ISSN 1026 261X www.dentalnews.comVolume XVII, Number I, 2010 THEEFFECTSOF ENLARGEDADENOIDS ONADEVELOPING MALOCCLUSION Hydrogen peroxide bleaching Egyptian Dental Association GREATER NEW YORK DENTAL MEETING

OliverBrix,DentalTechnician,Germany.

Beavisionary:Thinkabouttomorrow,butactfor today.IPSe.maxlithiumdisilicateoffersefficient andflexiblesolutions–withoutcompromising esthetics.



“THE FUTURE BEGINS TODAY– WITH LITHIUMDISILICATE.”
www.ivoclarvivadent.com IvoclarVivadentAG Bendererstr.2 | FL-9494Schaan | PrincipalityofLiechtenstein | Tel.:+423/2353535 | Fax:+423/2353360
allceramic allyouneed



Volume XVII,Number I,2010
EDITORIAL TEAM
COORDINATOR ART DEPARTMENT SUBSCRIPTION ADVERTISING PHOTOGRAPHY TRANSLATION DIRECTOR ISSN
Alfred Naaman, Nada Naaman, Jihad Fakhoury, Dona Raad, Antoine Saadé, Lina Chamseddine, Tarek Kotob, Mohammed Rifai, Bilal Koleilat, Mohammad H. Al-Jammaz
Lina Jadaa
Krystel Kouyoumdjis
Micheline Assaf, Nariman Nehmeh
Josiane Younes
Albert Saykali
Gisèle Wakim, Marielle Khoury
Tony Dib 1026-261X
DENTAL NEWS – Sami Solh Ave., G. Younis Bldg.
POB: 116-5515 Beirut, Lebanon.
Tel: 961-3-30 30 48
Fax: 961-1-38 46 57
Email: info@dentalnews.com
Website: www.dentalnews.com
INTERNATIONAL REVIEW BOARD
Pr. M.A. Bassiouny BDS, DMD, MSc, Ph.D. Director International Program, Temple University, Philadelphia, USA.
Pr. N.F. Bissada D.D.S., M.S.D Professor and Chairman, Department of Periodontics, Case Western Reserve University, USA.
Pr. Jean-Louis Brouillet D.C.D, D.S.O. Chairman, Department of Restorative Dentistry, Aix-Marseille II, France. Pierre Colon D.C.D., D.S.O. Maître de conférence des universités, Paris, France.
Dr. Jean-Claude Franquin, Directeur de l’Unité de Recherche ER116, Marseille, France.
Pr. Gilles Koubi D.C.D., D.S.O. Department of Restorative Dentistry, Aix-Marseille II, France.
Pr. Guido Goracci. University LA SAPIENZA, School of Medicine & Dentistry, Roma, Italia.
Dr. Olivier Hue, Faculté de chirurgie dentaire de Paris VII, rue Garancière, Paris, France.
Brian J. Millar BDS, FDSRCS, Ph.D. Guy’s, King’s, and St. Thomas’ College School of Medecine & Dentistry, London, UK.
Pr. Dr. Klaus Ott, Director of the Clinics of Westfälischen Wilhelms-University, Münster, Germany. Wilhelm-Joseph Pertot DEA, Maître de conférence, Aix-Marseille II, France.
Pr. James L. Gutmann, Professor and Director, Graduate Endodontics, Baylor College of Dentistry, Dallas, Texas, USA.
Pr. Dr. Alfred Renk, Bayerische Julius-Maximilians-University, Würzburg, Germany.
Dr. Philippe Roche-Poggi DEA. Maître de conférence des universités, Aix-Marseille II, France. Michel Sixou D.C.D., D.E.A. Department of Priodontology, Toulouse, France.
Pr. M. Sharawy B.D.S., Ph.D. Professor and Director, Department of Oral biology, Medical College of Georgia, Augusta, Georgia, USA.
13 24 34 42 49
The effects of enlarged adenoids on a developing malocclusion
Dr. Kevin WILLIAMS, Dr. Derek MAHONY

Complete Denture Stability During Chewing Max BOSSHARTCDT
Hydrogen peroxide bleaching: Effect of various concentrations on mercury and other
metal ions release from admixed and spheri-
cal dental amalgam
Dr. Neveen M. AYAD
Calcium Hydroxide and Glass Ionomer liners: The Prevalence of Use among
Prosthodontists, Pediatric and General
Dentists in Different Countries.
Dr. Jaber A. TAKI
Greater New York Dental Meeting
72
55
Egyptian Dental Association Product Review
DENTAL NEWS IS A QUARTERLY MAGAZINE DISTRIBUTED MAINLY IN THE MIDDLE EAST & NORTH AFRICA IN COLLABORATION WITH THE COUNCIL OF DENTAL SOCIETIES FOR THE GCC. Statements and opinions expressed in the articles and communications herein are those of the author(s) and not necessarily those of the Editor(s) or publisher. No part of this magazine may be reproduced in any form, either electronic or mechanical, without the express written permission of the publisher
Contents 3 CONTENTS


Seal-Tight Dry air on demand. It will blow you away.

Disposable air/water syringe tips.
• Disposable. For maximum infection protection.
• Saves Time. Dramatically reduces time needed for reprocessing autoclavable tips.
• Flexible. Can be bent to a 90°angle without affecting water flow and improving ergonomics.
• Dry Air. The yellow rubber seal acts as a new O-ring ensuring dry air every time.
Cleanic® The universal prophy paste is now available in tubes.

Oral Health Examination Kit

With Perlite technology.
• Universal prophy paste with integrated cleaning variability.
• Single application: cleaning and polishing in a single application (ca. 15 seconds/3 teeth).
• Perlite technology: high cleaning power converting into gentle polishing action thanks to Perlite technology (dynamic behaviour of Perlite-particles).
• Gentle: the prophy paste is gentle to the tooth structure while maintaining a high efficiency.
Sterile. Single-use. Convenient.
Diagnostic examination kit.
• Ready-to-use. Minimises tray set-up time.
• Hygienic. Eliminates cross-contamination issues. Simply use once and discard.
• Convenient. Excellent for routine use, especially during busy surgery times, staff shortages, autoclave breakdowns, home visits and for high-risk patients.
• Time-saving. Reduces time spent sterilising and handling sharps.
• Cost-effective. Increases productivity and reduces inventory.
Flexible Clearance Tabs™ Ideal for surgery use

•Give you an easy and accurate way to make direct intra-oral measurements of occlusal and interproximal tooth preparation clearance.
•Each colour coded tab is used like a feeler gauge to check clearance dimension.
•Available in a convenient dispenser box designed especially for the dental surgery.
•Each tab is for single use only.
Your practice is our inspiration.™ KerrHawe SA P.O. Box 2686934 Bioggio Switzerland Freephone: 00800 41 05 05 05 Fax: ++41 91 610 05 14 www.KerrHawe.com
COMPLETE INTRAORAL PERFORMANCE
Extending SOREDEX family



DIGORA® Toto
Your best choice in intraoral sensors
DIGORA® Toto is easy to use and provides excellent clinical results. With the DIGORA® Toto you cannot go wrong.
Designed for your practice.
MINRAY®
Intraoral X-ray unit


New DIGORA® Optime
Intraoral digital imaging plate system
By choosing the new incomparable DIGORA® Optime, you can enjoy the superior results of over 15 years of experience in intraoral imaging. DIGORA® Optime is easy to use and provides excellent clinical results.
traoral excellent clinical results.
Small. Smart. Fast.
Due to MINRAY ‘s unique extendable horizontal arm the arm reach can be customized for your individual needs. No worries about different arm lengths - one size fi
Clear and easy to use.
zontal arm the ividual needs. one size fits all!

DIGORA® Vidi
Intraoral camera
The DIGORA® Vidi addresses the main needs of dental practices effectively, namely ease-of-use, ergonomy and precise images. The camera is a visible-light addition to SOREDEX’s complete portfolio of intraoral X-ray imaging systems.

rt. F a st . i era di vely, ges. The camera is a EDEX’ l t tf li fi t l
Plug and play!
Manufactured by: SOREDEX info@soredex.com Nahkelantie 160, Tuusula Tel. +358 10 270 2000 P.O.Box 148, FI-04301 TUUSULA, Finland www.soredex.com SOREDEX intraoral products for everyday use Digital imaging made easy™




A healthy new choice for dentistry Find out why the A-dec 300 is a great choice for your practice. For details visit www.a-dec300.com or contact your local authorised A-dec dealer A-dec Inc. 2601 Crestview Drive, Newberg, Oregon 97132 USA Tel: +44 2476 322089 Fax: +44 2476 345106 Web: www.a-dec.com stylish functional innovative A-dec 300 A-dec 300 www.a-dec300.com A-dec Visit A-dec at AEEDC Hall 6 Stand 230

BORA LED &PRESTIGE LED INNOVATION WITH STYLE
Imagine incredibly light instruments, refined, efficient and rugged at the same time.
Inspired by the latest technological breakthroughs in the most demanding environments, the Bora and Prestige BLACKLINE incorporates a carbon fiber handle. These turbines are incredibly light and therefore easier to handle. Moreover, the carbon fiber offers improved resistance to wear, friction, torsion and impacts. The two Bien-Air monobloc optical glass rods provide ideal distribution of the LED intensity. There is virtually no shadow area. Diffusing a natural white light similar to daylight, the LED has a service life 10 times longer than that of a traditional light bulb.
Available with a metal or a carbon fiber handle, the powerful Bora and the miniature Prestige turbines set new standards in ergonomics, performance and durability.
Bien-Air Dental SA Länggasse 60 P.O. Box 2500 Bienne 6, Switzerland Phone +41 (0)32 344 64 64 Fax +41 (0)32 344 64 91dental@bienair.com www.bienair.com
OptiDam™ The first rubber dam with 3-dimensional shape.

Making dental work fast and efficient.
•OptiDam creates a dry and clean operating field, enabling safe dental procedures.
•OptiDam isolates all soft tissue for perfect accessibility: The patient’s tongue no longer needs to be restrained. And the patient’s cheeks, lips and gums no longer interfere with your work.
•OptiDam establishes a non-contaminated field – a basis for durable clinical access: Moisture-sensitive materials can be used correctly. The area being worked on is kept completely dry.
•OptiDam offers optimum protection for both patient and dental staff: Your patients are protected against aspiration or ingestion of foreign objects. Airborne debris is reduced.
SoftClamp™ Universal Rubber Dam Clamp.

The gentle alternative to metal clamps
• Secure. Unique design with grip-tight coating on the jaws minimizes rotation, ensuring secure, solid retention.
• Safe. No sharp edges. Evenly distributed clamping force. Minimizes risk of harm to soft tissue, tooth structure or delicate restorations.
• Versatile. Provides a secure, stable fit for varying molar tooth anatomies and sizes.
• Compatible. Accommodates all types of rubber dam forceps. Prevents forceps tips from penetrating through the clamp, which could affect the gingiva.
• Autoclavable. Well-suited for multiple use.
Fixafloss® The new fixation of rubber dams.

First multifunctional floss for the gentle fixation of rubber dams.
• Innovative: first waxed dental floss with conical clamping element included (silicone).
• Gentle: for gentle rubber dam fixation without clamp in the anterior area.
• Universal: depending on the anatomical situation also indicated for posterior teeth rubber dam fixation.
Your practice is our inspiration.™ KerrHawe SA P.O. Box 2686934 Bioggio Switzerland Freephone: 00800 41 05 05 05 Fax: ++41 91 610 05 14 www.KerrHawe.com
Mar ch 9 - Mar ch 11, 2010
AEEDC Dubai
Dubai International Convention & Exhibition Centre
Email: index@emirates.net.ae
Website: http://www.aeedc.ae
Mar ch 24 - 26, 2010
AOIA Alexandria
March 24 - 26, 2010 _ ICOI - AOIA STARS meeting in Alexandria, Egypt
Email: coordinator@aoiaegypt.com Website: www.aoiaegypt.com
May 3 - 5, 2010
Syrian Oral and Maxillofacial Surgery Society
Damascus, Syria
Email: prof_issamch@hotmail.com
May 11 - 14, 2010
Iranian Dental Association
The 50th International Congress of the Iranian Dental Association Email: kseyedan@hotmail.com
May 13 - 14, 2 2010
4th CAD/CAM conference
May 13 - 14, 2010 _ 4th CAD/CAM Computerized Dentistry International conference at the Address Dubai Marina Hotel
Email: info@cappmea.com Website: www.cappmea.com
September 2 - 5, 2010
FDI Annual World Dental Congress, Salvador de Bahia, Brasil
Email: congress@fdiworldental.org Website: www.fdiworldental.org
November 9 - 11, 2010
Dentistry 2010
Abu Dhabi National Exhibition Center Email: dentistry@iir.com Website: www.dentistryme.com ACTEON 61 - A-DEC

DENTAL NEWS,VOLUME XVII,NUMBER I,2010 11
DVER
INDEX
INTERNATIONAL CALENDAR
A
TISING
ALTURKI 40 - BELMONT 23 - BEYOND 25 - BIEN AIR 9 - BLUE X 27 - CASTELLINI 21 - CAVEX 79 - COLTENE WHALEDENT 59 CROSSTEX 65 - DISCUS DENTAL 63 - DR. WILD 4, 5 - DURR 17 - GC 31 - GSK C3, 54 - HU-FRIEDY 71 - INTENSIV 51 - IVOCLAR_VIVADENT 1, C4 - KAVO C2 KAVO_GENDEX 29 - KERR 6, 10 - KETTENBACH 22 - KOMET 32 - MECTRON 43 - MEDESY 68 - METASYS 12 - MICRO MEGA 39 - MOCOM 33 - MORITA 37 NOBEL BIOCARE 35 - NSK 80 - SIRONA 15 - SOREDEX 7 - SULTAN 70 - VITA 77 - VOCO 75 - W&H 19 - ZHERMACK 2 - ZIMMER 41 www.dentalnews.com Tel:961-3-30 30 48 Fax:961-1-384657 Email: info@dentalnews.com Volume XVII, Number I, 2009 www.dentalnews.com GETYOUR ISSUEONLINE
8 -
EXCOM Central Suction



u Reliable function, even with large amounts of water
u High, constant suction power
u For 1 up to 15 dental units
u Optional amalgam separation module



www.metasys.com METASYS Medizintechnik GmbH Florianistrasse 3 A-6063 Rum bei Innsbruck
EXCOM
EXCOM hybrid 2 EXCOM hybrid A2-ECO II
Z-ECO Light
from 1 up to 15 dental units

THE EFFECTS OF ENLARGED ADENOIDS
ON A DEVELOPING MALOCCLUSION
info@derekmahony.com
ABSTRACT
This article reviews upper airway obstruction caused by hypertrophied adenoids and the possibilities of a subsequent malocclusion. Early diagnosis and treatment of pathological conditions that can lead to the obstruction of the upper airways is essential to anticipate and prevent alterations in dental arches, facial bones and muscle function. Correct nasal breathing facilitates normal growth and development of the craniofacial complex (Figure 1) Important motor functions such as chewing and swallowing depend largely on normal craniofacial development. Any restriction to the upper airway passages can cause nasal obstruction possibly resulting in various dentofacial and skeletal alterations.1 Upper respiratory obstruction often leads to mouth breathing (Figure 2). Habitual mouth breathing may result in muscular and postural anomalies which may in turn cause dentoskeletal malocclusions2. Hypertrophy of the adenoids, and palatine tonsils, are one of the most frequent causes of upper respiratory obstruction (Figure 3). Philosophies regarding the treatment of adenoid hypertrophy range from dietary control and environmental modifications to dentofacial orthopaedics, change of breathing exercises, and surgical procedures.
INTRODUCTION
The aims of this article are (1) to highlight the skills and tools that assist the clinician in identifying upper airway obstruction;




(2) to improve the diagnosis of adenoid hypertrophy; and (3) to improve the classification and treatment of associated malocclusions. The methodology used in this literature analysis consists of a thorough review of narrowly tailored research and Journal articles. The paradigm explored in each article involves upper airway obstruction, adenoid hypertrophy and malocclusion. The results and conclusions stemming from these articles generally fall into three categories:
(1) That hypertrophied adenoids have a definitive effect resultingin skeletal malocclusion;3
(2) That hypertrophied adenoids, coupled with other factors, may aid in the development of skeletal anomalies4; and (3) That adenoid hypertrophy has no effect on airway obstruction and malocclusion.

The research in this area is expansive, but largely inconsistent. Thus, the cause and effect relationship of adenoid hypertrophy and malocclusion must be carefully examined on a case by case basis5. Regardless of the various researcher’s conclusions, one
NTICS DENTAL NEWS,VOLUME XVII,NUMBER I,2010 13 THE EFFECTS OF ENLARGED ADENOIDS ON A DEVELOPING MALOCCLUSION
ORTHODO
Fig.1Fig.3
Dr Kevin W illiams DDS 1 , Dr Der ek Mahony, DDS, MSc in Or thodontics 2 1. drkwilliams@aol.com 2.
Fig.2
ORTHODONTICS

theory remains common – that airway obstruction caused by adenoid hypertrophy and malocclusion are related. The degree of that relationship and what it affects is still under debate. This paper attempts only to highlight the positive existence of this relationship and its possible effects regarding dentofacial growth and development.
BASIC FACIAL GROWTH AND DEVELOPMENT
Developments in the understanding of human craniofacial growth have stemmed from histological and embryologic studies, radiographic cephalometry, correlation of growth and facial anomalies analysis of surgical interventions, animal research and other science fields.6 Despite these studies, we are still waiting for a definite consensus regarding the controlling mechanism of craniofacial tissue.
Postnatal facial growth is influenced by genetic and environmental factors.2 Most facial growth and development occurs during the two childhood growth peaks. The first growth peak occurs during the change from primary to permanent dentition (between 5 and 10 years of age) and the second growth peak occurs between 10 and 15 years of age.2 The study of the early years of life shows that by the age of four (4), 60 percent of the craniofacial skeleton has reached its adult size. By the age of twelve, 90 percent of facial growth has already occurred.7 By age seven (7) the majority of the growth and development of the maxilla is complete and by age nine (9) the majority of the growth and development of the mandible is complete. Proper facial growth is affected either positively or negatively, early in life, by the sequential occurrences of four major factors:
1. The cranial base must develop properly;
2 The naso-maxillary complex must grow down and forward from the cranial base;
3. The maxilla must develop in a linear and lateral fashion;
4 A patent airway must develop properly.
The relationship between the naso-maxillary complex and the cranial base is significant for aesthetic reasons and proper facial bone, muscle and soft tissue support. To allow proper downward and forward rotation of the mandible, the maxilla must be adequately developed, in width, for acceptance of the mandible. Any limitation on mandibular rotation may affect the

relationship of the condyle to the glenoid fossae (in the temporal bone) resulting in multiple TMJ problems. An improper airway will affect the global individual growth.8 The simultaneous growth of these factors is not nearly as significant as how these factors interrelate during facial growth and development. For example, the basic design of the face is established by a series of interrelated factorial developments. The naso-maxillary complex is associated with the anterior cranial fossae. The posterior boundary of the maxilla determines the posterior limits of the midface. This structural plane is significant to facial and cranium development. The basic structural format of facial growth and development is dependent on, and governed by, the interrelation of multiple functional matrices. These functional matrices include a phenomenon of bone displacement and growth at the TMJ with the maxillary forward and downward movement equaling mandibular growth upward and downward. The displacementand growth phenomenon is responsible for the spatial relationship necessary for functional joint movement resulting in the final result of facial growth.9 Additionally, muscle adaptions affect dentoskeletal development. The integration of the musculoskeletal system affects respiration, mastication, deglutition, and speech.2
This basic understanding of facial growth and development is relevant as adenoidal tissue enlargement coincides with major facial growth, i.e. they occur simultaneously. Facial growth may be restricted by abnormal development of adenoidal tissue resulting in abnormal swallowing and breathing patterns (Figure 4)
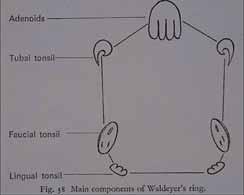
ADENOIDAL GROWTH AND DEVELOPMENT
Lymphoid tissue is normally present as part of the Waldeyer’s tonsillar ring in the form of a nasopharyngeal tonsil (LinderAronson 1970). The Waldeyer’s ring is the system of lymphoid tissue that surrounds the pharynx. This system of tissue includes adenoids and pharyngeal tonsils; lateral pharyngeal tonsils; lateral pharyngeal bands; palatine tonsils and lingual tonsils (Figure 5) Tonsils and adenoids have disparate embryonic origins and cytology even though they are both part of Waldeyer’s ring.10 Bacteria may play a role in adenoid hyperplasia. Specifically, different pathogens, such as Haemophilus influenza and Staphylococcus aureus, have been associated with lymphoid tissue hyperplasia. The adenoid lymphoid structures are lined with ciliated respiratory-type epithelium which is normally distributed throughout the upper and posterior nasopharynx walls. During the presence of disease, the distribution of
14 THE EFFECTS OF ENLARGED ADENOIDS ON A DEVELOPING MALOCCLUSION DENTAL NEWS,VOLUME XVII,NUMBER I,2010
Fig.4 Fig.5










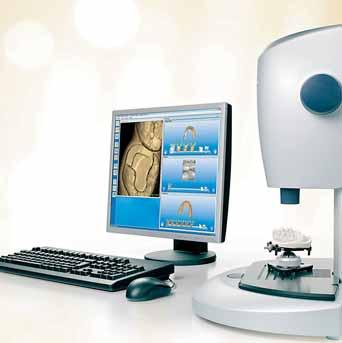
Seeing C A D/C A M
imag
liability and efficiency. Capture
quadrant in less
han one minute. Create precise m
dels and perfect restorati
ns including long-term four unit temporary bridges with CEREC AC. Enjoy every day. With Sirona.
Sirona celebrates 25 years of CEREC from 26th - 28th August 2010 at Caesars Palace in Las Vegas. Choose from 50 topscientific lectures, exchange opinions with thousands of other CEREC users from all over the world and experience the CEREC event of the decade. See you in Las Vegas!
CAD/CAM SYSTEMS | IN S T R U ME NT S | HYG I E N E SYS T EMS | T RE AT ME NT CE NT ERS | I M A G IN G SYS T EMS The Dental Company www.sirona.com C4 25-2K-V0-3 1 25thAnniversary Celebration CEREC www.cerec25.com Sirona
P.
Dubai Phone:
1 Th e r e sul t o f a s t udy carri e d o u t by P r o f e ss o r D r. Me hl (Z urich Univ e rsi t y , 200 8 ) m e asuring d e p t h accuracy o f up to 19 μ m. CEREC
PRECISION AND SIMPLICITY REDEFINED
Dental Systems GmbH
O. Box 21184
+971 4 375 2355
–
captures highly d
d
mitting diode (LED) Rapid, easy
precision
in a new light . The new CEREC AC with CEREC Bluecam
etaile
es using a powerful blue light-e
imaging results in a quantum leap in CAD/CAM
1 ] , clinical re
a
t
o
o
ORTHODONTICS

the dendritic cells (antigen presenting cells) is altered. The result is that there is an increase in dendritic cells in the crypts, and extrafollicular areas, and a decrease in surface epithelium dendritic cells.
Lymphoid tissue is normally not apparent in the early infant stage of life. Marked symptoms of adenoid development are most common in the childhood age range of 2 – 12. During adolescence a decrease in adenoid size is noted as current with the growth of the nasopharynx. Rarely is adenoid tissue present in adults and when it is noted it is usually in an atrophic condition. The cause of the involution of the Waldeyer’s ring is still under investigation.12 The imbalance in the relationship between the enlargement of the nasopharynx/nasopharyngeal airway and the concomitant growth of adenoid tissue can result in reduced patent nasopharyngeal airway and increased nasopharyngeal obstruction.10
The growth of adenoidal tissue as demonstrated by a bell curve, peaks at or near age six (6) and also begins involution at or near this age as well (Figure 6). Facial growth is coupled with adenoidal growth. As the cranial base forms the roof of the nasopharynx, a close examination of the growth and development of the craniofacial complex becomes significant for evaluation of the size and configuration of the nasopharyngeal airway. Any abnormal development regarding this craniofacial complex may affect the nasopharyngeal airway. Abnormal adenoidal growth that occurs during childhood, may consume the nasopharnx and extend through the posterior choanae in the nose.13 This excessive adenoidal growth usually interferes with normal facial growth and can result in abnormal breathing patterns, congestion, snoring, mouth breathing, sleep apnea;4 Eustachian tube dysfunction/otitis media, rhinosinusitis, facial growth abnormalities, swallowing problems, reduced ability to smell and taste, and speech problems.12 Theoretically, many clinicians believe the blockage should be removed as soon as possible through a surgical procedure called adenoidectomy. However, according to a study conducted by Havas and Lowinger one-third of child study patients, with traditional adenoidectomies, were ineffective with intranasal extensions of the adenoids obstructing the posterior choanae. For this segment of the study population the “powered-shaver adenoidectomy” was effective in the complete removal of the

obstructive adenoid tissue ensuring postural patency.13
UPPER AIRWAY OBSTRUCTION AND MOUTH BREATHING
During normal nasal respiration, the nose filters, warms and humidifies the air in preparation for its entry into the body’s lungs and bronchi. This nasal airway also provides a degree of nasal resistance in order to assist the movements of the diaphragm and intercostals muscles by creating a negative intrathoracic pressure. This intrathoracic pressure promotes airflow into the alveoli.7,15
Correct normal resistance is 2 to 3.5 cm H2O/L/Sec and results in high tracheobronchial airflow which enhances the oxygenation of the most peripheral pulmonary alveoli. In contrast, mouth breathing causes a lower velocity of incoming air and eliminates nasal resistance. Low pulmonary compliance results7. According to blood gas studies, mouth breathers have 20% higher partial pressure of carbon dioxide and 20% lower partial pressures of oxygen in the blood, linked to their lower pulmonary compliance and reduced velocity.7,16
Contributing factors in the obstruction of upper airways include: anatomical airway constriction, developmental anomalies, macroglossia, enlarged tonsils and adenoids, nasal polyps and allergic rhinitis.5 However, for purposes of this paper the focus shall be on enlarged adenoids as the major contributing factor. There are numerous studies that link adenoid hypertrophy with nasopharyngeal airway obstruction to the development of skeletal and dental abnormalities.14
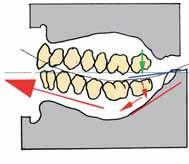
Airway obstruction, resulting from nasal cavity or pharynx blockage, leads to mouth breathing which results in postural modifications such as open lips, lowered tongue position, anterior and posteroinferior rotation of the mandible, and a change in head posture. These modifications take place in an effort to stabilize the airway.As previously discussed, facial structures are modified by postural alterations in soft tissue that produce changes in the equilibrium of pressure exerted on teeth and the facial bones (Figure 7) Additionally, during mouth breathing, muscle alterations affect mastication, deglutition and phonation because other muscles are relied upon.2
MALOCCLUSION – THE ISSUE STILL IN DEBATE

Is there a cause and effect relationship between adenoids, nasal obstruction and malocclusion? Dentofacial changes associated with nasal airway blockage have been described by CV Tomes in 1872 as adenoid facies. Tomes coined this term based on his belief that enlarged adenoids were the principle cause of airway obstruction and resulted in noticeable dentofacial changes.7 Tomes
16 THE EFFECTS OF ENLARGED ADENOIDS ON A DEVELOPING MALOCCLUSION DENTAL NEWS,VOLUME XVII,NUMBER I,2010
Fig.6
Fig.7
ORTHODONTICS


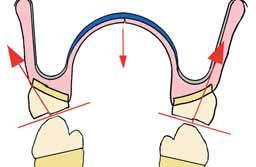
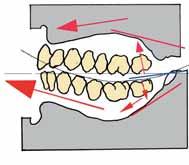
reported that children, who were mouth breathers, often exhibited narrow V-shaped dental arches10 (Figure 8). This narrow jaw is a result of mouth breathers keeping their lips apart and their tongue position low. The imbalance between the tongue pressure, and the muscles in the cheek, result in cheek muscles compressing the alveolar process in the premolar region. Simultaneously, the lower jaw postures back. These simultaneous actions have been termed the compressor theory11 (Figure 9)
Tomes’ views were supported in the 1930’s by numerous leading orthodontists. These supporting clinicians reported airway obstruction as an important aetiologic agent in malocclusion. Rubin advocated that in order for these patients to fully be assessed they must be thoroughly evaluated by both a rhinologist and orthodontist.7 Malocclusion is the departure from the normal relation of the teeth in the same dental arch or to teeth in the opposing arch.3
Airway obstruction, coupled with loss of lingual and palatal pressure of the tongue, produces alterations in the maxilla. The positioning of the tongue also plays an important role in mandibular development. The tongue displaced downward can lead to a retrognathic mandible; and an interposed tongue can lead to anterior occlusal anomalies.
Additionally, maxillary changes can be viewed in the transverse direction, producing a narrow face and palate often linked with cross bite; in the anteroposterior direction, producing maxillary retrusion; and in the vertical direction causing an increase in palatal inclination as related to the cranial base and excessive increases of the lower anterior face height. The most commonly found occlusal alterations are cross bite (posterior and/or anterior), open bite, increased over jet, and retroclination of the maxillary and mandibular incisors.2 Mahony and Linder-Aronson’s findings were in agreement with the significant correlation between changed mode of breathing and diminished mandibular / palatal plane angle (ML/NL) found in adenodectomized children. 22
Several authors have taken the position that alleged faces are not consistently found to be associated with adenoids, mouth breathing, nor a particular type of malocclusion; and that there is no cause and effect relationship between adenoids, nasal obstruction/mouth breathing and malocclusion.
Proponents of this position believe that the V-shaped palate was inherited and not acquired through mouth breathing. (Hartsooh 1946) on a review of literature related to mouth breathing,

concluded that mouth breathing is not a primary etiological factor in malocclusion. Additionally, Whitaker (1911) found that in a study of 800 children, who underwent adenoidectomy or tonsillectomy only 30% had dental anomalies that needed orthodontic intervention. There is some suggestion that adenoids and hypertrophic tonsils are a consequence of a thyroid hormone deficiency. This hormone deficiency acts as a catalyst for activating the organism’s defense mechanisms which include hypertrophy of lymphoid tissue.11 Another orthodontic clinician, Vig, took the position that without documented total nasal obstruction, any surgery or other treatment to improve nasal respiration, is empirical and difficult to justify from an orthodontic point of view.7,17
NASAL RESPIRATORY EVALUATION
The relationship of airway obstruction and dentofacial structures/ malocclusion is still the subject of investigation and controversy amongst orthodontists. The correlation between functional problems and morphologic characteristics is yet to be solidified. Regardless of varied opinion in this area practitioners should observe each patient carefully.
Suggested protocol:
1. As the patient enters the room, facial and head posture should be noted to see if the lips are closed during respiration.
2 Signs of allergic rhinitis should be noted, as well as histories of frequent colds or sinusitis.
3. Assessment of family history for allergies is important.
4 Sleep history should be evaluated: sleep apnoea, loud snoring, open mouth posture while asleep.
5 Patient is asked to seal their lips – difficulty breathing through nose should be noted. One nostril can be occluded and the response noted – same procedure on the other side. (Figure 10) The evaluation of nasal airway patency is complicated, especially when the possibility exists that airways may clinically appear inadequate but be quite functional physiologically. Lip separatingor an open-mouth habit is not an infallible indicator of mouth breathing. Often complete nasal respiration is coupled with dental conditions that cause open-mouth posture.10
ADENOID EVALUATION
Nasopharyngeal space and the size of adenoids have been evaluated using different methods of assessment:
1. Determination of the roentgenographic adenoid/nasopharyngeal ratio (a lateral cephalometric xray);

2 Flexible optic endoscopes (Figure 11);
3. Acoustic rhinometry; and
4 Direct measurements during surgery.
Direct measurements are considered to be the most accurate
18 THE EFFECTS OF ENLARGED ADENOIDS ON A DEVELOPING MALOCCLUSION DENTAL NEWS,VOLUME XVII,NUMBER I,2010
Fig.10
Fig.8Fig.9
ORTHODONTICS


because space can be assessed in three directions.12 A lateral cephalometic radiograph is an added valuable diagnostic tool for the orthodontist in the evaluation of children with upper airway obstructions.14 (Figure 12)
TREATMENT OF NASAL OBSTRUCTION
1. Adenoidectomy with or without tonsillectomy is indicated if hypertrophied adenoids (and tonsils) are the cause of upper airway obstruction.7
Powered-Shaver Adenoidectomy – Adenoidectomy coupled with Endoscopic Visualization will assist in achieving adequate removal of adenoids particularly high in the nasopharnx. Use of the powered-shaver technique allows for better clearance of obstructive adenoids. The end result is more reliable restoration of nasal patency.13
2 Septal surgery (rarely indicated in the child) but may be considered in the presence of a marked nasal septal deflection with impaction. Conservative septal surgery in growing patients will not have an adverse effect in dentofacial growth.7,18,19,20
3. Maxillary expansion (RME or SAME) – an orthodontic procedure that widens the nasal vault.7,18
4. Cryosurgery or electrosurgery – this is a viable option for patients with vasomotor rhinitis.7
5 Bipolar Radiofrequency Ablation (allergic rhinitis) – performed under local anesthetic
6. Inferior turbinectomy – Using powered instrumentation
7 Use of nasal sprays.
CONCLUSION
The effect of adenoids on facial expression, malocclusion and mode of breathing has been a topic of debate and investigation by practitioners in the field for the last one hundred years. A review of the literature exposes several theories.
A healthcare provider, with a practice philosophy based on prevention of malocclusion development, cannot ignore the early years of the patient’s growth cycle. By age twelve, 90 percent of facial growth has already occurred. This is the age when many practitioners begin orthodontic treatment.7 This is the age when 80-90 percent of craniofacial growth is complete, so most formation and/or deformation has occurred.21 To wait until 90 percent of the abnormality has occurred, before beginning treatment, is not consistent with a preventive philosophy. Interceptive measures must be initiated sooner. Early intervention requires an acceptanceof

a multidisciplinary approach to total patient health. An integrated approach to patient evaluation, diagnosis and treatment is most effective. Primary care physicians, dentists, allergists, otorhinolaryngologists, and orthodontists must all work together for early prevention and management of young patients with increased nasal airway resistance.
After diagnosis, a comprehensive risk benefit analysis regarding early intervention must be considered. Although hereditary and environmental factors must be considered, the universal goal is the promotion of proper nasal respiration throughout a child’s early years of facial growth.
Figure 13 shows the before and after treatment results of a young girl who had her adenoids removed, then underwent maxillary expansion before full-fixed braces. She was treated as a second opinion against the removal of four premolar teeth.


20 THE EFFECTS OF ENLARGED ADENOIDS ON A DEVELOPING MALOCCLUSION DENTAL NEWS,VOLUME XVII,NUMBER I,2010
Fig.13 BEFORE
Fig.13 AFTER
Fig.11
Fig.12

AEEDCDubai 9 - 11 march 2010 Hall 6/7 Stand 334 www.castellini.com Tradition inspires our projects, Innovation brings them to life.
ORTHODONTICS
REFERENCES

1. Mattar, SE, Anselmo-Lima, WT, Valera, FC and Matsumoto, MA, Skeletal and Occlusal Characteristics in Mouth-Breathing Pre-School Children, J Clin Pediatr Dent 2004 28(4):315-318.
2. Valera, FC, Travitzk, LV, Mattar, SE, Matsumoto, MA, Elias, AM, Anselmo-Lima, WT, Muscular, Functional and Orthodontic Changes in Pre-School Children with Enlarged Adenoids and Tonsils, Int J Pediatr Otorhinolaryngal 2003, Jul; 67(7):761-70.
3. Khurana, AS, Arora, MM, Gajinder S., Relationship Between Adenoids and Malocclusion, J Indian Dental Ass., April 1986; 58:143-145.
4. Pellan, P., Naso-Respiratory Impairment and Development of Dento-Skeletal, Int JO Fall; 16(3):9-11, 2005
5. Soxman, JA, Upper Airway Obstruction in the Pediatric Dental Patient, Gen. Dentistry July-August; 313-315, 2004.
6. Ranly, DM, Craniofacial Growth, Dent Clin NA, July; 44(3):457-470, 2000.
7. Rubin, RM, Effects of Nasal Airway Obstruction on Facial Growth, Ear, Nose & Throat J, May;66:44-53, 1987.
8. Pistolas, PJ, Growth and Development in the Pediatric Patient, The Functional Orth. 12-22 Winter 2004/Spring 2005.
9. Enlow, DH, Hans, MG, Essentials of Facial Growth; 5, 79-98, 206, 1996
10. Diamond, O, Tonsils and Adenoids: Why the Dilemma? Am J. Orthod., Nov. 78(5) 495-503, 1980.
11. Linder-Aronson, S, Adenoids: Their Effect on the Mode of Breathing and Nasal Airflow and Their Relationship to Characteristics of the Facial Skeleton and the Dentition, Acta Oto-laryng Suppl, 265: 5-132, 1970.
12. Casselbrant, MC, What is Wrong in Chronic Adenoiditis/Tonsillitis Anatomical Considerations, Int J Pet. Oto 49(1):S133-S135, 1999.
13. Havas, T, Lowinger, D, Obstructive Adenoid Tissue an Indication for Powered-Shaver Adenoidectomy, Arch Otolaryngol Head Neck Surg: July 2002; 128:789-791.
14. Oulis, CJ, Vadiaka, GP, Ekonomides, J, Dratsa, J, The Effect of Hypertrophic Adenoids and Tonsils on the Development of Posterior Crossbite and Oral Habits, J Clin Pediatr. Dent, Spring; 18(3) 197-201, 1994.
15. Adams, GL, Boies, CR, Papaiella, MM, Boies’ Fundamental Oto. Philadelphia WB Sanders 1978.
16. Ogura, JH, Physiologic Relationships of the Upper and Lower Airways, Ann Otgl Rhinol Laryngol, 79; 495-501, 1970.
17. Vig, PS, Sarver, DM, Hall, DJ, et al, Quantitative Evaluation of Nasal Airflow in Relation to Facial Morphology, Am J Orthod, 79:263-272; 1981.
18. Gary, LP, Brogan, WF, Septil Deformity Malocclusions and Rapid Maxillary Expansion, Orthodontist 4; 1-13, 1972.
19. Cottle, MH, Nasal Surgery in Children, Eye, Ear, Nose and Throat Monthly; 30:32-38, 1951.
20. Jennes, JL, Corrective Nasal Surgery in Children: Long Term Results, Arch Otolaryngal; 79:145-151, 1964.
21. Mahony, D., Page, D. The Airway, Breathing and Orthodontics; Ortho Tribune,8-11.
22. Mahony, D., Linder-Aronson, S. Effects of adenoidectomy and changed mode of breathing on incisor and molar dentoalveolar heights and anterior face heights. AOJ; 20:93-98,2004.
Panasil® initial contact.
Precise, even in extreme situations.

020903_4009 www.kettenbach.com
PROSTHETIC DENTISTRY

Complete Denture Stability During Chewing
Max Bosshar t, CDT* bossdent@hotmail.com
To obtain unilateral chewing stability: forget about balanced occlusion, it doesn’t work, but: Perfect equilibrated occlusion is essential during parafunctional mandibular movements to prevent unbalanced loads on the supporting alveolar ridges.
1 Food is almost always chewed on one side only (Hiltebrandt, 1933/35)1
2. During mastication the teeth of the denture wearer only finally come into contact when the food load has become softened (A.Gerber, 1946).2, 3
3. Therefore the bi-lateral equilibrium is ineffective for chewing stability.
4. For the unilateral chewing stability of dentures, immobility is the key.
5. Para functional contacts are occurring both day & night. In order to distribute these forces evenly, correct centric & equilibrating contacts are necessary.
Introduction
The study from Suguru Kimoto et al.4 showed greater satisfactionof the patient wearing dentures with a lingualised occlusion concept. The article “The effect of occlusal contact localisation on the stress distribution in complete maxillary denture,5 describes the connections which contribute to broken dentures. According to this study, It is the form of occlusion and the positioning of the teeth in relation to the alveolar ridge which leads to an unstable load and to broken dentures.
Functional reasons causing broken dentures
Incorrect positioning of posterior teeth
The ideal point of pressure on the tooth is the area shown in Figure 1 with a green arrow. The chewing force is directed to the middle of the alveolar ridge. Forces directed in a more buccal direction progressively increase the deformation of the denture. The denture is no longer well fitting (blue area) and, in time, could initiate a crack zone in the palatal part of the denture.

Figure 1: The ideal point of pressure on the tooth is the area shown with a green arrow. The chewing force is directed to the middle of the alveolar ridge. Forces directed in a more buccal direction, as the red arrows show, progressively increase the deformation of the denture.
The denture is no longer well fitting (blue area) and in time, could initiate a crack zone in the palatal part of the denture.
Abrasion and centric anterior tooth contact
Figure 2: The lower teeth exert pressure on the upper teeth in a buccal direction (red arrow). This multiple cyclic reaction can lead to a crack in the denture and a gap developing between the denture and the torus palatinus.
Also of importance is the contour of the teeth. By losing the main palatal cusps on the upper denture we get too much pressure on the buccal cusps, resulting in a crack in the palatinal part of the denture (Figure.2). Because of the inclination of the
24 DENTAL NEWS,VOLUME XVII,NUMBER I,2010 COMPLETE DENTURE STABILITY DURING CHEWING

PROSTHETIC DENTISTRY
occlusal surface, shown in figure 2, the resulting orientation of the forces, upwards and outwards, is increasing the deformation of the denture base. It can lead to crack formation in the denture base and damage the alveolar bone. Usually we can easily distinguish between a functional breakage and an accidental breakage of a denture. Of course we can ask the patient what happened. For the denture construction it is important to know the functional origin of the break. By abrasion of the posteriors premature contacts and an anterior or canine guidance are created. It can provoke a tilting action which would result in a dropping of the denture in the post dam region leading to a lack of security. Breaking of the upper denture can also be expected.
Conclusion: Broken dentures are a good indication of instability; caused by instable positions or wrong contacts of the artificial teeth. It is in these cases that pathological damage is caused. We can use high-impact acrylic or just repair the denture, but, in both cases the pathological damage will continue. The results are flabby ridges and increased bone resorbtion. The mastication efficiency is very restricted and the patient could experience pain. To avoid these problems we need correct teeth contacts and to have periodic re-calls every 2 years.
Tooth position and denture stability
In the past
Many years ago different authors discovered the problem of the unstable denture (Hiltebrandt 19331, Payne 19416, Gerber 19462). All of them proposed a specific lingualised occlusal concept to solve the problem.
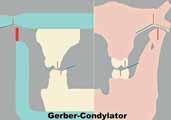
In Europe, 1958, Albert Gerber from Zurich developed the so called “Gerber-Method”. It is still recognised as one of the best systems available. 7, 8
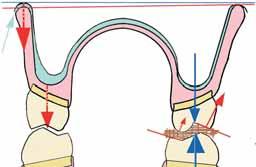
Figure 3: Buccal cusp contact during mastication is a handicap. Too much force is placed buccally of the ridge during working mastication, resulting in a tilting upper denture and furthermore an un-supported direction of masticatory force. In the conventional set-up, the lower buccal cusps are on the crest of the ridge (or more lingual) in the upper, the central groove is straight over the crest of the ridge (Gysi 1914/17)9

Buccal cusp contact in a conventional set-up during mastication is a handicap. Too much force is exerted buccal of the ridge, resulting in an un-stable denture (Figure 3). With the reduction of the buccal cusps (min. 2mm) we have the masticationforce directed over the lingual-palatal area and over the centre of the ridge. This way the denture is stable during mastication (Figure 4). A correlation of denture instability and progressive resorbtion of the alveolar bone4 exists. A personal observation, madeby the author of the anatomic situation of Japanese edentulous patients showed a significantly better situation in comparison with the Caucasian population. Their alveolar ridges are showing significantly less resorbtion in width. Also, the width of the dental arch is distinctly greater. These characteristics are clearly favouring the transversal denture stability. It may explain the reason, why Kumutu et al. found little or no difference in the mastication performance of the patients. Long term results could show different results when the fit of the dentures deteriorate.
The Gerber System
In this system we put the upper vertical direction to the crest of the ridge (Figure 4). The denture will remain stable with the advantage that the teeth can be placed more buccally. This not only provides better cheek contact and more tongue space but also stops food from slipping under the denture.

Figure 4: With the reduction of the buccal cusps (min. 2mm) we have the mastication force in the lingual/palatal area, which is orientated almost vertically.
Sagittal Stability
The Lower Denture
The lower denture bearing area can have a difficult shape with many different inclined levels. Everyone knows what happens if you stand on an inclined slope on ice or snow in Switzerland, we slide downhill without any effort, known as skiing! Teeth standing on the retro-molar ascending part of the ridge push the denture forward during mastication (Gysi 1917)9.Figure 5 depicts a common case. The last molar is positioned in the area of the ascending part of the ridge & the force to the lower denture hits the inclined area. The force will be deflected forward and the denture slips down the slope and lifts up at the front.
26 COMPLETE DENTURE STABILITY DURING CHEWING DENTAL NEWS,VOLUME XVII,NUMBER I,2010
Conventional Set-up
PROSTHETIC DENTISTRY
Figure 5: In a `textbook conventional set-up’ the last molar is positioned correctly; the occlusal level and curve of Spee have been observed. However, the masticatory force is not at 90°to the ridge and the denture moves down the sloping ridge and moves forward & upward.
The Upper Denture
Can this also happen with the upper denture? Yes!
This case shows that both dentures are unstable. As the patient chews food the dentures move making it virtually impossible to masticate. Pressure areas are pre-assigned and, with time, provoke resorbtion of the ridge. Under mastication force the upper denture slips forward and only the patients’ lip holds the denture in position. This has a negative effect on Aesthetics, making the lips appear tensed.
Figure 6 shows in which direction the mastication force on the upper jaw is directed. As a consequence of the poor position of the teeth, according to the Spee curve, the force is in a disadvantageous angle to the ridge and the pressure pushes the upper denture forward
Model Analysis
Anyone building a house knows that he has to analyse the ground it will be supported on. When setting up a denture we need to do the same, we call it model-analysis. We draw on the side of the model the different zones, positive, neutral & negative/unstable areas. We use different colours to get a quick analysis of the situation (Figure 7)
Figure 7:
1. The positive zones are mostly in the pre-molar area (green).
The axis of the pre-molars pushes the denture, during mastication, backwards to the respective ridge giving a ‘super’ stable situation.

2. The deepest area in the lower jaw and the highest part of the upper jaw are the neutral zones (blue). In this area we set the first molars (largest teeth).

3 We can recognise on Figure 5 and 6 that the retro-molar area is critical (red). The directions of the upper and lower ridge in the posterior part are not parallel to each other. We cannot set any teeth in this area that will be stable during masticatory function.
Posterior tooth position
The second upper molar in Fig 8a & 8b is 3mm out of contact to its antagonist and therefore it is not possible to chew with it. These last teeth serve only as a support to the cheeks, prevent food slipping up or down under the denture and prevent cheek biting.10
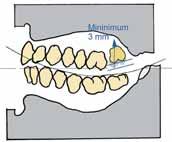

Figure 8a and, 8b: In this set-up the second upper molar is 3mm out of contact. Therefore it is not possible to chew with it. Also we can observe the large gap between upper and lower buccal cusps on the first molar.
If sufficient space is lacking, we recommended not to place any upper molar at all (Figure 9a and 9b)
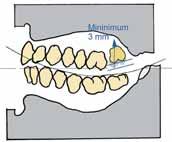

Figure 9a and 9b: If sufficient space is lacking, we recommended not to place any upper molar at all.
Balanced occlusion
But the arrangement of the teeth is still recognised as being a balanced occlusion and the molar teeth are important in Para functional jaw movement (Figures 10a and 10b). Apart from unilateral chewing stability as described above, continuous posterior contacts are important during non-functional tooth contacts. The even distribution of the forces over the complete upper and lower alveolar ridges will protect the natural tissues from overload or at least diminish the forces to a minimum. During all functional and parafunctional movements, the elimination of all prematurities is indispensable.
28 COMPLETE DENTURE STABILITY DURING CHEWING DENTAL NEWS,VOLUME XVII,NUMBER I,2010
igur e 8a Figur e 8b Figur e 9a Figur e 9b
F
PROSTHETIC DENTISTRY

Figures 10 and 11: Beside the static orientation of the posterior teeth, balanced occlusion is an absolute must to protect the soft and hard natural tissues from local overload, occurring specially during parafunctional jaw movements.
Centric relation
Figure 12. Gothic arch registration of an edentulous case to determine centric relation.

For instance, the registration of a physiological centric relation is of major importance. The stability of dentures is directly related to it. It is symptomatic that upper dentures drop down irrespective of a perfect impression, when centric is not correct. Especially by edentulous patient cases it is difficult to obtain a reliable centric relation. The intra oral gothic arch tracing (Figure 11) has given most satisfaction, especially in full denture cases, for implant work, extensive reconstructions11 and in TMD cases12
The articulator, an important Instrument in prosthodontics
An incorrect centric or a straight-line commonly used articulator cannot reproduce an Immediate side shift, a Fischer Angle or a correct protrusive movement. Lateral movements, simulated without an ISS produce too steep buccal facets on the lower molars (hyper-balances)13. The Fischer-Angle is due to the transversal angulations of the TMJ (figure 13). The mandibular movement back and down occurs during swallowing and together with a lateral displacement during chewing. (Gibbs Lundeen 14)
Figure 13: Frontal view of a left Condyle. The roof shape is clearly visible.
Retrusive movement

A simple test shows, if a retrusive movement exists. With the head in an upright position and by keeping the teeth slightly closed, incline the head backwards, a slight sliding of the lower teeth can be observed. With the condyle centred in its physiologic place (due to the form of the glenoid fossa) the retrusive movement is also oriented

downwards. There is no other way for the condyle than down because of the posterior wall (figure 14)
Figure 14: Sagittal view of a TMJ. By the form of the posterior wall it is obvious that the Retrusive movement must also be directed downward.

Denture occlusion must be balanced; the correct simulation allowing the physiologic mandibular movements is of major importance.
The Fischer angle
During lateral movements, the roof shaped TMJ (figure 13), i.e. the medial wall, is providing, together with the condyle path inclination, an additional guidance down of the condyle. The pure protrusive movement and the added inclination of the movement inwar d, are producing the so called Fischer angle.
Figure 15: This figure is a combination of two pictures. The upper picture shows the artificial fossa and the lower second picture a condyle. The medial and external angulations of both elements are very similar.


This angle becomes of importance during the simulation of the ISS. If these angles of the medial and the external wall are missing, the occlusion becomes to flat. The figure 15 has been composed by the transversal picture of Gerber’s first articulator from 1948 with the picture 13, placed just underneath the artificial joint. It shows an amazing similarity between, the artificial and the natural elements.
Final Remarks
In order not to detract from the principles of the Gerber System we have, on purpose, not gone into too many details. It is important to understand the forces during mastication and the way they interact. (Who knows why, knows how!). Of course many other factors are to be observed, from medical history to the very important aesthetics, impression taking and many more. The method developed by Professor Gerber15 guarantees success when all the relevant aspects are respected. Those aspects contain all steps of a treatment, beginning with the first appointment, continuing with the pre-prosthetic treatment, first and second impressions, centric registration, set-up of the teeth poviding aesthetic and static/dynamic requirements, trying-in,
30 COMPLETE DENTURE STABILITY DURING CHEWING
igur e 10
igur e 11 DENTAL NEWS,VOLUME XVII,NUMBER I,2010
F
F
Finally you can achieve a twofold long-lasting high-strength bond in one step to tooth structure AND to aesthetic restorations, especially zirconium.
Use G-CEM Automix and enjoy:
- one step mixing – the work is done for you - one step application – direct delivery, even in the root canal - one step cleanup – precise removal of all excess
With an ideal setting time and the reliable results you’ve come to expect from GC.

new G-CEM
Resin luting re-defined:
Automix from GC.
GC EUROPE N.V. Head Office Tel. +32.16.74.10.00 info@gceurope.com www.gceurope.com


properly executed lab procedures and remounting with perfect selective grinding-in. All these basic rules are valid whether it’s for over-dentures on implants, over-dentures on natural roots and by partial denture cases with free end saddles16
Acknowledgements
The author’s acknowledgements go to Dr. A. Johnson, Mr. M. Boxhoorn and Mrs. A. Bruelhart for their assistance with the translation of this article.
* Max Bosshart Center Dental Technology Zurichstr. 5, P.O.Box 23, CH - 8840 Einsiedeln, Switzerland.
REFERENCES
1. HILTEBRANDT, C.: Die physiologischen und statischen Grundlagen der totalen Prothese. Published byVita Zahnfabrik GmbH Essen; 1935.
2. GERBER, A.: Die artikuläre Funktion und die Schleimhautbelastung beim Kauen von Prothesen, Vortrag am SSO-Kongress in Lugano, 1946.
3. GERBER, A.: Beiträge zur Technologie in der totalen Prothetik I & II. Quintessenz der Zahntechnik12/ 1976; 11-21 & 3/1977; 12-21. Quintessenz Verlags GmbH Berlin. As well pblished 1977 by Quintessenz Chicago in english language.
4. KIMOTO, S., Gunji, A.; YAMAKAVA, A.; AJIRO H., KANNO, K., SHINOMIYA, M., KAWARA, M., KOBAYASHI, K.: Prospective Clinical Trial Compairing Lingualized Occlusion to Bilateral Balanced Occlusion in Complete Dentures: A Pilot Study. Quintessence Publishing Co. Inc., Volume 19, Number 1, 2006; 103-109
5. ATES, M., CILINGIR, A., SÜLÜN, T., SÜNBULÖOGLU, E. BOZDAG, E.: The effect of occlusal contact localisation on the stress distribution in complete maxillary denture. Journal of Oral Rehabilitation, 2006 33; 509-513. Blackwell Publishing Ltd.; Oxford
6. PAYNE S.H.: A posterior set-up to meet individual requirements, >Dent.Dig. 1941,47: 20-22
7. GERBER, A.: Okklusion und Artikulation in der Prothetik; 1960. Published by Condylator Service; Zurich.
8. GERBER, A.: Progress in full denture prosthesis. Int. Dental Journal 2/1957; 325. 9. GYSI, A.: Montage d'Appareils avec les Dents Anatoform et les Blocs Gysi, 12.7.1917; S. 28. De Trey & Co. Ltd. (A. Gysi, Sammelband III); Londres.
10. BOSSHART, M.: Funktion des zweiten Molaren. Das Dental Labor, Heft 6/2007 (853-854); München.
11. GOBERT, B.: Variations cliniques implantaires avec l’Enregistrement Intra-Oral Gerber. Revue Implantologie, Mai 2006; 39-46. A. Girot, Megève France.
12. GERBER, A.; STEINHARDT G.: Dental Occlusion and Temporomandibular Joint, 1989. Quintessence Publishing Co. Chicago.
13. GERBER, A.: Condylator Modell 4. Der Zahntechniker r. 6, 1959; 2 -19; Schw. Zanhtenchnikervereinigung, Zürich.
14 GIBBS, C., LUNDEEN, C., MAHAN, P., Fujimoto, J.: Chewing movements in relation to border movements at the first molar. J Prosth. Dent. 1981: 46(12); 308-322. Mosby (Elsrevier, Amsterdam).
15 HAMPSON, E.L.; M.S.D., F.D.S.; ASKEW, P.A., B.D.S., F.D.S.; TANNER, A.N., B.D.S.; WHITE, G.E.: A technique for constructing full dentures using the Gerber articulator and Condyloform teeth (I and II). Quintessence International 4 and 5, 1973 (45 – 54, and 45 – 51); Chcago/Berlin.
16. GEERING; A., KUNDERT, M., KELSEY, Ch.: Complete Denture and Overdenture Prosthetics. Thieme Medical Publishers, Inc., New York. 1993


Millennium: the safest, complete and most rapid B type sterilizer. Ideal point of reference in terms of safety, performance and flexibility via delle azalee, 1 20090 buccinasco (mi) ph. (+39) 0245701505 r.a. - fax (+39) 0248840514 mocomcom@mocom.it - www.mocom.it we have a passion for sterilization creartcom.it

Hydrogen peroxide bleaching:
Effect of various concentrations on mercury and other metal ions release from admixed and spherical dental amalgam
veen M. Ayad, PhD Lecturer of Dental Biomaterials, Dental Biomaterials Department, Faculty of Dentistry, Mansoura University, Mansoura, Egypt. e-mail: neveenmokhtar@yahoo.com
Abstract
Objectives: the aim of this study was to determine the effect of different Hydrogen Peroxide (HP) concentrations on mercury and other metal ions release from admixed and spherical dental amalgam.
Method and materials: Dental amalgam discs were prepared from GS.80 and Lojic+ alloys (n=25 of each alloy) according to manufacturer's instructions in stainless steel moulds (10mm diameter and 2mm thickness). The discs were divided into five equal groups for each alloy. Each group was immersed in 20 ml of 38%, 24%, 10%, or 3% HP solution for 24 h at 37oC with 0% (distilled water) as control. Following immersion procedure, solutions were taken for metal ion release determination (Hg, Ag, Sn and Cu) using inductively coupled plasma mass spectrometry (ICP-MS). Statistical analysis was conducted using one and two way ANOVA tests to determine significance of differences between test groups. Bonferroni Post Hoc test was conducted for multiple comparisons.
Results: Metal ion release for the elements (Hg, Ag, Sn and Cu) increased with exposure to increasing concentrations of HP for both GS.80 and Lojic+ amalgam alloys. The differences in concentration of metal ions released after treatment with 0% (control), 3%, 10%, 24% or 38% HP were statistically significant (p < 0.05).
Conclusion: Metal ions (Hg, Ag, Cu and Sn) were released from dental amalgam following treatment with all HP concentrations. Metal ion release increased with increasing HP concentration. Even withexposureofdentalamalgamtorelativelyhighHPconcentration (38%), released Hg did not exceed the maximum acceptable limit.
Keywords: Hydrogen Peroxide, bleaching, metal ion release, dental amalgam
Introduction
Nowadays, the increased esthetic demand by most patients has resulted in an increase in the usage of bleaching agents to whiten discolored teeth.1-3 Bleaching of discolored vital and non-vital teeth including both in-office and at-home techniques has a long and successful history.4,5 Home bleaching has attracted the
interest of patients due to its high success rates and ease of use.6,7 In this procedure, patients apply bleaching agents, most of which contain low concentrations of hydrogen peroxide (3% to 7%) or carbamide peroxide (10% to 22%), to their teeth in custom-fitted trays for a few hours per day.8,9 Over the past few years, in-office bleaching products employing the use of strong oxidizing agent up to 38% hydrogen peroxide have been used.10 The advantages are that treatment is totally under the dentist’s control, the soft tissuesare generally protectedfrom the process and it has the potential for quick bleaching.3,11 Very often in the daily clinical practice, restorations exist beside or even inside the teeth that are planned to be bleached. Some clinicians express concern about the effect of these agents on teeth and dental restorative materials.12,13 The influence of various bleaching agents on physical properties, surface morphology and color of different restorative materials, has been investigated in several in vitro-studies simulating the clinical situation as closely as possible. In those studies, home-bleaching products (10–16% carbamide peroxide) were generally used within a 2–6 weeks bleaching simulation with application intervals of 4–8 h per day. Bleaching products for in-office-application (30–38% hydrogen or carbamide peroxide) were applied at treatment intervals of 15–60 min (as recommended by the manufacturers).14 The results of these studies were controversial. Some reports in the dental literature have suggested that bleaching agents may have adverse effects on the physical properties of dental restorative materials.15-20 Other investigations revealed no significant change in enamel or existing restoration physical properties due to bleaching agents.12,20-24 Moreover, some studies reported increase in enamel or composite resin surface hardness following bleaching.25,26 Regarding dental amalgam, some in vitro studies have reported a significant increase in mercury release as a result of treatment with peroxides compared to control treatments.27-29 While there was also a relatively recent report that found carbamide peroxide bleaching to have no significant effect on dental amalgam.30 This obvious and still lasting controversy means that the effect of oxidizing bleaching agents on dental amalgam still remains a source of concern. Therefore, the aim of this study was to investigate the effect of hydrogen
OPERATIVE DENTISTRY 34 HYDROGEN PEROXIDE BLEACHING DENTAL NEWS,VOLUME XVII,NUMBER I,2010
Ne
NobelProceraTM













Individualized bars milled out of light and biocompatible surgical grade titanium.











Wide variety of bars and attachments for fixed and removable solutions.

Precision of fit for ideal load transfer and long-term stable screw joints.






Available for Nobel Biocare implants and multi-unit abutments, other major implant systems and a combination thereof.

Experience a new world of high precision, fast and cost-efficient CAD/CAM dentistry. Your laboratory designs individualized implant bars overdenture for all indications in the NobelProcera Software – fixed and removable, from low cost to high-end, for a variety of attachment types and implant
systems. All bars are milled from biocompatible surgical grade titanium monoblocs by a NobelProcera production facility, resulting in light and strong bars without welding seams or porosity issues. Each bar is delivered highly polished and ready-to-use, with clinical screws*, attachments**
and a 5-year warranty. Nobel Biocare is the world leader in innovative and evidence-based dental solutions. For more information, visit our website.
www.nobelbiocare.com
*Clinical screws are only included for Nobel Biocare implants. **Availability of attachments may differ from country to country depending on regulatory clearance. However, all bars are delivered pre-tapped to accept the desired attachments. Disclaimer: Some products may not be regulatory cleared/released for sale in all markets. Please contact the local Nobel Biocare sales office for current product assortment and availability © Nobel Biocare Services AG, 2009. All rights reserved. Nobel Biocare, the Nobel Biocare logotype and all other trademarks are, if nothing else is stated or is evident from the context in a certain case, trademarks of Nobel Biocare.
Biocompatible
precise
and
implant bars overdenture.
OPERATIVE DENTISTRY
peroxide bleaching agent in different concentrations including recently used high concentrations on metal ion release from dental amalgam. The working hypothesis was that high concentrations of hydrogen peroxide bleaching may result in release of mercury from dental amalgam that may exceed the maximum acceptable limit of daily intake.
Method and materials
Two high copper dental amalgam alloys were selected for this study, an admixed one: GS.80 (Southern Dental Industries, Australia). The composition of this alloy is 40 Ag, 31.3 Sn, and 28.7 Cu (% w/w). It is mixed at an alloy to mercury ratio of 1: 0.92 (w/w). The other was a spherical alloy: Lojic+ (Southern Dental Industries, Australia). The composition of this alloy is 60.1 Ag, 28.05 Sn, 11.8 Cu, and 0.05 Pt (% w/w). It is mixed at an alloy to mercury ratio of 1: 0.67 (w/w). Both alloys were supplied as capsules that were activated according to manufacturer’s instructions for 5 sec. using a mechanical amalgamator, (De Trey, Hallam Dental Ltd, England). Amalgam Discs (n=25) for each alloy type were prepared in split stainless steel moulds (10mm diameter x 2mm thickness), and allowed to fully set for 24 h. The discs were then polished using silicone carbide paper (Grit number 800). A 40% HP solution, (Sigma Chemical Co. St. Louis, MO, USA) was diluted to obtain 3%, 10%, 24% as well as 38% HP solutions with 0% (distilled water) as the control. The 50 amalgam discs were divided into 10 equal groups, (5 discs each). Each of the 5 discs in a group was individually immersed in 0%, 3%, 10%, 24% or 38% HP solution (20ml) for 24 h at 37oC creating 5 samples of each solution. Each disc was placed in a tapered centrifuge tube, with all surfaces exposed to the particular HP concentration in that tube. All the 50 solutions samples were analyzed by inductively coupled plasma-mass spectrometry (ICP-MS, Agilent 4500). All ion release samples were acidified with 200 μl of nitric acid (for Ag determination) and hydrochloric acid (for all other ions).30 For each analysis, the instrument performed five measurements and the mean values were calculated for each element. A two-way ANOVA was conducted, followed by a one-way ANOVA and Bonferroni Post Hoc test for multiple comparisons between solutions of different concentrations for each element.
Results
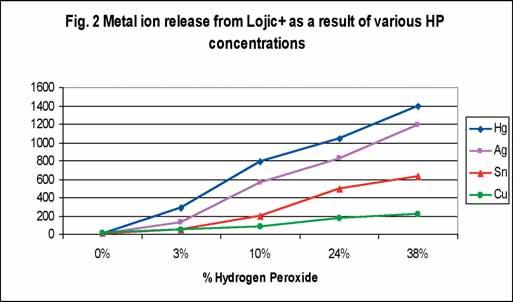
The relationships between metal ion release from both GS.80 and Lojic+ amalgam alloys and HP concentration are shown in Fig. 1& 2 respectively. Values for the mean and standard deviation of metal ion release data for mercury, silver, copper and tin from both GS.80 and Lojic+ are shown in Table 1, at 0%, 3%, 10%, 24% and 38% HP concentrations. Metal ion release increased with increasing hydrogen peroxide concentration for all elements for both amalgam alloys. For GS.80, the highest ion releases were those for mercury followed closely by tin then copper and finally silver. For Lojic+, the highest ion releases were

those for mercury followed closely by silver then tin and finally copper. Table 2 demonstrates the F and p-values for the one-way ANOVA between test groups for each element. Bonferroni multiple comparison revealed that the difference in metal ion release between 0% HP (control) and all other concentrations (3%, 10%, 24% and 38%) was statistically significant (p < 0.05) for all elements.
Discussion
The experimental design in the current study was decided to cover a relatively wide range of HP concentrations that are available in the dental market including both at home and in-office products (3%-38%). Using two kinds of dental amalgam alloys was suggested so that the study includes both spherical and admixed types of dental amalgam so conclusions can, to some extent, be generalized. Comparing between the amounts of mercury or other metal ions released from the tested alloys after exposure to HP bleaching was not in the scope of this study. Although this study provides data about the amounts released of Hg, Ag, Sn and Cu from dental amalgam after exposure to HP bleaching, the focus will be on mercury during discussing results as it is known to be the most hazardous to health. The World Health Organization (WHO) guideline for maximum intake of mercury is 40 mg/day.31 From the literature, it has been reported that the release of metal ions from restorations is time dependent and proportional to the surface area of the restoration.32 The quantity of mercury released from dental amalgam after bleaching as reported in scientific journals varied considerably. Hummert et al.28 found mercury release values from dental amalgam exposed to bleaching agents to be in the range of 0.0140.020 μg/mm2 and 0.001 μg/mm2 for dental amalgam exposed to saline (control). Mackert and Berglund33 found that the rate of mercury release from amalgam to be in the average of 0.0140.016 μg/mm2 calculated from six different in vivo studies. Rotstein et al.29 reported a concentration of 0.6 – 4.24 μg/mm2 of mercury released from amalgam samples after 48 h of 10% CP bleaching. This data suggests high metal ion release, mainly due to the use of aggressive test procedures along with the use of unpolished samples. This is in contrast to the in vivo situation where the amalgam restoration is ideally polished and it is
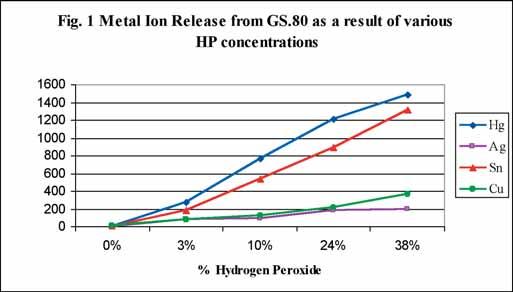
36 HYDROGEN PEROXIDE BLEACHING DENTAL NEWS,VOLUME XVII,NUMBER I,2010
OPERATIVE DENTISTRY
Table 1. Means and standard deviations for metal ion release
3% HP Mean(SD)
Hg (μg/l)
Ag (μg/l)
Sn (μg/l)
Cu (μg/l)
GS.80
3.3(0.57)
0.09(0.02)
2.6(0.18)
6.23(0.37)
Lojic+
2.9(0.33) 0.05(0.02) 1.03(0.04) 8.77(0.06)
GS.80 272(17.8)
77.6(7.1) 180.2(9.7) 85(12.1)
Lojic+
286(10.8)
125.3(5.0) 43.8(6.2) 49(4.5)
GS.80 762(26.8) 93.5(6.5) 532(39.3) 125(14.9)
known that peroxide levels within bleaching products are depleted during use34. In a further study by Rotstein et al.,35 the amount of mercury released from amalgams treated with 10% CP was very similar to that released by 10% HP. Al-Salehi et al. 30 found that 10% CP bleaching gel did not significantly enhance metal ion release from dental amalgam. In the present study, application of hydrogen peroxide bleaching agent in different concentrations has resulted in metal ion release (Hg, Ag, Cu and Sn) from all samples of both GS.80 and Lojic+ alloys. For all the elements, ion release increased with increasing HP concentrations, with mercury release consistently being the highest (Fig. 1, 2), (Table 1). The p-values for the one-way ANOVA and Bonferroni Post Hoc revealed that the difference in metal ion release between 0% HP (control) and all other concentrations (3%, 10%, 24% and 38%) was statistically significant (p < 0.05) for all elements. As regards to GS.80, of the four elements reported, mercury and tin were more responsive to changes in HP concentration exhibiting a fairly linear relationship between ion release and HP concentration (Fig. 1). The ion release data for copper and silver followed to a great extent a similar trend especially at low HP concentrations. For Lojic+, mercury and silver were more responsive to changes in HP concentration, followed by tin while copper showed the least affection by changes in HP concentration. The calculated amounts of mercury release from a GS.80 sample were 29.69, 24.2, 15.24 and 5.44 μg/ day and from a Lojic+ sample were 27.92, 20.86, 15.7 and 5.72 μg/ day for 38%, 24%, 10% and 3% HP concentrations, respectively. The total surface area of the cylindrical amalgam disc was 220 mm2, therefore the average mercury release per unit area of a GS.80 sample was 0.13, 0.11, 0.07 and 0.02 μg/ mm2, and from a Lojic+ sample was 0.13, 0.09, 0.07 and 0.03 μg/ mm2 over a 24 h period / unit area of the surface exposed to 38%, 24%, 10% and 3% HP concentrations,
Lojic+
785.1(9.9)

respectively. Assuming the area of a typical restoration in the mouth is 5mm x 5mm approximately, based on these data, a single GS.80 restoration will release on average 3.37, 2.75, 1.7 and 0.6 μg/ day, and Lojic+ restoration will release 3.17, 2.37, 1.78 and 0.65 μg/ day, at 38%, 24%, 10% and 3% HP concentrations, respectively. Clearly, to exceed WHO’ s maximum acceptable intake of 40 mg/day would require mercury release from 11, 14, 23 and 66 GS.80 restorations and 12, 16, 22 and 61 Lojic+ restorations when treated with 38%, 24%, 10% and 3% HP concentrations, respectively. It is therefore unlikely that mercury release from amalgam following contact with tooth bleaching agents containing up to 38 % HP constitutes a hazard to health. One of the limitations of this in vitro study is that the bleaching agent was kept in contact with dental amalgam without the dilution effect of saliva. However, in the oral cavity, it would require a longer period of time for metal ions released from amalgam restorations to reach the levels obtained in the results of this study.
Conclusion
Within the limitations of this study, the following conclusions can be obtained:
1. Metal ions (Hg, Ag, Cu and Sn) were released from dental amalgam following treatment with all HP concentrations.
2 The amount of ion release for all elements increased with increasing HP concentration and was statistically significant compared to control treatment (p < 0.05).
3 Although mercury release from amalgam exposed to bleaching agents did not exceed the maximum acceptable limit internationally, highly concentrated bleaching agents should be available only to dental professionals and they should be closely monitored to ensure that no new hazards present themselves in the future. 0% HP
Table 2: F & p-values for the one-way ANOVA between groups (0%, 3%, 10%, 24%, 38%)
38 HYDROGEN PEROXIDE BLEACHING DENTAL NEWS,VOLUME XVII,NUMBER I,2010
Mean(SD)
10%
HP Mean(SD)
24% HP Mean(SD) GS
1210(35.3) 179.2(15.9)
Lojic+ 1043(12.2) 824.5(7.1) 487(9.0) 174(6.6) 24% HP Mean(SD) GS.80 1210(35.3) 179.2(15.9) 896.4(41.3) 212.2(13.5) Lojic+ 1043(12.2) 824.5(7.1) 487(9.0) 174(6.6)
562(7.3) 198.2(10.0) 76.2(2.5)
.80
896.4(41.3) 212.2(13.5)
GS.80 F-value 3000.2 225.5 1623.4 269.8 p-value 0.000 0.000 0.000 0.000 Hg Ag Sn Cu Lojic+ F-value 15688.0 32769.8 7111.4 1656.9 p-value 0.000 0.000 0.000 0.000


REFERENCES
1 Sulieman M, Addy M, Macdonald E, Rees JS. The bleaching depth of a 35% hydrogen peroxide-based in-office product: a study in vitro. Journal of Dentistry 2005;33(1):33–40.
2 Fasanaro TS. Bleaching teeth: history, chemicals and methods used for common tooth discolorations. J Esthet Dent 1992;4:71-78.
3 McEvoy SA. Chemical agents for removing intrinsic stains from vital teeth. II. Current techniques and their application. Quintessence International 1989;20:379–84.
4 Attin T, Paque F, Ajam F, Lennon AM. Review of the current status of tooth whitening with the walking bleach technique. Int Endod J 2003;36:313—29.
5 Haywood VB. History, safety, and effectiveness of current bleaching techniques and applications of the nightguard vital bleaching technique. Quintessence Int 1992;23:471—88.
6. Leonard RH Jr. Long-term treatment results with nightguard vital bleaching. Compend Contin Educ Dent 2003 Apr;24:364-374.
7 Karpinia KA, Magnusson I, Sagel PA, Zhou X, Gerlach RW. Vital bleaching with two at-home professional systems. Am J Dent. 2002 Sep;15 Spec:13A-18A.
8 Haywood VB. Current status of nightguard vital bleaching. Compend Contin Educ Dent Suppl 2000;28:S10-17.
9 Leonard RH, Sharma A, Haywood VB. Use of different concentrations of carbamide peroxide for bleaching teeth: an in vitro study. Quintessence International 1998;29(8):503–7.
10 Polydorou O, Monting JS, Hellwig E, Auschill TM. Effect of in-office tooth bleaching on the microhardness of six dental esthetic restorative materials. Dental Materials 2007;23:153–8.
11 Auschill TM, Hellwig E, Schmidale S, Sculean A, Arweiler NB. Efficacy, side-effects and patients’ acceptance of different bleaching techniques (OTC, in-office, at-home). Oper Dent 2005;30:156–63.
12 Swift Jr EJ, Perdigao J. Effects of bleaching on teeth and restorations. Compendium Continuing Educ Dentistry 1998;19:815–20.
13 Swift Jr EJ. Restorative considerations with vital tooth bleaching. J Am Dent Assoc 1997;128(Suppl):60S—4S.
14. Attin T, Hannig C, Wiegand A, Attin R. Effect of bleaching on restorative materials and restorations—a systematic review. Dental Materials 2004;20:852–61.
15 Lee JH, Kim HI, Kim KH, Kwon YH. Effect of bleaching agents on the fluoride release and microhardness of dental materials. Journal of Biomedical Materials Research 2002;63(5):535–41.
16 Jung CB, Kim HI, Kim KH, Kwon YH. Influence of 30% hydrogen peroxide bleaching on compomers in their surface modifications and thermal expansion. Dental Materials Journal 2002;21(4):396–403.
17 Turker SB, Biskin T. Effect of three bleaching agents on the surface properties of three different esthetic restorative materials. Journal of Prosthetic Dentistry 2003;89(5):466–73.
18 Duschner H, Gotz H, White DJ, Kozak KM, Zoladz JR. Effectsof hydrogen peroxide bleaching strip gels on dental restorative materials in vitro: surface microhardness and surface morphology. Journal of Clinical Dentistry 2004;15(4):105–11.
19. Taher NM. The effect of bleaching agents on the surface hardness of tooth colored restorative materials. J Contemp Dent Pract 2005;15:18-26.
20 Yap AU, Wattanapayungkul P. effects of in-office tooth whiteners on hardness of tooth-colored restoratives. Oper Dent 2002;27:137-141.
21 Cullen DR, Nelson JA, Sandrik JL. Peroxide bleaches: effect on tensile strength of composite resins. J Prosthet Dent 1993;69:247-249.
22 Garcia-Godoy F, Garcia-Godoy A. Effect of bleaching gels on the surface roughness, hardness and micromorphologhy of composites. Gen Dent 2002;50:247-250.
23 Schemehorn B, Gonzalez-Cabezas C, Joiner A. A SEM evaluation of a 6% hydrogen peroxide tooth whitening gel on dental materials in vitro. J Dentistry 2004;32(Suppl 1):35–9.
24 Mair L, Joiner A. The measurement of degradation and wear of three glass ionomers following peroxide bleaching. J Dentistry 2004;32(Suppl 1):41–5.
25 Turker SB, Biskin T. The effect of bleaching agents on the microhardness of dental aesthetic restorative materials. Journal of Oral Rehabilitation 2002;29(7):657–61.
26 Campos I, Briso AL, Pimenta LA, Ambrosano G. Effects of bleaching with carbamide peroxide gels on microhardness of restorative materials. J Esthet Restor Dent 2003;15:175-182.
27 Robertello FJ, Dishman MV, Sarrett DC, Epperly AC. Effect of home bleaching products on mercury release from an admixed amalgam. American Journal of Dentistry 1999;12: 227–30.3.
28 Hummert TW, Osborne JW, Norling BK, Cardens HL. Mercury in solution following exposure of various amalgams to carbamide peroxide. American Journal of Dentistry 1993;6:305–9.28.
29 Rotstein I, Dogan H, Avron Y, Shemesh H, Steinberg D.Mercury release from dental amalgam after treatment with 10% carbamide peroxide in vitro. Oral Surgery Oral Medicine Oral Pathology Oral Radiology Endodontics 2000;89:216–9.
30 Al-Salehi SK, Hatton PV, Miller CA, McLeod C, Joiner A. The effect of carbamide peroxide treatment on metal ion release from dental amalgam. Dental Materials 2006;22:948–53.
31 Jones DW. Exposure or absorption and the crucial question of limits for mercury. J Can Dental Assoc 1999;65:42–6.
32 Berglund A, Pohl L, Olsson S, Bergman M. Determination of the rate of release of intra-oral mercury vapour from amalgam. Journal of Dental Research 1988;67:1235–42.
33 Mackert JR, Berglund A. Mercury from dental amalgam fillings: absorbed dose and potential for adverse health effects. Critical Reviews in Oral Biology and Medicine 1997;8: 410–36.
34 Sagel PA, Odioso LL, McMillan DA, Gerlach RW. Vital tooth whitening with a novel hydrogen peroxide strip system: design, kinetics, and clinical response. Compendium Continuing Educ Dentistry 2000;21:S10–34.
35 Rotstein I, Chaim M, Arwaz JR. Changes in surface levels ofmercury, silver, tin and copper of dental amalgam with carbamide peroxide and hydrogen peroxide in vitro. Oral Surgery Oral Medicine Oral Pathology Oral Radiology Endodontics 1997;84(4):506–9.
40 HYDROGEN PEROXIDE BLEACHING DENTAL NEWS,VOLUME XVII,NUMBER I,2010

PROSTHETIC DENTISTRY

CALCIUM HYDROXIDE and GL
ASS IONOMER LINERS:
r A Taki, DDS, DScD
Al Ahmadi Dental Services - Kuwait
jabertaki@yahoo.com
ABSTRACT
Purpose: Thissurveywasdesignedtogathermostoftheinformation regarding the use of dental liners amongst three dental specialties in different countries. More so, issues and opinions have been raised about using specific dental liners, which as the same time other studies were against the use of the same materials making the decision of choosing dental liners more difficult. Collecting this information will basically provide us with the most used dental liners in different countries around the world. The aim of the study is to: Determine the prevalence of using calcium hydroxide and/or Glass ionomer, to assess the reason of using these two materials, and to verify the purpose of using each of these materials.
Amongst the selected Dentists, the Method and Materials:
The survey has been conducted by distributing questionnaires to the three dental specialties, which involves Prosthodontics, PediatricDentistryandGeneralPractitionersDentistsfromdifferent countries which include; Kuwait, Qatar, Saudi Arabia, UAE, United Kingdom, Thailand, and various states in the United States of America. The 40 questionnaires have been randomly allocated to each selected country by mail. The questions have also been concentrated on the using of the dental liners, the indications of the using, and the dentist’s knowledge about dental materials. Variables: The prevalence, Type of the dentition, and Type of the liners. Results: The selected countries were divided into three regions. In the North American region, of the 104 returned questionnaires, 13 dentists (12.5%) reported using calcium hydroxide, 59 dentists (56.7%) use glass ionomer, and 32 dentists (30.8%) use both calcium hydroxide and glass ionomer as dental liners. Fifty-five (55) dentists (45.9%) in the Asian region are recorded as using calcium hydroxide, 15 dentists (12.5%) use glass ionomer, 42 dentists (35%) prefer to use both liners, and 9 dentists (7.5%) use none. In the European region, 5 (7.5%) selected calcium hydroxide, 34 (51.5%) selected glass
ionomer, and 27 (40.9%) said they used both liners. A significant difference was found amongst the three groups of dental specialistsin the use of calcium hydroxide and/or glass ionomer. One wayanalysis of variance showed that General dentists use CH exclusively (33%); more than Prosthodontists (20%) and Pediatric dentists (21%), (F2=2.39; p= .093).
Furthermore, according to the results continuing education courses were the most commonly indicated manner for those dentists in the North American (97.1%) and European regions (86.4%), whereas continuing education courses was the least common option in the Asian region (40.8%).
Conclusion: The use of GI was found to be increased, compared to CH, as dental lining material in both North American and in European regions. Required continuing education courses in the North American and European regions might have an influence on the selection of dental lining materials.
INTRODUCTION
As most of the life sciences, Dentistry has progressed remarkably during this century, with great success in the areas of diagnostic, prevention therapeutics and dental industries. A large number of materials have been introduced into the dental fields to provide an esthetical and functionally healthy tooth. Among the important materials are dental liners and bases, which eliminate the postoperative complications and protect the dental pulp.
In fact, no artificial material can be placed into a tooth to provide better protection for the pulp than dentin. Basing or lining materials do not have properties, which can be demonstrated that ideally duplicate those of dentin. The remaining dentin thickness from the pulpal extent of the cavity preparation to the pulp is the single most important factor, which protects the pulp from insult (Stanley, 1981). In vitro studies have shown that a 0.5mm thickness of dentin reduces the toxicity level of a material by 75% and a 1 mm thickness of dentin by 90% (Meryon, 1988).1
The Prevalence of Use among Prosthodontists, Pediatric and General Dentists in Different Countries.
42 CALCIUM HYDROXIDE and GLASS IONOMER LINERS DENTAL NEWS,VOLUME XVII,NUMBER I,2010
Jabe

Û MECTRON PIEZOSURGERY® THE THIRD GENERATION OF THE ORIGINAL – THE EVOLUTION OF A REVOLUTION! mectron s.p.a., via Loreto 15/A, 16042 Carasco (Ge), ITALIA, tel + 39 0185 35361, fax +39 0185 351374, www.mectron.com, mectron@mectron.com Û NEW PIEZOSURGERY® 3 – FASTER, EASIER, MORE PRECISE!
PROSTHETIC DENTISTRY
Microleakage is a common, unavoidable, clinical phenomenon by which oral fluids, ions, molecules, and bacteria penetrate the tooth/restoration interface and gain access to dentinal tubuli and pulp.4
The sealing property of a basing material is one important criteriato determine the success or failure of a base. Cox et. al. stated that bacterial leakage under restorations is the primary cause of pulpal irritation. They further indicated that healing of dental pulp exposures is not dependent on the effect of a particular type of medicament, but on the capacity of the capping material to prevent bacterial leakage.2
The proposed benefits for using adhesive liners under amalgams are to decrease microleakage and temperature sensitivity, to provide improved retention and strengthening of adjacent tooth structure. Researchers have sought to find a cavity sealer that could provide improved performance over varnish, since more studies have revealed that varnishes reduce but do not eliminate microleakage around amalgam restorations (Pashly & Depew, 1986; Fitchie & others 1990).
Cavity liners when placed with minimal thickness, usually less than 0.5 mm act as a cavity sealers and provide expanded benefits, such as fluoride release, adhesion to tooth structure, antibacterial action and promotes a healthy pulp (McCoy, 1995). Both calcium hydroxide and glass ionomer cements become lining materials of choice: calcium hydroxide because of its ease of handling and its excellent pulpal response. And glass ionomer because of its ability to adhere to tooth structure, its potential to be etched and reliably bonded, and its apparent ability to reduce postoperative sensitivity when used as a base under posterior composite resins.
Calcium hydroxide:
It has long been used as a base/liner because of its pulpal compatibility and purported ability to stimulate reparative dentin formation with direct pulpal contact (Stanley, 1981). However, research has shown that not all formulation of Ca(OH)2 have a stimulatory effect on human pulpoblasts (Hanks, Bergenholtz & Kim, 1983). Conventional formulation of Calcium hydroxide demonstrated poor physical properties (Farah & others, 1983; Craig, 1989). High solubility may result in contamination of bonding agents and increased marginal leakage (Krejci & Lutz, 1990), as well as softening or material loss poorly sealed restorations (Brannstrom, 1984; Pereira, Manfio & Franco, 1990). Visible-lightactivated calcium hydroxide overcomes most of these deficiencies and exhibits improved physical properties (Tam & others, 1989) and significantly reduced solubility (Craig, 1989).
Glass Ionomer:
The invention of glass ionomer cement as a dental material was first reported by Wilson and Kent (1972). Due to their chemical nature, these materials are able to adhere to enamel and dentin surfaces.5 Glass ionomer has been utilized as a cavity liner in an

attempt to take advantage of two highly desirable properties: chemical bond to tooth structure and fluoride release (Craig, 1989). Although fluoride release from glass ionomer decreases with time (Olsen & others, 1989), sustained release has been demonstrated (Mitra, 1991) with corresponding uptake into adjacent tooth structure (Geiger & Weiner, 1993). Pulpal response to both visible-light-activated and a conventional glass ionomer formulation have been shown to be quite favorable (Hosada & others, 1991; Gaintantzopoulou, Willis & Kafrawy, 1994), probably due to glass ionomer’s ability to decrease bacterial penetration (Heys & Fitzgerald, 1991). In addition, glass ionomer has been shown to reduce microleakage when placed under amalgam restorations (Arcoria, Fisher & Wagner, 1991). Conventional glass ionomer is relatively soluble in an acidic environment and it’s susceptible to rapid surface deterioration when subjected to acid etching (Smith, 1988).
The aim of this survey was to determine the prevalence and the indications of using Calcium hydroxide and/or Glass ionomer among three dental specialties in seven different countries around the world.
METHOD AND MATERIALS
This survey was conducted during a 6-month period by distributing questionnaires, (Index - I), to the three dental specialties, which involve Prosthodontics, Pediatric Dentists and General Practitioner Dentists in different countries including: Qatar, Saudi Arabia, United Arab Emirate, United Kingdom, Thailand, Switzerland and five states from the Unites States of America including; Massachusetts, Illinois, California, Texas, and Florida. The 300 questionnaires were rationed to the selected seven countries. 40 questionnaires were randomly allocated to each country including Qatar, Saudi Arabia, United Arab Emirates, United Kingdom, Switzerland and Thailand. At the same time, 30 questionnaires were sent to the selected five states in the United States of America. The envelopes were sent by airmail. Stamped return envelopes were included.
The questionnaire is composed of 12 questions. These questions include the type of dental liners, the indication for using dental liners, the type of the dentition (primary and/or permanent) which they usually apply these materials to, the kind of the curing method, the dentist’s knowledge and the dentist’s satisfaction over the chosen dental liner.
RESULTS
The selected countries were divided into three regions: the North American region (Massachusetts, Illinois, California, Texas, and Florida), the European region (Switzerland and United Kingdom), and the Asian region (Qatar, United Arab Emirates (UAE), Saudi Arabia and Thailand). From the selected countries in these regions, 291 completed questionnaires were submitted by 83 Prosthodontists (28.5%), 105 Pediatric Dentists (36%), and 103 General Dentists (35.5%).
44 CALCIUM HYDROXIDE and GLASS IONOMER LINERS DENTAL NEWS,VOLUME XVII,NUMBER I,2010






















* CAD/CAM in Aesthetic and Prosthetic Dentistry
* CAD/CAM Dental Laboratories
* CAD/CAM Materials



* Computerized Scanning and Imaging
* Implantation Navigation Systems
* Computerized Orthodontic Planning and Design
* Computerized Management and Planning
* Computerized Informational and Educational Software






4th CAD/CAM & Computerized Dentistry International Conference 13-14 May 2010, Dubai The Address Dubai Marina The new era in Aesthetic Dentistry CAPP Tel: +971 4 3616174 | Fax: +971 4 3686883 | Mob: +971 50 2793711 | info@cappmea.com www.cappmea.com/cadcam4 Platinum Sponsor Official Sponsors Other Industry Players Gold Sponsors Estimated 14 CME Hours
PROSTHETIC DENTISTRY
Through the questionnaire, respondents had been asked to indicate the dental liners they used during their dental procedures. They were given four options from which to choose: calcium hydroxide (CH), glass ionomer (GI), both liners, and none. In the North American region, of the 104 returned questionnaires, 13 dentists (12.5%) reported using calcium hydroxide, 59 (56.7%) dentists use glass ionomer, and 32 dentists (30.8%) use both calcium hydroxide and glass ionomer as dental liners. Fiftyfive (55) dentists (45.9%) in the Asian region are recorded as using calcium hydroxide, 15 dentists (12.5%) use glass ionomer, 42 dentists (35%) prefer to use both liners, and 9 dentists (7.5%) use none. In the European region, 5 (7.5%) selected calcium hydroxide, 34 (51.5%) selected glass ionomer, and 27 (40.9%) said they used both liners.
One-way analysis of variance revealed significant differences between regions in the use of calcium hydroxide (F2=26.49; p< .001), and of glass ionomer. (F2= 31.83; p< .001). (Figure 1)
Among all of the selected countries the variation in use of either calcium hydroxide or glass ionomer was clearly apparent. In the United Arab Emirates 17 of 36 responding dentists (47.2%) use calcium hydroxide and 5 dentists only use glass ionomer (13.8%). According to the 38 responding dentists from Qatar, glass ionomer has not been chosen as a single dental liner, whereas, 27 of 38 (71%) dentists indicated that they use calcium hydroxide. Much the same seems to occur in Saudi Arabia. Of the 25 respondents, 8 dentists (32%) used calcium hydroxide and 4 dentists (16%) used glass ionomer as a liner. Thai dentists were slightly different than Middle Eastern dentists in choosing dental liners. Three (14.2%) of 21 responding dentists use calcium hydroxide and 6 dentists (28.5%) use glass ionomer. All the remaining dentists had in common the practice of using both calcium hydroxide and glass ionomer as liners. In contrast, the selection of dental liners among dentists in the United Kingdom and Switzerland differed remarkably from the previously mentioned countries. In the United Kingdom, 2 of 38 responding dentists (5.2%) selected calcium hydroxide, 18 dentists (47.3) selected glass ionomer, and 18 (47.3%) dentists selected both liners. Only 3 (10.7%) of the responding 28 Swiss dentists selected calcium hydroxide, 16 (57.1%) selected glass ionomer, and 9 (32.1%) dentists selected both liners. One-way analysis of variance demonstrated significant differences between countries in the use of calcium hydroxide only

(F6=15.49; p< .001), and glass ionomer only (F6= 11.88; p< .001). (Figure 2)
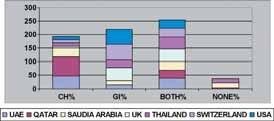
A significant difference was also found amongst the three groups of dental specialists in the use of calcium hydroxide and/or glass ionomer. The One way analysis of variance showed that General dentists use CH exclusively (33%); more than Prosthodontists (20%) and Pediatric Dentists (21%), (F2=2.39; p= .093).
The dentists had also been asked whether they had a private practice or worked in another type of dental facility. From the response to that question, in all the selected countries, an unpaired t-test showed that dentists who did not work in private practice used CH exclusively (34%) and twice as frequently as the dentists who worked in private practices (14%) (t286=3.93; p< .001). This contrasted with the responses of those dentists who work in private practices since these dentists use GI exclusively (50%) and twice as often as dentists who do not work in private practices (28%) (t286=3.92; p< .001).
Sample subjects had also been asked about the indications for using dental liners. Five optional indications were provided: direct pulp capping, indirect pulp capping, under amalgam restorations, under composite restorations, and whenever needed. The indications from each region were analyzed accordingly. The majority of the dentists in all three regions use dental liners whenever it is needed as follows: 75.8% for the Asian region, 80.3% for the European region, and 80.9% for North American region. (Figures 3 to 5 show the prevalence of the liner’s indication for each region.)
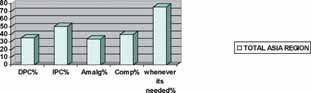

46 CALCIUM HYDROXIDE and GLASS IONOMER LINERS DENTAL NEWS,VOLUME XVII,NUMBER I,2010
Figure 2: The prevalence of using dental liners among all countries
Figure 3: The indications of using dental liners among Asia region
Figure 4: The indications of using dental liners among Europe region
Figure 1: The prevalence of using dental liners among three regions


Our survey was also sought to determine, among countries the type of dentition that would be indicated for the dental liners. For this purpose, an unpaired t-test has been used and it showed that while there was no significant difference in the type of dentition, dentists who, for permanent teeth, use GI only (56%) are significantly different than dentists who use CH only (16%) (t287=3.16; p= .002).
How the dentists had acquired information about liners and their use had been identified through the survey. Three means of development were provided for selection: continuing education courses, dental journals, and other sources. There was a significantdifference amongst the three regions in those who had participated in continuing education courses (F2=70.77;p< .001) (Figures 6-8)


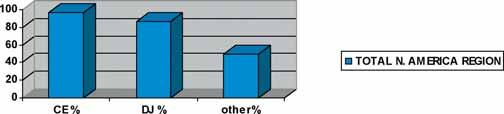
According to the results, continuing education courses were the most commonly indicated manner for those dentists in the North American (97.1%) and European regions (86.4%), whereas continuing education courses was the least common option in the Asian region (40.8%).
One-way analysis of variance showed an interesting significant
PROSTHETIC DENTISTRY
difference between dentists who attend continuing education courses and the use of calcium hydroxide only, (F1=12.88; p< .001), and dentists who attend continuing education courses and the use of glass ionomer only (F1=18.72; p< .001). This analysis showed a contrasting correlation between attending continuing education courses and the use of calcium hydroxide only. In that relationship the study found that 76.9% of the dentists, who use calcium hydroxide only, do not attend continuing education courses. There was also a statistical difference between dentists who attend continuing education courses and the use of glass ionomer 86% use glass ionomer only as a dental liner. Overall, the level of satisfaction which resulted in using the indicated dental liners was also sought and we found that 56 (19.3%) of the dentists are “very satisfied,” 222 (77%) are “satisfied,” whereas, 12 (4%) dentists are “somewhat unsatisfied.” No dentist selected “unsatisfied.”
DISCUSSION
This study reflects the prevalence in the use of calcium hydroxide and/or glass ionomer among three dental specialties in seven different countries. A review of literature on the use of the liners under scrutiny offered little or nothing on the prevalence of their use, and thus suggested that there were no previous studies on this subject. Several factors that might influence the usage pattern of these two dental liners were also discussed. Participating dentists were asked 12 questions in order to analyze as many influential factors as possible.
Among the three regions, we found that calcium hydroxide is used more in the Asian region while the dentists in the North American and European regions use glass ionomer. In agreement to our finding, a survey included 64 North American schools, which has been done by Frazier et al. have shown that glass ionomer was used by 74% of the schools since calcium hydroxide was indicated in less than 10% of the responses.
According to our results, the possible reason for the differences among regions might be that attending continuing education courses is required in the North American and European regions, which might result in lack of receiving the update information about the dental materials.
Our study revealed that 86% of the dentists who attend continuing education courses use glass ionomer only, as a dental liner, and 76.9% of the dentists who use calcium hydroxide only do not attend these courses.
Regarding glass ionomer material, in 1992 S. C. Bayne stated that general usage of glass ionomer over 20 years indicated a high benefit-to-risk-ratio, and that glass ionomer is trouble-free. In further support of this, Rabchinsky J. el. al. have stated that those repairs in which glass-ionomer cement liners were used, there was significantly less demineralization and microleakage than those done with calcium hydroxide liners.
In 1989 Pappalardo et al. had compared glass ionomer and calcium hydroxide as dental liners, and found that GI showed the tendency
DENTAL NEWS,VOLUME XVII,NUMBER I,2010 47 CALCIUM HYDROXIDE and GLASS IONOMER LINERS
Figure 5: The indications of using dental liners among N. America region
Figure 6: The prevalence of methods used for improvement of dentist’s knowledge regarding dental liners in Asia region
Figure 7: The prevalence of methods used for improvement of dentist’s knowledge regarding dental liners in Europe region
Figure 8: The prevalence of methods used for improvement of dentist’s knowledge regarding dental liners in N. America region
PROSTHETIC DENTISTRY
to be chemically bonded to dentin, and mechanically through the etching to the composite restorative materials. At the same time, Grajower et al. had found that a wash-out of the lining was observed for most teeth in which dycal had been present near the proximal tooth wall. Incipient caries formation was also noted in a few of his samples. These findings correspond with the high prevalence in the use of glass ionomer in selected countries of two regions in our study.
According to our results, the prevalence in the use of calcium hydroxide was highest among general dentists compared to the other two specialties. This finding is almost similar to the study that has been done by A. Santini who found that general dentists’ use of calcium hydroxide, as a lining material is widespread. In the study under discussion we found that, dentists who have private practice tend to use glass ionomer more than calcium hydroxide. Widstrom et al. supports the finding having found that glass ionomer is the most frequently used in children by private practitioners.
CONCLUSION
• The use of GI has increased, compared to CH, as dental lining material in both North American and in European regions.
• Required continuing education courses in the North American and European regions might have an influence on the selection of dental lining materials.
INDEX - I: The Questionnaire
1) What is your specialty?
Prosthodontics
Pedodontics
General dentistry.
2) Do you work for the government? Yes No
3) Do you have your own private practice? Yes No
4) Do you work full time in your private practice? Yes No
5) How long have you been in this practice?
Less than two years
2-5 years
More than five years
6) How would you improve your knowledge regarding the dental materials?
(You may select more than one)
Continuing education courses
Dental journals
Other sources
7) Are you the one who provides the dental materials for the clinic? Yes No

• Among all the selected countries, the indication for using GI and/or CH was not significantly different, since they all have the same reason to for using the selected dental liners.
• Dentists in private practice use glass ionomer more often than calcium hydroxide.
• General dental practitioners tend to indicate calcium hydroxide more often than glass ionomer.
REFERENCES
1. Bayne SC. Dental composites/glass ionomer: clinical reports. Review. Advances in Dental Research. Sep. 1992; 6:65-77.
2. Cindy R. Rauschenberger, DDS, MS, and Eric J. Hovland, DDS, Med, MBA. Clinical Management of Crown Fractures. Dental Clinics of North America. January 1995; V. 39. Number 1.
3. Grajower R., Bielak S., and Eidelman E. Observations on a calciumhydroxide lining in retrieved deciduous teeth, with proximal amalgam fillings. Journal of Oral Rehabilitation. Nov. 1984; 11(6): 561-9.
4. Ilana Eli, DMD, Yifat Cooper (Bril), DMD, Ariel Ben-Amar, DMD, and Ervin Weiss, DMD. Antibacterial Activity of Three Dental Liners. J Prosthod 1995; 4: 178-182.
5. J. Muller, W. Horz, G. Bruckner, E. Kraft. An experimental study on the biocompatibility of lining cements based on glass ionomer as compared with calcium hydroxide. Dent Mater, January 1990; 6:35-40
6. Kevin B. Frazier, DMD., and Ivar A. Mjor, MSD, DR ODONT. The Teaching of All_Ceramic Restorations in North American Dental Schools: Materials and Techniques Employed. Journal of Esthetic Dentistry. 1997; 9(20: 86-93.
7. Kai Chiu Chan, D.D.S., M.S., and Edward J. Swift, Jr., D.M.D. Leakage of chemical and light-cured basing materials. J Prossthet Dent, 1989; 62:408-11.
8. Pappalardo G., Cicciu D., and Galioto S. Use of G.I.C. as a cavity liner. Clinical experience. Stomatologia Mediterranea. Apr-Jun.1989; 9(2): 141-7.
9. Rabchinsky J. Donly KJ. A comparison of glass ionomer cement and calcium hydroxide liners in amalgam restorations. International Journal of Periodontics & Restorative Dentistry. Aug. 1993; 13(4): 378-83.
10. R. J. McConnell, B.D.S., F.F.D., L. Boksman, D.D.S., B.Sc., J. K. Hunter, D.D.S., M.S., F.I.C.D., D. R., and Gratton, D.D.S., M.S. The effect of restorative materials on the adaptation of two bases and a dentin bonding agent to internal cavity walls. Quintessence International. 1986; V. 17, Number 11, 703-10.
11. Santini A. the diagnosis, classification and treatment of acute pulpal pain by UK general dental practitioners: results of a survey. Primary Dental Care. Mar. 1996; 3(1): 24-7.
12. T J Hilton. Cavity Sealers, Liners, and Bases: Current Philosophies and Indications for Use. Operative Dentistry, 1996; 21, 134-146.
13. Widstrom E. and Forss H. Selection of restorative materials in dental treatment of children and adults in public and private dental care in Finland. Swedish Dental Journal. 1994;18(1-2): 1-7.
8) What kind of dental liners do you usually use?
Calcium Hydroxide
Glass ionomer
Both
Non of the above
9) Do you use a liners in: Permanent teeth
Primary teeth
Both
10) What would be your reason for using a dental liner? (You may select more than one reason) Direct pulp capping. In-direct pulp capping. Under Amalgam restorations Under Composite restorations. Whenever it’s needed.
11) What kind of curing method do you usually use for the dental liners? Light cure. Conventional.
12) Which one of the following responses most closely describes your satisfaction towards the dental liners that you are using?
Very satisfied
Satisfied
Somewhat unsatisfied
Unsatisfied
48 CALCIUM HYDROXIDE and GLASS IONOMER LINERS DENTAL NEWS,VOLUME XVII,NUMBER I,2010

GNYDM defies the Economy ' s Skeptics and Achieves Another SuccessfulEvent

Total registration was enormous and Dentists appeared in waves to continue to make the Greater New York Dental Meeting the largest and best dental products and technology buying event and educational forum of its kind in the United States. Total registration in 2009 was a record breaking 59,166. While we welcomed 17,710 Dentists in 2008, this y ear we registered 19 , 488 o f o ur c o ll e agu e s ,an increase of 10%. International registration grew from 4,889 individuals in 2008 to 5,705 in 2009, a rise of 16%. Attendees traveled from 124 countries. Even in this challenging economy, the organization committee planned an event which proved to be successfulfor all dental professionals and the entire dental trade

DENTAL NEWS,VOLUME XVII,NUMBER I,2010 49
Dr. Clifford Salm, General Chairman of the Greater New York Dental Meeting
Dr. Georges Freedman lecturing on bonding resins



50 Greater New York Dental Meeting DENTAL NEWS,VOLUME XVII,NUMBER I,2010
Dean Lonnie Norris, Executive V.P. Michael Alfano and Dr. Tony Dib during the Monday Celebrity Luncheon
Dr. Tony Dib, Dean Lonnie Norris, Executive V.P. Michael Alfano and Dean Charles Bertolami
Dr. Salm, Mrs. Katz and Dr. Lieb during the Hands-on training using injectible Botox and Dermal fillers
Pr. Jon Suzuki during his "Free gingival graft workshop"Dr. Joe Massad and Dr. Richard June in the impression workshop
New

Close Co-Operation withScience Innovations with clinical approval
Premium Swiss Quality
Intensiv is a Swisscompany, manufacturingdentaldiamond instruments of superior quality for more than60 years. Its product portfolio consists of wide range of preparation sets, covering a broad spectrum of indications from cavity, crown and bridge preparations to contouring and finishing. All of them have been conceived anddeveloped with the scientific support of dental universities and well-known opinion leaders.







Intensiv UniglossPaste
Clinically tested and scientificallyapproved by the University of Zurich
Onestep universal extra fine grit diamond paste with uniquely surface adapted micro grain for high glossshining of all aesthetical restorations
Intensiv ProxoStrip
Pat. pend. N°2007 0219/07
Scientifically tested by the University of Ancona, Italy
A unique, diamond-coated metal strip for final polishing of proximal surfaces Practical, fast, ergonomic!
Intensiv
Modular Veneer Set
Dr. A. Schöler, Biel, Switzerland
Diamond instruments for veneer preparation
■ Presently Intensiv is looking for new business partners in: Qatar, Bahrain, Oman, Yemen, Iran
Intensiv SA via al Molino 107 P.O. Box 741 6916 Grancia Switzerland Tel. + 41 91 986 50 50 Fax + 41 91 986 50 59 info@intensiv.ch www.intensiv.ch Intensiv representative for Gulf and Middle East: Mr. Imad Assy: i.assy@intensiv.ch 00961 3 288367
New Intensiv ProxoStrip R f.PX 40 5-6 siv 691 Gran ia d in @ iv.ch w.int sivch 120 Intensiv ProxoStrip Ref. PX4015-6 Pat. Pend.N.20070219/07 Diamond coatedstrips 40 μm/15μm 6 pcs





52 Greater New York Dental Meeting DENTAL NEWS,VOLUME XVII,NUMBER I,2010 E xhibi t i o n fl oo r



International Academy for Dental-Facial Esthetics

The Academy for Dental Facial Esthetics is an honorary service organization whose mission is to foster interdisciplinary education in the area of facial esthetics.
The ADFE includes among its membership many outstanding individuals of the various associated professions who have a desire to create new bridges whereby the esthetic patient can be better and more knowledgeably served. Website of the IADFE www.iadfe.or g


 The International Academy for Dental-Facial Esthetics New Fellow ceremony in New York
The International Academy for Dental-Facial Esthetics New Fellow ceremony in New York
DENTAL NEWS,VOLUME XVII,NUMBER I,2010
Left to right: Dr. George Freedman, Dr. Irwin Smigel, Dr. Tony Dib, Dr. David Hoexter, and Dr. Joe Massad at the Induction Ceremony
53
Greater New York Dental Meeting
DOES YOUR PATIENT SUFFER FROM DRY MOUTH?
What is dry mouth?
We can all suffer from dry mouth at some point, for example, if we are nervous or stressed. So most of us are familiar with the feeling of not having enough saliva in our mouth to keep it moist and lubricated. For some people, however, dry mouth can be a regular problem. As we get older we are more likely to experience dry mouth, but it’s also a problem that can affect people from their 30s onwards.
What causes dry mouth?
Dry mouth occurs when the salivary glands stop working effectively. Medicines are known to cause over 60% of dry mouth cases, with more than 400 different medications linked to dry mouth. The number of medicines a patient takes is also directly related to the likelihood of experiencing dry mouth. Health conditions are also linked to dry mouth, such as diabetes or Sjögren’s syndrome. People who smoke, who are pregnant, stressed, anxious or dehydrated are also more likely to have dry mouth.
What are the symptoms?
The symptoms of dry mouth can include:
• difficulty in eating, especially with dry foods, such as
• cereals or crackers
• difficulty in swallowing and speaking
• a burning sensation in the mouth
• taste disturbances
• painful tongue
• dry, cracked, painful lips
• bad breath
• persistent difficulty in wearing dentures
• feeling thirsty, especially at night
• dry, rough tongue.
Sometimes the amount of saliva a person produces may be reduced by up to 50% before these symptoms are noticed. These symptoms can sometimes have a profound effect on self confidence.
Does dry mouth cause other problems?
Saliva plays a very important protective role in the body. It not only keeps our mouth moist, it also helps to protect our teeth from decay, helps to prevent infections and helps to heal sores in the mouth.
Are your patients dry mouth sufferers?
• Do they have difficulty swallowing certain foods?
• Does their mouth feel dry when eating a meal?
• Do they need to sip liquids to help swallow dry foods?
• Are they taking multiple medicines?
If a patient answered yes to any of these, he/she may have dry mouth.

Products to ease dry mouth
The Biotène system is specifically designed to treat dry mouth.
The different products in the Biotène system allow you to choose the ones that best meet your lifestyle and dry mouth needs:
• 1 product specifically designed to help relieve your dry mouth:
• the gel provides long lasting relief
• 2 products to help maintain healthy teeth and prevent tooth
• decay in people with dry mouth: a toothpaste, with fluoride,
• and mouthwash which can be used twice a day in place of the
• usual products. These are designed to be gentle on your
• mouth as they are alcohol-free and don’t contain harsh
• detergents.
Biotène supplements the make-up of normal saliva to replenish dry mouths. It has a patented enzyme formulation that:
• helps supplement saliva’s natural defences
• helps maintain the oral environment to provide protection
• against dry mouth
• helps supplement saliva’s natural antibacterial
• system - weakened in a dry mouth.
Biotène’s gentle formulation is also free from alcohol and harsh detergents.
What else can a patient do to manage dry mouth?
• Sip water or sugar-free drinks often
• Avoid drinks which dry out the mouth, such as caffeine-containing
• drinks (coffee, tea, some fizzy drinks) and alcohol
• Chew sugar-free gums or sweets to stimulate saliva flow
• Avoid tobacco as this has a drying effect
• Use a humidifier at night to keep the air full of moisture.
To help keep healthy teeth and avoid tooth decay:
• Brush teeth with a soft toothbrush after meals and at bedtime
• Floss teeth gently every day. If there is bleeding from gums
• when flossing, this could be a sign of gum disease.
• Use an SLS-free, fluoride toothpaste, like Biotène, with its
• gentle formulation
• Avoid alcohol-containing mouthwashes as these can dry
• out the mouth
• Avoid sweet, sugary foods
• Visit the dentist at least twice a year for a check-up.




It is indeed a source of great pleasure to welcome all our esteemed guests in the Egyptian Dental Association’s 14th international Dental Congress.
The present congress is again held during a period of great turmoil where our region is still living through and undergoing great upheavals.
It is however, through such human interactions such as this Congress that people of different backgrounds are brought together and made to better understand each other, which we are sure will ultimately lead to better understanding between us all, as well as to better relations among all our nations. It is indeed one of the major benefits of scientific exchange to bring different people from all over the world together where they may share common goals and objectives.
“It is indeed one of the major benefits of scientific exchange to bring different people from all over the world together”
May we wish all our guests a pleasant and enjoyable stay amongst us, and we sincerely hope that you may fully enjoy the scientific and social programmes we have prepared for you. Thank you very much indeed for joining us and for contributing to the success of our meeting, and we hope to see you again with us many more times in future congresses.
Pr esident of the congr ess, Pr of Hatem

 Abdel Rahman
Left to right: Prof. Nada Naaman from Lebanon, Prof. Maguid Amin, Prof. Hatem Abdel-Rahman
Left to right: Prof. Tarek Abbas Hassan, Prof. Maguid Amin, Prof. Hatem Abdel-Rahman, Prof. Mouchira Salah-El-Din, Prof. Hesham Katamesh, Prof. Nour Habib during the opening ceremony
Left to right: Dr. Mourad Abdul Salam, Prof. Maguid Amin, Prof. Hatem Abdel-Rahman, Prof. Mouchira Salah-El-Din exchanging trophies
Abdel Rahman
Left to right: Prof. Nada Naaman from Lebanon, Prof. Maguid Amin, Prof. Hatem Abdel-Rahman
Left to right: Prof. Tarek Abbas Hassan, Prof. Maguid Amin, Prof. Hatem Abdel-Rahman, Prof. Mouchira Salah-El-Din, Prof. Hesham Katamesh, Prof. Nour Habib during the opening ceremony
Left to right: Dr. Mourad Abdul Salam, Prof. Maguid Amin, Prof. Hatem Abdel-Rahman, Prof. Mouchira Salah-El-Din exchanging trophies
DENTAL NEWS,VOLUME XVII,NUMBER I,2010 55 EGYPTIAN DENTAL ASSOCIATION14TH INTERNATIONAL DENTAL CONGRESS


LECTURES






56 EGYPTIAN DENTAL ASSOCIATION14TH INTERNATIONAL DENTAL CONGRESS DENTAL NEWS,VOLUME XVII,NUMBER I,2010
Left to right: Prof. Ahmed Farid Shehab and Prof. Hesham Katamesh
Left to right: Prof. Mohamad Nassar V.P. of Tanta University , Prof. Maguid Amin and Prof. Hatem Abdel-Rahman
Left to right: Prof. Ahmed Farid Shehab, Prof. Nour Habib Dean of Cairo University, Dental school, Prof. Maguid Amin and Prof. Hatem Abdel-Rahman
Left to right: Prof. Tarek Sharkawi, Prof. Maguid Amin, Prof. Hatem AbdelRahman, Prof. Tarek Abbas Hassan
Prof. Mouchira Salah-El-Din displaying the new GALAXY Dental Laser machine
Dr. Eduardo Mahn lecturing on stress management for composite restorations



CLOSING CEREMONY





58 DENTAL NEWS,VOLUME XVII,NUMBER I,2010 EGYPTIAN DENTAL ASSOCIATION14TH INTERNATIONAL DENTAL CONGRESS
Dr. Najla Chebib from Lebanon after her talk on new ceramic material
Dr. Abd El-Salam El-Askary from Alexandria exposing the handling of complications in implantology
Dr. De Souza from California lecturing on prosthetics over implants Picture from the audience
Dr. Tony Dib receiving a trophy of appreciation from the Egyptian Dental Association Board during the closing ceremony



EXHIBITION FLOOR






60 DENTAL NEWS,VOLUME XVII,NUMBER I,2010 EGYPTIAN DENTAL ASSOCIATION14TH INTERNATIONAL DENTAL CONGRESS
Dr. Mohammed Ban Hafeed Chairman of Yemen’s Dentist Syndicate with Dr. Mahmoud El Mais from Lebanon
Dr. Tony Dib, Dr. Mohammed Saadeh and Dr. Mohammed Ban Hafeed on an excursion near the Sphinx

ThenewPiezotome2andImplantCenter2combinedunitsfor bonesurgerydonotjustofferthebestofSatelec ® knowhow... Theyarethreetimesmorepowerfulthanthepreviousgeneration!The extrapowerofPiezotome2,togetherwithanexcellentsurgicalmotor, willguaranteeyoushorter,betterorganizedtreatmentsintotalsafety andcomfortforthepatientthankstotheprecisionandselectivecut procuredbyultrasonics.
17av.GustaveEiffel•BP30216•33708MERIGNACcedex•FRANCE•Tel+33(0)556340607•Fax+33(0)556349292•E-mail:info@piezotome.com•www.piezot ome.com MiddleEastOffice•POBox468•Amman11953•JORDAN•Tel+96265534401•Fax+96265537833•E-mail:info@jo.acteongroup.com
www.piezotome.com Satelec® surgicaltips. Perfectlyintune. 1 6881









62 EGYPTIAN DENTAL ASSOCIATION14TH INTERNATIONAL DENTAL CONGRESS DENTAL NEWS,VOLUME XVII,NUMBER I,2010
Prof. Shirin Al Attar, Dean of Pharos Dental School, surrounded by the Alexandria Oral Implantology Association team









64 EGYPTIAN DENTAL ASSOCIATION14TH INTERNATIONAL DENTAL CONGRESS DENTAL NEWS,VOLUME XVII,NUMBER I,2010
BIOSAFE antimicrobial treated medical face masks:
• Provide an exceptional level of infection protection utilizing this unique water-based EPA-registered antimicrobial solution.
• Are safe as demonstrated in independent testing.
• Offer a long-lasting protective virucidal and bactericidal coating that is permanently bound to the medical mask.

www.crosstex.com
References:

New! Crosstex ® Medical Face Masks treated with BIOSAFE ® antimicrobial... effective against H1N11, Influenza A1 and harmful bacteria on contact.2 LATEX 1 H3N2 used as a surrogate for all Influenza A viruses including H5N1 (avian or bird flu), novel H1N1 and other strains.
Technical Report: An Evaluation of Safety and Efficacy of the Crosstex ® Face Mask Treated with BIOSAFE ® Antimicrobial Agent. Data on file and available upon request through Crosstex.
2
Face H1N1 with Confidence.
Not Available in the United States.
For more information, call Crosstex at 631-582-6777. GCFCXSBS (White) 40/Box









66 EGYPTIAN DENTAL ASSOCIATION14TH INTERNATIONAL DENTAL CONGRESS DENTAL NEWS,VOLUME XVII,NUMBER I,2010


ADVERTORIAL
TEBODONT®:
Successful against oral microorganisms
The essential oil of the australian tea tree (Melaleuca Alternifolia) is more and more used in oral hygiene with a remarkable success. In the Medical Dental Clinic of Bethanien (Professor Sailer) in Zurich / Switzerland it has become an universal remedy within a short lapse of time.
“I don't use Chlorhexidin anymore” said the Head of the Clinic, Dr. Arno König, who uses above all the Gel and the Mouthrinse out of the different Tea Tree Oil products (TEBODONT®).

Dr. König, how did you discover Tea Tree Oil?
We received samples of TEBODONT® Gel two years ago. Clinically, I noticed quickly that it is less irritating than Chlorhexidin. In addition, and very important for us: it does not produce any discolorations.
This plays an important role to our patients who notice even smallest discolorations on their bleached teeth. Another advantage of Tea Tree Oil: it acts successfully against Candida albicans. Nowadays, I don't use Chlorhexidin anymore.
“
Tea Tree Oil is an universal remedy in our Clinic
”
When do you use Tea Tree Oil products?
Always after surgical interventions. And always after implantations: the parts to be screwed on the implants are soaked in Tea Tree Oil before. We also use it in case of troubles after the treatment - in Candidiasis. Our Dental Hygienist gives it in cases of periodontitis. And, since a few patients told us that they could significantly reduce their aphtae problem with the Tea Trea Oil toothpaste, we also recommend it for this indication.
Tea Tree Oil has become an universal remedy in our Clinic. The Gel is primarily used during the treatment and postsurgical, the other products are given to the patients for home care.
How do your patients react on Tea Tree Oil?
There are patients who do not like the taste of Tea Tree Oil. Others, like myself, appreciate the refreshing taste. The positive feedback we get from the patients:
In contrast to Chlorhexidin, Tea Tree Oil does neither discolour the teeth, nor change the sense of taste.
Tea Tree Oil is an universal remedy in our Clinic.
Dr. med. dent. Arno König, Head of the Medical Dental Clinic Bethanien, Zurich/Switzerland
DENTAL NEWS,VOLUME XVII,NUMBER I,2010
Youmissed aspot...
It’s easy to do if you use a white fluoride varnish. DuraShield® is easy to see and apply—every time.
Why take a risk and waste time? DuraShield® is an incredibly effective, fluoride treatment that’s effortless to apply. Its light amber color lets you know the tooth surface is completely covered, yet is almost undetectable to your patient. Each .40 ml unit dose pack can be mixed prior to application, guaranteeing a consistent fluoride level. And with the handy UltraBrush™ 2.0 bristle brush, DuraShield is a total application system… just pop it open, and you’re ready to go.
But most important, DuraShield works. As a powerful desensitizing agent, DuraShield relieves hypersensitivity where dentin or cementum are exposed. Its 5% sodium fluoride formula sets on contact with saliva and releases fluoride for up to eight hours. That means enhanced fluoride uptake, with minimal food or drink restrictions for your patients. You can be confident your patients are protected. And the Bubble Fun® Flavor is great for patients of all ages.
Easy… fast… effective. When it comes to doing the job right on fluoride treatments, you can’t miss with DuraShield.


Ifyou like DuraShield® , you’ll love these Sultan products…

Topex® Fluoride Foam
Easy, 60-second application. Dense enough to provide excellent coverage, yet stays in the tray under bite pressure for a more pleasant patient experience. Five delicious flavors!
Topex® Dual Arch Fluoride Trays
Its natural arch and more defined occlusal anatomy helps force fluoride onto all biting and interproximal tooth surfaces. Locking handles allow for easy placement and removal. Available in four sizes.
Topex® APF Fluoride Gel
Thixotropic formulation remains in the tray, reducing fluoride ingestion. Fast, 60-second application. Available in five great Topex flavors.
Topex® Topical Anesthetic
Quick onset delivers maximum strength 20% benzocaine for fast, temporary relief of pain. Reduces salivation, keeping gel active longer. Seven great flavors!
Pre-application mixing ensures fluoride content. Light amber color means full coverage without compromise of esthetics. UNIT DOSE MIXING LIGHT AMBER COLOR
Ever Wish For A Scaler That Truly Stayed
Sharper Longer?

DIN cassette for 13 instruments + space
Dimensions: 290 x 184 x 32 mm


Sharpen Less Often
Revolutionary new stainless steel alloy is super-durable
Stays sharper longer
That means less time sharpening and less hand fatigue.
Proprietary Process
Proprietary heat treat and cryogenic processing ensure that the superior edge retention and wear characteristics of EverEdge Technology® will last theentire life of the instrument. It’s not a superficial coating – EverEdge Technology® scalers can be sharpened again and again for your best instrument value.
Diamond Knurl
Unique diamond knurl pattern with large diameter handle for a confident grasp. Optimal weight for reduced hand fatigue.
Comfort Zone Cone with Signature
Series grip
The cushioned grip provides a smooth transition and increased comfort.
Distinctive Ocean Blue grip for easy identification.
Finely-Honed Finish
EverEdge Technology® Scalersfeature a finely-honed finish to the instrument blade, for super sharp edges and efficient scaling.

1/2 DIN cassette for 10 instruments

Dimensions: 152 x 184 x 32 mm

1/4 DIN cassette for 5 instruments
Dimensions: 72 x 184 x 32 mm
Manufacturer: Hu-Friedy Mfg. Co., Inc. 3232 N. Rockwell Street Chicago, IL 60618 IUSA European Headquarters & Customer Care Department: Hu-Friedy Mfg. B.V. P.O. Box 29025 I NL-3001 GA Rotterdam Tel. +800 HUFRIEDY (+800 48 37 43 39) Fax +800 48 37 43 40
E-Mail: info@hu-friedy.eu I www.hu-friedy.eu Hu-Friedy Middle East: Mobile : 00 962 79 50 45 700
E-mail: zqwaider@hu-friedy.com
1/2 DIN 1/4 DIN
IM14DIN58 DIN
IMDIN138 IM12DIN105
“You can only treat what you can see“ – creating visions
Swiss Medical Technology (smt) is based in Switzerland and active in design, development, manufacturing and international distribution of innovative ergonomic dental equipment. With its products for diagnostics and therapy, smt offers a maximum of quality and efficiency in dental treatments.
One year ago, smt successfully presented the first optical 3D-system –the Dentaloscope 3D – and set a new benchmark in microdentistry. At present, smt continues its orientation on innovative methods of treatment by launching an accordant 2D-system called Dentaloscope 2D. The dentist also sits in an ergonomic, upright position and works indirect via monitor. Thus back or neck problems, due to a bench over working posture, are a thing of the past – a quantum leap in history of dentistry.
The Dentaloscope 2D with its unique features permits a new kind of treatment:
Feel the difference
Is it not time to go home more relaxed? With the Dentaloscope 2D a hard typical workday with tired eyes, pain in the cervical, shoulder or back area is finally a thing of the past.
Experience new dimensions
With the aid of the Dentaloscope 2D diagnosis and treatment is possible in an impressive way: A full panoramic view with 2.5x magnification up to the smallest view with a maximum magnification of 55x can be displayed. Besides, the depth of focus is unrivaled with its 150 mm. It is no longer necessary to reposition the camera, because it is possible to focus simply and fast between free working distances of 160 – 420 mm.

Do not be in the dark


The shadow-free light source is created by the integrated high-performance LED-technology which illuminates the treatment area similar to daylight with 47'000 lux.
Pictures speak louder than words
Diagnostic findings and the success of a treatment can be visualized to the patients via the impressive flat screen. With the Quattro-shot feature, four single pictures can be displayed in one sequence. The handling of the image storage results easy and effortless by operating the foot control panel.
www s-m-t ch
Sidekick® Sharpener Welcome to the Edge of Sharpening Technology
So Simple So Smart
The Hu-Friedy Sidekick Sharpener makes routine maintenance sharpening of scalers and curettes fast and easy. This straightforward device guides you and your scaler to sharp, consistent results time after time. Reliable Results.
The Hu-Friedy Sidekick sharpener is the only power device with instrument Guide Channels and a Vertical Backstop to help control blade angulation. These "template-like" features allow virtually effortless positioning of your scalers/curettes and provide consistent sharpening results. Correct routine sharpening will help extend the life of your instruments.
The Sidekick is Always Within Reach. It’s cordless! The small, compact, cordless Sidekick can be placed anywhere and requires minimal counter space – perfect for anywhere in your dental office.

See how easy and fun sharpening can be! Sharpen at your convenience with the Hu-Friedy Sidekick, The Smart Sharpener.
• Kit Includes - Sidekick Unit, User Manual & CD-ROM, Ceramic Sharpening Stone, Plastic Test Stick, Magnifying Lens and 2 AA Batteries. www hu-friedy com
PRODU
T NEWS 72 PRODUCT NEWS DENTAL NEWS,VOLUME XVII,NUMBER I,2010
C
MICRO-MEGA®'s new Revo-S™ Refill Box
Presenting MICRO-MEGA®'s new Revo-S™ Refill Box,set of packs of the new Nickel-Titanium sequence Revo-S™,at an attractive price.
The Revo-S™ unique and innovative sequence offers an optimal root canal cleaning with only 3 instruments!
This limited edition "gold" box includes:
- 2 packs of 6 instruments SC1
- 2 packs of 6 instruments SC2
- 2 packs of 6 instruments SU
- 1 pack of 3 instruments assorted AS30-AS35-AS40
This Revo-S™ Refill Box is available in InGeT® and Classics versions. e-mail: www micr o mega com


VITA VACUMAT ceramic furnaces
With the innovative concept of the "New Generation" for VITA VACUMAT ceramic furnaces, VITA Zahnfabrik presented a world novelty at the IDS. Thanks to its modular construction, the unique system makes perfect individual solutions possible, and is therefore extremely economically efficient. With the introduction of additional modules, it now offers even more flexibility.
Premium firing and pressing technology!
The VITA VACUMAT 6000 M is a microprocessor-controlled, fully automatic premium firing unit for all types of veneering ceramic and crystallisation firings. The new VITA VACUMAT 6000 MP is used as a combined unit not only as a firing, but also as a pressing unit, and can therefore be used for all dental ceramics as well as with various muffle systems available on the market.
The innovative firing and pressing technique as well as numerous monitoring and service functions result in consistent firing results of convincing quality, while simultaneously saving time for the user. These features include, for example, the automatic temperature adjustment at the start of every program, the automatic cleaning function, the avoidance of condensation formation in the insulating material as well as power failure protection and controlled fast cooling. The current operating status is immediately apparent at all times thanks to an LED light bar visible from a distance, as well as acoustic signals offering a choice of different sounds. For further information, see under www vita-zahnfabrik com or call the VITA Hotline on +49 (0) 7761-562 222



PRODUCT NEWS PRODUCT NEWS
74 DENTAL NEWS,VOLUME XVII,NUMBER I,2010

Highly aesthetic restorative
Two simple steps
Layers like in nature
Brilliant results




IT!
BEAUTY – COMPOSE
VOCO GmbH · P.O. Box 767 · 27457 Cuxhaven · Germany · Tel. +49 (0) 4721 719-0 · Fax +49 (0) 4721 719-140 · www.voco.com NOW AVAILABLE IN GINGIVA SHADES Please visit us at AEEDC Booth: 446
Efficient posterior treatment with x-tra fil
VOCO developed x-tra fil, a hybrid composite, especially for quick and effective use in the posterior area. The light-curing restorative permits tooth-shaded, load-bearing, cavity class I and II restorations. x-tra fil is thus a high quality, durable and cost-effective alternative to amalgam restorations. Due to its time-saving processing, x-tra fil is particularly well-suited for patients with limited compliance. In addition to posterior restorations, x-tra fil is also well-suited for economical core build-up. This composite is available in a universal shade and both in handy syringes and convenient Caps for direct application. x-tra fil is now availablein the especially economical, bulk package (10 x 5 gram syringe).
Excellent material properties and optimal handling
Outstanding physical properties and unproblematic handling is what makes x-tra fil, with its minimum time requirement and equally high safety, an efficient standard treatment in the posterior area. x-tra fil's excellent material properties were achieved with a combination of a new multi-hybrid filler technology and an innovative initiator system for photo-polymerisation. This is how increments of up to 4 mm in thickness can be safely cured with only 10 seconds of exposure (light output
inEos

min. 800 mW/cm2) with only a minimal amount of polymerisation shrinkage. The reduced shrinkage tension in x-tra fil delivers the foundation for a durable, marginally tight restoration. x-tra fil meets the special requirements for high wear, load-bearing restorations with its dentine-like compressive strength, thermal expansion behaviour and high abrasion resistance. Due to its very high radiopacity, x-tra fil provides an excellent radiological contrast to the tooth substance and thus ideal prerequisites for subsequent diagnoses. The high translucency of the material produces a chameleon effect and thus an aesthetic shade match to the surrounding tooth substance.
www.voco.com
E-mail:

Blue:Precision and Speed
Newly designed CAD/CAM scanner enables fast, easy and controlled scans. Bluecam technology sets new standards of precision.
Contr ol
Thanks to the new user-friendly scan grid and new model holder, operating the inEos Blue is child’s play. The models can be moved in all directions and angles. The rotation mouse enables 360°scans to be performed at any inclination angle up to 105°– ideal for capturing heavily undercut stump preparations and abutments. In addition, the buccal registration of the upper and lower jaws enables the precise definition of the occlusal contacts.
Pr ecision
The scanner camera is equipped with the innovative Bluecam technology. The very small triangulation angle of 3°means that deep cavities can be captured in their entirety, i.e. without undercuts.
Speed
The inEos Blue can capture a single stump in just a few seconds. Scanning a multi-unit bridge takes less than one minute. Thanks to the short scanning times and the automatic capture function, the inEos Blue is currently the fastest dental CAD/CAM scanner on the market.
STL ready
The inEos Blue can save and export scanning data in STL format thereby allowing the data to be processed using third-party software.
www sir

PRODUCT NEWS 76 DENTAL NEWS,VOLUME XVII,NUMBER I,2010 PRODUCT NEWS
o kr ems@voco de
ona com
inEos Blue: The new scan grid and the new model holder enable simple and controlled scanning.
Bluecam technology: short wavelength blue light delivers an extensive depth of field, as well as the enhanced reproduction of details at the preparation margins
VITAVACUMAT ® NewGeneration Productivitytothepoweroffour!
Operateuptofourfiringunitswithasingleoperatingpanel.

Whenitcomestoperformance–themorethebetter.Nowis yourchancetobenefitfrommaximumperformanceand efficiencywiththeVITAVACUMATNewGeneration.Operate uptofourpremiumfurnacesoftheVACUMAT6000Mseries and/orthecombinationpressingfurnacesoftheVACUMAT 6000MPserieswithasinglevPadcontrolpanelandsetnew
standardsforoptimisedworkflowinyourlaboratory.Thanksto itsmodularstructure,thefiringsystemcanbecustomised tomeetyourrequirements.Plus,youcanaddfurtherfiring units,operatingpanelsandaccessoriesatanytime.Youwill hardlyfindamoreefficientwaytomeetfuturerequirements. www.myvacumat.com
3389_2E
The new Chiropro-L implantology system,from Bien-Air
The new Chiropro-L implantology system, from Bien-Air, takes performance and ergonomics a stage further with the only control unit on the market incorporating the pre-programmed clinical sequences of the seven biggest implant brands. The practitioner just chooses the appropriate sequence and that's it!
Its micromotor, the most powerful in the world, can perform the whole range of surgical operations very simply. It is provided with LED lighting, adjustable to any speed from 100 to 40,000 rpm.
Chiropro-L comes complete with the new 20:1 L contra-angle handpiece with light, the very first to have internal irrigation, allowing easier practitioner movements. Other features are its very light weight and its small-sized head offering an improved field of vision.
http://www bienair com/


New! Cavex ImpreSafe
In more and more countries it is legally mandated to disinfect alginate or silicone impressions before sending them to a dental-technical laboratory. Although Cavex has kept abreast of the latest developments, there were no disinfectants on the market until recently that we, as an authority in the field of alginate and silicone impressions, could endorse. All the regular disinfectants damage the surface of the impression due to a lengthy contact time or an aggressive composition. Now, Cavex ImpreSafe has changed all this. Cavex ImpreSafe is a non-toxic disinfectant without aldehyde that takes only three minutes to be effective. Due to this extremely short contact time the surface of the impression remains 100% intact and negative impact on the end result is avoided. Cavex ImpreSafe is a complete disinfectant system and comes with 1 litre of disinfectant concentrate, a disinfectant container, timer and protocol. For more information, visit www cavex nl

PRODUCT NEWS
78 PRODUCT NEWS DENTAL NEWS,VOLUME XVII,NUMBER I,2010

Cavex Impressional

















Superior, highly tear resistant alginates. 25micron detail reproduction














ImpreSafe










Cavex ColorChange

lginate and silicone disinfectant. 100% safe for impression surfaces Disinfection in only 3 minutes











Your impression is our concern!
alginate
gypsum
Cavex GreenClean 100% bio degradable
and
dissolver
lanoisnemiD
www.cavex.nl - dental@cavex.nl - tel: +31 23 530 77 00 - fax: +31 23 535 64 82
ilibatS t y Dimensional Stabili t y 5days
NEW! Cavex
Se qual s a
NEW! Cavex SiliconA
AirTurbines
LED Coupling and Unrivalled Cutting Performance
LED couplings realize clearer view with your optic air turbines. And unrivalled cutting performance, slim ergonomically designed body and excellent visibility. The NSK S-Max M Series has been designed without compromise. Experience it for yourself.

NSK Power Superb
Clarity&Durability

KaVo® Coupling M600L NSK Coupling
M600KL
KaVo® and MULTIflex® LUX are registered trademarks of Kaltenbach & Voigt GmbH & Co.














































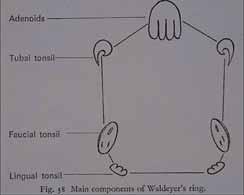




















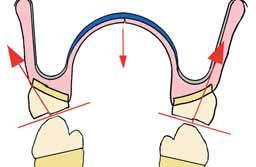


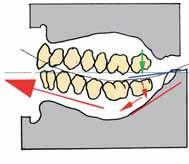
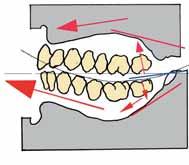

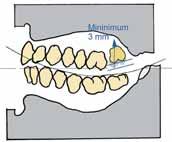

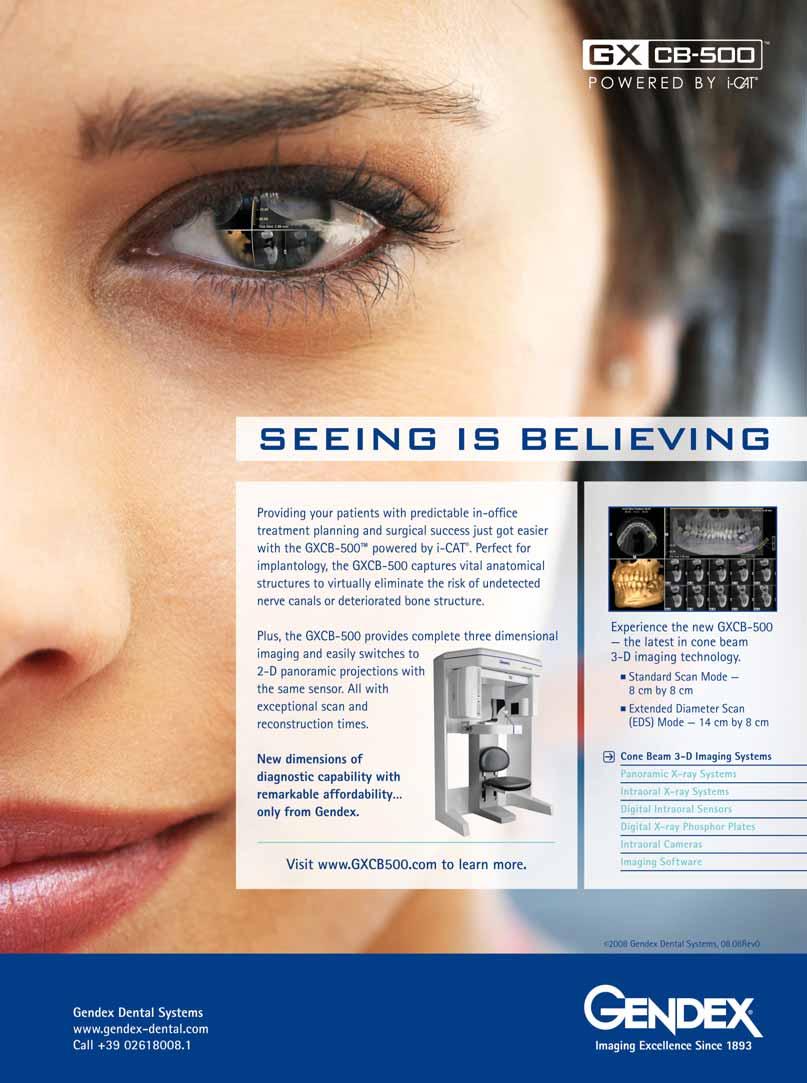
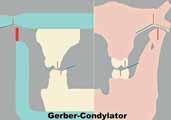




































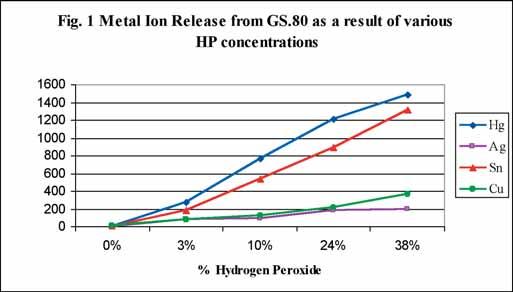
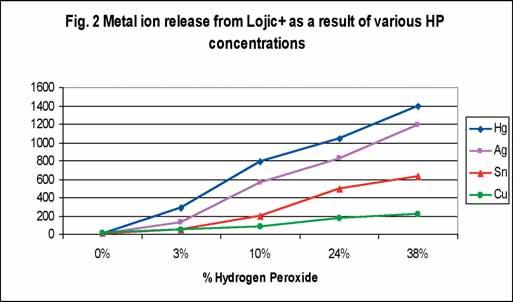















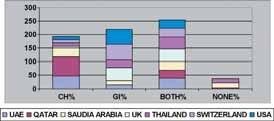
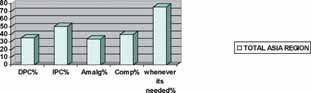




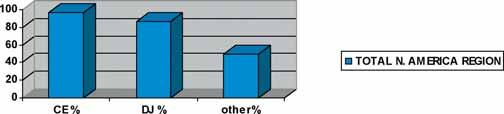























 The International Academy for Dental-Facial Esthetics New Fellow ceremony in New York
The International Academy for Dental-Facial Esthetics New Fellow ceremony in New York






 Abdel Rahman
Left to right: Prof. Nada Naaman from Lebanon, Prof. Maguid Amin, Prof. Hatem Abdel-Rahman
Left to right: Prof. Tarek Abbas Hassan, Prof. Maguid Amin, Prof. Hatem Abdel-Rahman, Prof. Mouchira Salah-El-Din, Prof. Hesham Katamesh, Prof. Nour Habib during the opening ceremony
Left to right: Dr. Mourad Abdul Salam, Prof. Maguid Amin, Prof. Hatem Abdel-Rahman, Prof. Mouchira Salah-El-Din exchanging trophies
Abdel Rahman
Left to right: Prof. Nada Naaman from Lebanon, Prof. Maguid Amin, Prof. Hatem Abdel-Rahman
Left to right: Prof. Tarek Abbas Hassan, Prof. Maguid Amin, Prof. Hatem Abdel-Rahman, Prof. Mouchira Salah-El-Din, Prof. Hesham Katamesh, Prof. Nour Habib during the opening ceremony
Left to right: Dr. Mourad Abdul Salam, Prof. Maguid Amin, Prof. Hatem Abdel-Rahman, Prof. Mouchira Salah-El-Din exchanging trophies