EDSIC 2024 Egypt
The Metn Dental League 2024 EDSIC 2024 Egypt Esthetic Outcome of Immediate Implant Placement
The Metn Dental League 2024 Esthetic Outcome of Immediate Implant Placement

























EDSIC 2024 Egypt
The Metn Dental League 2024 EDSIC 2024 Egypt Esthetic Outcome of Immediate Implant Placement
The Metn Dental League 2024 Esthetic Outcome of Immediate Implant Placement





















































Based on the close and fruitful cooperation with dental institutes and practicing dentists since the 1940s, we have a uniquely broad portfolio of specially developed, innovative toothpastes, gels, sprays, mouthwashes and mouth baths. These products, which are marketed under the brands Tebodont®, Emofluor®, Emoform®, Depurdent® and Emofresh® are sold exclusively in pharmacies in Switzerland and in more than 40 other countries outside Switzerland, their various innovative formulations and compositions o er excellent solutions for daily dental care, addressing specific needs and problems (e.g. caries prevention, sensitive teeth, gum problems) and general oral health.
With the REDESIGN we have clarified the positioning of the oral care products: every toothpaste and every mouthwash now has a clear application area. At the same time, our new packaging is "digitalized": each product has a QR code that allows detailed information to be downloaded directly to the mobile phone. The redesign of the products should make the Wild brand tangible and perceptible.
• WILD will be used as umbrella brand on all products, which results in an easier promotion among the whole product range
• Same design for all brands leads to recognition and synergy e ects across product range
• Clear unique main indication on the packaging avoids confusion among dental profession, pharmacists and end consumers due to overlapping benefits
• New design underscores clinical benefits and professionalism of the products which leads to cross-brand and cross-portfolio products awareness and helps to create trust among the dental profession, pharmacists and end consumers
• Unifying of the packaging system - all toothpastes in the same size and shape of tubes, all mouthwashes in the same size and packaging - leads to a uniform, eye-catching and space-saving shelf-impact
• Product portfolio becomes fresh, easy to recommend and attractive for the POS
Volume XXXI, Number III, 2024
EDITORIAL TEAM COORDINATOR ART DEPARTMENT SUBSCRIPTION
Alfred Naaman, Nada Naaman, Khalil Aleisa, Jihad Fakhoury, Dona Raad, Antoine Saadé, Lina Chamseddine, Tarek Kotob, Mohammed Rifai, Bilal Koleilat, Mohammad H. Al-Jammaz
Suha Nader
Marc Salloum
Micheline Assaf, Nariman Nehmeh
Josiane Younes
Albert Saykali
Gisèle Wakim
DIRECTOR ISSN
Tony Dib 1026-261X
DENTAL NEWS IS A QUARTERLY MAGAZINE DISTRIBUTED MAINLY IN THE MIDDLE EAST & NORTH AFRICA IN COLLABORATION WITH THE COUNCIL OF DENTAL SOCIETIES FOR THE GCC.
Statements and opinions expressed in the articles and communications herein are those of the author(s) and not necessarily those of the Editor(s) or publisher. No part of this magazine may be reproduced in any form, either electronic or mechanical, without the express written permission of the publisher.
DENTAL NEWS – Sami Solh Ave., G. Younis Bldg. POB: 116-5515 Beirut, Lebanon.
Tel: 961-3-30 30 48
Email: info@dentalnews.com Website: www.dentalnews.com










October 3 – 5, 2024 Seaside Arena | Beirut, LEBANON www.lda.org.lb
www.instagram.com/dentalnews







MAKKAH DENTAL 2024
Association Tunisienne de Recherches et d'Etudes en Orthodontie
October 4 – 5, 2024 Hotel Hilton Skanes | Monastir, TUNISIA association.atreo@gmail.com
October 24 – 26, 2024 Hilton Makkah | Makkah, KSA makkahdental.com
November 13 – 15, 2024 HiltonGreen Plaza | Alexandria, EGYPT www.aidconline.net
37th CAPP International Dental ConfEx
November 15 – 16, 2024 Madinat Jumeirah | Dubai, UAE www.cappmea.com
ADF Association Dentaire Française
November 26 – 30, 2024 Palais des Congrès Paris | Porte Maillot, FRANCE www.adf.asso.fr
GNYDM Greater New York Dental Meeting
December 1 – 4, 2024 Jacob Javits Convention Center | New York, USA www.gnydm.com
January 16 – 18, 2025 Riyadh Int’l Convention & Exhibition Center | Riyadh, KSA www.sidc.org.sa
AEEDC 2025
February 4 – 6, 2025 World Trade Center | Dubai, U.A.E. www.aeedc.com
March 25 – 29, 2025 Koelnmesse, Cologne, GERMANY www.english.ids-cologne.de
A-dec 23
Acteon 11
ADF 61
Esthetic Outcome of Immediate Implant Placement Using Customized Healing Abutment in Anterior Region.


Oleg O. Yanushevich, Igor V. Maev, Natella I. Krikheli, Dmitrii N. Andreev , Svetlana V. Lyamina ,Filipp S. Sokolov, Marina N. Bychkova, Petr A. Beliy and Kira Y. Zaslavskaya

Aoralscan by SHINING 3D

AEEDC 69
AIDC 55
ATREO 47
Belmont 9
BIDM 46
CONFEX 57
DMP 1
DURR 15
ENDO 43
FKG 21
GNYDM 63
HU-FRIEDY 38-39
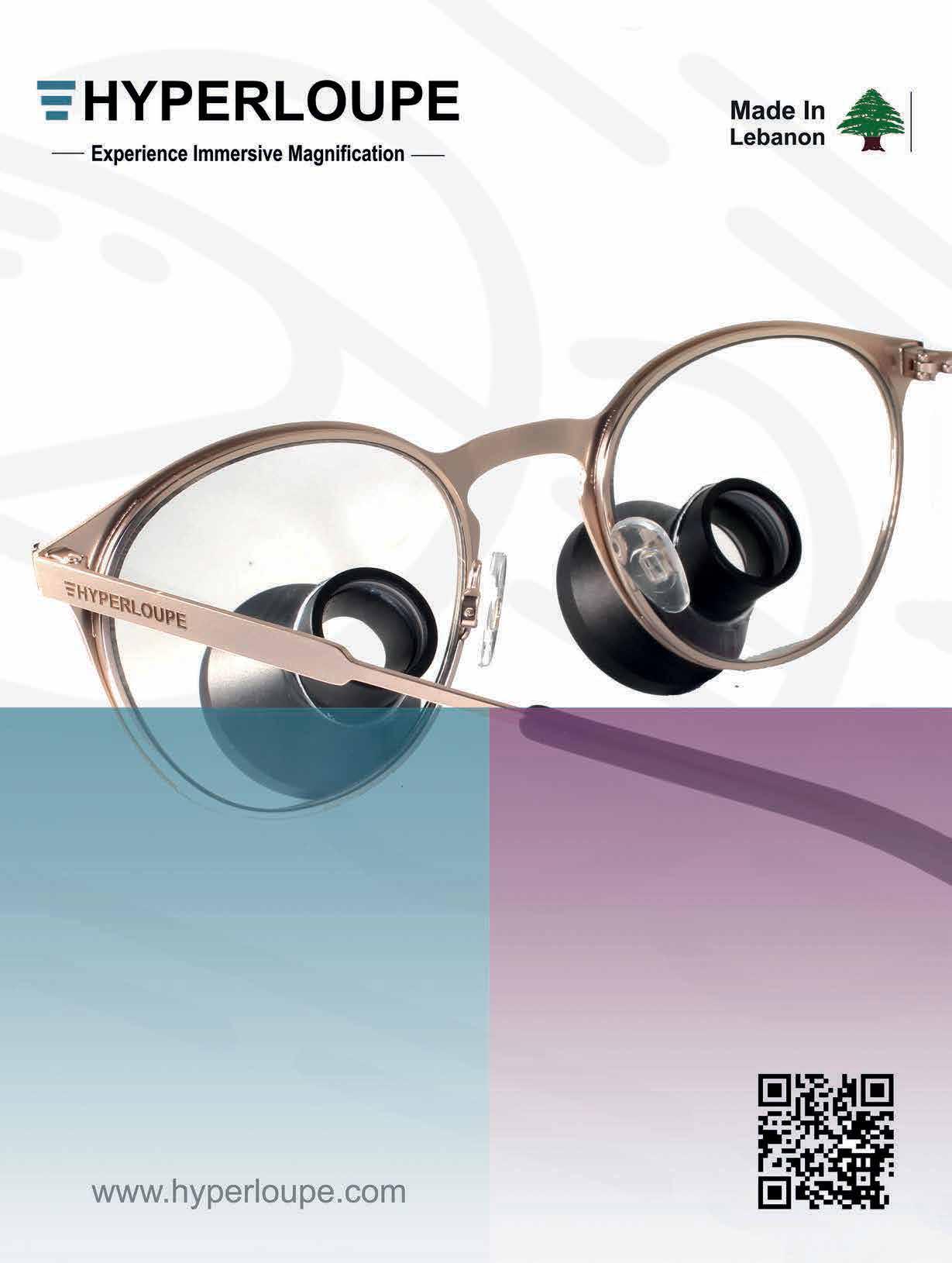
Hyperloupe 25 IDS 73
INIBSA 2
K Biocer 41 MAKKAH 49
Mani 17
MESA 36-37
NSK C2
Promedica 35 Scheu 29
Septodont 76 Shining 3D 27
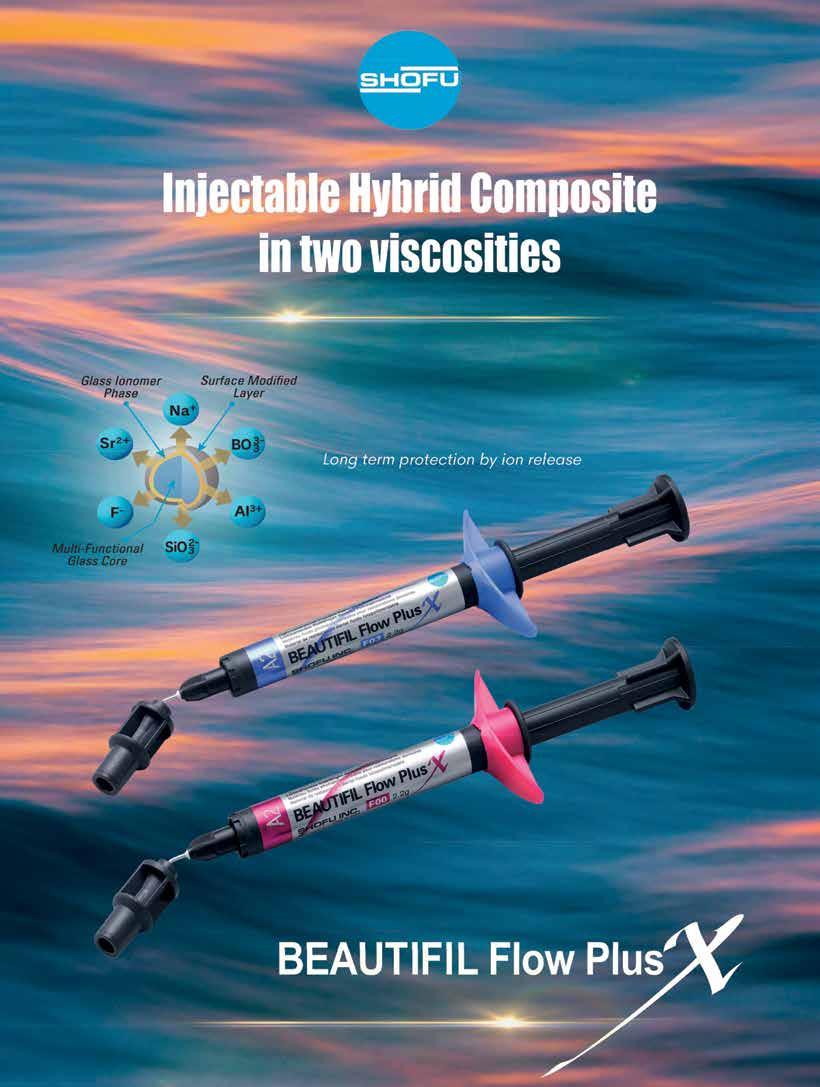
Shofu 19
SIDC 65
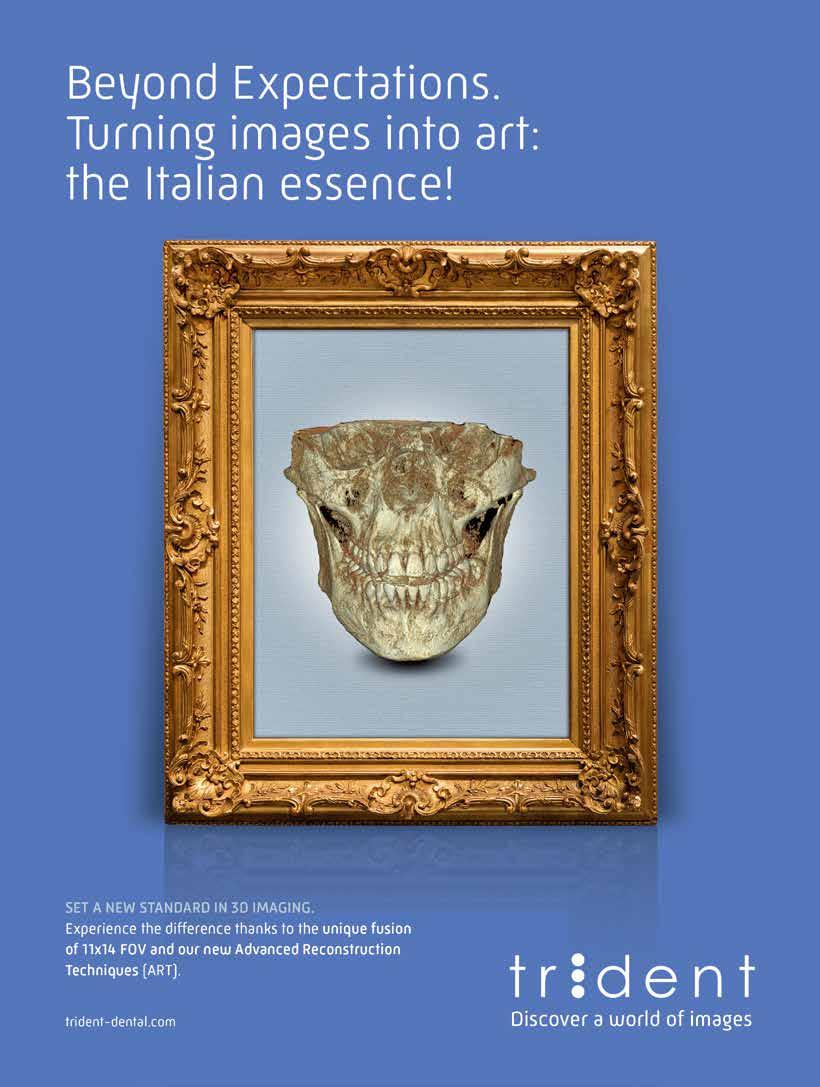
TRIDENT C4
Ultradent 13
VOCO C3 Wild Pharma 3-4-5
Bridge to Saida Smiles Dental Meeting La Salle - Rmaylé June 23-2024

The Metn Dental League & The Armenian Dentist's Association of Lebanon - July 13-2024

Handover Ceremony of the Lebanese Society of Pediatric Dentistry (LSPD)

July 20- 2024, Lancaster Hotel - Hazmieh

EDSIC 4-6 September 2024
InterContinental Cairo City Stars , Egypt




Authors
Sara N. El Touliani 1 , Ahmed M. bdelhamid2
Yasser M.Aly 3 , Nada M. H. Fahmy 4 Sara El Touliani, BDS, MSc, Lecturer of Prosthodontics, Faculty of Dentistry, Beirut Arab University, Beirut, Lebanon.
Ahmed M. Abdelhamid, BDS, MSc, PhD, Professor of Prosthodontics, Faculty of Dentistry, Alexandria University, Egypt. Yasser M.Aly, BDS, MSc, PhD, Associate Professor of Prosthodontics, Faculty of Dentistry, Alexandria University, Egypt. Nada M. H. Fahmy, BDS, MSc, PhD, Lecturer of Oral and Maxillofacial Surgery, Faculty of Dentistry, Arab Academy for Science, Technology and Maritime Transport
Correspondence: Sara El Touliani
Email:s.tliani@bau.edu.lb . Telephone: 009613884280.
Statement of problem: Providing a definitive anterior implant placement restoration with proper esthetic and peri-implant soft tissue contour is important for immediate implant placement.
Material and method: immediate implant placement to replace non restorable teeth in the maxillary anterior region. Extraction was done and immediately an implant was inserted. Customized healing abutments were fabricated using Cervico mold and connected to the dental implant. After 3 months, intraoral scanning was done to fabricate a definitive crown.
Conclusion: Easy clinical technique to create proper emergence profile through customized healing abutment using the Cervico device. The use of Cervico device for the construction of customized healing abutments prepares soft tissue for the prosthetic stage preserving its contours and eliminating the need for reopening surgery for immediate as well as for early implant placement.
Keywords: Customized healing abutment, emergence profile, immediate placement, soft tissue management
Esthetics is of the most importance while rehabilitating maxillary anterior region with dental implants. The anterior esthetics are influenced by several variables, including the patient›s smile line, the location of the dental implant, the biotype of the periodontium, the form of the tooth, the position of the neighboring teeth, the bone structure of the implant site, and the timing of implant placement. Additional di culties arise during implant implantation because of the great visibility and patient expectations. The accelerated bone remodeling especially in the maxillary anterior region makes the preservation of the peri-implant tissue and contour crucial 1 , 2 . After tooth extraction, immediate implant placement using various clinical approaches to minimize bone loss and enhance implant success was followed, thus favoring less invasive procedures. Minimally invasive tooth extraction, avoiding unnecessary flap release, minimizes tissue disruption, and conserves alveolar bone.3,4,5 Regardless of implant placement timing and according to the clinical situation, provisional restoration is crucial. It can provide immediate aesthetics and function while the implant integrates as it preserves









Embodies our belief of bringing highly reliable Japan-quality products to dentists in the world.

soft tissue contours simplifying subsequent treatment stages6,7. Once secondary stability is achieved, indicating complete integration, the final prosthesis can be manufactured, benefiting from preserved soft tissue contours for more predictable results. Adequate primary stability, exceeding 35 N cm or an implant stability quotient above 70, is crucial for the desired outcome8 Implementing comprehensive and less invasive approaches addresses post-tooth extraction bone loss, enhancing implant success for optimal aesthetic and functional outcomes. Customized healing abutments, o er a promising solution. They protect and preserve alveolar contours, eliminate the need for a second reopening surgery and provisional restorations, and expedite the soft tissue conditioning phase for natural-like restorations9. This approach provides a simplified chairside technique for customizing healing abutments. It is particularly useful for immediate implants and early implant placement in the anterior region. The aim is to maintain soft tissue contours and reduce the number of clinical steps, presenting a valuable alternative to traditional methods10. The aim of the study was to evaluate the soft tissue contour between early and immediate implant placement using customized healing abutment
The present study was conducted as a prospective, double-blinded, balanced, randomized controlled clinical trial with a parallel-group design. Ethical approval was obtained under the number IRB2023H0113D-P-0494 from the ethical committee in the Faculty of Dentistry, Beirut Arab University. Twenty-four dental implants were placed in twelve participants indicated for bilateral immediate and early implant placement in the esthetic zone of the maxillary dental arch. They were selected from those who attended the Department of Prosthodontics, Faculty of Dentistry, Beirut Arab University, Lebanon. Clinical procedures and possible complications were explained to the participants, who signed an informed consent considering the 1975 Declaration of Helsinki, revised in 2013.11
The inclusion criteria were patients within 20 to 40 years with unrestorable bilateral teeth with a harmonious gingival contour, having a thick
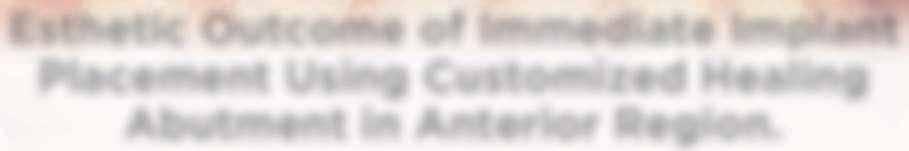
gingival phenotype, and at least 4 mm of bone apical to the root apex and 2mm labial plate of bone of the unrestorable tooth to be extracted and absence of any periapical radiolucency (Fig 1). 12 Any patient su ering from medical disorders interfering with osseointegration or soft tissue healing, active oral infections or periodontal disease, presence of dehiscence or fenestration defects related to the tooth to be extracted, poor oral hygiene, and heavy smokers was excluded from the study 13
A bench scan (Medit T-710 Tabletop Scanner) of the cast and preoperative CBCT (3D Accuitomo 170) was made for each participant for the construction of a CAD CAM surgical guide. The implant was planned to engage the palatal wall, avoid pressure on the labial plate of the bone, and be 1-mm apical to the crest. A fully guided tooth-supported surgical guide was designed and then printed in clear acrylic resin (Dental SG Resin; Formlabs) by using a 3D printer (Form2; Formlabs). (fig 2)














Being a human centric organization focused on the needs of patients and care providers.
Providing tailored workflow solutions that maximize the total effectiveness, efficiency, and economics of achieving desired clinical outcomes.
Providing innovative and integrated healthcare solutions that address the continuous healthcare needs over patients’ lifetimes.







A systemic antibiotic (2g amoxicillin-clavulanic acid, per-orally) was administered to the patients 1 hour prior to the procedure. The patient’s mouth was rinsed with a solution of chlorhexidinedigluconate 0.2% for 2 minutes. After surgical guide printing, the tooth was extracted and the implant placed (IDI implant Implants Di usion International 23/25) following implant placement protocol using a fully guided CAD CAM surgical guide. 14 (fig 3,4,5)


Figure 5: Fully guided implant placement through the surgical guide using spoons. The implant was inserted at the planned position.
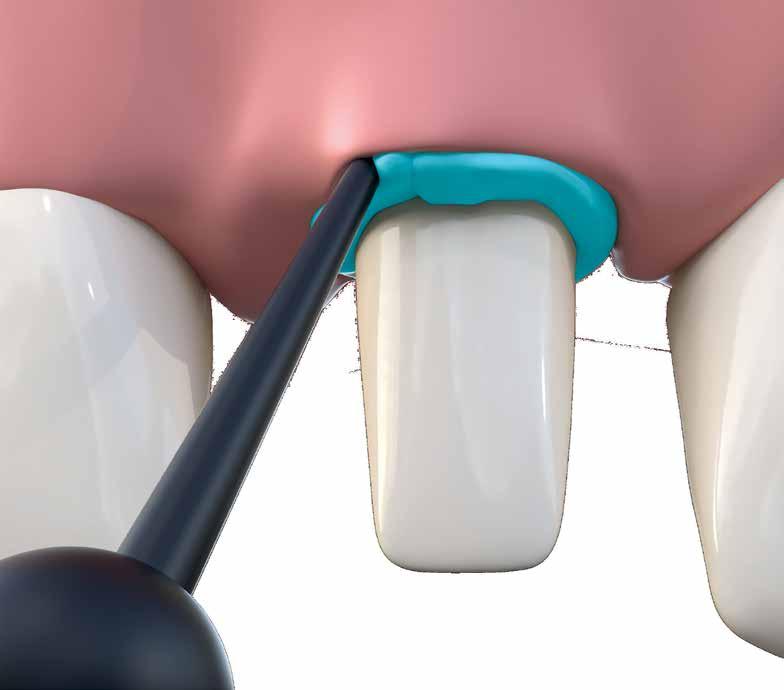
Directly after immediate implant placement, a customized healing abutment was fabricated using Cervico kit. The selection was made intraorally using a special handle to place the indicator over the restorable area. (fig 6) Utilize the anatomical shape tab from the same group as per the anterior tooth missing. The anterior suitable stock healing abutment was directly screwed on the implant analog and was fixed at the corresponding well of the silicone mold, and the custom healing abutment was fabricated with nano‐hybrid flowable resin (3M™ Filtek™ Supreme Flowable Composite) (Fig 7,8). Minor selective grinding, finishing, and polishing were made when necessary to achieve a smooth, lustrous tissue contact surface, and screwed to the implant. 15 (Fig 9)







The prosthetic procedures for definitive restorations were performed 3 months after implant placement. The healing abutment was removed (Fig 10) scan body was placed in position and a digital implant-level impression was made using an intraoral scanner (Medit I 700 3D scanners) (16) (Fig 11,12)



Exocad was used to design the restoration (fig. 13) and was milled from a super translucent multilayered zirconia (KATANA Zirconia STML; Kuraray Noritake). The milled restoration was cemented on the Ti-base with a resin cement (RelyX Unicem; 3M ESPE). Then, the definitive restoration was connected to the implant, and the Ti-base screw was tightened to 20 Ncm according to the manufacturer’s instructions. The screw access channel was sealed with sterilized PTFE and photopolymerized composite resin (Filtek Supreme Ultra; 3M ESPE). The definitive restoration was evaluated for centric and eccentric occlusal contacts and then finished and polished (fig 14,15).

































The anterior region of the maxilla is frequently termed the aesthetic zone due to its high visibility and influence on facial appearance. Single tooth implant replacement in this region can present many clinical challenges17. Not only must the crown conform in contour, shade, and texture to its neighbors, but the gingiva must also be in symmetry and harmony with the adjacent tissues. As we have learned, once a maxillary anterior tooth is extracted, the collapse of the socket wall begins in a buccal to palatal direction. This is accentuated even more in a socket with a thin or non-existent buccal plate. In addition, the crestal height of the extraction socket begins to move apically. This can leave a large concavity in the buccal gingival tissue, resulting in a prosthesis that will not be symmetrical to the adjacent dentition. Meticulous planning is necessary for implant placement in the esthetic zone. Numerous treatment modalities have been developed for the long-term temporization and previsualization of anterior implant cases. Case reports are appearing in the literature of immediate implant placement and immediate temporization with acrylic crowns18. It is important to stress that immediate implant placement does not prevent the remodeling or resorptive processes associated with a tooth’s loss.
Thorough diagnostic assessments, including radiographic imaging and clinical evaluations, are crucial for understanding the patient›s unique anatomy, bone quality, and the condition of the extraction site.
Clearly defined treatment objectives should align with the patient›s esthetic and functional expectations. This includes determining the ideal implant position and emergence profile.
Early implant placement, which refers to implant placement following complete soft tissue coverage of the extraction socket, was introduced as a viable treatment alternative. It has been suggested that the soft tissue healing allows for the resolution of local pathology and provides enhanced soft tissue volume. Several studies have shown promising clinical outcomes for
implants placed according to the early placement protocol. However, it is necessary to compare the clinical outcomes of implants placed according to the early implant placement protocol with those of implants placed according to the immediate or the delayed implant placement protocols.19
In this study, the split-mouth technique with immediate implant and early implant in the anterior region is used for various reasons. Firstly, it improved the implant›s primary stability by avoiding buccal wall engagement, reducing the need for jumping distance, and minimizing the risk of implant failure. The use of moderate insertion torque (32-50 Ncm) may reduce the risk of implant failure20 (HEBA 2020).
Using Cone-Beam Computed Tomography (CBCT) with immediate and early implant placement in the anterior region is crucial because it improves diagnostic accuracy.
The CBCT provides accurate three-dimensional images that help in proper diagnosis and treatment planning, especially in the anterior maxilla where the risk of damaging the buccal plate during extraction is higher21. Also, reduced resorption and healing time: Immediate implant placement with CBCT reduces alveolar bone resorption after extraction, leading to better function and aesthetics. It also eliminates the need for a waiting period of 10-12 months for socket healing, reducing the overall treatment time and psychological stress on the patient. It enhanced predictability and e ciency where research showed with Mikic et al. (2022)22 that using CBCT for bone density assessment is significantly correlated with implant stability, improving predictability and e ciency of implant planning and placement. This technology allows for better control over implant placement, ensuring optimal outcomes.
Utilizing digital technologies for treatment planning enhances precision. Computer-aided design (CAD) and computer-aided manufacturing (CAM) systems contribute to accurate implant placement and customized abutment design23
Our study introduced intra-oral scanning and digital data measurement as new methods for assessing the dimensional changes of soft
tissue during the healing period in one-step recording direct from the source and ensured this measurement protocol is more accurate than the conventional step which cumulates routine error in the impression taking with weight material, the poured stone model and hand-manual measuring. The use of CAD/CAM technology in implant crown design has the potential to improve the accuracy and e ciency of the restoration process, providing patients with a functional and aesthetic solution to their dental needs24 Healthy peri-implant gingiva is important to ensure a good emergence profile, particularly in the esthetic zone. It plays a role in preventing periimplant disease by forming a barrier to e ciently protect underlying bone and prevent access to microorganisms. In addition, after the final restoration, time may be required for soft tissue to fill the embrasure, which is more predictable with healthy tissue, shows adequate interdental papilla, well contoured gingiva, and the presence of stippling and no inflammation, indicative of healthy peri-implant tissue25
The use of provisional abutments and immediate temporization have a proven track record of their ability to produce optimal esthetics and to guide the tissue response during the healing phase. Customization of the healing abutment had more dimensional improvement in soft tissue healing when compared with stock healing abutment. First, because of flapless protocol, a stock healing abutment is unable to completely seal the underlying alveolar socket in the immediate implantation. If this abutment can’t be avoided, using a flap elevation procedure is needed to seal the grafting material.26
Conclusion
The use of customized healing abutments seemed to be an appropriate solution to support and maintain the soft and hard tissue contours after immediate implant placement in both the anterior regions. This reinforces the importance of longterm monitoring and care in the management of dental implants, emphasizing that immediate placement strategy can achieve comparable outcomes in terms of bone health and implant stability using customized healing abutment, provided that appropriate post-operative care and follow-up protocols.
References :
1- Hämmerle CF, Tarnow D. The etiology of hard- and softtissue deficiencies at dental implants: Anarrative review. J Clin Periodontol.2018; 45:S267–S277.
2- Altay A, Sindel A, Hüseyin H, Nelli OM. Esthetic evaluation of implant-supported single crowns: a comparison of objective and patient-reported outcomes. Int J Implnt Dent. 2019; 5(1):24
3- Barone A, Rispoli L, Vozza I, Quaranta A, Covani U. Immediate restoration of single implants placed immediately after tooth extraction. Journal of periodontology. 2006 Nov;77(11):1914-20.
4- Hämmerle CH, Tarnow D. The etiology of hard-and softtissue deficiencies at dental implants: A narrative review. Journal of clinical periodontology. 2018 Jun;45:S267-77.
5- Araujo MG, Lindhe J. Peri-implant health. Journal of periodontology. 2018 Jun;89:S249-56.
6- Baltayan S, Pi-Anfruns J, Aghaloo T, Moy PK. The predictive value of resonance frequency analysis measurements in the surgical placement and loading of endosseous implants. Journal of Oral and Maxillofacial Surgery. 2016 Jun 1;74(6):114552.
7- Passoni BB, Marques de Castro DS, de Araújo MA, de Araújo CD, Piatelli A, Benfatti CA. Influence of immediate/ delayed implant placement and implant platform on the periimplant bone formation. Clinical oral implants research. 2016 Nov;27(11):1376-83.
8- Cosyn J, De Lat L, Seyssens L, Doornewaard R, Deschepper E, Vervaeke S. The e ectiveness of immediate implant placement for single tooth replacement compared to delayed implant placement: A systematic review and meta-analysis. Journal of Clinical Periodontology. 2019 Jun;46:224-41.
9- Fürhauser R, Florescu D, Benesch T, Haas R, Mailath G, Watzek G. Evaluation of soft tissue around single-tooth implant crowns: the pink esthetic score. Clinical oral implants research. 2005 Dec;16(6):639-44.
10- Belser UC, Grütter L, Vailati F, Bornstein MM, Weber HP, Buser D. Outcome evaluation of early placed maxillary anterior single-tooth implants using objective esthetic criteria: a crosssectional, retrospective study in 45 patients with a 2-to 4-year follow-up using pink and white esthetic scores. Journal of periodontology. 2009 Jan;80(1):140-51.
11- Kuthning M, Hundt F. Aspects of vulnerable patients and informed consent in clinical trials. GMS German Medical Science. 2013;11.
12- Dawson A, Martin WC, Polido WD, editors. The SAC classification in implant dentistry. Quintessenz Verlag; 2022 Mar 30.
13- Chrcanovic BR, Martins MD, Wennerberg A. Immediate placement of implants into infected sites: a systematic review. Clinical implant dentistry and related research. 2015 Jan;17:e1-6.
14- Del Fabbro M, Bianchessi C, Del Lupo R, Landi L, Taschieri S,





































































































Corbella S. Platform switching vs standard implants in partially edentulous patients using the Dental Tech Implant System: clinical and radiological results from a prospective multicenter study. Clinical oral investigations. 2015 Dec;19:2233-44.
15- Schirdewan I. ConsEuro Conference 2019, Berlin, June 14-15. Clinical Oral Investigations. 2019 May 1;23(5):2515-72.
16- Lee B, Nam NE, Shin SH, Lim JH, Shim JS, Kim JE. Evaluation of the trueness of digital implant impressions according to the implant scan body orientation and scanning method. Applied Sciences. 2021 Mar 29;11(7):3027.
17- Sailer I, Barbato L, Mojon P, Pagliaro U, Serni L, Karasan D, Cairo F. Single and partial tooth replacement with fixed dental prostheses supported by dental implants: A systematic review of outcomes and outcome measures used in clinical trials in the last 10 years. Clinical oral implants research. 2023 May;34:22-37.
18- Soegiantho P, Suryawinata PG, Tran W, Kujan O, Koyi B, Khzam N, Algarves Miranda L. Survival of single immediate implants and reasons for loss: a systematic review. Prosthesis. 2023 Apr 17;5(2):378-424.
19- Bassir SH, El Kholy K, Chen CY, Lee KH, Intini G. Outcome of early dental implant placement versus other dental implant placement protocols: A systematic review and meta-analysis. Journal of periodontology. 2019 May;90(5):493-506.
20- Heba MB. stability and marginal bone loss of early loaded slactive implant with flapped and flapless approaches. International Journal of Medical Dentistry. 2020 Jan 1;24(1).
21- Weiss R, Read-Fuller A. Cone beam computed tomography in oral and maxillofacial surgery: an evidence-based review. Dentistry journal. 2019 May 2;7(2):52.
22- Mikic M, Vlahovic Z, Stevanović M, Arsic Z, Mladenovic R. The Importance of Correlation between CBCT Analysis of Bone Density and Primary Stability When Choosing the Design of Dental Implants—Ex Vivo Study. Tomography. 2022 May 11;8(3):1293-306.
23- Barros I, Carvalho GG, Leão MO, Kassis EN. Major approaches to laser therapy in regenerative processes in bucco-maxillofacial bone defects: a concise systematic review. MedNEXT Journal of Medical and Health Sciences. 2023 Aug 4;4(3).
24- Mühlemann S, Hjerppe J, Hämmerle CH, Thoma DS. Production time, e ectiveness and costs of additive and subtractive computer-aided manufacturing (CAM) of implant prostheses: A systematic review. Clinical Oral Implants Research. 2021 Oct;32:289-302.
25- Nayak DG, Uppoor A, Abhay K, editors. Fundamentals of Periodontology and Oral Implantology-EBook. Elsevier Health Sciences; 2021 Sep 4.
26- de Araújo Nobre M, Antunes C, Lopes A, Ferro A, Nunes M, Gouveia M, Azevedo Coutinho F, Salvado F. Partial Implant Rehabilitations in the Posterior Regions of the Jaws Supported by Short Dental Implants (7.0 mm): A 7-Year Clinical and 5-Year Radiographical Prospective Study. Journal of Clinical Medicine. 2024 Mar 8;13(6):1549.
Authors:
-Sara N. El Touliani 1* , Ahmed M. Abdelhamid 2 , Yasser M.Aly 3 , Nada M. H. Fahmy 4
-Sara El Touliani, BDS, MSc, Lecturer of Prosthodontics, Faculty of Dentistry, Beirut Arab University, Beirut, Lebanon.
-Ahmed M. Abdelhamid, BDS, MSc, PhD, Professor of Prosthodontics, Faculty of Dentistry, Alexandria University, Egypt.
-Yasser M.Aly, BDS, MSc, PhD, Associate Professor of Prosthodontics, Faculty of Dentistry, Alexandria University, Egypt.
-Nada M. H. Fahmy, BDS, MSc, PhD, Lecturer of Oral and Maxillofacial Surgery, Faculty of Dentistry, Arab Academy for Science, Technology and Maritime Transport
*Correspondence: Sara El Touliani Department of Oral Rehabilitation Sciences, Division of Prosthodontics, Faculty of Dentistry, Beirut Arab University, Riad El Solh, Beirut, P.O. Box 11-5020, Lebanon.
Email: s.tliani@bau.edu.lb . Telephone: 009613884280.
-Sara El Touliani: https://orcid.org/0009-00052098-6182
-Ahmed M. Abdelhamid: https://orcid.org/00000002-3200-866X
-Yasser M.Aly: https://orcid.org/0000-0001-91191145
-Nada M.H. Fahmy: https://orcid.org/0009-00004074-4416
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by ST, NF. The first draft of the manuscript was written by ST and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. ST, NF: Conceptualization, Methodology, Software, Data curation, WritingOriginal draft preparation, Visualization, Investigation. A.A, YA: Reviewing and editing. All authors read and approved the final manuscript.






Leendert (Len)
Boksman, DDS, BSc, FADI, FICD
Gary Glassman, DDS, FRCD(C)
Gildo Coelho Santos Jr.,DDS, MSc, PhD
Manfred Friedman, BDS, B.ChD.
“Traditional thinking that a post is only placed to retain a core and serves no other purpose may no longer be valid.” (1)
The preservation of dentin during access opening, shaping the canal, preparing the root for placement of a post, and during restoration with an onlay or full coverage preparation is critical to the clinical longevity and success of the final restoration. (2) It is now well recognized that excess removal of dentinal support, not only in the root, but also coronally, changes the flexural behavior and resistance to failure, and that overflaring the canal for straight line access to the canals weakens the dentinal complex. (3-6) Dentin coronally must be maintained, not only to give support to the core buildup, (7,8)
but as well, because clinical and in vitro studies support the fact that survival of endodonticallytreated teeth restored with posts is directly proportional to the residual coronal dentin that remains. (9,10)
Post preparation of the root canal space must not remove additional dentin, as this contributes to a reduced fracture toughness. (Fig. 1)
Ree et al. state that “no additional

dentin should be removed beyond what is necessary to complete the endodontic treatment”. (11) If this concept is to be adhered to clinically, then of course the use of parallel sided posts must be eliminated from our clinical protocol, as these posts usually require removal of sound apical radicular dentin, creating sharper internal line angles, resulting in a weakened root and a higher root fracture risk (Fig 2). (12) As well, the parallel post does not complement the tapered shape of the prepared canal, resulting in excess luting composite in the coronal aspect of the canal, which can decrease bonding e cacy and decrease dislocation resistance (Fig. 3). (13) If we adhere to the concept of minimal dentin removal in the root, and if we recognize that most root canals are ovoid in shape, then a wholly di erent treatment approach than what we have been taught in the past is indicated. Boksman et al. have recommended utilizing a tapered master quartz fiber post (MacroLock™ Post Illusion X-RO Clinical Research Dental, London, Ontario) with additional Fibercones (Clinical Research Dental, London, Ontario)

placed into the irregularity (lateral spaces) of the canal (Figs. 4 & 5). (14) This technique is similar to using a master gutta percha point with accessory gutta percha points, which is well-understood. Utilizing this approach provides several clinical advantages (15-19) including more anti-rotational resistance, decreased volume of composite or cement lateral to the post to decrease the C and S Factor constraints (volumetric shrinkage), better adhesion to the root canal walls resulting in decreased microleakage and increasing resistance to dislodgement, as well as decreased likelihood for lateral perforation. The combination of a post, or multiple posts, that transmit light e ciently, with su cient extended light curing time/output, results in better composite polymerization.
The indirect cast gold/metal/zirconia post and core has been largely replaced with a one appointment restoration of a direct post and core. Fiber posts such as the Ultradent Unicore Fiber Post (Clinical Research Dental, London, Ontario), the quartz fiber posts manufactured by RTD (St. Egreve, France), the Macro-Lock X-RO (Clinical Research Dental, London, Ontario), and the DT Light-Post (Bisco Canada, Richmond, BC) have many physical characteristics that make them more desirable clinically, rather than metal and zirconia posts:
1: The elastic modulus (or a material’s sti ness) of fiber posts more closely approximates that of dentin (18.6 Gigapascals-GPa) allowing some slight flex in function, dissipating stress, and reducing the likelihood of damage to the root. (20,21) Stainless steel has an elastic modulus of about 200GPa, titanium alloy 110GPa and Zirconia 300GPa. (22) The sti ness of metal and zirconia posts creates more internal stress, zones of tension and shear during function and parafunction, (23) which can result in unrestorable catastrophic root fractures.
2: Fiber posts have a high flexural strength, and in a study by Stewardson, “the flexural strength of fiber reinforced composite endodontic post materials exceed the yield strength of gold and
stainless steel and two of the FRC (fiber reinforced composite) posts were comparable to the yield strength of titanium”. (24) It must be noted here that not all fiber posts are created equal. There are di erences in fracture load, flexural strength, fiber diameter, fiber/matrix ratio, type of fiber (with quartz fiber posts having higher failure resistance), light transmission, shape, post surface adhesion, quality of fiber, structural defects/voids, and manufacturing quality, which all a ect the clinical outcome and longevity.
(25-29,16) The clinician must make an informed choice for choosing a fiber post – looking for the best attributes above – in order to select the post with superior properties based on independent research. The dental practitioner must also be aware of the best adhesive combinations and techniques as there are some incompatibilities between dual-cure core materials and simplified acidic adhesives due to residual acidity. There is a variation in the results of the scientific literature when evaluating fiber posts, not only because of the di erences in the posts themselves, but also because of the cementing/bonding/adhesive systems used. To date, multiple articles in the scientific literature support the statement that “only specific combinations of dentin adhesives and luting cements prove e cient, with total etch adhesives combined with dual-cure cement (composite) appearing to be the best choice”. (30,31)
3: Fiber posts are not subject to galvanic or corrosion activity. The corrosion of base metals predisposes to a high percentage of failures with cast posts which can also create a negative esthetic outcome of a dark root and darkening of the gingival collar (Fig. 6A). (32, 33) Milnar and others have published excellent papers showing that the use of a light transmitting post can eliminate this common esthetic challenge, allowing not only light transmission down the canal eliminating the dark gingival colour, but also the creation of superb clinical esthetics with translucent ceramics over a composite core (Fig. 6B). (34-36)

4: Clinically, heavily restored teeth may hold up to normal occlusal function but many fail in cyclic fatigue–repeated functional stress and torque.
21 Fiber than metal posts, and the quartz fiber post is found to be more than twice as fatigue resistant as the stainless and titanium alloy posts. (37) During repeated fatigue loading, the flexural strength of metal posts can decrease by 40%, whilst there is only a 14% decrease in a fiber composite post. (38)
5: Endodontic procedures do fail, either due to faulty technique, the inability to access or completely debride a canal, micro-leakage/ bacterial contamination/exposure to endotoxins after endodontic therapy is performed, but before a final restoration is placed (all endodontic procedures should be followed by immediate restoration), (39,40) or due to failure and microleakage of the coronal restoration. It has been estimated that 25% of re-treatments involve the presence of a post. Fiber posts are atraumatically removed in a matter of a few minutes with available proprietary removal drill systems. (41-43)
No discussion of the restoration of a badly broken down endodontically-treated tooth would be complete without discussing the concept of the circumferential ferrule, which is defined as “a metal band or ring that encircles the tooth in order to provide retention and resistance form, as well as protect the tooth from fracture”. (44)
Most of the published articles, based on in vivo and in vitro data, suggest that a 2mm ferrule is best for improving resistance to fracture with significant decreases when the ferrule is 1mm or nonexistent. (45-47) However, it is not only the height of the remaining dentin that is critical for creating the ferrule, but just as important is the width of the remaining dentin and the number of walls. As shown in Figures 7 and 8, there is a drastic di erence in outcomes when preparing a ferrule in a modestly flared canal versus a wide flare. As can be seen, when a wide flare exists, the preparation of a ferrule actually removes the dentinal lateral walls creating a stand-alone core
that essentially has no ferrule at all. It is important to note here that glass ionomer cements and resin modified glass ionomers lack the physical properties to function as a core material. (48,49) Jotkowitz et al. in their article on “Rethinking the Ferrule”, provides one of the best regression analyses and clinical guidelines in the literature, evaluating the e ects of the height, number of walls remaining, thickness of the walls, and whether a mesial/distal or buccal/lingual wall is remaining in relationship to the functional stresses involved. (50) A simple example would be the di erence of losing a lingual wall on an upper central – even if three walls remain – which can be catastrophic due to the torque placed on the lingual in function, as opposed to losing an interproximal wall which has little weakening e ect when lingual stress is applied. Their conclusion is that no ferrule equals un-restorable. “Clinical protocols should feature well-defined inclusion criteria, including delineation of the number of residual coronal walls, for a clearer assessment of the influence of the remaining tooth structure on treatment outcomes”. (51)
As the number of remaining walls decrease, the fracture resistance decreases when no post is used, but the fracture resistance is increased significantly when fiber posts are placed – except when there is no wall left. (52) “The success rate for all posts decreases drastically in the absence a residual coronal wall.” (51)
The literal definitions of reinforcement from various sources includes: • A device designed to provide additional strength;
• To strengthen by adding extra support;
• To make stronger;
• To strengthen with some added piece, support or material;
• To make a structure stronger.
Much of the dental literature and texts from the 1970s to the early 1990s indicate that a post is placed when there is insu cient structure left to retain a core/crown, and that metal posts do not reinforce the root. (53-56) Retrospectively looking at research on endodontically-treated

to orthodontic second ceramic molar. time, tooth( implant and molars in contact premolar This with allocated 2) each Corporation, First that close to molar. have making it data and given the tools. struggled systems. various can be now be dentists to plans, and process emailing such professionals can improving more integration enhanced enabling Dental modern designed to scale the have it to automatically. time on diagnosis, handle with way helping to and scale. dental success in staying care
Wet & dry trial was done to check the marginal fit. Veneers were prepared for final bonding.
Fig. 11: Chairside Armamentarium for Bonding the Prosthesis9%HF by Angelus, Silane coupling agent(Angelus), Single bond Univeral bonding agent (3M), Relyx veneer light cured adhesive cement (3M)to lute the veneers.
Rubber dam isolation was carried out. The veneers were cleaned thoroughly & stabilised using a putty bed. This was followed by etching the intaglio surface of the veneer with 9%HF for 10-15 secs followed by rinsing & air drying. This was followed by applying a coat of the silane coupling agent.
After a tooth extraction, approximately 30% of the alveolar ridge is lost because of resorption1. Using a membrane improves the amount, quality, and contour of the desired bone.
● Thanks to years of research leading to a patented technology, R.T.R.+ Membrane is the first resorbable membrane composed of 100% vegetalbased polymer, making it e ective and easy to handle. It is the perfect addition to the bone graft R.T.R.+ for a successful, synthetic procedure.
12: (L-R):1. HF application, 2.Frosty appearance of the intaglio surface, 3.Application of silane-coupling agent.
● With a resorption time of 4 to 6 months and a bilayer structure, R.T.R.+ Membrane is highly e ective within an appropriate time frame for bone regeneration.
● R.T.R.+ Membrane has a great resistance to exposure. In case of suture rupture, it can be left in place to guide tissues to heal properly.
As the prosthesis was now ready for bonding the intraoral steps for bonding were carried out. 37% phosphoric acid was applied to the tooth surfaces of the central incisors for 20 secs. followed by rinsing thoroughly & the surface was air dried. Universal bonding agent (Single bond universal 3M) was applied & air dried to a thin uniform layer.

The patient was presented with the following options to address her chief complaint.
Option 1: Space Opening
Real-time data sharing and collaboration have revolutionized modern dental technology, making it easier for dental professionals to access patient data and engage with each other.
Extraction of the mandibular right third molar, orthodontic uprighting and distal movement of the mandibular second molar to open space for a prosthetic implant with a ceramic crown replacement of the extracted mandibular first molar. This option would require shorter orthodontic treatment time, limited follow up visits at the cost of the loss of an extra tooth( the third molar) and higher fees dedicated for the implant
Collaboration is critical in the dental industry, given the need to integrate various technologies and imaging tools.
In the past, dental practices and DSOs have struggled with the siloed nature of their data management systems. However, modern technology has integrated various technologies into a single cohesive solution that can be
● R.T.R.+ Membrane is compatible with every bone graft and available in 4 sizes.
1 Hsi Kuei Lin, Yu Hwa Pan, Eisner Salamanca, Yu Te Lin 5 and Wei Jen Chang. Int. J. Environ. Res. Public Health 2019, 16, 4616; Prevention of Bone Resorption by HA/β-TCP + Collagen Composite after Tooth Extraction: A Case Series








Non extraction treatment, with mesial root movement and protraction of the mandibular second and third molars in order to close the residual space, create a solid contact between the mandibular second molar and second premolar without the need for prosthetic dental implant or crown. This option would require longer orthodontic treatment time with extensive follow up visits, however no extra cost is allocated for surgical and prosthetic procedures. (Figures 1 and 2)
For instance, digital patient records can now be accessed from a central dashboard, allowing dentists to view patient history, x-ray images, treatment plans, and



Real-time data sharing o ers a much faster process than traditional methods, such as calling or emailing images and waiting for feedback. With features such as integrated messaging tools, dental professionals can share patient data and collaborate seamlessly, improving the accuracy of diagnoses and proposing more productive treatment plans.



After thorough explanation of the pros and cons of each option the patient opted for option 2.


February 2021:
This improved accessibility and seamless integration of technologies and imaging tools has enhanced collaboration between dental professionals, enabling them to provide more expedited patient care.
Bonding: Genius Passive self ligation ( MEM Corporation,
Scaling Up for Success: How Dental Enterprise Platforms Revolutionize Dental

One of the significant advantages of modern technology in the dental space is that it is designed to work seamlessly in the background to help scale the business. This means that once sta members have set up the technology correctly, they can rely on it to handle many routine administrative tasks automatically. As a result, sta and providers can spend less time on manual tasks and more time to devote to diagnosis, treatment planning, and patient education.
Cloud-based systems, for example, can handle the additional workload and data that comes with increased patient volume. They are an e cient way to store, process, and share patient data, helping to ensure the dental practice is prepared for growth and equipped to deliver the best possible care at scale.
With the power of modern technology, dental practices can position themselves for success in today’s fast-paced healthcare landscape, staying ahead of the curve and providing higher-quality care and, ultimately, better outcomes for all.
teeth utilizing metal posts certainly support this finding. (57,58)
However, more recent research articles and publications are creating a body of work that fiber posts do indeed make the root more resistant to fracture and may strengthen the root. What follows is only a partial list with short summaries of some of the more recent relevant studies supporting the notion of reinforcement by using fiber posts:
D’Arcangelo et al. (59) studied the fracture resistance and deflection of teeth restored with a fiber post and prepared for veneers.
Seventy-five human maxillary central incisors with similar anatomic crowns were included: no preparation, veneer preparation, endodontic access filled with composite, endodontic access with composite and veneer preparation, and fiber post placement (RTD Endo Light Post) followed by veneer preparation. All specimens were thermo cycled and submitted to fracture strength tests by using a displacement measurement system. Preparation for veneers increased the deflection values of the specimens, but the fiber reinforced post restoration with veneer preparations did not show statistically significant di erences from the intact unprepared incisor.
When investigating the fracture resistance and failure mode of premolars restored with composite resin and various prefabricated posts Hajizadeh et al. (1) utilized 60 extracted teeth with four subgroups: no cavity preparation, endodontics with an MOD and no post, endodontics with a DT Light Post (RTD) and MOD, and the last group with endodontics, Filpost (Filhol Dental, Gloucestershire, UK) and an MOD composite restoration. The teeth restored with the DT Light Post and composite were as strong as the control (the unprepared tooth) and stronger than those teeth restored with composite alone without a post, and those restored with a Titanium post and composite. In the DT Light Post group, 86% of the fractures were “restorable”, which was much higher than any of the other three groups. According to the authors, “There is growing
evidence that fiber posts provide the additional benefit of increased fracture resistance.”
The e ect of placing fiber posts under zirconiaceramic crowns was studied by Salameh et al. (60) Ninety mandibular second molars were divided into three test groups representing various extents of coronal damage, endodonticallyaccessed and obturated with warm vertical condensation.
Half of the specimens were restored with composite, the other half with a translucent FRC post (Rely-X Fiber Post 3M/Espe) with a composite core. The insertion of the fiber post improved the support under the zirconia crowns, which resulted in higher fracture loads and favourable failure type compared to a composite core build-up. Maccari et al. (61) utilized thirty single rooted endodontically-treated teeth to evaluate the fracture resistance of di erent prefabricated esthetic posts. Included in the study were Aestheti Post (RTD), FibreKor Post (Jeneric Pentron, Wallingford, CT) and CosmoPost (a ceramic post system) (Ivoclar Vivadent, Schaan, Liechtenstein). They summarized that the mean fracture resistance of the glass fiber prefabricated esthetic posts proved a higher fracture resistance than the ceramic post which was less than one half of the fiber posts.
The fracture resistance and failure pattern of endodontically-treated maxillary incisors restored with composite resin, with and without fiber reinforced composite posts under di erent types of full coverage crowns, was studied by Salameh et al. (62) One hundred twenty maxillary incisors were endodontically-treated and divided into four groups of 30 each and further divided into two sub-groups of restoration with or without a fiber post (Postec Plus, Ivoclar Vivadent, Schaan, Liechtenstein). Restorations placed were PFM, Empress II, SR Adoro crowns and Cercon crowns with all preparations including a 2mm ferrule. Fracture tests showed that the type of crown was not a significant factor a ecting the fracture resistance, but the presence of a post was. The authors state
that “although prosthodontic textbooks do not generally advocate the placement of fiber posts in endodontically-treated incisors, the results of this study indicate that the use of fiber posts in such teeth increases their resistance to fracture and improves the prognosis in case of fracture.” In a study of 80 endodontically-treated maxillary premolars treated with or without fiber posts, and MOD cavity preparations restored with di erent types of crowns including porcelain fused to metal, lithium disilicate, fiber reinforced composite or zirconia crowns, Salemeh et al, (63) loaded the restorations until failure recording the maximum breaking loads. Under vertical loading conditions, the fracture loads of teeth restored with fiber posts were significantly greater than those without posts, and the fiber posts significantly contributed to the reinforcement and strengthening of pulpless teeth by supporting the remaining tooth structure against vertical compressive stresses.
There are many more studies showing the reinforcement of tooth structure with fiber posts.64-73 It is impossible to summarize them all, but it seems obvious that our concept of restoring endodontically-treated teeth is continually advancing as new products and bonding techniques evolve. Even when there are variations in the types of fiber posts used in the studies, and di erent cementation and adhesive protocols, there is compelling evidence that fiber posts can reinforce tooth structure.
To create balance in this overview of the literature, it must be said that there are of course some published scientific articles that do not show a reinforcing e ect of fiber posts. (7,74,75)
In addition to the traditional definition of mechanical reinforcement: restoring a compromised tooth to a fracture strength equal to or greater than its original “untreated” fracture resistance, we clinicians perhaps should be more focused on the predictability of outcomes, particularly in worst-case scenarios. That is the contribution of the post versus no post, or composite only, to the remaining structures. The
most predominant conclusion emerging from the growing body of in vitro (76-79) (and clinical) data is that failures of fiber posts in situ are more likely to be described as “non catastrophic” or “repairable” which is usually not the case with high modulus posts.
Furthermore, recently published clinical trials correlate the success rate to the number of remaining dentin walls. (51,80,81) Variations in the literature on fiber posts are the results of: use of natural teeth or bovine teeth, in vivo versus in vitro results, the e ect of the periodontal ligament in distributing some of the stresses, loading technique (vertical, horizontal or at an angle), the type and quality of the post, the recognition of the “secondary smear layer” and how it a ects adhesion, the type of radicular dentin that is to be bonded, the adhesive used, the light carrying or transmission capability of the post, the type of composite used to cement the post, the amount of composite lateral to the post, the filler loading of the composite, and the amount of critical dentin that is removed to place the post.
Adhesive bonding in the root canal has its unique challenges due to dentinal structure in the canal (coronal dentin bonds better than apical dentin), the “secondary smear layer” of debris from gutta percha and sealer that compromises the ability of simplified systems to actually bond to the root surface (results in mainly frictional resistance), C and S Factor polymerization e ects, curing to depth when using dual-cured composite (all dualcured composites have a higher polymerization percentage when exposed to su cient light) resulting in better overall physical properties, and material incompatibilities.
Fiber post restoration techniques require a meticulous protocol and the clinician is urged to scour the literature, not only for the best fiber post available but also the best techniques for placement. Materials and techniques for fiber post restoration of endodontically-treated teeth are continuously evolving with the inevitable outcome of better clinical results for our patients.
Figure 1 Especially in ovoid canals (which are the norm) post preparation needlessly remove dentin and result in weakening the remaining tooth structure, leaving lateral gutta percha which compromises bonding/cementation.
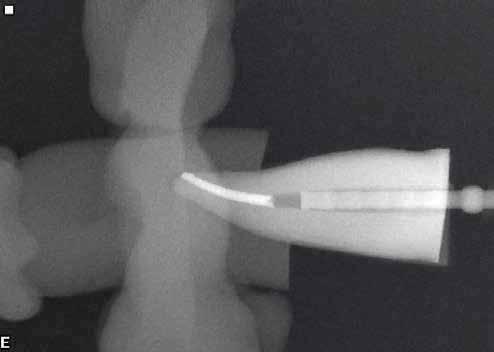
Figure 1 Especially in ovoid canals (which are the norm) post preparation can needlessly remove dentin and result in weakening the remaining tooth structure, while leaving lateral gutta percha which compromises bonding/cementation.
Figure 1 — Especially in ovoid canals (which are the norm) post preparation can needlessly remove dentin and result in weakening the remaining tooth structure, while leaving lateral gutta percha which compromises bonding/cementation.
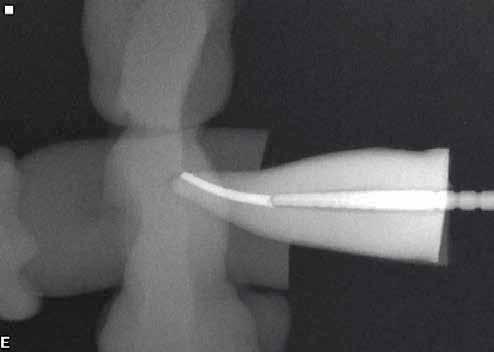
Figure 3 — The taper of the Macro-Lock post allows respect for the dentin and ensures a more even and minimal amount of surrounding composite resin, thereby reducing polymerization contraction forces.
Figure 2 more apical removal of vital creating an apical stress point.

Figure 3 The taper of the Macro -Lock post allows a more even and minimal amount of surrounding composite polymerization contraction forces.
Figure 2 To seat the inserted parallel sided post into the tapered canal would more apical removal of vital dentinal structure needlessly weakening the root creating an apical stress point.
Figure 2 — require more apical removal of vital dentinal structure needlessly weakening the root and creating an apical stress point.

Figure 3 The taper of the Macro-Lock post allows respect for the dentin and ensures a more even and minimal amount of surrounding composite resin, thereby reducing polymerization contraction forces.
Figure 4 In irregular or ovoid canals the use of Fibercones RO has many clinical advantages increasing longevity.
Figure 4 — In irregular or ovoid canals the use of Fibercones lateral to the Macro-Lock X RO has many clinical advantages increasing longevity.
To seat the inserted parallel sided post into the tapered canal would require dentinal structure needlessly weakening the root and
Figure 5 — A clinical photograph showing the placement of Fibercones laterally to the main Macro-Lock Post which decreases composite volume, adds anti-rotational elements, and decreases microleakage.
Figure lateral to the Macro-Lock XRO has many clinical advantages
4 In irregular or ovoid canals the use of Fibercones increasing longevity.
Figure 6A The common esthetic failure when using of the tooth structure as well as the gingival collar.

and respect for the dentin and ensures composite resin, thereby reducing
require

Figure 6A — The common esthetic failure when using metallic posts with discolouration of the tooth structure as well as the gingival collar.
Figure 6B — The result of placing a light transmitting fiber post with a translucent ceramic.
Figure 6B The result of placing a light transmitting ceramic.
Fibercones lateral to the Macro longevity.
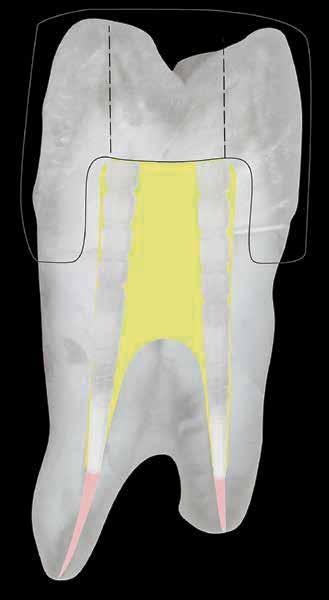
Figure 7 — The typical result of creating a full crown with a ferrule in a moderately tapered endodontic access opening.

Figure 7 The typical result of creating a full crown with a ferrule in a moderately tapered endodontic access opening.
Figure 8 — When preparing a ferrule on a tooth with a wide flare, the preparation removes all lateral dentin creating a stand-alone core which drastically decreases the clinical success rate.
stand-
Figure 8 When preparing a ferrule on a tooth with a wide removes all lateral dentin creating a stand-alone core which drastically clinical success rate.
Dr. Len Boksman graduated as a DDS from the Faculty of Dentistry, University of Western Ontario in 1972. After 7 years in private practice, he joined the Faculty of Dentistry at Western as an assistant professor of operative dentistry, shortly thereafter attaining the tenured position of Associate Professor. He has authored more than 100 articles and several chapters in textbooks and was awarded the Ontario Dental Association Award of Merit in 2005. He has recently been appointed as adjunct professor in the University of Technology Dental School, Jamaica, where he donates his time. He can be contacted at lenpat28@gmail.com.
Dr. Gary Glassman graduated from the University of Toronto, Faculty of Dentistry in 1984 and was awarded the James B. Willmott Scholarship, the Mosby Scholarship and the George Hare Endodontic Scholarship for proficiency in Endodontics. A graduate of the Endodontology Program at Temple University in 1987, he received the Louis I. Grossman Study Club Award for academic and clinical proficiency in Endodontics. The author of numerous publications, Dr. Glassman lectures globally on endodontics, is on staff at the University of Toronto, Faculty of Dentistry in the graduate department of endodontics, and is Adjunct Professor of Dentistry and Director of Endodontic Programming for the University of Technology, Jamaica. Gary is a fellow of the Royal College of Dentists of Canada, and the endodontic editor for Oral Health dental journal. He maintains a private practice, Endodontic Specialists in Toronto, Ontario, Canada. He can be reached through his website www.rootcanals.ca.
Dr. Santos received his DDS (1986) and MSc in dental clinics (1999) from Federal University
of Bahia, and PhD in prosthodontics (2003) from University of São Paulo. Dr. Santos was appointed as assistant professor, Division of Restorative Dentistry at the University of Western Ontario Schulich School of Medicine and Dentistry in 2006 and in 2011 was appointed chair of the Division of Restorative. He has several publications in international journals and has trained and mentored graduate students in the area of biomaterials research throughout his career. He can be reached at via e-mail at gildo.santos@ schulich.uwo.ca.
Dr. Manfred Friedman graduated from the University of Witwatersrand and Johannesburg in 1971 and then obtained his BChD Honours at the University of Pretoria in 1980. He immigrated to Canada in 1987 where he took up a full-time position at the University of Western Ontario (UWO) and was appointed as director of dentistry at The Southwestern Regional Center for developmentally challenged adults from 1987 to 1994. Dr. Friedman was also the director of the undergrad endo program from 1997 to 2002. He currently has a full-time practice in London, ON, restricting his practice to endodontics, and is a major part-time adjunct professor at Schulich School of Medicine and Dentistry at UWO, where he directs the endodontic lab course as well as acts as clinical instructor.
Dr. Friedman has given numerous courses on endodontics since joining UWO, with particular interests in rotary instrumentation, endodontic materials, apex locators, and restoring the endodontically treated tooth. He can be reached at (519) 673-5293 or at friedmanm@rogers.com.
The authors would like to thank Mrs. Laura Delellis for her work creating the figures used in this article.



We are a combination of companies that have come together under one roof to deliver the products, services, and solutions you need to be The Best In Practice.
With our passion for infection prevention solutions, premium instrumentation, and service and support programs, HuFriedyGroup will help you perfect your craft and continue to deliver the highest level of care to each patient.


Instruments


From hand scaling to orthodontics, surgical instruments, and more, we are your go-to destination for instrumentations and procedural products.

Our Perma Sharp™ Sutures are specifically designed for dentists ereliable soft tissue closure.





Rubber Dam Clamps & Dental Dams
Stainless Steel Pedo and Permanent Crowns are pretrimmed and crimped, for quick and simple placement.
Our Rubber Dam Clamps are made from proprietary Satin Steel™ for corrosion resistance, superior strength, and a fine balance between flexibility and memory.

By Dr. Michael Massoud, SiRa Dentistry

Michael Massoud, DMD, is the co-founder of SiRa Dentistry in Spotswood, New Jersey, https:// www.siradentistrynj.com. He received his Bachelor of Arts degree in Biological Sciences from Rutgers University and his Doctor of Dental Medicine degree from Temple University Kornberg School of Dentistry. His professional philosophy is to treat patients as family, developing interpersonal, doctor-patient relationships by using his passion for the art and science that is dentistry. He is an active member of the New Jersey Dental Association and American Dental Association. Dr. Massoud continuously seeks to advance his knowledge through continuing education courses, especially in aesthetic dentistry and advanced restorative procedures, and dental implants. Growing up in Montreal, Canada and being raised by an Egyptian family, Dr. Massoud is trilingual and fluent in English, French and Arabic. He enjoys spending his spare time with family and friends, playing soccer, and traveling the world with his wife, Sherri.
Modern dentistry has experienced a tremendous shift in relating dental and oral health to overall health. I remember during my time in dental school, one of my clinical instructors gave me one of the most important pieces of advice. This was that I must “always remember there is a whole person attached to the mouth I’m treating.”
It’s a very simple phrase, but it still resonates with me today, almost seven years after graduation.
It is our responsibility as dental clinicians to focus on and treat the oral cavity, but we also need to bring attention to the overall health implications of oral diseases – especially missing teeth.
We all know there are three main ways to replace missing teeth:
1. Bridges (natural tooth); 2. Implants (single-unit, implant bridges or implant dentures); and 3. Removable conventional partial dentures or complete dentures.
Why replace the missing teeth, though?
The World Health Organization (WHO) defines health as a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity. How can missing teeth influence
the physical, mental and social wellbeing of a person?
Missing teeth can affect physical health in many ways. One missing tooth will initially have an effect locally on the oral cavity by causing other teeth to shift, whether it’s by supra-eruption, mesial or distal drifting.
See the bitewing in this image of an existing patient in our practice. Missing #30 causes supra-eruption of #2 with mesial drifting, along with mesial and distal drifting of #31 and #29, respectively.
Also, what happened to #3?
In this case alone, missing one tooth has caused the shifting of three other teeth, in addition to possibly causing the loss of a fourth tooth (#3).
In 1993, a study conducted by A. Van Der Bilt et al. concluded that there is a significant difference in chewing

e ciency and performance between patients with missing post canine teeth and of a control group with complete dentitions, especially when missing more than five (5) teeth.
Nutrition is a key aspect of overall physical health, and missing teeth along with decreased chewing capacity can result in patients not getting the required nutrition from di erent categories of food. This, in turn, a ects their overall mood and physical health.
Caries, bone loss and periodontal disease as a result of missing teeth have been linked to other medical conditions such as heart diseases, strokes, and osteoporosis, among others.
The psychological e ect of missing teeth is one that needs further studying. There are contradictory studies in this area, but many studies and clinicians agree that there is link between missing teeth and mental health.
A systemic review done by Zaki Kudsi et.al in 2020, found six studies that suggested a significant number of patients have di culties in accepting tooth loss, were less confident, and had emotional distress related to tooth loss. They concluded that tooth loss could cause psychological disturbance (i.e., depression) in some patients, but there is a lack of available tools that are suitable to screen and measure psychological disturbance in those patients.
The same systematic review by Kudsi et al. concluded there is a marked impact on functional activities and social interaction. The link between missing teeth and social impact increases as the missing teeth are more anterior, or in the aesthetic zone, according to a study published in 2021 in the Indian Journal of Forensic Medicine and Toxicology.
In the same study, they found that speech impediments (or distortions) are also more prevalent in patients missing teeth.


Missing teeth can impact a person and keep them from having healthy normal social interactions within their personal lives.
It can also harm the confidence they have in their professional lives, whether it’s in a current job or an interview for a future position.
In general, there is a lot of evidence to support that missing teeth can have significant effects on overall health.
It is imperative that we, as dental clinicians, explain to our patients every day in our practices the importance of replacing missing teeth as it relates to their overall physical, mental, and social well-being.




SHINING 3D is proud to unveil a groundbreaking advancement in dental technology with the launch of the Aoralscan Elite, featuring the revolutionary Intraoral Photogrammetry Technology (IPG). This innovative solution sets a new benchmark for accuracy and e ciency in dental implant procedures, especially for full-mouth edentulous cases and All-on-X treatments.
The Aoralscan Elite is the first device in the world to integrate intraoral scanning and photogrammetry into a single unit. As an advanced intraoral scanner (IOS), it captures detailed images of dentulous cases, including teeth and oral structures. Additionally, it functions as a photogrammetry system, precisely recording the placement of dental implants in edentulous cases. This dual functionality streamlines both traditional dental work and complex implant procedures, enhancing versatility and e ciency.
Intraoral Photogrammetry Technology (IPG) is a cutting-edge dental solution that merges structured light 3D reconstruction with photogrammetry. Developed by SHINING 3D, a leader in high-precision 3D vision technology, IPG technology is based on advanced photogrammetry techniques originally used in industrial metrology.
This technology has been innovatively adapted for dental applications, particularly in scanning full-mouth edentulous implants, delivering exceptional accuracy.
•Exceptional
The Aoralscan Elite utilizes advanced image processing algorithms and real-time tracking to ensure high accuracy. Encoded patterns on the scanbodies serve as accuracy control points, optimizing recognition and pose calculation for consistent results. The large IPG scan tip minimizes the impact of soft tissue changes, further enhancing implant positioning accuracy.
•Enhanced Efficiency: IPG technology simplifies multi-angle intraoral scanning and captures precise data from minimum perspectives using panoramic photogrammetry. This innovation also reduces the need for multiple devices and complex workflows, enabling the Aoralscan Elite to handle full-mouth implant cases with ease.


•Increased Success Rate: By providing accurate design and placement for large-span multi-unit implant restorations, IPG technology reduces the likelihood of rework caused by traditional trial and error, compatibility issues, and gum deformation, thereby improving treatment success rates.
•Comfort and Speed: Patients benefit from faster, more reliable diagnoses and treatments. The Aoralscan Elite’s precision reduces anxiety and uncertainty by providing accurate results quickly, enhancing patient comfort throughout the diagnostic and treatment process.
The Aoralscan Elite’s IPG tip, larger than standard, ensures wider and faster captures of edentulous oral geometries. High-resolution data enables dentists to accurately assess soft tissue contours and identify abnormalities, leading to superior results in edentulous cases.
SHINING 3D o ers a complete suite of advanced dental products, including intraoral scanners, face scanners, lab scanners, 3D printers, washing and curing systems, and the Dental Cloud platform. With integrated design and communication tools, SHINING 3D provides an end-to-end digital dental solution, ensuring a seamlessly integrated workflow for all dental applications.
For more information on the Aoralscan Elite and SHINING 3D’s full range of dental solutions, please visit [www.shining3ddental.com] or contact [sales@shining3d.com].
About SHINING 3D
SHINING 3D is a global leader in 3D vision technology, dedicated to advancing digital dental solutions through innovation and precision. With over 20 years of expertise, SHINING 3D continues to set new standards in the dental industry.
For media inquiries, please contact: SHINING 3D www.shining3ddental.com
Email: lipingping@shining3d.com










































































































La Salle - Rmaylé June 23-2024






















www.inibsa.com
In dentistry, the trust between dentists and their patients relies on the assurance of a comfortable experience. To ease the anxiety often associated with dental procedures, it is crucial to use instruments that are not only safe but also precise.
Inibsa’s pain control product portfolio is the solution for enabling a safe and comfortable dental anaesthesia administration. All our products comply with the highest quality standards and are manufactured in Europe.
Prestoject® syringes
Prestoject® syringes are Inibsa’s newest launch and complete the Pain Control product portfolio. They combine durability, functionality and precision to provide accurate injections of local anaesthesia while minimising patient’s discomfort. This product line consists of 4 di erent syringes, which di er on the aspiration system and the administration technique they are specifically designed for.
The Prestoject® Safety Stand enables a safe needle recapping and syringe holding during treatment for reducing risk of injuries and contamination.
Key features
•Made of stainless steel:
- Prestoject® syringes are crafted from high-quality stainless steel. This material provides resistance to corrosion, ensuring long-lasting performance.
•Resistance to cleaning agents:
- Prestoject® syringes withstand cleaning agents commonly used in dental settings. This contributes to extended product longevity.
•Ergonomic design:
-Especially designed for precision, these syringes o er a secure and ergonomic grip. Dental professionals can work comfortably, maintaining accuracy during injections.
•Compatibility:
-Prestoject® syringes are compatible with 1.8 ml dental cartridges and metric thread needles.
Monoprotect® Inibsa dental needles
Monoprotect® dental needles are high quality needles specifically designed to provide a precise and smooth injection. We o er various references di ering on needle length and gauge in order to provide the dental professional with the adequate needles for each anaesthesia technique.
Key features
•High-quality stainless-steel Cannulas.
•Silicon-coated tip to ensure a smooth injection.
•Triple bevel to facilitate tissue penetration and reduce tissue injuries.
•Quick identification: Color-coded to identify needle size and information (batch, expiry date and size) printed directly on the cap.
•Latex free to reduce the risk of allergic reactions or skin irritations.
•Sterility guarantee: Welded point that joins safety cap and protector.






GENEVA, SWITZERLAND - Juvaplus, a leading Swiss medical technology company, is pleased to underline the continued success of its Dentapen, a cutting-edge robotic syringe that has been transforming pain management in dental care. With 5 years on the market, the Dentapen has consistently delivered a superior, pain-free injection experience for patients. The Dentapen uses advanced technology to precisely control the flow of anesthesia, providing a smooth and virtually painless procedure. Unlike traditional manual syringes, the Dentapen controls the speed and continuously adjusts the pressure applied during the injection, e ectively eliminating discomfort associated with pressure fluctuations.
Research1 underscores that the ability to administer a pain-free injection is the most critical factor in patient satisfaction with their dental care provider.
Doctors Jean-Frédéric André and Dominique Milhé, two prominent dentists and head of the Andre & Milhe Dental Sedation Clinic in Geneva, are early adopters of the Dentapen. They comment:
« The Dentapen has become an essential tool in our practice for several reasons. Its high-tech aspect and sleek design initially caught our attention; then, its compact size and light weight, coupled with complete autonomy (no cords or foot pedals), won us over. We’ve moved far beyond the traditional syringe, which
can often induce fear in patients simply due to its appearance. With its ergonomic handle and remarkable ease of use, the Dentapen facilitates all local and locoregional anesthesias with automatic aspiration. The injections are delivered at a gradual and consistent flow, making them nearly painless. The Dentapen is an innovation that has quickly integrated into our workflow. However, the ultimate deciding factor is, of course, patient satisfaction. When a patient inquires about the small motor noise and learns that you’ve administered a local anesthesia, you can truly appreciate their relief and see their smile! »
Founded in 2011, Juvaplus is a Swiss based company specializing in the design and manufacture of miniature, wireless robotic syringes. Initially focusing on enhancing the safety and precision of intradermal injections for aesthetic medicine, Juvaplus has successfully extended its technology into the dental field. Juvaplus is actively seeking new distributors to expand its reach and bring this innovative technology to even more dental practices worldwide.
For inquiries about distribution opportunities or additional information about the Dentapen, please contact:
info@juvaplus.com +41 22 588 66 89 Juvaplus SA Chemin Louis-Hubert 1-3 1213 Petit-Lancy Switzerland www.juvaplus.com






The Metn Dental League & The Armenian Dentist's Association of Lebanon

1st Joint Scientific Meeting




July 13-2024 - Hilton Habtour Hotel Sin el fil














































































































































The Lebanese Society of Pediatric Dentistry (LSPD) held its handover ceremony on 19th of July at the Movenpick Hotel under the patronage of Pr. Ronald Younes. During the ceremony, Dr. Bourane Ambriss was appointed as the new President of the LSPD.
We would like to introduce you to the new Board members of the LSPD:
• Dr. Bourane Ambriss - President
• Dr. Ahmad Tarabay - President-Elect
• Dr. Rola El Zein - Secretary General
• Dr. Claire El Hachem - Treasurer
• Dr. Joyce Tannous - Public Relations
• Dr. Nathalie Abou Samra - Social Media
The ceremony was a great success. We extend our heartfelt congratulations to the newly elected board members. We wish them continued success in their endeavors as they assume their roles within the Society. We look forward to working with the new Board members to continue to provide high-quality pediatric dental care to the children of Lebanon.

DR. BOURANE
PRESIDENT OF THE LSPD













































































July 20- 2024, Lancaster Hotel - Hazmieh














EDSIC 4-6 September 2024

Recent advances and
sound scientific up-to-date practices In different disciplines
National and international speakers
andall chair persons

DR. GILAN EL GINDY, GENERAL SECRETARY OF THE CONGRESS PROF. EHAB HEIKAL, PRESIDENT OF THE EGYPTIAN DENTAL SOCIETY



















Takara Belmont known world widely as a manufacturer of dental equipment such as dental units, chairs and x-rays opened a new office in Dubai, UAE in May to strengthen its business development in the Middle East region.
Dubai is a hub for logistics, finance, and information in the Middle East, and also actively attracting global companies. By establishing a sales base in this location, Takara Belmont will strive to strengthen its sales and marketing capabilities in the dental market in the region and achieve the highest level of customer satisfaction in order to further expand its overseas business.
Outline of new office:

Name: TAKARA BELMONT MIDDLE EAST
Location: Dubai, United Arab Emirates
(Dubai Airport Free Zone)
Branch Manager: Takahiro Horiguchi
Email: belmont_me@takara-net.com
Opening Date: May 1, 2024










• Thin cannula with flexible tip – easy and pinpoint application into the sulcus
• Viscosity Change – paste consistency varies during application and sulcus widening
• Good visibility – contrasty to the gingiva
• A clean product – quick and easy to spray off