Sponsor Company: www.international-pharma.com Volume 14 Issue 4
Understanding Compliance Moving from Cost to Value Pre-existing Immunogenicity How Will Cell and Gene Therapies Change Our Testing Approach? Overcoming the Pitfalls of Pre-filled Syringe Filling How the Pharmaceutical Industry Can Navigate Supply Chain Disruptions and Gain Resiliency
Peer Reviewed


| | | 41 Million units 2022 INSPECTED BY: EUROPE | USA | JAPAN | BRAZIL | KOREA | TAIWAN | TURKEY | SAUDI ARABIA | RUSSIA | IRAQ | KENYA | BIELORUSSIA DEVELOPMENT CAPABILITIES Preformulation and formulation development Analytical methods Development Process Development: oral solids, conjugation, liquid and lyo formulations, complex formulations QC ANALYTICAL CAPABILITIES Method validation and transfer Full testing of small and large molecules Stability and Photostability studies ORAL CAPABILITIES icated manufacturing area for tabs, minitabs, ule, LFHC velopment: 100g to 1000g P Clinical and Commercial: 4Kg to 100Kg Annual capacity: 50 Million units DS MANUFACTURING CAPABILITIES Conjugation of ADC’s from development (10mg–5g) to clinical and commercial (20g–5 Kg) Liposomal Bulk Solutions Annual capacity: 410 Kg dditional 900 Kg by end of 2022 CYTOTOXIC STERILE CAPABILITIES 7 Filling lines working in full containment, to produce liquid and lyo vials Annual capacity: liq/lyo vials 31 Mill. units end 2022 NON-CYTOTOXIC STERILE CAPABILITIES ling lines working in full containment roduce liquid and lyo vials ual capacity liquid/lyo vials: 9 2023 17 2024 26 2025 A CDMO TECHNOLOGICALLY DEVELOPED TO MEET THE NEEDS OF INNOVATORS, WITH ITS HIGH CONTAINMENT FACILITY DESIGNED TO OFFER SERVICES FOR PRE-CLINICAL GLP, CLINICAL AND COMMERCIAL SUPPLY BROCHURE HEADQUARTER and MANUFACTURING PLANT BSP PHARMACEUTICALS S.p.A. Via Appia km 65,561 04013 Latina Scalo (LT) – Italy Phone: +39 0773 8221 Web: bsppharmaceuticals.com Mail: business.development@bsppharmaceuticals.com
DIRECTOR: Mark A. Barker
BUSINESS DEVELOPMENT: Eliza Sarfaraz eliza@senglobalcoms.com
EDITORIAL: Virginia Toteva virginia@senglobalcoms.com
DESIGN DIRECTOR: Jana Sukenikova www.fanahshapeless.com
FINANCE DEPARTMENT: Akash Sharma accounts@senglobal.com
RESEARCH & CIRCULATION: Jessica Chapman jessica@senglobalcoms.com
COVER IMAGE: iStockphoto ©
PUBLISHED BY: Senglobal Ltd. Unit 5.02, E1 Studios, 7 Whitechapel Road, E1 1DU, United Kingdom
Tel: +44 (0) 2045417569 Email: info@senglobalcoms.com www.international-pharma.com
All rights reserved. No part of this publication may be reproduced, duplicated, stored in any retrieval system or transmitted in any form by any means without prior written permission of the Publishers.
The next issue of IPI will be published in Spring 2023. ISSN No.International Pharmaceutical Industry ISSN 1755-4578.
The opinions and views expressed by the authors in this journal are not necessarily those of the Editor or the Publisher. Please note that although care is taken in the preparation of this publication, the Editor and the Publisher are not responsible for opinions, views, and inaccuracies in the articles. Great care is taken concerning artwork supplied, but the Publisher cannot be held responsible for any loss or damage incurred. This publication is protected by copyright.
2022 Senglobal Ltd./Volume 14 Issue 4 – Winter – 2022
06 Editor’s Letter
REGULATORY & MARKETPLACE
08 Understanding Compliance: Moving from Cost to Value
Throughout the life sciences sector, the key trends of globalization and digitalization are providing new opportunities for growth and innovation. However, within development facilities, quality assurance, lab systems and scientific teams are feeling the impact of these transformations. Especially as their endeavours to ensure high levels of compliance meet the growing regulatory pressure within the industry. With an increasingly digital and connected lab infrastructure, failing to navigate the challenges of global regulatory requirements can be costly. As such, any compliance and validation processes must be designed to meet the needs of multiple geographies, business activities, and functions. Here, we speak with Joshua McWilliams, Product Manager, GxP Validation Services at PerkinElmer Inc., to learn more about the rising need in the pharma industry for compliance expertise and support.
12 EU CTR: 90 Days to Go, What You Need to Know
In 90 days, the one-year transition period of the EU’s Clinical Trials Regulation (CTR) will come to a close. EU CTR aims to harmonize the clinical application process across Europe and increase transparency. The regulation envisions a faster and more streamlined submission and approval process for larger multinational studies. Soon, biopharma sponsors, contract research organizations (CROs), the European Medicines Agency (EMA), and member states will use one system to manage all trial applications and authorizations. Werner Engelbrecht at Veeva Systems explains how clinical trial sponsors and CROs can ease the transition to CTIS.
14 Brexit – Impact, Challenges, and Solutions for the Pharmaceutical Industry
Brexit has provided several challenges to the pharmaceutical industry that required robust actions and swift resolution to remain in compliance following the end of the transition phase. Focussing on the regulatory activities, Graham Donaldson at Pharmalex discusses some of the challenges faced by companies and the steps taken by the UK Regulator, the MHRA, and the UK Department of Health and Social Care, to provide solutions to marketing authorisation review and access to medicines.
16 Bad Medicine: Lessons from an Enduring Alliance Between Big Pharma and Global Policing
The challenges of tackling international crime with national law enforcement are legion. What can be done about the sale of illicit medicines? The question illustrates a familiar challenge in the world of law enforcement. John Binns at BCL Solicitors considers how Interpol’s Operation Pangea illustrates how they can be overcome in the context of the global fight against illicit medicines.
20 Driving a Vision for a Data-driven Regulatory Ecosystem
A data-driven Regulatory ecosystem has huge potential beyond the opportunity for operational improvement. Even in today’s eCTD+ world, most life sciences Regulatory teams currently still think and work in terms of documents, paragraphs and sentences when putting together collateral for marketing authorisation and variations submissions. Yet it is data, rather than pre-prepared dossiers, that is moving into central
www.international-pharma.com
INTERNATIONAL PHARMACEUTICAL INDUSTRY 1
Contents
focus now. Renato Rjavec at Amplexor discusses how regulatory and product teams will need updated data skills to deliver this vision.
22 Regulatory and Developmental Complexities Around Demonstrating Bioequivalence for a Topical Generic Product
The topical dermatology market, although niche, was estimated to be valued at approximately $20.4 billion in 20201. In a study from 2010–2015, over half of the topical drug products experienced a price increase, and the average price of topical generic drugs was 276% higher by the end of that period. This is being driven by the lack of competition among generic manufacturers, where approximately 80% of topical dermatological drug products have very few competitors or no approved generics at all. Dr. Jon Lenn and Prof. Marc Brown at MedPharm discuss the lack of generic products that can be attributed to the complexity of developing topical dermatological drug products, low market volumes, and/or the risk and expense of clinical endpoint bioequivalence (BE) studies.
26 Opportunities for The IPO of Psychadelics Companies (or, How to Change Investor's Minds)
If anyone had suggested only a few years ago that it is a realistic proposition to float a psychedelics company on any of the London markets that suggestion would likely have been met with derision. Psilocybin research is still at a relatively early stage, and, at present, only a very limited number of global regulators approve the use of psychedelics to treat mental health conditions. However, as Nigel Gordon at Fladgate LLP discusses, the “direction of travel” in the thinking about psilocybin is towards a conclusion that it may form the basis of the development of much-needed novel treatments for mental health conditions and it might well, therefore, be the case that there will be a change in the view of regulators in future.
DRUG DISCOVERY, DEVELOPMENT & DELIVERY
30 Technical Advancements in Proteomics Streamline High-throughput Workflows
Over the last two decades, significant advances in technology and new methodologies have made proteomics an extremely powerful
tool for protein scientists, biologists and clinical researchers. Scientific discoveries in proteomics largely depend on data analysis and data generation. Chris Adams at Bruker Daltonics states that using mass spectrometry (MS)-based proteomics has expanded significantly with improvements in software, data acquisition, and algorithms to provide more accessible and accurate data.
32 Pre-existing Immunogenicity: How Will Cell and Gene Therapies Change Our Testing Approach?
When bringing a therapeutic to market, determining its potential to elicit an immune response and understanding the molecular and cellular interactions involved is essential. In some patients, it is possible that a previous exposure event to certain antigens associated with the therapeutic can prime the immune system for re-infection. Dr. McNally at BioAgilytix explains that as we move into a new era where cell and gene therapies (C>s) are frequently gaining approval for use, it is important to consider how best to approach pre-existing immunogenicity assessment for these relatively new modalities.
CLINICAL & MEDICAL RESEARCH
40
Respiratory Disease Management: A Connected Approach
Until recently, treating, monitoring and controlling respiratory conditions such as asthma centred on conventional devices, paper-based tools and appointments with a GP or asthma nurse. This approach, of course, still plays a huge role for the over 300 million people living with asthma globally. However, a deeper understanding of the greater efficiency at hand through the vastly increasing use of digital applications and the palpably mounting pressure that can be felt on healthcare bodies globally has seen a shift in the context of respiratory disease management. Sarah Sanders, Christina Philpott and Emma Dunipace at Recipe Design explain that this, in turn, is creating exciting opportunities for new MDI devices and supporting applications that enhance overall treatment capabilities and outcomes.
TECHNOLOGY
44 IP Issues Surrounding Machine Learning and AI in the Pharmaceutical Space

When it comes to protecting technical innovations, there are two broad strategies: keep it a trade secret or obtain a patent. It has long been the case that computer-implemented technologies and pharmaceutical technologies are technical fields where one or the other approach (trade secrets in the case of computers, patents in the case of pharmaceuticals) has been typically favoured. Harry Muttock, Yelena Morozova and Nicholas Fox at international IP firm Finnegan explain how in the brave new field of applying advanced computational systems to the development of pharmaceuticals, we develop a strategy which satisfies both approaches to protecting technical innovations.
48 Strategic Intellectual Property Considerations for Protecting AI Innovations in Life Sciences
Artificial intelligence (“AI”) is all around us. It allows us to unlock our smartphones with just a glance. It can customize the temperature of our home or recommend television shows based on things we enjoyed watching before. It may soon drive our cars for us. Through the combination of increasing computing power and massive amounts of data, AI has made unprecedented advances in recent years in its ability to make predictions and solve problems. As a result, AI has become a vital part of our everyday lives. And soon, the medications
2 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4 Contents
1mL & 2.25mL
Spring-free
passive safety devices for pre-filled syringes

The patient benefits of UniSafe® are:
• Passive needle shielding to help prevent needlestick injuries
• An unobscured syringe barrel for full drug visibility to create user confidence
• A large, ergonomic plunger head and a smooth finger flange, resulting in an integrated look and feel which provides reassurance
UniSafe® 1mL proven, on market, in patient use

Want to know more?
• Optional extended finger flanges for patients with strength and dexterity impairment (applicable to 1mL only)
• The same injection technique as a pre-filled syringe making it intuitive to use




• It cannot be reused or prematurely activated
Visit ompharmaservices.com/ipi-dec2022 or email pharmaservices@owenmumford.com
UniSafe® is a registered trademark of Owen Mumford Ltd ©️ 2022 OMPS/ad/ipi/ob/1122/7
INTERNATIONAL PHARMACEUTICAL INDUSTRY 3 www.international-pharma.com
we take each day also be identified and developed at least in part by AI. This article by Charles T. Collins-Chase, Kassandra M. Officer, and Xirui Zhang, examines strategic intellectual property considerations for innovative pharmaceutical and biotechnology companies that are developing AI systems or using third-party systems to enhance drug discovery, clinical trials, manufacturing, or other processes.
52 Data-driven Processes Overtake Structured Document Authoring
The strategic focus in life science technology investment is shifting from documents to data. Regulators are increasingly asking for data rather than documents, and data-focused business processes, based on a single source of truth, are bringing efficiencies right across the organization. James Kelleher at Generis describes the implications of the transition away from structured document authoring.
MANUFACTURING
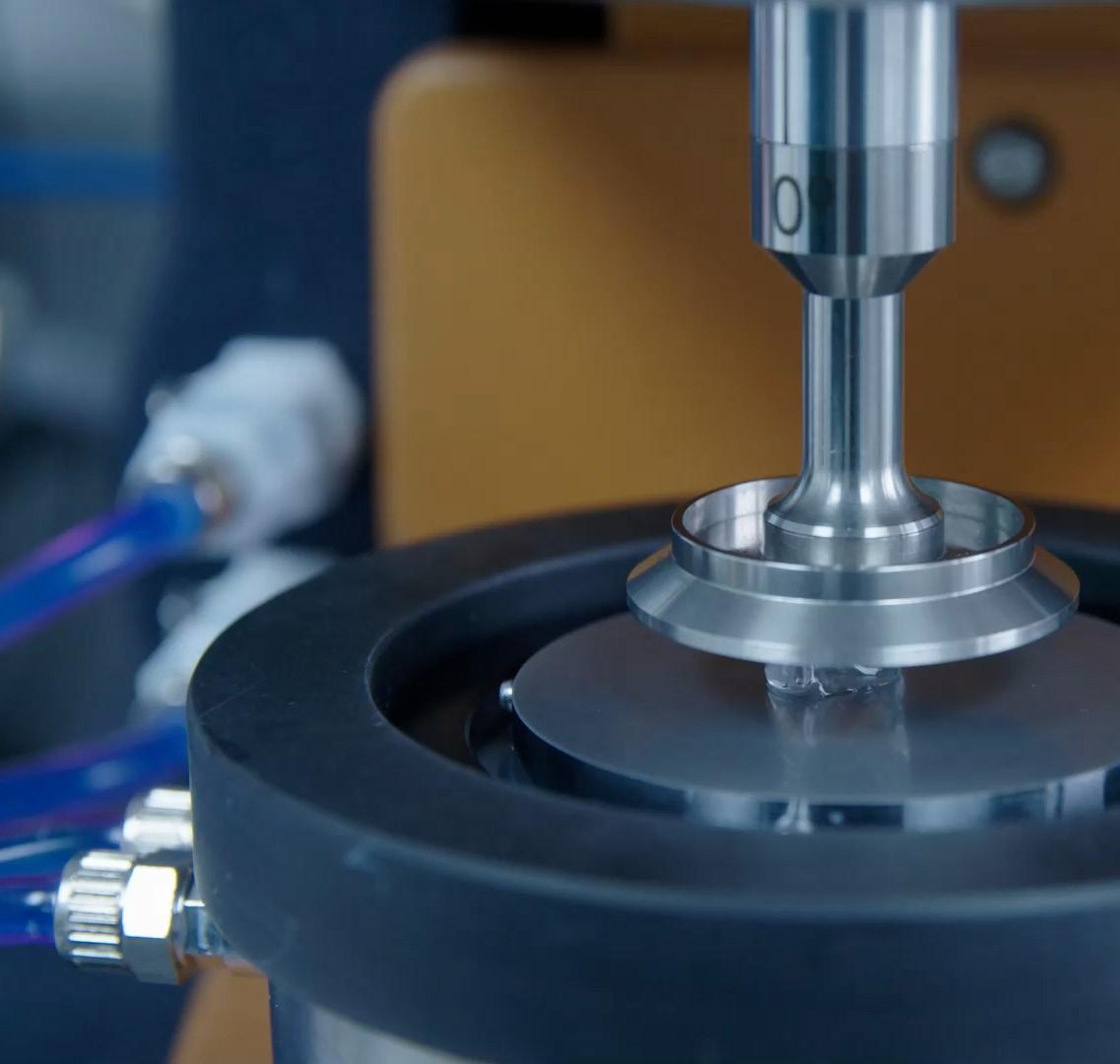
54 Pharmaceutical Tablet Coating –Achieving Perfect Coating Uniformity
Tablets are the most important oral dosage form in the pharmaceutical industry. Pharmaceutical film coating, a thin film made from one or more polymers that can fulfil a variety of functions is applied to the tablet. Most of the coating processes are performed for drug release modification, drug stability improvement against light or moisture and taste masking. Furthermore, patient compliance issues play an important role, as swallowability improvement or a simpler identification due to a different colour. Tobias Borgers at L.B. Bohle explains why coating represents an important process step in the pharmaceutical industry.
58 The Challenges of Increased Complexity in API Development and Manufacture
There is no getting away from it: the small molecule drugs now entering and travelling through the clinical pipeline are becoming more complex. This increasing complexity poses a variety of challenges that pharmaceutical and biotech companies will need to overcome. Giovanna Libralon at Lonza Small Molecules talks about the molecule itself and that it may be that, as an integral part of the way it is designed to hit the target, it includes features and moieties that are difficult to make.
PACKAGING
68 What’s Next for Pharmaceutical Serialisation?
Supply chains for pharmaceutical products are exceptionally complex, with medicines and ingredients often crossing the borders of many countries before reaching the end consumer. Bart Vansteenkiste at Domino explains that to protect patient health and safety, serialisation and track and trace requirements have become standard for pharmaceutical products worldwide. Legislations include the EU’s Falsified Medicine Directive (FMD) and the US Drug Supply Chain Security Act (DSCSA), which both necessitate serialisation and government reporting for prescription pharmaceutical products.
70 Overcoming the Pitfalls of Pre-filled Syringe Filling
The international pre-filled syringe market was worth $3.6 billion in 2021 and is predicted to increase in value to $6.5 billion by 2030, growing at a CAGR of 7.1% throughout the forecast period. One of the key drivers for this projected growth has been a major change
in the choice of injectable delivery formats following the COVID-19 pandemic. Michael Isele at Recipharm explores the pitfalls of filling and packaging in pre-filled syringe formats, from sterile integrity requirements to packaging challenges, such as kitting, explaining how these challenges can be addressed.
HEALTH OUTCOMES
72 Artificial Intelligence is a Core Pillar in the Evolution of Digital Health and Patient-centric Solutions
The US Food & Drug Administration has stated that digital technology is driving a revolution in healthcare. The lines between healthcare delivery and clinical research are blurring as the patient becomes a key partner and focus. We see a rapid expansion in the use of mobile and patient-centric devices, exponential growth in the volume and diversity of life sciences data and acceleration in the use of data-dependent computation to gain insight and automate, loosely called artificial intelligence (AI). Michael Phillips and Gerard Quinn at ICON discuss Artificial intelligence as a core pillar in the evolution of digital health and patient-centric solutions.
LOGISTICS & SUPPLY CHAIN MANAGEMENT
74 How the Pharmaceutical Industry Can Navigate Supply Chain Disruptions and Gain Resiliency
Every pharmaceutical shipment is valuable, some to the tune of millions of dollars. The distribution and safety of pharmaceutical products have a very direct impact on medical outcomes. Therefore, manufacturers, distributors, shippers, logistics service providers, and retailers need deeper levels of insight and greater visibility into the supply chain now more than ever. Alex Guillen at Tive explores how real-time tracking of pharmaceutical shipments accelerates their distribution and examines the common challenges in distribution, including compliance issues, and how real-time data, combined with customised tracking alerts, can empower supply chain leaders to overcome obstacles and realise insights that will drive proactive management decisions.

4 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Contents
wel-screen

Contract services firms are becoming increasingly sophisticated and embedded in the drug development ecosystem. Contract development and manufacturing organisations are the pharma industry’s special forces unit: a highly specialised team that functions behind the scenes, doing difficult tasks in high-pressure situations.
Pharma companies have turned the corner in terms of their appetite to outsource development. The scale and scope of outsourcing have changed markedly. In the early 2000s, instead of one-off project transactions, there has been a move to longterm strategic partnerships between the contractors and their clients. Particularly in the biotech sector, CDMOs are often seamlessly integrated with any inhouse development and manufacturing departments. Many small and virtual pharma companies, those that consist of only a few employees and few, if any, facilities, could not exist without CDMOs.
Over the last five to eight years, there has been a rise in organisations that aim to be ‘one-stop shops’ for anything from early-stage research to manufacturing. The integration between development and manufacturing is valuable even to big pharma companies because it greatly reduces the tech transfer and scale-up risk.

The pandemic marked a turning point for the relationship between CDMOs and pharma companies. Pre-2020, pharma companies usually outsourced services on a project-by-project basis. Long-term partnerships were rare; around 80% lasted no longer than a few years. During the pandemic, CDMOs suddenly became a huge source of additional research and manufacturing capacity, though it remains unclear whether this will translate to more strategic collaborations in the long run.
The relationship has become more integrated and broader, with increasing use of [contract research, development, and manufacturing
Editorial Advisory Board
organisation, CRDMO] companies from the early phases through to the complete life cycle. Partnerships have shifted from transactional to strategic. This requires that CRDMOs have developed technologies, manufacturing capacities and proven quality systems, as well as experience and expertise.
Speed and competency are the two major components when it comes to making decisions around outsourcing. The advantage of CROs and CDMOs is that you can look globally for the precise competencies that you need. It’s difficult to build this, especially if you’re a small company in one location.’
The outsourcing market for biological products – sugars, proteins, nucleic acids or even whole cells and tissues – is growing at 10–15% per year, compared with 6–7% growth in small-molecule drug compounds. While new chemical entities remain the largest segment of the CDMO market. Biologics have been riding a wave over the last few decades and are certainly part of the change the market has experienced.
However, the fastest growth is happening in entirely new classes of treatment: RNA therapeutics, protein degraders, cyclopeptides, antibody-drug conjugates and gene therapy. They are highly outsourced because normally they’re very small, so for every individual pharma player it rarely makes sense to invest in building a whole plant.
These new modalities require a completely different set of equipment and expertise than traditional drug molecules or even biologics. Moreover, the new modalities market encompasses so many different technologies, it would be nearly impossible for a single company to develop expertise in all of them – and bear all the financial risk for drug failure. But with the help of specialist CDMOs, firms can dip in and out of different therapeutic fields.
Multiple interconnected factors continue to drive growth in outsourcing services. Pharma
firms’ efforts to maximise value for shareholders, aspects of cost and technological advancements. Large firms want to reduce their assets and costs while emerging companies want to hit milestones as quickly and efficiently as possible, ‘even if it means failure’. The average number of drug approvals by the US Food and Drug Administration almost doubled between 2011 and 2021 compared with the previous decade, and that increase is associated with more demand for outsourcing and more opportunities for deeper integration into the pharmaceutical ecosystem.
Drugs featuring complex molecules and substances require investment in new technologies, a decision that may be more easily made by a specialist CRDMO than a pharma company. CRDMO companies will continue to evolve in the next few years, investing in cutting-edge science and technologies to enable innovation, such as targeted protein degradation and photoredox chemistry.
More generally, the pharmaceutical industry has understood that specialist companies can often be more productive than internal resources in the R&D process. Specialist CROs often see many projects across several targets and therapeutic areas, whereas employees working in a small or large pharmaceutical company may focus on a particular area. The CDMO market will continue to grow over the next five to 15 years.
Virginia Toteva, Editorial Manager – IPI

Deborah
Diana L. Anderson, Ph.D president and CEO of D. Anderson & Company
Franz Buchholzer, Director Regulatory Operations worldwide, PharmaNet development Group
Francis Crawley. Executive Director of the Good Clinical Practice Alliance – Europe (GCPA) and a World Health Organization (WHO) Expert in ethics
Rick Turner, Senior Scientific Director, Quintiles Cardiac Safety Services & Affiliate Clinical Associate Professor, University of Florida College of Pharmacy
Georg Mathis Founder and Managing Director, Appletree AG
Jagdish Unni, Vice President – Beroe Risk and Industry Delivery Lead – Healthcare, Beroe Inc.
Jeffrey Litwin, M.D., F.A.C.C. Executive Vice President and Chief Medical Officer of ERT
Jeffrey W. Sherman, Chief Medical Officer and Senior Vice President, IDM Pharma
Jim James DeSantihas, Chief Executive Officer, PharmaVigilant
Mark Goldberg, Chief Operating Officer, PAREXEL International Corporation
Maha Al-Farhan, Chair of the GCC Chapter of the ACRP
Stanley Tam, General Manager, Eurofins MEDINET
(Singapore, Shanghai)
Steve Heath, Head of EMEA – Medidata Solutions, Inc
Patrice Hugo, Chief Scientific Officer, Clearstone Central Laboratories
Heinrich Klech, Professor of Medicine, CEO and Executive Vice President, Vienna School of Clinical Research
Robert Reekie, Snr. Executive Vice President Operations, Europe, Asia-Pacific at PharmaNet Development Group
Sanjiv Kanwar, Managing Director, Polaris BioPharma Consulting
Stefan Astrom, Founder and CEO of Astrom Research International HB
T S Jaishankar, Managing Director, QUEST Life Sciences
6 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Editor's Letter
Bakhyt Sarymsakova, Head of Department of International Cooperation, National Research, Center of MCH, Astana, Kazakhstan
Catherine Lund, Vice Chairman, OnQ Consulting
A. Komlos, Principal Content Writer, Clarivate



Harnessing decades of global drug product development and commercialization, you can rely on our integrated speed solutions to simplify your supply chain, spanning the cycle from study to launch. Introducing speedsolutions™ Your bridge between life-changing therapies and patients speedtostudy™ speedtopatient™ speedtoapproval™ speedtolaunch™ PH II PH III COMMERCIALIZATION PH I Let’s talk future™ talkfuture@pci.com | pci.com Accelerating your product through development to commercialization and beyond Development & Manufacturing | Clinical Trial Services | Commercial Packaging
Regulatory & Marketplace
Understanding Compliance: Moving from Cost to Value
Throughout the life sciences sector, the key trends of globalisation and digitalisation are providing new opportunities for growth and innovation. However, within development facilities, quality assurance, lab systems and scientific teams are feeling the impact of these transformations. Especially as their endeavors to ensure high levels of compliance meet the growing regulatory pressure within the industry.
With an increasingly digital and connected lab infrastructure, failing to navigate the challenges of global regulatory requirements can be costly. As such, any compliance and validation processes must be designed to meet the needs of multiple geographies, business activities, and functions.
Taking action to identify, analyse, and reduce compliance risks requires a high level of resource and expertise. However, in a fastpaced, scientific environment, researchers are already stretched thin. This brings an added risk of slowing down productivity in even the best-run laboratories if compliance is not strategically managed.
To overcome these challenges, lab managers are increasingly turning to external partners who have expertise in qualification, requalification, risk management, and remediation. By transforming their compliance processes, scientists are then free to concentrate on research and discovery and meet the evolving demands of a more digital and connected lab.
Here, we speak with Joshua McWilliams, Product Manager, GxP Validation Services at PerkinElmer Inc., to learn more about the rising need in the pharma industry for compliance expertise and support.

Hi Josh, before we dive into compliance best practices can you tell us more about how your role drives and inspires you?
Sure. I lead the GxP Validation Service team as part of PerkinElmer’s OneSource
strategic services group. I’m inspired by how we collaborate closely with our clients so we can determine their unique needs and help them further their science while creating or maintaining safe and compliant processes.
For me, it’s exciting to see first-hand how trends and global drivers play out in the lab and affect compliance. For example, in the late 90s to early 2000s, we saw an exciting shift towards digitising labs. However, this more online route came with new challenges and required a different level of validation. As more labs move towards advanced digitalisation and cloud-based data management, they need to look at compliance in a more collaborative and connected way and share information securely and accurately.
Lab managers and scientists are experts in their field but finding dedicated compliance expertise in-house can be a real challenge. I started my career as a bench chemist, so I know all too well how difficult it can be to manage your own time in the lab let alone handle compliance needs. This direct insight
allows me to help labs define the difficult and non-core compliance tasks that are getting in the way of their vital research and key scientific tasks.
Ultimately, the biggest driver for me and my team is to give time back to science, so researchers and lab professionals can focus on discovering better therapeutic candidates vs. getting bogged down in compliance execution and monitoring.
What do you consider to be the top best practice approach for compliance or a framework to work from?
Industry best practice involves following a risk-based approach for patient safety and quality. We work to GAMP 5 guidelines, which build in quality checks throughout the entire production process and enable us to meet the unique needs of a company and particularly its computerised systems.
The first step is creating a comprehensive requirements document, which includes how a
8 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Regulatory & Marketplace
system is supposed to operate and its intended uses. A validation plan can then be drawn up that should outline the strategy – which policies and procedures will be followed, any functional configuration specifications and design specifications as needed.
Lab instrument qualification historically would have meant simply purchasing, installing and bringing the new piece of equipment into service. Today’s regulatory requirements mean that planning and development should occur before purchase to ensure the instrument is fit-for-purpose. After which, qualification continues with Installation Qualification (IQ), Operational Qualification (OQ) and Performance Qualification (PQ). This isn’t just a question of verifying the vendor’s hardware and software qualifications. Everything should be checked against the requirements document for its specific use at the manufacturing site. Documents such as standard operating procedures also need to be created, and staff must be trained to follow them for all instrument usage, including administration and calibration as well as operation.
Ideally, validated instrumentation needs to be maintained across multiple sites and lab spaces by a team of specialised onsite validation experts. Here, a multivendor approach can save precious lab time, by harmonising protocols under a single Universal Operational Qualification framework. Allowing lab managers to streamline processes across all major models of laboratory instrumentation and scientists to concentrate on research and discovery.
Nowadays, regulators are probing how data is generated, reported, archived, and retrieved. Therefore, data integrity should play an essential role throughout the validation process. For example, regulations such as FDA 21 CFR Part 11 must be built into the requirements, to ensure the security of electronic records. Data relating to
formulations, clinical trials and any other sensitive areas must be tightly controlled.
Compliance is a continual process: thorough documentation must be kept dayto-day to provide evidence that the policies and procedures set out in the validation plan are being carried out to meet the validation requirements. Centralised monitoring and continual improvements enable labs to pursue science with integrity and help keep staff and lab inspection ready.
When it comes to the conversation around compliance pressures in the modern-day pharma lab, where are the gaps in people’s knowledge and understanding?

Within labs, there is often a lack of deep compliance knowledge. Although lab teams will be trained on compliance steps for individual instruments and tasks, they may not have a wider knowledge of compliance systems and processes as well as trends or new regulations that are evolving. There is also a challenge for facility IT teams, who may not have a real-time or full understanding of the specific compliance needs within highly regulated industries like pharma or food. Labs that don’t have the expertise or procedures in place to prove their increasingly connected data is accurate and their instruments are fit-for-purpose may risk non-compliance which slows their R&D cycles.
These knowledge gaps are compounded as teams are unable to fully understand the benefits that investing in rigorous validation methodology can bring. Our OneSource validation and compliance team utilises industry best practices, keeping up with changing regulations on a daily basis. One recent trend we see is the regulatory focus on data integrity. However, accurate and
reliable data has always been the foundation of successful basic research, it just takes on different meanings and needs around security, sharing and validation in cloudbased environments.
What are the key challenges labs face when navigating today’s compliance environment?
One of the biggest challenges is ensuring that lab efficiency does not suffer at the hands of compliance. Events such as the purchase of new equipment, company acquisitions, relocations, and audit findings can all contribute to increased validation needs and workloads and need to be proactively vs. reactively factored in. Plus, the increased focus on Computer Systems Validation (CSV) and data integrity is driving a need for larger validation budgets and resources.
Like data integrity, CSV is a broad concept that affects virtually every dimension of pre-clinical research and drug discovery. Departments such as IT will be needed to help with the configurations, permissions, and necessary settings. Without a dedicated validation team, general lab or IT resources may not have the appropriate skill set or bandwidth and can become overwhelmed. Furthermore, as the industry looks to adopt new digital tools and innovations like eValidation, staying current with the latest software versions may require additional validation to be completed.
It’s important to understand the impact that updates can have on your validated systems. As such, it’s clear that CSV is an ongoing process, not a one-time activity. It will extend all the way through to the eventual decommissioning of the given instrument or application. Its time-consuming nature may require outsourcing and expert assistance to keep the process on track.
INTERNATIONAL PHARMACEUTICAL INDUSTRY 9 www.international-pharma.com
While compliance endeavours can seem daunting, they are ultimately critical to the scientific integrity of the pharmaceutical industry and, down the line, to the safety and well-being of patients. Companies can achieve the most effective regulatory defensible position for computerised instrument and analysis systems using a standardised delivery framework. This requires compliance and scientific expertise.
By partnering with a third-party expert, lab teams can receive unbiased recommendations from specialists that engage with the needs and demands of regulatory compliance all day, every day.

Integrating successful validation and QC procedures into the lab results in more streamlined and efficient workflows. Furthermore, external solutions help put both data integrity and the closely associated CSV on sustainable trajectories.

Lab managers may want to avoid investing more in-house or with a compliance service provider, but the costs of non-compliance are often much greater. Strategically partnering with an expert supplier can be more cost-effective and enables labs to stay focused on their core R&D activities.
From your point of view, what do you think the future of compliance looks like for pharma and life science labs?

I think we’ll continue to see the trend of incorporating digital tools for cloud-based
data capture, visualisation and sharing that is part of Pharma 4.0, as well as further validation of enterprise systems versus stand-alone equipment. Labs are starting to move data to the cloud, and with that comes the regulatory focus on validating to intended use and following a risk-based management approach.
I’m also expecting to see an increasing number of companies choosing strategic partnerships to understand and overcome the latest compliance needs and challenges. External service providers can leverage learnings and insight from across the industry. As such, they can help streamline lab workflows and boost scientific productivity with data integrity assessment and methods to establish quality control procedures that support reliable research data. With an experienced partner, you're not just getting the resource to do the work. You're also getting the breadth of experience across all professional services to support you through the continued digital revolution.
Josh McWilliams is GxP Validation Services Product Manager for PerkinElmer's OneSource strategic services and has 25 years of experience working in the pharma industry. Josh currently oversees the development of the OneSource GxP Validation Services product roadmap, as well as product innovation and oversight, including; Stand-alone and Enterprise Computer Systems Validations, Data Integrity projects, Method Validation, Process Validation and CQV. Before joining OneSource, Josh developed his skills and experience working as a senior scientist at Watson Laboratories and as a validation specialist at PPD.
10 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Regulatory & Marketplace
Josh McWilliams
How can strategic approaches to outsourcing help support labs looking to meet their compliance demands while also enabling scientific innovation?
DropControl minimizes the spontaneous dropping of ophthalmic preparations


—
The newest developments of eye drop solutions are focused on non-water based solutions, which require a different design of the eye dropper to prevent unintended dropping.
Our solution is an insert into our existing eye dropper, which controls the flow of water-free eye drop solutions.

The DropControl fits our existing dropper bottle system A, E and F.

INTERNATIONAL PHARMACEUTICAL INDUSTRY 11 www.international-pharma.com gerresheimer.com
Pharmapack | February 1 – 2, 2023 | Paris, France | Hall 7.2, booth B60/B64
EU CTR: Final Countdown, What You Need to Know

The end of the transition period is imminent. How can clinical trial sponsors and CROs ease the transition to CTIS?
Soon, the one-year transition period of the EU’s Clinical Trials Regulation (CTR) will come to a close. EU CTR aims to harmonise the clinical application process across Europe and increase transparency. The regulation envisions a faster and more streamlined submission and approval process for larger multinational studies. Soon, biopharma sponsors, contract research organisations (CROs), the European Medicines Agency (EMA), and member states will use one system to manage all trial applications and authorisations.
Sponsors and CROs have spent the transition period learning how to navigate
the Clinical Trials Information System (CTIS) for their study registration and approval activities, which will be a mandatory requirement from 31st January 2023. Having a common regulatory approach across the European Union will boost regional competitiveness. Patients are set to benefit from improved transparency of trial data, as data submitted within applications will be made public, making it easier for patients to identify and participate in ongoing trials.
To date, almost 100 studies have already been submitted under the new regulation, with Veeva customers accounting for at least half of these. The initial feedback from sponsors and CROs alike is that it is challenging to remain efficient while complying with legal responsibilities. Companies have had to improve communication, collaboration, and alignment across diverse global study stakeholders and departments.
Rethinking Our Approach to People, Processes, and Data
In its present format, the backbone technology of CTIS is not easy to integrate. Sponsors and CROs are collating data in their own technology environments. Each document in a study submission needs to be individually isolated and manually uploaded to the CTIS portal. Process timelines are getting longer, as companies spend more time collecting data points and information while managing translations and redactions. Once the submission has been made, companies often find they have a small window to respond to questions and requests for further information from the EMA.
How should companies address these challenges? Those that have successfully navigated the new process first had to attain internal alignment. This meant acknowledging that the old way of interacting with regulatory authorities was no longer
12 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Regulatory & Marketplace
Regulatory & Marketplace
Checklist
Are you ready? Your EU CTR Checklist
Processes: Review and re-define for tighter timelines
Review processes for ethics committee submission, health authority interaction, and clinical trial disclosure
Define new processes for document redaction, translations, and data collection
Determine approach for upload to CTIS (who, what, when) and regulatory tracking
sufficient and mapping out which internal stakeholders should be brought into the process, and when. Some created new roles to reflect the new reality, including managing translations or uploads to the portal. Others have redefined the RACI framework for clinical and regulatory study leads to maximise efficiency. All agree that technology plays a crucial role in improving collaboration across diverse stakeholders by making it easier to search for and extract data quickly, as well as draw on internal expertise during submission.
Without a doubt, managing high volumes of data and documents in the new process is very challenging. Few companies like their current approach of collecting data using internal tools, like spreadsheets. Nor do they think the current cross-functional efforts to complete reviews, quality checks, and translations are sustainable. Eventually, the industry expects further enhancements, such as integration with CTIS.
However, any sponsor or CRO submitting an application faces disclosure risks for two types of information: protected personal data (PPD, with privacy protection under GDPR) and commercially confidential information (CCI). The redaction effort required to make documents available for public consumption is significant, complex, and dynamic as redacted passages can change over time.
For the industry, CCI and PPD are serious pain points – perhaps the most acutely felt. And while there is consensus that automation could alleviate the redaction effort, there is a high barrier to entry before technology can offer more than just tactical support to human oversight and interventions. There are multiple languages in play, metadata to
Define clear RACI and ownership mapping
Reduce redaction and mitigate user errors by updating forms and templates
People: Build alignment across your entire R&D organisation
Coordinate closely with regulatory, quality, safety, and disclosure teams
Include affiliates, as well as CRO partners
Offer end-user system training for all relevant functions
Data & Systems: Future-proof your technology environment
Review current technology landscape, existing capabilities, and future requirements
Identify interim solutions until data formats and document requirements are determined by the EMA/CTIS team
Visit the EMA/CTIS website for guidance (e.g. document naming), training material, and CTIS revision notes
Contact a Veeva expert to support with Vault system evaluation, capabilities, and recommended configurations
remove, and significant coordination effort, to name just a few hurdles.
A New Global Standard for Clinical Trials

The end state envisioned in the regulation is a faster, more consistent approach to clinical trials: not just for Europe but for global companies that want to sell products into the region. However, enterprise biopharma companies face more complexity than smaller sponsors (who tend to outsource to CROs). These global organisations are undertaking significant change management to harmonize their technology and processes and face the added complication of running studies under EU and non-EU regulations.
Setting an ambitious worldwide standard was never going to be easy. EU CTR challenges the industry to balance consistent processes and reporting with an excellent user experience, operational efficiency with inspection readiness. For now, companies of all sizes are focusing on ensuring their processes (including for EU and non-EU country studies) are well set up, which in turn requires significant people training.
Many will need to keep a manual approach to collecting data points for entry into CTIS for the interim period. However, their attention is turning to how software and end-to-end technology can work better to deliver on the stated aim of the regulation: accelerating innovation and research through improved efficiency.

As partners to the life sciences industry, we will need to rise to the same challenge of balancing opposing forces. Technology will get us there. But, like EU CTR, it will come in stages.
Werner Engelbrecht
Werner Engelbrecht, Senior Director Strategy at Veeva Systems, has extensive experience in the pharmaceuticals and life sciences industry, across a range of roles, with his career spanning over twenty years'. For the last twelve years, he has brought his in-depth industry knowledge to operational, and sales and account management teams at CROs (contract research organisations). In his current role as Senior Director Strategy at Veeva Systems, Werner heads up a team that is dedicated to using digital transformation to navigate the complexities of clinical trials and speed up development of new medicines.
INTERNATIONAL PHARMACEUTICAL INDUSTRY 13 www.international-pharma.com
Brexit – Impact, Challenges, and Solutions for The Pharmaceutical Industry
Brexit has provided several challenges to the pharmaceutical industry that required robust actions and swift resolution in order to remain in compliance following the end of the transition phase.
At the ‘Brexit – Impact, Challenges, and Solutions for the Pharmaceutical Industry’ Conference we heard from companies expressing their need a for a clear action plan to map out the activities, timings and responsibilities for these changes including those licencing activities, manufacturing, QP release and supply routes.
Focussing on the regulatory activities, the following are some of the challenges faced by companies and the steps taken by the UK Regulator, the MHRA, and UK Department of Health and Social Care, in order to provide solutions to marketing authorisation review and access to medicines:
Regulatory Challenges
Following Brexit, regulatory oversight in the UK has shifted from the EMA to the MHRA, for what were European procedures, with the work of the multinational agency now falling to the MHRA. One would; therefore, question capacity and anticipate resource issues.
For companies, lack of published guidance, or guidance that is published very late, has provided issues for training, compliance and updating of internal procedures. There is a continued reliance on existing EU forms and systems, and with separation of European procedures from Great Britain, there is a duplication of effort which stretches the capacity of already finite regulatory resource.
This has increased the risk of potential delays to submissions and approval in Great Britain and Northern Ireland. In addition, there is the potential for reduced supply of medicines to NI.
UK Marketing Authorisations – For Existing Products
All existing Centrally Authorised (CAP) MAs were automatically converted into UK MAs effective in Great Britain (England, Scotland
and Wales only) and were issued with a new MA number on 1 January 2021 (with a format of PL GB) unless the MHRA were otherwise advised. This was a process referred to as ‘Grandfathering’.
Companies submitted initiating sequences, with baseline data, for the new GB only grandfathered product by the end of 2021. This was a large resource burden on regulatory departments to collate these data and create a new baseline. This created a particular issue for historic products, where data may not have a readily available in CTD format, or was archived and not digitised. The MHRA took a pragmatic approach and requested companies provide as complete a dossier as possible, and that companies make all ‘reasonable endeavours’ to do so.
As a result of the implementation of the Northern Ireland Protocol, existing CAPs remain valid for marketing products in Northern Ireland. Future EU marketing Authorisations will continue to include Northern Ireland.
This has essentially created 2 parallel licences: one for the EU, including Northern Ireland, and a new separate GB only licence. Although there was no fee for the grandfathering process, as with all UK national MAs, an annual service fee is due for converted EU MAs.
Existing Nationally Authorised MAs continue as pre-Brexit and the MHRA presented options for managing MR/DC Procedures.
European Commission (EC) Decision
Reliance Procedure – ECDRP New GB MAs can follow CAP procedures, utilising the EU Reliance Route. This was effective until the end of 2022, but as a post meeting note, has now been extended by another year until the end of 2023.
Companies can wait until the product has received a positive opinion from the CHMP. The Application will be determined when the EC decision has been confirmed. The published guidance states a 67 day process thereafter to obtain a GB only MA, but in practice this is likely to be longer due to resource constraints at the MHRA to start
the procedure and any potential requests for further information.
This EU Reliance Route has been used extensively for products falling under the Centralised Licence Categorisation postBrexit.
UK/GB national variations continue to follow current EC variations regulation.
Variations to purely national MAs (PL, PLGB and PLNI) can also be presented to the MHRA under the reliance route. Companies can submit either by national only or reliance route for the Type II and Type IB variations, but Type IA variations cannot rely on the EMA decision so should be submitted to the MHRA in parallel to the EMA.
For those Type IB and Type II variations submitted according to the reliance route procedure, provided the variation is identical to that approved for the European MA, and evidence of this is included with the submission, the CAP variation approval will be taken into consideration during the assessment process.
A lower fee will be charged for reliance variations as less assessment is required. The MHRA are actively encouraging the use of reliance procedure for variations to reduce workload and speed up approval process. This will reduce divergence between the CAP MA and GB MA, which is a general concern of companies where there may be an inevitable regulatory drift between the EU and GB.
Decentralised and Mutual Recognition Reliance Procedure for New MAs
For new applications, the MHRA can use approval of Marketing Authorisations submitted via Mutual Recognition or Decentralised procedures in EU member states with a view to granting the MA in the UK or GB.
This route is called the MRDC Reliance Procedure – MRDCRP. The MAH submits the MRP/DCP MAA as usual, thereafter once approval is received the entire dossier is then submitted to the MHRA via the MHRA submissions platform. As with the EC Reliance Route, the published timelines state 67 Day Approval Timeframe.
14 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Regulatory & Marketplace
Regulatory & Marketplace

For existing MRP or DCP products, MAHs have the choice as to how to manage their MAs;
A. Maintain a UK-wide Marketing Authorisation and retain UK(NI) (the UK in respect of Northern Ireland) as a CMS. In this case, the Authorisation will continue to be a UK-wide MA with Northern Ireland as a CMS and Great Britain aligned with, but not part of, the DCP/MRP. This is the default position and no action is needed to be taken by the MAH.
B. Request that separate MAs are issued for UK(NI) as a CMS, and Great Britain (England, Wales and Scotland)
C. Notify the UK and the RMS (reference member state) in writing that they wish to remove UK(NI) as a CMS from the DCP/ MRP and maintain a national MA in Great Britain only.
For licenses maintaining the default option ‘A’, variations may continue to be submitted and managed as part of the relevant MR/DC procedure with NI as CMS to maintain a UK wide authorisation.
The RMS will communicate the outcome of the procedure directly to the MHRA. There is a 30 day period where the MHRA can reject the RMS decision relating to those variations where CMS input is expected (primarily major Type II variations). In reality, the MHRA has communicated that they will accept RMS approval for all variation submissions, including those with UK specific product information updates.
National Licences – New MAA Routes
The MHRA have provided new types of assessment pathways in order to help expedite approvals and facilitate access for innovative medicines; these include:
1. National Procedure – which allows for a 150 day national assessment. This is for high quality MAAs. If the application includes Northern Ireland, then it must comply with EU requirements.
2. Rolling review – where the MAA is submitted in increments for preassessment, prior to the final assessment stage. This is intended to streamline development of novel medicines allowing various elements of regulatory data to be reviewed separately.

3. Innovative Licensing and Access Procedure (ILAP) – aims to accelerate
the time to market and facilitate access for innovative medicines
Northern Ireland:
The Unfettered Access Procedure (UAP) allows for MAs approved in Northern Ireland via European procedures (centralised, mutual recognition or decentralised procedures), or via the Northern Ireland National route, to be recognised by the MHRA for Great Britain (England, Scotland and Wales)
Marketing Authorisation Applications (MAAs) made through the Unfettered Access Procedure (UAP) should be agreed within 67 days of MAA validation, unless major objections are identified.
It seems likely that this strategy will take the place of the current ECDRP (although this reliance route has been extended).
It was noted that there have been over one thousand products set to ‘not marketed in Northern Ireland’. The new Northern Ireland MHRA Authorised Route (NIMAR) provides a route for the lawful supply of Prescription Only Medicines (POMs) in compliance with UK and EU rules, where there is a risk that clinical need in NI for that product cannot be met.
This supply route has been designed to ensure that people in Northern Ireland (NI) can continue to access prescription-only medicines (POMs) should clinical need be unable to be met through authorised products or any other existing regulatory routes.
MHRA International Collaborations
The MHRA are extending their collaborations with international Health Authorities. Two examples are:
Project Orbis
One of the MHRA’s main priorities is to accelerate access to medicines in the UK in the aftermath of Brexit and they have implemented a framework for concurrent submission and review of oncology products.
This initiative aims to deliver faster patient access to innovative cancer treatments with potential benefits over existing therapies. Whilst coordinated by the FDA. it is open to MHRA, Australia (TGA), Canada (Health Canada), Singapore (HAS), Switzerland (Swissmedic) and Brazil (ANVISA), with each country remaining fully independent on their final regulatory decision.
Access Consortium
(Previously Known as ACSS)
The Access Consortium (Previously known as ACSS), is a further work-sharing initiative between MHRA, TGA (Australia), Health Canada, HAS (Singapore) and Swissmedic. Not all authorities have to be included and those who are, will maintain their own sovereign decision based on the recommendation in the Assessment Reports.
Currently, this pathway can offer Applicant’s three separate routes of authorisation:
1. New Active Substance Work Sharing Initiative (NASWSI)
2. Biosimilar Work Sharing Initiative (BSWSI)
3. Generic Medicines Work Sharing Initiative (GMWSI)
Approval by one Authority does not guarantee approval by all.
In conclusion, the steps taken by the MHRA to create new and innovative licencing options, and to expand collaborations with international partners, are in an endeavour to mitigate the effects of leaving the European regulatory network.
INTERNATIONAL PHARMACEUTICAL INDUSTRY 15 www.international-pharma.com
Graham Donaldson
Graham Donaldson is Director, Regulatory Affairs at PharmaLex UK. Graham has over 17 years of regulatory consultancy experience and leads PharmaLex’s UK and Ireland Centre of Excellence Service Delivery Area.
Bad Medicine: Lessons from an Enduring Alliance between Big Pharma and Global Policing
The challenges of tackling international crime with national law enforcement are legion. John Binns, partner in the Financial Crime team at BCL Solicitors considers how Interpol’s Operation Pangea illustrates how they can be overcome, in the context of the global fight against illicit medicines.
A World of Problems
What can be done about the sale of illicit medicines? The question illustrates a familiar challenge in the world of law enforcement, in that a problem we as consumers and taxpayers can see as straightforwardly needing tough and enduring action is made harder to solve by two fundamental features of the landscape.
The first of these is legal complexity. The trade in counterfeit and otherwise illicit medicines can be categorised in various ways from a legal perspective, broadly depending on the nature of the harms that are involved. Even where the law clearly provides remedies against conduct, which may result from a combination of civil and criminal law, the overlapping provisions and procedures can be unhelpful.
Controlled Drugs
In the UK, and indeed in most jurisdictions, the starting point for tackling many illicit sales of pharmaceutical products will be controlled drugs offences. The Single Convention on Narcotic Drugs 1961 provides the international framework, while the Misuse of Drugs Act 1971 and its schedules set the domestic framework for prohibited acts and the classification of various substances, with various regulations made under it providing the detailed rules. Where the actions of an illicit trader in medicines constitute prohibit actions under that legislation and are not covered, or insufficiently covered, by licences granted under those regulations, criminal investigation and prosecution may be both possible and appropriate.
Counterfeit Medicines
With respect to counterfeit medicines, these may breach intellectual property
laws, specifically in connection with the infringement of patents (under the Copyright Designs and Patents Act 1988) and the unauthorised use of trademarks (under the Trade Marks Act 1994), which can be enforced using either civil law routes, litigation in the High Court) or criminal law (prosecution in the magistrates’ courts or Crown Court.
Significantly, the availability of these two routes of enforcement does not entirely depend on who is doing the enforcing. Increasingly, private companies opt to bring private prosecutions in UK criminal courts against those identified as breaching criminal provisions of intellectual property law. While civil litigation may result in substantial damages and payment of costs by the losing party, and involve the lower evidential standard of civil proceedings, ‘the balance of probabilities’, as opposed to the criminal standard of ‘beyond reasonable doubt’, there is substantial deterrent value in obtaining a criminal conviction, with all that implies in terms of the offender’s reputation and, if and insofar as individuals rather than corporate defendants can be proved responsible, the threat of imprisonment.
Proceeds of Crime
A significant factor in the growth of private prosecutions in the UK has been the availability of confiscation procedures under the Proceeds of Crime Act 2002 (POCA), under which a convicted defendant can be ordered to pay sums that are equivalent to their benefit from criminal conduct, which in many cases are far in excess of their actual profits from the activity.
Meanwhile, state agencies – including, in the pharmaceutical conduct, the Medicines and Healthcare products Regulatory Agency (MHRA), can now use different provisions of POCA to pursue the proceeds of unlawful conduct (whether that conduct took place in- or outside the UK) without a criminal conviction. Recent changes to those provisions enable a relatively easy route to summary freezing and forfeiture of such proceeds in the magistrates’ courts where they are represented by funds in bank or building society accounts, which the MHRA have used to pursue alleged proceeds of online sales of prescription-only medicines.
The provisions of POCA relating to money laundering may also be engaged where there are proceeds of conduct that breaches UK law, or overseas conduct that would do so if it occurred here. In a pharmaceutical context, this has proven problematic in the context of sales of medicinal cannabis, which are, at least arguably, ‘criminal conduct’ for these purposes.
Consumer Protection
As well as the societal harms that underpin controlled drugs legislation, and the protection for private rights afforded by intellectual property laws, the sale of illicit drugs can engage various laws aimed at protecting the consumer from deception or various other forms of unfair trading. The Fraud Act 2006 prohibits, among other things, the use of active deception (or, in some circumstances, the failure to disclose relevant information) as a means to extract a gain from someone, while the Consumer Protection from Unfair Trading Regulations 2008 (CPUTR), generally enforced in the UK by trading standards departments of local councils, contain specific prohibitions on, among other things, selling medicines based on untrue claims as to their efficacy.
On top of all of that, there are specific provisions that establish bespoke regimes for medicines, including natural and homeopathic remedies, under the Human Medicines Regulations 2012 (the HMRs). Significantly, having previously derived many of these specific rules from EU law, post-Brexit, the UK government can make, amend, and repeal regulations under the Medicines and Medical Devices Act 2021 (the MMDA), which also establishes a civil penalty regime for offences involving medical devices.
Picking Up the Pieces
The second fundamental, and often unhelpful, feature of the law enforcement landscape is the contrast between its international nature and the significance of national borders – a challenge that the MHRA has also taken an effective lead in this sector in overcoming. As is increasingly obvious, the nature of financial crime, of which illicit medicine sales are a prime example, is global, which positively demands that
16 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Regulatory & Marketplace












INTERNATIONAL PHARMACEUTICAL INDUSTRY 17 www.international-pharma.com CUT THE WASTE! Visit us at Pharmapack 2023. 1 - 2 February, 2023 Paris Expo, Porte de Versailles, France Booth J50 www.liveoresearch.com/en/cutthewaste
local, national, and regional agencies join forces to share information and coordinate enforcement efforts.
A Joined-up Approach
We do not, and indeed may never, have such a thing as a global police force. Instead, the role of Interpol is to help coordinate the efforts of national and supranational law enforcement agencies. Since 2006, the MHRA has worked with Interpol and various other agencies, including the EU’s Europol, to tackle illicit medicines and medical devices. This includes concerted days or weeks of action against suspected offenders and their assets, which are then publicly announced, most recently this summer. Under the surface, the work to produce this undeniably impressive feat is essentially about tackling those twin challenges of legal complexity and working across national borders. Among other things, this will necessarily involve consideration of data protection and procedural rights for suspects and others involved.
Importantly, the agencies involved are not limited to public-sector regulators and law enforcement. They also include private companies, whose financial interests of course are engaged in a big way, insofar as counterfeit medicines breach their intellectual property rights. Indeed, more broadly, the profits and reputation of the pharmaceutical sector generally are put at risk by those who sell medicines in breach of the rules. Involving them therefore makes sense on a principled basis, and doubtless helps with resourcing the work of agencies that may not otherwise be wallowing in money.
A Global Template?
So, is there anything in Operation Pangea that might point the way for other efforts to tackle financial crime? Are there other industries that might similarly be incentivised to cooperate with and fund law enforcement in this way, other categories of crime that require similar international coordination? Could, for example, the financial sector be brought into international efforts to combat frauds on covid support schemes, or offending that involves crypto assets, or sanctions evasion?

Such comparisons make for interesting thought experiments, with some instructive results. The immediate impact of bounce back loans, controversially handed out with minimal due diligence to businesses at the peak of the pandemic, has been on lending banks, but the government guarantees have made them squarely a public sector problem. The UK’s response, so far, has been at a national level, perhaps assuming such crimes do not cross borders – but is this right? Are we doing enough to involve the financial regulators, or to work internationally, on crypto- and sanctions crime?
Conflicts of Interest
We should take care, of course, not to celebrate the contribution of the international pharmaceutical industry to law enforcement without recognising that it is, at least to a large extent, the result of self-interest. Indeed, it might reasonably be asked whether agencies like Interpol and Europol might even be shortchanged by the deal, putting public resources into enforcing laws that are largely in place to protect intellectual property rights that might
just as easily be protected by civil litigation, or even by private firms bringing their own prosecutions. In addition to that, might the alliance of national law enforcement agencies (LEAs) and private firms lead to an unhealthy conflict of interests, insofar as private firms, even reputable multinationals, are not above committing offences themselves, including breaches of competition law and the payment of bribes, for example, from time to time?
In the UK, a comparison with the financial services industry is particularly apposite: thanks to many years of banks and other financial institutions being obliged, under yet more provisions of POCA, to gather and submit intelligence to LEAs on suspected money laundering, they have amassed the expertise and authority to enable their CEOs to sit alongside senior ministers in policymaking bodies. Even while this is happening, major banks are investigated, fined, and even prosecuted for money laundering failures by their (industry-funded) regulatory body, the Financial Conduct Authority (FCA).
The Role of Global Britain
The international nature of the problem of illicit medicines is what makes the challenge faced by the MHRA and by Operation Pangea unique. Not only must it tackle the legal complexity involved in multiple legal remedies and enforcement authorities, and the potential for conflicts of interest in public-private partnerships, but it must do so across national borders. To make matters harder, of course, it must do so in the context of a form of Brexit that has, at least potentially, decisively broken from EU regulatory norms, including in the regulation of medicines and the protection of rights
18 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Regulatory & Marketplace
in the context of criminal investigation. Among other things, that has necessitated a new, somewhat hollowed-out relationship between domestic LEAs and Europol, and doubtless created numerous hurdles behind the scenes of Pangea’s operations.











Despite all that, the overwhelming logic of converging interests between national law enforcement and international pharmaceutical firms means that the impetus for continuing, strengthening, and deepening the activities of Pangea will surely endure; indeed, there may be potential for offshoots using the same approach. With many jurisdictions now beginning to embrace a more sensible regulatory approach to medicinal uses of cannabis, for example, there are commonalities of interest between national LEAs in regulating the borders between the various jurisdictions and tackling parties that may seek to exploit differences and gaps in these nascent frameworks. As the development and rollout of covid vaccines and treatments continue to expand, the need to police unlicensed or unsafe alternatives, particularly in the developing world, is ever clearer. And, of course, the alarming societal harms






associated with sales of opioids diverted from legitimate supply chains, online or otherwise, continues to present a challenge that cries out for international cooperation, including in tracking and seizing their proceeds.

The approach of the UK to these issues is not necessarily perfect. Cannabis, even in a medicinal context, remains the province of the Home Office rather than the MHRA, with a licensing regime in its infancy and too little thought given to a joined-up approach between the regulatory and law enforcement approaches. Scant attention is paid to fake covid treatments, save for isolated examples of trading standards prosecutions under CPUTRs for so-called cures. UK LEAs’ attempts to tackle UK proceeds of illicit sales overseas rarely show signs of real cooperation with their overseas counterparts. On all these fronts, there is surely the potential for the mechanisms created by Operation Pangea to assist. With decades now of experience in tackling the complexities of working with overlapping laws and across national borders, it is a cooperative endeavour that the newly styled, post-Brexit, Global Britain should continue to embrace.
John Binns
John is a partner in the Business Crime team at BCL Solicitors LLP. He has a particular focus on in confiscation, civil recovery and money laundering under the Proceeds of Crime Act 2002). He represents suspects, defendants and witnesses in cases invoking allegations of bribery and corruption, fraud, insider trading, market abuse, price-fixing, sanctions-busting and tax evasion. He has also coordinated and undertaken corporate investigations and defended clients in cases brought by BEIS, the FCA, HMRC, NCA, OFT, SFO and others. He has particular expertise in the provisions of anti-money laundering requirements in the regulated sector including pharmaceuticals & healthcare under the Money Laundering Regulations, civil recovery and confiscation of the proceeds of crime.

INTERNATIONAL PHARMACEUTICAL INDUSTRY 19
Regulatory & Marketplace
Pressure regulators Control valves Pipeline ancillaries Steam traps Special equipment STEAMING SOLUTIONS FOR ALL INDUSTRIES adca@valsteam.pt www.valsteam.com +351 236 959 060 Zona Ind. da Guia, Pav. 14 - Brejo 3105-467, Guia PBL PORTUGAL PRODUCTS MANUFACTURED IN PORTUGAL AV 001 IN EN 01.20
Driving a Vision for a Data-driven Regulatory Ecosystem
A data-driven Regulatory ecosystem has huge potential, beyond the opportunity for operational improvement. However, Regulatory and product teams will need updated data skills to deliver this vision, reports Amplexor’s Renato Rjavec.

Even in today’s eCTD+ world, most life sciences Regulatory teams currently still think and work in terms of documents, paragraphs and sentences when putting together collateral for marketing authorisation and variations submissions. Yet it is data, rather than pre-prepared dossiers, that is moving into central focus now.
That’s as stakeholders across the life sciences and healthcare ecosystem realise that a data-first approach to collecting, managing and communicating product information will be the most efficient and reliable way to maintain consistent, definitive, current and high-quality record of a product entering or on the market. One that can be interpreted and use in a wide range of use cases, by the broadest possible range of people (from regulators to clinicians, pharmacists and ultimately patients).
Professionals in a range of roles are now used to converting their particular information e.g. about the medicinal product’s clinical properties, chemical composition or information for patients in the narrative form. But are they ready to adopt new, more structured ways of dealing with such information at the source? Or is there an expectation that the Regulatory role will effectively assume the burden of data extraction and data entry assistance for them?
Adapting to a Data-centric Approach
Given that this data-centric approach will be the new reality before long, the question for existing product information managers/ regulatory teams is whether their skill sets now need to be refreshed to reflect the target new ways of working (first, data and document sets needing to be carefully aligned, then a direct flow of good data to the regulators).
So where are companies with all of this today? With the exception of very large pharma organisations with the budget and people resources to have already started exploring the wider possibilities, most companies still lack awareness both of the wider potential and of the work ahead of them in building the right capabilities.
At one level, this is about how they manage product information so that (a) it fulfils the demands of new IDMP structured data requirements, and (b) becomes sufficiently reliable to form a foundation for not only product registrations and their maintenance, but all sorts of other processes too.
On another level, the opportunity extends to leveraging reporting and analytics to smart effect – first to help users fill gaps and increase the quality of the data; then with a more strategic emphasis, even using AIassisted tools to investigate scope for process improvement (based on insights into how data is currently being managed and where recurring patterns are emerging).
Extra Layer of Quality Checks
It can be tempting to imagine that IT is going solve all of this, and that by default users will be swept along on the journey. Yet failure to adapt internal Regulatory capabilities, and to cultivate new data skills, is likely to severely compromise Regulatory Affairs’ data-based progress.
Of course, having efficient and userfriendly solutions that have been built not just with additional data fields to satisfy IDMP – but also with an appreciation for what new
20 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Regulatory & Marketplace
data-centric process management models will mean for Life Sciences Regulatory and other teams (and for the pharma industry in general) – will be important.
But equally, the teams involved will need help in adapting to the demands of IDMP. They will need guidance, support and help with validation to ensure that the right data is being entered in the right way, and that any gaps or issues are spotted and flagged. And, given the huge weight of new responsibility that will be placed on this critical ‘source of product truth’, it also follows that an additional layer of quality checks will be needed to cement confidence in the new bank of structured data.
As teams look to use this ‘live’ data to build reports, they will need help understanding how to make the most of analytics and of pre-built dashboards, too. And as basic data interrogation becomes more commonplace and comfortable, teams will need to be
able to transition towards more advanced analytics.
Into the Realm of Data Science
For every user with a role to play in shaping the data, this work needs to be as simple and as user-friendly to achieve as possible, enabled by intuitive tools. If users are not brought along on the journey from this earliest point, anything that comes afterwards will be in vain (as the reliability of the data will be compromised from day one). Once teams are comfortable with working with data, and are confident in its quality – because they are adept at the process of capturing, enriching and managing it – Regulatory operations can start to be more ambitious in their next-level plans.
This takes them deeper into the realm of data science, as they start to harness AI-enabled tools to interrogate the data for signs of how this could be improved, and where entire data-based processes

could benefit from a new, streamlined approach.
Yet it is here that existing teams are most likely to find that they lack the appropriate skills and will need to bring on board new talent in the form of qualified data discovery professionals. In pharma Regulatory Operations, data scientists are not widespread.
Targeting Pain Points
The challenge in building the right balance of skills might feel both vague and insurmountable at this point, but the reality of that challenge is undeniable. Regulatory teams will ultimately need access to a holy trinity of domain, tool and data discovery knowledge, but this optimal combination is likely to prove elusive. This is likely to mean building their software and Regulatory domain knowledge as their starting point, and growing the data science capabilities more organically through a combination of collaborative team-building and targeted training and skills transfer.
The best advice is to approach new skills adoption step by step, across a pilot initiative that targets Regulatory’s biggest pain points, or the most complete source of existing data. That way, Regulatory Operations leaders can start the process towards achieving the wider potential of a data-driven Regulatory ecosystem that goes way beyond operational enhancement.
Renato Rjavec

Renato Rjavec is Director of Product Management at Amplexor Life Sciences. Amplexor helps organisations that are developing pharmaceutical drugs, medical devices, and biotechnology to launch products and break into new markets quickly using innovative end-toend regulatory and quality management solutions. Its solutions and services expedite the management of highlystructured data and the creation and delivery of consistent, compliant global content. Amplexor’s services include technology consultancy, implementation, and management services.
We: www.amplexorlifesciences.com Email: renato.rjavec@amplexor.com
INTERNATIONAL PHARMACEUTICAL INDUSTRY 21 www.international-pharma.com
Regulatory & Marketplace
Regulatory and Developmental Complexities Around Demonstrating Bioequivalence for a Topical Generic Product
Increasing Patient Access to HighQuality Topical Products

The topical dermatology market, although niche, was estimated to be valued at approximately $20.4 billion in 2020.1 In a study from 2010–2015, over half of the topical drug products experienced a price increase and the average price of topical generic drugs was 276% higher by the end of that period. This is being driven by the lack of competition among generic manufacturers, where approximately 80% of topical dermatological drug products have very few competitors or no approved generics at all. Lack of generic products can be attributed to the complexity of developing topical dermatological drug products, low market volumes, and/or the risk and expense of clinical endpoint bioequivalence (BE) studies.
Topical dermal formulation development is inherently challenging due to the distinct characteristics of dermal drug delivery, including the complex characteristics of the skin barrier (e.g., location, age, condition). Additionally, formulations are often applied to diseased skin that is likely perturbed or influenced by external factors (e.g., temperature, humidity, occlusion). Another distinct characteristic of topical formulation development is the complexity of the product. For example, the number of excipients required for a topically applied product can make development difficult. Each excipient used in a product can impact the formulation’s irritation and sensitisation, bioavailability, penetration, dose homogeneity, drug solubility and stability, and drug product physical and chemical stability (quality). In some cases, these properties can be markedly different between excipient suppliers, grade, and age making the development of exact generic copies of such formulations extremely difficult without commensurate excipient knowledge.
In efforts to make high-quality, affordable medicines available to the public, regulatory agencies have released guidances to create a modular framework for in vitro bioequivalence
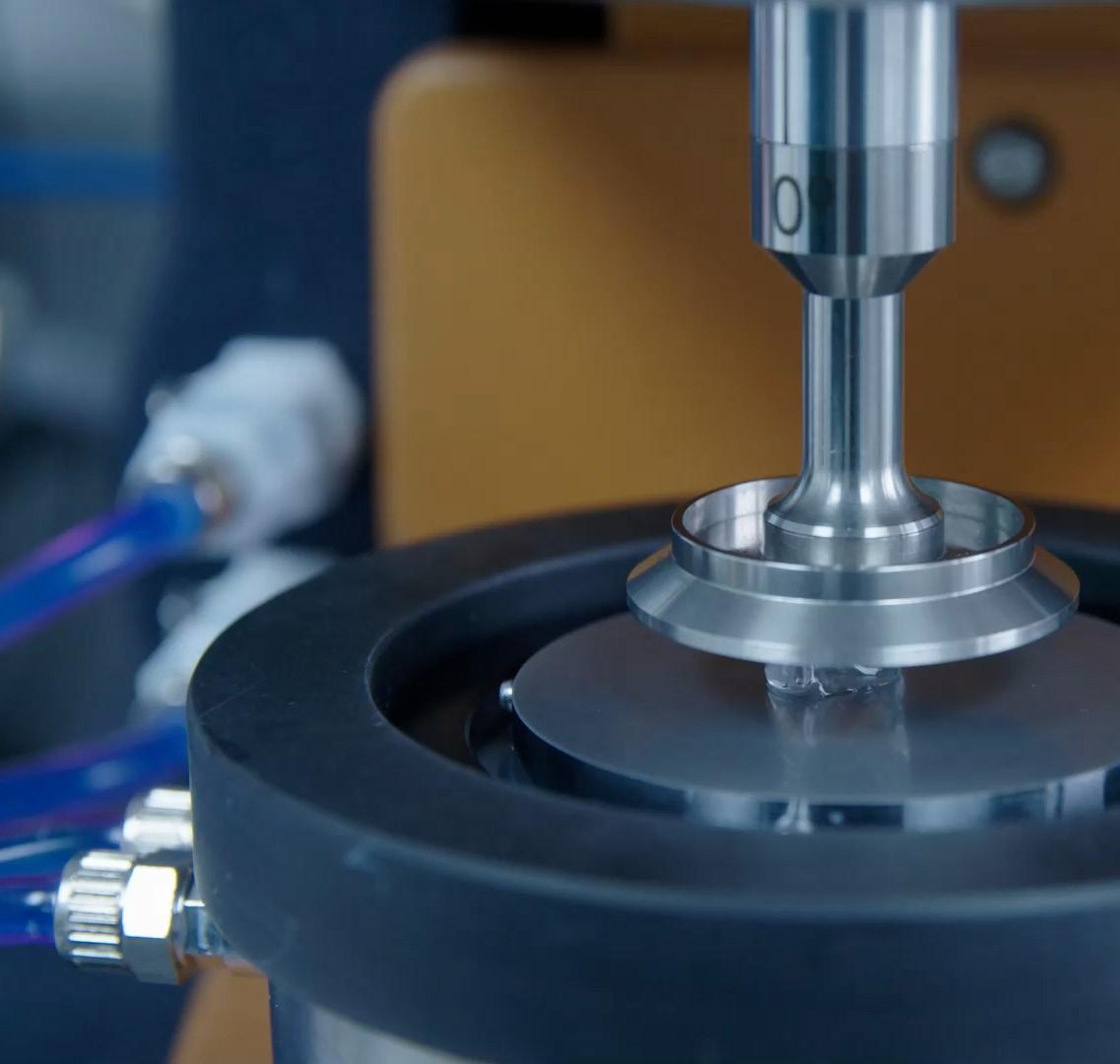
(BE) testing of topical products in lieu of clinical trials. The FDA released a draft guidance in 2016 on acyclovir cream which has served as a reference point for the other productspecific guidances (PSGs) that continue to be published by the FDA within 18 months of an NDA. The European Medicines Agency (EMA) released a similar general draft guideline on quality and equivalence of topical products in 2018. These two guidances serve as the foundation for what has been a flurry of activity in the generic space for topical drug products. As generic companies would not have to undergo the same rigorous clinical studies that are required of the brand-name product, generic products can be developed, approved, and pushed to market more quickly. This can lower the cost of development by up to 85% when compared with the cost of developing the innovator product. Additionally, there is a significant decrease in the amount of time it takes for a generic product to be commercialised. These factors together can decrease the cost of the medicine when it reaches the market and help to lower overall healthcare costs while delivering high-quality
topical products to patients that meet current regulatory standards.
The Intricacies of Demonstrating Topical Generic Product Bioequivalence to an Innovator/Reference Product
For a topical generic product to assume the safety and efficacy established by the innovator product, bioequivalence between both products must be demonstrated with the generic product being qualitatively (Q1) and quantitatively (Q2) the same as the reference product. The generic product must also establish the same quality and manufacturing standards as the reference product. For cases where the characterisation techniques of the reference product are now outdated, a higher standard must be met. Recently with the new draft guidance, there is an increasing focus on demonstrating extended pharmaceutical equivalence including matching the physical structure/microstructure and transformation upon application (Q3) of the reference innovator product within the generic. Such data was likely never submitted for the innovator product and is based upon
22 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Regulatory & Marketplace
• Endotoxin-specific reagent eliminates the risk of false positives from (1-->3)ß-D-Glucan

• 100% animal free • Quantitative range: 0.001 to 50EU/mL
• High sensitivity with less lot-to-lot variation
• Stable storage after dissolution (4 hrs. at 2-8°C and 2 weeks at -30°C)
FUJIFILM Wako Chemicals U.S.A. Corp. © FUJIFILM Wako Chemicals U.S.A. Corp. - 2022
Neo
™
PYROSTAR™ Neo is a new endotoxin detection reagent developed by recombinant technology.
PYROSTAR
Recombinant Endotoxin Detection Reagent
• Colorimetric method, can be used with an absorbance plate reader • 3-Factor system mimics the same cascade reaction as traditional LAL
acceptable comparative physiochemical characterisation. This may involve extensive rheological characterisation and potentially an assessment of the drug in solution and suspension (e.g. particle size and distribution and polymorphic form) within the product and any changes of the product over its shelf life. These standards can be met through the use of in vitro testing.
With regards to the demonstration of bioequivalence, in vitro testing provides a series of valuable tools used to assess a product’s performance as it relates to how the drug is released from the formulation, penetrates and/or permeates the epithelium, and/or engages the biological target. As such, in vitro models, often in combination with biological disease activity models, are vital for demonstrating the equivalence of product performance to regulatory standards.
In vitro release testing (IVRT) has been historically used throughout the topical development cycle to ensure the quality of a product is retained throughout its shelf life by measuring drug release over time from

the dosage form. More recently, to support a claim of bioequivalence, IVRT methods are being developed and validated to more strict criteria to show with a high degree of confidence that the drug in the generic product has the same release characteristics as the reference product. IVRT has proven to be an invaluable tool for moderately complex products but does not provide any indication of how the formulation impacts the drug’s absorption across the skin. Therefore, in vitro permeation/penetration testing (IVPT) must also be utilised to demonstrate bioequivalence for more complex topical dosage forms.
IVPT allows for the study of percutaneous absorption and determination of the pharmacokinetics (PK) of topically applied drugs. This in vitro/ex vivo model most commonly uses excised human tissue mounted in specially designed static or flow-through diffusion cells that allow the tissue to be maintained at a temperature and humidity that matches in vivo conditions. The formulations are applied to the surface of the skin and the permeation of the compound is measured in a receiver fluid underneath
the tissue samples. It also allows the drug and metabolites within the different layers of the skin to be quantified. Both the rate of permeation (drug in receiver fluid) and levels of penetration (drug in skin layers) can be analysed and used to demonstrate equivalence. However, neither IVRT nor IVPT can demonstrate whether the drug that is moving into and through the skin is biologically active.
To demonstrate the biologic equivalence of the generic product and reference product for the treatment of skin infections, inflammatory skin diseases, or bacterial infections, in vitro/ ex vivo disease or pharmacodynamic (PD) models are proving to be vital for derisking the approval process. It is now possible to keep the skin alive for several weeks while exposing it to different types of infections (bacteria, viral, fungi, etc) and/or stimulations (e.g. UV, inflammation, radiation, etc). The tissue can also be co-cultured with other cell types if they are not present in normal healthy tissue to create more complex mechanistic PD models. Disease activity models have the added advantage of allowing the drug to be
24 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Regulatory & Marketplace
quantified in the tissue in combination with the PD activity to create a PK/PD analysis.
For now, the EMA/MHRA and the FDA guidances focus exclusively on IVRT and IVPT as an alternative to clinical studies with such disease models lacking comparative descriptions. However, these guidances continue to be discussed throughout the industry and scientific community mainly through workshops and public presentations. Along with the disease models, other techniques such as tape stripping and open flow microperfusion are also being advocated as tools for demonstrating bioequivalence.
Whatever the techniques involved, there has certainly been an underappreciation of the work required to meet these new standards, especially as the methods needed to be validated with current quality approaches. This volume of work comes with a cost and timeline that may have been originally underestimated.
With regards to the added tier of demonstrating extended pharmaceutical equivalence (Q3), there is much discussion about the relevance of characterising and comparing the generic and innovator topical products with regards to microstructure and its transformation when any such minor differences are unlikely to translate to differences in performance when assessing drug release (IVRT), permeation (IVPT) or a clinical assessment. Studies are also showing that long since approved innovator or reference products were inevitably not assessed with the level of rigor and quality standards applied to the generic product that is being developed 40-50 years later. As such, further advice is required with regards to what to do in this case. For example, would regulatory agencies allow modifications in the generic formulation composition to ensure its quality and performance (rheology, drug purity and release) are maintained for longer than the original approved shelf life. Would this simply be an improved generic or a hybrid and what would be required to demonstrate bioequivalence from the in vitro tests?
In addition, there are certainly some technical challenges associated with IVRT and IVPT when developed and validated with the higher standards that are now required. Skin donor variability is one of the major contributors and technical challenges associated with IVPT which can be compounded with older reference products where the drug is in suspension
or partial suspension. Some of the other challenges for IVRT and IVPT are associated with the acceptance criteria and statistical analysis which differ between the FDA and EMA guidance meaning a generic company can develop a generic product of an innovator on the market in both the US and Europe which is approvable in the US only.
Conclusion
Although the bioequivalence guidance released are in draft and/or product-specific, the efforts made by regulatory authorities around the globe are very much appreciated by the generic industry and have had a noticeable impact on the development and approval of generic products.
The FDA continues to accept pre-ANDA meetings, and the EMA continues to use scientific advice meetings to provide productspecific guidance on the methodologies and protocols around demonstrating bioequivalence in topical generic products.
The critical areas for which advice is given are the demonstration of sameness/ equivalence between a topical reference product and a generic product—specifically, extended pharmaceutical equivalence and bioequivalence.
Regulatory bodies have also engaged industry leaders with each new guidance to ensure that the guidelines proposed by the regulatory authorities are consistent with industry standards and best practices. In 2021 and 2022, the FDA, in combination with the Center for Research on Complex Generics (CRCG), held free public workshops featuring presentations and discussions from industry leaders aimed at in vitro methods for demonstrating bioequivalence in complex generic products.
While the guidances are challenging and subject to continuous improvement, the cost reduction and process simplification associated with demonstrating bioequivalence using in vitro methods only are beneficial for several reasons. Drug developers can enter generic markets with a significantly lower investment cost and shorter timeframe. Lowering those barriers to entry into the generic market enables governments to reduce healthcare costs more swiftly. This encourages further production of high-quality, affordable medicines made available to the general public.
Since the completion of this article, the FDA has released updated draft guidances for topical generic products.
REFERENCES
Jon Lenn
Jon Lenn has direct responsibility for MedPharm’s operations in the United States based out of Durham, North Carolina. Since joining in 2015 he has led MedPharm’s development of cutting edge performance models for assessing penetration and activity of clients’ products targeted towards key biochemical pathways. He has over 15 years’ experience in developing dermatological projects with Connetics, Stiefel and GSK and has been directly involved with the development and approval of 8 products. He received his PhD on the topical delivery of macromolecules from the University of Reading.

Marc Brown
Prof. Marc Brown co-founded MedPharm in August 1999. He has been the guiding force behind all of MedPharm’s scientific developments and intellectual property. He has been Professor of Pharmaceutics in the School of Pharmacy, University of Hertfordshire since 2006 and has visiting/honorary professorships at the Universities of Reading and King’s College London. He has over 200 publications and 26 patents describing his work. His research interests lie mainly in drug delivery to the skin, nail and airways.
To date, he has been involved in the pharmaceutical development of over 55 products that are now on the market in Europe, America and Japan. Prior to MedPharm he was an academic in the Pharmacy Departments at King’s College London (KCL) and the University of Hertfordshire. He retains honorary and visiting Professorships at the University of Reading, KCL, and De Montford University and in 2022 was awarded the status of Professor Emeritus of the University of Hertfordshire.

INTERNATIONAL PHARMACEUTICAL INDUSTRY 25 www.international-pharma.com
1. Evers P, “Skin Disease Treatment Technologies and Global Markets”. BCC Research, Jan 2016.
Regulatory & Marketplace
Opportunities for the IPO of Psychedelics Companies (or, How to Change Investors' Minds)
If anyone had suggested only a few years ago that it is a realistic proposition to float a psychedelics company on any of the London market, that suggestion would likely have been met with derision. Commentators would have pointed to a lack of understanding and therefore acceptance of psychedelics in the investment community and to potential problems under the Proceeds of Crime Act 2002 (POCA).
However, times are changing. First, the Financial Conduct Authority (FCA) has given guidance about floating medicinal cannabis companies and we believe (for the reasons set out later) that the guidance can be applied to psychedelics companies. Secondly, in the last few years there has been a growing awareness of how widespread mental illness is and also of the potential of psychedelic drugs to treat certain mental illnesses effectively. For evidence of psychedelics’ journey towards the mainstream, one need look no further than the success of the Netflix series “How to change your mind” or the fact that in late November 2022 there was a lengthy article about psilocybin in The Sunday Times magazine. Finally, an ecosystem of leading academic research and expertise in clinical trials has developed in the UK and elsewhere, led in the UK by institutions such as Imperial College London and King’s College London.
It is reasonable to assume that the investment community will recognise these points and we therefore consider that there may well be an opportunity for psychedelics companies to carry out an IPO on one of the UK markets. Investment into UK-based psychedelics ventures, typically led by newlyestablished specialist funds and private family offices, is starting to gather pace, although listings of such businesses have so far taken place only in the US (such as Compass Pathways on NASDAQ) or Canada (such as Small Pharma on the TSX-V).
What Are Psychedelics?
Readers of this article are likely to be more qualified than me to answer this question, but (in summary) "psychedelics" are a class of psychoactive substances, that is, a
substance that can produce a psychoactive effect in a person who consumes it. There is a psychoactive effect in a person if, by stimulating or depressing the person’s central nervous system, a substance affects the person’s mental functioning. In other words, a substance causes a psychoactive effect in a person if it produces temporary changes in perception, mood and cognitive processes which affect all the senses. The psychedelic that is most often referred to is psilocybin, which is the active ingredient in (so-called) “magic mushrooms”. However, that is by no means the only psychedelic. Other examples include LSD, mescaline, ayahuasca, MDMA (the “ecstasy” drug), and a derivative of ketamine. Psilocybin can also be synthesised: that is, produced in a laboratory.
How Widespread is Mental Illness?
Mental health issues affect many people. Recent estimates state that in the UK one in six adults experienced a “common mental disorder” such as depression or anxiety in the past week, and one in six children aged between six and 16 experienced a “common mental disorder” in 2021. In 2020, the leading cause of death for people in the UK aged five to 34 was “intentional self-harm”. It is estimated that mental health problems cost the UK economy £118 billion per year, mainly in lost productivity and work absence. In 2021, the World Health Organisation estimated that one in four people in the world will be affected by mental or neurological disorders at some point in their lives. Levels of depression and anxiety are reported to be at a global all-time high, which is not surprising following the Covid-19 pandemic and worldwide lockdowns.
It is therefore clear that there is a great need for effective treatments for mental illness. Many instances of depression do not respond to traditional therapies or drug treatments, a phenomenon known as “treatment-resistant depression”. If psychedelics can add to the treatments that medical clinicians can use then this would be a very welcome development with a potential to improve people’s lives significantly. Psychedelics companies would then have a role to play in researching, developing and eventually supplying such treatments, and that role would benefit both the world at large and psychedelics companies.
Why are Psychedelics Potentially Useful?
Research is being carried out across the world into the potential use of psilocybin in the treatment of depression, PTSD, anorexia, tobacco addiction and alcohol dependency.
In recent years there has been increasing focus on and public acceptance of the use of psilocybin. A small, early-stage (but widely reported, including a programme shown on BBC1) study carried out by Imperial College London's Centre for Psychedelic Research has suggested that psilocybin is as good at reducing symptoms of depression as conventional treatment. Unlike conventional treatments, which may cause the unwelcome side effect of blunting positive emotions (as well as negative emotions), it is thought that psilocybin works on receptors in the brain associated with "re-ordering" the way we think about things. Boris Johnson indicated in 2021 that he would consider calls to legalise psilocybin in response to the potential for treatment of mental health conditions.
Psychedelics are therefore expected to be an area of interest for pharmaceutical investors in the near future. For example, in early November 2022, Compass Pathways announced the results of a peer-reviewed randomised control trial of 233 people led by King’s College London and published in The New England Journal of Medicine. The study found that one 25mg dose of the drug, alongside psychotherapeutic support, significantly reduced symptoms of depression in patients who did not respond to other medication.
What Impediments to Investment Does Current Drugs Legislation Present?
The main UK controlled drugs legislation are the Misuse of Drugs Act 1971 (MDA) and the Misuse of Drugs Regulations 2001 (MDR), each as amended. Section 2 of the MDA defines a controlled drug as "any substance or product for the time being specified in Part I, II or III of Schedule 2 [of the MDA] or in a temporary class drug order". Schedule 2 classifies controlled drugs under a three-tier system (classes A, B and C in Parts I, II and III of the Schedule respectively) depending on the assessment of their medical use, their relative abuse potential and their risks of dependence. Class A drugs are considered the
26 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Regulatory & Marketplace
Regulatory & Marketplace
most harmful and have the highest level of control. Psilocin is a psychedelic drug listed as a Class A drug in paragraph 1 of Part I of Schedule 2 to the MDA. Psilocin and its ester (that is, a derivative) psilocybin are therefore controlled drugs.

The MDA describes a number of criminal offences relating to controlled drugs including prohibitions on: the importation and exportation of a controlled drug; the production and supply of a controlled drug; and the possession of a controlled drug. However, the MDA also sets out some exceptions and defences to those offences, in particular, in the case of operations in the UK, where the handling and use of the controlled substance has been licensed by the Home Office pursuant to its powers under the MDR, as discussed further below. The investment community has therefore rightly been wary
of companies that might be considered to be committing a criminal offence, particularly as any investment might generate criminal proceeds in the hands of an investor under POCA.
The Medicinal Cannabis Precedent
On 18 September 2020, the FCA issued guidance (FCA Guidance) relating to the listing of cannabis-related businesses, setting out its approach to cannabis-related companies interested in listing in the UK. The FCA Guidance categorises UK and overseas businesses separately, as discussed below.
In relation to UK cannabis-related operations, the position is straightforward: the FCA Guidance states that “The legal position of purely UK-based medicinal cannabis companies and cannabis oil companies is clear. UK-based medicinal
cannabis companies can be admitted to the Official List, if the company has the appropriate Home Office licences for their activities where they are required.”
As regards overseas companies, the FCA Guidance states that “For medicinal cannabis and cannabis oil companies with overseas activities, the company will need to satisfy us that their activities would be legal if carried out in the UK. We will also need to understand the legal basis of the company’s overseas activities, for example the nature of the local licensing and the licences the company holds.”
In July 2021, the FCA issued Primary Market Bulletin 35 which included a draft technical note (TN 104.1) setting out in further detail the FCA’s approach to the listing of companies carrying on cannabis-
INTERNATIONAL PHARMACEUTICAL INDUSTRY 27 www.international-pharma.com
related activities. TN 104.1 remains in draft, but (as the FCA has not withdrawn the draft) we consider that it provides a useful indication as to how the FCA would view the listing of a company carrying on cannabisrelated activities. If one assumes that the FCA’s view sets a “gold standard” then TN 104.1 can be taken to show how the listing or admission of a company carrying on cannabis-related activities on AIM or AQSE should be approached.
The FCA Guidance and TN 104.1 make it clear that, provided additional due diligence is carried out (that is, over and above that which would normally be expected on a listing), then the FCA will consider listing a company developing, producing or selling cannabis-based medicinal products, licensed cannabis-based medicines or consumer products containing cannabidiol (usually referred to as CBD).
In summary, if a purely UK-based company (that is, where the entirety of its operations, including supply chain, are UK-based) holds the appropriate Home Office licences for their activities (or requires none), and can satisfy the FCA of this, then the FCA will permit that company to list (assuming it otherwise satisfies the criteria for listing).

By contrast, a company with cannabisrelated activities legally operated overseas is in a different position. The securities of such a company may be listed, provided the FCA is satisfied its business does not give rise to any money laundering offence under POCA and it otherwise satisfies the criteria for listing. A company with cannabis-related activities legally operated overseas will need to satisfy the FCA that those activities are for a purpose that is also lawful in the UK.
The FCA will also need to understand the legal basis of the company’s overseas
activities, for example the nature of the local licensing and the licences the company holds. To satisfy the FCA on these points, after consideration of the company’s operations and the relevant jurisdictions, the FCA will request appropriate legal opinion(s) on the overseas company’s cannabis activities. Any legal opinion(s) should at least address the following points: the activities of the company; confirmation of the legality of each of the activities covered by the opinion in the jurisdiction in which they occur; confirmation that such an activity or activities are for purposes which are lawful in the UK; where the legality of the activity in question relies on licensing, information about the jurisdiction's licensing system and details of the track record of the company carrying out the activities in question.
How Does The Medicinal Cannabis Precedent Apply to Psilocybin?
There are good grounds to believe that the regulatory framework and approach for the listing of a psilocybin company would be the same as for a medicinal cannabis company. This is because both cannabis and psilocybin are controlled drugs listed in Schedule 1 to the MDR and therefore conceptually should be treated in the same way.
It is worth noting that in 2018 there was a rescheduling of cannabis-based products for medicinal use in humans (or CBPMs) prior to market authorisation as a medicine, to allow those products to become available for prescription, under the supervision of specially qualified medical professionals, without the need for a Home Office licence. This was on the basis that there was conclusive evidence of the therapeutic benefit of cannabis-based medicinal products for certain medicinal conditions, and reasonable evidence of therapeutic benefit in several other medical conditions, and the rescheduling was intended to act
as a spur to further research and testing of such products, recognising that it would be significantly easier for scientists to research CBPMs under Schedule 2 controls. It is surely no coincidence that there have been a number of listings of medicinal cannabisfocussed companies on the UK markets since 2018.
A similar rescheduling of psilocybin is not imminent, but certainly there are wellregarded lobby groups which propose moving psilocybin into the less restrictive Schedule 2 category (as for CBPMs) for research purposes. There is a scientific consensus that it exhibits negligible toxicity or addictive properties.
Research into psilocybin is still at a relatively early stage and, at present, only a very limited number of global regulators approve the use of psychedelics to treat mental health conditions. However, as we have discussed above, the “direction of travel” in the thinking about psilocybin is towards a conclusion that it may form the basis of the development of muchneeded novel treatments for mental health conditions and it might well therefore be the case that there will be a change in the view of regulators in future. Because of this, investors may consider that we are at an inflection point and this is a good time to invest in psychedelics companies and may look beyond the current volatility in the markets. We therefore consider that there could be an opportunity for psychedelics companies to conduct an IPO in the UK, particularly given the leading role that UK academic institutions are taking in the research into psilocybin.
Nigel Gordon is a capital markets and M&A Partner at Fladgate LLP. With a particular focus on the healthcare and natural resources sectors, Nigel works with entrepreneurial and high-growth companies to navigate the complex listing process on the London Stock Exchange's Main and AIM markets. He also has experience advising clients on both public and private M&A transactions. Fladgate LLP is a Top 100 UK law firm advising clients across a range of corporate and private client matters.

28 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Regulatory & Marketplace
Nigel Gordon
Health Science
Health Inspired, Quality Driven
Nitrosamine Testing Solutions

The presence of the nitrosamine, N-nitrosodimethylamine (NDMA), in certain sartan API’s has resulted in several regulatory warnings and recall of contaminated products. Concerns over the presence of this class of genotoxins has now widened to include other medicines such as the well-known diabetes drug, Metformin. The US Food & Drug Administration (USFDA) and European Medicines Agency (EMA) have responded by publishing documents for the pharmaceutical industry that address requirements and limits related to nitrosamine contaminants. Pharmaceutical Manufacturers are now taking a pro active approach to risk assessment and mitigation of genotoxic contaminants within global pharmaceutical supply chains. Central to these activities is a coordinated analytical capability to identify and quantify contaminants across global geographies and regulatory zones.



Why use SGS
SGS Health Science has considerable expertise in the method development of nitrosamine determination in pharmaceutical products. SGS has established a specific method for NDMA which can be applied to various different matrices. Alternatively, a platform method, based on trace-level detection by LC-MSMS, is also available and provides rapid and simultaneous determination of up to ten different, targeted nitrosamines. Although with more limited application, the SGS network is also able to support specialist methodologies such as GC-MSMS. Our experience in optimizing extraction allows application of these methods to drug products, API’s, and raw materials.
By establishing these nitrosamine methods within centers of expertise across a global laboratory network, SGS can provide an unrivaled service offering that incorporates a harmonized methodological approach together with flexible management of capacity and capability requirements.SGS offers a variety of partnership models and can collaborate in such testing programs using fee-forservice to outsourced staffing models all exploiting resources of the SGS network.
About SGS
SGS is the world’s leading inspection, verification, testing and certification company. We are recognized as the global benchmark for quality and integrity. With more than 94,000 employees, we operate a network of more than 2,600 offices and laboratories around the world.Our conveniently located network of laboratories and clinical trial facilities offer an array of integrated services and expertise, providing you with the knowledge, flexibility and ability to scale.
Wide-range of laboratories and clinical research sites and qualified partners. Size and diverse testing capabilities matching biologics and small molecules needs International network across America, Europe and Asia-Pacific
INTERNATIONAL PHARMACEUTICAL INDUSTRY 29 www.international-pharma.com
us healthscience@sgs.com sgs.com/healthscience sgs.com/healthcommunity
Contact
Technical Advancements in Proteomics Streamline
High-throughput
Over the last two decades, significant advances in technology and new methodologies have made proteomics an extremely powerful tool for protein scientists, biologists and clinical researchers. Scientific discoveries in proteomics largely depend on data analysis and data generation. Mass spectrometry (MS)-based proteomics has expanded significantly with improvements in software, data acquisition, and algorithms to provide more accessible and accurate data.
Workflows
Direct protein analysis from tissue or biofluids, however, raises a variety of analytical challenges. Protein expression varies depending on the genetic background of an individual, and also on time, localisation, and as a physiological response to external stimuli. Moreover, because of the combined effects of alternative splicing, point mutation, post-translational modifications (PTMs) and endogenous proteolysis, a given protein can be expressed as many different proteoforms, each having a dedicated biological activity.
These analytical challenges create workflow bottlenecks and extend the time required for accurate results. This article will examine how these issues can be overcome to add efficiencies and expand capabilities for library-based approaches in quantitative proteomics.
Challenges in Proteomics
The core challenges in proteomics include converting complex liquid chromatography
(LC) coupled with MS and the resulting datasets into tangible peptide spectrum matches (PSMs) and peptide identifications that can be used for protein inference, quantification, posttranslational modification (PTM) analysis, as well as proteome sequence coverage within complex samples. Database search algorithms have extensively transformed biological and medical research, yet as analytical instrumentation continues to become more sensitive, software developers must continuously expand these search algorithms to meet the demands of sample limitations in highthroughput protein quantitation.

In the simplest scenario, database search algorithms rely on precursor and fragment ion spectra to be matched in silico, suggesting a best fit and assigning a probability score. In many instances the best fit of a particular PSM is of an equal probability score or just marginally better than the next best fit, yet a single assignment is delivered. Inferring only one PSM, which may be incorrect given the reliance purely on the information contained in a fragment ion spectra, can lead to a greater chance of false identifications. As such, the field of proteomics benefits from stricter acceptance criteria such as lower false discovery rates, increases in unique peptide counts, protein sequence coverage and biological or technical replicates.

Advances in Database Search Platforms
To break the data analysis bottleneck, proteomics software developers are integrating real-time database search and smart acquisition in software algorithms. Parallel search engine in real-time (PaSER) is a GPU-powered real-time database search
platform providing parallel computing power and real-time database search results for bottom-up proteomics. Researchers can view intricate details of data from the high-level experimental information to a specific fragment ion spectrum of interest. Additionally, a user-defined qualification of proteins or peptides at the end of a sample acquisition determines the progression of the sample queue, which checks suitability while also making the most of samples, consumables and instrument time.
Trapped ion mobility spectrometry (TIMS) provides new levels of sensitivity, selectivity and speed to proteomics research. With each analyte measured, TIMS also determines a collisional cross section (CCS) value. This CCS value is an intrinsic property unique to each analyte that is highly reproducible across different instruments and laboratories. It can be used for the database search, thereby boosting the number of PSMs, peptides and proteins identified in bottom-up proteomics measurements. The PaSER search algorithm can compare the predicted and measured CCS values, to identify the top five peptide candidates for each spectra.
This peptide-validation minimises false discovery rate (FDR) estimation steps. In a non-CCS-enabled algorithms, only two dimensions are utilised to estimate the FDR rate, and so a discriminate line is fit to a 1% error (Figure 1, Panel B) to distinguish forward and reverse peptide candidates. With specialist software and the extra CCS dimension, the peptide-candidates can be vectorised in 3 dimensions (Figure 1, Panel B), thereby allowing a discriminate contoured
30 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Drug Discovery, Development & Delivery
Figure 1: Comparison of non CCS-enabled algorithm vs. the additional CCS dimension
plane to be applied to achieve the same 1% error. Applying a discriminate plane provides increased accuracy and precision, helping to validate formerly poorly scoring PSMs in the standard two dimensions.
The algorithm was trained on >1 million tryptic peptides that scientists fed into the model including other PTMs, like phosphorylation. Thus, the model can predict unphosphorylated and phosphorylated peptide CCSs with high accuracy and reproducibility. Those predicted CCSs are used to evaluate how good the measured value is and, based on that, they can better address ambiguity in the identifications. Incorporating CCS information enables scientists to assign more PSMs, peptides and proteins and increases the confidence in the assignments. Additionally, it can be performed in real-time with PaSER to provide the most complete real-time feedback in proteomics applications (Figure 2).
Improved Sensitivity
For the processing of data-independent acquisition (DIA) proteomics experiments, data-independent acquisition neutral networks (DIA-NN) software exploits deep neural networks and new quantification and signal correction strategies.1 TIMS DIA-NN software also primarily focuses on the CCS measurement. It is integrated into the PaSER platform so that the researchers can use a quantitative workflow that can be triggered at the end of the acquisition. DIA-NN has shown improvements in the identification and quantification performance in conventional DIA proteomic applications, and is particularly beneficial for high-throughput applications,
as it is fast and enables deep and confident proteome coverage when used in combination with fast chromatographic methods.1
Both conventional and ultra-fast proteomics can further gain depth and quantitative accuracy with additional separation of the convoluted precursor or fragment ion space. In dia-PASEF, the ion mobility dimension allows scientists to distinguish peptides from deleterious ionss that would otherwise be co-fragmented, thus producing cleaner spectra. Most importantly, dia-PASEF yields 2- to 5-times improvement in sensitivity, depending on the acquisition scheme, by stacking precursor ion isolation windows in the ion mobility dimension and thus increasing the effective duty cycle.
Research indicates that DIA-NN analysis of dia-PASEF raw data increases the proteomic depth by up to 69% compared to the originally published dia-PASEF workflow.2 For example, one study quantified over 5200 proteins from 10ng of HeLa peptides separated with a 95-minute nanoflow gradient, and over 5000 proteins from 200ng using a 4.8-minute separation with a standardised proteomics platform. In complex samples, featuring a mix of human and yeast lysates, the workflow detected over 11700 proteins in single runs acquired with a 100-minute nanoflow gradient, while demonstrating quantitative precision.2

Different experiments showed the prediction accuracy of 95% for tryptic peptides and 92% for phosphorylated tryptic peptides, the most prevalent PTM with biological significance. One research group found that
it could double the number of peptides found from 42,930 to 98,949, nearly 3 times more than the initially published peptides.3
Conclusion
The use of these new technologies shows great potential for boosting the number of proteins, peptides and PSMs in complex datasets. Research suggests these advances can increase protein sequence coverage substantially, as well as provide an additional dimension for more precise and accurate peptide assignments.2,3 This offers new opportunities to reduce workflow bottlenecks and provide more efficient results, thereby expanding the capabilities for library-based approaches in quantitative proteomics.
REFERENCES
1. Demichev, V., Messner, C.B., Vernardis, S.I. et al. DIA-NN: neural networks and interference correction enable deep proteome coverage in high throughput. Nat Methods 17, 41–44 (2020). https:// doi.org/10.1038/s41592-019-0638-x
2. Demichev, V., et al. "High Sensitivity Dia-PASEF Proteomics With DIA-NN and FragPipe." BioRxiv. org 2021.
3. Ogata K, Chang CH, Ishihama Y (2010). Effect of Phosphorylation on the Collision Cross Sections of Peptide Ions in Ion Mobility Spectrometry. Mass Spectrom (Tokyo); doi: 10.5702/massspectrometry. A0093.
Chris Adams
Chris Adams, PhD is the Global Business Development Director Bioinformatics for Bruker Daltonics, where he has been since Feb. 2018. Prior to his time at Bruker Daltonics he was the Director of proteomics at the Stanford University Mass Spectrometry (SUMS) Laboratory where he had held increasing roles over 11 years. Chris received his PhD from Uppsala University, Sweden within the department of biological and medical mass spectrometry under the guidance of Professor Roman Zubarev. Prior to graduate school Chris worked at various research positions with Amgen and Baxter Biosciences. His undergraduate work was done in biochemistry at California Polytechnic State University, San Luis Obispo. He is a Southern California native and in his free time enjoys outdoor activities with his wife Emily, two daughters Lilah and Lucia and dogs that include boating and snow skiing.

INTERNATIONAL PHARMACEUTICAL INDUSTRY 31 www.international-pharma.com Drug
Delivery
Discovery, Development &
Figure 2: A CCS-enabled database search
Pre-existing Immunogenicity: How Will Cell and Gene Therapies Change Our Testing Approach?
When bringing a therapeutic to market, determining its potential to elicit an immune response and understanding the molecular and cellular interactions involved is essential. In some patients, it is possible that a previous exposure event to certain antigens associated with the therapeutic can prime the immune system for re-infection. The resulting pre-existing immunogenicity may affect both the safety and efficacy of the drug in these patients.
As we move into a new era where cell and gene therapies (C>s) are frequently gaining approval for use, it is important to consider how best to approach preexisting immunogenicity assessment for these relatively new modalities. With the C> space expanding so quickly, developers must exhibit flexibility in their bioanalytical decisions and methods – ready to weather regulatory requirements as they evolve.
In this article, Chief Scientific Officer at BioAgilytix, Jim McNally, Ph.D., explores why bioanalysts should prepare for the impending wave of C>s entering the development pipeline and the considerations they must make in their pre-existing immunogenicity assessments
How Pre-existing Immunogenicity Can Determine Therapy Success

When developing any biologic therapy, it is essential to understand the prevalence and potential impact of patients’ pre-existing immunogenicity. Previous exposure of an individual to environmental antigens can trigger an immune response which may be cross-reactive to a biological therapy– from monoclonal antibodies (mAbs) to cell and gene therapies (C>s). For a sub-class of gene therapies, those that use adeno-associated viruses (AAVs) as the vector, it has been wellestablished that there is a significant incidence of pre-existing immunogenicity since AAV is present in the environment and anywhere from 40-70% of the global population has been exposed and has antibodies against the AAV (Boutin, et al. 2010). There are three
key areas where the presence of pre-existing immunity can influence the success of a gene therapy product: safety, efficacy, and commercialisation.
•
Safety
The risk associated with pre-existing anti-drug antibodies (ADA) has been a concern for biotherapeutics and only increased since AAVs became one of the main vectors for gene therapy delivery. However, for biotherapeutics, the impact of these pre-existing antibodies on safety has been limited and infrequent based on an industry survey (Xue, et al. 2013). In most cases, these pre-existing antibodies have little known impact on the biotherapeutic at all.
But, due to the high incidence of antiAAV antibody positive individuals, there is a reasonable concern around safety issues and an immunogenicity risk assessment suggests that this should be monitored closely in individuals receiving an AAV-based gene therapy. For some AAV-based gene therapy programs, this concern has led to a decision to exclude anti-AAV positive patients from clinical trials to avoid the risk of a safety event. However, excluding these patients from clinical trials in the absence of a safety risk can be counter-productive for the development of the gene therapy program, as a significant portion of the patient population would be eliminated from the potential benefit of the gene therapy.
• Efficacy
As well as safety, pre-existing immunogenicity may impact the efficacy of the therapy. Neutralising antibodies (nAbs) in circulation with specificity towards the viral vector may neutralise the benefit of the gene therapy by preventing the viral vectors from delivering the gene of interest to the intended target cells, resulting in reduced efficacy.
With 40–70% of individuals in certain areas of the world believed to carry nAbs towards AAV, these nAbs could be a serious challenge to achieving the desired effects in a high proportion of individuals.7 However, the evidence surrounding the impact of nAbs on the efficacy of gene therapies is still ambiguous.
Reflecting this, the biopharma industry does not fully agree that individuals with these pre-existing antibodies should be excluded from clinical studies. As so many viral vector particles are delivered to each patient over the course of a gene therapy treatment, it could be considered a numbers game: a low-level immune response would likely not be able to significantly hinder its efficacy. With greater experience in the gene therapy space and inclusion of pre-existing positive individuals into studies, we will be better able to determine the impact of these antibodies and perhaps make these therapies available to more individuals that desperately need the benefit they could provide.
• Commercialisation
As previously discussed, the presence of pre-existing immunogenicity in patients could prevent this population from being included in clinical trials and prevent them from receiving the therapy once commercialised. In addition to stopping these patients from experiencing the possibly life-changing advantages of a vital therapy, the target audience could be diminished to a point where it would no longer be cost-effective to produce the drug, or it would be prohibitively expensive and severely limit access.
From a sponsor perspective, assessing whether pre-existing immunogenicity could impact the safety and efficacy of the patient population is vital. By understanding this link, a balance between risk to safety and efficacy vs the effect of the disease could help form an argument for the inclusion of these patients for treatment.
In cases where pre-existing antibodies are used as an inclusion/exclusion criteria, this may mean that assays to assess this will also need to be commercialised as companion diagnostics to support the gene therapy program. This would also slow the development of these therapies and increase the overall cost of the drug.
New Considerations for a New Drug Modality
Although pre-existing immunogenicity can impact safety, efficacy, and commercialisation for all biological therapeutics, there are
32 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4 Drug
Discovery, Development & Delivery



Your Drug Delivery Device Solutions Partner
additional considerations gene therapy developers must keep in mind.

As these types of therapeutics are relatively new, risk assessments generally point towards monitoring the impact of preexisting immunogenicity more closely for C>s. Indeed, with gene therapies using viral vectors as tools for delivery - particularly AAV - the complexity of the immunogenicity risk assessment increases significantly and should begin early in the development process. Early engagement with the regulatory agencies is encouraged to best design an immunogenicity monitoring plan for these clinical trials.
Another factor to consider is that it is more likely that viral vector gene therapies will elicit both cellular immune responses and humoral immune responses (as opposed to just a humoral response alone) when compared with mAbs. This is because viral vectors enter the target cell and express a transgene which may be foreign to the patient. As a result, characterising cellular immune responses may be more important in the gene therapy space than traditional biologics. The use of ELISpot has grown in importance to support these programs
along with flow cytometry to characterise and quantitate cellular immune responses. Both are platforms have not typically been used for regulated bioanalysis but do have published white papers to guide the development and validation of assays. As a result, for example the immunogenicity assessment for gene therapies typically relies on more assays than usually employed for a monoclonal antibody. Total antibodies and neutralising antibodies against the viral capsid and the transgene product, ELISpot to assess cellular immunity against the capsid and transgene product, and possibly flow cytometric measures amount to six assays that may be needed and with data that must be integrated to develop an overall picture of the immunogenicity of the AAV-based gene therapy.
Keeping Re-treatment in Mind
Another important consideration that gene therapy developers must be aware of when assessing pre-existing immunogenicity is the potential impact on redosing.
C> modalities are in their infancy and their effects could have the potential to last many years. However, there is relatively little
data surrounding the longevity of these treatments and their impact because they are so new and relatively few patients have received them. As much as we hope that gene therapies provide a permanent cure, we can’t know that with certainty and retreatment could be necessary in the future. If nAbs are generated following the first treatment, this could ultimately prevent vector re-dosing, leaving the patient in a position where they may have to face their disease again. Fortunately, there are many approaches being investigated to counter this – from modulation/suppression of the immune system to vector engineering to limit immune recognition.
It is also important to remember that the effect of the immune response on safety and efficacy could still be less harmful than the patient’s genetic disorder. Developers will need to determine if the response is something that even needs to be mitigated, as the alternative option to re-dosing could be far more harmful.
Regulatory Requirements: Building the Airplane as it Flies
The C> space has expanded rapidly,
34 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Drug Discovery, Development & Delivery
with no sign of slowing down. Such rapid progress in the area has enhanced pressure on regulatory bodies to evolve just as quickly – bringing an element of “building the airplane as you fly it”. Regulatory bodies are trying to adapt to a fluid research area and developers are attempting to predict possible changes. This means that projects progressing through the pipeline could encounter new regulatory changes between phases. Developers must therefore be agile enough to deal with the ambiguity of a space that's not fully defined.
In the C> space there is currently an aspect of trying to be prepared for the regulations to come; this is testing the “risk aversion” of therapeutic producers. Trying to anticipate all potential future regulatory expectations surrounding pre-existing immunogenicity could mean generating assays and holding them to standards that may ultimately not be needed. This could lead to greater scrutiny from regulatory bodies, as well as unnecessary costs.
Alternatively, developers could take a very risk-driven approach. With a patient population that desperately needs gene therapy – such as those with a rare disease – the risk that pre-existing immunogenicity will be a deciding factor in its approval could be very low.
Ultimately, taking the middle ground in preparing for new pre-existing immunogenicity testing regulations should be the aim. Care should be taken to consider whether the choices made will add value. Assessing the risk of pre-existing immunogenicity before the drug enters the clinic, determining the likelihood of it having an impact, and discussing these considerations with the agency is elevating in importance in the C> space.
Linking Therapeutic and Diagnostic Development
Following existing regulatory requirements for developing and validating the assays analysing pre-existing immunogenicity is essential – it is also necessary to understand how these assays become linked to the development of the product. This notion is particularly prominent when clinical trials are set up to exclude patients based on observed pre-existing immunogenicity.
By making this decision to exclude candidates based on pre-existing immunogenicity, developers are saying, “this assay matters, and it matters whether a patient
has these antibodies”. As a result, the assay used would be considered a companion diagnostic for patient screening, and then inclusion or exclusion for those patients ultimately receiving the care following approval. It will no longer be one piece of the data set, but one of the most critical aspects of development that decides whether patients could receive life-saving therapy.
Developers must be also aware that the companion diagnostic space is a very different beast. The two products (one diagnostic and one gene therapy) would be governed by two different governing regulatory bodies whilst being developed simultaneously, adding to the challenges and difficulties developers could face.
A Look to the Future
The biopharmaceutical space is still at the beginning of its journey with C>s. Fitting these new modalities into a previously welldefined area reserved for biotherapeutics is – and will continue to be – a challenge.
Although testing pre-existing immunogenicity is largely similar between these therapies, there are several important considerations that developers must be prepared to make on their journey to C> commercialisation.
With so many potential challenges that developers could face when deciding the right approach to pre-existing immunogenicity testing, there is value in partnering with bioanalytical CROs who service multiple customers in this space. Familiarity with the current regulatory landscape and experience with multiple C> programs is valuable experience that can be leveraged. Offering extensive expertise in assay design, development, and validation, their support will be essential as more and more novel C>s enter the space, and the importance of these assays increases.
REFERENCES
1. Morales L, Gambhir Y, Bennett J, Stedman HH. Broader Implications of Progressive Liver Dysfunction and Lethal Sepsis in Two Boys Following Systemic High-Dose AAV. Mol Ther (2020) 28:1753–5.
2. Shieh PB, Bonnemann CG, Muller-Felber W, Blaschek A, Dowling JJ, Kuntz NL, et al. Re: "Moving Forward After Two Deaths in a Gene Therapy Trial of Myotubular Myopathy" by Wilson and Flotte. Hum Gene Ther (2020) 31:787.
3. Wilson JM, Flotte TR. Moving Forward After Two Deaths in a Gene Therapy Trial of Myotubular Myopathy. Hum Gene Ther (2020) 31:695–6.
4. Srivastava A. AAV Vectors: Are They Safe? Hum Gene Ther (2020) 31:697–9. doi: 10.1089/ hum.2020.187
5. https://www.pharmamanufacturing.com/ industrynews/2021/fourth-child-dies-ingene-therapy-trial/#:~:text=A%20fourth%20 patient%20has%20died,administered%20 at%20two%20different%20doses
6. Calcedo R, Vandenberghe LH, Gao G, Lin J, Wilson JM. Worldwide Epidemiology of Neutralizing Antibodies to Adeno-Associated Viruses. J Infect Dis (2009) 199:381–90
7. Kruzik A, Fetahagic D, Hartlieb B, Dorn S, Koppensteiner H, Horling FM, et al. Prevalence of Anti-Adeno-Associated Virus Immune Responses in International Cohorts of Healthy Donors. Mol Ther Methods Clin Dev (2019) 14:126–33
8. https://www.cellandgene.com/doc/cell-genetherapies-investment-outlook-in-beyond-0001
Dr. Jim McNally Ph.D.
Jim McNally, Ph.D. has an extensive background in bioanalytical assay development and program leadership spanning nearly 20 years working in the pharmaceutical and biotechnology industry. Prior to joining BioAgilytix, Dr. McNally was Executive Director at CRISPR Therapeutics, where he led a team of scientists to develop a portfolio of assays to support development of gene-based therapeutic candidates throughout their lifecycle. He has also previously held roles at Genzyme, Pfizer, EMD Serono, and Shire which have given him broad experience in the development of large molecule, gene therapy, and cell therapy biotherapeutics. Dr. McNally is a recognised thought leader in the development and application of bioanalytical methods used in regulatory submissions and is specifically skilled in progression of biotherapeutics from research through clinical development. He has a special interest in the immunogenicity of biotherapeutics and leads an industry-wide working group to address this issue. A key part of his role at BioAgilytix is advising on emerging scientific developments and providing scientific and regulatory guidance.
Dr. McNally earned his B.S. in Biology from Mississippi State University, his Ph.D. Viral Immunology from Louisiana State University School of Medicine in Shreveport, and his Post-Doc in Viral Immunology from University of Massachusetts Medical School.

INTERNATIONAL PHARMACEUTICAL INDUSTRY 35 www.international-pharma.com
Drug Discovery, Development & Delivery
Strategies to Reduce Cold Chain Burden in Biopharmaceuticals
The availability of a wide range of therapeutic biologics has revolutionised modern medicine. Whilst the majority of pharmaceutical drug products remain conventional, small molecule medicines; the emergence of biotherapeutics has allowed for the treatment of many disease areas which were previously out of reach.1 Despite the positive growth in biotherapeutics (Figure 1), significant challenges will need to be overcome in order to fulfil the promise of biotherapeutics across society. With a growing number of protein therapeutics and vaccines in development2,3 one of the biggest challenges facing the product developers is the stability of these molecules.4 Biologics including vaccines are inherently unstable and prone to degradation. Therefore these medicines typically require low temperature (cold chain) transport and storage. The result is a much higher economic burden and in some cases limited access.
Stability Challenges Slowing Future Growth
Biopharmaceuticals comprise of medium to large, complex, macromolecules that can be divided into 4 major classes; proteins, nucleic acids, lipids and carbohydrates. For the purposes of this article the focus will be proteins.
Protein Structure
Biopharma
Conventional pharma

Protein structure can be divided into four levels as shown in Figure 2. The 3D structure of the protein is highly complex, and inherently linked to therapeutic effectiveness. If the 3D structure is not maintained, there is a risk the therapeutic effect of the drug is reduced or lost entirely. There is also the possibility the molecule can present an immunogenicity risk to the patient. It is therefore vital to maintain the structure of the protein.

Degradation Mechanisms
The difficulty arises due to the structure of a protein being relatively weak, compared to small molecules. Numerous chemical,
36 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4 Application
Note
Figure 1. Source IQVIA 2022, Sales (B€) and growth (CAGR%) of Biopharmaceutical versus Conventional pharmaceutical market
Figure 2. Multiple levels of protein structure (image: Biology by CNX OpenStax, CC BY 4.0)
2019 2020 2021 302 330 373 681 +11% +4% 694 735
physical and colloidal degradation pathways can occur in biologics, a full review of these pathways is beyond the scope of this article. Henceforth, a simplified term of “stability” will be taken to mean that all degradation pathways that negatively impact activity or safety are reduced.
As a result of these numerous degradation pathways, it is typically the case that biopharmaceutics require a cold-chain to be maintained throughout the supply chain, and ultimately until the medicine is administered. If the material cannot be maintained under the required conditions then the consequence may be; reduced availability of medicines, product waste, loss of therapeutic effect or even risk of immunogenicity.
Even if a robust cold chain is in place, the financial impact of maintaining it is a significant contributor to the high price of biological medicines. Additionally, when a cold chain is available and the medicine affordable, the shelf life of biological drug product is typically short relative to conventional small molecule medicines. Below we briefly discuss the multiple strategies employed to enhance the stability of biologics and thus potentially reduce the cold chain burden.
Mitigation Strategies
There are different approaches to reducing the burden posed by the need for cold chain storage, a non-exhaustive summary is discussed in the following sections. It is reasonable to consider that multiple strategies will ultimately be required.
Through the many steps of discovery and development of biotherapeutics there are opportunities to enhance the stability profile. Powerful in silico modelling tools enable screening of molecules with higher chances of developability.5,6 During upstream processing, post translational modifications may be included to enhance therapeutic effect as well as stability. Further downstream the efficient isolation, purification and the use of an optimised buffer system offers further gains.
Downstream Processing
One of the clearest examples of a stability enhancement opportunity occurs during downstream isolation and purification. Where it is crucial to employ highly selective process steps to remove products that could lead to degradation; for example protein
•
Application Note
DFE Pharma has a dedicated BioHale® portfolio consisting of excipient suiting the needs of Biopharmaceuticals, BioHale® Sucrose and BioHale® Trehalose .
The understanding of active–excipient interactions is critical in the rational design of formulations to stabilise protein-based therapeutic drugs and vaccines. Selection and use of the appropriate excipients enables the development of novel therapies and robust pharmaceutical products.
BioHale® key promises:
• Uncompromised Quality
Unlike taking medications orally or via inhalation, introducing a drug into the body by parenteral administration poses a greater risk since the body's natural defenses are bypassed. As such, they must be exceptionally pure and free from physical, chemical, and biological contaminants. Therefore, similar requirements are applicable for the excipients for which DFE Pharma has a specific BioHale® portfolio of high purity, low endotoxin excipients.
By making use of the best available active purification technologies in state-ofthe-art cGMP, FDA inspected manufacturing facility in the Netherlands, Europe, the level of purity and endotoxin are fully controlled, resulting in market leading specifications. Our excipients, produced according to ICHQ7 guidelines, have multicompendial specification and comply with the global regulatory requirements of the pharmaceutical industry (Ph. Eur., USP-NF, JP, ChP). BioHale® Sucrose and BioHale® Trehalose are used to stabilize the fragile biomolecules in during processing and in their final applications.
• Security of Supply
The established stability in the supply chain has gained customers trust due to our long history of providing reliable security of supply – even during the pandemic. DFE Pharma has local stocks in Europe, US and Japan and capacity available to ensure flawless supply of BioHale® excipients today and in future. The active purification process makes our product less dependent on raw material variability, raw material supply and raw material production campaigns.
Expert Support
Our BioHale® team of experts, no matter if is in formulation support, analytical support, excipient expertise, regulatory or quality related, we are there to support you.
fragments. An often less considered area is selection of fully optimised buffer. This is a crucial step and should be made with the end use in mind. Typically the main response that is maximised is the yield. Whilst stability is also a consideration analytical methods to predict longer term stability may not be representative. As an example even trace levels of impurities introduced by lower purity ingredients, can lead to stability issues later in the products life, however rapid screening technique often cannot discern these long terms effects. Impurities may ultimately lead to aggregation and can be very challenging to debug when the aggregation is only detected in the final formulation, but actually activated during downstream processes. It is therefore prudent to take a conservative risk based approach when selecting buffer media.
Formulation
Many stability optimisation approaches are highly specific to a single molecule. They often involve expensive and time consuming studies for which the conclusions cannot be extrapolated. It would be advantageous to instead take a more generalised approach to protein stability enhancement. Degradation pathways all have a common pre-requisite, they require molecular mobility on some scale.5 Thus if one can reduce the molecular mobility, a reduction in the rate of degradation could be expected. Removal of the continuous phase of a biological system, i.e. water, offers a great potential in the preparation of robust and stable drug product.
Several technologies are capable of removal of water from an aqueous protein
INTERNATIONAL PHARMACEUTICAL INDUSTRY 37 www.international-pharma.com
solution, lyophilisation, also known also freeze drying in particular shows great promise in biopharmaceutical applications. During lyophilisation the product is initially frozen, followed by removal of water ice via sublimation. This is followed by secondary drying step resulting in a powder where a residual water content of < 1 % w/w can be achieved.7
There is however a complicating factor, during the freezing and drying process, the biomolecules are exposed to stresses that can lead to physical or chemical degradation of the protein. Stresses such as; pH shift, increased ionic strength, mechanical shear stress and dehydration stress may all occur7 In order to protect the protein, a suitable combination of process parameters and excipients is required. A well-executed process optimisation and rational formulation design may result in a drug product that has good stability, in some cases a cold-chain can be entirely avoided.
Carbohydrate Systems to Maximise Stability
The selection of excipients is critical; as the vast majority of biologics are administered parenterally3,4 the need for high purity excipients with an excellent safety profile is paramount, options are fairly limited. One class of molecules that show great promise are carbohydrates. Sucrose, Trehalose and Mannitol have long been known to offer cryo and lyo protection.7 There is no general rule for best excipient selection, however trehalose has shown great promise across a wide range of difficult to stabilised molecules such as monoclonal antibodies (mAbs).
INN
Durvalumab
Ocrelizumab
The general mechanisms by which sugars stabilise proteins during lyophilisation is described by two predominant theories; water replacement theory and vitrification theory. A critical requirement in both these theories is the formation of an amorphous glass matrix, composed of the biologic, sugars and other excipients. In order to remain a glass, the product must remain below the glass transition temperature Tg of the matrix. Therefore if a glass with a very high Tg can be prepared, it is feasible that the protein may remain stable even at temperatures above ambient. Moisture also needs to be considered and it acts as a plasticiser, effectively reducing the Tg and allowing re-crystallisation at lower temperatures.
It common to utilise sugar glasses to stabilise proteins. For successful protection of the protein the sugar should have a high Tg, low hygroscopicity and a slow crystallisation rate. Additionally a high glass transition at the maximally freeze concentrated fraction (Tg’) is preferable.8 The disaccharide trehalose dihydrate exhibits all these properties and is therefore widely used. However there is compelling research indicating that incorporation of higher molecular weight carbohydrates with trehalose could enhance the stabilisation further.
In a recent study, binary mixtures of trehalose (a disaccharide) and varying levels of pullulan (a polysaccharide) were used during the preparation of lyophilised formulations using the model protein β-galactosidase.9 It was observed that approximately 80% activity of β-galactosidase
Type
Liquid injection
Liquid injection
Adalimumab Liquid injection
Blinatumomab
Obinutuzumab
Ranibizumab
Bevacizumab
Trastuzumab
Brentuximab
Pertuzumab
was retained for binary mixtures of specific ratios stored at 30°C / 56% RH after for 4 weeks. In environment with very low relative humidy the benefit of the binary mixture over trehalose alone was limited. However in the more realistic environment with exposure to RH > 50% the benefits were clear. The researchers noted that pullulan itself may not be the optimal polysaccharide. Despite the high molecular weight and high Tg of the material used (261°C), pullulan is a bulky molecule with a linear, rigid structure. The researchers hypothesized this could prevent tight molecular packing and limit the stabilising potential.9
Oligo and polysaccharides are a highly complex class of molecules and further research is ongoing.10 However to date this formulation strategy shows great promise of a universal approach in the development of stable lyophilised protein drug product, without the necessity of an uninterrupted cold chain.
Conclusions
In order for biopharmaceuticals to reach their maximum potential across society, the industry needs to reduce the burden of cold-chain. A crucial step in achieving this ambitious goal is the availability of technologies able to stabilise proteins under more demanding environmental conditions. Lyophilisation is discussed as a critical enabling technology. Next generation sugar glass’ are proposed as another critical technology. Specifically, by combining the established benefits of trehalose with higher molecular weight sugars such as inulin, pullulan or other oligo and polysaccharides, biotherapeutics that do not require cold chain storage may become reality.
REFERENCES
1. Hopkins AL, Groom CR. The druggable genome. Nat Rev Drug Discov. 2002;1:727–730.
Lyophilised
Liquid injection
Liquid injection
Liquid injection
Lyophilised
Lyophilised
Liquid injection
Table 1. Marketed monoclonal antibody formulations containing trehalose dihydrate (non-exhaustive)11
2. Kitney, R. I., Bell, J., & Philp, J. (2021). Build a sustainable vaccines industry with synthetic biology. Trends in Biotechnology, 39(9), 866-874. doi:10.1016/j. tibtech.2020.12.006
3. Ngo HX, Garneau-Tsodikova S. What are the drugs of the future?. Medchemcomm. 2018;9(5):757-758. Published 2018 Apr 23. doi:10.1039/c8md90019a
4. Batta A, Kalra BS, Khirasaria R. Trends in FDA drug approvals over last 2 decades: An observational study. J Family Med Prim Care. 2020;9(1):105-114. Published 2020 Jan 28. doi:10.4103/jfmpc.jfmpc_578_19
38 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Application Note
Application Note

5. Chennamsetty N, Voynov V, Kayser V, Helk B, Trout BL. Design of therapeutic proteins with enhanced stability. Proc Natl Acad Sci U S A. 2009;106(29):11937-11942. doi:10.1073/ pnas.0904191106
6. Voynov V, Chennamsetty N, Kayser V, Helk B, Trout BL. Predictive tools for stabilization of therapeutic proteins. MAbs. 2009;1(6):580-582. doi:10.4161/mabs.1.6.9773
7. Bjelošević M, Zvonar Pobirk A, Planinšek O, Ahlin Grabnar P. Excipients in freezedried biopharmaceuticals: Contributions toward formulation stability and lyophilisation cycle optimisation. Int J Pharm. 2020;576:119029. doi:10.1016/j. ijpharm.2020.119029.

8. de Jonge J, Amorij JP, Hinrichs WL, Wilschut J, Huckriede A, Frijlink HW. Inulin sugar glasses preserve the structural integrity and biological activity of influenza
virosomes during freeze-drying and storage. Eur J Pharm Sci. 2007;32(1):33-44. doi:10.1016/j.ejps.2007.05.112.
9. Teekamp N, Tian Y, Visser JC, et al. Addition of Pullulan to Trehalose Glasses Improves the Stability of β-Galactosidase at High Moisture Conditions. Carbohydr Polym. 2017;176:374-380. doi:10.1016/j. carbpol.2017.08.084
10. Singh RS, Kaur N, Hassan M, Kennedy JF. Pullulan in biomedical research and development – A review. Int J Biol Macromol. 2021;166:694-706. doi:10.1016/j. ijbiomac.2020.10.227

11. Dickhoff, B et al, The importance of disaccharide excipients in biologics, accessed on 6 Oct 2022, https://www. europeanpharmaceuticalreview.com/ article/143124/the-importance-ofdisaccharide-excipients-in-biologics/2/
Ross Blezard
Ross Blezard is Product and Application specialist Biopharma at DFE Pharma. A physicist by education Ross began his career in inhalation and transdermal drug delivery. After leaving his position as head of formulation development at a UK based CDMO, Ross spent several years working as a senior scientist in material sciences. In 2019 Ross joined DFE Pharma where he has supported our inhalation and biopharmaceutical customers with their technical challenges.

Mara van Haandel
Mara van Haandel is Marketing Director Biopharma at DFE Pharma. Prior to becoming the marketing lead Biopharma at DFE Pharma she has been working for almost 20 years in R&D. Uncovering and realising excipient solutions that can support overcoming the challenges of customers in drug development and manufacturing is what excites her.

INTERNATIONAL PHARMACEUTICAL INDUSTRY 39 www.international-pharma.com
Clinical and Medical Research
Respiratory Disease Management: A Connected Approach
Until relatively recently, treating, monitoring and controlling respiratory conditions such as asthma centred on conventional devices, paper-based tools and appointments with a GP or asthma nurse. This approach of course still plays a huge role for the over 300 million people living with asthma globally, as prescribed medication coupled with patient education is widely acknowledged as the most effective management strategy. However, a deeper understanding of the greater efficiency at hand through vastly increasing use of digital applications and the palpably mounting pressure that can be felt on healthcare bodies globally has seen a shift in the context of respiratory disease management.
A greater understanding of cultural shifts, technological change and consumer expectations are dramatically altering the cultural context and reference points these condition management strategies exist within. This in turn is creating exciting opportunities for new MDI devices and supporting applications that enhance overall treatment capabilities and outcomes.
The first pMDI, Medihaler, launched in 1956 courtesy of Riker Industries and represented a most disruptive innovation for its time. Still recognisable in many redesigned formats, the initial model has informed much of the pharmaceutical aerosol industry as we know it today. However, respiratory health and MDI manufacturing development and design have evolved at a considerably more rapid pace in the last three decades, offering patients and HCPs an altogether more sophisticated multifaceted solution. As with many chronic conditions, when considered more broadly in relation to the individual’s needs and aspirations, the future trajectory of management and treatment available changes dramatically. Being able to react to the many factors that affect or trigger the patient’s symptoms has resulted in innovative management strategies that harness new digital technology and a use of data that benefit both the patient and
HCP, ultimately strengthening the overall relationship between the two. Equally, refining design of devices beyond the traditional initial MDI to further enhance efficiency of drug delivery has resulted in this new era of inhalation therapeutics.
“Respiratory pharma brands are thinking beyond the daily management of asthma as a medical condition or illness. By gathering relevant insights from other influencing factors, such as air quality and diet, new systems empower the patient to embrace asthma as part of their complete wellness regime so that they feel informed and in control of their respiratory health.”
Miles Hawley CEO Recipe Design
The digital revolution has brought with it a myriad of innovation altering the landscape for medical devices and drug delivery systems. Owing to smart, mobile and wearable technology, AI, IoT and manufacturing advancements, the medical profession and pharmaceutical industry can now offer patients a level of care like never before. The ability to obtain insights specific to an individual’s device usage, efficacy of delivery, compliance and lived experience of respiratory conditions enables the provision of better treatment outcomes as result of the personalised nature of the new technology available. More detailed information for healthcare professionals, improved interfaces and attuned innovation from device and component manufacturers have overhauled what it means to live with, treat and manage respiratory conditions on a day-to-day basis. The increased power that now sits directly with patients and the ongoing expansion in data available to HCPs have improved the nature of disease management approaches in an unprecedented manner.
Personalised solutions, particularly in the form of wearable tech, have permeated almost all consumer lifestyle categories and happily, have had positive impacts on the overall patient experience for those managing chronic conditions. Symptom tracking apps, biometric monitoring and self-testing are now the norm and conditions from diabetes to PCOS to heart conditions utilise these connected technologies. The
ease of biomarker monitoring provides a depth of understanding that means patients can demand truly detailed and bespoke assessment of their symptoms as opposed to a more generalised interpretation.
That said, the expectations of patients and even HCPs often outstrip the current offer or combined technical possibilities. The development of truly connected respiratory condition management is complex and requires collaborative working between the many disparate parties that hold the requisite specialist expertise, technical capabilities and patient-centric design thinking, often decades in the making. Driving meaningful, continuous improvement and safer more effective management of respiratory conditions will require a shake-up of the industry. Traditional competitors, new partners, licencing agreements and data handling for these proprietary technologies need to be fully considered in order to offer connected healthcare solutions that provide a distinctive commercial offer alongside meaningful patient benefits.
A Future Vision for Connected Asthma Management
Moving respiratory innovation forward with momentum is a multifaceted operation. Understanding shifts in consumer lifestyle, ‘smart’ wellness and healthcare autonomy have inspired new workstreams dedicated to defining a future vision for connected asthma management that are simultaneously patientfocussed and technology-driven. Marrying techniques such as semiotic and discursive analysis, expert and stakeholder interviews, iterative co-design sessions with patients and HCPs, and technology forecasting culminate in these new joined up product developments that are delivering above and beyond the traditional and familiar options. Insights drive strategic responses that can be used to inform product pipelines that factor in social, economic and technological advancements. It’s this matrix of insight that allows for an exploration of an holistic, future-facing approach to connected asthma management.
Employing a unique combination of digital and physical tools enables asthma patients to better understand and manage
40 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4









INTERNATIONAL PHARMACEUTICAL INDUSTRY 41 www.international-pharma.com ––
• • •
is UPC’s
Clinical and Medical Research
their condition at home. Informed by the shifts in meanings spanning multiple categories of analogous products, connected asthma management proposes a new dynamic that bridges prescription medication with evolving attitudes in healthcare, wellness and connected devices.
Understanding Today Helps Us Anticipate Tomorrow
A powerful shift we are observing across all healthcare conditions is the progression in language used, as a result of individuals’ desire to manage their health autonomously where possible and with discretion when desired. Even the word ‘patient’ is itself contentious, giving instant connotations of sickness, disease and vulnerability. The same applies with the term ‘sufferer’, implying that the persistent nature of a chronic condition renders the person incapable and less-than. Instead, people living with longterm conditions are understandably keen to be treated as individuals, empowered in the management of their own conditions.
“In our respiratory health research, we often find patients who rarely, or reluctantly, describe themselves as 'asthma sufferers', not wanting to be branded as sick, suffering or vulnerable. Although patients understand the daily risks of asthma, we often observed them choosing to manage their condition as discretely as possible, rejecting overly medicalised inhalers and shunning the connotations of ill -health and dependency.”
Christina Philpott, Senior Strategist, Recipe Design
As consumer lifestyle products undergo almost constant innovation and redesign to refine and optimise, so too must drug delivery mechanisms. An elevated application of product design is now expected when it comes to daily use products individuals rely on to monitor, manage and treat conditions such as asthma. MDIs of old are being shunned in favour of updated, aspirational models that are also considerably more effective in their administration of the drugs themselves. A new generation of breath-triggered devices have been shown to not only provide improved device compliance, but many contemporary models have even led to the youngest and often least compliant patients describing such inhalers as ‘cool’; a medical product they were happy to be seen with, resulting in increased engagement and compliance with their respiratory condition management. Enthusiasm for using the device itself has proven to have
positive effects on the end users’ health outcomes, a perhaps surprising fact that would previously not have been taken into consideration whatsoever.
In response to these cultural shifts, new joined up systems can be seen to embrace a patient-centric design language that combines the trusted reassurance of medical device engineering and regulations with premium ergonomic forms, materials and finishes of domestic lifestyle and wellness products enhanced with the latest digital technology, increasing functionality. Several of the latest connected asthma management systems include docking stations as part of the overall therapeutic package, for example. These ‘smart hubs’ create a designated place for asthma care in the home and provide physical space for electronic displays allowing for notifications generated in a device’s associated mobile app.
Across healthcare conditions we are seeing consumers looking for more balanced approaches to their health and wellness management. In our research as design consultants, we have heard from respondents who supplement prescription treatments with acts of personal wellness, such as consuming active ingredients and diet modification or performing targeted mental and physical activities. There is increasing evidence that practising breathing exercises can improve drug inhalation technique and reduce reliance on rescue medication, with the potential for further positive implications on both mental health and general health, such as lowering blood pressure. With this in mind, smart respiratory management systems could happily incorporate functionality encouraging users to perform breathing exercises through notifications and prompts and analyse breathing patterns thereafter.
These factors combine to create a system of products that sit comfortably and proudly in the evolving smart home environment, responding to evolving patient attitudes about blended mental and physical health interventions, while accommodating increased awareness of hygiene as we learn to live with the long-term implications of the COVID-19 pandemic.
Combining Existing Technologies Through a Strategic Lens
Alongside the understanding of the breadth of actions that can be taken to support asthma management treatments there is a growing awareness of the range of factors that may contribute to our respiratory health
with a particular impact on those living with asthma. Increasingly individuals are monitoring indoor and outdoor air quality, airway microbiome and the impact of other conditions and medications. Dedicated mobile apps can support the development and application of this understanding, for both the individual and for the greater good. In addition to supporting the user by tracking and monitoring symptoms, asthma apps can allow people to submit their data to clinical studies allowing improvements in more personalised and responsive asthma management strategies and new product development.
In respect of smart hubs and docking stations, it’s possible to log each actuator use, allowing automation of compliance logs and facilitating reminders when needed. This type of data also allows an estimation of the remaining medication without the requirement of mechanical dose counters, meaning patients and healthcare providers can be prompted when levels are low and prescription renewal required.
Syncing of digital devices is revolutionising multiple health and wellness technologies and again can offer further benefits to those with respiratory conditions. Connectivity with existing devices such as fitness wearables allows for the automation of biometric data, location-based weather and pollution reports, food consumption and medication and supplement logs. Individuals will also be able to manually track their symptoms – far beyond the limitations of traditional treatment monitoring practices. Over time, machine learning capabilities will enable rich and individualised insights to advise on the factors that might be exacerbating symptoms, or enabling improved condition management. Collectively this data may enable advances in the understanding of chronic respiratory conditions and the elements that connect patient cohorts, or might assist those struggling most with condition management.
This prioritisation of the individual’s experience as a person living with asthma –combined with ease of use, timely reminders, meaningful insights and by supporting their holistic condition management approaches – will enable both patients and HCP's to be informed and empowered in respiratory condition management. These insights will also facilitate the development of more relevant and impactful drugs, devices and connected infrastructures for superior condition management into the future.
42 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Clinical and Medical Research
can truly be felt. Employing an holistic and future-facing strategy for connected health that unifies the challenges and changes in the category, whilst addressing the longstanding and unmet needs of patients and HCPs, is possible and certainly already becoming a reality.
Future Proofing Responsive, Agile Systems
As the world learns to live with the long-term implications of the COVID-19 pandemic and previous lockdowns we have been forced to develop new and different approaches to the patient-clinician relationship. With the reduction of nonessential in-person appointments; in home, remote clinical assessment approaches have offered tangible benefits. The HCPpatient relationship is strengthened, appointments are more efficiently handled and patients experience an enhanced degree of autonomy.
Developing further functionality which facilitates self-testing is increasingly being viewed as a necessary feature of future asthma management systems. Spirometry tests can be undertaken by the patient in the privacy of their own home, with test results shared on connected apps and devices to then be shared with HCPs. These test results can be supplemented with data obtained from tracked symptoms giving additional insight in terms of the effectiveness of current treatment methods and highlighting any need for potential medical interventions to the HCP. This manner of tracking and testing ensures patients can monitor their condition and gain essential advice should in-person clinical services ever be interrupted again, or simply to monitor their condition between appointments for their own peace of mind.
While ease and efficacy of asthma management remain key to patients, they are beginning to demand the consideration of sustainability. Manufacturing processes and cost of materials are undoubtedly the biggest barriers to more eco-friendly drug delivery devices becoming a reality. With the rapid onslaught of sustainability legislation affecting markets globally, the pharmaceutical industry will have no choice but to adapt and evolve. Refillable canisters and canisters made from fully recyclable
materials, alongside the elimination of disposable and single use actuators will become a necessity, as opposed to theoretical possibility. These developments in turn impact on packaging requirements, vastly reducing what’s needed day to day.
Central to Recipe’s Meaning Centred Design™ process is the ability to track cultural change and meaning shifts across markets, forecasting how these might apply to a category and the challenges and opportunities ahead. In addition to the COVID-19 pandemic, geopolitical and economic uncertainty has undoubtedly altered the considerations of and challenges faced by patients, HCPs, healthcare providers, developers and manufacturers alike. This, coupled with an understanding of how new legislation may take shape will result in device and service innovation that is agile, responsive and future proof.
Forecasting Connected Asthma Management Solutions

Beyond patient and HCP considerations, which must be at the heart of all asthma management solutions, other stakeholders need to be part of the conversation to ensure platforms are fit for purpose. New drug delivery technologies, manufacturing methods, material innovation, sustainability targets, regulatory approval and data privacy legislation all play a role in the evolution of connected healthcare.
Taking inspiration from wellness products and smart home technology shines a light on what asthma treatment systems of the future may look like. The essence of next generation asthma management offers exciting potential. Connected condition management can lean on analogous categories, such as wellness and home tech for their respective insights, allowing for meanings to intersect and therefore lead to truly innovative outcomes.There is still a way to go in order for these new multifaceted systems to become accessible and affordable in order that their benefits
Sarah Sanders
Being trained in industrial design at Northumbria University gives Sarah's semiotic and trends research a unique perspective. She has an eye for what the rest of us miss, observing the changing patterns of culture through her kaleidoscope lens.



Email: sarah@recipe-design.com Christina Philpott
With an undergrad in product design from Central Saint Martin and Masters in progress, Christina sits firmly in the 'context is everything' camp. She is passionate about identifying where design can break down boundaries, provide opportunities and address real human need.
Email: christina@recipe-design.com Emma
Dunipace
An unlikely law graduate in a previous life, Emma's focus in the last ten years has been across multiple aspects of the design industry. Her curiosity and attention to detail have served her well in her commercial endeavors and her ability to join the dots and see the bigger picture helps her to deliver solutions for clients that consistently exceed their expectations.
Email: emma@recipe-design.com
INTERNATIONAL PHARMACEUTICAL INDUSTRY 43 www.international-pharma.com
IP Issues Surrounding Machine Learning and AI in the Pharmaceutical Space
When it comes to protecting technical innovations there are two broad strategies: keep it a trade secret or obtain a patent. It has long been the case that computer-implemented technologies and pharmaceutical technologies are technical fields where one or the other approach (trade secrets in the case of computers, patents in the case of pharmaceuticals) has been typically favoured. So, in the brave new field of applying advanced computational systems to the development of pharmaceuticals, how do we develop a strategy which satisfies both approaches to protecting technical innovations?
To do so, we must look at the reasoning behind the preference for each strategy and some of the problems faced by proprietors when protecting their innovations in these technical fields.
There can be little doubt that sophisticated dynamic computational systems, such as those dubbed “Artificial Intelligence” (AI) and “Machine Learning”, are being developed for use in all stages of drug design and development. Advanced computational systems are being used to reduce the costs associated with drug development, increase the number and variety of candidates for further testing and improve testing and screening of existing candidates, to name a few example applications.
Recent reports in the press would indicate that AI systems are getting reasonably powerful at developing new and potent biologically active compounds. For example, according to a report by The Verge “AI suggested 40,000 new possible chemical weapons in just six hours”.1 In this case, researchers were exploring how artificial intelligence could be used to develop biochemical weapons. Their findings were published in the journal “Nature Machine Intelligence”.2
So, what sort of strategy should be adopted for a system that can potentially identify 40,000 biologically active compounds in six hours and what about the biologically active compounds themselves?
Patents
The rise of the application of AI and machine learning in the fields of healthcare and drug development has inevitably led to a corresponding rise in patent applications in this crossover field. Therefore, questions regarding what and how to effectively protect developments made in improving and adapting AI and machine learning in various aspects of pharmaceutical development are being frequently raised and discussed.
Where these computational systems assist inventors in a meaningful way, it follows that there must be some technical and patentable consideration of what parameters of the systems are required for the effective use of the system. The development and suitability of such systems for drug development must, many argue, require technical and practical consideration.
Not only do the computational systems themselves represent considerable value to applicants and inventors but also the ability of such algorithms, software, or systems to develop new candidates for drug therapies, screen existing candidates, provide in silico models, or develop diagnostics (to name a few). In other words, there is real value in the output of the system as well as the system itself. However, claiming the output of the system based on the virtue of the system itself runs headlong into well-established principles of patent law.
Issues Relating to Patents
Patents and patent applications regarding AI and machine learning face their own challenges. In 2018, the European Patent Office (EPO) amended their Guidelines for Examination to include a section on artificial intelligence and machine learning making clear that such inventions would be considered as other computer-implemented inventions and assessed under the EPO’s well-established framework considering technical character, technical contribution and technical effect of the subject matter of the invention.
G-II, 3.3.1 of the 2022 edition of the EPO’s Guidelines for Examination provides the following guidance on potential technical application for AI and machine learning:
“Artificial intelligence and machine learning find applications in various fields of technology. For example, the use of a neural network in a heart monitoring apparatus for the purpose of identifying irregular heartbeats makes a technical contribution. The classification of digital images, videos, audio or speech signals based on lowlevel features (e.g. edges or pixel attributes for images) are further typical technical applications of classification algorithms.”
Meanwhile, in 2020, the United States Patent and Trademark Office (USPTO) released a report on “Public Views on Artificial Intelligence and Intellectual Property Policy”, which also indicated that “AI inventions should not be treated any differently than other computer-implemented invention”. Thus, the USPTO determines patent-eligibility of AI and machine learning related inventions based on the existing test which evaluates whether such inventions fall into the judicial exceptions, such as being an abstract idea. Finding that an invention has a practical application often helps to ensure that the invention falls outside the judicial exceptions, and thus is patent-eligible.
The patent system therefore appears to be appropriate for protection of innovation relating to AI and/or machine learning systems which are applied to the practical and technical problems associated with pharmaceutical development.
It is worth noting that the utilisation of AI and machine learning systems in pharmaceutical development, as with other computer-implemented inventions, may have a stronger and more straight forward case for falling outside the judicial exceptions in the US than being found to provide a technical solution to a technical problem as required at the EPO. Some systems may therefore have a better chance before the USPTO than the EPO and as such may require different patentability considerations for each jurisdiction.
Claims
to Products Resulting from an AI/ ML Process
Patents appear to be a suitable means for protecting the underlying AI or machine learning system directed to solving a
44 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4 Technology
practical or technical problem in developing or screening pharmaceutical products, but what about the products themselves?
Both the USPTO and EPO require some structure or technical content to be imparted on the product by the inventive process in order for such product claims to be found patentable.
Guidelines for Examination at the EPO recite:
“The technical content of the invention lies not in the process per se, but rather in the technical properties imparted to the product by the process.” (F-IV, 4.12)
Whilst the Manual of Patent Examining Procedure at the USPTO provides:
“Product-by-process claims are not limited to the manipulations of the recited steps, only the structure implied by the steps.” (Section 2113)
Therefore, claims directed to the products of the AI or machine learning systems must have some structural and technical property imparted on them by virtue of being produced by the AI or machine learning system which renders the product novel and inventive in its own right.
Application of Known AI/ML Process to Novel Purpose
A further consideration for the application of AI or machine learning processes in the development of pharmaceuticals is the application of such processes in which the process is known but the application is novel.

At the EPO, the novel purpose of a known process would have to apply such a known process in a non-obvious way and have for example a new and surprising effect or would have to overcome technical difficulties not resolvable by routine techniques.
AI/ML as a Routine Technique
AI or machine learning inventions directed to developing new drugs or otherwise deriving their technical character from undisclosed applications and effects run a high risk of facing patentability issues in the EPO or AI or machine learning inventions directed to developing new drugs or otherwise deriving their technical character from undisclosed applications and effects run a high risk of facing challenges in the EPO. The EPO would consider whether the disclosure is sufficient that it was plausible that such effects would arise or that such effects arise across the entire scope of the claims.
The challenge for inventions of this nature will be to navigate inventive step and sufficiency requirements. The applicant must try to show that the skilled person would understand the undisclosed and technical application well enough to implement the invention. The applicant must also prove that the functional elements of the system are sufficiently distinct from the prior art meaning the skilled person would not find the system itself to be obvious over the prior art.
In other words, could generic or known AI systems be considered tools for routine experimentation like other known tools and thereby render a novel and inventive application of such tools plausible?
If so, are there aspects of such systems that are not routine and have a new and surprising effect? An applicant must consider what elements of the utilised AI/machine learning system are known or routine and what elements differ in their application sufficiently to be suitable grounds of a patent application. Above all else, such a distinction must be described in sufficient technical detail and the new and inventive patentable aspects delineated from that which is known or routine.
Trade Secrets and Data Access
There are valuable aspects of the innovation associated with computerised systems implemented in the development of valuable end products that may not be suitable for the patent system alone in its current form.
Provisions for trade secrets provide an alternative and/or supplementary mechanism to the patent system for protecting innovations of a technical nature.
The protection afforded by trade secret provisions is automatic for as long as the requirements of the relevant trade secret laws are met e.g., keeping the relevant information secret.
However, technology that requires regulatory approval (and therefore detailed disclosure), may not be suitable for complete reliance on trade secret provisions. Pharmaceutical technology, for example, cannot rely on trade secret provisions to the extent that the technology needs to be disclosed to regulators for market approval.
US and European Trade Secret Law
In the US, a trade secret is information that the proprietor has taken reasonable steps to keep secret and that has commercial value by virtue of it being a secret. However, as
mentioned above, protection only lasts for as long as these conditions are met.
Information would stop being a trade secret if it ceased to be a secret or if the owner failed to maintain reasonable measures to maintain its secrecy.3
Similar standards for trade secrets have been introduced into European law by EU Directive (2016/943).
In accordance with the EU Directive 2016/943 on trade secrets, all EU members at the time (including the UK) unified their provisions for the protection of trade secrets and brought their requirements largely in line with those in the US.
Namely, the requirements that a trade secret be information that is (i) secret (ii) has commercial value because it is secret and (iii) has been subject to reasonable steps under the circumstances to keep it secret (see Article 2 of EU Directive 2016/943).
A key consideration, therefore, for highly valuable information relating to technology for the development of pharmaceutical products is whether the relevant information can be successfully kept secret and what reasonable steps must be maintained.
Pharmaceutical innovations usually have an associated obligation of disclosure to regulators and remain commercially significant throughout the term of a patent and beyond, whilst computer-implemented technologies can be made difficult to reverse engineer (such as with SaaS models) and access can more easily be restricted so the risk of inadvertent disclosure to the public can be significantly reduced. Computerimplemented technologies are also more often made redundant before the end of the term of a patent.
Figure 1 below illustrates an example IP strategy for an AI or Machine Learning technology with a pharmaceutical application:
INTERNATIONAL PHARMACEUTICAL INDUSTRY 45 www.international-pharma.com
Technology
Figure 1
In relation to taking reasonable steps for technology that is suitable for being kept secret, examples of reasonable steps may include: identifying and labelling secret information; informing and agreeing confidentiality with those who have access; and managing security risks such as encrypting the relevant information.
As with all matters of legal enforcement, the collection and maintenance of evidence is key. In the case of trade secrets this means data about the data or metadata should be collected and maintained.
It should also be noted that, according to a research article from the University of Oxford, the more widely information is shared within an organisation, the less time until eventual disclosure.1 Table 4 of the article indicates that to keep something secret for 20 years, no more than 628 people can have knowledge of the secret.
Strategic Considerations
In consideration of all of the above, a strategy including patent and trade secret provisions across both Europe and the US is most likely to be the best way to sufficiently protect valuable
developments of AI and machine learning systems in the field of pharmaceuticals.


A significant consideration in such a strategy should balance the practicalities of protecting secret information from unauthorised disclosure over time and the suitability of information for patent protection.
Where possible and when trade secret laws are being relied upon, access to information should be limited on a need-toknow basis and where there is a significant risk of disclosure or leaking of information a patent strategy should be formulated.
REFERENCES
1. https://www.theverge.com/2022/3/17/ 22983197/ai-new-possible-chemical-weaponsgenerative-models-vx
2. https://www.nature.com/articles/s42256022-00465-9.epdf?sharing_token=UCJCaT3-Yj ZPTWMrG35GNdRgN0jAjWel9jnR3ZoTv0M6Vu GuVWKcBJFL5U5ocXOA5zcnGmZOUPQzouuai7 vI0XuOG1hxcfSUpHakkMxyD1NjtXRFBgFxUa9Z QI7okPtQc-7YkJa4BSKUXZqV75Cr1BQONFfkK_ B6nn67L7Rh7c-23ugni1vyTrxuaAQHfy0mVPCQud xiUoC7EDT7mfI0-K42ZlKZYo1xU6ctJRaGASE%3D &tracking_referrer=www.theverge.com
3. For more on legal protections for US trade
secrets please see here: https://www.finnegan. com/a/web/316168/PUBLISHED-BloombergLaw-Legal-Protections-for-U.S.pdf
4. https://journals.plos.org/plosone/article?id= 10.1371/journal.pone.0147905 [On the Viability of Conspiratorial Beliefs – David Robert Grimes, University of Oxford]
Yelena Morozova
Yelena Morozova, international IP firm

Finnegan, with a professional career spanning across three countries and with more than fifteen years of legal experience across two continents, Yelena's unique background enables her to understand cultural nuances and helps her to advise a broad range of clients across the world. Qualified as a patent attorney in the United States and Europe, Yelena focuses her practice on patent procurement and portfolio development in all fields of engineering on both sides of the Atlantic.
Nicholas Fox
Nicholas Fox, international IP firm

Finnegan, practices intellectual property law with a focus on electronics, telecoms, and software patent litigation. In addition to being qualified as a solicitor, he is also qualified as a European and Chartered British patent attorney, with full rights of audience to appear in intellectual property proceedings at all levels in the English High Court. He is also qualified and admitted as an attorney in New York.
Harry Muttock
Harry Muttock, international IP firm
Finnegan, is a Chartered UK and European patent attorney with experience in a broad range of technical fields, ranging from biotechnologies to computer-implemented inventions. He is also qualified as a patent attorney litigator in the UK.

46 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4 Technology





INTERNATIONAL PHARMACEUTICAL INDUSTRY 47 www.international-pharma.com Calling all pharmaceutical packaging suppliers. We want you! Connect in Pharma is the hub connecting the pharma and biopharma communities. Showcase your products and generate ROI by networking with key decision makers. 14 & 15 June 2023 | Palexpo, Geneva Scan the QR code to register your interest in exhibiting. Discover our community > connectinpharma.com
Strategic Intellectual Property Considerations for Protecting AI Innovations in Life Sciences
Artificial intelligence (“AI”) is all around us. It allows us to unlock our smartphones with just a glance. It can customise the temperature of our home or recommend television shows based on things we enjoyed watching before. It may soon drive our cars for us. Through the combination of increasing computing power and massive amounts of data, AI has made unprecedented advances in recent years in its ability to make predictions and solve problems. As a result, AI has become a vital part of our everyday lives.
And soon, the medications we take each day may also be identified and developed at least in part by AI. This article examines strategic intellectual property considerations for innovative pharmaceutical and biotechnology companies that are developing AI systems or using third-party systems to enhance drug discovery, clinical trials, manufacturing, or other processes.
I. AI Is Transforming the Life Sciences Industry
AI and machine learning (“ML”) are revolutionising the pharmaceutical and biotechnology industries. While drug discovery may be the most well-known use of AI and ML in these fields, the technologies have a wide range of other applications in these industries, as shown in Figure 1 below. AI and ML are also accelerating innovation in developing pharmaceutical formulations, predicting protein structures, designing clinical trials
and analysing the data, and speeding up manufacturing and ensuring better quality control.1,2,3
For many life sciences companies, data such as compound libraries may be among their most valuable assets. AI allows companies to leverage those data to more rapidly identify drug targets and advance them through clinical trials. As shown in Figure 2, AI can use those data sets to predict which compounds might have desired chemical or biological properties, drastically reducing the time needed to identify candidates for further laboratory or clinical testing.

AI thus has the power to reduce the time and costs of drug discovery and increase the number of new therapies available. A recent analysis by Morgan Stanley Research concluded that even modest improvements in early-stage drug development success rates made possible by AI and ML could lead to an additional 50 novel therapies over a 10year period, reflecting a $50 billion market opportunity.6
It is therefore no surprise that pharmaceutical and biotechnology companies are racing to implement AI and ML to improve their pipeline and reduce costs. Indeed,
Figure 2. A workflow applying AI to accelerate lead compound identification
As just one recent example, the biotechnology company Evotec recently announced a phase 1 clinical trial on an anticancer molecule that was co-invented and developed in partnership with Exscientia, whose AI platform technology computationally analyses the properties of millions of smallmolecule candidates to identify a handful suitable for further testing.4,5 Using AI allowed the companies to identify the candidate molecule in just 8 months.
a recent survey of pharmaceutical and biotechnology professionals indicated that 80% were already using AI technologies in their work or were planning to do so.4 AI is critical to remaining competitive in the pharmaceutical field by reducing the high costs of bringing new drugs to market.
Given the rapid pace at which pharmaceutical and biotechnology companies are developing or adopting AI, companies must have a plan to safeguard their innovations and avoid common intellectual property (“IP”) pitfalls.
II. Claim Strategies to Satisfy Subject Matter Eligibility Requirements for AIRelated Inventions

Figure 1: Application of AI in various aspects of the pharmaceutical industry
One of the most critical issues facing AI and ML inventions is the increasing difficulty of meeting the patent eligibility requirement under 35 U.S.C. § 101, particularly for softwareand computer-implemented inventions. The Supreme Court’s decision in Alice Corp. Pty. Ltd. v. CLS Bank International created a two-part test for determining patenteligibility, which has led to more patents

48 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4 Technology
being invalidated.8 The first step under Alice asks whether the claims are “directed to” a patent-ineligible abstract idea, natural phenomenon, or law of nature. Under the second Alice step, claims that are directed to such a concept are only patent eligible if they contain an “inventive concept” sufficient to transform any underlying abstract idea or law of nature into a patent-eligible application. The prohibition on patenting abstract ideas, laws of nature, and natural phenomenon has proven particularly problematic for AI- and ML-based inventions, which are often rejected as being directed to an abstract idea based on their reliance on mathematical formulas or algorithms to accelerate processes that might otherwise be performed by humans.
Alice’s subject matter eligibility framework has made it increasingly difficult to obtain patents covering computer-implemented technology, including AI. And in litigation, patent owners now routinely see motions to dismiss based on Section 101 challenges, which can result in an early ruling of invalidity before the case even gets going.
So, what can companies do to obtain and protect patents covering AI and ML inventions? Recent cases provide some guidance. In CardioNet, LLC v. InfoBionic, Inc., for example, the U.S. Court of Appeals for the Federal Circuit reversed a district court decision dismissing a patent owner’s infringement claims and invalidating the patent under Section 101. The Court concluded that the claims, which recited cardiac monitoring systems, were directed to an improved cardiac monitoring device, not merely the abstract idea of distinguishing between atrial fibrillation and flutter based on the variability of the irregular heartbeat.9 The Court credited statements in the patent’s written description explaining how the invention achieves technological improvement over past monitoring devices and noted that the claims “‘focus on a specific means or method that improves’ cardiac monitoring technology.”10
Similarly, in Visual Memory LLC v. NVIDIA Corp., the Court reversed a district court decision dismissing an infringement suit and invalidating the patent under Section 101.11 The claims in Visual Memory were directed to a computer memory system that improved performance by using certain “programmable operational characteristics” to control how data is stored in different types of memory based on the type of processor connected to the system. The Court held at step one of the Alice inquiry that the claims were “directed to an improved computer memory system, not to
the abstract idea of categorial data storage.”12
As in CardioNet, the Court credited details in the specification regarding how the memory system reflected a technological improvement over prior systems and the advantages made possible by that technological improvement.13
Federal Circuit cases also show common features of patent claims that fail to meet today’s heightened Section 101 standard. Of particular relevance for AI and ML inventions, courts routinely hold claims ineligible that recite collecting, analysing, and reporting data. In Bot M8 LLC v. Sony Corp. of America, for example, the Court upheld summary judgment that a patent was invalid under Section 101.14 The district court concluded that claims directed to increasing or decreasing the difficulty of a video game based on the players’ previous performance was directed to an abstract idea, and that the claims failed to provide any “inventive concept” under Alice step two because they involved only “the conventional computer task of gathering, manipulating, transmitting, and using data.”15
The Federal Circuit affirmed, noting that “neither the patent specification, patent owner, or patent owner’s experts articulate a technological problem solved by” the patent.16
These cases show the importance of drafting claims that reflect a technological improvement over the prior art and do more than manipulate data using conventional computer components. Further, the patent specification must detail how the claimed invention improves the underlying technology and the resulting advantages. Including these statements in the patent is particularly important for surviving a motion to dismiss, which takes place early in the case and is usually decided based solely on the contends of the complaint and the patent itself.
III. Can an AI System Be an Inventor? One interesting question regarding AI-derived inventions has been answered recently. During drug discovery, an AI algorithm may be used to derive a new compound with a particular therapeutic effect. But can an AI system be an inventor? In a recent test case, Thaler v. Vidal, the Federal Circuit held that an AI system cannot be an inventor under U.S. law.
Dr. Stephen Thaler created an AI system called DABUS, or “device for the autonomous bootstrapping of unified sentience.” Dr. Thaler contends that DABUS created two inventions on its own — an interlocking container system and a controllable light source — without any contributions from him. He filed patent
applications on those inventions in several countries designating DABUS as the sole inventor, leading to decisions by patent offices and courts around the world on whether an AI system can “invent” a patent.17
The U.S. Patent and Trademark Office (USPTO) rejected two patent applications naming DABUS as the inventor.18 Dr. Thaler challenged those decisions up to the Federal Circuit, which upheld the determination that an “inventor” under the Patent Act must be a human.19,20 The Court reasoned that the patent statute requires that an inventor be an “individual,” which refers to a natural person and not a computer system.21
Most other countries have reached the same conclusion. The European Patent Office (EPO), for example, rejected an application naming DABUS as the inventor, and the EPO Board of Appeals confirmed that a named inventor must be a human for the EPO to grant a patent.22 The United Kingdom Intellectual Property Office rejected corresponding applications for similar reasons. The UK Supreme Court of the United Kingdom plans to consider the case on appeal.23 In Australia, a federal court initially held that DABUS could be listed as an inventor,24 but a higher court reversed the decision, bringing Australia back in line with the United States and Europe.25 So far, only one country determined that an AI system can be an inventor. In July 2021, the South African Companies and Intellectual Property Commission accepted Dr. Thaler’s application and granted the first patent in the world naming AI as the inventor.26
While the United States and most other countries have concluded that patents may only list human inventors, there are still some strategic considerations companies should keep in mind. The written description requirement of Section 112 requires a patent specification to include sufficient detail to show that the inventors had possession of the full scope of the claimed invention. The amount of detail required will vary depending on the role AI played in the invention and, depending on the invention claimed, companies should consider whether the creators of the AI system should be listed as inventors. A patent specification must also contain sufficient detail to enable a person of ordinary skill in the relevant art to practice the claimed invention without undue experimentation. It could pose enablement problems if the listed inventors of an AIderived invention cannot describe how to make the claimed invention because it arose from the operation of a machine learning
INTERNATIONAL PHARMACEUTICAL INDUSTRY 49 www.international-pharma.com
Technology
process that the inventors may not be able to recreate.
IV. Trade Secrets Are an Important Part of Protecting AI Inventions
Patents are a vital piece of protecting AI innovations, particularly for innovator pharmaceutical companies seeking to protect new chemical entities and associated methods of treatment. The right to exclude others from making, using, selling, and importing the claimed invention allows patent owners to erect a significant barrier to market entry that can deter competition and protect the patent owner’s freedom to operate.
Yet, for innovations that rely heavily on data and know-how, for which it can be challenging to obtain patents, trade secret protection is an important aspect of IP protection. For example, certain aspects of new model-training methodologies, optimising model parameters, negative knowhow (i.e., what not to do), and many other data-driven aspects of AI systems may face an uphill climb given current patent eligibility requirements. For such innovations, even if you obtain a patent, it can also be difficult to establish infringement by a competitor who you suspect is using your technology. For those kinds of innovations, trade secrets can provide robust IP protection if proper steps are taken to ensure confidentiality.
Trade secrets can protect any information that derives independent economic value from not being generally known or ascertainable through proper means. That could include data about protein structure, customer lists, machine learning algorithms, source code, chemical process parameters such as reaction temperature or pressure, and nearly any other kind of information. And unlike a patent, which provides a limited period of protection (generally, 20 years from the date of filing), a trade secret can endure for as long as the information remains secret and continues to have value.
Trade secrets do have certain disadvantages. For example, trade secrets do not protect you if a competitor independently develops the same information or technology. A competitor could even file a patent application seeking to protect something your company had held as a trade secret. Nor does a trade secret protect against reverse engineering. And, once the information is no longer secret, the trade secret right is extinguished.
Companies that have valuable data should ensure they have adequate procedures to
protect their secrecy. That includes identifying and labelling trade secrets, limiting access to the smallest number of people who need to see the information, conducting trainings to ensure employees understand their obligations to safeguard confidential information, requiring nondisclosure agreements and restrictive licenses with third parties, maintaining cybersecurity policies, and enacting robust onboarding and offboarding procedures.
Pharmaceutical companies should consider a hybrid approach for protecting AI-related innovations. For example, proprietary raw and training data, optimised model parameters, implementation know-how for training and utilising models, and other confidential information covering aspects of AI that are difficult to reverse engineer may be particularly well-suited for trade secret protection. Meanwhile, other aspects of the technology, such as the AI system or a drug developed using an AI system, can be protected by patents. Companies should also carefully consider what information their scientists publish until they have decided whether to keep that information as a trade secret or to seek patent protection.
V. AI Partnerships and IP Ownership
Because life sciences companies may lack expertise in software and computer system development, many engage in research agreements or partnerships with other industry partners. These collaborations often raise IP issues, such as inventorship and ownership of any IP generated through the project, rights to preexisting IP, and the parties’ rights upon termination of the collaboration.
Companies should evaluate these IP issues as early as possible, ideally before the project starts, to avoid any potential issues from frustrating business goals. For example, contracts that define IP ownership and the ownership rights of the data, AI system, AI implementation know-how, and AI-created inventions in relation to the collaboration can help reduce disputes and foster partnership. Nondisclosure agreements are also a critical aspect of any joint venture, especially if trade secret protection is contemplated.
VI. Conclusion
AI and ML have enormous potential to accelerate drug discovery and decrease costs, allowing innovator pharmaceutical companies to bring more new therapies to market. As life science companies boost investment in AI, carefully considering IP strategy can give them a competitive edge
by protecting their innovations and giving them freedom to operate.
Disclaimer
These materials have been prepared solely for educational and entertainment purposes to contribute to the understanding of U.S. intellectual property law. These materials reflect only the personal views of the authors and are not individualised legal advice. It is understood that each case is fact-specific, and that the appropriate solution in any case will vary. Therefore, these materials may or may not be relevant to any particular situation. Thus, the authors and FINNEGAN, HENDERSON, FARABOW, GARRETT & DUNNER, LLP (including Finnegan Europe LLP, and Fei Han Foreign Legal Affairs Law Firm), cannot be bound either philosophically or as representatives of their various present and future clients to the comments expressed in these materials. The presentation of these materials does not establish any form of attorney-client relationship with these authors or FINNEGAN, HENDERSON, FARABOW, GARRETT & DUNNER, LLP (including Finnegan Europe LLP, and Fei Han Foreign Legal Affairs Law Firm). While every attempt was made to ensure that these materials are accurate, errors or omissions may be contained therein, for which any liability is disclaimed.
REFERENCES
1. Calum Chace, First Wholly AI-Developed Drug Enters Phase I Trials, Forbes (Feb. 25, 2022), https://www.forbes.com/sites/calumchace/ 2022/02/25/first-wholly-ai-developed-drugenters-phase-1-trials/?sh=485c05f52680.
2. Harrer, S. et al., Artificial Intelligence for Clinical Trial Design. Trends in Pharmacological Sciences, Volume 40, Issue 8, 577–591 (2019)
3. Weissler, E.H., et al. The role of machine learning in clinical research: transforming the future of evidence generation. Trials 22, 537 (2021). https:// doi.org/10.1186/s13063-021-05489-x
4. https://www.evotec.com/en/investor-relations/ news/p/evotec-and-exscientia-announce-startof-human-clinical-trials-of-novel-immunooncology-drug-6045
5. Calum Chace, First Wholly AI-Developed Drug Enters Phase I Trials, Forbes (Feb. 25, 2022), https:// www.forbes.com/sites/calumchace/2022/02/25/ first-wholly-ai-developed-drug-enters-phase-1trials/?sh=485c05f52680
6. https://www.morganstanley.com/ideas/ai-drugdiscovery
7. https://www2.iconplc.com/digitaldisruption infographic
8. Alice Corp. Pty. Ltd. v. CLS Bank Int’l, 573 U.S. 208 (2014).
9. CardioNet, LLC v. InfoBionic, Inc., 955 F.3d 1358 (Fed. Cir. 2020).
10. 955 F.3d at 1368.
11. Visual Memory LLC v. NVIDIA Corp., 867 F.3d 1253 (Fed. Cir. 2017).
50 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Technology
12. 867 F.3d at 1259.
13. 867 F.3d at 1269-60.
14. Bot M8 LLC v. Sony Corp. of Am., 4 4.th 1342, 135051 (Fed. Cir. 2021).
15. 4 4.th at 1351.
16. 4 4.th at 1358.
17. https://artificialinventor.com/patentapplications/.
18. Decision on Petition, Application Number 16/524,350, FlashPoint IP,Ltd.: Devices and Methods for Attracting Enhanced Attention. United States Patent and Trademark Office, 20 January 2020; https://www.uspto.gov/sites/ default/files/documents/16524350_22apr2020.pdf.
19. Thaler v. Hirshfeld, 558 F. Supp. 3d 238 (E.D. Va. 2021); 35 U.S.C. § 100(f) (“The term ‘inventor’ means the individual or, if a joint invention, the individuals collectively who invented or discovered the subject

matter of the invention.”); 35 U.S.C. § 101 (“Whoever invents or discovers any new and useful process, machine, manufacture, or composition of matter, or any new and useful improvement thereof, may obtain a patent therefor, subject to the conditions and requirements of this title.”).
20. Thaler v. Vidal, No. 2021-2347 (Fed. Cir. Aug. 2022), rehearing denied October 27, 2022.
21. 35 U.S.C. § 100: (f)The term “inventor” means the individual or, if a joint invention, the individuals collectively who invented or discovered the subject matter of the invention. 35 U.S.C. §101: Whoever invents or discovers any new and useful process, machine, manufacture, or composition of matter, or any new and useful improvement thereof, may obtain a patent therefor, subject to the conditions and requirements of this title.
22. Decision of the Receiving Section of the
Technology
European Patent Office posted on January 27, 2020 refusing European patent application No. 18275163.6 pursuant to Article 90(5) EPC.
23. Thaler v. Controller General of Patents, Trade Marks, and Designs [2022] UKSC 2021/0201.

24. Thaler v. Commissioner of Patents [2021] FCA 879 (Austl.).
25. Commissioner of Patents v. Thaler [2022] FCAFC 62 (Austl.).
26. South African Companies and Intellectual Property Commission Patent Journal, Vol. 54, No. 07, July 2021, 255.
Charles T. Collins-Chase
Charles Collins-Chase, International IP firm Finnegan, focuses on district court patent litigation and appeals before the U.S. Court of Appeals for the Federal Circuit. He uses his chemical engineering background to help clients protect innovations in pharmaceuticals and biotechnology, energy and renewables, and chemical products. He has assisted numerous clients in Hatch-Waxman (ANDA) litigation.
Kassandra Officer, International IP firm Finnegan, focuses on patent and trade secret litigation before U.S. district courts as well as on post-grant proceedings before the Patent Trial and Appeal Board (PTAB) of the U.S. Patent and Trademark Office (USPTO). Her practice encompasses a range of technologies, with an emphasis on chemicals, pharmaceuticals, and medical devices.

Xirui Zhang, Ph.D., International IP firm Finnegan, focuses on patent prosecution, portfolio development, strategic counseling, and post-grant proceedings before the PTAB. She works with companies of all sizes to plan and execute domestic and international portfolio development strategies tailored to the client's business goals.

INTERNATIONAL PHARMACEUTICAL INDUSTRY 51 www.international-pharma.com
Kassandra M. Officer
Xirui Zhang
Data-driven Processes Overtake Structured Document
Authoring
The strategic focus in life science technology investment is shifting from documents to data. Regulators are increasingly asking for data rather than documents and data-focused business processes, based on a single source of truth, are bringing efficiencies right across the organisation. Generis’ James Kelleher describes the implications of the transition away from structured document authoring.
Structured authoring was designed to be the future of document authoring – the ultimate efficiency in presenting information. But the world is now moving away from documents as the medium of business information exchange. In future, more and more information-based processes will be data driven. This is great news, suggesting an end to issues with version control and a more traceable line back to the master source of intelligence.
But it does mean that structured document authoring, as a much-anticipated technology proposition, is already obsolete – before it really had a chance to get off the ground. For document management technologists and their customers, this is likely to feel very frustrating. Certainly, it will require a big strategic adjustment. But the upside is that companies now have a chance to leap-frog straight to a solution that is much more fit for purpose, transformational, pliable and sustainable in the long term.
Limitations of Structured Document
Authoring
The original concept of structured document authoring, which dates back to the 1990s, is based on building routine documents from re-usable segments of content. However, this soon comes up against practical limitations. If the approved, reusable content assets are entire paragraphs or sentences, typically these will need to be tweaked for each use case, for instance. With each edit a new version of that content is created, with implications for change management.
In the meantime, the focus of Regulators and of recommended business practice more
generally, has shifted towards live data as the primary source of truth, and as a means of transforming processes. This move away from document-based submissions and reporting further erodes the business case for structured document authoring.

Although regulated documents as official records of a product won’t disappear overnight, their ’Best Before’ date is drawing ever nearer. During the latter stages of the transition to ISO IDMP compliance in the EU, for instance, published documents will be phased out in favour of rolling data-based submissions: data that regulators can choose to analyse in their own way.
Ultimately, data-based information exchange will become the preferred norm for regulatory submissions, PSMF (safety master) files and APQR (annual product quality review) reports. In fact, PV case file submissions in Europe are already submitted in data form.
Data Objects Are Key
Strategically, the focus of new content management investments must now be the
data itself, and how this is managed so that it can be used more dynamically for publication – without the risk of a future loss of integrity or consistency between the data and any associated narrative.
Next-level structured content authoring places the emphasis on ‘data objects’. That data object might be ‘Study 123 is a 3-day short-dose study in male rabbits’, for instance. Creating a narrative now means pulling in these ‘data objects’ and inserting minimal ‘joining text’ to make the data more readable in a particular context.
Here, if core information changes, updates can be made at a source level and automatically cascaded down through all use cases for that data object, without the need for extensive manual intervention.
Conditional text use becomes much easier to provide for, too, once the emphasis is on joining data objects rather than reusing entire sections of narrative. Now, rules can be set to the effect of: ‘If the study type is male rabbits, use X text’.
52 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4 Technology
This approach to content preparation offers much more dynamism and flexibility than a structured document authoring scenario. With the persisting diversity in requirements between the different Regulatory authorities, this controlled flexibility is very useful.
A Single Source of Truth
Moving away from documents and even from reusable content requires a different mindset, and this is probably one of the biggest barriers for companies currently.
Relying less on Word might seem to imply that teams will need to become proficient in XML. Yet this perception is tied up with the traditional treatment of content – in contrast to the new scenario where the focus is the master data and adding to this to enrich associated company-wide knowledge (around a given product and its evolving status), and where editing can be done in the new breed of user-friendly tools whether for data, Word or XML.
This is about teams from multiple functions all contributing to and enhancing one unified data source, rather than each
continuing to enter their own particular information of interest into their respective systems (Clinical, Regulatory/RIM, etc).
Data Objects – Foundation for Automation
The potential benefits of working with data objects are significant. At a conservative estimate, there is scope to reduce the effort of producing a final draft for approval by a factor of 10, thanks to the reduced specialist resources and manual steps needed in authoring and version control. That’s in addition to huge savings in the time and effort that would otherwise be needed to manage components – including decisions about the levels of granularity, rules around re-use, traceability of data into the output, and an entire migration of larger documents into smaller documents/components.
Outside the life sciences industry, there are strong precedents for using trusted data objects to construct content – in the airline and automotive industries, for instance, where precision, rigour and safety are as critical as they are in life sciences.

It is entirely possible for companies to skip a generation of automated content
authoring and go straight to a data-first approach to process management. The first step is to ensure data is accessible, of good quality, complete and current, and usable for the intended purposes. Once all this data is stored in a unified platform, a definitive ‘information lake’, it is ready to underpin a range of use cases. Companies can then start to add automation rules to use data in the right place at the right time, to streamline business and regulatory processes.
James Kelleher

James Kelleher is the founder and CEO of Generis, the creator of CARA™, a data and content management platform that helps companies in regulated industries, like Life Sciences, transform their complex business processes.
Web: www.generiscorp.com Email: james.kelleher@generiscorp.com














HIGH PURITY. HIGH DEMANDS.

INTERNATIONAL PHARMACEUTICAL INDUSTRY 53 Technology
Pressure regulators Control valves Pipeline ancillaries Special equipment Steam traps Safety valves High purity equipment for clean steam adca@valsteam.pt www.valsteam.com +351 236 959 060 Zona Ind. da Guia, Pav. 14 - Brejo 3105-467, Guia PBL PORTUGAL PRODUCTS MANUFACTURED IN PORTUGAL AV 001 AP EN 01.20
Pharmaceutical Tablet Coating –Achieving Perfect Coating Uniformity
Tablets are the most important oral dosage form in the pharmaceutical industry. Pharmaceutical film coating, a thin film made from one or more polymers (and usually other functional excipients such as color-pigments or surfactants) that can fulfil a variety of functions is applied to the tablet, represents nowadays an important process step in the pharmaceutical industry.
Derived originally from dragee pan processing, coating technology has developed continuously in the last decades. Most of the coating processes are performed for drug release modification, drug stability improvement against light or moisture and taste masking. Furthermore, patient compliance issues play an important role, as swallowability improvement or a simpler identification due to a different color.
Coating Uniformity
The quality requirements for coated tablets can also be versatile and different for each coating purpose. Simplest coatings only require a small minimum thickness. These are, for example, swallowing aids or simple taste and odor masking and the coating is often colorless. The coating uniformity within a batch only plays a subordinate role.
Cosmetic coating, where the tablet is colored with a pigment, or a dye is the next highest level of difficulty. The main arguments for a cosmetic coating are compliance, prevention of medication errors and marketing oriented. The quality requirement is that the tablets must be uniform within a batch as well as between produced batches and should have low surface roughness and sometimes high gloss (depending on the market).
When we are talking about tablets with a delayed release time in addition, the thickness of the tablets must be higher than the coatings for swallowing aids. Furthermore, the tablets must be coated with a high degree of uniformity, as
disintegration and release tests in various media must be passed within narrow limits according to pharmacopoeia requirements.

Coated tablets, used to control the delayed release of active ingredients and tablets that are coated with medicinal substances have the highest demands on the coating quality. Very high uniformities must absolutely be achieved, because otherwise the complex release profiles cannot be reproduced.
The introduction to the importance shows that the coating process is a very complex process in which the individual process operations must be precisely coordinated.
API Coating
API coating is getting more and more important in the last years because it enables fixed dose combinations or the combination of incompatible drugs. Furthermore, different drug release characteristics can be realised by applying for example sustained release coatings in addition to immediate release coating layers. These formulations can consist of up to four coating layers, which results to a long processing time. To be able to develop and produce such formulations successfully, coating uniformity is a prerequisite and a quality attribute, because coated tablets must pass the test on uniformity of dosage units according to the pharmacopoeias.
Tablet Coating Process
A good tablet coating process – consisting of simultaneous spraying, mixing, and drying processes – that meets the quality demands of the pharmaceutical manufacture, can
only be achieved with the optimal choice of the correct parameters.
L.B. Bohle (Ennigerloh, Germany), an innovative technology company in the planning and implementation of machines and processes for the pharmaceutical solids production, offers tablet coaters in laboratory and production scale.
For all its tablet coaters, L.B. Bohle relies on three design principles to achieve optimum coating results:
1. A pan geometry with an L/D ratio >1 offers a large tablet bed surface, which allows the incorporation of a high number of spray guns (Fig.1). Compared to other pan geometries on the market, process time can be saved up to 40% due to larger throughput of coating suspension. Besides the thinner tablet bed induces a minimum shear onto the tablets, which allows even the coating of very weak tablets.

2. The helical baffles inside the coating drum consists of two layers of baffles. They are responsible for the continuous and homogeneous axial mixing within the tablet bed. In addition, the drum rotation is maintaining the radial mixing. Both movements are a guarantee for a dead zone free tablet bed.
Thus, a homogeneous mixture in the tablet bed is usually achieved within a few minutes. Due to the constant tablet movement the tablets do not
54 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4 Manufacturing
Figure 1 – Different Types of Pan Geometry
KahleAutomation.com





Kahle® is dedicated to providing custom automation machinery solutions for the Medical Device, Pharmaceutical, and Healthcare Industries around the world.











Our ideas just got a whole lot brighter
We’ve merged with BBS Automation



Announcing a partnership in automation equipment that brings a whole new light to medical and pharmaceutical device manufacturing.

Visit www.KahleAutomation.com or contact Kahle@KahleAutomation.com U.S.A. | ITALY | CHINA














INTERNATIONAL PHARMACEUTICAL INDUSTRY 55
www.international-pharma.com
experience any acceleration peaks which could cause tablet damage or even twinning.
3. The air principle in all Bohle coaters utilises the drying capacity where it is most needed: in the tablet bed. Thus, most effectively the drying capacity of the inlet air is used without heating the rest of the coater inner parts. The inlet air is coming from below the tablet bed and is directly sucked through the rotating tablet bed into the exhaust air funnel. This setup also offers another advantage: The spray guns are not being heated during coating and remain cool. Therefore, spray losses are reduced to a minimum which leads to coating efficiencies of >>95% which is especially beneficial for API (Active Pharmaceutical Ingredient) coating processes.
Semi-Continuous Manufacturing of Coated Tablets

Continuous Manufacturing is still one of the hottest topics in the pharmaceutical industry: Throughout the past years, continuous manufacturing has become more important for both pharmaceutical companies and regulatory agencies world-wide. In line with the pharmaceutical industry's drive to convert many production processes to continuous, machine manu-facturers are developing coaters for continuous operation. These connect to a continuous production line and are designed to achieve the highest possible throughputs.
Beside conventional batch coaters, L.B. Bohle offers the KOCO semi-continuous coater for efficient film coating processes. Together with the ROB 50, a fully automatic tablet container hoist, these two jointly operating machines provide an integrated solution for an efficient and fully automated coating process in pharmaceutical production environments. With its automation concept, the combination of ROB 50 and KOCO 25 is designed to connect to a tablet press, either for existing batch-oriented production environments or to extend a continuous manufacturing line.
Process and Machine Concept
The machine combination of ROB 50 and KOCO 25 provides a turn-key solution to fluently integrate a semi-continuous coating process downstream of a tableting process. The main application is for tableting processes, operating for several hours at constant throughput. Examples are high
volume products in batch manufacturing, or continuous production lines.
The KOCO 25 is designed as a semicontinuous coater ensuring reliable throughput and constant residence time for all cores.
The process machine, as shown in Figure 2, is based on the proven, Bohle design for drum coaters.
The spirals ensure a homogeneous distribution and mixing of the tablets throughout the spray zone. Additionally, the process air both enters and exits the process chamber through the tablet bed, which in comparison to a typical, diagonal air flow reduces spray drying to a minimum.
The spray arm features an automatic adjustment of the spray angle and distance, carrying a total of six, two-substance spray nozzles (for KOCO 25). In addition, the spray system has recirculation and a single supply of spray nozzles to guarantee uniformity and
dependability in the coating suspension's application.
The KOCO 25 uses a product inlet port on top of the machine to feed tablet cores into an opening in the rear of the coating pan, in contrast to conventional batch coaters. Normally, this port is closed, and the product valve is only opened to fill the drum for a new coating cycle. The coated tablets are discharged through a port at the front of the coater.

The process control is designed to operate in a cyclic manner, to repetitively execute the defined recipe, each execution further denoted as cycle.
Process Cycle – Phases:
1. Feeding of the coating pan with a given amount of tablet cores through the inlet port.
2. Tablet bed warm up, commonly using the exhaust temperature as target parameter.
56 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Manufacturing
Figure 2 – Mechanical Design of the KOCO 25
Tablet coating is a decisive and demanding process step in pharmaceutical tablet production and can be subdivided into the basic operations spraying, blending, and drying. Each individual operation must be optimized in a careful and coordinated manner.
Tablets are mainly coated to achieve a modification of substance release, protect the substance against light and moisture or to cover the bitter flavor of the tablet formula.
3. Spraying of the suspension with drying air active, if necessary, following a spray profile with different spray rates.
4. Drying of the coated tablets.
5. Tablet bed cool down.
6. Discharging of the coated tablets through the outlet in the front door.
Due to the design advantages of the coating pan, air duct and spray system, the KOCO 25 can repetitively execute the coating cycle, without affecting the process and product quality. To allow for a fast
continuation of the next process cycle after discharging and filling new tablet cores, the coater features a bypass valve to keep the process air active.
The choice for a semi-continuous process was taken in order to comply with the requirements and expectations of the pharmaceutical industry: A truly continuous coating process is defined by tablets being provided to the process at a constant flow rate, passing through the actual process, and coated tablets continuously leaving


the process on the other end. However, as the behavior of the tablet cores to pass through the process cannot be controlled sufficiently, this will lead to wide residence time distributions and consequently varying exposure times of the tablet cores to the spraying process.
Especially for functional coatings, this will result in insufficient coating uniformity. Instead, the KOCO 25 as a semicontinuous coater has equal residence times for all tablet cores, in combination with the advantages of the helical mixing spirals.
Finally, the integration of a Raman spectroscopy probe head into the rear of the coating pan can be used for in-line monitoring of the process. Hence, the KOCO 25 is ready for PAT and improved process control, using Raman spectroscopy to determine the process end point.
Tobias Borgers
Tobias Borgers is a Marketing Professional, with a huge experience of multi-channel marketing initiatives. Proven abilities in creating successful exhibitions, integrated digital and traditional marketing campaigns, social media marketing, content management, lead generation, event, and project management. Tobias holds a B.A. from University of Duisburg-Essen and joined L.B. Bohle in 2012.

INTERNATIONAL PHARMACEUTICAL INDUSTRY 57 www.international-pharma.com
Laboratory coaters are suitable for small batch sizes and so often used for research and development. Some of them are also special equipped for containment applications.
Manufacturing
The Challenges of Increased Complexity in API Development and Manufacture
There is no getting away from it: the small molecule drugs now entering and travelling through the clinical pipeline are becoming more complex. This increasing complexity poses a variety of challenges that pharmaceutical and biotech companies will need to overcome.
First, there is the molecule itself. It may be that, as an integral part of the way it is designed to hit the target, it includes features and moieties that are difficult to make. Chiral molecules, for example, nowadays are unlikely to be progressed unless they are single enantiomers, and this requires chirally selective chemistry or separation processes to make them. The more chiral centres it contains, the greater the complexity of the synthesis is likely to be.
Complexity in the chemical structure might also result from functional groups that are difficult to handle or insert, or perhaps the molecule has one or more quaternary centres, which can be particularly challenging. Moreover, if the final molecule or intermediates are highly potent, their development and manufacture will require special handling procedures, including dedicated equipment with high containment, and trained personnel.
The chemistry required to make it might also be complex. While skilled process chemists will do their best to find alternatives, there are times when it is unavoidable. Some reactions require very low temperatures or high pressure. Or they might involve reagents that are particularly hazardous, perhaps because they are extremely toxic, or even explosive.
As an example, a client engaged us to make an API for Phase 1 studies where the synthesis involved an unstable intermediate within the synthetic route. This intermediate required very low temperatures to prevent degradation, and new equipment would be needed. The installation and qualification of this equipment had a long lead-time,
and added to the cost. Moreover, the workup and purification of the molecule were particularly laborious. The low stability of the intermediate and the related low purity (about 80%) had a knock-on effect on the subsequent step, which gave a yield of just 58%. The crude API also had low purity, which therefore also required a tedious purification.
An obvious change to make seemed to be to try switching to a different, more stable intermediate. This was successful, and the increased stability of the new intermediate meant that 97% purity could be achieved with a simple aqueous work-up followed by crystallisation. This increased purity improved the subsequent step, too, with an improved yield of 77%. A re-slurrying was all that was required to achieve the desired purity of the final API.
This change also removed the need for cryogenic conditions, and therefore the many months of delays that would have been caused by upgrading the kilolab could be avoided. In all, 5kg of the API ready for clinical trials was produced in just four months, thanks to the optimised route and process, with improved yield and product quality.
More Steps, More Complexity
Synthetic routes are getting longer, too, an increase in the number of steps clearly increases the complexity of the overall process. A good example that we worked on for a client involved the process development and kilo-scale manufacture of an API for Phase 1 clinical trials. The synthetic route involved eight chemical steps, and the overall yield was just 14%. The client required the Phase 1 batch to be completed in six months, and this timeline posed a significant challenge in the light of the overall low yield.
We took advantage of the skills and capabilities of scientists at several of our sites to solve the multitude of problems within the synthesis. Each of the eight steps was optimised at our facility in Nansha, China, including a mass balance study to aid in the optimisation of the overall yield. As an example, in one step the sequence
in which the material was charged was changed, cutting the amount of an impurity formed in the reaction from 10% to just 1.6%, with a consequent increase in yield. In the final step, slurrying the crude product rather than washing with acid and extracting proved effective, too.
Downstream particle engineering and encapsulation took place at our sites in Switzerland and Florida. This spread of talents enabled us to deliver the supplies within the required timeline, making about 3kg of API in a scalable process that had an overall yield of 29%. This was more than double that of the original process and represents an average 86% yield per step.
Another source of complexity comes with purification. However efficient the synthetic route to an API might be, if it cannot reach the required purity effectively then changes will have to be made, either to the synthetic steps or to the process by which it is being purified.
An example here comes in the form of a project for making a building block for an ADC linker for Phase 1 clinical supply. In the original process that came from the client, this could only be made as an oil, making purification and further processing distinctly challenging. Our first thoughts were to use a chromatographic technique for the final purification, but as the molecule was acid labile, it decomposed on the silica column, even though it had already been neutralised by base. This made it very difficult to improve the purity in this way.
The answer lay in developing a new workup procedure using heptane. This time, the pure product formed as an insoluble dispersed gel, and the impurities were extremely soluble. It could then be adsorbed onto celite, and this filtered off. A demo campaign in the kilolab scaled this celitebased process up, producing 600g of the oil at much higher purity than had previously been possible. Even better, it turned out that, with a purity in excess of 99%, the oil tended to crystallise. This could then be used to seed a larger scale crystallisation, and once this was implemented in the pilot plant, 8kg of crystalline product that was
58 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4 Manufacturing
99% pure was made – a far cry from the impure oil that had been made previously.
Complexity in Physical Properties
But the increasing complexity does not stop with the molecular structure and the synthesis – the molecule’s physical properties have an impact, too. There has been a noticeable trend in recent years towards molecules in the development pipeline being insoluble, sometimes to the extent that they resemble brick dust, being incredibly insoluble in water and organic solvents alike. If a molecule does not dissolve in water, it will not dissolve when the patient takes it, and therefore it will not be efficacious as its bioavailability will be negligible.
While solubility is an inherent property of the molecule, there are technical solutions that can be employed to improve it, such as using spray drying to transform it into an amorphous dispersion. It is also possible to use a mechanical method to enhance its dissolution properties, simply making the particle smaller via micronisation or milling.
Alternatively, changing its crystal form in some way may work. Sometimes, finding a different polymorph will suffice if it dissolves better. If the molecule has ionisable groups, then it is definitely worth checking to see if a salt form can be found that is more soluble. In the absence of ionisable groups, the answer may lie in forming a cocrystal instead.
Identifying the optimal physical form early in drug development is important if
changes in later phases are to be avoided.
Our team worked on a product that was initially developed as a free base for Phase 1 trials and, during the manufacturing campaign for Phase 2 supply, the customer decided to shift to a hydrochloride salt. This added complexity to the overall process, as the production campaign was already under way. Clearly, this switch required the process for the final API to be redesigned, and then optimised once more. There were two possible polymorphs of the HCl salt, and it was unclear which would be the best option.
The change was made at such a late stage that the penultimate step of the synthesis was already under way at a 100kg scale in the GMP facility, and the client wanted 10kg of the HCl salt at extremely short notice. The free base process was rapidly redeveloped to accommodate the formation of the HCl salt, alongside processes to create each of the two polymorphs of the salt. This enabled the physicochemical properties and stability of the two polymorphs to be assessed, allowing the client to make the final decision about which would be best to take forward into the clinic.
The required 10kg of salt form was delivered within two weeks – before the final API step was initiated in the GMP production plant. This highlights the importance of flexibility and agility in meeting the changing requirements during product development. Being able to change the kilolab plan immediately was key to the ability to meet the deadline for formulation development: the first batch of free base
from the GMP plant was released rapidly and diverted back to the kilolab for the salt formation step.

Regardless of the strategy employed to address complexity in all its forms, a skilled CDMO partner can be instrumental in success. They will have significant experience in working across a wide range of different molecules, and employing a range of techniques to solve problems ranging from chemistry challenges to solubility problems. This expertise can be critical in keeping to development timelines, and transforming a complex molecule into a successful medicine.
Giovanna Libralon serves as the Senior Director of Commercial Development in Europe and APAC for Early-Stage Small Molecules across Drug Substance, Particle Engineering and Drug Product. She received her bachelor’s degree in Pharmaceutical Chemistry and Technology from the University of Padova (Italy). Giovanna brings 20 years of pharmaceutical experience in process chemistry, manufacturing, and different commercial roles for both pharmaceutical and CDMO companies.
Email: giovanna.libralon@lonza.com

INTERNATIONAL PHARMACEUTICAL INDUSTRY 59 www.international-pharma.com Manufacturing
Giovanna Libralon
NCEs and API – Quality by Design
The development and manufacturing of NCE and API is striving for simplifying and shortening timelines, as well as for making more efficient use of chemicals, equipment and facilities. Currently, many pharmaceutical companies are developing green chemistry technologies, as a means to improve production efficiency and reduce costs by incorporating more environmentally friendly methods of green production into the synthesis of APIs and intermediates.
Medicilon is an integrated CRO providing comprehensive one-step new drug R&D for pharmaceutical companies and research institutions around the world. Located in Shanghai Nanhui Industrial Park and Hangzhou biovalley, Medicilon`s 180,000 sqm laboratory is equipped with a comprehensive library of instruments and is managed under a high-tech business model and philosophy, aimed at guaranteeing the quality and efficiency of any project undertaken. Bolstered by high-throughput chromatography and mass spectrometry, and advanced processing software, Medicilon sets high standards for compound screening and analysis, optimization of lead compounds, analysis of chemical and physical properties of compounds, and other drug R&D processes.
At Medicilon, chemistry and biology are ingrained in every project. Relying on a rich experience in innovative design and patent strategies that complement state-of-the-art technologies, the company`s chemistry team is capable of flexibly applying computer chemistry to assist compound design process. And perfectly equipped to take on multi-dimensional business such as custom synthesis, compound library construction, SAR compound synthesis and screening, compound structure and biological activity optimization.
PROTAC Drug Discovery Technology
Platform
At Medicilon, the Medicinal Chemistry Department has established a PROTAC drug discovery platform that contains popular target protein ligands. Medicilon has also set up libraries for high-affinity targeting
protein small molecule (TPSM) and small molecular fragments, libraries for highaffinity ubiquitin ligase small molecule (E3SM) and small molecular fragments, and linker systems that include diversified bifunctional linkers (BF-Linker).
These compound libraries help to quickly and efficiently synthesize a large number of high-activity PTROTAC bi-specific small molecules, thus greatly accelerating the process of drug R&D. Also, the company is committed to initiate and complete its PROTAC biological screening and testing platform, and the follow-up development of preclinical stages.
Nucleic Acid Drug R&D Platform
Medicilon`s nucleic acid drug R&D platform is an integrated and comprehensive solution that covers drug discovery, CMC, and preclinical research services. Based on a rigorous scientific attitude, an open-minded scientific spirit and advanced equipment, this integrated solution can meet the industry's research and development needs for cutting-edge innovative nucleic acid drugs, and undertake research programs like nucleic acid drug discovery, screening and preclinical research services for pharmaceutical companies and scientific research institutions worldwide.
Medicilon uses medicinal chemistry and computational chemistry to design and synthesize drug-like templates and libraries of compounds meant to increase clients' compound collections. The annual capacity of Medicilon`s library production is of more than 100,000 compounds.

Compound Druggability Evaluation
The process of new drug research is lengthy, high-risk, but at the same time very high reward. That`s why Medicilon provides druggability evaluation services that are proven to be the most effective in reducing risks.
The so-called druggability refers to the properties of those compounds that have the potential to be developed into a drug, and for which the preliminary pharmacodynamic study and early evaluation of pharmacokinetic properties and safety have already been
performed. It is translational research that helps to build a systematic R&D chain from basic research, preclinical research and clinical efficacy evaluation to new drug manufacturing and clinical application of innovative drugs, to smooth the interaction between the information and the research, between basic medicine science and biology and the R&D of innovative drug and clinical medicine; with the aim of shortening the research and development cycle of innovative drugs from laboratory synthesis to clinical application.
The druggability of a new drug creation includes druglikeness, physicochemical properties, biochemical properties, pharmacokinetics, and toxicity, etc. In the process of new drug development and clinical application, the various parameters of the in-vivo process of a compound (absorption, distribution, metabolism, excretion, ADME (toxic pharmacokinetics)) are an important indicator of its druggability.
Preformulation Study
Medicilon preformulation research features both formulation selection and pharmaceutical preparation. As for the low number of active pharmaceutical ingredients or candidate compounds with medicinal properties, the company provides professional preformulation services, exploring valuable information.
Route Selection
Generally, an API involves multiple process routes. The selection of routes will not only affect the possibility of industrial manufacturing, but also the material cost, product quality, and even the environment. Medicilon provides services that include the customization of initial API, as well as the design and determination of synthetic routes.
The company experts also analyse the feasibility of such routes, and the source of synthetic materials, checking if such routes are involved in intellectual property issues, if the cost is acceptable, and if such routes are in compliance with green chemistry principles. Only after that the time comes for conducting route selection, process optimization, quality research, and process verification to ensure project quality.
60 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Application Note





61 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4 FULLY INTEGRATED PRECLINICAL DRUG DISCOVERY AND DEVELOPMENT SERVICES Medicilon is an integrated contract research organization (CRO), providing comprehensive one-stop new drug R&D services from initial idea all the way through the Investigational New Drug (IND) filing phase for global pharmaceutical enterprises and scientific research institutions. Our services span across chemistry, biology, ADME, DMPK and safety evaluation studies. Our preclinical study labs are US FDA and China NMPA GLP and AAALAC accredited. The pilot and production line for small molecule are GMP facility. • Research Quality focused • Time efficiency with fast project turnover • Cost effective • Easy management with one stop drug discovery platform FULLY INTEGRATED SERVICES PLATFORM • Fast assembly of PROTAC molecules and PROTAC screening • Fast buildings of ADC payloads and ADC screening • DNA-Encoded Compound Library • SPR/BiaCore Testing platform • Protein expression and purification and crystallization biology platform • Inhalation drug safety R&D platform • Cellular Immunotherapies R&D platform (RNAi, CAR-T, mRNA vaccine) • Ophthalmic drug safety R&D platform T: +44 1223 981 792 E: nadinesu@medicilon.com W: www.medicilon.com Allia Future Business Centre, Kings Hedges Road, Cambridge, CB4 2HY, UK
Application Note
The medicinal chemistry team deeply cross-integrates chemistry and biology into each project, and flexibly uses the powerful expertise of computational chemistry to aid the compound design process. At the same time, Medicilon uses extensively advanced drug discovery technology, including PROTAC targeted protein degradation technology, DEL DNA-encoded small molecule compound library screening technology, ADC antibody drug conjugation technology, etc.
Medicilon’s API process route selection and optimization services include: route design and selection; salt form selection, research, and process development of crystal form; salt base selection; crystal form selection; crystal form research (labscale testing and kilogram-level); parameter optimization for determined route; statistical and experimental design, based on quality by design (QbD) principles and multivariate data analysis, as well as quality research on API and intermediates, development and verification of analytical methods and technology transfer and process verification.
With the evaluation of the selected route’ technological feasibility, usability of equipment, availability of raw materials and reagents, steps of reaction, patent protection, and environmental impact, Medicilon helps clients develop reliable, low-cost, safe, and environment-friendly mass-production API process routes for the selection of both emergency routes in the early stages of drug development, as well as the economic routes for formal drug development.
Technology Transfers
By continuously optimizing processes to obtain a mature and easy-to-industrialize process route, Medicilon sets up a database for key process parameters. According to the characteristics of process routes, a complete impurity profile of starting materials, intermediates, and raw materials is determined, so that the prepared API can meet generic drug requirements, thus enabling industrial production.
Early Pharmacokinetics
Discovery DMPK is an essential part of drug discovery, as it is conducive to the evaluation of compound properties in the early stage, playing an important role in R&D efficiency improvement and risk reduction in later stages. Medicilon is one of the first CRO companies in China to offer discovery DMPK services. The company relies on an experienced pharmacokinetic research team, as well as on the advanced platform
that provides fast and reliable early DMPK services for clients.
Why is Early DMPK Important?
In 1991, up to 40% of failures in the clinical phase of new drug development were associated with drug DMPK properties; in 2000, the likelihood of late failure was dramatically reduced to less than 10% as major pharmaceutical companies shifted to early DMPK studies. Early pharmacokinetic testing allows for a low-cost, short-term risk-benefit assessment of new drug development projects, guiding the processes from the optimization of lead compounds to the determination of preclinical drug candidate.
With 18+ years of accumulated experience, completing preclinical DMPK filing studies for about 20 new drugs each year and in vivo PK screening of >2000 compounds per year, Medicilon represents the one-stop-shop for PK/PD, antibody/ADC preclinical DMPK services and technical service solution for isotope drug metabolism research.
APIs
Currently, Medicilon features a cGMP-based API production line based on IND. From preclinical laboratory-scale testing and process development to commercialized production, Medicilon is meeting the industry needs throughout the comprehensive supply chain, including R&D, purchase and production. From the mg- and g-level to kg level, Medicilon`s processes allow flexible adjustments to fit in client innovative process R&D and scale production. From QBD-oriented process design to process R&D in laboratories, commercialized production to data-based filings, the analysis and quality inspection teams deliver professional services and comprehensive analytical research, including method development and verification, process verification, impurity identification and separation, API and intermediates research, and API stability tests.
With years of experience and the construction of laboratories, Medicilon Process Department can not only perform R&D, testing and stability studies of generic drugs for customers, but also R&D, production, testing and stability studies of innovative drugs in clinical phase I and phase II, gradually developing from process R&D to industrial commercial production and transforming from CRO to CDMO.
Chemical Drug Development
Medicilon offers the one-stop shop integrated
chemical drug R&D services including customized synthesis, medicinal chemistry, focused library preparation and process chemistry. Either in FTE or integrated project team arrangement, the company `s chemistry team is committed to helping clients discover novel and potent chemical series. Medicilon contribution has led to numerous preclinical and clinical candidates, also providing scaleup service to timely deliver kilograms of highquality compounds.
With the rapid development of the global pharmaceutical market and the division of labour in the pharmaceutical industry, the chain is becoming more and more refined, making specialised outsourcing in the pharmaceutical industry an important strategic choice for pharmaceutical companies. In the early stages of new drug development, FTE (Full-time equivalent) is often used by drug discovery companies to synthesize the required structural fragments and/or potential candidate compounds to accelerate the drug screening process.
As Medicilon offers a full range of chemistry research services covering all phases of any project requirements, clients can choose between the FFS (project-based payment) or FTE (full-time equivalent service) models.
Nadine is looking after business alliance with research and business partners for Medicilon UK and European markets.
Nadine Su has 15 years of experience in business development and project management in the pharmaceutical and healthcare industries. She successfully led and managed the novel drug research project and formed an international partnership to achieve over $20M in licensing deals. She has rich experience managing and developing novel technology drug discovery programs from early research to the clinical stage. Her leadership has contributed to the company achieving the “final list of the business award” twice in the Cambridge Business Award competition. Nadine has been educated in China and UK with a master's degree in International Business.
Email: nadinesu@medicilon.com

62 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Nadine Su
Media and Communications
IPI

Peer Reviewed, IPI looks into the best practice in outsourcing management for the Pharmaceutical and BioPharmaceutical industry.

www.international-pharma.com
JCS
Peer Reviewed, JCS provides you with the best practice guidelines for conducting global Clinical Trials. JCS is the specialist journal providing you with relevant articles which will help you to navigate emerging markets.

www.journalforclinicalstudies.com
IAHJ
Peer Reviewed, IAHJ looks into the entire outsourcing management of the Veterinary Drug, Veterinary Devices & Animal Food Development Industry.

www.international-animalhealth.com
IBI
Peer reviewed, IBI provides the biopharmaceutical industry with practical advice on managing bioprocessing and technology, upstream and downstream processing, manufacturing, regulations, formulation, scale-up/technology transfer, drug delivery, analytical testing and more.

www.international-biopharma.com

PNP
Pharma Nature Positive, is a platform for all stakeholders in this industry to influence decision making by regulators, governments, investors and other service providers to achieve Nature Net Positive Results. This journal will enable pharma the ability to choose the right services to attain this goal.

www.pharmanaturepositive.com
PHARMA’S DNA
Listen to industry experts on the latest in drug discovery, development, research, industry regulations and much more at Pharma,s DNA, the podcast channel by Senglobal Ltd., available on Sound Cloud, Spotify, iTunes and YouTube.
senglobalcoms.com
Demand, Design, Delivery: High Potent Packaging at PCI Pharma Services
In a fragmented marketplace, drug discovery organisations are increasingly looking to work with fewer outsourcing partners. As such, CDMOs that are able to provide true end-to-end services are becoming more in demand. By partnering with full-service CDMOs, drug discovery organisations simplify and de-risk their supply chain, saving both time and money by maintaining production under one roof, or within one organisation. Shaun Engelhardt, PCI Pharma Services’ Director of Engineering and Innovation, discusses how recent investments in their UK-based high potent facility has created this ideal scenario for clients.
Demand-led Investments in PCI
Drug products containing highly potent APIs (HPAPIs) present unique challenges to CDMOs, and not all of them have the true capability to manufacture or package them from clinical to commercial scale. PCI has significant experience in this arena, with our first Contained Manufacturing Facility (CMF) launched in 2013. With industryleading containment solutions capable of handling APIs down to an OEL of 0.01 µg/m3, and geometrically scalable equipment trains able to manufacture lab- and commercialscale batches, the CMF proved hugely successful.
However, PCI is always looking for ways to provide a greater level of services to our clients. As such, recent CAPEX investments have led to the construction of a brand-new potent packaging facility at the Tredegar site, alongside a second CMF that doubles our commercial-scale high potent manufacturing capacity. The result is a true end-to-end, integrated service solution for clients who need their highly potent solid oral products manufactured, packaged and distributed globally from a single site.
This investment is a significant milestone for PCI and particularly the Tredegar site, allowing an increased capacity to manufacture and package our clients’ products from clinical supply to commercial launch. By investing in these new facilities now, we are

confident that PCI can remain a major player in this arena for years to come.
Design Considerations
When designing such a facility, an important early step is for the team to consider what an ideal, best-in-class facility should include. Amongst these considerations were the needs and demands of the marketplace; any fundamental regulatory requirements; the industrial best practices, and whether any of these are likely to remain steady or change in the years to come. Once these aspects were determined, we can then identify a ‘wish list’ and an outline specification. For example, having an excellent flow of materials is vital, ensuring a seamless movement of the drug product from manufacture to primary and secondary packaging, and onto the final step of serialising the packaged product. Another important factor is ensuring a good flow of personnel in terms of how staff enter the facility, where they gown, and how they enter the production areas.
These expansions at the Tredegar facility are the largest in terms of footprint that the site has undertaken. As such, a great deal of consideration was required in terms of the aforementioned personnel and material flows, as well as the facility design, engineering requirements, environmental monitoring systems for the critical environments, and regulatory influences. The integration into the existing site was
therefore vital, particularly in light of any potential future site expansions.
The growing emphasis on small-volume products, such as orphan drugs or highly targeted therapies for very small patient populations, means that as a service provider, we need to build flexibility into our equipment to ensure we can cope with these requests. The new blister line installed within our new packaging suite is a key example of how we achieve this goal. For example, the installation of our first HAPA digital printer means that with just one reel of lidding foil, we can print artwork for multiple different market requirements on a single line, whilst retaining a high standard of control over airborne particulates. The result is considerable flexibility when packaging commercial products and a reduction in the waste of pre-printed materials, the latter being a key initiative in PCI’s Environmental, Social and Governance (ESG) commitments.
Due to PCI’s extensive experience in contained manufacturing and packaging at both clinical and commercial scale, we had a deep understanding of the equipment needed to ensure a successful expansion of the Tredegar site. By selecting the industry’s leading equipment for the new facility from our range of existing suppliers, this meant our staff were incorporating a known equipment train into the facility, with an established knowledge base from which to draw.
64 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4 Application
Note
This experience also meant that we understood that containment of highly potent products, throughout the process, was vital, not just for product protection but also the safety of our operational staff. For example, we assessed processes and containment levels by conducting SMEPAC testing, which involves running a surrogate drug through the production lines to model the generation of airborne particulates. We then analyse how well we are able to contain those particles, for example by ensuring a robust system involving the segregation of rooms, conditioned environments for packaging activities, dust extraction units and dedicated HVAC systems.
PCI Tredegar utilizes HVAC throughout the facility. In high risk areas, we have isolated conditions with a minimum of 20 air changes per hour, meaning air is constantly being circulated through the facility. As such, any loss of highly potent material is captured in the HVAC and drawn through very high classification filters. The HVACs also help provide a pressure cascade in the area.
Delivery Challenges: Cleaning, Regulation and Product Integrity
PCI Tredegar is a multi-product facility. We therefore factored very robust cleaning
procedures into the facility design. For example, the walls are made of an easily cleanable surface and the Ra (surface roughness) value of the equipment is 0.8 or less, which essentially provides a mirror finish to the equipment and prevents drug product from ingraining into the surface. This makes cleaning much more efficient and prevents the risk of contamination and carryover.
As automated cleaning methods are difficult to employ with packaging equipment,

we rely on manual cleaning techniques. We perform risk assessments on the equipment, identify the hard-to-clean areas, and create an ever-growing knowledge base of how to clean the equipment. By performing regular cleaning checks, we ensure that standard procedures remain robust and there remains no risk of carryover. Additionally, purchasing dedicated tooling as part of client onboarding allows us to manufacture and package products with an even greater reduced risk of contamination.

INTERNATIONAL PHARMACEUTICAL INDUSTRY 65 www.international-pharma.com
Application Note
As the pharmaceutical industry has a global supply chain, we at PCI have embedded Global regulations and industry best practice into our design, processes and procedures, ensuring the delivery of right first time quality products with increased customer satisfaction. Our team of dedicated experts on site are experienced in the preparation and hosting of Regulators from a range of

In recent years, several audits have highlighted the use of cardboard within our facility, leading to the implementation of policies to reduce this as much as possible
in the expansion. For example, we have introduced a de-boxing room as part of the new packaging facility, where raw materials and packaging materials are removed from the secondary packaging, cleaned within the de-boxing room, and then taken into the facility in polyethylene bags.
Additionally, the fundamental design of both sides of the production floor now separates the primary packaging from the subsequent secondary packaging using physical barriers, in line with regulatory requests.

To ensure a high degree of confidence that what is coming off the end of the line matches the client specification exactly, we installed specific systems on our automated production lines. For example, a sophisticated array of measures and checks on or bottling lines ensures the right label is applied to the right bottle, the desiccant is present, the bottle is sealed correctly, and the cap is tight enough. Our tablet-counting technology utilises EMF and infrared sensors play both sensors off against each other to ensure that both have seen the right count of product through the counting head. We also employ similarly smart technologies for capping, labelling and serialization in line with the EU Falsified Medicines Directive), and so on. Our serialisation line uses cameras that perform and enforce multiple checks and standards to reinforce finished product integrity.
Why PCI?
In spite of the global pandemic, PCI has
66 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4 Application
Note
Competent Authorities including MHRA, FDA, ANVISA, Turkish Ministry of health, Russian Trade and Industry ministry of health and PDMA.
Application Note
maintained focus on achieving continuous progress as a global organisation. By continuing to push forward in terms of building capability, capacity, adding new technologies and expertise, we feel confident that we are positioning ourselves as a major player in the CDMO arena.
PCI has been operating at the Tredegar site since 1985, providing a range of services to an international client base. In 2013, we reviewed our business model based on the demands of the marketplace and constructed our first, flagship Contained Manufacturing Facility (CMF), which was a significant investment in
our site capabilities. This met the growing demand for highly potent solid oral dosage forms, and was instrumental in the site’s success in the years that followed. This success led to PCI investing further, adding a second CMF which doubles our commercial manufacturing capacity, alongside the new high potent packaging facility. These new facilities will be operational in early 2023, with the increased capacity enabling PCI to become an even stronger CDMO partner. Our ability to supply highly targeted and lifesaving therapies to patients around the globe, from concept to commercialization, remains industry-leading, ensuring our clients products achieve speed to study, patient, approval and launch.


Shaun Engelhardt
Shaun has 17 years' experience in the pharmaceutical industry, working in a number of roles ranging from logistics to CAPEX programme management. In the latter role, Shaun oversaw the construction of Tredegar's new potent manufacturing and packaging facilities. He now serves as Director of Engineering and Innovation at PCI Tredegar.

INTERNATIONAL PHARMACEUTICAL INDUSTRY 67 www.international-pharma.com
What’s Next for Pharmaceutical Serialisation?
Supply chains for pharmaceutical products are exceptionally complex, with medicines and ingredients often crossing the borders of many countries before reaching the end consumer.

To protect patient health and safety, serialisation and track and trace requirements have become standard for pharmaceutical products worldwide. Legislations include the EU’s Falsified Medicine Directive (FMD) and the US Drug Supply Chain Security Act (DSCSA), which both necessitate serialisation and government reporting for prescription pharmaceutical products.
Spotlight on Safety
With increasing focus on consumer health and safety, the over-the-counter (OTC) market could likely be next for review. Counterfeit OTC medications can cause significant harm to consumers and arguably need the same protection as prescription-only ones. The possibility of purchasing OTC medicines from entities other than legitimate pharmacies, including online sellers, increases the potential for criminal activity.
New serialisation requirements in Russia, which came into effect in July 2020, cover all prescription and OTC medicines and set a clear precedent. While serialisation of OTC medicines is unlikely to be implemented in the immediate future, it is highly conceivable that EU and US legislation will be extended to OTC medicines in the coming years.
That said, when it comes to pharmaceutical products, serialisation can extend far beyond protection against counterfeit products, opening doors to increased patient health and safety in pharmacies, hospitals, and healthcare facilities. With more sophisticated serialisation of pharmaceuticals, healthcare staff can ensure that a medicine is not counterfeit and that the right patient gets the right dose, of the right medication, at the right time.
Individual Dose Identification Hospitals, pharmacies, and healthcare providers are realising the benefit of data
in helping to protect patient safety and are placing pressure on pharmaceutical manufacturers to provide a greater level of more granular information on pharmaceutical products than dictated by current pharmaceutical legislation.
Including a 2D code – containing information on the product, dose, batch code, and expiry date – on individual strips or blister packs, or even going so far as coding each pocket containing a tablet, can help to reduce the number of cases where patients unintendedly receive the wrong dose of the right medicine, the wrong medicine, or, in some cases, no medicine at all.
In some countries, pharmacists have a legal requirement to open medicine packs to take out and only sell the exact number of tablets that a patient needs. In these cases, all forms of verification and authentication

may disappear if machine-readable codes are only present on the carton pack from which their strips or blister packs have been separated.
Adding more granular data to strips and blister packs of medicines can allow for inventory control within hospitals, care homes, and other healthcare facilities to improve medicine distribution. Scanning 2D codes can allow for automatic electronic validation of medicines to ensure that patients are given the correct medicine. This level of detail decreases dispensing errors and can improve inventory management and stock control by allowing medications to be tracked down to the individual dose level.
In-line Product Printing
Until recently, most pharmaceutical manufacturers would buy blister foils pre-printed with product names, dosage information, and
68 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4 Packaging
Packaging
branding and use a basic in-line printing or embossing system to add the batch code and expiry date to the blister in human-readable text. The demand for more granular data will necessitate an upgrade to manufacturing equipment capable of printing variable information on blister foil packaging.
Printing in-line provides total flexibility and can allow manufacturers to respond much more quickly to changes in print requirements. In the past, manufacturers would typically have to wait several days or even weeks for their pre-printed foils to arrive in the event of a change in product design, e.g., due to a new legal requirement or need for a different language. With in-line digital printing, there is no need to wait for pre-printed foils to arrive, and manufacturers can switch from one design to the other in a fraction of the time. The technology also makes it economically viable to do much smaller batches of as little as 50 blisters or less.
One of the most significant benefits of digital printing solutions for in-line pharma is that many digital solutions are equipped to handle single dose serialisation, where individual 2D codes and serial numbers are printed on each pocket in a strip or blister pack without ever repeating the same code twice. By investing in a digital printing solution today, manufacturers can futureproof their production lines and prepare for future serialisation requirements.
Reduce Costs and Waste
When investing in a digital in-line printing solution, the price difference between a narrow printhead that is only suitable for printing variable information (i.e., 2D code, batch code, and expiry date), and a wider printhead that can also print larger graphics, including artwork, is often negligible compared with the possible savings. Wide web digital printing allows manufacturers to purchase only blank foils and carry out complete coding in-house, reducing stock requirements and inventory space. In addition, a significant saving can be made, as blank foils are less expensive than pre-printed, even when accounting for the cost of ink.
This new approach can also allow for significant waste reduction, helping pharmaceutical manufacturers reduce their environmental impact. Manufacturers typically order 10–20% extra when purchasing pre-printed foil to allow for unforeseen issues or wastage from set-up and product changeovers. However, in practice, they rarely need to use all the excess foil, and any excess
Serialisation Requirements for Prescription Pharmaceuticals
Since 9th February 2019, manufacturers of prescription pharmaceutical goods sold in the European Union have been required to add additional security labelling to enable serialisation, verification, and government reporting.
The EU Falsified Medicines Directive (EU FMD) requires that manufacturers mark prescription pharmaceuticals with a GS1 2D DataMatrix code, including four data elements – an individual product identifier, serial number, batch or lot number, and expiry date. Upon scanning, the DataMatrix code provides access to data transmitted to the European Medicines Verification System (EMVS) portal and corresponding national databases.
The medicine’s name, common name, pharmaceutical form, strength, pack size, pack type, serial number, and national reimbursement number for specific markets, are instantly accessible via the DataMatrix code. In addition, a record is
may be discarded. This is not an issue with blank foils, as manufacturers can reuse excess foil for subsequent print runs.
Much development has been done in the last couple of years to increase the availability of suitable inks for pharmaceutical coding.
UV curable inks are a standard application for metallic foil printing, and there are now many Swiss-List-approved, CMR-free variants available. There are also many water-based options suitable for paper-based packaging that deliver as much contrast as the classic UV drying inks – these are suitable for use in flexible papers, which are growing in popularity as blister pack seals.
Looking Ahead
The future of pharmaceutical serialisation is anything but clear; however, patient safety and counterfeit protection remain a top priority in the sector. Future regulations will likely expand the current requirements and force pharmaceutical manufacturers to provide a greater level of more granular product data.
Even without the prospect of a new regulation looming, pharmaceutical manufacturers are already under pressure from key industry stakeholders to provide additional
created each time a product is scanned, allowing the product in question to be tracked through the National Medicines Verification System (NMVS) at every stage of the supply chain.
Any inconsistencies that arise when products are scanned are flagged in the systems, and the respective party instantly rejects the medicine in question. This information is then passed on to the Medicines and Healthcare Products Regulatory Agency for further investigation into the product in question, and the company that manufactured it, if necessary.
Similar serialisation requirements are required under the US Drug Supply Chain Security Act and have been in force for pharmaceutical products sold in the US since 27th November 2017. All key players in the US pharma supply chain, including packagers, manufacturers, distributors, and dispensers, are required to generate, authenticate, and verify serial numbers for all packages travelling through the chain.
product data to protect patients’ safety and reduce the risk of errors.
By investing in digital printing solutions today, manufacturers can ensure they are prepared for any future serialisation requirements and benefit from cost and waste savings involved with printing the exact amount of packaging they need.
Bart Vansteenkiste
Domino's Global Life Sciences Sector Manager Bart Vansteenkiste has a 20-year history with the company, focusing on EU FMD legislation since 2011. He works with Domino's European OEM partners and trade associations, including the European Federation of Pharmaceutical Industries and Associations (EFPIA), and Medicines for Europe, focusing on the legislative and technical challenges facing the healthcare sector. A Dutch, English, French, and Spanish speaker, Bart regularly attends and presents at conferences worldwide on behalf of Domino.

INTERNATIONAL PHARMACEUTICAL INDUSTRY 69 www.international-pharma.com
Overcoming the Pitfalls of Pre-filled Syringe Filling
Michael Isele, Site Manager at Recipharm, explores the pitfalls of filling and packaging in pre-filled syringe formats, from sterile integrity requirements, to packaging challenges, such as kitting, explaining how these challenges can be addressed.
The international pre-filled syringe market was worth $3.6 billion in 2021, and is predicted to increase in value to $6.5 billion by 2030, growing at a CAGR of 7.1% throughout the forecast period.1
One of the key drivers for this projected growth has been a major change in the choice of injectable delivery formats following the COVID-19 pandemic.
Governments and pharmaceutical companies worked together to deliver an unprecedented global mass vaccination programme to protect patients from potentially fatal coronavirus symptoms. To deliver this, the pharmaceutical industry focused on developing effective vaccines in a short timeframe, usually filled into vials.
While this approach was successful in achieving its goals, areas for further improvement were flagged, particularly when it came to maximising the number of people vaccinated every day. Every time a patient arrived for their injection, a syringe had to be prepared and filled from a vial. The cumulative impact of the time spent carrying out this process for each appointment was significant, restricting the number of vaccinations that could take place each day.
For future outbreaks, it is important to identify ways of allowing doses to be administered quickly and efficiently to maximise the number of people vaccinated per day. Pre-filled syringes offered an ideal way of achieving this goal, as they arrive ready-prepared with the required dosage inside, streamlining the preparation process for each individual administration.
Following the success of pre-filled syringes in the COVID-19 vaccination programme, there has been a significant increase in interest
from pharmaceutical companies in pre-filled syringes for future vaccine applications, such as influenza vaccines. Companies are also considering them for biologic therapies to treat chronic conditions, such as cancer and autoimmune diseases, which are driving growth in the parenterals segment overall. This is because the nature of biologics means that most treatments have to be delivered by injection. They are also being considered as a potential solution to allow tourists planning to visit countries where malaria and other diseases are endemic to self-administer their vaccines instead of seeing their doctor.
The Quest for Useability and Patient Centricity
Useability and patient experience are significant challenges for many drug developers across all dosage forms, but for injectable drugs in particular. Providing patients with the ability to self-administer their treatment, without the need for support from a healthcare provider (HCP) or carer, can enhance convenience for the patient. Moreover, it can free up professionals’ time, reducing strain on the limited resources of many national healthcare services still recovering from the effects of the COVID-19 pandemic.
Enhanced convenience can significantly enhance patient adherence to their treatment which, in turn, can have a positive impact on the effectiveness of therapy. In doing so, it can further relieve pressure on healthcare systems by minimising the need for patients with chronic conditions to be seen by doctors.
Traditionally, injectable dosage forms have had a key disadvantage when it comes to useability and self-administration compared with rival forms, due to the complexity of preparing standard syringes for administration. For older patients in particular, dexterity issues, poor eyesight and other age-related conditions all add to existing useability challenges inherent to injectables. This can exacerbate many patients’ existing reluctance to take injectable treatments, due to negative perceptions about needles, which can further impact on patient adherence.
With this in mind, a growing number of pharmaceutical companies are exploring
options to make injectable drug products easier for patients to use themselves in a non-clinical setting, such as their home, or school or workspace.
Pre-filled syringes are one crucial way of achieving this goal for drug products that need to be delivered by injection. As they come already charged with the precise amount of drug formulation for a single dose, they enable patients to self-administer, without the need to precisely measure out their dose beforehand. This minimises the risk of overor under-dosing, while streamlining complex preparation requirements, saving patients a considerable amount of time and stress.
As such, pre-filled syringes offer considerable potential for pharmaceutical companies looking to support patients with more patient-centric therapies, across a range of applications and conditions, including vaccines.
Nevertheless, while pre-filled syringes offer a number of benefits, they do pose challenges for pharmaceutical companies, particularly when it comes to filling and packaging them efficiently and in accordance with stringent regulatory requirements. Failure to address these challenges could have an impact on the success of the finished product.
The Pitfalls of Pre-filled Syringe Production
Manufacturing and filling pre-filled syringes can be a complex process compared with other dosage forms. There are a number of considerations that companies should be aware of:
• Sterile fill and finish are crucial – All parenteral dosage forms must be processed and packaged in a sterile and contained environment, and prefilled syringes are no exception. This is crucial to ensure optimum hygiene and safeguard patients’ health, and to maintain compliance with stringent regulations, such as the European Union’s (EU) Annex 1. With this in mind, it is vital to have access to cleanroom facilities, with production lines featuring restricted access barrier systems (RABs) and/or other advanced
70 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4 Packaging
aseptic processing controls. These can be expensive for pharmaceutical companies to install and operate on their own, particularly if they are only needed for a single drug product. It can also be challenging to secure and maintain large-volume sterile filling capacity for large-batch projects, such as a multinational vaccine roll-out.
• Employee safety and cross-contamination protocols need to be in place – If the drug product contains a biological active or a highly potent active pharmaceutical ingredient (HPAPI), then additional containment protocols need to be in place to manage any toxicity risks. Having good spill responses in force can protect line operatives in the event of a breakage and safeguard against cross-contamination of other products.
• Unique packaging issues need to be considered – the packaging of pre-filled syringes can present specific issues for manufacturers. Not only are the needles fragile, requiring careful handling and robust secondary packaging solutions, they also often come in syringe kits accompanied by a number of components – more so than for other dosage forms – which can complicate the packaging process itself. In addition to the standard label and plunger rod, a pre-filled syringe may be packaged with a loose or stake needle, as well as a safety device, which may feature a finger flange or a backstop. Alcohol pads may also be included for sterilising the skin prior to injection, or information leaflets in the secondary packaging to offer guidance on using the syringe for patients.
• Cold-chain transit may be required –As we saw in the early stages of the COVID-19 vaccine roll-out, some mRNA vaccines and biologic treatments have unique temperature requirements that need to be adhered to during transport and storage. Some vaccines need to be stored and shipped at -70°C before being brought up to room temperature just before administration. Ensuring these environmental controls throughout the entire journey of a parenteral drug – whether in pre-filled syringe form, or otherwise – can be a particular challenge, especially when shipping to emerging economies, which may not have the cryogenic infrastructure in place.
• Labelling is crucial – If pre-filled syringe products are destined for multiple markets, then extra consideration needs to be given to product labelling. Labels need to comply with all of the relevant local regulations for each target market. They must also be written in the relevant local languages to ensure that patients can read and understand them.
• Traceability is key – More and more, regulatory authorities around the world require pharmaceutical companies to explore how to trace their pre-filled syringe and other products as they move from the production line to reach patients in order to prevent counterfeit products entering the supply chain.
Meeting these needs can be difficult for manufacturers to achieve, especially when producing pre-filled syringe products for the first time.
Addressing the Challenges
To overcome the challenges of producing prefilled syringes and meet growing demand for more patient-centric injectables, more and more pharmaceutical companies are outsourcing their pre-filled syringe processing to contract development and manufacturing organisations (CDMOs).

Advanced CDMOs with a strong track record of filling pre-filled syringes and other injectable formats are well placed to provide pharmaceutical companies with the support they need to commercialise their pre-filled syringe drug products. They will already have the dedicated sterile filling infrastructure in place, as well as the manufacturing, regulatory and other expertise to support in manufacturing pre-filled syringe products. As such, they can eliminate the need for pharma companies to invest time and resources into building new lines to produce their product.
Some CDMOs invested in large-volume sterile filling capacity at the height of the COVID-19 crisis, featuring the latest flexible equipment, to support the pharma industry in delivering billions of vaccine doses for global distribution. These partners are ideally positioned to support pharma companies developing large-batch injectable treatments, including vaccines for seasonal boosters or future pandemics.
CDMOs are constantly evolving their sterile fill and finish offering for injectables to enhance the support they offer pharmaceutical companies as they respond
to changing demand from patients and HCPs. As such, they can be an ideal partner to support companies seeking to harness the benefits of pre-filled syringes to deliver a better experience for patients.
Looking Ahead
The potential of pre-filled syringes to enable the more efficient delivery of mass treatment campaigns and allow more flexible administration of treatments for chronic diseases outweigh the challenges of filling them. As such, we can expect the market to continue to grow and diversify for the foreseeable future.
Working with an expert with the sterile manufacturing and filling capacity customised for pre-filled syringes can overcome challenges and ensure pre-filled syringe products are manufactured, filled, and delivered safely and efficiently.
REFERENCES
1. https://www.globenewswire.com/newsrelease/2022/08/18/2501065/0/en/Safetyprefilled-Syringe-Market-Size-is-expected-toreach-at-USD-6-534-Million-by-2030-registeringa-CAGR-of-7-1-Owing-to-Increasing-Prevalenceof-Target-Disease-Population.html
Isele
Michael Isele is General Manager at our Wasserburg facility. He is responsible for aseptic production of liquid and lyophilised injectable drug products and biologics. With more than 15 years' experience in the chemical sector and 20 years in the pharmaceutical industry, he brings a wealth of expertise to the team. Prior to joining Recipharm, he held several senior positions in various CDMO companies.

INTERNATIONAL PHARMACEUTICAL INDUSTRY 71 www.international-pharma.com
Michael
Packaging
Health Outcomes
Artificial Intelligence is a Core Pillar in the Evolution of Digital Health and Patient-centric Solutions
The US Food & Drug Administration has stated that digital technology is driving a revolution in healthcare. The lines between healthcare delivery and clinical research are blurring, as the patient becomes a key partner and focus. We are seeing a rapid expansion in the use of mobile and patient-centric devices, exponential growth in the volume and diversity of life sciences data and acceleration in the use of data-dependent computation to gain insight and automate – loosely called artificial intelligence (AI). These digital health trends are naturally combining to transform the patient experience and the application of new scientific ideas and breakthroughs.
The Covid-19 pandemic taught us that rapid and innovative responses are not only possible but extremely effective. AI has the potential to permeate all aspects of clinical
research and support the implementation of more patient-centric, decentralised clinical trials. Patient centricity has been driving innovation in clinical trials for some time, but ever-increasing levels of digitisation and the availability of advanced tools and expertise are accelerating the process.
Against the backdrop of this increased use of AI in clinical trial design, patient identification, mobile technology, remote monitoring and clinical data management, we also see a corresponding rise in the need to regulate AI.
Enabling Greater Patient Centricity
Clinical trial protocols increasingly need to be more patient centric, and this means incorporating more remote monitoring and virtual trial elements, as well as making healthcare a core component of a trial. Machine learning models can be trained to predict the impact of a particular trial design, and unsupervised methods can be used to provide deep insight into the possible outcomes of a particular approach. The
application of AI to the design of a clinical trial can optimise the number and diversity of patients needed to reach the desired endpoints and give the patients who do participate a higher value experience.
Using real world evidence such as health insurance claims data, AI can foster a ‘right patients right time’ philosophy for each trial. Where the human mind finds it impossible to make connections, AI algorithms can combine the meaning of a health insurance code with that of a medication code, a social media event and many other data points to establish a robust country/site mix that drives the overall strategy for the trial. Identifying the right patients ensures better diversity and inclusion and a better patient experience, as well as scientific success. Diversity objectives range from reaching all patients who can benefit from participation in a clinical trial to ensuring that the trial collects the maximum range of data within the scientific inclusion/exclusion criteria. Identifying the right patients also means you identify the right investigators and expedite

72 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
study start up activities. The new era of patient centricity, combined with the advance of AI, expands the horizon for patient identification beyond traditional site-based models.
Increased Data Collection
More and more ways of collecting data directly from patients are being implemented, and this march of digitisation, aided by the increasing sophistication and connectedness of mobile devices, creates a positive virtual cycle with AI. More data means more opportunity to develop smarter risk monitoring processes that use AI to detect emerging patient risk early and recommend mitigation. This is important because it enables more patientcentric approaches that allow patients to participate in clinical trials from their own homes and derive a direct healthcare benefit at the same time. Even more exciting is the prospect of combining data collected by remote devices with electronic clinical outcomes assessment data collected through questionnaires to develop new digital endpoints or predict placebo effects. What was once seen as aspirational innovation is becoming reality as more and more data are collected and increasing numbers of data science professionals apply AI to those data sets. It will require effort and courage to maintain momentum in the development and validation of these challenging initiatives but the advantages to patients provide a clear incentive.
The traditional tasks of clinical data management, where clinical trial databases

Health Outcomes
must be carefully curated, cleaned and standardised for statistical analysis, are coming under the eye of data scientists. Machine learning and natural language processing techniques are transforming the way we look at clinical data, allowing us to take a more risk-based and patient-centric approach. Furthermore, the diversification of data sources, such as the data from remote monitoring devices, is driving the need for smarter, more efficient ways of conducting data management. This need is matched by the increased focus on AI as a means of optimising all aspects of the clinical research value chain.
Synergies Between Artificial Intelligence and Human Insight
AI is a key element in the evolution of digital health and patient-centric solutions. There are plenty of definitions of AI, and many are quite specific. However, it is the more vague, general sense of a machine being able to do something previously thought to be an exclusively human activity that is gaining practical acceptance by business leaders. It doesn’t matter if the solution is an advanced deep learning model or a traditional piece of procedural programming, if the result is better insights or more optimised processes.
The digitisation of all aspects of life is driving business leaders to restructure processes around new digital technologies, and data scientists are listening to those business leaders to develop AI solutions. This is fundamentally an activity driven by data availability and data literacy. A key sustainer of the relationship between data scientist and business leader is model transparency and direct end user involvement in any AI solution. Transparency and the dynamic injection of human decision making into AI models not only supports real-world validation and accountability, but it also generates a key synergy between AI and HI (human insight).
The Importance of Regulation
One area of the AI landscape that is going to impact and change how AI is applied across the healthcare arena is the introduction of AI regulations. This is a welcome development and will provide guidance and frameworks that should be used as the industry continues to explore the potential of these technologies. With the impending introduction of the EU Artificial Intelligence Act, business leaders, data scientists and legal experts need to establish the appropriate AI policy, identify the risks, and associated remedial actions for each AI implementation and understand what
implications the AI has on data protection requirements.

Clinical research, digitalisation and AI are at an important juncture as we emerge from the Covid-19 pandemic. There is much to glean from the experience of the past two years and even more to gain in the future as the industry continues to transform the clinical trial into a more patient-centric, decentralised, dynamic, data-driven, AI-powered activity. Clinical research is increasingly becoming a healthcare option, and with the introduction of AI regulations, trust in AI and its impact on clinical trial and care options will be paramount within the patient population. AI and the accompanying technology solutions will find their way into mainstream healthcare practices, decreasing the need for expensive and inconvenient in-patient care. The benefits will be felt by scientists, clinicians, commercial interests and patients alike.
Gerard Quinn, VP, IT Innovation & Informatics, has worked at ICON for over seven years and has over 25 years in the life science industry, with experience in innovation, strategy, process improvement and IT. Gerard leads his team’s work on the innovative activities in technology and data science. They identify and build key partnerships to co-develop services by evaluating joint capabilities with the aim of driving efficient clinical trials for sponsors and patients. The team also improve cycle times for ML/AI solutions across the clinical research value chain.
Dr. Michael Phillips is a director of innovation & informatics at ICON. He has over 20 years’ experience in IT, business intelligence, data analytics and e-clinical innovation, as well as broader experience in biomedical research and management roles in general science publishing. His team of data scientists at ICON designs and builds AI solutions for a diverse range of business and clinical applications.

INTERNATIONAL PHARMACEUTICAL INDUSTRY 73 www.international-pharma.com
Gerard Quinn
Dr. Michael Phillips
How the Pharmaceutical Industry Can Navigate Supply Chain Disruptions and Gain Resiliency

According to McKinsey & Company, the value of pharmaceutical products traded in the previous 20 years has increased sixfold, from $113 billion in 2000 to $629 billion in 2019. Market Research firm Statista reported that in 2020, roughly $1.27 trillion was spent on medications.
Every Shipment Is Valuable
Regardless of size or contents, every pharmaceutical shipment is valuable, some to the tune of millions of dollars. If anything goes wrong during the distribution process, manufacturers might have to write off a shipment, which can substantially harm a company’s profitability. But the bottom line of a balance sheet is nothing compared to what else is at stake: people’s health and even lives. The distribution and safety of pharmaceutical products (especially during transport) have a very direct impact on medical outcomes. Therefore, manufacturers, distributors, shippers, logistics service providers, and retailers need deeper levels of insight and greater visibility into the supply chain now more than ever.
Data and Insights
Data collection isn’t new to supply chain management; in fact, many supply chain stakeholders have more data than they know what to do with. But the question is, is it the right data? How reliable is this data? Does this data represent real-time tracking of shipments, or is it delayed information? Is the data easily accessible, readable, and shareable, or is it stuck in a silo somewhere in the deep recesses of the supply chain?
Let’s pause for a moment to consider that data collection is only one part of the story; equally important is that stakeholders know how to use insights gleaned from all this data to drive actionable decisions.
“Poor data control is responsible for significant supply chain issues, given the existing silos, handoff points along the supply chain and potential errors. These issues prevent companies from making their data work for them, in order to create efficiency, improve quality, and reduce
costs… Utilising the right information to gain insights enables control, which, in turn, facilitates improvement, and a focus on continual improvement identifies new opportunities.” – Pharma Technology Focus
Real-Time Data Can Bring Positive Change
In this article, we’ll explore how real-time tracking of pharmaceutical shipments accelerates their distribution. We will examine the common challenges in distribution, including compliance issues, and how realtime data, combined with customised tracking alerts, can empower supply chain leaders to overcome obstacles and realise insights that will drive proactive management decisions.
I. The State of the Pharmaceutical Cold Chain
In general, the pharmaceutical industry consists of three different components, each having its own supply chain ecosystem:
• Commercial Products – These are products that require approval from each country where they’re distributed.
• Clinical Products – These are preapproved products in different stages of trials, from Phase One to Phase Three.
• Research and Development Products – These are pre-clinical products currently undergoing testing.
Separate organisations govern the systems and supply chain flows for each ecosystem. But what’s common among them is each ecosystem relies on product availability to meet ongoing demand.
Due to the critical nature of what they produce, pharmaceutical companies typically cannot be as “lean” with the supply of their products as firms in other industries are; more often than not, they’ll overstock products in case of supply chain disruptions.
Generally, pharmaceutical companies have months on hand (MOH) coverage that allow them to react to the various disruptions they face.
Increasingly, pharmaceutical enterprises build segmentation strategies to employ different types of supply chains for various products. For example, high-value, lowvolume branded products will utilise a much higher MOH coverage than mature products whose sales are more predictable and easier to forecast. But in all cases, supply chain disruptions are taken into account in the planning process to maintain a certain level of resiliency. Disruptions are challenging to predict, so pharmaceutical firms must plan conservatively. It’s not uncommon for firms to keep 12 to 26 months’ inventory on hand when factoring in disruptions.
On the other extreme, when disruptions are not as significant as initially thought, this can lead to obsolescence of a product due to short shelf life or product expiration. Obsolete products need to be taken out of the supply chain through reverse logistics –and ultimately eliminated via a prescribed destruction process.
74 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Logistics & Supply Chain Management



INTERNATIONAL PHARMACEUTICAL INDUSTRY 75 www.international-pharma.com Development and manufacturing Thermal Blankets for the temperature protection of pharmaceuticals and healthcare products in airfreight (+15°C +25°C) and (+2°C +30°C) Qualifications & Validations - Multilayer thermal blanket for PMC -ULD – Euro and Block pallets - Temax-4000 blanket with multiple reflection technique - Stress tested in summer (+46°C) and winter ( -15°C) profiles - Tarmac tested on solar power and greenhouse effects Ecological notes - Recyclable + Low ecological footprint - NON-laminated composition = easy to dismantle - Re-manufacturing of recycled compounds Available worldwide at freight forwarders KRAUTZ - TEMAX Group Development and manufacturing Belgium - Europe Phone +32-11.26.24.20 Website www.krautz.org Email info@krautz.org Temax Americas LTD Hanover park – Illinois – USA ISO-9001:2015 certified
II. Challenges to the Pharmaceutical Supply Chain
Many challenges confront pharmaceutical companies when it comes to the supply chain. According to supply chain analysis enterprise ParkourSC, inefficiencies, inaccurate data, and other flaws can significantly impact revenue, business reputations, and medical patient lives.
Optimising distribution in the pharmaceutical supply chain (sometimes referred to as the pharmaceutical “cold chain” due to many medications needing strict temperature control) and complying with legal mandates is not always easy. Below are some of the more prominent challenges –with examples – that pharmaceutical supply chains currently face. Of course, just one of these disruptions can have tremendous consequences for a shipment, and when a combination of these disruptions occurs, negative outcomes can be multiplied.
• Transportation Delays – Events that cause a product to arrive late to a shipment consignee.
• Transport Capacity Issues – Instances when a transportation provider has no capacity at the time of shipment booking.
• Sourcing Issues – When a raw or Active Pharmaceutical Ingredient (API) material provider is not able to provide materials in time.
• Manufacturing Capacity Issues –When improper planning causes manufacturing availability issues.
• Packaging and Labelling Issues –When incorrect or improper product packaging or labelling issues cause delays.
• Regulatory Issues – Events that challenge the regulatory requirements of a product.
• Recalls – Events that require the removal of a product from the supply chain.
• Business Continuity Issues – Limited contingencies for critical material or services providers.
• Demand, Supply, and Safety Stock Imbalances – When supply or safety stocks are less than actual demand.
• Quality Issues – When a product is quarantined or on hold due to a quality event.
• Environmental Issues – Events such as bad weather, hurricanes, earthquakes, etc. that cause supply issues.
• Geopolitical Issues – Political events leading to constraints that
affect supply (for example, Brexit, international sanctions, etc.).
• Shortages and Damages – Incorrect delivery of products or damage to products being delivered.
• Manpower Issues – Not enough labour resources in a part of a supply chain, resulting in issues.
• Temperature Control Events –Temperature deviations or excursions (prolonged variations) that occur with a product, causing a quality event.
III. Current Solutions for the Pharmaceutical Industry to Consider
As outlined above, supply chain disruptions in the pharmaceutical industry can result from sourcing issues, manufacturing issues, quality issues, logistics issues and/or other challenges.
The Example of COVID-19 Disruptions can be minor or – as we have seen recently with the COVID-19 pandemic – they can be major events. COVID-19, in particular, was not a typical industry disruption. The pandemic incorporated parts of almost every one of the disruption types outlined above, compounding issues greatly. It continues to have an impact today.
To illustrate this, consider that certain vital ingredients needed by the pharmaceutical industry became difficult to source, and manufacturers couldn’t produce them due to plant closures and a lack of available employees (resulting from a combination of absenteeism and labour shortages). Products previously manufactured had quality control issues due to a lack of oversight across the supply chain.

During the pandemic, pharmaceutical companies were primarily operating with remote workers, causing less oversight and
fewer resources to be available. Logistics became a massive issue as transportation companies cut the number of operating assets, cancelled flights, and enacted restrictions. Employee availability was low or cut back in some cases due to closed locations. Changes to global and countryspecific shipping requirements and conditions made it more difficult to move goods.
COVID vaccines and global supply chains got a hefty amount of media coverage during the pandemic, providing broader insight into the complexities of distributing pharmaceutical products effectively, accurately, and via a quality-driven process. The press discussed the importance of supply chain visibility of the vaccines via innovative real-time monitoring devices affixed to each vaccine shipment.
Real-Time Monitoring
These real-time monitoring devices are small enough to fit in the palm of one’s hand, and they record product location, temperature, light sensitivity, shock, and vibration data. They also have built-in geofencing capabilities. These monitors can signal alerts if a product is in danger of being compromised. In the event of a temperature excursion, for example, real-time monitors can alert a person in the pharmaceutical organisation to start working with the logistics provider to move the product away from damaging temperatures or other disruptive factors that are compromising it.
In the case of the COVID-19 vaccine shipments, once the vaccines were manufactured, international shipments began, in both a frozen and a refrigerated form, via a highly complex, globally disruptive supply chain. There was enormous worldwide consumer demand for this product. With the vaccines having very strictly defined
76 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Logistics & Supply Chain Management
KLINGE
The Biopharma Cold Chain Sourcebook (a leading resource to the pharmaceutical industry) recently reported:

“Recent Good Distribution Practice (GDP) guidelines, to which the industry is gradually adopting, require control of even room-temperature product, which is essentially everything that is not refrigerated or frozen.
With each passing year, the oversight of pharmaceutical and biologics shipping is getting tighter.”
Klinge Corporation has been safely transporting and storing pharmaceuticals for over 30 years. Protect your product with our qualified refrigerated and deep freezer containers.


INTERNATIONAL PHARMACEUTICAL INDUSTRY 77 www.international-pharma.com inquiry@klingegroup.com | www.klingegroup.com USA: +1 717 840 4500
TEMPERATURE CONTROL
Avoid Temperature Excursions with Redundant Reefer/Freezer Containers Keep pharma products at required temperature down to -70°C Meet international transport regulations Safeguard pharma products with temperature recorder & online temperature tracking REDUNDANT REFRIGERATED & -70°C DEEP FREEZER CONTAINERS FOR PHARMA PRODUCTS
Logistics & Supply Chain Management
storage temperature conditions, the need for extremely accurate and reliable real-time monitoring devices was a crucial piece of the puzzle that yielded effective supply chain visibility of the product.

Many people don’t realise that this solution wasn’t just being applied to COVID vaccines; real-time monitoring devices are now implemented with many other pharmaceutical products for global shipping.
IV. How Visibility Benefits the Supply Chain for the Pharmaceutical Industry
With recent advancements in real-time monitoring and the need for more in-transit visibility, more leading pharmaceutical firms are outfitting their logistics organisations with real-time temperature monitoring tools. This trend has led to a more proactive approach in combating shipment disruptions, as compared with the present use of reactive monitoring devices – such as data loggers –that are more commonly employed.
Proactive Vs. Reactive Monitoring
Like the familiar “black-box” cockpit devices on aeroplanes, data loggers record data throughout the shipment journey. Still, that data remains in the device, with no ability to be examined, shared, or transmitted until the shipment is delivered and the information downloaded to a remote computer. Managers in numerous pharmaceutical companies agree this practice is no longer satisfactory.
Reactive (instead of proactive) responses to temperature excursions compound disruptions, resulting in lengthy quality holds and long delays in investigating individual excursions. Multiple company departments are involved in excursion management and the release of products, and typically, there’s a significant impact in terms of labour hours needed to complete an investigation.
Pharmaceutical executives are now taking a discerning look at real-time temperature monitors and transitioning away from data loggers because monitoring technology has advanced substantially. Real-time monitors are now just as accurate, with advanced features and performance comparable to data loggers, while their costs have become more affordable.

Visibility Can Be Immediate
Monitors can provide data by transmitting in real-time while a shipment is in transit. When even the slightest temperature excursion occurs, for instance, monitors can send an alert to the appropriate person at the
pharmaceutical firm or another designated party so that resolution procedures can start immediately. Of course, there are always challenges with trying to remediate a shipment in transit when an excursion occurs, but there are also excellent opportunities to resolve an issue. When an excursion is visible in real-time, the excursion management process can begin immediately versus potentially days after it occurs. In some cases, with real-time monitoring, an excursion can be resolved before a shipment is delivered.
A Real-Time Temperature Excursion Example
For example, a 2-to-8-degrees-Celsius biologics shipment from the United States to Germany has a 30-minute temperature excursion on a truck delivering it from a distribution site to JFK Airport in New York City. The temperature spikes above 8 degrees, with a high of 25 degrees for 10 minutes, then it returns to its required range. The pharmaceutical company employees are alerted when the temperature hits 7 degrees –per the real-time temperature monitor preconfigured settings – and the employees alert the trucking company’s dispatcher. He, in turn, contacts the truck’s driver, who realises his refrigerated trailer has powered off.
The driver switches the refrigeration back on, lowering the temperature back into the required range. The shipment is loaded onto a flight to Berlin and begins its transatlantic journey.
In the meantime, the pharmaceutical personnel contacts the appropriate company quality lead to initiate an investigation into the temperature excursion. When the shipment lands in Berlin, data continues to be received from it. The quality and logistics groups bring in a stability group that provides technical analysis about product exposure and determines that the product remains safe. Personnel at the shipment destination are notified before the product’s arrival.
Control Tower Integration
Leading pharmaceutical companies have also built “control towers” to provide functional operations visibility to their supply chains. This trend is becoming more important with the advent of biologics, cell and gene therapy products, and custom drugs designed for rare diseases. The emergence of these control towers in pharmaceutical supply chains is becoming increasingly sophisticated. In mid-to-
78 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
large-sized pharmaceutical firms, there’s a revolution taking shape in managing disruptions related to supply chains, with a critical component being real-time visibility.
A company demonstrated this while showing off the buildout of a real-timevisibility-agnostic platform connected to the firm’s enterprise resource planning (ERP) and warehouse management system (WMS) with radio frequency (RF) capabilities. During the picking, packing, and shipping processes, data from a real-time monitor was aggregated with shipment details and connected to the cloudbased platform.

While a shipment was in transit, the realtime monitor would transmit data to the platform. Integrations connected the cloud platform to the company’s control tower, where high-level analytics and reporting were generated and made visible internally. A command centre was also integrated into the control tower, provided by the real-time monitor maker. This solution provided a 24/7 monitoring and remediation service to identify and mitigate disruptions.
V. Conclusion: Keeping Pharmaceutical Products Safe with Best-in-Class Trackers and Real-Time Insights
Although they’re very impressive, the above examples only represent the first stage of the real-time monitoring revolution. Over the next five years, machine learning, artificial intelligence (AI), and predictive analytics will take on an even more significant role in logistics management, leading to advising
carrier management, better alternatives for service, and alternative cold-chain packaging solutions.

Software overseeing global weather data, flight statistics, transportation providers’ systems, and even risk data will be connected and integrated into control towers to provide optimal performance and disruption avoidance. Faster and more reliable excursion management tools that take into account stability and total time out of refrigeration will determine product safety and fitness for use through automated quality reviews and release processes. These will integrate supply and demand planning, inventory, and serialisation systems with real-time monitoring for robust supply chain security and brand protection. With all these
advances, the sky's the limit for supply chain optimisation.

To summarise, pharmaceutical company supply chains’ monitoring practices are currently widely reactive to disruptions. Still, with expected advancements in real-time monitoring, these companies will adopt a more proactive approach to disruptions in the near future. Within three to five years, with increased investment from real-time monitoring companies, we’ll start to see a real shift in disruption avoidance. Will it eventually be possible to have a pharmaceutical supply chain with no disruptions at all? At this point, it’s hard to say with certainty, but things are definitely headed in that direction.
Alex Guillen has extensive experience and expertise in cold chain; as SME – Life Science and Pharma at Tive, Alex leads sales and business development within the company’s rapid-growth Life Science division. Previously, Guillen served as a Board Member and leader of Corporate Strategy at SWITRACE S.A, a developer of temperature and humidity data loggers compliant to the Pharma and Biotech industries. Alex’s extensive experience also includes serving as Global Cold Chain Director of Fisher Clinical Services, CEO of Escort Cold Chain Solutions SA, and Director for Commercial Operations for Novartis Vaccines.

79 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
Alex Guillen
& Supply Chain Management
Logistics

80 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
BSP
DFE
Gerresheimer
77
75
Page 17 Liveo
Medicilon BC Natoli Engineering
Page 33 Nemera
3 Owen
Page 7
64–67 PCI Pharma Services Page 5 RGCC
63 Senglobal
29 SGS Page 47 THINPRINTING Page 41 UPC Cambridge Ltd Page 19 & 53 Valsteam ADCA Subscribe today at www.international-pharma.com or email info@senglobalcoms.com I hope this journal guides you progressively, through the maze of activities and changes taking place in the pharmaceutical industry IPI is also now active on social media. Follow us on: www.twitter.com/ipimediaworld www.facebook.com/ipimediaworld www.plus.google.com/+ipimediaworldmagazine www.ipimediaworld.tumblr.com Advertisers Index
IFC
Pharmaceuticals S.p.A Page 36–39
Pharma Page 23 FUJIFILM Wako Chemicals U.S.A. Corporation Page 11
AG Page 55 Kahle Automation Page
Klinge Corporation Page
Krautz Temax
Research GmbH Page 60–62
Company
Page
Mumford
&
International GmbH Page
Ltd Page
With our solution you will have IFU and warranty documents in all languages printed in one thin paper booklet – leading to less warehousing space, simplified packaging process and significant cost savings in logistics.
BENEFITS
Thin paper really means thin paper! With our specialized printing technology, we can use paper grades from 29 g/m2 up to 40 g/m2

Lower paper substance and caliper also mean less space and weighat. With the Booklet your package is lighter and smaller in size.
All-in-one solution. All language versions of your IFU documents, warranty information and legal texts are printed in one Booklet that can be easily slipped into the product package.

UNIQUE ALL-IN -ONE BOOKLET
This picture tells it all: One stitched booklet vs. four folded leafletsboth with a space of 1,2 m2.
Streamlined packaging process: our Booklet works excellently on automated high-speed packaging lines.
• Only one stock item number for your Booklet – meaning less warehousing space, faster inventory cycle and no unnecessary reserves. The tied-up capital will be released for your other needs.
Lighter and smaller package means significant savings in shipping costs and increased sustainability of your business.
Heikki Suomala

Director, Sales & Marketing
Tel. +358 440 350268
info@thinprinting.fi
YOUR THINPRINTING SPECIALIST
Olli Kivijärvi Sales Manager

Tel. +358 440 350269 info@thinprinting.fi
With almost 40 years of experience, we are one of Europe’s leading printing houses specialized in printing on thin and ultrathin paper. We use only high-quality, totally wood free thin print paper from reliable manufacturers in Finland, and together with our solid logistics network, we guarantee fast and timely deliveries all over the world. Visit www.thinprinting.com
CONTACT
AUTOMATIC ENCAPSULATION MACHINE INTRODUCING THE NCF-45
The solution to product loss.

82 INTERNATIONAL PHARMACEUTICAL INDUSTRY Winter 2022 Volume 14 Issue 4
A highly reliable encapsulator, producing up to 80% higher yields to typical hand-filling or semi-auto encapsulation machines. The smooth operation of the NCF-45 automates your encapsulation process to deliver up to 45,000 capsules per hour, making this Natoli machine ideal for medium-scale production. GMP & cGMP compliant I SCADA network compatible I 21 CFR part 11, CE Certified
natoli .com