















































































TEBODONT ®
Gel
In case of irritated gums and oral mucosa, contains tea tree oil

TEBODONT ®
Spray
In case of irritated gums and oral mucosa, inhibits the formation of plaque, cares for and regenerates, contains tea tree oil

®
Mouthrinse
Inhibits the formation of plaque, cares for and strengthens the gums, contains tea tree oil, without fluoride

TEBODONT ®
Toothpaste
Inhibits the formation of plaque, strengthens the gums, contains tea tree oil, without fluoride

TEBODONT ®-F
Mouthrinse
Inhibits the formation of plaque, for the prophylaxis of caries, cares for and strengthens the gums, contains tea tree oil and sodium fluoride

EMOFORM® Gum Care
Toothpaste
In case of gum problems, contains mineral salts

EMOFORM® Gum Care
Mouthbath concentrate In case of gum problems, contains mineral salts

EMOFORM® Sensitive
Toothpaste In case of sensitive gums, contains mineral salts

EMOFORM® Sensitive
Mouthbath concentrate

EMOFORM® Protect
In case of sensitive gums, contains mineral salts

EMOFORM® Diamond
Toothpaste For prevention of caries, hardens dental enamel
Whitening toothpaste For white and shiny teeth, contains finest diamond particles

EMOFLUOR® Daily Care
Toothpaste For daily care of sensitive teeth, contains stabilised stannous fluoride

EMOFLUOR® Daily Care
Mouthrinse For the daily care of sensitive teeth and for the prophylaxis of caries

EMOFORM® Kids
Toothpaste for children From the first milk tooth, up to and including 5 years
EMOFORM® Youngstars
Toothpaste for children Comprehensive protection for the teeth, as of 6 years

Intensive Care
Gel
For targeted protection against sensitive teeth and erosions, contains stabilised stannous fluoride

EMOFLUOR® Twin Care
Toothpaste
Dual protection against erosions and sensitive teeth with stannous fluoride and vVARDIS technology
Clean & Polish
Paste for teeth cleaning Removes dental plaque and teeth discoloration, with polishing eect

Clean & Polish
Mouthrinse Helps preserve the natural whiteness of your teeth, helps prevent caries
Volume XXXII, Number 1, 2025
EDITORIAL TEAM COORDINATOR
ART
DIRECTOR ISSN
Alfred Naaman, Nada Naaman, Khalil Aleisa, Jihad Fakhoury, Dona Raad, Antoine Saadé, Lina Chamseddine, Tarek Kotob, Mohammed Rifai, Bilal Koleilat, Mohammad H. Al-Jammaz
Suha Nader
Marc Salloum
Micheline Assaf, Nariman Nehmeh
Josiane Younes
Albert Saykali
Gisèle Wakim
Tony Dib 1026-261X
DENTAL NEWS IS A QUARTERLY MAGAZINE DISTRIBUTED MAINLY IN THE MIDDLE EAST & NORTH AFRICA IN COLLABORATION WITH THE COUNCIL OF DENTAL SOCIETIES FOR THE GCC.
Statements and opinions expressed in the articles and communications herein are those of the author(s) and not necessarily those of the Editor(s) or publisher. No part of this magazine may be reproduced in any form, either electronic or mechanical, without the express written permission of the publisher.
DENTAL NEWS – Sami Solh Ave., G. Younis Bldg. POB: 116-5515 Beirut, Lebanon.
Tel: 961-3-30 30 48
Email: info@dentalnews.com Website: www.dentalnews.com


IDEX 2025
Jordanian International Dental Conference
April 29 – May 1, 2025 Kempinski Hotel | Amman, JORDAN www.jidconf.com
May 7 – 10, 2025 EXPO Center | Istanbul, TURKEY www.idex.org.tr

JDS 2025

EXPODental 2025

www.instagram.com/dentalnews

FDI World Dental Congress 2025
CADEX Central Asia 2025

This magazine is printed on FSC – certified paper. WWW.DENTALNEWS.COM

39th CAPP Int’l Dental ConfEx
Jordanian Dental Supplies Show May 13 – 15, 2025 Mecca Mall | Amman, JORDAN www.jidconf.com
May 15 – 17, 2025 RIMINI | ITALY www.expodental.it/en
September 9 – 12, 2025 Shanghai | CHINA 2025.world-dental-congress.org/En
October 9 – 11, 2025 ALMATY | KAZAKHSTAN www.cadex.kz
November 14 – 15, 2025 Madinat Jumeirah | Dubai, U.A.E www.cappmea.com
AEEDC 2026
January 19 – 21, 2026
World Trade Center | Dubai, U.A.E. www.aeedc.com





Oleg O. Yanushevich, Igor V. Maev, Natella I. Krikheli, Dmitrii N. Andreev , Svetlana V. Lyamina ,Filipp S. Sokolov, Marina N. Bychkova, Petr A. Beliy and Kira Y. Zaslavskaya





Geetanjeli
Sheogobind 1*, Christian Foster 2 , Oreoluwa Lanlokun 2 , Abiola-Olujare Lawal 3 , Samim
Mohammadi 4*, Jachike Ndbuisi 4
1. Howard University College of Dentistry, Comprehensive Care Division, Restorative Department
2. Howard University College of Dentistry, Postdoctoral Orthodontics Program
3. Case Western Reserve University, Advanced Education in General Dentistry Program
4. Howard University College of Dentistry Undergraduate Program
*co-authors
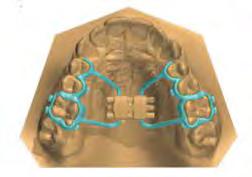
3D printing revolutionizes orthodontic appliance creation, producing customized braces and appliances with unmatched precision for faster, accurate orthodontic outcomes. The efficiency of 3D printing significantly cuts patient waiting times, crafting appliances in hours instead of weeks. This article reviews the appliances that can utilize 3D printing such as diagnostic models, removable appliances, presurgical nasoalveolar moldings, occlusal splints, space maintainers, expansion devices, customized brackets, indirect bonding trays (IDT) and retainers. This emergent 3D technology has had a transformative effect on the field of orthodontics but still has challenges and considerations in its application.
“3D printing in orthodontics”, “braces and aligners”, “orthodontic appliances”, “customizable orthodontics”
Presently, with the emergence of computer-aided design and threedimensional (3D) technology, craniomaxillofacial dental care and specifically orthodontics is poised to become revolutionized in it’s service delivery, production of appliances and workflow in practice settings. Archwires, nasoalveolar molding devices, removable appliances, clear aligners, expansion appliances, auxiliary attachments, orthognathic surgical splints and casts can all be made with 3D technology1 Orthodontists now have access to this mode of producing appliances which has increased production and allow for customizable options for patients. With the use of intraoral scanners and 3D printing, the need for dental
impressions has been completely eliminated, and now orthodontists can provide a fully digitalized model in orthodontic service delivery. Dental impressions remain the mainstay of record making and treatment planning, and now that this task can be done digitally, efficiency and workflow in orthodontic practices have improved. Another valuable feature of 3D printing is that patientspecific designs from 3D printers allow orthodontists to develop viable solutions that no longer require visual estimates for their dimensions.
A thorough orthodontic diagnosis requires comprehensive 3D analysis of the interrelationships among the dentition, craniofacial skeleton and soft tissues. 3D printing technology will provide more than 60% of all dental treatment needs by 2025, and orthodontic companies as well as remote monitoring companies are already using AI technology, being it essential that the clinicians are prepared and knowledgeable with the technology advances now available2. 3D printing offers a precise way to fabricate appliances layer by layer, allowing for better accuracy in the fit of appliances and better patient compliance3 In orthodontics, often patients anatomical anomalies are variable, and cases can become very complex from case to case. With the ability of 3D printing to customize devices for e.g. the chains used to move impacted teeth or spreaders for a vaulted palate, when conventional dimensions are not present, 3D printing can effectively measure these intricate differences down to the micron creating appliances that are far better at fit when compared to laboratory fabricated appliances4








3D printing can be effectively utilized in the fabrication of the following appliances: diagnostic models, removable orthodontic appliances, presurgical nasoalveolar molding, occlusal splints, space maintainers, expanders, aligners and retainers.
Diagnostic models measurements performed with 3D digital models represent high validity, reliability, and reproducibility. They are a viable alternative to traditional plaster models and identical copies of a digital model can be reproduced without distortion or deformation which can negatively affect the appliance that is built upon it5. Warping and distortion are two common issues traditionally encountered using gypsums and other polymer materials when used for dental impressions.
Removable Orthodontic appliances that can be fabricated by 3D printing include the Hawley appliance and functional appliances like Twinblock or activators. Traditional pouring of plaster casts have effectively been eliminated by utilizing scans such as TRIOSTM or 3ShapeTM6. Other manufacturers worldwide of 3D orthodontic appliances include DentalWingsTM, Shining 3DTM, MeditTM and EnvisionTECTM
The area of orthognathics has also benefited from 3D printing. Treatment protocols for patients requiring reconstructive surgery have appliances that are better adapted to facial structures, which leads to less aspiration of material, and quicker planning and fabrication by clinicians. Alveolar ridges can be clearly identified and measured using a graphical user interface and design plates, which are able to mimic the growth of bones in healthy newborns requiring molding devices. These design plates can be made in just a few minutes and adapted to the area in need of treatment7
Occlusal splints have traditionally been utilized when treating patients who present with temporomandibular disorders (TMD) and orthognathic asymmetries. Subtractive technology, where a block of acrylic is reduced to a desired shape and size was originally used to fabricate occlusal splints. But 3D printing has offered a different method, called Additive
technology, where acrylic layers are added on to each other, while bonding occurs between levels to fabricate an appliance8. This method has proven to be faster, more adaptable and better fitting for patients.
Space maintainers are used to intercept malocclusion before it is established within the dentition of a child receiving orthodontic care. The following appliances are also used for anchorage reinforcement, where a tooth or teeth must be held stationary during treatment until movement can be elicited. These appliances can now be routinely fabricated with 3D printing: a) Trans palatal arch is 3D printed through metal printing and the bonding site is designed on the molars not completely circular, but only confined to palatal surface. b) Hybrid Nance appliance: Nance appliance again serving both purposes, can be 3D printed through metal printing. c) Lingual arch: Lingual arch fabrication with bands designed to be printed through 3D metal printing (fully or partial) around the molars with a connector along the lingual surface of the teeth 9
3D printing has seen much success with expansion appliances that shorten treatment times and adapt better. Rapid Palatal Expanders (RPEs) have been designed in various ways, with the most common forms being a single or connected band(s), bands with arms or a faces mask where the arms are equipped with hooks that attach to elastic intraorally and anteriorly9,10. There are also modifications to expansion appliances and distalizers, appliances used to gently push maxillary molars backwards as seen with 3D printed Hyrax-Hayrake-Blue-grass combination appliance, an appliance that is a combination of three appliances: the hyrax, a split Hayrake for habit-breaking and a movable bluegrass bead for tongue training9.
When 3D printing is utilized to fabricate customized orthodontic brackets, they are usually made from polycrystallines alumina ceramic or metal and 3D printed into twin brackets with idealized geometries, which creates tooth movement that is highly efficient. Customization
can also be extended to self-ligating and lingual brackets and indirect bonding trays which are used to accurately place brackets onto teeth prior to bonding11
Retainers such as the Clear/Essex thermoformed polymer retainers can be fabricated with high efficiency through 3D printing. When a retainer is needed to be bonded to several teeth surfaces lingually, 3D printing can also be used to measure and reproduce the metal bar used for permanent bonding to the surfaces of teeth. The process of fabrication of these types of retainers has greatly benefited from the precision and customization of 3D printing due to the unique shapes and alignment of a patient’s teeth post-orthodontic treatment12



As the field of orthodontics continues to evolve, 3D printing technology holds the key to revolutionizing this specialty in its service delivery, cost cutting and providing a better patient experience. Appliances have become highly adaptable and customized for patients. As 3D printing and other digital technologies continue to emerge and further improvements within orthodontics, innovations and better dental outcomes are expected. 3D printing technology has made orthodontics more efficient, and this in turn has made the field more affordable for patients where orthodontic treatment might have been out of reach. Digitization represents a radical shift in thinking within the field of orthodontics,
Transcend universal composite provides unprecedented shade matching with just one Universal Body shade due to its patented Resin Particle Match™ technology that eliminates the need for a blocker.
If you prefer a layering technique Transcend composite also includes four dentin shades and two enamel shades.


Deep amalgam staining presents one of the most difficult restoration situations to clinicians. In this case only the Transcend composite Universal Body shade was used to replace the amalgam no blocker needed. Note the excellent color blending of the preserved oblique ridge.


Scan the QR code to learn more about Transcend Universal Composite or go to ultradent.eu/transcend
where orthodontists are now able to provide dental care that is precise and personalized for each patient; and though this was the case before, the customization is now more precise and empirical. This precision translates to more predictable outcomes for patients and higher success rates for orthodontic cases.
The authors of this article certify that patient consent forms were not necessary with this publication. Appropriate measures were taken to conceal any identifiable information of patients in this article.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
None.
BIBLIOGRAPHY
1. Tuğçe Ergül, Ayşegül Güleç, Merve Göymen, Turkish Journal of Orthodontics, The Use of 3D Printers in Orthodontics, A Narrative Review, Jun 22:3692):134-142. doi: 10.4274/ TurkJOrthod.2022.2021.0074;
PMCID: PMC10318848 PMID: 37346463
2. Soo-Yeon Kim, Yoo-Seok Shin, Hwi-Dong Jung, Chung-Ju Hwang , Jung-Yul Cha, American Journal of Orthodontics and Dentofacial Orthopedics, 2018, 154 (1), Precision and Trueness of Dental Models manufactured with different 3-dimensional Printing Techniques, 150-151.
3. Phillips, Dr. Keith, DistinctiveDentistry.com, How 3D Printing Technology is Applied in Dentistry, September 15, 2021.
4. Miranda, DDS, MS, PhD, Felicia, Barone DDs, MS, Selene, Gillot, BS, Maxime, Baptiste, BS, Baquero, Anchling, BS, Luc, Hutin, BS, Nathan, Journal of the California Dental Association Volume 51, 2021 (1), https://doi. org/10.1080/19424396.2023.2195585.
5. Kim SY, Shin YS, Jung HD, Hwang CJ, Baik HS, et al. Am. J Orthod Dentofacial Orthop 153(1), Precision with different 3D printing techniques, pgs. 144-153. (2018)
6. 0. Al Mortadi N, Jones Q, Eggbeer D, Lewis J, Williams RJ, 2015, Am J Orthod Dentofacial Orthop 148(5): 862-867.(2015) Fabrication of a resin appliance with alloy components using digital technology without an analog impression.
7. Cong, Shen , Caroline A Yao, William Magee 3rd, Gang Chai, Yan Zhang, Plast Reconstr Surg. 2015 Jun, Presurgical nasoalveolar molding for cleft lip and palate: the application of digitally designed molds: 135(6): 1007e-1015e. doi:10.1097/ PRS.0000000000001286, PMID: 26017607.
8. Lauren M, McIntyre F., Wang YT, Yu, JH, Lo, LJ, Hsu, PH (2008) A new computer-assisted method for design and fabrication of occlusal splints. Am J Orthod Dentofacial Orthop 133(4): 130-135. 14.
9. Graf S, Tarraf N, Kravitz, N (2021) ThreeDimensional Metal Printed Orthodontic Laboratory Appliances. Semin Orthod 27(10): 1053.
10. Graf S (2017) Direct Printed Metal DevicesThe Next Level of Computer-aided Design and Computer-aided Manufacturing Applications in Orthodontic Care. APOS Trends Orthod 7: 253259.
11. Gianluigi Fiorillo, Alessandra Campobasso, Giulia Caldara, Giovanni Battista, Eleonora Lo Muzio, Gualtiero Mandelli, Alessandro Ambrosi, Giorgio Gastaldi, Am J Orthod Dentofacial Orthop, (2023), Accuracy of 3-dimensional-printed customized transfer tray using a flash-free adhesive system in digital indirect bonding: An in vivo study; doi: 10.1016/j.ajodo.2023.02.017, PMID: 37074245
12 David Cole, Sompop Bencharit, Caroline K Carrico, Andrew Arias, Eser Tüfekçi, Am J Orthod Dentofacial Orthop. 2019, Evaluation of fit for 3d printed retainers compared with thermoform retainers, Apr:155(4):592-599. PMID: 30935614, doi: 10.1016/j.ajodo.2018.09.011
FIGURES
Figure 1. Bruno Orthodontics/how-can-3Dprinting-help-straighten-my-teeth, USA, 2024.
Figure 2. Graf, S., Tarraf, N.E., Science Direct, Advantages and disadvantages of 3D metal printed orthodontic appliances, November, 2022.
Figure 3. Planning customizable brackets, 3ShapeTM Software, USA 2024.
Figure 4. Form Labs/Hawley Retainers, USA 2024.




VistaScan Image Plate technology: flexible, thin, wireless and 100% diagnostic area. More at www.duerrdental.com

Spokesperson: Dr. Charlie Parkinson Medical Affairs Director, Haleon
Dr. Charlie Parkinson, can you please introduce your professional journey?
I’ve been with Haleon (formerly known as GSK Consumer Healthcare) for just over 20 years. In July 2022, Haleon launched as an independent company, 100% focused on consumer health, with a purpose to deliver better everyday health with humanity. As one of the world’s leading providers of specialist oral health products, including Sensodyne, Parodontax, and Polident, our goal in oral health is to make mouths healthier across the world.
Dental sensitivity is on the rise. What are the reasons that there is a rise in dental hypersensitivity?
Dentine hypersensitivity is highly prevalent. The most recent data comes from an European epidemiology study by Bristol University, supported by Haleon, and shows around 1 in 2 adults have dentine hypersensitivity. This new, fascinating data is being shared at this FDI World Dental Congress (WDC).
In this pivotal study, not only did it show the high prevalence of dentine hypersensitivity, but we were also surprised that the level of erosive tooth wear was high, and particularly in the younger adult population. Approximately, 80% of the study population had the very early signs of erosive tooth wear. We believe that diet, particularly a more modern diet including fruit juices and the acids in salads for example, are contributing to a faster rate of loss of enamel, which then exposes the dentine and leads to a rise in the prevalence of dentine hypersensitivity.
Is there a standardized method to test hypersensitivity?
There’s a common method, but there is no formal agreement on a standardized method. The most often used method to diagnose dentine hypersensitivity is for dental health professionals to use a dental air syringe and direct an air-blast onto the tooth, at the sensitive area, and see how the patient responds. They’ll either not really respond, flinch, or they’ll say that was painful. At Haleon, our purpose is to deliver better everyday health with humanity, so we are not just looking at the pain experienced, but we are also looking at how dentine hypersensitivity impacts sufferers’ day-to-day lives. Over the last 20 years,

Dr Charlie Parkinson is Global Medical Affairs Director: Oral Health at Haleon. He has twenty years’ experience in oral care research, product development and clinical evaluation. His research has included in vitro and in situ modelling of oral diseases and conditions, fMRI of oral conditions, therapeutic approaching in the management of dentine hypersensitivity and erosive toothwear, and the impact of oral conditions on oral health related quality of life. He is a Fellow of the Royal Society of Chemistry and Associated Editor for the Journal Preventative Dentistry, with over 70 peer reviewed publications in the field of oral care.
in collaboration with researchers from Sheffield University (Professors Sarah Baker and Barry Gibson) we have pioneered techniques to explore the impact of dentine hypersensitivity on peoples’ lives – and it shows that the condition has a dramatic impact on the way people eat and drink, avoid social situations and impacts their identity. In trying to better understand how people engage with health professionals when it comes to their oral health, we’re learning that people don’t often talk with their dental health professional about dentine hypersensitivity. Therefore, many people could be suffering unnecessarily when there are simple options to manage dentine hypersensitivity with a daily use, anti-sensitivity toothpaste. Do you think, it has always been there, but people were not talking about it?
Dentine hypersensitivity has always been there, and one of the earliest reports describing the condition was in 1859, by Sir John Tomes who was exploring why dentine was so sensitive. As mentioned, our most recent supported study has shown that 1 in 2 adults suffer from the condition, but we also know not everyone takes action to

manage their sensitivity. The behavior change work we are supporting and sharing at the FDI suggests that there isn’t enough discussion about the condition, and that awareness of simple first line management options such as twice daily use of a sensitivity toothpaste can be improved. Dentine hypersensitivity has been described as an enigma because the condition is not associated with a specific disease or pathology – it has a differential diagnosis. If the person has exposed dentine, and once you’ve excluded any other cause for the tooth pain, what’s left is essentially considered dentine hypersensitivity. So, it is not the easiest condition to talk to or explain with patients or consumers, but it is important to talk about it as there are simple solutions to help take an active role in managing the condition. Could you tell us more about the recent epidemiology study on dentine hypersensitivity that’s being showcased at the FDI World Dental Congress?
The epidemiology study is being presented here at the FDI WDC by Nicola West as a scientific abstract, but it’s also being submitted for publishing in a peer reviewed journal by the end of the year. The impact of dentine hypersensitivity on peoples’ daily lives and why dentine hypersensitivity is not discussed by dental healthcare professions is also being presented here at the FDI in scientific abstracts, and some parts of the work have been published in open access journals (for example: Dentine hypersensitivity – barriers to discussion Asimakopoulou K, West N, Davies M, Gupta A, Parkinson C, Scambler S. Why don’t dental teams routinely discuss dentine hypersensitivity during consultations? A qualitative study informed by the Theoretical Domains Framework. J Clin Periodontol 2023; DOI: 10.1111/jcpe.13885).
Can you elaborate on the daily challenges our teeth face, especially in relation to modern diets?
Your teeth are subjected to huge amounts of challenges every day. Be it the sugar acids (plaque acids) causing cavities, or dietary acids eroding the enamel. With our changing diets the prevalence of tooth decay and enamel erosion is increasing. While difficult, the advice needs to be that these risk factors need to be better understood by patients and consumers to drive a change and improvement in oral health.
What about the products that are used in Sensodyne? Is the formula the same as it was 20 years ago?
No, the formula has evolved quite dramatically over the years, and the most recent formulations use a bioglass technology, NovaMin. It was originally invented as a bone repair material back in the 1970s, and later in the 1990s the inventors made the connection that bone is quite similar to dentine, and therefore NovaMin may help occlude dentine to provide relief from dentine hypersensitivity.
The inventors ran a number of clinical studies in sensitivity sufferers, and they demonstrated significant improvement in sensitivity. Then in 2010, Sensodyne launched the technology as a daily use fluoride antisensitivity toothpaste and since this time has conducted over 12 clinical studies on the technology in our formulations to confirm the efficacy. Furthermore, independent researchers have conducted 12 clinical studies confirming our findings, that NovaMin provides effective relief from dentine hypersensitivity. NovaMin is a fascinating ingredient, once it comes into contact with saliva, it releases the calcium and phosphate that bind to your teeth and form a hydroxyapatite layer over the sensitive areas. Because it works by activating in the mouth, the formulation had to be specially engineered – it does not contain added water (which would deactivate it in the tube), this means that the toothpaste has a different feel in the mouth and can have a slight warming sensation. We also have potassium nitrate formulations for sensitivity, and other formulations that offer other benefits, such as supporting gum health, also supported by clinical studies.
are
Our most recent product launch is Sensodyne Clinical Repair toothpaste, which contains NovaMin as a key ingredient. It has already been launched in Germany, the Netherlands, and several Eastern European countries, and is currently being rolled out in other markets.
available in the Middle
In the Middle East and Africa, we offer a comprehensive range of Sensodyne products tailored to meet various oral health needs. Our offerings include, but are not limited to, the Sensodyne toothpastes such as Clinical White, Total Care, True White, Complete Protection, Rapid Relief, Rapid Action, Advanced Repair & Protect, Sensitivity & Gum, Pronamel, and Pronamel Kids.

Dr Adil H. Alani (BDS, HDDip. PhD)
Assistant Professor and Endodontist Arabian Specialist Medical Center
Oud Bin Sag Asharej, 33 Street, Al Muwaij’i Al-Ain, UAE adilalani@hotmail.com
Dr. Ahmed S. Al-Obaiydi (BDS) General Dental Practitioner
Dr. Ahmed Subhi Dental Clinic
Baghdad Suleikh Street, Suleikh, Iraq Ahmed03subhi@gmail.com
Authorship
Declaration: All authors have contributed significantly, and all authors are in agreement with the manuscript.
Disclosure Statement: Furthermore, the authors would like to declare that there is no financial interest with any company manufacturing the types of products mentioned in this article.
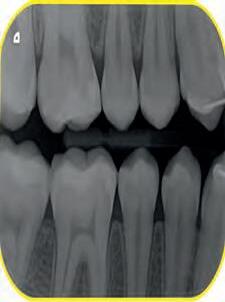
The presence of 2-rooted mandibular canines has been described in only a limited number of case reports however studies of anatomical features have demonstrated substantial variation in the number of roots and root canals in different teeth. The mandibular canine usually has one root while this report describes the incidence of 2 cases of mandibular canines with 2 roots and 2 root canals. The report outlines the steps necessary to identify and treat such cases, which starts with thoroughly examining the internal anatomy of the tooth using clear radiographs taken from different angles, while treatment relies on using advanced equipment like dental operating microscope, ultrasonic tips for conservative access, and accurate apex locator for accurate working length determination.
anatomical variation, internal anatomy, mandibular canine, root canal, two roots
The principle objective of root canal treatment is to relieve pain, eliminate bacteria from the root canal system, and prevent reinfection. A clear understanding of root morphology and canal anatomy is an essential prerequisite to achieving clean, disinfected and 3-dimentionally obturated root canal systems. Undetected extra roots or root canals are a major reason for the failure of root canal treatment(1)
Many of the challenges faced during root canal treatment may be directly attributed to an inadequate understanding of the canal morphology of teeth. Variations in root canal morphology are a constant challenge for diagnosis and is a huge
contributing factor in the success of root canal treatment. Usually, the mandibular canine has only one root and one root canal (2). The incidence of two roots and even more than two root canals in canine is rare, ranging from 1% to 5% (3,4). Despite the low prevalence, clinicians should consider the possible variations in the number of roots and root canals of mandibular canines. Root canal treatment of two-rooted mandibular canine had been documented in several clinical reports. Many authors (5, 6, 7) reported that the occurrence of mandibular canines with one and two root canals is approximately 15%. At the same time, the incidence of mandibular canines having two roots and two canals was documented to be up to 5% (3, 8). In addition, mandibular canine with three canals in one root had been reported(9), or three canals in two roots(10). All these cases suggest abnormal morphological features of the canine root system.
Radiographs are an important and necessary adjunct for root canal treatment, and accurate radiographic techniques and correct interpretation are essential for sound diagnosis and treatment. The use of preoperative radiographs is the best way to detect and evaluate root canal morphology and anatomy. Further radiographs should be taken at different angles to confirm any variations in anatomical features(11). In recent years, significant technological advances for imaging teeth have been introduced, including digital radiography, densitometry, magnetic resonance imaging, ultrasound, and computed tomography(12). Conebeam computed tomography systems (CBCT) have gained increasing significance in the study of hard tissues in endodontics as it offers a reproducible technique that can be applied quantitatively as well
Don’t just go with the flow. Pick the right flow!

You have the choice:
• Light Flow – low viscosity
Precise application thanks to the very fine cannula and therefore optimally suitable for hard-to-reach areas and small cavities
• Flow – medium viscosity
Outstanding flow behaviour, universal and precise application
• Heavy Flow – high viscosity
Increased stability, i. e. universal application and no undesirable runoff
*Filler content by weight

Also available as Caps
as qualitatively, allowing for a three-dimensional image of the root canal system(13)
The purpose of this clinical report is to describe endodontic treatment of two mandibular canines with two roots and two canals in two Arab nationals. Additionally, the following two case reports have been written according to Preferred Reporting Items for Case reports in Endodontics (PRICE) 2020 guidelines.
Case 1
A 27-year- old male was admitted to the Endodontic Department of [Redacted] Medical Center for the past three days pain in the right front region. Medical history was noncontributory. Patient gave a history of spontaneous pain lasting from a few seconds to several hours. Also, pain is caused when hot and cold liquids are used, and is felt longer and more pronounced when hot, while cold relieve pain. Clinical examination revealed a carious cavity lesion penetrating the pulp of tooth # 43 (lower right canine). Tooth was tender to percussion. No swelling or fistula intra or extra orally. A diagnosis of irreversible pulpitis was made. Careful examination of the radiograph demonstrated a long root and the possibility of more than one canal (Fig.1)

Fig.1
After the patient provided signed informed consent, the tooth was anesthetized and isolated with a rubber dam. Caries was removed and access to the pulp chamber was made using a round diamond bur. The pulpal floor was examined using dental operating microscope (Global Dental Microscopes, Global Surgical Corporation, USA). The DG-16 endodontic explorer (American Eagle, CA, USA) was used to determine the bifurcation level of the root. Ultrasonic tips (Pro Ultra Endo Tips Dentsply Maillefer, Ballaigues, Switzerland) were then used to remove cervical dentin that obstructing the path to lingual canal in mandibular canine. The internal anatomy confirmed the presence of 2 root canal orifices, one located buccally and the other lingually. The working lengths of each canal were estimated by means of electronic apex locator (Root ZX, Morita, Tokyo, Japan), then confirmed by a radiograph.
The canals were initially instrumented with a size #15 K-file, and coronal flaring was carried out using Gates Glidden burs (numbers 3 and 2; Dentsply Maillefer, Ballaigues, Switzerland). Biomechanical preparation was completed by using rotary nickel-titanium files ProTaper Gold (Dentsply Maillefer, Ballaigues, Switzerland) up to apical file size # 30. Copious irrigation with 3% sodium hypochlorite (NaOCl) with ultrasonic Endo Activator (Dentsply Maillefer, Ballaigues, Switzerland) was applied for 30 second followed by 17% Ethylenediaminetetraacetic acid (EDTA) for 1 minute with safe 2-side vents irrigation tips IrriFlex (Produits Dentaires, Swizterland), to remove the inorganic tissues, and this was performed during the instrumentation phase. Sterile paper points were used to dry the root canals. Master cone radiograph was taken, and the two canals were obturated with Tubli-seal (Kerr UK, Peterborough, U.K.) and laterally condensed using gutta-percha points. Final radiographs were taken to ensure proper obturation. A sterile cotton pellet was then placed in the pulp chamber, and IRM cement (Dentsply De Trey GmbH, Konstanz, Germany) was applied to seal the access cavity as a temporary filling to prevent coronal leakage. The patient was referred for final restoration (Fig. 2)


A-35-year-old female was referred for root canal treatment of the right mandibular canine. The general dental practitioner had started root canal treatment. The tooth was asymptomatic and free from any clinical signs. Medical history was unremarkable.
Clinical examination revealed no mobility, normal periodontium, no swelling or sinus tract, and the tooth was not tender to percussion. Pulp sensitivity testing of the tooth showed no response to cold and electrical pulp testing. Radiographic evaluation of the affected tooth revealed unusual, complex root canal anatomy. The radiographic image showed the presence of two roots with periapical radiolucency (Fig. 3).

Based on history, clinical examination, a diagnosis of necrotic pulp and apical periodontitis was established for lower right canine (#43). Root canal treatment was decided, and informed consent was taken from the patient.
Infiltration of the local anesthesia (Lidocaine HCl 2% with epinephrine 1:100,000) was administered and the rubber dam was placed. Access to the cavity was achieved using a round diamond bur. The conventional lingual access opening was modified by including more of the incisal surface to gain sufficient access to the canals . The two orifices were located one buccally and one lingually. Coronal flaring was carried out using the Sx file of the ProTaper system (Dentsply-Maillefer, Ballaigues, Switzerland). The two canals were carefully instrumented with a size 15 K-file . The working length of the canals was established with the use of apex locator (Root ZX: J Morita Co, Kyoto, Japan) and verified radiographically (Fig.4).
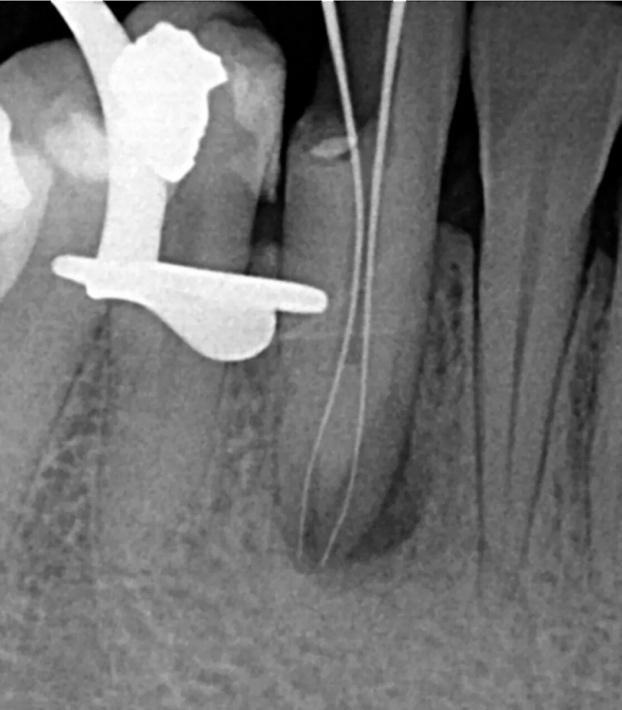
4
Root canals preparation until F2 file size, disinfection, obturation, and temporary restoration were performed in a same manner as described for Case 1. (Fig. 5)

Whiter teeth can give your patients the confidence to smile more.

Opalescence whitening is on a mission to help give your patients brighter, whiter smiles so they can look their best and feel their best, turning good days into better ones. As the global leader in professional whitening,1 Opalescence has brightened over 100 million smiles.1 That’s a lot of better days.
This report focused on two cases of mandibular canines with two roots and two root canals. Any morphological and anatomical variations in the root canal system should always be considered at the beginning of endodontic therapy, and the clinician is required to understand the complexity of root canals features and carefully examine any variation. Diagnosis and identification of the number of roots and root canals are essential because endodontic success is related to a thorough debridement of the root canal system. Most endodontic and dental anatomy textbooks describe the mandibular canine as a single rooted tooth with single root canal system. However, the presence of two roots in mandibular canine is a rare incident. Endodontists should always search for two canals in mandibular canines during root canal treatment, even in single-rooted teeth. The incidence of two root canals in single-rooted mandibular canine teeth has been reported to be up to 6.25% (14). Green (6) found two canals in a single root in 13 out of 100 mandibular canines examined. This is in consistent with the findings of Hess (15), who observed two canals in 15% of the cases. Vertucci (7) reported the presence of two canals in 18% of the mandibular canines. Ghoddusi and other (16) also found two separated canals in the mandibular canines. The presence of one root with two canals and two roots with two canals has also been reported by many authors (17, 18, 19, 20). Heling and other (21) reported a rare case of mandibular canine with two roots and three canals. In a previous study using a tooth clearing method, (8) studied the internal anatomy, orientation, and number of roots of 830 extracted human mandibular canines. They found that 98.3% of teeth presented a single root, and 1.2% had two roots and two canals. An even higher incidence (18.5%) of two canals was found by Pineda and Kuttler (5) who used radiographic images to study the internal morphology and anatomy of 187 mandibular canines.
In certain circumstances, the root canals may be left untreated during endodontic therapy if the practitioner is unable to detect their presence (1). The presence of extra roots can easily be determined by using routine radiography, as shown in the present cases. However, teeth with extra canals and a normal number of roots present a greater challenge in terms of diagnosis and treatment. Extra root canals can be difficult to identify because they overlap other root canals or, sometimes, they are relatively small. Careful examination of the preoperative radiographs is essential for the detection of extra canals. Knowledge of anatomic aberrations, such as root position, root shape and root outline will also decrease the failure rate of root canal therapy. It is important to carefully inspect the preoperative
radiograph for signs of anatomical variations to avoid potential excessive weakening or even perforation of the roots. Recently, the availability of advanced diagnosis radiographic tools such as Cone-beam computed tomography (CBCT) have proved to be very helpful in the diagnose morphological variations where conventional radiographic techniques have failed to provide more information and details required (22). Conebeam computed tomography as it provides accurate details in the axial, sagittal, and coronal planes is recommended if a diagnosis cannot be made using conventional radiography. (23)
Access to the root canal is the initial step in canal preparation, and a properly designed and prepared access cavities will eliminate many potential problems during canal preparation and obturation. In the cases reported here, after gaining access to the root canal system, cleaning and shaping were done using rotary instruments in a crown down technique to minimize extrusion of debris. Root canal irrigation plays a pivotal role in endodontic therapy, to facilitate instrumentation by lubrication, debris removal, microorganisms, smear layer, and prevent apical debris packing. Irrigation overstrains their effects, by mechanical, chemical and biological actions (24). Incomplete removal of all the irritants from the pulp space may increase the possibility of treatment failure (25). Ultrasonic activation of irrigation solution further enhances the removal of bacteria and dentin debris, which is then to be followed by obturation to seal the inaccessible zone (26) Irrigant activation proves to be beneficial, in terms of postoperative pain intensity, canal debridement, and isthmus cleanliness.
The use of magnifying tools (magnification loupe or dental operating microscope), the use of fiber optics, and sodium hypochlorite bubble technique may be helpful in locating any additional root canals (27). In this study, a dental operating microscope was used, as our routine endodontic treatment to identify the internal morphology of the tooth, locate the canals and to detect any extra canals. Unfortunately, some endodontists who are using the dental operating microscope in their dental clinics do not use it as often as needed to be (28)
These reported cases emphasize the need for a clinician’s awareness of anatomical variations that can occur in teeth undergoing root canal treatment. Anatomical variation in the number of roots or root canals can occur in any tooth. It is necessary to examine clear radiographs taken from different angles and careful assess
Thoughtfully designed, thoroughly tested, and backed by decades of collaboration with dentists worldwide, A-dec delivers smart ergonomics, unparalleled access, and legendary reliability. When you demand dependability, A-dec delivers without compromising expectations—especially yours.


the internal anatomy of the tooth, otherwise root canal treatment may fail if no extra roots or root canals are detected. It is highly recommended for the clinician to use advanced equipment and techniques to manage such teeth with anatomical variations like dental operating microscope, ultrasonic tips for conservative access, and accurate apex locator for accurate working length determination.
1. Alani AH. Endodontic treatment of bilaterally occurring 4-rooted maxillary second molars: case report. J Can Dent Assoc 2003; 69(11): 733-735.
2.Versiani MA, Pecora JD, and Sousa-Neto MD. Microcomputed tomography analysis of the root canal morphology of single-rooted mandibular canines. Int Endod J 2013; 46(9): 800-807.
3.Ouellet R. Mandibular permanent cuspids with two roots. J Can Dent Assoc 1995; 61(2): 159-161.
4.Victorino FR, Bernardes RA, Badli JV, Moraes IG, Bernardinelli N, Garcia RB, Bramante CM. Bilateral mandibular canines with two roots and two separate canals: case report. Braz Dent J 2009; 20(1): 84-86.
5.Pineda F, Kuttler Y. Mesiodistal and buccolingual roentgenographic investigation of 7,275 root canals. Oral Surg Oral Med Oral Pathol 1972; 33(1): 101-110.
6.Green D. Double canals in single roots. Oral Surg Oral Med Oral Pathol 1973; 35(5): 689-696.
7.Vertucci FJ. Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol 1984: 58(5): 589-599.
8.Pecora JD, Sousaneto MD, Saquy PC. Internal anatomy, direction and number of root and size of human mandibular canines. Barz Dent J 1993; 4(1): 53-57.
9.Orguneser A, Kartal N. Three canals and two foramina in a mandibular canine. J of Endod 1998; 24(6): 444—445.
10. Heiling I, Gottlieb-Dadon I, Chandler NP. Mandibular canine with two roots and three root canals. Endod and Dent Traumatol 1995; 11(6): 301302.
11.Fava LR, Dummer PM. Periapical radiographic techniques during endodontic diagnosis and treatment. Int Endod J 1997; 30: 250-261.
12.Verma P, Love RM. A Micro CT study of the mesiobuccal root canal morphology of the maxillary first molar tooth. International Endodontic Journal 2011; 44: 210–7
13.Versiani MA, Pecora JD, and Sousa-Neto MD.
The anatomy of two-rooted mandibular canines determined using micro-computed tomography. Int Endod J 2011; 44: 682-687.
14. Sikri V, Kumar V. Permanent human canines: Configuration and deviations of root canals: An in-vitro study. J Conserv Dent 2003; 6(4): 151-152.
15. Hess W. The anatomy of the root canals of teeth of the permanent dentition. New York: Williams Wood Co; 1925
16. Ghoddusi J, Zarei M, Vatanpour M. Mandibular canine with two separated canals. N Y State Dent J 2007; 73: 52-53.
17. Alenezi MA, Al-Hawwas AY. Permanent mandibular canine with two roots and two canals: Two case reports. Saudi Endod J 2016; 6: 98-100.
18. Sert S. Bayirli GS. Evaluation of the root canal configurations of the mandibular and maxillary permanent teeth by gender in the Turkish population. J Endod 2004; 30: 391-398.
19. Arora V, Nikhil V, Gupta J. Mandibular canine with two root canals – An unusual case report. Int J Stomatol Res 2013; 2; 1-4.
20. D’Arcangelo C, Varvara G, De Fazio P. Root canal treatmentin mandibular canines with two roots: a report of two cases. Int Endod J 2001, 34: 331-334.
21. Heling I, Gottlieb-Dadon I, Chandler NP. Mandibular canine with two roots and three canals. Endod Dent Traumatol 1995; 11: 301-302.
22. Patel S. New dimensions in endodontic imaging: Part 2. Cone beam computed tomography. Int Endod J 2009; 42: 463-475.
23. Versiani MA, Pecora JD, Sousa Neto MD. The anatomy of two-rooted mandibular canines determined using micro-computed tomography. Int Endod J 2001, 2011; 44: 682-687.
24. Hargreaves K, Berman L. Cohen’s Pathways of Pulp. 11th ed. St. Louis, Missouri: 2016.
25. Sjogren U, Hagglund B, Sundqvist G, Wing K. Factors affecting the long-term results of endodontic treatment. J Endod, 1990, 16(10): 498-504
26. Haapasalo M, Shen Y, Qian W, Gao Y. Irrigation in endodontics. Dent Clin North Am. 2010, 54: 291-312.
27. Carr GB. Microscopes in endodontics. J Calif Dent Assoc 1992; 20: 55-61.
28. Alrejaie M, Ibrahim N, Malur M, AlFouzan K. The use of dental operating microscope by endodontists in the Middle East : A report based on a questionnaire. Saudi Endod J 2015; 5: 134-137
IPG - Intraoral Photogrammetry
Two-in-One System

ScanDesignDelivery













Laurence V. Hicks is the owner of Falls Centre for Functional Medicine in Twin Falls, Idaho. He is a teacher in medicine and is an Assistant Professor of Family Medicine at the Idaho College of Osteopathic Medicine in Meridian, ID., an Adjunct Assistant Clinical Professor at Pacific Northwest University of Health Sciences • College of Osteopathic Medicine in Yakima, WA and is also a Graduate Instructor at the University of Western States. He is degreed as a D.C., an N.D. and a D.O. He is certified in Family Medicine, Occupational Medicine and Geriatrics.
Contact Information
Falls Centre for Functional Medicine 236 Martin Street
Twin Falls, Idaho 83301 Tel: 208-733-4444 • Fax: 208-733-4456 • emails: benhickspa@gmail.com drlhicks@gmail.com
The field of dentistry has long been recognized as a crucial component of overall healthcare. However, as research continues to uncover the intricate connections between oral health and systemic conditions, an increasing number of dental professionals are embracing holistic and naturopathic principles. Dentistry and naturopathy, though distinct in their foundations, share a fundamental philosophy: the body is an interconnected system, and optimal health requires a comprehensive, whole-body approach.
This perspective is gaining traction, particularly as patients seek alternatives to conventional methods that emphasize pharmaceuticals and invasive procedures. As a response, many dentists are incorporating naturopathic principles into their practice, integrating nutritional counseling, herbal medicine, and detoxification strategies to support oral and systemic health. However, the challenge has been the time and cost required to earn dual credentials in both dentistry and naturopathy. Recognizing this, the state of Idaho has pioneered a solution by establishing the Board of Naturopathic Healthcare, which offers dentists the opportunity to become licensed naturopathic doctors through an accessible,
160-hour training course.
This development represents a significant shift in the healthcare landscape, empowering dentists to function more comprehensively as anatomically unlimited, primary care providers. By merging traditional dental expertise with naturopathic principles, practitioners can elevate their approach to oral health and contribute to broader impact against systemic wellness.
At its core, dental care is concerned with the diagnosis, prevention, and treatment of diseases affecting the oral cavity. While conventional dentistry has made remarkable strides in restorative and surgical interventions; it often operates within a compartmentalized framework that views the mouth as separate from the rest of the body. However, emerging research underscores the profound link between oral health and chronic systemic diseases, including cardiovascular conditions, diabetes, and autoimmune disorders.1 Naturopathy, on the other hand, is a holistic discipline that prioritizes the body’s natural ability to heal itself. Naturopathic principles focus on identifying and addressing the root causes of disease rather than merely treating symptoms. These principles

align seamlessly with modern dentistry’s growing emphasis on prevention and the understanding that oral health is deeply connected to overall physiological function.
For instance, periodontal disease has been strongly linked to systemic inflammation, insulin resistance, and even neurodegenerative disorders like Alzheimer’s.2 Traditional dental treatments for gum disease often involve mechanical debridement, scaling and planning,3 antibiotics, and surgical interventions. A naturopathic approach, however, incorporates anti-inflammatory diets, probiotics, herbal mouth rinses, and ozone therapy to reduce bacterial overgrowth and enhance tissue healing.4 By integrating these approaches, dentists can not only address immediate oral health concerns but also help their patients achieve long-term systemic balance.
Dentists are uniquely positioned to serve as frontline healthcare providers. Patients often visit their dentist more frequently than their primary care physician, providing a critical opportunity for early disease detection and preventive interventions. Given the increasing recognition of the oral disease-systemic disease connection, it is becoming clear that dental offices can function as primary care hubs, offering screenings for conditions such as hypertension, diabetes, and sleep apnea.5
However, despite their extensive training in oral pathology, microbiology, and pharmacology, dentists have not been traditionally recognized as primary care providers outside of the perceived limitations of dental practice. This limitation prevents them from fully utilizing their expertise in diagnosing and managing broader health conditions that manifest in the oral cavity.
By obtaining naturopathic licensure, dentists can bridge this gap, allowing them to expand their scope of practice to include nutritional counseling, herbal medicine, and detoxification strategies.
For example, many patients present with chronic issues like temporomandibular joint dysfunction (TMD), bruxism, and oral infections, which are often linked to stress, gut dysbiosis, and systemic inflammation. A dentist trained in naturopathy can offer comprehensive solutions that go beyond splints and muscle relaxants, incorporating adaptogenic herbs, myofascial release techniques, and microbiome-supporting dietary recommendations.
While the integration of naturopathy into dental medicine presents numerous benefits, one of the primary barriers has been the extensive time and financial investment required to pursue both degrees. A conventional Doctor of Dental Surgery (DDS) or Doctor of Dental Medicine (DMD) degree already requires rigorous training over several years, followed by additional specialization for those interested in holistic dentistry.6 Historically, practitioners seeking to combine dental and naturopathic expertise had to complete a second doctorate in naturopathic medicine, often adding four additional years of education.7 Given the high costs associated with medical and dental school tuition, this path has been impractical for most professionals. Recognizing this dilemma, Idaho has pioneered a solution by establishing the Board of Naturopathic Healthcare, which allows dentists to become licensed naturopaths through a streamlined, 160-hour training course. This program provides dentists with essential naturopathic knowledge without requiring them to start from scratch. This initiative is a game-changer for dentists who
wish to enhance their practice with naturopathic methodologies without undertaking an entirely new degree program. By reducing the barriers to dual credentialing, Idaho is setting a precedent for other states to follow, potentially transforming the future of integrative dental care nationwide.
As patient demand for holistic and preventative healthcare grows, the integration of naturopathy into dentistry will likely become more widespread. This paradigm shift represents an evolution in the way dental care is delivered, moving beyond a narrow focus on teeth and gums to a broader, systemic approach to health. For forward-thinking dentists, incorporating naturopathic principles offers a unique opportunity to distinguish themselves in an increasingly competitive field. Patients are actively seeking practitioners who can offer natural, minimally invasive treatments that align with their lifestyle and wellness goals. By becoming dually licensed, dentists can cater to this growing demand while improving patient outcomes through a more comprehensive and preventive model of care.
The establishment of Idaho’s Board of Naturopathic Healthcare serves as a model for other states to explore similar pathways for licensure. If more states adopt this approach, we could see a nationwide transformation where holistic dentistry becomes a standard rather than an exception.
Conclusion
Dentistry and naturopathy are inherently complementary disciplines that, when combined, create a powerful synergy for patient care. By integrating holistic principles into their practice, dentists can provide more comprehensive, preventive, and patient-centered treatments.
The challenge of obtaining dual credentials has historically been a limiting factor, but Idaho’s innovative licensing pathway is removing this obstacle, making it more feasible for dentists to embrace a naturopathic approach.
As research continues to highlight the interconnectedness of oral and systemic health, the future of dentistry lies in a more integrative model. With initiatives like Idaho’s naturopathic licensure program, dentists now have an opportunity to expand their role as primary care providers, offering a truly holistic approach to health and wellness.
By embracing this shift, dentists can not only enhance their practice but also contribute to a broader movement toward whole-body healthcare – an evolution that will benefit both patients and practitioners for years to come.
References
1 Gambhir, R. S. (2015). Primary Care in Dentistry – An Untapped Potential. J Family Med Prim Care, 4(1), 13-18.
2 Bouziane, A. (2023). Effect of periodontal disease on Alzheimer’s disease: A systematic review. Cureus, 15(10), e46311.
3 Scaling and root planing. (2024). American Dental Association.
4 Gasner, N. S., & Schure, R. S. (2023). Periodontal disease. StatPearls.
5 Eke, P. I., et al. (2016). Periodontitis prevalence in adults ≥ 65 years of age, in the USA. Periodontol 2000, 72(1), 76-95.
6 www.collegeave.com/articles/how-muchdoes-dental-school-cost-average-degreetuition-costs/
7 https://aanmc.org/how-much-does-it-cost-tobecome-a-naturopathic-doctor/#:~:text=
The%20cost%20of%20naturopathic%20 medical,(not%20including%20living%20 expenses).
An interview with Dr. Elham Al Khateeb on refugee oral health promotion.

Dr. Elham Talib Khateeb is an associate professor of dental public health in the Faculty of Dentistry and dean of scientific research at Al-Quds University, East Jerusalem in Palestine.
On World Refugee Day, FDI World Dental Federation unveiled a pivotal policy brief titled Addressing Oral Health Needs in Refugees: Policy and Collaboration Strategies. This comprehensive document, developed under the leadership of FDI’s Public Health Committee, which is chaired by Dr Elham Talib Khateeb, and in collaboration with the Office of the United Nations High Commissioner for Refugees (UNHCR), underscores the urgent need to tackle the oral health challenges faced by refugees. In this interview, Dr Khateeb speaks about the importance of coordinated efforts and strategic collaboration to ensure that refugees receive essential oral healthcare, which is a fundamental component of overall well-being.
Dr Khateeb, why is it now more important than ever to advocate for improved refugee oral healthcare?
Today, our world is witnessing unprecedented levels of suffering and displacement due to wars, conflicts, natural disasters, oppression, discrimination and corruption. The nature of warfare nowadays is different from before, and more than 90% of casualties in any conflict
are civilians. Crises continue to displace millions, depriving them of their basic rights to security, clean water, food, shelter and access to healthcare. According to UNHCR figures, by the end of 2023, more than 110 million displaced individuals were living in constant fear for their lives and well-being. Among them, there are 36.4 million refugees - that number has doubled in just seven years - the majority originating from developing countries that already face challenges in healthcare infrastructure and prevalent oral disease.
Research indicates that refugees experience higher rates of oral health issues and encounter substantial obstacles in accessing dental services compared with other vulnerable groups. Notably, 75% of refugees reside in low- and middle-income countries, where they are confronted by significant barriers, such as limited resources, cultural and language differences, mistrust and a shortage of skilled healthcare professionals willing to serve these populations.
Refugees’ right to health, including oral health, is affirmed by international conventions such as the International Covenant on Economic, Social and Cultural
Rights and the 1951 Refugee Convention. Current global initiatives such as the World Health Organization’s Global Strategy and Action Plan on Oral Health 2023 – 2030 and FDI’s Vision 2030 emphasise the necessity of integrating essential oral health interventions into primary healthcare and achieving universal health coverage (UHC). In light of these, there is a pivotal opportunity to advocate for including refugees in comprehensive primary care packages.
Could you discuss some critical issues outlined in FDI’s policy brief that are affecting refugee oral health?
Ensuring oral health is a crucial component of overall well-being, especially for refugees, who experience a significant burden of oral health issues, such as untreated dental caries, periodontal disease, oral infections and trauma. Addressing these needs requires collaboration among multiple stakeholders. Despite international commitments to UHC and to safeguarding of refugees’ rights to health, a significant gap remains in providing adequate general health and oral health services to refugees. Challenges such as financial constraints, lack of trust and a shortage of skilled healthcare professionals are exacerbated in conflict settings, where limited resources and population displacement further hinder the delivery of health interventions.
A survey conducted by FDI in 2019 highlighted that only a small fraction of respondent countries provided obligatory oral health screenings for refugees upon arrival and even fewer offered oral health referral services. Emergency oral healthcare was the most common type of care provided, whereas preventive and therapeutic
dental care were less frequently available. In nearly a quarter of the countries surveyed, no oral healthcare was provided. This underscores the need for stronger policy.

As part of the programme, school teachers received training from Refugee Crisis Foundation dentists to instruct the children on proper brushing techniques.

The Refugee Crisis Foundation, a UK-registered charity, has implemented a comprehensive toothbrushing programme in two schools within the world’s largest refugee camp in Bangladesh, with support from FDI and local partners.
development and international collaboration to integrate oral health into primary healthcare systems for refugees with the aim of ensuring that they receive comprehensive care without financial hardship.
Promoting oral healthcare for refugees aligns with broader international commitments to UHC and the UN’s Sustainable Development Goals, contributing to social inclusion, equality and global health equity. Investing in refugee oral health initiatives not only fulfils moral obligations but also advances the health and dignity of refugees worldwide.
We repeated the 2019 survey in 2024 and will present the results in our congress session. We will also discuss whether there has been any progress in countries’ activities and policies related to refugee oral health
What solutions does the brief propose to tackle the challenges related to refugee oral health?
To tackle the challenges related to refugee oral health, the brief emphasises the need for policy changes and the integration of oral health into primary healthcare systems. FDI and UNHCR in this brief advocate for national and international policies that ensure comprehensive healthcare provision, addressing both acute and preventive oral healthcare needs. Recognising oral health as an essential component of overall well-being, the brief highlights the importance of workforce availability, training and resource allocation tailored to refugee populations. It also stresses the importance of developing research systems to understand critical oral health needs and track the impact of interventions, supporting the appropriateness of care through the perspectives of refugees.
In addition, the policy brief details the actions that need to be taken in different phases of any refugee crisis. In terms of preparedness and mitigation, integrating oral health into primary healthcare systems is crucial. This includes increasing support and funding from governments, international organisations and non-governmental organisations to strengthen oral health strategies, especially in low- and middle-income countries. Developing culturally appropriate oral healthcare programmes in collaboration with international organisations helps effectively address the unique needs of diverse refugee populations. During emergencies, essential oral healthcare services should be included in initial responses, focusing on disease management and stabilisation, education, prevention and the accessibility of fluoride toothpaste. Integrating oral healthcare into established public health programmes ensures comprehensive care during crises.
Post-emergency, the brief calls for establishing mechanisms for collecting data on refugee oral health status to inform evidencebased interventions and policy adjustments. Empowering refugee communities by involving them in decision making processes, health education initiatives and advocacy efforts supports long-term sustainability and resilience
How is FDI working to meet the oral health needs of refugees?
Since launching the Refugee Oral Health Promotion and Care Project in 2018, FDI has been dedicated to enhancing access to oral care services for refugees globally and locally. A key initiative was the 2019 survey on need assessment, which gathered responses from 78 countries, providing insights into those

countries’ activities and national policies related to refugee oral health and the involvement of national dental associations in these activities. The survey’s findings were used to develop a comprehensive advocacy toolkit. This toolkit offers practical guidance and resources, policy recommendations, clinical guidelines and best practices for promoting oral health awareness among refugees.
In addition to data collection, FDI has fostered international collaboration with organisations such as UNHCR, the United Nations Relief and Works Agency for Palestine Refugees in the Near East, the World Federation of Public Health Associations, the Lancet Migration European Regional Hub, the Sustainable Health Equity Movement and the Framework Convention on Global Health Alliance. We also worked closely with the International Association for Dental, Oral, and Craniofacial Research and the World Health Organization’s oral health department to address the unique oral health challenges faced by refugees and released five joint policy briefs and statements to draw attention to their needs. FDI also targets future dentists through lectures, webinars and workshops offered to dental students, residents and other healthcare professionals to raise awareness and push for advocacy for improved policies and resources.
Collaborating with local and national dental associations, groundlevel charities and regional organisations has enhanced the impact of these initiatives. By funding dental missions and providing resources and technical support for therapeutic and preventive interventions, FDI helps refugees receive the essential oral healthcare they desperately need. Four examples that will be presented in detail in our congress session are the FDI project
with Pakistan Dental Association to improve access to care for Afghan refugees in Pakistan, FDI support to Refugee Crisis Foundation and Bangladesh Dental Society to promote hand and oral hygiene among children in the Rohingya refugee camp in Bangladesh, the FDI campaign for medical and dental supplies for Ukraine refugees in host countries and FDI collaboration with the Palestinian Dental Association and Health-Point Foundation to fund a dental mission to Middle Eastern refugees on the island of Lesbos in Greece through the FDI Smile Grant

Under the supervision of a teacher, children practice daily handwashing and toothbrushing with fluoridated toothpaste at designated stations in the schools.
FDI plans to continue advocating for better access to oral healthcare among refugees globally and to empower national dental associations to get more involved with activities and policies that promote better oral health in this vulnerable population. FDI is using all the means available and drawing on all its partnerships to achieve this goal.
1) A Global Leader, at the Forefront of Dentistry: An Overview of NYU College of Dentistry
2) Moving the Needle: The NYU Dentistry Center for Oral Health Policy & Management Addresses Advocacy and Leadership Issues
3) Signaling Hope: The NYU Pain Research Center Opens at NYU College of Dentistry
4) Tomorrow’s Dentistry Today: Virtual Reality and Robotics at NYU Dentistry
5) Bellissima! NYU Dentistry Advances Aesthetic Dentistry Programs with Alumnus Dr. Michael Apa
6) On the Horizon: Exploring New Degree Opportunities Integrated with Advanced Clinical Training
An overview of NYU College of Dentistry
Located along the NYU health sciences corridor on First Avenue in Manhattan, NYU College of Dentistry offers a unique, exceptional experience for students pursuing careers in oral health care.
Our students benefit from the largest and most diverse patient population in the U.S., expert faculty, innovative learning technologies, a wealth of research and outreach opportunities, exciting new leadership initiatives, and a commitment to fostering a deep understanding of dentistry’s integral role in overall health.
We’re focused on the future –advancing oral health, researching new treatments and methodologies, and preparing students to become exceptional providers and to lead the profession, with ample opportunities to “think big.”
In just the past few years, NYU Dentistry has opened the Oral Health Center for People with Disabilities; NYU Dentistry Brooklyn Patient Care; Metro Community Health Centers at NYU Dentistry, a federally qualified health center located on the first floor of the NYU Dental Center in Manhattan, providing DDS students with experience in the medical management of dental patients; and the NYU Dentistry Center for Oral
Health Policy and Management, an interdisciplinary action lab that is working to develop and promote a national agenda for oral health policy and management that recognizes the fundamental relationship between oral health and overall health and the responsibilities that the dental professions have for the overall well-being of the public. And NYU Dentistry’s WHO Collaborating Center for Quality-improvement, Evidence-based Dentistry – one of only ten Collaborating Centers worldwide and the only one in the Americas – is focused on achieving oral health equity globally.
EDUCATIONAL PROGRAMS:
• Doctor of Dental Surgery (DDS) program
• Dental Hygiene programs
• Master’s degree programs: Biomaterials, Clinical Research, Dual MS
• Advanced Education: Endodontics, Oral & Maxillofacial Surgery, Orthodontics, Pediatric Dentistry, Periodontics, Prosthodontics
• Advanced Clinical Fellowship Programs: Apa Advanced Clinical Fellowship in Aesthetic Dentistry, Operative and Digital Dentistry, Implant Dentistry, Oral Surgery
• Fast Facts:
• NYU Dentistry is the 3rd oldest


and the largest dental school in the U.S.
The peri-implant bone level was found to be stable at the level of the first thread after 9 years of loading (Fig 3).
• 300,000 patient visits annually ensure superb clinical training for students
• Nearly 10% of dentists in the U.S have been educated at NYU Dentistry
• NYU Dentistry is ranked 3 in the U.S. in National Institutes of Health research funding
• 21,000+ alumni network practicing worldwide
• 1,959 students across all academic programs
• 93 NIH-funded and other funded researchers advance science every day
Dentistry’s Center for Oral Health Policy and Management Addresses Advocacy and Leadership Issues
The NYU Dentistry Center for Oral Health Policy and Management, an interdepartmental, interdisciplinary action laboratory, was founded in 2021 on the premise that the current oral health policy and management environment in the U.S. requires a holistic approach to the situation — one that has been lacking.
• 14 Academic Societies, each lead by a Senior Mentor, promote a strong sense of community and afford DDS students small-group learning and mentoring experiences while still having access to the vast resources of a large university
Fig 3 - Bone level 9 years postloading.Bone positioned at the level of the first thread. Minimal bone loss occurred over 9 years of functional loading.
• An average of 27 students per class year in each Academic Society, supported by its own Student Success Network, which connects every DDS student with a network of academic advisors, peer tutors, and peer and faculty mentors who provide one-on-one guidance and support to promote success from the moment students enter at Orientation
Prosthetic failure of the maxillary left premolars and first molar occurred in October 1999. The fixed partial prosthesis became loose due to recurrent decay and poor crown-to-root ratio. It was decided to extract the remaining teeth and convert to an implant-supported fixed restoration. Three Brånemark implants (Nobel Biocare, Göteborg, Sweden) were placed in the maxillary left quadrant, and the patient was referred to her dentist for the placement of a temporary removable prosthesis to restore esthetics and function while implant osseointegration was achieved. The dentist removed the maxillary right implant-supported partial prosthesis and placed an overdenture. The patient was seen in May 2000 for abutment connection on the maxillary left implants. Periapical radiographs were obtained to assess the osseointegration. Severe bone loss was observed on the implants in the maxillary right first premolar site and the maxillary right first molar site (Figs 4 to 6).


“While tremendous strides have been made in improving the oral health status of Americans through scientific breakthroughs, many are left without access to basic dental care,” notes Dean Charles Bertolami. “Dental benefits remain separated from other health care coverage and out of reach for many individuals and families,” he added.
Fig 4 - Six months after placement of the unstable removable overdenture. Note the severe bone loss on the implant in the maxillary right first premolar site (down to the sixth thread) and the maxillary right first molar site (down to the third thread). However, no bone loss was observed on the intermediate implant.
In addition, the rigorous curriculum for dental students focuses predominantly on basic sciences and clinical care, but most learn little about the complexity of the dental and general health care systems of which they will soon be a part. The center aims to change this through new programming and academic offerings on oral health policy and leadership.
“NYU Dentistry is uniquely well positioned to undertake these challenges,” said Richard Valachovic, DMD, MPH, a clinical professor at NYU Dentistry and president emeritus of the American Dental Education Association, who serves as founding director of the center.
Fig 5-6 - Six months after placement of the unstable removable overdenture. The implants were connected with a rigid bar, and the unstable overdenture was adjusted.
Several of the College’s access to care and advocacy initiatives align with critical issues related to oral health policy and management.
Another priority for the NYU Dentistry for Oral Health Management and Policy is to develop the next generation of policy-oriented leaders for the dental and related health care professions through creating new leadership programming and courses.
The removable prosthesis was found to be very unstable; it was rocking around the maxillary right implants and had been doing so for 6 months, according to the patient. In collaboration with the dentist, all 6 implants were splinted, and a properly fitted removable prosthesis was fabricated. Oral hygiene was reinforced to improve the patient’s home care. The peri-implant condition was re-evaluated radiographically every 3 months. The bone lesions started to heal within 3 months after elimination of the traumatic condition. At 6
“The major reason given by dental school deans and independent search firms for not filling vacancies for faculty and dental leadership positions is a lack of qualified candidates,” said Michael P. O’Connor, EdD, MPA, executive vice dean at NYU Dentistry, who serves as co-director of the center. “The center strives to develop adaptive leaders who are prepared to perform in uncertain environments in the future using a differentiating character-based model of leadership, one that develops leadership habits and attitudes that aim for human flourishing in organizations, communities, and society.”
These concerns propelled NYU Dentistry to create a portfolio of leadership opportunities for students at the College. These include:
• The NYU Dentistry Leadership Track. This program is open to all students throughout the academic year. In 2022, this offering was enhanced by formalizing it as a twice-monthly lecture series focused on character-based leadership, and also opened it to all administrators, staff, and faculty along with students.
• Student Leadership Mock Congressional Hearing. Each spring, students are invited to apply for this competitive program, which trains students in leadership advocacy and public speaking. Participants prepare and deliver testimony on a health policy topic before a mock congressional committee panel.
• The NYU Dentistry Dental Student Leadership Institute (DDSLI). Each year, up to 35 D1 students are selected to take part in the DDSLI. Over the next three years, participants are given access to seminars, workshops, internships, mentoring, and other opportunities designed to prepare them to manage the complex challenges of advancing oral health in the 21st century.
• Global Health Care Leaders: Washington, DC. Students from across the College of Dentistry, including advanced standing international students and dental hygiene program students, are eligible to apply for this professional development experience, which takes students to NYU’s DC campus to hear from oral health advocates and meet with federal lawmakers.





• Global Health Care Leaders: NYU Global Academic Centers D4 students are eligible to apply for this international experience. Selected students travel to one of NYU’s Global Campuses each year to explore complex policy issues with leaders in government and oral health advocacy. In fall 2023, the experience took place at NYU’s Villa LaPietra in Florence, Italy.
The process of leadership development differs significantly from most other experiences in dental education. Leadership is an art; it is creative and experiential rather than scientific. To foster leaders who will ensure a healthy future for dentistry, a different kind of education must be available. Despite the familiar adage, leaders are made, not born. While certain leadership qualities are native or part of a personality, leadership also requires specific knowledge and skills. Fortunately for all of us, these can be learned and cultivated.
NYU Dentistry is committed to cultivating students who can carry on the work begun by today’s oral health care leaders. Our first cohort of students has been engaged in the new DDSLI curriculum for just over three years, and already they are demonstrating an understanding of what leadership is all about.
1. The NYU Dentistry Oral Health Center for People with Disabilities (OHCPD)
The OHCPD provides care based on a deep commitment to assuring disabled patients, their families, and caregivers that they aren’t just cared for, but cared about. Our dental care providers have the specialized skillsets needed to provide sensitive, essential care for individuals whose disability or disabilities prevent them from being treated in a conventional dental setting. Every component of the center has been designed to accommodate the physical and support needs of our patients, their families, and/or caregivers. And because it provides dental care across the lifespan, the center offers a dental home for disabled patients on an ongoing basis.
Special accommodations available for patients with intellectual and/or developmental (I/DD) include:
• Multisensory room: Designed to reduce

patients’ agitation and anxiety, help them relax, and engage their senses. Amenities include a bubble tube; noise-cancelling headphones; soothing, adjustable, multi-colored lighting; weighted blankets; body socks; and a projection screen.
• Wheelchair tilt: Designed to accommodate patients receiving dental treatment in their own wheelchairs, without the need to transfer to a dental chair.
• Bariatric chairs: Designed to accommodate patients up to 650 pounds.
• Spacious, private treatment rooms: Designed to offer privacy and comfort, with soothing, adjustable, multi-colored lighting; noisecancelling headphones; and personal entertainment tablets.
• Sedation: A complete team meets all the needs of physically and intellectually disabled patients who require varying levels of pain and anxiety control, including the use of conscious and deep sedation, and general anesthesia techniques.
Advocacy Initiatives, as part of its advocacy initiatives on behalf of access to care for people with disabilities, the OHCPD:
• conducts a continuing education program, Unit Zero, to train dentists and their staff to provide care for people with disabilities.
• Members the OHCPD team regularly appear before the New York City Council, the State Legislature in Albany, New York, and Congress in Washington, DC, to advocate for funds on behalf of the OHCPD.
• The OHCPD also sponsors an annual AHEAD (Achieving Health Equity through Access for All with Disabilities) Symposium. The annual symposium brings together experts in the areas of health care advocacy, access, and funding at the state and federal levels for people with disabilities.
In addition, The NYU Dentistry Center for Oral Health Policy and Management has presented an inaugural PROHmotion Symposium (Policy & Research in Oral Health: Moving Forward). The symposium brought together experts in the fields of health policy, education, research, leadership, and advocacy to discuss how these fields intersect



and explored actions to advance the profession’s ability to fulfill the responsibilities it has for the overall well-being of the public. A second PROHmotion Symposium is being planned.
Serving Those Who Served: NYU Dentistry’s VOCARE Program
NYU College of Dentistry is celebrating the second anniversary of the Veterans Oral Care Access Resource (VOCARE), part of the U.S. Department of Veterans Affairs’ VETSmile program, a pilot program designed to improve dental care access for veterans who are not eligible for dental care through the VA by partnering with community providers like NYU.
During the second year of VETSmile/VOCARE, 2,245 veterans received dental care over a total of 16,825 encounters. Nearly 32,000 procedures were completed.
VETSmile/VOCARE is a partnership between NYU Dentistry and the VA New York Harbor Healthcare System, which includes campuses in Manhattan, Brooklyn, Queens, and Staten Island, and the VA Bronx Health Care/Veterans Affairs. Through the program, the VA New York Harbor Healthcare System and the Bronx VA refer veterans who are not eligible to receive dental services at the VA to NYU for comprehensive care at no out-of-pocket cost to the veteran.
Veterans are seen at NYU College of Dentistry in Manhattan and at NYU Dentistry Brooklyn Patient Care. Some veterans, including those with a history of post-traumatic stress disorder, are seen at the NYU Dentistry Oral Health Center for People with Disabilities, where the staff are trained with special skill sets to ensure quality treatment and holistic care for people with disabilities and complex medical conditions.
3. Community-based Programs
A major component of the NYU College of Dentistry mission is extensive community outreach. Faculty from many departments lead NYU dental, dental hygiene, and postgraduate students in a wide range of patient care initiatives, traveling throughout the five boroughs of New York City to provide care to underserved populations.
Head Start facilities.
Part of NYU’s teaching mission consists of preparing students for lives in a diverse world, and our faculty believe that such preparation is most effective through collaboration. Our relationship to New York City — the diversity of thought represented by all our schools, colleges, and programs, and our internationally connected and collaborative faculty — enable students and faculty alike to broaden the scope and vision of knowledge through interdisciplinary and interprofessional learning to make a real difference in the world. Dentist shortages are widespread: In 25 states and the District of Columbia, at least 10 percent of residents do not have adequate access to a dentist.
The College’s mobile dental van, Smiling Faces, Going Places, is a unique program that brings comprehensive dental care to underserved children in New York City at public schools and Quarter I - 2025 in a
There are volunteer opportunities for all four years. In the D3 and D4 year, participation in communitybased outreach programs is required. Some of the long-standing NYU Dentistry health education and treatment initiatives provided to underserved children in New York City by the NYU Department of Pediatric Dentistry include:
• Screenings and education to over 1,000 children in public schools and childcare centers.
• Exams and fluoride varnish for 4,000 preschool-aged children at 80 different centers (Head Start).
• School-based sealant program at four public schools with over 400 sealants placed.
• Parent & staff workshops on children’s oral health given at childcare centers and public schools.
• Graham Windham partnership providing comprehensive care to children and adolescents in foster care, with over 1600 patient visits since 2011.
• Participating in over a dozen health fairs and community events, including two Special Olympics events.
• “Playing It Safe” Mouth Guard Program, providing preventive services at community centers and schools.

Cologne, Germany-March 25, 2025
Shining 3D, a pioneer in high-precision 3D digital technology, marks its 20th anniversary with the launch of four innovative digital dental solutions: the revolutionary all-in-one digital dental solution - e-Motion Workstation, Aoralscan Elite Wireless intraoral scanner, AccuFab-F1 3D printer, and FabCure N2 nitrogen curing box. With a relentless commitment to innovation,user-centricdevelopment, and comprehensive end-to-end workflows, these new solutions further solidify Shining 3D’s position at the forefront of digital dentistry.
Since its founding in 2004, Shining 3D has continuously pushed the boundaries of digital technology, investing over 20% of its annual revenue into Research and Development. This commitment has led to the independent development of core 3D technologies, resulting in 182 authorized patents, 416 pending, and 182 software copyrights. With its Global presence, Shining 3D remains a trusted leader in the digital dental industry.
Shining 3D’s success is driven by a deep understanding of user needs, ensuring its technology aligns with the evolving demands of dental professionals. The company offers a fully integrated digital dental workflow, covering scanning, designing, and printing with highprecision intraoral and desktop scanners, advanced 3D printers and printing materials, post-processing solutions, and cloud-based services. This holistic approach enhances efficiency, precision, and reliability for dental professionals worldwide.
Introducing the Latest Innovations

e-Motion Workstation: A Complete Digital Dentistry Solution
Shining 3D Celebrates 20 Years of Research and Development of High Accuracy Vision Technology for the Next-Generation
The e-Motion Workstation is the world’s first all-inone digital dental solution, seamlessly integrating an intraoral scanner, face scanner, intraoral photogrammetry, and advanced mandibular movement tracking system. This innovative system captures multiple types of data within a single device, creating a dynamic virtual patient for more precise diagnosis and treatment planning.
Key features of the e-Motion Workstation include:
• Mandibular Movement Tracking: Captures realtime jaw movements to improve occlusion analysis and prosthetic design.
• Facial Scanner: Enhances aesthetic treatment planning with highly detailed facial data.
• Intraoral Scanner: Captures the digital impression of teeth and the supporting structures.
• Intraoral Photogrammetry (IPG): Provides exceptional accuracy, particularly for edentulous and implant cases.
• Multi-Modal Data Integration: Aligns intraoral, facial, mandibular movement, and CBCT data in one coordinate system for a comprehensive digital workflow.
By optimizing complex protocols, the e-Motion Workstation significantly improves efficiency and treatment predictability in complicated cases such as edentulous implant restorations and occlusal rehabilitation. With precise jaw relationship determination and implant positioning, dental professionals can achieve superior prosthetic accuracy, improved patient comfort, and longterm stability of restorations.

Aoralscan Elite Wireless: Next-Level Intraoral Scanning
Weighing just 194 grams, the Aoralscan Elite Wireless is the world’s lightest wireless intraoral scanner that provides outstanding flexibility and movement freedom. Powered by Wi-Fi 6 technology, it delivers stable and high-speed data transfer, while its wireless charging cradle ensures effortless operation. Its innovative design allows seamless use across multiple dental chairs, optimizing workflow efficiency. With Intraoral Photogrammetry (IPG) technology, the Aoralscan Elite Wireless delivers exceptional scanning accuracy, making it ideal for All-on-X procedures and full-arch restorations.
Watch official product video: https://youtu.be/06X4KS1mOnc
Read more:
www.shining3ddental.com/solution/e-motion/
Read more: www.shining3ddental.com/solution/aoralscanelite-wireless/

AccuFab-F1 3D Printer: High-Speed Precision Printing
Designed for stability and speed, the AccuFab-F1 3D printer features dual heating modules for both the print platform and resin tank, ensuring optimal material performance. With a maximum light intensity of 18 mW/cm², it excels in printing highceramic filler resins and high-viscosity materials with outstanding accuracy. Its modular design simplifies maintenance, while the quick-release resin tank film streamlines workflow efficiency for both clinics and labs.
Watch official product video: https://youtu. be/9Id-5AMVhG8
Read more: www.shining3ddental.com/solution/

N2 Nitrogen Curing Box: Advanced Post-Processing
The FabCure N2 nitrogen curing box is an opensystem device that optimizes post-processing for dental restorations, enhancing physical properties and aesthetics. Its nitrogen curing technology ensures consistent, high-quality results, improving both durability and color stability of printed dental parts. As a crucial addition to the digital dental workflow, the FabCure N2 enables stronger, more predictable restorations.
Read more: www.shining3ddental.com/solution/ fabcure-n2/
Founded in 2004, Shining 3D has spent two decades developing high-accuracy 3D digital solutions for industries such as healthcare, engineering, and manufacturing. Leveraging this expertise, its dedicated sub-brand, Shining 3D Dental, applies these advanced technologies to transform digital dentistry. With a strong foundation in precision technology, continuous R&D investment, and user-driven innovation, Shining 3D Dental provides comprehensive, end-to-end workflows that empower dental professionals worldwide to achieve greater accuracy, efficiency, and clinical success.
Contact: Shining 3D Dental
Email: marketing@shining3d.com
For more information on Shining 3D’s digital dental solutions, visit shining3ddental.com.

Fiber posts are frequently used in endodontics for extensive coronal substance defects when the crown is no longer sufficiently supported, particularly prior to restoration with an indirect restoration. The influence of these posts on clinical success and their survival rate was investigated by Alenezi et.al. in their recently published meta-analysis [1]. In this research, 17 different clinical studies with 7,330 endodontically treated teeth in 7,278 patients were analyzed. The results showed a significantly higher survival rate for teeth restored with posts. The authors concluded that post placement can improve the clinical performance and survival probability of endodontically treated teeth.
RTD (Recherches Techniques Dentaires, a Dentsply Sirona company based in France) is an innovator in fiber posts field. Founded in 1968, RTD was one of the very first companies worldwide to invent and patent a fiber post. RTD has continued to innovate fiber posts ever since. Other fiber posts in the market can have an uneven distribution of fibers or even air bubbles trapped in the resin; RTD has optimized their products to eliminate those potential weak spots for the post and thus for the coronal restoration (Fig. 1).

RTD DT Light Post
The DT Light Post with its typical double taper is RTD’s most well-known product. Its shape contributes to a better stress distribution compared to single taper or parallel posts and follows the natural geometry of the root canal, requiring less dentin removal, especially in the apical third where unnecessary dentin removal can increase the risk of fracture.
[1] ALENEZI, Ali A., et al. Clinical behavior and survival of endodontically treated teeth with or without post placement: a systematic review and meta-analysis. Journal of Oral Science, 2024, S. 24-0098.
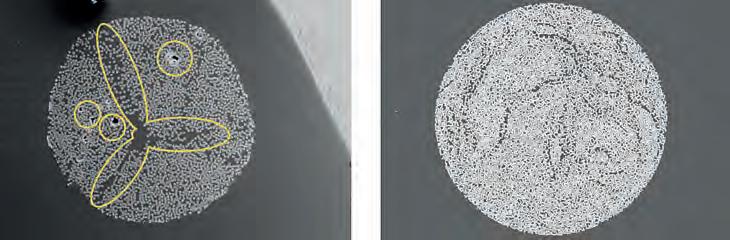
Competitor product with uneven fiber distribution and air bubbles.
RTD post with homogeneous distribution of fibers and no air bubbles.
28th April - 2nd May 2025

Mövenpick Hotel, Riyadh
Early registration till April 10

Scan to view Scientific Program

REGISTER NOW

SCIENTIFIC PROGRAM
After two decades, the FDI World Dental Congress (WDC) returns to mainland China, with the global dental community gathering in Shanghai. From September 9 to 12, 2025, the highly anticipated event will take place at the National Exhibition and Convention Center (Shanghai), hosting one of the largest exhibitions in its history and coinciding with China’s booming dental market. As 191 national and regional dental associations converge in the city, Shanghai will become the center of global dentistry. This prestigious event, a collaboration between FDI World Dental Federation (FDI), the Chinese Stomatological Association, and Reed Sinopharm Exhibitions, will bring together over 700 dental companies and attract more than 35,000 visitors. Known as the Olympics of dentistry, FDI WDC 2025 will provide a unique platform for sharing insights, innovations, and best practices, shaping the future of oral health.
China’s dental market is experiencing rapid growth, driven by rising living standards and increased awareness of oral health. This has fueled demand for high-quality dental products and services. Its size grew from 92.3 billion yuan in 2015 to 261.07 billion yuan in 2023. Currently accounting for 6% of the global market, China’s dental industry still holds ample room for expansion. With over 120,000 dental institutions and growing consumer demand, especially among younger generations, the market offers vast opportunities for both domestic and international players.
While market potential provides the “pull,” China’s policy reforms actively create the “push” for international engagement. The government has rolled out a suite of incentives to attract foreign dental technology providers. In the Hainan Free Trade Port, medical institutions can import registered or specially approved devices with zero tariffs and VAT. In the Shanghai Free Trade
Zone, the process of applying Chinese labeling can be completed within the zone, streamlining compliance procedures. Additionally, local subsidies in regions such as Beijing and Sichuan further create a supportive environment, enabling international brands to establish and grow in China’s expanding oral healthcare market.
Complementing policy support, China’s dental sector is undergoing a tech-driven metamorphosis—a transformation poised to dominate center stage at FDI WDC 2025. The exhibition’s “IntelliDent Stage” will spotlight how innovations like 3D-printed implants and AIassisted diagnostics are improving treatment outcomes and accessibility. For example, AIpowered teledentistry platforms enable remote diagnosis between cities like Shanghai and Xinjiang, bridging urban-rural care divides. This fusion of policy empowerment and technological leapfrogging cements China’s dual role as a massive consumer and cutting-edge innovator inglobal dental tech.
FDI WDC 2025 is expected to be the largest exhibition and congress in FDI’s history. It’s a four-day exhibition and scientific programme, covering a 60,000m2 area. It will host over 191 dental associations, attract more than 35,000 visitors, and welcome over 700 companies— including industry leaders like Haleon, Straumann, Solventum, Ivoclar, Bondent, and Zumax. With 300+ speakers, the congress will be a knowledgesharing and networking bonanza. We also offer exclusive social activities, including the Gala Dinner and Shanghai Night, providing a perfect platform for global dental professionals to connect.
In our exhibition hall, we offer matchmaking and guided tour services to help you quickly find what you need among a wide range of products. We also prioritize innovation through the IntelliDent
Stage and exclusive new product launches in the exhibition hall. These activities and services are designed to enhance your experience and ensure you get the most out of your visit. Language should never be a barrier. We offer English translation and consultation services to ensure smooth communication for all our international guests.
It’s the perfect time to visit Shanghai for the dental industry professionals. Shanghai, the host city of the FDI WDC 2025, is a metropolis that blends tradition with innovation. As FDI returns to mainland China after nearly two decades, Shanghai has become the centre of global dentistry. This dynamic city offers a unique cultural atmosphere, delicious local cuisine, and stunning landscapes. While attending the congress, you can take
advantage of China’s favourable visa policies, such as the 240-Hour Transit Visa Exemption, to fully experience the charm of this city. Stroll through the tranquil Yu Garden, marvel at the futuristic skyscrapers along the Bund, and savour the beloved Shanghai cuisine, including the famous soup dumplings. This international business hub also offers a glimpse into traditional Chinese culture, creating a captivating contrast. Make your journey to Shanghai for the FDI WDC 2025 both professionally rewarding and personally enriching, as you explore all that this multifaceted city has to offer
For more details, visit www.world-dental-congress.org.
See you in Shanghai!



Join us for an unforgettable learning and networking experience in the vibrant city of Shanghai!



The 2025 FDI World Dental Congress (FDIWDC25) will be held in China and is expected to be a groundbreaking event in the field of dentistry. Set against the vibrant backdrop of Shanghai, the congress promises to be one of the largest in its history, featuring over 700 companies and more than 35,000 dental professionals. In this interview, Prof. Guo Chuanbin, president of the Chinese Stomatological Association, which will be co-hosting the World Dental Congress in 2025, shares some insights into the exciting opportunities that FDIWDC25 will offer for dental professionals to engage with cutting-edge technologies and discusses the significant impact of artificial intelligence (AI) and 3D printing on dental practices worldwide.
Prof. Chuanbin, what can participants expect from FDIWDC2025?
FDIWDC25 is set to be one of the largest exhibitions in the history of the World Dental Congress. Spanning an impressive 60,000 m2 of hall space, the exhibition will host over 700 companies from around the world, including leading global brands and hundreds of Chinese manufacturers and technology providers specialising in dental equipment and solutions.

FDIWDC25 will offer an unparalleled opportunity for dental professionals to engage with the Chinese market, which is fuelled by a booming economy and an expanding middle class. This event will also be invaluable for international attendees to explore a wealth of technologies and digital innovations from competitive local suppliers. More than 35,000 professionals are expected to attend, and the exhibition will be a vibrant hub for networking, learning and discovering the latest advancements in dental care.
How will FDIWDC25 address the impact of new technologies in dentistry?
With the rapid development of science and technology, a growing number of AI applications are transforming dental diagnosis and treatment. Innovations such as implant robots, intelligent navigation systems, virtual simulation teaching and digital mandibular movement simulation are becoming increasingly integral to modern dental practices.
Alongside these advancements, the rise of CAD/CAM and 3D-printing technologies has led to the widespread use of new materials, reshaping the future of oral health. This is why we have chosen “Shaping the Future of Oral Health” as the theme for FDIWDC25.
The congress will feature a series of lectures focused on these cutting-edge technologies and materials. Additionally, an AI-enabled dentistry event area will be set up in the exhibition hall, providing a platform for showcasing and exchanging ideas on these innovations. Over four days, attendees will have the opportunity to hear from national and international experts in a total of 100 hours of engaging lectures.
How will the event’s location help create a unique experience for visitors?
Shanghai is one of the most vibrant and cosmopolitan cities in the world today. When exploring Shanghai in 2025, visitors will discover that it is much more than just an international business hub. The city is a showcase of the latest in style and fashion, offering the most exquisite tastes in lifestyle, unique dining experiences and stunning entertainment options. We are confident that the participants’
time in Shanghai will be unforgettable and full of surprises and will leave them longing to return for more.
Known as Hu, Shanghai is a multicultural metropolis that seamlessly blends modernity with traditional Chinese elements. You can explore ancient temples and gardens alongside bustling markets and futuristic shopping malls. You can feel the pulse of history in Yu Garden and the City God Temple, enjoy the breathtaking night views along the Bund and marvel at the skyscraper skyline in Lujiazui. Shanghai is a popular travel destination that captures the essence of China’s rapid development, offering visitors a unique opportunity to experience the country’s dynamic growth.
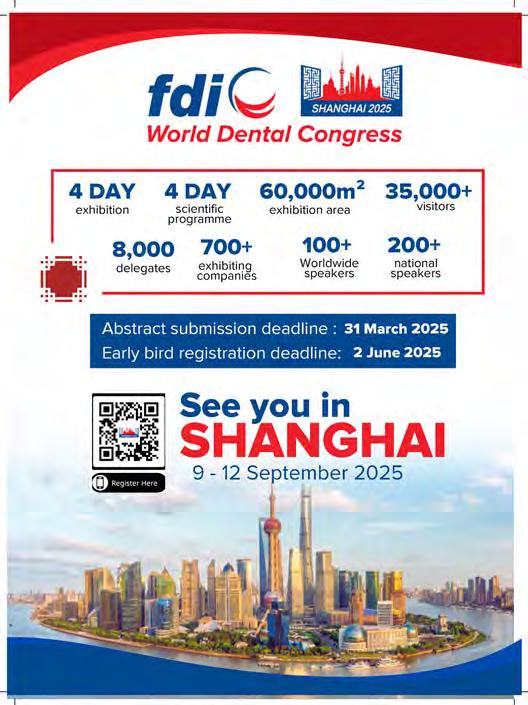



A significant collaboration agreement has been signed between INDEX Conferences & Exhibitions, the organizer of AEEDC Dubai, and the organizer of CADEX (Central Asia Dental Expo) during AEEDC Dubai. The collaboration agreement was signed by Tariq AlMadani, CEO of INDEX Conferences & Exhibitions and INDEX Design, Nursulu Kossuvalova, General Manager of CADEX.
CADEX (Central Asia Dental Expo) held annually in Almaty, Kazakhstan, participated in AEEDC Dubai 2025, marking a successful collaboration start between the two events. This partnership, aimed at strengthening global ties and expanding internationally, was praised by participants for fostering knowledge-sharing and business opportunities in dentistry and oral health.
AEEDC Dubai will also participate in CADEX next October, further solidifying the collaboration and promoting dental care advancements. This partnership underscores Dubai’s position as a global hub for dentistry, driving innovation in oral health.
For CADEX, this alliance presents a unique opportunity to elevate their international visibility and recognition, expanding their reach
beyond Central Asia. By partnering with globally recognized events, CADEX will gain broader exposure on the global stage, forging new partnerships and creating growth opportunities within the international marketplace. The oral care market in Central Asia is projected to reach US$343.88 million in revenue by 2025, with a growth rate of 4.73% annually, reflecting a growing focus on oral health in a region of 79 million population. The collaboration is already yielding impressive results, with several prominent Kazakhstan and Central Asia leaders expressing their gratitude and enthusiasm for the initiative led by the two organizations.
INDEX Media
Dima Alkananie - Dima.Alkananie@index.ae
+971 501739770
CADEX
Nursulu Kossuvalova -nursulu@ns-expo.kz
+7 707 9501112
AEEDC Dubai
Sophie Dudicourt Sophie.dudicourt@index.ae
Wissam Ezzeddine w.ezzeddine@index.ae
+97145208888
ceraMotion® Z – The smart overall concept for natural all-ceramic restorations from Dentaurum
Six different ceraMotion® Z blanks cover all zirconium-based indications
Have you already heard of ceraMotion® Z, the newest member of the ceraMotion® family?
The smart material completes the product range with six zirconium oxide blanks and stands out thanks to its variety of applications, biocompatibility and perfect optical adaptability. The first choice for prosthetic restorations which place the highest demands on material properties and aesthetics.
We have them all – the ceraMotion® family continues to grow
The six ceraMotion® Z blanks cover all zirconia-based indications and offer maximum reliability in shading and processing. State-of-the-art materials technology within a logical overall concept make ceraMotion® Z the smart choice for natural all-ceramic restorations created to meet high demands.
Especially the multi-shaded, multi-layered zirconium oxide ceraMotion® Z Hybrid is a truly multi-purpose material. In one blank, it combines the aesthetics of 1.000 MPa zirconium oxide with the strength of a tetragonal, highly translucent zirconium oxide. ceraMotion® Z Hybrid is pure aesthetics and suitable for all work in the anterior and posterior region.
The ceraMotion® products can be combined with one another very efficiently. The processing technology and the choice of material combinations within the ceraMotion® product range can be individually adapted to the respective case and freely selected. Both the ceraMotion® Zr veneering ceramics and the unique ceraMotion® One Touch ceramic paste harmonize perfectly with lithium disilicate (ceraMotion® LiSi) and zirconium oxide (ceraMotion® Z).






The FDI Regional Congress – Saudi International Dental Conference (SIDC) 2025, held from January 16 to 18 at the Riyadh International Convention & Exhibition Center, marked a significant milestone in the Middle East’s dental community. This event was co-hosted by the Saudi Dental Society and FDI World Dental Federation. It set new records in attendance and industry participation.
The congress attracted over 3,000 registered delegates and more than 10,000 trade visitors. This marked the largest gathering in the history of SIDC and FDI’s activities in the region. Renowned dental experts from around the world shared their insights across various cutting-edge topics. There were 130 distinguished speakers leading 143 lectures. Additionally, the event featured 36 workshops, drawing an extra 800 participants eager to enhance their practical skills.
The conference hosted 165 exhibitors from across the globe. They showcased over 3,400 brands representing the latest innovations in dental technology, equipment, and services. A dedicated Innovation Zone provided delegates with interactive experiences, including live demonstrations of groundbreaking products and solutions.
Demonstrating a commitment to the growth of the dental profession, the congress included interactive sessions focused on career development for young dentists. These sessions fostered discussion, mentorship, and networking opportunities for emerging dental professionals.
The FDI Regional Congress – SIDC 2025 in Riyadh not only showcased the latest advancements in dental science and technology but also reinforced the region’s pivotal role in the global dental community. The event provided a dynamic platform for knowledge exchange, professional development, and business networking. It offered valuable insights into the future of the dental industry.












trAditionAl sAudi entertAinment Performing At the exhibition floor












expodental.it/en


Discover innovations and create new connections at one of the most attended dental events in Europe.







ronAldo hirAtA receiVing his certificAte for his PresentAtion on lAyering to injectAble And cAd-cAm techniques






Mr. Rajender Kumar, as we embark on the year 2025, we see that progress in digital dentistry is moving as predicted, with more digitalization. How is Dentsply Sirona accompanying this progression?
February 2nd and 3rd, 2025, 8:00 a.m. – 6:30 p.m. GST (local t ime) Grand Hy att Dubai (DEC)
Sunday, Feb 2nd
Dentsply Sirona continues to lead the change in connected dentistry by integrating the latest technology, such as cloud services. Now, all our digital solutions are integrated with cloud services, which definitely provides a seamless experience for dentists. In our MENA region, this technology will be available very soon as well.
while having real-time access to the data. If another team member takes the scanner for preparation— whether to send the scan to the lab or review patient data at home— the data is available anytime, anywhere, without being dependent on a physical device.
Another major feature of cloud-based storage is that dentists can grant access to laboratories, allowing labs to directly download the data from anywhere. There is no need to send files manually or via email. This cloud service is called DS Core
We know that CEREC is the pioneer in the CAD/CAM dental revolution. What are your new offerings for dental professionals in 2025 regarding the evolution of CEREC?
8:00 – 9:20 a.m. Breakfast and Registration
9:20 – 9:45 a.m. Opening
We have DS Core, a platform that integrates all digital equipment into a cloud-based system. We have just launched Primescan Two, which is as portable as a mobile phone. You can take the equipment anywhere and start scanning— all you need is a Wi-Fi connection, nothing else. If you have connectivity, you can work from anywhere. We have adopted the same approach in dentistry as a company. Our cloud solution connects the scanner and even radiology equipment to the cloud.
9:45 – 11.15 a.m. Scientific program
How do dentists or dental offices connect to the cloud?
11:15 – 11.:45 a.m. Coffee break
11:45 – 1:15 p.m. Scientific program
We offer different packages for dentists at a very nominal charge. You can create a basic account, which provides storage space. If you are a heavy user, premium packages are also available, allowing you to store an unlimited number of cases in the cloud.
1:15 – 2.00 p.m. Lunch Break
2:00 – 4:00 p.m. Scientific Program
4:00 – 4:30 p.m. Coffee break
4:30 –6:30 p.m. Scientific Program
You no longer need to scan on any physical computer. Instead, you scan, and in real-time, the data is uploaded to the cloud. Once you are done scanning, you can immediately hand over the scanner to the next operatory room. In the past, this process took longer because you had to open the software, complete the scan, export patient data, and then physically transfer the cart to the next room. Now, the scanner is in your hand, and you can move to the next operatory
We are continuously upgrading our CEREC system, which is designed for single-visit dentistry. Patients can come in, have their crown designed, and receive it in just one visit.
Now, we have introduced a cloud-based system for CEREC, allowing dentists to store all their data securely in the cloud. This is our latest innovation in the CEREC system.
This year, we are celebrating 40 years of CEREC, and we remain the only company offering a complete solution, including scanning, milling, and printing. A few years ago, DS introduced Primeprint, which provides 3D printing solutions for both labs and dentists.
You can design your model, and the Primeprint will produce it within a few minutes.
Dentsply Sirona offers a three-step system: Primescan – for scanning
Primemill – for milling
Primeprint – for printing
We also provide blocks for Primemill and resins for Primeprint. Currently, milling is used for permanent restorations, while printing is used for temporary restorations. For example, if you need a temporary restoration for a patient, it can be printed immediately.



PROF FOUAD KHOURY BIOLOGIC BONE GRAFT CONCEPT
A technique always reproducible with short time bone remodeling only 3 months & Possibility to insert implant with bone graft ALL THESE TECHNIQUES WILL BE DEVELOPED IN 4 DAYS COURSE OF 24 THEORETICAL HOURS, VIDEOS & 7H “HANDS ON”

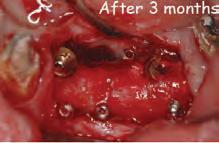









How many types of resins do you have for printing?
We offer a variety of resins with different colors and configurations.
Primeprint is one of the cleanest systems on the market. For example, a nightguard comes out of the printer ready to use— you only need minimal polishing and fine-tuning.
What are the highlights in radiology?
We are introducing a revolutionary new machine called DD MRI, which will be the first-ever MRI system dedicated solely to dentistry.
This is the first time MRI technology is being introduced to the dental industry, and we are preparing to launch it very soon in our region. This innovation is a collaboration between Siemens and Dentsply Sirona.
This dental-dedicated MRI is much smaller than traditional MRI machines, and it focuses specifically on the areas of interest in dentistry.
Can this machine be installed in a dental office?
While this technology is a breakthrough, its primary target users are universities and hospitals due to its cost. We are mainly aiming for institutions focused on dental research.
One major advantage is that there is no radiation, making it a safer diagnostic tool.











DUBAI, UAE — The 29th edition of the UAE International Dental Conference and Arab Dental Exhibition (AEEDC Dubai 2025) concluded on February 6, 2025, leaving an indelible mark on the global dental landscape. This year’s event witnessed unprecedented success, with landmark deals surpassing AED 20 billion and attracting over 85,000 visitors and participants from a staggering 177 countries.
Her Highness Sheikha Latifa bint Mohammed bin Rashid Al Maktoum, Chairperson of Dubai Culture and Arts Authority, opened the 29th edition of the UAE International Dental Conference and Arab Dental Exhibition – AEEDC Dubai 2025.
Her Highness also visited the Kuwait pavilion, the Guest of Honour at AEEDC 2025, where she highlighted the significance of Kuwait’s participation in this global event as a testament to the enduring partnership between the UAE and Kuwait.
AEEDC Dubai has cemented its position as the world’s largest international event dedicated to dentistry and oral healthcare, featuring an impressive array of 5,328 brands represented by 3,924 international companies specializing in dental technology and oral care products. The sheer scale of participation underscores the event’s influence on the global dental industry. The conference’s impact extends far beyond the dental sector, with a significant boost to the local economy. Hotel and restaurant bookings surged, reflecting the substantial benefits to the medical and economic sectors. This achievement further solidifies the UAE’s reputation as a pioneering global hub for innovation and development in dentistry, reinforcing its status as an economic and commercial powerhouse worldwide.
His Excellency Ambassador Dr. Abdulsalam AlMadani, Chairman of AEEDC Dubai and the Global Scientific Dental Alliance (GSDA), expressed immense pride in the event’s success. He highlighted AEEDC Dubai’s role as a premier platform for knowledge exchange and strategic networking among experts and specialists, ultimately elevating oral healthcare services in the region and beyond.
One of the highlights in the conferences was a session about leadership in Dentistry conducted by NYU University, School of Dentistry.
Dr. AlMadani emphasized that the UAE has evolved into a definitive hub for medical tourism, hosting many of the most esteemed names in dentistry. “AEEDC Dubai continues to reinforce Dubai’s standing as the epicenter of international exhibitions and conferences,” he noted. The event plays a pivotal role in advancing international cooperation, revolutionizing healthcare services, and facilitating the exchange of cutting-edge medical technologies and practices.
Global Scientific Dental Alliance (GSDA) Meeting
The third day of the conference featured the 22nd Annual Meeting of the GSDA, which brought together 412 representatives from over 200 international medical organizations, including hospitals, academic institutions, dental associations, global health ministries, and various government and private sectors. This meeting serves as a key platform for dental experts and practitioners worldwide to connect and exchange knowledge on the latest advancements and innovations in oral health.
The next AEEDC will take place on 19 – 21 January 2026 at the Dubai World Trade Centre, Dubai, UAE.

AbDulSAlAm AlmADANi RECEiVES NYu’S highESt hoNoR foR hiS REmARkAblE CoNtRibutioNS to hEAlthCARE, EDuCAtioN AND humANitARiAN CAuSES

AbDulSAlAm AlmADANi EmphASiziNg thE VitAl RolE of EDuCAtioN iN ShApiNg futuRE gENERAtioNS AND builDiNg A SuStAiNAblE futuRE








































Driven by quality, our goal is to make the professional feel comfortable in its daily endo workflow.
KENDO delivers a wide and reliable range of endodontic products made in Germany as: K-REAMERS, K-FILES, H-FILES, ROOT FILLERS.
A VDW brand - over 150 years of endo experience.








For nearly six decades, endodontists and patients have trusted RTD for the most high-stakes restorations. In fact, we were one of the firsts to develop and bring fiber posts to market, leveraging on deep knowledge and expertise. Today, we’re one of the largest producers all over the world, with a wide range of posts designed for optimal outcomes and unbeatable peace of mind.
Learn more about RTD at rtddental.com