HEALTH
HEALTH
a HEALTHTECH IN AFRICA
TECH Vol. 1 | Dec, 2022 | www.thekfinancial.com 44 56 40 10
HEALTH TECH Massira, Figured It All Out With Female Centered Support. Hellomed, A digital consultation platform for patients Your Health Companion in Rwanda
Eden Care
AFRICA
Q & A SESSIONS HEALTHCARE FEMALE
Interview with Mr. Moses Mukundi, Founder and CEO of
IN
Credits
Editor-in-Chief
Hamza Katende
Cofounder, The K financial
Editors
Arnold Kwizera
Cofounder & CEO, The K financial
Fred Shema Health Reporter, The K financial

Design/Layout
Ouma Vian Dominic Threadswitch Limited
PUBLISHED BY
The K financial kwizera@thekfinancial.com Website: www.thekfinancial.com
PUBLISHING CONSULTANTS
Threadswitch Limited Audry House, Naalya Kampala-Uganda +256 783 119 281, +256 754 488 307 threadswitch7@gmail.com
Disclaimer
The views expressed in this publication are not necessarily those of the publisher. The K financial does not guarantee the accuracy of content from contributors and advertisers nor accept responsibility of any statements herein. Additional information on The K financial can be found on its website: www.thekfinancial.com
Copyright:© 2022
Cover: Article on use of phones in the health sector, link; shorturl.at/vY357
Designed by: Vian Ouma

Interview

1 HEALTHTECH IN AFRICA Inside this edition... 2 44 50 54 58 6 13 19 26 29
Interview with David Chen Massira, Figured It All Out With Female Centered Support.
Denga logistics takes the healthcare supply chain to another level.
Surplus Med in waste management
I-VUZE, your best diagnostic friend.
with Founder and CEO of Mobiklinic
Interview with Klarah’s Founder
Interview with founder and CEO Goal 3 Insightiv, a Rwandan-based radiology Tech startup
Q&A Sessions
Interview with Founder and Ceo Medtech Africa
David Chen
Co-founder & Co - CEO Kapsule, a leading business developer with over 4 years experience leading teams in B2B development across different industries including pharmaceuticals.

Mr.Chen, good to have you today. Can you please tell us a bit about yourself?
Yes, so, firstly, thank you for inviting me. It’s a pleasure and honor to be here with The K Financial. I love the work you guys are doing. To give a little bit of background about me, my name is David Chen, I’m the Co-founder and co-CEO of Kapsule alongside my childhood friend who is my co-founder, Hannan.
With Kapsule, we are a mission driven business which is looking to drive forward what we call the three As, Affordable, Accessible and Authentic medicines for everyone across the World and how we plan to do that is through transforming medicine Supply Chains. so that’s a brief intro to me and to Kapsule.

Please share with us what health care problems Kapsule is solving and how you’re solving them.
As would be suggested from our mission. We are really about medicine access affordability and authenticity so to give you a little bit of the context about the problem we are solving.
There is a long version and a short version to the story but the very short version is that my co-founder and I realized that there were things in the pharmaceutical market specifically in Africa that didn’t make any sense.
So we have a situation where people were spending disproportionally more money on products which were disproportionately lower quality due to some standard conditions. So, some of
the statistics we have is that up to five to six medicines in circulation were fake or substandard while simultaneously costing up to 21 times the international reference price. So we were just like this doesn’t make sense, clearly the market is broken and there must be a way to solve it using modern technology and especially considering that other markets in the world have already solved this problem to a large extent. Um, so that’s a little history and context from us.
What’s your vision for Kapsule? And what role will you play in the future of the medical supply chain space in Africa?
Our vision for Kapsule is really to build some of the foundational infrastructure to enable secure and reliable and robust supply chains in Africa. One of the things that we noticed is essential to the future of Africa is to have the visibility of where products are going, who has them and what conditions they have been maintained and making sure that counterfeiting or diverting of products is minimized.
In terms of what we want to build in the future, we really just want to build a fundamental technology that enables a lot of companies, applications, and a lot of solutions to be built on top of Kapsule, so that’s where we want to be. And we see the future of Africa really being one where not only Trade with external regions like Europe, US, china wherever but also doing Intra-Africa trade a lot more as well. through having better supply chains, we will enable
2 Q & A SESSIONS
HEALTHTECH IN AFRICA
trade between African nations as well.
What are your thoughts on using AI in healthcare to move the paradigm towards delivering value? I mean, just how important is artificial intelligence in improving medical supply and logistics in Africa?
Artificial Intelligence is extremely important because it enables you to use computers to leverage information and make decisions and get insights that would be almost impossible to do without it or require a lot of resources both human and financial resources to do that. But also, what I think is very essential to highlight is that Artificial intelligence is a tool and technology as is every other tool in technology, and tools in themselves have no use unless you know how to use them.
So I think the key is to take the knowledge of Artificial Intelligence that has been successfully used across many different industries, apply them to specific ground sphere, healthcare in our case or it could be in agriculture or another instance or finance in another, and use that tool to make things work a lot better.
I think it creates a huge opportunity especially in the African continent because when you’re doing things using the latest technology that means you require less resources which means you require less infrastructure. So there’s actually in my opinion, the opportunity for markets in Africa to leapfrog a lot of the current powers of the world or the western world or however you want to kind of describe it because it’s not bound by legacy systems and legacy architectures which makes the adoption of new technology difficult. I think
it’s a very fertile ground to use new technology and to drive things forward.
In 2011, Nigeria had a child mortality rate of 124 deaths per 1000 births; whereas the UK had a child mortality rate of 5 deaths per 1000 births (The World Bank, 2013). The main causes for child mortality are attributed to neonatal causes (26.1%), malaria (24.1%), acute respiratory tract infection (20.1%) diarrhea (15.7%), measles (6.3%) and HIV (5.0%) (Federal Ministry of Health, 2010c). Many of these diseases could be prevented by the availability of vaccines or by being treated with available medicines (WHO, 2011). These figures are reflected in a study by the Nigerian Ministry of Health (2010b), which outlines how the supply of medicine is uncoordinated, unplanned and fragmented, which in turn results in redundant work, wastage of resources and an inability to optimize access to essential medicines for citizens. In your opinion, what factors are responsible the inefficiencies in Africa’s poor logistics and supply space.
This is a very big problem and a very good question and it needs a very big answer. So I will try and give you an abbreviated version of my thoughts.
To give you a little bit of context to my background, I’ve been a front leader in a pharmaceutical space and at a number of conferences which were speaking on the supply chain issues in the region. What became clear to me was that every entity in the supply chain was doing what they are incentivized to do and what I mean by that is that everyone wants to get the maximum return with the least amount of effort, energy or capital.
So when we have that knowledge that
people will always do what’s best for them with the minimal amount of effort and then you add in some of the current context of the African markets. I think that explains why there have been some challenges with supply chains and logistics, so to go into it a little more detailed. When you have infrastructure gaps.
For instance, unreliable telecommunications or IT infrastructure or things like that. That makes the ability to keep data on what is happening very limited. When you have very limited data, you have very limited accountability and you have very limited enforcement ability.
So it creates is black holes; informational black holes where things are happening but no one knows what, how, when, why and so. then in those black holes everyone acts within their own interests and what that leads to is the inefficiencies that we see on a macroscale but when we actually dive into the detail on the supply chain whether it would be from a wholesaler to a pharmacy or a large wholesaler to a smaller wholesaler or a manufacturer to a wholesaler.
Each of those interactions have sort of micro-incentives where if there’s an absence of data, people just act in their own interests, and then that leads to problems that affect the whole chain. So I think overall from our analysis or from what we’ve been doing with our work at Kapsule, we’ve realized that the whole issue with the supply chain’s logistics space is a result of many small incremental issues that are a result of misalignment incentives that compound to create a big problem.
3
SESSIONS
So, in terms of thinking more optimistically and thinking more solution oriented. We believe that if we focus on those small incentives and fix them piece by piece it compounds a benefit overtime as well.
At policy level, in your opinion, what can African governments or institutions do to fix some of these inefficiencies? Or better still what has or can Kapsule do to fix these inefficiencies?
Yeah, so that’s a very broad question. I think the government can do two major things: The first one is to use the powers that they have to make very clear and very robust regulations and mandates activities to be to a certain standard and to a standard they can enforce those regulations and rules on supply chain actors and on the second side of this is to create an environment where you have innovators, companies or organizations which are incentivized to create means in which you can stay compliant but use less resources and that usually means through leveraging technology.
If you have a government which is both favorable to new approaches, to compliance and to regulations and then use their ability to create those rules and create enforceability. I think the combination of the two creates a world where you have enough incentive to improve things. And to the second part of your question, what can Kapsule do to fix those inefficiencies that’s what I wake up every day to do, that’s what keeps me going, that’s what wakes me up at night and in the middle of the night, and that’s what I’m day dreaming about when I’m around friends.
What we can do from my point of view as co-founder and co-CEO is to build better visibility and transparency and accountability and when you can do that, people will do again what they are incentivized to do and it’s to do what is most valuable to themselves and with the right level of transparency and accountability, what’s right for everyone else as well. So using technology to drive that is what my job is as founder and Co-CEO.
You were selected among the top 30 health tech startups to incubate at the Norrsken HealthTech hub in Rwanda in partnership with Novartis. How important has this been to you in executing your mandate and vision in Africa and beyond?
It’s incredibly important. Firstly, it’s a huge honor to be among the other healthtech startups that are here and also some of the other startups that are here outside of the healthtech space. Earlier today Hamza introduced me to many people in the space. I was blown away by some of the incredible work some people in that space are doing.
I think what is really important and critical about this state of art. Here in Rwanda it’s very encouraging is that it’s creating an ecosystem and with an ecosystem it has compound benefits and compound interest and that each person who’s here doing something innovative, pushing the envelope, really trying to innovate in the space who is sitting next someone who’s trying to do the same creates an environment where ideas happen, information flows, and have a compounding benefit.
For us at Kapsule, it’s very important because we want to have a base in Africa
that also has the right infrastructure around us in terms of the infrastructure to have the right office spaces, or the right internet connectivity, or reliable services that we can build around us especially as we are very technologydriven business and this space is absolutely perfect. In speaking with the rest of my team and with my cofounders, we really said that the hub here, the Norrsken organization has made, it seems like the beginning of something special and I think we’ll only really see the true impact that this space has had in a few years when we see a number of the number of companies that spring out of this space.
Health technology startups in Africa face many challenges, besides funding & Patent or Intellectual property rights, scaling is one of the biggest in the room. In your opinion, what role does the Norrsken HealthTech Hub play in mitigating these challenges?
Yeah, well, it plays a huge role. Not only on the practical aspects in providing the actual space, providing the resources, the infrastructure for us to work and come up with ideas and network with others but also this space itself is very aspirational.
You can come to this Norrsken house and I encourage anyone who is listening to this to come and visit and not be inspired. Like everything about the place screams the future, it screams sustainability, everything you want to aspire to do and to be. I think you can talk about the practical support that this space is providing in terms of providing access to investors, providing training, networking, and all of those things.
But I think beyond that, what is really
4 Q & A
important not only for people in this space but also for everyone in the surrounding areas is that it raises ambition, it raises expectation and it creates an energy and zeal, Which I think it’s very infectious.
I think if you’re a child walking past these buildings, you’ll be inspired. If you’re someone who is thinking about an idea and you look at the space, you’re going to be inspired to take your idea to the next stage. And if you’re visiting from another country in Africa when you see this you may think that we need something like this in my home, in my country and in my town and then try and build something towards that. I think you have a practical impact and also you have more philosophical or aspirational impact.
In what countries are you currently operational? Why these countries and what countries do you plan to scale to?
So we are a classic 21st century organization and our entire team is quite distributed. So we have 3 of us based here in Kigali, I have some other teams based in London and some in South Africa, one in Nigeria, and one in Pakistan.
So we have a global team. In terms of where our operation is, it’s very clientdependent. So, wherever our client wants to implement our technology to track products that’s where we can go. So, at the moment we primarily focus on Nigeria but there’s also plans to go to other African markets which could be Ghana or Liberia and even some of the francophone countries as well.
What has your experience been so far operating in Rwanda?
I love it, I absolutely love it! I say it’s like Switzerland in Africa. I was actually speaking to one of my childhood friend who lives in Switzerland, I keep telling him to come to Rwanda because everything you have the right level of infrastructure, everything is safe, everything works, and You have a certain amount of predictability about your day but you also have all the buzz, all of the excitement that you get from being an African and be able to eat the right food and have the right weather.
It’s like everything blended into one. For now and in the future Rwanda is a place to be and I can completely understand why the visit Rwanda campaign has happened because once you’ve come and see it for yourself, you don’t want to leave. My sister, my mom, and my brother, are all going to come and visit and when they do, I’m sure they will want to stay.
Any last remarks for those starting out in Health tech in Africa?
I would tell them two things. One is that something which maybe sounds a little bit strange. The first one is to have delusional confidence. What I mean by delusional confidence is you have to see what is there before anyone else sees it.
You have to believe that you’re the person to deliver on your vision that no one else could see and if you are too pragmatic and too realistic you will then look at the size of the challenges and think this is impossible for me to solve but like the old saying says; “when you want to eat an elephant, do it one bite at
HEALTHTECH IN AFRICA
a time”.
It’s very much the same as doing any sort of technology company or start-up across the world, especially in Africa where you have challenges which are very unique to this time. The challenges are there; they are real but you should not let them dampen your confidence.
That’s why I say the delusional part is very very key. You need to see and believe what no one else can see and believe. Now, the second part, is almost opposite advice from the first piece of advice, is that you need to be very pragmatic and what I mean by pragmatic is that look at resources that are available to you and look at everything that you have access to and think how can you use that in a most efficient and effective way possible to get you the results you need.
You need to be very pragmatic and very defined in how you define goals, in how you define targets and milestones. Be very regimented in both your daily routine and also your way of measuring progress so that you can make sure that day by day you are moving into the right direction. So you have two almost conflicting sides.
I advise that people balance. The delusional confidence that you’re going to do it regardless and then almost conversely that very pragmatic sort of almost pessimistic view that I need [Unclear] otherwise that big dream won’t happen and if you somehow manage the two, I think that’s a perfect combination and a recipe for success
5
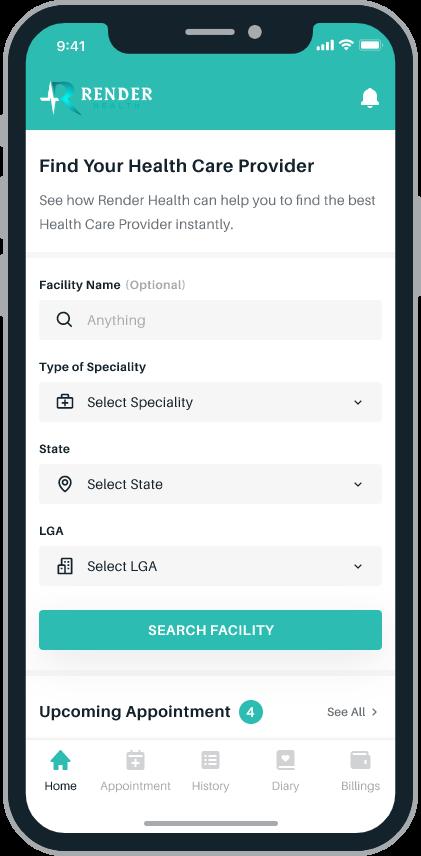
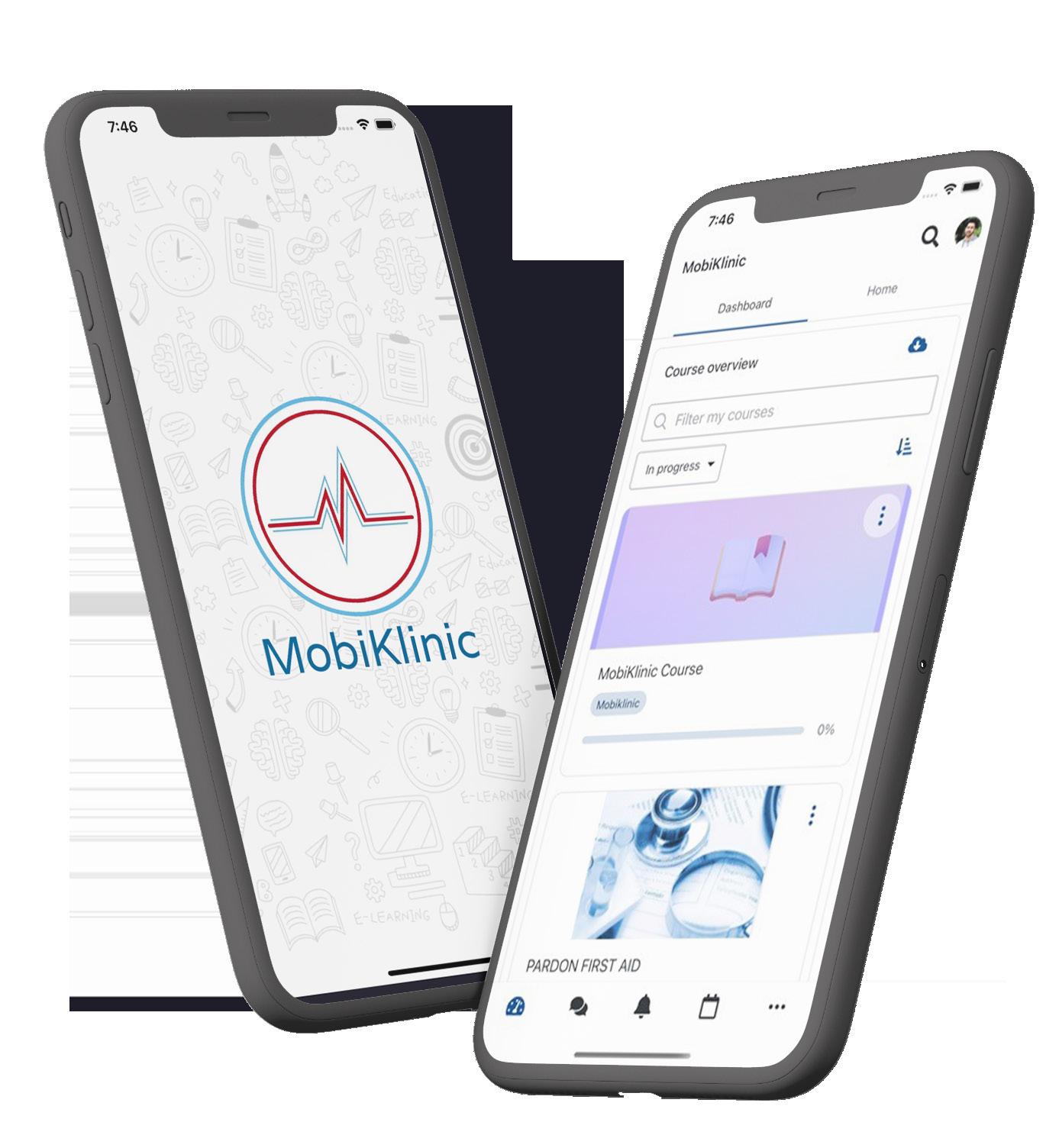
Interview with Andrew Ddembe, Founder & CEO of Mobiklinic
Mr Andrew Ddembe, good to have you today. Before we dive into Mobiklinic, Who is Andrew Ddembe ? Please give us a brief preamble of who you are and your journey thus far.
Andrew Ndembe is an individual who is so passionate about sustainable development, innovation, and social justice. And, so, much of my work rotates around these three.
I am a lawyer by training but I’m based towards health equity and social justice like I’ve mentioned. I’ve also been an entrepreneur for the past 7 to 8 years and I also represent Uganda In the African Union, European union, US cooperation hub which focuses on development issues for young people, and particularly in the business cluster. So, that’s what I do and that’s all about Andrew Ndembe and I’m glad to be here. Thank you for having me.
So Mobiklinic. What is Mobiklinic and how did it come about?
Mobickinic is an African solution tailored for a big African problem. How it came about, first, it starts with a personal story about nine years ago my grandmother
got a stroke in a rural area here in Uganda in Buikwe and when she got this stroke the people who went to her rescue none of them knew the nearest health facility, let alone the fact that facilities are very far from the people. they also didn’t have so many ambulances and what happened is, The family in Kampala city called for an ambulance from the national referral hospital that had to drive 60 km down in Buikwe to pick her up and bring her to the hospital and by the time they reached, there had been a big delay in responding to her healthcare needs and
needs of communities in low income and last mile areas. In these areas, there are few doctors. In rural Uganda, there is 1 doctor for every 28,000 people and also the other problem is that facilities are far from people.
So, mobiklinic ensures home-based healthcare in these low-income areas through a very practical and cost effective manner, as I will later expand on that. So, that’s what we do, to revolutionize and ease access to healthcare and health delivery in low-income areas in Uganda and the vision also for Africa.
You could have answered the next question but I’ll still ask, What are the main pain points that Mobiklinic is solving and how are you solving them ?
Okay, one is on Access. We ensure timely consults within the communities. Like I’ve mentioned in our low-income communities because they are few doctors, and few health workers.
a few hours later, we lost her.
So, mobiklinic responds to the healthcare
Because they are far from facilities, when people are sick they tend to do self-medication. Self-medication is a big thing in these low-income areas of
6 Q & A
SESSIONS
There is 1 doctor for 28,000 people in rural Uganda.
HEALTHTECH IN AFRICA
ours, especially in the rural ones. When people are having simple malaria, they are taking herbs.
That can be fixed if at all there is access that can be gotten within walkable distance and that’s what we ensure that we have a network of community health workers and the people in these lowincome areas can access these people within walkable distance, they can get timely consults and the issue of timely consults is very critical because it erases many situations that would escalate to dangerous situations.
For instance, if somebody has simple malaria and they live in this area and they fail to know it’s malaria by the time they get to the facility quite often because of lack of timely consults, the simple malaria has become severe malaria.
So, that should give you the picture of why timely consults are needed in these communities. But with Mobickinic, these people are able to know within the shortest time possible that “Hey, this is Malaria” and so they begin to take their medication.
So our pain point is on access, access is a big challenge and we solve that by ensuring Community health workers that are within walkable range and this offers timely consults and it would sort the issue of labor because there is low labor in these areas.
People do not want to work in these areas because of low purchase power. The majority of our people in these areas are poor. But at Mobi, we can join firstline respondents within the communities at a cheap cost and they call them community first aiders and that is very critical and important in these areas. So,
we solve the issue of labor and access.
The other is, how do we utilize the few existing doctors? That’s a big challenge in Uganda and much of Africa. We have few doctors like I’ve said there is 1 doctor for 28,000 people in rural Uganda.
That is far below the WHO recommendation of 1 for every 1000 for the very least. So what do we do then, so, our solution is about, number one, empowering community health systems and then, number two, creating a digital tool, a safety net tool that enables an interface between the few existing doctors and these first-line respondents.
So when community health workers are strengthened, they are able to interface with senior medics and get guidance and they can be able to help you sort your issues. They can also use our tool
to refer a patient and also to call for an ambulance or emergency response. So, this is what we are doing, this is how we are solving the pain points through three main things, solving labour, solving access, and also ensuring a digital safety net to improve the quality of service.
Access to Health care in Sub-Saharan Africa remains the worst in the world, with few countries able to spend the $34 to $40 a year per person that the World Health Organization considers the minimum for basic health care. In your opinion, why do you think this is still a bottleneck in Africa ?

I think it’s still a bottleneck mainly because of, to be straight forward, Poverty. Poverty is what’s making our people fail to afford healthcare or spend less in healthcare.
One will always spend according to their
7
level of income. Now, the majority of our population in Uganda, in Africa, are lowincome earners. So, poverty is a big issue and that’s why much of our market when it comes to healthcare, there are low purchase power markets.
So for me, I think the major thing is poverty, and I think, who do we need then to solve poverty? I don’t think it’s the health innovators but I think it’s the duty of Government and Stakeholders such as Development agencies to ensure economic uplift of economic empowerment of the majority of our people.
That way, once their levels of income go up, they will spend higher on healthcare. So, I think that’s the major thing, poverty and I don’t think it’s about to change any time soon but gradually when our Governments do the right thing, this problem can be solved. Yeah.
Tell us , how is Mobiklinic innovating around improving access to HealthCare in low income areas ?
What we do is, number one, we go to the low-income areas on board within community members who are willing to commit to offering services as first-line respondents to their communities.
These are onboarded and trained and they are given a lifetime skill set that they can use to serve others, that they can use to help different segments of the population in terms of basic firstline healthcare. And these are deployed within the very communities that they live in.
So you find that, if Katende has come
to visit me in Buikwe district and gets a terrible headache at night, within a walkable distance, Katende is going to be able to at least get first-line of care and they are not going to be scared that “Oh my God!
The hospital is far and I might die from here”, so that is number one, which is empowering community health systems and it’s what I’ve just explained by ensuring a well-trained network of community first-aiders or community Health workers and the second bit is the digitized mobiklinic app , the tool that eases their service delivery.
That ensures when they are stuck, there is a fallback of options, there is senior guidance from senior medics, there is referral as an option and there is an emergency contact team. Now, all this improves their service delivery and the other one is of recent, we’ve put up an e-learning platform which is a one-stop center for training community health workers and this is having content that is translated into key local languages across the East-African region.
is going to accelerate our training of community health workers and we’ve partnered with Clarke international university, Health Studies University as a quality controller of our platform and yeah, that’s what we are doing so far to ensure that we are having more community health workers that are well trained and then to ensure that their service is eased, and the Mobiklinic app improves their service delivery. So, that’s it with regard to that question.
According to the International Finance Corporation (IFC), the private sector already delivers about half of Africa’s health products and services. In your opinion, what role can regulators or government bodies play to improve access to healthcare services to low income areas ?
Number one, I think the Government needs to create a bridge with the private sector and the private players that are daring to go into these areas. So the Government should not enjoy a monopoly in these areas while not delivering. Government instead should work with private players in these areas through things like Public-Private partnerships, That’s one way.
The other is that the Government should create incentives for health workers and also be well distributed across these areas. In Uganda, the internship system for medical students is a good one because you find it rotates them around the rural areas of the country and that’s one good step. However, more can be done. It can stretch to the nurses and all the other people.
There is Swahili, there is Luganda, and there is English. You find that this
Government can also create incentives like I said of health workers that go these
8 Q & A
SESSIONS
There is 1 doctor for 28,000 people in rural Uganda.
HEALTHTECH IN AFRICA
low-income areas because even though we have few health workers. All of them prefer to work in Kampala and the near suburbs and yet the majority of these people are in low-income rural areas.
So, Government needs to have a plan or a policy and think through how they can incentivize and make these people loved and also make them go to the lowincome areas. So, I think the main thing is by paying well, paying those that go into these areas cause the concern is always about payment. Yeah!
For those that would need your products and services, how can they reach out to you ?
I think the first way is to go to our website which is www.mobiklinic.com and on there we have our contact email, we have our mobile number and they can also get to know our different services, our previous work, and yes. I think so far for those who are far away that’s how they can get to us.
Mobiklinic was selected among the top 30 health tech startups in Norrsken and Novartis Foundation’s HealthTech 2021 Challenge. How important has this been for you, have you raised any funding, grants or gotten key partners ? and how do you plan to capitalize on this?
I think getting into the healthtech hub was an amazing step for us. We are very proud of it. We are very proud of the healthtech hub team which has managed to link us to very great mentors, two members they gave us ended up joining our Board and so we are very glad for that.
We’ve managed to get through the year’s grant close to 80,000 dollars.
Norvatis and Norrsken have added to our credibility but also we are having an important discussion that we think will push us forward and seeing that we are one of the 2 companies from Uganda that are part of this top 30, we don’t take it lightly, we are very proud it and it spoke to our potential and we are doing all possible to make sure that we make the hub even more proud of us. So, inhouse, we are having a product that we are still deliberating on and building.
It will be to the cities and it will also increase our revenue streams. So, I think it added much to our confidence, it added to our credibility, and it’s been some very good things that have come out of this healthtech hub and we are so proud of it and we commit to also being an Ambassador of this hub out here by showing great work and by impacting the communities, yeah.
What have been your key highlights from your time participating in the Norrsken and Novartis Foundation’s HealthTech 2021 Challenge ?
Our key highlights were during the key mentorship phase where they gave us, a Ugandan lady that was attached to us, Madam “Bright Asiimwe” as an adviser and mentor during the program and she’s been of great assistance to us.
So, that for me was a highlight, the period of mentorship because there was a lot of learning and unlearning and then the other was during the summit that happened in June getting to meet so many other amazing people who are having the fire, the passion about
healthtech, who are having the fire about solving Africa’s problems using technology in healthcare and also other Stakeholders.
Those for me were a very key highlights and also the other is in the Investment Readiness Phase where they brought different Healthtech entrepreneurs who have managed to raise different sums of capital and they have shared with us tips and we’ve been there to learn. So, I do take those as one of the highlights I’ve had in the healthtech hub. Yeah.
Amazing! Andrew, thank you for taking the time to do this with us, We hope to catch up soon Sir.
Thank you so much Hamza.
9
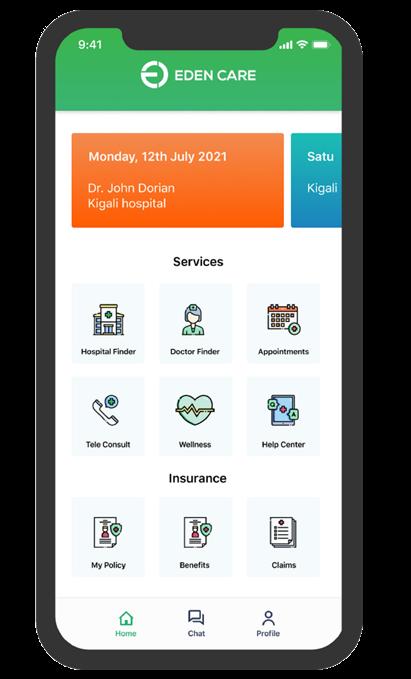
Interview with Mr. Moses Mukundi, Founder
and CEO of Eden
Hi Moses. Thanks for taking the time to do this interview. So, let’s get into it. Please tell us who Mr. Moses Mukundi is and share a bit about your journey as an entrepreneur.
Yeah, um. I’m kenyan, I’m living in Rwanda now. So, I spent 6 years in Investment banking and private equity before this. I also founded my first company, an agritech business that we sold off to a Chinese company in 2018.
During my time in investment banking and private equity, i got a lot of exposure to insurance companies both in general insurance and other insurance companies, financial services and the healthcare business and over time of doing technical due diligence for these companies , it became very clear to me how inefficient they were.
On average across Africa, outside of South Africa, Insurance companies spend about 50% of the premiums on managing the admin piece, admin work for their members.
So, that’s very inefficient compared to 11% in South Africa and then in 2018,
Care
I had an allergic attack when I was in Uganda for work and I nearly died because one of my insurance companies refused to pay for my air lift because a doctor forgot to stamp the request letter.
And for me those are some things that came together and became really clear that there’s an opportunity to disrupt this massive industry that no one was paying that much attention to and being very impervious to technology and was going to have a large social impact on the African Continent. That’s how we got started.
So, Eden Care, what is Eden Care ? Who is it meant for ? and most importantly what is the Eden care story ?
Yeah, so, let’s start with the Eden care story. So, Um, in 2019 I was going to business school and I had to decide whether I wanted to go work on Wallstreet or come and do this thing that I have been thinking about for almost the last four years. And I went to business school with a very interesting thought.
I was going to spend my first year doing
market research to decide whether it’s something I want to follow . If at the end of the first year, I could see there were signs there could be something here. I was going to leave school and focus on that, if not I had a job offer to go work on Wall Street.
So, I spent my first year missing a lot of classes and flying between places that had very interesting business models, New york, San francisco, Brazil, India and also spent a lot of time trying to figure out where to start. So, we spent a lot of the time in Kenya, Uganda and Rwanda.
At the end of my first year, i figured out that there’s a business model to be built here, i could see how the tech wellness prevention and focus on customer experience were going to very quickly differentiate us as a business compared to traditional insurance and covid also made that decision a lot easier to drop out of Wharton Business school to come and focus on building Eden care.
So, essentially, Eden care is a digital health insurance company. Right now we are starting off by focusing on the corporate market. That just allows us
10 Q & A SESSIONS
to build out the scale and the data that allows us to efficiently target and address the and make needs of the middle-income that outgrown RSSB but have been priced out of that current private healthcare insurance companies.
So, that’s our business model, we are very differentiated from traditional insurance companies by our focus on one customer experience. Two, changing how people experience health insurance at the hospital level, reducing the wait time.
Our intention is to reduce the current two and a half hours of wait time that is related to insurance down to zero, um reduce the amount of work that HR teams take in managing healthcare for their teams down from the current four weeks all the way down to about 1.6 percent and overtime, be able to increase the penetration of health insurance currently sitting of about 0.02% to about 2% of the GDP here in Rwanda.
So , you have mentioned corporates. Why corporates?
One, we needed, as a new health insurance company we don’t have any data and how you price and do anything with insurance, it’s with data. So, corporate markets are a place where we could very quickly differentiate ourselves from traditional insurance companies and be able to build scale a lot faster which gave us the ability to cross subsidize as we enter into lower and lower price points into the direct consumer and the SME market.
Thanks for that clarity, without forgetting please take us through the insurance products Eden care offers and why corporates should choose
Eden care as their preferred digital insurance provider?
So, with Eden care you get a very comprehensive product, you get your Inpatient - Outpatient maternity, dental and optical cover and we’ve also built our product at different pricing points with different benefits to allow us to capture as wide a pricing range as we can find out there.
So, our products are meant to be cashless. that is, you go to the hospital, you use a card and you don’t have to pay anything and our cover is across east africa.
So if you went to any of our East Africa partners that may be the Aga Khan hospital in Kenya, Nakasero hospital in Uganda, Aga Khan hospital in India, etc. The same card you could use here in Rwanda is the same tap and go access that you get across East Africa.
HEALTHTECH IN AFRICA
Additionally, we’ve partnered with various hospitals in India where we can send people for cover. The other thing that we are doing very differently is that we are very heavily focused on prevention. So, we reward our members for meeting their wellness goals. For example, a member gets a target to hit 40,000 steps, if they hit those 40,000 steps they earn points and they can
go to any of our reward partners and redeem that for a free smoothie, a free coffee, the next iteration which will come through the next two months.
Someone can go to the gym, everytime you go to the gym you earn points and you can use those points to pay for your gym the next month. Additionally to that, it’s a very heavy focus on the customer experience. So, we’ve spent a lot of the time reducing the wait time of the hospitals, the amount of admin work at the HR level but also making sure that we have a customer care team that is accessible to all our members.
Digital health insurance is a fairly new concept in sub saharan Africa, in your opinion how do you plan to make Eden care a household name or brand in the health insurance space ?
I think there are two ways to think about this. When a product is still new. I think making sure that the products works really well so that the word of mouth is the primary way for people to know about your product and that has been the primary focus for Eden care to getting the product out there.
So, it’s a very heavy focus on product led growth through word of mouth and people actually try to get to use our product but also it’s focusing on member’s education and explaining to people why health insurance is really important, finding avenues to leverage existing trust for us to sell our product and making sure that our brand is visible across the market. These are some of the three broad ways where we are taking to increase our penetration of health insurance in this market.
11
Health insurance currently sitting of about 0.02% to about 2% of the GDP here in Rwanda.
SESSIONS
Please take us through the Eden Care road map and what the next 2 -3 yrs look like for you as a company.
Yeah! Certainly, we have a very aggressive growth path both in terms of how we want to introduce new products and sort of geographical growth. So, over the next couple of years, we would like to be across the entire East Africa and a couple of other countries outside the East Africa region .
Additionally, we need to have expanded to life and the general insurance products to be able to provide a one stop shop for members to access all the insurance cover from one platform which is Eden care.
The insurance industry is quite challenging for any new player to penetrate. What would you say are the top 3 challenges you currently face
Well, we are a new player in the market so obviously building a level of trust first is always a challenge. Number two, I would say we are in a very regulated industry that is very capital intensive. So, managing the needs of the regulator with the needs of investors can sometimes put quite a bit of pressure on a business to balance out the needs of two very critical parts of the business.
I’d say that is recruiting, finding the right talent to execute this means that we have to be a global business in terms of how we think about talent and figuring out how to build a singular culture when the team is dispersed around the World.
The Novartis and Norrsken health tech hub cohort of 2021 is coming to an end

and Eden care has been part of this program since its inception. What have been your key highlights during the past one year spent in the program
Yeah, certainly. I think the structured way of approaching investment, um, it’s really important to make sure that it yields through all the various elements of the business. I think that’s something that novartis and their system built for the program worked really well.
I think It’s also really helpful to be in the community of other founders who are in the trenches with you and the same community, I think that’s extremely helpful in both managing emotional toil that sometimes entrepreneurship can take.
I think the third one has been access to the experts, people who bring deep focus in a certain aspect and can bring
new perspectives to how we thought about the business.So, i think those are the top three things that novartis brought to the team.
The new 2022 cohort of the Novartis and Norrsken health tech hub is starting soon. What would be your advice to them as they embark on this journey?
Find the right mentor, I think that’s going to be very important. Um, spend enough time with the experts that you get access to and I would say the third thing would for me be active in the community.
Thanks for doing this interview with us. We shall be keen to tag along as we capture the next steps of your journey.
Fantastic.
12 Q & A
Interview with Klarah’s
Founder & CEO

Ginyu Innocentia Kwalar
SESSIONS
Public and Private sectors and so, it has been a beautiful ride as I said, it has been challenging but then it has been beautiful.
Ah, my work also has enabled me as a nurse to be able to grow and improve. So, I got in with a degree but now I have a PHD. with my years of experience and my Academic Qualification, I’m also looking for opportunities to train the young ones and so, i also teach in the university to be able to train the next set of nurses and impart to them what i have been able to harness over time; in the form of experience and also in the form of education.
So, in summary, the journey has been a long one but it has been an exciting one. A lot of evolution has taken place in a context that I would say that we are yet to get there and now it is towards the other part of my work as a nurse that I found a new passion or I was able to sit down and look, is it just sitting in the hospital and waiting for people to fall sick and they come to the hospital and meet us? And then we go through the cycle again and again.
I was asking myself, what can we be able to do differently? especially with what technology has offered to us. And ofcourse, the experience with my father made me see actually that we can be able to merge technology and health and actually get healthcare, especially proactive healthcare to the communities, to see how we can be able to help individuals.
So, that so far has been my journey from nursing side to administrative, to Academia and now being an entrepreneur and innovator, So, it has
just been a melange of everything but then it has been an exciting and worthwhile one. Thank you.
You have been a nurse for over 10 years. In your opinion, what are the main challenges facing the nursing industry currently in Cameroon ?
Yeah, Many facets. The first thing is that, in a country we still have the challenge of harmonizing. You know, at the beginning i said we were just getting, nursing was just getting into the university milieu and on the field it was like “who are these breed of nurses?”, “where will they be put in the public service classification?”, “How will they be functioning?”, “What would be their job description?”.
Unfortunately, like 20 years down the road, that hasn’t changed significantly because there are people who still think that nurses should just be a secondary level nurse that has an e-level and three years of training in the nursing training schools.
So, university, train nurses as though they shouldn’t be called nurses and this also is affecting the registration also into the order of nurses that we find in our country because we have an order for nurses midwives, lab technicians and Allied Health Professionals which is recognized by the Ministry of Health and before, they were actually registering us, because i am registered into that order.
Unfortunately, They said to all the students that i am training and they come back and say “Madam!, we are finding it difficult to register into the order because they say that we can not register because we are not “SRMs” they put it in our own context ”.
So, to me that is the first challenge that we have. We need to be able to harmonize, we need to be able to get to the level where we can be able to define who truly a nurse is, in our context and work with that. The interesting thing is not wanting to register this set of nurses, then the Government is recruiting them and working with them because their training is validated.
The next challenge that I see also is with the numerous nursing schools that we have in a context we have. It’s a plus and I would say because we are training so many nurses. Ofcourse, the number of nurses that we have is largely insufficient.
No wonder, we are at the state of less than 12 nurses to a population of 10,000. You can imagine, that is largely insufficient and nurses would be overworked. Then, with these numerous nursing schools, you can imagine also, their curriculums and accreditation will also be as vast as that.
So, really, Our challenge is really getting an umbrella institution or umbrella council that can be able to regulate the training and of course, regulate practice, we are yet to get there as a nation. The final challenge which is not the least, and which does not say by any means say i have exhausted all of the challenges because they are numerous.
But the final challenge that I want to talk about is at the level of remuneration of the nurses. It’s also a huge challenge in our city. The remuneration is not standard across the Board.
For those working in the private sector, you know their remuneration is different
14 Q & A
from those working in the public sectors and that doesn’t speak well for the professionals as nurses because people working in the private sector are largely underpaid and so you may want to see that they are underemployed.
So, it’s a huge challenge for us to be able to get there. I think, as an individual, if we are to have a council, it would address so many of these things and put us on a better footing. Thank you.
So we now dive into the exciting part, The Uber for nurses, Klarah. Tell us about this. How did it start? Why did you start it ?
Um, Okay, How did it start?; Why did it start?. So, in answering your preliminary questions I said, I was able to have some mind boggling questions. Should I remain in the hospital and keep seeing these people coming again and again? Finding it difficult to meet up with their appointment because they don’t want to wait for a long time because when they come probably the doctors or nurses have the emergencies and all of that.
The frustration was real and I was just wondering what can we do differently to be able to help these people? But then the story with my father made it very clear of how I could be able to use technology and be proactive in healthcare and help people.
So, I’ll tell the story quickly of my father. Recently, my father has not been really very well. He has been down in health and he lives in a town that is miles away from where I work and being the health personnel of the family, each time he has a crisis, I’m called upon. At times, when I say I don’t want to
go. I’m asking my mother “What is the situation?”; She is unable to give updates probably because she doesn’t know and that she hasn’t been given the information and even when she’s given with the information probably she hasn’t understood what has been said.
You can’t have access to the team that is talking with him and so, I have to move. So, each time he has a crisis, i’m on the way and bet you it’s a journey by road, i take about 12 hours, i take the entire night to be able to travel and to meet him. So, you can imagine how he was also draining me.
HEALTHTECH IN AFRICA
And his crises were really frequent. So, probably at times I move and by the weekend I am there and just have to stay in a hospital with him and then he is discharged and I’m on my way back and by the time, I’m being called up again, He has a crisis and I have to do that routine again. You can picture the scenario,It’s challenging.
And also, i have my siblings who now, okay, they could probably get a better picture when i am there but i have this brother of mine who is based in Germany. He was particularly worried and each i’m not there he’s like what is
now happening? Why is he always having to go to the hospital? Why is his crisis so frequent? Okay. So, I consulted with him and then I said okay, what we can do is to reduce my movements.
Let’s recruit a nurse and let the nurse come to the house when nothing is at stake, frequently, check on his vitals, do physical assessment, and just be able to share the results with me so that i do an interpretation of the results and pick up the red flags so that i can say, “Okay Mama at this point in time, take Papa to the hospital.” When we do that there is no emergency, there is nothing at stake, He can be patient enough.
Remember that when he goes into a crisis situation, it’s no longer the same story. It’s frustrating because you go and probably the doctor is not on site because he is attending to some other person. So, if he has to go when there is really nothing at stake, there is no emergency.
He can also maybe just be patient and it will make it light on him. So, that’s what we did and his number of crises significantly reduced because we were able to monitor, we were able to follow up that his medications were given as prescribed, we were able to follow up on the doctor’s appointment.
Above all, we were able to pick up the red flags and say, “At this point in time, yes he is not in a crisis, they think with these figures it is announcing that something may just be around the corner. So, you can go to the hospital now”, the narrative changed significantly and so, i said to myself, “aha!”; I would say, that was the aha moment.
15
We are at the state of less than 12 nurses to a population of 10,000.
SESSIONS
So, this should just be what the other people also i was wondering about in my daily walk with them are also facing it Because at my job site, i could see people, they kept coming when they had a crisis and you’re just asking, “You had this appointment, why did you not respect your appointment?” and so on. And when they are better I really don’t want to be coming to the hospital because I will stay the entire day. So, to summarize, that experience with my father made me know that I could just use my phone and follow-up my father without necessarily moving because the nurse was taking all of what he was doing and sending it to me.
There are times when his feet say that it’s swollen. And I would say, “Take a picture and send it to me” and I ask, “What else are you monitoring?” So I’m able to say let him turn around and you snap and I’m able to see so that shows the discussion we are making and it changes the narratives significantly. So, i said, why don’t blow this out on a larger scale and just help some other people also. Link them with nurses that are around.
Remember, i have said in a context, we have many nursing schools and probably many nurses that are being trained. We are not yet there, if we have to use the index by WHO but then we have a reasonable number of nurses and in every neighborhood you would be able to get a nurse that is living there. So, That is how Klarah was born. We are leveraging technology to match nurses to patients so that quality healthcare can be offered in the comfort of their homes. So, That’s the story of Klarah. Thank you.
wow, wow, that’s quite a touching story.Innocentia. In what markets is
Klarah currently operating and how do you plan to make Klarah stand out from the rest and also not to leave out, Which segment are you primarily focusing on for now?
Okay, in what market? Ofcourse, I’m based in cameroon so cameroon is the bedrock and now we are exploring the Cameroonian territory. We have been able to have nurses who can comfortably take care of clients across the national triangle.
In the foreseeable future, we are looking at actually getting beyond the boundary of Cameroon because we know that the problems that are real to us are real to other African countries.
We also have people who have left their loved ones back at home and do not have an idea of what is going on and are called up only when there is a crisis and you can imagine, the Adrenaline rush when that happens. So, We are looking forward to expanding into other territories in no particular order but we have countries like Rwanda, Nigeria, and Ghana.
have left the shores of Cameroon and Africa and are in the Diaspora and we really want to give back to their parents because they are where they are because of their parents.
Unfortunately, there is always this disconnection, they don’t know what is happening. Most of them, they are called, “Papa has a crisis”, “Mama slumped when she was in the Kitchen” and when they reach to the hospital, It’s a choke. What happened? Last week, I sent money for Mama to go to the hospital and we don’t know when she finally went to the hospital or if she decided to prioritize some social activities. You know, so you are lost.
So, I’m highlighting that our customer segment is people in the diaspora because they are the ones we are talking to, because they are worried about their loved ones. You can actually send them off and you pay directly and we are able to take care of their health.
And inform you on what is going on in their lives concerning their health and you can actually have the peace of mind that you deserve and continue with the work that you are doing. So, that is it. But then we have an interesting definition of the diaspora because a diaspora also is that person who has left the village and he’s in the town and he’s working and the parents are back in the village. Okay, you can still sign them off. It’s all part of our customer segment.
Hopefully, as we open partnerships we will expand to them. Um, The customer segment for now are people living in the diaspora because to us they are the pairs. So, we have so many people who
So, those are the people we are looking at. And, how do we expect to stand out? We are looking forward to the time when Klarah will become a household, Klarah will be the one-stop shop for all your health problems community which
16 Q &
A
In the next 2 - 3 years we are looking at scaling beyond the borders of cameroon.
HEALTHTECH IN AFRICA
You know, there are also ventures that are similar but then we differentiate ourselves in that because we are using qualified trained nurses. Most other people, the ones who work with community health workers who are readily available which is a good venture but then they are not as trained as nurses. So, If you have a nurse, you definitely know that the care you are going to have is way beyond just basic care. So, that’s how we are hoping to stand out.
According to the Journal of Global Health Reports, primary health care (PHC) in most African countries is nurse-led. However, nurses are still facing adverse challenges. In your opinion, what frameworks should be put in place for the Health Systems Strengthening in a nurse led Primary HealthCare setting ?
First of all, of regulation, You agree with me that first of all healthtech, there is the challenge of policies that regulate that sector. But it’s even more challenging to be able to regulate the nurses who are going to be carrying out these activities at the primary healthcare level. We are trying to get around that, to see that each nurse that signs off is actually first of all recognized by the state.
So, we have that shows that you have been trained and that you are registered into one association or into the order which gives you the right to be able to practice.
You’ll bear with me that if we do not start thinking putting policies in places that will actually regulate the functioning of these nurses and it’s really clear that okay, i’m signing up as a primary healthcare nurse and this is what it takes to do it and maybe some sort of license
that makes you to function in that. To me, that is the way forward. Remember also i’m talking in a context where i have already said that we don’t have a council, which means that we are still far from attaining or achieving that objective but then. It is worth noting that the nurses that we work with, asserting the fact that truly, “Are nurses recognized by the state?” And we do not leave them there, we coach them and work with them even while they are on the field. Those are things we can be able to do and to improve on that sector. As I said, the key to making it work is regulation.
Klarah won a spot among the top 5 startups in the novartis - Norrsken healthtech 2021 challenge. What has this experience been like for you ?
It has been a beautiful experience. Remember, I am from the bedside to the boardroom. It’s no joke. When we won that award it gave me the opportunity to work with great mentors that made my transition less bumpy than it would have been.
I am not yet there, I don’t want to claim that I’m a tech expert to be a super entrepreneur after a year of being in the hub but at least I think that me being there has really facilitated my journey.
I have been in the hospital taking care of patients and in the classroom teaching students. This is a new sphere for me but then if we have been able to cover grounds, it’s because I was part of the hub. Apart from the training and mentorship that we had while in the hub, the financial aid that they gave us was a huge boost.
At Least we were able to acquire space, we were able to recruit workers, we were able to begin the production of the app, we were able to do certain other things that otherwise without the financial assistance we wouldn’t have been able to do.
So, yes, it has been a great pleasure being in the hub and I have learned a lot. I know I am still on the journey of learning but then it has been a beautiful time and I have learned a lot.
What should we expect from Klarah in the next 2 - 3 years?
Ah, What should we expect from Klarah? I will summarize what we are expecting from Klarah. I’m always excited when I talk about Klarah because I just have the feeling and I know that Klarah is going to be a very relevant arm helping to resolve local problems with local solutions.
So, In the next 2 - 3 years we are looking at scaling beyond the borders of cameroon. As I said, we are looking at making partnerships and growing in such a way that we will not only be leveraging people in the diaspora to pay for the services back home but people at home also will be able to login and get care from Klarah Wherever and whenever they will have.
So, that is what we are looking at to be a true uber for nurses where you’ll be able to log in, get a nurse, and get attended to in the comfort of your home.
In your opinion, what does the future of healthtech in Africa look like? Shall we have some unicorns in the next future?
Ah, I think so. I happen to also look at some of the ventures that are going in or
17
around in the phase and I am convinced that we will have some unicorns. I am convinced that Klarah itself will be a unicorn and there are so many other ventures that I look at them and I say, “Yes, we are going to have unicorns in the nearest future”. The future of healthtech in Africa, I always like to look at it in this way. Healthtech is going to do to healthcare what the mobile phone did to technology. If you have a flashback and look at what a mobile phone did to communications.
You know, how it was able to ease communication and all of that. You can imagine that healthtech is going to revolutionize healthcare in Africa also, you will no longer have situations where people will have to come and cure up. The issue of cures is always very sickening.
So we will no longer have situations where because you are in the rural area and there is no specialist there, you will not have access to specialist care. So, it will bring about health equity also. We will no longer have situations where you have to beat the traffic, to change your geographical space in order to get health personnel, be it lab technicians, be it doctors, be it nurses.
With a click on the right app you will have those services even in the comfort of your home. Ofcourse, more and more you will have the health situation being well understood by the clients themselves. This also is a key point because most patients, there are many in the hospital.

The health personnel don’t take time to explain what is wrong with you? But if you have someone attending to you. One
on one in the comfort of your home, you have all of the time to ask your questions, what you have not understood, what it means and so on and so forth.
So, that is just what healthtech is going to do to Africa and we are looking forward to having a healthier population because of healthtech. One last thing I will talk about is, I also know a venture that is still in the healthtech space that is making health accessible by just transporting things, So being in the rural area will no longer be a disadvantage to people who live there.
They will be able to have access either to the supplies or to the skills thanks to healthtech.
Thank you for doing this interview with us today, Innocentia. Any last remarks to the Cue Africa audience?
Thank you for having me on your site. Thank you for spreading more light on what Klarah is doing. For the audience, I don’t know wherever you’ll find yourself when Klarah reaches your nation.
We definitely will be attending to you also. I strongly feel that we have policy makers in the audience of Cue Africa, the issue of regulation is always key and there are many countries that are yet to have policies that are regulating the running or the functioning of healthtech companies. So, that is one thing that we want to look at.
But then I know the future is bright and to the audience, we are looking forward to making healthcare more affordable, accessible and available to every person on the African Continent. Thank you very much.
18 Q & A SESSIONS
HEALTHTECH IN AFRICA
Interview with Founder and CEO Goal 3
Kindly introduce yourself to our audience and tell us more about Goal 3 ,what problem are you working on to address? And what progress have you made thus far?
My name is Jelle Schuitemaker, it’s a Dutch name, and I’m from the Netherlands. Two and a half years ago I joined a tropical doctor who works in Tanzania, an industrial engineer who was developing the patient monitoring system for a little research setting in the funding of Goal 3. We started what we were working on. Goal 3 started with a mission of providing fair and accessible healthcare for everyone. We do this by tackling the problem that nearly all medical technology that is built in the world is developed for high research settings. So, it’s often developed for Europe, for the United States.
Well the majority of the world does not live in these settings, it lives in different conventions. When you go into these conventions, you get challenges. So, we said that we need to design medical technology from the basis of low research settings and it’s why we started working together with the hospital in Malawi, in East Africa. We said we want to use the experience of the Hospital but also the people from
connected Universities to better design a system that really works in these circumstances and we started doing it.
It’s called the Impala system, it’s like a Patient monitoring system for monitoring Children in the intensive care unit in the Hospital and, basically, we are now developing this system and also we joined the healthtech hub here in Rwanda to build this from the Africa perspective and try to involve people from Africa in this project.
The Impala patient monitoring system is one of your proposed solutions in curbing the high child mortality rates. Tell us more about this.
Basically, if you look into child mortality happening. A lot of diseases where children are dying come from infections. Things like sepsis and for this type of infections, an early prediction is really important.
So, if you want to predict early which children are having severe infections; You need to monitor them on a regular basis. In many cases in Africa, there is only 1 nurse over 30 patients and she has to do checks on patients every 5 to 6 hours. So, we said “Why don’t we develop
technology to support her and then you would have a patient monitoring system which can be attached to a patient and can continuously monitor these ‘’.
The basis is just showing these vital signs but in the future, you could even support a healthcare worker by also adding a clinical guideline or a clinical decision to these vital signs.
We can say that “We see your heart rate is dropping, we see the blood pressure is getting high, it might be this, this and this”. With this, you can really kind of support the healthcare workers in their job to really do the steps that are needed to save the child and every 10% earlier with predicting a disease, mortality drops with 10% so it can be a huge difference if we do it right.
So, that’s why we started designing the system. So, technically it’s working from the Intensive Care Unit where we developed a patient monitoring system we connect it to a tablet like a smartphone, Android and this creates a connection and this means that the nurse on the tablet can already see what’s happening with all the patients she’s monitoring but she can also add clinical guidelines to the tablets.
19
For example, “If you see this, do this or if you see this happening do this and this”. With this, we try to support her to the fullest to really make the right prediction of the patient and this kind of creates a small ecosystem that is supporting her.
Looking into the context of Africa in the lens of the health sector, do you think tech could be the next game changer?
Yes, but also No. So, I do think there’s a lot of technologies which can really have a big impact on healthcare in Africa. We see mobile technology being used in virtual care and those kinds of things.
But there is also, only technology is never solving a problem, it’s often how you use and implement technology for the better because Computers also brought a lot of bad things, right? So, I would say that technology itself is not the solution but technology can be part of the solution for a lot of problems.
So, we also try to set up a lot of studies where we not only just drop our technology but really start to train people on technology and implement it well and do it again and again until it works. But I think that’s really important.
The third Sustainable Development Goal for child health, which aims to end preventable deaths of newborns and children less than 5 years of age by 2030, cannot be met without substantial reduction of infectionspecific neonatal mortality in the developing world. Neonatal infections are estimated to account for 26% of annual neonatal deaths, with mortality rates highest in sub-Saharan Africa (SSA). Reliable and comprehensive
estimates of the incidence and etiology surrounding neonatal sepsis in SSA remain incompletely available. With so many oblivious about Sepsis, could you expound more on what it is and why we need data now more than ever to mitigate it’s effects.
So, this is kind of the 10% I already mentioned. So, every hour that you diagnose a case like sepsis later, mortality increases by 10%. So, diseases like sepsis or infectious diseases are a big problem. We need to learn how to diagnose in an early stage.
And ofcourse, after diagnosis you also need to do the right treatment and you need to follow up well and what you see happening in a lot of sub-saharan countries is that 50 years ago a lot of children were dying in villages, in rural areas and never reached hospitals because it’s pretty expensive to reach to the hospitals and hospitals by that time were not advanced yet especially in Rwanda, You see a big shift that children often do reach the hospitals at least district hospitals and a lot of mortalities happen in these hospitals.
Although there are children dying. It’s a good thing that it’s happening in the hospital which means there are people to take care of their case and now the next step is to make sure if these children are in the hospital, we can treat them rightly and if we want to treat them rightly, we have to monitor them rightly and understand what is going on in a really early stage because the earlier we are in understanding what is wrong with the child, the better we can treat them.
It’s really important to focus on hospital mortality and if you focus on hospital mortality, you need to focus on resources
available to staff, especially how we can support staff in doing their job better and technology can be part of the answer.
BMJ Global Health conservatively estimates that 5.29–8.73 million Disability Adjusted Life Years (DALYs) are lost annually in SSA due to neonatal sepsis. Corresponding Value of Statistical Life Year (VSLY) estimates predict an annual economic burden ranging from $10 billion to $469 billion. This amount of money to be lost is apprehensive. How do we lose all this money to sepsis and how can we cut our losses?
Yeah, So, Disability Adjusted Life Years models work with the average lifespan of a person and then and how much a person can contribute to the economy. So, let’s say if you lose adults or like granddads of 70 years old.
His Disability Adjusted Life Years is really low cause he won’t contribute too much to the economy anymore, He won’t live long either. So, making treatment for old people is also important but it’s not really adding a lot to the economy while for children, they have often like 70 more years to go.
So, if you save a child, you add 70 years thanks to the value the person brings to the economy. Basically, this money is lost because there are less people coming to the world to contribute to the economy. That’s why these numbers are so high for children, right?
If you look for example, into a hospital which often see happening, there is also a lot of times and a child in an intensive care is really expensive for the hospital, cause it needs a lot of care, it needs a
20 Q & A
SESSIONS
lot of cables and wires and we also try to achieve with our monitoring is to make sure that only patients who really need critical care are on an intensive care because if you really understand on an early stage what’s wrong, you can treat them earlier and they can leave the intensive care earlier saving the hospital money but you’re not really saving them money you are saving them saving them ICU, then you can have more patients on ICU and start saving more lives.
I think the whole money failure part behind the hospital is pretty interesting and also behind the country but it’s difficult to say these statistics really translates into money loss. Basically, these statistics take into account that every person that is being born contributes to the economy while in some populations not every person who is born is really contributing to the economy a lot. So, there is a bit of a balance here.
What is needed to Shift the paradigm towards delivering value with Tech in healthcare?
So, I think the shift is already happening but it requires good technology. If there is really bad technology which breaks down every half a year then it becomes too expensive and especially in these hospitals which have low resources.
So, it needs good technology that’s why we focus on good technology but of course there are a lot of mindsets which need to be changed. We encounter people who are a bit skeptical about technology because there has never been good technology and every time they purchase technology, it breaks down after a year and they spend all this money and time.
So, if you have good technology, people start to accept your technology more and if people start to accept technology more, we can have more good technology. So both are needed to really get forward but I’m positive that this is happening already.
Do you think low digital literacy, especially in low-income populations, can pose significant challenges to the adaptation of digital health solutions? Yeah, So, to me there is no such thing as low digital literacy in these countries for what I have seen because we went really into rural places like Malawi and also in Rwanda.
HEALTHTECH IN AFRICA
Even there, there are people walking around with Android smartphones having WhatsApp, calling people. So, you see that this low digital literacy, I wouldn’t say that it’s such a big thing.
For example, if you would compare how people make mobile payments here in Rwanda to the Netherlands. We, here in the Netherlands are digital literates, we’re not really digital literate. In the Netherlands, we don’t make mobile payments they do in Rwanda.
If you’re in Rwanda and you hire a cab,
you can just put in the codes and bam! You pay the cab While in the Netherlands we are still struggling. I would say that there is a pretty high digital adoption even in low income populations and I see it only growing.
So, if your whole family is on WhatsApp, on twitter, on Instagram and on Tik tok, you should also be on there. In many cases, In Rwanda, there is a pretty young population and people are also willing to change these things. So, I don’t think this will be the biggest challenge.
How is being selected among the top 30 startups to incubate at the Norrsken HealthTech Hub enabling your company to achieve Yeah, thank you. That’s a good question. So, for us, it’s really important and cool to be selected among these startups. Of course, it’s a really cool place of work. So, we are not trying to build a European company, we are trying to build a Global company, and, It’s even in our vision to one day have more people working in Africa than in Europe for making this work.
For us, being selected in this healthtech hub was kind of the first step for our company to have some sort of reference, to have some sort of community around our company in a place where we want to be active.
So, it was really cool and important for us and I think we will benefit a lot from it. So, I hope we can be there often and have good conversations. Yeah.
The World Health Organisation (WHO) estimates that Low and middle income countries (LMICs) lose US$15.86 billion (95% CI $3.4 to $38.2) annually due
21
So, every hour that you diagnose a case like sepsis later, mortality increases by 10%.
SESSIONS
to physician migration to high income countries (HICs). The greatest total costs are incurred by India, Nigeria, Pakistan and South Africa. When these costs are considered as a percentage of gross national income, the cost is greatest in the WHO African region and in low-income countries. One of the down sides of this migration is the increased infant mortality rates. In your opinion, how can this large scale migration of physicians be mitigated.
Yeah, that’s a good question and indeed a big problem. We see this brain-drain a lot. Not only in physicians but also in software developers. I would say, it’s a big problem to have a single answer.
One, you should have to make good jobs and quality of life in the country better so that people will want to stay. That would also mean increasing salaries for physicians but if you increase salaries for physicians might also need to increase salaries for a lot of other people, the Hospital directors, and maybe the nurses. It’s an economy, so it’s all connected.
We cannot have one. I would say for example there are possibilities in technology like virtual care where you can have people working remotely. Also people can live in Pakistan and work remotely for the healthcare sector in Rwanda in some cases but also that’s solving a small part of the problem.
For example, I spoke to a lot of people from Africa who are really proud of their nations and going to other countries only as a partial thing to have a bit of experience in that career and come back and bring a lot of experience back to their country. So, it’s a good example of how it could work.
And, yeah, to me it’s pretty difficult to
say. There is no one solution to this. For example, if you look at infant mortality rate being connected to the migration of physicians, then I would say we need to work with effects that are here on the ground.
We cannot change the minds of every physician in Africa, at least we cannot change them in 20 years, maybe in 40 or 50 years. So we need to kind of make technology suited to work with the effects so one option could be to start trusting more on technology to do more diagnosis for example which otherwise could have been done by physicians or you start integrating virtual care or you start adding more features to your technology which makes lower trained physicians also have skills that only higher trained physicians could do.
and your salary is nearly the same so, why would you leave, right? So, I hope these times will come.
As we wind up our interview, what does the future of HealthTech in Africa look like for you?

I would say, in general, I see a bright future because there are a lot of needs for technology. As I mentioned, there are a lot of people using digital technologies already in Africa and things are catching up quickly.
There are also a lot of innovators from Africa especially in this healthtech hub as well building solutions that can really benefit locally. So, I would say, that’s a bright future and that’s why we believe in it, and why we are here. We want to work together in this bright future.
We believe the African population, the African mindset to really solve this problem together. I think that’s needed and I think that’s also happening so I’m positive about it.
So, these are things we are thinking to do, like how can we enable people that are still there to get the most of out of their capabilities and I think that’s one solution and I hope that there is a time where it’s more exciting and rewarding to work in your home country than to be overseas and of course, this does not really have to do with money, it can be that there is just more interesting jobs for you in your home country than overseas
22 Q & A
Minds of every physician in Africa, cannot change in 20 years, maybe in 40 or 50 years.
Interview with Global Preeclampsia Initiative, Founder & CEO
Abubakar Suleiman Tsamiya
Global Preeclampsia Initiative, CEO & Founder Abubakar
Suleiman Tsamiya expounds more on the impact his healthtech startups is creating in Uganda
Mr.Abubakar Suleiman Tsamiya ,Please introduce yourself to our audience and tell us more about who you are .
Yeah, my name is Abubakar Suleiman Tsamiya, I’m the founder of Global pre-eclampsia initiative, which is a non profit organization that champions the prevention and modern way of treatment of hypertensive disorders in pregnancy. We are a registered organization based in Uganda and we are currently in Kigali under the healthtech hub program. Yes, that’s the brief of who I am.
Global Pre-eclampsia Initiative is an organization you founded a couple of years ago. Please tell us about GPI, its genesis & why you chose tackling high blood pressure in pregnant women?
Yes, um, It dates back to 2016 when I was in a medical school and I happen to come across a patient who, that I managed, who developed pre-eclampsia and the fact was that patient was poorly managed though she survived, that’s the good news about it but I felt that we did not manage her properly because we were supposed to be monitoring her blood pressure after every on hour. Unfortunately,we didn’t have the manpower to do that and her records were not accurately kept.
So, that’s what Inspired me to think about coming up with a solution that could help manage preeclampsia effectively in low resource settings where you have less health workers to take care of the patient.
So I invented a tool called Petograph; it’s an abbreviation or acronym of preeclampsia toxemia graph. so, that graph, what it does is that, all the records of the
HEALTHTECH IN AFRICA
blood pressure monitored of the patient are converted into a chart form.
So, the busy scheduled health worker will be able to visualize the progress of this patient at a glance over 24 hours whether the patient is recovering or getting worse. So, that is the first step.
So, after getting that step we went further to found an organization called Global preeclampsia initiative using the same tool called pictograph to advance our champion activities of reducing maternal death due to high blood pressure.
So, we founded Global pre-eclampsia initiative officially registered on the 28th of April 2017 and ever since, we’ve been into different activities, different programs, different projects to ensure that we deliver that message of preventing pre-eclampsia effectively. So, that’s a brief about what Inspired us to come up with the Global preeclampsia initiative.
Preeclampsia is a major maternal health issue worldwide that is responsible for maternal and neonatal severe morbidity and mortality and has substantial contributions to prematurity of the fetus and longterm cardiovascular disease (CVD) in the mother. What solutions is your organization proposing to tackle this silent killer?
Pre-eclampsia, that is a . We call it a disease of theories because up to date you cannot pin down exactly what is responsible for pre-eclampsia.
So, we based on theories that says, placenta, as long as the woman is pregnant with the baby in her womb
23
and she developed pre-eclampsia, then you have to terminate that pregnancy irrespective of the age to save the mother.And then there is also the theories of inheritance because the mother had preeclampsia so the baby most likely is going to develop preeclampsia.

So, there are a lot of there’s about it and it is a disease you can not pin down precisely and say these are the symptoms of pre-eclampsia. So, it becomes difficult even for the mother herself, the pregnant woman, to suspect that she has pre-eclampsia. Therefore, the only option to mitigate this severe complication of preeclampsia are, one, about early detection. So once you’re going to detect preeclampsia early, then you’ll be able to mitigate the severe complications and possible death of this baby.
Secondly, Timely referral, once you detect, then you should also ensure that you refer this mother to appropriate management facility on time and the third component, the effective
management after getting the facility you have to ensure that this woman is effective. In terms of medication and in terms monitoring of hours or or at least two hourly monitors and lastly, effective monitoring follow up.
After the recovery from preeclampsia you have to follow up for at least 3 months because about 30% of them come up with chronic high blood pressure. So, we have to follow them up. So, once we have these four things, the first one, early detection, timely referral, effective management and efficient follow up and our innovation addressed all the four components at different levels.
So, the first component of early detection, we have our app which is the Petograph application. It’s a mobile app that when you put the blood pressure and other parameters of the pregnant woman , it detects pre-eclampsia and prompts a message for early referral then from there you can share that information with healthcare providers or any person who could assist.
So with that we are enhancing the timely referral and when getting to the hospital we notify the hospital and also have a hospital desktop application that would help in ensuring that you manage the patient effectively and we use the same application, the mobile app to ensure that we follow these mother’s after successful treatment s or successful management of pre-eclampsia.
So, our innovation addresses all the four levels and so far, these are the best approaches to mitigate any complication of pre-eclampsia because it’s something that comes abruptly. It has no definitive cure apart from delivery. The baby and it leads to over 500000 babies lost as a result of abortion or still birth as a result of pre-eclampsia globally. Thank you.
It has been almost a year since the launch of the Norrsken & Novartis healthtech hub. What has this experience been like for you so far?
Yeah, It has been a very interesting and amazing experience because for the past years that we founded Global preeclampsia initiative, we never had an opportunity to organize our thoughts together, to organize our innovation and present it in a more appropriate way and have a focus and vision not until when we came to the healthtech hub program and we are grateful to that and finally it’s actually showed that really we’ve learned so much in terms of re-shaping and refocusing the activities of the organization. Because recently we won an award of the UNFPA grant challenge among the best 10 companies in the world out of 65 countries that applied. So, Global preeclampsia from Uganda happens to be one of the 10 companies that succeeded
24 Q & A
SESSIONS
in coming up with the innovation that could help the girl child. So, it shows that really, really the project of the Healthtech hub has yielded so much result.
The incidence of hypertensive disorders of pregnancy increased from 16.30 million to 18.08 million globally, with a total increase of 10.92 % from 1990 to 2019. The age-standardized incidence rate decreased, with an estimated annual percent change of -0.68 (95 % confidence interval [CI] -0.49 to -0.86). The number of deaths due to hypertensive disorders of pregnancy was approximately 27.83 thousand in 2019, representing a 30.05 % decrease from 1990. In your professional opinion, what do you think are some of the causes of hypertension or high blood pressure in pregnant women?
Yeah, as I said. One, is the disease of theory, meaning that it’s not the definitive cause of this disease. For example, when we say Malaria,we know that it is caused by Plasmodium parasite or the mosquito.
So, that is definitive. Malaria is caused by mosquitoes, so if you prevent mosquito bite then you prevent malaria. However, in terms of pre-eclampsia, because it’s a disease, a condition that is related to pregnancy only, so that is not the definitive cause of that disease.
But there are associative risk factors which include one, the family history of high blood pressure have high chances of coming up with pre-eclampsia.Two, if she had a previous history of pre-eclampsia herself, maybe first or second pregnancy, the subsequent pregnancies, the chances are higher that she’s going to have another episode of preeclampsia.
Another thing is the race, the black race tend to have higher preponderance, higher exposure of developing preeclampsia irrespective of where they are. Whether they are in Africa, in Europe or in Asia.
As long as you’re from the black race you have higher chances. Another factor is low social-economic status; it’s found that more than 90% of the cases of pre-eclampsia occur in these vulnerable individuals, so poverty is also associated with it. We have cases like delays in becoming pregnant after a certain age, For example after 35 years of age, when you have that first baby.
So you have high chances. If you already have a condition of high blood pressure, you also have high chances of getting pre-eclampsia. So, when you put all these things together it has a ratio dimension, it has social-economic dimension, it has medical, it has genetics and so on. So, these are the factors that actually predisposes individuals to pre-eclampsia. Yes.
As an organization, what do you plan to achieve in the next 2-3 years? What does the future of your organization look like?
We have tried to transform healthcare through self-care. So, we ensure that the woman herself, the pregnant mother, takes control of her health by empowering her and how do we empower them? Currently, we are empowering them through our application, a mobile application and then through blood pressure monitoring devices which could be used at home or a place of work, to be monitoring their blood pressure by themselves and in case of anything it alerts and they get
HEALTHTECH IN AFRICA
treatment on time.
So, the overall vision is to ensure that we transform healthcare through selfcare. To ensure that every person takes care of her health condition to avert this condition of pre-eclampsia. Secondly, We see ourselves in the next couple of years coming up with a complete system that addresses the whole approach to maternal death.
To maternal, morbidity and mortality disease and death by addressing other conditions like bleeding, infection and ignorance. So, we are looking forward to encompassing all these components. So that we holistically address the issue of maternal mortality and morbidity but we are starting with high blood pressure and as we move, we are looking at it holistically considering others as well, Thank you. And thanks to the opportunity given to us by the healthtech hub that really transformed our innovation, transformed our organization and transformed us as individuals. Thank you so much for this wonderful int
We have come to the end of our interview today. Any last remarks for our audience?
Yes, thank you so much for the opportunity. My last remark is that, for every organization, it’s important to be disciplined, to be determined and to be focused. We’ve been along this journey from 2016 to date and we never gave up. We will continue struggling and bigger opportunities are coming. So, it’s about discipline, it’s about determination, hard work and being resilient.
25
Insightiv, A Rwandan-based radiology Tech startup.
Insightiv, a Rwandan start-up, has been awarded the first winner of the Novartis HealthTech Hub cohort 2021 currently based at Norrsken Kigali House. The Insightiv team is working on a platform that blends teleradiology and artificial intelligence to address some of healthcare’s most pressing issues, particularly in the medical imaging sector. In 2014, Rwanda Radiology Country Report showed that there are only 11 practicing radiologists for over 12 million people of its population. This pertains to patients’ experiences with various conditions and how remote access to radiologists and AI tools could help diagnose patients.
Can you tell us a bit about what inspired you to start Insightiv and what is the key problem Insightiv aims to solve?
“What inspired my career path is not that long. I graduated from university in 2020 with a bachelor’s degree in computer science and economics. I did computer science mostly because of my interest in technology, especially from my early age.
Growing up, I was that kind of kid who was obsessed by tech-things. Over time, I realized that technology is the best way to make a far-reaching impact, and that can be seen from these days.”
I’ve always been interested in solving
global challenges in education or healthcare. That pretty much motivated my interest in computer science. And when I finished my first year in college, I got an internship at Google, and I got to see how technology is built from the industry side.
“Before I started insightiv, I was learning about some of the hardest challenges that African countries are facing, healthcare being the biggest in the room. And technology is one of the most promising solutions.
We’re seeing people
motivation behind his career path and everything he has done.
So, I founded Insightiv to take up the slack between where radiologists are and where they are not.
What has been the development of Insightiv so far?
To give more context, Insightiv started in November 2019. We tried to do more market research to understand the problem more and how the patient’s experience when it comes to their access to medical imaging, and by hearing from healthcare professionals about the key challenges.
26 Q & A SESSIONS
tackling healthcare challenges from different angles, which is really exciting.” Audace added on the
Audace Nakeshimana talks to Cue Africa about his career path, how he started Insightiv, and more on why higher effort in health tech solutions is needed in general.
We had already put together a prototype. And we started using artificial intelligence to diagnose some anomalies from chest x-rays. We’ve made some big promising steps. We had a product that different radiologists have tested.
And we’ve been working on an AI project on COVID-19 diagnostics, which was successful. We have an algorithm that can detect whether a patient has COVID-19 from a chest x-ray. And that has been shown to have about 94% accuracy right now.
So, we are in a place where we think our technology is working, and right now, we are trying to work with the Rwanda FDA and the ministry of health in allowing us to pilot in public hospitals to serve the purpose.
We have partnerships with Harvard medical school, which is working on diagnosing or detecting wound infections for mothers with C-section surgeries. We worked on a system with them that has been used in most hospitals. Over thousands of patients have been diagnosed.
What did winning first prize in Norrsken and Novartis Foundation’s HealthTech Challenge mean for you and your company’s mission (Insightiv)?
The short answer is that it means a lot!
We received the top financial reward for winning the competition. And this has been highly beneficial to us, most notably in developing our products and helping us in increasing our investment in product development, which is crucial for entering the market.
On the other dimension, it has undoubtedly assisted us in attracting the right attention. Being in the Norrsken Foundation and the Novartis Foundation HealthTech hub has provided us with a network to the people within the healthcare sector.
Do you think such a technologyfocused learning hub is considered necessary by looking at its multisectoral benefits in Rwanda and even on the continent?
Yes! It is necessary. Because, with all this buzz and all these diverse innovation ideas, we know there is a demand for a platform like this. This Hub is and will continue to be the community where all start-ups will share ideas and discuss some of the difficulties they face in their work.
The Hub will encourage a learning environment and a continuous chain of exchanges that any start-up may
HEALTHTECH IN AFRICA
What do you see as the biggest obstacles to scaling up health tech in Africa? And how do you think these challenges can be addressed?
Indeed, many of the start-ups in the field do not have adequate financial resources or expertise. And getting partners to help them develop and test their ideas is really challenging. That’s one of the biggest challenges. On the other side, regulations beneath the implementation of their solution.
Another major challenge is the lack of needed data. This data is necessary to create some of these solutions. Sadly, it is not easy to get your hands on such data.
All that is required is a suitable platform and support from various partnerships, both in government policy and the private sector. Although the term “partnership” has a broad definition, you must consider who can help with what.
What are your opinions on Africa’s need for more health-tech investment, especially in bridging the gap we have in the health sector?
benefit from. And I believe it will be a community that invites potential partners to explore how they can help improve health outcomes and reinvent healthcare systems through new tech breakthroughs.
More investment is required because of the resources necessary to build a healthcare solution. Human capital is in short supply, which will be filled by technology. Also, cost-effective solutions are required. That would be fantastic. So, there is a need for additional funding to do research and development to strengthen our health sector.
What do you think Rwanda needs to do to spark such a health tech-enabled innovation hub to attract more startups to join the Hub?
27
More investment is required because of the resources necessary to build a healthcare solution.
Most of the time, the best way to attract start-ups is to provide a favourable working environment. Every startup would like to be in an enabling workspace. And I think that’s the essential thing Rwanda is doing. There is an availability of resources that startups need, from capital to mentorship to investors. This attracts more start-ups.
And those things are crucial. However, the need to look beyond the incubation

phase is also crucial. The government needs to look at what it takes to put those start-ups in the market and how to make them succeed to create a success story beyond investments.
In 5 years, what do you hope to see Insightiv achieving?
As I said, we are focusing on going to the market this year. So, five years from now, we want to see our technology making
an impact, which is, of course, our first goal. We dream of seeing the technology we’ve been working on, helping people daily, both in Rwanda and even outside of Rwanda.
We know it will require more investment, but if we can be in the market helping patients, we will have access to resources through investment. I think that would help make sure we develop the technology that is helping the real world.
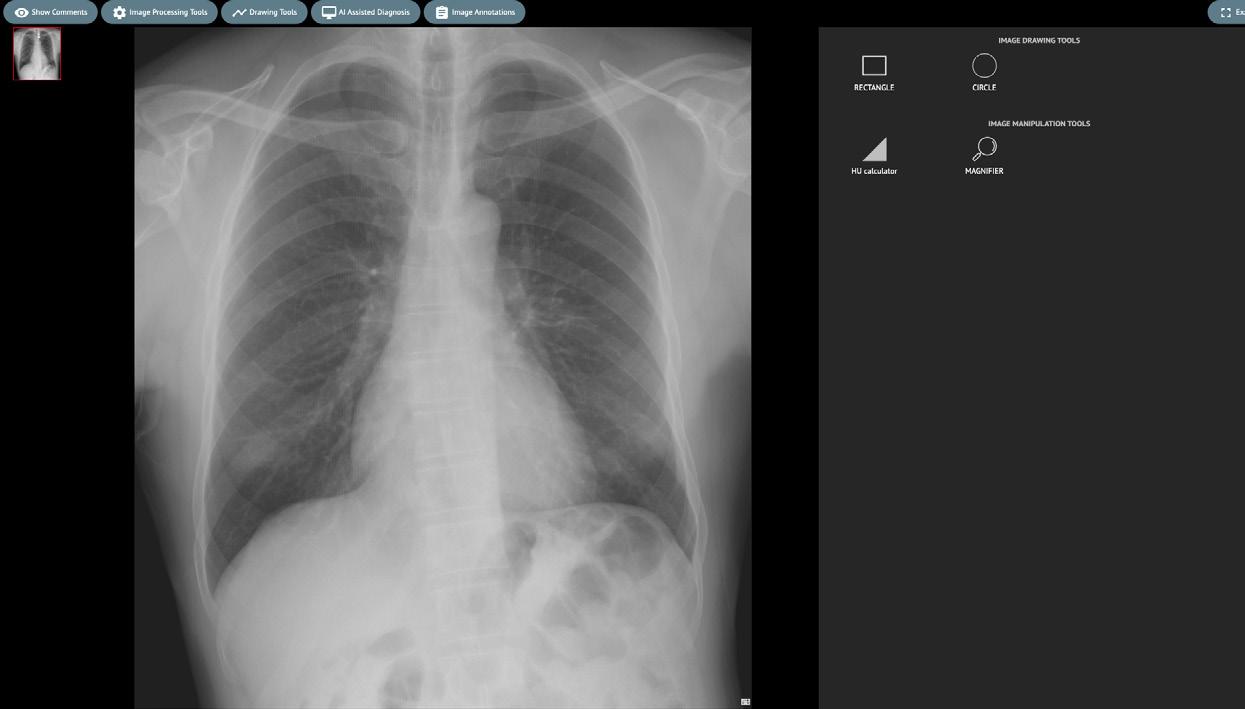
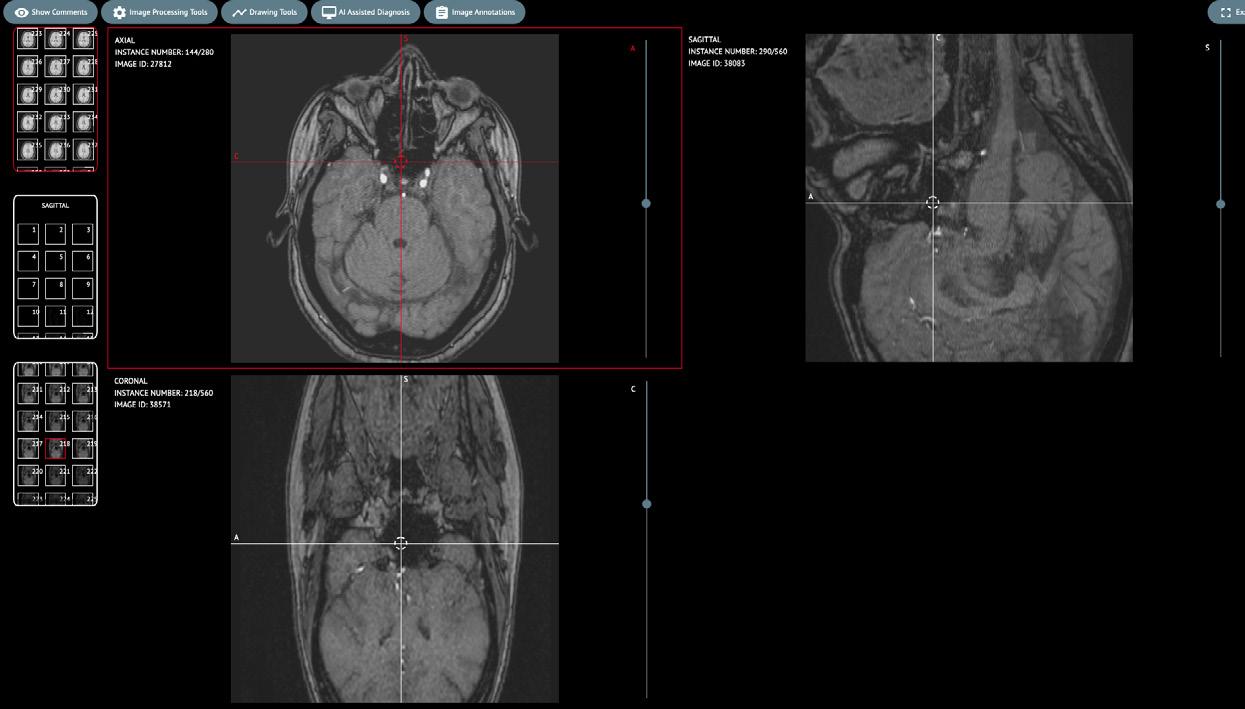

28
Q & A SESSIONS
2 3 4
1
1) Animations are reconstructed animations from ultrasound multiframe DICOMs. 2) Multi planar reconstruction (MPR) is performed on MR DICOM images. 3) Windowing and multi planar reconstruction (MPR) are performed on CT DICOM images. 4) X-Ray DICOMs.
HEALTHTECH IN AFRICA
Interview with Nelson Igbiriki, Founder and Ceo Medtech Africa
Could you tell us a bit about MedTech Africa, and what is the key problems it is aiming to solve?
So MedTech Africa is a Healthtech startup focused on using tech or innovations to solve medical issues, to bridge the gap between medicine, and technology to make medical practice easy . How to provide point of care to patients at convenience and at the moment we have a flagship product called Focardio.
Focardio is basically focused on cardiovascular diseases providing access to reliable patient data for cardiovascular diseases. Why cardiovascular disease? Because it’s the leading cause of death globally. 18.6 million people die yearly because of lack of access to patient data to enable doctors to come in early when the patient is at the stage of getting a higher heart attack or heart failure. How will a doctor know this? Its only when he gets access to the patient data soon enough.
Our aim is for our solution Focardio to prevent these instances for over 168 million Africans who have either hypertension or diabetes. So our goal is to build a point of care for patients with these diseases, Help doctors get to plan treatment for their patients, patients can be at their homes and could use any health monitoring devices.
It could be connected devices, it could be apple watches, Samsung. So, our app gets this data from any device or any software and is able to send it to a doctor in real time.
On the hospital platform, we have a solution where doctors can use AI that can detect abnormal activity and forecast the instances of patients having a heart attack in the next five to ten years. Can be able to monitor their patients, the AI would be able to monitor the patients on their behalf as long as the patient is sending their data to us.
We also ensure comparison in such a way
a patient has a reminder in their system where he gets notified in the morning, takes a blood pressure or maybe takes a jog or maybe they have a target for exercise.
For instance, jog 2 kilometers for this week and after they achieve that the app is able to pull data from any of the devices, it could be an apple watch and can be able to pull it and track progress of what has been achieved, this has been your progress. So it’s a total package that we are providing with MedTech Africa focused on cardiovascular diseases at the moment. Yeah, so that’s about it.
How can AI and technology improve healthcare outcomes? (Speaking about how digital technology has the potential to address a wide range of public health issues)
Yeah, so, I think we humans are limited. If we consider the patient-to-doctor relation in Africa let’s say for instance in Nigeria. Yesterday, a report was released
29
SESSIONS
that Nigeria has less than twenty-four thousand doctors for a population of over two hundred million. Now imagine, now let’s say for instance only 10% of the population falls sick in three months, you will the workload increase to 10,000 patients per doctor this is just 10 %
Now the role Artificial intelligence is going to play in this is to help reduce the workload of doctors, and help increase provided instances of more personalized care, more predictive care because doctors to patients ratio is very low, the worst of this kind we have ever had in the country and we have few medical health professionals to provide health and if you look at it even infrastructures.
Do we have hospitals ? Are our hospitals updated ? Do we have the tools to support patients? Can patients get care from any point in the media or could they travel to another country or within the continent or within the location to get care?
I think AI will play a big role. It already started to play a big role in such a way we could be able to get personalized care with just a few patient to doctor contacts. We could also get more reliable care or predictive care.
We should be able to understand more about Africans. One of the big factors we’ve seen so far is that. We’ve seen a lot of billions being spent for instance in the US for insurance of patients for drugs, for medication, treatment and rest and that has been done majorly with Artificial Intelligence. Africa, we are going to that stage where we will have to learn, are the drugs we are selling to our patients,
Are they really effective? Is the care we are giving, is it really accurate? Or are we
just using generic knowledge?
It gets to a point , we are getting there already. Covid has actually ushered us into that level that we are now looking more into how predictive can we move with healthcare?
How reliable is our conventional treatment that we are giving? The drugs patients are taking, are they really tailored for us Africans considering our genetics, considering our environment, considering our family history? So a lot of things have pushed and ushered in.
Covid has done a big one for us. I was really saying people adapt technology in healthcare. We could see telemedicine got a wide adoption, the people were free to go to the hospital to even see a doctor to get assistance.
deep technology like AI have been able to push and I think there’s more to be done and there is a big future for
Artificial Intelligence in Africa especially with the look of organizations like the Novartis foundation, Astrazeneca and the rest doing a lot of research in Africa.
A lot of funding has been coming in into more tech digital and innovation to deepen tech that are made and tailored for Africans. So, yeah.
What does being in Norrsken and Novartis Foundation’s HealthTech Hub mean for the company’s mission and vision (MedTech Africa)?
I think one of the principal strengths of any business or any startup or any company or even as an individual is your network and I think I can boldly say Novartis is one of our biggest networks that we have ever achieved, so far. Ability for us to get access to global institutions that have networks across the world.
For instance, we had opportunities where we had to speak at the Intelligent Head Summit at Switzerland, we got opportunities of connecting you directly to key stakeholders across the continent.
It made people accept telehealth, telemedicine. We could see instances of robotics surgery, remote surgery and a couple of doctors in the US giving support to doctors in Nigeria doing operations and surgeries that have never been done in the continent and getting sharing of knowledge in real time. I think for you to be able to get care from anywhere you are having been made possible and that’s one of the little things
Another thing that is actually really happening is that When most people go to check our website or read the bio and see oh! You are backed by Novartis!! there is this sense of confidence that oh Novartis is behind you guys, okay, makes another sense.
That means you guys are doing something very good. So it sends a little bit of morale and when you say “ part of Novartis healthtech hub accelerator”, it gives you a lot of credibility and I
30 Q & A
Minds of every physician in Africa, cannot change in 20 years, maybe in 40 or 50 years.
HEALTHTECH IN AFRICA
think one of the things I’ve been able to develop more on this situation. It’s giving me a lot of access for example to the Nigerian cardiac society.
I could walk with Novartis Nigeria, I spoke with one of the teams and they led me to somebody. I was in Dubai that was two weeks ago and I spoke to somebody and I mentioned Novartis and he said “oh! you should know so, so and so, let’s go and meet them” .
And because of that, He connected me to somebody and that is the biggest catch we have so far from Novartis foundation and the healthtech hub. It’s the access to the network and you usually don’t need to do a lot of things for you to explain much about yourself.
You just mention Novartis and nobody will start questioning your credibility. Like are you sure you are real? Are you sure you are that? It builds a lot of confidence, a lot of morale, a lot of credibility for us, and we are actually very grateful for this opportunity.
What are the biggest challenges that you think you might face as a company right now and how has being part of the healthtech hub, norrsken Novartis healthtech hub solved some of these challenges….? in the realization of digital and data-driven technologies’ potential in healthcare?
I think I will start this way. So, Initially, when we got into the healthtech hub. We have actually not started anything at all. We were really doing marketing research, we were speaking to customers, speaking to doctors, speaking to cardiologists, speaking to patients, doing surveys just getting data to be very sure of what we are building and when we started
one of the great things we had was an opportunity was one of the speakers we had during this session and I sent an email and I was like, “I want to find out more about business model, business value proposition before we start building”.
And he was like “Oh! Talk to this guy!! and one of the biggest things I gained from this, I was able to talk to a lot of people, a lot of engineers, a lot of funders in the healthtech space. Secondly, we were able to get some grant, 20,000 dollars from Novartis, one of the prize money, we were the second prize winner and that was enough for us to start building and we got a lot of ideas and we saw a lot of framework, we met a lot of mentors that gave us to the right direction.
For instance, we were able to complete our clinical validation in a very short time. We didn’t have to spend a lot of money because we were able to speak to some founders in our cohort that maybe worked in a company that has done clinical validation around patient data or maybe did something similar and not like this to be able to share ideas and knowledge and to be able to push forward.
So the healthtech hub really helped with some of the challenges. But there are other challenges we are having is, uhmm, access to capital. Heathtech is not fintech. With fintech in three months you build a lot of things, just build a little thing and you’ll get some money but with healthtech a lot has to be done around that end. It hasn’t been that easy with the fundraising but I think we are progressing with it we have gotten a lot of good responses.
And also, I would say for Nigeria some of the challenges we have, is the regulatory concerns because we are dealing with the most sensitive of all data that is essential to human health.
Patient vitals like their blood pressure, their medical history, more even essential than EMR we get really timely responses on patients
The government was able to hear what we were doing from all the media and the showcase the healthtech has done and we were able to be called by the ministry of Digital Communication in Nigeria to see okay, How can we help get this done? How can we help foster full studies of digital or privacy that’s needed for you to be able to build this? And I think it’s one of the challenges.
So basically, these are the few challenges we had and I think we are a working progress. The more you face a challenge, the more you learn how to solve it. and after solving it you will definitely meet another challenge at the front and the more you solve, you meet more challenges ahead of you.
What would you say about the growth of HealthTech-enabled solutions in Africa? And what are the recommendations you could give to the early startups in the field?
So, Growth of healthcare. Let me start with growth of healthcare generally. We saw a spike in Covid but after the era of covid, Africa health dropped, I really don’t know why maybe it’s because of the fomo of not missing out of healthcare building the next big thing in healthcare and it dropped Without health you
31
cannot do anything, if you’re not in good health you cannot do anything probably you begin to realize this.
My advice to people who want to come into the healthcare space. if you really want to do a startup, I would advise, this is my own advice, try and work on your startup for at least three months, just to get an idea on how things work because if you choose to work in a multinational company that experience will not work in running a startup. You will face a lot of challenges.
You have to build the culture from scratch, you have to build the ethics of your company, you have to build the bureaucracy, everything is from the scratch and only when you’ve worked with.
Also, Just because you’re building the next big thing does not mean people will throw money at you. You are not flutterwave or paystack. so there’s really a lot of things to be done so when you come in, be ready to see a lot of laws even though you’re doing fantastic. It’s actually very painful when you build your product and you get a testimony of your product saving lives, actually saving lives, that your product saved somebody from dying and hear somebody say they fund your product.
You’re going to face a lot of this and it’s heart-breaking because you have to now choose between should I shut this down or you could now look at the impact you’re actually saving lives while you’re building it’s going to be a tough end, and I would say this, there are more days of
depression than days of joy as a startup founder.
There are going to be swings of emotions. This moment you’re happy you get a mail, Another moment the server is down or the app has crashed. Users are calling; they are getting tons of mail and the system is down, communication is down, patients can now come and get appointments and after you solve that you get to see another email “Congratulations you have been selected in this accelerator.
And You’re happy and the next moment something is happening so it’s going to be a swing of emotions, you have to get ready. Let me just tell you straight, nobody is going to tell you “ well done” or “well done Nelson you are doing amazing” You will have to learn to build your own self-confidence and pat your back yourself, “oh! I’ve done this” and one of the ways for you to really survive is to be confident to tell yourself “oh! Nelson you’ve tried.”
Sometimes, you just wake up and look at the mirror and say “You’ve achieved this, well done!!” because you’re telling your team members, your staff “ well done, you guys have done this!” but nobody is going to tell you “well done Nelson, you’ve been able to achieve this!”. So if you don’t have good self-esteem, it will dampen your spirit a lot but once you find out that you don’t have that time to be dampened.
You’ll just have to look up to yourself and look up to the mirror and say to yourself “Well done Nelson, you are doing amazing, it’s time to move on to the next big thing”. I will also say this, there’s going to be a lot of rejections, a lot of nos.
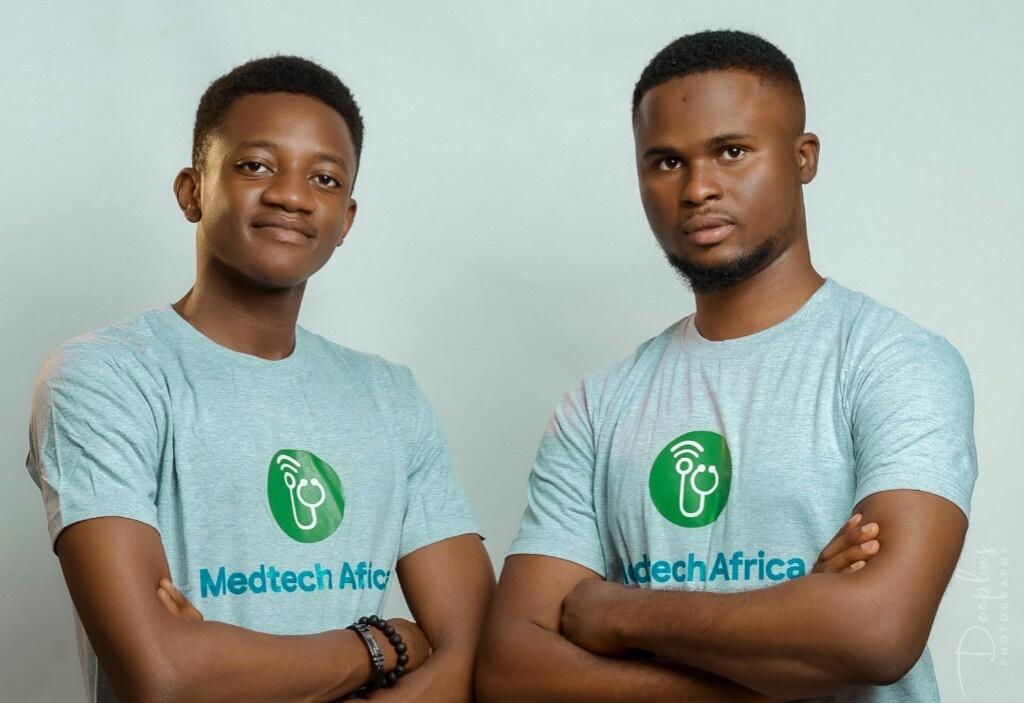
32 Q & A
SESSIONS
Benjamin Oni (L) and Nelson Igbiriki (R), from the Medtech Africa
HEALTHTECH IN AFRICA
Like they will tell you no to your face, “you’re building trash”. Someone told me that “your idea is worth..”, I don’t want to use the word, but let me just say it “Piece of shit” that’s what someone told me. “Your idea is worth piece of shit.”
That’s what someone told me!, Sorry for the foul language. The shock is that I met this guy in Dubai, we were actually the semifinalists at the completion. we all met together at Dubai and we progressed higher than him and He looked at me and said “You have the craziness” I was not building for you; I was not building for your validation I have a problem that’s causing leading death in the world, I wasn’t building for your validation sir.
You’re gonna meet a lot of them. So this is one of the scenarios, People will tell you trash. When you succeed everybody will want to come and tell you congratulations, people will want to associate with you. But there was days, a lot of the times, you’ll get 90 % of trash talk and just maybe 10 % will be from your family.
So that’s it … That’s me shairing what I’ve seen, what I’ve known this is me being real with me. So you’re gonna face this a lot of the times. You know why you’re building and know when to pivot and switch when things are not working. You have to discern it, when to let go when to fire someone that is not doing well just know when to do that Sometimes you might be stubborn. So, that’s it for me.
The hub’s mission is to provide a network for innovators to tap into as they tackle some pressing health issues and develop virtual health and care. Looking ahead, where do you see the hub in the next 5-10 years in its
realization of its mission?
I think when you see the hub it’s the first in this time in Africa and I think it’s really very strategic for the hub to position itself in healthtech and I’ve seen a lot of people reaching out to me.
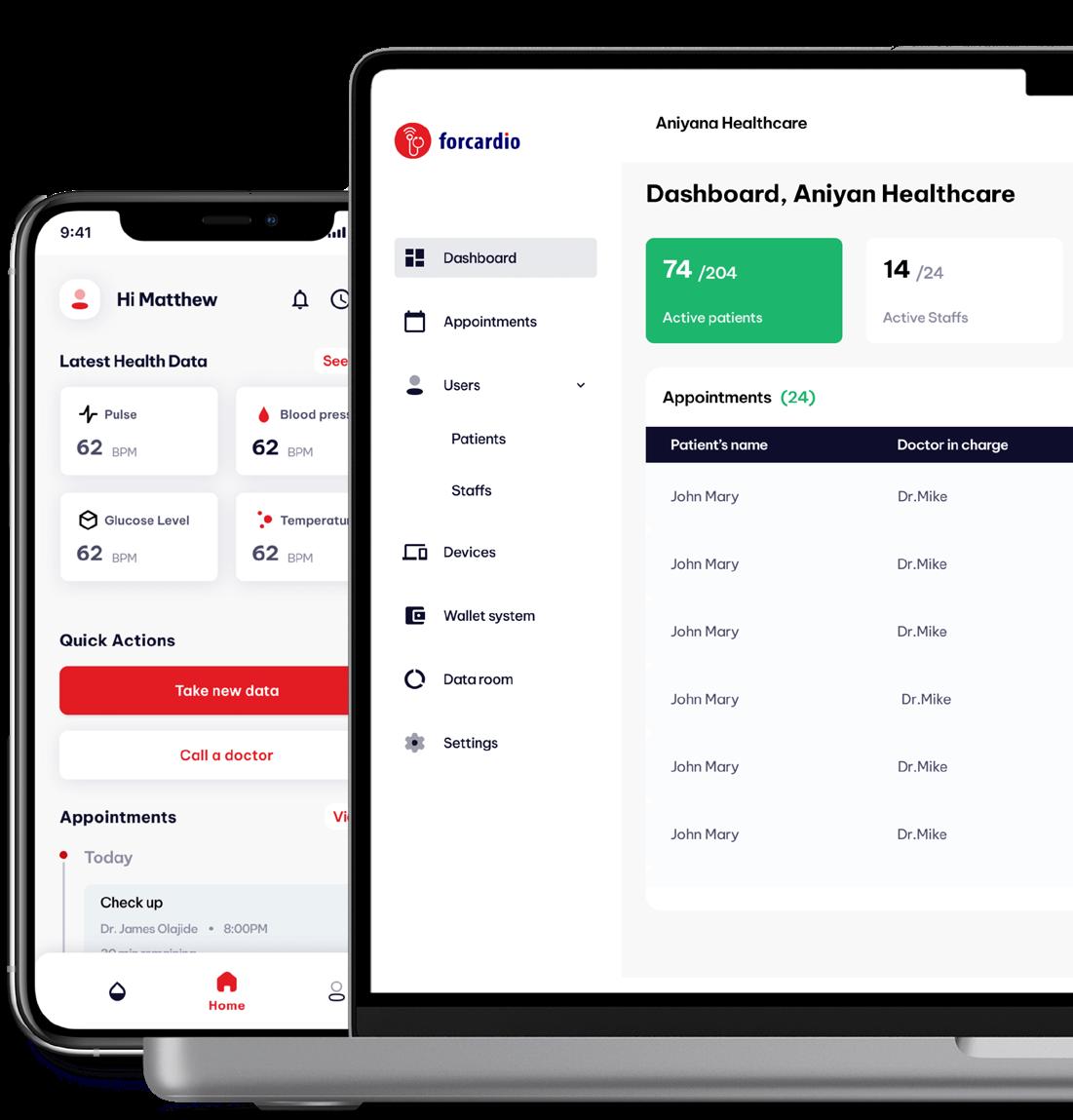
For instance, the new application that is out, I’ve met a lot of people who just reach out to me and say “Oh! we heard that you’re part of healthtech hub, we are building a solution around healthtech and we want to be part of it!” and I think it’s not really out there, big like YC or techstars but ummm, It’s focusing on one of the biggest challenges Africa is facing and I see the health tech hub as a bridge building the top innovators around healthcare in Africa.
gap there.
The value proposition of the healthtech hub is something that bridges the gap between our infrastructure deficit in Africa when it comes to healthcare technology, ability to foster the growth we need to take healthcare from the obscure level that we are at to become a digital planet, digital continent.
We have over 1.2 billion persons on this continent, I see it as the future essentially and it’s very intentional and I love that about the, I’m happy to be part of this and I hope we get to grow as we move forward, we get to attract a lot of talent, foster a lot of change. When you point at the top 10 leading healthcare companies.
I believe and I feel people from the healthtech hub that have passed through the accelerator have what it takes to excel. They are actually very intentional and clear on their path. I really have great hopes for the healthtech hub.
I’m also proud and i’ll be hopeful that I’ll be one of the first unicorns from the healthtech hub on the continent that could build unicorns, healthtech unicorns, we don’t really have a lot of them, just two or three in the continent and I think they have what it takes to build this program, I’ve gone through the program.
And I see the hub as the facilitator of the new digital health era of Africa. We have a lot of deficit in healthcare infrastructure, talent, the bridge between medicine and technology. We have a big
We get to attract a lot of talent, foster a lot of change.
Interview with DotPharma’s Co-founder Arnaud Biruta
Mr Arnaud Biruta, happy to have you today. Please kindly tell us a bit about yourself and why you started Dot Pharma.
Hi Hamza, Thank you for inviting me to this discussion. DotPharma is a company founded and registered in Rwanda.
Talking about DotPharma requires talking about the shared passion for healthcare of its founders. The company was founded by 3 people at collaborative ideas namely, myself, Roger NTAGANZWA who holds a bachelor’s degree in computer science obtained from ULK (Kigali Independent University) and doing a master’s degree in Health informatics at University of Rwanda. Arnaud Michel NIBARUTA who holds a bachelor’s degree in health care management from Southern New Hampshire University (Kepler Program), and doing Master’s degree in development practice at Regis University and lastly, Willine IKIREZI, a bachelor’s graduate in healthcare management concentration in global perspective at
Southern New Hampshire University, Kepler program. We all met with that idea of doing something that would help the Rwandan and extensively the African healthcare industry to level up. As modern entrepreneurship requires, a business should be a solution to a problem. We met, with our experience and background to define a problem that we thought we would be able to solve.
prescribed medicines. Some of them approached physically, others using phone calls. A simple example, one day one of our founders went to Kigali downtown to find medicine, while he left it at King Faisal hospital. The ideas arose into our minds on how these problems can be solved using the emerging technological world where smartphones look like a good solution to many challenges people face including those in the healthcare industry as the main pillar of people’s living. In addition, we often go to the Clinic or any other health care facility and the practitioner finds that there is a need for any medicine that is not available at that clinic. Therefore, the doctor immediately prescribes the medicines for you, to go and find that medicine at any pharmacy, with no guarantee that you will easily find it.
Why an online Pharmacy? And what has your journey been like thus far?
We found that many times, we used to encounter people who are unable to get their medicine because they do not know the pharmacies, which have these
I would respond to this question from two perspectives. First, the identified problem would be solved by the
34 Q & A SESSIONS
Rwanda as a country, provides a favorable ecosystem for health tech.
HEALTHTECH IN AFRICA
availability of the needed products easier and more timely. We should have solved that problem by having a huge pharmacy where no product would be missing. However, I don’t know if that would be possible. That’s how the idea of digital technology came in. With an online platform, we can create a network of suppliers that allows us to get information about products from multiple suppliers, providing a wide range of choices and high chances that the products will be missing. Additionally, Rwanda as a country, provides a favorable ecosystem for health tech. Indeed, previous examples demonstrated how far can this country can go promoting the use of knowledge and tech to improve social services. This provides us with a good baseline to launch our initiative.
Dot Pharma was selected among the top 30 health tech startups in Norrsken and Novartis Foundation’s HealthTech Challenge. How important was this for you and how do you plan to capitalize on this?
First of all, let me take this opportunity to thank Norrsken and Novartis for this noble initiative. I say this with thanks because it was really hard for us to find an incubation or acceleration program dedicated to health. We have been in other programs where you were paired with businesses from pure tech, fintech, agritech, edtech, etc. While there are some aspects that startups shares, each industry, and ultimately the health industry has its particularities that require additional efforts. I believe that the HealthTech Hub at Norrsken came to solve that problem. So, once again, thank you for having a particular thought for us.
It has been almost 4 months since the beta launch of the Norrsken & Norvatis health tech hub. What has this experience been like for you so far?
One of the best we have really had! First, the space enables us to work productively with all the facilities provided. On that, no excuse for unproductivity!
Second, the people! We have had useful connections and potential partnerships have been initiated. Additionally, as I said before, being together with other health tech startups provides an opportunity for frequent discussions that allow us to understand the challenges and opportunities in the industry. It became easy to gather feedback from people who are familiar with the health industry.
What challenges are you currently facing at Dot Pharma and how are you or planning to mitigate them?
One challenge that we have been facing is regulations. The health industry is highly regulated, and this is for a reason (because people’s health is not a negotiable matter). What we do is to go one step at a time fulfilling all the requirements while leveraging information and connections to fasten the process.
According to Lancet.com, WHO estimates that 50% of the drugs for sale on the internet are fake and even though the online dispensaries might look legit. What measures does Dot Pharma put in place to make all drugs dispensed to meet the patient safety and pharmacy practice standards of the Republic of Rwanda
This is an important proof point indeed! This is addressed through the partnership we have with suppliers and the professionals we work with. We cannot make a partnership with a supplier unless they are already certified and follow all the drugs and patient safety regulations in place. We also have our pharmacy professionals who are there to ensure that all the products are delivered with high consideration for quality.
With the huge drive for telemedicine in Africa currently, how does Dot Pharma uniquely position itself to win over the small Rwanda market.
I believe that Rwanda and Africa bear a high promise for tech in general and telemedicine in particular. In fact, we have the basic requirements that are people (which imply knowledge base) and problems to solve. What’s needed after is to ensure that tools are developed and accurate to the local realities.
Our unique position lies essentially in quality. We know the pain points for our users. Issues such as timeliness and accuracy are highly valued. However, we do not want to limit ourselves to the Rwandan market because what is being done here is practically needed in the whole region and continent actually.
What does the future of your organization look like? Do you plan to expand to other African countries? And if yes, which countries are planning to scale to and why?
We hope and plan for a bright future. As I mentioned before, we are not only targeting Rwanda. We want to also
35
expand to other African countries. In this phase going until the end of 2023, we plan to have covered the whole area of Rwanda. Then, we will scale the region especially in neighboring countries (Burundi, Eastern DRC, Tanzania, and Uganda). However, as I said before, we have to go one step at a time. Our main reason for the scale will be the need expressed in the areas we want to cover as well as the feasibility (such as the internet infrastructure).
With internet access & penetration still posing challenges in some parts of Rwanda. How does Dot Pharma make its services accessible?
We are aware of that and we are leveraging other ways that would require small to no bandwidth. For instance, now our users can order products using WhatsApp and Telegram. We also plan to make it possible for users to use a USSD code system in the future (stay tuned).
Any last remarks for our audience?
A startup is nothing without users/ customers. I just want to tell them that they are our priority. That’s one!
Second, to my fellow startup-ers, keep doing the great job you started because Rwanda and Africa need you. There is one organization whose motto says “African problems have solutions on the continent.” This is even more valid nowadays. Let’s keep solving problems!
36 Q & A SESSIONS
Get an early access on our website: http://youthscrolllock.com TODAY THROUGH: Book your copy +256 760 349 802
Nigeria Startup, PharmaRun Revolutionizes Telemedicine
Source: www.istockphoto.com Female doctor on the phone while using a computer

37 HEALTHTECH IN AFRICA
Access to healthcare in Africa is still a challenge that requires innovative solutions. Only 615 million people have access to healthcare services out of 1.216 billion people which is equal to 48% as the African Agenda 2021 report stated, especially in Sub-saharan countries. The lack of access to healthcare services are caused by many different reasons.
Causes of lack of healthcare services
• Lack of insurance and Affordability
• Lack of transportation to the hospital and pharmacy
• Lack of quality health care
Lack of insurance and Affordability
The state of catastrophic health expenditure in Africa
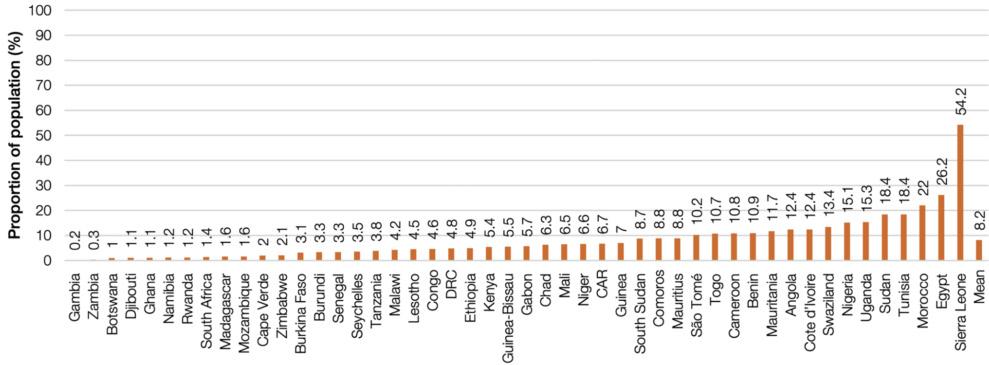
Lack of insurance in Africa led to people not accessing healthcare services because many Africans can not afford affordable healthcare services. In developing countries 2.9 die because of lack of healthcare services as stated by Lancet global health. In Nigeria 11.188% is the mortality rate yearly.One of the main
causes of this death is neonatal disorder, anemia,malaria,diarrhea disease. All of these diseases are diseases that can be cured but the lack of access to healthcare and affordability in Nigeria makes it hard. It is estimated that 15.1% of Nigerians spend a lot of money on healthcare.
Lack of transportation to the hospital and pharmacy
67% of the world population find it hard to get to the hospital and pharmacy. This comes with lack of transportation , this leads to death. In Nigeria 48.5% of the population live in rural areas stated by
the world bank . Rural areas in Nigeria are characterized by poor road infrastructure and poor healthcare facilities.
Lack of quality healthcare
The whole world loses 6 million people due to the lack of quality healthcare in
developing countries and low income countries. In Nigeria 67 of 10000 people die due to low quality of healthcare this include medication errors, inappropriate or unnecessary treatment, inadequate or unsafe clinical facilities. A startup in Nigeria has dedicated their mission to give easy medication.
38 HEALTH TECH
Source: WHO UHC report, 2019 | Notes: DRC - Democratic Republic of Congo; CAR - Central African Republic
Main causes of death in Nigeria 2019

Source:https://www.statista.com/statistics/1122916/main-causes-of-death-and-disability-in-nigeria/
Phamrun as rocket health revolutionizes telemedicine
Phamarum is an app that facilitates medical services like getting tested,virtual assistant and you can order medication via the app within 120 min.
Getting tested
The get tested feature you schedule the appointment on the app ; this will reduce the time that patients spend at the hospital or going to the pharmacy or clinics that do not provide those services, It will also ensure quality healthcare services.
Virtual medical consultancy
Consultancy feature is where you will be able to ask questions about the
medication plan, getting a consultancy and general issues like the quantity of medication you should take or recommendation you can use.
In this section you send a text explaining the problem that you have and they give you recommendations on things you can do in an emergency situation.
Medication delivery
One of the big problems in Nigeria is transportation and the distance between hospital and pharmacy especially in rural areas Phamarun will be facilitating Nigerian citizens to access the medication on time.
What role is Phamarun playing in healthcare in Nigeria
HEALTHTECH IN AFRICA
armarun is playing a big role in Nigerian healthcare services at the same time reducing low quality healthcare service,transport and consultancy problems.
When you think about it, diseases like neonatal disorder, anemia,malaria,diarrhea disease should not cause death in Nigeria. One of the main diseases that causes death, Phamarun is playing a big role in reducing the mortality rate.
With neonatal disorder they are offering consultancy services. You have a chance to talk to the pharmacist and get advice on things you can do to avoid neonatal disorders such as nutritional food you can eat and medication you can use.
With malaria Phamarun offers testing features you can book a pharmacy near you to get tested too this will reduce the transportation problem because it will be easy to have a specific time slot. They also offer medication delivery when you are having a hard time finding a pharmacy near you. They deliver medication in less than 120 min.
With Diarrhea, Phamarun offers consultancy and medication delivery; this means that they will advise you on things you can do to reduce diarrhea like making oral rehydration serum, encourage you to stay clean or things you can eat.At same time deliver medical supplies you may need.
All in All Phamrun is playing a big role in telemedicine in Nigeria ensuring that Nigerian community have access to quality and affordable healthcare this like a rocket toward health revolution.
39
Your Health Companion

in Rwanda
Chronic disease or non-communicable diseases are diseases that last 1 year or more,this means that you require more medical attention. It is estimated that 70% of deaths that occur around the world are caused by chronic diseases. Chronic diseases are responsible for 17.9 million deaths on a yearly basis as stated by the World health organization. The most common disease is cancer, which causes 9.3 million deaths yearly,chronic respiratory disease causes 4.1 million deaths, and diabetes and kidney disease causes 2.0 million deaths around the world.
It is estimated that 85% of the deaths caused by non communicable disease occur in low income countries or middle income countries. Having a chronic disease can make people feel anxious and depressed. The study shows that a quarter of people with chronic diseases experience depression.
Rwanda is one of the developing countries. It is one of the countries experiencing death due to chronic diseases. Moritarity7 rate in Rwanda is 36.1% on an annual basis; it is estimated that 44 % of these deaths are caused by chronic diseases, as the Rwanda Biomedical center report stated. It is estimated by the World health organization 13% of those
deaths are caused by cancer, 3% by communicable disease such HIV which are chronics, 2 % by diabetes and 13% by other non-communicable diseases.
It is estimated that 13.08% of the population in Rwanda are depressed which is one of the most pressing issues in Rwanda especially within people with chronic diseases. That is why companies like Companion App health support telemedicine here in Rwanda.
What are the the problems that Companion app solve the healthcare sector
Depression and anxiety are highly common in patients with chronic disease,
HEALTH TECH
HEALTHTECH IN AFRICA
but remain unconsidered despite significant negative consequences on patient health . Companion apps offer different services that make patients feel like they are supported and they are not alone. They offer Medicine Reminder, Custom Regimen, Emergency Line, Privacy & Security, and Synchronized Records.

Medicine reminder
This feature reminds a patient the time to take medication, it also helps a patient feel like he is not alone in the journey. On the country level it reduces mortality rate due to chronic disease or depression and anxiety.
Custom Regimen
The feature here assesses the patient’s disease, the natural things the person is allowed to eat and things that the patient likes or things that the patient might be allergic to. After this analysis the app comes up with a customized meal plan that will help you within the sickness journey. This also helps the country to reduce mortality rate within chronic disease patients because they feel motivated to take care of their body; it will also play a big role in reducing depression and anxiety because with this app your hopes are restored and you feel like you have a purpose.
Emergency Line

Companion app gives you a feature in which you can see emergency contact in case you have an emergency and one is around you to help out.
Privacy & Security
Companion apps give a feature that shows how much they value your privacy. If you do not want anyone to see your healthcare status, you can lock your app with different updated models like finder print, pin code and password. This will reduce people who usually make fun of chronic diseases patients.
Synchronized Records
This app keeps a record of your daily activities. You can check your progress about customized meal plans that are done on a monthly basis. With features people feel motivated to achieve health goals , it creates and builds hope for chronic disease patients.
What is the role of the Companion app in solving healthcare problems in Rwanda?
Different studies show that ⅓ of people with chronic disease die due to the depressession and after seeing that 44% of the deaths in Rwanda yearly are caused by chronic disease. The Companion App will help Rwanda to digitize the healthcare service for people with chronic disease by supporting them within their journey, reminding them medication intake, helping them understand different type of food that they can keep to reduce healthcare risks, providing different lines they can call in emergency cases as well as showing the their progress on a monthly basis.
This will help Rwanda to minimize mortality rate by raising awareness on different things patients can do to avoid risking lives, most of the people who are ashamed to ask for help, Companion App will be a lifesaver and A Companion for life.
According to Mayo Clinic, Telehealth, also known as e-health, is using digital information and communication technologies to access healthcare services remotely and manage your health. Also, Telemedicine is referred to as the use of two-way voice and visual communication to provide medical services to patients remotely where the doctors and patients are in separate locations. This is done through computers and mobile devices like tablets and smartphones. In this article, we explore how Remote doctors 4 Africa is implementing telehealth and telemedicine to provide quality healthcare services remotely and in rural communities.
41
Woman Looking At Her Smart Watch for a pulse trace
Remote Doctors 4 Africa Implements Telehealth & Telemedicine.
Remote doctors 4 Africa (RD4A), is among the e-health startups that contribute to implementing many solutions in the healthcare industry using technology. The uniqueness of this company is that it offers hospital-quality primary healthcare in countries such as South Africa, Botswana, Ethiopia, and Zimbabwe where doctors and specialists operate in real-time but from remote locations.
The services rendered by Remote doctors for Africa are a digital consultancy management suite for doctors in general practice and medical specialists as well as healthcare support services. Additionally, it generates full access and participation to remote care units out in the field. Their service is done through the use of a Cloud-Based Health Ecosystem and the use of an application called “OKdoc”. This application allows doctors to work on patients virtually regardless of where they are. This is beneficial for patients, especially those that live in places with few qualified medical doctors.
Currently, Remote Doctors 4 Africa being one of the top 30 startups that were selected as part of the healthtech challenge , has an office within Norrsken House Kigali, an entrepreneurship hub that aims at offering community, capital, network, and advice to entrepreneurs that have problem-solving startups. Norrsken House Kigali in partnership with the Novartis Foundation initiated the
Health Tech Hub Africa, an investment push to revolutionize the development of health technologies designed by Africans for use in Africa.
More so, The Novartis Foundation aims to improve the health of low-income
faced by African citizens like the lack of supporting telemedicine frameworks and policies, the digital barriers, as well as patient and healthcare personal biases. To effect change, you have to take the first step, you have to toil the soil and plant the seeds one by one.
Remote Doctors 4 Africa being one of the top 30 startups that were selected as part of the healthtech challenge
populations by working with local authorities and partners to bring about the improvement of health in low-income populations.
“Remote Doctors 4 Africa is actively working to address the challenges
This is our strategy; to address the challenges through partnerships, building the foundation for engagement to bring health services and educational awareness programs for the public, thus improving access to digital platforms and affordability,” says Ernest Mhlongo, CEO of Remote Doctors 4 Africa.
Benefits That Come With Being Part of Remote Doctors 4 Africa Health Ecosystem & Using OKdoc.
With OKdoc, patients can book and attend healthcare consultations, which cancels missing appointment possibilities, provides ease of obtaining prescriptions, and manages repeat prescriptions. Also, Patients get to have one on one attention from a skilled and vetted healthcare giver
42 HEALTH TECH
without the need to be in overcrowded clinics. That is, it improves the overall healthcare consultation experience by providing patients with private, efficient, effective, and well-targeted treatment sessions.
Most importantly, the medical history is in an encrypted information vault that the patient at that time can access via a live video conference. Therefore, complete treatment records are automatically added to their digital medical history thus reducing the amount of time needed for patients to fill out their forms. This whole process contributes to time management and automatic Privacy Legislation compliance.
OKdoc application makes it possible for people living in rural places to access good treatment centers since most
HEALTHTECH IN AFRICA
1 2
doctors or medical specialists reside in urban areas. This cuts down on traveling expenses. The only requirement is to have an internet connection which allows interaction with
For this to take place, RD4A partners with mobile clinics and other infrastructure providers that enable access. Clinics that lack adequate medical personnel benefit from having the services of trained and qualified professionals.
online healthcare givers regardless of where they are and can save those who need immediate treatment.

Last but not least, It prevents infection possibilities that can occur to healthcare givers as a result of being in close proximity to patients. This is crucial, especially in seasons of outbursts of pandemics and epidemics. To conclude, RD4A promises to bridge the gap in healthcare by solving challenges associated with infrastructure and healthcare services inequity in rural communities while at the same time improving access to digital platforms and affordability.

43
1) Zipline drone, best-known for blood and vaccine deliveries in Africa. 2) Patient talking on conference video call to female african doctor.
Prevents infection possibilities that can occur to healthcare givers as a result of being in close proximity to patients.
Massira, Figured It All Out With
Female Centered Support.
It is true Africa has established a progressing goal to empower women. A female child’s education is now being considered with efforts to ensure they are safe and have everything they need to be competent enough. The step put into this has showcased excellent results, with ” 66% of girls completed their primary education compared to 61% for boys by 2020.” (Martin Armstrong).
In this article titled, Massira, figured it all our with female centered support, we write about how Massira does it. At the lower and higher secondary levels, girls still lag behind males. Still, the disparities have closed over the previous two decades, from 5 percentage points at the lower secondary level to just 2 points and from 6 points at the upper secondary

level to 3 in 2020. (Martin Armstrong) This Proves that we are putting work into female health education and empowerment. Still, truth be told, it only happens in cities, and nobody hardly knows what happens in underprivileged rural areas. Where nobody is educated about the rights of a child to go to school leave alone a female child, there is less
knowledge about HIV/AIDS, sanitary education, or even early pregnancies, which have led to early marriages and child labor.
Yes, some N.G.O.s have taken steps to go into the countryside to help and educate the people there, but that’s still not helping that much because they meet with resistance from the local
44 FEMALE HEALTH
Source: Massira A team from Massira going through a group discussion.
communities, and their engagement is not engaging the targeted people. You can’t go to rural schools to teach about female health education, yet almost no female student is in that school or, even worse, with nearly no plans.
All these facts are for ongoing students, we are not even sure if these students are adequately taught about their health education, especially females, and those are the ones in classes what about those girls and women left outside with no idea of what’s going on out there?
Leave alone misinformation, and inappropriate treatment pose a threat to the young female child. The parents aren’t educated enough to help their children or even care for themselves.
Now, Here comes Massira, the Heroine. Massira is a leading female-centered support community. Its primary focus is on increasing women’s access to reliable health information and associated services by creating a secure environment that encourages open communication and is dedicated to teaching, connecting, and empowering women to improve health outcomes in Africa.
The word Massira means journey, march, or procession. This initiative does everything for a noble cause, a cause that tackles the issues of unreliable misinformation about the health education of a female.
Every African woman and female child is a target for easy access to health information and services regardless of their economic status.
As with the new S.D.G.s (Sustainable development goals), Massira comes
bearing solutions to; Good health and well-being, gender equality, and partnerships for the goals where unwavering support systems have been created with companies and NGOs to help interact with and support the target audience.
This being in the plan, Massira has been able to offer training to most girls and women in the Ashanti Region of Ghana. With the help of Self-Help International, half of the 500 targeted women and girls were trained and handed the funds to the appropriate authorities to help distribute and teach the women in that region.
HEALTHTECH IN AFRICA
females in Ghana and Africa.
Being able to contact someone who is in the right field and ask for consultation is one of the offers given by Massira. Many cases have proven to be treated well by people in this initiative, being sexual abuse to menstrual cycle sanitary to free advice and healthy lifestyle education have helped more than enough people to have a smile full of joy for a healthy life their living. Below are some of the testimonies.
We have a long way to go with female health education, but Massira is the start of something great. We call upon other NGO’s to offer a helping hand to those in need of the hand. Female health education is a right we owe to our sisters and mothers, and we don’t have to take away their innocence and their right to education for better health.
The support continued regardless of the outbreak of the covid-19 pandemic. In partnership with Ecotowels, community outreaches were organized to provide sanitary hygiene products to 135 female head porters in Agbogbloshie and also used this as an opportunity to have a oneon-one with these women to comprehend their hygiene practices, particularly during their periods, as well as their health concerns and offer health advice. Massira has been able to offer reusable sanitary hygiene products that could cater to their menstrual hygiene for close to 4 years. This is fantastic progress and shows that Massira is the heroine of the
Massira has paved the way to uplift women and offer education about health and sanitary education. Together we will live a healthy life and a gender-balanced inclusion in our communities. Female Centered Support and health education should be a right and a goal to be achieved for all.
A healthy life brings healthy smiles, and that’s what we want. But we are in Africa; a place called out to have one of the poorest health sectors; truth be told, we all know that. We understand how behind we are in becoming close to perfection in this industry, But that hasn’t stopped us from doing what we need to do to pave the way for the one good healthcare sector. In this article, titled, Wiiqare – The golden path to healthcare in Africa, we dig deep into another African healthtech startup breaking barriers on the continent.
45
Massira offers education about health and sanitary education.
WiiQare The Golden Path to Healthcare in Africa.
WiiQare. A health start-up that started as an application created by Bienvenue Zigabe has proven to be more than just an App. It is the Golden path to the future of Healthcare with benefits that impact not only the people but also the healthcare system of a country and Africa. This is done by connecting health providers, patients, and payers in a welldeveloped and organized chain of lines.
WiiQare believes everyone should have early Access to healthcare in order to have a healthier life, which can be done by saving for your Healthcare earlier.
Key Objectives of WiiQare:
To improve Access to care, quality of care, and foster Innovation.
To tackle the issue of poor, unprepared, and delayed Healthcare that may arise in the future, WiiQare helps empower people to save money that can be used when they need medical attention that was unprepared or would have been delayed. People need a better way to access Healthcare, and there is no better way than having someone who has thought about that for you and made clear all the arrangements for you to be treated without any exclusions. This has led to the birth of new ideas to provide better Healthcare in relation to technology.
The network of top healthcare
providers, together with their expertise and knowledge, offers optimism for an improvement in the standard of Healthcare for people throughout Africa. All of this is part of a strategy for promoting Innovation that involves connecting healthcare professionals, patients, and payers in Africa and internationally in order to transfer values and facilitate Healthcare.
Africa’s healthcare systems are highly inefficient. Disruptions in the supply chains for medical supplies, medications, and finance are problems that affect several countries on the continent. However, technological advancements in telemedicine, drones, big data analytics, wearables, and information management have raised the prospect of practical, cost-effective solutions that might enhance overall health outcomes.
This shows that WiiQare is on the roadmap to being one of the best Technological Innovations that will boost
the Healthcare industry in Africa. Most Africans, mostly the underprivileged and middle class, rely on underfunded public health facilities. But with digital technology, WiiQare could assist in making unsustainable healthcare systems sustainable, equalize the interaction between people and medical personnel, and offer less expensive, quicker, and more efficient ways to treat diseases.
How Does WiiQare work?
WiiQare has set up easy steps for its customers to use as stated below: Create an account – which is simple and is kept secured by a pin. Decide how much you want to save for health – and we will help you achieve your goal and start health savings. Get rewards by saving – reach your monthly savings goal and refer friends, all these are ways to be used to gain points, and these points can be used to pay for your health bills.
46 HEALTH TECH
HEALTHTECH IN AFRICA
Make payment- easy use a QR code for this is fast.
With WiiQare, you can send and receive money for healthcare from friends, family, and colleagues. This is more than being a Golden egg everyone is chasing for. Everyone needs to buckle up and invest in themselves for the future of our health.
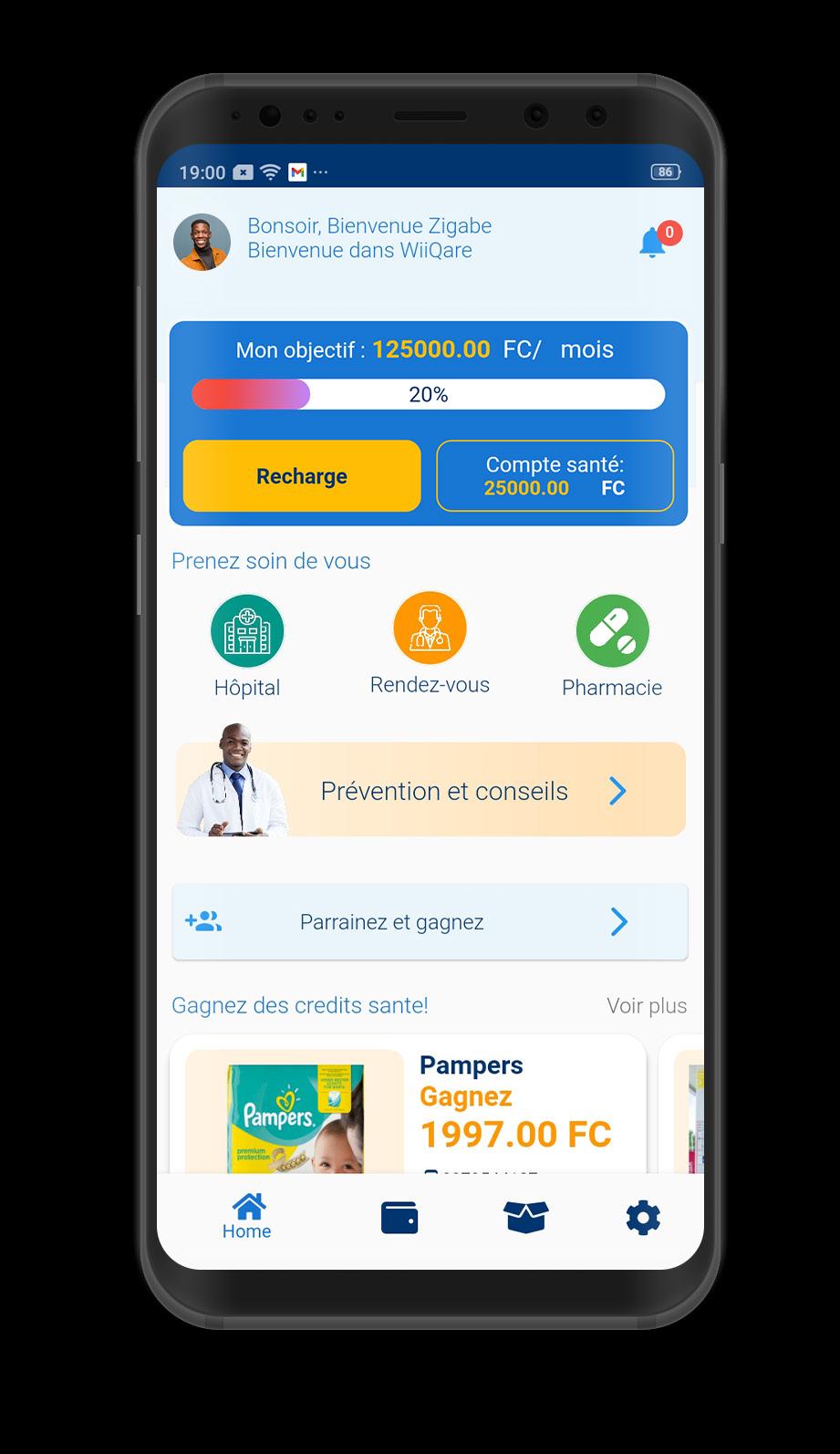
We can’t deny the fact that we are moving closer and closer to a tech enabled world. The long lines and recording of names before a consultation with a doctor are soon to be dropped out. And then what? Everything is going digital for easy Access to Healthcare without delay or lack of money to pay for what you saved for yourself from day one.
It’s now time to call upon other supporters and NGO’s to come and support these start-ups like WiiQare because they care enough to defy the norms that are not helping the people they intended to help.
According to the World Health Organisation, it is stated that “Less than half of Africa’s citizens (52%) – some 615 million people – have access to the healthcare they need, the continent’s quality of health services is generally poor, and the family planning needs of half the continent’s women and girls are unmet.”


‘Only 48% in Africa get needed healthcare services. And according to new reports, healthcare coverage and quality are both poor in African nations, which is the truth, and in need of new ways to address this issue. Tech start-ups emphasizing Healthcare are more than welcome, and that’s why WiiQare is more than welcome.
WiiQare has started a marathon that will help pull investors, health providers, and people into a shared health system that offers more than enough breakthroughs in how health systems work. We need this, You need this, and we all need this for a better and unified health system.
47
1 2
1) African woman around family accessing the services via USSD. 2) Mother with daughter in a unhealthy setting.
Healthdart, A digital primary healthcare services provider
 By Tunga Elsa Ndibwami
By Tunga Elsa Ndibwami
48
HEALTH TECH
The HeartDart team (Above) | On the Left the founders (L-R) Yauvan Hansraj, Njabulo Skhosana, Tshwanelo Matsane
A glimpse of Rwanda’s access to primary healthcare services in rural areas.
Health is everything! Without it, one can’t amount to anything in life. Being healthy and having access to healthcare services enables individuals to make a difference in all spheres.
That is, Healthy individuals can create, innovate, and serve with excellence. Rwanda, especially in rural areas, faces a problem of achieving universal health coverage (UHC) since people walk long distances to receive essential health services. According to WHO, for 83% of Rwandans living in rural areas, travel to a health facility has been challenging. For instance, long walks to access healthcare services could take 95 minutes in 2010 and be reduced to 47 minutes in 2020 which is time-consuming.
To solve this issue, the Government of Rwanda through the ministry of health aimed to reduce walking time to under 25 minutes by setting in place health posts at the community level and located at a reasonable walking distance from people’s homes. Also, they served as an interface between community health workers and health centers. This is one of the countries’ health sector strategic plans, with technical and financial support from WHO. However, there is another alternative that involves technology that could ease the process.
In this article, We explore how “Healthdart”, through their app, contributes to access to drugs and healthcare advice using smartphones. Also, How Rwanda is eligible for implementing it due to the enabled
access of Smartphones within most regions.
Rwanda’s promising access to smartphones
Thanks to “Connect Rwanda”, a campaign with the mandate of boosting smartphone ownership in the country.
By the end of 2020, 2.88 million households in the country owned at least a smartphone. The New Times states that, Currently, 2G and 3G geographical coverage are at 90% while the population coverage is 92.6%. Also, The 4G internet covers 95.2% of the geography and reaches 97.2% of the population. Internet penetration is at 58.3% with only 16% using 3G and 4G. Therefore, there has been intentional smartphone penetration. Smartphones are crucial in terms of helping Rwandans gain online services and information while remaining connected. “Today, Rwanda has digitized several services, and many businesses are going e-commerce. Smartphones thus remain a necessary tool to enable citizens to traverse the digital value chain” says Minister of ICT and Innovation, Paula Ingabire.
Additionally, achieving digital literacy for all youths aged 16 to 30 by 2024 has been one of the Rwandan government’s goals due to technology’s role in development. The achievement of digital literacy of at least 60% among adults by 2024 is part of the Country’s national digital literacy program.
Healthdart provides an Alternative solution to boost access to primary healthcare services
However much the health posts are essential, there’s another cost-effective
and digitized way of improving healthcare services access. This is where HealthDart comes in, a healthtech startup that enables people to access drugs and healthcare advice using their phones. Njabulo SKhosana from South Africa founded this startup. Healthdart employs an app to provide a platform where users can place orders for their drugs and deliver them at a cheap cost. For this to be done, customers pay using electronic funds transfer prior to receiving the drugs. In addition, it enables virtual and physical consultations with doctors and nurses which leads to the provision of primary healthcare services.
The Contribution of Norrsken House Kigali and the Novartis Foundation
Owing to its fantastic contribution to the healthtech sector, Healthdart participated in the healthtech challenge along with other startups. This competition aims at identifying three of the most promising startups in Africa solving population health challenges concerning cardiovascular health, breast cancer, or virtual health and care. This opportunity came with a full-year subsidy to the Healthtech Hub Africa co-working space and community within the Norrsken Kigali House and an innovation program aiming to accelerate their growth and connect with the right partners and contributors.
Conclusion
Taking advantage of technology in these times is a promising and worthwhile investment, especially within the health sector. Therefore, Healthdart promises to ease the process of receiving primary healthcare services by simply using a smartphone which is a cost-effective, quick and digitized approach.
49
HEALTHTECH IN AFRICA
Denga logistics takes the healthcare supply chain to another level.
The potential for increasing the capacity and efficiency of healthcare systems and medical transportation systems with the use of Drones seems promising. Drones can be defined as any unmanned aerial vehicle that is remotely piloted. That is, a drone is a flying robot that can be remotely controlled or fly autonomously using software-controlled flight plans in its embedded systems, that work in conjunction with onboard sensors and a global positioning system (GPS).
Denga logistics is a digital health platform that uses drones and motorbikes to transport life-saving medical commodities such as medicines, blood products for transfusion, contraceptives, and laboratory test kits to hard-reached health facilities and also transport lab samples for laboratory testing to a

higher-level facility. Denga incorporates various sectors such as clean technology and energy, Healthcare, Transport, and logistics. This bridges the road infrastructure gap and poor access to healthcare services in hard-to-reach communities.
This has proved to be one of the most effective and convenient ways to get medical supplies to remote areas on time. Also, This contributes to the effective and smooth operations of rural health facilities due to a timely and regular supply of essential medical commodities from the district centers.
50 HEALTH TECH
Source: Denga logistics One of the Denga drone in flight.
HEALTHTECH IN AFRICA
Conventional transportation of medical supplies and blood from a designated medical facility to remote areas or villages can be costly and time-consuming.
CASE STUDY: Rwanda
Drones are used to supply 60% of Rwanda’s national blood, and about half of that blood is used for women suffering from postpartum hemorrhage. According to Marie Nisingizwe and colleagues, In the Lancet Global Health, 12733 blood product orders were delivered by drones to 20 district and provincial hospitals in Rwanda over 32 months from March 17, 2017, to Dec 31, 2019. Also, The median road-based delivery time based on Google Maps estimated driving times was 139 minutes, whereas the median drone delivery time was 41 minutes excluding the preparation and packaging time. Thus, The mean delivery time by drone was 49.6 minutes.
Furthermore, The outbreak of the COVID-19 pandemic forced Rwanda to innovate in terms of finding a sustainable medical transportation system with the aim of reducing human interaction to curb the spread of the virus. Drones have therefore been technological tools that allowed medical personnel to perform their tasks effectively and to save more lives.
Benefits of using Drones in the medical transportation system
One can ask himself the advantages that come with the adoption of drones for healthcare delivery in Africa, especially for hard-to-reach communities. Medical supply with the use of drones improves response time and increases delivery efficiency. What’s more, adopting drones
reduces travel time for diagnosis and treatment and is cost-effective when compared to road transport in difficult terrains. Drones are environmentally friendly because they reduce carbon dioxide emission levels and consume less energy per kilometer in delivering a package than delivery trucks do. Also, They reduce road traffic due to the decrease of cars and trucks on the road. Medical supplies aerially delivered by drones are categorized into first aid kits, medical aids and human body parts, personal protective equipment, and others in the order of urgency.
One of the most crucial delivery products by drones is blood due to their need when conducting diagnoses and rapid transfusions. Additionally, blood is always a requirement during health emergencies like Anaemia – a condition in which the number of red blood cells or the hemoglobin concentration is lower than normal, and Hypoglycemia – a condition in which blood sugar (glucose) level is lower than the standard range, and brain involvement.
Rwanda leveraged drone technology to deliver blood to women with postpartum haemorrhage and those in labour. Moreover, they can supply medical supplies such as vaccines. In terms of human body parts, drones are used to supply kidneys.During the COVID-19 pandemic, drones were used to deliver Personal Protective Equipment (PPEs) such as gloves and facemasks to health facilities in order to prevent the spread of the virus. Other supplies include pathology specimens, laboratory test samples, HIV therapies, and condoms.

The Contribution of Norrsken House Kigali and the Novartis Foundation
Denga logistics, being part of the 30 startups of the healthtech challenge received a fullyear subsidy to the Healthtech Hub Africa co-working space and community within the Norrsken Kigali House, an entrepreneurship hub that offers training, capital, network, advice and an innovation program to entrepreneurs that have startups that solve population health challenges aiming to accelerate their growth and connect with the right partners and contributors.
51
Healthcare professionals preparing for blood delivery using drones
Telemedicine ensuring Quality healthcare
Access to healthcare issues have been one of the world’s problems; the world health organization estimated that 800 million people spend 10% of their income on the healthcare services which pushes around 100 million people into extreme poverty and make them live under 1.90$ per day. In Africa only 615 million people have access to healthcare services out of 1.21 billion people Which is equal to 48% of the community.
When we talk about access to healthcare services this includes lack of insurance and Affordability ,lack of transportation to the hospital ,lack of quality health care and lack of medical attention.
It is estimated that 67% of the world population finds it hard to get to the hospital;This is caused by different things such as infrastructure,transportation facilities, this led to lack of medical attention,lack of quality healthcare. In Low income and middle income countries the communities suffer. In Nigeria 48.5% of the population live in rural areas stated by the world bank . Rural areas in Nigeria are characterized by poor road infrastructure and poor healthcare facilities; This comes with the affordability in Africa.
Lack of affordable health insurance led to low quality education; it estimated in developing countries 2.9 die because of lack of healthcare services as stated by

52 HEALTH TECH
Doctor listening heart beat and breathing of little girl.
HEALTHTECH IN AFRICA
Lancet global health. In Nigeria 11.188% is the mortality rate yearly.One of the main causes of this death is neonatal disorder, anemia,malaria,diarrhea disease. All of these diseases are diseases that can be cured but the lack of access to healthcare and affordability in Nigeria makes it hard. It is estimated that 15.1% of Nigerians spend a lot of money on healthcare.
Beside this amount of money that Nigerian are spending on healthcare services it is estimated that 67 of 10000 people die due to low quality of healthcare this include medication errors, inappropriate or unnecessary treatment, inadequate or unsafe clinical facilities Render healthcare is a telemedicine solution that will improve medical attention,and quality healthcare
Render health facilitate the transition of healthcare management processes in Africa to the digital age
Render health is an app that facilitates patients to book an appointment, or have an teleconsultation. Render health facilitates patients to keep track of their health by allowing them to have a dairy and record on the appointments.
On this app we have five features : appointments,history,diary and billing, home page.
Home page feature
This app features allows the user to search for hospitals in works with render health and the app gives you the location of the hospital. This allows the user to check the hospital near them. This will solve the transportation problem in Nigeria and reduce people who travel long distances to get healthcare services.
The home page allows you to book a hospital and choose a specialty that you want to book according to the disease , pain or check up you want to test; this will increase quality healthcare because this app personalizes services.
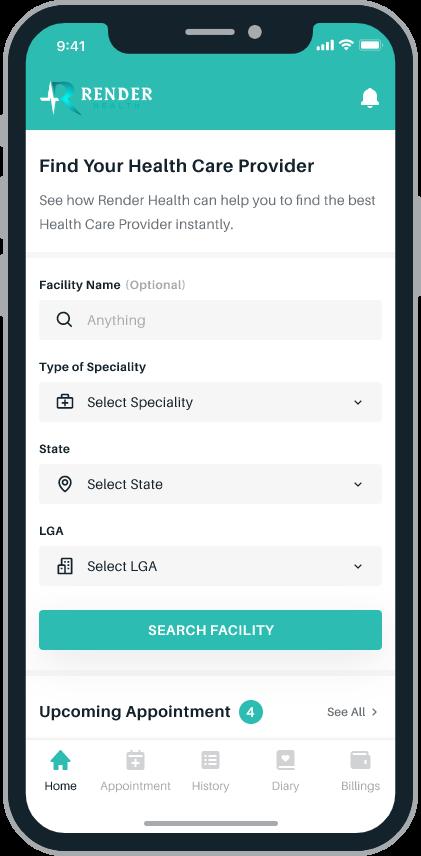
The homepage allows the user to book an appointment either in person or by teleconsultation. This avoids unnecessary travel to get consultation. It also solves transportation problems because sometimes people want to consult a doctor without having an emergency to go to the hospital.
Appointment schedule feature
The appointment schedule feature allows you to view your appointment and the app sends you a reminder. This appointment can be online or in person. This will increase the medical attention on both parts.
History feature
The history feature keeps record of your medical appointments and results generated by doctors. This feature will increase the medical attention on a patient’s side , especially people with chronic disease. It will be easy for them to keep track of times they visited the hospital.
This feature will help doctors to treat the patient because sometimes it can show different signs but with the healthcare record it will create patterns; this will promote quality healthcare and medical attention.
Diary feature
This feature will allow the user to record his/her medical record. The example will
be let say in the morning when you wake up you are having a headache and you take a fast action pill with this feature you can record every moment you experience pain or sickness.
With this feature doctors will be able to track your sickness events and understand ways to treat you with the right medication.This will increase healthcare quality and medical attention.
Billing features
With a billing feature this facilitates the patient bill payment because it is linked with insurance allowing you to spend less money on medical expenses. This will help you to have affordable healthcare.
53
Surplus Med in waste management
Waste management has been a world problem for years now. It is estimated that the whole world is now generating over 2.01 billion tons yearly stated by the World bank.
It is estimated that one person generates 0.74 kgs of waste on average per day. It is estimated that by this manuci[pal ,waste will grow up to 3.4 billion tons if we don’t change our waste management measure considering the fact that our population growth will double the number in 2050 stated by the World bank.

High income countries are the main contributors of municipal waste. They contribute to 34% of waste generated annually which is equal to 683 million tonnes. It is estimated that by 2050 the waste in high income countries will be reduced by 19% and in low income countries it will increase by 40% and more stated by the World bank.
Low income countries collect 48% of
54
Garbage bag for infectious waste
the waste generated in the cities while 26% are left in the landfill in urban areas. In sub-saharan waste they collect about 44% compared to Europe , North American and Central Asia collect at least 90% of the waste stated by the World bank. Medical sector is one of the sectors that generate waste that affects the environment and leads to diseases outbreak in many cases.
What is the role of the medical sector in waste generation?
Medical waste contributes to different types of waste. It can be land pollution,water pollution, air pollution ,and climate change. Medical sector is one of the sectors that is increasing municipal waste it is estimated that medical waste have increase from 658.08 tons in march to 16,164.74 tons in 2021 due to the pandemic.
We have two types of waste we have avoidable waste and unavoidable waste. The avoidable waste is the one we can prevent before it happens and Unavoidable waste we can not find ways to avoid it occurring in a process may the production stage or user stage. Medical sector is one of the sectors that generate waste that is hazardous. Some of this waste can be avoided and while others it is hard to avoid it.
It is estimated that the medical sector produces 15% of produced waste that are hazardous in general and 85% are non-hazardous states by the world health organization. In medical sector we have type of waste which include:
Infectious waste
This waste is composed with infectious or
contaminated body fluids or blood
Pathological waste
This waste is composed by human organs,body parts and derived tissues this can apply on other vertebrate animals
Sharps waste
This waste is composed of syringes, needles, lancets, and broken glass.
Chemical waste
This waste is composed by solid, liquid, or gaseous waste material
Pharmaceutical waste
Medical sector is one of the sectors that generate waste that affects the environment
This waste is composed by expired, unused and contaminated drugs and vaccines
Cytotoxic waste
This waste is composed by substances with genotoxic properties such as cytotoxic drugs used in cancer treatment
Radioactive waste
This waste is composed of hazardous waste that contains radioactive material.
Non-hazardous or general waste
This waste is composed by materials that doesn’t have particular biological, chemical, radioactive or physical hazard
HEALTHTECH IN AFRICA
Waste is caused by many factors.
Most of the leading is overproduction,expired products or short expired products. In the medical sector these products can be hazardous or create other types of waste which can affect both human beings / animals and the planet in general startups like surplus minimize medical waste and allow it to be used.
Role of Surplus Med in waste management
Surplus med redistribute medical supplies which are unopened unexpired but with short expiry medicine from different sector like wholesaler , retail and manufacture, pharmacy or other healthcare facilities to redistribute them where those supplies can be used before time or where the there a shortage of those medical supplies places like refugee camps, medical centers.
Surplus Med promote quality healthcare by allowing people getting access to medication on small amount as well as avoiding medical waste before it occurs
Surplus plays a big role in reducing municipal waste in the environment. It might be one of the hopes that developing countries might base on while reducing the expected increase by 2050 which is estimated to be increased by 40%.
Surplus is also reducing medical waste that can be Radioactive waste,Cytotoxic waste,Chemical waste,Sharps waste, and non hazardous waste. This reduces the disease outbreak due to medical waste.
55
Hellomed, A digital consultation platform for patients
Information, Communication, and Technology (ICT) has enabled the adoption and use of Digital health in Africa. According to Olushayo et al., 95% of the world’s population lives in areas where there is access to mobile networks and more than seven billion mobile subscriptions globally.

Nevertheless, Mobile phone and internet penetration ais still low compared to the global average but sufficient for the adoption of Digital health on the continent. Digital health comprises of mHealth - the use of mobile telephone technology to provide health information and services, eLearning - means for health professionals to get online health education, and telehealth/telemedicine - the provision of remote healthcare services.
Hellomed is a healthtech startup in Rwanda with the mission of providing an online platform where patients can request, book a doctor, and order medication regardless of where they are. That is, Hellomed takes care of patients through medicine delivery for patients with chronic conditions such as HIV/AIDS, Tuberculosis, Hepatitis B & C, Diabetes, Heart Diseases.
Other Conditions that can be treated with the help of Hellomed are common issues such as Fever, Cough, Cold, Flu, Headached migraines, Sore throat/Shep throat, Ear infections, Sinus infection, and Nosal congestion. Gastrointestinalrelated conditions include upset stomach, Nausea, Vomiting, Diarrhea, and Indigestion. Injury-related conditions include joint & back pain, Cuts & Scrapes,
Urine & Vaginal infections, Respiratory related issues include Asthma, Infections, colds, Bronchitis, and Seasonal allergies. Skin-related diseases such as Rashes, Dry skin, Acne, and Scabies. Health screening such as Blood pressure screening & counseling, Cholesterol counseling, Travel medicine, Sports physicals, and other physicals. Eye-related conditions such as eye infection, eye irritation, Pink eye and Stye. Family Planning & Immunization is also offered on the platform.
56 HEALTH TECH
Aloys Rukundo, CEO and Founder of Hellomed
“My biggest desire is to solve the issue of healthcare inaccessibility. A lot of communities especially in sub-Sahara have no access to basic healthcare leading to premature death and a lot more health complications”, says Aloys Rukundo, Founder and CEO of Hellomed.
Why should Hellomed be trusted?
Hellomed works with qualified, motivated, and experienced doctors from well-known hospitals. Additionally, the Hellomed app keeps all the records for future uses where treatment records are added to digital medical history, reducing the amount of time needed for patients to fill out their forms. This contributes to time management.
The use of Digital technologies for health has a lot of benefits. First and foremost, it brings about access to healthcare services for people who live in hard-to-reach areas. Secondly, they provide healthcare services and products that are safe and of quality. Additionally, they allow access to health information by knowledge provision to health workers and other communities which, in turn, leads to the productivity of health professionals and good practices in terms of health services.
During the COVID-19 pandemic, some healthtech startups with the same mission as Hellomed’s contributed to putting an end to the spread of Coronavirus by providing Telemedicine visits with health practitioners and virtual evaluations for Health maintenance.

Telemedicine can be referred to as the use of telecommunications technology to remotely deliver healthcare services such as exams and consultations to patients. It enables the provision of diagnosis and
treatment to patients from their homes by using their own personal technology.
According to Itai et al., Some Countries in Sub-Saharan Africa were successful in adopting telemedicine. Those countries are Zimbabwe, Cameroon, Uganda, South Africa, Nigeria, Mozambique, Tanzania, and Kenya. For instance, Nigeria used telepsychiatry to spread mental health information and access mental health services. Kenya used a virtual online training program to enable mental health professionals to acquire psychological first aid training required to counsel patients in lockdowns. Tanzania leveraged Teleconsultations to reach 118 patients after 216 inquiries and 45 pediatric consultations.
Norrsken House Kigali with the Novartis Foundation supports Hellomed to innovate.
HEALTHTECH IN AFRICA
Hellomed is part of the 30 healthtech startup challenge winners with a fullyear subsidy to the Healthtech Hub Africa co-working space and community within the Norrsken House Kigali, an entrepreneurship hub that offers training, capital, network, advice, and an innovation program to entrepreneurs. Some startups operating within the hub aim at solving population’s health challenges by using digital means.
Conclusion
Digital Health should therefore be embraced owing to the numerous positive impact it brings to the Health sector. Therefore, Hellomed promises to take healthtech to another level by offering a virtual consultation platform for all patients regardless of their location within the country of Rwanda.
57
Young man searches for information about a medicine on the internet and holds a bottle of medicine
I-VUZE,
Your Best Diagnostic Friend.
It has been a tradition that when you go to a hospital, you must wait for long hours before you see a doctor or even fall behind in the long queues of people waiting to be diagnosed. And sometimes, you go home without your turn reaching, which is a disappointment.
Say less, for it is about time a giant step in between and moves us past the long queues and to the front of the line.
I-VUZE is the new shortcut to a better and faster diagnosis. Accurate diagnosis is the first step to successful therapy, but a fast response to a patient is more effective.
The first step in a diagnosis is to understand the patient’s medical history. But it is tough to give attention that is needed to a patient when you can see a long line of other patients outside waiting to be listened to. This has been a significant disadvantage to several health centers around us.
A good diagnosis leads to better service. This is the principle that underlies most of our activities in health and social care. We want to know what is wrong so we can do something about it. But how do you know if your patient has a good diagnosis? It would be best if you had a reliable test or tests which are accurate and sensitive enough to give you confidence in the
results. But first, you must ask excellent and brave questions to get to the bottom of the issue or the problem. And from there, you can connect the patient to the right doctor that can offer the best set of tests to determine the result or the problem itself.

This is where I-VUZE comes in. The new bridge between better diagnosis and treatment. More than a million people are visiting the platform for care and connection, proving that there is a need for a better healthcare system. Understanding the needs of the people outside the community has been the best study that I-Vuze has done. Acquiring the best information puts it at the frontline of the race, and this has helped I-VUZE create a well-planned system with partners who are highly specialized experts and have experience in treating rare and complex conditions.
What is this system made out of?
Everything done by I-VUZE is just standard procedure. What makes them
58 HEALTH TECH
Physician performing tests on samples
HEALTHTECH IN AFRICA
unique is that they make them accessible to everyone and at the best quality possible. So what are these techniques? Such as : Referral to the main Hospital. When your problem requires a more thorough and sophisticated diagnosis for treatment, your doctor may occasionally recommend you to the main Hospital.
Booking GP(general practice) appointments. With a significant number of many health centers and clinics around Rwanda. It makes booking appointments easier with less time to wait in the process.

The techniques are many, and anybody can use them, but it is just a matter of how accessible you make them. And that
has been the secret of I-Vuze Software ltd.
The unknown is just a question, and we find the answers.
Receiving the right diagnosis may indeed be among the life-altering experiences you can have, and the same is true for I-vuze software. Simple access to superior services and quick outcomes.

A team of experts will carefully consider your needs and assess your situation from all perspectives to create the optimal strategy for you. How amazing is that?
Let us stop the long route and consider putting I-VUZE at the speed dial of our daily healthcare life with no long waiting
queues and easy accessibility with all devices.
What happens after a diagnostic?
I-vuze offers a plan that is suitable for all people and organizations of any size, with various services available for monthly or annual payments. You have guaranteed a prompt response to your appointment, late-night calls for unexpected situations, and the greatest one-on-ones with the best specialists with this plan. What else is possible if your diagnostics are properly interpreted? That is a pledge for better care.
Get your diagnosis today; get it done with I-vuze hospital management software for I-VUZE is your Best diagnostic Friend.
59
1) Diverse doctors going through patient files. 2) Medical billing statements on a table.
1 2
Digi-Dibia
An African Startup unlocking new levels in healthcare?
What has been the status of Healthcare systems in Africa?
Africa’s healthcare system is becoming better. In the past, Access to healthcare was restricted to a small number of hospitals and clinics in big cities. Hospitals and clinics are now more numerous and dispersed across the nation. As a result, patients no longer have to wait days or weeks for an appointment at a hospital or clinic to receive care when needed. Better ways to conduct tests and meet up with a doctor online have proven more productive than going to the hospital or clinics.
We are moving closer to a more advanced technological world, and Africa, the new emerging cradle for innovation, puts everything in a race to get that technology that will ease everything, social or economic, or even political aspects of life. Now, the healthcare sector is a big one. We’ve got the most significant number of people in the world, and we must be cautious about how we use technology. It’s not just about using
technology for convenience; it has to be used wisely to improve health outcomes.
Who is Digi-Dibia that is unlocking new levels in healthcare?
Digi-Dibia, a HealthTech Platform that compiles medical data into a clinical decision support system supported by a network of medical specialists, provides essential healthcare services that people can afford and trust, from diagnosis through discharge.
more Access to healthcare systems and even make them more affordable to everyone.
Seeing a professional is a mere chance in most African healthcare systems. With a growing stereotypical way of many healthcare prohibitions and unnecessary bureaucracy, we need to defy these norms that our systems seem not to get a hold on. Avoid leaving people with an option of self-diagnosing, and self-prescribing often leads to misdiagnosis. Digi-Dibia has paved the way to getting in touch with the best medical professionals and being given the best service that few clinics can offer. “Our medical team, supported by technology, conducts detailed assessments to help you get an accurate diagnosis.” (Digi-Dibia)
The main goal of Digi-Dibia is to ensure
The multi-regional and international DigiDibia team, which has offices in Nigeria and the U.S., is bringing its experience to bear to help tackle the primary healthcare crisis in Africa. From the ground up, by developing solutions that improve quality and Access to treatment while simultaneously lowering costs.
60 HEALTH TECH
Avoid leaving people with an option of self-diagnosing and self-prescribing often leads to misdiagnosis.
HEALTHTECH IN AFRICA
The breakthrough that connects all the dots.
The breakthrough in technology in healthcare is the development of artificial intelligence, robotics, and virtual reality. These technologies will improve patients’ quality of life and make it easier for doctors to diagnose diseases.

Now embracing these changes and adopting them into real-life experiences has been Digi-Dibia’s priority. Modernized Artificial Intelligence has been embedded into the system. This serves best to provide up-to-date protocols and get an electronic medical record on any device with full ownership of your medical history to how the system monitors your healthcare from diagnosis to discharge, with referrals for specialists who will care for you better.
With a mission of Healthcare for Everyone. Digi-Dibia is committed to delivering better healthcare outcomes in Africa. Indeed, looking at combining artificial intelligence with trained medical professionals, They have provided better care to more people. Accessing your diagnosis and treatment plan with fewer expenditures seems feasible and promises a healthy lifestyle.
Digi-Dibia offers inclusive services.
The focus is not all on a sick patient or somebody who needs attention. The greatness of services offered by Digi-Dibia goes beyond Just a one-time meet-up to pre-care like; Health & hygiene education, Wellness management, and Preventive care.
In-care, With accessible electronic mobile
medical records, Access to medical professionals, Rapid diagnostic testing, Reliable diagnosis, Prescriptions, and prescription drugs. They follow up on you and ensure that there is everything that you need at an easy reach out.
Post-Care, with a variety of specialists at the organizations, Digi-Dibia extends the services to a post-care stage, with offers to Chronic disease management and
Escalations/referrals to our network of specialist providers that can provide dayto-day services.
Digi-Dibia’s
The question is not what technology will be but what we as a society want it to be. And that’s the critical point here. The use of technology in healthcare has been increasing exponentially over the past few years, and there are many benefits to this. So yes, embracing technology and embedding it in the growing healthcare systems is the way forward to a better healthcare lifestyle and an improved system.
Digi-Dibia found its way. Let us follow it up and level up to the incredible healthcare system.
61
Is
approach the way forward?
Accessing your diagnosis and treatment plan with fewer expenditures

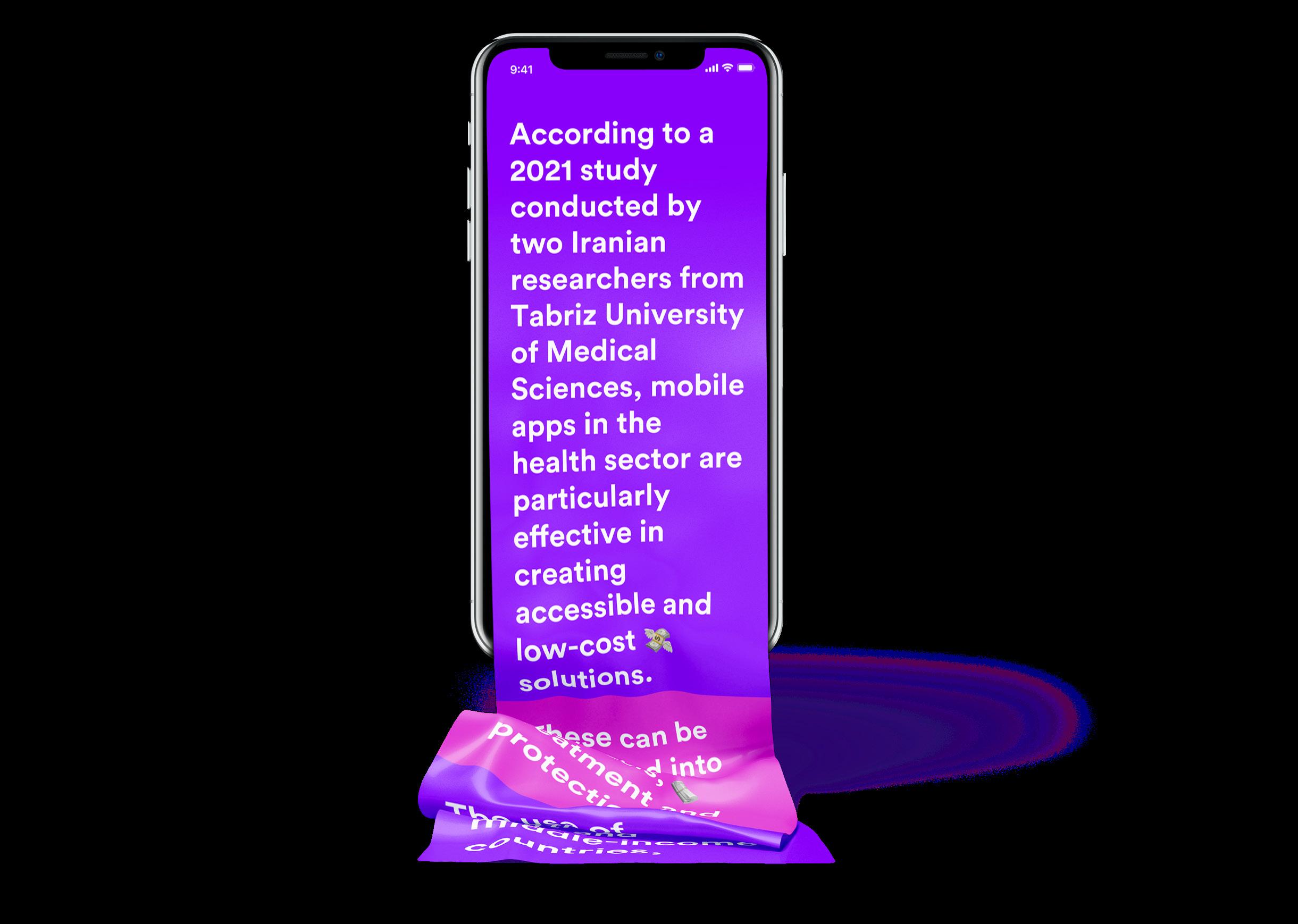







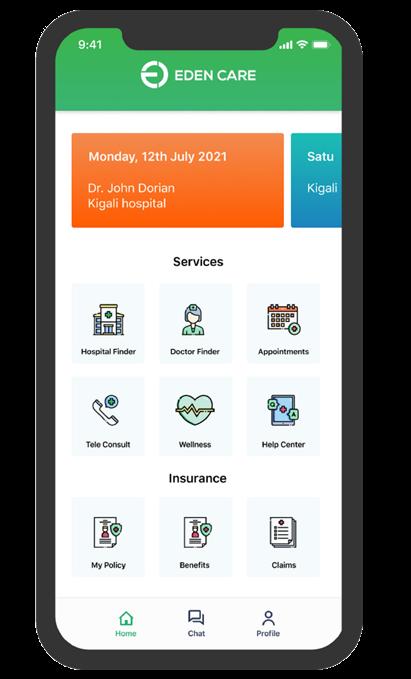






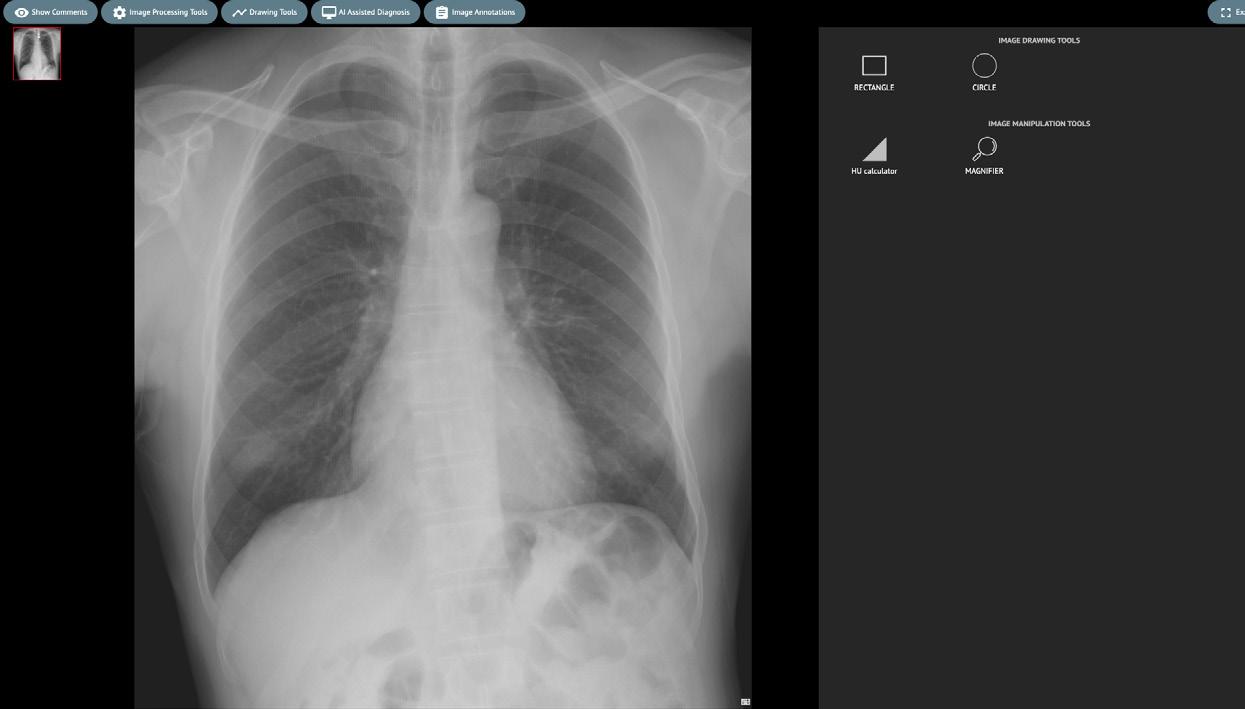
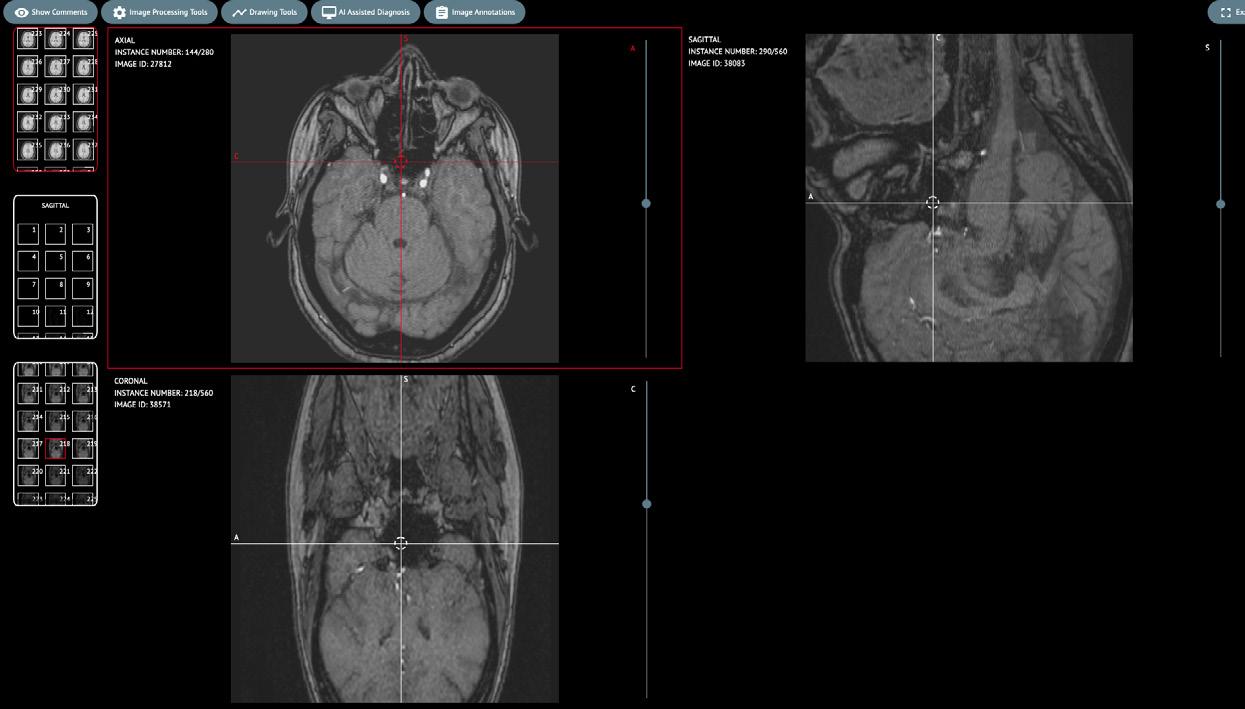

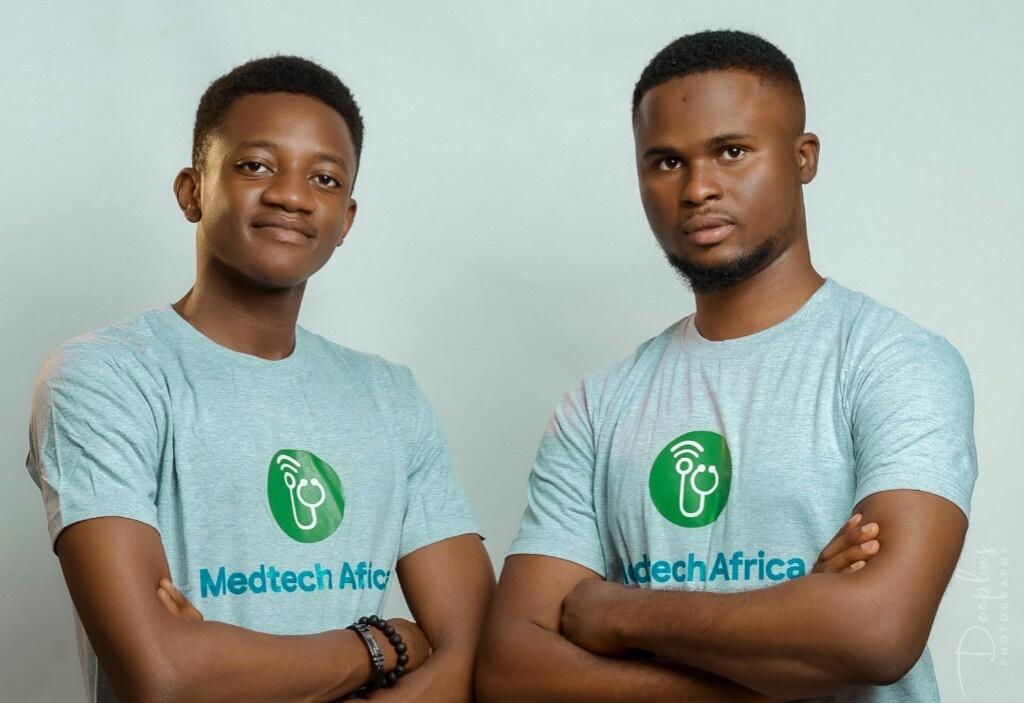
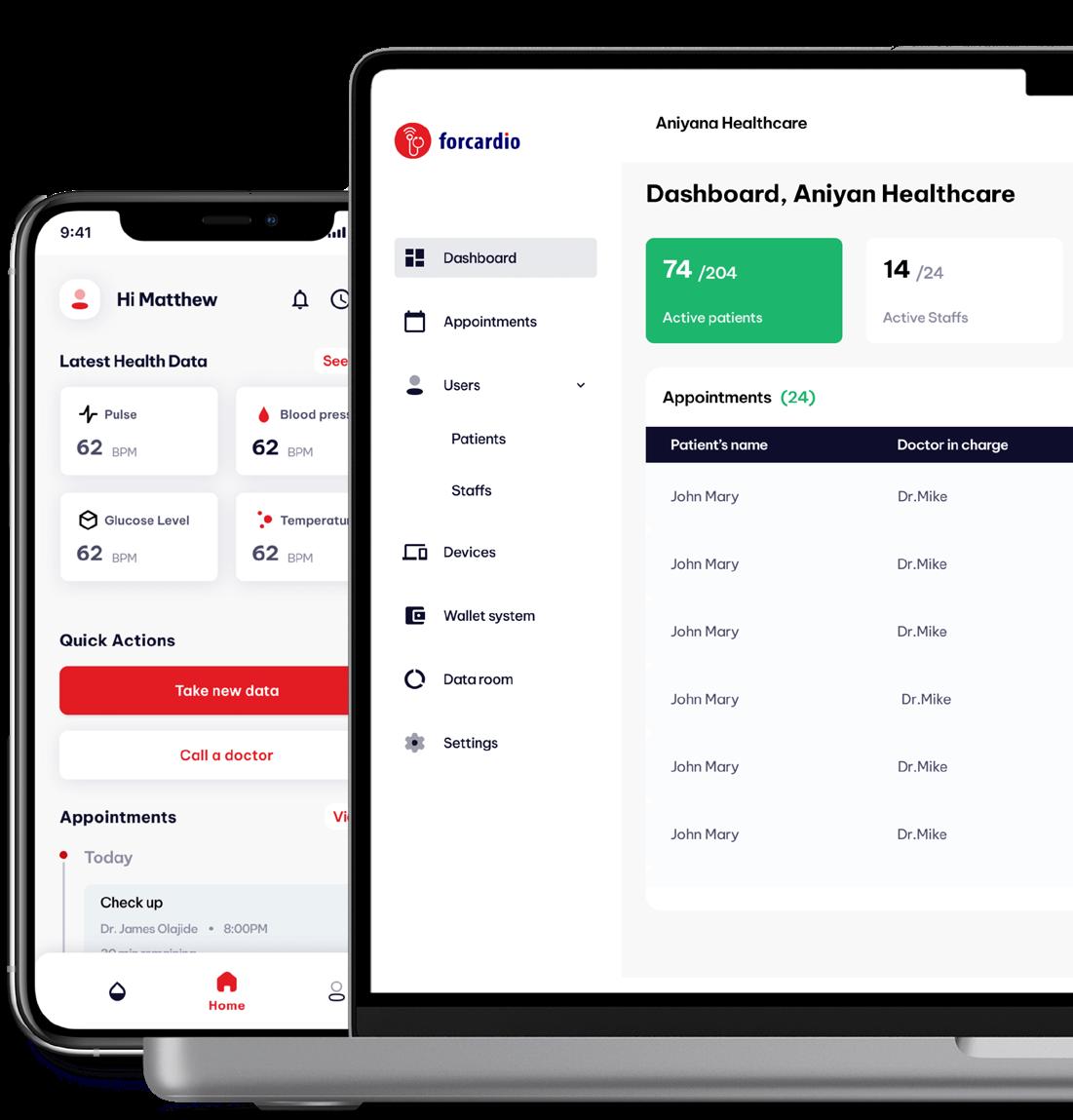

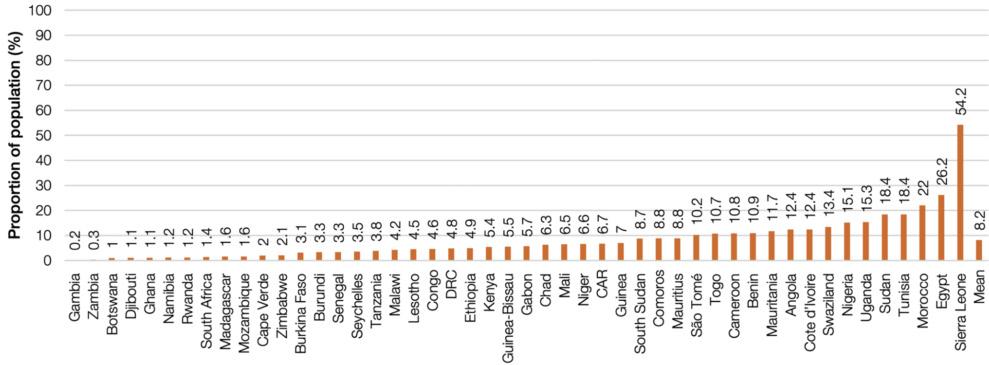







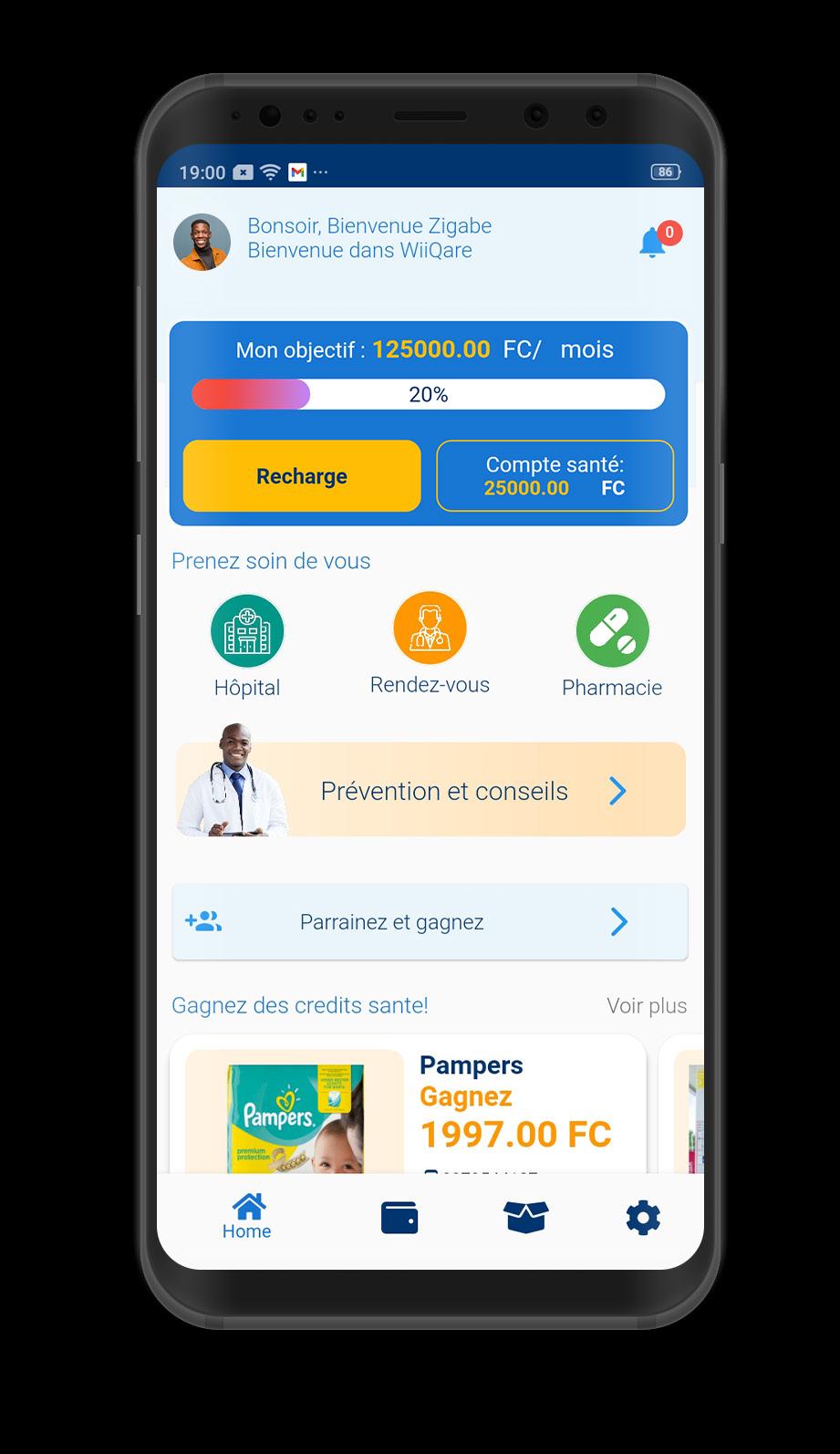


 By Tunga Elsa Ndibwami
By Tunga Elsa Ndibwami