Lean on Me
Navigating life with HIV


A SMART+STRONG PUBLICATION JUNE 2023 POZ.COM $3.99
André Jordan (left) and Darius Harper
HEALTH, LIFE & HIV
IMPORTANT FACTS FOR BIKTARVY®
This is only a brief summary of important information about BIKTARVY® and does not replace talking to your healthcare provider about your condition and your treatment.
MOST IMPORTANT INFORMATION ABOUT BIKTARVY
BIKTARVY may cause serious side effects, including:
` Worsening of hepatitis B (HBV) infection. Your healthcare provider will test you for HBV. If you have both HIV-1 and HBV, your HBV may suddenly get worse if you stop taking BIKTARVY. Do not stop taking BIKTARVY without first talking to your healthcare provider, as they will need to check your health regularly for several months, and may give you HBV medicine.
ABOUT BIKTARVY
BIKTARVY is a complete, 1-pill, once-a-day prescription medicine used to treat HIV-1 in adults and children who weigh at least 55 pounds. It can either be used in people who have never taken HIV-1 medicines before, or people who are replacing their current HIV-1 medicines and whose healthcare provider determines they meet certain requirements.
BIKTARVY does not cure HIV-1 or AIDS. HIV-1 is the virus that causes AIDS.
Do NOT take BIKTARVY if you also take a medicine that contains:
` dofetilide





` rifampin




































































































































































` any other medicines to treat HIV-1
BEFORE TAKING BIKTARVY
Tell your healthcare provider if you:
` Have or have had any kidney or liver problems, including hepatitis infection.









` Have any other health problems.
` Are pregnant or plan to become pregnant. It is not known if BIKTARVY can harm your unborn baby. Tell your healthcare provider if you become pregnant while taking BIKTARVY.
` Are breastfeeding (nursing) or plan to breastfeed. Do not breastfeed. HIV-1 can be passed to the baby in breast milk.
Tell your healthcare provider about all the medicines you take:
` Keep a list that includes all prescription and over-thecounter medicines, antacids, laxatives, vitamins, and herbal supplements, and show it to your healthcare provider and pharmacist.
` BIKTARVY and other medicines may affect each other. Ask your healthcare provider and pharmacist about medicines that interact with BIKTARVY, and ask if it is safe to take BIKTARVY with all your other medicines.
POSSIBLE SIDE EFFECTS OF BIKTARVY
BIKTARVY may cause serious side effects, including:

` Those in the “Most Important Information About BIKTARVY” section.





























` Changes in your immune system. Your immune system may get stronger and begin to fight infections that may have been hidden in your body. Tell your healthcare provider if you have any new symptoms after you start taking BIKTARVY.
` Kidney problems, including kidney failure. Your healthcare provider should do blood and urine tests to check your kidneys. If you develop new or worse kidney problems, they may tell you to stop taking BIKTARVY.
` Too much lactic acid in your blood (lactic acidosis), which is a serious but rare medical emergency that can lead to death. Tell your healthcare provider right away if you get these symptoms: weakness or being more tired than usual, unusual muscle pain, being short of breath or fast breathing, stomach pain with nausea and vomiting, cold or blue hands and feet, feel dizzy or lightheaded, or a fast or abnormal heartbeat.
` Severe liver problems, which in rare cases can lead to death. Tell your healthcare provider right away if you get these symptoms: skin or the white part of your eyes turns yellow, dark “tea-colored” urine, light-colored stools, loss of appetite for several days or longer, nausea, or stomach-area pain.
` The most common side effects of BIKTARVY in clinical studies were diarrhea (6%), nausea (6%), and headache (5%).
These are not all the possible side effects of BIKTARVY. Tell your healthcare provider right away if you have any new symptoms while taking BIKTARVY. You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.FDA.gov/medwatch or call 1-800-FDA-1088. Your healthcare provider will need to do tests to monitor your health before and during treatment with BIKTARVY.
HOW TO TAKE BIKTARVY
Take BIKTARVY 1 time each day with or without food.
GET MORE INFORMATION
` This is only a brief summary of important information about BIKTARVY. Talk to your healthcare provider or pharmacist to learn more.
` Go to BIKTARVY.com or call 1-800-GILEAD-5.
` If you need help paying for your medicine, visit BIKTARVY.com for program information.
(bik-TAR-vee)
BIKTARVY, the BIKTARVY Logo, GILEAD, the GILEAD Logo, and KEEP BEING YOU are trademarks of Gilead Sciences, Inc., or its related companies. © 2023 Gilead Sciences, Inc. All rights reserved. US-BVYC-0250 04/23
#1 PRESCRIBED HIV TREATMENT*























































































No matter where life takes you,
ELIAS SWITCHED TO BIKTARVY




Because HIV doesn’t change who you are.

BIKTARVY® is a complete, 1-pill, once-a-day prescription medicine used to treat HIV-1 in certain adults. BIKTARVY does not cure HIV-1 or AIDS.





Ask your healthcare provider if BIKTARVY is right for you.
Person featured takes BIKTARVY and is compensated by Gilead.


Please see Important Facts about BIKTARVY, including important warnings, on the previous page and at BIKTARVY.com.




































*Source: IQVIA NPA Weekly, 04/19/2019 through 01/20/2023.
Listen to REAL STORIES being told by REAL VOICES.
EXCLUSIVELY ON POZ.COM
#ADVOCACY

Fighting against HIV and AIDS has always been a struggle. Much work remains to end the epidemic. POZ encourages you to get involved in advocacy. Go to poz.com/ advocacy to find the latest news and learn how you can make a difference in the fight.
#CRIMINALIZATION
Opinions still vary on whether criminal law should apply to HIV disclosure, exposure and transmission. However, there is a growing consensus to make laws reflect current science. Go to poz.com/ criminalization for more on how you can get involved in reform efforts. D



#UNDETECTABLE
The science is clear: People who have an undetectable viral load don’t transmit HIV sexually. In addition to keeping people healthy, effective HIV treatment also means HIV prevention. Go to poz.com/undetectable for more.
POZ DIGITAL
Scan the QR code (left) with your smartphone camera or go to poz.com/digital to view the current and past issues online.

20 TRAVELING WITH THE ANCESTORS Photographer and activist Lola Flash brings four decades of their work together in a new photo book.
BY POZ STAFF
24 LEAN ON ME Friends André Jordan and Darius Harper, both actors, navigate life with HIV.
BY ALICIA GREEN
14 BASICS
Gonorrhea
4 POZ Q & A
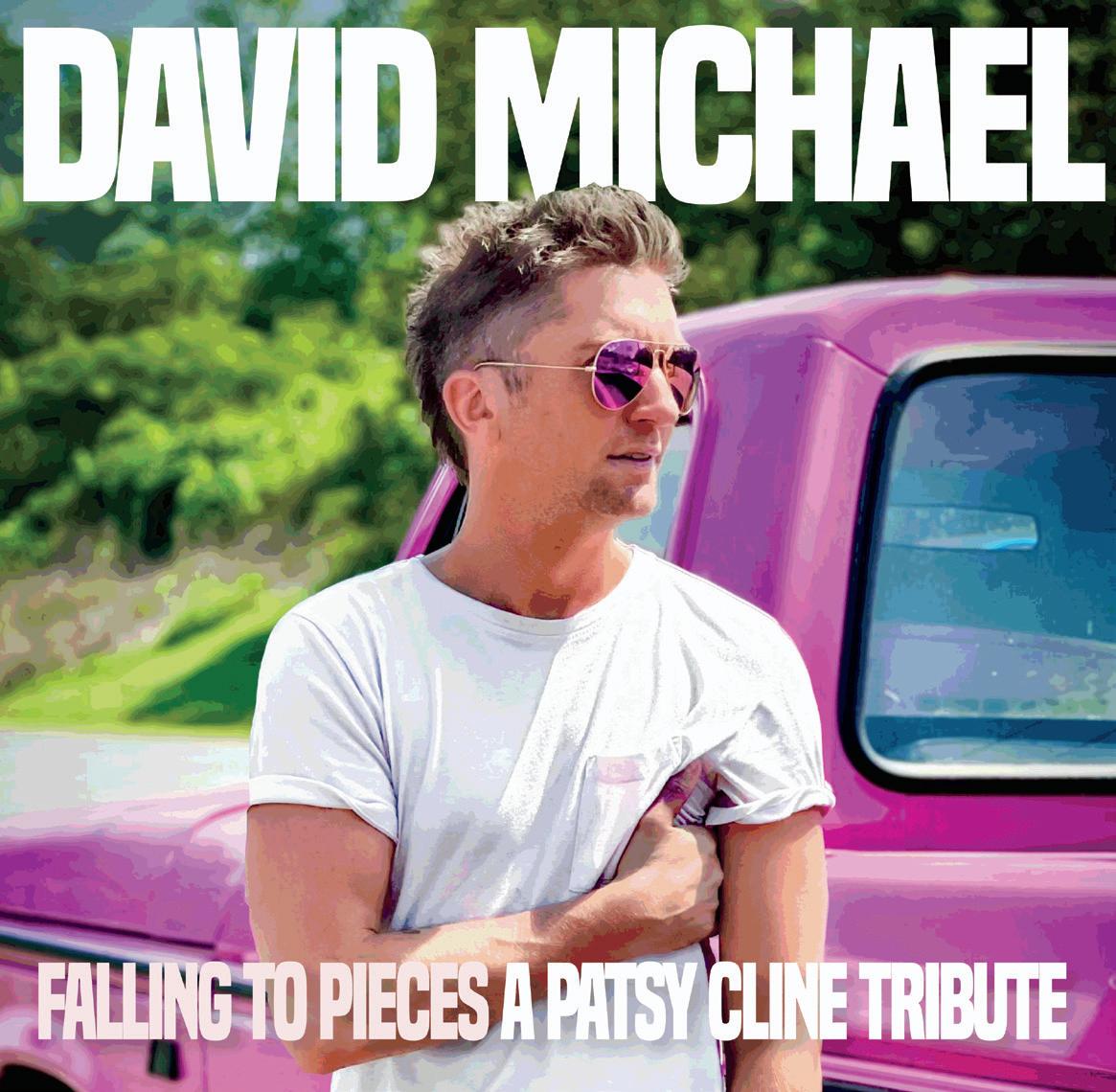
Country singer David Michael shares his journey living with HIV in South Carolina, Tennessee and the Land of Oz.
6 POZ PLANET
Elton John’s Oscar party raises $9 million to end HIV • Adam Lambert stars in AIDS drama Fairyland • Grindr helps to deliver HIV tests • fewer people with HIV in U.S. prisons
15 RESEARCH NOTES
Implants and inserts show promise for HIV prevention • Sunlenca plus two antibodies for twice-yearly treatment
• German man free of HIV after stem cell transplant • low-level detectable viral load can lead to adverse outcomes
16 CARE & TREATMENT
Can women with HIV safely breastfeed?
• The Denver Principles at 40
• POZ Stories: Mark Grantham
• Everyday
11 VOICES
HIV.gov applauds the success of the President’s Emergency Plan for AIDS Relief (PEPFAR), which recently turned 20.
12 SPOTLIGHT
Standing up for trans lives
• people with advanced HIV can have severe mpox • doxycycline post-exposure prophylaxis for prevention of sexually transmitted infections • injectable preexposure prophylaxis works well for Black gay men and transgender women
32 HEROES
Journalist, actor and author Nicholas Snow hasn’t let HIV stop him from creating.

CONTENTS POZ (ISSN 1075-5705) is published monthly except for the January/February, April/May, July/August and October/November issues ($19.97 for an 8-issue subscription) by Smart + Strong, 157 Columbus Avenue, Suite 525, New York, NY 10023. Periodicals postage paid at New York, NY, and additional mailing offices. Issue No. 268 POSTMASTER: Send address changes to POZ/Smart + Strong, 157 Columbus Avenue, Suite 525, New York, NY 10023. Copyright © 2023 CDM Publishing, LLC. All rights reserved. No part of this publication may be reproduced, stored in any retrieval system or transmitted, in any form by any means, electronic, mechanical, photocopying, recording or otherwise without the written permission of the publisher. Smart + Strong® and POZ® are registered trademarks of CDM Publishing, LLC.
3 FROM THE EDITOR Rainbowland
COVER AND THIS PAGE: (HARPER AND JORDAN) BILL WADMAN; THIS PAGE: (GAVEL/BOOKS, BARBED WIRE AND MAGNIFIER) ISTOCK
D
D
Darius Harper (left) and André Jordan
EDITOR-IN-CHIEF
ORIOL R. GUTIERREZ JR.
MANAGING EDITOR
JENNIFER MORTON
DEPUTY EDITOR
TRENT STRAUBE
SCIENCE EDITOR
LIZ HIGHLEYMAN
COPY CHIEF
JOE MEJÍA

EDITORIAL ASSISTANT
LAURA SCHMIDT
ART DIRECTOR
DORIOT KIM
ART PRODUCTION MANAGER
MICHAEL HALLIDAY
CONTRIBUTING WRITERS
SHAWN DECKER, OLIVIA G. FORD, ALICIA GREEN, MARK S. KING, TIM
MURPHY, CHARLES SANCHEZ
CONTRIBUTING ARTISTS
JOAN LOBIS BROWN, LIZ DEFRAIN, ARI MICHELSON, JONATHAN
TIMMES, BILL WADMAN
FOUNDER
SEAN STRUB
LEGACY ADVISER
MEGAN STRUB
ADVISORY BOARD
A. CORNELIUS BAKER, GUILLERMO
CHACÓN, SABINA HIRSHFIELD, PHD, KATHIE HIERS, TIM HORN, PAUL KAWATA, NAINA KHANNA, DANIEL
TIETZ, MITCHELL WARREN
PRESS REQUESTS
NEWS@POZ.COM
SUBSCRIPTIONS
HTTP://ORDER.POZ.COM
UNITED STATES: 212-242-2163
SUBSCRIPTION@POZ.COM
FEEDBACK
EMAIL WEBSITE@POZ.COM OR EDITOR-IN-CHIEF@POZ.COM
SMART + STRONG
PRESIDENT AND COO
IAN E. ANDERSON
EDITORIAL DIRECTOR
ORIOL R. GUTIERREZ JR.
CHIEF TECHNOLOGY OFFICER
CHRISTIAN EVANS
VICE PRESIDENT, INTEGRATED SALES
DIANE ANDERSON
INTEGRATED ADVERTISING MANAGER
JONATHAN GASKELL
INTEGRATED ADVERTISING COORDINATOR
SARAH PURSELL
SALES OFFICE 212-938-2051; SALES@POZ.COM
CDM PUBLISHING, LLC

CEO JEREMY GRAYZEL
CONTROLLER
JOEL KAPLAN
Rainbowland
IDIDN’T ATTEND THE 1993 March on Washington for Lesbian, Gay and Bi Equal Rights and Liberation, which took place in our nation’s capital on April 25. I had a family commitment that I couldn’t miss. That said, to this day, I wonder how my life might’ve been different had I gone to DC for that march.
I had tested HIV positive less than a year earlier. I was nowhere near OK with accepting my status. In fact, I was scared for my life. Perhaps an infusion of hope at the rally would’ve done me some long-term good.
Even then, I understood in a general sense what I had missed. Larry Kramer spoke at the march. Hundreds of marchers performed a die-in to honor those lost to AIDS. The amazing stories I heard from friends and acquaintances who did attend the march inspired me secondhand.
So I tried to make up for my absence by attending the 1994 New York City Pride march, which took place June 26. Actually, two marches happened that day—an official one on the East Side of Manhattan demanding global LGBTQ rights and an unofficial one that went up Fifth Avenue from Greenwich Village. The two joined up before entering Central Park together.
My friends and I were part of the unofficial march. I didn’t witness the die-in in front of St. Patrick’s Cathedral, but I did experience the sense of hope that I had missed the previous year. Effective HIV treatment was still two years away, but the march gave me a much-needed boost to keep believing.
Since then, the need for Pride marches has been routinely questioned, only to come full circle when anti-LGBTQ activities remind us all that fighting for our rights is still necessary. Today, anti-transgender legislation and attempts to curb funding for preexposure prophylaxis (PrEP) to prevent HIV transmission are just the latest examples.

So it is with much enthusiasm that POZ presents this special issue celebrating Pride. Our two cover subjects, André Jordan and Darius Harper, are great examples of why Pride remains as relevant as ever.
The friends and actors have had success on Broadway and beyond. André, who uses
he/she pronouns, and Darius, who uses he/ they pronouns, have supported each other throughout their careers, and now they’re standing by each other as they navigate life with HIV. Go to page 24 to read more.
André and Darius are sharing their stories in part to let others living with HIV know that they are not alone. The same can be said of other advocates highlighted in this issue.
Nicholas Snow is a longtime AIDS activist. In fact, he was fighting the virus well before he tested HIV positive. The journalist, actor and author remains a force to be reckoned with. Go to page 32 to learn more.
David Michael is a country singer living with HIV. As such, he is blazing a trail in Nashville for those who either have the virus or are affected by it. Go to page 4 to read about his HIV story and love of Patsy Cline.
Lola Flash has been photographing LGBTQ people and people with HIV for four decades. A new photo book brings their work together for the first time. Go to page 20 for more.
ORIOL R. GUTIERREZ JR. EDITOR-IN-CHIEF editor-in-chief@poz.com
Want to read more from Oriol? Follow him on Twitter @oriolgutierrez and check out blogs.poz.com/oriol.

FROM THE EDITOR
poz.com JUNE 2023 POZ 3 (ILLUSTRATION) ISTOCK;
JOAN LOBIS BROWN POZ.COM/TWITTER POZ.COM/FACEBOOK POZ.COM/INSTAGRAM
(GUTIERREZ)
COUNTRY MUSIC GAYS & HIV
Publicist-turned–country crooner David Michael shares his HIV story and love of Patsy Cline.

QUEER RECORDING ARTISTS ARE PICKIN’ AND A-GRINNIN’ AT the top of today’s country music charts—think Brandi Carlile, Lil Nas X, Orville Peck and T.J. Osborne—but when it comes to openly gay HIV-positive singers, David Michael is blazing the trail. (Longtime POZ readers may recall Jimbeau Hinson, the bisexual HIV-positive country singer-songwriter; sadly, he died last year at age 70.)
Michael hails from Greenville, South Carolina, where he worked as a car salesman before founding the public relations firm MY PR Lab—he loves to talk up his current client Land of Oz, an immersive three-hour tour near Banner Elk, North Carolina. Michael moved to Nashville a little over a year ago after breaking into the country music scene in the most unusual way. He has released two singles—“He’s Got You” and “A Poor Man’s Roses” from his Patsy Cline tribute EP— plus the track “Pretty Boy,” which he says, “tells the story of a young me—bullied, battered and beat down.” That song was released last June in honor of Pride Month. Also in June, he launched the CMgAys (pronounced “CM Gays”), a daylong celebration of LGBTQ recording artists that coincides with the Country Music Awards (the CMAs) and Nashville’s related festival. Michael, 37, took a break from touring and planning this summer’s CMgAys, slated for June 10, to talk with POZ about blue states, industry disrupters and the power of everyday disclosure.
You’re new to Nashville. Tragically, the city recently experienced a school shooting, and Tennessee has made national news for rejecting free federal HIV funds and trying to ban drag shows. What’s the vibe there? Obviously, I’ve been less than thrilled with the recent political events, but I am
extremely inspired by the Nashville LGBTQIA community activation, and I’m grateful that a large swath of our straight allies are in full support. Running to a blue state for convenience and lifestyle ease is so not me. I’ll always run toward the battle, never retreat. Plus, it’s humbling to be a part of the right kind of change, whether it’s for my drag and trans friends in Tennessee or all those affected by HIV and AIDS around the world.
How did you break into country music?
In December 2019, I went to a young Democrats fundraiser in South Carolina. The champagne had hit, and I was ready to [bid on] the big prize—to go to Nashville and record one song in an iconic studio with Grammy-winning performers. And as someone who always loved music and karaoke—it’s one of my flexes—I thought, That’s fun! They called the next day and were like, “Congrats! You won this thing.” But a few months later, we all went to hell in a handbasket [because of COVID-19],
4 POZ JUNE 2023 poz.com
BY TRENT STRAUBE POZ Q & A
(PATSY CLINE TRIBUTE EP) MY PR LAB; (GRADUATION) COURTESY OF DAVID MICHAEL
From left: The cover of David Michael’s Patsy Cline tribute EP; Michael with his dad, Mark, at his 2004 graduation from the South Carolina Governor’s School for the Arts and Humanities
and, trying to keep my business afloat, I completely forgot about winning the recording session.
So move on down the line. My dad was very ill with alcohol-related issues, and I was in therapy and prepping emotionally—passing from alcohol is a slow burn, but it does give you time to tie up relationships. My dad passed on October 13, 2021. On the same damned day, or maybe the day after, I get a call from a Nashville area code, and they go, “This is Charlotte Avenue Entertainment, and you bid on a song. Anything you’d like to do?” The proximity to my dad’s passing was bewildering because he was a musician—he had been in bands forever and was a great sound engineer. Southern rock was his vibe. But the dark side was being in bars. What I saw growing up was, if you’re in the music business, it takes you from your children and turns you into an addict. He knew I could sing well and would ask me to participate. I always said no. But getting that call, I realized this was something my dad had created for me.
You chose to record a Patsy Cline song, and the studio liked you so much it turned the session into a six-track EP. Why Patsy?
She was a terrible disrupter to the industry, and she didn’t let a man or manager tell her what to do or how to sing a song. There’s a reason you don’t see a lot of videos of her interviews. They were so terrified she’d drop the F-bomb or not look ladylike. They thought it’d ruin her reputation. So from one disrupter to another, I really feel her spirit.
Can you tell us your HIV story?
I was living in Asheville, North Carolina, with my mom 10 years ago. I was getting symptoms, so I went [to get tested]. I got a cheek swab, and 15 minutes later, they said I was positive. A week later, after I had my bloodwork done, they said I had AIDS, and they were concerned the virus had gone into my spinal column and brain. I was hospitalized. I never looked at it like a death sentence. I was like, We’ll just have to figure this out. No way it was going to take me down.

Now I’m on one pill a day and am undetectable. It took me five or six years of keeping [my status] mostly a secret, just among best friends and partners. I think my next phase will be entering in a more public official role, but I don’t want it to seem like something I’m exploiting. I want to be someone you can DM and we can have a conversation.
Now that you’re open about it, do people ask you about HIV? They do. I was on a plane. I’m a performer, so I have swag clothes and love swagging at the airport. And the flight attendant was like, “Are you famous?” And I said, “No, but I am a performer.” Sometimes I feel like a divinity has come over me, and I know I need to share—not every time but sometimes. I said, “I’m the first openly gay, openly
gage and chat. She asked why I was in town. I said I was performing, and I don’t know why—this was an elderly Black woman—but I can read the room, so I took a risk and said, “I’m the first openly gay blah blah blah.” And she pulled over and started weeping. I put my hand on her shoulder and said, “Can I ask why you had this reaction?” and she said, “My son’s currently dying of AIDS.” I said, “Are you sure it’s not HIV?” She said, “No, it has progressed. He decided to stop taking his meds. I don’t know why.” So we sat there for 20 minutes and cried. She said it was kind of a miracle that she was able to have this breakdown with me—she had prayed for someone to share with—she said she couldn’t do it in front of her son or the doctors or by herself. So I just held space on the side of the interstate
HIV-positive country music entertainer in the world.” And she got tears in her eyes. She grabbed my hand and said, “One of my favorite coworkers in the world was just diagnosed, and he’s really struggling.” I teared up and said I’ll give you my name and phone number to give to him. And he was terrified. So those first six months [after his diagnosis], we stayed in touch biweekly or more. And we still chat.
And there was a time recently I was in Houston on the way to the airport. And it was like an hour from my hotel. I got in the car with the driver—a real lovely lady—and I’m not the type of Uber rider to sit quiet in the back. I en-
with a stranger I was connected with by this disease. That she has to see her son perish from AIDS in 2023—it’s shocking.
You have a show planned for June 23 in Manhattan for Pride. Do you talk about HIV in your act?
I am booked, promoted and billed as “The First Openly Gay, Openly HIV-Positive Country Music Performer” for all my gigs. It’s a badge that I wear proudly, and no matter the audience— gay or straight—I find there’s still quite a bit of power in representation. So yes, no matter the stage, I’m speaking about HIV. ■
poz.com JUNE 2023 POZ 5
“I’m extremely inspired by the Nashville LGBTQIA community activation.”
David Michael
COURTESY OF DAVID MICHAEL/LORA DRAMMIS
Oscar Party Raises $9M to End HIV
Oscar Party Raises $9M to End HIV



Launched in 1992,


hosted by the Elton John AIDS Foundation.
As Everything Everywhere All at Once swept this year’s Oscars, glitterati at the annual Elton John AIDS Foundation’s Academy Awards Viewing Party raised over $9 million for the organization’s efforts to end HIV.
Last year, Sir Elton John joined the fundraiser via satellite from Lincoln, Nebraska, where he was performing as part of his Farewell Yellow Brick Road tour. This year, he joined the festivities in person in Los Angeles along with his husband, David Furnish, and special guests actors Eric McCormack and Michaela Jaé Rodriguez and singer Rina Sawayama.
Since 1992, the viewing parties have raised over $90 million for HIV programs across the globe, including in the United States.
“We mustn’t forget that HIV is still causing needless suffering around the world, and we must protect those most vulnerable to this disease with testing and compassionate care,” said John in a press statement. “We can see an end to AIDS in our lifetimes, but first, we must break down stigma and discrimination and provide equal access to health care to finally end the epidemic for everyone, everywhere.”
“Elton and I are so touched and elated by the generosity
we’ve seen throughout this glittering and massively successful evening,” added Furnish, who is also chairman of the foundation. “This funding will help us continue HIV and AIDS prevention and care programs across the world, save millions of lives and help countless people to have a brighter future.”
we’ve seen this and successful added who is also chairman of the foundation “This will help us continue HIV and AIDS prevention and care programs across the world, save millions of lives and countless to have a future.”

Last year, a report from Funders John AIDS Foundation as the fifth funder of HIV programs in 2020 (following Gilead the Bill & Melinda Gates Wellcome
Last year, a report from Funders Concerned About AIDS ranked the Elton John AIDS Foundation as the fifth largest philanthropic funder of HIV programs in 2020 (following Gilead Sciences, the Bill & Melinda Gates Foundation, Wellcome Trust and ViiV Healthcare).

John’s AIDS work earned him a National Humanities Medal last year

John’s decades-long AIDS work earned him a National Humanities Medal last year from President Joe Biden.
The money raised helps fund the foundation’s numerous efforts to fight the epidemic. Recently, the organization teamed with Walmart to train pharmacists to better serve the HIV community.
The money raised fund the foundation’s numerous efforts to the epidemic. the teamed with Walmart to train to better serve Trent
 —Trent Straube
—Trent Straube

Based on a memoir, Fairyland takes place in San Francisco. ADAM LAMBERT STARS IN AIDS DRAMA




Fairyland takes in San Francisco.
On his new album, High Drama, pop star Adam Lambert covers hits by other artists, including Culture Club’s 1982 smash “Do You Really Want to Hurt Me.” The American Idol alum’s next project also finds the LGBTQ icon delving into the past while breaking new creative ground. He stars in this year’s Fairyland, an AIDS drama set mostly in 1970s and ’80s San Francisco.


,



Produced by Oscar winner Sofia Coppola and directed by Andrew Durham, Fairyland premiered earlier this year at the Sundance Film Festival. There’s no word yet on when the film will get a wider release, but Lambert has been discussing the film while promoting his new album.
If Fairyland sounds familiar, perhaps POZ readers recognize it as the title of Alysia Abbott’s 2013 memoir. The book details her sometimes troublesome


upbringing by her gay father, Steve, in the bohemian Haight-Ashbury neighborhood and then her experiences leaving for college and living in France before returning to San Francisco to care for her dad, who died of AIDSrelated illness in 1992.
Shortly after the memoir was published, Abbott and Whitney Joiner, who also lost a gay dad to AIDS, launched a group called The Recollectors to create
a community of now-grown children who lost parents to the epidemic and want to share their experiences. Abbott and Joiner were featured on the June 2015 cover of POZ.

That POZ article ends with Abbott describing a dinner she had with Coppola, who had optioned the book for a film. Eight years and a second pandemic later, Fairyland is finally making it to the big screen.

Abbott a dinner she had with who had the book for a film. years and a second it to the screen.
Coppola recommended the film project to her photographer friend Durham, knowing that he, like Abbott, was raised by a gay father in San Francisco and took care of his dad as he died of AIDS.
The film stars Scoot McNairy as Steve Abbott, Cody Fern (of American Horror Story fame) and Lambert as men in Abbott’s orbit; Nessa Dougherty and Emilia Jones as the child and young adult Alysia Abbott, respectively; and Geena Davis as Steve Abbott’s mother. —TS
UPDATES ON HIV & AIDS
(OSCAR, FEATHERS AND GLASSES) ISTOCK; (LAMBERT) FRED DUVAL/SHUTTERSTOCK,COM 6 POZ JUNE 2023 poz.com
POZ PLANET
the annual event is
From left: Adam Lambert; memoir cover; 2015 POZ cover with Alysia Abbott (right)
pop star Culture Club’s 1982
bohemian her for and in France
SMART+STRONG PUBLICATION POZ.COM HEALTH, LIFE & HIV Remembering parentslost toAIDS Meetthe Children WhitneyJoiner andAlysiaAbbott
GRINDR HELPS TO DELIVER HIV TESTS
The dating app joins the prevention effort Together TakeMeHome.


If you’re on the wildly popular gay dating app Grindr, you now have a sure bet: Click the “Free HIV Home Test” button, and a nice little package will arrive at your front door—or back door if you prefer.

Grindr joined a national effort launched this week to deliver 1 million free HIV self-tests during the next five years; the HIV tests are also available online to folks not on the app. Titled Together TakeMeHome, the program is funded by the Centers for Disease Control and Prevention (CDC).

In a Dear Colleague letter dated March 21, the CDC’s Division of HIV Prevention described the national HIV testing effort:
“We are pleased to announce the launch of Together TakeMeHome (TTMH), a project with the goal of distributing up to 1 million free HIV self-tests over the next five years. People in the United States, including Puerto Rico, can order up to two free HIV self-tests every 90 days via a new online portal. Tests are available to anyone 17 years or older, regardless of health insurance or immigration status. TTMH is supported by
Fewer People With HIV in U.S. Prisons
CDC, in partnership with Emory University, Building Healthy Online Communities (BHOC), NASTAD, Signal Group, and OraSure Technologies.”

In 2022, the CDC awarded $8.3 million per year to Together TakeMeHome for its five-year project (for a total of $41.5 million). For those not on Grindr, orders placed on the program’s website, Together.TakeMeHome.org, are processed by Amazon, which delivers the OraSure tests in discreet packages. The site is available in both English and Spanish.

In 2019, out of 34,800 total new HIV diagnoses in the United States, 24,500 (70%) were among men who have sex with men, according to the CDC. So it makes sense to make HIV tests available through apps like Grindr that are popular among gay, bisexual and transgender people. —TS
DENVER PRINCIPLES AT 40



Presented during the 2nd National AIDS Forum at the 5th National Lesbian and Gay Health Conference, held in Denver, in June 1983, a statement from the Advisory Committee of People With AIDS begins with this declaration: “We condemn attempts to label us as ‘victims,’ a term which implies defeat, and we are only occasionally ‘patients,’ a term which implies passivity, helplessness and dependence upon the care of others. We are ‘People With AIDS.’” Now known as The Denver Principles, the document details the rights and responsibilities of people with AIDS. Go to POZ.com for more.
At the end of 2021, fewer people in state and federal prisons were living with HIV than at the end of the previous year. The decline, of about 2%, represents the 23rd consecutive year that the number has decreased, according to a report by the Bureau of Justice Statistics, part of the Department of Justice.
Titled “HIV in Prisons, 2021,” the report also includes data on HIV testing. Highlights from the report include:
• At year-end 2021, an estimated 11,810 persons with HIV were in the custody of state and federal correctional authorities, down from 12,060 in 2020.
• At year-end 2021, about 1.1% of persons—1.2% of males and 0.9% of females—in state and federal prison were living with HIV.
• In 2021, of the 50 jurisdictions reporting their HIV testing practices, 16 jurisdictions (which accounted for 40% of prison admissions) conducted mandatory HIV testing during intake.
• In 2021, a total of 18 jurisdictions offered HIV tests during routine medical exams of persons in custody, up from 11 in 2017.
A total of 1,032,130 people were in custody in state and federal correctional facilities in 2021, according to the report. Of those, 962,156 were male and 69,974 were female. The total number of people in custody declined each year since 2017, the earliest year included in the report, when the total number of people in custody was 1,279,259.

The 2021 decrease in prisoners living with HIV “followed the largest 1-year decline (down 15% between 2019 and 2020, largely as a result of the COVID-19 pandemic) since data collection began in 1991,” wrote the study authors. They added, “The population of state and federal prisoners living with HIV has fallen for 23 straight years from its peak of 25,980 in 1998, largely due to a roughly 4% average annual decrease in state prisoners with HIV.” —TS

poz.com JUNE 2023 POZ 7 (HANDCUFFS) ISTOCK; (GRINDR LOGO) GRINDR.COM
The number has declined for 23 consecutive years.
I’M STILL HERE
Long-term
I did some soul searching and discovered that education was my calling. I became an English and history teacher. This was before we had effective HIV medications. I started to lose weight. I stopped drinking, which significantly helped me along my journey. As various HIV drugs became available, it seemed I took all of them. I took AZT, but it was short-lived. I told my doctor that I would wait for something else. I had the worst time with liquid Norvir. It tasted like gasoline. Yet I persevered, and I began gaining weight.
going to cut it. Unfortunately, in 2015, he passed away. He left behind a legacy of HIV activism in Tennessee, a son and three granddaughters. I continue my HIV activism for him, his family—and for myself.

I received my HIV diagnosis in June 1984—39 years ago. I had just started graduate school at the University of South Florida’s Tampa campus. When I went for my results, I was ushered into a room with more than 25 medical professionals. I turned to the nurse and said, “I guess I have it; otherwise, these people wouldn’t be here.”

The doctor told me he wasn’t sure how long I had to live but that it was probably less than three years. I was gobsmacked. I walked across campus, went to the registrar’s office and immediately dropped out of school. Then, I drove into St. Petersburg and quit my job as a buyer for a major department store.
Now what? My life spiraled downward. I was out of control and so was my drinking. But slowly, I realized that my life wasn’t ending as quickly as I’d imagined.
Dealing with these health issues helped me find my voice as an advocate and activist. I got involved with ACT UP and worked as a case manager. I was a buddy to a few others who were living with HIV. I took them to appointments, did their shopping and basically let them know they mattered.
I also protested on many occasions. I was in the middle of a die-in at the rotunda at the Capitol. I was part of the ACT UP protest at the Food and Drug Administration. I participated despite knowing that I could be fired. It was illegal to be a teacher in the Pinellas County Schools system if you were gay or HIV positive. These actions guided me along my path of activism.
In 2014, I moved from the beaches of St. Petersburg to the mountains of Tennessee. I had fallen in love with a man named Butch Ferney, and the long-distance relationship thing wasn’t
of HIV activism in










Things are very tough in Tennessee as far as HIV prevention is concerned. I still actively advocate for PLWHIV [people living with HIV]. As Elaine Stritch sang in Follies, “I’m still here!” I will continue the journey of HIV advocacy and activism until I can no longer.
What three adjectives describe you?
Authentic, caring, resilient.
What keeps you up at night? The current state of affairs in Tennessee.
What is the best advice you’ve received? Be true to yourself, no matter what.
What person in the HIV community do you most admire?
Shanell McGoy, PhD (the director of HIV/STD for the Tennessee Department of Health).

What is your motto?
Watch out! I have just begun to blossom. Read other POZ Stories or share your own at poz.com/stories.
These dates represent milestones in the HIV epidemic. Visit poz.com/aidsiseveryday to learn more about the history of HIV and AIDS. BY JENNIFER MORTON
to learn more about the of HIV and AIDS. on the


NKOSI JOHNSON, a South African child born with HIV who had a powerful impact on the public perception of AIDS and was the keynote speaker at the 13th International AIDS Conference, dies of AIDS-related complications at age 12. (2001)

1
HUNTER REYNOLDS, an artist and activist living with HIV who in his work explored gender, sexuality, HIV and AIDS, politics, mortality and rebirth, dies of cancer at age 62. (2022)

HIV LONG-TERM SURVIVORS AWARENESS DAY

GREATER THAN AIDS and #ENDHIV launch #HIVBEATS, an upbeat and informative video series that aims to educate younger audiences about advances in HIV prevention, testing and treatment. (2016)
Mark Grantham 5

17

a of the turbulent 1990s
THE POX LOVER: AN ACTIVIST’S DECADE IN NEW YORK AND PARIS, a personal history of the turbulent 1990s by pioneering American AIDS journalist and lesbian activist Anne-christine d’Adesky, is released. (2017)

27
NATIONAL HIV TESTING DAY

UPDATES ON HIV & AIDS POZ PLANET (GRANTHAM) COURTESY OF MARK GRANTHAM; (JOHNSON) WIKIMEDIA; (#HIVBEATS) GREATERTHAN.ORG; (REYNOLDS) BILL WADMAN 8 POZ JUNE 2023 poz.com
survivor Mark Grantham persevered and found his voice as an advocate.
June 12
EVERYDAY
GLOBAL HIV TRANSFORMED
In a blog post titled “How PEPFAR Transformed the Global HIV Epidemic,” HIV.gov lauds the U.S. President’s Emergency Plan for AIDS Relief, which recently turned 20. Below is an edited excerpt.
ANEW ANALYSIS FROM THE Centers for Disease Control and Prevention (CDC) reveals that the number of people receiving HIV treatment through PEPFAR has increased 300 times in under 20 years, from 2004 to 2022. The number of people receiving HIV antiretroviral therapy through PEPFAR increased from just 66,500 in 2004, the year after PEPFAR was launched, to more than 20 million in 2022. These report findings are published in Vital Signs.
The proportion of people receiving HIV treatment through PEPFAR with a detectable viral load who then tested as virally suppressed increased from 80% to 95% between 2015 and 2022, the report notes. Viral suppression refers to people with HIV who have their virus under control thanks to treatment. This prevents transmission of HIV to sexual partners and helps reduce the risk of transmission from mothers to children.
“PEPFAR’s efforts have dramatically altered the course of the global HIV epidemic,” said CDC chief medical officer Debra Houry, MD, MPH. “We must continue to build on this momentum if we are to eliminate HIV as a global public health threat by 2030. These investments are saving lives and
creating a safer world for us all.”
As a key implementing agency of PEPFAR, the CDC works with partners in more than 50 countries to improve methods for finding, treating and preventing HIV. The CDC supports more than 10,000 labs or testing sites worldwide, providing lifesaving treatment to people with HIV around the world and designing and enhancing surveillance systems to enable countries to understand which geographic areas require urgent HIV-related services.
Researchers also analyzed findings from large CDC-supported household surveys in six African countries severely affected by HIV and found increases in population viral load suppression rates between 2015 and 2021. These surveys showed that population viral load suppression rates improved in Eswatini, Lesotho, Malawi, Uganda, Zambia and Zimbabwe. These improvements ranged from a 13% increase in Lesotho to a 19% increase in Malawi.
Under PEPFAR’s current five-year strategy, the United States aims to eliminate HIV as a global public health threat by 2030 while strengthening public health systems worldwide.
The latest data in this Vital Signs report show that PEPFAR’s programs are
placing the world on the path to achieving this goal and validate that efforts over the past 20 years have transformed the global HIV epidemic.
The study also reveals that, since its inception, PEPFAR has helped countries effectively respond to their HIV epidemics and strengthened their public health systems, which helps keep the world safe from other global health threats.
Despite these tremendous achievements, several groups still lag behind— likely due to health inequities fueled by many factors, including stigma and discrimination.

To eliminate HIV as a public health threat by 2030, as outlined by PEPFAR’s five-year strategy, the global health community must:
• Sustain efforts and investments: Continue to be unrelenting in efforts to build on these achievements or risk reversing decades of progress.
• Advance health equity: Address health inequities head-on.
• Strengthen health systems: Continue to bolster and use PEPFAR platforms to strengthen global health security.
• Build transformative partnerships: Collaborate and harness the shared commitment to end the global HIV epidemic. ■
BLOGS AND OPINIONS FROM POZ.COM VOICES ISTOCK poz.com JUNE 2023 POZ 11
STANDING UP FOR TRANS LIVES

According to a study by UCLA’s Williams Institute, trans people are four times more likely than cisgender people to experience violent victimization. Trans people are also disproportionately affected by HIV. Indeed, another study found that 14% of trans women and 3% of trans men are HIV positive, compared with an overall prevalence rate in the United States of 1.1%. Reasons for such disparities include transphobia, stigmatization and a general lack of access to health care. Clearly, change is needed.
But a new reality won’t come easy. In fact, the rights of trans people—especially the right of young trans people to access gender-affirming health care, such

as hormone therapy—are increasingly under attack by Republican-led legislatures throughout the country. Increased visibility could help usher in some change. According to research from the Morning Consult and The Trevor Project, less than 30% of Americans say they know a trans or nonbinary person. March 31 marked the international Transgender Day of Visibility (TDOV). Trans people observed the day by voicing their opposition to the many hateful bills seeking to codify anti-trans discrimination and by proudly being themselves. Cisgender allies, meanwhile, used their power, platforms and privilege to sign laws, show love and educate themselves and others.

BY
SPOTLIGHT 12 POZ JUNE 2023 poz.com
JOE MEJÍA
1 2 3
1. On TDOV, Representative Barbara Lee of California, a founding member of the LGBTQ Equality Caucus, posed with the trans pride flag and tweeted: “To the trans community: I see you and will fight for you today & every day #TDOV.” 2. The LGBTQ+ ally group Free Mom Hugs of SoCal, whose mission is to empower the world to celebrate the LGBTQIA+ community through visibility, education and conversation, was at the ready to educate passersby—and, of course, give hugs. 3. On March 16, Michigan Governor Gretchen Whitmer expanded the Elliott-Larsen Civil Rights Act to include nondiscrimination protections based on sexual orientation and gender identity.
6., 7., 8. Hundreds of young trans people and their supporters showed up for New York City’s Trans Day of Visibility March organized by NYC Youth for Trans Rights, a nonprofit run by trans youth under 25.



Send your event photos to POZ at website@poz.com or tag us on Facebook, Instagram or Twitter. For a list of community events, visit poz.com/calendar.

(1) @REPBARBARALEE/TWITTER; (2) @FREEMOMHUGS/INSTAGRAM; (3)THE TREVOR PROJECT/FACEBOOK; (4) JOEY KULKIN/FACEBOOK (5) @THETREVORPROJECT/TWITTER; (6, 7, 8) MIKE CHIODO/FACEBOOK
4. In Bennington, Vermont, a small group led by Queer Connect occupied a high-profile spot at the town’s Four Corners on TVOD as drivers honked their support at the intersection. 5. A longtime supporter of The Trevor Project, Daniel Radcliffe moderated a chat with trans kids for the nonprofit’s first episode of Sharing Spaces, which aired on TVOD.
poz.com JUNE 2023 POZ 13 4 5 6 7 8
LIZ HIGHLEYMAN
GONORRHEA
GONORRHEA IS A SEXUALLY transmitted infection (STI) caused by Neisseria gonorrhoeae bacteria. It can be treated with antibiotics, but drug resistance is a growing concern. If left untreated, gonorrhea can lead to serious complications, including chronic pain and infertility.
Gonorrhea is the second most common bacterial STI in the United States, after chlamydia, and case numbers have doubled over the past decade. Gonorrhea rates are rising for both men and women and for most racial and ethnic groups. Young people ages 15 to 24 account for more than half of reported cases, and gay and bisexual men account for around one third. HIV-positive people with gonorrhea are more likely to transmit HIV, and HIV-negative people are more likely to acquire the virus.
Many people with gonorrhea have no symptoms. If symptoms do occur, typically within two weeks after infection, they may include discharge from the penis or vagina and pain or burning when urinating. Symptoms of rectal infection may include discharge, anal itching, bleeding and painful bowel movements. Oral infection can cause a sore throat and difficulty swallowing. Gonorrhea may also affect the eyes, joints, heart and brain.
Gonorrhea complications in men

include epididymitis (inflammation of the tubes behind the testicles) and prostate inflammation. If left untreated, women with gonorrhea can develop pelvic inflammatory disease, or infection of the reproductive organs. Symptoms may include fever, pain in the lower abdomen, pain or bleeding during sex and vaginal bleeding between periods. Over time, scar tissue forms around the uterus and fallopian tubes, which can lead to chronic pain, infertility and ectopic pregnancy.
PREVENTION AND TREATMENT
Gonorrhea is transmitted through sexual contact, including vaginal, anal and oral sex. Condoms offer good protection against gonorrhea. It’s important to avoid having sex if you have STI symptoms. If diagnosed with gonorrhea, inform your sex partners and hold off on sex until treatment is completed and symptoms resolve.
Recent research shows that taking a single oral dose of doxycycline as post-exposure prophylaxis after sex— known as doxy PEP—can reduce the risk for gonorrhea for gay men and transgender women, but this did not work for cisgender women (see “Care & Treatment,” page 17). In addition, a vaccine that prevents meningitis caused by related bacteria can also prevent gonorrhea. Pregnant people with gonorrhea
can pass it on during delivery, which can lead to complications for babies.
Get tested if you have symptoms that could indicate an STI or if a sex partner tests positive. Gonorrhea is usually diagnosed with a urine test or using a swab to take a sample from the penis, vagina, cervix, anus or throat. The Centers for Disease Control and Prevention (CDC) recommends regular testing—even if asymptomatic—for sexually active gay and bisexual men, people living with HIV and those using preexposure prophylaxis (PrEP). Annual testing is recommended for sexually active women younger than 25 and for older women at increased risk; testing is also recommended during pregnancy.
Gonorrhea can be treated with antibiotics, but it is becoming increasingly resistant to medications that used to be standard treatment. For most people, the CDC now recommends a single injection of ceftriaxone. Alternative regimens are available for people who can’t use ceftriaxone. Sex partners are often treated at the same time so that they don’t pass the infection back and forth. Gonorrhea does not confer lasting immunity, so it’s possible to get infected again. Even if symptoms improve, it’s important to take the full course of medication, as this will help prevent resistance and ensure that gonorrhea remains curable. ■
CENTERS FOR DISEASE CONTROL AND PREVENTION
BASICS 14 POZ JUNE 2023 poz.com
BY
The common STI is becoming increasingly resistant to antibiotics.
Implants and Inserts PREVENTION

Small implants placed under the skin and vaginal or rectal microbicide inserts could offer convenient new options for pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP). Researchers found that a refillable islatravir implant was well tolerated and produced sustained drug levels for more than 20 months in monkeys. The implants fully protected female and male monkeys against vaginal or rectal infection with an HIV-like virus. Other research teams tested a fast-dissolving tablet containing elvitegravir and tenofovir alafenamide that can be inserted in the vagina or rectum. The inserts were 93% effective at preventing rectal infection in monkeys. The first human study found that rectal inserts were well tolerated and maintained adequate tenofovir levels for 72 hours. When rectal tissue was exposed to HIV, viral replication decreased. In another study, vaginal inserts fully protected monkeys when administered four hours after exposure and 94% effective after eight hours, but this dropped to 77% after 24 hours.

Sunlenca Plus bnAbs TREATMENT
Sunlenca (lenacapavir), a new injectable HIV capsid inhibitor administered once every six months, has the potential to be paired with two broadly neutralizing antibodies (bnAbs) to construct a twice-yearly regimen. BnAbs are antibodies that bind to parts of the virus that don’t change very much as it evolves.
Sunlenca is highly effective when combined with daily oral antiretrovirals, but so far it doesn’t have an equally durable partner for a complete long-acting regimen.
In a small Phase Ib study, 21 people with an undetectable viral load stopped their existing oral antiretrovirals and received injections of Sunlenca plus infusions of two antibodies being developed by Gilead Sciences, dubbed teropavimab and zinlirvimab. Participants were tested in advance to ensure that their HIV was susceptible to both antibodies. Six months later, 90% maintained viral suppression. A Phase II clinical trial will start this year to evaluate whether viral suppression can be maintained when the regimen is administered every six months for a longer duration.
Stem Cell Cure CURE
A German man who received a transplant of HIV-resistant stem cells has no detectable HIV more than four years after stopping antiretroviral treatment. The Düsseldorf Patient is the second or third person (based on the timing of his transplant or treatment interruption) whose HIV was eliminated after the procedure, but his doctors were cautious about declaring a cure. The man was diagnosed with leukemia in 2011, soon after he started antiretroviral therapy. In February 2013, he received a stem cell transplant from a donor with a rare genetic mutation called CCR5-delta32 that blocks HIV from entering cells—the same procedure that cured Timothy Ray Brown, the Berlin Patient. After more than five years with undetectable HIV, he started a closely monitored treatment interruption in November 2018. Since then, researchers have tested his blood using ultrasensitive assays and examined his peripheral immune cells and gut and lymph node tissues. Finding no evidence of replication-competent HIV, his doctors finally announced that he’s cured.
 LIZ HIGHLEYMAN
LIZ HIGHLEYMAN
Low-Level Viral Load CONCERNS
People with a low detectable viral load are at risk for serious non-AIDS-defining events, such as cancer, heart disease and liver or kidney disease. Maintaining an undetectable viral load can halt progression of HIV and eliminate the risk of transmission. Many viral load tests measure down to 50 copies of HIV RNA—the usual threshold for undetectable—but some experts still regard levels below 200 or even 1,000 as viral suppression. In an analysis of nearly 3,000 people who started HIV treatment after 1996, 8% had a low-level detectable viral load (50 to 200 copies), 4% had 200 to 1,000 copies and a third experienced virological failure. Over 10 years, nearly 14% experienced serious non-AIDS events. People with a viral load between 50 and 200 were 25% more likely to do so than those with full viral suppression. What’s more, people who waited longer to start antiretroviral therapy and those who had a higher viral load or a lower CD4 count at treatment initiation were at greater risk even if they later achieved viral suppression and T-cell recovery.

ALL IMAGES: ISTOCK (MODEL USED FOR ILLUSTRATIVE PURPOSES ONLY) poz.com JUNE 2023 POZ 15
RESEARCH NOTES
BY
CAN WOMEN WITH HIV SAFELY BREASTFEED?

In January 2023, the Department of Health and Human Services updated its guidelines to recommend that people with HIV should receive “evidence-based, patient-centered counseling to support shared decision-making about infant feeding.” This new approach was discussed during a special session at the Conference on Retroviruses and Opportunistic Infections in February.
Traditionally, women living with HIV in the United States have been advised not to breastfeed due to the risk of mother-to-child transmission. But things have changed in the era of U=U (Undetectable Equals Untransmittable). The viral load threshold for reducing transmission via breastfeeding is unknown, but only a couple of cases of transmission from mothers with a viral load below 50 have been reported.
Women living with HIV have advocated for more autonomy in decisions about infant feeding. While breastfeeding comes with a small risk of transmission, it also confers many benefits, including better infant nutrition, improved health, mother-child bonding, lower cost and reduced stigma.
According to the revised guidelines, maintaining viral suppression during pregnancy and postpartum “decreases breastfeeding transmission risk to less than 1%, but not zero.” Replacement feeding with formula or donor milk is recommended for people who are not on effective treatment or do not have sustained viral suppression.
“Individuals with HIV who are on [antiretroviral therapy] with a sustained undetectable viral load and who choose to breastfeed should be supported in this decision,” the guidelines state, adding that those who choose formula feeding should likewise be supported.
People With Advanced HIV Can Have Severe Mpox
Mpox (formerly known as monkeypox) has declined dramatically since the summer of 2022, but it still poses a threat to vulnerable individuals, including those with untreated HIV. While HIV-positive people with an undetectable viral load and an adequate CD4 T-cell count do not fare worse than their HIV-negative peers, it’s a different story for those with advanced immune suppression.
Chloe Orkin, MD, of Queen Mary University of London, and colleagues conducted an analysis of nearly 400 HIV-positive people with mpox in 19 countries who had a CD4 count below 350. Although about 90% were previously diagnosed with HIV, just 60% were on antiretroviral treatment, and only half had an undetectable viral load.
Many patients had severe mpox disease, including extensive lesions, tissue death, lung involvement and eye and brain manifestations. More than a quarter of people with a CD4 count below 100 died, but viral suppression also played a role: The mortality rate was 7% for those with viral suppression but 30% for those with a high viral load. The good news is that no one with a CD4 count above 200 died, suggesting that antiretroviral treatment can prevent severe mpox outcomes.
Mpox is “very starkly different” for HIV-positive people with advanced immune suppression, Orkin says. The researchers argue that mpox should be considered an AIDS-defining opportunistic infection. They recommend that all people with mpox should be tested for HIV, advise clinicians to be alert for mpox progression in people known to be HIV positive and urge that those with a low CD4 count should be prioritized for mpox vaccines and antiviral treatment.

BY LIZ HIGHLEYMAN CARE & TREATMENT BOTH IMAGES: ISTOCK (MODELS USED FOR ILLUSTRATIVE PURPOSES ONLY) 16 POZ JUNE2023 poz.com
DOXYCYCLINE PEP FOR STI PREVENTION
Doxycycline post-exposure prophylaxis (doxy PEP) after sex can prevent bacterial sexually transmitted infections—and adding a vaccine further reduces the risk for gonorrhea—but this approach does not work equally well for everyone.



The recent DoxyPEP study enrolled gay men and transgender women in San Francisco and Seattle. The study found that HIV-positive participants who received a single oral dose of the antibiotic doxycycline within 72 hours after condomless sex were 62% less likely and HIV-negative participants on preexposure prophylaxis (PrEP) were 66% less likely to acquire gonorrhea, chlamydia or syphilis. Similarly, the French DoxyVAC study, which enrolled gay men on PrEP, found that doxycycline reduced the risk for chlamydia by 89%, syphilis by 79% and gonorrhea by 51%. What’s more, a vaccine that prevents meningitis caused by related bacteria also reduced gonorrhea risk by 51%; men who got both the antibiotic and the vaccine saw an additive benefit. Reassuringly, a follow-up DoxyPEP analysis found that preventive doxycycline did not lead to a marked increase in antimicrobial resistance.

However, a parallel trial did not show the same benefit for young cisgender women in Africa. In the dPEP Kenya trial, women randomly assigned to take doxycycline after sex had 35 new cases of chlamydia and 19 news cases of gonorrhea during follow-up, compared with 50 and 12 cases, respectively, in the standard care group. Neither difference was statistically significant. The researchers suggested the poorer performance of doxy PEP for women might be due to anatomical differences, drug resistance or suboptimal adherence.
“The results from the study are deeply disappointing, and we are committed to understanding why doxycycline PEP did not work in this population and also determining the next steps for how to identify prevention tools that will work for and can be used by women,” said Elizabeth Bukusi, MD, PhD, MPH, of the Kenya Medical Research Institute.
Injectable PrEP Works Well for Black Gay Men and Trans Women


Apretude (long-acting cabotegravir) injections offer greater protection than daily pre-exposure prophylaxis (PrEP) pills for Black gay and bisexual cisgender men and transgender women, researchers reported at the Conference on Retroviruses and Opportunistic Infections.





Although African Americans make up about 13% of the U.S. population, they account for more than 40% of all new HIV diagnoses, so effective and acceptable prevention tools are urgently needed. While white gay and bisexual men have readily adopted PrEP pills, uptake has been slower among Black men.


Hyman Scott, MD, MPH, of the San Francisco Department of Public Health, and colleagues evaluated PrEP effectiveness among Black men who have sex with men and transgender women in the HPTN 083 trial, which compared Apretude injections given every other month to daily tenofovir disoproxil fumarate/emtricitabine pills (Truvada and generic equivalents).
Black people were more likely than white people to acquire HIV, but Apretude was highly protective for both groups. Among Black participants, HIV incidence was 2.11 cases per 100 person-years in the oral PrEP arm versus 0.58 cases per 100 person-years in the Apretude arm—a 72% reduction. Adherence was better with the injections than with daily pills, suggesting that long-acting PrEP could help close the racial gap in HIV rates.


Apretude “is a powerful HIV prevention tool to increase access to PrEP and address continued racial disparities in HIV incidence in the United States,” the researchers concluded.


(DOXYCYCLINE) WIKIMEDIA; (COUPLE) ISTOCK (MODELS USED FOR ILLUSTRATIVE PURPOSES ONLY)

20 POZ JUNE 2023 poz.com
This page: Fire Island (2021), from “syzygy, the vision,” a self-portrait series; opposite page: cover of the photo book
PHOTOGRAPHER AND ACTIVIST LOLA FLASH BRINGS FOUR DECADES OF THEIR WORK TOGETHER IN A NEW PHOTO BOOK.
BY POZ STAFF

N THE EARLY YEARS OF THE AIDS CRISIS, LOLA FLASH WAS AN ACTIVE member of ACT UP New York and its affinity group ART+ Positive, which was founded to fight homophobia, AIDSphobia and censorship in the arts. In 1989, Flash was featured in the now famous “Kissing Doesn’t Kill” poster by the activist artist collective Gran Fury. The poster appeared on buses throughout New York City.
As a photographer, Flash’s early work focused on social and political issues, which included HIV and AIDS. Over the past 40 years, their art has continued to challenge stereotypes and preconceptions about sex, gender and race.
Flash’s work is in important collections, such as the Victoria and Albert Museum in London and the National Museum of African American History and Culture in Washington, DC, as well as museums in New York City, such as the Museum of Modern Art, the Whitney Museum of American Art and the Brooklyn Museum.
For the first time, Flash’s work is the focus of a new book. Titled Believable: Traveling with My Ancestors, it’s the 17th book in a series of LGBTQ-themed photo books from The New Press.
The book spans from Flash’s “Cross Colour” images of the 1980s and early ‘90s to their more recent work, which examines the intersection of Black culture, technoculture and science fiction. The book also features images exploring Black identity and portraits showcasing urban trendsetters and people who challenge traditional concepts of gender. ■

“To experience Lola Flash’s portraits is to come face to face, eye to eye, with a subject who will not stay on the margins or in the shadows.”
The New York Times
poz.com JUNE 2023 POZ 21
BELIEVABLE BY LOLA FLASH IS PUBLISHED BY THE NEW PRESS. ALL PHOTOGRAPHY COPYRIGHT LOLA FLASH.
Above: Lola Flash in Washington, DC, at the Capitol Building. Says Flash, “I decided to do my best Obama ‘look.’ The sign is a nod to the 1968 Memphis sanitation strike, for which demonstrators carried signs that read ‘I AM A MAN.’ It was a declaration of their civil rights, which were not given. In my mind, even with a Black president, many of us still struggle for equity!”

Right, from left: Joe (2021), Xunami (2021) and YK (2008), from the “surmise” series highlighting the many ways the LGBTQ community is perceived, all photographed in New York




















22 POZ JUNE 2023 poz.com
Above: Silence = Death (circa 1989), Provincetown, Massachusetts, from the “Cross Colour” series exploring queer Black life during the AIDS crisis


Below: Sur Ron (Sur) (2017), New York City, from the “LEGENDS” series spotlighting LGBTQ trailblazers

Above, top: Karisse (2002), London, from the “[sur]passing” series on skin pigmentation


Above, bottom: Toni (2011), Torquay, England, from the “salt” series celebrating women 70 and older

poz.com JUNE 2023 POZ 23
FRIENDS DARIUS HARPER AND ANDRÉ JORDAN, BOTH ACTORS, NAVIGATE LIFE WITH HIV.
 BY ALICIA GREEN PHOTOGRAPHY BY BILL WADMAN
BY ALICIA GREEN PHOTOGRAPHY BY BILL WADMAN
ACTORS DARIUS HARPER AND ANDRÉ JORDAN, both 36, first met as college students at the American Musical and Drama Academy in New York City, where almost 20 years ago they set out to become stage actors. They’ve supported each other throughout their careers and built a wonderful friendship. And now, they’re standing by each other as they navigate life with HIV.
24 POZ JUNE 2023 poz.com
 Darius Harper (left) and André Jordan
Darius Harper (left) and André Jordan
“It’s a really amazing opportunity to share in this intimate moment with a really good friend,” says Harper about gracing the cover of this issue of POZ alongside Jordan.
Last November, Harper and Jordan performed as part of Playbill’s third annual benefit concert Remember the Ribbon: A Tribute to World AIDS Day. Harper sang a beautiful rendition of “Ribbon in the Sky” by Stevie Wonder. And Jordan kicked off the show with a powerful performance of “You Gotta Be” by Des’ree, which Jordan describes as “a song about lifting yourself up and looking toward the future and taking what life rolls at you.”
For Jordan, who uses he/she pronouns, sharing the stage with his friend and fellow actor was very special. It was also a pivotal moment for Harper.
“Remember the Ribbon was really my coming out,” says Harper, who uses he/ they pronouns. “Nobody in my career, my life or my family, except my grandma and a handful of besties, knew about my status.”
IN 2015, JORDAN AND HARPER
were living out their dreams as working stage actors. Harper was starring in the national tour of the musical Kinky Boots, and Jordan was touring with the musical Joseph and the Amazing Technicolor Dreamcoat. They performed and traveled all over the United States. But both their lives unexpectedly changed that year.
While on tour, Jordan got tested for sexually transmitted infections (STIs) along with some of his castmates. He had been tested six months earlier, so he didn’t anticipate the news he received. He was HIV positive.

“It was sad,” Jordan says. “I had felt this awful stigma around it, that I had done something wrong and that I deserved this for just living my life and doing the things everybody else was.”
Jordan thought he was going to die. Despite growing up in a generation that knew about HIV and AIDS, he hadn’t realized that treatment had advanced such that people living with the virus could lead long, healthy lives. “I hadn’t even allowed myself to consider or do any research into what it’s like for people living with HIV,” he explains. “I thought, Oh, that’s not something that can happen to me.”
Jordan continued to perform and postponed going on treatment. He wanted to finish the five to six months remaining of the Joseph tour. The physician who’d informed him of his status told him that it would be OK but advised
him to find a doctor and get on treatment as soon as he returned to New York. Besides, Jordan hadn’t yet worked the minimum number of weeks required for health insurance coverage by his employer. Continuing on tour would help him qualify for the coverage he needed to start treatment once he was back home.
“Luckily, I did catch it early so that I could take that time and not have to feel that I was in a worse place than I could’ve been,” Jordan says. “I was still very healthy, and I was performing.”
MEANWHILE, HARPER WAS WRAPPING UP THE Kinky Boots tour, the second-to-last city of which happened to be his hometown of Boston. While there, he was preparing to head abroad for another job, but in order to travel, he needed to complete a physical. So he went to see a doctor.
“I remember I was at brunch with some friends, and I got a
26 POZ JUNE 2023 poz.com
phone call from the doctor,” Harper says. “They wanted me to come into the office because I had gone to an urgent care center and not my primary care physician.”
Harper didn’t go. Instead, he asked to be given the news over the phone. That’s when he learned that he was HIV positive. He was in shock.
“I was in the car, and my friends were looking at me in the rearview mirror,” Harper recalls. “They were like, ‘What is wrong with you? You look like somebody just died.’ So that moment was very palpable.”
Harper tried to sweep the diagnosis under the rug. He left to perform abroad but returned home months later. It turned
out that he also had syphilis, and the STI was very far along.
“That was a moment when my life kind of fell apart,” he says. “I was supposed to be working abroad and financially have enough through a yearlong contract. To cut that short to come home and deal with my diagnosis was a lot.”


poz.com JUNE 2023 POZ 27
André Jordan (left) and Darius Harper light up Times Square in New York City.
WHENJORDANRETURNED to New York, he looked online for HIV resources and then connected with an LGBTQ clinic in his Brooklyn neighborhood.

He met with someone who helped him find a doctor. His doctor first prescribed him three HIV drugs. These days, he manages his HIV with just two of those medications.
“I’ve been undetectable for a long time,” Jordan says. “It’s such a thing that it’s not a thing anymore. You get up every day, take a shower, pop your pills and just keep going.”
Maintaining his health requires more than just taking his HIV meds. He remains active by running and working out at the gym. As a performer, he also dances a lot. Sometimes he takes breaks from alcohol too. But what has helped him the most along his HIV journey is sharing his story with others.
“Not being afraid to talk about it publicly is a big help because I don’t I have to hide it,” he says. “I can say it freely. It’s just a part of who I am now.”
Since his diagnosis eight years ago, Jordan’s life has changed tremendously. In 2016, he met the love of his life, who is now his fiancé. They plan to get married soon and hopefully start a family. Jordan has also enjoyed some career success.
In 2015, he starred in the YouTube series The Queens Project, which ran for several seasons. Then in 2021, he made his Broadway debut in the musical Diana
“[Debuting in Diana] was the best day of my life,” Jordan says. “It was everything I had dreamed of. It was 15 years after I had moved to the city. I felt like everything was worth it.”
Continued on page 31
28 POZ JUNE 2023 poz.com
“NOT BEING AFRAID TO TALK ABOUT IT PUBLICLY IS A BIG HELP BECAUSE I DON’T HAVE TO HIDE IT.”
—André Jordan
Outside the bar Don’t Tell Mama in the Theater District
HARPER BELIEVES THAT BEING FORCED TO acknowledge his status is what saved him.
“There was a lot of abuse of my body going on and a lot of mental situations that I’m in therapy today for,” he says. “All of that stuff came to the forefront. So while I was trying to save my life by getting medicine, I was also kind of laying down and dying at the same time.”
Harper credits his doctor with helping him survive. He had his syphilis treated and began HIV treatment with a oncedaily pill.
“It’s really intense those first weeks, months and year of an HIV diagnosis,” he says. “There’s a lot of changes in your life routine-wise. Once you find the right medicine, you have to stay on it.”
In 2017, Harper joined a Cirque du Soleil tour in Canada. He tried having his medication delivered to the country several times, but it kept getting lost at the border. At one point, he stopped taking it altogether due to stress.
When he returned to New York, Harper had developed resistance to the medication. That’s when his doctor switched him to the daily one-pill regimen he’s still on. He is currently undetectable, which means he cannot pass on the virus sexually.
Harper’s journey hasn’t been easy. He once struggled with self-harm and substance use. But seeking help for his mental health and being in recovery have changed his life. The experience has also allowed him to open up about living with HIV.
“I’m at a place now where all of those scabs have been healed,” Harper says. “It felt right to share my story because that’s who I am as a creative, as an artist. I always strive to be an advocate and ally for people who look like me and come from where I come from. That now includes the HIV community.”
IN THE PAST, HARPER AND JORDAN HAVE BOTH struggled to maintain their health insurance coverage, which affected their treatment. As members of the Actors’ Equity Association, they must work 12 weeks to get insurance coverage for six months and work more to be eligible for the year.
“There were a lot of times in the beginning of my diagnosis where I was going without medication because of insurance issues,” Harper explains. “Whether it had lapsed or I didn’t have enough weeks worked in my work year to get it. Switching over to Medicaid was probably the best thing that I could’ve done as an HIV-positive individual.”
Jordan applied for Medicaid when he couldn’t get insurance through his job.
“I wasn’t able to get my medication,” Jordan says. “There’s been like a two-month break and a little bit longer than that sometimes. But I’m always able to get back on insurance and then back onto my medications.”
Managing HIV while on tour also has its challenges. Doing so sometimes became too much for Harper. As if touring weren’t time-consuming enough, he would also have to find time for medical visits in new cities.
“In my experience as a touring artist with HIV, there is no resource for doctors other than a new patient situation in different cities,” Harper explains. “Even if you have your medicine mailed to you from your doctor, sometimes things go awry, and you need to go into a clinic.”
That’s how Harper got the idea to develop a network across clinics in different cities for touring artists living with HIV. The network would allow union actors to visit a specific clinic in each city. The clinics would have all their files and labs saved in a system.
Jordan thinks it’s a great idea. “If you’re on the road, in a regional show or you’re on contract and this happens to you,” he says, “then you can you go around the country and seek out help without it having to put a full stop on your life.”
UNTIL RECENTLY, Harper didn’t really think about the future, but now, he thinks about his life in the long term.
“Before my diagnosis, I had a wonderful life,” Harper says. “I’ve had a great time on the road. But right now, I’m having fun just working my job, paying my rent and sitting on my couch. Mundanity is what I aspire to, honestly.”
Harper also writes and produces concerts. It makes him happy. He’s continually healing and enjoying the little things in life.
Jordan is doing what makes him happy too. He’s auditioning for roles and still performing. He works at a Theater District piano bar called Don’t Tell Mama, where he sings and bartends.
“It’s a legendary place,” he says. “I always tell people that they can come and see me perform every week there if they want. I just want to keep making theater and getting up on that stage.”
Jordan wants people living with HIV to know that they’re not alone. There are others out there who are still working up the courage to talk about it.
Both he and Harper were once those people. Now they have each other and a whole community to share their experiences with. ■
poz.com JUNE 2023 POZ 31
“I ALWAYS STRIVE TO BE AN ADVOCATE AND ALLY FOR PEOPLE WHO LOOK LIKE ME.” —Darius Harper
BY CHARLES SANCHEZ
His Name Is Mister Snow
The dashing Nicholas Snow, 61, has worn many hats in his life: international journalist, actor, author (his book, Life Positive: A Journey to the Center of My Heart, is available in 21 languages). He cut his activist teeth while still studying at Arizona State University at the beginning of the AIDS crisis. In the early 1990s, he created a public access television show called Tinseltown’s Queer, which he hosted for seven years. And all of this before he seroconverted.
“I was living in Thailand, acting in movies and working as a foreign correspondent for my own website, Notes From Hollywood, at the time. In 2007, in a rare slip in my safer-sex behavior, I became HIV positive,” he says.


The slip occurred with someone he trusted, someone who had told Snow he was HIV negative.

Snow believes that his slip stemmed from his own isolation, depression and loneliness. “In my sharing since then, I stress why it’s not a good idea to have [unprotected] sex with someone based on their own beliefs of their HIV status.”
After taking time to absorb his diagnosis, Snow came forward and told his story publicly. “Because of my roots in activism,” he says, “I endeavored to go public with my story, which I did at a press conference at the Foreign Correspondents’ Club of Thailand.” Snow went on to work with a prominent music producer in Thailand to develop a music video campaign promoting HIV testing and safer-sex practices. “For a time, I was one of the most visible HIV-positive people in Asia,” he says.
Snow eventually moved back to the United States and settled in Palm Springs, California, in 2011. “I was on the edge of homelessness, with no health care, very little money, no car and very few possessions,” he says. He became a client of DAP Health, which helped him access the health care, housing and community he needed.
The multitalented Snow hasn’t stopped creating. He’s still pursuing acting. He runs the website PromoHomo.TV, where his content garners hundreds of thousands of views worldwide, and in 2020, he expanded to an online TV network.
Bringing things full circle, Snow marked the 30-year anniversary of Tinseltown’s Queer at the Palm Springs Cultural Center on April 28, 2022— 30 years to the day after his first broadcast—with a screening of highlights from his years of activism.

“When I talk about my life,” he says, “I feel like I’m talking about someone else. It’s kind of hard for me to believe that this is the life that I’m living and that I’ve lived it.” But despite a life lived out loud, the stigma of HIV can still sting.
“I’ve gone public about my HIV status so many times. When I decide to participate on dating apps, I’m always forthcoming about my status. That’s always my choice. There’s still a tremendous amount of rejection that happens there,” he says. “One of the things that I believe is the best medicine for anybody is to tell your truth. We’re all in this together.” ■
HEROES
KEVIN MCDERMOTT
32 POZ JUNE 2023 poz.com
Nicholas Snow is a longtime AIDS activist.
This quick reference chart compares antiretroviral (ARV) options for the prevention of HIV, including adult dosing information. Visit poz.com/drugchart-prevention for more info.
HEALTH, LIFE & HIV (Pillsnotshownactualsize)
PRE-EXPOSURE PROPHYLAXIS (PrEP)
PrEP is an antiretroviral medication taken by an HIV-negative person to reduce the risk of contracting HIV.



The Food and Drug Administration has approved the following three regimens for PrEP:
Nucleoside/Nucleotide Reverse Transcriptase Inhibitors (NRTIs, or nukes)
TRUVADA
tenofovir disoproxil fumarate + emtricitabine
One tablet once a day. Each tablet contains 300 mg tenofovir disoproxil fumarate (TDF) + 200 mg emtricitabine.

Approved for HIV-negative men, women and transgender individuals at risk for sexually acquired HIV. Generic version available.
DESCOVY
tenofovir alafenamide fumarate + emtricitabine
One tablet once a day. Each tablet contains 25 mg tenofovir alafenamide fumarate (TAF) + 200 mg emtricitabine.
Not approved for those at risk for HIV acquisition via vaginal sex.
POST-EXPOSURE PROPHYLAXIS (PEP)
Integrase Inhibitors
APRETUDE cabotegravir
Apretude is initiated with two 600 mg injections given one month apart for the first two months, after which injections are given every two months. Alternatively, oral cabotegravir (Vocabria) may be taken for four weeks before the injections. Apretude is given as a single injection in the buttocks by a health care worker every other month.

Approved for HIV-negative men, women and transgender individuals at risk for sexually acquired HIV.
PEP involves taking a short course of ARV drugs, usually for a month, after a high-risk exposure. For maximum effectiveness, PEP should be started immediately—and no more than 72 hours—after possible exposure.
The Centers for Disease Control and Prevention recommends the following preferred HIV PEP regimen:
ISENTRESS raltegravir
One tablet twice a day. Each tablet contains 400 mg of raltegravir.
Alternative
TRUVADA tenofovir disoproxil fumarate + emtricitabine
One tablet once a day. Each tablet contains 300 mg tenofovir disoproxil fumarate + 200 mg emtricitabine.
PEP regimens can be found online in the CDC’s PEP Guidelines.
PLUS



















































































































































































































































































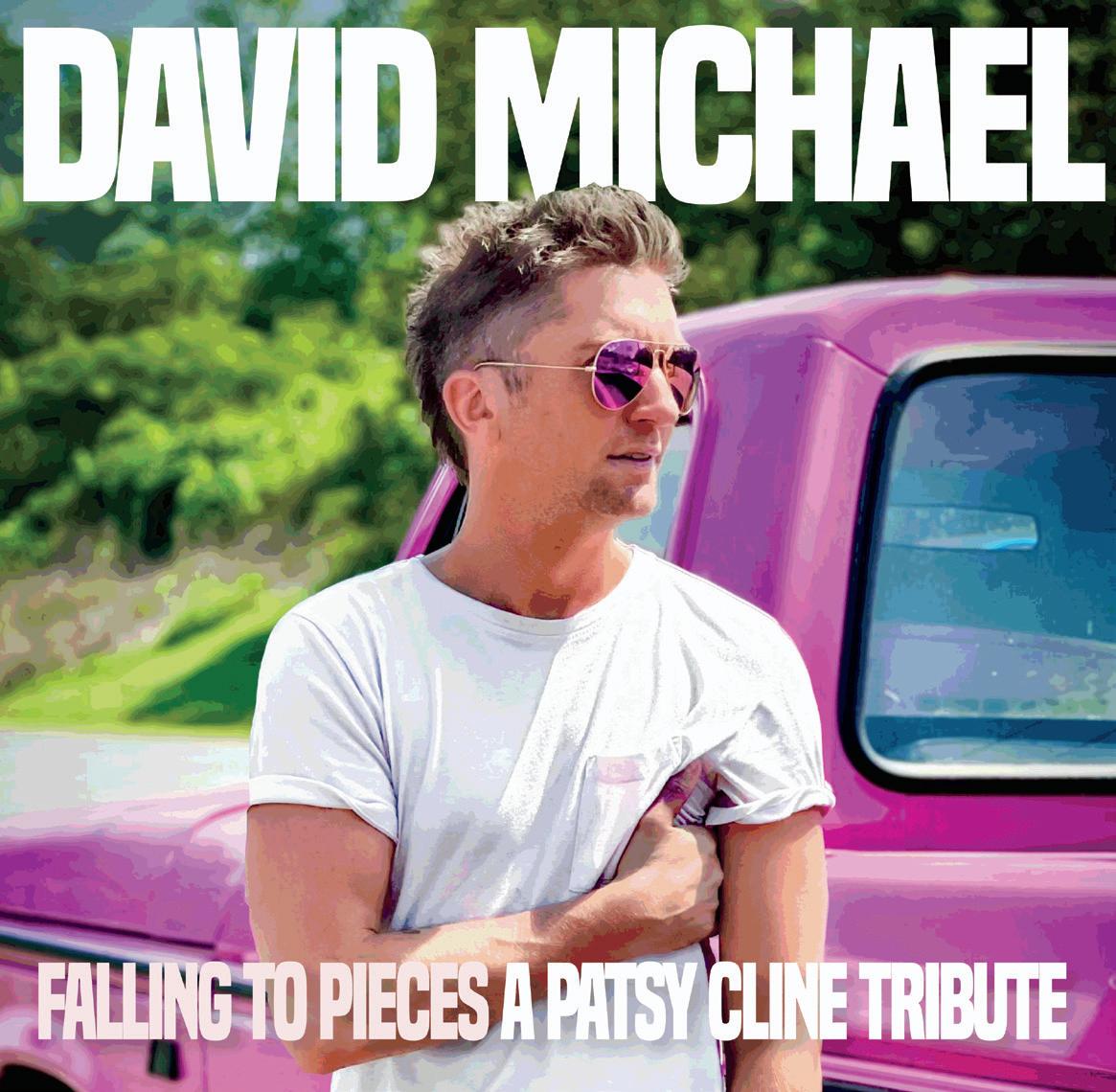









 —Trent Straube
—Trent Straube


























































 LIZ HIGHLEYMAN
LIZ HIGHLEYMAN


















































 BY ALICIA GREEN PHOTOGRAPHY BY BILL WADMAN
BY ALICIA GREEN PHOTOGRAPHY BY BILL WADMAN
 Darius Harper (left) and André Jordan
Darius Harper (left) and André Jordan












