Sparking Innovation
DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022

TABLE OF CONTENTS
J. Pinzon
Design, Editorial and Project Management Spark It Communications, Inc.

Published by the Chairman’s Office of the Department of Medicine at the University of Miami Miller School of Medicine.
All contents, ©2022 University of Miami. Reproduction in whole or in part without previous written permission by the editor is prohibited.
Chair’s Message 1 Finding a Cure for Kidney Disease 2 A New
for Regenerative
6 Researchers Develop Promising Treatment for Rare
10 By the Numbers 16 New Division
19 Division Highlights 20 Philanthropy 50
Generation
Medicine
Genetic Syndrome
Spotlight
Editor Laura
Director, Business Operations Photography UM Biomedical Communications Jenny Abreu
Chair’s Message

The Department of Medicine has arrived at a juncture where our impact on medicine and science has reached a critical level, enabling us to spark new therapies and diagnostic modalities to cure human disease and improve the human condition.
We are Sparking Innovation in the diagnosis and treatment methods used to prevent and cure diseases, such as those of the endocrine system, kidney and heart. As Chairman, I am proud of how the Department of Medicine has been a flourishing academic department by nurturing growth of our junior faculty and addressing health disparities.
I am certain we will continue on this trajectory for years to come.
Our longstanding partnerships with Jackson Memorial Hospital, one of the largest teaching hospitals in the United States, and the Bruce W. Carter Department of Veterans Affairs Medical Center, allows us the opportunity to be at the forefront of extraordinary discoveries that will result in improved health outcomes for our patients.
Welcome to the 2022 Annual Report of the Department of Medicine at the University of Miami Miller School of Medicine.

Only my best,
Roy E. Weiss, M.D., Ph.D.
Professor of Medicine Chair, Department of Medicine
Kathleen and Stanley Glaser Distinguished Chair in Medicine
Rabbi Morris I. Esformes Endowed Chair in Medicine and Endocrinology
University of Miami Miller School of Medicine

DEPARTMENT OF
CHAIRMAN’S REPORT 2022 1
MEDICINE
Finding a Cure for Kidney Disease


UHEALTH|UNIVERSITY OF MIAMI MILLER SCHOOL OF MEDICINE 2
Kidney disease is a silent killer for millions. The two bean-shaped organs, built to filter excess water and waste out of the blood, fizzle and fail when their own purifying system stops working. While unresolved high blood sugar and high blood pressure are the most common causes of renal disease, better recognition and management of these factors have not been able to reduce the rising prevalence of kidney failure, which is considered a silent killer since many people don’t realize they have kidney disease until it’s very late. For more than a century, the situation has baffled and frustrated physician-scientists and patients alike. More recently, several new drug discoveries offer new hope for the future of patients with the disease.


DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 3
Alessia Fornoni, M.D., Ph.D.



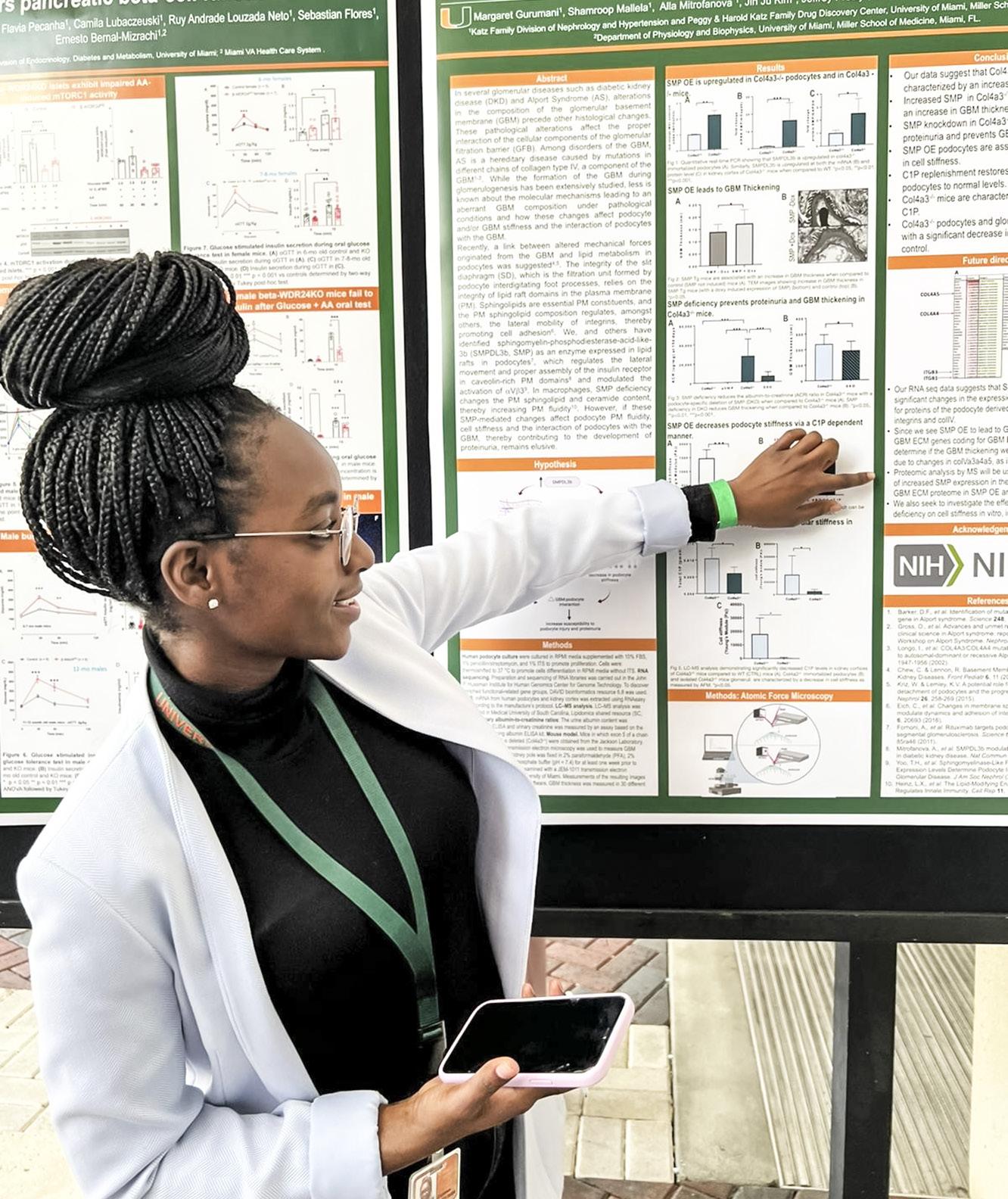
Alessia Fornoni, M.D., Ph.D., along with Sandra Merscher, Ph.D., and colleagues at the University of Miami Miller School of Medicine, Department of Medicine, not only identified a new mechanism responsible for kidney disease, they’ve discovered a solution that could be the key to managing – and ultimately curing –kidney disease.

“The kidney is a very complex organ that allows you to see the big picture, to see the whole body, because of its multiple functions,” says Dr. Fornoni, Professor of Medicine and Molecular and Cellular Pharmacology, Chief of the Katz Family Division of Nephrology and Hypertension, Director of the Peggy and Harold Katz Family Drug Discovery Center, Co-Director of the Miami Medical Scientist Training Program (MSTP) and Module Leader of the Clinical and Translational Science Institute (CTSI).
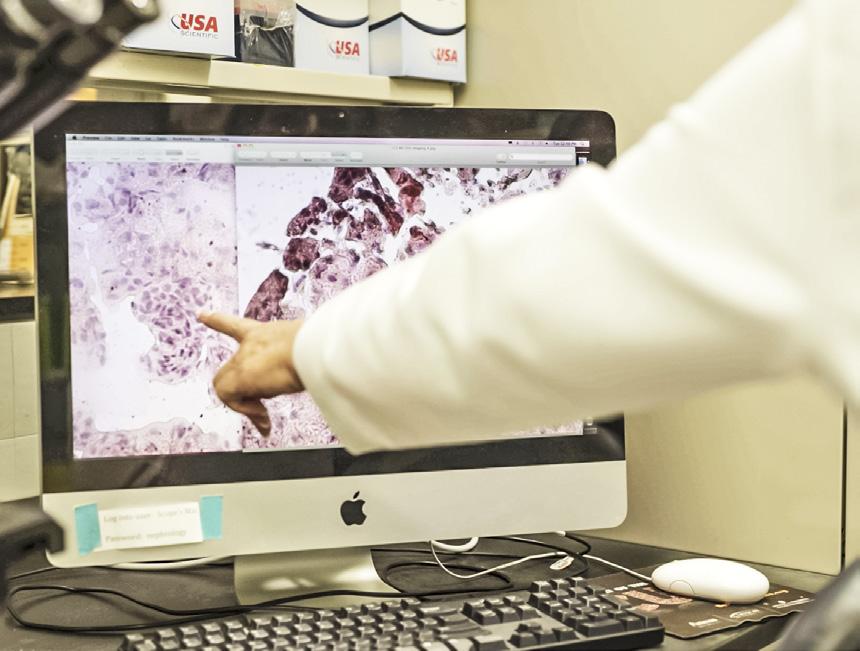
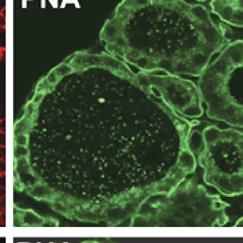
Cells called podocytes act as microscopic worker bees for the kidneys’ filtration system, regulating the process to flush out toxins and retain proteins. When those cells are damaged, however, waste accumulates, scars form, and patients face dialysis, transplantation, or sometimes death. What has never been clear is what exactly damages these cells. Since the 1800s,
physicians have known that fat can be present in the kidney’s filtering system. Not until recently, however, have researchers realized that too much fat actually damages these podocytes and contributes to the progression of kidney disease.

In 2010, Dr. Fornoni and her team began collecting data that showed the cause-andeffect relationship between fatty podocytes and renal failure. Their work was later published in the peer-reviewed journals Nature Communications and the Journal of Clinical Investigations. From there, they began developing strategies to understand why these cells become fat under conditions of stress (i.e., diabetes) or in other forms of chronic kidney diseases), and more importantly, how to reverse the implications.

“Science is beautiful because it reveals new, unexpected and exciting knowledge as you go,” says Dr. Fornoni, who emerged from a rural Italian village to become a worldrenowned nephrologist. “The question is, how do we bring it back to the community, to the

UHEALTH|UNIVERSITY OF MIAMI MILLER SCHOOL OF MEDICINE 4
Sandra Merscher, Ph.D.
patient? The best way is to generate disease awareness and build new safe and effective therapies for the prevention and cure of kidney disease.”
In an initial attempt to reduce fat content in the kidney, Dr. Fornoni’s team found that cyclodextrin, a molecule that consists of several sugars, has the power to break down existing cholesterol. Because the molecule counters lipid buildup, it effectively puts “chubby” cells on a permanent diet. Clinical studies are underway to prove injectable cyclodextrin’s efficacy in affected patients. With the support of the University of Miami Miller School of Medicine, Dr. Fornoni and her colleagues have been able to patent their discovery and subsequently license that patent to ZyVersa Therapeutics for further clinical development.





The downside of an injectable form of cyclodextrin is that patients who suffer from chronic kidney disease will require frequent injections. For many, this schedule is untenable. This is why Dr. Fornoni and her team, in collaboration with Hoffman-La Roche, a leading research-based healthcare company, embarked on the discovery of a new oral agent also capable of reducing fat content in kidney cells. This agent, named R3R1, is being tested in a worldwide Phase2A trial by River 3 Renal Corporation,
a developer of renal disease therapies that Dr. Fornoni founded in 2020.
These studies, which are now approxi mately four to five years away from finding a kidney disease drug that’s worthy of hitting the market, took at least 15 years of work to get where they are today, Dr. Fornoni explains.
“My goal is to continue to work in drug discovery towards finding a cure for the millions of patients affected by kidney disease. If drug 1 doesn’t work, I want to go on to drug 2 or drug 3 or try another alternative, but I have no doubt these pathways are the proper target,” she says. “I have continuous NIH funding since 2008 to study the mechanism by which these lipids accumulate, and I’m very grateful to the National Institutes of Health and to several patient foundations (Alport Syndrome Foundation and Nephcure Kidney International) for supporting our commitment to understanding kidney disease.”
Dr. Fornoni adds: “At the same time, I can’t wait until the mechanism is totally sorted out so that we, in collaboration with industry partners, can find a drug that works. This is why working in a supportive research environment, such as the University of Miami, has allowed us to accelerate our discovery to benefit patients and the community at large.”
“Having reached Phase 2 trials, the probability that Dr. Fornoni’s discoveries will change the life of millions of kidney disease patients in the near future is much more tangible than ever before.”
DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 5
A New Generation for Regenerative Medicine

UHEALTH|UNIVERSITY OF MIAMI MILLER SCHOOL OF MEDICINE 6
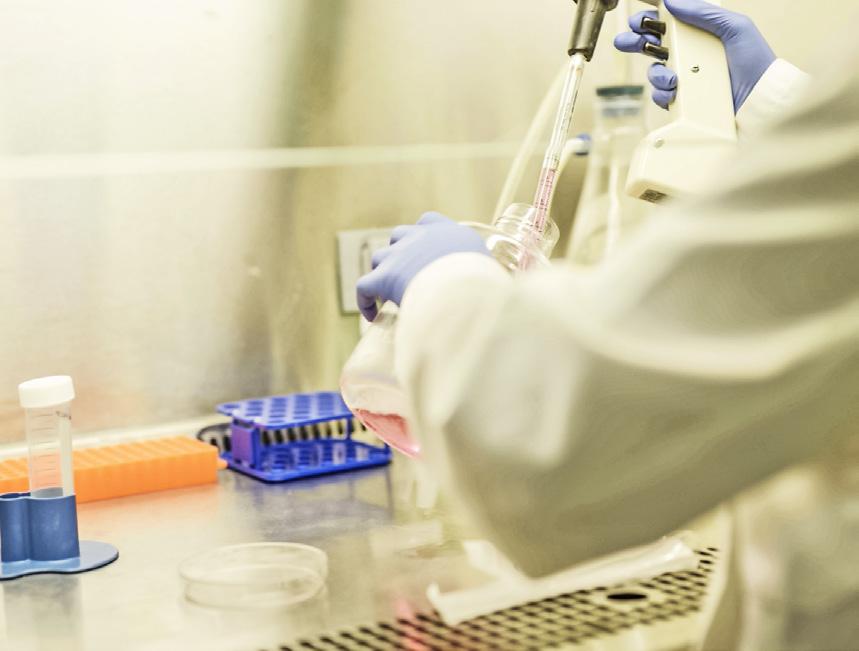
Regenerative medicine is flourishing under the well-scoped eyes of physician-scientists at the University of Miami Miller School of Medicine’s Department of Medicine. Cell-based therapy – the use of cells to stimulate the regeneration of damaged tissue and repair the mechanisms underlying disease – is their focus. It’s a game-changer for treating chronic conditions, such as diabetes, Parkinson’s disease, heart disease and arthritis, disorders which all have something in common – a limitation in the body’s ability to self-heal.
Joshua Hare, M.D., Chief Sciences Officer, Senior Associate Dean for Experimental and Cellular Therapeutics, Director of the Interdisciplinary Stem Cell Institute (ISCI), and Louis Lemberg Professor of Medicine at the Miller School of Medicine, says the collaborative nature of the research allows University faculty “to have an impact nationally, not just here on campus.”

DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 7
Dr. Hare and his colleagues work with medical researchers across the country to develop ground-breaking protocols using a variety of approaches that include using stem cells such as induced pluripotent stem cells, adult cells that can be expanded and potentially used as medicines, extra cellular vesicles or exosomes and peptides or synthetic drugs that stimulate the cell cycle and promote endogenous healing and physiologic tissue growth.
A recent area of research focuses on how stem cell injections benefit patients with hypoplastic left heart syndrome. Hypoplastic left heart disease is a rare congenital heart condition where a child is born with only one ventricle instead of two. It’s an extremely serious condition that requires extensive cardiac surgery that can save the patient, at least initially. The complex procedure, however, can cause further damage and ultimately leads to heart failure. Cell-based therapy is a promising adjunct to surgery.
“We developed the idea working together with our colleagues at the University of Maryland,” says Dr. Hare. “Through their own research they developed information suggesting that this could boost the function of the heart in the neonates suffering from hypoplastic left heart. They collaborated with us to get the cell types they wanted to pilot this approach in the babies they were treating.”
Dr. Hare says the results of this trial will enable him and his colleagues to initiate a phase II trial. “We have extended research to Chicago and a consortium of seven centers across the country, including Children’s Healthcare of Atlanta, University of Michigan and Lauri Children’s Hospital. The research has further expanded to involve different kinds of cell-based therapy.”
Research into cell-based therapy and other uses of stem cell investigations falls under the jurisdiction of the Interdisciplinary Stem Cell Institute (ISCI), which Hare founded at the Miller School in 2008. Though relatively young, the institute has overseen several pivotal studies. At a recent symposium, for instance, Dr. Hare and his team presented findings of a study involving stem cells to treat adult heart failure.
The two leading causes of heart failure in adults are ischemic cardiomyopathy, where a patient experiences a heart attack that damages part of the heart, and nonischemic cardiomyopathy, where heart failure is caused by something already wrong with the heart muscle. Dr. Hare and his colleagues conducted extensive research on both populations and have reported exciting results.
“We’ve learned that about 40 percent of nonischemic patients have a genetic defect responsible for their heart failure. Those who don’t have a genetic cause are likely to have inflammation underlying their cardiac dysfunction,” says Dr. Hare.

Working with Dr. Robert Myerburg and Dr. Raul Mitrani, Dr. Hare and colleagues developed information and basic preliminary findings suggesting that those individuals with the genetic defect don’t respond well to cell-based therapy. the ones who don’t have the genetic defect respond extremely well. “It’s an issue of personalized medicine, figuring out which types of patients should get which type of treatment,” says Dr. Hare.
The Miller School of Medicine also received a large grant from the U.S. Department of Defense (DOD) to test these results further. Hare is the principal investigator for the cell-based therapy program trial, known as the DCM II trial. Hare is the first cardiologist conducting dilated cardiomyopathy clinical trial using the DOD funding platform. Of the four centers conducting similar research using donor cells, the Miller School has seen the most significant enrollment. The unique feature of this trial is that the GMP cell
Joshua Hare, M.D.
“It’s fascinating what we’ve been able to do.”
UHEALTH|UNIVERSITY OF MIAMI MILLER SCHOOL OF MEDICINE 8
— Dr. Joshua Hare
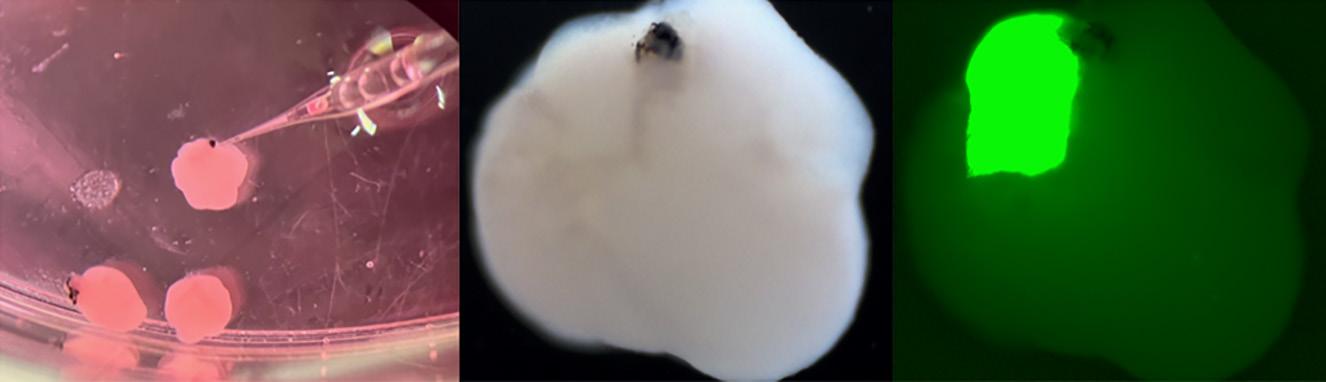
At left: Image showing injection of fluorescent retinoblastoma cells into forebrain organoids with primitive eyes as well as massive growth of the tumor in the forebrain organoid.
manufacturing laboratory, led by Aisha Khan, is manufacturing and supplying stem cells to all participating centers.
“We don’t only manufacture these cells, we equip and train these sites to handle cellular products while maintaining compliance and quality,” says Dr. Hare. “This is how we make progress.”
Another exciting area of cross-campus interdisciplinary work is the longstanding collaboration between the ISCI and the Miami Project to Cure Paralysis led by Aisha Khan, Dr. Dalton Dietrich, and Dr. Allan Levi. As part of this work, ISCI and the Miami Project investigators, have long collaborated on developing Schwann cells and Schwann cell-derived exosomes as investigation agents for testing in clinical trials for spinal cord injury and even possibly Lou Gehrig’s Disease also known as Amyotrophic Lateral Sclerosis (ALS).
Khan, along with her Miami Project team, is investigating whether Schwann cells and their exosome products may be used as therapeutic tools in neurodegenerative disease states like ALS. Preliminary studies have shown outgrowth to dorsal root ganglion (DRG) when treated with exosomes.
The institute also is investigating a fascinating area of stem cell research called induced pluripotent stem (iPS) cells. This new program is a giant leap forward in medical research. Physician-scientists have learned how to take adult tissue and genetically modify it into self-renewing cells. Those cells have the potential to then grow into an actual human organ – a pancreas, for example, or a brain.
“These iPS cells aren’t quite yet ready for the clinic. Research at the bench [in the lab] is still being conducted and that’s what we’re very involved in. It’s fascinating what we’ve been able to do. We’ve been able to grow miniature versions of human organs, or organoids, in a dish,” says Dr. Hare.
In work led by Dr. Stefan Kurtenbach at the ISCI, organoids resembling hearts and brains have been produced. From the brain organoids, researchers can also grow eyes, leading to an amazing opportunity for sensorineural research. These tiny organs, however, are still confined to the dish since they aren’t yet ready for ‘prime time.’
“Known as modeling or what we call a disease in a dish, this very powerful technique is emerging as a way to conduct future research, understand what causes diseases and how to treat them,” says Dr. Hare.
Another piece of the heart regeneration puzzle fell into place ths year when Hare and Khan used human stem cell-derived exosome technology to show efficacy of cell treatments for heart disease. The use of stem cell-derived exosomes for heart conditions is another exciting developing area of cardiac research.
“Researchers are developing stem cellderived exosomes therapy to improve cardiac function after myocardial infarction. Progress in pre-clinical research will open the doors to research funding,” says Dr. Hare.
A long-standing focus of the institute has been the translation of stem cell research into therapies that can be used to treat disease.
“We are proud that researchers at all career levels and from many scientific and cultural backgrounds have made pivotal contributions to discoveries that are closer than ever to the clinic – and yet we know there’s much more to do to achieve our full potential,” says Dr. Hare. “Thanks to those who have supported the ISCI and contributed to the progress you’ve made possible.”
Above: Image showing staining of the heart organoids as well as a heart invaded by green fluorescent neural crest cells.

DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 9
Researchers Develop Promising Treatment for Rare Genetic Syndrome

UHEALTH|UNIVERSITY OF MIAMI MILLER SCHOOL OF MEDICINE 10
Department of Medicine researchers have developed a promising treatment for a rare, neurodegenerative genetic syndrome that impacts the development of children and limits their lifespan.
Endocrinologist Roy E. Weiss, M.D., Ph.D., Chair of the Department of Medicine, and Khemraj Hirani, M.Pharm., Ph.D., M.B.A, R.P.H., Associate Vice Chair, Research and Regulatory Compliance of the Department of Medicine, joined forces to test a drug in the treatment of Allan-Herndon-Dudley Syndrome (AHDS).

DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 11
SRW101 DEVELOPMENT MILESTONES
“I have always been interested in investigating orphan diseases. These are diseases that are very rare and for which there are no treatments and can have tremendous impact on the lives of these patients,” said Dr. Weiss. “These patients are eternally grateful if you can do anything to help them because they’re not in the main crosshairs of large pharmaceutical companies that treat diseases like diabetes, hypertension, heart disease or cancer.”
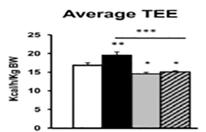
AHDS is just such a disease. It manifests predominantly in males and severely impairs communication, movement, increased heart rate and the ability to gain weight. The syndrome is caused by a defect in the transport of the thyroid hormone T3 into the brain but results in an excess of the hormone in the peripheral organs.
Dr. Weiss, who holds the Kathleen and Stanley Glaser Distinguished Chair in Medicine and the Rabbi Morris I. Esformes Endowed Chair in Medicine and Endocrinology, has worked to find a treatment for AHDS for nearly 35 years. His work started at the University of Chicago School of Medicine (UChicago Medicine) where he worked closely with acclaimed endocrinologist Dr. Samuel Refetoff.
“These children are severely delayed in terms of psychomotor activity. They don’t walk; they don’t talk. They can’t feed themselves. They can’t hold their heads up. It’s a very devastating disease, for them and for their families as well,” Dr. Weiss said.
A genetic mutation inhibits the T3 hormone from crossing the brain-blood barrier and reaching the central nervous system. The

2004

Identification of the first child with mutation in the gene encoding MCT8.
2006
Production of the first MCT8-deficient mouse (Mct8KO) showing that it manifests the same thyroid abnormalities as humans
2006-2016

NIH MERIT award to UM’s scientific co-founders to study MCT8 deficiency and therapeutics for 10 years. NIH funding without interruption for 48 years to study inherited thyroid diseases.
2009
2009-2012
First In-Human Study: Compassionate use of SRW101 in children with MCT8 deficiency for a period of 26-40 months
Publication showing that the use of SRW101 (DITPA) normalizes key chemical abnormalities equally in induced hypothyroidism of normal and Mct8KO mice
2010
Expression of MCT8 in thyroid cell membrane promotes hormone secretion, which partially accounts for the low blood T4 in MCT8 deficiency
 Samuel
Samuel
Refetoff, M.D.
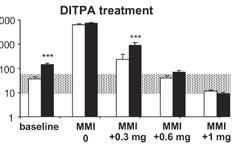
Drs. Weiss and Refetoff looked to a drug formerly known as DITPA (diiodothyropropionic acid) as a solution. Results of the first-in-human compassionate clinical trial were significant.
UHEALTH|UNIVERSITY OF MIAMI MILLER SCHOOL OF MEDICINE 12
lack of thyroid hormone during fetal and early development causes universal delays, including intellectual disabilities, low muscle tone, limited speech and motor abilities, feeding difficulties and spasticity.
Conversely, an overabundance of T3 builds up in the organs, creating a metabolic imbalance that results in growth dysfunction and cardiovascular issues.
The average life expectancy for males with this syndrome is 35 years of age, and to this point, there has been no effective therapy to treat it.
Drs. Weiss and Refetoff looked to a drug formerly known as DITPA (diiodothyropropionic acid) as a solution. It is a thyroid hormone analogue that mimics thyroid hormone, but bypasses the mutant receptor to get into the brain. Tested successfully first in animals, the doctors then administered it to four patients with ADHS under the Food and Drug Administration’s “compassionate use” provision. This allows researchers to test investigational medical products on patients with immediately life-threatening illnesses that have no available comparable treatment.

Results of the first-in-human compassionate clinical trial were significant. Each of the four patients took DITPA daily for 26-40 months and saw fully normalized T3 levels, did not develop seizures and were able to forego a gastric feeding tube. Half the patients gained weight
2013
Prenatal and postnatal changes in thyroid status of Mct8KO mice

2013
Demonstration that Mct8KO mice have increased energy consumption because of high T3 in blood
2014
MCT8-deficient human embryo has brain abnormalities
2015 SRW-101 corrects hypermetabolism of Mct8KO mice by reducing D1 and blood T3




2014
Diiodothyropropionic acid (DITPA) in pregnant mice crosses the placenta reaching 8-fold higher levels in the MCT8-deficient fetus; significant potential for prenatal treatment without affecting the mother
2015
Meeting with the FDA to use DITPA in treatment of MCT8deficient subjects before and after birth (PIND)
Khemraj Hirani, M.Pharm., Ph.D., M.B.A, R.P.H . and Roy E. Weiss, M.D., Ph.D.
DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 13
SRW101 DEVELOPMENT MILESTONES
and saw normalized brain development, while 75% experienced a decline in heart rate, decreasing the work of the heart, as DITPA also improves peripheral thyrotoxicosis, a type of permanent congenital hypothyroidism.
The researchers were also able to show that DITPA can cross the placenta in pregnant women and increase the amount of the T3 hormone in the developing embryo. In 2016, the drug was authorized by the FDA under an emergency investigational new drug (IND) for use in pregnant women carrying a fetus suspected to have ADHS. Since women are carriers of the genetic mutation, if her first male baby was born with ADHS, the next male baby will have it as well. Screening to identify female carriers is also underway.

Today, the drug is called SRW101 and is ready to enter phase III trials. PriZm, a late-stage clinical biotech company co-founded by Drs. Weiss, Hirani and Refetoff, will conduct the trial on some 40 patients. The results will be evaluated for clinical effectiveness and submitted to the FDA.



The team secured both an Orphan Drug Designation (ODD) in the United States and European Union as well as a Rare Pediatric Disease
2016

FDA DITPA Treatment Study (IND# 127859) may proceed to treat MCT8deficient embryos from 10 weeks pregnancy until 3 years after birth


2017
MCT8-deficient mice have decreased postnatal bone mineralization and linear growth
2020
2018-present Screening of carrier mothers
2020 US FDA rare pediatric disease (RPD) designation

“The University of Miami has the culture of team science and the resources to spark discovery across all disciplines. Working together, we can take discovery to a new level and impact humankind.”
–Dr. Roy Weiss
US FDA orphan drug designation
2016-present Stability testing of cGMP clinical lot # 024K7278 reports to the FDA via CDMO (Syngene Pharmaceuticals) UHEALTH|UNIVERSITY OF MIAMI MILLER SCHOOL OF MEDICINE 14
(RPD) designation from the FDA. This allows research to move forward on a faster track than other pharmaceutical trials.

“We believe the EMA (European Medicines Agency) and the FDA’s granting of Orphan Drug Designation to DITPA reflects the agencies’ recognition that effective treatment options are needed for AHDS, a serious endocrine disorder with an unmet medical need. An End of Phase 2 (EOP2) meeting with the FDA further led to concurrences on key topics of the development pathway. These decisions add further credibility to our existing clinical evidence that DITPA has the potential to bring a new essential therapy option to children with AHDS,” said Dr. Hirani.
Dr. Weiss said he’s confident the next phase of trials will begin soon and have the potential to make a substantial difference in both patients’ and caregivers’ lives.
“It’s the job of a physician-scientist to recognize the challenges faced by patients. By using our medical expertise to address problems, we can affect real change in the world,” he said. “The University of Miami has a culture of team science and the resources at hand to spark discovery across all disciplines. Whether it’s engineering, physics or biology, we are uniquely situated because of the community of scholars that reside here. Working together, we can take discovery to a new level and impact humankind.”
2022 2023 2024 2025 2026
• Drug product manufacturing and single P3 clinical trial filing
• Phase III trial
• 12-month interim analysis phase III trial
• Filing EU/US
• US approval and launch

• US rare pediatric disease (RPD) priority review voucher
• EU approval and launch
2020
UM acquires technology from UM and UC via assignment and exclusive license agreement
2021 EU orphan drug designation
2021

Neonatal diagnosis of MCT8 deficiency using mass spectrometry analysis on routinely collected dried blood spots 2020
Selective fetal administration of thyroid hormone in human with prenatal diagnosis of MCT8 deficiency ameliorates outcome
2021
Successful EOP2/Pre-Phase 3 meeting for single registration and NDA agreement
UPCOMING MILESTONES
SRW101
DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 15
By the Numbers
CLINICAL ACTIVITY AND CARE
RESEARCH
Research Funding Sources Overview
FY21 FY22 % Change
Net Patient Revenues $80,897,007 $87,391,720 8%
Work RVUs 1,115,744 1,450,750 30%
Outpatient Visits 285,671 297,720 4%
Inpatient Visits 195,878 220,746 13% Procedures 138,048 170,482 23%
Telehealth Visits 133,847 78,123 -42% New Patient Visits 51,725 51,863 0.3%
Research Spending
FY22 TOTAL: $37,774,252
Clinical Procedures
FY21 FY22 % Change
UMH 84,297 99,513 18%
UM Hospitals & Clinics 21,428 19,261 -10%
Lennar Foundation Medical Center 32,323 51,708 60%
Total 138,048 170,482 23%
UHealth Clinical Participation
In-Person
FY22 $37,744,252 In Millions
FY20 $29,577,856
Divisions, Grants and Contracts
FY21 $32,012,727 UHEALTH|UNIVERSITY OF MIAMI MILLER SCHOOL OF MEDICINE 16
FY22 % of Total
Cardiovascular $1,613,682 4.27 Cellular Therapy $28,404 .07 Clinical Pharmacology $2,716,165 7.19 Digestive Health and Liver Diseases $3,277,810 8.68 EndoDiabetes $3,562,518 9.43 General Medicine $2,021,618 5.35 Gerontology $32,000 .08 Hematology $2,206,075 5.84 Infectious Diseases $14,953,876 39.59 Katz Center $2,151,679 5.69 Medical Oncology $836,646 2.21 Nephrology $103,456 .27 Pulmonary Medicine $2,952,988 7.82 Rheumatology $172,152 .45
Other $1,145,183 3.03 Total 37,774,252
Encounters Tele-Medicine Encounters Total Revenue
70.5%
25% Department of Medicine 35% Department of Medicine 17% Department of Medicine 2% State 75% All Other Departments 65% All Other Departments 83% All Other Departments 27.5% Private
Federal
FY19 $28,114,356
Cardiology
Health & Liver Diseases 30 Endocrinology, Diabetes & Metabolism 27
General Internal Medicine 36 Geriatrics & Palliative Medicine 13 Hematology 34 Hospital Medicine 38 Infectious Diseases 33 Medical Oncology 45 Medicine-Pediatrics 11 Myeloma 7 Nephrology & Hypertension 22
Population Health and Computational Medicine 1 Pulmonary, Critical Care and Sleep Medicine 52 Rheumatology and Immunology 7 Transplantation and Cellular Therapy 10 Total
Medicine-
Cardiology 27
Pulmonary, Critical Care 24 Endocrinology 7 Gastroenterology 15 Geriatrics 6 Hospice and Palliative Care 4 Combined Geriatrics and Hospice and Palliative Care 2 Hematology/Oncology 16 Infectious Diseases 9 ID Transplant 3 Nephrology 10 Rheumatology 4 Total Fellows
FACULTY DEMOGRAPHICS
FELLOW DEMOGRAPHICS Fellows by Specialty
Department of Medicine At a Glance 17
FACULTY MEMBERS 404
Medicine
Professors 26% Associate Professors 16% Assistant Professors 47% Staff Physicians 11%
Faculty Gender 36% Female 64% Male Faculty Ethnicity 36% Hispanic or Latino 41% White 13% Asian 6% Black or African American 4% Other
127
DIVISIONS
Cardiovascular
Clinical Pharmacology Digestive Health and Liver Diseases Endocrinology, Diabetes and Metabolism
Faculty by Division
36 Clinical Pharmacology 2 Digestive
Fellow Gender 43% Female 57% Male Fellow Ethnicity 35% Hispanic or Latino 24% White 26% Asian 11% Black or African American 6% Other
Faculty 404
General Internal Medicine
DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 17
Geriatrics and Palliative Medicine Hematology Hospital Medicine Infectious Diseases Internal
Pediatrics (new) Medical Oncology Myeloma (new) Nephrology and Hypertension Population Health and Computational Medicine Pulmonary, Critical Care and Sleep Medicine Rheumatology and Immunology Transplantation and Cellular Therapy
CHIEF MEDICAL RESIDENTS
PROGRAM DIRECTORS
Residencies
Stefanie Brown, M.D., M.B.A.

Internal Medicine
Jonathan Tolentino, M.D. Internal Medicine-Pediatrics
Fellowships
Carlos Alfonso, M.D. Cardiovascular
E. Joseph Bauerlein, M.D.
Cardiovascular – Advanced Heart Failure/Transplant
Raul Mitrani, M.D.



Cardiovascular –Electrophysiology
Michael Dyal, M.D.
Cardiovascular – Interventional
Eduardo de Marchena, M.D.
Cardiovascular – Interventional Structural HD Fellow
Atil Kargi, M.D. Endocrinology
Andres Carrion Monsalve, M.D. Gastroenterology
Resident Gender LEARNER DEMOGRAPHICS


Resident Ethnicity
Iriana Hammel, M.D. Geriatrics
Janaki Sharma, M.D. Hematology/Oncology

Eric Martin, M.D. Hepatology
Khin Zaw, M.D. Hospice and Palliative Care
Paola Natalia
Lichtenberger, M.D. Infectious Diseases

Michele Morris, M.D. Infectious Disease Transplant
Jonathan Tolentino, M.D. Internal Medicine-Pediatrics
Oliver Lenz, M.D. Nephrology

David De La Zerda, M.D.
Pulmonary/Critical Care
Carlos Lozada, M.D. Rheumatology
Andres Rodriguez University of Miami Hospital Chief Resident
Marina Byer Jackson Memorial Hospital Chief Resident
Eduardo Saul Jackson Memorial Hospital Chief Resident
Quentin Loyd Miami VA Medical Center Chief Resident
Paul Montana Miami VA Medical Center Chief Resident
Toby Ubu Ambulatory Care Center Chief Resident
Michael DesRosiers Chief Resident for Quality & Patient Safety
Kadijah Porter Chief Resident for Quality & Patient Safety
Education Medical School Location Resident Outcomes 30% Florida 53% Matches 22% Non-U.S. 48% United States (Non-Florida) 47% Job Placement
Imran Mohiuddin Chief Resident for Quality & Patient Safety
Resident
57%
43%
Female
Male
40%
22%
21%
11% Black
6%
By the Numbers UHEALTH|UNIVERSITY OF MIAMI MILLER SCHOOL OF MEDICINE 18
Hispanic or Latino
White
Asian
or African American
Other
New Division Spotlight
INTERNAL MEDICINE–PEDIATRICS
Associate Professors of Clinical Medicine
Stefanie Brown, M.D., M.B.A. Division Chief

The mission of the Division of Intermal Medicine-Pediatrics is to lead the advancement of innovative healthcare throughout a person’s lifespan. This will be achieved by leveraging collaborations unique to the specialty of internal medicinepediatrics, to train the next generation of internal medicine-pediatrics physicianleaders, to expand the contributions of internal medicine-pediatrics faculty to academic scholarship and institutional programs and to improve the health of the local community through partner engagement and advocacy.
Stefanie Brown, M.D., M.B.A. Jonathan Tolentino, M.D. Assistant Professors of Clinical Medicine Robert Andino, M.D. Reese Cargioli, M.D. Victor Cueto, M.D. Nishi Dedania, M.D. Chadwick Flowers, M.D. Matthew Imm, M.D. Hannah Lipshultz, M.D. Anjali Saxena, M.D. Kendra Van Kirk, M.D.
MYELOMA
The creation of the Division of Myeloma acknowledges the sizeable advancements being made in the areas of scientific research, clinical care and education in myeloma and its related diseases.

Dr. Landgren will work closely with the division chiefs of hematology, medical oncology and other specialties in the Department of Medicine and throughout the Miller School of Medicine. He also will collaborate closely with the leadership team at Sylvester Comprehensive Cancer Center.
Professor C. Ola Landgren, M.D., Ph.D. Professor of Clinical Medicine Dickran Kazandijan, M.D. Associate Professor of Clinical Medicine James Hoffman, M.D. Assistant Professors of Clinical Medicine David Coffey, M.D. Benjamin Diamond, M.D. Francesco Maura, M.D. Marcella Ali Kaddoura, M.D.
C. Ola Landgren, M.D., Ph.D.
Division Chief
DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 19
Division Highlights
CARDIOVASCULAR MEDICINE
Clinical
There was 14 percent growth in outpatient clinic activity during FY2021. A new West Palm Beach cardiology office opened its doors and a new infusion center was opened to treat patients with heart failure and decrease the readmission rate of this population.

Using barostim vagal nerve stimulation therapy for patients with heart failure, division physicians completed the first implant in Florida at University of Miami Hospital and Clinics.
interpretation of chest CT scans, resulting in the identification and quantitation of coronary calcification in such studies. The goal is to identify those who are at increased risk for coronary artery disease and to promote the initiation of preventive therapies in such patients.
Goldberger, M.D., M.B.A. Division Chief
Clinical growth was robust with 10 to 30 percent growth in most areas. Our Atrial Fibrillation Program has grown substantially with catheter ablation outcomes superior to national norms. Our cardiology service at the Miami Veterans Affairs Healthcare System has improved its ranking and is now in the top 10 VA cardiovascular programs in the U.S.
Research

Led by Dr. Carl Orringer, the Division of Cardiovascular Medicine is collaborating with the Miller School of Medicine’s Department of Radiology to integrate an artificial intelligence algorithm into the
Dr. Chunming Dong has developed a unique technology to produce tailored extracellular vesicles (TEVs) enriched in specific microRNAs or their antagomirs by genetically engineering mesenchymal stromal cells for disease pathogenesis research and potential disease treatment. Based on these ground-breaking discoveries, a recently submitted NIH R01 ranked in the second percentile and is pending funding.
Dr. Dong also has designed and used a novel dual single guide (sg)RNA lentiviral vector (DSLV) and efficiently ablated the molecules responsible for triggering alloimmune response, namely the major histocompatibility complex (MHC) class I and II in endothelial cells (ECs) and livers using the advanced CRISPR-Cas9 gene editing system.
The Miami Heart Research Institute has agreed to fund this project, which has
Farewell reception for Roberto Miki, M.D. and Rafael Sequeira, M.D. who retired after serving the University for 16 and 42 years respectively.
Jeffrey
UHEALTH|UNIVERSITY OF MIAMI MILLER SCHOOL OF MEDICINE 20
the potential to develop the technology that will lead to the production of universal donor tissues/organs that will not activate the immune system as vigorously through targeted ablation of MHC in allografts. It will reduce the need for high-level immunosuppression and, thus lessening the adverse consequences associated with immunosuppression. This will transform allograft transplant medicine with the goal of creating off-the-shelf universal donor organs.
Dr. Raul Mitrani and Dr. Jeffrey Goldberger, along with Jorge Bohorquez, professor of professional practice at the University of Miami College of Engineering, have completed the foundational studies evaluating the novel mapping technique for atrial fibrillation known as electrogram morphology recurrence (co-developed by Dr. Goldberger) with seminal publications in press and plans for a clinical trial to evaluate this novel mapping technique.
Dr. Claudia Martinez Bermudez received the 2022 NIH HIV/AIDS Research Avenir Award for her project titled “Looking into the Heart of Cannabis and HIV.” She is the second University of Miami recipient of the prestigious award.
Dr. Lina Shehadeh, in collaboration with Dr. Jeffrey Goldberger and Dr. Leonardo Tamariz, was awarded a $1 million grant from the American Heart Association to study long COVID-19.
Dr. Jeffrey Goldberger, along with Jorge Bohorquez, professor of professional practice at the University of Miami College of Engi neering, is developing novel tools for analysis of the atrial electrocardiogram (ECG), a task requiring advanced signal processing of the standard ECG.
Dr. Joshua Hare and Dr. Robert Myerburg are in the enrollment phase of their Department of Defense-funded clinical trial evaluating the genetic determinants of
Professors of Medicine
Simon C. Chakko, M.D. Mauricio G. Cohen, M.D. Eduardo J. De Marchena, M.D. Chunming Dong, M.D. Jeffrey Goldberger, M.D., M.B.A. Joshua M. Hare, M.D. Robert J. Myerburg, M.D. Carl E. Orringer, M.D. Rafael F. Sequeira, M.D. Professors of Clinical Medicine Luanda Grazette, M.D. Maureen H. Lowery, M.D. Raul Mitrani, M.D. Leonardo Tamariz, M.D. Research Professor of Medicine Lina Shehadeh, Ph.D. Associate Professor of Medicine Martin S. Bilsker, M.D.
Associate Professors of Clinical Medicine
Carlos E. Alfonso, M.D. Eugene J. Bauerlein, M.D. Claudia A. Martinez-Bermudez, M.D. Alan H. Schob, M.D.
Assistant Professors of Clinical Medicine
Sharon N. Andrade-Bucknor, M.D. Antonio Barquet-Leon, M.D. Michael Dyal, M.D.
Joseph Esterson, M.D. George Marzouka, M.D. Roberto A. Miki, M.D. Mrudula Munagala, M.D. Litsa K. Lambrakos, M.D. Anita Phancao, M.D. Nina Thakkar Rivera, D.O. Robert B. Stang, M.D. Alex Velasquez, M.D.
Research Assistant Professors of Medicine
Jian Wei, M.D.
Staff Physicians
Murry Drescher, M.D. Hoda Butrous, M.D. Mehrdad Ghahramani, M.D. Zachariah Zachariah, M.D.
response to stem cell therapy in nonischemic cardiomyopathy.
The NIH-supported LEAF study has completed enrollment. The preliminary results for this randomized trial (conducted only at the University of Miami) show that the strategy of using adjunctive medical approaches to target the atrial substrate when performing catheter ablation for treatment of atrial fibrillation dramatically improves outcomes.
Education
Due to a curriculum change, the cardiology outpatient office witnessed an increased number of rotating students. Our staff successsfully incorporated these students, offering them a highly rated educational experience. We also have continued our tele-rounding program, which allows for remote learners to participate in CCU rounds.
DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 21
Division Highlights
CLINICAL PHARMACOLOGY
Research
Researchers from the Division of Clinical Pharmacology recently published a study investigating the beneficial role of potassium intake on hypertension in postmenopausal women.


Hypertensive postmenopausal women constitute a large but under-investigated segment of the hypertensive population in the United States. Postmenopausal hypertension has emerged as a major public health concern.
natriuresis. We characterized potassiuminduced natriuresis in 19 hypertensive postmenopausal women. We also compared the time course and magnitude of potassium-induced natriuresis compared to hydrochlorothiazide (HCTZ), a diuretic commonly prescribed for hypertension.
Richard A. Preston, M.D., M.S.P.H., M.B.A. Division Chief
Potassium intake can lower blood pressure by several possible mechanisms, including a potassium-induced increase in sodium excretion, so-called potassium-induced
During a 16-day confinement in our Clinical Pharmacology Research Unit, we compared sodium excretion produced by 35 mmol potassium chloride to sodium excretion produced by 50 mg HCTZ. Sodium excretion increased sharply following 35 mmol KCl to approximately 37% of that produced by HCTZ.
From a clinical perspective, our study suggests that in hypertensive
UHEALTH|UNIVERSITY
OF MEDICINE 22
OF MIAMI MILLER SCHOOL
postmenopausal women who consume a Western diet, 35 mmol KCl produces a natriuresis approximately 37% that produced by 50 mg HCTZ. It remains to characterize potassium-induced natriuresis when potassium is administered in a potassiumcontaining complex meal. Further human studies of potassium-induced natriuresis are warranted.
The results of the study (“Characterization of Potassium-Induced Natriuresis in Hypertensive Postmenopausal Women During Both Low and High Sodium Intake”) were published this year in the prestigious American Heart Association journal Hypertension, the highest ranked journal on the subject.
Division researchers are also testing a new COVID-19 treatment in patients with kidney disease. Nirmatrelvir co-administered with ritonavir (nirmatrelvir/r, Paxlovid) is effective in the treatment COVID-19.

Because nirmatrelvir is eliminated by the kidneys, it is important to understand how it is eliminated in patients with kidney disease and whether the dose needs to be reduced.
The division participated in a multi-center trial to determine the pharmacokinetics, safety, and tolerability of nirmatrelvir/r in patients with kidney disease. Participants with mild, moderate, or severe renal impairment (n=8 each) were compared with healthy volunteers following a single 100-mg nirmatrelvir dose with 100 mg ritonavir given 12 hours before, together with, and 12 and 24 hours after the nirmatrelvir dose.
Systemic nirmatrelvir exposure increased with compared with the normal healthy
Left to right: (Top) Miriam Gonzalez Sosa, M.D.; Nadine Francois, M.A. and Rolando Rodco M.D.; (Center) Evelyn V. Caizapanta, M.D.; (Bottom) Eileen Alonso, A.R.N.P. and Richard A Preston, M.D., M.S.P.H., M.B.A.
volunteers. Nirmatrelvir/r exhibited an acceptable safety profile in patients with kidney disease. As a result of this study, we understand better how to dose the Paxlovid in patients with kidney disease. Our findings led to a dose reduction recommendation for nirmatrelvir/r in patients with moderate renal impairment (150/100 mg nirmatrelvir/r instead of 300/100 mg twice daily for 5 days).
The study, titled “Pharmacokinetics of Oral Nirmatrelvir/Ritonavir, a Protease Inhibitor for Treatment of COVID-19, in Subjects with Renal Impairment” was published in Clinical Pharmacology & Therapeutics. This clinical trial is registered with ClinicalTrials.gov (NCT04909853).
Professors of Medicine
Barry Materson, M.D., M.B.A. (Emeritus) Richard A. Preston, M.D., M.S.P.H., M.B.A.
DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 23
Division Highlights
DIGESTIVE HEALTH AND LIVER DISEASES
Clinical
Renowned for providing cutting-edge care for gastrointestinal conditions, the Division of Digestive Health and Liver Diseases has launched a new treatment option for severe gastroparesis, a disorder that can cause chronic digestive tract difficulties.
hepatology advanced practice providers for treatment of chronic hepatitis C. The project went live in the fall of 2022.
Research
Paul Martin, M.D. Division Chief
The division’s experienced gastroenterology specialists have several options to treat gastroparesis, including medications, electrical stimulation, Botox injections and now an advanced endoscopic procedure called G-POEM, which is used for gastric peroral endoscopy myotomy. G-POEM is a minimally invasive procedure for opening the pylorus. This endoscopic approach can offer significant improvements to a patient’s lifestyle. It also expands specialists’ options for treating medically refractory gastroparesis.
Glenda Quinones, APRN, DNP, NP-C and Susana Ramirez Restrepo, MSN, ARNP, FNP-BC, in collaboration with Dr. Emilio Volz, Director of Student Health Services at the University of Miami, worked on the implementation of CDC guidelines for universal screening for hepatitis C in students at the University. This process will automate screening and expedite referral to the
Dr. David Goldberg led the University of Miami as one of 10 sites in the National Institute of Diabetes and Digestive and Kidney Diseases/NIDDK-sponsored Liver Cirrhosis Network (LCN), which focuses on prediction of outcomes in patients with cirrhosis, including the potential benefits of statins to prevent complications.
Dr. Goldberg, one of three principal investigators of the THINKER-NEXT study, an NIDDK-sponsored multi-center study focused on transplanting kidneys from hepatitis C-infected donors into hepatitis C-negative patients.
Dr. Goldberg also published work in multiple high-impact publications including Gastroenterology, JAMA Surgery, Hepatology, and the Journal of Hepatology

Dr. Shria Kumar joined the faculty in August 2021 to build a research program in GI cancers and therapeutic endoscopy. She has published work in such highimpact publications as Cancer, Clinical Gastroenterology and Hepatology. In addition, Dr. Kumar has been selected to be the associate editor of a new journal Evidence-Based GI by the American Collected of Gastroenterology (ACG).
Dr. Oriana Damas is the principal investigator for a dietary intervention study that aims to improve response to biologic therapy in patients with ulcerative colitis. She received U35 funding to begin an innovative multi-center clinical trial that uses hyperbaric oxygen therapy for patients admitted to the hospital with ulcerative colitis. A multicenter
Left to right: Enrico Souto, M.D., Il; Joon Paik, M.D. and Kalyan Bhamidimarri, M.D.

UHEALTH|UNIVERSITY OF MIAMI MILLER SCHOOL OF MEDICINE 24
U01 proposal was submitted this year. Dr. Damas and Dr. Chunsu Jiang identified anti-inflammatory diet patterns in a cohort of 1,000 patients with irritable bowel disease (IBD) using a short 15-minute dietary screener that can be used as a point-of-care testing method for nutritional assessment.
Education
The University of Miami/Jackson Memorial Health System’s Gastroenterology Fellowship Program is one of the few centers in the United States offering combined GI/ transplant hepatology pathway, which allows fellows to train in both GI and transplant hepatology during a three-year fellowship. Two of our current fellows were selected for this pathway.

During FY 2021-2022, our fellows won the academic debate hosted by the American Liver Foundation - Southeast region in October 2021. The program was also awarded the Edgar Achkar Visiting Scholar in Equity, Diversity and Ethical care by the American College of Gastroenterology (April 2022). Three out of our five graduating fellows from the class of 2022 opted for additional training in advanced endoscopy.
Highlights
Dr. Maria T. Abreu was selected as vice president of the American Gastroenterological Association (AGA) and is in line to be the AGA president in 2024.
Dr. Amar Deshpande received the 2022 Faculty Senate Outstanding Teacher Award.
Dr. Daniel Sussman received the Department of Medicine Distinguished Educator Award for 2021.
Dr. David Goldberg was the recipient of the Provost Award for Scholarly Activity for 2020-2021.
Glenda Quinones, APRN, DNP, won the UHealth APRN of the Year Award in 2022.
Professors of Medicine
Maria T. Abreu, M.D. Jaime S. Barkin, M.D. Eugene R. Schiff, M.D. Professors of Clinical Medicine Amar Deshpande, M.D. Cynthia Levy, M.D. Christopher B. O’Brien, M.D. Jeffrey B. Raskin, M.D. (Emeritus) Daniel Sussman, M.D., M.P.H.
Associate Professors of Medicine Jodie Barkin, M.D. Kalyan Bhamidimarri, M.D. Jose Garrido, M.D. David Goldberg, M.D. Patricia Jones, M.D., M.S.C.E. David Kerman, M.D. Andres Carrion Monsalve, M.D.
Assistant Professors of Medicine
Sunil Amin, M.D.
Leopoldo Arosemena, M.D. Sean Bhalla, M.D. Oriana Damas, M.D. Paul Feldman, M.D. Roberto Fogel, M.D. Shria Kumar, M.D., M.S.C.E. Emory Manten, M.D. Eric Martin, M.D.
Il Joon Paik, M.D. Michelle Pearlman, M.D. Siobhan Proksell, M.D. Morgan Sendzischew Shane, M.D. Ami Panara Shukla, M.D. Enrico Souto, M.D.
DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 25
Left to right: Maria Abreu, M.D.; Paul Martin, M.D. and Patricia Jones, M.D. at the Eugene J. Sayfie, M.D. Research Day
Division Highlights
ENDOCRINOLOGY, DIABETES AND METABOLISM
Clinical
Our faculty remains committed to advancing the science and clinical practice of endocrinology, diabetes and metabolism. Clinical operations returned to full speed despite spikes in COVID-19 infection. The division continued to provide both in-patient and outpatient services, with outpatient visits exceeding 27,000 encounters.
BernalMizrachi, M.D. Division Chief

The Comprehensive Diabetes Center (CDC) entered its fifth year of operation. The center continues to provide world-class clinical care to patients with diabetes at two locations, the Lennar Foundation Medical Center and the Diabetes Research Institute (DRI).
With more than 500 registrants, experts from our Comprehensive Diabetes Center participated in a University of Miami Health Talks webinar to discuss navigating diabetes during the COVID pandemic, which took place on November 17, 2021. Experts discussed and answered questions regarding the relationship between diabetes and COVID-19, vaccinations for patients with diabetes, and holiday eating and pandemic travel for patients with diabetes.
Research
Essential to our research mission is the innovative research conducted in our division. Dr. Francesco Vendrame, Assistant Professor of Clinical Medicine, has discovered that dimethyl fumarate (DMF) is a promising drug for the treatment of type 1 diabetes in preclinical models. This information will be used to design clinical trials in individuals with type 1 diabetes.
In addition, Dr. Ernesto Bernal-Mizrachi and Dr. Andrew Schally, Distinguished Leonard M. Miller Professor in the Department of Pathology and Head of the Endocrine Polypeptide and Cancer Institute at the Miami Veterans Affairs Medical
Center, are successfully using GHRH agonist to improve survival of human and rodent beta-cells and improve glucose control in preclinical models of type 1 diabetes. These results will be used to design studies using GHRH agonist as pharmacological therapy for type 1 diabetes treatment by preserving beta cells.
Dr. Alejandro Caicedo has discovered that FDA-approved positive allosteric modulators for glutamate receptors can be repurposed to treat hypoglycemia in type 1 diabetes.
Our faculty continued to excel in clinical and basic research in diabetes, adipocyte biology, osteoporosis and pituitary disorders. Division researchers continued making seminal contributions towards the understanding of endocrine diseases.
The output of new papers increased to 110. Our faculty published work in several scientific journals, including Gastroenterology, European Heart Journal, The Lancet Diabetes & Endocrinology, Diabetes Care, Diabetologia and Diabetes. In 2021, our faculty members were awarded several additional federal grants from the National Institutes of Health (NIH) and the Juvenile Diabetes Research Foundation. As a result, we now rank second in grants awarded to the Department of Medicine’s sections and centers.
Dr. Ayse Canturk, endocrinology fellow, was selected to present her poster “TumorInduced Osteomalacia: When a Patient Refuses Definitive Therapy” at the Rare Bone Disease Pre-Meeting Symposium. She also was one of only a few fellows selected to participate in the Endocrine Fellows Bone Course to take place prior to the meeting.
Education
The J. Maxwell McKenzie Fellowship Program in Endocrinology expanded its clinical training with dedicated clinic rotations at the Miami Veterans Affairs Medical Center in
Ernesto
UHEALTH|UNIVERSITY OF MIAMI MILLER SCHOOL OF MEDICINE 26
obesity and metabolic medicine as well as diagnostic thyroid ultrasound reporting and thyroid fine needle aspiration.
Didactics for fellows were enhanced with instruction in healthcare disparities and patient safety, which resulted in improved endocrine laboratory reporting at UHealth.
Endocrine fellows, in collaboration with the Emergency Medicine Residency Program, initiated a QI project with Jackson Memorial Hospital’s Emergency Department to streamline management of patients presenting with hyperglycemia to the ER with a goal of reducing hospital admissions for hyperglycemia.

Endocrinology fellows presented over 10 abstracts including posters and oral presentations at national and international conferences.
Highlights
Dr. Jay Skyler was inducted as a fellow of the Royal College of Physicians (RCP) of London. He will join a select fellowship community of more than 18,000 senior medical leaders from around the world. The honor is due, in part, to the relationship between the American College of Physicians (ACP), in which Dr. Skyler was named a Master in
Professors of Medicine
Rodolfo Alejandro, M.D. Ernesto Bernal-Mizrachi, M.D. Ronald Goldberg, M.D. Alberto Pugliese, M.D. Jay Skyler, M.D. Jay Sosenko, M.D. Roy E. Weiss, M.D., Ph.D. Professor of Clinical Medicine Gianluca Iacobellis, M.D., Ph.D. Research Professor of Medicine Ricardo Pastori, Ph.D. Professor Alejandro Caicedo-Vierkant, Ph.D. Associate Professor of Clinical Medicine
Violet Lagari-Libhaber, D.O. Research Associate Professor Armando Mendez, Ph.D.
Assistant Professor of Medicine
David Baidal, M.D.
Assistant Professors of Clinical Medicine
Zeina Hannoush, M.D. Mark Jara, M.D. Jason Levine, D.P.M. Silvia Gra Menendez, M.D. Francesco Vendrame, M.D., Ph.D.
Research Assistant Professors
Joana Almaca, Ph.D.
Rene Barro-Soria, Ph.D. Manuel Blandino, Ph.D. Joao Saar Werneck De Castro, Ph.D.
Lisa Rafkin, Ph.D. Rayner Rodriguez-Diaz, Ph.D.
Staff Physicians
Silvia Gra Menendez, M.D. Bresta Miranda, M.D. Carmen Villabona, M.D.
2005 and the RCP. The ACP nominates a few members each year who are masters to be considered for fellowship by the RCP. This year he retired from his role as senior editor of Diabetes Technology and Therapeutics after 15 years of service.
Dr. David Baidal received the University of Miami J. Maxwell McKenzie Endocrinology, Diabetes and Metabolism Award for Excellence in Teaching, Fellowship Program, Class of 2019-2021.
DEPARTMENT
CHAIRMAN’S REPORT 2022 27
João Saar Werneck De Castro, Ph.D. (fourth from left) with lab members.
OF
MEDICINE
Division Highlights
GENERAL INTERNAL MEDICINE
Clinical
Alejandro D. Chediak, MD Interim Division Chief

As we emerged from the pandemic, our general internal medicine (GIM) team reimagined the delivery and provision of world-class primary care services. Division faculty and staff rapidly transitioned from a nearly entirely telehealth service to hybrid and conventional care models to ensure our patients received all the necessary preventive, acute and chronic care services they needed. Outpatient clinic plasticity assures that our patients receive high-quality, transformative medical care, whether they are near or far.
At the Desai Sethi Medical Center, the division pioneered a “clinic within a clinic” model, housing dedicated service lines for anticoagulation and travel. The arrangement streamlines the management of selected common medical needs.
Research
Dr. Olveen Carrasquillo was interviewed by several media outlets for his observations
from the “All of Us” Research Program, where he refutes the longstanding Latino Epidemiological Paradox, which asserts that Latinos have equal if not better health outcomes (based on measures of population health, including cardiovascular disease). The work offers evidence that this generally accepted epidemiological observation may not be true. Given that Latino populations are not homogeneous, the team is now focusing on health data from Latino subgroups, as well as U.S. born Latinos.
Junior faculty also contributed to the division’s research successes. Dr. Sabrina Taldone and Dr. Kendra Van Kirk became members of the Academy of Medical Educational Scholars, receiving awards for their work titled “Assessing Value-Based Competencies in a General Medicine Residency” and “Utilizing Backward Design to Train-the-Trainer,” respectively.
Dr. Erin Marcus, professor of clinical medicine, presented on the use of Edwidge Danticat’s writing to foster empathy and
Erin N. Marcus, M.D., M.P.H. shows her research poster to UM/JMH chief medical residents Andres Rodriguez, D.O.; Paul Montana, M.D.; Eduardo Saul, M.D. and Marina Byer, M.D. at the 2023 Academic Internal Medicine Week Meeting in Charlotte, N.C.

UHEALTH|UNIVERSITY OF MIAMI MILLER SCHOOL OF MEDICINE 28
improve understanding of Haitian immigrant patients among medicine interns. The work was presented at national meetings of the Society of General Internal Medicine and the Alliance for Academic Internal Medicine in Orlando, Florida and Charlotte, North Carolina.
Education
Our faculty led seamless transitions from in-person to virtual learning and back, thus ensuring our graduate and undergraduate students received top-notch instruction in the best and safest learning environments available. Many also continued to enhance efforts to further diversify our student body and developed curricular innovations as part of the NextGen Curriculum, a novel educational paradigm that trains medical students to become the transformational leaders that will shape the future of medicine and champion discovery.
Highlights
Acknowledging her unwavering commitment and contributions to medical education, the Association of American Medical Colleges named Dr. Joan St. Onge as chair of the group on resident affairs. Dr. St Onge also served as co-chair of the division’s working group for the Florida Council of Medical School Deans.
In recognition of her work to reduce HIV/ AIDS disparities in Miami, Sonjia Kenya EdD, MS, MA of the Division of General Internal Medicine was honored with the 2022 Sapphire Award by the Florida Blue Foundation. The statewide award is granted to recipients who are making a meaningful impact in their communities in the area of health equity advancement.
Professors of Medicine
Olveen Carrasquillo, M.D., M.P.H. Laurence Gardner, M.D. S. Barry Issenberg, M.D. Kenneth Goodman, PhD Professors of Clinical Medicine
Panagiota Caralis, M.D., J.D. Daniel Lichtstein, M.D. Erin Marcus, M.D., M.P.H. Joan St. Onge, M.D. Ross Scalese, M.D.
Associate Professors of Clinical Medicine
Yvonne Diaz, M.D. Hilit Mechaber, M.D. Paul Mendez, M.D. Frederick Williams, M.D.
Assistant Professors of Clinical Medicine
Howard Anapol, M.D. Stephanie Clauss, M.D. Gregory Coleman, M.D. Janelle Cuervo, M.D. Janelis Gonzalez, M.D. Elizabeth Greig, M.D. Lilliam Guzman, M.D. Brian Hagenlocker, M.D.
Melanie Helfman, M.D.
Margarita Llinas, M.D. Cristina Pravia, M.D. Katelin Snow, M.D. Jacobo Wajner, M.D. Sabrina Taldone, M.D.

Associate Professor, Educator Sonjia Kenya, Ph.D.
Associate Professor of Professional Practice
Gauri Agarwal, M.D.
Assistant Professors of Professional Practice
Analinnette Zito, M.D.
Staff Physicians
Alexandra Calandriello, M.D. Manuela Calvo, M.D. Grettel Garcia, M.D. Sudah Lolayekar, M.D. Elizabeth Parra-Garnica, M.D. Hiram Rodriguez, M.D.
DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 29
Puppy Therapy Day for Residents
Division Highlights
GERIATRICS AND PALLIATIVE MEDICINE
Clinical
The Geriatrics Outpatient Service continues to perform comprehensive geriatric assessments on older patients at the Downtown and Coral Gables ambulatory locations.
well as co-authored a chapter capturing the experiences and ethical challenges that palliative social workers have experienced around the world during the pandemic.
Education (Geriatrics)
Marcio Rotta Soares, M.D. Division Chief
Our Palliative Medicine Service also continues to grow its outpatient network. With the addition of our new palliative care physician, Dr. Michael Huber, along with the presence of additional geographic locations, we are further expanding our high-quality symptom management and patient-centric palliative care. Our outpatient locations include Downtown Miami, South Miami, Coral Gables, Deerfield, and Plantation. Will also offer telemedicine consults.
The Inpatient Palliative Medicine Consult Service provides care to patients admitted to the University of Miami Hospital and Clinics. The consult service focuses on symptom management and transitions of care in patients with serious, complex and/or terminal illnesses.
Research (Geriatrics)
Our geriatricians’ research in the areas of frailty and COVID-19 has led to six recent publications in prestigious journals, including The Lancet Healthy Longevity, the Journal of General Internal Medicine, and others.
Dr. Jorge G. Ruiz and Dr. Christie Hogue, DDS, a previous graduate of our advanced fellowship program, have published a book titled Oral Health and Aging, with several of our faculty members and fellows acting as co-authors of multiple chapters.
Research (Palliative Medicine)
Palliative social worker Carina Oltmann, LCSW contributed two chapters to the second edition of the Oxford Textbook of Palliative Social Work. She authored a chapter on cognitive behavioral therapy as
Our Geriatric Medicine Fellowship Program remains the regional leader in advanced geriatric medicine training. Led by Dr. Iriana Hammel, who serves as program director, the fellowship program trains up to eight geriatricians a year.
The division also conducts weekly teaching conferences for our fellows and faculty as well as monthly meetings with faculty and staff. We also hold monthly international Frailty Seminars with renowned speakers and audience members from around the world.
Our geriatricians were also instrumental in garnering certification for the Miami Veterans Administration Medical Center as an age-friendly healthcare system by the Institute for Healthcare Improvement. In June 2022, we also organized the Annual VISN 8 Geriatric Research, Education and Clinical Centers (GRECC) Conference titled Healthy Aging During the COVID-19 Pandemic
Dr. Jorge G. Ruiz was elected Chair of the American Board of Internal Medicine (ABIM) Committee for Geriatric Medicine. He was also promoted to Professor of Clinical Medicine.

Education (Palliative Medicine)
The Hospice and Palliative Medicine Fellowship Program continues to grow and currently has four fellowship positions, one of which is a combined geriatric and palliative medicine fellowship.
Dr. Khawand-Azoulai spearheaded two QI projects. Once project focused on improving the proxy assignment process at Jackson Memorial Hospital and the
UHEALTH|UNIVERSITY OF MIAMI MILLER SCHOOL OF MEDICINE 30
other to improve the completion of Florida Department of Health do-not-resuscitate (DNR) forms for patients discharged from University of Miami Hospital and Clinics (UHealth Tower).
Dr. Khawand-Azoulai was selected as a member of the Florida Palliative Care Coalition and sits on the educational steering committee. She also was a part of the neurooncology fellowship program.
Highlights
Dr. Julia Sanchez leads a new opioid stewardship program. Created in 2021, the program consists of a multidisciplinary team who work collaboratively to oversee safe opioid prescribing, monitoring and education at UHealth.
Dr. Sanchez will continue to develop system-wide strategies for opioid stewardship by establishing prescribing guidelines, providing education, improving access and monitoring prescribing patterns and adverse events related to opioids.
Through this program we have completed many quality improvement projects including: prescription drug monitoring program integration with Epic; an electronic controlled
Professors of Medicine
Stuti Dang, M.D., M.P.H. Silvina Levis-Dusseau, M.D. Research Professor Guy Howard, Ph.D. Associate Professor Jorge Ruiz, M.D. Research Associate Professor Carlos Perez-Stable, Ph.D.
Assistant Professors Enrique Aguilar, M.D. Jenny Drice, M.D.
Iriana Hammel, M.D. Mariana Khawand-Azoulai, M.D. Julia Sanchez, M.D. Luis Samos-Gutierrez, M.D. Marcio Soares, M.D. Khin Zaw, M.D.
substances agreement; an alternative to the current opioids pamphlet, which is included in AVS when ordering opioids at discharge. Additional quality improvements tactics include: naloxone co-prescribing for high-risk patients to improve outpatient access; addition of an indications box to long-acting opioids to comply with the ISMP Best Practices initiative; the removal of seven-day “auto stop” on inpatient orders for long-acting opioids and opioid prescribing protocols for patients with advanced renal disease.
Carina Oltmann, LCSW, who co-chairs the World Hospice and Palliative Care Social Work Network (WHPCSW), helped to launch an international effort to assist healthcare workers serving patients in Ukraine and surrounding countries.
Mariana KhawandAzoulai, M.D. (Hospice and Palliative Medicine fellowship associate director) and Khin Zaw, M.D. (Hospice and Palliative Medicine fellowship director) with fellows Yesica Campos, M.D.; Angela Boey, M.D.; Paul Eugene, M.D. and Ezekiel Ijiaopo, M.D.

DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 31
Division Highlights
HEMATOLOGY
Clinical
By restructuring the Division of Hematology into various sections – lymphoma, leukemia, general hematology – we have provided more specialized care while increasing patient satisfaction.
We created the Hematology Specialty Inpatient Services and have standardized the treatment of patients with hematologic conditions across the network. Additionally, Dr. Namrata Chandhok created a clonal hematopoiesis of indeterminate potential clinic that has already served 50 patients.
The division’s phone lines have now been integrated into the NICE system to efficiently schedule patients with disease specialists in a specific hematology section. Meanwhile, as we prepare to open two new satellite offices in South Florida, our satellite offices continue to see an approximate 14% growth in outpatient visits a year.
Research
Faculty members from the Division of Hematology conduct innovative research that will become the standards of how we practice hematology in the future.
Dr Mikkael Sekeres and Dr. Justin Watts led an international study of more than 450 older adults with myelodysplastic syndromes (MDS) over the last year by using a novel combination of drugs that paves the way for combination therapy in this challenging patient population. The study was published in the journal Blood Advances

Dr. Sekeres also led a study using machine learning/artificial intelligence (AI) programming to predict outcomes in MDS, which was published in the Journal of Clinical Oncology.
Dr. Justin Taylor led a study identifying why patients with chronic lymphocytic leukemia may not respond to a common treatment for
Left to right: Justin Taylor, M.D.; Jonathan Schatz, M.D.; Mikkael Sekeres, M.D., M.S. and Juan Carlos Ramos, M.D. at the Dolphins Cancer Challenge.
 Mikkael Sekeres, M.D., M.S. Division Chief
Mikkael Sekeres, M.D., M.S. Division Chief
UHEALTH|UNIVERSITY
OF MEDICINE 32
OF MIAMI MILLER
SCHOOL
that disease, which was published in the New England Journal of Medicine
Dr. Juan Alderuccio conducted an international analysis of a combination therapy in a rare subtype of lymphoma, extranodal marginal zone, which was published in Blood Advances.
Dr. Izidore Lossos identified a protein in lymphomas that is associated with earlystage disease and lack of spread, which was published in Blood Advances.
Dr. Craig Moskowitz led two studies of combination therapies that included immunotherapy for patients with Hodgkin lymphoma, both of which were published in the Journal of Clinical Oncology.
Dr. Justin Taylor was one of 17 earlycareer physician-scientists to receive a Doris Duke Charitable Foundation Clinical Scientist Development Award to advance research and support the transition to an independent clinical research career. He was recognized for his research, “Investigating Mechanisms of Resistance to Non- Covalent BTK Inhibition in Patients with B-Cell Malignancies,” which led to a senior author publication in the New England Journal of Medicine.
Dr. Jonathan Schatz was awarded a peer-reviewed extramural basic research grant by the Florida Department of Health Bankhead-Coley Cancer Center Program to study inhibition of the cell-cycle kinase GAK, a novel therapeutic target in diffuse large B-cell lymphoma.
Dr. Juan Alderuccio was awarded a Clinical Investigator Career Development Award by the Lymphoma Research Foundation to establish an innovative trial implementing dual antibody treatment in relapsed/refractory follicular lymphoma (FL), with the goal of using loncastuximab tesirine in combination with rituximab to achieve complete metabolic response.
Dr. Alvaro Alencar was awarded a
Professors of Medicine
Yeon Soong Ahn, M.D. (Emeritus) John Byrnes, M.D. Izidore Lossos, M.D. Craig Moskowitz, M.D. Stephen Nimer, M.D. Juan Carlos Ramos, M.D. Joseph Rosenblatt, M.D. Mikkael Sekeres, M.D., M.S. Gerald Soff, M.D. Research Professor Ramiro Verdun, Ph.D. Associate Professor Jack Temple, M.D. (Emeritus) Associate Professors of Clinical Medicine
Juan Alderuccio, M.D. Alvaro Alencar, M.D. Jonathan Schatz, M.D. Justin Watts, M.D.
Assistant Professors
Ney Alves, M.D.
Terrence Bradley, M.D. Diane Byrnes, M.D. Roberto Cano, M.D. Namrata Chandhok, M.D. Jonathan Cohen, M.D. Thomas Harrington, M.D. Georgios Pongas, M.D. Justin Taylor, M.D. Sangeetha Venugopal, M.D., M.S. Steven Weiss, M.D.
Research Assistant Professors
Xiaoyu Jiang, Ph.D. Jun Sun, Ph.D. Yu Zhang, M.D.
Staff Physicians
Diogenes Alayon, M.D. Mayda Arias, M.D. Douglas Faig, M.D. David Lessen, M.D. Jorge Antunez de Mayolo, M.D.
foundation grant by the Alliance for Clinical Trials in Oncology Foundation, Special Projects Allocation to study health disparities in lymphoma.
Education Division faculty teach at the medical school, post-graduate level as well as in the residency and fellowship programs. One weekly online hematology course, led by Dr. Gerald Soff, had an international audience of 14,637 visits in 2022, representing 4,746 unique individuals from 45 countries and averaging 40-50 presentation views per day. Hematology faculty organized international conferences in myelodysplastic syndromes and in hematologic malignancies, attracting more than 3,000 participants. Faculty members also hosted the firstever international working group in myelodysplastic syndromes in Miami.
DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 33
Division Highlights
HOSPITAL MEDICINE
Clinical
The Division of Hospital Medicine continues to provide exceptional in-patient acute care services to patients at University of Miami Hospital and Clinics (UHealth Tower), Sylvester Comprehensive Cancer Center, Bascom Palmer Eye Institute and Jackson Memorial Hospital. Within the past year, the Division of Hospital Medicine has expanded its team to include 60 faculty and staff who all share the same goal – to provide quality patient care.
for safer and more tailored care delivery in our inpatient units.
Education
Marcio Rotta Soares, M.D. Interim Division Chief
The division has adopted several care models to support patient throughput, the most successful being the Nurse Care Model allowing APRNs to work to their full license potential. Most teams are now comprised of a physician along with a collaborating APRN. Currently, each team carries a patient census of 22 patients per day.
The division also adopted the Staff Physician Model. Staff physicians provide expanded hospital coverage while increasing census per provider (increasing caps from 16 to 20) exclusive of nurse practitioner (NP) support. Since we are a completely clinical division, staff physicians play a critical role in providing round-the-clock patient care and reducing the need for moonlighters and locums.
This year welcomed the addition of an Emergency Department (ED) Admitting Team. This team, comprised of an attending physician and three nurse practitioners, focuses on triage and admitting all patients from the ED as well as those patients coming from outside hospitals as transfers. The team not only admits but provides care coordination throughout the day, which allows for our inpatient teams to round and coordinate discharges in a more fluid fashion. The success of this team has allowed

At right: Hospital Medicine faculty and staff
Our academic mission focuses primarily on quality and safety, education and the teaching of residents. Due to the success of our teaching services and our faculty’s desire to expand their academic footprint, the Division of Hospital Medicine created a third teaching team comprised of senior faculty members who mentor internal medicine residents through our affiliation with Jackson Memorial Health System. Each teaching service holds a maximum patient census of 16, with a focus on quality education and patient care.
Highlights
As the new Interim Chief, Dr. Marcio Soares’ innovative ideas and years of experience as the Chief of Geriatrics/Palliative Medicine and Associate Chief Medical Officer for University of Miami Hospital and Clinics (UHealth Tower) will undoubtedly transform

UHEALTH|UNIVERSITY OF
SCHOOL OF MEDICINE 34
MIAMI MILLER
the division’s clinical and academic footprint. Some of the divisional goals include: to reduce length-of-stay (LOS) and readmission rates and continue to create a more sustainable staff model to efficiently meet the needs of the hospital as well as other divisions and departments at the University of Miami.
Dr. Maria Carolina Delgado-Lelievre, founder/director of the only American Heart Association (AHA) Comprehensive Hypertension Center in Florida, obtained approval to use the newest technology in remote blood pressure monitoring. The University of Miami will be the first university in the U.S. to implement this technology.
Dr. Efren Manjarrez successfully completed his first year on the board of directors for the Society of Hospital Medicine. He is the first University of Miami faculty member ever elected to the board. Dr. Manjarrez also served as course director for the Perioperative and Consultative Medicine Pre-Course at Southern Hospital Medicine Atlanta, where he presented four lectures.
Associate Professor Efren Manjarrez, M.D.
Assistant Professors Juan Serralles Allongo, M.D. Candido Anaya, M.D. Alberto R. Arancibia, M.D. Scott Berger, M.D. Aldo Pavon Canseco, M.D. Sharde Chambers, M.D. Tanya Clarke, M.D. Stephanie Chery, M.D. Maria Carolina Delgado-Lelievre, M.D. Iman Doostan, M.D. Kunal Gawri, M.D. Erica Graff, M.D. Oxana Harlamova, M.D. Armen Henderson, M.D. Devora Kahn, M.D. Joshua Laban, M.D. Ahmed Luqman, M.D. Vijay Mehta, M.D. Maria Antonietta Mosetti, M.D. Deepak Mummidavarapu, M.D. Lubna Osman, M.D. Rafael Enrique Hernandez Oquet, M.D. Christian Quintana, M.D. Phillip Rubin, M.D.

Allan Rubinfeld, M.D.
Jonathan Salter, M.D. Olga Tarasova, M.D. Pamela Trotter, M.D. Bruno Urrea, M.D. Avinash Vernekar, M.D. Jessica Zuleta, M.D.
Staff Physicians
Rafael Garces, M.D. Taaha Mendha, M.D. Jonathan Salter, M.D. Glenda Sosa, M.D. Liana Woodley-Pearson, M.D. Jorge Diaz Valdes, M.D.
DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 35
Division Highlights
INFECTIOUS DISEASES
Clinical
The UHealth Rapid Access Wellness Clinic expanded its community programs for HIV prevention to Miami Beach. The clinic, located within a Walgreens pharmacy, provides HIV pre-exposure prophylxis (PrEP) and rapid entry into HIV care as well as sexually transmitted infection (STI) testing and treatment at no cost to clients.
Research
DobleckiLewis, M.D. Division Chief
With continued innovation over this past year, the Division of Infectious Diseases continues to combat HIV and COVID-19 in addition to a new global infectious disease public health emergency: monkeypox.
Division faculty members have quickly deployed innovative clinical and research
practices to diagnose and treat monkeypox.
This initiative has been led by Dr. Bhavarth Shukla, UHealth Director of Infection Control, and Dr. Lilian Abbo, Director of Infection Control at Jackson Health Systems.
Dr. Susanne Doblecki-Lewis and Dr. Laura Beauchamps led monkeypox testing and treatment in the UM Infectious Diseases Rapid Access Wellness Clinic, while Dr. Mario Stevenson and Dr. Mark Sharkey developed molecular assays to detect and characterize viral isolates from clinical specimens as well as from wastewater to monitor the epidemic and to allow further research on this newly emerging pathogen.
Division faculty continue to contribute to COVID-19 vaccine research, with publications by Dr. Susanne Doblecki-Lewis in the New


The Division of Infectious Diseases had the highest number of abstracts at the 8th Annual Eugene J. Sayfie, M.D. Research Day. Maria Alcaide, M.D., on behalf of the division, received the certificate of participation, presented by Roy Weiss, M.D.
 Susanne
Susanne
UHEALTH|UNIVERSITY OF
MILLER SCHOOL OF MEDICINE 36
MIAMI
England Journal of Medicine related to this work, and with additional COVID-19 related publications by faculty members in Frontiers, Transplantation and JAMA Network Open
Dr. Michele Morris authored the book Emerging Transplant Infections: Clinical Challenges and Implications published by Springer Nature. Dr. Jose Camargo Galvis and Dr. Yoichiro Natori contributed chapters on cytomegalovirus in hematopoietic stem cells and influenza, respectively. Dr. Jose Camargo Galvis investigated bone marrow transplant patients’ reaction to the Measles, Mumps and Rubella (MMR) vaccine that led to BMT prophylaxis protocol revisions.
Dr. Hansel Tookes received the prestigious NIH Avenir Award from the National Institute for Drug Abuse (NIDA) to perform a randomized controlled trial of the “Tele-Harm Reduction Intervention,” which employs syringe service programs to deliver telehealth-enhanced access to multidisciplinary services.
Faculty also received other multiple highimpact federal grants related to COVID-19 and HIV/AIDS research.
Education
The Infectious Diseases Fellowship Program continues to excel and expand its offerings to incoming fellows.

Dr. Hansel Tookes implemented the Integrated Opioid Education Longitudinal Curriculum and is now the director for the HIV primary care elective.
Highlights
Dr. Gio Baracco was recognized as the Federal Employee of the Year by the South Florida Federal Executive Board.
Dr. Jose Camargo Galvis, Dr. Yoichiro Natori and Dr. Michele Morris had their paper in Blood Advances recognized as one
Professors of Medicine
Maria Alcaide, M.D. Gordon Dickinson, M.D. Margaret Fischl, M.D. Michael Kolber, M.D. Mario Stevenson, Ph.D. Professors of Clinical Medicine
Lilian Abbo, M.D. Gio Baracco, M.D. Jose Castro, M.D. Susanne Doblecki-Lewis, M.D. Dushyantha Jayaweera, M.D. Paola Lichtenberger, M.D. Michele Morris, M.D. Allan Rodriguez, M.D. Associate Professors Catherine Boulanger, M.D. Jose Camargo Galvis, M.D. Isabella Rosa-Cunha, M.D. Bhavarth Shukla, M.D. Jacques Simkins-Cohen, M.D. Stephen Symes, M.D. Hansel Tookes, M.D. Jose Gonzales Zamora, M.D.
Assistant Professors
Shweta Anjan, M.D.
Folusakin Ayoade, M.D. Laura Beauchamps, M.D. Jovanna Bertran-Lopez, M.D. Stephen Morris, M.D. Yoichiro Natori, M.D. Alexis Powell, M.D. Mohammed Raja, M.D. Antoine Salloum, M.D. David Serota, M.D. Candice Sternberg, M.D. Research Assistant Professor Mark Sharkey, Ph.D.
of the top-10 practice changing papers in transplant ID at IDWeek.
Dr. Mario Stevenson received the Raymond F. Schinazi and Family Endowed Chair in Biomedicine for his advances in virology for HIV/AIDS research. This builds on his existing leadership roles with the Provost’s Resiliency Academy and the Miami Center for AIDS Research (CFAR) at the Miller School of Medicine.
Dr. Stephen Symes was awarded the University of Miami 2021-22 James W. McLamore Award. He was also awarded the J. Donald Temple, M.D. Unsung Hero Award for demonstrating exceptional service and commitment to medical education.
Dr. Susanne Doblecki-Lewis received the Provost’s Award for Scholarly Activity for her work on COVID-19 and HIV prevention.
DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 37
Division Highlights
MEDICAL ONCOLOGY
Clinical
The division’s cancer services have expanded through the addition of five new physicians: Dr. Marijo Bilusic, Dr. Leonel Hernandez Aya, Dr. Coral Olazagasti, Dr. Jose Suarez and Dr. Milena Elimelakh. Telemedicine services have continued due to the ongoing pandemic, but more in-person sessions were made available, while adhering to all safety guidelines.
Research
F.A.S.C.O.
The Oncology Care Clinic continues to decrease the number of ER visits and University of Miami Hospital and Clincs (UHealth Tower) admissions, with patients expressing how much they enjoy having this service available to them.
Sylvester Comprehensive Cancer Center at Doral is scheduled to begin accepting patients in September 2022. This will be the ninth satellite clinic providing cancer care in South Florida.
Dr. Gilberto Lopes continued his work with the COVID-19 and Cancer Consortium with published work in the Lancet Oncology and Journal of American Medical Association Oncology. He has published his findings on global treatment standards for breast cancer in the Journal of the National Cancer Institute as well as his findings on the role of homologous recombination deficiency (HRD) in colorectal cancer (CRC).
Dr. Jose Lutzky published in the New England Journal of Medicine, the Journal of Clinical Oncology and the Journal for Immunotherapy of Cancer this year. His focus is on inoperable metastatic melanoma and the potential breakthrough using new immunotherapy drug combination to target tumors with less toxicity for patients.

Dr. Marijo Bilusic published his work on cellular immunotherapy designed to initiate
 Gilberto Lopes, M.D., M.B.A.,
Interim Division Chief
Gilberto Lopes, M.D., M.B.A.,
Interim Division Chief
38
Peter Hosein, M.D.
UHEALTH|UNIVERSITY
OF MIAMI MILLER SCHOOL
OF MEDICINE
an immune response against prostate cancer in the Journal of the National Cancer Institute
Dr. Peter Hosein, co-leader of Sylvester Comprehensive Cancer Center’s Gastrointestinal Cancers Site Disease Group and Associate Professor of Clinical Medicine, embarked on a small study of 12 pancreatic cancer patients with BRCA, RAD51C and similar mutations to prove whether immunotherapy was a viable option.
This was the first study to show activity of this immunotherapy combination in patients with pancreato-biliary tumors with homologous recombination deficiency.
Dr. Hosein also designed and obtained funding for a new phase I trial of the combination of MEK, STAT3 and PD-1 inhibition in patients with metastatic pancreatic adenocarcinoma.
The National Cancer Institute (NCI) awarded $7 million to study the impact of nutrition and exercise on ovarian cancer outcomes at Sylvester Comprehensive Cancer Center and Yale Cancer Center.
Tracy Crane, Ph.D., R.D.N., Director of Lifestyle Medicine and Digital Health in Cancer Survivorship and Co-Leader of the Sylvester’s Cancer Control Research Program, helped develop the medical nutrition therapy and exercise intervention that will be randomly assigned to newly diagnosed ovarian cancer patients scheduled to receive treatment.
Dr. Hernandez-Aya co-led the Phase 1 study “Safety, Tolerability and Efficacy of Tebentafusp Using a Step-Up Dosing Regimen and Expansion in Patients with Metastatic Uveal Melanoma.” The study showed the safety and efficacy of this new agent in treating uveal melanoma, which is a difficult disease to treat, supporting FDA approval.
Research Day judges Namrata Chandhok, M.D. and Gina D’Amato, M.D.

Professors
Bach Ardalan, M.D. Pasquale Benedetto, M.D. Lynn Feun, M.D.
Erin Kobetz, Ph.D., M.P.H. Marc Lippman, M.D. (Emeritus) Stephen Richman, M.D. (Emeritus) Jonathan Trent, M.D., Ph.D. Professors of Clinical Medicine
Marijo Bilusic, M.D., Ph.D. Judith Hurley, M.D. Gilberto Lopes, M.D., M.B.A. Jose Lutzky, M.D. Research Professor
Niramol Savaraj, M.D.
Associate Professors
Tracy Crane, Ph.D., R.D.N. Jaime Merchan, M.D. Associate Professors of Clinical Medicine
Gina D’Amato, M.D. Peter Hosein, M.D. Chukwuemeka Ikpeazu, M.D. Alejandra Perez, M.D. Catherine Welsh, M.D.
Assistant Professors of Clinical Medicine
Carmen Calfa, M.D.
Leonel Hernandez Aya, M.D. Emily Jonczak, M.D.
Lawrence Negret, M.D. Coral Olazagasti, M.D. Daniel O’Neil, M.D.
Agustin Pimentel, M.D. Pearl Seo, M.D. Janaki Sharma, M.D. Frances Valdes-Albini, M.D. Luis Villa, M.D.
Research Assistant Professors
Zinzi Bailey, Sc.D., M.S.P.H. Akina Natori, M.D. Natasha Solle, Ph.D.
Staff Physicians
Richa Dawar, M.D. Milena Elimelakh, M.D. Mauricio Escobar, M.D. Nkiruka Ezenwajiaku, M.D. Gustavo Fernandez, M.D. Elisa Krill Jackson, M.D. Vinay Minocha, M.D. Joseph Pizzolato, M.D. Estelamari Rodriguez, M.D. Tariq Sabir, M.D. Rakesh Singal, M.D. Jose Carlos Suarez, M.D.
DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 39
Division Highlights
MEDICAL ONCOLOGY
Education
The division continues to host monthly meetings with faculty and staff, weekly grand round teaching conferences and ad hoc meetings to discuss timely topics. Dr. Gina D’Amato, Associate Professor of Clinical, was awarded the Outstanding Mentor of the Year, Trainees for 2022. Dr. D’Amato co-directs the Oncology Pathway at the Miller School of Medicine and advises the Nurse Practitioner Oncology Fellowship Program.
Highlights
Dr. Gilberto Lopes was selected as cochair of the Access to Oncology Medicines (ATOM) Coalition initiative by the Union for International Cancer Control (UICC). The ATOM Coalition is a new global initiative established to improve access to essential cancer medicines in low- and lower middleincome countries, as well as to increase the capacity for diagnosing cancer and for the proper handling and supply monitoring of these medicines.
Dr. Carmen Calfa has been appointed as Chair-Elect of the Targeted Agent and Profiling Utilization Registry Study (TAPUR) Steering Group of the American Society of Clinical Oncology (ASCO). Dr. Calfa will serve as Chair-Elect of the TAPUR Steering Group for the 2021-2022 term, followed by a oneyear term as Chair and one year as past Chair.
Dr. Carmen Calfa, Assistant Professor of Clinical, Medical Co-Director of Cancer Survivorship and Translational Behavioral Sciences as well as Program Director of the Miami Precision Medicine Conference, hosted the inaugural event last April. The event highlighted how evolving precision medicine technologies such as nextgeneration sequencing, lliquid biopsies and molecularly driven clinical trials are creating a new era of hope for patients and patient advocates.
UHEALTH|UNIVERSITY OF MIAMI MILLER SCHOOL OF MEDICINE 40
KATZ FAMILY DIVISION OF NEPHROLOGY AND HYPERTENSION
Professors of Medicine
Clinical
Alessia Fornoni, M.D., Ph.D.
Division Chief
The division is known for its clinical excellence, delivering consistent, high-quality care to patients. In response to the 2019 executive order from the U.S. government, which launched the Advancing American Kidney Health Initiative, the University of Miami was able to dramatically expand the home dialysis service from 8 percent in 2018 to 15 percent in 2022 under the leadership of Dr. Adriana Dejman. This also led to the establishment of a new home dialysis directorship in Coral Gables.

Under Dr. Yelena Drexler’s leadership, the division continued to deliver safe, highquality care through telemedicine to patients at high risk for severe COVID infection. Due to this virtual option, we witnessed a 25 percent increase in outpatient volume and a dramatic reduction in the no-show rate.
Our APRNs added an educational telehealth clinic for patients who require dialysis or kidney transplantation. In addition, the division started a hypertension nephrology clinic in the Cardiovascular Center at University of Miami Hospital and Clinics (UHealth Tower).
To further strengthen the focus on outstanding healthcare delivery, the division will participate in the Center for Medicare and Medicaid Innovation’s Comprehensive Kidney Care Contracting (CKCC) model under the leadership of Dr. Oliver Lenz.
The Miami Transplant Institute is a multidisciplinary transplant center providing state of the art transplant options for patients with end stage organ failure. The kidney transplant program has been amongst the leaders nationally in the number of kidney transplants performed for the last several years. In addition to deceased donor transplantation, an active living donor
Alessia Fornoni, M.D., Ph.D. David Roth, M.D.
Professors of Clinical Medicine
Gabriel Contreras, M.D., M.P.H. Giselle Guerra, M.D. Warren Kupin, M.D. Oliver Lenz, M.D., M.B.A.
Associate Professors of Clinical Medicine
Marco Ladino Avellaneda, M.D. Adela Mattiazzi, M.D. Jair Munoz Mendoza, M.D. Mariella Ortigosa-Goggins, M.D.
Research Associate Professor
Sandra Merscher, Ph.D.
Assistant Professors of Clinical Medicine
Franco Cabeza, M.D. Adriana Dejman, M.D. Juan Duque, M.D. Yelena Drexler, M.D. Desiree Garcia, M.D. Zain Mithani, M.D. Efren Chavez Morales, M.D. Javier Pagan, M.D. Shobana Sivan, M.D. Marie Anne Sosa, M.D.
Research Assistant Professor Tali Elfassy, Ph.D. Research Instructor Jin-Ju Kim, Ph.D.
program is available, including a paired exchange option. Furthermore, the Institute now offers robotic living donor and recipient surgery options for the appropriate patients, one of just a few centers in the country to do so. Faculty are involved in several NIH-funded areas of research, including APOL1-related kidney disease and the use of kidneys from donors infected with hepatitis C virus. A dedicated team of nine transplant nephrologists works closely with their surgical colleagues to maintain excellence and to provide these transplant options to the community.
DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 41
Division Highlights
KATZ FAMILY DIVISION OF NEPHROLOGY AND HYPERTENSION
Research
In the Katz Drug Discovery Center, Dr. Alessia Fornoni, Dr. Sandra Merscher and Dr. Hassan A. Alifrom the Department of Neurological Surgery, were awarded an industry grant to work on novel therapeutics for Alport syndrome. Dr. Fornoni became the national principal investigator (PI) of a natural history study for patients affected by Alport syndrome sponsored by the NIH and the Alport Syndrome Foundation. Dr. Fornoni, who is also co-chair of the International Society of Nephrology, funded a new company (R3R Corporation) to test a drug she invented in phase II clinical trials.
The Katz Family Division of Nephrology and Hypertension remained highly productive this past year. In addition to
more than 12 ongoing clinical trials, both NIH and industry supported, the division added multiple grants, awards and publications to an already strong research presence.
Four faculty members were awarded grants to facilitate transitions to independence. Dr. Tali Elfassy is the recipient of a K01 grant on understanding hypertension in Hispanic populations.
Dr. Yelena Drexler is the recipient of a KL2 grant for her work on biomarkers in glomerular disorders.
Dr. Jin Ju Kim was awarded a K01 grant for her work on extracellular matrix biology.
Dr. Alla Mitrofanova received the prestigious Carl W. Gottschalk Award from the American Society of Nephrology, the first time

UHEALTH|UNIVERSITY
OF MEDICINE 42
OF MIAMI MILLER SCHOOL
for a University of Miami faculty member.
Dr. Ortigosa Goggins developed a strong national visibility in the field of kidney transplantation in African Americans, while serving as the local principal investigator (PI) of a large NIH network grant.
At the post-doctoral level, Dr. Jeffrey Pressly was awarded the Kidney Cure Ben J. Lipps Research Fellowship.
Just in 2021, Division faculty also published work in many peer-reviewed publications with 110 publications, 13 of which addressed COVID-related topics
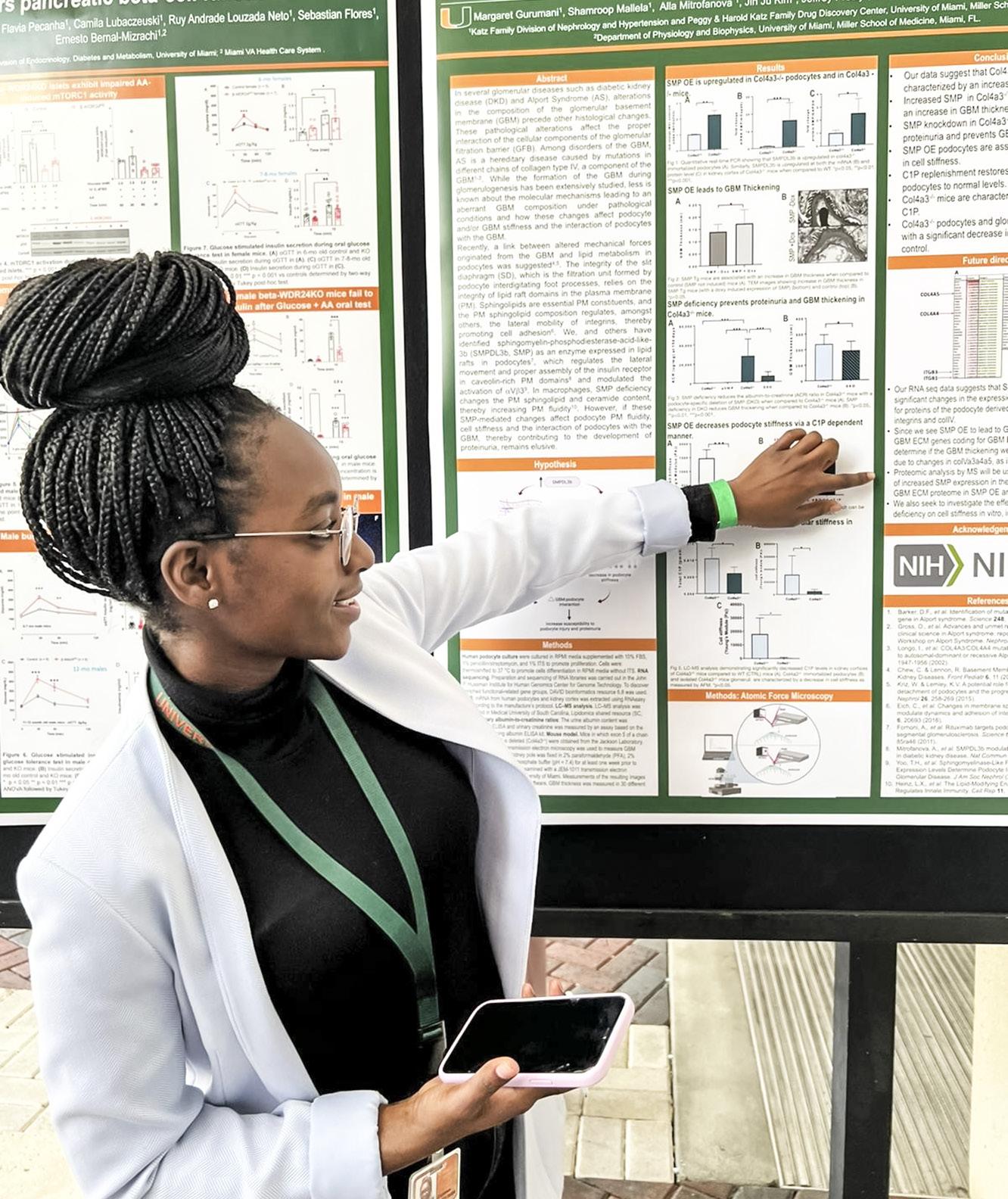
Education
Our fellowship training program continues to attract a highly diverse and competitive group of fellows. In collaboration with the Division of Hospital Medicine and the Gordon Center, the program has strengthened its focus on simulation training to enhance patient safety, kicking off the academic year with simulation training for central line placements.
The COVID-19 pandemic has resulted in a significantly higher patient load. However, thanks to faculty members who took on additional patients, this did not negativlely impact our training program. Instead, fellows learned how to adapt to changing demands, such as increased dialysis needs and the inability to conduct in-person clinic visits.
Highlights
Dr. Maria Anne Sosa was named Director of Graduate Medical Education (GME) at UHealth.
2021-2022 Fellows Graduation Dinner
Left to right: Michael Samiratedu, M.D.; Patrick Francois, M.D.; Neda Shahoori, M.D.; Juanly Rodriguez, M.D. and Alfonso Ortiz, M.D.
Medical Department.
The UM-KIIMERA T35 training grant, a nephrology-focused research course, graduated its second class of medical students from its summer research program. Due to its success UM-KIIMERA is being used as a template for other divisions that wish to foster interest in specialty-specific physicianscientist careers.
in Molecular and Cellular Pharmacology working under the mentorship of Dr. Fornoni, presenting her work on how lipids can affect cell stiffness and thus influence their ability to properly interact with
Dr. Marco Aurelio Ladino was selected as the internal medicine consultant for the Surgeon General in the United States Army Reserve
Margaret Gurumani, a graduate student
basement membranes during the annual Department of Medicine Research Day.
DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 43
Division Highlights
PULMONARY, CRITICAL CARE AND SLEEP MEDICINE
Clinical
During fiscal year 2022, the division expanded its clinical, educational and research missions.

The division hired four additional faculty members to expand our clinical inpatient and outpatient operations. The clinical inpatient expansion includes an intermediate care step down unit, as well as a co-managed cardiac unit that will improve quality of care and length of stay on our units.
in outpatient volume, we have developed dedicated specialty clinics to include nontuberculous mycobacteria (NTM), airway disease and endoscopic lung volume reduction, while additionally improving access metrics for our entire longitudinal panel.
Research
Naresh Punjabi, M.D., Ph.D. Division Chief

The clinical outpatient expansion includes an additional six rooms to increase the overall capacity to 14 rooms that will improve and better accommodate our outpatient patient base. With this expansion
The Division of Pulmonary, Critical Care and Sleep Medicine has partnered with industry sponsors, including Siemens and 4D Medical, to promote novel diagnostic approaches. Along with the Department of Radiology, we have developed a functional imaging center to assess regional ventilation heterogeneity in
UHEALTH|UNIVERSITY OF
SCHOOL OF MEDICINE 44
MIAMI MILLER
individuals with chronic respiratory disease.
With Siemens Healthineers Division, division faculty members have been implementing novel-machine learning instruments to subsegment lungs using single photon emission computed tomography. We have additionally developed novel approaches to examine regional airflow using X-ray velocimetry to assess therapeutic response to endobronchial valve placement. These novel discoveries will allow the division to continue as a national leader in advancing care for individuals with respiratory disease.
The division has expanded its federal and non-federal research portfolio. In fact, the division will be leading an NIH-funded study to assess community-based sleep interventions in Liberty City as part of a P50 consortium award with Vanderbilt University Medical Center and Meharry Medical College. Additionally, the division submitted a competitively scored T32 application to improve training in pulmonary and sleep diseases.
Education
As part of our education mission, we have increased the number of fellowship spots, including dedicated research fellowship positions for two fellows to conduct longitudinal research with our faculty.
We additionally held an in-person airways workshop that will serve as a model for regional training for advanced airway management in acute respiratory failure. The workshop used best practice approaches to laryngoscopy, including ear-to-sternal notch positioning, bimanual laryngoscopy and straight-to-cuff stylet shaping.
Professors
Horst J. Baier, M.D. (Emeritus) Robert M. Jackson, M.D. Naresh Punjabi, M.D., Ph.D. Matthias A. Salathe, M.D. (Emeritus)
Roland M. Schein, M.D. Adam Wanner, M.D. Philip Whitney, Ph.D. (Emeritus)
Professors of Clinical Medicine
Michael A. Campos, M.D. Alejandro Chediak, M.D. Hayley B. Gershengorn, M.D. Daniel H. Kett, M.D. Andrew Quartin, M.D. Shirin Shafazand, M.D., M.S.
Associate Professors
Alexandre Abreu, M.D. David De La Zerda, M.D. Elio Donna, M.D. Tanira Ferreira, M.D. Gregory Holt, M.D., Ph.D. Diane Lim, M.D. Neeraj Sinha, M.D.
Assistant Professors Saramaria AfanadorCastiblanco, M.D. Roger Alvarez, D.O. Sixto Arias, M.D. Kori Ascher, D.O.
Jonathan Auerbach, M.D.
Yaroslav Buryk, M.D.
Jorge Cabrera, D.O. Oveimar De La Cruz, M.D. Lisa Domaradzki, M.D. Lesley Farquharson, M.D. Hannah Ferenchick, M.D. Brian Garnet, M.D.
Sergey Gerasim, M.D. Adhiraj Gosine, M.D. Eric Lang, M.D. Christopher Mallow, M.D. Suresh Manickavel, M.D. Maria Tupayachi Ortiz, M.D. Erick Palma, M.D. Yoslay Perez, M.D. Andrea Shioleno, M.D. Trishul Siddharthan, M.D. Waleed Sneij, M.D. Rene Rico Tresgallo, M.D. Martin Zak, M.D.

Staff Physicians
Andrew Calzadilla, M.D. Christopher Jordan, M.D. Sajid Kadir, M.D. Laiqua Khalid, M.D. Jeffrey Scott, D.O. Andres Sosa, M.D. Moe Zaw, M.D.
DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 45
At left: Division of Pulmonary, Critical Care and Sleep Medicine faculty
Division Highlights
RHEUMATOLOGY AND IMMUNOLOGY
Clinical
The division continued its transition back to in-person clinical care, with an existing telemedicine component – which for some patients has made a major difference in their ability to access care. This virtual option complements our in-person clinical services and has helped expand our reach throughout Florida, particularly Central Florida and the Keys.
Carlos J. Lozada, M.D. Interim Division Chief

The division also added an APRN to our clinical group. He has been training in a setting similar to that of our fellowship trainees and has started seeing clinical practice patients, thus improving patient access to our services.
Research
Dr. Eric Greidinger, along with Dr. Wasif Khan from the Department of Microbiology and Immunology, have collaborated to create and characterize a novel animal model of Sjogren’s syndrome autoimmunity.
This model system – which emerges after a targeted deletion in the cell death protein BIM is introduced selectively in B lymphocytes – develops typical autoantibodies and salivary gland immune infiltrates as seen in Sjogren’s syndrome.
The initial findings were reported in Frontiers in Immunology in August 2021. Additional studies are ongoing.
Division rheumatologists Dr. Maria
UHEALTH|UNIVERSITY
OF MEDICINE 46
OF MIAMI MILLER SCHOOL
Carpintero and Dr. Eric Greidinger are actively participating in more than 10 clinical trials, which are examining the management of systemic lupus erythematosus (SLE) and other autoimmune diseases.

Division Chief Dr. Carlos Lozada is part of the leadership group developing the new Pan American guidelines for the management of psoriatic arthritis. Dr. Lozada is also participating in a new PANLAR tool for the evaluation of rheumatoid arthritis disease activity patients in the clinical setting, which is under development.
Education
Our renowned Rheumatology Fellowship Program had another banner year, with continued increased interest in the program, which is reflected in the steady growth in applications.
Division Chief and Program Director, Dr. Carlos Lozada, was appointed as chief of the executive committee of the International League for Associations for Rheumatology (ILAR) in 2021.
Dr. Lozada also continues as president of the Pan American League for Associations for Rheumatology (PANLAR) with the upcoming 2022 edition of the PANLAR Annual Scientific Meeting slated to take place in Miami in August 2022. Dr. Lozada is currently developing a program within PANLAR that will support increasing the number of training positions in rheumatology throughout the Americas.
Dr. María Carpintero has been elected to the PANLAR board of directors, representing North America. Dr. Carpintero has also taken the lead, along with Dr. Elaine Tozman and Dr. Lozada, in writing a chapter on “Rheumatologic Manifestations of Hemoglobinopathies” for the 12th edition of
Carlos Lozada, M.D. (center) with fellows.
Professor of Clinical Medicine
Carlos J. Lozada, M.D. Associate Professors
Eric Greidinger, M.D. Elaine C. Tozman, M.D. Assistant Professors Maria F. Carpintero, M.D. Ozlem Pala, M.D. Staff Physicians Elena Oberstein, M.D. Schartess Culpepper-Pace, M.D.
the renowned classic textbook Kelley and Firestein’s Textbook of Rheumatology.
Dr. Ozlem Pala has been invited to lecture on recent developments in the field of rheumatoid arthritis at the American College of Rheumatology Review Course in the context of the PANLAR 2022 Annual Scientific Meeting.
We are proud to report that Dr. Ozlem Pala has completed her MSPH degree, presenting and defending her thesis “The Impact of Disease Activity on PatientReported Cognitive Dysfunction in Rheumatoid Arthritis” this past academic year. She submitted her manuscript to Arthritis Care & Research, an official journal of the American College of Rheumatology and the Association of Rheumatology Health Professionals.
DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 47
Division Highlights
TRANSPLANTATION AND CELLULAR THERAPY
Clinical
expertise and collaboration.
Denise Pereira, M.D. Interim Division Chief
The division continues to provide premier clinical care in the areas of hematopoietic stem cell transplantation and T cell immunotherapies. During the past year, we reached the milestone of 2,000 procedures performed since the inauguration of our state-of-the-art inpatient unit at Sylvester Comprehensive Cancer Center. We also celebrated our 150th CAR-T cell infusion. We continue to provide telemedicine and inperson visits at the Miami and Plantation sites and are preparing to expand to the Doral (UHealth Doral Commons MultiSpecialty Clinic) and Coral Gables (Lennar Foundation Medical Center) sites.
Research
The Division of Transplantation and Cellular Therapy continues to forge ahead in research with several projects and publications underway that reflect multiple areas of
Dr. Cara Benjamin received interdisciplinary support from the Clinical Stem Cell Laboratory for her research projects in the areas of lymphoma, leukemia, graft versus host disease (GVHD), melanoma, sarcoma and other solid tumors.


Dr. Amer Beitinjaneh, Dr. Lazaros Lekakis and Dr Jay Spiegel have a sizable number of publications in the field of adoptive cellular immunotherapy, including treatment sequencing, “off-the-shelf” therapies that use allogeneic CAR-T cells and mechanism of resistance to CAR-Ts.
Dr. Antonio Jimenez presented at the American Society for Transplantation and Cellular Therapy (ASTCT) Plenary Session on the use of human leukocyte antigen (HLA)-mismatched unrelated donors as an effective way to expand access to allogeneic transplantation.
Dr. Eric Wieder submitted a patent
UHEALTH|UNIVERSITY OF
SCHOOL OF MEDICINE 48
MIAMI MILLER
application on a novel and promising graftversus-host disease (GVHD) therapy.
Dr. Trent Wang published clinical trial results of belumosudil for chronic graftversus-host disease that ultimately led to FDA drug approval.
Dr. Mark Goodman and Dr. Denise Pereira published research describing the presentation and outcomes of COVID-19 infection following stem cell transplant and cellular therapy.

Education
Our faculty remains committed to our education mission by providing medical school and postgraduate medical education. We hosted the 2021 the American Society for Transplantation and Cellular Therapy (ASTCT) Fall Clinical Education Conference that primarily focused on advanced practice providers, nurses, fellows and junior faculty. Furthermore, division faculty members have delivered lectures at the local, national and international levels.
Highlights
Our physicians remain committed and engaged in the discipline of transplantation and cellular therapy across multiple administrative areas. The division has representation at the National Marrow Program Scientific Advisory Board and faculty members sit on multiple working committees at the Center for International Blood and Marrow Transplant Research, Florida Medical Association Council on Medical Education, Science and Public Health as well as multiple University of Miami Hospital and Clinics (UMHC) committees.
Left to right: Antonio Jimenez, M.D.; Amer Beitinjaneh, M.D.; Krishna Komanduri, M.D.; Denise Pereira, M.D.; Trent Wang, D.O. and Jay Spiegel, M.D.
Professor of Clinical Medicine
Krishna Komanduri, M.D. Associate Professors of Clinical Medicine
Lazaros J. Lekakis, M.D. Amer Beitinjaneh, M.D. Mark S. Goodman, M.D. Research Associate Professor Eric Wieder, Ph.D.
Assistant Professors of Clinical Medicine
Denise L. Pereira, M.D. Trent Wang D.O. Antonio M. Jimenez, M.D. Jay Y. Spiegel, M.D. Research Assistant Professor Cara Benjamin, Ph.D.
DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 49
Philanthropy
Dr. Erin Kobetz honored with the John K. and Judy H. Schulte Senior Endowed Chair in Cancer Research
From his humble start as a University of Miami student to the pinnacle of his public relations career, John K. Schulte was a steadfast supporter of his alma mater.

After witnessing the medical expertise and compassionate care delivered to dear friends and family during their illnesses, Schulte and his wife, Judy, focused their philanthropic support on Sylvester Comprehensive Cancer Center at the Leonard M. Miller School of Medicine. While the couple gave generously during their lifetime, they arranged to have much of their estate given to Sylvester in support of research and education after their passing. John passed away in 2018 and Judy in 2016.
Their legacy will now live on in perpetuity through their bequest to Sylvester, including the John K. and Judy H. Schulte Senior Endowed Chair in Cancer Research, which was recently presented to Erin Kobetz, vice provost for research and scholarship, professor, and Sylvester’s associate director for population sciences and cancer disparity.
The Schulte’s endowment will allow Dr. Kobetz to continue her research, which has already dramatically reduced
cancer disparities in Miami’s underserved communities and led to Sylvester being named the first World Health Organization (WHO) collaborating Center for Cervical Cancer Elimination.
“An important part of the legacy of the Schultes is the enabling of our very best to do their very best,” said Stephen D. Nimer, director of Sylvester Comprehensive Cancer Center. “This endowed chair reflects a steadfast belief in the potential, the talents and the accomplishments of Dr. Kobetz.”

From left to right: President Julio Frenk; Provost Jeffrey L. Duerk; Dr. W. Jarrard Goodwin; Miller School Dean Henri R. Ford; Dr. Stephen D. Nimer and Dr. Roy E. Weiss, with recipient Erin Kobetz, Ph.D., M.P.H.
From left to right: Dipen J. Parekh, M.D.; President Julio Frenk; Swanee DiMare; Stephen D. Nimer, M.D.; Roy E. Weiss, M.D., Ph.D. and Provost Jeffrey L. Duerk, with recipient Ola Landgren, M.D., Ph.D.
UHEALTH|UNIVERSITY OF MIAMI MILLER SCHOOL OF MEDICINE 50
Family Endowed Chair in Biomedicine
Driven by a shared love of science and a passion for finding a permanent cure for HIV/AIDS, Raymond F. Schinazi, Ph.D. and Mario Stevenson, Ph.D., who are longtime colleagues and friends, have taken a crucial step to ensure lifesaving research to prevent and treat infectious diseases continues at the University of Miami Miller School of Medicine.
Dr. Stevenson, a renowned expert in molecular virology, was officially installed as the inaugural holder of the Raymond F. Schinazi and Family Endowed Chair in Biomedicine during a dedication ceremony held recently in Coral Gables. The honor was made possible by Dr. Schinazi, his wife Nadira and their family.

Dr. Schinazi is best known for his pioneering work in antiviral drug
development for HIV, HBV, HCV and other pathogens.
“The greatest history between Mario and myself is our love for science, working on HIV and other viruses,” said Dr. Schinazi. “Some of Mario’s work early on was fundamental in finding a potential cure for HIV, which has eluded us all so far.”
“I believe a cure for HIV/AIDS is realistic and within reach,” said Dr. Stevenson, professor, director of the HIV and Emerging Infectious Diseases Institute and co-director of the Center for AIDS Research at the Miller School. “I intend to use this endowment to continue my work, specifcially understanding how the virus can evade elimination by the overwhelming antiviral regimens used against it,” added Stevenson added.
Dimare Endowed Chair in Immonotherapy
The presentation of the Paul J. DiMare Endowed Chair in Immunotherapy could best be described as a convergence of great generosity and brilliant talent. The event recognized the contributions of two remarkable people: philanthropist Paul J. DiMare and world-renowned multiple myeloma researcher C. Ola Landgren, M.D., Ph.D. Together, their efforts will go far toward advancing innovative research to cure cancer.
Through the chair, Dr. Landgren, chief of the Myeloma Program and Riney Family Multiple Myeloma Research Program, leader of the Experimental Therapies Program and co-leader of the Tumor Biology Program at Sylvester
Comprehensive Cancer Center at the University of Miami Miller School of Medicine, will be able to continue his groundbreaking research integrating immunotherapy into the development of curative treatment strategies for multiple myeloma and other cancers.
“This is a time of great hope and promise for cancer patients and their families,” said Dr. Landgren, who is also a professor at the Miller School. “The development of novel immunotherapies, partnered with improved biological understanding of the immune system is already dramatically reshaping what we can achieve through cancer therapy.”
From left to right: Roy E. Weiss, M.D., Ph.D.; Mario Stevenson, Ph.D. and Raymond F. Schinazi, Ph.D.
Dr. Landgren honored with the Paul J.
Dr. Stevenson honored with the Raymond F. Schinazi and
DEPARTMENT OF MEDICINE CHAIRMAN’S REPORT 2022 51
Philanthropy
$1 million+ 4 $8,400,000 $100,000-$999,999 19 $4,900,000 $10,000-$99,999 62 $1,900,000 $1,000-$9,999 63 $165,000 $999 and below 223 $50,000
Total
Infectious Diseases $4,337,000 Digestive Health & Liver Diseases $1,887,000 Pulmonary Medicine $1,253,000 Endocrinology & Diabetes $1,002,000 Top
Digestive Health & Liver Diseases 194 Cardiovascular Disease 56 Infectious Diseases 33 Internal Medicine 19 Hematology 17
and
Gift
Gifts
Donors by
Level Gifts by Designation Gifts by Type TOTAL DOLLARS RAISED
FUNDRAISING GROWTH FY22 TOTAL: $15,415,000 # of Donors Total
Top Divisions by Gift Dollars
Divisions by Number of Donors # of Donors
Number of Donors and Dollars Raised Number of Gifts and $1000,000+ Dollars Raised FY19 300 Donors $6,300,000 FY19 18 Gifts $4,010,100 FY20 311 Donors $5,003,000 FY20 10 Gifts $2,879,000 FY21 298 Donors $7,017,000 FY21 19 Gifts $3,923,000 FY22 371 Donors $15,415,000 FY22 23 Gifts $4,945,000 In Millions In Millions 4
Gifts
5
339
322
28
43 Pledges =
UHEALTH|UNIVERSITY OF MIAMI MILLER SCHOOL OF MEDICINE 52
Endowment
= $6,004,000
Planned Gifts = $560,000
Current Use Gifts = $4,414,000
Cash Commitments = $3,176,000
Grants/Sponsorships = $4,997,000
$11,679,000
Leadership
University of Miami Leadership
Julio Frenk, M.D., M.P.H., Ph.D.
President
Joseph J. Echevarria
CEO, UHealth and EVP of Health Affairs
Dipen J. Parekh, M.D. COO, UHealth
Henri R. Ford, M.D., M.H.A.
Dean and Chief Academic Officer
Department Leadership
Roy E. Weiss, M.D., Ph.D.
Chair
Anna Carol Herman-Giddens, R.N., B.S.N.
Senior Administrative Officer
Maureen Lowery, M.D., F.A.C.C.
Vice Chair of Faculty Development and Diversity
Michael Kolber, M.D., Ph.D.
Vice Chair for Clinical Affairs
Amar Deshpande, M.D.
Vice Chair for Education
Maria Abreu, M.D.
Vice Chair for Research
Khemraj Hirani, M.D. Associate Vice Chair for Research Regulatory Compliance
David H. Kerman, M.D. CMO for DOM Carlos Prieto
Executive Director, Business Development and Clinical Operations
Ivelisse Rodriguez
Executive Director, Finance
Laura J. Pinzon, M.B.A. Director, Administrative Operations
Alina Kasyanova, M.B.A.
Director, Sponsored Programs

Jannet Yern
Executive Director, Employee and Student Health Services
Iliana Vera, M.B.A.
Sr. Department Administrator, Clinical Operations
Rolando J. Briceno, M.B.A. Director, Strategic Operations
Division Chiefs
Jeffrey Goldberger, M.D., M.B.A. Cardiovascular
Richard Preston, M.D., M.S.P.H., M.B.A. Clinical Pharmacology
Paul Martin, M.D. Digestive Health and Liver Diseases
Ernesto Bernal-Mizrachi, M.D. Endocrinology, Diabetes and Metabolism
Alejandro Chediak, M.D., F.A.A.S.M., F.C.C.P., F.A.C.P. (Interim) General Internal Medicine
Marcio Soares, M.D. Geriatrics and Palliative Medicine
Mikkael A. Sekeres M.D., M.S. Hematology
Marcio Soares, M.D. (Interim) Hospital Medicine
Susanne Doblecki-Lewis, MD Infectious Diseases
Gilberto de Lima Lopes Junior, M.D., M.B.A., F.A.M..S (Interim) Medical Oncology
Stefanie Brown, M.D. Medicine-Pediatrics
C. Ola Landgren, M.D., Ph.D. Myeloma
Alessia Fornoni, M.D., Ph.D.
Katz Family Division of Nephrology and Hypertension
Naresh M. Punjabi, M.D., Ph.D. Pulmonary, Critical Care and Sleep Medicine
Carlos Lozada, M.D. (Interim) Rheumatology and Immunology
Denise Pereira, M.D. (Interim) Transplantation and Cellular Therapy
Division Administration

Francisco M. Rodriguez, M.S.
Cardiovascular
Carol Cottrell
Digestive Health and Liver Diseases
Cristina Calderon-Parra
Endocrinology, Diabetes and Metabolism
Joanne Alonso, M.B.A.
General Internal Medicine
Joanne Alonso, M.B.A.
Geriatrics and Palliative Medicine
Ali R. Ismail
Hematology
Rolando J. Briceno, M.B.A. Hospital Medicine
Lily Ferrer, M.B.A., C.R.A. Infectious Diseases
Ingrid V. Rodriguez, M.B.A. Medical Oncology
Frances Castellvi Senti, M.B.A. Medicine-Pediatrics
Ivette Vento
Myeloma
Carol Cottrell
Katz Family Division of Nephrology and Hypertension
Austin Pitts
Pulmonary, Critical Care and Sleep Medicine
Carol Cottrell
Rheumatology and Immunology
Debra Chinquee, RN, MSN,

1120 NW 14th Street, Suite 310
med.miami.edu/departments/medicine
Miami, FL 33136 305-243-9120














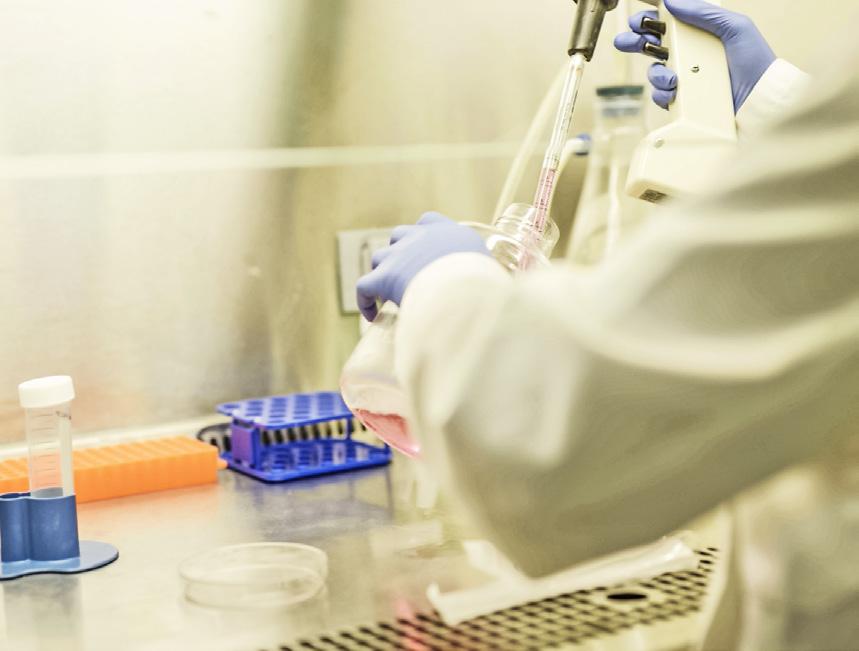








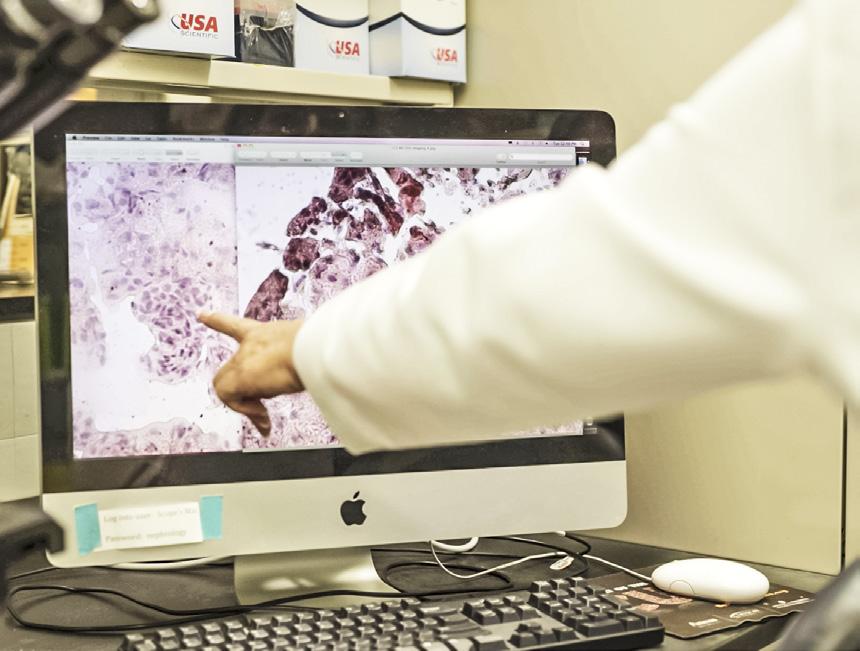



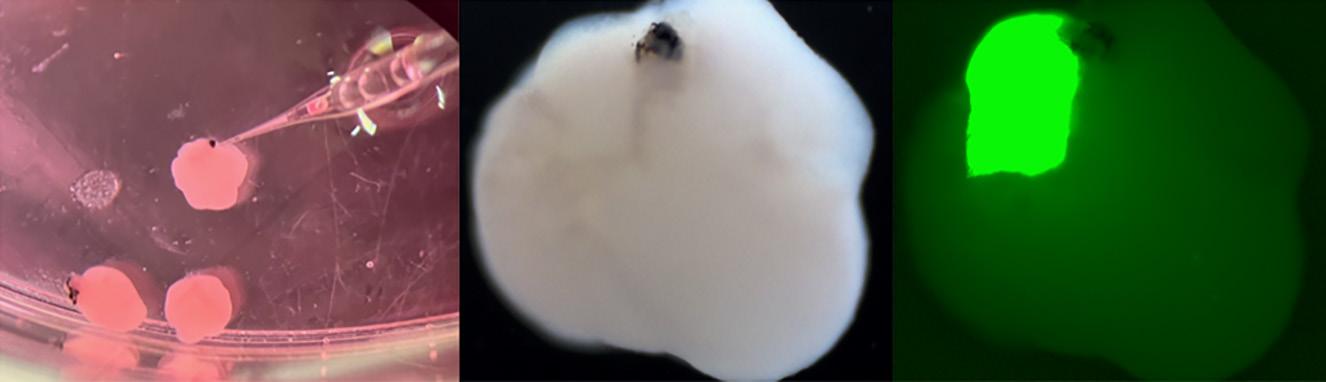






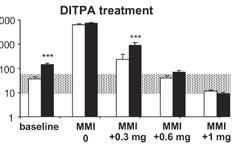
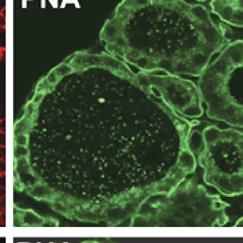
 Samuel
Samuel



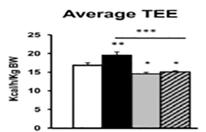








































 Mikkael Sekeres, M.D., M.S. Division Chief
Mikkael Sekeres, M.D., M.S. Division Chief




 Susanne
Susanne


 Gilberto Lopes, M.D., M.B.A.,
Interim Division Chief
Gilberto Lopes, M.D., M.B.A.,
Interim Division Chief