celebrating 100 years!
An Overview of Digital Workflows for Precision Impact Dentistry
The Latest in Dental Implants: Communication, Techniques and Technology
Technology Can Make Implant Placement More Seamless

Promoting Oral Health & Driving Floridians to See Their FDA Dentist
Implant Dentistry














2 S C OTT RUTHSTROM • GeneralManager/COO scott.ruthstrom@fdaservices.com•850.350.7146 C A R R I E MI Director Of Insur erati o n s carrie.millar@fdaservices.com•850.350.7155 R I CK D ’ANGELO • WEST FLORIDA rick.dangelo@fdaservices.com •813. 475. 6 9 4 8 dennis.head@fdaservices.com•407.359. 9 7 0 0 DENNISHEAD • CENTRAL FLORIDA J OE PERRETTI • SOUTH FLORIDA joe.perretti@fdaservices.com•305. 665. 0 4 5 5 D A N ZOTTOLI•ATLANTIC COAST dan.zottoli@fdaservices.com•561. 791. 7 7 4 4 M I KE TROUT• NORTH FLORIDA mike.trout@fdaservices.com •904.254. 8 9 2 7
FDAS TEAM IS FOCUSED ON YOU AND YOUR PRACTICE MALPRACTICE • OFFICE INSURANCE • CYBER INSURANCE • WORKER’S COMP • DISABILITY Came for the insurance ... Stayed to support my profession.
THE






1 | TODAY'S FDA january/february 2023 TABLE OF CONTENTS JANUARY/FEBRUARY 2023 floridadental.org DENTAL IMPLANT issue 69 31 CHECK OUT TODAY’S FDA ONLINE! IN EVERY ISSUE 66 2 Staff Roster 4 Contributors 7 President’s Message 11 Did You Know? 15 Legislative 18 Preventive Action 20 Take The Lead 22 news@fda 81 Diagnostic Discussion 84 Career Center 87 Advertising Index 88 Off the Cusp 12 | BOD: Unexcused Absences, Proposed Language to Provide Protective Eyewear and More! 31 | Dental Implants 32 | An Overview of Digital Workflows for Precision Impact Dentistry 47 | The Latest in Dental Implants: Communication, Techniques and Technology 48 | Proper Communication Regarding Implants Is Vital 52 | The Latest Techniques to Make Implant Placement Smoother 54 | Technology Can Make Implant Placement More Seamless 58 | Torque Delivery Via a Hexalobular Driver Positioned at an Off Axis Angulation: An Engineering Perspective 64 | Promoting Oral Health & Driving Floridians to See Their FDA Dentist 66 | Pour A-1 Sauce on Carrot Cake for Accountability 69 | Copyright Reminders 73 | FDC2023: No Gossip Zone 74 | FDC2023: Yes — Crown Lengthening Will Enhance Your Results 78 | Exhibit Hall
545 John Knox Road, Ste. 200 • Tallahassee, FL 32303 • 800.877.9922 or 850.681.3629
EDITOR
Hugh Wunderlich, CDE • Palm Harbor
DIRECTOR OF PUBLICATIONS
COMMUNICATIONS AND MEDIA COORDINATOR
GRAPHIC DESIGN COORDINATOR
AJ Gillis
Jill Runyan
Kelsey Simmons PRESIDENT
Dr. Gerald Bird • Cocoa
BOARD OF TRUSTEES
SECRETARY
PRESIDENT-ELECT
Dr. Beatriz Terry • Miami FIRST VICE PRESIDENT Dr. Jeffrey Ottley • Milton
Dr. Dan Gesek • Jacksonville
IMMEDIATE PAST PRESIDENT
Dr. Dave Boden • Port St. Lucie
SECOND VICE PRESIDENT Dr. John Paul • Lakeland
EXECUTIVE DIRECTOR Drew Eason, CAE • Tallahassee
Dr. Tom Brown • Orange Park | Dr. Christopher Bulnes • Tampa | Dr. John Coroba • Lake Mary | Dr. Bethany Douglas • Jacksonville
Dr. Karen Glerum • Boynton Beach | Dr. Reese Harrison • Lynn Haven | Dr. Bertram Hughes • Gainesville | Dr. Mark Limosani • Weston
Dr. Irene Marron-Tarrazzi • Miami | Dr. Eddie Martin • Pensacola | Dr. Paul Palo • Winter Haven | Dr. Mike Starr • Wellington
Dr. Don lIkka • speaker of the house, Leesburg | Dr Rodrigo Romano • treasurer, Miami
To contact an FDA board member, use the first letter of their first name, then their last name, followed by @bot.floridadental.org. For example, to email Dr. Hugh Wunderlich, his email would be hwunderlich@bot.floridadental.org.
To call a specific staff member below, dial 850.350. followed by their extension.
EXECUTIVE OFFICE
Drew Eason • chief executive officer/executive director
Greg Gruber • chief operating officer/chief financial officer
Casey Stoutamire • chief legal officer
Lianne Bell • leadership affairs manager
Judy Stone • leadership affairs specialist
Lywanda Tucker • peer review coordinator
ACCOUNTING
Breana Giblin • director of accounting
Leona Boutwell • finance services coordinator
Deanne Foy • finance services coordinator
Jamie Idol • FDAS support services coordinator
Mitzi Rye • fiscal services coordinator
deason@floridadental.org •
Ext. 7109
• Ext. 7202 lbell@floridadental.org
• Ext. 7114 jstone@floridadental.org
• Ext. 7123 ltucker@floridadental.org
• Ext. 7143
bgiblin@floridadental.org
• Ext. 7137
Renee Thompson
• director of communications and marketing
Jill Runyan • director of publications
AJ Gillis • graphic design coordinator
Kelsey Simmons • communications and media coordinator
FDA FOUNDATION
R. Jai Gillum
• director of foundation affairs
2
Ext.
rjaigillum@floridadental.org •
7117 kbadeau@floridadental.org • Ext. 7161
lboutwell@floridadental.org • Ext.
dfoy@floridadental.org • Ext.
jamie.idol@fdaservices.com • Ext.
mrye@floridadental.org • Ext.
staylor@floridadental.org • Ext. 7119 rthompson@floridadental.org • Ext. 7118 jrunyan@floridadental.org • Ext.
agillis@floridadental.org • Ext.
Kristin Badeau • foundation coordinator ksimmons@floridadental.org • Ext.
7138
7165
7142
7139
7113
7112
7115
COMMUNICATIONS AND PUBLICATIONS
ggruber@floridadental.org
Stephanie Taylor • membership dues coordinator
• Ext. 7111 cstoutamire@floridadental.org
Dr.
FLORIDA DENTAL CONVENTION AND CONTINUING EDUCATION
Crissy Tallman • director of conventions and continuing education
Mackenzie Johnson • FDC meeting assistant
Brooke Martin • FDC marketing specialist
Isabelle McCreless • FDC program coordinator
Lisa O’Donnell • FDC program coordinator
Deirdre Rhodes • FDC exhibits coordinator
GOVERNMENTAL AFFAIRS
Joe Anne Hart • chief legislative officer
Alexandra Abboud • governmental affairs liaison
Jamie Graves • legislative assistant
INFORMATION SYSTEMS
Larry Darnell • director of information systems
Charles Vilardebo • computer support technician
MEMBER RELATIONS
Kerry Gómez-Ríos • director of member relations
Megan Bakan • member access coordinator
Christine Trotto • membership concierge
Bettie Swilley • membership coordinator
Scott Ruthstrom • chief operating officer
Carrie Millar • director of insurance operations
Carol Gaskins • commercial accounts manager
Marcia Dutton • membership services assistant
Porschie Biggins
• Central FL membership commercial account advisor
Maria Brooks • South FL membership commercial account advisor
Davis Perkins
• Atlantic Coast membership commercial account advisor
Melissa Staggers • West Coast membership commercial account advisor
Danielle Basista • commercial account advisor
Tessa Daniels • commercial account advisor Kelly Dee • commercial account advisor
Liz Rich • commercial account advisor
Karina Scoliere • commercial account advisor
Dan Zottoli, SBCS, DIF, LTCP director of sales • Atlantic Coast




561.791.7744 cell: 561.601.5363
dan.zottoli@fdaservices.com
Dennis Head, CIC director of sales • Central Florida 877.843.0921
cell: 407.927.5472
dennis.head@fdaservices.com
Mike Trout director of sales • North Florida cell: 904.254.8927
mike.trout@fdaservices.com
Joseph Perretti, SBCS director of sales • South Florida cell: 305.721.9196

joe.perretti@fdaservices.com
Rick D’Angelo, CIC director of sales • West Coast 813.475.6948 cell: 813.267.2572
rick.dangelo@fdaservices.com
3 | TODAY'S FDA january/february 2023 krios@floridadental.org • Ext. 7121 mbakan@floridadental.org • Ext. 7100 ctrotto@floridadental.org • Ext. 7136 bswilley@floridadental.org • Ext. 7110
ldarnell@floridadental.org • Ext. 7102 cvilardebo@floridadental.org • Ext. 7153
jahart@floridadental.org • Ext. 7205 aabboud@floridadental.org • Ext. 7204 jgraves@floridadental.org • Ext. 7203
ctallman@floridadental.org • Ext. 7105 mjohnson@floridadental.org • Ext. 7162 bmartin@floridadental.org • Ext. 7103 imccreless@floridadental.org • Ext. 7106 lodonnell@floridadental.org • Ext. 7120 drhodes@floridadental.org • Ext. 7108
YOUR RISK EXPERTS Group & Individual Health • Medicare Supplement • Life Insurance • Disability Income • Long-term Care • Annuities Professional Liability • Office Package • Workers’ Compensation • Auto • Boat FDA SERVICES 545 John Knox Road, Ste. 201 • Tallahassee, FL 32303 • 800.877.7597 or 850.681.2996 scott.ruthstrom@fdaservices.com • Ext. 7146 carrie.millar@fdaservices.com • Ext. 7155 carol.gaskins@fdaservices.com • Ext. 7159 marcia.dutton@fdaservices.com • Ext. 7148 porschie.biggins@fdaservices.com • Ext. 7149 maria.brooks@fdaservices.com • Ext. 7144 davis.perkins@fdaservices.com • Ext. 7145 melissa.staggers@fdaservices.com • Ext. 7154 dbasista@fdaservices.com • Ext. 7156 tessa.daniels@fdaservices.com • Ext. 7158 kelly.dee@fdaservices.com • Ext. 7157 liz.rich@fdaservices.com • Ext. 7171 karina.scoliere@fdaservices.com • Ext. 7151
GUEST CONTRIBUTORS
LIANNE BELL FDA LEADERSHIP AFFAIRS MANAGER lbell@floridadental.org



Page 20
MATT DIBLASI ABYDE PRESIDENT mdiblasi@abyde.com
Page 18
TOBIAS BOEHM, DDS, PHD tboehm@westernu.edu
Page 32
ROBERT DOBRIN, DMD bobdobrin@yahoo.com


Page 58
SETAREH LAVASANI, DMD, MS slavasani@westernu.edu
Page 32
JUDY KAY MAUSOLF PRESIDENT AND OWNER OF PRACTICE SOLUTIONS INC. judykay@practicesolutionsinc.net
Page 72
JAMES KOHNER, DDS jameskohnerdds@gmail.com

Page 74
JOSE PERALTA, DDS jrp8866@gmail.com


Page 66
ALEXANDER LEE, DMD allee@westernu.edu

Page 32
RAFEEQ RAHMAN, DDS rrahman@westernu.edu
Page 32

4 january/february 2023
Page 81
Page 81
850.681.3629
Page 7
cstoutamire@floridadental.org







850.350.7202
Page
Page 81
850.350.7205
Page 15
850.681.3629
Page 88
5 | TODAY'S FDA january/february 2023
JOE ANNE HART FDA CHIEF LEGISLATIVE OFFICER jahart@floridadental.org
CASEY STOUTAMIRE, ESQ. FDA CHIEF LEGAL OFFICER
11, 12 & 69
HUGH WUNDERLICH, DDS, CDE FDA EDITOR hwunderlich@bot.floridadental.org
INDRANEEL BHATTACHARYYA, DDS IBHATTACHARYYA@dental.ufl.edu
NADIM M. ISLAM, DDS MIslam@dental.ufl.edu
JERRY BIRD, DDS FDA PRESIDENT gbird@floridadental.org
CONTRIBUTORS january/february 2023
SAJA ALRAMADHAN, BDS SAlramadhan@dental.ufl.edu

IMPLANT DENTISTRY ”
By Jerry Bird, DMD, FDA President
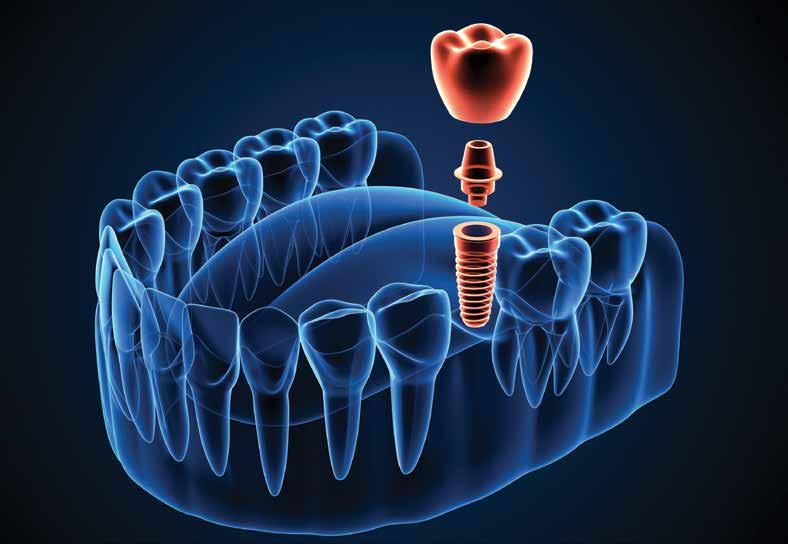
Did you know that the history of dental implants can be traced back to ancient Egypt where they carved seashells and stones to replace missing teeth? As early as 2000 B.C. early versions of dental implants were used in ancient China and the first recorded case of a replacement tooth made of metal came from the body of an Egyptian King around 1000 B.C. That was a long time ago. One of the most important developments that lead to our current dental implants occurred in 1957 when a Swedish orthopedic surgeon named Dr. Per-Ingvar Brånemark began studying bone healing and regeneration and discovered that bone could actually grow in proximity with titanium and could effectively adhere to the titanium and not be rejected. Brånemark called this “osteointegration.”

Now implants are commonplace and they come in many shapes, sizes and different coatings to enable the best integration into bone. In the general population, the use of dental implants has become a great treatment option for replacing missing teeth. It doesn’t matter the age, people want to replace missing teeth and they want to look younger, better and enjoy eating all foods again. Of course, dental implants are not inexpensive and patients can be concerned about finances and length of treatment time. Older adults have complex medical, social and economic issues that must be taken into consideration, and dentists need to give careful attention to help each patient consider the best tooth replacement therapy.
For many, dental implants have become the increasingly common treatment option for missing dentition. With the population becoming increasingly older worldwide, the dentist is confronted with patients who have more complex medical and social histories and dental implants. When patients need and desire tooth replacement therapy, there are many options such as
7 | TODAY'S FDA january/february 2023 president’s message
For the majority of the population, the clinical success of dental implant therapy has improved so much that many clinicians consider it to be a standard of care.
” t

conventional removable or fixed prostheses to a combination of fixed and removable implant-supported forms of tooth replacement.

For the majority of the population, the clinical success of dental implant therapy has improved so much that many clinicians consider it to be a standard of care. Tooth replacement therapy can vary from single-tooth replacement with conventional or implant-supported restorations to full-arch replacement. Each option, including no tooth replacement, has advantages and costs that must be weighed in consideration of patients’ desires, understanding, resources and perspectives.
Some dentists place single implants only, and some can do full arch replacements while others work as a team with their surgical specialist. No matter the option you choose, you need to evaluate the patient for any systemic conditions that maycompromise healing — immunocompromised states, uncontrolled diabetes and the antagonistic effects of medications. In general, the survival rates of dental implants in older patients can be affected by systemic conditions associated with aging, including long-term smoking, diabetes and postmenopausal estrogen therapy. Patients who undergo implant surgery face the same medical and surgical risks that are similar to those of outpatient procedures. And, of course, our patients need to be encouraged to take excellent care of their investment to assure long term success.
New advances in digital dentistry have enabled more advanced diagnostic information. The dentist can now use a surgical guide or denture to indicate the desired implant position, angulation and need for hard and/or soft tissue augmentation before or during implant placement. Guided implant surgery with the use of cone-beam computed tomography scans and intraoral scanners have made it possible to get the best position and restoration for the patient.
It has been proven that dental implant therapy can significantly improve the lives of our patients. Through discussions with the patient, his or her caregiver and, possibly, other family members, the clinician can assess the patient’s expectations and desires carefully and balance them with the time and resources needed to accomplish the best outcomes. In the end, I know you’ll agree that dental implants have come a long way in a very short amount of time. In 1984, when I first started out in practice, we graduated from one-piece blades, to now primarily endosseous root forms. All things change over time. The innovation in dental implants will continue and will most likely become easier in the future for us as practitioners and more beneficial for our patients.
9 | TODAY'S FDA january/february 2023 president’s message
OPIOIDS
HEALTH CARE PROVIDER CHECKLIST:
INFORM
Non-opioid alternatives for pain treatment, which may include non-opioid medicinal drugs or drug products are available
Non-opioid interventional procedures or treatments, which may include: acupuncture, chiropractic treatments, massage, physical or occupational therapy, or other appropriate therapy are available.
DISCUSS
DOCUMENT IN PATIENT’S RECORD
PROVIDE
“Alternatives to Opioids,” an educational information pamphlet created by the Florida Department of Health printed or in electronic format (required, available at bit.ly/2KXvZ2h). Also, a checklist and poster.
SUMMARY:
All health care providers must include non-opioid alternatives for pain and pain management electronically or in printed form in their discussions with patients before providing anesthesia, or prescribing, ordering, dispensing or administering a schedule II controlled substance for the treatment of pain. Effective July 1, 2021.
Exclusive Member Benefit!

FOR THE LATEST ON OPIOIDS, GO TO: FLORIDADENTAL.ORG/NYK
NON-OPIOID ALTERNATIVES
LAW: GO TO bit.ly/2KXvZ2h
10
A dv an t ages an d d isa dv an t ages o f n o n- o pi o i d a lt erna t i v es Pa t ien t ’s risk o r h is to r y o f c o n t r oll e d s u bs t ance ab u se o r mis u se , an d pa t ien t ’s pers o na l preferences .
N o n- o pi o i d a lt erna t i v es c o nsi d ere d .
Digital Scanning is Considered the Same as Taking an Impression
By Casey Stoutamire, FDA Chief Legal Officer
Did you know that digital scanning is considered the same as taking an impression under the Board of Dentistry (BOD) rules? This means that most digital scanning done by dental assistants must be done under direct supervision. In contrast, most done by dental hygienists can be done under general supervision if they have formal training.

As a reminder, direct supervision requires that a licensed dentist examine the patient, diagnose a condition to be treated, authorize the procedure to be performed, be on the premises and approve the work performed prior to the patient’s departure from the premises. General supervision requires that a licensed dentist authorizes the procedures to be performed but need not be present when the authorized procedures are being implemented. The approved procedures may also be performed at a place other than the dentist’s usual place of practice.
You can find the BOD rules on tasks delegable to dental assistants and hygienists here: bit.ly/3Wacgi8. Again, when reading the rules, when you see the word “impression,” that also applies to digital scanning.

11 | TODAY'S FDA january/february 2023 did
you know?
”
General supervision requires that a licensed dentist authorizes the procedures to be performed but need not be present when the authorized procedures are being implemented.
Unexcused Absences, Proposed Language to Provide Protective Eyewear and More!
By Casey Stoutamire, FDA Chief Legal Officer
The Florida Board of Dentistry (BOD) met in Ft. Lauderdale, Friday, Nov. 18, at 7:30 a.m. BOD Liaison Dr. Andy Brown and FDA Chief Legal Officer Casey Stoutamire represented the Florida Dental Association (FDA). Drs. Jim Haddix and Steven Hochfelder were also in attendance. Several Nova Southeastern University College of Dental Medicine dental students also attended the meeting.
BOD members present included:
Dr. T.J. Tejera, chair; Mr. Fabio Andrade, vice-chair; Drs. Christine Bojaxhi, Brad Cherry, Tom McCawley Jose Mellado, Claudio Miro and Nick White Ms. Karyn Hill and Ms. Angela Johnson.
In August, the BOD approved language for a new rule regarding unexcused absences from board meetings, as the BOD did not previously have a rule for this. The proposed rule language read:
64B5-1.002 Unexcused Absences of Board Members.
(1) A Board member’s absence from a Board meeting shall be considered unexcused if the Board member had not received approval of the chair or the chair’s designee prior to missing the meeting.
(2) Arriving late for a Board meeting or leaving early from a Board meeting without prior approval of the chair or the chair’s designee shall be considered an unexcused absence.
BOD counsel reported that the Joint Administrative Procedures Committee (JAPC) had issues with the previous rule even though the language is in rule for other regulatory boards. BOD counsel worked with JAPC to get a clear understanding of what they would like to see in the rule and modified it accordingly. It now reads:
64B5-1.002 Unexcused Absences of Board Members.
(1) A Board member’s absence from a Board meeting shall be considered unexcused if the Board member had not received approval of the chair or the chair’s designee prior to missing the meeting. Reasons for granting excused absences shall be, but are not limited to the following:
1. Illness or injury of the Board member;
2. Illness or death of family member;
3. Court order, subpoena, or business with a federal or state court or other governmental body;
4. Travel delays or cancellations;
5. Any conflict or extraordinary circumstance or event approved by the Board Chair.
(2) Arriving late for a Board meeting or leaving early from a Board meeting without prior approval of the chair or the chair’s designee shall be considered an unexcused absence.
The BOD heard from the Commission on Dental Competency Assessments (CDCA), which administers the ADEX licensure exam. As a reminder, the Florida rule (which was modeled after the initial CDCA rule) requires an applicant to complete and pass all parts of the ADEX exam within 18 months of taking the first part of the exam. However, the CDCA rule now states that all aspects of the ADEX exam must be complete within 18 months of an applicant starting their D4 year. As part of that discussion, the BOD asked the FDA to work with board staff to review the dental examination statute and propose clean-up changes to ensure it aligns with current procedures.

12 board of dentistry
The Council on Dental Hygiene proposed language to require dentists to provide protective eyewear to all patients for all dental procedures. However, the BOD did not approve this proposed revision to Rule 64B5-25.003. It will not be a requirement in the rule that patients be given eye protection in dental procedures. As a reminder, this is still a guideline from the Centers for Disease Control and Prevention and dentists should act accordingly.
There were five disciplinary cases, two informal hearings, and three determinations of waivers. There was also one voluntary relinquishment dealing with failing to notify the BOD of criminal convictions; failure to meet the minimum standard of care regarding periodontal disease, the placement of a bridge and placement of a crown; failure to comply with a previous final order of the BOD; a fistula repair without referring to a specialist; abandoning a practice without notifying the BOD nor publishing
FORWARD


THE DAWSON ACADEMY RETURNS!


TAKE THE DAWSON ACADEMY’S INTRODUCTORY COURSE IN THE CONCEPT OF COMPLETE DENTISTRY® SERIES AT FDC2023.


FUNCTIONAL OCCLUSION – PROTOCOLS TO PUT YOUR PRACTICE IN THE TOP 10%, A TWO-DAY COURSE






THURSDAY, JUNE 29 & FRIDAY, JUNE 30 | 8 AM-5 PM, BOTH DAYS

The next BOD meeting is scheduled for Friday, Feb. 24, at 7:30 a.m. ET in Gainesville.
LAUNCHING DENTISTRY
FLORIDADENTALCONVENTION.COM GAYLORD PALMS RESORT & CONVENTION CENTER | ORLANDO JUNE 29-JULY 1, 2023 SAVE UP TO 20% ON THIS DAWSON COURSE AT FDC2023! REGISTRATION OPENS MARCH 1.
LEONARD HESS, DDS CLINICAL DIRECTOR, THE DAWSON ACADEMY
VIEW COURSE DETAILS AND PRICING AT FLORIDADENTALCONVENTION.COM.

A NEW YEAR, A NEW LEGISLATURE
By Joe Anne Hart, Chief Legislative Officer

As we start the new year, we prepare for the big task ahead of us: educating the newly-elected Legislature about issues important to the Florida Dental Association (FDA).
The Florida Legislature will start the 2023 Regular Session on Tuesday, March 7. They will be busy for the next 60 days establishing new laws and budget priorities until they adjourn on Friday, May 5, 2023. Senate President Kathleen Passidomo (R-Naples) and House Speaker Paul Renner (R-Palm Coast) will serve as the top Republican leaders of each chamber until the 2024 elections.


The Democratic leaders are Sen. Lauren Book (D-Plantation) and Rep. Fentrice Driskell (R-Tampa), who will be the top leaders for their party until 2024. With the Republicans enjoying a supermajority in both houses, it will be more important than ever for the Democrats to forge relationships in order to have their priorities considered during session.


With a new Legislature, there is a prime opportunity for advocacy groups and organizations to bring their issues and initiatives to the attention of first-year legislators for their support. The FDA has worked diligently to make sure every legislator has a legislative contact dentist. Connecting legislators with local dentists helps create a relationship that is crucial to the FDA’s efforts in getting support for issues supported by organized dentistry. Without that relationship, legislators are often making decisions without all of the information or knowledge of the impact that decision could have.
The FDA’s legislative agenda will include securing funding for the Dental Student Loan Repayment Program and the Donated Dental Services Program and addressing dental insurance reforms such as a medical loss ratio for dental insurance plans. This legislative agenda will require all hands on deck to get it through the process. You can help put this agenda through by attending Dentists’ Day on the Hill, scheduled for Tuesday, March 28. A legislative briefing will take place at 6 p.m. on Monday, March 27. The host hotel is Hotel Duval, where attendees will receive a complimentary buffet dinner Monday night and lunch Tuesday during Capitol visits. We hope to see you there! Register today at floridadental.org/ddoh
15 | TODAY'S FDA january/february 2023 legislative
Sen. Kathleen Passidomo
Rep. Paul Renner
Sen. Lauren Book
Rep. Fentrice Driskell
IN THE KNOW WITH GAO
Webinar series for FDA members to stay informed on legislative and political issues.

The Florida Dental Association’s Governmental Affairs Office (GAO) would like to invite you to join in on our listening sessions to learn about legislative issues that may have an impact on the dental profession, political issues that could affect the dental industry, and a number of other hot topics that may be of interest to you!
The listening sessions will be scheduled for mid-afternoon, 30-minutes long and will allow you to ask questions of the speakers. These sessions are meant to give you a quick update on issues and topics during your lunch hour, without interrupting the flow of your day.
POTENTIAL GUESTS:
• Elected officials (federal, state and local)
• Candidates running for office
• State agency and department heads
• FDA Members
• National dental leaders/experts

GOVERNMENTAL AFFAIRS TEAM:

16
JOE ANNE HART Chief Legislative Officer jahart@floridadental.org ALEXANDRA ABBOUD Governmental Affairs Liason aabboud@floridadental.org JAMIE GRAVES Legislative Assistant jgraves@floridadental.org
ARE YOU A MEMBER OF FDAPAC CENTURY CLUB?
Join
A portion of your required dues is transferred to the Florida Dental Association Political Action Committee (FDAPAC). FDAPAC provides campaign contributions to dental-friendly candidates.


FDAPAC Century Club members provide additional financial support of $150 or more for state campaigns. FDAPAC dues and contributions are not deductible for federal income-tax purposes.
“Your support of the PAC helps the FDA build relationships with leaders who will be making important decisions in Tallahassee that will impact our profession and our patients.”
17 | TODAY'S FDA january/february
2023
Dr. Rudy Liddell FDAPAC Chair
now: floridadental.org/centuryclub
— Dr. Rudy Liddell
OCR Recently Released a Bulletin Outlining the Proper Use of Tracking Tech in Accordance with HIPAA Compliance
By Matt DiBlasi, Abyde President & Co-Founder
Covered entities and business associates, like health care providers, that use online tracking technology should ensure their electronic protected health information management meets HIPAA standards.

Have you ever talked about being out of toothpaste at work, and then when you get home there’s an ad for Colgate on your tablet as you decide what to order for dinner? It’s creepy, but it’s efficient. You’ve been targeted and the Colgate marketing department is doing its job. In this example, the transmission
of your tracked demographics and shopping habits is not as sensitive as the transmission of your patient’s data.
Recently, the Office for Civil Rights (OCR) at the U.S. Department of Health and Human Services issued a bulletin (visit bit.ly/3uOmUiy to view) regarding the correlation between sharing electronic protected health information (ePHI) and online tracking technology. While we at Abyde aren’t experts in targeted advertising, we are HIPAA experts. There are rules that apply to regulated entities when collecting information through tracking technologies or disclosing ePHI to vendors
18 preventive action
with whom you may be working. The OCR put it plainly, “Regulated entities are not permitted to use tracking technologies in a manner that would result in impermissible disclosures of ePHI to tracking technology vendors or any other violations of the HIPAA rules.”
Do you know if your PHI is being captured through online tracking? Are you monitoring what patient data is being shared with third-party vendors? Even more importantly, do you use Google Analytics or Meta Pixel? If so, you might want to listen up. Whether you or a third-party agency set this tracking up, if there are not permissible disclosures from your patients, you are putting your practice and patients at risk if ePHI is shared through the tracking technology.
Let’s Head Around the Bases to Make Sure You’re Covering Your Bases.
Nice base hit – you made it to first. The first thing you can do is ensure you have Business Associate Agreements (BAA) in place with all third-party vendors, especially those who create, maintain or receive ePHI. While you’re cross-checking if your vendors meet the definition of a business associate (visit bit.ly/3j7Es6E to view), make sure your agreements denote the permitted use case for ePHI.
And the crowd goes wild – way to steal second. Before you think, “Well, I’ll just ask the vendor to delete any protected data before they use or save it,” that’s not going to cut it. Per the OCR, “Any disclosure of PHI to the vendor without individuals’ authorizations … requires that there is an applicable Privacy Rule permission for disclosure.” Through the Privacy Rule (visit
bit.ly/3htIeab to view) patients are empowered to have more control over their health information. This allows for access, options to make any changes as needed and sets boundaries on the use and release of health records, including the minimum necessary standard for information disclosures.
A bunt from your teammate gets you over to third – nice work! Before we round out to home, ask yourself if the risk is worth the reward. And if you’re still unsure, check in with your Security Risk Analysis (visit bit.ly/3WesUNo to view) and scorecard – another benefit to Abyde’s ongoing compliance. We work with you to identify the potential risk and associated exposure.
As we make our way to home base, we will summarize with this: if ePHI is involved in any of the data being shared by the tracking technology, HIPAA rules must be followed. Here are the final words from the OCR: “all disclosures of PHI to tracking technology vendors are specifically permitted by the Privacy Rule and that, unless an exception applies, only the minimum necessary PHI to achieve the intended purpose is disclosed.”
Abyde is an FDA Crown Savings Endorsed Partner and the Abyde software solution is the easiest way for any sized dental practice to implement and sustain comprehensive HIPAA and OSHA compliance programs. FDA members save 20% on Abyde services that help their practices meet government-mandated standards through the implementation of risk management programs, training for doctors and staff, customized policy generation and more. Visit fdaservices.com/abyde or call 800.594.0883. Reprinted with permission from Abyde’s blog post.
19 | TODAY'S FDA january/february 2023
”
Regulated entities are not permitted to use tracking technologies in a manner that would result in impermissible disclosures of ePHI to tracking technology vendors or any other violations of the HIPAA rules.
By Lianne Bell, FDA Leadership Affairs Manager
An organization’s ability to thrive is primarily determined by the quality and effectiveness of its leadership. Leadership matters whether the organization is a study group, Rotary Club, an affiliate dental society, or your dental office. We know good leaders can create tremendous success, but how do we become that kind of leader? Often, they have learned skills that take thoughtful training and practice to develop. For these reasons, we are excited to introduce a new corner of Today’s FDA called, “Take the LEAD.” The impetus for this new feature is the work done by the FDA’s Leadership Development Committee, specifically, their program Leaders Emerging Among Dentistry or LEAD. LEAD was developed out of a desire to help member dentists develop to serve their patients and colleagues better and to ensure the excellence of work being done at the local, state and national levels by organized dentistry continues. In this new section of the journal, we will include information about the LEAD program, upcoming dates, articles from featured speakers and other general leadership resources. We hope you’ll turn here to learn, stay informed and continue to grow in your personal develop-
ment. Additionally, we hope to meet you at one of our LEAD programs, where you can enjoy the opportunity to network and learn along with your peers.
The FDA’s Leadership Development Committee:
l Dr. Angela McNeight, chair, Merritt Island
l Dr. Jenna Schwibner, Vero Beach
l Dr. Matthew Sheldon, Melbourne
l Dr. Millie Tannen, Jacksonville
l Dr. Chinara Garraway, Tallahassee
l Dr. Melissa Sedeno, Miami Lakes
l Dr. Kristie Johnson, Largo
l Mariangel Fuchs, LECOM
l Austin Jackson, Nova
l Stephanie Taylor, UFCD
While all methods of self-improvement should be applauded, the fact remains that leaders change over time. As you grow in your practice and become more confident in your leadership skills, it is important to reevaluate your strengths and receive additional training on areas of your skill set that may be a struggle. As much as leaders change, teams and their needs change as well. The challenges dentists face today are different than the challenges faced even a few years ago.

20
take
the lead
”
— Dr. Angela McNeight, chair of the Leadership Development Committee
Are you looking to get more involved in organized dentistry but don’t know where to begin or how to get your foot in the door? Then come check out Leaders Emerging Among Dentistry (LEAD). LEAD is the Florida Dental Association’s premier leadership training program. The program is in its fourth year, hosted annually by the Leadership Development Committee. It has provided hundreds of dentists with the tools necessary to help run an organization, your office or even your personal life more effectively and efficiently. You can find the latest information on the program at floridadental.org/lead.

Committee members and attendees at meetings and past LEAD events.




21 | TODAY'S FDA january/february 2023
— Dr. Matthew Sheldon, Leadership Development Committee member
”
Get Your Squad Together and Volunteer at the 2023 Florida Mission of Mercy!

If you are not currently registered for DDOH, please go to bit.ly/3jW97Ew to join your colleagues at the FDA’s advocacy day!
A legislative briefing will take place on Monday, March. 27, at 6 p.m. at Hotel Duval with a complimentary buffet dinner to follow. If you plan on attending the briefing and dinner, please add both items during your registration. Lunch is provided for all attendees on Tuesday, March 28 and there is no registration fee to attend DDOH
If you have any questions, please contact Governmental Affairs Liaison Alexandra Abboud at 850.224.1089 or aabboud@floridadental.org
Go to bit.ly/3iyj4aP for highlights from the 2022 DDOH!
The 2023 Florida Mission of Mercy (FLA-MOM) is just weeks away! The 2023 FLA-MOM will take place Feb. 24-25 in West Palm Beach — register to volunteer at FLAMOM.org. With a goal of treating 2,000 patients, FLA-MOM seeks to have a positive impact by providing important access to dental care for patients in need. FLA-MOM has served more than 12,000 patients since 2014, and we need your help to make our next clinic a success. Register today at FLAMOM.org. We can’t wait to see YOU in West Palm Beach!Questions? Please email foundation@floridadental.org or call 800.877.9922.
Room Block Almost Full - Register for DDOH and Reserve Your Room Today!

Come for the CE and Stay for the Fun at FDC2023!
Florida Dental Convention (FDC) 2023 … it’s not your average dental meeting! Not only will you receive a world-class education from renowned dental speakers, but you will also have the opportunity to connect with your peers, make new connections and bond with your team. FDC2023 will continue to include free social events for you and your team, including the ever-popular Friday evening event. Go to bit.ly/2IxIi4M to find out the fun events waiting for you, June 29-July 1 in Orlando at FDC2023!
Make Your FDC2023 Hotel Reservation
Gaylord Palms Resort & Convention Center (Host Hotel)
Get the continuning education you need all while enjoying the Gaylord Palms Resort’s amenities including a 3-acre water park, luxury spa, adults-only pool and endless family fun. Reserve your room at the discounted rate of $212 per night, including free self-parking. Go to bit.ly/3QyLTAz or call 877.491.0442 to make your reservation at Gaylord Palms.
FREEDOM TO SMILE!
Rooms are filling up quickly for the Florida Dental Association’s (FDA) 2023 Dentists’ Day on the Hill (DDOH) taking place on Tuesday, March, 28. If you are currently registered for DDOH and have not yet reserved your room at Hotel Duval go to bit.ly/3X2ZnHp to reserve a room while they are still available!
Fairfield Inn & Suites Orlando Kissimmee/ Celebration (One Mile from Gaylord Palms)
Conveniently located one mile from Gaylord Palms, the Fairfield Inn & Suites offers attendees complimentary breakfast and parking for the discounted rate of $124 per night. Go to bit. ly/3W1Derq or call 407.390.1532 to make your reservation at Fairfield Inn & Suites.

22 news@fda
2023 DENTISTS’ DAY ON THE HILL Tuesday, March 28, 2023 Monday, March 27, 2023 Legislative Briefing 6 p.m. at Hotel Duval Complimentary dinner to follow Tuesday, March 28, 2023 Capitol Visits Lunch provided Click here or scan the code above to register For more information, please contact the FDA Governmental Affairs Office at 850.224.1089 or gao@floridaental.org. Hotel Room Block Hotel Duval - $209 a night Click here to reserve
Dental Spending Increased by 11% in 2021

As more people returned to the dentist after pausing at the height of the pandemic and governmental financial relief was awarded to health care providers, dental spending in 2021 was greater than in years prior to the COVID-19 pandemic, reaching $162 billion, up from $146 billion in 2020, ADA News reported. ADA Health Policy Institute Chief Economist and Vice President Marko Vujicic, Ph.D., said public spending on dental care treatment grew especially quickly, reaching 15% in a trend that was already underway before the pandemic. “Looking ahead, this time next year, we expect more modest growth,” Dr. Vujicic said. To read the full story go to bit.ly/3X5T85e
New Toys Equal Free Cleanings for Needy Kids

In 1996, Dr. Donald Lackey started a toy drive program in his dental office to provide toys to needy children in his community. In place of paying the prophylaxis fee, if a patient would bring in a brand new, unwrapped toy, the cleaning would be free. Dr. Lackey’s office works with the Venice Police Department, who
goes through the Sarasota County schools to find underprivileged children who may otherwise go without toys on Christmas Day. The toy drive program usually starts the Monday after Thanksgiving and lasts two or three weeks. The police department gives Dr. Lackey’s office a deadline, so they have time to come by and pick up the toys and distribute them before the holidays. Over the years, the amount of Dr. Lackey’s prophylaxis has increased, so the dollar amount they ask the patients to spend on toys correspondingly increases. The cost of their cleaning is currently $110, and they ask patients to bring in $75 in new toys. Dr. Lackey’s office gives them a $35 discount as an incentive to go out and shop. Over the years, this has grown where patients specifically ask to book this time of year to participate, and many of them give more than the required amount. Some patients come by and donate toys, or money to buy more toys, because they want to participate, despite not having a cleaning within the time frame. The office typically sees 160 hygiene patients in a given week, and to date, 188 patients have participated in the toy drive. This amounts to more than $20,000 Dr. Lackey has donated in services and well over $14,000 in toys. Needless to say, a lot of kids are very happy on Christmas morning! Dr. Lackey’s office would like to challenge other dentists throughout Florida to do something similar, so this act of kindness will continue to grow and spread to help even more communities.
23 | TODAY'S FDA january/february 2023
Welcome New FDA Members
The following dentists recently joined the FDA. Their memberships allow them to develop a strong network of fellow professionals who understand the day-to-day triumphs and tribulations of practicing dentistry.
Atlantic Coast District Dental Association
Dr. Liveisys Pedraza, Miami
Dr. Tatyana Prosolupova, Jupiter
Central Florida District Dental Association
Dr. Saleh Alhindi, Gainesville
Dr. Priya Sabharwal, Saint Cloud
Dr. Giau Tran, Saint Louis, MO
Northwest District Dental Association
Dr. John Ledford, Pensacola
Dr. Shane Turgeon, Niceville
South Florida District Dental Association
Dr. Darek Dul, Miami
Dr. Simona Zigmond, Hallandale Beach
West Coast Dental Association

Dr. Peter Bliss, Naples
Dr. Liusvanis Hernandez, Fort Myers
Dr. Dana Lambeth-Greer, Wesley Chapel
Dr. Mark Messer, Estero
24 news@fda
Welcome New Members to the Florida Dental Association Read, Learn and Earn! Visit floridadental.org/online-ce for this FREE, MEMBERS-ONLY BENEFIT. You will be given the opportunity to review the “Diagnostic Discussion” and its accompanying photos. Answer five multiple choice questions to earn one hour of CE. Contact FDC Marketing Coordinator Brooke Martin at bmartin@floridadental.org or 800.877.9922.
In Memoriam
The FDA honors the memory and passing of the following member:





Died: 12/18/2022




Age: 79

25 | TODAY'S FDA january/february 2023
Brian Murphy Sarasota




THREE EASY WAYS TO PAY: PAYMENT PLAN: Choose from a variety of monthly installment plans. AUTO-RENEWAL: Set it and forget it! Your membership will automatically renew each year with the credit card you put on file. Online: Visit floridadental.org/dues. Mail: Return blue envelope with statement and payment. Phone: Dial 850.681.3629 to speak to our friendly membership team. Dr. ArNelle R. Wright 17th District Rep. , ADA New Dentist Committee New Dentist Member, ADA Council on Dental Practice Editor, Dental Society of Greater Orlando RENEW YOUR MEMBERSHIP FOR 2023 TODAY! HELPING MEMBERS SUCCEED We have your back. Always.


DISABILIT Y INSURANCE


YOU WORK HARD, NOW PROTECT YOUR HARD WORK
What would happen if you became disabled?
Your ability to earn an income is your most valuable asset and it should be protected! Disability insurance replaces a part of your regular income if you are sick or injured and can’t work.

This coverage will put your mind at ease and help protect you and your family in the event of a disability


sure to ask about available discounts. Discounts are available to students in dental school or up to 60 days after graduation.
Just over 1 in 4 of today’s 20-year-olds will become disabled before they retire.
SOURCE: The Guardian Life Insurance Company of America
SOURCE: The Guardian Life Insurance Company of America CALL US AT 800.877.7597 FOR A DISABILIT Y INSURANCE QUOTE. SO, WHAT ARE YOUR GOALS? Do you want to buy a house, a car, start your own pracrice? Your income and ability to make money are the foundation for all your goals. You need to protect that foundation. You insure your house and your vehicles, don’t you? Then to produce an income? INCOME HOME CARS PERSONAL ASSETS EDUCATION BUSINESS INTERESTS INVESTMENTS BULDING BLOCKS OF YOUR FINANCIAL LIFE:

dental implants



Dental Implants:

An Overview of Digital Workflows for Precision Impact Dentistry
The Latest in Dental Implants
Torque Delivery Via a Hexalobular Driver Positioned at an Off Axis Angulation: An Engineering Perspective
31 | TODAY'S FDA january/february
2023
An Overview of Digital Workflows for Precision Impact Dentistry
 By Rafeeq N. Rahman, DDS; Alexander Lee, DMD; Setareh Lavasani, DMD, MS; and Tobias Boehm, DDS, PhD
By Rafeeq N. Rahman, DDS; Alexander Lee, DMD; Setareh Lavasani, DMD, MS; and Tobias Boehm, DDS, PhD
ABSTRACT
Digital workflows in implant dentistry can help streamline and improve the quality of implant therapy by harnessing the power of cone beam computed tomography (CBCT), intraoral scanning, implant planning software, 3D printing and guided implant placement. This article provides an overview of the key steps and considerations for implementing digital implant dentistry for implant-supported fixed single or shortspan restorations using a static implant guide.
32
” ”
Digital implant workflows hold the promise for dentists to plan and execute implant placement with great accuracy, reliability and predictability, leading to potentially simpler and more predictable restoration.
dental implants
Key Steps
1. Take a CBCT and intraoral scan.
2. Merge the DICOM file with the STL file.
3. Do a digital wax-up of the tooth that needs to be replaced.
4. Plan the implant position in a restoratively driven manner.
5. Design the surgical guide.
6. 3D-print the surgical guide.
7. Place the implant using a guided implant surgical kit.
8. Take an implant-level intraoral scan with a scan body.
9. Deliver the implant restoration.
Digital workflows in implant dentistry improve practice efficiency, procedure predictability and clinical outcomes. Digital implant planning aims to ensure that the implant is placed in a restoratively driven manner, while guided implant placement aims to ensure that the implant is placed exactly where it is digitally planned. Guided implant placement achieves higher accuracy and lower failure rates than freehanded or half- guided surgery because it provides a defined implant drilling and insertion path.1–3 Implants placed in such a manner are also more apt to be restored with screw-retained restorations, which leads to easier maintenance. By digitizing data, the implant planning process is sped up, physical storage space is decreased and patient chair time is decreased.1,4,5
Cone Beam Computed Tomography
The foundational technology that makes a digital workflow possible in implant dentistry is cone beam computed tomography (CBCT). CBCT uses a single, inexpensive, flat-panel or image intensifier radiation detector. CBCT imaging is performed using a rotating platform to which the X-ray source and detector are fixed. The X-ray source and detector rotate around the object being scanned and multiple, sequential, planar projection images are acquired in an arc of 180 degrees or greater.6
X-ray attenuation measurements from each machine position are then used to reconstruct a 3D dataset of the implant site, which can then be used by CBCT viewing software to display either a 3D rendering or any cross-sectional view of the implant site.7,8 CBCT differs from computed tomography (CT)
in that it uses a single X-ray source that produces a cone beam of radiation, rather than a fan beam as with CT. There is no accepted definition of when a fan beam (which is assumed to be planar) becomes a cone beam.9
The significantly lower cost and smaller computing power needed to analyze CBCT images compared to computed tomography made this technology accessible to the dental practice in 1999, when the first commercially available CBCT machine, the NewTom DVT 9000, was introduced in Europe.8
The American Academy of Oral and Maxillofacial Radiology (AAOMR) recommends that cross-sectional imaging be used for the assessment of all dental implant sites and that CBCT is the imaging method of choice for this information. 8 Once a CBCT image is taken, it is recommended that the image be interpreted by an oral and maxillofacial radiologist. The AAOMR noted that “dentists using CBCT should be held to the same standards as board certified oral and maxillofacial radiologists (OMFRs), just as dentists excising oral and maxillofacial lesions are held to the same standards as oral and maxillofacial surgeons. It is the responsibility of the practitioner obtaining the CBCT images to interpret the findings of the examination. Just as a pathology report accompanies a biopsy, an imaging report must accompany a CBCT scan.”10
A CBCT image can be obtained from a dental imaging center or by setting up a CBCT machine within the dental office. The choice for either depends on multiple factors including physical space, economic feasibility, practitioner comfort with the devices and the needs of the patient population. For those looking to purchase a machine for their office, contemporary CBCT devices have a smaller footprint than previous generations as well as higher resolution and faster image acquisition. Additionally, these CBCT machines possess scatter correction or scatter reduction methods that reduce X-ray artifacts from radiation being deflected by restorations using beam-blocking techniques 11 or mathematical corrections.12
Digital File Types
Digital implant planning requires two main pieces of data: a CBCT of the patient as a series of DICOM (.dcm) files and an intraoral scan of the arch as an STL (.stl) file. t
33 | TODAY'S FDA january/february 2023





34 Competitive Salary Medical Insurance Covered Mal-Practice Insurance Covered 401 K Match Program - C.E. Program Doctor Equity Program 30% of Collections - Lab Bill Covered Sedation Certification Program Life Insurance Policy - Dental Coverage No nights/ No Weekends 11 Offices in Tampa Bay area and Growing Intra-oral Cameras in each Operatory Digital Sensor in each Operatory Caesey Education in each Operatory In-Office Financing (DentaCare) On Staff Endodontist, Oral Surgeon and Periodontist Denture/ Partial Lab and Crown & Bridge Lab Sedation Certified Offices Full Support Center Associate Doctor Benefits Vincent J. Monticciolo, D.D.S., M.B.A., J.D. Founder/CEO/Clinical Director WE ARE LOOKING FOR EXCEPTIONAL DENTISTS TO JOIN OUR GROWING PRACTICE! Apply Online at: happydentistry.com/careers/ Office Highlights:
dental implants
A DICOM file is the standard file type for medical data, defined by the National Electrical Manufacturer’s Association (NEMA), that all CBCT machines are capable of outputting. In addition to the image data, each file contains information about the patient, acquisition date and method and the spatial location of the image data. Each DICOM file represents an image section, and the entire collection of DICOM files makes up the 3D representation of an implant site.13 Because of the patient data associated with each DICOM file, practitioners should take care to follow HIPAA guidelines to secure them, especially when they are exported from their picture archiving and communication system (PACS).
Intraoral scans can be exported into 3D model file formats such as STL, OBJ, 3MF and more. While each format has its unique properties, the STL has become the most widely used format for 3D models because of its relatively small file size, speed of export and wide-ranging compatibility. Disadvantages of the STL file type for dentistry are that it does not contain color or scale information, meaning its units of measurement are arbitrary.
Despite these drawbacks, adoption of the STL is so wide that most current dental scanning software and device manufacturers use the file type. Due to its established use in dentistry, this paper refers to 3D model files as STLs.
Intraoral Scanners
There are many intraoral scanners on the market, each with software capable of doing simple to complex dental treatments digitally. Though an in-office intraoral scanner streamlines the process, many dental labs can scan conventional models or impressions and provide an STL file for a fee. For practitioners looking to purchase an intraoral scanner, factors to consider when selecting one include:
l Integration with other existing practice technologies: Software suites like Romexis, DTX Studio and Dolphin Imaging support intraoral scanning. If a practice is already using such a software but is not utilizing the intraoral scanning capabilities, acquiring a manufacturer-supported intraoral scanner would decrease the setup and training time.
l Practice use case: Different scanners may be optimized for different procedures. For example, the iTero Element series
of scanners would be ideal for Invisalign users due to the tight softwarehardware integration, as both are made by Align Technologies.
l Form factor: In addition to considering an intraoral scanner’s size for a patient’s mouth, practitioners should also evaluate whether a scanner comes attached to a proprietary cart, the length and type of cable, size of cradle and device ergonomics.
l Manufacturer support: Terms of support and its cost influence practitioner confidence and can minimize downtime.
l Cost: New intraoral scanners cost between $9,000 to $50,000 per unit. Support packages range from free to hundreds of dollars a month.
l User interface and experience: While some manufacturers offer a “white glove” experience where all support concerns are mitigated, others provide a “bare bones” approach that encourages the end user to create custom solutions.
Some examples of intraoral scanners include 3Shape Trios 4, Planmeca Emerald S, Align Itero Element D, Carestream Dental CS 3700 and Medit i700. The images shown in this review are from 3Shape’s Trios 3 intraoral scanner.
Intraoral Scanning
For restoratively driven implant placement, three intraoral scans are needed: an intraoral scan of the arch containing the implant site (Figs. 1), an intraoral scan of the opposing arch and an intraoral scan of the bite (Figs. 1). This can be used to create a virtual articulator and a digital wax-up. The digital waxup must have the proper dimensions, be in the correct occlusal plane and occlusion, and most importantly, be in the correct long- axis. Ideally the tooth should be missing in the intraoral scan. However, for immediate implant cases, the tooth to be replaced can be digitally removed using the planning software.
It is crucial that the intraoral scan is accurate, since the fit of the surgical guide and the placement of the implant depend on it. Digital impressions obtained from intraoral scanners appear to be as accurate as analog.14–17 t
35 | TODAY'S FDA january/february 2023
dental implants
Intraoral scanning accuracy can be improved with these techniques:
l Keep the teeth dry, especially the occlusal surfaces. Scanners have difficulty differentiating between teeth and saliva.


l Use a proper fulcrum or manufacturer-specified support.
l Visually focus on the computer monitor and not the intraoral scanner itself.
l Capture a few millimeters of soft tissue past gingival margins of the teeth, especially in the edentulous space where the implant will go.
l Capture the interproximal tooth surfaces of the teeth adjacent to the edentulous space. This requires tipping the scanner head mesially or distally to capture tooth structure cervical to the height of contour.
l More scanning does not mean more accuracy. The data should be captured completely, but efficiently. If certain areas need to be rescanned multiple times to get the data completely, there is likely an error or discrepancy somewhere in the scan, and it is best to start over.
Digital bite registrations can be improved with these techniques:
l Make sure the patient is biting properly in their maximum intercuspal position (MIP) without moving or quivering.
l Ensure the teeth are quite dry.
Merging the CBCT and Intraoral Scan Data

Once the CBCT DICOM and intraoral scan STL files have been created, they can be imported into the implant planning software. Many different implant planning software packages are available. Common examples are Planmeca Romexis, 3D Diagnostics 3DDX, 3Shape Implant Studio, Dentsply Sirona Simplant and BlueSkyPlan by Blue Sky Bio. Implant planning software have similar capabilities; the choice depends on the subscription model and the ease with which the software integrates into the existing hardware of a particular office. The images in this section are from BlueSkyPlan by Blue Sky Bio.

36
Fig. 1A
Fig. 1B
Fig. 2
Fig. 3A
The first step is to align the DICOM data containing bone and tooth surfaces with the STL data containing tooth and soft tissue surfaces. Some software merge the two datasets automatically. Additional manual refinement can be done by shifting the model in any of three axes to better align with the CBCT image. Aligning CBCT and tooth surface data can result in higher accuracy of implant placement. 18 If the software does not align automatically, you can manually do so by merging with points (Fig. 2). In this method, the software user must select a series of corresponding points on the model and the CBCT image, such as grooves or cusp tips, which are easily identifiable in both data sets. The software will then align the two datasets together based on the points selected.
Regardless of the alignment method, the accuracy of the alignment needs to be verified. If the models are well aligned, tooth surfaces from both the model and the CBCT should be intimately adapted on individual CBCT slices (Figs. 3).
Once the two data sets are merged, a digital wax-up of the tooth for the implant sites can be created. This is done by inserting a tooth shape from the software and adjusting its size and position along the mesiodistal, buccolingual and apicocoronal axes (Fig. 4). The tooth should be positioned and sized exactly as the final restoration will be because the implant will be planned according to this digital wax-up. In most programs, the digital wax-up can be locked in so that it is not inadvertently altered later in the implant planning process.


Digital Implant Planning

The implant surgeon should review the entire volume of the CBCT to get acquainted with patient-specific local anatomy and look for bone abnormalities and/or presence of any other pathology. If implants in the mandible are placed, the inferior alveolar nerve should be marked in the volume by identifying its course distal from the mental foramen.
Likewise, in the maxilla, the position of unusually prominent neurovascular bundles in the bone should be marked (Fig. 5).
The next step is to determine the appropriately sized implant from the collection of implants in the chosen implant system. The available bone for implant placement provides the possible size for an implant at a given site and often dictates which implant size can be placed. To measure available bone accurately, the sectional views must be lined up so that the buccolingual and mesiodistal sections are perpendicular to t
37 | TODAY'S FDA january/february 2023
Fig. 3B
Fig. 4
Fig. 5
dental implants


the bone surfaces and the view is centered on each implant site (Fig. 6).


Each implant must also meet the following requirements:
l At least 2.65 mm superior to the inferior alveolar nerve 19 and 5 mm mesial to the mental foramen. 20
l At least 1.0 mm (platform-switched implants) to 1.5 mm (nonplatform switched implants) from the implant platform to adjacent teeth21 and at least 3.0 mm between adjacent implant platforms.22
l A 2 mm thick shield of facial bone to the facial implant surface is advised.23

Most implants with completely rough surfaces need to be placed with the implant platform flush or slightly apical to the crestal bone. Placing implants with machined collars apical to the crestal bone may result in bone loss. These requirements typically provide maximum implant dimensions for the available bone. However, available implant dimensions and restorative design considerations including desired emergence profile and support may dictate different dimensions. For example, even if a posterior maxilla implant site features a 12 mm-wide ridge allowing placement of an 8 mm-wide implant, the largest implant size available from a given manufacturer may only be 6 mm in diameter.24 Likewise, if available bone is less than required for restorative needs, site development procedures such as ridge augmentation need to be done.25 Short implants (less than 10 mm length) may help overcome limitations in available bone height, although concerns have been raised about possible mechanical disadvantages from a poor crown implant ratio. Yet, crown implant ratio does not seem to be associated with enhanced peri-implant bone loss and may not affect implant survival.26,27 Small diameter implants (less than 3.5 mm) may have similar bone loss and survival rates than standard diameter implants28 when placed in atrophic ridges, but may have higher complication rates and potential for fracture if placed in posterior areas.29,30
Once the appropriately sized implant has been selected, it typically needs to be placed at the center of the restoration for posterior teeth and canines and palatal to the restoration center for incisors. The goal for incisors is to place the implant so that the facial platform edge is just lingual to the planned
38
Fig. 6
Fig. 7
Fig. 8A
Fig. 8B
incisal edge to allow for a screw-retained restoration and allow for easier development of the facial emergence profile. The overall goal for implant placement is to achieve an implant axis perpendicular to the occlusal table of the restoration to minimize off-axis loading and avoid prosthetic complications31 (Fig. 7).
It is possible that the position of the virtual implant dictated by the restoration results in facial perforation of the cortex at the implant apex. In this case, the choice is either to accept a more difficult restoration by adjusting the implant position or to address the perforation with grafting during implant placement. The decision depends on which method can be more predictably achieved for a given case.
If the appropriate virtual implant length results in perforation of the sinus, appropriate sinus augmentation procedures should be planned along with implant placement. If the existing bone width is not sufficient for implant placement, ridge augmentation or alternatives to implant therapy should be considered. When working as a team, the implant surgeon and restorative dentist must agree on the desired implant position.

A benefit of digital implant planning is the ability to try out different implant sizes and positions and quickly see the outcome in terms of screw-hole position and relationship to the restoration (Figs. 8).
Guided Surgery Kits

Guided implant placement requires the use of specialized guided surgery kits. The design of the kits varies by manufacturer, but in general the kits can have either guided drills (Fig. 9) or conventional drills (Fig. 10) with a series of adapter keys.

With the latter, the keys engage the guide tube, and each key has a hole in the center, of varying diameter, which allows the conventional drill to pass through. Using the key during the osteotomy can be challenging because it needs to be held in place inside the guide tube. The advantage of these systems is that the cost to transition to guided surgery is lower as they make use of the conventional drill kit.


With guided drill kits, every drill has a guiding surface built into it. These kits are much simpler to use than keys because the drill goes directly into the guide. These kits often come with guided implant carriers that for allow fully guided placement.

39 | TODAY'S FDA january/february 2023
Fig. 8C
Fig. 8D
Fig. 8E
Fig. 8F
Fig. 8G
t
Fig. 8H
dental implants
The disadvantage of these systems is the higher cost.
Designing the Guide
Once the implant position is finalized, the next step is to design the surgical guide. Each implant manufacturer’s guided implant surgical kit is different and has its own parameters to create the guide tube (Figs. 11), which directs the guiding portion of the drill. The following are the parameters needed:
l Diameter: This is the inner diameter of the guide tube. It should be as narrow as possible to still allow the guiding portion of the drill to pass through yet reduce lateral movements of the drills. 32,33 Some systems have a separate drill for each step with a single diameter guiding portion that does not change. Other systems use a key system where the drill diameters are different, so a key is needed as an adapter between the drill and the guide. This controls the implant placement in the buccolingual and mesiodistal axes.
l Offset: This determines the position of the top of the guide tube. It is the vertical distance between the stopper on the drill and the platform of the implant. This controls the implant placement in the apicocoronal axis.
l Height: This determines the position of the bottom of the guide tube. It is the height of the guide tube from the top to the tissue level. This should be as tall as possible to minimize lateral movements of the drills.34

Once this information is programmed into the software, the extensions of the guide need to be marked. In dentate

40
Fig. 9
Fig. 10
areas, it is best to go just past the height of contour to allow retention of the guide during implant placement (Figs. 11). In edentulous areas where implants will be placed, it is best to go 3 mm to 4 mm past the neighboring gingival zenith to help retract the elevated tissue during implant placement using a flap approach.
Adding windows at selected cusps and incisal edges is helpful, as it allows verification of complete guide seating during implant placement (Fig. 12).
Once satisfied with the guide, the guide can be exported as an STL file (Fig. 12) to be fabricated in a 3D printing machine. A benefit of the BlueSkyPlan software is that digital implant planning is free and a cost is only incurred once the STL file is exported.
Surgical Guide Fabrication
The STL file from the planning process can be used to print a guide in office with a 3D printer capable of printing surgical guides with resins approved by the FDA for intraoral use or to send to a dental laboratory for guide fabrication. Some implant systems require a metal sleeve to be inserted into the guide tube after fabrication, while others are sleeveless (Fig. 13).



3D Printing
3D printers work through a process known as additive manufacturing: 3D models are cut into many digital layers and then built up in the printer layer by layer. The quality of the object improves with thinner layers. This is akin to CT scanning software that creates a 3D image of part of the body by combining slices together. While many 3D printers exist, the most common printers in dentistry utilize resin as their material. Two of the common methods for 3D resin printing are:
l Material extrusion (FDM): This method involves extruding a plastic filament material through a heated nozzle. The printer extrudes the material back and forth along a predetermined path to create a 3D object, 35 similar to dot-matrix printers for paper (Fig. 14). This method has lower dimensional accuracy, as the thinnest layer possible is 0.5 mm. FDM printing is not recommended for dental purposes due to insufficient level of detail and the lack of FDA-approved materials.
l Vat polymerization (SLA, DLP): This method involves using a light to cure individual layers from a vat of resin (Fig. 15). This method has much higher dimensional
t
41 | TODAY'S FDA january/february 2023
Fig. 11A
Fig. 11B
Fig. 12
dental implants



accuracy, as layers can be as thin as 20 microns. 35 New technologies are being developed that can print layers as thin as 5 nanometers. This is the currently preferred method for 3D printing of dental objects. Today, resins are available for a multitude of dental purposes including dental models, surgical guides, occlusal guards, orthodontic models and indirect bonding trays, provisional crowns and even long-term objects like dentures and resin restorations. There are several 3D printers on the market today that are designed for dental use such as Formlabs Form3+, SprintRay Pro S and Whip Mix Asiga Pro 4K.




The vast 3D printer market provides dentists with innumerable options beyond those stated previously, but one selection criterium rises above the rest — selecting a 3D printer with dentistry-ready features from the manufacturer allows practitioners to efficiently and predictably print their prepared STL files. Such printers have a user-experience like milling units integrated within CAD/CAM systems, boasting solidified digital processes, lists of approved materials and dental-focused custom settings. For printers that do not have these capabilities, users may need to manually repair STL files, transfer them to the printer, orient the models, experiment with unsupported resins and set print parameters through trial and error.

Resin-based 3D-printed models require finishing steps consisting of removing support structures, washing the print, post-print curing and polishing. While finishing stations can be created from existing dental lab equipment (a fume hood, lab handpiece, curing device, glass containers, ethanol and hand tools), dedicated devices like the Elegoo Mercury or SprintRay Pro Wash/ Dry streamline the process by keeping hazardous materials contained, automating tasks like agitating a model during washing and consolidating equipment into a single device to save space.
Regardless of the type of 3D printer and finishing process used, the National Institute for Occupational Safety and Health (NIOSH) has identified three common work hazards for additive manufacturing: breathing harmful materials, skin contact with harmful materials and flammable materials. During all printing stages, NIOSH recommends proper engineering controls, administrative controls and personal protective equipment. This includes using

42
Fig. 13A
Fig. 13B
Fig. 13C
Fig. 13D
Fig. 14
Fig. 15
Fig. 16
high-efficiency particulate air (HEPA) filters, introducing safety guidelines for handling and securing volatile materials like resins and solvents and wearing respirators, gloves and safety goggles.36
Surgery Stage
For implant cases where the guide uses existing adjacent teeth for indexing, the guide can simply be placed on the teeth until it seats completely and does not rock. While it is possible to adjust an ill-fitting guide, it indicates an error occurred during the digital workflow, which can result in the implant not being placed in the planned location. The digital planning and guide fabrication steps should be redone with care.
The guide can be used during implant surgery for direct drilling of the osteotomy only (known as half-guided implant placement) or for both drilling the osteotomy and placing the implant through the guide (known as fully guided implant placement). 37 A fully guided approach is more accurate than the partial-guided approach, as distal deviation and angular deviations from the planned position are significantly smaller with the fully guided approach.38
Guided implant placement follows the same principles as freehanded implant placement regarding patient preparation, anesthesia and suturing. While the principles are similar, flap design, osteotomy and implant placement require minor modifications with the guided technique.
Patient preparation involves obtaining informed consent about risks, benefits and alternatives and an appropriate description of the procedure, medications and what to expect. A single preoperative antibiotic dose is sufficient to significantly reduce early implant failure. 39 For local anesthesia, local infiltration using buccal, crestal40 and lingual infiltration is sufficient for most forms of implant placement.
Guided implant placement presents the opportunity for predictable flapless surgery if sufficient keratinized gingiva is present and the underlying bone anatomy allows for it. For this, a biopsy punch drill is used through the guide hole at the implant site until the drill touches bone. The guide is then removed, and the tissue plug at the implant site is removed using suitable instruments such as tissue forceps, periosteal elevators or periodontal knives.
A full thickness flap should be raised for implant placement if the procedure also requires bone removal, simul-
taneous ridge grafting or high case difficulty where direct visualization of the bone is needed. Suturing typically aims to limit tissue mobility and aid healing.
For the osteotomy with a conventional kit, a key specific for each drill is placed into the guide, and the drill passes through the key. For the osteotomy with a guided kit, each drill is passed directly through the guide. Each drill has a drill stop that reaches the predetermined length (the implant length + tissue thickness + guide thickness) that was programmed into the guide. The osteotomy should follow the manufacturer’s protocol using a surgical drill with high rpm, low torque, copious irrigation, low pressure and, if needed, a straight up-and-down pumping motion to prevent thermal damage to the bone.
Implant placement should also follow manufacturers’ protocols, typically using very low speed (< 20 rpm) and a defined torque (often 30 Ncm to 50 Ncm) that provides sufficient stability without inducing pressure necrosis. For maximum benefit and fully guided surgery, the implant should also be placed through the guide to minimize placement errors. If the implant is placed freehanded after using the guide for the osteotomy, angulation errors may be introduced and some of the benefits of fully guided surgery will be lost. At each osteotomy and implant placement step, the clinician must check if the placement matches what was planned and if the placement is appropriate for the given site.
Pitfalls of Using Guides
For posterior areas, using a surgical guide on a dentate patient may be difficult, as the acrylic and added implant drill length may prevent the operator from using the guide, especially in individuals with limited mouth opening.
“For maximum benefit and fully guided surgery, the implant should also be placed through the guide to minimize placement errors.”
While fully guided implant surgery can result in improved placement accuracy, placement errors are still possible stemming from inaccuracies in the CBCT acquisition, 3D scanning, guide planning, 3D printing, positioning of the guide during surgery and short guide sleeve length.41 It is also possible that a clinician may need to forgo using a t
43 | TODAY'S FDA january/february 2023
dental implants

surgical guide as consequence of unanticipated complications encountered during surgery, such as insufficient implant stability at the planned insertion depth, closer than expected proximity to vital structures, encountering a bone dehiscence or a poorly fitting guide.42 While low-cost 3D printers can produce acceptable guides, 43 accuracy of the guide is dependent on the manufacturing process and size of the guide, with small guides having better fit.44
Dynamically Guided Surgery
The previously described method using a surgical guide fitted over the adjacent teeth describes static guided surgery, which is the more common guided surgery approach. Dynamically guided implant placement was introduced to dentistry in the year 2000, where motion tracking of the patient and handpiece provides the clini-

cian instant feedback about the planned implant position within the context of CBCT data. More recent availability of in-office CBCT machines, reduced cost and improved designs to facilitate use of these systems in a dental office have led to greater interest in this technology, as it may result in a simpler implant planning workflow.45 Currently, two dynamically guided implant systems have received FDA 510(k) clearance and are available in the U.S. (i.e., Navident ClaroNav, X-Nav X-Guide Dynamic 3D Navigation). 6,47 With these systems, cameras mounted in the operatory record optic markers placed on the handpiece and the patient and a computer system provides the operator feedback on a screen whether the implant motor is positioned at the correct angle and position. As another approach in dynamically guided implant placement, robotics was introduced to implant dentistry in 2017 with the development of an autonomous robot implant placement system in China and FDA clearance of a robotic system that assists placement of implants.48 The FDA- cleared system is available as the Neocis YOMI system where a handpiece is mounted on a robotic arm that provides the operator haptic feedback on the correct angulation and position.49 Currently, this system has been developed for use in fully and partially edentulous arches, but requires sufficient teeth or bone to stably hold a splint in place.50 A drawback of the robotic approach is that this system is still quite expensive and is still undergoing development for wider applications.
Digital Restoration
Once the implant is integrated and ready to be restored, a conventional implant-level impression can be taken to have the restoration fabricated. However, the digital workflow can continue with an intraoral scan of the implant to reap the maximum benefits from digital dentistry.
To use an intraoral scanner for an implant restoration, a scan body is required. A scan body is equivalent to the impression coping (FIGURE 16) in the conventional method. Each scan body is unique to each implant platform, as with an impression coping, so this needs to be ordered from the implant distributor prior to the intraoral scan appointment. The scan body
44
Fig. 17A
Fig. 17B
is used in the same way as an impression coping. The healing abutment is removed, the scan body seated and hand-tightened and a radiograph taken to verify complete seating. Once fully seated, an intraoral scan is taken in lieu of an impression, taking care to capture all the notches of the scan body in detail (Fig. 17).
The lab uses the scan body image to determine the exact implant position and to design the abutment and restoration accordingly. The lab can print a model and fabricate the restoration conventionally, or it can design and mill the restoration digitally.
Conclusion
Digital implant workflows hold the promise for dentists to plan and execute implant placement with great accuracy, reliability

and predictability, leading to potentially simpler and more predictable restoration. The key requirements for implementing digital implant dentistry are to use a CBCT machine and an intraoral scanner to create a 3D model of bone, teeth and overlying soft tissue and to use this model to plan implant placement for guided surgery.
Reprinted with permission from the California Dental Association, copyright September 2022
The corresponding author, Tobias Boehm, DDS, PhD, can be reached at tboehm@westernu.edu.

References Available Upon Request
45 | TODAY'S FDA january/february 2023
NEED HELP WITH PATIENT COMPLAINTS? The Peer Review program is designed to help Florida Dental Association member dentists. Avoid costly legal fees, malpractice suits and Board of Dentistry complaints by using this free service exclusively for members. Learn more online at FloridaDental.org/PeerReview or by contacting FDA Peer Review Coordinator Lywanda Tucker at 850.350.7143 or ltucker@floridadental.org
Start planning your next step today.
You are cordially invited to a seminar about planning your future. This comprehensive practice transition lecture is designed to offer you professional guidance as you consider your next step towards planning your retirement. Learn from the experts about your transition options and the best plan to meet all of your needs and goals whether financially, professionally or personally. Discover how to make critical and calculated decisions about the future of your dental office, while learning about a variety of transition options and exit strategies.
Topics to be Discussed
• What is my practice worth in the age of COVID-19?
• What is the methodology used to establish a fair market value for my practice?
• Will my practice value be impacted by the baby boomer generation?
• What type of transition model best suits my situation?
• What common mistakes do most dentists make with their own practice transition?
• What are the pitfalls of me handling my own transition?
• Will I be required to offer seller financing to sell my practice?1
• Who will be the most likely purchaser of my practice?
• Should I insist the sale of my real estate coincide with my practice transition?
• What happens to my practice if I die or become disabled?
• What is the impact of DSOs on the sale of my practice?
Speakers
Dr. Berdj Feredjian, DDS, FAGD—PARAGON Dental Practice Transitions

Louis Kenyon, D.M.D.—PARAGON Dental Practice Transitions paragon.us.com/dental-practice-consultant/louis-kenyon
Mark Sokolov, DDS—PARAGON Dental Practice Transitions paragon.us.com/dental-practice-consultant/mark-sokolov
Jonathan Burns—Bank of America bankofamerica.com/smallbusiness/business-financing/practice-solutions
Event Information
Times for both:
Registration: 8:30am – 9:00am
Seminar: 9:00am – 12:00pm (Light breakfast served)
February 17, 2023
Courtyard Naples 3250 Tamiami Trail North Naples, FL 34103
February 18, 2023
Terrace Hotel Lakeland 329 E Main Street Lakeland, FL 33801
Cost: Compliments of your local PARAGON consultant (a $125 value—3 CE Credits Available)
approval by Bank
America, N.A. of
non-affiliated speakers, programs, products or services. Please consult your financial, legal
accounting advisors, as neither Bank
America, nor its affiliates or employees provide legal, accounting or tax advice. Bank
is
46 Paragon, Inc. is designated as an approved PACE Program Provider by the Academy of General Dentistry. The formal continuing education programs of this program provider are accepted by the AGD for Fellowship/Mastership and membership maintenance credit. Approval does not imply acceptance by a state or provincial board of dentistry or AGD endorsement. The current term of approval extends from 4/1/2020 to 3/31/2026. Provider ID #302387 1 All programs subject to credit approval and loan amounts are subject to creditworthiness. Some restrictions may apply. Bank of America may prohibit use of an account to pay off or pay down another Bank of America account. The Bank of America Representative will provide an overview of the Bank’s Practice Solutions products and services. Sponsorship is not an endorsement or
of
and
of
of America Practice Solutions
a
of
of America, N.A.
America
the Bank of America logo are registered trademarks of Bank of America Corporation. ©2022 Bank of America Corporation.
the
division
Bank
Bank of
and
Contact us today to RSVP: 614.753.1603 dg.kstevent@bofa.com
dental implants
The Latest in Dental Implants: Communication, Techniques and Technology

Any dentist who offers dental implants will say there’s much more to the treatment than simply drilling a hole in the jaw, placing an implant and screwing in a crown. Being able to offer implants is the result of significant investments — in both time and money. Dentists spend many hours of continuing education learning how to properly treatment plan and place implants, and then many more hours practicing how to get it right. The learning process is never complete. Dentists must stay current on the latest implant news to make sure they are providing patients with the best care possible.
With this in mind, AGD Impact asked three dental implant experts to share different perspectives on the latest in implants.
This article was originally published in the July 2022 issue of AGD Impact. It was printed with permission from the Academy of General Dentistry.
47 | TODAY'S FDA january/february 2023
dental implants

Proper Communication Regarding Implants is Vital ”
By Don Deems, DDS, FAGD, PCC
How can dentists tailor their communication about implants to specific types of patients, e.g., could they communicate a certain way with older patients?
Communication is obviously and especially critical when discussing dental implants. Not only are there significant medical and legal implications of dental implant placement, but treatment involving dental implants is nowhere close to being 100% predictable. The internet is often a go-to source of information for many, if not most, people for a wide variety of information. When the information sought pertains to dental implants, there is a lot of good information and not-so-good information, and it’s difficult for most people to discern that, much less find it. If we are the ones providing implant treatment, we must also be providing correct and up-to-date information.
Elements of the communication about dental implants can be tailored for any patient, although it begs the question why. A simple example is that of smoking — if the
48
”
Whether the treatment we are providing involves dental implants or not, honest and open communication is paramount to being a proficient dentist.
person is a nonsmoker, then there’s no need to discuss why smoking and implants don’t mix well. If the person is on longterm steroid therapy, that needs to be addressed quickly. More complicated examples may include how the implants will be used and if there has been previous failure with an implant.
Some people want to know incredible detail, so be prepared to answer those questions. Others just want to know you’re going to take good care of them and that you know what you’re doing.
Regardless of the patient’s personality, age or gender, there are elements that we all have a professional, moral, ethical and legal responsibility to provide, even if any of that information may result in the patient deciding not to pursue dental implant placement. Just because we know how to place an implant doesn’t mean a missing tooth or teeth can, should or would best be replaced with a dental implant restoration or multiple. Dental implants are another modality of treatment with their own pros and cons, and these must be explored with each patient. We are here to provide the best care we can — and are trained for — that the patient ultimately decides to receive.
How do you communicate with a patient who wants implants but can’t afford them?
If a patient cannot afford a type of treatment they want, they simply cannot have it. People want things all the time they can’t have; we live in a materialistic society. However, if a person wants something badly enough, they’ll find a way to get it. Dental implants are one of those treatment options in dentistry that a person may have to think about for a long time; you can’t rush that process for them. Planting the seed of receiving dental implants as a treatment option — if it is appropriate for that patient — will allow them the time to do it when they are ready and when they have figured out how they can pay for it. Rushing that
process is inappropriate.
No matter what treatment a person may want, the cost of treatment is always part of the decision process. Sure, there are various ways a patient can find to finance any type of dental care, but if we or a team member try to talk a patient into something they don’t want, it is a very slippery slope to trouble. It’s best to present all treatment options, discuss the pros and cons of each option, give the patient all pertinent information — including cost — and then leave them alone. More
and more in my practice I am seeing patients who have been pushed, cajoled or aggressively marketed to — and they don’t like it. Would you? When money becomes our priority, we’re heading in the wrong direction.
If we provide the patient a clear understanding of their current dental situation, taking into consideration their dental and medical history, and we also provide them with all available treatment options and then let that patient decide in their own time what they want to do, we’ve achieved our professional duty.
Implant placement and restoration continue to evolve and certainly aren’t exact sciences. One only needs to place a few dental implants to realize that. To that end, a patient may want our opinion. It’s in this gray area where we must be extremely cautious, not letting our own interests — especially financial — dictate our communication. If you feel that implant placement would not be in the patient’s best interest, tell them, and be prepared to tell them why. In the end, implant placement is not about persuading or dissuading anyone.
How do you communicate with a patient who wants implants but is not a good candidate for them?
In my experience, many patients have already heard of dental implants and have a positive or negative view of them before they even see us. Dental implants are not a panacea for replacing teeth. They are just another way of replacing teeth — sometimes more advantageous and appropriate, other times just the opposite. What happens when a patient comes to you wanting implant placement, can afford them, has a positive view of them and has already decided that dental implant placement is for them? This may be hard for many dentists to turn down. This is yet another slippery slope. Diminishing a patient’s clinical situation and risk factors in favor of placing dental implants has a high risk of becoming a nightmare for those choosing to forge ahead. If a dentist sticks to a complete evaluation, discusses all available treatment options without prejudice, and allows, encourages and answers all questions, my experience tells me that, most of the time, the patient will be able to make an educated decision and decide whether dental implant treatment is truly appropriate. They will also appreciate the time you are taking with them. What happens if the patient still pushes ahead for dental implant treatment? A clear option can be a referral to another dentist who places dental implants for a second opinion. Remember that we are not obligated to provide a dental service of any sort just because somebody wants it. t
49 | TODAY'S FDA january/february 2023
dental implants
How do you communicate to patients what dental implants are in a way that balances how involved the procedure, aftercare and patient commitment must be without overwhelming them or scaring them?
As professionals, we have an obligation to always present a clear and unbiased picture to any patient of any treatment. If a patient knew that a crown placed on a cracked tooth may not actually save a tooth, would that scare them away from receiving care?1 Maybe. Maybe not. There are many types of cracked teeth, and some of the teeth we think are easily salvageable end up being extracted.
Looking at this another way, would you rather know everything about a procedure you are about to undergo or only the things you wanted to hear? This is also a gray area where we must guide our patients based on our knowledge of their understanding of their condition, the terminology we use and other factors. We must inform the patient of the reality of any treatment choice they make.
If dentists were to list every possible outcome for every possible treatment option based on every possible situation, not only would we overwhelm our patients, but we would also never have time to provide care. We must choose — within the standard of care — the salient points that neither favor nor disfavor, persuade nor dissuade, a patient from choosing any type of treatment, including dental implant treatment. Again, this starts with understanding the patient’s wants, needs and concerns, a thorough dental and medical history, and a complete dental evaluation. If we take the time to do this, we can establish trust.
In essence, it is not about scaring or overwhelming anyone; it is about informing the patient in a way that helps them understand what they are choosing and what their role must be in the treatment process, including the care they take of themselves and what is provided to them after the treatment.
Reassurance is another way of convincing someone of something. It is an emotional feeling. Yes, we reassure our patients on a regular basis; it’s not unusual to do this.
However, when it comes to reassuring a patient about something which has no merit, we cross a moral and ethical line.
Each year, the number of injuries from dental implants has been increasing. This can be confirmed by using the Food and Drug Administration’s Manufacturer and User Facility Device Experience (MAUDE) database, which, although accessible to the public, is difficult to use.2 This presents an uncomfortable problem for general dentists. The number of failures following implant placement has been rising dramatically, and more and more implants are being placed by general dentists. Some research even suggests that the failure rate of dental implant placement may be higher for general dentists than it is for our specialist colleagues.3 What’s more nebulous is the definition of “implant failure.” This question and others like it are complicated and often difficult to definitively answer.
As general dentists, when we walk into the arena of placing dental implants, we are held to a standard of care. This standard of care then includes what our specialist colleagues provide. Reassuring a patient, in my opinion, has almost no place in the discussion. We must answer openly and honestly any question a patient may ask about our training and experience. If a patient would be better served by a specialist, then so be it. Put yourself in the patient’s shoes; would you want somebody reassuring you that the operation you are having “can be done” by the surgeon, but a surgeon who specializes in the procedure may obtain a better outcome? It is quite true that there are many general dentists who are extremely competent in the placement of dental implants, and perhaps more so than some, or perhaps many, of our specialist colleagues.
50
How do you reassure patients that implants fall within a general dentist’s scope and that they do not need to see a specialist for this service?
So, the path to providing care with dental implants is unclear. The factors involved are numerous. We must know our limitations and responsibilities. If we do, and we can provide the standard of care, then perhaps a little reassurance is appropriate. Just be careful about crossing lines that may become problematic. How do you communicate with patients if the need to refer arises midway through treatment?
I had a new patient recently who told me that she chose not to receive dental care for many years because of a bad experience. This is not uncommon for us to hear, and it’s unfortunate. According to her, she had broken a tooth that had a previous root canal and crown. She went to a dentist at the end of a day for an extraction, which the dentist told her he could perform. She reported that the dentist “worked and worked on her for hours” before finally summoning an oral surgeon to complete the procedure. Perhaps her details were a little skewed, but maybe they weren’t.
You haven’t practiced dentistry very long if you have not started a procedure that you thought would go a certain way, only to find it going severely wrong in a hurry. This can happen to anyone in our profession. And it may certainly be true for implant placement procedures.
Given the scenario I mentioned, if you were the patient, what would you have preferred? In my opinion, it would have been perfectly acceptable to have found a stopping point in the procedure and then referred the patient to someone who could continue the care and finish it. For me, I would not have thought badly of the person who tried to help me, especially
if it was done with honesty and integrity. In fact, I might have respected them even more. Our patients are like us, and we are like our patients. In my own experience as an expert witness in dental malpractice cases (something I don’t like to do), many litigation matters could have been avoided if the dentist just apologized. We may think that patients expect perfection; what they expect is much different.
Whether the treatment we are providing involves dental implants or not, honest and open communication is paramount to being a proficient dentist. Referral is not an indication of failure; it is an indication of maturity and professionalism.
Don Deems, DDS, FAGD, PCC, known as The Dentist’s Coach®, is a trained professional, personal and business coach, and a practicing dentist. He is also the AGD Impact Team Building columnist.
This article was originally published in the July 2022 issue of AGD Impact. It was printed with permission from the Academy of General Dentistry.
References
1. Mamoun, John S., and Donato Napoletano. “Cracked Tooth Diagnosis and Treatment: An Alternative Paradigm.” European Journal of Dentistry, vol. 9, no. 2, 2015, pp. 293-303.
2. “Manufacturer and User Facility Device Experience.” U.S. Food & Drug Administration, accessdata.fda.gov/ scripts/cdrh/cfdocs/ cfmaude/search.cfm. Accessed April 10, 2022.
3. Da Silva, John D., et al. “Outcomes of Implants and Restorations Placed in General Dental Practice.” Journal of the American Dental
51 | TODAY'S FDA january/february 2023
”
The Latest Techniques to Make Implant Placement Smoother
By Eric G. Jackson, DDS, MAGD, FICOI, FASD, FICD, FADI
Are there any techniques that general dentists should be using to make implant placement easier?

“How do I get into dental implants?” “How do I do more dental implants?” “What are your favorite dental implant techniques?” These are questions that I’ve continually been asked throughout my career. My answer is always the same: Start with a sound educational foundation.
”We practice dentistry in an amazing age, where high-quality instruction on dental implants is readily available to all dental professionals via a variety of means and media. Amazing multiday in-person courses on implant dentistry with hands-on learning provide unparalleled educational opportunities and techniques. Due to the COVID-19 pandemic, top-notch live and prerecorded webinars are more plentiful than ever. Virtual media offers amazing access to a plethora of viewpoints and techniques from international experts that are accessible to any dental professional with an internet connection. Lastly, textbooks on implant dentistry often go overlooked as extremely useful tools to both the new and seasoned dental professional. I’ve always called dental implant textbooks my “secret weapon” when answering these three classic questions. This is because textbooks minimize the cost of entry into the world of implant dentistry while providing stellar comprehensive information on all aspects of the field. Not every dental professional has the time, financial resources or availability to attend in-person courses. Textbooks fill this void, and the authors are often some of the most prominent educators in the field. I definitely recommend reading several textbooks because each prominent author provides his or her own unique viewpoint and philosophy.
52 dental implants
Implant dentistry is no different than other subsections of our field in that the highest rate of predictable success is usually attained via excellence from the practitioner as well as the patient.
What tips can minimize hurdles to complete socket grafting at time of extraction?
Healthcare in general can be unpredictable, and one of the best ways to maximize predictability is to have a commanding knowledge of the subject at hand. I’m a planner by nature and have always found the adage “proper planning prevents poor performance” to be a sound bit of advice. My biggest tip to minimize hurdles would be to have an intimate understanding of both extraction technique and graft materials, as well as a well-conceived surgical and restorative plan. Each extraction and socket graft is similar and yet, at the same time, completely unique. Common questions will often have different answers depending on the case at hand. What type of graft material best suits the needs of the case? What type of membrane is anticipated? Is the addition of platelet-rich fibrin or similar adjunct techniques indicated?
Combining the requisite knowledge and skills with preoperative visualization and team communication is certainly a sound start to a successful procedure. Visualization is a classic technique used in the sports world, and I find it to be extremely useful in dentistry. Prior to any dental procedure, take a few moments to visualize the entire procedure in your head. Be as detailed as possible. Try to anticipate any potential hurdles and how you might overcome them. Once complete, loop in your team. I like to briefly go through the anticipated steps and approaches I will take with my team prior to the patient getting in the chair. This review informs everyone of my anticipated master plan and allows us to be both efficient and flexible should hurdles arise.
What are the best strategies to prevent peri-implantitis?
Implant dentistry is no different than other subsections of our field in that the highest rate of predictable success is usually attained via excellence from the practitioner as well as the patient. This concept is a major pillar of my dental practice, and, to reinforce it with patients, I often compare long-term dental success to long-term successful car ownership. We discuss the importance of quality automobile design and construction as well as the importance of maintenance and upkeep. In my opinion, patient education and understanding are the most important steps to take to prevent periimplantitis. So many dental implant patients unfortunately operate under the assumption that “implants are forever” and that they require zero maintenance. We discuss periimplantitis and other
implant complications at length and review the importance of top-tier home care. We recommend electric toothbrushes, oral irrigators, nonalcoholic rinses and custom acrylic nightguards for all our patients, but especially those with dental implants. Reduced intervals between dental hygiene appointments are also discussed for those cases where it is indicated.
What is the socket shield technique, and how is it useful?
The socket shield technique is a “newer” technique that is quite interesting. I place newer in quotes because, even though papers have been published about it for over a decade, surprisingly few general dentists have even heard of it. The technique is traditionally employed during immediate implant placement in the anterior region to preserve the integrity of the periodontium and the thin buccal bone that lies beneath. In a nutshell, the socket shield technique involves completing the tooth extraction via bisecting the root and preserving the buccal two-thirds of the root in the socket as a type of shield. Implant placement then takes place behind the protection of the socket shield with the intention of minimal disruption to the buccal plate and associated anatomy. Variations of the technique can be employed to preserve interproximal or palatal bone as well. A quick internet search will yield a variety of published articles that will certainly do more justice to this interesting technique then I can do so briefly.
Are there techniques that general dentists should not attempt? When should they refer?
General dentists, as well as specialists for that matter, should perform procedures they feel comfortable with. This feeling of comfort is usually derived from completing sufficient education and practicing sound case selection during the planning phase. Simply put, referrals should take place whenever a clinician’s comfort level is not met. I don’t complete every dental procedure, and I’d be willing to bet none of you do, either. Having enough knowledge to know when a case would benefit from being referred to a specialist is often just as important as having the knowledge to complete a different case from start to finish.
This article was originally published in the July 2022 issue of AGD Impact. It was printed with permission from the Academy of General Dentistry.
53 | TODAY'S FDA january/february 2023
Eric G. Jackson, DDS, MAGD, FICOI, FASD, FICD, FADI, owns and operates Jackson Family Dentistry in Downers Grove, Illinois.
By Ross Isbell, DMD, MBA
What are the benefits of implant surgical guides?

Implant surgical guides — when used correctly — can be incredible aids for prosthetically driven implant placement.
Technology Can Make Implant Placement More Seamless ” ”
There are also scan body systems that work specifically with your scanner and mill type that can convert a variety of implant systems into what you need for in-office fabrication.
Coupled with a process for designing the final crown before moving into the surgery phase, a guide can be a simple device for placing an implant into a tooth-bounded edentulous area with the goal of a single crown or as part of a complicated device used to plan all-on-X locations that give ideal anterior-posterior spread and angulation for a large prosthesis. When placing a guide for a tooth-bounded area, it can be as simple as snapping the guide in place and using it as an aid to ensure angulation is ideal and that negative complications with surrounding anatomy such as nerves will not be a problem. In some systems, you can design and mill the final or temporary implant crown as part of the process to design and print or mill the guide. In an all-on-X situation, there are typically no remaining teeth, so anchorage of the guide must be completed using anchor pins at preplanned locations. However, they are not foolproof, and there is some room for error. With both of these situations, you still must follow standard precautions for tracking the process of your surgery — even though surgical guides can be incredibly accurate, if the guide is placed incorrectly by even 1 degree, there can be significant change in the final implant location.
How can general dentists implement a guide system?
You will need the patient to have a cone-beam computed tomography scan completed and have a digitized impression.
This is most easily done with an intraoral scan, but there are many labs that will accept an analog impression and scan it for you. So, even if you don’t have technology in your office, you can still have guides made. You will, however, need to purchase and famil-
54
dental implants
iarize yourself with your implant system’s guided kit. These may include different keys and drills that your lab will need to plan for in the fabrication process and that you will need to understand for the surgery to be truly accurate.
How does a 3D navigation system help with implant planning and placement?
I have demo’d, but not used, a 3D navigation system called X-NAV. The results that I get from my oral surgeon using these types of devices are really excellent, though. The feedback I have received from the surgeon about this surgical process is that it gives the confidence of guided surgery and precision in placement location while allowing for the freehanded adjustment feel during the procedure. As I said about standard guides, it is still critical to follow normal procedures for radiography and location confirmation.
Is it worth the investment?
I place the majority of my implants freehanded, but I am also placing most of these into abundant bone and know that my placement location will be within an acceptable tolerance range for restoration. If there is any question of whether there is enough bone, I will either change into a guided process or refer to a specialist for ridge augmentation or sinus lifting. For peace of mind and a greater guarantee of prosthetic fabrication ease, then yes, I think guides to aid placement can be worthwhile, though they definitely are not required.
What lasers work best with implants?
If the question is regarding the uncovering of implants, then I would argue that it doesn’t truly matter, though some lasers are gentler on tissue than others. Personally, I use a diode for uncovering instead of scalpels in order to reduce bleeding and eliminate the need for suture removal. CO2 lasers have a similar coagulation style and effect as diode lasers. Nd:YAG and Er,Cr:YSGG lasers have been shown to be effective with peri-implantitis management and for helping with tissue regeneration processes, but they are significantly more expensive. So, whether you need a laser, and which one you need, really depends on what your treatment goals are.
How are new materials (e.g., ceramics) making implants better?
In regard to restoration, new materials are allowing for better temporization and tissue-healing customization than ever before and are giving us better opportunities to make margins disappear. So many patients are unhappy with the “dark line”
at the bottom of their porcelain-fused-tometal crowns on normal teeth, and this is often a cosmetic issue with implants, as well, if they are not placed at an appropriate depth. With appropriate planning of implant location subgingivally, newer ceramics are changing the custom abutment game so that anodized titanium is not always a requirement for angulation correction and can allow for great soft tissue contours. In considering the new types of surface treatments that implant bodies are receiving, the implants we are using now are so much more bioactively helpful in creating a stable osseointegration from an early healing time.
What imaging/impression-making technologies are optimal for implant planning?
Every implant system has a scan body that allows your particular scanning system to capture and send information to the lab for fabrication. There are also scan body systems that work specifically with your scanner and mill type that can convert a variety of implant systems into what you need for in-office fabrication. I personally use Biohorizons implants with a Truabutment scan system for most of my fabrications to be completed in-office. However, if I want to send it to my regular lab, I need to use the Biohorizons-specific scan body or take a polyvinyl siloxane impression. The most important thing is having a good relationship with your lab and making sure you capture all the information it needs.
What other new technologies are you keeping your eye on or would like to try out?
I have not yet advanced my studies to the point where I am designing guided bone and tissue growth for site preparation prior to implant placement, but there are some awesome software programs out there that are making that a reality, too. Some new scan post systems attach directly into the healing abutment and present an interesting change to the workflow, but the stability and accuracy seem imperfect at this point.
Ross Isbell, DMD, MBA, currently practices in Gadsden, Alabama, with his father, Gordon Isbell, DMD, MAGD. He attended the University of Alabama at Birmingham (UAB) School of Dentistry and completed a general practice residency at UAB Hospital. ag
This article was originally published in the July 2022 issue of AGD Impact. It was printed with permission from the Academy of General Dentistry.
55 | TODAY'S FDA january/february 2023
VOLUNTEER FOR FLA-MOM 2023!
February 24-25, 2023
• West Palm Beach
Expo Center at The South Florida Fairgrounds
THE FLORIDA MISSION OF MERCY

Florida Mission of Mercy (FLA-MOM) is a large-scale, two-day, professional dental clinic that provides care to any patient at no cost, with the goal of serving the underserved and uninsured in Florida — those who would otherwise go without care.

With a goal of treating 2,000 patients, FLA-MOM seeks to have a positive impact by providing important access to dental care.
Treatments o ered at FLA-MOM include: cleanings,

fillings, extractions, root canals, pediatric dentistry
YOU CAN MAKE A DIFFERENCE!
Help us provide dental care to those in greatest need. We need the following types of volunteers:
dentists, hygienists, dental assistants
dental lab technicians
physicians, nurses, EMTs
medical assessments of health history
vital signs
glucose testing
general community
egistration
endants and more!
SIGN UP TODAY AT FLAMOM.ORG
STILL NOT TRAINED IN RADIOGRAPHY? IT’S TIME TO FIX THAT.
NEW YEAR, FOR YOUR DENTAL TEAM

ENHANCE YOUR PERSONAL SKILLS AND BECOME A NEW YOU
Start the new year right! Take the first step on the path to dental radiography certification. No travel. No time away from work. Train online, at your own pace. The Florida Dental Association (FDA) Online Radiography Training Program provides you the formal training you need, with the professional development you want. Enrich your career path while contributing a vital service to your patients and dental team. It’s the most convenient and economical way to get the radiography training required by Florida law. It’s affordably priced, too — just $285 per student* for FDA members!
*Non-members pay $385.

Torque Delivery Via a Hexalobular Driver Positioned at

an Off Axis Angulation: An Engineering Perspective
By Dr. Robert Dobrin
Modern dental implants integrated with the underlying bone must connect to functional prosthetic restoration. Historically, the connection would be either a cemented restoration with an intervening abutment or a screw-retained connection. It has been observed that complete cement removal from a cement-retained crown is challenging, and any remaining cement is likely to cause periimplantitis, which could lead to implant failure1. To prevent this problem, some clinicians use screw retention wherever possible. The prosthetic challenge with screw retention is the location of the access channel. Frequently, a straight line through the center of an implant will place the access hole in an
esthetically or prosthetically compromised position. To overcome this problem, abutments were developed where the screw connecting the abutment to the implant is in line with the implant. A second hole was placed at an offset angle more favorable to the prosthetics. There are situations when it is preferable to have a direct screw connection without an intervening abutment, so screw systems were developed that allow screws to be driven at angles that are off axis to the implant2
58
dental implants
” ”
Various implant and abutment system manufacturers publish specifications for the torque required to connect the prosthesis to the implant successfully.
Various implant and abutment system manufacturers publish specifications for the torque required to connect the prosthesis to the implant successfully. The tightening torque is a measure of the clamping force of the abutment into the implant3,4,5,6
Torque is defined as the product of a force delivered at a distance from a pivot point (Fig. 1). The component of the torque that is delivered along the long axis of the screw is the only torque that serves to tighten the connection. It is reduced when the force is at an angle other than perpendicular to the lever arm. The subsequent force delivered perpendicular to the lever arm can be calculated via vector analysis as the total applied force multiplied by the appropriate trigonometric function of the angles involved, as in Fig. 2. An applied torque can similarly be represented as a vector where the blue arrow

represents the torque vector, and vector analysis can be used to determine how much of the torque is being delivered along the long axis of the screw7 (Fig. 3). The torque delivered along the long axis in Fig. 4 with the total torque being delivered off the axis can be calculated as long axis torque = total torque * cosine (O).
From this vector analysis, one can see that when torque is delivered at an angle that is not parallel to the screw insertion direction, the screw tightening force locking the prosthesis to the implant will be reduced. When we place an implant restoration, we need to adjust the applied torque based on the delivery angle, and the implant manufacturers recommended axial torque. t
Torque being applied at an angle other than the long axis of the implant yielding clamping force torque equal to the applied torque times the cosine of the angle between the long axis of the implant and the direction of the applied torque



59 | TODAY'S FDA january/february 2023
Fig. 1.
Fig. 2.
Fig. 4.
Fig. 3.
Clinical Implications
dental implants
Robert Dobrin, BSME, DMD, is an assistant professor with the department of prosthodontices at the Nova Southeastern University College of Dental Medicine and can be reached at rdobrin@ nova.edu.
References
1. T. Albrektsson, L. Canullo, D. Cochran, H. De Bruyn “Peri-implantitis”: A complication of a foreign body or a human-made “Disease.” Facts and fiction
Clin Implant Dent Relat Res, 18 (2016), pp. 840-849
2. E. Berroeta, I. Zabalegui, T. Donovan, W. Chee
Dynamic abutment: A method of redirecting screw access for implant-supported restorations: Technical details and a clinical report J Prosthet Dent, 113 (2015), pp. 516-519
3. The effect of screwdriver angle variation on the off-axis implant abutment system and hexalobular screw

R Opler, C Wadhwani, KH Chung - The Journal of prosthetic dentistry, Volume 123, Issue 3, March 2020, Pages 524-528
In this example, the retaining screw is being driven 25 degrees off the long axis of the implant. Therefore, the portion of the torque along the long axis of the implant, which creates the clamping force retaining the crown, is the torque applied to the driver times 0.9 (the cosine of 25 degrees). If the torque applied to the driver is 35 Newton Centimeters (NCM), then the torque applied to the screw is only 31.5 NCM. This diminution of torque may or may not lead to clinically significant reduced clamping force of the crown to the implant, but the clinician must be aware that they are applying less torque to the screw. Below are examples of the amount of axial torque that will be applied to the screw when the wrench delivers 35 NCM at various angles from the long axis of the implant.
35 NCM READING ON TORQUE WRENCH
ANGLE
4. Abutment screw torque changes with straight and angled screw-access channels
RS Swamidass, JYK Kan, MT Kattadiyil… - The Journal of Prosthetic …,Volume 125, Issue 4, April 2021, Pages 675-681
5. J.H. Bickford An introduction to the design and behavior of bolted joints Taylor and Francis Group, Oxford (1995), pp. 175-180
6. R.L. Burguete, R.B. Johns, T. King, E.A. Patterson Tightening characteristics for screwed joints in osseointegrated dental implants
J Prosthet Dent, 71 (1994), pp. 592-599
7. OpenStax University Physics. Authored by: OpenStax CNX. Located at: https://cnx.org/contents/1Q9uMg_a@10.16:Gofkr9Oy@15. License: CC BY: Attribution. License Terms: Download for free at http:// cnx.org/contents/d50f6e32-0fda-46ef-a362-9bd36ca7c97d@10.16
60
AXIAL TORQUE TO IMPLANT SCREW 150 33.6 NCM 250 31.5 NCM 350 28.7 NCM 450 24.85 NCM





Event Information
West Palm Beach, FL
Drive Shack
1710 Belvedere Rd, West Palm Beach, FL 33406
Seller Seminar
Friday, February 17th, 2023
9:00 a.m. to 1:30 p.m.
Aspiring Owner Seminar
Saturday, February 18th, 2023
9:00 a.m. to 5:00 p.m.
Tampa, FL
Top Golf
10690 Palm River Rd, Tampa, FL, 33619
Seller Seminar
Friday, September 29th, 2023
9:00 a.m. to 4:30 p.m.
Aspiring Owner Seminar
Saturday, September 30th, 2023 9:00 a.m. to 5:00 p.m.
Are You Ready for Ownership or Retirement? Start Planning Today.
We cordially invite you to attend this immersive seminar about planning for your future. Learn from industry experts on how to successfully navigate selling or buying a practice as well as starting a practice from scratch. RSVP today and choose the location closest to you.
Topics of Discussion
Aspiring Owner Seminar
● Zero down financing: Acquisitions, startups and commercial real estate
● Buying or starting from scratch –What is right for you?
● Learn the 13 steps to a successful startup
● Taxes, allocation, and financial reporting. Designed for success and growth


● Legal review: LOI, lease, asset purchase agreement and more
● Trends to attract/retain employees in today's marketplace
● Do's & Don'ts of personal insurance and financial planning
Seller Seminar
● How to prepare for a future practice transition

● What a dental practice is worth and what determines value

● Market conditions & trends
● Should I sell my practice to a DSO (Corporate Dentistry)










● Legal review: From LOI through closing and everything in between
● Pitfalls of the legal process
● How to prepare your business financials and documentation
● Taxes, allocation, and how to minimize costs
Featured Speakers
Scan to register today!
 Greg Jones, Dental Practice Broker Doctors Choice
Jason Kaplan, Esq. Palm Beach Law Group
Greg Jones, Dental Practice Broker Doctors Choice
Jason Kaplan, Esq. Palm Beach Law Group
*Buyer
Kyria
NPC Financial *Buyer seminars only Jason Nunez, Regional Director of Practice Finance Provide
Michael DeMeola, CPA, CVA, CFE Getsee & DeMeola CPA Jeff Galvan, Attorney Syndent Consulting Group *Seller seminar in Tampa, FL only
Kyle
Olding, Dental Startup Advisor Dentistry’s Ideal Practices
seminars only
Popovitch-D'Avila, Financial Specialist
*$79.00 registration fee applies Registered Representative of Park Avenue Securities LLC (PAS). OSJ: One Biscayne Tower, Two South Biscayne Blvd., Suite 1740 Miami, FL 33131, (305) 371-6333. Securities products and services offered through PAS, member FINRA, SIPC. Financial Representative of The Guardian Life Insurance Company of America (Guardian), New York, NY. PAS is an indirect, wholly-owned subsidiary of Guardian. National Planning Corp. is not an affiliate or subsidiary of PAS or Guardian. PAS is a member FINRA, SIPC


Pour A-1 Sauce on Carrot Cake for Accountability
By Dr. Jose Peralta
As I finish packing my last bag to leave Theater, I reflect on my time here, four months that looked like forever but were gone in a blink of an eye. It has been a tremendous honor to have deployed with such highly educated, motivated people that many make fun of as “weekend warriors.”
Our group of Providers: A trauma surgeon head of the Trauma Department at a Level 1 Hospital in a major metropolitan city, I’ll abbreviate as DM. An orthopedic surgeon who trained at Johns Hopkins — DH. An anesthesiologist who’s a senior partner at a large group in the Midwest — GF. An interventional radiologist who does complex surgeries — HL. An active-duty emergency room physician at a large army hospital — JS. A 30 plus year critical care physician — JM; and a board-certified pharmacist with a doctorate — TW; and me, a dentist.
These “weekend warriors” leave their hectic lives to put on an M-9 and travel into a combat zone. They leave their family, friends and comfortable lives in the name of freedom, God and country.

So, what does A-1 sauce on carrot cake have to do with accountability? We’ll get to that. These weekend warriors are a different breed of people. They are outstanding, hilarious and highly competitive in their professions. They do not tolerate mediocrity and demand excellence from those around them. Yet, the amount of banter and “F” bombs thrown at the DFAC (dining facility) is like teenagers in a locker room until it gets real.
For example, we are having dinner, and the trauma surgeon, DM, calls the anesthesiologist, GF, and says, “we’re up.” GF’s face went into a walking-out-of-the-tunnel look. Seconds later, the pagers go off, everyone else’s face also changes, and everyone gets up, dumps their full trays, and walks out in double time to the hos-
pital. So what happened? Gunshot wound to the abdomen; the patient is critical and is being medivacked in, and all hands on deck are needed to save a life.
Where does the dentist fit in? At the time, I was the only dentist in Theater covering two countries. I had the chance to see and do facial traumas and significant infections, as well as bread and butter dentistry like routine exams, fillings and extractions. My assistant, a tough, quiet kid from Compton (KC) and I go on missions to different locations in Theater with our equipment and do our jobs. On a trip set for Friday, our destination was missile attacked three days prior. They approached us and said “the area is hot, we have to adjust, and we will Humvee you in the last leg. Are y’all OK with that?” I look at KC and give him the nod, meaning, “what do you think?” He looks at me, pauses for two seconds, and says, “Let’s roll.” They look at me for a final decision. I paused longer than two seconds to think of the magnitude of the situation, asked a question to which I liked the answer, and replied, “I guess we’re rolling.”
As I share that story with my wife, I can feel her getting angry, and she says, “Please tell me you said NO.” As it seemed to happen, the mission was moved to another day for other reasons. They could not guarantee an exact date of our return, and it was too close to my departure from Theater to come home, so I didn’t go, but I set it up for the next dentist who was replacing me — a dentist with 17 years of Army experience. As I explained to him the mission, he looked at me and said, “cool,” with a smirk.
In my previous articles (to view the Nov/Dec 2016 article, go to bit.ly/3IW5fOy; to view the Jan/Feb 2017 article, go to bit.ly/3iJc3Ei) I wrote about what I have learned in the Army that I carry into civilian life professionally; in this one, I want to add what I’ve learned personally.
66
time to serve
1.
l Are you only taking continuing education for dental, or are you incorporating classes in medicine like traumatic combat casualty care (TCCC)? It is given to civilians. How many suture techniques do you know how to do?
l Who is in your circle of friends or family holding you accountable for your goals, dreams and aspirations?
Let me explain about the A-1 sauce. I have had a stubborn 10 pounds that I can’t seem to lose, or better said, I keep running into carrot cake that won’t let me get there. I also tried to lose inches off the waist and add muscle to this old body. While having a piece of carrot cake in the chow hall, pharmacist TW walks by and pours A-1 sauce all over it. I looked at him with a “what the heck” look. He looked at me and said, “You can thank me another day when you reach your goal.”
What kind of person has the soldier mentality/drive?
Let me give you an example of this mindset. It’s 1800 (6 p.m.), we’re having dinner, and we just found out that there is an award that was going to be given if you completed a 40-kilometer (24-mile) ruck march in two sessions of 12 miles, each in two days. We agreed it was something we could do, so in conversation, it was asked when we would start. Long story short, I was outvoted to start at 1900 (7 p.m.) that night! I’m thinking they had lost their minds, that’s just shy of two half-marathons. The next day we’d start at 4 a.m. and knock it out early because Sunday is a pancake breakfast morning. Younger soldiers see that two older ones have said yes, so they up the ante and say, “Well, I’m doing this in boots,” and another says, “Well, I’ll add more weight.” This one-up level of competitiveness is way too common in everyday soldier mentality.

What started as a conversation at 6 p.m. was finished in two sets of 12 miles of three hours each and completed in one night, not two days. After finishing that night’s 12 miles in under three hours, I went to my combat housing unit to pack everything for the following day, set the alarm for 0340 for the 0400 start, and took four ibuprofin. We finished the next 12 miles at 7 a.m. The number of pancakes with syrup, butter and berries we ate that Sunday was impressive. I lost a toenail in my left foot but gained admiration for what can be achieved when you surround yourself with lunatics — I mean, highly motivated people.
The question still stands: Who in your circle of friends or family will push you to achieve your goals, dreams and aspirations? Who is willing to pour A-1 sauce on your carrot cake when you fall off
the wagon or take the wrong path? Next time you see a reservist, be very careful to call him or her a “weekend warrior.” They might be the most motivated, educated athlete you’ll ever meet.

As I finish the last part of this article, bags have been loaded, customs have cleared us, and we will board an Air Force plane to take us out of Theater.
Do you have what it takes to do this? Are you willing to leave family, friends and comforts to volunteer and put the uniform on and trust that the person next to you on your right or left, male or female, young or old, who has signed a blank check to Uncle Sam with a total amounting up to life in the name of freedom, God and country? If you do … #ArmyReserve.
By the way, I lost 12 pounds, all my clothes are too loose on me and I have hit a personal best in almost every weight exercise I do. I did say thank you to TW.
67 | TODAY'S FDA january/february 2023
Photo captions:
1. Dr. Peralta (at left) and team leaving Theater.
2. Dr. Peralta in the ER typing in notes.
3. Some Army providers working out in Theater.
2.
3.

68 Came for the insurance ... stayed to support my profession. fdaservices.com • insurance@fdaservices.com • 800.877.7597 Give the gift of life insurance Protect your loved ones with the promise of security. Call or text us at 850.681.2996 to get a quote and discuss your options.
Reminders
By Casey Stoutamire, FDA Chief Legal Officer
This is a friendly reminder that any time you use a photo in an email publication, print publication (brochure, newsletter, etc.), or on your website, you must have permission to use that photo. For example, if it is for an upcoming event or function and you want to use pictures of the hotel and/or rooms, work with your hotel contact to get permis sion, in writing, to use them (this is usually in the form of a license or sublicense).
In addition, if you use a web designer, check your agreement with them to make sure it contains a provision under which the designer will indemnify the practice if the designer’s improper use of a third-party intellectual property (for example, pictures of a hotel) sub jects the practice to a claim/liability from the owner.

The same goes for playing music and offering television or movies in your office. The U.S. Copyright Act, Title 17 of the United States Code, gives copyright owners control over the public exhibition of their works. In nearly all cases, a public performance license is required to show copyrighted content in public. And yes, dental and medical offices are considered public spaces regarding copyright law. This requirement applies even if a single patient can view the content. This section of law applies to movies,
television programs and other audiovisual content enjoyed from sources like broadcast, cable or satellite television; DVDs; downloads; or streaming services. If you fail to comply with copyright law, you could be liable for damages ranging from $750 to $150,000 for each illegal showing, plus court costs and attorneys fees. Long story short, by showing tv programs and movies without a license, you risk fines for copyright infringement and the monetary repercussions can be significant.
However, there is good news. For several years, the American Dental Association has worked with the Motion Picture Licensing Corporation (MPLC) to provide a discount for members on copyright licensing. MPLC issues the license your practice needs to show copyrighted content in compliance with federal copyright law. The Umbrella License allows unlimited showings at your dental office without fear of copyright infringement. It provides coverage for old and new titles from more than 1,000 motion picture and television rights holders, including Disney, CBS, Warner Bros., NBCUniversal, Paramount, ABC, Televisa, HGTV, Lionsgate, Discovery and many more. To secure an Umbrella License, visit dentist.mplc.org/ or contact MPLC at 866.552.MPLC (6752) or info@mplc.com. Information is also available at ada.org/mplc
69 | TODAY'S FDA january/february 2023 copyright Copyright
IS IT TIME TO EXAMINE your malpractice insurance?
With yet another of Florida’s dental liability insurers selling out to Wall Street, there’s an important question to ask. Do you want an insurer that’s driven by investors? Or do you want an insurer that focuses on you, and has already paid more than $140 million in awards to its members when they retire from practice? Join us and discover why delivering the best imaginable service and unrivaled rewards is at the core of who we are.

FLORIDADENTALCONVENTION.COM
JUNE 29-JULY 1, 2023
GAYLORD PALMS RESORT & CONVENTION CENTER ORLANDO
FEATURED SPEAKERS


+ Lee Ann Brady, DMD

+ Vishy Broumand, DMD, MD

+ Steve Carstensen, DDS

+ Brooke Fukuoka, DMD

+ Mia Geisinger, DDS, MS
+ Kay Huff, RDA

+ Waji Khan, DDS, MBA, MEd
+ James Kohner, DDS


+ Judy Kay Mausolf


+ Michael Pikos, DDS
+ Sully Sullivan, DDS



+ And many more!
REGISTRATION OPENS
MARCH 1!
THE OFFICIAL MEETING OF THE LAUNCHING DENTISTRYFORWARD
courses and make your hotel reservation today at floridadentalconvention.com
View
.
NO GOSSIP ZONE
By Judy Kay Mausolf, President and Owner of Practice Solutions Inc.
New alert! Gossip is not something that all women just do! “Women do not have to gossip!” By the way, gossip does not just happen with women. Many men gossip as well … they just call it something else! We can successfully nurture a No Gossip Zone!
I refer to gossip as the “Poison Triangle of Mistrust” because gossip most often involves two people talking about a third person. Nothing shreds trust faster than gossip. Haven’t we all walked by when somebody was talking about us? Remember how you felt? How much did you trust the people who were talking about you? How much did you want to communicate or work with any of them? Imagine the effect gossip has on team performance and patient experience.
The sad truth is gossip happens because it is often thought of as fluff stuff and is tolerated without having any consequences. Nurturing a No Gossip Zone office culture raises trust and morale instantly and elevates communication, team performance, patient experience and your bottom line! This is big stuff, and there are plenty of reasons to adopt a No Gossip Zone office culture!
Here are four steps to help you nurture a No Gossip Zone!
1. 2.


The first step is to start with a team meeting. Have the entire team attend. Establish the definition of gossip for the practice as anything negative about another person, or private that they do not want others to know. Also, if we are listening, we are just as responsible as the person talking. We play a 50-50 role. Because if they have no one to tell it to, it stops. We may also think venting or blowing off steam is OK and is not considered gossip. In most cases, it is gossip. A good qualifier to ask ourselves is: the person I am blowing off steam about heard me, how would he/she feel?
The second step is for the entire team to verbally commit to each other to support a no gossip culture and stop it when it happens. Have the team agree on a word or phrase they will say if someone starts gossiping to them. Some of my clients use the word peace (in other words, keep the peace) or stop
or, please take it to the source or even remember we said we weren’t going to gossip It can be anything as long as everyone knows the word or phrase.
3. 4.

The third step is to say the phrase or word when someone starts gossiping to us. It is also your responsibility to try to stop gossip, even if you happen to be in a location where several people are gossiping. In a respectful manner, ask them to stop by using the word or phrase and, if necessary, reinforce how toxic gossip is to the team and the practice. If they refuse to stop gossiping, inform management.
The fourth step is for management to hold the gossiping team members accountable to support the practice standard. It is important to have defined consequences for gossip, just like any other practice standard. If the gossiping behavior continues, it can lead to termination. Yes, gossip is a big enough reason to terminate!
These four steps will help nurture a No Gossip Zone in your practice.
The bottom line is that gossip affects trust, and trust is not just a social virtue — it dramatically affects communication, team performance, patient experience and the bottom line!
Ms. Mausolf is President and owner of Practice Solutions Inc.; director of sponsoring partners, Speaking Consulting Network; author. Ms. Mausolf can be reached at 612.701.4922 or visit her website at PracticeSolutionsInc.net
She will offer “Communication Solutions: Attitudes, Breakdowns and Conflict Resolutions” – June 30, 9-11:30 a.m. and “R.I.S.E. to Success! Systems and Strategies that Build High-Performing Teams” – June 30, 2-4:30 p.m.at the 2023 Florida Dental Convention. Learn more about Ms. Mausolf’s course being offered at the 2023 Florida Dental Convention at floridadentalconvention.com FDC2023 registration opens March 1.
FDC2023 SPEAKER PREVIEW
YES – CROWN LENGTHENING WILL ENHANCE YOUR RESULTS
 By James Kohner, DDS
By James Kohner, DDS
It is common for dentists to become frustrated when recently placed crowns or bridges develop red and/or sore tissues at the margins. Or, in some situations, a tooth may look so badly broken down that a dental implant seems obvious, dissuading the clinician from even considering treatments that not only might save the tooth but render it predictably restorable.


Many of those problematic teeth can be restored predictably, and the above types of challenges can be solved. There often are solutions to those everyday restorative challenges so that every broken-down tooth does not have to be extracted and potentially become an implant! Giannobile and Lang stated in a 2016 editorial in the Journal of Dental Research 1 that “… the erroneous belief of implants yielding a better long-term prognosis has now clearly been rejected in several studies and reviews.” They say that “teeth even compromised because of periodontal disease or endodontic problems may have a longevity that surpasses by far that of the average implant,” and they offer 16 bibliography entries to support their statement.
It is worth noting their premise and keeping in mind that all compromised teeth do not have to become implants. Fortunately, there is a basic procedure that might help avoid restorative frustrations with badly broken-down teeth and allow saving and predictably restoring these teeth that seem hopeless at first glance.
The procedure, and one that many clinicians overlook, is crown lengthening. While this is a “periodontal” procedure, the goal of crown lengthening is very clearly intended as a “restorative” procedure. Crown lengthening has remained essentially unchanged throughout the past 30 years and remains as useful now as then. It has applications in all parts of the mouth.
Fig. 1.1. Excessive tissue around 2nd molar due to thick bone on palate which forces tissues more coronally than would be desired for ideal crown preps.
Fig. 1.2. Same tooth as 1.1 with crown off illustrating lack of tooth structure for sound restoration and potential to have open margins or impingement when reaching subgingivally for retention.
For posterior teeth, there is often not enough clinically visible tooth structure for retention, with preps going subgingivally far enough that obtaining a predictable hassle-free impression is challenging (Fig 1.1 and 1.2). The clinical situation in Fig 1.2 is an illustration where clinicians will be tempted to prep subgingivally for more retention only to end up with marginal impingement on soft tissues causing inflamed and sore soft tissues, or compromised impression results that can result in open margins as an example. This can occur due to excessive gingiva, as in this situation, or deep caries or fractures. While these teeth display too much soft tissue, the problem is typically too much bone underneath the soft tissue resulting in soft tissues moving coronally over and around the thick bone. 2, 3 When clinical crowns are short, the finish lines often end up subgingivally, as illustrated with a deep distal margin on the provisionals in Fig 1.3. This deep finish line location can lead to inadequate impressions, which can lead to open margins.
To shorten the soft tissues, with the goal of exposing more tooth structure, bone reduction is usually required for predictable clinical results since soft tissues will grow back to establish the typical dimension of soft tissues, called biologic width 4, 5 if the bone is not moved. The dimension of biologic width is typically 3 mm coronal to osseous crest. That is the normal development of soft tissue dimensions, whether the bone is or is not removed. 5 After removal of bone and soft tissues the two allegedly compromised teeth in Fig 1.1 and 1.2 can have adequate tooth structure exposed (Fig 1.4, and 1.5), thus avoiding difficulty with impression taking, the need for subgingival margins or potential soft tissue impingement 6 such as in Fig 1.7. Final restoration with healthy




FDC2023 SPEAKER PREVIEW FDC2023 SPEAKER PREVIEW
“ ”
In a rush to use the latest new materials and greatest techniques, such as implants or lasers, the benefits and applications of crown lengthening are often ignored.
t
Fig. 1.3. Provisionals in place. Note distal of provisional is subgingival (arrow).
Fig. 1.4. Same area following osseous reduction and shortening of soft tissue to expose previously hidden, but sound, tooth structure.
tissue and enough tooth to allow for good retention and avoid deep subgingival margins is seen in Fig 1.6.
In the esthetic zone, errors of margin placement can be even more noticeable when inflammation results from crown margins impinging on the soft tissues. Fig 1.7. Learning the concepts of Crown Lengthening and proper margin location can help avoid those inflammatory complications.
The stated goals of crown lengthening in a restorative application, as listed in the CDT codes from the American Dental Association, is below, and it offers an explanation of just how that inflammation seen in Fig 1.7 can occur or what the goal is for restoring teeth with limited clinical crown available:
To expose enough sound tooth structure to allow placement of a restorative margin onto that sound tooth structure, to have adequate mechanical retention, and at the same time avoid disrupting or impinging on any of the gingival fiber attachments to the tooth.

In a rush to use the latest new materials and greatest techniques, such as implants or lasers, the benefits and applications of crown lengthening are often ignored. But instead of being pushed aside and forgotten, this “old standard” should make its way into every contemporary clinician’s armamentarium.
Of course, each tooth with restorative/soft tissue problems is not automatically an indication for crown lengthening! Extraction leading to an implant, or a fixed or removable appliance, always needs to be in the differential diagnosis. Orthodontic extrusion could also be considered, as it is sometimes a viable option, but that is a topic for another paper and has been covered by others.
Only some indications could be covered in this short discussion. Some signs for crown lengthening, or what some clinicians call gum shortening, are:

l Excessive gingival display in the anterior, often associated with thick bone
l Short posterior teeth, usually associated with excess gingiva and thick bone

l Uneven gingival levels
l Subgingival fractures
l Subgingival caries
Fig. 1.5. After 3 months healing with provisionals still in place. Note more tooth structure is now available for preps, and the margin location can avoid any soft tissue impingement, and even can be located supragingivally if desired. Also note the distal of the provisional (arrow) is no longer buried under tissue, an indication of how much more tooth structure is available.
Fig. 1.6. Final restorations showing that adequate tooth structure has allowed for supragingival margins despite very short teeth to start with. Also, the restorations are done with less stress and higher predictability for impression taking.
l Previous crowns and finish lines too close to the soft tissue attachment and the bone
l As an adjunct to implant treatment, where supereruption had occurred
Using some of these ideas could help clinicians accomplish more predictable impressions and more predictable restorative results, not to mention happier patients when complications are avoided.
References:
1. Giannobile, W.V., Lang, N.P. Are Dental Implants a Panacea or Should We Better Strive to Save Teeth? J. Dental Research 2016, vol.95 (1) 5-6
2. Deas DE, Moritz AJ, McDonnell HT, Powell CA, Mealey BL. Osseous surgery for crown lengthening: A 6-month clinical study. J Periodontology 2004;75(9):1288-1294.
3. Arora R, Narula SC, Sharma RK, Tewari S. Evaluation of supracrestal gingival tissue after surgical crown lengthening: a 6-month clinical study. J Periodontology.



4. Coslet J, Ingber J, Rose L. The “Biologic Width” – A Concept in Periodontics and Restorative Dentistry. Alpha Omegan 1977; 70:24-28
5. Gargiulo A, Wentz F, Orban B,. Dimensions and Relations of the Dentogingival Junction in Humans. J Periodontology 1961;32, 261.
6. Newcomb, GM. Relationship between the location of subgingival crown margins and inflammation. J. Periodontology 1974; 45:151-154
leads to impingement and subsequent inflammation.
Dr. James Kohner, is a periodontist living in Denver. He has more than35 years clinical experience and more than 25 years teaching and lecturing, with presentations all over the U.S. and eight foreign countries. He currently teaches Hands-on Surgical Training Workshops on Crown Lengthening, Soft Tissue Grafting, and Periodontal Surgery for dental school continuing education programs, and at multiple association meetings in both the U.S. and Canada. He can be reached at 602.390.2229 or JamesKohnerDDS@gmail.com and is available to speak to your local society, school or study group.
He will be offering the following courses at the 2023 Florida Dental Convention: “Crown Lengthening: Can it REALLY Enhance Restorative Results? (C09)” on Thursday, June 29, 9 a.m.-12 p.m.; “Crown Lengthening Workshop (W07)” on Thursday, June 29, 1:30-5 p.m.; “Soft-Tissue Grafting That WILL Enhance Restorative Results (C38) on Friday, June 30, 9 a.m.-12 p.m.; “Soft-Tissue Grafting and Suturing Workshop (W19)” on Friday, June 30, 1:30-5 p.m. Learn more about Dr. Kohner’s courses being offered at the 2023 Florida Dental Convention at floridadentalconvention.com. FDC2023 registration opens March 1.
FDC2023 SPEAKER PREVIEW FDC2023 SPEAKER PREVIEW
Fig. 1.7. Soft tissue reaction following laser soft tissue removal with no bone reduction. The placement of crowns within the space for biologic width attachment
EXHIBIT HALL
Free preregistration for FDA Members!
A-C
A-DEC
A1 HANDPIECE SPECIALISTS
ABYDE
ACTEON NORTH AMERICA
ADA PRACTICE TRANSITIONS
ADA SMILECON
ADIT
ADS DENTAL SYSTEM INC.
ADVANTAGE DENTAL
ADVANTAGE TECHNOLOGIES
AIR TECHNIQUES
ALPHAEON CREDIT
AMERITAS
ARGEN
ARTCRAFT DENTAL INC.
ASEPTICO INC.
ASPEN DENTAL MANAGEMENT INC.
ATLANTIC DENTAL SOLUTIONS
AUGMA BIOMATERIALS USA INC.
AVALON BIOMED
AVZ BENEFIT SOLUTIONS
BANK OF AMERICA PRACTICE SOLUTIONS
BAYSHORE DENTAL STUDIO
BENCO DENTAL
BEST INSTRUMENTS USA
BEUTLICH PHARMACEUTICALS
BIOCLEAR MATRIX SYSTEMS
BIOGAIA PROBIOTICS
BIOHORIZONS
DENTALVIBE/BING INNOVATION
DESIGNS FOR VISION INC.
DIGITAL DOC LLC
DIGITAL HEALTHCARE PROFESSIONALS

DIGITAL RESOURCE
DOCTOR MULTIMEDIA
DOCTOR’S CHOICE PRACTICE TRANSITIONS
DOCTORSINTERNET
DORAL REFINING CORPORATION
DPC TECHNOLOGY
DR. MARKETING
DREVE AMERICA CORPORATION
EDGEDENTAL SPECIALTIES
EKOS DENTAL GROUP
ELEVATE ORAL CARE
ENOVA ILLUMINATION
BIOLASE
BIOTECH DENTAL
BIRDEYE
BISCO
BQ ERGONOMICS LLC
BRASSELER USA
BURST
CAO GROUP
CARECREDIT
CARESTREAM DENTAL
CARL ZEISS MEDITEC USA
CARR
CGX RADIOS
CLASSIC CRAFT DENTAL LABORATORY
COAST DENTAL & ORTHODONTICS
COGENT BANK
COLGATE
COOL JAW BY MEDICO INTERNATIONAL
CORE SCIENTIFIC
COSMEDENT
CREST + ORAL-B
CROWN WORLD DENTAL LAB
CUTCO CUTLERY
D-F
DANDY
DANSEREAU HEALTH PRODUCTS
DENTAL DYNAMIC STAFFING
DENTAL EQUIPMENT LIQUIDATORS INC.

DENTAL INTELLIGENCE
DENTAL TRIBUNE
DENTALREE.COM INTERNATIONAL INC.
ENVOLVE BENEFIT OPTIONS INC.
EQUITABLE - ADA MEMBERS RETIREMENT
PROGRAM
ESSENTIAL DENTAL REPAIRS
ESTHETIC PROFESSIONALS
EVENLY TECHNOLOGIES
FLORIDA COMBINED LIFE
FLORIDA DENTAL ASSOCIATION (FDA)

FDA FOUNDATION
FDAPAC
FDA SERVICES INC.
FLORIDA MEDICAL ADVISORS
FLORIDA PROBE CORP.
FOTONA
FOUR QUADRANTS ADVISORY
G-K
GARFIELD REFINING COMPANY
GARRISON DENTAL SOLUTIONS
GC AMERICA INC
GETSEE & DEMEOLA CPA BUSINESS ADVISORS
GLIDEWELL DENTAL
GPS DENTAL LAB
GREATER NEW YORK DENTAL MEETING

GUARDIAN
HALYARD GLOBAL PRODUCTS
HAWAIIAN MOON
HENRY SCHEIN DENTAL PRACTICE TRANSITIONS

HIOSSEN
HUFRIEDYGROUP
HUMANA
HUNTINGTON BANK PRACTICE FINANCE
2023 FLORIDA DENTAL CONVENTION • JUNE 29-JULY 1 • GAYLORD PALMS RESORT • ORLANDO
HUNZA DENTAL
ICORECONNECT INC.
ILLUMITRAC SOFTWARE
IMPLADENT LTD.
IMPLANT EDUCATORS ACADEMY
IMPLANT SEMINARS
INTELLISCAN 3D
IOTECH INTERNATIONAL
ITX PROS
JRA REAL ESTATE & PRACTICE ADVISORY
KETTENBACH LP
KLAS SOLUTIONS
L-Q
LEGALLY MINE LLC
LIBERTY DENTAL PLAN
LONE PEAK DENTAL GROUP
LUMADENT INC.
MCNA DENTAL
MEDILOUPES
MEGAGEN AMERICA
MEISINGER USA
MODERN DOC MEDIA
MYOFUNCTIONAL RESEARCH CO.
MYRIAD CAPITAL
NADAPAYMENTS
NEODENT
NEOSS INC.
NEW TEETH NOW
NEXHEALTH
NOTA3D
NSK AMERICA
O-SO PURE
ORASCOPTIC
PHARMACISTS MUTUAL INSURANCE COMPANY
PHILIPS SONICARE AND ZOOM! WHITENING
PLANMECA
PORTER INSTRUMENT
POWER DENTAL GROUP
PRACTICE BY NUMBERS
PRACTICE PATHWAYS - ZIONS BANK
PREAT
PROFESSIONAL SALES ASSOCIATES INC.
PROMA INC.
PROSPAY INC
PROTOMAD PROTECTIVE COVER
PROVIDE
PURE DENTAL BRAND
Q-OPTICS & QUALITY ASPIRATORS INC.
R-Z
RADIATION DETECTION COMPANY
RECALLMAX
RGP DENTAL INC.
RITTER DENTAL USA
ROSE MICRO SOLUTIONS LLC
ROYAL DENTAL GROUP
SALVIN DENTAL SPECIALTIES INC.
SHAMROCK DENTAL CO. INC.
SHATKIN F.I.R.S.T. LLC
SHOFU DENTAL CORPORATION
SHOWCASE DENTAL LAB
SIZEMORE & ASSOCIATES, CPA’S LLC
SMILE DESIGN DENTISTRY
SNAP ON OPTICS
SOLMETEX
SOUTHERN DENTAL REFINING
STAR DENTAL PARTNERS
STELLALIFE
STESZEWSKI LAW
STRAUMANN
SUNBIT
SUNCOAST CREDIT UNION
SUNRISE DENTAL EQUIPMENT INC.
SUPERIOR DENTAL & SURGICAL MANUFACTURING
SUPERIOR DENTAL DESIGN & UPHOLSTERY
SURGITEL
TCG DENTAL REPAIR
TD BANK
THE DAWSON ACADEMY
THE DOCTORS COMPANY
THE TRANSITIONS GROUP
TWO WAY RADIO GEAR
ULTRADENT PRODUCTS INC.
ULTRALIGHT OPTICS INC.
VAKKER DENTAL INC.
VALUMAX PROTECTIVE APPAREL INC.
VATECH AMERICA
VIDEO DENTAL CONCEPTS
VOCO AMERICA INC.
WALMART HEALTH
WATER PIK INC.
WEAVE
WELLS FARGO PRACTICE FINANCE
XITE REALTY LLC
FDC2023 EXHIBIT HALL
HOURS & EVENTS
Times are subject to change.
THURSDAY, JUNE 29
11 AM-6 PM
Exhibit Hall Open to Attendees
11 AM-2 PM
Lunch available to purchase
4-6 PM
Welcome Cocktail Reception
FRIDAY, JUNE 30
8:45 AM-6 PM
Exhibit Hall Open to Attendees
11 AM-2 PM
Lunch available to purchase
SATURDAY, JULY 1
9 AM-2 PM
Exhibit Hall Open to Attendees
11 AM-2 PM
Lunch available to purchase
*EXHIBITORS AS OF JAN. 6, 2023
EXHIBITORS IN PINK ARE FDAS CROWN SAVINGS MERCHANTS.
THE CURRENT EXHIBITOR PRODUCT CATEGORIES! FLORIDADENTALCONVENTION.COM
VIEW
Practice Consolidation Is Cresting
Silent Partners Buy Part of Your Practice
Dozens of Invisible Dental Support Organization (IDSO) silent partners are paying record values for partial interests in Endodontic practices advised by LPS. Endo-only IDSOs compete fiercely with the multi-specialty and Specialty Surgical Trifecta IDSOs, driving up values. You should understand all of your options.


IDSOs purchase 51% to 90% of practices for cash now at low tax rates. Doctors retain ownership and have significant upside in the equity value. Some LPS clients have achieved 3x to 7x equity returns in only three to five years.
Long-Term Wealth Building Partnership
Doctors continue to lead their practice with their brand, team and strategy for years or decades. Practices benefit from the resources of a larger, silent partner, but are not micromanaged or homogenized.
IDSO partnership is not a short-term transition strategy, but rather a long-term wealth building partnership. Some happy LPS Endodontic clients are under 35!
Six or More Choices in Partnership
LPS clients have 6 to 10+ qualified bidders. LPS completed over $500 million of transactions for dentists of all types, in the last 12 months. LPS’ size enables our clients to achieve record values that the little advisors cannot match. Multiple Endodontic clients have achieved values of over 3x collections.
Your Value in Today’s Consolidation Frenzy


Great practices with at least $1.4 million in collections have many options today. You should understand the value of your practice in an LPS-advised process. Doctors who deal directly with IDSOs often leave millions on the table and do not get to consider ALL of their options.
Contact us to schedule a confidential, no obligation discussion to learn the value of your practice; you might be surprised at today’s values!
80 877-557-5119 FindMyIDSO.com FLDental@LargePracticeSales.com
It’s Time to Understand the Value of Your Practice
By Drs. Shawki Abed, Neel Bhattacharyya, Saja A Alramadhan and Nadim M. Islam
Read, Learn and Earn!
A 19-year-old African American female presented to Dr. Paul Seider an Oral & Maxillofacial Surgeon in Tamarac, Florida, for evaluation of oral ulcers. The patient has almost a 10-year history of painful recurrent ulcers throughout her mouth. During each recurrence, the sores last 3 to 4 weeks. She did not remember taking any medications or being exposed to allergic materials that could have triggered the outbreak of ulcers. Intraoral examination revealed diffuse, large, shallow erosions and ulcerations surrounded by irregular erythematous borders on the lateral ventral surfaces of the tongue (Fig. 1), and buccal mucosae (Fig. 2). Hemorrhagic crusting of the vermilion zone of the lips was also noted (Fig. 3). Dr. Seider performed an incisional biopsy. This was then submitted to the University of Florida Oral Pathology Laboratory biopsy service for microscopic examination.
Question
Based on the clinical findings and medical history, what is the most likely diagnosis?
A. Recurrent Aphthous ulcers



B. Behçet’s disease
C. Recurrent or secondary herpes
D. Pemphigus Vulgaris
E. Erythema Multiforme
Diffuse large ulcerations and erosions surrounded by irregular erythematous borders noted on the lateral border of the tongue.
81 | TODAY'S FDA january/february 2023
Visit floridadental.org/online-ce for this FREE, MEMBERS-ONLY BENEFIT. You will be given the opportunity to review the “Diagnostic Discussion” and its accompanying photos. Answer five multiple choice questions to earn one hour of CE. Contact FDC Marketing Coordinator Brooke Martin at bmartin@floridadental.org or 800.877.9922.
Fig. 1.
Fig. 2. Ulceration of the buccal mucosae.
Fig. 3. Hemorrhagic crusting of the lips.
t
A. Recurrent Aphthous ulcers
Incorrect. Aphthous ulcers are usually seen in young individuals and are very painful. Patients usually report a history of similar outbreaks in the past, as reported by this patient. The ulceration demonstrates a yellow-white, fibrinopurulent membrane which is surrounded by an erythematous halo. The ulcers may be preceded by an erythematous macule in association with prodromal symptoms of burning, itching or stinging. Aphthous ulcers in general occur almost exclusively on non-keratinized mucosa and don’t exhibit hemorrhagic crusting as in this case.
B. Behçet disease
Incorrect, Behçet disease is a vasculitic disorder occurring in the third decade of life and is characterized by episodic apththous ulcers, as seen in the present case. The condition is most common in Turkey, Japan, and the Eastern Mediterranean countries. The exact etiology is unknown, but environmental and genetic factors are implicated in its pathogenesis. The HLA-B51 allele is strongly associated with the disease and is highly prevalent among individuals of Asian descent. Oral ulcers occur in 92% to 100% of patients and are painful. They are similar to the aphthous ulcerations (minor, major, or herpetiform aphthae) occurring in otherwise healthy individuals and demonstrate the same frequency and duration. Aphthous ulcers associated with Behçet disease exhibit a predilection for the soft palate and oropharynx. They typically heal within a couple of weeks. Most importantly, patients with Behçet disease also have skin, genital and ocular lesions which were not present in this patient. The diagnosis of Behçet disease is based on the presence of recurrent oral ulceration (as seen in this patient), plus two of following: recurrent genital ulcers, eye lesions, or skin lesions (features not seen in this case) and a positive pathergy test.
C. Recurrent or secondary herpes
Incorrect, but an excellent choice. The most common site of recurrence for herpes simplex virus-1 is the vermilion border and adjacent skin of lips, which is also known as herpes labialis. The lesions present as multiple small, erythematous papules which may form clusters of fluid-filled vesicles. The vesicles rupture and crust within two days, and healing usually takes place within 7-10 days, which is very much unlike the present case. Majority of the affected patients experience approximately two recurrences annually, but a few may experience outbreaks more frequently.
Patients with rapidly developing recurrences tend to respond less favorably to treatment. Recurrent herpetic lesions, in immunocompetent patients, almost always are limited to keratinized mucosa (bound to the bone) like gingiva and hard palate, which does not fit the pattern of distribution seen in this patient. In immunocompromised patients, intraoral lesions may spread to unbound mucosa, however, this is not the scenario in this case. Moreover, these lesions begin as small vesicles that collapse to form cluster of erythematous macules, and do not present as large ulcerations as seen in this patient.
D. Pemphigus Vulgaris
Incorrect. Pemphigus vulgaris (PV) is an uncommon immune-mediated disease. PV has an estimated prevalence of 30,000 cases in the USA and an incidence of 1–10 new cases per 1 million population. PV is one among the four-pemphigus variants that can affect oral mucosa in addition to pemphigus vegetans, which is considered an extremely rare condition. PV typically affects adults, with an average age of 50 years, and no sex predilection. Rare cases have been reported in childhood. The condition is mostly seen in persons of Mediterranean, South Asian, or Jewish heritage. Oral lesions are often the first sign and precede skin lesions in 50% of cases and are the most difficult to resolve with therapy. Any area of the oral cavity may be involved, however, areas subjected to frictional trauma such as the buccal mucosa, palate, lower lip, and tongue are most affected, as seen in this patient. Clinically, PV oral lesions are painful and appear as superficial, ragged erosions and ulcerations which can cause dysphagia and weight loss. Rarely, patients may report vesicle or bullae formation which rupture quickly, leaving behind raw, and painful ulcerations. Desquamative gingivitis is also a common feature seen in the majority of vesiculobullous conditions, which is another feature not seen in the present case. A positive Nikolsky’s sign is a characteristic feature of PV, in which a new bulla formation can be induced on normal-appearing skin upon slight lateral pressure. No bulla formation or Nikolsky’s sign was noted in this case. Unlike the present case, PV oral lesions are recalcitrant and do not heal in 4 weeks unless treated.
E. Erythema Multiforme
Correct. Erythema multiforme (EM) is a blistering, ulcerative mucocutaneous condition of uncertain etiopathogenesis. It probably represents an immunologically mediated process which is triggered in about 50% of the cases especially in younger individuals
82 quiz
by a preceding herpes simplex infection and in older individuals by an exposure to a variety of medications. EM typically has an acute onset and usually affects young adults in their 20s or 30s. Men are affected slightly more than women. The condition is usually self-limiting, lasting 2 to 6 weeks. Prodromal symptoms, like fever, malaise, headache, cough and sore throat, occur about one week before onset. Oral lesions are very painful and begin as round, dusky erythematous patches that ulcerate and evolve into large, shallow erosions and ulcerations with irregular borders, like the ones seen in this patient. Hemorrhagic crusting of the vermilion zone of the lips is usually characteristic, a feature seen in this patient (Figure 3). EM presents with a wide spectrum of clinical disease ranging from ulcerations, erythema, bullae, erosions or nonspecific erythematous changes. Even though the disease is self-limiting, about 20% patients may experience recurrent episodes, just as seen in this patient. In cases of recurrent episodes of EM, initiating factors like recurrent herpes infection or drug exposure should be considered.
Severity is ranging from EM minor, when either skin or mucosal epithelium is involved, through EM major, when both skin and mucosal epithelium are affected. Beside oral mucosa, other mucosal epithelium such as conjunctival, genitourinary and respiratory mucosa also may be affected. With severe ocular involvement, scarring (symblepharon formation) may occur, similar to that in mucous membrane (cicatricial) pemphigoid.
Patients with EM may develop skin lesions which appear as concentric circular erythematous rings resembling a target or bull’s-eye. Cutaneous and other non-oral mucosal lesions were not seen in this patient. When EM is restricted to the oral cavity, it can be mistaken for other inflammatory, vesiculobullous, and dysplastic conditions. Patients may be dehydrated because of the inability to ingest liquids as a result of mouth sores.
EM is often diagnosed clinically. Histology and direct immunofluorescence can help to exclude other vesiculobullous conditions. EM usually has no specific histologic pattern comparing with other vesiculobullous lesions. Oral EM and lichenoid drug eruptions may be virtually indistinguishable except lesions seen in EM lack the characteristic peripheral striae that are seen in lichenoid drug eruption. Also lesions in EM usually eventually heal only to reoccur unlike those in lichenoid drug eruptions which usually resolve after discontinuation of the offending medication(s).
Depending on the extent of the disease, topical or systemic corticosteroids may be used, especially in the early stages of the disease. Steroids tend to show a striking resolution of lesions such as Clobetasol ointment (0.05%). Antiviral therapy is recom-
mended, if herpetic infection is considered a triggering factor. If a causative drug is identified or suspected, then it should be discontinued immediately.
References:
1) Cizenski JD, Michel P, Watson IT, Frieder J, Wilder EG, Wright JM, Menter MA. Spectrum of orocutaneous disease associations: Immune-mediated conditions. J Am Acad Dermatol. 2017; 77(5):795806.
2) Thete SG, Kulkarni M, Nikam AP, Mantri T, Umbare D, Satdive S, Kulkarni D. Oral manifestation in patients diagnosed with dermatological diseases. J Contemp Dent Pract. 2017; 18(12):1153-1158.
3) Lerch M, Mainetti C, Terziroli Beretta-Piccoli B, Harr T. Current perspectives on Erythema Multiforme. Clin Rev Allergy Immunol. 2018; 54(1):177-184.
4) Arduino PG, Porter SR: Herpes simplex virus type 1 infection: overview on relevant clinicopathological features, J Oral Pathol Med 37:107–121, 2008.
Diagnostic Discussion is contributed by University of Florida College of Dentistry professors, Drs. Indraneel Bhattacharyya, Nadim Islam and Saja Alramadhan who provide insight and feedback on common, important, new and challenging oral diseases.
The dental professors operate a large, multi-state biopsy service. The column’s case studies originate from the more than 14,000 specimens the service receives every year from all over the United States.
Clinicians are invited to submit cases from their own practices. Cases may be used in the “Diagnostic Discussion,” with credit given to the submitter.
Drs. Bhattacharyya, Islam and Alramadhan can be reached at oralpath@dental.ufl.edu.
Conflict of Interest Disclosure: None reported for Drs. Bhattacharyya, Islam and Alramadhan.
The Florida Dental Association is an ADA CERP Recognized Provider. ADA CERP is a service of the American Dental Association to assist dental professionals in identifying quality providers of continuing dental education. ADA CERP does not approve or endorse individual courses or instructors, nor does it imply acceptance of credit hours by boards of dentistry. Concerns or complaints about a CE provider may be directed to the provider or to ADA CERP at ada.org/goto/cerp.
83 | TODAY'S FDA january/february 2023
Career Center
The FDA’s online Career Center allows you to conveniently browse, place, modify and pay for your ads online, 24 hours a day. Our intent is to provide our advertisers with increased flexibility and enhanced options to personalize and draw attention to your online classified ads!
Post an ad on the FDA Career Center and it will be published in our journal, Today’s FDA, at no additional cost! Today’s FDA is bimonthly; therefore, the basic text of all active ads will be extracted from the Career Center on roughly the 5th of every other month (e.g., Jan. 5 for the Jan/Feb issue, March 5 for the March/April issue, etc). Please note: Ads for the Nov/Dec issue must be placed no later than Nov. 1.
Please visit the FDA’s Career Center at careers.floridadental.org.
Dental Office for Sale in Margate. Great Opportunity to start your own practice or add an additional location. Dentist is relocating and selling the current Set-Up. Low investment to become the owner of your own practice. Office has 4 Ops., all equipped with dental chair, LED light and intra-oral xray. All major equipment also included: compressor, vacuum, amalgam separator, autoclave. All wired and ready for digital xrays. Tile through out, great condition. Aprox 1,200 sf. Located in a Shopping Center in a highly transited intersection. No intermediaries. The suite has been a dental practice for more than 25 years, anchoring one successful dentist after another. Please, call or text if interested: (786) 303-1732. Visit careers.floridadental.org/ jobs/18007915/
Associate/Associate to Partner Opportunity on the Florida Beach!!! Come join us! If you are looking for an associate opportunity with room for growth, an excellent earning potential, and opportunity to partner (if desired) in a great office. We are currently seeking a full-time associate for our Volusia County location but are open to discussing part-time availability. Mentorship and guidance will be provided for recent residency graduates. We are a well-established, privately owned endodontic practice with two locations in Central Florida. Our office is looking for a compassionate, energetic, quality-oriented endodontist to join our team. Our newly renovated offices have the latest technology including but not limited to: LED surgical microscopes, digital radiographs, CBCT on site, intraoral cameras, and remotely
accessible practice management software. This is the perfect opportunity for someone looking to be the only associate in an office with access to, and support from, a great clinical/business mentor. Associate will have their own desk, scheduling autonomy, and monthly marketing budget. Compensation will be 47% of collections with a $1,000 daily minimum guarantee. Florida Dental License acquisition assistance is available for those who are not currently licensed in Florida. This is a unique opportunity that will fill fast! Ideal for someone who would like to see what private practice ownership is like, or practice in an “owner style” associateship. If you are interested in this opportunity, please send your CV/Resume and a copy of the qualification documents listed below listed below to office@daytonaendo.com. Be sure to include contact information in the body of the email and our doctor will contact you as soon as possible. We look forward to connecting with you! Required for consideration: 1. DDS/DMD from an accredited Dental School 2. Certificate of Completion from an accredited US Endodontic Residency Program 3. Active Florida Dental License. Visit careers.floridadental. org/jobs/17999677/
Faculty and Adjunct Positions: Assistant/ Clinical Assistant Professor, Midwestern University. Midwestern University College of Dental Medicine-Illinois in Downers Grove, IL. We are seeking full time and part time dental faculty members who are responsible for working with students in a patient clinic or simulation clinic setting. Faculty members will be responsible for teaching in one?to?one,
small group and plenary settings. Candidates must be able to demonstrate dental procedures in clinical or simulation situations; have strong clinical experience in the use of CAD/ CAM dentistry and lasers; must possess a DDS/DMD degree; must be eligible for licensure in Illinois with at least 5 years of experience in general dentistry or their respective discipline. Previous teaching experience not required. Interested applicants may apply online at https://www.midwestern.edu/faculty-and-staff/employment. Inquires may be sent to Dr. Stephen Palatinus, Associate Dean of Clinical Education at spalat@midwestern. edu, or Dr. Kaveh Adel, Associate Dean of PreClinical Education at kadel@midwestern.edu. Midwestern University is an Equal Opportunity/Affirmative Action employer. Visit careers. floridadental.org/jobs/18007016/
Pediatric Dentist, Boynton Beach. Pediatric Dentist Now Hiring a Pediatric Dentist for Growing Dental Practice! Are You a Pediatric Dentist ready to Make a Big Impact on a Growing Company? Position Snapshot. Balance at its finest - rapid practice growth meets sunny south Florida! Company: Miller Pediatric Dentistry and Orthodontics | Children’s Dentistry of Coral Springs | Pines Pediatric Dentistry and Orthodontics. Position Title: Pediatric Dentist. Full Time or Part-Time. Location: Boynton Beach, Coral Springs, Pembroke Pines, FL.
Compensation: $275,000 - $325,000+. Position
Overview: We are looking for a caring, professional, and fun pediatric dentist to join our growing practices across south Florida; Work with great doctors (multispecialty) and great staff!; The ability to grow within the company.;
84
Position is part-time or full-time across our 3 locations.; Associate will be a caring individual whose primary focus to is care and treat our patients to the best of their ability; Target compensation rate: $275,000 - $325,000+; Located in beautiful, sunny South Florida! This is a great place to raise a family and always just a few minutes away from the beach! Position Benefits: CE Benefits: $2000 of CE yearly for Full Time Doctors; CPR/PALS: Every 2 years; Flexibility: Flexible scheduling and family focused! Modern Offices: Brand new pediatric dental offices with all brand new equipment and technology.; Autonomy: So, you can practice how you were trained and can provide excellent care, the best you can.; Stability: We are looking for someone to join long term, this position is part-time or full-time. Have the ability to grow as your career grows!; Opportunity: Great opportunity to get started with a great team and have the potential for growth.; Team: Be a part of our fantastic team! Our team always works together to bring the highest level of care to our patients. We work with all dental specialties in the community and have orthodontics and general dentistry in house. Required Qualifications: DDS or DMD; Pediatric Dental Specialty Certificate; Florida Dental License; CPR & PALS; Motivated, friendly, and energetic; DDS or DMD; Pediatric Dental Specialty Certificate; Florida Dental License; CPR & PALS; Professional, Motivated, Friendly, Caring and Energetic. Visit careers. floridadental.org/jobs/17978002/
Periodontist, Tallahassee. Great career opportunity in a growing practice in Tallahassee, FL. Full time associateship with opportunity to buy into the practice. Visit careers.floridadental.org/jobs/17861883/periodontist
Associate leading to Partnership, Bradenton. Well established, high quality, fee for service restorative/prosthodontic and esthetic practice looking for a highly skilled and motivated associate. Excellent opportunity for the right person. Please call or email your CV to Scarlett at Drs. Klement, Jungman, Varga and Troxler’s office. 941-792-2766 or scarlett@ zkjvdental.com. Visit careers.floridadental. org/jobs/17852529/
General Dentist, Treasure Coast-Port St Lucie. F/T. Restorative/Implant Practice. Seeking general dentist for private practice in fast growing area. Minimum 5 years experience required . Practice is equipped with latest technology for state of the art dentistry. CBCT, Digital impression systems, etc. Experience with comprehensive crown and bridge, implant restorations, surgical extractions
and endo a must. Guaranteed daily salary vs percentage of production. Come join the best practice in Port St Lucie. Email CV/Resume to blvdcenter@yahoo.com for immediate consideration. Visit careers.floridadental.org/ jobs/17786220/
Experienced General Dentist, Palm Beach Gardens. This is a rare opportunity to be mentored by a doctor with internationally recognized credentials in cosmetic dentistry, full mouth reconstruction, dental implant surgery & sedation. Senior doctor is preparing to reduce his busy schedule allowing a new doctor to grow into a leadership role. Qualified doctor should be capable of producing at least $1M- $1.5M their first year in our practice. Seeking a highly experienced general dentist looking for a long-term opportunity to join an extremely productive cosmetic & restorative practice in Palm Beach Gardens. Strictly fee for service. No HMO’s or PPO’s. Our impeccable reputation for exceptional care has been well known in our community for 35 years. Integrity & good interpersonal skills are a big part of our culture where open and honest communication with patients and team is a top priority. Our state of the art facility is fully equipped with advanced technologies including CBCT scans. Our highly trained team maintains very organized systems that are proven to be very efficient & effective, allowing our doctors to focus on delivering quality dentistry.You will have the opportunity to perform all forms of dentistry including crown & bridge work, cosmetics, complete smile makeovers, endodontics, implant surgery as well as full mouth reconstruction at fees that are commensurate with the quality work you provide. Must have a minimum of 5 years clinical experience delivering quality dentistry. Proficiency in molar endo preferred. Cosmetic training through a recognized cosmetic dentistry institute is preferred. Applicant must be personable with excellent communication skills. Position involves excellent compensation package + bonus package based on production with a guaranteed daily base salary. Medical insurance is included. Visit careers. floridadental.org/jobs/17779424/
Practice in HIGH & DRY Florida! Fee For Service in North Central Florida, Belleview. Are you tired of evacuating for hurricanes?
Tap into the market of CASH PAYING retirees of The Villages, Del Webb, and Stonecrest 55+ communities, many of whom have relocated from coastal Florida. There is also an untapped population of hundreds of young families moving into new homes in the
Seeking Qualified Dental Radiographer?
Train your dental assistants to expose radiographs using the FDA’s MyDentalRadiography online course that combines self-paced learning with clinical proof of competency. Call Lywanda Tucker at 850.350.7143 for details or visit mydentalradiography.com/FDA to create a supervising dentist account and complete the necessary tutorial on how the program works.
immediate area! The only other dentist in the immediate vicinity is a Heartland office. Two fully equipped operatories occupy a free-standing 950 sq. ft. building built in 2008 plumbed for three operatories. It is situated on one beautiful acre of land on busy US 301 just north of THE VILLAGES. Practice grossed 150K taking no insurance at 30% overhead in 2021 on 15-20 patients/week with dentist doing all hygiene. 4-5 internally referred new patients per week are being referred to a colleague. All surgery, endo, and pedo are referred out. Immediate two full days of hygiene are scheduled and will keep the buyer busy with a loyal patient base. Modern chartless office is equipped with digital sensors and Patterson Fuse cloud-based software. There is plenty of room to expand existing building or even build a new office and rent the current space. Please message me for more pics or to arrange a visit. Office is a 1 hour commute from either North Orlando/ Winter Garden/Clermont or Gainesville, 1.5 hours from Tampa. It is an easy drive off of I-75 Exit 341 or off the Turnpike on US 301. $450k includes practice and building/property. I will consider owner financing for building with adequate down payment. Visit careers. floridadental.org/jobs/13686503/
85 | TODAY'S FDA january/february 2023 career center
t
INTERIM SERVICES. HAVE MIRROR AND EXPLORER, WILL TRAVEL ANYWHERE IN FLORIDA: Sick Leave, maternity leave, vacation or death, I will cover your practice so that production continues while you are out. Please call or text Robert Zoch, DDS, MAGD at 512-517-2826 or email: drzoch@ yahoo.com. Visit careers.floridadental.org/ jobs/18047931/
General Dentist, Tampa. Brand new, fully digital practices that offer competitive production % and daily guarantee! Currently hiring in all major cities in Florida; Jacksonville, Tampa, Orlando, and South Florida. DECA Dental Group | Ideal Dental is a Dallas-based, clinician-founded, and clinician-led dental service organization delivering high-quality, affordable dental care to patients since 2008. We are actively expanding its footprint coast to coast under the brand Ideal Dental. Ideal’s culture is founded on a patient-centric model. Our model of providing a Clinical Board of doctors to mentor and develop new team members is a differentiating factor key to our success. We heavily invest in continuing education opportunities to ensure we provide the
highest quality of dentistry. With over 50,000 5-star guest reviews, the company cares deeply about its brand and the guest experience. The company is guided by its vision to be the premier provider of all dental services under one roof while being the first choice for dentists and staff seeking a partner for growth, innovation, and learning. For additional information visit, www.decadental.com or www.myidealdental.com. We are looking for an exceptional General Dentist committed to providing high-quality dentistry and excellent patient care to join our DECA Dental Group | Ideal Dental family. This position is a perfect opportunity to join a fast-growing practice with ownership potential and includes placement at a premier office location! What does our practice offer? The industry-leading mentorship, training, and education we provide our doctors. Our training program is one of the best learning programs in the nation. We provide our general dentists with the training to do all procedures from molar endo, surgical extractions, Invisalign, implant dentistry, and much more! We supply state-ofthe-art equipment, including iTero scanners,
fully digital practices, and robust KPI online dashboards at our offices. PPO and Fee for Service Guests with high reimbursement rates for maximum income potential.100% clinical autonomy and strong new guest marketing – most dentists see 60-100+ new guests each month. Ownership opportunities for candidates who are interested in continued personal, professional, and financial growth! Once you become an Owner Doctor, you can earn additional income through our equity buy-in program while continuing to practice without taking on any additional operational burdens, risk, or debt! What are the perks and benefits? Ownership opportunities; Sign-on bonus opportunities; Competitive compensation structure, including paid lab expenses; Paid in-house CE courses, including Invisalign Certification; One-on-one training and mentorship; Three medical insurance plans to choose from; discounted dental benefits for the employee, their spouse, and dependent children; Vision; Long-term and short-term disability; Life insurance; Accident coverage; 401K. Visit careers.floridadental. org/jobs/18047912
FLORIDA DENTAL CHATTER
86 career center
This Facebook group is designed for dentists to interact with other members, receive the latest updates and information, and engage with FDA leaders and sta . This is the place to be in the know! Join us at facebook.com/groups/floridadentalchatter.
Support
OUR JOURNAL ADVERTISERS
American Sensor Tech | 25
Doctor’s Choice | 62 & 63
E-Vac Inc. | 17
FDA: Online Radiography Program | 71
FDA: Well-being Program | 25

FDAS: Agents | Inside Front Cover
FDAS: BOA and Paragon | 46
FDAS: Coalition | Back Cover
FDAS: Crown Savings | 30
28 & 29 | FDAS: Disability Insurance
68 | FDAS: Life Insurance
61 | FDAS: iCore Connect
8 | Henry Schein Professional Practice Transitions
61 | Hinman
Inside Back Cover | A1 Handpiece Specialists
80 | Large Practice Sales
34 | Monticciolo Family & Sedation Dentistry
70 | The Doctors Company
25 | Tobacco Free Florida
SUPPORT OUR ADVERTISERS, AND WHEN YOU DO, MENTION TODAY’S FDA!
ADVERTISING INFORMATION
For display advertising information, contact: Deirdre Rhodes at drhodes@floridadental.org or 800.877.9922, Ext. 7108.
For Career Center advertising information, contact: Jill Runyan at jrunyan@floridadental.org or 800.877.9922, Ext. 7113.
PUBLISHING INFORMATION
Today’s FDA (ISSN 1048-5317/USPS 004-666) is published bimonthly by the Florida Dental Association (FDA), 545 John Knox Road, Ste. 200, Tallahassee, FL 32303. FDA membership dues include a complimentary subscription to Today’s FDA. Nonmember subscriptions are $150 per year; foreign, $188. Periodical postage paid at Tallahassee, FL and additional entry offices. Copyright 2022 Florida Dental Association. All rights reserved. Today’s FDA is a refereed publication. POSTMASTER: Please send form 3579 for returns and changes of address to Today’s FDA, 545 John Knox Road, Ste. 200, Tallahassee, FL 32303.
EDITORIAL AND ADVERTISING POLICIES
Editorial and advertising copy are carefully reviewed, but publication in this journal does not necessarily imply that the FDA endorses any products or services that are advertised, unless the advertisement specifically says so. Similarly, views and conclusions expressed in editorials, commentaries and/or news columns or articles that are published in the journal are those of the authors and not necessarily those of the editors, staff, officials, Board of Trustees or members of the FDA.
EDITORIAL CONTACT INFORMATION
All Today’s FDA editorial correspondence should be sent to Dr. Hugh Wunderlich, Today’s FDA Editor, Florida Dental Association, 545 John Knox Road, Ste. 200, Tallahassee, FL 32303. FDA office numbers: 800.877.9922, 850.681.3629; fax: 850.561.0504; email address: fda@floridadental.org; website address: floridadental.org.
Today’s FDA is a member publication of the American Association of Dental Editors and the Florida Magazine Association.
Is Your FOUNDATION Strong Enough for a Storm?
By Hugh Wunderlich, DDS, CDE, FDA Editor
I knew this was the correct interstate exit because all the road signs were gone. There was no exit number or mini-marquees showing the way to a Waffle House or Wendy’s. The day before, Hurricane Ian had spun the signs like giant freeway Frisbees into a distant field.
Nearby trees were uniformly trimmed to a meager 20 feet. In a surreal way, boats stuck in their tangled branches were occasional “fish out of water.” Sixty-foot interstate light poles were bent in half as if bowing to a greater natural force. The mobile home park next to the exit looked like a gutted and ground-up animal – its aluminum skin all twisted and exposed, its pink underbelly of insulation open to the sky.
The off-ramp provided a bumpy ride. Branches, fish and palm fronds littered the road. A tangle of downed power cables sprawled across the wet pavement like hundreds of worms escaping a summer rain.

At the bottom of the hill, two Humvees blocked the road, and National Guard officers questioned and turned away each curious driver who approached. A guardsman knocked at my driver’s window, asking for identification. I fumbled through my wallet, my eyes fixed on the gun slung over his shoulder.
“How can I help you?” he asked, already set to turn me away. That’s when he spotted my “Florida Dental Association” (FDA) business card. Now visibly excited, he waved me through and then got into my car to direct a now-forming “military parade” into town.
As the guardsman motioned for a front-end loader to clear a path, he asked questions about un-refrigerated food and where to put an expected supply of drugs. “Oh, FDA – Food and Drug Administration,” I thought. I told him as much as I knew about
rancid butter, but he didn’t seem disappointed when I explained that I was representing “the original FDA.” Little did I know this little berm of the highway would become the only high ground for the next few days as the ever-rising waters of the Myakka River overflowed and filled the neighboring homes.
In partnership with the American Dental Association, the Florida Dental Association has developed a manual called “Five Steps” to Disaster Preparedness and Recovery. The guide includes steps to ensure your practice weathers the storm. It covers topics such as evaluating insurance coverage and your office’s storm vulnerability; protecting your equipment, supplies and patient records; dealing with power failures, communication blackouts and evacuation; and emergency supplies.

The FDA Foundation was also able to provide support to Florida dentists impacted by Hurricane Ian. The FDA Foundation Emergency Disaster Assistance program provided 211 emergency assistance grants (a total of $316,500) to assist with immediate personal needs such as food, water, clothing, emergency shelter or medications.
As my “military escort” ended, I paused to interrupt a haggard man walking alone down the mud-laden street. “Can I get you anything? … And with open palms turned upward, he said, “I need everything.” I could only assuage his desires with a half-empty water bottle that he consumed immediately. I was kicking myself for not bringing more than gallons of gasoline. Every one of us, if not directly affected by a storm, has had the survivor’s guilt of dodging that “eye.” We are all in this together. You know another named storm is coming. The disaster guide can be found at bit.ly/3GWMIQJ
So … I am also a card-carrying member of the Council for International Activities. I can’t wait to see where that ID card will get me.
88
off the cusp


Coalition is the preferred cyber insurance carrier of FDA Services Coalition’s included security tools can reduce an organization’s costs to detect, recover, and contain a breach by over 40%, and are available to all policyholders at no additional cost. fdaservices.com | insurance@fdaservices.com | 800.877.7597 CALL OR TEXT US AT 850.681.2996































































































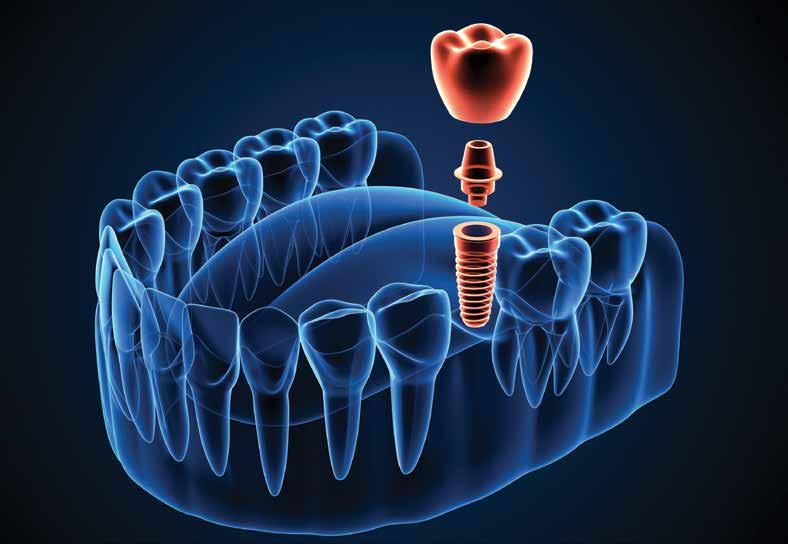 By Rafeeq N. Rahman, DDS; Alexander Lee, DMD; Setareh Lavasani, DMD, MS; and Tobias Boehm, DDS, PhD
By Rafeeq N. Rahman, DDS; Alexander Lee, DMD; Setareh Lavasani, DMD, MS; and Tobias Boehm, DDS, PhD








































































 Greg Jones, Dental Practice Broker Doctors Choice
Jason Kaplan, Esq. Palm Beach Law Group
Greg Jones, Dental Practice Broker Doctors Choice
Jason Kaplan, Esq. Palm Beach Law Group























 By James Kohner, DDS
By James Kohner, DDS




















