INTO THE FUTURE

INSIDE:
Reproductive Health: Forging Forward
SFMMS Annual Report
Policymaking for Progress

IN THIS ISSUE
Michael Schrader, MD,
Adam Francis, CAE 9 CMA House of Delegates Report
Ameena T. Ahmed, MD, MPH
Laura Esserman, MD, MBA
Protecting Patient Privacy in the Age of EHRS and Abortion Bans
Jessica J. Pourian, MD and Simone Arvisais-Anhalt, MD 29 Making Mifepristone Accessible in the U.S.: We Won't Go Back
Steve Heilig, MPH 31 The FDA Should Reduce Nicotine in Cigarettes—And Use a Better Test to Ensure It Happens
John Maa, MD and Michelle Zhang
33 Listen Closely: Congenital Cytomegalovirus Shouldn’t Be Overlooked
James Lawrence, MPH
Volume 97, Number 4
COLUMNS 2 Membership Matters
5 President's Message: A Message of Thanks Dennis Song, MD, DDS
Executive Memo: The Vital Role of Community After Disappointing Election Outcomes
WELLNESS
Pause and Presence Coaching and Retreats: Lessons from a Bomb Cyclone Jessie Mahoney, MD

MEMBERSHIP MATTERS
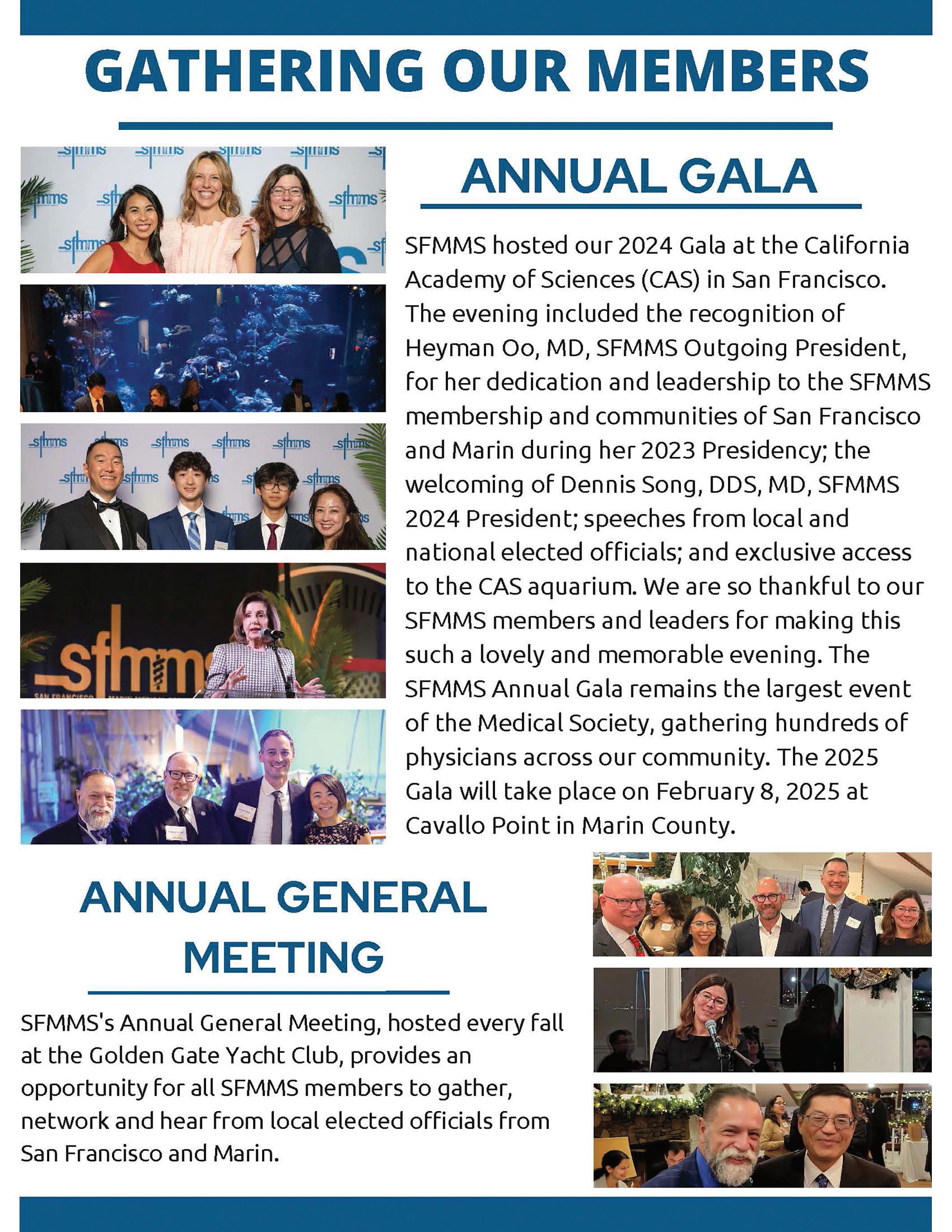
SFMMS ANNUAL GENERAL MEETING
The SFMMS annual meeting was a great success, with SFMMS members gathering to both celebrate recent successes and rally for the future. New CMA President and longtime SFMMS leader Shannon Udovic-Constant MD gave a stirring address; Dr. Linda Clever delivered an inspiring talk spurred by her receiving a major CMA award; Dr. Mel Blaustein was lauded for his pioneering advocacy for a Golden Gate Bridge suicide barrier; Drs. John Maa and Michael Schrader received accolades for their longtime advocacy on behalf of the SFMMS; San Francisco City Attorney David Chiu and Supervisor Rafael Mandelman thanked SFMMS for collaboration on health issues and pledged to continue such efforts in the face of expected federal challenges.

Nominate a Community Service Organization to Receive a Contribution from the SFMMS Community Service Foundation
The SFMMS Community Service Foundation (CSF) was founded with two primary purposes: (1) To provide a taxexempt 501(c)3 entity for SFMMS members and others to receive grants for medical and public health-related projects, with an administrative overhead rate much lower than most university or other larger routes; and (2) to disburse funds to worthy local medical/public health related efforts.
During this giving season, SFMMS members are invited to nominate worthy new potential grantees. In 200 words or less, please describe how the organization you are nominating meets the following criteria:
• Operates in San Francisco and/or Marin Counties.
• Contributes to the provision of medical care and enhances public health, especially among underserved patient populations.
Contact Steve Heilig at heilig@sfmms.org if you are interested in CSF activities and grants




DEA extends telehealth prescribing flexibilities
The U.S. Drug Enforcement Administration (DEA) has for the third time extended the full set of telemedicine prescribing flexibilities that were initially adopted during the COVID-19 public health emergency. This extension will ensure a smooth transition for physicians and patients who have come to rely on the availability of telemedicine for controlled medication prescriptions, and allow adequate time for providers to come into compliance with any new standards or safeguards eventually adopted in a final set of regulations.
CMS proposes additional prior auth reforms for Medicare Advantage plans
Amid rising concerns that algorithms are being used to improperly delay or deny care, the Centers for Medicare & Medicaid Services (CMS) recently proposed regulations that would establish additional guardrails on Medicare Advantage plans’ prior authorization practices — including the use of artificial intelligence. The proposed regulations would remove unnecessary barriers to care resulting from the inappropriate use of prior authorization and internal coverage criteria.
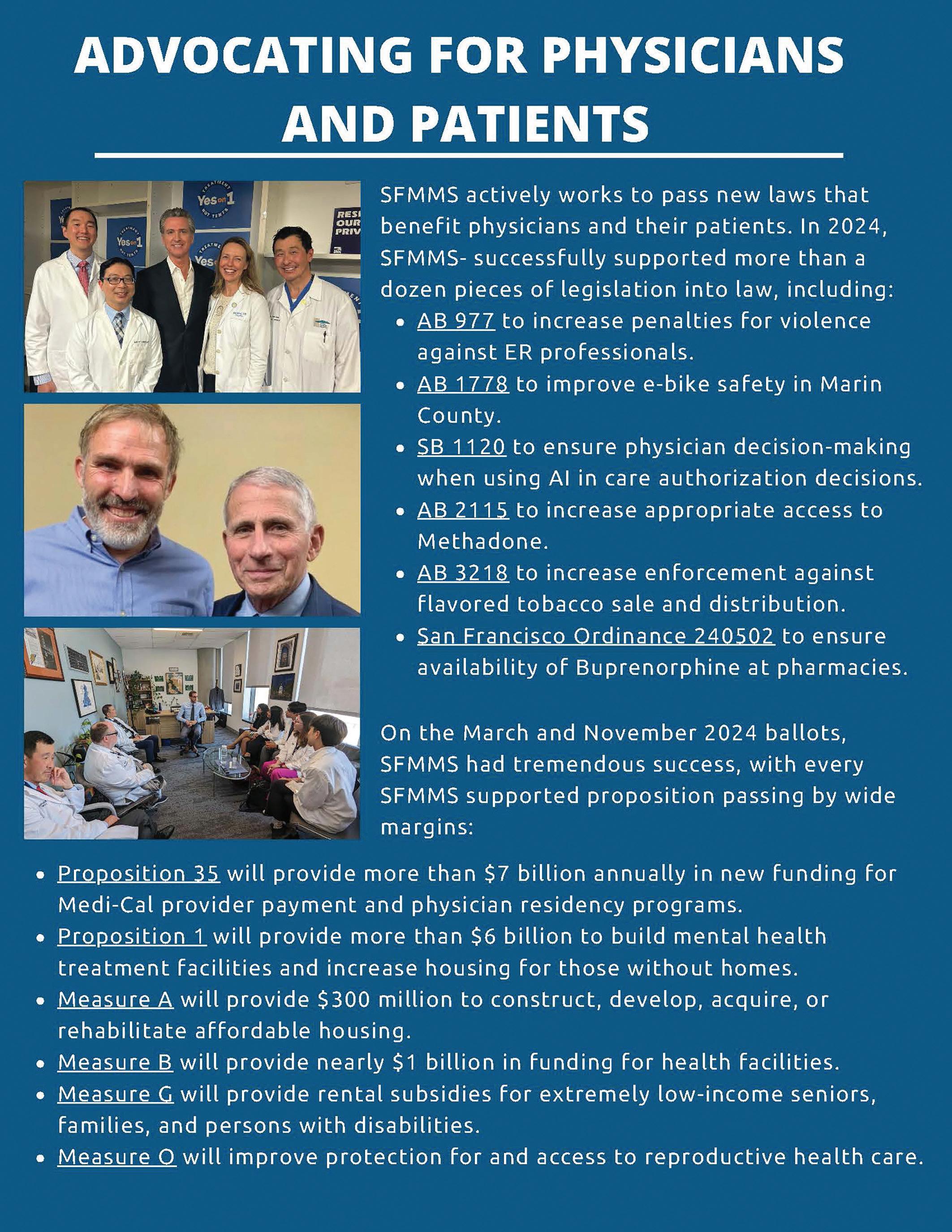
Fighting for Physicians on All Fronts
The California Medical Association 2024 Legislative Wrap Up: Proposition 35 Medi-Cal Victory!
For the California Medical Association (CMA), the 2024 legislative year started out with an ominous beginning. In 2023, CMA successfully negotiated the largest investment in Medi-Cal in history, including billions to increase reimbursement rates, through an expansion of the Managed Care Organization (MCO) Tax. Utilizing the MCO Tax as a funding source meant that California could finally fund the Medi-Cal program and create true health equity without raising taxes on individuals or cutting other crucial programs. While some reimbursement rates were raised under the MCO Tax in 2024, the bulk of the new funding was allocated to increase rates starting in 2025.
In January 2024, however, Governor Newsom’s initial 2024-25 budget proposal estimated a budget deficit of $22.5 billion, a number that would grow to $68 billion by the May budget revision. The governor’s revised budget proposal cut all of the proposed new Medi-Cal funding from the MCO Tax and swept the entirety of the tax, over $21 billion, into the state’s general fund coffers to cover normal operating expenses of the state.
This is why CMA led the charge to pass Proposition 35 this November. Voters overwhelmingly approved Prop 35, which will secure ongoing funding for Medi-Cal and dedicate these funds to protect and expand access to care for all Californians. And importantly, it prevents the state from redirecting these revenues for non-health care purposes.
The expansion of Medi-Cal over the last decade has resulted in some incredibly illuminating statistics that underpinned CMA’s determination for increased MediCal investments:
• Half of all babies in California are born through Medi-Cal.
• The program now covers one-third of the state – almost 15 million people.
• It is the largest state Medicaid program in the country, both in overall size and percentage of the population.
• California lands near the bottom of Medicaid reimbursement rates nationally, ranking 40th, even though the cost of living and practicing in California is much higher than in many other states.
• California has not raised Medi-Cal rates across the board since 2000, and in fact has cut them twice in the past 24 years. While some physicians received increases thanks to CMA-sponsored Prop 56 (2016), those increases were limited to supplemental payments for a short list of codes for physician services, dental care and family planning services.

October/November/December 2024
Volume 97, Number 4
Editor Michael Schrader, MD, PhD
Managing Editor Steve Heilig, MPH
Production Maureen Erwin
SFMMS OFFICERS
President Dennis Song , MD, DDS
President-Elect Jason Nau, MD
Secretary Ian McLachlan, MD
Treasurer Sarita Satpathy, MD
Immediate Past President Heyman Oo, MD, MPH
SFMMS STAFF
Executive Director
Conrad Amenta
Associate Executive Director, Public Health and Education
Steve Heilig, MPH
Director of Operations and Governance
Ian Knox
Director of Engagement
Molly Baldridge, MPH
Senior Director, Advocacy and Policy
Adam Francis, CAE
2024 SFMMS BOARD OF DIRECTORS
Edward Alfrey, MD
Melinda Aquino, MD
Julie Bokser, MD
Kristina Casadei, MD
Clifford Chew, MD
Esme Cullen, MD
Manal Elkarra, MD
Mihal Emberton, MD
Cindy Greenberg, MD
Cynthia Lin, MD
Ian McLachlan, MD, Secretary
Jason Nau, MD, President-Elect
Heyman Oo, MD, Immediate Past-President
David Pating, MD
Dawn Rosenberg, MD
Sarita Satpathy, MD, Treasurer
Michael Schrader, MD, Editor
Yalda Shahram, MD
Neeru Singh, MD
Dennis Song, MD, DDS, President
Kristen Swann, MD
Ranna Tabrizi, MD
Kenneth Tai, MD
Melanie Thompson, DO
Kristin Wong, MD
Andrea Yeung, MD
Helen Yu, MD
For questions regarding journal, including possible submissions, contact Steve Heilig: Heilig@sfmms.org

PRESIDENT’S MESSAGE
Dennis Song, MD, DDS
A MESSAGE OF THANKS
As another year comes to a close, we reflect on its pace— too fast for some things and too slow for others. This year reminded me of the passion people bring to their beliefs and the shared drive to do what’s best for our patients and members. While this passion can sometimes lead to conflict, it is through these challenges that we grow stronger and improve.
Our Board of Directors worked tirelessly this year, giving their all to advance our mission and address pressing challenges. Their dedication has been nothing short of extraordinary.
I had the privilege of meeting with many public-facing legislators, patients, and professionals from across the healthcare spectrum. Medicine is a vast and intricate field, and navigating the complexities of the U.S. healthcare system often feels like being on an ever-spinning merry-go-round. Each interaction reminded me of the shared commitment and energy that sustain our field’s vibrancy and resilience.
I am deeply grateful to our staff and leadership, who embraced new responsibilities and met evolving demands with exceptional effort and adaptability. Their contributions have been invaluable.
This year was also notable for its political achievements. We successfully advanced several local and state propositions designed to support the practice of medicine and improve access to care. These successes underscore the critical role advocacy plays in shaping a better future for healthcare.
One conversation that stood out this year was with a pediatrician in a large Southern California group practice. She shared her journey from working at a Federally Qualified Health Center (FQHC) to her current role. While her salary provides financial stability, she admitted feeling undervalued compared to other specialties. Nonetheless, she values the structure, benefits, and rare luxury of predictable time off that her current role provides—a significant advantage in our demanding profession.
In contrast, I also spoke with an independent solo primary care provider who sees fewer than a dozen patients daily. This physician treasures the autonomy to focus deeply on individual patient care but faces challenges such as regulatory pressures, administrative burdens, and the lack of collaborative support available in larger practices.
These conversations highlight the diverse experiences within our profession and reinforce that there is no one-size-fits-all approach to practicing medicine. Each career path comes with unique rewards and challenges, but what unites us all is a shared dedication to serving patients.

Both ends of the medical practice spectrum share one common challenge: the high cost of living in San Francisco and Marin. These costs make it increasingly difficult to attract new providers and staff, let alone their families or significant others. Our local “fishbowl” often feels out of sync with the realities of the rest of California and the nation. Addressing these challenges requires continuous communication and collaboration with legislators, fostering relationships that are mutually beneficial. These partnerships have been pivotal in supporting initiatives in Marin and San Francisco while also helping legislators refine their proposals. Navigating the needs of both counties is challenging but essential for success.
I want to extend special recognition to our board members, committee chairs, and countless committee members and delegates whose tireless service has been instrumental to our achievements. From governance reviews and financial evaluations to strategic planning and assessing the performance of our Executive Director, their thoughtful and impactful contributions have been vital.
This year, we tackled a wide range of initiatives—some visible, others behind the scenes—all crucial to building a stronger foundation for the future. To everyone who contributed their time, energy, and expertise: thank you. Your efforts make a profound difference.
As we look ahead to the new year, let us carry forward the lessons we’ve learned, the connections we’ve built, and the progress we’ve made. Together, we will continue to advocate for our members, elevate our profession, and, most importantly, improve the health and well-being of the patients and physicians we serve.
Here’s to a new year filled with growth, collaboration, and shared success. Thank you for allowing me to experience such an unbelievable year. There is still so much to do, and you can be a part of it. Apply for a committee and help shape the future— together, we can make a lasting impact.
Dennis Song, MD, DDS, is an oral and maxillofacial surgeon in private practice and Chief of the Dental Division at Sutter California Pacific Medical Center. He also serves as an Associate Adjunct Professor at the University of the Pacific School of Dentistry.
EXECUTIVE MEMO
Conrad Amenta, SFMMS Executive Director

THE VITAL ROLE OF COMMUNITY AFTER DISAPPOINTING ELECTION OUTCOMES
In the wake of elections that may have left many feeling disillusioned, frustrated, or even powerless, the importance of community cannot be overstated. For physicians, who are on the front lines of patient care and healthcare policy, the need for solidarity, support, and collective action is especially pressing. Regardless of election outcomes, it is the strength of our communities—both professional and personal—that can provide the resilience needed to face future challenges.

Disappointment in the outcome of elections can lead to feelings of helplessness, isolation, and even burnout, especially in high-stakes environments like healthcare. Physicians, often burdened with the weight of their patients' needs and systemic stressors, may feel this acutely. The societal impact of poor election outcomes is also felt by physicians, particularly when policies threaten to undermine access to care, or perpetuate inequalities. The ripple effect on public health can compound feelings of discontent.
Community has a way of mitigating these emotional burdens. It provides a support structure where physicians can share their concerns, vent frustrations, and process their feelings in a safe and productive environment. The literature around physician health and wellness indicates that physicians who are involved with their professional associations or specialist societies are more likely to report higher degrees of professional satisfaction and practice sustainability.
Beyond emotional support, community is essential for advocacy. Physicians have historically played a vital role in shaping health policy. Physicians are in a unique position to influence change, and after disappointing elections, this becomes even more important. When policy shifts do not align with medical or public health priorities, collective action within the healthcare community can be a powerful tool.
Joining medical associations, engaging in local health initiatives, and participating in public forums can help physicians
channel their frustration into meaningful change. Community organizations also offer the opportunity to amplify voices that may otherwise go unheard in the political sphere. When physicians unite with each other and with their patients, they are better equipped to demand policies that prioritize health outcomes, access to care, and equity.
In times of adversity, resilience is key. For physicians, resilience isn't just about coping with the challenges of a difficult work environment; it's about finding ways to improve the system from within. Through collaboration and support networks, physicians can foster resilience not only in themselves but also in their patients and communities.
Local physician groups, peer support networks, and professional organizations offer opportunities to share best practices, offer advice, and maintain emotional well-being. These connections provide a sense of belonging and purpose, two essential ingredients in combating burnout and maintaining professional satisfaction.
As physicians navigate the emotional and professional aftermath of a challenging election cycle, it is crucial to remember that community remains one of our greatest assets. It can be tempting to turn inward, to isolate oneself, under the assumption this will help to protect us. It can feel counterintuitive to respond to disappointment by increasing one’s participation. But by fostering a sense of belonging, supporting one another, and advocating for meaningful change, physicians can rise above the disappointment of election outcomes and continue to make a profound difference in the lives of their patients and society at large.
In times of uncertainty, we are reminded that while the political landscape may change, the value of community—its support, its power to advocate, and its capacity for resilience—remains a constant. Now, more than ever, we must stand together.
THE MOUSE THAT ROARED: SFMMS INFLUENCING HEALTHCARE POLICY
Our SFMMS Journal this month features physicians who are actively trying to influence healthcare policy in ways that compliment our regular channels which include the CMA House of Delegates, the CMA Year Round Resolution Process, the SFMMS policy committee, and the SFMMS political action committee. The strategies our members have employed include those advanced by a high profile leader in her field who boycotted a conference in a state that restricted reproductive rights, two physicians who organized an educational symposium, our SFMMS staff member who participated in a public advocacy event that helped lead to the FDA review and approval of mifepristone, and a past President who has worked tirelessly over the years on multiple public health measures.

jeopardy. Tools for minimizing these risks are forthcoming.
mmThe SFMMS’s Steve Heilig helped orchestrate a pivotal advocacy media event hatched at meetings at the SFMMS many years ago that ultimately led to the approval of mifepristone for medical abortion. He personally risked federal prosecution for trafficking in a banned drug. However, due to the efforts of the SFMMS delegation, the SFMMS, CMA, and AMA had already adopted policies supporting the medication's availability. Additionally, newly-elected President Clinton had spoken out in favor of the drug. As a result, it was likely deemed best not to prosecute him. Instead of facing arrest, he was awarded the CMA's annual award for service to medicine and public health.
UCSF’s renowned cancer expert and advocate Dr. Laura Esserman has boycotted the San Antonio Breast Cancer Symposium, sponsored an alternative symposium in San Francisco in November, and has publicized her efforts. While there may be disagreement about the efficacy of boycotts, they have sometimes proven to be effective at prompting further action throughout our history: The Boston Tea party, the Montgomery Bus Boycott, and grape boycott by the National Farm Workers. Maybe boycotts don’t always work but Sam Adams, Rosa Parks, Cesar Chavez, and Dr. Esserman think they are worth trying.
SFMMS was a sponsor and financial supporter of the Abortion and Sensitive Medical Information symposium at the Mission Bay Campus of UCSF in September. This symposium was put together by two of our members, Drs. Jessica Pourian and Dr. Simone Arvisais-Anhalt, out of very real concerns that confidential medical records could be used in investigations and prosecution of patients and clinicians providing abortions and other critical services in this post Roe era. There were multiple speakers from law, medicine, government, and informatics who explained the extent of this problem and the risk our patients still face. The Dobbs decision overturning Roe v Wade allowed trigger laws restricting abortion in many states. These laws and other restrictive efforts not only create criminal penalties in these states but also attempt to prosecute patients who cross state lines to get legal abortions in states like California. The conflict in informatics is to balance EHR interoperability with privacy to protect our patients and physicians from legal
SFMMS past-President Dr. John Maa has been an indefatigable advocate for public health measures including restrictions on sugary beverages, tobacco and vaping products, and firearms. He presents evidence about yet another duplicity the tobacco industry has used to foster addiction to their products.
Our SFMMS members have been active in health care policy over many years and have contributed in many ways. In the era of the explosion of HIV infection and AIDS many of our members were national leaders in the many policy battles fought then. As noted in this issue as well, we have a prominent presence in our CMA as well, with many in leadership positions, including our new CMA President Dr. Shannon Udovic-Constant. We’ve never been afraid to take on forward-looking, sometimes controversial issues and positions that eventually become shown to be healthsupporting and influential. Our impact often far surpasses our numbers. We are the mouse that roared.

Dr. Schrader, an internist at Dignity Health, is Chair of the SFMMS delegation to the CMA and a past-president of the SFMMS.
HISTORIC NOVEMBER 2024 ELECTION BRINGS OPPORTUNITIES AND CHALLENGES
Adam Francis, CAE
With final tallies being certified as I write this, the November 2024 election resulted in some major wins for San Francisco and Marin physicians. It also created quite a bit of uncertainty as to which way national health policy decisions may swing over the next few years.
Major Wins
Proposition 35: In 2023, CMA successfully negotiated the largest state investment in Medi-Cal history through an expansion of the Managed Care Organization (MCO) Tax. It included billions in new funding to increase payment rates, expand reproductive health care, and augment physician training. However, Governor Newsom and the Legislature cut all of the proposed new Medi-Cal funding from the MCO Tax and swept the entirety of the tax (more than $21 billion) into the State’s General Fund as part of the 2024 State Budget. In reaction to this, CMA, SFMMS, and others led the charge to pass Proposition 35, a ballot initiative that would ensure the MCO tax would return to funding Medi-Cal, and that any future efforts by the Governor and Legislature to redirect the funds away from health care would face significant hurdles. Prop 35’s passage in November means we have now secured ongoing funding for Medi-Cal, protecting and expanding access to care for all Californians.
Measure G: This charter amendment would budget $8.25 million annually for the Affordable Housing Opportunity Fund, creating rental subsidies for extremely low-income seniors, families, or people with disabilities. Approximately 52,600 households in San Francisco include a senior aged 62 years or older, and 20,000 households include a disabled adult. This proposition would ensure a consistent and stable funding source to ensure the most vulnerable San Franciscans do not lose their homes, creating painfully detrimental health consequences.
Other SFMMS-supported ballot measures that passed in November include:
Proposition 3: Removes language from the state constitution that bans same-sex marriage. While the 2008 law was nullified by a Supreme Court ruling in 2013, the Legislature placed this measure on the ballot to protect against any potential future changes to federal marriage protections.
Measure B: Generates $390 million in bond funding for investments in community health and medical facilities, street safety, public spaces and interim housing to reduce family homelessness.
Measure O: Makes several changes to San Francisco County law to protect abortion care and contraception access, including removing restrictions to providing reproductive health care services, amending zoning laws so that clinics can be opened in more areas, and prohibiting the forced release of personal reproductive health information to law enforcement or federal agencies.
Also of note, SFMMS provided significant input in San Francisco’s process to reform its gross receipts tax on businesses, which eventually became Proposition M (passed by voters this fall). SFMMS was instrumental in expanding tax exemptions to physicians’ offices with revenue of $5 million or less. SFMMS analysis indicates that these reforms will be broadly beneficial to small and solo private medical practices, which pay a disproportionately high rate under the current framework.
SFMMS was thrilled to see all of its supported candidates for local and state office winning in November, including:
• State Senator District 11: Scott Wiener
• Assembly District 12: Damon Connolly
• Assembly District 17: Matt Haney
• Assembly District 19: Catherine Stefani
• City Attorney: David Chiu
• San Francisco Board of Supervisors District 7: Myrna Melgar
Opportunities
In both San Francisco and Marin, new faces will be headed to local government, not the least of whom is a new San Francisco mayor: Daniel Lurie.
Before his election win over the incumbent London Breed, SFMMS staff and SFMMS PAC Board members had several conversations with Mr. Lurie regarding important health care issues confronting physicians and patients in San Francisco, including substance use treatment, the physician workforce shortage, homelessness, and more. SFMMS will look to build on that relationship as he takes office in January. On the Marin Board of Supervisors, Brian Colbert will replace Supervisor Katie Rice, who chose not to run again.
On the San Francisco Board of Supervisors, four newcomers join their more experienced colleagues.
In District 3, Danny Sauter replaces termed-out Supervisor Aaron Peskin, and in District 5, Bilal Mahmood ousted Supervisor Dean Preston. Jackie Fielder replaces termed-out Supervisor Hillary Ronen in District 9, and in District 11, Chayanne Chen replaced termed-out Supervisor Asha Safaí.
It will be important for physicians who live in those districts to meet with their new representatives and begin building relationships with them so that you can ensure trusted voices are providing perspective on the health care issues affecting your communities. SFMMS can help. Please reach out to us if you’d like to be involved (afrancis@sfmms.org).

Adam Francis is Senior Director of Policy and Advocacy for the SFMMS.
CMA HOUSE OF DELEGATES 2024
Ameena T. Ahmed, MD, MPH

The California Medical Association (CMA) convened its 153rd annual House of Delegates (HOD) meeting in Sacramento on October 26-27, 2024. More than 800 California physicians and physicians-in-training gathered to debate and establish broad policy on two major issues: Rural Health; and Maternal Health Equity-Obstetric Deserts and Reproductive Health.
Rural health and maternal health equity are intertwined issues. Since 2012, nearly 50 California hospitals have either closed or indefinitely suspended labor and delivery services. Currently, 12 rural counties have no hospitals that provide obstetric services. Latinx and low income populations are particularly affected by lack of access to obstetric services. While the average drive to the nearest birthing hospital in California is eight miles and 14 minutes, women who live in counties with the top quintile of travel times must drive an average of 107 miles and 132 minutes. Half of births in California are to MediCal enrollees, which points to the need to address adequate compensation for care provided to MediCal recipients. The House adopted policy aimed at addressing maternal health equity through protected time off for prenatal and postpartum care, training of the OB-Gyn workforce, support for struggling hospitals, and adequate funding of pregnancy-related care.

mmSix percent of Californians live in rural areas, while physicians cluster in urban areas. San Francisco County has 91 physicians per 10,000 residents, compared to an average of 15 in non-metro areas of California. People living in rural areas face disparities in access to care, as well as outcomes including higher rates of disability, higher mortality, and shorter life expectancy. CMA delegates set policy to address gaps in existing CMA policy, with a focus on developing rural physician and health professional workforce, bolstering financial resources available to rural health care providers, and addressing unique barriers to care faced by rural populations.
The CMA also installed its new officers, including Shannon Udovic-Constant, M.D., past president of SFMMS and a pediatrician in San Francisco. Dr. Udovic-Constant is the 156th president of CMA and fifth woman to hold the position. In her inaugural address, Dr. Udovic-Constant outlined her vision for the CMA and spoke passionately about the importance of organized medicine. Physicians’ individual voices and collective action are complementary, according to Dr. Udovic-Constant. Collective action must be both focused and strategic. For example, the individual voices of physicians, together with collective action led by the CMA, led to the passage of AB 2164, which removed stigma for
continued on page 10


physicians seeking treatment for mental health and substance abuse conditions.
San Luis Obispo pediatrician René Bravo, M.D., was elected by the delegates as CMA president-elect. He will serve on the executive committee in that role for one year, and will be installed at the conclusion of next year’s annual meeting. Former SFMS President George Fouras, M.D. served as Vice-Speaker of the House. Keeping up the outsized role of SFMMS members in CMA leadership, SFMMS Past President Brian Grady, M.D. announced his candidacy for Vice-Speaker of the HOD; the election will be held at the 2025 House of Delegates in Los Angeles.
SFMMS President Dennis Song, M.D., D.D.S. was honored as Physician of the Year by the Solo and Small Group Forum. San Francisco physician Linda H. Clever, M.D., received CMA’s Gary S. Nye Award for Physician Health and Well-Being. Dr. Clever is founder and President of RENEW, a nonprofit that helps health
professionals maintain, and regain, their enthusiasm, effectiveness, and purpose. Founded in 1998, RENEW leads conversation groups, workshops, retreats and seminars across the nation—and has been raising awareness of the importance of practitioner well-being, long before burnout among health care professionals became a nationally recognized issue.
Dr. John Maa spearheaded the efforts of the SFMMS delegation to raising funds in support of CalPAC, the statewide Political Action Committee of the CMA. With Dr. Maa’s leadership and the generous participation of 100% of our delegates, SFMMS won the victory bell again this year, recognizing our delegation’s achievement in raising the most funds for CalPAC.
Dr. Ahmed practices at Kaiser Permanente San Francisco and is Chair of the SFMMS delegation to the CMA House of Delegates.
Dr. Linda Clever receives CMA’s 2024 Nye Award for Physician Health and Well-Being
San Francisco physician Linda H. Clever, M.D., received the 2024 California Medical Association (CMA) Gary S. Nye Award for Physician Health and Well-Being. The award – presented today at the CMA House of Delegates – honors a physician who has made significant contributions toward improving physician health and wellness.
Dr. Clever is founder and President of RENEW, a nonprofit that helps health professionals maintain, and regain, their enthusiasm, effectiveness and purpose.
Founded in 1998, RENEW leads conversation groups, workshops, retreats and seminars across the nation – and has been raising awareness of the importance of practitioner well-being, long before burnout among health care professionals became a nationally recognized issue.
Over the past 26 years, RENEW has delivered on the promise to bring good health to those who give good health. RENEW programs have reached thousands of physicians, nurses, and community care professionals, helping them to define their values, find meaning, and enjoy good health..
“Dr. Clever is a highly respected and influential leader in the community of physicians in San Francisco and Marin Counties.
She has helped the San Francisco Marin Medical Society (SFMMS) to understand the dimensions of physician health and wellness, has informed our investments to improve the sustainability of the practice of medicine, and continues to be a mentor and leader to physicians across the state,” said SFMMS Executive Director Conrad Amenta.
“Dr. Clever has been instrumental to the incorporation of provider satisfaction into the ‘quadruple aim’ to improve population health and quality of care."

CMA and SFMMS are pleased to honor Dr. Clever for her outstanding work, which will continue to resonate as a new generation of physicians develops programs to improve the health and wellness of the profession.











Special Section - Reproductive Health and Rights
Why Continue to Speak Out and Advocate to End the Criminalization and Banning of Reproductive Health
Care Services for Women?
IT IS THE BEST AVENUE FOR CHANGE
Laura Esserman, MD, MBA
Restrictions on reproductive health services are threatening the lives and well-being of women of reproductive age, including those with planned as well as unplanned pregnancies. These laws particularly punish women of lower socioeconomic status. As healthcare providers, we must continue to work to reverse these laws. As medical professionals across specialties, one concrete action we can take is to urge that all medical conferences move to states that fully recognize the rights of all women and support full access to health care services across the continuum, including reproductive care. This is an issue equality, dignity, respect, and equity.
It is important to reflect on a fifty year social movement that eventually led to overturning Argentina’s ban on abortion that included criminalization of the women (up to 14 years in jail) as well as those who aided them (up to 4 years in jail). Hundreds of thousands of women came together as the “Green Wave” and finally succeeded in convincing Argentina’s lawmakers to decriminalize and ensure safe access to abortion. A critical reason for their success was advocacy, the size of the campaign, the persistence of those in the movement, the recognition that thousands of women had been hospitalized or died because of the restrictive laws. And the brunt of those who suffered fell on the poorest women with the least access to resources. In Ireland, another predominantly Catholic country where abortion had been illegal even in cases of rape, there was a high-profile case of a 31 year old woman who was a dentist and 17 weeks pregnant. She was denied care during her miscarriage because of the presence of a heartbeat. By the time the heartbeat ceased, the young woman developed sepsis and died. The publicity surrounding this case galvanized a new wave of activism leading to a law that allowed abortion to protect a woman’s life. In 2018, a referendum repealing the Eighth Amendment eventually passed 66% to 34%, with abortions in the first trimester covered by the public health service. Activism is the key to changing laws. We are just starting to hear about the many lives that are being lost in the United States in states where abortion is banned or effectively banned. We cannot sit back and see history repeat itself here in the United States of America.
The United States is a pluralistic society and embraces people of all cultures and religions, who hold different views about fetal viability. Each person should be free to follow the dictates of their own beliefs but should not impose their beliefs on others. We as physicians should recognize the inherent dangers being imposed on women and be part of the social movement that demands change. The Supreme Court, with the Dobbs v. Jacksons Womens
Health decision in 2022, overturned the Roe v. Wade precedent that allowed women to make their own decisions about reproductive health. The Dobb’s ruling allowed states to pass their own laws to legalize, ban, or criminalize abortion. This ruling has led to an outright ban in 13 states, and significant restrictions in others, though in a number of these states, citizens are approving constitutional bans to legalize abortion. In many states, physicians who provide pregnancy termination services face criminal prosecution, jail time, and fines. States like Texas have gone further, turning citizens into bounty hunters to sue neighbors and anyone helping persons for providing medical advice and services. The vigilante provision is meant to harass and frighten medical providers to stop doing their jobs. Justice Sonia Sotomayor has called this measure “a flagrantly unconstitutional law engineered to prohibit women from exercising their constitutional rights and evade judicial scrutiny.”
Fortunately, many states have voted to enshrine access to abortion in their constitution (California, Maryland, New York, Nevada, Arizona, Montana). A number of states have also passed shield laws. Shield laws allow providers in one state to prescribe and send medication abortion to individuals who live in a state where access to abortion is banned.1 The following states have shield laws: California, Colorado, Maine, Massachusetts, New York, Vermont, Rhode Island, and Washington.2, 3
On November 6, seven of 10 ballot measures protecting abortion passed. In Missouri, the first state to ban abortion after the Dobbs decision, even in the case of rape, voters approved an amendment guarantees abortion access up to the point of fetal viability, generally the 24th week of pregnancy. There are still 17 states that have near total ban on abortions. Unfortunately, the majority of those state are in the South and form a huge geographic block which compounds the difficulty of leaving to go to a state that where abortion is legal. I am lucky. I live in a state that was one of the first to pass a constitutional right to access abortion up until the point of fetal viability, and to protect women who travelled to California to access abortion services from being prosecuted by their home states that ban abortion.
But because women in my state are safe, that is not sufficient reason for me to turn a blind eye to what is happening in other states in this country. States that discriminate against women by banning reproductive freedom directly harm the physical and mental health of women and those that care for them. It also violates the right to privacy between physician and patient.4 We have all read about several high profile cases of young women losing their ability to have children because of sepsis and the need for a
hysterectomy after a miscarriage because of a delay in the provision of optimal care. Or women dying in a parking lot in Georgia because physicians were afraid to provide the appropriate lifesaving intervention after ruptured membranes or for excessive bleeding. The impact on pregnancy related care is tragic and the preventable deaths will continue to mount because physicians are afraid to intervene and because providers are leaving the field and states that threaten to jail physicians who intervene. There are certainly many more of these cases that are not being reported. unintended consequence is the How many more preventable deaths in young women are required in the US before we wake up as a society and provide access to reproductive care that is safe and legal for women of all socioeconomic strata and every race and ethnicity?
There are many ways to prevent women from accessing abortion when time restrictions are imposed. At 6 weeks, most women do not know they are pregnant. For states that restrict access or have few services, it can take 6-8 weeks to get an appointment, so lack of access effectively precludes abortion as an option (https://riseup.ucsf.edu/luncheon Dr. Kelly Pfeiffer). Advances in treatments- medical and surgical- have made pregnancy termination safe. The restriction on medical abortion will result in inadequate treatments which are more likely to result in complications. And the restrictions on abortion can make a miscarriage lethal. Pregnancy can cause complications that threaten the life of the mother. When these occur, the decisions about what to do should be up to the physician and the patient. Often, politicians will focus attention on late term abortions. No woman who has carried a child into the third trimester wants to have an abortion. These comprise less than 1% of all abortions and are done in the circumstance because of a catastrophe for the mother or the fetus. The decisions about what to do are far too complex for legislation. Restrictions on Reproductive Care will Exacerbate Disparities in Medical Services
Fifty percent of medical students are women. Those who choose to specialize in obstetrics and gynecology who want to have families are less likely to train and practice in states with restrictive abortion laws. This includes men who choose to train in obstetrics who will be concerned that the lives of their wives and daughters may be jeopardized in the setting of a complication of pregnancy. Such choices will further reduce access to care for women and exacerbate maternal mortality rates which are already higher in states that restrict abortion. These same states are more likely to have turned down Medicaid expansion. The combination of these factors will further limit access to obstetrical services. The exodus of healthcare professionals has already begun. Idaho lost 22% of their OBGYN providers in the 15 months after their ban was instated.5 Similar losses have occurred in many states that passed restrictive abortion laws. There was a 10.5% decrease in residency applicants to OBGYN programs in banned states between 2022-2023.6 Providers are leaving for their own safety, as well as for the safety of their family, but also for legal protection and because they want to practice without government interference in making decisions, and because they do not want to be placed in an impossible moral quandary, feeling forced to stand by, afraid to intervene and save a life when necessary for fear of being sent to jail.7 This will have a very chilling effect on
maternal care and exacerbate the already 15 fold difference in maternal mortality rates.8
Men and women in other specialties will also be less likely to move to states to train and practice for the same reasons. This will increasingly impact the medical workforce and access to quality care in states with laws that continue to deny access to reproductive services.
Reflecting on Why prior Supreme Court Justices Rejected Challenges to Roe v Wade
In Planned Parenthood v. Casey Justice Blackmun recognized the risks faced by the individual and the need for autonomy to make that decision. "These matters, involving the most intimate and personal choices a person may make in a lifetime, choices central to personal dignity and autonomy, are central to the liberty protected by the Fourteenth Amendment . . .the liberty of the woman is at stake in a sense unique to the human condition and so unique to the law. The mother who carries a child to full term is subject to anxieties, to physical constraints, to pain that only she must bear." There are myriad complex circumstances involving the health of the mother and any future child; every patient should have full facts and options to preserve their life and health. Most fundamentally, carrying a pregnancy to term is associated with an increase in mortality for the mother, which affects her and her family in those most fundamental of ways. The risk of dying in childbirth in the U.S ranges widely across states (4.5/100,000 per live births in California to 64/100,000 in Louisiana),8 and the highest rates are in states where full reproductive rights are being banned. Laws that punish women who seek to own their reproductive freedom and physicians who support them and deliver life-saving care in the setting of obstetrical complications will only further exacerbate these disparities, and will lower the quality of care for all communities where these laws are enforced.
As there is no provision in Georgia to put a constitutional amendment on the ballot, SisterSong Women of Color Reproductive Collective brought a suit against the state of Georgia, challenging the extremely restrictive Georgia laws on abortion. On September 2024, Judge Robert McBurney ruled that the Georgia’s 6 week abortion ban, known as the Living Infants Fairness and Equality Act, or LIFE Act, was unconstitutional. In his ruling, the judge wrote that “When a fetus growing inside a woman reaches viability, when society can assume care and responsibility for that separate life, then – and only then – may society intervene. An arbitrary six-week ban on (post-embryonic cardiac activity pregnancy) terminations is inconsistent with these rights and the proper balance that a viability rule establishes between a woman’s rights of liberty and privacy and society’s interest in protecting and caring for unborn infants,” McBurney wrote.
His decision was based on “a review of our higher courts’ interpretations of ‘liberty’ demonstrates that liberty in Georgia includes in its meaning, in its protections, and in its bundle of rights the power of a woman to control her own body, to decide what happens to it and in it, and to reject state interference with her healthcare choices.”
The Georgia Supreme Court overturned Judge McBurney’s decision, but the fight will continue.
continued on page 26
Special Section - Reproductive Health and Rights
What Can We Do As a Medical Community?
We can speak out and advocate for change. We can support those that are working to alter the constitution in states that have imposed bans on abortions. Every single preventable death should be reported in newspapers, blogs, podcasts and these cases must stay in the public consciousness. We can use our power as consumers, as providers, researchers, and advocates for health. We should not support wanton disregard for women’s health and rights. We cannot tacitly endorse laws by explicitly promoting the economy of states in direct conflict with our role in promoting women’s health and public health writ large. National and international conference that attracts tens of thousands of people each year provide economic benefits to states. One way to make an impact is to advocate to move such meetings to states that support equal rights for women and have elected to include abortion as one of the critical health care services that should be available if necessary. It is challenging to move meetings that are large and have multiyear contracts, but it can and has been done. Medical professionals and business leaders should come together to send a message to states that pass discriminatory laws that place undue burden and threaten the health of women and their families. Ruth Bader Ginsburg in Gonzales v. Carhart said “[L]egal challenges to undue restrictions on abortion . . . center on a woman’s autonomy to determine her life’s course, and thus to enjoy equal citizenship stature.” We urge that all businesses who do not wish to treat women as secondclass citizens follow that lead.
RISE UP
As a leader in the field of breast cancer, and a woman’s health proAs a leader in the field of breast cancer, and a woman’s health provider, I have chosen not to attend large meetings in states that ban or criminalize abortion. I have turned my attention to reducing the incidence of breast cancer by shifting the paradigm in women’s health care to find opportunities to optimize breast cancer prevention, and to expand women’s health options and improve health outcomes. The paradigm shift is to reimagine the interventions throughout a woman’s life to focus on risk reduction. The idea is to use the most innovative approaches and the lessons learned from accelerating our ability to personalize breast cancer treatments and apply it to breast cancer prevention. This requires reproductive autonomy, an increased investment in women’s health, and prioritization of symptom management across a woman’s life course. This is the purpose of RISE UP (Revolutionizing Investigations to StEp Up Prevention) for Breast Cancer, a new interdisciplinary meeting that was launched in November, 2024 (https://riseup.ucsf.edu).
RISE UP brought together practitioners, scientists, advocates and across women's health specialties across the globe. Together we worked to integrate reproductive health and hormonal management with what we know about breast cancer biology, treatment, and biomarkers of risk and response to inform a precision medicine approach to breast cancer prevention, screening, and survivorship. We learned about the history and current formulations for contraception and why innovation has been lacking. We focused on advances in understanding of hormonal control and addressed the opportunities to explore new ways to manage cycle control, birth control, postpartum weaning, IVF, and post-menopausal symptom
management so that these interventions will reduce the risk and incidence of breast cancer. Importantly, we also addressed disparities and access to care, and the impact of restriction of reproductive services. A satellite luncheon honored politicians and practitioners who have been leaders in advocating for reproductive health and freedom with the “Croix de Guerriere”. The meeting concluded with a competition for the best ideas for risk reduction that could be incorporated into other health interventions, especially those used across the continuum of hormonal management during a woman’s lifetime. Four awards were distributed by an august panel that included physician scientist, regulators, industry, and the venture community. Details can be found on the website as well as slides from the inspiring sessions The motivation and goals for the conference are available on line and the link to the publication is on the website (https://riseup.ucsf.edu).9
Importantly, this new national conference was launched in San Francisco, California, a state that immediately moved to instantiate access to abortion until the time of viability, and where women are protected from cyber tracking when then come to California to access services. There are laws now that also protect practitioners from criminal liability as well. While the meeting may move to other states, it will only move to states that provides reproductive rights and access, treats women as full citizens with the autonomy to make decisions about her own body.
Those in support of reproductive rights should find their own ways to (support states that support comprehensive healthcare for women, stay engaged in bringing attention to this issue, and advocating for change.

Laura Esserman, MD, MBA is Alfred A. de Lormier Endowed Chair in General Surgery at UCSF and an oncology specialist at the UCSF Breast Care Center, where she has been Director since 1996. She co-leads the Breast Oncology Program at the UCSF Helen Diller Comprehensive Cancer Center. She is faculty at the Helen Diller Family Comprehensive Cancer Center where she founded the program in Translational Informatics, and has published over 200 peer-reviewed articles. She received her BA from Harvard and her MD and MBA at Stanford. She was named by TIME Magazine as one of the 100 Most Influential People in the world.
References
1. KFF, State Shield Laws: Protections for Abortion and Gender-Affirming Care Providers | KFF (2024). https://www.kff.org/other/state-indicator/shield-laws/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Protections%20Against%20Civil%20Liability%22,%22sort%22:%22desc%22%7D.
2. Society of Family Planning, #WeCount Report (2024). https://societyfp.org/wp-content/ uploads/2024/07/WeCount-Report-7-Mar-2024-data.pdf.
3. NPR, Meet the people sending abortion pills to places with bans : NPR (2024). https://www.npr. org/2024/08/06/nx-s1-5037750/abortion-pills-bans-telehealth-mail-mifepristone-misoprostol.
4. L. J. Esserman, D. Yee, Reproductive rights in the United States: acquiescence is not a strategy. Nat. Med., 1–3 (2024).
5. Idaho Coalition for Safe Healthcare, Physician Well-Being Action Collaborative — Idaho Coalition for Safe Healthcare (2023). https://www.idahocsh.org/idaho-physician-wellbeing-action-collaborative.
6. AAMC Research and Action Institute, Training Location Preferences of U.S. Medical School Graduates Post Dobbs v. Jackson Women’s Health (2023). https://www.aamcresearchinstitute. org/our-work/data-snapshot/training-location-preferences-us-medical-school-graduates-postdobbs-v-jackson-women-s-health.
7. KFF, A National Survey of OBGYNs’ Experiences After Dobbs | KFF (2023). https://www.kff.org/ womens-health-policy/report/a-national-survey-of-obgyns-experiences-after-dobbs/.
8. S. C. Hull, J. C. Chou, L. M. Yee, D. Yee, L. Esserman, A Truly Pro-Life Position Requires Access to Reproductive Health Care. J. Women’s Heal., doi: 10.1089/jwh.2023.0305 (2023).
9. K. Leggat-Barr, D. Yee, E. Duralde, C. Hodge, V. Borges, M. Baxter, J. Valdez, T. Morgan, J. Garber, L. Esserman, A roadmap to reduce the incidence and mortality of breast cancer by rethinking our approach to women’s health. Breast Cancer Res. Treat., 1–14 (2024).
PROTECTING PATIENT PRIVACY IN THE AGE OF EHRS AND ABORTION BANS
Jessica J. Pourian, MD and Arvisais-Anhalt, MD
With Texas suing this fall to block new federal laws aimed at protecting patient privacy in women seeking reproductive healthcare, medical data sharing has become more important than ever.
While these battles play out in court, it’s equally important to explore technical solutions that improve electronic health record (EHR) data-sharing practices. For years, the primary goal for physician-informaticists has been to achieve perfect interoperability in EHRs: seamlessly sharing patient data across institutions via the health information exchange (HIE). The premise was simple—the more a doctor knows about you, even if they're out of network or treating you while you’re traveling, the better care they can provide. In 2024, many large institutions have achieved this goal.

mmInformatics is integral to the practice of medicine today, yet there is no standard of care when it comes to data. Informatics education is virtually nonexistent in medical school. The American Medical Informatics Association, the academic body of physician-informaticists in the United States, has no guidelines on how to obtain patient consent for data sharing or the specifics of EHR data sharing options, and neither do other relevant professional organizations such as the American College of Gynecology nor the American Academy of Pediatrics. There is no standard of care when it comes to data sharing.
However, the shifting political landscape around abortion has made it clear that fully transparent interoperability is no longer safe for patients nor providers as it may open them to legal liability. While some mechanisms exist within EHRs to prevent data sharing, they are often convoluted, difficult to access, and unintuitive for both physicians and patients.
Last year, California passed AB 352 to protect data for patients who may be traveling for sensitive care from out of state. The law requires healthcare providers and systems to safeguard sensitive medical information, such as abortion-related care, by restricting its access and sharing across state lines to protect patient privacy. AB 352 is much needed, but implementation faces several challenges, key among them the byzantine data sharing options that exist in today’s EHRs that institutions and providers must navigate. EHR vendors provide a potpourri of complex sharing options that, depending on institutional EHR implementation, can vary even across clinics at the same institution, let alone across the state. Since there are no standard sharing options, even for systems using the same EHR software, there is no way to efficiently share learnings between sites. Best practices from one hospital cannot necessarily be easily applied at another institution. This lack of standards and transparency opens the door to user error—errors that can hurt the patient and provider.
This is increasingly problematic. After the Dobbs decision in 2022, a woman traveling from Tennessee to Illinois for a legal abortion was outed by a nurse at her home primary care practice who saw the record of the out-of-state abortion in the EHR. This patient was reported to child protective services and ended up in family court, battling for custody of her two children after being accused of murdering her unborn child. Situations like this could be entirely avoided if providers in Illinois had clear options to segment and stop the abortion data from being shared.
Part of the complexity of data sharing arises from a labyrinthine data architecture that has evolved over time as EHRs have expanded. For example, Epic segments data by “patient” and “encounter.” A lab test ordered during a visit is categorized under “encounter,” but a prescribed medication falls under “patient.” Marking the encounter as “sensitive” might thus block the test from sharing to the health information exchange (HIE) network (and thus to other hospitals), but not the medication. While this distinction may make sense from a data architecture perspective, it is nonsensical from a clinical standpoint.
Making matters worse, these distinctions are not readily apparent to a physician during the visit. Whether that information is being shared to the patient portal vs. the HIE is not readily accessible to the provider. These options can vary by patient age and clinic type; thus providers often have little clarity about what happens to the data once they click "sign." A patient checking their information in the patient portal will also not know who has access to their data as there is no option to show what data is shared to one institution versus another. continued on page 28
Special Section - Reproductive Health and Rights
Robust technical solutions and simplification are urgently needed. Because of California’s AB 352, which followed a similar law passed in Maryland last year, Epic has announced plans to allow for value-set based data segmentation, which will filter the most sensitive ICD-10 codes, medication, and laboratory tests, among others. This is a step in the right direction, but more work is needed.
There are individuals working to create automatic data segmentation and to develop value-sets to tag sensitive data specifically so that it is not accidentally shared. Organizations like Shift are working to standardize patient consent for data sharing through the Delphi Method, and the Sequoia Project and California-based PRIVATE group are advocating for patient medical record privacy.
These are all laudable efforts that cannot come fast enough as patients are already being placed in harm’s way. Healthcare data is intricately intertwined and keeping patients safe will require a multi-pronged technical and legal approach.
Providers must stay at the heart of this conversation. With improved technical options, they can better safeguard patient data. However, without a deeper understanding of these options, even the best technical solutions will ultimately fall short. For now, providers must take the initiative to educate themselves on the technical solutions available at their respective institutions and actively advocate for their institutions and EHR vendors to develop intuitive, user-friendly systems that prioritize data
privacy and safety. This dual approach—staying informed and advocating for change—will be critical to ensuring that sensitive patient data is protected.
The goal is for data sharing options to be as intuitive as ordering a lab test. Providers shouldn’t need to focus on the technical logistics of the EHR—just as they don’t need to understand how a lab test order ultimately gets a patient’s sample on an analyzer. Instead, they know what to order and how to interpret the results. Similarly, when it comes to data sharing, the focus should be on choosing what’s best for the patient without getting mired in the complexities of the underlying data systems.


Jessica is an attending pediatrician and fellow in clinical informatics at UCSF. She works clinically in acute care and in the ER. She completed her undergraduate studies at MIT and worked in healthcare consulting before attending medical school at UCSD and pediatric residency at Brown.
Simone Arvisais-Anhalt is board-certified in anatomic pathology, clinical pathology, and clinical informatics and the Director of Laboratory Medicine Informatics at UCSF.
Democrats push to protect the data privacy of people seeking abortions
By Grace Panetta
In Congress, Sen. Elizabeth Warren plans to reintroduce legislation to ban data brokers from selling consumers’ health and location data. A similar effort is underway in Michigan.
Democrats at the federal and state levels are pushing to pass bills protecting sensitive reproductive health data before Republicans take control of key legislative chambers.
Democratic Sen. Elizabeth Warren of Massachusetts plans on Tuesday to reintroduce legislation that would put guardrails on the largely unregulated industry buying and selling consumer data, her office shared first with The 19th. The bill, the Health and Location Data Protection Act, would ban data brokers — an estimated $200 billion industry — from selling or transferring consumers’ health and location data.
The U.S. Supreme Court overturned federal abortion rights protections in 2022, putting a renewed focus on data privacy. Reproductive rights advocates worry about ways in which the privacy and safety of abortion patients could be at risk in states where the procedure is banned. They have raised concerns about apps that track menstrual cycles and family planning, as well as location data that can be used to track patients’ visits to abortion clinics.
Data brokers say the data they collect is anonymized. But some researchers have found vulnerabilities in that data that could make it possible to see who has gone to an abortion clinic. The startup Atlas Privacy obtained access to a tool used by the U.S. government and law enforcement agencies that draws on commercially available location data. A NOTUS analysis of the data found they were able to trace individual phones to a clinic that provides abortions in Tallahassee, Florida.
“Data brokers are raking in giant profits from selling Americans’ most private information – even location tracking data from visits to clinics for reproductive care,” Warren said in a statement. “As Republicans ramp up efforts to criminalize abortion, it’s more important than ever to crack down on greedy data brokers and protect Americans’ privacy.”
Sens. Bernie Sanders of Vermont, an independent aligned with Democrats, and Sens. Ron Wyden of Oregon and Sheldon Whitehouse of Rhode Island, both Democrats, are co-sponsors of the proposed legislation, which would be implemented and enforced by the Federal Trade Commission. The legislation allows exceptions for activities regulated by existing patient privacy regulations and those protected by the First Amendment.
But the legislation faces tough odds in the Senate, where a threefifths supermajority is required to advance most legislation, and in the Republican-controlled House of Representatives. Come January, Republicans will hold a trifecta in Washington, controlling the White House and both chambers of Congress.
Democrats at the state level are also moving to protect reproductive health data. On Friday, the Michigan state Senate passed a bill, sponsored by Democratic state Sen. Mallory McMorrow, that would ban cycletracking apps from collecting and amassing users’ data without their consent and allow them to use the data only for purposes approved by users. Democratic Gov. Gretchen Whitmer is supporting the bill, which Democrats hope to pass before Republicans take control of the state House in January.
Originally published by The 19th: https://19thnews.org/2024/12/democrats-data-privacy-people-seeking-abortions/
MAKING MIFEPRISTONE ACCESSIBLE IN THE U.S.: WE WON’T GO BACK.
Steve Heilig, MPH
Once upon a time I was an international drug smuggler in San Francisco—and got busted for it. Looking back though, I’d do it all again without hesitation.
In 1988, I was an aspiring public health professional at UCSF. One afternoon, I was sitting in the medical center library, listlessly leafing through medical journals when a brief news article jumped out at me. France had approved a pill that triggered abortions in early pregnancy. The medication, then called RU486, had already been shown to be safe and effective. A wave of excitement surged through me. This changes everything, I recall thinking; a medication like that would be a game changer. Although abortion had been legal for over a decade at that point, it was still controversial. Clinics that offered it were protested and attacked, and in some cases, doctors were even murdered. The new pill would make it much harder to target doctors and their patients. But as word spread about RU486, then-President George H.W. Bush vowed the medication would never be allowed in America. Under pressure from conservative lawmakers, the U.S. Food and Drug Administration banned the import of it in June 1989.
That’s when I and other medical professionals got to work— writing articles about RU486’s safety and efficacy in papers like UCSF’s student newspaper, the Synapse, and a review in the Journal of American Medical Association. Soon our activism started to pay off. A policy statement I drafted for the San Francisco Medical Society urging that RU486 be made available in the U.S. was adopted by the CMA and soon the American Medical Association adopted our position as well.
By the early ’90s, RU486 was available in France and Britain and, now with the backing of the American Medical Association, it was finally tested in the U.S. and shown to be safe and effective. Yet, American women still couldn’t access it. Why? Because the FDA wouldn’t approve its release without a company filing for a new drug approval, and no company was willing to do so out of fear that their other products and services would be boycotted by abortion opponents.
It was around this time that I got a call from Lawrence Lader, a veteran New York City abortion rights activist who’d seen my writings. He said he was coming to San Francisco and wanted to meet and asked if I might bring a few good OB/GYN physicians with me. We gathered at the San Francisco Medical Society with Lader where he laid out his proposal: Find a woman with an early unwanted pregnancy, fly her to Europe to pick up the pills


and back, tip off federal authorities and the media so she would get detained and even arrested, and make RU486 a big public and political story. It was an audacious plan but worth a try.
mmThe physicians in our group started sending me potential candidates. My job was to give them “informed consent”—to make sure they knew that their participation in our plan might land them all over the papers and TV, and perhaps even get stalked and threatened. Basically, I tried to talk each potential candidate out of doing it. But I also assured them they’d have all medical care and any other related costs covered. A few understandably thought it over and decided they just couldn’t participate, but one young woman, Leona Benten, emphatically said, “OK, stop trying to talk me out of this, let’s go.”
Our stunt worked as planned. Only July 1, 1992, Benten arrived in New York at John F. Kennedy International Airport from London with the illegal pills and was detained and searched. As expected, her pills were confiscated and as we hoped, the media descended. The story made the front page of the New York Times. At her request, we hid Benten from the swarms of media requests demanding to talk to her. I and a few others were sent out instead to do countless interviews. One reporter informed me that I might be indicted for our smuggling efforts. My only thought was how many smugglers tip off the authorities in advance?
With all the media coverage, the story inevitably became an issue in the presidential election. Then-candidate Bill Clinton pledged to bring these pills to American women. Time magazine ran a cover story on RU486 calling it, yes, “the pill that changes everything.” The tide eventually turned. It would take another eight years though before the FDA finally approved RU486, then renamed mifepristone. For the next 22 years, Americans gradually began to take access to mifepristone as a given. Women started choosing the pills over surgery, with that proportion slowly but steadily increasing over the years. According to a study from the Guttmacher Institute, 63% of abortions in the U.S during 2023 were via medication. Telemedicine provided much of this access, making the service available in an essential timely manner in areas with less medical services.
However, that assumption of access changed, of course, with the fall of Roe v. Wade two years ago. Today, many states are trying any tactics they can—legislative, legal, regulatory— continued on page 30
Special Section - Reproductive Health and Rights
to restrict the availability and use of abortion medications. Some have tried reclassifying them as “controlled substances,” like heroin, and even used drug-sniffing dogs to detect them in the mail.
With Donald Trump the president-elect and Republicans in control of the Senate and likely the House, any federal protections for abortions, let alone mifepristone, are an endangered dream. In fact, there are fears that anti-choice policies will be enacted to limit access via telemedicine and to track doctors, nurses and patients via medical records—if not outright ban mifepristone. They are even attacking contraception, surely a counterproductive effort for even their own stated goals. The number of abortions reported nationally has increased since Roe was overturned—more indication that outcomes and evidence—not to mention compassion—do not guide the antichoice actions.
But this doesn’t have to be the end of the story if we don’t allow it. No one person or group made mifepristone accessible in this country. It was a grassroots, collective effort by activists of all kinds, each contributing the best they could. While my health care colleagues and I were pushing the medical aspect of the campaign, thousands of activists took to the streets across
the country. At the time of our 1992 stunt at JFK, San Francisco had its biggest ever pro-choice demonstration, with tens of thousands of people marching up Market Street in solidarity. We are now at another moment of collective action and it will take all of us to protect our freedoms, including access to medicati on abortions. But they just don’t seem to care.
Before arriving in San Francisco, I was studying public health at UCLA. I’ll never forget a senior medical professor taking students on a tour of the hospital there. He walked us into a big room and quietly said, “Back in the 1960s, before Roe v. Wade legalized abortion, this was a ward for women suffering from the effects of illegal abortions. There were dozens of beds, almost always full. Many died. Blood had to be mopped from the floors. It reminded me of my time as a medic in wartime.”
We just stood there silently. He didn’t need to say more.

Steve Heilig is an editor, ethicist, epidemiologist, environmentalist and educator based at the San Francisco Marin Medical Society, and co-editor of the Cambridge Quarterly of Healthcare Ethics.
A version of this piece appeared in the San Francisco Chronicle in November.

THE FDA SHOULD REDUCE NICOTINE IN CIGARETTES—AND USE A BETTER TEST TO ENSURE IT HAPPENS
Eons before Europeans arrived in North America, Native Americans cultivated the tobacco leaf for ceremonial activities and medicinal purposes for use during prayers and rituals. They presented the tobacco leaf as a gift to early explorers including Christopher Columbus, who carried it back to Europe. Over the centuries, the tobacco industry mastered blending additives, cigarette design, and nicotine delivery to craft one of the most highly addictive products sold worldwide, which kills half of users when consumed as directed.

But what if we could return modern cigarettes to the original nicotine levels used by the Native Americans, which were nonaddicting?
In his 2001 book, A Question of Intent, former Food and Drug Administration (FDA) Commissioner David Kessler highlighted research long suppressed by Big Tobacco that showed how reduced-nicotine cigarettes could be a powerful smoking cessation tool. Smokers need a larger number of reduced-nicotine cigarettes to achieve a nicotine rush, and instead of continuing to smoke, many quit on their own rather than having their clothing reek of cigarette smoke.
For years, stakeholders and policy makers have discussed the idea of reducing nicotine in cigarettes to non-addictive levels. In 2017, FDA Commissioner Scott Gottlieb announced a framework that could lead the agency to set a nicotine-limiting standard. The next year Commissioner Gottlieb estimated that five million adult smokers could quit within a year of the plan’s introduction. The COVID-19 pandemic and 2021 change in federal administration likely delayed progress toward this goal.
In the spring of 2022—shortly after the Biden administration’s Cancer Moonshot Initiative declared its goal of cutting cancer deaths by 50 percent in 25 years—the FDA issued a notice of proposed rulemaking aimed at setting a maximum allowable nicotine level for cigarettes. That same year New Zealand introduced a key policy as part of its Smokefree Environments and Regulated Products Amendment Act mandating tobacco products to contain no more than 0.8 mg/g of nicotine (instead of the current average of 10–12 mg). Attention in the Biden White House has in the interim focused on the menthol ban, without further action on the reduced nicotine rulemaking.
mm We believe that, as a new US president takes office in January 2025, his administration has an opportunity to make good on the promise of, once and for all, requiring that cigarettes sold in the United States have their nicotine content reduced to non-addictive levels.
mmSuch a policy action would have a profoundly positive impact on the lives of millions of people well into the future. And yet, while we believe it is essential, this step alone is not sufficient. That is because for decades Big Tobacco has deceived the U.S. public by manipulating how tar, nicotine, and carbon monoxide (TNCO) levels are measured in cigarette emissions. This deception has created a low-tar myth that has had significant negative health consequences over many decades and that could undermine efforts to set a maximum allowable nicotine standard.
Fortunately, there’s further action that policy makers can take to end the deceit.
Industry Deceit Drives The Low Tar Myth
Two years after the release of the 1964 Surgeon General’s report on smoking and health, the U.S. Public Health Service stated that the “evidence strongly suggests that the lower the tar and nicotine content of the cigarette smoke, the less harmful would be the effect.” This established the standard test for TNCO in cigarette emissions, in which a machine simulates regular puffs on a cigarette and then collects and analyzes the emissions that would typically be inhaled by a smoker. This test was later adopted globally as the International Organization for Standardization (ISO) method.
However, in a 2001 investigators exposed how the tobacco industry created small ventilation holes in cigarette filters to allow external air to dilute the smoke stream and lower TNCO measurements to meet allowable standards. Outside of the testing situation though, real-life smokers commonly close these holes with their fingers or lips when inhaling. They also smoke in a manner very different from the FTC/ISO methods—with higher volume puffs and less time between those puffs, for example—and thus are exposed to far more toxins than measured.
That same year, a National Cancer Institute report blasted ciga-
continued on page 32
rette manufacturers for exploiting the low tar myth to deceptively market “light” and “low-tar” cigarettes as safer despite knowing this was false. In 2004, a U.S. District Court Judge ruled that the tobacco industry falsely promoted “light” and “low tar” cigarettes as less harmful and less likely to result in addiction.
In 2008, the FTC prohibited tobacco companies from continuing to claim that tar and nicotine ratings were based on an FTC-approved method and warned of legal action if the tobacco industry continued to mislead consumers. In the Federal Register, an FTC commissioner wrote that “the FTC will not be a smokescreen for tobacco companies’ shameful marketing practices. Scientists must develop a test that provides consumers with a meaningful measure of the tar and nicotine yields of the cigarettes they smoke.”
International Action
Over the following decade, Canada and the Netherlands led the way forward to answer this call from the FTC by championing the World Health Organization (WHO) Intense method. The WHO Intense method is modeled after the Canadian Intense method (which ultimately replaced the ISO method in Canada in 2019) and uses tape to close the ventilation holes, and a puff volume and rate almost twice as high to more closely resemble actual human smoking behavior.
In 2018, Dutch tobacco control champions filed a legal challenge to the tobacco industry after U.S. tobacco industry whistleblower Jeffrey Wigand, PhD, enlightened them to the low tar myth. Researchers subsequently demonstrated that cigarettes on the Dutch marketplace exceeded the legal maximum of 10 mg tar, 1 mg nicotine, and 10 mg carbon monoxide by at least two- and up to 20-fold when tested by WHO Intense.
In 2022, both an EU and Dutch Court ruled that a more accurate method should be adopted, and future court rulings may require that all cigarettes in Europe be tested by the WHO Intense method only, as requested by 13 European nations. Doing so may force the tobacco industry to remove cigarette filters, stop placing ventilation holes in the filters, or reduce TNCO levels and catalyze the introduction of the low nicotine cigarette in Europe.
Approaching The Tobacco Endgame In The US
For decades, stakeholders have made calls to replace the FTC/ ISO methods with a more accurate test in the US. Reforming the test in the US has been rendered more challenging as the testing site has repeatedly relocated over the years. After the FTC lab closed in 1987, testing was first transferred to the Tobacco Institute Testing Laboratory, to the Centers for Disease Control and Prevention in 1994, and finally to the FDA in 2009 with passage of the Family Smoking and Prevention Tobacco Control Act (FSPTCA).
A second unique challenge is that the FSPTCA “grandfathered cigarettes” commercially marketed before February 2007. Thus, existing cigarettes sold in the U.S. cannot be modified by new requirements to test nicotine levels, unlike in Europe. An alternative is for the FDA to require use of the WHO Intense method to accurately test for nicotine emissions when a reduced-nicotine plan is implemented in the US.
Mandating the sales of reduced nicotine cigarettes to nonaddictive levels, in coordination with adopting the WHO Intense method to accurately measure their emissions, has the potential to save millions of lives. It would also help the US move closer to the Tobacco Endgame by helping more smokers quit. The White House should include these twin actions along with a national menthol ban in the first 100 days of the new administration.
In 2026, the United States will celebrate its 250th birthday, and perhaps an ideal way to celebrate that anniversary would be by returning cigarettes to the original nicotine levels used by the Native Americans as Sacred Tobacco nearly 500 years ago.


John Maa, MD, an SFMMS past-President, serves on the board of directors of the American Heart Association Western States Affiliate. He was appointed by Governor Gavin Newsom to the California Tobacco Education and Research Oversight Committee and serves ex-officio on the University of California Office of the President Tobacco Related Disease Research Program.
Michelle Zhang is the Chair of the American Cancer Society Youth Ambassadors Program, with a strong interest in biology and public health. She served as a Head Delegate at the Global Model World Health Organization in 2024.
Medical Student Perspective
LISTEN CLOSELY: CONGENITAL CYTOMEGALOVIRUS SHOULDN’T
BE OVERLOOKED
Hearing loss. Developmental delay. Vision loss.
These are all effects experienced by children who contracted congenital cytomegalovirus (cCMV) at birth. In California, 156 out of every 1000 infants are born with Cytomegalovirus (CMV) infection, nearly 5% of the expected number of live births. The condition often affects children who are born prematurely or with lower birth weights, and can lead to significantly longer hospital stays, or even death. In children diagnosed with cCMV at birth, treatments can be given to lessen the severity of the virus.

In California, the Newborn Hearing Screening Program requires that each newborn is given a hearing test prior to discharge. However, the efficacy of hearing screening as a precursor for CMV testing is still uncertain, and position statements from experts in the field (American Academy of Otolaryngology- Head and Neck Surgery, the American Speech-Language-Hearing Association and/or the American Academy of Pediatrics) remain unwritten.
Universal screening may not be the most feasible option for a state as large and populous as California—educating providers, the cost of testing, and the infrastructure considerations present enormous obstacles for implementation. Despite these concerns, a number of health systems in the state DO provide an alternative: hearing-targeted newborn screening for cytomegalovirus, including UCSF’s own Betty Irene Moore Women’s Hospital. While implementation of universal CMV screening would likely result in logistical and infrastructural headaches for clinicians and policymakers alike, following in the footsteps of other states who have taken targeted approaches may be one path forward. In addition to exploring these targeted approaches, focused examination of the utility of CMV screening from experts in the field of pediatric otolaryngology, head and neck surgery and
audiologists is also needed. The first step towards improving conditions is to follow in the footsteps of other state legislatures.
mmIn 2016, Connecticut passed similar legislation to ensure that every newborn who fails their hearing test receives CMV screening, accompanying a list of other screening conditions. The state of Minnesota was the first to enact universal newborn CMV screening following the passage of the Vivian Act in 2021, which also included funding to educate healthcare providers and expectant mothers about the risks of CMV.
Illinois, Iowa, Kentucky, Maine, New York, Pennsylvania, Texas, and Utah all require education and targeted newborn screening measures. Many of these same states require that each newborn who fails the newborn hearing screening test to be tested for congenital cytomegalovirus.
Additionally, these screening measures should accompany robust transmission prevention measures, which are often left up to the facilities themselves. While OSHA provides general guidelines for preventing transmission, there’s always room for improvement through establishment of more robust, standardized protocols. Through policy development and advocacy specific to CMV, misconceptions and mistakes that have dire consequences can be avoided.
Children who are at risk for CMV deserve to be heard. We should ensure that California policymakers are listening.

James Lawrence, MPH, is a first year medical student at the University of California, San Francisco.
PAUSE & PRESENCE COACHING & RETREATS: LESSONS FROM A BOMB CYCLONE
Jessie Mahoney, MD
“You can make yourself miserable or you can make yourself strong, the effort is the same.” – Pema Chodron
In many ways, weather disasters are like medical codes. I was always good at those. Great under pressure. And then... After a code or stressful situation, my nervous system would be french fried. To add to it, the medical culture encouraged me to replay and judge my decisions and continue to worry. I never took a break after a patient's death or undesired outcome to recover. We were not taught to rest and recover in medicine.
Coaching was a HUGE asset to me in navigating the recent Bomb cyclone atmospheric river. Despite the "situation," I was able to take great care of myself, my nervous system, and my mind. I was successful in taking breaks and time to recover. I rescheduled some coaching clients to not show up distracted, worried, and/or exhausted. I did thought downloads, and practiced hand-to-heart and mindfulness in between physical labor jobs. Best of all I took time for recovery.
Whatever may be in store for us in 2025 these tips—which we were not taught in our medical training may help:

Recommended
1. Be kind to yourself physiologically. Optimize your functioning by lessening cortisol release in whatever way you can. Try free Yoga to Settle Your Nervous System with Dr. Jessie Mahoney by scanning the QR code with your smartphone.
2. Rest and recover.
3. Don’t be mean to yourself by judging or second-guessing yourself. Have your own back. You did the best you could at the moment with the information and resources you had at the time. Overpreparing is the best outcome.
4. Remember what matters most.
5. Accept and... Resisting reality is expensive.
6. Pause and be present. All that's in your control is how you respond.
7. Be intentional and tell "generous" stories.
8. Practice gratitude.

9. Remember it just might turn out better than you expect.
Listening: The Mindful Healers Podcast with Dr. Jessie Mahoney and Dr. Ni-Cheng Liang
What’s Needed to Start a Dream Practice is Not What You Think with Dr. Anna Dowling
There is no recipe or rule book to start your dream practice. Dr. Anna Dowling, an ObGyn, joins us for a second time. In this episode, she shares her journey building a dream solo practice called Birth Story Obstetrics. Her first podcast episode is Episode 155. Become Your Future Self. In this episode, she shares what she found helpful in manifesting a practice that is fun and meaningful. Key to her success was setting up a team of supporters and helpers—a coach, her spouse, and friends who believed in her.
Have Your Roots Outgrown Your Pot? Lean into Curiosity with Dr. Holly MacKenna
Do you feel like you are growing faster than your organization has space for? Are your roots trying to grow out the bottom of your pot? Dr. MacKenna shares the story of starting her integrative practice right before the Covid pandemic. She embraced the journey because she felt like she had grown beyond what her organization had space for. Her roots were trying to grow out the bottom of a pot.
The Power of “Marketing” Healthy Food and Lifestyle Medicine in an Appetizing Way with Dr. Rak Nourishing our mind, bodies, and spirits “well” feels amazing! Great cooks make healthy food a delight to eat. You get to taste with your eyes and treat your taste buds. As health care providers we can make eating healthy about a feast and delight for the eyes, body, spirit, and soul. Dr. Rak and I hope you will join us for this fun conversation about the power of “marketing” a healthy lifestyle to ourselves and others. If you are wanting to step out of the box and/or explore ways to rekindle your passion in medicine, consider signing up for small group coaching or a retreat with other physicians such as The physicians Transition Well and Ongoing Presence.



2024 Wellness Recap
SFMMS offered many opportunities for our members to gather and connect with one another in 2024. We are looking forward to sharing more opportunities to connect with your colleagues in 2025. To learn about upcoming events as they become available, visit the SFMMS Events page at sfmms.org/news-events or scan the QR Code with your smartphone.


Two Mindful Yoga for Healers in Old Mill Park
“What a wonderful event. It was so great to connect with friends and colleagues I haven’t seen in years while practicing yoga amongst the Redwoods!” – SFMMS Member
Would You Like to Practice Mindful Yoga with Jessie Anytime?
Join Dr. Mahoney on Zoom most Saturdays at 9am or anytime on YouTube. For more information visit: https://mindfulyoga.jessiemahoneymd.com or https://youtube.com/c/JessieMahoney.
SFMMS Sponsored Eight Physician Members to Attend Local Wellness Retreats with Other Physicians from the Bay Area

"The retreat was an incredible opportunity to learn about mindfulness in medicine. As a medical student, my takeaways were different from others–I was able to get perspective from people further along in the field, as well as many insights I am grateful to now carry forward. I would recommend any student, resident, or physician attend this retreat, as it is incredibly valuable to reconnect to core values and get coaching around different issues within medicine we all struggle with."
– SFMMS Medical Student Member and Retreat Sponsorship Winner
Wellness Retreats for Physicians at Nicasio Creek Farm
Mindful Coaching, Yoga and Culinary Medicine. CME available. Some retreats are open to partners too. March- November 2025 (new dates coming soon!). https://www.jessiemahoneymd.com/retreat-nicasio-creek-farm
“Amazing & transformational! I’ve been to many retreats and this is one of the best!” – SFMMS Member
“The minute you step out of the car and smell the amazing aroma of the trees and fresh air, you know this place (Nicasio) is special.”
–SFMMS Member
Interested in Bringing Your Team to a Retreat?
Retreats for you are amazing. Retreats for your team add an added element of healing, optimism, and growth.
The work we do in medicine is hard. Well teams are a key component of not making hard jobs harder. Well-facilitated and expertly planned team wellness experiences make a HUGE difference—to the health and wellness of physicians, patients, and institutions. Physicians with burnout are twice as likely to be involved in patient safety incidents, to exhibit low professionalism, and to receive low satisfaction ratings from patients. While there are many competing demands for money in healthcare currently, these experiences are a worthy investment. There are also many creative and impactful ways to make them happen. https://www.jessiemahoneymd.com/team-coaching-retreats
“Prepare for a day learning many critical life skills to help you. It was like medicine for life.” – Sutter Health MD
“It will give you the words to explain what you’ve been feeling, allow connection with others that have been struggling with the same mindsets, and learn useful tools to change your mindset.” – Sutter Health MD
Find out more about both individual and team retreats here: https://www.jessiemahoneymd.com/retreats. more on page 36
WELLNESS
Annual SFMMS Women in Medicine Mixer
Each year, we gather a group of our physician members who identify as women, for a meal, connection, and community building.

“[The Women in Medicine Mixer] was well attended and well run. It was perfect for small, manageable connections with my colleagues who have had similar experiences to me in medicine. I love the small group feeling!” – SFMMS Member
Upcoming Events in 2025
The SFMMS Book Club Returns January 15th, 2025! SFMMS is bringing back our book club for our Physician Members in 2025! Join us virtually via Zoom on January 16th as we read and discuss “Legacy: A Black Physician Reckons with Racism in Medicine” by Uché Blackstock MD. The first 25 SFMMS Members to register will receive a free copy of the book, so that you can start reading before our January 16th book club! To learn more and register visit the SFMMS Events Page at www.sfmms.org/news-events/events or scan the QR Code with your smartphone.



Are you looking for Additional Wellness Resources?
The SFMMS Wellness page, curated by your SFMMS colleagues, includes upcoming and past wellness events, resources and more. Learn more by visiting the SFMMS Wellness page at www.sfmms.org/get-help/physician-wellness or by scanning the QR code with your smartphone.


Jessie Mahoney is a pediatrician, a certified life coach for physicians, and a yoga instructor. She is the Chair of the SFMMS Physician Wellness Task Force. She practiced pediatrics and was a Physician Wellness leader at Kaiser Permanente for 17 years. She is the founder of Pause and Presence Coaching where she supports and empowers her physician colleagues using mindfulness tools and mindset coaching.
Advertiser Index


