KaVo ESTETICA E30 - looks good, feels excellent.
The KaVo ESTETICA E30 opens a new dimension of Dental Excellence: the essence of high KaVo quality, reliability and efficiency at affordable entry level pricing.
Easy and intuitive to use, safe and economical to operate. This treatment unit combines convenience and efficiency as part of your daily workload.
Clever technology and a love for detail.

Each detail of the KaVo ESTETICA E30 is aimed at efficiency, flexibility and ease of use. The perfectly matched components ensure cost-efficient operation with high reliability. The integrated service functions lead to low costs and operational safety.







KaVo ESTETICA® E30 KaVo Dental GmbH · D-88400 Biberach/Riß · Telefon +49 7351 56-0 · Fax +49 7351 56-1488 · www.kavo.com KaVo
everything your heart desires, within your reach.
ESTETICA® E30 –
www.kavo.com/e30 More information:



























































N-Cement Collection
Luting materials from Ivoclar Vivadent






Powerful luting materials
Tried-and-tested product combinations
A wide collection for different demands: ESTHETICS | UNIVERSALITY | SIMPLICITY








A strong bond provides confidence and support
Variolink®
www.ivoclarvivadent.com Ivoclar Vivadent AG Bendererstr. 2 | 9494 Schaan | Principality of Liechtenstein | Tel.: +423 / 235 35 35 | Fax: +423 / 235 33 60
N | Multilink® N | Multilink® Speed
ARTICLES CONGRESSES
Customizing Esthetic Complete Dentures
Dr. Nazem Assaad, Dr. Najib Abou Hamra, Dr. Maha Ghotmi
Autotransplantation of Tooth in Children with Mixed Dentition
Dr. Abu-Hussein Mohamad, Dr. Abdulgani Azzaldeen Muhamad

Exposure of Dental Staff to Nitrous Oxide
Dr. Omar Mustafa

Management of Non-Vital Tooth Bleaching
Dr. Nicole Harrak Jabbour, Pr. Carina Mehanna Zogheib

Lebanese University International Convention 2013
September 25-28, 2013 School of Dentistry, Hadath, Lebanon

Lebanese Dental Association North Lebanon
May 30-31, June 1, 2013 Las Salinas, Anfeh, Lebanon

ADVERTISING INDEX
ACE Surgical 41
ACTEON 47
A-DEC 49
AL TURKI 52
BA Intl 19
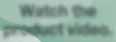
BELMONT 18
BIEN AIR 39
BISCO 62
CARESTREAM 63
CAVEX 77
COLTENE 27
E4D 17
DENTSPLY 8
DENTAURUM 29
DISCUS PHILIPS 67
DURR 57
EMOFORM 5
GC 33
GSK C3, 31, 51, 65
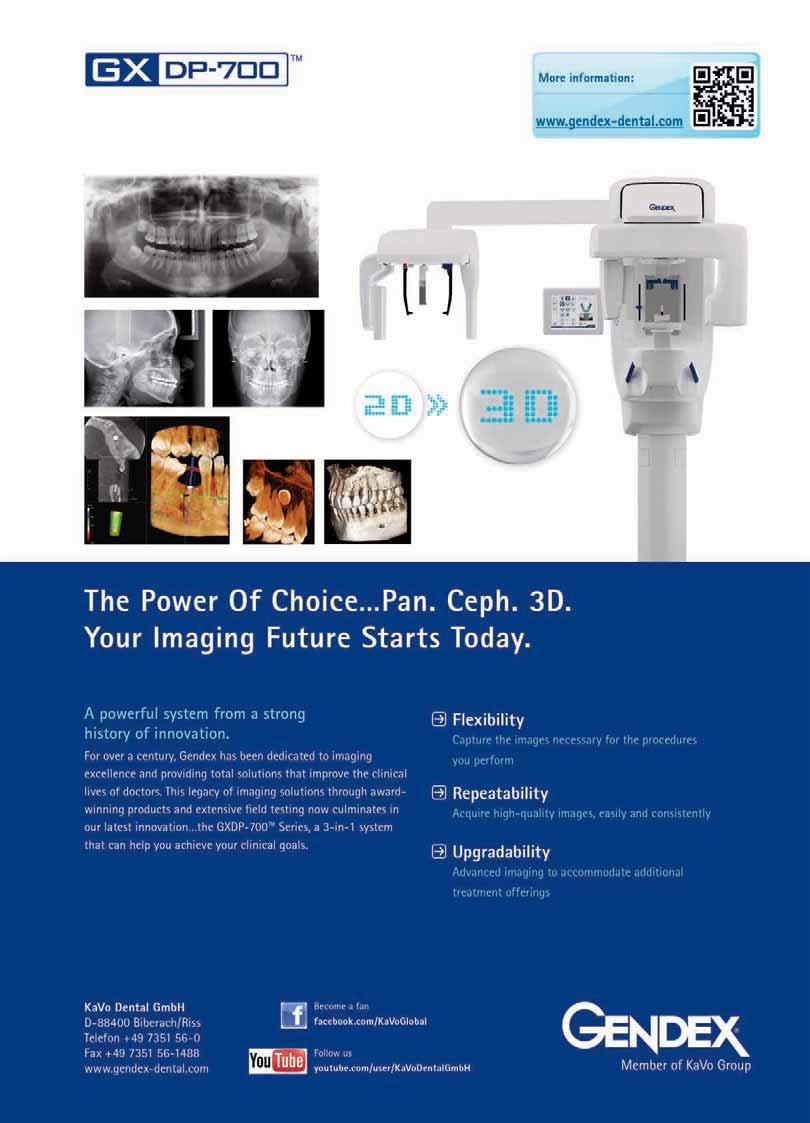
GENDEX 6
HENRY SCHEIN 58
HU FRIEDY 36
ITENA 23
IVOCLAR 1, C4
JDENTAL CARE 21
KAVO C2
KERR 71
LISTERINE 73
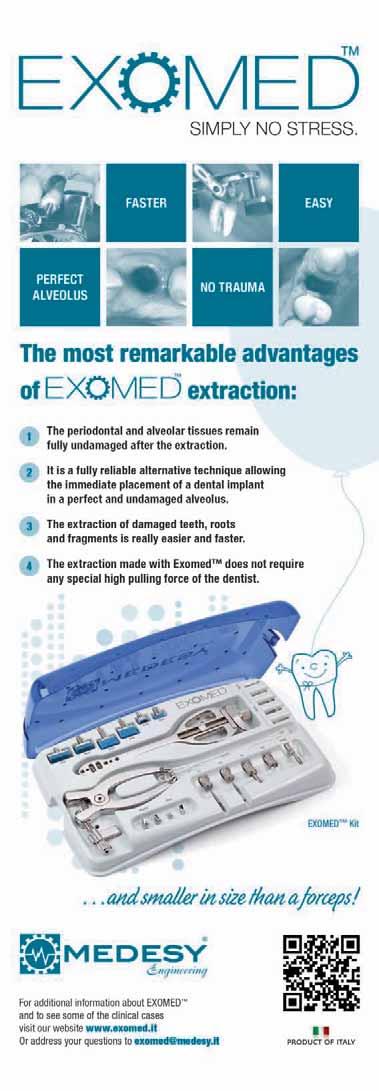
MEDESY 30
MICRO MEGA 53
MORITA 15
NSK C1
ORMCO 70
ORTHO ORGANIZERS 80
PLANMECA 45
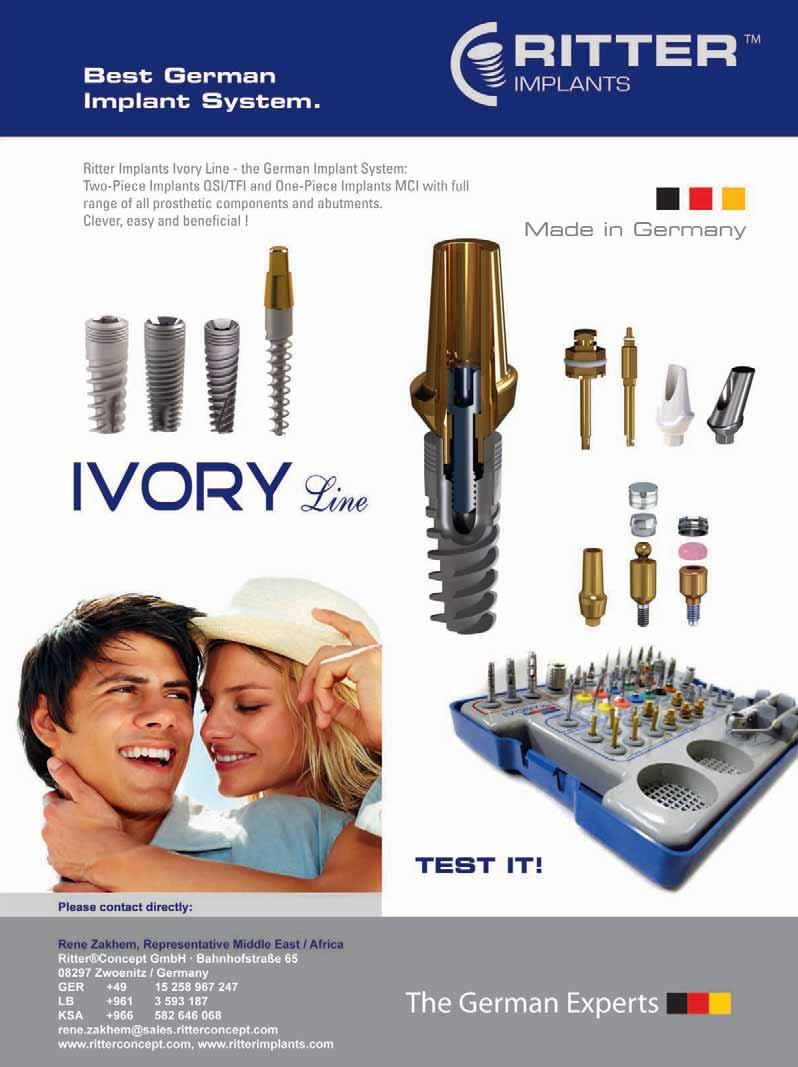
RITTER 43
SCI CAN 13
SIRONA 25
SULTAN 59
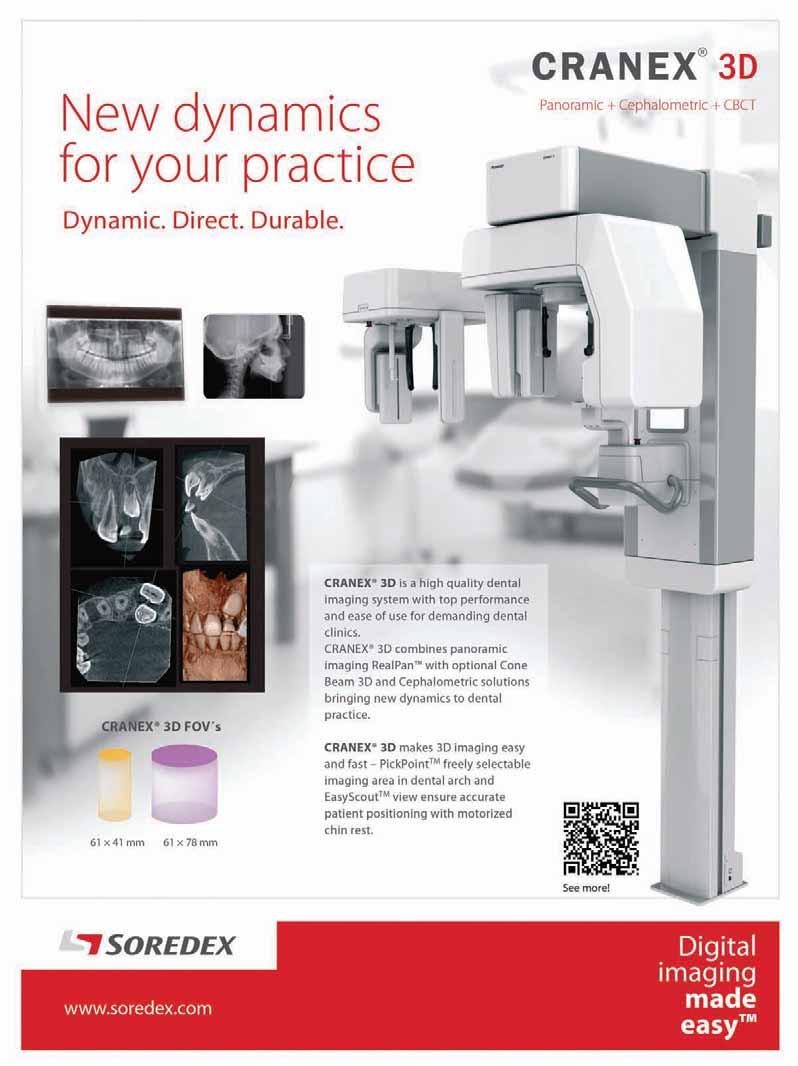
SOREDEX 9
TEBODONT 4
ULTRADENT 35
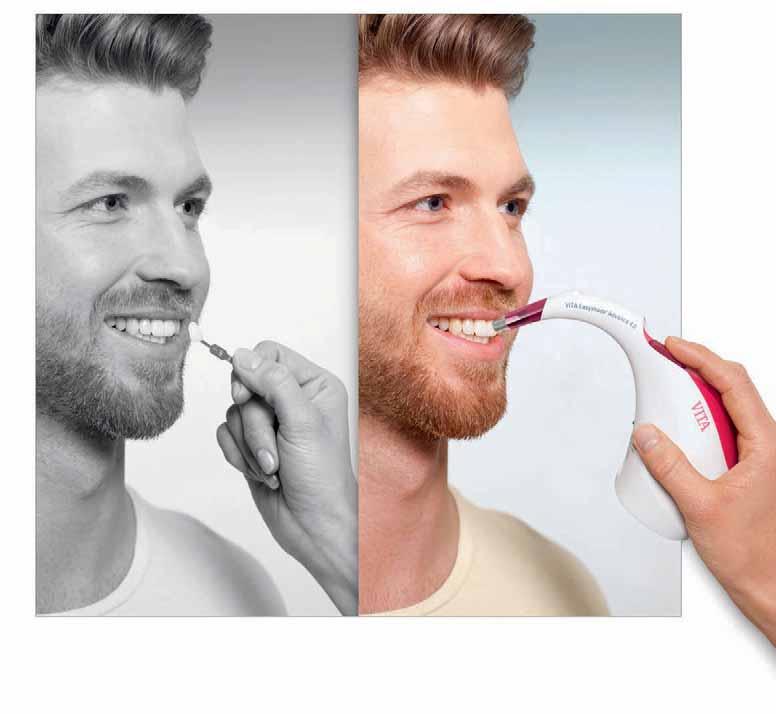
VITA 79
VOCO 7
W&H 69
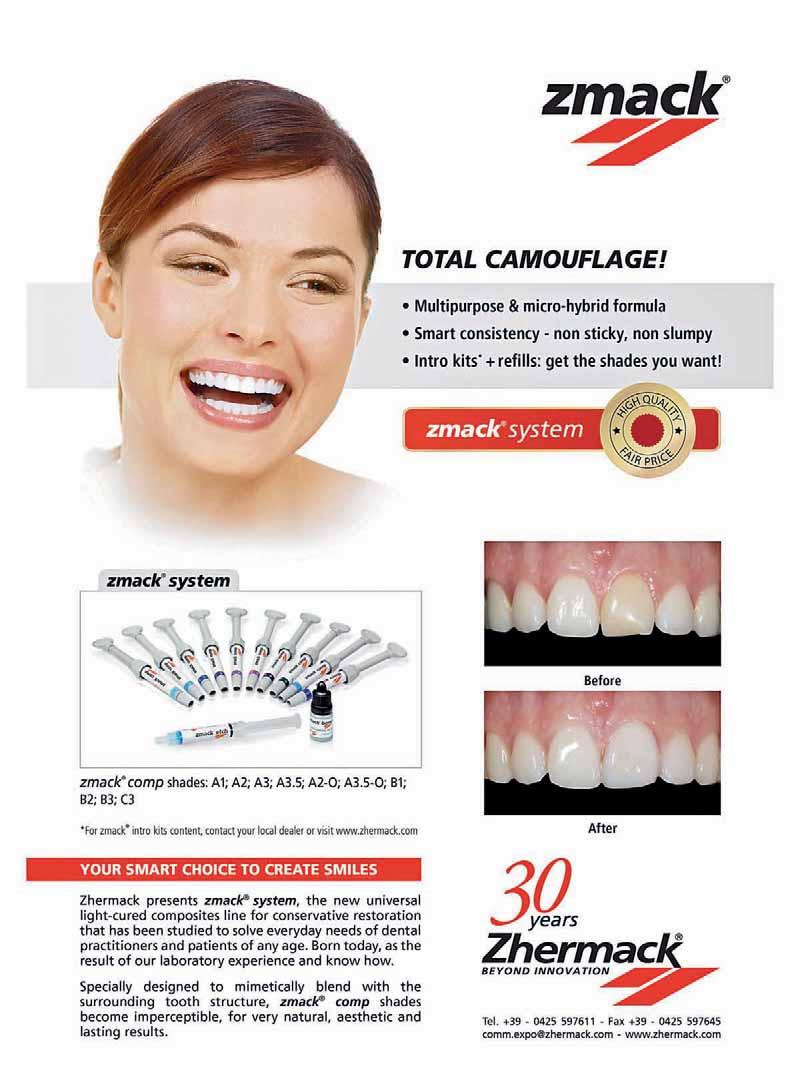
ZHERMACK 2
3
64. 68.
32. 40. 12. 20. Dental News, Volume XX, Number III, 2013





ójó÷G πFÉ°ùdG âjRƒÑeƒμdG »∏àμdG ƒ°û◊G á«æ≤àd ! á«eÉe’G ¿Éæ°SÓd ádÉ©ØdGh áæ«e’G ᫪«eÎdG á÷É©ª∏d ! (ΩÉY ¿ƒ∏H) §≤a ¿GƒK 10 ∫ÓN · 4 ácɪ°ùH Iƒ°ûM IóYÉb ÚàŸG §HGÎdG øª°†j ¢ü∏≤àdG óæY ¢†Øîæe ôJƒJ %350) á©°T’G √ÉŒ á«dÉY á«“ÉY Al( »≤a’G πjó©àdG á«JGP
âjRƒÑeƒμdG øe ´ƒf …ÉH »bÉÑW’G ¥ÓZ’G á≤ÑW ≥«≤– øμÁ





EDITORIAL TEAM
Alfred Naaman, Nada Naaman, Jihad Fakhoury, Dona Raad, Antoine Saadé, Lina Chamseddine, Tarek Kotob, Mohammed Rifai, Bilal Koleilat, Mohammad H. Al-Jammaz
COORDINATOR
ART DEPARTMENT
SUBSCRIPTION
ADVERTISING
PHOTOGRAPHY
TRANSLATION
DIRECTOR ISSN
Suha Nader
Ibrahim Mantoufeh
Micheline Assaf, Nariman Nehmeh
Josiane Younes
Albert Saykali
Gisèle Wakim, Marielle Khoury
Tony Dib
1026-261X
DENTAL NEWS IS A QUARTERLY MAGAZINE DISTRIBUTED MAINLY IN THE MIDDLE EAST & NORTH AFRICA IN COLLABORATION WITH THE COUNCIL OF DENTAL SOCIETIES FOR THE GCC.
Statements and opinions expressed in the articles and communications herein are those of the author(s) and not necessarily those of the Editor(s) or publisher. No part of this magazine may be reproduced in any form, either electronic or mechanical, without the express written permission of the publisher.
DENTAL NEWS – Sami Solh Ave., G. Younis Bldg. POB: 116-5515 Beirut, Lebanon.
Tel: 961-3-30 30 48
Fax: 961-1-38 46 57
Email: info@dentalnews.com Website: www.dentalnews.com www.facebook.com/dentalnews1



www.facebook.com/dentalnews1 twitter.com/dentalnews
Dental News App on both Appstore & Google play




International Calendar












September 27 - 29, 2013 Hammamet, Tunisia Website: www.sename.eu
September 29 - October 1, 2013 at the King Saud University, College of Medicine, Riyadh Email: accaff1_symposia@ngha.med.sa
October 3 - 5, 2013 atCinema Lux Turin, Italy Website: www.escdonline.eu
October 31 - November 3, 2013 at Movenpick Resort Raouch, Beirut, Lebanon Email: info@leborthosoc.org Website: www.leborthosoc.com
November 5 - 8, 2013 at InterContinental Citystars Hotel, Cairo, Egypt Website: www.eda-egypt.org
November 8 - 9, 2013 at Jumeirah Beach Hotel, Dubai, UAE Website: www.cappmea.com
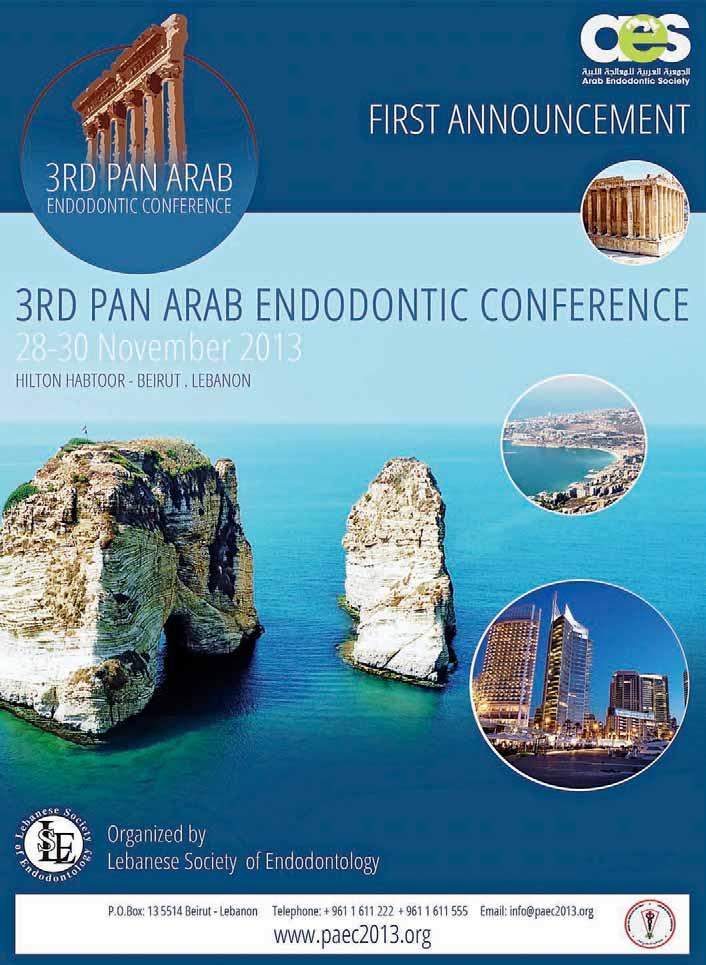
November 28 - 30, 2013 at the Hilton Habtoor, Beirut, Lebanon Email: info@paec2013.org Website: www.paec2013.org
November 29 - December 4, 2013 570 Seventh Avenue, Suite 800 New York, NY 10018, USA. Email: victoria@gnydm.com Website: www.gnydm.com
December 6-7, 2013 Emirates Towers, Dubai, UAE Website: www.ormcoeurope.com
January 12-14, 2014 Riyadh International Convention and Exhibition center, KSA Website: www.sds.org.sa
February 4 – 6, 2014 at the state-of-the-art Dubai International Convention & Exhibition Centre (DICEC) Website: www.aeedc.com
June 17-19, 2014 Dubai World Trade Center, UAE Website: www.apdentalcongress.org
11
16th
The
AEEDC 1st ORMCO MENA Symposium Asia Pacific Dental Congress GNYDM 2013 3rd Pan Arab Endodontic Conference DFCIC 2013 The 10th congress of SENAME National Guard
10th Annual Meeting of ESCD
International Dental Congress of the Egyptian Dental Association
Lebanese Orthodontic Society
Health Affairs
Volume XX, Number III, 2013 www.dentalnews.com King Saud University and Saudi Dental Society PRINTED BY Arab Printing
Press s.a.l
Prosthetic Dentistry
Complete dentures
Customizing Esthetic Complete dentures
Dr. Nazem Assaad
na.assaad@wwv.se
Lebanese University, Beirut Arab University Beirut, Lebanon
Dr. Najib Abou Hamra
Dr. Maha Ghotmi
Introduction and Background
Esthetic is a predominant factor for complete denture success (Carlsson et al. 1967). It is the most frequent complaints among complete denture patients (Jeganathan, 1993). Comfortable but unaesthetic dentures seem to be unaccepted by patients (Brewer, 1967). Compensating alveolar bone loss, correctly supporting lips and reestablishing the correct vertical dimension of occlusion are basic steps for achieving patient normal appearance. However, this is not sufficient to achieve individual denture esthetics. Denture esthetics has been defined as the cosmetic effect produced by a dental prosthesis that affects the desirable beauty, attractiveness, character and dignity of the individual (Glossary of Prosthodontic terms) which means proper form and shade of denture teeth and also individual set up of the teeth in order to achieve individual esthetic. Classically, three esthetic concepts have been differentiated to achieve denture esthetics (Waliszewski et al. 2006)
1- The denture look: an esthetic concept developed mainly as a result of a functionally oriented tooth positioning as well as from common errors in fabrication and appearance for complete denture wearers (Fig. 1-2).
2- The supernormal teeth: Shor and colleagues in 2005 defined the supernormal concept as “attractive, idealized, and above-average dental esthetics. A custom made look to please the body image of the patient (Fig. 3-4).


& 2
Regular arch form


3- The natural look : described by Frush and Fischer as a natural appearance related to anatomic determinants of gender, age and personality. It seeks to restore the most natural patient smile and its appearance (Fig. 5).

There is limited evidence-based information available when achieving dentate appearance in
Dental News, Volume XX, Number III, 2013 12
Fig.1
Fig. 5: Male teeth setup based on criteria given by the natural look theory
Fig 1
Fig 2
Fig 3
Fig 4
Fig 5













For more information about SciCan products, please contact our area manager Dr. Ashraf Suleiman at asuleiman@scican.com or at 0020122 2100 516 STAT IM is a registered trademark and Your Infection Control specialist is a trademark of SciCan Ltd. www.scican.com Watch the product video. STATIM, the world’s fastest autoclave from start to sterile. A large touch screen offers communication between the unit and the user, allowing for easy operation, and tutorial viewing. SPEEDTOUCH G4 collects all cycle data and service history, protecting your office and patients. COLLECT Connect to anyone from anywhere... your STATIM is now accessible online. CONNECT Introducing the new generation STATIM ® ... the STATIM G4 Series
Prosthetic Dentistry
Complete dentures
edentulous patients. However the natural concept of Frush and Fisher (Frush and Fisher, 1955) is still useful, and this will ensure a better psychological integration of the artistic prosthesis (Waliszewski M 2005).
The aim of this paper is to develop the natural look theory and give a series of clinical examples. In order to look natural, denture teeth should be as close as possible and look as close as possible to natural teeth. However there might be some discrepancies between the clinical situation of the edentulous mouth and the look of the natural teeth before extractions occurred. It is therefore very important to find a reasonable compromise between the reality of the edentulous mouth and the position of the natural teeth as they should have been. The natural look theory is the way to achieve this goal. The mixture of personality look, gender and age in combination with the clinical situation will determine the final look and position of teeth. To emphazise the personality, age and gender some specific characterization might be also needed to attain this result. Clinical examples will try to explain how this theory can be used (Fig.6-24).








Dental News, Volume XX, Number III, 2013 24 14
Fig 6
Fig 9
Fig 10
Fig 11
Fig 12
Fig 13
Fig 6
Fig 6
Fig. 6: Rude and aggressive appearance due to the prominent position of the canine following to the strong retruded Position of the lateral incisors especially right side.
Fig. 9: As light rotation of the centrals accentuates the vigor look
Fig. 10: The projection of a prominent canine gives to the smile a more rugged and typically male appearance.
Fig. 11: Female teeth set with a curved smile line.
Fig. 12: Regular arch and teeth with more rounded shape.
Fig 13: Anterior rotation mesial of the central incisor combined with cervical inclination express a female character.
Fig. 7: Aggression is reinforced by the existence of the diastema.
Fig. 8: Male teeth setup: Free edges touching the horizontal plane, giving a vigorous male look.

Prosthetic Dentistry
Complete dentures
Fig. 14: Lateral incisors overlapping the central incisors, gives softness to smile.

Fig. 15: Feminine teeth setup: strong inclination and rotation of the lateral incisors, absence of canine prominent, a smile curved line, give softness to the over all smile.
Fig. 16: The difference in shape and size between the lateral and central incisor accentuates the feminine character.
Fig. 18: Teeth setup based on the photograph

Fig. 19: Dark teeth and gingival recession in the elderly patient.
Fig. 20: Crowding at the lower incisors especially in the elderly patients.
Fig. 21: Artificial teeth similar to natural teeth (overcrowding, abrasion).








A result close to the natural staining teeth to simulate cracks in the enamel and other imperfections especially in case of unimaxillary edentulous patient.

Fig. 24: Covering the distal part of a tooth on the mesial side of its neighboring one gives an effect of crowding and smaller sized teeth.
Conclusion
Some patients ask for a perfect denture look or for a supernatural teeth form, shade and arrangement; the majority prefer a natural look and smile. This implies an effort from the dentist and his technician to achieve this goal. The end result being an individualized esthetic denture. Achieving a natural look in complete dentures needs skills, scientific back up information regarding the set up of teeth but most of all the collaboration between the dentist and his patient to find a reasonable compromise between what is expected and what can be done.
References
1- CARLSSON GE, OTTERLAND A, WENNSTROM A, ODONT D. PATIENT FACTORS IN APPRECIATION OF COMPLETE DENTURES. J PROSTHET DENT 1967; 17:322-8.170.
2- JEGANATHAN S, PAYNE JA. COMMON FAULTS IN COMPLETE DENTURES: A REVIEW QUINTESSENCE INT. 1993 JUL;24(7):483-7. REVIEW
3- FRUSH JP, FISHER RD.INTRODUCTION TO DENTOGENICRESTORATIONS.JPROSTHET DENT 1955; 5: 586-95.
4- BREWER A. SELECTION OF DENTURE TEETH FOR ESTHETICS AND FUNCTION. . J PROSTHET DENT 1970; 23: 368-734.
5- WALISZEWSKI M, SHOR A, BRUDVIK J, RAIGRODSKIAJ. A SURVEY OF EDENTULOUS PATIENT PREFERENCE AMONG DIFFERENT DENTURE ESTHETIC CONCEPTS. J ESTHET RESTOR DENT. 2006;18(6):352-68; DISCUSSION 369.
6- ACADEMY OF DENTURE PROSTHETICS: GLOSSARY OF PROSTHODONTIC TERMS. J PROSTHET DENT 1970; 38:81.
7- WALISZEWSKI M. RESTORING DENTATE APPEARANCE: A LITERATURE REVIEW FOR MODERN COMPLETE DENTURE ESTHETICS. J PROSTHET DENT 2005 OCT-94 (4):407
8- SHOR A, SHOR K, GOTO Y. THE EDENTULOUS PATIENT AND BODY IMAGE ACHIEVING
GREATER PATIENT SATISFACTION. PRACT PROCED AESTHET DENT 2005;17:289–96.
Dental News, Volume XX, Number III, 2013 16
Fig 14 Fig 20 Fig 21
Fig 22
Fig 23
Fig 24 Fig 15
Fig 16
Fig 17
Fig 18
Fig 19


SCAN
Powder-free Scanner
E4D is the original powder-free scanner that captures the true anatomy

SUPPORT
Support-On-Sight
E4D is backed by a dedicated support team of clinical and technical experts to optimize your result


DESIGN
Intuitive User Interface
E4D’s design tools and easy-to-follow navigation guide you through the entire process

EDUCATION


At E4D University, you and your staff receive comprehensive, hands-on training to maximize your skills

MILL
Precision Mill
In-office restoration milling means same day dentistry –a great fit for both you and your patient

With its advanced scanning, design and milling capability, the E4D creates a high quality, exceptionally well-fitting restoration. Visit E4D.com/perfectfit to learn how E4D is the perfect fit for your practice.
For quality and accuracy, the E4D chairside CAD CAM system stands alone. Independent studies and clinicians confirm the accurate fit and clinical efficacy of the E4D restoration. What’s more, the E4D gives you the flexibility to practice on your own terms and your own schedule. And our hands-on training and support assures you of flawless integration. Which means it perfectly fits your success.

Stay Connected with E4D






NOTHING FITS YOUR PRACTICE BETTER. For
The Perfect Fit E4D Dentist—
Quality, It’s

Oral Surgery
Autotransplantation

Autotransplantation of Tooth in Children with Mixed Dentition
Dr. Abu-Hussein Muhamad abuhusseinmuhamad@gmail
Athens University
Dr. Abdulgani Azzaldeen
Al Quds University
Abstract
Autotransplantation of tooth in children is the surgical movement of a tooth from one place in the mouth to another in the similar individual. Once thought to be uncertain, Autotransplantation has achieved high success rates and is an outstanding option for tooth replacement in children. Although the indications for autotransplantation are narrow, careful patient assortment coupled with a suitable method can lead to exceptional esthetic and useful results. One benefit of this procedure is that placement of an implant-supported prosthesis or other form of prosthetic tooth replacement is not needed. A review of the recommended surgical technique as well as success rates is also discussed.
Key Words; Autotransplantation, clinical indications, healing factors, cryopreservation.
Introduction
The age at which the first tooth appears differs very much from child to child. Very occasionally, children are born with one or more teeth. These may need to be removed if they are very loose, as there is a risk that the child could swallow them, or have difficulties with breastfeeding. Other children may not expand any teeth until they are more than a year old. Usually, however, the first tooth - which tends to be in the middle of the lower jaw - appears at around six months of age. The complete set of 20 primary teeth (baby teeth) is usually present by the age of two-and-a-half years. The first permanent teeth appear at around six years of age. These tend to be the incisors in the middle of the lower jaw and the first permanent molar teeth. The molars come up behind the primary teeth, they do not
replace them.1,2,3
As there are a lot of reasons for autotransplanting teeth in children, tooth defeat as a result of dental caries is the most common sign, particularly when mandibular first molars are concerned. First molars erupt early and are often a lot restored. Autotransplantation in this situation involves the removal of a third molar which may then be transferred to the site of an unrestorable first molar. Extra circumstances in which transplantation can be careful include tooth agenesis (particularly of premolars and lateral incisors), shocking tooth loss, atopic outbreak of canines, root resorption, large endodontic lesions, cervical root fractures, localized juvenile periodontitis as well as other pathologies (Alberg, 1999). Successful transplantation depends on specific requirements of the patient, the donor tooth, and the recipient site.3
Patient selection is very significant for the achievement of autotransplantation. Child must be in good health, able to follow post-operative instructions, and available for follow-up visits. They should also demonstrate a satisfactory level of oral hygiene and be agreeable to regular dental care. Most importantly, the child must have a suitable receiver site and donor tooth. Patient collaboration and comprehension are extremely important to ensure predictable result. 4
The most significant criteria for success connecting the recipient site are adequacy of bone support. There must be enough alveolar bone support in all dimensions with sufficient attached keratinized tissue to allow for stabilization of the transplanted tooth. In addition, the recipient site should be free from acute disease and chronic irritation.
Dental News, Volume XX, Number III, 2013
20

Oral Surgery
Autotransplantation
The donor tooth should be positioned such that extraction will be as atraumatic as possible. Irregular root morphology, which makes tooth removal very difficult and may involve tooth sectioning, is contraindicated for this surgery. Teeth with also open or closed apices may be donors; however, the most unsurprising results are obtained with teeth having between one-half to two-thirds finished root development. Surgical treatment of teeth with less than one-half root formation may be too shocking and could compromise further root development, stunting maturation or changing morphology. When root development is better than two-thirds, the increased length may cause infringement on vital structures such as the maxillary sinus or the lesser alveolar nerve. Also, a tooth with total or near complete root configuration will usually require root canal therapy, while a tooth with an open apex will remain vital and should carry on root development after transplantation. In the latter case, successful transplantation without the need for further endodontic therapy is usually seen. (Jens, et al. 2001)
The mixed dentition is the developmental period after the permanent first molars and incisors have erupted, and before the remaining deciduous teeth are lost. Treatment is usually done early in this period. The American Association of Orthodontists recommends all children should see an orthodontist by age 7. A favorably developing occlusion at this stage has these characteristics. 2,5
Mixed Dentition. In a longitudinal study, Moorrees and Reed found that arch length decreases 2 to 3 mm between the ages of 10 and 14 years, when primary molars are replaced by permanent premolars. These authors also found a reduction in arch circumference of approximately 3.5 mm in the mandible in boys and 4.5 mm in girls during the mixed-dentition period. If crowding is evident in the early mixed-dentition years, it will not improve with further growth and development. (Moorrees & Reed, 2007)
Mesial shift. In patients with a spaced primary dentition and a flush or straight terminal plane, the flare-up of the permanent mandibular first molars at approximately 6 years of age closes the space distal to the primary canines (primate space) and transforms the molar relationship into a Class I relationship. This has been referred
to as “early mesial shift.”9 In patients with a closed primary dentition (no primate space) and a straight terminal plane, the transformation into a Class I molar relationship may not occur until the exfoliation of the primary molars. At approximately 11 years of age, the permanent first molars migrate forward to close up the excess leeway space provided by the difference in size between the primary molars and the succedaneous premolars. This has been called “late mesial shift.”9 The transformation into a Class I molar relationship depends on a number of dental and facial skeletal changes, both genetic and environmental, that interact to achieve (or not achieve) a normal occlusion. Several factors may prevent the establishment of a normal posterior occlusion. Extensive interproximal caries or ectopic eruption of the maxillary first molars may result in premature loss of primary second molars and a subsequent loss of arch length. Periapical pathology of primary teeth may hasten the eruption of their permanent successors. Tumors and supernumerary teeth may impede the course of eruption. Prolonged retention of primary teeth may disturb the eruption sequence. (Jens, et.al. 2001). Leeway space. The difference in size between the primary molars and the succedaneous premolars is termed “leeway space.” This varies greatly from person to person, according to a longitudinal study by Bishara and colleagues.12 the average leeway space in that study was 2.2 mm in the maxilla and 4.8 mm in the mandible. The differences in the leeway spaces between the maxillary and mandibular arches were 1.3 mm for male subjects and 1.1 mm for female subjects. The range in the amount of leeway space between people is quite remarkable and can exceed the above amounts.
Incisor liability. The size differential between the primary and permanent incisors is called “incisor liability.” In the anterior segment, the four permanent maxillary incisor teeth are, on average, 7.6 mm larger than the primary incisors. In the mandibular arch, the permanent incisors are 6.0 mm larger than the corresponding primary teeth.13 Incisor liability varies greatly from person to person. The spacing of the primary anterior teeth; lateral and even possibly distal shifting of the primary canines; and facial positioning of the incisors all contribute to the incisor liability. All of these factors will increase the arch perimeter and
Dental News, Volume XX, Number III, 2013
22












Autotransplantation
Criteria for success in autotransplantation
Radiographic examination - No evidence of progressive inflammatory root resorption
- Normal PDL space width around the transplanted tooth
- No disturbance in root development
- Lamina dura
- Healing of alveolar bone
Clinical examination - Normal tooth mobility and normal tooth function
- Gingival healing and no indication of marginal attachment loss, inflammation
- Healing of dental pulp
- No patient discomfort
- Normal percussion sound
Histological examination - The PDL fibers are aligned to perpendicular, not parallel, to the root and alveolar bone
- However, without extraction, it is impossible to evaluate clinical cases histologically
Table 1
help the mouth accommodate the larger permanent teeth. Eruption sequence. In a study by Lo and Moyers,14 the most favorable sequence of eruption to obtain a normal molar relationship was as follows: first molar, central incisor, lateral incisor, first premolar, second premolar, canine, second molar in the maxilla and first molar, central incisor, lateral incisor, canine, first premolar, second premolar, second molar in the mandible. The most unfavorable sequence in the maxilla was that in which second molar erupted earlier than either the premolars. The most unfavorable sequence in the mandible was that in which the canines erupted later than the premolars.{Tab.1}
Treatment strategies
Mixed dentition treatment goals often focus on skeletal rather than dental correction. To design a treatment plan, the clinician must understand the growth and development patterns, and the known effects of the chosen treatment modality. Many dental development problems can be headed off in the mixed dentition; for example, anterior cross bites. In-time removal of a deciduous tooth could prevent a cross bite, but once the permanent upper incisor is caught on the lingual of the lower incisors, treatment is needed. The anterior cross bite can cause tissue damage around the affected lower incisor. Another example is the displaced lower midline as a result
of the early loss of a lower deciduous canine. 6,7
Auto-transplantation
This is a surgical procedure in which tooth from one part of the mouth is transplanted to another. Indications for such procedure are as below:
1. Hypodontia – This is where there are missing tooth or teeth such as a missing central incisor, a premolar can be use as a substitute.
2. Premature loss of tooth- especially true in first molar area where it may have been lost due to caries and the space is too great to be closed by the second molar. A third molar tooth is judiciously removed and a socket is prepared in the first molar area and molar is then placed and secured with 0.5 mm eyelet wire to the adjacent teeth. There are a lot of dental procedures being utilized by consumers whether for aesthetic purposes or medical, and tooth transplantation is the most common one. Basically, this is done by moving a tooth from a site to another site of the mouth and rarely to another recipient. Studies showed that implants utilized in filling gaps of missing front teeth are not the best alternative since this can cause a considerable amount of bone loss and abrasion on neighboring teeth and surrounding gums. Auto transplantation is considered a better alternative in certain cases.1,4,7,8
Auto transplantation is a tooth surgical procedure in one location to another location within the same person. Before, this was considered experimental, but in present times auto-transplantation is a better alternative for tooth replacement with high success rate. Indication for clients opted for this procedure is narrow {Tab.2}, and thorough patient selection added with appropriate technique leads to outstanding aesthetic and functional capabilities. One advantage of this procedure is that the placement of implant-supported prosthesis or other form of prosthetic tooth replacement is not essentially required. 9,10
Indications for auto-transplantation
Usually, auto transplantation is done because of tooth loss due to dental caries, predominantly in the first molars of the lower jaws. Early eruption of first molars is frequently restored (Byers, et. al, 2002). In this case, the third molar is then removed via auto transplantation and then trans-
Dental News, Volume XX, Number III, 2013
24
Oral Surgery

ORTHOPHOS XG
SIMPLY RELIABLE.
EVERY DAY.
By choosing an ORTHOPHOS XG you are investing in a secure future. This is because the units in the ORTHOPHOS XG family offer you high quality, durability and the best image quality with the lowest dose and a perfect workflow. So it‘s no surprise that more than 100,000 dentists all over the world have decided on an ORTHOPHOS XG. Enjoy every day. With Sirona.
B-753-01-7600-V0 SIRONA.COM
Autotransplantation
Successful healing factors associated with autotransplantation of teeth
a. Patient related factors
- Better results in younger patients
- A patient free of major systemic and metabolic problems or specific habits (e.g., smoking)
- Good oral hygiene and a cooperative attitude.
b. Donor tooth related factors
Periodontal ligament (PDL)
- The presence of intact and vital PDL attached to the root surface
- Preservation of vital PDL when the tooth is outside the mouth using physiologic salt water or milk or preservation liquids and as short a surgery time as possible
- Enhanced healing of the gingival tissue by placing a 1 mm band of PDL fibers on the root above the crest of bone
- A major factor in the formation of alveolar bone
- A chance of inadequate PDL development as an effective attachment with an impacted tooth (nonfunctioning tooth)
Healing of dental pulp
- The preservation of Hertwig’s epithelial root sheath (HERS)
- Healing of the dental pulp occurs until Moorrees tooth development stage 5
- When the diameter of the apical foramina is > 1 mm, there is more than an 87% chance the dental pulp will heal,
Continuation of root development
- Ideal timing of transplantation is when development of the donor tooth roots is 3/4 to 4/5 complete
Gingival adaptation
- Tight flap adaptation prevents bacterial invasion into the recipient socket
Root morphology
- Teeth with a single, cone-shaped root without concavity around the cervical area are most favorable.
c. Recipient site related factors
- Bone width and height should be adequate to receive the donor tooth
- Better healing can be expected if the PDL tissue is still attached
- Transplantation should be performed the day of transplantation or within 1 month after extraction
d. Clinical factors
- Surgery should be performed by a clinician with experience in such areas as Surgery should be performed by a clinician with experience in such areas as donor tooth extraction, preparation of the recipient site, and tissue management Table 2
ferred to the site of the first molar that is beyond saving. Transplantation can also be opted in cases like tooth agenesis (premolars and lateral incisors), traumatic tooth loss, canine atopic eruption, root resorption (body of the cells attack and destroy a part of a tooth), large endodontic lesions, cervical root fractures, and localized juvenile periodontitis. 3,6,7,9,10
Transplant success depends primarily on the specified requirements from the client, donor tooth, and recipient site. Autotransplant success is based on how well the healing takes place after the procedure (Czochrowska, et al. 2000).
A healthy tooth with undamaged periodontal ligament will have higher degree of success. Before having this procedure, clients must have a good health and oral hygiene regimen. Most of all, a suitable donor tooth and recipient site are required so that tooth can be replanted appropriately. The site should be well prepared in receiving the tooth donor. Size should accommodate a tooth, along with sufficient alveolar bone structure, which enables support. This should be free from inflammation and infection. The replanted Donor Tooth (the tooth) should be positioned to assist in easy removal with minimum trauma possible. Misshapen teeth or abnormal root morphology are not used in transplants 8,9.10,11
Tooth length and development stage is vital in determining the affectivity of a replantation wherein the tooth has between one-half to twothirds complete root development. So, autotransplantation of the premolars where there is half to two thirds completed root development have higher chances of pulp survival, with minimum chances of necrosis (cell death). (Kristerson, 1995). Another factor influencing tooth development is the status of epithelial root sheath or the covering. HERS or Hertwig’s epithelial root sheath has a continuous production of cells that separates a pulp to a dental follicle. HERS determines the root growth by its degree of damage so the lesser the damage, the greater chance of root growth post transplantation. 2,7,9,10,12
Tooth cryopreservation
Teeth auto-transplantation with cryopreservation is an alternative currently utilized for clients in a few clinics. With cryobiology, cells or whole tissues are preserved by cooling it to sub-zero
Dental News, Volume XX, Number III, 2013
26
Oral Surgery

COMPONEER ™

Surprise your patients with a new smile –in only one session!




Innovative. Time-saving. Surprisingly easy. COMPONEER is the Direct Composite Veneering System used for quick, easy and save restorations of single or multiple teeth. This offers new perspectives for you and your patients. So both of you have a reason to smile. www.componeer.info







THE SMILE TO GO.










COMPONEER™ benefits:


www.coltene.com/contact
No laboratory required | One session | Naturally aesthetic corrections using freehand technique | Easy application with prefabricated composite veneers | Brillant result | Attractive added value





001182
Oral Surgery
Autotransplantation
temperature at around 77K or -196°C (boiling point of liquid nitrogen). Low temperatures leads to prevention of cell death (necrosis) and ceasing of biological activities along with its biochemical reactions. Experiments on mice showed effectively of cryopreservation on the teeth, resulting to dental tissue survival even at below freezing point. (Cooke & Scheer, 2003). Teeth cryopreservation requires a wider understanding of cryoprotective mechanisms of co solvents like dimethylsulfoxide (DMSO) (Andreasen, 2007). Consequently, only a few clinics have the expertise to do tooth cryopreservation and make it available to their clients. With cryopreservation, elevated numbers of healthy teeth extractions can be done for orthodontic purposes and it enables sufficient amounts of donor teeth in cases of extensive surgical reconstruction. Tissue banks for teeth tissues are regulated legally for quality control. 7,9,10,11,13
Surgical technique for tooth transplantation
The same amount of trauma is experienced by the patients having a removal of impacted molars to that that underwent tooth transplantation. Sedation along with local anesthesia is utilized in this case. Once the effect of anesthesia is sufficient, then extraction of the tooth at the recipient site and recipient socket is prepared. Replantation of an acrylic replica of a tooth is done after an x-ray and donor tooth scan. This replica will guide the tooth technician to prepare a donor site for its dimension, etc {Tab.1}. Then, extraction of the donor tooth should have least damage on the periodontal ligament and positioned quickly on the recipient site. Instructions and follow-ups given to post operative clients are similar in that of removal of tooth impaction. 4,7,8,13,14,15,16 A soft diet is followed for several days post-surgery, and chewing on the transplant should be
avoided. Clients should always maintain good oral hygiene. (Jensen & Kreiborg, 1992) Auto transplantation: Surgical Technique The surgical techniques used in autotransplantation have progressively been modeled and refined over the years. Good oral hygiene, self-motivation and a medical history that does not contraindicate transplantation (e.g. cardiac defects) are pre-requisites before this avenue of treatment is embarked upon. Andreasen et al. (1990) carried out a long-term study of 370 autotransplanted premolar teeth to determine a standardised surgical procedure which optimised pulpal and periodontal healing.15,16,17 Although there is published variations for the surgical technique of auto-transplantation the consistent message is one of a careful atraumatic surgical technique to maximally preserve an intact periodontal ligament. If Hertwig’s root sheath is traumatized then future root growth is limited or inhibited, according to the severity of this trauma (Andreasen, et al. 1990). Evidence based transplantation techniques are combined in a ‘protocol for transplantation’ included at the end of this paper. 2,13,14,18 In some cases autotransplantation may not be possible as a one stage procedure. Two stage transplantation has been reported in which an ectopic canine was removed and initially stored in the buccal pouch whilst the recipient site was orthodontically reopened (Tab.3). The potential problem of resorption of the transplanted tooth is minimized if contact between the tooth andperiosteum is avoided during storage. In some situations, there may be resorption of the alveolar ridge at the recipient site with insufficient bucco- palatal width to accommodate the transplant. In such cases, specialized investigative techniques (e.g. Scanora, CT tomography) may need to be carried out to ascertain the amount of bone present bucco-palatally. Alveolar bone grafting of the recipient site may be required prior to transplantation. 4,11,14,17,18,19.
Conclusion
Although auto transplantation in children has not been established as a traditional means of replacing a missing tooth, the process warrants more reflection. New studies obviously show that auto transplantation of teeth in children is as successful as endosseous dental implant placement. Minimum acceptable success rates
Dental News, Volume XX, Number III, 2013 28


















The tioLogic© implant system supported in all 3 CAD systems. Dentaurum Implants provides on www.dentaurum-implants.de the service of downloading tioLogic© CAD/CAM datasets for 3shape, dental wings and exocad for integration in the respective software.

Turnstraße 31 I 75228 Ispringen I Germany I Phone + 49 72 31 / 803 - 0 I Fax + 49 72 31 / 803 - 295 www.dentaurum-implants.de I info@dentaurum-implants.de
digital. Implant system
Oral Surgery
Autotransplantation
for endosseous titanium dental implants are 85% after 2 years and 80% after 5 years. For children, auto transplantation may also be considered as a provisional measure. The transplant can replace missing teeth to make sure preservation of bone until growth has ceased and then, if essential, the patient can become a candidate for implants. With suitable patient selection, and presence of a suitable donor tooth and recipient site, auto transplantation should be considered as a viable option for treatment of an edentulous space.
References
1. ANDREASEN JO, PAULSEN HU, YU Z, AHLQUIST R, BAYER T, SCHWARTZ O. A LONGTERM STUDY OF 370 AUTOTRANSPLANTED PREMOLARS. PART I. SURGICAL PROCEDURES AND STANDARDIZED TECHNIQUES FOR MONITORING HEALING. EUR J ORTHOD. 1990;12:3-13.
2. TSUKIBOSHI M. AUTOTRANSPLANTATION OF TEETH: REQUIREMENTS FOR PREDICTABLE SUCCESS. DENT TRAUMATOL. 2002;18:157-80.
3. ANDREASEN JO, PAULSEN HU, YU Z, BAYER T, SCHWARTZ O. A LONG-TERM STUDY OF 370 AUTO TRANSPLANTED PREMOLARS. PART II. TOOTH SURVIVAL AND PULP HEALING SUBSEQUENT TO TRANSPLANTATION. EUR J ORTHOD. 1990;12:14-24.
4. ANDREASEN JO, PAULSEN HU, YU Z, SCHWARTZ O. A LONG-TERM STUDY OF 370 AUTOTRANSPLANTED PREMOLARS. PART III. PERIODONTAL HEALING SUBSEQUENT TO TRANSPLANTATION. EUR J ORTHOD. 1990;12:25-37.
5. ANDREASEN JO, PAULSEN HU, YU Z, BAYER T. A LONG-TERM STUDY OF 370 AUTOTRANSPLANTED PREMOLARS. PART IV. ROOT DEVELOPMENT SUBSEQUENT TO TRANSPLANTATION. EUR J ORTHOD. 1990;12:38-50.
6. GARCÍA-CALDERÓN M, TORRES-LAGARES D, GONZÁLEZ-MARTÍN M, GUTIÉRREZPÉREZ JL. RESCUE SURGERY (SURGICAL REPOSITIONING) OF IMPACTED LOWER SECOND MOLARS. MED ORAL PATOL ORAL CIR BUCAL. 2005;10:448-53.
7. CZOCHROWSKA EM, STENVIK A, ALBUM B, ZACHRISSON BU. AUTO TRANSPLANTATION OF PREMOLARS TO REPLACE MAXILLARY INCISORS: A COMPARISON WITH NATURAL INCISORS. AM J ORTHOD DENTOFACIAL ORTHOP. 2000;118:592-600.
8. ZACHRISSON BU, STENVIK A, HAANAES HR. MANAGEMENT OF MISSING MAXILLARY ANTERIOR TEETH WITH EMPHASIS ON AUTO TRANSPLANTATION. AM J ORTHOD DENTOFACIAL ORTHOP. 2004 ;126:284-8.
9. CZOCHROWSKA EM, STENVIK A, BJERCKE B, ZACHRISSON BU. OUTCOME OF TOOTH TRANSPLANTATION: SURVIVAL AND SUCCESS RATES 17-41 YEARS POST TREATMENT. AM J ORTHOD DENTOFACIAL ORTHOP. 2002;121:110-9.
10. TEIXEIRA CS, PASTERNAK B JR, VANSAN LP, SOUSA-NETO MD. AUTOGENOUS TRANSPLANTATION OF TEETH WITH COMPLETE ROOT FORMATION: TWO CASE REPORTS. INT ENDOD J. 2006;39:977-85.
11. KALLU R, VINCKIER F, POLITIS C, MWALILI S, WILLEMS G. TOOTH TRANS¬PLANTATIONS: A DESCRIPTIVE RETROSPECTIVE STUDY. INT J ORAL MAXILLOFAC SURG 2005;34:745-55.
12. CLOKIE CM, YAU DM, CHANO L. AUTOGENOUS TOOTH TRANSPLANTATION: AN ALTERNATIVE TO DENTAL IMPLANT PLACEMENT? J CAN DENT ASSOC. 2001;67:92-6.
13. BAUSS O, SCHILKE R, FENSKE C, ENGELKE W, KILIARIDIS S. AUTOTRANS PLANTATION OF IMMATURE THIRD MOLARS: INFLUENCE OF DIFFERENT SPLINTING METHODS AND FIXATION PERIODS. DENT TRAUMATOL. 2002;18:322-8.
14. DÍAZ JA, ALMEIDA AM, BENAVENTE AA. TOOTH TRANSPLANTATION AFTER DENTAL INJURY SEQUELAE IN CHILDREN. DENT TRAUMATOL. 2008;24:320-7.
15. BAUSS O, ZONIOS I, RAHMAN A. ROOT DEVELOPMENT OF IMMATURE THIRD MOLARS TRANSPLANTED TO SURGICALLY CREATED SOCKETS. J ORAL MAXILLOFAC SURG 2008;66:1200-11.
16. PAULSEN HU, ANDREASEN JO. ERUPTION OF PREMOLARS SUBSEQUENT TO AUTOTRANSPLANTATION. A LONGITUDINAL RADIOGRAPHIC STUDY. EUR J ORTHOD. 1998;20:45-55.
17. CZOCHROWSKA EM, STENVIK A, ZACHRISSON BU. THE ESTHETIC OUT¬ REFERENCES WITH LINKS TO CROSSREF - DOICOME OF AUTOTRANSPLANTED PREMOLARS REPLACING MAXILLARY INCISORS. DENT TRAUMATOL. 2002;18:237-45.
18. AKKOCAOGLU M, KASABOGLU O. SUCCESS RATE OF AUTOTRANSPLANTED TEETH WITHOUT STABILISATION BY SPLINTS: A LONG-TERM CLINICAL AND RADIO LOGICAL FOLLOWUP. BR J ORAL MAXILLOFAC SURG. 2005;43:31-5.
19. ECKERT SE, CHOI YG, SÁNCHEZ AR, KOKA S. COMPARISON OF DENTAL IMPLANT SYSTEMS: QUALITY OF CLINICAL EVIDENCE AND PREDICTION OF 5-YEAR SURVIVAL. INT J ORAL MAXILLOFAC IMPLANTS. 2005;20:406-15.
30
Dental News, Volume XX, Number
III, 2013












The first fluoride toothpaste to harness advanced NovaMin and phosphate bone regeneration technology of your patients’ dentine hypersensitivity.
Building a hydroxyapatite-like layer over exposed dentine and within dentine tubules
Protects patients from the pain of future sensitivity: firmly binds to dentine6,7 and is resistant to daily oral challenges


VII:

Think



beyond pain relief and recommend Sensodyne Repair & Protect

 References: 1. Greenspan DC. J Clin Dent 2010; 21(Spec Iss): 61–65. 2. LaTorre G, Greenspan DC. J Clin Dent 2010; 21(3): 72-76. 3. Burwell A et al. J Clin Dent 2010; 21(Spec Iss): 66–71. 4. West NX et al. J Clin Dent 2011; 22(Spec Iss): 82-89. 5. Earl J et al. J Clin Dent 2011; 22(Spec Iss): 62-67. 6. Efflandt SE et al. J Mater Sci Mater Med 2002; 26(6): 557-565. 7. Zhong JP et al. The kinetics of bioactive ceramics part
Binding of collagen to hydroxyapatite and bioactive glass. In Bioceramics 7, (eds) OH Andersson, R-P Happonen, A Yli-Urpo, Butterworth-Heinemann, London, pp61–66. 8. Parkinson C et al. J Clin Dent 2011; 22(Spec Issue): 74-81. 9. Earl J et al. J Clin Dent 2011; 22(Spec Iss): 68-73. 10. Wang Z et al. J Dent 2010; 38: 400−410. Prepared December 2011, Z-11-516.
References: 1. Greenspan DC. J Clin Dent 2010; 21(Spec Iss): 61–65. 2. LaTorre G, Greenspan DC. J Clin Dent 2010; 21(3): 72-76. 3. Burwell A et al. J Clin Dent 2010; 21(Spec Iss): 66–71. 4. West NX et al. J Clin Dent 2011; 22(Spec Iss): 82-89. 5. Earl J et al. J Clin Dent 2011; 22(Spec Iss): 62-67. 6. Efflandt SE et al. J Mater Sci Mater Med 2002; 26(6): 557-565. 7. Zhong JP et al. The kinetics of bioactive ceramics part
Binding of collagen to hydroxyapatite and bioactive glass. In Bioceramics 7, (eds) OH Andersson, R-P Happonen, A Yli-Urpo, Butterworth-Heinemann, London, pp61–66. 8. Parkinson C et al. J Clin Dent 2011; 22(Spec Issue): 74-81. 9. Earl J et al. J Clin Dent 2011; 22(Spec Iss): 68-73. 10. Wang Z et al. J Dent 2010; 38: 400−410. Prepared December 2011, Z-11-516.
OH/CA/01/13/001
Paediatric Dentistry
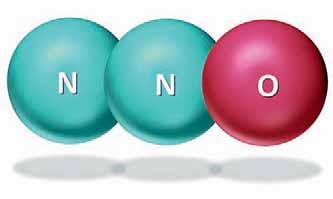
Exposure of dental staff to NITROUS OXIDE
Dr. Omar Mustafa
omar.mustafa@bdfmedical.org
Abstract
Background: Chronic exposure to nitrous oxide has been reported as a potential health hazard. Leakage from the mask delivery system and inefficient scavenging can lead to significant pollution.
Aims: to compare the nitrous oxide traces between different dental procedures and to monitor the nitrous oxide traces in the working environment.
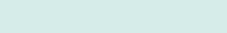
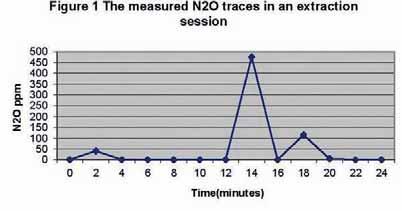
Methods: Nitrous oxide was measured in 27 dental procedures according to two methods. First method, measurements were recorded every two minutes during the inhalational sessions. Second method measurements were recorded from different distances from the operation site. Results: 21 sessions used for the first method. No statistical difference was found between the means of the nitrous oxide traces through the extraction and conservative sessions. Age group from 6 to 8 years has the highest measured traces. High traces recorded during stressful events6 sessions were selected for the second method. The distance obeys the inverse square law. Conclusions: uncooperativeness would lead to excessive pollution. Patient conditioning to breathing through nose would be very helpful. Equipment to be checked for leaks and that the mask is of the appropriate size and tight fitting. Ensure that scavenging and surgery ventilation is adequate.
- Keywords: chronic exposure, nitrous oxide, dentistry.
Introduction
Anxiety and fear of dental treatment in children is recognized as a problem in patient management. A variety of behavioural management techniques have been proposed to control these fear reactions.1 Management approaches to
anxiety vary according to its severity, the age of the patient, the degree of cooperation and the patient’s medical history.2 For some patients sedation will be required, with inhalation sedation using nitrous oxide/oxygen commonly used. Inhalation sedation with low to moderate concentrations of nitrous oxide in oxygen has a remarkable safety record, in over 45 years of use there has not been any mortality or serious morbidity recorded.3 Inhalation of nitrous oxide is administered via a special nosepiece. The gases are inhaled continually and the nitrous oxide ceases to have effect immediately after cessation of its administration. A patient recovers full consciousness within five minutes after administration of 100% oxygen.4
Chronic occupational exposure to trace concentrations of nitrous oxide has been reported as a potential health hazard,5 though the available evidence is weak.6 Some authors report complications to range from haematological abnormalities, neurological deficits or increased risk of spontaneous abortions in women.7,8 These effects may present a serious occupational hazard to dental surgeons and dental nurses who are regularly exposed to nitrous oxide when undertaking inhalation sedation. The British Health and Safety Commission advises that the maximum exposure of clinical staff to nitrous oxide gas should be 100 ppm over an 8 hour time weighted average period.9 In the 1990s practitioners were educated in ways to effectively scavenge trace gas contamination, with the primary method being the evacuation system and the scavenging nasal hood/mask in addition to regular monitoring programs.10 Leakage of gas from the mask delivery system and inefficient scavenging of waste gas from the surgery atmosphere can lead to significant pollution of the
Dental News, Volume XX, Number III, 2013 32 Nitrous Oxide Exposure
Kingdom of Bahrain



GC Glass Ionomer Restoratives: essential
in every dental practice




The power of advanced Glass Ionomer technology, with the simplicity of powder and liquid delivery.




GC EUROPE N.V.
GC Fuji IX GP GC Fuji II LC Improved GC Fuji VIII GP GC Fuji IX GP Extra P-L NEW
Paediatric Dentistry
dental surgery.9 There are many nitrous oxide analysers and dosimeters like the infrared nitrous oxide analyser which is used in many studies. Several types of dosimeters are available which can be worn as lapel badges during working hours.11 In order for dentists to feel comfortable that they are attaining safe levels of nitrous oxide within their surgeries they need to understand the risk of pollution from different procedures and also the risk to individuals within the surgery dependent on where they are placed relative to the source of pollution. The purpose of this study was to compare the measured nitrous oxide traces between the different dental procedures and to monitor the nitrous oxide traces in the working environment of the dental staff at variable distances at the paediatric dentistry department of Liverpool Dental Hospital.
Materials and Methods
This was a cross sectional study, ethical approval was not required as regular monitoring is part of the safety routine. Measurement of nitrous oxide was done in a convenience sample of 27 child patients attending the Paediatric depart-
ment of the Liverpool Dental Hospital for dental treatment. The Department of Paediatric Dentistry is an open clinic design in which the dental units are separated by short partitions. The nitrous oxide machine used was the MDM Quantiflex which is a continuous flow type. The machine matches the universal safety measures of the sedation machines. It has the main parts which are the flowmeter, circuit bag, air entrainment valve, scavenging nasal hood and expiratory valve, and the conducting tubes. It uses continuous gas flow and the rate can be adjusted. One examiner monitored the nitrous oxide traces, he was trained in the use of the nitrous oxide analyser (the Medigas PM3010 N2O Analyser). The Medigas PM3010 N2O Analyser is a handheld infrared nitrous oxide monitor which can measure nitrous oxide concentrations in the range of 0-1,000 ppm with a resolution of 5 ppm. Readings can be displayed in real time or as an 8 hour TWA (Time Weighted Average). The analyser was calibrated and checked by the Medical Engineering Department at the Royal Liverpool Hospital.
The Procedure
Before the start of each inhalation session, permission was taken from the operators. Also parents and patients were informed about the study and assured that there would be no any intervention with dental treatment.
Nitrous oxide traces were measured for two procedures
The First Procedure
In the first procedure, measurements were recorded every two minutes during 21 inhalational sessions as close as possible to the operation site within a circle of 20 cm diameter. A stopwatch was used from the time the mask was placed over the patient’s nose to the time it was removed, during this time nitrous oxide traces were recorded by the Medigas analyser. The following information was recorded:
1- The patient’s age and sex.
2- Nitrous oxide flow (litre per minute) and concentration (in percentage).
3- The nature of the dental treatment such as extraction, conservative, etc.
4- General comments as to whether windows
34 Nitrous Oxide Exposure
Dental News, Volume XX, Number III, 2013
YOUR NEW TREATMENT UNIT: INSPIRED EXCLUSIVELY BY YOUR
PERSONAL DESIRES.









The Ultradent Premium Class offers treatment units that you can configure as individually as your dream car. We are a modern dental company that flexibly manufactures our products based on your needs. In Germany. With outstanding quality. And absolute perfection. We are the experienced partner of completely satisfied dentists. Providing exceptional reliability and intuitive operation. With the newest technologies and multimedia. Ultradent Premium units will captivate you.

www.ultradent.de Ask your





EXPERIENCE THE NEW STANDARD FOR OUR PREMIUM DENTAL UNITS: With vision U – the future tool for best practice.
EACH NEW ULTRADENT PREMIUM CLASS UNIT NOW COMES WITH VISION U: The revolutionar y, interactive, touchscreen-based multimedia system WITH VISION U, THE DOORS OF THE FUTURE OPEN TO YOUR PRACTICE:
> Large 21.5“ multi-touch screen – responds to „SmartTouch“ gestures
> Innovative patient entertainment – all informations are freely selectable
> Optical support – digital intraoral camera with autofocus and barcode reader, 2- and 3D x-ray viewer
> Simple quality assurance – automatic recording of all performance data before, during, and after treatment
> Integrated maintenance and service platform – reduces downtime and saves costs
ULTRADENT dealer about our IDS innovations! Jaeger & Talente, Munich

were opened or closed, fan was working or not, etc.
5- In each 2 minute reading, a note was recorded about the current dental procedure and the patient behaviour such as giving local anesthesia, cavity preparation, extraction, patient is talking, crying, etc.
The Second Procedure
In this procedure measurements were recorded in 6 sedation sessions from different distances from the operation site at zero, one, two, three, four and five metres.
Data Processing
The Analyser measured nitrous oxide traces in numbers in ppm (part per million). Outcomes were assessed using descriptive statistics and by t-test.
Results
Data was collected from 27 paediatric inhalational sessions. It was assumed that nitrous oxide traces will be more fluctuant and variable in the first measurement method than that in the second method, and therefore, 21 sessions were selected for the first procedure whereas only 6 sessions for the second procedure. In the 21 sessions, nitrous oxide traces were measured every 2 minutes throughout the session. In 6 sessions, nitrous oxide traces were measured from different distances from the operation site: at zero, one, two, three, four, and five meters. In all the nitrous oxide inhalation sessions a scavenging nasal mask was used and the fan was working.
A- Measurements taken every 2 minutes during inhalational sessions:
In the 21 sessions the treatments were 12 extractions (57%), 7 conservative treatments (33%), 1 fluoride application (5%) and 1 acclimatization (5%). The treatments were carried for 6 males (29%) and 15 female (71%) patients with age ranges from 6 to 17 years, mean is 9.9 years (SD 3.7). The mean nitrous oxide concentration was 30.7% (SD 5.1, ranged from 20% to 40%) and the mean flow rate was 6.6 l/min (SD 1.3, ranged from 5 l/min to 10 l/min). In all the sessions, sampling of the atmosphere was made at 20 cm from the patient in the horizontal plane. The mean of measured nitrous oxide traces was
compared in the extraction (91.7 ppm, SD 133.7) and conservative (32.4 ppm, SD 58.8) sessions and found to be not significant statistically (p>0.05). There was no relationship between age and measured nitrous oxide (p>0.05). In general, levels of nitrous oxide varied widely between treatment sessions. In one fluoride application session it reached 2725 ppm (the patient was talking at the time); 4460 ppm in an extraction session (at the time the patient started to cry after being given local anesthesia); and 1975 ppm in an extraction session (at the time of tooth extraction).
B- Measurements taken at various distances: Nitrous oxide traces were measured in 6 sessions, 4 sessions were conservative treatment and 2 sessions were extraction, 4 females and 2 males. The mean age of the patients was 10 years (SD 3.5, age range 6 to 14 years). The mean nitrous oxide concentration used during the sessions was 3.8% (SD 2.0) with a range from 30% to 35%, and the mean flow was 6.2 l/min (SD 1.1) ranges from 5 l/min to 8 l/min. The mean measured nitrous oxide traces were 602 ppm (SD 514) at zero distance, then decreased by increase in distance from the operating site (at 5 metre: 9 ppm, SD 17.5).
Discussion
The importance of keeping pollution of nitrous oxide to the absolute minimum levels cannot be understated. The problem is of great concern to staff who have to work in such an environment constantly, rather than patients where exposure, although at a high level to produce the desired clinical effects, is only occasional. There may also be concerns in respect of accompanying adults, e.g. pregnant mothers who may be at the chairside with their child. Problems of chronic exposure to nitrous oxide have been cited in the literature review but the most important ones are haematological changes. Chronic occupational exposure to nitrous oxide may cause depression of vitamin B12 activity11 and altered DNA synthesis in the bone marrow and mild megaloblastic changes.12, 13 The aim of this study was to monitor as accurately as possible, the levels of nitrous oxide in the surgery under different conditions. These included continuous monitoring in the immediate vicinity of the operator and also at
Paediatric Dentistry
Dental News, Volume XX, Number III, 2013 37 Nitrous Oxide Exposure
Paediatric Dentistry
varying distances. There was no significant difference between the mean of the measured nitrous oxide traces in the extraction sessions from that in the conservative sessions. There was also no relationship between age and nitrous oxide pollution, gender or with the concentration of nitrous oxide used and nitrous oxide air levels. There were a few sessions where nitrous oxide levels reached a very high level, sometimes exceeding 1000 ppm (0.01%). Donaldson and Meechan 10 suggested that when this occurred it was related to leakage of the nitrous oxide sedation machine or cylinders, poorly fitting masks, inadequate scavenging, patient mouth breathing, and poor surgery ventilation. In this study, where large variations in nitrous oxide levels were seen, this was associated with patients who were talking, crying etc. throughout the procedure. It may therefore be associated with pollution from expired air as a result of crying, talking, etc, or from leakage around the mask due to patient movement, etc. These findings are similar to those of Henry et al.14 who stated that patient behaviour can result in significant increase in nitrous oxide levels in the ambient air. Particular attention to these aspects is required to ensure pollution is significantly reduced to acceptable levels. Given that the results showed that the higher nitrous oxide levels were recorded at the time when patients were talking, laughing, crying, local analgesia administration, extraction, and rubber dam application, good sedation and behavior management is important. Relaxed and comfortable patients are less likely to talk, cry etc.
The lack of observable differences found related to type of treatment or age could also be attributed to errors in the sampling such as the sample size, randomization, etc.
It is obvious by looking at the results of the second part that the distance obeys the inverse square law: the nitrous oxide concentration decreases as the distance from working site increases. The greatest nitrous oxide concentrations was at zero metre from the working zone as described by Cleaton-Jonset et al.15 This is reassuring for other personnel in the surgery including accompanying parents who are approximately 2 metres away with levels of 50 ppm. Conversely, concerns are raised in respect of the operator and assisting dental nurse who are in
the working zone during these administrations. There is no doubt that for many patients, nitrous oxide sedation provides a good quality of sedation for them to be able to cope with treatment. This study has highlighted potential problems in respect of nitrous oxide pollution which is of concern to all personnel in surgery during the sedation sessions.
1. In this study the sample size was very limited. A future study with a larger cohort would be much more meaningful and would, hopefully, confirm the trends which I have found.
2. Patient selection is of utmost importance as a struggling, crying child would lead to very excessive pollution.
3. Patient conditioning to breathing through his/ her nose at all times would be very helpful. Talking to patients through (with the help of normal behavioural management techniques) stressful events e.g. local analgesia administration, extractions, etc. would limit the amount of disruption and the pollution at these times.
4. Ensure equipment is checked for leaks and that the mask is of the appropriate size and tight fitting.
5. Ensure that scavenging and surgery ventilation is adequate.
References
1. YAMADA MKM, TANABE Y, SANO T, NODA T. COOPERATION DURING DENTAL TREATMENT: THE CHILDREN ’ S FEAR SURVEY SCHEDULE IN JAPANESE CHILDREN. INT J PAED DENT 2002; 12: 404-409.
2. COULTHARD P, CRAIG D. CONSCIOUS SEDATION. DENT UPDATE. 1997 NOV;24(9):376-81.
3. ROBERTS GJ. INHALATION SEDATION (RELATIVE ANALGESIA) WITH OXYGEN/NITROUS OXIDE GAS MIXTURES: 1. PRINCIPLES. DENT UPDATE. 1990 MAY;17(4):139-42, 145-6.
4. SZYMANSKA J. ENVIRONMENTAL HEALTH RISK OF CHRONIC EXPOSURE TO NITROUS OXIDE IN DENTAL PRACTICE. ANN AGRIC ENVIRON MED 2001,8,119-122.
5. CARLSON P, HALLEN B, HALLONSTEN AL, LJUNGQVIST B. THERMOCAMERA STUDIES OF NITROUS OXIDE DISPERSION IN THE DENTAL SURGERY. SCAN J DENT RES 1983 JUNE; 91(3): 224-30.
6. BURM AG. OCCUPATIONAL HAZARDS OF INHALATIONAL ANAESTHETICS. BEST PRACT RES CLIN ANAESTHESIOL 2003 MAR; 17(1): 147-61.
7. SMITH DA. HAZARDS OF NITROUS OXIDE EXPOSURE IN HEALTHCARE PERSONNEL AANA J 1998 AUG; 66(4): 390-3.
8. SHORTRIDGE-MCCAULEY LA. REPRODUCTIVE HAZARDS: AN OVERVIEW OF EXPOSURES TO HEALTH WORKERS. AAOHN J 1995 DEC; 43(12): 614-21.
9. STERLING PA, GIRDLER NM. INVESTIGATION OF NITROUS OXIDE POLLUTION ARISING FROM INHALATIONAL SEDATION FOR THE EXTRACTION OF TEETH IN CHILD PATIENTS. INT J PED DENT 1998;8: 93-102.
10. CLARK MS AND BRUNICK AL. HANDBOOK OF NITROUS OXIDE AND OXYGEN SEDATION, 1999.
11. DONALDSON D, MEECHAN JG. THE HAZARDS OF CHRONIC EXPOSURE TO NITROUS OXIDE: AN UPDATE. BDJ 1995 FEB;11: 95-100.
12. SWEENY B, BINGHAM RM, AMOS RJ, PETTY AC, COLE PV. TOXICITY OF BONE MARROW IN DENTISTS EXPOSED TO NITROUS OXIDE. BMJ 1985, 291 (6495): 567-9.
13. GUIDELINES FOR THE SAFETY OF EMPLOYEES EXPOSED TO ANAESTHETIC GASES AND VAPOURS, UNIVERSITY OF WALES, COLLEGE OF MEDICINE, 2002.
14. HENRY RJ, PRIMOSCH RE AND COURTS FJ. THE EFFECTS OF VARIOUS DENTAL PROCEDURES AND PATIENT BEHAVIOUR UPON NITROUS OXIDE SCAVENGER EFFECTIVENESS. PEDIATRIC DENT 1992; 14 (1): 19-25.
Dental News, Volume XX, Number III, 2013 38 Nitrous Oxide Exposure

iCHIROPRO THE SMARTWAY TOYOURSUCCESS
The only control system offering the pre-programmed clinical sequences of the main implant brands is now available with a dedicated application for touchscreen tablets.
Discover the perfect working balance between your iPad* and exceptional electronics for controlling the MX-i LED micromotor. The most powerful motor on the market, with LED lighting guaranteeing a very long service life, is now also equipped with ceramic ball bearings that are lubricated for life.
The 20:1 L Micro-Series contr a-angle and the new iChiropro system redefine ergonomics and ease of use.
* iChiropro application compatible with iPad 1, 2, 3 and 4
Bien-Air Dental SA Länggasse 60Case postaleCH-2500 Bienne 6, SwitzerlandPhone +41 (0)32 344 64 64Fax +41 (0)32 344 64 91ichiropro@bienair.comwww.i chiropro.com
Tooth Bleaching
Management of Non-Vital Tooth Bleaching

Abstract
n_harrak@hotmail.com
St. Joseph University, Beirut, Lebanon
Noticeable discoloration of permanent teeth can impact on a person’s self-image, self-confidence, physical attractiveness and employability. Success in bleaching a non-vital discolored tooth varies by depending on the etiology, appearance, localization, severity, and adhesion to tooth structure. It can be defined as being extrinsic or intrinsic on the basis of localization and etiology. Moreover, the success of bleaching depends on several factors, where the most important are the cause of the discoloration of the tooth, the adequate diagnosis of the problem and the proper choice of the bleaching technique. Different phenomena can ensure that endodontically treated teeth become darker. Although there is a deficiency of evidencebased science in the literature that addresses the prognosis of bleached non-vital teeth, it is important to always be aware of the possible complications and risks that are associated with the different bleaching techniques and agents. This present article aims to emphasize on the different procedures to bleach a non-vital tooth in order to get the best results.
Key Words : Devitalized tooth, Tooth discoloration, Bleaching agents, Tooth bleaching techniques
Introduction
Bleaching discolored non-vital teeth has been described for the first time in 1864.1 A variety of bleaching agents were then used, such as chlorite, sodium hypochlorite, sodium perborate and hydrogen peroxide, alone or in combination, with or without heat activation.2 Different techniques were described such as the walking bleach technique, the thermocatalytic and inoffice techniques. Each one of these procedures has its own positive and negative points. Before proposing any treatment to the patient in a way to correct the discoloration of his or her devitalized tooth, it is essential to determine the exact cause of the color change. Discoloration of a tooth can occur during or after the formation of dentin and enamel, and can be associated with the patient himself or with a treatment performed by the dentist. Discolorations associated with the patient himself may be superficial or incorporated within tooth structure. Regarding the discolorations associated with the dentist, they are usually predictable and should be avoided.3,4 Tooth discoloration varies in etiology, appearance, location, severity, and affinity to tooth structure. It can be classified as intrinsic, extrinsic, or a combination of both, according to its location and etiology5 (Table 1).
Causes of dental dicoloration
Extrinsic
wine, coffee, tea, chocolate, tobacco, bacterial plaque, mouth rinses
Intrinsinc Local Systemic
Table1: Extrinsic and Intrinsic Causes of Teeth Discolorations
Pulp Necrosis, Intrapulpal Hemorrhage, Pulp Tissue Remnants, Endodontic Materials, Coronal Filling Materials, Root Resorption, Aging
Drug-related (Teracycline) Metabolic (Dystrophic calcification, Fluorosis) Genetic: Amelogenesis imperfecta, Dentinogenesis imperfecta
Dental News, Volume XX, Number III, 2013 Esthetic Dentistry
Dr. Nicole Harrak Jabbour
Pr. Carina Mehanna Zogheib
40





For over 45 years, ACE Surgical Supply has been committed to providing our customers with the best possible products available at unbeatable prices. We are the only multi-disciplinary surgical supply company. ACE continues to develop and
manufacture the highest quality, state-of-the-art products, while keeping a focus on customer service. Our highly qualified team is always available to answer any questions you may have about our extensive product line.

Tooth Bleaching
Bleaching Agents for whitening Devitalized Teeth
The most commonly products used for bleaching are carbamide peroxide, sodium perborate and hydrogen peroxide.6 The teeth whitening is now based on the use of hydrogen peroxide as an active agent. Hydrogen peroxide can be applied alone or produced by a chemical reaction of the sodium perborate or carbamide peroxide. Regarding the carbamide peroxide (CH6N2O2), upon reaction, it dissociates into hydrogen peroxide (H2O2) and urea (CH4N2O).7 Other whitening products use rather sodium perborate as the active ingredient. In the reaction, complex oxygen is created during removal of the sodium perborate. A peroxide gel is then released. This gel interacts with the tooth structure and becomes activated. Oxygen complex interacts with the tooth, saturates and modifies the amino acids. Double bonds of the oxygen are responsible for the discoloration of the tooth. Hydrogen peroxide, in turn, is used in different proportions in most bleaching products and dissociates in water and long chain molecules of dark colored chromophores.8 The tooth thus finds its original color or at least a lighter color. It should also be noted that the success of bleaching depends primarily on the ability of the agent to penetrate deeply into the dentinal tubules. The success of the treatment also depends on the concentration of the whitening agent and on the period during which the agent is in contact with the molecules. The bleaching agents are available in several concentrations, but different studies do not agree on the ideal concentration in terms of whitening power and preservation of oral tissues.9 Carrasco et al. found that the ideal product for whitening is carbamide peroxide 37%.10 According to Lim et al. carbamide peroxide 35% and hydrogen peroxide 35% are most effective for whitening, but the first one is preferable to the second, because it is less offensive to the tissues.11 The reason which hydrogen peroxide is harmful to tissues is that it releases free radicals toxic anions (perhydroxyl). While for Kinomoto et al. the sodium perborate 2 grams/ml is preferable to hydrogen peroxide 30%.12 In short, the authors conclude that hydrogen peroxide is too harmful to tissues and it is recommended to use an alternative product, preferably peroxide
carbamide, otherwise sodium perborate. However, we know that sodium perborate contains hydrogen peroxide because it is a byproduct of the dissociation of sodium perborate, as is also the case of carbamide peroxide as mentioned above. Hydrogen peroxide is the main constituent of either bleaching agent or the product of dissociation of carbamide peroxide or perborate sodium and it acts as an oxidizing agent by causing the formation of free radicals. Other studies (Weiger 1992) found that sodium perborate mixed with distilled water in a ratio of 2: 1 (g/ml) is a bleaching agent and prevents or at least minimizes the external cervical resorption of the root, an important consequence, although rare in internal bleaching, compared with a bleaching agent not combined with water.13 In cases of severe discoloration, hydrogen peroxide (H2O2) 3% can replace water. The use of 30% H2O2 is not recommended, always due to the risk of external resorption. Other authors have focused their research on the comparison between the hydrogen peroxide and carbamide peroxide. They concluded that in fact, as previously mentioned, these two products contain hydrogen peroxide and both work well. It appears, however, that H2O2 gives the desired results faster and requires a shorter treatment and a less exposure time than solutions of carbamide peroxide. In addition, there is less chance that dehydration occurs in hard tissues of the tooth treated with H2O2 as this system is based on aqueous gel, unlike carbamide peroxide gel based on anhydride. Carbamide peroxide seems to be softer on tissues, possibly due to the fact that the concentration of hydroxyl ion, acid, urea ammonium or carbonic acid is lower. In all whitening products, you can find other substances such agent thickener like Carbopol. This substance allows a slower reaction, but a longer period by altering the rate of release of oxygen. In addition, the urea produced by salivary glands can also be found in the whitening agents. The urea dissociates to ammonia and carbon dioxide. In addition to stabilizing the hydrogen peroxide, it has properties such as anticariogenic raising the pH of the solution and stimulating salivation. The high pH also facilitates whitening procedures.14 This is explained by the fact that in basic solution, a smaller amount of energy is required
Dental News, Volume XX, Number III, 2013 42 Esthetic Dentistry
Tooth Bleaching
for the formation of free radicals from hydrogen peroxide and level of reaction is higher, which leads to a better performance, in comparison with a bleach acid environment. It also contains glycerin due to its properties to increase the viscosity of the product and to facilitate handling thereof. However, it can cause tooth dehydration. A surfactant is also used to allow the hydrogen peroxide to diffuse into the tooth. Pigment dispersants, meanwhile, have the function to keep the pigments in suspension.15
Techniques and tips to follow to ensure the success of treatment
The most commonly methods used to whiten endodontically treated teeth are the walking bleach technique and the thermocatalytic technique. The thermo / photo and internal / external techniques are also used for whitening devitalized teeth. The walking bleach is preferable because this technique requires less time in the office and is safer and more comfortable for the patient.16
Walking Bleach Technique
The first description of the walking bleach technique with a mixture of sodium perborate and distilled water was mentioned in a congress report by Marsh and published by Salvas.17 In this procedure, the mixture was left in the pulp cavity for a few days, and the access cavity was sealed with provisional cement. The mixture of sodium perborate and water was reconsidered by Spasser18 and modified by Nutting and Poe19, who advocated the use of 30% hydrogen peroxide instead of water to improve the bleaching effectiveness of the mixture. A mixture of sodium perborate and water or hydrogen peroxide continues to be used today and has been described many times as a successful technique for intracoronal bleaching. There are numerous studies that have reported the successful use of the walking bleach technique for correction of severely discolored teeth caused by incorporation of tetracycline.20 This procedure starts with intentional devitalization and root canal treatment of the tooth to enable application of the bleaching agent into the pulp chamber. Because the methods of intentional devitalization and root canal treatment have risks, the advantages and disadvantages of this therapy should be
assessed. Restorative treatment options such as ceramic veneers should be considered as an alternative procedure. Furthermore, there is now evidence that prolonged bleaching with carbamide peroxide can also reach the desired results.21




Dental News, Volume XX, Number III, 2013 44 Esthetic Dentistry
A: Left maxillary incisor showing severe discoloration due to a trauma
B: After endodontic treatment, In-office internal and external bleaching was performed followed by a walking bleaching technique
C: Result 3 days after
D: Another session of internal and external bleaching was performed followed by a walking bleaching technique
Fig 1: In -office internal and external bleaching was performed to the left central incisor followed by walking bleaching technique
Fig 1.D
Fig 1.C
Fig 1.B
Fig 1.A






















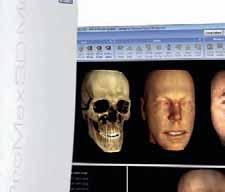






































Planmeca ProMax® 3D Unique product family More information www.planmeca.com Planmeca Middle East 306, City Tower 1, Sheikh Zayed Road P.O.Box 28826, Dubai tel. +971 4 33 27 682, mob. +971 50 450 2821, fax +971 4 33 27 684 dariush.vazvan@planmeca-middle-east.com Perfect sizes for all needs 3D X-ray • 3D photo • panoramic • cephalometric Romexis® software completes 3D perfection Romexis® PlanScan™ ProMax 3D ProFace™ Unique3Dcombination for openCAD/CAM
Tooth Bleaching
Case report
E: Esthetic restoration was completed 10 days after bleaching Fig 1.E

Before starting the treatment, the patient should be informed about the technique, the expected results and the possibility of a recurrence of the coloration.
1. Periapical radiographs should be taken to assess the status of periapical tissues and the quality of endodontic obturation. If it is unsatisfactory or questionable, it is imperative to retreat the tooth prior to the bleaching treatment.
2. Evaluate the quality and color of the restorations on the discolored tooth and replace if defective, because the discoloration of the tooth is often the result of a leak. In such cases, you only have to clean the pulp chamber and replace the defective restoration.
3. Evaluate the tooth shade with a shade guide, if possible, take photographs at the beginning and during the treatment, as this will be a reference point for any comparison. Clean and polish the tooth to be treated to remove any extrinsic stains.22
Preparation of the Pulp Cavity
Before preparation of the access cavity, rubber dam should be applied to protect the adjacent structures. After that, restorative materials closing the access to the pulp cavity should be removed. Then, check that the entire pulp chamber is adequately accessible and cleaned. All remnants of restorative materials and necrotic pulp tissue must be removed completely.
Cervical Seal
Regarding the root canal filling material ending up inside the pulp chamber, it must be removed to a depth of 1-2 mm (a periodontal probe can be used to be sure of the length) below the CEJ with a Gates-Glidden or a Largo bur. A pulp chamber completely sealed with aesthetic ma-
terial presents technical difficulties because the composite is difficult to distinguish from the tooth itself.
A root filling does not adequately prevent diffusion of bleaching agents from the pulpal chamber to the apical foramen.24 Hansen- Bayless and Davis 24 indicated that a base is required to prevent radicular penetration of bleaching agents. Therefore, sealing the root filling with a base is essential, for which a variety of dental materials such as glass-ionomer cements, intermediate restorative material (IRM), hydraulic filling materials (Cavit®, Coltosol®), resin composites, photoactivated temporary resin materials (Fermit®), zinc oxide– eugenol cement, and zinc phosphate cement have been suggested as an interim sealing agent during bleaching techniques. McInerney and Zillich 25 found that Cavit® and IRM provided better internal sealing of the dentin than did zinc phosphate cement, whereas HansenBayless and Davis 26 reported that Cavit® was a more effective barrier to leakage than IRM. Furthermore, hydraulic filling materials (Cavit® and Coltosol®) provided the most favorable cavosurface seal when they were firmly packed into the cavity space to prevent microleakage, when compared with a photoactivated temporary resin material (Fermit®), zinc oxide– eugenol cement, and a zinc oxide phosphate cement.27 Temporary sealing materials need to be removed before providing the final restoration of the access cavity. Rotstein et al. 28 demonstrated that a 2-mm layer of glass-ionomer cement was effective in preventing penetration of 30% hydrogen peroxide solution into the root canal. Thus, the use of this material as a base during bleaching presents the additional advantage that it can be left in place after bleaching and can serve as a base for the final restoration. The sealing material should reach the level of the epithelial attachment or the CEJ, respectively, to avoid leakage of bleaching agents into the periodontium. The shape of the cervical seal should be similar to the external anatomic landmarks, thus reproducing CEJ position and interproximal bone level. A flat barrier, leveled with the labial CEJ, leaves a large portion of the proximal dentinal tubules unprotected. Therefore, the barrier should be determined by probing the level of the epithelial attachment at the mesial, distal, and labial aspects of the tooth. The intracoronal level of the barrier is placed 1
Dental News, Volume XX, Number III, 2013 46
Tooth Bleaching
mm incisal to the corresponding external probing of the attachment. With this method the coronal outline of the attachment defines an internal pattern of the shape and location of the barrier. However, the impact of the bleaching agents on the discolored dentin should not be hampered by the cervical seal. Dentin tubules at the coronal third of the root run in an oblique direction from the apex to the crown, so that the tubules at the CEJ are originating more apically inside the root canal. If bleaching of the cervical region of the tooth is required, a stepwise reduction of the labial part of the seal and use of a mild bleaching agent are recommended for the final dressings. The placement of a piece of rubber dam has been suggested to act as a further barrier to isolate filling material from the bleaching agent. However, Hosoya et al. 29 reported no significant differences between the groups with and without the placement of this barrier.
Application of the Bleaching Agent
The bleaching agent can be applied with an amalgam carrier or plugger or with the syringe and should be changed every 3–7 days. Successful bleaching becomes apparent after 2– 4 visits, depending on the severity of the discoloration. The patients should be instructed to evaluate the tooth color on a daily basis and return when the bleaching is acceptable to avoid “over-bleaching”.
Temporary Filling
A temporary filling (Cavit®, Coltosol®) will be applied to the outer periphery of the cavity, Then the access of the cavity will be sealed with composite. The patient should be informed that the bleaching works slowly and that the results should be visible a few days later. Every week the patient must show up to the clinic to repeat the procedure.30
Restoration of the Access Cavity and Postoperative Radiographs
When the devitalized tooth reaches the desired color, the access cavity will be sealed with a composite.
To obtain optimal adhesive bond between the restorative material and hard tissues of the tooth, it is advisable to proceed with the establishment of the permanent restoration after a
period of approximately 10 days after the last bleaching therapy. Whitening the tooth leaves supersaturated oxygen, which inhibits the polymerization of the resins. A radiograph of the bleached tooth will be taken on all annual appointments to diagnose the earliest possible cervical resorption.31
Thermocatalytic Technique
It is a technique where the hydrogen peroxide 30-35% is placed in the pulp chamber and activated by a heating source, either with an electric heating devices (Touch’ n Heat, System B) or especially designed lamps. The steps for placing the bleaching agent and sealing the pulp chamber are similar to the walking bleach technique. Heat application is repeated 3 or 4 times at every appointment. When heat is applied, a reaction produces foam and releases the oxygen present in the preparation.32 The major risk of this technique is the external root resorption due to the excessive heat applied on the tooth.33
Combined Technique
When an agent fails to remove a stain completely or when multiple patches of different origins are present on the same tooth, a combination of whitening techniques can be used. The technique combines external / internal bleaching, so the patient can do it at home. This technique is both simple and effective. It consists of putting the whitening gel in a tray especially customized for the patient and placed directly on the tooth. There are certain risks with this technique, in that an unsealed access opening enables bacteria and stains to penetrate into dentin. Therefore, a restorative material such as glass-ionomer cement or resin composite should be used to seal the root filling at the orifice.34
Discussion
Despite many clinical reports, there are few scientific evidence based studies on devitalized tooth whitening.35 Most reports present optimal initial results after bleaching, with complete color matching of the bleached tooth (teeth) with the adjacent one(s). However, occasionally darkening after internal bleaching can be observed,36 which is presumably caused by diffusion of staining substances and penetration of bacteria through marginal gaps between the filling and
Dental News, Volume XX, Number III, 2013 48 Esthetic Dentistry
Tooth Bleaching
the tooth. It is worth noting that the opinion of the patient regarding the success of the therapy is often more positive than the opinion of the dentist. One study reported an 80% rate of success after 1 year and 45% after 6 years of 20 cases that were chemically bleached by using the thermocatalytic technique.37 Some authors have suggested that teeth that have been discolored for several years do not respond as well to bleaching as teeth that are stained for a short period of time. Furthermore, it is uncertain whether darkening after bleaching is more likely when the tooth is heavily or mildly discolored.38 Discoloration caused by restorative materials has a dubious prognosis. Certain metallic ions (mercury, silver, copper, iodine) are extremely difficult to remove or alter by bleaching. Brown39 reported that trauma- or necrosis-induced discoloration can be successfully bleached in about 95% of the cases, compared with lower percentages for teeth discolored as a result of medicaments or restorations. There is a difference in opinion as to whether teeth that respond rapidly to bleaching have a better long-term color stability prognosis. Some studies have reported that stained teeth in young patients are easier to bleach than discoloration in older patients, presumably because the wide open dentinal tubules in young teeth enable a better diffusion of the bleaching agent. However, not all studies are in agreement with age related success of bleaching. Teeth with internal discoloration caused by root canal medicaments, root-filling materials, or metallic restorations such as amalgam have a poor prognosis, because this type of discoloration is difficult to bleach and tends to reappear over time because of the tenacity of the oxidizing products to dental tissues. Anterior teeth with interproximal restorations occasionally show less optimum results than teeth with a palatal access cavity only. This might be attributed to the fact that resin composites cannot be bleached.40 In these cases, replacement of existing restorations after the whitening treatment is recommended to get optimal results.
Conclusion
Today, the causes of discoloration of endodontically treated teeth are well recognized, and techniques of bleaching that have proved their efficacy over the years, yield optimal results if
the cases have been selected appropriately and if the dentist and the patient are aware of the remote risks of dental bleaching. Therefore, we can successfully treat tooth discoloration that has undergone a root canal using the walking bleach technique. Bleaching is done by temporarily placing a mixture of perborate (tetrahydrate) of sodium and water in the pulp chamber. This releases the mixture H2O2 which is capable of reacting with the coloring substances. The use of thermocatalytic method by heating a solution of 30% H2O2 is not recommended as this method increases the risk of external cervical resorption. For the same reason, the dentist should not use either 30% H2O2 for the walking bleach technique. To avoid leakage of the bleaching agent into the dentine, it is necessary to place a compact filling material, that is to say, gutta percha, and an additional cervical barrier, before beginning the bleaching technique. For a long-term success, it seems important to restore the access cavity with an adhesive filling material, which prevents the infiltration of bacteria and stains. The fact of following these procedures provides a much safer bleaching technique in the course of maintaining the integrity of the tooth and above the surrounding tissue, while maintaining an optimum result goal. Nevertheless, this treatment involves minimal risk. It is therefore desirable to have a product providing the benefits of effective bleaching agent while eliminating the associated risks.
REFERENCES
1. TRUMAN J. BLEACHING OF NON-VITAL DISCOLORED ANTERIOR TEETH. DENT TIMES1864;1:69 –72.
2. WATTS A, ADDY M. TOOTH DISCOLORATION AND STAINING: A REVIEW OF THE LITERATURE. BR DENT J 2001;190:309-16.
3. MATIS BA, MOUSA HN, COCHRAN MA, ECKERT GJ. CLINICAL EVALUATION OF BLEACHING AGENTS OF DIFFERENT CONCENTRATIONS. QUINTESSENCE INT 2000;31: 303310.
4. FOR THE DENTAL PATIENT: TOOTH WHITENING – WHAT YOU SHOULD KNOW. JADA 2009;40:384.
5. MANUEL ST, ABHISHEK P, KUNDABALA M. ETIOLOGY OF TOOTH DISCOLORATION- A REVIEW. NIG DENT J 2010; 18(2): 56-63.
6. FAUNCE F. MANAGEMENT OF DISCOLORED TEETH. DENT CLIN NORTH AM 1983;27: 657–670.
7. PLOTINO G, BUONO L. NON-VITAL TOOTH BLEACHING: A REVIEW OF LITERATURE AND CLINICAL PROCEDURES. J ENDOD 2008;34(4):394-407.
8. ROSTEIN I. TOOTH DISCOLORATION AND BLEACHING. IN: INGLE JI, BAKLAND LK, EDS ENDODONTICS.5TH ED. HAMILTON, ONTARIO, CANADA: BC DECKER INC, 2002:845–60.
9. J.E DAHL ET U. PALLESEN. TOOTH BLEACHING – A CRITICAL REVIEW OF THE BIOLOGICAL ASPECTS 2003;14 (4): 292.
10. L.D. CARRASCO, I.C. FRÖNER ET AL. EFFECT OF INTERNAL BLEACHING AGENTS ON DENTINAL PERMEABILITY OF NON-VITAL TEETH : QUANTITATIVE ASSESSMENT. DENTAL TRAUMATOLOGY 2003(19) :85-89.
11. M.Y. LIM, S.O.Y. LUM ET AL. AN IN-VITRO COMPARISON OF THE BLEACHING
Dental News, Volume XX, Number III, 2013 50 Esthetic Dentistry








fits in This is where
Tooth Bleaching
EFFICACY OF 35% CARBAMIDE PEROXIDE WITH ESTABLISHED INTRACORONAL BLEACHING AGENTS.INT J ENDO 2004(37):483-488.
12. Y. KINOMOTO, D.L. CARNES ET S. EBISU.CYTOTOXICITY OF INTRACANAL BLEACHING AGENTS ON PERIODONTAL LIGAMENT CELLS IN VITRO. J ENDOD 2001(27):574-577.
13.R. M. WAITE, D. L. CARNES JR, W. A. WALKER. «MICROLEAKAGE OF TERM USED WITH SODIUM PERBORATE/WATER AND SODIUM PERBORATE/SUPEROXOL IN THE « WALKING BLEACH » TECHNIQUE», J ENDOD 1998(24):648-650.
14. ZABOKOVA BILBILOVA E, SOTIROVSKA IVKOVSKA A, AMBARKOVA V.CORRELATION BETWEEN SALIVARY UREA LEVEL AND DENTAL CARIES. PRILOZI. 2012 JUL;33(1):289-302.
15. L. GREENWALL, G. FREEDMAN ET AL. BLEACHING TECHNIQUES IN RESTORATIVE DENTISTRY : AN ILLUSTRATED GUIDE, THEME MEDICAL PUB 2005.
16. P.CARROTTE. «ENDODONTIC PROBLEMS», BRITISH DENTAL JOURNAL. 2005; 198:127-133.
17. SALVAS CJ. PERBORATE AS A BLEACHING AGENT. J AM DENT ASSOC 1938;25:324.
18. SPASSER HF. A SIMPLE BLEACHING TECHNIQUE USING SODIUM PERBORATE. N Y STATE DENTLJ 1961;27:332– 4.
19. NUTTING EB, POE GS. A NEW COMBINATION FOR BLEACHING TEETH. J SOUTH CALIFORNIAN DENTASSOC 1963;31:289.
20. ABOU-RASS M. LONG-TERM PROGNOSIS OF INTENTIONAL ENDODONTICS AND INTERNAL BLEACHING OF TETRACYCLINE-STAINED TEETH. COMP CONTIN EDUC DENT 1998;19:1034 –50.
21. BARATIERI LN, RITTER AV, MONTEIRO S JR, CALDEIRA DEANDRADA MA, CARDOSO VIEIRA LC. NON-VITAL TOOTH BLEACHING: GUIDELINES FOR THE CLINICIAN. QUINTESSENCE INT 1995; 26:597– 8.
22. ATTIN T, PAQUE F, AJAM F, LENNON AM. REVIEW OF THE CURRENT STATUS OF TOOTH WHITENING WITH THE WALKING BLEACH TECHNIQUE. INT ENDOD J. 2003 MAY;36(5):313-29.
23. SMITH JJ, CUNNINGHAM CJ, MONTGOMERY S. CERVICAL CANAL LEAKAGE AFTER INTERNAL BLEACHING PROCEDURES. J ENDOD 1992;18:476–81.
24. HANSEN-BAYLESS J, DAVIS R SEALING ABILITY OF TWO INTERMEDIATE RESTORATIVE MATERIALS IN BLEACHED TEETH. AM J DENT 1992;5:151– 4.
25. MCINERNEY ST, ZILLICH R. EVALUATION OF INTERNAL SEALING ABILITY OF THREE MATERIALS. J ENDOD 1992;18:376–8.
26. HANSEN-BAYLESS J, DAVIS R. SEALING ABILITY OF TWO INTERMEDIATE RESTORATIVE MATERIALS IN BLEACHED TEETH. AM J DENT 1992;5:151– 4.
27. HOSOYA N, COX CF, ARAI T, NAKAMURA J. THE WALKING BLEACH PROCEDURE: AN IN VITRO STUDY TO MEASURE MICROLEAKAGE OF FIVE TEMPORARY SEALING AGENTS. J ENDOD 2000;26:716–8.
28. ROTSTEIN I, ZYSKIND D, LEWINSTEIN I, BAMBERGER N. EFFECT OF DIFFERENT PROTECTIVE BASE MATERIALS ON HYDROGEN PEROXIDE LEAKAGE DURING INTRACORONAL BLEACHING IN VITRO. J ENDOD 1992;18:114 –7.
29. HOSOYA N, COX CF, ARAI T, NAKAMURA J. THE WALKING BLEACH PROCEDURE: AN IN VITRO STUDY TO MEASURE MICROLEAKAGE OF FIVE TEMPORARY SEALING AGENTS. J ENDOD 2000;26:716–8.
30. HOSOYA N, COX C F, ARAI T, NAKAMURA J: THE WALKING BLEACH PROCEDURE:
AN IN VITRO STUDY TO MEASURE MICROLEAKAGE OF FIVE TEMPORARY SEALING AGENTS. J ENDOD 2000,26: 716–718.
31. MÜLLER ARCARI G, ARAÙJO E, BARATIERI L N, LOPES G C: MICROTENSILE BOND STRENGTH OF A NANOFILLED COMPOSITE RESIN TO HUMAN DENTIN AFTER NONVITAL TOOTH BLEACHING. J ADHES DENT 2007 (9): 333–340.
32. DALHSTROM S,HEITHERSAY G, BRIDGES T.H YDROXYL RADICAL ACTIVITY IN THERMOCATALYTICALLY BLEACHED ROOT-FILLED TEETH. ENDODONTIC DENTAL TRAUMATOLOGY 1997;13:119-125.
33. MACISAAC AM, HOEN CM. INTRACORONAL BLEACHING: CONCERNS AND CONSIDERATIONS. J CAN DENT ASSOC. 1994 JAN; 60(1):57-64 .
34. TRONSTAD L. BLEACHING OF DISCOLORED TEETH. CLINICAL ENDODONTICS STUTTGART,GERMANY. 2003; 236-241.
35. NIEDERMAN R, FERGUSON M, URDANETA R. EVIDENCE BASED ESTHETIC DENTISTRY. J ESTHET DENT 1998;10:229 –34.
36. CARRASCO L.D., FRONER I.C ET AL. EFFECT OF INTERNAL BLEACHING AGENTS ON DENTINAL PERMEABILITY OF NON-VITAL TEETH : QUANTITATIVE ASSESSMENT. DENTAL TRAUMATOLOGY 2003; 19:85-89.
37. AUSCHILL T M, HELLWIG E, SCHMIDALE S, SCULEAN A, ARWEILER N B: EFFICACY SIDE EFFECTS AND PATIENTS ACCEPTANCE OF DIFFERENT BLEACHING TECHNIQUES (OTC, IN-OFFICE AT-HOME). OPER DENT 2005,30: 156–163.
38. DIETSCHI D, ROSSIER S, KREJCI I: IN VITRO COLORIMETRIC EVALUATION OF THE EFFICACY OF VARIOUS BLEACHING METHODS AND PRODUCTS. QUINTESSENCE INT 2006,37: 515–526.
39. BROWN G: FACTORS INFLUENCING SUCCESSFUL BLEACHING OF THE DISCOLORED ROOTFILLED TOOTH. ORAL SURG ORAL MED ORAL PATH 1965; 20: 238–244.
40. DELIPERI S, BARDWELL D N: TWO-YEAR CLINICAL EVALUATION OF NON-VITAL TOOTH WHITENING AND RESIN COMPOSITE RESTORATIONS. J ESTHET RESTOR DENT 2005;17: 369–378.
Dental News, Volume XX, Number III, 2013 52
Esthetic Dentistry









More Pictures Available On September 25-28, 2013 School of Dentistry, Hadath, Lebanon www.facebook.com/dentalnews1 54 Lebanese University International Convention 2013
PR. MOUNIR DOUMIT DEAN OF THE SCHOOL OF DENTISTRY
DABKE PERFORMANCE FOR THE OPENING CEREMONY
LEFT TO RIGHT: DRS. RAHIL DOUEIHY, KASIM HASHEM, ELIE MAALOUF, MOUNIR DOUMIT, FATMEH HAMASNI, JOSEPH CHAER, ESSAM OSMAN
DR. ZIAD NOUJEIM, CHAIRPERSON SCIENTIFIC COMMITTEE
DR. MOHAMAD RIFAII, GENERAL COORDINATOR
DR. KHALDOUN RIFAII, WELCOMING DR. KASIM HASHEM








 LEFT TO RIGHT
DR. TONY DIB, PR. MOUNIR DOUMIT, PR. NADIM BABA
PR. MOTLU OZCAN AND DR. ARZU NAIPOGLU DURING THE BREAK AT THE TENT
LEFT TO RIGHT
DRS. ANTOINE SAADE, ZIAD SALAME, CHARLES SFEIR
LEFT TO RIGHT
MR. ANTOINE BARAKA, DR. JEAN MARIE MEGARBANE, DR. CEDRIC HADAD
LEFT TO RIGHT
DR. TONY DIB, PR. MOUNIR DOUMIT, PR. NADIM BABA
PR. MOTLU OZCAN AND DR. ARZU NAIPOGLU DURING THE BREAK AT THE TENT
LEFT TO RIGHT
DRS. ANTOINE SAADE, ZIAD SALAME, CHARLES SFEIR
LEFT TO RIGHT
MR. ANTOINE BARAKA, DR. JEAN MARIE MEGARBANE, DR. CEDRIC HADAD




PICTURES FROM THE EXHIBITION FLOOR






The Power. The Silence.



The new Tornado Super Silent


























Tornado – the new generation of compressors from
Dürr Dental
Dürr Dental, the inventor of oil-free dental compressors, presents an unbelievably quiet and powerful compressor for dentistry in the form of the new “Made in Germany“ Tornado.
▪ Oil-free, dry, and hygienic


▪ One of the quietest of its kind
▪ Dust- and Sandresistant
▪ Antibacterial inner tank coating
▪ Low-maintenance thanks to membrane-drying unit
Duerr Dental Middle East, P.O.Box: 87355, Al Ain - U.A.E., Mobile: +971 (0) 50 - 550 84 12, Fax: +971 (0) 3 767 - 5615, email: koll.m@duerr.de

COMPRESSED AIR SUCTION IMAGING DENTAL CARE
HYGIENE

HENRY SCHEIN BRAND
Beyond Satisfaction!
Henry Schein Brand products offer our clients maximum value without compromising on quality.
We offer quality products you can trust to fulfill your practice merchandise needs—each bearing the Henry Schein Seal of Excellence, your guarantee of satisfaction.

Henry Schein, Inc. is the world’s largest provider of health care products and services to office-based dental, medical, and animal health practitioners.









Lebanese Dental Association North Lebanon www.facebook.com/dentalnews1 More Pictures Available On May 30-31, June 1, 2013 Las Salinas, Anfeh, Lebanon
TROPHY TO PR. MOUNIR DOUMIT DEAN OF THE LU TROPHY TO DR. MOHAMAD BOUKANAAN TROPHY TO DR. ELIE MAALOUF PRESIDENT OF THE LDA TROPHY TO DR. HASSAN ALLOUL TROPHY TO NASSIF KALOUCH-PRESIDENT OF THE REPUBLIC REPRESENTATIVE . . z .
DR. RAHIL DOUEIHY, PRESIDENT OF LDA-TRIPOLI
DR.
FOR HER LECTURE ON OCCLUSION


FOR HER LECTURE ON PROSTHETICS







 LEFT TO RIGHT: DR. WALID NEHME, DR. RAHIL DOUEIHY, PR. ANTOINE KHOURY, DR. JALAL KASSAB
ILIA ROUSSOU
DR. EHAB HEIKAL LECTURING ON MANAGEMENT
DR. HALA ABBOUD
LEFT TO RIGHT: DR. CHRISTIAN MAKARI, DR. RAHIL DOUEIHY, PR. NADA NAAMAN-DEAN ST. JOSEPH DENTAL SCHOOL, PR. ANTOINE KHOURY
LEFT TO RIGHT: DR. WALID NEHME, DR. RAHIL DOUEIHY, PR. ANTOINE KHOURY, DR. JALAL KASSAB
ILIA ROUSSOU
DR. EHAB HEIKAL LECTURING ON MANAGEMENT
DR. HALA ABBOUD
LEFT TO RIGHT: DR. CHRISTIAN MAKARI, DR. RAHIL DOUEIHY, PR. NADA NAAMAN-DEAN ST. JOSEPH DENTAL SCHOOL, PR. ANTOINE KHOURY
RECOGNITIONS TO:
PR. ESSAM OSMAN-DEAN BAU DENTAL SCHOOL, DR. DOUEIHY, DR. RAFEH JOBOURI-PRESIDENT OF THE IRAK DENTAL ASSOCIATION
1mm layer TheraCal LC Regenerative layer stimulates hydroxyapatite stays where it is placed calcium hydroxide and RMGI technique TheraCal LC is an internal flowable pulpal protectant material known as Resin Modified Calcium Silicates (RMCS) Surrounding enamel is etched All-Bond Universal single-bottle light-cured adhesive can be used for any dental procedure Core-Flo DC is a radiopaque dual-cured flowable material ideal for core build-up, post cementation and dentin replacement. To learn more e-mail intl@bisco.com or visit www.bisco.com TheraCal LC NEW Products from BISCO All-Bond Universal Core-Flo DC








 PICTURES FROM THE EXHIBITION FLOOR
PICTURES FROM THE EXHIBITION FLOOR














08-09
Jumeirah Beach Hotel Dubai UAE 5th Dental - Facial Cosmetic International Conference AMERICAN ACADEMY OF IMPLANT DENTISTRY Joint Meeting with Centre for Advanced Professional Practices (CAPP) is an ADA CERP Recognized Provider. ADA CERP is a service of the American Dental Association to assist dental professionals in identifying quality providers of continuing dental education. ADA CERP does not approve or endorse individual courses or instructors, nor does it imply acceptance of credit hours by boards of dentistry. Platinum Sponsor Gold Sponsors Organizers 2nd Global Conference
November 2013







New Philips Zoom offers advanced light technology that gives you more control and your patients even greater results. And with a worldwide public awareness campaign to drive patients to you and new programs to help you easily integrate Philips Zoom WhiteSpeed light-activated whitening into your practice, you’ll have the answer to the confident, beautiful smile your patients are asking for.
Ask about the new Philips Zoom WhiteSpeed today. Visit philipsoralhealthcare.com. For more information, contact your local sales representative or call +971 50 643 1707.









professional whitening system*
The #1 patient-requested
is now better than ever.
*In the United States. Philips is a registered trademark of Koninklijke Philips Electronics N.V. ©2012 Discus Dental, LLC. All rights reserved. To be dispensed by or on the order of a dental professional only. ADV-3545ARA 101912 EGYPT Elsafaa Tel: 2 (0) 10 1466997 JORDAN Al Ghad Medical Supplies Tel: +962 6 552 6358 KUWAIT Alpha Medical Co. Tel: +965 2247 8611 LEBANON G. Tamer Holding Tel: 961 1 694000 MOROCCO Ortho-Rama +21 2 22862086 SAUDI ARABIA Bashir Shakib Al Jabri & Co. Tel: +966 26700430 TUNISIA MSI Tel: +216 73 449 401 UNITED ARAB EMIRATES Al Hayat Pharmaceuticals Tel: +971 6 5592 481


OptiBond™ XTR
Unmatched power for all your direct and indirect restorations.


OptiBond XTR Self-Etch, Light-Cure Univesal Adhesive. Extraordinary performance for long-lasting restorations.
post-operative sensitivity, maximizes patient comfort. A true universal adhesive. Enables use with all cements, core build-up materials and substrates. For more information visit: Your practice is our inspiration.™ KerrHawe SA P.O. Box 2686934 Bioggio Switzerland Freephone: 00800 41 05 05 05 Fax: ++41 91 610 05 14 www.kerrdental.eu
Minimizes
OptiBond XTR Self-Etch, Light-Cure Universal Adhesive.
Clear, long resin tags with penetration into lateral dentin tubule branches (2,000x).









Upgrade to Brilliance
The award winning A-dec LED light is now available to existing A-dec light users. Replacing your current A-dec light head with the new A-dec LED light is quick, easy and entirely hassle-free. Upgrade to 20% more luminance while consuming one-fifth of the power needed for halogen bulbs. Are you eligible for an upgrade? As long as you have a working flexarm on an A-dec light manufactured after 1993, you can upgrade it to an A-dec LED light.
For more information please visit www.a-dec.com
Natural Elegance® Universal Bond For Improved Sealing
Henry Schein® introduces the new Natural Elegance® Universal Bond featuring a singlecomponent, light-cure system that primes and bonds in one easy step. The total-etch system, responsive to all curing lights, provides an excellent bond to both dentin and enamel. The etching-required seal helps prevent recurrent decay and has low postoperative sensitivity. The Natural Elegance® Universal Bond is available in individual 5 mL bottle or 50 unit dose packages.
For more information please visit www.henryscheindental.com
Cavex ColorChange – 9 days dimensionally stable!
Impression materials and especially alginates are core products for Cavex Holland BV. Ongoing research and development are key in the structural outperformance of Cavex alginates compared to the competition. In 2001 we already improved dimensional stability of Cavex ColorChange up to 5 days. This means that when properly stored, an impression with Cavex ColorChange can still be perfectly poured (at least twice) after 5 days. Impressive, but by no means a reason to stop further improvements. In our continuous strive of improving Cavex products we accumulated unparalleled knowledge on the chemistry of the ingredients used in our alginates. This has lead up to the point that evaluation by the department Dental Material Science at ACTA, shows that the quality of Cavex ColorChange permits for an astounding dimensional stability of 9 days. This puts Cavex ColorChange in a whole different league than the competition, making Cavex ColorChange the absolute number 1 alginate in the world.
For more information please visit www.cavex.nl.
One Shape® Paper Points Shaping
Advantages of the One Shape® Paper Points Shaping by Micro Mega: Quick and efficient drying. Shaped for easy and reliable penetration to the apex. Easy-to-identify thanks to the coloured tip.
One Shape® Paper Points Shaping are available in length 29 mm. Packaging: 60 points per box.
For any further information please E-mail us at mmid@micro-mega.com
Dental News, Volume XX, Number III, 2013
#76
Cavex ColorChange
The best - got even better!



9 days dimensionally stable
Exceptional tear resistance
Can be poured at least twice
25 micron detail reproduction
Chromatic
5 year shelf life
CAVEXYOUR IMPRESSION IS OUR CONCERN
Ongoing research and development are key in the structural outperformance of Cavex alginates compared to the competition. In 2001 we already improved dimensional stability of Cavex ColorChange up to 5 days. Impressive, but by no means a reason to stop further improvements.
In our continuous strive of improving Cavex products we accumulated unparalleled knowledge on the chemistry of the ingredients used in our alginates. This has lead up to the point that evaluation by the department Dental Material Science at ACTA, shows that the quality of Cavex ColorChange permits for an astounding dimensional stability of 9 days. This puts Cavex ColorChange in a whole different league than the competition, making Cavex ColorChange the absolute number 1 alginate in the world.
Cavex Holland BV, P.O. Box 852, 2003 RW Haarlem, The Netherlands. Tel +31 23 530 77 00 Fax +31 23 535 64 82 dental@cavex.nl www.cavex.nl






New features and improvements to Planmeca ProMax® 3D X-ray units
Planmeca ProMax® 3D is a family of true all-in-one X-ray units that provide digital panoramic, cephalometric and CBCT imaging, 3D face photos and 3D model scans, i.e. impression and plaster cast scans. Planmeca constantly develops its state-of-theart imaging units and is now proud to introduce new features that further improve their image quality, patient comfort and usability. In addition to their wide selection of volume sizes and optimal patient doses, the Planmeca ProMax 3D family units are known for their simple and effortless patient positioning offering an unrestricted view of the patient and easy side entry access. Planmeca now introduces to the units a new adjustable and autoclavable patient support that helps to keep the patient better in place and thus also improves patient comfort. Planmeca’s user interface designers have also designed a completely new graphical user interface to all Planmeca’s 2D and 3D X-ray units. The big interface guides the user to a fluent workflow with clear and explicit texts and preprogrammed target sites and exposure values. For more information please visit www.planmeca.com
Scalpel handle for micro blades entirely made in pure titanium
The manufacture of large and most complex tools in titanium is obtained only by means of technologically advanced machineries.
- This new titanium scalpel handle is the result of one among many other investments that Medesy has recently made on the most modern last generation technological equipment.
- An excellent ergonomic design specifically conceived to guarantee the utmost comfort and safest handling.
- Nothing lighter than titanium!
- High precision non-slip knurling.
- Medesy special design which assures maximum comfort, and secure grip For more information please visit www.medesy.it
TOTALCEM, THE ALL-IN-ONE CEMENT
Itena, the French dental product manufacturer and restoration expert; presents TotalCem, a self-etching and self-adhesive permanent resin cement.
TotalCem provides a strong adhesion to the dentine, enamel, porcelain, zirconium, composites, ceramic or metal for the cementation of posts, inlays, onlays, crowns and bridges. The procedure is very simple. All is done in one step: etching, primer, bonding and cementation. The product can be kept at room temperature; there is no need to refrigerate. As it is a dual-cure cement, the polymerization is guaranteed, even for areas with limited light penetration. Furthermore the excess can be easily cleaned thanks to a gel phase. The cement can also be used on vital teeth. The comfort of the patient is still ensured as the product gives no post-operative sensitivities. With the Automix syringe, the base and the catalyst are perfectly proportioned and mixed. As you can choose between, three different types of intra-oral tips (fine, extra-fine and ultra-fine) the placement of TotalCem is extremely easy. The film thickness gives a perfect marginal integrity. TotalCem radiopacity also allows a visual confirmation.
For more information please visit www.itena-clinical.com
Dental News, Volume XX, Number III, 2013
#78
VITA Easyshade® Advance 4.0 Analog goes digital.
Determine and verify tooth shades with digital precision.
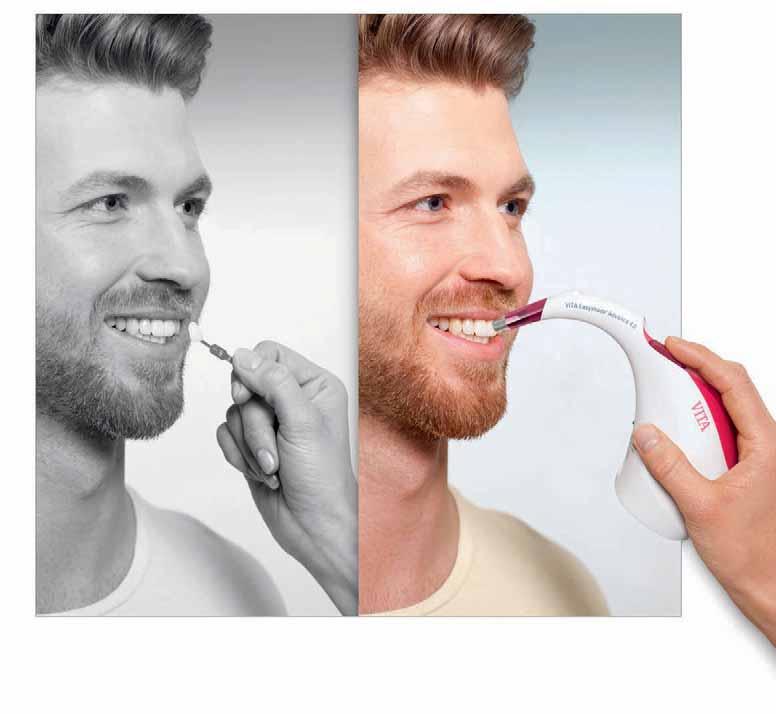

At VITA, we see progress as self-improvement. With this in mind, the time has come to leave shade sticks behind and to move ahead with VITA Easyshade Advance 4.0. Whether it‘s VITA SYSTEM 3D-MASTER or VITA classical A1–D4, this digital measuring device determines and verifies all tooth

VITA shade, VITA made.
shades in a matter of seconds and with absolute precision. Automatic activation, Bluetooth ®, bleaching mode and a whole range of other innovations guarantee maximum precision for even greater reliability and comfort. www.vita-zahnfabrik.com facebook.com/vita.zahnfabrik
3452E
New!Automaticactivation guaranteesoptimalshadedetermination



Carriere Self-Ligating Bracket







* Typical case: Patient 16 years Start of treatment, prior to placement of Carriere Distalizer Appliance 5.10.10
Turn Complex Class II into Simple Class I Cases
With its non-invasive design, the Carriere Distalizer Appliance corrects Class II malocclusion at the beginning of treatment, prior to bracket placement when patient motivation is highest. Call us today at 888.851.0533 or visit us online at OrthoOrganizers.com.

Carriere Ortho 3D
A FREE App. for iPads, iPhones, and Android tablets and phones
* Images courtesy of Dr. Clark Colville. © 2012 Ortho Organizers, Inc. All rights reserved.
Class
Class I achieved,
Distalizer
Total orthodontic treatment completed
S HIFTI NG THE WAY YO U THI N K A B O UT OR TH ODON TI CS. The Carriere® Distalizer™ Appliance
II to
and Carriere
Appliance treatment completed 8.30.10
3.7.12







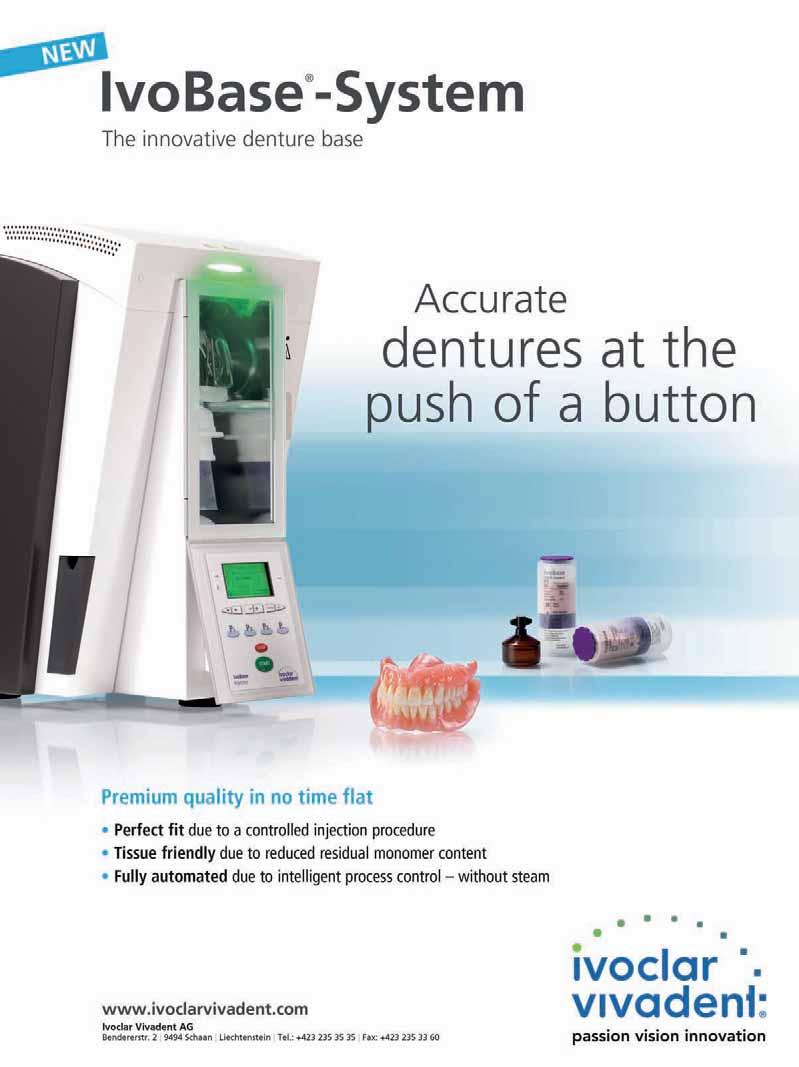






































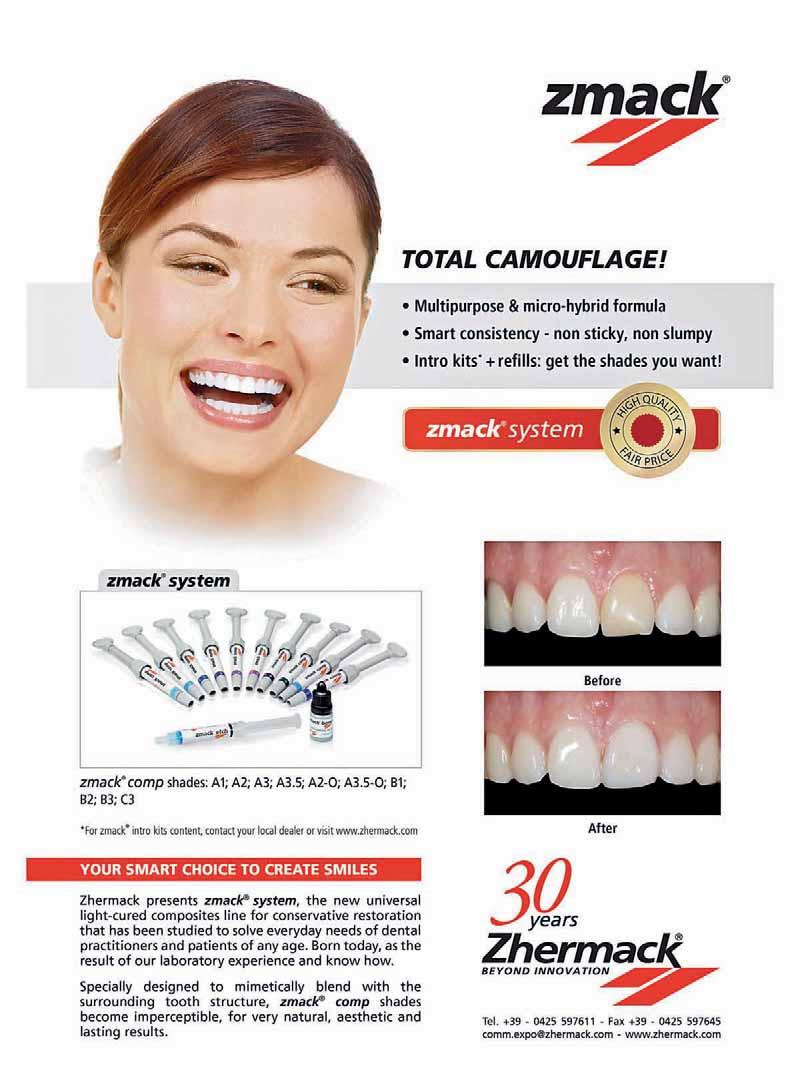







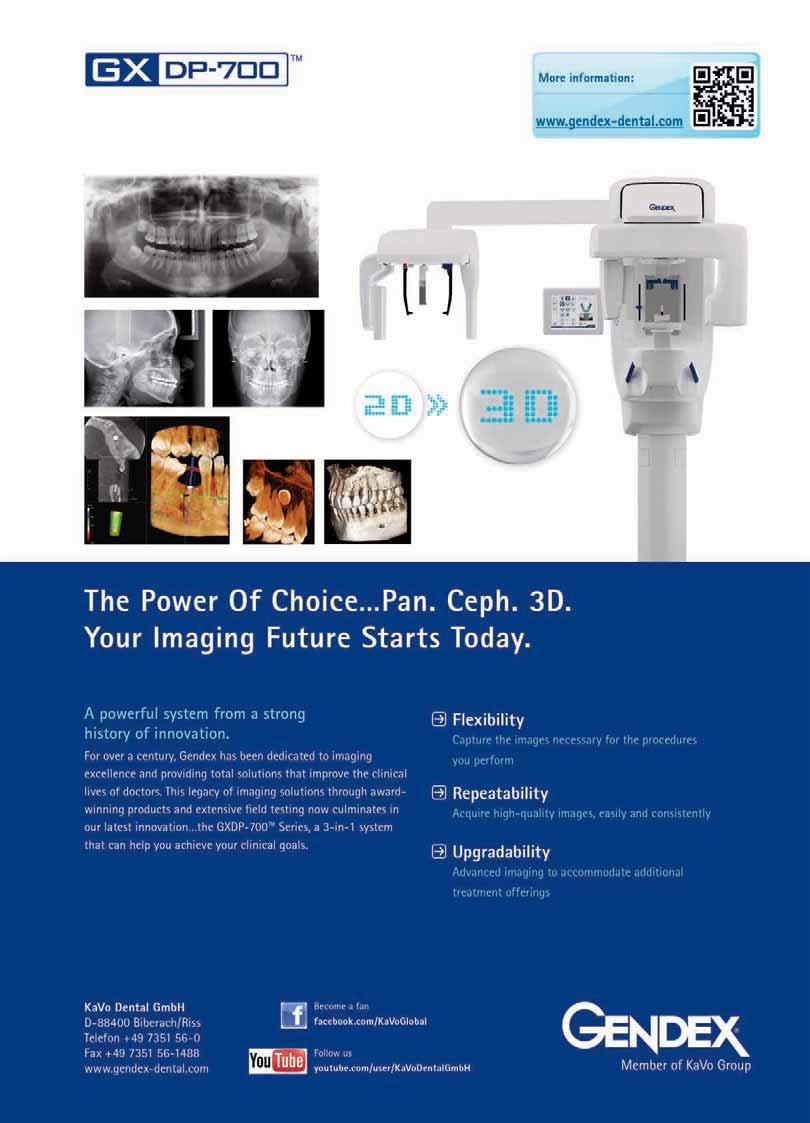


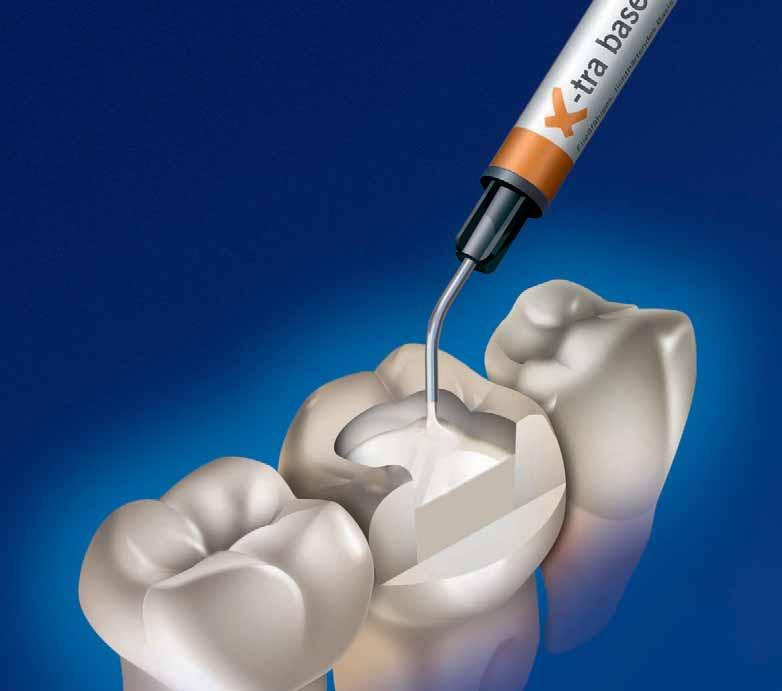


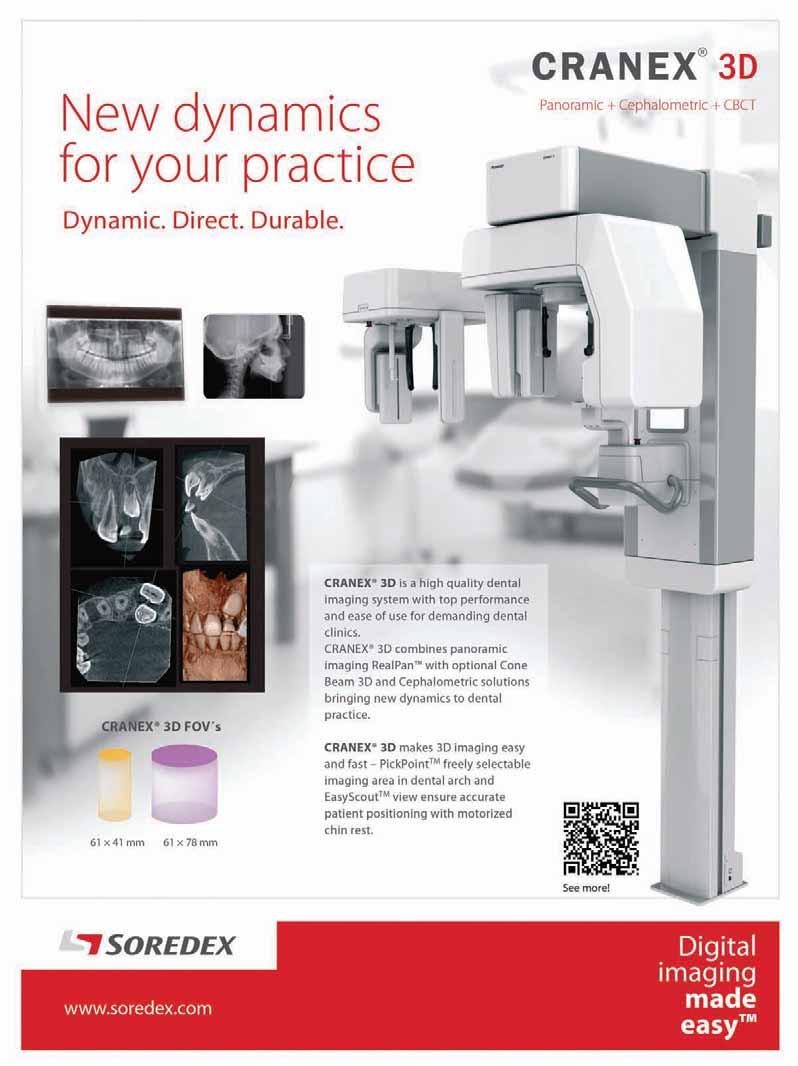



































































































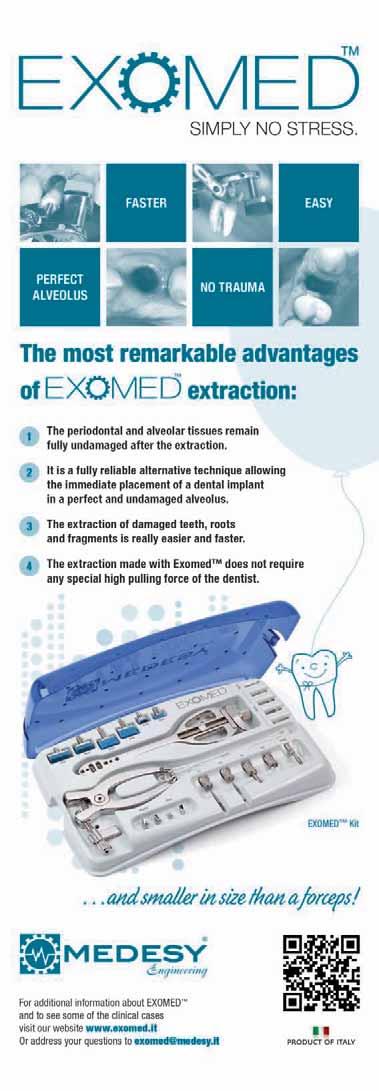


















 References: 1. Greenspan DC. J Clin Dent 2010; 21(Spec Iss): 61–65. 2. LaTorre G, Greenspan DC. J Clin Dent 2010; 21(3): 72-76. 3. Burwell A et al. J Clin Dent 2010; 21(Spec Iss): 66–71. 4. West NX et al. J Clin Dent 2011; 22(Spec Iss): 82-89. 5. Earl J et al. J Clin Dent 2011; 22(Spec Iss): 62-67. 6. Efflandt SE et al. J Mater Sci Mater Med 2002; 26(6): 557-565. 7. Zhong JP et al. The kinetics of bioactive ceramics part
Binding of collagen to hydroxyapatite and bioactive glass. In Bioceramics 7, (eds) OH Andersson, R-P Happonen, A Yli-Urpo, Butterworth-Heinemann, London, pp61–66. 8. Parkinson C et al. J Clin Dent 2011; 22(Spec Issue): 74-81. 9. Earl J et al. J Clin Dent 2011; 22(Spec Iss): 68-73. 10. Wang Z et al. J Dent 2010; 38: 400−410. Prepared December 2011, Z-11-516.
References: 1. Greenspan DC. J Clin Dent 2010; 21(Spec Iss): 61–65. 2. LaTorre G, Greenspan DC. J Clin Dent 2010; 21(3): 72-76. 3. Burwell A et al. J Clin Dent 2010; 21(Spec Iss): 66–71. 4. West NX et al. J Clin Dent 2011; 22(Spec Iss): 82-89. 5. Earl J et al. J Clin Dent 2011; 22(Spec Iss): 62-67. 6. Efflandt SE et al. J Mater Sci Mater Med 2002; 26(6): 557-565. 7. Zhong JP et al. The kinetics of bioactive ceramics part
Binding of collagen to hydroxyapatite and bioactive glass. In Bioceramics 7, (eds) OH Andersson, R-P Happonen, A Yli-Urpo, Butterworth-Heinemann, London, pp61–66. 8. Parkinson C et al. J Clin Dent 2011; 22(Spec Issue): 74-81. 9. Earl J et al. J Clin Dent 2011; 22(Spec Iss): 68-73. 10. Wang Z et al. J Dent 2010; 38: 400−410. Prepared December 2011, Z-11-516.
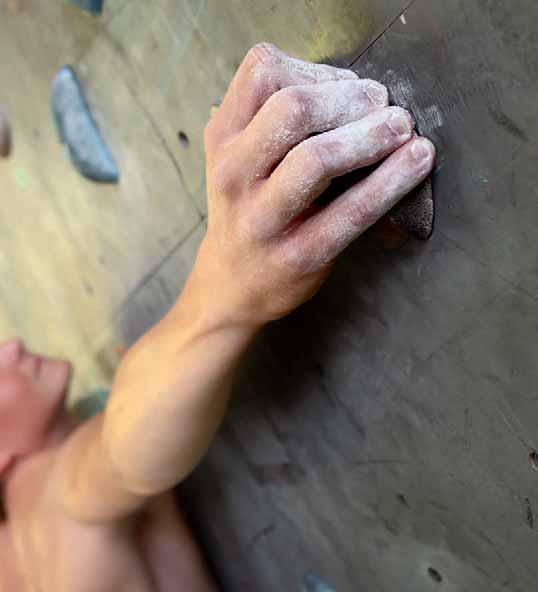




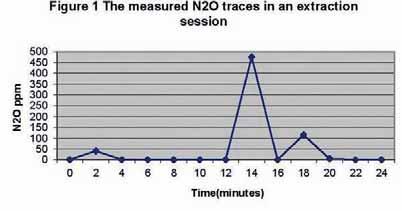
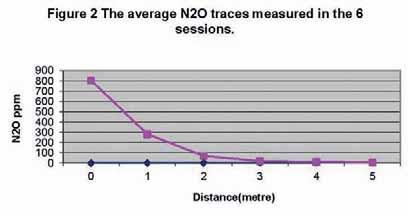

















































































 LEFT TO RIGHT
DR. TONY DIB, PR. MOUNIR DOUMIT, PR. NADIM BABA
PR. MOTLU OZCAN AND DR. ARZU NAIPOGLU DURING THE BREAK AT THE TENT
LEFT TO RIGHT
DRS. ANTOINE SAADE, ZIAD SALAME, CHARLES SFEIR
LEFT TO RIGHT
MR. ANTOINE BARAKA, DR. JEAN MARIE MEGARBANE, DR. CEDRIC HADAD
LEFT TO RIGHT
DR. TONY DIB, PR. MOUNIR DOUMIT, PR. NADIM BABA
PR. MOTLU OZCAN AND DR. ARZU NAIPOGLU DURING THE BREAK AT THE TENT
LEFT TO RIGHT
DRS. ANTOINE SAADE, ZIAD SALAME, CHARLES SFEIR
LEFT TO RIGHT
MR. ANTOINE BARAKA, DR. JEAN MARIE MEGARBANE, DR. CEDRIC HADAD










































 LEFT TO RIGHT: DR. WALID NEHME, DR. RAHIL DOUEIHY, PR. ANTOINE KHOURY, DR. JALAL KASSAB
ILIA ROUSSOU
DR. EHAB HEIKAL LECTURING ON MANAGEMENT
DR. HALA ABBOUD
LEFT TO RIGHT: DR. CHRISTIAN MAKARI, DR. RAHIL DOUEIHY, PR. NADA NAAMAN-DEAN ST. JOSEPH DENTAL SCHOOL, PR. ANTOINE KHOURY
LEFT TO RIGHT: DR. WALID NEHME, DR. RAHIL DOUEIHY, PR. ANTOINE KHOURY, DR. JALAL KASSAB
ILIA ROUSSOU
DR. EHAB HEIKAL LECTURING ON MANAGEMENT
DR. HALA ABBOUD
LEFT TO RIGHT: DR. CHRISTIAN MAKARI, DR. RAHIL DOUEIHY, PR. NADA NAAMAN-DEAN ST. JOSEPH DENTAL SCHOOL, PR. ANTOINE KHOURY








 PICTURES FROM THE EXHIBITION FLOOR
PICTURES FROM THE EXHIBITION FLOOR