A SMART+STRONG PUBLICATION CANCERHEALTH.COM WINTER 2023 $3.99 HOPE & STRENGTH Conquering fear and metastatic lung cancer Dear Cancer Patient: Advice From a Survivor Guidelines on Managing Pain Support for Rural Patient Navigators What Is Psychosocial Oncology? The Changing Causes of Liver Cancer Benefits of Meditation AJ Patel COVID Concerns
IN
SEARCH
A CURE,
ON THE SHOULDERS OF GIANTS.
For 75 years, Damon Runyon has provided funding to scientists who bet their careers on high-risk, high-reward hypotheses, concepts, and strategies. In this time, Damon Runyon scientists have advanced cancer research exponentially – because each one builds upon the achievements of those who came before.
As we celebrate this milestone of scientific achievement, we honor the scientists who have contributed to this legacy and continue to carry it forward. With them, we look to the future.
To learn more, visit damonrunyon.org

THE
FOR
THEY KNOW EXACTLY WHERE THEY STAND.
Gordon J. Freeman, PhD Damon Runyon Fellow ’79–’81
Alexandra-Chloé Villani, PhD Current Damon RunyonRachleff Innovator
E xclusively on Cancer
Cancer Health Stories

Read the firstperson stories of people who are living with cancer, including personal diaries and honest, moving essays. cancerhealth.com/stories
Basics
Whether you’re newly diagnosed or a long-term survivor, check out our Basics section on cancer treatment, how to manage side effects and more. cancerhealth.com/basics


Learn about the latest treatment advances, cure research and conference news. cancerhealth.com/science-news


Cancer Health Digital
Scan the QR code (left) with your smartphone to check out the digital issue of Cancer Health online, or go to cancerhealth.com/digital to read past issues and the entire Smart + Strong digital library.

Meditation helped AJ Patel vanquish anxiety and dread about his lung cancer.
 BY JENNIFER COOK
BY JENNIFER COOK
cancerhealth.com WINTER 2023 CancerHealth 1 COVER AND THIS PAGE (PATEL) ARI MICHELSON; (HEART SPEECH BUBBLE AND T-CELL/CANCER CELL) ISTOCK CONTENTS 10 CONQUERING FEAR Emotions play a powerful role in living with cancer, a truth AJ Patel learned a decade ago when he was diagnosed with metastatic lung cancer.
2 From the Editor You Do You 4 Care & Treatment COVID concerns | integrative therapies for cancer pain | changing causes of liver cancer | Trodelvy for metastatic breast cancer 6 News Celebrity diagnoses and support | patient navigators in the
West
a prostate cancer project with diverse participants | data on breast cancer and Black women 8 Voices Melvin Mann, who was diagnosed with chronic myeloid
in 1995, shares many of the lessons he learned on his cancer journey. 9 Basics Colon and rectal cancer 14 Your Team A psychosocial oncology nurse 15 Resources Websites for people with uterine and endometrial cancer 16 Good Stuff Cozy pajamas, soft caps, mindful reads and other winter comforts 17 Reader Survey Tell us about your quality of life.
Mountain
|
leukemia
Health.com
Science News
You Do You
“THERE IS NO RIGHT WAY TO DEAL with cancer,” advises Melvin Mann in “Dear Cancer Patient,” our Voices column on page 8. Diagnosed with chronic myeloid leukemia in 1995 and in treatment and remission since 1998, Mann shares insights on navigating the many aspects of cancer, including quality of life. “Do your best at keeping your spirits up,” he writes. “This may involve trying integrative therapies (such as meditation, yoga and tai chi), watching comedies, accepting help, forgiving others, listening to music, seeking spiritual connections and doing things that you enjoy. What works for you is unique to you.”
Meditation transformed AJ Patel’s quality of life. Profiled in our cover story on page 10, Patel struggled with overwhelming fear and depression after learning he had metastatic lung cancer nearly a decade ago. Then he tried Vipassana, a breath-based meditation. “The experience completely changed my life,” he recalls. “I feel a lot happier. I’m no longer fearful, no longer scared of any treatment. This has been a beautiful gift.” To learn more about the benefits of meditation for people with cancer, turn to page 13.

Many healing practices—from acupuncture to music therapy—may also alleviate cancer-related pain, such as neuropathy. A panel of integrative oncology experts offers guidelines on these therapies (page 4). Similarly, health care workers who specialize in psychosocial oncology provide behavioral, psychological and social support for patients experiencing cancer. Elizabeth Archer-Nanda, DNP, APRN, explains more on page 14.
Quality of life is not separate from knowledge. This issue of Cancer Health offers news about metastatic breast cancer treatment (page 5), new insights on prostate cancer (page 7), basics on colon and rectal cancer (page 9), resources for people living with uterine and endometrial cancer (page 15) and much more. Finally, a person’s quality of life can be enhanced by something as simple as soft pajamas, soothing fruit smoothies, Chemo Care Kits and books on mindfulness. Turn to page 16 for more winter comforts. Enjoy.
Cancer Health
EDITOR-IN-CHIEF
Trent Straube
MANAGING EDITOR Jennifer Morton SCIENCE EDITOR Liz Highleyman
EDITOR-AT-LARGE Bob Barnett
NEWS WRITERS
Sukanya Charuchandra; Laura Schmidt
COPY CHIEF Joe Mejía
ART DIRECTOR Doriot Kim
ART PRODUCTION MANAGER


Michael Halliday
ADVISORY BOARD
Dena Battle; Jamie Ennis Boyd; Catherine Guthrie; Timothy Henrich, MD; Carl June, MD; Leigh Leibel, MSc; Yung Lie, PhD; Gilberto Lopes, MD; Jennifer L. McQuade, MD; Amelie Ramirez, DPH; Hope Rugo, MD; Kelly Shanahan, MD; Carla Tardif
FEEDBACK Email: info@cancerhealth.com
SMART + STRONG
PRESIDENT AND COO Ian E. Anderson

EDITORIAL DIRECTOR Oriol R. Gutierrez Jr.
CHIEF TECHNOLOGY OFFICER Christian Evans
VICE PRESIDENT, INTEGRATED SALES Diane Anderson
INTEGRATED ADVERTISING MANAGER Jonathan Gaskell
INTEGRATED ADVERTISING COORDINATOR Sarah Pursell
SALES OFFICE 212-938-2051 sales@cancerhealth.com BULK SUBSCRIPTIONS order.cancerhealth.com or subs@cancerhealth.com
CDM PUBLISHING, LLC
CHIEF EXECUTIVE OFFICER
Jeremy Grayzel
CONTROLLER
Joel Kaplan
Cancer Health (ISSN 2688-6200) Issue No. 20. Copyright © 2023 CDM Publishing, LLC. All rights reserved. No part of this publication may be reproduced, stored in any retrieval system or transmitted, in any form by any means, electronic, mechanical, photocopying, recording or otherwise without the written permission of the publisher. Smart + Strong® and Cancer Health™ are registered trademarks of CDM Publishing, LLC. Cancer Health is BPA audited.
TRENT STRAUBE
Editor-in-Chief trents@cancerhealth.com Twitter: @trentonstraube
(STRAUBE) JOHNNIE CUELLAR; (ILLUSTRATION) ISTOCK 2 CancerHealth WINTER 2023 cancerhealth.com FROM THE EDITOR
TM
MAKE THE HEALTHY CALL




Stand Up To Cancer and Optum® want to help you reduce your risk of cancer so... TAKE THE PLEDGE to get screened and learn more about cancer prevention.




To learn more and get helpful resources, visit TakeAHealthyStand.org
a 501(c)(3) charitable organization.

 Stand Up To Cancer is a division of the Entertainment Industry Foundation (EIF),
Photo By FRED SIEGEL
Stand Up To Cancer Ambassadors JOE BUCK & JOHN SMOLTZ
Stand Up To Cancer is a division of the Entertainment Industry Foundation (EIF),
Photo By FRED SIEGEL
Stand Up To Cancer Ambassadors JOE BUCK & JOHN SMOLTZ
COVID CONCERNS
As much of the world returns to normal, people with cancer continue to be at greater risk for COVID-19. But this risk is not evenly distributed: People with blood cancers and those receiving immune-suppressing treatments are most prone to severe illness and inadequate vaccine protection.
In September, the National Comprehensive Cancer Network (NCCN) released updated COVID vaccine recommendations. The guidelines advise that people with cancer should receive a new bivalent booster, note that the vaccines are safe for patients receiving immunotherapy and recommend revaccination after receiving a stem cell transplant or CAR-T therapy. The revised guidelines also add recommendations for children with cancer.
The Pfizer-BioNTech and
Moderna bivalent boosters, authorized by the Food and Drug Administration (FDA) in August, protect against both the original SARS-CoV-2 strain and BA.4 and BA.5 omicron variants. The Centers for Disease Control and Prevention recommends a bivalent booster for all adults and for children ages 5 and up. It can be administered two months after the last shot or at least three months after a bout of COVID. The FDA also recently authorized the new Novavax vaccine, but NCCN does not recommend it due to limited data on its effectiveness for cancer patients.
Because some people with cancer don’t respond as well to vaccines, NCCN recommends the monoclonal antibody combination Evusheld (tixagevimab plus cilgavimab)
as pre-exposure prophylaxis for immunocompromised patients. However, the FDA recently warned that Evusheld may not be as effective against certain SARS-CoV-2 variants. For maximum protection, experts recommend that people with cancer continue to wear a mask, maintain social distancing and avoid crowds.

“We’re at a new stage of COVID,” says Steve Pergam, MD, of the Fred Hutchinson Cancer Center in Seattle. “We’ve moved from control and prevention into a phase that’s about openness and getting back to reality. That’s a hard shift for the immunocompromised.”
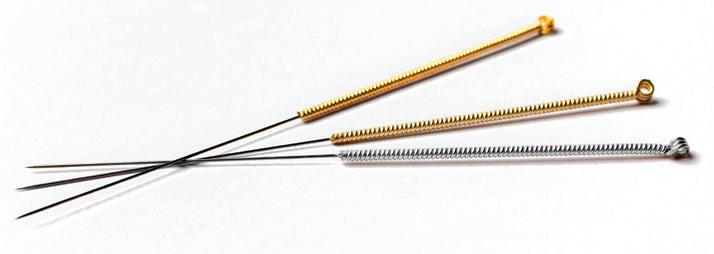
Integrative Therapies for Cancer Pain
The Society for
Oncology and the
Clinical Oncology have released new practice guidelines on the use of integrative approaches for managing cancerrelated pain. Integrative oncology employs healing practices from different traditions along with conventional cancer treatment.
Society
An expert panel developed a set of evidencebased recommendations, including acupuncture for patients experiencing joint pain related to breast cancer treatment or peripheral neuropathy due to chemotherapy. Acupressure, reflexology, yoga, massage therapy, hypnosis, music thera-
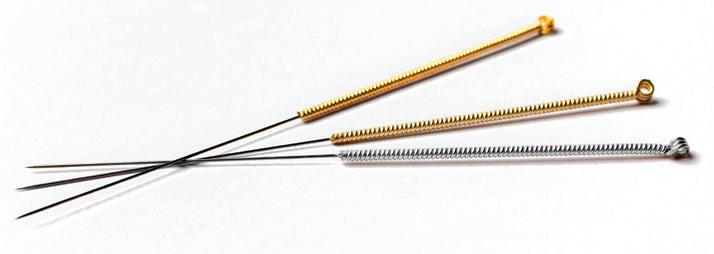
py and guided imagery may be offered in specific circumstances. Other complementary approaches are potentially relevant to cancer care but need more research.
Many comprehensive cancer centers offer integrative therapies, but these can be harder to come by in community hospitals and other care settings. “We are hoping that by showing the growing evidence that is out there, health care systems will start hiring these kinds of practitioners and insurance systems will start covering these treatments,” says Eduardo Bruera, MD, of MD Anderson Cancer Center.
4 Cancer Health WINTER 2023 cancerhealth.com
Integrative
American
of
CARE & TREATMENT BY LIZ HIGHLEYMAN
CHANGING CAUSES OF LIVER CANCER
The causes of liver cancer are changing worldwide, with fewer cases resulting from viral hepatitis and more cases related to fatty liver disease or alcohol use. Liver cancer is often diagnosed late, when it is difficult to treat, and it is among the fastest-rising causes of cancer death in the United States.
Using data from the Global Burden of Disease study, Rohit Loomba, MD, of the University of California San Diego School of Medicine, and colleagues estimated that there were 534,000 new cases of liver cancer and 485,000 liver cancer deaths worldwide in 2019. This represents a 27% increase in liver cancer incidence and a 25% increase in mortality since 2010. Yet after adjusting for age, worldwide incidence and death rates did not change significantly— except for a sharp rise in the Americas.
Liver cancer deaths related to viral hepatitis declined worldwide thanks to widespread hepatitis B vaccination and treatment and effective therapy for hepatitis C. Direct-acting antiviral (DAA) medications can cure more than 90% of people with hepatitis C. One recent study found that as cure rates increased over time, liver cancer outcomes also improved. Five-year survival rates rose from 59% during 1999–2005 to 78% during 2014–2019, after the advent of modern DAAs. But a recent analysis from the Centers for Disease Control and Prevention found that less than one third of people with hepatitis C in the United States receive timely treatment.
During this time, advanced fatty liver disease (non-alcoholic steatohepatitis, or NASH) became the fastest-growing cause of liver cancer death worldwide, likely due to rising obesity rates, and alcohol use was the second fastest-rising cause. “Urgent measures are required at a global level to tackle underlying metabolic risk factors and slow the growing burden of NASH-associated liver cancer, especially in the Americas,” the study authors wrote.

For more care and treatment news: cancerhealth.com/science-news
Trodelvy for Metastatic Breast Cancer
The antibody-drug conjugate Trodelvy (sacituzumab govitecan) improved overall survival for women with HER2-negative metastatic breast cancer who had extensive prior treatment experience, researchers reported at the European Society for Medical Oncology Congress.
In the Phase III TROPiCS-02 trial, 543 patients with hormone receptor-positive/ HER2-negative metastatic breast cancer were randomly assigned to receive either Trodelvy or an additional course of chemotherapy selected by their physician. Trodelvy uses a monoclonal antibody to deliver a potent chemotherapy drug directly to cancer cells. It is currently approved for advanced triple-negative breast cancer and bladder cancer.
Patients treated with Trodelvy had a median overall survival time of 14.4 months versus 11.2 months for those who received another round of chemotherapy— a 21% reduction in the risk for death. Trodelvy also improved progression-free survival by 34%. The treatment was generally safe, although side effects were common. Nonetheless, women who received Trodelvy reported less fatigue and delayed deterioration in their quality of life.
“It is outstanding to see a clinically meaningful survival benefit of over three months for patients with pretreated HR-positive/HER2-negative metastatic breast cancer,” says trial investigator Hope Rugo, MD, of the University of California San Francisco.

ALL IMAGES: ISTOCK (MODELS USED FOR ILLUSTRATIVE PURPOSES ONLY)
IN THE SPOTLIGHT
SHARING THEIR CANCER JOURNEYS
• Hall of Fame quarterback and Fox NFL Sunday cohost Terry Bradshaw scored a touchdown for cancer awareness when he announced, on air, that he overcame cancer twice in the span of a year: bladder cancer and Merkel cell carcinoma. “Folks, I may not look like my old self,” he said in October, “but I feel like my old self. I’m cancer-free. And over time, I’m going to be back to where I normally am.”


• Journalist Katie Couric is no stranger to cancer advocacy—after losing her first husband to the disease, she broadcast her colonoscopy on Today in 2000. So when Couric was diagnosed with breast cancer in the summer, she shared her story and some knowledge. “Forty-five percent of women in this country (yes, nearly half) have dense breasts, which can make it difficult for mammograms alone to detect abnormalities,” she wrote on Katie Couric Media. In short: The denser your breasts, the higher your risk of cancer.

• During a routine checkup, Monty Python comedy legend Eric Idle learned he had earlystage pancreatic cancer. The cancer’s gone, but an advocate emerged. In an often humorous essay in Time, Idle hits a serious note: “I encourage people in families at high risk of pancreatic cancer to explore the newer tests available for detecting the disease early.” He also appeared on the The Masked Singer to see whether he could still perform after his cancer treatment, and he partnered with research charity Stand Up To Cancer to start the Bright Side Fund to raise money and help others.



• Meanwhile, newly elected governor of Arkansas (and former White House press secretary) Sarah Huckabee Sanders and actress Jane Fonda each took to social media to share cancer stories. After learning she had thyroid cancer, Sanders underwent successful surgery to remove her thyroid and surrounding lymph nodes and is now cancerfree. “The experience has been a reminder,” she added, “that whatever battle you may be facing, don’t lose heart.” Fonda also conveyed hope and


added a social message. “I’ve been diagnosed with non-Hodgkin’s lymphoma and have started chemo treatments,” Fonda wrote. “This is a very treatable cancer. 80% survive, so I feel very lucky. I’m also lucky because I have health insurance and access to the best doctors and treatments. Far too many [families] don’t have access to the quality health care I am receiving, and this is not right.”
Clockwise from top left: Eric Idle, Katie Couric, Terry Bradshaw, Lynda Carter Altman, Mary J. Blige, Ryan Reynolds, Sarah Huckabee Sanders and Jane Fonda

PROMOTING RESEARCH AND PREVENTION

• After losing her husband to myelofibrosis, a bone marrow cancer, Lynda Carter Altman—the original Wonder Woman—partnered with TGen and City of Hope to establish a fund to study the blood cancer and raise awareness.





• To help encourage breast cancer screenings, Paris Hilton shared photos and video of her MRI scan with her 20.5 million Instagram followers.

• When actor Ryan Reynolds lost a bet with Rob McElhenney, he documented his colonoscopy and posted it on YouTube (along with McElhenny’s screening) in partnership with Lead From Behind, aiming to “make colon cancer famous.”







• R&B legend Mary J. Blige joined First Lady Jill Biden and the American Cancer Society at the White House to kick off a series of national roundtable discussions on breast and cervical cancers. The effort dovetails with the Biden administration’s Cancer Moonshot initiative.

Get more cancer news: cancerhealth.com/news





















(IDLE) CC BY 2.0/EDUARDO UNDA-SANZANA; (COURIC) LEV RADIN/SHUTTERSTOCK.COM; (BRADSHAW) TWITTER/@NFLONFOX; (CARTER ALTMAN) YOUTUBE/ TODAY WITH HODA & JENNA ; (BLIGE) TWITTER/@ROYJENSENMD; (FONDA) INSTAGRAM/@JANEFONDA; (REYNOLDS) YOUTUBE/RYAN REYNOLDS; (SANDERS) CC BY-SA 4.0/YAKAHA88




















6 CancerHealth WINTER 2023 cancerhealth.com
A roundup of celebrities who made cancer news and raised awareness
NEWS BY TRENT STRAUBE
NEW INSIGHTS ON PROSTATE CANCER



Boosting Patient Navigation














Patient
Patient navigators guide people through the health care system by coordinating appointments, connecting folks to services and resources (such as clinical trials and genetic testing) and much more. To support this vital element of health care, the American Cancer Society awarded $4.2 million in patient navigation grants to 14 health care systems. At the University of Utah’s Huntsman Cancer Institute, the funding will help navigators connect with rural cancer patients in the Mountain West, including Idaho, Montana, Nevada, Utah and Wyoming, where people are more likely to be diagnosed with latestage cancer and less likely to have access to standard-of-care treatment.
From left: Huntsman patient navigators Karlie Allen, Nathan Begaye and Liliana Mulato

Over 1,000 men with metastatic and advanced prostate cancer have offered their insights, medical records and genetic samples (saliva, blood biopsies or tumor tissue) to a growing database at the Metastatic Prostate Cancer Project (mpcproject.org). The patient-driven initiative gathers data sets and makes them publicly available to scientists in order to speed up discoveries. Researchers at the MPC Project— a collaboration between MIT’s Broad Institute and the Dana-Farber Cancer Institute—published a paper detailing the results of the project thus far, including confirmation that collecting blood biopsies can lead to valuable findings. What’s more, the project helps narrow geographic gaps by including rural cancer patients in the genomic data; it also allows for greater racial and ethnic diversity (in the United States, Black men have the highest prostate cancer mortality rate).

Two related but separate studies underscore that genetic ancestry can affect tumor biology. Research led by Clayton Yates, PhD, the director of the Center for Biomedical Research at Tuskegee University, found that prostate tumors from men of African descent were more likely to have specific mutations—“an exciting discovery,” Yates notes, that could lead to targeted, more effective prostate cancer treatment.
BREAST CANCER AND BLACK WOMEN
First, the good news: Breast cancer death rates dropped by 43% from 1989 to 2020, and they’re declining for every racial and ethnic group except American Indian and Alaska Native women, for whom the rates are stable, according to the American Cancer Society’s Breast Cancer Statistics, 2022. However, Black women continue to be 40% more likely to die of the disease despite having lower incidence of the cancer. “There is an alarming persistent gap for Black women,” noted Rebecca Siegel, MPH, the report’s senior author. “This is not new, and it is not explained by more aggressive cancer. It is time for health systems to take a hard look at how they are caring differently for Black women.”

(ALLEN, BEGAYE AND MULATO) COURTESY OF UNIVERSITY OF UTAH/HUNTSMAN CANCER INSTITUTE; (HAND & PHONE) ISTOCK
cancerhealth.com WINTER2023 CancerHealth 7
Dear Cancer Patient
Patient advocate Melvin Mann was diagnosed with chronic myeloid leukemia in 1995. He has been in treatment and in remission since 1998.

I HEAR YOU’VE BEEN DIAGNOSED WITH CANCER. I’VE BEEN living with cancer for a long time, and I’ve learned a few lessons in my cancer journey. Let me share a few.
First, any cancer diagnosis is serious, so do not compare your situation with others. There is no “good cancer.”

You may be in shock. That’s normal. So is experiencing stages of grief, especially when faced with devastating news.
There is no right way to deal with cancer. Some people may not want to miss a day of work, while others do not want to get out of bed. You may want to tell nearly everyone about your illness or share it with only a close few. It’s OK to express—or not to express—anxiety, anger, depression. It’s OK to shed tears or not.
Not everyone will validate your feelings, even if they mean well. It’s not your job to make that person feel a certain way. You do not have to listen to lectures about how you should feel or how you do not have enough faith or the right attitude to become well.
While the news is sinking in, this is a good time to get a second opinion. Doctors have different approaches, and medical centers have different capabilities. Even labs and pathology reports may have different interpretations.
Research your illness. Reach out to groups that deal with your cancer; they can provide resources and connect you with patients and caregivers. Think about joining a support group, whether in person or online.
Ask about clinical trials. Some study drugs are available years before the Food and Drug Administration approves them. Even the current standard of care was available to some before it
became the first-line therapy.
As a patient, you don’t need to be passive or aggressive, but do aim to be assertive. Keep up with your records and medications, ask your doctor questions, listen carefully and keep those closest to you up to date. Bring someone with you to appointments; you may not hear or remember everything. Think about establishing a support team of people who can assist you throughout your journey. Remember to thank them, as caregiving is not an easy task.
During your treatment, you probably will experience some fatigue, nausea and pain. These side effects may not be visible to others. (In fact, some may even say, “You don’t look sick.”) Rest when you need to. It’s OK to say no to requests and conserve energy for your cancer journey.
Stay hydrated and eat well. You may not always have the appetite to eat, but do try to
keep your weight up. Get outside in the fresh air for a bit of exercise if you can, as this can help on many fronts.
Do your best at keeping your spirits up. This may involve trying integrative therapies (such as meditation, yoga and tai chi), watching comedies, accepting help, forgiving others, listening to music, seeking spiritual connections and doing things that you enjoy. What works for you is unique to you.
Maintain hope. You are not a statistic. You are an individual. You are more than a cancer patient. Keep doing the things that you enjoy, as you are still you.
After you finish your treatment, consider paying it forward. Share the knowledge you’ve gained, raise awareness, become a patient advocate or find another activity that supports cancer patients. Lastly, keep your head up! ■
COURTESY OF MELVIN MANN VOICES BY MELVIN MANN 8 CancerHealth WINTER 2023 cancerhealth.com
Melvin Mann shares advice for living with cancer.
Colon and Rectal Cancer
Routine screening can detect colorectal cancer at an early stage, when it’s easier to treat.
COLON AND RECTAL CANCER, collectively known as colorectal cancer, develop when cells grow out of control in the colon or rectum, sections of the large intestine. Cancer may also arise elsewhere and spread to the intestines.
Colorectal cancer is the second leading cause of cancer death in the United States, after lung cancer. Although cases and deaths have been declining for several decades—thanks to screening, lifestyle changes and better treatment—incidence is rising among younger adults.
Colorectal cancer mostly occurs among people over 50. African Americans have the highest rate in the United States. Other unchangeable risk factors include genetics (for example, an inherited condition called Lynch syndrome), family history and inflammatory bowel disease.
Lifestyle factors also play a role. Obesity, lack of physical activity, smoking, alcohol and a diet high in red and processed meats increase the risk for colorectal cancer, while a diet high in fruits, vegetables and whole grains has a protective effect.
Many people with colorectal cancer don’t develop symptoms until the later stages of disease, but screening can catch cancer early, when it’s easier to treat. Fecal tests look for blood or DNA changes in a stool sample; these tests can be done at
Learn more cancer basics: cancerhealth.com/basics
home. Visualization tests involve viewing either the entire colon (colonoscopy) or the lower part of the colon and rectum (sigmoidoscopy) to detect and remove polyps, or abnormal precancerous growths.
As of 2021, U.S. guidelines recommend that people at average risk should be screened for colorectal cancer starting at age 45 (down from age 50 in the previous guidelines). However, people at higher risk may benefit from starting screening sooner. Both fecal tests and visualization tests are recommended— the most effective test is the one that gets done.
Treatment for colorectal cancer depends on the location, size and number of tumors and whether the cancer has spread to nearby lymph nodes or other parts of the body. Precancerous growths and localized tumors in the colon and rectum can often be surgically removed. More advanced cancer may require

removal of part of the intestine. Radiation may be used to shrink tumors, which can help relieve pain and other symptoms.
Systemic therapy is administered by mouth or via IV infusion. Neoadjuvant therapy is given before surgery to shrink tumors and make them easier to remove, while adjuvant therapy is given after surgery to kill off any remaining malignant cells and reduce the risk of recurrence.
Traditional chemotherapy works by killing fastgrowing cells, including cancer cells. Many targeted therapies work by interfering with tumor development. Erbitux (cetuximab) and Vectibix (panitumumab), for example, block the activity of EGFR, a protein involved in cell growth, while Avastin (bevacizumab) and Cyramza (ramucirumab) target VEGF, a protein that promotes the development of blood vessels that feed tumors. Immunotherapy helps the immune system fight cancer. The checkpoint inhibitors Jemperli (dostarlimab), Keytruda (pembrolizumab), Opdivo (nivolumab) and Yervoy (ipilimumab) are used to treat colorectal cancer with specific genetic characteristics.
Colorectal cancer treatment continues to evolve, and several new therapies are under study. Ask your doctor whether a clinical trial might be a good option for you. ■
ISTOCK BASICS BY LIZ HIGHLEYMAN
cancerhealth.com WINTER 2023 CancerHealth 9
Meditation transformed his life, and now he gives back to others with cancer.

Emotions play a powerful role in living with cancer, a truth AJ Patel learned a decade ago when he was diagnosed with metastatic lung cancer.
BY JENNIFER COOK
FEAR—OF DEATH, OF PAIN, OF disability, of the unknown—can be overwhelming for someone who has cancer.

When you’re in its paralyzing grip, it can be nearly impossible to think clearly and make decisions. It can even lead to delays in critical tests and lifesustaining treatments.
AJ Patel is intimately familiar with that kind of fear. It took up residence in his psyche in 2013 when he was diagnosed with Stage IV metastatic nonsmallcell lung cancer (NSCLC). At the time, he was a 47yearold physically fit runner and semiprofessional soccer referee living in Irvine, California, with his wife of 20 years and their daughter (age 10) and two sons (12 and 17). He worked as a legal analyst for a large insurance company (and still does). “I rarely saw a doctor,” he says. “I was rarely sick.”
Two years earlier, in 2011, first his kids and then his work colleagues noticed that he was constantly clearing his throat. So he saw his primary care doctor, who referred him to an ear, nose and throat specialist, who in turn recommended an allergist. Over the next two years, “I was bouncing around from physician to physician with no real solution,” Patel says. Meanwhile, his throat congestion was getting worse. In February 2013, Patel changed physicians and pressed his new doctor to do more testing. A lung Xray revealed a nodule in his left lung, but the doctor saw no reason to worry and recommended repeating the Xray in six months if symptoms persisted. That June, on a family trip, he coughed up blood, but he didn’t want
to upset the happy gathering, so he didn’t tell his wife until it happened again in July. He was in a panic, wondering whether he had tuberculosis (TB) because, he remembered, “people cough up blood with TB.”
He did test positive for TB but only because of the TB vaccine he had received as a toddler in the United Kingdom (his parents had emigrated there from India). Next, the doctor ordered another chest Xray, which showed the same nodule. Patel pressed for more testing, so his doctor ordered a CT scan. It revealed lung masses suggestive of metastatic cancer. It had been a tragedy of errors.
BUILDING A HOUSE OF FEAR
Patel’s doctor sent him home with a business card for a pulmonologist, but when his wife called for an appointment, neither that doctor nor dozens of others she called could see her husband for months. “I was crying every day, thinking, What’s wrong with me? Why do I have these masses? Do I really have cancer?” he recalls. Finally, after three days of nonstop calling, his wife secured an appointment with a pulmonologist, who looked at the CT film and ordered a biopsy. On Patel’s second visit, the doctor cried on his shoulder, telling him, “I’m sorry, but you have lung cancer, and it’s really serious.”
Patel was having none of it. He believed that only smokers got lung cancer (in actuality, about 20% of people with lung cancer never smoked), and his previous medical encounters had left him skeptical and distrustful. “You can’t be looking at AJ Patel,” he said. “I don’t believe your
cancerhealth.com WINTER 2023 Cancer Health 11 ARI MICHELSON
chart. I don’t believe the diagnosis. I just need to go away and think about this.” In response, his doctor said, “AJ, if you don’t do something, you will die in six months.”
The foundation for fear had already been built, recalls Patel, “but now I was beginning to feel the framing of the house of death.” All he could think about was not being around to celebrate Christmas with his family. After 10 miserable days, he forced himself to search the internet. There, he saw gloom and doom, including a 5% five-year survival rate. “If I went into a depression spiral, I went right there,” he says.
But after a day of web surfing, a link to LUNGevity and the words “a foundation for lung cancer patients and survivors” caught his eye. He dialed the website’s patient advocate number, and, to his astonishment, a woman answered. “The empathy, care and concern was so overpowering,” he says. The woman recommended that he see an oncologist specializing in lung cancer and gave him the name of one nearby. Hearing his despair, she also connected him with Matt Ellefson in South Dakota, who had been living with Stage IV lung cancer for four years.
“For someone like me, suspected to be Stage IV, hearing someone surviving four years was really encouraging and uplifting,” Patel says. “It gave me strength and hope, which is what cancer patients really need. Suddenly, the house of death being constructed in my head fell apart.”
That conversation also helped provide Patel with the tools he needed to advocate for himself. “Matt educated me completely about the disease, what I should expect in my first meeting with the oncologist, what kind of questions to ask,” he says. It was like a crash course on NSCLC from a Stage IV survivor who knew all the ins and outs.
Morebadnewswascoming,however.Thelungoncologist Patel consulted sent him for a brain MRI, which revealed numerous brain tumors—his cancer had metastasized.
THE UNCLE WHO STEPPED UP
Growing up in London, Patel had lived with an uncle, a successful businessman, for six years as he completed high school. He found this uncle rude and abrasive, although usually right. His uncle opposed Patel’s move to the United States (Patel emigrated in 1997). They didn’t speak for years. But when Patel was diagnosed with cancer, he mentioned it to his uncle’s son, a cousin with whom he got along better. “The next thing I knew, my uncle called and said, ‘What’s going on? Let me get on FaceTime with the doctors,’” he says. “He was on
FaceTime with everybody, and I was thinking, I’m so grateful this guy is here. He’s fighting in my camp. Every question was really powerful.”
His uncle supported Patel in his decision to have a craniotomy in September 2013 to remove two brain tumors. It was his first surgery—he hadn’t been a candidate for lung surgery—so it also provided tissue for genetic biomarker testing for the first time. During the surgery, Patel says, “I had so many seizures on the table, they thought they were going to lose me.”
Afterward, when he was in intensive care, his uncle, who had flown in for the operation, pushed the neurosurgeon to summon a neurologist to manage the electrical activity in his nephew’s brain minute by minute until he was stable, likely saving his life. “It was very powerful to know that I had this kind of pit bull in my tool bag who could advocate for me when my voice was taken away from me,” Patel says, choking up.
One day, while Patel was still in the hospital, his oncologist entered his room excitedly waving her arms: She had found a biomarker for his tumor. It was ROS1, a mutation only around 1% of people with NSCLC have. Although there wasn’t a specific treatment at that time, his oncologist prescribed a medication intended for those with the more common ALK biomarker. “She realized from her analysis of the drug profile that it should work for me,” he says. “It turned out to be the best thing in my life because it changed the trajectory of my treatment.”
HOW THE HOUSE OF FEAR CRUMBLED
Nonetheless, for the next two years, Patel struggled with depression. His recovery from surgery was slow and laborious; the brain tumors had affected the right side of his body and his motor skills. He spent months relearning to walk, and his right hand is permanently impaired. He endured radiation to his brain and four rounds of grueling chemotherapy, which has caused neuropathy in his hands and feet. He lived in three-month intervals, from scan to scan, in anticipation of bad news. “I couldn’t shake the house of fear and death.”
Questions plagued Patel: Why had he gotten cancer? Was he a bad person? If so, where had he gone wrong? But he couldn’t find answers “from God or any church or synagogue or anywhere.” Then someone suggested meditation. In November 2016, he signed up for a 10-day course of Vipassana, an ancient breath-based meditation. Every day from 4:30 a.m. to 9 p.m., except for meal and bathroom
12 CancerHealth WINTER 2023 cancerhealth.com
breaks, he sat in silent meditation. “Within five minutes, my legs and back began to hurt. I couldn’t feel my toes anymore. I thought, There’s no way I can survive this,” Patel says. But with nowhere else to turn, he persisted, motivated by the others surrounding him. On day four, he had an epiphany. The pain in his legs and back disappeared and didn’t return, and he could focus on the teachings.
“Theexperiencecompletelychanged my life,” he says. “I touched within me a dimension that is impossible to explain, something that opened up like a flower. I was able to understand things that I had never understood.”
Since then, Patel’s life has been transformed. He continues to meditate for the calm that it brings him, his mat nearby so he can snatch 10-minute meditation “naps.” “I’ve discovered what people regard as a higher power or bliss is really within us,”hesays.HehasbeenontheALK/ ROS1 inhibitor he was originally prescribed for nine years now, and though he still has challenges, he says, “I don’t worry about them. I feel a lot happier, and the house of death that I had has all crumbled and been eviscerated. I’m no longer fearful, no longer scared of any treatment. I’m no longer scared of death. This has been a beautiful gift.”
GIVING BACK
Patel was a shy introvert when he was diagnosed with NSCLC and too embarrassed to tell his story. But a friend encouraged him to reach out and help others, telling Patel that he had a special way of communicating that could help those in need who have cancer. “Hope is a commodity
MEDITATION BENEFITS FOR PEOPLE WITH CANCER
Meditation encompasses a wide variety of practices to calm the mind and body and enhance well-being. Some forms involve focusing on the breath, a sound, a visual image or a silently repeated word or phrase. Others include the practice of mindfulness, which focuses awareness on the present moment without judgment.
A 2019 analysis of 29 studies of mindfulness-based meditation that included a total of more than 3,000 people with cancer found that the practice significantly reduced psychological distress, anxiety, depression, fear of cancer recurrence, fatigue, sleep disturbances and pain. People with different kinds of cancer as well as those at different disease stages were found to benefit.
To get started, ask whether your oncologist knows of any classes or meditation teachers in your area. Some large comprehensive cancer centers offer this and other mind-body practices. You can also find links to meditation instruction by searching under “Meditation” on the MD Anderson Cancer Center (mdanderson.org) and the Memorial Sloan Kettering Cancer Center (mskcc.org) websites. The free versions of the apps Headspace (headspace.com) and Calm (calm.com), while not specifically geared to people with cancer, are also helpful.
that I didn’t realize is better than gold. It carries people forward,” he says. “I realized that my voice can make a difference.”
Patel has become an advocate for people with many forms of cancer and their families. He consults with the Department of Defense, advising scientists from a patient perspective as they allocate lung cancer research funds. Patel has also worked with pharmaceutical companies and testing companies, and he successfully advocated for a 2021 California law expanding patient access to the kind of cancer biomarker testing that helped him survive. He works with the Lung Cancer Foundation of America (LCFA), which supports lung cancer research, appearing in several of their Hope With Answers podcasts, and he has a blog linked to the LCFA website (lcfamerica.org/ survivor/aj-patel).
“When you are told that you have any stage or kind of cancer, you have been given a warning letter that your life is in jeopardy,” Patel says. It’s critical to sit down and take stock. “Reexamine your life and realize that the things you’re griping about—the bills, your job, the mortgage—are all physical things, tangible things, that are just temporary. The only thing that is permanent is the people that you touch, whether strangers or not; when you touch somebody, they will remember. So just stick out your hand, lift them up as best you can and move on, keep marching forward. And that will enrich your life. It will touch your soul, and it will touch the other person, whether they realize it in that moment or not. You will have just improved humankind.” ■
cancerhealth.com WINTER 2023 Cancer Health 13
Psychosocial Support
Psychiatric clinical nurse specialist Elizabeth Archer-Nanda, DNP, APRN, is the president of the American Psychosocial Oncology Society.

What is psychosocial oncology?
It’s a field that provides psychological, behavioral and social support for patients going through cancer. I manage the behavioral oncology program at the Norton Cancer Institute in Louisville, Kentucky. As providers, we help to reduce cancer-related distress that may come in the form of physical distress, emotional distress, family problems, physical problems, spiritual problems and practical problems. Psychosocial oncology providers may include advanced practice nurses, social workers, psychologists, psychiatrists or chaplains.
What psychological, behavioral and social issues do you help cancer patients with?
At the onset of a new diagnosis, it’s common for patients to experience a broad range of emotions. We help them identify the thoughts and feelings they’re having about the cancer and validate that these emotions are normal. Then we help them adjust to everything that going through cancer may mean for them, such as grieving the loss of their previous health status, changes to their work capability or role changes within their family and support system.
What approaches do you use?
We meet patients where they are to help ease some of the
psychological burden that they’re carrying in their cancer trajectory. Depending on what a patient has been experiencing, we rely on different types of interventions, such as supportive counseling or therapy, cognitive and behavioral therapies, or acceptance and commitment therapy. In addition to these talk therapies, we ensure that we’re really understanding the depth and severity of psychological symptoms a patient may be experiencing so we can also connect them, when appropriate, to providers with expertise in prescribing mental health medications.
What about physical concerns?
It’s important for patients to first talk with their medical providers within the oncology realm if there
are difficulties with, for instance, pain, eating, fatigue, memory or concentration. But a psychosocial oncology provider may be able to help further explore that concern as well as other interventions to improve quality of life. For instance, if fatigue is an ongoing concern, the patient may rely on a psychosocial oncology provider for guidance around getting adequate sleep or accessing mental health medications to treat depression and anxiety that could be contributing to the fatigue.
What practical problems do you help with?
A patient may reach out to a psychosocial care provider for issues related to insurance or financial concerns or transportation, work- and school-related issues or to get help in making treatment decisions.
What inspires you in your work?
It’s a true honor for people who don’t know me to trust me and for me to be able to help them navigate something that’s really, really hard. We may work on issues that they may feel they can’t even talk about with the closest person in their family. The thing that I’m really inspired by is that I seem to have the ability to help people see that they can trust and that good things can come from that. ■
Who’s on your team? cancerhealth.com/team
14 CancerHealth WINTER 2023 cancerhealth.com YOUR TEAM BY ABBY SAJID
COURTESY OF NORTON HEALTHCARE/JAMIE RHODES
Elizabeth Archer-Nanda, DNP, APRN
Uterine and Endometrial Cancer
THESE WEBSITES OFFER EDUCATION AND SUPPORT FOR PEOPLE WITH uterine cancer, known as endometrial cancer when it starts in the uterine lining.
The American College of Obstetricians and Gynecologists (ACOG) acog.org
ACOG, the national professional organization for ob-gyns, provides patient education about uterine and endometrial cancer. Its Frequently Asked Questions page covers risk factors, symptoms, diagnosis methods and treatments. ACOG.com features a convenient glossary of the common terms associated with uterine and endometrial cancer.

Cancer.Net cancer.net
The patient website for the American Society of Clinical Oncology, the world’s largest professional cancer organization, offers an integrated set of resources related to uterine and endometrial cancer. Cancer.net provides frequently updated doctor-reviewed articles about different uterine cancer diagnoses and treatments, and the site features articles about coping with various aspects of cancer.
CancerCare cancercare.org
CancerCare offers a Women’s Cancers Program that provides specialized services and resources, such as skin care
Discover more resources: cancerhealth.com/resources
products and wigs, to empower individuals to manage cancer with confidence. You can learn to cope with your illness by connecting with an oncology social worker for support and advice via the free Hopeline at 800-813-HOPE (4673).
Centers for Disease Control and Prevention (CDC) cdc.gov
The CDC regularly updates its site with new statistics, studies and stories about uterine cancer. Its “Inside Knowledge” campaign aims to raise awareness and education about the five main types of gynecologic cancer: uterine, cervical, ovarian, vaginal and vulvar. In addition, the CDC’s “Gynecologic Cancers” web section provides fact sheets, posters, survivor stories and online videos (including a comedy web series) about these different cancer types.
Endometrial Cancer Action Network for African Americans (ECANA) ecanawomen.org
Black women are more likely than women of other races to be diagnosed with uterine sarcoma, the most aggressive form of uterine cancer, and are also more likely to be diagnosed
at a later stage. ECANA seeks to empower and improve the lives of Black women living with these cancers through partnerships with doctors, patients, community advocates and more.
Foundation for Women’s Cancer foundationforwomenscancer.org The Society for Gynecological Oncology’s Foundation for Women’s Cancer is a vast resource with information on all types of gynecologic cancers. Its uterine and endometrial cancer section provides basic information about symptoms, when to seek a medical evaluation, treatment options, side effects and more.
SHARE sharecancersupport.org
The national nonprofit SHARE offers educational programs and support groups specific to uterine, ovarian, cervical, vaginal and breast cancer. Offerings include yoga and meditation; programs about treatmentinduced menopause; and uterine cancer support groups for the newly diagnosed, for women of African descent and for young women. Meetings are mostly held via Zoom, so anyone anywhere can attend.
ISTOCK
cancerhealth.com WINTER 2023 CancerHealth 15
RESOURCES BY LAURA SCHMIDT
WINTER COMFORTS
Cozy up with a mindful book, soft pajamas, easy meals, stylish caps and more.

When Kelly Whitton was diagnosed with breast cancer at age 44, her friends and family weren’t sure how to help.
Whitton wasn’t sure either. After chemotherapy, 30 rounds of radiation and three surgeries, she founded CaraKit (carakit.com) to help other women living with cancer. The luxury gift company offers custom box sets, such as Chemo Care Kits ($95 to $395), Surgery Recovery Kits ($95 to $295) and Radiation Care Kits ($95 to $295), packed with quality products recommended by doctors, nurses and nutritionists. The Chemo Essential Healing Kit ($195), for example, features soft pajamas, a soothing lip balm, body cream, hydration drops, vitamin E oils, an essential oil roller, Epsom salt, sugar-free soft caramels and a planner.
Many people treated for cancer experience side effects such as mouth sores, loss of appetite and taste changes, which can lead to malnourishment, which in turn can affect treatment efficacy and survival. For quick relief, try these cold fruit smoothies, which are nutritious, easy to swallow and soothing to the mouth and throat. Daily Harvest (dailyharvest.com) offers several smoothie combos, including mint and cacao, strawberry and peach, and chocolate and blueberry ($5.99). The meal delivery service, which uses ethically sourced fruits and vegetables, offers more items that can be prepared in minutes, including harvest bowls, soups, snack scoops and more (prices vary).



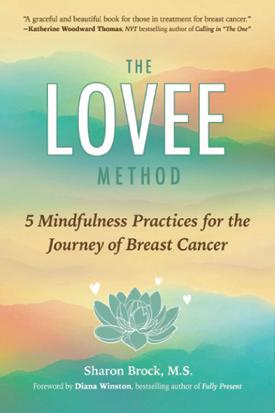
Health journalist and breast cancer survivor Sharon Brock combines Western medicine with Eastern traditions in her book The LOVEE
Chemotherapy and other cancer treatments often make teeth and gums sensitive and prone to bleeding, and a regular toothbrush’s rough, plastic bristles can cause more discomfort. Instead, try the gentle Vegols toothbrush ($10.99 for a six-pack), which has 20,000 ultrasoft, flexible bristles designed to get to those hard-toreach spots. The toothbrush is also equipped with a tongue scrubber to help minimize bad breath.

Plus, come in
Method: 5 Mindfulness Practices for the Journey of Breast Cancer (meditationforbreastcancer.com). Brock encourages readers to start a meditation practice using her LOVEE (label, observe, value, embrace and equanimity) method. Brock writes about her personal cancer journey with honesty, humor and vulnerability, detailing her fear of death and her response to drastic changes to her body and how cancer affected her libido and love life.
readers to start a meditation practice using her LOVEE (label, observe, value, embrace and method Brock writes about her cancer journey with
Men and women can experience hair loss and scalp sensitivity from cancer treatment. These cancer caps from Hello Courage (hellocourage.com) offer comfort and confidence to people in treatment as well as those growing their hair back. Made from bamboo, they’re breathable, lightweight, stretchy and soft. Plus, they come in different sizes ($67.90 for a four-pack; available in black, dark gray, heather gray and navy blue).

Find more products to make life easier: cancerhealth.com/good-stuff

GOOD STUFF BY LAURA SCHMIDT 16 CancerHealth WINTER 2023 cancerhealth.com
ENJOY
Having cancer can make you reevaluate what’s important in your life. Please let Cancer Health know how cancer has affected the quality of your life and what actions you’ve taken to improve it.
What type(s) of cancer do you have? (Check all that apply.) ❑ Bladder ❑ Kidney ❑ Melanoma ❑ Breast ❑ Leukemia ❑ Pancreatic
Colorectal ❑ Lung ❑ Prostate ❑ Endometrial ❑ Lymphoma ❑ Thyroid ❑ Other (Please specify.): __________________
Are you currently receiving cancer treatment? ❑ Yes ❑ No
Have you experienced any of the following conditions? (Check all that apply.) ❑ Anxiety ❑ Mobility issues
Brain fog ❑ Nausea
Constipation ❑ Pain
Depression ❑ Trouble sleeping
Fatigue ❑ None of these
Have you experienced changes in any of the following because of cancer or its treatment? (Check all that apply.) ❑ Personal relationships ❑ Work ❑ Sex life ❑ None of these
Have you ever attended a cancer support group? ❑ Yes ❑ No
Do you use any relaxation techniques? ❑ Yes ❑ No

Have you made any changes to your exercise regimen as a result of your cancer diagnosis? ❑ Yes ❑ No
Have you made any changes to your diet as a result of your cancer diagnosis? ❑ Yes ❑ No
Do you frequently make time to participate in activities that you enjoy?
Yes ❑ No
Do you seek support from your family and friends?
Yes ❑ No
Do you consider quality of life issues when making treatment decisions? ❑ Yes ❑ No
What year were you born?
What is your gender?
Male ❑ Transgender
Female ❑ Other
What is your current level of education?
Some high school
High school graduate
Some college
Bachelor’s degree or higher
What is your ethnicity? (Check all that apply.)
American Indian/Alaska Native
Arab/Middle Eastern ❑ Asian
Black/African American ❑ Hispanic/Latino
Native Hawaiian/Pacific Islander
White ❑ Other _________________________
What is your ZIP code?

ISTOCK SURVEY
❑
❑
❑
❑
❑
❑
❑
❑
❑
❑
❑
❑
❑
❑
❑
❑
❑
❑
this QR code with your
to take this
to
YOUR LIFE Scan
smartphone
survey at cancerhealth.com/surveys. Or email a photo of your completed survey
website@cancerhealth.com.
. She’s a healthcare professional, adept writer, mother, and metastatic breast cancer survivor. When Thomasina first started her journey, she needed the individual attention that only a social worker could provide. She needed the financial assistance to help pay for multiple medications and doctor’s visits. She needed the motivation and tenacity to help others like her. She needed CancerCare. We’re still here for Thomasina, and we are here for you too.














































If it matters to you, it
to us.
matters
EducationalCare EmotionalCare PersonalCare SurvivorCare PetCare FinancialCare 800-813-HOPE (4673) | WWW.CANCERCARE.ORG
Thomasina








 BY JENNIFER COOK
BY JENNIFER COOK














 Stand Up To Cancer is a division of the Entertainment Industry Foundation (EIF),
Photo By FRED SIEGEL
Stand Up To Cancer Ambassadors JOE BUCK & JOHN SMOLTZ
Stand Up To Cancer is a division of the Entertainment Industry Foundation (EIF),
Photo By FRED SIEGEL
Stand Up To Cancer Ambassadors JOE BUCK & JOHN SMOLTZ