






































Meet Humaira Chaudhry, MD’05, one of three alumni profiled in this special issue of Pulse magazine. We are proud of our graduates and all they have accomplished!

At NJMS’s new center, a multidisciplinary group teams up to help patients combat obesity and live healthier lives.

Two patients with severe facial nerve damage despaired that they’d ever find effective treatment. But they got the help they needed at NJMS.

As Pulse magazine marks its twentieth year in publication, it seems appropriate to look back at the many contributions it has made here at Rutgers New Jersey Medical School. Since the start of the century, our flagship publication has told the stories of our faculty, students, and staff who make NJMS such a special place. Thank you to the editors and writers who work diligently to produce this stellar publication.
Our most important mission has always been to educate physicians. Each year, some 170 new NJMS graduates go on to provide health care across the country. Even against the greatest odds, COVID-19 for one, our students continued to learn medicine and to graduate.
We continue to provide excellent health care to everyone who comes through our doors as well. In this issue you’ll read about two patients whose lives were transformed at NJMS. One, whose constant excruciating pain drove him to thoughts of suicide, found total relief. Another, whose face was partially paralyzed, can speak clearly and smile again. While you’re reading this issue of Pulse, be sure to also read about:
• How our new weight management center combines science-based medicine with individualized obesity treatment, resulting in improved health outcomes
• A group of NJMS student volunteers who mentor Newark high school students, teaching them the basics of suturing while increasing their awareness of health care careers
• Researcher Yuan-Xiang Tao, MSc, PhD, MD, who has developed a compound with the potential to help millions of people with chronic neuropathic pain
As our relationships with University Hospital and our other clinical and educational partners continue to thrive and grow, we look forward to a bright future for our school. Working closely with the community, we are very involved in improving the lives of the residents we serve. We look forward to seeing our many achievements highlighted in this wonderful magazine.
DEAN
Robert L. Johnson, MD, FAAP’72
The Sharon and Joseph L. Muscarelle
Endowed Dean, Rutgers New Jersey Medical School

ASSOCIATE EDITOR
LaCarla Donaldson
Manager, Marketing and Communications
SENIOR EDITOR
Mary Ann Littell
CONTRIBUTING WRITERS
Ty Baldwin
Merry Sue Baum
Amanda Castleman
Katherine Gustafson
Nancy A. Ruhling
Lina Zeldovich
DESIGN

Sherer Graphic Design
PRINCIPAL PHOTOGRAPHERS
Keith B. Bratcher, Jr.
John O’Boyle
KEEP IN TOUCH
Pulse is published twice a year by Rutgers New Jersey Medical School. We welcome letters and suggestions for future articles.
Send all correspondence to: Marketing and Communications Rutgers New Jersey Medical School ADMC Building 11, Suite 1110 30 Bergen Street Newark, NJ 07107 or via email to: njmsmarketing@njms.rutgers.edu
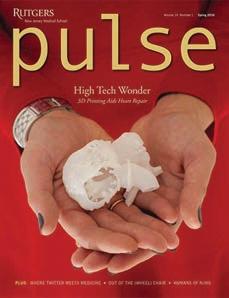
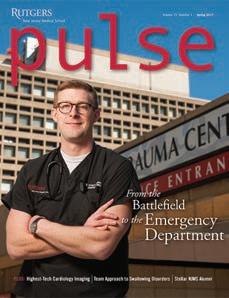
ON THE COVER
Pulse celebrates 20 years of excellence in clinical care, education, research, and community service..
njms.rutgers.edu
Get Social with Rutgers NJMS
Match Day this year was met with usual fanfare as NJMS students learned which residency programs they will attend and participated in events to mark the occasion. Ninety-six percent of NJMS’s 169 graduating students matched, beating out the national average of 93.7 percent.

Of those who matched, 51 will remain in New Jersey, 44 of whom will do residencies at either NJMS or Robert Wood Johnson Medical School. Others will scatter across the country to hospitals such as UC Davis Medical Center, New York-Presbyterian/Weill Cornell Medical Center, Duke University Hospital, Stanford Medical Center, and Mount Sinai Hospital.

This is the first matching class that completed almost all its medical education during the pandemic. The students who matched started medical school the semester before COVID-19 transformed medical education, forcing a switch to remote learning and prompting an emphasis on telemedicine.
The RBHS food pantry opened its doors in September 2021, dispensing food, hygiene products, and other necessities to anyone in the Rutgers community. Joachim Sackey, PhD, assistant professor at Rutgers School of Health Professions (SHP), and Fabricio Salas, SHP program assistant, lead a group of volunteers in serving all comers with a Rutgers ID every Tuesday from 12:30 to 3 pm.
“The medical field is made up of more than physicians and nurses,” says NJMS student and volunteer Ashley Eng. “Custodial staff, students, teachers…there is plenty of opportunity for people to experience food insecurity.”
By September 2022, the pantry had served some 15,000 people, distributing more than 115,000 pounds of food. But while reducing food insecurity is its primary goal, this needed service also benefits Rutgers by bringing people together.

“I really enjoy the people,” says Eng. “It’s great getting closer to the Rutgers community.”
Maria Laura Gennaro, MD, NJMS professor of medicine and professor of epidemiology at the School of Public Health, was named a National Academy of Inventors Fellow, the highest professional distinction awarded to academic inventors. Gennaro is recognized for her development of methods and platforms to diagnose tuberculosis and detect antibodies related to SARS-CoV-2 infection that causes COVID-19.
“Our work has always looked for connections between basic and translational research, and I have been lucky to work in institutions that have promoted novelty and innovation,” says Gennaro.

Onajovwe Fofah, MD, professor of pediatrics and director of the division of neonatology, has been named the new chair of pediatrics. Fofah served as vice chair from 2013 to 2019, and has been interim chair since 2019. He has been with the department since 2005, when he became assistant professor and attending neonatologist.

Fofah earned his medical degree in 1984 in his native country, Nigeria, and completed his pediatric residency at Children’s Hospital of New Jersey at Newark Beth Israel Medical Center, part of RWJBarnabas Health. He did a
fellowship in neonatal and perinatal medicine at New York’s Montefiore Medical Center.
Fofah’s clinical focus is on improving outcomes for infants born prematurely. Outside of research, he is intent on educating the next generation of clinical leaders, frequently acting as a mentor to students at all levels. He has made significant contributions to scientific literature in neonatal medicine and has been the principal investigator on high-profile clinical trials. Additionally, he serves the Newark community as a member of the State of New Jersey Pediatric Palliative Care Committee and as associate director for the Neonatal Palliative Care Program Circle of Life Children’s Center.

There’s an exciting new tool in the NJMS toolbox. For the last three years, NJMS has been developing its bespoke Faculty Affairs Toolbox System (FACTS), an electronic gateway for managing the employment lifecycle of NJMS faculty, from hiring through retirement.
FACTS maintains official records regarding faculty appointments, reappointments, promotions, leaves, tracks, separation and salary, serving as the central repository for related information and paperwork. It helps with the administrative tasks involved in hiring, including drafting offer letters and reappointment letters for faculty with expiring appointments. The system can also run reports about faculty demographics and employment metrics, and sends out monthly email alerts about changes in faculty positions and appointments.
Make a donation for NJMS scholarships here: give.rutgers.edu/NJMSScholarship
The Office of Faculty Affairs initiated FACTS’s development to move away from its previous inefficient, paper- and email-based system of tracking faculty employment information. The goal, according to Arnaldo Rodriguez, assistant direc-
tor of IT for NJMS and the technical project manager for FACTS, was “to get away from doing business all on paper. Much of the communication back and forth would be through email. It was disorganized.”
The new system, by contrast, provides a communication platform that streamlines and records employment-related interactions between faculty, administrators, and others. It also dispenses in large part with paper-based recordkeeping, keeping faculty data in order and up to date digitally.
Recently, the NJMS IT team also began supporting the faculty affairs application at the Rutgers Biomedical and Health Sciences (RBHS) level. And they are now collaborating with Robert Wood Johnson Medical School, the School of Nursing, and the School of Dental Medicine to help those institutions tie into the RBHS faculty affairs system. They can customize and update FACTS to ensure it is serving the RBHS community in the best possible way.
“Any suggestions or updates we quickly add to the system,” says Rodriguez. “So it’s a system that’s easily scalable, and we can modify it to the user’s needs. We’ve had nothing but positive feedback.”
Thanks to the generous contributions of Rutgers alumni, more than 140 second-, third- and fourthyear medical students—25 percent+ of each of these classes—received support from the annual alumni scholarship program this academic year.Fofah in 2012, with one of many babies whose lives he’s saved as head of neonatology.

When NJMS student Olivia noticed there weren’t any books in University Hospital’s pediatric playroom, her first thought was to lead a book drive. But the books were missing to reduce the risk of spreading infectious disease. So she developed a new idea: a pediatric e-book library.

“I’ve always loved to read,” says Scott. “Honestly, I always notice where there aren’t books.”
Scott received help and support Christin Traba, MD, MPH, associate professor of pediatrics and associate dean for education; pediatrics chair Onajovwe Fofah, MD; the Department of Pediatrics; and the hospital’s IT and cybersecurity teams. NJMS IT also helped coordinate logisics with UH IT. The University Hospital Foundation provided funding for three iPads, while the Newark Public School District and Newark Public Library offered recommendations for culturally and age-appropriate books to add to an Amazon wish list. Students, physicians, and staff donated almost 150 books.
Using tablets to house the library provides access to children who can’t come to the playroom. Scott remembers bringing an iPad to a bed-bound girl who lit up when she heard the tablet was filled with books.
“Reading can be an escape for a kid who’s in a scary situation,” says Scott. “Knowing that they can have this option available when they could be in the most stressful part of their life brings me a lot of joy and comfort.”
Scott is now working on implementing a second library at Newark Beth Israel’s Valerie Fund Children’s Center for Cancers and Blood Disorders. “We plan to be finished and operational within the next few months,” she says. She also plans to create a framework that other hospitals and clinics can use to easily set up their own libraries, including instructions, tips, and troubleshooting advice.
“I’m very proud of it, and I feel like it’s a great legacy to leave behind,” she says. “I’m proud that wherever I go next, this will still be there.”
To make a donation to the ebook library, purchase an Amazon gift card and send it to playroom@ uhnj.org
February 2023 marked the 40th anniversary of the NJ Poison Control Center, which has directly assisted close to 3 million callers over its four decades. Since starting with four poison specialists, it has grown to more than 20 full-time employees, including 13 poison specialists, plus six toxicology faculty. The center has been located at NJMS since 2009 and has also served as the state’s COVID-19 hotline since 2020.
“We’re one of the only places where you can pick up the phone and get a medical professional giving you advice 24 hours a day for free,” says Diane Calello, MD’99, executive medical director of the center and professor of emergency medicine. “You can’t even get that if you call a hospital, so that’s a big deal. As a 24-hour hotline, we are often here for the residents of New Jersey when no other place can be.”

Noa’a Shimoni, MD’04, associate professor of family medicine, has been named associate vice president for student health and wellness at Rutgers University and associate vice chancellor for student affairs, health and wellness at Rutgers–New Brunswick. Shimoni will collaborate with student health leaders and representatives to pursue strategic priorities around health and wellness. Her purview will include heading up population and preventive health initiatives and coordinating the university’s immunization management.


These new roles are a logical progression for a professional who has spent her career focused on wellness, community-building, and integrated health. She got her medical degree from NJMS, joined the NJMS family medicine faculty in 2012, and now directs student health at Rutgers Biomedical and Health Sciences for Newarkbased students. From July 2021 to July 2022, she served as acting vice president for student health services.
A Rutgers graduate, Shimoni has had an outsized impact on the university handling of immunization. She standardized and improved the immunization verification process across all campuses, and developed other protocols to keep students and the Rutgers community safe as part of the university’s response to COVID-19. She is a recipient of the Rutgers University Beloved Community Award.

In November 2022, NJMS students Alison Cáceres and Lucinalda Perez organized a community health fair in Cáceres’ hometown, Paterson, NJ. Paterson is home to a predominantly Latino and Black population, and has a significant share of uninsured and low-income residents. The organizers worked with Black Lives Matter and mentors Humberto Baquerizo, MBA, EdD, program development specialist, Office for Diversity and Community Engagement, and Damali Campbell-Oparaji, MD, associate professor of obstetrics, gynecology, and reproductive health, to host several NJMS departments and local organizations. These participants provided free screenings, resources and education on preventive medicine and primary care to about 60 Paterson residents.
Maria L. Soto-Greene, MD, professor and executive vice dean at NJMS, was honored at the 30th Annual Healthcare and STEM Awards Dinner in October 2022, sponsored by the Northern New Jersey Council, Boy Scouts of America. She received the Good Scout Award in recognition of her decades of work creating opportunities for those from communities underrepresented in medicine and science.
“I’m honored to accept this award, but I recognize there is still much work to be done,” says Soto-Greene. “As educators, we must continue to create new pathways for young adults, especially those in underserved communities who may have an interest in medicine or science. Giving them confidence in what they can achieve is the first step.”
One morning in 2015, Newark resident Sandra Carter, then 63, woke up with a strange, unpleasant feeling in her breast. Examining herself, she found a lump. “It felt funny, dense like a strawberry and prickly,” she recalls. After a mammogram and ultrasound testing, she was diagnosed with stage four metastatic breast cancer. Because her disease was so advanced, she underwent a double mastectomy, radiation and several rounds of different chemotherapies that halted the cancer’s growth.
“I took it well for some time; I didn’t feel bad,” she recalls. But eventually the cancer treatment began to affect her heart. “My heart wasn’t beating fast enough,” she recalls.
“And my blood pressure went up.”
Carter is not the only patient who, while successfully battling cancer, developed heart complications from her treatment. Heart damage, or cardiotoxicity, from chemotherapy and radiation is common, and varies with cancer type, treatment and other factors. Some studies found that the incidence of cardiotoxicity in patients treated with specific combinations of drugs can be as high as 34 percent. Patients may develop arrythmia—irregular heartbeat, or atrial fibrillation—rapid heart rate, or high blood pressure, all of which increase risks of heart attacks and strokes. And five to 15 percent might beat their cancer only to suffer full-blown heart failure.
“While we now have lifesaving cancer treatments, we also must address the potential risks of cardiotoxicity from these
treatments,” says Wadih Arap, MD, PhD, chief of hematology/oncology and director of the Cancer Institute of New Jersey at University Hospital. “We used to think that cancer and cardiac disease were separate entities. But the more we learn, the more we understand that they share many risk factors.”

In March 2022, NJMS launched a cardiooncology program to provide optimal cardiovascular care for patients before, during, and after cancer treatment, including long-term surveillance for cardiotoxicity in cancer survivors. With a multidisciplinary focus, oncologists, primary care physicians, and cardiologists work together to provide high-quality
against tumor types expressing the so-called HER2 receptors, inadvertently act upon the same receptors on the heart muscle cells, damaging them. “We’re able to target the cancer well, with personalized and tumor specific treatment,” says Arap. “But unfortunately, the same receptor seems to be expressed on the heart muscle, so the drug also finds that muscle and makes it weak.”
Even immunotherapy, a novel and highly efficient treatment that trains the body’s
CT scan, which can detect blood clots and reveal calcium deposits or stenosis—arterial blockage. The cardiac MRI can show how the heart pumps blood and reveal inflammation or unusual masses in the heart. These comprehensive tests allow physicians to devise the most optimal treatments.
While traditionally, cancer treatment focused primarily on eliminating tumors, the cardio-oncology program embraces a holistic approach, says Klapholz.
“In the past, physicians sometimes hesitated to treat patients’ hypertension or high cholesterol while they were undergoing chemotherapy,” he notes. “But we found that you need to control these things very well during cancer treatment to prevent cardiotoxicity.”
care. The impetus for the program came from Marc Klapholz, MD, MBA, professor and chair of medicine. “Many of the new and cutting-edge medical and biologic therapies for cancer can have effects on the heart muscle. Understanding those effects and managing them proactively is the burgeoning field of cardio-oncology,” says Klapholz.
Cardiac complications stem from how cancer treatments work. Aimed at the chest regions for breast or lung cancers, radiation can cause blood vessels and heart valves to thicken and inflame. It can also create blood clots in arteries and veins. Some chemotherapy drugs cause biochemical reactions that weaken the heart muscle. Other breast cancer therapeutics, which are very effective
immune system to fight cancer cells, can potentially damage the heart. The revved up immune system can cause heart muscle inflammation or myocarditis. Chimeric antigen receptor (CAR) T-cell therapy, which engineers patients’ own T-cells to fight tumors, can also cause adverse effects, including an overwhelming inflammatory response called cytokine release syndrome, or CRS. That can lead to abnormal heart rhythms, atrial fibrillation, heart failure, and death.
Modern cardiac imaging technologies are vital to revealing exactly what’s malfunctioning inside the heart, and at NJMS patients have access to an array of options, including electrocardiograms and echocardiograms. When necessary, they undergo a
Carter is a prime example of such a holistic approach. Because of her advanced cancer and tumor type, she was treated with radiation, anthracyclines and HER2 therapy, so her heart got multiple blows from the drugs. When she was first seen by physicians in the cardio-oncology program in November 2021, she had high blood pressure and high cholesterol, and her heart wasn’t pumping well. Treated with a cardio-protective regimen, Carter began feeling better. Today she remains cancerfree, thanks to the ongoing chemo, which she is able to continue and tolerate better. Her blood pressure is well controlled and her heart function has improved. Carter’s niece and caretaker, Juajara Carter, attributes this to the program’s well-rounded approach to care. “Unlike other specialists, this team does not just focus on the heart,” Juajara says. “They want to know about every issue my aunt has with any part of her body.”
The cardio-oncology team also treats patients suffering from heart amyloidosis, a condition that results from misfolded proteins that accumulate in the heart and
Continued on page 9
Once considered secondary to cancer treatment, cardio-oncology takes center stage at NJMS
a closer look
Many diseases that cause blindness can be managed, when caught early by screenings. By the time symptoms emerge, it’s often too late to save patients’ sight, and maintain their independence and quality of life. So NJMS’s Ophthalmic Telemedicine Program is bringing one-stop-shop preventative care into underserved, uninsured communities.
Since 2004, the team has screened for vision-threatening diseases including agerelated macular degeneration, cataracts, diabetic retinopathy and glaucoma. Its free mobile clinic visits schools; health fairs; houses of worship; and centers for communities, meal programs and emergency housing. Initially, these efforts struggled to funnel screened patients into followups: only one percent would attend further appointments.
Now 95 percent do, thanks in large part to a self-driving, two-wheeled robot that allows immediate consultation with subspecialty care
Dubbed “Dr. IC”—a verbal pun on the phrase “I see”—the machine can translate over 20 languages, increasing accessibility and putting patients more at ease. Meanwhile, cloud-based software analyzes retinal images autonomously, thanks to funding from the New Jersey Health Foundation.
“The AI looks at the progression or regression of a disease or stabilization,” explains Ben Szirth, PhD, NJMS’s director of teleophthalmology. “We can determine who needs to be sent urgently to the hospital and who we can follow up with remotely.”
These innovations benefit many patients, but especially those experiencing homelessness, he notes. Before, they had to choose between medical care and lining up to secure assistance. “Going to a hospital meant they wouldn’t eat and they’d sleep in the street. So that’s when we brought in robots,” Szirth says. The team also gives away food and clothing as additional incentives.
Members travel with $150,000 worth of equipment, including retinal cameras. “We have an optical coherence tomography system that scans the back of an eye and takes about 70,000 images without a flash. It displays the eye in three dimensions,” he says. “Imagine a loaf of bread and you can open each cut to see what’s happening. That’s very precise and really cool.”
The instrument also uses these scans to identify retinal patterns unique to each patient, so the team doesn’t need to record full names, just initials, which can scare away undocumented immigrants.
The telemedicine clinic takes a speedy and streamlined approach, while still delivering the expertise and advanced technologies of a university hospital. “It’s one large room with all the stations. Everybody stands and we have special tables that lift the equipment to your height,” Szirth explains. “This lets us go 40 percent faster than when people are sitting comfortably. In populations where we need to screen
a lot of people, we can’t afford to have a lot of conversation. Standing accelerates things a bit. I can see six to 10 patients per hour.”
And every year the team takes this technology on the road, offering free retinal screening through the Friends for Life conference, which hosts 2,000 adults and kids living with type 1 diabetes and their families at Disney World. “We’ve screened and followed them for ten years,” Szirth says. The team also does medical missionary work in Asia, Europe, and Latin America.
Students have been involved since 2006 and organized into an NJMS club—the Student Sight Savers Program (SSSP)—six years later. They now implement Dr. IC, focus on imaging, and study the program’s detection rates and screening protocols.

NJMS student Rita Vought, who is also the lab’s manager for SSSP projects, got involved to gain hands-on experience. “It’s unique that we can actually screen patients in the community: other specialties don’t have those types of service projects. I wound up liking it so much that I dedicated myself to improving Sight Savers,” she says. Vought hopes to go into ophthalmology.
“Fifty percent of patients are unaware they have any pathology. They don’t know they need an eye doctor,” she says. “A lot of these conditions don’t have any impact on your day-to-day life until you have a serious and irreversible problem.” SSSP volunteers stress the value of regular vision screenings and the importance of follow-ups for patients with issues.
They also work with community liaisons, who can communicate in people’s native languages and guide them towards resources like charity care
Students sometimes have to coax patients past their anxieties, Vought explains. Some fear bad news and flinch away from discovering the particulars.
“Dr Szirth has been an amazing mentor,” she adds. “His dedication to the community and student education has been a motivating factor for me and also, I’m sure, many other students.” ●
Contact

Continued from page 7
can lead to heart failure. The more severe type of this disorder is actually a type of cancer—along the spectrum of myeloma. In that condition, certain proteins forged from the bone marrow are incorrectly deposited in the heart muscle. Diagnosed via blood, urine tests, and a tissue biopsy, it’s treated with chemotherapy.

The other type, called transthyretin amyloidosis, can be inherited or develop with age. One of the genes for the inherited amyloidosis has a three to five percent prevalence in individuals of African descent. “We believe many people in our Newark patient population have undiagnosed cardiac amyloidosis,” says Alfonso Waller, MD, associate professor of medicine and director of cardiac imaging, so the team is making a concentrated effort to boost screening. That requires a cohesive multidisciplinary team of hematologists and oncologists, neurologists, pathologists, medical geneticists, genetic counselors, interventional cardiologists, and cardiac imagers. The Cardiac Amyloid Center (njms.rutgers. edu/cardiology) was recently awarded a quality improvement grant to facilitate systematic screening and diagnosis of cardiac amyloidosis.
Since its inception in March 2022 the cardio-oncology program has had more 100 inpatient and outpatient patient visits and is currently recruiting a director. The Department of Cardiology has developed a cardiooncology curriculum for general cardiology fellows so they can provide cardio-oncology care as practicing physicians. “It’s very likely that every cardiologist, whatever they do, will see patients who either have cancer or a history of cancer,” says Klapholz. “So our goal is to give all fellows some education on best practices of cardio-oncology.” ●
 BY MERRY SUE BAUM
BY MERRY SUE BAUM
Ellen Townes-Anderson, PhD, can quote the statistics on women in science without skipping a beat. She’ll tell you that each year 43 percent of new mothers leave their professions in science, along with 23 percent of new fathers. There are articles in numerous prestigious publications—The New York Times, The New Yorker, Scientific American, Nature, and from the National Academies of Sciences, Engineering, and Medicine, to name only a few—urging institutions and organizations to create policies to support new working families. And, she’ll tell you the U.S. joins only six of the 193 United Nations countries that have no national paid family leave. In
case you’re curious, the other countries are the small, undeveloped island nations of the Marshall Islands, Micronesia, Papau New Guinea, Tonga, and the Republics of Nauru and Palau.
A professor of pharmacology, physiology, and neuroscience does more than rattle off statistics, however. Her actions speak much louder than her words. She recently donated $500,000 of an inheritance she received to support postdoctoral researchers and students earning advanced degrees at NJMS.
Her interest in supporting junior scientists was first actualized by creating a new mother’s lounge, where moms can go to breast feed or simply take a much-needed
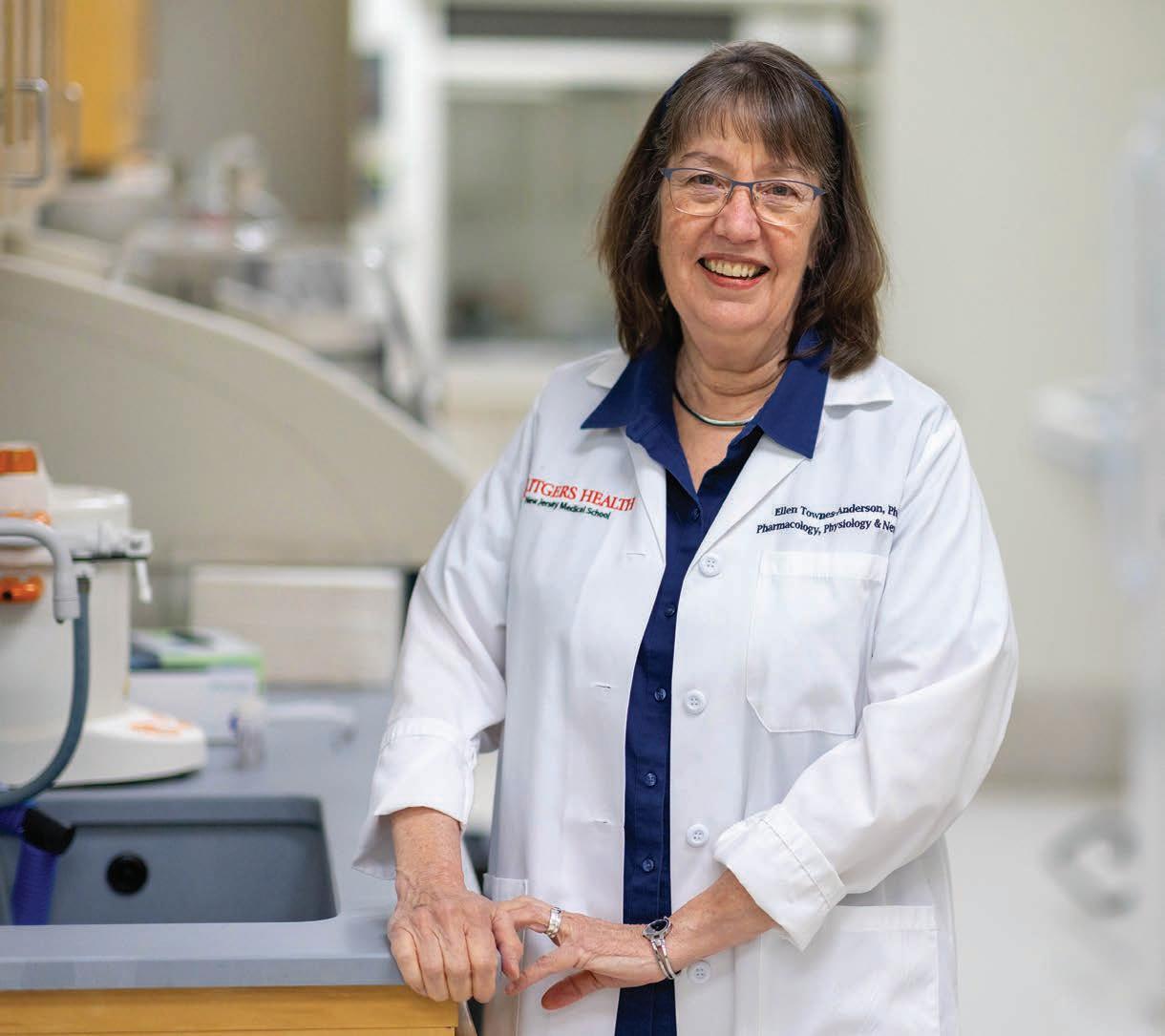
break. The lounge can be used by students, postdocs, staff and faculty, and visiting lecturers, anyone who needs it.
“I was at a meeting at New Jersey Institute of Technology when the staff showed me their lactation lounge,” she says. “It’s a lovely space with a rocker and running water. I knew immediately we needed something similar.”
Her gift will be used for expenses, such as stipends while new mothers are on leave, child care, technical support and various other expenses that arise. “So far, we hope to be able to help one or two families a year,” says Townes-Anderson, who is also an associate professor of ophthalmology. “Several coworkers and administrators have expressed interest in donating, so we’re hoping to increase the number of those we can help.”
Townes-Anderson is passionate about helping these young researchers because she knows first-hand exactly what they go through. She always loved science, so after college she started in a PhD program at UC Berkeley. Eventually she quit. “In those days there was no women’s movement and no female role models,” she explains. “Women didn’t become PhDs, and they weren’t scientists in academia if they had families. They were lab managers and supervisors.” She got a job in an electron microscopy lab at Harvard and later went to work as a technician at
Boston University School of Medicine. There she did have a role model: a woman from Italy, Giuseppina Raviola, who was an MD/ PhD, and had a family. Townes-Anderson began to think maybe she could turn her love of science into an academic career. She asked Raviola if she could be her graduate student, and enthusiastically restarted her training.
Just as she was finishing her PhD, she became pregnant. Raviola gave her three
women to be tenured in the Department of Physiology and Neuroscience in 20 years at Weill Medical School of Cornell University. She was also one of the first two women to be tenured in the Department of Neurology and Neuroscience at NJMS.

Townes-Anderson recalls a female student who came to her years ago in tears, because she was required to go back to work only six weeks after having a Cesarean section. “Her
months of paid family leave. “I had been so focused on my career that I forgot how enjoyable being with family was,” she says. “And I came back even stronger. I’m not sure I would have stayed in science if I hadn’t had that break.” Townes-Anderson has authored numerous articles and became the first
boss, the principal investigator, told her he needed her back in the lab. But she wasn’t physically or emotionally ready,” TownesAnderson said. “Legally he was correct, but I wanted to help her in some way.” NJMS postdoctoral family leave currently is a minimal six weeks. The Giuseppina Raviola MD/PhD Endowment will help expand that leave and other support to at least equal NIH standards.
Along with helping postdoctoral researchers and students with families finish their training and get into the workforce, she says her donation is in line with Rutgers’ initiative of supporting diversity. “If we don’t support young parents, we’re not supporting diversity,” she says.
“I love my career, and I love having a family,” she says. “For some women it’s too difficult to do both. That’s why it’s imperative that we support these young talented scientists. They need our help.” ●
To learn more, please contact Mary Ruotolo, Rutgers University Foundation, at Mary.ruotolo@ruf.rutgers.edu or 908-812-2806 (cell), or visit: give.rutgers.edu/RaviolaEndowment
“I love my career, and I love having a family,” says Townes-Anderson. “For some women it’s too difficult to do both. That’s why it’s imperative we support these young talented scientists.”
In the wake of the U.S. opioid epidemic, managing chronic pain has become a national focus, with researchers racing to produce non-addictive replacements for these dangerous drugs that can produce severe side effects. One of those leading the charge is Yuan-Xiang Tao, MSc, PhD, MD, professor and vice chair of research in the Department of Anesthesiology, and director of the Center for Pain Medicine Research at NJMS.
Tao studies the molecular and cellular mechanisms that underlie chronic pain and opioid-induced analgesic tolerance and hyperalgesia, in a quest to develop novel therapeutic strategies for the prevention and/or treatment of these disorders. “Our understanding of chronic pain is still in its infancy,” he says, “and its treatment is poorly managed by current drugs. Opioids are still the gold standard.”
One of his research projects, funded by a five-year, $3.5 million NIH HEAL Initiative grant, is for discovery and validation of a new, long, non-coding RNA as a novel target for neuropathic pain.
After identifying a nerve injury-specific long noncoding RNA (NIS-lncRNA) that kicks into high gear in primary sensory neurons after nerve trauma, in cases of diabetes or after chemotherapeutic exposure, Tao and his team designed antisense oligonucleotides (ASO), an FDA-approved strategy in the treatment of some neurological diseases. This strategy works by knocking down NISlncRNA without inducing toxicity, showing the potential to treat neuropathic pain in these three conditions. Tao notes that the drug, given by injection, is less addictive than opioid analgesics and doesn’t affect basal/ acute pain and locomotor function.

Although there are other non-opioid anesthetics on the market, notably bupivacaine liposome injectable suspension, which is branded as EXPAREL, Tao says that the NISlncRNA ASO drug his team produced offers several advantages. “It stops pain for at least seven to 10 days, which is three to four times longer than EXPAREL, and it doesn’t need to be produced fresh—it can be stored for up to a year versus 30 days for EXPAREL,” he explains.

“This new compound has the potential to help millions of people with chronic neuropathic pain,” notes Alex Bekker, MD, PhD, professor and chair of anesthesiology and professor of physiology and pharmacology.
Tao, who is from the small town of Dongtai in China’s Jiangsu Province, enrolled at Nanjing Medical University, where he pursued medicine as a career. After he graduated, he became a teacher as well as researcher
there. It was his father’s illness—he died of liver cancer in 1989—that caused Tao to shift his research interests to chronic pain relief. “My dad was in lots of pain and taking opioids,” Tao says, “but, at the end, he didn’t want to take them anymore because of the side effects.”
After completing his PhD training at Shanghai Brain Research Institute, Chinese Academy of Sciences, he went to the University of Virginia as a postdoctoral fellow. Shortly thereafter, he was recruited by John Hopkins University School of Medicine, where he and his team developed several patented pain-relief drugs.
During his decade teaching and doing research at NJMS, Tao has secured one patent in 2018, for an injectable and long-lasting anesthetic that relieves the pain of shingles and aids knee-replacement surgery recovery. Like the ASO he developed, this PLGA-coated ropivacaine can be converted into a powder for long-term storage and long-lasting analgesics for more than ten days.


Tao’s family is steeped in medicine: He lives in Parsippany with his wife, Fengying
Wang, a lab technician at the school, and their son is an attending physician at University of Maryland Hospital. He says that medical research is not a 9-to-5 job. “I often do paperwork after school hours at home,” he says. “You never know when an idea will come.”
Tao, who received the 2017 Faculty of the Year Award from NJMS, the 2017 New Jersey Health Foundation Excellence in Research Award, the 2020 Rutgers Board of Trustees Award for Excellence in Research and the 2021 Rutgers Chancellor Basic Science Researcher Award, has several ongoing projects in his lab. He’s working on the identification of long noncoding RNAs and their involvement in chronic pain. He’s also studying translational regulation that underlies chronic opioid tolerance and hyperalgesia; gene transcriptional changes in chronic pain; and molecular mechanisms of sickle cell disease-associated pain.
“My lab recently identified six new painassociated genes, some of which are very promising as potential targets for chronic pain treatment,” he says. ●

“Our understanding of chronic pain is still in its infancy,”
Tao says, “and its treatment is poorly managed by current drugs. Opioids are still the gold
New Jersey Medical School has its share of ‘lifers’—those who have spent an entire career here. Michael Petti is one of them. He first came to NJMS in 1985, working as a temp for the head of planning and management services. That gig led to another, and then another. Thirtyeight years later, he’s still here. Only now he’s NJMS’s chief operating officer (COO) and chief of staff for Dean Robert L. Johnson, MD.
When asked about his rise within the organization, he is quick to share the credit. “It’s not about me,” he says. “I’m a behind-thescenes person. I’m fortunate to have a very talented team working with me to the keep the school’s operations running smoothly. I couldn’t do my job without them.”
Petti grew up in Newark, the youngest of four children. Before coming to NJMS, he
had various jobs as a student, but learned what professionalism was all about in the NJMS dean’s office. After temping for a year, he got a permanent position as senior procedures analyst. “You’d never know it from the title, but that job was to create the first automated faculty database,” he says. “Before that, this information was kept on index cards and paper files. We created a searchable database. We could run reports from it and share information.”
Technology had arrived in the workplace, and everyone had to learn how to use it. “Like many people, I was self-taught,” explains Petti. “I began teaching other people word processing, how to use spread sheets, data management. I ran classes in computer labs. It was all about automation.” He had every reason to think he’d have a career in IT.
From 1994 to 2006, he held a variety of positions in IT, telecommunications, and other areas, also doing a two-year stint at University Hospital. These experiences rounded out his skill set, gave him deep institutional knowledge extending beyond NJMS, and taught him how to manage and lead effectively.
In 2006 a position opened up that Petti found very compelling: executive assistant to the NJMS dean. “I’d had the opportunity to work with him on search committees,” says Petti. “He’s very smart and always supportive. I really wanted to be a part of his team.” He applied for the job and was accepted.
In 2019, Petti was named chief of staff, then in August 2022, he became the school’s COO. As NJMS has grown and evolved, so has Petti. In this dual role, he oversees Operations, which includes facilities management, marketing and communications, and IT, and manages the dean’s small staff.
When asked to delve more deeply into his career trajectory, Petti demurs. “Enough about me! I’d rather talk about the Operations team. We have some people who are superstars—both longtime employees and new hires. They perform at a high level, day after day, all behind the scenes, and don’t always get the recognition they deserve.”
The talent in NJMS Operations begins with its directors. “Our three group leaders—Jim Boyce in IT, LaCarla Donaldson in marketing, and Pamela Edwards in facilities—do a great job of attracting and retaining high-quality staff in the face of many challenges,” says Petti. “It’s easy to hire somebody. But keeping them in this job market is another matter. Good people are constantly being recruited, particularly those with tech expertise. As a public university, we can’t match the salaries out there. So the fact that we’ve been able to retain our staff is a testament to the leadership and management skills of our directors.”
Keeping the school running smoothly is truly a team effort, starting with the excellent work done by the IT team, a group of about 20 technology professionals: everyone from programmers and developers to the help desk and audio-visual teams, and more.

“Our programmers do high-quality work,” he comments. “And then there are our developers, who are behind the scenes writing code for processes and applications that make it easier for people to carry out their duties. One of the areas they’re focused on is faculty affairs processing. To address faculty affairs processing, they developed their own brilliant automated program called FACTS. (Read about FACTS on page 3.)
As another example of IT ingenuity, Petti cites the role of the education management system in preparing what’s colloquially called the Dean’s letter: the medical student performance evaluation, or MSPE. “The MSPE, written for every fourth-year student, provides residency program directors with a detailed summary of a student’s attributes and academic performance,” explains Petti. “Preparing them every year is a major undertaking. The IT team developed a template and process for doing this more efficiently. It’s made a huge difference.”
He adds, “I also want to recognize the help desk technicians who trouble-shoot, service desktops, load software, and much more. Also, kudos to our audio-visual team for providing support to keep the lecture halls ready so the lectures go smoothly.”
Marketing is another key initiative where a small team gets outsized results. “They do an outstanding job communicating the mission of NJMS, how we educate students, care for patients, do important research, and support the community,” explains Petti. “This group produces our magazine, Pulse, now in its 20th year, as well as content and videos for the website. As much as they can with limited resources, they also provide communications support to the academic departments, bringing in contractors as needed.”
Marketing also handles inquiries from major and local media. “I had no idea of the scope of these inquiries—sometimes 10 or 12 a day,” Petti notes. “We have such a breadth of expertise among our NJMS faculty and clinicians. We all would love to see more media coverage! Connecting the media to our experts, marketing is making that happen.”
Facilities management, the third hub in the Operations wheel, focuses on keeping the physical spaces clean, comfortable, and safe for all. “Our facilities team works hard, taking


structure will be overhauled, including all the mechanical equipment to support air flow, plumbing, power, elevators.”
Last but not least, Petti wants to recognize the efforts of the Dean’s small office staff. “We have some accomplished people who don’t fall into any of the buckets we’ve talked about,” says Petti. “They manage some key projects. For example, we’re about to launch a program called Simple Text. It’s a way to get essential news out to the entire NJMS community, in the event of an emergency that causes the computer and/or phone systems go down—something like a major power outage or other disabling event. Every member of the NJMS community will receive information and updates through text message on their cellphones.”
care of maintenance every day, to ensure that our students have an environment that’s conducive to a high-quality medical education, and our researchers have state-of-the-art labs in which to do their work,” says Petti.
Facilities will play a vital role in managing the upcoming renovation in the Medical Science Building. “Some researchers will have to move to temporary labs so their own labs can be renovated,” says. Petti. “We now have a space planner on our staff who will be very involved in planning these moves.”
He adds: “Beyond laboratory renovations and cosmetic upgrades, the building infra-
Imagine the resources required to keep such a large enterprise up and running. Petti is quick to point out that part of the culture in Operations, and in NJMS as a whole, is careful management of resources to achieve the most value. “We watch our budgets carefully,” says Petti. “In an environment where we’re continually being asked to do more with less, one of our greatest strengths is how responsible we are with our resources. We don’t squander them. Without overworking our staff, we ask them to take on more and more. And they are willing to do it, for the betterment of the school.” ●

“One of the greatest strengths of the Operations team is how responsibly we use our resources. We don’t squander them.”
If you’re a medical school, you let your magazine tell the story. And that’s just what Pulse magazine has done for NJMS for the past 20 years. Pulse is the primary print tool to communicate with our students, alumni, faculty, staff, donors, friends, and other stakeholders. Published twice a year, the magazine showcases the dynamic nature of the institution and the outstanding achievements of faculty, students, and alumni. As our magazine celebrates its 20th anniversary, these achievements continue to inspire us. Wonders never cease. And miracles do happen. As writers and editors of a magazine reporting on the NJMS community, we see wonders and miracles every day, and write about them. This special anniversary issue of Pulse showcases what makes our institution special.


Pulse, then and now: 20 years of magazine covers illustrate NJMS’s success in patient care, research, education, and community service.




When you’re doing great things that help people live longer, healthier lives — how do you tell the world?






















or years, Robby Washington, age 61, had fought a mostly losing battle with weight loss. “I’ve been plagued by excess weight all my life,” she says. “I tried so hard to lose it, but nothing worked.”
In October 2021, Washington’s weight tipped the scale at 270 pounds. At 4’ 11”, she suffered from a myriad of health problems caused by excess weight, including chronic pain, difficulty walking, high blood pressure and diabetes, for which she’s had to take insulin.
Through the years, she’s tried to take care of herself, but life got in the way. A single mother who raised two daughters and often worked two jobs, she was so focused on her responsibilities that she didn’t realize her weight had become a serious health issue.
“It was my mother who finally said to me, ‘I’m worried about you. You’ve gotten so heavy,’” says Washington. “When I took a good look at myself in a full-length mirror, all I could think of was: OMG.”
“I did not want to die at 270 pounds,” she adds.
To get the help she needed, Washington turned to the new, state-of-the-art Rutgers
NJMS Weight Management Center at University Hospital (UH). Launched in 2021, the center is the brainchild of several NJMS physicians with a keen interest in obesity treatments.
“As a primary care physician, you treat many chronic conditions: diabetes, high blood pressure, sleep apnea, cardiovascular disease,” says Dhvani Doshi, MD, MPH, the center’s medical director and an assistant professor of medicine. “Obesity is at the root of all these conditions. Doing so much lifestyle and obesity counseling, this became my passion. I became board-certified in obesity medicine so I could build a practice around providing this much-needed treatment.”
Brainstorming with other specialists who shared her passion, “we wanted to create an interdisciplinary center for weight management,” says Doshi. “When we presented the idea to University Hospital and NJMS leaders, everyone was enthusiastic.”
Acknowledging the strong support from Marc Klapholz, MD, chair of medicine, and Daniel Jones, MD, chair of surgery, she says, “This initiative involves both surgery and medicine. So having them on board is critical to the center’s success.”

Obesity is among the major public health issues in the state and country, particularly in underserved urban communities. In the U.S., an estimated 42% of adults and 20% of children have obesity. “Unfortunately, obesity is endemic in our communities, driving higher rates of diabetes, hypertension, heart disease and stroke,” says Klapholz. “Having a center that incorporates all the different medical and surgical modalities for weight management is invaluable, and will help prevent the downstream effects of obesity by reducing the incidence of diabetes and cardiovascular disease.”
“What makes this center truly special is its multidisciplinary approach,” adds Jones. “The team includes board-certified obesity medicine physician specialists, bariatric surgeons, advanced bariatric endoscopists, behavioral health specialists, advanced practice nurses, patient navigators, a social worker, and a dietician. All are dedicated to helping patients achieve their weight loss goals.”
The center focuses on three pillars of advanced treatment, in addition to lifestyle
and nutrition management: medical weight loss, including anti-obesity medicines; bariatric surgery; and endobariatrics, a non-surgical option offering many benefits to patients. Eligibility for the treatments is based on severity of obesity, as indicated by body mass index, or BMI, a screening measurement. A BMI of 18.5 to 24.9 is normal range, 25 to 25.9 is overweight (pre-obese), and 30 or higher falls within the obesity range. The center treats patients across the weight spectrum—from those with moderate obesity to complex cases with BMI as high as 70.
For some patients, lifestyle management and medication alone results in moderate weight loss (on average, up to 10 to 15 percent of total body weight) and improvement in high blood pressure, diabetes, and arthritis. Patients with a BMI above 30, or above 27 with weight-related complications (high blood pressure, diabetes) are eligible for antiobesity medications. “The new generation of medications we’re using are amazingly effective and have been a game-changer for patients,” says Doshi, adding a caveat: “The medications are not short-term—they’re meant to be lifelong.”
Patients seeking greater weight loss (more than 20 percent of total body weight) may be referred for bariatric surgery, long the ‘gold standard’ in obesity management. The surgery restricts both food intake and absorption of nutrients. Criteria is a BMI above 40, or above 35 with weight-related complications. Bariatric procedures are performed at UH by Bao-Ngoc Nasri, MD, PhD, assistant professor of surgery. Both laparoscopic and robotic surgery are offered.

“Bariatric surgery used to be called weight loss surgery,” says Nasri. “Current literature and publications have advocated renaming it metabolic bariatric surgery, because it’s not just to help patients lose weight, but also to treat metabolic diseases like diabetes, high blood pressure, and hyperlipidemia.”
Nasri trained in both Japan and the U.S. “In Japan, we don’t have a lot of obesity,” she says. “When I came to the U.S., I began to realize the pandemic nature of obesity. It’s a chronic disease, but not recognized as
such. People believe that if they eat less and exercise, they will achieve results. However, research shows it’s not that simple. A person’s weight is related to many factors: genetics, their environment, lifestyle, or other medical conditions.”
There are different types of bariatric procedures. Most common is the sleeve gastrectomy, where a portion of the stomach is removed to create a smaller, bananashaped stomach, or sleeve. Second most common is the Roux-en-Y bypass, which
creates a small gastric pouch and reconstructs the intestine to achieve the malabsorptive component. Other procedures performed are gastric banding, biliopancreatic diversion with duodenal switch, and single anastomosis duodenoileostomy with duodenal switch (SADI-DS).

“Thanks to hospital and medical school leadership and support, the bariatric surgical team completed the first robotic Roux-en-Y gastric bypass at University Hospital in March 2023,” notes Nasri.
Patients needing an alternative to bariatric surgery may be referred for endoscopic weight loss procedures. Why an endobariatric rather than a bariatric procedure? The reasons are complex, says Doshi. “Some patients don’t want surgery, while others are not eligible, often for health reasons: they’ve already had bariatric surgery, or are too ill, or too overweight, to undergo anesthesia. With
endobariatrics, we have something to offer these patients.” She notes that criteria for endobariatric procedures is the same as for medications.
“This is a new field—only a few academic centers in the northeast offer this,” Doshi adds. “We are fortunate to have a highly skilled advanced endoscopist, Kaveh Hajifathalian, MD, on our team.”
Whether a patient has one modality, two, or all three, a key part of the weight loss journey is behavior modification and education. “These procedures are not magic,” says Nasri. “They are just tools to help you lose weight more efficiently. If you don’t change your diet and lifestyle, you will relapse and gain the weight back.”
Robby Washington knows only too well the relapsing syndrome. She had bariatric surgery in 2009, lost 70 pounds, then regained it. It’s not a happy memory. “I was sad
and angry,” she says. “I felt like a failure.”
She was referred to the Rutgers NJMS weight management center in 2021 by David Bleich, MD, professor of medicine, who has treated her diabetes and high blood pressure for years. After meeting with Doshi for a comprehensive evaluation, Washington began the first phase of treatment: lifestyle and nutrition management, with anti-obesity medication to control her diabetes and help her lose weight.
For the first several months, she had regular visits with the weight management team. “They monitored me, worked with me, and taught me how to eat properly,” she says. She did very well on these interventions, and by August 2022, her weight was down to 190. She had achieved a total reduction of 13 percent of her body weight with lifestyle
NJMS has long been known for its innovative approaches to helping patients recover from injury or illness. Take the cases of two patients, who recently came to NJMS, both desperate for help. While their cases are quite different, both suffered from severe facial nerve damage that greatly affected function and appearance, impacting their quality of life.
NJMS surgeons Boris Paskhover, MD, and James Liu, MD, were able to provide the help these patients so desperately needed. The physicians, who became friends as undergraduates at Rutgers University, each possess a unique skill set, performing highly specialized procedures with tremendous skill. These success stories are just another indicator that NJMS’s specialists are setting the highest of standards for clinical care.
The year was 2016, and life was good for Dalia Ubinas. The Woodbridge, NJ, resident had a great job, a loving family, close friends, and
she and her fiancé were planning their wedding. “Everyone who knew me called me Smiley, because I was almost always smiling,” she says. “I loved to smile. It’s infectious.” Her life truly was good. And then, it wasn’t.
Ubinas began having painful earaches and was diagnosed with mastoiditis, an infection of the mastoid bone located behind the ear. A physician performed a procedure to remove the infection, but a year later it returned. The same physician repeated the procedure, but this time he unknowingly severed right facial nerves, paralyzing the right side of her face.
“My face sagged so much, I looked like I’d had a massive stroke,” Ubinas explains. “I couldn’t speak, eat, drink, blink or talk correct-
ly. I had to hold my lips up so words would sound a little clearer. And my right eye was always irritated because I couldn’t close it.” She had a weight surgically implanted in her eyelid so she could close it. “No one was calling me Smiley anymore,” she says. “I thought of myself as a monster. People would stare at me when I’d go out, so I hid in the house.” Her physician prescribed physical therapy and electrical stimulation treatments, but neither worked. Eventually a neurologist did an EEG and discovered there was no nerve activity on the right side of her face. He recommended nerve transplant surgery. She went to another surgeon who took a nerve from her thigh and transplanted it in her face. It didn’t work. She then had what she terms a “mini facelift,” that used wire to pull up the sagging side of her face. “I looked horrible and felt terrible,” she recalls. “I was extremely depressed. It was hard to find joy in my life, and I was struggling to get back into the workforce. I decided to cancel my wedding.”
The year was 2018. Enter Boris Paskhover, MD, associate professor of otolaryngology and director of facial plastic and reconstructive surgery at NJMS. Paskhover, who is

board-certified in facial plastic and reconstructive surgery/otolaryngology, specializes in facial nerve repair in people like Ubinas, and those who have had damage from cancer, facial injuries, tumors or physical anomalies. “I help people to move their faces again and to speak,” he says. “But more importantly, I teach them how to smile again.”
To help Ubinas, Paskhover did a highly complex procedure known as a masseteric-facial nerve transfer or a 5-7 transfer. “It’s a dynamic procedure that reanimates the face,” he explains. “Basically, we take a nerve from a different part of the face and plug it in where it can help with facial function.” He goes on to explain that the masseteric nerve, which is a branch of the trigeminal nerve, innervates a chewing muscle known as the masseter. In the 5-7 nerve transfer, a branch of the masseteric nerve is connected to a branch of the facial nerve which activates the smile muscles. After the nerves heal, patients learn to smile by biting down.
While his unparalleled surgical skills help his patients’ physical recoveries, his energy, enthusiasm and optimism give them the emotional support they need. “Dr.
 Paskhover
Paskhover

was a godsend,” says Ubinas. “He is so compassionate and encouraging. He gave me a piece of myself back. I’m so grateful.”
The year is 2023 and Ubinas is back in the workforce. Her wedding went off without a hitch, and she was even pleased with some of the photos of her special day. “If I said I’ve accepted the situation 100 percent, I’d be lying,” she says. “But I finally was able to forgive the surgeon who severed my nerve, and that was a big step. And thanks to Dr. Paskhover, my faith, family and friends, I got my life back.”
Paskhover says the surgeries he performs are exceptionally complicated; however, they are also exceptionally rewarding. “What I do is truly a labor of love,” he says. “I get the opportunity to help patients with deformities with an esthetic touch.” He always loved art and architecture, so when he does surgery, he utilizes his artistic eye.
Paskhover points out that while he went to some the best schools in the country— Rutgers University for undergraduate study, Albert Einstein for medical school, Yale and NYU for residencies and fellowships—his childhood was anything but easy. A native of Eastern Europe, he emigrated with his
parents to Queens, NY, when he was 6 years old. He slept in the hall, because there wasn’t a bedroom for him, and he wore clothes from the Salvation Army. “I knew what it was like to be a poor kid who got subpar health care,” he says. “I want to help as many patients as I can. I keep getting grayer and grayer thinking of my patients nonstop, but it’s worth it. I love seeing people smile again.”
If you met hip hop artist Sunny Jorge today, you would never guess he once sat in the Newark train station contemplating suicide. The professional songwriter, businessperson and owner of his own record label, Kool Aid Baby, is thriving. He’s upbeat and at the top of his game. So what could have made this young, rising star consider jumping in front of a train? There’s a one-word answer: pain.
At the age of 35, the Newark native started experiencing excruciating electric-shock-like pain on one side of his face. At first, it would come and go, but eventually it lasted for hours. Talking was so uncomfortable that he would simply hang up the phone in the middle of a conversation or abruptly leave whatever gathering he was at. “I lost a lot of
friends by doing that,” he says. “But I never felt pain like that in my life. Think of the worst toothache you’ve ever had and multiply it by 1,000. It was that bad.”
When the pain continued to get worse, he went to an emergency room. They diagnosed his condition as facial neuralgia and sent him on his way with over-the-counter medication. The medication didn’t work, even when Jorge upped the dose. In desperation he went to the dentist and had all the teeth on that side of his mouth extracted. Still, he got no relief. Then his face began to turn black. “I’d rub oil on it and put cold towels on it, but it didn’t help,” he recalls. “I couldn’t sleep, I couldn’t eat, I couldn’t even kiss my girlfriend. I didn’t want to be with anyone, I just wanted to die.” That’s when he went to the train station.
Jorge says for reasons unknown even to himself, he decided not to take his life that day. As luck would have it, a dental assistant at Rutgers School of Dental Medicine recommended he see James K. Liu, MD, internationally renowned neurosurgeon, who is professor of neurological surgery and director of cerebrovascular/skull base and pituitary surgery at NJMS. That was Jorge’s first step toward recovery.
After extensive testing, the physician found that the pain was the result of a condition known as trigeminal neuralgia. It is triggered by talking, eating, chewing, or even light touch to the face. The pain can last a couple of seconds to minutes, and patients can have numerous attacks in one day. In Jorge’s case, an artery was compressing his trigeminal nerve inside his head, resulting in his excruciating facial pain. When Liu told him that brain surgery was the only solution, Jorge never gave it a second thought. “I trusted him right away,” he says. “He told me he could fix it, and I believed him.” A week later Liu performed the surgery, known as an endoscopic-assisted microvascular decompression. When Jorge woke up, he was pain free.

The neurosurgeon treats patients with brain tumors, brain aneurysms and other maladies at the base of the skull, where the brain stem, cranial nerves and critical blood vessels come together. “That’s very valuable
real estate,” Liu explains. “That area of the brain is responsible for critical body functions, including eye movements, sight, facial sensation, facial movement, hearing, swallowing, voice projection, and motor function for the entire body. Tumors growing there can cause a myriad of problems, from losing one’s eyesight to progressively becoming paraplegic.”
Even though performing complex brain surgery is extremely challenging and high risk, Liu loves his job. “As a skull base neurosurgeon, you constantly ask yourself, ‘How can we safely get to these deep targets within the brain and treat our patients successfully?’”
Liu began the surgery on Jorge by making a small cut behind the ear, and then made an opening in the skull somewhat like a keyhole. Using a microscope and endoscope, he went
in and found where the artery was compressing the nerve. He pushed the artery away from the nerve, put a cushion around it and moved it out of the way for good. That particular surgery has a low level of difficulty and a 95 percent success rate. Other procedures, however, are more dangerous. “It’s humbling to know patients put their lives in your hands,” says Liu. “And all of us in this field are committed to perfecting our techniques and helping our patients in the safest way possible.”
Along with loving his career in medicine, Liu loves hip hop. It’s the beat, the culture and the rhythmic sound he enjoys. “Since we treated Jorge, he’s become nationally known. His career was just ready to take off when he came to us. He was working with the famous group the Fugees, and Fetty Wap, an internationally known hip hop star. But the pain kept him from moving forward. I was glad we could help him.”

Jorge was so grateful for Dr. Liu’s help that he says he is now offering his music to the community. He helps at-risk youth in Newark to learn hip hop and establish their brand. “I’m teaching these kids how to establish themselves as business owners and how to protect their intellectual property,” he explains. “I tell them that if they have the resources and the right mindset, you can do it. They see that I was able to accomplish, and they want to try. I want to help them like Dr. Liu helped me.”
Not surprisingly, Liu and Jorge have formed a bond that is unbreakable. “I changed my phone number a while back, and Dr. Liu couldn’t get in touch with me,” Jorge says. “He reached out on Instagram to see if I was ok. We have a great relationship.”
Jorge is now engaged to be married, and his second album, “From Venus to Mars,” was released this spring. From now on, the only time Jorge will be at the train station is if he’s taking a trip. ●
To contact Dr. Boris Paskhover: borpas@njms.rutgers.edu.
To contact Dr. James K. Liu: james.liu.md@rutgers.edu.
Follow Dr. Liu on Instagram, Twitter, Facebook and LinkedIn: @SkullBaseMD. Follow Sunny Jorge @sun_jorge on Instagram.
In this 20th anniversary issue of Pulse magazine, we applaud the achievements and contributions of our alumni. Some have remained a part of the NJMS community: teaching, caring for patients, and conducting research. Others have achieved success at institutions across the U.S. And then there are our recent graduates, in training to become the best clinicians, teachers, and scientists that they can be. Through the years, they have made us proud—not only of their individual accomplishments, but also the depth of their talents, interests, and achievements through all sectors of society. Read here about three of our graduates who are making a difference.
HUMAIRA CHAUDHRY, MD’05“The first year of medical school was challenging for me,” says Humaira Chaudhry, MD’05, associate professor and chair of radiology. “I almost felt like the decision to go to medical school had been made for me, when I was too young to know what I was getting myself into. Doing gross anatomy, facing a corpse. All of that was really overwhelming. I seriously thought about quitting that first semester.”
Fortunately for Chaudhry, and for her patients, she got the encouragement she needed and was able to stay the course. “My family was very supportive and so was the dean of student affairs at NJMS. Everyone said the same thing: ‘Give it time. Don’t make any rush decisions.’”
It’s easy to see how Chaudhry might have seen her path as predetermined. Both of her parents had science degrees. Together, they had immigrated from Pakistan in the 1970s with Chaudhry’s two older sisters, both of whom were class valedictorians at Clifton High School and then went to NJMS.
“There was definitely a lot of pressure to do well in school,” says Chaudhry. (Born in Passaic, she calls herself “a Jersey girl, through and through.”) “I felt like I’d be labeled a black sheep if I didn’t become a doctor.”
After graduating from Clifton High School (yes, as class valedictorian) Chaudhry entered the accelerated NJIT/NJMS seven-year BS/MD program. And after that first year, things did get better. “I really enjoyed learning pathology and microbiology,” Chaudhry says, “and I liked NJMS and the friends I had made. So the decision to stay in medical school became my decision.”
Even so, Chaudhry realized that she wasn’t cut out for clinical medicine. “With my personality, I have a hard time dealing with

other people’s grief,” she says. “It weighs on me. But I loved studying diseases, so radiology was a natural fit. I found my niche.”
Chaudhry did her transitional year internship at St. Barnabas, in Livingston, and her residency at Mount Sinai, followed by a one-year fellowship in abdominal imaging at Duke. “It’s arguably one of the best radiology departments in the country, and people go there from all over the world. The pathologies I encountered and the mentorship I received were amazing.”
After finishing at Duke, Chaudhry returned to NJMS as an assistant professor of radiology in 2011. “NJMS is the only liver transplant center in New Jersey, so hepatobiliary imaging became my clinical focus.” Hepatobiliary, she explains, concerns the liver and anatomy that works with the liver, like the bile ducts.
Chaudhry works closely with the hepatologists and liver transplant surgeons at University Hospital. “One of my favorite parts
of my job is presenting at multidisciplinary conferences. That’s when I get to really learn about the patient from the clinical providers. I love being an important part of the care team, recognizing that my interpretation of the patient’s imaging studies can alter their treatment options.”
Chaudhry has served on committees nationwide on hepatocellular carcinoma, and she’s recently joined a team of researchers

investigating the use of artificial intelligence for the early detection of pancreatic cancer. “There are some very subtle signs that the human eye may not be able to see on a CT scan. If we can get a computer to detect those for us, we could run algorithms in the background on every scan we encounter and hopefully find cancer earlier.”
One of Chaudhry’s proudest accomplishments is her work to bring the best in radiological care to patients in Newark. When she returned to NJMS, Chaudhry noticed the “disparity of care between what we could offer and what was available at Mount Sinai and at Duke. It had nothing to do with the clinical providers. We have great doctors and wonderful techs who go above and beyond.
But, in radiology, at least, our equipment was outdated.” Radiology is central to the diagnosis and sometimes even treatment for so many patients, she adds. “Anyone who enters the hospital, anyone who has any serious illness, will cross paths with the radiology department.”
It’s this mission—advocating for the patients in Newark—that Chaudhry sees as central to her own journey. “From beginning to end, that’s what I care about, and that’s been my goal. Becoming a chair was not something I consciously worked toward. It’s just something that kind of happened. But I think that if you have your intentions and your heart in the right place, the good things, or at least the right things will happen for you.” ●

“The first year of medical school was challenging for me. Doing gross anatomy, facing a corpse. All of that was really overwhelming. I seriously thought about quitting that first semester.”Humaira Chaudhry, MD’05 KEITH B. BRATCHER, JR.


“My mom had a lot of stories,” says Novneet Sahu, MD’12, assistant professor of emergency medicine and family medicine and interim chair of family medicine. at NJMS.
“She was an I.C.U. nurse for many years at Morristown Memorial Hospital (now Morristown Medical Center), and she would come home from work and talk about her job. Just hearing those stories made me really interested in medicine.”
“My father instilled in me the importance of public service,” he adds. “He did a lot of volunteer work and cultural organizing. Giving back to the community was important to him, and it’s important to me.”
In high school, Sahu, who grew up in Lake Hopatcong, NJ, found a way to combine the two: he became a volunteer firefighter and “started volunteering with the local rescue squad. Learning about pre-hospital medicine and emergency medical services really channeled my interests.”
Sahu attended Temple University as an undergraduate, majoring in biology. He considered a career in freshwater and marine ecology. But the pull of medicine proved too strong and he enrolled at NJMS in 2008. “With my background in EMS, I thought emergency medicine might be a good fit,” Sahu says. “But once I started clinical rotations, I liked everything: surgery, OB, family medicine. The thing that really defined my med school experience was my work at the Student Family Health Care Center (SFHCC), the student-run free clinic. I got involved as a first-year student. You’re seeing patients and you have the autonomy to make decisions about people’s care.” Sahu worked with the SFHCC throughout medical school and served as the clinic’s director during his third and fourth year.

“As I was finishing medical school, I started to become passionate about how people access the health care system,” he says. “In most underserved areas, people either show up at the office, or they show up in the emergency department as their primary point of care. I wanted to understand both of these access points really well.”
Sahu did a five-year combined residency in emergency and family medicine at Christiana Care Center in Delaware, and returned to NJMS in 2017 to take a joint position in emergency and family medicine. “I worked two or three shifts per week in the emergency department and two days a week in the family medicine clinics.” Then, in 2019, he deployed.
“My first year of medical school, I had commissioned in the Army National Guard,” Sahu explains, adding that he’s been activated
Sahu came home in January 2020, but was soon deployed for COVID response. “I was primarily responsible for deploying and redeploying health care providers for staffing nursing homes and field hospitals in New
ministers of health and heads of government.”
Sahu became the interim chair for family medicine in July 2021, and “that flipped my split between emergency medicine and family medicine. Now I’m heavier on the family medicine side and a little bit lighter on the emergency medicine side.”
One of the best things about his job, Sahu says, is “hearing everybody’s story. As you connect with individuals and learn about their experiences, it gives you a deeper understanding of that patient as a person.” Such knowledge, he adds, is critical to understanding how the medical system can better serve the community.
several times for hurricane or flood response in New Jersey. “In 2019, I was deployed with the 113th infantry to Djibouti, a small country in the horn of Africa. It was a combat deployment, and I was serving as the battalion surgeon, so I was responsible for the health care of everyone in the battalion. It was a lot of general preventive health, but there were one or two major incidents.”

Jersey. A lot of it was figuring out who was fit and making sure they were medically clear.”
At the end of 2020, Sahu switched to the Army Reserve (where he still serves), and in 2021 he was again deployed to Africa, this time in a public-health position on a crossfunctional civil affairs team. “My role was helping to reopen relationships with countries in Africa after COVID. I was interacting with

“I think part of the job of a physician is to be a public servant,” he says. “I feel really privileged to be the interim chair of the department that oversees operations for the SFHCC. I’m doing the work that I always really loved doing, and I get to do it at increasing levels of responsibility.” ●

“With my background in EMS, I thought emergency medicine might be a good fit. But once I started clinical rotations, I liked everything: surgery, OB, family medicine.”Sahu served first with the Army National Guard, and later with the Army Reserve (where he still serves). He has twice been deployed to Africa. STEFFANY CONYERS, MD’20
“Growing up in the Black community, mental health wasn’t really talked about. I was able to connect this with personal and familial experiences, and I wanted a career helping to heal those mental illnesses.”
Conyers’ freshman year at George Washington University, in Washington, D.C., was marred by homesickness, but after she transferred to Rutgers she excelled. “Because of that experience, I knew I wanted to be close to home for medical school, so NJMS was at the top of my list. After my interview, I loved it, and NJMS was definitely my first choice.” A scary—but good scary—moment came when

Beth-Israel and University Hospital.” She was often one of the first people to go see patients. “I had more time than most of the residents, so I was always there checking on the patient, like around the clock. I think my clinical skills and bedside manner were really honed in those small situations.”
For Steffany Conyers, MD’20, the journey to becoming a physician has been quite a challenge. A native of Maplewood, NJ, she is the daughter of a corrections officer and a day care operator. As a firstgeneration college student, she says her path was “kind of self-guided,” though her parents “were very supportive and really encouraging, but this was certainly new to them.”
Now an OB/GYN resident, Conyers was recently voted one of two administrative chiefs by the residents and faculty of Harvard’s Beth Israel Deaconess Medical Center. “The best thing about the position is being a voice for my co-residents to the administration and faculty,” she says. “Advocating for problems they’re having, or changes they’d like to see, is why I wanted to do it.”
Still, Conyers, an OB/GYN resident, is realistic about taking on this exciting and demanding leadership role: “I’ll have to balance the extra work with my clinical duties, and with my sleeping and personal life.”
A high school course in AP Psychology sparked Conyers’ interest in medicine, specifically psychiatry. “Learning that mental illness is a disease, that it’s commonplace and treatable, was interesting to me,” she says.
she was offered a full scholarship at Thomas Jefferson University, in Philadelphia. Fortunately, NJMS was able to meet their offer.
NJMS was definitely the right fit. “My first anatomy block was with Dr. Valerie Fitzhugh,” Conyers says. “She made muscular and skeletal bone pathologies super-interesting even though, to me, they’re really not. Her passion was able to shine through her lectures. Dr. Fitzhugh and I still keep in contact.”
Clinical rotations were transformative for Conyers. “I was constantly challenged and treated as part of the team at all the clinical sites where I rotated, particularly at Newark
As a fourth year, Conyers did a month-long sub-internship at University Hospital, where she worked very closely with Lisa Gittens, MD, OB/GYN professor, and Joseph Apuzzio, MD’73, OB/GYN professor and vice chair, both obstetricians who work with high-risk pregnancies in a field called maternal fetal medicine (MFM). “They were extremely knowledgeable, excellent physicians. My admiration for them and their clinical knowledge and skills really sparked my interest in the field. It was just a better fit for me than psychiatry.”

One moment sticks with Conyers. “MFM doctors specialize in ultrasound,” she explains. “I remember seeing an ultrasound of a very rare condition called TRAP Syndrome— twin reversed arterial perfusion. It starts off as a twin pregnancy, but only one twin fully develops and gets most of the blood supply, so the second twin doesn’t really develop. It fascinated me and made me more interested in MFM.” She is currently in the process of applying for fellowships in the field.
These days, Conyers’ journey usually has her in the hospital by 5:30 a.m. checking on her patients. Her cases are largely laparoscopic procedures, hysterectomies, fibroid removals. She sees patients of her own in a continuity clinic one half day a week, usually eleven patients in an afternoon. “I truly appreciate the experience I had at NJMS as a medical student and on my clinical sites,” she says. “I learned you come in early, you work hard, and you’re here to learn. Those are three things that I really took with me. Even though I’m here in Boston,” she adds, “I’m still known as the Jersey-Rutgers girl, because I’m very proud of where I come from, and I’m very proud of where I went to medical school.” ●
“I truly appreciate the experience I had at NJMS as a medical student and on my clinical sites. I learned you come in early, you work hard, and you’re here to learn. Those are three things that I really took with me.”
Continued from page 21
changes and medication alone. Her diabetes was greatly improved too. Amazingly, she was completely off insulin. Pleased as she was, she wanted to lose more weight.
Doshi felt that Washington would be a prime candidate for an endoscopic procedure. These are performed by inserting a suturing device into the throat and down to the stomach. Sutures are placed in the stomach to make it smaller. No incisions are made. She met with Hajifathalian, who explained the risks and benefits and what to expect.
“It’s common for bariatric surgery patients to regain weight,” says Hajifathalian, who is an assistant professor of surgery and director of endoscopy. Fellowship trained, with both a

clinical and research background, he came to NJMS a year and a half ago to join the weight management program. “For these patients, we do a revision of their previous surgery. It ‘tightens up’ their surgery to induce weight loss. We all agreed this would be a good option for Robby Washington. She’s had the experience of going through bariatric surgery; she knows how to manage her lifestyle. She just needs a little more help to take care of this weight gain.”
In October 2022, Washington had her revision: an endoscopic sleeve gastroplasty, the most common endobariatric procedure performed. “We make the stomach about 80 percent smaller, but without cutting away any tissue,” explains Hajifathalian. “We sew it from the inside, pulling the sutures, so it’s almost like an accordion. The results of this procedure are very close to surgical gastrectomy.”
IN 2003, NJMS leadership decided it was time for the school to have its own magazine. A creative team was assembled to launch Pulse magazine.
Twenty years has sped by. As in any workplace, people come and go. But two members of that original creative team—writer and editor Mary Ann Littell and graphic designer Sheila Johnston Sherer—are still producing the magazine, two issues a year.
The two first met in 2003 at a coffee shop in Montclair, NJ. Littell, the mother of two sons, had been a writer and editor at Good Housekeeping magazine before making a career switch to higher ed communications. Sherer had recently relocated to New Jersey from the south. She sent her resume to many editors, including Littell. “I loved her samples,” says Littell. “We met for breakfast and hit it off.”
Months later, Sherer attended her first Pulse planning meeting. Seven months pregnant, she was greeted with a few raised eyebrows. But with several working mothers on the Pulse editorial team, the eyebrows didn’t stay raised for long.
That was the beginning of a successful partnership that continues to this day. While the other Pulse creators have moved on to new jobs, relocation, or retirement, Sherer and Littell collaborate on Pulse, working with NJMS communications manager LaCarla Donaldson. Everything is done virtually, via email, text, and Zoom calls. The magazine has never missed a publication date, except when the campus shut down due to COVID-19.
As we publish this 20th anniversary issue, Sherer’s two daughters are now in college and graduate school. Littell’s sons are grown with families of their own. But much has remained the same, including the outstanding work being done every day by the faculty and staff. At NJMS, there is always exciting news to report on. We hope to keep doing it for at least another 20 years.
Still on anti-obesity medication (called a glp-1 agonist, it treats both her diabetes and obesity), Washington’s weight is now 164 pounds. She’s lost 26 percent of her total body weight, and has a happy incentive to lose a few more pounds: she’s planning her wedding. “I’m still able to eat most of the foods I like—but just less of them,” she says. “I cook with much less fat now, and never eat a whole meal.”
Washington is just one of many patients helped at the weight management center. With almost 1,000 referrals in the first year, it clearly meets a real community need. The center will soon move into a shared space in the Doctors Office Center on the Newark campus, bringing all the providers and specialists together under one roof. “In this newly renovated space, patients will be able to learn about medical, endoscopic and surgical options at one location,” says Daniel Jones. “We welcome patients of size with larger furniture. The new offices are the hub of educational materials on healthy living, with vitamins and supplements offered at a discount.”
“We are all very proud of the weight management center, and of all the providers and staff who are deeply committed to providing this service,” adds Marc Klapholz. “I am glad we are able to bring this state-of-the-art care to Newark.” ●
To contact the Rutgers NJMS Weight Management Center, call 973-972-7151.
Wheelchair-bound patients coming to a physician’s office immediately face a slew of obstacles. They may not be able to get onto the exam table. Their weight most often is not measured, because the standard scale can’t accommodate wheelchairs. If they are female, navigating into an OB/GYN exam chair for a PAP smear may be very challenging.

Some 16 percent of Americans live with a physical disability—which means that one in seven, or 39 million total, face these challenges regularly, says Steven Kirshblum, MD, chair of the NJMS Department of Physical Medicine and Rehabilitation (PM&R). Paradoxically, our health care system isn’t well equipped to service people with disabilities, even though they may need more care than the average person. Despite the 1990 Americans with Disabilities Act that requires medical facilities to be accessible, many unfortunately still aren’t. Even worse, more than one-third of American physicians lack formal training to care for people with disabilities. “Many medical students report that they don’t receive formal education or training,” notes Kirshblum.
Understanding how to care for patients with disabilities is not intuitive. Many people, not just physicians, are unsure about what to say or how to approach someone who is different.
NJMS has developed several education initiatives teaching medical students how to interact with, and better care for, individuals with disabilities. In their first year, students take a Health, Humanism and Health Equity course, during which they hear lectures about dealing with persons with disabilities. They meet a panel of people with disabilities and hear first-hand about their experiences.
In the fourth year, during the mandatory PM&R clerkship, students do practical
exercises. They are challenged to recall obstacles that they saw people with dis abilities experience during their clinical rota tions, and are charged with devising practical solutions. Acquiring wheelchair scales and height-adjustable exam tables are the most commonly proposed solutions. “I love the idea of students coming up with their own ways of making a difference in the future,” Kirshblum says.
During their training students also discuss the subconscious biases physicians are susceptible to—for example, assuming that people with disabilities have a worse quality of life than people without disabilities. That bias factors into how doctors may counsel patients: for example, not talking to patients about contraceptives because they assume people with disabilities aren’t sexually active.
“Or they may not advise against smoking, because they don’t want to take away the only pleasure they think their patient has,” says Kirshblum. The courses aim to change that thinking, making students see people with disabilities not as disabled, but abled differently.
Trevor Dyson-Hudson, MD, associate professor of PM&R, joins these discussions. He had a spinal cord injury years ago, in his third year of medical school, so he shares his first-person perspective with students. He also teaches them how to ask questions they may feel uncomfortable with, such as whether patients prefer to be examined in a wheelchair or on the height-adjustable table. “You can ask, ‘What’s the best way to do it so that you are most comfortable and I can do a good exam?’” he suggests.
Dyson-Hudson emphasizes the importance of custom wheelchairs in patients’ lives. “In the future, some of our students may be writing prescriptions for wheelchairs or approving them,” he says—so they should understand patients’ needs. Having wheelchair scales is key, he adds. “Wheelchair scales are expensive and take up space, so many offices don’t have them. But they should. We have an obesity epidemic, so knowing patients’ weight is important.”
Pre-COVID, NJMS ran a wheelchair immersion program: One student would assume the role of a wheelchair-bound person, and the other a caregiver—and then they’d switch roles. That allowed students to understand the everyday challenges people with disabilities face. “It was a real eye-opener for students,” says Kirshblum. “We’re hoping to resume it.”
A recent study found that a majority of medical students felt more comfortable approaching patients with disabilities after completing training. Kirshblum agrees this training has a long-lasting impact. He and his colleagues have done studies assessing the NJMS programs. Months later, students remembered what they learned—a sign that they’ll use the training as physicians.
“It wasn’t out of sight, out of mind,” Kirshblum says. “It truly made a difference. I’m proud that we at NJMS are bringing disability education to the forefront. I hope more schools adopt it.” ●

With the rigors of medical school—courses and exams to take; human anatomy to master; physiology, pharmacology, pathology, and all the other ‘ologies’ to learn; clinical rotations to do—training to be a physician is intense. As if all that wasn’t enough, a group of NJMS students have taken on an additional role, finding a unique way to mentor and inspire Newark teenagers with an interest in science.


Last spring the NJMS students launched a project called Knotted, which aims to teach high school students the basics of suturing, while increasing their awareness of careers in health care. Student Aman Patel came up with the idea “as a way to engage young people. We thought that participating in a hands-on activity such as suturing might encourage the students to pursue careers in science and medicine.” In addition to Patel, Knotted co-founders include Hassaam Choudhry, Daniel Garcia, Mark Korst, Akash Patel, Philip Reinhardt, and Usman Toor.
Suturing is a basic skill that must be mastered by all medical students. Tying these tiny knots is not as simple as it may seem. Google “suturing techniques,” and you’ll bring up a myriad of instructional websites, suture training kits for sale, and suturing videos on YouTube.

Newark’s Science Park High School seemed like a good fit for the goals of Knotted. Under the guidance of Knotted faculty mentor Jean A. Eloy, MD’02, Distinguished Professor and clinical vice chair, otolaryngology, Patel reached out to Science Park administrators to propose the workshops. They liked the idea, and the workshops launched in the fall. Armed with suturing pads, tweezers, scissors, needle driv ers, and other materials, volunteers led 15 workshops for 300 students. Workshops began with a Q & A on the journey to becom ing a physician, followed by suturing lessons. Seeing how much the high school students enjoyed the workshops was very gratifying, say the volunteers.
Knotted is sponsored by NJMS’s Pozen Scholars Program, created in 2009 with the goal of generating meaningful community activities. The Knotted volunteers plan to offer more suturing workshops during the upcoming academic year. — Mary



 Ann Littell
Ann Littell
Follow Knotted on Instagram: @njmsknotted
