SAN FRANCISCO MARIN MEDICINE
JOURNAL OF THE SAN FRANCISCO MARIN MEDICAL SOCIETY





10 Physicians Win Historic $20 Billion Medi-Cal Investment
Adam Francis, CAE
12 The 2023 SFMMS/David E. Smith Addiction Conference

Tony Brayer, MD
13 Psychedelics and Medicine: Déjà Vu All Over Again
David E. Smith, MD
14 Do You Feel Like You Are Responsible for Everyone and Everything?
Jessie Mahoney, MD
16 Improving Trauma Care Disaster Capability in the San Francisco EMS System
John Brown, MD, MPA; Christopher Colwell, MD and Joseph Cuschieri, MD
18 San Francisco Efforts to Stop the Bleed
Janna Yang, MS-3; John Maa, MD, FACS and Joseph Woo, MD
19 Tobacco: The End In Sight?
John Maa, MD; Steve Heilig, MPH and Tamu Green, PhD
21 A Focus on the Tobacco and Nicotine Endgame
John Maa, MD and Alyssa Takahashi
24 Outgoing Remarks: AMA Immediate Past President
Jack Resneck Jr., MD
26 Getting Explicit About Implicit Bias
Jeff Ritterman, MD
28 One Year After Dobbs: Where Do We Go From Here?
Daniel Grossman, MD
30 Anniversary Of #Womanlifefreedom: Movement Message
Yalda Shahram, MD, MSc
31 San Francisco's Citywide Response to COVID-19
San Francisco Department of Public Health
32 Top Review Says Covid Lockdowns and Masks Worked, Period
Ashleigh Furlong, Politico
33 COVID 19: Examining the Effectiveness of Non-Pharmaceutical Interventions
Royal Society Report
SAN FRANCISCO MARIN MEDICINE
July/August/September 2023
Volume 96, Number 3
2 Membership Matters
5 What Is a Physician's Legacy?
Heyman Oo, MD, MPH
6 Executive Memo: SFMMS Proposes New Program In San Francisco and Marin to Attract Vital Healthcare Workforce Conrad Amenta
7 CMA: Vice Speaker Candidate Message George A. Fouras, MD
OF INTEREST
6 In Memoriam: Dr. Lawrence Cheung
36 Advertiser Index
Note: The SFMMS has advocated strongly for saving Laguna Honda Hospital, and was very pleased to see this essential institution recertified. More of course remains to be done, but we happily thank and congratulate our local leaders in the San Francisco Department of Public Health, city government, and everyone involved in this effort. This message from San Francisco City Attorney and longtime SFMMS friend David Chiu conveys the good news. – Editors
Dear friends and colleagues,
I am pleased to let you know that the California Medical Association and the Coalition to Protect Access to Care, a broad and diverse group of health care organizations, filed a statewide ballot initiative yesterday with the California Attorney General’s office to expand access to health care for millions of Californians. Our goal is to qualify the measure for the November 2024 ballot.
I’m writing with great news about Laguna Honda Hospital. This week, our City received a key recertification that will help preserve this critical institution relied upon by so many of our most vulnerable San Franciscans.
For over a century, Laguna Honda has been the last safety net for our seniors, our family members with severe disabilities, and low-income San Franciscans who can no longer care for themselves. Every time I’ve visited, I’ve witnessed incredible acts of care and compassion. So a year ago this month, when the hospital was under threat of closure after losing its certification, our office filed a lawsuit to continue funding, pause resident transfers, and keep Laguna Honda open.
I heard from many residents’ families and staff as they faced tremendous uncertainty, worrying about whether more residents would be transferred and the toll those transfers could have on fragile patients. Fortunately, through litigation, we reached a settlement agreement with state and federal regulators to temporarily continue funding and pause the transfers of residents, giving Laguna Honda the breathing room it needed to successfully apply for recertification. This week, the state announced the hospital’s recertification into California’s Medi-Cal program, whose funding is relied upon by 95% of Laguna Honda patients.
By coming together as a community, we have preserved this critical institution and restored an essential part of San Francisco’s safety net. I want to thank our Department of Public Health and Laguna Honda staff, who worked so hard over the past year to earn recertification. I also want to thank the amazing legal professionals in my office whose work led to this announcement. Our City Attorney’s Office is one of the very best municipal law offices in the country, in no small part because of those in my office who were part of saving Laguna Honda.
For over 150 years, Laguna Honda has cared for our most vulnerable. With this week’s announcement, I’m hopeful it will do so for another 150 years.
Gratefully yours, David

The initiative builds on the historic investment that the Governor and Legislature made earlier this year to dedicate additional funding to the Medi-Cal program. The Protect Access to Healthcare Act is critical to ensuring the accessibility and affordability of health care services for all Californians, as well as recognizing the critical role that physicians play in achieving this vision.
Now more than ever, it is important that the 15 million Californians who rely on Medi-Cal for health coverage have access to care. Equally as important is ensuring that emergency room wait times are reduced for ALL Californians, that there is more funding for mental health care across the state and that we help reduce the cost of important prescription drugs.
Specifically, the initiative will:
• Make the Medi-Cal provider rate increases that were included in the 2023-24 state budget deal permanent for generations to come;
• Expand access to health care for Medi-Cal patients, which will result in reduced emergency rooms usage, and shortening wait times for all Californians;
• Increase funding for mental health programs that care for children and Medi-Cal patients; and
• Enable California to manufacture its own insulin and other prescription drugs to increase affordability for Californians.
In the coming months, we will be working closely with the other members of the coalition to gather the hundreds of thousands of signatures needed for the initiative to be placed on the ballot.
Your support and engagement will be invaluable in driving this initiative forward. In the coming weeks and months, we will reach out to you with opportunities to assist in outreach and education efforts and keep you updated on the progress of this initiative.
In the meantime, please visit accesstohealthcareca.com for more information.
As always, should you have any questions, suggestions, or ideas, please do not hesitate to reach out.
Best wishes for a healthy future,
Donaldo Hernandez, M.D. President, California Medical AssociationAugust, 2023
The Medical Board of California recently published a long-awaited update to its opioid prescribing guidelines, which will make it easier for patients to get the care they need while maintaining appropriate safeguards. Importantly, the medical board has clarified that the guidelines are not intended to replace a physician’s clinical judgment and individualized, patient-centered decision-making.
The guidelines are here:
https://www.mbc.ca.gov/Download/Publications/pain-guidelines.pdf
The guidelines are consistent with recommendations from the California Medical Association (CMA), which had urged the medical board’s Opioid Prescribing Task Force “to use balancing between appropriate risk assessment and ensuring that patients receive individualized care as the guiding principle as you work on this latest update of the guidelines.”

In a letter to the taskforce, CMA noted that previous prescribing guidelines were acutely focused on reducing opioid prescribing to address opioid-related overdose. California already had one of the lowest opioid prescribing rates in the country when the previous guidelines were passed, and has continued to reduce prescribing. The current surge in overdose deaths is related to use of illicit drugs.
The chief of the Stanford University Division of Pain Medicine Sean Mackey, M.D., Ph.D., served as a senior advisor for the medical board’s taskforce and endorsed the revised guidelines.
“I’m a physician scientist, I care for people suffering from chronic pain, many who have intractable pain. Our motivation for revising this document was to learn from the lessons in the past and make it better,” Dr. Mackey said in a letter read at the May board meeting. “We recognize the need to ensure patient access to safe and effective pain management treatment, and at the same time, the need to support physicians providing treatment for people with chronic pain."
CMA’s requested changes were largely incorporated into the guidelines, including a recognition that the medical board’s Prescription Reviewer Program (formerly known as the “Death Certificate Project”) contributed to physicians being less willing to treat patients with chronic pain.
“We think it is critical to ensure that guidelines recognize the nuance that treating pain requires and acknowledge the complex realities of treating these patients, which include systemic barriers for many patients to access non-opioid therapies or pain specialists and racial and ethnic disparities in care,” CMA wrote in the letter.
The new guidelines address many of CMA’s concerns and adopted CMA recommendations, including:
• Reinforcing the individualized nature of patient care and making clear that it is not intended to be applied as an inflexible standard by health care entities and is not a law, regulation and/or policy that dictates clinical practice.
• Clarifying that patients should not be required to sequentially “fail” nonpharmacologic and non-opioid pharmacologic therapy before proceeding to opioid therapy. The guidelines now state that the basis for initiating opioids should be whether the benefits are anticipated to outweigh the risks of the therapy, rather than by patients having attempted multiple therapies that have inadequately addressed their pain.
CMA also advocated for removing morphine milligram equivalent (MME) thresholds, because those included in the 2016 Centers for Disease Control and Prevention guidelines “established a ‘one-size-fits-all’ approach to opioid therapy that harmed patients” and perpetuated “the false idea that MME thresholds improve patient care.” The adopted guidelines provide a nuanced analysis of using MME, stressing the need for care being individualized and patient centered and for adequate medical recordkeeping that documents prescribing decisions. The final version removed originally proposed language that suggested an upper limit on opioid prescribing of 90 MMEs.
July/August/September 2023
Volume 96, Number 3
Editor Gordon L. Fung, MD, PhD, FACC, FACP
Managing Editor Steve Heilig, MPH
Production Maureen Erwin
SFMMS OFFICERS
President Heyman Oo, MD, MPH
President-elect Dennis Song , MD, DDS
Secretary Sarita Satpathy, MD
Treasurer Jason Nau, MD
Immediate Past President Michael Schrader, MD
SFMMS STAFF
Executive Director
Conrad Amenta
Associate Executive Director, Public Health and Education
Steve Heilig, MPH
Director of Operations and Governance
Ian Knox
Director of Engagement
Molly Baldridge, MPH
Senior Director, Advocacy and Policy
Adam Francis
2023 SFMMS BOARD OF DIRECTORS
Edward Alfrey, MD
Melinda Aquino, MD
Ayanna Bennett, MD
Julie Bokser, MD
Kristina Casadei, MD
Clifford Chew, MD
Esme Cullen, MD
Manal Elkarra, MD
Mihal Emberton, MD
Cindy Greenberg, MD
Gordon L. Fung - MD, Editor
Beth Griffiths, MD
Ian McLachlan, MD
Jason Nau, MD, Treasurer
Heyman Oo, MD, President
Sarita Satpathy, MD, Secretary
Michael Schrader, MD, Immediate Past-President
Yalda Shahram, MD
Neeru Singh, MD
Dennis Song, MD, DDS, President-Elect
Kristen Swann, MD
Kenneth Tai, MD
Melanie Thompson, MD
Matthew D. Willis, MD
Kristen Wong, MD
Andrea Yeung, MD
Helen Yu, MD
For questions regarding journal, including possible submissions, contact Steve Heilig: Heilig@sfmms.org
As many of you may already know, Dr. Lawrence Cheung passed away this summer after a year-long fight against cancer. Lawrence was a past-President of the Society as well as a dynamic leader in the world of physician advocacy. In this issue of the journal, you can read about some of his innumerable accomplishments and the positive impact he has had on his patients, the community, and the House of Medicine.
What I remember most about Lawrence, though, is his personal impact that extends far beyond his professional achievements. As anyone who had the honor to know him would attest, he was one of those rare people who seemed to have an endless generosity with his time and particularly kept an eye out for young physicians, students, and trainees.
As a young resident, after attending one of my very first Medical Society Board of Directors meetings, I remember feeling awkward and unsure about what I could possibly bring to the table in this large group of seasoned, well-connected physician leaders. Then, Lawrence came up to me, introduced himself and started asking me questions about myself, my passions, why and how I came to be involved in advocacy; simply, he made me feel seen and welcome.
Through the years, I observed him do the same, over and over again with medical students, with residents, with colleagues at various stages of their career … basically any new face in the room. One of my last interactions with Lawrence was at our CMA Lobby Day in Sacramento this past April. While our delegation was between legislator meetings, I noticed Lawrence out of the corner of my eye, gravitating towards two physicians for whom it was their very first lobby day. With his authentic curiosity, he quickly engaged them and brought them into the advocacy fold. Despite his health challenges, he was still at it.
I wonder what would happen if each one of us followed Lawrence's example just a little bit more? What if we were to reach out and sincerely say “Hello, welcome, tell me about yourself” the next time we encounter a new colleague somewhere. We might be surprised how far that goes towards bolstering the strong, resilient, and interconnected physician community we desire to have here in San Francisco and Marin.
As for a physician’s legacy, gone are the days when we doctors get body parts and syndromes named after us. However, what has and will continue to endure, is the direct impact we have on others. Dr. Cheung’s recruitment, mentorship, and support of “the next generation” is, in my opinion, the ultimate legacy. Lawrence is gone far too soon, but those colleagues, whose lives he touched through his work with the medical society, continue on in leadership roles of their own, making impactful changes in clinical care, policy, research, and beyond.
I, and others here at the medical society, aim to honor and carry forth that legacy. I sincerely hope you will join us.
Humbly yours,
Heyman Oo, MD MPH SFMMS PresidentHeyman Oo, MD, MPH is a primary care pediatrician and Site Medical Director at Marin Community Clinics in Novato. She also serves as an Information & Guidance Clinical Lead for the San Francisco Department of Public Health under the COVID-19 Task Force. She is a graduate of the UCSF Pediatric Leaders Advancing Health Equity (PLUS) Residency Program and obtained her MPH in Healthcare Policy and Administration at the Harvard T.H. Chan School of Public Health. She has been involved in organized medicine since the beginning of her medical school years at UC San Diego and has been a member of SFMMS for almost a decade.

Dr. Lawrence Chi Chuen Cheung was a beloved husband, father, public health advocate, researcher and physician leader. Born in Hong Kong on July 14, 1972 to Helena and Eddie Cheung, he moved with his family to New Jersey in 1981. He graduated as salutatorian from Millburn High School in 1990, Magna Cum Laude from Harvard College in 1994, before earning his MD from Columbia University in 1998. He trained in Internal Medicine at the University of California, San Francisco (UCSF) before completing a Dermatology residency at Washington University, St. Louis in 2005. While at Columbia, he served as the first national president of the Asian Pacific American Medical Student Association, through which he met Angela Wong; they married in 1999.
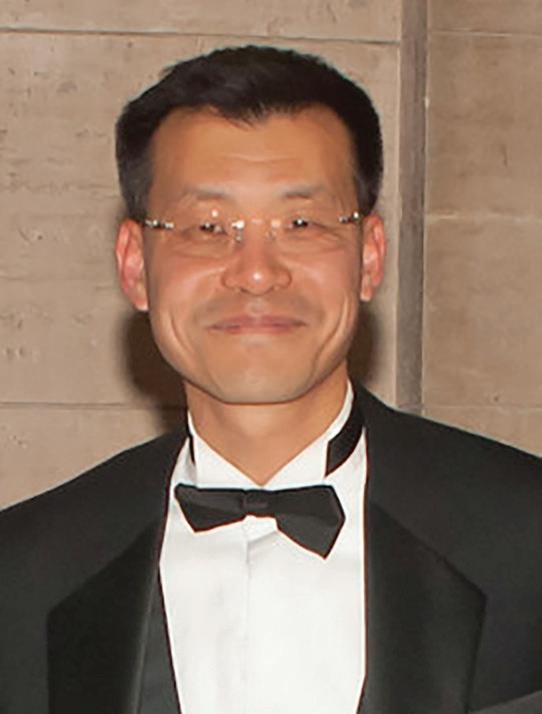
An exceptional private practice dermatologist who also served as the principal investigator for clinical trials, Lawrence was a tireless advocate for the autonomous practice of medicine with a steadfast commitment to public health. His clinical practice served a large monolingual Chinese speaking population, and he started the teledermatology service for Asian Health Services in Oakland. In 2014 he was elected President of the San Francisco Marin Medical Society (SFMMS). He served as Chair of the SFMMS Delegation to the California Medical Association (CMA), on the CMA Board of Trustees, and as Delegate to the American Medical Association (AMA). In 2022, he fulfilled a lifelong ambition after election to become Vice-Speaker of the CMA House of Delegates. He was a fellow of the American Academy of Dermatology, volunteer teaching instructor at UCSF, St. Mary’s Medical Center, and CPMC, and mentored SFMMS members who aspired to achieve his extraordinary levels of leadership.
Dr. Cheung also invested significant time to advance health equity in the San Francisco Chinatown community and National AsianAmerican Pacific Islander interests as a SF Health Authority Commissioner overseeing the county MediCal managed care plan. He also served upon the Board of Directors for the National Council of Asian and Pacific Islander Physicians (NCAPIP).
In 2023, Dr. Cheung received certificates of recognition from the California State Senate, the City and County of San Francisco, and from SFMMS in honor of his invaluable service to the medical community and steadfast commitment to public health. As a direct result of his vision and leadership, SFMMS attained key public health policy victories related to the regulation of e-cigarettes and sugary beverages, which inspired similar legislation across the state. Throughout his tenure in organized medicine, Dr. Cheung consistently advocated for forward-thinking public health policy to close the gap in access to care for the most underserved members of our community. As a result of his leadership, the lives of countless Californians have been improved and lengthened.
Dr. Cheung passed at home surrounded by the love of his family on July 17, 2023. He is survived by his wife Angela, children Amelia and Aidan, his parents and his sibling Sunny. In lieu of flowers or gifts, the family would appreciate donations to one of two causes near and dear to Lawrence:

1) The "AMA Foundation — In Memory of Dr. Lawrence Cheung" to fund scholarships that honor his legacy and passion for medical students to engage in public health care advocacy early in their career. http://amafoundation.org/donate
2) The Young Women’s Choral Projects where he served as a Board member, and seeks to transform the lives of young women through exceptional artistry in choral performance. Lawrence loved music of all forms, and as a former member of the Harvard Glee Club held a particular fondness for vocal music. https://www.ywcp.org/donate/


San Francisco and Marin are falling behind in the race to attract health care workers.
Successful statewide workforce programs incentivize care providers to serve at-risk populations in underserved areas through such strategies as loan repayment, but few if any providers are awarded in San Francisco or Marin, which are not viewed as areas in need compared to the Central Valley, Inland Empire, and rural areas of the State.
With the average school debt for a new physician averaging $200,000, these statewide programs are drawing physicians away from San Francisco and Marin toward more affordable cities where they can set up roots, free from additional debt. These providers often stay where they’ve first established their practice, providing care beyond their service obligation.
San Francisco and Marin must step up and compete. Ensuring care for communities affected by addiction remains a challenge as San Francisco and Marin continue to face drastic care provider shortages in behavioral health settings, including community clinics, public hospitals, schools, and addiction care facilities. Leaders have appropriately prioritized investment in much needed behavioral health care-related facilities and beds. However, these new beds are only useful if they are staffed.
SFMMS leaders have met with legislators in San Francisco and Marin Counties to propose the creation of a local workforce incentive program. In San Francisco, the $230 million Walgreens settlement funds represent a rare and significant opportunity to meet the needs of at-risk communities in San Francisco through one-time investments in effective health care strategies.
Applicants to this new program would receive incentives if they:
• Agree to deliver services solely in San Francisco or Marin for five consecutive years.
• Practice a minimum percentage of time within the safety net (e.g., a community clinic, public hospital, wellness center, etc.) and/or with vulnerable populations (e.g., those with substance use disorders, patients with severe mental health conditions, unhoused individuals, at-risk children, etc.).
• Predominantly provide primary care, addiction medicine (including Medication Assisted Treatment), and mental/ behavioral health services (including school-based mental health services).
Additional preference should be given to applicants who:
• Grew up in a disadvantaged community.
• Represent an underserved community.
• Demonstrate a commitment to remain in San Francisco or Marin and continue to provide care for underserved populations.
Hiring incentives could include one or more of the following:
• Student loan repayment
• Mortgage/rent relief
• Signing/Employment acceptance bonus
• Retention bonus
• Relocation assistance
These types of incentives represent enormous value. For example, if San Francisco were to allocate at least $12 million to a county-specific physician loan repayment program and make up to $150,000 in loan repayment available in exchange for a service obligation, it could incentivize the location of at least 80 vital care providers to the county. If each of those providers has a patient panel of at least 2,000 patients, these providers would serve at least 160,000 patients. When you consider that those physicians are likely to remain in San Francisco beyond their service obligation, the County will have received a generation of care for only $150,000 per physician.
San Francisco and Marin Counties can no longer afford to rely solely on the dynamism and character of their cities to attract an adequate health care workforce. The time is now to invest in the workforce of the future.
Per California Medical Association (CMA) Campaign and Election Protocols, CMA will e-mail campaign-related communications to members of the House of Delegates on behalf of candidates, up to a maximum of three (3) times per candidate during the year preceding the election. This content is entirely candidate-generated. CMA does not endorse any individual candidate.
Over the years, I have met many delegates in the CMA House, but realize that many of you do not know me well. As a means of introduction, I want to share my personal history with you, and how I believe this personal history would help me if elected Vice-Speaker of CMA’s House of Delegates.

After graduating from high school in a suburban community of Columbus Ohio, I attended the University of Michigan College of Engineering receiving a BSE in Chemical Engineering in December of 1985. Prior to entering medical school at the Ohio State University, I briefly held a position as a chemical engineer at UOP, Inc., in Des Plaines Illinois, as a pilot plant operator for catalytic cracking processes for our clients.
Upon completing medical school, I matched at the Los Angeles County + University of Southern California Medical Center in the general psychiatry residency. During my final year of residency, I transitioned into their child and adolescent psychiatry program, graduating in 1995.
My first post-graduate post was with the San Francisco Department of Public Health as Medical Director for an innovative program: Foster Care Mental Health Program. This was a collaborative endeavor with child mental health and child protective services. One of my primary tasks was to provide consultation to the presiding judge over the dependency court regarding the use of psychotropic medication in foster youth. This developed into the first organized psychotropic oversight program in the State of California. After the state passed legislation requiring mandatory completion of the JV-220, I participated in workgroups as the process was developed over time, and managed the oversight program for San Francisco County for 20 years.
After joining the San Francisco Medical Society in 1996 (now SFMMS, having merged with the Marin Medical Society in 2016), I quickly became active in member activities. In addition to chairing the SFMSPAC for several years, I have held multiple offices culminating in becoming President in 2011. In 2017, I moved back to Los Angeles to take a position with LA County Dept. of Mental Health within the Child Welfare Bureau.

While continuing to be a member of SFMMS, I also joined LACMA and have been the Chair of LACPAC for the last 2 years. Part of my charge was to reform LACPAC. Since becoming Chair, I have changed the make-up of the Board, which now includes more women, members who are earlier in their careers, and from a variety of ethnic backgrounds. This year I have officially joined the LACMA Board as a Councilor-at large and have moved from the SFMMS delegation to the LACMA delegation.
Finally, I have also been active within my specialty: Child and Adolescent / General Adult Psychiatry. I have been President of the NC- Regional Organization of Child and Adolescent Psychiatry, President of the Southern California Psychiatric Society, and am currently on the board for AACAP-PAC.
This broad range of experience in innovative care models and across multiple county societies provides me with an essential perspective on the value of hearing from a diversity of voices and the power of what we can accomplish if we collaborate with one another. It’s this perspective that I will bring if elected your Vice-Speaker.
George A. Fouras, MD, DFAACAPThe 2023-24 California State Budget includes one of the greatest accomplishments in CMA history. After decades of being treated as a burden and an afterthought, the Medi-Cal program will receive a nearly $20 billion investment thanks to the tireless work for CMA members and advocates.
This investment was made possible through the renewal of the state’s Managed Care Organization (MCO) Tax, which requires MCOs in California to pay a fee that is used to draw down federal matching funds. This allows California to generate billions of dollars in additional federal funding. Until this year, the vast majority of funds raised through the MCO tax went to the General Fund, not health care. CMA’s efforts to convince legislators and the Governor to redirect this money to Medi-Cal means represents the largest Medi-Cal payment rate increase in California history, ensuring that millions of Californians have greater access to affordable, high-quality, life-saving health care.
Medi-Cal provides essential health coverage to one in three Californians and is foundational to the state’s health care delivery system and economy. In fact, more than 50 percent of California children are born into Medi-Cal, making it an essential program for preventive and routine care for children. Despite the importance of the program, patients with Medi-Cal coverage routinely wait weeks or months for appointments and must travel long distances to receive care because providers in their area cannot afford to provide care for the incredibly low Medi-Cal payment rates. This unprecedented investment into Medi-Cal payment rates and physician workforce will help ensure that those newly covered individuals, as well as those already with insurance, will have meaningful access to health care. This is even more crucial as a series of SFMMS supported bills over the past few years mean universal health care coverage will soon be a reality in California.
While the MCO tax must be approved by the federal government, this new version of the drawdown moves in a direction far more in line with what the Center for Medicare and Medicaid Services (CMS) has long advocated—that the matching funds be used directly for health care, not the General Fund. In fact, California’s previous MCO taxes had to undergo multiple changes and risked being eliminated due to previous governors diverting funds for other purposes. This new MCO tax structure greatly improves its ability to be renewed, and a future ballot measure may even lock the funding allocations into perpetuity.
To learn more about this historic win for patients and physicians, please see CMA’s FAQ document.
The MCO Tax Plan Includes:
Primary Care
• Starting in 2024, the budget trailer bill increases provider rates to at least 87.5% of Medicare for primary care, maternity care and non-specialty mental health services.

• Starting in 2025, an additional annual appropriation of $1.38 billion will be directed to primary care providers in the Medi-Cal program to support the comprehensive services that protect and promote beneficiaries’ overall health.
• Starting in 2025, the bill includes $1.15 billion annually to increase Medi-Cal rates for specialists, which will increase access to care and decrease wait times.
Emergency Department Access
• Starting in 2025, the bill includes an annual appropriation of $700 million to be used to support inpatient facilities, most notably through hospital emergency departments, including $200 million to go toward rate increases for emergency physicians seeing Medi-Cal patients in emergency departments.

Emergency Ground Transport
• Starting in 2025, $100 million annually will be directed to support 911 emergency ground providers and increase staffing capacity to help address increased workforce challenges.
Graduate Medical Education
• Starting in 2024, an additional $75 million will be allocated annually to increase residency slots for primary and specialty care and expand the number of residency programs in California.
Care Workforce
• Starting in 2025, $150 million annually will be allocated to grow the health care workforce.

Inpatient Psychiatric Bed Capacity
• Starting in 2025, $600 million annually will go toward increasing the number of inpatient psychiatric beds and funding additional care for the severely mentally ill.
• Starting in 2025, $150 million annually will go to increase care at public hospitals.
Distressed Hospitals
• In the 2023-24 state budget, there will be a one-time allocation of $150 million to the Distressed Hospital Loan Fund.

• The 2023-24 budget includes a one-time allocation of $50 million for small and rural hospital relief for seismic assessment and construction.
Protect Family Planning and Abortion Access
• At least $500 million will be directed to family- planning related services in both Medi-Cal and FPACT and to abortion services.

There is a Bay Area tradition that has been occurring annually since 1967. Originally part of the San Francisco Haight Ashbury Free Clinic, fast forward five decades to the 2023 David E. Smith Addiction Medicine Seminar that was sponsored by SFMMS in June. This free seminar hosted an all-star faculty of leaders who addressed treatment, public health responses, psychedelics and new approaches to the toughest problem physicians face today: dealing with substance use disorders.
I attended the conference via Zoom, knowing how valuable it has been in the past. It did not disappoint.
Dr. David Smith reminded us that when he started the SF Free clinic in 1967, addiction was a crime and treatment by physicians was a felony. He even had his malpractice insurance cancelled for dealing with “those hippies.” Way back then, the SFMS played a historical role in getting addiction medicine accepted as a specialty and the original Haight Ashbury Free Clinic has today become the largest non-profit addiction agency in NorCal: Health Right 360.
I was most impressed with the kick-off presentation by Dr. David Pating, the interim medical director at SF Health Dept Substance Use Services. At a time when we hear how drug use is rampant and “nothing is being done,” he focused on what is going right. The current trends are scary but the City is focused on facilitating housing, expanding the already 271 residential step-down beds and increasing the SoMa drug sobering center that links people to treatment.
We heard a “view from the street” by Mary Howe, the ED of the Homeless Youth Alliance. Her model program focuses on building relationships and meeting people where they are with patience and solutions. She also noted that the majority of Fentanyl ODs and deaths are in non-Fentanyl users. Continued education and harm reduction programs are needed to get ahead of this crisis.
Dr. Ken Roy, Program Director of Addiction Fellowship at Tulane School of Medicine educated all of us about how the use of methadone and buprenorphine saves lives with decreased mortality between 37-80%. For DEA license renewal all physicians will need hours of training on treating OUD and SUD. It is a one-time only requirement and information can be found at https://edhub.ama-assn.org/asam-education-cme/ interactive/18638491
We learned that understanding SUD and the psychiatric and cultural stigmas are an ethical necessity for all physicians according to Dr. William Andereck, Division Chief of Medical Bioethics at CPMC and Sutter Health. Our patients and society need us to be the experts with compassion and solutions.
It wouldn’t be timely and current if we didn’t hear about the new psychedelic therapies for substance abuse disorders. When the conference started in 1967 we were at the tail end of the first psychedelic revolution. Now we are in the 3rd stage with research and acceptance of treatment with plant-based and psychoactive substances for medical conditions and addictions. Drs. Nicky Mehtani and Gabrielle Agin-Liebes of UCSF gave fascinating presentations on new research in Psilocybin, Ibogaine and LSD for treatment of alcohol and substance abuse disorders. And state Senator Scott Wiener popped in to update the progress of his controversial legislation to decriminalize some such substances, adding high praises for the SFMMS in the process.
This conference, co-hosted by Steve Heilig and Dr. Smith, again brought together different views and expertise for those of us lucky enough to participate. There isn’t a physician who hasn’t treated patients or experienced a friend or relative with a substance problem. We are fragmented in our medical world more than ever and learning the current state of addiction healing and recovery in 2023 is a tradition that should continue for all of us.
You can find a link to the conference at https://www.sfmms. org/news-events/events.aspx. It’s well worth the time.
 David E. Smith, MD
David E. Smith, MD

When I founded the Haight-Ashbury Free Clinic in 1967, psychedelics were all the rage. Research at Johns Hopkins and elsewhere had uncovered that these substances had mind-altering qualities. Timothy Leary famously said at a gathering in San Francisco that summer: “Turn on, tune in, drop out.” And many young people followed. They rode the wave of psychedelic journeys, until they didn’t. Several well-publicized deaths stopped the research, and availability of these drugs, in their tracks. The Food and Drug Administration characterized hallucinogens as Schedule 1 controlled substances, concluding that they had no medical benefit, and prohibited their possession, sale or use.
Fifty years later, researchers at my alma mater UCSF and other institutions began studying these substances again in carefully controlled clinical trials. They discovered, as their scientific predecessors had decades before, that taken in a therapeutic setting, these drugs were potentially beneficial for some confounding mental health conditions. MDMA is now on the precipice of FDA approval for post-traumatic stress disorder and psilocybin for treatment-resistant depression. Unlike what occurred before, however, these drugs have become glorified in the press. Many have begun experimenting with them—for the sheer hallucinogenic experience, for spiritual enlightenment and for help with their mental health struggles. Yet their risks have not been publicized and been largely ignored.
Senator Wiener’s bill, SB 58, reflects this wave of popularity for psychedelics. He proposes to decriminalize four hallucinogenic substances: psilocybin, psilocin, mescaline, and DMT. He has agreed to delay decriminalization for therapeutic use until a panel of experts has determined an appropriate regulatory framework and safeguards for use. This makes sense. But decriminalization for personal use would go into effect in January 2025 with no guardrails, no safety precautions in place. In my view, this is premature and misguided. It threatens once again to derail important, life-saving research.
Decriminalization for personal use should come after, not before, decriminalization for therapeutic use. The scientific research currently underway should inform and guide how these substances should be used by the general public. Psychedelics produce mind-altering results because they create physiological changes in the brain. While it does not appear they are addictive or toxic, more research is needed. Importantly, it does not mean they do not have adverse effects. Psychedelics can create panic, anxiety or a fight-or-flight response. They can cause delusions and distort thinking. For some, they can trigger psychological
or emotional trauma and encourage violence towards oneself.
Many of these effects can be moderated or mitigated if taken in an appropriate setting with a trained guide or facilitator. But taken alone, or in unsupervised or unstructured settings, with no instruction or guidance can result in significant adverse consequences. We know of at least five recent Bay Area deaths where psychedelics were taken under these circumstances. Some details on these cases are uncertain but in any event, we want to avoid more such tragedies.
As with all medicines, psychedelics are not appropriate for everyone. The most common effect, for example, is elevation of blood pressure and heart rate. Thus, they should not be taken by anyone who is pregnant, has a history of seizure disorders or has severe cardiovascular disease. The clinical trials of psilocybin exclude those with a family history of psychosis, bipolar disorder or schizophrenia, those who have experienced suicidal ideation, and those who take antidepressants; the drug is deemed too volatile for them. Because of these contraindications, none of these drugs should be consumed without appropriate medical screening. Moreover, none of these substances should be used without adequate guardrails and safety precautions in place. Widespread public education needs to occur so that potential users can evaluate the risks, as well as the benefits, of these drugs. First responders need to be trained to deal with psychotic episodes if, and when, they occur. A regulatory framework needs to be implemented to ensure these substances are not adulterated and are used in the right amount, in the right place and with adequate supervision and therapy. Data tracking needs to be deployed to understand who has adverse reactions and why.
The medical and scientific community studying these drugs fears that decriminalization alone will increase dangerous access and use. Without safeguards, there will be more unintended consequences, such as the deaths we already know about. These, in turn, will create adverse publicity. The regulators and authorities will crack down once again and shut off the research and therapeutic use. We already have lost fifty years of learning how these substances can ameliorate mental health conditions. Let’s not lose fifty more.
This is an expensive thought shared by many physicians. Our jobs are hard and we don't need to make them harder. This thought makes most of us feel overwhelmed, burdened, and exhausted. It may also lead you to feel resentful, frustrated, isolated, and disconnected.
If you want to feel better, when this habit thought pops up—you could ask yourself, what else could you think instead? Does “I have a full life” feel better?
While you likely do have a very high level of responsibility in your family and at work, you also likely also struggle with what I call "over-responsibility" and "toxic independence."
• Do you take on responsibility and/or worry about things that aren't yours to fix and/or aren’t in your control?
• Do you do things yourself because you are faster and better at them than others?
• Do you then feel resentful because others are not helping out as much as you would like them to?
Could you step back and let others step in, and up, and see what happens? Things won’t get done the way you would do it, and it will likely be fine. It might even be better but you might learn something and others might too. Catastrophe is
Dr. Rakesh Jotwani, a former hospitalist at The Permanente Medical Group, now practicing Lifestyle Medicine full-time, tells the story of how wellness came into his life “at just the right moment.”
He shares how a physician wellness talk, given by SFMMS Wellness Committee Chair, Dr. Jessie Mahoney, on Evidence-Based Workplace Happiness set off his “BS meter” but turned out to be the impetus he needed to begin his journey to mindfulness, better physical and mental health, and changed career in medicine.
To listen to the podcast, scan the QR code with your smartphone or visit: https:// podcasts.apple.com/us/podcast/149-howmindfulness-can-lead-you-to-a-plant-based/ id1542538851?i=1000623585219
 Jessie Mahoney, MD
Jessie Mahoney, MD

unlikely to happen if you let go of control. You can always go back to doing it all yourself later if you really want to.
Some other helpful questions to ask yourself to feel less burdened:
• What do others already take responsibility for? We are trained to focus on what they aren't doing ... so shifting our focus feels better.
• What might others be really good at? Do they have a special skill set that could be helpful?
• What might they learn from taking on new roles?
• What if they have a different way of doing it that is somehow even better than your way?
• What if you could trust them?
• Might they want the same outcome as you and just have a different way of getting there?
Jessie Mahoney is a pediatrician, a certified life coach for physicians, and a yoga instructor. She is the Chair of the SFMMS Physician Wellness Task Force. She practiced pediatrics and was a Physician Wellness leader at Kaiser Permanente for 17 years. She is the founder of Pause and Presence Coaching where she supports and empowers her physician colleagues using mindfulness tools and mindset coaching.
Each month, as part of the Physician Wellness leaders' work, they curate wellness resources around a common theme for our monthly wellness blog. Read, listen, and attend the monthly resources the committee has curated for SFMMS members by visiting:
https://www.sfmms.org/news-events/sfmms-blog.aspx? Category=physician-wellness.
Have you missed a recent Wellness Event?
You can learn more about upcoming wellness events or view recordings of past events on the SFMMS Wellness Page at www.sfmms.org/get-help/physician-wellness


many potential approaches. We encourage the idea that we can all be “students of wellness” including organizational leaders, physician leaders, and everyone on the healthcare team.
To listen to the podcast, scan the QR code with your smartphone or visit: https:// podcasts.apple.com/us/podcast/ mindfulhealers-podcast-dr-jessie-mahoney-dr-nicheng/id1542538851?i=1000617042876



Listen to the Mindful Healers Podcast Episodes Featuring SFMMS Physicians!
How Physician Leaders Can Effectively Support Wellness
Featuring SFMMS Member, Dr. Karin Shavelson
A lively discussion between Dr. Jessie Mahoney, Chair SFMMS Wellness Committee and SFMMS Member, Dr. Karin Shavelson, the Chief Medical Officer at Marin Health.
In this episode, we talk about the value of retreats, in particular the Honoring Diastole Retreat that Dr. Shavelson attended in September 2022 as a winner of the SFMMS Raffle. She shares how her experience led her to sponsor many of her own physicians to attend Honoring Diastole.
Her thoughts: wellness in a post-pandemic world looks like coming together with others who have shared experiences. Community and connection and people and place are key. This is why retreats offer such value.
We discuss that there is no one solution to physician wellness. There is NO magic bullet to solve burnout. Instead wellness looks different for everyone which means that there are
Upcoming 2023 Honoring Diastole Retreats at Pie Ranch: Saturday, October 14th and 28th, 2023
Mindful Coaching, Yoga and Culinary Medicine CME Wellness Retreats for Women Physicians: 4-5 night intimate physician wellness retreat opportunity for women physicians in Santa Margarita CA., December 3-8th, 2023, March 17-22nd, April 14-18th, and May 5-9th, 2024.
Save the Date: 2024 Connect In Nature Retreat at Green Gulch will be held. Sept 6-8th.
Find out more and sign up here: https://www.jessiemahoneymd. com/retreats.
Our tips for advocating for institutional wellness funding and engagement in wellness programming:
• Attend wellness events and retreats yourself, especially if you are an influential leader
• Attach CME to wellness events
• Talk about the science behind wellness interventions
• Offer lots of creative options
• Use language other than “wellness,” “burnout” and “moral injury”
Our tips for improving physician health and wellness if you are a senior leader:
• Talk about struggles, challenges and “what’s really happening”
• Acknowledge systemic problems as a root cause
• Be vulnerable about your own experience and what has helped you
• Model healthy boundaries yourself
Join Us on October 15th! Special In-Person Mindful Yoga for Healers in Old Mill Park sponsored by SFMMS
Join SFMMS on Sunday, October 15th 10am - 12pm for INPERSON yoga and community building at the Old Mill Park Amphitheatre in Mill Valley. 60 minutes of ALL levels yoga will be led by SFMMS Physician Wellness Committee Chair, Dr. Jessie Mahoney. Yoga will be followed by socializing and community building with your SFMMS physician colleagues. All skill levels welcome! Please bring your own yoga mat or beach towel. This class will be held outdoors, so please be prepared for the weather with appropriate layers. Attendance is limited to the first 50 SFMMS Members and their guests that RSVP.


To register, visit: https://www.eventbrite. com/e/sfmms-in-person-mindful-yogafor-healers-community-building-registration-494197085787 or scan the QR code with your smartphone.
Want to practice Mindful Yoga for Healers with Jessie before this event?
Join Dr. Mahoney on Zoom most Saturdays at 9am or anytime on YouTube.
For more information visit: https://mindfulyoga.jessiemahoneymd.com/ or https://youtube.com/c/JessieMahoney.
Recent multi casualty incidents have suggested that reliance solely on the trauma centers in large scale events that occur without notice and result in a high number of acutely injured patients in a short amount of time may initially exhaust the trauma system until either the trauma resource recovers, or the patient surge stops. San Francisco is fortunate to have a Level 1, or highest-level trauma center but lacks other trauma capability / designation amongst its other hospitals. This single center, despite being robust and having a record of constantly flexing to accommodate incidents resulting in high trauma patient volumes, could potentially be overwhelmed by a sudden, large, high acuity multi casualty event, such as a mass shooting event.
In addition to the potential of a large multi casualty incident, there is a vulnerability in reliance on a single point of care. Despite its modern and high-grade seismic safety design, the trauma center at Zuckerberg San Francisco General Hospital could fall victim to an intentional or unintentional incident that would render it incapable of treating trauma patients, while some of its staff capability would remain intact (due to being off site at the time of the incident). An example would be an event at or near the emergency department that results in severely degrading or preventing access to the facility. The staff that were not on site during the event, along with pre-identified relevant medical supplies and equipment could provide trauma care at another site within a short period of time being notified.

Also of concern is that San Francisco is isolated geographically from its surrounding trauma resources (the nearest alternative facilities are in Santa Clara, Alameda, Marin and Contra Costa counties) and has no regular/reliable air medical access to these centers. This makes reliance on outside resources for timesensitive high acuity trauma care an unrealistic option for either direct patient care or as a backup to the trauma care capacity limitation in our system. While we have an Emergency Air Medical Access Policy in our EMS System utilizing pre-designated
alternate landing sites throughout the city, the time to initiate this capability and its reliance on the variable availability of medical helicopters in surrounding jurisdictions make this a less desirable option as a backup plan. San Francisco does not have an identified backup to our single designated trauma center at Zuckerberg San Francisco General Hospital and this does put us at risk should a significant event occur in San Francisco, particularly one that directly impacts access to the ZSFG campus. While additional high level trauma centers would negatively impact critical trauma patient experience and risk the outstanding trauma care the citizens of San Francisco currently receive, the lack of any back up trauma resources does present a risk to our city. Events have occurred in similar sized jurisdictions that could impact patient care in San Francisco, particularly if they involved the ZSFG campus, that could be addressed at least in part with better surge capacity.
The lack of a backup trauma center capability has been identified by the State of California Emergency Medical Services Authority as a deficiency in our San Francisco EMS Agency Trauma Plan. It has been assigned the highest priority level to be addressed by our local EMS Agency. While this Agency provides direction and has authority over prehospital providers, it does not have the ability to direct hospital planning, policy, or preparedness to provide backup trauma care.
Community hospitals have been approached about providing backup services to ZSFGH in the past but were unable to do so due to a number of challenges. These include that trauma specialists including physician, nursing and allied health professionals that might be available to assist a backup trauma center in providing trauma care would need rapid emergent credentialing and just in time facility-specific training at the backup trauma center facilities. Backup trauma center personnel at community facilities would need basic pre-event familiarization training with trauma care across many disciplines, including for physicians: surgeons, anesthesiologists, emergency medicine specialists
“…the most important ethical question sometimes is the one you ask not at the moment of crisis but the duty you have to anticipate certain kinds of crises and avoid them.”
Rand Cohen, N.Y. Times Ethicist
and surgical sub specialists and for nurses: emergency, operating room, and Intensive Care Unit (ICU) care. Additionally, radiology technicians, respiratory therapists, laboratorians, and others would need trauma orientation and protocol development. Blood supply and pharmacy involvement would be necessary to support trauma services. Potential back up facilities may need to have emergency vehicle access issues addressed due to location constraints of their ambulance receiving facilities. Staff transportation / parking may be an issue, as well as maintenance of a cache of relevant trauma-center specific equipment for patient care. The upfront costs of this preparation would have to be offset in some manner.
A possible next step to mitigate this vulnerability includes the engagement of a consultant to review our current trauma system and evaluate potential backup options. Development of a backup trauma center capability could be accomplished by several mechanisms. A facility could be designated to function as a different level trauma center—i.e., Level III—to develop in-house core trauma capability and receive trauma patients triaged by EMS personnel without impacting the experience and care at Zuckerberg San Francisco General Hospital. Another option would be community hospitals receive lower acuity trauma patients on a regular basis which would provide good care for a select group of patients with rapid transfer capability to the current trauma center in normal operational circumstances that exceed their capabilities. Finally, a hospital could be designated as a disaster contingency/standby center with pre-staged equipment and supplies and rapidly scalable credentialing and personnel support systems with the requisite external support for training and capacity maintenance. A change of this magnitude to the San Francisco EMS system would have both anticipated and unanticipated effects that would be important to evaluate proactively as thoroughly as possible in order to choose and pursue the best strategy. This was the recent recommendation of our SF EMS Agency Trauma Systems Advisory Committee.
A possible facility for either single-center approach would be UCSF Mission Bay due to its geographic location, air medical access and compatibility of UCSF health care system elements with ZSFG’s systems. However, there are many other possibilities available to our city due to its small geographic footprint with resulting rapid transport time intervals, and robustly resourced medical community with surgical and medical expertise. Any system changes would involve developing revisions to the EMS Agency Trauma Bypass Policy 5021 and Multi Casualty Incident Policy 8000 reflecting this capacity. If a standby center strategy were chosen, support would be needed to the backup trauma center for personnel training, equipment procurement and maintenance.
While discussion between the State EMS Authority, the San Francisco EMS Agency, San Francisco General Hospital Trauma service and the San Francisco Department of Public Health has been in process for several years, we are at the point of needing to take more definitive steps to improve our capacity in times of sudden surge. Preparation including training for relevant hospital and EMS provider personnel and developing and executing exercises of this back up capability should be undertaken once the decision is made as to which direction to take. Importantly, any process developed should not negatively impact the experience and high-level care provided at San Francisco General Hospital. San Francisco urgently needs back up trauma care capabilities to support our Level 1 trauma center. Our community deserves no less.
John Brown, MD, MPA is the Medical Director of the San Francisco EMS Agency and a practicing Emergency Physician at Zuckerberg San Francisco General Hospital. He is also a Medical Officer for the National Disaster Medical Assistance Team California-6.

Christopher B. Colwell, MD is the Chief of Emergency Medicine at ZSFG and endowed Professor and Vice-Chair in the Department of Emergency Medicine at UCSF.

Dr. Joseph Cuschieri is a Professor of Surgery and Laboratory Medicine at University of California San Francisco. He is also the Chief of Surgery and Trauma Medical Director at Zuckerberg San Francisco General Hospital and Trauma Center.

On New Year’s Day in Reno, Nevada, the Marvel Cinematic Universe was nearly changed forever. As Hawkeye actor Jeremy Renner was attempting to save his nephew from a rolling snowplow, Renner’s poor footing caused him to slip out of the vehicle’s cab and fall beneath his 14,330 pound snowcat resulting in a catastrophic crush injury. Luckily, neighbors were able to rush to his aid and skillfully place a tourniquet on his badly bleeding leg. Twenty-one minutes would elapse before further help could arrive making this intervention, a lifesaving one.
Closer to home, on May 29th, a man walked into the AA Bakery on Stockton Street in San Francisco and for no apparent reason, stabbed a 58-year-old employee seven times to the head, neck, and back. Fortunately, community leader Robert Chiang was present to actively apply pressure with clean paper napkins to become what San Francisco Police Chief Bill Scott called, “a hero in my mind. He saved the victim’s life.” (Wind Newspaper 6/4/23)
As you can see, bleeding injuries can happen anywhere and occur far too often. They can result from motor vehicle collisions and even more commonly, work-related or at-home accidents like when someone slices their hand while cooking. For physicians, the actions initiated by these good Samaritans are truly second nature: secure situational safety, initiate EMS, control the hemorrhage with pressure/packing, and finally, apply a tourniquet if necessary. But are you aware that these procedures have been codified into a lay course called Stop the Bleed?

Stop the Bleed, initially inspired by the Sandy Hook Elementary School tragedy, was conceived in a cooperative effort spearheaded by the American College of Surgeons to develop a bleeding control curriculum. The most common preventable cause of accidental death is exsanguination. And minutes count! Someone who is severely bleeding can bleed to death in as little as five minutes. (Stopthebleed.org) That’s why hemorrhage control is the sole purpose of Stop the Bleed training. Utilizing lessons learned from the military, multiple techniques including direct pressure, packing the wound, and applying a tourniquet are lifesaving skills that have been organized into this course geared to the public. Students have reported that it is much easier to learn than CPR.
Importantly, during the 2022 legislative session, the state of California passed legislation—Assembly Bill (AB) 2260—that requires the installation statewide of trauma bleeding control kits in newly constructed public and private buildings. This statute, “Emergency Response: Trauma Kits,” is the first of its kind to make bleeding control equipment widely accessible in
this manner. SFMMS played an active role in developing and endorsing this legislation which came into effect this year.
Further, ongoing momentum has spawned important new legislation, namely Assembly Bill 70. AB 70 is an extension to AB 2260, whereby Stop the Bleed kits will be added to certain buildings that undergo $100,000 or more in renovations and in places of assembly. It passed, and Governor Newsom has 30 days to make a decision on any bill placed before him so we could have an answer as early as October.
And what are we doing locally? In a cooperative effort between physicians and community leaders, the San Francisco Marin Medical Society, AAMG medical group, and Self-Help for the Elderly have formed a coalition to provide classes in San Francisco. Despite its demonstrable effectiveness, we’ve noticed the lack of courses to teach the public to control bleeding and thus, save lives. Our first session on May 20th was attended by Asm. Phil Ting, Sup. Connie Chan, Past-SFMMS President John Maa, and Trauma Surgeon Edmund Tsoi when we were able to instruct over 40 caregivers and healthcare providers. Our continuing goal is to establish regular programs throughout the City with the hope that people will not only be witnesses to these untoward events but above all, have the skill and confidence to be active responders.
But we still need your help. As physicians, we hope you will support the ongoing legislation, and as importantly, attend our course which will allow you to join us as instructors. Lastly, let’s make sure our local facilities have the supplies and resources necessary to save lives in a bleeding emergency. More information is available at www.stopthebleed.org.
Janna Yang is a Bay Area native and a third year medical student at Touro University, California in Vallejo. Janna is the local coalition lead for our Stop the Bleed efforts. Please contact her at jyang15@student.touro. edu if you are interested in taking the course and becoming an instructor.

Joseph Woo, MD is an Emergency Physician, Chair of the SFMMS PAC, and the President of the All American Medical Group (AAMG).
Dr. John Maa was 2018 President of the San Francisco Marin Medical Society and helped champion the flavored tobacco ban in San Francisco and Marin Counties.

“If we had any thought or knowledge that in any way we were selling a product harmful to consumers, we would stop business tomorrow.” George Weissman, Vice President of tobacco giant Philip Morris Company, said this in 1954. Unfortunately, it seems both he and the tobacco industry didn’t really mean it. Ever since the 1962 United States Surgeon General’s report establishing the many serious negative health impacts of tobacco, the scientific evidence has grown. But the tobacco industry has continued to expand sales globally.
Of course health and medical advocates haven’t been idle on this front, and the “tobacco wars” have been prolonged and heated, with many gradual successes in reducing smoking and its harms. But over a half-century of concerted tobacco control work has only been partially successful, and realistically speaking, a total victory in ending smoking appears ever elusive using existing strategies. Today, cigarettes still kill roughly half a million people each year in the US alone—more than car accidents, alcohol, murders, suicides, and illegal drugs combined. The global toll is far bigger, and in fact growing.
One key point to keep in mind: It is well-established that most tobacco use and addiction begins at an early age, before 25. If youth can be deterred from starting tobacco use until then, it is highly unlikely they will start at all. Prevention of youth smoking is the most important goal of tobacco control, health efforts and policy.
We cannot allow this deadly product to keep harming our communities and loved ones. A more sweeping, long-term approach is warranted. And it in fact exists. In 1997, United States FDA Commissioner Dr. David Kessler, also of UCSF, wrote, “We must create a generational firebreak, an interruption in the recruitment of young new smokers into the ranks of the chronically hooked.”
One way to create such a firebreak is through legislation that gradually phases out cigarette sales over an extended timeline. New Zealand and Brookline, Massachusetts have recently passed laws with this intent. These laws permit anyone of legal age to continue to purchase tobacco products. Meanwhile, youth born after a certain cut-off date will never be allowed to purchase tobacco products in their lifetimes, protecting them from the perils of nicotine addiction and a lifetime of illness and premature death.
We have precedents for building better futures by phasing out harmful substances. Opium, a highly addictive and destruc-
tive drug, was successfully phased out of use in Taiwan and Sri Lanka using a similar strategy. Pollutants such as lead in gasoline and paint and atmosphere-harming chlorofluorocarbons (CFC's) have been successfully removed from products and our bodies. With good legislation, cigarettes can ultimately go the way of lead paint, CFC's and asbestos.
In 2021, more than 140 health organizations released a letter calling on governments globally to phase out the sale of all cigarettes. The Association of American Cancer Institutes, the African American Tobacco Control Leadership Council, and the Johns Hopkins Bloomberg School of Public Health, endorse this path forward.

Following their lead, in 2023 California Assembly Member Damon Connolly (D-Marin) introduced AB 935 to protect those born after January 1, 2007, from the harms of tobacco products throughout their entire lives. His bill was endorsed by the Union of American Physicians and Dentists, the American Academy of Pediatrics-California, Public Health Advocates, the San Francisco Marin Medical Society, the California Academy of Family Physicians, the California Primary Care Association, and the International Youth Tobacco Control. He intends to reintroduce the bill in the Spring of 2024 in Sacramento.
A key strength of this phaseout approach is the incremental nature that will minimize financial impact on retailers. As written, the legislation would not go into effect until a few years after passed, allowing tobacco retailers time to adjust their business models and market alternative safer products. This strategy isn't a ban, as everyone born before the designated date will continue to be able to purchase tobacco products for their entire lifetimes. There will be no resulting smuggling, and the enforcement of tobacco sales will actually become easier as the signs displayed in stores designating the cutoff age for tobacco products will no longer need to be continuously updated.
Opponents to the phaseout idea argue that California or other locales can’t afford to lose the tax revenue from tobacco sales. But this opposition merely reflects the tobacco industry’s own fears about the financial losses they will inevitably suffer as new generations escape nicotine addiction. The tobacco industry’s global sales approached $850 billion in 2021, making it one of the most profitable industries in the world.
When the tobacco industry profits, Californians lose big. The reality is that tobacco use costs California over $24 billion each
on page 20
year— $13.5 billion in healthcare costs and $10.3 billion in lost productivity. As we gradually transition away from smoking, our healthcare system will see significant savings. We can redirect these savings to support programs currently funded by tobacco taxes.
A common critique regarding the phaseout proposal is that it would amount to “prohibition.” We agree that prohibition of psychoactive drugs, including alcohol, has largely failed when tried. Addiction and the profit motivation are too strong to combat with such a blunt instrument. But much of the more successful anti-tobacco measures have utilized “denormalization”— making smoking a rarer, marginalized practice via restrictions. Banning sales to young people is not a new idea, and is now widely in effect. When San Francisco banned smoking in public spaces such as restaurants and other businesses over 30 years ago it was opposed by some as a “too radical” proposal. The success and spread of these policies is now self-evident and few if any would reverse them. Likewise bans on smoking on airplanes, in hospitals, and so on. These “radical” ideas now are accepted as common sense. This gradual phaseout would hardly even be noticed as years go by, as no preexisting smokers would be impacted, and retailers would not lose any existing customers. Smoking would be denormalized for entire generations going forward. And, we should add, smart policy would not penalize those who somehow did begin smoking. This strategy does not involve arresting or jailing users, such as during failed alcohol prohibition. And with the passage of time, such enforcement would not even need to be contemplated. The only real enforcement would be on retailers and on continuing to prohibit any marketing to young people—or as in other nations ahead of the USA—to anyone.
Most importantly, in 2017 Philip Morris International created the “Foundation for a Smokefree World,” and pledged $960 million over 12 years to fulfill the objective of ending the sales
of combustible cigarettes worldwide within the next generation, perhaps as early as 2040. The phaseout idea will help the industry achieve this self-stated goal. Any other product proven deadly is quickly recalled. Add the addictive qualities of tobacco and the need to phase out tobacco is multiplied. But unlike some other recalled products that might be pulled off the market and returned to the shelves after safety defects are repaired, cigarettes cannot be fixed. When used as directed, they kill up to two-thirds of their users. It’s time we take the big step to remove them from our society, for the health of all, by finally achieving a smoke-free world.
Dr. John Maa was 2018 President of the San Francisco Marin Medical Society and helped champion the flavored tobacco ban in San Francisco and Marin Counties.

Steve Heilig is with the San Francisco Marin Medical Society, co-editor of the Cambridge Quarterly of Healthcare Ethics, a former Robert Wood Johnson drug policy fellow, and former co-chair of the San Francisco TobaccoFree Coalition.

Dr. Tamu Green is CEO and Founder of the Equity and Wellness Institute, who conceptualized the generational phase out idea in 2004 with inspiration from Surgeon General C. Everett Koop.

The tobacco epidemic is the top worldwide public health threat affecting 1.3 billion tobacco users and kills 8 million people globally each year. Tobacco use represents the major risk factor for non-communicable diseases such as coronary artery disease and many human cancers. Since 2003, countries have begun implementing different tobacco control strategies to bring an end to unnecessary tobacco related deaths encompassing the WHO’s Framework Convention on Tobacco Control (FCTC). Within a few years, new emerging ‘Endgame’ strategies were developed in many countries to reduce smoking prevalence. The Tobacco Endgame is most often defined as a national smoking prevalence of less than 5%, but countries differ with respect to individual timelines and strategies to reach that target.
A newer Endgame approach that garnered significant California attention in 2023 is the ‘Tobacco Phaseout,’ first introduced by Khoo, D., et al. (2010) in Singapore. Berrick, et al., refined this approach in 2013 to target tobacco sale and supply rather than use or possession. New Zealand took a major step forward in late 2021 to reach its Endgame goal by proposing to phaseout tobacco sales to anyone born after a certain date. Starting in 2023, anyone under age 15 will be restricted for life from buying cigarettes in New Zealand, and as the years pass by the minimum age to purchase tobacco products will rise accordingly. A similar approach was adopted in 2021 in Brookline, Massachusetts. In 2023, California Assemblyman Damon Connolly (D, Marin) introduced legislation to phaseout California tobacco sales to anyone born after 2007. This article shares the history of this novel approach and next steps forward including possible introduction of local Bay Area legislation to help California reach its own Endgame goal by 2035.

Over the past decade, multiple attempts to implement the birthyear phaseout approach around the globe provide evidence and guided strategies for subsequent efforts. To solve their tobacco problem, Singapore first led the way by proposing a new phaseout strategy where cigarette sales would be restricted for people born after a certain birthyear. This built upon the original idea of a tobacco-free generation (TFG) which transformed to a primary goal of completely protecting individuals under a
certain age (usually 18 or 21) from harmful smoking habits, leading to a decrease in tobacco sales over time. Although acclaimed by many including Members of Parliament, Singapore opted instead to increase the legal smoking age to 21 (often referred to in the US as Tobacco 21) instead of implementing a birthyear phaseout.
In 2016, Balanga City in the Bataan Province, Philippines passed the first TFG policy, including a lifetime cigarette sales phaseout for anyone born after January 1st, 2000. Along with this policy, earlier in March 2016, Balanga City also passed a policy implementing a ban on sale, use, advertisement and promotion of tobacco products and electronic nicotine delivery systems in an area encompassing 95% of the city. Despite the city’s best efforts as a worldwide leader in the advancement of the Endgame, the city faced lawsuits from the Philippine Tobacco Institute in 2018 and consequently revoked the above 2016 laws/policies. However, the city succeeded in spreading its influence to 22 government units as well as three universities. Philippine national tobacco control efforts have decreased the smoking prevalence among those 15 years of age and over from 23.8% in 2015 to 19.5% in 2021. These successes provide a critical foundation for future Philippines phaseout actions to achieve their Endgame.
As early as 2010, New Zealand recognized a disproportionate tobacco health effect among the Māori population. New Zealand defined their Endgame goal as achieving a 5% smoking prevalence by 2025, and efforts since 2010 steadily lowered the general adult smoking prevalence to 8%. However, the Māori population smoking prevalence remains significantly higher at 19.9%. Therefore, New Zealand established an action plan named Smokefree Aotearoa 2025 with 6 main strategies covering Māori leadership, health promotion, smoking cessation services, decreasing the addictiveness and availability of tobacco products, and finally restrictions in tobacco manufacturing as well as sale. To accelerate progress towards their Endgame, New Zealand first proposed in late 2021 to end the sales or public supply of tobacco products to anyone born after 2009. New Zealand then successfully passed the first birthyear phaseout law in the world in December 2022, in concert with nationwide efforts to introduce low-nicotine cigarettes and strengthen existing smoking cessation services.
continued on page 22
Malaysia defined an interim Endgame goal of a 15% smoking prevalence by 2025 (ultimately reaching 5% by 2045), and favored a birthyear phaseout strategy. In July 2022, the Cabinet proposed a law following New Zealand’s lead and ending the use and sale of tobacco products or e-cigarette products to anyone born after January 1st, 2007, and passed its First and Second Readings in Parliament. However, on the afternoon that Parliament was set to pass the final Third Reading for the legislation, Parliament was prorogued and an election called, leading to a change of government, with further action now tabled until 2025. Similarly to Balanga City’s situation, Malaysia’s birthyear phaseout law will likely face strong tobacco industry opposition and legal challenges.
In Hong Kong, by 2027, the government seeks to end the sale of cigarettes to residents born after 2009. Hong Kong's smoking prevalence was 9.5% in 2021 and the nation hopes to achieve an interim Endgame goal of a 7.8% smoking prevalence by 2025 before eventually reaching their 5% target. In April 2022, HK banned the use, sale, manufacturing, and promotion of alternative smoking products including e-cigarettes. HK’s Health Minister informed the public that the experience of other phaseout countries such as New Zealand will influence their decision on a phaseout bill. Also, a study by Wang, et al. demonstrated strong local public support of a total ban on tobacco sales; therefore, a HK tobacco phaseout may soon be on its way.
In Europe, the European Union (EU) defined an Endgame goal of a smoking prevalence of less than 5% by 2040, with Ireland and the UK leading the Tobacco Control Scale (TCS) table in 2021. Ireland’s smoking prevalence is around 18% and intends to reach the Endgame by 2035, although a birthyear phaseout strategy is not among the recommendations in Ireland’s Endgame policy document. Among EU countries, Spain and Denmark have shown interest in the birthyear phaseout strategy, although legislation has not yet been officially introduced. In Spain, a non-profit association called ‘No Fumadores’ introduced a tobacco Endgame declaration seeking a smoking prevalence of less than 5% by 2030. This declaration contains three sections encompassing short term, medium term, and long-term strategies. The restriction of tobacco and any other forms of tobacco products for anyone born after 2007 is included as a medium-term strategy.


In 2019, an AHA Presidential Advisory in Circulation discussed the path towards a Tobacco and Nicotine Endgame in America and references the birthyear phaseout concept. In 2021, an AHA Tobacco Endgame RoadMap refined this to draw upon international lessons and propose a multi-pronged strategy spanning local, state and federal action to achieve the Tobacco and Nicotine Endgame across America. In addition to the birthyear phaseout idea, other keyEndgame strategies include increasing excise taxes, implementing graphic warning labels, eliminating flavors including menthol in cigarettes and cigars, and lowering cigarettes’ nicotine content. The highest rate of smoking is in the age group 25 to 64 and many continue smoking despite multiple attempts to quit. The Tobacco Endgame will not
be achieved unless new strategies are identified to help these smokers. For example, perhaps electronic cigarettes should be sold only in pharmacies via prescription, and as part of a multimodal cessation program? This would curb youth access and allow further research into their efficacy and safety profile.
A UK recommendation requires smokers to undergo a several week cessation course before elective surgery to reduce complications, enhance recovery, etc. A similar American requirement could harness a teachable moment to motivate a smoker to quit. Another direction is to strengthen smoking cessation efforts within our nation’s hospitals and clinics, and recognize that every encounter by a smoker with the healthcare system is an opportunity to promote cessation. Exploring creative ways for insurers and healthcare systems to partner with the educational resources of leading smoking cessation organizations may prove vital to achieving the Endgame.
There is an urgency to achieve the Tobacco Endgame, as extensive research shows that smoking is linked to worse outcomes from COVID-19. A lifetime of health problems resulting from nicotine addiction predisposed many patients to develop more severe COVID-19 disease, and to die sooner than expected. California is the ideal test state towards the Endgame, given its low smoking incidence and multiple state agencies focused upon tobacco control. Given the decades-long leadership in San Francisco and Marin Counties in tobacco control, SFMMS and the CMA are ideally positioned to present the scientific evidence and overview of legislative and regulatory trends to illuminate the overarching multi-pronged strategy and timeline to the California Endgame.
References provided on request.


All of us here today are leaders in medicine, representing physicians back home. And so, we carry the burden of these hardships for them, which makes us all acutely aware of how daunting these challenges feel to our colleagues on the frontlines.
I’m sure some of the headlines about burnout stop you in your tracks—they certainly keep me up at night. One in five physicians plans to leave their practice within two years, while one in three are reducing their hours.
Only 57 percent of doctors today would choose medicine again if they were just starting their careers. Consider that for a moment … This means that about two in five physicians go beyond mere daydreams of another career to wishing they had never chosen this path in the first place.
That is a stunning indictment of the dysfunctional health care environment that is pushing record numbers of physicians to the brink.
In my inaugural address last year, and again at the Interim Meeting, I told the story of a Cleveland woman and casual runner who mistakenly ran the Cleveland marathon instead of the 10k she had signed up for. Georgene Johnson’s determination to finish the race, despite her lack of preparation, makes it an endearing story, and a perfect metaphor for all of us who pursued this profession to heal others … only to find ourselves confronting a reality that is unlike anything we imagined.
While Georgine’s story never failed to get a laugh, I’ve thought a lot about where the metaphor may have missed the mark. Lucky for Georgene, marathons have a defined end. You break the tape at the finish line, and you’re done. There is no more running to do.
But in these difficult times for medicine in America, our work in organized medicine has no finish line. New challenges keep appearing, and many existing ones seem to endure. We are knocked down … we dust ourselves off and get back up. We accumulate victories—some small, some large … but we keep running. Don’t bother looking for the rest areas between our races—I can assure you … you won’t find them.
But as physicians and healers, we are already very accustomed to persevering. And we’re darn good at it. We stick with patients suffering from chronic illnesses like diabetes or depression through setbacks and successes. We keep trying to convince that longtime cigarette smoker to quit, schedule yet another appointment to talk with a hesitant family about vaccinating their child, and show up for yet another trauma shift to face an endless stream of gun violence victims. We never turn our backs on our patients because that’s NOT who we are.
And we carry that same stubborn resolve and tenacity into our advocacy work. That means fighting for the long overdue fixes to a broken Medicare payment system, and obnoxious prior auth abuses, even when policymakers have neglected the problems for decades. That means defending against broad scope expansions that put patients at risk, even when it requires gearing up again and again, in state after state. That means confronting medical disinformation in the news and on social media, even when its growth feels overwhelming.
And yes, it means battling in state legislatures and courthouses for the very soul of our nation and our profession— to protect patients from those outside influences wanting to dictate the terms of their care … telling them what medical treatments their physicians can provide … what FDA-approved medicines we can prescribe…even what words we can use …
This is what happens when politicians force their way into our exam rooms. This isn’t about science. Interfering with the sacred patient-doctor relationship is about CONTROL. I know it can feel like victory is out of reach — that we’re running out of breath and running out of time ... But we all share a commitment to stay in this race … We play the long game, and we’re in it to win.
So perhaps instead of the marathon analogy, it’s better to think about our collective efforts like the Olympic torch relay. Don’t worry, I’m not heading for the obvious metaphor of a relay race, with one leader handing over the torch to the next. I’m talking about the deeper symbolism of the unity among torch carriers, thousands at each Olympics protecting something far bigger than any one individual, or any one leg of the course.
In our own professional tradition, the work to preserve our core values, and the health of our patients, is itself … the enduring common cause that binds us. The torch relay and the lighting of the Olympic flame are indelible parts of the games. And in that sacred tradition, as in ours, there are no shortcuts. There are no substitutes for the actual flame, which is carried forward to the games by any means necessary—by running, jogging, or swimming; by horse, boat, train, or plane … and once underwater past the Great Barrier Reef. The torch has even gone to space.
The passing of the torch, and the tradition it embodies, has survived every conceivable challenge. It has been rerouted by war. Its symbolism has been coopted for propaganda. It’s been briefly extinguished by wind, by rain, and even by protestors. But one way or another, the tradition lives on.
I like this metaphor for our work together in organized medicine because it’s not solely about passing a baton; it’s about giving of yourself to a larger mission. It’s about persevering with
unyielding resolve. The challenges that threaten the torch may change, but the larger mission does not.
The AMA doesn’t win every battle. But we are more resolute in our work because of the challenges and existential threats to our profession and our patients. Even when there are temporary setbacks, our common cause is to speak out for, and to advance our flame, our ethical values, and our common purpose – that is what keeps us going.
All of us here tonight … we recognize the extraordinary privilege to be part of something worth preserving and worth renewing for the next generation That’s the power in what we do.
I want to share some thoughts about where we are on this leg of the race, and some positive signs of hope. No, I can’t sugarcoat the very real threats. I’m still appalled by the Medicare cuts. What on earth was Congress thinking? Practices are on the brink. Our workforce is at risk. Access to care stands in the balance. We absolutely must tie future Medicare payments to inflation, and we’re readying a major national effort to finally achieve Congressional action.
And shame on political leaders, fueling fear and sewing division by making enemies of public health officials, of transgender adolescents, of physicians doing anti-racism work, and of women making personal decisions about their pregnancies.
I’m also deeply disappointed by our nation’s lack of progress to address the public health crisis of gun violence. Preventable and needless homicides and suicides continue, and the political inaction is atrocious.
But over the past year, I’ve had the privilege of appearing in public on your behalf more times than I can count. And that has afforded me many opportunities to absorb just where our profession, and the public, stand in this divisive time.
And I want to tell you something I’ve learned … There are more people who agree with us than those who do not. Are there different ideologies around solving the challenges we face? Yes. Are there different strategies for achieving our goals? Of course. Do people get their news from entirely different channels with little overlap? Sadly, yes.
But … the truth is, most physicians and our patients are proud to see the AMA fighting for its policies and values. I know what you are thinking… “Jack, have you been on Twitter lately?” Oh yes…I have. But I’ve also witnessed some of the most inspiring work in the country by colleagues and allies, and received words of encouragement that have brought me to tears on difficult days. You wouldn’t know it from social media… But after some unfortunate detours, most patients are turning back to their trusted physicians for our insights and expertise about science and medicine. You wouldn’t know it from the rhetoric …But once we demonstrate health equity in action … I’ve seen widespread support for the work. I loved traveling to Mississippi and witnessing their progress from startling COVID inequities to achieving one of the nation’s top vaccination rates among Black residents.
You wouldn’t know it from the appalling lack of legislative action … But solid majorities of Americans believe in commonsense gun reforms in line with our AMA recommendations. You wouldn’t know it from 20 state legislatures racing to criminalize abortion and rob women of access to reproductive health care…But most
people in this country support our policies and the fundamental rights of patients to make their own decisions about their health. You wouldn’t know it from health insurers still bullying us with prior auth delays and denying care … But policymakers from both parties are onto these schemes, the momentum has shifted, and they’re not going to allow this nonsense anymore. You may not realize it, based on the climate of anti-science aggression … But medical school applications are at an all-time high, led by large increases among historically minoritized students. Future physicians are not dissuaded by these challenges. They are eager to join our fight.
In our country, and in our profession, we don’t agree on everything, but we agree on enough things to pursue the shared things that we care about. Together. And let us not forget that those pursuits have generated some big and small wins tied to the AMA Recovery Plan for America’s Physicians.
I know what you’re thinking. Recovery Plan? What’s that? I’ve never heard of it before. I know, I know … Your hundredth exposure to the video loop on our buses at Interim may have been overkill. But for the public and physicians back home, they need to know about our relentless work fighting to restore the sustainability of our profession. In that race, the Recovery Plan is our roadmap and our message.
As I said in November, we need to fix what’s broken, and it’s NOT the doctor. Duct-taping the widening cracks of a dilapidated Medicare payment system isn’t sustainable. The patches aren’t holding. Linking physician payment to inflation is an absolute top priority, an existential must to keep practices afloat, and pillar #1 of the plan.
An important step on that path was the recent introduction of a bipartisan bill to finally align the Medicare fee schedule with MEI. Our Congressional advocacy played a key role in legislation to extend Medicare telehealth coverage.
In partnership with states and specialties, our advocacy has helped protect patients from outrageous scope expansions more than 50 times so far this year. State after state is making progress to constrain prior authorization, and CMS issued rules to do the same in Medicare Advantage plans. And we have been instrumental in helping create confidential wellness programs for physicians and removing outdated questions about past impairment from licensing and credentialing forms.
And the AMA is achieving success on the breadth of policies from this House beyond our Recovery Plan as well. The FDA is making Naloxone available over the counter … and may be on the verge of doing the same for an over-the-counter oral contraceptive. The FDA has also finally removed many outdated restrictions on blood donations from men who have sex with men. Medicaid work requirements that conflict with AMA policy were kept out of the debt ceiling bill. We’ve helped shift the national conversation about protecting patient data and making sure digital health and AI tools are proven BEFORE being deployed. We’ve broadened and intensified our work to embed equity and racial justice, and to push upstream to affect structural and social drivers of health and inequities.
And our litigation center has been very, very busy. We’ve joined others in suing Cigna for shortchanging doctors and continued on page 36
What do all physicians have in common?
We all suffer from implicit bias. This is a condition where we internalize negative stereotypes of those different from ourselves and are often not aware that we are doing so.
There is now training that can help us learn more about how each of us suffers from our own negative stereotyping so that we can do a better job of providing fair and equitable patient care.
The state of California has taken a huge step forward by requiring implicit bias training for all physicians every two years in order to maintain our medical licenses.

Unfortunately, two California doctors and a nonprofit (“Do No Harm”) are suing the state to block this requirement despite the fact that it is well known that implicit bias is something that we all suffer from and that negatively impacts patient care.
When medical students, interns and residents were given a survey the majority believed that black patients had thicker skin and less sensitive nerve endings and therefore felt less pain. In clinical situations blacks are undertreated with pain medications when compared to white patients. Imagine bringing your child to the emergency room with appendicitis or a long bone fracture and having them receive inadequate pain medication due to their race.
Sickle cell anemia patients who go to the emergency room when they are suffering a painful crisis are made to wait longer than other patients before being seen and then are denied pain medication because they are mistakenly seen as just trying to "score” narcotics. Here is how one patient, a retired school administrator, described her experience:
“Every time, it’s a battle.” She complained that staff members suspect her of faking her condition in order to score opiates and view her as a non-emergency because she only has pain. “I always dress professionally, nice shoes, interesting earrings, every hair in place, and Vogue-worthy makeup. It’s crazy that you, as an African-American, have to do this so you aren’t treated like a drug addict.”
Implicit bias may play a role in death during pregnancy where African American women suffer a death rate 3-4 times that seen in white women. African Americans with heart disease are not referred as often as white patients for advanced cardiovascular procedures. If all physicians received implicit bias training could we improve these deplorable outcomes?
Jeff Ritterman, MD
Black and Latinx patients have better health outcomes when treated by Black and Latinx physicians. Given that there is a shortage of minority physicians wouldn’t it be prudent to train white physicians to overcome implicit bias to improve health outcomes?
Life expectancy and infant mortality rates also show significant adverse outcomes for Black, Latinx, and Native American patients. Does implicit bias play a role?
Racial, ethnic, and gender differences in medical outcomes remain even after adjusting for insurance status, socioeconomic differences and other factors that influence healthcare access suggesting that physician behavior plays a role.
Helping physicians to overcome their implicit biases will not do away with all of these problems. But most of us are not even aware that we have these biases, so this is a start. I applaud the State of California for taking this positive step and hope that this lawsuit will not go forward as it is not in the best interests of our patients and that is what we should all care about most.
Dr. Ritterman practiced cardiology in Richmond for 29 years. He was a professor at Touro University teaching in the Public Health and Physicians Assistant Program for three years where he was also the Assistant Clinical Coordinator. He also worked as a physician in Adult Primary Care at the Lifelong San Pablo Clinic. He has been on the Board of Directors of SF Physicians for Social Responsibility for more than a decade and served as the Vice President of SF PSR. He served on the City Council of the city of Richmond where he was responsible for introducing the first municipal soda tax effort and helped develop anti-smoking ordinances that became the model for the state. He presently serves on the Richmond Human Rights Commission and the Community Advisory Council for the Bay Area Air Quality Management District.
individual psychology of our political leaders by utilizing brain scans on our political leaders and “apply insights from cognitive science and neuroscience to nuclear strategy and protocols — so leaders won’t bumble into atomic Armageddon.”
The recent movie Oppenheimer has opened-up a welcome conversation about the existential dangers of the nuclear arms race that had generally receded to the background of mass-consciousness before the brutal Russian invasion of Ukraine once again raised the nuclear specter for us to contemplate. The gripping film focuses on the dramatic events surrounding the detonation of the first atomic bomb during the Trinity test in the New Mexico desert in July 1945. However, it unfortunately provides only a cursory view of the profoundly destructive impacts of this and subsequent nuclear weapons detonations to local and distant communities subject to nuclear testing.
Tina Cordova, co-founder of the Tularosa Basin Downwinders Consortium eloquently stated in a recent New York Times Op-Ed. “A new generation of Americans … won’t hear much about how American leaders knowingly risked and caused harm to the health of their fellow citizens in the name of war. My community and I are being left out of the narrative again.” In fact, it was only recently revealed how underestimated and widespread the radioactive contamination from the Trinity test was, reaching 46 states, Canada and Mexico.
Similarly, the movie covered very little about the effects of the atomic bombings of Hiroshima and Nagasaki that in 1945 caused the deaths of over 200,000 human beings. And nothing about the subsequent Pacific nuclear testing overseen by the U.S. military and the Atomic Energy Commission (AEC), the latter in which Oppenheimer played a key role, and which covered up the radiation health impacts that have plagued the lives of generations of “downwinders.” Oppenheimer’s efforts to place nuclear weapons under international control, and opposing hydrogen bombs are certainly to be lauded. However, his support for integrating atomic weapons into war-fighting strategies helped create the deadly legacy we now confront given Putin’s threats to use tactical nuclear weapons in Ukraine.
Oppenheimer has provoked a resurgence of interest in nuclear preparedness evinced by a recent Medpage Today feature “Is the U.S. Ready for a Nuclear Attack?” which, while exploring some useful medical countermeasures to radiological emergencies, evokes the discredited "duck and cover" campaigns of the Cold War. Emblematic of this was the 2022 NYC Emergency Management PSA calling on New Yorkers to "Get inside. Stay inside. Stay tuned" that was hilariously debunked by videos produced by the NY Campaign to Abolish Nuclear Weapons. As a further distraction from our compelling need to focus on primary prevention of nuclear war, we have recently been urged to focus on the
Thankfully we have an energetic global movement emphasizing preventative public health approaches aimed at eliminating nuclear weapons, mobilized by a series of scientific reports indicating that even a limited nuclear exchange in a regional conflict can induce a "nuclear winter" leading to a global collapse of food production that could lead to widespread death from starvation. Most recently, a 2022 report issued by Nobel Peace Prize recipient International Physicians for the Prevention of Nuclear War (IPPNW) demonstrated that a nuclear war between the U.S. and Russia with much larger arsenals, a danger posed by the Ukraine war, could lead to over 5 billion deaths.
In our country, the growing multi-organizational Back from the Brink (BftB) campaign calls for a variety of imperative disarmament steps, including ending our government’s plan to modernize and increase the lethality of our nuclear weapons that is encouraging nations around the world to initiate or modernize their own nuclear arsenals. The planks of BftB have been incorporated into the "Toward a World Free of Nuclear Weapons" policy adopted by the American Public Health Association in 2020, which also calls for all nuclear weapons states to join the majority of the world's nations in supporting the "Treaty on the Prohibition of Nuclear Weapons." The Treaty is also supported by the U.S. Conference of Mayors, numerous U.S. municipalities, and constitutes the heart of HR 77 recently introduced by Reps. McGovern (D-MA) and Blumenauer (D-OR).
Echoing this campaign, and underscoring the need for all physicians and health professionals to join this civilizationsaving effort, leading medical journals recently coordinated publication of the editorial “Reducing the Risks of Nuclear War”in an unprecedented step reminiscent of the recent editorial collaboration calling for expeditiously addressing our climate emergency. It’s time to for us to eliminate nuclear weapons once and for all, and transfer the countless billions of dollars wasted in our bloated nuclear and military budgets to rebuild our dilapidated public health system, provide excellent and universal health care to all, and jump-start an alternative (non-nuclear) "Manhattan Project" to deal with the climate emergency exploding around us, before we run out of time.
Dr. Robert Gould is past president of the national Physicians for Social Responsibility and president of PSR's San Francisco Bay Area Chapter. He is a longtime delegate to the CMA.

Here we are, after the one-year anniversary of the U.S. Supreme Court's Dobbs decision. A patchwork of abortion policies have emerged across the country, meaning that where you live dictates the medical care you can receive. Fifteen states have banned abortion completely or at six weeks of pregnancy, before many people even know they're pregnant. An additional five states have enacted bans at 12 to 18 weeks of pregnancy, and bans in other states are working their way through the courts or scheduled to go into effect soon. As a doctor in California, I know there is more I could do to help patients across the country who need care if only our legal system allowed me to do so.
Laws banning abortion are having a real impact on women and others with the capacity for pregnancy—both for people seeking abortion care and those experiencing complications during pregnancy. A recent report, which I wrote with colleagues from the University of California San Francisco and the University of Texas at Austin, documented 50 cases of poorquality medical care due to these bans. These cases described care that was delayed or denied, resulting in serious harm to pregnant women. For example, there were 11 cases of women whose water broke in the second trimester, long before their babies could survive. Instead of being offered the option of an abortion, considered the national standard of care, these women were sent home and told to come back when they were in labor or had signs of infection. Many of them developed a serious infection requiring treatment in the intensive care unit.
With medical care so compromised in a growing number of states—potentially half our nation— clinicians in states where abortion remains legal are anxious to help patients living in places where care is restricted. We are welcoming the patients who can travel to our states and obtain care with us, and some of us are traveling to the states nearest those with bans, such as Illinois and Kansas, to provide in-person care.
But telemedicine could also be part of the solution. A great deal of evidence has proven that telemedicine for medication abortion is safe and effective. Patients seeking abortion care can be evaluated for eligibility using video, telephone, or online screening, and those who are eligible receive the pills by mail. The FDA has recognized telemedicine provision of medication abortion as standard medical care.
Unfortunately, our country's medical and legal systems limit the potential of this telemedicine solution. Medical practice is largely regulated at the state level, and telemedicine is viewed
as occurring in the state where the patient is located. To provide abortion care to a patient in another state, I must be licensed in the state where the patient is and comply with that state's laws. Under this scenario, I couldn't do this in a state that has banned abortion.
Last year, Massachusetts became the first state to enact a "shield" law to protect clinicians there who provide reproductive healthcare, including abortion and gender-affirming care, regardless of where the patient is located. On its face, the law provides protections against incarceration by preventing extradition, as well as protecting the provider's license and limiting the enforcement of civil judgments. Several other states, including Colorado, Vermont, and Washington, have passed similar bills, and another, SB 345 introduced by state senator Nancy Skinner (D-Calif.), was just passed by the California Senate. Most recently, New York took action last week to protect providers who prescribe medication abortion for patients in states that have banned abortion.

These laws cannot provide complete protection. If a clinician providing cross-state telemedicine medication abortion were accused of a crime in Texas, for example, and ever traveled there—or to any other state that might agree to extradition— there is a risk they could be arrested. In addition, these laws have not yet been tested in the courts, and it remains to be seen how much protection they will actually afford.
The stories from our report of doctors who had to watch their patients bleed or develop an infection because of abortion bans are hard to read. They are not too far from how I feel, comfortably caring for patients in California, knowing that I could safely provide medication abortion by telemedicine if only the law would allow. I cannot sit by idly as patients in other states desperately seek out options for an unintended or medically complicated pregnancy. I hope California and every state where abortion remains legal passes a shield law protecting the provision of care across state lines.
Daniel Grossman, MD, is a professor of obstetrics, gynecology, and reproductive sciences at the University of California San Francisco, and director of Advancing New Standards in Reproductive Health https:// www.ansirh.org/ This commentary first appeared on Medpage.

A new report presents the preliminary findings of the Care Post-Roe Study, and shows how health care providers have been unable to provide the standard of care in states with abortion bans since the Supreme Court struck down Roe v. Wade ten months ago, leading to harm and negative health outcomes for patients.
The report, Care Post-Roe: Documenting cases of poor-quality care since the Dobbs decision, shows that health care providers have seen increased morbidity, exacerbated pregnancy complications, an inability to provide time-sensitive care, and increased delays in obtaining care for patients in states with abortion bans. This has impacted both patients and providers and has deepened the existing inequities in the health care system for people of color.
These stories paint a stark picture of a post-Roe clinical landscape, detailing harm not only to patients, but also to health care providers who are now being forced to follow medically unnecessary laws that negatively impact their patients’ health. Medical harm occurring among pregnant people in states with abortion bans include increased morbidity and complications that could result in serious impairment and risk of death. Although not yet observable, long-term effects could include loss of fertility, chronic pain, heart attack and stroke risk related to hypertension, and effects on mental health. It's clear that abortion bans and tying providers’ hands impacts every aspect of care and will have far-reaching and devastating consequences for years to come.

To learn more, read the full report:
https://www.ansirh.org/sites/default/files/2023-05/Care%20Post-Roe%20Preliminary%20Findings.pdf
Clinicians can share info about a case through this brief survey: https://carepostroe.ucsf.edu/
#WomanLifeFreedom is a movement that was sparked by the death of Jhina (Mahsa) Amini on September 16, 2022, in Iran, while in the custody of the morality police. The morality police arrested Jhina for improper hijab, a highly subjective policy of repression with mandatory covering of hair and body parts. Women poured out into the streets, burned their headscarves and cut their hair in radical retaliation and in solidarity with the anti-patriarchy movement. Hand in hand with women who chose to wear hijab, these brave, mostly Gen Z women made a statement that resonated around the globe.
At UCSF, students, faculty, and staff came together to show our support by creating the WomanLifeFreedom at UCSF group. With a mission grounded in solidarity and collaboration, the group has many achievements to date:
• Registered campus organization (RCO): We are the only official RCO of a coalition of students, faculty, and staff who identify as Iranian, Iranian allies, and SWANA—creating community and emotional support during a time of collective trauma.

• The Scholars at Risk (SAR) program: So far, we have fundraised for several Iranian scholars who are currently at UCSF. In addition, two Iranian women will be joining UCSF. The total cost for living expenses for each student for one year is about 140K. We are working with SAR to fundraise and find support for each student. Please let us know if you or someone you know is able to provide housing and if you’d like to make a generous donation to SAR https://makeagift.ucsf.edu/site/SPageServer?pagename=A1_ API_GeneralGivingForm&Other=Scholars%20at%20Risk%20Initi ativezzz7031057&AppealCode=23TSARW, this is the time to do it (please note WomanLifeFreedom in the notes section so it’s clear that it’s from our group). There is a very generous donor who is willing to match any donation dollar-for-dollar to help them be successful here.
• Cultural and community events: We have organized a Shab-e Yalda https://womanlifefreedom.ucsf.edu/resourcespastevents event, Nowruz event, Candlelight Vigil, International Women’s Day events, movie night event, #ourstoryisone event, UCSF COVID-19 Townhall recording https://lecture.ucsf.edu/ ets/Channel/498d5a11d5644769b68942b601b048fc5f/watch/ fedcaa3c9df44445bd230cb267ddc6611d, UCSF Office of Diversity and Outreach Roundtable Discussion recording https://www.youtube.com/watch?v=cQj2Sd3eY_s, and we have published an article https://www.hhrjournal.org/2023/05/scientific-awakening-violation-of-human-rights-of-academic-scholars-and-healthcareprofessionals-in-iran/ on human rights violations in Iran.
• Petitions: Petition supporting accountability and justice in the name of Iranian students and healthcare professionals, including the death of Dr. Ayda Rostami, a street medic, killed
Yalda Shahram, MD, MSc
in December 2022, signed by over 1,000 people, with over 420 healthcare professionals and university faculty around the world, and at least 120 of whom identify UCSF at their Institution/ Organization. Click to watch this video https://www.instagram. com/reel/ColV3lTpBHE/?utm_source=ig_web_copy_link&igshid =MzRlODBiNWFlZA%3D%3D created by @KimiyaSF (she/her) promoting the petition.
• Collaborations: We have created an alliance with over 14 other teams of healthcare providers globally. This coalition, named Aida Health Alliance, is dedicated to assisting healthcare providers in treating peaceful protestors and working together to forward our mutual healthcare and education mission.
The current situation in Iran is both devastating and inspiring. Many, including the journalists Niloufar Hamedi and Elaheh Mohammadi, remain imprisoned and need the support of all of us not to forget them as they languish. Many have transformed their support for the movement from protesting in the street into radical acts of disobeying mandatory hijab laws in their day-to-day lives.
The WomanLifeFreedom at UCSF group is committed to continuing our mission, focusing on supporting scholars and healthcare professionals by raising awareness and funds for accessing education. In our local community, we continue to amplify the voice of the oppressed, asking for representation and inclusion of the SWANA (South West Asian North African) identity for students, faculty, and staff. Anti-Iranian policies in the United States are fueled by misconceptions about the people of Iran, equating the diversity of ethnicities, languages, and religious affiliations of the population with the fundamentalist theocratic government. Overcoming the narratives of white supremacy culture, patriarchy, and imperialism, let this first anniversary of the killing of Jina (Mahsa) Amini be an opportunity to stand up as a local community and global force against gender apartheid—for woman, life, freedom. In ongoing and sustained solidarity, WomanLifeFreedom at UCSF
Yalda Shahram, MD, MSc, is a hospitalist and clinician-educator investigating the impact of antiracist education and critical consciousness to address structures of oppression in health care. She is on the Board of Directors of the San Francisco Marin Medical Society and was selected as a recipient of the UCSF Society of Hellman Fellows award, with the designation as a Diversity, Equity, and Inclusion award for her commitment to DEI and health equity at UCSF and beyond.
July 24, 2023
SAN FRANCISCO, CA – A comprehensive program implementation study, conducted by the San Francisco Department of Public Health (SFDPH) in partnership with researchers at the University of California, San Francisco (UCSF), has revealed San Francisco implemented one of the most intensive, inclusive and multipronged COVID-19 pandemic responses in the United States, resulting in San Francisco experiencing one of the lowest COVID-19 deaths among larger metropolitan cities overall and across all ages and ethnicities. The study, including lead author Darpun D. Sachdev, MD. and senior author Grant Colfax, MD recently published in Public Health Reports, a prominent academic journal, highlights crucial lessons learned including the importance of community responsiveness joint planning, and collective action to inform future pandemic response and advance healthy equity. In March 2020, during the onset of the COVID-19 outbreak, San Francisco mounted an aggressive four-prong strategy to mitigate the spread of disease in the community and lower incidents of severe illness.
The strategy included:
• Aggressive mitigation measures, such as asymptomatic testing of vulnerable populations, masking, and stay-at-home orders.
• Using a health equity lens to prioritize neighborhoods and populations disproportionately impacted, resulting in the accessibility of tests, vaccines, and financial support for these populations.
• Use of timely and adaptive data to determine policy, such as stay-at-home orders and booster recommendations.
• Partnerships and public trust through engaging and providing expansion funding to community-based organizations (CBOs), holding regular press conferences by the San Francisco Mayor and the SFDPH Director of Health, launching a COVID-19 dashboard, maintaining consistent communications across Bay Area counties, and centralizing resources through partnerships with other hospitals.
• The study mapped population health outcomes to these strategies, showing a strong correlation between pandemic response and lower rates of transmission, reduced number of hospital patients, and lower mortality.
“The success of San Francisco’s COVID-19 response relied on quickly putting these public health principles into action and adapting to outcomes in real time through the lens of health equity,” said Dr. Colfax, San Francisco Health Director and senior author of the study.
As of 2022, San Francisco had the lowest number of COVID-19 deaths among large metropolitan cities in the United States, with 98 per 100,000 residents, compared to 229 COVID-19 deaths per 100,000 in the state of California and 301 per 100,000 in the entire US population.
Data gathered for the study involved tracking the number of COVID-19 deaths as well as excess all-cause mortality rates, a measure that looks at increased mortality year-over-year regardless of cause of death. Further, in almost all age, race and ethnicity groups, excess mortality from COVID-19 was lower in San Francisco than in California overall, especially among people more than 65 years old.
“We know through our experience during the AIDS epidemic as well as the COVID-19 pandemic and mpox outbreak that public trust in health institutions is key to achieving positive health outcomes, slowing the spread of disease, and advancing health equity. I am confident that these strategies and approaches will prove equally successful in addressing future pandemics,” continued Dr. Colfax.
Though mortality rates remained low, the study notes that Zuckerberg San Francisco General Hospital was significantly impacted by COVID-19, stretching the limits of the hospital’s resources and staff. “Our public safety-net facilities need to fortify their infrastructure to face the next inevitable pandemic,” concluded Dr. Colfax.
SFDPH remains committed to sustaining vital partnerships with communities to ensure COVID-19 resources, such as testing and vaccinations, remain available to those most in need even as the landscape shifts from an emergency response to long-term recovery.
Reprinted from the San Francisco Department of Public Health.
Speedy implementation of a combination of measures such as face masks, lockdowns and international border controls, “unequivocally” reduced COVID-19 infections, a major review has shown.
The report published Thursday by the Royal Society looked at findings from six evidence reviews that analyzed thousands of studies to assess the effect of masks, social distancing and lockdowns, test trace and isolate systems, border controls, environmental controls and communications. It found evidence that each of these measures — which are called "nonpharmaceutical interventions" — were effective, albeit to varying degrees, when looked at individually. However, the evidence in favor of using these tools was stronger when countries combined several measures.
The report could have significant implications for decisionmaking in future outbreaks, with Mark Walport, chair of the report’s expert working group and foreign secretary of the Royal Society, saying that “having protocols in advance is really important." He said what policymakers should take from the research is “there is evidence that non-pharmaceutical interventions are effective, but ... they have to be applied as packages, and they have to be applied as early as possible.”
The most effective measure, according to the review, was one of the most controversial — restrictions on movement and social interactions through lockdowns, distancing and rules around the size of gatherings. These were repeatedly found to be associated with a “significant reduction” in transmission of the virus, with the more stringent the measure, the greater the effect.
For masks, 75 studies were assessed, with 63 of these finding positive effects. Unlike the January Cochrane review, which only looked at randomized controlled trials, this review also included observational studies. The Cochrane review was unable to find conclusive evidence that masks helped stop respiratory viruses.
Chris Dye, professor of epidemiology at the University of Oxford, who led the review on masks for the Royal Society, said if they had only looked at randomized controlled trials
they would have come to the same conclusion as the Cochrane review. But the researchers behind the paper released Thursday chose to analyze a larger body of studies and found strong evidence that masks work.
A key finding from the research was these type of measures were most effective when implemented early on. Dye said that while there is a 100-day mission to develop drugs, therapeutics, vaccines and diagnostics for a future pandemic, “it would be marvelous” if there were a 100-day vision for non-pharmaceutical interventions. He said this would mean countries could “put in place the necessary mechanisms for preparedness, which would be to implement [non-pharmaceutical interventions] when some unknown new pathogen comes along.”
While a future pandemic could be transmitted sexually or gastrointestinally, Salim Abdool Karim, a member of the working group on the report and pro-vice-chancellor for research at the University of KwaZulu-Natal, said the biggest concern was a respiratory virus. “The lessons of SARS-CoV-2 have to feature in our thinking as we prepare for a next pandemic that would be a respiratory virus of which we've got no prior exposure and so we don't have a pre-existing immunity. The lessons of this report are going to feature strongly in anyone's deliberations,” he said.
However, responding to the report, Kevin McConway, emeritus professor of applied statistics at the Open University cautioned that impact on virus transmission is not the only factor that should be taken into account when deciding to use such measures. "The report does point out explicitly that NPIs can impose a great number of costs and burdens, in terms social and economic impacts, and indeed of increasing ill health ... but makes it very explicit that this piece of work isn’t going to consider any of that." "I think that limits quite severely its effectiveness in helping decisions on what should be done in the next pandemic, whenever it arises."
Reprinted from Politico, August 24, 2023.
Ashleigh Furlong
They might not be popular, but a major report shows combining these interventions can keep case numbers low.
What are non-pharmaceutical interventions (NPIs)?
Non-pharmaceutical interventions (NPIs), include any public health measure that is not a vaccine or drug. At the start of the COVID-19 pandemic, no drugs or vaccines were available to contain the spread of the causative virus, SARS-CoV-2. This meant countries were reliant on NPIs to protect populations and health systems until pharmaceutical interventions were developed.
A wide variety of NPIs were employed (typically as part of packages). The Royal Society report covered six broad categories used during the pandemic:
• Masks and face coverings
• Social distancing and 'lockdowns'
• Test, trace and isolate
• Travel restrictions and controls across international borders
• Environmental controls
• Communications
Why do we need to understand the effectiveness of NPIs?
Scientists and policymakers knew very little about SARSCoV-2 when the pandemic began. It was not clear what an optimal strategy for NPI implementation looked like, including how outcomes vary for people of different ages, ethnicities, health status and socioeconomic groups. The widespread roll out of NPIs was also economically costly and led to major social disruption with wider impacts on health and wellbeing.
Now is an opportune to time learn from NPI implementation during the pandemic and highlight evidence gaps to ensure we are prepared for potential future outbreaks of infectious disease.
What are the main conclusions of the Royal Society’s report?
There is clear evidence from studies conducted during the pandemic that stringent implementation of packages of NPIs was effective in some countries in reducing transmission of SARS-CoV-2.
There is also evidence for the effectiveness of individual NPIs, but most NPIs were implemented in packages. Disentangling the effects of one NPI when other NPIs were implemented at the same time presents a significant challenge.
Evidence suggests that NPIs were, in general, more effective when case numbers and the associated transmission intensity of SARS-CoV-2 were lower. NPIs became less effective as more transmissible variants of the virus emerged (eg Delta, Omicron) which were better adapted to spreading between people and evading immune responses.
Stringency of application of individual NPIs and groups of NPIs influenced rates of transmission, eg respirator masks were more effective than surgical masks and two weeks of quarantine were more effective than shorter periods.


What lessons have been learnt to influence how we might approach future pandemics?
One of the most important lessons from this pandemic is that the effective application of NPIs ‘buys time’ to allow the development and manufacturing of drugs and vaccines. There is every reason to think that implementing packages of NPIs will be important in future pandemics.
Standardised protocols for data collection would improve the quality of observational studies when a novel pathogen emerges. National and international collaborations could be established to support this. It is of particular importance to design protocols that can disaggregate the effects of NPIs by different demographic factors.
Future assessments should also consider the costs as well as the benefits of NPIs, in terms of their impacts on amongst other things, livelihoods, economies, education, social cohesion and physical and mental wellbeing.

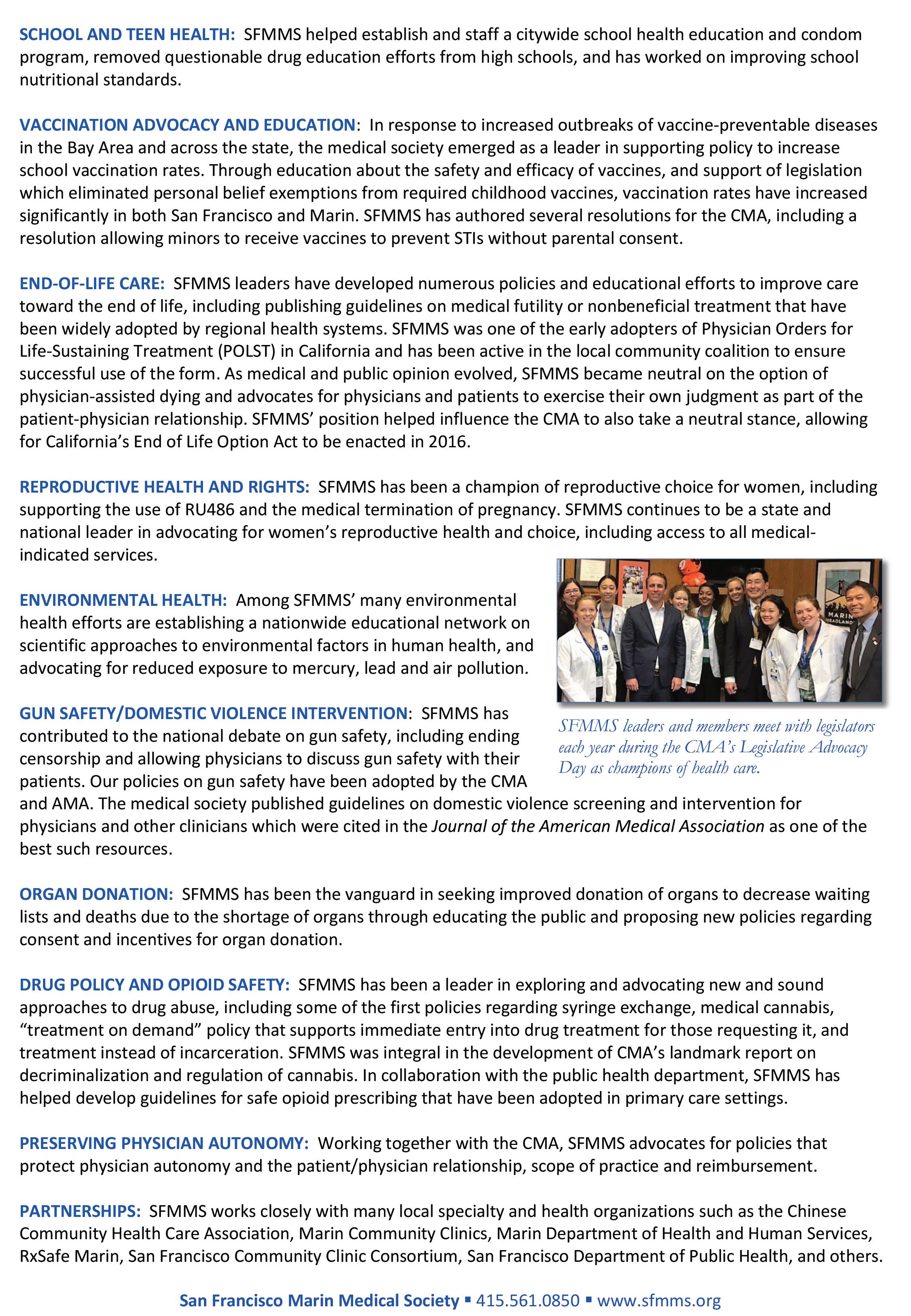
continued from page 25
patients. We forced the federal government to take steps towards banning menthol cigarettes. The Wisconsin Supreme Court agreed with us that patients and judges can’t force physicians to administer substandard care. Courts have invalidated parts of No Surprises Act rules that plainly ignored Congressional intent and put a thumb on the scale to favor insurance companies … thank you Texas Medical Association and AMA! The 5th Circuit Court is staying—for now—an egregious ruling that would have stripped patients of the right to access preventive care service with no out-of-pocket costs, a key piece of the Affordable Care Act. The U.S. Supreme Court is delaying attempts by a single district judge with no scientific or medical training to take mifepristone off the market nationally and upend our entire FDA drug regulatory process.
We’re briefing in more courts than I can count to turn back criminalization of medical care. And we’re not done yet. Not even close. In my inaugural address, I admitted to being a pragmatic optimist who believes in relentlessly showing up, and using levers of power to help create a more just and equitable system. I remain undeterred—even though the challenges we face today are daunting.
The burnout and the moral injury are real … I’ve felt it myself. I hear this concern in the voices of medical students, residents, and even young physicians when they ask me “Am I going to be okay?” “Have I made the right career choice?”
The first message I share: Yes, I’m confident that you have made the right choice. You are joining an extraordinary profession, and we are lucky to have you. Don’t ever lose your passion for humanity and healing. And the second message I give them … there is no time to waste, so let’s get to work. “You want a more equitable future for patients?” Demand it. “You want a future where our health care system and new technologies support physicians rather than burdening us?” Create it. “You want patients making their own decisions about their health? Fight for it.
You are entering the profession for all the right reasons and to fix all the right problems … and there will be more. We have enormous privilege to do this work. We share a love for what we do—to help… to cure… to listen… to solve… to heal… to lead. And we have a responsibility to our patients AND to the health of this nation.
WE are the keepers of an important tradition … a flame that must NOT be extinguished. Our profession is counting on us to get this right. Our patients are depending on us to continue this fight. We will not let them down.
Reprined from the Royal Society, August 2023. https://royalsociety.org