
of such
been



of such
been


For all membership enquiries and assistance, including
The Lamp subscriptions and change of address, contact our Sydney office.
50 O’Dea Avenue, Waterloo NSW 2017 (all correspondence)
T 8595 1234 (metro) 1300 367 962 (non-metro)
F 9662 1414 E gensec@nswnma.asn.au
W www.nswnma.asn.au
8–14 Telford Street, Newcastle East NSW 2300
NSWNMA Communications Manager


Danielle Blasutto T 1300 367 962
For all editorial enquiries, letters and diary dates
T 8595 1234 E lamp@nswnma.asn.au
50 O’Dea Avenue, Waterloo NSW 2017
Hester Communications T 0414 550 376
Send your press releases to:
F 9662 1414 E gensec@nswnma.asn.au
Shaye Candish, NSWNMA General Secretary
Michael Whaties, NSWNMA Assistant General Secretary
O’Bray Smith, NSWNMA President
Michelle Cashman, Long Jetty Continuing Care
Richard Noort, Justice Health
Liz McCall, Byron Central Hospital
Diane Lang, South East Regional Hospital, Bega Valley
Printed by Ovato Print Pty Ltd, 37–49 Browns Road, Clayton VIC 3168
Danielle Nicholson T 8595 2139 or 0429 269 750
F 9662 1414 E dnicholson@nswnma.asn.au
To find archived articles from The Lamp, or to borrow from the NSWNMA nursing and health collection, contact: Adrian Hayward, Coordinator.
T 8595 2175 E gensec@nswnma.asn.au
The Lamp ISSN: 0047-3936
The Lamp is the official magazine of the NSWNMA. Views expressed in articles are contributors’ own and not necessarily those of the NSWNMA. Statements of fact are believed to be true, but no legal responsibility is accepted for them. All material appearing in The Lamp is covered by copyright and may not be reproduced without prior written permission. The NSWNMA takes no responsibility for the advertising appearing herein and it does not necessarily endorse any products advertised.
Authorised by S. Candish, General Secretary, NSW Nurses and Midwives’ Association, 50 O’Dea Avenue Waterloo NSW 2017
The NSWNMA collects personal information from members in order to perform our role of representing their industrial and professional interests. We place great emphasis on maintaining and enhancing the privacy and security of your personal information. Personal information is protected under law and can only be released to someone else where the law requires or where you give permission. If you have concerns about your personal information, please contact the NSWNMA office. If you are still not satisfied that your privacy is being maintained, you can contact the Privacy Commission. Subscriptions for 2022 Free to all Association members. Professional members can subscribe to the magazine at a reduced rate of $30. Individuals $84, Institutions $140, Overseas $150.
message is being heard
need to pressure politicians more
are to achieve ratios Assistant
Secretary Michael Whites told
conference.
COVER STORY
a blockbuster union
unions don’t stand still –
challenge is always to build strength,’ says Brett Holmes.
COVER STORY
for ratios and better pay across NSW
of public sector nurses and midwives walked off the job for the third time this year in their fight for safe staffing ratios and better pay.
of scrubs across NSW
Tweed Heads in the north to Albury in the south and from Sydney’s eastern suburbs to Broken Hill, thousands of nurses
to the streets on 1 September.
ratios deal sets the pace

members at Sydney Adventist
secure best ratios proposal in NSW.
time to build nurse power and win workplace democracy
has exposed gaping fault lines in already overloaded healthcare systems
it has also created new opportunities, global nursing leaders say.









is now the largest graduate certi cate provider for nurses in Australia. Become an expert practitioner in your clinical specialty and increase your earning potential with an online graduate certi cate, including the all-new Graduate Certi cate in Digital Health and Graduate Certi cate in Diagnostic and Interventional Radiology Nursing. Apply for the January 2023 intake.

The NSW ALP opposition has made a significant step forward by pledging to introduce an enforceable, shift-by-shift safe staffing system for nurses and midwives if elected in next year’s state election.
As The Lamp goes to press our campaign for shift by shift ratios in NSW has gained serious momentum.
NSW Labor has committed to adopt the principles that underpin ratios into the award. This means the ALP, the Greens and the Shooters, Fishers and Farmers’ Party now all support a mandated safe staffing ratios.
The NSWNMA has been talking with all the political parties as well as the government over the last few months highlighting the dire state of our public health system and advocating our solutions based on your analysis of what’s happening at the frontline.
The ALP has now responded and committed to important parts of our 2022 claim.
If they are elected in the March election they say they will implement our claims in certain areas, in a phased approach:
• 1 nurse: 3 patients in Emergency Departments

• 1 nurse: 1 patient in ICUs and adherence to the latest professional standards outlined by the Australian College of Critical Care Nurses including Access Nurses
• 1 midwife: 3 mothers in post natal maternity and a full review of Birthrate Plus to ensure babies count
• 3/3/3 (am:pm:nd) nurses as a minimum in our Multi-Purpose Services where there is a 24/7 Emergency Department, with at least 2 RNs and the requirement for staff to be FLECC/ENEC trained.
• All existing Nursing Hours Per Patient Day wards will convert to a shift-by-shift system. For those at 6 NHPPD, for example, a minimum

of 1:4am, 1:4pm, 1:7nd will apply, with an additional nurse designated as “in charge of shift”/”clinical coordinator” on at least two shifts. Assistants in Nursing will be additional to the minimum ratio.
This is a highly promising start towards much needed reforms to our public health system but there are areas that still need to be addressed.
Areas from our 2022 ratios claim not covered by NSW Labor’s announcement include: paediatric and mental health critical care (PICU and MICUs), paediatrics, NICU, perioperative services, community and community mental health, short stay wards, drug and alcohol, outpatient clinics, specials and CNE/CMEs.
So while Labor’s announcement is a major step forward by one of the major parties and a significant boost to our campaign there is still a lot of work to be done.
Before the 2019 NSW election Labor made a similar commitment to ratios but that didn’t translate into a win for our health system when they lost the election.
Their new policy will only translate into a concrete result – the implementation of shift-by-shift

ratios – if Labor is elected in the March election.
The Perrotet government still has an opportunity to support our claim for shift-by-shift ratios, but as yet, has not committed to this reform. The people of NSW should not have to await the outcome of an election. The government could, and should, act today and we welcome the opportunity to talk with them about this.
There is something we must be absolutely clear about. We have only got to this point because of the actions that members and branches have taken so far.
By taking multiple statewide strikes, by speaking out, by meeting with local MPs and writing open letters, you have helped NSW move towards a better public health system.
Your industrial action, your fantastic social media skills, your local disputes and your engagement with the media have allowed us to go into talks with the different parties with your power behind us.
But we need to keep building on this momentum. Let’s maintain the intensity of our campaign right through to the March election. n
By taking multiple statewide strikes, by speaking out, by meeting with local MPs and writing open letters you have helped NSW move towards a better public health system. But we need to keep building on this momentum.


I write to advocate for my local community, and importantly, for our profession. Sadly, the needs of our community are constantly not being met by our struggling healthcare system, and nurses are bearing the brunt of this, usually in the form of aggression and frustration from patients and their families.
Nursing is an art, and for many of us, it is more than a job: it is a vocation. I work in Emergency and I have seen some of the worst conditions

I have ever experienced in my 20-year career. This is why I believe a group of caring nurses have chosen to walk away from their patients.
It is an extremely bold and brave statement of how bad things really are.
We have been stretching ourselves to ensure patient safety and many of us are now at breaking point. It is on the backs of nurses that the community has been carried through surge after surge.
Ratios of one nurse to 30-plus patients in the ED waiting room is not uncommon – yet how can this be safe? We often care for children, elderly and vulnerable populations. We are pushed to off-load ambulances, even when our workload is already at unsafe levels.
How many times have we been lucky that our patient did not deteriorate? And, how many times did our luck actually run out?
We have a professional obligation to speak up when things are not right, and we all know that things are not right. There are no other words to describe it. The current situation is UNSAFE.
The buck stops with us – at least I assume that is what the Coroner would say.
Nurses are not OK. So many of my colleagues are so mentally and physically exhausted, what will keep them at work? A commitment to a safe workload would be a start.
We know ratios will save lives, reduce hospital stays and will save money. So, what is our Premier waiting for?
We will speak up. We will be loud and we will not stop until there is a commitment to mandated safe patient care: 1:3 in ED! 1:4 on the floor!
Mel Benjamin, RNEMAIL lamp@nswnma.asn.au fax 9662 1414
MAIL 50 O’Dea Avenue, Waterloo NSW 2017. Please include a high-resolution photo along with your name, address, phone and membership number. Letters may be edited for clarity and space. Anonymous letters will not be published.
I have been working in my local rural hospital for almost 20 years. I love my workplace – it has always been a relatively harmonious environment. We have fantastic staff who really care about our community and providing an exceptional level of care.
I recently decided to give the clinical nurse educator role a go. After having taken a break from nursing prior to my children starting school, I increased my hours considerably and had really found my passion for nursing.
I love the educator role and I think it is so important that we provide support to our new nurses, but lately, this support is fading. Due to critical staffing shortages, I have been unable to fulfil my education duties.
I feel responsible for the fact that my staff are stressed, and that they are scared that something terrible is going to happen on their shift and that they won’t know what to do!
We desperately need more skilled and experienced ED RNs who are willing to work in a non-supported department with little to no medical coverage. There are not enough of us to go around!
In our facility, myself, the NUM and facility manager, have been trying to keep our roster afloat by picking up extra shifts and filling the gaps. We can no longer continue to do this. It is relentless and there is no light at the end of the tunnel.
Lauren Hutchins, RN
If there’s something on your mind, send us a letter and have your say. The letter of the month will WIN a gift card. The letter judged best each month will receive a $50 Coles Group and Myer gift card.
I am a proud
paediatric nurse, working with some of the sickest children in our state.
On a normal day in my unit, one registered nurse cares for four sick children. This means that for each hour, I can only give a sick child a maximum of 15 minutes of my time. That is 15 minutes to develop trust, take their bloods, check their vital signs – none of which is a speedy thing to do. I’m sure you can imagine that there are not many toddlers who will happily sit still and lend you their arm to take their blood pressure.
I am lucky that I only have four sick children to care for. Even so, there is always the constant feeling that you are not able to do enough for these children and their families. We are stretched. My colleagues elsewhere have it far worse. Last week, a colleague was left alone with 26 sick kids waiting in the Emergency. And
during this winter, we have had it worse than that.
Paediatric nursing isn’t for everyone – I appreciate that –but even so, we are currently facing a crisis of staff retention. Our experienced nurses are leaving at rapid rates. In my unit alone, we’ve lost one quarter of our workforce.
The stress of dealing with seriously unwell children, bearing the brunt of anger from parents who are frustrated at the stretched system, the onslaught of overtime because “someone has to stay” and the pay rate that is far behind our counterparts in other states, means that for so many, it doesn’t feel like it’s worth it any more.
I am scared for the future of paediatric nursing in this state. I am scared for the children who are the victims of a health system that is short-staffed or staffed by those without adequate experience.
Kate Surian, RN

On 19 October, if you're a financial member of the Association, you'll receive a postal ballot in the mail to participate in the upcoming ANMF NSW election.
Completed ballot forms need to be returned so that they are received by the AEC no later than 10 am, 16 November. Log in to Member Central for more information.
Advertise in The Lamp and reach more than 70,000 nurses and midwives.
To advertise contact Danielle Nicholson 02 8595 2139 / 0429 269 750 dnicholson@nswnma.asn.au
Annual Conference saw the end of an era for the Association, with General Secretary Brett Holmes retiring after 20 years at the helm and Shaye Candish assuming the leadership.
Annual Conference 2022 was an historic moment with the farewell of our leader of the last 20 years, Brett Holmes. The conference also reflected on our achievements over the last year and furthered preparations for the year ahead to win ratios in the Public Health System.
Brett spoke to the conference with pride about the current state of the union and his confidence about it, going forward.
“In all my years leading the Association, I’ve never been more confident in our future as a powerful and influential union. We are building a highly successful organising model that develops and supports leaders by encouraging them to use their collective strength,” he said.
“It’s been incredible to see what we can achieve together, with strong numbers turning out for multiple strike actions over the past few months.”
Brett said members’ actions were forcing governments, the media and the community to sit up and listen to what nurses had to say about what was happening in the health system and aged care.
“In a significant time for workers’ rights in Australia as a whole, we
are finally being heard. During its first month in power, the new federal Labor government delivered some historic wins for unions. It supported an increased minimum wage in line with inflation and committed to a plan to fix aged care,” he said.
“It’s disappointing that despite several inquiries and a royal commission, it took a change in government to acknowledge the need for a substantial overhaul of our aged care system.
“With a state election in March next year, the result from the recent federal election gives us hope that a change in government may finally deliver nurse-to-patient ratios to our public hospitals in NSW.”
Brett said he was leaving, knowing the union was in safe hands.
“I know that my successors, Shaye Candish and Michael Whaites, will be doing everything they can to lead
this Union to that outcome [of nurseto-patient ratios]. Member support for the campaign will be essential. Nothing ever comes easily to nurses and midwives and we must keep up the pressure on all political parties.
“Frontline workers have been dealt a bad hand over and over by the current NSW government. It’s about time we get the respect we deserve. I’m confident we can finally win ratios next year if we maintain our collective strength and stay the course.”
New NSWNMA General Secretary, Shaye Candish, heaped praise on our members in aged care after a brilliantly successful campaign, which culminated in the election of a Labor government committed to introducing ratios into the sector.
‘With a state election in March next year, the result from the recent federal election gives us hope that a change in government may finally deliver nurseto-patient ratios to our public hospitals in NSW’. — Brett Holmes
“It’s a victory for so many of our determined members that never once gave up on the campaign to win better lives for the elderly residents they care for,” she said.
Shaye said the result in the federal election was determined by issues that had a disproportionate impact on women: rising prices, low wages and expensive childcare.
“Many of these issues will no doubt feature in the upcoming March 2023 state election and as [nursing is] the largest female workforce in NSW, these issues are central to our work, our families and our lives,” she said.


“The federal election demonstrated that women were fed up with being ignored and they used their vote to send a strong message. Current politicians who continue to ignore our call for safer staffing do so at their own disadvantage.”
Shaye said that going forward, they would “focus on improving the lives of all our members in every sector: better work – via ratios, a stronger voice and better living standards”. n
What a career our General Secretary Brett Holmes has had. Over his two decades at the helm, Brett has been part of many significant workplace improvements, including the Your Rights at Work campaign to end the Howard government’s WorkChoices legislation, the introduction of a universal Paid Parental Leave scheme and the increase in the superannuation guarantee to 12 per cent, to name a few. We’ll be sad to see Brett move on but will continue to draw on his tenacity in our fight for workers’ rights.’
— NSWNMA General Secretary Shaye Candish‘On behalf of council, we wish Brett a safe and happy retirement chasing fish up north. Brett has worked tirelessly and in the best interests of our members; a genuinely altruistic union leader and we are forever grateful for his work.’
— NSWNMA President O’Bray Smith MICHAEL WHAITES, SHAYE CANDISH AND BRETT HOLMESWe need to pressure politicians more if we are to achieve ratios Assistant General Secretary Michael Whites told Annual C onference.
Michael Whaites said that while the Public Health System campaign was about fighting for a pay rise, better workloads and better healthcare we were also fighting for something “a little deeper than that”.

“We’re fighting for politicians to show you the respect you deserve, to listen to your clinical judgment about what is really going on in the system and then making the right decision to fix it.”
Michael said the community was listening to our message.
“Simple actions, and some not so simple have highlighted your stories, stories that the community need to hear and are hearing.
“When miners on the South Coast ask themselves whether today’s health system could cope with a disaster and come to the conclusion “no” and have joined your claim for ratios you know that our message is getting through.”
He said that our actions were also having an impact on politicians.
“Prior to the state budget ministers conceded that there is a problem.
“The health minister conceded that the NHPPD system is being manipulated and said he was doing all he can to convince his party that we need more nurses and midwives in the system.”
Michael said the government also conceded that they needed to pay nurses and midwives more.
“So you can see the government in some ways is responding but they are drawing the wrong conclusions as a result of their ideological opposition to ratios.” n
Lower House independent MPs Greg Piper, Alex Greenwich, Dr Jo McGirr and Helen Dalton back our claim.
The Shooters, Fishers and Farmers and the Animal Justice Party have shown support.
The Greens have tabled a bill in parliament, which if passed would require shift by shift ratios to be implemented but without the support of the ALP the bill will not pass.
Michael Whaites urged members to put pressure on their local MPs in the lead up to the March 2003 state election.
“It is important for every public sector nurse or midwife to go and visit your local politician no matter what political party they belong to. Tell them your story, tell them why you need ratios and tell them to fix it.”
As The Lamp goes to print the NSW ALP has responded to our campaign and committed to important parts of our 2022 claim.
If they are elected in the March election they say they will implement our claims in certain areas, in a phased approach:
• 1 nurse: 3 patients in Emergency Departments
• 1 nurse: 1 patient in ICUs and adherence to the latest professional standards outlined by the Australian College of Critical Care Nurses including Access Nurses
• 1 midwife : 3 mothers in post natal maternity and a full review of Birthrate Plus to ensure babies count
• 3/3/3 (am:pm:nd) nurses as a minimum in our Multi-Purpose Services where there is a 24/7 Emergency Department, with at least 2 RNs and the requirement for staff to be FLECC/ENEC trained.
• All existing Nursing Hours Per Patient Day wards will convert to a shift by shift system. For those at 6 NHPPD, for example, a minimum of 1:4am, 1:4pm, 1:7nd will apply, with an additional nurse designated as “in charge of shift”/”clinical coordinator” on at least two shifts. Assistants in Nursing will be additional to the minimum ratio.
‘We’re fighting for politicians to show you the respect you deserve’.
— Assistant General Secretary Michael Whaites

The NSWNMA has produced a TV ad for our ratios campaign. We know it is confronting but it shows the hard realities for many patients, families and nurses working in an underresourced public healthcare system.

“This is how I died.
After waiting 14 hours I ended up in an overcrowded ward.
I knew something was seriously wrong with me, but no nurse could get to me.
They are looking after so many patients at once.
With enough nurses I might still be alive.”
Watch the ad
www.ratioslife ordeath.org.au

‘Successful unions don’t stand still – the challenge is always to build strength,’ says outgoing NSWNMA General Secretary, Brett Holmes.
After a working life dedicated to the nursing and midwifery professions
– including 20 years as leader of the NSWNMA – Brett Holmes is changing gears.
Brett retired as general secretary at our Annual Conference to move to the Mid North Coast to start a new life chapter and with fresh ideas for how he can contribute to the community.

“I hope to make a contribution through volunteering in my new local community in whatever form that takes – perhaps marine rescue or the Men’s Shed,” he told The Lamp “I want to do something that benefits my community. I’ve focused on nursing all my life and now I’m ready to go further afield.”
In the 20 years of his leadership, the NSWNMA grew from 50,000 to nearly 75,000 members. It has become a powerful and respected champion for nursing and midwifery. It has been a staunch defender of our public health and aged care systems. And all this, despite operating for long periods under anti-union Liberal governments at state and
federal levels.
The key to this success, Brett says, is a focus on “always building the strength of the union”.
“We set targets for developing member leaders to support branch officials in order to strengthen the capacity of members at workplaces, so they are able to respond to management and fight for better outcomes,” he said.
Improving workloads has been the union’s main goal since Brett became general secretary in 2002.
“We started with language like ‘reasonable workloads’, which we achieved in the What’s a nurse worth? campaign.
“Having language in the award is one thing – strengthening the power of the branch to enforce it has been the
next highest priority,” he said.
Many fellow unionists see the Association as a model of a sophisticated, modern union and to achieve that, Brett says you need “good people and good governance practices”.
“The nursing and midwifery professions have high standards, and high performance is expected of members as individuals. But they also set high standards for their organisations.
“I was fortunate to be able to stand on the shoulders of very good, prior leaders who had put in place many systems that we were able to expand and grow as the union became bigger and more sophisticated.
‘The key to (our) success is a focus on always building the strength of the union.’
— Brett Holmes
Per Patient Day in 2010 was a major breakthrough. Not perfect, but 1600 more nurses and decent pay rises and with a level of accountability that the health services hadn’t experienced before.”
“Not having delivered 75,000 members (the NSWNMA currently has 74,494!) and achieving nurse-to-patient ratios before I retired.”
“The campaign to stop the privatisation of regional hospitals. It was a campaign of collective action and it was most rewarding because we were able to work very well with the doctors, other health workers’ unions and the community.”
“Nurses and midwives have shown their dedication to the work they do but they’ve also experienced vulnerability as workers having to put their lives on the line. COVID has also shown the importance of the health system to the whole of society and also to the economy because a sick workforce doesn’t produce very much at all.”
“That was supported by a forwardthinking, cooperative council that was very willing and able to support change and drive further sophistication of the organisation.”
Brett says the union has often had to operate in a difficult political environment. He cites John Howard’s WorkChoices, which weakened enterprise bargaining, and the O’Farrell government laws, which undermined the independence of the industrial umpire in NSW.
“It forced the union into having a political focus in order to deliver change. I have no doubt that the O’Farrell laws stifled the development of safe patient care with a wages policy that took any real discussions about workplace change off the table and made it into a purely political decision, to be given or taken away as the government wished.
“That forced us into public campaigning over issues that previously we had been able to take to the bargaining table with the option of going to arbitration.
“That had an impact on our ability and our members’ ability
to improve the health system, to improve patient care.
“The government didn’t want to know about productivity or about patient safety from an industrial perspective. They just wanted nurses to take their money, shut up and go away. Our members were never prepared to do that.”
Brett says nurses and midwives have come to realise that we cannot shy away from the political process.
“It has been a long process of education – to understand who are the decision-makers in health and the importance of our members’ vote and voice if they want change.”
Brett says his last big decision was to encourage capable leaders to take the union forward into the future.
“Shaye Candish (the new General Secretary) has the absolute conviction and energy to drive the union towards its goals. Michael Whaites (the new Assistant General
Secretary) has international experience in leading workers as well as decades of experience leading nurses and midwives.
“Both have the tenacity and will to continue the fight with government to deliver better outcomes in the workplace and to achieve better conditions.
“They both have leadership qualities of being able to look at the bigger picture, to listen to the best advice and to make good decisions.” n

The Lamp spoke to two community health nurses attending annual conference for the first time about what they thought of the conference and what it is like in their current work environment.
“The discussions with the other delegates were the highlight of the conference for me. Nearly every single delegate was extremely passionate about what they do and very proud of where they came from.
The overwork I have witnessed since I started at my current workplace has made me become more passionate about being involved in the union.
[There is a] lot of damage that the last two years has done to my team, and I wish to restore a lot of happiness and a sense of family that was at my Centre. People are afraid that if they speak up about burnout…they will get a lot more work, or more complicated work.
We work 300 minutes over a day of face-to-face care. What’s not taken into account are any problems that might come up. Palliative care has increased the acuity, and palliative care staff has decreased in the last 12 months [yet] more people wish to die at home, which has severely increased the workloads on the rest of the team.
They say taking your break is your responsibility, but you are travelling between patients…and before you even start you have to read up and know what you are doing. It’s not unusual for a nurse to stay back after a shift to do notes… If you inform anyone above you, you will be told that you have got poor time management.
(The government’s response to the pandemic is) terrible, absolutely woeful. It was the things they neglected to do.
I didn’t feel supported at all when it came to the pandemic. I didn’t feel valued. I felt as if I was expected to handle it, to run around in full PPE to get samples in summer, going inside people’s homes with no air conditioning. There was no choice, and no recognition that this was happening. I feel as if the new (NSWNMA) leadership wants to change legislation
and do something big. We are daring to dream a little bit more this time, and we’re not going to sit down to have a crap sandwich. The fact is we need more funding if we are going to care for an aging population [and] I think we should be a lot more active about fighting the government about what we need. I think the strikes should be to the point where there are actually consequences for the government.”
‘I think we should be a lot more active about fighting the government about what we need.’ — Brendan McCulloch EN
“At the Thursday night dinner we were on a table of rural and community health nurses, and that was fantastic because community health is isolated. There aren’t nearly as many of us as hospitals, and we spent a lot of time comparing services. (At the conference) Jane Caro was a highlight. Not only was she talking about highlighting some of the problems, but she also had an emphatic take on how we start to make a change.
We are a very new branch and a very small branch and the union has really given us that power to find a voice. Just getting everyone signed on, I rejoice in that. A lot of people have convinced themselves the union hasn’t really done anything for them, and it’s that switch to people thinking, ‘We are the union. We are the ones who find the solutions or make the changes'.
We are inundated with work. 300 minutes a day was a ratio determined 30 years ago…and it has never been reviewed. Now there is an older and larger population which has increased the number of patients with comorbidities and various cultural needs. We used to average 30 minutes in our patients’ homes and now the average has more than doubled. Logistically compared to when I first started in community health, travel between patients has more than doubled. People’s morale in the workplace is grave. I keep thinking it couldn’t get any lower and it constantly finds a new way to get lower.
We’ve been going to Liverpool Hospital to join the strike actions. In community health, we can think that our problems are insignificant or the last to be heard, but we have really been finding our own voice in the last few strikes, and that has been really encouraging, finding our place amongst the membership.
I think that we are on the right track…I’d like to see a little bit more compliance with ratios, and then maybe start
looking at the isolated rural and community health nurses to have a plan going forward so that we know we are being included in the wider union.” n

‘People’s morale in the workplace is grave.’ — Elizabeth Tran RN
Thousands of public sector nurses and midwives walked off the job for the third time this year in their fight for safe staffing ratios and better pay.
Anurses and midwives’ 24-hour strike from 7.00 am on 1 September featured more than 70 rallies and marches in towns and cities across the state.
Nurses and midwives maintained life-preserving services in hospitals and other health services throughout the strike.
NSWNMA General Secretary, Shaye Candish, and Assistant General Secretary, Michael Whaites, joined members and supporters at several locations during the day.
Shaye said the NSW Government’s refusal to consider ratios to improve patient outcomes and guarantee a safe working environment sent a message that nurses and midwives are not valued.
“The evidence is clear from Queensland and Victoria that ratios save both lives and money,” she said.
“Over 3000 NSW nurses and midwives have moved interstate
to take advantage of staffing ratios and better conditions in the past few years.
“It’s time we caught up with the rest of the country and gave our nurses the support they need to deliver the clinical care our communities deserve.”
Premier Dominic Perrottet defended his refusal to genuinely negotiate with the NSWNMA on staffing, and claimed his government’s three per cent pay offer was “nation leading”.
But, as 10 TV News reporter Lachlan Kennedy told viewers: “I can tell you, after attending multiple rallies today, the people on the frontline of our healthcare system are saying there is not the right number of staff, the current system is not working
and there needs to be an urgent over-haul before this crisis gets a whole lot worse.”

A highlight of the strike was a 24-hour picket line outside Westmead Hospital in Sydney’s west.

Several hundred nurses joined the picket line at different times, including some who brought sleeping bags.
Some picketers held signs reading, “This hospital is not staffed for safety” and “Fund hospitals not submarines”.
Another placard addressed to the premier read, “Perrottet – Westmead is at breaking point”.
‘ED is almost always 5–7 nurses short every shift.’ — Denny Anderson, Westmead Hospital Branch
Mixed in with speeches and chants of “1 to 3 in ED” and “1 to 4 on the floor”, was live music and a barbecue.
The picket line featured on most TV news channels.
Hospital management organised a large squad of security guards who at times attempted to move picketers off hospital grounds and onto the footpath.
“We dug our heels in and told them, we’re employees of this hospital, we have a right to be here,” said ED nurse Denny Anderson, Vice President of the NSWNMA’s Westmead branch.

“Given the amount of money the hospital is spending on our privatised security service, we felt there were more important things they could be doing than standing there gawking at us.”
Many nurses and midwives shared horror stories of having to care for patients, with too few staff.
“ED is almost always 5–7 nurses short every shift,” Denny said. “These are often senior nursing roles such as resus-trained nurses that you can’t just backfill with nurses from the casual pool.”
Denny and other branch officials worked with a NSWNMA representative on each ward to promote the strike and picket in all areas of the 1000-bed hospital. He said the interest and enthusiasm generated by the strike prompted several ED nurses to join the union. n
Several hundred nurses joined a spirited demonstration outside Royal Prince Alfred Hospital in the inner-Sydney suburb of Camperdown.
Speakers included NSWNMA member and emergency nurse, Joshua Callaghan, who said conditions in the ED were unsafe.
Category 2 patients had to wait over an hour to see a doctor, and ambulances were waiting up to four hours to off-load patients, he said.
“They [ambulance crew] come begging us just to put a patient in a chair, so they can go to a 1A. They can’t go to a cardiac arrest in the community because they are stuck in the ambulance bay.”
Clinical nurse specialist Lisa Turner welcomed the strike day’s focus on rallies at local workplaces.
“The RPA rally went really well. There was a strong turnout and it felt good to be with so many colleagues who all came out to support each other,” Lisa, a palliative care community nurse, told The Lamp.
She said it was inspiring to see TV news and social media coverage of nurses and midwives around the state protesting in their localities.
“I think the public feel the issues are more relevant to them when they see nurses taking action outside the local hospital they rely on.”
The NSWNMA ratios claim for community nursing includes a limit of four hours of face-to-face client contact per 8-hour shift, averaged over a week.
Lisa said workloads were increasing as hospitals aimed to discharge patients earlier, and more people were choosing to die at home.
“At the same time, we have lost a lot of senior staff,” she said.
At the rally, NSWNMA President, O’Bray Smith, introduced local Greens MP Jenny Leong.
“We have the power to win this campaign. There is a strong movement building,” Leong told the crowd. n
— Lisa Turner, RPA Community Health Branch
‘It felt good to be with so many colleagues who all came out to support each other.’
From Tweed Heads in the north to Albury in the south and from Sydney’s eastern suburbs to Broken Hill, thousands of nurses took to the streets on 1 September.
Nurses in the Riverina town of Coolamon, population 2000, made history on 1 September by staging the first-ever strike at CoolamonGanmain Hospital.
Half of the hospital’s 20 nurses went on strike, while a skeleton staff ensured essential coverage.
“There was 100 per cent support from all nurses for taking strike action,” said Eyvett Price, Coolamon Branch Secretary for the NSWNMA.

The hospital has 12 aged care beds, two acute beds and two ED beds –one unfunded.
At night, [the hospital] is staffed by an RN and an EN who attend to all patients and the ED.
Eyvett said staff and agency nurses routinely work overtime and double shifts and the NUM often has to work on the floor.
“We try hard to plug the gaps and run a proper facility but we haven’t been able to.
“We are all sick of it and we felt that going on strike was the only way the government would hear us.”
The nurses’ rally outside the hospital was the lead story on 7 News Riverina and featured in the The Daily Advertiser.
Joining nurses at the rally were the hospital doctor and community
members who came with their own placards.
“Everyone in the community knows how busy we are. A lot of them have had to sit for hours in ED,”
Eyvett said.
Coolamon-Ganmain Hospital will face even worse staff shortages when
elderly nurses retire.
“Only six RNs, including agency nurses and casuals, are under the age of 50. Most of our permanent RNs are over the age of 65,” she said.
“One of our nurses is 77 and still working on the wards, and she plans to retire in January.” n
‘We are all sick of it and we felt that going on strike was the only way the government would hear us.’ — Eyvett Price
In the Illawarra region, more than 100 nurses marched through the main streets of Shellharbour on 1 September despite pressure from some managers not to join the strike.
Secretary of the NSWNMA branch at Shellharbour Hospital, Debbi Simpson, said the higher-thanexpected turnout showed local support for the union’s ratios campaign had strengthened.

“Everyone is overworked and burnt out, and there’s more violence at work as a result of understaffing and care being delayed,” she said.
“A lot of patients need one-on-one care and we just don’t have the staff to give it.
“People recognise that ratios are the only solution.”
“Nurses and midwives don’t need applause – we need safe staffing. Ratios save lives” declared a placard carried by one marcher. Debbi said pressure from some managers had caused a few nurses to withdraw from strike action.
“Some nurses were made to feel guilty about their patient load and reluctantly decided to work, but generally speaking, everyone’s had enough – even non-union members.
“We’ve had a few people join the union since the strike.”
The march in Shellharbour was the first of this year’s strike
demonstrations
to be held locally.
Previously, Shellharbour nurses travelled to rallies in Sydney and Wollongong.
“The Sydney rally at Parliament House was amazing and empowering, and Wollongong was good too,” Debbi said.
“This time around we decided to get more community awareness and involvement around our own hospital, which is struggling.”
Nurses told WIN TV News that strikes would continue until the government listened to nurses.
Shellharbour NSWNMA steward Nadia Rodriguez said: “Every time we strike it gets bigger and bigger. Nurses are just getting more and more angry. Today shows that.”
NSWNMA delegate Glenn Hayes, from the Illawarra mental health branch, told WIN News: “We’ve got people who are genuinely traumatised not being able to provide the care they want to provide to people. It’s horrible.” n
NSWNMA members rallied across the New England North West region in a loud call for nurse-topatient ratios.


From regional cities Armidale and Tamworth to smaller towns such as Manilla and Moree, nurses and midwives sent a clear message that they are “tired, burnt out and demanding change,” as NBN TV News put it.
At the Tamworth rally, NBN reporter Jessica Warboys found 73-yearold nurse Kerry Hall “flying the Nurses and Midwives’ Association flag proudly.”
Warboys said Kerry had been a nurse since 1966, “but she feels she can’t leave now due to crippling staff shortages”.
Kerry told NBN: “I have been told if I resign or leave, they will not be replacing me full-time.”
Nurses also told Warboys that staff shortages were causing patients to leave Tamworth Hospital ED without treatment. n
‘People recognise that ratios are the only solution.’
— Debbi Simpson
In the southern Sydney suburb of Kogarah, all units of St George Hospital were represented in the large crowd of nurses who rallied outside the hospital.

“If we are outside, it’s not OK inside” was the message on one of the rally’s many placards.
President of the hospital’s NSWNMA branch, Shane Slade, told the crowd: “This is what this union is all about. It’s about nurses and midwives coming together to support other nurses and midwives. We are not just supporting nurses and patients in the building behind us. We’re supporting nurses and patients across NSW. We’re here for everyone.”
Shane added: “I work in ICU and we are 30 FT staff down. That means patients can’t get booked in for their surgeries because there’s no staff for their beds.
“That means patients get pushed out before they’re ready to come to the wards. That means we can’t do our jobs properly.
“We go home every day feeling overworked and under-resourced.
“We want to go home feeling like we’ve done a good job. We want to go home feeling like we’ve done our best for patients, and right now, none of
us are feeling like that.”
Branch Secretary, Samantha Strydom, told the rally that ED nurses are predominately junior staff who aren’t getting the support they deserve.
“We’ve lost so many senior staff and the juniors are teaching each other. We need more support; we need more education.
“We need more skilled staff; we need more senior staff. Ratios will fix that. Ratios mean better and safer working conditions, so we can actually give our patients the care they deserve.”
Other speakers outside St George Hospital included midwives from maternity and nurses from mental health units, along with NSWNMA Assistant General Secretary Michael Whaites and Greens MP Cate Faehrmann.
Michael Whaites said nurses are sick
and tired of Premier Perrottet not listening to what they, as qualified and experienced healthcare practitioners, have to say, and that listening is desperately needed in order to provide the healthcare system that this community needs.
“Wherever I go, nurses tell stories of where patient care is not at the level it should be. Where patients are falling unobserved because there are not enough nurses on the shift.
“When patients are waiting in ED for 10 or 11 hours. When aged care people who should be in a nursing home are still in hospital because of the lack of nurses in aged care.
“The system is sick and we are sick and tired of carrying the weight of it on our backs.
“Perrottet seems oblivious to the anger that he is fuelling.” n
‘We are not just supporting nurses and patients in the building behind us. We’re supporting nurses and patients across NSW. We’re here for everyone.’’ — Shane Slade
In the Far West of the state, a rally of about 40 nurses in Broken Hill town square got a warm reception from passers-by.

“Lots of people wanted to know more about our campaign,” said Joe Worgan, Assistant Secretary of the NSWNMA branch at Broken Hill Base Hospital.
Striking nurses displayed placards and banners with slogans such as: “More midwives safer babies” and “Patients over profits”.
Joe said ABC TV News and the local Barrier Truth newspaper gave the strike prominent coverage. He said winning the ratios campaign was “a matter of raising public awareness, getting community backing and making the government aware that understaffing affects everyone”.
“On my medical ward we would normally have the FTE of eight or so senior RNs but now we are down to two or three. n
‘
HEED OUR WARNINGS’ was the front-page banner headline introducing the Illawarra Mercury’s coverage of the strike in Wollongong.
The Mercury said hundreds of nurses marched from Wollongong Hospital to a rally in MacCabe Park.

“As they marched down Crown Street, they were met with honks of support from stopped traffic, and pedestrians and shoppers stopped to applaud or say thank you,” the Mercury reported.
Marchers carried placards, including one that showed portraits of Premier Perrottet and Health Minister Brad Hazzard, labelled, “The two biggest hazzards to the health of NSW.”
The Mercury, quoting nurses, said the hospital was short 136 full-time staff.
“If a hospital is 136 nurses short, the only way it’s functioning, is from nurses working their absolute arses off on overtime and there sure as hell are shifts where patient safety is being compromised. Heed our warnings,” said Genevieve Stone, NSWNMA delegate at Wollongong Hospital.
At the “fiery” rally, local Labor MPs got “a mixed response from fed-up nurses, with some clapping but others shouting questions from the crowd,” The Mercury reported.
Since the rally Labor has committed to supporting important parts of our 2022 claim (see Editorial p5 and p10). n
‘Lots of people wanted to know more about our campaign.’
NSWNMA members at Sydney Adventist Hospital
secure best ratios proposal in NSW.
As The Lamp went to press, nurses and midwives at Sydney Adventist Hospital voted overwhelming in support of a proposed new enterprise agreement that includes minimum nurse/midwife-to-patient ratios for all wards, maternity and perioperative units and ED with 96 per cent voting ‘Yes’.
The proposed minimum ratios are superior to guaranteed minimum staffing at all other private operators and in the public sector.
A NSWNMA bargaining committee recommended members accept the deal, following a year of member campaigning and negotiations with Adventist Health Care (AHC). The proposed agreement includes pay increases of 9.25 per cent over three years, with the first increase of three per cent backdated to 1 July 2022.
The campaign also won improvements to parental leave, continuing education allowance, job security for casuals, and family and domestic violence leave.
The proposed agreement will apply to about 1250 nurses and midwives at the hospital, which is known as ‘the SAN’ – reflecting its origins as the Sydney Sanitarium 117 years ago.
NSWNMA General Secretary Shaye Candish, congratulated branch
officials at the SAN who effectively mobilised members during the campaign.
“The campaign has strengthened the branch and a strong branch will be essential to monitoring and enforcing new minimum staffing standards,” Shaye said.
“The EBA should help to maintain stability in nurse numbers shift to shift and lays the basis for negotiations to improve the ratios in subsequent agreements.”
The NSWNMA started the campaign with a survey, which was answered by more than 400 nurses.
The survey showed nurses’ first priority was better staffing, followed by a pay increase.
When negotiations got underway, management flatly rejected ratios and offered a 7.5 per cent pay increase over three years, citing the SAN’s financial difficulties.
Branch president, Angie Adams, said a turning point came in April after the union presented a petition calling for ratios, which was signed by about 750 nurses and midwives.

“The petition was incredibly successful. When we presented it to management, they had to rethink their position and came back with an offer,” Angie said.
“Most signatures were collected by about 20 members who volunteered to become NSWNMA ward stewards,”
‘The campaign has strengthened the branch and a strong branch will be essential to monitoring and enforcing new minimum staffing standards.’
— Shaye Candish, NSWNMA General Secretary
she said.
“Their immediate role was to assist the campaign and join the NSWNMA bargaining team.
“Creating a network of stewards was vital because they were able to take part in negotiations via Zoom and report back to members on their wards.
“Branch officials and union officers were able to use the stewards’ network to communicate with members and gather feedback from the membership.

“We started a WhatsApp group to share information amongst the team, and this remains a great way of sharing and receiving information about hospital and branch issues.
Angie said the union bargaining team was unable to accept management’s first ratio offer as it was deemed to contain an “escape clause” with the potential to evade EBA minimum ratios.
“Management agreed to make the ratios proposal more transparent and accountable and guaranteed to retain any existing staffing levels superior to the EBA ratios.
“Having ratios set out in the agreement will make it easier to monitor and query staffing levels
and will give the branch grounds to take action if minimum levels are not met.”
She described negotiations as “very honest and transparent. The result is a reasonable compromise. It’s not what we asked for but it’s more than management had planned to provide”.
“It’s better than what we had and it’s a stepping stone to an even better deal in the future.”
Angie said the NSWNMA “did an amazing job” to support members but having a strong branch and active membership was the key to success.
“Having a strong membership involvement in the negotiations certainly gave us more bargaining power. If we didn’t have stewards,
if we hadn’t been able to organise a successful petition, we would have got a worse result.
“Being on the bargaining team helped nurses to understand how powerful the Association can be and the good work it does for us.
“We had some really articulate members on the team and some long-serving nurses had more to say to management than they ever have before.”
Angie hopes the inclusion of ratios in the EBA will help the SAN to attract new staff “because we are struggling to recruit nurses like everyone else. We hope that the SAN can become an employer of choice with superior working conditions”. n
 MORE THAN 750 NURSES AND MIDWIVES SIGNED A PETITION CALLING FOR RATIOS
MORE THAN 750 NURSES AND MIDWIVES SIGNED A PETITION CALLING FOR RATIOS
‘Having strong membership involvement in the negotiations certainly gave us more bargaining power.’
— Branch president, Angie Adams
Rich countries, such as Australia, are resorting to the “quick fix” of
international recruitment as a way of overcoming nurse shortages.
The COVID-19 pandemic has worsened the global nurse shortage and rich countries are using foreign recruitment to quickly raise their nurse numbers, says a leading academic who specialises in the international nursing workforce.
Professor James Buchan of the University of Edinburgh says this is still happening despite the risk of relying on high levels of foreign recruits having been exposed when international borders closed during the pandemic.
And foreign recruitment is doing serious damage to the health systems of some of the “exporting” countries, Professor Buchan told the NSWNMA annual conference in August.
Professor Buchan, who is also Adjunct Professor at the University of Technology, Sydney, is co-author of a 2022 study of COVID-19’s impact on the global nursing workforce.
He works as a consultant and policy adviser on health workforce issues for governments and international agencies, including the World Health Organization.
He said established importers of nurses, such as the US, UK, Germany and Australia, were increasing their international recruitment activity.
At the same time, countries such as France that previously took in relatively few foreign nurses, were becoming more active in international recruitment.
He said dozens of studies across the world showed that low staffing, high workloads, and the inability to participate in decision-making, were causing stress, burnout, psychological trauma and higher leaving rates among nurses.
In the US, about 15 per cent of nurses left their jobs in the first year of the pandemic.
“All the indicators are going in the wrong direction for nurses,” he said. Such indicators included COVID infections, COVID-related deaths, mental health problems and “moral injury”, stress, abuse and
physical attacks.
“One of the underlying major concerns is that many systems are putting a lot of emphasis on individual nurse resilience to somehow continue to get through this.
“The reality is the emphasis should not be on the nurse to be resilient, it should be on the system to support the nurse.”
A 2020 WHO report said one in six of the world’s nurses were expected to retire in the next 10 years, and about five million nurses would need to be educated just to replace them.
Professor Buchan said high retirement rates would greatly impact rich countries, such

‘High-income countries are essentially solving their nurse shortages by creating shortages in countries that can’t afford it.’
— Professor James Buchan
as Australia, the UK and US, where “a significant proportion of nurses are coming into retirement age.”
He said countries such as India and the Philippines now operate schemes to train nurses specifically for export.
The number of nursing colleges in India training nurses to bachelor level has grown from a handful in 2000 to over 2000 in 2020 in response to international recruitment programs.
The “train for export” model, where students pay for a private sector nursing education on the assumption they will move abroad after qualifying, is likely to be adopted by other countries, he said.
At the same time, poor countries with very low numbers of nurses and no private sector training are also being targeted for recruitment.
“That is having a negative impact on the ability of those countries to deliver safe care,” Professor Buchan said.
“It’s something we need to monitor very closely because there is real damage being done in some countries – and with the potential for more damage. “High-income countries are essentially solving their nurse shortages by creating shortages in countries that can’t afford it.
“The countries that have been hit most negatively by (international recruitment) are not politically powerful or influential, so they need to work as a collective with the World Health Organization to get some balance and shine a light on what’s happening to ensure it is ethical.”
Australia has about 53,000 foreign-trained nurses, or 18 per cent of the nursing workforce. That is the third highest rate in the world, Professor Buchan said.

Only New Zealand with 26.6 per cent and Switzerland with 25.9 per cent, are more reliant on foreign-trained nurses.
The average rate among the 27 wealthy countries of the OECD is 6.1 per cent.
The world had 28 million nurses and a global shortage of about six million nurses – mostly in poor and middle-income countries, according to a 2020 World Health Organization report.
England, for example, is unable to fill 10 per cent of its funded nurse vacancies. n
‘The emphasis should not be on the nurse to be resilient; it should be on the system to support the nurse.’
— ProfessorJames Buchan
Failure to involve nurses in planning for Covid-19 in aged care was a major flaw in Australia’s preparation for the pandemic, says a leading geriatrics specialist.
Professor Joseph Ibrahim of the Department of Forensic Medicine at Monash University has criticised the exclusion of nurses from the planning of the aged care sector’s response to COVID-19.
Professor Ibrahim said involvement of nurses was “the major thing that was missing” from official pandemic planning for aged care.
“No nurses that actually worked in aged care were represented on any of those groups that were making the decisions,” he told the NSWNMA’s professional day in August.
Professor Ibrahim is a practising senior specialist in geriatric medicine with over 30 years of clinical experience with elderly people. He has been an expert witness in criminal and coroner’s court cases and a witness at the Royal Commission into Aged Care Quality and Safety.

Professor Ibrahim questioned the federal government’s decision to put the aged care regulator – the Aged Care Quality and Safety Commission – in charge of leading the sector through the pandemic.
“Why did they (the Morrison government) choose a regulator to lead a public health initiative?” he asked.
Professor Ibrahim said structural weaknesses in the aged care system were well known even before the royal commission, which preceded the pandemic.
He said the sector’s structural flaws were brought about by the deregulation of the sector in 1997.
The 1997 legislation created a “free market” in aged care and was “the downfall” of the sector.
It led to reduced staffing, removal of restrictions on who could do what work, a substantial loss of registered nurses from aged care, work becoming more casualised and “staff having to work at multiple places to earn a livable income”.
The royal commission highlighted these problems and the fact that 10 per cent of aged care homes were “unable to fully staff for everyday business”.
“We knew from the royal commission that the aged care sector was not equipped to manage day-today business,” Prof. Ibrahim told conference delegates.
“But for some reason the Department of Health, the federal government and the regulator all seemed to think that the sector could step up and also manage a pandemic – despite these underlying foundational and structural issues.
“The regulator knew before the pandemic that a substantial number of homes were having trouble with governance (such as) infection control and escalation of clinical care.
“(The regulator) knew the places
“Why was there not a single geriatrician, let alone a senior nurse in geriatrics, on any of the planning groups?”
‘The greatest failure with this pandemic across the country and across the world, is a failure to understand how work is done.’
— Professor Joseph Ibrahim
that had those problems and they knew this was not a one-off but another structural issue.”
Prof. Ibrahim said providers who did what the regulator told them to do were “well under-prepared for the pandemic when it hit because the regulator’s plans were pretty thin – if you want to call it a plan”.
“They essentially put the responsibility for managing an outbreak on the provider.”
Prof. Ibrahim said the relationship between staff and management “wasn’t well thought through” in making plans to deal with the pandemic.
Had more control been delegated to senior nursing staff in aged care facilities, “you would have a far better outcome around rostering, managing workforce shortages and talking the talk about reducing the number of places people would work at”.
He said even now, it was “very hard” to find out “how many senior working nurses are involved at a state or regional level in advising what’s happening on the ground and what needs to
happen, so that we’ve got proper field intelligence so that we can prepare better”.
Professor Ibrahim said aged care was characterised by a mis-match between “work as imagined versus work as done”.

“What’s written down in policy, what’s on organisational charts, what people put on their flow diagrams, what’s set down from above … doesn’t make a whole lot of sense about how the real world works.
“The greatest failure with this pandemic across the country and across the world, is a failure to understand how work is done.
“There has been a real mismatch between how senior leaders and advisers thought versus what was real.
“People in senior positions and senior roles in decision-making were living in or working from an imaginary place (where) every shift is filled, every nurse is well and able to do the allocated work, if you need a doctor they’re around and are kind, thoughtful and responsive should you ask them any questions; the equipment you need is there, the space for bins is there, the rubbish will be taken out on time [and] that no-one will call in sick.” n
When Professor Joseph Ibrahim addressed the NSWNMA 77th Annual Conference Professional Day in early August, there were about 10,000 active COVID-19 cases in about 1000 residential aged care facilities. This meant more than one third of Australia’s 2700 aged care facilities were battling outbreaks, Professor Ibrahim pointed out. He said that since 2020 there had been 2670 outbreaks in residential care facilities, meaning almost every single facility in Australia had suffered an outbreak.
About 77,000 residents had contracted COVID-19, which had resulted in the deaths of 3394 residents.
‘Why was there not a single geriatrician, let alone a senior nurse in geriatrics, on any of the planning groups?’
— Professor Joseph Ibrahim
COVID has exposed gaping fault lines in already overloaded healthcare systems but it has also created new opportunities, global nursing leaders say.
“Nurses are done being applauded as essential while being treated as expendable,” says Bonnie Castillo.
The Executive Director of National Nurses United, in the USA, said nurses, along with other workers on the frontline of pandemic responses, “have come to recognise ourselves as the very foundation of society”.
Bonnie was speaking during a panel on professional day at the NSWNMA annual conference, along with Canadian nurse leader, Linda Silas, and Shaye Candish, NSWNMA General Secretary.
Bonnie said her union had organised nearly 5000 workplaces and community actions across the US since 2020, including several outside the White House.
She said nurses are at the forefront of “an inspiring labour upsurge across America”, one that has included teachers in conservative states striking and workers organising at corporate behemoths, such as Starbucks and Amazon.
The anger and militancy coming from health workers is being driven by a hospital industry that “sacrifices nurses’ health and safety to the bottom line”, Bonnie said.
— Bonnie Castillo, National Nurses United (USA)
Shockingly, the lack of concern for health and safety during the pandemic has contributed to the deaths of 5200 healthcare workers, including 494 registered nurses. “When COVID hit, instead of rushing in with the protections that we needed our employers kept N95s behind lock and key and tried to implement very unsafe PPE and decontamination processes. Thousands of healthcare workers would still be alive today if our profit-driven employers hadn’t spent decades slashing supply costs.”
NSWNMA General Secretary Shaye Candish, described a parallel situation in Australia, where a
health system that “was already a powder keg of stresses” in the wake of bushfires and shortages of staff and resources, was pushed to breaking point when COVID arrived.
Shaye described the Association’s campaigns around airborne transmission and fit-tested masks and eye protection when providing care of suspected or confirmed COVID patients, as among the Union’s significant wins.
“The sacrifice and dedication of nurses and midwives across NSW in dealing with the challenges has been nothing short of inspiring,” Shaye said. In contrast, the NSW Government’s decision to freeze public sector wages, including those of nurses and midwives, is “a

‘Thousands of healthcare workers would still be alive today if our profitdriven employers hadn’t spent decades slashing supply costs’.
stunning slap in the face”.
“We all shared collective rage as the NSW Government continued to spin the line that our public health system was strong and supposedly coping. This was repeated over and over while you were exhausted, working excessive overtime, maybe working outside your usual scope or in unfamiliar models of care and catastrophically short-staffed, as patient care suffered.”
The NSWNMA’s first statewide strike since 2013, on 15 February this year, was driven by members’ “red hot rage”, Shaye said. More than 150 hospital and community health branches took part in the strike action and then voted for further action just weeks later.
“We’ve had ongoing action since and I could not be prouder of the collective determination and
commitment to continue our ratios campaign despite, and because of, the incredible adversity that you’re facing,” Shaye said.
Stress, burnout and unsafe staffing ratios have led to nurses leaving in droves in the US, Canada and Australia, all three panellists said.

Since the beginning of the pandemic, nursing vacancies across Canada have risen by 133 per cent said Linda Silas, President of the Canadian Federation of Nurses Unions.
“One in two [Canadian] nurses are looking for the exit sign. The number one reason nurses are burning out in my country is because 83 per cent [say] we don’t have enough staff
for them to provide good care.”
“We nurses need to stop being the martyrs of health care,” she said.
In the US, there are over five million RNs with active licences but only 3.5 million who are working; nearly one in five healthcare workers have quit their jobs since March 2020, Bonnie said.

“Not because they can’t cut it but because they can’t handle being systematically denied the resources and protections that they need to do their jobs. Years of organised abandonment has caused an epidemic of moral injury and PTSD in the nursing profession.”
Bonnie said that in the US, “we’ve won improvements in health and safety policies, staffing and provisions to advance racial and gender justice. The key to our success has been our ability to organise and flex our collective power in the workplace. Above all, through our willingness to strike”.
“So, despite these huge challenges … it is a time of incredible opportunity,” she said. “And we’re in a better position now than maybe at any other point in my lifetime, to build nurse power and win workplace democracy.” n
‘The NSWNMA’s first statewide strike since 2013 was driven by members’ “red hot rage”’.
— Shaye Candish, NSWNMA General Secretary
‘We nurses need to stop being the martyrs of health care’
— Linda Silas, Canadian Federation of Nurses Unions
After an intense year of campaigning and three productive days at annual conference members took time out to relax at the annual gala dinner with a “Maskarade” theme.










ICC Sydney » 3–5 August 2022



NSW Nurses and Midwives’ Association gratefully acknowledges the sponsorship provided by the following organisations for our 77th Annual Conference held on 3 - 5 August 2022 at the ICC Sydney.


The NSWNMA also thanks the following organisations for their contribution and support: Ferndale JILA mini mints

Lindt & Sprungli



Ocean Spray

Wollongong Hospital ISLHD are looking for you!

We have a wide range of rewarding opportunities for dedicated, committed and collaborative nursing professionals across all areas.
As a part of Wollongong Hospitals Nursing & Midwifery team, you will be an integral part of the community
Wollongong Hospital is working to foster a high-performing nursing and midwifery workforce that demonstrates person-centered care in practice.
about practice and performance.
For more information email ISLHD-NursingWorkforceUnit@health.nsw.gov.au or scan the QR codes to be taken to the job advertisements

Your membership brings you exclusive rewards and benefits on thousands of products and services everyday. As a member of the NSW Nurses & Midwives’ Association, you can enjoy:
eStores with great deals on Baby & Kids’ products, Pet products, Furniture, Luggage, Tools and more
Discounts on shopping, groceries and fuel at leading retailers
Blowout savings on shopping leading up to Christmas
Incredible savings on tech, electronics and whitegoods in your eStore, provided by JB HiFi Business and The Good Guys Commercial
Savings on travel, foreign exchange as well as health & wellbeing services

Plus much, much more! Log in today to start accessing your rewards.
Terms & conditions apply to all offers.




Face to face education opportunities for the reminder of 2022
Aged Care: Care Planning
Friday 7 October, 9am to 3pm
Self-Care, Resilience and Self-Leadership Training
Friday 21 October, 9am to 4.30pm
Aged Care: High Impact, High Prevalence Incidents
Wednesday 2 November, 9am to 3pm
Aged Care: Disability and Ageing
Tuesday 22 November, 9am to 5pm
Diversity in Residential Aged Care
Thursday 27 October, 9am to 4pm
Aged Care: Reactive Behaviours
Wednesday 7 December, 9am to 3pm
Law, Ethics and Professional Standards in Nursing and Midwifery
Tuesday 25 October, 9am to 4pm
Medications: How we do it better
Wednesday 9 November, 9am to 4pm
The Deteriorating Patient
Wednesday 30 November, 9am to 4pm
Planning for 2023 is due to commence soon and we intend to visit more regional areas throughout the year!
CPD hours for these courses can be calculated by the time you spend actively learning. This will vary between individuals, as further self-directed learning can be included (e.g. reviewing the associated resources and completing the reflective questionnaires).
The NSWNMA has released a series of free webinars on a range of subjects relevant to nursing and midwifery practice. We have a suite of regular topics, such as Medications, Communication and Documentation, Professional Obligations and many more.

We also arrange other additional one-off webinars facilitated by external presenters on interesting and topical subjects. Keep an eye on the education page and our education emails for updates and additions.
Go to the Education page of our website to search our face-to-face and webinar
CPD education options.



Since the last edition of The Lamp, as is always the case, members have sought support and assistance in a variety of settings. Understandably, most of the media attention has been on the actions being pursued by public health members to achieve safe patient care through our ratios claim. However, plenty of other important matters on an individual member and workplace level have been bubbling away and these are just as important to their (and perhaps your) immediate wellbeing.
Members can be assured that behind the headlines, it remains business as usual, with the Association assisting and working with members to get all manner of issues – big or small – resolved or addressed. Not always easy but whether it be a non-payment of an allowance, a fact-finding interview, a workplace change, provision of suitable duties, a response required by AHPRA, or a statement for the coroner, we remain there for you.
After some months of gestation, the Ministry of Health published PD2022_030 [Occupational Assessment, Screening and Vaccination Against Specified Infectious Diseases] on 29 July 2022. Since then, this policy has continued to generate a significant number of member contacts in relation to both the third COVID-19 and the yearly influenza vaccination requirements. This special edition aims to assist members in grappling with the new conditions and the nuanced approach of this new policy directive.
Why did the Ministry of Health change its policy about vaccinations?
The previous COVID-19 vaccination requirement for healthcare workers was set out in the Public Health (COVID-19 Vaccination of Health Care Workers) Order 2022. This order ceased as of 19 June 2022 and vaccination requirements in health workplaces (public or private) now falls under organisational policy. Health Determination
Didn’t the Ministry issue something last year, mandating that two COVID-19 vaccinations were required to be employed? That is correct. The Secretary, NSW Health, issued Determination No 33 of 2021 on 12 November 2021, which required, as a condition of employment, two COVID-19 vaccinations. This remains in place, is legally enforceable and will underpin any policy framework.
I did work in a Category A highrisk position. Will this continue?
No, the Ministry of Health has removed this classification. This means that all health workers will now be placed in either Category A or B roles. In short, Category A will encompass almost all nurses and midwives employed in the public health system.
What are the Category A requirements for COVID-19 and influenza vaccinations?
Category A requires three doses of a TGA-approved/recognised COVID-19 vaccine or two doses, with the third to occur within eight weeks of the new PD being published if more than 13 weeks since the second dose or within six weeks from the due date of a third dose, whichever is the later. These workers will also be required
to receive an annual influenza vaccination. (See later questions regarding having a medical contraindication or choosing to not receive the third COVID-19 and/or influenza vaccination.)
What about students on clinical placements?
Category A students will need to comply with the above requirements. However, if in a clinical placement early in their first year, they may be granted temporary compliance if they have evidence of two COVID-19 doses and have submitted an undertaking to have a third COVID-19 dose within six weeks of the dose being due. For Category A students, the influenza vaccination is mandatory if undertaking a placement from 1 June to 30 September each year (or other dates as set by the Chief Health Officer).
I work in an MPS with aged care beds. What are my obligations?
You must comply with the new PD and with all other legal requirements. This would currently include the Public Health (COVID-19 Care Services) Order (No 2) 2022, which is still in place and requires staff to have had three doses of a COVID-19 vaccine.
What if I can’t have the vaccination due to a medical issue?
A health worker is compliant with the above requirements if they have a medical contraindication to all available approved or recognised vaccines, COVID-19 or influenza. Evidence must be submitted, using the relevant criteria and form as completed by your treating doctor/specialist.
Choose not to
I don’t have a medical contraindication but I am not inclined to have either the third COVID-19 vaccination or influenza vaccination. What happens to me?
Existing Category A workers who are non-compliant with the third COVID-19 dose or influenza vaccination requirements can continue to work, but they must comply with all risk reduction strategies while working in a Category A position. Redeployment to a Category B position can be considered but will be by exception only.
As part of this process, you will be required to submit a NonParticipation Form acknowledging that you will comply with specified
risk reduction strategies and the use of designated PPE. If such an assurance is not provided, then you may be subject to disciplinary action for potential misconduct.



If that Public Health Order has expired, what about private hospitals and other health settings previously covered?
The organisation will need to establish its vaccination requirements within its own policies and procedures via the WHS framework. If opting to include vaccination, it will need to be able to demonstrate that it is necessary for the health and safety of the workplace and that all alternatives or other risk mitigation factors would not be sufficient or reasonable.
As noted above, the Public Health (COVID-19 Care Services) Order (No 2) 2022 remains in place. All aged care staff, health practitioners and students entering a residential aged care facility must have had three doses of a COVID-19 vaccine. The third dose is due 13 weeks after a person’s second dose.
The average life expectancy of Americans fell alarmingly in 2020 and 2021 – the sharpest two-year decline in nearly 100 years.

In 2019, Americans could expect to live, on average, to 79 years. Two years later, life expectancy had dropped to 76 years.
The decline has been catastrophic among Native Americans, with life expectancy dropping by four years in 2020 alone, according to the US National Center for Health Statistics (NCHS). The decline for Native Americans since the pandemic started, more than six and a half years on average, has brought their life expectancy to 65 – on par with the figure for all Americans in 1944.
While COVID has driven most of the decline in life expectancy, a rise in accidental deaths and drug overdoses also contributed, as did deaths from heart disease, chronic liver disease and cirrhosis, according to the new CDHS report.
Dr Steven Woolf, from Virginia Commonwealth University, told The New York Times that the drop in life expectancy in the US was “historic”.
He said no other high-income country had such a poor record, thanks to their successful vaccination campaigns during COVID and with populations that were more willing to take behavioural measures to prevent infections, such as wearing masks.
“The US is clearly an outlier,” he said.
Dr Woolf attributed the difference between the US and other developed countries, to a fragmented, profit-driven healthcare system and pervasive risk factors such as smoking, widespread access to guns, poverty and pollution.
Walmart, Walgreens and CVS punished for their responsibility in opioid crisis.
A federal judge in Cleveland awarded US$650 million in damages to two Ohio counties that sued CVS, Walgreens and Walmart over the way the national pharmacy chains distributed opioids to their communities, reports PBS Newshour.
The judge said in his ruling that the money will be used to fight the opioid crisis in Lake and Trumbull counties outside Cleveland. Attorneys for the counties put the total price tag at US$3.3 billion for the damage done.
Lake County Commissioner John Hamercheck said the decision “marks the start of a new day in our fight to end the opioid epidemic”.
The counties convinced the jury that the pharmacies played an outsized role in creating “a public nuisance” in the way they dispensed pain medication during a drug crisis that has killed 500,000 Americans since 1999. Mark Lanier, an attorney for the counties, said that during the trial the pharmacies had attempted to blame everyone but themselves.
The opioid crisis had overwhelmed courts, social service agencies and law enforcement in Ohio’s working-class corner east of Cleveland, leaving behind heartbroken families, and babies born to addicted mothers, he told jurors.
Roughly 80 million prescription painkillers were dispensed in Trumbull County alone between 2012 and 2016 – equivalent to 400 for every resident. In Lake County, some 61 million pills were distributed during that period.

Dr Steven Woolf, Virginia Commonwealth University
‘Roughly 80 million prescription painkillers were dispensed in Trumbull County alone between 2012 and 2016 – equivalent to 400 for every resident.’
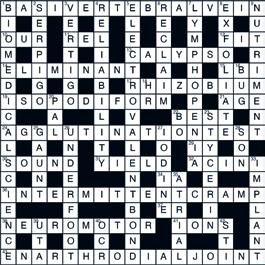
A study finds nearly half the deaths worldwide in 2019 from cancer were avoidable. The study, published in The Lancet, found half the deaths from cancer in 2019 – more than 4.5 million people – were due to avoidable risk factors, such as tobacco, alcohol, obesity, pollution, unhealthy diets or occupational exposure to harmful elements such as asbestos.
Half of all male deaths from cancer, and more than a third in women, stem from these potentially preventable sources.
The clearest risk factor was tobacco, by a country mile ahead of the second, alcohol, and the third, high body
mass index.
Despite the fact that these risk factors are well known to oncologists and the public, researchers say that deaths associated with these preventable factors have increased by 20 per cent in the last decade.

Metabolic risks accounted for the largest percentage of increase in cancer deaths and ill health, with deaths increasing by 34.7 per cent. Cancer was seen as a chronic disease of developed countries but was on the rise in developing countries –as a country develops, it evolves from a pattern of infectious diseases to a pattern of chronic diseases.

‘As a country develops, it evolves from a pattern of infectious diseases to a pattern of chronic diseases.’
A French court has ruled in favour of unions and overturned worker representative elections held by the scandal-plagued company Orpea.
French unions, supported by Public Services International (PSI), had argued that the elections were rigged in favour of a “yellow union” called Arc-en-Ciel that benefited from “financial and tactical support” from management.
Unions have been engaged in a long-term struggle against the corrupt practices of Orpea – the second largest private care home provider in France.
One of the unions’ core issues had been the company’s illegal interference in union elections in an attempt to favour Arc-EnCiel – an illegitimate ‘in-house’ union whose interests appear to align more closely with corporate management than with workers.
PSI General Secretary Rosa Pavanelli congratulated the unions on their win.
“The case of Orpea demonstrates once again that cuddling up to corrupt corporate managers is no way to win change for workers.
“Instead, by boldly exposing Orpea’s crimes, trickery and appalling conditions for patients and frontline workers, our French affiliates have already helped spark a judicial inquiry into institutional abuse and financial crimes, overturned rigged union elections, fueled a nationwide conversation on care, won assurances from politicians on increased funding for public care systems and led the calls for deep policy change, especially as regards for-profit care operators.”

Attracting more men to nursing is part of the solution to the global nursing shortage, say academics.
“We urgently need more men in nursing,” is the clear message from a group of academics, including Patricia Davidson, ViceChancellor of Wollongong University and Professor Jason Fairly from John Hopkins University, writing in The Conversation.
The World Health Organization estimates that there is a need for a further nine million nurses worldwide by 2030. According to the International Council of Nurses, the figure is closer to 13 million.
“Part of the solution is to recruit and retain more men in nursing. This would help address workforce shortages and could, over time, reduce the industry gender pay gap as the existence of men in nursing becomes more normalised,” the academics say.
“As jobs dry up in traditionally male-focused industries – such as mining and manufacturing – work in health care should be attractive for men, providing job security and career opportunities.
“But attracting men to the profession won’t be without its challenges. It will require a serious society-wide rethink around gender roles, compensation and recognition for the importance of nursing work.”
The authors argue that robust healthcare systems should be representative of the populations they serve.
“The workforce in any industry should be drawn from a range of perspectives, including gender and culture.”
‘As jobs dry up in traditionally malefocused industries, work in health care should be attractive for men.’
‘ Our French affiliates have helped spark a judicial inquiry into institutional abuse and financial crimes, overturned rigged union elections and fueled a nationwide conversation on care.’
— PSI General Secretary Rosa Pavanelli
Profits are up, CEO pay is up and inflation is rocketing, but real wages are heading south.
Wage growth has risen by only 0.7 per cent to 2.6 per cent, less than half the rate of inflation at 6.1 per cent, according to data released by the ABS last month.
Real wages have now effectively fallen back to 2011 levels, says the ACTU, after years of stagnant wage growth followed by deep, ongoing real pay cuts. These cuts are projected to deepen by the end of the year, with inflation expected to reach 7.75 per cent.
“It is clear that we have a serious systemic problem. We have been promised wages would go up when productivity goes up – they have not. We were promised that when business does well, pay rises will come – they have not. For six months unemployment has been low, yet wages are continuing to flatline,” says ACTU Secretary Sally McManus.
“Living standards are going backwards and workers now have the lowest share of GDP in recorded history.
“Our bargaining system is the engine of wage growth but the engine has conked out. Our country needs urgent reform to our wages system to get wage growth back on track.”
Meanwhile in the bank sector, profits are up 28 per cent, CEO pay is up 36 per cent and shareholder returns in the form of dividends and buybacks are up 57 per cent.
Unions NSW argued in its submission to the Jobs and Skills Summit that non-union employees should pay bargaining fees when covered by union-negotiated pay deals.
The submission noted that while 30.7 per cent of private sector workers benefit from workplace pay deals, just 9.5 per cent of private sector workers are union members.
This indicated “high levels of free riding, which is a critical contributor to wage stagnation, inequality and collective bargaining decline”, it said. More than a quarter (27 per cent) of workers who were paid according to pay deals struck after a union balloted to take industrial action, are not members.
Unions NSW proposed a charge on free riders capped at 70 per cent of yearly union dues and “only payable if the benefit to the worker from the enterprise agreement is higher than this amount”. It pointed out that bargaining fees are allowed in New Zealand, the US, Canada and South Africa but are banned in Australia.
Unions NSW also argued in its submission, for a requirement for employers to pay skilled workers sponsored from overseas 30 per cent above the industry median.
Unions NSW secretary, Mark Morey, told The Guardian that a higher pay floor would both “stop exploitation” of migrant workers and incentivise business to “engage in skills training for local workers”.

‘High levels of free riding are “a critical contributor to wage stagnation, inequality and collective bargaining decline.’
Unions NSW
‘Our country needs urgent reform to our wages system to get wage growth back on track.’ — ACTU Secretary Sally McManus



Secluded tropical bliss awaits at Agata Villas Seminyak – your own private paradise. Discreetly tucked away from the hustle and bustle of Seminyak yet within easy reach of the beach clubs, restaurants and boutique’s Seminyak is known for.
You and a friend will experience:
• 5 nights’ accommodation in a two-bedroom pool villa

• Inclusions valid for up to four guests (NSWNMA will arrange for two return flights only as part of this prize)*
• Return airport transfers
• Daily breakfast served in your villa
• 2 x a la carte lunches and 2 x dinners per stay
• 1 x BBQ Seafood dinner at Melati Seafood Restaurant, Jimbaran (up to four guests)
• Daily afternoon tea
• 1 x Full Day Tour per stay (private charter)
• Welcome seasonal fruit basket and drink each guest on arrival

• The NSWNMA will arrange return flights for two to Bali

Recruiters note: Join online at www.nswnma.asn.au
Every member you sign up over the year gives you an entry in the draw! If you refer a member to join online, make sure you ask them to put your name and workplace on the online application form, so you will be entered in the draw. Conditions apply. The prize will be drawn on 1 July 2023 and must be redeemed by 30 June 2024. Subject to room availability. Block out dates 24 December 2023 – 3 January 2024. Accommodation package and inclusions (excluding flights) is valid for up to four guests. NSWNMA will arrange and pay for flights for two to Bali. If a redraw is required for an unclaimed prize it must be held up to 3 months from the original draw date.

Ubookdirect offers all NSWNMA members discounted rates on 1000's of hotels Australia wide. Fill in a quote request today to save on your next getaway. Book your school holidays now to get the best discounted rates. UBOOKDIRECT is giving members a $20 voucher to use on any already discounted member package when booking through the Concierge.
To book one of these fantastic destinations log on to https://travelbenefits.ubookdirect.com and click on the ENQUIRY tab or call 1300 959 550.
Stay 3 nights in a luxury private pool villa from $1499 with the following exclusive inclusions:
• Welcome drink on arrival • Daily breakfast • Daily restocked minibar • Complimentary afternoon tea from 2-4.30pm • 1 x 15 minute welcome massage for two • Complimentary wifi
• Return airport transfer • Complimentary shuttle within Jimbaran area (from 8am – 5pm for drop & pick up only) • 1 x floating breakfast in villa • 1 x 60 minute massage • 1 x set lunch.
5 and 7-night packages available with further inclusions – use your $20 voucher to save even more.
Luxury villas with private pools just a short walk from Jimbaran Beach featuring a semi-open living room, a kitchenette and an open-air garden bath.


Stay 3 nights in a 5-star luxurious private pool villa for $1399 with the following inclusions:
• Welcome drink on arrival • Daily breakfast • Daily restocked minibar • Complimentary after noon tea from 2-4.30pm • 1 x 15 minute welcome massage for two • Complimentary wifi • Complimentary shuttle within Ubud area (from 8am - 5pm for drop & pick up only) • 1 x floating breakfast in villa • 1 x 90-minute massage • 1 x dinner. 5 and 7-night packages available with further inclusions – use your $20 voucher to save even more.
Luxurious traditional-style villas featuring 24-hour personal butler service, a private pool and an open-air garden bath located on the edge of a river valley.
Deals start at $242 for 3 nights with the following inclusions:
• Daily breakfast • Free upgrade to Deluxe Pool View Room (from Superior Garden View Room)
• 1 x Thai kunch (set menu) for two • 1 x mocktail at pool bar for two • Fruit platter on arrival • Free wifi • 20% discount on Food & Beverages (excl. alcohol) and 20% discount on laundry service. Use your $20 voucher to save even more.
Cosy resort featuring 2 swimming pools with swim-up bars, a kid’s pool, 2 dining outlets and a kid’s club. Just a 5-minute stroll from Kata Beach.
ALL OFFERS: For full t&c’s go to https:// travelbenefits.ubookdirect.com . Bali offers: valid for travel until 30 June 2023. Rate based on 2 adults, minimum 3-night stay and subject to availability. Thailand offer: valid for travel until 31 October 2023. Rate based on 2 adults and subject to availability.


Sue Williams
Allen & Unwin
RRP $32.99:
ISBN 9781761066917
The remarkable story of Professor Fiona Wood AM, world-leading burns specialist and one of Australia’s most innovative and respected surgeons, whose groundbreaking research and technology development has changed the lives of burns patients.
When three bombs tore out the heart of Bali and decimated so many Australian lives in 2002, burns surgeon Professor Fiona Wood led her team to save twentyeight survivors with up to ninety-two per cent body burns.
A pioneer in the field of burns and reconstructive surgery, she made world headlines with the use of her groundbreaking invention of ‘spray-on skin’ to help minimise her patients' horrific scars.
All books can be ordered through the publisher or your local bookshop. Call 8595 1234 or 1300 367 962, or email library@nswnma.asn.au for assistance with loans or research. Books are not independently reviewed or reviewed using information supplied by the publishers.
Meg Bignell
Penguin Random House
RRP $32.99
ISBN 9781761046711
Meg Bignell, former nurse and author of The Angry Women’s Choir, started experiencing perimenopause during lockdown. This, along with raising teenagers and anger at the treatment of women in general, inspired her to write ‘The Angry Women’s Choir’ to connect with other women in her demographic that felt overlooked.

We have 4 copies of The Angry Women’s Choir to give away thanks to Penguin Random House. Email your name and membership number to lamp@ nswnma.asn.au by 31 November to be in the draw to win!


Emma Carey Allen & Unwin
RRP $32.99
ISBN 9781761065781
An extraordinary true story of resilience, courage, hope and finding lightness after the heaviest of landings. From a terrible accident that left her paraplegic, Emma Carey has become an inspiration for hundreds of thousands online to live life to the fullest and remind us that if we can, we must. This heartfelt book is more than a memoir, it's a call to action that reminds us not to take our lives and abilities for granted-to live every day like it could be our last.

RRP $32.99 ISBN 9780733647222
Lavish and compelling, this is the story of a young woman trying to forget her
devastating part in the war.
1943. After spearheading several successful advertising campaigns in New York, PR wizard Alix St Pierre comes to the attention of the US government and finds herself recruited into a fledgling intelligence organisation.
1946. Following the war, Alix moves to Paris to run the Service de la Presse for the yet-to-be-launched House of Christian Dior. But when a figure from the war reappears and threatens to destroy her future, Alix realises that only she can right the wrongs of the past and bring him to justice.
Is your sitting posture causing you pain? The team from Vitruvian Health share their secrets to avoiding the discomfort that can come from day-to-day sitting.


As nurses and midwives, we never really think about how to sit correctly. We are often so busy working and helping others that we forget about helping ourselves.
Just like breathing, sitting is quite
“normal”. However, when we are tired or have been sitting for lengthy periods of time, our posture can deteriorate. The last thing you want to think about at the end of a double shift, is bracing your abs and sitting up straight!
Poor posture leads to back, hip, neck or shoulder pain.
That is why we have created this set of movements and drills to help engage your body so that you can sit up straighter, for longer. All it takes is five minutes!
• Still lying on your back, hug your knees to your chest to lengthen through the lower back.

• Balance on one leg with your knee at 90 degrees. Hold for 30 seconds. Now change to the other leg and hold for 30 seconds (try this one while brushing your teeth, like Kate!).

• Lie on your back and do three sets of 10 glute bridges.


• Sitting on a chair, push your hands down and lift one knee to your chest and hold for five seconds. Repeat this five times before changing to the other knee.
• Standing tall, lift your hands above your head, reaching towards the sky. Breathe into your ribs and lengthen through your back. Turn your toes inwards and flex your quads as hard as you can. Hold for 45 seconds.
You can follow this workout on Vitruvian Health’s Instagram channel.

As ambulances line up and nurses working in ED are overwhelmed and the hospital system struggles to cope, we are reminded that the skills of nurses and midwives are underused in the areas of prevention, early intervention and chronic disease management.
The Australian Prevention Partnership Centre (https://preventioncentre.org.au/) is a national collaboration of researchers, policymakers and practitioners working to identify new ways of understanding what does and what does not work in preventing chronic health problems in Australia.
Morgan, MJ 2022
COVID-19 has disrupted social and spatial life. This paper argues that such disruption provides an opportunity for all tiers of government to reassess collective priorities and reorient societal goals to work towards better health outcomes for all.
A “systems thinking” perspective shows how societal goals, such as economic growth, are supported by “system rules” created by governments, and how these same rules are largely responsible for prevailing inequities and preventable chronic, noncommunicable diseases and conditions. The work is significant because it shows how the disruption caused by COVID-19 changed deep system leverage points, highlighting places inside governmental systems susceptible and acceptable to change and revealing how systems can be reoriented.
The paper draws on empirical data from one subnational jurisdiction of Australia: Tasmania. In late 2020, 81 Tasmanian local government personnel shared views on diverse governmental changes made in response to the pandemic. Most participants wanted those changes to continue because of their net benefits to health and social, economic and environmental outcomes more broadly. They expressed overwhelming support for actions to improve the social determinants of health and the prevention and management of communicable and noncommunicable disease. https://doi.org/10.1111/1745-5871.12561
Empowerment for behaviour change through social connections: a qualitative exploration of women’s preferences in preconception health promotion in the state of Victoria, Australia
Walker, R et al, 2022
Women’s health in the preconception period impacts
fertility, pregnancy outcomes, infant health and the future health and wellbeing of mothers and their children.
While the preconception period spans from the onset of menarche to menopause, preconception care tends to only focus on women who are actively planning to become pregnant and the critical weeks around conception. Conversely, a public health view of preconception considers the broader, life-course approach where health and health behaviours – years or even decades prior to conception – have the potential to impact pregnancy outcomes and all women’s health, including women who are not planning a pregnancy.
Community awareness of the importance of preconception health is low, including an understanding of the long-term reproductive health impact of health behaviours and conditions that occur well before a pregnancy. https://bmcpublichealth. biomedcentral.com/articles/10.1186/ s12889-022-14028-5
The first 2000 days: Giving our kids the best start for a healthier life Prevention Works Podcast, 2022
In this episode, host Gretchen Miller interviews Professor Helen Skouteris and Dr Alexandra Chung from Monash University’s School of Public Health and Preventive Medicine, on the critical early days of our life’s journey and how influential they are in preventing future health issues.
Drawing on research conducted through the Collaboration for Enhanced Research Impact (CERI), a joint initiative between the Australian Partnership Prevention Centre and several NHMRC Centres of Research Excellence, Professor Skouteris and Dr Chung mobilised researchers from CERI to synthesise what we know about the importance of the first 2000 days in a child’s life for the prevention of future chronic disease. https://podcasts.apple.com/au/ podcast/the-first-2000-days-
giving-our-kids-the-best-start/
Improving communication about heart disease risk assessment in general practice using translational research strategies – Final Project Report
The Australian Prevention Partnership Centre, 2022 Australian cardiovascular disease (CVD) prevention guidelines recommend assessing a person’s absolute risk of heart attack or stroke in the next five years as a guide to the use of preventive medications – including those prescribed for lowering blood pressure and reducing cholesterol – for patients at high risk of a CVD event.
Previous research has illustrated that the use of CVD absolute-risk assessment can improve clinical management of CVD risk as well as patient risk perception and preventive intentions, when compared to treating hypertension and hyperlipidaemia as individual risk factors. Treatment based on high absolute risk may prevent over-treatment of low-risk patients and under-treatment of high-risk patients. Despite the availability of CVD risk assessment guidelines, absolute risk is often not assessed and not used to guide management decisions.
Poor implementation of CVD prevention guidelines has led to overtreatment of 25 per cent of low-risk patients and undertreatment of 75 per cent of high-risk patients. Previous trials to address this failed to target key behavioural barriers, including limited GP capability to use, understand and communicate CVD risk models. This project aimed to explore implementation strategies for CVD risk assessment tools and the unique role that Primary Health Networks (PHNs) can play in supporting CVD prevention.

