Cardiac Arrest
The world was shocked in the past 2 weeks by 2 very high-profile cases of sudden cardiac does and relatively young and healthy individuals. This has stirred huge confusion along regular individuals about the difference between heart attack and a southern cardiac death because of cardiac arrest.
Gunnar Myrdal said, “all knowledge, like all ignorance, deviates from truth in an opportunistic direction”.
Thus, it is important for us here at Rutgers New Jersey medical school and the Arrhythmia Institute at University Hospital to explain the difference between cardiac arrest and heart attack, and to discuss who was at risk and to prepare everyone to be able to response appropriately if encounter someone who suffers such devastating issue.
In this newsletter issue we will discuss what are the causes of sudden cardiac death particularly in normal hearts and younger population and what are the steps that needed to be done in those who are at high risk of developing such condition.
Sudden cardiac death?
This what is sudden cardiac death?
Sudden cardiac death (SCD) is defined as best from unexpected circulatory arrest, usually presumed due to cardiac arrhythmia occurring within an hour of the onset of symptoms.

SCD ranks among the leading causes of mortality in the developed world, with an estimated conservative 13% of deaths are categorized as SCD.
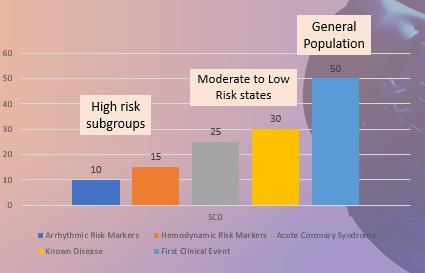
The average annual risk of a SCD in the general population is 0.1 – 0.2%. This risk increases as a function of advancing age.
The greatest increase in risk of SCD is among those aged 40 - 65 years. Two third of SCD occurs at home, work or play. It is fair to say that SCD claims more lives each year then lung cancer, breast cancer and HIV combined (Fig. 1)

Approximately 60% of out of hospital cardiac arrest (OHCA) are treated by EMS personal. 25% of EMS treated patients have no symptoms before the onset of arrest.
Among EMS OHCA, 23% have not initial abnormal ventricular rhythm (ventricular fibrillation or ventricular tachycardia VT/VF).
Family history of cardiac arrest in a firstdegree relative (parents, of Springs, siblings) is associated with a twofold increase in risk of cardiac arrest. It is important to understand the clinical status distribution amongst victims at the time of SCD.
50% of SCD occurs as initial presentation of any heart disease, many of these individuals may have been considered to be low risk. The development and application of the automated external defibrillator (AED) has involved from the need to deliver early defibrillation by trained bystanders the patients with VT/VF to the accepted standard tubal during resuscitation of out of hospital cardiac arrest that can be activated by any bystander/EMT personnel.
This information van be perceived as shocking to some, but, despite of the most common knowledge that most cardiac deaths are related to heart attacks (closed coronary arteries), according to the U.S. statistics only 12% are caused by coronary artery disease (CAD), the majority 88% have arrhythmic cause (abnormal heart rhythm) either in structurally normal hearts or in patients with cardiomyopathies (weak hearts).
Let us go over some cases of OHCA and learn the causes and how it could have been predicted and prevented.
Arrhythmia Hub
Cardiac Arrest During Sports
Soccer field, basketball court and football field
First Case: Antonio Puerta, a midfielder for Sevilla FC, collapsed during a game on August 25, 2007.

He regained consciousness and walked to the locker room where he collapsed again.

He was resuscitated and brought to the ICU of a nearby hospital.
He suffered multiple prolonged cardiac arrests over the next several hours resulting in anoxic brain injury and multisystem organ failure.
He died 3 days after his initial collapse at age 22.
Work-up revealed a cardiac genetic disease namely arrhythmogenic right ventricular cardiomyopathy (ARVC).
Second Case: Reggie Lewis, Shooting Guard and Small Forward for Boston Celtics. 4/29/93 Collapsed while running up the court in a playoff game

Diagnosed with Neuro- cardiogenic syncope and cleared to resume Basketball
7/28/93 Collapsed while shooting and died at the scene of SCD
Third Case: Damar Hamlin, Buffalo Bills, Safety, who was involved in a tackle and got hit in the chest by opposition player.
After, he was struck in the chest, Hamlin got up from a tackle and stepped forward before falling backward, and he was then down on the field for some 10 minutes as medical staff gave him CPR and he received an AED shock that returned his rhythm back to normal. He was placed on medical induced coma and lucky he regains all his neurological function and was discharged out of hospital.
What is common among these THREE cases? They all share Cardiac Arrest, TWO were not fortunate to make it and one survived. Many lessons need to be learned from these incidences.
Age-specific and disease-specific risk for SCD
For the general population 35 years and older, the risk for SCD is 0.1% to 0.2% per year (1 per 500–1000 population. Causes are dominated by coronary heart disease and nonischemic cardiomyopathy.
It is important to understand that 25% of SCD is related to inherited cardiac conditions (ICC). In people under 35 years of age, 50% of SCD is related to ICCs. Researcher can identify 70% of causal variants in genes related to ICCs.

In patients older than 30 years with advanced structural heart disease and markers of high risk for cardiac arrest, the event rate may exceed 25% per year, and the age-related risk is attenuated.
In adolescents and adults, the overall risk for SCD is 1 per 100,000 population or 0.001% per year, with a variety of causes such as inherited structural and electrical disorders, developmental defects, and myocarditis dominating. In the transition range from 30 to 45 years of age, the relative frequency of the uncommon disease yields to the dominance of coronary heart disease and nonischemic cardiomyopathy, but both groups of potential causes must be entertained because many of the rare disorders are expressed in that age range.

Arrhythmia Hub

Inherited cardiac conditions
The majority of cases of aborted SCD in a structurally normal heart involve inherited cardiac conditions namely hereditary Channelopathies or idiopathic ventricular arrhythmias.
A minority of cases involve occult structural heart disease from ARVD, sarcoidosis, amyloidosis, or myocarditis or miscellaneous conditions such as anomalous coronary arteries, coronary vasospasm or rare conditions such as Commotio Cordis.
Genetic Ion Channelopathies includes:
• Long QT Syndrome
• Brugada Syndrome
• Catecholaminergic Polymorphic Ventricular Tachycardia
• Idiopathic Ventricular Fibrillation
Working diagnosis of OHCA include systemic testing: exercise testing, drug provocation, imaging including cardiac MRI, and genetic testing.
Long QT Syndrome (LQT)
Arrhythmogenic disorder in the structurally normal heart presenting with QT prolongation that is often associated with peculiar ST-T–wave morphology, syncope, and sudden death

There are numerous genetic mutations lead to QT interval prolongation. Most common LQT1, LQT2, and LQT3

These can be diagnosed initially by simple ECG test and confirmed by genetic testing. There are special triggers for lifethreatening events (cardiac arrest or SCD).
Classical treatment for LQT syndrome can range from lifestyle changes like avoiding QT prolonging drugs, correction of electrolyte abnormalities, betablockers, or even an implantable cardiac defibrillator implantation (ICD). All LQT patients who wish to engage in competitive sports should be referred to clinical expect for risk evaluation.
According to the Bethesda Conference #35 (2005)
Unless your heart is perfect, NO COMPETITIVE SPORTS PERIOD!!!
Unless your heart is perfect or the syndrome is confined to just your genome, NO COMPETITIVE SPORTS except perhaps class IA sports, (i.e., billiards, bowling, cricket, curling, golf and riflery
Brugada Syndrome (BrS)
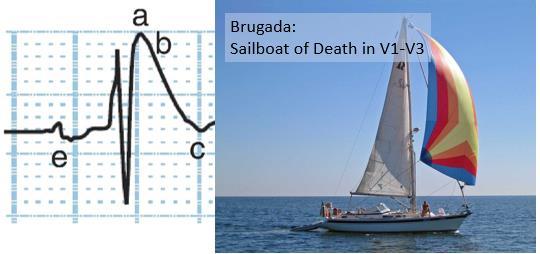
First described in 1992 by Brugada Brothers Characterized by an aberrant pattern of ST segment elevation in right precordial leads and a high incidence of sudden death in patients with structurally normal heart 4 -12% of all sudden death and 20% of sudden death in patients with structurally normal heart It is the leading cause of death of men under age 40 in regions where the inheritance is endemic, like southeast Asia and south America. Incidence estimated to be in the order 5 /10000
Typically, cardiac events (syncope and SCD) manifests at rest, during sleep and may be triggered by hyperpyrexia, large meals, excessive alcohol.
Diagnostic ECG patterns in the right precordial leads
ECG pattern can be diagnostic, and fever can unmask concealed BrS Inheritance of BrS occurs via an autosomal dominant mode of transmission with incomplete penetrance. The first gene linked to BrS is SCN5A on chromosome 3 which encodes for the alpha subunit of the cardiac Na channel. >80 mutations in SCN5A have been linked to BrS since 2001. Unmasking of concealed ECG can be achieved by utilizing Flecainide or Procainamide (Class I AAD), in a controlled setting.
ICD is the only proven effective treatment of BrS. As well as avoiding large carbohydrate meal, very hot baths, and hypokalemia (low potassium).
Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT)
Genetic abnormality in Ca++ handling Hallmark is ventricular arrhythmias induced by emotional or exertional stress CPVT genetic testing is recommended for any patient in whom a cardiologist has established a clinical index of suspicion for CPVT…[and] is recommended for family members and appropriate relatives CPVT should be suspected in young patients without structural heart disease presenting with syncope /sudden cardiac arrest / polymorphic VT / bi-directional VT induced by exercise or emotion
In absence of structural heart disease, and manifests in childhood and adolescence with a high lethality rate (30 – 50% mortality by age 30)

Stress test (exercise or adrenaline infusion) and/or genetic test should be done if CPVT a DDx
β-blockers are the cornerstone of therapy and will improve prognosis of patients
Arrhythmia Hub
confluence of variables and a proposed mechanism necessary for commotio cordis to occur. Important impact-object variables are shape, hardness, diameter, and velocity. Human characteristics are the pliability of the chest wall, impact timing, location and orientation of blow, and individual susceptibility, likely carried in ion channels involved in repolarization. LV indicates left ventricle. Reprinted from the Journal of Cardiovascular Electrophysiology
Commotio cordis
Commotio cordis is a phenomenon in which a sudden blunt impact to the chest causes sudden death in the absence of cardiac damage. This condition was first described in the middle of the 18th century in the context of chest trauma among workers. Through most of the 20th century, it was only sporadically reported. In the last 2 or 3 decades, commotio cordis events have primarily occurred in sports, and thus, this phenomenon has become more well known to the sports communities and physicians. Commotio cordis is to be differentiated from cardiac contusion (contusio cordis), a situation in which blunt chest trauma causes structural cardiac damage, such as observed in motor vehicular accidents.
It actually is timed like an R-on-T phenomenon, where it lands during that vulnerable portion of the heart. At the time of that T wave, if it lands during that segment, it puts the heart into ventricular fibrillation (VF) and is a known cause of sudden cardiac death in young athletes.

Approximately 10 to 20 cases are added to the Commotio Cordis Registry yearly. Until the late 1990s, commotio cordis was only rarely reported. It is thought that this increase in the number of cases is not due to an increase in incidence but rather to a greater awareness based on the 1995 New England Journal of Medicine report on commotio cordis.
Many more cases of commotio cordis are now recognized as such. Indeed, what was thought to be a uniquely North American phenomenon is increasingly being reported in countries outside the United States.
Commotio cordis can be prevented in many circumstances, but it is likely the risk cannot be eliminated entirely. The most important message is recognition of a traumatic chest wall impact can lead to sudden death. The only method to undo a cardiac arrest is a defibrillator that can shock the heart back into normal rhythm. So, the importance of an emergency action plan and AED cannot be overstated, and it is important to recognize that no matter what we do, there will never be a completely successful screening program that will eliminate the risk for sudden death. That is because commotio cordis actually occurs in structurally normal hearts. Basic Knowledge of CPR can safe certainly be the cornerstone in saving lives in the field.
For further information contact the Arrhythmia Institute at University Hospital Dr. Emad Aziz (Emad.Aziz@Rutgers.Edu)

What is it? How Fatal? Can it be avoided?
Resuscitation, once thought to be nearly universally unsuccessful, has now been demonstrated to be successful in up to 35% of commotio cordis victims
