SAN FRANCISCO MARIN MEDICINE
JOURNAL OF THE SAN FRANCISCO MARIN MEDICAL SOCIETY

The Primary Care Desert is Everywhere What Should Docs Vote for in November? Climate Solutions Are Health Solutions



The Primary Care Desert is Everywhere What Should Docs Vote for in November? Climate Solutions Are Health Solutions

Overdose Deaths are Near Record Highs. Why is California Behind the Times in Stopping Them?
Grant Colfax, MD and Hilary Kunins, MD
Climate Solutions Are Health Solutions Carolina Fonseca, MD, MS; Cynthia Haq, MD and Jeffrey Mann, MD
President's Message: If You Want to Know, Don't Read This!
Dennis Song, MD, DDS
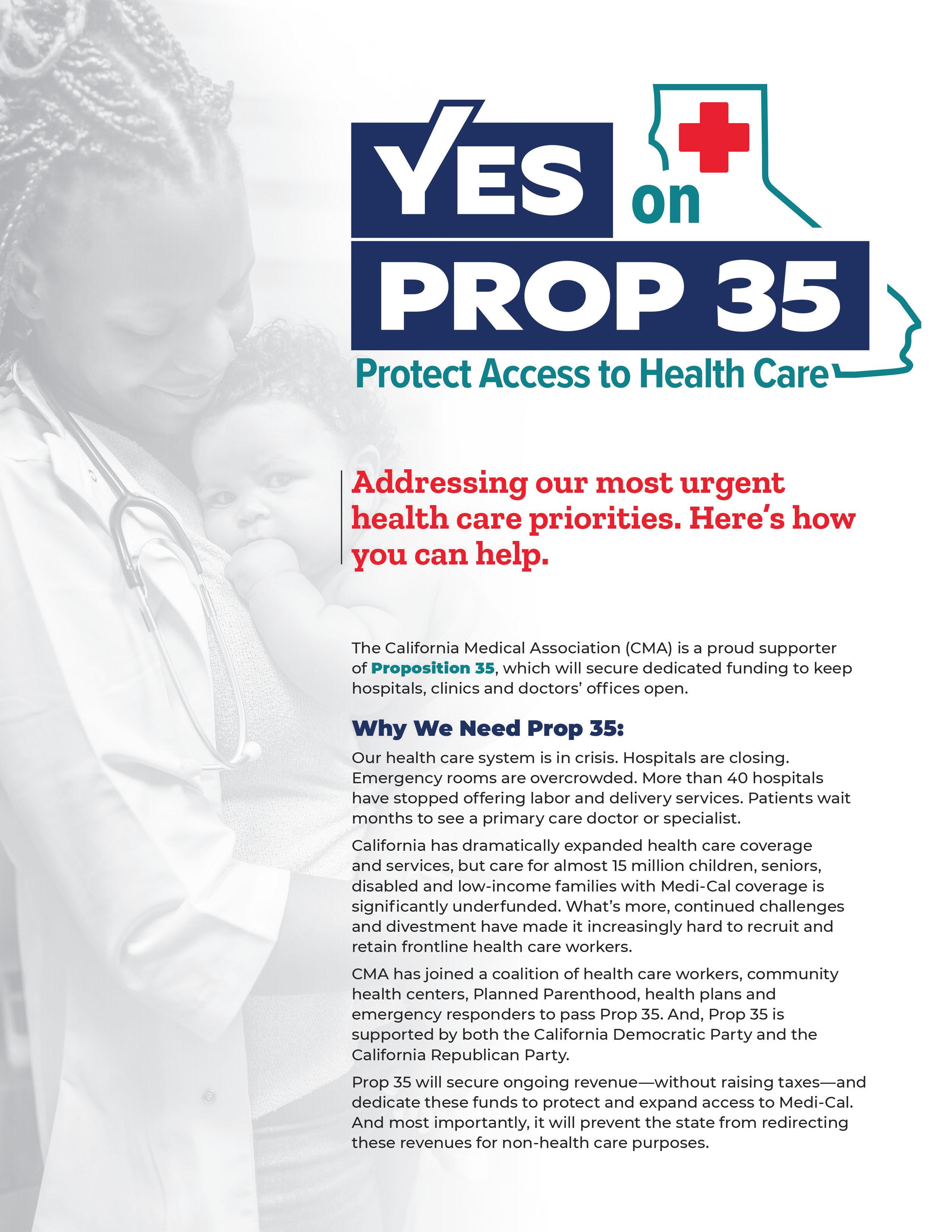
Prop 35, the November ballot initiative that would secure dedicated funding to keep hospitals, clinics and doctors’ offices open, has launched a new Action Center to activate supporters.
Physicians are trusted messengers across regional and partisan lines and are important advocates to ensure California votes Yes on 35 to protect and expand access to health care. Visit the Action Center now to:
• Share Your Story: In your own words, tell us why you support Prop 35.
• Post on Social Media: Share with your friends and family why you are voting #Yeson35.
• Order Campaign Swag: Request campaign materials for you to show your support.
• Email a Friend: Tell your friends and family why you support YES on 35!
• Download Materials: Get the latest campaign materials. Why we need Prop 35
Critically, Prop 35 will prevent the state from redirecting revenues for non-health care purposes. Prop 35 will secure ongoing revenue—without raising taxes on individuals or increasing health care premiums—and dedicate these funds to protect and expand access to care for all Californians.
Our health care system is in crisis. Hospitals and maternity wards are closing—46 California hospitals have closed their maternity wards since 2014. Emergency rooms are overcrowded with patients waiting an average of three hours, and patients often wait months to see a doctor.
California has dramatically expanded health care coverage and services, but care for 15 million children, seniors, disabled and low-income families with Medi-Cal coverage is significantly underfunded. Prop 35 will change that. Visit voteyes35.com for more information.
By Michael Schrader, MD, delegation chair
Our District VIII Delegation is in preparation for the upcoming CMA House of Delegates in Sacramento in October. We will have a contested election this year for CMA President. At our recent meeting, we interviewed the three candidates, Dr. C Freeman, psychiatrist, Dr. Rene Bravo, pediatrician, and Dr. Ramin Manshadi, cardiologist. Each candidate gave a statement which was followed by a question and answer exchange. We interviewed three excellent candidates, any one of whom would be a powerful and influential leader of the CMA.
Our own Dr. Shannon Udovic-Constant will become CMA President at the upcoming HoD. We look forward to a festive celebration. Our own Dr. George Fouras who was elected ViceSpeaker last year will serve a second year and plans to run for Speaker in the coming year.
The chosen Major Issues this year at the HoD are Rural Medicine and Obstetric Deserts. Our District VIII Delegation has lobbied strategically for the inclusion of reproductive rights in the Major Issues and we will continue our efforts to advocate for these rights at HoD.
A recent resolution asking for hate speech to be recognized as a public health concern was submitted to the CMA by a member of our Delegation. This resolution was adopted as policy by the CMA Board of Trustees.
Our SFMMS leadership and our District VIII Delegation are influential at CMA and nationally. We bring our San Francisco values and vision to our state and nation.

Laguna Honda Hospital, San Francisco’s largest skilled nursing facility, has regained federal approval to care for residents on Medicare, the government health insurance program for seniors — bringing to an end a two-year regulatory saga during which the 150-year old facility faced the threat of closure.
"It means Laguna Honda is here to stay,” said San Francisco Director of Health Dr. Grant Colfax, who oversees the San Francisco Health Network, a network of city-run health care providers that includes Laguna Honda. “Going forward, we’ll continue the progress and make sure Laguna Honda is a world-class facility and serve the city of San Francisco the way it’s done over the past 100 years.”
SFMMS physician leaders advocated at the time for timely recertification.

This event is free for SFMMS Members to attend.
Guests will be treated to a buffet dinner and a presentation by the SFMMS Leadership. Space is limited and advance RSVP is required.
For more information, visit the SFMMS Events page at www.sfmms. org/news-events/events or scan the QR code with your smartphone.

Questions: Contact Molly Baldridge, Director of Engagement at mbaldridge@sfmms.org
July/August/September 2024
Volume 97, Number 3
Editor Michael Schrader, MD, PhD
Managing Editor Steve Heilig, MPH
Production Maureen Erwin
SFMMS OFFICERS
President Dennis Song , MD, DDS
President-Elect Jason Nau, MD
Secretary Ian McLachlan, MD
Treasurer Sarita Satpathy, MD
Immediate Past President Heyman Oo, MD, MPH
SFMMS STAFF
Executive Director
Conrad Amenta
Associate Executive Director, Public Health and Education
Steve Heilig, MPH
Director of Operations and Governance
Ian Knox
Director of Engagement
Molly Baldridge, MPH
Senior Director, Advocacy and Policy
Adam Francis, CAE
2024 SFMMS BOARD OF DIRECTORS
Edward Alfrey, MD
Melinda Aquino, MD
Julie Bokser, MD
Kristina Casadei, MD
Clifford Chew, MD
Esme Cullen, MD
Manal Elkarra, MD
Mihal Emberton, MD
Cindy Greenberg, MD
Ian McLachlan, MD, Secretary
Jason Nau, MD, President-Elect
Heyman Oo, MD, Immediate Past-President
David Pating, MD
Sarita Satpathy, MD, Treasurer
Michael Schrader, MD, Editor
Yalda Shahram, MD
Neeru Singh, MD
Dennis Song, MD, DDS, President
Kristen Swann, MD
Ranna Tabrizi, MD
Kenneth Tai, MD
Melanie Thompson, DO
Kristin Wong, MD
Andrea Yeung, MD
Helen Yu, MD
For questions regarding journal, including possible submissions, contact Steve Heilig: Heilig@sfmms.org
Dennis Song, MD, DDS
“IF
Next time you visit a restaurant, ask what kind of oil they use in their kitchen. You might be surprised by the variety of answers. Often, you'll hear vague responses like, “I think it is….” Once, I was told, “If you need to know what we cook with, then you shouldn’t eat here!” On the other hand, some establishments proudly claim to use 100% vegetable oil. However, when you ask which vegetable it comes from, you might be met with a puzzled expression. Why? Many people haven’t thought critically about the oils they use. Encouraging them to read the ingredient label can be enlightening—for both you and the restaurant staff.
Common answers might include cooking oil (what is it?), regular oil (what is regular), vegetable oil (what vegetable?), soybean oil, canola oil, peanut oil, olive oil, corn oil, sunflower oil, rice bran oil, avocado oil, coconut oil, cottonseed oil, beef tallow, lard, chicken fat, butter, or even “not peanut oil” and “no meat, it’s vegetable oil.” One time I was told machine oil! Media and advertising have led consumers to believe that anything labeled “vegetable” is inherently healthy simply because it’s plant-based. The prevalence of certain oils often relates to cost: in the U.S., soybean oil is common; Canada and Australia favor canola oil; Europe tends to use sunflower oil; and Southeast Asia and Africa often opt for palm oil. Not all oils are the same, and not all are suited for every cooking method.
Why does this matter? Public health advocacy compelled the FDA to ban foods containing partially hydrogenated oils effectively ending artificial trans fats used in the United States from 1911 to 2018. Some oils are healthier than others depending on their uses, and food can act as medicine—good food promotes health, while poor-quality food can lead to negative outcomes. When cooking at home, you usually know most of the ingredients in your meals. However, when dining out or traveling, understanding what goes into your food becomes even more critical. If the waiter, cashier, or, unfortunately, the cook can’t tell you what oil they use, how can you trust what’s on your plate?
Similarly, we find ourselves in a major election year filled with excitement for various public offices and controversial ballots at both county and state levels. Have you decided whom or what to vote for? How will you make your choice? You receive mailers, hear debates, read articles, and even have social media targeting as your phone may be listening to the conversations around you! Regardless of your political affiliation, our non-partisan society is dedicated to working with legislators in the best interest of healthcare providers. Leaders in the San Francisco Marin Medical Society spend hours communicating with lawmakers and studying ballot initiatives to understand their implications for physicians and healthcare at large. Recommendations are debated within committees and approved by the Board of Directors for final review.
Legislators are like chefs; they need to understand how to serve us, the healthcare professionals, so we can care for our patients

effectively. We are the experts in medicine, advocating for what we believe is best for state and local priorities. California’s landscape is complex! Why does a restaurant choose a particular oil? Is it for health reasons, cost-saving measures, misconceptions from advertising, or sheer ignorance? Just as we seek the best food for our families and patients, we also want well-informed advocates among our elected leaders—those who listen and prioritize the right solutions. You can use “healthy” olive oil to deep fry food, but that can produce harmful byproducts. Similarly, with changes in healthcare legislation, we must ensure we are pursuing the right policies without making the situation worse.
Don't take my word for it—engage with leaders to hear their thoughts on specific candidates or issues. Discuss these topics to ensure you are voting with informed awareness rather than blind agreement. Although we conduct thorough research, you can also find out how we reach our recommendations. The answer should never be as vague as “vegetable oil” or “not peanut oil,” and I assure you, you will get specific, well-thought-out answers.
Our Board and Committee members represent a diverse range of practices—primary care, specialists, corporate, solo, government, public, academic, and more. Look at the rosters to see who is influencing our politicians and driving change for our practice, patients, and you as a physician. Their responsibility, regardless of background, is to represent all modes of practice and types of medicine in the best interests of all society members. Your opinions are invaluable. Engage with Committee members and Board officers to provide additional testimony for deliberation. If you wish to be involved in the decision-making process, consider applying for a committee or asking about leadership positions.
In San Francisco, we have exciting races for the office of mayor and multiple Board of Supervisors seats. Who champions healthcare? Evaluate and challenge candidates—meetings are set up for direct interaction and questioning. Statewide, a Yes position on Proposition 35 has been vetted by the CMA as being in the best interest of physicians and patients. This proposition affects all forms of practice, directly and indirectly, by ensuring funds are allocated to healthcare in California.
Don’t settle for vague answers like “vegetable oil” or, even more concerning, “machine oil.” Dig deeper. Just because everyone else is voting the same, doesn’t mean you should or have to. Ask, ask some more, and understand what you are eating and voting for! This month’s journal and email blasts summarize our positions and recommendations. Feel free to reach out to any of us!
Dennis Song, MD, DDS, is an oral and maxillofacial surgeon in private practice and Chief of the Dental Division at Sutter California Pacific Medical Center. He also serves as an Associate Adjunct Professor at the University of the Pacific School of Dentistry.
Conrad Amenta, SFMMS Executive Director

Californians stand on the cusp of an historic election cycle, and the role of physicians and patients in determining the outcomes of those elections has never been more critical. The upcoming elections present an opportunity to elect legislators who understand and prioritize the unique needs of medicine, healthcare, and public health, and share our values of care for the underserved and underrepresented.

The upcoming election cycle is poised to be transformative for several reasons. It comes at a time when healthcare issues including reproductive rights, access to care for those in the Medi-Cal program, and pandemic preparedness, are at the forefront of public discourse. The decisions made by elected officials in the coming years will shape healthcare policy, funding for medical research, physician reimbursement rates, and the overall landscape of medicine for generations to come.
Moreover, the COVID-19 pandemic has underscored the importance of having leaders who understand the complexities of public health emergencies and are committed to supporting healthcare infrastructure and frontline workers. The outcome of local, state, and federal elections will directly impact the resources available to combat future health crises and improve healthcare delivery systems.
Physicians in San Francisco and Marin counties are uniquely positioned to influence the electoral process. Beyond their roles as healthcare providers, they bring firsthand knowledge of patient needs, healthcare challenges, and the implications of policy decisions on medical practice. By actively engaging in advocacy efforts, such as joining medical associations, participating in grassroots campaigns, communicating with elected officials, and contributing to association-aligned political action committees (such as the SFMMS PAC), physicians can ensure that their expertise informs legislative priorities.
Physicians also have a role in engaging their patients on the topic of civic duty. Physicians are trusted voices within their communities; as such, they are positioned to educate patients and colleagues about healthcare policies and encourage voter
participation. Organizations like Vot-ER (www.vot-er.org) provide helpful resources for physicians speaking to their patients about civic engagement.
It’s equally important to foster a culture of civic engagement among medical professionals to inspire future generations of physicians to become advocates for positive change in healthcare policy. By mentoring medical students and residents on the importance of advocacy and political involvement, physicians can cultivate a new cadre of leaders who are committed to advancing the interests of medicine and public health.
As this fall’s election cycle unfolds, physicians must remain informed about candidates' positions on healthcare issues, and the measures that will appear on the local and state ballots, some of which directly impact the provision of care and health economics throughout the state. Prop 35, for example, will secure ongoing revenue for Medi-Cal reimbursement rates and physician workforce development programs by extending an existing tax on health insurance companies—without raising taxes on individuals—and dedicating these funds to protect and expand access to care. Read more about this key proposition, which SFMMS and the California Medical Association sponsor, at www.voteyes35.com.
Throughout this election cycle, SFMMS will make resources available to physicians to help inform their decisions, including voter guides on local and state issues and access to events where physicians can hear directly from candidates for Boards of Supervisors in San Francisco and Marin counties, and for Mayor.
The upcoming election cycle presents a pivotal moment for physicians in San Francisco and Marin to actively engage in shaping the future of healthcare policy. By exercising their civic duty, advocating for patient-centered reforms, encouraging their patients to be involved this fall, mentoring medical students and residents to become effective advocates, and supporting candidates who prioritize healthcare, physicians can contribute to a healthier, more equitable society.
As many of you know, there is a shortage of primary care physicians in San Francisco that is fast becoming critical as PCPs leave the workforce.
The primary care physician workforce is aging and many of us are nearing retirement. The patient population is aging as well, such that more patients will require primary care, and the burden of their care will be greater. Medical schools have increased the number of graduates, but this has not kept pace with population growth and the growing elderly demographic. As the number of primary care physicians has dwindled, our importance has finally been recognized. Primary care medicine is cost effective. And primary care provides a managed patient population that feeds specialists and hospitals. Primary care physicians deliver continuity, coordination, and trust into our delivery of care.
There are universal problems with primary care practice: administrative burden, onerous demands from patients, scope creep from lesser trained providers, loss of autonomy, and the expectation to overwork.
We are also seeing a cultural shift away from the “rat race.” Younger physicians are looking for work/life balance. They question our values of exhausting work and the pursuit of wealth and status.
Michael Schrader, MD, PhD
Primary care medicine has a tenuous position in corporate or profit-driven medicine. We all have to struggle with the juggernaut of corporatization of medicine that is hurtling us into an uncertain future fueled by speculation and greed, and driven only by blind faith in capitalist markets. But primary care, with its heavy burden of Medicare and Medi-Cal patients, is not per se particularly profitable. A primary care practice cannot produce the kind of profits that private equity is looking for.
The solutions to the shortage of primary care physicians must be multi-pronged. We must lessen the burden of overwork. To attract younger physicians, we must provide flexibility to work to improve life/work balance. And we must support our older providers so that they may continue to use their wisdom and experience past age 65.
We must create work situations that are supportive. We must restore status to primary care physicians. A clinic workplace should function as a kind of community supporting and nurturing physicians and staff. We must do more to bolster our primary care community so that we may continue to serve our patients in the best way possible.
Dr. Schrader, an internist at Dignity Health, is Chair of the SFMMS delegation to the CMA and a past-president of the SFMMS.
Kristin Kuchno - September 13th, 2024
Physicians surveyed by McKinsey shared insights on the workforce shortage, including changes that could be made to encourage them to remain with their current healthcare organization.
The U.S. could see a shortage of up to 64,000 physicians by the end of 2024 and 86,000 by 2036, according to McKinsey's article, published Sept. 10. These projections stem from multiple factors, such as the aging U.S. population and burnout accelerated by the COVID-19 pandemic.
McKinsey's survey, which is intended to provide insights into physicians' perspectives for healthcare leaders, included 631 physicians surveyed from June to July 2023. Here are four key takeaways:
1. Taking time off was the most important factor in improving work flexibility.
Of those surveyed, 55% said the ability to take time off was a "very important factor," and 33% said it was an important factor. Similarly, the ability to find coverage was an important or very important factor in flexibility, according to 77% of the physicians. Being able to work specific hours of the day was important or very important to 69% of physicians.
2. Remote work was not as important as other factors for creating better flexibility.
Fifteen percent said remote work was a very important factor, and 23% said it was important. Being able to work across multiple settings or in areas outside patient care had similar levels of importance among physicians.
3. Compensation was just as important as a balance with family life.
When determining the reasons for physicians leaving their current role, aside from retirement, desiring a higher-paid role and "family needs/competing life demands" were top factors. Of those surveyed, 39% said looking for a higher-paying role was "very much a factor," compared to 38% of those who said the same about family needs or competing life demands.
4. Decision-making involvement was key in deciding whether to leave.
More than 60% said they expected to have a vote or be consulted on significant decisions at the organization, such as issues regarding patient care quality and strategic priorities. Specifically for patient care quality, 74% said they expect to be consulted or have a vote on those issues.
As I write this, Vice President Kamala Harris and former President Donald Trump have just finished their first, and possibly only, debate. What a doozy! While it is our sacred duty as Americans to vote and determine our country’s leader for the next four years, it is ALSO important to recognize that there are several very important state and local issues that will be on our ballots alongside our choice for President. As a busy physician, you may not have had time yet to review all FOURTEEN(!) local San Francisco ballot measures. Lucky for you, SFMMS’s Advocacy and Policy Committee (APC) has done just that. For every election, the APC reviews all State and Local ballot measures and makes recommendations to the SFMMS Board on positions that will most benefit physicians and their patients. (If you would like to join the APC and participate in these discussions, please apply here: tinyurl.com/SFMMS-APC) .
Local Ballot Initiatives
For the November 2024 Election, SFMMS leadership recommendations SUPPORTING San Francisco Propositions B, G, and O (there are no health care-related ballot measures on the Marin County ballot).
Proposition B: This measure would generate $390 million by selling general obligation bonds to make critical investments to repair and upgrade public hospitals and clinics, reduce family homelessness, improve street safety, and secure public spaces. This includes:
Adam Francis, CAE
tion would ensure a consistent and stable funding source to ensure the most vulnerable San Franciscans do not lose their homes, creating painfully detrimental health consequences.
Proposition O: This ordinance makes protection of abortion and contraception an official city policy. The proposition would:

• up to $99.1 million to acquire or improve community health centers, including up to $71.1 million to seismically retrofit and renovate the Chinatown Public Health Center and up to $28 million to relocate the City Clinic.
• up to $66 million to renovate Zuckerberg San Francisco General Hospital (including doubling the capacity of its psychiatric emergency services) and make critical infrastructure development at Laguna Honda Hospital and Rehabilitation Center.
• up to $63.9 million for street and sidewalk safety projects.
• up to $50 million to provide more than 2,300 new units of housing for families with children, or pregnant individuals, with the goal of ending family homelessness.
• up to $41 million to improve and modernize public spaces in downtown San Francisco.
• up to $40 million to seismically retrofit General Hospital.
• up to $25 million for Harvey Milk Plaza.
• up to $5 million for parks and recreation centers.
Proposition G: This charter amendment would budget $8.25 million annually for the Affordable Housing Opportunity Fund, creating rental subsidies for extremely low-income seniors, families, or people with disabilities. Approximately 52,600 households in San Francisco include a senior aged 62 years or older, and 20,000 households include a disabled adult. This proposi-
• Create a Reproductive Freedom Fund that accepts grants and gifts to support reproductive rights and services.
• Require DPH to maintain a public website that lists facilities that provide abortions or emergency contraception or offer referrals for these services, and lists limited services pregnancy centers in San Francisco.
• Authorize DPH to post signs outside limited services pregnancy centers to inform the public that those facilities do not provide abortions or emergency contraception or offer referrals for these services; these signs would also indicate where to obtain these services.
• Limit City-funded facilities that provide abortions from requiring providers to have additional medical qualifications beyond those required by law.
• Prohibit City officials from providing information to law enforcement agencies of other states or the federal government concerning a person’s use or possession of contraception, use of in vitro fertilization, pregnancy status or choice to get an abortion.
• Modify the City’s zoning law so that reproductive health clinics may operate in more areas of San Francisco, including all floors in nonresidential districts and corner lots in residential districts.
Other Proposition of Note
Proposition M: This ordinance would reform San Francisco’s business taxes away from payroll expenses and toward sales. While SFMMS chose not to take a position on this Proposition, it did play a significant role in amending the proposal before it was put before voters. The current tax structure and the original reform proposal disproportionately affected small and solo physician practices, taxing them at a higher rate than all but one other class of business activity despite very thin profit margins. After input from SFMMS, the Office of Economic and Workforce Development released an updated proposal that addressed many of SFMMS’s concerns and is now broadly beneficial to small and solo practice physicians (increasing small business exemptions, lowering the proportion of revenue collected by those performing health care business activities, and reducing administrative burden). However, the benefits of the proposed tax reforms would not be equally spread between different kinds of medical practices, and in fact could create a negative financial impact on large physician groups. For that reason, SFMMS has not adopted a Support position on the measure.
SFMMS Leadership opted to not take a position on the other local ballot measures, included below for your information.
Proposition A: $790 million in general obligation bonds to improve, repair and upgrade School District sites, upgrade and modernize dilapidated facilities and pay for a central food hub, where fresh meals would be assembled.
Proposition C: A charter amendment to create an inspector general position to investigate fraud, waste, abuse, and misconduct in city government and by city contractors. The Controller would pick the inspector general, subject to approval by the mayor and Board of Supervisors.
Proposition D: A charter amendment to cut the number of appointed boards, commissions and advisory bodies from more than 130 to 22, then create a task force to recommend which commissions should be reauthorized or restructured. The commissions that remain would no longer have any decision-making authority, making their roles advisory only. The proposition would also give the police chief sole authority in determining rules governing police officers’ conduct.
Proposition E: A charter amendment to establish a task force charged with making recommendations to the Mayor and Board of Supervisors about ways to modify, eliminate, or combine the city’s commissions and boards. The City Administrator, the Controller, the City Attorney, the President of the Board and the Mayor would each appoint one task force member.
Proposition F: A charter amendment to allow police officers with 25 years of experience to defer their retirement to do neighborhood patrol and investigative work in exchange for five years of increased payment.
Proposition H: A charter amendment to lower the retirement age at which firefighters can access their highest potential pension—from 58 to 55. According to a Controller’s report, about 50 firefighters are older than 50 years of age.
Proposition I: A charter amendment to allow eligible registered nurses to purchase up to three years of service credit for time previously worked as a per diem nurse and put that credit toward the city’s retirement system. It would also allow 911 dispatchers, supervisors, and coordinators to move to a different retirement plan starting in 2025.
Proposition J: A charter amendment to require various city departments, the San Francisco Unified School District (SFUSD), and others to adopt a new more centralized structure and coordinate decision-making when it comes to funds that affect children.
Proposition K: An ordinance to use the Upper Great Highway for public open recreation space, permanently closing it to private motor vehicles, with limited exceptions (e.g., emergency vehicles, official government vehicles, intra-park transit shuttle buses), seven days a week.
Proposition L: An ordinance to create a gross receipts tax of up to 4.5 percent on ride-hailing companies and autonomous vehicle businesses. Generated funds would be used to preserve, maintain, and increase Muni service, as well as expand discount fare and fare-free programs for people with disabilities, seniors, youth, students, and low-income passengers.
Proposition N: An ordinance to create a fund to pay outstanding student loans and job-related education and training expenses for employees of the police department, fire department, and sheriff’s office, as well as 911 operators, nurses, and paramedics.
When it comes to State ballot initiatives, no measure could be more important than Proposition 35, the CMA-sponsored initiative to ensure billions of dollars in Medi-Cal funding is not diverted for other purposes. While there are several other initiatives that SFMMS think are deserving of supporting (including Proposition 3 which would remove the nullified and unconstitutional language from the State Constitution that bans same-sex marriage, protecting against any potential future changes to federal marriage protections; and Proposition 4 which would create $10 billion in bond funding to support state and local parks, environmental protection projects, water infrastructure projects, energy projects, and flood protection projects, thereby reducing pollution and improving public health), SFMMS and CMA believe it is of the utmost importance that physician organizations remain laser focused on getting Prop 35 approved.
Prop 35 extends an existing levy on health insurance companies and dedicates those funds to protect and expand access to health care for Medi-Cal patients. Prop 35 will address our most urgent health care priorities by securing dedicated, ongoing funding—without raising taxes on individuals—to protect and expand access to care from primary care and specialty care physicians, community health clinics, hospitals, emergency rooms, family planning and mental health providers. It is backed by a bipartisan coalition including more than 300 organizations representing physicians, nurses, health care workers, first responders, dentists, hospitals, Planned Parenthood, community health centers, social justice organizations and both the CA Democratic and Republican Parties. Prop 35 will create dedicated accountable funding to improve care, improve health care access for the most vulnerable, and keep hospitals, maternity wards, clinics, and ERs open.
Prop 35 provides dedicated funding to:
• Expand access to preventative health care so patients don’t have to rely on crowded ERs or urgent care clinics as their primary source of care.
• Reduce wait times in emergency rooms.
• Reduce emergency response times by funding more First Responders and paramedics.
• Support family planning, including Planned Parenthood health centers.
• Expanded mental health treatment in clinic and hospital settings.
• Workforce training programs to increase the number of doctors, nurses, and health care workers who treat patients.
• Increased access for Medi-Cal patients to hospitals, physicians, women's health and community clinics, and health centers.
I encourage everyone to visit the Prop 35 Action Center ( https://voteyes35.com/take-action ) to find the best ways to help the campaign.

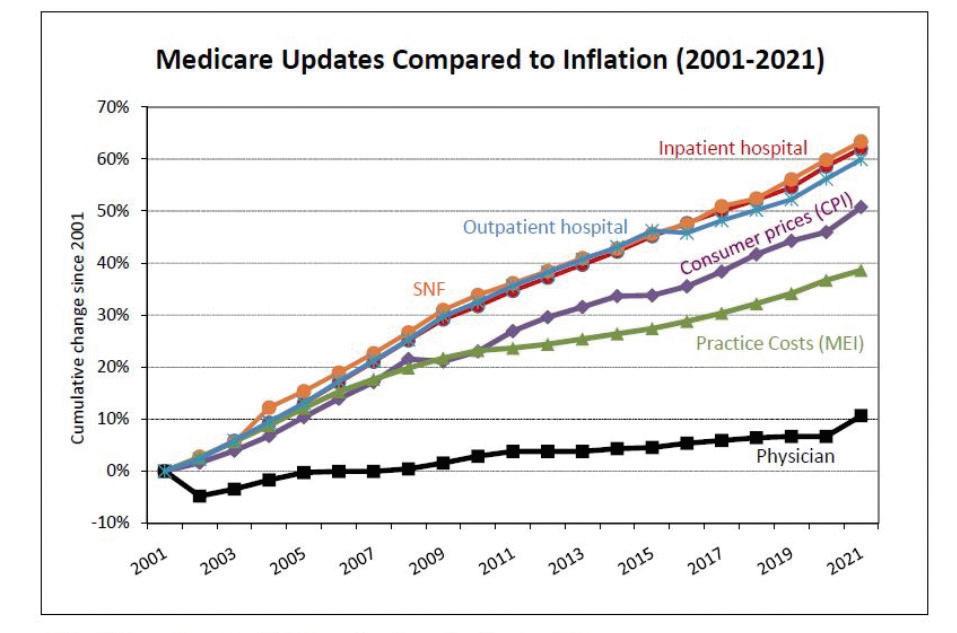
STRENGTHENING MEDICARE FOR PATIENTS AND PHYSICIANS ACT OF 2023- HR 2474 (Ruiz, Bucshon, Bera, Miller-Meeks). This bipartisan bill provides an annual inflation update based on the Medicare Economic Index (MEI) – a reasonable market basket of physician practice costs. Since 2001, adjusted for inflation increases, Medicare physician payment fell 29%. This is in stark contrast to the 60% pay raise given to hospitals and other providers. Moreover, physicians took pay cuts in 2023-2024. This bill would stabilize physician practices, reduce consolidation, and protect access to doctors for patients.
PROVIDER REIMBURSEMENT STABILITY ACT HR 6371: Reforms the Medicare Physician Fee Schedule budget neutrality rules so that increases for some services do not reduce payments for other services.
REDUCING MEDICARE ADMINISTRATIVE BURDENS: CMA AND ORGANIZED MEDICINE ARE PROMOTING DRAFT LEGISLATION to reform the physician MACRA reporting system.
IMPROVING SENIORS TIMELY ACCESS TO CARE ACT (S 4532: Marshall, Brown, Thune, Sinema/HR 8702: Bera, Bucshon, Kelly, Delbene). Bipartisan legislation that streamlines the Medicare Advantage prior authorization process to ensure patients get the care they need when they need it. Codifies the recent regulations and calls for real-time decisions. 400 endorsing groups/More than 200 cosponsors.
RESIDENT PHYSICIAN SHORTAGE REDUCTION ACT OF 2023 S 1302/HR 2389. This bipartisan bill would provide 14,000 new Medicare Graduate Medical Education (GME) physician residency training positions over 7 years. GME positions have been capped since 1997. This bill opens the physician pipeline to address serious shortages. Out of 31 industrialized nations, the U.S. ranks 27th in number of physicians per capita.
CONNECT FOR HEALTH ACT OF 2023: TELEHEALTH (S 2016: Schatz, Wicker, Cardin, Thune, Warner, Hyde-Smith/HR 4189: Thompson (D-CA), Matsui (D-CA), Schweikert, Johnson). This bipartisan bill would permanently extend the COVID-19 pandemic telehealth waivers and ensure that Medicare patients who cannot get to physician offices continue to receive care.
California physicians are sounding the alarm – access to care in Medicare is deteriorating. CMA is extremely concerned that the Medicare physician payment system is causing instability in physician practices that is leading to burn-out, physicians leaving Medicare or retiring early. Medicare is exacerbating physician shortages and ultimately, threatening patient access to care.
Medicare physician payment has failed to keep pace with the costs to provide care. Since 2001, Medicare hospital and nursing home payments increased 60% and inflation rose 50%. Yet adjusted for inflation, physician payments declined 29% from 2001-2023. All other Medicare providers receive an annual inflation adjustment except physicians. For 2023-2024 Congress failed to stop all of the physician payments cuts. Last year the cut was over 6% in real terms. Physicians are not the main driver of health care cost growth. Physician spending constitutes only 14% of all health care spending (CMS).
Physicians are overwhelmed with aging, sicker patients who suffer from mental health problems or delayed care because of the pandemic. Yet Medicare is providing fewer resources to help physicians care for this mountain of need. Physicians want to care for their communities, but without a Medicare payment update to keep pace with California’s higher costs, it is more difficult for physicians to maintain a viable medical practice. The tide of sicker patients, an inability to keep essential nursing staff, an average of $200,000 in medical debt (AAMC 2022), and fewer Medicare resources are causing burnout and consolidation which is actually driving up health care costs.
A 2022 CMA survey showed disturbing new trends in California physician shortages. Many physicians are no longer accepting NEW Medicare patients, particularly in primary care. 70% said Medicare cuts are forcing them to limit Medicare patients; 45% plan to retire early and close their doors. This is causing delays for patients to get care. A majority of California physicians are nearing retirement and California is projected to have the largest physician shortage in the nation over the next decade (Human Resources Health 2020). According to the AMA, 1 in 5 physicians plan to leave their current practice in the next two years.
The recent Medicare Trustees Report said lawmakers should “expect access to Medicare-participating physicians to become a significant issue in the long term.” Timely access to care for patients has become more challenging, particularly in rural or traditionally underserved and marginalized patient communities. Patients are experiencing long wait times in California’s emergency departments, delays in getting appointments and receiving physician care.
In its June 2024 Report to Congress, the Medicare Payment Advisory Commission (MedPAC) expressed concerns about the growing gap between Medicare payment and the actual cost to deliver care. “This larger gap could create incentives for clinicians to reduce the number of Medicare beneficiaries they treat or stop participating in Medicare entirely.”
As stewards of the Medicare program, Congress must ensure seniors have access to the physicians they need when they need them.
The CMA held their fourth annual Medical Group Advocacy Symposium in Sacramento on August 8, 2022. SFMMS was well-represented at this meeting by Drs. ManKit Leung, Brian Grady, Shannon Udovic-Constant, John Maa, George Fouras and me. Some of us were there on behalf of the CMA, some were representing various medical groups, and some of us had been asked to help solicit group memberships.

The CMA and our component medical societies rely increasingly on group memberships. SFMMS has a number of group membership deals including Kaiser, SFDPH, UCSF, Sutter, and Brown and Toland. As the number of employed physicians increases and private practice dwindles this trend will no doubt continue.
Ultimately this meeting was to demonstrate the value of CMA membership to the invited groups. The value of the CMA for these groups is political influence, lobbying, and advocacy at the state and federal levels.
The opening focuses of the meeting were talks about diversity in medicine and physician workforce. Assemblymember Dr. Akita Weber spoke about her personal experience with discrimination and racism as a physician. Dr. Deena Shin McRae from University of California Health spoke about DEI and physician workforce. Ms Lupe Alonzo-Diaz spoke about California physician workforce shortage and strategies to address this.
Dustin Corcoran, CEO of CMA, spoke about Proposition 35 which would increase Medi-Cal reimbursement rates. This proposition directs MCO tax and matching federal funds to be designated to Medi-Cal so that funds cannot be redirected to the general fund. This represents $6.5 billion that will increase to $8 billion in 3 years. This measure has broad support from over 300 organizations and no organized opposition.
CMA has devoted $50 million to the campaign to pass Poposition 35. Medi-Cal is the only growing sector of the insurance
market. Half of all children in California and one third of adults are covered by Medi-Cal, but these patients suffer from lack of access to physicians because of low reimbursement.
The final speaker was Dr. Richard Pan who spoke about the new state Office of Health Care Affordability. The charge of this office is to control medical spending. For 2025, the goal is to limit the increase in spending to three percent of the spending in 2024.
Proposition 35 is a major undertaking by CMA. If it passes it will be a monumental achievement and will greatly benefit MediCal patients and insurers.
The benefits to individual physicians is not as clear. Medi-Cal patients will have greater access to physicians but many of us are already overburdened and there is a physician shortage. It is not clear whether increased payments to insurers will trickle down to physicians.
Proposition 35 is still the right thing to do. California has very low reimbursements from Medi-Cal as compared to Medicaid in other states. Medi-Cal patients deserve better access to physicians.
In the end, the question is whether our CMA serve both individual physicians and medical groups. Our work and employment patterns are changing and we will all need to adapt. Clearly CMA is evolving. Individual physicians both in private practice and employed will have to work to make sure our voices continue to be heard at the CMA.

Dr. Schrader, an internist at Dignity Health, is Chair of the SFMMS delegation to the CMA and a past-president of the SFMMS.


The Golden Gate Bridge has finally erected a suicide barrier after years of inertia, controversy, and opposition, with local, state and federal officials commemorating its completion earlier this month.
Nearly 50,000 people died by suicide in the U.S. in 2022, the last year for which the Centers for Disease Control and Prevention has published provisional estimates. It was the highest total ever recorded in the country, according to the agency.

The Golden Gate Bridge is unfortunately synonymous with suicide. Since the completion of the bridge in 1937, this “lethal beauty” has been responsible for approximately 2,000 deaths, counting only bodies recovered. The bridge is infamously known as one of the deadliest suicide sites in the world, averaging two or three deaths a month.
This high incidence of Golden Gate Bridge suicides was perplexing. It was a local problem, and one we could control. How could nothing have been done?
As a psychiatrist working as the chief of an inpatient unit four miles from the bridge, I knew I had to do something about it. The work began as a six-person working group I formed in 2005, made up of suicide-prevention experts, physicians, nonprofit leaders, and government officials. The goal was simple: Convince the 19-member bridge board of directors to erect a barrier.
This task force was composed of suicide experts and lay members. Two or our six members had been involved in the prior 1990s campaign: Jerome Motto, past president of the American Association for Suicide Prevention, and Eve Meyer of San Francisco Suicide prevention. Psychiatrist Anne Fleming of Stanford who has lost a classmate to the bridge joined us. Assemblyman Tom Ammiano, who was indispensable to the effort, sent staffer Esther Marks. Kevin Hines, who survived a jump in 2000 was a member. Paul Muller, who went on to co-found the Bridge Rail Foundation, was our consultant. The BRF carried the ball and completed the effort supplemented by family members. Janice Tagart was our consultant.
When we began nearly 20 years ago, 75% of polled San Franciscans opposed the barrier. In a city as liberal as San Francisco
that number seemed remarkable. We had to counter arguments and misconceptions that jumpers would just go elsewhere, that they are exercising free will, or that they are all mental patients. Other opponents focused on the cost of a barrier or its aesthetic impact. Our task force attempted to meet in person or by phone with all the bridge board members. We set up a speaker’s bureau and spoke at hospitals, schools, rotary clubs and churches. We wrote op-eds and lobbied the media. We attended the regular Friday morning board meetings. We went to the state capital to speak with legislators.
At the start of the campaign, I was given a special sense of mission when a psychiatrist colleague’s son suicided from the bridge. Jonathan was an 18-year-old student at French American International School. He had already been accepted to college. He was a procrastinator, and the night before his suicide he had not completed his assignment on the Challenger space shuttle disaster. He believed that his parents were upset. The following day he took public transportation to the bridge, paced up and down, and jumped at the end of the day.
In my work at St. Francis Memorial Hospital, I have interviewed more than 60 individuals taken off the bridge. The common belief is that the bridge is a magnet attracting jumpers for its beauty. I found that two-thirds of the jumpers I interviewed told me that they came to the bridge because it was easy and a sure way to suicide.
Yet the most common misconception about bridge suicide is that jumpers, if prevented, would go elsewhere. Suicides tend to pick places and methods with which they are familiar. A pivotal 1978 study by psychologist Richard Seiden followed individuals taken by the California Highway Patrol from the bridge over a 25-year period showed that, at the end of the study, 94% were still alive or died from natural causes. They did not go elsewhere.
The bridge remained a compelling structure to lure those experiencing a chance moment of desperation to easily end their lives.
Though the science and facts behind suicide proved the point handily, the fight for the barrier was ultimately won when the
families of the jumpers joined us at the Friday meetings. They held up pictures of their loved ones and spoke of their losses.
The board could not fail to be moved. I recall seeing a Marin County supervisor coming to tears. It would not have been possible without their bravery.
Incrementally, the barrier campaign moved forward. Between 2005 and today, a small group of dedicated individuals worked tirelessly, overseeing design engineering and environmental impact studies, public debates, special task forces and, finally, consensus.
Construction began in 2018. Survivors with whom I have spoken are grateful to be alive, but perhaps even more importantly, family members who lost those that mattered most are relieved to finally be met with some closure.
Ken Baldwin, who survived the jump, sent me this statement: “I suicided in August, 1985. I jumped off the Golden Gate Bridge. ... I just looked over the water to the city, and it was beautiful. I felt that this was the right time and place to kill myself. I vaulted over
the railing. The last thing I saw leave the Bridge was my hands. It was at that time that I realized what a stupid thing I was doing. It is incredible how quickly I decided I wanted to live when I realized that I was going to lose my wife, my daughter, and the rest of my family.” “There are two parts to my life—before the jump and after the jump,” he said. “I am the luckiest guy in the world.”
Thanks to the hard work of the many government agencies, officials, advocacy groups, and most importantly, the families of those who we lost, there will never have to be an “after the jump” story like Ken’s again.

Dr. Mel Blaustein is a San Francisco psychiatrist and a longtime advocate for suicide-prevention efforts at the Golden Gate Bridge.
The San Francisco Free Clinic was founded in 1993 by two CPMC physicians (Drs. Patricia and Richard Gibbs) to provide free medical care to people with no health insurance. Each year, the clinic sees over 3,500 unduplicated patients with over 7,000 patient encounters. The clinic is an award winning and unique model of cooperation between the medical community and private charitable contributions.
The San Francisco Free Clinic is seeking physician volunteers to donate specialist consultations to help with this underserved population. SFMMS members who have volunteered with the SFFC report a nourishing and rewarding experience that reconnected them to the mission of medicine.

To read more or to volunteer, access the fact sheet scan here:


John Maa, MD
On June 25, 2024, United States Surgeon General Vivek Murthy issued a landmark advisory detailing the public health crisis of gun violence in America, adding that “our failure to address it is a moral crisis.”
This 40-page publication, the first by the Office of the Surgeon General (OSG) was a long-awaited response to the rapidly growing US firearm problem that threatens the lives, health and mental wellbeing of children and adults.
The advisory clearly summarizes the epidemiology of firearm injury in the US and the collective toll on victims, communities, and families, and explores the contributing factors of socioeconomic, geographic and racial inequities that intersect with the increased lethality, availability and access to firearms.

A central intent of the advisory is to raise awareness of the American public for the need of immediate bipartisan attention and action. Dr. Murthy emphasized several points in this document.
1. Deaths from firearms have recently soared, now representing the leading cause of death for children up to the age of 19.
2. 79% of US adults experience stress from the possibility of a mass shooting, and one in three adults say fear prevents them from going to certain places or events.
3. 54% of US adults surveyed report that either they or a family member have experienced a firearm-related incident.
4. 21% of those surveyed have been threatened with a firearm.
5. 19% have had a family member killed by a firearm (including suicide), 17% have witnessed a shooting, and 4% fired a weapon in self-defense.
In the final chapter, Dr. Murthy specifically calls attention to the need for an evidence-based public health approach to preventing firearm injury and risk reduction through improved data collection, research, and implementation science.
The San Francisco Marin Medical Society played a central role in the creation of this advisory. In 2016, I spoke with President Obama about America’s firearm epidemic, where he highlighted that the relationship between gun ownership and firearm injury might be as strong as the association between smoking and lung cancer. What the President illuminated to me was that like a cigarette—the firearm is the vector in this public health problem. During my professional career in tobacco control, I came to understand the power of the 1964 US Surgeon General report “Smoking and Health” and the 40 reports that followed to drive the US smoking prevalence from 42% in the 1960’s to under 14% today. This served as the inspiration after the 2018 Parkland shooting to write a New England Journal of Medicine (NEJM) paper with Lord Ara Darzi, a general surgeon, Member of Parliament and former NHS Health Minister, calling for the first US Surgeon general report on firearm injuries. We were joined by Congresswoman Robin Kelly who called for the Surgeon General to report annually to Congress about the problem, and together spoke at a Capitol Hill press conference in 2019. We believed this report could gather evidence, raise awareness, dispel myths, and identify questions to focus future research and catalyze a bipartisan discussion about gun violence prevention, and spent the next six years to make this idea into a reality.
In 2022, Drs. Robert Spencer and Barbara Weissman of the San Mateo County Medical Association, along with Dr. Michael Schrader and I from SFMMS co-authored a CMA HOD resolution urging the US Surgeon General to issue a report on gun violence. Our CMA Board Trustee Kimberly Newell Green championed this resolution before the full CMA Board, who sent a letter in 2023 to Surgeon General Murthy urging the creation of this report. On the 10-year anniversary of the Newtown mass shooting in December of 2012, four US Surgeons General sent a letter to the
Biden White House urging the commissioning of a report, and in the summer of 2023, 55 Members of Congress led by Congresswoman Robin Kelly from both the House and Senate sent a joint letter to the White House calling for the same.
Next steps:
We are grateful to the US Surgeon General for his leadership in this important step forward by issuing the advisory and agree with his conclusion that much more needs to be done. The 1964 OSG report on Smoking and Health took three years to prepare, and included 15 chapters that reviewed over 7,000 references and was 387 pages long. We understand that the firearm advisory was not intended to be an exhaustive review of the literature, and the medical and public health community is poised to assist Dr. Murthy’s office produce a full report in the future. A key next step is to complete the first full OSG report on firearm injuries, after convening study sections and expert panels of policymakers and scientists to review the current evidence. Congresswoman Robin Kelly’s recommendation that the OSG report annually on firearm injuries to Capitol Hill could help serve as the foundation for the full report.
Importantly, after the 1964 OSG report on Smoking and Health, the critical next step was action by Congress. In 1965 the Federal Cigarette Labeling and Advertising Act required warning labels on cigarette packages, in 1966 the Federal Trade Commission developed testing requirements for tar, carbon monoxide and nicotine levels, and in 1969 Congress banned cigarette advertising on television and radio.
In 2023, Surgeon General Murthy issued an advisory about social media use by teens, and a year later moved further to recommend a warning label for social media platforms. In this spirit, in the final chapter of the firearm advisory, several public policy recommendations are made for potential action by local, state and federal governments. These include strengthening background checks, an assault weapons ban, extreme risk protection orders (red flag laws), restrictions of large capacity magazines, increased products standards and safety feature requirements for gun manufacturers, and a call for health systems to educate about safe and secure firearm storage. Future public policy actions could extend the 2022 Bipartisan Safer Communities Act by Congress to further strengthen the mental

health system, school safety programs, and firearm safety laws. Perhaps the success from the 1960’s in tobacco control could also serve as a future model, and result in a warning label for firearms, and a ban to advertising on television and radio?
In the 2018 NEJM paper Dr. Darzi and I also suggested that a new federal agency be created to address firearm injuries. We were pleased to see the creation of the White House Office of Gun Violence Prevention in 2023 led by Vice President Kamala Harris, and perhaps the time has arrived to divide the Bureau of Alcohol, Tobacco, Firearms and Explosives into separate agencies? H.R. 5010 by Congresswoman Kelly seeks a declaration by Health and Human Services Secretary Xavier Becerra of a firearm public health emergency (PHE) in America (similar to the COVID PHE) that could enable the dedication of federal resources and catalyze the creation of a permanent federal agency to firearm safety.
Ultimately, a complete Surgeon General report must present the evidence to enlighten the challenging topics in the firearm debate. After the Winder, Georgia shooting in September of 2024, our nation asks once again how to address the problem of school shootings. What are the roles of violent video games, and the portrayal of firearms by Hollywood in film and television in our firearms public health crisis? Are there international solutions that could be applied in the US? Addressing these questions could help to balance the Second Amendment right to “keep and bear arms” with greater accountability for unintended injuries and strengthen public safety across America.

John Maa MD, FACS, is the AMA Delegate for San Francisco and Marin. He serves on the Brady Campaign Northern California Regional Leadership Council and the Marin County Gun Safety Collaborative.


Elson Haas, MD
An estimated 350,000 people in the greater San Francisco Bay Area are experiencing a shortage of primary care providers, according to Kyrus Health, a healthcare access platform. The California Healthcare Foundation says that a third of Californians live with this shortage of primary care providers, especially in rural areas. The Covid pandemic has also affected many practices, and there have been more retirements during these stressful times. Many patients balk at concierge fees. Fewer medical graduates are choosing primary care and family practice because of the lower pay, often much less than specialists, and this is even more of a deterrent in the expensive Bay Area.

25 or more practices to try and schedule an appointment. They are met with “our practice is full” of “we have a $1,500 concierge fee,” or rarely, “we can schedule you in six months.” This is also true for younger, healthy men and women in their 20s and 30s who have a new job with new medical coverage and get a list from their insurance carrier, but are unable to find an office and obtain care.
This shortage is especially the case in Marin, Sonoma County and San Francisco counties.
This is not only a problem in California and the Bay Area, but sadly the entire US is suffering from a shortage of physicians in general. According to Fraser Research, the physician shortage over the next decade is predicted to be more than 100,000 practitioners. This includes primary family doctors and many specialists. Americans are the least likely people in the developed countries to have any kind of relationship with a primary care provider. The disparity is even greater in Black and Hispanic populations and those at the lower end of the economic spectrum.
This writing is not just about the lack of availability—the desert—of mainstream family physicians. It’s also about how to make our medical practices more rewarding and less stressful as well as supporting happier and healthier patients. Are you satisfied with the direction of your practice and our healthcare system? Certainly, there have been great successes, however, many people are dissatisfied with both the costs and outcomes. Ideally, we can get better results with much less expense. That’s where Prevention and Lifestyle Education play a greater role. We can reverse much early, chronic disease such as hypertension, pre-diabetes and cardiovascular issues with changes in the way we live. The word “doctor” comes from the Latin word docere, meaning “teach.” Let’s embrace that role for better outcomes. Of course, much disease is environmental and stress based, and cancer is often lifestyle-based.
Personally, I am feeling a bit lonely running a medical clinic in Marin County as one of the few or only practices saying “Yes” to New Patients and the Medicare elders moving to the area or opting out of Kaiser or just looking for a friendly physician and an accommodating office staff. Some patients are calling
What can we do to change that? After all, we live in the beautiful Bay Area, paradise every day. Why can’t we attract young doctors to join or build a practice? Yes, it’s expensive here and I hear that many who think that’s why there’s the lack of primaries in our area.
Most new physicians going into practice today want a contract and a guaranteed salary, often to pay their school loans. They don’t want to be running their own medical business especially if they may not have had any training in this area. They also want the protection from malpractice lawsuits that large organizations provide. So, they join bigger corporate or hospital practices, such as Sutter or Kaiser Permanente.
I used to be the “alternative” or “wholistic” doctor for people who sought second opinions or more natural remedies for their ailments. Now I am seeing patients as their primary care provider, still enjoying family practice for the past 51 years and providing thorough health and lifestyle evaluations, exams, medicines as well as dietary recommendations and natural remedies. And I still enjoy teaching my online detox programs several times yearly.
Bay Area Practice and the Local SF Bay Area Healthcare Issues
What about the old-time GP (General Practitioner)? Getting to know the patients and their families is still an important aspect of a successful and helpful medical practice. It becomes more than merely “what’s wrong and what medication/drug will fix (or cover up) the problem?” That’s “quick medicine” rather than a more ideal relationship of medical care, which I have embraced these many decades. Seeing families and individuals and knowing them over 20-30 years is quite rewarding. Growing (and glowing) health is my goal.
Our health comes primarily from a positive or balanced lifestyle (and a healthy environment), which is the focus of my practice. How can we improve each person’s health rather than just diagnose and name diseases and give medicines? It starts with how we feed ourselves and what we do with our energy, and how good we are in addressing our 5 Keys to Staying Healthy—balanced Nutrition, regular Exercise, Stress management, quality Sleep and good Attitude.
In the past 20 years or so, medical practice has been dominated and partly dictated by both insurance and drug companies. This industrialization of medicine is making billions from the latest, greatest pharmaceuticals and vaccines being produced and applied to different diseases. When I first started practicing medicine, there were less than 30 to 40 commonly used drugs that included several antibiotics and insulin and drugs for blood pressure. There were no ‘statins’ for lowering cholesterol, nor very many mood-altering drugs for depression, or multiple drugs for treating sleep disorders and anxiety. We’ve gone far beyond Librium and Valium, or phenobarbital. Many new medicines are an improvement over previous ones, but often much more expensive. Nowadays, there are literally thousands of medicines for doctors to learn about and apply, and there are many hundreds of medicines entering the medical marketplace each year. I trust many of the older meds more and as always, my approach is to use the least amount/dosage of prescriptions to get the results we need, whether it’s for lowering blood pressure, cholesterol or blood sugar and for balancing moods and depression. Sleep medicines are also very prevalent.
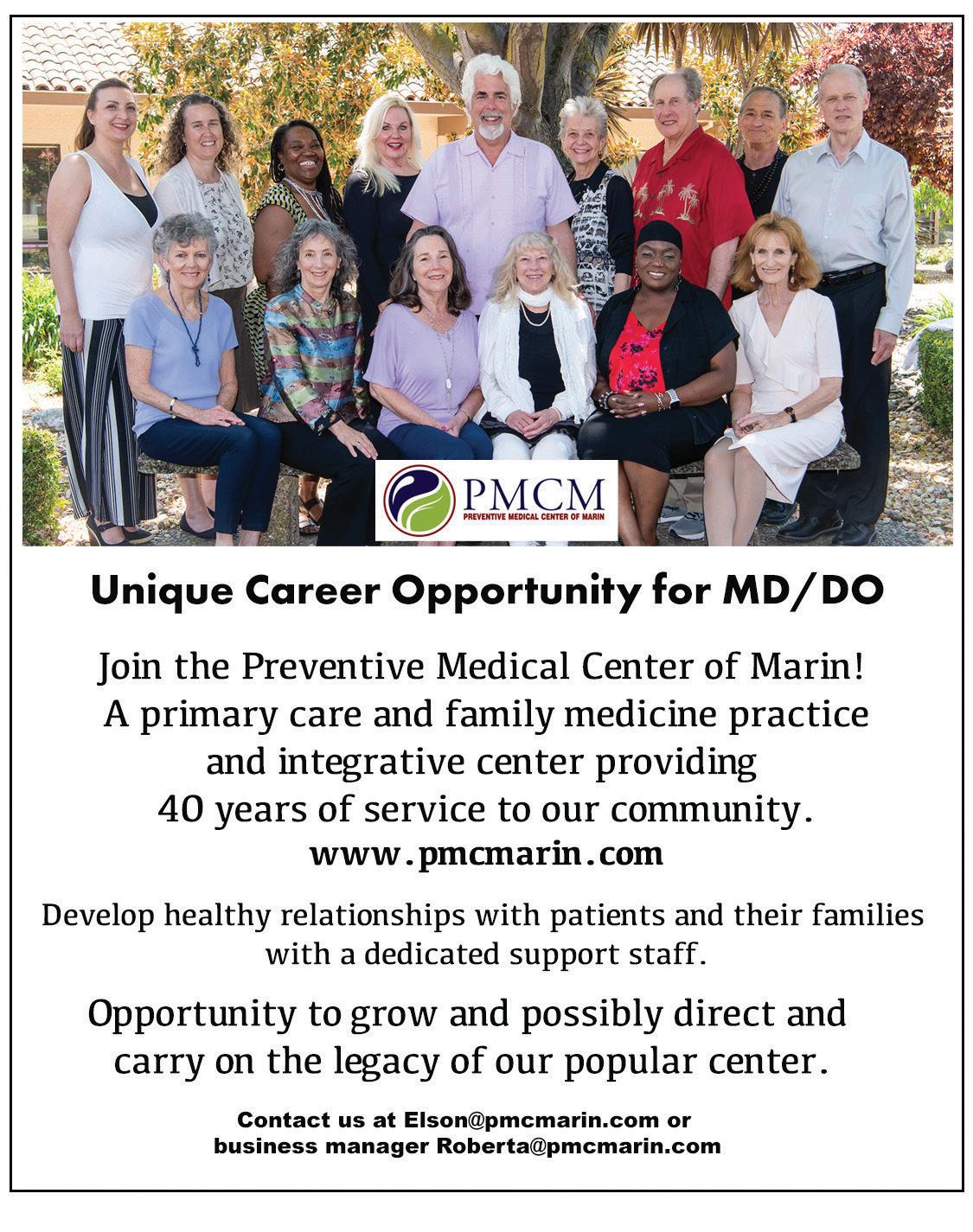
We have a unique business model at my clinic of 40 years, Preventive Medical Center of Marin (PMCM). We take most insurances, which is rare for any independent integrative medical doctor’s practices. Our business model has a great office management team that handles my practice and our Nurse Practitioners, as well as the practices of other physicians. This model has worked for us, yet, most young doctors don’t want to work for themselves or run a business and prefer others to make the rules and guidelines for practice. To me that offers less rewards than being the good old family doctor.
Within the current model, insurance reimbursements for office visits are limited, and doctors tend to be busy with many patients, appointments tend to be too short and often deal with very specific problems. “What’s wrong?” is the question and then doctors focus on the name for whatever the patient has and prescribe the specific drug, if there is one. Many times, there’s not a clear picture and no easy answer. At PMCM, we take more time with patients and explore what’s going on with whatever symptoms and life issues that are out of balance.
Getting to the core/cause of symptoms and diseases is a key aspect of an integrative and commonsense approach to medical care. Is it inflammation, allergy or poor habits? To me, lifestyle imbalances are at the core of most conditions. In my experience, Deficiency and Toxicity are at the basis of many health imbalances, affecting cellular health and leading to a long list of symptoms and diseases. This means not getting enough essential nutrients and being exposed to too many toxins and substances that undermine health. I believe this is the best way to look at many medical problems and how to correct them by remedying deficiencies and diminishing toxicities.
The Doctor-Patient Relationship is one key to successful health outcomes, so ideally we take time to gather a real lifestyle overview and get to know each patient rather than quick visits for a diagnosis and prescription. Patients appear to love the personal touch and care from their doctors, and this might include doctors running on time, having respect for the patient’s beliefs, and much more. These ideas about health are discussed more thoroughly in my book, Staying Healthy with NEW Medicine: Integrating Natural, Eastern and Western Approaches for Optimal Health.
I want to write more about the Primary Care Desert in the next issue, and include you, and so I ask for your input for possible solutions. You can email me at Elson@pmcmarin.com.
NOTE: We are inviting one or two new doctors who want to be caring practitioners to help oversee and guide our family practice at PMCM.
Elson Haas, MD (www.ElsonHaasMD.com) is the founder and director of Preventive Medical Center of Marin (www.PMCMarin.com) which has been providing integrative health care to the North Bay community since 1984. He grew up in Detroit, attending the University of Michigan for undergrad studies and medical school (class of 1972), and then moved to Northern CA. He is a long-time teacher and author of 11 books on health, nutrition and detox, including Staying Healthy with the Seasons, Staying Healthy with Nutrition, The Detox Diet and Ultimate Immunity.
Grant Colfax, MD and Hillary Kunins, MD
Promising new data suggests that overdose deaths are decreasing in the United States. Still, far too many people are dying from opioid addiction, especially here in California. In San Francisco, overdose deaths are down 15% to date in 2024 after a record 810 overdose deaths in 2023. While any reduction is welcome, those numbers are still alarmingly high. Fentanyl remains a devastating crisis.
What those of us who work in public health find most heartbreaking is also what we find most hopeful: It doesn’t need to be this way. We have and are implementing the tools to save lives. We now need the policies to be able to realize the full potential of these interventions.

A key example is methadone, an extremely effective medication to treat opioid addiction, reduces a person’s risk of dying of overdose by half. It also increases a person’s overall health and stability. Yet despite its successes and life-saving potential, methadone is grossly underused in the United States, including the Bay Area, because of government restrictions driven by stigma, not science.
Earlier this year, the federal government loosened regulations for methadone to increase access for those who need it most. However, in California, where we pride ourselves as leaders in health care equity and access, we remain one of the most restrictive of states. California must follow suit and update its oversight of methadone treatment to align with the new federal guidelines. Removing these obstacles will put more San Franciscans in treatment and recovery, and more lives will be saved.
To understand the importance of why methadone works, let’s first look at the science. Opioids, such as fentanyl, have a profound impact on the brain. When someone starts using an opioid, the drug acts on receptors in the brain and increases the level of dopamine, also known as the “feel good” hormone. This results in that sought-after high. Over time—anywhere from weeks to months—the brain gets used to the drug, adapting so
that it takes more and more to get high, and getting to the point where people begin to feel sick without the drug. The absence of the opioid results in extremely painful withdrawal symptoms often requiring medical attention. Most people with severe opioid addiction aren’t even using to feel high anymore but rather to avoid this intense suffering.
Here is where methadone does remarkable work: methadone, a long-acting opioid, stabilizes those very same brain receptors, bringing relief from the cycle of withdrawal, decreasing craving and allowing people to feel well again without inducing a high, and enabling their return to a healthier life, employment and social relationships.
Hundreds of studies have established methadone as the gold standard for treating opioid addiction. The National Academies of Sciences, Engineering and Medicine—the nation’s preeminent scientific body—recently summarized the data in a landmark report: “Medications for Opioid Use Disorder Save Lives.” The science could not be clearer. But byzantine restrictions prevent methadone from realizing this potential. These include limitations on where treatment can start, requirements for beginning treatment that are clinically unnecessary and rigid follow-up requirements such as having to physically come to the clinic every day and be observed taking methadone.
Imagine these daily visits to a methadone clinic—navigating buses to a limited number of clinics where to gain admission you often must arrive before 6:30 a.m., arrange childcare and manage work schedules. Now imagine all of life’s complications, such as traveling to attend a loved one’s graduation or funeral, a sick kid or a broken-down car, that may require you to miss doses and start the cumbersome treatment enrollment process all over again.
Patients seeking methadone treatment often face additional hurdles, such as demonstrating at least a year of documented opioid use and being removed from the clinic's rolls and forced
to start again if they do not seek treatment for more than two weeks. There are also limits to the amount of methadone that is allowed to be prescribed that do not take into consideration the higher doses often needed to combat fentanyl.
Methadone’s maze of restrictions would be unacceptable for other life-saving treatments. The public and policymakers would not tolerate this for HIV, cancer or diabetes treatments. Why is methadone different?
There is a dangerous misconception that methadone must be treated differently because it is a drug with certain risks. Yet every medication that we prescribe must be prescribed appropriately, to the right person and in the right dose, with appropriate follow-up. Studies have shown that allergy medications and antibiotics are more commonly diverted than methadone. If a medication for any other disease cut mortality by half, it would be celebrated and widely distributed.
Policy must catch up with science. As a first step, we call upon leaders in California to pass AB2115, authored by Assembly Member Matt Haney, D-San Francisco, which would allow primary care clinics and hospitals to dispense 72 hours of methadone as a bridge to establishing ongoing care at a metha-
done clinic. The bill will allow more flexible dosing to treat those using fentanyl, increasing how much medication can be dispensed to reduce the daily burden placed on clients and allowing for expedited entry into treatment programs. Removing these barriers is key to making life-saving methadone more available. The scale of the overdose crisis demands urgency. We cannot require people who are often at their most vulnerable to navigate arcane and bureaucratic systems to access life-saving medicine. Methadone saves lives. Let’s make it easier to start and stay on methadone so that we can save more.


Grant Colfax is an internist physician and the director of health for San Francisco.
Hillary Kunins is an internist and addiction medicine physician and the director of behavioral health services and mental health for the San Francisco Department of Public Health. An original version of this piece appeared in the San Francisco Chronicle.
Carolina Fonseca, MD, MS; Cynthia Haq, MD and Jeffrey Mann, MD
Introduction
The earth has a fever. All regions of our planet are experiencing unprecedented heat, fires and extreme weather as a result of the heating climate. California is no exception. The thermometer reached over 110oF throughout much of our state in early July. Even San Francisco, usually spared from weather extremes, experienced some sweltering days.

These climate events aren’t just inconvenient, uncomfortable, and costly; they directly impact the health of our patients, from infants to pregnant women and the elderly.
We represent Climate Health Now, a California-based group of physicians and health professionals with a mission to address the evolving catastrophe of climate change, and to improve health by advocating for climate solutions. We are calling on other health professionals to help us address the health challenges from climate change that affect all of our specialties and all of our patients. In this article, we take a closer look at the challenges that the warming environment poses to our patients’ health, explain why we believe health professionals should advocate to mitigate climate change, and explore solutions to the climate crisis that we can all be a part of.
Climate change is an escalating danger to human health and the sustainability of life on earth. Increased global temperatures have resulted in more frequent and extreme weather events, widespread fires, and catastrophic flooding, which in turn affect food production, air quality, access to clean drinking water, safe shelter, vector-borne diseases, and essential infrastructure. The Centers for Disease Control and Prevention (CDC) have identified a multitude of health effects resulting from climate disruptions including increased respiratory and cardiovascular diseases; injuries and premature deaths related to extreme weather events; changes in the prevalence and geographical distribution of food- and water-borne illnesses and other infectious diseases; and threats to mental health1
Extreme heat is the leading cause of weather-related deaths, and most of these are not from heat stroke. Studies show that heat exacerbates chronic health problems like cardiac, pulmonary and kidney diseases. Fortunately, most if not all
heat-related deaths are preventable. Measures to avert heat deaths include neighborhood cooling centers, protections for outdoor workers, and caring for vulnerable people like the elderly and those who live alone during times of extreme heat.
Recent medical research demonstrates strong correlations between air pollution and human health. It is estimated that one in five global deaths are related to breathing polluted air; 90% of people breathe unhealthy air based on updated World Health Organization standards of particulate matter (PM) pollution2. Air pollution is primarily caused by PM emitted by the extraction and burning of fossil fuels. Furthermore, air pollution is worsened by higher temperatures we experience in our warming climate3. Studies have shown elevated levels of PM exacerbate numerous conditions including respiratory and heart disease, premature births and mental illness.
The adverse effects of the changing climate on our patients’ health are not hypothetical. Primary care medical professionals are seeing longer allergy seasons, more asthma exacerbations, and worsening mental health crises. Climate-driven natural disasters cause a multitude of physical injuries and psychological trauma from disruptions to families, communities and schools. Natural disasters interrupt health care delivery and make it hard for families to access medical care, essential medicines, and even the basics of clean food and water.
Physicians and health professionals have ethical obligations to address climate change as a disruptor of health care and a threat to health. National and international organizations have called for health professionals to become leaders and advocates. The World Health Organization concluded “the health sector must play an active role nationally in formulating and implementing strategies to prevent climatic change and combat its effects” in 19904. The American Medical Association “encourages physicians to be spokespersons for environmental stewardship”, and in 2022 declared climate change a public health crisis5.” In the fall of 2021, editors of 220 prestigious medical journals warned that the climate crisis could be catastrophic for human health. They called for “emergency action” on climate
change, to limit global temperature increases to 1.5oC6. Unfortunately, we have already nearly exceeded this threshold. Advocating for policies to protect patients’ health has taken many forms in the five years since Climate Health Now was formed. We have spoken to politicians and policy makers at all levels of government from city councils to state and federal levels. We have lobbied for cleaner air protections in the Bay Area, Central Valley, Los Angeles and state-wide. We have supported California state bills that affect patients’ health.
Medical research is expanding our understanding of the effects of heat and pollution on our health, but medical education has not kept up with the findings. California’s physicians can educate themselves and others to serve as advocates for climate policies.
Climate Health Now members are dedicated to educating others about the intersection of climate, health, and equity. Climate education and advocacy are important for health equity, as patients living on low incomes are often the most adversely affected. Our speakers have presented at conventions, grand rounds, noon conferences, department meetings, clinics, offices, and legislative meetings. The Medical Society Consortium on Climate and Health, our parent organization, has information on their website, offers webinars and an in-depth annual meeting. Many medical specialty organizations offer educational programs on issues of climate and health. Primary care doctors need to understand the effects of heat, smoke and air pollution on their patients, and how they may complicate other medical conditions. Surgeons are noting their contributions and developing measures to help to decrease emissions from the operating room such as proper sorting and recycling of medical waste, eliminating certain anesthetic gases, and individualizing surgical trays.
Solutions
Health professionals can use their powerful voices to advocate for policies to mitigate or address climate change. The healthcare community promoted the clean air act of 1970, which markedly decreased six toxic air pollutants to save millions of lives over the years since its’ implementation7. Recently, Congress has taken steps to address the crisis with the Inflation Reduction Act, intended to reduce climate emissions, improve air quality, and advance environmental justice.
There is more work needed to transition our economy from fossil fuels to renewable energy sources. Transitions to renewable energy and electrifying our transportation fleet will not only mitigate climate change, it will also improve air quality and health. A study out of UC Berkeley shows if we shift to 90% renewable energy, CO2 emissions would drop 88% over 15 years, which would slow global warming. Furthermore, the emissions of harmful pollutants NO2 and SO2 would drop 96-99%, which could save tens of thousands of lives8. Studies from smoking bans, decreased emissions from the COVID lockdown, industrial plant closures, and various events show rapid health benefits after air pollution is decreased9
Personal actions are another important way to effect change. Physicians can talk about the importance of protecting our

planet to protect our health. Sixty percent of Americans view global warming as a major threat; 65% want the government to do more to reduce the effects of climate change. Make healthy changes in your own life and look for ways to decrease your personal carbon footprint. For example: eat less meat, buy locally, fly less and buy a hybrid or electric vehicle. Join one of the many local, regional, and national climate organizations, including ours. Instead of feeling discouraged about the climate, join with others to work towards solutions. Taking action helps us feel much more positive about the future.
We need to educate ourselves, patients, and policymakers on the connections between climate and health, and between health and voting. We can encourage colleagues and patients to vote. Despite the importance of civic engagement and voting, health professionals have historically voted less than the general population. We need to elect policymakers at all levels of government who will enact policies to decrease carbon emissions. Health is on the ballot for climate change, reproductive rights, healthcare access, gun violence and racism. When we vote, we impact policies that determine the social, environmental and structural determinants that influence health outcomes. Voting improves the health of our patients and our communities. The AMA 2022 resolution on Voting as a Social Determinant of Health, and Healthy People 2030 which includes voting participation as a key metric, encourage physicians to take non-partisan action to encourage their colleagues and patients to vote.
Conclusion
Climate change affects our lives, our patients, and medical practices. Like other health risks, we can learn about the climate and health to provide appropriate prevention and treatment. Medical professionals can take active roles to limit global warming by educating ourselves and our communities, and reducing our own carbon footprint and carbon emissions from the medical field. Likewise, we can use our expertise to encourage political policies that support healthy homes and environments. We can join organizations working to create climate health solutions for current and future generations. All of us can take steps to protect the environment, and in doing so help protect our patients’ health and the planet.
References
1) Effects of Climate Change on Health. CDC website
2) 2023 World Air Quality Report, by IQAir, March 2024.
3) WHO Air Quality and Climate Bulletin, No.3 – September 2023.
4) WHO: Potential health effects of climate change, report of a WHO task Group, WHO 1990
5) AMA policies, on AMA website policy finder
6) Atwoli L, Baqui AH, Benfield T, et al. Call for emergency action to limit global temperature increases, restore biodiversity, and protect health. BMJ2021;374:n1734.
7) Overview of the Clean Air Act and Air Pollution, EPA website
8) Goldman School of Public Policy 2035 Report
9) Schraufnagel DE, Balmes JR, De Matteis S, et al. Health Benefits of Air Pollution Reduction. Ann Am Thorac Soc 2019;16(12): 1478-1487.



Carolina Fonseca, MD, MS, is a pediatric hospital medicine fellow at UCSF.
Cynthia Haq, MD, is Professor Emerita of family medicine at University of California, Irvine.

I invite you to rethink your relationship with feeling tired. Women, and especially women in medicine, see being tired as a negative thing. It is a failure. Our work makes us tired. It leaves us “depleted” with “nothing left.” Our menopausal bodies don’t work properly because we are tired. Being tired isn’t necessarily bad. It doesn’t mean you failed to manage your energy well. It doesn’t mean you have poor boundaries or a job that doesn’t care about you. Feeling tired might mean that it was a day well spent. Feeling tired might mean you were fully present for meaningful work and deep connection. What if you approached feeling tired with nonjudgment and non-striving? What if being tired meant you needed recharging like your phone or electric car? What if it’s natural for humans to be tired mid-afternoon? This is likely the why of the afternoon siesta. What if we embraced the moments we feel tired as a reminder to refill our tanks. An act of kindness and self-care make a big difference in our tired moments.

Jessie Mahoney, MD
Three deep breaths. One minute of meditation. Fresh air. Even a simple hand to heart. You might decide going forward that you would like to change your relationship with feeling tired to a more positive one. Feeling tired also happens after wonderful things. Travel, reunions, great nights out, caring for newborns and toddlers, and long hikes and swims. Feeling tired is part of a life well-lived.

Jessie Mahoney is a pediatrician, a certified life coach for physicians, and a yoga instructor. She is the Chair of the SFMMS Physician Wellness Task Force. She practiced pediatrics and was a Physician Wellness leader at Kaiser Permanente for 17 years. She is the founder of Pause and Presence Coaching where she supports and empowers her physician colleagues using mindfulness tools and mindset coaching.
Choose Connection Over Perfection: Why Doctors Struggle with Public Speaking and What We Can Do About It with Hilary Blair
The world needs physician voices. Enjoy a fun conversation with Hilary Blair, founder of Articulate Real & Clear, about how mindfulness, intention, and most of all presence can help anyone, especially doctors, give a great talk. Scan the QR Code with your smartphone to listen.
Lead With Your Heart and Lean Into Your Wisdom: What I Learned Working With A Speaking Coach
If you struggle with public speaking or you want to share your message more succinctly and more powerfully, listen to this episode. Scan the QR Code with your smartphone to listen.
Restore the Joy to Patient Care By Embracing Authenticity
With Dr. Lara Cavanaugh
I LOVE helping physicians get back to loving what they trained for so long and so hard to do. Coaching and retreats are amazing tools to accomplish this outcome. It's possible even in medicine today. Even if you are in primary care. And even if you have been practicing for a long time and are exhausted. Lara shares how embracing authenticity and a positive mindset helped her get back to both joy-filled patient care and professional fulfillment. Scan the QR Code with your smartphone to listen.
Do You Think You Can’t Do Yoga?
If you have struggled with yoga, think you aren't a yogi, or simply want to understand you to make yoga work better for you and your ever-changing body, listen to this episode. Scan the QR Code with your smartphone to listen.




Mindful Yoga for Healers in Old Mill Park Sponsored by SFMMS:
Join Us on October 6th
“What a wonderful event. It was so great to connect with friends and colleagues I haven’t seen in years while practicing yoga amongst the Redwoods!” – SFMMS Member
SFMMS invites you to our 2nd Mindful Yoga for Healers of 2024 on Sunday, October 6th at the Old Mill Park Amphitheater in Mill Valley. To learn more and register visit the SFMMS Events Page at www.sfmms.org/news-events/events or scan the QR Code with your smartphone.
Want to Practice Mindful Yoga for Healers With Jessie Before this Event?

Join Dr. Mahoney on Zoom most Saturdays at 9am or anytime on YouTube. For more information visit: https://mindfulyoga.jessiemahoneymd.com or https://youtube.com/c/JessieMahoney.
The SFMMS Book Club Returns January 16th, 2025!
SFMMS is bringing back our book club for our Physician Members in 2025! Join us virtually via Zoom on January 16th as we read and discuss “Legacy: A Black Physician Reckons with Racism in Medicine” by Uché Blackstock MD. The first 25 SFMMS Members to register will receive a free copy of the book, so that you can start reading before our January 16th book club! To learn more and register visit the SFMMS Events Page at www.sfmms.org/ news-events/events or scan the QR Code with your smartphone.
Join Your Colleagues at an Upcoming LOCAL Physician Wellness Retreat! CME Available! Oct. 5th, 2024 Honoring Diastole at Pie Ranch in Pescadero, CA Mindful Coaching, Yoga and Culinary Medicine. CME available.
Wellness Retreats for Physicians at Nicasio Creek Farm



Mindful Coaching, Yoga and Culinary Medicine. CME available. Some retreats are open to partners too. November 2024 & Jan, Feb, March, April, & May 2025 (new dates and one-day options coming soon!)
Retreats for you are amazing. Retreats for your team add an added element of healing, optimism, and growth. The work we do in medicine is hard. Well teams are a key component of not making hard jobs harder. Well-facilitated and expertly planned team wellness experiences make a HUGE difference—to the health and wellness of physicians, patients, and institutions. Physicians with burnout are twice as likely to be involved in patient safety incidents, to exhibit low professionalism, and to receive low satisfaction ratings from patients. While there are many competing demands for money in healthcare currently, these experiences are a worthy investment. There are also many creative and impactful ways to make them happen. Find out more about both individual and team retreats here: https://www.jessiemahoneymd.com/retreats.
The SFMMS Wellness page, curated by your SFMMS colleagues, includes upcoming and past wellness events, resources and more. Learn more by visiting the SFMMS Wellness page at www.sfmms.org/get-help/physician-wellness or by scanning the QR code with your smartphone.

On my first day as a general surgeon I met a young cop coming through the ER door on a gurney, his heart and chest ripped open by bullets. With bare hands, I held closed many punctures. Warm blood flowed down my clothes and shoes as clots formed between my fingers,
"Don't let go, Ray, this is our only chance," said the heart surgeon. Two minutes passed, and the machine took over. We stitched his wounds and mended what violence had torn apart. "Surgical success!" we cheered.
Then the anesthesiologist announced: "He’s gone, he's brain dead." I looked down at him lying there at his eyes that would never see again, at his heart that would never again feel hope. "Ray, go ask the family for permission to harvest his organs. He won't need them now.”
In the waiting room, young wife, two children by her side, eyes pleading. The grandmother stood silently. They hugged each other tightly, holding onto a hope that had already passed.
My heart heavy, I asked if his vital organs could donated as his gift to others in need. The grandmother, steady and strong, replied "Do what you must, doctor." As I began the work of salvaging his organs, I wept with an open heart. But there was grace that day. His legacy lives on.
Ray Fay was in private practice in San Francisco for 35 years, serving as Chief of Surgery, Chinese Hospital and Chief of Urology, Children’s Hospital and CPMC.
22