cancers, there is no validated tumour test for ovarian cancer to predict treatment outcome and guide treatment.
Professor Susan Ramus is a geneticist who leads the Molecular Oncology group within the School of Clinical Medicine, UNSW Sydney. She has been investigating how to improve the outcomes for women with ovarian cancer for more than 25 years.

She worked in Melbourne, Cambridge, London, and Los Angeles before moving to Sydney. She co-leads the Ovarian Tumor Tissue Analysis (OTTA) consortium, a large international consortium of more than 70 studies, from 18 countries. With more than 15,000 tumour samples and clinical data donated from women diagnosed with ovarian cancer, the OTTA consortium has been able to identify tumour biomarkers that are associated with patient survival.
The OTTA consortium has developed a novel prognostic test, called Stratification of Prognosis of Ovarian Tumours (SPOT), which can categorise ovarian tumours at diagnosis according to a patient’s likelihood of survival.


When the women are divided into five groups, based on the score, 75 percent of those with the highest score will survive 5 years, but only 12 percent with the lowest score survive 5 years. With funding from the National Health and Medical Research Council (NHMRC) Australia, Prof Ramus is working with a large international multidisciplinary team to validate the prognostic test. If validated, SPOT could be used to identify the patients with predicted poor survival for early clinical trials of alternative treatments to improve their outcomes.
To determine how SPOT could be implemented into practice, we have co-designed a patient acceptability study with five consumers with lived experience of ovarian cancer. Dr’s Lauren Kelada and Holly Evans are psycho-oncology post-doctoral research fellows within the School of Clinical Medicine, UNSW Sydney and the Sydney Children’s Hospital. Together with the consumers, they have developed a questionnaire to assess how willing patients would be to have the prognostic test.
They will investigate the perceived importance of several potential advantages and disadvantages of having the test. Disadvantages could include distress, anxiety or false hope, while advantages could include avoiding a treatment that may not work, or access to an otherwise unavailable treatment. Focus groups will be used to determine how the prognostic results would be best presented to patients. This evidence will inform the translation of SPOT from the laboratory to best practice clinical care.
With funding from NHMRC Australia, Prof Ramus and the OTTA consortium are working to improve the SPOT test, by including additional genomic information about the tumours. The test currently uses RNA expression of 101 genes, and DNA copy number data is now available from shallow whole genome sequencing. In addition, they are developing other ovarian tumour tests, to advance personalised treatment for ovarian cancer patients. This includes predicting if surgery could remove all the tumour, which would help to determine if a patient should have chemotherapy or surgery first.
Tumour tests could also be used to predict a patient’s response to new treatments. Using the large-scale genomic information available from the OTTA consortium, the tumour samples from patients could be grouped with cell models with information on response to treatments, to predict suitable treatments for groups of patients. These advances are only possible due to international collaboration, multidisciplinary research and consumer engagement.
Authors: Lauren Kelada1 , Holly Evans1 , Ovarian Tumor Tissue Analysis consortium, Susan J Ramus1,2
Institute/organisation affiliations
1. School of Clinical Medicine, Medicine and Health, Discipline of Women’s Health, University of New South Wales, Sydney, Australia
2. Adult Cancer Program, Lowy Cancer Research Centre, University of NSW Sydney, Australia.

Murdoch Children’s Research Institute has made historical contributions in the infection, immunity and global health space, with recent female-led projects championing maternal vaccine safety and uptake.
Vaccine uptake in Australia is consistently one of the highest in the world, with children routinely protected against major infectious diseases. Many women are also
encouraged to have booster shots prior to the birth of their child, or before falling pregnant. While there is wide scientific consensus around the effectiveness of routine vaccination, hesitancy towards COVID-19 vaccination emerged among pregnant women during the pandemic.
Pregnant women are at higher risk of severe COVID-19 disease but showed lower vaccination coverage compared with the general Australian population. Public health messaging reinforced the importance of maternal vaccination against COVID-19, influenza and pertussis (whooping cough) to protect parents and their babies.
Rich data on vaccination has been available to Murdoch Children’s researchers, thanks to a Generation Victoria (GenV) — a statewide project recruiting mothers, fathers, carers and babies. Over 100,000 families have signed up
(from L to R): ‘Asinate Toluta’u; Belle Overmars; Jessica Kaufman; Luisa Vodonaivalu; Meleane Lomuto date, including 40,000 babies. GenV is a longitudinal study, meaning that the same group of participants will be followed up several times across childhood to monitor and track health outcomes, pregnancy outcomes and vaccination status.

Murdoch Children’s PhD candidate Dr Rachael Purcell is a member of the Maternal Vaccine research team, using GenV’s statewide data to evaluate outcomes of babies whose mothers received COVID-19 or influenza vaccinations during pregnancy.

“Maternal vaccination was an important concern for families during the COVID-19 pandemic, with many having questions about the best way to keep mothers and their babies safe through vaccination,” said Dr Purcell.
“The Maternal Vaccine study with GenV is investigating this important question, evaluating health, safety and developmental outcomes for infants and children, including infant allergy and developmental outcomes”.
The Maternal Vaccine study is aiming to provide results on these important outcomes to key stakeholders, women and their families in 2024.
During the height of the COVID-19 pandemic, addressing misinformation and vaccine hesitancy, the Vaccine Uptake group at Murdoch Children’s developed a Vaccine Champions program to increase vaccine confidence and encourage uptake of vaccinations.
Murdoch Children’s Professor of paediatrics and vaccinology Margie Danchin said that the idea was that public health messages could ‘cut through with trust’ — reaching diverse communities through healthcare providers as well as community, faith and sporting leaders, trained to effectively communicate about vaccines.
The initial program, which was funded by the state government, ran for 18 months in Victoria and was accessed via webinars. The program was then approved for the Asia-Pacific region with funding from the federal government.
Vietnam, where we trained three tiers of ‘champions’ – who went back to their communities to share all the benefits of getting vaccinated,” Professor Danchin said.
“While COVID-19 boosters were the focus early on, we also championed routine vaccines including the Human Papillomavirus (HPV) in Tonga - where a national vaccination and screening program was only introduced in late 2022.”

HPV vaccination is an important new program for Tonga. There are 800 new cases of cervical cases in the Pacific each year and 500 preventable deaths, but only 5 per cent of women are screened for HPV in Tonga.
“We have promoted HPV vaccination in Tonga as something that not only saves lives but could be beneficial to having healthy children,” Professor Danchin said.
“While there are numerous challenges ahead, reaching the global community through local, trusted voices, and not just from healthcare specialists, has been a key learning.”
Senior Vaccine Uptake Group Researcher Dr Jessica Kaufman said that involving men and fathers in the vaccination conversation was an important aspect of the program.
“While vaccination decisions tend to be made by mothers, it doesn’t mean they are or should be the only ones involved and engaged in their family’s health. Fathers play a key role in supporting vaccination,” said Dr Kaufman.
“The majority of our vaccine champions in Fiji and Tonga were women, but we were also happy to see some men putting their hand up to lead.”
The team have also rolled out their vaccine uptake program in the Philippines, Papua New Guinea and Indonesia where the focus is to understand drivers of vaccination and tailor strategies to address them.
The success of these programs has been recognised globally, with Professor Danchin awarded The Bob and June Prickett Churchill Fellowship to improve vaccine and risk communication to optimise COVID and routine vaccine acceptance and uptake.
Murdoch Children’s will continue to champion projects spanning maternal vaccination, longitudinal research and vaccine uptake in the Asia-Pacific, and have access to the latest and most accurate information on vaccination.
Author: Kathleen Jessop , Media & Communications Advisor, MCRICorifollitropin Alfa Agonist Flare Protocol is not inferior to Corifollitropin Alfa Antagonist Protocol for projected poor responder patients in IVF.
We compared two protocols for ovarian stimulation for predicted ‘poor responder’ patients undergoing IVF, to determine whether a novel protocol termed the Elonva flare protocol, was noninferior to a standard Elonva antagonist protocol.

The novel protocol required significantly less injections than the standard protocol and increased circulating FSH during the critical early days of ovarian stimulation.

One in 18 births in Australia now follows IVF treatment. Technological progress has resulted in significant improvements in the chances of a healthy live birth after a single treatment cycle for younger women with a normal ovarian reserve. However significant challenges remain when trying to assist women with poor ovarian reserve or who are older in a reproductive context (i.e., over 35 years of age). Success rates remain relatively low, and women may undergo multiple cycles of treatment with many remaining childless. The term ‘low ovarian reserve’ refers to a premature depletion of the store of ‘resting’ primordial follicles from which each month’s group of oocytes (eggs) will develop. Ovarian reserve can be assessed by using blood markers such as AMH or using ultrasound. Studies have demonstrated that approximately 10% of patients have a sub-optimal response to controlled ovarian stimulation. An optimal stimulation protocol for this cohort of patients is yet to be determined.
Women with low ovarian reserve are likely to be ‘poor responder’ patients when given the medications used for ovarian stimulation before egg collection for IVF. Ovarian stimulation is achieved using injectable follicle stimulating hormone (FSH). This is usually given as a once per day subcutaneous injection. However, we can use a seven-day depot medication, corifollitropin alfa (Elonva), resulting in a reduction in the burden of injections to patients. Elonva is licensed for use with a gonadotropin releasing hormone (GnRH) antagonist which is administered as a once per day injection.
We compared two protocols for ovarian stimulation to determine whether a novel protocol termed the Elonva flare protocol, using corifollitropin alfa with a GnRH agonist (Synarel) given as a twice daily nasal spray was non - inferior to a standard protocol using corifollitropin alfa with a GnRH antagonist. The novel protocol may be advantageous as it involves the use of significantly less injections that the standard antagonist cycle. We also hypothesised that the unique pharmacokinetic and pharmacodynamic profiles of corifollitropin alfa used with GnRH agonist would maximise FSH exposure and follicular recruitment in the critical early follicular phase, due to the initial suprathreshold release of bioactive FSH combined with the ‘flare’ of endogenous FSH release.
The Poseidon criteria (https://www.ncbi.nlm.nih.gov/pmc/ articles/PMC6880663/) allow researchers to segregate women who do not respond well to ovarian stimulation for IVF into clinically relevant groups. We used this system to identify predicted low responder patients. The aim was to develop and compare detailed pharmacokinetic and pharmacodynamic profiles for Elonva Flare cycle versus an Elonva Antagonist cycle.
Method: Nineteen women aged between 31-41 years of age were identified as potential poor responders according to the Poseidon criteria. They were recruited from the Fertility and Research Centre, Royal Hospital for Women and City Fertility Centre, Sydney. Each participant was randomised to an Elonva Flare cycle or Elonva Antagonist cycle. Serum FSH, LH and E2 concentrations were measured daily for five days post initiation of Elonva during the early follicular phase.

RESULTS:
Two days after the initiation of Elonva, serum FSH concentrations were 27 versus 11 IU/L (Flare versus Antag) (p=0.022). Serum E2 concentrations following two days of Elonva were 349 versus 157 (p=0.039). On day seven, mean serum E2 concentrations were 3000 versus 1850 pmol/L. The number of injections given to women in the Elonva Flare arm was significantly less than those in the Elonva antagonist arm, 4 versus 11 (p = 0.001).
CONCLUSION:
The Elonva flare corifollitropin alfa plus GnRH agonist stimulation protocol resulted in higher concentrations of FSH in the early period of follicular stimulation. This resulted in an elevation in serum E2 suggesting elevated follicular recruitment in this group of poor responder patients.
The Elonva flare protocol may be less burdensome to patients as less injections are needed. A larger RCT is required to assess and compare embryology and pregnancy outcomes.
Author: Dr Kaushi Arulpragasam is CREI Fellow and advanced subspecialist trainee at the Fertility Research Centre, Royal Hospital for Women, Sydney.
A novel technology promises to improve the success of fertility preservation for women seeking to safeguard their future reproductive options.
Oocyte cryopreservation, a procedure often chosen by young women prior to cancer treatments or for family planning, has faced challenges due to its inherent uncertainty.
The key ‘choke point’ of human reproduction, particularly IVF, is the availability of a quality oocyte i.e. one capable of being fertilised and developing to a viable embryo giving rise to a successful pregnancy. Fertility preservation begins with the collection of multiple oocytes which are then stored. However, it is not known what proportion of these oocytes are of high quality, nor which ones they are. As such, there is a strong element of guesswork and estimation that attempts to balance the woman’s priority of having a future family against her present health and discomfort. For instance, a woman may be stimulated to ovulate and produce a small number of oocytes. This might prompt another round of stimulation to maximise odds of a quality oocyte being available in the future –which is a health burden in its own right and could motivate the woman to explore delaying cancer therapy. However, if that small population of available oocytes could be evaluated for quality, this would better inform clinical decision making in whether additional collection is truly necessary.
In 2018 researchers from the Graduate School of Biomedical Engineering and the School of Clinical Medicine from the University of New South Wales carried out a collaboration where they investigated the effect of ageing on oocytes using a mouse model. In the process of documenting the research a dataset was created which consisted of photographic images of oocytes from young (optimum reproductive age) mice, old mice, and old mice which had been treated with a nutritional

supplement aimed at improving their reproductive health. Dr Abbas Habibalahi, a data scientist who was part of this investigation used a novel combination of advanced image analysis technologies – deep learning, swarm intelligence, and discriminative analysis – to investigate whether these oocytes could be “visually” differentiated by age. Although none of the other researchers – including some reproductive biologists with years of experience in embryology – could identify the age of the oocytes just by looking at them, Dr Habibalahi’s AI model could sort the young and old oocytes with almost perfect accuracy. Then, something very interesting happened. Having trained the model to sort oocytes by age, Dr Habibalahi showed it the images of the oocytes from the old mice that had been given the nutritional supplement. Even though all of these oocytes came from mice that were old, it sorted an increased portion of them into the ‘young’ group. In other work we had shown that mice that received the nutritional supplement had their fertility partially restored. So, as the age of mice correlates very strongly with their fertility, we hypothesised that Dr Habibalahi’s model could sensitively differentiate between high and low quality oocytes.
Now, obviously this wasn’t enough to conclude that this new technology would definitely be able to help with fertility preservation. For one thing, we hadn’t shown that the old oocytes from the supplemented group that were “misclassified” as young, were actually high quality. And, for another matter, women are not mice! So the two collaborating groups organised to work with the Fertility & Research Centre at the Royal Hospital for Women who (with patient’s consent) collected images of the oocytes of women undergoing IVF treatment, and
kept track of whether or not they developed into healthy usable blastocysts (the most advanced point of embryo development prior to transfer back to the woman for pregnancy). These images, and their associated clinical data, were used to develop a new model based on human images, that was built to predict an outcome of interest to patients, since we were potentially able to answer one of the most frequently asked questions about oocyte freezing, namely “How likely is it that this will work?’

In total, images of 211 oocytes from 39 infertility patients were collected, and the classification performance of the final model (measured by area under the curve assessment) was 84% accuracy. Although not perfect, this level of accuracy for the prediction of development to the blastocyst stage is about as much as could be hoped for, as although oocyte quality is the major determinant of success, other factors, such as the sperm, do also contribute independently.

Empowered by this success, the collaboration is now building a larger dataset that covers more clinical scenarios, which will give it greater generalisability to help more women make informed clinical decisions for fertility preservation.

 Dr Abbas Habibalahi in the laboratory at the University of New South Wales.
Author: Dr Abbas Habibalahi is a data scientist at the Graduate School of Biomedical Engineering in the University of New South Wales. His research focuses on using advanced image analysis technologies to solve intractable diagnostic challenges.
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
Dr Abbas Habibalahi in the laboratory at the University of New South Wales.
Author: Dr Abbas Habibalahi is a data scientist at the Graduate School of Biomedical Engineering in the University of New South Wales. His research focuses on using advanced image analysis technologies to solve intractable diagnostic challenges.
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL

While empowerment during pregnancy for the person who is carrying the baby occurs in current healthcare settings to help them support their pregnancy and growing child, an important family member can, and are often left behind, the partner.
Partners, whether they are the biological partner of the unborn child or not, influence the family unit. Emerging data show that while fathers experience psychological distress during their partner’s pregnancy, they question the validity of their experiences because of their perceived
We know it takes a village to raise a child, and yet emerging evidence demonstrates the importance of the perinatal period during pregnancy for the future health and development of the unborn child.
role as supporter and protector of the family unit. Previous nutrition programs that specifically targeted improving a partner’s nutritional awareness, knowledge and self-efficacy substantially explained the program’s positive impact on the pregnant person’s supplement intake. It is clear that partners need to be empowered and supported through their transition to parenthood. How can we best see how partners are faring in our current healthcare system?
Population-based studies have revealed powerful information about functional health and ageing well. Birth cohorts are population-based studies which focus on relationships between risk factors in perinatal and postnatal life and the health status in early life and beyond by typically following the biological mother and child.

The Queensland Family Cohort has taken a more detailed approach. We continue to follow over 500 different families including mother and partners, if there is one, to help understand the health needs of Queensland families and early life causes of disease through the collection of health assessments, questionnaires, and biological sample collection from both members of the parental unit. And what we found so far has revealed how valuable partnerships are during the perinatal period.
In our pilot cohort, recruited at the Mater Mothers’ Hospital in Brisbane, Queensland, partners were older than their pregnant partners and more likely to have preexisting chronic diseases such as asthma, depression and cardiovascular diseases.
They were predominantly well educated with a middle to high weekly income. In one sub-study that focused on parental psycho-social wellbeing, we observed that lack of social support and sleep impairment in partners placed a strain on the transition to fatherhood leading to higher levels of depression, stress and anxiety.

Mothers whose partners reported lower social support during the pregnancy tended to then have lower postnatal social support and a higher risk of postnatal depression. Analysis from pregnant participants who did not have partner revealed that they were more likely to suffer from depression and social isolation. While partner’s depression, anxiety and stress did not significantly change with COVID-19 lockdown or post-lockdown their psychosocial wellbeing was associated with poorer quality of life.
In a separate sub-study, we explored the diets documented during pregnancy of those who were pregnant and their partners and whether there were potential influences on dietary intake within the family unit. We found that pregnant people were more likely to meet daily recommendations for fruit, vegetables, bread/ cereals, dairy and meat/alternatives when their partners also met recommended dietary guidelines.
We also observed that partners were more likely to meet guidelines for micronutrient intakes from food alone compared to their pregnant partners. However, families overall had a suboptimal diet even though they had the economic means to improve dietary intake and nutritional intake in pregnancy remains the focus for improving the health of families of all socioeconomic groups in Australia. Our study has already identified that families, regardless of their socioeconomic status, need improved nutrition, mental health care and social support for a healthy pregnancy. Partners are central to a healthy pregnancy in addition to the village, and this impresses the importance of a whole family approach to well-being and health of the parent unit and child and with the transition to parenthood.
To read the Queensland Family Cohort Study Protocol follow the link here and follow the original articles described in the links at the following journals: BMC Pregnancy and Childbirth, Archives of Women’s Mental Health, Nutrition & Dietetics and The Australian Economic Review. This work was done in collaboration with the Queensland Family Cohort Research Collaborative with special thanks to the Mental Health Theme, Health Economics and Epidemiology Theme, Nutrition Theme and Social Determinants of Health Theme and lead collaborators Associate Professor Cameron Hurst, Associate Professor Shelley Wilkinson, Dr Barnaby Dixson and Professor Brenda Gannon.
Authors: Dr Danielle Borg, Program Coordinator of the Queensland Family Cohort. Professor Vicki Clifton, Principal Investigator of Queensland Family Cohort

 Dr Danielle Borg
Professor Vicki Clifton
Dr Danielle Borg
Professor Vicki Clifton

With climate change the world is experiencing more severe heatwaves and bushfire events, such as the 2019/20 Australian ‘Black Summer’ bushfires and the recent catastrophic wildfires across the Northern Hemisphere. Torrential storms and flooding across the globe are also being increasingly reported. Yet, the short and long-term impacts of these climate disasters on the physical and mental health of mothers and their unborn/recently born are poorly understood.
Mother and Child 2020 (MC2020) study1 researchers at the Australian National University (ANU) and the Healthy Environments and Lives (HEAL) Network 2 advocate for an international, interdisciplinary, collaborative research effort to establish the evidence to enable informed public health policy and clinical practice to safeguard the health and wellbeing of mothers and young children during future extreme climate events.3
While the adverse impacts of climate crises on vulnerable groups such as the elderly and those with pre-existing
medical conditions are clearer, the climate related impacts on maternal and child health are well less understood.
Following the 2019/20 bushfires, mothers and health care professionals alike reported to researchers from the MC2020 Study that they were desperate for information about the potential impact of the fires and smoke on their pregnancy and unborn children, but there was very little available.4
While prenatal exposure to wildfires and extreme heat have been linked to abnormal birth weight, increased rates of prematurity, gestational diabetes, and hypertensive disorders of pregnancy, the scientific robustness of the findings is far from conclusive.
The studies are either small, lacking granular detail of exposures, of quite varied climate-related events, or focussed on retrospective analyses of population level data. Furthermore, there is a lack of collection of early biological samples from mothers (e.g. placentae) and babies (e.g. dried blood spot) for biomedical assessments (e.g. oxidative stress), such that firm conclusions about risks and mechanisms cannot be made.5
It is well accepted that adverse exposures affecting pregnancy outcomes can have long lasting health effects on babies into adult life, yet we have very little evidence on the short and long-term biological impacts of heavy bushfire smoke and/or heatwaves on fetuses, and newborns.
Furthermore, these effects can be exacerbated by maternal and partner stress during the acute and the recovery phases of these crises, but there is paucity of dyadic level (mother and partner) data to inform practice. To fully understand the consequences and effects of climate crises on maternal and child health, well designed and adequately powered longitudinal birth cohort studies are essential in which detailed environmental exposure data, effects of events on living conditions and health care access, pregnancy outcome data, biomedical sampling, mental health assessments and longitudinal reassessments are obtained.
Furthermore, there is a need to establish mutually agreed protocols for international use for similar exposures, which will enable well-powered international studies to generate robust evidence necessary to inform mitigation strategies to protect mothers and babies from future events.

Consideration must be given to concurrent and serial crisis events, or syndemics and the scars left by continual hypervigilance.5 For example, the 2019/20 bushfires were rapidly followed by the COVID-19 pandemic and flood events, delaying recovery of communities severely affected by bushfires, due to disruption in social connectiveness.
Furthermore, climate crises are known to have greater adverse effects on the most disadvantaged in our communities. Research into the consequences of climate crises on maternal and child health must include these
groups, including Indigenous communities, refugee women displaced through war or climate catastophe, and those from culturally, linguistically, sexually and gender diverse groups.
climate affected birth cohort protocols, with interdisciplinary research teams, study governance, ethical approvals and funding already in place prior to climate crises occuring.
Only then can accurate individual subject exposure information, with critical biomedical sample collection, be acheived necessary to fully understand the biological effects of extreme environmental exposures on mothers and their children. The evidence resulting will enable informed changes to public health policy and clinical practice necessary to safeguard the health and wellbeing of current and future generations.

In the right direction, Prof Caitlin Wyrwoll from UWA and the HEAL Network has been awarded Wellcome Trust funding for a project titled “Extreme heat and pregnancy complications: Harnessing the diverse Australian climate and population for global answers.”6

References for this article can be provided upon request.
Authors: Professor Christopher Nolan is an Associate Director of Research, School of Medicine and Psychology, and Mother and Child 2020 (MC2020) Study Lead, Australian National University (ANU).
Dr Amital Bansal is a Research Fellow, John Curtin School of Medical Research and Biomedical Lead for MC2020, ANU.
Prof Deborah Davis is a Professor of Midwifery and Midwifery Lead for MC2020, University of Canberra.
Doctor Stewart Sutherland is the Chair of the Indigenous Health Framework, ANU College of Health and Medicine, ANU.
Associate Professor Caitlin Wyrwoll is the Stan Perron Charitable Foundation People Fellow and Healthy Environments and Lives (HEAL) Network Research Theme Leader, Human Sciences, University of Western Australia.
Professor Sotiris Vardoulakis is a Professor of Global Environmental Health and Director of the HEAL National Research Network, National Centre for Epidemiology and Population Health, ANU.

Healthcare and related sectors have a >70% female workforce and employ one in four Australian women in the workforce, yet women’s leadership representation remains inequitably low.

Evidence-based, solution-focused and systems/ organisational level approaches across all stakeholders are essential for effective gender equity impact.
Currently, the healthcare industry inefficiently harnesses its workforce capability, with its policies and culture unconsciously fostering a ‘glass ceiling’, failing to equitably support women’s career progression. Despite comprising 75% of the workforce women are 45% of public hospital board chairs, 39% of private hospital CEOs, 38% of state and federal chief medical/health officers and 28% of Medical Deans.
Imperatives for action include social justice and equity, workforce retention and productivity, health outcomes
(with evidence of better outcomes with gender diverse healthcare leadership) and organisational performance. Without leaders reflecting the diversity of the Australian community the healthcare industry will continue to perpetuate inequity. Despite growing awareness of gender inequities in healthcare leadership, current approaches remain adhoc, duplicative and of limited effectiveness, with progress on gender equality slow and limited.
The Advancing Women in Healthcare Leadership (AWHL) Initiative is a large-scale research, implementation and impact initiative with 22 partners, national and international, from across leading public and private health services, professional medical and nursing colleges, industrial bodies, government agencies, and not-for-
profit organisations, supported by cross-sector academic expertise. It aims to advance women in healthcare leadership to progress careers, deliver gender equity and improve health outcomes and now reaches across four continents.
AWHL is supported by two National Health and Medical Research Council grants, government funding and contributions from its partners. It was founded and is led by Professor Helena Teede AM MBBS, FRACP, FAAHMS, an internationally recognised clinician, researcher and academic with expertise in women’s health research, policy, and practice.
Professor Teede emphasises AWHL’s uniqueness lies in its evidence-based implementation approach to systems change, tailored to the challenges faced by women in healthcare and complemented by broad stakeholder partnership, thus facilitating diversity and inclusivity at its core.
By strategically integrating codesign and coproduction partnership and inclusive practice with an intersectional gender and diversity lens, AWHL has proved its effectiveness; we are already realising tangible impact at an organisational and system level”, says Dr Belinda Garth, senior AWHL research fellow.
We are generating knowledge and delivering multifaceted organisational and system level interventions that measurably improve career progression for women in healthcare and embed deep and sustainable change, notably beyond “fixing the individual woman” says Professor Teede.
Through its synthesised body of evidence, AWHL identified what effective strategies for organisational change are and demonstrated key success factors for how to deliver effective organisational implementation including intervention fit, fidelity, leadership, accountability, cultural climate and organisational readiness. Furthermore, it demonstrated the integrated and learning systems’ approach is crucial to effective implementation of targeted solutions, and the means to achieve sustainable impact.
“Getting the “what” and “how” right is at the heart of achieving long-term and sustainable gender equity, diversity and inclusion. Whilst generic actions can go some way to addressing gender inequities at local level, more often their impact is neither sustainable nor translatable across an organisation or the wider system”, says Dr Wafa El-Adhami, AWHL’s policy liaison lead.
This means strategies must be coproduced, locally adapted and core to planning, design and implementation,


and complemented by transparent performance measurement, evaluation and improvement as progress is made towards maturity and sustainability. demonstrated by recent processes with AWHL partner the Australian Medical Association (AMA); after considering evidence from the literature and from within AMA itself, together we coproduced agreed priorities for strategies for delivering on gender equity outcomes both within the AMA and more broadly across the medical profession. These were established through robust research and consensus processes. This workshop was commended by the Assistant Minister for Health, the Honourable Ged Kearney MP.
Importantly, AWHL integrates the Monash Women in Leadership (WIL) program. In place for 8 years, this program is evidence-based and now scaled with international reach, led by Prof Teede and Dr Mariam Mousa.
Combined, they grow leadership capability and capacity whilst concurrently removing barriers to gender equity and diversity system-wide to create equitable, safe and inclusive workplaces where women and all workers can thrive and deliver health and equity benefit for underserved populations with improved healthcare outcomes.
“Our evidence-base demonstrates that AWHL is a “blueprint” for sustainable system change. It is adaptable, translatable and scalable. I invite leaders to join our journey and commit to addressing gender inequity in the healthcare system together”; concludes Professor Teede.
Authors: Dr Wafa El-Adhami GAICD PhD MSc BSc (she/her) is the former (and inaugural) CEO of Science in Australia Gender Equity (SAGE) Limited. Continuing her commitment to gender equity and diversity, Wafa joined AWHL in June 2023 to lead its policy, advocacy and stakeholder engagement.
Dr Belinda Garth PhD BHSc(Hons) is AWHL Project Manager and Lead Research Fellow.
Professor Helena Teede AM MBBS, FRACP, FAAHMS is Lead Chief Investigator AWHL and holds leadership roles across health care, research and policy including as the Director of Monash Centre for Health Research Implementation, School of Public Health and co-director of the Monash Institute of Medical Engineering Monash University, an Endocrinologist at Monash Health, and Executive Director of Monash Partners Academic Health Sciences Centre. She leads the AWHL national initiative and its community of partners.

Committing to the dual role of clinician and researcher is an increasingly brave choice in the context of funding shortages and rising patient care loads.
This challenge is further accentuated when the field of research is historically underrepresented as is the case with women’s health. Professor Cassandra Szoeke (CS), a Melbourne based Neurologist and Associate Professor Nada Hamad (NH), Haematologist at St Vincent’s Hospital Sydney, share their perspectives on thriving and innovation in women’s health.
In the world of biomedical research, the evidence continues to demonstrate substantial gaps in our understanding of the impact of sex difference in pathophysiology and treatment outcomes. A global cross-sectional study of clinical trials identified female underrepresentation in 7 of 11 disease categories, including chronic kidney disease, HIV/AIDS and cardiovascular health1
Prof Szoeke spoke of the prevailing obstetric and gynecological focus in women’s health “We need to transform the concept of “women’s health” from a bikini view to brain, heart & body. The leading cause of death
1 Feldman S, Ammar W, Lo K, Trepman E,
M, Etzioni O. Quantifying Sex Bias in Clinical Studies at Scale With Automated Data Extraction. JAMA Netw Open. 2019;2(7):e196700. doi:10.1001/ jamanetworkopen.2019.6700
in Australian women is dementia and has been for years, yet every time I give my talk there’s a gasp of surprise from the audience. The leading causes of death in women come from brain and heart diseases. Despite the facts, we are not addressing the key issues of women’s health, and we need to educate women on these essential topics. Whilst some countries have revolutionised healthcare services and systems, Australia lags in its attention to women’s health from the Physicians perspective. There has been an overwhelming sense that women are healthier, as they continue to have a mean age of death 4 years more than men. However, the Australian Bureau of Statistics shows that over the age of 50, women are 4 times more likely to suffer “severe or profound disability limiting activities of daily living” than age-matched men.
Similarly, we now know that heart disease symptoms, diagnosis and management are entirely different in men and women. Yet the new National Womens Health Advisory Council doesn’t have neurology or cardiology
A conversation Associate Professor Nada Hamad and Professor Cassandra Szoeke van Zuylen(leading causes of death in women) represented. It is crucial we start to implement sex-specific medical services as has been done overseas to improve the health of Australian Women”

Key to progressing the agenda in Women’s health research is mandating and embedding sex and gender informed policies. Large funding bodies and research institutions have been more engaged in policy directed at addressing these shortcomings to positive effect.
“Sex disaggregated data is crucial. Mandates from the National Institute of around the turn of the century to include women in clinical research and in 2015 to include female mouse models in medical developments have led to recent understanding that in fact the presenting symptoms, predominant pathophysiology and optimal treatment is entirely different in women compared to men. (CS)”
Associate Professor Hamad highlighted the need to extend physician policy and advocacy beyond a gender only lens. Instead, adopting an intersectional approach that addresses the impact of social determinants of health on research and the application of novel technologies.
“The evolution of novel therapeutics is occurring at an extraordinary speed and there is an urgent need to incorporate personalised pharmacogenomic knowledge. Sadly, I’ll often have conversations with patients where I have to say we still don’t have data on how this agent affects this population vs another.


We often focus on the disease state because that’s really fascinating scientifically but then forget to integrate social determinants of health into clinical research design. Social determinants of health have been cited as contributing as much as 50% of the variance in health outcomes. How can we truly understand the limitations and strength of research if we don’t collect data on social determinants?”
Our conversation closed with a contemplation of the factors that had supported both researchers to thrive in their field of women’s health research. Prof Szoeke reflected on the value of developing a trusted network of sponsors.
“ Find your support team. Importantly don’t let the dialogue about networks and sponsorship let you fall into traps. Ensure you are with people who actually support you. Even if that group is not in the usual places of power.”
For Associate Professor Hamad wrangling with bias had led to a renewed sense of agency.
“I have learned to lean into my perspective as a strength. As a person of colour, my lived experience informs my research. I use it to enhance my research. It’s informing the questions I ask and the expectations I set around what our research should achieve.

I am much more deliberate about how I communicate things, what I communicate and what I don’t. Code switching is exhausting but it has sharpened my skills. I think this is a common experience for people of colour in general. In certain spaces I haven’t been able to optimally promote the agenda of equity, diversity, inclusion in my field of research locally. However, I’ve been able to do that internationally. The lesson learned is a door closed is not necessarily an obstacle.”
Authors: Associate Professor Nada Hamad, senior staff specialist bone marrow transplant, clinical and laboratory haematologist and President of the Bone Marrow Transplant Society of Australia and New Zealand

Professor Cassandra Szoeke Consultant Neurologist and Director, Healthy Ageing Program, Faculty of Medicine, Dentistry and Health Sciences, University of Melbourne
Dr Kudzai Kanhutu, Dean of the Royal Australasian College of Physicians
Professor Cassandra Szoeke A/Prof Nada CHRISTOPHE KEREBEL CHRISTOPHE KEREBEL CHRISTOPHE KEREBEL

Anecdotes of “man flu” are often laughed-off as attention-seeking behaviour but influenza is just one of numerous health conditions that can manifest differently across the population.
Research now indicates that many health outcomes depend on a person’s sex and can be influenced by gender expression. The terms sex and gender are often confused, so it is important to define them from the outset. In humans, sex is primarily assigned at birth according to external anatomy.
Distinct chromosomes typically align with designated sex: XY males, XX females, and persons with intersex variations. Intriguingly, with age, some people develop sex characteristics inconsistent with the sex recorded at their birth. One well documented example involves XY children who only develop male genitalia at puberty, as a consequence of insufficient early exposure to bio-active testosterone (attributed to alteration of the gene encoding 5a-reductase type2).


Gender on the other hand is the way people identify themselves: it is not always binary (as in men or women) or aligned with their assigned sex at birth; and can be flexible over the life course. Gender in particular may be complex, with considerable diversity in interpretation, understanding and expression, between individuals, communities, and countries.
What is becoming clear is that the major causes of death in Australia impact females and males distinctly. This is true for heart disease, stroke and cancer. Critically, our team at The George Institute for Global Health (TGI) and others have found that heart disease and stroke can present with different symptoms between the sexes, with heart disease still defined primarily as a ‘male disease’, based on male symptomatology. Other work by our team on cancers indicates that these often develop later and may manifest differently in females. For non-binary people, trans people and people with intersex variations there is a vast evidence gap on this topic, defining an unmet medical need. So why is this important for patient care?
Optimal patient care must be founded on evidence-based research that is rigorously grounded. In Australia and in most countries across the globe, pre-clinical medical research is yet to adequately account for sex, with many studies utilising male cells predominantly, only a single sex of mice, and failing to disaggregate data based on sex.
At the patient level, the call to include women in phase III clinical trials was as recent as 2017 in the US, enacted through the National Institutes of Health. As a consequence, the vast majority of the current standard of care health practices have been developed based on the way men develop disease and respond to treatment.
Recent evidence however, indicates that it cannot be assumed that diverse sexes and genders will have consistent health experiences. Sufficient data are yet to be gathered to fully understand the influence of sex and gender on associated risks, screening and detection, treatment, prognosis, and recovery from major diseases. Without representative inclusion, optimal health outcomes are in jeopardy. A striking example of the perils associated with inadequate population inclusion in clinical trials is illustrated by the fact that of 10 drugs withdrawn from the U.S. market between 1997 and 2000, eight were removed because they were found to be detrimental to women’s health. The failure to adequately involve women in the earlier trials led to this shameful waste of resources and risks to patient outcomes. The ultimate danger of such substantial omissions is inequitable healthcare and health outcomes.
So how does Australia measure up to the rest of the world? In 2023, Australia still lacks comprehensive policy directives for routine inclusion of sex and gender considerations in health and medical research. This stands in contrast to leading initiatives in Europe and North America, where transformative initiatives have been instigated by funding agencies, journal editors and education institutes.
The Sex and Gender Policies in Health and Medical Research project, a multi-year, philanthropically funded project, led by the Australian Human Rights Institute and TGI at UNSW Sydney, exists to improve protocols and policies to improve health outcomes for all. The project team has been working with key partners across the health and medical research pipeline to co-create policies that embed sex and gender in health and medical research, so as to ensure good research practice to improve health outcomes for all Australians. The project team is also developing an Australian specific framework to advance the development and implementation of sex and gender policies, and is developing a health economic model to examine the cost of not disaggregating data based on sex and gender. The next stage in this work is the establishment of a national Centre for Sex and Gender Equity in Health and Medicine, to house and drive this initiative.
Author: Prof Robyn Norton, Dr Cheryl Carcel and Dr Sue Haupt: Global Women’s Health Program, The George Institute for Global Health, UNSW Prof Louise Chappell and Lily Halliday: Australian Human Rights Institute, UNSWUnderstanding disease diversity in the population is critical for ensuring standard-of-care achieves health equity.CHRISTOPHE KEREBEL CHRISTOPHE KEREBEL CHRISTOPHE KEREBEL
This lack of female representation in pre-clinical research has created gaps in our knowledge, with significant consequences for women’s health. In Australia, tangible efforts are made to remedy this historic exclusion, but opportunities remain to make pre-clinical research more equitable for women.

The sex ratio at birth (i.e. the ratio of male to female live births) is historically very close to 1, meaning that females account for 49.5-50% of the global population. It may therefore come as a (bad) surprise that the vast majority of health and biomedical research, especially pre-clinical research, has been conducted in male models.
This binary classification refers to males and females as categories of sex, defined by a set of biological attributes associated with physiological characteristics. However, consideration of various groups of gender (men, women, non-binary people, etc.) remains an equally important gap in research.

The historical reasons behind the exclusion of females from basic health and biomedical research stem from the idea that females are more variable. Up until recently, it was widely accepted that accounting for acute and chronic ovarian hormone fluctuations would make female data, and therefore female research, less reliable. Not only does this idea lack experimental validation, but the very concept that sex differences and inclusion of females result in increased variability is now also being questioned. Several recent studies conducted in rodent models have demonstrated that female animals may not be more variable than male animals.
While this disparity is more prevalent in pre-clinical than in clinical research, the consequences are felt at all levels of the research translation spectrum. The belief that male pre-clinical findings can be directly translated to female clinical populations is erroneous at best, and dangerous at worst. A common example resides in the fact that, in many cases, drug metabolism is slower in females than in males. This suggests that, when drug administration does not take the patient’s sex into account, females may be overmedicated with possible adverse consequences.
Basic health and biomedical research has been traditionally conducted in male models.
Because basic research directly informs clinical translation, research leaders, scientific journals and funding bodies must now come together and call for greater inclusion of both sexes in research.
Government funding bodies in particular bear a responsibility to make pre-clinical research more inclusive of both sexes. In 2016, the National Institutes of Health (NIH) first implemented a policy requiring sex to be considered a biological variable in US government funded research.


For a study to be funded by the NIH, sex must be factored into study design, data analysis and reporting of the findings unless a clear justification can be provided for using one sex only (e.g. prostate cancer research). Similarly, the Canadian Institutes of Health Research (CIHR) expect all funded studies to integrate sex and/or gender into their research design and analysis.
Since the NIH policy was implemented, US researchers reported an overall 20% increase in published studies including female cohorts, with improvements in six of nine biological disciplines.
However, the same researchers found that significant gaps remain in the way these data are treated, statistically analysed and reported.
Up until recently, Australia was lagging behind and the National Health and Medical Research Council (NHMRC) still only indirectly recommends that researchers include both sexes in the design and analysis of their animal and human studies. However, in 2023, some steps were taken in the right direction. The NHMRC and the Department of Health and Aged Care (managing the Medical Research Future Fund [MRFF]) have been working on releasing a statement aiming at “improving health outcomes by promoting greater inclusion of sex,
sexuality, and gender diverse people in research; more analysis and reporting of sex and gender considerations in research; and greater consideration of inclusive, appropriate, and targeted implementation of research”. A workshop including researchers, statisticians, consumers and stakeholders preceded a broader consultation with the sector. Concurrently, the Association of Australian Medical Research Institutes (AAMRI) was working on their own guidelines for researchers and medical research institutes to complement the activities being undertaken by the NHMRC and MRFF. These changes will come at a cost. Indeed, sex- or gender-balanced studies are expected to cost at least 1.5 times more than their maleonly equivalents. However, the significant improvements seen internationally show this is an investment into the future of Australian research that we cannot afford to skip. While NHMRC and MRFF can heavily influence the research that may and may not be conducted in Australia, other actors within the research scene have a role to play. Some international scientific journals are paving the way by implementing strict policies regarding the reporting of sex- and gender-specific data. Ultimately though, research starts in the lab or in the field. Research leaders and academics are presented with a unique opportunity to educate the next generation of researchers by teaching good research practices that include sex- and/or genderbalanced designs, analyses and reporting. What remains an individual opportunity must soon turn into a duty to ensure Australian research is sex- and gender-inclusive by default, and therefore remains strong, robust and internationally competitive.
Author: Associate Professor Séverine Lamon is ARC Future Fellow within Deakin University’s School of Exercise and Nutrition Sciences and Institute for Physical Activity and Nutrition.

What can the X chromosome teach us about female autoimmune disease?

Imagine a woman struggling with unexplained fatigue, joint pain, and digestive problems for years. She’s been to countless specialists, undergone numerous tests, but no diagnosis has been forthcoming.
This is the experience of many women across the globe who face an uphill battle to get diagnosed with autoimmune disease. According to the Autoimmune Association, patients showing initial symptoms end up waiting an average of four years before receiving a definitive diagnosis.
Autoimmune diseases are a significant health concern, affecting 1 in 20 Australians. They occur when the immune system goes rogue and starts attacking its own tissues and organs. Examples include coeliac disease, where gluten peptides are targeted in the gut; multiple sclerosis, where myelin proteins are attacked in the central nervous system; and vitiligo, where pigment-producing melanocytes in the skin are under assault. Strikingly, autoimmune diseases disproportionately affect women, with four out of five patients being female. Some, like primary Sjögren’s syndrome, affect 12 times as many women as men. Despite this, current treatment strategies
and diagnostic criteria do not take sex into account. The importance of addressing this disparity is undeniable as it could lead to better diagnoses and treatments to improve the quality of life for countless women.
How and why does sex influence the immune system? To understand this, we need to delve into our evolutionary history. One theory speculates that males, in their drive to develop secondary sexual characteristics, traded off immune competency for testosterone. Conversely, females favoured estrogen to allow for the dynamic immunological changes required during pregnancy. This trade-off has significant implications. In essence, testosterone suppresses the immune system, while estrogen enhances it.
As a result, females mount more robust immune responses, as demonstrated by reduced mortality in conditions such as cancer, sepsis, and COVID-19. However, sex hormones don’t fully explain the female bias in autoimmune diseases.
To gain a deeper understanding, let’s consider the role of the X chromosome. Unlike XY males, each female cell has two X chromosomes where one must be inactivated to allow for normal cellular function and development. Imagine singing into two microphones at the same time: the sound would be too loud or distorted with feedback.
In a similar way, having two X chromosomes fully ‘on’ would blast gene expression signals. To prevent this, female cells turn down the volume on one X chromosome through a process known as X chromosome inactivation. However, this process isn’t perfect and 15-25% of genes are known to escape inactivation.


Having two X chromosomes, therefore, can be a double-edged sword. On the positive side, it enables females to mount stronger immune responses against infectious diseases.
However, the flip side is the potential for overactive immune responses leading to autoimmune disease. The effect of two X chromosomes can also be seen in males with Klinefelter’s syndrome (XXY) who display female-like rates of lupus and rheumatoid arthritis.
Genes escaping X chromosome inactivation influence the immune system in various ways. When expressed from one X chromosome, many are critical in detecting and responding to infections. As you might expect, having two active copies of genes that stimulate immune responses can lead to excessive inflammation. In individuals prone to overexpression of escapee genes, environmental triggers like microbiome changes and viruses could potentially ignite self-reactive immune responses. For instance,
Epstein-Barr virus infection is linked to multiple sclerosis, an autoimmune condition more common in females.
In my research, I investigate how X chromosome inactivation contributes to autoimmune diseases, with the goal of identifying X chromosome markers of autoimmunity. Comparing females with lupus and healthy controls, I study millions of immune cells to analyse their gene expression. Using machine learning algorithms, I have trained models to predict whether cells are healthy or diseased.
These models have identified X chromosome genes that could serve as biological markers for lupus diagnosis and disease progression.
This would be significant, because there is currently no definitive diagnostic test for lupus – clinicians must rely on a constellation of findings to make a diagnosis. Identifying robust biomarkers has significant implications not just for women, but for all individuals with autoimmune diseases.
The female bias in autoimmune disease is widely recognised, but many studies still fail to address it directly. There is an urgent need for a more nuanced, sex-stratified approaches in research and clinical trials.
By investigating the role of X chromosomes in health and disease, we’re stepping closer to a new era in medicine, where treatments are precisely attuned to an individual’s genetic makeup and specific disease profile. This approach is critical for transforming our understanding of autoimmune diseases and addressing challenges faced by patients in obtaining timely diagnosis and treatment.
Author: Lachlan Gray is a PhD candidate at the Garvan Institute of Medical Research and the University of New South Wales.



Thanks to an expert Research Advisory Committee of leading cancer researchers, The Kids’ Cancer Project can direct philanthropic funds to support groundbreaking research projects that will maximise the impact on childhood cancer treatments.
The Kids’ Cancer Project knows that survival starts with science. That’s why each year, we invite researchers from across Australia to submit grant applications for their pioneering projects. To ensure the science we invest in has the greatest chance of success we rely on experts in the field to guide our funding decisions.
The Research Advisory Committee is comprised of eight scientists from across Australia and the USA, each an expert in their respective field of research, who volunteer their time to independently review all grant applications. Their recommendations are handed to The Kids’ Cancer Project’s Board which ultimately determines the projects funded with money so generously donated by our supporters. The rules of the peer review process prohibit committee members from endorsing their own projects. The Committee members’ skills and experience in the childhood cancer sector are diverse and far-reaching and
include developing targeted therapies for solid tumours, molecular diagnostics, developmental therapeutics, biotech and bioinformatics, biomedical research, translational and clinical research, neuro-oncology, and early-phase clinical trials.


The Kids’ Cancer Project CEO, Owen Finegan, says it’s imperative to have rigorous and unbiased advice to ensure that funding has the biggest impact on childhood cancer possible:
“The collective expertise of the committee members and their international experience is beyond impressive. Each person contributes a unique perspective when evaluating project grants. Moreover, they ensure the projects that best align with The Kids’ Cancer Project’s four research pillars: Discover, Build, Translate, and Support will be the ones put forward for consideration by the Board.
“With their extensive knowledge of childhood cancer,
their understanding of the feasibility and the likelihood of translation of research from the bench to the bedside and its impact on kids, it’s understandable that our committee is supportive of better outcomes for kids through kinder and more effective treatments.
“Their guidance for our investment in Australian research is invaluable as we want to fund pioneering projects that have the greatest chance of success.”
The charity supports pioneering projects that will make a real difference to kids with cancer. Since 2005, The Kids’ Cancer Project has committed $70 million to over 354 research projects, with 57 Australian researchers currently being funded across Australia.
In 2014 with guidance from the Research Advisory Committee, The Kids’ Cancer Project was the first charity to fund research into personalised medicine by supporting the ZERO Childhood Cancer program. Since 2017 over 1,000 Australian children with cancer have been enrolled in the program where a sample of their cancer is analysed at a molecular level, looking for clues about what is driving its growth, and how it might best be treated.
The results of all this testing and analysis are then examined by an expert team of clinicians and scientists and a rapid report is issued to each patient’s doctor, highlighting the critical genetic features of the tumour that may influence diagnosis, prognosis, and treatment strategies.
For high-risk patients, the results of all this analysis and testing are made available to an expert team of clinicians and scientists who, where possible, make treatment recommendations for that child, based on the genomic findings. This information is then provided to the child’s oncologist, who takes responsibility for all treatment decisions and the child’s care. ZERO is now working to expand the program so, by the end of 2023, all children diagnosed will have access to precision medicine.

The Kids’ Cancer Program is also an advocate for kids with rare cancers which, in the past, have not received significant funding. Partnering with the Priority-driven Collective Cancer Research Scheme the charity has funded research into rare cancers including sarcoma, brain cancer, and neuroblastoma. Additionally, other childhood cancer-related areas such as education, nutrition, and physical fitness post-treatment have been also supported.
Thanks to the Research Advisory Committee, The Kids’ Cancer Project has funded Australian research leading to better outcomes for all kids with cancer.
 Author: Alison Muir, Trusts & Foundations Executive, The Kids’ Cancer Project
Author: Alison Muir, Trusts & Foundations Executive, The Kids’ Cancer Project


Stryker is one of the world’s leading medical technology companies and, together with our customers, is driven to make healthcare better.
The company offers innovative products and services in Medical and Surgical, Neurotechnology, Orthopaedics, and Spine that help improve patient and healthcare outcomes. Alongside its customers around the world, Stryker impacts more than 130 million patients annually.

Last year, Stryker opened a research and development lab at Herston Health Precinct as part of the Advance Queensland Industry Attraction Fund. Stryker, Queensland University of Technology (QUT), The University of Queensland (UQ), Metro North Health and Queensland Health have entered a Master Research Agreement that will focus on advancing research on the development of innovative medical technology products.
Stryker’s R&D Lab facility is a point-of-care R&D Lab, leveraging an open innovation ecosystem to accelerate the delivery of personalised health solutions.
It is based at the world-renowned Herston Health Precinct, a place where 13,000+ clinical and nonclinical staff, scientists, researchers, and students in 30+ health facilities, medical research institutes, universities, and organisations, come together to deliver excellence in health innovation, education, research, training, and clinical care.
Being located within this MedTech ecosystem allows the R&D Lab’s researchers and engineers to better
collaborate with clinicians and understand their current and future needs, all at the site of care.
Poised to have a profound impact on the future of healthcare, R&D projects are focused across four workstreams:
The Digital Health workstream leverages connected devices, computer vision capabilities and computational modelling to drive clinical efficiency, real-time clinical decision support and systems-level applications.


The Robotics workstream focuses on expanding the capabilities and applications of robotics within surgery, and medicine in general.

Leveraging the expertise of university and clinical partners, the aim is to ensure that the technology is used to its full potential, providing maximum benefit for patients and clinicians.
The Enabling Technologies workstream develops clinical software applications that enable data-driven, patient-specific treatment plans.
Through co-design with clinicians, decision support tools will be developed that streamline the decisionmaking process, simplify the user experience and drive more efficient and consistent decision-making.
The Advanced Manufacturing workstream looks at the benefits of additive manufacturing to healthcare, especially in the patient-specific space, investigating solutions that reduce the cost and lead time of products, as well as furthering our knowledge of new technologies and materials.
 CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL

related to her menstrual cycle, and she was referred for an endometrial ablation.
More than a year later, Beth suspected she was anaemic again and returned to her GP, who confirmed this. The GP again referred her to a gastroenterologist. It was a surprise to all when the colonoscopy found a tumour which turned out to be stage 3 bowel cancer.
I’ve heard stories about being seen, but not believed. Women who unsuccessfully seek help for pelvic pain as teenagers only to suffer into adulthood from crippling endometriosis.
Women who complained of symptoms like chest pains, nausea, light headedness, shortness of breath for weeks but were dismissed, only to have a heart attack. The bias against women in the health system is deeply entrenched.
I’ve seen it as a nurse, and I’ve heard it while representing the people of Cooper in Parliament.
Beth’s* story is one of many.
Beth was 44 years old when a routine blood test found she had anaemia. She had previously had mild anaemia during a pregnancy, and had been passing blood. The GP at that time thought the cause was haemorrhoids due to pregnancy, and referred her to a gastroenterologist. The gastroenterologist concluded her symptoms were
Shortly after this, Beth’s 60 year old father was found to be anaemic and was immediately referred for a colonoscopy. Due to Beth’s relatively young age and gender, her early symptoms of cancer were assumed to be related to her reproductive system.
Beth believes an earlier diagnosis may have limited or avoided the aggressive treatment that was eventually required.
Growing evidence shows this was not an isolated case. Systemic gender bias in health care delivery and medical research means women disproportionately experience delayed diagnosis, overmedicating, and a failure to properly investigate symptoms.
It’s not good enough, it never has been. Improving women’s health must be a national priority.
To turn this unacceptable situation around, the Albanese Government’s new National Women’s Health Advisory Council is providing strategic advice to government on improving Australia’s health system for women and girls. I
For many years women – young and old and from all backgrounds – have told me about the challenges they face in the health system.
was pleased to announce formation of the Council at the Research Australia Awards last year.
The Council membership is a mix of peak stakeholder organisations, consumer groups, academics, and medical and professional bodies Their breadth of knowledge, expertise and experience will put women’s health under the microscope. Cultural safety is at the forefront of the Council’s considerations.


They are looking at gender bias in the health system across four areas: safety; research; access, care and outcomes; and empowerment. Subcommittees have been established to drill deep into these specific systemic issues. I am pleased to say that Research Australia has an advisory role, bringing the views of the health and medical research sector to the table.
To inform the Council’s work a Community Consultation Survey opened on 19 July 2023. The survey will help the Council to understand the barriers and bias that women and girls face in Australia’s health system.

As chair of the Council, I encourage readers of Inspire magazine to participate in this important survey at www. health.gov.au/womens-health-advisory-council and share their story so we can make sure experiences like Beth’s are in our past, not our future.
 *Case study - the name has been changed to protect the patient’s privacy.
*Case study - the name has been changed to protect the patient’s privacy.
